
For OSUWMC USE ONLY. To license, please
contact the OSU Technology Commercialization
Office at https://tco.osu.edu.
ACHILLES TENDON REPAIR
CLINICAL PRACTICE GUIDELINE
Background
Achilles tendon repair is performed after injury occurs to the Achilles tendon. The injury is often accompanied
by an audible and palpable pop with limited ability to push off of the injured limb. For best outcomes, the
Achilles tendon repair is typically performed within 2 weeks of the injury and recovery is expected to take
between 6 to 9 months. Return to sport may take 9 to 12 months depending on the severity of injury and nature
of the sport the patient desires to play.
These rehabilitation recommendations are based upon the guidance of content experts and evidence-based
practice. Progression through each phase is based on the patient demonstrating readiness by achieving
functional criteria rather than the time elapsed from surgery. The times frames identified for each phase of
rehabilitation are approximate times for the average patient, NOT concrete guidelines for progression.
Disclaimer
Progression is time and criterion-based, dependent on soft tissue healing, patient demographics, and clinician
evaluation. Contact Ohio State Sports Medicine at 614-293-2385 if questions arise.
For OSUWMC USE ONLY. To license, please
contact the OSU Technology Commercialization
Office at https://tco.osu.edu.
Summary of Recommendations
Risk Factors
for Rupture
• Age (30-50 years)
• Male
• Fluoroquinolone use
Precautions
1. Recommend WBAT in protective device at post-op week 2 (NWB days 0-14 or as directed)
2. No aggressive stretching of Achilles or gastrocnemius-soleus complex before 12 weeks
Outcome
Tools
Collect the Lower Extremity Functional Scale (LEFS) at each visit.
Consider collecting one of the following outcome tools. Be consistent with which outcome tool is
collected each visit.
1. The Foot and Ankle Ability Measure (FAAM)
2. The Achilles Tendon Total Rupture Score (ATRS)
Criteria to
Discharge
Walking Boot
1. ROM: Able to achieve 0˚ DF
2. Weight Bearing: Demonstrates pain-free ambulation without antalgic gait
3. Timeframe: Full discharge from boot and heel lifts by Week 8
Criteria to
Initiate
Return to
Running and
Jumping
1. ROM: 95% symmetry ROM (DF/PF) compared to uninvolved limb
2. Anthropometrics: 95% symmetry calf circumference at 10 cm distal to tibial tubercle
compared to uninvolved limb
3. Weight Bearing: Normalized gait and jogging mechanics
4. Strength: 25 single leg heel raises with heel height within 20% of uninvolved limb
5. Timeframe: Initiate between Weeks 12-16
Criteria for
Return to
Sport
1. ROM: 95% symmetry ROM (DF/PF) compared to uninvolved limb
2. Weight Bearing: Normalized gait and jogging mechanics
3. Strength: <10% plantarflexor asymmetry at 0˚ DF and <25% asymmetry at 20˚ PF with
handheld dynamometer compared to uninvolved limb (Appendix A)
4. Neuromuscular Control: 90% symmetry between limbs on Y-balance test with appropriate
lower extremity mechanics
5. Functional Hop Testing: 90% symmetry SL hop testing (Appendix B)
6. Physician Clearance
7. Timeframe: Initiate between 6-9 months
For OSUWMC USE ONLY. To license, please
contact the OSU Technology Commercialization
Office at https://tco.osu.edu.
Red Flags
Red flags are signs/symptoms that require immediate referral for re-evaluation.
Red Flags
• Signs of DVT (Refer directly to ED)
o Localized tenderness along the distribution of deep venous system
o Entire LE swelling
o Calf swelling >3cm compared to asymptomatic limb
o Pitting edema
o Collateral superficial veins
Protection Phase (Post-op - 2 weeks)
Precautions
• Maintain post-operative splint or cast per surgeon (if splint or cast is not removable, then
treatment will only be initiated at proximal joints)
• NWB x 2 weeks (or as directed by surgeon)
ROM
• Joint mobilizations: improve accessory motion at subtalar, distal tibiofibular, midfoot, and
forefoot joints as needed
• Initiate PROM
o PF as tolerated
o DF to minimal stretch, DO NOT aggressively stretch
*Only performed if patient is in removable splint or cast
Weight
Bearing
• NWB x 2 weeks (or as directed by surgeon)
o Refer to surgeon’s post-operative report or office visit note for specific instructions on
weight bearing
Therapeutic
Exercise
• Initiate foot intrinsic exercises:
o Toe taps
o Arch doming
o Toe spreading
• Towel crunches
• Ankle AROM/alphabets
• SLR 4-way
*All exercises should be pain-free; only performed if patient is in removable splint or cast
Goals
• Reduce edema
• Ensure closure of incision
• Educate on DVT/thromboembolism
For OSUWMC USE ONLY. To license, please
contact the OSU Technology Commercialization
Office at https://tco.osu.edu.
