
Stte of Helth n the EU
Luxembour
Countr Helth Profle 2021

2
Stte of Helth n the EU Luxembour Countr Helth Profle 2021
The Countr Helth Profle seres
The Stte of Helth n the EU’s Countr Helth Profles
provde concse nd polc-relevnt overvew of
helth nd helth sstems n the EU/Europen Economc
Are The emphsse the prtculr chrcterstcs nd
chllenes n ech countr nst bcdrop of cross-
countr comprsons The m s to support polcmers
nd nfluencers wth mens for mutul lernn nd
voluntr exchne
The profles re the ont wor of the OECD nd the
Europen Observtor on Helth Sstems nd Polces,
n cooperton wth the Europen Commsson The tem
s rteful for the vluble comments nd suestons
provded b the Helth Sstems nd Polc Montor
networ, the OECD Helth Commttee nd the EU Expert
Group on Helth Sstems Performnce Assessment (HSPA)
Contents
1 3
2 4
3 6
4 7
5 11
51 Effectveness 11
52 Accessblt 13
53 Reslence 16
6 22
Dt nd nformton sources
The dt nd nformton n the Countr Helth Profles
re bsed mnl on ntonl offcl sttstcs provded
to Eurostt nd the OECD, whch were vldted to
ensure the hhest stndrds of dt comprblt
The sources nd methods underln these dt re
vlble n the Eurostt dtbse nd the OECD helth
dtbse Some ddtonl dt lso come from the
Insttute for Helth Metrcs nd Evluton (IHME), the
Europen Centre for Dsese Preventon nd Control
(ECDC), the Helth Behvour n School-Aed Chldren
(HBSC) surves nd the World Helth Ornzton
(WHO), s well s other ntonl sources
The clculted EU veres re wehted veres of
the 27 Member Sttes unless otherwse noted These EU
veres do not nclude Icelnd nd Norw
Ths profle ws completed n September 2021, bsed on
dt vlble t the end of Auust 2021
Demographic factors Luxembourg EU
Populton sze (md-er estmtes) 626 108 447 319 916
Shre of populton over e 65 (%) 145 206
Fertlt rte (2019) 13 15
Socioeconomic factors
GDP per cpt (EUR PPP) 79 223 29 801
Reltve povert rte (%, 2019) 175 165
Unemploment rte (%) 68 71
1 Numbr of chldrn born pr womn gd 15-49 2 Purchsng powr prt (PPP) s dfnd s th rt of currnc convrson tht qulss th
purchsng powr of dffrnt currncs b lmntng th dffrncs n prc lvls btwn countrs 3 Prcntg of prsons lvng wth lss thn 60 %
of mdn quvlsd dsposbl ncom Sourc Eurostt dtbs
Dsclmer The opnons expressed nd ruments emploed heren re solel those of the uthors nd do not necessrl reflect the offcl vews of
the OECD or of ts member countres, or of the Europen Observtor on Helth Sstems nd Polces or n of ts Prtners The vews expressed heren
cn n no w be ten to reflect the offcl opnon of the Europen Unon
Ths document, s well s n dt nd mp ncluded heren, re wthout preudce to the sttus of or soverent over n terrtor, to the delmtton
of nterntonl fronters nd boundres nd to the nme of n terrtor, ct or re
Addtonl dsclmers for WHO ppl
© OECD nd World Helth Ornzton (ctn s the host ornston for, nd secretrt of, the Europen Observtor on Helth Sstems nd
Polces) 2021
Demographic and socioeconomic context in Luxembourg, 2020

3
Stte of Helth n the EU Luxembour Countr Helth Profle 2021
1 Hhlhts
Luxembourg has seen a continuous increase in life expectancy up to 2019, but there was a significant fall in 2020
because of deaths due to COVID-19. Behavioural risk factors contribute to more than one third of all deaths, with
high alcohol consumption and growing obesity rates of particular concern. Luxembourg’s population enjoys good
access to health care, with a broad benefits package and low out-of-pocket payments. Luxembourg reacted rapidly
to the COVID-19 pandemic with implementation of a large-scale testing strategy, teleconsultations, a national
reserve of health professionals and a reorganisation of primary care.
Health Status
Life expectancy at birth in Luxembourg increased by nearly two years
between 2010 and 2019. Although it then fell by nearly one year in 2020
during the COVID-19 pandemic, it is still above the EU-wide average.
Despite reductions in ischaemic health disease and stroke rates, they
remain the leading causes of death, along with lung cancer.
Risk factors
Behavioural risk factors – especially poor nutrition, smoking, physical inactivity
and alcohol consumption – are major drivers of morbidity and mortality in
Luxembourg. One in three adults report binge drinking behaviour, which is
the third highest rate in the EU. Overweight and obesity levels and physical
inactivity among 15-year-olds are above the EU average. On a more positive
note, smoking levels have declined since 2001 for both adults and adolescents.
Health system
In 2019, Luxembourg spent EUR3742 per capita on health (adjusted for
purchasing power parity), which is relatively high compared to the EU
average of EUR3523. The public share of total health spending (85%) was
also above the EU average. In 2020, public spending on health increased
sharply in response to the COVID-19 pandemic.
Effectiveness
Preventable mortality is lower
than the EU average, reflecting
the effectiveness of prevention
policies. Treatable causes of
mortality are also low, indicating
that the health system provides
effective primary and acute care
for potentially fatal conditions.
Accessibility
Coverage of health services in
Luxembourg is generally good, and
unmet needs for care are among
the lowest in the EU. However,
during the first 12 months of
the COVID-19 pandemic, one
in five people reported forgoing
medical care – slightly lower
than the EU average. Growing use
of teleconsultations helped to
maintain access to care during the
various waves of the pandemic.
Resilience
Luxembourg responded rapidly
to the pandemic, and set up
various measures such as large-
scale testing and effective contact
tracing. The vaccination campaign
was rolled out in six phases. As of
the end of August 2021, 56% of
the population had received two
doses of COVID-19 vaccine (or
equivalent).
LU EU
Option 1: Life expectancy - trendline Select a country:
Option 2: Gains and losses in life expectancy
Luxembourg
80.8
82.4
82.7
81.8
79.8
80.5
81.3
80.6
2010 2015 2019 2020
Yea rs
Luxembourg
Life expectancy at birth
2.8
1.9
-0.9
2.5
1.5
-0.7
2010/2019
2019/2020
2000/2010
Lf xpctnc t brth, rs
Ag-stndrdsd mortlt rt
pr 100 000 populton, 2018
Preventble
mortlt
Tretble
mortlt
EEffffeeccttiivveenneessss -- PPrreevveennttaabbllee aanndd ttrreeaattaabbllee mmoorrttaalliittyy Select country
Country code Country Preventable Treatable
AT Austria 157 75
Treatable mortality
BE Belgium 146 71
Preventable mortality
BG Bulgaria 226 188
HR Croatia 239 133
CY Cyprus 104 79
FFoorr ttrraannssllaattoorrss OONNLLYY::
CZ Czechia 195 124
DK Denmark 152 73
EE Estonia 253 133
FI Finland 159 71
FR France 134 63
DE Germany 156 85
GR Greece 139 90
HU Hungary 326 176
IS Iceland 115 64
IE Ireland 132 76
IT Italy 104 65
LV Latvia 326 196
LT Lithuania 293 186
LU
Luxembourg
130 68
MT Malta 111 92
NL
Netherlands
129 65
NO Norway 120 59
PL Poland 222 133
PT Portugal 138 83
Original (don't change)
Austria
Belgium
Germany
Croatia
Cyprus
Bulgaria
Czechia
Denmark
Estonia
Finland
France
Greece
Hungary
Iceland
Treatable mortality
Preventable mortality
Age-standardised mortality rate per 100 000 population, 2018
92
160
68
130
Treatable mortality
Preventable mortality
Luxembourg EU
Age-standardised mortality rate per 100 000
Shr of totl populton vccntd gnst
COVID-19 up to th nd of August 2021
SShhaarree ooff ttoottaall ppooppuullaattiioonn vvaacccciinnaatteedd aaggaaiinnsstt CCOOVVIIDD--1199
Note: Up to end of August 2021
Source: Our World in Data.
Note for authors: EU average is unweighted (the number of countries included in the average varies depending on the week). Data extracted on 06/09/2021.
54%
56%
62%
64%
0%10%20%30%40%50%60%70%80%90%100%
EU
Luxe
Two doses (or equivalent) One dose
LU
EU
0% 50% 100%
Two doses (or equvlent) One dose
Overweight
and obesity
Smoking
Binge drinking
0 20 40
0 20 40
0 20 40
Smoking
% of adults
Overweight and
obesity
% 15-year-olds
Binge drinking
% of adults
1
LU EU Lowest Hhest
Pr cpt spndng (EUR PPP)
LU EU
Luxembourg EU
€ 4 500
€ 3 000
€ 1 500
€ 0
LU EU
Accessibility - Unmet needs and use of teleconsultations during COVID-19
Option 1:
Croatia
Option 2:
39%
42%
% using
teleconsultation
during first 12 months
of pandemic
21%
25%
Croatia EU
% reporting forgone
medical care during
first 12 months of
pandemic
0
10
20
30
Croatia
% reporting forgone medical
care during first 12 months
of pandemic
% using teleconsultation
during first 12 months of
39%
42%
% using
teleconsultation
during first 12 months
of pandemic
21%
25%
Croatia EU
% reporting forgone
medical care during
first 12 months of
pandemic
% reporting forgone
medical care during first
12 months of pandemic
% using teleconsultation
during first 12 months of
pandemic
% reporting forgone medical
care during first 12 months
of pandemic
% using teleconsultation
during first 12 months of
pandemic
0% 1% 2% 3% 4%
L
EU
High income
All
Low income
LU
EU
% rportng unmt mdcl cr nds, 2019
Hh ncome All Low ncome

