
Medicare Benefit Policy Manual
Chapter 13 - Rural Health Clinic (RHC) and
Federally Qualified Health Center (FQHC) Services
Table of Contents
(Rev. 11803, 01-26-23)
Transmittals for Chapter 13
Index of Acronyms
10 - RHC and FQHC General Information
10.1 - RHC General Information
10.2 - FQHC General Information
20 - RHC and FQHC Location Requirements
20.1 - Non-Urbanized Area Requirement for RHCs
20.2 - Designated Shortage Area Requirement for RHCs
30 - RHC and FQHC Staffing Requirements
30.1 - RHC Staffing Requirements
30.2 - RHC Temporary Staffing Waivers
30.3 - FQHC Staffing Requirements
40 - RHC and FQHC Visits
40.1 - Location
40.2 - Hours of Operation
40.3 - Multiple Visits on Same Day
40.4 - Global Billing
40.5 - 3 Day Payment Window
50 - RHC and FQHC Services
50.1 - RHC Services
50.2 - FQHC Services
50.3 - Emergency Services
60 - Non RHC/FQHC Services
60.1 - Description of Non RHC/FQHC Services
70 - RHC and FQHC Payment Rate
70.1 - RHCs Billing Under the AIR
70.2 - RHC Payment Limit and Exceptions
70.2.1 - Payment Limits Applicable to Independent RHCs, and Provider-Based
RHCs in a Hospital with 50 or More Beds, and New RHCs
70.2.2 – Payment Limits Applicable to Provider-Based RHCs in a Hospital
with Less than 50 Beds
70.2.2.1 - Determining Payment Limits for Specified (that is,
Grandfathered) Provider-Based RHCs with an AIR Established for
RHC Services Furnished in 2020
70.2.2.2 - Determining Payment Limits for Specified (that is,
Grandfathered) Provider-Based RHCs that did not have an AIR
Established for RHC Services Furnished in 2020
70.3 - FQHC PPS Payment Rate and Adjustments
70.4 - FQHC Payment Codes
80 - RHC and FQHC Cost Reports
80.1 - RHC and FQHC Cost Report Requirements
80.2 - RHC and FQHC Consolidated Cost Reports
80.3 - RHC and FQHC Cost Report Forms
80.4 – RHC Productivity Standards
90 - RHC and FQHC Charges, Coinsurance, Deductible, and Waivers
90.1 - Charges and Waivers
90.2 - Sliding Fee Scale
100 - Commingling
110 - Physician Services
110.1 - Dental, Podiatry, Optometry, and Chiropractic Services
110.2 - Treatment Plans or Home Care Plans
110.3 - Graduate Medical Education
120 - Services and Supplies Furnished “Incident to” Physician’s Services
120.1 - Provision of Incident to Services and Supplies
120.2 - Incident to Services and Supplies Furnished in the Patient’s Home or Location
Other than the RHC or FQHC
120.3 - Payment for Incident to Services and Supplies
130 - Nurse Practitioner, Physician Assistant, and Certified Nurse Midwife Services
130.1 - NP, PA, and CNM Requirements
130.2 - Physician Supervision
130.3 - Payment to Physician Assistants
140 - Services and Supplies Furnished Incident to NP, PA, and CNM Services
150 - Clinical Psychologist and Clinical Social Worker Services
160 - Services and Supplies Incident to CP Services
170 - Mental Health Visits
180 - Physical Therapy, Occupational Therapy, and Speech Language Pathology Services
190 - Visiting Nursing Services
190.1 - Description of Visiting Nursing Services
190.2 - Requirements for Furnishing Visiting Nursing Services
190.3 - Home Health Agency Shortage Area
190.4 – Authorization for Visiting Nursing Services
190.5 – Treatment Plans for Visiting Nursing Services
200 - Telehealth Services
210 - Hospice Services
210.1 - Hospice Attending Physician Services Payment
210.2 - Provision of Services to Hospice Patients in an RHC or FQHC
220 - Preventive Health Services
220.1 - Preventive Health Services in RHCs
220.2 - Copayment and Deductible for RHC Preventive Health Services
220.3- Preventive Health Services in FQHCs
220.4 - Copayment for FQHC Preventive Health Services
230 – Care Management Services
230.1 - Transitional Care Management Services
230.2 - General Care Management Services – Chronic Care Management, Principal
Care Management, and General Behavioral Health Integration Services
230.2.1 – Chronic Care Management (CCM) Services
230.2.2 – Principal Care Management (PCM) Services
230.2.3 – Chronic Pain Management (CPM) Services
230.2.4 – General Behavioral Health Integration (BHI) Services
230.2.5 – Payment for General Care Management Services
230.3 - Psychiatric Collaborative Care Model Services
240 – Virtual Communication Services
Index of Acronyms
(Rev. 10729, 04-26-21)
AIR – all inclusive rate
AWV – annual wellness visit
BHI – behavioral health integration
CCM – chronic care management
CCN – CMS certification number
CNM – certified nurse midwife
CoCM – collaborative care model
CP – clinical psychologist
CSW – clinical social worker
DSMT – diabetes self-management training
EKG – electrocardiogram
E/M – evaluation and management
FQHC – Federally qualified health center
FTE – full time equivalent
GAF – geographic adjustment factor
GME – graduate medical education
HCPCS – Healthcare Common Procedure Coding System
HHA – home health agency
HHS – Health and Human Services
HPSA – Health Professional Shortage Area
HRSA – Health Resources and Services Administration
IPPE – initial preventive physical exam
LDTC – low dose computed tomography
LPN – licensed practical nurse
MAC – Medicare Administrative Contractor
MEI – Medicare Economic Index
MNT – medical nutrition therapy
MSA – metropolitan statistical area
MUA – Medically-Underserved Area
MUP – Medically-Underserved Population
NCD – national coverage determination
NECMA – New England County Metropolitan Area
NP – nurse practitioner
OBRA - Omnibus Budget Reconciliation Act
PA – physician assistant
PCE - Primary Care Exception
PCM – Principal Care Management
PFS – physician fee schedule
PPS – prospective payment system
PHS – Public Health Service
RHC – rural health clinic
RN – registered nurse
RO – regional office
RUCA – Rural Urban Commuting Area
SLP – speech language therapy
TCM – transitional care management
UA – urbanized area
USPSTF – U.S. Preventive Services Task Force
10 - RHC and FQHC General Information
(Rev.239, Issued: 01-09-18, Effective: 1-22-18, Implementation: 1-22-18)
10.1 - RHC General Information
(Rev. 11803; Issued: 01-26-23; Effective: 01-01-23; Implementation: 02-27-23)
Rural Health Clinics (RHCs) were established by the Rural Health Clinic Service Act of
1977 to address an inadequate supply of physicians serving Medicare beneficiaries in
underserved rural areas, and to increase the utilization of nurse practitioners (NP) and
physician assistants (PA) in these areas. RHCs have been eligible to participate in the
Medicare program since March 1, 1978, and are paid an all-inclusive rate (AIR) for
medically-necessary primary health services, and qualified preventive health services,
furnished by an RHC practitioner.
RHCs are defined in section 1861(aa)(2) of the Social Security Act (the Act) as facilities
that are engaged primarily in providing services that are typically furnished in an
outpatient clinic. RHC services are defined as:
• Physician services;
• Services and supplies furnished incident to a physician’s services;
• NP, PA, certified nurse midwife (CNM), clinical psychologist (CP), and
clinical social worker (CSW) services; and
• Services and supplies furnished incident to an NP, PA, CNM, or CP
services.
RHC services may also include nursing visits to patients confined to the home that are
furnished by a registered professional nurse (RN) or a licensed professional nurse (LPN)
when certain conditions are met. (See section 190 of this manual)
To be eligible for certification as an RHC, a clinic must be located in a non-urbanized
area, as determined by the U.S. Census Bureau, and in an area designated or certified
within the previous 4 years by the Secretary, Health and Human Services (HHS), in any
one of the four types of shortage area designations that are accepted for RHC
certification. (See section 20 of this manual)
In addition to the location requirements, an RHC must:
• Employ an NP or PA;
• Have an NP, PA, or CNM working at the clinic at least 50 percent of the time the
clinic is operating as an RHC;
• Directly furnish routine diagnostic and laboratory services;
• Have arrangements with one or more hospitals to furnish medically necessary
services that are not available at the RHC;
• Have available drugs and biologicals necessary for the treatment of emergencies;
• Meet all health and safety requirements;
• Not be a rehabilitation agency or a facility that is primarily for mental health
treatment;
• Furnish onsite all of the following six laboratory tests:
○ Chemical examination of urine by stick or tablet method or both;
○ Hemoglobin or hematocrit;
○ Blood sugar;
○ Examination of stool specimens for occult blood;
○ Pregnancy tests; and
○ Primary culturing for transmittal to a certified laboratory.
• Not be concurrently approved as an FQHC, and
• Meet other applicable State and Federal requirements.
RHCs can be either independent or provider-based. Independent RHCs are stand-alone
or freestanding clinics and submit claims to a Medicare Administrative Contractor (A/B
MAC). They are assigned a CMS Certification Number (CCN) in the range 3800-3974
or 8900-8999. Provider-based RHCs are an integral and subordinate part of a hospital
(including a critical access hospital (CAH)), skilled nursing facility (SNF), or a home
health agency (HHA). They are assigned a CCN in the range 3400-3499, 3975-3999, or
8500-8899. (NOTE: A provider-based CCN is not an indication that the RHC has met
the qualifications for the special payment rules applicable to payment limits discussed
in section 70.2 of this chapter.)
The statutory requirements for RHCs are found in section 1861(aa) of the Act. Many of
the regulations pertaining to RHCs can be found at 42 CFR 405.2400 Subpart X and
following, and 42 CFR 491 Subpart A and following.
For information on claims processing, see Pub. 100-04, Medicare Claims Processing
Manual, chapter 9, http://www.cms.gov/Regulations-and-
Guidance/Guidance/Manuals/downloads/clm104c09.pdf
For information on certification requirements, see Pub. 100-07, State Operations Manual,
Chapter 2, and Appendix G, https://www.cms.gov/Regulations-and-
Guidance/Guidance/Manuals/Downloads/som107c02.pdf
10.2 - FQHC General Information
(Rev.239, Issued: 01-09-18, Effective: 1-22-18, Implementation: 1-22-18)
Federally Qualified Health Centers (FQHCs) were established in 1990 by section 4161 of the
Omnibus Budget Reconciliation Act (OBRA) of 1990 and were effective beginning on October
1, 1991. As with RHCs, they are also facilities that are primarily engaged in providing services
that are typically furnished in an outpatient clinic. FQHCs were paid an AIR for primary
health services and qualified preventive health services until October 1, 2014, when they began
to transition to the FQHC prospective payment system (PPS). Beginning on January 1, 2016,
all FQHC are paid under the provisions of the FQHC PPS, as required by Section
10501(i)(3)(B) of the Affordable Care Act.
FQHC services are defined as:
• Physician services;
• Services and supplies furnished incident to a physician’s services;
• NP, PA, certified nurse midwife (CNM), clinical psychologist (CP), and clinical
social worker (CSW) services;
• Services and supplies furnished incident to an NP, PA, CNM, or CP services;
and
• Outpatient diabetes self-management training (DSMT) and medical nutrition
therapy (MNT) for beneficiaries with diabetes or renal disease.
The statutory requirements that FQHCs must meet to qualify for the Medicare benefit are in
section 1861(aa)(4) of the Act. No Part B deductible is applied to expenses for services that
are payable under the FQHC benefit. An entity that qualifies as an FQHC is assigned a CCN
in the range 1800-1989 and 1000-1199.
FQHC services also include certain preventive primary health services. The law defines
Medicare-covered preventive services provided by an FQHC as the preventive primary health
services that an FQHC is required to provide under section 330 of the Public Health Service
(PHS) Act. Medicare may not cover some of the preventive services that FQHCs provide, such
as dental services, which are specifically excluded under Medicare law.
There are 3 types of organizations that are eligible to enroll in Medicare as FQHCs:
• Health Center Program Grantees: Organizations receiving grants under section 330 of
the PHS Act, including Community Health Centers, Migrant Health Centers, Health
Care for the Homeless Health Centers, and Public Housing Primary Care Centers;
• Health Center Program Look-Alikes: Organizations that have been identified by HRSA
as meeting the definition of “Health Center” under section 330 of the PHS Act, but not
receiving grant funding under section 330; and
• Outpatient health programs/facilities operated by a tribe or tribal organization (under
the Indian Self-Determination Act) or by an urban Indian organization (under Title V of
the Indian Health Care Improvement Act).
NOTE: Information in this chapter applies to FQHCs that are Health Center Program
Grantees and Health Center Program Look-Alikes. It does not necessarily apply to tribal or
urban Indian FQHCs or grandfathered tribal FQHCs.
An FQHC must:
• Provide comprehensive services and have an ongoing quality assurance program;
• Meet other health and safety requirements;
• Not be concurrently approved as an RHC; and
• Meet all requirements contained in section 330 of the Public Health Service Act,
including:
o Serve a designated Medically-Underserved Area (MUA) or Medically-Underserved
Population (MUP);
o Offer a sliding fee scale to persons with incomes below 200 percent of the federal
poverty level; and
o Be governed by a board of directors, of whom a majority of the members receive
their care at the FQHC.
Additional information on these and other section 330 requirements can be found at
http://bphc.hrsa.gov/.
Per 42 CFR 413.65(n), only FQHCs that were operating as provider-based clinics prior to 1995
and either a) received funds under section 330 of the PHS Act or b) were determined by CMS
to meet the criteria to be a look-alike clinic, are eligible to be certified as provider-based
FQHCs. Clinics that do not already have provider-based status as an FQHC are no longer
permitted to receive the designation.
For information on claims processing, see to Pub. 100-04, Medicare Claims Processing
Manual, chapter 9, http://www.cms.gov/Regulations-and-
Guidance/Guidance/Manuals/downloads/clm104c09.pdf, and Pub. 100-07, State Operations
Manual chapter 2, sections 2825 and 2826, http://www.cms.gov/Regulations-and-
Guidance/Guidance/Manuals/downloads/som107c02.pdf.
20 - RHC and FQHC Location Requirements
(Rev.239, Issued: 01-09-18, Effective: 1-22-18, Implementation: 1-22-18)
To be eligible for certification as an RHC, a clinic must be located in 1) a non-urbanized area,
as determined by the U.S. Census Bureau, and 2) an area designated or certified within the
previous 4 years by the Secretary, HHS, in any one of the four types of shortage area
designations that are accepted for RHC certification as listed in section 20.2.
A clinic applying to become a Medicare-certified RHC must meet both the rural and
underserved location requirements. Mobile clinics must have a fixed schedule that specifies
the date and location for services, and each location must meet the location requirements.
Existing RHCs are not currently required to continue to meet the location requirements. RHCs
that plan to relocate or expand should contact their Regional Office (RO) to determine their
location requirements.
FQHCs may be located in rural or urban areas. FQHCs that are Health Center Program
Grantees or Look-Alikes must be located in or serve people from a HRSA-designated MUA or
MUP.
20.1 - Non-Urbanized Area Requirement for RHCs
(Rev. 220, Issued: 01-15-16, Effective: 02-01-16, Implementation: 02-01-16)
The U.S. Census Bureau determines if an area is an urbanized area (UA). Any area that is not
in a UA is considered a non-urbanized area. A clinic located in an area that is not a UA would
meet the RHC requirement for being in a non-urbanized area. Information on whether an area
is in an urbanized area can be found at http://factfinder.census.gov; or
http://www.raconline.org; or by contacting the appropriate CMS RO at
http://www.cms.gov/RegionalOffices/.
20.2 - Designated Shortage Area Requirement for RHCs

(Rev. 220, Issued: 01-15-16, Effective: 02-01-16, Implementation: 02-01-16)
The HRSA designates areas as MUAs/MUPs and/or Health Professional Shortage Areas
(HPSAs). To be eligible for RHC certification, a clinic must be located in an area that has one
of the following types of shortage area designations:
• Geographic Primary Care HPSA;
• Population-group Primary Care HPSA;
• MUA (this does not include the population group MUP designation); or
• Governor-Designated and Secretary-Certified Shortage Area (this does not include a
Governor’s Medically Underserved Population designation).
No other type of shortage area designation is accepted for purposes of RHC certification. The
designation cannot be more than 4 years old in order to meet the requirement of being in a
currently designated area. For RHC purposes, the age of the designation is calculated as the
last day of the year 4 years from the date of the original designation, or the date the area was
last designated. For example, a clinic that is located in an area that was most recently
designated or updated on June 1, 2010, would be considered as meeting this location
requirement through December 31, 2014.
