Print Advisory – Document Pages: 72
Revised: 02/28/2022
A Guide to Fellowship Training Programs
in Surgical Critical Care and Acute Care Surgery
Third Edition
Developed by the
Surgical Critical Care Program Directors Society
EDITORS
William C. Chiu, MD, FACS, FCCM
Associate Professor of Surgery
University of Maryland School of Medicine
Director, Surgical Critical Care
Fellowship Program
R Adams Cowley Shock Trauma Center
University of Maryland Medical Center
Baltimore, Maryland
Samuel A. Tisherman, MD, FACS, FCCM
Professor of Surgery
University of Maryland School of Medicine
Director, Center for Critical Care
and Trauma Education
Director, Surgical Intensive Care Unit
R Adams Cowley Shock Trauma Center
University of Maryland Medical Center
Baltimore, Maryland
Kimberly A. Davis, MD, MBA, FACS, FCCM
Professor of Surgery
Chief, Division of General Surgery, Trauma,
and Surgical Critical Care
Yale University School of Medicine
Trauma Medical Director
Yale-New Haven Hospital
New Haven, Connecticut
David A. Spain, MD, FACS
David L. Gregg, MD Professor
Chief of Acute Care Surgery
Associate Chief, Division of General Surgery
Department of Surgery
Stanford University School of Medicine
Stanford, California
Robert A. Maxwell, MD, FACS
Associate Professor of Surgery
University of Tennessee College of Medicine
Director, Surgical Critical Care
Fellowship Program
University of Tennessee Health Science Center
Chattanooga, Tennessee
Krista L. Kaups, MD, FACS
Professor of Clinical Surgery
University of California (San Francisco) / Fresno
Director, Surgical Intensive Care Unit
Community Regional Medical Center
Fresno, California
Charles A. Adams, Jr., MD, FACS, FCCM
Associate Professor of Surgery
Chief, Division of Trauma and Critical Care
Warren Alpert Medical School
Brown University
Providence, Rhode Island
Surgical Critical Care
Program Directors Society

[Table of Contents] SCCPDS Fellowship Guide 2
Contributors
James E. Babowice, DO
Surgery Chief Resident
Allegheny General Hospital
Pittsburgh, Pennsylvania
16. Fellowship Interviews
Jacqueline J. Blank, MD
Surgical Critical Care Fellow
University of Pennsylvania Health System
Philadelphia, Pennsylvania
17. Coaches, Advisors, Mentors, and Confidantes: What You Need and Why
Michelle R. Brownstein, MD, FACS
Associate Professor
Department of Surgery
Division of Acute Care Surgery
Associate Program Director, Surgical Critical Care Fellowship
East Carolina University
Greenville, North Carolina
21. Re-entry Applicants
Clay Cothren Burlew, MD, FACS
Professor of Surgery
Director, Surgical Intensive Care Unit
Program Director, Surgical Critical Care Fellowship
Program Director, Trauma & Acute Care Surgery Fellowship
Denver Health Medical Center
University of Colorado School of Medicine
Denver, Colorado
1. Acute Care Surgery
Robert A. Cherry, MD, MS, FACS, FACHE
Adjunct Professor of Surgery
Chief Medical and Quality Officer
UCLA Health
Los Angeles, California
10. Geographic Considerations
William C. Chiu, MD, FACS, FCCM
Associate Professor of Surgery
University of Maryland School of Medicine
Director, Surgical Critical Care Fellowship Program
R Adams Cowley Shock Trauma Center
University of Maryland Medical Center
Baltimore, Maryland
Preface
Preface to Second Edition
Preface to First Edition
SAFAS Applicant Instructions
5. How Many Years of Fellowship Training?
25. Web Sites of Interest
26. Acknowledgment

[Table of Contents] SCCPDS Fellowship Guide 3
Daniel J. Cucher, MD
Dignity Health
Chandler Regional Medical Center
Chandler, Arizona
9. What Do Fellows Do, Day In, Day Out?
Kimberly A. Davis, MD, MBA, FACS, FCCM
Professor of Surgery
Chief, Division of General Surgery, Trauma, and Surgical Critical Care
Yale University School of Medicine
Trauma Medical Director
Yale-New Haven Hospital
New Haven, Connecticut
1. Acute Care Surgery
Matthew L. Davis, MD, FACS (posthumous)
Assistant Professor of Surgery
Texas A&M Health Science Center College of Medicine
Trauma Medical Director
Scott & White Hospital and Healthcare
Temple, Texas
3. Surgical Critical Care or Acute Care Surgery Fellowship?
4. Should I Do An Elective At An Institution That I Am Considering?
Therese M. Duane, MD, MBA, CPE, FACS, FCCM
Professor of Surgery
Texas Christian University
University of North Texas Health Science Center
Academic Chair and Program Director for General Surgery
Texas Health Resources
Fort Worth, Texas
5. How Many Years of Fellowship Training?
Linda A. Dultz, MD, MPH, FACS
Assistant Professor of Surgery
Program Director, Surgical Critical Care Fellowship
University of Texas Southwestern Medical Center
Medical Director, Surgical Intensive Care Unit
Parkland Memorial Hospital
Dallas, Texas
16. Fellowship Interviews
Paula A. Ferrada, MD, FACS
Professor of Surgery
Medical Director, Surgical and Trauma ICU
Director, Surgical Critical Care Fellowship
Division of Trauma, Critical Care, and Emergency Surgery
Virginia Commonwealth University Health System
Richmond, Virginia
3. Surgical Critical Care or Acute Care Surgery Fellowship?

[Table of Contents] SCCPDS Fellowship Guide 4
Laura N. Godat, MD, FACS
Associate Professor of Clinical Surgery
Program Director
Surgical Critical Care and Acute Care Surgery Fellowship
Medical Director, Surgical Intensive Care Unit
Assistant Trauma Director
University of California San Diego Medical Center
San Diego, California
16. Fellowship Interviews
Shea C. Gregg, MD, FACS
Chief, Section of Trauma, Burns, and Surgical Critical Care
Yale New Haven Health – Bridgeport Hospital
Bridgeport, Connecticut
6. What Things Should I Look For At Each Program?
David A. Hampton, MD, Meng, FACS
Assistant Professor
Division of Trauma and Acute Care Surgery
Department of Surgery
Associate Program Director, Adult Surgical Critical Care Fellowship
Associate Clerkship Director, Surgery
University of Chicago Pritzker School of Medicine
Chicago, Illinois
7. International / Overseas Surgical Rotations
16. Fellowship Interviews
Lewis J. Kaplan, MD, FACS, FCCM, FCCP
Professor of Surgery
Division of Trauma, Surgical Critical Care and Emergency Surgery
University of Pennsylvania Perelman School of Medicine
Chief, Section of Surgical Critical Care
Philadelphia Veterans Affairs Medical Center
Philadelphia, Pennsylvania
17. Coaches, Advisors, Mentors, and Confidantes: What You Need and Why
Mansoor A. Khan, MBBS (Lond), PhD, FRCS(GenSurg), FEBS(GenSurg), FACS, AKC
Surgeon Commander, Royal Navy
Consultant Trauma Surgeon
Associate Professor in Military Surgery
Royal Naval Medical Services
St. Mary’s Hospital
Imperial College Healthcare NHS Trust
London, United Kingdom
24. International Physicians
Uzer S. Khan, MBBS, FACS
Associate Professor of Surgery
Director, Surgical Critical Care Fellowship Program
Associate Director, Trauma Intensive Care Unit
Division of Trauma, Critical Care, and Acute Care Surgery
Allegheny General Hospital
Pittsburgh, Pennsylvania
16. Fellowship Interviews

[Table of Contents] SCCPDS Fellowship Guide 5
Jennifer C. Knight Davis, MD, FACS
Associate Professor
Division of Trauma, Emergency Surgery and Surgical Critical Care
Department of Surgery
West Virginia University School of Medicine
Trauma Medical Director
Jon Michael Moore Trauma Center
Morgantown, West Virginia
11. Family Considerations
Stefan W. Leichtle, MD, FACS
Associate Professor of Surgery
Program Director, Surgical Critical Care Fellowship
Medical Director, Trauma Intensive Care Unit
Division of Acute Care Surgical Services
Virginia Commonwealth University
Richmond, Virginia
12. Applying to Fellowship Programs
16. Fellowship Interviews
Alexander L. Marinica, DO
Clinical Instructor
University of Texas Southwestern Medical Center
Parkland Memorial Hospital
Dallas, Texas
16. Fellowship Interviews
Joshua A. Marks, MD, FACS
Associate Professor of Surgery
Division of Acute Care Surgery
Program Director, Surgical Critical Care Fellowship
Associate Program Director, General Surgery Residency
Sidney Kimmel Medical College
Thomas Jefferson University Hospital
Philadelphia, Pennsylvania
13. Application Chronology
William A. Marshall, MD
Surgical Critical Care and Acute Care Surgery Fellow
University of California San Diego Medical Center
San Diego, California
16. Fellowship Interviews
Niels D. Martin, MD, FACS, FCCM
Associate Professor of Surgery
Vice Chair, Diversity & Inclusion
Chief, Section of Surgical Critical Care
Director, Traumatology & Surgical Critical Care Fellowship Programs
Perelman School of Medicine
University of Pennsylvania
Philadelphia, Pennsylvania
12. Applying to Fellowship Programs
13. Application Chronology
16. Fellowship Interviews

[Table of Contents] SCCPDS Fellowship Guide 6
Maureen McCunn, MD, MIPP, FASA, FCCM
Professor
Department of Anesthesiology
University of Maryland School of Medicine
Division of Trauma Anesthesiology
R Adams Cowley Shock Trauma Center
Baltimore, Maryland
23. Anesthesiologists
Benjamin J. Moran, MD, FACS
Assistant Professor of Surgery
Sidney Kimmel Medical College
Thomas Jefferson University
Associate Director
Surgery Residency Program
Einstein Healthcare Network
Philadelphia, Pennsylvania
8. What to Expect in a Fellowship Program
David S. Morris, MD, FACS
Associate Medical Director, General Surgery
Intermountain Healthcare
Salt Lake City, Utah
2. Acute Care Surgery Traits
5. How Many Years of Fellowship Training?
6. What Things Should I Look For At Each Program?
14. Preparing Your Personal Statement
15. Letters of Recommendation
Chet A. Morrison, MD, FACS, FCCM
Associate Professor of Surgery
Central Michigan University College of Medicine
Trauma Medical Director
Attending Trauma and Critical Care Surgeon
Ascension St. Mary’s Hospital
Saginaw, Michigan
20. What is the Post-Fellowship Job Outlook?
Nathan T. Mowery, MD, FACS
Associate Professor of Surgery
Director, AAST Acute Care Surgery Fellowship
Wake Forest School of Medicine
Wake Forest Baptist Medical Center
Winston-Salem, North Carolina
6. What Things Should I Look For At Each Program?
Catherine S. Nelson, MD
Arnot Medical Services, PLLC
Arnot Ogden Medical Center
Elmira, New York
12. Applying to Fellowship Programs
13. Application Chronology
14. Preparing Your Personal Statement
15. Letters of Recommendation

[Table of Contents] SCCPDS Fellowship Guide 7
Mary Noory, MD
Surgery Chief Resident
State University of New York Downstate Medical Center
Brooklyn, New York
16. Fellowship Interviews
Samuel Osei, MD
Surgery Chief Resident
Beaumont Hospital
Royal Oak, Michigan
16. Fellowship Interviews
Jose L. Pascual, MD, PhD, FACS, FRCSC, FCCM
Professor of Surgery
Division of Trauma, Surgical Critical Care and Emergency Surgery
University of Pennsylvania Perelman School of Medicine
Philadelphia, Pennsylvania
17. Coaches, Advisors, Mentors, and Confidantes: What You Need and Why
Susan E. Rowell, MD, MBA, MCR, FACS
Professor of Surgery
Director, Surgical Critical Care Fellowship Program
Co-Director, Surgical Intensive Care Unit
University of Chicago Medicine
Chicago, Illinois
16. Fellowship Interviews
Joseph V. Sakran, MD, MPH, MPA, FACS
Associate Professor of Surgery
Associate Chief, Division of Acute Care Surgery
Director, Emergency General Surgery
Vice Chair of Clinical Operations
Department of Surgery
The Johns Hopkins Hospital
Baltimore, Maryland
2. Acute Care Surgery Traits
5. How Many Years of Fellowship Training?
6. What Things Should I Look For At Each Program?
14. Preparing Your Personal Statement
15. Letters of Recommendation
Edgardo S. Salcedo, MD, FACS
Professor of Surgery
Interim Vice Chair of Education
Program Director, General Surgery Residency
Program Director, Surgical Education and Simulation Fellowship
Division of Trauma, Acute Care Surgery, and Surgical Critical Care
University of California, Davis Medical Center
Sacramento, California
2. Acute Care Surgery Traits
5. How Many Years of Fellowship Training?
6. What Things Should I Look For At Each Program?
14. Preparing Your Personal Statement
15. Letters of Recommendation

[Table of Contents] SCCPDS Fellowship Guide 8
David A. Spain, MD, FACS
David L. Gregg, MD Professor
Chief of Acute Care Surgery
Associate Chief, Division of General Surgery
Department of Surgery
Stanford University School of Medicine
Trauma Medical Director
Stanford Health Care
Stanford, California
20. What is the Post-Fellowship Job Outlook?
Gary A. Vercruysse, MD, FACS
Professor of Surgery
Director of Emergency General Surgery
Division of Acute Care Surgery
University of Michigan Medical School
University of Michigan Health System
Ann Arbor, Michigan
5. How Many Years of Fellowship Training?
James F. Watkins, MD, MSc, FACS
Executive Director
Rocky Mountain Trauma Society
Snowmass Village, Colorado
19. How to Prepare for the SCC Board Certifying Examination
Julie Mayglothling Winkle, MD, FACEP, FCCM
Associate Professor
Department of Emergency Medicine
Department of Anesthesiology, Division of Critical Care
University of Colorado School of Medicine
Aurora, Colorado
22. Emergency Physicians
Salina M. Wydo, MD, FACS
Assistant Professor of Surgery
Cooper Medical School of Rowan University
Program Director, Surgical Critical Care Fellowship
Division of Trauma, Surgical Critical Care and Acute Care Surgery
Cooper University Hospital
Camden, New Jersey
18. Identifying and Developing Your Interests
[Table of Contents] SCCPDS Fellowship Guide 9
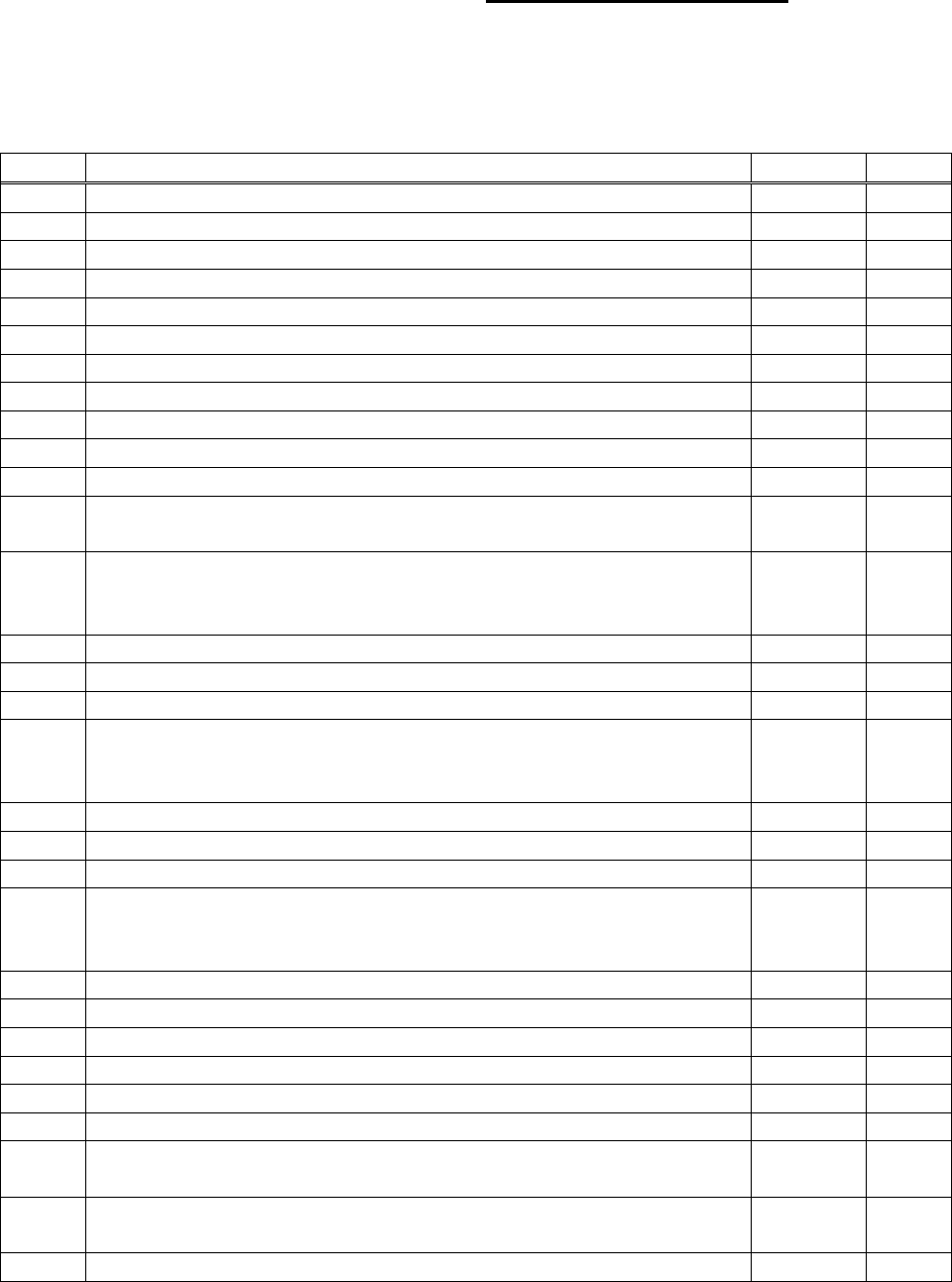
Table of Contents
Chapter
Title
Authors
Page
Cover
1
Contributors
2
Table of Contents
9
Preface
Chiu
11
Preface to Second Edition
Chiu
12
Preface to First Edition
Chiu
13
SAFAS Applicant Instructions
Chiu
14
1
Acute Care Surgery
K. Davis
Burlew
15
2
Acute Care Surgery Traits
Morris
Sakran
Salcedo
17
3
Surgical Critical Care or Acute Care Surgery Fellowship?
Ferrada
18
M. Davis
19
4
Should I Do An Elective At An Institution That I Am Considering?
M. Davis
19
5
How Many Years of Fellowship Training?
Salcedo
Morris
Sakran
20
Duane
21
Vercruysse
22
Chiu
23
6
What Things Should I Look For At Each Program?
Salcedo
Morris
Sakran
24
Gregg
26
Mowery
28
7
International / Overseas Surgical Rotations
Hampton
29
8
What to Expect in a Fellowship Program
Moran
30
9
What Do Fellows Do, Day In, Day Out?
Cucher
32
10
Geographic Considerations
Cherry
34
11
Family Considerations
J. Knight
Davis
35
12
Applying to Fellowship Programs
Leichtle
Martin
36
Nelson
37
[Table of Contents] SCCPDS Fellowship Guide 10
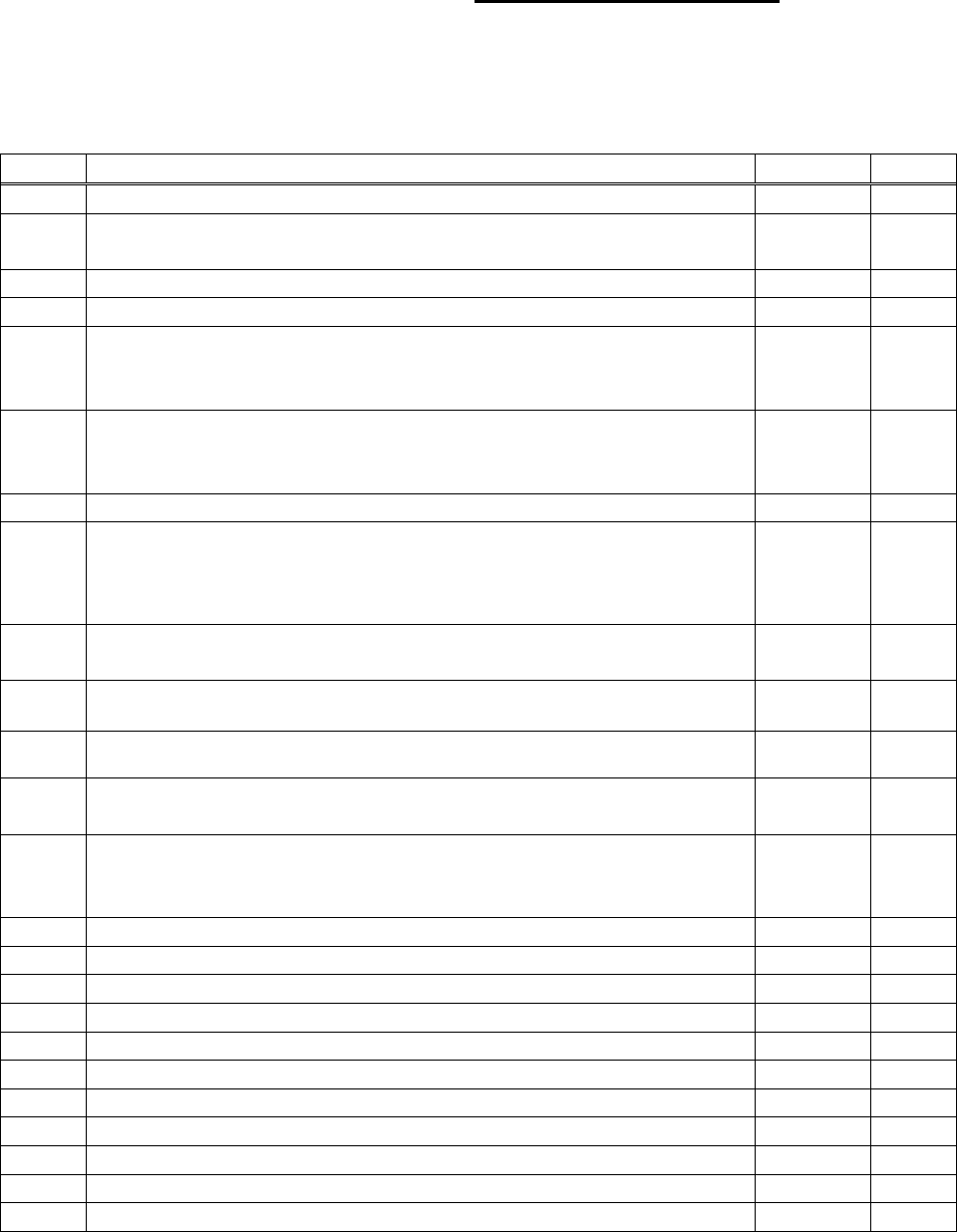
Table of Contents (continued)
Chapter
Title
Authors
Page
13
Application Chronology
Marks
Martin
39
Nelson
40
14
Preparing Your Personal Statement
Nelson
41
Sakran
Salcedo
Morris
42
15
Letters of Recommendation
Sakran
Salcedo
Morris
43
Nelson
43
16
Fellowship Interviews
Noory
Osei
Rowell
Hampton
44
Leichtle
Martin
46
Marinica
Dultz
48
Babowice
Khan
52
Marshall
Godat
54
17
Coaches, Advisors, Mentors, and Confidantes:
What You Need and Why
Blank
Pascual
Kaplan
56
18
Identifying and Developing Your Interests
Wydo
61
19
How to Prepare for the SCC Board Certifying Examination
Watkins
62
20
What is the Post-Fellowship Job Outlook?
Morrison
63
Spain
64
21
Re-entry Applicants
Brownstein
65
22
Emergency Physicians
Winkle
66
23
Anesthesiologists
McCunn
69
24
International Physicians
Khan
71
25
Web Sites of Interest
Chiu
72
26
Acknowledgment
Chiu
72

