The Mental Health Strategy
for Canada
:
A Youth Perspective
PAGE i
In March 2013, the Mental Health Commission
of Canada’s Youth Council (YC) came up with
the idea to rewrite or “translate,” from a youth
perspective, Changing Directions, Changing Lives:
The Mental Health Strategy for Canada. Although
every effort was made during the writing of the
Strategy to reach as many audiences as possible,
the YC decided to rewrite it to resonate better
among their friends and peers — or anyone else
interested in mental health discussions in Canada.
The main aim of their project was to develop
a supplemental document that highlights the
experiences and vision of young people working
toward system change, ultimately making the
original Strategy a more accessible document
to all.
Over the course of two years, the YC met in
person four times to work through the Strategy,
page by page. Using a critical youth lens, they
rewrote all six strategic directions, drawing on
personal experiences to make sense of a large
policy document and turn it into something
original. To our knowledge, never before has
a group of Canadian youth designed a project
of this scope or contributed to the eld of
knowledge exchange by translating a policy
document written largely for, and by, adults.
While the Strategy team consulted with hundreds
of youth and their families during the initial
writing process, the policy focus of the document
meant that many people could nd it challenging
to access. The YC hopes that the new version
helps to overcome this challenge.
The original Strategy is geared toward people of all ages and outlines a few specic recommendations for action
on child and youth mental health. For example, the Strategy recommends that we:
> Increase comprehensive school health and post-secondary mental health initiatives that promote mental
health for all students and include targeted prevention efforts for those at risk (from Strategic Direction 1).
> Remove barriers to full participation of people living with mental health problems or illnesses in
workplaces, schools (including post-secondary institutions), and other settings (from Strategic Direction 2).
> Remove nancial barriers for children and youth and their families to access psychotherapies and clinical
counselling (from Strategic Direction 3).
> Remove barriers to successful transitions between child, youth, adult, and senior mental health services
(from Strategic Direction 3).
FOREWORD
PAGE ii
This document builds on these recommendations and others in order to advance dialogue among mental
health advocates, activists, students, community mental health workers, policy makers, or anyone interested
in transforming Canada’s mental health system. We hope that you nd this document useful for becoming
even more engaged in policy discussions that directly impact people of all ages.
Despite being written by youth who highlight youth-specic examples, the report you are about to read is not a full
mental health strategy for youth, nor is it intended to take the place of the original Strategy. If you are interested in
more detailed policy recommendations on child and youth mental health, take a look at these other reports from the
MHCC: Evergreen: A Child and Youth Mental Health Framework for Canada, School-Based Mental Health in Canada:
A Final Report, Taking the Next Step Forward, and, of course, The Mental Health Strategy for Canada.
The YC also understands and appreciates the range of experiences people have with mental illness and do not
intend to use the term in any uniform way. For the purposes of this document, the YC chose “mental health issues”
as a way of encompassing the vast range of diagnoses and lived experiences with mental health problems and
illnesses. People living with schizophrenia, for example, may be at different stages of recovery than someone
living with depression or may require much more complex services than others. Some people may have so few
resources or support that conversations about recovery seem impossible. Either way, the YC acknowledges the
diversity of experiences and understands, through their own lived experience, the complexity of mental illness
and the range of services and supports our system needs in order to advance recovery for everyone.
FOREWORD

PAGE iii
On behalf of the Mental Health Commission of Canada (MHCC), we are delighted to share
with you The Mental Health Strategy for Canada: A Youth Perspective.
The MHCC’s Youth Council worked tirelessly to adapt Changing Directions,
Changing Lives: The Mental Health Strategy for Canada into a highly accessible
format. Their enthusiastic effort saw the transformation of a 150-page – often
technical – document into an engaging, fresh, and relevant take on mental health
in this country.
Harnessing their keen minds, our Youth Council highlights issues and experiences
unique to young Canadians. Yet, their worldview is broad enough to encompass
the needs of ALL Canadians. Displaying an innate sensitivity to Canada’s diverse
population, they have created a resource that we believe will spur meaningful
dialogue from coast-to-coast-to-coast.
It isn’t enough to hear young people.
They have far too much to offer to simply be a voice at the table. They must be
active participants in setting the course for mental health policy and practice in
Canada. The MHCC is privileged to bene t from the wisdom and experience of
these thoughtful emerging leaders.
Now, our nation’s dialogue on mental health is richer for their contribution.
So please, read on.
Louise Bradley & the Hon. Michael Wilson, P.C., C.C.
MESSAGE FROM THE CHAIRMAN OF THE BOARD AND THE PRESIDENT AND CEO

PAGE iv
.............................................................................................................. page i
................ page iii
................................................................................................. page iv
............................................................................................... page 1
......................................................................................................... page 2
1: ......................................................................... page 6
STRATEGIC DIRECTION 2: RECOVERY ...................................................................... page 10
STRATEGIC DIRECTION 3: ACCESS ........................................................................... page 13
STRATEGIC DIRECTION 4: DIVERSITY ...................................................................... page 18
STRATEGIC DIRECTION 5: FIRST NATIONS, INUIT & MÉTIS ........................................ page 23
STRATEGIC DIRECTION 6: COORDINATION & COLLABORATION .................................. page 27
CALL TO ACTION .................................................................................................... page 30
TABLE OF CONTENTS

PAGE 1
The Mental Health Commission of Canada’s Youth Council (YC) has many people to thank for helping to make
this project a reality. When we decided to write a youth-translated version of the Mental Health Strategy for
Canada, we were not prepared for how much work that would actually entail. After almost two years since we
decided to do this project and after countless revisions, consultations, in-person meetings, brainstorming sessions,
more revisions, graphic design, knowledge exchange planning, we are nally able – and delighted – to share this
document with you.
The following people and organizations were instrumental in helping nish this project:
> The Assembly of First Nations National Youth Council, the Inuit Tapiriit Kanatami Youth Council, and
youth volunteers from the Métis Nation of British Columbia: thank you for helping us write certain sections
of this document from culturally relevant and safe perspectives.
> Sam Bradd, our image guy: thank you for bringing the Strategy to life with your amazing graphics.
> Former YC members: thank you for your ideas and help on the early parts of this project and for your
unconditional support from afar.
> Original developers and writers of the Strategy: thank you for helping us keep our messages in line with
Changing Directions, Changing Lives: The Mental Health Strategy for Canada.
Sincerely,
Kristen Zaun (YC Chair)
Amanee Elchehimi (YC Vice-Chair)
Ally Campbell
Dustin Garron
Aaron Goodwin
Patricia Laliberté
Simran Lehal
Don Mahleka
Katie Robinson
Jack Saddleback
Marta Sadkowski
Nancy Savoie
Vanessa Setter
ACKNOWLEDGMENTS

PAGE 2
The Mental Health Strategy for Canada
:
A Youth Perspective
DID YOU KNOW...
MORE THAN TWOTHIRDS OF YOUNG ADULTS LIVING WITH A MENTAL HEALTH
PROBLEM OR ILLNESS SAY THEIR SYMPTOMS FIRST APPEARED WHEN THEY
WERE CHILDREN?
That makes child and youth issues an especially important topic in mental health, one that the Mental Health
Commission of Canada (MHCC) recognized early on when it created the Youth Council in 2008.
WHO ARE WE?
The MHCC’s Youth Council (YC) represents young people with lived experience of mental health issues, whether
personally or through family or friends. YC members are selected from across Canada with consideration given to
the following: age and gender; province or territory of residence; cultural background; First Nations, Inuit, or Métis
background; linguistic background; siblings or family members of persons with mental illness; experience with the
child welfare system; sexual orientation and/or gender identities; or youth at risk with issues in housing, addictions,
and/or the justice system.
WHAT DO WE DO WITH THE MHCC?
>
Advocate for young people with mental health issues.
> Get involved with local, provincial, and national youth mental health networks.
> Bring a youth perspective to MHCC projects.
> Speak on behalf of youth at MHCC events.
> Promote recovery and inspire other youth at public events.
> Make sure youth have a voice in the decisions being made about Canada’s
mental health services and policies.
introduction
PAGE 3
in 2013, we got to thinking…
SO WHY MAKE A DIFFERENT VERSION OF THE STRATEGY?
The Mental Health Strategy for Canada was published in 2012. It took over ve years to research and write, with
thousands of Canadians being consulted in the process. It looks at a lot of issues and recommends ways to improve
the mental health system — but it’s over 150 pages long and can be technical sometimes.
We thought — let’s make sure these important messages reach as many people as possible. Young people, youth
advocates, service workers, and the general population need to equip themselves with the right knowledge so that
they can have an informed say in issues that affect Canadians now and in the future! We hope this document makes
mental health policy more accessible to anyone advocating for system or service level changes.
HOW DID WE DO IT?
It took us two years to write this version. We looked at every priority and recommendation in the Strategy and rewrote
them keeping our target audience in mind - Canadians who might not nd current mental health policy documents
accessible. We highlighted youth-specic examples to reect our own experiences, but certainly there are more that
could have been included to reect the needs of people of all ages. Before starting, we had to think about a number
of things:
> How can mental health policies be written to make better sense to Canadians directly
affected by the mental health system, services, and supports?
> What examples of best practices could make the Strategy more meaningful to
anyone engaged in mental health policy discussions across Canada?
> What parts of the Strategy’s recommendations are most relevant to youth?
> How can a youth perspective on the Strategy inspire mental health system
change and a sense of hope and optimism in young people?
In order to reect the histories of First Nations, Inuit, and Métis (FNIM) in Canada, the YC also consulted with FNIM
youth groups who helped us write certain sections from culturally relevant and safe perspectives. We understand
that in order to truly transform Canada’s mental health system, the needs and challenges of Canada’s FNIM populations
must be recognized and reected in future mental health policies. We expand on what we mean by this in Strategic
Direction 5.
INTRODUCTION
PAGE 4
WHAT DO YOU NEED TO KNOW BEFORE READING OUR REPORT?
The priorities and recommendations in the Mental Health Strategy for Canada are grounded in mental health
and recovery terminology. That means you have to understand these terms in order to really “get” the rest of
this document.
GOOD MENTAL HEALTH AND MENTAL HEALTH ISSUES
Mental health is a state of wellbeing in which you can realize your own potential, cope with the normal stresses of life,
work productively, and make a contribution to your community. Good mental health protects us from the stresses of
our lives and can even help reduce the risk of developing mental health issues.
It’s important to recognize that good mental health is not the same as “not having a mental health issue.” Even if you
develop a mental health issue, you can still experience good mental health and make progress along your personal
journey toward recovery.
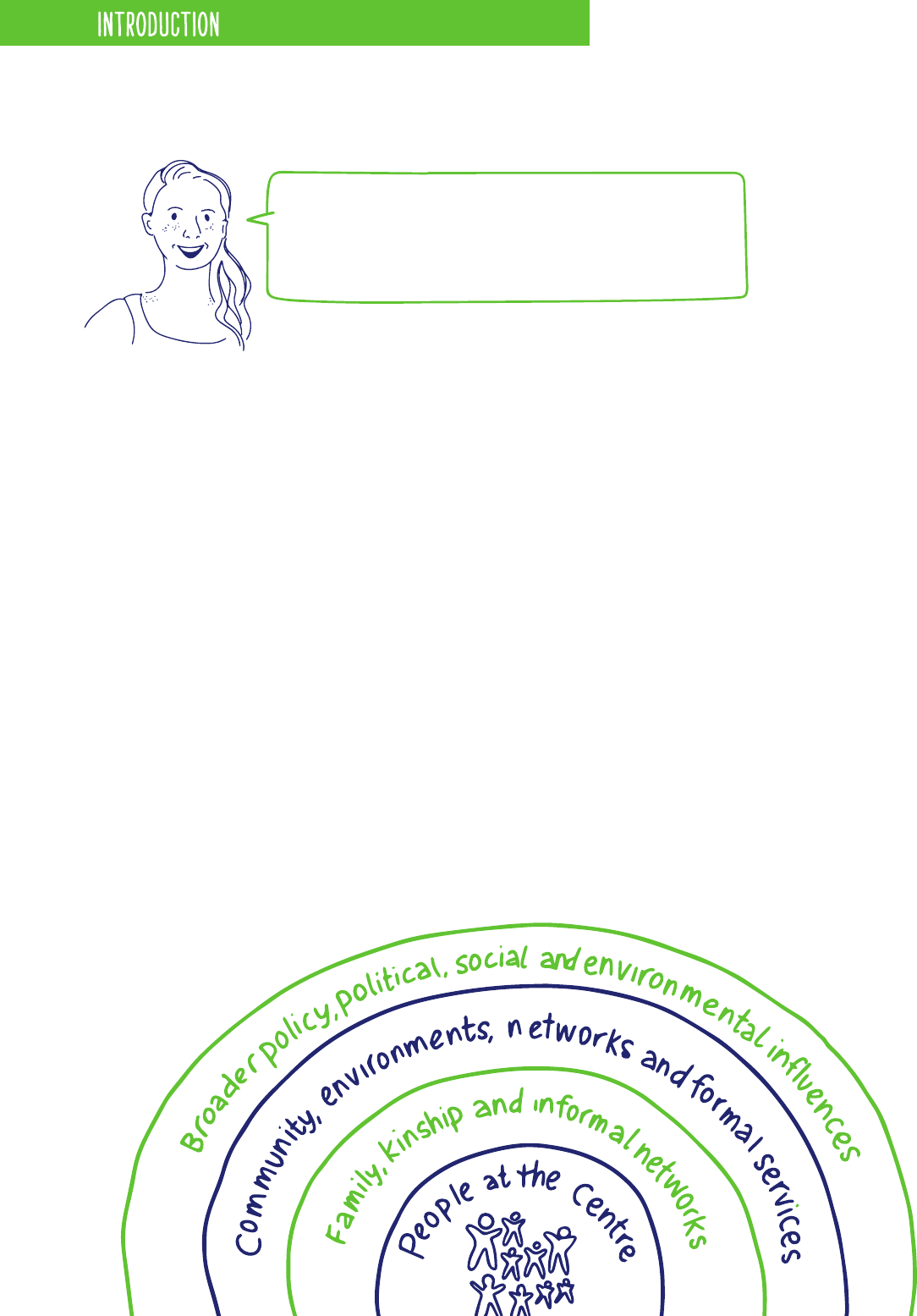
There is no single cause of any mental health issue. Whether a mild mental health problem or a severe mental illness,
mental health issues are the result of a complex mix of social, economic, psychological, biological, and genetic factors.
“THE YOUTH COUNCIL IS A BRIDGE BETWEEN THE MHCC AND
YOUTH EXPERIENCING MENTAL HEALTH ISSUES. WE MAKE
SURE YOUTH ARE REPRESENTED IN MHCC’S DECISION-MAKING
SO CHANGES IN THE MENTAL HEALTH SYSTEM WILL BENEFIT
YOUTH.” – MARTA S.
