
FUTURE HOSPI - CASH
POLICY WORDINGS
UIN:IRDA/NL-HLT/FGII/P-H/V.I/75/13-14
FGH/UW/RET/67/02

INTENTIONALY LEFT BLANK
FUTURE HOSPI-CASH
CUSTOMER INFORMATION SHEET
(Description is illustrative and not exhaustive)
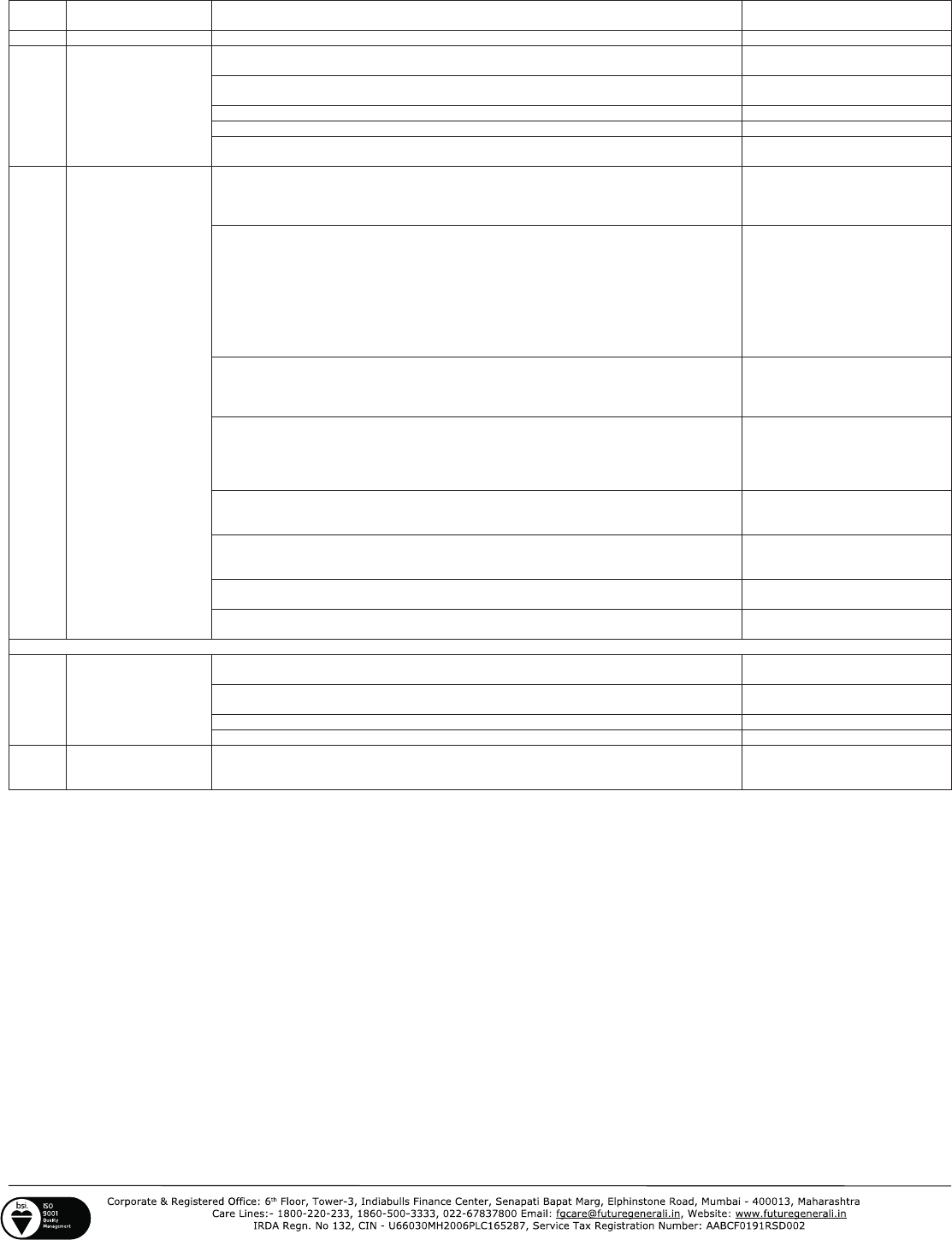
S.NO
TITLE DESCRIPTION
REFER TO POLICY
CLAUSE NUMBER
1
Product Name
Future Hospi-cash
2
What am I covered
for:
Hospital admission longer than 24 hrs
Section A (4) and Section B (I,
II and III)
Hospital Cash benefit for each continuous and completed period of 24 hours for a
maximum of 30 days / 60 days / 90 days/ 180 days as per the schedule
Section B (I)
2 times benefit payable for ICU within the city.
Section B (II)
3 times benefit payable for ICU outside the city.
Section B (III)
a fixed amount towards convalescence for Hospitalisation beyond 10 consecutive
days which is payable only once per hospitalisation event
Section B (IV)
3
What are the major
exclusions in the
policy:
Benefits will not be available for Any condition, ailment or injury or related
condition(s) for which You have been diagnosed, received medical treatment, had
signs and / or symptoms, prior to inception of Your first Policy, until 48 consecutive
months have elapsed, after the date of inception of the first Policy with Us.
Section C (1)
Without derogation from the above point no. (1), any Medical Expenses incurred
during the first two consecutive annual Periods
during which You have the benefit of
a Health Insurance Policy with Us in connection with cataracts, benign prostatic
hypertrophy, hernia of all types, hydrocele, all types of sinuses, fistulae,
hemorrhoids, fissure in ano, dysfunctional uterine bleeding,
fibromyoma
endometriosis, hysterectomy, all internal or external tumors/cysts/nodules/polyps of
any kind including breast lumps ( except malignant conditions), surgery for
prolapsed inter vertebral disc unless arising from accident, surgery of varicose veins
and varicose ulcers.
Section C (2)
Without derogation from the above point No. (1), any Medical Expenses incurred
during the first annual period during which You have the benefit of a Health
Insurance Policy with Us in connection with any types of gastric or duodenal ulcers,
stones in the urinary and biliary systems, surgery on ears/tonsils/adenoids.
Section C (3)
Medical Expenses incurred during the first three consecutive annual periods during
which You have the benefit of the Policy with Us in
connection with joint
replacement surgery due to Degenerative condition, Age related osteoarthritis and
Osteoporosis unless such joint replacement surgery is necessitated by accidental
Bodily Injury.
Section C (4)
Medical Expenses incurred for any illness diagnosed or diagnosable within 30 days,
of the commencement of the Policy Period except those incurred as a result of
accidental Bodily Injury.
Section C (5)
Injury or Disease directly or indirectly caused by or arising from or attributable to
War, Invasion, Act of Foreign Enemy, War like operations (whether war be declared
or not).
Section C (6)
Dental treatment or surgery of any kind unless requiring hospitalisation as a result
of Accidental Bodily injury
Section C (9)
General debility, ‘’Run-down’’ condition or rest cure, sexually transmitted disease,
intentional self-injury.
Section C (12)
(Note: the above is a partial listing of the policy exclusions. Please refer to the policy clauses for the full listing).
4
Waiting period
Initial waiting period: 30 days for all illnesses (not applicable on renewal or for
accidents)
Section C (5)
Specific waiting periods :
24 months for Cataract, Hernia etc diseases
Section C (2)
36 months for Joint Replacement Surgeries
Section C (4)
Pre-existing diseases: Covered after 48 months
Section C (1)
5
Renewal Conditions
The policy is renewable lifelong.
In case of renewal, grace period of 30 days is admissible.