[Table of Contents] SCCPDS Fellowship Guide 11
Preface
Impact of the COVID-19 Pandemic on the Interview Process
and the New Application Chronology/Timeline
In the spring of 2020, the Coronavirus Disease 2019 (COVID-19) pandemic
resulted in widespread implementation of lockdowns, stay-at-home orders, and travel
restrictions for public health and safety. The pandemic also altered the process of
Residency and Fellowship applications, with the greatest impact being on the format of
interviews. Fellowship Programs had already started to convert traditional in-person
education and conferences to virtual and online teaching.
In April 2020, under the leadership of President Kimberly Davis, the Surgical
Critical Care Program Directors Society (SCCPDS) Board of Directors recommended
that all Fellowship interviews be conducted using a virtual format for that recruitment
cycle. We learned that there were many benefits for both Programs and applicants to
the virtual interview process. The following year, in 2021, we endured the Delta variant
surge that necessitated continuing virtual interviews for another recruitment year. In this
third edition, based upon these experiences, we have included a new chapter on
Fellowship Interviews. Several groups of SCCPDS members have contributed their
perspectives, focusing primarily on virtual interviews, what to expect, tips for preparation
and standing out, do’s and do not’s.
The Application Chronology and timeline for this year has changed compared to
the past six years. In March 2021, the SCCPDS Match Committee, under the direction
of Chair Niels Martin, embarked on an effort to optimize the Application to Match
timeline, with an initial objective of reducing the duration of the application period. The
proposal was made to open the Surgical critical care and Acute care surgery Fellowship
Application Service (SAFAS) on March 1. Furthermore, it was also proposed to move
the National Resident Matching Program (NRMP) Surgical Critical Care (SCC) Match
Day approximately one month earlier.
The new shortened timeline proposal was distributed to the SCCPDS
membership for an open comment period, followed by approval with a majority vote
from SCC Fellowship Program Directors. In this third edition, the chapters on Applying
to Fellowship Programs and Application Chronology have been substantially revised to
reflect the new timeline. We hope that this Guide to Fellowship Training Programs will
continue to be a useful resource and provide essential information for applicants.
William C. Chiu, MD
President
Surgical Critical Care Program Directors Society
February 28, 2022

[Table of Contents] SCCPDS Fellowship Guide 12
Preface to Second Edition
History of the Surgical critical care and Acute care surgery
Fellowship Application Service (SAFAS)
The first informal meetings of Surgical Critical Care (SCC) Fellowship Program Directors were held in
conjunction with the annual meeting of the American Association for the Surgery of Trauma (AAST) in 2003 and
2004, organized by William Cioffi, AAST Critical Care Committee Chair. The primary topics discussed were common
issues in training SCC Fellows, including curriculum updates, ACGME competencies, and possibly developing a
Fellowship Match program. After several meetings, it became clear that a concerted effort was needed from the
Program Directors. Independent meetings were held during the American College of Surgeons Clinical Congress
starting in 2005. In 2008, the Surgical Critical Care Program Directors Society (SCCPDS) was formally incorporated
in the State of Rhode Island as a 501(c)(6) non-profit organization, with Dr. Cioffi as Founding President.
In those early years of SCCPDS, the Fellowship application process had not yet begun to evolve.
There were separate Fellowship listings on the Web sites for the Accreditation Council for Graduate
Medical Education (ACGME), Eastern Association for the Surgery of Trauma (EAST), AAST, and
SCCPDS. Back then, Residents with an interest in a SCC Fellowship were required to conduct their own
research on available programs. They were required to contact each Program individually, most often by
regular postal mail and occasionally by telephone. At the time, most Programs did not yet have a
significant Web presence, so Programs typically sent out application forms by mail. Since each
Program’s application forms were different, applicants were required to complete each one separately,
either in handwriting or rarely using a typewriter. Completed applications were sent by mail.
Recommenders were provided a list of Program addresses to send personalized letters of
recommendation by mail. Mail navigated through institutional channels, and arrived in Fellowship
Program offices without delay, only when lucky.
In 2010, David Spain, SCCPDS Treasurer, first introduced the idea of SCC Fellowship Programs
using the Electronic Residency Application Service (ERAS
®
). At the 2011 SCCPDS Annual Meeting,
under President Frederick Luchette, members discussed and endorsed the use of ERAS, with Secretary
Samuel Tisherman leading the implementation process. In 2013, many SCC Fellowship Programs
started using ERAS, but several major concerns became evident. SCC Fellowship Programs had
historically accepted applications beginning in the spring, but ERAS would not open until July annually.
This allowed for a short application season, with the National Resident Matching Program (NRMP
®
) Rank
Order List deadline in September annually. Moreover, ERAS did not alert Programs to new application
submissions, forcing Programs to log in to ERAS daily to check for updates. These issues doomed ERAS
for SCC, and members unanimously voted to discontinue participation in ERAS after the one-year trial.
In November 2013, the SCCPDS Board of Directors began discussion on a combined SCC and
Acute Care Surgery (ACS) standard application service. In February 2014, with the assistance of our
freelance Web site developer, the Surgical critical care and Acute care surgery Fellowship Application
Service (SAFAS) was “under construction.” By May 2014, SAFAS underwent beta testing, but several
key issues (system glitches) could not be resolved. In February 2015, SCCPDS abandoned the project
with the freelancer, and contracted with a professional developer. FluidReview
®
, a subsidiary company of
SurveyMonkey
®
, was the leading online application management platform on the Web, powering the
application processes of organizations, educational institutions, and foundations around the world. With
the one-year development experience struggle behind us, customization and implementation of SAFAS
on FluidReview became an easy one-month process. SAFAS, sponsored by SCCPDS, launched on
March 2015, and has since been the application service utilized by all ACGME-accredited SCC
Fellowship Programs and AAST-approved ACS Fellowship Programs.
William C. Chiu, MD
President-Elect
Surgical Critical Care Program Directors Society
November 19, 2018

[Table of Contents] SCCPDS Fellowship Guide 13
Preface to First Edition
On February 11, 2010, Eastern Association for the Surgery of Trauma (EAST)
President Donald Jenkins extended a “thought for the EAST website” to Bruce Crookes
(EAST Information Management and Technology Committee Chair) and me. One of his
fourth-year Surgery Residents from the Mayo Clinic, Nicole Krumrei was an EAST
Oriens Award applicant, and had submitted a personal essay on “This is Why I Want a
Career in Trauma.” The story that President Jenkins related was that there seemed to
be a lack of clarity or central location of information for Residents applying for Trauma
Fellowships, and it was surprising that there wasn’t more information on the process.
The EAST Web site has emerged as the leading resource for Fellowship
information in our specialty. The EAST Fellowships Listing originated from the Trauma
Care Fellowships booklet, published by the Fellowship Task Force of the Careers in
Trauma Committee in 1996. In 1997, this booklet was converted to electronic format for
the EAST Web site. The EAST Fellowships Listing has represented a current database
of the most comprehensive descriptive information available on Fellowships in Trauma,
Critical Care, and Acute Care Surgery.
When I was a Surgery Resident, I had a copy of the “little red book,” a resource
to medical students who were applying for Residency Programs in Surgery, a guide to
finding and matching with the best possible Surgery Residency. This book was created
by Drs. Kaj Johansen and David Heimbach, both from the University of Washington.
The book has since been adapted to an electronic format with expanded content, and is
available on the American College of Surgeons Web site.
This current Fellowship guide will uniquely represent the only comprehensive
resource available offering subjective advice for prospective Fellows in our specialty,
and will have a staged development plan. The initial effort will be presented in Portable
Document Format (PDF), available on the EAST Web site. With the renovation of the
EAST Web site, we hope to eventually progress with a transition to an interactive
electronic resource.
On May 5, 2011, Michael Rotondo, EAST Past President and Past Careers in
Trauma Committee Chair offered me a “thought” on what he envisions as the future
development of a Fellowships guide (similar to TripAdvisor
®
,
“Read Reviews from Real
People. Get the Truth. Then Go.”) This initiative should continue to sustain the EAST
Web site as the definitive information resource for Residents interested in Fellowship
Training in Trauma, Critical Care, and Acute Care Surgery.
William C. Chiu, MD
Chair, Careers in Trauma Committee
Eastern Association for the Surgery of Trauma
May 30, 2011
[Table of Contents] SCCPDS Fellowship Guide 14
Surgical critical care and Acute care surgery
Fellowship Application Service (SAFAS)
www.safas.smapply.io
APPLICANT INSTRUCTIONS
Please print and read all instructions prior to beginning application process.
REGISTER and CREATE ACCOUNT:
1. On the SAFAS Home page, go to “Register” for an Account.
2. Complete the Registration form.
3. You will receive a confirmation E-mail.
4. Click on the hyperlink in the E-mail to confirm Registration.
CREATE and EDIT APPLICATION:
5. Log In to SAFAS.
6. On Applicant Home Page, click on “View Programs”.
7. On Programs page, click on “MORE >” and then click on “APPLY”.
8. SAFAS Application Form: Complete all 4 sections.
9. You may Save, Log Out, and Continue Editing later.
UPLOAD SUPPORTING DOCUMENTS:
10. Upload your Photograph, Curriculum Vitae, and Personal Statement.
11. Upload a copy of your USMLE and ABSITE Scores (or equivalent).
12. The preferred image type is JPG and document type is PDF.
13. Extra Comments/Documents is optional.
REQUEST RECOMMENDATIONS:
14. Give your Recommenders advanced notice.
15. Recommendation Letters: Enter 3 Names and 3 different E-mail addresses for 3 Recommenders.
16. Each Recommender will receive an automated E-mail request.
17. Each Recommender will be requested to complete 2 tasks:
Separate and Standardized Letter of Recommendation.
18. You will receive an automated E-mail notification upon completion of the recommendation.
19. If Recommender’s institutional firewall blocks Web-generated E-mails, Contact SAFAS Administrator.
SELECT PROGRAMS and FEE:
20. Select the Programs you wish to receive your application materials.
21. Your Recommenders will have access to view:
All of your completed and uploaded documents in-progress.
Your Fellowship Programs Selection Form, if completed.
22. Programs selected will NOT have access to your Programs Selection Form.
23. The Application Fee is $10 for each Fellowship Program selected.
SUBMIT APPLICATION:
24. Submit your Application - Do NOT wait for Recommenders to complete Letters.
25. Upon Submitting your Application, it becomes Locked from Editing.
26. You will receive an automated E-mail confirmation.
27. Each Program selected will receive an automated E-mail notification.
28. You may “Download” Application as a PDF document.
29. To Edit/Withdraw Locked Application, Contact SAFAS Administrator.
SUBMIT APPLICATION TO ADDITIONAL PROGRAMS:
30. You may Create another Submission by returning to Applicant Home Page.
31. Your Application Form and most Supporting Documents are reusable.
32. You may edit your Application Form and Supporting Documents.
33. Do NOT re-enter Recommenders, unless you wish to edit them.
34. Select new Programs – Do NOT select Programs previously selected.
HELP and SUPPORT:
35. Resources, Links, and Contact information at the SAFAS Home page.
Revised: 02/24/2022
Surgical Critical Care
Program Directors Society

[Table of Contents] SCCPDS Fellowship Guide 15
1. Acute Care Surgery
02/15/2022 Kimberly A. Davis, MD, MBA, FACS, FCCM (New Haven, CT),
Clay Cothren Burlew, MD, FACS (Denver, CO):
Although often used interchangeably, “emergency general surgery” and “acute
care surgery” have different meanings. Whereas emergency general surgery (EGS)
refers to acute general surgical disorders, acute care surgery (ACS) includes surgical
critical care and the surgical management of severely ill patients with a variety of
conditions including trauma, burns, surgical critical care or an acute general surgical
condition. The challenges in caring for these patients include around-the-clock
readiness for the provision of comprehensive care, the often-constrained time for
preoperative optimization of the patient, and the greater potential for intraoperative and
postoperative complications due to the emergency nature of care. Doubling as surgical
intensivists, acute care surgeons provide not only a much-needed service but a
continuity of care; the acute care surgeon combines both operative care of the acute
surgical disorder as well as postoperative management for the critically ill patient. This
combination of skill and breadth of care is not matched in any other field.
There are two routes of training for surgeons interested in a career in ACS.
Some will choose to participate in the RRC-accredited one-year training program in
surgical critical care. Others may choose a two-year fellowship, either under the
auspices of the American Association for the Surgery of Trauma (AAST) approved
fellowship programs, or other programs that may offer either additional trauma or burn
training. Which route of training often depends on the fellow’s prior training and career
goals. Graduating chief residents may feel ready to operate independently and thus
question the additional year of surgical training. Alternatively, they may acknowledge
the importance of added training to best position for a highly competitive faculty
appointment. These decisions are deeply personal and should be made in conjunction
with advice from trusted mentors.
The core components of ACS are trauma, surgical critical care and EGS; the
fellowship training paradigm designed by the AAST is designed to create a versatile
surgeon able to confront a host of acute surgical disease processes. Recent curricular
changes in the fellowship included the identification of a minimum number of operative
cases needed in specific body regions, similar to defined case volumes for general
surgery. These cases may be obtained either through defined rotations on subspecialty
services, through a more experientially based method, or a combination of both. Each
fellowship individualizes the fellows’ training components to capitalize on local expertise
and rotations to optimize the fellows’ educational experience both in and out of the
operating room. Additionally, there is a list of desired cases for the fellows; these
provide guidance to the fellows, program directors and subspecialty colleagues as to
the types of cases deemed important for the fellows' training. The fellowship is designed
to assure competence in the management of complex surgical disease in patients with
significant underlying comorbidities. The fellowship curriculum includes operative cases
and bedside procedures as well as nonoperative management of complex trauma and
EGS conditions.

[Table of Contents] SCCPDS Fellowship Guide 16
The AAST ensures that ACS fellowships will continue to build on the strong
foundation of process and structure that already exist. A comprehensive core curriculum
provides didactic information on trauma and EGS topics and state-of-the-art media
dedicated to complex surgical exposures. Additionally, key areas will have added
“pearls from the experts” with technical tricks for complex operative procedures; these
tips may be particularly advantageous for patients who, due to severity of illness, do not
have the luxury of preoperative physiologic restoration.
The goals of training acute care surgeons are to demonstrate mastery in the field
of ACS, expanding on the basics learned in a general surgery residency. Those trained
in ACS fellowships are eligible for board certification in surgical critical care through the
American Board of Surgery. Added certification in ACS following the 2 year fellowship is
currently offered through the AAST. Currently there are twenty-nine approved ACS
programs. Unlike most specialty training, this paradigm strives to create a broad-based
surgical specialist, specifically trained in the treatment of severely ill patients with acute
surgical disease across a wide array of anatomic regions.
Our most critically ill surgical patients have benefited from the evolution of ACS,
with improved outcomes, more efficient care, and decreased mortality. The training
paradigm for ACS fellows will continue to ensure that fully trained acute care surgeons
are comfortable with a wide variety of anatomic exposures across all body regions.
Acute care surgeons are uniquely positioned to decrease health care costs and improve
care in the United States as mandated by the Affordable Care Act of 2010. Cost savings
can be actualized, and the system for care delivery can be optimized by focusing on
efficiency and the use of standardized, evidence-based, consistent care. Acute care
surgeons stand at the front line of care delivery for the patients who are most critically ill
and injured. Getting the right patient to the right venue at the right time is the paramount
skill that the acute care surgeon, through training and experience, adds to the value
equation.

[Table of Contents] SCCPDS Fellowship Guide 17
2. Acute Care Surgery Traits
02/20/2022 David S. Morris, MD, FACS (Salt Lake City, UT),
Joseph V. Sakran, MD, MPH, MPA, FACS (Baltimore, MD),
Edgardo S. Salcedo, MD, FACS (Sacramento, CA):
Surgeons who choose Acute Care Surgery as a career come from a wide variety
of backgrounds with ultimate career goals that may be vastly different as well. Several
traits are common among those in the field. Chief among these is an interest in multi-
organ system physiology, a desire to operate in many areas of the body, and a love of
caring for the most acutely ill patients. In general, acute care surgeons are drawn to
managing the challenging or unexpected case and are accustomed to being called to
help when there’s no one left to call.
As a resident, did you find yourself thinking often about the complexities of
human physiology as you cared for your patients? Did you enjoy the time you spent in
the ICU? Did you ever find yourself wishing that you could really understand how to
manage a difficult ventilated patient, or balance the sometimes-competing requirements
of failing organ systems? Surgeons who choose to do a critical care fellowship
generally enjoy the medical aspects of surgical care. The acute care surgeon is a
further extension of this principle. Fellowship training in surgical critical care affords the
opportunity to maximize one’s knowledge of medical care and augments the surgical
skills one has worked hard to develop as a resident.
The acute physiology learned in the ICU portion of fellowship becomes the
foundation for trauma training. Trauma surgery involves many decisions that must be
made quickly, often without complete information. Unlike elective surgery, where
anatomy drives the decision-making, trauma surgery is driven by physiology. As a
trained trauma surgeon, one is qualified to use the knowledge of acute physiology to
intervene on behalf of very sick patients. This intervention knows no anatomic bounds –
if the physiology requires the opening of the chest, or exposure of peripheral
vasculature, the trauma surgeon will go there. The physiology dictates the extent and
timing of the operative repairs required.
In many cases, the trauma surgeon will wish to call for the assistance of
specialists. One key reason to pursue training in acute care surgery, however, is to
prepare oneself for the day (or more likely night) when such assistance is not available.
Trauma surgeons are trained to handle the middle of the night disaster and to put forth
the heroic effort to save a patient against all odds. Surgeons who require a fixed
schedule and predictable workday will do better in another field.
In summary, the work of the acute care surgeon is hard, with long, unpredictable
hours. The work is often thankless and definitely not glamorous in most cases. But the
satisfaction of saving the life of a patient in extremis makes the time and effort
worthwhile.