4
Stte of Helth n the EU Luxembour Countr Helth Profle 2021
2 Helth n Luxembour
1. Includes deaths with and from COVID-19 in all settings (hospitals, nursing homes and at home).
Life expectancy in Luxembourg is
relatively high, but COVID-19 had
an important impact in 2020
In 2020, life expectancy at birth in Luxembourg
stood at 81.8 years, over one year higher than the EU
average, but below other EU countries such as Ireland,
Malta and Italy (Figure 1). Life expectancy increased
from 80.8 to 82.7 years between 2010 and 2019, but
following the outbreak of the COVID-19 pandemic,
it fell temporarily by 11 and a half months in 2020
compared to the average in the EU of nearly 8 months.
The gender gap in life expectancy was an estimated
4.8 years in 2020, which is smaller than the EU
average of 5.6 years.
Figure 1. Life expectancy in Luxembourg is still well above the EU average
Not Th EU vrg s wghtd Dt for Irlnd rfr to 2019
Sourc Eurostt Dtbs
Circulatory diseases and lung cancer are the
main causes of mortality, along with COVID-19
Circulatory diseases account for almost 30% of all
deaths in Luxembourg, followed by cancer (26%).
Looking at more specific diseases, ischaemic heart
disease was the leading cause of mortality in 2019,
accounting for 7% of all deaths, followed by lung
cancer (5.3%), which remained the most frequent
cause of death by cancer, and stroke (4.8%) (Figure 2).
Over the last decade, Luxembourg’s death rates have
been falling for nearly all causes. The increase in life
expectancy until 2019 resulted in particular from a
reduction in premature deaths from circulatory and
cerebrovascular diseases, as well as a decrease in
the number of suicides and road traffic accidents. In
contrast, mortality rates for breast cancer, chronic
obstructive pulmonary disease (COPD), diabetes and
Alzheimer’s and other dementias remained roughly at
the same level during this period.
In 2020, COVID-19 accounted for about 500 deaths
in Luxembourg (11% of all deaths). An additional
330 deaths were registered by the end of August
2021. Most deaths occurred among older people (see
Section 5.3). The mortality rate from COVID-19
1
up
to the end of August 2021 was about 17% lower in
Luxembourg than the average across EU countries
(about 1325 per million population compared with
about 1590).
LLiiffee eexxppeeccttaannccyy aatt bbiirrtthh,, 22000000,, 22001100 aanndd 22002200
Select a country:
GEO/TIME 2000 2010 2020
22000000 22001100 22002200
Norway 78.8 81.2 83.3 0 #N/A #N/A #N/A
Iceland 79.7 81.9 83.1 0 #N/A #N/A #N/A
Ireland 76.6 80.8 82.8 0 #N/A #N/A #N/A
Malta 78.5 81.5 82.6 0 #N/A #N/A #N/A
Italy 79.9 82.2 82.4 0 #N/A #N/A #N/A
Spain 79.3 82.4 82.4 0 #N/A #N/A #N/A
Sweden 79.8 81.6 82.4 0 #N/A #N/A #N/A
Cyprus 77.7 81.5 82.3 0 #N/A #N/A #N/A
France 79.2 81.8 82.3 0 #N/A #N/A #N/A
Finland 77.8 80.2 82.2 0 #N/A #N/A #N/A
Luxembourg
83.3
83.1
82.8
82.6
82.4
82.4
82.4
82.3
82.3
82.2
81.8
81.6
81.5
81.3
81.2
81.1
81.1
80.9
80.6
80.6
78.6
78.3
77.8
76.9
76.6
75.7
75.7
75.1
74.2
73.6
65
70
75
80
85
90
2000 2010
Years
2020
Luxembourg
EU
80.8
82.4
82.7
81.8
2010 2015 2019 2020
Life expectancy at birth, years

5
Stte of Helth n the EU Luxembour Countr Helth Profle 2021
Figure 2. In 2020, COVID-19 accounted for a significant share of deaths
Not Th numbr nd shr of COVID-19 dths rfr to 2020, whl th numbr nd shr of othr cuss rfr to 2019 Th sz of th COVID-19 box s
proportonl to th sz of th othr mn cuss of dth n 2019
Sourcs Eurostt (for cuss of dth n 2019) ECDC (for COVID-19 dths n 2020, up to w 53)
2. It should be noted that these estimates were made before the COVID-19 pandemic; this may have an effect on cancer incidence during 2020.
Prostate and breast cancers are the most
diagnosed cancers in Luxembourg
According to estimates from the Joint Research
Centre based on incidence trends from previous years,
around 3000 new cases of cancer were expected in
Luxembourg in 2020
2
. The age-standardised incidence
rates for all cancer types were expected to be lower
than the EU averages for both men and women.
Figure 3 shows that the main cancer sites among men
are prostate (24%), lung (15%) and colorectal (11%),
while among women breast cancer is the leading
cancer (37%), followed by colorectal (11%) and lung
cancer (8%).
Figure 3. Nearly 3000 people in Luxembourg were estimated to have cancer in 2020
Not Non-mlnom sn cncr s xcludd Utrus cncr dos not nclud cncr of th crvx
Sourc ECIS – Europn Cncr Informton Sstm
COVID-19
506 (108%)
Ischemc hert
dsese
287 (70%)
Lun cncer
219 (53%)
Chronc obstructve
pulmnr dsese
198 (48%)
Pneumon
111 (27%)
Pncretc
cncer
87 (21%)
Dbetes
83 (20%)
Brest
cncer
97 (24%)
Colorectl cncer
119 (29%)
Stroe
199 (48%)
Others
Non-Hodgkin
lymphoma
Pancreas
Skin melanoma
Bladder
Colorectal
Lung
Prostate
After new data, select all and change font to 7 pt.
Adjust right and left alignment on callouts.
Enter data in BOTH layers.
Others
Ovary
Uterus
Thyroid
Skin melanoma
Lung
Colorectal
Breast
31%
4%
4%
5%
6%
11%
15%
24%
27%
4%
4%
4%
5%
8%
11%
37%
Men
1 601 new cases
Age-standardised rate (all cancer)
LU 673 per 100 000 populton
EU 686 per 100 000 populton
Age-standardised rate (all cancer)
LU 474 per 100 000 populton
EU 484 per 100 000 populton
Women
1 356 new cases

6
Stte of Helth n the EU Luxembour Countr Helth Profle 2021
3 Rs fctors
3. Binge drinking is defined as consuming six (five for Luxembourg) or more alcoholic drinks on a single occasion for adults.
Behavioural risk factors are a major driver
of mortality
More than one third of all deaths in Luxembourg in
2019 can be attributed to behavioural risk factors,
such as tobacco smoking, dietary risks, alcohol
consumption and low physical activity, while
environmental issues like air pollution also contribute
to a sizeable number of deaths from circulatory
diseases, respiratory diseases and some types of
cancer (Figure 4). About 17% of all deaths were due to
tobacco smoking (including direct and second-hand
smoking), a share similar to the EU average. Dietary
risks (including low fruit and vegetable intake, and
high sugar and salt consumption) are estimated to
account for about 13% of all deaths in Luxembourg.
About 7% of all deaths can be attributed to alcohol
consumption, while about 2% are related to low
physical activity. Air pollution in the form of fine
particulate matter (PM
2.5
) and ozone exposure alone
accounted for about 2% of all deaths in 2019.
Figure 4. Tobacco, dietary risks and alcohol are major contributors to mortality in Luxembourg
Not Th ovrll numbr of dths rltd to ths rs fctors s lowr thn th sum of ch on tn ndvdull, bcus th sm dth cn b
ttrbutd to mor thn on rs fctor Dtr rss nclud 14 componnts such s low frut nd vgtbls dt, hgh sugr-swtnd bvrgs
consumpton Ar polluton rfrs to xposur to PM
25
nd ozon
Sourcs IHME (2020), Globl Hlth Dt Exchng (stmts rfr to 2019)
Poor nutrition and low physical activity
contribute to rising obesity among adolescents
About one in six adults reported being obese in 2019
– a rate equal to the EU average. More than one in five
15-year-olds were overweight or obese in Luxembourg
in 2018 – a higher proportion than in most EU
countries, and a significant rise since 2006. Boys are
more likely to be overweight or obese than girls.
In Luxembourg, as in other countries, poor nutrition
is the main factor contributing to being overweight
or obese. Fruit and vegetable consumption is less
common than in most other EU countries, with only
about 40% of adults eating fruit or vegetables every
day. Altogether about 65% of 15-year-olds reported
in 2018 that they did not eat any fruit or vegetables
every day. Low physical activity also contributes to
weight problems. Regular physical activity among
adults is similar to the average among EU countries
(63% compared to a 64% EU average). Among
adolescents, only one in eight (12%) 15-year-olds
reported doing at least moderate physical activity
every day in 2018 – a lower proportion than the EU
average (14%).
Excessive alcohol consumption in adults
is among the highest in the EU
Limited progress has been achieved in tackling
excessive alcohol consumption, and it continues
to be a major public health problem. Although, in
general, alcohol consumption has declined slowly
over the last two decades, the percentage of adults
reporting heavy episodes of alcohol consumption
(“binge drinking”
3
) is the third highest in the EU after
Denmark and Romania, with more than one in three
adults reporting such behaviour on a regular basis in
2019 (see Section 5.1). On a more positive note, only
one in ten 15-year-olds reported having been drunk
at least twice in their life in 2018 – the second lowest
rate in the EU.
Dietary risks
Luxembourg: 13%
EU: 17%
Tobacco
Luxembourg: 17%
EU: 17%
Alcohol
Luxembourg: 7%
EU: 6%
Air pollution
LU: 2%
EU: 4%
Low physical activity
LU: 2%
EU: 2%

7
Stte of Helth n the EU Luxembour Countr Helth Profle 2021
Smoking among adults and teenagers
has declined
The proportion of adults smoking on a daily basis
has decreased in Luxembourg compared to 20 years
ago. Only one in nine adults smoked daily in 2019,
compared with over one in four in 2001
4
. Similarly,
smoking rates among adolescents have decreased
over the last decade: 13% of 15-year-olds reported
smoking in the past month in 2018, down from 21%
in 2013-14, and a lower proportion than in most EU
4. The results from the Luxembourg Cancer Foundation Survey show higher rates of daily smokers among adults (around 17% in 2019 and 2020), with a slight
increase over the past five years.
countries (and the EU average of 18%) (Figure 5).
Some of this decrease could be attributed in part to
the anti-tobacco initiatives launched over the past
few decades, such as the smoking ban in public
places in 2006 (see Section 5.1). Although the smoking
ban contributed to a reduction in socioeconomic
inequalities in smoking (Tchicaya, Lorentz &
Demarest, 2016), the difference between the lowest
and highest income groups persists.
Figure 5. Rising child obesity and high alcohol consumption among adults are important public health issues
Not Th closr th dot s to th cntr, th bttr th countr prforms comprd to othr EU countrs No countr s n th wht “trgt r” s thr s
room for progrss n ll countrs n ll rs
Sourcs OECD clcultons bsd on HBSC surv 2017-18 for dolscnts ndctors EU-SILC 2017 nd EHIS 2019 for dults ndctors
4 The helth sstem
The social health insurance system is
administered by two ministries
Luxembourg operates a compulsory social health
insurance (SHI) system. The responsibility for
financing and purchasing of health services lies
with the National Health Insurance Fund – Caisse
Nationale de Santé (CNS) – which covers three
schemes: health care, sickness leave and long-term
care (LTC) insurance. Responsibility for health system
governance is highly centralised and split between
the Ministry of Social Security and the Ministry
of Health. The latter develops health policy and
oversees planning and regulatory functions, as well as
licensing of providers. Its Health Directorate oversees
public health issues. The Ministry of Social Security
supervises the public institutions funding health care,
sickness leave and LTC. The Ministry of Family Affairs
oversees LTC facilities, home care networks and care
services for disabled people. During the COVID-19
pandemic, governance mechanisms were put in place
to manage the crisis, with the Ministry of Health
primarily in charge of coordinating the health system
response (Box 1).
6
Vegetable consumption (adults)
Vegetable consumption (adolescents)
Fruit consumption (adults)
Fruit consumption (adolescents)
Physical activity (adults)
Physical activity (adolescents)
Obesity (adults)
Overweight and obesity (adolescents)
Binge drinking (adults)
Drunkenness (adolescents)
Smoking (adults)
Smoking (adolescents)
Select dots + Effect > Transform scale 130%
OR Select dots + 3 pt white outline (rounded corners)

