

Paving the Way to Equity: A Progress Report (2015-2021)
2
Centers for Medicar e & Medicaid Services
Office of Minority He alth
2015-2020
Table of Contents
Executive Summary .................................................................................................................. 3
Introduction ............................................................................................................................... 6
The CMS Equity Plan for Improving Quality in Medicare ..................................................... 7
CMS Equity Plan for Medicare: Priority Areas ..................................................................... 9
Measuring Progress ................................................................................................................ 10
Evaluation Goal ................................................................................................................ 10
Evaluation Questions ........................................................................................................ 11
Limitations of This Report ................................................................................................. 11
Increasing Understanding and Awareness of Disparities .................................................... 11
CMS Expanded the Collection, Reporting, and Analysis of Standardized Data ................. 12
CMS Developed Resources to Increase the Health Care Workforce’s Understanding of
Disparities ......................................................................................................................... 15
Gaps, Needs, and Next Steps To Increase Understanding and Awareness of Disparities . 17
Developing and Disseminating Solutions to Achieve Health Equity ................................... 18
CMS Evaluated Disparities Impacts and Integrated Equity Solutions across CMS
Programs .......................................................................................................................... 18
CMS Developed and Disseminated Promising Approaches to Support the Health Care
Workforce in Addressing Health Disparities ...................................................................... 20
Gaps, Needs, Next Steps to Achieve Health Equity By Developing and Disseminating
Solutions ........................................................................................................................... 25
Implementing Sustainable Actions to Achieve Health Equity.............................................. 25
CMS Leveraged Qualitative and Quantitative Research Findings to Improve Programs and
Policies to Reduce Disparities ........................................................................................... 26
CMS Convened and Mobilized Partners to Take Action on Disparities .............................. 28
Gaps, Needs, and Next Steps to Implement Sustainable Actions ..................................... 30
Paving the Way to Equity: A Progress Report (2015-2021)
3
Executive Summary
Disparities in health and health care persist despite decades of research and widespread efforts
to improve health in the United States.
i
Certain populations – including racial and ethnic
minorities, sexual and gender minorities, people with disabilities, and individuals living in rural
areas – are more likely to experience worse health outcomes, limited access to health care
services, and lower quality of care than the general population.
ii,iii,iv,v
These disparities are
reflected among vulnerable Medicare beneficiaries. These individuals typically have lower
preventive care utilization, limited access to chronic disease management, lower patient
experience scores, and higher rates of hospital readmissions and chronic disease compared to
their non-minority counterparts.
vi,vii,viii
In 2015, in recognizing these disparities and seeking to close gaps in health care access,
quality, and outcomes among those CMS serves, the agency developed the first-ever CMS
Equity Plan for Improving Quality in Medicare (CMS Equity Plan for Medicare). This plan
provides an action-oriented, results-driven path for achieving health equity by focusing on
populations that experience disproportionately high burdens of disease, worse quality of care,
and barriers to accessing care – specifically, racial and ethnic minorities, sexual and gender
minorities, people with disabilities, and individuals living in rural areas. CMS developed this
strategic approach to addressing disparities to support and advance work already underway
within the agency and among partners. This includes CMS’ network of quality improvement
partners, federal, state, local, and tribal organizations, health care providers, health plans,
individuals and families, researchers and policymakers, and other stakeholders invested in
achieving health equity among Medicare beneficiaries. The CMS Equity Plan for Medicare
focuses the agency and external stakeholders on results, unleashing innovation, and
empowering patients, while eliminating disparities among those we serve.