[Table of Contents] SCCPDS Fellowship Guide 18
3A. Surgical Critical Care or Acute Care Surgery Fellowship?
08/22/2018 Paula A. Ferrada, MD, FACS (Richmond, VA):
Why do an extra year? Why Acute Care Surgery Fellowship?
Acute Care Surgery (ACS) includes three specialties in one: Trauma, emergency
general surgery, and critical care. ACS is not a new concept, however, ACS fellowship
is relatively new. The AAST has several approved fellowships in ACS currently, each
one with different strengths and opportunities.
The concept of ACS was born many years before it was recognized as a
specialty because of the need to have further specialized training in general surgery.
There is a real necessity to train surgeons to take care of emergencies with proficiency,
and to recognize the immense and growing demand for emergency and critical care
surgical coverage that exists globally.
Having an extra year of ACS training will help you maintain an ample scope of
practice and make you more marketable. This is true if you want to go to the community
or stay in academics. In the community, the surgeon that takes care of trauma also
provides care to all the other surgical emergencies, and sometimes including critical
care. These surgeons are the backbone of rural hospitals and emergency general
surgery is an important source of revenue. In the academic setting, the extra year will
help you by offering you more technical exposure and time for research, as well as time
to reflect on your academic path after your training.
The extra year consists of 1-3 months rotations of different services with you
acting as the fellow (transplant, thoracic, vascular). This will enhance your technical
abilities. In some places, an added training or mentoring in research is also available for
ACS Fellows. This extra time makes you more comfortable as a technician and can help
when you join a group as junior faculty. You will feel the benefits of this extra time in the
OR within your first few months of junior faculty. This is true even if you had ample
cases during residency. Your role changes as you continue to grow in training.
Some fellowships offer the possibility of doing international rotations. If you can
take the opportunity to travel abroad, this is an amazing experience. Not only it gives
you exposure to different procedures and techniques, it allows you to understand
trauma systems differently, as well as to have a new appreciation for what we take for
granted in the United States. Some of these international rotations are trauma heavy,
some offer more experience in emergency general surgery or burns. You will learn to
take care of patients with different resource allocation. I believe this experience can
offer more than technical training, it can help you develop as a leader of a team that can
function in difficult circumstances.
In summary, the extra year that I spent as an ACS fellow can offer a vast
operative experience, time for research, but most important a different perspective to
help you build an academic career.
[Table of Contents] SCCPDS Fellowship Guide 19
3B. Surgical Critical Care or Acute Care Surgery Fellowship?
06/22/2011 Matthew L. Davis, MD, FACS (Temple, TX):
ACS vs Surgical critical care alone
In deciding whether a surgical critical care or an acute care surgery fellowship is
right for them, trainees also must consider their training background. Was their general
surgery residency completed in a place that had a large amount of emergency general
surgery, in addition to well-balanced specialty cases? How many cases did he/she
complete during their five years of clinical general surgery training? It is also important
that trainees be honest with themselves regarding their comfort level caring for complex
general surgical emergencies. In many residencies, trainees are mainly a spectator or
first assist during the vast majority of training. In others, a high level of operative
responsibility and autonomy is built in early. Those trainees who, after honest
introspection, feel that they need more experience to be comfortable with a wide variety
of surgical emergencies should definitely look at an acute care surgery fellowship.
4. Should I Do An Elective At An Institution That I Am Considering?
06/22/2011 Matthew L. Davis, MD, FACS (Temple, TX):
Elective at the prospective fellowship institution
Doing an elective rotation at an institution that you are really interested in can
have multiple advantages. First of all, you are able to see for yourself how the institution
functions on a day to day basis. You are able to watch the staff-staff, staff-fellow and
fellow-fellow interactions and get a feel for how you and your personality fit in at that
institution. Each training center has a distinct personality and it helps to know if that
personality meshes well with your own. Often, programs have developed a reputation or
have a name that, once you visit, you may feel is not deserved and that will lead you to
look elsewhere. Experiencing rounds, cases, management of trauma victims and sitting
in during didactic sessions can give you a real feel for an institution. If it is good for a
month, it is likely really good. Anything can be dressed up for interview day. Next, it
gives you the opportunity to show yourself off. When a program gets to know that you
are bright, willing to work hard and have a strong interest in their program, they will
remember that at match time. Be cautious though – if your performance is below
standard, they will remember that as well. I have seen several candidates lose their
chance of joining fellowships due to a lackluster performance. If your life is unsettled or
the rotation is closely following the birth of a child, near a board exam or other areas of
personal turmoil, it is best to either not do the rotation, or re-schedule for a better time.

[Table of Contents] SCCPDS Fellowship Guide 20
5A. How Many Years of Fellowship Training?
02/20/2022 Edgardo S. Salcedo, MD, FACS (Sacramento, CA),
David S. Morris, MD, FACS (Salt Lake City, UT),
Joseph V. Sakran, MD, MPH, MPA, FACS (Baltimore, MD):
All ACGME-accredited fellowship training programs for Surgical Critical Care complete the
Surgical Critical Care portion of the training in one year. Many programs offer a second year of training.
The second year is not accredited by the ACGME and is not monitored by the RRC. The American
Association for the Surgery of Trauma (AAST) approves programs for a two-year fellowship in Acute Care
Surgery (ACS) that incorporates the first year of Surgical Critical Care fellowship. In most cases, the
structure of that second year of fellowship is set up to emulate your first year of practice as a junior
attending.
The goal of the second year is to refine surgical skills and decision making in managing the
complex presentations of acute surgical disease, as seen in trauma, surgical critical care, and emergency
general surgery. The AAST ACS Fellowship aims to provide fellows with advanced operative
experiences in trauma and emergency surgery. Rotations in thoracic, vascular, and complex
hepatobiliary pancreatic procedures are expected clinical experiences for AAST ACS Fellowships with
experiences in neurosurgical injuries, orthopedic injuries and interventional radiology techniques
encouraged. Not all 2
nd
years of fellowship are AAST approved. Second year fellows at many programs
will function as attending surgeons, taking independent calls with admitting and OR privileges.
Choosing to proceed with a second year depends on the foundation you have built. General
Surgery residency programs will have widely variable emergency general surgery and trauma
experiences. If you trained at a place where penetrating trauma was rare, going to a program with a
second year where penetrating trauma is more common will help you gain experience and confidence in
managing those injuries. Even if you may not practice in a place where these injuries are common, the
principles employed when managing such cases are invaluable and applicable in many arenas. The
same is true if you trained at a place with minimal volume of trauma activations and resuscitations.
Practicing in a center where it is common to run multiple resuscitations simultaneously may be an
invaluable experience that helps polish off your training.
The second year of fellowship offers a tremendous career-development opportunity to practice at
a clinically busy, often Level 1 Trauma Center with a proven record of academic productivity. Such
programs allow fellows to tailor their second-year experience consistent with their ultimate career
aspirations. For those interested in pursuing an academic career, the additional year provides the time to
learn and hone the skills necessary to complete research projects and present them to the academic
community. The second year of training is also valuable for those destined for less traditionally academic
positions. Surgeons who wish to be trauma directors at regional centers, perhaps more community-
based, would do well to consider an extra year to finish off their training. The inner workings of what it
takes to run a trauma center smoothly can be learned from mature institutions that have been serving
their communities for decades. The details of these logistics may not be in place at non-trauma center
residency training programs, or if they were, adequate time was not available to help develop those skills
as you were focused on becoming a competent general surgeon. The second year offers the unique
opportunity to witness, “how the experts do it” both clinically and from a systems level viewpoint.
The decision to target programs with a second-year fellowship experience (and whether it is a
AAST ACS Fellowship) is a personal one. It requires applicants to consider their clinical and career
development experiences before embarking on fellowship training and their career aspirations after
completing training. As you weigh the various factors that will inform your decision, be sure to ask
questions about how each of these experiences you are considering is set up. Understanding the clinical
and career development opportunities each program offers will help you decide which ones are best
suited to your training history and your future plans.

[Table of Contents] SCCPDS Fellowship Guide 21
5B. How Many Years of Fellowship Training?
01/03/2022 Therese M. Duane, MD, MBA, CPE, FACS, FCCM (Fort Worth, TX):
Careers in Trauma: Choosing 1 vs 2 years of fellowship.
My original contribution to this effort was almost 4.5 years ago and the focus was on whether 1 or
2 years of fellowship training was necessary for a successful career when looking at a strictly surgical
critical care fellowship, not an acute care surgery fellowship which includes the one year of surgical
critical care and is always two years. I think there are pros and cons to both the one and two year, and it
has to be based on the individual’s career goals. However, here is my general advice as someone who
was intending to do two years and changed my mind in the middle of my first year.
The fellows who benefit from two years are those who ultimately want to pursue an academic
career in which research and publishing will be an integral part, yet they have done very little during their
training. The extra year provides dedicated time to gain the skills necessary to learn how to execute
clinical trials, prepare IRB documents, develop research protocols as well as data collection and
manuscript preparation. All of these skills can only happen through practice, and once out in practice it is
difficult to find the time to learn all of these skills as well as gain the confidence necessary to get these
projects going. The time is even more important for fellows interested in bench science, as this absolutely
requires dedicated time in a lab to learn techniques and become facile with basic science research.
The fellows for whom a second year is not necessary, although still an option, are those who
have already taken research time during their training. This is true even if it was in fields other than
trauma, as the skill sets are similar. If the individual feels comfortable with the process of developing
study questions and seeing them answered to fruition, then an additional year may not be necessary.
This needs to be couched with the person’s goals, objectives, financial and family situation. The other
fellows who may not need a second year would be those whose intention is to work in a non-academic
setting in which he/she does not intend to continue a research focus.
Since I last offered the advice above in the previous edition, I have held more leadership roles in
departments as Chair and am now building a new academic department and general surgery program.
These experiences have provided me a new perspective and has somewhat changed my opinion on
duration of fellowship. The additional time for research as discussed is very important for those going into
academics if their experience during their general surgery program is limited. However, with the work hour
limitations and restructuring of training programs, I would highly encourage individuals who want to be
facile in trauma, especially those doing full acute care surgery with complex emergency general surgery,
to do a second year of an acute care surgery fellowship. In order to be comfortable with a wide variety of
cases and operative exposures, this second year provides an opportunity to work as junior faculty with
closer supervision than graduates receive once they are in their first position. Acute Care Surgery (ACS)
service lines are designed by nature to be a supportive team environment, so new recruits will always
have oversight and back-up by their more senior team members. However, in new ACS programs and
growing academic hospital systems unaccustomed to this model, having additional experience is
incredibly important to engender confidence in this “one stop shop” approach to handling all of the injuries
and issues which minimizes outside consultations, thereby streamlining care while optimizing resource
utilization. ACS is a high pressure environment, so having that extra year to build confidence and hone
skill sets will always be to the advantage of the trainee.

[Table of Contents] SCCPDS Fellowship Guide 22
5C. How Many Years of Fellowship Training?
03/06/2018 Gary A. Vercruysse, MD, FACS (Ann Arbor, MI):
One vs. Two Year Fellowship Programs
This is some advice for the fellow candidate pondering a one year or two year
fellowship in trauma/surgical critical care (SCC). I am a graduate of a one year
fellowship with an optional second year (I did only the first year.) I now work at a
program that has a one or two year fellowship. Either a one or two year fellowship can
lead to a successfully trained Trauma/SCC surgeon. There are benefits and drawbacks
to both, and ultimately the choice is a personal one that should be made after some
serious consideration. What follows are simply one surgeon’s opinion.
For me, the great thing about a one year fellowship was that it was over in one year. As
a resident, I felt like I had adequate operative experience (but graduated before the
implementation of the 80 hour work week) and mostly needed to work on my critical
care skill set. An added benefit was that I could start making an attending salary after
only 6 years of post-graduate training. The downside of the one year fellowship for me
was that I did not have adequate time to accomplish any research whatsoever, not even
one case report. I have since built some skills in research and have accomplished
several successful projects that have led to grant funding etc., but it was not easy to
accomplish without early mentorship (that may have occurred during my second year of
fellowship). Having said all that, I still feel that my personal decision to pursue a one
year fellowship was a good one.
After working at several institutions that have mandatory two year programs, I
can definitely see some good things about the two year plan as well. Firstly, having a
whole year dedicated to trauma surgery, fellows get to do several hundred operations in
order to hone their skills at complex trauma surgery. In the post 80 hour work week
age, with less resident operative experience, this could be interpreted as a benefit.
Secondly, the fellows also get an extra year of critical care exposure as they co-manage
patients in the SICU with the SCC fellows their trauma year, and are primarily
responsible for the SICU patients in their SCC year. Thirdly, all fellows get ample
opportunities to begin to acquire the skills necessary to have a successful academic
career by becoming actively involved in research projects that stretch over both
fellowship years.

[Table of Contents] SCCPDS Fellowship Guide 23
5D. How Many Years of Fellowship Training?
02/28/2022 William C. Chiu, MD, FACS, FCCM (Baltimore, MD):
For many Fellowship applicants, the decision on a one- or two-year program is
frequently based upon the perceived extent of training and experience that is needed to
achieve independent competence and confidence. Many other applicants are burdened
by an overwhelming sense of educational debt, and are most influenced by the need to
begin earning a salary that will enable the start of loan repayment. I have had Fellows
who had initially committed to two years, and then changed minds mid-year, and found
jobs after one year. I have also had Fellows who were initially planning for just one
year, and then decided to pursue a second year. My advice to prospective applicants
would be to first choose the best program and institution as a priority, and then assess
the personal benefits and options for additional years.
American Association for the Surgery of Trauma (AAST)-approved Acute Care
Surgery (ACS) Fellowships are mandatory two-year programs. The minimum duration
required by the Accreditation Council for Graduate Medical Education (ACGME)
Surgery Residency Review Committee (RRC) for a Surgical Critical Care (SCC)
Fellowship is one year. The majority of SCC Fellowships are one-year programs, with
or without an optional second year. Some programs have separate tracks for one-year
and two-year curricula. Some programs may spread the ACGME required SCC one-
year experience into two years. There are some two-year mandatory SCC programs,
and some with an optional third year.
With the exception of AAST-approved ACS programs, those SCC Programs that
have a mandatory or optional second year have a variety of curricula, with no national
consistency or regulatory oversight. These second year curricula are not monitored by
the ACGME, and may include required clinical experience as a Fellow or a senior
Fellow, attending responsibilities, research, academics, and various formats and
arrangements. Some programs offer opportunities to pursue additional educational
degrees, such as a Master’s Degree in Public Health (MPH) or Business Administration
(MBA), or Certificate Programs.

[Table of Contents] SCCPDS Fellowship Guide 24
6A. What Things Should I Look For At Each Program?
02/20/2022 Edgardo S. Salcedo, MD, FACS (Sacramento, CA),
David S. Morris, MD, FACS (Salt Lake City, UT),
Joseph V. Sakran, MD, MPH, MPA, FACS (Baltimore, MD):
The Surgical Critical Care (SCC) year and the optional second year of training
can be evaluated separately. Only the SCC year is addressed here. The previous
section addresses second year fellowship programs in more detail. When assessing the
features of the SCC year at various programs it is important to understand what your
role will be within the Intensive Care Unit (ICU) and ultimately, what you are looking to
gain at this stage of your training. At some programs you will be the first-call for all
patient care questions for anything from a missing Tylenol order to the coding patient.
At other programs you will be overseeing residents and advanced practitioners. One
might be expected to conduct teaching rounds, and mentor other trainees in bedside
procedures (e.g., central line placement, bronchoscopy). Some programs require in-
house call, while others take only home call. The calls themselves may be strictly
covering the ICU in one program and helping provide trauma and emergency general
surgery coverage in another.
The composition of the ICU attending staff is also important to consider. Some
institutions have units that are run solely by trauma surgeons while others have units
that are run by surgeons, anesthesiologists, and medical intensivists. It is our
perspective that it is valuable to see how different specialists manage critically ill
patients. While unifying literature exists for some conditions to direct practice patterns,
each practitioner brings a different perspective to the bedside and the more exposure
you have to different thought processes the more informed you will be when forming
your own management approach.
While fellowship programs are required to have clinical rotations for the entire
year, they are not required to rotate you in their SICU for all 12 months. Learning about
what other rotations each program offers besides the core time spent in the SICU is
important. Some institutions will have separate critical care teams for pediatric,
neurologic, cardiothoracic, burn and pulmonary / medical patients. The opportunity to
rotate with these other services is another way to gain new perspectives on critical care
issues. Learn about the different elective opportunities for each program you visit and
the flexibility of the various elective rotations within the schedule. For example, does
the institution have a strong practice in Burn Surgery and/or Burn ICU care, or is it a
busy liver transplant center. Details like these will provide you with an idea of the
clinical experience available at each respective program.

[Table of Contents] SCCPDS Fellowship Guide 25
The ICU’s place within the health system’s care paradigm may also be important.
Fundamentally, you want to know if the unit is closed or open, if the ICU team is primary
or consulting and the flow of the orders you write and the decisions you make for each
of the patients on your unit. That said, every ICU, wherever you practice, should always
adhere to principles of transparency and open communication between surgical and
ICU teams in the care of critical patients.
It’s important to know what patients are admitted to the SICU for the SCC
Service to manage. Are all the patients from the general surgery sub-specialties
(surgical oncology, colorectal, thoracic, vascular, transplant, etc.) being covered by the
SICU and the SCC Fellows? Similarly, are there clinical relationships with other
surgical specialties that routinely require critical care level services for their patients
(spine surgery, orthopedics, etc.)? Although trauma and emergency general surgery
patients will often provide enough clinical material for a rich and broad SCC Fellowship
experience, the opportunity to see patients with conditions related to other surgical
specialties is valuable.
The educational program for the SCC year will be mostly uniform at different
institutions because the training program is monitored by the ACGME and RRC. All
programs will provide educational opportunities at the bedside while caring for individual
patients and some places will have more established lectures and conferences
available to their trainees. If there are multiple critical care services in the system, the
programs may have varying degrees of inter-disciplinary educational activities as part of
their curriculum. Discuss these issues with current fellows during your interview
process. This is probably one of the best ways to really find out what takes place at the
program you might be interested in pursuing.
Finally, the size of the program is another feature that may be important to
consider. Fellowship programs will have anywhere from one fellow for the year up to
nearly ten in a class. Indeed, the size of the class will necessarily reflect the size of the
center where the fellowship is run to some degree. That said, it is worth reflecting on
the kinds of learning environments where you have thrived in the past and the kind of
environment you are seeking for your next level of training. On the one hand, as a
program’s only fellow you are, in a way, the collective project of the faculty. For a
program with multiple fellows, the camaraderie of shared intense experiences typical of
training in our field is both memorable and motivating.
[Table of Contents] SCCPDS Fellowship Guide 26
6B. What Things Should I Look For At Each Program?
02/21/2018 Shea C. Gregg, MD, FACS (Bridgeport, CT):
What is the specialty of Surgical Critical Care?
A Surgical Critical Care specialist receives additional training in the management of acute, life
threatening or potentially life threatening surgical conditions.
1
Specific knowledge that is gained during
fellowship will include the following: physiology of tissue injury from trauma, burns, operation, infections,
acute inflammation, or ischemia and their relation to other disease processes.
1
Additional topics that
fellows are typically exposed to include ICU administration, infection control, palliative care, organ
donation procedures, declaration of brain death, ICU billing and compliance and national quality
improvement guidelines.
Where to start: Residency considerations
Fellowship is meant to solidify your knowledge base in the physiology of critical illness, augment
your command of the technologies currently employed in management, and expand your appreciation of
outcomes among intensive care patients. With residents having varying degrees of exposure and comfort
managing critically ill patients, one should perform a self-evaluation of their previous residency training
prior to researching fellowship programs: What were the strengths and weaknesses of my residency
program in regards to the trauma, critical care, and/or emergency general surgery experiences? After you
define educational objectives, the following questions may be useful when evaluating individual fellowship
programs:
General considerations:
-Where is the program located?
-Will I be managing a diverse group of patients?
-Will I be rotating in academic and/or community-based hospitals?
-How well does the program adhere to work-hour regulations?
-How many fellows are in the program? Is there competition for educational experiences?
-How collegial are the faculty? Administrators? Nursing staff? Ancillary staff? Fellows? Residents?
-Are faculty engaged in the educational process?
-Do fellows find mentors/coaches during their fellowship training?
-Are the Program Director and/or Division Chief well-established? Are they active in the educational
process?
-Does the program participate in the National Resident Matching Program (NRMP)?
-How competitive is it to get accepted into the fellowship?
-Is the fellowship accredited by the Accreditation Council for Graduate Medical Education (ACGME)?
-What is the regional, national, and international reputation of the fellowship?
-Are women and/or minorities comfortable in the fellowship?
Family considerations:
-How many years is the fellowship?
-Will the family be happy in the chosen fellowship location?
-Where do fellows live?
-How is the commute?
-Will the fellowship salary and benefit package adequately support your family over the course of the
fellowship training experience?
-Are there local job opportunities for your spouse?
Educational considerations:
-How formalized is the didactic curriculum?
-Is there protected time for lectures?
-How formalized are teaching rounds?
-What opportunities are there to participate in simulation-based education?
-What educational opportunities exist outside of the institutional curriculum (i.e. courses sponsored at
national meetings, Advanced Trauma Life Support, Advanced Trauma Operative Management, etc.)?