8
Stte of Helth n the EU Luxembour Countr Helth Profle 2021
Luxembourg’s health system scheme
provides universal coverage
Luxembourg’s SHI scheme is compulsory for everyone
who is economically active or receiving social security
payments from the state. It covers family members,
including minors and students who have no other
5. A significant proportion of GDP in Luxembourg consist of profits from foreign-owned companies that are repatriated. Thus, gross national income may be a more
meaningful measure for the capacity to pay for health care, but even that is not a true measure of the productive capacity of the domestic economy.
health insurance coverage. The CNS’s large reserves
facilitate a broad benefits package (see Section 5.2).
People who only work occasionally in Luxembourg (i.e.
less than three months per calendar year) are exempt,
but may choose to pay voluntary contributions. People
working for European institutions or international
organisations, who represent an important share of
the population, are covered by their employers’ health
insurance schemes. Official data show that 100%
of the resident population are covered by health
insurance; however, a few people are without coverage
(see Section 5.2).
Health spending per capita is relatively high,
and the share of public funding is above
the EU average
Spending on health is high in Luxembourg. Health
expenditure per capita stood at EUR3742 in 2019
(adjusted for differences in purchasing power) –
about EUR220 higher than the EU average (Figure 6).
In contrast, Luxembourg spends only 5.4% of its
GDP on health, the lowest share in the EU (9.9%).
This statistic reflects Luxembourg’s strong overall
economic performance
5
. Public financing is based
on a system of shared contributions: 40% is paid by
the state, and the rest is shared between the insured
population and employers. Public expenditure
accounts for 85% of the total, a share that has
increased since 2012 (82.8%) and is above the EU
average (79.7%). Due to the very broad coverage
of the SHI scheme, out-of-pocket (OOP) spending
is low, at 9.6% compared to EU average of 15.4%.
Complementary voluntary health insurance (VHI)
represents only 4.1% of health expenditure, although
it is purchased by two thirds of the population.
Figure 6. Luxembourg is among the highest spenders on health in the EU
Not Th EU vrg s wghtd
Sourc OECD Hlth Sttstcs 2021 (dt rfr to 2019, xcpt for Mlt 2018)
Box 1. An inter-ministerial crisis unit was
established for the COVID-19 response
The Hh Commsson for Ntonl Protecton,
under the remt of the Prme Mnster nd
Mnster of Stte s responsble for coordntn
crss mnement nd plnnn the ntonl
protecton pln, whch stte mnstres, ences
nd deprtments re requred to mplement
In ddton, n nter-mnsterl crss unt ws
estblshed n md-Mrch 2020 under the Mnster
of Helth’s drecton to ssess the stuton
contnuousl, te necessr mesures nd
coordnte nttves cross mnstres Wthn
the Mnstr of Helth, n nternl crss unt
ws qucl set up to nlse the stuton n
the countr, set enerl response strtees
nd coordnte mplementton of ll mesures
relted to the crss The crss unt comprses 10
worn roups tht oversee nd mne dstnct
res (such s communcton, survellnce,
dnostcs nd trcn, testn nd prmr cre)
Ths unt coordntes ll efforts wthn hosptls,
lbortores, prmr cre, phrmces, nursn
homes nd cre networs, s well s mnn
lostcs, medcl equpment, helth worforce
suppl nd crss communcton
Sourc COVID-19 Hlth Sstms Rspons Montor
CCoouunnttrryy
GGoovveerrnnmmeenntt && ccoommppuullssoorryy iinnssuurraannccee sscchheemmeess VVoolluunnttaarryy iinnssuurraannccee && oouutt--ooff--ppoocckkeett ppaayymmeennttss TToottaall EExxpp.. SShhaarree ooff GGDDPP
Norway 4000 661 4661 10.5
Germany 3811 694 4505 11.7
Netherlands 3278 689 3967 10.2
Austria 2966 977 3943 10.4
Sweden 3257 580 3837 10.9
Denmark 3153 633 3786 10.0
Belgium 2898 875 3773 10.7
Luxembourg 3179 513 3742 5.4
France 3051 594 3645 11.1
EU27 22880099 771144 3521 9.9
Ireland 2620 893 3513 6.7
Finland 2454 699 3153 9.2
Iceland 2601 537 3138 8.5
Malta 1679 966 2646 8.8
Italy 1866 659 2525 8.7
Spain 1757 731 2488 9.1
Czechia 1932 430 2362 7.8
Portugal 1411 903 2314 9.5
Slovenia 1662 621 2283 8.5
Lithuania 1251 633 1885 7.0
Cyprus 1063 819 1881 7.0
2019
0.0
2.5
5.0
7.5
10.0
12.5
0
1 000
2 000
3 000
4 000
5 000
Government & compulsory insurance Voluntary insurance & out-of-pocket payments Share of GDP
% GDP
EUR PPP per capita
0.0
2.5
5.0
7.5
10.0
12.5
0
1 000
2 000
3 000
4 000
5 000
Government & compulsory insurance Voluntary insurance & out-of-pocket payments Share of GDP
% GDP
EUR PPP per capita

9
Stte of Helth n the EU Luxembour Countr Helth Profle 2021
Spending on outpatient care has decreased,
while spending on inpatient care has gone up
The largest category of health spending in
Luxembourg is outpatient care (including home care)
(Figure 7), which accounted for one third (32.9%)
of all health spending in 2019 and is above the EU
average (29.5%). Slightly less than one third (29.1%) is
spent on inpatient care, which is equal to the average
in the EU as a whole. Despite the 2010 health reform
law that aimed to contain rising health expenditure
in hospital care and to strengthen primary care, the
share of spending on inpatient care increased by 2.5
percentage points between 2010 and 2019, partly
as a result of collective labour agreements in the
hospital sector. Conversely, the share of outpatient
care spending fell by 5.1 percentage points during the
same period. Spending in the other categories has
remained fairly stable. Luxembourg spent slightly
more on LTC per capita than the EU average (EUR708
compared to EUR617). However, per capita spending
on pharmaceuticals, medical devices and prevention
is lower than the EU averages (Figure 7).
In 2020, additional financial allocations of
EUR194million were made to the health system
as part of the government’s COVID-19 fiscal
package. Resources were used to create outpatient
health centres for COVID-19 care, acquire medical
equipment, boost testing capacities and to cover
temporary accommodation expenses for cross-border
health and social care workers who needed to stay in
Luxembourg during the pandemic (see Sections 5.2
and 5.3).
Figure 7. Luxembourg spends more on outpatient, inpatient and long-term care than the EU averages
Not Th costs of hlth sstm dmnstrton r not ncludd 1 Includs hom cr nd ncllr srvcs (g ptnt trnsportton) 2 Includs
curtv-rhblttv cr n hosptl nd othr sttngs 3 Includs onl th hlth componnt 4 Includs onl th outptnt mrt 5 Includs onl
spndng for orgnsd prvnton progrmms Th EU vrg s wghtd
Sourcs OECD Hlth Sttstcs 2021, Eurostt Dtbs (dt rfr to 2019)
A substantial share of health services
are provided outside Luxembourg
About one third of those covered by the CNS (35%)
are cross-border employees (who make up nearly half
of Luxembourg’s workforce). As these non-residents
mostly seek health care in their country of residence,
many health services covered by the CNS are provided
outside Luxembourg – mainly in Germany, Belgium
and France. In 2019, 8677 patients (residents and
non-residents) requested authorisation by the CNS
for care outside Luxembourg, mainly for hospital
treatment (45%) and consultations and examinations
(33%). The costs for treatment in neighbouring
countries accounted for 20% of total health
expenditure in 2019 (IGSS, 2021; CNS, 2020).
Patients in Luxembourg enjoy a free choice of
providers and unrestricted access to all levels of care
(general practitioners (GPs), specialists and hospitals).
Hospital care is provided by four general and two
specialised hospitals, with 4.3 hospital beds (and 3.3
acute care beds) per 1000 population, which is below
the EU average of 5.3 per 1000 population. Hospital
bed rates have declined steadily by 34% since 2004,
mostly due to population growth. Meanwhile, the
average length of stay has increased by half a day
since 2011 – up to 9.3 days in 2019, which is well
above the European average (7.4 days). During the
COVID-19 pandemic, Luxembourg’s acute hospitals
were required to postpone or cancel procedures and
reorganise services to free up 270 acute beds and
about 100 intensive care unit (ICU) beds for COVID-19
1 022
1 010
617
630
102
0
0
0
0
0
1 231
1 088
708
495
92
Luxembour
Preventon Phrmceutcls
nd medcl devces
Lon-term cre Inptent cre Outptent cre
0
200
400
600
800
1 000
1 200
1 400
EU27EUR PPP per cpt
33%
of totl
spendn
29%
of totl
spendn
19%
of totl
spendn
13%
of totl
spendn
2.5%
of totl
spendn

