
1
Global Fund
Prospective Country
Evaluation
2021 SYNTHESIS REPORT
19 February 2021
Myanmar
Knowledge
Management
CAMBODIA
DEMOCRATIC
REPUBLIC OF THE
CONGO
GUATEMALA
MOZAMBIQUE
MYANMAR
SENEGAL
SUDAN
UGANDA
ii
DISCLAIMER
Views expressed in this report are those of the author. The author has been commissioned by
the Technical Evaluation Reference Group (TERG) of the Global Fund to Fight AIDS,
Tuberculosis and Malaria (the Global Fund) to conduct an assessment to provide input into
TERG’s recommendations or observations, where relevant and applicable, to the Global Fund.
This assessment does not necessarily reflect the views of the Global Fund or the TERG.
This report shall not be duplicated, used, or disclosed – in whole or in part without proper
attribution.
DISCLAIMER
Views expressed in this report are those of the author. The author has been commissioned by
the Technical Evaluation Reference Group (TERG) of the Global Fund to Fight AIDS,
Tuberculosis and Malaria (the Global Fund) to conduct an assessment to provide input into
TERG’s recommendations or observations, where relevant and applicable, to the Global Fund.
This assessment does not necessarily reflect the views of the Global Fund or the TERG.
This report shall not be duplicated, used, or disclosed – in whole or in part without proper
attribution.
DISCLAIMER
Views expressed in this report are those of the author. The author has been commissioned by
the Technical Evaluation Reference Group (TERG) of the Global Fund to Fight AIDS,
Tuberculosis and Malaria (the Global Fund) to conduct an assessment to provide input into
TERG’s recommendations or observations, where relevant and applicable, to the Global Fund.
This assessment does not necessarily reflect the views of the Global Fund or the TERG.
This report shall not be duplicated, used, or disclosed – in whole or in part without proper
attribution.
DISCLAIMER
Views expressed in this report are those of the author. The author has been commissioned by
the Technical Evaluation Reference Group (TERG) of the Global Fund to Fight AIDS,
Tuberculosis and Malaria (the Global Fund) to conduct an assessment to provide input into
TERG’s recommendations or observations, where relevant and applicable, to the Global Fund.
This assessment does not necessarily reflect the views of the Global Fund or the TERG.
This report shall not be duplicated, used, or disclosed – in whole or in part without proper
attribution.
DISCLAIMER
Views expressed in this report are those of the author. The author has been commissioned by
the Technical Evaluation Reference Group (TERG) of the Global Fund to Fight AIDS,
Tuberculosis and Malaria (the Global Fund) to conduct an assessment to provide input into
TERG’s recommendations or observations, where relevant and applicable, to the Global Fund.
This assessment does not necessarily reflect the views of the Global Fund or the TERG.
This report shall not be duplicated, used, or disclosed – in whole or in part without proper
attribution.

iii
Authorship
Alexander Marr
Allison Osterman
Audrey Batzel
Dr. Bernardo Hernandez Prado
Bethany Huntley
Casey Johanns
Christen Said
Emily Carnahan
Francisco Rios Casas
Dr. Herbert Duber
Dr. Juliann Moodley
Dr. Kate Macintyre
Dr. Katharine D. Shelley
Dr. Louisiana Lush
Matthew Cooper
Dr. Matthew Schneider
Dr. Nicole A. Salisbury
Patric Prado
Dr. Saira Nawaz
Thomas Glucksman
UCSF
PATH
IHME
IHME
IHME
IHME
UCSF
PATH
IHME
IHME
EHG
EHG
PATH
EHG
EHG
IHME
PATH
UCSF
PATH
IHME

iv
Contents
Authorship ................................................................................................................................................................................ iii
Acronyms .................................................................................................................................................................................... v
Executive Summary ............................................................................................................................................................ vii
Chapter 1 .................................................................................................................................................................................... 1
1.1 Introduction ................................................................................................................................................................. 1
1.2 Grant cycle approach ............................................................................................................................................... 1
1.3 Focus topics .................................................................................................................................................................. 2
1.4 Methods .......................................................................................................................................................................... 3
Data ..................................................................................................................................................................................... 3
Budget variance ............................................................................................................................................................ 3
Indicator performance tracking ............................................................................................................................ 4
Root cause analyses .................................................................................................................................................... 4
RSSH Support vs. Strengthening “2S” analysis .............................................................................................. 4
Analytical approach to synthesis .......................................................................................................................... 4
Chapter 2: NFM2 grant cycle ............................................................................................................................................ 5
2.1: NFM2 funding request to grant making ........................................................................................................ 5
2.2: NFM2 grant implementation .............................................................................................................................. 9
Implementation Progress ........................................................................................................................................ 9
The role of revisions during implementation .............................................................................................. 14
Chapter 3: Lessons learned NFM2 to NFM3 ............................................................................................................ 22
Chapter 4: Discussion and conclusions ..................................................................................................................... 35
Chapter 5: Strategic recommendations/considerations ................................................................................... 36
References ............................................................................................................................................................................... 39
Annexes .........................................................................................................................................................................................I
Annex 1. Summary of countries eligible for matching funds in NFM2 and NFM3 by type. .............I
Annex 2. Qualitative data collected by PCE countries .......................................................................................I
Annex 3. Approach to identification of human rights, gender, and other equity-related
investments .......................................................................................................................................................................... II
Annex 4. PCE 2020 Guidance on Operationalizing the 2S Framework ................................................... X
Annex 5. Supplemental figures of budget changes by disease and RSSH ........................................ XVII
Annex 6. Table of cumulative absorption by year for all modules, RSSH modules, and HRG-
Equity-related modules.............................................................................................................................................. XIX
Annex 7: Application of the Global Fund’s performance-based funding model ............................. XXI

v
Acronyms
ACT
Artemisinin-based combination therapy
APE
Agente Polivalente Elementars
AGYW
Adolescent girls and young women
ART
Antiretroviral therapy
C19RM
COVID-19 Response Mechanism
CCM
Country Coordinating Mechanism
CCS
Collaborating Centre for Health [Mozambique]
CEP
Country Evaluation Partner
CRG
Global Fund Communities, Rights, and Gender Team
COE
Challenging Operating Environment
CSO
Civil society organization
CSS
Community Systems strengthening
CT
Country Team
DGS/DAGE
Direction Générale de la Santé/Direction de l’Administration Générale et de
l’Equipement [Sénégal]
DHIS2
District Health Information System 2
DRC
Democratic Republic of the Congo
EDT
Essential Data Tables
EHG
Euro Health Group
FEW
Female Entertainment Worker
FSW
Female sex worker
GAC
Grant Approvals Committee
GEP
Global Evaluation Partner
HMIS
Health Management Information System
HRG-Equity
Human rights, gender, equity
IHME
Institute for Health Metrics and Evaluation
ISD
Integrated service delivery
KII
Key informant interview
KVP
Key and vulnerable population
LFA
Local Fund Agent
LIC
Low-income country
LLIN
Long-lasting insecticide-treated net
LMIC
Lower-middle income country
M&E
Monitoring and evaluation
MDR-TB
Multidrug-resistant tuberculosis
MMT
Methadone maintenance treatment
MoH
Ministry of Health
MoHA
Ministry of Home Affairs [Myanmar]
MoU
Memorandum of Understanding
MSAS
Ministère de la Santé et des Affaires Sociales [Sénégal]
MSM
Men who have sex with men
NFM2
New Funding Model 2 (2017-2019 funding cycle)
NFM3
New Funding Model 3 (2020-2022 funding cycle)
NSP
National Strategic Plan
OBR
Official Budget Revision
OIG
Office of the Inspector General

vi
OPN
Operational Policy Note
PAAR
Prioritized Above Allocation Request
PCE
Prospective Country Evaluation
PLHIV
People living with HIV
PMTCT
Prevention of mother-to-child transmission
PR
Principal Recipient
PSM
Procurement and supply chain management
PU/DR
Progress update and disbursement request
PWID
People who inject drugs
QA
Quality Assurance
RAI3E
Regional Artemisinin-resistance Initiative 2 Elimination Program
RCA
Root cause analysis
RSSH
Resilient and sustainable systems for health
SO
Strategic Objective
SR
Sub-recipient
STC
Sustainability, transition, and co-financing policy
TERG
Technical Evaluation Reference Group
TRP
Technical Review Panel
UCSF
University of California, San Francisco
UHC
Universal health coverage
UMIC
Upper middle income country
UNOPS
United Nations Office for Project Services
UQD
Register of Unfunded Quality Demand
VfM
Value for Money
WPTM
Work Plan Tracking Measures

vii
Executive Summary
Introduction
In 2020, the Prospective Country Evaluation (PCE) took a comprehensive look at the Global Fund
grant cycle, assessing how business model factors have facilitated or hindered the achievement
of objectives during implementation of grants approved through New Funding Model 2 (NFM2;
2017-2019 funding cycle), including around Resilient and Sustainable Systems for Health (RSSH),
sustainability and equity, and whether lessons learned during the current grant have informed
the next funding cycle. In this report, we present our synthesis of findings from eight PCE
countries: Cambodia, DRC, Guatemala, Mozambique, Myanmar, Senegal, Sudan and Uganda. The
objective of the grant cycle analysis was to understand what, when, why and how grant
investments change over time, including significant factors that influenced the implementation of
and changes to the original grant. In each country, this was assessed using focus topics as lenses
to evaluate the grant cycle and to better understand drivers of change. This report follows the
grant cycle, first presenting synthesis findings from NFM2, including the funding request and
grant making process and implementation, followed by how the NFM3 (2020-2022 funding cycle)
grant design process was informed by lessons from NFM2. Conclusions related to grant design
and implementation are discussed in Chapter 4, focusing primarily on RSSH and human rights,
gender and other equity-related investments (HRG-Equity), paralleling Global Fund Strategic
Objectives 2 and 3.
1
NFM2 funding request to grant making
The PCE found that grant design and budgets did not change significantly during the NFM2 grant
making process from the Global Fund’s Technical Review Panel (TRP)-approved funding
requests, although proportionally more changes were made to investments in HRG-Equity and
RSSH areas. In the majority of PCE countries, investments in reducing HRG-Equity barriers
declined during grant making, whereas RSSH budgets show large increases in some countries and
declines in others. Factors that influenced prioritization and changes during grant making
included Country Team support and input, catalytic matching funds investments and TRP review
and comments, among others.
NFM2 grant implementation
NFM2 grant implementation has been uneven, including start-up delays during Year 1, primarily
as a result of the lengthy selection and contracting processes for sub-recipient implementers.
After grant start-up, absorption performance increased in Year 2, although weak grant
coordination and issues with performance monitoring constrained ongoing implementation
progress. The PCE found that early implementation delays disproportionately affected RSSH and
HRG-Equity activities and absorption remained particularly low in some RSSH and HRG-Equity-
related investment areas. However, regular progress reviews and grant coordination meetings
among key stakeholders helped accelerate implementation of the grants. During Year 3, the onset
of the COVID-19 pandemic caused significant disruption, particularly for HRG-Equity
investments, which required agile adaptations. Grant revision processes introduced to support
1
Building from this 2021 PCE Synthesis Report, the TERG commissioned a three-month extension phase
(April-June 2021) to focus on deeper analysis. Key areas explored included: NFM2 grant revision issues
and lessons learnt from the Global Fund’s response to COVID-19; Health systems support and
strengthening; Reasons for the limited uptake of RSSH coverage indicators; and NFM3 grant making,
including drivers of budgetary shifts and transparency, country ownership and inclusion. Additional
findings and recommendations are being produced.
viii
the COVID-19 response were flexible and a reasonably ‘light lift’ for country stakeholders,
enabling rapid implementation adjustments in 2020.
In contrast, grant revisions are usually perceived as burdensome and administratively complex.
Additional funding revisions tended to occur earlier in the grant lifecycle, initiated by the
Secretariat and negotiated between the Country Teams (CTs), Country Coordination Mechanisms
(CCMs) and grant recipients, and were based on reviews of high-priority activities from the
register of unfunded quality demand (UQD). Program revisions (‘reprogramming’) to the scale or
scope of grants were uncommon, occurring in only four PCE countries. Evidence from some PCE
countries suggests that some potential program revisions (e.g., where new evidence became
available) were not undertaken during NFM2 and were instead shifted for inclusion in NFM3
funding requests—in part due to the burdensome program revision process and the short three-
year implementation cycle. PCE countries most frequently made budget revisions (‘reallocation’)
as a financial management tool to influence absorption. In most PCE countries, this resulted in a
cumulative shifting of unused resources to later in the grant cycle, rather than undertaking a more
substantial program revision, particularly for low absorbing RSSH and HRG-Equity interventions.
Using budget revisions systematically to shift unutilized resources from Year 1 to Years 2 and 3,
and subsequently from Year 2 to Year 3, has significant potential to reduce allocative efficiency.
The lack of sufficient programmatic performance data upon which to guide revision decisions
likely contributes to the emphasis on using budget revisions to influence absorption.
The annual funding decision does not appear to be working as intended to operationalize the
principle of performance-based funding. Specifically, disbursements often varied dramatically
from the total agreed budget for each reporting period and, even when performance against grant
targets and indicators was weak, disbursements were often above or a relatively high proportion
of the total grant budget. As such, it is unclear if or how disbursements are being used to
incentivize performance.
Lessons learned NFM2 to NFM3
Ensuring grants are well designed at the time of the grant award is critical. In most PCE countries,
the NFM3 funding request process was an improvement over NFM2. With some variation, it was
more streamlined, efficient and flexible, characterized by improved country ownership,
participation by a wider group of stakeholders and with a range of business model factors used
effectively to influence grant priorities. However, despite greater inclusivity, transparency and
country ownership during funding request development, this tended to decline during the grant
making stage, where key decisions were often taken. Nonetheless, KVP representatives reported
feeling more included in NFM3 funding request processes than in NFM2, in some cases helped by
having gained experience from previous processes and having received support to build their
capacity. The efficiency of the Matching Funds application process also improved for NFM3
compared to NFM2. TRP recommendations (made both on NFM2 and NFM3 funding requests)
informed NFM3 grant designs, often with implications for HRG-Equity and RSSH related
investments. However, across all application approaches, COVID-19 changed the way the funding
request and grant making processes were managed, with both positive and negative implications.
The Global Fund’s successful Sixth Replenishment, alongside a commitment to ‘do things
differently’ offered an important opportunity to ‘change the trajectory’ in NFM3. NFM3 funding
requests included significantly larger budgets and focus on some—but not all—of the areas
where a change in trajectory is needed to meet the Global Fund Strategic Objectives.
ix
HRG-Equity: PCE countries show evidence of NFM3 funding requests being designed with
explicitly more focus than in NFM2 on improving equitable access to health services and
allocating resources to intervention approaches that are known to contribute to greater
programmatic sustainability. However, in some cases, efficiency and/or effectiveness
considerations appear to have taken precedence over equity considerations in NFM3 grant
design. For instance, in response to concerns with efficiency, some countries adjusted NFM3 PR
and SR implementation arrangements with potentially negative consequences for equity. On the
other hand, several PCE countries used better-quality and/or more recent data on KVPs during
NFM3 compared to NFM2, which enabled grants to set up new interventions to target KVPs more
precisely or widen the geographical distribution of places that KVPs would receive services.
However, the quality of data (particularly the accuracy of KVP population size estimates)
continues to constrain these decisions and overall allocative efficiency.
RSSH: Most PCE countries increased their allocation to RSSH in NFM3, although, compared to
NFM2, a greater proportion of these investments are designed to support rather than strengthen
health systems. As such, it is unclear how the NFM3 grants are intended to ‘change the trajectory’
for the achievement of SO2. Evidence suggests that the Global Fund’s RSSH guidance “to shift from
a focus on short-term, input-focused support...towards more strategic investments...that build
capacity and lead to sustainable results”(1) is not being systematically operationalized. In some
countries, NFM3 RSSH investment design builds upon progress made during NFM2, especially in
HMIS/M&E, but most PCE grants did not appear to use the NFM3 funding request process to link
RSSH investments more strategically with sustainability plans. In some countries, NFM3 grants
are shifting RSSH intervention approaches, with greater emphasis on community systems
strengthening for improving access to and quality of service delivery. Several countries show
governance adaptations to improve coordination and implementation of crosscutting RSSH
investments. Despite extensive new guidance, most NFM3 grant performance frameworks do not
appear to include many of the new RSSH coverage indicators, suggesting that monitoring RSSH
performance and progress toward meeting SO2 will remain a challenge. Coverage indicators
rarely capture aspects of system strengthening (such as data use for decision-making) and some
RSSH investment areas do not map well to available indicators.
Conclusions
Grant design
1. Improvements to the business model between NFM2 and NFM3 contributed to more
efficient and inclusive funding request processes. However, NFM3 saw limited adoption
of changes in the design of performance monitoring, particularly for HRG-equity and
RSSH.
2. In NFM3, both RSSH and HRG-Equity investments rose, in many cases as a result of
overall allocation increases. An increased proportion of RSSH investment is directed
toward activities that support rather than strengthen the health system.
Grant implementation
3. Implementation of NFM2 grants faced significant start-up delays and COVID-19
interruptions. Absorption was overall weaker for RSSH and HRG-Equity interventions.
4. Multiple barriers and challenges exist for undertaking revisions to the scope and/or
scale of grants mid-cycle, such as in response to new evidence or emerging performance
issues.
x
Recommendations
Recommendation 1: Improve grant-specific performance monitoring to inform
implementation decisions.
• Establish routine grant review processes at the country level with a quality improvement
lens, emphasizing grant-specific performance data and drawing on emerging evidence
and data to better inform revisions that maximize impact. (PRs, Grant Management
Division including Country Teams)
• Implement proposed reforms of the grant rating system to reflect both grant-specific
performance and contribution of Global Fund grants to national program performance.
Additionally, this should draw upon qualitative inputs, including expertise of the CCM,
LFA, Country Team and wider Secretariat. (Grant Management Division, Strategy
Committee, Board)
• Based on the revised grant rating system, the Secretariat should also develop a set of
indicative options to demonstrate how good and poor performance could be responded
to, and a framework for deciding when and how to introduce these measures in different
contexts and circumstances (Grant Management Division, Strategy Committee, Board).
• Strengthen the use of revised RSSH indicators to address delayed implementation and
potential deprioritization throughout grant implementation. (PRs, Grant Management
Division including Country Teams)
Recommendation 2: Build in more flexibility and responsiveness in implementation by
simplifying grant revision processes to encourage their use throughout the grant cycle.
• Consider flexibilities and streamlining of material program revision process to
encourage/reward earlier introduction of innovative programming that maximizes
impact and limits non-strategic budgetary shifts to later in the 3-year grant cycle.
(Secretariat)
• Introduce flexibilities to PR and SR contractual arrangements and performance
frameworks that can be used to introduce mid-term changes as required. (PRs, Grant
Management Division)
• Through the Secretariat’s planned grant revision review (mid-2021), examine how
countries could strengthen data-driven revision decisions (thereby avoiding the over-
reliance on financial data to guide revision decisions), in line with establishing a more
streamlined, flexible process for program revision. (Secretariat)
Recommendation 3: In order to reduce gaps between policy guidance and grant design,
improve communication around how to invest more strategically in RSSH, including CSS.
• In the next Strategy, the Global Fund board in collaboration with the Secretariat should
clarify their position on whether the primary objective of RSSH is to support the three
disease programs or to invest more holistically in health systems strengthening. (Board,
Secretariat RSSH team)
• Clarify specific Global Fund RSSH priority areas and what strengthening as opposed to
supportive investment would look like for these, including specific purpose, indicators
and targets in performance frameworks. (Secretariat RSSH team, Country Teams)
• To facilitate integration and strengthening RSSH, ensure proper engagement and
ownership from health system planning experts and leaders to support health sector-
wide programming decisions, including alignment of grant design and sustainable
financing within wider national health, health system and UHC policy context, and the
timelines associated with broader strengthening efforts. (PRs, Country Teams)
xi
Recommendation 4: In order to improve grant contribution to equity and SO3, explicitly
promote grant investments in these areas, including through more direct measurement
of the drivers of inequity and of outcomes of human rights and gender investments.
• Invest more in data and data use, including up-to-date KVP surveys as well as other data
sources that shed light on socio-economic, gender, geographical and ethnic differences in
disease burden and access to services that grants are aiming to contribute to. (Country
Teams, national stakeholders)
• Ensure performance frameworks incorporate existing data including on human rights
and political commitment as well as disease burden and service access amongst different
population groups and use this data effectively to monitor grant contribution to both SO3
and SO1 or disease impact. (Country Teams, national stakeholders)
• Recognizing the success of strategic initiatives and/or matching funds in incentivizing
grant investments in reducing equity, human rights and gender related barriers to
accessing services, prioritize scaling up across the portfolio and incentivizing such
investments through mainstream grant management operations. This should include
explicit efforts to improve implementation and where necessary, timely revisions to
maximize grant contribution to reducing barriers to care and disease impact. (Grant
Management Division, Strategic Initiatives team)
1
Chapter 1
1.1 Introduction
The Prospective Country Evaluation (PCE) is an independent, multi-year prospective evaluation
of the Global Fund, commissioned by the Global Fund’s Technical Evaluation Reference Group
(TERG). The goal of the PCE is to evaluate how the Global Fund business model operates in eight
countries in order to generate evidence that will accelerate progress towards meeting the Global
Fund Strategic Objectives (SOs). The PCE is led by two Global Evaluation Partners (GEPs), in
collaboration with eight Country Evaluation Partners (CEPs). The Euro Health Group/University
of California San Francisco (EHG/UCSF) consortium supports Cambodia, Mozambique, Myanmar
and Sudan; the Institute for Health Metrics and Evaluation (IHME)/PATH consortium supports
the Democratic Republic of the Congo (DRC), Guatemala, Senegal and Uganda. These eight
countries, although not selected to be formally representative of the Global Fund portfolio overall,
comprise approximately 20% of the investment during the 2017-2019 allocation period (US$2.2
billion) and 2020-2022 allocation period (US$2.5 billion), and present an array of disease
epidemics, geographies, development statuses and Global Fund support (Table 1, with additional
details available in Annex 1). Among the countries, only Guatemala is transition-eligible for
malaria and TB in the next funding cycle.
Table 1. PCE Portfolio Characteristics (US$)
Characteristic
CAM
DRC
GTM
MOZ
MYN
SEN
SDN
UGA
Total
World Bank Income Group
LMIC
LIC
UMIC
LIC
LMIC
LIC
LIC
LIC
High Impact Portfolio
X
X
X
X
X
5
Core Portfolio
X
X
X
3
Challenging Operating Environment (COE)
X
X
2
AGYW Priority Country
X
X
2
Matching funds eligible (NFM2, millions)
NA
$16.0
NA
$19.7
$19.3
$2.5
NA
$9.4
$66.9
Matching funds eligible (NFM3, millions)(2)
$6.0
$12.6
NA
$22.4
$12.3
$1.3
NA
$23.5
$77.9
Table Notes: LIC = low income country; LMIC = lower-middle income country, UMIC = upper middle income country
1.2 Grant cycle approach
Each year, the PCE synthesizes country findings to present a more comprehensive assessment of
the Global Fund business model. During the 2020 evaluation phase, the approach was informed
by the TERG’s interest in understanding how the Global Fund grant cycle has facilitated or
hindered the achievement of grant objectives during implementation within the New Funding
Model 2 (NFM2) grant cycle (2017-2019 funding cycle), including around Resilient and
sustainable systems for health (RSSH), sustainability and equity, and whether lessons learned
during the current grants have informed the New Funding Model 3 (NFM3) (2020-2022 funding
cycle). Applying a mixed-methods approach, information was collected from a variety of
quantitative and qualitative data sources; through analysis and data triangulation, the PCE
generated results that elucidate how the Global Fund business model plays out in-country.
The objective of the grant cycle analysis was to understand what, when, why and how grant
investments change over time, including significant factors that influenced the implementation of
and changes to the original grant. We examined aspects of grant design and implementation, and
specifically aimed to evaluate:
● how and why the NFM2 grants were modified along the grant cycle (during grant making,
implementation, and grant revision);
● how the Global Fund business model facilitated or hindered modifications along the grant
cycle; and
2
● whether and how grants contributed to achieving progress towards (or away from)
equity, sustainability and/or health systems strengthening objectives.
In addition, the PCE assessed the 2020 funding request and grant making process for NFM3 on
five themes, relative to the NFM2 process where relevant: (1) Differentiated applications: tailored
review, program continuation, and full review; (2) Transparency, inclusion, and country
ownership; (3) Moving beyond ‘business as usual’ to change in trajectory for achieving impact;
(4) Data use and target setting; and (5) Value for money.
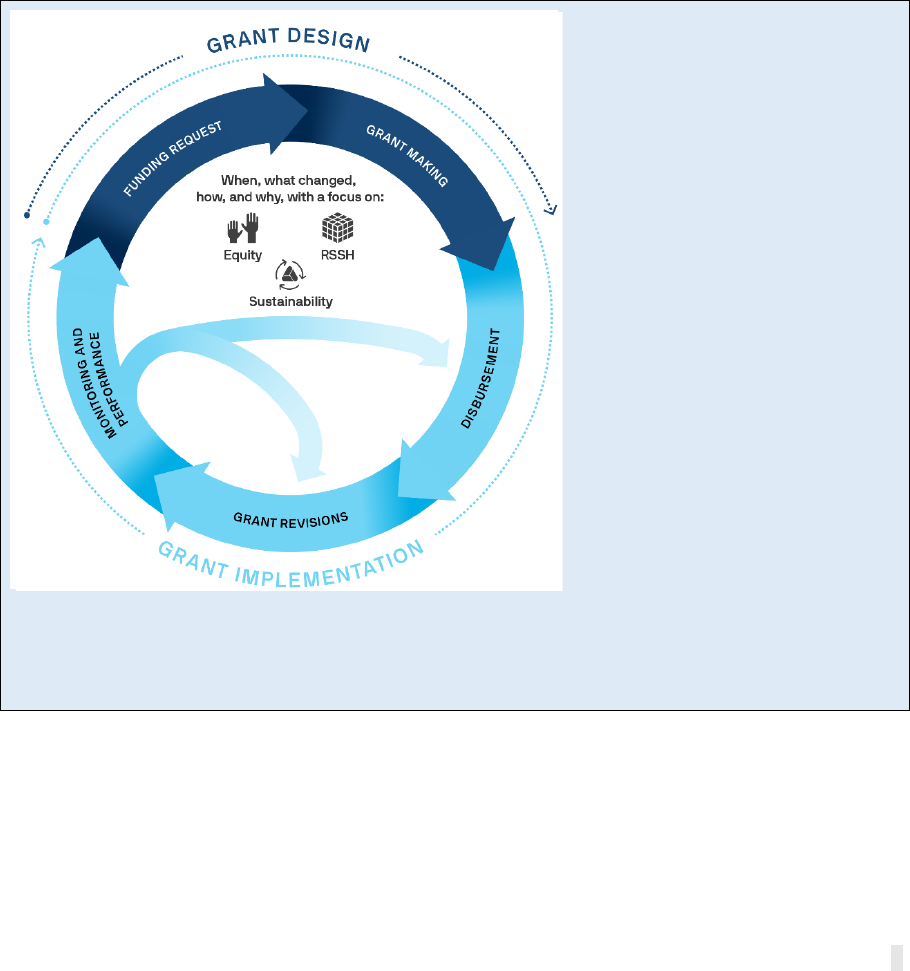
The PCE used a Grant Cycle framework (Figure 1) as the primary evaluation framework for
organizing 2020 data collection and analysis. The Global Fund grant cycle begins with the funding
request development leading to grant making, grant award, and grant signing. This process takes
eight to nine months and is followed by a three-year implementation period during which funds
are disbursed, activities are implemented, grants are modified through revision processes, and
progress is monitored. During the third and final year of implementation, the next funding
request development and grant making process begins for the upcoming grants and aims to be
informed by lessons learned from the current grants.
Figure 1. Grant cycle framework
NFM2 grant design: Little is known
about shifts between the Technical
Review Panel (TRP)-reviewed
funding request and grant making.
We examine shifts during the grant
making process as they relate to
Global Fund strategic objectives,
including prioritization of equity and
RSSH in funding requests and shifts in
equity and RSSH-related investments
during grant making.
NFM2 implementation: We examine
performance against grant and
national program indicators and
targets, Global Fund strategic
objectives, and implementation
progress, including the barriers and
facilitators to implementing RSSH
and equity-related investments. We
further examine budgetary shifts and
the role of grant revisions in
enhancing or detracting from RSSH
and equity investments.
NFM2 vs. NFM3: Global Fund’s 2019 replenishment set commitments to change the trajectory to meet
2030 disease goals. We compare NFM2 and NFM3 investments and interventions, exploring whether
lessons learned in NFM2 are informing the NFM3 funding request processes and grant design, with a
particular focus on equity, RSSH, and sustainability.
1.3 Focus topics
The PCE used a series of focus topics as lenses through which to evaluate the grant cycle and to
better understand drivers of change and results at the country level (figure 2). Focus topics were
selected with relevance to equity, RSSH and, in limited instances, sustainability considerations.
Through these focus areas, we examined how and why grants were modified along the grant cycle,
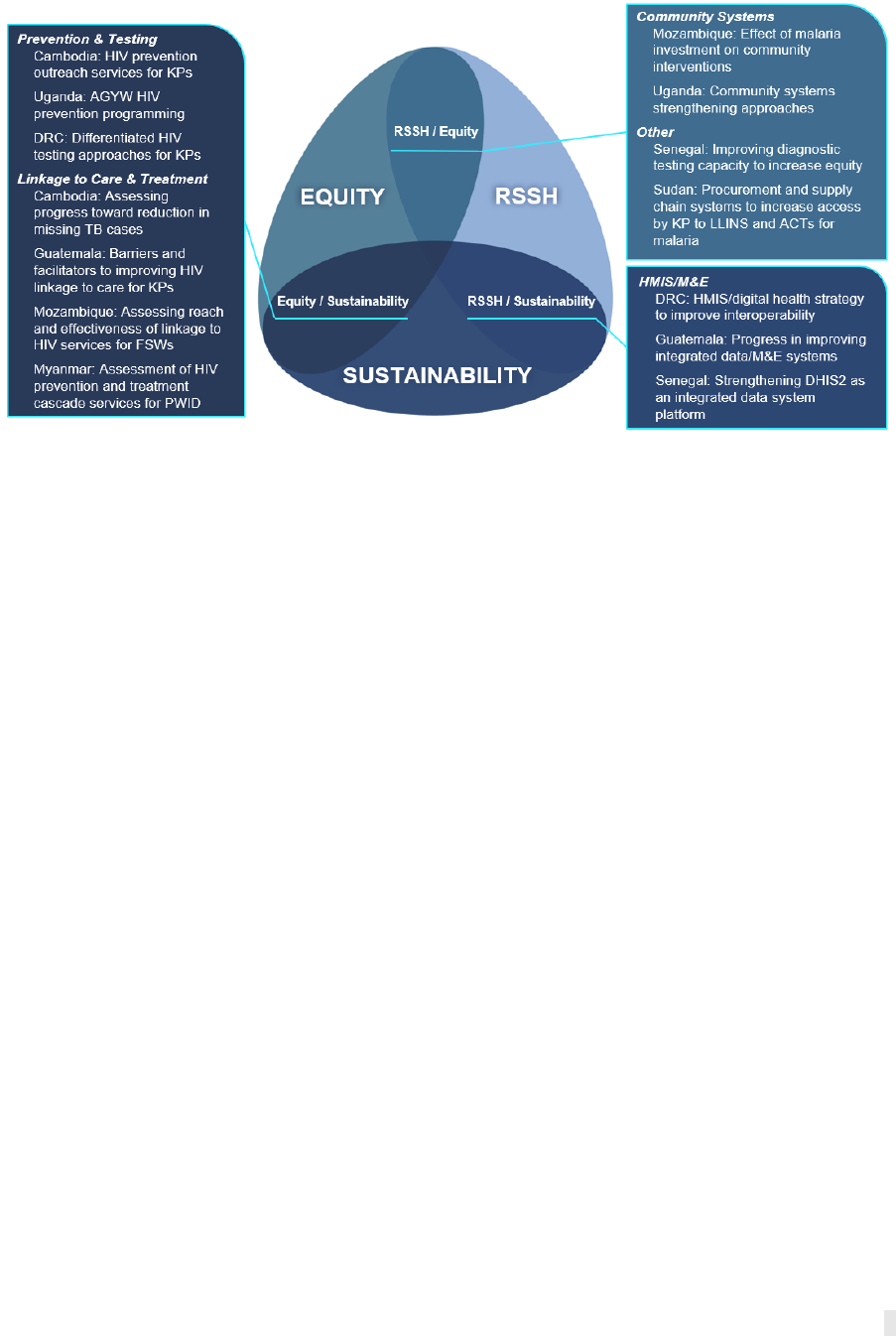
3
successes and bottlenecks to implementation, and results achievement against grant
performance targets.
Figure 2. Focus topics by country and theme
1.4 Methods
The PCE employed a mixed methods approach to assess how Global Fund business model factors
influence performance of grants throughout the stages of the grant cycle. Relying upon analyses
using both quantitative and qualitative data, the PCE examined and sought to explain changes in
planned resources and activities throughout the grant making process, revisions and
performance during grant implementation, as well as changes to the next grant window.
Triangulation of data across multiple sources and analytic approaches was used to ensure
robustness of findings, and interpretation of findings was commonly based on more than one
analysis. The EHG/UCSF consortium used contribution analysis to structure the interpretation of
findings against evaluation questions focused around the contribution of grant inputs (resources
and other inputs) to national disease program outcomes, as well as to assess the degree to which
this also enabled the achievement of Global Fund Strategic Objectives.
Data
Primary data were collected through meeting observations and key informant interviews (KIIs)
to explore issues in-depth; in addition, fact-checking interviews were conducted to fill
information gaps (Annex 2). KIIs elicited stakeholder perspectives on global and country-specific
evaluation questions and allowed the PCE to better understand grant cycle processes, including
barriers and facilitators. Interviews were also used to triangulate, interpret and validate results
generated through quantitative analyses and document review. Interview transcripts and
meeting notes were coded according to key themes.
The PCE obtained detailed budgets for all available active and planned grants from the Global
Fund Secretariat for funding requests, approved grants, awarded for grant making, and official
revisions (with corresponding Implementation Letters). In addition to detailed budgets, local
fund agent (LFA)-verified progress update/disbursement requests (PU/DRs) were obtained.
Budget variance
The PCE conducted detailed financial analyses of Global Fund budgets throughout the grant cycle
for NFM2 grants as well as available budgets from funding requests to grant making during NFM3.