Section D (9) (a)
Section D (9) (c)
(LEGAL DISCLAIMER) NOTE: The information must be read in conjunction with the product brochure and policy document. In case of any conflict
between the CIS and the policy document the terms and conditions mentioned in the policy document shall prevail.
UIN:IRDA/NL-HLT/FGII/P-H/V.I/75/13-14
FGH/UW/RET/67/02

FUTURE HOSPI- CASH
This Policy is issued to You based on Your Proposal to Us and Your
payment of the premium. You are eligible to be covered under this
Policy if Your age is between 6 months to 65 years with lifelong
renewability. This Policy records the agreement between Us and sets out
the terms of insurance and the obligations of each party.
A. DEFINITIONS
The following words or terms shall have the meaning ascribed to them
wherever they appear in this Policy, and reference to the singular or to
the masculine shall include references to the plural and to the female
wherever the context so permits:
1. Accident is a sudden, unforeseen and involuntary event caused by
external, visible and violent means.
2. Injury/ Bodily Injury means accidental physical bodily harm
excluding Illness or disease solely and directly caused by external,
violent and visible and evident means which is verified and certified
by a Medical Practitioner.
3. Hospital means any institution established for in-patient care and
Day Care Treatment of Illness and/ or injuries and which has been
registered as a Hospital with the local authorities under Clinical
Establishments (Registration and Regulation)Act,2010 or under
enactments specified under the Schedule of Section 56(1) of the
said Act OR complies with all minimum criteria as under:
í has qualified nursing staff under its employment round the
clock;
í has at least 10 in-patient beds in towns having a population of
less than 10,00,000 and at least 15 inpatient beds in all other
places;
í has qualified medical practitioner(s) in charge round the clock;
í has a fully equipped operation theatre of its own where surgical
procedures are carried out
í maintains daily records of patients and will make these accessible
to the insurance company’s authorized personnel
4. Hospitalisation means admission in a Hospital for a minimum
period of 24 In patient Care consecutive hours except for specified
procedures/ treatments, where such admission could be for a period
of less than 24consecutive hours.
5. Intensive care unit means an identified section, ward or wing of a
Hospital which is under the constant supervision of a dedicated
medical practitioner(s), and which is specially equipped for the
continuous monitoring and treatment of patients who are in a critical
condition, or require life support facilities and where the level of care
and supervision is considerably more sophisticated and intensive than
in the ordinary and other wards.
6. You, Your, Yourself means the Insured person shown in the
Schedule.
7. We, Our, Us, Insurer means Future Generali India Insurance
Company Limited.
8. Family means and includes You, Your Spouse & Your dependent
child/ children (up to the age of 25 years)
8.1. The maximum number of days of Hospitalisation
as
mentioned in the Schedule would float over all the members
under the Family Floater Policy.
8.2. In the event of more than one Family member being
hospitalised at the same time, the number of days each
member has been hospitalised would be added, and the
maximum allowable for the whole Family would be restricted
to the number of days as mentioned in the
Schedule
(maximum number of days would float over the
Family)
under the Family Floater Policy.
9. Schedule means that portion of the Policy which sets out Your
personal details, the type of insurance cover in force, the period and
the sum insured. Any Annexure or Endorsement to the Schedule
shall also be a part of the Schedule.
10. Proposal means that portion of the Policy which sets out Your
personal details, the type of insurance cover in force, the period and
the sum insured.
11. Policy means the complete documents consisting of the Proposal,
Policy wording, Schedule and Endorsements and attachments if
any.
12. Policy Period means the period between the commencement date
and the expiry date specified in the Schedule and includes both the
commencement date as well as the expiry date.
13. Medical Practitioner is a person who holds a valid registration from
the Medical Council of any State or Medical Council of India or Council
for Indian Medicine or for Homeopathy set up by the Government of
India or a State Government and is thereby entitled to practice
medicine within its jurisdiction; and is acting within the scope and
jurisdiction of his licence. The registered practitioner should not be
the insured or close Family members.
14. Pre-existing Condition means any condition, ailment or Injury or
related condition(s) for which You had signs or symptoms, and / or
were diagnosed, and / or received Medical Advice / treatment
within 48 months to prior to the first
Policy issued by the Insurer.
15. Illness means a sickness or a disease or pathological condition
leading to the impairment of normal physiological function which
manifests itself during the Policy Period and requires medical
treatment.
16. Home City means the city of residence.
17. Other than Home City means the city which is other than the
residential city of the Insured.
18. Day Care Treatment refers to medical treatment, and/or Surgical
Procedure which is:
18.1. undertaken under General or Local Anesthesia in a
Hospital/Day care centre in less than 24 hrs because of
technological advancement, and
18.2. which would have otherwise required a Hospitalisation of
more than 24 hours.
Treatment normally taken on an out-patient basis is not included in
the scope of this definition.
19. Deductible
is a cost-sharing requirement under a health insurance
Policy that provides that the Insurer will not be liable for a specified
rupee amount in case of indemnity policies and for a specified
number of days/hours in case of Hospital cash policies which will
apply before any benefits are payable by the Insurer . A Deductible
does not reduce the sum insured.
20. Dependent child refers to a child (natural or legally adopted), who
is financially dependent on the primary insured or proposer and does
not have his / her independent sources of income.
21. Grace Period means the specified period of time immediately
following the premium due date during which a payment can be made
to renew or continue a Policy in force without loss of continuity
benefits such as waiting periods and coverage of pre existing
diseases. Coverage is not available for the period for which no
premium is received.
22. Inpatient care means treatment for which the insured person has to
stay in a Hospital for more than 24 hours for a covered event.
23. Surgery or Surgical Procedure means manual and/ or operative
procedure (s) required for treatment of an Illness or Injury,
correction of deformities and defects, diagnosis and cure of diseases,
relief of suffering or prolongation of life, performed in a Hospital
or
Day care centre by a medical practitioner.
24. Medical Advice: Any consultation or advice from a Medical
Practitioner including the issue of any prescription or repeat
prescription.
25. Maternity expense shall include –
a. medical treatment expenses traceable to childbirth (including
complicated deliveries and caesarean sections incurred during
Hospitalisation)
b. expenses towards lawful medical termination of pregnancy during
the Policy period.
26. Dental Treatment is treatment carried out by a dental practitioner
including examinations, fillings (where appropriate), crowns,
extractions and Surgery excluding any form of cosmetic
surgery/implants.

27. Any one illness means continuous Period of Illness and it includes
relapse within 45 days from the date of last consultation with the
Hospital/Nursing Home where treatment may have been taken.
28. Congenital Anomaly :Congenital Anomaly refers to a condition(s)
which is present since birth, and which is abnormal with reference to
form, structure or position
a. Internal Congenital Anomaly- Congenital Anomaly which
is not in the visible and accessible parts of the body.
b. External Congenital Anomaly- Congenital Anomaly which
is in the visible and accessible parts of the body.
29. Condition Precedent shall mean a Policy term or condition upon
which the Insurer's liability under the Policy is conditional upon.
30. Unproven/Experimental treatment: Treatment including drug
experimental therapy which is not based on established medical
practice in India, is treatment experimental or unproven .
31. Disclosure to information norm: The Policy shall be void and all
premium paid hereon shall be forfeited to the Company, in the event
of misrepresentation, mis-description or non-disclosure of any
material fact.
32. Renewal defines the terms on which the contract of insurance can be
renewed on mutual consent with a provision of Grace Period for
treating the Renewal continuous for the purpose of all waiting
periods.
33. Portability means transfer by an individual health insurance
policyholder (including Family cover ) of the credit gained for Pre-
existing conditions and time-bound exclusions if he/she chooses to
switch from one Insurer to another.