Early Loading Phase (2-6 weeks)
Precautions
• DF P/AROM to minimal stretch, DO NOT aggressively stretch
ROM
• Initiate pain-free AROM plantarflexion, inversion, eversion; continue PROM
• Joint mobilizations: improve accessory motions at subtalar, distal tibiofibular, midfoot, and
forefoot joints as needed
Weight
Bearing
• Initiate WBAT with crutches in CAM walker boot starting post-op Week 2
o 2 heel lifts: remove 1 lift every 1-2 weeks per surgeon’s note
• Discharge crutches by Week 4
• Week 4: Initiate weight shifts out of boot as tolerated
Therapeutic
Exercise
• Submaximal ankle isometrics all planes
• Seated heel raises
• BAPS board seated as tolerated
• Recumbent bike with CAM boot
• Gluteal and lumbopelvic strength and stability
• Initiate at 4 weeks:
o Progressive resisted PF, inversion, and eversion with theraband
o Seated heel raises with light weight
o Initiate balance/proprioceptive training on stable surface once able to weight bear in
neutral ankle position out of boot
o Standing BAPS board as tolerated: PWB FWB
o Light weight double leg press
All exercises should be pain-free
Other
Suggested
Interventions
• May initiate soft tissue mobilization and incisional mobility after adequate wound closure
• Pool therapy may begin at post-op week 4 (if wound closed and able to weight bear in
neutral ankle position out of boot)
• Neuromuscular Electrical Stimulation at 4 weeks in standing when patient able to equally
bear weight
Goals
• Initiate ankle strengthening
• DF P/AROM to 0˚ with knee extended
For OSUWMC USE ONLY. To license, please
contact the OSU Technology Commercialization
Office at https://tco.osu.edu.
Strength Phase (6-12 weeks)
Precautions
• DF P/AROM to minimal stretch, DO NOT aggressively stretch
ROM
• Achieve full PROM/AROM plantarflexion, inversion, eversion
• Joint mobilizations: improve accessory motion at subtalar, distal tibiofibular, midfoot, and
forefoot joints as needed
Weight
Bearing
• Week 8: Begin to wean out of boot, initiate walking in shoe/neutral ankle position
o Use of heel wedges (≤2) in shoe as needed: start with number of wedges where no
pain is felt and patient demonstrates proper gait mechanics, remove as able
Therapeutic
Exercise
• Initiate balance training on unstable surfaces
• Continue BAPS standing as tolerated within pain-free ROM, increasing level as able
• Closed chain hip and knee strengthening per patient’s tolerance
• Recumbent bike in shoe
• Initiate calf raise progression on shuttle:
o Double leg
2 up 1 down single leg
o Starting position: neutral ankle dorsiflexion
• Week 8: Initiate standing heel raise progression as able
o Double leg 2 up 1 down single leg
o Starting position: neutral ankle dorsiflexion
• Week 10:
o Initiate step holds with focus on lower extremity alignment and balance (within available
DF)
o Initiate heel taps (within available DF)
All exercises should be pain-free
Criteria to
Discharge
Walking Boot
1. ROM: Able to achieve 0˚ DF
2. Weight Bearing: Demonstrates pain-free ambulation without antalgic gait
3. Timeframe: Full discharge from boot and heel lifts by Week 8
Goals
• Initiate weight bearing strengthening exercises
• Gradual wean from boot and lifts with goal of ambulation in supportive shoe by Week 8
• > 10 single leg heel raises with heel height within 20% of uninvolved limb
For OSUWMC USE ONLY. To license, please
contact the OSU Technology Commercialization
Office at https://tco.osu.edu.