4
Budgets were analyzed by recipient, disease, module, intervention, and focus topic.
2
Observed
changes in financial resources and prioritization between activities were triangulated using
qualitative data collected during KIIs, document review, and additional interviews. Using the
Global Fund’s modular framework, the PCE tracked resources for RSSH and human rights, gender,
and other equity (HRG-Equity) related interventions. HRG-Equity modules and interventions
were identified using Global Fund’s disease-specific technical briefs on gender, human rights, and
key populations; gender technical briefs; and validated through conversations with the Global
Fund Secretariat’s Community, Rights and Gender (CRG) team. Additional details can be found in
Annex 3, including a complete table of modules and interventions included in the PCE analysis of
HRG-Equity.
An analysis of financial absorption (expenditure as a percentage of budget) within and across
grants was conducted using PU/DRs, examining trends in absorption by semester, module, and
intervention. Similarly, absorption for RSSH- and HRG-Equity-related modules and interventions
were tracked throughout the grant cycle.
Indicator performance tracking
Indicator achievement against targets are reported within the LFA-verified PU/DRs during grant
implementation. These data were also compiled and tracked over the grant cycle to understand
changes in performance across grants, focus topics, and RSSH and HRG-Equity. Insights from
indicator trends over time were used to guide KIIs and fact checking interviews to triangulate
how the Global Fund business model facilitated or hindered performance.
Root cause analyses
The PCE used root cause analyses (RCA) to further explore, analyze and understand the root
causes underlying observed challenges or successes identified through a variety of triangulated
data sources (KIIs, secondary data analysis, document review).
RSSH Support vs. Strengthening “2S” analysis
The PCE analyzed RSSH activities in NFM2 and NFM3 according to whether they contributed to
“systems support” or “system strengthening,” drawing on definitions from Chee et al. (2013). (3)
We developed a coding methodology, aligned to Global Fund’s RSSH modules in the modular
framework, to designate each RSSH activity in the budget as either predominantly support or
strengthening. Three parameters—scope, longevity, and approach—were examined for each
RSSH intervention/activity pair, adapted from the methodology previously used by the TRP’s
examination of RSSH in the 2017-2019 funding cycle.(4) Two coders independently applied a
determination of support or strengthening after reviewing each intervention and activity
description, and any relevant text in the funding request narrative, and cost category. Details on
the methodology used are available in Annex 3.
Analytical approach to synthesis
Drawing from country analyses and annual reports, the GEPs compiled quantitative and
qualitative evidence into matrices organized by grant cycle stage and RSSH, equity, and
sustainability thematic areas. Evidence was drawn from focus topics as well as grant- and
country-level analyses. The evidence matrices helped identify patterns in the data across
countries and informed further discussion and analytical triangulation with cross-country budget
variance data. Due to the variation of focus topics, not all findings were able to be substantiated
across the eight countries; wherever possible, findings were supported by additional country
focus topics and portfolio-level analyses. Early synthesis findings were validated with CEP teams
for feedback and additional data interpretation.
2
Some budgets were not included in the synthesis as these grants were not subject to analysis at the country level
during the course of 2019-20, namely: Sudan HIV/TB, Cambodia malaria, and Myanmar malaria.
5
Chapter 2: NFM2 grant cycle
2.1: NFM2 funding request to grant making
This section presents findings on the changes that were made during 2017/2018 to NFM2 grant
designs between the country funding request submissions and the final approved grant award—
i.e., through the grant making process. This includes analysis of how and why changes were made,
who suggested that they be made, and whether these changes were in line with the Global Fund
guiding policies and priorities.
Key message 1: Overall grant designs and budgets did not change significantly during the
2017 grant making process (NFM2). More substantial changes were made to investments
supporting the achievement of SO2 (RSSH) and SO3 (HRG), although not necessarily to
prioritize these areas (despite being consistently highlighted through the PCE and other
analyses as requiring more attention).
In general, during NFM2, relatively few major changes in overall grant design and budgets
occurred between funding requests and final approved grant awards for PCE countries (as seen
in Annex 5 figures 5.1, 5.2 and 5.3). Proportionally (given investments in these areas are relatively
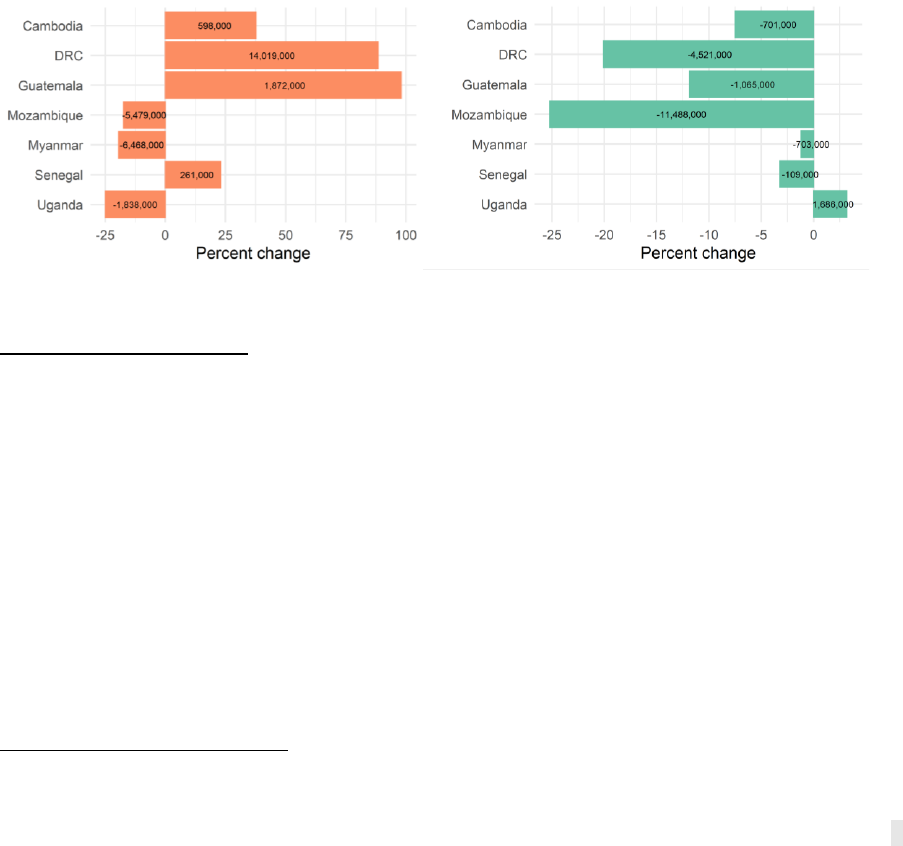
small compared to the overall grants), more significant changes were made to investments in
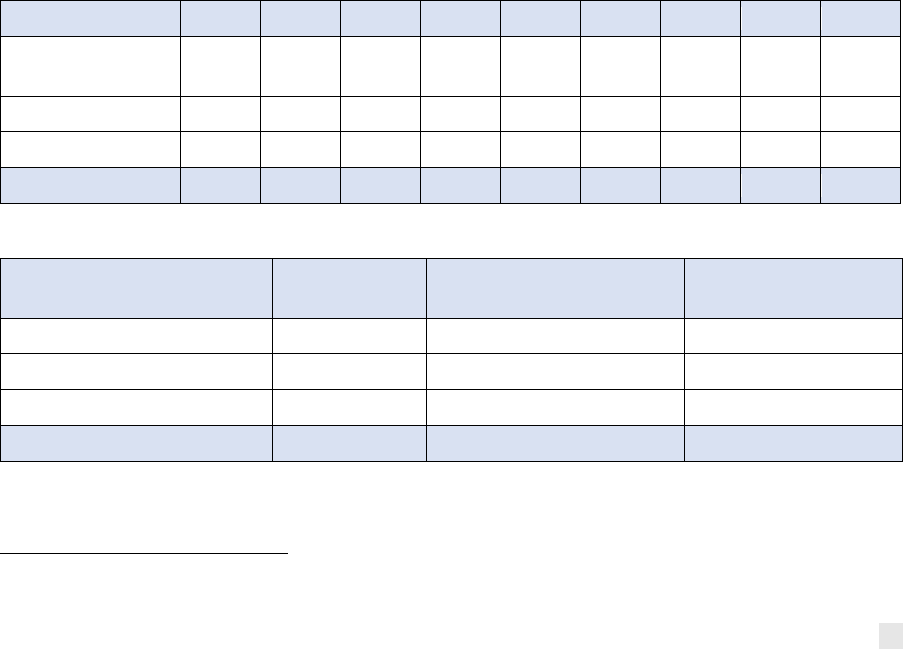
HRG-Equity and RSSH for most PCE countries during the NFM2 grant making process (Figure 3).
Figure 3. Percent change in RSSH (left) and HRG-Equity (right) investments from NFM2 funding
request to grant award
3
Source: Global Fund detailed budgets
HRG-Equity Investments
Analysis of all investments that seek to address HRG-Equity-related barriers to access and/or
health outcomes show that the budget for these areas declined in six of the eight PCE countries
during the grant making process. While no clear patterns emerged for TB and malaria (for which
these types of investments are small and difficult to track), HIV grant budgets mostly declined,
particularly for prevention among key and vulnerable populations (KVPs). Specifically, in all
countries that included some budget allocation for the following modules, the budget decreased
between the funding request and grant award:
● Prevention for Men who have sex with men (MSM): Substantial declines in
Mozambique, DRC and Guatemala.
● Prevention for People who inject drugs (PWID): Almost complete removal in
Mozambique and heavy cuts in DRC.
3
To ensure comparability, we restricted the grants to only those with full and tailored review (excludes continuation
grants for malaria in DRC, Mozambique, Senegal and Sudan, as well as HIV in Senegal and Sudan, and TB in Sudan).
6
● Prevention among prisoners: Complete removal in Mozambique and heavy cuts in
Cambodia and Guatemala.
The budget for prevention for female sex workers (FSW) also reduced or stayed the same in three
out of five countries, only increasing in Cambodia, where there was focused effort to increase
targeted programming to this group (and other KVPs) via improved management and support for
outreach workers.
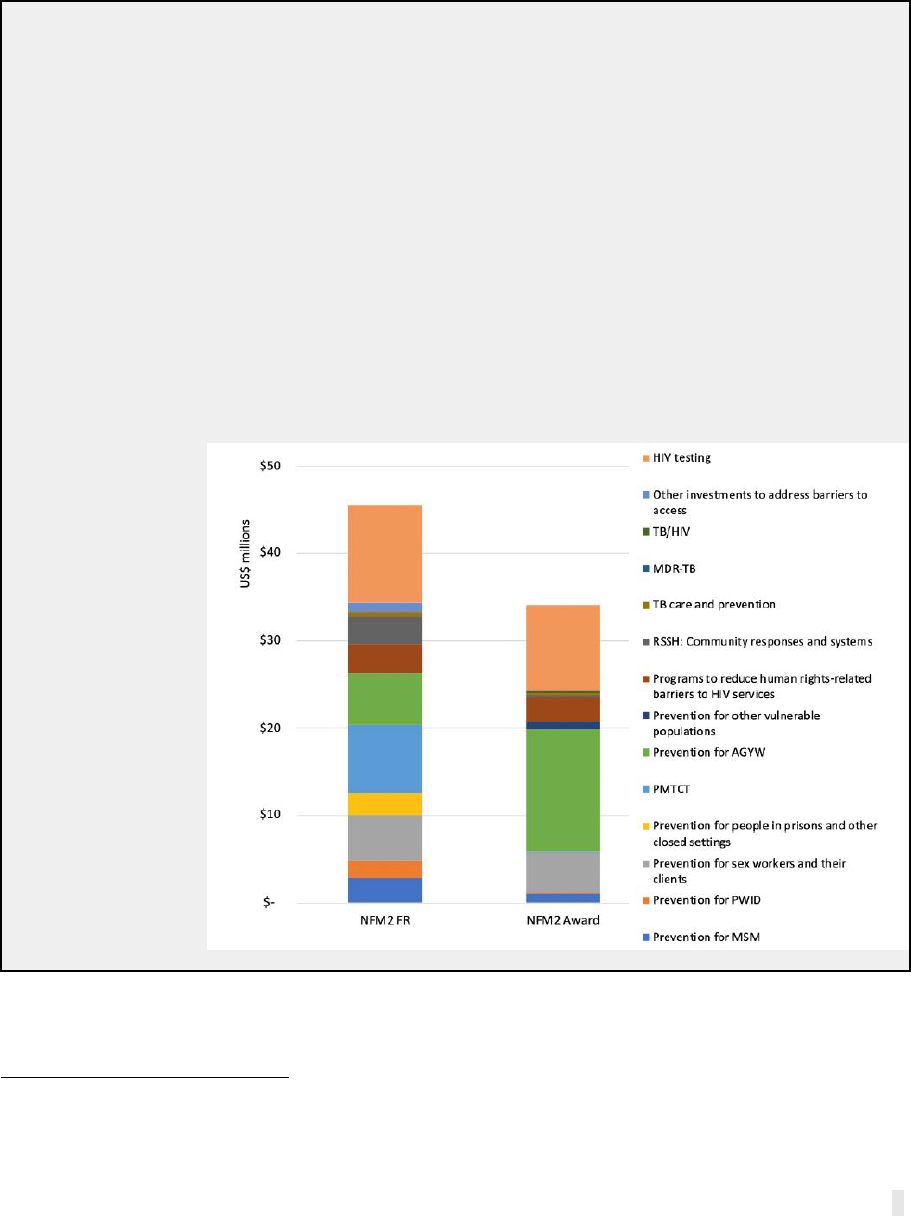
Box 2.1: Mozambique HIV/TB investments to address equity-related barriers.
The NFM2 grant making process reduced investments to address HRG-Equity-related barriers
in Mozambique by 25% (from US$46m to US$34m), mainly driven by a US$6m (68%) reduction
in HR-related investments and a US$3m (30%) reduction in wider KVP investments.
4
These
reductions were partly offset by a substantial increase in funding for prevention among
adolescent girls and young women (AGYW), from US$6m to US$14m, in response to emergent
evidence of increasing incidence among this group. Of note, anticipated matching funds for
human rights (US$4.7m) were added after the grant award, so appear in the first
implementation letter. For human rights, it was felt the strategy was not complete and the
implementation therefore was also not ready, so the Grant Approvals Committee (GAC) agreed
to delay the start and reduce the budget from the core allocation without jeopardizing eligibility
for matching funds. For AGYW, the budget from the core allocation was increased to support
more activities for this group.
Figure 4. NFM2 HIV/TB funding request and grant award budget variance analysis of investments
designed to address HRG-Equity or other barriers to accessing health services and/or achieving
health outcomes:
Source: Global Fund
detailed budgets
4
There was also a US$8m (98%) reduction in funding for Prevention of mother-to-child transmission (PMTCT) —
reflecting the shift from Option B+ to test and start. The related increases in testing and treatment costs were included
in other budget lines, notably treatment care and support, which is not included in our estimates of equity-related
investments at grant award.