INTRODUCTION
PAGE 5
RECOVERY
The Mental Health Strategy for Canada denes recovery as living a satisfying, hopeful, and meaningful life, even
when there are ongoing limitations caused by mental health issues. With the right combination of services and supports,
many people who are living with even the most severe mental illnesses can experience signicant improvements in
their quality of life.
Recovery does not imply a “cure.” Yes, the full remission of symptoms may be possible for some. But for others, mental
health issues should be thought of in the same way as diabetes or other chronic health problems — something that has
to be managed over the course of your life but does not prevent you from leading a happy, fullling life.
At its core, the concept of recovery is about hope,
empowerment, self-determination, and responsibility.
Good mental health and wellbeing are important for all of us — no matter our age and whether or not we experience
mental health issues. The principles of recovery apply to everybody. With children and youth, for example, a key focus
should be on becoming resilient and attaining the best mental health possible as they grow. For seniors, it’s about
addressing the additional challenges that come with aging.
Our goal in doing this work was simple. We wanted to bring to life a document that is
accessible to everyone, including youth, with the hope of sparking the minds of Canadians
to want to be a part of changing the mental health policy landscape.
“I ALWAYS THOUGHT BEING MENTALLY ILL MADE ME A BAD PERSON, EVEN
BROKEN, BUT WHEN I REACHED RECOVERY I WAS ABLE TO SEE EVERYTHING
THAT MY ILLNESS TAUGHT ME: COMPASSION, EMPATHY, APPRECIATION, AND
RESILIENCY. WHEN I LEARNED TO LIVE AND THRIVE WITH IT, I REALIZED IT
MADE ME A BETTER AND STRONGER PERSON IN THE END.” NANCY S.
“THE YOUTH PERSPECTIVE ENRICHES THE WORK OF MHCC AND OTHER
MENTAL HEALTH GROUPS. BECAUSE THERE ARE GAPS IN SERVICE PROVISION
AND PROMOTION, THERE NEEDS TO BE MORE YOUTH LEADERSHIP,
COORDINATION, EVIDENCEINFORMED STRATEGIES, AND PARTICIPATION IN
THESE SERVICES. YOUTH WITH LIVED EXPERIENCE NEED TO BE ENCOURAGED
TO SPEAK OUT MORE ON VARIOUS ISSUES TO INSPIRE AND GIVE DIRECTION
FOR BETTER CHANGE.” DON M.
INTRODUCTION
PAGE 6
ENCOURAGE LIFELONG MENTAL HEALTH IN ALL SOCIAL ENVIRONMENTS
WHERE PEOPLE LIVE OR SPEND TIME AND PREVENT MENTAL HEALTH
ISSUES AND SUICIDE WHEREVER POSSIBLE.
Mental health issues can have many causes, ranging from the biological (such as chemical changes in the body) to
the environmental (such as stressful life events). No one can predict for sure who will experience them and who
won’t. What we do know is that efforts to promote mental health, and to treat and prevent mental health issues
and suicide, are more successful when they do the following:
When people live in a healthy and
supportive environment, they tend to
have better mental health and less risk
of mental illness.
STRENGTHEN PROTECTIVE FACTORS
& REDUCE RISK FACTORS
STRATEGIC DIRECTION 1
KNOW WHO TO REACH
Prevention efforts work better when
they’re designed for one specic group –
for example, people with the same age or
from the same community.
PAGE 7
STRATEGIC DIRECTION 1
The Mental Health Strategy for Canada in Action
The TAMI (Talking About Mental Illness) Coalition’s Stomping Out Stigma campaign in Durham, Ontario has been called a “best-in-class” example of mental
health awareness and prevention for middle and high school students. It uses contact-based education to decrease stigma about mental health issues and
promote help seeking. Speakers with lived experience go into schools giving teachers and students the opportunity to meet and interact with real people
who have experienced mental health challenges. The program’s website has helpful links for students, parents, and teachers, with separate curricu-
lum-based teaching guides and toolkits specically for middle school (Grades 7 and 8) and high school students. http://tamidurham.ca/
KEY WORDS
Risk factor: Any-
thing that makes
a person more
likely to suffer
from mental health
issues.
Protective factor:
Anything that
helps a person to
keep their mental
health.
Stigma: Negative
attitudes and
behaviours that
make people with
mental health
issues feel judged
and ashamed.
Ageism: Being
prejudiced against
someone because
of their age — old
or young.
Contact-based
education: Meeting
people who have
experienced mental
health issues and
are willing to share
their stories of
recovery.
SET CLEAR GOALS
Knowing in advance what the goals are
helps to measure success down the road.
Communities have the potential to take
care of people – as long as they have
the right tools and enough resources.
GIVE COMMUNITIES WHAT
THEY NEED TO TAKE ACTION
PLAN FOR THE LONGTERM
The best initiatives are those that last a
long time, giving them more of a chance
to be effective.
We all have a part to play in improving mental health. It isn’t just something for therapists
and clinics to deal with. Mental health must be addressed anywhere people spend their time —
including home, school, and work.

PAGE 8
PRIORITIES
1.1 HELP PEOPLE UNDERSTAND HOW TO ENCOURAGE MENTAL HEALTH,
REDUCE STIGMA, AND PREVENT MENTAL HEALTH ISSUES AND SUICIDE.
Being mentally healthy helps us to do better at school, make a good living,
and be physically well.
As youth, we have a unique opportunity to be young leaders — lend a hand,
make a point to connect with others, take part in group recreation when
possible. In our various communities, having access to programs that foster
better mental health is a must.
Many people with mental health issues experience stigma.
One of the best ways to break down stigma is through contact-based education.
It’s important that people get support as soon as possible when experiencing mental health issues.
We all need to be educated to be able to recognize symptoms of mental health issues in ourselves
and others. For youth, for example, it’s especially important that front-line workers have this
expertise because people like teachers, coaches, and community workers are the ones young
people usually turn to rst.
1.2 HELP FAMILIES, CAREGIVERS, SCHOOLS, POSTSECONDARY INSTITUTIONS, AND
COMMUNITY ORGANIZATIONS ENCOURAGE CHILD AND YOUTH MENTAL HEALTH AND
INTERVENE EARLY WHEN SIGNS FIRST EMERGE.
70 per cent of young adults with mental illnesses report that their symptoms rst started
in childhood. It's kind of a no-brainer that encouraging good mental health early in life
is important.
The best places to reach youth are at home, school, community centres and in the places
where youth work.
We should have programs that take a very broad approach to mental health and more
targeted programs that specically address children and youth who have a high risk of
mental health issues —due to poverty, family violence, or a parent having a mental health
or substance use problem.
“DURING THE PROCESS OF MY RECOVERY, I HAVE COME TO REALIZE THAT
WE HAVE A RESPONSIBILITY AS INDIVIDUALS, COMMUNITIES, AND LEADERS
WITHIN COMMUNITIES TO ADVOCATE FOR THE PREVENTION, PROMOTION,
AND ACCESS TO QUALITY MENTAL HEALTH SERVICES FOR CHILDREN, YOUTH,
AND ALL CANADIANS. TOGETHER, THROUGH THE STRENGTH OF OUR DIVER
SITY AS CANADIANS, WE CAN CREATE A DIALOGUE THAT IS NECESSARY
TO FOSTER COLLABORATION AND INNOVATION FOR TANGIBLE, IMPACTFUL
CHANGES IN MENTAL HEALTH.” KRISTEN Z.
STRATEGIC DIRECTION 1
The Mental Health Strategy for Canada in Action
The Thunder Bay Youth Suicide Prevention Task Force (TBYSPTF) is made up of 30 organizations working together to address the issues of youth suicide.
Their goals are to increase awareness of issues related to youth suicide, to work collaboratively to prevent suicides in our community, and to mobilize
services to respond quickly to a youth suicide or other tragic event. The Task Force has run public health campaigns for teachers, coaches, and parents,
with posters and quick-reference cards about spotting early warning signs of mental illness plus tips on what to say and where to get help. Check out
their web site at http://www.heresthedeal.ca
PAGE 9
1.3 CREATE MENTALLY HEALTHY WORKPLACES.
Just as mentally healthy schools are important for children and youth, mentally healthy
workplaces have a signicant inuence on the mental health of everyone who spends
time at work. We need to make sure workplaces inuence in a positive and not a negative
way, otherwise they can also contribute to the development of mental health issues like
depression and anxiety.
To encourage good mental health and ght stigma, workplaces need to:
> Have strong leaders and managers willing to make change happen
and to play their part in stopping bullying and harassment.
> Implement management training, employee assistance, and promotion
and prevention programs.
> Encourage a positive work-life balance.
> Support recovery for employees living with mental health issues.
1.4 ENCOURAGE GOOD MENTAL HEALTH IN SENIORS.
Many of you can probably remember a time when you or someone you know has been stereotyped or
discriminated against because of their age (ageism). This can affect people at all stages of life.
Take depression for example. Many people don’t take depression later in life
seriously (including seniors themselves) because they think it goes hand in hand
with the aging process. If we want to stop stereotypical attitudes based on age,
we need to challenge the idea that mental illness
is just a normal part of aging. We need to better
understand the difference between age and illness.
A range of efforts is needed to help promote physical and mental wellness in
seniors and to prevent mental illness, dementia, and suicide wherever possible.
STRATEGIC DIRECTION 1
The Mental Health Strategy for Canada in Action
National Standard of Canada for Psychological Health and Safety in the Workplace
Championed by the Mental Health Commission of Canada, and developed by the Canadian Standards Association and the Bureau de normalisation
du Québec, the Standard is a voluntary set of guidelines, tools and resources focused on promoting employees’ psychological health and
preventing psychological harm due to workplace factors.
HOW ARE YOU?
PAGE 10
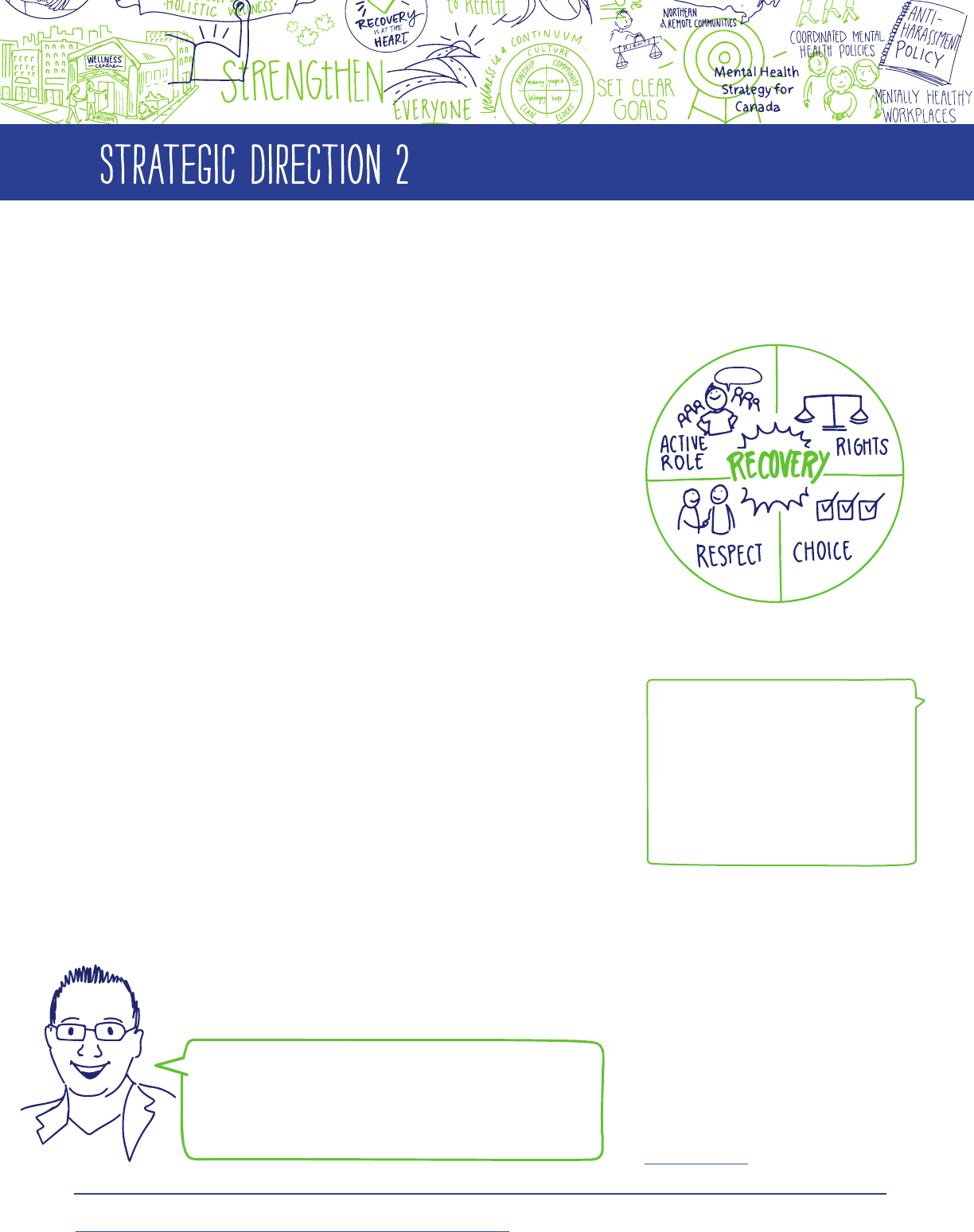
FOCUS THE MENTAL HEALTH SYSTEM ON RECOVERY AND
WELLBEING FOR PEOPLE OF ALL AGES AND PROTECT THE
RIGHTS OF PEOPLE WITH MENTAL HEALTH ISSUES.
Recovery is an important concept in mental health, but it is
not always well understood. When a mental health system is
focused on recovery, it helps those with mental health issues
to live satisfying, hopeful, and meaningful lives (as dened by
each individual person).
Recovery and wellbeing are for everyone — people living with
mental health issues, their families and communities, and the
country as a whole. In 2006, the Out of the Shadows at Last
report
1
said recovery should be “at the centre of mental health
reform” in Canada. But even today, our mental health system is
still not focused enough on the full range of services, treatments,
and supports that promote recovery and wellbeing. That means
there’s still a lot of work to be done.
To truly put recovery at the centre of the system, we need to
make sure that:
> People with lived experience are able to play an
active role alongside mental health professionals.
> The rights of people with mental health issues
are protected.
> People with mental health issues are treated with
respect in every setting and situation.
> People can choose the service, treatment, and support
options that work for them.
