
Health Plan
Shopping Guide
1
Use this guide to help you choose a health insurance plan
through the Massachusetts Health Connector.
Step 1: Know which plans you qualify for
First, you’ll need to know which plans are available to you. If you applied
online, you’ll be able to see your plan choices after you complete your
application and click the Find a Plan button. If you applied by paper
application or by phone, you can search for plans available in your area by
going to MAhealthconnector.org and clicking on Browse Plans halfway
down the homepage. You can also call Customer Service.
Step 2: Compare costs
The total cost of your coverage will include your monthly premium payments
and your out-of-pocket costs. In general, the lower your monthly premium, the
higher your out-of-pocket costs will be when you get covered services. You can
nd a list of benets included in all Health Connector plans on page 4.
Our plans are organized by metallic tiers (levels) to make plan premiums
and out-of-pocket costs easier to compare. Learn more about metallic tiers
on page 5.
Use our worksheet on page 3 to see how much your out-of-pocket costs might
be, based on health services you think you’ll need during the plan year.
Step 3: Check the providers and prescription medicines
covered by plans
Once you’ve narrowed your plan choices down, check to see if providers you
want to use for care (such as doctors, hospitals, or health centers) and any
prescription medicines you need are covered by a plan before you enroll. To
nd out which plans cover your providers and medicines, use our online tool
at PlanFinder.MAhealthconnector.org.
Step 4: Choose your new plan and enroll!
After you’ve learned more about a plan’s costs and checked to see if
the providers you want are in its network, you will need to complete your
enrollment. You can enroll online at MAhealthconnector.org, or call
Customer Service to enroll by phone. After you choose a plan, you’ll need
to pay your rst premium to complete enrollment. Payment is always due
by the 23rd of the month before your coverage begins.
Questions to help you get started
Answer the questions below before you start shopping for health insurance. Your answers
will help you decide which health plans are best for you and your family. Your answers will
also help you know how much you might have to pay in out-of-pocket costs for the year.
1. Think about how often you and anyone on your
plan usually access health care services. Health
care services are things like going to the doctor, or
having an operation. Write down how many times
a year you expect to:
Visit a Primary Care Physician (PCP)
__________
Visit a specialist __________
Have tests, like blood tests or MRIs,
as part of managing a chronic condition
__________
Have a planned surgery, birth,
or other procedure
__________
If you get health care services often, you may
want to choose a plan with a higher monthly
premium, but lower out-of-pocket costs.
2. Do you have prescription medications that you
and anyone on your plan take regularly? If so, for
each medicine write:
Medicine 1 exact name _____________________
The number of pills or dose that you have
lled at the pharmacy each month
_________________
Medicine 2 exact name _____________________
The number of pills or dose that you have
lled at the pharmacy each month
_________________
Medicine 3 exact name _____________________
The number of pills or dose that you have
lled at the pharmacy each month
_________________
Medicine 4 exact name _____________________
The number of pills or dose that you have
lled at the pharmacy each month
_________________
Make sure that any plan you are interested
in covers all of your medicines and nd out
what their costs will be. You can nd this
information with our online tool at:
PlanFinder.MAhealthconnector.org
3. Are there any doctors or specialists that you
or anyone on your plan will want to be able to see
for appointments? If so, list those doctors here.
___________________________________________________________
___________________________________________________________
___________________________________________________________
___________________________________________________________
___________________________________________________________
___________________________________________________________
4. Do you have a hospital or health center that you
or anyone on your plan will want to be able to go
to if you need care? If so, what is the name of the
hospital or health center?