[Table of Contents] SCCPDS Fellowship Guide 27
-What are the American Board of Surgery-Surgical Critical Care examination pass rates for previous
fellows?
-How does fellowship prepare you for the board examination?
-Are there international rotations/opportunities?
-Are there opportunities to work towards advanced degrees as part of the fellowship (i.e. Master’s in
Public Health, Master’s in Business Administration, etc.)
-Is there a curriculum dedicated to leadership training? ICU administration? Billing and compliance
issues? Critical incident stress debriefing? Quality improvement? Infection control? Palliative care?
Geriatrics?
Research considerations:
-What are the research expectations?
-Is there protected time to conduct research?
-Are there basic science and/or clinical research opportunities?
-What is the previous fellow experience with completing and presenting research at meetings?
-Is there support to attend conferences and/or national courses pertaining to surgical critical care?
Details of the critical care training:
-What technologies are being employed in the intensive care unit (i.e. Advanced airway management,
open-lung ventilation strategies, adjuncts to managing ARDS, damage control methods, renal
replacement therapies, ultrasound, extracorporeal membrane oxygenation, bedside procedures, etc.)?
-Are subspecialists managing these technologies or do fellows manage them?
-Do simultaneous rotators (i.e. medical students, residents, other fellows, etc.) compromise the
educational experience?
-“Closed” versus “open” intensive care unit?
-What patients will you be caring for: Medical? Surgical? Trauma? Cardiac?
Details of the trauma experience:
-What is the patient volume?
-What is the operative experience?
-What are the call expectations?
-Will simultaneous rotators be competing for cases?
-What is the penetrating versus blunt trauma experience?
-Is there any experience managing severe burns?
Details of the emergency general surgery experience:
-What is the patient volume?
-What cases will I be performing?
-What are the call expectations?
-Is there an outpatient experience?
-Is there any experience managing necrotizing soft tissue infections?
Career considerations:
-Where do fellows find jobs?
-How difficult is it to get a job after completing fellowship?
-Is there an opportunity to become a faculty member at the institution where fellowship is being
completed?
Summary:
Finding the right fellowship in Surgical Critical Care can be intimidating given that everyone’s
circumstances and experiences are diverse. By using the above questions as a basis for evaluation, you
will hopefully find a fellowship that will maximize your educational experience and accommodate your
lifestyle outside the hospital.
Bibliography:
1. “Specialty of Surgical Critical Care Defined.” Absurgery.org. March, 2008. Web. Accessed: 2/20/2018.
http://www.absurgery.org/default.jsp?aboutsccdefined

[Table of Contents] SCCPDS Fellowship Guide 28
6C. What Things Should I Look For At Each Program?
04/11/2018 Nathan T. Mowery, MD, FACS (Winston-Salem, NC):
Once you have made the decision to seek out additional training in Surgical Critical Care
you must sort through the abundance of well-qualified programs available. In the end your
focus must be on selecting the program that will make you the best possible attending physician
but also keeps all career options available to you. At the beginning of fellowship you may still
be struggling to decide between an academic career and a private practice job. You may not
have decided if you want to go to a place that requires significant research or one that would
allow you to focus solely on patient care. You may decide mid training that you want to switch
from one track to another. I would encourage you to pick a fellowship that can train you in all
those areas so that you will not limit your future employment choices. It is important to keep
focus on the fact that you are choosing a program that addresses not only your strengths but
potentially can make some of your weaknesses into strengths. Did you train at a residency
without a significant penetrating trauma experience? Now could be a time to seek out an urban
program that can round out that experience. Have you not gotten a chance to experience
research? Now would be a time to find a program that is familiar with mentoring inexperienced
fellows and that has multiple projects at various stages of development. Everyone wants to be
in an environment where our strengths are amplified but often a critical assessment of what you
need to improve in your weakest areas will lead you to be a better physician.
It is also important to consider what type of career you want after fellowship. Selecting a
fellowship that can train you for that job and has the networking connections to place you into it
is invaluable. If you plan to move to a geographic area with limited penetrating trauma and
practice surgical critical care you would be ill served to do a fellowship at a location that is heavy
in penetrating trauma and whose critical care experience consists mainly of the care of sick
trauma patients. Also, it is important to look at the track record of programs in placing fellows in
jobs they desire. You do not want your job search to be limited to jobs that are readily
advertised but instead to be able to pick your “dream location” and have a realistic chance of
them hiring you. If you do not know what type of practice you will want at the completion of your
fellowship I would encourage you to select a training program that will keep as many options
open to you as possible. It would stand to reason that programs that have sought out the
highest available designation from our parent organizations would be more likely to hire fellows
who had chosen to train at centers that also carried that designation.
Do not discount the advantages that a certain geographic location can afford you and
potentially your family outside of the hospital. You have no doubt worked hard to have options
available to you and should not feel bad in having the location of the training program factor into
your decision. There are fantastic programs available in all parts of the country that offer a
variety of activities outside the hospital. Surgeons often feel guilty about letting our
extracurricular activities influence our career paths, but with strong programs in a variety of
settings (urban vs. rural, warm vs. cold, beach vs. mountains) there is no reason to
compromise. Take advantage of the benefits your efforts to this point have netted you and
select a program that meets both your professional and personal needs.
[Table of Contents] SCCPDS Fellowship Guide 29
7. International / Overseas Surgical Rotations
01/24/2022 David A. Hampton, MD, MEng, FACS (Chicago, IL):
An international surgical rotation is an educational opportunity which can enhance your
Fellowship experience. Depending on the location, it has the potential to provide a high level of
independence, challenge your clinical and technical skills in a resource-limited environment, and
expose you to end-stage surgical pathology that may not be routinely seen at your home
institution. Aside from the surgical duties, the opportunity to explore a new country, experience
its culture and food, and discuss world events with your newly found colleagues are added
benefits that can only occur while abroad.
Several United States (US) Fellowship programs have established relationships with
international medical centers. Their respective US institutions have vetted these sites to ensure
they maintain an expected clinical and educational standard. Depending upon the relationship,
your surgical cases and procedures may be applied toward your ACGME requirements.
In preparation for your excursion, navigating the host country’s medical licensure
pathway will be your first undertaking. Several US-based organizations, such as the Electronic
Portfolio of International Credentials (EPIC), www.ecfmgepic.org , are documentation
repositories which will verify your credentials’ authenticity and forward them to the host nation’s
licensure board. The duration of this process is variable and may take several months to over a
year. Once your decision to travel abroad is entertained, this process should begin.
Any domestic or international trip has an associated level of personal risk which needs to
be considered. The US Department of State, www.state.gov/travelers , monitors countries
around the world and can provide information regarding political stability, areas of increased
personal violence, or health concerns. The COVID-19 pandemic has significantly changed
national and international travel. Understanding the potential movement restrictions when
embarking upon your trip and the quarantine requirements for a positive test result could
potentially change your plans. Additionally, notifying your home institution and close contacts,
as well as preparations for a new travel itinerary should be enacted in the event an extended
unforeseen stay is required.
Even though you will be working in a host nation medical facility participating in an
academic relationship with your home institution, worldwide standards of care are variable. In
the event you require medical care or a potential hospital admission, organizations such as
International SOS, www.internationalsos.com , can assist with liaising with local physicians and
surgeons, or personal extraction to higher levels of care or to your country of record.
Having gone through the aforementioned process, I spent 5 weeks at Groote Schuur
Hospital, a University of Cape Town, South Africa, training facility. Our international team
consisted of medical professionals from the US, Canada, Estonia, Switzerland, Libya, UAE,
Tanzania, Zimbabwe, Mauritius, and South Africa. We received over 900 trauma activations and
performed over 200 procedures. It was a personally and professionally enlightening rotation and
resulted in numerous life-long friendships.
With a modicum of forethought, an international surgical opportunity can be a fruitful
endeavor. It has the potential to change your care pathways, help establish and develop
professional connections, and build your confidence as an independent surgeon. All Surgical
Fellows should consider this opportunity.

[Table of Contents] SCCPDS Fellowship Guide 30
8. What to Expect in a Fellowship Program
02/16/2022 Benjamin J. Moran, MD (Philadelphia, PA):
It is important to understand that not all fellowship programs are identical. Each
program will provide all the experiences and cases required to pass your surgical critical
care boards, but each program will vary with respect to the amount of trauma, types of
trauma (blunt vs penetrating, operative vs non-operative), critical care (surgical,
medical, cardiac, transplant and neurosurgical), ECMO, and acute care surgery
experience they offer. The amount of in-house call, home call, and responsibility will
differ as well. Fellows may be required to run trauma activations, lead rapid response
and code blue teams or be the junior acute care surgeon. Whatever the differences in
each fellowship, it is critical to take a review of oneself and decide how much of each
factor you want and what opportunities you need to become an expert in critical care.
Day one of your fellowship, you will not be expected to be an expert in surgical
critical care or acute care surgery. The reason why you are in a fellowship is to learn
the art of critical care and acute care surgery. However, the earlier you show the staff
that you are a capable, confident, and knowledgeable physician with a willingness to
learn and improve, the sooner you will be treated like an expert and the better
experience you will have.
It is also important to remember that as a fellow you are not a ‘glorified resident’
but a board eligible or boarded general surgeon who knows the ins and outs of general
surgery but is honing their intensivist skills. Your job is to act like an attending and
assume the role of a surgical intensivist alongside someone who has the experience to
guide you. You will become an educator, team leader, and be ultimately held
responsible for the patient. Your attending may treat you like a resident at first, but do
not take this personally as they are testing your skills and assessing your knowledge
base. You will need to initially work with your attendings to develop patient care plans,
but the earlier you distinguish yourself from the role of a follower to that of a team
leader, the sooner you will garnish respect and accrue more responsibility. Remember
the trust and respect of your attending staff, colleagues and junior staff should be
earned, not demanded and certainly not expected.
It is important to see yourself as a patient care leader in the ICU. Expect to lead
and communicate your patient care plans with the entire ICU team and the patient’s
family. This includes the ICU staff, nurses, social workers, clergy, physician extenders,
respiratory therapists, and all others involved in patient care. Remember, utilize the
experience of the staff around you to help plan and provide the best patient care.
Additionally, part of developing your surgical critical care skills and undertaking the role
of an attending is to accept the responsibility of your patient’s care. Your attendings will
expect you to make sound assessments, provide team leadership and instruction, and
deal with the trials and tribulations of patient care.

[Table of Contents] SCCPDS Fellowship Guide 31
If a case you participated in is selected for a morbidity and mortality review,
expect to be an integral part in presenting and reviewing the case. You are expected to
speak with your patient and their family prior to the operating room, post operation and
additionally in the ICU. You will be responsible for explaining any complications to the
patient and family and discuss the next plans of action. In the ICU you will develop your
own style of communicating with patients and families and learn how to deliver bad
news and lead discussions in end-of-life care.
As a future educator and clinical leader, expect to be involved in resident
education. You will instruct residents informally at the bedside and during rounds but
also you may be required to give formal didactic sessions. Additionally, you will guide
residents through bedside procedures and cases in the operating room. The fellowship
will help you develop your own teaching style, where you allow residents enough
distance to learn but provide enough supervision and guidance to provide adequate
patient care. This is the ultimate transition from a follower to leader and educator.
Lastly remember that you are in fellowship to learn. On a daily basis you will be
pulled in a multitude of directions; from leading ICU rounds, to performing bedside
procedures, operating, or stabilizing a trauma patient. Remember to stay humble and
have a willingness to learn. Each attending will have a different background and can
provide a new perspective to patient care. You may not like all of it but incorporate
pieces into your skillset and your style of practice. Remember that attendings are not
the only teachers; you have nurses, respiratory therapists and physician extenders that
have a wealth of experience and knowledge that you can tap into on a daily basis. No
matter what fellowship you matriculate into, you will be surrounded with knowledgeable
and compassionate people who will work with you to become an expert surgical critical
care physician.

[Table of Contents] SCCPDS Fellowship Guide 32
9. What Do Fellows Do, Day In, Day Out?
06/01/2018 Daniel J. Cucher, MD (Chandler, AZ):
The way you spend your days and nights as a Surgical Critical Care fellow will vary greatly
depending on which institution you attend for fellowship, your rotation schedule, and the people you work
with. The intention of this chapter is not to orient you to working in an ICU, or list your daily
responsibilities. By the time you start fellowship, post-Surgical, Anesthesia or Emergency Medicine
training, you have already spent time as an intern and resident in the ICU taking care of trauma patients
and the critically ill. The purpose of this chapter is to describe how to maximize your training by
approaching the daily and nightly activities as a Surgical Critical Care fellow and embracing your new role
in patient care and education.
Pre-rounds
Regardless of your variable role in presenting patients, co-attending morning rounds, or fully
leading rounds, a degree of pre-rounds is advisable. Just as it is impossible to present a patient on
rounds without updated information on your patient’s condition, it is difficult to lead rounds relying entirely
on what you see and hear presented in the morning. Unlike a resident, however, knowing your patients’
lab values and precise I/O data before rounds is not as important as ascertaining a big-picture concept of
how your patients are doing in respect to their major physiologic ailments. Doing this efficiently is
contingent on a solid knowledge of your patients’ chronic and acute medical problems. A tremendous
amount of information can be gleaned by simply walking around the unit in the morning. Why is there a
code cart outside a patient’s room? Why have the infusion pumps multiplied by a patient’s bedside? Why
are there three nurses and an RT in a room? Who is still or newly intubated? Which patients are sitting up
and appear ready to transfer out of the ICU? Pre-rounds as a fellow may sometimes look like residency,
but the goal is to hone your ability to rapidly assess and determine what needs to be discussed on
rounds.
New Admissions
Whether you are at the bedside when a new patient shows up in the ICU or you discover them in
the morning when you arrive, every new patient requires a complete and accurate assessment. When
you first meet a new patient, try to anticipate all that he needs in order to transfer out of the unit. Although
it may change as your patient’s disease state evolves, make a plan of action early and see to it that your
ICU team is making progress with that patient.
Triage
Critical Care fellows often bear the responsibility of being gatekeepers to the precious and limited
ICU beds. The starting point for this job is to understand how bed flow works in your institution. Where do
patients come from, and where can they go when they leave the ICU? What other critical care areas are
there in the hospital? How is overflow managed? You must also know which patients in your unit are
appropriate to transfer, and who must stay in the ICU. When you cross-cover a unit, make sure it is clear
in your hand-off which patients you can transfer.
Every bed request you get is a call for help. Your first responsibility is to the patient, regardless of
the ICU census. If you truly feel that a patient needs an ICU bed and your unit is full, and all of your
patients are too sick to transfer out, know who you can call to advocate for the patient. There is often a
ranking faculty member who can move mountains to make a critical care bed available somewhere in the
hospital for a patient in need.
When you receive a bed request, your primary objective is to determine “What are this patient’s
critical care needs?” Sometimes, you won’t be able to come up with anything except that the primary
team members are uncomfortable managing the patient and feel overwhelmed. A call from a surgical sub-
specialty intern at 3 am because a post-operative patient has a “borderline respiratory status” may
indicate a crashing patient who needs to be intubated, or perhaps a stable patient with chronic respiratory
issues who just needs to be more tightly managed on his home regimen. Go see the patient and figure
out what he needs. If you don’t feel an ICU bed is warranted, this is a good opportunity to educate the
resident and make management recommendations.

[Table of Contents] SCCPDS Fellowship Guide 33
Rounds
Your role on rounds is likely to vary depending on your rotation and attending. Whether you are
presenting patients, an “expert consult” for the residents, co-attending rounds, or leading rounds by
yourself, your goal is always to learn how to lead rounds as an attending. Know the literature behind your
management decisions, and be familiar with national practice guidelines. As an attending, you don’t want
to manage, for example, ventilator weaning a certain way just because that’s the way you did it in
residency training. Much has been written on virtually every important topic, and it will serve you well to
be familiar with the literature and be able to defend your practice with data. Be open to learning from
everyone on rounds.
Procedures
If you are not already proficient in a wide range of bedside procedures when you start fellowship,
now is the time to gain that expertise. Balance your need and desire to do procedures with your
responsibility to teach residents how to do them safely and efficiently. Know when to take over a difficult
procedure, and which patients’ procedures need to be handled by the one who is most experienced.
Evening Rounds
If you are in charge of evening rounds, keep them brief and try to walk around the unit. The goals
are to see if your team has made progress with the patients and anticipate any impending crises before
the unit turns over to the night team. This is a good opportunity to circle back to important clinical and
educational questions asked on morning rounds. At the end of evening rounds, recap which patients
you’re most concerned about so that your team can exercise appropriate vigilance.
Hand-offs
Unfortunately, due to ACGME regulations, you can’t be on call 24 hours a day and 7 days a
week. This necessitates handing off your patients to another fellow, and also cross-covering ICUs where
you aren’t familiar with the patients. It is in everyone’s best interest to keep an up-to-date patient list with
pertinent information well maintained. As the team leader, make sure that the things you think are
important about each patient are on that list.
Other tasks
The previous version of this chapter by Marcin A. Jankowski DO included an excellent summary
of the many things you may find yourself doing during Surgical Critical Care fellowship. We have reprinted
it here for your benefit.
- supervise or perform bedside procedures
- attend to all SICU emergencies
- prepare fellow lecture series or PowerPoint presentations for students and junior house staff
- schedule Fellows Conference guest speakers
- prepare morbidity and mortality presentations
- read critical care texts
- perform research and literature reviews
- update educational resources
- review and update current management protocols
- staff, supervise or assist with OR cases
- perform bedside junior staff lectures
- present lectures at weekly Fellows Conference
- log operative cases and complete any related required fellowship paperwork
- attend staff meetings
- update families and significant others
- attend end-of-life family meetings

[Table of Contents] SCCPDS Fellowship Guide 34
10. Geographic Considerations
02/02/2018 Robert A. Cherry, MD, MS, FACS, FACHE (Los Angeles, CA):
Choosing the right location for your fellowship training is an important
consideration and should not be underestimated. There are numerous factors to
consider that might impact your personal lifestyle and professional career path. For
instance, access to indoor and/or outdoor recreational activities, shopping, restaurants,
sporting events, museums, theatres, and schools will carry varying degrees of weight
depending on your lifestyle. Cost of living and affordable housing may be an issue
depending on your financial resources. Spouse and child preferences are important
since family satisfaction often influences the degree to which you are engaged and
finding value in your work. Whether or not you have a significant other, a built-in
support system may be important to you during your training. Proximity to immediate
and/or extended family and in-laws may therefore drive your decision-making with
respect to location.
Some people choose a particular geographic area that they plan to live in after
completion of their fellowship training. If this is your situation, then it will be important to
know if there are ample employment opportunities for you and any significant other.
Geographic variations may also have a significant influence on the trauma and critical
care population that you will be caring for. Population density, socioeconomic factors,
local culture, seasonal variations, and market competition may profoundly define your
clinical, educational and research experience, including trauma center volume, injury
patterns, and acute care surgery presentations.
Nevertheless, a robust commitment to your education by a highly regarded group
of faculty - in a location that you find personally and professionally desirable - should
compensate for any geographic differences between fellowship programs over the long
term.