10
Stte of Helth n the EU Luxembour Countr Helth Profle 2021
patients, which represented 13% of Luxembourg’s
total acute bed capacity and two thirds of its intensive
care capacity (see Section 5.3).
The COVID-19 pandemic stressed the
challenge of Luxembourg’s dependency
on foreign health professionals
Luxembourg has the second lowest number of doctors
in the EU, with approximately 3 physicians per 1000
population in 2019 (compared to 3.9 across the EU;
Figure 8) despite an increase of 39% since 2000. The
low density of doctors mostly relates to the absence
of medical training in the country, which makes
it dependent on foreign-trained doctors. The first
national degree in general medicine started in 2021.
The share of doctors living outside the country but
practising in Luxembourg nearly doubled between
2008 and 2017 (from 15.6% to 26.4%), and only about
half of all practising doctors are national citizens
of Luxembourg (IGSS, 2021). GPs account for about
one third of physicians, which is higher than the EU
average (21%). The physician workforce is ageing:
more than half of practising GPs (54.4%) and nearly
two third of specialists (60%) were over the age of 50
in 2017 (Lair-Hillion, 2019) (see Section 5.2).
In contrast, the number of nurses in Luxembourg has
increased continually over the last few years, and its
density is one of the highest in the EU (approximately
11.7 compared to an EU average of 8.4 per 1000).
More than two thirds of practising nurses live in the
neighbouring countries of France (29%), Germany
(24%) and Belgium (12%) (Lair-Hillion, 2019), but are
attracted by higher remuneration and good working
conditions in Luxembourg. This made Luxembourg
particularly vulnerable to border closures during the
first lockdown of the COVID-19 pandemic in 2020.
Figure 8. Luxembourg has sufficient nurses, owing to cross-border supply, but has very low numbers of
physicians
Not Th EU vrg s unwghtd In Portugl nd Grc, dt rfr to ll doctors lcnsd to prcts, rsultng n lrg ovrstmton of th numbr
of prctsng doctors (g of round 30% n Portugl) In Grc, th numbr of nurss s undrstmtd s t onl ncluds thos worng n hosptls
Sourc Eurostt Dtbs (dt rfr to 2019 or th nrst r)
2 3 4 5 6 6.55.54.53.52.5
0
2
4
6
8
10
12
14
16
18
20
Practicing nurses per 1 000 population
Practicing doctors per 1 000 population
EU average: 8.4
EU average: 3.9
Doctors High
Nurses Low
Doctors High
Nurses High
Doctors Low
Nurses Low
Doctors Low
Nurses High
NO
DK
BE
CZ
LT
LU
IE
SI
RO
PL
EE
SK
LV
IT
ES
CY
BG
SE
DE
IS
AT
PT
FI
HU
HR
EU
NL
MT
EL
FR
11
Stte of Helth n the EU Luxembour Countr Helth Profle 2021
5 Performnce of the helth sstem
51 Effectiveness
Public health interventions in Luxembourg have
had a positive impact on preventable deaths
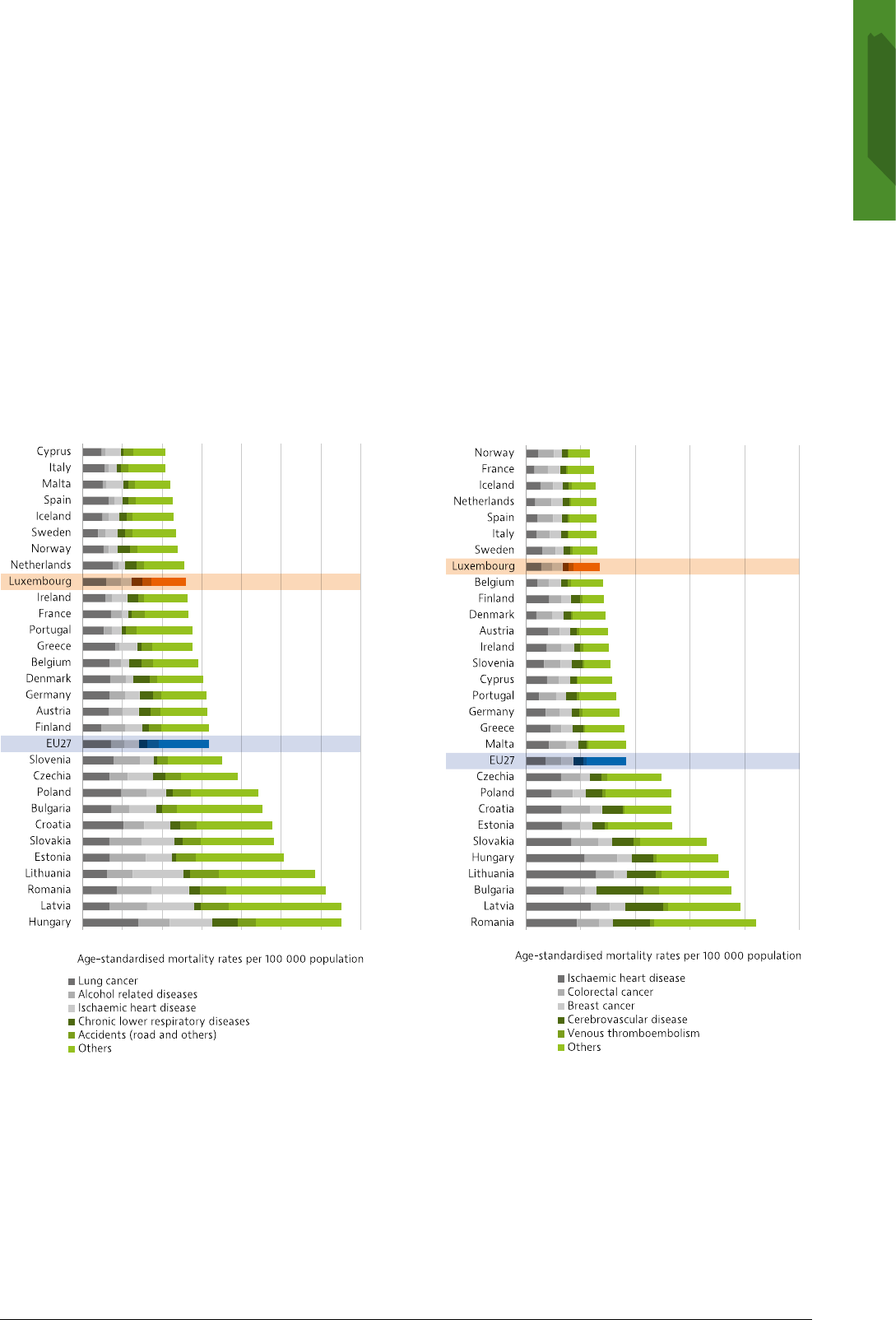
Luxembourg compares favourably with the EU as
a whole for mortality from both preventable and
treatable causes (Figure 9). In 2018, preventable
mortality accounted for 130 deaths per 100000
population, the main causes being lung cancer,
alcohol-related diseases, chronic lower respiratory
disease and ischaemic heart disease. To support
decreasing levels of preventable deaths, preventive
health policies remain a priority. In 2019, Luxembourg
launched its first National Plan against Cardio-
neuro-vascular Diseases (2020-24) to reduce related
preventable deaths. The main measures include
prevention of risk factors, screening and improvement
of patient pathways.
Figure 9. Mortality from preventable and treatable causes is among the lowest in the EU
Not Prvntbl mortlt s dfnd s dth tht cn b mnl vodd through publc hlth nd prmr prvnton ntrvntons Trtbl mortlt
s dfnd s dth tht cn b mnl vodd through hlth cr ntrvntons, ncludng scrnng nd trtmnt Hlf of ll dths for som dsss
(g schmc hrt dss nd crbrovsculr dss) r ttrbutd to prvntbl mortlt th othr hlf r ttrbutd to trtbl cuss Both
ndctors rfr to prmtur mortlt (undr g 75) Th dt r bsd on th rvsd OECD/Eurostt lsts
Sourc Eurostt Dtbs (dt rfr to 2018, xcpt for Frnc 2016)
The comparatively low levels of preventable
deaths from causes such as lung cancer and road
traffic accidents registered in Luxembourg may be
explained in part by strong public health policies,
such as smoking bans in public places, bars and
cafés and awareness-raising campaigns for road
safety implemented in 2006 and 2014. The effect of
more recent anti-tobacco measures – such as public
104
104
111
113
115
118
120
129
130
132
134
138
139
146
152
156
157
159
160
175
195
222
226
239
241
253
293
306
326
326
59
63
64
65
65
65
66
68
71
71
73
75
76
77
79
83
85
90
92
92
124
133
133
133
165
176
186
188
196
210
0 50 100 150 200 250 300 350
0 50 100 150 200 250
Preventable causes of mortality Treatable causes of mortality

12
Stte of Helth n the EU Luxembour Countr Helth Profle 2021
awareness campaigns under the Anti-Tobacco Plan
2016-20, the rise in the legal age for purchasing
tobacco products in 2017 and tax increases – have
helped to reduce smoking rates, particularly among
adolescents (see Section 3), but will take time to
translate into reduced preventable mortality. Despite
these early signs of improvement, the fight against
tobacco consumption remains a public health priority.
In 2008, the Ministry of Health and the CNS set up
a stop smoking programme that covers two doctor
consultations and half of the costs for substitutes
(capped at EUR100). Despite its long existence,
participation in the programme remains limited.
Frequent alcohol consumption continues to be a
public health issue, despite relatively low preventable
mortality specifically due to alcohol-related deaths.
Luxembourg has very high levels of binge drinking
(see Section 3), particularly among men. In 2020, the
National Alcohol Plan (2020-24) was finally adopted,
after being initiated in 2012, to reduce alcohol misuse
and harm and to create supportive environments
that enable people to adopt healthy and sensible
drinking behaviours at all ages. However, owing to
the COVID-19 pandemic, implementation had to be
postponed.
Cardiovascular disease and cancers play a
large role in mortality from treatable causes
Overall, mortality that can mainly be avoided through
health care interventions has decreased since 2011
and, at 68 deaths per 100000 in 2018 was below the
6. Other survey data from the European Health Information Survey (EHIS) indicate that 78% of women reported to have received breast cancer screening in 2019.
EU average of 92 deaths per 100000 (see Figure 9). The
main causes of treatable mortality in Luxembourg
were ischaemic heart disease, colorectal cancer,
breast cancer and stroke, and all rates were below the
EU averages.
Cancer screening is based on national
recommendations and has a central role in improving
survival outcomes and lower overall rates of mortality
from treatable causes. The rates of cervical cancer
screening across the country increased from 51%
to 70% between 2013 and 2019. However, the
participation rates in breast cancer screening, which
was introduced in 1992, have decreased over the last
decade from 64% in 2009 to 53% in 2019 – below
the EU average (Figure 10)
6
. While data on cancer
mortality and screening rates for most types of cancer
are available, evaluating the quality of cancer care
is more difficult, as data on five-year survival rates
are not systematically collected. Luxembourg has,
however, adopted a second National Cancer Plan for
the period 2020-24, which aims to improve prevention
and treatment (Box 2).
Due to the COVID-19 pandemic many cancer
screenings, operations and non-essential
examinations were postponed in 2020. A recent survey
among cancer care providers revealed that during the
first lockdown the number of radiotherapy sessions
fell by almost one third and even after lockdown
(between July and October 2020) they remained below
usual levels (Backes et al., 2021).
Figure 10. Only about half the women in Luxembourg participate in recommended mammography screening
Not Th EU vrg s unwghtd For most countrs, th dt s bsd on scrnng progrmms, not survs
Sourcs OECD Hlth Sttstcs 2021 nd Eurostt dtbs
Selected country
95
83
81
80
77
76
75
74
72
72
69
66
61
61
61
60
60
59
56
54
53
53
50
49
39
39
36
31
31
9
0
10
20
30
40
50
60
70
80
90
100
2009 (or nearest year) 2019 (or nearest year)
% of women aged 50-69 screened in the last two years