7
RSSH Investments
Analysis of RSSH budget changes during grant making shows large increases in some countries
and significant declines in others, as well as substantial shifts between modules/program areas
in many countries. Three PCE countries increased the overall RSSH allocation from funding
request to grant award (Cambodia, DRC, Guatemala) and three countries decreased the overall
RSSH allocation (Mozambique, Myanmar, Uganda). In all countries, the final agreed level of RSSH
investment was below what was recommended by the Secretariat (which varied from 5% to 11%
of total grant value across countries) and the vast majority of the agreed NFM2 RSSH investments
were designed to support rather than strengthen the health system.(4)
RSSH module budgets shifted in different ways during grant making. Four out of seven PCE
countries with available data (excluding Sudan) increased resources for the Health Management
Information System and Monitoring and evaluation (HMIS/M&E) module and three countries
increased resources for Procurement and supply chain management (PSM)—two areas critical to
supporting core disease grant implementation. Guatemala introduced a substantial increase in
HMIS and M&E in response to TRP comments (discussed further below). In Mozambique,
investments for integrated service delivery (ISD) and quality improvement, which were relatively
limited in most PCE countries, declined significantly during grant making. Three countries
reduced resources allocated to community responses and systems between the funding request
and grant award, with negative implications for equity, given the role of these systems in reaching
the most vulnerable, and for achieving sustainability objectives. Value for Money (VfM)
considerations sometimes drove reductions. In Uganda, for example, per diem allocations for
community systems strengthening (CSS) outreach were reduced in alignment with the
government’s policy on rates.
Key message 2: Several business model factors, including the role of the Secretariat
Country Teams (CT), matching funds and the TRP review process, influenced prioritization
during grant making.
A range of country-specific and Global Fund business model factors affected prioritization
decision making during the grant making process. As compared to the relatively open and
transparent funding request development process, grant making was difficult to observe from an
evaluation perspective, with many discussions taking place in private between senior Secretariat
staff and country stakeholders. Nonetheless, evidence suggests that the most significant business
model factors influencing the design of grants were:
Role of the Secretariat: Across all PCE countries, qualitative evidence suggests that the
Secretariat played an important role in working alongside country stakeholders to guide
prioritization decision making. This included working with country stakeholders to revise initial
funding request submissions prior to TRP review, and in interpreting the recommendations made
by the TRP and GAC to finalize grant designs and budgets. In some countries, the Secretariat has
a ‘hands on’ role, such as in the DRC, where the budget for HIV testing among KVPs was reduced
during grant making to accommodate a Secretariat request to partake in the Supply Chain
Transformation Project, and the CT asked Principal Recipients (PRs) to identify budget cuts
across various modules to make US$10m available.
Matching funds: Five out of eight PCE countries received catalytic matching funds that served to
increase total investment in HRG-Equity-related areas. However, evidence is mixed on whether
these funds had the desired effect of increasing the level of investment to these areas made from
the core country allocations. Although in Mozambique, the human rights budget reduced (Box
1.1), for most countries receiving human rights matching funds (DRC, Senegal, Uganda), the total
budget from the core allocation increased for this priority area during grant making. By contrast,
of the three PCE countries that received matching funds for RSSH/data systems, the related
8
budget from the core allocation decreased in Mozambique, while in DRC it increased. In Myanmar,
although the allocation to RSSH from the HIV budget increased, the overall allocation to RSSH
declined due to TB grant reductions.
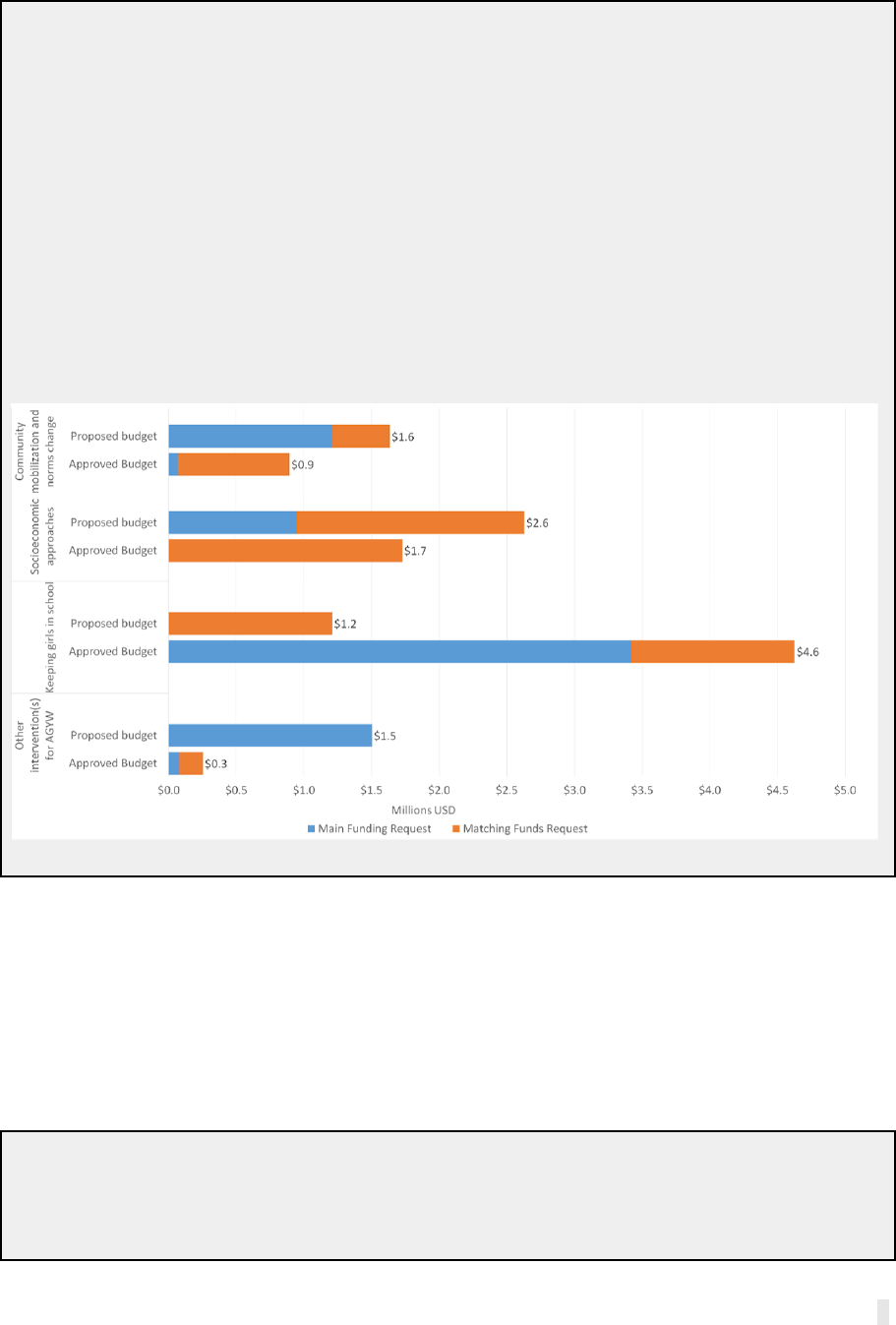
Box 2.2: Drivers of AGYW intervention shifts during grant making in Uganda.
The total investment in interventions within the AGYW module remained relatively unchanged
after grant making, decreasing 1% from US$5.0m to US$4.96m. However, there were substantial
shifts across four of the seven AGYW intervention areas budgeted, mainly in response to TRP
comments on the matching funds application requiring iteration. Per the TRP comments, the
proposed matching funds were spread across too many interventions and geographies, and
some interventions were unrelated to the proposed outcomes. During grant making, the PRs
and CCM adjusted the AGYW interventions in the HIV grant’s main allocation and revised the
matching funds submission to remove activities that did not contribute directly to accelerating
progress and enhancing outcomes among vulnerable AGYW. The reductions in the
socioeconomic approaches, community mobilization, and other AGYW interventions created
room for an increase of US$3.4m in the main HIV grant activities focusing on keeping girls in
school interventions, which had no allocation in the original funding request.
Figure 5. NFM2 funding request to grant making budget variance for select AGYW interventions:
Source: Global Fund detailed budgets in Uganda
TRP review process: TRP comments and recommendations influenced the grant design and
budget in several countries. For instance, following the TRP comments in Mozambique, during
grant making the PR placed significant emphasis on prevention among AGYW and reduced
budgets for prevention among other KVPs. TRP comments in Uganda contributed to narrowing
the focus of AGYW intervention areas during grant making with the aim of maximizing investment
into interventions with a strong evidence base, that would significantly reduce the HIV risk
among AGYW. Another example from Myanmar is provided in Box 2.3.
Box 2.3: Effect of TRP comments on equity investments during grant making in Myanmar.
One of the TRP comments on the NFM2 funding request was a request to expand service
coverage for HIV testing and methadone maintenance treatment (MMT) for PWID. Following
grant negotiations with the Secretariat, the two PRs increased targets for reaching PWID with
9
HIV prevention, testing and MMT for the NFM2 grant period through cost efficiencies in
prevention activities: PWID HIV prevention targets increased by 16%; the PWID tested target
increased by 32%; and the PWID on MMT target increased by 38%. The revised targets were
confirmed by the GAC for the grant award.
Box 2.4: Effect of TRP comments on RSSH design during grant making in Guatemala.
During grant making, the HMIS budget more than doubled in direct response to comments from
the TRP. Noting persistent weaknesses in the ability of the national HMIS to track program
indicators and monitor progress, the TRP requested a detailed plan to strengthen HMIS and
better monitor progress toward epidemic control and recommended consideration of DHIS2 as
a platform. As a result, the PR INCAP added US$500,000 to the program and data quality
intervention, to support the strengthening of the national HMIS and develop a system to enable
to PR to track relevant community level indicators. This targeted investment for the PR was
aligned with a national HMIS strengthening plan that had identified DHIS2 as an option for wider
HMIS strengthening endeavors and was presented by the CCM and PR as the response to the
TRP comments. Despite the increased investment in HMIS, no additional relevant indicators
were added to the performance framework.
2.2: NFM2 grant implementation
Implementation Progress
Key message 3: A number of Global Fund business model factors influenced grant start-up
and early implementation, especially: lengthy selection and contracting processes for
implementers and CT support. Early implementation delays disproportionately affected
RSSH and HRG-Equity activities.
NFM2 grant implementation was significantly disrupted, both by delays to start-up in Year
1 and by the onset of the COVID-19 pandemic in Year 3. Across PCE countries, a number of
Global Fund business model factors resulted in initial start-up delays in Year 1 of NFM2 grant
implementation, discussed further below. Overall Year 1 absorption for all modules across all
grants ranged from a low of 54% in Cambodia to a high of 74% in Myanmar, with an average of
68% (Figure 6). Implementation progress accelerated in Year 2 in nearly all PCE countries as
implementers overcame start-up delays and in some cases put in place accelerated or ‘catch-up’
implementation plans. Average absorption across PCE countries was 81% (see Figure 6 and
Annex 6). Based on available data for the first half of Year 3 (2020) in a subset of countries (DRC,
Senegal, Uganda), we observed lower absorption compared to Year 2. Evidence suggests that this
is partly due to challenges in implementation resulting from the COVID-19 pandemic. However,
the cumulative effect of budget revisions resulting in unutilized budgets from earlier years being
shifted to the final year of grant implementation also contributed to low absorption in Year 3.
Compared to the grants’ overall average progress, implementation remained particularly
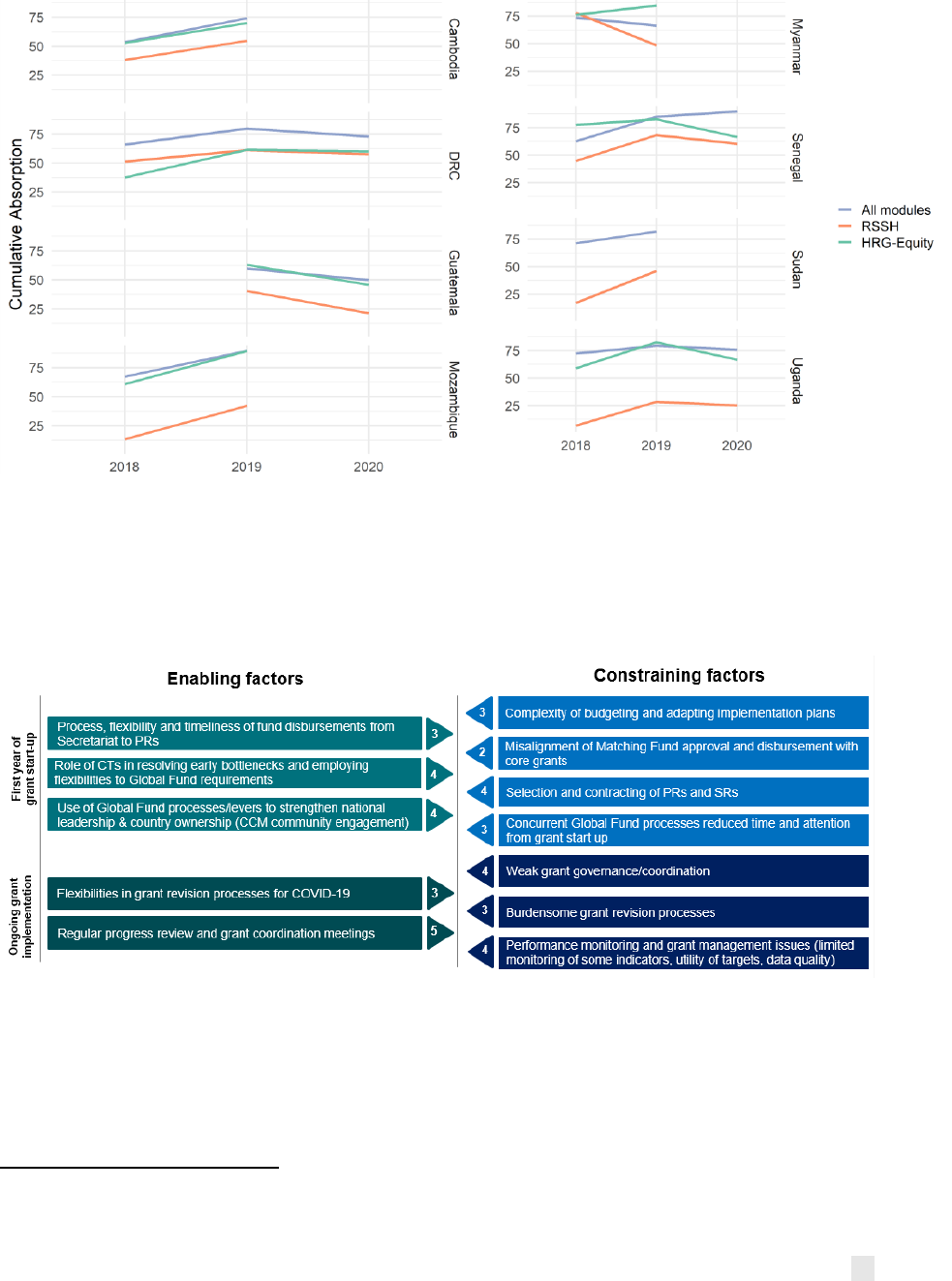
slow in some RSSH and HRG-Equity-related investment areas. At the most recent time point
where data are available (2019 S2 or 2020 S1, depending on the country), seven of eight PCE
countries had lower cumulative absorption for HRG-Equity investment areas compared to the
overall grants, and all eight PCE countries had significantly lower cumulative absorption for RSSH
investments compared to the overall grants (see Figure 6).
5
Financial absorption is defined as the
percentage of the budget that was spent within a given time period. However, as noted in previous
PCE reports, absorption is an imperfect measure of implementation progress as it does not
5
RSSH absorption was 15 or more percentage points below total absorption in all countries, and in half of the PCE
countries (Mozambique, Senegal, Sudan, Uganda) it was 30 or more percentage points lower.
10
capture the quality of implementation and may incentivize implementers to focus on activities
that are more quickly absorbed.
Figure 6. NFM2 cumulative absorption over time for all modules, HRG-Equity-related
investments, and RSSH investments
Figure note: 2020 absorption only includes S1; Guatemala grants began NFM2 implementation later.
Source: PU/DRs
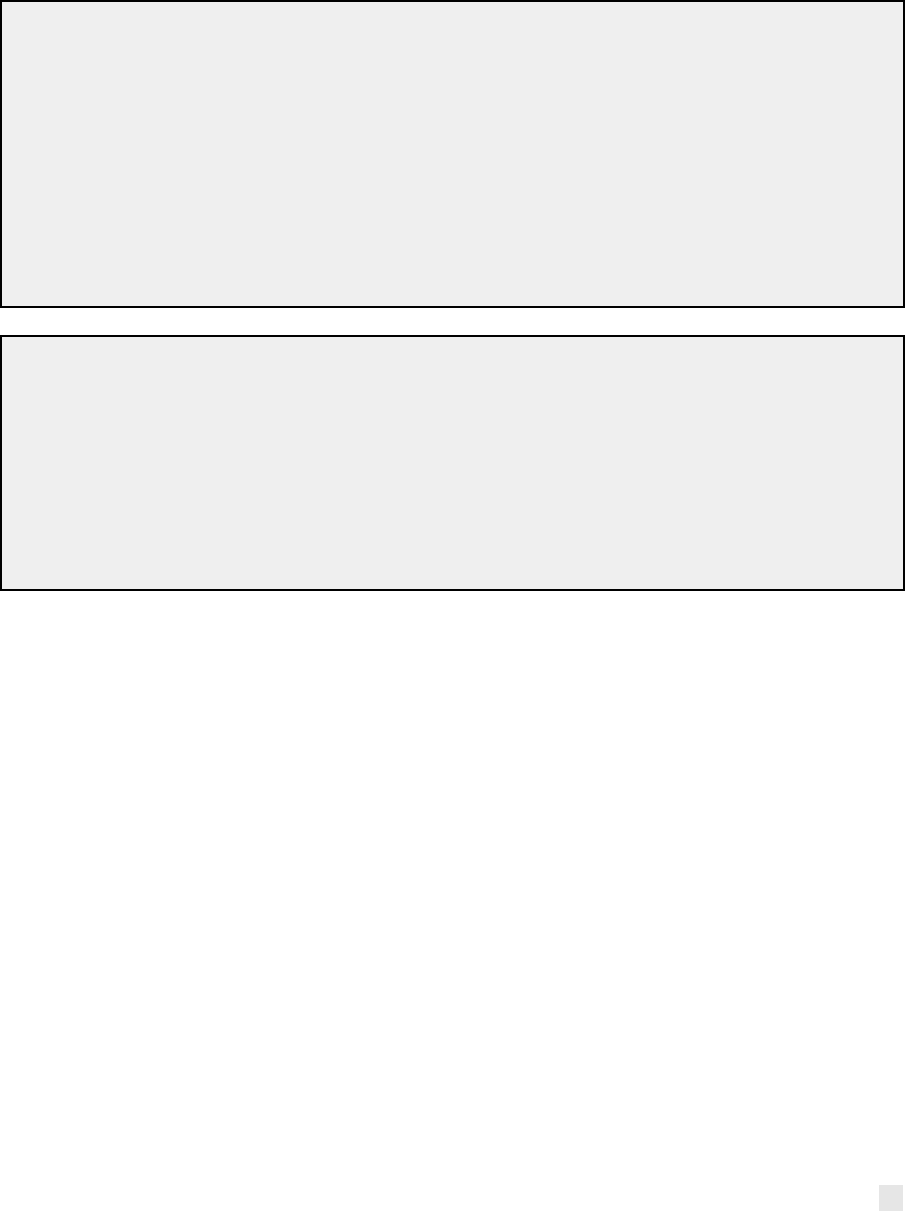
As summarized in Figure 7, and explored in more detail below, a number of Global Fund business
model factors influenced implementation progress during NFM2, with some particularly affecting
the grant start-up phase in Year 1.
Figure 7. Global Fund business model factors influencing implementation progress
6
Lengthy selection and contracting of implementers, particularly SRs by PRs, delayed
implementation of activities in the majority of PCE countries. In Sudan, the new PR undertook
capacity assessments with 14 new SRs and Implementing Units but not sufficiently in advance of
grant implementation, causing significant delays. In Cambodia, DRC, Mozambique, Senegal and
Uganda, disbursements to SRs did not occur until the second or in some cases third quarter of
2018 as a result of SR contracting delays due to weak capacity. SR contracting delays during grant
6
Each of the factors have been weighted in the form of a score based on their relative level of influence over grant
implementation, where five (5) is the most important and one (1) the least (noting that the least important factors are
not included to aid readability).
11
start-up particularly affected the implementation of HRG-Equity activities as PRs often rely on
SRs with community experience to deliver KVP, HR and gender interventions and these
organizations have less experience with Global Fund management systems. In other cases, new
government PRs, appointed to enhance sustainability, had relatively little experience with Global
Fund processes, resulting in early implementation delays. For example, Cambodia appointed the
Ministry of Finance as PR for NFM2 to promote national ownership and sustainability, which led
to a slow grant start-up in year 1 due to disbursement delays, but subsequently implementation
picked up pace (see also Senegal example in Box 2.5).
Box 2.5: Senegal new government PR lack of familiarity with Global Fund processes.
For NFM2, Senegal moved to consolidate and centralize responsibility for grant management
within the Ministry of Health to create efficiencies and streamline ownership. As recommended
by the CCM, the Secretariat awarded PR-ship of the TB/RSSH grant to the Direction Générale
de la Santé/Direction de l’Administration Générale et de l’Equipement (DGS/DAGE), while the
national TB program, the former PR, became a sub-recipient. These implementation
arrangement changes affected roles and responsibilities across different Ministry of Health
actors, and, along with the DAGE’s relative inexperience with Global Fund procedures as a new
government PR, caused implementation delays, which stakeholders attributed to the absence
of a transition phase between allocation cycles and inadequate consideration of onboarding
needs to support new PRs.
Box 2.6: Sudan new PR lack of familiarity with Global Fund processes inhibited malaria
grant implementation.
Under NFM2, the PR for the malaria grant transitioned to the Ministry of Health (MoH),
although government financial and management systems did not fully meet standard Global
Fund requirements. Throughout NFM2, extreme political and economic upheaval severely
impacted on the delivery of the malaria program, partly due to PR lack of familiarity with the
Global Fund business model. Together, these factors limited disbursement and delayed
implementation and absorption, particularly for routine LLIN distribution. Despite these
problems, in 2019 the GAC approved a budget of $25 million for LLIN mass distribution.
Concurrent Global Fund processes were a barrier to implementation progress. Most PCE
countries spent the first six months of NFM2 grant start-up simultaneously closing NFM1 grants.
These concurrent processes were reported as time-consuming in several PCE countries (Sudan,
Myanmar, Uganda) and reduced time and attention from grant start-up activities, even in the case
of program continuation grants.
Aligning budgets and implementation plans for Global Fund grants was a highly complex
process. As observed across all PCE countries, the advantages of input-based budgeting in terms
of risk management did not outweigh the complexity of subsequent changes to implementation
plans. In Myanmar, budgetary management tools inhibited implementation in a number of ways.
For instance, the managed cash flow system, introduced as a financial risk mitigation measure,
contributed to low budget absorption, alongside high program management costs. Intensive
reporting and data verification processes also took significant time for PRs to deal with,
detracting their focus from implementation.
Finally, some countries did not approve Matching Funds and related disbursements until well
into the NFM2 grant implementation period. This misalignment with the main grant approvals
negatively affected the implementation of those activities and had a significant effect on RSSH and
HRG-Equity activities, as they rely more on matching funds and take significant time to plan. In
DRC for example, the Secretariat processed matching funds for RSSH/data systems separately
from the main grant and they did not go through GAC approval until eight months into NFM2
12
implementation. Similarly, in Uganda, misalignment of timing of matching funds for AGYW and
Human Rights, due to the matching funds request sent back from TRP for iteration, delayed
signing of MoUs with public sector SRs, causing further implementation delays. Senegal also
experienced significant delays in the incorporation of matching funds.
Influential enablers of early implementation progress during NFM2 included the role of CTs in
resolving early bottlenecks and employing flexibilities to Global Fund requirements and the
process, flexibility and timeliness of fund disbursements from the Global Fund Secretariat to
PRs—most PCE countries received initial disbursements on time. In Uganda, DRC, Cambodia and
Senegal, the CTs played an important role in allowing for flexibility in the disbursement of funds
to avoid disruption to grant implementation. In Myanmar, stakeholders reported that alignment
with the National Strategic Plan (NSP) and the CCM coordinating partners also supported
implementation.
Key message 4: After grant start-up, weak grant coordination as well as issues with
performance monitoring constrained ongoing implementation progress. Again, these
factors particularly affected RSSH and HRG-Equity-related activities. Conversely,
stakeholders’ engagement in regular progress reviews and grant coordination meetings
facilitated implementation.
As summarized in Figure 7 above, a number of Global Fund business model factors influenced
implementation progress in Years 2 and 3. Most notably:
Weak coordination within and between grants, with other program teams and between donors,
constrained implementation in multiple PCE countries (Cambodia, DRC, Guatemala, Senegal and
Sudan). Coordination challenges particularly affected RSSH investments, in part due to resources
for RSSH activities being spread across grants, and because responsibility for the aspects of health
systems being targeted often lies outside of the disease programs. As a result, a diverse set of
stakeholders needed to be involved in grant design and implementation, which evidence suggests
was lacking in many countries. Where RSSH funds and activities were provided through the
disease-specific grants, stakeholders found it challenging to implement activities that were
intended to be integrated across diseases (see Box 2.7). In DRC, governance and coordination
challenges stymied implementation of digital health interventions following the government’s
creation of a new digital health agency with responsibilities overlapping those of the national
health information systems agency. In Senegal (Box 2.7), the Secretariat lacked an accountability
mechanism for ensuring follow-through and/or intervention, although between NFM2 and NFM3,
a strategic shift centralized management of TB and Malaria grants under a single unit within the
MoH, which may help address both coordination and leadership issues in the future. These
examples highlight that coordination and leadership are needed to implement activities with
objectives beyond the disease grants.
Box 2.7: Senegal RSSH coordination challenges. In Senegal, each disease program grant was
expected to contribute 10% of its RSSH budget to support the multi-sectoral RSSH platform,
created to improve coordination and harmonization of crosscutting RSSH activities under the
Ministère de la Santé et des Affaires Sociales (MSAS) Direction Générale de la Santé (DGS),
which was selected as the PR of the TB/RSSH grant. However, only the TB program allocated a
portion of their funds, while the HIV and Malaria programs did not because they were unclear
how the funds would be used. This contributed to the platform’s already weak financial and
logistical management capacity, and undermined efforts to integrate RSSH investments across
all three disease programs.
Some PCE countries have examples of successful approaches to overcoming coordination
challenges. In Mozambique, initial delays in recruitment of an RSSH lead delayed implementation
of critical RSSH investments. However, once that position was filled, their leadership facilitated
13
RSSH implementation progress. In other countries (DRC, Guatemala), support and/or persistent
follow-up from the CT supported RSSH implementation progress.
While weak grant coordination was identified as a common implementation constraint, a number
of other mechanisms strengthened these functions and leveraged national leadership and
country ownership over grant implementation. In some cases, the CCM ensured broad and
diverse engagement of stakeholders in a number of countries, particularly in Myanmar.
Regular progress reviews and grant coordination meetings, supported by CTs, also enabled
progress. In DRC, Uganda and Senegal, these reviews and meetings at national and/or subnational
levels facilitated coordinated implementation progress. In Mozambique, coordination of the grant
with the wider MoH program similarly facilitated implementation. Conversely, where there are
examples of lack of political support and the above levers were not suitable and/or used to good
effect, this negatively affected implementation—for instance, with a lack of progress made in
implementing activities to strengthen DHIS2 in Senegal.
Issues with performance monitoring and grant management inhibited implementation
across PCE countries. The Global Fund has designed performance frameworks to include
indicators that are helpful for tracking overall country progress but less useful as indicators to
measure grant implementation progress or results. Moreover, NFM2 performance frameworks
lacked specificity on key RSSH and HRG-Equity investments. Where indicators were proposed,
poor data quality often hampered their use (see Box 2.10 and 2.11).
The grant revision process, discussed in more detail in the section below, was also a barrier to
implementation progress. While the Global Fund intended grant revisions processes to enable
implementation adjustments to maximize impact, in practice, stakeholders found the process
burdensome and have sought to avoid undergoing significant changes that would trigger a TRP
review. In contrast, the grant revision processes for COVID-19 revisions were perceived as more
flexible and a lighter lift for country stakeholders, which has enabled rapid implementation
adjustments in 2020 (see Box 2.8), and may be a source for lessons learned in addressing some
limitations of the standard revision processes.
Box 2.8: Grant implementation and COVID-19 disruptions. Evidence from the PCE countries
underscores how COVID-19 particularly affected HRG-Equity investments in NFM2. For
example, the social distancing measures in Uganda as part of the COVID-19 response included a
ban on social gatherings and movement, as well as school closures, which affected activities like
dialogues, sports campaigns, outreach, and in-school activities that targeted AGYW to reduce
gender barriers to HIV prevention, care, and treatment. COVID-19 also affected HIV services for
KVPs in Cambodia, as described further below.
14
Equity implications of COVID-19 on delivery of HIV
services for key populations in Cambodia. By the
end of 2019, KVP outreach targets had largely been
met and/or exceeded, with the exception of PWID
(not shown). As a result, in 2019, the grant increased
resources for these services through portfolio
optimization and revisions, shifting funds to the
stronger performing interventions targeting Female
Entertainment Workers (FEW), MSM and
transgender people. However, during 2020, COVID-
19 restricted achievement of targets for all key
populations, especially FEW and PWID (not shown).
Entertainment venue closures triggered FEW to
migrate, which disrupted outreach contact. Some
stakeholders expressed concern around the capacity
of implementers to deliver on additional services
under COVID-19 and its effect on absorption.
Global Fund business model flexibilities were
critical in channeling additional resources to the COVID-19 national response through
grant savings and the COVID-19 Response Mechanism (C19RM). Countries used flexibilities
within the NFM2 grants through a mix of ‘true’ savings (e.g., delayed implementation over Year
1-2, lower unit costs, over-budgeting, etc.) and savings from activities that could not be
implemented during lockdowns (e.g., outreach, training, meetings, supervision, school-based
activities), revising US$26m from current grants. An additional US$209m was approved
through C19RM. PRs and SRs undertook various implementation adaptations in responding to
COVID-19 disruptions. For example:
● Cambodia: COVID-19 was predicted to affect antiretroviral therapy (ART) attendance, so
implementation shifted to providing multi-month scripting for all stable ART patients to
ensure maintenance.
● Guatemala: To limit face-to-face outreach interactions, a SR switched to online outreach for
KVPs, with early evidence of improved performance.
● Myanmar: Additional procurement for ARV buffer stock through October 2021, treatment
for opportunistic infections and methadone maintenance, rapid test kits.
● Senegal: Strengthen procurement and supply of laboratory equipment and reagents in
reference labs and potentially increasing use of GeneXpert for COVID-19 testing.
● Uganda: Innovations that leverage Global Fund investments, such as using the bed net
campaign database to guide distribution of facemasks to households, or utilizing community
health volunteers to support medication refill and distribution.
Table 2. Approved grant flexibilities and C19RM ($US millions).(5)
Mechanism
CAM
DRC
GTM
MOZ
MYN
SEN
SDN
UGA
Total
Flexibilities
$0.52
$0
$2.3
$2.6
$6.3
$2.2
$1.6
$10.5
$26.1
C19RM
$0
$55.1
$1.1
$60.5
$27.3
$4.9
$8.7
$51.9
$209.5
The role of revisions during implementation
As per the Operational Policy Manual: “The goal of a grant revision is to allow Global Fund
investments to adjust to programmatic requirements during grant implementation, in order to
ensure the continued effective and efficient use of Global Fund resources invested to achieve
Figure 8. Percentages of FEW reached and
tested by KVP outreach program
15
maximum impact in line with the Global Fund’s 2017-2022 Strategy. A grant revision may also occur
due to other changed circumstances and arrangements.”(6) Grant revisions include:
7
● Additional funding revisions: When the total approved funding is adjusted, including
through ‘portfolio optimization’ and additional donor pledges.
● Program revisions: When programmatic changes in the scope (changing goals,
objectives, or key interventions) and/or scale (increasing or decreasing targets) are
applied to the grant (formerly referred to as “reprogramming”).
● Budget revisions: When the budget is adjusted but the total approved funding does not
change, nor is there any effect on the performance framework.
In addition, subject to its review of grant performance, the Secretariat makes an annual funding
decision that determines the proportion of the grant budget that will be disbursed in the following
period. This is in effect how the Global Fund’s performance-based funding model is
operationalized—i.e., the full budget is disbursed where grant performance is strong, but a
proportion of the budget is withheld where grant performance is weak (see Annex 7). As such, in
theory these decisions also influence whether and how grant revisions are made. The cumulative
effect of these various processes is a grant budget that is frequently subject to change and highly
complex. We explore the implications of these processes for grant management and
implementation in the findings below.
Key message 5. The burdensome revisions process, alongside management incentives on
PRs and CTs to maximize absorption, resulted in revisions being used predominantly as a
financial management tool, rather than necessarily to maximize impact. The cumulative
effect was that grants shifted resources to later in the cycle rather than undergoing
significant restructuring to the scope and/or scale of grants, having the potential to reduce
allocative efficiency.
PCE countries made frequent budget revisions (N=38) and additional funding revisions
(N=37), but program revisions (N=17) to scale or scope were uncommon (Table 3).
Table 3. Number and type of grant revisions during NFM2
`
CAM
DRC
GTM
MOZ
MYN
SEN
SDN
UGA
Total
Additional Funding
Revision
1
11
2
11
0
3
4
5
37
Budget Revision
3
0
5
8
4
5
3
10
38
Program Revision
0
8
0
1
6
2
0
0
17
Total
4
19
7
20
10
10
7
15
92
Table 4. Number of grant revisions and length of approval process by revision type during NFM2
Type of revision
Number of
revisions
Average revision approval
duration (days)
Average revision
approval date
Additional Funding Revision
37
132
11/7/2019
Budget Revision
38
57
4/22/2020
Program Revision
17
52
12/5/2019
Grand Total
92
87
1/15/2020
7
The PCE did not examine the other two types of revisions defined in the Operational Policy Manual: Extensions (End
Date Revisions) and Administrative Revisions.

16
As shown in Figure 9, a range of incentives drove grant revision decision making. Additional
funding revisions tended to occur earlier in the grant lifecycle, be initiated by the
Secretariat and negotiated between the CTs, CCMs and grant recipients, and were based on
reviews of high-priority activities approved in the register of unfunded quality demand
(UQD). Decision makers used funds to fill gaps and reinforce approved grant strategies, including:
increasing the investment in community TB care delivery in Cambodia; maintaining vector
control coverage and covering the 2020 ART gaps in Mozambique; providing emergency funding
for refugee LLINs and filling case management gaps in ACTs, in Sudan, alongside filling gaps in
IRS and LLIN mass campaigns in year 3; expanding geographic coverage of the LLIN campaign
and HIV testing and treatment in DRC; and incorporating funds from Comic Relief to ramp up
efforts to eliminate mother-to-child transmission of HIV in Guatemala.
Evidence from Cambodia suggests that the process for selecting what activities/interventions are
supported with the additional funding can be problematic. Specifically, despite national
stakeholders being encouraged by the Secretariat to put forward innovative programming
proposals, the Country Team aligned with TRP approved proposals, although the process through
which these decisions were made became a source of frustration and disillusionment among
national stakeholders
Figure 9. Available information and incentives drive decisions and influence grant revision
processes.
Most PCE countries undertook frequent budget revisions (reallocation), in order to
improve financial performance and maximize absorption. In Cambodia, for instance, where
the PR shifted funds away from poorly absorbing (and performing) PWID activities and into
better absorbing (and performing) FEW/MSM/transgender interventions. DRC was a notable
exception because it did not undergo any budget revisions, but, compared to other PCE countries,
had the most program and additional funding revisions. Tracking budget revisions is time-
consuming and lacks a systematic process of documentation, which has implications for
transparency beyond the PRs and LFA. Implementation letters (when official budgets are
updated) did not generally document budget revisions, which meant PCE teams examined budget
revisions through detailed comparison of official budgets over time.
Only four PCE countries executed program revisions. Revisions resulted from various triggers
(e.g., changes in implementation arrangements, in response to absorption issues, and/or
administrative issues—such as shifting funding between PRs in DRC due to changes in commodity
and freight unit costs). DRC had the most program revisions compared to other PCE countries,
which is likely a reflection of the portfolio size and complexity. However, the broader trend across
PCE countries suggests that program revisions were an underutilized mechanism for executing
changes in programmatic scope and scale. At the midpoint of the grant lifecycle, PRs did not want
funds to be withdrawn from their grant budgets, nor did they want to introduce new
programmatic activities (particularly for RSSH) that would be difficult to implement and may not
align with grant performance framework targets. Furthermore, the burdensome grant revision

17
process, particularly for program revisions, acted as a disincentive to undertaking substantial
grant revision. As shown in Table 4, program revisions took on average 52 days for approval.
However, this average duration does not include any ‘material’ program revisions requiring TRP
or GAC reviews, as none occurred in PCE countries in part due to the perceived burdensomeness
of the process; material program revisions would likely have taken longer on average. Limitations
to programmatic evidence available to inform grant revisions also restricted the ability of PRs,
CCMs and CTs to revise grants based on data/evidence about programmatic results or impact (in
line with the objective to ‘maximize impact’).
8
Box 2.9: AGYW investments in Uganda underwent frequent budget revisions by the civil
society PR, whereas the government PR appeared to miss opportunities for revision. The
civil society PR made budget revisions within the AGYW module, in some instances resulting in
a 60% increase/decrease to intervention totals, but did not introduce changes to targets. They
viewed budget revisions as necessary to improve absorption and responding to AGYW
beneficiaries’ preferences for vocational training offerings (with sustainability implications of
improving AGYW livelihood opportunities). Despite several budget shifts, the overall total
investment remained roughly stable at US$10m. Stakeholder interviews indicated that they
viewed matching funds as ‘protected’ or ‘sacred’—and that this drove efforts to ensure any
budget reallocation retained the funds within the AGYW module. The government PR did not
undertake similar budget revisions for AGYW interventions, despite ongoing delays in
implementation through 30 months of the grant, and only three of six interventions registering
any expenditure as of S1 2020 (cumulative 1.49% absorption). However, in September 2020, the
Ministry of Education, an SR, in consultation with the government PR, proposed 38% of its AGYW
module allocation be reallocated toward the prevention of gender-based violence, which was
approved by the CT. This example highlights evidence of COVID-19-related revisions aiming to
incorporate equity considerations, including programming to address the indirect impacts on
young people resulting from COVID-19, including increased gender-based violence, teenage
pregnancies and HIV infections among AGYW.
Box 2.10: Mozambique did not use grant revisions to rectify a known issue with the budget
versus target linking HIV+ FSWs to care. The recently established FSW program had funding
doubled during NFM2 grant making, but with targets set low based on relatively out-of-date KVP
data estimates (in spite of the TRP’s recommendation to scale up targets). The SR, FDC, initially
overachieved targets for outreach and testing, so grant performance was rated high. However,
partly because of the way targets are calculated in the prevention cascade, in reality the program
missed many HIV-positive FSW for linkage to care. In addition, FDC responsibility for linkage
ended with one visit to the closest health center, and they made no effort to follow up or ensure
clients fully entered into treatment. During implementation, the CT did not revise linkage targets
upwards as the budget did not increase and no grant revision took place. The CT did draw
attention to the women missed for linkage to ART, so FDC are altering their model of service
delivery for NFM3.
Box 2.11: DRC did not use grant revisions to adjust differentiated HIV testing targets
following new data on HIV incidence. DRC submitted a tailored review NFM2 funding request
for HIV/TB because the HIV component remained largely unchanged due to NFM1 grant delays
8
In particular, this refers to data on absorption being a weak proxy for implementation progress, limited quantitative
and standardized evidence available on grant implementation progress, grant performance framework indicators not
reflecting grant-specific results and not having any indicators in some important areas of the grants (often for RSSH),
and limited utilization of Work Plan Tracking Measures (WPTMs).
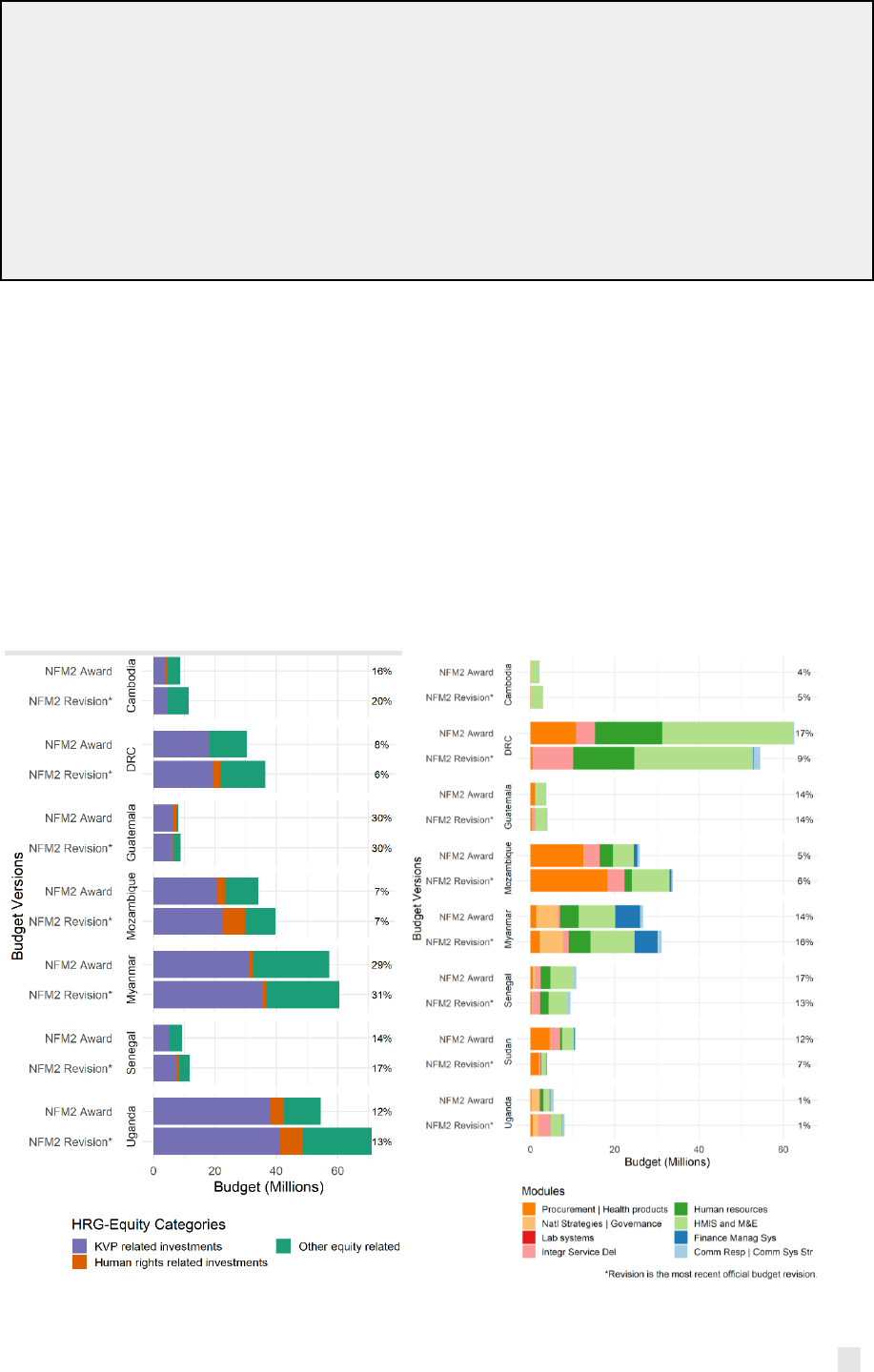
18
and lack of new epidemiological data. HIV grants were thus approved by the GAC with the
understanding that KVP testing targets would be updated during grant implementation
following the results of the 2017 HIV incidence study. However, by the time the new data on HIV
incidence were released in Q1 of 2020, development of the NFM3 funding request was already
underway and both the CT and PR considered it too late in the NFM2 grant cycle to undergo a
grant revision. This example highlights challenges with the business model of responding quickly
to new data and changes in programmatic and epidemiological context, but also raises
limitations in monitoring grant performance. For example, by semesters 3 and 4, HIV tests
administered to KVPs largely exceeded grant targets although it was acknowledged that the
under-estimated targets were driving the indicator performance.
In most PCE countries, PRs and CTs responded to low absorption of RSSH and HRG-Equity
budgets by shifting unused resources to later in the grant cycle rather than to higher-
absorbing program areas. For HRG-Equity-related areas, grant revisions mostly had the net
effect of increasing the budget. As depicted in Figure 10 (left), at the beginning of implementation,
investments related to HRG-Equity made up between 7% and 30% of PCE country budgets, with
an average of 16%. Of these investments, across countries the majority consisted of KVP-related
investments, followed by other equity-related investments and lastly, human rights. At the most
recent official revision observed by the PCE, funds for HRG-Equity had increased in all countries.
Grant revisions had a mixed effect across countries on the budget for RSSH. RSSH-related
investments during implementation decreased or remained fairly constant in half the PCE
countries while the other half observed increases (Figure 10, right). However, as a share of total
budgets, RSSH investments on average decreased from 11% to 9% across all countries.
Figure 10. HRG-Equity (left) and RSSH (right) related investments during implementation
Source: Global Fund detailed budgets
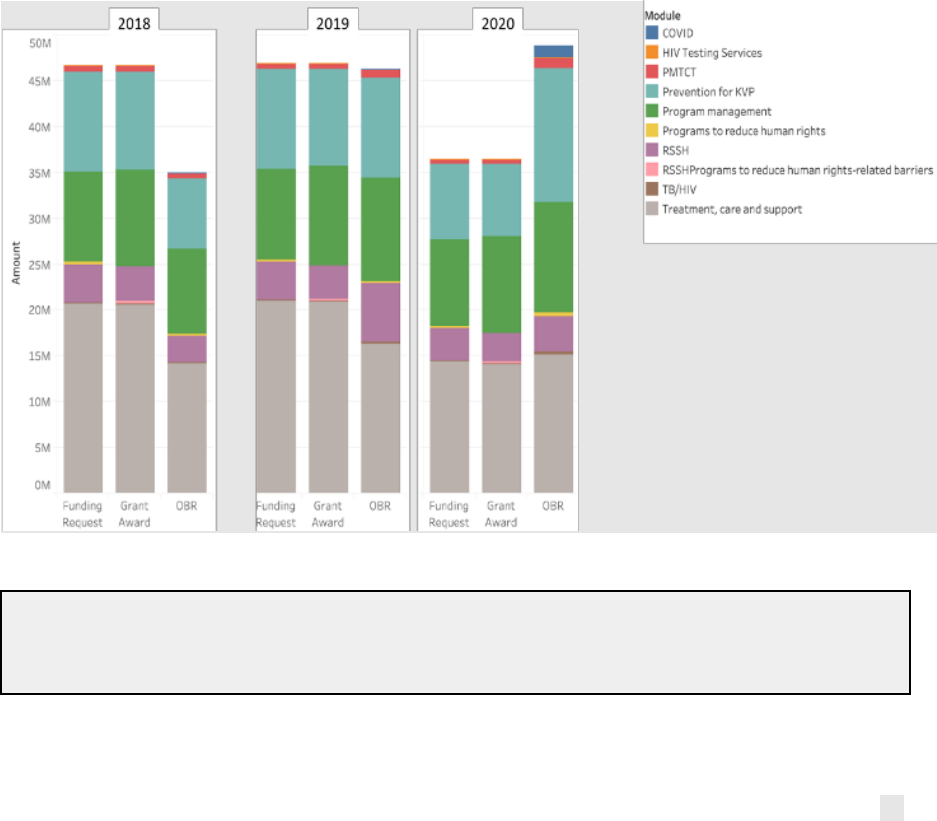
19
Using budget revisions systematically to shift unutilized resources from Year 1 to Years 2
and 3, and subsequently from Year 2 to Year 3, has potential to reduce allocative efficiency.
For example, in Myanmar (Figure 11), the HIV/TB grant budget reduction in Year 1 raised
absorption against the originally approved grant budget, with implications for grant
management. While it makes sense to shift resources to later in the grant cycle if this ensures that
they are well used, substantial sums were involved (around US$15m in the Myanmar example)
and the processes in place to make budget revisions were informal and did not require any form
of approval outside of the CT. When resources are moved around mid-cycle, the significant
benefits of the NFM model in terms of the predictability of funds are also eroded. Furthermore,
the accumulation of budget in the last year of the grant cycle places additional pressure on PRs
and SRs to avoid the Secretariat reallocating the resources through portfolio optimization.
Although the PCE has not yet been able to collect evidence on this as 2020 budgets had not been
published at the time of writing, other reviews, including SR2020, linked this situation to a
dramatic increase in spending on commodities in the final year of NFM1 grants and questioned
whether this was a good use of funding.
Analysis shows that the effects noted above were more pronounced for modules and/or
intervention areas where absorption is low in the early years of implementation. As shown above,
this affects both RSSH and HRG-Equity-related investments, which also often require more time
to plan for and implement than other investment areas. Box 2.12 provides an example from
Mozambique.
Figure 11: Comparison of the Myanmar HIV/TB grant budgets between Funding Request, grant
award and latest Official Budget Revision (OBR) (2019).
Source: Global Fund detailed budgets
Box 2.12: Delayed implementation of RSSH interventions in Mozambique. The budget for
RSSH within the HIV grants for 2018-20 was US$23m at grant award and US$27m as per the
latest grant revision, including an additional US$3m from matching funds. Based on cumulative
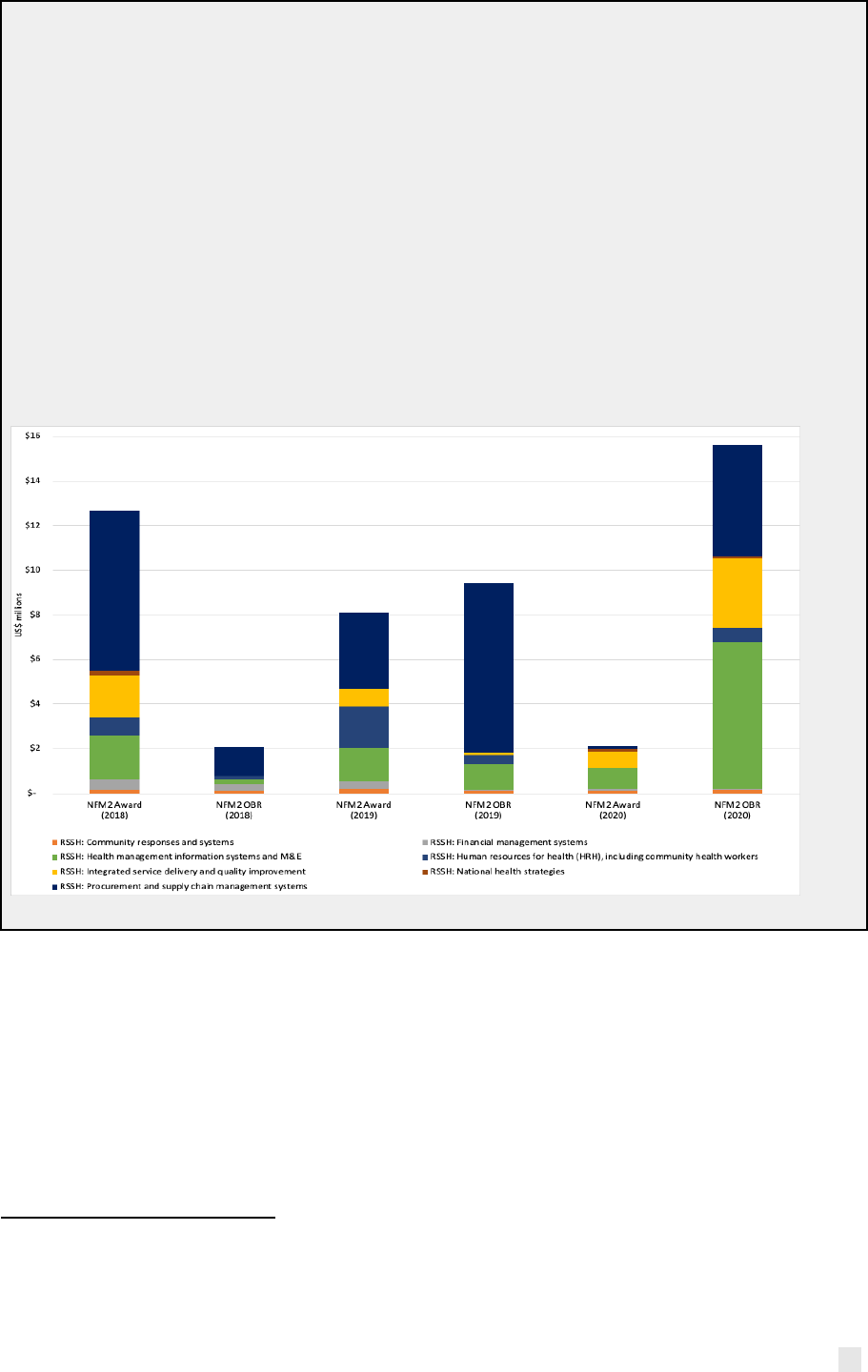
20
rate of absorption at mid-year in final year of grant, which was approximately 50%
9
, a large
amount of the funds would be unspent by the end 2020. At mid-2020, expenditure for the largest
investments—activities primarily designed to support health systems—was below budget, but
investment areas designed to strengthen the health system were even worse. The exception is
community responses and systems, for which the budget was reduced during grant making. Low
absorption partially stems from the delay of appointing a coordinator/lead for RSSH until May
2020. Despite low absorption, the grant did not use revisions to shift funds away from RSSH to
other programmatic areas, as funds were already committed in RSSH procurement processes.
Rather, as shown in Figure 12 below, the PR and CT shifted unused resources to later in the
grant. Despite this, a significant increase in resources for RSSH is planned during NFM3.
Stakeholders report that, although the NFM business model has increased predictability for
RSSH funding, the three-year cycle does not lend well to strengthening and sustaining
improvements in the health system.
Figure 12: Budget variance for Mozambique NFM2 HIV grants, RSSH modules only, 2018-2020,
by year
Source: Global Fund detailed budgets
Key message 6: Global Fund disbursements to countries often varied from the total budget
for each period but were not linked to indicator or grant performance ratings. As such, this
element of the business model does not appear to be working as intended to incentivize
performance.
The Global Fund seeks to incentivize performance, in part, by linking disbursement amounts to
the achievement of grant targets (summarized through an indicator rating, which informs an
overall grant rating).
As shown in Annex 7, disbursements often varied dramatically from the total agreed budget for
each reporting period.
10
Even where performance against the indicators within each grant
9
Information provided following the end of data collection for this report suggests absorption was over 90% by end of
December 2020, reportedly due to a significant increase in expenditure at the end of the grant cycle related to
procurement of commodities.
10
For instance, as shown in Annex Table 6.3, disbursements for 2018/19 exceeded the total original budget for this
period in 15 out 30 grants.
21
performance framework was weak (e.g., for some grants in Mozambique, Uganda and Senegal),
Secretariat disbursements were often above or a relatively high proportion of the total grant
budget.
11
Although indicator performance provides only a ’starting point’ for determining
disbursements, the lack of any relationship across all grants in PCE countries suggests that the
annual funding decision is not working as intended to operationalize the principle of
performance-based funding.
As noted in the sections above, analysis conducted through the PCE and elsewhere (e.g., SR2020)
suggests that this may be a function of:
a) The grant monitoring system being focused mostly on reporting progress against national
program-wide indicators rather than reporting the results of the Global Fund grant
specifically, and therefore not being a good proxy for grant implementation and
performance;
b) Limitations of grant performance frameworks, for instance where they include
weak/unrelated indicators with unrealistic targets, and/or where important investment
areas are omitted from the performance framework (e.g., human rights, RSSH), reflecting
wider measurement challenges.
12
(7,8) This is particularly true when considering how few
indicators are reported for some semesters.
The quantitative evidence on which to base disbursement decisions (and decisions on grant
revisions) to ensure they incentivize appropriate and optimal behavior is therefore limited. The
Mozambique example in Box 2.10 highlights a specific example of the difficulties faced in
measuring grant-specific progress. A number of PCE CEPs also reported that disbursement
decisions are made primarily based on financial needs, and possibly also qualitative information
on performance. The Secretariat may also consider it inappropriate to reduce funding to poorly
performing grants after only a year of implementation.
13
Nonetheless, the lack of clarity over how
the system works and how funding decisions are made may undermine the performance-based
funding model.
Box 2.13 provides an example of how disbursements decisions were made for a grant in
Mozambique.
Box 2.13: Disbursement decisions encouraged the achievement of results for a grant in
Mozambique with a troubled start
The Collaborating Centre for Health (CCS) HIV/TB grant achieved an indicator and grant rating
at the end of 2018 of B2 (inadequate but potential demonstrated). Correspondingly, the OPN
suggests that between 30% and 59% of the cumulative budget for 2018 and 2019 should be
disbursed in 2019.(6) While this is indicative and can be adjusted, analysis shows that
disbursements were much higher, at 94%. The CT confirmed that disbursement decisions were
made to manage financial resources, as well as performance. However, reducing funding to low
performing grants may not be the best way to maximize results. The indicator and overall grant
rating for this grant increased dramatically to A2 (meeting expectations) by the end of 2019.
11
As shown in Annex Table 6.3, the level of disbursements made is substantially different to the indicative funding
range for 19 out of 30 grants.
12
Ref previous PCE synthesis report, SR2020. For example, previous OIG analysis of 27 grants found that nearly 30%
of the budget was not reflected in the performance framework.
13
It is also worth noting that doing so may affect grants with a strong focus on activities that take more time to plan
and start implementation (e.g. those focused on RSSH, human rights, etc.).
22
Chapter 3: Lessons learned NFM2 to NFM3
As shown in Chapter 2, the ability of grant managers (both Secretariat teams and country
stakeholders) to adjust grants mid-term is fairly constrained, in part due to burdensome formal
revision processes and the significant disruption that these revisions potentially pose for
implementation. As also shown in Chapter 2, grant managers have few incentives to undertake
revisions that include scope/scale adjustments to grants; and instead tend to shift the unutilized
budget to later years in the grant cycle and delay major structural decisions until the next funding
request application. Ensuring grants are well designed at the time of the grant award is therefore
critical.
In this chapter, we therefore explore PCE findings on how the grant design process was informed
by lessons from NFM2, NFM3-specific elements of the business model, and new information and
policy to determine grant priorities, budget allocation and performance framework elements.
Key message 7: In most PCE countries, the NFM3 funding request process was an
improvement on NFM2: more streamlined, efficient and flexible; characterized by
improved country ownership and participation by a wider group of stakeholders; and with
a range of business model factors used effectively to influence grant priorities.
NFM3 ‘Tailored for NSP’ and ‘Full Review’ processes were found to be more efficient than
NFM2 ‘Full Review’ processes. Just two PCE countries, Myanmar and Uganda, submitted
tailored for NSP funding requests during NFM3, and stakeholders reported the process to be
more efficient than the NFM2 full review. Both countries reported that information generated
during NSP development consultations fed directly into funding request processes. In
Myanmar, both processes were embedded in the CCM structures that facilitated coordination
and synergies. In Uganda, because the NSP priorities were still ‘fresh’ in the minds of those
developing the funding request, they referred to the NSP more frequently, promoting greater
alignment and harmonization, and thus improving sustainability. However, the finalization of
the disease NSPs occurred concurrently with the funding request development processes,
which created some challenges for key actors and in determining how priorities from both
processes would be harmonized. Box 3.1: Process improvements through Tailored for NSP
funding request in Myanmar.
The MoH was keen to ensure that the NSP was well integrated with a wider national health
strategic plan and focused on the overall objective of universal health coverage (UHC). They
therefore worked hard to make diverse stakeholder participation more meaningful through
the Tailored for NSP approach: the CCM Secretariat was better embedded in the MoH and
shared information widely on timelines for NSP and funding request development, well ahead
of the actual process; UN agencies facilitated community networks’ engagement, including on
matching funds and community system strengthening; and a smaller, more strategic working
group led the process, operating on a tighter, more compressed timeline.
However, NFM3 full review processes were not always more efficient, compared to ‘lighter
touch’ processes for NFM2. Three PCE countries—DRC, Mozambique and Sudan— moved from
‘lighter touch’ approaches (e.g., program continuation and tailored review) in NFM2 to full review
applications in NFM3. In DRC, stakeholders regarded the 2017 program continuation and tailored
review processes as being restricted because interventions were predetermined and, as such,
they preferred the NFM3 Full Review process, which gave them greater latitude to propose new
interventions and strategies based on data, context and NFM2 lessons learned. In Mozambique,
the NFM3 process allowed for building on a recent NSP mid-term review, to incorporate its
findings into the new NSP and funding request. On the other hand, Sudan reported the 2020
process to be significantly more burdensome than their program continuation application in