34. Alternative treatments are forms of treatments other than
treatment "Allopathy" or "modem medicine" and includes Ayurveda,
Unani, Sidha and Homeopathy in the Indian context.
35. Day care centre means any institution established for Day Care
Treatment of Illness and / or injuries or a medical set -up within a
Hospital and which has been registered with the local authorities,
wherever applicable, and is under the supervision of a registered and
qualified Medical Practitioner AND must comply with all minimum
criteria as under:-
í has qualified nursing staff under its employment
í -has qualified medical practitioner/s in charge
í -has a fully equipped operation theatre of its own where surgical
procedures are carried out
í -maintains daily records of patients and will make these
accessible to the Insurance company’s authorized personnel.
B. POLICY BENEFITS:
In the event of Accidental Bodily Injury or Illness first occurring or
manifesting itself during the Policy Period and causing the Insured’s
Hospitalisation for Inpatient care within the Policy Period, the
Company will pay:
I. the Hospital Cash benefit for each continuous and completed
period of 24 hours of Hospitalisation necessitated solely by
reason of the said Accidental Bodily Injury or Sickness, for a
maximum of 30 days / 60 days /90 days/ 180 days as per the
Schedule
OR
II. two times the Hospital Cash benefit for each continuous and
completed period of 24 hours required to be spent by the Insured
in the Intensive care unit of a Hospital situated in the Home
Cityof the Insured, during any period of Hospitalisation
necessitated solely by reason of the said Accidental Bodily
Injury or Sickness for a maximum period of 10 days for each
Hospitalisation and 20 days during the Policy period
OR
III. three times the Hospital Cash benefit for each continuous and
completed period of 24 hours required to be spent by the Insured
in the Intensive care unit of a Hospital situated in a city other
than Home Cityof the Insured, during any period of
Hospitalisation necessitated solely by reason of the said
Accidental Bodily Injury or Sickness for a maximum period of 10
days for each Hospitalisation and 20 days during the Policy
period.
* In case of Section II and III the maximum benefit payable in
case of ICU whether in Home City/ other than Home City , is
limited upto 10 days for each Hospitalisation and maximum of
20 days for all Hospitalisations put together in the Policy
period. In case of the same Hospitalisation involving ICU stay in
both Home City as well as other than Home City, the benefits
under the “other than home city” would have precedence over
benefits under Home City while adjudication of claim.
** In case of Sec I, II and III the maximum benefits would
however be restricted to 30/ 60/ 90 /180 days as per the plan
opted for each Hospitalisation or all Hospitalisations during
the Policy period.
***In case the
Hospitalisation
exceeds the maximum stipulated
under Sec I as per the selected plan while adjudicating any claim
the benefits under ICU would have precedence over non ICU
Hospitalisation.
**** In case the Hospitalisation in ICU exceeds the per
Hospitalisation maximum limit of 10 days or the per Policy
period limit of 20 days, the remaining period of Hospitalisation
in ICU will be paid as per non ICU Hospitalisation benefits
subject to the overall Policy maximum of 30/ 60/ 90 or 180 days.
IV. A fixed amount towards convalescence for Hospitalisation
beyond 10 consecutive days which is payable only once per
Hospitalisation event. This benefit is payable only if there is an
admissible claim under any of the daily benefits.
C. EXCLUSIONS
We will not pay for any expenses incurred by You in respect of claims
arising out of or howsoever related to any of the following:
1 Benefits will not be available for Any condition, ailment or Injury or
related condition(s) for which You have been diagnosed, received
medical treatment, had signs and/or symptoms, prior to inception of
Your first Policy, until 48 consecutive months have elapsed, after
the date of inception of the first Policy with Us.
This Exclusion shall cease to apply if You have maintained the Policy
with Us for a continuous period of a 48 months, without break from
the date of Your first Hospital Cash Policy with Us.
The period of this exclusion would stand reduced if this Policy is a
continuous Renewal of an earlier Hospital cash/Daily allowance
Policy of the same per day benefit amount of another Insurer. The
period of exclusion would stand reduced by the period of continuous
existence of the earlier Policy with another Insurer of which this
Policy is a Renewal.
This Exclusion shall apply only to the extent of the amount by which
the benefit amount has been increased if the Policy is a Renewal of
a Hospital cash Policy without break in cover.
2 Without derogation from the above point no. (1), any
Hospitalisation during the first consecutive 24 months during which
You have the benefit of a Health Insurance Policy with Us in
connection with cataracts, benign prostatic hypertrophy, hernia of all
types, hydrocele, all types of sinuses, fistulae, hemorrhoids, fissure in
ano, dysfunctional uterine bleeding, fibromyoma, endometriosis,
hysterectomy, all internal or external tumors/ cysts/ nodules/ polyps
of any kind including breast lumps (except malignant conditions),
Surgery for prolapsed inter vertebral disc unless arising from
Accident, Surgery of varicose veins and varicose ulcers.
This exclusion Period shall apply for a continuous Period of 48 months
from the date of Your first Hospital Cash Policy with Us if the above
referred Illness were present at the time of commencement of the
Policy and if
You had declared such Illness at the time of proposing
the
Policy for the first time.
The period of this exclusion would stand reduced if this Policy is a
continuous Renewal of a earlier Hospital cash/ Daily allowance
Policy of the same per day benefit amount of another Insurer. The
period of exclusion would stand reduced by the period of continuous
existence of the earlier Policy with another Insurer of which this
Policy is a Renewal.
This Exclusion shall apply only to the extent of the amount by which
the benefit amount has been increased if the Policy is a Renewal of
a Hospital cash Policy without break in cover.

3 Without derogation from the above point No.(1), any
Hospitalisation during the first 12 months during which You have
the benefit of a Health Insurance Policy with Us in connection with
any types of gastric or duodenal ulcers, stones in the urinary and
biliary systems, Surgery on ears/ tonsils/ adenoids.
This exclusion period shall apply for a continuous period of 48 months
from the date of Your first Hospital Cash Policy with Us if the above
referred Illness were present at the time of commencement of the
Policy and if You had declared such Illness at the time of proposing
the Policy for the first time.
The period of this exclusion would stand reduced if this Policy is a
continuous Renewal of a earlier Hospital cash / Daily allowance
Policy of the same per day benefit amount of another Insurer. The
period of exclusion would stand reduced by the period of continuous
existence of the earlier Policy with another Insurer of which this
Policy is a Renewal.
This Exclusion shall apply only to the extent of the amount by which
the benefit amount has been increased if the Policy is a Renewal of
a Hospital cash Policy without break in cover.
4 Hospitalisation during the first consecutive 36 months during which
You have the benefit of the Policy with Us in connection with joint
replacement Surgery due to degenerative condition, Age related
osteoarthritis and Osteoporosis unless such joint replacement
Surgery is necessitated by accidental Bodily Injury.
This exclusion period shall apply for a continuous period of 48 months
from the date of Your first Hospital Cash Policy with Us if the above
referred Illness were present at the time of commencement of the
Policy and if You had declared such Illness at the time of proposing
the
Policy for the first time.
The period of this exclusion would stand reduced if this Policy
is a
continuous Renewal of a earlier Hospital cash/Daily allowance Policy
of the same per day benefit amount of another Insurer. The period
of exclusion would stand reduced by the period of continuous
existence of the earlier Policy with another Insurer of which this
Policy is a Renewal.
This Exclusion shall apply only to the extent of the amount by which
the benefit amount has been increased if the Policy is a Renewal of
a Hospital cash Policy without break in cover.