13
Stte of Helth n the EU Luxembour Countr Helth Profle 2021
The government ordered more influenza
vaccines in 2020 to increase vaccination rates
The COVID-19 pandemic raised the importance
of increasing vaccination rates against seasonal
influenza to avoid having another virus spreading
widely and to reduce pressures on hospitals. The
objective of the 2020/21 campaign was to vaccinate
30000 more people than in the previous year and
to avoid a shortage of influenza vaccine, which
Luxembourg experienced in 2018. To that end, up to
120000 shots in total were ordered by government
and the private sector. In the past, the influenza
vaccination rate among the population at highest risk
(over 65 years) has been low, despite health insurance
coverage and broad awareness-raising campaigns.
About 40% of the population over 65 received the
vaccination in 2019, which is slightly below the EU
average (42%). In contrast, high coverage is observed
for the universal childhood vaccination programme,
with centralised public procurement of vaccine
products and direct delivery to physician practices.
The low number of avoidable hospitalisations
points to effective primary care
Luxembourg’s rate of avoidable hospital admissions
for chronic conditions is lower than in many other
EU countries, suggesting that primary care and
outpatient secondary care are effective at managing
chronic diseases. Indeed, avoidable hospital
admissions for asthma and COPD, remained stable
7. The data from the Eurofound survey are not comparable to those from the EU-SILC survey because of differences in methodologies.
8. People on low incomes may apply for the benefit-in-kind model: local social welfare offices certify eligibility on an annual basis for medical and dental treatment
costs to be directly covered by the CNS. Patients’ co-payments are paid by local social welfare offices.
between 2007 and 2015 and are below the EU average.
Avoidable hospitalisations for diabetes decreased
in this period, although they are still above the EU
average. The outdated data on avoidable hospital
admissions and the data gaps on hospital quality
indicators such as 30-day in-hospital case fatality
rates, as well as cancer survival rates, point to gaps in
data collection. The new National Health Observatory
that Luxembourg is setting up aims to centralise
and harmonise health-related data, such as data on
health status and health provision (see Section 5.3).
52 Accessibility
Unmet needs for medical care have been low
but rose during the COVID-19 pandemic in 2020
Since health coverage is universal and the benefits
package is fairly comprehensive, before the COVID-19
pandemic, very few residents in Luxembourg (0.2%)
reported having experienced unmet needs for medical
care due to cost, distance or waiting times – a share
well below the EU average, and with little difference
between income groups (Figure 11). The share of
people reporting unmet needs for dental care was
also among the lowest in the EU (0.4% compared to
2.8%). However, unmet needs for medical care may
have risen in 2020. According to the Eurofound (2021)
survey
7
, during the first 12 months of the COVID-19
pandemic, 19% of respondents reported having
forgone medical care compared to 21% across the
EU as a whole although due to the small sample size,
these results should be viewed with caution.
Despite universal coverage some gaps and
access barriers remain
Despite compulsory health insurance, some
population groups remain without coverage and
have very limited access to health care – namely,
homeless people, residents whose welfare benefits
are ending and undocumented migrants. At least 880
people were reported to be without health insurance
or faced financial difficulties obtaining it in 2019
(Médecins du Monde, 2019). In 2013, Luxembourg
introduced a “benefit-in-kind model”
8
for vulnerable
groups who encounter difficulties paying in advance
for outpatient services. A third-party payment system
is planned for the entire population from 2023, which
will mean that the CNS, rather than patients, will pay
the reimbursed tariff directly to providers for services
at the point of care.
Box 2. Luxembourg has adopted a second
National Cancer Plan for 2020-24
Luxembour’s second Ntonl Cncer Pln
(2020-24) contnues the efforts nd mesures of
the frst Ntonl Cncer Pln lunched n 2014
The mn prortes re dtlston of dt
exchne nd expnson of nformton sstems,
mplementton of modern enetcs nd moleculr
ptholo nd the structurn of ptent pthws
nto competence networs Bolstern the
pplcton of reserch nd the centrl role of the
Ntonl Cncer Insttute re lso e elements
The Ntonl Cncer Pln follows the
recommendtons of the Europen Prtnershp
for Acton Anst Cncer nd the pllrs of the
Europe’s Betn Cncer Pln, whch sets out new
EU pproch to tcle the entre dsese pthw,
from preventon nd screenn to tretment nd
qult of lfe of cncer ptents nd survvors
(Europen Commsson, 2021)

14
Stte of Helth n the EU Luxembour Countr Helth Profle 2021
Figure 11. Before the pandemic, Luxembourg
recorded among the lowest levels of unmet needs,
with little variation by income
Not Dt rfr to unmt nds for mdcl xmnton or trtmnt
du to costs, dstnc to trvl or wtng tms Cuton s rqurd n
comprng th dt cross countrs s thr r som vrtons n th
surv nstrumnt usd
Sourc Eurostt Dtbs, bsd on EU-SILC (dt rfr to 2019, xcpt
Iclnd 2018)
The benefits package provides good
coverage for most health services
Individuals covered by the compulsory SHI scheme
enjoy a very broad benefits package, which goes
well beyond essential services and continues to
be extended gradually, especially for therapeutic
services. The SHI scheme covers most inpatient
treatments directly, with the exemption of a per
diem levied on all adults. Most outpatient services
are currently based on reimbursement: patients pay
providers in advance and are later reimbursed by the
CNS at different rates, ranging from 60% to 100%.
Usually, 88% of costs for medical and dental services
are reimbursed by the CNS, and the first EUR66.50 of
costs for dental care per year is also paid by health
insurance. Medicines included in the positive lists are
reimbursed at three different rates (100%, 80% and
40%). Cost-sharing exemptions apply for people with
disabilities or severe chronic conditions, children and
pregnant women, or if cost-sharing exceeds 2.5% of
annual gross income.
The shares financed by public spending for selected
health services and medical goods reflect the limited
cost-sharing requirements described above, and are
well above the EU averages (Figure 12). To cover OOP
payments or services not included in the benefits
package, such as acupuncture or single rooms in
hospitals, about 65.5% of the population purchases
VHI.
Figure 12. Extensive public coverage of services reflects comprehensive benefits coverage
Not Outptnt mdcl srvcs mnl rfr to srvcs provdd b gnrlsts nd spclsts n th outptnt sctor Phrmcutcls nclud prscrbd
nd ovr-th-countr mdcns s wll s mdcl non-durbls Thrputc pplncs rfr to vson products, hrng ds, whlchrs nd othr
mdcl dvcs
Sourc OECD Hlth Sttstcs 2021 (dt rfr to 2019 or nrst r)
0 5 10 15 20
Estonia
Greece
Romania
Finland
Latvia
Poland
Iceland
Slovenia
Slovakia
Ireland
Belgium
Denmark
Italy
Portugal
EU 27
Bulgaria
Croatia
Lithuania
Sweden
France
Cyprus
Hungary
Norway
Czechia
Austria
Germany
Luxembourg
Netherlands
Spain
Malta
Low incomeTotal populationHigh income
% reporting unmet medical needs
Hh ncome Totl populton Low ncome
Unmet needs for medical care
LLuuxxeemmbboouurrgg
89%
93%
0% 50% 100%
EU
LU
Inpatient care
75%
88%
0% 50% 100%
Outpatient medical
31%
47%
0% 50% 100%
Dental care
57%
71%
0% 50% 100%
Pharmaceuticals
37%
43%
0% 50% 100%
Therapeutic
Inpatient care
Outpatient
medical care Dental care Pharmaceuticals
Therapeutic
appliances
Publc spendn s proporton of totl helth spendn b tpe of servce

15
Stte of Helth n the EU Luxembour Countr Helth Profle 2021
Luxembourg has very low out-of-pocket
spending, but pharmaceutical payments can
be substantial
The proportion of OOP payments in total health
spending is the second lowest among EU countries
(9.6%) after France, and well below the EU
9. The data from the Eurofound survey are not comparable to those from the EU-SILC survey because of differences in methodologies.
average (Figure 13). As a share of final household
consumption, it is one of the lowest in the EU (1.6%
compared to a 3.1% EU average). However, OOP
payments can still be substantial for pharmaceuticals,
LTC and dental care. About one third of OOP spending
is devoted to pharmaceuticals (29%), and about one
fifth each to LTC, outpatient and dental care.
Figure 13. Out-of-pocket spending in Luxembourg is well below the EU average
Not Th EU vrg s wghtd VHI lso ncluds othr voluntr prpmnt schms
Sourcs OECD Hlth Sttstcs 2021 Eurostt Dtbs (dt rfr to 2019)
Reorganisation of health care training aims
to increase the attractiveness of some health
professions
As noted in Section 4, Luxembourg has low
numbers of doctors; this has the greatest impact
on ambulatory care. To address potential scarcities
of health professionals in the longer term, various
initiatives have aimed to decrease dependence
on foreign health care professionals and improve
the attractiveness of the medical profession. For
example, specialised medical training for doctors
who have completed their studies has been expanded
in the areas of oncology and neurology, and a new
bachelor’s programme in general medicine starts in
2021. In the next few years, the government also plans
to offer new academic nurse training programmes to
enhance the profession, including bachelor’s degrees
in nursing care, midwifery and radiology medical
technical assistance and four specialised nursing
bachelor programmes. An advanced four-year nursing
degree is also being planned. The new professions
will allow more collaborative working environments,
in which care is provided by multidisciplinary teams,
and the opportunity to alleviate doctor shortages
through task-shifting. The creation of a digital registry
of health professionals is also planned; this will aid
creation of work placements in areas of need.
A newly created teleconsultation platform
has helped to maintain provision of services
At the outbreak of the COVID-19 pandemic,
Luxembourg acted quickly to ensure that health
services were maintained while preventing
transmission of the virus to vulnerable populations
and health professionals. In March 2020, the
Ministry of Health reorganised the model of primary
health care, establishing four different care patient
pathways: teleconsultations; medical visits within
residential care facilities and at patients’ homes;
advanced care centres for COVID-19 patients; and
emergency department visits (see Section 5.3).
Teleconsultations played a key role in maintaining
access to non-COVID-19 health services. In mid-March
2020, a teleconsultation platform was set up to allow
patients to consult their treating physicians, dentists
or midwives via telephone or teleconsultation,
as well as to obtain a certificate of incapacity for
work or medical prescription. By 9April, about 600
doctors and more than 4000 patients had registered
with the e-consult platform, and almost 3000
teleconsultations had been carried out. According to
the Eurofound (2021) survey, 44% of the population
reported having a medical teleconsultation (above
the EU average of 39%) in the first 12 months of the
pandemic
9
.
Government/compulsory schemes 85.0%
VHI 4.1%
Inpatient 0.6%
Outpatient medical
care 1.7%
Pharmaceuticals 2.8%
Dental care 1.7%
Long-term care 1.9%
Others 0.9%
Government/compulsory schemes 79.7%
VHI 4.9%
Inpatient 1.0%
Outpatient medical
care 3.4%
Pharmaceuticals 3.7%
Dental care 1.4%
Long-term care 3.7%
Others 2.2%
Luxembourg
Overall share of
health spending
Distribution of OOP
spending by function
OOP
9.6%
EU
Overall share of
health spending
Distribution of OOP
spending by function
OOP
15.4%