___________________________________________________________
___________________________________________________________
___________________________________________________________
Before you enroll in a plan, check to make
sure the providers (like doctors and hospitals)
you want are in the plan's network. You can
nd this information with our online tool at:
PlanFinder.MAhealthconnector.org
2
3
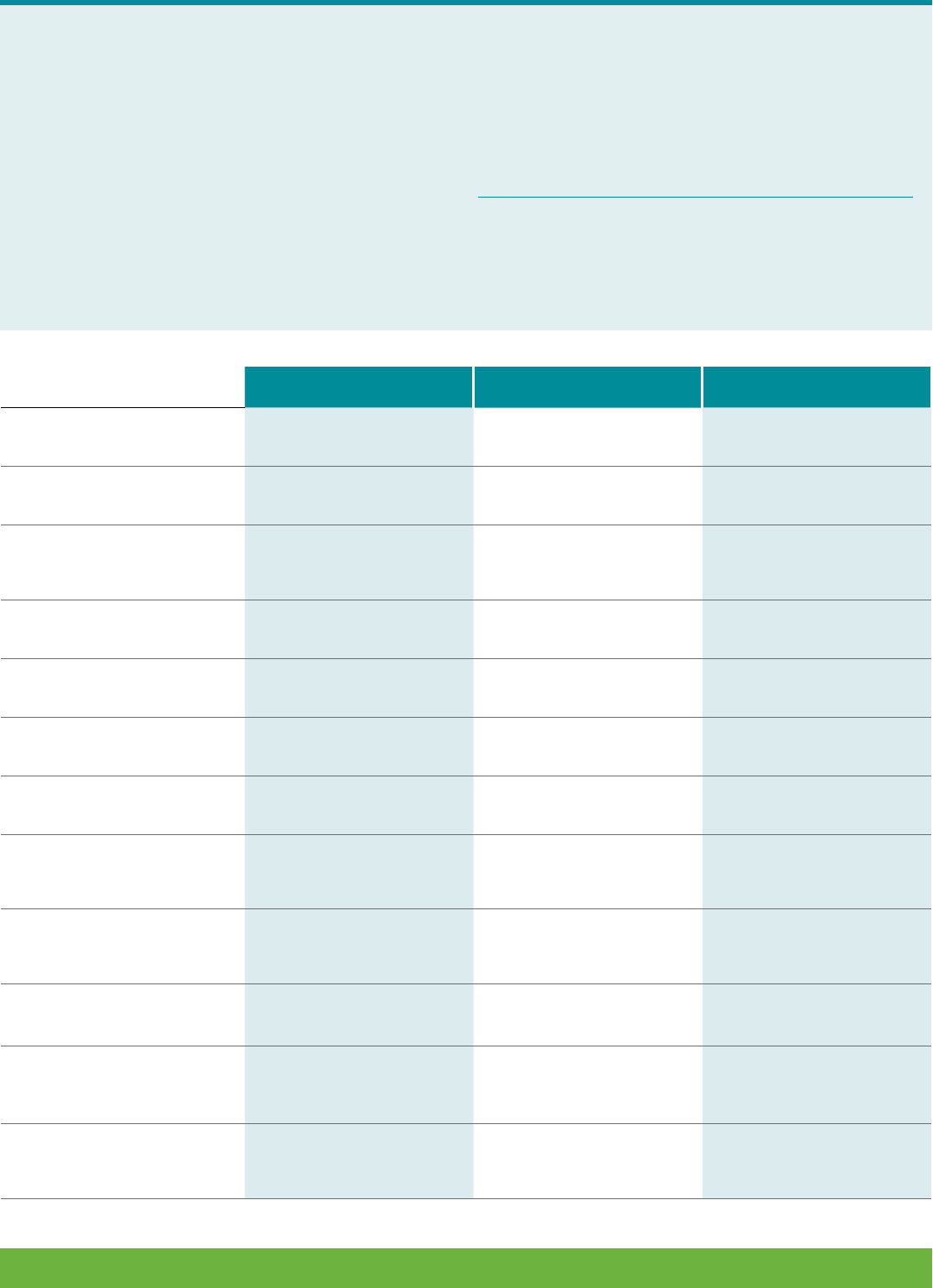
Compare your choices
Use this chart to compare up to three plans.
Use the rest of this guide to answer questions you
have while you are lling out the chart.
To ll out the chart, you’ll need to look at the
Summary of Benets and Coverage (SBC) for each
plan. You can nd the summaries on the plans’
websites, as well as MAhealthconnector.org on the
Plan Information page of the website's Learn section.
You will also need to know if your providers are in
the plans. You can nd out by using our online tool at
PlanFinder.MAhealthconnector.org.
You can also check the insurer's (insurance company)
website or call the insurer directly.
To help you gure out-of-pocket costs for the year
with different plans, you can multiply the co-pays
you list below for each plan by the number of visits
or prescriptions that you listed on page 2.
Plan A Plan B Plan C
Name of plan
Monthly premium
Are the providers and
hospitals you want in the
plan network?
Yes No Yes No Yes No
Deductible amount
Maximum out-of-pocket
(MOOP) amount
Is dental coverage included?
Yes No Yes No Yes No
Is there co-insurance for any
services you may need?
Yes No Yes No Yes No
¡ If you answered “Yes”
above, how much
is the co-insurance?
How much are co-pays for
visits to a Primary Care
Physician (PCP)?
How much are co-pays for
visits to specialists?
Are the prescription
medications you take
covered by this plan?
Yes No Yes No Yes No
¡ If yes, how much is
the co-pay for the
prescriptions you need?

Answers to help you choose a plan
These commonly asked questions can help you understand the different plans and costs,
and help you decide which plan is right for you.
1. What benets do the health plans cover?
All of the health plans you can choose through
the Health Connector offer these health benets:
¡ Outpatient care
–
Treatment you get without
being admitted to a hospital
¡ Inpatient care
–
Treatment you get in the hospital
¡ Emergency room treatment
¡ Prenatal/postnatal care
–
Care before and after your
baby is born
¡ Mental health and substance use disorder
services
–
This includes behavioral health treatment,
counseling, and psychotherapy
¡ Prescription drugs
¡ Services and items to help you recover if you are
injured, or have a disability or chronic condition
–
This includes physical and occupational therapy,
speech-language pathology, psychiatric rehabilitation,
and more
¡ Lab tests, such as bloodwork or Pap smears
¡ Preventive services
–
Services to help keep you
healthy, like counseling, screenings, vaccines,
and routine eye exams
¡ Pediatric services
–
Services for children, including
vision care
2. How do the health plans differ?
Differences between plans include:
¡ Which health insurance company offers the plan
¡ Provider networks (the doctors, hospitals, and
other providers in the plan)
¡ Costs, including monthly premium, and
out-of-pocket costs like co-pays and deductible
In Questions to help you get started, you wrote the
names of doctors and hospitals you want in the plan
you choose. Before you enroll in a plan, use our online
tools at PlanFinder.MAhealthconnector.org to make sure
the providers you want and the prescription drugs you
need are in the plan’s network.
You can also call the insurance company directly for this
information.
When you search or call an
insurance company to ask
about a provider, be sure to
give the plan’s full name. For
example, say:
“Fallon Health Select Care
Platinum Connector” and not
just “Fallon Health.”
3. What kinds of costs do health plans have?
There are ve kinds of costs in health plans:
¡ Premium: This is the cost you pay each month, whether
or not you use health care services. You will pay
your monthly premium bill to the Health Connector. The
premium is always due by the 23rd of the month.
¡ Deductible: This is the total cost you must pay in
a plan year before your plan will pay for part or all of
your services.
¡ Co-pay: This is the cost you pay at the time you get
certain health care services. Usually, you start to pay
co-pays after you meet your deductible.
¡ Co-insurance: If a health care service has co-
insurance,
you pay a percentage (part) of the cost for that service.
Usually, you start to pay co-insurance after you meet
your deductible. It is not a xed cost like a co-pay. The
amount depends on the total cost of the service.
¡ Maximum out-of-pocket cost (MOOP): This is the
most you pay in one year for health care services.
Once you have paid this amount, your plan pays for all
of your covered services for the rest for the year.
4. What is the difference between Platinum,
Gold, Silver and Bronze health plans?
The Health Connector’s plans are in tiers (levels) named
after metals. The metallic tiers are Platinum, Gold,
Silver and Bronze. The tiers make it easier for
you to compare the plans.
4
Here’s how it works:
¡ Platinum and Gold plans have the highest premiums
(monthly cost) but the lowest costs (deductibles
and co-pays) when you get health care services.
¡ Silver plans have premiums that are usually lower
than Gold plans but have higher costs when you get
health care services.
¡ Bronze plans have the lowest premiums but the
highest costs when you get health care services.
5. What is Catastrophic coverage?
Catastrophic plans are only available to certain people.
To qualify, you must be less than 30 years old or
have a qualifying hardship exemption from the federal
government. Catastrophic plans only cover you in
a major health event. They have very high deductibles.
You must pay for almost all of your health care until
you reach the deductible. If you enroll in a Catastrophic
plan you will not be able to get help paying for your
coverage, even if you would otherwise qualify.
6. Which metallic tier (Platinum, Gold, Silver or
Bronze) should I choose?
To choose a tier, think about how often you use health
care services. You may want to pay less each month
and pay more when you get care. Or you may want to pay
more each month and pay less when you get care.
A Platinum or Gold plan may be best for you if:
¡ You have a chronic condition (like diabetes) or think
you will use a lot of health care services (like going to
the doctor, getting a prescription lled, or having an
operation).
¡ You would rather pay a higher premium each month
so you pay less in co-pays and co-insurance when you
use health care services.
A Silver plan may be best for you if:
¡ You use some health care services and don’t
want to pay very high out-of-pocket costs when
you get care.
A Bronze plan may be best for you if:
¡ You do not use many health care services, except for
preventive care.
¡ You would rather pay less for your premium each
month and pay more when you use health care
services.
¡ You can afford to pay a high deductible and high
out-of-pocket costs if you need care.
7. What is a Health Savings Account (HSA)?
A Health Savings Account (HSA) is a way to set aside
money before taxes, to use for certain medical costs.
A few plans available through the Health Connector
are "HSA compatible," which means that you may be able
to set up an HSA if you are enrolled in one of
those plans. You can usually set up an HSA at a nancial
institution, like a bank. To learn more about HSAs, go
to IRS.gov and type "HSA" in the search tool.
8. How do I compare my choices?
Once you choose a metallic tier (Platinum, Gold, Silver or
Bronze) it will be easier to compare your plan choices.
If you are shopping for a plan at MAhealthconnector.org,
you can choose up to three plans to compare online.
9. What does Limited or Smaller Network mean?
A Limited or Smaller Network is a plan with fewer
providers and lower premiums than other plans offered
by the same insurer (insurance company). When you
shop for plans online, you will see “Network Note”
appear if you are looking at one of these plans. It may
be a good choice for you if it has the providers you want.
Before you enroll, use the Find a Provider tool to see if
your providers are in the plan.
Answers to help you choose a plan (continued)
CO-PAYS AND
DEDUCTIBLES
PREMIUMS
Usually, the lower the premium,
the more you have to pay when you
get health care services.
5

Co-insurance
If a health care service has co-insurance, you pay a
percentage (part) of the cost for that service. Usually,
you start to pay co-insurance after you meet your
deductible. It is not a xed cost like a co-pay. The amount
you pay depends on the total cost of the service.
Co-pay
A xed price you pay when you get certain health care
services. Not all services require a co-pay.
Deductible
The total amount you must pay in a plan year before
your plan will pay for part or all of your services. Some
services may not have a deductible. They may be free
or just have a co-pay, even though you haven't met the
deductible yet.
HMO
HMO stands for Health Maintenance Organization. If you
choose a plan that is an HMO, you must use in-network
providers in order to get your services covered. If you go
to an out-of-network provider, the plan won’t cover the
cost of your care, except in an emergency.
If you enroll in an HMO, you will also need to choose
a primary care provider (PCP). You may need to get
a referral from your PCP if you need care from specialists.
Most of the plans offered through the Health Connector
are HMOs.
Maximum out-of-pocket cost (MOOP)
The most you pay in one year for health care services.
Once you pay this, your plan pays for all of your covered
services for the rest of the year. You still need to pay your
premium each month.
Premium
The amount you pay each month for your health
insurance. You must pay your premium every month,
whether or not you use health care services. The
Health Connector will send you a bill for your premium
each month. The premium will always be due by the 23
rd
of the month.
Primary Care Physician (PCP)
The doctor who gives you health care and services,
such as referrals to specialists. If you enroll in an HMO
or EPO, you will need to choose a PCP.
Provider network
A provider network is a group of doctors, hospitals and
other providers that works with the health plan to give
you care. Each plan has a network. There are different
types of networks.
¡ In-network means the provider is part of the health
plan network. If you get care from an in-network
provider, it will cost you less.
¡ Out-of-network means the provider is not part of
the health plan network. If you get care from an
out-of-network provider, your plan may not pay for
those services and you could have to pay all or
part of the cost yourself.
Standardized Plans
We offer standardized plans within each metallic tier
(level). Standardized plans have a set of 21 major
benets with the same out-of-pocket costs, to make
them easier to compare.
Non-standardized plans can have varying out-of-pocket
costs for all benets and are also offered within each
metallic tier. If you see the word "Standard" in a plan
name, it means that the benets are standardized
and the plan may be easier to compare with other
standardized plans in the same metallic tier.
Glossary of Terms
Below is a list of terms you will see and hear when choosing your health plan. These terms
may be new to you. Learning them will help you better understand your health insurance.
Questions? Visit MAhealthconnector.org or call 1-877 MA ENROLL (1-877-623-6765)
or TTY: 1-877-623-7773.
6