STRATEGIC DIRECTION 2
1
The Out of the Shadows at Last report, produced by the Senate of Canada in 2006, can be viewed online at:
http://www.parl.gc.ca/Content/SEN/Committee/391/soci/rep/rep02may06-e.htm.
The Mental Health Strategy for Canada in Action
Student-athletes can face incredible pressure
to perform in sport and in the classroom and,
like many youth, they can also be reluctant to
talk about their mental health. The Student-Athlete
Mental Health Initiative (SAMHI) was created
to protect and promote the mental health of
student-athletes and to support those struggling
with mental illness. Because one of the keys to
recovery is opening up and realizing other people
have been through the same journey, a highlight
of SAMHI’s work is the “SAMHI Champion Series.”
Student-athletes are invited to write about their
real-life experiences with recovery and mental
illness on the blog so others can learn from their
challenges and victories. The blog also provides
links to help connect student-athletes with
counselling resources and other mental
health services.
http://www.samhi.ca
“WHEN YOU RECOGNIZE THE IMPORTANCE OF YOUR MENTAL
HEALTH, YOU CAN DETERMINE THE BEST ROUTE TO ATTAINING
GOOD MENTAL HEALTH. FOR ME, THIS INCLUDED HOSPITALIZATION
AND SEEING A THERAPIST. FOR OTHERS, THIS MIGHT INVOLVE
PHYSICAL ACTIVITY OR MEDICATIONS. WE CAN GET TO THE SAME
DESTINATION BY TAKING DIFFERENT ROUTES.” DUSTIN G.
Recovery: The process through which a
person is able to live a satisfying, hopeful,
and meaningful life (as dened by that
individual), even when there are ongoing
limitations caused by mental health issues.
Wellbeing: The physical and emotional
state that comes from living a balanced,
fullling life. Wellbeing can mean different
things to different people and can even
change depending on where a person is in
his or her recovery journey.
KEY WORDS
PAGE 11
PRIORITIES
2.1 PUT RECOVERY AND WELLBEING AT THE HEART OF MENTAL
HEALTH POLICIES AND PRACTICES.
Canada’s mental healthcare system needs to shift its focus to
recovery and wellbeing. Guidelines, indicators, tools, standards, on-
going training, and leadership are all essential pieces in creating this
shift from the current policies and practices to recovery-oriented ones.
There also needs to be greater collaboration between those who provide services and those who use them. People
living with mental health issues must be actively involved in developing and managing their own care plans.
Families and friends need information, resources, and supports to be partners in the recovery journey, while
respecting people’s right to keep things condential. For youth, siblings and peer networks are often important
members of the circle of care and those siblings and friends need supports and services themselves.
2.2 ACTIVELY INVOLVE PEOPLE LIVING WITH MENTAL
HEALTH ISSUES AND THEIR FAMILIES.
Anyone who has experienced or been close to someone affected by mental
health issues has unique expertise and perspective that can help change the
mental health system.
People with lived experience should be actively involved on boards and advisory
bodies that make decisions about the system and welcomed into the mental
health workforce — not just as peer support workers but at all levels within an
organization. Who better to help guide the changes that need to be made to the
system than individuals who have gone through the process themselves and
know where the pitfalls lie?
“RECOVERY IS A JOURNEY.
THE ONLY THING I SEE ON THE
MAP IS WHERE I AM TODAY
AND THE DISTANCE FROM
MY STARTING POINT. IT’S
ALSO ABOUT GIVING MYSELF
PERMISSION TO STRUGGLE
AND HAVING THE SUPPORT
AND COPING RESOURCES TO
GET THROUGH THAT STRUGGLE
FOR A LITTLE LONGER EACH
DAY.” ALLY C.
STRATEGIC DIRECTION 2
The Mental Health Strategy for Canada in Action
Youth advocates are changing lives across Canada and around the world. Youth with lived experience can play a major role in the recovery process.
Consider Kevin Breel, a Vancouver stand-up comic whose TED talk on depression has received more than three million views — highlighting how
youth can give voice to their struggles with suicide in a way that resonates with others around the world.
http://www.ted.com/talks/kevin_breel_confessions_of_a_depressed_comic
PAGE 12
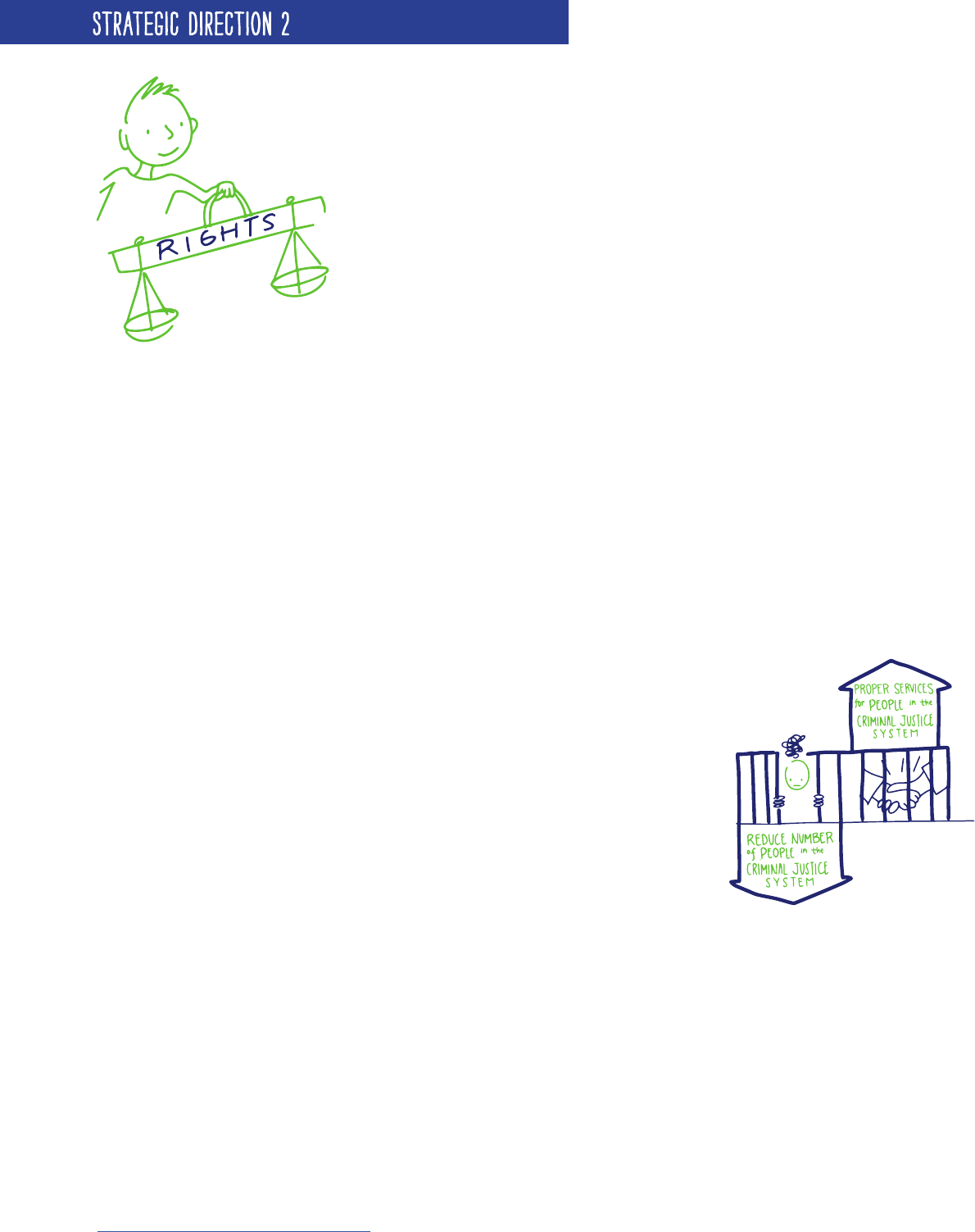
2.3 RESPECT AND PROTECT THE RIGHTS OF PEOPLE LIVING
WITH MENTAL HEALTH ISSUES.
Canada signed the United Nations Convention on the Rights of Persons
with Disabilities (CRPD) in 2010. The CRPD is a commitment to making
sure our laws and regulations include and protect the human rights of
all people with disabilities, including those with mental health issues.
What exactly do we mean?
Here’s an example: When police are called in to respond to a mental
health crisis, information about the incident may be recorded and then
disclosed in police record checks, which can make it difcult for the
person to get a job or travel outside the country. Some police agencies
have already stopped this practice. Now we need to make sure they
all do.
When mental health issues cause people to be potentially harmful to
themselves or others, the CRPD says safety measures should be the least
“intrusive” and “restrictive” possible. That is, any decision to restrain the
individual, whether physically or through the use of medication, or to
isolate them, should be evaluated in terms of his or her human rights.
The caregiver needs to ask, “Are human rights being respected?”
2.4 REDUCE THE NUMBER OF PEOPLE IN THE CRIMINAL JUSTICE SYSTEM
LIVING WITH MENTAL HEALTH ISSUES AND PROVIDE PROPER SERVICES AND
SUPPORTS TO PEOPLE ALREADY IN THE SYSTEM.
Most people living with mental health issues have no involvement with the criminal
justice system. But those who do are “over-represented” — meaning there are more of
them in the system than the general average. Where youth are concerned, it’s hard to
know exactly how common mental health issues are because many young people are
not diagnosed until they leave jail and are placed in group homes or foster care.
Changing this trend will require:
> A focus on prevention and early intervention, which can help keep youth
out of the criminal justice system for their entire lives. How? By preventing
mental health issues from developing and by providing help quickly when
they do.
> Adequate access to professional mental health services in correctional settings.
> A “continuity” of services — from a person’s rst interaction with the justice
system all the way through to when he or she returns to life in the
community — that involves more than just a check-in with a parole ofcer.
> More training and resources for police and corrections workers,
teaching them how to interact with people living with mental health
issues, including youth.
STRATEGIC DIRECTION 2
The Mental Health Strategy for Canada in Action
Putting mental health at the front lines of police response: The Mental Health Emergency Services Program run by Vancouver Coastal Health features
a mobile response unit called Vancouver’s Car 87 which pairs police ofcers with registered psychiatric nurses to provide onsite interventions for
people experiencing mental health crises. The nurses and ofcers respond to calls together and then work as a team in assessing, managing, and
deciding the most appropriate action. Similar steps are taken by Toronto’s Mobile Crisis Intervention team, which has its own crisis line supported by
crisis workers, specially trained police ofcers, and mental health nurses who provide secondary responses to calls for people in crisis.
http://www.torontopolice.on.ca/community/mcit.php
Convention on the Rights of Persons with Disabilities:
Article 1 – Purpose
The purpose of the present Convention is to promote,
protect, and ensure the full and equal enjoyment
of all human rights and fundamental freedoms by
all persons with disabilities and to promote respect
for their inherent dignity. Persons with disabilities
include those who have long-term physical, mental,
intellectual, or sensory impairments which in
interaction with various barriers may hinder their
full and effective participation in society on an
equal basis with others.

PAGE 13
GIVE PEOPLE ACCESS TO THE RIGHT SERVICES, TREATMENTS, AND
SUPPORTS WHEN AND WHERE THEY NEED THEM.
Everybody should be able to access the full range of mental health services, treatments, and supports.
Yet for a lot of people, the mental health system often feels like a maze, one with lots of cracks that are
easy to fall through.
Because each person’s recovery journey is unique, there will never be a “one-size-ts-all” solution for mental
health services. Still, there’s much that can be done to ensure “every door is the right door” — meaning no
matter where a person enters the system, they can get the care they need.
In order to improve the ow and efciency of mental health services, it’s helpful to think of the system in
tiers (or as having levels). Each represents a cluster of services of similar intensity. In order for the system
to function in a way that makes sense, access to all services should be available to everyone with no barriers
to entry and exit.
STRATEGIC DIRECTION 3
INTEGRATING AND COORDINATING
Doctors, teachers, police ofcers, and social workers should all work together with mental health service
providers to help people along the journey to recovery — whether that means providing timely access to
medication, affordable housing, professional counselling, or peer support.
PAGE 14
STRATEGIC DIRECTION 3
KEY WORDS
Barriers: Anything that
keeps people from access-
ing services or moving
through the system in
the way they want.
Primary Healthcare:
Healthcare provided by
family doctors, nurses, and
other health profession
-
als, often in collaborative
teams.
Peer Support: People
who have experience
with mental health issues
offering support, encour-
agement, and hope to each
other when facing similar
situations.
Recovery First: A recov
-
ery-oriented approach that
focuses on providing per-
manent, independent hous-
ing and additional supports
to homeless populations in
order to end homelessness.
The Mental Health Strategy for Canada in Action
Combining the skills and experiences of a wide range of professionals is key to delivering effective
services. This is especially true at the Nova Scotia Early Psychosis Program (NSEPP), a specialized,
community-focused outpatient program for youth experiencing a rst episode of psychosis. NSEPP
involves a team of psychiatrists, nurses, occupational therapists, social workers, people with lived
experience, and more, all working together to provide timely care in any form required. NSEPP also
provides art therapy programs as well as follow-up services and continuity of care for up to ve
years — along with courses that encourage family members to become more involved in the
recovery process. http://earlypsychosis.medicine.dal.ca/
PRIORITIES
3.1 GIVE PRIMARY HEALTHCARE A LARGER ROLE IN MENTAL HEALTH.
Mental and physical health are deeply connected and people are more likely to
talk to their family doctor about a mental health issue than any other healthcare
provider. Fortunately, many of the same approaches primary healthcare providers
use to deal with chronic illnesses like
heart disease and diabetes can be
applied to mental health. These include
working in multidisciplinary primary
healthcare teams (that is, teams of
people with different skills and training)
and giving people the tools they need to
better manage their own health.
Technology can also help in a big way.
Electronic health records and video chats
are all making it easier for doctors to provide people with the information they
need. New kinds of online and mobile services are also helping connect people to the care they need, with many
of them designed specically for youth.
What family doctors, nurses, and other healthcare professionals need now are stronger mental health skills and
training as well as a clear recovery approach in their work — all shaped by input from people with lived experience.
Mental Health Strategy for Canada in Action
Distance Treatment Service for Families, Nova Scotia
Strongest Families is a program developed by the IWK Health Centre in Halifax and now run by the Strongest Family Institute. This program helps
parents and children in four Nova Scotia health districts, as well as in B.C., Alberta, and Ontario, to learn to deal with the challenge of common childhood
behaviour and anxiety problems. Families receive handbooks and skill-demonstration videos and work through step-by-step modules at home, supported
by telephone consultations with trained coaches. Research using randomized controlled trials found that Strongest Families was more effective than
usual care services. The treatment drop-out rate was less than 10 per cent and children in the Strongest Families program were signicantly less likely to
still have a diagnosable illness after eight and twelve months. In addition, positive treatment effects were sustained at a one year follow-up and parents
reported high satisfaction with the quality of services.