16
Stte of Helth n the EU Luxembour Countr Helth Profle 2021
Simultaneously, a remote monitoring tool for
COVID-19 patients was launched throughout
Luxembourg to follow up patients who had been
discharged and were in isolation at home. Monitoring
was carried out by a team of professionals from
the Health Directorate: within the first month of its
operation, 388 patients were recuperating at home
using this new tool (Ministry of Health, 2020a). As
part of Luxembourg’s ongoing consultation process
to develop a national health plan, initiated in 2020
and known as “Gesondheetsdësch”, the monitoring
tool will be expanded into a permanent telemedicine
solution, integrated into e-health services.
Draft legislation aims to improve patients’
access to pharmaceuticals
Luxembourg is currently the only EU country without
its own medicines authorisation agency. This leads
to challenges in pharmaceutical negotiations and a
lack of transparency in pricing and reimbursement
decisions. To ensure access to medicines, the
government adopted a draft bill in 2019 that provides
for the creation of a National Agency for Medicines
and Health Products, with comprehensive functions
such as monitoring the quality and safety of
10. Currently, marketing authorisations are issued by the Ministry of Health, and reimbursement pricing is determined by the Ministry of Social Security.
11. In this context, health system resilience has been defined as the ability to prepare for, manage (absorb, adapt and transform) and learn from shocks (EU Expert
Group on Health Systems Performance Assessment, 2020).
medicines, authorisation and control of activities of
biotech companies, administration of clinical trials
and price determination of medicines and medical
devices. The aim is to improve patient access to
medicines that have not yet been authorised in
Luxembourg
10
. Addressing medicines shortages
aligns with one of the key planks of the European
Commission’s pharmaceutical strategy for Europe,
which sets out enhanced co-operation between
national authorities on pricing, payment and
procurement policies, with a view to improving the
affordability and cost–effectiveness of medicines
(European Commission, 2020).
Use of generics as a means of widening access to
medicines is low in Luxembourg. In 2014, the country
introduced a system of generic substitution by
specifying two pharmacotherapeutic groups to be
eligible for mandatory substitution for the lowest
priced generic alternative, regardless of what the
doctor has indicated on the prescription. Even so, the
country has the lowest generic penetration in the EU
by volume (Figure 14) and by value: only 5.6% of the
publicly funded pharmaceuticals market consists of
generics.
Figure 14. Use of generics in Luxembourg continues to be low
Not Dt rfr to th shr of gnrcs b volum
Sourc OECD Hlth Sttstcs 2021
53 Resilience
This section on resilience focuses mainly on
the impacts of and responses to the COVID-19
pandemic
11
. As noted in Section 2, the COVID-19
pandemic had a major impact on population health
and mortality in Luxembourg, with just over 830
COVID-19 deaths recorded between January 2020 and
the end of August 2021. Measures taken to contain the
pandemic also had an impact on the economy, but
Luxembourg’s GDP fell by only 1.3% in 2020, which is
lower than the drop of 6.2% across the EU as a whole.
Various mitigation measures were implemented
throughout successive waves of the pandemic
After the first cases of COVID-19 were identified in
early March 2020, the government released several
recommendations and containment measures, such
as calling off large public events with more than
1000 people, restrictions on travel, suspension of
face-to-face teaching and restrictions on hospital
and care home visits (Figure 15). By mid-March, when
a state of emergency was declared, the parliament
endorsed a full lockdown, with shop closures and
restrictions on mobility. In April and May, these
Select a country Luxembourg
Select comparator
countries
Spain
Germany
0
10
20
30
40
50
60
70
80
90
Luxembourg Spain Germany EU16
%

17
Stte of Helth n the EU Luxembour Countr Helth Profle 2021
measures were lifted gradually, accompanied by
a large-scale testing and preventive measures
such as mask-wearing in public spaces and social
distancing. From summer 2020 onwards, Luxembourg
experienced a second wave of cases, although
numbers were less pronounced than in some other
European countries. In response, the government
implemented restrictions on gatherings, which were
further tightened in October 2020 when case numbers
again surged, followed by new mitigating measures
in November and a second lockdown in December
12. Since 2005, the IHR have provided an overarching legal framework that defines countries’ rights and obligations in handling public health events and
emergencies. Under the IHR, all Member States are required to develop public health capacities to prevent, detect, assess, notify and respond to public health risks.
The monitoring process of IHR implementation status involves assessing, through a self-evaluation questionnaire, 13 core capacities.
2020 (including a night curfew and non-essential
shops closures). Most of these restrictive measures
extended well into the new year and were gradually
lifted between January and May 2021. The government
also implemented the “CovidCheck” digital (or
paper) certificate, which is applicable for hospitality
establishments, events and a range of activities. The
certificate provides proof that the registered user
has been vaccinated against COVID-19, has received
a negative COVID-19 test or has recovered from the
disease.
Figure 15. Containment measures have brought down COVID-19 case numbers
Not Th EU vrg s unwghtd (th numbr of countrs usd for th vrg vrs dpndng on th w)
Th numbr of COVID-19 css n EU countrs ws undrstmtd durng th frst wv n sprng 2020 du to mor lmtd tstng
Sourc ECDC for COVID-19 css nd uthors for contnmnt msurs
Luxembourg was relatively well prepared
for a public health emergency
Luxembourg had a very rapid initial response to
the COVID-19 pandemic. Although the country was
confronted with similar challenges to those seen
throughout Europe, such as shortages of personal
protective equipment (PPE) and health care workers,
public actors from various governance levels
(including communities and the fire and rescue corps)
rapidly joined the national effort to respond to the
crisis. Luxembourg’s small size helped it to put public
health measures in place quickly, and health system
actions (including mask-wearing, testing, contact
tracing, marshalling hospital infrastructure and
medical equipment, and organising COVID-19 care)
were centrally coordinated by the crisis unit at the
Ministry of Health (see Section 4).
According to the International Health Regulations
(IHR) framework
12
, Luxembourg recorded above-
average scores for indicators of self-reported capacity
to detect and manage public health risks (Figure 16).
This ample capacity was on display as the country
swiftly created ambulatory service points providing
testing and care for suspected COVID-19 cases, as well
as central procurement of laboratory equipment and
a centralised data monitoring system. At the Health
Directorate, a central contact tracing unit for early
detection of cases and clusters and notifications was
set up in March 2020. Laboratory capacities were
limited in the beginning but were quickly scaled
up with a large-scale testing strategy. Furthermore,
prior to the COVID-19 pandemic, Luxembourg had
no national PPE emergency stockpile, which mostly
affected nursing homes and primary care providers.
However, the government procured material from Asia
and received stock from the EU.
Weekly cases per 100 000 population
0
100
200
300
400
500
600
700
800
Luxembourg European Union
1st locdown
16/03 Closure of ll non-essentl
shops, school closure, lmted trffc,
bnnn mss therns of 100
people, confnement
2nd locdown
30/10 Nht curfew t 11pm, contct restrctons
26/11 Closure of resturnts nd lesure fcltes
26/12 Nht tme curfew t 9pm nd closure of
non-essentl shops
Esn of locdown
11/01 Reopenn of shops, cnems, thetres,
ms under certn condtons
16/05 Re-openn of resturnts nd cfés
M Esn of locdown
11/05 Return of clsses on rotton
bss, ese of contct restrctons,
reopenn of culturl venues
29/05 Reopenn of resturnts
nd most busnesses

18
Stte of Helth n the EU Luxembour Countr Helth Profle 2021
Figure 16. Prior to the pandemic, Luxembourg
reported better IHR public health emergency
capacities than the EU average
Not Th EU vrg s unwghtd
Sourc WHO IHR (dt rfr to 2019)
A long-term, large-scale testing strategy was
launched early on
From the onset of the COVID-19 pandemic,
Luxembourg pursued an ambitious large-scale testing
policy free of charge for everybody, resulting in a
very high testing rate (Figure 17). From May to July
2020, the entire population and cross-border workers
were invited for PCR testing, with the aim of lifting
lockdown restrictions based on reliable information,
and to gain a longitudinal perspective on household
transmission. The population was divided into three
categories depending on their risk of being exposed
to the virus, with each category invited at different
frequencies. Second and third testing phases were
rolled out in September 2020 to February 2021 and in
March to July 2021.
For this population-wide testing, Luxembourg had to
build the highest testing capacity in the EU, reaching
a weekly maximum of 23321 tests per 100000
population by mid-July 2020 – far above Denmark,
another country with a high testing rate (Figure 17).
All passengers entering the country from the end
of May 2020 were offered free COVID-19 testing
on arrival at Luxembourg’s airport. Until summer
2020, family gatherings made up a large part of
Luxembourg’s identified clusters, while cross-border
workers accounted for 16% of infections (ECDC, 2020).
When large-scale testing started in May and June 2020
and testing rates increased, positivity rates remained
stable and below 1%. During the second wave starting
in October 2020 testing declined somewhat and
positivity rates rose accordingly, peaking at between
6% and 8% (Figure 17).
Figure 17. Luxembourg achieved the highest testing rate in the EU early on, while positivity rates remained
lower
TTeessttiinngg aaccttiivviittyy
Note: The EU average is weighted (the number of countries included in the average varies depending on the week).
Source: ECDC.
Data extracted from ECDC on 15/03/2021 at 12:41 hrs.
CCoouunnttrryy 1100//0022//22002200 1177//0022//22002200 2244//0022//22002200 0022//0033//22002200 0099//0033//22002200 1166//0033//22002200 2233//0033//22002200 3300//0033//22002200 0066//0044//22002200
Austria #N/A #N/A #N/A #N/A #N/A #N/A #N/A #N/A 139
Belgium #N/A #N/A 1 38 86 148 236 333 464
Bulgaria #N/A #N/A #N/A #N/A #N/A #N/A #N/A #N/A #N/A
Croatia 0 0 4 3 13 48 103 158 218
Cyprus #N/A #N/A #N/A 7 2 26 43 40 43
Czechia 0 0 1 7 40 116 248 399 422
Denmark 0 0 6 14 85 126 172 485 478
Estonia 0 0 4 18 91 201 557 840 726
CCoouunnttrryy
Austria
Belgium
Bulgaria
Cyprus
Czechia
Denmark
European Union
Finland
France
Greece
Hungary
Iceland
Italy
Latvia
Lithuania
Malta
Netherlands
Norway
Portugal
Romania
Slovakia
Spain
Sweden
0
5 000
10 000
15 000
20 000
25 000
Denmark European Union
Luxembourg
Weekly tests per 100 000 population
WWeeeekk
30-Dec-19
6-Jan-20
13-Jan-20
20-Jan-20
27-Jan-20
3-Feb-20
10-Feb-20
17-Feb-20
24-Feb-20
2-Mar-20
9-Mar-20
30-Mar-20
6-Apr-20
13-Apr-20
20-Apr-20
27-Apr-20
4-May-20
11-May-20
18-May-20
25-May-20
1-Jun-20
8-Jun-20
29-Jun-20
6-Jul-20
13-Jul-20
20-Jul-20
27-Jul-20
3-Aug-20
10-Aug-20
17-Aug-20
24-Aug-20
31-Aug-20
7-Sep-20
28-Sep-20
5-Oct-20
12-Oct-20
19-Oct-20
26-Oct-20
2-Nov-20
9-Nov-20
16-Nov-20
23-Nov-20
30-Nov-20
7-Dec-20
28-Dec-20
4-Jan-21
11-Jan-21
18-Jan-21
25-Jan-21
1-Feb-21
8-Feb-21
15-Feb-21
22-Feb-21
Select dots + Effect > Transform scale 130%
OR Select dots + 3 pt white outline (rounded corners)
Select dots + Effect > Transform scale 130%
OR Select dots + 3 pt white outline (rounded corners)
Points
of entry
Risk
communi-
cation
Health service
provision
Nationalhealth
emergencyframework
Human resources
availability
Surveillance
Laboratory
IHR Coordination
Legislation
and Financing
100
60
40
20
0
80
Luxembourg EU average