23
2017, due to delays in developing the NSP, which further interrupted the funding request
submission.
Compared to NFM2, the NFM3 process benefitted from greater inclusivity, transparency
and country ownership during funding request development, but not during grant making
where key decisions were often made. CCMs were reported to be smaller, more informed and
organized, and with better coordinated technical working groups across Sudan, Myanmar,
Guatemala and Mozambique, mainly due to better government leadership and wider
participation. Sudan and Myanmar reported a reduced role needed by UN agencies as government
stakeholders showed greater leadership. For the early stages of the funding request development
process, engagement and ownership by national stakeholders extended beyond the usual
Ministry of Health program leads, including Ministries of Finance (Mozambique, Uganda),
Education and Gender Ministries (Uganda), subnational or provincial stakeholders (Cambodia,
DRC, Mozambique, Myanmar), and civil society organizations (CSOs) and KVP representatives
(DRC, Senegal, Guatemala, Mozambique), suggesting a shift toward greater integration of the
grants across national health budget processes and health systems, compared to NFM2.
However, later on in the process, (i.e., during budget allocation and priority setting) stakeholders
in most countries reported lower transparency for crucial decisions. For example, in Guatemala,
although participation in early meetings was wide, final prioritization and budget allocation
decisions were made by the PR and MoH and did not include KVP representatives. CTs also
appeared to exert a strong influence during the latter stages of the funding request process, with
countries reporting significant pressure to absorb Global Fund priorities into grants. This was
also a finding of the 2017/2018 PCE Synthesis Report.(9)
A number of KVP representatives reported feeling more included in NFM3 funding request
processes than in NFM2, in some cases helped by having gained experience from previous
processes and support to build their capacity. In DRC, KVP representatives reported that their
earlier participation in the National Program Review in 2019 strengthened subsequent
contributions to the funding request process. In Uganda, a KVP consortium organized separate
meetings and a system of email inputs which assisted a much wider group to participate than
previously, as well as technical assistance from CRG SI to civil society actors involved in the
writing process to help better articulate their priorities. Other countries where KVP
representatives reported better participation included Guatemala, Myanmar and Senegal. Uganda
and Myanmar, with Tailored for NSP funding requests, reported increased participation by KVPs
across both NSPs and the funding request, with potential implications for the design of more
sustainable and effective responses to the diseases.
Irrespective of differentiated application approaches, COVID-19 changed the way the
funding request and grant making processes were managed, with both positive and
negative implications. In response to COVID-19-related restrictions, many countries conducted
funding request and grant making meetings online, which stakeholders in some countries
reported as increasing transparency and participation by a wider range of organizations. For
example, in Mozambique, an online platform enhanced transparency compared to NFM2, and the
CCM used online surveys to achieve greater consensus. Based on lessons learned in the
development of the C19RM funding request in virtual engagement of youth across regions,
Uganda’s CCM is considering the continued use of virtual consultations to increase targeted
constituency engagement going forward. However, these approaches depend on stakeholders
having good access to internet connections, which was not always the case.
The process of applying for matching funds improved for NFM3 compared to NFM2. As
noted in earlier PCE reports, in many PCE countries, the NFM2 separate application processes for
matching funds led to their budgets not being aligned to other grant implementation cycles. For
NFM3, stakeholders reported significant efficiencies from integrating matching funds processes
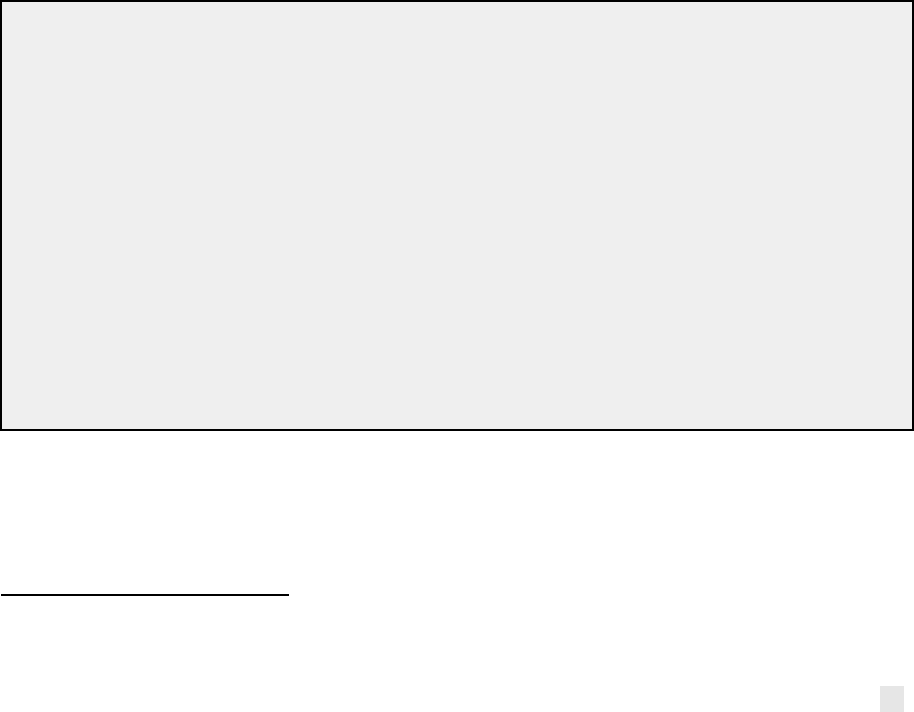
24
within the main grant applications. As explored below, matching funds for NFM3 (as for NFM2)
also appear to be helping to ensure that Global Fund strategic priority areas are addressed within
country grants, with some countries even exceeding the match requirement (for example, 2:1
matching for Uganda’s AGYW investments and marginal increase over requirements for AGYW in
Mozambique).
TRP recommendations (made both on NFM2 and NFM3 funding requests) informed NFM3
grant designs, with particular implications for HRG-Equity and RSSH related investments.
For example, Sudan in NFM3 is investing in strengthening HMIS data; prioritizing programs to
reach Internally displaced people, refugees and nomadic populations in remote states; addressing
acute gender barriers in these groups; and expanding investment in Community health
workers—all areas the TRP recommended during NFM2. In Mozambique, the NFM2 comments
from the TRP recommended increased coverage for services targeting FSWs. This was responded
to in NFM3 by increasing the performance framework target for the proportion of FSW reached
with prevention services from 13% by 2020 to 46% (67% in total including PEPFAR support) by
2023.
14
However, during NFM3, the TRP has again commented that coverage targets for FSW are
insufficient to reach epidemic control. In DRC, similar to comments provided in 2017, the TRP
again noted a lack of detail in the NFM3 HIV/TB funding request on differentiated HIV testing
strategies for KVPs. Although the applicant proposed numerous strategies such as HIV self-testing
at the community level, inadequate detail was included on other potential high-impact strategies
(e.g., index testing, online recruitment, and HIV case analysis from Enhanced Peer Outreach
Approaches). In response, the applicant provided a robust response with details regarding
additional high-impact strategies that will be implemented. In Uganda, there were no
recommendations related to CSS in the NFM2 request, but in NFM3 the applicants have been
responsive to a TRP recommendation to shift institutional capacity building, planning and
leadership development from the PAAR to the main allocation, which increased the RSSH CSS
allocation by 15%.
Box 3.2: TRP comments on the Myanmar 2020 funding request call for a stronger
evidence base on PWIDs to guide NFM3. During NFM2, overall HIV grant performance was
generally on track with the majority of grant coverage targets for KVPs being overachieved,
except for PWID. Despite a grant revision that significantly increased resources for PWID during
NFM2, absorption of PWID interventions addressing stigma, discrimination and violence, and
community empowerment was weak and the program achieved relatively low coverage. TRP
comments in both 2017 and 2020 highlighted the need for better evidence in relation to PWID
service coverage, access to methadone maintenance treatment and linkage to care. In response,
in 2020, the Myanmar CT requested the PCE Myanmar CEP to assess these issues to inform the
NFM3 planned expansion of PWID interventions. Findings were presented to a large group of
national stakeholders in November 2020, at an all-day meeting dedicated to the topic. As a result,
under the NFM3 grant, allocation to human rights and gender interventions has increased from
23% to 32% of the grant, including specific investments in strengthening community systems,
and resources for interventions specifically designed to address human rights barriers for PWID
have doubled from US$0.8 to US$1.6m under NFM3.
Key message 8: NFM3 funding requests included significantly larger budgets and focus on
some but not all of the areas where a change in trajectory is needed to meet the Global
Fund Strategic Objectives, largely as a result of the overall increase in country allocations.
14
We note a decrease in the denominator (from 97,712 in NFM2 to 86,000 in NFM3), which reflects the FSW size
estimates in the districts where the Global Fund grants are operating and is important to interpreting the scale of the
increase in the percentage of FSW targeted. The target may be subject to change in the final performance framework.
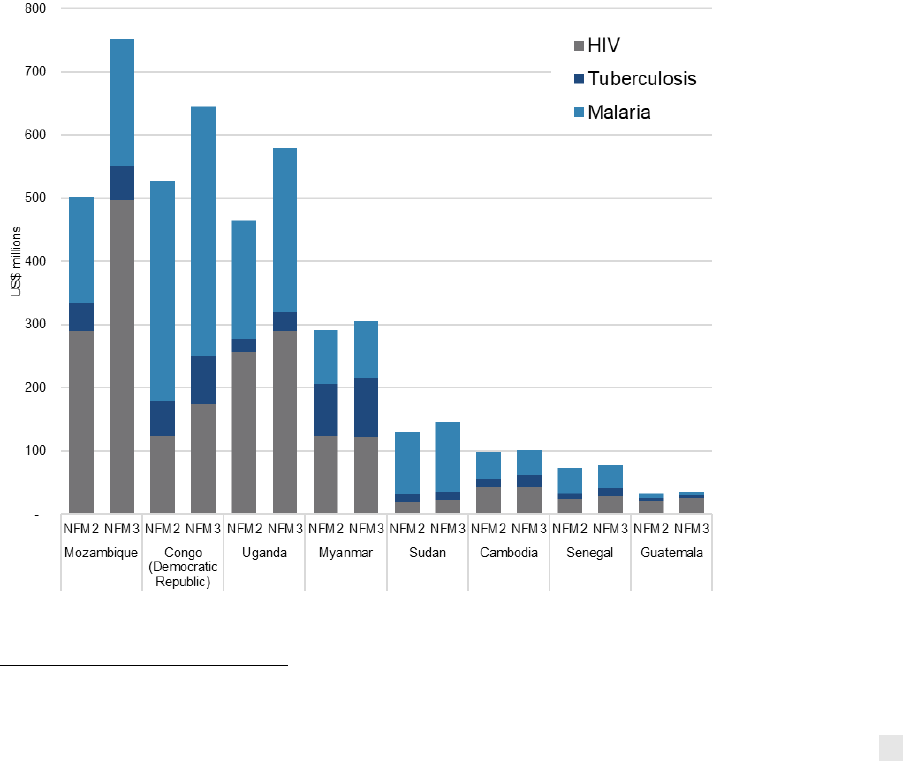
25
The successful Sixth Replenishment alongside a commitment to ‘do things differently’
offered an important opportunity to ‘change the trajectory’ in NFM3. The Global Fund’s 2019
investment case, used as the basis for the Sixth Replenishment to fund NFM3 grants, made a
compelling case to ‘do things differently’ in order to meet its Strategic Objectives.(10,11)
Specifically, it called for greater innovation, collaboration and effective execution, with a
particular emphasis in HIV on scaling up effective prevention to KVPs and AGYW, and significantly
more investment in overcoming HRG-related barriers to accessing health services. For TB, the
investment case called for expansion in both case finding and treatment of drug-sensitive and
MDR-TB cases, and for malaria, it called for expansion in the distribution of bed nets alongside
interventions to ensure they are used, as well as in testing and treatment. Lastly, it called for a
scaling up of investments to build RSSH. In addition, a series of applicant resources (12), including
information notes on HIV, TB, malaria and RSSH, and technical briefs on key areas of the Strategy
(human rights, gender equity, value for money, etc.), were updated to support countries in
operationalizing priorities as articulated in the Investment Case.
The 2019 Global Fund replenishment led to increases in total NFM3 allocations for all PCE
countries. As per the indicative program splits provided by the Global Fund (Figure 13), more
than half (55%) of the increased funding available in NFM3 is intended for HIV, with 35% for
malaria, and 10% for TB, with some variation by country. For example:
● Cambodia: 100% of the additional funding available in NFM3 is intended for malaria.
● Uganda: 63% of the additional funding available in NFM3 is intended for malaria.
● Mozambique: 83% of the additional funding available in NFM3 intended for HIV.
● Myanmar: 68% of the additional funding available in NFM3 is intended for TB, with a 1%
decline in funding for HIV.
Figure 13: PCE country allocations with indicative program split
15
Source: Global Fund detailed budgets
15
Data accessed through the Global Fund Data Service Allocations dataset.(13) Accessed on 25 November 2020. Actual
funding request budgets for the RAI3E included for Cambodia and Myanmar.
26
HRG-Equity
Key Message 9: PCE countries show evidence of NFM3 funding requests being designed
with explicitly more focus than in NFM2 on improving equitable access to health services
and allocating resources to intervention approaches that are known to contribute to
greater programmatic sustainability.
Nearly all PCE countries increased investments (both in absolute terms and as a
proportion of their NFM3 budgets) in prevention and KVPs compared to NFM2 budgets
(Figure 14). Overall, HIV prevention budgets increased in Cambodia, Guatemala, Mozambique,
Myanmar and Uganda (Annex Figure 5.1). In Cambodia and Myanmar, this was made possible by
governments taking on increasing responsibility for financing treatment costs, related to the STC
Policy, which freed up Global Fund resources for other purposes.
16
In DRC, Guatemala,
Mozambique and Uganda, the increase in budget for prevention emerged from the increased
NFM3 HIV allocation rather than by sacrificing other aspects of the grant (Annex Figure 5.1). Only
Senegal saw relatively small or no increases in KVP or HRG-related investments, as the planned
responses for KVPs in the HIV program were not considered sufficiently comprehensive by the
TRP or ambitious to achieve proposed 2022 targets, even though KVP targets increased between
NFM2 and NFM3. Smaller gains were notable for programming to address human rights barriers
in countries eligible for crosscutting human rights matching funds, including DRC, Mozambique,
Senegal and Uganda. Global Fund business model drivers of expansion in equity-related
investments, including the overall larger allocations, matching funds incentives, and improved
data sources to guide target setting, are discussed below. Likewise, for TB, as well as general
increases in funding for case finding (supported through matching funds), TB care and prevention
and MDR-TB, five PCE countries included TB-specific human rights-related investments in NFM3
(Cambodia, DRC, Mozambique, Myanmar and Senegal).
Box 3.3: Mozambique’s substantial increase in equity-related investments in NFM3 as a
result of increased overall allocation. The budget for activities to address HRG-Equity-related
barriers in the NFM3 HIV/TB funding request (US$78m) is significantly higher than under NFM2
(US$46m at funding request; US$34m at grant award; and US$40m as per the latest official
budget revision), reflecting the huge increase in the overall NFM3 allocation. The NFM3 budget
includes US$15m for human-rights-related investments, US$23m for wider KVP investments
and US$40m for other equity-related investments. Similarly, reflecting concerns around
increased HIV incidence in Mozambique, the prevention budget, excluding PMTCT, more than
doubled, from US$18m in the NFM2 funding request to US$46m in the NFM3 funding request,
most notably for prevention among AGYW: from US$6m in the NFM2 funding request to
US$14m through NFM2 grant implementation and to US$20m in the NFM3 funding request.
16
In Cambodia for example, the government commitment to ARV procurement has increased from US$9m under NFM2
to US$20m under NFM3.
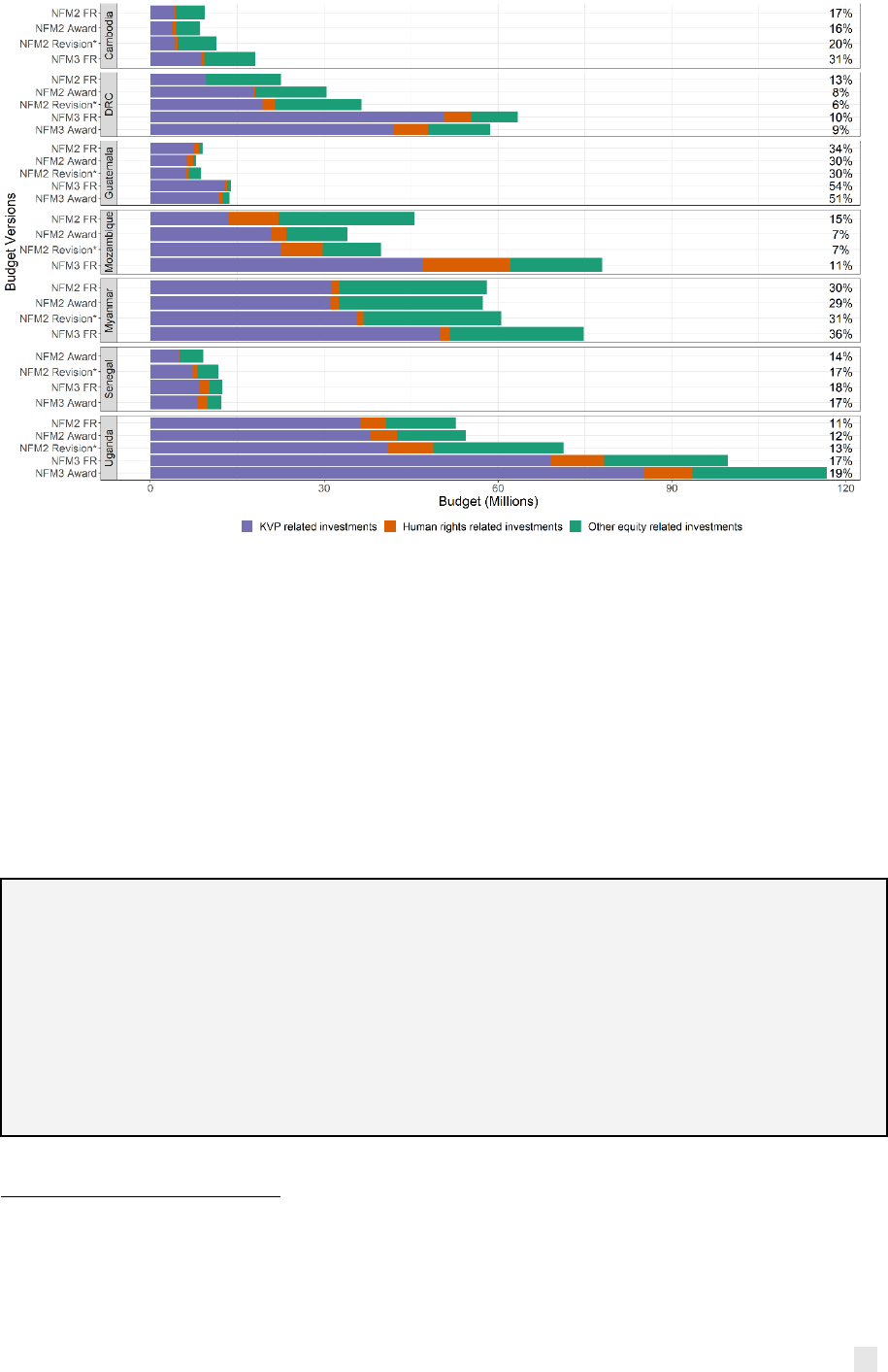
27
Figure 14: Changing budgets for HRG-Equity-related investments across NFM2 and NFM3.
17
Source: Global Fund detailed budgets
In some cases, efficiency and/or effectiveness considerations appear to have taken
precedence over equity considerations in the design of NFM3 grants. For example, compared
to NFM2, NFM3 grants cut subsidies for linkage to care (Guatemala) and patient living support
(Cambodia, Myanmar)—both critical to ensuring that the poorest can afford to access services.
Cambodia and Myanmar cut resources for PLHIV living support in order to prioritize more
efficiently targeted KVP HIV testing and increased budget for prevention. Guatemala reduced the
budget for travel subsidies and sub-recipient peer promoters due to concerns about the
effectiveness of promoters in identifying new HIV cases during NFM2. Although the Global Fund
issued new guidance on VfM to inform grant design, stakeholders in some countries (Cambodia,
Sudan) reported that VfM guidance had mainly been used by in-country consultant drafting teams
rather than reflecting improved discussion on VfM and/or equity among national stakeholders.
Box 3.4: Concerns about perceived inefficiency of peer promoters in Guatemala during
NFM2 seemed to outweigh equity considerations in NFM3. During the NFM3 funding request
development, updated KVP prevalence data were unavailable due to delays, which was a barrier
to improved intervention targeting. With limited data on KVPs, the PR relied on data from a
report, commissioned by the CT, on the productivity of peer promotors in NFM2 which found
low productivity in detecting and linking new cases to care. These findings informed a decision
by the PR to cut the budget for promotors in NFM3 and it is unclear whether potential
consequences on equitable access by key populations were given equal weight to efficiency
concerns.
17
Figure notes: *Revision is the most recent official budget revision. Percentages show the share of total grant budgets
that HRG-Equity makes up. Sudan is excluded from the figure, as the malaria grant did not include HRG-Equity
investments. Guatemala data include the HIV grant only. NFM2 funding requests (FR) in Senegal and DRC do not include
Program Continuation, specifically malaria grants in DRC and HIV and malaria in Senegal. In NFM2, due to the delayed
incorporation of catalytic matching funds after grants were approved, catalytic funds are reflected in the most recent
revision, except in Myanmar where they are included in the NFM2 funding request.
28
In response to concerns with efficiency, and given the lessons learned during NFM2 related to SR
selection and contracting issues that delayed implementation start-up, several countries are
retaining well performing SRs into NFM3 (Cambodia, DRC, Uganda), which will help promote
‘implementation readiness’ of approved grants—particularly for equity-related investments
carried out predominantly by SRs. In line with the Secretariat’s new guidance on preparing for
implementation ready grants, in early 2021 LFAs are conducting verification of implementation
readiness to quickly assess whether grant implementation is on track and the reasons why
(recognizing that COVID-19 is likely to have impacted plans around implementation readiness).
NFM3 grants have not substantially changed their orientation toward human rights,
gender and other elements of equity that would promote more sustainable impact on
services access and disease outcomes. Importantly, a disconnect remains between grant
‘equity’ indicators (which focus largely on budgetary contributions to human rights and KVP
interventions in addition to being heavily weighted toward HIV-relevant indicators) and wider
understanding of inequality in access to health services or health outcomes, which could better
inform an understanding of the equitable distribution of grant investments. A stronger
consideration for geographic accessibility was, however, evident in several countries. For
example, Senegal will expand diagnostic tools during NFM3 (GeneXpert, PCR, microscopy) to
address a lack of access in some high-burden areas. In Mozambique, malaria modeling and
surveillance results are being used to target higher-burden areas (see Box 3.5). In Sudan, the
malaria program has expanded to reach a wider number of provinces, many of which have large
internally displaced populations and refugees that were previously not reached.
Box 3.5: Mozambique’s VfM considerations in prioritizing malaria investments. During
NFM2, where the Agente Polivalente Elementars (APE) community health worker malaria
program operated, it performed well against mortality performance metrics. However, APE
distribution was not determined by malaria burden of disease, with some geographic areas
being under-resourced, thus limiting its overall impact. Under NFM3, the grant is expanding
community diagnosis and treatment for malaria, and community awareness through
conducting social and behavioral change communication activities designed to encourage
greater impact as well as continued provision of supply kits to the APEs for diagnosis and
treatment. NFM3 responds to new malaria modeling and surveillance results, which revealed
the need to target high-burden areas with more effective interventions, thereby prioritizing
equity as well as efficiency.
Several PCE countries used better-quality and/or more recent data on KVPs during NFM3
compared to NFM2, which enabled grants to set up new interventions to target KVPs more
precisely or widen the geographical distribution of places that KVPs would receive
services. However, ongoing concerns on the quality of data (particularly the accuracy of
KVP population size estimates) continue to constrain allocative efficiency. In some PCE
countries, the NFM3 funding request development process was more data-driven than that of
NFM2, largely because new data, particularly on KVPs, had become available. For example, based
on newly available data in Uganda and Mozambique, NFM3 grants are significantly expanding HIV
prevention programming for AGYW to include new geographies and increased overall coverage
targets. In Uganda, a baseline AGYW assessment completed during NFM2 informed the NFM3
design, including a strategic shift toward scale-up to achieve the ‘saturation’ required to reduce
incidence among AGYW, coupled with stronger integration of sexual and reproductive health and
HIV services for adolescents, both of which contributed to incorporation of US$59m for AGYW in
the Prioritized Above Allocation Request (PAAR).
In addition, the Essential Data Tables (EDT) (a new tool introduced by the Secretariat to improve
the funding request process by providing applicants with pre-populated and up-to-date data
29
related to demographics, the three diseases and other relevant crosscutting information)
informed NFM3 planning. DRC, Senegal and Myanmar reported using the new EDT to inform
NFM3 planning. Stakeholders in DRC considered the EDTs to contribute to a more efficient
process by reducing the time required to consolidate various data sources. In Senegal, although
stakeholders used the EDTs, they continued to question the accuracy of KVP estimates. In
Guatemala, implementation delays for HIV prevalence studies in NFM2 meant that those studies
were not available to inform NFM3 design. Both Guatemala and Senegal included investments in
NFM3 to improve KVP estimates.
Box 3.6: Using data to inform prioritization of human rights and gender investments in
DRC. NFM3 grants will prioritize equity through the sizable scale-up of activities targeting KVPs
and the expansion of interventions to reduce HRG barriers to services. DRC’s indicative HIV
allocation increased by 42% in NFM2, from US$123m to US$174m. Drawing upon updated KVP
size estimates that revealed a six times larger KVP population than previous estimates, in
consultation between the CT, country stakeholders, and technical partners, the PR decided to
intensify prevention activities that have historically been under-prioritized. NFM3 HIV testing
targets for all KVP categories are significantly higher than NFM2, which will address the current
low percentage of people living with HIV that know their status. The TRP review of the 2020
funding request noted strengthened and expanded HRG interventions compared to previous
rounds. Key facilitators included the use of data to define strategies for addressing HR barriers;
the Global Fund-supported Breaking Down Barriers initiative that produced a baseline
assessment and convened stakeholder consultations leading to the development of a five-year
costed HRG National Plan with priority activities; and availability of catalytic matching funds.
RSSH
Key Message 10: Most PCE countries increased the overall allocation to RSSH in NFM3,
although, compared to NFM2, a greater proportion of these investments are designed to
support rather than strengthen health systems. As such, it is unclear how the NFM3 grants
are intended to ‘change the trajectory’ for the achievement of SO2, which is intended to
increase strengthening investments and enhance RSSH.
The budget for RSSH modules increased significantly in NFM3 in several PCE countries
(Cambodia, Mozambique, Senegal, Uganda), while in other countries the RSSH budget
remained relatively stable (Guatemala) or declined slightly compared to NFM2 approved
budgets (DRC, Myanmar, Sudan). However, only Cambodia, Guatemala and Myanmar saw
increases in strengthening investments from NFM2 to NFM3 (Figure 15), and they were
minor.
18
In most PCE countries, the proportion directed to strengthening activities actually
decreased from NFM2 to NFM3. While a higher allocation to supportive investments may be
appropriate in some countries (e.g., Uganda, Mozambique, DRC) given their place on the
development continuum, this is not the case in other countries that are closer to transition (e.g.,
Cambodia, Guatemala).
As such, evidence suggests that the Global Fund’s RSSH guidance “to shift from a focus on
short-term, input-focused support...towards more strategic investments...that build capacity
and lead to sustainable results” is not being systematically operationalized.(1, p. 5) This is
partially explained by the shorter (three-year) funding period, lack of domestic and donor
funding sources for RSSH (other than the Global Fund), use of funds for commodities, and the
persisting vertical nature of the three disease programs. It is worth emphasizing that despite the
18
Building from the “2S“ framework proposed by Chee (2013) (3) and the “4S” work in the TRP’s RSSH Review (2018)
(4), the PCE developed a simplified coding “2S” application to analyze support and strengthening activities. See Annex
4 for protocol guidance. The 2S analysis compares the final NFM2 approved budgets with the NFM3 funding request
budgets (because at the time the analysis was conducted the NFM3 grant making budgets were unavailable).
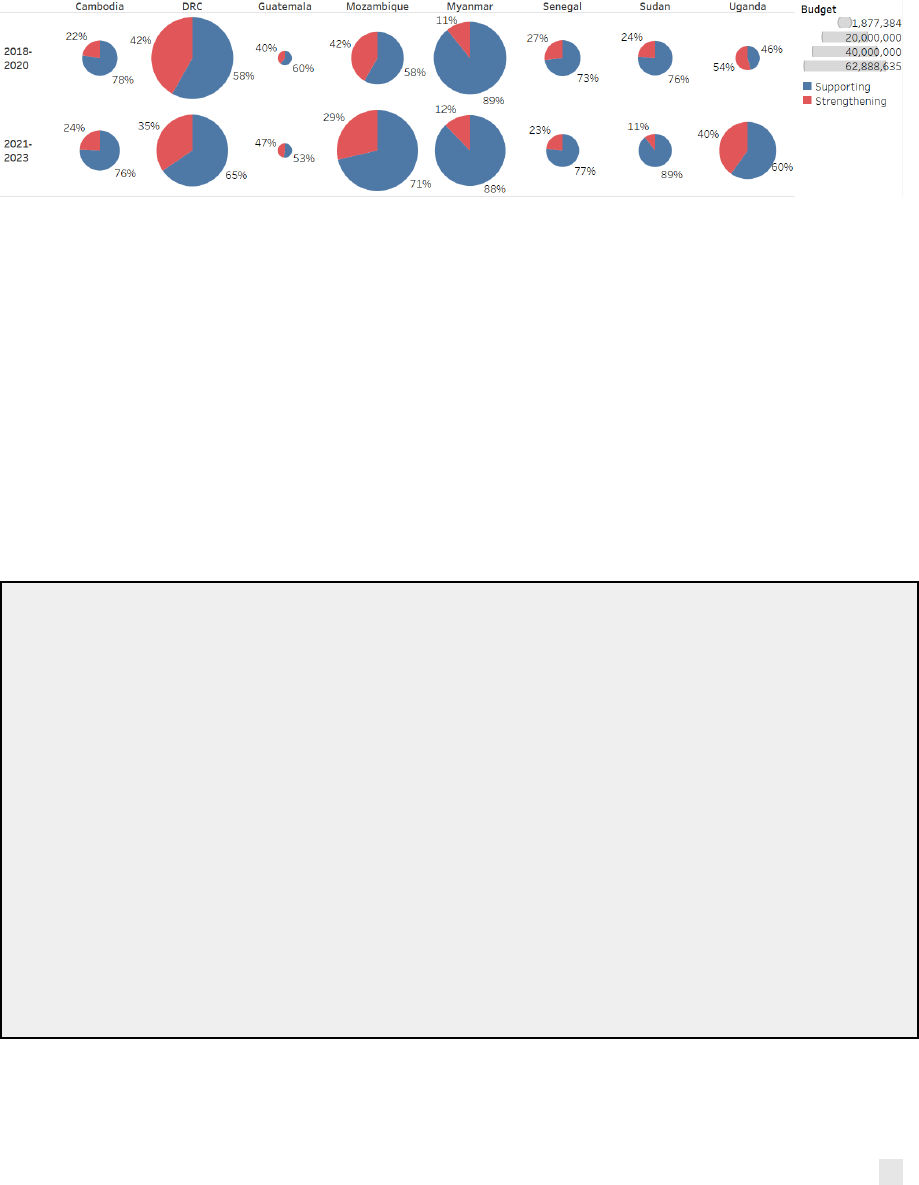
30
stated desire by the Global Fund to invest in more strategic strengthening interventions, many
PCE countries still require some level of investment in systems support (indeed, inputs-oriented
investments may be a precursor to some longer term strengthening efforts). If the Global Fund
truly intends its investments to be primarily strengthening RSSH, rather than supporting disease
program functions, PRs and country-level program managers require more information for how
to distinguish support and strengthening investments and also how to operationalize the
guidance to invest more in strengthening activities.
Figure 15. Comparison of RSSH budget between approved grants (NFM2) and funding request
budgets (NFM3), including shifts in proportion for supporting vs. strengthening activities.
Source: Global Fund detailed budgets
Note: Circles are sized according to overall RSSH budget size, as indicated by key with grey bars to the right.
In some countries, NFM3 RSSH investments are designed building on progress made
during NFM2, especially in HMIS/M&E. In DRC, Mozambique, Myanmar, Senegal and Sudan,
work in NFM2 to develop, roll out and expand DHIS2 (e.g., through an eHealth platform in
Myanmar) intends to be expanded upon in NFM3, where the focus is more oriented toward
expanding routine data collection, assessing data quality and training of technicians to improve
its application. In Mozambique, plans include a shift in PSM/HPM investments from support for
warehouse infrastructure and commodity storage capacity in NFM2 toward in-country
distribution and regulatory/QA support to combat counterfeit or low-quality drugs in NFM3. In
Sudan, investments in laboratory systems also appear to have evolved from infrastructure and
rehabilitation costs in NFM2 to improving the efficiency and quality of laboratory functions in
NFM3.
Box 3.7: Strengthening HMIS and digital health investments in DRC. In NFM3, DRC’s
investments in digital health, although smaller than in NFM2, received the largest portion of the
RSSH budget (the HMIS/M&E module represents 56% of the total RSSH budget). While DRC’s 2S
analysis showed an overall decrease in strengthening investments from 42% to 35% between
the NFM2 approved budget and NFM3 funding request, the HMIS/M&E module was the
exception where strengthening investments increased from 50% to 55%. In part, this is
explained by NFM3 digital health interventions that build upon lessons learned during NFM2.
For example, NFM3 grants increased focus on improving HMIS data quality and data use. While
NFM2 investments were successful in improving systems integration and reporting by all disease
programs in DHIS2 (achieving greater than 90% data completeness), gaps remain in data quality,
reporting timeliness and data use for program management that will be addressed during NFM3.
In addition, DRC also aims to enhance coordination between public and private sectors in NFM3
with integration of private sector data in DHIS2 as a key priority. Related investments include
developing official guidelines and standard operating procedures for how private health
establishments will be integrated into national policy and information systems, including at the
provincial level, which will further promote data system sustainability.
31
Box 3.8: Sustainability considerations in strengthening HMIS in Guatemala. Despite a large
investment in NFM2 to deploy DHIS2 to facilitate monitoring and reporting by the non-
governmental PR, and encouragement by the CT, TRP and others to build upon this, the PCE
found that certain stakeholders were against adoption of open-source technologies such as
DHIS2 and favored the development a new informational system for the national HIV program
using an Oracle platform. However, recently, the Minister of Health has stated an interest in
scaling up DHIS2 for the whole MoH. Many HIV program stakeholders, including the PR, were
unaware of the Minister’s interest until the end of 2020. While greater country ownership and
political will is indeed positive, these more recent developments could slow the Global Fund
HMIS investments as they will need to be aligned to the still nascent strategy of the MoH.
Considering that malaria and TB are entering transition during NFM3, delays to HMIS
strengthening presents risks.
Most PCE grants did not appear to use the NFM3 funding request process to link RSSH
investments more strategically with sustainability plans. In PCE countries, in addition to
findings above on the type of RSSH investments, few countries appeared to have prioritized
alignment of funding requests and NSPs with wider health plans, and transition plans did not
appear to be used systematically to guide domestic RSSH investments. In addition, few PCE
countries reported successful grant investments in structural or institutional shifts toward a
more sustainable approach to addressing their disease epidemics, as is confirmed in other
assessments of policy strength, an exception being Cambodia, where a 2019 proclamation aimed
to facilitate government contracting with NGOs.(16) PCE evidence suggests the NFM3 funding
request process may therefore have missed an opportunity to move national disease programs
toward eventual transition away from dependence on external funds. This finding aligns with
sustainability challenges raised by the TRP, many of which overlap with RSSH: 1) limited planning
of domestic resources for pooled procurement and integrated service delivery across programs
(Cambodia, DRC, and Uganda), for maintaining KVP outreach and programming (Guatemala), and
to meet financing gaps for NSP (Cambodia); 2) gaps in capacity of national entities to identify
efficiencies and cost savings (DRC, Guatemala, Mozambique, Myanmar); and 3) lack of M&E for
sustainability roadmaps (Cambodia, Myanmar), Health Financing Strategies (DRC, Mozambique),
and other program-specific sustainability plans (Cambodia, Uganda).
Box 3.9: Mixed progress on sustainability in Myanmar. During NFM2, the national HIV
program introduced significant policy reform to increase equitable access to treatment and
prevention services for KVPs, including legal reforms to reduce punitive measures for KVPs;
shifting the National Drug Control Policy toward a public health approach to improve PWID
access to harm-reduction services; launching a Prison SOP in collaboration with Ministry of
Home Affairs (MoHA) to improve HIV services in prisons; initiating guidelines for new
combination of prevention interventions for KVPs; and revising township classification for
HIV programming based on HIV burden to ensure key populations in remote and hard-to-
reach areas are not left behind. The Global Fund is the major financier of all these efforts, and
the NFM2 grant prioritized treatment and prevention service coverage in high-burden areas.
However, despite progress, root causes of the barriers remain unaddressed: armed conflicts
and security situations in Kachin, Shan and Rakhine continue to prevent the full
implementation of TB and HIV programs; and poverty, external and internal migration, and
language barriers in ethnic minority states continue to pose as barriers to accessing services.
Advocacy efforts for protection of violence against women have become visible in recent
years, but no legal framework exists to prevent and protect from intimate partner violence.
TRP comments in both 2017 and 2020 highlighted limited progress in building long-term
program sustainability beyond the grant period, particularly human resources for health and
community system strengthening and contracting.
32
In some countries, NFM3 grants are shifting RSSH intervention approaches, with greater
emphasis on community systems strengthening for improving access to and quality of
service delivery. Several countries substantially expanded CSS investment under NFM3,
including DRC, Mozambique, Myanmar, Senegal and Uganda (in line with broader NFM2 TRP
observations).(17) Both Senegal and Uganda included investment in community-level data
collection and reporting into DHIS2. Some countries are building integration and equity
considerations into RSSH investment design. In Senegal, for example, addressing laboratory
services gaps will help improve overall diagnostic testing service availability to KVPs. In DRC, the
NFM3 funding request includes stronger emphasis on integrating across disease programs,
including greater support for community-based organizations involved in comprehensive health
prevention and promotion; integrated supervision tools for the three diseases and other maternal
and child health interventions; and capacity building for provincial health authorities. In
Cambodia, most CSS investments coded as ‘strengthening’ in NFM2 were outsourced to a CSO
partner to coordinate KVP meetings. Stakeholders reported limited added value for this as a
primary activity and, although it was retained in NFM3, it was moved from the RSSH CSS module
and re-assigned to the ‘removing human rights barriers’ module.
Box 3.10: Investing in stronger community systems in Uganda. The RSSH allocation for the
CSS module increased seven-fold from the NFM2-approved grants (US$830K) to the NFM3
approved grants (US$6.9m), driven by several factors including increased civil society advocacy
and active engagement in the funding request process, as well as previous PCE findings
highlighting limited Global Fund investment in CSS. During NFM3 grant making, an additional
US$908K was added in response to a TRP recommendation to move the “institutional capacity
building, planning and leadership development” intervention from the PAAR to the main grant.
However, given that CSS investments during NFM2 have been extremely delayed in
implementation (absorption <30% as of June 2020), PRs will need to ensure more effective
grant start-up to avoid delays. The 2S analysis of the CSS RSSH module suggests a marginal
improvement toward increased strengthening investments, from 32% in NFM2 to 40% in
NFM3. An infusion of US$3.0m through matching funds for community health data science will
support strengthening community reporting, including through digitization efforts
interoperable with DHIS2 systems, thereby promoting stronger use of data for decision-making
and programmatic sustainability.
Several countries show governance adaptations to improve coordination and
implementation of crosscutting RSSH investments. In Senegal, for example, grant
implementation arrangements are structured so that ownership of RSSH investments is more
centralized under a single government PR and a civil society PR implementing community-based
activities. Similarly, in Uganda, a stronger coordination structure with the government PR
providing oversight and implementation of crosscutting RSSH investments, while the civil society
PR manages and coordinates CSS interventions was developed. Both Cambodia and DRC have
applied for stand-alone RSSH grants in NFM3. In DRC, this was proposed by the CCM to deliver
more integrated RSSH interventions and elevate health systems issues to the Secretary General
and MoH, who will be managing the grant. In Cambodia, RSSH resources come from the regional
malaria grant (RAI) and, in order to integrate it better with other disease grants, the CCM decided
to continue implementation through the MoH Lead Implementing Team, but have the grant
managed by the Ministry of Economy and Finance rather than UNOPS, which is anticipated to
improve governance and coordination.