5 Hospitalisation for any Illness diagnosed or diagnosable within 30
days (1month), of the commencement of the Policy Period except
those incurred as a result of accidental Bodily Injury.
6 Injury or Disease directly or indirectly caused by or arising from or
attributable to War, Invasion, Act of Foreign Enemy, War like
operations (whether war be declared or not).
7 Circumcision unless necessary for treatment of a disease not
excluded hereunder or as may be necessitated due to an Accident.
8 Vaccination (unless post bite) inoculation, cosmetic treatments (for
change of life or cosmetic or aesthetic treatment of any description),
plastic Surgery other than as may be necessitated due to an
Accident or as a part of any Illness, refractive error corrective
procedures, Unproven/ Experimental treatment, investigational
or unproven procedures or treatments, devices and pharmacological
regimens of any description.
9 Dental Treatment or Surgery of any kind unless requiring
Hospitalisation as a result of Accidental Bodily Injury.
10 The treatment of obesity (including morbid obesity) and other weight
control programs, services and supplies.
11 Hospitalisation towards treatment of Illness/disease/condition
arising out of abuse of alcohol, substance or drugs.
12
Hospitalisation for General debility, “Run-down’’ condition or rest
cure, sexually transmitted disease, intentional self-Injury.
13 Hospitalisation for Invitro fertilization (IVF), Gamete intrafallopian
transfer (GIFT) procedures, and zygote intrafallopian transfer (ZIFT)
procedures, and any related prescription medication treatment;
embryo transport; donor ovum and semen, voluntary medical
termination of pregnancy; any treatment related to infertility and
sterilization.
14 Maternity expense for Hospitalisation or treatment arising from or
traceable to pregnancy, childbirth, miscarriage, abortion or
complications of any of this, including caesarian section. However,
this exclusion will not apply to abdominal operation for extra uterine
pregnancy (Ectopic Pregnancy).
15 Hospitalisation arising out of any condition directly or indirectly
caused to or associated with Human T-Cell Lymphtropic Virus type III
(HTLB-III) or Lymphadenopathy Associated Virus (LAV) or Human 5
Immunodeficiency Virus or the Mutants Derivative or Variations
Deficiency Syndrome or any Syndrome or condition of a similar kind
commonly referred to as AIDS.
16 Congenital Internal and /or external Illness/disease/defect anomaly.
17 Hospitalisation primarily for diagnostic, X-ray or laboratory
examinations not consistent with or incidental to the diagnosis and
treatment of the positive existence or presence of any ailment,
sickness or Injury, for which confinement is required at a Hospital/
Nursing Home.
18 Injury or Disease directly or indirectly caused by or contributed to by
nuclear weapons/materials.
19 Costs incurred on all methods of treatment including Alternative
treatments other than Allopathy.
20 Genetic disorders and stem cell implantation/surgery/storage.
21 Any Hospitalisation arising from Insured’s participation in any
hazardous activity including but not limited to scuba diving, motor
racing, parachuting, hang gliding, and rock or mountain climbing.
22 Any treatment received in convalescent home, health hydro, nature
care clinic or similar establishments.
23 Hormone replacement therapy, Sex change or treatment which
results from or is in any way related to sex change.
24 Any treatment including Surgery to remove organs from the donor in
case of a transplant surgery.
25 Hospitalisation for any mental Illness or psychiatric Illness.
26 Any
Hospitalisation received out of India.
D. CONDITIONS
1Due Care
Where this Policy requires You to do or not to do something, then
the complete satisfaction of that requirement by You or someone
claiming on Your behalf is a precondition to any obligation under this
Policy. If You or someone claiming on Your behalf fails to
completely satisfy that requirement, then We may refuse to consider
Your claim. You will cooperate with Us at all times.
2 Insured
Only those persons named, as the Insured in the Schedule shall be
covered under this Policy. The details of the Insured are as provided
by You. A person may be added as an insured during the Policy
Period after his application has been accepted by Us, an additional
premium has been paid and Our agreement to extend cover has been
indicated by it, issuing an endorsement confirming the addition of
such person as an Insured. Cover under this Policy shall be
withdrawn from any Insured upon that Insured giving 14 days written
notice to be received by Us.
3 Cost of pre-insurance medical examination
We will reimburse 50% of the cost of any pre-insurance medical
examination once the Proposal is accepted and the Policy issued for
that insured. We shall maintain a list of and the fees chargeable by,
institutions where such Pre-insurance medical examination may be
conducted, the reports from which will be accepted by Us. Such list
shall be furnished to the prospective policyholder at the time of pre-
insurance medical examination.
4 Communications
a) Any communication meant for Us must be in writing and be
delivered to Our address shown in the Schedule. Any
communication meant for You will be sent by Us to Your address
shown in the
Schedule.
b) All notifications and declarations for Us must be in writing and sent
to the address specified in the Schedule. Agents are not authorized
to receive notices and declarations on Our behalf.
c) You must notify Us
of any change in address.
5Claims Procedure
If You meet with any accidental Bodily Injury or suffer an Illness/
sickness that may result in a claim, then as a Condition Precedent to
Our liability, You must comply with the following:
a) You or someone claiming on Your behalf must inform Us in writing
immediately, and in any event within 48 hours of the aforesaid
Illness or Bodily Injury. You must immediately consult a Medical
Practitioner and follow the Medical Advice and treatment that he
recommends.
b) You must take reasonable steps or measures to minimise the
quantum of any claim that may be made under this Policy.
c) You shall expeditiously provide the Company with any and all
information and documentation in respect of the Hospitalisation.
The claim and/ Our liability hereunder that may be requested, and
You shall submit Yourself for examination by the Company’s
medical advisors as often as may be considered necessary by Us.
The cost of such medical examination will be borne by Us.
d) You or someone claiming on Your behalf must promptly and in any
event within 30 days of discharge from a Hospital give Us the
documentation (written details of the quantum of any claim along
with certified copies of discharge card, Hospital bill and receipt.)
and other information if We ask for, to investigate the claim or Our
obligation to make payment for it.
e) In the event of the death of the insured person, nominee claiming
on his/ her behalf must inform Us in writing immediately and send
Us a copy of the post mortem report (if any) within 14 days.
f) Mandatory necessary documents required to process claim are
i. Completely filled Future Hospi-Cash Claim form ( original )
ii.
Discharge certificate/ card from Hospital (photocopy)
iii. Final Hospital bill with receipt (photocopy)
g) The periods for intimation or submission of any documents as
stipulated under (d) and (e) will be waived in case of any hardships
being faced by the insured or his representative which is supported
by some documentation.
6 Settlement of Claims
i. Our
doctors will scrutinize the claims and flag the claim as
settled/ Rejected/ Pending within the period of 30 days of the
receipt of the last ‘necessary’ documents.
ii. Pending claims will be asked for submission of incomplete
documents.
iii. Rejected claims will be informed to the Insured Person in
writing with reason for rejection.
iv. Upon acceptance of an offer of settlement as stated in sub-
regulation (5) of the (Protection of Policyholders’ Interest)
Regulations, 2000 by You, We will make payment of the
amount due within 7 days from the date of acceptance of the
offer by the insured. In the cases of delay in the payment,
We shall be liable to pay interest at a rate which is 2% above
the bank rate prevalent at the beginning of the financial year.
7 Basis of claims payment
a) If You suffer a relapse within 45 days of the date when You last
obtained medical treatment or consulted a Medical Practitioner
and for which a claim has been made, then such relapse shall be
deemed to be part of the same claim.
b) If the claim event falls within two Policy periods, the claims shall be
paid taking into consideration the available sum insured in the two
Policy periods, including the Deductibles for each Policy period.