19
Stte of Helth n the EU Luxembour Countr Helth Profle 2021
Not Th EU vrg s wghtd (th numbr of countrs ncludd n th vrg vrs dpndng on th w)
Sourc ECDC
The effective contact tracing system did
not necessitate an accompanying app
In March 2020, the Health Directorate set up a contact
tracing unit that identifies contacts, administers
quarantine and isolation and manages clusters of
infections. The contact tracing team comprised 220
people, including 68 employees from the national
airline, who were redeployed for this purpose. Owing
to rapidly rising positive cases in November 2020,
the Health Directorate simplified and sped up its
procedure by asking people who had tested positive
for COVID-19 to provide contact names through an
online form without having to wait to be contacted
by the contact tracing unit. People were also asked
to transfer a link and their reference number to their
high-risk contacts.
Luxembourg’s contact tracing system was very
effective: the time between identification of
laboratory-confirmed cases and notification was
generally 24-48 hours. Because of the effective contact
tracing system, Luxembourg did not set up a contact
tracing app, unlike most other EU countries. However,
from June 2020 residents could use other European
apps, such as Germany’s Corona-Warn-App.
Luxembourg had sufficient infrastructure and
workforce to manage COVID-19 patients
To meet the increased demand for health care due to
the COVID-19 pandemic, the government carried out a
mandatory census of all licensed health professionals
in March 2020, including residents, students, retirees
and people on unpaid leave. In parallel, it set up a
platform for medical and non-medical volunteers.
Based on these databases, Luxembourg started to
build up a medical reserve. Volunteers were also
deployed to other settings, such as hotlines, contact
tracing, sampling centres and COVID-19 consultation
centres.
Luxembourg is well equipped with acute and ICU
hospital beds, with rates above the EU averages (see
Section 4). The government asked hospitals to make
capacity available for COVID-19 patients, mostly by
delaying planned and elective procedures, as well
as by creating additional ICU beds. The operation
of hospital services was centrally coordinated and
defined by four phases according to the COVID-19
surge capacity plan in place. As a result, the available
capacities of acute and ICU beds were not exhausted
during the first and second wave of the COVID-19
pandemic (Figure 18). In fact, COVID-19 patients
from neighbouring countries such as France were
transferred to Luxembourg for treatment.
Four advanced ambulatory care centres
expanded capacity during the COVID-19
pandemic
Early in the COVID-19 pandemic (mid-March 2020),
the government and health professional organisations
set up four advanced care centres. These aimed to
provide specific care for COVID-19 patients, to reduce
pressure on hospitals and to keep patients away from
emergency departments and general practices. The
centres operated daily from 08:00 to 20:00, and had
two strictly separate channels of consultation: the
first for patients with signs of COVID-19 infection;
the second for those without (Ministry of Health,
2020b). Patients with a positive test result were either
sent home for isolation or transferred to a hospital
if necessary. The patient’s information was also
transferred to the Health Directorate’s contact tracing
unit to ensure appropriate contact tracing.
%
2%
4%
6%
8%
10%
12%
14%
16%
18%
20%
Denmark European Union Luxembourg
ccoouunnttrryy
Austria
Cyprus
European Union
Greece
Italy
Malta
Portugal
Spain
Positivity rate

20
Stte of Helth n the EU Luxembour Countr Helth Profle 2021
Figure 18. Hospitals had sufficient intensive care unit capacity for COVID-19 patients
Not Onl ncluds ICU bds for lvl 3 n 2020 (th most ntnsv cr) othr ICU bds t lvls 1 nd 2 r not ncludd
Sourc Mnstr of Hlth
Consultations in advanced care centres were free of
charge, irrespective of a person’s health insurance
coverage. Outside these centres, COVID-19 tests
were carried out upon presentation of a medical
prescription, social security card and identity card.
With decreasing case numbers, the advanced care
centres were successively closed by early summer
2020 – and two consultation centres reopened
in October and November 2020 for patients with
COVID-19 symptoms or a COVID-19 diagnosis, with
the aim of relieving pressure on GPs and reducing the
risk of transmission.
Nursing homes were strongly affected
during the first wave, but the response
improved immediately afterwards
As in many countries, residential LTC facilities in
Luxembourg were particularly affected by the first
wave of COVID-19. Between March and the end of
May 2020, nearly half (46%) of all COVID-19 deaths
in Luxembourg were among LTC residents (OECD,
2021). A working group devoted to nursing homes set
up various safety and hygiene measures to prevent
transmission within these facilities. Training and
guidance on use of PPE, infection control, hygiene
measures and testing for care professionals were as
important as inspections and recommendations by
hygienic teams on care quality, and safety measures
to ensure separate patient flows and non-COVID-19
areas within nursing homes.
The new organisational model for primary care
during the COVID-19 pandemic (see Section 5.2) also
included the establishment of on-call GP services
during weekends and public holidays for residential
facilities. The 24/7 availability of doctors aimed
to reduce hospital admissions and deliver better
continuity of care within nursing homes. Due to these
positive experiences, the government started a pilot
project in July 2020 that aims to continue the 24/7
on-call medical system in the future.
Luxembourg started vaccinating health
professionals and care home residents in
December 2020
The country’s vaccination strategy consisted of six
phases with different risk groups. The first phase
started at the end of December 2020: it targeted
health care professionals and staff in hospitals and
residential facilities, as well as care home residents.
The subsequent phases included population groups
by age and pre-existing health condition. Vaccinations
were carried out in six vaccination centres (for the
general population) and hospitals. Mobile teams
carried out vaccinations for older people in their
homes and in nursing homes. By the end of August
2021, more than half (56%) of the population had
received two doses of the vaccine (or equivalent)
(Figure 19).
Per 100 000 population
Feb
Mar
Apr
May
Jun
Jul
Aug
Sep
Oct
Nov
Dec
ICU COVID-19 patients
0
2
4
6
8
10
12
14
16
18
ICU bed capacity prior to COVID-19 ICU bed surge capacity during the first wave of COVID-19 ICU COVID-19 patients
Per 100 000 population
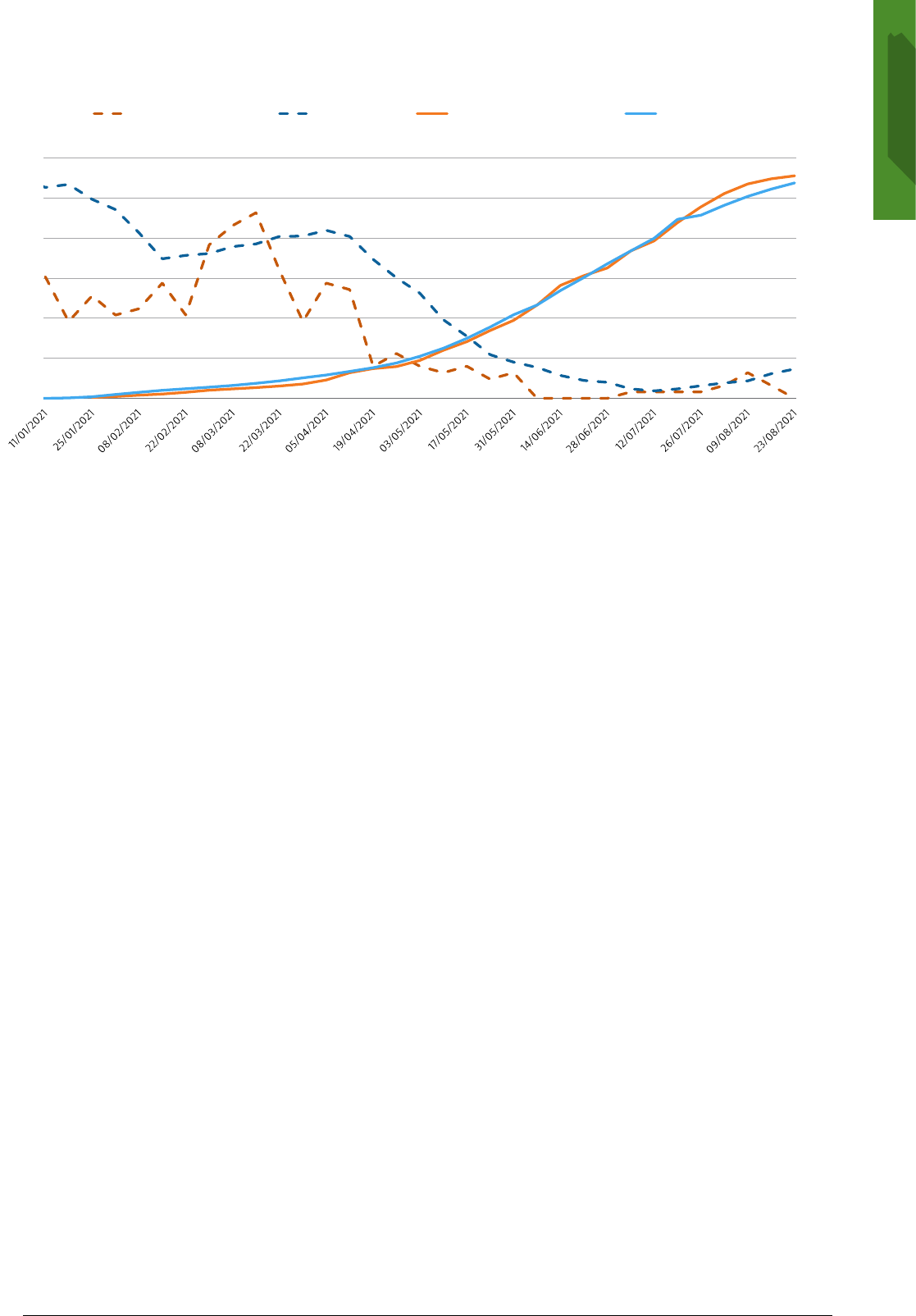
21
Stte of Helth n the EU Luxembour Countr Helth Profle 2021
Figure 19. Vaccination rates in Luxembourg have kept pace with EU-wide vaccination progress
Not Th EU vrg s unwghtd (th numbr of countrs usd for th vrg vrs dpndng on th w)
Sourcs ECDC for COVID-19 css nd Our World n Dt for vccnton rts
The COVID-19 pandemic revealed the need
for an improved health information system
The development of real-time monitoring of available
resources and epidemiological surveillance during
the COVID-19 pandemic showed that centralised
and timely collection of health-related data and data
exchange between health care providers is essential
for a functioning and responsive health care system.
Luxembourg’s new National Health Observatory,
established in 2021, will play a central role in the
development of health data and information systems.
Its activities include collecting and analysing disease
and death registries data.
Moreover, the Luxembourg Centre for Systems
Biomedicine is involved in the European Health Data
Space initiative, which is designed to promote better
exchange and access to different types of health data,
including electronic health records, genomics data
and data from patient registries, to support health
care delivery, as well as health research and policy-
making (European Commission, 2021b). In particular,
Luxembourg is supporting the development of the
future European Health Research and Innovation
Cloud, a decentralised digital health infrastructure,
which is the cornerstone of the European Health Data
Space
Resilience is being strengthened
through financial reserves and the EU’s
Recovery and Resilience Facility
The CNS has registered continuous revenue surpluses
over the past few decades, building up a large
financial reserve, which facilitated rapid mobilisation
of resources during the COVID-19 pandemic.
Despite additional expenses as part of the
government’s pandemic response, such as extended
family leave, sick leave payments and new payment
rates for doctors and dentists the CNS estimated a
surplus of EUR6.7million for 2020 and a reserve of
26.3% of current expenditure in 2021. This surplus is
also made possible by an additional financial injection
from the state of EUR200million in 2020.
In addition, as part of its National Recovery
and Resilience Plan, Luxembourg has dedicated
EUR1.2million to strengthening the resilience of
the health care system. In particular, health sector
investment will support reforms in bolstering the
competencies of health professionals. Specific
measures include broadening skills, expanding
domestic training and creating a register of health
care professional for better health planning
(EUR0.34million). Moreover, there is a focus on the
challenges identified in the Gesondheetsdësch to
future-proof the health system. Among these, the
digitalisation of health care will be addressed by
proposed investments in telemedicine solutions
(EUR0.83million) (Ministry of Finance, 2021).
COVID-19 weekly mortality and vaccination rates
Note: The EU average is unweighted (the number of countries used for the average varies depending on the week).
0
10
20
30
40
50
60
0
1
2
3
4
5
6
Luxembourg-deaths EU-deaths Luxembourg-vaccination EU-vaccination
Weekly deaths per 1 000 000 population
% of the population with two doses (or equivalent)