33
Despite extensive new guidance, most PCE NFM3 grant performance frameworks do not
appear to include many of the new RSSH coverage indicators,
19
suggesting that monitoring
RSSH performance and progress toward meeting SO2 will remain a challenge. The Global
Fund updated the modular framework in 2019 with extensive revisions and additions to coverage
indicators for each of the RSSH modules: expanding from 13 to 24 RSSH coverage indicators, 22
of which were newly added.
20
However, beyond standard HMIS and M&E module indicators,
adoption of other RSSH indicators aligned to major investment areas was infrequent in
performance frameworks submitted with funding requests (consistent with the TRP Window 2
review findings regarding an inadequate range of indicators for coverage, outcome and impact of
RSSH investments)(15) (Table 5). For instance, in Guatemala, where HMIS comprises the majority
of the RSSH investment within the HIV grant, no RSSH coverage indicators were included in the
performance framework. There does, however, appear to be more progress for CSS
investments—for instance, three countries prioritizing CSS investments (DRC, Senegal and
Uganda) included one of the two newly added CSS indicators from the modular framework.
Several funding request performance frameworks included Work Plan Tracking Measures
(WPTM) for monitoring investments in CSS (Cambodia, Uganda), laboratory strengthening
(Cambodia, Mozambique), and HMIS/M&E (Mozambique). Additional WPTMs were also
introduced during grant making, for example for monitoring integration of private sector
reporting into DHIS2 (DRC), and improvements in the comprehensiveness and quality of routine
reporting (Myanmar), among others.
Coverage indicators rarely capture aspects of system strengthening (such as data use for
decision-making) and some RSSH investment areas do not map well to the available indicators.
Beyond performance framework indicators, some countries may include complementary in-
depth RSSH assessments to measure aspects of systems strengthening and performance, which
was an approach undertaken in NFM2 for equity-related investments. Some countries included
custom RSSH indicators in performance frameworks to better fit the monitoring needs of their
RSSH investment areas and stronger opportunities to measure aspects of systems strengthening.
For example, according to stakeholders in DRC, there was a concerted effort to develop indicators
beyond output measurement (such as facilities that receive supportive supervision), but also
capture the quality of those supervision visits according to national standards and guidelines.
Following funding request submission, the TRP did not provide feedback for amending, including,
or strengthening RSSH indicators. Additional investigation is warranted to understand the
limited uptake of RSSH indicators in some countries.
19
The PCE has previously reported challenges in performance monitoring of Global Fund RSSH investments, wherein
NFM2 grants reported against only three RSSH coverage indicators: M&E-1: Percentage of HMIS or other routine
reporting units submitting timely reports according to national guidelines (Cambodia, Myanmar, Senegal, Sudan,
Uganda); M&E-2: Proportion of facility reports received over the reports expected during the reporting period
(Cambodia, DRC, Mozambique); and PSM-2: Percentage of health facilities with essential medicines and life-saving
commodities in stock (Senegal).
20
Of the 13 RSSH coverage indicators in the 2017 modular framework, 11 were discontinued and only two were
retained in the 2019 modular framework, which contains 22 new RSSH coverage indicators. All RSSH impact indicators
were removed and four new RSSH outcome indicators were included. Of the PCE countries, DRC (HSS O-6, HSS O-7,
HSS-O8, and a custom HSS outcome indicator) and Sudan (HSS O-5) are the only to incorporate RSSH outcome
indicators into NFM3 funding request performance frameworks.

34
Table 5. Coverage indicators in NFM3 funding request performance frameworks by RSSH module
and proportion of RSSH investment in each RSSH module, per country.
21
Table Notes: Percentages and color gradient represent the amount of the total country RSSH budgets each module
comprises. Indicator definitions: M&E-2a Completeness of facility reporting: Percentage of expected facility monthly
reports (for reporting period) that are actually received; M&E-2b: Timeliness of facility reporting: Percentage of
submitted facility monthly reports (for reporting period) that are received on time per the national guidelines, M&E-
4: Percentage of service delivery reports from community health workers integrated into HMIS; M&E-5: Percentage of
facilities which record and submit data using the electronic information system; PSM-3: Percentage of health facilities
providing diagnostic services with tracer items available on the day of the visit or day of reporting; PSM-4: Percentage
of health facilities with tracer medicines for the 3 diseases available on the day of the visit or day of reporting; SD-5:
Percentage of facilities that receive supportive supervision at least 1 per quarter; CSS-1: Percentage of community-
based monitoring reports presented to relevant oversight mechanisms; HSG-1: Percentage of district health
management teams or other administrative units that have developed a monitoring plan, including annual work
objectives and performance measures. Custom indicates countries included a custom indicator. WPTM = Work Plan
Tracking Measures. Myanmar and Cambodia include budget and indicators for TB/HIV grants only.
21
In Cambodia, the TB/HIV grant and the separate RSSH grant are now supervised by the same CT. Both grants use the
PMTCT module and both grants apply RSSH specific modules. The TB/HIV grant used three RSSH modules in NFM2
and in NFM3. The RSSH grant used three RSSH modules in NFM2 and five modules in NFM3. NFM3 grant retained the
NFM2 activity (sole CSO) under RSSH-CRS, although shifted to the Removing Human Rights Barriers module. Modules
in the stand-alone RSSH grant are implemented by separate departments within the MOH, and performance indicators
in this grant are linked only to the PMTCT module. PMTCT procurement of RDT is made via the TB/HIV grant previously
included via Treatment Care Support module but now shifted to the PMTCT module in NFM3. Meanwhile training and
related ANC activities are channeled via the PMTCT module in the RSSH grant.

35
Chapter 4: Discussion and conclusions
In this chapter we set out our overall conclusions in relation to how the Global Fund business
model is facilitating and impeding the achievement of Strategic Objectives across the grant cycle.
The focus is primarily on RSSH and HRG-equity, paralleling Global Fund SO2 and SO3, and
examining the degree to which business model incentives that operate through these areas
indirectly affect the achievement and acceleration of sustained impact on the three diseases
(SO1). Overall, the PCE evidence suggests that the Global Fund business model has facilitated
improvements across the grant cycle in design and implementation during these past 3-4 years.
However, these trends appear unlikely to deliver the sustained improvements in equity and/or
health system strengthening needed to achieve the Strategic Objectives and 2030 goals.
Grant Design
Conclusion 1: Improvements to the business model between NFM2 and NFM3 contributed
to more efficient and inclusive funding request processes. However, NFM3 saw limited
adoption of changes in the design of performance monitoring, particularly for HRG-equity
and RSSH.
The NFM3 funding request process was generally more efficient and benefited from changes that
meant a wider set of stakeholders were included, despite COVID-19 interruptions to the process.
The tailored to NSP and full review differentiated application approaches were viewed positively
relative to NMF2, particularly as relates to inclusion, although stakeholders reported inclusion
declined at later stages of grant making. Most PCE countries also showed evidence of increased
national ownership of Global Fund grants and disease programs, perhaps reflecting gradual
country familiarity and adaptation during the third round of NFM grants. Incorporating matching
funds within the main funding request in NFM3 improved alignment and the efficiency of the
design process, a key improvement over NFM2, as well as catalyzed increased investment for
HRG-Equity. However, despite some increases in data quality and use, particularly for KVPs,
performance frameworks, indicators and targets changed surprisingly little—particularly for
HRG-Equity and RSSH interventions. Measuring Global Fund impact on other areas of equity
beyond KVP service delivery, whether due to socioeconomic status, gender barriers or ethnic
group discrimination, remains challenging.
Conclusion 2: In NFM3, both RSSH and HRG-Equity investments rose, in many cases as a
result of overall allocation increases. An increased proportion of RSSH investment is
directed toward activities that support rather than strengthen the health system.
Many new grants include large increases in KVP HIV prevention investments but smaller
increases in reducing HRG barriers (from a lower base). Despite revised guidance and greater
emphasis in the funding request template, it remains unclear if or how VfM considerations are
systematically and holistically considered in prioritization and decision making. The funding
requests do demonstrate some evidence of growing expertise and investment in areas of the
health system (CSS, HMIS, PSM), but overall there was a lack of clear and consistent consensus on
the ultimate purpose of RSSH investments. RSSH investments continue to be owned and designed
by disease-specific stakeholders, with limited evidence of an integrated and aligned approach
within wider health planning and financing systems, which likely contributed to a tendency
toward designing supporting rather than strengthening interventions. Collectively, the PCE
country NFM3 funding requests demonstrated relatively little evidence that they were designed
specifically to promote programmatic sustainability beyond the grant horizon, even in countries
close to transition.