Such eligible claim amount to be payable to the insured shall be
reduced to the extent of premium to be received for the
Renewal/due date of premium of health insurance Policy, if not
received earlier.
c) We shall make payment in India in Indian Rupees only.
d) The Company shall only make payment under this Policy to the
Insured or in the event of death or total incapacitation of the
Insured to the Proposer/ Nominee. Any payment made in good faith
by the Company as aforesaid shall operate as a complete and final
discharge of the Company’s liability to make payment under this
Policy for such claim.
e) A continuous and completed period of less than 24 hours of
Hospitalisation or Day Care Treatment consequent upon an
insured event shall be deemed to be a continuous and completed
period of 24 hours if such period extends to at least 12 hours.
8Fraud
If You or any of Your Family member make or progress any claim
knowing it to be false or fraudulent in any way, then this Policy will
be void and all claims or payments due under it shall be lost and the
premium paid shall become forfeited.
9 Renewal & Cancellation
a) Your Policy shall be renewable lifelong except on grounds of fraud,
moral hazard or misrepresentation or non-cooperation by the
insured.
b) This Policy may be renewed by mutual consent every year and in
such event, the Renewal premium shall be paid to Us on or before
the date of expiry of the Policy or of the subsequent Renewal
thereof.
c) In case of 0ur own Renewal a Grace Period of 30 days is
permissible and the Policy will be considered as continuous for the
purpose of Two year waiting period/Four year waiting periods. Any
Hospitalisation as a result of
Accident/disease contracted during
the break period will not be admissible under the Policy
.
d) In case of Hospi-Cash Policy, there will be no loading on premium
for adverse claims experience (except for Group policies ) .
e) We may cancel this insurance by giving You at least 15 days
written notice, and if no claim has been made then We shall refund
a pro-rata premium for the unexpired Policy Period.
f) You may cancel this insurance by giving Us at least 15 days written
notice, and if no claim has been made then We shall refund
premium on short term rates for the unexpired Policy Period as per
the rates detailed below.
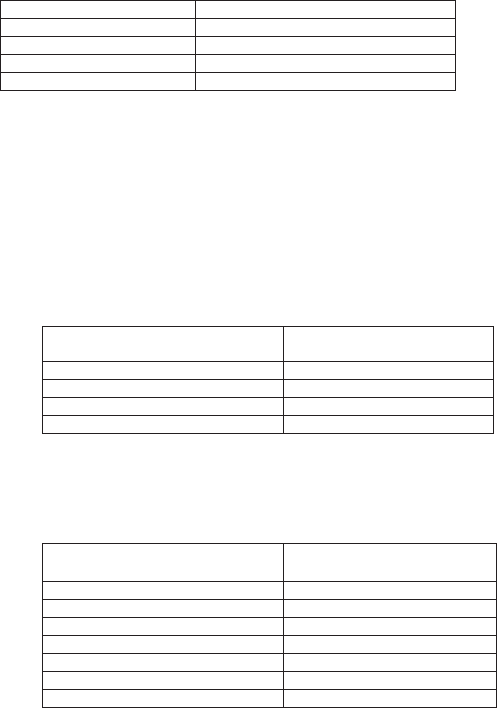
Period on risk
Rate of premium refunded
Up to one month
75% of annual rate
Up to three months
50%of annual rate
Up to six months
25% of annual rate
Exceeding six months
Nil
g) For Family floater policies, in the event of the death of any of the
insured members, the cover ceases to exist for that insured and the
remaining members would continue to have the coverage until the
end of the Policy period.
h) In case of group policies the following would apply
i. Discount Percentage for favorable claim ratio (BONUS):Low
claim Ratio Discount at the following scale will be allowed on
the Total premium at Renewal only, depending upon the
incurred claims ratio for the entire group insured under the
Group Future Hospi-cash Policy for upto preceding three
years.
Incurred Claim Ratio under
the Group Policy
Discount Percentage
(%)
Up to 20 %
20
21-35%
15
36-50%
10
51-55%
5
ii. Loading Percentage for high claim ratio (MALUS):The Total
Premium payable at Renewal of the group Policy will be
loaded at the following scale depending upon the incurred
claims ratio for the entire group insured under the Group
Hospi-cash Policy for upto preceding three years.
Incurred Claim Ratio under
the Group Policy
Loading Percentage
(%)
Between 71% and 80%
25
Between 81% and 100%
50
Between 101% and 125%
85
Between 126% and 150%
115
Between 151% and 175%
150
Between 176% and 200%
180
Over 200%
Cover to be reviewed
i) The brochure/ prospectus mentions the premiums as per the age
slabs/ Sum Insured and the same would be charged as per the
completed age at every Renewal. The premiums as shown in the
brochure/ prospectus are subject to revision as and when approved
by the regulator. However such revised premiums would be
applicable only from subsequent Renewals and with due notice
whenever implemented.
10 Free Look Period
a. The insured will be allowed a period of at least 15 days from the
date of receipt of the Policy to review the terms and conditions
of the Policy and to return the same if not acceptable.
b. If the insured has not made any claim during the free look
period, the insured shall be entitled to-
i. A refund of the premium paid less any expenses incurred by
the Insurer on medical examination of the insured persons
and the stamp duty charges or;
ii. where the risk has already commenced and the option of return
of the Policy is exercised by the policyholder, a deduction
towards the proportionate risk premium for period on cover or;
iii. Where only a part of the risk has commenced, such
proportionate risk premium commensurate with the risk
covered during such period.
11 Portability
i. Portability will be granted to policy holders of a similar
Hospital Cash Policy (Fixed daily benefit Policy) of another
Insurer to Future Hospi Cash Policy as per Portability
guidelines.
ii. Portability will be granted subject to the Policyholder desirous
of porting his Policy to Future Hospi Cash Policy applying to
Future Generali India Insurance Company Ltd at least 45 days
before the premium Renewal date of his/her existing Policy.
iii. We will not be liable to offer Portability if policyholder fails to
approach Us at least 45 days before the premium Renewal
date.
iv. Where the outcome of acceptance of Portability is still awaited
from Us on the date of Renewal the existing policyholder
should extend his existing Policy with the existing Insurer on
a short period basis as per the Portability guidelines.
v. Portability will be allowed for all individual Hospital Cash
policies (Daily Benefit policies) issued by non-life insurance
companies including Family floater policies
vi. Individual members, including the Family members covered
under Group Future Hospi Cash of Future Generali India
Insurance Company shall have the right to migrate from such a
group Policy to an individual Future Hospi Cash Policy or a
Family Floater Policy
with the same Insurer.
12 Dispute Resolution
a) Any and all disputes or differences, which may arise under or in
relation to this Policy, relating to the quantum of any claim, liability
otherwise being admitted, shall be referred to arbitration in
accordance with Arbitration and Conciliation Act, 1996, within a
period of 30 days of either the Company or the Insured giving notice
in this regard.
b) The applicable law in and of the arbitration shall be Indian law.
c) The expenses of the arbitrator shall be shared between the parties
equally and such expenses along with all reasonable costs in the
conduct of the arbitration shall be awarded by the arbitrator to the
successful party, or where no party can be said to have been wholly
successful, to such party, as substantially succeeded.
d) It is agreed a Condition Precedent to any right of action or suit
upon this Policy that an award by such arbitrator or arbitrators shall
be first obtained.
e) In the event that these arbitration provisions shall be held to be
invalid then all such disputes shall be referred to the exclusive
jurisdiction of the Indian Courts.