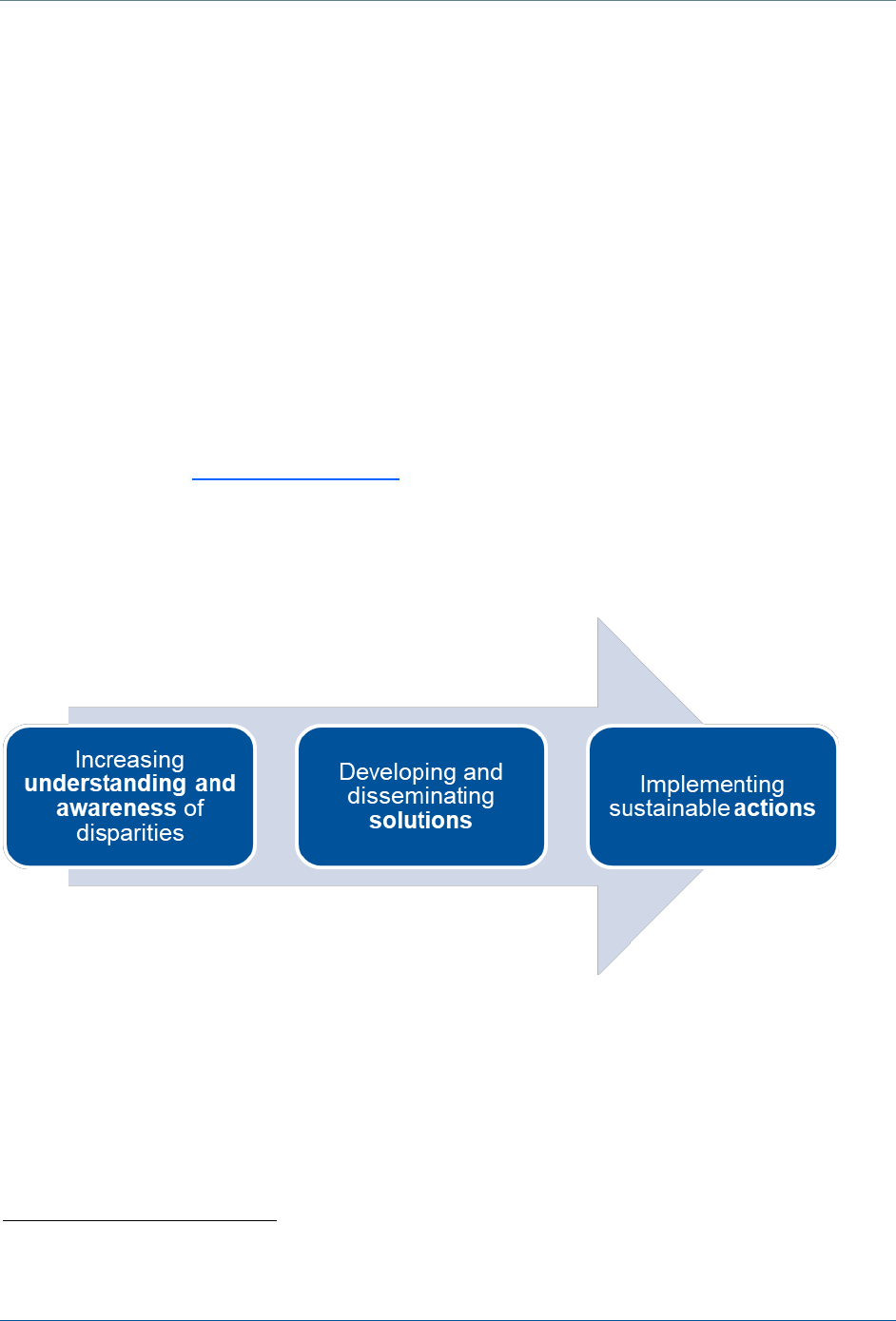
The CMS Equity Plan for Medicare reflects CMS’ Path to Equity, an organizing framework with
three core elements: 1) increasing understanding and awareness of disparities; 2) developing
and disseminating solutions to achieve health equity; and 3) implementing sustainable actions
to achieve health equity. CMS uses this framework to guide health equity work within the
agency and with external partners. This report describes some of the key ways CMS has
demonstrated progress on the Path to Equity between 2015 and 2021, including:
Paving the Way to Equity: A Progress Report (2015-2021)
4
Increasing Understanding and Awareness of Disparities
► CMS expanded the collection, reporting, and analysis of standardized data through
publication of reports, public data sets, increased access to CMS data for researchers,
and data visualization products. These resources allow users to see variations across
communities. They also empower users to enhance their own data collection and analysis
to deliver results. For example in 2016, CMS began annually releasing data and reports on
the Medicare Advantage (MA) population stratified by race and ethnicity. In 2018, CMS
expanded this effort with the annual publication of its Rural-Urban Disparities in Health
Care in Medicare report. These tools and reports are broadly used – as of October 2020,
the Mapping Medicare Disparities Tool has been used by over 39,800 individuals to learn
more about local health disparities and identify opportunities for improvement.