36
Grant Implementation
Conclusion 3: Implementation of NFM2 grants faced significant start-up delays and COVID-
19 interruptions. Absorption was overall weaker for RSSH and HRG-Equity interventions.
The NFM introduced a fixed implementation period compared to the previous round’s system
and, alongside the introduction of portfolio optimization, strong incentives to maximize resource
utilization within a relatively short three-year time period. The increased predictability of funds
is perceived as a positive development, although the NFM grant cycle has also had some
unintended consequences linked to Conclusion 4. The Global Fund Country Team structure is a
critical element of the business model that generally works to support grant implementation,
particularly where regular reviews and coordination meetings, tailored to the country context,
take place.
However, a number of areas of the business model were less supportive of efficient grant start-
up, including lengthy selection and contracting processes for implementers and issues with
disbursements between PRs and SRs, as well as weak coordination functions, which particularly
affected RSSH and HRG-Equity interventions.
Conclusion 4: Multiple barriers and challenges exist for undertaking revisions to the scope
and/or scale of grants mid-cycle, such as in response to new evidence or emerging
performance issues.
Incentives acting on grant implementers to achieve high levels of absorption, which is rigorously
measured and reported on, are relatively strong. In contrast, incentives for grant managers to
undertake substantial mid-cycle program revisions to the grant scope (objectives or key
interventions) or scale (targets) to maximize impact are relatively weak. Firstly, the
administrative requirements for doing so are burdensome; and secondly, grant-specific
performance monitoring data to guide revision decision making is fairly limited.
As a result, two unintended consequences emerged during NFM2:
● decisions around grant revisions appear driven by the short implementation cycle and the
associated need to maximize absorption, and instead PRs and Country Teams tend to rely
on multiple, smaller budget revisions to influence implementation and for financial
management to maximize absorption; and
● where new survey and evaluation data emerged, grant revisions to scope or scale appear to
have been deferred to the NFM3 funding request cycle, rather than undergoing burdensome
but innovative revisions.
Revisions were often used to shift budgets to later in the grant cycle, having the effect of making
absorption appear higher in earlier years. Overall, in PCE countries, the cumulative effect was
small net increases allocated to HRG-Equity interventions, compared to grant awards, but a more
mixed picture for RSSH with decreases in some countries and increases in others. It remains to
be seen how these shifts will affect Year 3 budgets and absorption, in the context of COVID-19.
Chapter 5: Strategic recommendations/considerations
The purpose of these recommendations is to engage in a dialogue with the TERG and the
Secretariat on ways to respond to the conclusions in Chapter 4.
Recommendation 1: Improve grant-specific performance monitoring to inform
implementation decisions.
● Establish routine grant review processes at the country level with a quality improvement
lens, emphasizing grant-specific performance data and drawing on emerging evidence and

37
data to better inform revisions that maximize impact. (PRs, Grant Management Division
including Country Teams)
● Implement proposed reforms of the grant rating system to reflect both grant-specific
performance and contribution of Global Fund grants to national program performance.
Additionally, this should draw upon qualitative inputs, including expertise of the CCM, LFA,
Country Team and wider Secretariat. (Grant Management Division, Strategy Committee,
Board)
● Based on the revised grant rating system, the Secretariat should also develop a set of
indicative options to demonstrate how good and poor performance could be responded to,
and a framework for deciding when and how to introduce these measures in different
contexts and circumstances (Grant Management Division, Strategy Committee, Board).
● Strengthen the use of revised RSSH indicators to address delayed implementation and
potential deprioritization throughout grant implementation. (PRs, Grant Management
Division including Country Teams)
Recommendation 2: Build in more flexibility and responsiveness in implementation by
simplifying grant revision processes to encourage their use throughout the grant cycle.
● Consider flexibilities and streamlining of material program revision process to
encourage/reward earlier introduction of innovative programming that maximizes impact
and limits non-strategic budgetary shifts to later in the 3-year grant cycle. (Secretariat)
● Introduce flexibilities to PR and SR contractual arrangements and performance frameworks
that can be used to introduce mid-term changes as required. (PRs, Grant Management
Division)
● Through the Secretariat’s planned grant revision review (mid-2021), examine how countries
could strengthen data-driven revision decisions (thereby avoiding the over-reliance on
financial data to guide revision decisions), in line with establishing a more streamlined,
flexible process for program revision. (Secretariat)
Recommendation 3: In order to reduce gaps between policy guidance and grant design,
improve communication around how to invest more strategically in RSSH, including CSS.
● In the next Strategy, the Global Fund board in collaboration with the Secretariat should clarify
their position on whether the primary objective of RSSH is to support the three disease
programs or to invest more holistically in health systems strengthening. (Board, Secretariat
RSSH team)
● Clarify specific Global Fund RSSH priority areas and what strengthening as opposed to
supportive investment would look like for these, including specific purpose, indicators and
targets in performance frameworks. (Secretariat RSSH team, Country Teams)
● To facilitate integration and strengthening RSSH, ensure proper engagement and ownership
from health system planning experts and leaders to support health sector-wide programming
decisions, including alignment of grant design and sustainable financing within wider
national health, health system and UHC policy context, and the timelines associated with
broader strengthening efforts. (PRs, Country Teams)
Recommendation 4: In order to improve grant contribution to equity and SO3, explicitly
promote grant investments in these areas, including through more direct measurement of
the drivers of inequity and of outcomes of human rights and gender investments.
● Invest more in data and data use, including up-to-date KVP surveys as well as other data
sources that shed light on socio-economic, gender, geographical and ethnic differences in
disease burden and access to services that grants are aiming to contribute to. (Country Teams,
national stakeholders)
● Ensure performance frameworks incorporate existing data including on human rights and
political commitment as well as disease burden and service access amongst different

38
population groups and use this data effectively to monitor grant contribution to both SO3 and
SO1 or disease impact. (Country Teams, national stakeholders)
● Recognizing the success of strategic initiatives and/or matching funds in incentivizing grant
investments in reducing equity, human rights and gender related barriers to accessing
services, prioritize scaling up across the portfolio and incentivizing such investments through
mainstream grant management operations. This should include explicit efforts to improve
implementation and where necessary, timely revisions to maximize grant contribution to
reducing barriers to care and disease impact. (Grant Management Division, Strategic
Initiatives team)

39
References
1. The Global Fund. Building Resilient and Sustainable Systems for Health (RSSH)
Information Note [Internet]. 2019. Available from:
https://www.theglobalfund.org/media/4759/core_resilientsustainablesystemsforhealth_infon
ote_en.pdf
2. The Global Fund. Eligibility & Allocations Archive [Internet]. [cited 2021 Jan 22]. Available
from: https://www.theglobalfund.org/en/archive/eligibility-allocations/
3. Chee G, Pielemeier N, Lion A, Connor C. Why differentiating between health system
support and health system strengthening is needed. Int J Health Plann Manage. 2013;28(1):85–
94.
4. Technical Review Panel. Report on RSSH Investments in the 2017-2019 Funding Cycle
[Internet]. The Global Fund; 2018. Available from:
https://www.theglobalfund.org/media/8093/trp_rssh2017-2019fundingcycle_report_en.pdf
5. The Global Fund. “Funding Approved for COVID-19 Response” database. Flexibilities data
(12/21/20) and C19RM data (12/24/20). [Internet]. [cited 2021 Jan 13]. Available from:
https://www.theglobalfund.org/en/covid-19/
6. The Global Fund. Operational Policy Manual, Issue 2.27 [Internet]. 2020. Available from:
https://www.theglobalfund.org/media/3266/core_operationalpolicy_manual_en.pdf
7. EHG, ITAD, UCSF. Strategic Review 2020 Final Report: Vol 1 [Internet]. 2020. Available
from: https://www.theglobalfund.org/media/10498/terg_strategicreview2020_report_en.pdf
8. EHG, ITAD, UCSF, IHME, PATH, Johns Hopkins University, Bloomberg School of Public
Health. Global Fund Prospective Country Evaluation: 2019 Synthesis Report. 2019 Feb.
9. EHG, ITAD, UCSF I. Global Fund Prospective Country Evaluation: 2018 Synthesis Report.
2018.
10. The Global Fund. The Global Fund Investment Case 2019, Presented by Peter Sands
[Internet]. 2019 [cited 2021 Jan 22]. Available from:
https://www.youtube.com/watch?app=desktop&v=ieTyzTvDG38
11. Step up the fight: Investment Case, Sixth Replenishment 2019 [Internet]. Geneva,
Switzerland: The Global Fund; 2019. Available from:
https://www.theglobalfund.org/media/8279/publication_sixthreplenishmentinvestmentcase_r
eport_en.pdf
12. The Global Fund. Applicant Guidance [Internet]. 2019 [cited 2021 Jan 22]. Available from:
/en/funding-model/applying/resources/
13. Data Service - The Global Fund to Fight AIDS, Tuberculosis and Malaria [Internet]. Data
Service. [cited 2020 Nov 25]. Available from: http://data-service.theglobalfund.org
14. The Global Fund. TRP Lessons Learned from Review Window 1 of the 2020-2022 Funding
Cycle [Internet]. 2020. Available from: https://www.theglobalfund.org/media/9811/trp_2020-
2022lessonslearnedwindow1_report_en.pdf
15. The Global Fund. TRP Lessons Learned from Review Window 2 of the 2020-2022 Funding
Cycle [Internet]. 2020. Available from: https://www.theglobalfund.org/media/10179/trp_2020-
2022lessonslearnedwindow2_report_en.pdf
16. HIV Policy Lab. Global HIV Policy Report [Internet]. Georgetown University; 2020.
Available from: https://www.hivpolicylab.org/reports/2020GlobalReport

40
17. Technical Review Panel Observations on the 2017-2019 Allocation Cycle [Internet].
Geneva, Switzerland: The Global Fund; 2019 Nov. Available from:
https://www.theglobalfund.org/media/9053/bm42_08-trppbservations2017-
2019allocationcycle_report_en.pdf?u=637319004066130000
18. The Global Fund. Technical Brief: Gender Equity [Internet]. 2019. Available from:
https://www.theglobalfund.org/media/5728/core_gender_infonote_en.pdf
19. The Global Fund. Technical Brief: Tuberculosis, Gender and Human Rights [Internet].
2020. Available from:
https://www.theglobalfund.org/media/6349/core_tbhumanrightsgenderequality_technicalbrie
f_en.pdf
20. The Global Fund. Technical Brief: HIV, Human Rights, and Gender Equality [Internet].
2019. Available from:
https://www.theglobalfund.org/media/6349/core_tbhumanrightsgenderequality_technicalbrie
f_en.pdf
21. Strategy Development, The Global Fund. Landscape Analysis - Human Rights, Gender
and Equity [Internet]. 2020 Jun 26. Available from:
https://www.theglobalfund.org/media/9839/strategydevelopment_2020humanrightsgendere
quity_landscapeanalysis_en.pdf
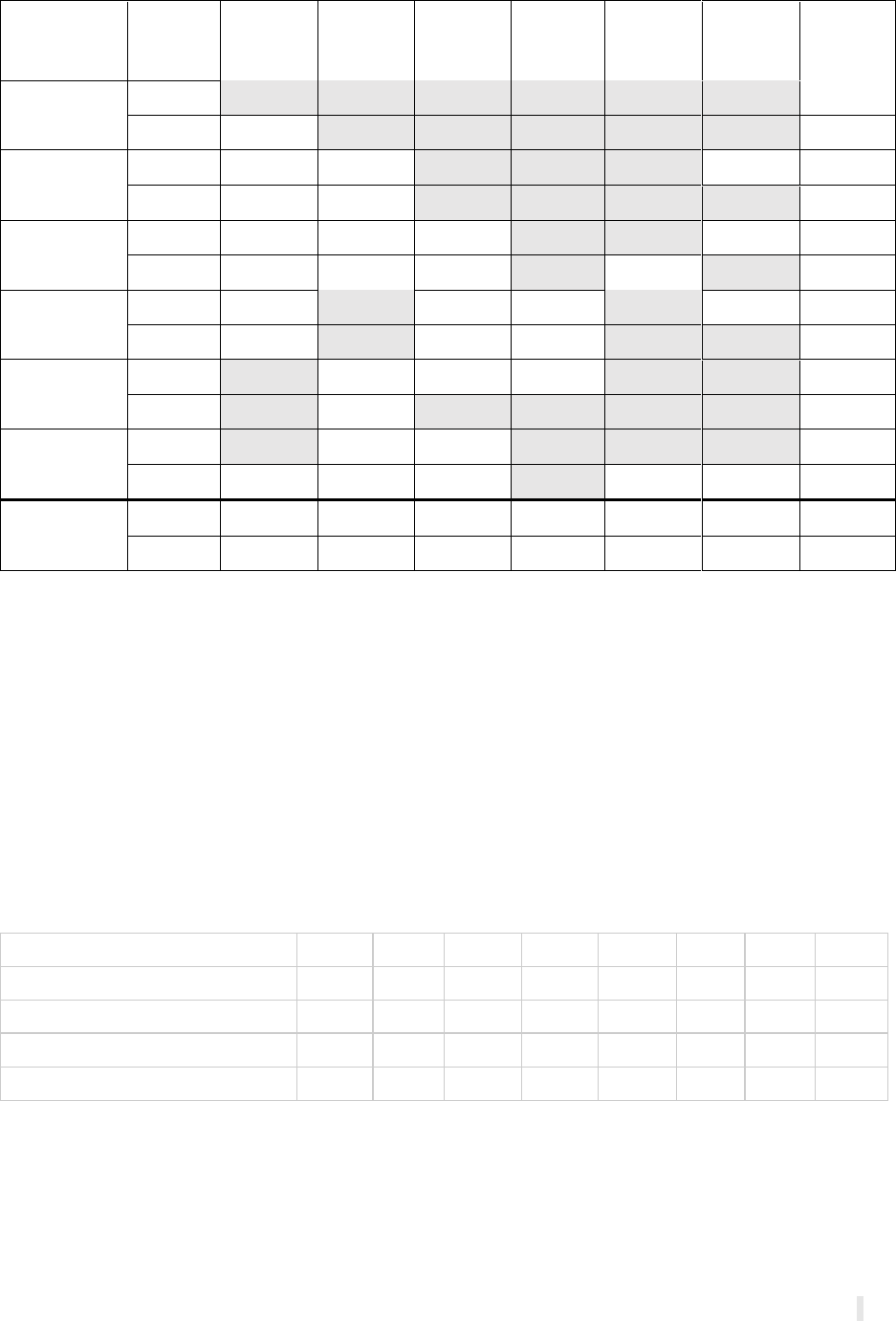
I
Annexes
Annex 1. Summary of countries eligible for matching funds in NFM2 and NFM3 by type.
Country
Funding
Cycle
TB:
Missing
cases
Human
Rights
HIV:
AGYW
HIV: KP
HIV:
self-
testing
RSSH:
Data
systems
Totals
Cambodia^
NFM2
$0.0
NFM3
$6.0
$6.0
DRC
NFM2
$10.0
$3.0
$3.0
$16.0
NFM3
$10.0
$2.6
$12.6
Mozambique
NFM2
$6.0
$4.7
$6.0
$3.0
$19.7
NFM3
$6.0
$4.0
$9.5
$2.9
$22.4
Myanmar^
NFM2
$10.0
$6.3
$3.0
$19.3
NFM3
$6.0
$6.3
$12.3
Senegal
NFM2
$1.5
$1.2
$0.0
NFM3
$1.2
$1.2
Uganda
NFM2
$4.4
$5.0
$9.4
NFM3
$6.0
$4.4
$7.2
$2.9
$3.0*
$23.5
Totals
NFM2
$26.0
$13.6
$11.0
$7.5
$0.0
$9.0
$67.1
NFM3
$34.0
$12.2
$16.7
$6.3
$5.8
$3.0
$78.0
*Improved data science in community health
^In NFM3, excludes catalytic element of multi-country RAI in Cambodia ($15 million) and Myanmar ($40
million)
Annex 2. Qualitative data collected by PCE countries
CAM
DRC
GTM
MOZ
MYN
SEN
SUD
UGA
KIIs
20
33
36
24
68
25
98
21
Fact checking
50
10
35
18
63
7
8
23
meetings observed
30
5
27
17
35
93
78
14
documents reviewed
150
116
135
60
102
81
100
60
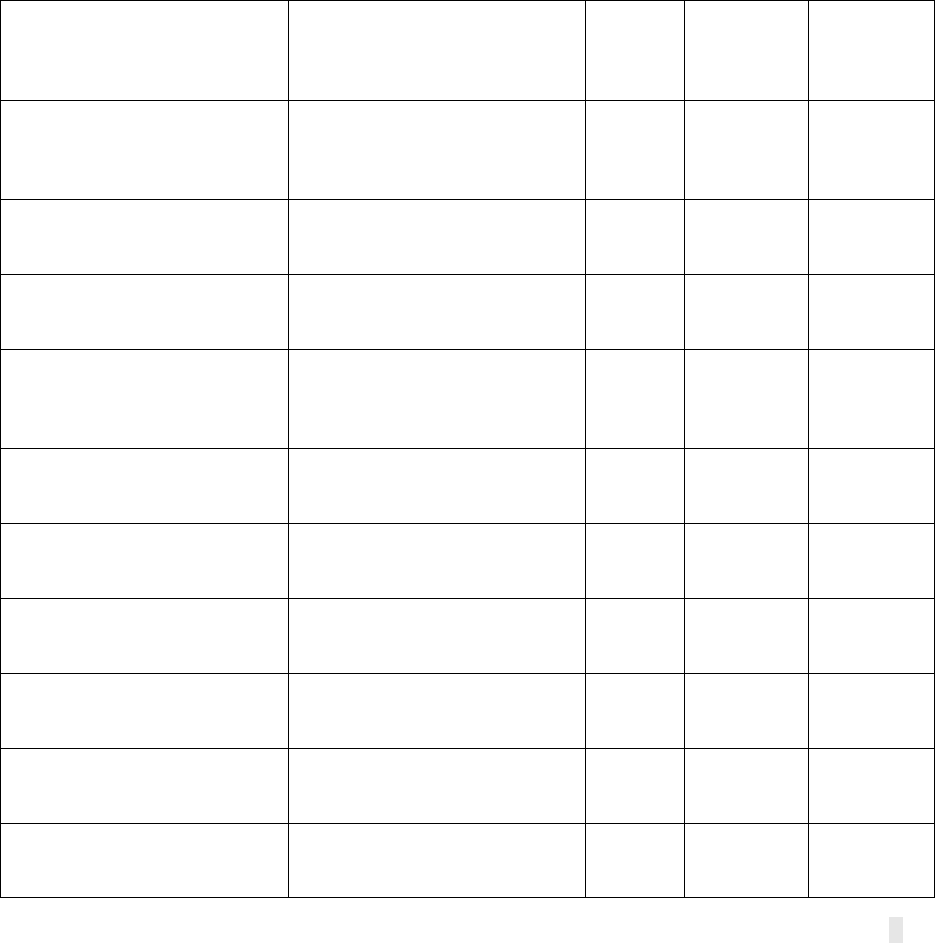
II
Annex 3. Approach to identification of human rights, gender, and other equity-related
investments
The PCE relied upon the Global Fund gender and human rights disease-specific technical briefs to
initially identify modules and interventions which contain investments related to human rights,
gender and other equity (HRG-Equity). (18–21) The list of these HRG-Equity-related modules and
interventions were shared with the Global Fund Secretariat and the Community, Rights and
Gender (CRG) team for review and feedback. After a consultative discussion and receiving a draft
methodology of how the CRG team has proposed tracking human rights-related investments, a
sub-categorization of these modules and interventions was included to allow for a clearer
understanding of the types of investments captured within the PCE’s HRG-Equity-related
investments. The sub-categories include 1) human rights-related investments, which align with
the CRG’s proposed methodology of “Opt-in modules and interventions,” 2) key and vulnerable
populations-related investments, and 3) other equity-related investments. Table 2.1 below shows
examples of modules and interventions included in each category; while the full list is extensive
(138 module/interventions pairs in total) and unable to be included in the text of the report, it
can be made available upon request.
Annex Table 2.1
Module
Intervention
Human
rights
funding
Key and
vulnerable
populations
funding
Other
equity
related
investments
Comprehensive prevention
programs for men who have
sex with men
Addressing stigma,
discrimination and violence
against men who have sex with
men
TRUE
FALSE
FALSE
Comprehensive prevention
programs for men who have
sex with men
Behavioral interventions for
men who have sex with men
FALSE
TRUE
FALSE
Comprehensive prevention
programs for men who have
sex with men
Condoms and lubricant
programming for men who
have sex with men
FALSE
TRUE
FALSE
Comprehensive prevention
programs for men who have
sex with men
Diagnosis and treatment of
sexually transmitted infections
and other sexual health services
for men who have sex with men
FALSE
TRUE
FALSE
Comprehensive prevention
programs for men who have
sex with men
HIV testing services for men
who have sex with men
FALSE
TRUE
FALSE
Comprehensive prevention
programs for men who have
sex with men
Interventions for young men
who have sex with men
FALSE
TRUE
FALSE
Comprehensive prevention
programs for people who
inject drugs and their partners
Behavioral interventions for
people who inject drugs
FALSE
TRUE
FALSE
Comprehensive prevention
programs for people who
inject drugs and their partners
Community empowerment for
people who inject drugs
FALSE
TRUE
FALSE
Comprehensive prevention
programs for people who
inject drugs and their partners
Condoms and lubricant
programming for people who
inject drugs
FALSE
TRUE
FALSE
Comprehensive prevention
programs for people who
inject drugs and their partners
Diagnosis and treatment of
sexually transmitted infections
FALSE
TRUE
FALSE
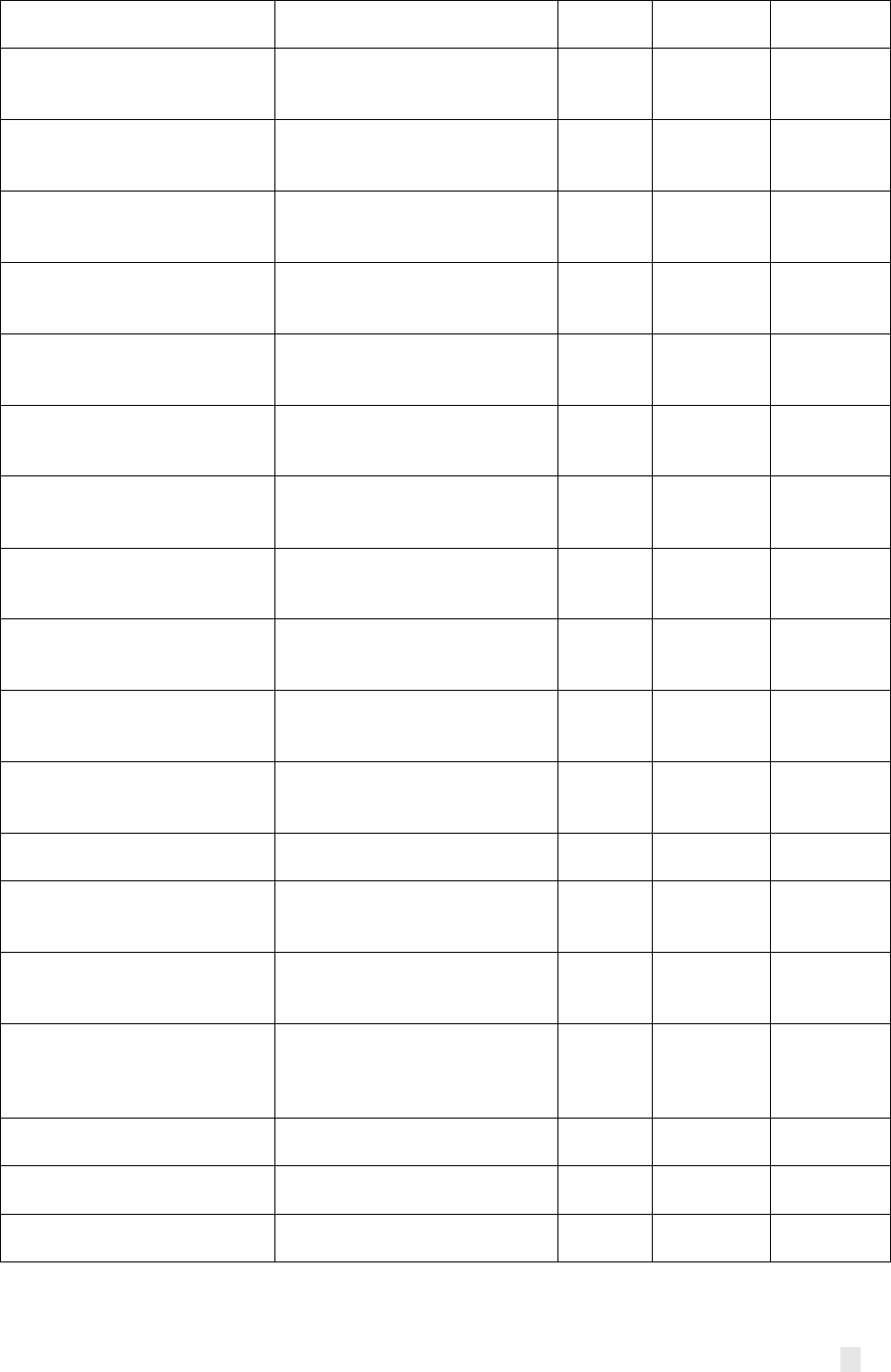
III
and other sexual health services
for people who inject drugs
Comprehensive prevention
programs for people who
inject drugs and their partners
HIV testing services for people
who inject drugs
FALSE
TRUE
FALSE
Comprehensive prevention
programs for people who
inject drugs and their partners
Interventions for young people
who inject drugs
FALSE
TRUE
FALSE
Comprehensive prevention
programs for people who
inject drugs and their partners
Needle and syringe programs
for people who inject drugs and
their partners
FALSE
TRUE
FALSE
Comprehensive prevention
programs for sex workers and
their clients
Behavioral interventions for sex
workers
FALSE
TRUE
FALSE
Comprehensive prevention
programs for sex workers and
their clients
Condoms and lubricant
programming for sex workers
FALSE
TRUE
FALSE
Comprehensive prevention
programs for sex workers and
their clients
HIV testing services for sex
workers
FALSE
TRUE
FALSE
Comprehensive prevention
programs for sex workers and
their clients
Interventions for young people
who sell sex
FALSE
TRUE
FALSE
Comprehensive prevention
programs for transgender
people
Behavioral interventions for
transgender people
FALSE
TRUE
FALSE
Comprehensive prevention
programs for transgender
people
Condoms and lubricant
programming for transgender
people
FALSE
TRUE
FALSE
Comprehensive prevention
programs for transgender
people
HIV testing services for
transgender people
FALSE
TRUE
FALSE
Prevention of mother-to-child
transmission
Prong 1: Primary prevention of
HIV infection among women of
childbearing age
FALSE
FALSE
TRUE
Prevention of mother-to-child
transmission
Prong 3: Preventing vertical
HIV transmission
FALSE
FALSE
TRUE
Prevention of mother-to-child
transmission
Prong 4: Treatment, care and
support to mothers living with
HIV, their children and families
FALSE
FALSE
TRUE
Prevention programs for
adolescents and youth, in and
out of school
Other interventions for
adolescent and youth
FALSE
FALSE
TRUE
Prevention programs for
general population
Gender-based violence
prevention and treatment
programs for general
population
FALSE
FALSE
TRUE
Prevention programs for other
vulnerable populations
Behavioral interventions for
other vulnerable populations
FALSE
TRUE
FALSE
Prevention programs for other
vulnerable populations
HIV testing services for other
vulnerable populations
FALSE
TRUE
FALSE
Prevention programs for other
vulnerable populations
Male and female condoms for
other vulnerable populations
FALSE
TRUE
FALSE
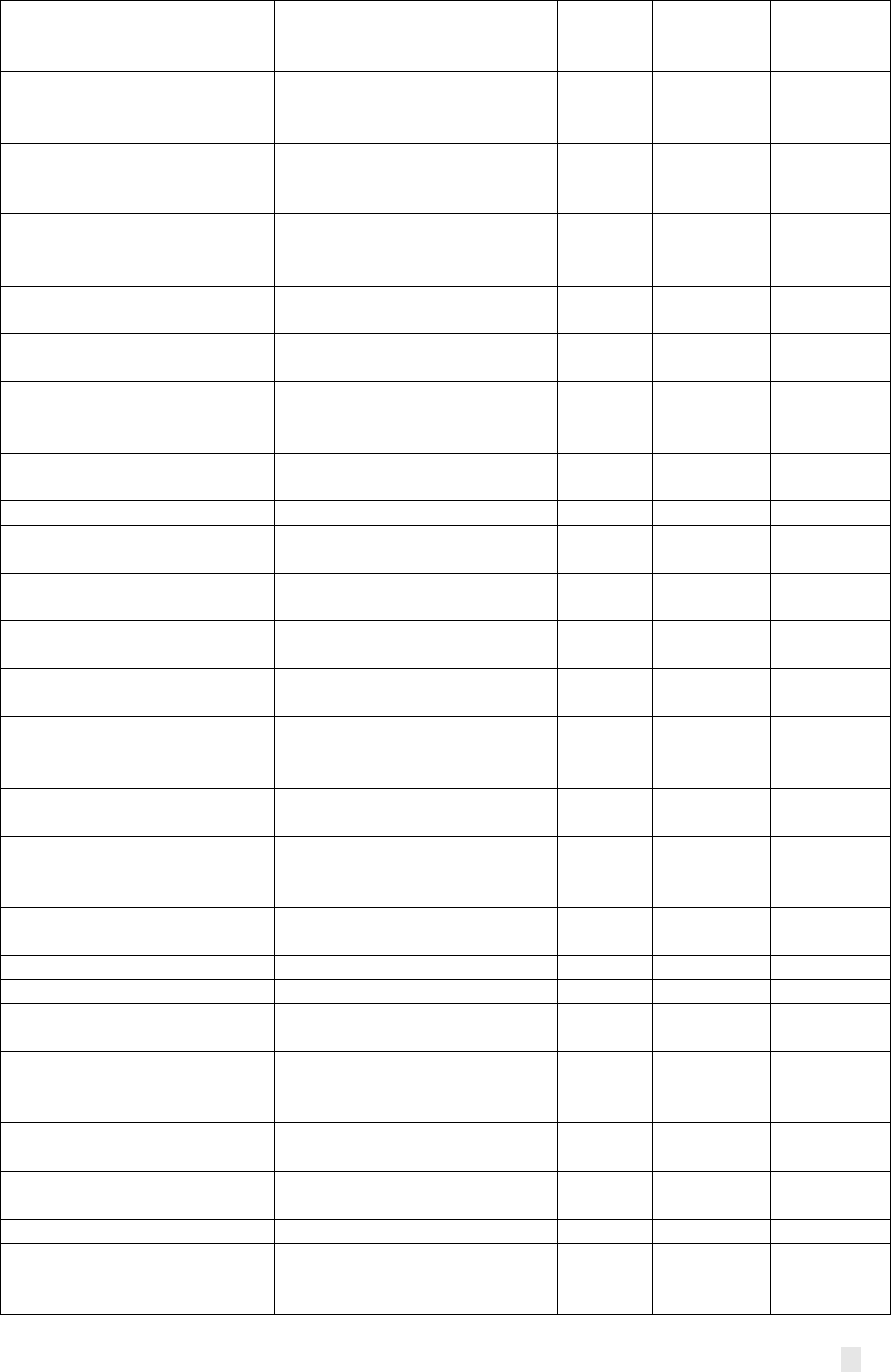
IV
Programs to reduce human
rights-related barriers to HIV
services
HIV and HIV/TB-related legal
services
TRUE
FALSE
FALSE
Programs to reduce human
rights-related barriers to HIV
services
Improving laws, regulations and
polices relating to HIV and
HIV/TB
TRUE
FALSE
FALSE
Programs to reduce human
rights-related barriers to HIV
services
Sensitization of lawmakers and
law enforcement agents
TRUE
FALSE
FALSE
Programs to reduce human
rights-related barriers to HIV
services
Stigma and discrimination
reduction
TRUE
FALSE
FALSE
TB/HIV
Key populations (TB/HIV) -
Others
FALSE
TRUE
FALSE
TB/HIV
Key populations (TB/HIV) -
Prisoners
FALSE
TRUE
FALSE
Treatment, care and support
Prevention, diagnosis and
treatment of opportunistic
infections
FALSE
FALSE
TRUE
Multidrug-resistant TB
Community MDR-TB care
delivery
FALSE
FALSE
TRUE
TB care and prevention
Community TB care delivery
FALSE
FALSE
TRUE
TB care and prevention
Key populations (TB care and
prevention) – Others
FALSE
TRUE
FALSE
Differentiated HIV Testing
Services
Community-based testing
FALSE
TRUE
FALSE
Differentiated HIV Testing
Services
Facility-based testing
FALSE
TRUE
FALSE
Differentiated HIV Testing
Services
Self-testing
FALSE
TRUE
FALSE
PMTCT
Prong 2: Preventing unintended
pregnancies among women
living with HIV
FALSE
FALSE
TRUE
PMTCT
Prong 3: Preventing vertical
HIV transmission
FALSE
FALSE
TRUE
PMTCT
Prong 4: Treatment, care and
support to mothers living with
HIV, their children and families
FALSE
FALSE
TRUE
Prevention
Addressing stigma,
discrimination, and violence
TRUE
FALSE
FALSE
Prevention
Behavior change interventions
FALSE
TRUE
FALSE
Prevention
Community empowerment
FALSE
TRUE
FALSE
Prevention
Condom and lubricant
programming
FALSE
TRUE
FALSE
Prevention
Gender-based violence
prevention and post-violence
care
FALSE
FALSE
TRUE
Prevention
Harm reduction interventions
for drug use
FALSE
TRUE
FALSE
Prevention
Interventions for young Key
Populations
FALSE
TRUE
FALSE
Prevention
Needle and syringe programs
FALSE
TRUE
FALSE
Prevention
Opiod substitution therapy and
other medically assisted drug
dependence treatment
FALSE
TRUE
FALSE
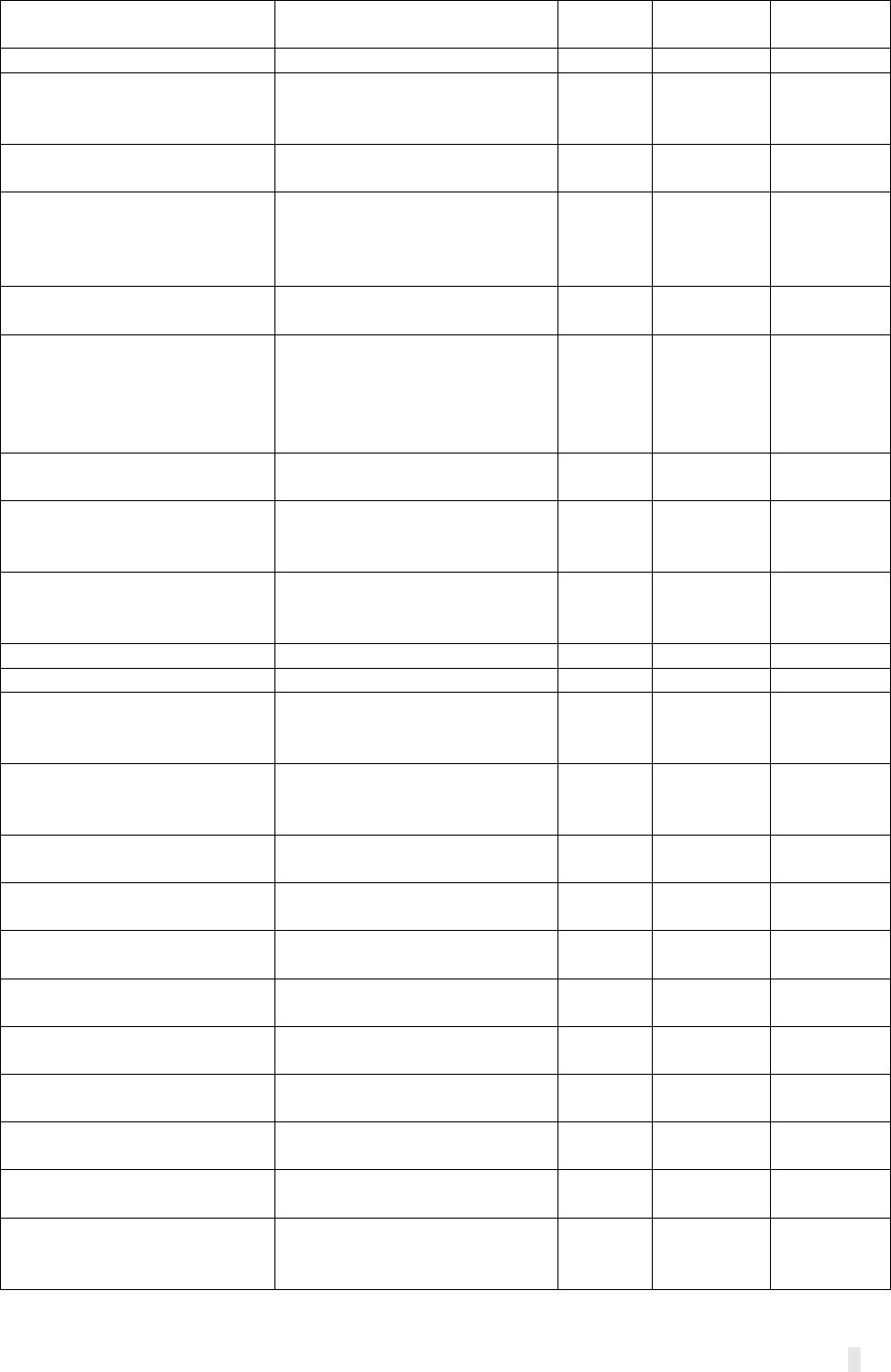
V
Prevention
Overdose prevention and
management
FALSE
TRUE
FALSE
Prevention
Pre-exposure prophylaxis
FALSE
TRUE
FALSE
Prevention
Prevention and management of
co-infections and co-
morbidities
FALSE
TRUE
FALSE
Prevention
Sexual and reproductive health
services, including STIs
FALSE
TRUE
FALSE
Reducing human rights-related
barriers to HIV/TB services
Human rights and medical
ethics related to HIV and
HIV/TB for health care
providers
TRUE
FALSE
FALSE
Reducing human rights-related
barriers to HIV/TB services
Legal Literacy (""Know Your
Rights"")
TRUE
FALSE
FALSE
Reducing human rights-related
barriers to HIV/TB services
Reducing HIV-related gender
discrimination, harmful gender
norms, and violence against
women and girls in all their
diversity
TRUE
FALSE
FALSE
Reducing human rights-related
barriers to HIV/TB services
Stigma and discrimination
reduction
TRUE
FALSE
FALSE
Treatment, care and support
Prevention and management of
co-infections and co-
morbidities
FALSE
TRUE
FALSE
Removing human rights and
gender related barriers to TB
services
Legal aid and services
TRUE
FALSE
FALSE
TB care and prevention
Key populations - Children
FALSE
TRUE
FALSE
TB care and prevention
Key populations - Prisoners
FALSE
TRUE
FALSE
PMTCT
Prong 1: Primary prevention of
HIV infection among women of
childbearing age
FALSE
FALSE
TRUE
Reducing human rights-related
barriers to HIV/TB services
Improving laws, regulations,
and policies relating to HIV and
HIV/TB
TRUE
FALSE
FALSE
Community responses and
systems
Community-led advocacy
FALSE
FALSE
TRUE
Case management
Integrated community case
management (iCCM)
FALSE
TRUE
FALSE
Specific prevention
interventions
Intermittent preventive
treatment – In pregnancy
FALSE
TRUE
FALSE
Specific prevention
interventions (SPI)
Intermittent preventive
treatment (IPT) - In infancy
FALSE
TRUE
FALSE
Specific prevention
interventions (SPI)
Intermittent preventive
treatment (IPT) - In pregnancy
FALSE
TRUE
FALSE
Integrated service delivery and
quality improvement
Quality of care
FALSE
FALSE
TRUE
TB/HIV
Community TB/HIV care
delivery
FALSE
FALSE
TRUE
TB/HIV
Key populations (TB/HIV) –
Prisoners
FALSE
TRUE
FALSE
Removing human rights and
gender related barriers to TB
services
Human rights, medical ethics
and legal literacy
TRUE
FALSE
FALSE
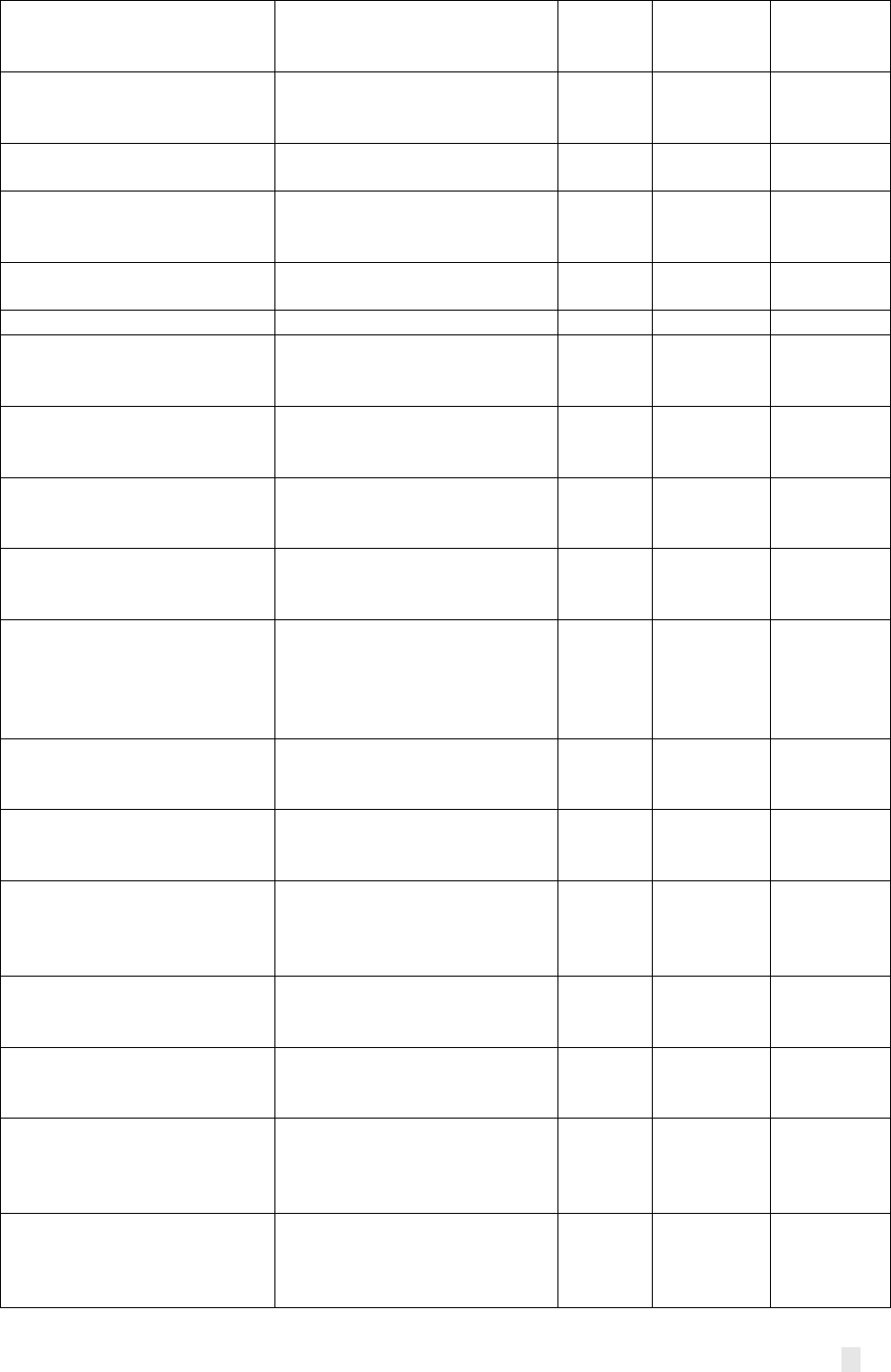
VI
Removing human rights and
gender related barriers to TB
services
Reform of laws and policies
TRUE
FALSE
FALSE
Removing human rights and
gender related barriers to TB
services
Stigma and discrimination
reduction
TRUE
FALSE
FALSE
TB care and prevention
Key populations - Miners and
mining communities
FALSE
TRUE
FALSE
TB care and prevention
Key populations - Mobile
populations: refugees, migrants,
and internally displaced people
FALSE
TRUE
FALSE
Community systems
strengthening
Community-led advocacy and
research
FALSE
FALSE
TRUE
TB/HIV
Key populations - Children
FALSE
TRUE
FALSE
Comprehensive prevention
programs for men who have
sex with men
Community empowerment for
men who have sex with men
FALSE
TRUE
FALSE
Comprehensive prevention
programs for men who have
sex with men
Other interventions for men
who have sex with men
FALSE
TRUE
FALSE
Comprehensive prevention
programs for men who have
sex with men
Pre-exposure prophylaxis
(PrEP) for men who have sex
with men
FALSE
TRUE
FALSE
Comprehensive prevention
programs for men who have
sex with men
Prevention and management of
coinfections and co- morbidities
men who have sex with men
FALSE
TRUE
FALSE
Comprehensive prevention
programs for sex workers and
their clients
Diagnosis and treatment of
sexually transmitted infections
and other sexual and
reproductive health services for
sex workers
FALSE
TRUE
FALSE
Comprehensive prevention
programs for sex workers and
their clients
Other interventions for sex
workers and their clients
FALSE
TRUE
FALSE
Comprehensive prevention
programs for transgender
people
Community empowerment for
transgender people
FALSE
TRUE
FALSE
Comprehensive prevention
programs for transgender
people
Diagnosis and treatment of
sexually transmitted infections
and sexual health services for
transgender people
FALSE
TRUE
FALSE
Comprehensive prevention
programs for transgender
people
Interventions for young
transgender people
FALSE
TRUE
FALSE
Comprehensive prevention
programs for transgender
people
Other interventions for
transgender people
FALSE
TRUE
FALSE
Comprehensive prevention
programs for transgender
people
Pre-exposure prophylaxis
(PrEP) and other biomedical
interventions for transgender
people
FALSE
TRUE
FALSE
Comprehensive prevention
programs for transgender
people
Prevention and management of
co-infections and co-
morbidities for transgender
people
FALSE
TRUE
FALSE