13 Compliance with Policy Provisions
Failure by You or the Insured Person to comply with any of the
provisions in this Policy may invalidate all claims hereunder.
14 Territorial Limits and Law
a) We cover Hospital Cash benefit due to Accidental Bodily Injury or
Sickness sustained by the Insured Person during the Policy Period
anywhere in India only.
b) The construction, interpretation and meaning of the provisions of
this Policy shall be determined in accordance with Indian Law.
c) The Policy constitutes the complete contract of insurance. No
change or alteration shall be valid or effective unless approved in
writing by Us, for which approval shall be evidenced by an
endorsement on the Schedule.
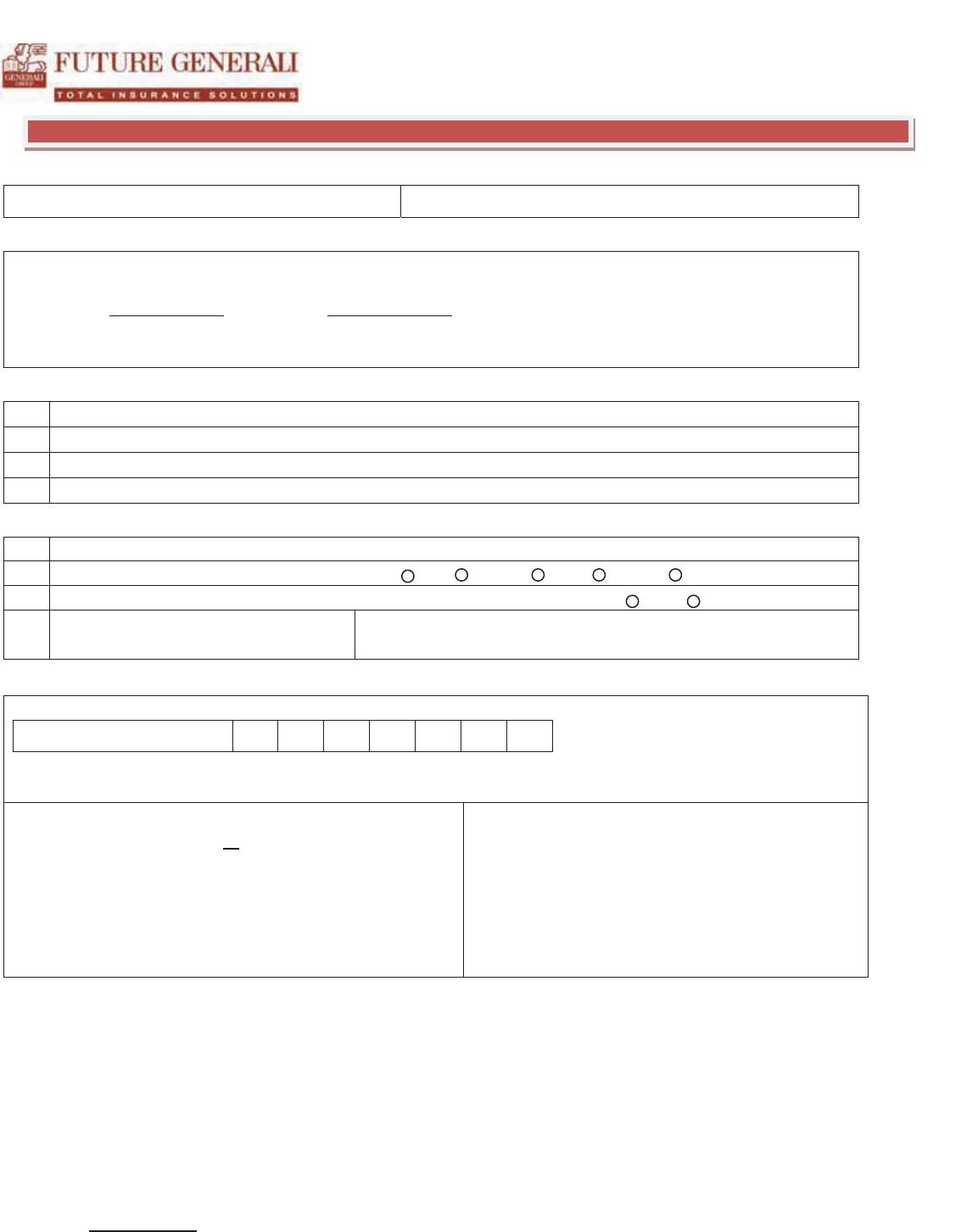
HEALTH INSURANCE CLAIM FORM
ALL FIELDS IN THIS FORM ARE MANDATORY AND THE CLAIM WILL BE NOT BE PROCESSED IF ANY OF THE DETAILS ARE MISSING
Claim Number (For FGH Use Only)
POLICY / INSURED DETAILS
Policy No : _______________________________________________ Health Card No. of Patient ____________________________________________
Policy Start Date
_________________ Policy End Date __________________ Date of Joining the Policy
__________________________________
Corporate Name : ________________________________________________(Only for Group Policies) Employee ID ________________
_________
PERSONAL DETAILS OF EMPLOYEE/PROPOSER
1
Name of the Employee / Individual:
2
E
-Mail address of the Employee/Individual:
3
Mobile No:
4
Permanent Account Number (PAN):
CLAIMANT / PATIENT DETAILS
1
Name of the Patient:
2
Relationship with the Employee / Proposer Self Spouse Child Parent Others _________________
3
Date of Birth of Claimant: _______________________ Age _____________________ Years Gender Male Female
4
Residential Address
CLAIM DETAILS
CONSENT REQUIREMENT FOR ACCESS TO TREATMENT PAPERS / INDOOR CASE SHEETS / MEDICAL RECORDS / INVESTIGATOR VISIT
I hereby authorize Future Generali India Insurance or any agency / individual authorized by them to obtain copies or review in person all my medical records
including but not limited to admission notes, treatment sheets, indoor case papers, investigation reports, prescriptions and all other documents present in the
hospital case file. Details related to my past hospitalisations in your hospital can also be provided / shown to Future Generali or its authorized representatives. I
agree that all information provided above by me in the claim documents is true and that if I have provided any false or untrue information, my right to claim the
reimbursement of expenses shall be absolutely forfeited.
Name of Patient / Relative: ______________________________________________________
Relationship with Patient: ______________________________________________________
Signature of Patient / Relative: __________________________________________________
Date: DD_/_MM_/_YYYY
Total Claimed Amount: B
Claimed Amount in Words: Rupees ( B____________________________________________________________________________________________
1. Diagnosis
______________________________________
_________________
2.
Admission Date: _______________ __Discharge Date :
_________________
3
. Name of Treating Doctor: ______________________________________
___
4. Mobile No.
of Treating Doctor
: _____________________________________
5.
Name of Family Physician: ________________________________________
6. Mobile No.
of Family Physician: ___________________________________
Enclosure Check List :
1. Original Discharge Summary containing all relevant details
2. All Original Bills and their Receipts
3. Copies of all Reports & prescriptions
4. First Prescription / Consultation Letter from your Doctor.
5.
Original Money Receipt duly signed with a Revenue Stamp.
6.
Copy of Proposer/Employee Photo ID Proof & Address Proof
TOLL FREE PHONE: 1800 103 8889
TOLL FREE FAX: 1800 103 9998
E MAIL: fgh@futuregenerali.in
Please attach this form in Original to the hospital bill and other claim documents. Separate claim form required for each claim. PLEASE ENCLOSE A PHOTOCOPY OF THE
FUTURE GENERALI HEALTH ID CARD.