[Table of Contents] SCCPDS Fellowship Guide 35
11. Family Considerations
02/09/2018 Jennifer C. Knight Davis, MD, FACS (Morgantown, WV):
Balancing Work and Life in Fellowship
Fellowship is a different experience than residency. Balancing work and life
remains challenging and if this is an important factor for you, special considerations
should be made. A fellowship program will have varied responsibilities and
expectations unique to each program, like call schedules, patient loads and vacation
options. Time commitments will vary. Some programs have at-home call and you come
in for special circumstances, while others have in-house call. Realistically exploring
each of these may affect the appeal of a fellowship and as an applicant you should ask
these questions during your interview. The current fellows can shed light on specifics
and asking them is helpful.
A few things to consider:
Factoring in the "others" in your life like a significant other, children or pets is
needed. Depending on the length of the fellowship, having career options for your
significant other is important. Some fellowships in established GME programs have
established support systems for these endeavors. Smaller programs may be more
limited. There will likely be more options in an urban setting versus rural. If you are
planning for a long-distance relationship during your fellowship, you should look into
transportation options. Airports, train stations, highways etc. Living close to an airport
can make this more convenient.
If you have children, some programs have amenities like day care. Finding at-
home help for childcare in an urban setting will likely be more expensive. Combining at-
home childcare could be an option if coworkers are in a similar situation. Urban areas
will have wait lists for pediatricians and if the hospital system that your fellowship is
affiliated with can provide that care, it might be easier to get an appointment.
Planning ahead for healthcare and insurance will prevent gaps. Now that most
fellowships start August 1, gap coverage will be necessary. Your residency program
coordinator can help with options for gap coverage supplied by your institution.
Extracurricular activities should be considered. With fellowships all over the
country, coastal, mountainous, urban and rural options are there. The lifestyles in each
setting can be picked to suit various interests.
How much of a factor each of these challenges poses will be different by the
program and the applicant.
[Table of Contents] SCCPDS Fellowship Guide 36
12A. Applying to Fellowship Programs
01/10/2022 Stefan W. Leichtle, MD, FACS (Richmond, VA),
Niels D. Martin, MD, FACS, FCCM (Philadelphia, PA):
1) List of Surgical Critical Care, Trauma, and Acute Care Surgery Programs
There are approximately 150 Surgical Critical Care Fellowship programs in the U.S.
Each year, there are a few new programs and a few programs that close or intentionally
don’t fill for various reasons. Beyond word of mouth from your mentors, there are
several sources that can be used to find programs and learn of their highlights. Keep in
mind, not every program updates every site, so be sure to look at when listings were
updated.
• The ACGME website offers a list of all ACGME-accredited programs by specialty at
https://apps.acgme.org/ads/public/.
• A more detailed but not comprehensive list can be found on the website of the Eastern
Association for the Surgery of Trauma (EAST) at https://www.east.org/education-career-
development/career-management/fellowships. This website provides additional details
on number of positions, trauma volume and composition, and contact information.
• The American Association for the Surgery of Trauma (AAST) maintains a list of currently
approved Acute Care Surgery Fellowship training programs at
https://www.aast.org/acute-care-surgery/new-program-directors-program-
coordinators/approved-sites in addition to more information on content and curriculum of
the AAST-approved Acute Care Surgery fellowship.
• The Surgical Critical Care Program Directors Society (SCCPDS) provides a list of
approved Surgical Critical Care (SCC) and Emergency Medicine SCC programs, as well
as a list of unfilled positions after the Match, in addition to other useful information for
current and future SCC fellows at https://sccpds.org/future-fellows.
2) The Application
The SCCPDS maintains the electronic and central application process “SAFAS” (SCC
and ACS Fellowship Application Service) at https://safas.smapply.io, that allows for the
upload of CV, letters of recommendation, transcripts, and all other documents
necessary for application. All programs participate in SAFAS.
3) The Match
After application via SAFAS and interviews with the programs, all applicants need to
register with the National Resident Matching Program (NRMP). The NRMP website
(https://www.nrmp.org/fellowship-applicants/) offers description of the process and a
timeline for SCC https://www.nrmp.org/fellowship/surgical-critical-care/.
[Table of Contents] SCCPDS Fellowship Guide 37
12B. Applying to Fellowship Programs
01/20/2022 Catherine S. Nelson, MD (Elmira, NY):
1) The Surgical Critical Care Program Directors Society has created a central
application process for both the Surgical Critical Care and Acute Care Surgery
Fellowships called SAFAS (https://safas.smapply.io). This allows you to apply to
multiple sites via the same application packet. General information can be found on
their Future Fellows webpage (https://www.sccpds.org/future-fellows) as well as
significant application deadlines. From their website:
(Dates will change in subsequent years)
Appointment Year 2023:
SAFAS will Open on March 1, 2022
- Do not start new application prior to March 1
SAFAS application deadline on July 31, 2022
SAFAS will remain Open for post-Match Unfilled Positions
In addition to the basic application form you will need to fill out, you will also need to
upload the following documents:
Photograph
Curriculum Vitae
Personal statement
USMLE (or equivalent)
ABSITE scores (or equivalent)
Names and contact info of three people writing you letters of recommendation.
Finally you will need to select the programs you wish to apply to. Additional programs
can be added after your first submission if you wish.
2) Many of the national bodies maintain lists of current programs
Surgical Critical Care Program Directors Society (www.SCCPDS.org) hosts information
for SCC candidates under their “future fellows” page. https://www.sccpds.org/future-fellows
List of SCC programs: https://www.sccpds.org/future-fellows/fellowship-programs
List of EM-SCC programs: https://www.sccpds.org/future-fellows/approved-programs
List of unfilled programs: https://www.sccpds.org/future-fellows/unfilled-positions
The American Association for the Surgery of Trauma maintains a list of currently
approved Acute Care Surgery Fellowship training programs which can be found under
the “Acute Care Surgery” section of their main menu at aast.org or at:
https://www.aast.org/acute-care-surgery/new-program-directors-program-
coordinators/approved-sites
[Table of Contents] SCCPDS Fellowship Guide 38
The Eastern Association for the Surgery of Trauma (EAST) maintains the
www.east.org/career-management/fellowships website where programs are organized
by state or by type (critical care only, acute care surgery only, combined). Each
program’s entry includes program director, university affiliation, hospital data,
information on the fellowship, ratio of blunt to penetrating trauma, and number of spots
available per year.
3) The National Resident Matching Program (www.nrmp.org/fellowships/surgical-
critical-care-match) organizes the combined program match that surgical critical care
and acute care surgery participate in. They maintain a list of important dates for the
match process on their website
(https://www.nrmp.org/match-calendars/fellowship-calendars/).
(Dates will change in subsequent years)
For Appointment year 2023:
Jun 22 Match opens
Jul 13 Rank order list opens
Aug 24 Rank order list deadline
Sep 07 Match day
They also publish a helpful Match check list https://www.nrmp.org/wp-
content/uploads/2021/08/SMS-Applicant-Checklist.pdf and a report on the outcomes of
the previous year’s match.
NRMP surveyed program directors regarding factors they consider when selecting
applicants for interviews and ranking in 2016. This information is made public in a
publication which can be found on their page Fellowship Match Data & Reports:
https://www.nrmp.org/wp-content/uploads/2021/08/2016-PD-Survey-Report-SMS.pdf

[Table of Contents] SCCPDS Fellowship Guide 39
13A. Application Chronology
01/22/2022 Joshua A. Marks, MD, FACS (Philadelphia, PA),
Niels D. Martin, MD, FACS, FCCM (Philadelphia, PA):
The application for surgical critical care fellowship takes place the year prior to
admission. This means applicants should start preparing the application in January of their
fourth year of residency. The following is an approximate guideline of when and what you
should be doing:
January - February
- Research programs and begin figuring out which programs you are interested in / which
are right for you and your needs and wants
o Determine why you plan to complete the followship; what are your needs?
(SEE CHAPTER 5)
▪ SCC or ACS?
▪ 1 year or 2 year?
o Visit websites, talk to colleagues and mentors
- Start working on your personal statement
- Update your curriculum vitae
- Begin giving recommenders advanced notice for requesting letters of recommendation
o This is one of the most time-consuming steps. Start early!
March 1
- Applications open through SAFAS
o Applicants must create an account and register
March - April
- Fill out and submit applications online through SAFAS
- Request letters of recommendation in your SAFAS application
- Check on the status of your letters of recommendation
- Touch base with programs directly if you have not heard from them
o Applications may get lost in the mix
o Individual program timelines may differ
▪ Be sure to check if a program has an application submission deadline
that is earlier than the SAFAS deadline
April – July
- Interview at programs
o Many programs are likely to continue interviewing virtually
June
- The National Resident Matching Program (NRMP) conducts the Surgical Critical Care
and Acute Care Surgery Match - registration begins in June
o Applicants must separately register with the NRMP
July
- NRMP opens the rank order list submission function
July 31
- SAFAS application deadline
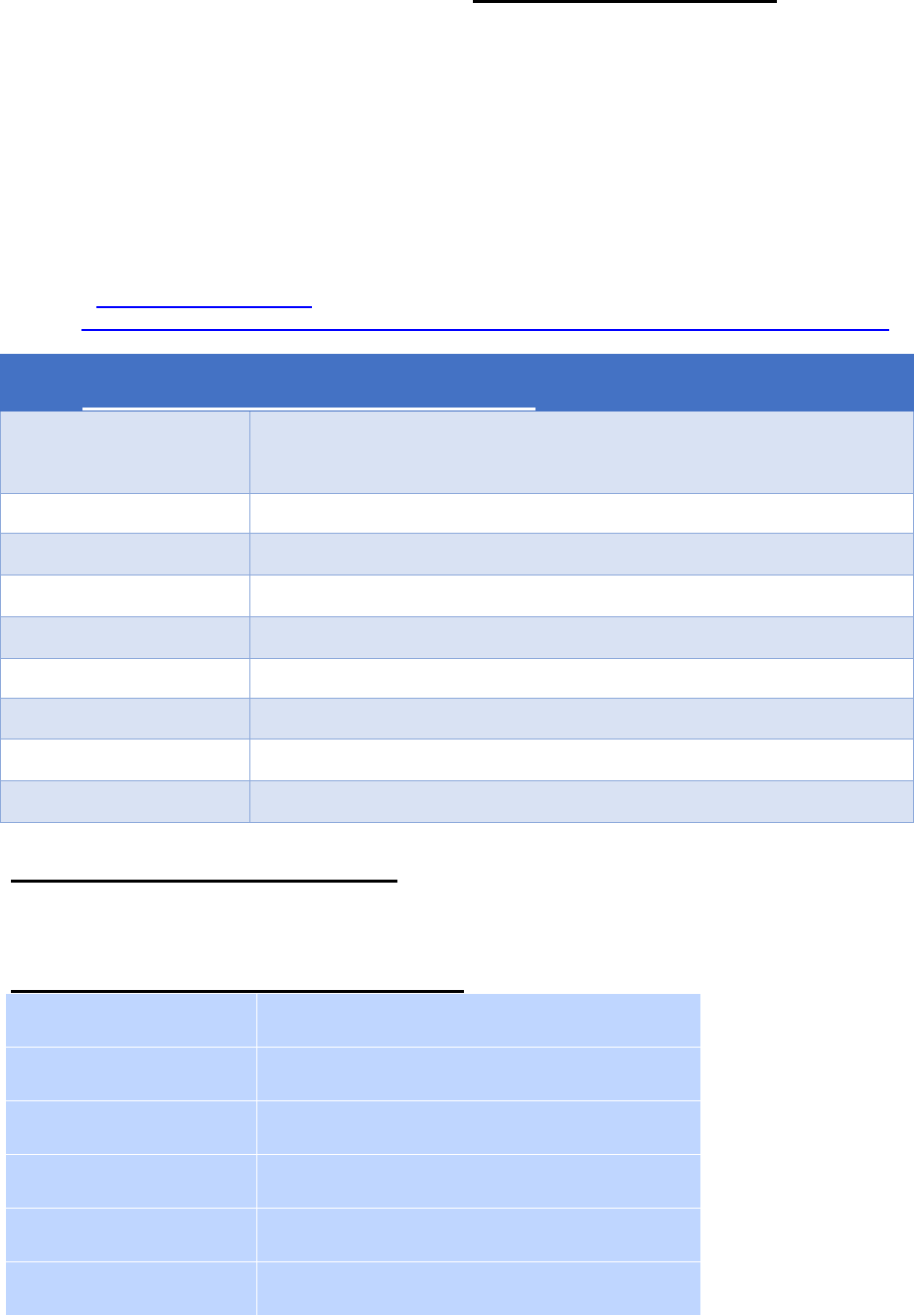
[Table of Contents] SCCPDS Fellowship Guide 40
August
- Start thinking about programs you are interested in / develop your rank list
- Have mentors call programs in which you are most interested / top choices
- Certify your rank order list by the deadline
September
- Match occurs early in the month
- Positions that are not filled/remain open will be listed on the NRMP and SAFAS websites
- SAFAS will remain open for post-match unfilled positions
All dates are subject to change and need to be verified directly:
SAFAS (www.safas.smapply.io)
NRMP (https://www.nrmp.org/fellowship-applicants/selecting-fellowships/surgical-critical-care-match)
SCC Application Timeline for Summer 2023 Appointments
(Dates will change in subsequent years)
January-February
Research programs for compatibility
Write personal statement and update CV
Give recommenders advanced notice
March 1, 2022
Applications Open Through SAFAS / Create Account
March-April
Submit Application and Request letters of recommendation
April-July
Interview at Programs
June 22
NRMP Match Opens / Register for NRMP
July 13
Ranking Opens
July 31
SAFAS Application Deadline
August 24
Rank Order List Deadline
September 7
Match Day
13B. Application Chronology
01/20/2022 Catherine S. Nelson, MD (Elmira, NY):
(Dates will change in subsequent years)
March 01, 2022
SAFAS opens/create account
June 22, 2022
NRMP opens/register
July 13, 2022
NRMP Ranking opens
July 31, 2022
SAFAS application deadline
August 24, 2022
NRMP Rank Order List deadline
September 07, 2022
Match day

[Table of Contents] SCCPDS Fellowship Guide 41
14A. Preparing Your Personal Statement
01/20/2022 Catherine S. Nelson, MD (Elmira, NY):
This is your chance to make yourself stand out from the pile of applications sitting
on a program director's desk. The average applicant will likely have equally good letters
of recommendation, experiences and/or research so you can use the personal
statement as a way of differentiating yourself from others. Don't waste space talking
about what everyone else will. Instead mention things that make your application
unique or memorable.
Your personal statement should be no more than one page in length, if it’s too long
readers will be more likely to skim though it. Consider the organization; you can devote
a paragraph to discussing why you are interested in acute care surgery or critical care.
Try to list specific examples of interesting patients or experiences. Make this personal.
Find aspects about the field that appeal to you as a career that others might not think
about. Talk about the teamwork or research into prevention, if those are things that
interest you.
Another paragraph can be spent on where you see yourself in the future. Are you
interested in general surgery and managing your own ICU patients? Do you want to
focus on trauma in a high-volume center? Are you interested in teaching or research?
This will give your reader a sense of your interests and also allow them to figure out if
you will be a good fit for their program. After all, they are going to be preparing you to
assume the role you will choose.
Once you are done writing your essay, find a good editor. This is arguably the most
important part. It goes without saying that your spelling and grammar need to be
accurate. Find someone who will also assess your essay for readability, flow, and
content. You need an editor who isn't afraid to tell you when things need to be rewritten
or removed. Be prepared to rewrite whole sections multiple times. Give yourself enough
time so that you do not rush through the editing process. You want to feel that you have
best presented yourself and your interests in the one page that you have to work with.
Your personal statement will often be referenced during your interview so be prepared
to talk about what you have written.

[Table of Contents] SCCPDS Fellowship Guide 42
14B. Preparing Your Personal Statement
02/20/2022 Joseph V. Sakran, MD, MPH, MPA, FACS (Baltimore, MD),
Edgardo S. Salcedo, MD, FACS (Sacramento, CA),
David S. Morris, MD, FACS (Salt Lake City, UT):
At this point in your career you have probably written a number of personal
statements that have gotten you into college, medical school, and residency.
Fellowship program directors will tell you that in general, the personal statement is
probably not going to hurt you and it’s probably not going to help you. This is not a
green light to not invest effort in putting together a top-notch narrative describing why
you are inspired to do the work you’ve sought out to do. What will hurt you is if the
person reading your statement stumbles across grammatical and/or spelling errors.
This simply demonstrates a lack of attention to detail. The other key in developing the
personal statement is to not regurgitate your curriculum vitae, which the program
already has access to. Tell us your story. Describe something that we may not know,
and why you as a person might stand out from all the other prospective applicants. This
is really an opportunity for the applicant to get across a point that might not be evident
from the application and can potentially provide insight as to the unique background and
qualities one might possess.

[Table of Contents] SCCPDS Fellowship Guide 43
15A. Letters of Recommendation
02/20/2022 Joseph V. Sakran, MD, MPH, MPA, FACS (Baltimore, MD),
Edgardo S. Salcedo, MD, FACS (Sacramento, CA),
David S. Morris, MD, FACS (Salt Lake City, UT):
This part of the application process is probably one of the most important steps.
The trauma/surgical critical care community is relatively small. Most of us know each
other or have interacted in a committee or at a meeting. While getting a letter from a
“big name” might draw attention to your application, it is also important to note that you
really want the individual to know you as a person. It is usually evident in the letter of
recommendation if the person really knows the applicant. This is the program’s
opportunity to get to know the individual from a somewhat objective standpoint. You
should always waive your right to see the letter. Don’t ask for a letter if you don’t think
they will write you a good one. Most individuals will let the applicant know if they don’t
feel like they are able to write them a letter that will help their application. Most
programs require three letters of recommendation. We always say ask for four. Why?
Well this allows you to have a safety net in case one of the letters falls through. Be
prepared; don’t ask for a letter of recommendation at the last minute. You should ask
months in advance. Make it easy for the person writing the letter. Supply them with
your personal statement and CV. Finally, after you have narrowed down the programs
you are really interested in, it usually is a plus if the person writing your letter will pick up
the phone and call the program director.
15B. Letters of Recommendation
01/20/2022 Catherine S. Nelson, MD (Elmira, NY):
Each program requires letters of recommendation from three attendings that you
have worked with. Ask early (March or April if possible), you will want to give your
recommender plenty of time to work on your letter; it also allows them to focus on your
performance so that they can add greater detail to your letter. Your recommenders
should be people that know you well and have worked with you. You should include a
Trauma/ACS/Critical care attending if possible. SAFAS (https://safas.smapply.io) will
require you to enter the names and email addresses of your three recommenders. It
will then send an automated request email to those people to submit a letter. You will
receive notification once your letter has been uploaded.
[Table of Contents] SCCPDS Fellowship Guide 44
16A. Fellowship Interviews
02/02/2022 Mary Noory, MD (Brooklyn, NY),
Samuel Osei, MD (Royal Oak, MI),
Susan E. Rowell, MD, MBA, MCR, FACS (Chicago, IL)
David A. Hampton, MD, MEng, FACS (Chicago, IL):
THE ERA OF VIRTUAL INTERVIEWS - WHAT TO EXPECT
Traditionally, fellowship interviews were conducted in person. The COVID-19
pandemic has compelled programs to conduct this process virtually. While most
fellowship programs have adjusted to this change, it is still a novel experience for
applicants. Before the era of virtual interviews, applicants could only accept a limited
number of interviews, primarily due to travel expenses, time off from work, and clinical
responsibilities. The absence of these barriers has allowed applicants to apply to
multiple programs. Virtual interviews at numerous programs enable applicants to
expand their options, seek out locations that may not have been logistically feasible,
and gain insight into training differences across the country.
Interview Preparation
Aside from the expected pre-interview preparation – reviewing the informational
package, researching the faculty, understanding their mission statement, and having an
extensive list of questions – there are several elements unique to the virtual interview
process.
1. Know the difference in time zones. There may be a significant difference in time
between your home and the interview location.
2. Utilize a secure and reliable internet service and connection. Using a computer
with a direct Ethernet connection as opposed to Wi-Fi will ensure a virtually
seamless interview.

[Table of Contents] SCCPDS Fellowship Guide 45
3. Familiarize yourself with various virtual meeting software platforms - Zoom, Cisco
WebEx, and Microsoft Teams. Unlike the in-person interviews, you may be asked
to navigate and virtually enter and depart various chat rooms.
4. Conduct your interview in a location without distractions. To ensure privacy, a
reserved office or call room may be the ideal location.
5. Do not have a distracting background. You are the center of attention. Animated
backgrounds should be avoided.
6. Practice looking directly at the camera and speaking in a plain voice. Conducting
a mock interview with a colleague will help identify mannerisms that are
accentuated by the camera.
Disadvantages of Virtual Interviews
One disadvantage of virtual interviews is the inability to visit the hospital and
interact with the staff. Program directors are aware of these concerns. Presentations
focused on daily interactions with the hospital staff, camaraderie amongst team
members, and extracurricular activities are usually given. Additionally, group sessions
with the current fellows and the Advanced Practice Providers were common ways to
mitigate this deficit.
Personal Experience With Virtual Interviews
All in all, the virtual interviews process was a positive experience. I participated in
all my interviews without missing a day of work. I would round in the morning with my
junior resident, formulate a treatment plan with my team, run the list with my attending,
and make it to the call rooms on time for my morning interviews. Depending upon the
interview time, I was able to cover operative cases. Virtual interviews allowed me to
interview with many programs because it did not affect my clinical responsibilities. I
interviewed with multiple programs across the country without significantly affecting my
finances. Lastly, interviewing with numerous programs across the country allowed me to
select programs that best fit my fellowship needs.
[Table of Contents] SCCPDS Fellowship Guide 46
16B. Fellowship Interviews
02/21/2022 Stefan W. Leichtle, MD, FACS (Richmond, VA),
Niels D. Martin, MD, FACS, FCCM (Philadelphia, PA):
1. “Virtual” is the new Normal
With the onset of the COVID pandemic in 2020, SCC fellowship interviews have moved
to virtual platforms such as Zoom, GoTo Meeting, or Microsoft Teams. It is unclear for
how much longer fellowship interviews will be held via videoconferencing platforms, and
it may well remain the standard in the future.
The virtual platform offers multiple advantages for both programs and applicants. Travel
for in-person interviews used to be expensive and time-consuming, particularly for
fellowship applicants, while virtual interviews are essentially free and only take up a few
hours per interview. Applicants can now easily apply and interview at more programs
than before, but this has conversely resulted in a much higher applicant to position ratio
and should be considered. Additionally, as interviews have become easier and cheaper
for both programs and applicants, it may be more difficult to ascertain the degree of
interest an applicant has in a program and vice versa.
2. Tips for Virtual Interviews
Virtual interviews represent a unique situation and the following points may help with
your preparation. There are also numerous helpful guides on how to prepare for (video)
interviews online.
Technical Issues
1. Be familiar with the interview platform. You may have become a “Zoom expert”,
but some programs use Microsoft Teams, GoToMeeting, or others. Most
importantly, remember that your video settings, virtual backgrounds, etc. do not
carry over from one platform to the other.
2. Make frequent eye contact with your camera (your interviewers’ “eyes”) and only
briefly look at the screen.
3. The “gallery view” in Zoom allows you to see all participants in a video
conference at the same time, not just the speaker.