VII
Comprehensive prevention
programs for transgender
people
Prevention and management of
co-infections and co-
morbidities for transgender
people
FALSE
TRUE
FALSE
Comprehensive programs for
people in prisons and other
closed settings
Behavioral interventions for
people in prisons and other
closed settings
FALSE
TRUE
FALSE
Comprehensive programs for
people in prisons and other
closed settings
Community empowerment for
people in prisons and other
closed settings
FALSE
TRUE
FALSE
Comprehensive programs for
people in prisons and other
closed settings
Condoms and lubricant
programming for people in
prisons and other closed
settings
FALSE
TRUE
FALSE
Comprehensive programs for
people in prisons and other
closed settings
Diagnosis and treatment of
sexually transmitted infections
and other sexual and
reproductive health services for
people in prisons and other
closed settings
FALSE
TRUE
FALSE
Comprehensive programs for
people in prisons and other
closed settings
Other interventions for people
in prisons and other closed
settings
FALSE
TRUE
FALSE
HIV Testing Services
Differentiated HIV testing
services
FALSE
TRUE
FALSE
Prevention of mother-to-child
transmission
Other interventions for PMTCT
FALSE
FALSE
TRUE
Prevention programs for
adolescents and youth, in and
out of school
Gender-based violence
prevention and treatment
programs for adolescents and
youth
FALSE
FALSE
TRUE
Programs to reduce human
rights-related barriers to HIV
services
Legal literacy (“Know Your
Rights”)
TRUE
FALSE
FALSE
Programs to reduce human
rights-related barriers to HIV
services
Other intervention(s) to reduce
human rights- related barriers
to HIV services
TRUE
FALSE
FALSE
Programs to reduce human
rights-related barriers to HIV
services
Training of health care
providers on human rights and
medical ethics related to HIV
and HIV/TB
TRUE
FALSE
FALSE
Integrated service delivery and
quality improvement
Supportive policy and
programmatic environment
FALSE
FALSE
TRUE
Reducing human rights-related
barriers to HIV/TB services
Community mobilization and
advocacy
TRUE
FALSE
FALSE
Reducing human rights-related
barriers to HIV/TB services
Sensitization of law-makers and
law-enforcement agents
TRUE
FALSE
FALSE
Community responses and
systems
Social mobilization, building
community linkages,
collaboration and coordination
FALSE
FALSE
TRUE
TB care and prevention
Key populations (TB care and
prevention) – Prisoners
FALSE
TRUE
FALSE
TB care and prevention
Removing human rights- and
gender-related barriers to TB
care and prevention
TRUE
FALSE
FALSE
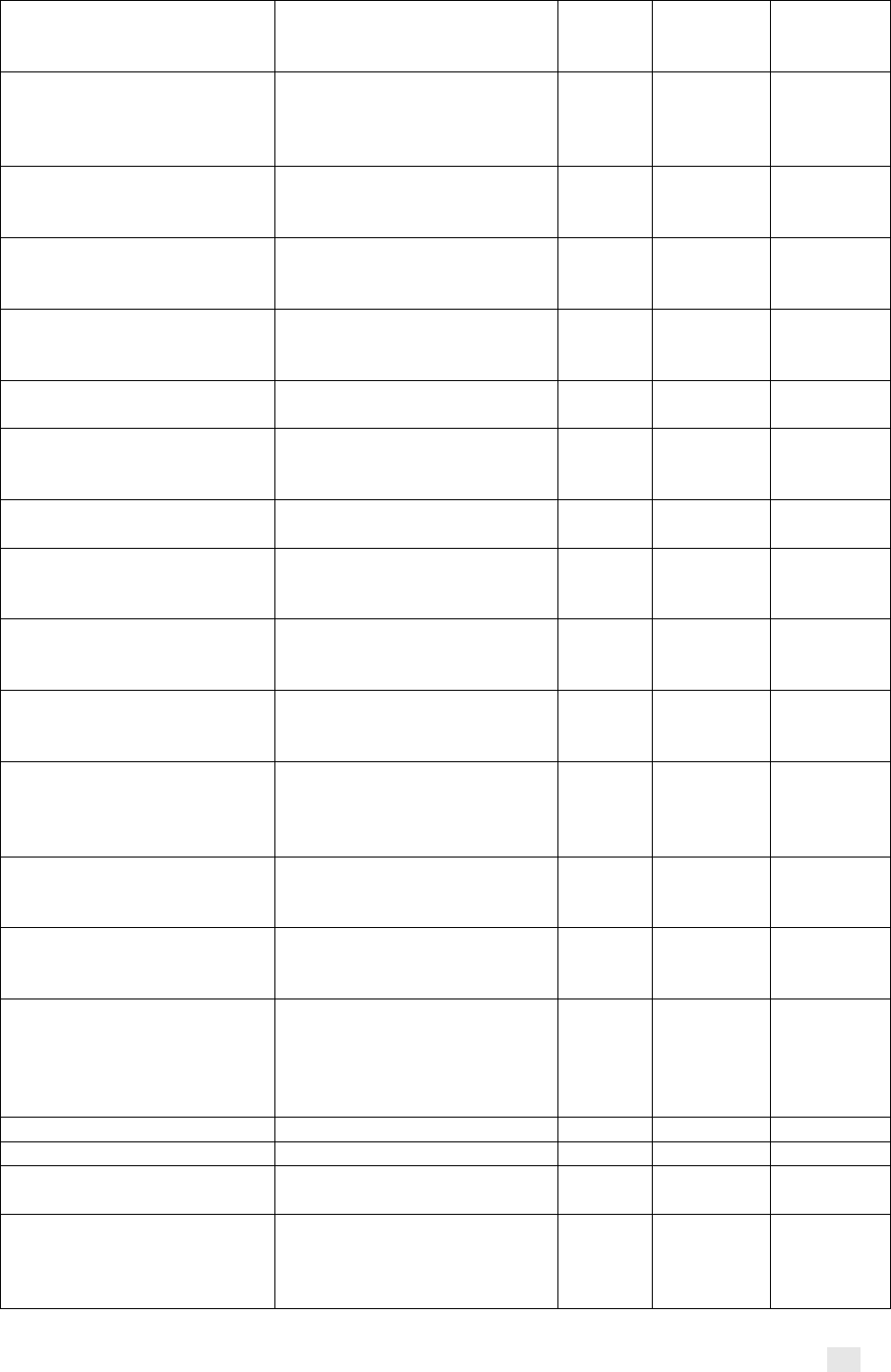
VIII
Comprehensive prevention
programs for people who
inject drugs and their partners
Addressing stigma,
discrimination and violence
against people who inject drugs
TRUE
FALSE
FALSE
Comprehensive prevention
programs for people who
inject drugs and their partners
Opioid substitution therapy and
other drug- dependence
treatment for people who inject
drugs
FALSE
TRUE
FALSE
Comprehensive prevention
programs for sex workers and
their clients
Addressing stigma,
discrimination and violence
against sex workers
TRUE
FALSE
FALSE
Comprehensive prevention
programs for sex workers and
their clients
Community empowerment for
sex workers
FALSE
TRUE
FALSE
Comprehensive prevention
programs for sex workers and
their clients
Pre-exposure prophylaxis
(PrEP) for sex workers
FALSE
TRUE
FALSE
Prevention programs for other
vulnerable populations
Other interventions for other
vulnerable populations
FALSE
TRUE
FALSE
Prevention
Integration into national multi-
sectoral responses of AGYW
programs
FALSE
FALSE
TRUE
Reducing human rights-related
barriers to HIV/TB services
HIV and HIV/TB related legal
services
TRUE
FALSE
FALSE
Community systems
strengthening
Social mobilization, building
community linkages, and
coordination
FALSE
FALSE
TRUE
Comprehensive prevention
programs for people who
inject drugs and their partners
Other interventions for people
who inject drugs and their
partners
FALSE
TRUE
FALSE
Comprehensive prevention
programs for people who
inject drugs and their partners
Overdose prevention and
management
FALSE
TRUE
FALSE
Comprehensive prevention
programs for people who
inject drugs and their partners
Prevention and management of
co-infections and co-
morbidities for people who
inject drugs
FALSE
TRUE
FALSE
Prevention programs for
adolescents and youth, in and
out of school
Behavioral change as part of
programs for adolescent and
youth
FALSE
FALSE
TRUE
Prevention programs for
adolescents and youth, in and
out of school
HIV testing services for
adolescents and youth, in and
out of school
FALSE
FALSE
TRUE
Prevention programs for other
vulnerable populations
Diagnosis and treatment of
sexually transmitted infections
and other sexual health services
for other vulnerable
populations
FALSE
TRUE
FALSE
MDR-TB
Key populations - Prisoners
FALSE
TRUE
FALSE
TB care and prevention
Key populations - Others
FALSE
TRUE
FALSE
TB/HIV
Key populations (TB/HIV) –
Others
FALSE
TRUE
FALSE
Prevention programs for
adolescents and youth, in and
out of school
Addressing stigma,
discrimination and legal
barriers to care for adolescents
and youth
TRUE
FALSE
FALSE
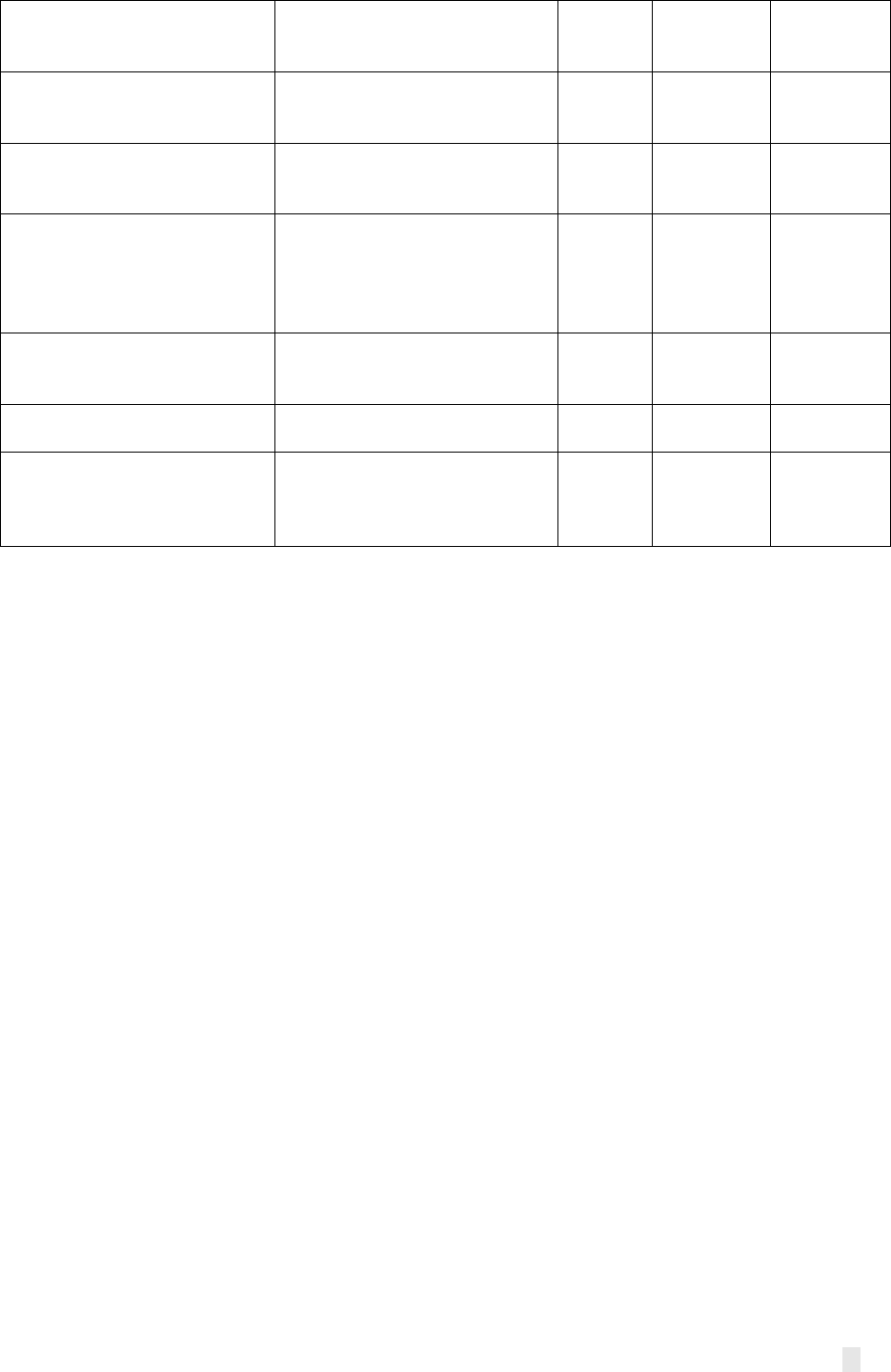
IX
Prevention programs for
adolescents and youth, in and
out of school
Community mobilization and
norms change
FALSE
FALSE
TRUE
Prevention programs for
adolescents and youth, in and
out of school
Keeping girls in school
FALSE
FALSE
TRUE
Prevention programs for
adolescents and youth, in and
out of school
Socioeconomic approaches
FALSE
FALSE
TRUE
Programs to reduce human
rights-related barriers to HIV
services
Reducing HIV-related gender
discrimination, harmful gender
norms and violence against
women and girls in all their
diversity
TRUE
FALSE
FALSE
Prevention programs for
adolescents and youth, in and
out of school
Linkages between HIV
programs and RMNCH
FALSE
FALSE
TRUE
Specific prevention
interventions
Intermittent preventive
treatment – In infancy
FALSE
TRUE
FALSE
Specific prevention
interventions (SPI)
Removing human rights and
gender related barriers to
specific prevention
interventions
TRUE
FALSE
FALSE
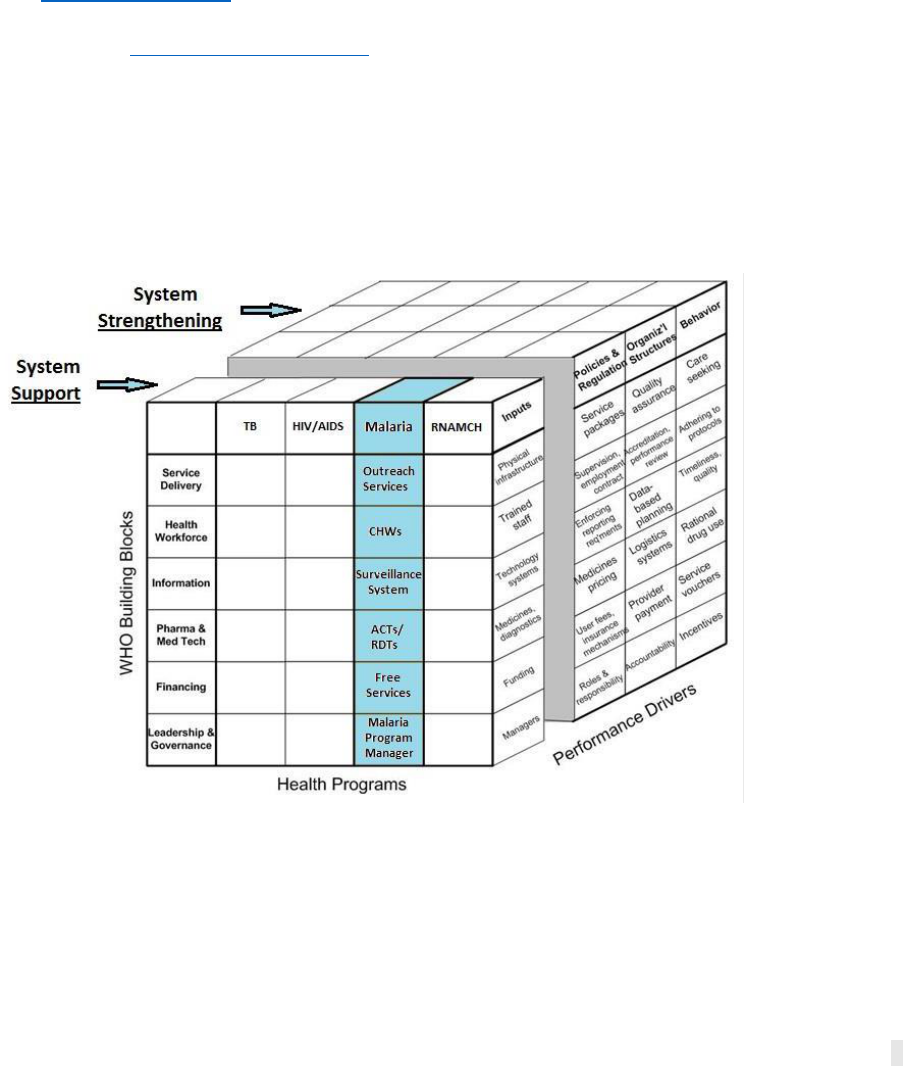
X
Annex 4. PCE 2020 Guidance on Operationalizing the 2S Framework
1. Purpose of this document
This document provides guidance for how to analyze whether “direct” RSSH investments in
current and upcoming Global Fund grants constitute health systems support or health systems
strengthening This guidance builds from references to 4S in both the RSSH and sustainability
guidance documents. Given the need for consistency in applying the framework to budgets in the
2017 and 2020 funding requests and across the four countries, GEP and CEP will work together
closely on the coding process. By examining the change over time, we will assess whether
countries have increased the proportion or Global Fund RSSH investments contributing to health
systems strengthening (versus support).
2. Health system investments: supporting vs. strengthening
The TRP report on RSSH investments in the 2017-2019 funding cycle applied the 4S framework
(start-up, support, strengthening, sustainability), which was an expansion of the framework
proposed by Grace Chee et al. (2013) describing systems support vs. systems strengthening
(hereafter “2S”) as visualized through the health systems cube (Figure 1). Through the TRP’s
review, it was noted that the ‘start-up’ and ‘sustainability’ categories of 4S (the outer two S) were
not applied very often, meaning that most Global Fund investments fell into either the ‘support’
or ‘strengthening’ categories (the middle two S) within the 4S continuum. For that reason, and in
consultation with the TRP, the PCE will apply the 2S framework, which will also help to increase
coding consistency by having fewer categories.
Figure 3.1. Systems Support and Systems Strengthening: Health Systems Cube (Chee et al. 2013).
The health system cube Y-axis includes the WHO building blocks, which are considered key
functions of the health system. The X-axis includes illustrative disease‐specific programs that
deliver critical services, while the third dimension along the Z axis includes performance drivers,
including inputs (systems support), policies, and regulations, organizational structures, and
behaviors (systems strengthening) (Chee et al. 2013). Our analysis will assess whether
proposed RSSH activities contribute to systems support versus system strengthening in
line with Figure 1 above. Per Chee et al. (2013):
XI
• “Supporting the health system can include any activity that improves services, from
distributing mosquito nets to procuring medicines. These activities improve outcomes
primarily by increasing inputs.”
• “Strengthening the health system is accomplished by more comprehensive changes to
performance drivers such as policies and regulations, organizational structures, and
relationships across the health system to motivate changes in behavior and/or allow more
effective use of resources to improve multiple health services.”
The TRP methodology notes that funding requests examples that were health systems support
oriented included requests for cars, computers, phones, travel costs for routine monitoring,
furniture and office equipment, payments for fuels and maintenance of vehicles, cost for regular
training or overseas training, software, reimbursement for importation, among others. Whereas
funding requests characterized by more health systems strengthening interventions included
requests for upscaling of volunteer networks; developing protocols for data quality monitoring;
developing standard operating procedures for quality control in laboratories; transferring of the
procurement system of Global Fund into the national procurement systems; digitizing HMIS data;
developing strategies to engage with the private sector; providing technical assistance for DHIS2
roll-out, improving procurement and supply chain procedures including e-LMIS, and establishing
medicine regulatory authority, among others.
3. Data Sources for RSSH interventions/activities
PCE will rely on up to three budget types as source documents for applying 2S, pending data
availability:
1. Final approved budgets following grant making (2017)
○ To be independently coded by two GEP and compared to review any inconsistencies
and reach consensus on 2S codes.
○ The final approved grant making budget is preferable to the funding request budget,
as it represents the RSSH allocation actually planned for implementation.
2. Funding request budgets submitted to TRP (2020)
○ To be independently coded by GEP and CEP (and then compared in small working
group to review inconsistencies in coding and to reach consensus on 2S codes).
3. Final approved budgets following grant making (2020) for HIV in GTM
○ This may not be available for all countries by the end of 2020. Where available
following grant making, to be independently coded by GEP and CEP (and then
compared to review inconsistencies in coding and to reach consensus on 2S codes).
In addition to the budget data, the funding request narrative description of RSSH investments
should be used as a secondary source for triangulating with budget information when examining
interventions (or activities) and applying the 2S framework. The funding request narrative is
often not well aligned with the budget, unfortunately, but can still often be helpful in
understanding the overall scope of the RSSH interventions.
4. Steps for operationalizing 2S application to RSSH activities in Global Fund grants
4.1 Review the RSSH budget data
Relevant budget data will be extracted by GEP for each country to ensure we are using a
systematic data format across countries. In line with the detailed budgets, the template includes
columns (shaded green) for the extracted data: Grant, Grant Period, Module, Intervention, Activity
Description, Cost Input, and Budget. Additional columns (shaded blue or purple) for data entry
XII
by coders include Scope, Longevity, Approach, Designation (Supporting vs. Strengthening) and
Justification.
Review budget data for each line item, examining the module, intervention, and activity
description. In addition, review the Cost Input categorization. Together, these four data elements
should yield sufficient information to understand the RSSH activity. In some cases, where this
data is insufficient, the funding request narrative can be referred to for additional description of
the RSSH interventions.
HMIS/M&E Investments
RSSH investments in many PCE countries contain substantial investments in HMIS/M&E modules.
While as for other modules, determining whether HMIS/M&E investments are strengthening or
supporting requires careful review of the activity description, our review of the 2017 budgets has
revealed a few patterns. Generally speaking, activities (meetings, etc) related to data validation
(especially when part of the analysis/review intervention category) can be considered
strengthening. Activities related to monitoring the performance of the Global Fund grants
themselves (as opposed to strengthening country M&E systems) should be considered supporting.
Some activities aimed at improving internet connectivity to support information systems
strengthening can also be considered strengthening because, although an input, efforts to improve
the collection and use of data is persistently hampered by poor connectivity, and therefore this
may be a foundational investment upon which broader strengthening efforts are dependent. Other
activities (training, supervision, etc) related to the roll-out of DHIS2 (or similar system) can be
considered strengthening.
4.2 Consider the Scope, Longevity, and Approach of each RSSH intervention/activity pair, and the
cost input category
Drawing from the TRP’s methodology, we will apply three criteria--scope, longevity, and
approach--to assess each RSSH intervention/activity pair in the budget. These three criteria,
along with the Cost Input categorization, will be taken together in determining the designation of
“supporting” or “strengthening”. With the exception of Justification (which requires the coder to
type a justification for why they selected supporting or strengthening, these columns all contain
dropdown menus for the definitions of Scope, Longevity, Approach, and Designation to ease the
coding process. The criteria for a system strengthening intervention include:
• Scope: activities have impact across health services and outcomes
• Longevity: effects will continue after activities end
• Approach: revise policies and institutional relationships to change behaviors and
resource use to address identified constraints in a more sustainable manner
The definitions of Scope, Longevity, and Approach included in the table below will be used for
determining whether an activity is systems support versus systems strengthening.
Parameter
System Support
System Strengthening
Scope
May be focused on a
single disease or
intervention
Activities have impact across health services and
outcomes; and systems may be integrated into the
overall health sector
Longevity
Effects limited to
period of funding
Effects will continue after funded activities end
XIII
Approach
Provide inputs to
address identified
system gaps
Revise policies and institutional relationships to change
behaviors and resource use to address identified
constraints in a more sustainable manner
In many cases, if the majority of the three (scope, longevity and approach) criteria are designated
support or strengthening (i.e. at least 2 out of 3), that will be sufficient to determine the final
designation for the row. There are some cases, where one or more of the criteria may be
designated as unclear, even after considering the cost input category (see below), resulting in a
1-1 tie. These instances will require more of a qualitative judgment to arrive at a final
determination and should be discussed between coders to ensure agreement.
Cost input categories
There are minimum budget requirements for Global Fund funding request submissions, including
modules and their related interventions (selected from prescribed list in the Modular Framework
Handbook) and cost groupings and cost inputs selected from a prescribed list (see Appendix 1, p.
77 of Global Fund guidelines for budgeting). In addition to considering the scope, longevity and
approach criterion in determining whether an activity is supporting or strengthening, certain cost
categories (as indicated in the Table below) can inform this categorization.
Cost Grouping
Cost Input Categories
Supporting / Strengthening
1. Human
resources
1.1 Salaries - program management
1.2 Salaries -outreach workers, medical
staff and other service providers
1.3 Performance-based supplements,
incentives
1.4 Other human resources costs
1.5 Severance costs (added to 2019
guidelines)
1.1/1.2 Considered supporting as
a health system input--including
payment for salaries and other
financial incentives
1.3 Performance-based
supplements and incentives are
the exception to this rule and can
be considered strengthening.
2. Travel-related
costs
2.1 Training-related per
diems/transport/other costs
2.2 TA-related per
diems/transport/other costs
2.3 Supervision/surveys/data
collection-related per
diems/transport/other costs
2.4 Meeting/advocacy-related per
diems/transport/other costs
2.5 Other transportation costs
Most often considered supporting
as a health system input.
2.1 Training-related per-
diems/transport/other costs
should be considered supporting,
unless activity description clearly
describes strengthening capacity
in relation to data use, data
validation meetings, financial
management, PSM, M&E, or other
systems strengthening related
area)
2.4 Meeting related costs
generally considered supporting
unless the activity description
indicates that the purpose is for
policy change or development.
XIV
3. External
professional
services
3.1 Technical assistance
fees/consultancy fees
3.2 Fiscal/fiduciary agent fees
3.3 External audit fees
3.4 Other external professional services
3.5 Insurance related costs
3.1 Technical assistance may be
considered strengthening but
this determination depends upon
review of the activity description.
4. Health products
-- pharmaceutical
products
4.1 Antiretroviral medicines
4.2 Anti-tuberculosis medicines
4.3 Antimalarial medicines
4.4 Opioid substitutes medicines
4.5 Opportunistic infections and STI
medicines
4.6 Private sector subsidies for ACTs
(co-payment to 4.3)
4.7 Other medicines
Most often considered supporting
as a health system input (e.g.
medicines for HIV, TB, malaria);
unlikely to be tagged within RSSH
modules
5. Health products
-- non-
pharmaceuticals
5.1 Insecticide-treated nets (long-
lasting insecticidal nets/insecticide-
treated nets)
5.2 Condoms –male
5.3 Condoms –female
5.4 Rapid diagnostic tests
5.5 Insecticides
5.6 Laboratory reagents
5.7 Syringes and needles
5.8 Other consumables
5.9 Private sector subsidies for rapid
diagnostic tests (Co-payments to 5.4)
Most often considered supporting
as a health system input (e.g.
bednets, condoms, RDTs,
insecticides, reagents, syringes);
unlikely to be tagged within RSSH
modules
6. Health products
-- equipment
6.1 CD4 analyzer/accessories
6.2 HIV viral load analyzer/accessories
6.3 Microscopes
6.4 TB molecular test equipment
6.5 Maintenance and service costs for
health equipment
6.6 Other health equipment
Unlikely to be tagged within RSSH
modules
7. Procurement
and supply chain
management costs
7.1 Procurement agent and handling
fees
7.2 Freight and insurance costs (health
products)
7.3 Warehouse and storage costs
7.4 In-country distribution costs
7.5 Quality assurance and quality
control costs
7.6 Procurement and supply
management customs duties and
clearance charges
7.7 Other procurement and supply
management costs
Cost inputs in this group are most
often considered supporting
7.5 (quality assurance and quality
control costs) and 7.7 (other
procurement and supply
management costs) are possible
exceptions which might be
considered strengthening,
depending on the activity
description
8. Infrastructure
8.1 Furniture
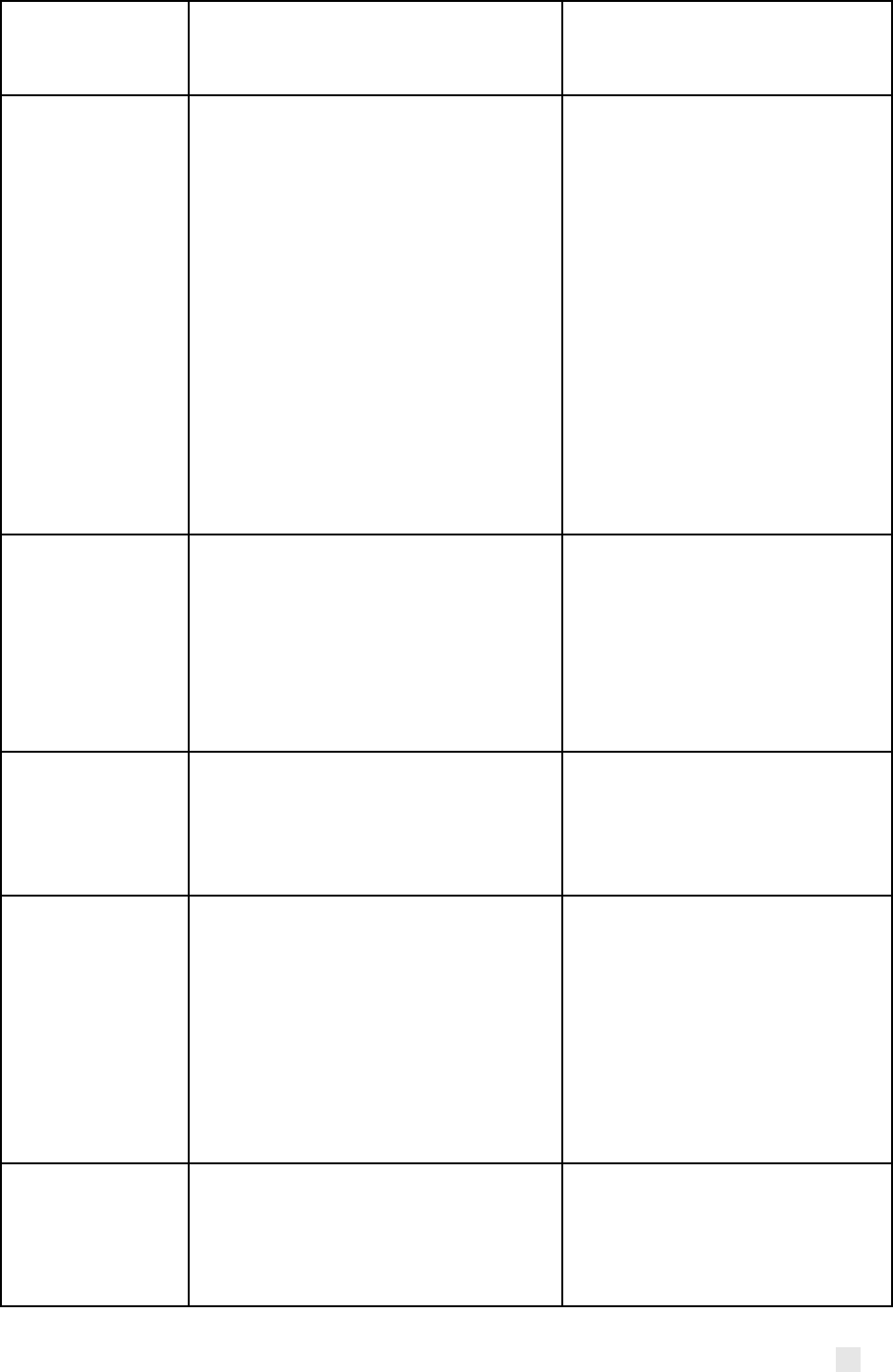
XV
8.2 Renovation/constructions
8.3 Infrastructure maintenance and
other infrastructure costs
9. Non-health
equipment
9.1 IT -computers, computer
equipment, software and applications
9.2 Vehicles
9.3 Other non-health equipment
9.4 Maintenance and service costs non-
health equipment
9.1 IT equipment can typically be
categorized as strengthening if it
is intended to build data systems
capacity. Equipment to facilitate
stand-alone disease-specific
activities may be considered
support, but we haven’t seen
examples of this yet.
9.2 Vehicles are always support.
9.3 Varies, so closely review
activity descriptions. Lab-
strengthening equipment
purchases are generally
considered to be strengthening,
and tend to fall within this cost
input category
10.
Communication
material and
publications
10.1 Printed materials (forms, books,
guidelines, brochure, leaflets, etc.)
10.2 Television/radio spots and
programs
10.3 Promotional material (t-shirts,
mugs, pins, etc.) and other
communication material and
publications costs
All inputs within this cost
grouping are generally considered
to be supporting
11. Indirect and
overhead costs
11.1 Office-related costs
11.2 Unrecoverable taxes and duties
11.3 Indirect cost recovery -% based
11.4 Other PA costs
11.5 Shared costs
All inputs within this cost
grouping are generally considered
to be supporting
12. Living support
to client/target
population
12.1 Support to orphans and other
vulnerable children (school fees,
uniforms, books, etc.)
12.2 Food and care packages
12.3 Cash incentives/transfer to
patients/beneficiaries/counselors/
mediators
12.4 Microloans and microgrants
12.5 Other costs related to living
support to client/target population
Unlikely to be tagged within RSSH
modules
13. Payment for
results
Added to 2019 guidelines:
13.1 Results Based Financing
13.2 Activity Based Contracts,
Community Based Organizations and
other service providers
13.1 and 13.4 are generally
considered to be considered
strengthening