YOUTH COUNCIL TIPS: GETTING THE MOST FROM YOUR DOCTOR APPOINTMENTS
A family doctor is often the rst place people go
with a mental health issue — but given the short
amount of time you usually have with your doctor,
it’s important to be prepared. Here are some tips to
make the most of your appointment.
> Don’t be afraid to ask questions. It might
help to write your questions down in advance
so you don’t forget any of them.
> Don’t be intimidated by the doctor and
remember that you’re allowed to bring a
parent or friend into your appointment if it
will help you feel more comfortable.
> Keep in mind that medication is only one type
of treatment option. Be sure to ask about all
of the options that might be available to you.
> Don't lose your voice. If you don’t understand
the doctor’s technical jargon, be sure to ask
for a simpler explanation.
> Only you know what’s going on inside your
head. Be totally honest and explain things as
clearly as possible; otherwise, your doctor
will have a harder time helping you.

PAGE 15
STRATEGIC DIRECTION 3
3.2 MAKE MENTAL HEALTH SERVICES MORE READILY AVAILABLE IN THE COMMUNITY FOR PEOPLE OF ALL AGES.
When mental health services and treatments aren’t available in the community, people
living with mental health issues can end up homeless, in jail, or constantly going to the
emergency room for support. Unfortunately, many communities are stretched to the limit.
Some no longer keep waiting lists for mental health services because it might give false
hope to people in need that eventually their turn for support will come.
Everyone should have the same access to a full range of services and care, no matter
how old they are, where they live, or their income level. If people can’t afford to pay,
they shouldn’t be prevented from getting services like psychotherapy that are mostly not
covered by provincial health plans. Children and youth stand to benet the longest from
better access to services and better youth mental
health means lower costs over the long-run for
governments as well.
Community services must also be better
coordinated so people can “navigate” between
them easily as their needs change. One way to do
this is to have people with mental health issues
work with service providers on personal plans
tailored to their individual recovery journey.
3.3 GIVE PEOPLE LIVING WITH COMPLEX MENTAL HEALTH ISSUES BETTER ACCESS TO THE SPECIALIZED
SERVICES AND TREATMENTS THEY NEED.
The mental health system must be able to meet everybody’s
needs, including those with complex mental health issues
like schizophrenia and people with multiple diagnoses —
for example, youth with both autism and anxiety.
In some cases, people with complex mental health issues
need “acute” (short-term but intensive) hospital services.
Others may require specialized, long-term services. There
is a major need for better coordination between health,
education, justice, and social services and for improved
skills and knowledge among service providers.
Because of this poor coordination, youth with complex
mental health issues often “fall through the cracks” as they age, losing access to services that may be unavailable
or difcult to access in the adult system. They might also encounter gaps because their move to adult services is
not properly organized.
“MY RECOVERY BEGAN WHEN I WAS ABLE TO BE HONEST WITH MYSELF ABOUT
WHAT WAS GOING ON AND TO BE ABLE TO VERBALIZE IT. IT WAS IMPORTANT TO
IDENTIFY THAT THIS WAS REAL AND WAS NOT JUST ALL IN MY HEAD.” VANESSA S.
PAGE 16
STRATEGIC DIRECTION 3
The Mental Health Strategy for Canada in Action
MHCC Youth Transitioning to Adult Mental Health Services Project
Identifying gaps and best practices in the mental health system leads to better services and outcomes for all people living with mental illnesses. This project is an
initiative of the MHCC launched to guide policy and practice that will improve how youth make the shift to adult mental health programs as they grow older.
3.4 INCLUDE PEER SUPPORT AS AN ESSENTIAL PART OF MENTAL HEALTH SERVICES.
A peer is someone who has something in common with you, such as
age, background, or qualications.
Peer support works because people who have experience with mental
health issues can offer encouragement and hope to each other — often
reducing hospitalization, providing social support, and improving
quality of life. It can also connect families experiencing similar
situations, helping them better understand the mental health system
and improving their ability to take care of their loved one’s needs.
Despite its effectiveness, peer support gets very limited funding.
Continuing to develop standards and guidelines will help make peer
support more credible and seen as a key part of the mental health
system. Because peers have such a signicant inuence on youth, the
contributions of younger peer support workers, including high school
students, must also be taken more seriously.
The Mental Health Strategy for Canada in Action
Guidelines for the Practice and Training of Peer Support
Published in 2013, the guidelines were created to provide direction to policy makers, decision makers, program leaders, and the public about the practice of
peer support and to help enhance the credibility of peer support as an essential component of a transformed mental health system. The guidelines focus on a
structured form of peer support that fosters recovery. Peer support workers from across the ten provinces and three territories came together to develop the
guidelines in conjunction with the MHCC.
Another barrier relates to the accessibility of medication, which is usually not covered by public insurance outside of
hospitals. This is a problem especially for people transitioning back into the community, when uninterrupted access
to medication is often critical. From the youth perspective, many are unable to afford their medications once they
become adults.
Striking the right balance of intensive services in community and institutional settings requires “benchmarks” to guide
planning. In other words, it’s about knowing what different people — children, youth, adults, seniors — require by way
of care. It also requires everybody with a role to play — police, doctors, social workers, families — to contribute in a
coordinated community-based support system.
PAGE 17
STRATEGIC DIRECTION 3
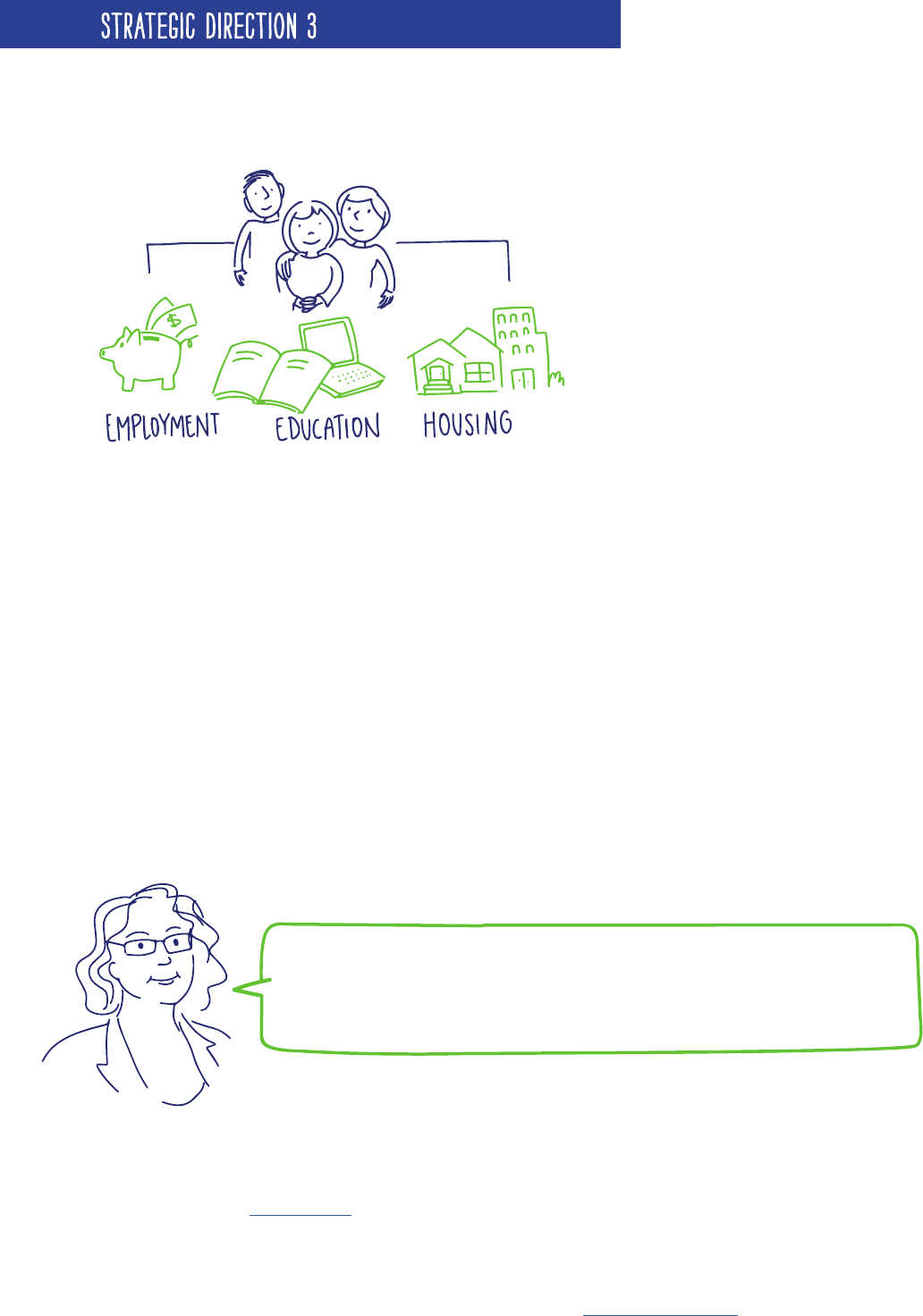
3.5 GIVE PEOPLE LIVING WITH MENTAL HEALTH ISSUES AND THEIR FAMILIES AND CAREGIVERS BETTER
ACCESS TO HOUSING, EMPLOYMENT, AND EDUCATION.
Recovery isn’t just about having access to mental
health care. It’s also about having a place in a
supportive community with everything a person
needs to ensure their wellbeing.
At least 100,000 people living with mental health
issues and their families will need access to affordable,
adequate housing and related supports over the next
ten years, with options that suit each family’s needs.
Specic initiatives are also needed to assist people
who are homeless and have mental health issues. For
example, housing rst programs provide housing and
other recovery-oriented supports without requiring
people to accept treatment as a condition of housing. From a youth perspective, these and other models should be
further explored to prevent long-term homelessness in youth specically.
Action is needed on other fronts, too. Today, people with serious mental health issues have high rates of
unemployment and often lack opportunities to develop their talents. Barriers that keep people out of the workforce
must be removed. At the same time, supports that help them obtain employment should be increased.
Canada also needs to improve the ways it handles disability benets. The current system often discourages people
from returning to work, taking away benets — such as medication coverage — when they try to do so. Youth often
nd it quite difcult to access disability benets because they don’t know how to navigate the system or even where
to begin. Many simply give up trying, putting themselves at nancial risk.
Caregivers, including relatives and friends, who provide unpaid care for a person living with mental health issues can
also be held back from participating in the workforce. An estimated 27 per cent of caregivers lost income because
of the time they spent caring for a family member. For youth, providing care to a sibling, parent, or partner not only
makes it difcult to hold down a job, but it can also take away time from their studies. Caregivers need access to
nancial supports like tax credits and caregiver allowances, as well as the support of school and workplace policies
like caregiver leaves and exible hours to help ease their burden.
The Mental Health Strategy for Canada in Action
In 2008, the Government of Canada allocated $110 million to the MHCC
to undertake a research demonstration project on mental health and
homelessness. The result? At Home/Chez Soi, a four-year project in ve
cities that aimed to provide practical, meaningful support to Canadians
experiencing homelessness and mental health problems. In doing so, the
MHCC is demonstrating, evaluating, and sharing knowledge about the
effectiveness of the "housing rst" approach, where people are provided
with a place to live and then offered recovery-oriented services and
supports that best meet their individual needs.
The Mental Health Strategy for Canada in Action
Halifax’s Laing House is a youth-driven, community-based organization
offering programs to help young people living with mental illnesses get
the support they need. Its Employment Program, for example, helps
with job searching, résumé writing and interview skills. Through its
Independent Living Program, Laing House helps youth develop the
skills to nd and maintain safe, affordable housing, with workshops on
apartment hunting, tenant rights and obligations, income assistance,
and more. Other programs include Creative Arts, Healthy Living, Family
Support Group, and Hospital and Community Outreach.
http://www.lainghouse.org/
“MY MENTAL HEALTH IS ABOUT BALANCE BETWEEN MY RELATIONSHIP
WITH OTHERS AND MY RELATIONSHIP WITH MYSELF. IT’S ABOUT BEING
ABLE TO EXPERIENCE A BROAD RANGE OF EMOTIONS AND STILL BEING
ABLE TO KEEP MY INDEPENDENCE.” PATRICIA L.
PAGE 18
ENSURE EVERYONE HAS ACCESS TO APPROPRIATE MENTAL HEALTH
SERVICES BASED ON THEIR NEEDS, ESPECIALLY IN DIVERSE AND
REMOTE COMMUNITIES.
Income, location, race, education, and many other factors have a profound inuence
on our physical and mental wellbeing. In general, people with higher incomes, more
education, and stronger relationships tend to be healthier than those who do not
have such advantages.
Because of these “social determinants of health,” different people face unique
realities and have different needs. Some groups in particular face more
discrimination and stigma, or require better access to services and supports.
These include:
> Immigrants and refugees
> Lesbian, gay, bisexual, transgender, two-spirit and queer
(LGBTTQ) communities
> Faith groups
> People with differing abilities
> Those living in the North or in remote communities.
We need to recognize the strengths of diverse peoples. Because every community is
different, the way services are delivered to each needs to be different. In fact, every
individual is different — meaning that community-specic services should be tailored
even further to provide a truly “person-centered approach” to mental health.
STRATEGIC DIRECTION 4
KEY WORDS
Social determinants of
health: Factors like income,
education, housing, etc.,
that affect opportunities
for health and wellbeing.
Person-centered approach:
Making sure any mental
health service meets the
specic needs of an indi
-
vidual instead of using a
“one-size-ts-all” model.
Health equity: Ensuring
that every person can
access the healthcare
programs and services they
need.
Racialized groups: Group
about whom others make
assumptions based on race.
The Mental Health Strategy for Canada in Action
The Positive Spaces Initiative (PSI) is a project of OCASI - Ontario Council
of Agencies Serving Immigrants. PSI supports the immigrant- and refugee-
serving sector in Ontario to work respectfully and effectively with LGBTQ+
(lesbian, gay, bisexual, trans, queer, intersex, asexual, etc.) newcomers. They
provide consultations, four modules of online/ofine training for service
providers, a Positive Space Assessment Tool, and an online database of
resources. PSI also participates in regional networks, partnerships, and special
events around Ontario to connect LGBTQ+ newcomers, staff, volunteers, and
community members. http://www.positivespaces.ca
“MENTAL HEALTH IS MORE THAN THE
ABSENCE OF MENTAL ILLNESS. IT
MEANS STRIKING A BALANCE AMONG
BEING EMOTIONALLY, MENTALLY,
PHYSICALLY, AND SPIRITUALLY WELL.