► CMS produced numerous resources to increase the health care workforce’s understanding
of disparities and of ways to improve patient experience, and disseminated research
findings on the drivers of disparities and best practices on the provision of culturally and
linguistically appropriate services (CLAS).
Developing and Disseminating Solutions to Achieve Health Equity
► CMS focused on results, evaluating disparities impacts and integrating equity solutions
across programs through the development and implementation of the CMS Disparities
Impact Statement. The CMS Health Equity Technical Assistance Program is available to
support quality improvement partners, providers, and all other CMS stakeholders.
Stakeholders can ask questions about how to embed health equity and reduce disparities
among enrollees and beneficiaries they serve. From its inception in 2017 through October
2020, the Health Equity TA team has responded to over 278 technical assistance requests
from stakeholders in 39 states as well as Washington, DC, and Puerto Rico.
► CMS developed and disseminated innovative and promising approaches to support the
health care workforce in addressing health disparities and improving the patient
experience through provider-focused, accredited trainings supported by the Medicare
Learning Network and other platforms. Nearly a dozen provider-focused guides have been
produced to help practices take strategic, step-by-step approaches to improving care for
vulnerable communities.
► CMS responded to the Coronavirus (COVID-19) pandemic and public health emergency
through listening sessions, creation of new resources, developing Medicare COVID-19
data snapshots to indicate impact on minority populations, and helping to accumulate all
existing resources for minority populations, providers serving minority populations, and
anything in additional languages.
Implementing Sustainable Actions to Achieve Health Equity
► CMS embedded a focus on health equity results in programs and policies through
standardized monthly and quarterly reporting on health disparities in the QIN-QIO and
Hospital Innovation and Improvement Network (HIIN) programs in the 11
th
Statement of
Work. The HIINs were also required to complete and update CMS Disparities Impact
Statements and action plans to monitor and reduce disparities.
Paving the Way to Equity: A Progress Report (2015-2021)
5
► CMS engaged with stakeholders, focusing attention on vulnerable and rural communities
who have been hardest hit by the public health emergency and COVID-19. CMS is
working with stakeholders and partners to identify barriers, solutions, and opportunities to
improve access to care and the quality of care in health settings including nursing homes
and hospitals.
► CMS convened and mobilized partners to take action to reduce disparities through the
CMS Health Equity Award focused on results and innovation. This recognition has
fostered dedicated communities of national stakeholders working together and
independently to close gaps in health care, access, and outcomes. In the 3 years this
recognition has been shared, nearly 90 organizations have applied for the award and six
have been profiled for their ability to reduce and eliminate disparities.
Each section of this report concludes by considering emerging opportunities to build on our
progress with a focus on CMS’ current strategic initiatives, HHS priorities, and areas in which
CMS quality improvement contractors will be in action moving forward. For example, CMS will
continue to rethink and improve its work in partnership with rural and other vulnerable
communities to ease the burden on local providers and focus on results, innovation, and patient
experience. We will build on successful work embedding evaluation, monitoring, standardized
data, and tools to reduce disparities for minority beneficiaries served by CMS programs, further
inspire our partners to collaborate to achieve health equity, and continue spreading resources
and innovative practices to reduce disparities across organizations and communities.
CMS will also enhance and strengthen existing work supporting providers in underserved and
rural areas as they move toward Merit-Based Incentive Payment, Advanced Alternative
Payment Models, and other value-based payment systems, to ensure that all individuals served
by CMS can reach their highest level of health. CMS will continue to explore opportunities to
advance health equity across all of the Agency’s programs and policies, broadening the reach
and impact of the CMS Equity Plan beyond the Medicare program to benefit the millions of
individuals we serve. COVID-19 has shed new light on the prevalence of disparities in access,
quality, and outcomes among minority and vulnerable communities, and has underscored the
importance of taking action to promote health equity. Although the Path to Equity is long and
challenging, CMS is committed to working with partners and communities to move the needle
on disparities and achieve health equity for all those impacted by CMS programs.

Paving the Way to Equity: A Progress Report (2015-2021)
6
Introduction
Health and health care disparities are related but unique concepts: health disparities typically
refer to higher burdens of illness, mortality, injury, or quality of life experienced by one group
relative to another, whereas health care disparities generally refer to differences between
groups in access to, use of, quality of care, or health coverage.
ix,x,xi,xii
These differences cannot
necessarily be explained by variations in health needs, preferences, or treatment
recommendations but are more likely to be related to social, systemic, and environmental
inequities or inequalities that affect individuals.
xiii,xiv,xv
For example, language barriers, how
health care is organized and accessed, provider bias, geography, affordability, transportation,
social isolation, housing, nutrition, access to technology, and other social risk factors that affect
individuals’ health behaviors, work together and independently to create gaps between and
among groups of varied socioeconomic status, age, location, gender, disability status, race and
ethnicity, and sexual identity and orientation. Disparities can affect any and all populations and
subgroups within populations, and may differ for communities across locations and over time.
xvi,
,xvii
Many communities face significant disparities in health care quality, outcomes, and access, but
racial and ethnic minorities, sexual and gender minorities, individuals with disabilities, and
individuals living in rural areas are disproportionately affected.
xviii,xix,xx
For example:
► In 2017, across nearly every state and territory Black, Hispanic, Asian Pacific Islander, and
American Indian and Alaska Native Medicare beneficiaries have a higher prevalence of
chronic conditions including hypertension, diabetes, chronic kidney disease, and heart
failure than Whites.
xxi
► The LGBTQ population has the highest rates of tobacco use, and certain LGBTQ
subgroups have more chronic conditions as well as higher prevalence and earlier onset of
disabilities than heterosexuals.
xxii,xxiii
► Individuals with disabilities experience worse health and poorer access to mental health
care services compared to people without a disability. Women with disabilities are less
likely to receive regular breast and cervical cancer screenings and are more likely to have
cancer and then be diagnosed at a later stage, than women without disabilities.
xxiv,xxv
► The prevalence of diabetes is 8.6 percent higher in rural areas than in urban areas, and
those diagnosed with diabetes in rural areas are at higher risk of amputations and
inpatient death. They are less likely to receive a professional foot exam, and less likely to
be able to access diabetes self-care education than their urban counterparts.
xxvi
Providers, government agencies, and researchers have worked for decades to understand and
reduce health and health care disparities. However, despite improvements in overall population
health, communities including racial and ethnic minorities, sexual and gender minorities,
individuals with disabilities, and those living in rural areas, experience a lower quality of care
and worse health outcomes than their non-minority counterparts.
xxvii,xxviii,xxix
Disparities persist,
and in some cases, continue to worsen, and affect individuals throughout their lifespan from
birth into older adulthood, often leading to complex and compound health conditions at later life
Paving the Way to Equity: A Progress Report (2015-2021)
7
stages.
xxx,xxxi
It is not necessarily a lack of effort or intention allowing these gaps to grow. Rather,
in many cases CMS has heard that organizations struggle with knowing where to begin to
address the driving forces of these disparities and how they can systematically change
communities’ and individuals’ social determinants of health and their health trajectory. In order
to effectively reduce disparities, government, providers, and health care organizations need to
work deliberately and collaboratively to address the factors driving these gaps, so that each
individual can achieve their highest level of health.
CMS is committed to quality improvement and reducing disparities while meeting the needs of
providers, individuals, and families. Though the Path to Equity is long, CMS and its many
partners will continue to work together to bring about long-term change. This report highlights
some of CMS’ progress from 2015 through 2021 and identifies areas of opportunity to achieve
health equity moving forward.