Return to Function Phase (12 weeks – Return to Sport/Activity)
Precautions
• None
ROM
• May initiate gastrocnemius-soleus complex stretching as needed to restore DF ROM
• Joint mobilizations and soft tissue mobility as needed
Weight
Bearing
• Normalized gait mechanics
• Reciprocal pattern with stair ascent and descent
Therapeutic
Exercise
• Emphasize strengthening at end-range PF
o Heel raises on decline board (starting in plantarflexed position)
o Resisted inversion and eversion in plantarflexed position (theraband or ankle weight)
o DL heel raises with theraband pulls into ankle inversion and eversion
o Toe walking
• Heels raises in knee flexion
• Continued progression of strength/stability/balance exercise on stable and unstable
surfaces to correct altered mechanics
• Initiate plyometric progression:
o Shuttle press: DL alternating SL
o FWB: DL straight plane diagonal plane rotational tuck jumps SL
• Step/hop holds for training on lower extremity landing mechanics for jogging
• Resisted jogging in place with resistance in all planes
• Sports specific exercise/agility progression, emphasis on proper mechanics
Criteria to
Initiate
Return to
Running and
Jumping
1. ROM: 95% symmetry ROM (DF/PF) compared to uninvolved limb
2. Anthropometrics: 95% symmetry calf circumference at 10 cm distal to tibial tubercle
compared to uninvolved limb
3. Weight Bearing: Normalized gait and jogging mechanics
4. Strength: 25 single leg heel raises with heel height within 20% of uninvolved limb
5. Timeframe: Initiate between Weeks 12-16
Criteria for
Return to
Sport
1. ROM: 95% symmetry ROM (DF/PF) compared to uninvolved limb
2. Weight Bearing: Normalized gait and jogging mechanics
3. Strength: <10% plantarflexor asymmetry at 0˚ DF and <25% asymmetry at 20˚ PF with
handheld dynamometer compared to uninvolved limb (Appendix A)
4. Neuromuscular Control: 90% symmetry between limbs on Y-balance test with appropriate
lower extremity mechanics
5. Functional Hop Testing: 90% symmetry SL hop testing (Appendix B)
6. Physician Clearance
7. Timeframe: Expected time frame between 6-9 months
For OSUWMC USE ONLY. To license, please
contact the OSU Technology Commercialization
Office at https://tco.osu.edu.
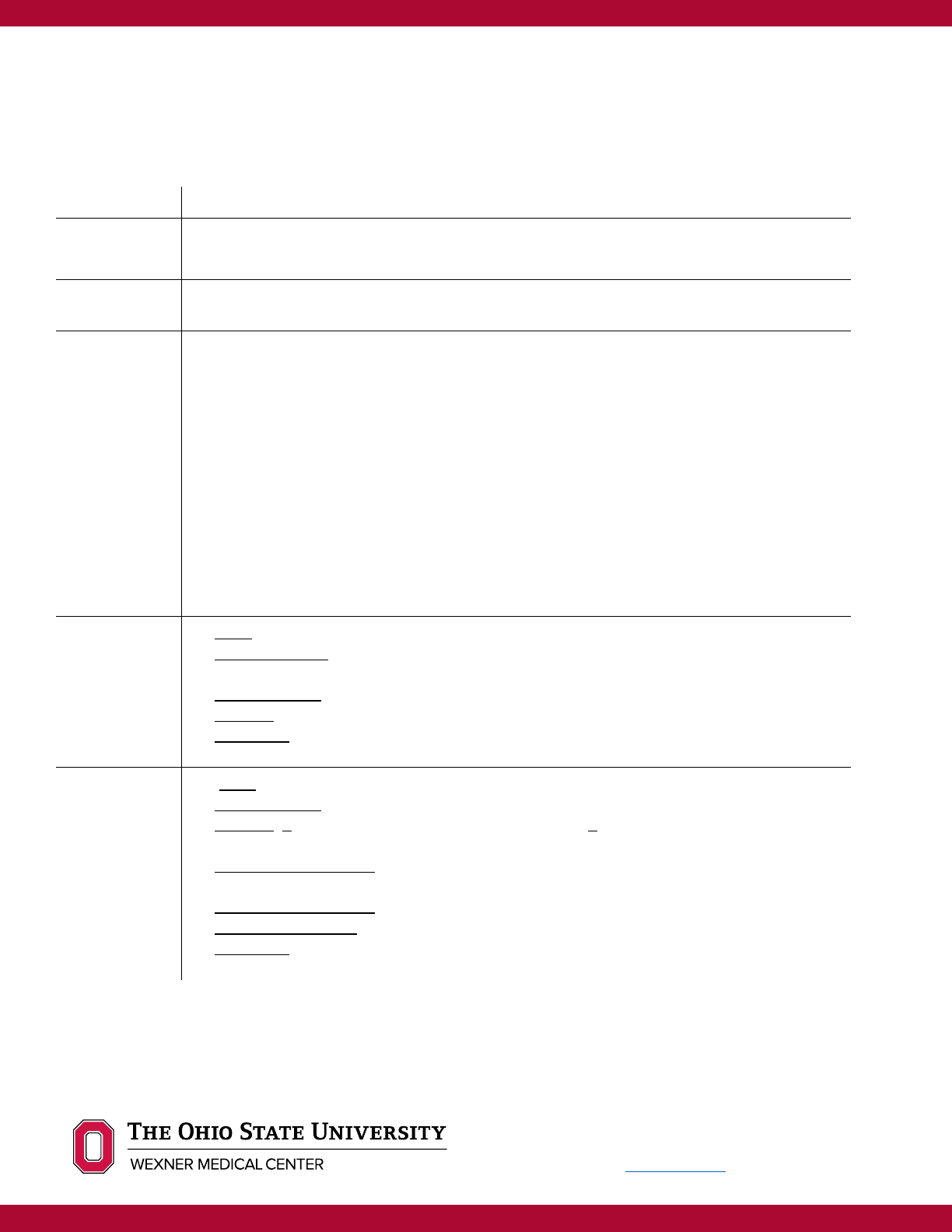
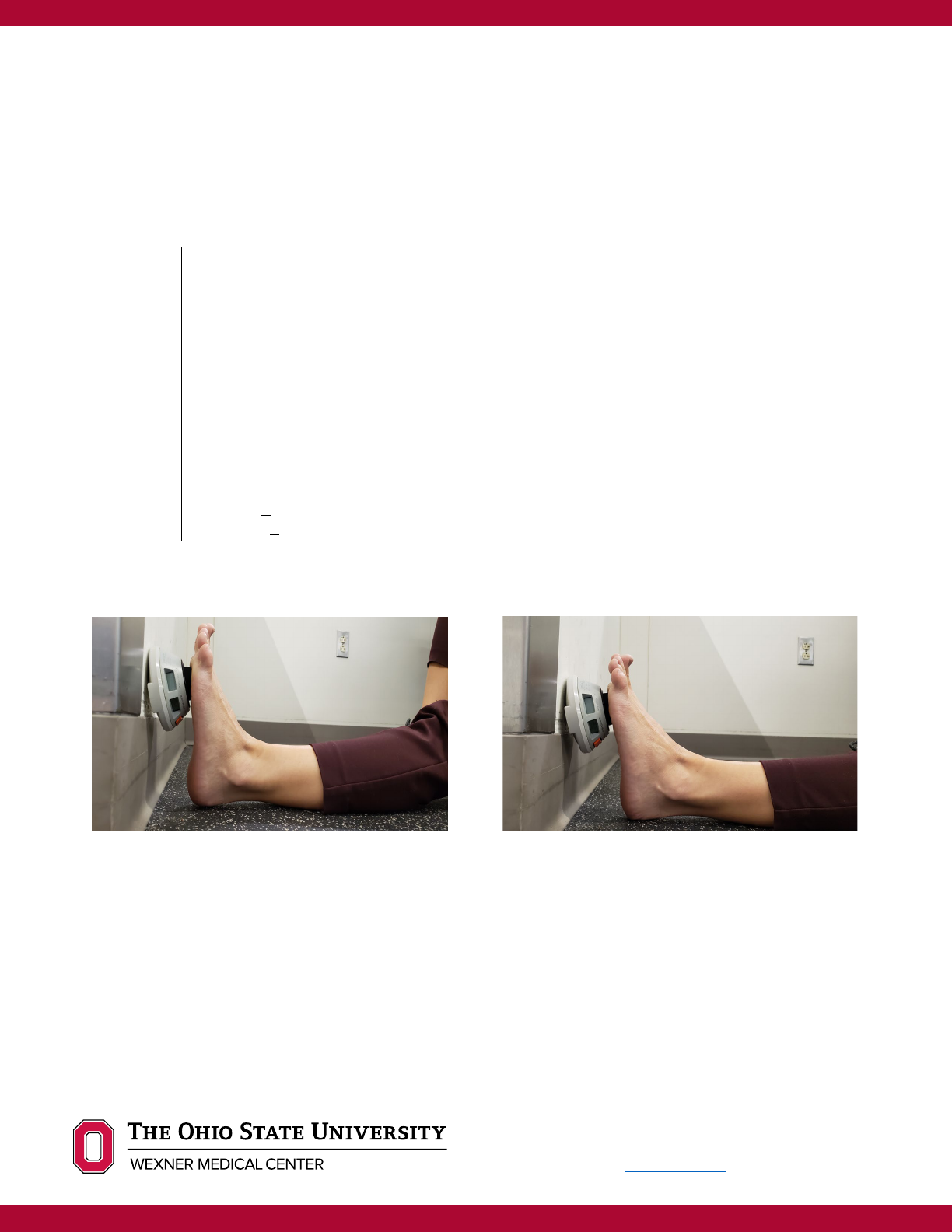
Appendix A: Hand-Held Dynamometry for Ankle Plantarflexion
Position
• Patient in long-sit position on non-slip floor with foot against wall; barefoot
• Knee is fully extended
Placement
• Hand-held dynamometer placed between wall and foot, against plantar surface of foot just
proximal to the metatarsal heads
• Stabilize lower leg just proximal to ankle as needed
Protocol
• Testing performed at 0° DF and 20° PF
• 3 isometric contractions performed in each position lasting 3-5 seconds each
•
Minimum 10 second rest between trials, 1 minute rest between testing angles
•
Take average of the 3 trials at each angle
•