Areas that are listed as “proposed for withdrawal” are considered designated. The designation
date is the date that the area was last updated, not when the area was proposed for withdrawal.
To determine the designation date of an area that is listed as “proposed for withdrawal”,
contact HRSA’s Shortage Designation Branch at [email protected] or call 1-888-275-4772.
30 - RHC and FQHC Staffing Requirements
(Rev. 166, Issued: 01-31-13, Effective: 03-01-13, Implementation: 03-01-13)
30.1 - RHC Staffing Requirements
(Rev. 239, Issued: 01-09-18, Effective: 1-22-18, Implementation: 1-22-18)
In addition to the location requirements, an RHC must:
• Employ an NP or PA; and
• Have an NP, PA, or CNM working at the clinic at least 50 percent of the time the clinic
is operating as an RHC.
The employment may be full or part time, and is evidenced by a W-2 form from the RHC. If
another entity such as a hospital has 100 percent ownership of the RHC, the W-2 form can be
from that entity as long as all the non-physician practitioners employed in the RHC receive
their W-2 from this owner.
The following are examples of situations that would NOT satisfy the employment requirement:
• An NP or PA who is employed by a hospital that has an ownership interest in the RHC
but is not physically present and working in the RHC;
• A CNM who is employed by the RHC;
• An Advanced Practice Registered Nurse who is not an NP or PA; or
• An NP or PA who is working as a substitute in an arrangement similar to a locum
tenens physician.
An RHC practitioner is a physician, NP, PA, CNM, CP, or CSW. At least one of these
practitioners must be present in the RHC and available to furnish patient care at all times the
RHC is in operation. A clinic that is open solely to address administrative matters or to
provide shelter from inclement weather is not considered to be in operation during this period
and is not subject to the staffing requirements.
An NP, PA, or CNM must be available to furnish patient care at least 50 percent of the time
that the RHC is open to provide patient care. This requirement can be fulfilled through any
combination of NPs, PAs, or CNMs as long as the total is at least 50 percent of the time the
RHC is open to provide patient care. Only the time that an NP, PA, or CNM spends in the
RHC, or the time spent directly furnishing patient care in another location as an RHC
practitioner, is counted towards the 50 percent time. It does not include travel time to another
location, or time spent not furnishing patient care when in another location outside the RHC
(e.g. home, SNF, etc.).
A clinic located on an island that otherwise meets the requirements for RHC certification is not
required to employ an NP or PA, although it is still required to have an NP or PA at least 50
percent of the time that the RHC is in operation (OBRA ’89, Sec 4024). An island is a body of
land completely surrounded by water, regardless of size and accessibility (e.g., bridges).
As of July 1, 2014, RHCs may contract with non-physician practitioners (PAs, NPs, CNM, CPs
or CSWs) if at least one NP or PA is employed by the RHC (subject to the waiver provision for
existing RHCs set forth at section 1861(aa)(7) of the Act).
It is the responsibility of the RHC to assure that all staffing requirements are met and that RHC
practitioners provide services in accordance with state and federal laws and regulations.
See section 80.4 of this chapter for information on productivity standards for RHCs.
30.2 - RHC Temporary Staffing Waivers
(Rev. 239, Issued: 01-09-18, Effective: 1-22-18, Implementation: 1-22-18)
An existing RHC may request a temporary staffing waiver if the RHC met the staffing
requirements before seeking the waiver, and either or both of the following occur:
• An NP or PA is not currently employed by the RHC.
• An NP, PA, or CNM is not furnishing patient care at least 50 percent of the time the
RHC operates.

To receive a temporary staffing waiver, an RHC must demonstrate that it has made a good faith
effort to recruit and retain the required practitioner(s) in the 90 day period prior to the waiver
request. Recruitment activities should begin as soon as the RHC becomes aware that they will
no longer be in compliance with this requirement. Good faith efforts can include activities
such as advertising in an appropriate newspaper or professional journal, conducting outreach to
an NP, PA, or CNM school, or other activities.
Staffing waivers are for a period not to exceed 1 year. The waiver cannot be extended beyond
1 year, and another waiver cannot be granted until a minimum of 6 months have elapsed since
the prior waiver expired. RHCs should continue their recruitment activities during the waiver
period to avoid termination when the waiver period ends.
An RHC will be terminated if any of the following occur:
• The RHC does not meet the staffing requirements and does not request a temporary
staffing waiver;
• The RHC requests a temporary staffing waiver and the request is denied due to a lack
of good faith effort to meet the requirements;
• The RHC does not meet the staffing requirements and is not eligible for a temporary
staffing waiver because less than 6 months have passed since the expiration of the
previous waiver;
• The RHC reaches the expiration date of the temporary staffing waiver and has not come
into compliance; or
• Other non-compliance issue.
30.3 - FQHC Staffing Requirements
(Rev. 239, Issued: 01-09-18, Effective: 1-22-18, Implementation: 1-22-18)
FQHCs must have a core staff of appropriately trained primary care practitioners and meet
other clinical requirements. It is the responsibility of the FQHC to assure that all staffing
requirements are met and that FQHC practitioners provide services in accordance with State
and Federal laws and regulations. Additional information on FQHC staffing requirements can
be found at: http://bphc.hrsa.gov/about/requirements/index.html.
40 - RHC and FQHC Visits
(Rev. 11803; Issued: 01-26-23; Effective: 01-01-23; Implementation: 02-27-23)
An RHC or FQHC visit is a medically-necessary medical or mental health visit, or a
qualified preventive health visit. The visit must be a face-to-face (one-on-one) encounter
between the patient and a physician, NP, PA, CNM, CP, or a CSW during which time
one or more RHC or FQHC services are rendered. However, effective January 1, 2022, a
mental health visit is a face-to-face encounter or an encounter furnished using
interactive, real-time, audio and video telecommunications technology or audio-only
interactions in cases where the patient is not capable of, or does not consent to, the use
of video technology for the purposes of diagnosis, evaluation or treatment of a mental
health disorder. A Transitional Care Management (TCM) service can also be an RHC or
FQHC visit. Services furnished must be within the practitioner’s state scope of practice,
and only services that require the skill level of the RHC or FQHC practitioner are
considered RHC or FQHC visits.
An RHC or FQHC visit can also be a visit between a home-bound patient and an RN or
LPN under certain conditions. See section 190 of this chapter for information on visiting
nursing services to home-bound patients.
Under certain conditions, an FQHC visit also may be provided by qualified practitioners
of outpatient DSMT and MNT when the FQHC meets the relevant program requirements
for provision of these services.
RHC and FQHC visits are typically evaluation and management (E/M) type of services
or screenings for certain preventive services. A list of qualifying visits for FQHCs is
located on the FQHC web page at https://www.cms.gov/Center/Provider-Type/Federally-
Qualified-Health-Centers-FQHC-Center.html.
40.1 – Location
(Rev. 11803; Issued: 01-26-23; Effective: 01-01-23; Implementation: 02-27-23)
RHC or FQHC visits may take place in:
• the RHC or FQHC,
• the patient’s residence (including an assisted living facility),
• a Medicare-covered Part A SNF (see Pub. 100-04, Medicare Claims Processing
Manual, chapter 6, section 20.1.1),
• the scene of an accident, or
• the location of the patient during a Hospice election, including a patient’s residence
or a Medicare certified facility
RHC and FQHC visits may not take place in:
• an inpatient or outpatient department of a hospital, including a CAH, or
• a facility which has specific requirements that preclude RHC or FQHC visits
(e.g., a Medicare comprehensive outpatient rehabilitation facility, a hospice
facility (except when the RHC/FQHC is furnishing hospice attending
physician services during a hospice election), etc.).
Qualified services provided to a RHC or FQHC patient are considered RHC or FQHC
services if:
• the practitioner is compensated by the RHC or FQHC for the services provided;
• the cost of the service is included in the RHC or FQHC cost report; and;
• other requirements for furnishing services are met.
This applies to full and part time practitioners, and it applies regardless of whether the
practitioner is an employee of the RHC or FQHC, working under contract to the RHC or
FQHC, or is compensated by the RHC or FQHC under another type of arrangement.
RHCs and FQHCs should have clear policies regarding the provision of services in other
locations and include this in a practitioner’s employment agreement or contract. RHCs
and FQHCs providing RHC or FQHC services in locations other than the RHC or FQHC
facility must continue to meet all certification and cost reporting requirements. Services
in other locations may be subject to review by the A/B MAC. RHC or FQHC services
furnished by an RHC or FQHC practitioner may not be billed separately by the RHC or
FQHC practitioner, or by another practitioner or an entity other than the RHC or FQHC,
even if the service is not a stand-alone billable visit. Services furnished to patients in any
type of hospital setting (inpatient, outpatient, or emergency department) are statutorily
excluded from the RHC/FQHC benefit and may not be billed by the RHC or FQHC.
40.2 - Hours of Operation
(Rev. 239, Issued: 01-09-18, Effective: 1-22-18, Implementation: 1-22-18)
RHCs and FQHCs are required to post their hours of operations at or near the entrance in a
manner that clearly states the days of the week and the hours that RHC or FQHC services are
furnished, and days of the week and the hours that the building is open solely for
administrative or other purposes, if applicable. This information should be easily readable,
including by people with vision problems and people who are in wheel chairs. Qualified
services provided to an RHC or FQHC patient other than during the posted hours of operation
are considered RHC or FQHC services when the practitioner is compensated by the RHC or
FQHC for the services provided, and when the cost of the service is included in the RHC’s cost
report.
Services furnished at times other than the RHC or FQHC posted hours of operation to
Medicare beneficiaries who are RHC or FQHC patients may not be billed to Medicare Part B if
the practitioner’s compensation for these services is included in the RHC/FQHC cost report.
(See Section 100 on Commingling).
This applies to full and part time practitioners, practitioners who are employees, practitioners
working under contract to the RHC or FQHC, and practitioners who are compensated by the
RHC or FQHC under another type of arrangement. RHCs and FQHCs should have clear
policies regarding the provision of services at other times, and include this in a practitioner’s
employment agreement or contract.
40.3 - Multiple Visits on Same Day
(Rev. 11803; Issued: 01-26-23; Effective: 01-01-23; Implementation: 02-27-23)
Except as noted below, encounters with more than one RHC or FQHC practitioner on the
same day, or multiple encounters with the same RHC or FQHC practitioner on the same
day, constitute a single RHC or FQHC visit and is payable as one visit. This policy applies
regardless of the length or complexity of the visit, the number or type of practitioners seen,
whether the second visit is a scheduled or unscheduled appointment, or whether the first visit
is related or unrelated to the subsequent visit. This would include situations where an RHC
or FQHC patient has a medically-necessary face-to-face visit with an RHC or FQHC
practitioner, and is then seen by another RHC or FQHC practitioner, including a specialist,

for further evaluation of the same condition on the same day, or is then seen by another
RHC or FQHC practitioner, including a specialist, for evaluation of a different condition on
the same day.
Exceptions are for the following circumstances only:
• The patient, subsequent to the first visit, suffers an illness or injury that requires
additional diagnosis or treatment on the same day (for example, a patient sees
their practitioner in the morning for a medical condition and later in the day has a
fall and returns to the RHC or FQHC). In this situation only, the FQHC would
use modifier 59 on the claim and the RHC would use modifier 59 or 25 to attest
that the conditions being treated qualify as 2 billable visits;
• The patient has a medical visit and a mental health visit on the same day (2
billable visits); or
• For RHCs only, the patient has an initial preventive physical exam (IPPE) and a
separate medical and/or mental health visit on the same day (2 or 3 billable visits).
NOTE: These exceptions do not apply to grandfathered tribal FQHCs.
40.4 - Global Billing
(Rev.239, Issued: 01-09-18, Effective: 1-22-18, Implementation: 1-22-18)
Surgical procedures furnished in an RHC or FQHC by an RHC or FQHC practitioner are
considered RHC or FQHC services. Procedures are included in the payment of an otherwise
qualified visit and are not separately billable. If a procedure is associated with a qualified visit,
the charges for the procedure go on the claim with the visit. Payment is included in the AIR
when the procedure is furnished in an RHC, and payment is included in the PPS methodology
when furnished in an FQHC. The Medicare global billing requirements do not apply to RHCs
and FQHCs, and global billing codes are not accepted for RHC or FQHC billing or payment.
Surgical procedures furnished at locations other than RHCs or FQHCs may be subject to
Medicare global billing requirements. If an RHC or FQHC furnishes services to a patient who
has had surgery elsewhere and is still in the global billing period, the RHC or FQHC must
determine if these services have been included in the surgical global billing. RHCs and
FQHCs may bill for a visit during the global surgical period if the visit is for a service not
included in the global billing package. If the service furnished by the RHC or FQHC was
included in the global payment for the surgery, the RHC or FQHC may not also bill for the
same service.
Services not included in the global surgical package are listed in Pub. 100-04, Medicare Claims
Processing Manual, chapter 12, section 40.1.B, and include, but are not limited to: initial
consultation by the surgeon to determine the need for major surgery; visits unrelated to the
diagnosis for which the surgical procedure is performed (unless the visit occurs due to
complications of the surgery); treatment for the underlying condition or an added course of
treatment which is not part of normal recovery from surgery; etc.
For additional information on global billing, see http://www.cms.gov/Regulations-and-
Guidance/Guidance/Manuals/downloads/clm104c12.pdf
40.5 - 3-Day Payment Window
(Rev.239, Issued: 01-09-18, Effective: 1-22-18, Implementation: 1-22-18)
Medicare’s 3-day payment window applies to outpatient services furnished by a hospital (or an
entity that is wholly owned or wholly operated by the hospital). The statute requires that
hospitals’ bundle the technical component of all outpatient diagnostic services and related non-
diagnostic services (e.g., therapeutic) with the claim for an inpatient stay when services are
furnished to a Medicare beneficiary in the 3 days (or, in the case of a hospital that is not a
subsection (d) hospital, during the 1-day) preceding an inpatient admission in compliance with
section 1886 of the Act.
RHCs and FQHC services are not subject to the Medicare 3- day payment window
requirements.
For additional information on the 3 day payment window, see http://www.cms.gov/Outreach-
and-Education/Medicare-Learning-Network-
MLN/MLNMattersArticles/downloads/MM7502.pdf
50 - RHC and FQHC Services
(Rev. 166, Issued: 01-31-13, Effective: 03-01-13, Implementation: 03-01-13)
50.1 - RHC Services
(Rev. 11803; Issued: 01-26-23; Effective: 01-01-23; Implementation: 02-27-23)
RHC services include:
• Physicians' services, as described in section 110;
• Services and supplies incident to a physician’s services, as described in section
120;
• Services of NPs, PAs, and CNMs, as described in section 130;
• Services and supplies incident to the services of NPs, PAs, and CNMs, as
described in section 140;
• CP and CSW services, as described in section 150;
• Services and supplies incident to the services of CPs, as described in section 160;
and
• Visiting nurse services to patients confined to the home, as described in section
190.
• Certain care management services, as described in section 230.
• Certain virtual communication services, as described in section 240.
RHC services also include certain preventive services when specified in statute or when
established through the National Coverage Determination (NCD) process and not
specifically excluded (see section 220 – Preventive Health Services). These services include:
• Influenza, Pneumococcal, Hepatitis B, COVID-19 vaccinations, and covered
monoclonal antibody products used as pre-exposure prophylaxis prevention of
COVID-19;
• IPPE;
• Annual Wellness Visit (AWV); and
• Medicare-covered preventive services recommended by the U.S. Preventive
Services Task Force (USPSTF) with a grade of A or B, as appropriate for the
09individual.
Influenza, pneumococcal and COVID-19 vaccines, and covered monoclonal antibody
products used as pre-exposure prophylaxis prevention of COVID-19 and their
administration are paid through the cost report, and payment for the hepatitis B vaccine
and its administration is included in an otherwise billable visit. The professional
component of the IPPE, AWV, and other qualified preventive services is paid based on
the AIR.
Note: Monoclonal antibody products used for the treatment or for post-exposure
prophylaxis of COVID-19 (when they are not purchased by the government) and their
administration are paid through the cost report until the end of the calendar year in which
the Emergency Use Authorization declaration for drugs and biological products with
respect to COVID-19 ends.
50.2 - FQHC Services
(Rev. 11803; Issued: 01-26-23; Effective: 01-01-23; Implementation: 02-27-23)
FQHC services include all of the RHC services listed in section 50.1 of this chapter.