AUTHORIZATION FOR TRANSFER OF CLAIM AMOUNT BY NATIONAL ELECTRONIC FUND TRANSFER
Name as per Bank Account
Bank Name
Branch Name & Address
Branch Phone No.
Branch MICR Code
Branch IFSC Code for NEFT
( Please attach a Photocopy of a cheque or a blank cheque of your bank duly cancelled for ensuring accuracy of the bank name, branch name, account
number & name of account holder printed)
Account Type (Please Tick)
Savings Current Cash / Credit
Account No. (as appearing in
Cheque Book)
HR Authorization & Stamp
Bank Authorization & Stamp
Date from which the mandate should be effective: _______________________
I hereby declare that the particulars given above are correct and complete and request you to remit any amount due to me, if any to the aforesaid bank account. I
herewith further declare that if any transaction is delayed or not effected at all or is wrongly credited to any other account for reasons of incomplete or incorrect
information as provided above, I shall not hold Future Generali India Insurance Company Ltd (“Company“) or any of its directors, employees or agents responsible
for the same. I also declare that the remittance of any dues to the aforesaid bank account shall be considered as full and valid discharge of its obligations by the
company. I also undertake to advise any change in the particulars of my bank account to facilitate updation of records for the purpose of credit of any amount
due, through NEFT.
Name of Employee / Proposer: ____________________________________ Signature of Employee / Proposer: _______________________ Policy No.
__________________________________ Claimant Name: ____________________________________ Date: __________________
FEEDBACK AND SUGGESTIONS
We thank you for choosing Future Generali as your Insurance provider. We always strive to ensure that our service levels exceed our customer’s expectations. In
the spirit of this endeavour, we will greatly appreciate your valuable inputs and feedback. Kindly provide your feedback on your experience with Future Generali
and any suggestions for improving our services. We value your time and promise to evaluate your suggestions for improvement of our service.
---------------------------------------------------------------------------------------------------------------------------------------------------------------------------------------------------
---------------------------------------------------------------------------------------------------------------------------------------------------------------------------------------------------
---------------------------------------------------------------------------------------------------------------------
-------------------------------------------------------------------------------------------------------------------------------------------------------------------------
---------------------------------------------------------------------------------------------------------------------------------------------------------------------------------------------------
Future Generali India Insurance Company Limited
Registered office address : Indiabulls Finance Centre, Tower 3, 6th Floor, Senapati Bapat Marg, Elphinstone (W), Mumbai - 400 013
Corporate Identity No (CIN): U66030MH2006PLC165287 Telephone No 022 4097 6666 and Fax No 22 4097 6900
Email: fgcare@futuregenerali.in website address www.futuregenerali.in FGH-CF-02
TOLL FREE PHONE: 1800 103 8889
TOLL FREE FAX: 1800 103 9998
E
MAIL: fgh@futuregenerali.in
Grievance Redressal Procedures
Dear Customer,
At Future Generali we are committed to provide “Exceptional Customer-Experience” that you remember and return to fondly. We encourage
you to read your policy & schedule carefully. We want to make sure the plan is working for you and welcome your feedback.
What Constitutes a Grievance?
A “Grievance/Complaint” is defined as any communication that expresses dissatisfaction about an action or lack of action, about the
standard service/deficiency of service from Future Generali or its intermediary or asks for remedial action.
If you have a complaint or grievance you may reach us through the following avenues:
Help
- Lines
1800-220-233 /
1860-500-3333 /
022-67837800
Email
Fg
care@futuregenerali.in
Website
www.futuregenerali.in
GRO at each Branch
Walk
-in to any of our branches and request to meet the Grievance Redressal Officer (GRO).
What can I expect after logging a Grievance?
x We will acknowledge receipt of your concern within 3 - business days.
x Within 2 - weeks of receiving your grievance, we shall revert to you the final resolution.
x We shall regard the complaint as closed if we do not receive a reply within 8 weeks from the date of receipt of response.
What do I do, if I am unhappy with the Resolution?
x You can write directly to our Customer Service Cell at our Head office::
Customer Service Cell
Customer Service Cell, Future Generali India Insurance Company Ltd.
Corporate & Registered Office:
- 6th Floor, Tower 3, Indiabulls Finance Center,
Senapati Bapat Marg, Elphinstone Road, Mumbai – 400013
Please send your complaint in writing. You can use the complaint form, annexed with your
policy.