[Table of Contents] SCCPDS Fellowship Guide 47
4. An artificial background is the most versatile choice for the interview setting.
Regardless of whether you interview from home, the call room, or any other
location, it avoids having to “set up” your background. While photographs of a
Caribbean beach can break up the monotony of some hospital meetings, for
interviews a neutral, non-distracting background is probably best.
5. Mute your microphone when you do not talk, and do not forget to unmute when
answering questions.
6. Check your username, especially if you share an account with someone or use a
hospital computer.
Communication and Interpersonal Issues
7. It is best to minimize the risk for interruptions by silencing your cellphone or
pager and closing the door to your room. However, if an unexpected interruption
occurs, do not let it throw you off – it happens!
8. With the camera focusing primarily on your head, there are few non-verbal cues
during virtual interviews and conveying enthusiasm and interest can be difficult.
Smile and try to act natural.
9. Virtual interviews make it much harder to have a natural flow of conversation.
Make deliberate pauses to allow your interview partner to speak up, make
comments, and ask questions.
10. Preparation for frequently asked questions (“what made you apply to this
program?”, “what is important to you for your fellowship training?” etc.) is
important, but attentive, active listening throughout the interview is even more so.
11. You may find it helpful to record yourself during a “mock interview” to check your
video settings and assess how you come across on camera.

[Table of Contents] SCCPDS Fellowship Guide 48
16C. Fellowship Interviews
02/22/2022 Alexander L. Marinica, DO (Dallas, TX),
Linda A. Dultz, MD, MPH, FACS (Dallas, TX):
Tips For Standing Out in a Virtual Interview
The COVID-19 pandemic brought many changes to our personal and professional
worlds. We have all grown accustomed to a new way of life defined by restrictions –
masks, vaccines, in-person gathering, travel – but one of the most profound changes
has been to the way we now interact with one another professionally. The virtual
platforms of Zoom, Teams and WebEx have taken the place of the grand-round lecture
halls in the basement of the hospital where we could expect stale bagels and watered-
down coffee. With a simple click of a few buttons, you can transport yourself from your
weekly educational lecture to a quick patient follow-up visit, then to a national
conference without even leaving the comfort of your bed. Some of these changes may
have been a necessary adaptation to a global pandemic and will dissolve away as we
gain more control over future variations of the disease, however, many of these
changes will become our new professional baseline.
One of the best adaptations we were forced to make during the pandemic is adopting
virtual platforms for meetings. Moreover, as some institutions return to in-person
gatherings and major academic organizations are again hosting in-person meetings, the
ease and cost savings a virtual meeting space provides cannot be overlooked. The
American Board of Surgery has announced that future oral board examinations will be
offered virtually after the successful administration of their first round of examinations.
Many national and international organizations have also announced that they will
continue to have a “virtual-attendance” option for their annual meetings, allowing those
constrained by travel cost and complicated coverage schedules to attend.
Like an old man fondly remembering a by-gone time, I’ve found myself reminiscing
about hitting the interview trail. And I mean the actual trail. I was part of the last class of
Surgical Critical Care Fellows that traveled the country for in-person interviews and
what an experience it was! I will admit openly, even though the begging to trade call
shifts, traveling post-call to save vacation days, the dread of cancelled flights, and total
cost of the experience placed monumental stress on my life, I loved the process. Like
someone who traveled for business I became an expert at packing light and changing in
airport bathrooms. I also got to meet so many interesting people, all going through the
same process, all who were to become my colleagues in the field of trauma, acute care
surgery, and surgical critical care and some who have become my best friends. Most of
all, I enjoyed meeting people on their home turf. Getting to watch the way coworkers
interacted, how the hospital staff went about their day and to step foot inside some the

[Table of Contents] SCCPDS Fellowship Guide 49
most celebrated departments in the surgical world gave me perspective on how I might
fit in to their work family.
Just like board exams, the virtual interview was forced out of necessity and seems to be
the new standard going forward. Having now participated in two cycles of virtual
interviews for the University of Texas Southwestern Surgical Critical Care Program,
where I am currently in my second year as a Clinical Instructor, I would like to offer
some tips and tricks to navigate this new world. Some may seem obvious, but as the
adage goes, you’d be surprised …
- Expect the best, prepare for the worst.
The preparation should start days before your scheduled interview. Make sure
you have a dependable computer and internet connection because without both,
you’ve missed your interview. If you are planning to interview from home, you
know the space and internet connection well (i.e. Do you spend most nights
waiting for your Netflix to buffer or can you binge uninterrupted on your post-call
day?), however, if you have to interview outside of your home make sure to pick
the space carefully. Make sure it is private and quiet and test the internet
connection before interview day. Many hospitals and medical schools have
designated spaces just for this purpose so make sure to check with your
institution far in advance to make sure you can reserve the space. If you are
unfamiliar with the virtual platform (Zoom, Teams, WebEx) ask a friend or
colleague to create a meeting and practice on the platform. The first time you see
yourself on these platforms should not be day of the interview. Have a Plan B. A
second laptop, a desktop that is hardwired for internet, or a phone that can serve
as a hotspot if the internet connection fails.
- Dress like the interviewer will see your shoes.
This point might be my favorite. Please, dress professionally from head to toe,
just as you would if you were meeting the interviewers in person. One unique
byproduct of the virtual platform is that you can still be at work on the same day
as your interview. This does not mean you are excused from dressing
professionally (i.e. no scrubs!). Also remember, screens and cameras have
amazing resolution so skipping the dry cleaning or not ironing your shirt may get
noticed and makes an impression. And please, wear the pants that match your
outfit! No gym shorts or sweatpants!
- Room without a view.
This point dovetails on the first two, minimizing distractions and staying
professional extends to your backdrop. An office or a room with some personal
effects in the background looks professional and offers a unique setting, but your
scotch collection on the shelf over your shoulder may rub some the wrong way.
Additionally, try not to use a virtual background if possible. While a professional
backdrop of your work institution is acceptable, the interviewers are not
interested if you are pretending to sit on a beach, it only offers distractions.

[Table of Contents] SCCPDS Fellowship Guide 50
Having a friend or coworker call you on one of the virtual platforms and critically
assessing your space will help keep you from making these embarrassing
oversights. Next, isolate yourself in your interview space so that family members
or pets don’t have the option to make an unexpected appearance on interview
day. Lastly, try and practice, or at the very least turn on your camera at the same
time of the day your interview is scheduled so you can assess the lighting and
noise level. The last thing you want is the sun directly over your shoulder
distracting both you and the interviewer!
- Make eye contact, with your camera.
I have found this point especially important. It is inherently awkward to stare into
a camera and look engaged, which is probably why you did not choose a career
as a broadcaster. Turn on your camera before the interview day and take note of
the angles. It is easy to be off center, and therefore have the interviewer see the
side of your face instead of being face-to-face. Try to fight the urge to look at
your screen or the small window that shows your camera view because it is
noticeable. My advice is to find your optimal position. Typically, that is back a
short distance from the computer screen, with the camera elevated at eye level.
A laptop stand can be purchased to achieve this, or simply stacking some of your
unopened medical textbooks will do just fine. You may be engaged and
engaging, but if the angle of your camera does not mimic the face-to-face
posture of an in-person interview, you may be in danger of coming off as
disinterested.
- Remember that virtual waiting rooms are not private.
When interviewing in person, candidates are typically placed in a large
conference room to wait in-between interviews. These rooms are typically
private, or at the very least you can easily see everyone who is present.
Reverting to casual talk with the other candidates is not only a way to de-stress,
but also helps you to get to know your fellow candidates through trading war
stories about your experiences. Virtual waiting rooms are not private, and many
times an administrator is there, camera off, waiting to shuffle the next group in
and out of the next round of interviews. You also don’t have the benefit of easily
spotting who is there to interview and who may be faculty or staff because every
name and video box will be foreign to you. My advice is to act as if the chairman
of the department is present – always stay professional.
- To eat or drink … that is the question.
A non-descript mug with some coffee, or a glass of water is perfectly acceptable
to have within view. However, just as if you were at an in-person interview refrain
from snacking or drinking until your designated breaks.
- Take notes, the old-fashioned way.
It may seem easier to take notes on your computer during the interview, but that
looks sloppy and cumbersome. Trying to navigate taking notes and having the
virtual platform open may accidently get you kicked out of your interview. I have

[Table of Contents] SCCPDS Fellowship Guide 51
found that keeping a notepad on the desk in front of me and writing a few notes
down, or having some questions prepared that I can quickly reference still looks
professional while also not creating a distraction for the interviewer. Lastly, do not
take notes on your phone (see next tip)!
- Silence your phones and watches.
It is never acceptable to use your phone, check your smart watch, respond to
messages on your computer, answer pages, or in any way engage in anything
but your interview. Better yet, turn all your devices off and set your computer
programs to “do not disturb” mode. Even if you’re at work, your colleagues and
co-residents should treat you as if you’re on vacation and have no way to reach
you. The people interviewing you have taken time out of their busy schedules to
get to know you, please show them the same courtesy.
- Guard against your mannerisms.
Small ticks – adjusting glasses, playing with hair, swiveling in a desk chair,
touching your face – are distracting habits we fight to control even during in-
person interviews. The difference is that we’ve developed comfort in dealing with
them out of repetition over the many years of interviewing in-person. The virtual
platform can distract us from engaging our defense mechanisms, so be honest
with yourself about your ticks and work to minimize them. If you swivel in your
desk chair, find a chair without wheels to sit in for your interview. Keep your
hands on the desk, fingers interlocked if you have the tendency to touch your
face or twist your hair.
- Take advantage of “on-site” visits, or “second-looks.”
Many programs are offering in-person “second-look” visits for candidates, so
don’t forget to ask the programs at the top of your list if they can make this
accommodation.
- Do all the things you would do in person.
Prepare just as you would for an in-person interview. Research the program and
the faculty that you will interview with and come prepared with thoughtful
questions about the program. Make sure to thank the interviewers at the end of
your private sessions and send thank you notes (either hand-written or email).
This list is not comprehensive. Ask ten different people and I am sure you would get
unique recommendations based on their own nuanced experience. The final piece of
advice I would offer is this: be yourself. The purpose of interviews is to get to know who
you are beyond the words we can read on your application. The virtual platform creates
a barrier that makes that interaction inherently more awkward and mechanical,
however, just remember that the insecurities you feel about interacting virtually are also
felt by the person on the other side of the screen. To borrow a sports analogy, both
teams are playing from their own home courts, so you can focus on representing who
you are without the distractions of feeling like you’re in a foreign place. Best of luck and
enjoy the process!

[Table of Contents] SCCPDS Fellowship Guide 52
16D. Fellowship Interviews
02/23/2022 James E. Babowice, DO (Pittsburgh, PA),
Uzer S. Khan, MBBS, FACS (Pittsburgh, PA):
The Virtual Fellowship Interview
The ongoing COVID-19 pandemic has spurred a transition from a totally in-person
fellowship interview season with candidates traveling to visit training programs to a
totally online process for both candidates and programs. While there are obvious
benefits to completing interviews online – in particular a marked decrease in travel costs
and travel time – the virtual interview process is novel for both candidates and programs
and so preparation and performance can potentially be more challenging for the online
interview format.
Preparing For a Virtual Interview
Scheduling
The first challenge for interview preparation among candidates will be scheduling and
coordinating clinical coverage during your interview time slots. The majority of virtual
fellowship interviews will occur during weekdays during regular daytime hours and will
last one half day. A minority will last a full day, occur in the evening, or occur on
weekends. Almost all fellowship programs offer more than one interview date. Most
programs have their interview scheduling through their program coordinator, who is
almost universally able to help you with scheduling conflicts or challenges if you can
address them well ahead of time.
Given that most fellowship candidates are senior and chief surgical residents they will
need to balance the clinical challenges of managing a busy surgical service with the
professional challenge of scheduling dedicated time for interviews. Plan ahead to create
a reasonable plan for continuity of care and surgical case coverage during your time
away to avoid the possibility of needing to interrupt your interview day for an
unanticipated clinical problem requiring your attention. In addition, don’t forget to
consider different time zones or changes to daylight savings time as it relates to the
start and end times for your interview day.

[Table of Contents] SCCPDS Fellowship Guide 53
Equipment, Interview Space, and Software
In addition to the universally good job interview advice to dress professionally, virtual
fellowship candidates will need to have an interview space and equipment coordinated
ahead of time. An interview space should be professional, clean, well lit, and with
minimal background noise. Good examples include a conference room or professional
office. Bad examples include a call room or bedroom. Necessary equipment is a laptop
or desktop computer with an absolutely reliable internet connection as well as a web
camera, microphone, and lighting. An example of a good equipment setup for interviews
would be a workplace laptop connected to your institution’s wireless internet, with a
high-definition web camera, a USB microphone, and a ring light for lighting in a
professional conference room. Equipment failure is inevitable, however, so in a pinch
your smartphone stabilized and angled on a stand or desk should be usable. It may,
therefore, be prudent to have access to the relevant Zoom links, etc. on your phone with
a pair of low-profile headphones.
Additionally the software clients used for virtual interviewing can be variable. The
majority of fellowship programs use Zoom for virtual interviews and a minority use
Microsoft Teams or other platforms. Reach out to your program coordinator to clarify
technical details and test your equipment on an unfamiliar platform prior to your
interview day in order to prevent missing or delaying meeting the trainees and faculty at
your desired fellowship.
The Interview
Most interviews will start in the morning with a group introduction to the program and
then separate into individual interviews with faculty and fellows at your desired program.
Interviews are normally 20-30 minutes and are the same as any in-person job interview.
If you have any preparation materials it would be worthwhile to print them ahead of time
as it can be difficult or distracting to toggle between your video interview and any
prepared materials on your computer screen.
After the Interview
One of the challenges of virtual interviewing is that it can be difficult to appreciate some
of the intangible features of a fellowship program that would be appreciable on an in-
person visit. Don’t hesitate to reach out to faculty, fellows, or staff to discuss any
additional questions you may have in order to gather information and make an informed
decision for your rank list. Depending on current conditions with COVID some programs
may be able to host you for an in-person second look as well.

[Table of Contents] SCCPDS Fellowship Guide 54
16E. Fellowship Interviews
02/23/2022 William A. Marshall, MD (San Diego, CA),
Laura N. Godat, MD, FACS (San Diego, CA):
Additional Virtual Interview Do’s and Do-not’s:
The interview process for surgical critical care can be an anxiety producing time. Try to
remember that the interview process is truly about getting to know you and finding the
fellow who will be the best fit for a program. In addition, you are looking for a program
that is the best fit for you. Below you will find a few items that we hope will be helpful for
you when preparing for the actual interview day.
• The vast majority of SCC interviews offer informal sessions (lunch Q&A, “social
hour”) with current fellows and residents – take advantage of this time! In my
experience, these sessions are paramount to get a good feel for the place that
you cannot physically visit in the current interview landscape. I had never
physically been on many of the campuses I interviewed at for SCC fellowship; I
relied heavily on the opinions of the non-faculty members I interacted with to get
a good “feel” for each program.
(As an aside, be wary of any program that does not make their current fellows or
residents available for these sessions. Transparency is a “must” when choosing
a program!)
• Have a set location in mind where you can complete your interview, and know
this location in advance to avoid any unforeseen stress on the day of your
interview. For me, I would structure as many interviews as possible around my
post-call days so that I could interview from within the confines of my own
household, but there were several days where I had to retreat to a call room in
the hospital for a few hours for an interview. Pick a location that’s quiet,
distraction-free, and comfortable.
• While these interviews seem less “formal” because they are completed virtually,
always dress and act in a professional manner. Just because your faculty
interviewer is wearing scrubs and a scrub cap does not mean that you should! A
suit is definitely still the appropriate choice for interview attire.

[Table of Contents] SCCPDS Fellowship Guide 55
• Take notes! If you thought it was difficult remembering your in-person interviews
at 10-15 different programs across different states for residency, well, this piece
of advice is for you. Unfortunately, virtual interviews all blend together after a
while, and interview fatigue is very real. It becomes incredibly difficult to
remember the nuances of each interview day unless you stay organized and
document what you liked and didn’t like at each of your programs, so be sure to
do this in real time at the end of each interview. You’ll be thankful once it comes
time to submit your rank list!
• Many of your faculty interviews will start with something that sounds like “Well,
what questions can I answer for you?” This can be a daunting question if you’re
not prepared for it, so be sure to commit several thought-provoking, non-generic
questions to memory before each faculty session. If you know who you are
interviewing with beforehand, try and glance through his or her CV ahead of time.
Be sure to engage your interviewer with comments and questions that
demonstrate that you’re a serious applicant who is strongly considering their
program.
• After your interview, I would strongly encourage you to stay in touch with the
programs you’ve interviewed with until you submit your rank list. Reach out to the
program directors, residents, faculty, etc., with any questions you may have so
that you can get the most complete, comprehensive picture about these
programs where you’ll be spending the next 1-2 years. Also, it is important to let
your favorite programs know that you are interested by sending a thank you
email.