While the following services may also be furnished in an RHC, the statute specifically
lists certain services as FQHC services, including but not limited to:
• Screening mammography;
• Screening pap smear and screening pelvic exam;
• Prostate cancer screening tests;
• Colorectal cancer screening tests;
• DSMT services;
• Diabetes screening tests;
• MNT services;
• Bone mass measurement;
• Screening for glaucoma;
• Cardiovascular screening blood tests; and
• Ultrasound screening for abdominal aortic aneurysm.
Influenza, pneumococcal and COVID-19 vaccines, and covered monoclonal antibody
products used as pre-exposure prophylaxis prevention of COVID-19 their administration
are paid through the cost report, and payment for the hepatitis B vaccine and its
administration is included in an otherwise billable visit. The professional component of the
IPPE, AWV, and other qualified preventive services is paid based on the lesser of the
FQHC’s charge or the PPS rate for the specific payment code, with an adjustment for IPPE
and AWV (see section 70.4 – FQHC Payment Codes).
Note: Monoclonal antibody products used for the treatment or for post-exposure prophylaxis
of COVID-19 (when they are not purchased by the government) and their administration are
paid through the cost report until the end of the calendar year in which the Emergency Use
Authorization declaration for drugs and biological products with respect to COVID-19 ends.
50.3 - Emergency Services
(Rev.239, Issued: 01-09-18, Effective: 1-22-18, Implementation: 1-22-18)
RHCs provide outpatient services that are typically furnished in a physician’s office or
outpatient clinic and generally provide only limited emergency care. Neither independent nor
hospital-based RHCs are subject to Emergency Medical Treatment and Active Labor Act
regulations. However, RHC practitioners are required to provide medical emergency
procedures as a first response to common life threatening injuries and acute illnesses and to
have available the drugs and biologicals commonly used in life-saving procedures. The
definition of a “first response” is a service that is commonly provided in a physician’s office.
If a patient presents at the RHC with an emergency when the RHC is not open for patient care
because a physician, NP, PA, CNM, CP, or CSW is not present, other staff may attend to the
patient until care of the individual can be transferred. Any care provided in this situation must
be within the individual’s ability, training, and scope of practice, and in accordance with state
laws, and would not be considered an RHC service.
During their regular hours of operations, FQHC practitioners are required to provide medical
procedures as a first response to common life threatening injuries and acute illnesses and to
have available the drugs and biologicals commonly used in life-saving procedures. After their
operating hours, FQHCs must provide telephone access to an individual who has the
qualifications and training to exercise professional judgment in assessing a patient’s need for
emergency medical care, and if appropriate, to refer the patient to an appropriate provider or
facility that is open.
Additional information on emergency preparedness requirements for RHCs and FQHCs can be
found 42 CFR 491.12.
60 - Non RHC/FQHC Services
(Rev.239, Issued: 01-09-18, Effective: 1-22-18, Implementation: 1-22-18)
RHCs and FQHCs must be primarily engaged in furnishing primary care services, but may also
furnish certain services that are beyond the scope of the RHC or FQHC benefit, such as
laboratory services or the technical component of an RHC or FQHC service. If these services
are authorized to be furnished by the RHC or FQHC and are covered under a separate
Medicare benefit category, the services must be billed separately (not by the RHC or FQHC) to
the appropriate A/B MAC under the payment rules that apply to the service. RHCs and
FQHCs must identify and remove from allowable costs on the Medicare cost report all costs
associated with the provision of non-RHC/FQHC services such as space, equipment, supplies,
facility overhead, and personnel.
60.1 - Description of Non RHC/FQHC Services
(Rev. 11803; Issued: 01-26-23; Effective: 01-01-23; Implementation: 02-27-23)
Certain services are not considered RHC or FQHC services either because they 1) are not
included in the RHC or FQHC benefit, or 2) are not a Medicare benefit. Non- RHC/FQHC
services include, but are not limited to:
Medicare excluded services - Includes routine physical checkups, dental care, hearing
tests, routine eye exams, etc. For additional information, see Pub. 100-02, Medicare
Benefit Policy Manual, Chapter 16, General Exclusions from Coverage, at
http://www.cms.gov/Regulations-and-
Guidance/Guidance/Manuals/downloads/bp102c16.pdf
Technical component of an RHC or FQHC service - Includes diagnostic tests such as x-
rays, electrocardiograms (EKGs), and other tests authorized by Medicare statute or the
NCD process. These services may be billed separately to the A/B MAC by the facility).
(The professional component is an RHC or FQHC service if performed by an RHC or
FQHC practitioner or furnished incident to an RHC or FQHC visit).
Laboratory services - Although RHCs and FQHCs are required to furnish certain
laboratory services (for RHCs see section 1861(aa)(2)(G) of the Act, and for FQHCs see
section 330(b)(1)(A)(i)(II) of the PHS Act), laboratory services are not within the scope of
the RHC or FQHC benefit. When clinics and centers separately bill laboratory services, the
cost of associated space, equipment, supplies, facility overhead and personnel for these
services must be adjusted out of the RHC or FQHC cost report. This does not include
venipuncture, which is included in the AIR when furnished in an RHC by an RHC
practitioner or furnished incident to an RHC service, and it is included in the per-diem
payment when furnished in an FQHC by an FQHC practitioner or furnished incident to an
FQHC service.
Durable medical equipment - Includes crutches, hospital beds, and wheelchairs used in
the patient’s place of residence, whether rented or purchased.
Ambulance services - The ambulance transport benefit under Medicare Part B covers a
medically necessary transport of a beneficiary by ambulance to the nearest appropriate
facility that can treat the patient's condition, and any other methods of transportation are
contraindicated. See https://www.cms.gov/Regulations-and-
Guidance/Guidance/Manuals/downloads/bp102c10.pdf for additional information on
covered ambulance services.
Prosthetic devices - Prosthetic devices are included in the definition of “medical and other
health services” in section 1861(s)(8) of the Act and are defined as devices (other than
dental) which replace all or part of an internal body organ (including colostomy bags and
supplies directly related to colostomy care), including replacement of such devices, and
including one pair of conventional eyeglasses or contact lenses furnished subsequent to each
cataract surgery with insertion of an intraocular lens. Other examples of prosthetic devices
include cardiac pacemakers, cochlear implants, electrical continence aids, electrical nerve
stimulators, and tracheostomy speaking valves.
Body Braces – Includes leg, arm, back, and neck braces and their replacements.
Practitioner services at certain other Medicare facility – Includes services furnished to
inpatients or outpatients in a hospital (including CAHs), ambulatory surgical center,
Medicare Comprehensive Outpatient Rehabilitation Facility, etc., or other facility whose
requirements preclude RHC or FQHC services. (NOTE: Covered services provided to a
Medicare beneficiary by an RHC or FQHC practitioner in a SNF may be an RHC or FQHC
service.)
Telehealth distant-site services - See section 200 of this chapter for additional
information on telehealth services in RHCs and FQHCs.
Hospice Services (with the exception of hospice attending physician services) – See
section 210 of this chapter for additional information on hospice services in RHCs and
FQHCs.
Group Services – Includes group or mass information programs, health education classes,
group therapy, or group education activities, including media productions and publications.
70 - RHC and FQHC Payment
(Rev. 252, Issued: 12-07-18, Effective: 01-01-19, Implementation: 01- 02-19)
RHCs and FQHCs must submit claims for RHC or FQHC services under the RHC or FQHC
payment methodologies and are not authorized to submit claims under the Physician Fee
Schedule (PFS) for RHC or FQHC services. Newly certified RHCs or FQHCs should work
with their A/B MAC to ensure that all claims filed for RHC or FQHC services are paid as RHC
or FQHC claims as of the date of their certification.
70.1 - RHC Payment
(Rev.239, Issued: 01-09-18, Effective: 1-22-18, Implementation: 1-22-18)
Medicare pays 80 percent of the RHC AIR, subject to a payment limit, for medically-necessary
medical, and qualified preventive, face- to- face (one-on-one) visits with an RHC practitioner
(as defined in section 30) for RHC services (as defined in section 50.1), unless otherwise
noted. The rate is subject to a payment limit, except for RHCs that have an exception to the
payment limit (see section 70.2). An interim rate for newly certified RHCs is established based
on the RHC’s anticipated average cost for direct and supporting services. At the end of the
reporting period, the A/B MAC determines the total payment due and reconciles payments
made during the period with the total payments due.
In general, the AIR for an RHC is calculated by the A/B MAC by dividing total allowable
costs by the total number of visits for all patients. Productivity, payment limits, and other
factors are also considered in the calculation. Allowable costs must be reasonable and
necessary and include practitioner compensation, overhead, equipment, space, supplies,
personnel, and other costs incident to the delivery of RHC services.
Services furnished incident to an RHC professional service are included in the AIR and are not
billed as a separate visit. The professional component of a procedure is usually a covered
service, but is not a stand-alone billable visit. The costs of covered services provided incident
to a billable visit may be included on the RHC cost report. To receive payment for qualified
services, HCPCS coding is required on all claims.
70.2 - RHC Payment Limit
(Rev. 11803; Issued: 01-26-23; Effective: 01-01-23; Implementation: 02-27-23)
Prior to April 1, 2021, the RHC payment limit was set by Congress in 1988 and was adjusted
annually based on the Medicare Economic Index (MEI). The payment limit was released
annually via Recurring Update Notifications.
Prior to April 1, 2021, a provider-based RHC that is an integral and subordinate part of a
hospital (including a CAH), as described in regulations at 42 CFR 413.65, could receive an
exception to the per- visit payment limit if:
• the hospital had fewer than 50 beds as determined at 42 CFR 412.105(b); or
• the hospital's average daily patient census count of those beds described in 42 CFR
412.105(b) did not exceed 40 and the hospital meets both of the following conditions:
o it was a sole community hospital as determined in accordance with 42 CFR 412.92
or an essential access community hospital as determined in accordance with 42 CFR
412.109(a), and
o it was located in a level 9 or level 10 Rural-Urban Commuting Area (RUCA). (For
additional information on RUCAs, see http://depts.washington.edu/uwruca/.
The exception to the payment limit applied only during the time that the RHC met the
requirements for the exception.
70.2.1 – Payment Limits Applicable to Independent RHCs, Provider-Based
RHCs in a Hospital with 50 or More Beds, and New RHCs
(Rev. 11803; Issued: 01-26-23; Effective: 01-01-23; Implementation: 02-27-23)
Beginning April 1, 2021, independent RHCs, provider-based RHCs in a hospital with 50
or more beds, and RHCs enrolled under Medicare on or after January 1, 2021 will
receive a prescribed national statutory payment limit per visit increase over an 8-year
period for each year from 2021 through 2028.
The national statutory payment limit for RHCs over the 8-year period is as follows:
● In 2021, after March 31, at $100 per visit;
● In 2022, at $113 per visit;

● In 2023, at $126 per visit;
● In 2024, at $139 per visit;
● In 2025, at $152 per visit;
● In 2026, at $165 per visit;
● In 2027, at $178 per visit; and
● In 2028, at $190 per visit.
Beginning in 2029 and each year thereafter the limit established for the previous year is
increased by the percentage increase in MEI applicable to primary care services furnished as
of the first day of such year.
We note that new RHCs are those that have submitted an application and are enrolled under
Medicare on or after January 1, 2021.
70.2.2 – Payment Limits Applicable to Provider-Based RHCs in a Hospital with
Less than 50 Beds
(Rev. 11803; Issued: 01-26-23; Effective: 01-01-23; Implementation: 02-27-23)
Beginning April 1, 2021, provider-based RHCs that meet a specified criteria are entitled to
special payment rules that establish a payment limit based on the provider-based RHC’s per
visit payment amount (or AIR) instead of the national statutory payment limit. For purposes of
this section of the manual, we use the term “specified” interchangeably with the term
“grandfathered” since those RHCs that meet the specified criteria are considered to be
“grandfathered” into the establishment of their payment limit per visit.
The specified criteria that an RHC must meet in order to be eligible for the special payment
rules are as follows:
• As of December 31, 2020, was in a hospital with less than 50 beds (not taking into account any
increase in the number of beds pursuant to a waiver during the Public Health Emergency
(PHE) for COVID-19); and one of the following circumstances:
o As of December 31, 2020, was enrolled in Medicare (including temporary enrollment during
the PHE for COVID-19); or
o Submitted an application for enrollment in Medicare (or a request for temporary enrollment
during the PHE for COVID-19) that was received not later than December 31, 2020.
Medicare Administrative Contractors (MACs) will calculate the payment limit per visit for
specified provider-based RHCs (that is, grandfathered RHCs) as discussed in sections
70.2.2.1 and 70.2.2.2 below.

A grandfathered provider-based RHC will lose this designation if the hospital does not
continue to have less than 50 beds. If this occurs, the provider-based RHC will be subject to
the statutory payment limit per visit applicable for such year for RHCs discussed in section
70.2.1 of this manual.
70.2.2.1 – Determining Payment Limits for Specified Provider-Based RHCs
with an AIR Established for RHC Services Furnished in 2020
(Rev. 11803; Issued: 01-26-23; Effective: 01-01-23; Implementation: 02-27-23)
Beginning April 1, 2021, specified provider-based RHCs that had a per visit payment amount
(that is, AIR) established for services furnished in 2020, the payment limit per visit shall be set
at an amount equal to the greater of:
1. the per visit payment amount applicable to such RHC for services furnished in 2020, increased
by the percentage increase in the MEI applicable to primary care services furnished as of the
first day of 2021; or
2. the national statutory payment limit for RHCs per visit (see section 70.2.1 of this chapter).
For subsequent years, the specified provider-based RHC’s payment limit per visit shall be
set at an amount equal to the greater of:
1. the payment limit per visit established for the previous year, increased by the percentage
increase in the MEI applicable to primary care services furnished as of the first day of
such subsequent year; or
2. the national statutory payment limit for RHCs (see section 70.2.1 of this chapter).
Note: For purposes of establishing the payment limit effective April 1, 2021 for specified
provider-based RHCs defined in section 1833(f)(3)(A)(i)(I) of the Act, that is, had an AIR
established for services furnished in 2020, MACs shall use the cost report ending in 2020 that
reports costs for 12-consecutive months. If the RHC does not have a 12-consecutive month cost
report ending in 2020, the MACs shall use the next available 12-consecutive month cost report
that reports costs for RHC services furnished in 2020. MACs should not combine cost report
data to equal a 12-consecutive month cost report.
70.2.2.2 – Determining Payment Limits for Specified Provider-Based RHCs
that did not have an AIR Established for RHC Services Furnished in 2020
(Rev. 11803; Issued: 01-26-23; Effective: 01-01-23; Implementation: 02-27-23)
Beginning April 1, 2021, specified provider-based RHCs that did not have a per visit payment
amount (that is, AIR) established for services furnished in 2020, the payment limit per visit
shall be at an amount equal to the greater of:
1. the per visit payment amount applicable to the provider-based RHC for services furnished in
2021; or
2. the national statutory payment limit for RHCs (see section 70.2.1 of this chapter).
For subsequent years, the provider-based RHCs payment limit per visit shall be set at an
amount equal to the greater of:
1. the payment limit per visit established for the previous year, increased by the percentage
increase in MEI applicable to primary care services furnished as of the first day of such
subsequent year; or
2. the national statutory payment limit for RHCs (see section 70.2.1 of this chapter).
Note: For purposes of establishing the payment limit effective April 1, 2021 for specified
provider-based RHCs defined in section 1833(f)(3)(A)(i)(II) of the Act (that is, those that
did not have an AIR established for services furnished in 2020), the MACs shall use the
cost report ending in 2021 that reports costs for 12 consecutive months. If the RHC does
not have a 12-consecutive month cost report ending in 2021, the MACs shall use the next
most-recent final settled cost report that reports cost for 12- consecutive months. MACs
should not combine cost report data to equal a 12-consecutive month cost report.
70.3 - FQHC PPS Payment Rate and Adjustments
(Rev.239, Issued: 01-09-18, Effective: 1-22-18, Implementation: 1-22-18)
Medicare pays 80 percent of the lesser of the FQHC’s charge or the FQHC PPS payment rate
for the specific payment code, unless otherwise noted. Except for grandfathered tribal FQHCs,
the FQHC PPS payment rate reflects a base rate that is the same for all FQHCs, a geographic
adjustment based on the location where services are furnished, and other applicable
adjustments as described below. The 2015 and 2016 FQHC PPS base rates were updated by
the MEI. Beginning in 2017, the FQHC PPS rate is updated annually by the FQHC market
basket. To receive payment for qualified services, HCPCS coding is required on all claims.