THE CMS EQUITY PLAN FOR IMPROVING QUALITY IN MEDICARE
CMS developed the CMS Equity Plan for Improving Quality in Medicare (CMS Equity Plan for
Medicare) in 2015, to support its commitment to achieving health equity through a focus on
results, innovation, and improving the patient experience. The CMS Equity Plan for Medicare
lays out an action-oriented, results-driven path for achieving health equity. It focuses on driving
improvement in communities with disproportionately high burdens of disease including chronic
conditions, worse quality of care, and barriers to accessing care. These vulnerable populations
include racial and ethnic minorities, sexual and gender minorities, people with disabilities, and
individuals living in rural areas. This strategic approach to disparity reduction advances work
underway at CMS’ network of quality improvement partners, federal, state, local, and tribal
organizations, providers of all types, health plans, beneficiaries and their families, researchers
and policymakers, and other stakeholders invested in achieving health equity among Medicare
beneficiaries.
To develop the plan, CMS conducted a literature review to identify evidence-based health care
interventions, quality improvement programs, and initiatives with potential to reduce disparities
among our priority populations. CMS also conducted an environmental scan to identify
promising health care interventions, programs, initiatives, and policies. Most importantly, CMS
gathered initial and ongoing input from stakeholders in a series of regional listening sessions
across the U.S. Over the last five years and into the future, CMS OMH has and will continue to
engage in conversations with national, regional, and local thought leaders to carve out a timely,
responsive, and actionable plan for a Path to Equity in Medicare.
Paving the Way to Equity: A Progress Report (2015-2021)
8
The CMS Equity Plan for Medicare is built around a framework that consists of three core
elements:
1. Increasing understanding and awareness of disparities;
2. Developing and disseminating solutions to achieve health equity; and
3. Implementing sustainable actions to achieve health equity.
CMS has termed this focus on understanding, solutions, and actions the Path to Equity. This
organizing framework is pictured in
Figure 1
, below, showing how these areas feed into each
other on a continuum, each one leading to the next. This report summarizes CMS’ progress
over the last four and a half years (September 2015 to January 2021)
1
in achieving health equity
through its policies and programs. It is illustrated with examples of how the agency has
increased understanding, solutions, and actions to reduce disparities nationwide. The examples
included in this report are not exhaustive, and CMS’ work is ongoing. We encourage