XVI
13.3 Incentives for Principal Recipient
and Sub-Recipients staff members
13.4 Incentives for Community Health
Workers (CHW), outreach workers,
medical staff and other service
providers
4.3 Review the funding request narrative to inform categorization
In some cases, the intervention/activity description and cost-inputs are very vague and provide
insufficient information on which categorize activities as supporting or strengthening. In these
instances, before making a final determination refer back to the funding request narrative to see
if there is additional context around interventions to help inform the final categorization. If no
such information exists, then apply the ‘unclear’ category. Note: In our review of the 2017 budgets,
we found very few interventions which required us to return to the funding request narratives, and
that could not be categorized after exhausting all of these options.
4.4 Review the other coder’s categorization and identify any discrepancies
Each budget will be coded twice, by one CEP and one GEP member. After completing coding of
the budgets, assign one person to compare and identify any lines where the final designation of
supporting vs. strengthening is not consistent between coders. Schedule a call to discuss each of
those discrepancies and align on the final designation. If needed, consult with other members of
the 2S working group to see if parallels can be drawn with other countries.
4.5 Quantify the proportion of the RSSH funds allocated to supporting vs. strengthening investments.
When final designations have been determined, quantify the proportion of funds going to
supporting vs strengthening investments. This can then be compared to 2017 investments to see
whether there is evidence of increased allocation of funds toward strengthening (which could be
considered evidence of a ‘changing trajectory’, or whether the allocations are similar to 2017
(which could be considered evidence of ‘business as usual’). Depending on what we find, we may
drill down to look in greater detail at change for specific modules or intervention categories
(which may be related to focus topics, e.g. HMIS/M&E) and may consider using Tableau to help
illustrate some of these findings. We will continue to build out our approach to this as we explore
the data and patterns or findings begin to emerge.
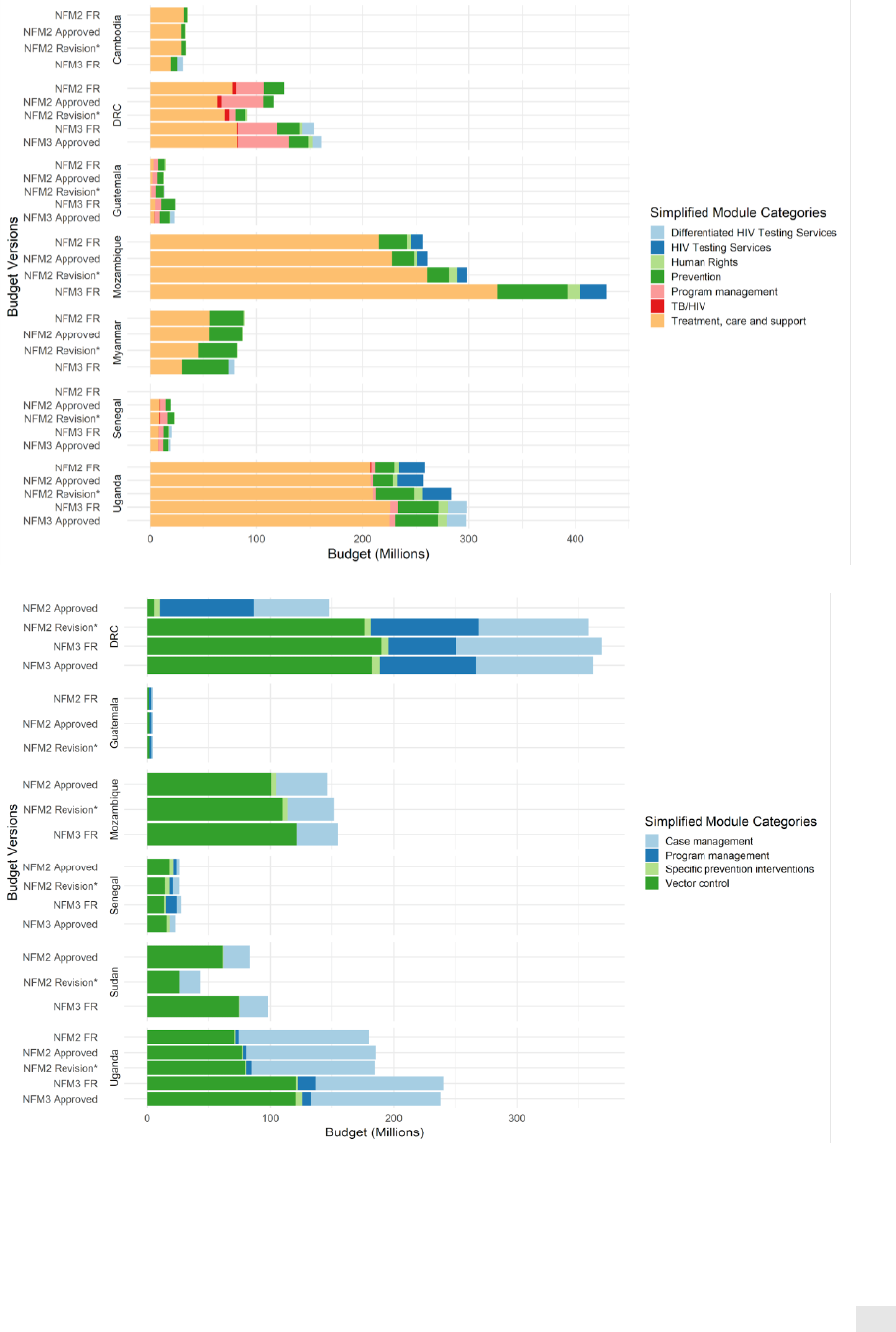
XVII
Annex 5. Supplemental figures of budget changes by disease and RSSH
In all figures, revision is the most recent official budget revision.
Annex Figure 5.1. Budget variance in HIV investments between NFM2 and NFM3.
Annex Figure 5.2. Budget variance in malaria investments between NFM2 and NFM3.
*Program Continuation in NFM2 did not require budget as part of the Funding Request; this data is not available for DRC, Mozambique,
Senegal and Sudan
**The first revision in DRC added an additional US$141,533,250 for the bed net mass distribution campaign that was originally going
to be implemented by PSI and was instead implemented by Global Fund PRs
***Funds for malaria, TB, and RSSH in Senegal remained unchanged between NFM3 FR and Approved Budgets. However, program
management funds for malaria are collapsed with those for TB in these figures due to the integration of some of the malaria component
within the TB/RSSH grant.
XVIII
Annex Figure 5.3. Budget variance in TB investments between NFM2 and NFM3.
Annex Figure 5.4. Budget variance in RSSH investments between NFM2 and NFM3
22
,
23
Figure note: Percentages represent the share of total budget RSSH modules made up for each respective
budget version. NFM2 Funding Requests (FR) could not be included for grants which were continuations
from NFM1—specifically for DRC, Senegal, and Sudan.
22
Given updates to the Modular Framework in 2019, for comparing similar RSSH modules across NFM2 and NFM3, we aligned across
funding cycles, e.g., “community responses and systems” (NFM2) comparable to “community systems strengthening” (NFM3);
“national health strategies” (NFM2) comparable to “health sector governance and planning” (NFM3); “procurement and supply chain”
(NFM2) comparable to “health products management systems” (NFM3). In addition, “laboratory systems” (red) was added as a
distinct module in NFM3, but in NFM2 was included as an intervention within the “Integrated Service Delivery” (pink) module.
23
The data presented does not include all disease components in some countries. Cambodia and Myanmar do not include data for
malaria. Sudan does not include data for HIV and TB. Only HIV is included for Guatemala in NFM3.
XIX
Annex 6. Table of cumulative absorption by year for all modules, RSSH modules, and
HRG-Equity-related modules
24
Country
Modules
Year
Cumulative
Expenditure
Cumulative Budget
Absorption
1
All Countries
All modules
2018
$ 435,221,116
$ 637,529,912
68%
2
All Countries
All modules
2019
$ 1,010,827,839
$ 1,243,020,973
81%
3
All Countries
All modules
2020
$ 774,919,591
$ 1,033,503,661
75%
4
All Countries
RSSH
2018
$ 24,252,479
$ 59,818,215
41%
5
All Countries
RSSH
2019
$ 40,085,859
$ 79,182,340
51%
6
All Countries
RSSH
2020
$ 38,861,769
$ 71,864,527
54%
7
All Countries
HRG-Equity
2018
$ 26,490,910
$ 54,175,617
49%
8
All Countries
HRG-Equity
2019
$ 81,579,875
$ 116,076,973
70%
9
All Countries
HRG-Equity
2020
$ 40,967,119
$ 80,258,075
51%
10
Cambodia
All modules
2018
$ 11,788,588
$ 22,030,647
54%
11
Cambodia
All modules
2019
$ 33,449,455
$ 45,208,043
74%
12
Cambodia
RSSH
2018
$ 269,245
$ 707,626
38%
13
Cambodia
RSSH
2019
$ 1,161,296
$ 2,127,055
55%
14
Cambodia
HRG-Equity
2018
$ 1,504,385
$ 2,855,512
53%
15
Cambodia
HRG-Equity
2019
$ 4,119,724
$ 5,901,577
70%
16
DRC
All modules
2018
$ 123,142,804
$ 187,137,531
66%
17
DRC
All modules
2019
$ 271,907,215
$ 341,325,377
80%
18
DRC
All modules
2020
$ 412,216,321
$ 565,885,160
73%
19
DRC
RSSH
2018
$ 11,745,365
$ 23,005,174
51%
20
DRC
RSSH
2019
$ 15,191,099
$ 24,878,992
61%
21
DRC
RSSH
2020
$ 31,165,051
$ 54,150,564
58%
22
DRC
HRG-Equity
2018
$ 4,771,951
$ 12,737,267
37%
23
DRC
HRG-Equity
2019
$ 14,521,128
$ 23,683,135
61%
24
DRC
HRG-Equity
2020
$ 16,915,414
$ 28,104,393
60%
25
Guatemala
All modules
2019
$ 12,568,696
$ 21,025,472
60%
26
Guatemala
All modules
2020
$ 6,653,971
$ 13,364,136
50%
27
Guatemala
RSSH
2019
$ 806,011
$ 1,998,652
40%
28
Guatemala
RSSH
2020
$ 441,170
$ 2,084,918
21%
29
Guatemala
HRG-Equity
2019
$ 2,218,054
$ 3,526,162
63%
30
Guatemala
HRG-Equity
2020
$ 3,108,291
$ 6,804,475
46%
31
Mozambique
All modules
2018
$ 90,247,014
$ 134,362,850
67%
32
Mozambique
All modules
2019
$ 319,921,010
$ 357,429,377
90%
33
Mozambique
RSSH
2018
$ 1,811,418
$ 13,645,166
13%
34
Mozambique
RSSH
2019
$ 11,349,364
$ 26,997,164
42%
35
Mozambique
HRG-Equity
2018
$ 3,841,326
$ 6,331,732
61%
24
HRG-Equity investments in Sudan were only analyzed for malaria, and were very small. Nonetheless, absorption
against these areas was 0%. 2020 expenditure, budget, and absorption figures only reflect the first semester.
XX
36
Mozambique
HRG-Equity
2019
$ 18,964,823
$ 21,238,368
89%
37
Myanmar
All modules
2018
$ 54,094,227
$ 73,507,181
74%
38
Myanmar
All modules
2019
$ 52,175,815
$ 78,649,237
66%
39
Myanmar
RSSH
2018
$ 7,362,593
$ 9,458,290
78%
40
Myanmar
RSSH
2019
$ 3,686,430
$ 7,620,775
48%
41
Myanmar
HRG-Equity
2018
$ 11,386,127
$ 14,968,265
76%
42
Myanmar
HRG-Equity
2019
$ 23,740,879
$ 28,033,573
85%
43
Senegal
All modules
2018
$ 18,994,323
$ 30,327,752
63%
44
Senegal
All modules
2019
$ 43,548,244
$ 51,378,861
85%
45
Senegal
All modules
2020
$ 77,008,620
$ 85,834,261
90%
46
Senegal
RSSH
2018
$ 2,026,230
$ 4,538,079
45%
47
Senegal
RSSH
2019
$ 5,037,052
$ 7,392,846
68%
48
Senegal
RSSH
2020
$ 5,705,050
$ 9,457,464
60%
49
Senegal
HRG-Equity
2018
$ 3,010,466
$ 3,892,393
77%
50
Senegal
HRG-Equity
2019
$ 6,747,325
$ 8,167,893
83%
51
Senegal
HRG-Equity
2020
$ 6,472,849
$ 9,754,681
66%
52
Sudan
All modules
2018
$ 28,408,002
$ 39,989,280
71%
53
Sudan
All modules
2019
$ 43,720,610
$ 53,498,940
82%
54
Sudan
RSSH
2018
$ 775,227
$ 4,552,725
17%
55
Sudan
RSSH
2019
$ 1,390,904
$ 3,017,984
46%
56
Sudan
HRG-Equity
2018
$ -
$ -
0%
57
Sudan
HRG-Equity
2019
$ -
$ 91,282
0%
58
Uganda
All modules
2018
$ 108,546,157
$ 150,174,671
72%
59
Uganda
All modules
2019
$ 233,536,793
$ 294,505,666
79%
60
Uganda
All modules
2020
$ 279,040,679
$ 368,420,104
76%
61
Uganda
RSSH
2018
$ 262,400
$ 3,911,156
7%
62
Uganda
RSSH
2019
$ 1,463,702
$ 5,148,873
28%
63
Uganda
RSSH
2020
$ 1,550,498
$ 6,171,580
25%
64
Uganda
HRG-Equity
2018
$ 44,551,947
$ 75,761,952
59%
65
Uganda
HRG-Equity
2019
$ 23,610,161
$ 28,606,493
83%
66
Uganda
HRG-Equity
2020
$ 33,098,451
$ 49,673,788
67%
XXI
Annex 7: Application of the Global Fund’s performance-based funding model
Introduction
The annual funding decision and disbursement processes are key to the Global Fund
Secretariat’s grant management function and performance-based funding model. The objective
of these processes is to: (6)
• review grant implementation progress (including achievement of programmatic targets,
and financial and management issues) and assign an overall grant rating;
• determine the funding to be disbursed for each grant for the following 12-month period;
and
• identify implementation issues, risks and mitigating measures.
The annual funding decision is intended to encourage grant recipients to focus on results and
timely implementation by being based on the principle of performance-based funding—i.e.,
where funding is reduced for poor performance and increased for high performance. (6)
Grant ratings in PCE countries
The grant rating is based on:
• Indicator rating: Quantitative assessment of progress against the targets in the
Performance Framework which is adjusted based on the Country Team’s understanding
of the quality of data and programmatic performance of the grant.
• Grant management issues: Qualitative assessment of whether issues exist across the
areas of M&E, program management, financial management and systems, and health
product management.
As shown in Table 1.1, across all grants in the eight PCE countries over the period 2018 to mid-
2020, the majority of grant ratings are applied to the B1 and A2 categories reflecting moderate
performance.
Annex Table 6.1: Frequency of grant ratings for all grants in PCE countries (2018-20)
Rating
Description
Frequency
%
A1
Exceeds expectations
11
9%
A2
Meets expectation
20
16%
B1
Adequate
83
65%
B2
Inadequate but potential demonstrated
12
9%
C
Unacceptable
2
2%
Of interest, and as partly shown in Annex Figure 6.1, grant ratings change dramatically between
semesters in some instances (such as the TASO TB/HIV grant in Uganda which moved from a C
rating in Jan-Jun 2018 to a B2 rating in Jun-Dec 2018 to a B1 rating in Jan-Jun 2019 to an A1 rating
in Jun-Dec 2019), although there are no clear trends to discern across all countries.
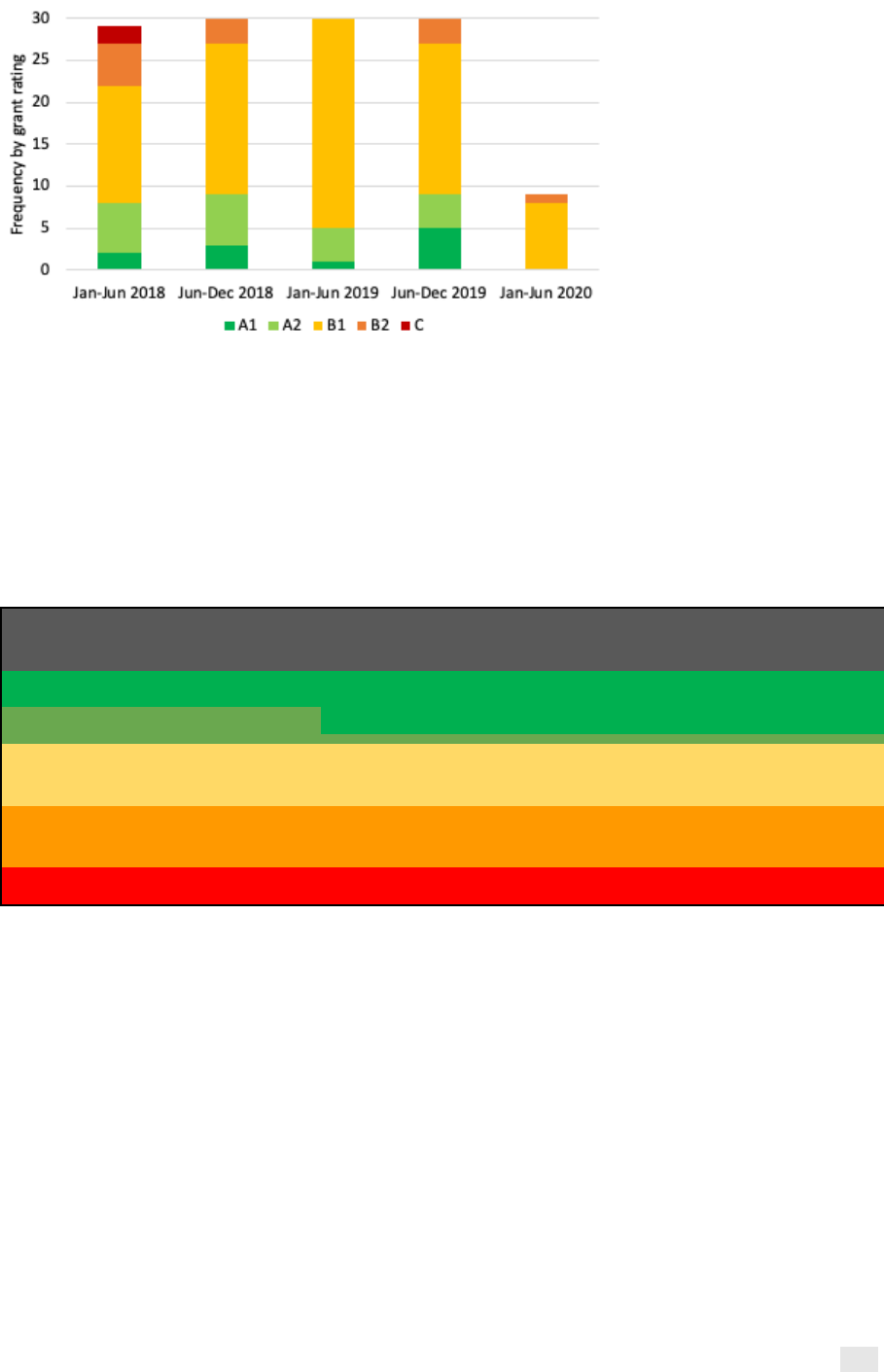
XXII
Annex Figure 6.1: Frequency of grant ratings by semester for all grants in PCE countries
Disbursements
According to the Operational Policy Note on Annual Funding Decisions and Disbursements, the
annual funding amount should be based on: (a) an indicative annual funding range based on the
indicator rating; (b) the rate of expenditure/absorption; and (c) the presence of grant
management issues. Table 1.2 sets out how the indicator rating is used to derive an annual
funding range, with a clear link between indicator performance and the proportion of the budget
to be disbursed in the following reporting period.
Annex Table 6.2: Use of indicator ratings to determine the indicative funding range
Indicator
rating
Target
achievement
Indicative funding range
a1
>100%
Between 90-100% of Cumulative Budget through the next
reporting period
a2
90-100%
b1
60-89%
Between 60-89% of Cumulative Budget through the next
reporting period
b2
30-59%
Between 30-59% of Cumulative Budget through the next
reporting period
c
<30%
To be discussed individually
As shown in Table 1.3, in the vast majority of instances where a grant attained an indicator rating
of b1 or b2 at the end of 2018, the level of funding disbursed in 2018 and 2019 exceeded the
indicative funding range, often dramatically. As such, the indicative funding range does not
appear to have influenced the annual funding decision and level of disbursements made. Rather,
evidence suggests that disbursement decisions are made by Country Teams primarily based on
financial needs, and possibly also qualitative information on performance.
Analysis suggests that this may be appropriate given that indicator performance is often not a
good proxy for what grants have implemented and achieved. It can also be reasonable not to
reduce funding to poorly performing grants after only a year of implementation. As such, the
utility of the indicator rating and how this is used to incentivize performance is unclear.
There are two important caveats to this analysis:
• The budgets used for this analysis are as at the grant award, and could have changed by
the time (i.e., after the end of 2018) the annual funding decision was made.
• The indicative funding ranges are designed to serve as a “starting point” for the Country

XXIII
Team in determining the annual funding amount, and there may be valid reasons for
disbursing outside these ranges. We would nonetheless expect the analysis to show
some pattern between the indicator rating and the level of disbursements made.
Annex Table 6.3: Actual % of budget disbursed in 2018-19 compared to indicative funding
range for 2018-19, based on the indicator rating at end-2018
Grant
Indicator rating
(end-2018)
Indicative funding range for
2018-19 budget
Actual % of budget
disbursed (2018-19)
KHM-C-MEF
b1
60-89%
105%
MOZ-C-CCS
b2
30-59%
92%
MOZ-H-FDC
b1
60-89%
128%
MOZ-H-MOH
a2
90-100%
61%
MOZ-M-MOH
a2
90-100%
62%
MOZ-M-WV
a1
90-100%
93%
MOZ-T-MOH
b1
60-89%
76%
MMR-H-UNOPS
b1
60-89%
83%
MMR-T-SCF
a2
90-100%
92%
MMR-H-SCF
a1
90-100%
93%
MMR-T-UNOPS
b1
60-89%
84%
SDN-H-UNDP
b1
60-89%
113%
SDN-T-UNDP
b1
60-89%
120%
SDN-M-MOH
b1
60-89%
107%
UGA-H-MoFPED
b1
60-89%
98%
UGA-T-MoFPED
a2
90-100%
110%
UGA-C-TASO
b2
30-59%
144%
UGA-M-MoFPED
b1
60-89%
165%
UGA-M-TASO
b1
60-89%
163%
SEN-Z-MOH
b2
30-59%
117%
SEN-H-ANCS
a1
90-100%
106%
SEN-H-CNLS
b1
60-89%
104%
SEN-M-PNLP
b1
60-89%
80%
GTM-T-MSPAS
b1
60-89%
310%
GTM-M-MSPAS
b1
60-89%
147%
COD-H-MOH
b1
60-89%
93%
COD-C-CORDAID
b1
60-89%
119%
COD-M-SANRU
a2
90-100%
93%
COD-M-MOH
a2
90-100%
99%
COD-T-MOH
b1
60-89%
99%