Geographic Adjustment: The PPS base rate is adjusted for each FQHC based on its location by
the FQHC Geographic Adjustment Factor (FQHC GAF). The PPS payment rate is the PPS
base rate multiplied by the FQHC GAF for the location where the service is furnished. Since
the FQHC GAF is based on where the services are furnished, the FQHC payment rate may
differ among FQHC sites within the same organization. FQHC GAFs are updated periodically
and can be found at: https://www.cms.gov/Center/Provider-Type/Federally-Qualified-Health-
Centers-FQHC-Center.html.
New Patient Adjustment: The PPS payment rate is adjusted by a factor of 1.3416 when an
FQHC furnishes care to a patient who is new to the FQHC. A new patient is someone who has
not received any Medicare-covered professional health service (medical or mental health) from
any site within the FQHC organization, or from any practitioner within the FQHC
organization, within the past 3 years from the date of service.
IPPE and AWV Adjustment: The PPS payment rate is adjusted by a factor of 1.3416 when an
FQHC furnishes an IPPE or an AWV to a Medicare beneficiary.
NOTE: These adjustments do not apply to grandfathered tribal FQHCs.
70.4 - FQHC Payment Codes
(Rev.239, Issued: 01-09-18, Effective: 1-22-18, Implementation: 1-22-18)
FQHCs set their own charges for services they provide and determine which services are
included in the bundle of services associated with each FQHC G code based on a typical
bundle of services that they would furnish per diem to a Medicare beneficiary. The FQHC
should maintain records of the services included in each FQHC G code and the charges
associated with the service at the time the service was furnished. Each FQHC decides what
documentation is appropriate to record the services included in each G-code pursuant to its
own determination. Charges must be reasonable and uniform for all patients, regardless of
insurance status. G code services and charges can be changed by the FQHC, but must be the
same for all patients and cannot be changed retrospectively.
FQHCs must include one or more of the FQHC payment codes listed below on claims to
receive payment for services furnished:
1. G0466 – FQHC visit, new patient: A medically-necessary medical, or a qualified preventive
health, face-to-face encounter (one-on-one) between a new patient (as defined in section 70.3),
and an FQHC practitioner during which time one or more FQHC services are rendered and
includes a typical bundle of Medicare-covered services that would be furnished per diem to a
patient receiving an FQHC visit.
2. G0467 – FQHC visit, established patient: A medically-necessary medical, or a qualifying
preventive health, face-to-face encounter (one-on-one) between an established patient and an
FQHC practitioner during which time one or more FQHC services are rendered and includes a
typical bundle of Medicare-covered services that would be furnished per diem to a patient
receiving an FQHC visit.
3. G0468 – FQHC visit, IPPE or AWV: An FQHC visit that includes an IPPE or AWV and
includes a typical bundle of Medicare-covered services that would be furnished per diem to a
patient receiving an IPPE or AWV.
4. G0469– FQHC visit, mental health, new patient: A medically-necessary, face-to-face
mental health encounter (one-on-one) between a new patient (as defined in section 70.3), and
an FQHC practitioner during which time one or more FQHC services are rendered and
includes a typical bundle of Medicare-covered services that would be furnished per diem to a
patient receiving a mental health visit.
5. G0470 – FQHC visit, mental health, established patient: A medically-necessary, face-to-
face mental health encounter (one-on-one) between an established patient and an FQHC
practitioner during which time one or more FQHC services are rendered and includes a typical
bundle of Medicare-covered services that would be furnished per diem to a patient receiving a
mental health visit.
80 - RHC and FQHC Cost Reports
(Rev. 220, Issued: 01-15-16, Effective: 02-01-16, Implementation: 02-01-16)
80.1 - RHC and FQHC Cost Report Requirements
(Rev. 11803; Issued: 01-26-23; Effective: 01-01-23; Implementation: 02-27-23)
RHCs are required to file a cost report annually in order to determine their payment rate
and reconcile interim payments, including adjustments for GME payments, bad debt, and
influenza, pneumococcal and COVID-19 vaccines, and covered monoclonal antibody
products used as pre-exposure prophylaxis prevention of COVID-19 and their
administration. If in its initial reporting period, the RHC submits a budget that estimates the
allowable costs and number of visits expected during the reporting period. The A/B MAC
calculates an interim rate based on a percentage of the per-visit limit, which is then adjusted
when the cost report is filed.

FQHCs are required to file a cost report annually and are paid for the costs of GME, bad
debt, and influenza, pneumococcal and COVID-19 vaccines, and covered monoclonal
antibody products used as pre-exposure prophylaxis prevention of COVID-19 and their
administration through the cost report. All FQHCs, including an FQHC that does not have
GME costs, bad debt, or costs associated with influenza, pneumococcal and COVID-19
vaccines, or covered monoclonal antibody products used as pre-exposure prophylaxis
prevention of COVID-19 and their administration, must file a cost report.
The RHC and FQHC cost reports were updated to reflect costs related to COVID-19 shots
and COVID-19 monoclonal antibody products and their administration.
Note: Until the end of the calendar year in which the Emergency Use Authorization (EUA)
declaration for drugs and biological products with respect to COVID-19 ends, CMS covers
and pays for these infusions or injections the same way it covers and pays for COVID-19
vaccines when furnished consistent with the EUA. That is, for RHCs and FQHCs COVID-19
monoclonal antibody products (when purchased from the manufacturer) and their
administration are paid at 100 percent of reasonable cost through the cost report. Effective
January 1 of the year following the year in which the EUA declaration ends, CMS will cover
and pay for monoclonal antibody products used for the treatment or for post-exposure
prophylaxis of COVID-19 in the same way we pay for other Part B drugs and biological
products. For RHCs, payment is through the All-Inclusive Rate and for FQHCs payment is
through the FQHC Prospective Payment System.
RHCs and FQHCs must maintain and provide adequate cost data based on financial and
statistical records that can be verified by qualified auditors.
RHCs and FQHCs are allowed to claim bad debts in accordance with 42 CFR 413.89.
RHCs may claim unpaid coinsurance and deductible, and FQHCs may claim unpaid
coinsurance. RHCs and FQHCs that claim bad debt must establish that reasonable efforts
were made to collect these amounts Coinsurance or deductibles that are waived, either due
to a statutory waiver or a sliding fee scale, may not be claimed.
80.2 - RHC and FQHC Consolidated Cost Reports
(Rev. 11803; Issued: 01-26-23; Effective: 01-01-23; Implementation: 02-27-23)
RHCs and FQHCs with more than one site may file consolidated cost reports if approved by
the A/B MAC in advance of the reporting period for which the consolidated report is to be
used. Once having elected to use a consolidated cost report, the RHC or FQHC may not
revert to individual reporting without the prior approval of the A/B MAC.
New RHCs (enrolled under section 1866(j) of the Act on or after January 1, 2021) are
permitted to file consolidated cost reports with:
• New RHCs that are provider-based,
• New RHCs that are independent,
• Existing independent RHCs, and/or
• Existing provider-based RHCs that are in a hospital that has more than 50 beds.
In addition, specified provider-based RHCs are not allowed to file a consolidated cost
report with a new RHC.
80.3 – RHC and FQHC Cost Report Forms
(Rev. 11803; Issued: 01-26-23; Effective: 01-01-23; Implementation: 02-27-23)
RHCs and FQHCs use one of the following cost report forms:
Independent RHCs and Freestanding FQHCs:
RHCs: Form CMS-222-17, Independent Rural Health Clinic Cost Report.
FQHCs: Form CMS-224-14, Federally Qualified Health Center Cost Report.
Provider-based RHCs and FQHCs:
Hospital-based RHCs: Worksheet M of Form CMS-2552-10, Hospital and Hospital Care
Complex Cost Report.
Hospital-based FQHCs: Worksheet N of Form CMS-2552-10, Hospital and Hospital Care
Complex Cost Report.
Skilled Nursing Facility based: Worksheet I series of form CMS-2540-10, “Skilled Nursing
Facility and Skilled Nursing Facility Health Care Complex Cost Report”.
Information on these cost report forms is found in Chapters 44 and 46; and 40 and 41,
respectively, of the “Provider Reimbursement Manual - Part 2” (Publication 15-2), which
can be located on the CMS Website at http://www.cms.gov/Regulations-and-
Guidance/Guidance/Manuals/Paper-Based-Manuals.html.
the patient’s condition without the interposition of a third person’s judgment. Direct
visualization includes review of the patient’s X-rays, EKGs, tissue samples, etc.
Except for services that meet the criteria for authorized care management or virtual
communications services, telephone or electronic communication between a physician and
a patient, or between a physician and someone on behalf of a patient, are considered
physicians’ services and are included in an otherwise billable visit. They do not constitute
a separately billable visit.
Qualified services furnished at an RHC or FQHC or other authorized site by an RHC or
FQHC physician are payable only to the RHC or FQHC. RHC and FQHC physicians are
paid according to their employment agreement or contract (where applicable).
80.4 – RHC Productivity Standards
(Rev.239, Issued: 01-09-18, Effective: 1-22-18, Implementation: 1-22-18)
Productivity standards are used to help determine the average cost per patient for Medicare
reimbursement in RHCs. The current productivity standards require 4,200 visits per full-time
equivalent physician and 2,100 visits per full-time equivalent non-physician practitioner (NP,
PA, or CNM). Physician and non-physician practitioner productivity may be combined. The
FTE on the cost report for providers is the time spent seeing patients or scheduled to see
patients and does not include administrative time.
The A/B MAC has the discretion to make an exception to the productivity standards based on
individual circumstances. All visits (Medicare, Medicaid, Managed Care, etc.) are included in
determining the productivity standards for the cost report.
At the end of the cost reporting year, the A/B MAC re-calculates the AIR by dividing the total
allowable costs across all patient types (i.e., the numerator) by the number of visits (as defined
in section 40) for all patient types (i.e., the denominator). If fewer than expected visits based
on the productivity standards have been furnished, the A/B MAC substitutes the expected
number of visits for the denominator and uses that instead of the actual number of visits. The
total allowable costs (numerator) would be divided by the higher, expected number of visits
(denominator). In this example, this would have the effect of lowering the AIR.
Physician services that are provided on a short term or irregular basis under agreements are not
subject to the productivity standards. Instead of the productivity limitation, purchased
physician services are subject to a limitation on what Medicare would otherwise pay for the
services under the Physician Fee Schedule (PFS), in accordance with 42 CFR
405.2468(d)(2)(v). Practitioners working on a regular, ongoing basis are subject to the
productivity standards, regardless of whether they are paid as an employee or independent
contractor.
FQHCs are not subject to the productivity standards.
90 - RHC and FQHC Charges, Coinsurance, Deductible, and Waivers
(Rev. 252, Issued: 12-07-18, Effective: 01-01-19, Implementation: 01- 02-19)
Except for certain preventive services for which the coinsurance is statutorily waived, the
beneficiary in an RHC must pay the deductible and coinsurance amount, and the beneficiary in
an FQHC must pay the coinsurance amount (there is no Part B deductible in FQHCs for
FQHC-covered services). For RHCs, the coinsurance is 20 percent of the total charges. For
FQHCs, the coinsurance is 20 percent of the lesser of the FQHC’s charge for the specific
payment code or the PPS rate. For claims with a mix of waived and non-waived services,
applicable coinsurance and deductibles are assessed only on the non-waived services. For both
RHCs and FQHCs, coinsurance for care management and virtual communication services is 20
percent of the lesser of submitted charges or the payment rate.
90.1 - Charges and Waivers
(Rev. 220, Issued: 01-15-16, Effective: 02-01-16, Implementation: 02-01-16)
Charges for services furnished to Medicare beneficiaries must be the same as the charges for
non-Medicare beneficiaries. FQHCs may waive collection of all or part of the copayment,
depending on the beneficiary’s ability to pay. RHCs may waive the copayment and deductible
after a good faith determination has been made that the patient is in financial need, provided
the waivers are not routine and not advertised. (See 42 U.S.C. 1320a-7a(6)(A))
90.2 - Sliding Fee Scale
(Rev. 239, Issued: 01-09-18, Effective: 1-22-18, Implementation: 1-22-18)
RHCs may establish a sliding fee scale if it is uniformly applied to all patients. An RHC that
chooses to offer a sliding fee scale must post the policy so that all patients are aware of the
policy. If the payment policy is based on an individual’s income, the RHC must document that
income information from the patient was obtained in order to determine that the patient
qualified. Copies of their wage statement or income tax return are not required, and self-
attestations are acceptable.
FQHCs that are approved by HRSA are required to establish a sliding fee scale in accordance
with statutory and HRSA requirements.
100 – Commingling
(Rev. 239, Issued: 01-09-18, Effective: 1-22-18, Implementation: 1-22-18)
Commingling refers to the sharing of RHC or FQHC space, staff (employed or contracted),
supplies, equipment, and/or other resources with an onsite Medicare Part B or Medicaid fee-
for-service practice operated by the same RHC or FQHC physician(s) and/or non-physician(s)
practitioners. Commingling is prohibited in order to prevent:
• Duplicate Medicare or Medicaid reimbursement (including situations where the RHC
or FQHC is unable to distinguish its actual costs from those that are reimbursed on a
fee-for-service basis), or
• Selectively choosing a higher or lower reimbursement rate for the services.
RHC and FQHC practitioners may not furnish or separately bill for RHC or FQHC-covered
professional services as a Part B provider in the RHC or FQHC, or in an area outside of the
certified RHC or FQHC space such as a treatment room adjacent to the RHC or FQHC, during
RHC or FQHC hours of operation.
If an RHC or FQHC practitioner furnishes an RHC or FQHC service at the RHC or FQHC
during RHC or FQHC hours, the service must be billed as an RHC or FQHC service. The
service cannot be carved out of the cost report and billed to Part B.
If an RHC or FQHC is located in the same building with another entity such as an unaffiliated
medical practice, x-ray and lab facility, dental clinic, emergency room, etc., the RHC or FQHC
space must be clearly defined. If the RHC or FQHC leases space to another entity, all costs
associated with the leased space must be carved out of the cost report.
RHCs and FQHCs that share resources (e.g., waiting room, telephones, receptionist, etc.) with
another entity must maintain accurate records to assure that all costs claimed for Medicare
reimbursement are only for the RHC or FQHC staff, space, or other resources. Any shared
staff, space, or other resources must be allocated appropriately between RHC or FQHC and
non-RHC or non-FQHC usage to avoid duplicate reimbursement.
This commingling policy does not prohibit a provider-based RHC from sharing its health care
practitioners with the hospital emergency department in an emergency, or prohibit an RHC
practitioner from providing on-call services for an emergency room, as long as the RHC would
continue to meet the RHC conditions for coverage even if the practitioner were absent from the
facility. The RHC must be able to allocate appropriately the practitioner's salary between RHC
and non-RHC time. It is expected that the sharing of the practitioner with the hospital
emergency department would not be a common occurrence.
The A/B MAC has the authority to determine acceptable accounting methods for allocation of
costs between the RHC or FQHC and another entity. In some situations, the practitioner’s
employment agreement will provide a useful tool to help determine appropriate accounting.
110 - Physician Services
(Rev. 252, Issued: 12-07-18, Effective: 01-01-19, Implementation: 01- 02-19)
The term “physician” includes a doctor of medicine, osteopathy, dental surgery, dental
medicine, podiatry, optometry, or chiropractic who is licensed and practicing within the
licensee’s scope of practice, and meets other requirements as specified.
Physician services are professional services furnished by a physician to an RHC or FQHC
patient and include diagnosis, therapy, surgery, and consultation. The physician must either
examine the patient in person or be able to visualize directly some aspect of the patient’s
condition without the interposition of a third person’s judgment. Direct visualization includes
review of the patient’s X-rays, EKGs, tissue samples, etc.
Except for services that meet the criteria for authorized care management or virtual
communications services, telephone or electronic communication between a physician and a
patient, or between a physician and someone on behalf of a patient, are considered physicians’
services and are included in an otherwise billable visit. They do not constitute a separately
billable visit.
Qualified services furnished at an RHC or FQHC or other authorized site by an RHC or FQHC
physician are payable only to the RHC or FQHC. RHC and FQHC physicians are paid
according to their employment agreement or contract (where applicable).
110.1 - Dental, Podiatry, Optometry, and Chiropractic Services
(Rev. 239, Issued: 01-09-18, Effective: 1-22-18, Implementation: 1-22-18)
Dentists, podiatrists, optometrists, and chiropractors are defined as physicians in Medicare
statute, and qualified services furnished by physicians are billable visits in an RHC or FQHC.
These practitioners can provide RHC or FQHC services that are within their scope of practice
and not excluded from coverage (e.g., Medicare coverage of chiropractic services is limited to
manual manipulation of the spine for a demonstrated subluxation).
An RHC or FQHC can bill for a face-to-face, medically necessary visit furnished by a dentist,
podiatrist, optometrist, or chiropractor if the service furnished is a qualifying visit for RHCs or
FQHCs and all other requirements are met. All services furnished must be within the state
scope of practice for the practitioner, and all HCPCS codes must reflect the actual services that
were furnished.

RHCs and FQHCs are required to primarily provide primary health care. Since dentists,
podiatrists, optometrists, and chiropractors are not considered primary care physicians, they do
not meet the requirements to be either i) a physician medical director or ii) the physician or
non-physician practitioner (NP, PA, or CNM) that must be available at all times the clinic is
open. Therefore, a dentist, podiatrist, optometrist, or chiropractor can provide a medically
necessary, face-to-face visit with an RHC or FQHC patient only when the statutory and
regulatory staffing requirements are otherwise met.
For additional information on these services, see Pub. 100-02, Medicare Benefit Policy
Manual, chapter 15 on Covered Medical and Other Health Service at
http://www.cms.gov/Regulations-and-Guidance/Guidance/Manuals/Downloads/bp102c15.pdf.
110.2 - Treatment Plans or Home Care Plans
(Rev. 239, Issued: 01-09-18, Effective: 1-22-18, Implementation: 1-22-18)
Except for comprehensive care plans that are a component of authorized care management
services (see section 230), treatment plans and home care oversight provided by RHC or
FQHC physicians to RHC or FQHC patients are considered part of the RHC or FQHC visit and
are not a separately billable service.
110.3 - Graduate Medical Education
(Rev. 263, Issued: Effective: 01-01-20, Implementation: 01-23-20)
Freestanding RHCs and FQHCs may receive direct graduate medical education (GME)
payment for residents if the RHC or FQHC incurs the salaries and fringe benefits (including
travel and lodging expenses where applicable) of residents training at the RHC or FQHC.
Allowable costs incurred by the RHC or FQHC for GME are paid on a reasonable cost basis
and are not subject to the payment limit. RHCs and FQHCs may claim allowable costs only
while residents are on their RHC or FQHC rotation.
RHCs and FQHCs that are receiving GME payment may not separately bill for an RHC or
FQHC visit provided by a resident, as the cost of these practitioners is included in the GME
payment. A medically-necessary medical, or a qualifying preventive health, face-to-face
encounter with a teaching physician who is an RHC or FQHC practitioner may be a billable
visit if applicable teaching physician supervision and documentation requirements are met.
Under Pub. 100-04, Chapter 12, section 100.1.1.C., the Primary Care Exception (PCE) only
applies in an outpatient department or an ambulatory setting where a hospital is claiming on the
cost report the residents for indirect medical education and direct GME purposes. Therefore,
in the instance where the RHC or FQHC is incurring the cost of the resident(s), the PCE would
not apply.
For additional information see 42 CFR 405.2468 (f) and 42 CFR 413.75(b).
120 - Services and Supplies Furnished “Incident to” Physician’s Services
(Rev. 239, Issued: 01-09-18, Effective: 1-22-18, Implementation: 1-22-18)
“Incident to” refers to services and supplies that are an integral, though incidental, part of the
physician’s professional service and are:
• Commonly rendered without charge and included in the RHC or FQHC payment;
• Commonly furnished in an outpatient clinic setting;
• Furnished under the physician’s direct supervision; except for authorized care
management services which may be furnished under general supervision; and
• Furnished by RHC or FQHC auxiliary personnel.
Incident to services and supplies include:
• Drugs and biologicals that are not usually self-administered, and Medicare-covered
preventive injectable drugs (e.g., influenza, pneumococcal);
• Venipuncture;
• Bandages, gauze, oxygen, and other supplies; or
• Services furnished by auxiliary personnel such as a nurse, medical assistant, or other
clinical personnel acting under the supervision of the physician.
Supplies and drugs that must be billed to the DME MAC or to Part D are not included.
NOTE: Payment for Medicare-covered Part B drugs that are not usually self-administered and
are furnished by an RHC or FQHC practitioner to a Medicare patient are included in the RHC
AIR or the FQHC’s PPS per diem payment. However, Section 1861(s)(2)(G) of the Act
provides an exception for RHCs when a physician prepares a specific formulation of an antigen
for a patient if the antigen is “forwarded to another qualified person (including a rural health
clinic) for administration to such patient…, by or under the supervision of another such
physician.” An RHC practitioner (physician, NP, PA, or CNM) acting within their scope of
practice may administer the drug and the cost of the administration may be included on the
RHC's cost report as an allowable expense. The cost of the antigen prepared by a physician
outside of the RHC is not included in the RHC AIR. Physicians who prepare an antigen that is
forwarded to an RHC should submit a claim for the antigen in accordance with instructions
from the contractor that processes their Part B claims and applicable CMS requirements.
120.1 - Provision of Incident to Services and Supplies
(Rev. 263, Issued: Effective: 01-01-20, Implementation: 01-23-20)
Incident to services and supplies can be furnished by auxiliary personnel. All services and
supplies provided incident to a physician’s visit must result from the patient’s encounter with
the physician and be furnished in a medically appropriate timeframe. More than one incident
to service or supply can be provided as a result of a single physician visit.
Incident to services and supplies must be provided by someone who has an employment
agreement or a direct contract with the RHC or FQHC to provide services. Services or
supplies provided by individuals who are not employed by or under direct contract with the
RHC or FQHC, even if provided on the physician’s order or included in the RHC or FQHC’s
bill, are not covered as incident to a physician’s service. Services that are not considered
incident to include the services of an independently practicing therapist who forwards his/her
bill to the RHC or FQHC for inclusion in the entity’s statement of services, services provided
by an independent laboratory or a hospital outpatient department, services furnished by a nurse,
medical assistant, or other auxiliary personnel who is not an employee of or working under
contract to the RHC or FQHC, including services provided by a third party under contract, etc.
Services and supplies furnished incident to physician’s services are limited to situations in
which there is direct physician supervision of the person performing the service, except for
authorized care management services (as described in section 230) which may be furnished
under general supervision. Direct supervision does not require the physician to be present in
the same room. However, the physician must be in the RHC or FQHC and immediately
available to provide assistance and direction throughout the time the incident to service or
supply is being furnished.
When services and supplies are furnished incident to an RHC or FQHC visit, payment for the
services are included in the RHC AIR or the FQHC PPS rate. An encounter that includes only
an incident to service(s) is not a stand-alone billable visit for RHCs or FQHCs.
120.2 - Incident to Services and Supplies Furnished in the Patient’s Home or
Location Other than the RHC or FQHC
(Rev. 239, Issued: 01-09-18, Effective: 1-22-18, Implementation: 1-22-18)
Except for authorized care management services, services furnished incident to a physician’s
visit by RHC or FQHC auxiliary personnel in the patient’s home or location other than the
RHC or FQHC must have direct supervision by the physician. For example, if an RHC or
FQHC nurse accompanies the physician to a patient’s home and administers an injection, the
nurse’s services would be considered incident to the physician’s visit. If the same nurse makes
the call alone and administers an injection, the services are not incident to services since the
physician is not providing direct supervision. The availability of the physician by telephone
and the presence of the physician somewhere in the building does not constitute direct
supervision. (This rule applies only to the incident to provision. It does not apply to visiting
nursing services described in section 190.) For additional information on supervision
requirements for Part B services incident to physician services see Pub. 100-02, Medicare
Benefit Policy Manual, chapter 15, section 60.1.
120.3 - Payment for Incident to Services and Supplies
(Rev. 239, Issued: 01-09-18, Effective: 1-22-18, Implementation: 1-22-18)
Services that are covered by Medicare but do not meet the requirements for a medically
necessary or qualified preventive health visit with an RHC or FQHC practitioner (e.g., blood
pressure checks, allergy injections, prescriptions, nursing services, etc.) are considered incident
to services. The cost of providing these services may be included on the cost report, but the
provision of these services does not generate a billable visit. Incident to services provided on a
different day as the billable visit may be included in the charges for the visit if furnished in a
medically appropriate timeframe.
Incidental services or supplies must represent an expense incurred by the RHC or FQHC. For
example, if a patient purchases a drug and the physician administers it, the cost of the drug is
not covered and cannot be included on the cost report.
If a Medicare-covered Part B drug is furnished by an RHC or FQHC practitioner to a Medicare
patient as part of a billable visit, the cost of the drug and its administration is included in the
RHC’s AIR or the FQHC’s PPS payment. RHCs and FQHCs cannot bill separately for Part B
drugs or other incident to services or supplies.
130 - Nurse Practitioner, Physician Assistant, and Certified Nurse Midwife
Services
(Rev. 252, Issued: 12- 07-18, Effective: 01-01-19, Implementation: 01- 02-19)
Professional services furnished by an NP, PA, or CNM to an RHC or FQHC patient are
services that would be considered covered physician services under Medicare (see section
110), and which are permitted by state laws and RHC or FQHC policies. Services may include
diagnosis, treatment, and consultation. The NP, PA, or CNM must directly examine the
patient, or directly review the patient’s medical information such as X-rays, EKGs and
electroencephalograms, tissue samples, etc. Except for services that meet the criteria for
authorized care management or virtual communication services, telephone or electronic
communication between an NP, PA, or CNM and a patient, or between such practitioner and
someone on behalf of a patient, are considered NP, PA, or CNM services, and are included in
an otherwise billable visit. They do not constitute a separately billable visit.
130.1 - NP, PA, and CNM Requirements
(Rev. 220, Issued: 01-15-16, Effective: 02-01-16, Implementation: 02-01-16)
Services performed by NPs, PAs, and CNMs must be:
• Furnished under the general (or direct, if required by state law) medical supervision of a
physician;
• Furnished in accordance with RHC or FQHC policies and any physician medical orders
for the care and treatment of a patient;
• A type of service which the NP, PA, or CNM who furnished the service is legally
permitted to furnish by the state in which the service is rendered;
• Furnished in accordance with state restrictions as to setting and supervision;
• Furnished in accordance with written RHC or FQHC policies that specify what services
these practitioners may furnish to patients; and
• A type of service which would be covered under Medicare if furnished by a physician.
130.2 - Physician Supervision
(Rev. 220, Issued: 01-15-16, Effective: 02-01-16, Implementation: 02-01-16)
RHCs and FQHCs which are not physician-directed must have an arrangement with a
physician that provides for the supervision and guidance of NPs, PAs, and CNMs. The
arrangement must be consistent with state law.
130.3 - Payment to Physician Assistants
(Rev. 239, Issued: 01-09-18, Effective: 1-22-18, Implementation: 1-22-18)
Section 1842(b)(6)(C) of the Act prohibits PAs from enrolling in and being paid directly for
Part B services. The only exception to this is found in Section 4205(d)(3)(B) of the Balanced
Budget Act (BBA), which amended Section 1842(b)(6)(C) of the Act to allow Medicare to
directly pay a PA when the PA was the owner of an RHC for a continuous period beginning
before the date of the enactment of the BBA, and ending on the date the Secretary determines
the RHC no longer meets the requirements of Section 1861(aa)(2) of the Act.
140 - Services and Supplies Furnished Incident to NP, PA, and CNM
Services
(Rev. 239, Issued: 01-09-18, Effective: 1-22-18, Implementation: 1-22-18)
Services and supplies that are integral, though incident to an NP, PA, or CNM service are:
• Commonly rendered without charge or included in the RHC or FQHC payment
• Commonly furnished in an outpatient clinic setting;
• Furnished under the direct supervision of an NP, PA, or CNM, except for authorized
care management services which may be furnished under general supervision; and
• Furnished by a member of the RHC or FQHC staff.
NOTE: The direct supervision requirement is met in the case of an NP, PA, or CNM who
supervises the furnishing of the service only if such a person is permitted to exercise such
supervision under the written policies governing the RHC or FQHC.
Services and supplies covered under this provision are generally the same as described in
section 120 as incident to a physician’s services and include services and supplies incident to
the services of an NP, PA, or CNM.
150 - Clinical Psychologist (CP) and Clinical Social Worker (CSW) Services
(Rev. 252, Issued: 12- 07-18, Effective: 01-01-19, Implementation: 01- 02-19)
A CP is an individual who:
• Holds a doctoral degree in psychology, and
• Is licensed or certified, on the basis of the doctoral degree in psychology, by the state in
which he or she practices, at the independent practice level of psychology to furnish
diagnostic, assessment, preventive, and therapeutic services directly to individuals.
A CSW is an individual who:
• Possesses a master’s or doctor’s degree in social work;
• After obtaining the degree, has performed at least 2 years of supervised clinical social
work; and
• Is licensed or certified as a clinical social worker by the state in which the services are
performed; or, in the case of an individual in a state that does not provide for licensure
or certification, meets the requirements listed in 410.73(a)(3)(i) and (ii).
Services may include diagnosis, treatment, and consultation. The CP or CSW must directly
examine the patient, or directly review the patient’s medical information. Except for services
that meet the criteria for authorized care management or virtual communication services,
telephone or electronic communication between a CP or CSW and a patient, or between such
practitioner and someone on behalf of a patient, are considered CP or CSW services and are
included in an otherwise billable visit. They do not constitute a separately billable visit.
CSWs are statutorily authorized (1861(hh)(2) of the Act) to furnish services for the diagnosis
and treatment of mental illnesses only.
Services that are covered are those that are otherwise covered if furnished by a physician or as
incident to a physician’s professional service. Services that a hospital or SNF is required to
provide to an inpatient or outpatient as a requirement for participation are not included.
Services performed by CPs and CSWs must be:
• Furnished in accordance with RHC or FQHC policies and any physician medical orders
for the care and treatment of a patient;
• A type of service which the CP or CSW who furnished the service is legally permitted
to furnish by the state in which the service is rendered; and
• Furnished in accordance with state restrictions as to setting and supervision, including
any physician supervision requirements.
160 - Services and Supplies Incident to CP and CSW Services
(Rev. 252, Issued: 12-07-18, Effective: 01-01-19, Implementation: 01- 02-19)
Services and supplies that are integral, though incident to a CP or CSW service are:
• Commonly rendered without charge or included in the RHC or FQHC payment;
• Commonly furnished in an outpatient clinic setting;
• Furnished under the direct supervision of the CP or CSW, except for authorized care
management services which may be furnished under general supervision; and
• Furnished by a member of the RHC or FQHC staff.
NOTE: The direct supervision requirement is met in the case of a CP or CSW who supervises
the furnishing of the service only if such a person is permitted to exercise such supervision
under the written policies governing the RHC or FQHC. Services and supplies covered under
this provision are generally the same as described in section 120 as incident to a physician’s
services and include services and supplies incident to the services of a CP or CSW.
170 - Mental Health Visits
(Rev. 11803; Issued: 01-26-23; Effective: 01-01-23; Implementation: 02-27-23)
A mental health visit is a medically-necessary face-to-face encounter between an RHC or
FQHC patient and an RHC or FQHC practitioner during which time one or more RHC or
FQHC mental health services are rendered. Effective January 1, 2022, a mental health
visit is a face-to-face encounter or an encounter furnished using interactive, real-time,
audio and video telecommunications technology or audio-only interactions in cases where
the patient is not capable of, or does not consent to, the use of video technology for the
purposes of diagnosis, evaluation or treatment of a mental health disorder.
The CAA, 2023 extends the telehealth policies of the CAA, 2022 through December 31, 2024 if
the PHE ends prior to that date
. The in-person visit requirements for mental health telehealth
services and mental health visits furnished by RHCs and FQHCs begin on January 1, 2025 if
the PHE ends prior to that date.
There must be an in-person mental health service furnished
within 6 months prior to the furnishing of the mental health service furnished via
telecommunications and that an in-person mental health service (without the use of
telecommunications technology) must be provided at least every 12 months while the
beneficiary is receiving services furnished via telecommunications technology for
diagnosis, evaluation, or treatment of mental health disorders, unless, for a particular 12-
month period, the physician or practitioner and patient agree that the risks and burdens
outweigh the benefits associated with furnishing the in-person item or service, and the
practitioner documents the reasons for this decision in the patient’s medical record.
RHCs and FQHCs are instructed to append modifier 95 (Synchronous Telemedicine
Service Rendered via Real-Time Interactive Audio and Video Telecommunications System)
in instances where the mental health visit was furnished using audio-video communication
technology and to append modifier 93 (Synchronous Telemedicine Service Rendered Via
Telephone or Other Real-Time Interactive Audio-Only Telecommunications System) in
cases where the service was furnished using audio-only communication.
Mental health services that qualify as stand-alone billable visits in an FQHC are listed on
the FQHC center website, http://www.cms.gov/Center/Provider-Type/Federally-Qualified-
Health-Centers-FQHC- Center.html. Services furnished must be within the practitioner’s
state scope of practice.
Medicare-covered mental health services furnished incident to an RHC or FQHC visit are
included in the payment for a medically necessary mental health visit when an RHC or
FQHC practitioner furnishes a mental health visit. Group mental health services do not
meet the criteria for a one-one-one, face-to-face encounter in an FQHC or RHC.
A mental health service should be reported using a valid HCPCS code for the service
furnished, a mental health revenue code, and for FQHCs, an appropriate FQHC mental
health payment code. For detailed information on reporting mental health services and
claims processing, see Pub. 100-04, Medicare Claims Processing Manual, chapter 9,
http://www.cms.gov/Regulations-and-
Guidance/Guidance/Manuals/downloads/clm104c09.pdf
Medication management, or a psychotherapy “add on” service, is not a separately billable
service in an RHC or FQHC and is included in the payment of an RHC or FQHC medical
visit. For example, when a medically-necessary medical visit with an RHC or FQHC
practitioner is furnished, and on the same day medication management or a psychotherapy
add on service is also furnished by the same or a different RHC or FQHC practitioner, only
one payment is made for the qualifying medical services reported with a medical revenue
code. For FQHCs, an FQHC mental health payment code is not required for reporting
medication management or a psychotherapy add on service furnished on the same day as a
medical service.
180 - Physical Therapy, Occupational Therapy, and Speech Language
Pathology Services
(Rev. 263, Issued: Effective: 01-01-20, Implementation: 01-23-20)
Physical Therapy (PT), Occupational Therapy (OT), and Speech Language Pathology (SLP)
services may be provided in the RHC or FQHC directly by a physician, NP, or PA, if included
in the practitioner’s scope of practice. A physician, NP, or PA may also supervise the
provision of PT, OT, and SLP services provided incident to their professional services in the
RHC or FQHC by a PT, OT, or SLP therapist. PT, OT, and SLP therapists who provide
services incident to a physician, NP, or PA visit may be an employee of the RHC or FQHC or
contracted to the RHC or FQHC. PT, OT, and SLP services furnished by an RHC or FQHC
practitioner or furnished incident to a visit with an RHC or FQHC practitioner are not billable
visits.
If the services are furnished on a day when no otherwise billable visit has occurred, the PT,
OT, or SLP service provided incident to the visit would become part of the cost of operating
the RHC or FQHC. The cost would be included in the costs claimed on the cost report and
there would be no billable visit.
190 - Visiting Nursing Services
(Rev. 220, Issued: 01-15-16, Effective: 02-01-16, Implementation: 02-01-16)
190.1 - Description of Visiting Nursing Services
(Rev. 239, Issued: 01-09-18, Effective: 1-22-18, Implementation: 1-22-18)
A visiting nurse provides skilled nursing services. The determination of whether a service
requires the skills of a nurse is based on the complexity of the service (e.g., intravenous and
intramuscular injections or insertion of catheters), the condition of the patient (e.g., a non-
skilled service that, because of the patient’s condition, can only be safely and effectively
provided by a nurse), and accepted standards of medical and nursing practice. All services
must be reasonable and necessary to the diagnosis and treatment of the patient’s illness or
injury within the context of the patient’s unique medical condition.
A service that can be safely and effectively self-administered or performed by a nonmedical
person without the direct supervision of a nurse, is not considered a skilled nursing service,
even if provided by a nurse.
A service which, by its nature, requires the skills of a nurse to be provided safely and
effectively continues to be a skilled service even if it is taught to the patient, the patient’s
family, or other caregivers. If a patient needs skilled nursing care and there is no one trained or
able and willing to provide it, the services of a nurse would be reasonable and necessary to the
treatment of the illness or injury.

The determination of whether visiting nurse services are reasonable and necessary is made by
the physician based on the condition of the patient when the services were ordered and what is
reasonably expected to be appropriate treatment for the illness or injury throughout the
certification period.
190.2 - Requirements for Furnishing Visiting Nursing Service
(Rev. 252, Issued: 12- 07-18, Effective: 01-01-19, Implementation: 01- 02-19)
RHCs and FQHCs are paid for visiting nursing services when G0490 is on an RHC or FQHC
claim and all of the following requirements are met:
• The patient is considered confined to the home as defined in section 1835(a) of the Act
and the Medicare Benefit Policy Manual, Chapter 7 (see http://www.cms.gov/Regulations-
and-Guidance/Guidance/Manuals/downloads/bp102c07.pdf;
• The RHC or FQHC is located in an area that has a shortage of home health agencies;
• The services and supplies are provided under a written plan of treatment;
• Nursing services are furnished on a part-time or intermittent basis only; and
• Drugs and biological products are not provided.
190.3 - Home Health Agency Shortage Area
(Rev. 239, Issued: 01-09-18, Effective: 1-22-18, Implementation: 1-22-18)
A shortage of HHAs exists if an RHC or FQHC is currently located in a county, parish or
similar geographic area in which the Secretary has determined that:
• There is no participating HHA under Medicare, or adequate home health services are
not available to RHC or FQHC patients even though a participating HHA is in the area;
or
• There are patients whose homes are not within the area serviced by a participating
HHA; or considering the area’s climate and terrain, whose homes are not within a
reasonable traveling distance to a participating HHA.
190.4 - Authorization for Visiting Nursing Services
(Rev. 220, Issued: 01-15-16, Effective: 02-01-16, Implementation: 02-01-16)
RHCs or FQHCs that are located in an area that has not been determined to have a current
HHA shortage and are seeking to provide visiting nurse services must make a written request
to the CMS RO along with written justification that the area it serves meets the required
conditions.
190.5 - Treatment Plans for Visiting Nursing Services
(Rev. 252, Issued: 12- 07-18, Effective: 01-01-19, Implementation: 01- 02-19)
For services and supplies that require a treatment plan, the treatment plan must be written and
reviewed by a supervising physician, NP, PA, CNM, or CP, as appropriate, at least once every
60 days; and meet other documentation requirements. If the patient does not receive at least
one covered nursing visit in a 60-day period, the plan is considered terminated for the purpose
of Medicare coverage unless:
• The supervising physician has reviewed the plan of treatment and made a recertification
within the 60-day period which indicates that the lapse of visits is a part of the
physician’s regimen for the patient, or
• Nursing visits are required at intervals less frequently than once every 60 days, but the
intervals are predictable (e.g., it is predictable that a visit is required only every 90 days
for the purpose of changing a silicone catheter, etc.).
Home nursing visits furnished before the plan is put into writing are covered if authorized in
writing by the supervising physician.
200 - Telehealth Services
(Rev. 239, Issued: 01-09-18, Effective: 1-22-18, Implementation: 1-22-18)
RHCs and FQHCs may serve as an originating site for telehealth services, which is the location
of an eligible Medicare beneficiary at the time the service being furnished via a
telecommunications system occurs. RHCs and FQHCs that serve as an originating site for
telehealth services are paid an originating site facility fee.
Although FQHC services are not subject to the Medicare deductible, the deductible must be
applied when an FQHC bills for the telehealth originating site facility fee, since this is not
considered an FQHC service.
RHCs and FQHCs are not authorized to serve as a distant site for telehealth consultations,
which is the location of the practitioner at the time the telehealth service is furnished, and may
not bill or include the cost of a visit on the cost report. This includes telehealth services that
are furnished by an RHC or FQHC practitioner who is employed by or under contract with the
RHC or FQHC, or a non-RHC or FQHC practitioner furnishing services through a direct or
indirect contract. For more information on Medicare telehealth services, see Pub. 100-02,
Medicare Benefit Policy Manual, chapter 15, and Pub. 100-04, Medicare Claims Processing
Manual, chapter 12.
210 - Hospice Services
(Rev. 230, Issued: 12-09-16, Effective: 03-09-17, Implementation: 03-09-17)
210.1 - Hospice Attending Physician Services Payment
(Rev. 11803; Issued: 01-26-23; Effective: 01-01-23; Implementation: 02-27-23)
Medicare beneficiaries who elect the Medicare hospice benefit may choose either an
individual physician, NP or PA to serve as their designated attending practitioner (Section
1861(dd) of the Act). Beginning January 1, 2022, under section 132 of the CAA 2021,
RHCs and FQHCs are authorized to serve in this role. A physician, NP, or PA who works
for an RHC or FQHC may provide hospice attending physician services during a time when
he/she is working for the RHC or FQHC (unless prohibited by their RHC or FQHC contract

or employment agreement). The RHC or FQHC would bill for these services as they would
for any other qualified service to be paid the RHC AIR or the FQHC PPS rate,
respectively.
A physician, NP, or PA who works for an RHC or FQHC may provide hospice attending
services during a time when he/she is not working for the RHC or FQHC (unless prohibited
by their RHC or FQHC contract or employment agreement). These services would not be
considered RHC or FQHC services and the physician or NP would bill for these services
under regular Part B rules using his/her own provider number. Any service provided to a
hospice beneficiary by an RHC or FQHC practitioner must comply with Medicare
prohibitions on commingling. (See section 100 of this chapter).
210.2 - Provision of Services to Hospice Patients in an RHC or FQHC
(Rev. 11803; Issued: 01-26-23; Effective: 01-01-23; Implementation: 02-27-23)
For hospice services that are not described above in section 210.1, RHCs and FQHCs can
treat hospice beneficiaries for medical conditions not related to their terminal illness.
However, if a Medicare beneficiary who has elected the hospice benefit receives care from
an RHC or FQHC related to his/her terminal illness, the RHC or FQHC cannot be
reimbursed for the visit, even if it is a medically necessary, face-to- face visit with an RHC
or FQHC practitioner, since that would result in duplicate payment for services, except
under either of the following circumstances:
• The RHC or FQHC has a contract with the hospice provider to furnish core
hospice services related to the patient’s terminal illness and related conditions
when extraordinary circumstances exist within the hospice. Extraordinary
circumstances are described as “unanticipated periods of high patient loads;
staffing shortages due to illness or other short-term temporary situations that
interrupt patient care; and temporary travel of a patient outside the hospice’s
service area” (42CFR 418.64);
• The RHC or FQHC has a contract with the hospice provider to furnish highly
specialized nursing services that are provided by the hospice so infrequently that
it would be impractical and prohibitively expensive for the hospice to employ a
practitioner to provide these services. For example, a hospice may infrequently
have a pediatric patient, and in those situations, contract with an RHC or FQHC
that has a pediatric nurse on staff to furnish hospice services to the patient.
In these situations, all costs associated with the provision of hospice services must be
carved out of the RHC or FQHC cost report, and the RHC or FQHC would be reimbursed
by the hospice. (42 CFR 418.64(b)(3)).
Any service provided to a hospice beneficiary by an RHC or FQHC practitioner must
comply with Medicare prohibitions on commingling. (See section 100 of this chapter).
220 - Preventive Health Services
(Rev. 230, Issued: 12-09-16, Effective: 03-09-17, Implementation: 03-09-17)

RHCs and FQHCs are paid for the professional component of allowable preventive services
when all of the program requirements are met and frequency limits (where applicable) have not
been exceeded. The beneficiary copayment and deductible (where applicable) is waived by the
Affordable Care Act for the IPPE and AWV, and for Medicare-covered preventive services
recommended by the USPSTF with a grade or A or B.
220.1 - Preventive Health Services in RHCs
(Rev. 11803; Issued: 01-26-23; Effective: 01-01-23; Implementation: 02-27-23)
Influenza (G0008), Pneumococcal (G0009) and COVID-19 vaccines, and certain COVID-
19 monoclonal antibody products
Influenza, pneumococcal and COVID-19 vaccines and covered monoclonal antibody
products used as pre-exposure prophylaxis prevention of COVID-19 and their
administration are paid at 100 percent of reasonable cost through the cost report. No visit
is billed, and these costs should not be included on the claim. The beneficiary coinsurance
and deductible are waived.
Hepatitis B Vaccine (G0010)
Hepatitis B vaccine and its administration is included in the RHC visit and is not separately
billable. The cost of the vaccine and its administration can be included in the line item for
the otherwise qualifying visit. A visit cannot be billed if vaccine administration is the only
service the RHC provides. The beneficiary coinsurance and deductible are waived.
Initial Preventive Physical Exam (G0402)
The IPPE is a face-to-face one-time exam that must occur within the first 12 months
following the beneficiary’s enrollment. The IPPE can be billed as a stand-alone visit if it is
the only medical service provided on that day with an RHC practitioner. If an IPPE
visit is furnished on the same day as another billable visit, two visits may be billed. The
beneficiary coinsurance and deductible are waived.
Annual Wellness Visit (G0438 and G0439)
The AWV is a face-to-face personalized prevention visit for beneficiaries who are not
within the first 12 months of their first Part B coverage period and have not received an
IPPE or AWV within the past12 months. The AWV can be billed as a stand-alone visit if it
is the only medical service provided on that day with an RHC practitioner. If the AWV is
furnished on the same day as another medical visit, it is not a separately billable visit. The
beneficiary coinsurance and deductible are waived.
Diabetes Self-Management Training (G0108) and Medical Nutrition Therapy (97802
and 97803)
Diabetes self-management training or medical nutrition therapy provided by a registered
dietician or nutritional professional at an RHC may be considered incident to a visit with an
RHC practitioner provided all applicable conditions are met. DSMT and MNT are not
billable visits in an RHC, although the cost may be allowable on the cost report. RHCs
cannot bill a visit for services furnished by registered dieticians or nutritional professionals.
However, RHCs are permitted to become certified providers of DSMT services and report
the cost of such services on their cost report for inclusion in the computation of their AIR.
The beneficiary coinsurance and deductible apply.
Screening Pelvic and Clinical Breast Examination (G0101)
Screening pelvic and clinical breast examination can be billed as a stand-alone visit if it is
the only medical service provided on that day with an RHC practitioner. If it is furnished on
the same day as another medical visit, it is not a separately billable visit. The beneficiary
coinsurance and deductible are waived.
Screening Papanicolaou Smear (Q0091)
Screening Papanicolaou smear can be billed as a stand-alone visit if it is the only medical
service provided on that day with an RHC practitioner. If it is furnished on the same day as
another medical visit, it is not a separately billable visit. The beneficiary coinsurance and
deductible are waived.
Prostate Cancer Screening (G0102)
Prostate cancer screening can be billed as a stand-alone visit if it is the only medical service
provided on that day with an RHC practitioner. If it is furnished on the same day as another
medical visit, it is not a separately billable visit. The beneficiary coinsurance and deductible
apply.
Glaucoma Screening (G0117 and G0118)
Glaucoma screening for high risk patients can be billed as a stand-alone visit if it is
the only medical service provided on that day with an RHC practitioner. If it is
furnished on the same day as another medical visit, it is not a separately billable visit.
The beneficiary coinsurance and deductible apply.
Lung Cancer Screening Using Low Dose Computed Tomography (LDCT) (G0296)
LDCT can be billed as a stand-alone visit if it is the only medical service provided on
that day with an RHC practitioner. If it is furnished on the same day as another medical
visit, it is not a separately billable visit. The beneficiary coinsurance and deductible
are waived.
NOTE: Hepatitis C Screening (GO472) is a technical service only and therefore it is
not paid as part of the RHC visit.
220.2 - Copayment and Deductible for RHC Preventive Health Services
(Rev. 239, Issued: 01-09-18, Effective: 1-22-18, Implementation: 1-22-18)
When one or more qualified preventive service is provided as part of an RHC visit,
charges for these services must be deducted from the total charge for purposes of
calculating beneficiary copayment and deductible. For example, if the total charge for
the visit is $150, and $50 of that is for a qualified preventive service, the beneficiary
copayment and deductible is based on $100 of the total charge, and Medicare would pay
80 percent of the $100, and 100 percent of the $50 (minus any deductible). If no other
RHC service took place along with the preventive service, there would be no copayment
or deductible applied, and Medicare would pay 100 percent of the payment amount.
220.3 - Preventive Health Services in FQHCs
(Rev. 11803; Issued: 01-26-23; Effective: 01-01-23; Implementation: 02-27-23)
FQHCs must provide preventive health services on site or by arrangement with another
provider. These services must be furnished by or under the direct supervision of a
physician, NP, PA, CNM, CP, or CSW. Section 330(b)(1)(A)(i)(III) of the Public Health
Service (PHS) Act required preventive health services can be found at
http://bphc.hrsa.gov/policies regulations/legislation/index.html, and include:
• prenatal and perinatal services;
• appropriate cancer screening;
• well-child services;
• immunizations against vaccine-preventable diseases;
• screenings for elevated blood lead levels, communicable diseases, and
cholesterol;
• pediatric eye, ear, and dental screenings to determine the need for vision
and hearing correction and dental care;
• voluntary family planning services; and
• preventive dental services.
NOTE: The cost of providing these services may be included in the FQHC cost report but
they do not necessarily qualify as FQHC billable visits or for the waiver of the
beneficiary coinsurance.
Influenza (G0008), Pneumococcal (G0009) and COVID-19 vaccines and certain
COVID-19 monoclonal antibody products
Influenza, pneumococcal and COVID-19 vaccines and covered monoclonal antibody
products used as pre-exposure prophylaxis prevention of COVID-19 and their
administration are paid at 100 percent of reasonable cost through the cost report. The
cost is included in the cost report and no visit is billed. FQHCs must include these
charges on the claim if furnished as part of an encounter. The beneficiary coinsurance is
waived.
Hepatitis B Vaccine (G0010)
Hepatitis B vaccine and its administration is included in the FQHC visit and is not
separately billable. The cost of the vaccine and its administration can be included in the
line item for the otherwise qualifying visit. A visit cannot be billed if vaccine
administration is the only service the FQHC provides. The beneficiary coinsurance is
waived.
Initial Preventive Physical Exam (G0402)
The IPPE is a face-to-face one-time exam that must occur within the first 12 months
following the beneficiary’s enrollment. The IPPE can be billed as a stand-alone visit if it
is the only medical service provided on that day with an FQHC practitioner. If an IPPE
visit is furnished on the same day as another billable visit, FQHCs may not bill for a
separate visit. These FQHCs will have an adjustment of 1.3416 to their PPS rate. The
beneficiary coinsurance is waived.
Annual Wellness Visit (G0438 and G0439)
The AWV is a personalized face-to-face prevention visit for beneficiaries who are not
within the first 12 months of their first Part B coverage period and have not received an
IPPE or AWV within the past12 months. The AWV can be billed as a stand-alone visit if
it is the only medical service provided on that day with an FQHC practitioner. If the
AWV is furnished on the same day as another medical visit, it is not a separately billable
visit. FQHCs that are authorized to bill under the FQHC PPS will have an adjustment of
1.3416 to their PPS rate. The beneficiary coinsurance is waived.
Diabetes Self-Management Training (G0108) and Medical Nutrition Therapy (97802
and 97803)
DSMT and MNT furnished by certified DSMT and MNT providers are billable visits in
FQHCs when they are provided in a one-on-one, face-to-face encounter and all program
requirements are met. Other diabetes counseling or medical nutrition services provided
by a registered dietician at the FQHC may be considered incident to a visit with an FQHC
provider. The beneficiary coinsurance is waived for MNT services and is applicable for
DSMT.
DSMT must be furnished by a certified DSMT practitioner, and MNT must be furnished
by a registered dietitian or nutrition professional. Program requirements for DSMT
services are set forth in 42 CFR 410 Subpart H for DSMT and in Part 410, Subpart G for
MNT services, and additional guidance can be found at Pub. 100-02, chapter 15, section
300.
Screening Pelvic and Clinical Breast Examination (G0101)
Screening pelvic and clinical breast examination can be billed as a stand-alone visit if it is
the only medical service provided on that day with an FQHC practitioner. If it is
furnished on the same day as another medical visit, it is not a separately billable visit.
The beneficiary coinsurance is waived.
Screening Papanicolaou Smear (Q0091)
Screening Papanicolaou smear can be billed as a stand-alone visit if it is the only medical
service provided on that day with an FQHC practitioner. If it is furnished on the same day
as another medical visit, it is not a separately billable visit. The beneficiary coinsurance is
waived.
Prostate Cancer Screening (G0102)
Prostate cancer screening can be billed as a stand-alone visit if it is the only medical
service provided on that day with an FQHC practitioner. If it is furnished on the same day
as another medical visit, it is not a separately billable visit. The beneficiary coinsurance
applies.
Glaucoma Screening (G0117 and G0118)
Glaucoma screening for high risk patients can be billed as a stand-alone visit if it is the
only medical service provided on that day with an FQHC practitioner. If it is furnished on
the same day as another medical visit, it is not a separately billable visit. The beneficiary
coinsurance applies.
Lung Cancer Screening Using Low Dose Computed Tomography (LDCT) (G0296)
LDCT can be billed as a stand-alone visit if it is the only medical service provided on that
day with an FQHC practitioner. If it is furnished on the same day as another medical
visit, it is not a separately billable visit. The beneficiary coinsurance is waived.
NOTE: Hepatitis C Screening (GO472) is a technical service only and therefore not paid
as part of the FQHC visit.
220.4 - Copayment for FQHC Preventive Health Services
(Rev. 239, Issued: 01-09-18, Effective: 1-22-18, Implementation: 1-22-18)
Under the FQHC PPS, coinsurance will generally be 20 percent of the lesser of the
FQHC’s charge or the PPS rate. When one or more qualified preventive services are
provided as part of an FQHC visit, the A/B MAC will use the lesser of the FQHC’s
charge for the specific FQHC payment code or the PPS rate to determine the total
payment amount. To determine the amount of Medicare payment and the amount of
coinsurance that should be waived, the A/B MAC will use the FQHC’s reported line-
item charges and subtract the dollar value of the FQHC's reported line-item charge for the
preventive services from the full payment amount.
For FQHC claims that consist solely of preventive services that are exempt from
beneficiary coinsurance, Medicare pays 100 percent of the lesser of the FQHC’s charge
or the FQHC PPS rate, and no beneficiary coinsurance is assessed.
230 – Care Management Services
(Rev. 11803; Issued: 01-26-23; Effective: 01-01-23; Implementation: 02-27-23)
Care management services are RHC and FQHC services and include transitional care
management (TCM), chronic care management (CCM), principal care management
(PCM), chronic pain management (CPM), general behavioral health integration
(BHI), and psychiatric collaborative care model (CoCM) services. The RHC and
FQHC face-to-face requirements are waived for these care management services.
Effective January 1, 2017, care management services furnished by auxiliary personnel
may be furnished under general supervision. (Note: General supervision does not
require the RHC or FQHC practitioner to be in the same building or immediately
available, but it does require the services to be furnished under the overall supervision
and control of the RHC or FQHC practitioner.) Except for TCM services, care
management services are paid separately from the RHC AIR or FQHC PPS payment
methodology. RHCs and FQHCs may not bill for care management services for a
beneficiary if another practitioner or facility has already billed for care management
services for the same beneficiary during the same time period. However effective
January 1, 2022, RHCs and FQHCs may bill for care management and TCM services
and other care management services (outside of the RHC AIR or FQHC PPS
payment), for the same beneficiary during the same time period. Coinsurance and
deductibles are applied as applicable to RHC claims, and coinsurance is applied as
applicable to FQHC claims.
230.1 - Transitional Care Management Services
(Rev. 11803; Issued: 01-26-23; Effective: 01-01-23; Implementation: 02-27-23)
Effective January 1, 2013, RHCs and FQHCs are paid for TCM services furnished by
an RHC or FQHC practitioner when all TCM requirements are met. TCM services
must be furnished within 30 days of the date of the patient’s discharge from a hospital
(including
outpatient observation or partial hospitalization), SNF, or community mental
health center.
Communication (direct contact, telephone, or electronic) with the patient or caregiver
must commence within 2 business days of discharge, and a face-to-face visit must
occur within 14 days of discharge for moderate complexity decision making (CPT
code 99495), or within 7 days of discharge for high complexity decision making (CPT
code 99496).
The TCM visit is billed on the day that the TCM visit takes place, and only one TCM
visit may be paid per beneficiary for services furnished during that 30 day post-
discharge period.
TCM services are billed by adding CPT code 99495 or CPT code 99496 to an RHC
or FQHC claim, either alone or with other payable services. If it is the only medical
service provided on that day with an RHC or FQHC practitioner it is paid as a stand-
alone billable visit. If it is furnished on the same day as another visit, only one visit is
paid.
230.2 – General Care Management Services
(Rev. 11803; Issued: 01-26-23; Effective: 01-01-23; Implementation: 02-27-23)
General Care Management Services include: Chronic Care Management (CCM),
Principal Care Management (PCM), Chronic Pain Management (CPM) and
general Behavioral Health Integration (BHI) services. A separately billable
initiating visit with an RHC or FQHC primary care practitioner (physician, NP, PA,
or CNM) is required before care management services can be furnished. This visit
can be an E/M, AWV, or IPPE visit, and must occur no more than one-year prior to
commencing care management services. Care management services do not need to
have been discussed during the initiating visit, and the same initiating visit can be
used for CCM, PCM, CPM and general BHI services as long as it occurs with an
RHC or FQHC primary care practitioner within one year of commencement of care
management services. Beneficiary consent to receive care management services
must be obtained either by or under the direct supervision of the RHC or FQHC
primary care practitioner, may be written or verbal and must be documented in the
patient’s medical record before CCM, PCM, CPM or general BHI services are
furnished. The medical record should document that the beneficiary has been
informed about the availability of care management services, has given permission
to consult with relevant specialists as needed, and has been informed of all of the
following:
• There may be cost-sharing (e.g. deductible and coinsurance in RHCs, and
coinsurance in FQHCs) for both in-person and non-face-to-face services
that are provided;
• Only one practitioner/facility can furnish and be paid for these services
during a calendar month; and
• They can stop care management services at any time, effective at the end
of the calendar month.
Beneficiary consent remains in effect unless the beneficiary opts out of
receiving care management services. If the beneficiary chooses to resume care
management services after opting out, beneficiary consent is required before care
management services can
resume. If the beneficiary has not opted out of care management services but
there has been a period where no care management services were furnished, a
new beneficiary consent is not required.
230.2.1– Chronic Care Management (CCM) Services
(Rev. 11803; Issued: 01-26-23; Effective: 01-01-23; Implementation: 02-27-23)
Effective January 1, 2016, RHCs and FQHCs are paid for CCM services when a
minimum of 20 minutes of qualifying CCM services during a calendar month is
furnished. CCM services may be furnished to patients with multiple chronic
conditions that are expected to last at least 12 months or until the death of the
patient, and that place the patient at significant risk of death, acute
exacerbation/decompensation, or functional decline.
CCM service requirements include:
• Structured recording of patient health information using Certified EHR
Technology including demographics, problems, medications, and
medication allergies that inform the care plan, care coordination, and
ongoing clinical care;
• 24/7 access to physicians or other qualified health care professionals or
clinical staff including providing patients/caregivers with a means to make
contact with health care professionals in the practice to address urgent
needs regardless of the time of day or day of week, and continuity of care
with a designated member of the care team with whom the patient is able
to schedule successive routine appointments;
• Comprehensive care management including systematic assessment of the
patient’s medical, functional, and psychosocial needs; system-based
approaches to ensure timely receipt of all recommended preventive care
services; medication reconciliation with review of adherence and potential
interactions; and oversight of patient self-management of medications;
• Comprehensive care plan including the creation, revision, and/or monitoring
of an electronic care plan based on a physical, mental, cognitive,
psychosocial, functional, and environmental (re)assessment and an
inventory of resources and supports; a comprehensive care plan for all
health issues with particular focus on the chronic conditions being managed;
• Care plan information made available electronically (including fax) in a
timely manner within and outside the RHC or FQHC as appropriate and a
copy of the plan of care given to the patient and/or caregiver;
• Management of care transitions between and among health care
providers and settings, including referrals to other clinicians; follow-up
after an emergency department visit; and follow-up after discharges from
hospitals, skilled nursing facilities, or other health care facilities; timely
creation and exchange/transmit continuity of care document(s) with other
practitioners and providers;
• Coordination with home- and community-based clinical service providers,
and documentation of communication to and from home- and community-
based providers regarding the patient’s psychosocial needs and functional
deficits in the patient’s medical record; and
• Enhanced opportunities for the patient and any caregiver to communicate
with the practitioner regarding the patient’s care through not only telephone
access, but also through the use of secure messaging, Internet, or other
asynchronous non- face-to-face consultation methods.
230.2.2– Principal Care Management (PCM) Services
(Rev. 11803; Issued: 01-26-23; Effective: 01-01-23; Implementation: 02-27-23)
Effective January 1, 2021, RHCs and FQHCs are paid for PCM services when a
minimum of 30 minutes of qualifying PCM services are furnished during a
calendar month. PCM services may be furnished to patients with a single high-
risk or complex condition that is expected to last at least 3 months and may have
led to a recent hospitalization, and/or placed the patient at significant risk of
death.
PCM service requirements include:
• A single complex chronic condition lasting at least 3 months, which is the
focus of the care plan;
• The condition is of sufficient severity to place patient at risk of
hospitalization or have been the cause of a recent hospitalization;
• The condition requires development or revision of disease-specific care plan;
• The condition requires frequent adjustments in the medication regiment; and
• The condition is unusually complex due to comorbidities.
230.2.3– Chronic Pain Management (CPM) Services
(Rev. 11803; Issued: 01-26-23; Effective: 01-01-23; Implementation: 02-27-23)
Effective January 1, 2023, RHCs and FQHCs are paid for CPM services when a
minimum of 30 minutes of qualifying non-face-to-face CPM services are furnished
during a calendar month. CPM services may be furnished to patients with multiple
chronic conditions that involve chronic pain, and may include a person-centered plan
of care, care coordination, medication management, and other aspects of pain care.
230.2.4– General Behavioral Health Integration (BHI) Services
(Rev. 11803; Issued: 01-26-23; Effective: 01-01-23; Implementation: 02-27-23)
BHI is a team-based, collaborative approach to care that focuses on integrative
treatment of patients with primary care and mental or behavioral health conditions.
Effective January 1, 2018, RHCs and FQHCs are paid for general BHI services
when a minimum of 20 minutes of qualifying general BHI services during a
calendar month is furnished to patients with one or more new or pre-existing
behavioral health or psychiatric conditions being treated by the RHC or FQHC
primary care practitioner, including substance use disorders, that, in the clinical
judgment of the RHC or FQHC primary care practitioner, warrants BHI services.
General BHI service requirements include:
• An initial assessment and ongoing monitoring using validated clinical
rating scales;
• Behavioral health care planning in relation to behavioral/psychiatric health
problems, including revision for patients who are not progressing or whose
status changes;
• Facilitating and coordinating treatment such as psychotherapy,
pharmacotherapy, counseling and/or psychiatric consultation; and
• Continuity of care with a designated member of the care team.
230.2.5– Payment for General Care Management Services
(Rev. 11803; Issued: 01-26-23; Effective: 01-01-23; Implementation: 02-27-23)
CCM services furnished between January 1, 2016, and December 31, 2017, are
paid based on the PFS national average non-facility payment rate when CPT
code 99490 is billed alone or with other payable services on an RHC or FQHC
claim.
CCM or general BHI services furnished between January 1, 2018, and December
31, 2018, are paid at the average of the national non-facility PFS payment rate for
CPT codes 99490 (30 minutes or more of CCM services), 99487 (60 minutes or
more of complex CCM services), and 99484 (20 minutes or more of general
behavioral health integration services), when general care management HCPCS
code G0511 is on an RHC or FQHC claim, either alone or with other payable
services.
CCM or general BHI services furnished on or after January 1, 2019, are paid at the
average of the national non-facility PFS payment rate for CPT codes 99490,
99487, 99484, and 99491(30 minutes or more of CCM furnished by a physician or
other qualified health care professional), when general care management HCPCS
code G0511 is on an RHC or FQHC claim, either alone or with other payable
services.
CCM, PCM or general BHI services furnished on or after January 1, 2021 are
paid at the average of the national non-facility PFS payment rate for CPT codes
99490, 99487, 99484, and 99491, and CPT codes 99424 (30 minutes or more of
PCM services furnished by physicians or non-physician practitioners (NPPs)) and
99426 (30 minutes or more of PCM services furnished by clinical staff under the
direct supervision of a physician or NPP), when general care management
HCPCS code G0511 is on an RHC or FQHC claim, either alone or with other
payable services.
CCM, PCM, CPM or general BHI services furnished on or after January 1, 2023 are
paid at the average of the national non-facility PFS payment rate for CPT codes
99490, 99487, 99484, 99491, 99424 and 99426 when general care management
HCPCS code G0511 is on an RHC or FQHC claim, either alone or with other payable
services. The payment rate for HCPCS code G0511 is updated annually based on the
PFS amounts for these codes.
Coinsurance for care management services is 20 percent of lesser of submitted
charges or the payment rate for G0511. Care management costs are reported in the
non- reimbursable section of the cost report and are not used in determining the
RHC AIR or the FQHC PPS rate. G0511 can be billed once per month per
beneficiary when at least 20 minutes of CCM services, at least 30 minutes of PCM
services, or at least 20 minutes of general BHI services have been furnished and all
other requirements have been met.
Only services furnished by an RHC or FQHC practitioner or auxiliary personnel
that are within the scope of service elements can be counted toward the minimum
20 minutes that is required to bill for CCM and general BHI services and the
minimum 30 minutes that is required to bill for PCM services, and does not include
administrative activities such as transcription or translation services.
230.3 – Psychiatric Collaborative Care Model (CoCM) Services
(Rev. 263, Issued: Effective: 01-01-20, Implementation: 01-23-20)
Psychiatric CoCM is a specific model of care provided by a primary care team consisting
of a primary care provider and a health care manager who work in collaboration with a
psychiatric consultant to integrate primary health care services with care management
support for patients receiving behavioral health treatment. It includes regular psychiatric
inter-specialty consultation with the primary care team, particularly regarding patients
whose conditions are not improving. The primary care team regularly reviews the
beneficiary’s treatment plan and status with the psychiatric consultant and maintains or
adjusts treatment, including referral to behavioral health specialty care, as needed.
Patients with mental health, behavioral health, or psychiatric conditions, including
substance use disorders, who are being treated by an RHC or FQHC practitioner may be
eligible for psychiatric CoCM services, as determined by the RHC or FQHC primary care
practitioner. A separately billable initiating visit with an RHC or FQHC primary care
practitioner (physician, NP, PA, or CNM) is required before psychiatric CoCM services
can be furnished. This visit can be an E/M, AWV, or IPPE visit, and must occur no more
than one-year prior to commencing care management services.
Psychiatric CoCM services do not need to have been discussed during the initiating visit,
and the same initiating visit can be used for psychiatric CoCM as for CCM and BHI
services, as long as it occurs with an RHC or FQHC primary care practitioner within one
year of commencement of psychiatric CoCM services. Beneficiary consent to receive
care management services must be obtained either by or under the direct supervision of
the RHC or FQHC primary care practitioner, may be written or verbal and must be
documented in the patient’s medical record before psychiatric CoCM services are
furnished. The medical record should document that the beneficiary has been informed
about the availability of care management services, has given permission to consult with
relevant specialists as needed, and has been informed of all of the following:
• There may be cost-sharing (e.g. deductible and coinsurance in RHCs, and
coinsurance in FQHCs) for both in-person and non-face-to-face services that are
provided;
• Only one practitioner/facility can furnish and be paid for these services during a
calendar month; and
• They can stop care management services at any time, effective at the end of the
calendar month.
Beneficiary consent remains in effect unless the beneficiary opts out of receiving care
management services. If the beneficiary chooses to resume care management services
after opting out, beneficiary consent is required before care management services can
resume. If the beneficiary has not opted out of care management services but there has
been a period where no care management services were furnished, a new beneficiary
consent is not required.
RHC or FQHC Practitioner Requirements
The RHC or FQHC practitioner is a primary care physician, NP, PA, or CNM who:
• Directs the behavioral health care manager and any other clinical staff;
• Oversees the beneficiary’s care, including prescribing medications, providing
treatments for medical conditions, and making referrals to specialty care when
needed; and
• Remains involved through ongoing oversight, management, collaboration and
reassessment.
Behavioral Health Care Manager Requirements
The behavioral health care manager is a designated individual with formal education or
specialized training in behavioral health, including social work, nursing, or psychology,
and has a minimum of a bachelor’s degree in a behavioral health field (such as in clinical
social work or psychology), or is a clinician with behavioral health training, including
RNs and LPNs. The behavioral health care manager furnishes both face-to-face and non-
face-to-face services under the general supervision of the RHC or FQHC practitioner and
may be employed by or working under contract to the RHC or FQHC. The behavioral
health care manager:
• Provides assessment and care management services, including the administration
of validated rating scales;

• Provides behavioral health care planning in relation to behavioral/psychiatric
health problems, including revision for patients who are not progressing or whose
status changes;
• Provides brief psychosocial interventions;
• Maintains ongoing collaboration with the RHC or FQHC practitioner;
• Maintains a registry that tracks patient follow-up and progress;
• Acts in consultation with the psychiatric consultant;
• Is available to provide services face-to-face with the beneficiary; and
• Has a continuous relationship with the patient and a collaborative, integrated
relationship with the rest of the care team.
Psychiatric Consultant Requirements
The psychiatric consultant is a medical professional trained in psychiatry and qualified to
prescribe the full range of medications. The psychiatric consultant is not required to be
on site or to have direct contact with the patient and does not prescribe medications or
furnish treatment to the beneficiary directly. The psychiatric consultant:
• Participates in regular reviews of the clinical status of patients receiving
psychiatric CoCM services;
• Advises the RHC or FQHC practitioner regarding diagnosis and options for
resolving issues with beneficiary adherence and tolerance of behavioral health
treatment; making adjustments to behavioral health treatment for beneficiaries
who are not progressing; managing any negative interactions between
beneficiaries’ behavioral health and medical treatments; and
• Facilitates referral for direct provision of psychiatric care when clinically
indicated.
Payment for Psychiatric CoCM
Psychiatric CoCM services furnished on or after January 1, 2019, are paid at the average
of the national non-facility PFS payment rate for CPT codes 99492 (70 minutes or more
of initial psychiatric CoCM services) and CPT code 99493 (60 minutes or more of
subsequent psychiatric CoCM services) when psychiatric CoCM HCPCS code, G0512, is
on an RHC or FQHC claim, either alone or with other payable services. This rate is
updated annually based on the PFS amounts for these codes. At least 70 minutes in the
first calendar month, and at least 60 minutes in subsequent calendar months, of
psychiatric CoCM services must have been furnished in order to bill for this service.
Coinsurance for psychiatric CoCM services is 20 percent of the lesser of submitted
charges or the payment rate for G0512. Psychiatric CoCM costs are reported in the non-

reimbursable section of the cost report and are not used in determining the RHC AIR or
the FQHC PPS rate. G0512 can be billed once per month per beneficiary when all
requirements have been met.
Only services furnished by an RHC or FQHC practitioner or auxiliary personnel that are
within the scope of service elements can be counted toward the minimum 60 minutes that
is required to bill for psychiatric CoCM services and does not include administrative
activities such as transcription or translation services.
240 – Virtual Communication Services
(Rev. 252, Issued: 12-07-18, Effective: 01-01-19, Implementation: 01- 02-19)
Virtual communication services are RHC and FQHC services and include
communications-based technology and remote evaluation services. The RHC and FQHC
face-to-face requirements are waived when these services are furnished to an RHC or
FQHC patient.
Effective January 1, 2019, RHCs and FQHCs receive an additional payment for the costs
of communication technology-based services or remote evaluation services that are not
already captured in the RHC AIR or the FQHC PPS payment when the requirements for
these services are met. Coinsurance and deductibles apply to RHC claims, and
coinsurance applies to FQHC claims for these services.
Requirements
The following requirements must be met for RHCs and FQHCs to bill for virtual
communication services:
• At least 5 minutes of communications-based technology or remote evaluation
services are furnished by an RHC or FQHC practitioner to a patient that has had a
billable visit in the RHC or FQHC within the previous year; and
• The medical discussion or remote evaluation is for a condition not related to an
RHC or FQHC service provided within the previous 7 days, and does not lead to
an RHC or FQHC service within the next 24 hours or at the soonest available
appointment.
If the discussion between the patient and the RHC or FQHC practitioner is related to a
billable visit furnished by the RHC or FQHC within the previous 7 days or within the
next 24 hours or at the soonest available appointment, the cost of the RHC or FQHC
practitioner’s time would be included in the RHC AIR or the FQHC PPS payment and is
not separately billable.
Payment for Virtual Communication Services
Virtual communication services furnished by RHCs and FQHCs on or after January 1,
2019, are paid at the average of the national non-facility PFS payment rate for HCPCS
code G2012 (communication technology-based services), and HCPCS code G2010
(remote evaluation services), when the virtual communication HCPCS code, G0071, is on
an RHC or FQHC claim, either alone or with other payable services. The payment rate
for HCPCS code G0071 is updated annually based on the PFS amounts for these codes.
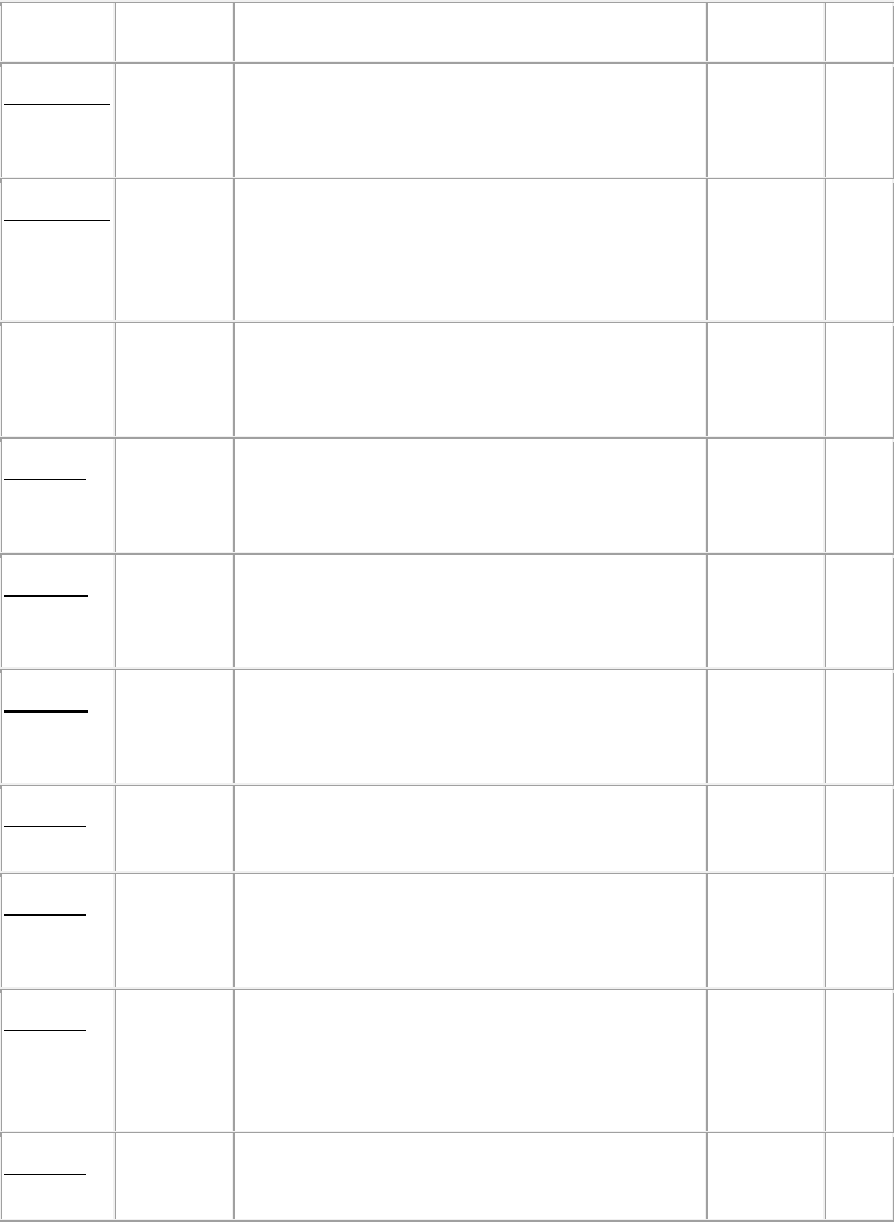
Transmittals Issued for this Chapter
Rev # Issue Date
Subject Impl Date CR#
R11803BP
01/26/2023
Rural Health Clinic (RHC) and Federally
Qualified Health Center (FQHC) Medicare
Benefit Policy Manual Chapter 13 Update
02/27/2023
13063
R10729BP
04/26/2021
Updates to Medicare Benefit Policy Manual for
Rural Health Clinic (RHC) and Federally
Qualified Health Center (FQHC) Services
(Manual Updates Only)
05/26/2021
12252
12/20/2019
Rural Health Clinic (RHC) and Federally
Qualified Health Center (FQHC) Medicare
Benefit Policy Manual Chapter 13 Update
01/23/2020
11575
R252BP 12/07/2018
Rural Health Clinic (RHC) and Federally
Qualified Health Center (FQHC) Medicare
Benefit Policy Manual Chapter 13 Update
01/02/2019
11019
R239BP 01/09/2018
Rural Health Clinic (RHC) and Federally
Qualified Health Center (FQHC) Medicare
Benefit Policy Manual Chapter 13 Update
01/22/2018
10350
R238BP 11/17/2017
Rural Health Clinic (RHC) and Federally
Qualified Health Center (FQHC) Medicare
Benefit Policy Manual Chapter 13 Update
02/15/2018
10350
R230BP 12/09/2016
Rural Health Clinic (RHC) and Federally
Qualified Health Center (FQHC) Updates
03/09/2016
9864
R220BP 01/15/2016
Rural Health Clinic and Federally Qualified
Health Center - Medicare Benefit Policy
Manual Update
02/01/2016
9442
R217BP 12/31/2015
Rural Health Clinic and Federally Qualified
Health Center - Medicare Benefit Policy
Manual Update – Rescinded and replaced by
Transmittal 220
02/01/2016
9442
R201BP 12/12/2014
Medicare Benefit Policy Manual - RHC and
FQHC Update - Chapter 13
01/05/2015
8981
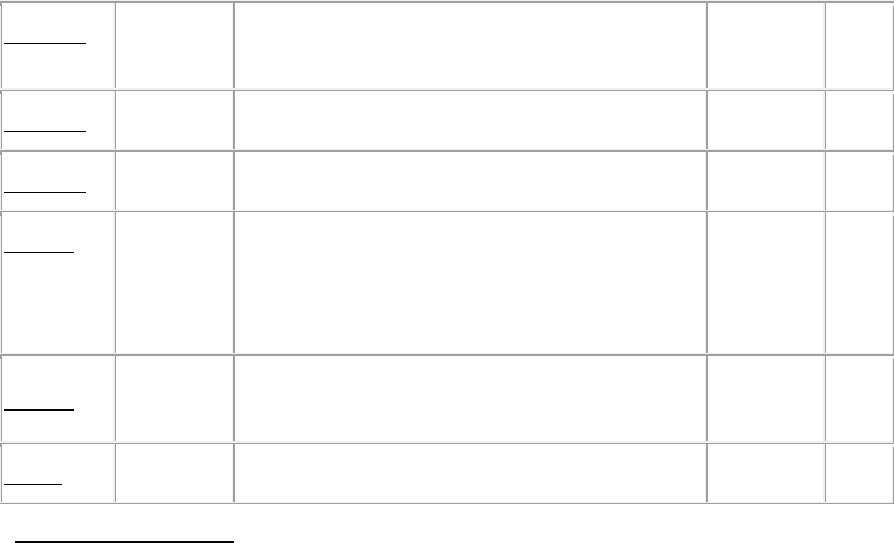
R173BP 11/22/2013
Medicare Benefit Policy Manual - RHC and
FQHC Update - Chapter 13
01/06/2014
8504
R166BP 01/31/2013
Reorganization of Chapter 13 03/01/2013
7824
R114BP 10/30/2009
Outpatient Mental Health Treatment Limitation 01/04/2010
6686
R49BP 03/31/2006
Payment of Federally Qualified Health Centers
(FQHCs) for Diabetes Self-Management
Training Services (DSMT) and Medical
Nutrition Therapy (MNT) Services
06/29/2006
4385
R40BP
11/18/2005
Skilled Nursing Facility Prospective Payment
System
02/16/2006
4079
R1BP 10/01/2003
Introduction to the Benefit Policy Manual N/A N/A
Back to top of Chapter