AND JUST AS FINGERPRINTS DIFFER
FROM ONE PERSON TO ANOTHER, SO
TOO DOES MENTAL HEALTH.”
SIMRAN L.
PAGE 19
STRATEGIC DIRECTION 4
PRIORITIES
4.1 IMPROVE MENTAL HEALTH BY IMPROVING PEOPLE’S LIVING CONDITIONS.
Poverty, a lack of affordable housing, underemployment, and other factors all affect people's risk of developing
mental health issues. Working towards better mental health goes hand in hand with working towards better
living conditions. For example, mental health can be improved through anti-poverty initiatives, which are often
collaborative efforts between public and private organizations and on-the-ground agencies.
Any new mental health policy or program should contribute to “health equity.“ A health equity approach makes sure
that all individuals are able to get the same degree of benets from a policy or program. Health equity is not about
giving everyone the same level of services. It's about making sure that everyone can get the services they need.
To know if vulnerable groups such as LGBTTQ or homeless youth are treated equitably, we need to gather more data.
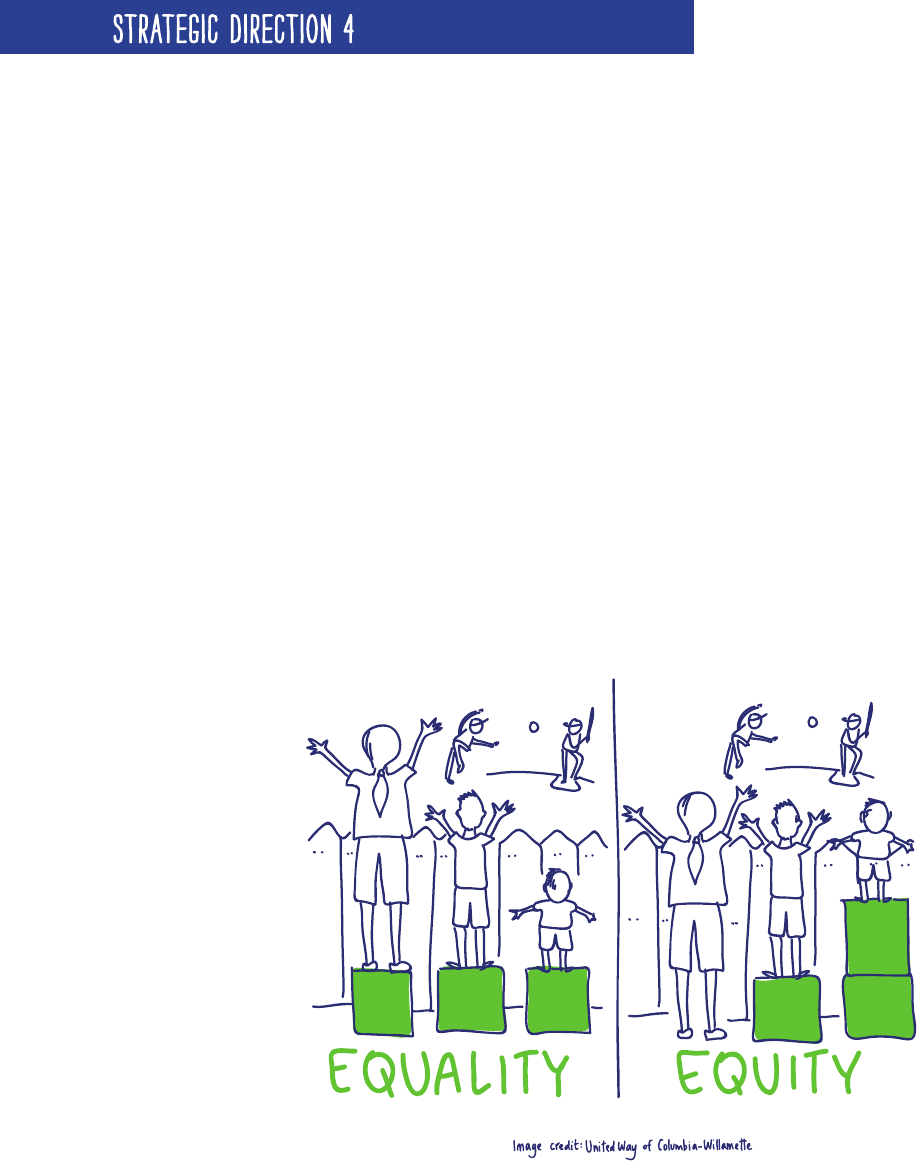
EQUALITY VS. EQUITY AND HEALTH EQUITY
Don’t understand what we mean by health equity? Take a look at the picture below to get a better understanding
of what equity is rst.
The same idea applies to "health equity" — it is not enough that the government provides equality (sameness)
in healthcare. There needs to be equity (fairness), meaning that barriers are removed that hinder people from
diverse or remote communities from getting the same care as the rest of the population.
Examples of these barriers include language, religion, culture, living conditions, and more.

PAGE 20
STRATEGIC DIRECTION 4
4.2 IMPROVE MENTAL HEALTH SERVICES FOR IMMIGRANTS, REFUGEES, ETHNOCULTURAL, AND
RACIALIZED GROUPS.
Different cultures often have unique ideas about mental health that can
sometimes make it difcult to start the conversation about mental health
issues. But, there are things we can do to make it easier.
Above all, stigma and stereotypes need to be eliminated. Mental health
professionals must have access to training in how to deliver culturally safe
and appropriate services and supports, so that their services are welcoming
to people from all backgrounds. This is especially helpful for youth who may
have to deal with family members who don’t understand the mental health
issues they face. These same youth may also feel that professionals are not
understanding them or their culture. People need to feel as though they can
get the help they need in a way that works for them. The value of traditional
knowledge and practices for healing and recovery must also be considered.
To be fully effective, this will require more than just service provider familiarity with cultural diversity. Service
providers must also acknowledge the inuence that social inequalities can have on a person’s wellbeing.

PAGE 21
STRATEGIC DIRECTION 4
4.3 TACKLE THE MENTAL HEALTH CHALLENGES FACED IN
CANADA’S TERRITORIES AND IN NORTHERN AND REMOTE
COMMUNITIES.
People living in Canada’s territories and northern or remote
communities have tremendous strengths. However, they also experience
some of the toughest social challenges in the country, including
overcrowded housing, poor access to clean water and affordable food,
and high rates of suicide and disease. Services to address mental health
needs are scarce or not offered at all. Some places receive doctor visits
only a few times a year.
To meet the requirements of these communities, we have to attract
skilled service providers such as doctors, nurses, and community
support workers to live in Canada’s territories or in northern or remote
communities. We must also train local people to ll these roles.
Technology can help by overcoming the isolation of communities even when a service provider can’t physically be
there. Telehealth and online “e-health” services are both good options for reaching people remotely. Youth especially
would be likely to take advantage of technology-based services. What’s required is infrastructure, faster networks,
and more reliable applications to make sure these kinds of services are readily available.
4.4 RESPOND BETTER TO THE MENTAL HEALTH NEEDS OF MINORITY FRANCOPHONE AND ANGLOPHONE
COMMUNITIES.
People should have access to services and treatments in their
language of preference to ensure that they are understood in
a culturally relevant way. Yet francophones living outside of
Quebec and anglophones living in Quebec can nd it hard to
access services in their rst language, especially in smaller
communities.
We need to encourage initiatives that improve access to
information, services, treatments, and supports in a person’s
rst language. This means launching programs to identify,
recruit, and keep French-speaking mental health service
providers in minority francophone communities and English-
speaking providers in minority anglophone communities.
The Mental Health Strategy for Canada in Action
Nunavut Kamatsiaqtut Help Line
Kamatsiaqtut means "thoughtful people who care" in Inuktitut. The Nunavut Kamatsiaqtut Help Line provides anonymous and condential telephone counselling
for Northerners in crisis. Trained volunteers are available 365 days a year and come from many different walks of life — and all of them are ready to provide a
listening ear in English, French, or Inuktitut. 1-800-265-3333, http://www.nunavuthelpline.ca
PAGE 22
STRATEGIC DIRECTION 4
4.5 MEET MENTAL HEALTH NEEDS RELATED TO
GENDER AND SEXUAL ORIENTATION.
Men and women face different mental health risks at
different stages of life. For example, while women are
more likely to experience anxiety and depression, men
are more likely to develop schizophrenia at a younger age.
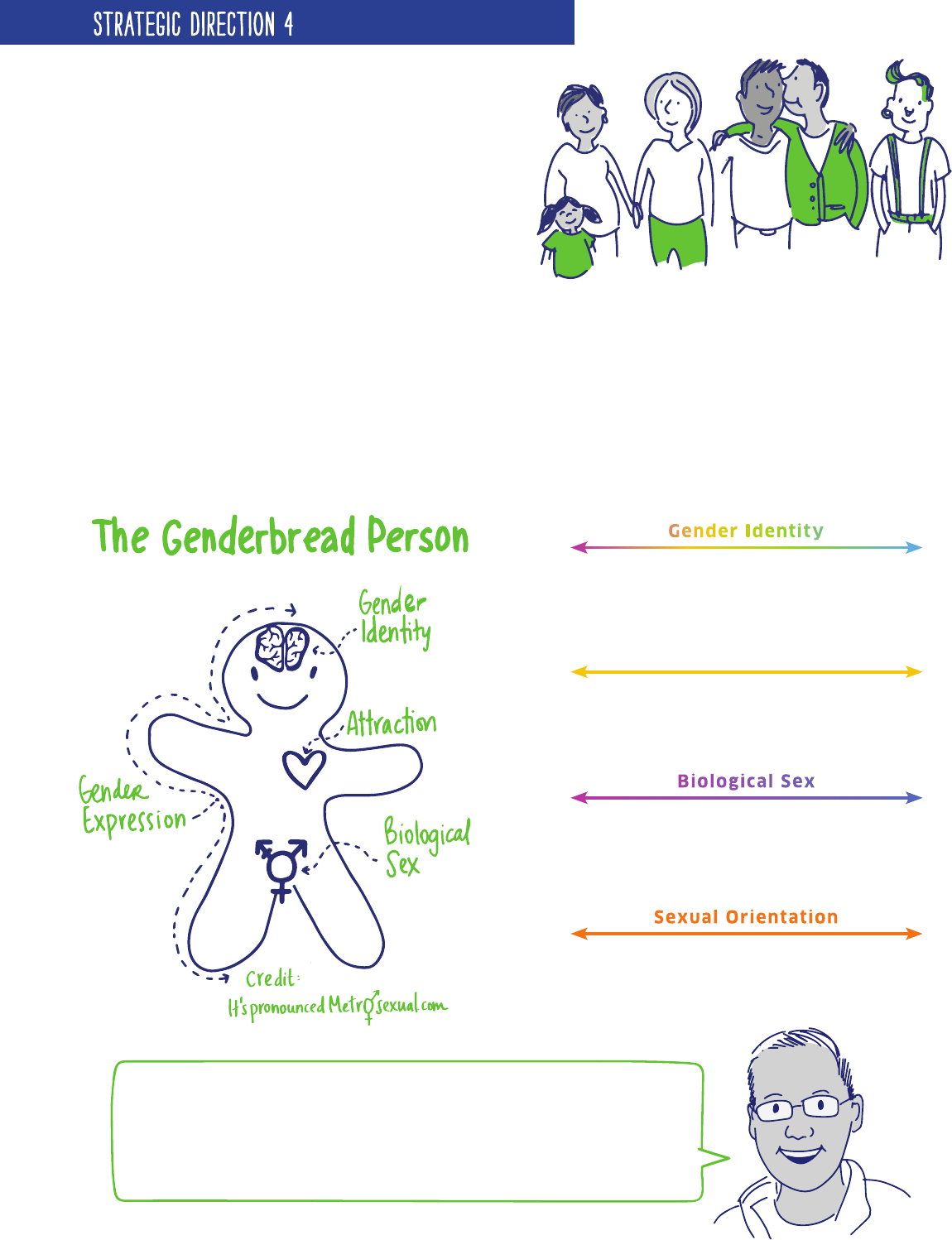
Our current system is especially difcult for trans-
identied people, as our society looks at gender as a
binary system (men/women) and not as a spectrum, which is inclusive of all peoples.
Sexuality and gender issues also affect a person’s risk for mental illness. LGBTTQ youth, for example, may be bullied
or assaulted. An accepting family and contact with other LGBTTQ youth can reduce risk for these young people; an
unaccepting family and no peer contact can increase risk. Stereotypes of all kinds can affect the way LGBTTQ people
living with mental health issues are treated by the mental health system.
Mental health service providers have to be careful not to stereotype or discriminate against LGBTTQ people. They
also need to better understand the impact discrimination and stigma can have on an LGBTTQ person’s mental health.
Woman
Gender Identity
Gender identity is how you, in your head, think about yourself. It's the
chemistry that composes you (e.g., hormonal levels) and how you interpret
what that means.
ManGenderqueer
Feminine
Gender Expression
Gender expression is how you demonstrate your gender (based on traditional
gender roles) through the ways you act, dress, behave, and interact.
Masculine
Androgynous
Female
Biological Sex
Biological sex refers to the objectively measurable organs, hormones, and
chromosomes. Female = vagina, ovaries, XX chromosomes; male = penis,
testes, XY chromosomes; intersex = a combination of the two.
Male
Intersex
Heterosexual
Sexual Orientation
Sexual orientation is who you are physically, spiritually, and emotionally
attracted to, based on their sex/gender in relation to your own.
Homosexual
Bisexual
“AT TIMES I FORGET THE FACES OF ALL THOSE WHO HELPED ME ALONG THE
WAY TO RECOVERY; IN THE NUMEROUS HOSPITALS, DOCTOR’S OFFICES,
COUNSELLING OFFICES, AND PSYCHIATRIC PRACTICES. BUT I WILL NEVER
FORGET THE FEELING OF BEING TREATED WITH KINDNESS, UNDERSTANDING,
AND COMPASSION. WHEN I GET ON THE EDGE OF RELAPSING BACK INTO
DEPRESSION AND SUICIDAL THOUGHTS, I REMEMBER THAT I AM NOT ALONE
AND THAT I DO HAVE PEOPLE TO TALK TO.” JACK S.
PAGE 23
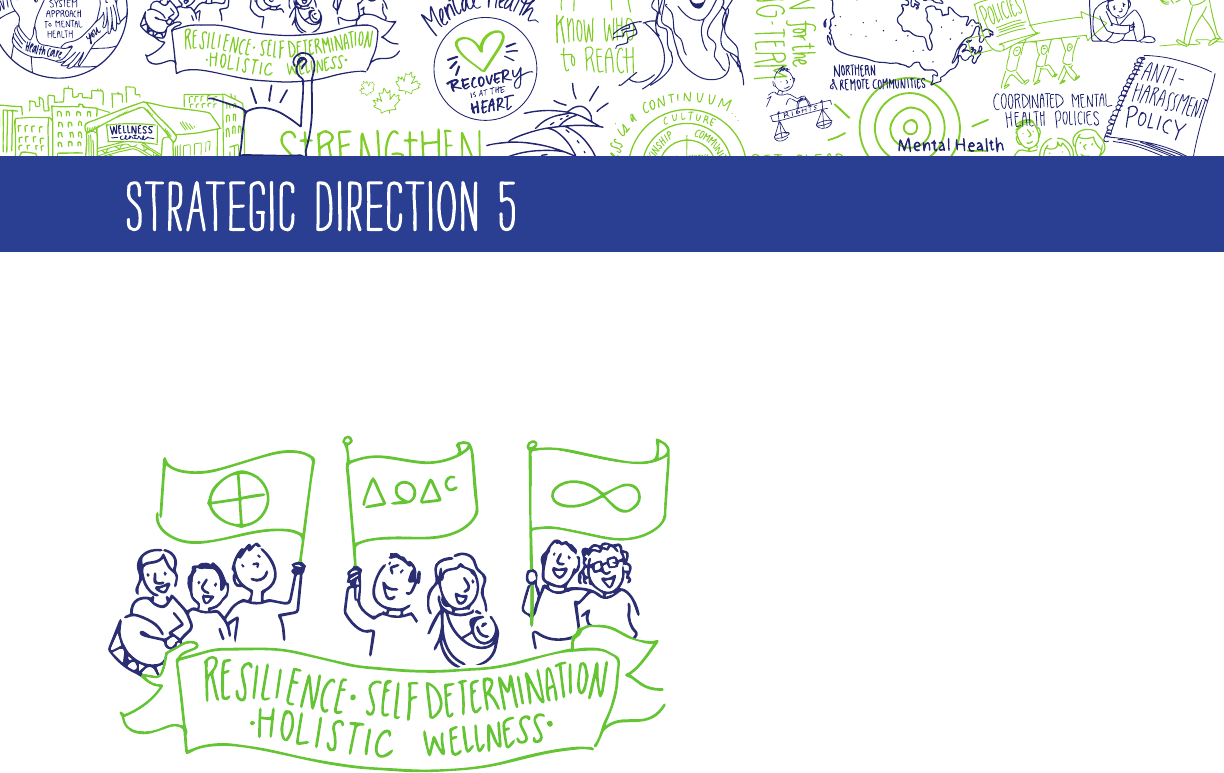
WORK WITH FIRST NATIONS, INUIT, AND MÉTIS TO MEET THEIR
DISTINCT MENTAL HEALTH NEEDS, WHILE RESPECTING THEIR UNIQUE
EXPERIENCES, RIGHTS, AND CULTURES.
This Strategic Direction highlights three
distinct streams for First Nations, Inuit,
and Métis, an approach that respects the
important differences in the cultures and
histories of each group. The three streams
identify the unique needs of, and complex
social issues affecting, First Nations,
Inuit, and Métis, and also highlight a few
common priorities regarding the mental
health of all people.
Working with concepts such as resilience,
self-determination, and holistic
understandings of wellness, First Nations,
Inuit, and Métis cultures have much to contribute to the transformation of the mental health system in Canada.
At the same time, the problems they often face are serious.
For example, although suicide is not a universal problem in First Nations, Inuit, and Métis communities, it is a
signicant challenge in many communities across Canada. First Nations youth die by suicide ve to six times
more often than non-Aboriginal youth. The suicide rates for Inuit are among the highest in the world, at 11
times the national average. For young Inuit men, those rates are 28 times higher. Less is known about suicide
rates for Métis youth. Mental health and suicide need to be addressed together through the promotion of good
mental health for all.
There is no “one-size-ts-all” answer, because every community has unique strengths and challenges. But we
need to do something, especially about:
> The harms caused by colonization, the residential school system, and other policies that kept First
Nations, Inuit, and Métis parents from passing their culture and history on to their kids.
> How hard it is for people in Canada’s territories and northern or remote areas to get mental health
professionals to live and work in their communities.
> How hard it is to access basic mental health services in Canada’s territories and northern or remote
areas, which often results in having to travel outside of one’s own community for support.
> The ongoing impact of racism, poverty, and other systemic issues on mental and physical wellbeing.
STRATEGIC DIRECTION 5
The Mental Health Strategy for Canada in Action
One of the keys to providing effective services to First Nations, Inuit, and Métis (FNIM) is to take an approach that involves all aspects of mental, physical,
emotional, and spiritual health. In downtown Calgary, the Elbow River Healing Lodge provides a range of primary health care services such as health
assessments and examinations, specialized services, advocacy for social supports, street outreach, and spiritual and cultural supports for FNIM people. An
Adult Aboriginal Mental Health team is also on site and provides culturally appropriate mental health services (assessment, treatment, information, referral,
and outreach). As part of a broader primary health care framework to ensure a culturally appropriate and respectful approach to health service delivery
adaptable to individual and community needs, the clinic is implementing Integrated Primary Care Standards. These standards are based on a holistic model
of care and treatment characterized by the integration of physical, emotional, spiritual, and mental components of health and wellbeing identied in First
Nations, Inuit, and Métis cultures.
PAGE 24
STRATEGIC DIRECTION 5
PRIORITIES
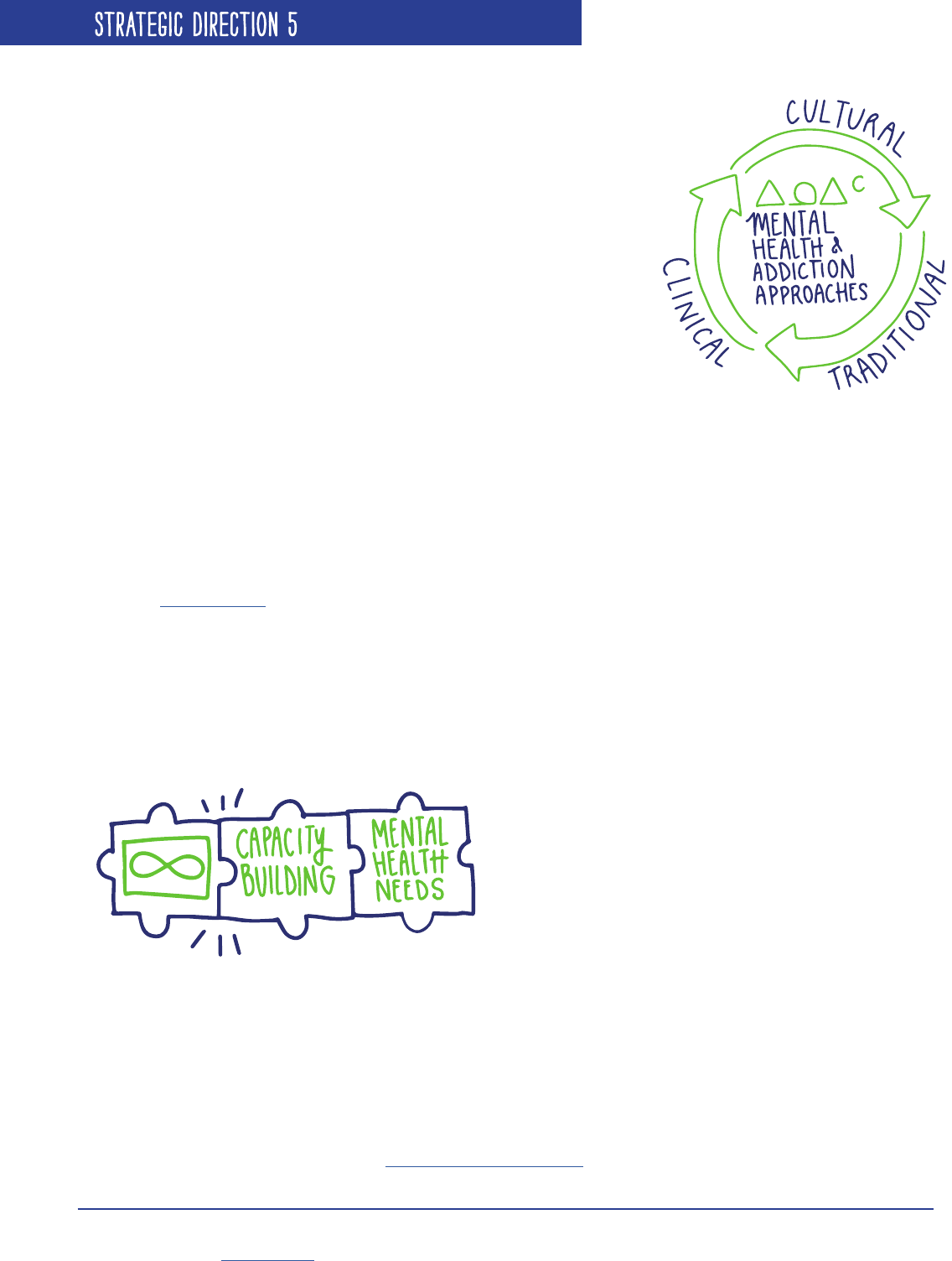
5.1 ADDRESS GAPS AND ENSURE GREATER COORDINATION BETWEEN MENTAL HEALTH AND ADDICTIONS
SERVICES FOR AND BY FIRST NATIONS, INCLUDING TRADITIONAL, CULTURAL, AND MAINSTREAM APPROACHES.
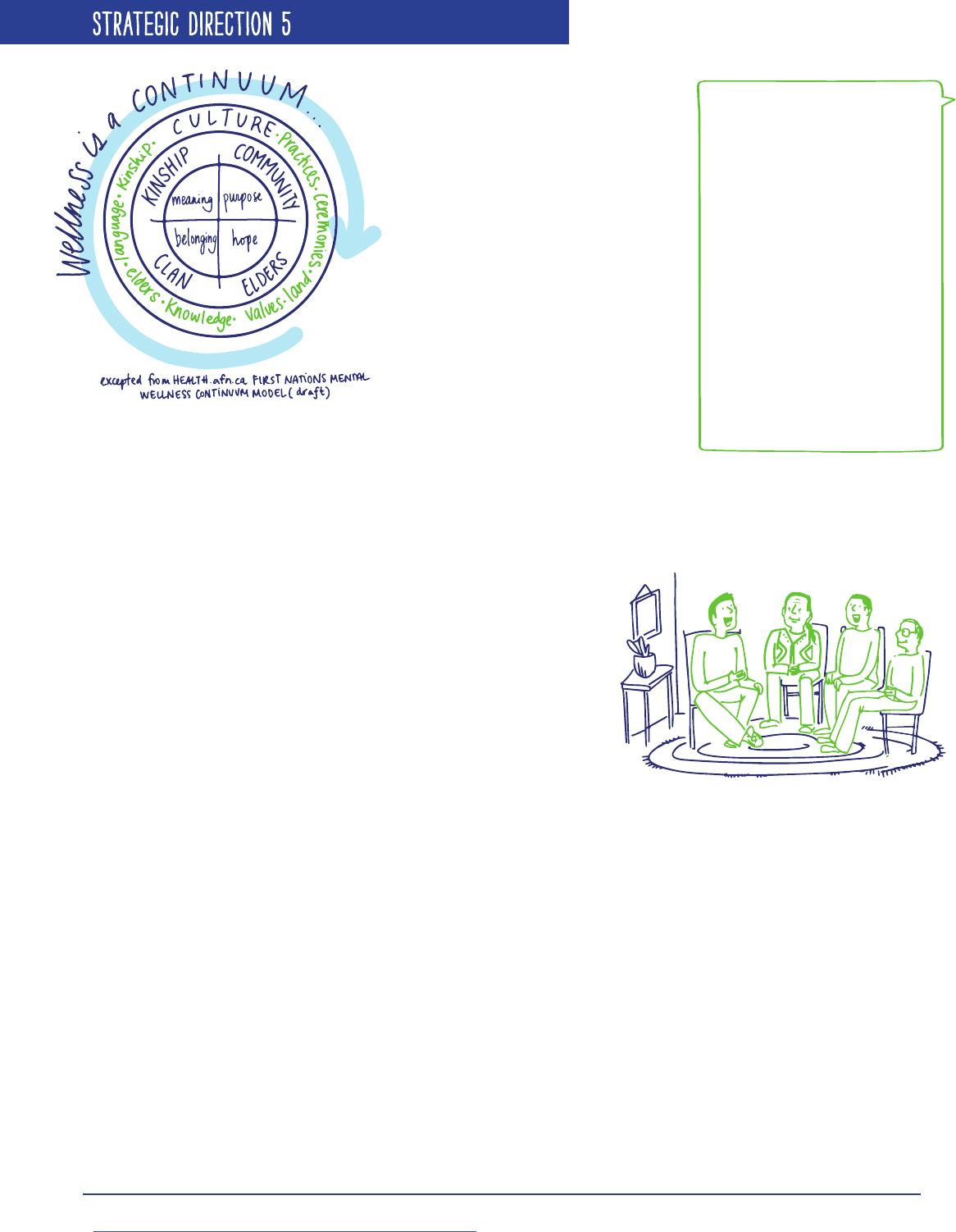
For First Nations, wellbeing is about balancing spiritual, mental,
emotional, and physical health. That way of life was nearly destroyed
by residential schools and the child welfare system. Combined with
poverty, poor housing, and a lack of educational opportunities, the
history of trauma suffered by First Nations has led to high rates of
mental health issues, substance use, suicide, and family violence in
many communities.
First Nations also have a hard time accessing mental health services
in all areas and regions of Canada, with rural and remote communities
nding it especially difcult to recruit and keep healthcare workers.
To promote their own healing, First Nations are using traditional, cultural, and mainstream approaches, including
recognizing the key role of Elders. At the same time, all mental health professionals who serve First Nations
communities must be trained in culturally safe practices.
First Nations collectively continue to pursue self-determination and strive to strengthen their relationships with
federal, provincial, and territorial governments. First Nations have long advocated for improved mental wellness
services, but progress has been slow. To create more meaningful change, a continuum of services that is coordinated
across jurisdictions is needed.
5.2 ADDRESS GAPS AND ENSURE GREATER COORDINATION OF MENTAL HEALTH AND ADDICTIONS SERVICES
FOR AND BY INUIT, INCLUDING TRADITIONAL, CULTURAL, AND CLINICAL APPROACHES.
Inuit dene mental wellness as “self-esteem and personal dignity owing from the presence of harmonious physical,
emotional, mental and spiritual wellness, and cultural identity.”