Kindly quote your policy number in all communication with us. This will help us to deal with the matter faster.
How do I Escalate?
While we constantly endeavor to promptly register, acknowledge & resolve your grievance, if you feel that you are experiencing difficulty in
registering your complaint, you may register your complaint through the IRDA (Insurance Regulatory and Development Authority).
x CALL CENTER: TOLL FREE NUMBER (155255).
x REGISTER YOUR COMPLAINT ONLINE AT: HTTP://WWW.IGMS.IRDA.GOV.IN/
Insurance Ombudsman:
If you are still not satisfied with the resolution to the complaint as provided by our GRO, you may approach the Insurance
Ombudsman for a review. The Insurance Ombudsman is an organization that addresses grievances that are not settled to your
satisfaction. You may reach the nearest insurance ombudsman office. The list of Insurance Ombudsmen offices is as mentioned below.
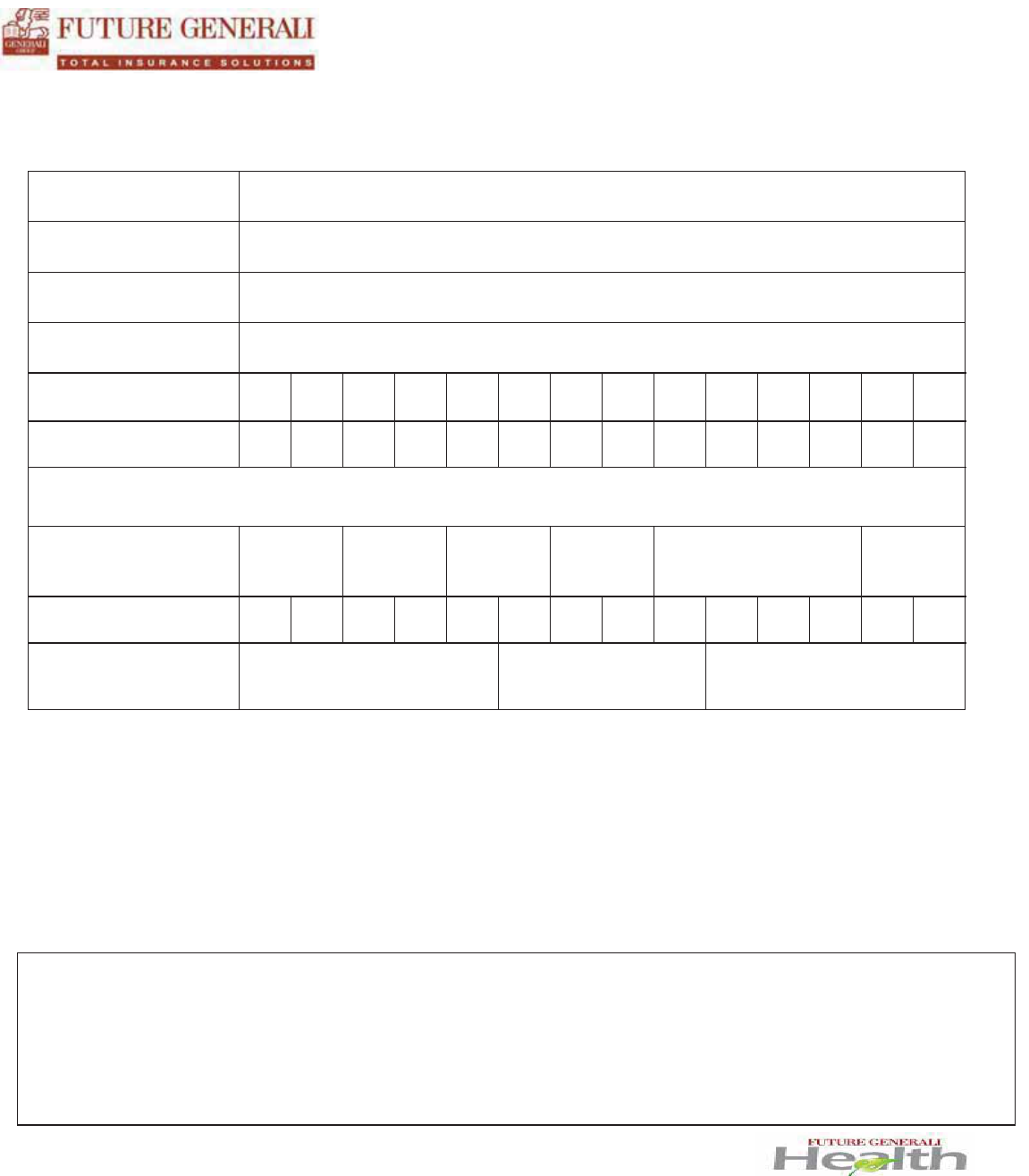
Office of the
Ombudsman
Contact Details
Areas of Jurisdiction
AHMEDABAD
Insurance Ombudsman Office of the Insurance Ombudsman
2nd Floor, Ambica House, Nr. C.U.Shah College, 5, Navyug Colony, Ashram Road,
AHMEDABAD -
380 014
Tel: 079- 27546840 Fax: 079-27546142 E-mail: ins.omb@rediffmail.com
Gujarat, UT of Dadra &
Nagar Haveli, Daman and
Diu
BHOPAL
Insurance Ombudsman Office of the Insurance Ombudsman
Janak Vihar Complex, 2nd Floor, 6, Malviya Nagar, Opp. Airtel, Near New Market,
BHOPAL - 462 023
Tel: 0755-2569201 Fax: 0755-2769203 E-mail: bimalokpalbhopal@airtelmail.in
Madhya Pradesh &
Chhattisgar
h
BHUBANESHWA
R
Insurance Ombudsman Office of the Insurance Ombudsman
62, Forest Park,
BHUBANESHWAR - 751 009
Tel: 0674-2596455 Fax: 0674-2596429 E-mail: ioobbsr@dataone.in
Orissa
CHANDIGARH
Insurance Ombudsman Office of the Insurance Ombudsman
S.C.O. No.101, 102 & 103, 2nd Floor, Batra Building, Sector 17
-D, CHANDIGARH - 160 017
Tel: 0172-2706468 Fax: 0172-2708274 E-mail: ombchd@yahoo.co.in
Punjab, Haryana, Himachal
Pradesh, Jammu &
Kashmir, UT of Chandigarh
CHENNAI
Insurance Ombudsman Office of the Insurance Ombudsman
Fatima Akhtar Court, 4th Floor, 453 (old 312), Anna Salai, Teynampet,
CHENNAI - 600 018
Tel:044
Tamilnadu, UT- Pondicherry
Town and Karaikal
(which are part of UT of
Pondicherry)
NEW DELHI
Insurance Ombudsman Office of the Insurance Ombudsman
2/2 A, Universal Insurance Bldg. Asaf Ali Road,
NEW DELHI - 110 002
Tel: 011-23239633 Fax: 011-23230858 E-mail: iobdelraj@rediffmail.com
Delhi & Rajashthan
GUWAHATI
Insurance Ombudsman Office of the
Insurance Ombudsman
Jeevan Nivesh, 5th floor Nr. Panbazar Overbridge, S.S. Road,
GUWAHATI - 781 001
Tel:0361
-2132204/5 Fax: 0361-2732937 E-mail: ombudsmanghy@rediffmail.com
Assam, Meghalaya,
Manipur,
Mizoram,
Arunachal Pradesh,
Nagaland and Tripura
HYDERABAD
Insurance Ombudsman Office of the Insurance Ombudsman
6
-2-46 , 1st Floor, Moin Court Lane, Opp. Saleem Function Palace, A.C.Guards, Lakdi-Ka-Pool,
HYDERABAD
- 500 004
Tel: 040-65504123 Fax: 040-23376599 E-mail: insombudhyd@gmail.com
Andhra Pradesh, Karnataka
and UT of Yanam
-
a part of
UT of Pondicherry
ERNAKULAM
Insurance Ombudsman Office of the Insurance Ombudsman
2nd Floor, CC 27/2603, Pulinat Building, Opp. Cochin Shipyard, M.G. Road,
ERNAKULAM - 682 015
Tel: 0484
-2358759 Fax: 0484-2359336 E-mail: iokochi@asianetindia.com
Kerala, UT of
(a) Lakshadweep,
(b) Mahe
- a part of UT of
Pondicherry
KOLKATA
Insurance Ombudsman Office of the Insurance Ombudsman
4
th
Floor, Hindusthan Bldg., Annexe, 4, C.R.Avenue, KOLKATA - 700 072
Tel: 033
-22124346 / (40) Fax: 033-22124341 E-mail : [email protected]n
West Bengal, Bihar,
Jharkhand and UT of
Andeman & Nicobar
Islands, Sikkim
LUCKNOW
Insurance Ombudsman Office of the Insurance Ombudsman
Jeevan Bhawan, Phase 2, 6th Floor, Nawal Kishore Road, Hazratganj,
LUCKNOW - 226 001
Tel: 0522
-2231331 Fax: 0522-2231310 E-mail: insombudsman@rediffmail.com
Uttar Pradesh and
Uttaranchal
MUMBAI
Insurance Ombudsman Office of the Insurance Ombudsman
Jeevan Seva Annexe, 3rd Floor, S.V.Road, Santacruz (W),
MUMBAI - 400 054
Tel: 022-26106928 Fax: 022-26106052 E-mail: ombudsmanmumbai@gmail.com
Maharashtra, Goa
The updated details of Insurance Ombudsman are available on IRDA website: www.irda.gov.in, on the website of General Insurance Council:
www.generalinsurancecouncil.org.in, our website www.futuregenerali.in
or from any of our offices.
Form for Request / Complaint / Feedback / Appreciation
I want to submit a REQUEST COMPLAINT SUGGESTION / FEEDBACK APPRECIATION
POLICY TYPE MOTOR HEALTH PERSONAL ACCIDENT OTHER
POLICY DETAILS POLICY NO CLAIM NO COVER NOTE HEALTH CARD EXISTING SERVICE REQUEST
CUSTOMER NAME
FIRST NAME MIDDLE NAME LAST NAME
ADDRESS
CITY PIN CODE
TEL NO. MOBILE NO.
Detailed description
D
D M
M
YYYY
Customer’s Signature Date
You may submit the form to the Nearest Branch Office or mail it to our Customer Service Cell at:
Customer Service Cell
Future Generali India Insurance Company Ltd.
Corporate & Registered Office: - 6th Floor, Tower 3, Indiabulls Finance Centre, Senapati Bapat Marg, Elphinstone Road, Mumbai – 400013
Care Lines: 1800-220-233 / 1860-500-3333 / 022-6783 7800 Email: fgcare@futuregenerali.in Website: www.futuregenerali.in
Office Use Only: Service / Case #
Comments:
