
FI N A L REPORT
Effects of the Affordable Care Act on
Safety Net Hospitals
November 2016
Laurie Felland
Peter Cunningham*
Annie Doubleday
Cannon Warren
Submitted to:
The Assistant Secretary for Planning and Evaluation
United States Department of Health and Human Services
200 Independence Avenue, SW
Washington, DC 20201
Project Officer: Andrew Sommers, PhD
Contract Number: HHSP23320095642WC/HHSP23337039T
Submitted by:
Mathematica Policy Research
1100 1st Street, NE
12th Floor
Washington, DC 20002-4221
Telephone: (202) 484-9220
Facsimile: (202) 863-1763
Project Director: Laurie Felland, MS
*Virginia Commonwealth University


iii
CONTENTS
I. INTRODUCTION / EXECUTIVE SUMMARY ................................................................................... 1
II. OVERVIEW OF PROJECT OBJECTIVES AND PROCESS ........................................................... 3
A. Policy context............................................................................................................................. 3
B. Project team............................................................................................................................... 3
C. Planning stage ........................................................................................................................... 4
D. Conceptual framework ............................................................................................................... 4
E. Study scope and methodology .................................................................................................. 5
F. Dissemination of findings ........................................................................................................... 6
III. KEY FINDINGS ................................................................................................................................ 7
A. Summary ................................................................................................................................... 7
B. Changes in patient volumes and mix ........................................................................................ 7
C. Experiences with alternative payment models and value-based payment initiatives .............. 12
D. Financial impacts ..................................................................................................................... 17
E. Additional observations about differences between the 2014 and 2015 semi-
structured discussions ............................................................................................................. 23
1. Quantitative findings.......................................................................................................... 23
2. Qualitative findings ............................................................................................................ 24
F. Limitations and challenges ...................................................................................................... 24
IV. CONCLUSIONS ............................................................................................................................. 27
APPENDIX 1: CONCEPTUAL FRAMEWORK .......................................................................................... 28
APPENDIX 2: TABLE OF HOSPITAL CHARACTERISTICS .................................................................... 32
APPENDIX 3: METHODOLOGY OVERVIEW ........................................................................................... 36
APPENDIX 4: FINANCIAL TABLE TEMPLATE......................................................................................... 45
APPENDIX 5: 10 SITE SUMMARIES ........................................................................................................ 49
APPENDIX 6: HOSPITAL PERFORMANCE ON CMS QUALITY MEASURES ........................................ 94

v
FIGURES
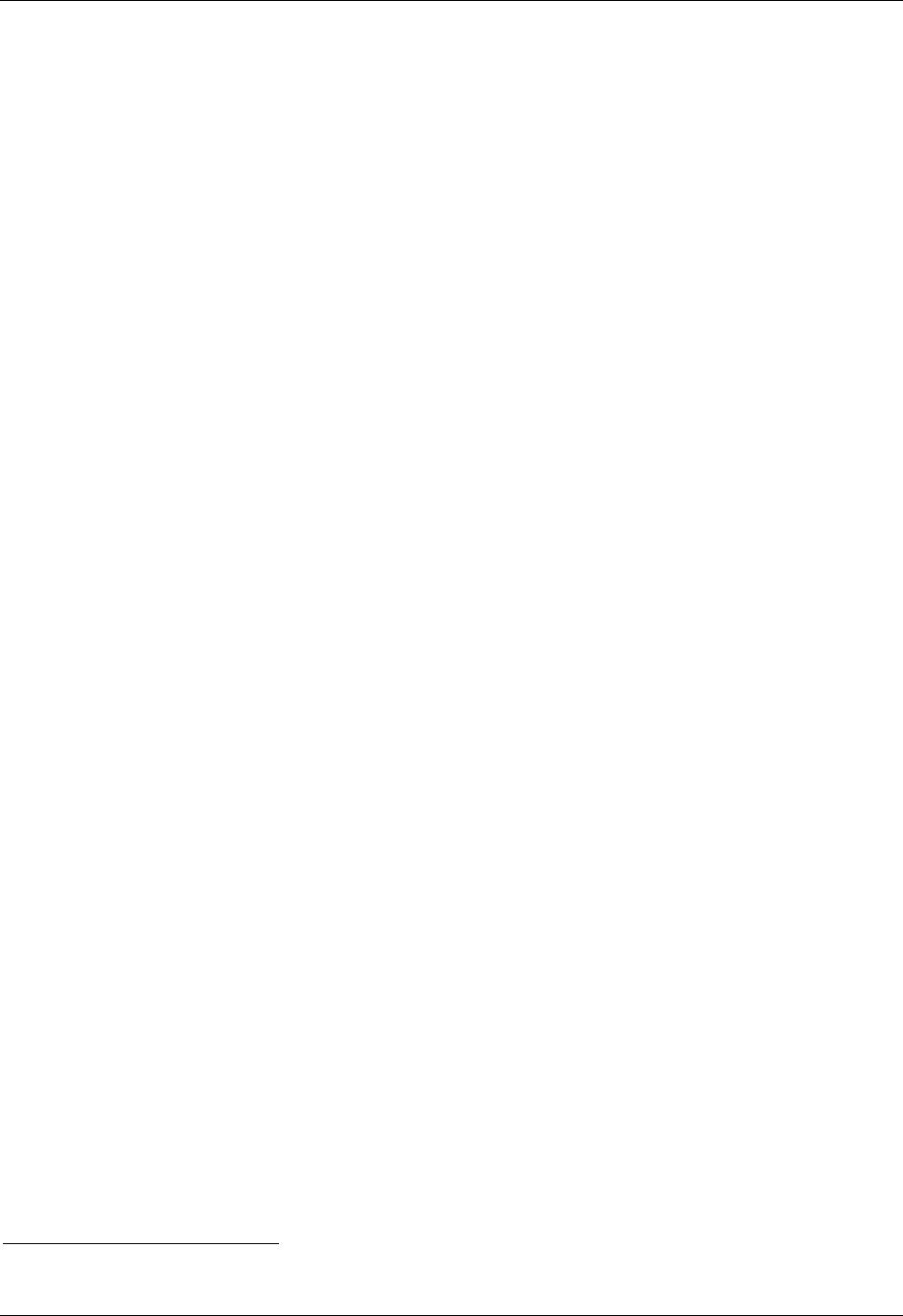
1 Average change in patient volumes by service between 2013 and 2015........................................ 8
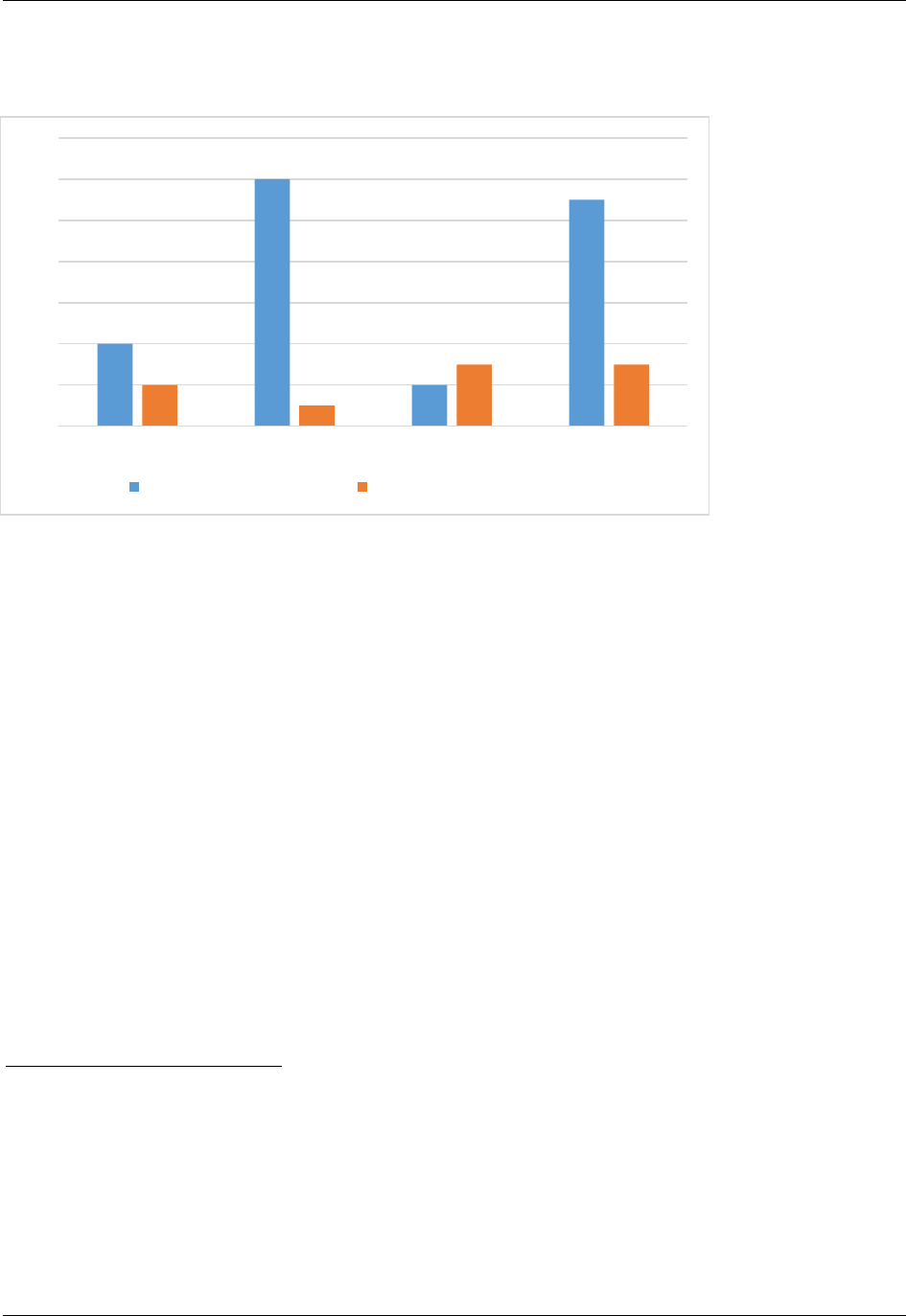
2 Average change in patient volume by payer source between 2013 and 2015 ................................ 9
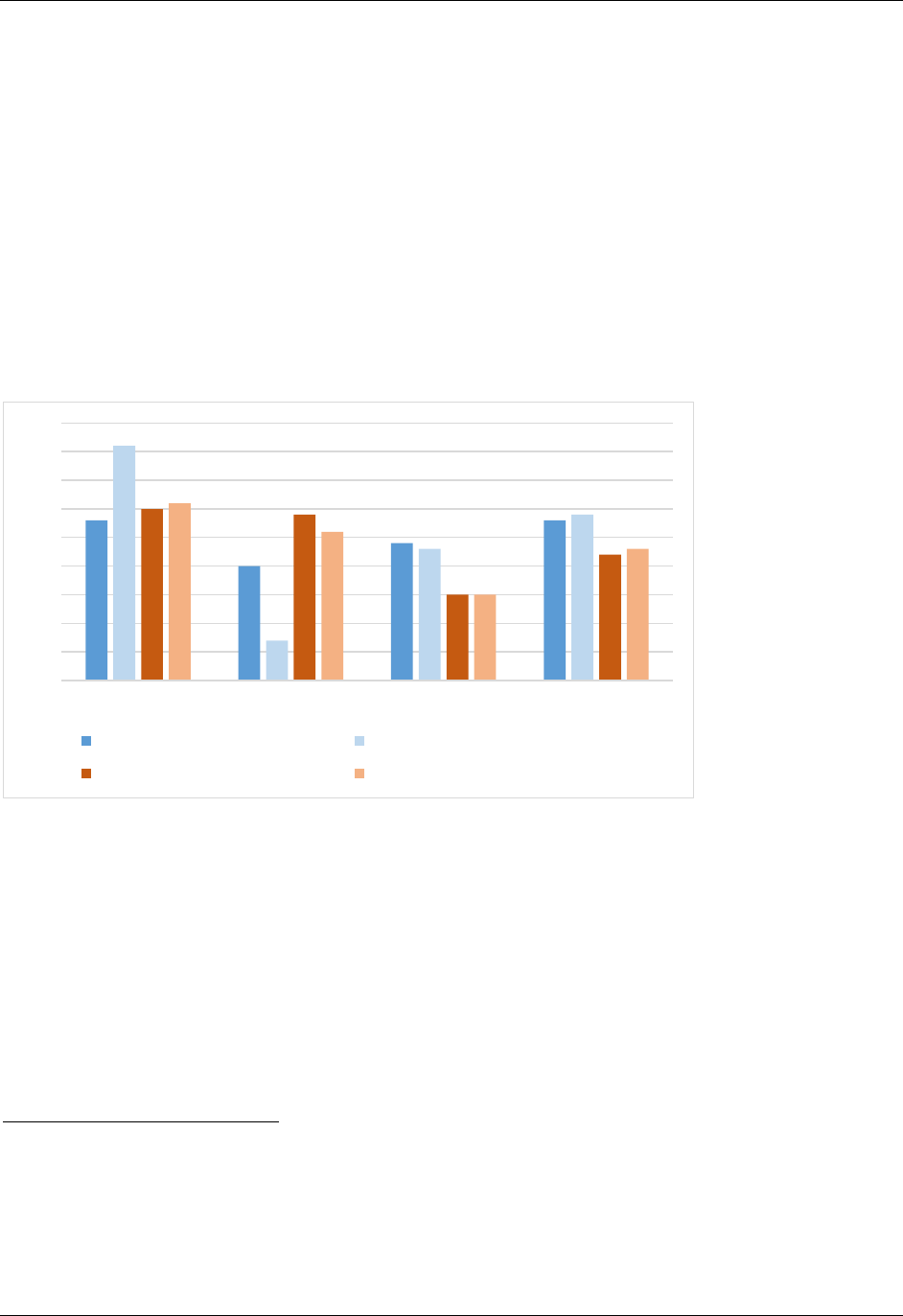
3 Average patient mix, 2013 and 2015 ............................................................................................. 10
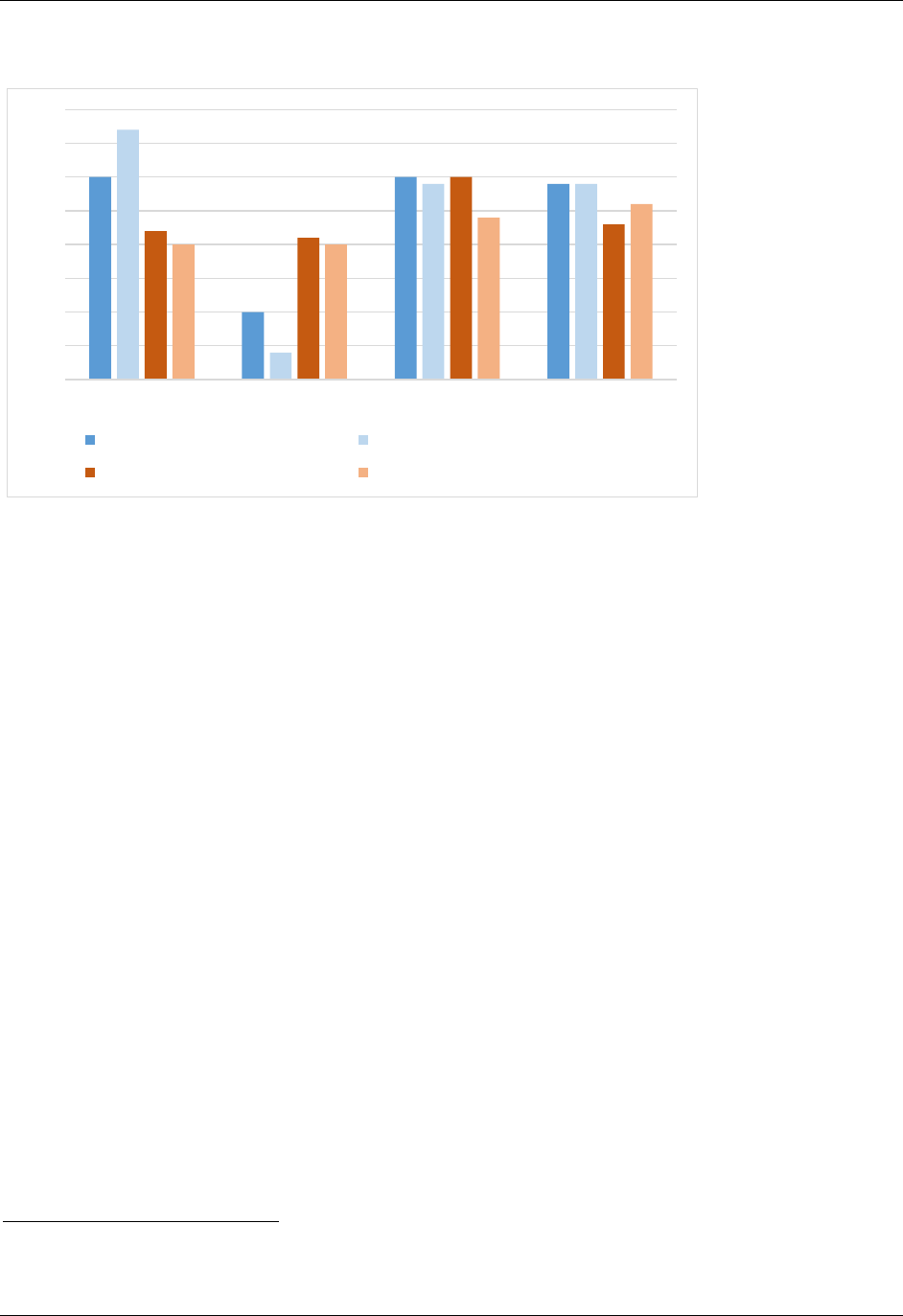
4 Average payer mix, 2013 and 2015 ............................................................................................... 18
5 Average financial margins, 2013 and 2015.................................................................................... 21

1
I. INTRODUCTION / EXECUTIVE SUMMARY
The Affordable Care Act (ACA) is expected to have profound effects on the health care
system in the United States, including the safety net hospitals that care for many low-income
uninsured people, Medicaid enrollees, and other vulnerable populations. Given the important role
safety net hospitals play in their communities, the Office of the Assistant Secretary for Planning
and Evaluation (ASPE) at the Department of Health and Human Services (HHS) contracted with
researchers from Mathematica Policy Research and Virginia Commonwealth University to study
the early effects of the ACA on 10 safety net hospitals, both in states that expanded income
eligibility for Medicaid under the ACA and those that did not. This primarily qualitative research
study, conducted between September 2013 and March 2016, provides an on-the-ground
assessment of the extent and nature of early changes in patient demand for services; hospital
capacity; preparations for payment and delivery system reforms; and changes in hospital
revenues, costs, and overall financial status.
In this final report, we summarize the objectives and process for designing and conducting
this study; the key findings, challenges, and limitations faced; the ways in which the results have
been disseminated; and the major conclusions and policy implications of these findings. Overall,
our research found that, on average, safety net hospitals in states that expanded Medicaid under
the ACA are treating significantly more insured and fewer uninsured patients than in 2013, and
that this shift has helped the hospitals financially. In contrast, the hospitals in states that did not
expand Medicaid typically experienced little change in their patient mix and increased financial
challenges. Overall, hospitals in both types of states experienced little effect from new
Marketplace coverage, faced declining subsidies, and are bracing for additional cuts, although
experience varied within the study set. The study also identified a number of challenges that
safety net hospitals face in adapting to payment and delivery system reforms; several of the study
hospitals have made progress in developing integrated delivery systems capable of assuming
financial risk, but others lag behind. The future viability of safety net hospitals may hinge on
potential changes to financial supports, as well as strategies to reduce hospital costs and better
manage care.

3
II. OVERVIEW OF PROJECT OBJECTIVES AND PROCESS
A. Policy context
Policymakers, health care providers, researchers, and others have expected the ACA to have
profound effects on the U.S. health care system, including the safety net hospitals that provide
health services to many low-income uninsured people, Medicaid enrollees, and other vulnerable
populations. Based on the assumption that as more people gain insurance coverage, hospitals will
receive increased revenue from insured patients and reductions in uncompensated care, the ACA
reduces Medicare and Medicaid Disproportionate Share Hospital (DSH) payments, although
these reductions have been delayed until 2018. To avoid a negative financial impact, safety net
hospitals likely will need to attain substantial changes in payer mix—that is, more insured
patients and fewer uninsured patients—to offset the loss of these subsidies. The degree to which
safety net hospitals fare well under health reform will also depend in part on whether they are
considered “essential community providers”
1
by health plans and the extent of competition with
other hospitals for newly insured patients.
The ACA also has called for major changes in the delivery and financing of health care.
These changes include a shift from paying for volume to paying for value and encouragement for
health care providers to accept greater financial risk for the care of patients. The ACA
encourages new forms of payment and care delivery—such as Accountable Care Organizations
(ACOs), value-based payment, bundled payments, and patient-centered medical homes (PCMH).
Given many of these new models are still in the relatively early stages of implementation,
limited evidence exists to date that alternative payment models can successfully improve quality
of care and lower health care costs on a national scale. In 2015, the Secretary of Health and
Human Services announced ambitious delivery system reform with the goals of tying 90 percent
of all Medicare fee-for-service payments to value-based payment programs by 2018, and making
50 percent of Medicare payments via alternative payment models in the same time frame.
2
Success under alternative payment models will require hospitals to function differently than
before, as payment is tied to performance on measures of quality and costs of care, and
accountability is shifted to the hospital for patient outcomes across the care continuum.
3
Safety
net hospitals in particular face a number of challenges to success under value-based payments
and alternative payment models, including more limited financial resources and a patient
population with more complex clinical and social needs.
B. Project team
The research team worked closely with Office of the Assistant Secretary for Planning and
Evaluation (ASPE) staff throughout all stages of the project. The principal investigators (Laurie
1
National Academy for State Health Policy. “Essential Community Providers: Tips to Connect with Marketplace
Plans.” April 2013. Available at http://www.nashp.org/sites/default/files/ecp.tips.connect.marketplace.plans.pdf.
2
Burwell, S.M. “Progress Towards Achieving Better Care, Smarter Spending, Healthier People.” Available at
http://www.hhs.gov/blog/2015/01/26/progress-towards-better-care-smarter-spending-healthier-people.html.
3
Centers for Medicare & Medicaid Services. “Better Care, Smarter Spending, Healthier People: Improving Our
Health Care Delivery System.” Available at https://www.cms.gov/Newsroom/MediaReleaseDatabase/Fact-
sheets/2015-Fact-sheets-items/2015-01-26.html.

II. OVERVIEW OF PROJECT MATHEMATICA POLICY RESEARCH
4
Felland from Mathematica and Peter Cunningham, formerly from Mathematica and now at
Virginia Commonwealth University)—collectively called the “project team” throughout this
report—discussed the project in regular biweekly calls with the project officer to provide updates
and seek guidance. The purpose of these calls was to report on progress, discuss issues that arose
over the course of the project, and seek input and comment from ASPE on key aspects of the
project and all deliverables. During the field period for the case studies, these calls also provided
an opportunity to share our early impressions with ASPE and report on any difficulties
encountered as we conducted our research. We also held several additional in-person meetings at
ASPE after the kickoff meeting, including one to discuss site selection, another to discuss the
earlier proposed quantitative study, and one on early findings from the qualitative data collection
effort.
C. Planning stage
Under Mathematica’s contract with ASPE, “Building Analytical Capacity for Policy
Analysis and Decision-Making,” the research team led a separate planning task in early 2013 for
conducting the case studies for this project. The planning phase consisted of four main
components: (1) an environmental scan to identify the key research questions and conceptual
framework for understanding the effects of health reform on safety net hospitals; (2) the metrics
and potential data sources that would be available for case studies; (3) a plan for conducting case
studies; and (4) convening an eight-member technical expert panel (TEP) meeting to provide
input to the plan. These activities informed the overall strategy as well as the specific
methodology for selecting the individual hospitals to study, identifying the types of organizations
and individuals with whom to speak, and specifying the content of the semi-structured
discussions and other information collected. In September 2013, Mathematica received the
contract to conduct the study and held a kickoff meeting with ASPE in November 2013.
D. Conceptual framework
The project team developed a conceptual framework during the planning stage to guide the
project (see Appendix 1). The framework draws on other efforts to develop a monitoring strategy
for safety net hospitals, such as the Agency for Healthcare Research and Quality’s (AHRQ’s)
Safety Net Monitoring Initiative, and an initiative by the Health Resources and Services
Administration (HRSA) to monitor the effect of state health insurance expansions on safety net
organizations.
4
We used the Institute of Medicine’s (IOM’s) definition of safety net providers:
“providers that organize and deliver a significant level of both health care and other health-
related services to the uninsured, Medicaid, and other vulnerable populations,” as well as
providers “who by mandate or mission offer access to care regardless of a patient’s ability to pay
and whose patient population includes a substantial share of uninsured, Medicaid, and other
vulnerable patients.”
5
4
Agency for Healthcare Research and Quality. “The Safety Net Monitoring Initiative: Fact Sheet.” August 2003.
Available at http://archive.ahrq.gov/data/safetynet/netfact.pdf; Harrington, Mary E., and Vivian L. Byrd.
“Monitoring the Impact of State Health Insurance Expansion on Safety Net Organizations. Final report submitted to
the Department of Health and Human Services, Health Resources and Services Administration, July 2009.
5
Institute of Medicine. “America’s Health Care Safety Net: Intact but Endangered.” Washington, DC: National
Academies Press, 2000.

II. OVERVIEW OF PROJECT MATHEMATICA POLICY RESEARCH
5
We adapted the conceptual frameworks used in these previous efforts to account for both
specific provisions of the ACA and recent changes in the health care delivery system, along with
issues specific to safety net hospitals. We also incorporated comments from the TEP. The
framework identified the key policies (other state and local policies and funding streams in
addition to the ACA provisions) that affect hospital demand, revenues, and costs, as well as the
types of contextual or “market” factors that influence hospitals’ responses to health reform, such
as community characteristics, the structure of the local health care delivery system, and
individual hospital attributes. Taken together, these policy and market factors contribute to
changes in the number of uninsured people in the community, which in turn affects demand for
care at safety net hospitals, and thus changes in these hospitals’ revenues and costs. These
changes, along with care delivery and payment reforms, affect a hospital’s “outcomes”; these
outcomes include its financial viability, ability to remain a safety net provider, array of service
offerings, and quality of care.
E. Study scope and methodology
ASPE and the research team purposively selected for study 10 safety net hospitals or
systems that range in size, role in their local safety net, ownership, and geographic location.
Some are single hospitals, some are hospital systems with several hospitals included in the
analysis (and other outpatient or other facilities), while others are part of larger hospital systems,
for which the other hospitals are separate from the analysis (either because they are in a different
community, focus on a limited set of services and/or are not deemed safety net hospitals).
Appendix 2 provides a table displaying key characteristics of these hospitals in more detail;
Appendix 3 provides details of our methodology.
Six hospitals are in states that expanded Medicaid under the ACA:
LAC+USC Medical Center in Los Angeles, California (flagship hospital of a four-hospital
county system)
Yale-New Haven Hospital in New Haven, Connecticut (part of the three-hospital Yale New
Haven Health System)
Denver Health in Denver, Colorado
University of Kentucky HealthCare (UK Health, three hospitals) in Lexington, Kentucky
Marcum and Wallace Memorial Hospital in Irvine, Kentucky
Lakewood Health System in Staples, Minnesota
Four hospitals are in states that have not expanded Medicaid:
Harris Health System (three hospitals) in Harris County (Houston), Texas
Regional One Health in Memphis, Tennessee
Froedtert Hospital in Milwaukee, Wisconsin (part of a three-hospital Medical College of
Wisconsin system)
II. OVERVIEW OF PROJECT MATHEMATICA POLICY RESEARCH
6
Homestead Hospital in Dade County, Florida (part of the Baptist Health South Florida
system)
The research team primarily used qualitative methods to understand the effects of the ACA
on these hospitals between early 2013 and 2015. Using a mix of in-person and telephone semi-
structured discussions, we spoke with the six hospitals from states that expanded Medicaid
(“Medicaid expansion states”) in both 2014 and 2015, and the other four hospitals in 2015 only.
The semi-structured discussions covered the following key topics: the hospitals’ role in the
local safety net; changes in their operational and financial well-being (including changes in
patient volumes for different service types, patient mix, system capacity, revenues and expenses,
and overall financial performance); factors contributing to these changes (ACA and other); and
the hospitals’ strategies, goals, and expectations for the future. The 2015 semi-structured
discussions also covered the hospitals’ experiences with Medicare value-based payment
initiatives—specifically, the Hospital Readmissions Reduction Program, Hospital-Acquired
Conditions (HAC) Reduction Program, and Hospital Value-Based Purchasing Program
6
—and
involvement in alternative payment arrangements, in which hospitals take on more financial risk.
We also gathered quantitative indicators directly from each hospital on patient volumes and
financial performance for the same time period, which informed both the semi-structured
discussions and the analysis (see Appendix 5). We analyzed the findings in two main stages: by
individual site (see Appendix 5 for the 10 summaries) and across sites (see below).
F. Dissemination of findings
We presented study findings (see next section) to several important audiences during the last
year of the project. Laurie Felland presented early findings from the original 6 sites at the June
2015 AcademyHealth Annual Research Meeting. Peter Cunningham presented key findings
across the 10 sites at the Annual AHRQ Research Conference in October 2015. We also
conducted a final study briefing for ASPE staff in April 2016.
The project team also summarized the findings of the cross-cutting analyses in two research
briefs. One paper examines the early effects of the ACA on the study hospitals’ patient volumes
and finances, while the second brief explores how the study hospitals are preparing for payment
and delivery system reforms.
6
See the CMS website for more information on these programs at https://www.cms.gov/Medicare/Medicare.html.

7
III. KEY FINDINGS
A. Summary
Study hospitals (Appendix 2) in states that expanded eligibility for the Medicaid program
experienced considerable patient volume increases from Medicaid enrollment expansions,
whereas they experienced little volume change from the ACA’s expansion of commercial
coverage through the federal and state Marketplaces. Despite concerns that they might lose many
newly insured patients to other providers, these study hospitals largely retained existing patients
and gained new ones. The growth in patient volume was especially notable for outpatient care,
and there were corresponding marked increases in the proportion of their patients with insurance
coverage. The growth in outpatient visits reflects in part safety net hospitals’ active efforts to
help uninsured patients enroll in coverage, expand primary care capacity, and improve their
facilities and systems to attract or retain patients as they gained coverage. Respondents (the
hospital executives and staff we spoke with for the study) reported that these changes both
supported their patients and the hospitals’ overall financial health. The words of one hospital
executive captured the sentiment of many: “The biggest success of the ACA is reducing our self-
pay [uninsured] patients and getting people the health care that they need. That to me has been a
great thing financially and a great thing for patients … we have anecdotal stories that people are
accessing care and identifying issues and getting better.”
In contrast, study hospitals in states that did not expand eligibility for Medicaid experienced,
on average, more modest increases in patient volumes and no overall change in patient mix, with
many of their patients remaining uninsured. On average, they experienced greater financial
challenges compared to the hospitals in states that expanded Medicaid (“expansion state
hospitals”); these challenges increased over the study period. Although hospitals in both types of
states experienced some declines in their subsidies to support care for the uninsured, all of them
are bracing for additional cuts.
B. Changes in patient volumes and mix
Patient volume grew overall but more so among expansion state hospitals. Most of the
study hospitals provided a higher volume of patient care in the first quarter of 2015 relative to
the first quarter of 2013. Respondents reported that this growth represents a mix of additional
services provided to existing patients who had previously been uninsured and services to new
patients. Overall, patient volumes increased more for expansion state hospitals than non-
expansion state hospitals, with the former reporting an average 11 percent increase and non-
expansion state hospitals reporting an average of 3 percent (Figure 1). The degree of increase
varied widely, from 2 percent to 22 percent, across all study hospitals. Outpatient volumes grew
more than other services (inpatient admissions and emergency department encounters) for
expansion state hospitals, by an average of 12 percent (the increases ranged from 4 percent to 24
percent across expansion state hospitals). In contrast, outpatient volumes did not change much at
non-expansion state hospitals: 1 percent on average (change across non-expansion state hospitals
ranged from -9 percent to 12 percent).
III. KEY FINDINGS MATHEMATICA POLICY RESEARCH
8
0%
2%
4%
6%
8%
10%
12%
14%
Inpatient Outpatient Emergency Dept. Total
Expansion-State Hospitals Non-Expansion-State Hospitals
Figure 1. Average change in patient volumes by service between Q1 2013
and Q1 2015
Expansion state hospitals’ outpatient growth reflects a variety of factors. Most of the
Medicaid expansion population receives care through managed care arrangements; the health
plans typically require new enrollees to choose a medical home (which provides primary care
and coordinates additional follow-up care) and encourage them to seek an appointment soon
after enrolling.
7
Also, many of the study hospitals had expanded outpatient capacity (see
Hospitals expanded ambulatory care section below) as they sought to redirect patients from their
emergency departments (EDs) and reduce or shift care away from inpatient facilities.
8
This
redirection occurred because of capacity constraints and the hospitals efforts to provide care in
less costly settings in preparation for new payment arrangements that reward value (better
outcomes at lower costs) over volume of services provided (see Experiences with Value-Based
Purchasing and Alternative Payment Models section.)
Overall, the study hospitals observed a 3 percent increase in ED volumes. Whereas changes
generally ranged from only small increases to small decreases, a couple of expansion state
hospitals saw larger (11–12 percent) increases in ED use. These increases are consistent with
studies that find that insured patients use EDs more than uninsured patients because EDs are
convenient and Medicaid patients typically face no cost sharing to use one;
9
access to primary
7
The extent to which Medicaid managed care plans use a strict gatekeeper model that authorizes referrals for
follow-up care varies by state/community, but the general concept is typically in place, whether the primary care
physician (PCP) has strict authorization authority or not.
8
Some apparent changes in volumes represent shifts among service categories. For Froedtert, part of the apparent
rise in outpatient cases is that the Medicare “two-midnight rule” shifted cases previously categorized as inpatient
into observation or outpatient cases.
9
Cunningham, Peter J., and Jessica H. May. “Insured Americans Drive Surge in Emergency Department Visits.”
Issue Brief No. 70, Washington, DC: The Center for Studying Health System Change, October 2003.

III. KEY FINDINGS MATHEMATICA POLICY RESEARCH
9
-60%
-40%
-20%
0%
20%
40%
60%
Medicaid Uninsured Commercial Medicare
Expansion-State Hospitals Non-Expansion-State Hospitals All Study Hospitals
and specialty care in outpatient settings may be more difficult. Some respondents were surprised
that ED visits did not increase more as people gained coverage.
ED use among non-expansion state hospitals also increased slightly. In addition to the slight
Medicaid volume increases, each non-expansion state hospital provided additional reasons for
the increase, from growth in commercially insured patients (Homestead), to population growth
(Harris) and greater severity in patients’ conditions, possibly linked to delayed care (Froedtert).
Inpatient volumes and average length of inpatient stay also did not increase much for
expansion state or non-expansion state hospitals.
10
This finding suggests that new patients were
not significantly sicker than previous patients. Although hospital executives reported more
chronic conditions and pent-up demand among their newly insured patients, many of those needs
reportedly were addressed on an outpatient basis.
Medicaid growth outpaced Marketplace growth. Overall, the Medicaid expansion was a
more significant contributor to volume growth at the safety net hospitals than the new
Marketplace coverage options for low-income people. The growth in patient volumes stemmed
from different sources for expansion state hospitals and non-expansion state hospitals: for the
former, primarily from Medicaid patients; for the latter, primarily from commercially insured
patients (Figure 2).
Figure 2. Average change in patient volume by payer source between Q1
2013 and Q1 2015
Medicaid volume grew more among expansion state hospitals in states that previously had
no or minimal Medicaid eligibility or other public coverage programs for childless adults
(California, Kentucky, and Colorado). A couple of the expansion state hospitals experienced
10
Only Marcum and Wallace had a significant increase (18 percent) in inpatient volumes, which mostly was
unrelated to the ACA or patient demand; rather, it reportedly represented a change in categorizing patients as
inpatients rather than observation stays.
III. KEY FINDINGS MATHEMATICA POLICY RESEARCH
10
0%
5%
10%
15%
20%
25%
30%
35%
40%
45%
Medicaid Uninsured Commercial Medicare
Expansion-State Hospitals 2013 Expansion-State Hospitals 2015
Non-Expansion-State Hospitals 2013 Non-Expansion-State Hospitals 2015
dramatic increases in Medicaid encounters
11
and significant (but lesser) drops in encounters from
uninsured patients: for LAC+USC, Medicaid encounters jumped by 150 percent, whereas
uninsured encounters plummeted 85 percent; for UK Health, Medicaid encounters grew by 80
percent, whereas uninsured encounters fell 55 percent.
As a result of the shifts in volume, the patient mix changed markedly (Figure 3). Medicaid
encounters (inpatient, outpatient, and ED) became a much larger portion of the services provided
in some expansion state hospitals, whereas uninsured encounters as a portion of total encounters
dwindled. On average, Medicaid grew from 28 to 41 percent of total patient encounters (a 46
percent increase); the proportion of uninsured encounters fell from 20 percent to 7 percent (a 65
percent decrease).
Figure 3. Average patient mix, Q1 2013 and Q1 2015*
*Calculated based on average of inpatient, outpatient and emergency department patient mix.
Patient mix unavailable for Denver Health.
For non-expansion state hospitals, Medicaid volumes grew modestly for some hospitals, but
typically with little effect on Medicaid as a proportion of overall encounters (on average, non-
expansion state hospitals experienced little change in their overall patient mix between 2013 and
2015). Respondents attributed some of this growth to the ACA sparking more outreach activities
that led people already eligible for Medicaid to apply (often referred to as a “woodwork” or
“welcoming mat” effect). Reportedly, general population growth and increased capacity
contributed to Harris’s increase, whereas a change in Wisconsin’s Medicaid program that
brought people from a waiting list into the program led to growth at Froedtert.
12
However,
11
Total volume of inpatient admissions, outpatient, and ED visits.
12
Wisconsin allowed childless adults to enroll in Medicaid before the ACA but, with implementation of the ACA,
reduced income eligibility from 133 percent to 100 percent to align with the income level at which federal subsidies
for Marketplace coverage kick in; the state then opened its enrollment cap. Many people who had been on the
waiting list reportedly lived in the Milwaukee area, contributing to a net increase in Medicaid patients and a
reduction in uninsured patients for Froedtert.

III. KEY FINDINGS MATHEMATICA POLICY RESEARCH
11
Medicaid volumes declined at Regional One, which executives attributed partially to Medicaid
patients aging into the Medicare program.
Although many study hospitals experienced some increase in commercially insured patients,
this source comprised more of non-expansion state hospitals’ volume growth than Medicaid (but
on average commercial as a percentage of overall patient mix remained stable and declined in
terms of overall revenue (Figure 4). Yet Marketplace coverage did not significantly affect either
expansion state or non-expansion state hospitals.
13
This finding is not especially surprising
because, in states that expanded Medicaid, enrollment typically far outpaced Marketplace
enrollment. Many of the study hospitals serve a very low-income population, so many existing
patients at expansion state hospitals qualified for Medicaid rather than Marketplace coverage,
and many non-expansion state hospitals’ patients live below the poverty line and are thus
ineligible for Marketplace subsidies. Also, a few hospitals reported challenges in obtaining
contracts with Marketplace health plans, either because they were not deemed “Essential
Community Providers” in their states and/or because they have historically lacked commercial
contracts as a basis for negotiation for inclusion in these plans’ provider networks.
Hospitals proactively worked to attract more patients. The growth in patient encounters
aligns with reported efforts by the study hospitals to retain and attract patients as they gained
coverage. Both expansion state and non-expansion state hospitals conducted in-reach (to existing
uninsured patients) and outreach (to find additional uninsured people in the community) to help
people apply for coverage. Some study hospitals gained ACA funding to assist in these efforts.
For example, UK Health participated in testing and implementing state outreach efforts in its
facilities, and a federally funded insurance navigator in Marcum and Wallace’s ED reportedly
helped many uninsured patients gain coverage.
The study hospitals made concerted efforts to improve their facilities, processes (for
example, appointment scheduling, wait times for appointments), and customer service so that
newly insured patients would select them over other providers. Many respondents referred to
these efforts as strategies to become “providers of choice, not last resort.” Also, some states
direct a large proportion of Medicaid enrollees who do not choose a health plan to those owned
by safety net providers; they also direct those who do not choose a medical home to safety net
providers. The study hospitals reported retaining many of their patients once they gained
coverage and also receiving new ones.
Hospitals expanded ambulatory care. Since many of these hospitals reportedly were
already operating close to or at capacity in their EDs and outpatient services before the ACA
coverage expansions, they needed to expand to treat more patients. With their focus on outpatient
services, most hospitals did not add inpatient beds; some even reduced staffed beds.
Whereas the study hospitals displayed a wide range in the extent of primary care they
provide, most had expanded primary care services between 2013 and 2015. As noted, primary
care capacity is vital if hospitals are to serve as medical homes in insurance networks; it also
helps them gain referrals for additional outpatient and inpatient services. In addition, primary
13
Many hospital executives noted difficulties in precisely parsing out Marketplace coverage from overall
commercial volumes to provide a percentage estimate of its total prevalence among commercial businesses.

III. KEY FINDINGS MATHEMATICA POLICY RESEARCH
12
care is an important component of preparing for value-based payments (see next section). The
study hospitals mainly boosted primary care by adding physicians and other staff (for example,
nurse practitioners) on site; at least one hospital (Yale) acquired physician practices in the
community.
Some hospitals also added physical capacity on the hospital campus or at clinics in the
community, or extended their primary care reach by collaborating with other community clinics.
Homestead had not traditionally provided primary care but recently started a clinic that provides
comprehensive visits to patients after they leave the hospital so as to reduce their reliance on the
ED for follow-up care. Froedtert is developing more community clinics and partnering with a
federally qualified health center (FQHC). With many patients presenting in their EDs for
behavioral health issues, some of the study hospitals also have added social workers and
psychiatric staff (Denver) and/or are working to integrate behavioral health into primary care
(Lakewood).
A couple of non-expansion state hospitals substantially increased their primary care services
in anticipation of a Medicaid expansion, which then did not occur; Harris Health built two large
primary care clinics. With Texas opting out of the Medicaid expansion, the clinics serve many
more uninsured patients than before and identifies many specialty care needs; addressing these
needs has reportedly strained Harris’s capacity and financial status.
Given the costs of adding physical capacity and staff, some hospitals increasingly have
turned to other ways to extend primary care and other services outside of traditional patient-
provider visits. For example, Froedtert started a virtual urgent care clinic, using Facetime and
Skype Internet technology. Some of these efforts are not captured in the hospital volume data. In
a key example, LAC+USC makes greater use of telephonic medical advice as well as an
EConsult system, in which PCPs consult with specialists electronically to gain advice on how to
treat a patient’s condition or refer the patient to the specialist; this system reportedly has reduced
the need for face-to-face visits with specialists by one-third.
C. Experiences with alternative payment models and value-based payment
initiatives
Although adapting to changes in volume, patient mix, and service capacity, the study
hospitals (Appendix 2) also were responding to payment and delivery system reforms, both in
the ACA and through other federal and state initiatives. Unlike the changes in patient volume
and mix, we did not find clear distinctions between hospitals in states that expanded Medicaid
and those that did not regarding their participation in and readiness for these new payment
arrangements.
Varied participation in alternative payment models. The eight study hospitals (we did
not include the two rural hospitals in this analysis because of their small size and exemption from
Medicare value-based purchasing requirements) vary considerably in the extent to which they are
moving toward risk-based payments under managed care or alternative payment models. The
two county hospitals with a broad set of integrated services appeared more advanced in these
arrangements for the Medicaid population than the smaller hospitals and the academic medical
centers.

III. KEY FINDINGS MATHEMATICA POLICY RESEARCH
13
LAC+USC and Denver Health are much further along the continuum of providing care
under risk-based payment arrangements than the other study hospitals. They already accept full
risk for their Medicaid patients (through capitation). Denver Health estimates that it currently
receives capitated payments for about 40 percent of patients (primarily through their Medicaid
and employee health plans). It is not pursuing ACO arrangements (typically involving sharing
risk with other providers) for any patient populations because “we think we are a bit ahead of
accountable care; we do full population health for the Medicaid population.” Crucially, both
hospitals exist in a state policy environment that is aggressively promoting payment and delivery
system reforms for Medicaid and public hospital systems. These reforms are Colorado’s
statewide Accountable Care Collaboratives for Medicaid beneficiaries and California’s Delivery
System Reform Incentive Payment (DSRIP) program targeting safety net hospitals, which
provides extra payments for these hospitals if they achieve quality improvement goals.
14
,
15
Also,
California provides the county hospitals with cost-based reimbursement for inpatient services for
new Medicaid enrollees, thus providing some protection from the risk-based arrangement.
Other study hospitals are participating in ACOs for their Medicare and/or commercially
insured patients but have yet to extend this approach to Medicaid patients. Froedtert in
Milwaukee is participating as a tertiary care provider in the Integrated Health Network of
Wisconsin, a “super ACO” comprising eight regional health systems and targeting Medicare and
commercially insured patients.
16
Northeast Medical Group, a physician practice owned by Yale-
New Haven Health System, is involved in a Medicare Shared Savings Program ACO.
Homestead has entered into an ACO with a major private insurance carrier (Florida Blue) for the
care of cancer patients. These hospitals tend to have higher volumes of Medicare and
commercially insured patients compared to the publicly operated systems described above.
The other study hospitals (UK HealthCare, Harris Health, and Regional One) are less
involved with alternative payment models for any payer type. They are more wary of accepting
greater financial risk for patients due to high uncompensated care levels and lack of Medicaid
expansion in their states (Harris Health and Regional One), or low Medicaid payment and lack of
integration with primary care and other services needed to manage and coordinate the care of
patients (UK HealthCare). These hospitals also cited a lack of political interest (both historically
and currently) at the state level in pursuing innovative Medicaid managed care programs and
payment models.
Patients’ social and clinical needs pose challenges. A major challenge for safety net
hospitals in value-based purchasing arrangements and new alternative payment models is that
many of the patients they serve are poor and low income, and have complex clinical and social
needs that require greater coordination with social services as well as other medical services.
These hospitals encounter greater difficulties with patients who are homeless or lack a permanent
address, lack social and family support in the community, have significant co-morbid mental
14
Colorado Department of Health Care Policy and Financing. Accountable Care Collaborative. Available at
https://www.colorado.gov/pacific/hcpf/accountable-care-collaborative.
15
California Department of Health Care Services. Delivery System Reform Incentive Payments (DSRIP). Available
at http://www.dhcs.ca.gov/provgovpart/Pages/DSRIP1.aspx.
16
Integrated Health Network of Wisconsin. Available at http://www.ihnwi.com/.

III. KEY FINDINGS MATHEMATICA POLICY RESEARCH
14
health and substance abuse problems, or have inadequate transportation to get to medical
appointments.
The socioeconomic mix of patients they serve creates challenges for safety net providers to
perform well on measures of quality of care and hospital readmission rates, which can lead to
higher penalties on their Medicare payments.
17
,
18
Respondents across the study hospitals reported
that the lack of adjustment for socioeconomic status puts them at a disadvantage relative to other
hospitals with respect to the quality measures used for the Centers for Medicare & Medicaid’s
(CMS’s) value-based purchasing programs. One specific example cited by multiple hospitals is
the relatively high rate of pressure ulcers in their facilities (included as a metric under the HAC
Reduction Program). Hospitals face more difficulty in preventing pressure ulcers among patients
who have been immobilized—for example, due to neurological injuries and wounds resulting
from violence, accidents, or other trauma; these hospitals care for many such patients.
Despite the hospitals’ concerns about the lack of adjustment for socioeconomic factors and
their perceived disadvantage, the study hospitals typically did not perform substantially worse on
the CMS quality measures compared to hospitals nationally (see Appendix 6). In cases in which
scores were relatively low, the penalties assessed tended to be modest and were of less concern
to these hospitals than other financial issues. In fact, some study hospitals have a low volume of
Medicare patients, which also limits the financial impact of these programs, either because these
hospitals are ineligible due to their small volume (the two rural hospitals in particular fall under
this category) or the amount of their penalty or bonus is modest.
In contrast, the challenges this set of safety net hospitals face tend to affect factors related to
patient satisfaction more than the quality of care provided. These hospitals tended to have
relatively low patient satisfaction scores based on the Hospital Consumer Assessment of Health
Plans (HCAHPS), which is administered to a sample of all patients, not just those under
Medicare.
19
Respondents believed that low HCAHPS scores reflected problems of access to care,
crowding in emergency and inpatient departments, and other resource constraints (for example,
inadequate staffing and customer service training, administrative and clinical information
systems) that affect patients’ experiences with the hospital. Initiatives were underway at a
number of hospitals to address these issues. In addition, many of them have been proactive in
improving interactions between clinicians and patients, including the use of outside consulting
groups that specialize in improving the patient experience.
Integrating primary care and addressing nonmedical needs are important. The
difficulty of transforming their delivery systems to improve integration and coordination with
other services and providers is a significant challenge for many of the study hospitals. Follow-up
for discharged patients who have no “medical home” was cited as particularly challenging,
17
Gilman, M., E.K. Adams, J.M. Hockenberry, A.S. Milstein, I.B. Wilson, and E.R. Becker. “Safety Net Hospitals
More Likely than Other Hospitals to Fare Poorly Under Medicare’s Value-Based Purchasing.” Health Affairs, vol. 4,
no. 3, 2014, pp. 398–405.
18
Joynt, K.E., and A. Jha. “Characteristics of Hospitals Receiving Penalties Under the Hospital Readmissions
Reduction Program.” Journal of the American Medical Association, vol. 309, no. 4, 2013, pp. 342–343.
19
Chatterjee, P., K.E. Joynt, E.J. Orav, and A.K. Jha. “Patient Experience in Safety-Net Hospitals.” Archives of
Internal Medicine, vol. 172, no. 16, 2012, pp. 1204–1210.

III. KEY FINDINGS MATHEMATICA POLICY RESEARCH
15
especially for a patient population with a high prevalence of mental and physical disabilities, low
health literacy, and inadequate transportation and housing.
Most study respondents felt that highly integrated delivery systems with a closed network of
providers was the optimal arrangement for managing the wide array of care needs for Medicaid
and uninsured populations. Among the study hospitals, the county-operated or supported systems
are more equipped for this approach. LAC+USC, Denver Health, Harris Health, and Regional
One typically employ their physicians (versus contracting with physicians in the community) to
align incentives. Also, they essentially “own the entire continuum of health care,” which helps
them achieve a high degree of integration between inpatient, primary care, and other outpatient
facilities. All of these hospitals believe that operating as an integrated system has allowed them
to keep 30-day inpatient readmission rates lower than they would be if the systems were more
fragmented—primarily because they facilitate greater communication and smoother handoffs
between different sectors within the system (see Appendix 6, which shows how the county-
operated hospitals tended to face lower readmission penalties than the private hospitals in the
study).
Denver Health, LAC+USC, and Harris Health have taken advantage of ACA-related grants
and programs to further increase the degree of integration and coordination of services they
provide. For example, Denver Health received a $19 million Center for Medicare and Medicaid
Innovation (CMMI) grant that supports patient navigators, programs to manage high utilizers,
co-location of primary and behavioral health services, and clinical pharmacists embedded in
primary care clinics. A major emphasis has been the use of patient navigators and dedicated staff
to proactively schedule primary care visits for patients with chronic illnesses who are at high risk
of readmission.
As part of reforms through California’s Medicaid waiver and DSRIP programs, LAC+USC
has focused on expanding access to primary care and assigning patients to medical homes in its
network, as well as greater integration of primary care and behavioral health. Also, LAC+USC
rented 600 units of supportive housing and opened 300 recuperative care beds for homeless
patients being discharged from the hospital. The estimated cost for the health system of
providing such housing, along with primary care and other supportive services ($1,200 per
patient per month), was less than the higher cost for inpatient readmissions and ED services that
could result without such support. However, capacity for these efforts remains limited,
reportedly leaving many patients with unmet primary care and behavioral health needs.
Harris Health has expanded primary care capacity and access within its system under
Texas’s DSRIP initiative, including the addition of nine primary care clinics. “Super-utilizers”
are being managed by sending medical teams out to patients’ homes to teach them how to
manage their chronic conditions. Care delivery reforms at the hospital also include identifying
patients at high risk for readmission and using case managers to follow up and encourage these
patients to see their primary care physician.
In contrast, the three academic medical centers in the study are much more limited in both
integration with primary care and other services used to address population health for their
Medicaid and/or uninsured populations. In general, their main strategy is to position themselves
as the tertiary and quaternary providers in ACO networks for Medicare and commercially

III. KEY FINDINGS MATHEMATICA POLICY RESEARCH
16
insured patients, rather than developing vertically integrated systems for these patients. These
systems have embraced ownership of physician practices in the community as a way to increase
their footprint for primary care and other specialties; however, these physicians primarily serve
Medicare and commercially insured patients. Instead of building primary care capacity within
their systems, they have focused on developing relationships with FQHCs to provide medical
homes for Medicaid and uninsured patients who use their EDs. For example, Froedtert recently
donated $15 million to a local FQHC to build an additional clinic site to expand access in the
community, and it has agreed to provide inpatient and specialty care for patients at the new
facility.
The Baptist Health Care System in South Florida (of which Homestead Hospital is a part)
also has little primary care capacity within its system. As a result, providing patients with follow-
up care after hospital discharge poses a major challenge for Homestead. In response, the hospital
has set up a “gap clinic”—a primary care center managed by a nurse practitioner and intended to
serve as a transitional center between inpatient and primary care for recently discharged patients.
Homestead has also tried to strengthen affiliations with local FQHCs to provide their patients
with a medical home for the longer term.
Electronic health record systems are essential for organizational and clinical
integration. All study hospitals agreed that having a system that maintains a single, integrated
electronic health record (EHR) for each patient throughout their system was essential for
coordinating patient care, documenting and analyzing the quality and costs of care, and
identifying operational changes that might be needed. Some hospitals were further along than
others in developing their EHR systems. With the exception of Regional One, all study hospitals
had (or had definite plans to implement) single EHRs linked to all providers in their system.
Some of the hospitals are also using outside consultants to develop systems for population health
management and patient engagement. Among the study hospitals, Regional One in Memphis
appears to lag furthest behind in adapting its information systems and enhancing its
administrative capabilities. It is the only study hospital that used different EHRs for different
departments, and still relies to some extent on paper records.
Despite system upgrades, the study hospitals appear to be limited in their understanding of
and ability to address cost drivers—both of which are key to long-term success under value-
based purchasing. For example, all facilities cited difficulties in attributing costs to patients,
service lines, or particular providers, which makes it challenging to understand the major cost
drivers in their health systems. The ability to hire staff devoted to collecting and analyzing data
on cost and quality performance varied across the hospitals; Harris Health and Regional One
identifying it as one of their major challenges, largely because of financial constraints.
For some hospitals, accurate documentation of patients’ condition(s) upon arrival and care
received can be as much of a challenge as implementing sophisticated EHR systems and
expanding analytical capabilities. For example, one hospital reported that it appeared to have a
high rate of accidental bowel lacerations during surgery (which factors into a CMS quality
indicator), which upon further investigation was a result of miscoding patients who arrived at the
hospital with that condition (for example, stabbing victims who arrived at the ED).

III. KEY FINDINGS MATHEMATICA POLICY RESEARCH
17
D. Financial impacts
Patient service revenue grew. Largely linked to the growth in patient volumes from
insured patients, operating revenues increased for expansion state hospitals (by an average of 17
percent) and, to a lesser extent, for non-expansion state hospitals (11 percent on average)
between 2013 and 2015. For expansion state hospitals, this increase came largely from Medicaid.
Revenue growth was especially large for the study hospitals that receive cost-based Medicaid
reimbursement (for at least some patients and/or services) from their states; these hospitals
include the rural critical access hospitals and LAC+USC (Appendix 2). For others, Medicaid
reimbursement is less than the costs of providing the services; however the hospitals previously
had been treating many of these patients as uninsured patients and so had received even less
reimbursement in the past.
Some hospital executives expressed concern that Marketplace products tend to reimburse
providers at rates considerably lower than traditional commercial coverage—at or closer to
Medicaid payment rates. One hospital detected lower payments as some patients switched from
employer-sponsored commercial coverage to Marketplace plans. Because Marketplace patient
volumes have been relatively low for these hospitals to date, however, the revenue impact has
been small overall.
Hospitals’ payer mix based on total patient revenues followed similar patterns to the shifts in
patient mix based on encounters (Figure 4). For both expansion state hospitals and non-
expansion state hospitals, commercial insurance revenues comprise a significantly larger
proportion of total revenues than commercial insurance encounters as a proportion of total
patient encounters, reflecting the higher payment rates for these services.
Hospital subsidies are on the decline. Longstanding federal, state, and local subsidies—for
example, from DSH programs, state provider taxes, or general county revenues—to safety net
hospitals began declining over the last few years, tempering their revenue growth. However, to
date some of these cuts have not been as large as the hospitals expected because of policymaker
decisions to phase them in more gradually, allowing hospitals to adjust to reform. Also payment
schedules typically lag behind the time frame during which the services are provided and shifts
in payer mix have occurred. That is, some safety net hospitals are temporarily benefiting from
stable subsidies based on a time frame during which they served more uninsured patients, even
as their uninsured numbers have since declined; in other words they are paid retroactively for
services provided. Some executives expect to have to repay some of these funds once the state
and/or federal government fully account for patient and payer mix changes.
III. KEY FINDINGS MATHEMATICA POLICY RESEARCH
18
0%
5%
10%
15%
20%
25%
30%
35%
40%
Medicaid Uninsured Commercial Medicare
Expansion-State Hospitals 2013 Expansion-State Hospitals 2015
Non-Expansion-State Hospitals 2013 Non-Expansion-State Hospitals 2015
Figure 4. Average payer mix, Q1 2013 and Q1 2015
In addition to direct patient revenues received from Medicaid programs and health plans,
safety net hospitals also typically receive additional Medicaid revenues through DSH. Most of
the study hospitals experienced either stable or declining Medicaid DSH payments between 2013
and 2015. Although the federal government has delayed the planned cuts to Medicaid DSH
several times (primarily because the initial schedule for reducing the payments preceded the
Supreme Court decision to allow states to opt out of the Medicaid expansion), states play a large
role in how these funds are allocated; some states changed their allocation formulas. Also, some
safety net hospitals’ allocations changed because their patient mix had changed.
Yet Medicaid DSH has not been a large funding source for some of the hospitals. Lakewood
and Homestead both receive less than $10,000 per year (less than 1 percent of revenues).
Marcum and Wallace reported the greatest decline in Medicaid DSH funds (55 percent between
2013 and 2015), but from a relatively small amount (from approximately $148,000 to $66,000).
Regardless of the amount, some of the study hospitals decided to no longer recognize DSH
payments as revenue; this strategy is intended to prepare for the upcoming cuts and out of
concern that they will need to repay much of the funds once their state assesses the change in
volumes and patient mix.
Medicare DSH payments to the study hospitals were either insignificant or did not change
substantially. However, Regional One’s Medicare DSH funds increased recently (amount not
available), reportedly related to the new allocation formula that distributes a portion of the 75
percent Medicare DSH fund reduction to hospitals with large numbers of uninsured patients.
20
Other common sources of Medicaid revenue for safety net hospitals are state programs that
redistribute funds generated by charging a fee to a broad set of providers; after receiving federal
20
Disproportionate Share Hospital (DSH). “The Medicare DSH Adjustment.” Accessed at:
https://www.cms.gov/medicare/medicare-fee-for-service-payment/acuteinpatientpps/dsh.html.

III. KEY FINDINGS MATHEMATICA POLICY RESEARCH
19
Medicaid matching funds, the state redistributes the funds to safety net hospitals. Denver
Health’s payments from such a fee program have been rising in the last few years. Homestead’s
$400,000 from Florida’s Low Income Pool has been stable over this period. After lengthy
negotiations over the future of the program, the state and federal governments came to an
agreement to continue this funding source, but at a lower level;
21
it is too early to know the
impact on Homestead’s funding levels. Yale’s experience with Connecticut’s provider fee
program differed, as the fee assessed on the hospital totaled more than the hospital received back
in enhanced Medicaid payments during the study period.
Federal Medicaid waivers are also important sources of funding for some safety net
hospitals. LAC+USC and Harris receive funds through the DSRIP component of their state’s
1115 Medicaid waivers, which has helped them to expand capacity in new ways, particularly for
primary care. The California waiver ended in October 2015, but a new waiver will extend the
DSRIP concept to 2020, with more expectations that hospitals will demonstrate that these funds
are helping them achieve better patient outcomes at lower costs. The Texas DSRIP program is
slated to end in 2016, unless the state’s Medicaid waiver (and the DSRIP program) is renewed.
The county-owned hospitals in the study appear more vulnerable than others because they
rely on additional state and local subsidies that also have started to decline. LAC+USC now
receives less funding through so-called realignment funds (sales tax and vehicle licensing fee
revenue that the state historically has provided to counties to provide health care to low-income
uninsured people); the state now directs more of these funds to social services.
Expansion state hospitals typically expected such funding reductions as their uninsured
populations declined, but the cuts are more painful for non-expansion state hospitals. County
funds (largely from property tax revenues) had made up almost half of Harris’s operating
revenue, but the county cut these funds by 13 percent (a reduction of $75 million annually)
starting in 2011. Reportedly, the county made this cut in anticipation of Texas expanding
Medicaid, which has not occurred. In contrast, Regional One’s county appropriation has been
steady over the last few years, and the hospital expects to receive an estimated 2 percent increase
this year. As a non-expansion state hospital executive suggested: “Medicaid expansion would
provide a better and more predictable funding stream” than the various subsidies on which the
hospital currently relies.
Uncompensated care expense fell. In line with reductions in uninsured patients,
uncompensated care (comprising both charity care and bad debt) declined by almost one-third
for expansion state hospitals.
22
Charity care tended to fall more than bad debt. In fact, some
study hospitals reported increases in bad debt, which hospital executives attributed to the
presence of more commercial insurance products with relatively high-cost sharing requirements
(deductibles and copayments) that patients cannot afford. The growth of such products started
before the ACA but has continued with the new Marketplace plans. Also, some of the newly
21
Associated Press. “Florida, Feds Agree to Extend Hospital Low-Income Pool Funds.” Modern Healthcare, June
24, 2015. Available at http://www.modernhealthcare.com/article/20150624/NEWS/306249975.
22
Although we attempted to gather uncompensated care costs in a consistent way across the study hospitals—as the
sum of charity care and bad debt—Yale also uses Medicaid shortfalls in its uncompensated care calculation, which
reportedly led to an increase in the amount.

III. KEY FINDINGS MATHEMATICA POLICY RESEARCH
20
insured patients might now be incurring bad debt for unpaid expenses that previously qualified
for charity care when the patient was uninsured.
The non-expansion state hospitals experienced mixed changes in uncompensated care. Both
Homestead and Harris experienced increases in uncompensated care—as much as 25 percent for
Harris—reflecting volume increases, general medical inflation, and the same bad debt issue.
However, Froedtert’s uncompensated care expense fell significantly (even as it increased the
upper-income limit for charity care eligibility) as more people gained coverage.
23
Overall
changes in uncompensated care at Regional One varied depending on time period (see Appendix
5).
Medicaid expansion helped financial performance. Most of the study hospitals started
with low or negative operating and total margins, and most of the expansion state hospitals saw
improved financial performance by 2015 (Figure 5). Reportedly, these improvements primarily
reflected gains in Medicaid patient revenue, but also some cost reductions (primarily through
staffing cutbacks). Between the first quarters of 2013 and 2015, average operating margins
across the six expansion state hospitals increased from -4 to 2 percent, and total margins
increased from 2 to 6 percent. Given their particularly large Medicaid enrollments in Kentucky,
UK Health and Marcum and Wallace stood out as experiencing significant gains, with margins
improving to more than 5 percent. LAC+USC’s margins improved but remained negative.
However, Yale faced declining margins, which executives attributed to reductions in the
hospital’s Medicaid reimbursement rates.
For most expansion state hospitals, much of the improvement in financial margins came
between 2013 and 2014; by 2015, margins typically had increased only slightly or even declined
from 2013. This fact likely reflects declining subsidies and increased costs, especially as
hospitals invested in more infrastructure to serve more patients and prepare for value-based
payments.
Non-expansion state hospitals’ average operating margins declined over the study period
and remained negative; total margins also fell but remained positive. The hospitals typically
attributed these losses to expenses (including investments in information technology, quality
improvement activities, and staff salaries) that outpaced relatively flat revenues. In contrast,
Froedtert had strong and improving operating margins, reflecting its relatively large growth (for
a non-expansion state hospital) in Medicaid volumes.
Financial constraints inhibited payment and delivery system reforms. Study hospitals in
states that expanded Medicaid have benefited financially from increased public insurance
revenue, which helped them address the new costs to develop infrastructure and implement other
needed changes to participate in value-based purchasing programs and alternative payment
models. As noted, participation in value-based purchasing programs has had little financial effect
23
Although Regional One’s uncompensated care appears to have increased in the quantitative data, the qualitative
information suggested an actual slight decline over the last few years (with the discrepancy attributed to the hospital
accounting for these expanses in batches throughout the year; also, the hospital first categorizes these accounts as
bad debt, then later determines what portion qualifies for charity care).

III. KEY FINDINGS MATHEMATICA POLICY RESEARCH
21
-50%
-40%
-30%
-20%
-10%
0%
10%
20%
2013 2015 2013 2015
Expansion-State Hospitals Non-Expansion-State Hospitals
Operating Total
on the study hospitals; for the hospitals engaged in alternative payment models, it is too soon to
know the longer-term financial impact.
The financially weaker hospitals lacked the resources to make these new investments and
are more focused on remaining viable and avoiding reductions in services. Harris Health and
Regional One reported that the lack of Medicaid expansion in their states significantly
contributed to their inadequate staffing and inability to upgrade electronic medical records
(EMRs) to improve quality and efficiency of care. One respondent summed up the trade-off
between costs and quality improvement efforts as follows: “When you are a safety net hospital,
you put [full-time equivalents] FTEs where they have to be, which is the clinical and regulatory,
and when you are trying to work on safety and quality, that’s where the FTEs are soft and you
start knocking the proposed ones off the budget.”
Figure 5. Average financial margins, Q1 2013 and Q1 2015*
*Margins unavailable for Homestead Hospital
Medicaid expansion also affected the study hospitals’ ability to continue with quality
improvement and other delivery system reform activities after initial funding through grants or
pilot programs had ended. Aided by its increase in Medicaid revenues, Denver Health intends to
continue with most of the activities funded by its CMMI grant—which ends in 2016—because
hospital leaders think that many of these changes pay for themselves through reductions in
inpatient admissions, ED visits, and other services.
In contrast, the DSRIP program in Texas has had mixed effects for Harris Health. DSRIP
funds enabled the hospital to expand primary care capacity in 2011 (by leasing space to operate
nine additional community clinics), with the expectation that the state would expand Medicaid—
but this preceded the 2012 Supreme Court ruling that made Medicaid expansion optional.
Texas’s decision not to expand Medicaid has meant that the hospital must now absorb increased
uncompensated care costs associated with its expanded network of primary care clinics and the
increase in specialty care and other referrals generated from primary care visits. The state’s

III. KEY FINDINGS MATHEMATICA POLICY RESEARCH
22
current Medicaid waiver ends in September 2016; if it is not renewed, the funding to operate
these clinics also could cease.
The level of Medicaid payment to hospitals affects not only their financial viability, but also
their willingness to assume financial risk for Medicaid patients and transform their delivery
systems. LAC+USC and other major safety net hospitals in California receive cost-based
Medicaid reimbursement for the Medicaid expansion population, which helps them to make
changes to their delivery systems. By contrast, Yale-New Haven faced recent cuts to its
Medicaid reimbursement (to address state budget deficits), which it estimates has decreased
Medicaid payment from 59 percent of costs in 2013 to 39 percent in 2015.
Active preparations for the future. Overall, improved financial stability has helped
expansion state hospitals to prepare for the future. The hospitals with greater financial security
now have more resources to help them continue expanding outpatient capacity, invest in
strategies to improve care coordination, and develop better infrastructure to monitor costs. All of
these actions are important for new payment arrangements, under which hospitals expect to
assume more financial risk for patient care and outcomes.
All of the study hospitals are cautious about spending, however. Many hospital executives
expressed concern that their recently improved financial status might be fleeting as subsidies
decline, and because Medicaid enrollment and payments could decline after 2017, when the
federal government no longer covers the full cost of the expansion.
24
As one said, “We’re in the
sweet spot of health reform.” Many non-expansion state hospitals have less of a financial margin
to pursue such investments; their executives express less confidence about their future.
Indeed, both expansion and non-expansion state hospitals are focused on ways to raise
additional revenues, primarily by diversifying their payer mix. Most hospital executives did not
expect to see many more of their uninsured patients gain coverage. Instead, they are focused on
pursuing new Marketplace and other commercially insured patients and, to a lesser extent,
Medicare patients. The academic medical centers have focused on expanding inpatient and/or
outpatient specialty services (tertiary and quaternary care) that appeal to a broader population.
For example, UK Health has added a new ambulatory building and inpatient beds to support this
strategy. Better branding and marketing is also important, respondents reported. For instance,
Regional One previously was known as Regional Medical Center and referred to as “the Med” in
the community; it adopted its new name as part of a rebranding strategy to reflect the broader
system of services it now provides (for example, primary care, outpatient surgery, and
rehabilitation).
The study hospitals are also focused on ways to cut costs. Those in non-expansion states are
more likely consider more significant changes to policies that could affect access. For example,
24
Starting in 2017, states must take on a portion of the cost, which will increase to 10 percent by 2020.

III. KEY FINDINGS MATHEMATICA POLICY RESEARCH
23
Harris Health has contemplated changing its charity care policy to reduce the number of people
eligible for free care.
25
E. Additional observations about differences between the 2014 and 2015
semi-structured discussions
Although the research team collected qualitative and quantitative information at two points
in time—2014 (reflecting back on 2013) and 2015 (reflecting back on both 2013 and 2014)—the
cross-site analyses discussed above generally focused on the overarching changes that the study
hospitals (Appendix 2) experienced between 2013 and 2015, rather than providing detail about
changes between 2014 and 2015. In response to ASPE’s request for more information about the
extent to which our findings differed between the 2014 and 2015 data collection periods, here we
summarize some common themes from both the quantitative and qualitative information (for the
qualitative piece, this summary represents only the six hospitals in the expansion states because
in 2014 we had not yet included the four hospitals in the non-expansion states).
1. Quantitative findings
The 2015 patient volume and financial indicators generally showed a continuation of what
had occurred in 2014. For hospitals in expansion states, Medicaid was a growing presence (in
patients and revenues); uninsured patients and uncompensated care costs were declining. Some
of those hospitals experienced more significant change between 2013 and 2014 than between
2014 and 2015. For others, the Medicaid expansion took more time to result in changes in
coverage and/or demand for care, and the degree of change between 2014 and 2015 exceeded
that of 2013 to 2014. However, these patterns often varied across service lines within an
individual hospital.
Still, many of the study hospitals in non-expansion states (and some in the expansion states)
experienced some fluctuation among the different time periods on different indicators. That is, in
a number of cases, patient volume in a certain category actually dipped a bit between the first
quarter of 2013 and 2014 but then showed more increase by 2015. Some respondents attributed
this development to more gradual coverage expansions in their states (especially if the state did
not expand Medicaid eligibility) but also to factors unrelated to the ACA. Such fluctuations
tended to be more prevalent among the Medicare and commercial volumes and payer/patient
mixes than in the Medicaid and uninsured categories.
Among hospitals in Medicaid expansion states, charity care steadily fell, but bad debt
fluctuated, in many cases rising between 2013 and 2014 and then falling to below 2013 levels in
2015. This finding could reflect initial increases in bad debt related to Marketplace and other
commercial insurance products that placed more cost-sharing requirements on consumers (for
example, through high-deductible products); whereas those products remained in place by 2015
and sometimes even grew more prevalent, coverage expansions may have caught up by 2015 to
reduce the number of people generating bad debt because they were uninsured (but did not
25
Hawryluk, Markian, “Harris Health considers cutting free care to close budget gap,” The Houston Chronicle, July
31, 2015. Available at http://www.houstonchronicle.com/news/health/article/Harris-Health-considers-cutting-free-
care-to-6416197.php.
III. KEY FINDINGS MATHEMATICA POLICY RESEARCH
24
qualify for charity care). Indeed, respondents generally seemed more concerned about rising bad
debt during the 2014 semi-structured discussions than semi-structured discussions in 2015.
For most of the study hospitals in expansion states, much of the improvement in financial
margins came between 2013 and 2014; by 2015, margins typically had increased only slightly or
even declined from 2013. This finding likely reflects declining subsidies and increased costs,
especially as hospitals invested in additional infrastructure to serve more patients and prepare for
value-based payments.
2. Qualitative findings
Overall, hospital executives’ thoughts about how the ACA was or was not affecting their
hospitals remained relatively consistent between 2014 and 2015. That is, for those areas about
which they were hopeful in 2014, they tended to remain hopeful in 2015 (for example, shifting
payer mix and revenues, preparations for value-based payments); for those areas about which
they were concerned in 2014, they generally remained concerned (for example, DSH cuts, not
receiving more commercially insured patients or even losing some of these patients).
However, there were some exceptions to this overall pattern. By 2015, hospital executives
reported less concern about competition with other providers for Medicaid patients. Also, some
had made less progress toward participating in alternative payment models than they had
expected in 2014. Whereas most hospitals did not expect their uninsured patient volumes/mix to
decline much more because they perceived most of these patients to be ineligible for coverage
based on their immigration status, at least one hospital (Denver Health) found it had initially
underestimated the number of people still eligible for coverage. Although not directly related to
the ACA, in 2014, the two rural hospitals were worried about potential changes to the definition
of a Critical Access Hospital (CAH) that might make them no longer eligible and were
concerned that their cost-based payments for Medicaid and Medicare would end even if they
remained a CAH; these concerns waned by 2015 because respondents perceived the changes
were no longer a focus of Congress.
F. Limitations and challenges
Given the limited research to date on the effects of the ACA on safety net hospitals, this
study provides an early look at the types of experiences these hospitals are experiencing in a
more timely way than larger evaluations. These larger evaluations typically take longer due to
the time needed for survey or other quantitative data to become available. Also, the in-depth
qualitative approach we used is valuable for understanding the varied contexts in which safety
net hospitals operate. This type of approach also provides a good view of how and why
hospitals’ experiences with the ACA may differ, as well as hospitals’ responses to new pressures
and other changes, which cannot be readily obtained through surveys or other quantitative
means. The study findings should be useful for forming hypotheses and research questions for
future quantitative and qualitative research.
Still, the study faced two key limitations. First, given the small sample size and purposive
sampling approach, the findings from these 10 study hospitals (Appendix 2) are not
representative of all safety net hospitals in the United States. Qualitative studies that rely on
open-ended semi-structured discussions with multiple respondents per study site are necessarily

III. KEY FINDINGS MATHEMATICA POLICY RESEARCH
25
limited in sample size and representativeness to allow for more in-depth understanding and
analysis of individual hospitals, and how they compare to hospitals that differ on important
organizational, regional, and state policy attributes. The findings cannot be generalized to all
safety net hospitals and should not be regarded as conclusive.
Second, the quantitative hospital data collected posed some limitations. Because we
collected quarterly rather than annual data, respondents cautioned that some changes could
represent normal period-to-period variation, rather than changes with practical significance. To
guard against overstating a level of change, we generally reported averages and ranges across
hospitals. Also, the research team was unable to obtain the release of information for some
indicators for certain hospitals, despite several attempts. However, the qualitative research
process enabled the researchers to offset some of these data omissions and other limitations by
capturing hospital executives’ perceptions of key changes and additional context and
information.

IV. CONCLUSIONS
Overall, the future viability of safety net hospitals may hinge on potential changes to their
financial supports, as well as adoption of strategies to reduce hospital costs and better manage
care so they can continue to serve both insured and uninsured patients, and fare well under
expanded payment reforms.
Although the hospitals in this study do not represent all safety net hospitals across the
country, their experiences highlight the types and degree of changes related to the ACA that
others might encounter. Overall, our findings suggest that the Medicaid expansion was a
significant, helpful change for these hospitals; also, this expansion in more states could help
bolster both the safety net hospitals operating in those states and access to care for their low-
income residents. Regardless of the state in which they operate, however, other Medicaid-related
funds and subsidies remain important to hospitals’ financial bottom lines, and they will face
challenges as they work to adapt to changes in funding streams and reduce costs of care—
particularly to fare well under payment and delivery system reforms.
Indeed, the study hospitals are trying to implement strategies that expand capacity and
access to new Medicaid enrollees and potentially attract other new patients while also adapting to
federal value-based purchasing programs and alternative payment models. Fortunately, many of
these strategies—including developing more primary care, creating information technology
systems to better track patient care and costs, and treating patients in new, more efficient ways
and for non-medical needs—appear consistent with both of these aims. Still, safety net hospitals
will need to be cognizant not to overextend their capacity or infrastructure in a way that
generates additional costs without bringing in adequate revenues, as well as not to economize to
the point of harming patient care.
Safety net hospitals across states face several potential funding challenges. With the federal
government soon passing along a portion of the cost of the Medicaid expansion to the states,
non-expansion state hospitals expressed concern that their states will become less inclined to
expand their Medicaid programs. Also, respondents at expansion state hospitals felt that this new
cost could lead some of their states to reduce Medicaid eligibility, benefits, or provider
payments. This possibility was a particular concern for the Kentucky study hospitals because
their Medicaid expansion was so large and because of a change in governor.
26
Such changes,
along with planned reductions in subsidies, could place some safety net hospitals in particularly
vulnerable positions.
26
Since the site visit, Kentucky has elected Matt Bevin as governor; he ran on a platform of repealing the Medicaid
expansion. Since his election, however, the governor has stated that he plans to retain the expansion but potentially
reduce benefits for new enrollees; he also plans to remove the state’s Marketplace (Kynect) and instead have
residents purchase coverage through the federal exchange. Barton, Ryland. “Kentucky Governor Tells Feds He Will
Dismantle State’s Insurance Exchange,” National Public Radio, January 12, 2016.
APPENDIX 1
CONCEPTUAL FRAMEWORK
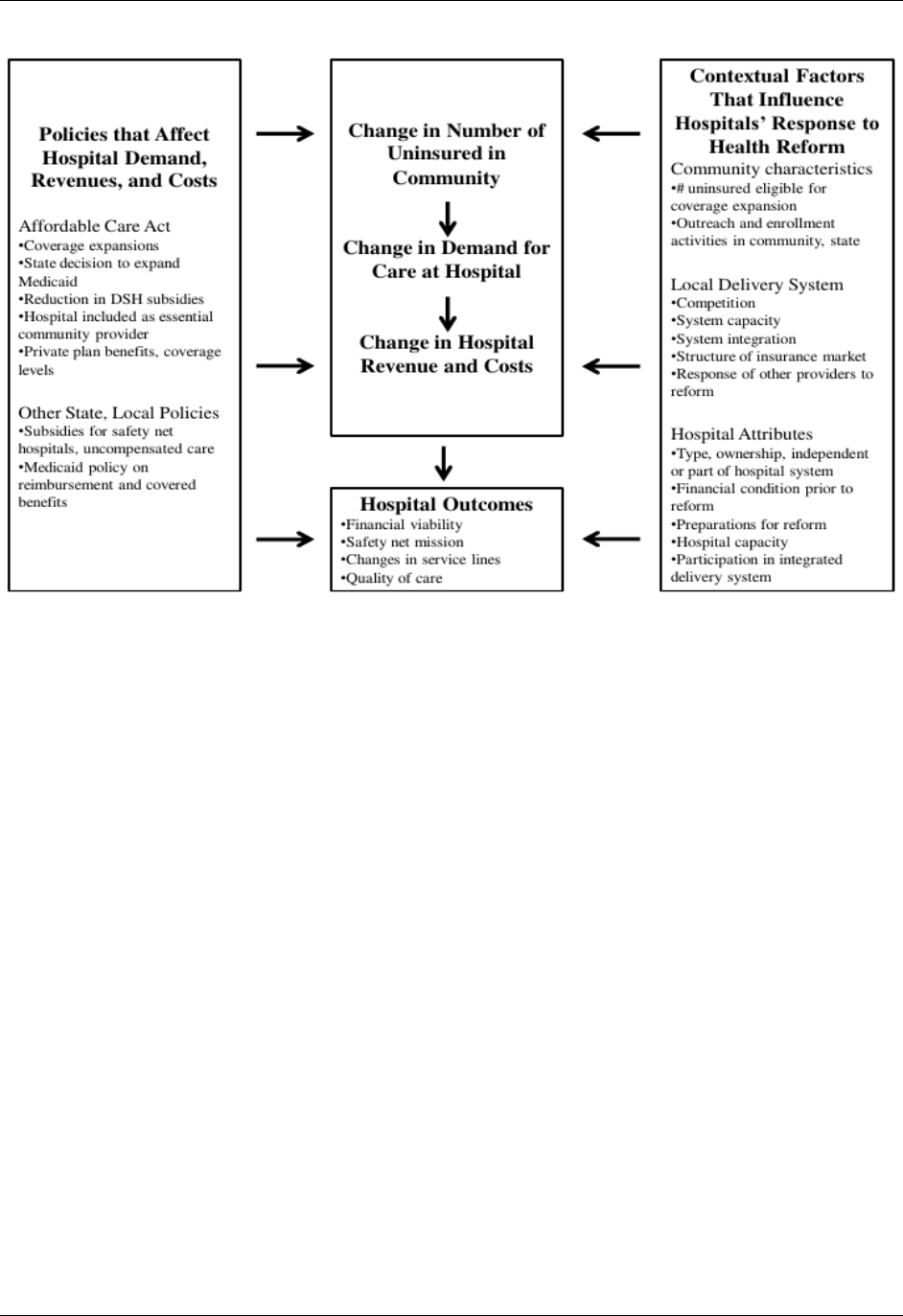
APPENDIX 1 MATHEMATICA POLICY RESEARCH
30
APPENDIX 2
TABLE OF HOSPITAL CHARACTERISTICS

APPENDIX 2 MATHEMATICA POLICY RESEARCH
34
Key Features of Study Hospitals
Hospital
Number
of Beds
Type
Position in local health care
market
DSH patient
percentage
prior to ACA
1
Share of total
uncompensated
care in county
prior to ACA
2
Denver Health Medical
Center
477
Publicly operated integrated delivery
system.
Dominant safety net system in
community
67.0
50.8
Froedtert Memorial Lutheran
Hospital (Milwaukee, WI)
509
Academic medical center (AMC)
affiliated with Medical College of
Wisconsin.
Competes with other major health
systems in area
31.7
20.3
Harris Health System (Harris
County, TX)
855
(3
hospitals)
Publicly operated integrated delivery
system
Dominant safety net system
.
.
Homestead Hospital
(Southern Miami-Dade
County, FL)
142
Part of not-for-profit system, affiliated
with Baptist Health South Florida
hospital system
Serves southern part of Dade county
not easily accessible to major public
system (Jackson Memorial)
68.7
6.3
LAC + USC Medical Center
(Los Angeles, CA)
600
Integrated delivery system that is part of
the LA County Department of Health
Services
Part of dominant safety net system
in community
84.9
20.6
Lakewood Health System
(Staples (Todd County), MN)
25
Independent, not-for-profit Critical
Access Hospital in an independent,
Integrated System includes primary,
specialty, behavioral health, and
long-term care and Level-3 trauma
center.
N/A
100
Marcum and Wallace
Memorial Hospital (Irvine
(Estill County), KY)
25
Critical Access Hospital part of not-for-
profit Mercy Health system
community’s sole health care facility;
limited outpatient and hospital
services (e.g., does not offer
surgical services)
N/A
100
Regional One Health
(Memphis, TN)
325
Not-for-profit system receiving support
from the county. Integrated delivery
system affiliated with University of
Tennessee Health Science Center
Dominant safety net system
75.0
18.3
University of Kentucky
HealthCare
(Lexington, KY)
945
(3
hospitals)
Academic Medical Center
Dominant health system in
community (safety net and
otherwise)
48.1
71.3
Yale New Haven Hospital
(New Haven, CT)
1,541
Academic Medical Center, primary
teaching hospital for Yale School of
Medicine
Dominant health system in
community (safety net and otherwise
42.9
72.2
APPENDIX 3
METHODOLOGY OVERVIEW

APPENDIX 3 MATHEMATICA POLICY RESEARCH
38
STUDY METHODOLOGY
A. Site and respondent selection
Key decisions regarding the selection of hospitals as sites for the 2014 case studies included
(1) the definition of a site; (2) whether to select the sites randomly or purposively; (3) whether to
include sites only in states that expanded Medicaid in 2014 or also include sites in states that did
not do so; and (4) whether sites should be restricted to the large public hospital systems or
include a diverse group of public hospitals, academic medical centers, and private not-for-profit
hospitals that provide an important safety net function.
Definition of a site. “Sites” could be defined either as individual hospitals or entire
communities (which would potentially include all safety net hospitals in those communities).
The community context (including population characteristics, organization of the health system,
and state and local policies) is important for understanding the effect of the ACA on safety net
hospitals, although the budget for this project precluded the amount of data collection needed for
understanding the effect of health reform on an entire community. Thus, this study defined sites
as individual hospitals, although we considered the context of the community when selecting
sites and in the analysis, to the extent possible.
Random versus purposive sampling of sites. Consistent with ASPE’s request for proposal
(RFP) for this project, the project budget initially covered four to five case study sites for 2014.
Although random selection typically has the advantage of greater representativeness and
generalizability of the study sites to other safety net hospitals in the U.S., such a small number of
sites would fall short of being statistically representative. Random selection of a small number of
sites also carries the risk that one or more hospitals would be selected that experienced little or
no change (for example, if there was little change in insurance coverage in the population despite
an expansion of Medicaid eligibility), thus reducing our ability to comment on how changes in
coverage are affecting safety net hospitals. For these reasons, we chose a purposive sampling
approach for site selection.
Restricting sites for 2014 discussions to states that expanded Medicaid in 2014. We
limited the sample for the 2014 case studies to states that expanded Medicaid in 2014 (at that
time, approximately half of the states). Although the research team and ASPE wanted to compare
the experiences of hospitals in expansion states with those in non-expansion states, the small
number of sites to be included for the 2014 case studies precluded analysis of differences
between these two groups. Including one or more hospitals from non-expansion states would also
greatly reduce our ability to examine change across a diverse group of hospitals facing the same
policy change.
Selection of hospitals in metropolitan areas. We selected four of the six study sites from
metropolitan areas. Based in part on input from the TEP convened in 2013 to help plan the
project, we restricted our selection of four of the sites to large hospitals or large hospital systems
in the top 100 metropolitan areas, since we expected that these hospitals were likely to be
experiencing the most change from the ACA. Because many metropolitan areas lack a county-
owned or -operated hospital system that typically serves a very strong safety net role by design,

APPENDIX 3 MATHEMATICA POLICY RESEARCH
39
we also included academic medical centers and private hospitals that provided an important
safety net function in the sample frame from which we selected the final case study sites.
We started the site selection process with a large universe of hospitals. Using data from the
Medicare Cost Reports, we computed the DSH patient percentage and uncompensated care costs
for all non-federal short-term general hospitals in the largest 100 counties in states that expanded
Medicaid. Within each county, we identified hospitals that provided the largest amount of
uncompensated care in the county and also had a high DSH patient percentage ((Medicare SSI
Days / Total Medicare Days) + (Medicaid, Non-Medicare Days / Total Patient Days)).
A variety of considerations guided the final selection of the four metropolitan hospitals for
study: how much state policy change likely was occurring (based on media reports, previous
research, and consultation with outside experts), with more change preferred; diversity by region
and type of hospital; and familiarity with various hospitals by project staff at Mathematica and
ASPE. Based on the project staff’s knowledge of specific hospital executives from other studies,
and in consultation with Bruce Siegel, President and Chief Executive Officer (CEO) of
America’s Essential Hospitals, we also considered the likelihood of hospital executives’
willingness to participate and how knowledgeable they would be about the effects of the ACA
and health policy in general.
The four metropolitan hospitals selected include the following: LAC+USC Medical Center
in Los Angeles, California; Yale-New Haven hospital in New Haven, Connecticut; Denver
Health in Denver, Colorado; and University of Kentucky HealthCare in Lexington, Kentucky.
California and Connecticut expanded Medicaid before 2014, and thus were likely to be
experiencing changes already due to coverage expansions. Denver Health is a large, fully
integrated safety net provider in a state active in promoting delivery system reform in its
Medicaid program through Regional Care Collaborative Organizations. University of Kentucky
HealthCare is the largest safety net hospital in one of the few southern states to expand Medicaid
in 2014. Also, the state-run health insurance marketplace in Kentucky (Kynect) reportedly was
highly successful in enrolling eligible uninsured people in coverage.
Selection of rural hospitals. The ASPE RFP requested that at least one of the 2014 study
sites be in a rural location. Selecting a suitable rural hospital presented special challenges due to
the large number and diversity of these hospitals; their small size (for example, CAHs have
fewer than 25 beds); and uncertainty as to how willing and able hospital officials would be to
participate, and their knowledge of the ACA and health policy in general. For this reason, we
consulted with rural health experts at the University of Iowa, University of Minnesota, the
National Rural Health Association, and the Health Resources and Services Administration about
suitable candidates for rural hospital sites.
We selected Lakewood Health System in Staples, Minnesota. Lakewood is an independent
CAH located about 135 miles northwest of Minneapolis and was highly recommended by rural
health experts we consulted because of its proactive implementation of a medical home model,
innovations in quality, health information technology, and value-based care. These rural health
experts also thought that Lakewood’s executives would be willing and knowledgeable study
participants. Lakewood has a particularly broad set of services for its size, from primary care to
long-term nursing care.

APPENDIX 3 MATHEMATICA POLICY RESEARCH
40
The rural health experts also recommended Marcum and Wallace Memorial Hospital in
Irvine, Kentucky, a CAH on the western edge of the Appalachian Mountains. This hospital is
part of the Mercy Health system and offers a fairly limited scope of services (inpatient and
emergency but no surgery, for example). The hospital president had recently won an American
Hospital Association Leadership award for rural hospitals. Although the original study objectives
called for only a single rural hospital, we decided to include Marcum and Wallace, given its
close proximity to the University of Kentucky HealthCare in Lexington, Kentucky, which could
be combined into a single site visit at a relatively low additional cost.
Selection of hospitals for the 2015 case studies. ASPE decided to exercise an option in the
contract (which coincided with a decision to divert resources from a previously planned
quantitative task) to conduct a second round of site visits in 2015. Neither the RFP nor our
proposal to ASPE specified whether we would conduct this second round of site visits with the
same group of hospitals we spoke with in 2014, or with a new group.
Based on the early findings from the 2014 site visits, ASPE and the research team decided
that it would be important to once again conduct semi-structured discussions with the initial set
of six study hospitals to determine whether their early experiences with the ACA were
continuing or had changed after an entire year had passed.
ASPE project staff also wanted to learn about the experiences of hospitals in states that did
not expand Medicaid and hear more about their experiences with payment and delivery system
reforms. They expected that hospitals would have valuable information to share about the latter,
even if they had experienced little change in utilization and payer mix due to a state’s reluctance
to expand Medicaid. The budget allowed the addition of four sites for 2015 if we conducted the
semi-structured discussions for all 10 sites by telephone. Apart from the new focus on hospitals
in states that had not expanded Medicaid, the same considerations that guided the selection of
sites in 2014 guided that of the four new sites.
The sites for 2015 were the following: Harris Health System in Harris County (Houston),
Texas; Regional One Health in Memphis, Tennessee; Froedtert Hospital in Milwaukee,
Wisconsin; and Homestead Hospital in Dade County, Florida. Harris Health and Regional One
are large county-operated or -supported safety net systems; Froedtert Hospital is an academic
medical center affiliated with the Medical College of Wisconsin; and Homestead Hospital is a
private, not-for-profit hospital that is part of Baptist Health South Florida hospital system.
Homestead exists in the shadow of a large county-operated system in Dade County (Jackson
Memorial Health System) but is located in a part of the county with significant need that is far
away from Jackson’s main facilities.
Selection of site visit respondents. The RFP and case study plan called for approximately
five to eight semi-structured discussions per site in 2014. We spoke with several types of
executives at each study hospital to capture the breadth and depth of information needed to
investigate the research topic areas, and to triangulate responses to ensure accuracy. The
executives typically included the CEO, the Chief Financial Officer (CFO), and the Chief Medical
Officer (CMO), but we included other executives, such as emergency department directors and
strategy executives, in some cases per the hospital’s suggestion. We also spoke with other health
care experts in the community to get an outsider’s perspective of a safety net hospital and further

APPENDIX 3 MATHEMATICA POLICY RESEARCH
41
triangulate our findings, capture the structure dynamics of the local health care system and state
and local health care policy, and understand the broader effect of the ACA on the community.
The organizations for which these individuals worked differed to some extent across the six
study sites but included the state Medicaid agency, community health centers, local health
foundations, and state hospital associations. We held semi-structured discussions with 46
individuals between June and August 2014.
We limited the 2015 semi-structured discussions to the core set of hospital executives.
(Based on the 2014 semi-structured discussions, we often targeted a smaller set of executives, as
we were familiar with their expertise from the first round or had developed more focused
discussion topics.) This decision was driven by budget limitations and because of the new
emphasis on hospital quality improvement initiatives and payment and delivery system reforms
taking place within a hospital; thus, we deemed the perspective of other community
organizations less critical. We held semi-structured discussions with 25 individuals between May
and September 2015.
B. Data collection
The 2014 semi-structured discussions focused on changes between the first part of 2013 and
first part of 2014 in patient demand and use of services, system capacity, revenues (operating and
non-operating), expenses (including uncompensated care), patient and payer mix, and financial
performance, and whether these changes were a result of the ACA or other factors. We also
discussed the hospital’s role in the local safety net; key strategies and goals with respect to the
ACA, including quality improvement initiatives, delivery system reforms, and the use of health
information technology; and how the mission and role of the hospital was likely to change
following implementation of the ACA. We asked about hospital executives’ expectations for the
future with respect to the ACA, especially the expected effects of the pending reductions in
Medicaid DSH payments.
Based on ASPE’s key areas of interest, the 2015 semi-structured discussions placed
considerably more focus and emphasis on the hospital’s experiences with Medicare value-based
payment initiatives, such as the hospital readmissions reduction and Hospital Acquired
Conditions programs. We also focused on the hospital’s experiences and plans regarding
alternative payment arrangements that pass more financial risk to the hospital, such as ACOs,
bundled payments, or capitation. To provide time in the semi-structured discussions to cover
these areas, we scaled back our focus on the general community context/local health care market
environment in which the hospital operates.
In both 2014 and 2015, we customized the discussions somewhat to fit the respondent type.
For example, the CFO semi-structured discussions focused primarily on changes in hospital
utilization, the payer mix and acuity level of patients, revenue and uncompensated care, and
hospital financial performance. The CMO semi-structured discussions focused primarily on
quality improvement initiatives, experiences with Medicare value-based payment initiatives, and
alternative payment models. The CEO semi-structured discussions covered many of these same
issues, but focused particularly on their view of the longer-term impacts of the ACA, how it
affects the hospital’s position in the local health care system, and the hospital’s strategy for
successfully adapting to it.

APPENDIX 3 MATHEMATICA POLICY RESEARCH
42
Quantitative hospital information. In advance of the semi-structured discussions, the
research team collected quantitative information on patient volumes and financial indicators
from each study hospital. To capture comparable and current information, the team requested
financial and performance data from the first quarters (January through March) of 2013 and
2014. Metrics included the number of inpatient admissions, ED visits and other outpatient visits,
as well as patient revenues, other operating and non-operating revenues, operating and other
expenses, and net margins. To maintain consistency across all hospitals as to the types and time
periods of information collected, we provided each hospital with a template to complete (see
Appendix 4). The researchers referred to this information during the hospital discussions to learn
about the degree of change across the volume and financial indicators, and the reasons behind
these changes or lack of changes.
The 2015 semi-structured discussions also asked for these same metrics. For the six
hospitals included in the 2014 semi-structured discussions, we ascertained whether the trends
observed between 2013 and 2014 continued into 2015, and the reasons for any change in the
trends. For the four new hospitals included in 2015, we obtained information on utilization and
finances for the first quarters of 2013, 2014, and 2015.
Conducting the site visits and semi-structured discussions. We conducted the site visits
between June and August 2014. Most semi-structured discussions occurred in person over two
days, with some conducted by phone for respondents who were not available during the two days
on site. The research teams for each site consisted of a senior researcher who led the semi-
structured discussions and a research assistant who took verbatim notes on a laptop computer.
(To facilitate respondent candor, we did not record the discussions.) Senior researchers included
the principal investigators for this project and, in 2014, Emily Carrier, at the time a senior
researcher at Mathematica. To facilitate a broad and deep understanding of each site, the same
senior researcher and research assistant team conducted all semi-structured discussions for a
given site. The discussions typically lasted an hour. At the start of each, we reminded
respondents that we would name their hospitals in our final publications, but in our public
documents we would not name the individuals we spoke with or attribute specific comments to
any particular individual. We also offered to keep confidential any information they shared with
us that they did not want included in a public document.
The research assistant cleaned and coded the notes from each discussion. (Coding involved
applying a code to each paragraph to indicate which topics the respondent discussed in that
paragraph.) The senior researcher reviewed and edited the notes to ensure they were complete
and accurate. We organized the notes using Atlas.ti, a qualitative software package, which allows
researchers to readily search semi-structured discussions for key topics and generate queries of
responses across respondents on a given code.
As noted earlier, we conducted all 2015 semi-structured discussions by phone. The semi-
structured discussions for each site took place over a two- to three-week period. The principal
investigators conducted all of the 2015 discussions. Otherwise, all of the procedures described
here for the 2014 site visits held for the 2015 discussions.

APPENDIX 3 MATHEMATICA POLICY RESEARCH
43
C. Analysis
The research team synthesized and analyzed the qualitative and quantitative information
through several steps and iterations. First, we synthesized the semi-structured discussions for
each site individually. Following each site visit, we reviewed the discussion notes and
supplemental information (for example, media reports, information provided by the study
respondents), and wrote a site summary synthesizing the major findings related to the key
objectives of the project. These site summaries also identified the three or four major themes that
described the effect of the ACA on the hospital. We repeated this process for the 2015 semi-
structured discussions; for the original six hospitals, the 2015 summaries essentially updated and
replaced the previous 2014 summaries to reflect the more recent semi-structured discussions (see
Appendix 5).
Comparing and contrasting key findings across the site summaries allowed us to identify
cross-cutting themes. In October 2014, the research team shared with ASPE a preliminary set of
five themes (on changes in payer mix, slight shifts from inpatient to outpatient utilization,
improving financial positions, concerns about the future, and strategies for the future) that
emerged from the 2014 visits and would be candidates for further cross-site analysis and
dissemination. Upon deciding to pursue additional sites and semi-structured discussions in 2015,
we determined, in collaboration with ASPE, to delay the development of the cross-site products
until those semi-structured discussions and site summaries had been completed.
In June 2015, we proposed four potential topics to develop for cross-cutting products. They
included the following: the effect of the ACA on the financial performance and viability of
safety net hospitals; experiences with quality improvement and care delivery innovations; efforts
by safety net hospitals to integrate with primary care and other providers in the community; and
how the role of safety net providers is changing as a result of the ACA. Discussions of these
topics with ASPE led to the decision to focus only on the first two topics and develop them as
research briefs. In collaboration with ASPE, we decided to pursue two cross-cutting analyses that
aligned closely with the major research questions for the project: (1) the effect of the ACA on
changes in demand for care, payer mix, uncompensated care, and financial performance; and (2)
experiences with payment and delivery system reforms. To analyze these topics in depth, the
research team organized and analyzed the qualitative and quantitative information in a variety of
ways. We analyzed the site summaries, reviewed the coded text from the discussion notes by
topic area, and created a table to examine the changes in volumes and finances across the
hospitals. We explored possible explanations as to why the safety net hospitals differed in their
experiences with the ACA through a review of the text and data, grouped by whether or not the
site was in a state that had expanded Medicaid, the type of hospital (county-owned or -operated,
academic medical center, private not-for-profit), and the hospital’s position in the local health
care system.

APPENDIX 3 MATHEMATICA POLICY RESEARCH
APPENDIX 4
FINANCIAL TABLE TEMPLATE

APPENDIX 5 MATHEMATICA POLICY RESEARCH
47
ASPE Study of Safety Net Hospitals
Financial Information
Please fill in the boxes (note that some cells have formulas built in to help generate totals
and sub-totals)
.
Three Months
Ended
March 31, 2013
Three Months
Ended
March 31, 2014
Three Months
Ended
March 31, 2015
A. Total Operating Revenue
.
.
.
.Inpatient revenue (total)
.
.
.
Medicaid
.
.
.
Medicare
.
.
.
Commercial insurance
.
.
.
Self-pay/uninsured
.
.
.
Other
.
.
.
Outpatient revenue (total)
.
.
.
Medicaid
.
.
.
Medicare
.
.
.
Commercial insurance
.
.
.
Self-pay/uninsured
.
.
.
Other
.
.
.
Operating revenue from state govt.
.
.
.
Operating revenue from city/county govt.
.
.
.
Other operating revenue
.
.
.
B. Total Non-Operating Revenue
.
.
.
C. Total Operating Expenses
.
.
.
Total Uncompensated Care Costs
.
.
.
Charity care costs
.
.
.
Bad debt
.
.
.
Other operating expenses
.
.
.
D. Total Non-Operating Expenses
.
.
.
Operating margin
.
.
.
.
.
.
Total margin
0
0
0
APPENDIX 5 MATHEMATICA POLICY RESEARCH
48
ASPE Study of Safety Net Hospitals
Utilization/ Patient Volume
Please fill in the non-shaded boxes (note that some cells have formulas built in to help
generate totals and sub-totals)
.
Three Months
Ended
March 31, 2013
Three Months
Ended
March 31, 2014
Three Months
Ended
March 31, 2015
Total Admissions
.
.
.
.
Medicaid
.
.
.
.
Medicare
.
.
.
.
Commercial insurance
.
.
.
.
Self-pay/uninsured
.
.
.
.
Other
.
.
.
Average Length of Stay (Days)
.
.
.
.
Medicaid
.
.
.
.
Medicare
.
.
.
.
Commercial insurance
.
.
.
.
Self-pay/uninsured
.
.
.
.
Other
.
.
.
Deliveries
.
.
.
.
Medicaid
.
.
.
.
Medicare
.
.
.
.
Commercial insurance
.
.
.
.
Self-pay/uninsured
.
.
.
.
Other
.
.
.
Emergency Department Visits
.
.
.
.
Medicaid
.
.
.
.
Medicare
.
.
.
.
Commercial insurance
.
.
.
.
Self-pay/uninsured
.
.
.
.
Other
.
.
.
Other Outpatient Visits
.
.
.
.
Medicaid
.
.
.
.
Medicare
.
.
.
.
Commercial insurance
.
.
.
.
Self-pay/uninsured
.
.
.
.
Other
.
.
.
APPENDIX 5
10 SITE SUMMARIES

APPENDIX 5 MATHEMATICA POLICY RESEARCH
51
ASPE Safety Net Hospital Study
2015 Site Summary for Denver Health
A. Summary of Denver Health
Denver Health is described as a vertically integrated delivery system with an acute care
hospital with some 500 beds, a level-1 trauma center, 8 federally qualified health centers
(FQHCs), and 15 school-based, dental, and other specialty clinics. The system also operates
the medical component of the Denver Department of Public Health.
Denver Health is the main safety net hospital in the city. The University of Colorado Health
system provides more specialized tertiary and quaternary services that Denver Health does
not provide.
B. Summary of the impact of the Affordable Care Act (ACA)
As a result of the ACA coverage expansions, Denver Health has seen substantial increases in
the number of patients, use (especially outpatient), patient revenues, total and operating
margins, and decreases in uninsured patients and uncompensated care.
The expansions in coverage and use have permitted expansions in capacity, including hiring
new staff, expanding certain service lines (for example, behavioral health, dental), and
building new facilities.
Denver Health has performed relatively well under the Centers for Medicare & Medicaid
Services (CMS) value-based purchasing (VBP) initiatives, which the health center attributes
to a relatively low number of Medicare fee-for-service patients, and an integrated delivery
system that stresses strong coordination between inpatient and primary care, and other
services. The Center for Medicare and Medicaid Innovation (CMMI) award has been helpful
with this.
Denver Health has no plans to start or join an ACO or bundled payment initiative. Instead,
they are focusing on full capitation in which they will be at full-risk for the cost of care to
their patients.
C. Changes in demand (Q1 2013 to Q1 2015)
Outpatient visits have increased 10 to 12 percent since 2013, and inpatient visits have
increased about 4 percent since then. Most of this increase reflects increased demand among
Medicaid patients.
Increased demand among Medicaid patients reflects new users as well as those who were
previously uninsured who enrolled in Medicaid. There was an increase of 27,000 new
patients in 2014 compared to 2013 (a 14 percent increase between 2013 and 2014), most of
whom were Medicaid patients. The number of uninsured patients has decreased
commensurately.
Service use related to behavioral health care has increased disproportionately. This reflects a
change in state Medicaid reimbursement policy, which allows providers to bill for
behavioral health and medical visits on the same day.

APPENDIX 5 MATHEMATICA POLICY RESEARCH
52
As of March 2015, Denver Health had 22,000 uninsured patients. Of this number, about
8,000 were estimated to be eligible for Medicaid; 1,000–2,000 were estimated to be eligible
for the health insurance exchanges; and 9,500 were undocumented immigrants. The
principal reason Medicaid-eligible patients are not signed up for the program is that they do
not follow through with the screening and enrollment process.
Take-up of private insurance through the health insurance marketplaces has been slower
than expected among Denver Health patients, but respondents believe it is now beginning to
accelerate due to efforts to improve patient experience, customer satisfaction, marketing,
and partnering with insurance companies.
D. Changes in capacity
Denver Health started ramping up for the ACA in 2013. They have focused especially on
expanding primary care and other specialty areas, such as behavioral health. They have
added physicians, advanced care nurse practitioners, psychiatric staff, social workers,
optometrists, and dental staff. (Colorado Medicaid began covering dental care in July,
2014.) In 2016, Denver Health will open a new outpatient clinic.
E. Changes in finances
Overall, inpatient revenues increased 8 percent between the first quarter of 2013 and 2015,
while outpatient revenues increased 22 percent. Most increased patient revenue is attributed
to Medicaid.
Consistent with the decrease in uninsured patients, self-pay revenue has decreased by more
than half since 2013, while charity care costs have decreased by 75 percent.
In terms of payer mix, Medicaid now comprises more than half of patient revenue (up from
35.8 percent in 2013), while self-pay revenue comprises 11.5 percent of revenue (down from
27.4 percent in 2013).
Revenue from commercial payers has also increased for outpatient care, although the share
of revenue from commercial insurance has not changed significantly (about 16 percent).
Colorado has a provider fee used to fund Medicaid Disproportionate Share Hospital (DSH)
and higher Medicaid reimbursement through the upper payment limit. This helps subsidize
care to the uninsured and allows Denver Health to receive close to 100 percent of Medicaid
costs. Revenue related to the provider fee has been increasing in the past few years, although
there is expectation that Medicaid DSH payments will begin to decrease in 2016 because of
decreases in uninsured patients (followed by additional ACA-related cuts that have been
delayed to 2018).
Financial performance has improved markedly since 2013, when the health system was
incurring losses and laying off staff. Operating margins improved from -1.5 percent in the
first quarter of 2013 to 3.4 percent in the first quarter of 2015. The improvement was
attributed mostly to the ACA coverage expansions.

APPENDIX 5 MATHEMATICA POLICY RESEARCH
53
F. Experience with Medicare VBP
Denver Health has relatively few Medicare fee-for-service patients, so the impact of VBP on
the health system has not been great. The financial impact has been about $400,000 annually
(out of total operating revenues of about $900 million in 2014).
Nevertheless, Denver Health has performed relatively well on VBP quality indicators for a
safety net hospital. They were only slightly above average for hospital readmissions and
incurred only a small penalty. Respondents attribute the relatively good performance on
readmissions to the fact that Denver Health is an integrated delivery system, which includes
primary care physicians, FQHCs, school-based clinics, and Denver’s Department of Public
Health. They are able to achieve a seamless flow of patients from the inpatient to outpatient
setting, good communication between inpatient and primary care providers, and a single
health information system. Respondents also attribute relatively low readmissions to
programs initiated with their $19 million CMMI award. Initiatives with this award focused
on better management of high-utilizing patients, funded patient navigators, medication
management, and integration of behavioral health into primary care settings.
Denver Health was not penalized under the hospital-acquired conditions (HAC) reduction
program in 2014. Although they did not identify any new programs as responsible for
helping to keep HAC rates low, they have emphasized that preventing falls as well as
controlling central and associated blood stream infections and surgical site infections as key
factors in reducing HAC.
Patient satisfaction scores have not been good in the past, but they have improved in the past
year. Respondents cited improved access to care (due to hiring of more staff) and shorter
waiting times as the main reasons for the improvement. Also, Denver Health has contracted
with the Studer group to redesign their approach to patient interactions. (The Studer group
has worked with about 900 hospitals in the country on this issue and reportedly has shown
good results.) This program just started, so it is too early to assess results.
Respondents mentioned some difficulty with CMS core measures based on chart review,
which they attributed to errors in documentation because their information systems are not
yet fully electronic. They expect this to improve with a new electronic health records system
coming online in 2016.
Respondents believe that having an integrated network of care and a single medical record
for every patient is crucial to being able to perform well under VBP. An emphasis on
population health, and being able to keep track of and contact patients when they are not in
the health system is also crucial. Being able to understand and analyze the data they have
acquired is also important.
Among the challenges of VBP, respondents expressed some frustration with the “explosion”
of quality metrics, and the frequency with which the measures change. They also report that
different reporting requirements between CMS and the Joint Commission take up
considerable staff time and resources. Respondents also believe that socioeconomic status
adjustments for safety net hospitals are required because of the unique needs of their
patients. One area that Denver Health struggles with is getting patients into post-acute care,
such as assisted living facilities and skilled nursing facilities, along with being able to
discharge patients with serious mental illness to a safe level of care.

APPENDIX 5 MATHEMATICA POLICY RESEARCH
54
G. Experiences with alternative payment arrangements
Denver Health does not participate in an ACO or bundled payment arrangements, and has no
plans to do so. But they are participating in full-risk capitation, primarily through their
Medicaid managed care plan, Medicaid Choice, which has 67,000 enrollees. Along with
commercially insured and Medicare patients, they estimate that 40 percent of their patients
are in fully capitated health plans in which the health system is at full risk—and they would
like to greatly expand that in the future. Because of their integrated care model, Denver
Health believes they do well under full capitation and are ahead of the curve with respect to
ACOs and other models.
To this end, Denver Health is implementing a care management program that is combining
social workers and use management so that a single case manager is working with patients
on all of their care transitions.
H. Participation in CMMI projects
As mentioned above, Denver Health received a $19 million award from CMMI to fund its
21st Century Care program, which includes a heavy emphasis on team-based care, care
coordination, integration of physical and behavioral health, and focusing on high- utilizing
patients. The grant ends this year (2015), but Denver Health is planning to continue with
much of the program (paid for through hospital operating costs) because they believe the
programs have great value and are self-sustaining.
I. Expectations for the future
Denver Health expects to see an increase in patients enrolled through the Marketplaces,
which is key to their strategy of diversifying their payer mix and changing their safety net
hospital image. However, they believe the state’s indigent care program, funded through
Medicaid DSH, discourages some people from enrolling in Marketplace plans because they
can essentially receive free care at Denver Health while uninsured. At the same time, cutting
or ending the indigent care program (of which there has been some discussion in the state)
will also negatively impact the health system.
Reductions in Medicaid DSH are a concern, not just the reductions related to the ACA that
have been delayed to 2018, but reductions based on their decreasing number of uninsured
patients. Denver Health is skeptical that increases in Medicaid patients— which they are
compensated for close to cost because of the provider fee and upper payment limit—will
fully offset the decrease in DSH funds used to pay for care for the uninsured.

APPENDIX 5 MATHEMATICA POLICY RESEARCH
55
ASPE Safety Net Hospital Study
2015 Site Summary for Froedtert Hospital
A. Overview of Froedtert Hospital
Froedtert Hospital is an academic medical center affiliated with the Medical College of
Wisconsin. Located in downtown Milwaukee, Froedtert is the flagship campus for this
health system, which also includes two other hospitals (St. Joseph and Community
Memorial), located in suburban areas. The health system also operates 25 specialty care and
primary care clinics throughout the Milwaukee metropolitan area.
Froedtert is a safety net hospital, primarily by virtue of its size. It provides about 20 percent
of all hospital uncompensated care in the county, although the proportion of uninsured and
Medicaid patients at the hospital is not as high as some other, smaller hospitals in the
community. A county-owned hospital that served as the main safety net hospital for the
county closed in 1995.
Froedtert views itself as the premier hospital system in the area that also provides a safety
net function, rather than viewing care for low-income people as its primary mission.
Froedtert is a strong competitor of the other major hospital systems in the Milwaukee area,
such as the Aurora health system and Columbia St. Mary’s (part of Ascension Health).
Froedtert is a tertiary and quaternary care provider in the Integrated Health Network of
Wisconsin (IHNW), a “super-ACO” comprising eight health systems throughout Wisconsin.
B. Summary of the impact of the Affordable Care Act
Wisconsin did not expand Medicaid coverage as part of the ACA coverage expansions of
2014. In 2014, however, the state expanded its BadgerCare program (a Medicaid expansion
from the late 1990s to cover uninsured children and families) by removing a cap on
enrollment for adults with family incomes up to the federal poverty line.
As a result of the BadgerCare expansion, Froedtert experienced changes in utilization and
finances similar to those in hospitals in Medicaid expansion states. Medicaid volumes and
revenue increased, whereas uninsured volumes and uncompensated care decreased.
C. Changes in demand (Q1 2013 to Q1 2015)
Froedtert’s overall patient volumes increased modestly, including 5 percent for inpatient
admissions, 3.3 percent for ED visits, and 2.7 percent for outpatient visits. The increase in
inpatient admissions occurred despite the implementation of Medicare’s “two-midnight”
rule, which resulted in more encounters being classified as outpatient rather than inpatient.
Despite Wisconsin not expanding Medicaid through the ACA, it changed its BadgerCare
program to allow more adults to enroll. The state removed the enrollment caps for adults
with incomes of less than 100 percent of poverty, which had resulted in a long waiting list,
especially in the Milwaukee area. As a result, Medicaid admissions increased by 21 percent,
Medicaid ED visits by 39 percent, and Medicaid outpatient visits by 13 percent. Utilization

APPENDIX 5 MATHEMATICA POLICY RESEARCH
56
by self-pay/uninsured patients declined commensurately, reflecting the fact that many of
these patients gained coverage through BadgerCare.
As a result, Froedtert’s patient mix also shifted. The share of admissions comprising
Medicaid patients increased from 17.5 percent to 20.2 percent, whereas the share of ED
visits comprising Medicaid patients increased from 29.8 percent to 40.1 percent.
Despite some previous types of inpatient stays now being classified as observation stays
(which tends to increase the length of inpatient stays because those remaining classified as
inpatients are sicker), Froedtert’s average length of stay actually decreased by about 5
percent. Hospital executives mostly attributed this to a concerted effort at better discharge
planning and “multidisciplinary rounding” since 2014 (explained more in the Medicare
value-based purchasing (VBP) section below).
D. Changes in capacity
One of Froedtert’s main strategies over the last few years has been to expand access points
in the community for both new and existing patients. It opened new clinics for primary and
specialty care in suburban Milwaukee (Oak Creek and New Berlin), implemented “virtual
urgent care” through FaceTime and Skype phone calls, and is considering partnerships with
grocery stores and pharmacies to establish retail clinics.
Froedtert donated $12 million to a local FQHC to open a new site, both to increase access to
care in the community and generate referrals for the hospital.
The hospital opened a new Center for Advanced Care in 2015, which will increase capacity
for outpatient and inpatient care, including a vascular and transplant center.
Froedtert also purchased an interest in an insurance plan (Network Health), which hospital
executives expect will help the hospital transition to a VBP system and allow them to
contract directly with employers.
E. Changes in finances (Q1 2013 to Q1 2015)
Froedtert’s total patient service revenue increased 32 percent between Q1 2013 and Q1
2015. This increase includes a 13 percent increase in inpatient revenue and a 38 percent
increase in outpatient revenue (reflecting expansions in outpatient capacity).
Medicaid inpatient revenue increased 77 percent, but Medicaid outpatient revenue was
stable (likely because the outpatient capacity expansions occurred in suburban areas where
fewer Medicaid patients live). As a result, the hospital’s percentage of inpatient revenue
from Medicaid increased from 9 to 14 percent, whereas its percentage of outpatient revenue
from Medicaid decreased from 8 to 6 percent.
According to a hospital executive, the hospital’s revenue growth is driven primarily by
increases in volume and, to some extent, higher patient acuity.
Froedtert’s uncompensated care costs declined 60 percent, reflecting the shift of many
uninsured patients to the BadgerCare program.
The hospital’s operating margins increased from 8.4 percent in Q1 2013 to 15.3 percent in
Q1 2015. However, a hospital executive expects revenues to decrease in the future (despite

APPENDIX 5 MATHEMATICA POLICY RESEARCH
57
higher volumes) due to decreased support from Medicaid DSH payments and the move
away from fee-for-service payments in Medicare and commercial insurance.
F. Experience with Medicare VBP
Froedtert’s quality-of-care measures as reported on Hospital Compare are generally similar
to or better than state and national averages. One problem area for the hospital has been
readmissions for hip/joint replacements, although the hospital’s executives believe this issue
has been resolved and subsequent years will show improvement.
The hospital also has patient satisfaction scores comparable to state and national averages;
Froedtert received four out of five stars on the new star rating system. To help its scores in
this area, Froedtert hired the Studer Group (a health care consulting/training organization) to
provide coaching and tutoring for providers.
Despite average performance, Froedtert executives see the hospital as at a disadvantage for
Medicare VBP because, as an academic medical center, it has higher risk scores than other
hospitals. They also cite a large indigent patient population as a disadvantage and suggest
the need for some type of socioeconomic risk adjustment.
Froedtert executives credit Wisconsin’s statewide health information exchange with
supporting quality improvement efforts. The exchange allows the hospital to view data on
service utilization at other health care providers in the state.
A major quality improvement effort for Froedtert has been to improve discharge planning to
reduce the length of stays. The hospital is using “multidisciplinary rounding,” which
involves a team of different medical providers visiting the patient at the same time rather
than different providers seeing the patient at different times during the day, thereby
improving communication and coordination among the providers. Froedtert attributes its
decrease in length of stay between 2014 and 2015 to this initiative.
G. Experiences with alternative payment models (APMs)
Froedtert Hospital is part of the IHNW, a “super ACO” that began in 2010 and comprises
eight largely hospital-based systems—including 45 hospitals and 5,700 providers throughout
the state.
From Froedtert’s perspective, the goal of IHNW is to “help us to move in the right direction
so that when Wisconsin converts to value-based care we have a system set up for
rationalization and have enough volume for all the systems to survive the change.”
(Reportedly, providers in Wisconsin still largely receive fee-for-service payments.) The
vision is of a horizontally integrated system with uniform care and quality improvement
processes that can be marketed to insurance companies.
IHNW has shared-savings contracts with Humana and United Healthcare. The organization
would like to expand such contracts to other plans and Medicare, but currently does not plan
to include Medicaid enrollees. Nevertheless, Froedtert executives stress that all patients will
benefit from the quality improvement processes they implement as part of the IHNW.

APPENDIX 5 MATHEMATICA POLICY RESEARCH
58
Executives report that care quality has improved since Froedtert joined IHNW, with key
examples including improvements in colonoscopy screening and pneumococcal vaccination
rates. However, they have yet to see any impact on costs.
H. Expectations for the future
As exemplified by its participation in the IHNW, Froedtert is pursuing a long-term strategy
to position itself to perform under VBP and other APMs for Medicare and commercially
insured patients. This strategy is partially in response to what hospital executives perceive
will be tighter revenue due both to the shift away from fee-for-service and decreasing
Medicaid payments (DSH).
Froedtert appears to be using a two-track approach to prepare for VBP and APMs: the
IHNW for commercially insured and Medicare patients, and affiliations with local FQHCs
for Medicaid and uninsured patients. Froedtert’s increase in inpatient, but stable outpatient
Medicaid revenues likely reflects the fact that (1) the majority of the hospital’s Medicaid
patients either are referred by FQHCs or come through the ED, and (2) Froedtert has
expanded outpatient capacity in suburban areas rather than in parts of the city where many
Medicaid patients live.

APPENDIX 5 MATHEMATICA POLICY RESEARCH
59
ASPE Safety Net Hospital Study
2015 Site Summary for Harris Health System
A. Summary of Harris Health System
Harris Health System is the primary safety net provider for Harris County, Texas, which
includes the city of Houston. It comprises three hospitals (Ben Taub, LBJ, and Quenyin
Mease) that include a total of 855 licensed beds. The system also includes 21 primary care
clinics, school-based clinics, dental clinics, mobile vans, and other services. It is affiliated
with two medical schools—Baylor College of Medicine and University of Texas Health—
that supply most of the medical staff.
The county provides about $600 million in tax support annually to Harris Health, accounting
for 47 percent of its operating revenue. The vast majority of patients (85 percent) are either
Medicaid or uninsured patients. Respondents believe that about one-third of the uninsured
are undocumented immigrants.
B. Summary of the impact of the Affordable Care Act
Given that the state of Texas has not expanded Medicaid, the Affordable Care Act has not
significantly affected Harris Health.
In anticipation of Medicaid expansion, which never materialized, Harris Health experienced
decreases in Medicaid disproportionate share hospital payments and county tax support. At
the same time, uncompensated care and other costs have increased, resulting in substantial
financial losses for the system and potentially leading to service cuts.
The Delivery System Reform Incentive Payment (DSRIP) program allowed Harris Health to
expand its primary care capacity, which contributed to increased patient volume. With the
expectation that Medicaid would be expanded, the system is now experiencing difficulty in
meeting the increased demand for specialty services generated by an increasing volume of
primary care visits (i.e., which lead to more referrals for specialty care).
The large uninsured and Medicaid population and relatively small number of Medicare
patients mean that Harris Health has limited exposure to penalties related to Medicare
Value-Based Purchasing Initiatives or opportunities to participate in alternative payment
methods, although respondents believe that, as an integrated health care system, Harris
Health is in a favorable position to perform well under these payment and delivery system
reforms.
C. Changes in demand (Q1 2013 to Q1 2015)
Despite the state’s failure to expand Medicaid, volume at Harris Health has increased since
Q1 2013 by 12 percent in inpatient stays and outpatient visits and by 5 percent in emergency
room visits.
Respondents attribute the increase to internal decisions to expand capacity (see below),
initiatives under the DSRIP program to increase access to care, and Harris County’s general
population growth (an increase of about 80,000 persons per year).
APPENDIX 5 MATHEMATICA POLICY RESEARCH
60
The number of commercially insured patients has been historically low (e.g., 2 percent of
inpatient stays in 2013) but is responsible for the greatest increase in patient load (66 percent
increase in inpatient stays), which, according to respondents, is the result of enrollment in
the new insurance marketplaces.
Nevertheless, respondents believe that marketplace enrollment has not been as great as it
could be because of Harris Health’s generous eligibility requirements for charity care (200
percent of poverty or lower); in fact, Harris Health is considering a reduction of the
eligibility requirement to 100 percent of poverty in order to encourage more enrollment in
the marketplaces.
D. Changes in capacity
Harris Health has been expanding capacity for the past 10 years or so with the goal of
increasing access to care in the community. Between 2007 and 2014, Harris Health built two
new “mega” clinics capable of handling 100,000 primary care visits per year.
Harris Health has also used the DSRIP program awarded to Texas to expand capacity,
including the addition of nine clinics that the health system leases. However, the health
system may lose the increased capacity if the program is not renewed in 2016.
Respondents mentioned that, without Medicaid expansion, they are unable to meet the
increased demand for specialty care generated by the increase in primary care capacity and
volume. Waiting times for primary care have decreased, but they have increased for
specialty care.
Given the system’s financial problems, Harris Health recently had to lay off 239 employees
and reduce the outsourcing of some services to other providers by about $7 million.
E. Changes in finances (Q1 2013 to Q1 2015)
Over the past several years, Harris Health has been experiencing financial losses—$24
million 2013, $17 million in 2014, and an expected $14 million in 2015. The system will
need to cut costs if it is to remain financially viable. Even after reducing staff, the system
has few options to cut more “fat” and instead is looking to cut back or limit services in the
future to cope with the financial problems. In fact, the system proposes a reduction in the
eligibility for charity care from 200 percent of poverty to 100 percent of poverty in order to
encourage patients to sign up for the health insurance exchanges.
Uncompensated care has been increasing (12 percent in the past two years) while Medicaid
DSH payments have been decreasing (13 percent). The increase in uncompensated care is
attributable to the general increase in volume, and reductions in Medicaid DSH funding
reflect decreases in the statewide pool that were negotiated as part of the Section 1115
waiver that also implemented the DSRIP. The reductions in DSH anticipated Texas’s
expansion of Medicaid (before the Supreme Court ruling made expansion an option).
Further compounding the system’s financial problems was a decrease in support from the
county beginning in 2011 (also in expectation of Medicaid expansion), resulting in a
revenue loss of $75 million.
APPENDIX 5 MATHEMATICA POLICY RESEARCH
61
F. Experience with Medicare Value-Based Purchasing
CMS’s programs have had only a small impact on Harris Health because Medicare
represents only about 9 percent of Harris Health patients.
Nevertheless, Harris Health has performed fairly well, with readmission rates and hospital-
acquired infection rates comparable to state averages. The system faced only a small penalty
associated with readmissions and no penalty associated with hospital-acquired conditions
(HAC). It expects HAC rates to increase along with an associated penalty, although the
reason at this point is not clear.
Respondents cite the advantage of Harris Health as an integrated system that is committed to
clinical coordination and case management for discharged patients. Efforts include
telephone calls within 48 hours after discharge, scheduling follow-up appointments with
primary care providers within 7 to 10 days of discharge, and managing “super utilizers.”
Under a DSRIP initiative (called Chronic Care/House Call), physicians and their teams visit
patients at home in cases of transportation or health barriers. Better utilization management
and review has reduced inpatients’ lengths of stay.
The one problem area is low patient satisfaction scores, which, according to respondents, are
attributable to resource constraints. Respondents believe that assigning four patients to a
room causes significant problems, particularly as related to noise and crowding. Satisfaction
scores are much better when only two patients occupy a room. As a result, the system has
undertaken a major initiative to increase semiprivate rooms throughout Harris Health.
Respondents view strong care coordination and discharge planning and follow-up as crucial
to performing well under value-based purchasing. In this respect, they believe that Harris
Health has an advantage, but they also cite resource constraints as barriers to expanding care
coordination/case management efforts. Lack of good data in understanding the system’s
patient population is another a barrier to improving quality-of-care measures.
G. Experiences with alternative payment arrangements (APM)
Harris Health does not participate directly in any ACOs or bundled payments despite some
interest in doing so. Respondents mention the poor payer mix (e.g., 64 percent uninsured
and 22 percent Medicaid) as a major barrier. In addition, Harris Health is not allowed by law
to accept capitation, although the Medicaid managed care plan (Community Health Choice)
operated by the system is able to accept capitation.
Harris Health is participating indirectly in an ACO through the faculty of the Baylor College
of Medicine, which, along with University of Texas Health, provides staff for Harris Health
facilities. Baylor is participating in an ACO with St. Luke’s Hospital in Houston, although
without realizing that some Harris Health patients would be attributed to Baylor physicians.
Baylor is trying to limit its ACO exposure to Harris Health’s uninsured patients by creating
two tax IDs: one for the public hospital it serves and another for its private side.
Other than poor payer mix, respondents believe that Harris Health can build on several
advantages that would allow it to perform well with APMs. First, it is an integrated system
that encompasses the entire continuum of care, including clinics that have earned NCQA
certification as patient-centered medical homes. Second, Harris operates a standardized

APPENDIX 5 MATHEMATICA POLICY RESEARCH
62
electronic health record throughout its system (Epic) and has learned how to operate
efficiently and on lean budgets. Third, it also believes that its Medicaid managed care plan
(which can accept capitation) offers potential opportunities for bundled payments or other
APMs.
In addition to citing poor payer mix and legal limits on compensation methods, respondents
mention difficulty in determining the true cost of services as a barrier to participating in
APMs. Further, the existing agreements with the two medical schools that staff Harris’s
facilities do not allow for incentives to reduce costs. Harris Health pays them on a salary
basis with a small “production incentive,” with no quality or performance incentives in the
contract.
H. Expectations
The greatest concern by far is that, without Medicaid expansion, Harris Health will continue
to be financially strained, leading to cuts in services and reduced access to care in the
community.
In addition to the cuts in county support and Medicaid DSH, respondents are bracing for the
ACA-related cuts in Medicaid DSH beginning in 2018.
Respondents are unsure about the renewal of DSRIP in 2016. Nonrenewal likely means that
the nine primary care clinics leased with DSRIP funding will cease operation.

APPENDIX 5 MATHEMATICA POLICY RESEARCH
63
ASPE Safety Net Hospital Study
2015 Site Summary for Homestead Hospital
A. Summary of Homestead Hospital
Homestead Hospital is a 142-bed hospital in the not-for-profit Baptist Health South Florida
hospital system. Homestead is the only hospital within a 20-mile radius in southern Miami-
Dade County. The hospital was rebuilt in 2007 and focuses on inpatient medical,
emergency, obstetrical, and diagnostic services. It provides little other outpatient care or
surgeries and no post-acute or long-term care. Homestead Hospital, which is located in a
low-income area, is part of a system that has a religious mission to serve the poor.
Consequently, the majority of its patients are low-income.
Respondents consider Homestead a de facto safety-net hospital because hospital receives
little public funding to support its safety-net role. Instead, the large county health system,
Jackson Health System, is the main safety-net hospital and receives dedicated local sales tax
revenues and significant state and federal funds. Jackson’s main campus is in downtown
Miami, but has a small hospital, Jackson South, in suburban Miami, the hospital closest to
Homestead.
Respondents reported a significant lack of primary care in Homestead’s service area.
Reportedly, it is economically difficult for physicians to survive in private practice here
because there are few commercially insured patients. A federally qualified health center
(FQHC) and three Baptist-operated community clinics serve the low-income population.
Homestead has not traditionally provided primary care services, but has recently started a
clinic in response to the population’s greater reliance on its emergency department (ED) for
non-emergency care. Approximately two-thirds of Homestead’s ED visits are for low-acuity
conditions.
B. Summary of the impact of the ACA
The ACA has had minimal impact on Homestead Hospital, primarily because Florida has
opted out of the Medicaid expansion. Homestead has many patients with incomes under 138
percent of poverty and would qualify for Medicaid, and many earn under the poverty level
so are ineligible for subsidies in the marketplace and remain uninsured. Although the
hospital receives little dedicated safety net funding, it is concerned about potential
reductions in its payments from the state’s Low Income Pool, as Florida’s governor
renegotiates this program with the Centers for Medicare & Medicaid Services (CMS).
The hospital has also struggled with patients who have gained coverage through the federal
marketplace. They report that a number of patients cannot afford the cost-sharing
requirements. And they have found that some patients are incurring bad debt or not using
their insurance and opting for the hospital’s sliding fee scale; that is, effectively acting as
uninsured patients. Also, the hospital reports challenges with some of their patients
continuing to present in their ED for care, even if they now have an assigned primary care
medical home provider elsewhere and/or Homestead is not in their health plan’s network for
hospital care.

APPENDIX 5 MATHEMATICA POLICY RESEARCH
64
Homestead performs well on quality indicators and has enjoyed bonuses from most of the
federal value-based payment (VBP) programs, although they do not represent a significant
amount of revenue to the hospital, which has relatively low numbers of Medicare patients.
Through its parent organization, Baptist Health, Homestead has entered an alternative
payment model through an accountable care organization (ACO) arrangement for cancer
care.
C. Changes in demand (Q1 2013 – Q1 2015)
Homestead has experienced little change in the volume of services it has provided over the
past two years, which respondents attribute to the lack of a Medicaid expansion and little
take-up of marketplace coverage. The hospital reports that over half of their patients have
incomes less than 200 percent of poverty and many of those earn less than 100 percent of
federal poverty so do not qualify for subsidies in the marketplace plans.
Homestead actually experienced a decline in Medicaid volume over the last two years,
which respondents attribute to the state’s 2014 expansion of Medicaid managed care to
virtually all Medicaid enrollees. Because Homestead participates in only 3 of the 10
Medicaid managed care plans in its region, the hospital lost some Medicaid volume.
Between Q1 2014 and Q1 2015, total Medicaid admissions declined almost 6 percent and
overall outpatient visits (ED, diagnostics and therapeutic services) fell 8 percent.
Respondents have somewhat different explanations for Homestead’s lack of managed care
contracts, with some stating that the health plans are losing money so they have renegotiated
contracts and narrowed their provider networks, choosing in many cases to exclude
Homestead. Another respondent thought it was more Baptist’s decision—that contracting
decisions are made at the system level with all products (commercial, Medicaid, and such)
of a given carrier in a single contract. As a result, these decisions affect each of the
individual hospitals in the system differently, depending on their payer mix.
ED visits increased 7 percent between FY2013 and FY2014
27
and the hospital expects a 3
percent increase this year. ED visits have been rising gradually since 2007 when the hospital
was rebuilt, with a larger ED, and relocated. With approximately 90,000 visits this past year,
the ED has significantly exceeded its planned capacity of 50,000 annual visits. Respondents
had not expected the recent spike in ED visits and reported that much of the increase is
related to a lack of primary care in the community and issues with insurance contracts:
- Some Medicaid and marketplace enrollees seek care in Homestead’s ED even though
Homestead is not their primary care medical home or possibly not in their covered
provider network at all. In a study of high ED users, Homestead discovered most of
these patients had Medicaid or other insurance, but they had never seen their designated
primary care physician (PCP). Some even provided the name of a Homestead ED
physician when asked who their PCP is. The hospital then has to refer these patients to a
contracted provider for ongoing care.
27
Note: much of the information the hospital provided on patient volumes and finances was not in the categories we
requested and difficult to interpret, so we relied heavily on information respondents provided in the semi-structured
discussions and follow-up emails.

APPENDIX 5 MATHEMATICA POLICY RESEARCH
65
- Respondents also detected patients coming to the ED who at that time had marketplace
coverage, but could not afford the cost sharing so instead use the sliding fee scale at
Homestead.
- The Baptist primary care clinics in the area are overwhelmed and uninsured patients face
high copayments at the local FQHC (reportedly typically $25 per visit), whereas
Homestead does not charge a copayment. Homestead tried to create a voucher program
in which they wanted to devote the $200,000 per year Baptist had been donating to help
support the FQHC’s general operations to instead help patients pay the out-of-pocket
costs of seeking care there, but, reportedly, the FQHC lost interest in this arrangement.
D. Changes in capacity
In response to rising ED volumes, Homestead recently started venturing into primary care
by creating a new clinic near the hospital called Baptist Health Follow-Up Care, which
handles post-discharge medical, pharmaceutical, and social needs for patients in
comprehensive 45-minute visits. These patients are then linked to a more permanent primary
care medical home in the community. Clinic staff also refer uninsured patients to a
community organization, Catalyst Miami, to determine their eligibility for coverage.
The Baptist system is providing funds to expand physical capacity and programs to help
provide more primary care and address the issues identified in a recent community needs
assessment that Baptist conducted as required by the ACA. That assessment identified
access to primary care and chronic disease prevention and management are areas for the
whole Baptist system to focus on, with Homestead needing to focus specifically on maternal
and child health and socioeconomic issues. New programs will include promoting
breastfeeding through lactation consultants and creating an OB/GYN hospitalist program so
there is an OB/GYN specialist on duty at all times).
E. Changes in finances (Q1 2013 – Q1 2015)
Homestead’s 2015 payer mix is roughly a third each Medicaid and commercial, Medicare in
the high teens, and uninsured in the low teens. The hospital had hoped to attract more
commercially insured patients when it rebuilt its facility because there was a lot of
residential development going on at the time, but then the housing bust and recession
followed and the area did not develop as many had anticipated. Payer mix has not changed
much in the past two years.
New marketplace coverage represents only 1.7 percent of Homestead’s overall business and
has not boosted hospital revenues. Homestead also found that many of its marketplace
patients were not newly insured, but rather switched from other commercial coverage to the
subsidized marketplace plans. And the hospital’s reimbursement from the marketplace plans
is lower than other commercial coverage. The hospital receives reimbursement for the out-
of-network care provided to the marketplace and Medicaid patients in its ED, but does not
have the opportunity to get the revenue from any needed admissions or follow up care
because those patients would be transferred to another hospital. Respondents report some
increase in uncompensated care expense due to patients with marketplace plans who cannot
afford to pay their cost sharing and incur bad debt.

APPENDIX 5 MATHEMATICA POLICY RESEARCH
66
The Florida Low Income Pool (LIP) is a sizable source of federal/state funding to help with
Homestead’s costs of caring for the uninsured. Respondents are relieved that the state
legislature finally approved a budget that keeps its LIP funds intact for now at
approximately $400,000 annually in the form of enhanced Medicaid payments. CMS and the
governor of Florida have been embroiled in a debate about these funds because the federal
government has plans to pare them back over the next few years, which the governor
contends is an effort to coerce the state into expanding Medicaid under the ACA.
Homestead receives a very small amount of disproportionate share hospital (DSH) funds
annually: approximately $6,000 this year. Respondents think they should be eligible for
more DSH and LIP funds because they reportedly provide more charity care as a percentage
of total revenues than Jackson Health System provides.
Homestead generally operates at a financial loss, which has not changed over the past two
years. Baptist subsidizes Homestead from the positive margins its other hospitals generate.
And, because these hospitals are larger and located in higher-income areas, they attract more
commercially insured patients.
F. Experience with VBP programs
Homestead performed better than average on VBP indicators. As one respondent said, “We
can’t do well financially because of our demographics, so we try to do well on quality.”
While Medicare is a relatively small portion of the hospital’s business, it did earn a $45,000
bonus this past year. Patient experience/satisfaction scores were particularly strong.
Respondents attributed the strong performance to good nursing and medical staff, as well as
case managers who not only work with patients but also conduct chart documentation and
review. The hospital has hardwired as much of the reporting requirements as possible into its
electronic health records.
Homestead incurred a slight penalty based on high diabetes and heart failure readmission
rates. Respondents think the lack of primary care in the community contributes to high
readmission rates and thinks the new clinic, and the addition of a certified diabetes educator
there, will turn this around next year. They cited a best practice of getting patients an
appointment with their PCP within 48 hours of discharge, which takes a heavy lift by their
social workers to achieve.
Respondents are concerned that Homestead will struggle with the new throughput measure
because of their high ED volumes/crowding.
G. Experience with alternative payment models
A few years ago, Homestead partnered with Florida Blue, a commercial Blue Cross Blue
Shield health plan, to create one of the first disease-specific ACOs. The health plan wanted
to reduce the high costs of caring for cancer patients by identifying best practices for care
management. The effort resulted in reduced ED visits and imaging in the patient population
as well as ensuring that ED visits made were necessary Respondents think that trusted
relationships, very forward thinkers and data sharing were vital to the success of this ACO.
Also, walk-in appointment availability at the oncology physician group in the ACO reduced
demand on the ED. Respondents considered this a great success from the utilization

APPENDIX 5 MATHEMATICA POLICY RESEARCH
67
standpoint, but Homestead itself assumed little financial risk. The hospital will replicate the
program and take on more financial risk with AvMed, another plan.
As a way of improving quality of care and encouraging efficiencies to reduce costs,
Homestead started an integrated network of physicians to reduce variation in how physicians
treat patients. The hospital plans to have physicians share in savings.
H. Participation in CMMI demonstration projects
Homestead does not participate in any CMMI demonstration projects.
I. Expectations for the future
Respondents do not expect significant changes in Homestead’s patient volume or financial
status over the next year, unless they lose LIP funds, which depends on the outcome of
negotiations between the state and the federal government. Even if these payments continue,
respondents indicated the state may require a hospital to contract with at least half of the
Medicaid HMOs to qualify for payments.
Homestead is looking into pursuing FQHC look-alike status for its new primary care clinic
to help both the hospital’s finances, through enhanced Medicaid payments, and patient
access, through low copayments, which are about $3. They think the health plans might be
more likely to contract with them if have this primary care structure in place, so patients
could select Homestead as a medical home.
Respondents were not aware of the essential community-provider designation and whether it
could help them gain inclusion in more marketplace plan provider networks.
As part of their strategic planning, Homestead is analyzing their outreach and enrollment
strategies for marketplace coverage so they can make any improvements for the next open
enrollment period. However, they are conflicted about encouraging patients to sign up
because they know many cannot afford the premiums, which are expected to increase, and
cost-sharing requirements.
In response, the hospital is looking for a way to provide patients financial assistance with
their out-of-pocket costs. The hospital has received conflicting guidance from different
branches of HHS about whether hospitals are allowed to do this, and respondents were
awaiting the US Supreme Court’s decision the constitutionality of providing insurance
subsidies through the federal marketplace (King v. Burwell) before pursuing the venture
further.

APPENDIX 5 MATHEMATICA POLICY RESEARCH
68
ASPE Safety Net Hospital Study
2015 Site Summary for LAC+USC
A. Summary of LAC+USC
LAC+USC remains the flagship acute care hospital of the four-hospital system owned and
operated by the Los Angeles County Department of Health Services. Under the Affordable
Care Act (ACA), this 600-bed, level-1 trauma center continues its role as the main safety net
hospital for Medicaid and uninsured patients in the county. The governance and operations
of the health department and LAC+USC are intertwined as an integrated delivery system,
which also includes 17 primary care clinics and an array of specialty care providers.
B. Summary of the impact of the ACA
The Medicaid expansion in the ACA has had a positive financial impact on LAC+USC to
date, mostly related to existing uninsured patients gaining Medicaid coverage in 2014; the
hospital has experienced little change in volume of services provided. Respondents caution,
however, that the hospital remains financially reliant on other funding streams in the state’s
Medicaid waiver, which is up for renewal this year, both to cover the costs of serving
Medicaid patients as well as the large number of immigrants not expected to gain coverage.
The hospital has struggled with patient satisfaction and some quality indicators and has
faced small penalties in the federal value-based payment (VBP) programs, but these have
had little financial impact because LAC+USC serves relatively few Medicare patients. The
county, which owns LAC+USC, assumes financial risk for Medicaid managed care patients,
so other alternative payment models (such as accountable care organizations) hold little
interest for the hospital.
C. Changes in demand (Q1 2013 to Q1 2015)
LAC+USC has experienced little overall change in patient volumes over the past two years.
Hospital data from the first quarters of 2013, 2014 and 2015 suggest a slight shift from
inpatient and emergency department (ED) care to outpatient visits in the last year. Inpatient
admissions changed little in the last two years, but declined about 4 percent over the past
year (related, in part, to a new state system to screen appropriateness of inpatient
admissions), and ED visits increased 3 percent over the past two years, but declined 4
percent over the past year. Outpatient visits grew 4 percent over the past two years.
However, respondents cautioned that these changes are small and were more comfortable
with concluding that these volumes are largely flat. In fact, one respondent detected a slight
recent dip in outpatient visits due to capacity constraints and efforts to decrease unnecessary
face-to-face visits with physicians (see later).
Volume by payer mix showed more change. Use by Medicaid patients grew across service
lines, while use by uninsured patients declined between 2013 and 2015. Medicaid
admissions increased 77 percent, deliveries 25 percent, ED visits grew 76 percent, and
outpatient visits almost doubled. Medicaid now represents about 3/4 of all inpatient

APPENDIX 5 MATHEMATICA POLICY RESEARCH
69
admissions and outpatient visits (compared to less than half of admissions and a third of
outpatient visits in 2013), and over half of ED visits (compared to a third in 2013).
These volume increases were larger between 2013 and 2014 than between 2014 to 2015
(after the Medicaid expansion) because of the Low Income Health Program (LIHP),
implemented in 2011 under California’s Bridge to Reform 1115 Medicaid waiver, which put
uninsured people into a Medicaid-like program to help them adjust to coverage and more
readily transition to Medicaid in 2014. LIHP patients were included in the Medicaid volume
numbers in 2013.
The commercial insurance expansions under the ACA have had little impact on the hospital.
Use by patients with commercial insurance was largely flat or even declining, except for ED
visits, which grew 23 percent. A respondent indicated that fluctuations in commercial
volume are typical and often related to their volume of trauma cases.
Although the hospital remains quite busy, respondents detect some competition with other
providers. As patients gain Medicaid, they need to select a medical home and become
empaneled to a primary care provider and network. Respondents report that they have
gained some Medicaid patients and lost others, perhaps because they have selected medical
homes closer to where they live. Also, LAC+USC is new to contracting with commercial
health plans and the private community health centers’ IPA, so the hospital has struggled to
receive referrals to provide specialty care or inpatient care to additional insured patients.
LAC+USC’s average inpatient length of stay increased 8 percent over the past two years
(although, again, one respondent considered it “steady”).
D. Change in capacity
Changes in capacity have been directed mainly at primary and specialty care. The county
added 10–15 primary care physician (PCP) full-time equivalents over the past year.
Respondents report that outpatient care volume has increased more than the numbers
indicate because the county has added capacity by implementing ways to treat patients
outside of traditional face-to-face visits, which are not reflected in volume indicators.
Telephone consults and programs in the community for primary care, as well as eConsult for
specialty care, are major examples of this.
28
E. Changes in Finances (Q1 2013 to Q1 2015)
LAC+USC’s overall financial status has improved slightly over the past two years, but the
hospital remains vulnerable, with a negative operating margin and no total margin. The
hospital experienced a 27 percent growth in total operating revenue, with outpatient revenue
increasing more than inpatient revenue (60 percent and 27 percent, respectively). Much of
this growth was from LIHP, then Medicaid, with LIHP/Medicaid inpatient revenues
increasing by 46 percent and outpatient revenues by 80 percent.
28
The eConsult system screens referrals online, with a specialist either informing a PCP how to proceed with a
patient’s condition or scheduling the patient for a consult. Approximately one-third of patients served through this
system are found to not need a face-to-face appointment with a specialist. Wait times for appointments reportedly
have improved from approximately nine months to 30 days for many specialties.

APPENDIX 5 MATHEMATICA POLICY RESEARCH
70
A respondent cited the new hospital presumptive eligibility policy as helping the hospital’s
finances significantly. The policy pays hospitals for services provided to patients who meet
Medicaid eligibility criteria but are awaiting official enrollment (up to 60 days).
The hospital did not see larger margins however because overall operating expenses also
grew (by 8 percent), even as uncompensated care expense declined 40 percent between
FY2011 and FY2013–14, mostly from declining charity care.
Also, while disproportionate share hospital (DSH) funding had been on the rise during the
several years leading up to the Medicaid expansion, Medicaid DSH then fell by over a third
between FY2013 and FY2014, from $167 million to $106 million. Medicare DSH grew
slightly between those years (from $24 million to $25 million). A respondent reported that
the county cannot draw down all of the DSH funds commensurate to the volume of services
provided because of a state cap.
F. Experience with VBP programs
VBP programs have had little impact on LAC+USC because the hospital has little Medicare
volume and the penalties have been small. The VBP penalty was 0.08 percent in 2014-15,
compared to the national average of 0.30 percent. The penalty for the county was about
$600,000, with LAC+USC’s share only about $150,000 (on total operating revenues of
approximately $325 million). As a respondent said, “We are making sure clinically that we
are providing the best care we can, but value-based payment penalties don’t drive that.”
While LAC+USC’s performance on many indicators was about average, it struggled with
patient satisfaction scores (received 2 out of 5 stars in 2014-15) and ED care, with patients
waiting longer than average among similar hospitals to be seen and admitted.
LAC+USC’s readmissions penalty was 0.13 percent compared to a national average of 0.49
percent. While the hospital’s readmission rate overall was relatively high, its readmission
rates for specific conditions tended to be average. The hospital treats many psychosocially
complicated patients, many of whom are homeless, and/or seriously mentally ill. It is
difficult to find skilled nursing facilities, other post-acute care services, and housing options
for them upon discharge from the hospital, which could lead to readmissions.
VBP could have more financial impact in the future because the hospital is trying to grow its
Medicare volumes, which have increased slightly. In fact, Medicare inpatient revenue grew
more than Medicaid inpatient revenues on a percentage basis over the last two years.
G. Experience with alternative payment models (APMs)
The county takes on full risk in Medicaid managed care, of which LAC+USC is a part.
However, the hospital receives cost-based reimbursement for some Medicaid patients, which
provides some financial protection, although these payments arrive approximately 18
months after the actual service is provided. Previous efforts to form Medicaid accountable
care organizations (ACOs) among other safety net providers in the county have not been
successful. Respondents questioned whether an ACO model would add value because the
county and LAC+USC already assumes risk for many lives.

APPENDIX 5 MATHEMATICA POLICY RESEARCH
71
One respondent reported that achieving the following was important for successfully
participating in APMs: attract a broader mix of patients (not just the sickest); be able to
provide care efficiently; use specialty care efficiently; avoid admitting patients when
possible; and discharge patients in a timely manner. Another respondent indicated that
having salaried physicians (which they have) as the key factor to ensure physicians do not
face incentives to produce more services than necessary.
To fare well under both VBP and APM, the hospital is devoting considerable effort to
customer service to retain and attract more patients over time. They have adopted the
patient-centered medical home model by placing patients with specific providers and
providing services in a more team-based model. These require internal culture and
workforce changes, new performance expectations, new work flows and labor issues (the
hospital is unionized), which they have found all take time to implement.
To both reduce readmissions and manage risk broadly, the hospital is making a “huge effort”
to develop complex case management and develop recuperative care and housing for this
population. The hospital opened 300 recuperative care beds and rented 600 units of
supportive housing and has saved money by housing patients who are heavy users of health
care services (e.g., a cost of $1,200 per month to house someone and provide community
services, compared to $3,500 per inpatient day). The hospital still struggles with the upfront
investment because housing is not an acceptable cost in the Medicaid program.
H. Participation in CMMI projects
LAC+USC has a small CMMI grant—$3-4 million over three years for a Strong Start grant
for maternal and prenatal care. One respondent considers it too much work to apply for these
grants and meet the ongoing reporting requirements for a small amount of money.
About three years ago, the hospital applied for a larger CMMI grant ($30 million over three
years) to develop a program to transition high users of ED care into outpatient care; they
received positive feedback but still were not selected.
I. Expectations for the future
LA County expects to have a large population (an estimated one million) who remain
uninsured due to immigration status or other reasons. Respondents do not expect the current
bill proposed by the California legislature to extend Medicaid (with state funds only) to
undocumented immigrants to pass.
LA County is heavily reliant on the state’s current Medicaid waiver for the funding sources
that to support not only care for the remaining uninsured but the costs of caring for the
Medicaid population, because the county is responsible for paying the state’s half of the
Medicaid matching funds. The state is in the process of renewing the waiver, which
otherwise will expire this fall. Because of expected declined in Medicaid managed care
payment rates (utilization by new Medicaid enrollees is lower than the state expected), DSH
and “realignment funds” (from state sales tax revenues and vehicle licensing fees) and other
funds, the hospital hopes a new waiver will, for example, extend its cost-based Medicaid
reimbursement and DSRIP funds, increase or remove the DSH cap and provide ways to
support housing and recuperative care. Respondents are concerned, however, with proposed

APPENDIX 5 MATHEMATICA POLICY RESEARCH
72
provisions that would distribute available funds more among private hospitals as well,
essentially diluting the county hospitals’ portion.
Still, in preparation for a potential net reduction in revenues, LAC+USC is trying to operate
more efficiently to reduce costs. It is focused on collecting and analyzing data in order to
fare well under insurance contracts and APMs, for example by implementing an electronic
medical record and improving other information systems to help calculate the costs of
providing a given service and document the volume of non-face-to-face visits provided.

APPENDIX 5 MATHEMATICA POLICY RESEARCH
73
ASPE Safety Net Hospital Study
2015 Site Summary for Lakewood Health System
A. Summary of Lakewood Health System
Lakewood Health System is an independent 25-bed CAH in Staples, Minnesota,
approximately 135 miles northwest of the Twin Cities of Minneapolis and St. Paul. As the
only provider in its immediate rural community, Lakewood serves the entire population and
plays a safety net role, given the relative low-income nature of the population. Lakewood
offers a broad spectrum of services, including primary care, behavioral health, medical and
surgical inpatient care, Level 3 trauma services, and post-acute and long-term care. As a
small hospital, it lacks highly specialized tertiary and quaternary care, however. Despite its
CAH status, Lakewood faces some competition from health systems in surrounding
counties, primarily over primary care clinics. Lakewood maintains a strong desire to remain
independent and avoid the need to merge with a larger health system, as many hospitals in
rural Minnesota reportedly have done.
B. Overview of ACA impact
Lakewood has not seen some of the more dramatic volume increases and patients shifting
from uninsured to Medicaid status that some study hospitals have experienced over the past
two years. This difference is largely because Minnesota had among the lowest rates of
uninsurance in the country before the ACA, due to relatively expansive Medicaid eligibility,
a state limited coverage program, and high rates of employer–sponsored coverage. Still,
Lakewood’s payer mix and financial margins have been helped by the state’s participation,
as of January 2014, in the full Medicaid expansion to all eligible adults with incomes under
138 percent of poverty.
On the other hand, the hospital is concerned about its loss of some commercial business,
attributed to higher patient cost-sharing requirements in employer-sponsored coverage and
the Marketplace plans.
As a CAH, Lakewood is exempt from participation in Medicare value-based purchasing
(VBP) programs, but reports some indicators and expects such participation to become a
requirement.
Lakewood has been preparing for alternate payment models (APMs) for the last few years,
primarily through leadership changes and other efforts to improve care coordination. Earlier
this year, it joined two ACOs, one for Medicare and one for Medicaid.
C. Changes in volumes (Q1 2013 to Q1 2015)
Lakewood’s total patient volumes increased 5 percent between 2013 and 2015, primarily
due to growth in outpatient care, which hospital respondents expected and hoped to see
because of their focus on PCMH and care coordination activities aimed at directing patients
to less expensive care settings. Indeed, ED visits fell 6 percent, but inpatient admissions did
not really change overall (a 1 percent increase). Average length of inpatient stay declined 14

APPENDIX 5 MATHEMATICA POLICY RESEARCH
74
percent. Deliveries declined 17 percent, which could be due to increased competition from
other hospitals (see below).
Lakewood did not provide actual breakdowns of volume by coverage type, although it
verbally reported an increase in Medicaid volumes and some decline in uninsured patients,
and reported that its revenues are a better indicator of how the payer mix has changed (see
Section E below).
Respondents were concerned about a loss of commercial inpatient stays and ED visits. They
think some of the loss could be attributed to patients going to other providers, but a more
prevalent situation is that more patients are forgoing care due to high out-of-pocket costs,
particularly as so many Marketplace plans have high patient cost-sharing requirements. (As
a sign of the prevalence of high deductible plans in this region, Lakewood now offers only
health savings accounts (HSAs) with high deductible plans to its own employees.)
D. Changes in capacity
Lakewood has moderately increased outpatient capacity. As part of its efforts to enhance
outpatient services and care coordination in preparation for new payment arrangements (see
below), the hospital has added a same-day clinic, increased care coordination staff (a
manager and several care coordinators), added 12 mental health providers, and integrated
behavioral health into the primary care setting. To help attract more commercial and
Medicare business, Lakewood has improved its oncology service, recruited two new
surgeons, added a dermatology clinic with a spa, and is selling more durable medical
equipment. Despite these changes, one respondent said that the overall number of physicians
has not really changed because some physicians have left.
E. Changes in finances (Q1 2013 to Q1 2015)
Overall, Lakewood received more revenue from Medicaid between 2013 and 2015, whereas
revenues from uninsured, commercial, and Medicare patients either were stable or had
declined.
Medicaid inpatient revenues increased 22 percent, whereas outpatient revenues increased 32
percent. As a proportion of total revenues, Medicaid grew from 17 to 21 percent on the
inpatient side and from 18 to 24 percent on the outpatient side. As a CAH, Lakewood
receives cost-based reimbursement for Medicaid outpatient services.
Lakewood has very little revenue associated with uninsured stays and visits; this situation
does not appear to have changed considerably over the last two years. Still, uncompensated
care costs fell 50 percent. Charity care declined significantly due to a reduction in people
applying for the program, even as the hospital expanded eligibility. Bad debt increased
overall between 2013 and 2015 (although declined between 2014 and 2015); respondents
reported that this number fluctuates considerably based on cyclical attempts to recover debt.
Lakewood is technically a district hospital but does not receive local tax revenues. Due to
this status, it does receive payments on debt through patients’ state tax returns, however.
Meanwhile, commercial inpatient revenues fell 35 percent or, as a portion of total, from 31
to 20 percent. However, commercial revenues from outpatient services were substantially
higher than for inpatient services, increasing 8 percent or, as a proportion of total outpatient

APPENDIX 5 MATHEMATICA POLICY RESEARCH
75
revenues, from 35 to 37 percent. Respondents attributed the decline in commercial inpatient
revenue to several factors: high cost sharing that might prevent some patients from seeking
care; a 30 percent cut in reimbursement rates from Blue Cross, its largest commercial
insurer; and reimbursement rates from Marketplace plans that are lower than typical
commercial rates. Although total commercial revenues did not really change over this
period, respondents were concerned that these changes signaled a growing issue.
Indeed, Lakewood does not receive any other subsidies to support care for the uninsured or
for Medicaid services not reimbursed at cost. Medicaid DSH payments remain very low—
about $10,000 annually since 2011. The hospital estimates that the cost of staff time to
report and claim these dollars exceeds $10,000, so it is considering forgoing these funds
completely. The hospital does not receive any Medicare DSH payments.
In total, Lakewood’s revenues increased 5 percent, whereas expenses increased 3 percent,
generating a slightly better operating margin—from -2 percent in 2013 to 0.23 percent in
2015. Respondents attributed the improvement mainly to changes in staff costs. Facing
relatively low patient volumes and negative margins in 2013, the hospital cut expenses
(mostly through layoffs of managers and other administrative staff) and generated a 4
percent margin in the first quarter of 2014. Since then, the hospital has added back staff
(mostly in care coordination and data/financial analysis), thus extracting some of the margin.
F. Experience with VBP programs
As a CAH, Lakewood currently is ineligible to participate in the Medicare VBP programs
but does report some indicators and expects that participation eventually will be required of
CAHs. Hospital executives think that the hospital provides high quality care but that its
current processes are not yet sufficiently standardized to appropriately “present the best
picture of what we are doing.”
- Lakewood’s performance on the measures it reported to Hospital Compare in 2014 were
mixed—at or above the national average on patient experience measures, at or slightly
below average on appropriate antibiotic prescribing, average for readmissions indicators,
and below average for appropriate imaging rates.
Respondents named several related investments needed for success in VBP programs (and
the same for APMs): one respondent stressed the importance of having an EHR and strong
data collection and analysis; another emphasized good cost management and care
coordination. A key strength Lakewood reportedly possesses is a strong relationship
between hospital executives and physicians. Indeed, administration worked with physicians
to encourage them to better document their patient care activities, which reportedly has
contributed to better scores in many areas—from the bottom decile to the 70th percentile.
G. Experience with APMs
In January 2015, Lakewood began participating in two ACOs, which currently cover about
10 percent of its total patient population:
- Accenture Medicare ACO. Lakewood joined in this ACO’s third year of a three-year
period. This initial period offers upside risk only, but in 2016, up to 15 percent of
Lakewood’s reimbursement in the ACO will be at risk. Lakewood has 1,000 attributed
patients; given its small size, the hospital is pooled with other providers.

APPENDIX 5 MATHEMATICA POLICY RESEARCH
76
- Minnesota’s Medicaid Integrated Health Partnership is used by Lakewood for 3,000
of its Medicaid patients (both fee-for-service and managed care patients). The hospital is
not pooled with other providers; it chose to take “a little bit of risk” in this first period.
The hospital is still in the early stages of transitioning to ACOs, but respondents state they
have “come a long way in a year.” The main ways it hopes to generate savings in the ACOs
are by increasing preventive/primary care visits and reducing ED, inpatient, and other high-
cost services.
Key activities to achieve this goal revolve around improved care coordination, both for
patients that need ongoing monitoring and healthy ones who still should be seen regularly.
In addition to the capacity changes mentioned earlier, Lakewood has restructured its senior
leadership team to align care coordination staff under a single vice president and added a
physician leader to each division; the CEO reportedly has relinquished some authority so as
to encourage new and creative ideas from others. It has also implemented a new EHR so all
providers are on the same system and is expanding and reconfiguring clinical space into
pods that house whole care teams, with the aim of promoting more use of nonphysician
clinicians.
Respondents named several challenges to doing well in APMs:
The hospital is still operating in a fee-for-service world, in which it faces financial
incentives to provide more services across the care spectrum. Some of the services they aim
to use less (for example, imaging, surgery) help subsidize primary care, so reducing
utilization in these areas also reduces revenues.
- Although reporting that Lakewood’s key strength for APMs is the strong relationship
between respondents and physicians, a respondent noted that getting and keeping
physician buy-in is difficult, as the preparations for APMs require a lot of work with no
immediate financial reward. Physicians reportedly have considerable leverage over the
hospital because it is difficult to recruit providers to this part of the state; also, they could
choose to move to another nearby provider organization. It reportedly took 10 months to
negotiate a new compensation model in which physician pay is linked to performance on
quality and value measures.
- Sorting out initial glitches with Medicare data and getting patients properly attributed to
Lakewood has taken time and investment. The hospital has started receiving claims data
on the patients attributed to these ACOs but is not sure it has the resources to adequately
analyze the data in house.
- Respondents expect initial data to show that the hospital has relatively low quality and
high costs. The former is because of inadequate documentation, as mentioned above.
They attributed the latter issue to the receipt of cost-based Medicare and Medicaid
reimbursement as they invest in care coordination. Lakewood’s cost structure reportedly
has made it less attractive to commercial ACOs.
- One respondent noted the need to rely less on adding staff to do more and instead find
tools to adjust processes for greater efficiency.
H. Participation in CMMI demonstration projects
Lakewood is not involved in any CMMI demonstration projects.

APPENDIX 5 MATHEMATICA POLICY RESEARCH
77
I. Expectations for the future
Respondents expressed considerable concern that more employers will drop their coverage
and instead have their workers enroll in Medicaid or purchase coverage through the
Marketplace, thus further reducing commercial hospital revenues. This is a particular
concern, since respondents expect cost-based Medicare and Medicaid reimbursement for
CAHs to be phased out in the next few years.
As a next step in achieving value-based care, the hospital is starting to engage in more
population health activities to prevent health care problems and drive down costs; these
activities include collaborating with schools on nutrition and obesity education, and
pursuing development of a wellness center, in which the costs of physical fitness and other
activities would be offset by physical therapy services for which the hospital can bill
insurers.
To the extent that Lakewood successfully shifts services from high- to low-cost venues, it
plans to downsize the higher-cost areas (for example, inpatient services). To help offset the
losses in revenues from those services, the hospital is considering adding more senior
services to incorporate into their ACO contracts, thus attracting more patients.

APPENDIX 5 MATHEMATICA POLICY RESEARCH
78
ASPE Safety Net Hospital Study
2015 Site Summary for Marcum and Wallace Memorial Hospital
A. Summary of Marcum and Wallace Memorial Hospital
Marcum and Wallace, a 25-bed critical access hospital (CAH) in rural Estill County, KY,
continues to be the community’s sole health care facility. Its primary and specialty care
clinics serve the broader region, as do a federally qualified health center (FQHC) and
independent private practice physicians. The hospital does not offer surgical services, so
patients must seek this type of care elsewhere; often this is in nearby Richmond, KY or
farther to Lexington, KY.
B. Overview of Affordable Care Act (ACA) impact
Kentucky’s large increase in Medicaid enrollment as a result of the ACA has had a more
consistently positive impact on Marcum and Wallace over the past year compared to the
year before, with payer mix continuing to improve as people gained coverage and financial
indicators stronger than before. “Our financial status has been great,” said one respondent.
This represents a considerable turnaround from pre-ACA when hospital finances were
strained related to rising numbers of uninsured patients. However, some of the financial
improvement is related to a growth in inpatient admissions that is not ACA related.
As a CAH, Marcum and Wallace is not required to participate in federal value-based
payment (VBP) programs, but it does report some indicators and would like to participate
more fully to better showcase its high-quality services. The hospital is also preparing for
ways it could take on more financial risk, although it considers itself too small to take full
risk or form an accountable care organization (ACO) on its own.
C. Changes in demand (Q1 2013 to Q1 2015)
Marcum and Wallace reports having only about 3 percent self-pay/uninsured patients now,
down from 13 percent at the end of 2012. The hospital largely credits the growth in covered
patients to its enrollment navigator stationed in the emergency department (ED), which was
supported through a Health Resources and Services Administration (HRSA) grant, as well as
help from enrollment staff from their hospital parent (Mercy Health) and collaboration with
the local FQHC.
The hospital reports seeing “some” patients with coverage from the state exchange.
Anecdotally, one respondent reported hearing of more residents considering early retirement
because they have the opportunity to buy insurance coverage that is not tied to an employer.
Volume growth has been mainly on the inpatient side and mostly by Medicaid patients.
Medicaid admissions more than doubled, compared with under 20 percent for all patients.
29
This growth does not, however, indicate that the hospital is now caring for sicker patients.
Instead, much of the growth in admissions is associated with the hospital’s adoption of a
29
Given the overall small numbers of patients the hospital treats, respondents guard against putting too much weight
on the precise percentage change numbers.
APPENDIX 5 MATHEMATICA POLICY RESEARCH
79
tool in the past year to help them determine when an admission is appropriate, rather than
keeping them in observation beds, which are counted as outpatient visits. Another
contributor to inpatient growth is the hospital’s increased use of swing beds as a way to keep
beds full and keep patients with longer-term needs in the community.
The switch from observation to inpatient status and other changes likely have masked the
growth in outpatient demand and utilization. Respondents think people are more likely to
seek appointments and procedures now that they have coverage. Outpatient visits grew just
5 percent over the two years, but had fallen in 2014, then increased about 15 percent by
2015.
Particularly bad winters in both 2014 and 2015 also may have tempered outpatient use.
Many patients live in the mountainous areas of Appalachia, and treacherous roads can
significantly impede travel. Also, radiology volumes decreased after the departure of a
primary care physician who tended to order tests at a higher rate than average.
While ED visits declined about 5 percent overall, Medicaid ED visits increased by a quarter.
D. Changes in capacity
Marcum and Wallace has not made major changes in capacity. However, the number of
physicians the hospital employs fluctuates. The more recent decline in outpatient visits is
attributed to a couple of physicians departing; more physicians have since been hired. A key
strategy for the hospital has been to improve physician alignment, primarily through
employing them, to both boost outpatient capacity and increase inpatient referrals.
E. Changes in finances (Q1 2013 to Q1 2015)
The hospital’s financial picture has improved considerably. Operating margin increased
from 1 percent to 7 percent and total margin increased from 4 percent to 17 percent
(confirm) (and does not include the hospital’s investment income).
A growth in Medicaid revenue linked to serving more Medicaid patients as well as the
change in observation/admissions policy, were the key factors in the improved financial
picture. As a CAH, the hospital receives cost-based reimbursement from both Medicaid and
Medicare.
- Between 2013 and 2015, gross Medicaid inpatient revenues increased almost three-fold
and gross outpatient revenues, including ED, increased 20 percent. Outpatient revenue
from other payers actually declined, which a respondent attributes to changes in their
charges. They had been out of compliance with some supply costs.
- The hospital gained considerable inpatient revenues from Medicare and commercial
payers as well, which is linked to the shift in admissions versus observation status
mentioned earlier.
- A respondent reported that overall net patient revenue increased almost 50 percent
between 2014 and 2015.
Uncompensated care costs fell 80 percent, with much of the decline due to plummeting
charity care costs. The hospital reported almost $1.9m in charity care in Q1 2013 and only
$300,000 in Q1 2015. Bad debt declined as well, but it fluctuates reportedly because the

APPENDIX 5 MATHEMATICA POLICY RESEARCH
80
collection activities are more “batched” now through outsourcing the collection activities.
Consequently, precisely matching debt to provision of services is difficult to do.
The hospital receives only Medicaid, not Medicare or disproportionate share hospital (DSH).
This funding appears to have been cut in half between 2013 and 2015, dropping from
approximately $148,000 to $66,000.
The hospital continues to struggle with payment denials or delays from Medicaid managed
care companies, but the situation appears to have improved somewhat from last year.
F. Experience with VBP programs
As a CAH, Marcum and Wallace is not required to participate in federal VBP programs.
However, for example, the hospital does submit patient-experience data to Hospital
Compare, on which it performs fairly well. Other indicators have been more difficult for the
hospital to collect, presumably because it would involve different charting and chart
abstracting. However, they just went live with Epic, an electronic health record (EHR),
which has all of the Hospital Compare indicators built in. ED physicians have started
documenting information with this system. The hospital is starting to monitor readmission
rates and other information because they want to be “ahead of the game” if reporting
becomes a requirement in the future.
Marcum and Wallace wants to be able to participate fully in VBP programs, that is, be
eligible for bonuses or penalties, because they believe they do provide high-quality care and
want to be able to demonstrate that a person can receive quality care in a small community
hospital. Participation would also help cover some of the costs of participation. Said one
respondent, “It would be nice to be rewarded for behavior and the positive things you’re
doing, as it does require resources. And maybe that would be a motivation to help others.
Maybe you could get 103 percent of costs versus someone who didn’t do as well and only
got 100 percent of costs.”
A respondent reported that care management, employing (rather than contracting with)
physicians, and a focus on primary care are important to faring well in VBP programs. But
having a small staff is a challenge. The hospital has one staff member who is focused on
quality improvement and care management and is spread thin across paperwork and patient-
care activities. Marcum and Wallace recently added a diabetic coordinator to work closely
with physicians.
The hospital is also implementing a patient-centered medical home (PCMH) initiative (see
below) to improve quality in its clinics. But having sufficient resources is a challenge
because the costs of many of these added initiatives in the community are not allowable
costs under the cost-based reimbursement structure.
A respondent named the National Rural Health Resource Center as a great resource for
strategies around quality and tools to help CAHs fare well on VBP indicators and to
implement PCMH initiatives.
G. Experience with alternative payment models (APMs)
Marcum and Wallace is not currently involved in APMs, but is trying to prepare for them
with the help of a consultant. Respondents expect that their new EHR will help obtain and

APPENDIX 5 MATHEMATICA POLICY RESEARCH
81
analyze the data needed to take on some degree of financial risk. However, because of the
hospital’s small size, they do not expect to have sufficient resources or patients to become
an ACO on its own or otherwise take full risk.
The hospital would be interested in participating in an ACO with a tertiary hospital in the
future—in an arrangement in which Marcum and Wallace could provide more of the routine
services. Respondents note, however, that some tertiary hospitals are interested in aligning
with more doctors, not necessarily with hospitals.
Marcum and Wallace is developing its primary care providers and pursuing a PCMH effort
in to attract more patients to choose Marcum and Wallace as their medical home, which
respondents think will also make the hospital an attractive partner to ACOs. The PCMH
effort is internal and the hospital currently receives no outside payments to support it.
However, respondents are trying to demonstrate cost savings to insurers and negotiate
payments to cover some of these investments by contending they could reduce costs to
insurers in the long run.
H. Participation in CMMI demonstration projects
Marcum and Wallace is not involved in any CMMI grants.
I. Expectations for the future
Marcum and Wallace respondents seem less concerned about the hospital’s future than they
were a year ago. Concerns about changing CAH payments/regulations remain, but have
subsided. The hospital is engaged in some strategic planning to continue to improve their
revenues and cut costs, but respondents do not expect payer mix to change much more.
One respondent noted concern about the “two-midnight rule,” which could hurt their
Medicare inpatient volumes. The rule requires physicians to certify that the patient would
need to stay in the hospital at least two nights to be considered an inpatient. The respondent
does not consider this good patient care, and is awaiting a Congressional fix. Note that
Medicare pays more for short inpatient stays than observation services.
30
Going forward, the hospital has made a decision to no longer recognize the DSH funds they
continue to receive as a revenue source because they expect the state to take back some of
the funds once they reconcile payments with actual volumes/costs of caring for the
uninsured. It is too early to know whether the increase in Medicaid revenues is balancing out
the loss in DSH. But it appears to be doing so as DSH funding is not that high.
Marcum and Wallace is also bringing in a new ED physician group this year, which they
hope will further improve quality scores and bring in more volume.
A respondent noted concern that the Medicaid expansion could be in jeopardy under a
potential change in governors and once full federal funding ends.
30
Cassidy, Amanda. “Health Policy Brief: The Two-Midnight Rule.” Health Affairs, January 22, 2015.

APPENDIX 5 MATHEMATICA POLICY RESEARCH
82
ASPE Safety Net Hospital Study
2015 Site Summary for Regional One Health System
A. Summary of Regional One
Regional One is the dominant safety net system in the Memphis area. It recently changed its
name from Regional Medical Center at Memphis (nicknamed “the Med). Historically, it has
served as a public hospital for the community but now is officially a 501(c)3 not-for-profit
system. Regional One is county supported and affiliated, as its board is appointed by the
Shelby County mayor and confirmed by the county commission. The county also provides
some financial support, especially in covering the costs of care to uninsured people.
Regional One also serves as a regional safety net provider for uninsured people in
neighboring counties in Tennessee, Arkansas, and Mississippi.
Regional One executives describe the organization as an integrated delivery system. The
system consists of an acute care hospital (the Regional Medical Center), extended care and
rehabilitation hospitals, an outpatient surgery center, four primary care centers, and other
outpatient services. Regional One has Centers of Excellence for trauma, burn, high-risk
obstetrics, and neonatal intensive care.
B. Summary of the impact of the Affordable Care Act
As the state of Tennessee elected not to expand Medicaid, study respondents reported that
the ACA has had virtually no impact on Regional One. (The governor had proposed a
Medicaid expansion in 2015, but it was voted down by the state legislature.)
Regional One has had mixed experiences with CMS value-based payment initiatives,
performing relatively well on measures of hospital readmissions but more poorly on
measures of HACs and patient satisfaction. Due to the low volume of Medicare patients at
the hospital, Medicare penalties are not large enough to pose a serious concern, although the
hospital has implemented a number of initiatives to improve performance.
Respondents cited the lack of Medicaid expansion as contributing to increasing financial
stresses that are impeding delivery system transformation, quality improvement initiatives,
and needed investments in physical plant, IT, and staff.
C. Changes in demand (Q1 2013 to Q1 2015)
Regional One’s service utilization, payer mix, and acuity level of patients reportedly have
been essentially flat for the past five to six years, with some year-to-year fluctuation.
The financial and utilization data that Regional One provided for this study differed from
what respondents reported (one executive attributed this difference to considerable
fluctuations in the quarterly data). Financial data provided by the health system show a 4.4
percent decrease in inpatient admissions between Q1 2013 and Q1 2015, but little change in
ED and outpatient visits (despite some fluctuation over the two-year period).