2
Because their traditional way of life centres on
working together to survive in the North, individual strengths — and those of the community — are very important.
Inuit experienced colonization recently and rapidly; many who are now adults grew up living off the land year-round.
Traumatic experiences, such as seeing children sent away to residential schools and being forcefully made to relocate
communities, have disrupted Inuit culture and language, resulting in high levels of depression, suicide, and addiction.
Just like all other Canadians, First
Nations, Inuit, and Métis need
equitable access to mental health
services, treatments, and supports,
wherever they live. They also
need access to services that are
appropriate to their distinct cultures
and traditions, no matter what
agency they go to.
All levels of government have to
work together to make this happen—
federal, provincial, territorial, and
Aboriginal, including the Assembly
of First Nations, Inuit Tapiriit
Kanatami, the Métis National Council, the Congress of Aboriginal Peoples, and the
Native Women’s Association of Canada.
KEY WORDS
Colonization: Settling among and
setting up political control over
the indigenous people of an area.
Residential schools: Church-run,
government-funded boarding
schools that separated Aboriginal
children from their families to
have them learn English, embrace
Christianity and adopt Canadian
customs. The rst school opened
in the 1840s; the last closed in
1996. Physical and sexual abuse
were widespread.
Cultural safety: When services
recognize Aboriginal experience,
power imbalances between
service providers and service
users, and systemic issues such as
racism and poverty.
2
Alianait Inuit-Specic Mental Wellness Task Group (2007). Alianait Mental Wellness Action Plan. Ottawa: Inuit Tapiriit Kanatami.
https://www.itk.ca/publication/alianait-inuit-mental-wellness-action-plan.
PAGE 25
STRATEGIC DIRECTION 5
Inuit mental wellness has to promote resilience as well as productive,
sustainable communities, based on traditional and cultural practices with
the support of clinical approaches. Yet many Inuit have to travel outside
their communities to receive even basic mental health services. More
Inuit need education and training so they can provide services to their
own people in their own language. Non-Inuit mental health workers also
require more training in cultural safety so they can deliver services in a
way that respects and understands Inuit culture.
Despite the challenges faced by Inuit communities, Inuit youth are
working towards raising awareness about mental health. The Inuit Tapiriit
Kanatami
3
(ITK) National Inuit Youth Council, for example, is developing
a strategy aimed at the following priority areas affecting Inuit youth in
all areas of Canada: suicide prevention; health and substance use; culture and language; youth political involvement;
youth facilities and resources; housing and poverty reduction; and education and research. These priority areas
build on ITK’s commitment to advancing Inuit knowledge in research and policy development within national and
international contexts.
3
Inuit Tapiriit Kanatami (ITK), formerly Inuit Tapirisat of Canada, is the national voice of 55,000 Inuit living in 53 communities across the Inuvialuit
Settlement Region (Northwest Territories), Nunavut, Nunavik (Northern Quebec), and Nunatsiavut (Northern Labrador), land claims regions.
More information here: http://www.itk.ca.
The Mental Health Strategy for Canada in Action
Ilisaqsivik Family Resource Centre
Located in Clyde River, Nunavut, this centre focuses on family healing and has a range of programs for people of all ages provided by Elders as well as family,
addictions and youth counsellors. The centre’s hip-hop program helps reduce self-harm and drug use among youth and is contributing to an overall decrease in
crime rates and suicidal thoughts. Programs are also offered that integrate mainstream and traditional approaches to help youth learn and experience traditional
ways of life. http://ilisaqsivik.ca/
The Mental Health Strategy for Canada in Action
MCFCS High Risk/At Risk Support Program
The Metis Child family and Community Services High Risk/At Risk Support Program focuses on helping Métis youth at risk because of gang involvement,
addiction, violence, sexual exploitation, and mental health issues. Taking a culturally based approach, the program focuses on working with the youth’s social
workers, caregivers, and supportive circle to provide stabilization, prevention, and safety oriented services and supports. The program is relationship and
strength-based and focuses on working closely with the youth and their supportive circle of caregivers, family, and peers to develop and implement strategies
to reduce the youth’s risk and enhance their potential. http://www.metiscfs.mb.ca/index.php
5.3 BUILD MÉTIS CAPACITY TO BETTER UNDERSTAND AND ADDRESS THEIR MENTAL HEALTH NEEDS.
The descendants of European fur traders and First Nations women, Métis people have a unique culture with their
own traditions, language, and way of life. For a number of reasons — such as the aftermath of the Métis uprisings
and the execution of Louis Riel — Métis people have tended not to acknowledge their ancestry openly. As well, it took
until 1982 for the federal government to recognize Métis as
one of the three distinct Aboriginal groups in Canada.
Even today, Métis have limited access to federally funded
mental health and addictions programs. Instead, they
continue to fall under provincial and territorial jurisdiction,
resulting in gaps in the availability and quality of Métis-
specic services.
More research is needed to understand how colonization has
affected the mental health of Métis people. What we do know
is that Métis people have many risk factors for mental health issues, including overcrowded housing, substance abuse,
and family violence. Fortunately, Canadian courts are increasingly recognizing Métis rights — and more and more
Métis are reconnecting with their culture and history, working together to improve their mental health and wellbeing.
PAGE 26
STRATEGIC DIRECTION 5
5.4 ADDRESS THE MENTAL HEALTH NEEDS OF FIRST NATIONS, INUIT, AND MÉTIS LIVING IN URBAN AND RURAL
CENTRES AND THE COMPLEX SOCIAL ISSUES THAT AFFECT MENTAL HEALTH.
More than 50 per cent of First Nations, Inuit, and Métis live in urban and rural centres, with considerable movement
to and from their home communities (typically these include First Nations reserves, remote Inuit communities, and
smaller Métis communities). The reasons for moving from smaller communities to larger cities and towns might be
better access to economic opportunities and employment, better access to health care, and the appeal of urban living.
For many, this choice does lead to improvements in key protective factors of mental health, such as better access to
education and employment.
Unfortunately, a signicant number of First Nations,
Inuit, and Métis continue to live in poverty. Even within
larger urban centres, there are problems with access to
services, such as long waiting lists, lack of transportation,
as well as lack of awareness and understanding of the
differences in cultures between service providers and
those receiving services.
Efforts to address factors like poverty and inadequate
housing in urban and rural centres have to be
coordinated across all levels of government. Better
support is also needed to deliver specialized mental
health services that integrate traditional, cultural, and mainstream approaches. Finally, more research is required
to deepen our understanding of the mental health issues faced by First Nations, Inuit, and Métis living in urban and
rural settings so that we can develop more effective mental health and substance use strategies.
At the same time, there are complex social issues that affect the mental health of First Nations, Inuit, and
Métis whether they reside in urban or rural centres, on First Nations reserves, in remote Inuit, or smaller Métis
communities. Three priorities are addressed here:
> Violence against women and girls: In some communities, up to 90 per cent of women are victims of violence.
With the causes of violence including poverty, racism, and discrimination, services must focus on community
and family healing.
> Over-representation in the child welfare system: While First Nations, Inuit, and Métis children represent
less than ve per cent of all children in Canada, they make up between 30 and 40 per cent of those living
in out-of-home care. Changing this requires First Nations, Inuit, and Métis families to be more involved in
the processes affecting their children. Culturally based approaches also need to be built into all aspects of
the child welfare system, with access to cultural activities and traditional teachings available whether the
child is “in care” or adopted.
> Over-representation in the criminal justice system: Greater access to culturally appropriate mental health
services is still needed in Canada’s correctional centres. More focus must be placed on programs that help
foster resiliency among youth to reduce their exposure to the criminal justice system in the rst place.
“CULTURE WAS A HUGE PART OF MY ROAD TO RECOVERY. BEING ABLE TO TAKE
PART IN CEREMONIES AND STAY CONNECTED TO MY COMMUNITY ALONG WITH
GOING TO THERAPY FOR MY DEPRESSION, HELPED TO CREATE A FEELING OF
BELONGING WHILE IN RECOVERY. MY FAMILY AND COMMUNITY WERE VITAL IN
HELPING ME CREATE A HOLISTIC EXPERIENCE OF THERAPY THAT RESPECTED MY
NEED FOR MY CULTURE.” JACK S.
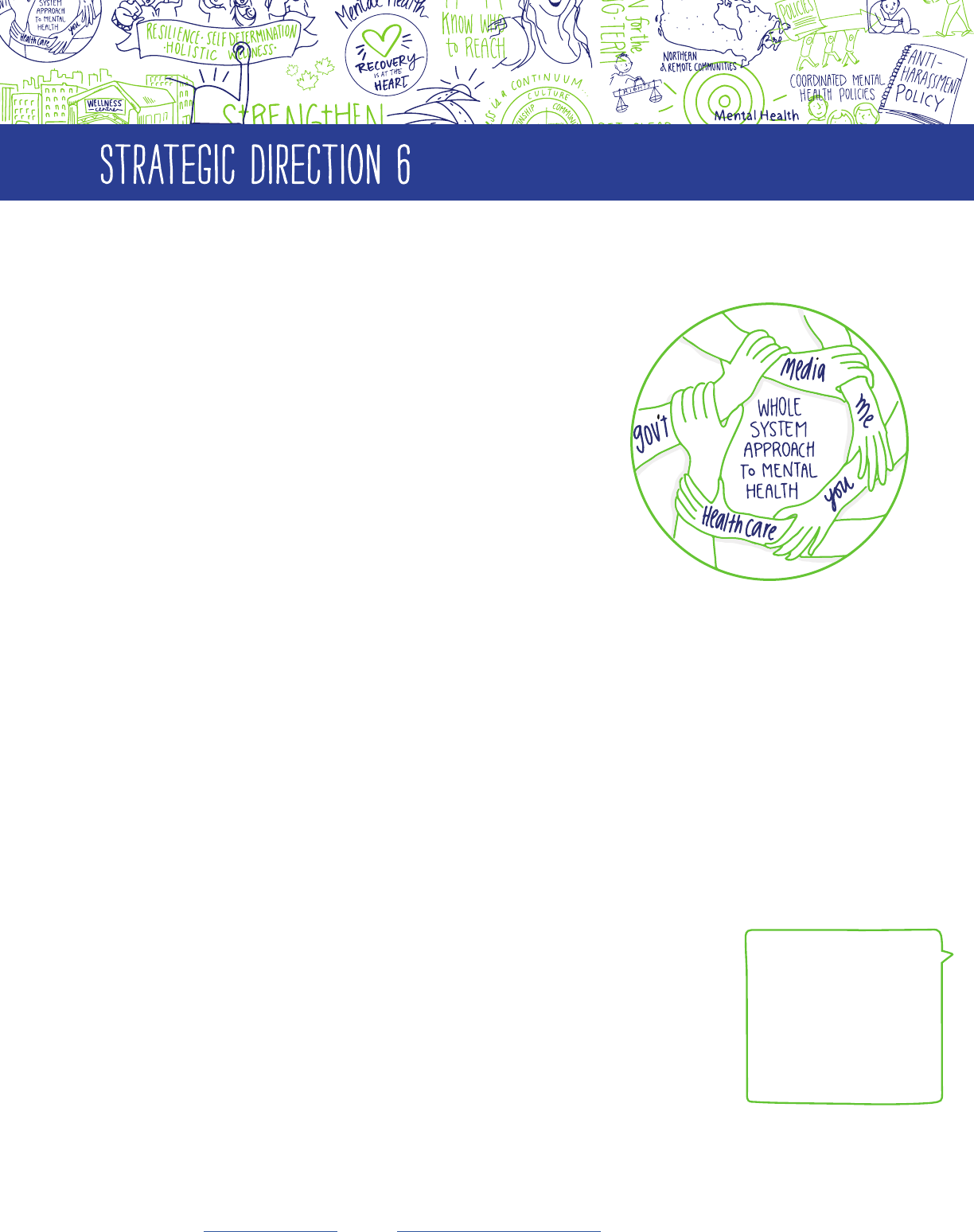
PAGE 27
INSPIRE LEADERSHIP, SHARE KNOWLEDGE, AND ENCOURAGE
COLLABORATION AT ALL LEVELS.
Mental health is getting more public attention in Canada than ever before,
from media, governments, and individuals all across the country.
We need to turn that attention into shared, collaborative action across all
levels of government and throughout the volunteer and private sectors.
An approach like this will help bring consistency to the ways mental
health issues are handled and ensure people don't fall through the cracks.
To make this integrated, coordinated approach to mental health a reality, we must:
> SHARE: nd better ways to share mental health information and best practices.
> RESEARCH: encourage more research so that we can learn what really works to improve mental
health and wellbeing.
> GUIDE: develop guidelines that will turn knowledge and evidence into action.
> COLLABORATE: increase collaborations with the addictions system since we know that drugs are a
common coping mechanism for people with mental health issues.
> EQUIP: communities and organizations need to have the right tools, skills, and resources available to
meet people’s needs and to adapt to new standards as they come into place.
> LEAD: give people with lived experience an opportunity to provide leadership
within the mental health system.
STRATEGIC DIRECTION 6
KEY WORDS
Knowledge exchange:
Gathering the best
knowledge available and
making it universally
accessible so it can be
acted on.
Knowledge translation:
Turning knowledge into
action.
The Mental Health Strategy for Canada in Action
Good things happen when young people with lived experience have the chance to be leaders. Ottawa’s Youth Net/Réseau Ado is a bilingual adolescent
mental health program that works from a strong youth engagement philosophy. As they say, “We are a, for youth, by youth organization.” Based within
the Children’s Hospital of Eastern Ontario (CHEO), Youth Net’s goal is to promote balanced mental health while decreasing the stigma that surrounds
mental illness and its treatment. They offer programs and services which focus on suicide prevention and intervention, mental health education, research,
and advocacy. Web: http://www.youthnet.on.ca Facebook: https://www.facebook.com/YNRAOttawa Twitter: @cheoyouthnet
PAGE 28
STRATEGIC DIRECTION 6
PRIORITIES
6.1 COORDINATE MENTAL HEALTH POLICIES ACROSS GOVERNMENTS AND SECTORS.
For best results, mental health policies need to be coordinated — across
government, in child and youth services, throughout the housing and criminal
justice systems, in workplace health and safety — so that the various promotion,
prevention, and treatment approaches work well together. Where First Nations,
Inuit, and Métis mental health policy is discussed, it is essential that they be
fully represented.
Volunteer organizations can help bring frontline experience into the mix.
There are voluntary organizations for service providers, families, various
health professions, specic illnesses, and for people living with mental health
issues. Collaboration among the volunteer organizations helps build shared
understanding, which makes stronger action possible.
Above all, clear leadership has to come from the highest levels of government. In Canada, that includes the prime
minister and provincial and territorial premiers.
The Mental Health Strategy for Canada in Action
Whole-of-Government Approach to Healthy Children, Manitoba
Established in 2000 by the Premier and under the leadership of the Healthy Child Committee of Cabinet, Healthy Child Manitoba (HCM) is a strategy to improve
outcomes for children across the province by coordinating and integrating policies and programs across government ministries. HCM has implemented evidence-
based programs for parents and children that have been shown to contribute to long-term improvement in health outcomes, such as the Families First Home
Visiting Program, the Triple P – Positive Parenting Program, Roots of Empathy, and PAX Good Behaviour Game. According to an HCM study, the implementation
of Roots of Empathy in Manitoba has yielded promising reductions in violent behaviour among children. HCM also collects data on early childhood development
to assist its network of Parent-Child Centred Coalitions in fostering local community initiatives. Legislation requires that a report on the status of Manitoba’s
children and youth be completed every 5 years.
The Mental Health Strategy for Canada in Action
This report is an innovative example of knowledge exchange with youth, for youth. By providing a youth perspective on the Strategy, members of the
MHCC’s Youth Council are equipping themselves to be leaders in mental health policy and helping other youth across the country to have an informed
say in mental health policy issues that affect them now and in the future.
6.2 IMPROVE MENTAL HEALTH RESEARCH AND KNOWLEDGE SHARING ACROSS CANADA.
Canada has come a long way in gathering evidence to drive change in the mental health system. But we still have
much further to go in being able to use this knowledge to measure progress and improve outcomes for people.
Compared to other areas of research — and considering how big an impact mental health issues have — mental health
research is seriously underfunded in Canada. We need a clear, committed research agenda that will explore questions
such as:
> What can we learn from the experiences of people living with mental health issues?
> How can we improve the transition from child and youth to adult mental health and addiction services?
> What are best practices for school-based mental health promotion?
> What can we learn from the traditional knowledge and customs of various cultures?
> What are the best ways to organize services and resources so they support people of all ages and
backgrounds on their journey toward recovery?
We also need better ways to track how the mental health system is performing and a way to monitor trends over
the long term. With better knowledge exchange, we can be faster about “knowledge translation” — that is, turning
research ndings into policy and practice. Developing in-depth guidelines and standards will also help improve the
quality of mental health services and better meet the needs of specic populations.
PAGE 29
STRATEGIC DIRECTION 6
6.3 STRENGTHEN MENTAL HEALTH HUMAN RESOURCES.
One of the keys to an effective mental health system is ensuring the right people with the right skills are in the
right places. Where youth are concerned, the “right people” are those who can deliver culturally safe mental health
services that are person-centered and relevant to, and appropriate for, youth.
Addressing the gaps related to mental health human resources will require us to:
> Establish a cross-country approach to workforce
training and development to ensure consistency in
mental health approaches.
> Embed recovery principles into workforce training
and development.
> Create opportunities for people living with mental
health issues to participate in the mental health
workforce.
> Increase the number of peer support workers
across Canada.
“THE YOUTH COUNCIL
ALLOWS US TO EXPRESS
OUR UNIQUE VIEW ON THE
SUBJECT OF MENTAL HEALTH.
WE ALL HAVE DIFFERENT
PERSPECTIVES AND
EXPERIENCES BUT SHARE ONE
COMMON GOAL: CREATING A
MORE ACCESSIBLE, EFFICIENT,
AND INCLUSIVE MENTAL
HEALTH SYSTEM.”
KATIE R.
“AS A GROUP, YOUTH ARE
TOO OFTEN EXCLUDED FROM
PROVIDING VALUE OR INPUT
INTO THE DECISIONMAKING
PROCESS. THE YOUTH COUNCIL
PROVIDES A FORUM FOR THE
YOUTH VOICE TO BE ENGAGED
IN MENTAL HEALTH ADVOCACY
AND POLICYMAKING ON A
NATIONAL SCALE.”
AMANEE E.
6.4 ENSURE PEOPLE LIVING WITH MENTAL HEALTH ISSUES HAVE A LEADERSHIP ROLE IN SETTING MENTAL
HEALTH POLICY.
Around the world, people living with mental health issues (and their families, friends, and support circles) are
helping transform mental health policies and promote recovery.
Strong leaders with lived experience, working within strong organizations, will not only contribute to the
transformation of service delivery, planning, and administration, but will also help to end stigma and discrimination.
Youth have an important voice to bring to the conversation — they just need more opportunities to make that
voice heard.
The Mental Health Strategy for Canada in Action
Supporting today’s youth leaders is incredibly important and so is identifying who the leaders of tomorrow will be. The New Mentality, a program of Children’s
Mental Health Ontario (CMHO), hosts an annual summer leadership camp called Disable the Label. Youth and adult allies come together from youth mental
health agencies across Ontario to brainstorm ideas and get training in leadership and facilitation. These youth then return to their communities to implement
projects that raise awareness of mental health and reduce stigma. http://thenewmentality.ca/
The Mental Health Strategy for Canada in Action
St Joseph’s Healthcare Youth Wellness Centre in Hamilton, Ontario focuses on youth
experiencing signs of mental health and/or addiction difculties for the rst time and
youth who need support moving from child and youth mental health and addiction
services to adult mental health and addiction services. This program helps to:
• Raise awareness of mental health and addiction issues through education and
outreach in the community, especially schools.
• Assess the symptoms and needs of youth and the areas of life affected by their
difculties, in order to provide the right kind of support as quickly as possible.
• Offer a thorough assessment for youth experiencing signs of mental illness
and/or addiction for the rst time and working with youth and their families on
a plan for recovery.
• Provide transition support and system navigation to youth who are moving
into the adult mental health and addiction system.
http://www.stjoes.ca/hospital-services/mental-health-addiction-services/mental-
health-services/youth-wellness-centre
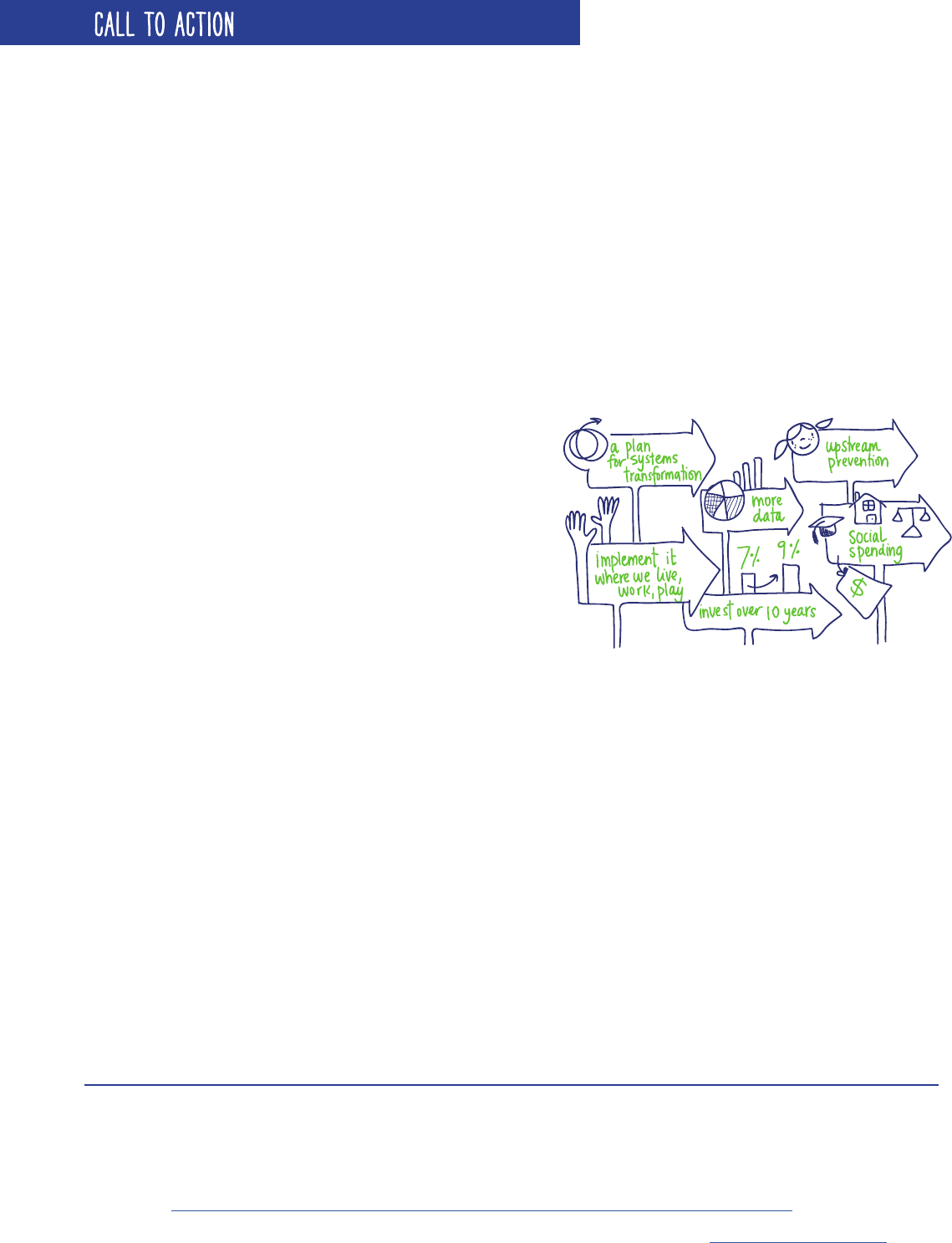
PAGE 30
CALL TO ACTION
The Mental Health Strategy for Canada: A Youth Perspective is intended to accompany the original Strategy, written
in 2012. The MHCC’s Youth Council hopes that this new version inspires others — especially youth — to become more
informed about mental health policy discussions in Canada, and more involved in changing perceptions of mental
health and wellbeing. If this document inspires you, we encourage you to read the full Mental Health Strategy for
Canada and think about how its contents can also help shape future discussions in your work.
It will take time to implement the many recommendations found in the Mental Health Strategy for Canada. Each
Canadian provincial and territorial government sets its own priorities. Provincial, territorial, or local governments
may nd some recommendations more useful than others at any particular time, and there is no one way for people
to use the Strategy to impact policy or practice. That is what makes the Strategy so important; it is a blueprint
for change. However, to change the system, we need people, organizations, and governments to champion and
implement its recommendations where they live, work, and play.
While everyone has a role in the implementation of the recommendations found in the Strategy, governments at all
levels have a particularly important responsibility. They have to invest more, and more efciently, in mental health.
Now is the time to invest more in mental health. Studies
suggest that the full economic impact of mental health
problems and illnesses in Canada is between $48.5
4
and
$51 billion per year.
5
No studies to date have been able to
measure the costs of mental illness on the criminal justice
system, on the education system, the costs borne by family
caregivers, or the cost of poor health to people who have
not experienced the symptoms of illness. Nevertheless,
the total costs of mental health problems and illnesses to
the Canadian economy are enormous and very likely to
increase unless action is taken soon.
Up to seventy percent of mental health problems and illnesses begin in childhood or adolescence and as many as
three in four children and youth with mental health problems and illnesses do not access services and treatments.
Children who experience mental issues are at much higher risk of experiencing them as adults and are also more
likely to have other complicating health and social problems. These numbers are alarming because the lifetime
economic cost of childhood mental health problems and illnesses is enormous – roughly $200 billion in Canada.
6
There are many things that can be done to make better use of the resources already being invested in the mental
health system. For example, improving a child’s mental health has been found to result in a lifetime savings of
$140,000.
7
Improved access to peer support, housing, and community-based services can increase one’s quality of
life and help to keep people living with mental health problems and illnesses out of hospitals and out of the criminal
justice system.
8
The Strategy calls for Canada to increase the amount spent on mental health from seven to nine per cent of health
spending over ten years. This investment should be accompanied with a system transformation guided by the
recommendations in the Strategy. We all have a shared role in advocating for greater and more efcient mental
health resources.
Mental health is not just a health issue, and any system transformation also benets from better investment in social
spending. This would mean, for example, increasing the amount spent on mental health by two per cent within the
education system, housing programs, and the criminal justice system.
4
Smith, P., Stiff, D., Briante, C., Adair, C., Ahmed, S., & Khan, M. (2011). The life and economic impact of major mental illnesses in Canada: 2011 to 2041.
Risk Analytica, on behalf of the Mental Health Commission of Canada.
5
Lim, K., Jacobs, P., Ohinmaa, A., Schopocher, D. & Dewa, C.S. (2008). A new population-based measure of the economic burden of mental illness in Canada.
Chronic Diseases in Canada, 28(3), 92-98.
6
Smith, J.P., & Smith, G.C. (2010). Long-term economic costs of psychological problems during childhood. Social Science & Medicine, 71(1), 110-115.
7
Friedli, L., & Parsonage, M. (2007). Mental Health Promotion: Building an Economic Case. Belfast: Northern Ireland Association for Mental Health.
Retrieved from http://www.chex.org.uk/media/resources/mental_health/Mental%20Health%20Promotion%20%20Building%20an%20 Economic%20Case.pdf
8
Community Support and Research Unit, Centre for Addiction and Mental Health, & Canadian Council on Social Development. (2011). Turning the key: Assessing housing and related
supports for persons living with mental health problems and illnesses. Calgary, AB: Mental Health Commission of Canada. Retrieved from http://www.mentalhealthcommission.ca.

PAGE 31
Measuring progress of mental health outcomes is also extremely important, and not enough data are currently
being collected to measure the critical elements of a recovery-oriented mental health system, such as quality of life,
satisfaction with services, and how involved people with lived experience are in making decisions at all levels. New
comprehensive data collection systems would make it possible to set and monitor clear targets for the availability
and effectiveness of services.
Committed leadership is needed if the Strategy is to have any impact. People with lived experience, youth, families,
and champions of mental health have an important, shared role in working together with governments and leaders
in all sectors to achieve the recommendations found in this document and in Changing Directions, Changing Lives:
The Mental Health Strategy for Canada.
CALL TO ACTION
The Mental Health Strategy for Canada in Action
The MHCC’s Informing the Future: Mental Health Indicators for Canada project aims to create a national set of mental health and mental illness indicators
that will identify gaps in service, allow stakeholders to gauge progress, and strengthen efforts to address the recommendations outlined in the Strategy.
Informing the Future represents a critical step in a larger conversation in Canada about the effective collection and use of data to support efforts in mental
health and recovery.

Mental Health Commission of Canada
Suite 1210, 350 Albert Street
Ottawa, ON K1R 1A4
Tel: 613.683.3755
Fax: 613.798.2989
info@mentalhealthcommission.ca
www.mentalhealthcommission.ca
The views represented herein solely represent views of the Mental Health Commission of Canada.
Production of this document is made possible through a nancial contribution from Health Canada.