stakeholders to visit CMS OMH’s webpage to navigate and explore the full suite of resources,
tools, and information that is publicly available.
Figure 1. CMS Path to Equity
1
Data on utilization of products and resources is reported as of October 2020.
Paving the Way to Equity: A Progress Report (2015-2021)
9
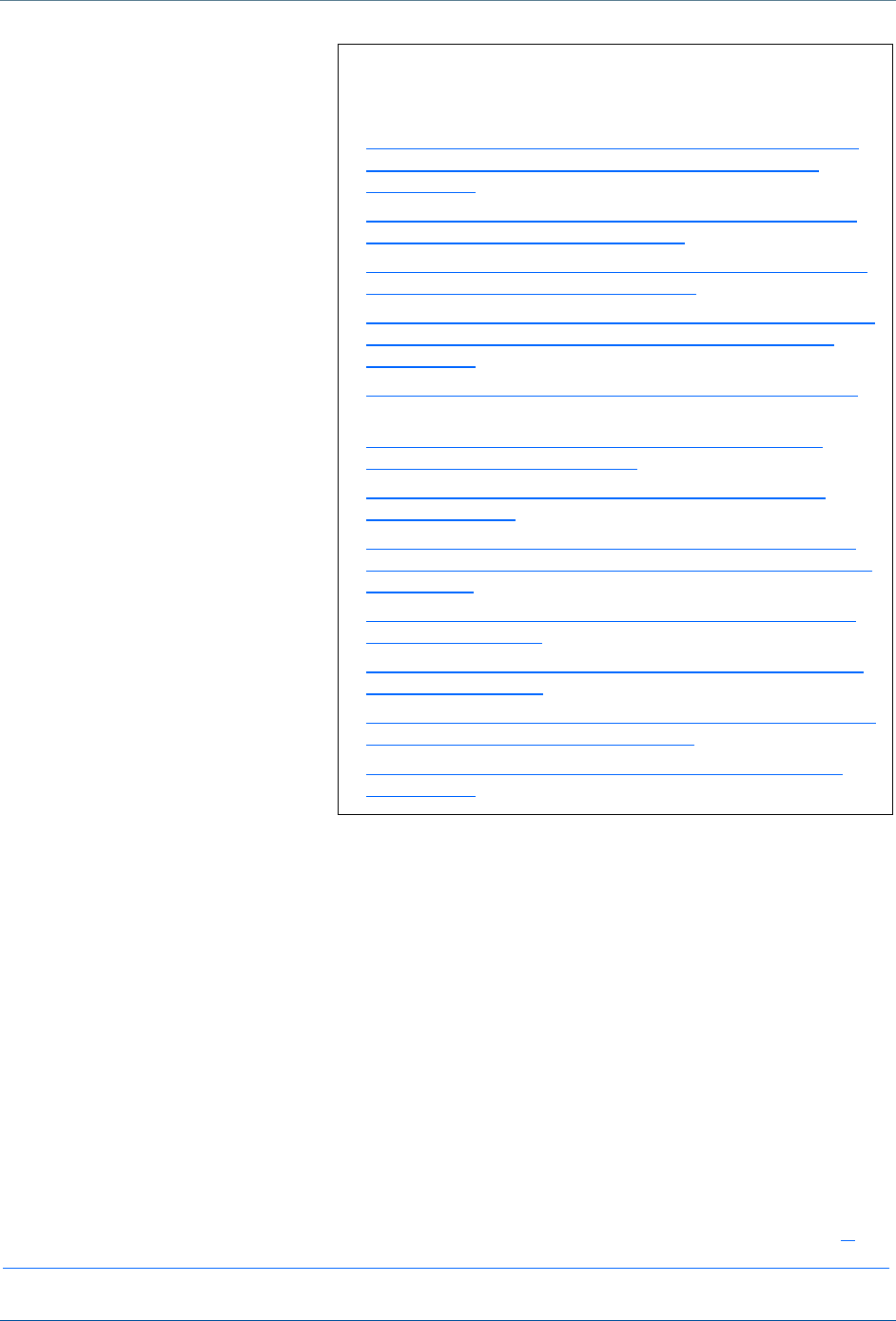
CMS EQUITY PLAN FOR MEDICARE: PRIORITY AREAS
On this foundation of understanding,
solutions, and actions, CMS has built up a
focus around six high-impact priority areas
identified by Agency stakeholders. These
priorities incorporate both community- and
systems-level approaches to achieving
health equity. They were established based
on stakeholder input and requests for
increased CMS support and direction, a
review of the evidence base, and
consideration of CMS’ role in the work
underway within the U.S. Department of
Health and Human Services (HHS). These
priorities were drafted in alignment with
existing CMS and HHS initiatives and were
designed with particular focus on how CMS
could best support QIN-QIOs and other
quality improvement contractors in the 11
th
Statement of Work. They are intentionally flexible to allow our work to adapt to our evolving
health care system. Activities related to these priorities cut across the three areas of the Path to
Equity. The six priorities embedded in the CMS Equity Plan for Medicare are listed in
Figure 2
and described in more detail below.
Priority 1: Expand the Collection, Reporting, and Analysis of Standardized Data. The focus of
Priority 1 is to increase the importance placed on collecting and analyzing standardized patient
data, and to develop solutions that enable stakeholders to collect and analyze data in their
communities. Comprehensive patient data, including race, ethnicity, language, sexual
orientation, gender identity, disability status, and geographic location are required to plan for
quality improvements and address changes among the target populations.
Priority 2: Evaluate Disparities Impacts and Integrate Equity Solutions across CMS Programs.
The focus of Priority 2 is two-fold: 1) to measure and understand the effects that CMS programs
and policies have on vulnerable populations and embed evaluation instruments into existing and
new CMS policies, programs, models, and demonstrations; and 2) to build solutions into the
fabric of the agency that will help close gaps in health care quality, access, and outcomes,
moving CMS and partners to take action together to reduce disparities. To achieve Priority 2,
CMS is always engaging partners to identify any gaps among vulnerable populations’ health
care quality, outcomes, and access and working to close those gaps through the agency’s
programs, policies, models, and demonstrations.
Priority 3: Develop and Disseminate Promising Approaches to Reduce Health Disparities. The
focus of Priority 3 is to develop promising solutions to achieve equity in Medicare quality and to
replicate and adapt effective models and strategies. Priority 3 activities identify and share best
Figure 2. CMS Equity Plan for Medicare:
Priority Areas
• Priority 1: Expand the Collection, Reporting,
and Analysis of Standardized Data
• Priority 2: Evaluate Disparities Impacts and
Integrate Equity Solutions across CMS
Programs
• Priority 3: Develop and Disseminate Promising
Approaches to Reduce Health Disparities
• Priority 4: Increase the Ability of the Health
Care Workforce to Meet the Needs of
Vulnerable Populations
• Priority 5: Improve Communication and
Language Access for Individuals with Limited
English Proficiency and Persons with
Disabilities
• Priority 6: Increase Physical Accessibility of
Health Care Facilities

Paving the Way to Equity: A Progress Report (2015-2021)
10
practices and promising approaches in the reduction of health disparities to complement the
work of other priorities in the CMS Equity Plan for Medicare.
Priority 4: Increase the Ability of the Health Care Workforce to Meet the Needs of Vulnerable
Populations. The focus of Priority 4 spans understanding, solutions, and actions. It aims to
increase the understanding of health care workforce innovations that reduce disparities for
vulnerable populations. Work under this priority also supports developing solutions to equip the
health care workforce to increase the provision of culturally and linguistically appropriate and
effective care for beneficiaries. Finally, this work drives actions to adopt and adapt promising
practices that enhance the workforce’s ability to improve quality of care and outcomes for the
individuals and communities they serve.
Priority 5: Improve Communication and Language Access for Individuals with Limited English
Proficiency and Persons with Disabilities. The focus of Priority 5 is to improve communication
and language access for Medicare and dual eligible beneficiaries. Through the development of
tools and resources, this activity supports organizations as they provide communication and
language assistance services to consumers to ensure they can actively participate in the care
they receive.
Priority 6: Increase Physical Accessibility of Health Care Facilities. Priority 6 focuses on building
shared understanding of the physical accessibility of health care facilities, identifying solutions,
and facilitating action to increase the physical accessibility of health care facilities.
Measuring Progress
To evaluate CMS’ progress toward achieving health equity among Medicare beneficiaries, we
established a goal and set of guiding questions. The Path to Equity is influenced by many
factors – some that CMS and our partners can influence directly and some that we cannot. This
makes evaluation and measurement a challenge. This progress report acknowledges that
improvements in health outcomes are slow to surface and difficult to attribute to a discrete
action, policy, or change. It gives the reader a snapshot into some of the key work that has been
done to move the needle since the CMS Equity Plan for Medicare was drafted in 2015. Moving
forward, CMS will continue to focus on results, identifying areas where success can be
measured qualitatively and quantitatively.
EVALUATION GOAL
The overarching goal for evaluating and monitoring CMS’ progress in achieving the aims of the
CMS Equity Plan for Medicare is to determine the extent to which CMS’ activities have
increased understanding and awareness of disparities, increased development and
dissemination of solutions, and accelerated the implementation of sustainable actions to
achieve health equity.
Paving the Way to Equity: A Progress Report (2015-2021)
11
EVALUATION QUESTIONS
To monitor CMS’ progress toward achieving health equity in Medicare, CMS developed four
evaluation questions. The first three align with the Path to Equity and help CMS determine how
its activities contribute to each of these aims. The fourth question helps inform opportunities for
CMS to improve its activities over time and work more effectively toward achieving health equity
among Medicare beneficiaries.
1. How are the activities in the CMS Equity Plan for Medicare increasing understanding and
awareness of disparities?
2. How are the activities in the CMS Equity Plan for Medicare supporting the development and
dissemination of solutions to increase equity in Medicare?
3. How are the activities in the CMS Equity Plan for Medicare leading to sustainable actions
that increase equity in Medicare?