[Table of Contents] SCCPDS Fellowship Guide 56
17. Coaches, Advisors, Mentors, and Confidantes: What You Need and Why
02/19/2022 Jacqueline J. Blank, MD (Philadelphia, PA),
Jose L. Pascual, MD, PhD, FACS, FRCSC, FCCM (Philadelphia, PA),
Lewis J. Kaplan, MD, FACS, FCCM, FCCP (Philadelphia, PA):
1. Why You Need a Guide
As you transition to a new role as a Fellow (or later as a Faculty member), you will
benefit from guidance regarding everything from orientation to goal setting. Guidance may come
from a coach, advisor, mentor, or confidante. These “guides” may help you during fellowship as
well as through your first few years as a junior attending; some find a guide (or guides) that
supports them throughout their career (more on that later). Guides may assist with both
professional and personal development. Your guide may help you decide which projects to
undertake, meetings to attend, societies to join, or jobs to consider. Furthermore, guides can
challenge you to expand the boundaries of how you think, the skills you acquire, and the goals
you set all while seeking to maintain life-work balance. Some of these domains are longer-lived
than others and one guide may be more appropriate than another for a specific period of your
career.
2. Advisors, Coaches, and Mentors
Perhaps the most common guide is an advisor. These are problem-oriented solution-
providers who help you answer specific questions and resolve individual and often time-
sensitive issues. Examples include which elective to select, which project to pursue, or where
to submit your review manuscript. While the advisor is invested in you – and your issues – their
role may be specifically defined by the boundaries of the problem at hand. A coach, on the
other hand, evaluates your performance in relation to a distinct task or activity, and provides
feedback to help you to improve. A coach’s duties are generally complete after you master the
goal at hand, such as the proper placement and use of a REBOA device. Advisors and coaches
may have overlapping roles and activities. Nonetheless, coaches generally provide solutions
within the confines of a specific task, while advisors often incorporate personal and professional
development in the guidance they provide.
A mentor is fundamentally different from an advisor or coach in several key aspects. A
mentor’s relationship with their mentee is fluid, longstanding, and ultimately bi-directional. First,
both the mentor and the mentee derive benefit from the relationship. Second, the relationship is
not assigned, but instead develops and matures as each dyad partner identifies important
aspects of the other. Mentors find that their mentee has qualities that they want to help develop.
Equally importantly, the mentor believes that they are able to help the mentee develop those
qualities. Examples include scientific inquiry, education, novel approaches to patient care, and
the like. Mentees often find that their mentor serves as an exemplar of both professional and
personal development demonstrating success along shared goals. Local leadership, service on
hospital committees, clearly balanced work-life dynamic, or leadership in medical professional
organizations provide common examples of such goals. Third, mentorship exceeds a
predetermined time period, and can sometimes be career spanning. Fourth, the goals for the
mentoring relationship change over time as each member grows. The relationship further
matures such that it responds to evolving needs rather than those present at the outset. Fifth,
mentorship extends guidance about life both in and outside work or career in a give-and-take
fashion. Sixth, while mentors and their mentees begin the relationship in a somewhat

[Table of Contents] SCCPDS Fellowship Guide 57
hierarchical manner, this evolves into one of equality as a goal and not as a matter of
happenstance. Perhaps most importantly, the mentor helps the mentee find their own path. A
common approach is for the mentor to raise questions that drive the mentee to explore
preconceived notions, personal values, and professional imperatives. These questions are
generated without a predetermined notion of where the mentee’s exploration will ultimately lead.
In a mature relationship, the mentee asks similar questions of their mentor.
3. Qualities of a Good Mentor
Good mentors share common traits. They are good listeners, ask appropriate questions
and dedicate time to their mentees. They are available in a scheduled fashion as well as on-
demand for urgent issues, have sufficient experience to represent different perspectives, can
relate to issues relevant to the mentee, and are dedicated to advocating for their mentee.
Moreover, they demonstrate cultural sensitivity, integrity, and ethical behavior. Individuals who
may serve as good mentors are often the individuals that others turn to in a dilemma, troubling
situation, or crisis. Such individuals are often – but not exclusively - Division or Section leaders.
This is not to be construed as the need for every mentor to be a Division or Section leader, but
rather to identify that successful leaders generally evidence some elements that characterize
good mentors. In particular, the faculty member who is NOT the Section or Division leader may
have more availability to engage in mentorship as a result of reduced administrative
encumbrance. Done well, the mentor should subtly and progressively challenge the limits of the
mentee’s comfort zone with regard to thinking, skill set, and perspective. A good mentor leads
the mentee to solutions and decisions by constructing a journey of introspection, analysis and
deductive reasoning that in most instances is a learning process for both. Mentorship requires
personal investment by both individuals and relies on significant trust in one another as well as
the processes of professional and personal development.
4. Qualities of a Good Mentee
In some ways it may initially be more difficult to be the mentee than the mentor. A good
mentee must also be a good listener, be willing and flexible to dedicate time to meet with their
mentor, as well as time to explore what their mentor proposes. The mentee should expect to be
challenged and, at times, uncomfortable. This process is key in driving growth and maturity.
Often the mentee needs to introspectively assess their values, likes, dislikes, cognitive focus,
and passion in order to clearly define future goals and paths. Time spent on service, academic
pursuits, suggested tasks, and personal pursuits may unwittingly create time conflicts that
should be specifically addressed with one’s mentor! Options for resolution that may not be
intuitively obvious - but may also be perfect solutions - may be initially opaque to the mentee.
The mentor may have previously trod this path and can share what they have learned. The
mentee needs to be open to hearing what the mentor has to say - even when what is being
shared is contrary to the mentee’s previously firmly held beliefs. Mentees also strengthen their
prospects as future mentors when they are open to the challenges set forth by their mentors;
one may only feel comfortable challenging others when one has experienced the merits of such
an approach. Specifically asking departing Fellows who has served them well is an excellent
way to gather information about a non-native institution’s faculty.
5. Where to Find Your Mentor
As a fellow, it is perhaps most straightforward to find your mentor within your Fellowship
Program, especially if it is a two-year program. One-year fellows may have insufficient time to
find a mentor and find it easier to embrace an advisor. Alternatively, they may identify a mentor
over the course of the year but find that their relationship blossoms only after graduation. If you
are a new faculty member, finding a mentor at your new institution is ideal as they are
conversant with your new home, the key individuals with whom you need to interface, as well as

[Table of Contents] SCCPDS Fellowship Guide 58
the relevant local issues that might impact your specific needs. Moreover, they are accessible in
the same time zone, and have likely faced many of the same challenges you will face in that
practice environment. Consider leveraging the summative experience of emeritus faculty who
are no longer clinically active but remain academically or administratively engaged. Their
availability and wisdom may be a superb starting point as one embarks on an academic career.
For those with a laboratory research focus, a basic science department with research scientists
aligned with your interests may yield a mentor who can help guide your scientific inquiry career.
During fellowship, mentors may less commonly be identified through professional societies. As
one advances through the faculty portion of one’s career, such societies are fertile grounds for
mentorship as membership in such a society leverages shared interests.
6. Mentors Within and External To Your Parent Specialty
Since mentorship is less about technical proficiency and more about professional and
personal development, finding a mentor outside of your parent specialty can succeed. This
approach often benefits from having subspecialty overlap that provides common goals and
experiences. For instance, many Acute Care surgeons have a mentor in Anesthesiology where
the overlap is the critical care aspect of their practice. Similarly, an increasing number of
Emergency Medicine faculty find Surgery mentors with overlaps in trauma and surgical critical
care. Occasionally, one may choose to have a mentor that is entirely unrelated to their specialty.
These relationships are generally organic, as the pairing is chosen not based on professional
alignment, but instead reflects finding an individual with the characteristics described above:
character, qualities, interests, availability, and ethics. Many permutations are possible as long
as the relationship works for both the mentor and mentee.
7. Local vs Long-distance Mentoring
While it is logistically easier to engage with a local mentor, long-distance mentoring can
be nonetheless successful. Digital platforms that facilitate video-based two-way discourse allow
the subtlety of facial cueing to remain an integral part of the relationship. The biggest challenge
in long distance mentoring is finding sufficient time such that what is set aside for mentoring is
not subject to interruption. Long-distance mentoring may impair the spontaneity that
characterizes some aspects of a local dynamic (i.e. leveraging the open office door for an
impromptu conversation). Physical separation between the mentor and mentee, however, may
sometimes foster excellent communication, as either member of the dyad may be motivated to
share sensitive thoughts without fear of repercussions at their home institution. Provided each
member is willing to devote the time and energy to maintain this relationship, the pairing may be
fruitful regardless of distance. Of course, one may concomitantly embrace a local as well as a
long-distance mentor.
8. More Than One Mentor
Early in one’s career a single mentor often suffices. However, as one develops and
one’s career becomes more complex, more than one mentor to help address different aspects
of your development may be quite appropriate. An alternative approach to the dedicated single
mentor-mentee relationship recognizes that time is a continually vanishing commodity and
instead leverages several mentors, often with slightly different focuses. This approach is termed
“mosaic mentoring” with mentors entering and exiting from different phases or aspects of one’s
career. One might envision a mentor assisting in research development who is different from
one assisting in medical professional organization advancement, and further different from one
for local administrative advancement. This approach runs the risk of developing into “mosaic
advising” but has its own merits, especially in a time constrained environment, or with a time
limited engagement such as during a single-year Fellowship.

[Table of Contents] SCCPDS Fellowship Guide 59
9. Divorcing Your Mentor
Both partners should regularly evaluate whether the relationship is working, and should
have a plan to discuss how the dynamic is progressing; indeed, a static relationship aids neither
party. An honest assessment of ongoing mentee development and success is important. When
each partner is benefitting and each person is continuing to develop, the partnership remains
successful. When this ceases to occur, investigating why the dynamic has changed is
essential. Often the inquiry leads to repair and some restructuring of the partnership. Even in
seemingly well-functioning relationships, over time, the mentor-mentee relationship may no
longer be mutually beneficial through no fault of the partners. One or both members of the
relationship may recognize that both parties have achieved their goals, or have reached the
limits of each other’s expertise and contributions. This is not a failure on either part, but rather
the astute observation that both members have successfully contributed to the other’s growth
and maturation up to that point in time. Recognizing that not all mentor-mentee relationships will
span a career, one should be prepared for that eventuality. Sometimes, no amount of repair will
be successful, or one partner may no longer wish to remain in their role. Retirement, disability,
relocation, and changes in life circumstance may all derail a successful partnership.
Unsurprisingly, most mentees have more than one mentor in their careers as a natural
consequence of career and life progression.
Accordingly, one must also be cognizant of “red flags” demonstrated by a failing mentor.
Lack of availability, inconsistent suggestions, anger, withdrawal, and wandering attention often
underscore a dysfunctional relationship. Moreover, not every pairing will result in an ideal
relationship, even if it seems otherwise functional. Differences in communication styles,
backgrounds, and life experiences may prevent a mentor-mentee relationship from progressing.
If either member feels that their needs are no longer being met, leaving the relationship is
preferable if there is no readily embraceable repair strategy. Failed mentor-mentee relationships
are nothing of which one should be ashamed; they should instead be viewed as learning
experiences that will help both the mentor and mentee elucidate both the important and
unimportant aspects of a relationship. Besides advisors, coaches, and mentors, many use
confidantes throughout their career.
10. Having a Confidante
A confidante serves as an ally and a listener, and may provide insight into circumstances
of consequences that the mentee may have not yet experienced. Often, a confidante serves as
a neutral party to whom the individual may share potentially uncomfortable thoughts or
questions, and from whom the individual believes there will be confidentiality. Having a
confidante in one’s Department may be useful as they will likely understand the unique aspects
that permeate rigorous training or practice with that specific set of individuals and in that precise
location. Conversely, one may choose a confidante outside of their Department for the purposes
of anonymity and impartiality. A confidante that is sufficiently separate from the mentee’s
working space may be able to better provide an unbiased perspective than one in the same
Department. Regardless, the relationship between a mentee and a confidante is never forced
but is borne out of necessity when the mentee desires advice, reassurance, or non-judgmental
listening as a form of emotional support. Unless there is a risk of emotional or physical danger
to the mentee, a confidante must never betray the trust of the mentee. Like the relationships
above, one may choose to have multiple confidantes throughout one’s career.
11. Diversity, Equity, and Inclusion (DEI) in Guides
There is no standard approach to DEI in working with a coach, advisor, mentor, or
confidante. Instead, the notion that what the guide provides to the mentee must meet the need
– or needs – of the mentee is paramount. Whether there is concordance in terms of gender,

[Table of Contents] SCCPDS Fellowship Guide 60
age, sexual orientation, ethnicity, and more is less important than the functionality of the
relationship. Mentors must be cognizant of DEI aspects that are important to the mentee – and
vice-versa!
12. Take Home Points
Everyone benefits from career guidance. A structured way to identify a guide – or
guides - and how they can help you is a point of embarkation. A useful way to characterize
guides you may encounter, or specifically seek, is as follows:
Coach: specific skill, task, solution for a specific problem (how to hit a fast ball)
Advisor: a more expanded solutions solver (how to grow to a level so that you can hit all pitches,
not just the fast balls)
Mentor: a guide for an active relationship that draws on your past, understands your vision for
the future, and helps to move you (does not direct you) to accomplish life's bigger goals,
especially fulfillment and happiness - both professionally and personally (helps you to become
the coach for the people who need to learn how to hit all the pitches). As such this is a long-term
relationship that benefits both mentor and mentee and may span an entire career.
Confidante: an impartial, trustworthy, grounded ally who provides emotional support and whose
relationship requires the utmost trust and confidence.
Being a good mentee helps prepare you to be a good mentor in the future!
References:
1. Burgess A, van Diggele C, Mellis C. Mentorship in the health professions: a review. Clin Teach.
2018;15(3):197-202.
2. Lovell B. What do we know about coaching in medical education? A literature review. Med Educ.
2018;52(4):376-390.
3. Kutsyuruba B, Godden L. The role of mentoring and coaching as a means of supporting the well-
being of educators and students. International Journal of Mentoring and Coaching in Education.
2019 Nov 21.
4. Sachdeva AK. Preceptoring, proctoring, mentoring, and coaching in surgery. Journal of Surgical
Oncology. 2021 Oct;124(5):711-21.
5. Sinclair P, Fitzgerald JE, Hornby ST, Shalhoub J. Mentorship in surgical training: current status
and a needs assessment for future mentoring programs in surgery. World Journal of Surgery.
2015 Feb;39(2):303-13.
6. Bettis J, Thrush CR, Slotcavage RL, Stephenson K, Petersen E, Kimbrough MK. What makes
them different? An exploration of mentoring for female faculty, residents, and medical students
pursuing a career in surgery. The American Journal of Surgery. 2019 Oct 1;218(4):767-71.
7. El-Gabri D, McDow AD, Quamme SP, Hooper-Lane C, Greenberg CC, Long KL. Surgical
coaching for advancement of global surgical skills and capacity: a systematic review. Journal of
Surgical Research. 2020 Feb 1;246:499-505.
8. Min H, Morales DR, Orgill D, Smink DS, Yule S. Systematic review of coaching to enhance
surgeons' operative performance. Surgery. 2015 Nov 1;158(5):1168-91.
9. West MA, Hwang S, Maier RV, Ahuja N, Angelos P, Bass BL, Brasel KJ, Chen H, Davis KA,
Eberlein TJ, Fong Y. Ensuring equity, diversity, and inclusion in academic surgery: an American
Surgical Association white paper. Annals of Surgery. 2018 Sep 1;268(3):403-7.
10. Meneses E, McKenney M, Elkbuli A. Diversity and inclusion among US general surgery residency
programs: Translating initiatives into action. The American Surgeon. 2021;87(1):166-7.
11. Thompson-Burdine JA, Telem DA, Waljee JF, Newman EA, Coleman DM, Stoll HI, Sandhu G.
Defining barriers and facilitators to advancement for women in academic surgery. JAMA Network
Open. 2019 Aug 2;2(8):e1910228-.

[Table of Contents] SCCPDS Fellowship Guide 61
18. Identifying and Developing Your Interests
11/06/2017 Salina M. Wydo, MD, FACS (Camden, NJ):
Identifying and Developing Your Interests
Development from resident to fellow to partner involves more than just exposure to
clinical medicine.
Fellowship is an opportunity to fill the gaps in your experience, refine the focus of your
future practice, and to do so in a structured, guided and supportive environment. For residents
who already have recognized and developed interests, it’s an opportunity to further hone your
skills and make connections in the large field of practicing specialty physicians. It is important to
seek a fellowship or faculty position at a program whose “hidden curriculum” explores and
identifies your interests and can help you cultivate your niche. Seek a mentor (or mentors, as
several may be needed to help you reach all of your goals) early in training or practice.
Important questions to ask yourself during the fellowship/job-seeking process are:
1. What has my experience been so far (e.g., have I trained at a facility that has had
research prospects; have I seen enough operative trauma; has our ICU been
technologically advanced, up-to-date with evidence-based medicine)?
2. What haven’t I done/seen/experienced (e.g., research projects; participated in
development of institutional protocols; taken the time to teach and get feedback on my
teaching; not enough operative trauma/penetrating trauma; have I been exposed to
ECMO, peri-operative cardiac surgery patients)?
3. What do I enjoy (e.g., trauma v. surgical critical care v. acute care surgery; direct patient
care v. administration; research; teaching);
4. Do I have non-clinical aspirations or interests within medicine, but outside of clinical
medicine?
a. Several common areas of non-clinical focus are research, education,
administration, and humanities.
1. Education – does my institution have a medical school and residency,
fellowship? Are there opportunities within the GME - committee/council
positions, teaching opportunities, faculty development?
2. Administration – Are there opportunities to have mentorship from the
administrative leadership -
3. Research – what are the opportunities at this institution (basic science only,
clinical science only, both; are there animal labs)? How involved are the
faculty? Do they have appreciable local resources (such as a dedicated
coordinator or faculty protected time)? Are there research requirements for
fellows and faculty? What is the representation at national meetings?
4. Humanities – mission work/care for underdeveloped nations, ethics and
palliative care
Know your strengths and interests, or have a plan to explore them with guidance. By
recognizing your strengths and interests, you can commit to activities that will benefit your
career, but not to those that don't offer value or personal satisfaction. Enjoyment is important,
but projects you enjoy but for which you lack an aptitude may take a disproportionate amount of
time and effort. The converse – things that come easily but offer no satisfaction - aren’t likely to
be meaningful and contribute to a long and fruitful career.
[Table of Contents] SCCPDS Fellowship Guide 62
19. How to Prepare for the SCC Board Certifying Examination
12/29/2021 James F. Watkins, MD, MSc, FACS (Snowmass Village, CO):
Most taking the Examination will have completed a surgery residency and so will have had
success with the ABSITE and the ABS Qualifying Examination, which are similar to the Surgical Critical
Care Certifying Examination. There is no oral component as there is in the General Surgery Certifying
Examination. If you had problems with prior examinations, you should probably make extra effort to
prepare for this one. The overall pass rate has fallen since 2018, when it was 98%, to 84%, according to
statistics posted on the ABS website. Conversely, the pass rate for the Qualifying Examination has
jumped and now hovers around 95%, although the Board does not offer any "comparables" or "risk-
adjusting" to help you debug whether the applicant pool has changed or there has been some quality
erosion. Your program should have statistics for pass rates for their recent graduates, although beware
the "small-numbers" problem. If you are taking the time to read this, I suspect you will do OK – not
because there is some magic, just that being organized tends to work.
If we assume that you've done OK on these sorts of exams before, then you probably know the
basics. Probably the most important thing is not to try to cram at the end. If you have problems with tests
and chose a very time-intensive program, then take a month or two off prior to starting work and just read.
Find a decent textbook and read it -- everyone has his or her favorite, and the partisans can be pretty
intense, so I'm not going to name one here -- ask peers or program director. Read the literature (your
program will have had journal clubs, and the citations in texts can guide you when trying to fill any gaps),
although you will not be expected to cite cutting-edge work in a written exam, it will help lead you to areas
of special interest, and the questions on the exam are posed by people, not some robot, so you ought to
be able to figure out what the areas of interest actually are. Ask recent examinees, particularly those
who've been through your program, what they found hard or received more emphasis than they expected,
and go there. Conversely, it is unlikely that you will be asked questions where the data are inconclusive or
lacking, such as whether one vent mode is better than another -- instead, they may ask about PEEP, tidal
volumes, and permissive hypercapnia, where there are data – I’d be willing to bet that ARDSNet will show
up. Be careful in reading the questions and tying them to your reading; just because you read a paper for
therapy X that hit a secondary endpoint in a famous trial is not the same as it being accepted as standard
of care, and similarly, it’s easy to misread the questions when you’re excited.
The question could easily be construed as asking if taking a review course is necessary. The
short answer is: “no.” I took the SCCM course, though, and thought it was worth every penny as it
provided a comprehensive review by experts from outside the cloister of the program I'd just completed.
You need to know, if you are considering that particular course, that it is aimed across multiple
specialties, and they mean it -- it's not called "Multiprofessional Critical Care Review Course" for nothing.
What this means in practice is that while the arrhythmia review may be awe-inspiring, it may be overkill for
most surgeons, unless you are working in an open-heart unit where they do maze procedures; the ABS
exam does not go into that kind of depth at all, although I am sure that the cardiologists are expected to
know this in minute detail. Aside from the fact that the course may not be specifically designed for the
ABS examination, it seems, to me, to be hard to beat. There are other courses about which I don't know
enough to form an opinion, so ask around, everyone loves to opine.
In terms of specific test answers, I saw no real trick questions, nor questions designed to see if
you spend your days reading Shock or J. Exp. Med. Just give them safe, reasonably up-to-date answers
that reflect widespread practice and you should do fine. It struck me in other ABS exams that the Board is
looking to assure safety, not measure brilliance, and my impression is that this holds for the Critical Care
exam as well. Good luck.
[Table of Contents] SCCPDS Fellowship Guide 63
20A. What is the Post-Fellowship Job Outlook?
02/21/2022 Chet A. Morrison, MD, FACS, FCCM (Saginaw MI):
The post-fellowship job outlook: The Secular growth Story Remains Intact
Glendower: I can call spirits from the vasty deep
Hotspur: Why so can I, or so can any man
But will they come when you do call for them?
Shakespeare Henry IV, Part 1
The term ‘secular growth story’ comes out of investment writing and generally means a
company or a stock that is expected to sustainably increase profits and earnings across
economic cycles, rather than being dependent on them. I think we can apply this term to the job
outlook in trauma/critical care and acute care surgery in that demand will continue to grow, and
has been growing since I graduated from my trauma and critical care fellowship; this has been
true not only across economic cycles, but also irrespective of changes within the health care
profession that have occurred. If anything, recent events including the SARS-CoV-2 pandemic
have more than confirmed that rather simple prophecy, and I believe that graduating fellows will
face a very robust job market that should allow them a range of geographic, economic and
practice choices, driven by an underlying demand for our services that should continue to grow
as the population ages and technological change highlights the need for savvy, dedicated
critical care professionals as well as trauma/acute care surgeons who, as the epigram states,
come when called. I also believe that the fellowship graduate can continue to look forward to a
generous salary that should provide lifelong financial security.
There are several reasons for this. The aging population, the rise of the numbers of
patients cared for in the ICU and the rise in cases of sepsis nationwide is a well-documented
phenomenon. As patients are living longer and more elaborate treatments are being offered for
previously untreatable conditions, the need for critical care specialists will have to rise in
parallel. Work done in the past decade by Dr. Young and colleagues, for example, suggests that
outcomes are better in ICUs managed predominantly by full-time intensivists. In their analysis, it
was estimated that full implementation of intensivist-model staffing would save approximately
53,850 lives each year in the United States. The authors further noted that “Because of potential
constraints related to the workforce and other resources, the feasibility of fully implementing
intensivist-model ICUs nationwide is uncertain”. Furthermore, intensivist staffing has been
shown to be cost effective and potentially cost saving in terms of decreasing costs associated
with intensive care and length of ICU stays. Unfortunately for the population, but perhaps
fortunately for the graduating fellow, a shortage of intensive care physicians is projected to be
as high as 35% in the next 20 years, according to well thought out models.
Paralleling this is the rising need for Acute Care/Trauma surgeons, who can effectively
manage the patients with acute injuries, the patients needing critical care services, the patients
needing emergency general surgery operations, and increasingly the patients needing some
kind of ‘surgical rescue’ to manage acute complications. This is in part driven by the aging
population, as well as the increasing number of patients who require emergency surgical care.
The Institute of Medicine released a report in 2006 that labeled hospital-based emergency care
“At the Breaking Point”. It was noted that three quarters of hospitals report difficulty finding
[Table of Contents] SCCPDS Fellowship Guide 64
specialists to take emergency and trauma calls.” And this was well before the Covid-19
pandemic which pushed a lot of hospitals and healthcare systems to the ‘breaking point’! Also, a
survey in 2009 found that there was a significant shortage of trauma surgeons nationwide, with
a mean of approximately two additional trauma surgeons per center and an average time a
position stood vacant of 19 months; this despite the compensation of a trauma surgeon which
often totals more than $400,000 per year (https://www.doctor-salaries.com/surgeon-
salary/trauma-surgeon-salary/). Contributing to the need for the acute care surgeon is the
decline of the non-specialized general surgeon. A substantial number of people in this country
live in a county that does not have a general surgeon. This is not a situation likely to change as
more and more graduates subspecialize and the number of surgical GME positions is not
expected to change. Thus another reason the need for acute care surgeons will grow
substantially in the future. Within the past seven years, numerous reports in the literature have
documented improved or equivalent outcomes in patients cared for under the new Acute Care
Surgery model, and it remains attractive to future surgeons due to the enhanced professional
satisfaction and also the potential for a controllable lifestyle. I expect then, as the specialty
refines itself further in the coming years, there should be increased institutional support for the
hiring of qualified physicians able to meet the demands of the Acute Care Surgery model.
I have already mentioned the current Covid-19 pandemic. It is also clear that mass
shootings, gunfire violence of all kinds and natural disasters have not shown any decline in the
past five years, and on some aspects may be increasing. Given this, services of the well-trained
acute care surgeon and critical care specialist will be essential; it has been noted that political
disaster planning tends to end at the hospital door. This has been shown to be grossly
inadequate; There will be future pandemics, and even well-equipped tertiary medical centers
with level one capabilities can be overwhelmed by one mass shooting event.
So, when one weaves these strands together one is led directly to the conclusion stated
at the beginning: that the future for the fellowship graduate in trauma, critical care and acute
care surgery is quite bright in the sense that our talents and skills will be needed for all kinds of
reasons, and the graduating fellow need have no doubt that his or her job prospects are
excellent and highly likely to stay that way for the foreseeable future. Bernard et al recently
documented that “ACS conditions together account for five to six million hospital admissions in
the USA per year, translating into $65 to $100 billion ($28 billion for EGS + $37–$80 billion for
trauma) for direct medical care” and that “The creation of an ACS care practice has been shown
to improve hospital contribution margin, patient throughput, and complication rates. This
observation remains even when considering patients with a high severity of illness” [Bernard A,
Staudenmayer K, Minei JP, et al “Macroeconomic trends and practice models impacting acute
care surgery, Trauma Surgery & Acute Care Open 2019”]. We bring unique and critically
needed skills to the healthcare profession, and as alluded to in the opening epigraph, we come
when called. Given this availability, our profession seems well secured for as long as we are
willing.
20B. What is the Post-Fellowship Job Outlook?
08/19/2018 David A. Spain, MD, FACS (Stanford, CA):
Fellows in 1 year programs have to be very organized and start the job hunting
process fairly early into the fellowship. I always emphasize that by X-mas time they
need to be sending out inquiries and assessing opportunities.
[Table of Contents] SCCPDS Fellowship Guide 65
21. Re-entry Applicants
01/07/2018 Michelle R. Brownstein, MD, FACS (Greenville, NC):
What about the applicant who is re-entering into practice after a hiatus from clinical practice?
Speaking from personal experience, the Surgical Critical Care (SCC) fellowship can be a
component of a reentry plan for someone who has taken time off from clinical practice. I took time away
from practice to focus on my family and was fortunate enough to have key mentors help me reenter when
the time was right.
I’m writing this piece not only for potential candidates, but also for program directors so they can
keep an open mind if approached by a colleague or an individual. Globally, reentering surgeons is one
way to address our workforce shortage needs. More granularly, it is a meaningful way to pay it forward
by realizing the shared investment made previously by that individual and all who had previously trained
him or her.
In order to be an appropriate candidate for a fellowship you will need to either maintain or
reinstate your board certification in general surgery and have an active medical license. This can be an
arduous task but it is not insurmountable. Anyone considering reentering into clinical practice will need to
evaluate critically their own circumstances to assess their personal knowledge and skill gaps. A general
resource to do is this website (http://physician-reentry.org/). Under the resources listed there you will find
issue briefs on the topic and in particular a schema for reentry to educational system that outlines the
basic needs. In addition to a needs assessment, the cornerstone is having a mentor/coach/champion
who will facilitate navigating the system.
Each state medical board has specific requirements regarding maintaining or regaining a medical
license with specifics for anyone who has been clinically inactive. Many have specific reentry
components depending on the time away and the reasons for that. My state does and my entire reentry
plan was dictated structurally by those requirements and included a graduated, proctored clinical
experience tailored to my needs followed by a 1 year SCC fellowship resulting ultimately in me being
recertified in general surgery and board certified in critical care. The Federation of State Medical Boards
(www.fsmb.org/) is a resource to assess the requirements of any state and also has a special committee
on reentry into practice. They released a Report of the Special Committee on Reentry into Practice in
2011.
Since 2012 the American Board of Surgery (ABS) has formalized the expectations for a surgeon
who wants to re-enter into clinical practice after a hiatus
(www.absurgery.org/default.jsp?policypracticereentry).
There are 5 components: Assessment of status of practice at departure, Re-entry pathway constructed by
the local physician champion, Proctoring plan, Outcomes assessment and ABS MOC. In special
situations, the SCC fellowship could serve as the sole clinical component of a re-entry plan depending on
how the fellowship is structured, the specific skill deficits of the surgeon and his/her ultimate practice
goals. Alternatively, a SCC fellowship can be coupled initially with an individualized period of time with
proctored opportunities to fill in missing skills prior to starting the fellowship. Anyone who wants to
consider completing the process will have an easier time if they have kept copies of all of their credentials
and certificates as well as maintain a current resume. If you are able to continue doing CME that will
facilitate the process as well.
Ultimately, you will need to work with the medical board in the state where you would do your re-
entry program and fellowship and also the ABS to meet all requirements. Plan ahead as acquiring all of
the necessary documents, finding an appropriate mentor and meeting all the requirements just to get
started requires 6 -9 months in advance at a minimum.