APPENDIX 5 MATHEMATICA POLICY RESEARCH
83
According to the financial data, Medicaid admissions decreased by almost 10 percent,
whereas Medicare admissions increased 20 percent. A hospital executive speculated that
these are related (that is, the Medicaid population is aging and transitioning to Medicare).
Inpatient admissions for commercial and self-pay (uninsured) patients also decreased (17
percent and 8 percent, respectively). Again, one executive’s own observation of trends in
volume seemed to contradict this decline, as he reported that volumes across all payers have
been flat.
D. Changes in capacity
In 2014, Regional One began a partnership with the University of Tennessee (UT) to create
UT Regional One Physicians, consisting of about 180 physicians and advanced care
practitioners. Most of the physicians are specialists who will practice at the Regional One
hospital and its other settings.
As part of “rebranding” its image as a public hospital over the past five years, Regional One
started a long-term care hospital, outpatient ambulatory care center, and outpatient surgery
center; expanded rehabilitation services; and added some beds, especially for burn patients.
E. Changes in finances (Q1 2013 to Q1 2015)
Regional One’s patient revenues have been essentially flat over the past four to five years,
with some fluctuations by payer source. The system experienced a 58 percent increase in
Medicare revenue (starting from a very low amount), which a hospital executive attributed
to increased Medicare volume and the new Medicare DSH formula (likely the fact that 75
percent of Medicare DSH funds are now redistributed to hospitals with large numbers of
uninsured patients).
A hospital executive reported that uncompensated care expenses have decreased slightly,
although the financial information provided to us showed a sizeable increase (24 percent)
between Q1 2013 and Q1 2015. A respondent attributed this discrepancy to the fact that the
financial information we requested shows only quarterly revenues and costs, which might
not include certain expenses documented in other quarters. Looking at annual data, the
respondent reported that charity care decreased by $3 million between 2014 and 2015,
whereas bad debt increased $6 million during the same period. The respondent did not know
the reason for the increase, other than suggesting that changes related to the new UT
physician group might have affected the payer mix.
Regional One has been receiving about $12 million in Medicaid DSH payments annually.
Tennessee is the only state in the country that does not have a permanent Medicaid DSH
program (due to a waiver negotiated to create the TennCare program in the 1990s). A DSH
pool was negotiated with the federal government in 2005, when TennCare coverage was cut
for about 300,000 people. With the advent of the ACA, respondents had been concerned that
CMS would not renew the DSH pool in 2015 as a way to pressure the state into expanding
Medicaid. Subsequently, the funding was renewed for 10 years, although Regional One
believes that funding levels will be reduced in future years.

APPENDIX 5 MATHEMATICA POLICY RESEARCH
84
Regional One receives an annual appropriation of about $27 million from the county to pay
for care for prisoners and indigent residents. The funding is expected to increase slightly (by
about 2 percent) in 2016.
Regional One’s operating margins have been decreasing in recent years, from a positive $51
million in FY 2012 to a projected loss of $7.9 million for FY 2016. This reflects stagnant
revenues and increased costs. A hospital executive attributes higher costs as being due to
investments in IT, quality improvement, deferred maintenance, and general increases in
salaries and supplies. Operating costs increased from $290 million in 2011 to $357 million
in 2014.
F. Experience with Medicare value-based pricing
Regional One has managed readmissions reasonably well, with readmission rates only
slightly above the national average, and incurring a Medicare penalty in FY 2015 of -0.01
percent. Hospital executives attributed the relatively low documented readmission rates in
part to low volumes of Medicare patients—the number of cases for many of the readmission
measures was too small to report.
The hospital system performed less well with HACs, particularly with respect to Methicillin-
resistant Staphylococcus aureus (MRSA) infections and pressure ulcers, and was among 718
hospitals that received penalties for HACs in FY 2015. A hospital executive cited the low
socioeconomic status of the patient population, the high number of accidents and injuries
coming through the trauma center, problems with coding arising from lack of resources, and
the types of patients they see as reasons for the high rates. For example, rates of pressure
ulcers are higher and more difficult to prevent among trauma and burn patients, who often
need to be immobilized.
Low patient satisfaction scores are also a problem, with the hospital scoring two stars on the
new five-star rating system. One hospital executive believes that low patient satisfaction in
part likely reflects some prejudices among hospital staff regarding low socioeconomic strata
patients, which need to be addressed (that is, the need to change the “public hospital”
mentality). To improve its scores, the hospital has hired the Studer Group (a health care
consulting/training organization) to provide coaching and tutoring for managers and nurses.
A respondent reported that the hospital’s scores had improved during the second quarter of
2015.
Regional One has implemented a number of other quality improvement initiatives. Among
the most important are medication reconciliation to reduce medication errors, changing the
culture to encourage more reporting of errors, and a program called TeamSTEPPS, an
AHRQ initiative designed to improve communication and teamwork skills among the
medical staff.
Hospital executives lamented that financial constraints have hampered their ability to hire
new staff to work on quality improvement (QI) initiatives and improve quality outcomes.
The lack of an EMR system across all hospital departments also hinders quality
improvement efforts. Although respondents reported that a single system interoperable
across all departments is desperately needed, the health system reportedly cannot afford it at
this time.

APPENDIX 5 MATHEMATICA POLICY RESEARCH
85
G. Experiences with alternative payment models (APM)
Regional One was not participating in any APMs at the time of our discussions with them.
However, the hospital is mandated to participate in the bundled payments initiative for hip
and knee replacements, which is set to begin April 1, 2016 (changed from January 1, 2016).
Hospital officials are concerned that they will not perform well in the joint replacement
initiative and will be penalized. This concern is due to the high number of these procedures
they perform on trauma patients, who are more costly and difficult to manage.
Respondents believe Regional One is at a disadvantage in being able to perform well under
alternative payment models due to the low socioeconomic status and poor payer mix of its
patient population, as well as an inability to invest in needed quality improvement and cost-
tracking activities, and an EMR.
As an example, the hospital has been making efforts to reduce the length of inpatient stays.
It has been unsuccessful, reportedly because of the difficulty in getting indigent care patients
placed in an appropriate setting following discharge, and because of some inefficient
throughput processes that the hospital has been unable to improve by hiring more staff.
Respondents believe that Regional One’s potential strength with APMs is its recent
affiliation with the University of Tennessee medical group. These physicians are currently
salaried, and there has been discussion about changing their compensation to be more risk
based and include performance-based incentives.
H. Expectations for the future
The biggest concern for Regional One executives is the lack of Medicaid expansion in the
state and the possibility that subsidies from federal, state, and county governments will
decrease, thereby putting the hospital in an untenable financial situation.
Medicaid expansion would provide the hospital with a better and more predictable revenue
stream, thereby making it easier to make the necessary investments in physical plant, IT, and
quality improvement to better position it for payment and delivery system reforms and allow
it to compete more actively for privately insured patients.
As part of its “re-branding” efforts, Regional One plans to continue efforts to change its
public hospital image, especially by trying to attract more privately insured patients in the
areas of cardiology, gastroenterology, and outpatient surgery.

APPENDIX 5 MATHEMATICA POLICY RESEARCH
86
ASPE Safety Net Hospital Study
2015 Site Summary for UK Health in Lexington, KY
A. Summary of UK Health
UK Health, part of the University of Kentucky, remains the main safety net system in the
Lexington area. This hospital, with almost 1,000 beds, is both the major provider for
Medicaid and uninsured patients as well as a tertiary/quaternary academic medical center for
the region at large.
B. Summary of the impact of the Affordable Care Act (ACA)
The ACA has continued to have a large, mostly positive, financial impact on UK Health,
stemming from many of the hospitals’ uninsured patients gaining Medicaid coverage and
from treating new Medicaid patients. Respondents attribute this growth to the significant
increase in Medicaid eligibility as well as to the state’s and UK Health’s strong outreach and
enrollment strategies and systems. The increase in Medicaid patients surpassed expectations.
As one executive said, “The degree and pace of Medicaid expansion has surprised everyone
here.”
UK Health has invested in improving performance for value-based payment (VBP)
programs and is in the early stages of exploring how it might fit into alternate payment
models. As one respondent said, the ACA has also “accelerated the path to value-based
care.”
C. Changes in demand (Q1 2013 to Q1 2015)
Over the past two years, total patient volumes increased in the emergency department (ED)
by 11 percent, while the volume of other outpatient visits increased by 15 percent. Inpatient
admissions increased just 3 percent. Medicaid patients accounted for most of the growth
with a 90 percent increase in outpatient visits, a 74 percent increase in ED visits, and a 39
percent increase in admissions.
Marketplace coverage has had less impact on UK Health. Indeed, commercial patient
volumes were negative, on the inpatient side, or rose only slightly on outpatient and in the
ED. Respondents reported that some patients moved from commercial to Medicaid
coverage.
UK Health is seeing many patients who are seeking care for the first time, are quite ill, or
have less severe but chronic issues. However, average length of stay for Medicaid patients
increased less than for Medicare and commercial patients. Respondents attribute the increase
to higher acuity and difficulty discharging patients, especially because the supply of post-
acute care beds in the community is relatively fixed.
D. Changes in capacity
The increased demand for care has led to strained capacity, largely demonstrated by
increased wait times for appointments and a greater increase in the ED over outpatient
volumes in the past year. In response, UK Health moved some practices to its new, larger

APPENDIX 5 MATHEMATICA POLICY RESEARCH
87
ambulatory center to provide them with more space. The hospital is adding “a lot of”
physicians and mid-level staff, and is working to improve clinic efficiency. Still, as a
primarily tertiary/quaternary hospital, UK Health has very limited primary care capacity.
UK Health also received certificate-of-need approval from the state to add 120 additional
beds (a 15 percent increase) over the past year to help ease their inpatient capacity
constraints.
E. Changes in finances (Q1 2013 to Q1 2015)
UK Health’s margins reached record levels over the past two years, with greatest gains
between 2013 and 2014, right after the Medicaid expansion. Its operating margin increased
from 6.7 percent to 10.4 percent, while total margins rose more, from 5.7 percent to 12.5
percent.
Medicaid outpatient (ED included) revenue increased 41 percent, compared to 50 percent
across all payers, and Medicaid inpatient revenue increased 58 percent, compared to 28
percent across all payers. Revenue increases align with changes in patient volumes and
payer mix. Self-pay/uninsured patients plummeted from 12-13 percent of patients before the
Medicaid expansion to about 2 percent this year.
The hospital has not yet faced cuts in disproportionate share hospital (DSH) funding because
the state payments lag actual activity level by about a year. The figures are incorporated in
the Medicare/Medicaid revenue numbers, so we are not able to determine its percentage of
the revenue.
Uncompensated care expense, especially charity care, fell significantly from about $55
million to $20 million during this period, while overall operating expenses rose in step with
rising patient volumes. These expenses are also linked to a new pharmacy initiative and
rising costs of specialty drugs.
F. Experience with VBP programs
UK Health has experienced little financial impact from federal VBP programs, but these
programs still create incentives to improve, from a patient care perspective. Respondents are
optimistic that they are responding in ways that will improve their performance.
- The hospital received a small bonus of 0.3 percent for VBP indicators, performing well
on most measures except timely ED care. A respondent reported that the main problem
is related to boarding patients who need to be admitted. UK Health recently opened up
an observation unit just off the ED and new cardiovascular floor to remove pressure
from the ED and reduce the need for inpatient beds.
- The hospital’s readmissions penalty was small at 0.42 percent (compared to a maximum
of 3 percent), slightly up from last year. According to a respondent, poor socioeconomic
status of many patients is a “huge factor” affecting readmissions and possibly other VBP
indicators. Risk adjustment helps in terms of accounting for age, gender, comorbidities,
but not past health care use (for example, if patient has never before seen a PCP). In one
key way to help reduce readmissions, UK Health is participating in Project Boost, a
Society of Hospital Medicine program to improve the discharge process.

APPENDIX 5 MATHEMATICA POLICY RESEARCH
88
- The hospital faced the largest possible hospital acquired conditions penalty at 1 percent.
The penalty was for the problem of catheter-associated urinary tract infections. The
problem has been tackled and the hospital is not expecting another penalty next year for
this problem.
UK Health expects to improve performance by focusing on two main components:
- Leadership will focus on the defined measures, set goals for these measures, and
establish a deliberate method to achieve them through tools such as LEAN or Six Sigma
- Leadership will ensure that administrative and clinical data can be accessed and is
analyzed thoroughly. In this spirit, UK Health recently launched an Office of Value and
Innovation in Healthcare Delivery, led by the chief medical officer and another
physician who have hired data engineers and analysts. The facility does have a data
warehouse.
A respondent thinks the Centers for Medicare & Medicaid Services (CMS) has
demonstrated due diligence in selecting the right measures to track but could do more to
help hospitals’ performance on them. A respondent reported that the Agency for Healthcare
Research and Quality (AHRQ) as being helpful by arranging collaboratives and other
strategies.
G. Experience with alternative payment models (APMs)
Commercial payers in the Lexington market have continued to demonstrate interest in
moving towards APMs and reportedly are discussing this with UK Health, but the hospital
has not yet adopted new payment arrangements.
- UK Health expressed interest in bundled payments because of the significant level of
tertiary/quaternary work they do, but noted the hospital is protected/isolated from
needing to take on full risk because they are the only hospital in the area offering trauma,
neonatal intensive care unit, and transplant services so they have significant negotiating
leverage with health plans on payment types and levels.
- Respondents indicate wanting to treat patients who are in others’ ACOs, but do not have
the full suite of services (namely significant primary care, post-acute care) to focus on
population health necessary to be a full partner in an ACO or form their own ACO.
- UK Health might experiment with APMs within its own employee health plan.
Kentucky Medicaid does not seem advanced enough yet to consider APMs. Medicaid
managed care is fairly new and health plans are focused on reducing overutilization (a
problem in the state) through strict payment authorizations. Payment delays and denials have
improved for UK Health over the past year.
UK Health is preparing for APMs, focusing on several key areas:
- Respondents visited Intermountain Healthcare and learned a hospital needs a lot of
confidence in care delivery and cost accounting systems to fare well
- One respondent named health information technology (HIT) infrastructure to integrate
data and the ability to manage patients across the care continuum as the most important
factors to faring well under APMs. UK Health has done a lot on HIT internally and has

APPENDIX 5 MATHEMATICA POLICY RESEARCH
89
electronic health records, but the state’s efforts to establish a health information
exchange have not been that robust. One respondent thinks a lot more work needs to
happen to control where services are provided across the care continuum and the hospital
is in the process of developing post-acute care relationships.
- Another respondent named patient compliance and education as the most important
factors to doing well. The hospital has put a lot of effort into medication compliance and
educating patients on when and where to seek care and reduce high utilization.
- Respondents think these components are important even if APMs do not proceed.
H. Participation in CMMI demonstration projects
UK Health is not involved with any CMMI grants.
I. Expectations for the future
UK Health does not expect much more change in payer mix: as one respondent said, “For
the most part those that would sign up [for coverage] are signed up.”
The respondents’ biggest concern is that the state might reduce Medicaid reimbursement
once the federal government no longer covers the full cost.
The respondents expect DSH funding to decline next year, but are unsure by how much, and
that it will eventually reach zero.
The hospital is working on a strategic plan to prioritize future spending by using the surplus,
most of which appears to be around saving some and expanding capacity. The hospital
continues to grapple with whether it should provide more primary care—either create their
own or partner with CHCs—even as they focus on becoming a tertiary hub. They also are
considering creating a clinic for chronically complex patients as a way to reduce
readmissions and ED visits.

APPENDIX 5 MATHEMATICA POLICY RESEARCH
90
ASPE Safety Net Hospital Study
2015 Site Summary for Yale New Haven Health System
A. Summary of Yale New Haven Hospital
Yale New Haven Hospital (Yale NH) is the flagship hospital of the three-hospital Yale New
Haven Health System. It is one of the largest hospitals in the country at 1,541 beds, and the
only hospital system in New Haven—one of the poorest cities in the state. It is the only
level-1 trauma center in southern Connecticut.
Yale NH is affiliated with Northeast Medical Group, which includes physicians employed
by the hospital (most of whom are primary care providers), and the Yale Medical Group, the
clinical faculty for the School of Medicine. The hospital has recently acquired other
physician practices.
B. Summary of the impact of the Affordable Care Act (ACA)
Although Yale NH has seen some increase in Medicaid patients, volume, and revenues due
to the ACA, these changes have been fairly small compared to most of the other hospitals in
the study that are in states that expanded Medicaid.
Although financial performance has generally been strong, a major concern for the hospital
is the increase in Medicaid shortfalls due to increases in provider taxes and cuts in state
subsidies to hospitals. An increase in patients in high deductible plans is also contributing to
an increase in hospital uncompensated care.
Yale NH has not performed especially well on Medicare quality measures and value-based
purchasing (VBP), which respondents attribute to the low socioeconomic status of their
patient population. The health system is active in alternative payment models, although it is
still too early to draw conclusions about the success of these initiatives.
C. Changes in demand (Q1 2013 to Q1 2015)
The patient population has remained largely stable since the implementation of the ACA.
There have been some increases in Medicaid and people enrolled in the marketplace plans,
and a small decrease in self-pay patients, but payer mix has remained largely stable. This
may reflect both a relatively small uninsured population prior to the ACA, and that
Connecticut began expanding its Medicaid program in 2010.
Respondents reported they were seeing a shift from employer-sponsored to marketplace
plans (“employers are creating a path for employees to access insurance through the
exchanges”), although they were not able to quantify the shift.
Inpatient and emergency department volumes have not changed much.
Outpatient use increased about 20 percent between Q1 2013 and Q1 2015, which
respondents attributed to the acquisition of mostly specialty physician practices by the health
system.

APPENDIX 5 MATHEMATICA POLICY RESEARCH
91
Respondents attribute some of the increase in Medicaid to investments by the hospital in
tertiary and quaternary care. They also attribute it to a new inter-hospital helicopter transport
for patients with complex needs, which has brought in more Medicaid patients as transfers
from other hospitals, and sizeable cuts in Medicaid reimbursements, which is causing
private practice specialists to no longer accept Medicaid patients. This is also resulting in a
much sicker and more complex patient mix that is contributing to increased length of stay.
Respondents reported that most of the remaining uninsured in the state are undocumented
immigrants, and therefore they do not expect to see major changes in payer mix in the future
due to the ACA.
D. Changes in capacity
The hospital has focused primarily on expanding tertiary and quaternary care capacity,
focusing especially on oncology and gastrointestinal diseases.
The hospital has been acquiring physician practices, focusing especially on specialists. Some
of this is in support of expanding oncology and GI services, but also appears to be part of a
strategy to have a wide network of hospitals and physician practices under a single umbrella
to provide more efficient and higher quality of care. This has generated some negative
criticism in the community and from state policymakers who are concerned that independent
physician practices are being squeezed out.
Yale NH has also started an inter-hospital transport for complex patients, which adds about
18-19 patients per day.
E. Changes in finances (Q1 2013 to Q1 2015)
Patient revenue increased by 5.3 percent over the two-year period, but most of this is driven
by increases in revenue from patients with commercial managed care.
Despite some increase in Medicaid revenue, Medicaid shortfalls have increased. The reason
for this is complicated, but it appears to be a combination of increased provider taxes, which
the state has used to match with federal funds, and cuts in the amount that the state is
sending back to hospitals (presumably in the form of Medicaid Disproportionate Share
Hospital (DSH). This has resulted in hospitals being taxed more than they receive in DSH
payments. As a result, Yale New Haven estimates that Medicaid payments have effectively
decreased from 59 cents on the dollar to 39 cents on the dollar.
The hospital has been able to offset lower Medicaid payments by increasing volume and
payment from private payers.
Uncompensated care costs increased 26 percent. Respondents attribute this to an increased
number of patients in high deductible plans (both employer plans and marketplace plans),
but it may also reflect the increase in the Medicaid shortfall, which they include as part of
their uncompensated care calculation.
Total and operating margins have fluctuated over the past two years, but they have remained
positive. Respondents expect margins to become smaller over the next few years, in large
part because of the Medicaid payment cuts.

APPENDIX 5 MATHEMATICA POLICY RESEARCH
92
E. Experience with Medicare VBP
In 2014, Yale NH lost about $3 million in penalties related to Medicare quality measures.
The largest penalties related to excessive readmissions, hospital- acquired conditions, and
HCAHPS scores on the patient experience. There has been some recent improvement in
readmission rates. Respondents believe they are at a disadvantage on these measures
because of the low socioeconomic status of much of their patient population. Specifically,
they feel they have little control over what happens to these patients when they are
discharged from the hospital, and there are few resources in the community to care for them.
To improve scores, respondents mentioned a major initiative to improve the patient
experience, although they did not give specific details. They also mentioned that they were
trying to create more integrated networks of providers that they believe will allow them to
perform better on quality scores, although they view this as a more long-term goal rather
than being geared toward producing results in the short term.
Respondents believe that in order to perform well in VPB programs, a hospital should have
a relatively homogeneous patient population that is well resourced (that is, well insured)
along with risk-based contracts and incentives to create closed medical systems with a high
level of care coordination. They mentioned Kaiser Permanente in California as an example,
but do not believe this model would work in Connecticut or other states. For example,
payment at Yale NH is virtually all fee for service, with only about 2 to 3 percent of the
revenue in some form of risk.
Respondents were adamant about the need to include a socioeconomic risk adjustment in the
quality measures. Moreover, they mention the difficulty of getting ahead of the measures
because they are constantly changing, and the measurement period has already passed by the
time the new measures come out.
Respondents also mentioned that it is important to address population health, but they do not
believe their hospital is set up or has the resources to address problems in the community
that contribute to low-quality scores, nor is it being compensated to address population
health issues.
F. Experiences with alternative payment arrangements (APMs)
Yale NH has been fairly active in pursuing alternative payment arrangements. Their
physician-owned practice, Northeast Medical Group that includes about 1,000 physicians,
participates in a Medicare Shared Savings ACO as well as shared savings programs with
some other commercial payers. This is fairly recent and so they do not know how it has
affected quality or costs, although their preliminary experience suggests they are having
difficulty meeting the medical loss ratio targets for the Centers for Medicare & Medicaid
Services (CMS) shared savings.
Yale NH is also participating in a CMMI bundled payment project for orthopedic services,
focusing especially on major lower joints. Although it is still too early to assess results, their
experience has not been very good, mentioning that “CMS is still working through many of
the operational logistics of the program.”
Yale NH cites a number of advantages they have in being able to perform well under APMs,
including a history of success in cross-continuum care management, dedicated physician

APPENDIX 5 MATHEMATICA POLICY RESEARCH
93
leadership, a single electronic medical record (Epic) across all parts of the system, an
employed physician group, engagement of third party technology for population
management (Conifer), and patient engagement (Emmi). Disadvantages or limitations
include a lack of a shared organization structure between inpatient and ambulatory care with
which to engage physicians, higher costs due to the academic focus, and lack of experience
among payers and providers in the state regarding risk or value-based contracts.
Respondents believe that to succeed with APMs, a hospital system needs a strong care
management staff (mix of registered nurses, social workers, and nonclinical navigators),
physician leadership in transforming clinical processes, technology such as outreach call
tools and patient portals, and actionable data analytics.
Respondents mentioned that CMS could better facilitate hospital participation in APMs by
providing timely and robust claims files for analysis, as well as funding for care
management infrastructure.
Yale NH is also participating in several PCMH initiatives focusing on their Medicaid and
uninsured populations, as well as a care management program for their employees, which
they are also attempting to expand to large employers.
G. Expectations for the future
By far the biggest concern among respondents is the future of Medicaid reimbursement.
Respondents believe that there will be difficulty in running the facility for the following
reasons: the recent increase in provider taxes and decreases in the amount of DSH funds
they are receiving in return, a sluggish economy, and what they view as a highly taxed and
regulated state (for example, Certificate of Need laws that require state approval for a
change in hospital ownership). For now they are able to essentially cost shift the Medicaid
shortfalls to private payers, but are concerned they will not be able to do so in the future.
The ACA-related Medicaid DSH cuts that begin in 2018 are viewed as “just piling on more
bad news based on a faulty premise.” They believe they can manage the planned cuts in
Medicaid DSH, but it is the unexpected cuts in Medicaid payment by the state that they have
the most difficulty and concern with.
APPENDIX 6
HOSPITAL PERFORMANCE ON CMS QUALITY MEASURES
APPENDIX 7 MATHEMATICA POLICY RESEARCH
96
Appendix 6. Medicare quality bonuses and penalties
Hospital
Value-based
purchasing Penalties,
Oct. 2014–Sept. 2015
Readmissions penalty
Oct. 2014–Sept. 2015
Received HAC penalty
for Oct. 2014–Sept. 2015
LAC+USC Medical Center
‐0.08%
‐0.13%
Yes
Denver Health Medical Center
‐0.20%
‐0.01%
No
Regional One Health
‐0.46%
‐0.01%
Yes
Harris Health System
‐0.15%
‐0.13%
No
Froedtert Hospital
‐0.22%
‐1.10%
No
University of Kentucky HealthCare
0.14%
‐0.42%
Yes
Yale-New Haven Hospital
‐0.39%
‐0.71%
Yes
Homestead Hospital
0.85%
‐0.39%
No
Source: CMS.
Note: Medicare exempts Marcum and Wallace Memorial Hospital and Lakewood Health System from reporting on
these indicators due to their small size as Critical Access Hospitals.

www.mathematica-mpr.com
Improving public well-being by conducting high quality,
objective research and data collection
PRINCETON, NJ ■ ANN ARBOR, MI ■ CAMBRIDGE, MA ■ CHICAGO, IL ■ OAKLAND, CA ■ WASHINGTON, DC
Mathematica
®
is a registered trademark
of Mathematica Policy Research, Inc.