Determine symmetry index for each angle: (involved/uninvolved)*100 = % symmetry
Goal
• 0° DF: < 10% asymmetry between limbs
• 20° PF: < 25% asymmetry between limbs
*Measurements obtained via hand-held dynamometry with always yield lower values than formal Biodex testing. The
numbers obtained from hand-held dynamometry are best utilized to determine level of symmetry between involved and
uninvolved limbs versus as an accurate representation of force production.
References
Marmon, Adam R, Federico Pozzi, Ali H Alnahdi, and Joseph A Zeni. (2013). “The Validity of Plantarflexor Strength
Measures Obtained through Hand-Held Dynamometry Measurements of Force.” International journal of sports
physical therapy 8(6): 820–27.
Orishimo, Karl F et al. (2018). “Can Weakness in End-Range Plantar Flexion After Achilles Tendon Repair Be
Prevented?” Orthopaedic journal of sports medicine 6(5): 2325967118774031.
Spink, Martin J., Mohammad R. Fotoohabadi, and Hylton B. Menz. (2010). “Foot and Ankle Strength Assessment Using
0° dorsiflexion
20° plantarflexion

For OSUWMC USE ONLY. To license, please
contact the OSU Technology Commercialization
Office at https://tco.osu.edu.
Hand-Held Dynamometry: Reliability and Age-Related Differences.” Gerontology 56(6): 525–32.
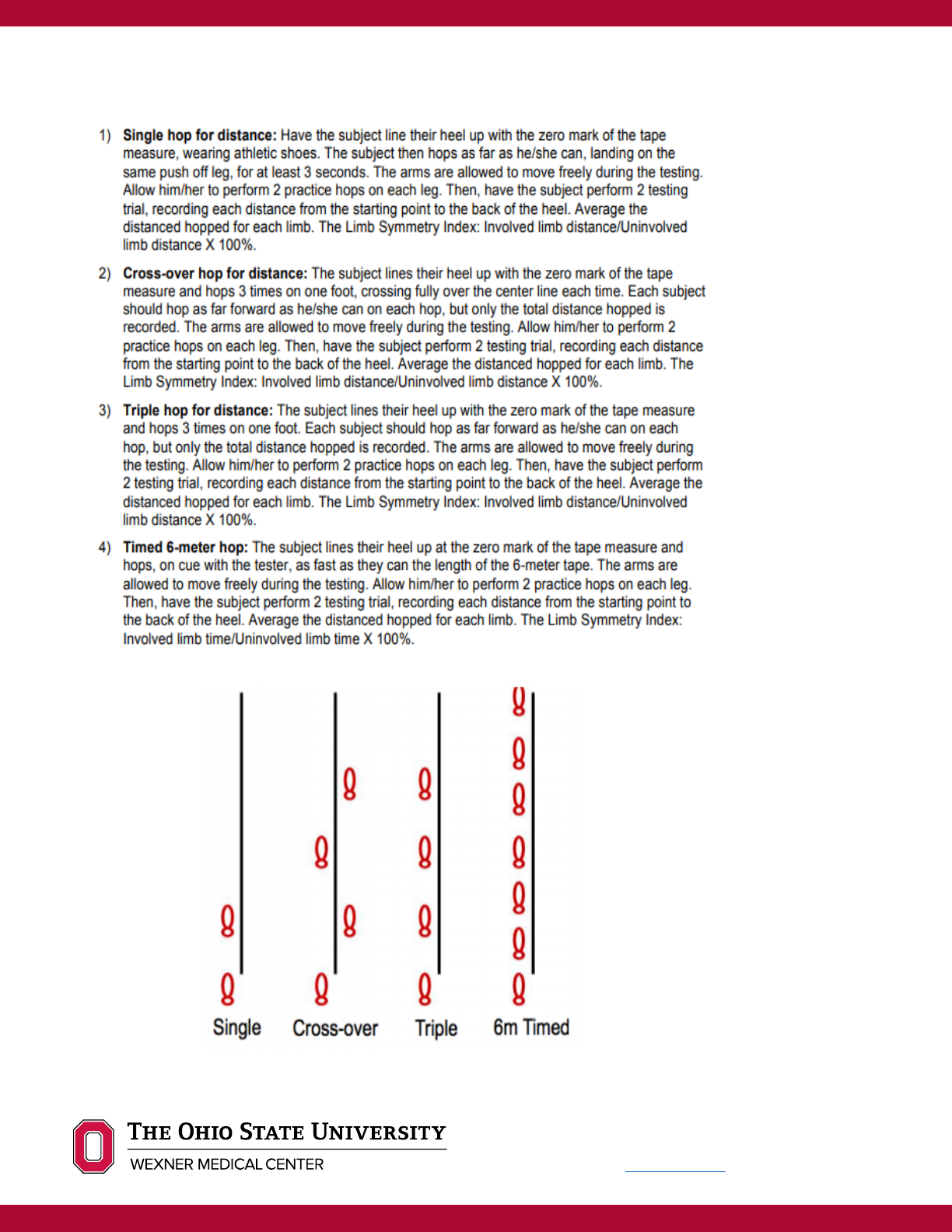
Appendix B: Single Leg Hop Series
For OSUWMC USE ONLY. To license, please
contact the OSU Technology Commercialization
Office at https://tco.osu.edu.