[Table of Contents] SCCPDS Fellowship Guide 66
22. Emergency Physicians
02/21/2022 Julie M. Winkle, MD, FACEP, FCCM (Aurora, CO):
CRITICAL CARE FELLOWSHIP TRAINING FOR EMERGENCY PHYSICIANS
FREQUENTLY ASKED QUESTIONS
1. Why do a surgical CC fellowship program?
Emergency Physicians (EP’s) report different reasons for wanting to pursue
critical care (CC) fellowship training. Current options include fellowships in surgical CC
(SCC), medical CC, anesthesia CC and neuro CC. Reasons stated for why EP’s may
train in CC include:
- Interest in taking care of critically ill patients and a wish to develop more of an
understanding and an expertise in the management of these patients
- Enjoying ICU rotations and a desire to practice in-patient CC
- Wanting a sub-specialty within Emergency Medicine (EM)
- A fascination with surgical pathology and the care of surgical patients, but not
wanting to be a surgeon
- A desire to improve the care of CC patients in the emergency department
- Affinity for procedures- SCC physicians can do bronchoscopy, percutaneous
tracheostomy and some feeding tubes, as well as central lines and chest tubes
- An interest in trauma and the possibility of combining post-graduate training in
both trauma and CC
2. How are the two years of surgical CC fellowship structured?
Currently, the American Board of Surgery (ABS) requirements state that EP’s
that have completed residency training must complete a preliminary year of surgical
training, followed by an ACGME-accredited SCC training program at the same
institution (https://www.absurgery.org/default.jsp?certsccce_abem).
One of the most common questions for EP’s considering a SCC training program
is in regards to the structure of this first year of training. Curricula and requirements vary
depending on the program, but the goal of this year is to give EP’s a fundamental
understanding of the pre-operative, intra-operative and post-operative conditions that
are encountered in caring for critically ill surgical patients
3
. Individual programs submit
their proposed curriculum for approval to ABS. Applicants are encouraged to ask
programs how this year is structured and what the EP’s role will be on surgical teams.
[Table of Contents] SCCPDS Fellowship Guide 67
3. Will I be board certified in CC after doing a surgical CC fellowship?
EP’s may become board certified in SCC by the ABS by meeting the following
requirements: successful completion of EM residency and achievement of ABEM board
certification, completion of a preliminary year of surgical training followed by an
ACGME-accredited SCC training program at the same institution, and successful
completion of the ABS board certifying exam in SCC.
4. What should I look for in a fellowship?
An important aspect for EP’s interested in a CC fellowship is to find a program
that is supportive of EM physicians practicing CC. EM trainees have a different skill set
entering CC fellowship - most tend to be more adept at certain topics such as
ultrasound, management of arrhythmias, acute coronary syndrome, neurologic
emergencies, and airway management; but may not have an extensive knowledge of
surgical pathology. It may be helpful to have supervising physicians that are aware of
that fact and have experience training EP’s. Important in any CC training program is a
comprehensive didactic program, a strong clinical experience consisting of a diverse,
critically ill patient population, and the opportunity to pursue elective or research
interests.
5. Which programs currently have ABS-approved 2-year fellowship programs?
The following is a list of fellowships that have been approved by ABS. This list may not
include all programs and applicants are encouraged to check the SCC Program Director
Society’s website for an updated list ( https://sccpds.org/future-fellows/approved-
programs ). EMRA also has a list of programs accepting EM applicants in the EMRA
fellowship guide: https://www.emra.org/books/fellowship-guide-book/5d-surgical-critical-
care/
• Albany Medical Center
• Carolinas Medical Center
• Johns Hopkins University
• Massachusetts General Hospital
• Medical College of Wisconsin
• Methodist Health System, Dallas TX
• St Luke’s Hospital
• Stony Brook University
• University of Iowa Hospitals and Clinics
• University of Maryland R Adams Cowley Shock Trauma Center
• University of Michigan
• University of Pennsylvania
• University of Texas Southwestern
[Table of Contents] SCCPDS Fellowship Guide 68
6. What are my options for practice after CC fellowship?
Over 250 EM physicians have done CC fellowships over the past 3 decades and
that number is increasing every year. Most of these dual trained physicians practice
both EM and CC. Now that there are pathways to board certification in CC, practice
options are wide for EP’s. Options for post-fellowship practice include academic,
community, and VA institutions, as well as surgical, surgical sub-specialty and
combined Medical-Surgical ICU’s. There are a growing number of Emergency
Department ICU’s (ED-ICU’s) as well as Resuscitation ICU’s that employ critical care
trained EP’s. National organizations such as ACEP and the Society of Critical Care
Medicine (SCCM) offer networking and mentorship to aid in finding post-fellowship
career opportunities.
Helpful References
1. Mayglothling JA, Gunnerson KJ, Huang DT. Current practice, demographics,
and trends of critical care trained emergency physicians in the United States.
Acad Emerg Med. 2010 Mar;17(3):325-9.
2. Huang DT, Osborn TM, Gunnerson KJ, Gunn SR, Trzeciak S, Kimball E, Fink
MP, Angus DC, Dellinger RP, Rivers EP; Society of Critical Care Medicine;
American College of Emergency Physicians; Society of Academic Emergency
Medicine; Council of Emergency Medicine Residency Directors; Emergency
Medicine Residents Association. Critical care medicine training and certification
for emergency physicians. Crit Care Med.2005 Sep;33(9):2104-9.
3. Tisherman SA, Alam HB, Chiu WC, Emlet LL, Grossman MD, Luchette FA,
Marcolini EG, Mayglothling JA; for the Surgical Critical Are Program Directors
Society Task Force on Emergency Medicine-Surgical Critical Care Training. J
Am Coll Surg. 2013;217(5): 954-9.e3
4. Parker BM, Foster MT, Menne A. Surgical Critical Care. In: EMRA Fellowship
Guide, 2
nd
Edition. Edited by Shafer, Krystle, Emergency Medicine Residents’
Association, 2018: 47-53
5. https://www.absurgery.org/default.jsp?certsccce_abem

[Table of Contents] SCCPDS Fellowship Guide 69
23. Anesthesiologists
09/17/2017 Maureen McCunn, MD, MIPP, FASA, FCCM (Baltimore, MD):
Trauma Anesthesiology and Acute Care Anesthesiology Fellowship Training
Anesthesiologists and surgeons are co-dependent in many aspects of their
practices, particularly in the operating room. Many anesthesiologists do not want to
practice, nor have an interest in, trauma care and very few are skilled or trained in the
management of the acutely ill patient in need of urgent operative intervention. If you are
the type of person who thrives in a high-intensity, high-stakes (life or death)
environment, is challenged by emergency cases, wants to develop a procedure-heavy
skill set, and are flexible, adaptable and calm under pressure, this is the field for you.
There are currently SIX trauma anesthesiology fellowships in the U.S.:
University of Maryland
http://www.umm.edu/programs/shock-trauma/services/clinical/trauma-anesthesiology
University of Texas
https://med.uth.edu/anesthesiology/education/fellowship/trauma-anesthesiology-
fellowship
University of Washington
http://depts.washington.edu/anesth/education/fellows/trauma.shtml
University of California, San Francisco
https://anesthesia.ucsf.edu/trauma-acute-care-surgery-anesthesia-fellowship
University of Alabama
https://www.uab.edu/medicine/anesthesiology/education/fellowships/trauma-and-acute-
care/applicant-information
Washington University
http://anest.wustl.edu/trauma/fellowship_overview
[Table of Contents] SCCPDS Fellowship Guide 70
What kind of job can you expect with this training?
Very few hospitals and medical centers can support a full-time practice in trauma
anesthesiology, so you may end up doing general OR and will have trauma/emergency
surgery cases intermittently. Critical care fellowships in anesthesiology are generally 1
year, but can be 2 or more, depending upon the fellow’s interest, such as cardiac,
neurocritical care, or trauma. A new concept has recently developed, similar to Acute
Care Surgery (trauma, emergency care and critical care) that is called “Acute Care
Anesthesiology”. (McCunn, et al) The proposed curriculum includes a minimum
requirement of 9 months of ICU training, and the program that you select may be
flexible in designing additional training in trauma, EMS/pre-hospital care, emergency
preparedness/disaster management, extracorporeal support modalities, research,
ultrasound, or global health. There are only a few trauma ICU’s in the country in which
to practice. However, the clinical proficiency that you obtain during a trauma/acute care
anesthesiology fellowship and the critical-thinking skills that you gain – in addition to
flexibility and readiness training – each add to your ability to work in a high-intensity and
readiness environment at all times.
Doing an elective rotation at an institution where you are considering a job or a
fellowship is beneficial to both you (do you like the staff, the system and the package)
and the program (do they like you, do your goals match their mission?).
The work hours, although limited by ACGME requirements, are usually longer
than those of an anesthesiologist in the OR, and during fellowship include in-house call
nights, weekends and holidays. Many programs fund a 2
nd
year of fellowship by having
the fellow work as an attending anesthesiologist in the OR part-time. If you complete
critical care fellowship training, after passing your boards you will have a certificate in
the subspecialty of critical care anesthesiology. There is no equivalent certification for
trauma or acute care anesthesiology, so it is highly recommended that you do a 9-
month critical care base year, and then focus on your area of interest, in order to be
eligible for the additional certification.
Reference
McCunn M
1
, Dutton RP, Dagal A, Varon AJ, Kaslow O, Kucik CJ, Hagberg CA, McIsaac JH 3rd, Pittet
JF, Dunbar PJ, Grissom T, Vavilala MS. Trauma, Critical Care, and Emergency Care Anesthesiology: A
New Paradigm for the "Acute Care" Anesthesiologist? Anesth Analg. 2015 Dec;121(6):1668-73.
[Table of Contents] SCCPDS Fellowship Guide 71
24. International Physicians
12/30/2017 Mansoor A. Khan, MBBS (Lond), PhD, FRCS(GenSurg),
FEBS(GenSurg), FACS, AKC (London, United Kingdom):
Guidance for Application from the UK for Fellowship in Trauma/Surgical Critical Care in the USA
Preparation for a fellowship in the USA is a time consuming process that requires a lot of
steps. I started my application process 2 years in advance! Prior to any
application/correspondence it is a good idea to have discussed this with your educational
supervisor, Programme Director and/or Postgraduate Dean as these individuals will have a big
say in whether you can get approval for the post to be recognized as Out of Programme
Experience (OOPE) or Out of Programme Training (OOPT) – more to follow on this later!
The initial decision is to decide where in the USA one should undertake the fellowship.
There are numerous sites on the internet, www.aast.org and www.east.org, all of which can
easily be accessed to help you decide which programme would be the best suited for you to
apply for.
It is imperative that you check eligibility criteria: do you possess the USMLE? Are you at
the right stage of residency (or equivalent)? Will this fellowship programme aid your career or do
you need to look at a different institution? If you do not possess the USMLE and it is a
requirement, then you must allow sufficient time to obtain this, as many institutions require this
before you even apply.
Remember, the key is to keep your UK programme faculty updated at all times. Once
you have decided to apply, you will require references. In my case, I obtained references from
my Educational Supervisor, Programme Director and Associate Postgraduate Dean.
Once all references are available, apply for the Fellowship and wait an interview date. If
successful at interview, then prepare for even more paperwork. I applied for my fellowship to be
recognized as OOPT, which is recognized training and counts towards a Certificate of
Completion of Training (CCT) – although I believe this option is no longer available.
Out of programme post approval process
In order to get any period of out of programme training approved, trainees should be
aware of the following process: once they have been offered a fellowship they must inform their
Deanery of their request. The deanery will then write a supporting letter in which you must state
the exact job description, roles and responsibilities, weekly timetable so that the Dean can seek
agreement from the relevant Royal College/faculty that the experience is appropriate and
relevant for the CCT.
Once approval from the relevant College is obtained, the Deanery can then apply to the
General Medical Council (GMC) and relevant Advisory Committee for approval for this training
to count towards CCT. This whole process can take a few months! In 2010, the PMETB has
merged with the GMC, however the application process still remains the same -
(http://www.gmc-uk.org/education/index.asp).
[Table of Contents] SCCPDS Fellowship Guide 72
25. Web Sites of Interest
02/28/2022 William C. Chiu, MD, FACS, FCCM (Baltimore, MD):
Accreditation Council for Graduate Medical Education (ACGME): www.acgme.org
American Association for the Surgery of Trauma (AAST): www.aast.org
American Board of Emergency Medicine (ABEM): www.abem.org
American Board of Medical Specialties (ABMS): www.abms.org
American Board of Surgery (ABS): www.absurgery.org
American College of Surgeons (ACS): www.facs.org
Eastern Association for the Surgery of Trauma (EAST): www.east.org
EAST Fellowships Careercasts:
www.east.org/education-career-development/career-
management/careercasts?categoryId=30
European Society of Intensive Care Medicine (ESICM): www.esicm.org
General Medical Council – United Kingdom (GMC-UK): www.gmc-uk.org
National Resident Matching Program (NRMP): www.nrmp.org
Society of Critical Care Medicine (SCCM): www.sccm.org
Surgical critical care and Acute care surgery Fellowship Application Service (SAFAS):
safas.smapply.io/
Surgical Critical Care Program Directors Society (SCCPDS): www.sccpds.org
26. Acknowledgment
02/28/2022 William C. Chiu, MD, FACS, FCCM (Baltimore, MD):
I am indebted to Dora Russell, SAFAS Administrator, for all of her dedication and
assistance in formatting the SCCPDS Fellowship Guide into an interactive PDF
document with hyperlinks to easily navigate to individual chapters.