22
Stte of Helth n the EU Luxembour Countr Helth Profle 2021
6 e fndns
• Life expectancy in Luxembourg has increased
by more than two years since 2010, reaching
81.8 years in 2020, which is well above EU
average. However, COVID-19 accounted for
an estimated 11% of deaths in 2020, which
contributed to a reduction of nearly 11
months in life expectancy compared with
2019. Risk factors, including smoking and
poor diet, account for one third of all deaths.
Public health policies such as smoking bans
and tax increases on tobacco products have
contributed to reducing smoking among
adolescents and adults. However, heavy
alcohol consumption in adults remains a
cause for concern.
• Low mortality rates from treatable causes
suggest that Luxembourg’s health system
provides effective health care interventions.
Mortality rates from heart attack, stroke and
cancer have declined in the last decade. The
mortality rate for breast cancer has remained
relatively stable, albeit close to the EU average.
Luxembourg’s second National Cancer Plan
(2020-24) aims to improve the use of modern
genetics and molecular pathology in treating
cancer.
• Health spending per capita in Luxembourg
is among the highest in the EU, although
it represents a relatively small share of its
GDP. The public share of health financing is
considerably higher than the EU average, at
85% in 2019. The population enjoys a broad
benefits package, and out-of-pocket spending
is the second lowest in the EU. Unmet needs
for medical and dental treatment are among
the lowest in Europe. However, out-of-pocket
spending for pharmaceuticals, dental care
and long-term care can still be substantial. To
further improve access to outpatient medical
care and streamline administration, the
government aims to extend the third-party
payment system from 2023.
• Luxembourg’s health workforce is marked
by strong dependence on neighbouring
countries. Around two thirds of nurses
and one quarter of doctors practising in
Luxembourg live outside the country. During
the early phase of the COVID-19 pandemic,
the reliance on foreign health professionals
made Luxembourg particularly vulnerable
to the risk of border closures with Belgium,
France and Germany. The government aims
to alleviate reliance on cross-border health
professionals by raising the attractiveness
of health professions among the resident
population, expanding medical training
opportunities and implementing skill-mix
approaches.
• The country acted rapidly in response to
the COVID-19 pandemic, and was relatively
well prepared. The crisis unit at the Ministry
of Health coordinated all related actions,
with support from other public services. The
public health surveillance system included
an efficient contact tracing and large-scale
testing strategy.
• The COVID-19 pandemic triggered rapid
progress and innovations in the organisation
of health care provision, while also
revealing persistent problems. For example,
Luxembourg started to use teleconsultations
extensively, created a reserve of health
professionals and fostered co-operation with
the Ministry of Family Affairs for support
and supervision of nursing homes. The
collaborative effort by public services, health
care providers, the armed forces and private
companies, as well as the financial reserves of
the National Health Insurance Fund, made it
possible to create dedicated structures, such
as the advanced care centres, testing centres
and new on-call GP services for nursing
homes. Some of these innovations will be
maintained in the long term.

23
Stte of Helth n the EU Luxembour Countr Helth Profle 2021
Countr bbrevtons
Austr AT
Belum BE
Bulr BG
Crot HR
Cprus CY
Czech CZ
Denmr D
Eston EE
Fnlnd FI
Frnce FR
Germn DE
Greece EL
Hunr HU
Icelnd IS
Irelnd IE
Itl IT
Ltv LV
Lthun LT
Luxembour LU
Mlt MT
Netherlnds NL
Norw NO
Polnd PL
Portul PT
Romn RO
Slov S
Sloven SI
Spn ES
Sweden SE
e sources
OECD/EU (2020), Hlth t Glnc Europ 2020 –
Stt of Hlth n th EU Ccl, Prs, OECD Publshn
WHO Reonl Offce for Europe, Europen Commsson,
Europen Observtor on Helth Sstems nd Polces
(2021), COVID-19 Helth Sstems Response Montor –
Luxembour
References
Bces C et l (2021) Lessons lerned from COVID-19
locdown for cncer cre ntonwde surve of
oncolosts n Luxembour Bulltn d l Soct ds
Scncs Mdcls du Grnd-Duch d Luxmbourg,
2020/2, Jnur 2021
CNS (2020), Dcompt d l’ssurnc mld-mtrnt
2019, Luxembour
ECDC (2020), Populton-wd tstng of SARS-CoV-2
countr xprncs nd potntl pprochs n th EU/
EEA nd th Untd ngdom Stocholm
EU Expert Group on Helth Sstems Performnce
Assessment (HSPA) (2020), Assssng th rslnc of
hlth sstms n Europ n ovrvw of th thor,
currnt prctc nd strtgs for mprovmnt
Eurofound (2021), Lvng, worng nd COVID-19 surv,
thrd round (Februr-Mrch 2021)
Europen Commsson (2020), A phrmcutcl strtg
for Europ
Europen Commsson (2021), Europ’s Btng Cncr
Pln
Europen Commsson (2021b), Th Europn Hlth
Dt Spc
IGSS (2021), Rpport gnrl sur l scurt socl u
Grnd-Duch d Luxmbourg 2020, Luxembour
Lr-Hllon ML (2019), Ett ds lux ds profssons
mdcls t ds profssons d snt u Luxmbourg
Rpport fnl t rcommndtons Luxembour, Snte
et Prospectves, Luxembour
Luxemburer Wort (2020), Plus d l mot ds dcs n
msons d rpos
Médecns du Monde (2019), Rpport nnul 2019
Mnstr of Helth (2020), Th tlconsultton
pltform nd th ptnt tlmontorng tool MAELA
Dgtlston n th fght gnst th COVID-19
pndmc, Luxembour
Mnstr of Helth (2020b), Orgnston du sstm d
snt n prod d pndm COVID-19, Luxembour
Mnstr of Fnnce (2021), Pln pour l rprs t l
rslnc du Grnd-Duch du Luxmbourg, Luxembour
OECD (2021), Rsng from th crss polc rsponss to
COVID-19 n long-trm cr, OECD Polc Bref
Tchc A, Lorentz N, Demrest S (2016), Socoeconomc
nequltes n smon nd smon cesston due to
smon bn enerl populton-bsed cross-sectonl
stud n Luxembour PLoS On Apr 2111(4)e0153966

Stte of Helth n the EU
Countr Helth Profle 2021
The Countr Helth Profles re n mportnt step n
the Europen Commsson’s onon Stt of Hlth n
th EU ccle of nowlede broern, produced wth the
fnncl ssstnce of the Europen Unon The profles
re the result of ont wor between the Ornston
for Economc Co-operton nd Development (OECD)
nd the Europen Observtor on Helth Sstems nd
Polces, n cooperton wth the Europen Commsson
The concse, polc-relevnt profles re bsed on
trnsprent, consstent methodolo, usn both
quntttve nd qulttve dt, et flexbl dpted
to the context of ech EU/EEA countr The m s
to crete mens for mutul lernn nd voluntr
exchne tht cn be used b polcmers nd polc
nfluencers le
Ech countr profle provdes short snthess of
· helth sttus n the countr
· the determnnts of helth, focussn on behvourl
rs fctors
· the ornston of the helth sstem
· the effectveness, ccessblt nd reslence of the
helth sstem
The Commsson s complementn the e fndns of
these countr profles wth Compnon Report
For more nformton see eceuropeu/helth/stte
Plese cte ths publcton s OECD/Europen Observtor on Helth Sstems nd Polces (2021), Luxmbourg
Countr Hlth Profl 2021, Stt of Hlth n th EU, OECD Publshn, Prs/Europen Observtor on Helth
Sstems nd Polces, Brussels
ISBN 9789264444966 (PDF)
Seres Stte of Helth n the EU
SSN 25227041 (onlne)