For OSUWMC USE ONLY. To license, please
contact the OSU Technology Commercialization
Office at https://tco.osu.edu.
Author: Tessa Kasmar, PT, DPT, OCS
Reviewers: Adam Groth MD, Timothy Miller MD, Kevin Martin MD, Tiffany Marulli, PT, DPT, OCS; Lucas
VanEtten, PT, DPT, OCS, Victoria Otto, PT, DPT
Completion date: May 2020
References
Achten, J., Parsons, N. R., Kearney, R. L., Maia Schlüssel, M., Liew, A. S., Dutton, S., … Costa, M. L. (2017). Cast versus
functional brace in the rehabilitation of patients treated non-operatively for a rupture of the Achilles tendon: protocol
for the UK study of tendo achilles rehabilitation (UK STAR) multi-centre randomised trial. BMJ Open, 7(10),
e019628. https://doi.org/10.1136/bmjopen-2017-019628
Agres, A. N., Gehlen, T. J., Arampatzis, A., Taylor, W. R., Duda, G. N., & Manegold, S. (2018). Short-term functional
assessment of gait, plantarflexor strength, and tendon properties after Achilles tendon rupture. Gait and Posture,
62(March), 179–185. https://doi.org/10.1016/j.gaitpost.2018.03.007
Bäcker, H. C., Yenchak, A. J., Trofa, D. P., & Vosseller, J. T. (2018). Strength Measurement After Achilles Tendon Repair.
Foot and Ankle Specialist, XX(X), 1–9. https://doi.org/10.1177/1938640018819779
Brumann, M., Baumbach, S., Mutschler, W., & Polzer, H. (2014). Accelerated rehabilitation following Achilles tendon
repair after acute rupture - Development of an evidence-based treatment protocol. Injury, 45(11), 1782–1790.
Chiodo, C. P., Glazebrook, M., Bluman, E. M., Cohen, B. E., Femino, J. E., Giza, E., … American Academy of
Orthopaedic Surgeons. (2010). Diagnosis and treatment of acute Achilles tendon rupture. The Journal of the
American Academy of Orthopaedic Surgeons, 18(8), 503–510. Retrieved from
http://www.ncbi.nlm.nih.gov/pubmed/20675643
Eliasson, P., Agergaard, A.-S., Couppé, C., Svensson, R., Hoeffner, R., Warming, S., … Magnusson, S. P. (2018). The
Ruptured Achilles Tendon Elongates for 6 Months After Surgical Repair Regardless of Early or Late Weightbearing
in Combination With Ankle Mobilization: A Randomized Clinical Trial. The American Journal of Sports Medicine,
46(10), 2492–2502. https://doi.org/10.1177/0363546518781826
Huang, J., Wang, C., Ma, X., Wang, X., Zhang, C., & Chen, L. (n.d.). Rehabilitation Regimen After Surgical Treatment of
Acute Achilles Tendon Ruptures A Systematic Review With Meta-analysis.
https://doi.org/10.1177/0363546514531014
Maffulli, G., del Buono, A., Richards, P., Oliva, F., & Maffulli, N. (2017). Conservative, minimally invasive and open
surgical repair for management of acute ruptures of the achilles tendon: A clinical and functional retrospective study.
Muscles, Ligaments and Tendons Journal, 7(1), 46–52. https://doi.org/10.11138/mltj/2017.7.1.046
Maffulli, N., Tallon, C., Wong, J., Peng Lim, K., & Bleakney, R. (2003). Early Weightbearing and Ankle Mobilization after
Open Repair of Acute Midsubstance Tears of the Achilles Tendon. The American Journal of Sports Medicine, 31(5),
692–700. https://doi.org/10.1177/03635465030310051001
Martin, R. L., Chimenti, R., Cuddeford, T., Houck, J., Matheson, J. W., Mcdonough, C. M., … Torburn, L. (2018). Clinical
Practice Guidelines Achilles Pain, Stiffness, and Muscle Power Deficits: Midportion Achilles Tendinopathy Revision
2018 Summary of Recommendations. J Orthop Sports Phys Ther, 48(5), 1–38.
https://doi.org/10.2519/jospt.2018.0302
McCormack, R., & Bovard, J. (2015). Early functional rehabilitation or cast immobilisation for the postoperative
management of acute Achilles tendon rupture? A systematic review and meta-analysis of randomised controlled
trials. British Journal of Sports Medicine, 49(20), 1329–1335. https://doi.org/10.1136/bjsports-2015-094935
Mullaney, M., Tyler, T. F., McHugh, M., Orishimo, K., Kremenic, I., Caggiano, J., & Ramsey, A. (2011). Electromyographic
analysis of the triceps surae muscle complex during achilles tendon rehabilitation program exercises. Sports Health,
3(6), 543–546. https://doi.org/10.1177/1941738111416911
Orishimo, K. F., Schwartz-Balle, S., Tyler, T. F., McHugh, M. P., Bedford, B. B., Lee, S. J., & Nicholas, S. J. (2018). Can
Weakness in End-Range Plantar Flexion After Achilles Tendon Repair Be Prevented? Orthopaedic Journal of Sports
Medicine, 6(5), 2325967118774031. https://doi.org/10.1177/2325967118774031
Saxena, A., Ewen, B., & Maffulli, N. (n.d.). Rehabilitation of the Operated Achilles Tendon: Parameters for Predicting
Return to Activity. https://doi.org/10.1053/j.jfas.2010.10.008
Spennacchio, P., Vascellari, A., Cucchi, D., Canata, G. L., & Randelli, P. (2016). Outcome evaluation after Achilles tendon
ruptures. A review of the literature. Joints, 4(1), 52–61. https://doi.org/10.11138/jts/2016.4.1.052
Zhao, J.-G., Meng, X.-H., Liu, L., Zeng, X.-T., & Kan, S.-L. (2017). Early functional rehabilitation versus traditional
immobilization for surgical Achilles tendon repair after acute rupture: a systematic review of overlapping meta-
analyses. Scientific Reports, 7, 39871. https://doi.org/10.1038/srep39871