4. What are the gaps, needs, and next steps to achieve equity in the Medicare program?
LIMITATIONS OF THIS REPORT
This progress report focuses on key results of CMS’ activities to achieve health equity in
Medicare. It does not report every initiative undertaken as part of the CMS Equity Plan for
Medicare or more broadly at CMS and HHS. Given the multi-faceted nature of community- and
systems-change and the potential for confounding factors, it is not possible to directly attribute
changes in health disparities among Medicare beneficiaries to CMS’ activities to achieve health
equity through its policies and programs at this time. However, the current and potential future
impact of these initiatives should not be ignored. The purpose of this progress report is to
describe key results and activities between September 2015 – January 2021 that are paving the
way to health equity and helping CMS and partners begin to move the needle on disparities.
Increasing Understanding and Awareness of
Disparities
The first step on the Path to Equity is increasing
understanding and awareness of disparities. CMS’
activities in this area respond to the research
question: How are the activities in the CMS Equity
Plan for Medicare increasing understanding and
awareness of disparities?
In this section, we explore two major areas of
progress: 1) expanding the collection, reporting, and
analysis of standardized data, and 2) increasing the
health care workforce’s understanding of disparities
by disseminating research findings on disparities,
Paving the Way to Equity through
Understanding involves:
• Identifying knowledge gaps across
CMS and partners about disparities
and their drivers;
• Filling knowledge gaps to better inform
programs, policies, and partners;
• Enhancing understanding of the drivers
of disparities; and
• Improving understanding of why
disparities matter and why it is
important to address them.
Paving the Way to Equity: A Progress Report (2015-2021)
12
their drivers, and best practices on the provision of culturally and linguistically appropriate
services (CLAS).
CMS EXPANDED THE COLLECTION, REPORTING, AND ANALYSIS OF
STANDARDIZED DATA
CMS has worked to achieve equity by making existing data more accessible as well as
increasing and improving the collection of standardized data. This helps quality improvement
partners and other stakeholders, as well as the providers they serve, identify where there are
gaps in health care quality, outcomes, and access. This can show where and how interventions
can be targeted to ensure all beneficiaries are receiving the highest and most equitable care
under the Medicare program. This approach enables CMS and our partners to focus on results,
and to tailor our work to improving patients’ experiences with the health care system.
CMS made existing data more accessible
The published literature suggests that increasing the collection of standardized patient
demographic and language data across health care systems, including race, ethnicity, language
preference, sexual orientation, gender identity, disability status, and geographic location is an
important first step toward improving population health.
xxxii,xxxiii
Equally important is ensuring that
these data are accessible to key stakeholders. As such, CMS is committed to making existing
data relevant, accessible, and easy to use for providers, researchers, quality improvement
professionals, health care organizations, and other stakeholders in support of their efforts to
access federal data to identify and address health disparities.
For example, in 2016, for the first time in its history, CMS released stratified data and reports on
the Medicare Advantage (MA) population. This is significant because Medicare Part C and D
plans cover nearly one-third of Medicare beneficiaries. These data and reports identify
variations in their clinical care outcomes and patient experiences. Because they provide
contract-level data, CMS’ annual publication of these reports encourages health plans to
respond to disparities within their member populations. CMS has published numerous reports
and products on these data, many of which are updated annually and as new data become
available. This provides the public with streamlined and easily accessible information on
disparities in health care by race and ethnicity, gender, and urban-rural location. Some of the
most recent include:
► Racial, Ethnic, and Gender Disparities in Health Care in Medicare Advantage (April 2020)
describes the quality of health care received in 2018 by Medicare beneficiaries enrolled in
Medicare Advantage (MA) plans nationwide (31.6 percent of all Medicare beneficiaries).
The report highlights racial and ethnic differences in health care experiences and clinical
care, compares quality of care for women and men, and examines racial and ethnic
differences in quality of care among women and men separately. This 2020 report is the
fifth in a series of reports that are updated annually.
Paving the Way to Equity: A Progress Report (2015-2021)
13
► Rural-Urban Disparities in Health Care in Medicare (November 2020) describes rural-
urban differences in health care experiences and clinical care received nationally in 2019.
In addition to comparing the quality of care delivered to rural and urban Medicare
beneficiaries overall, the report looks at how these differences vary by race and ethnicity
and by race and ethnicity within rural and urban areas.
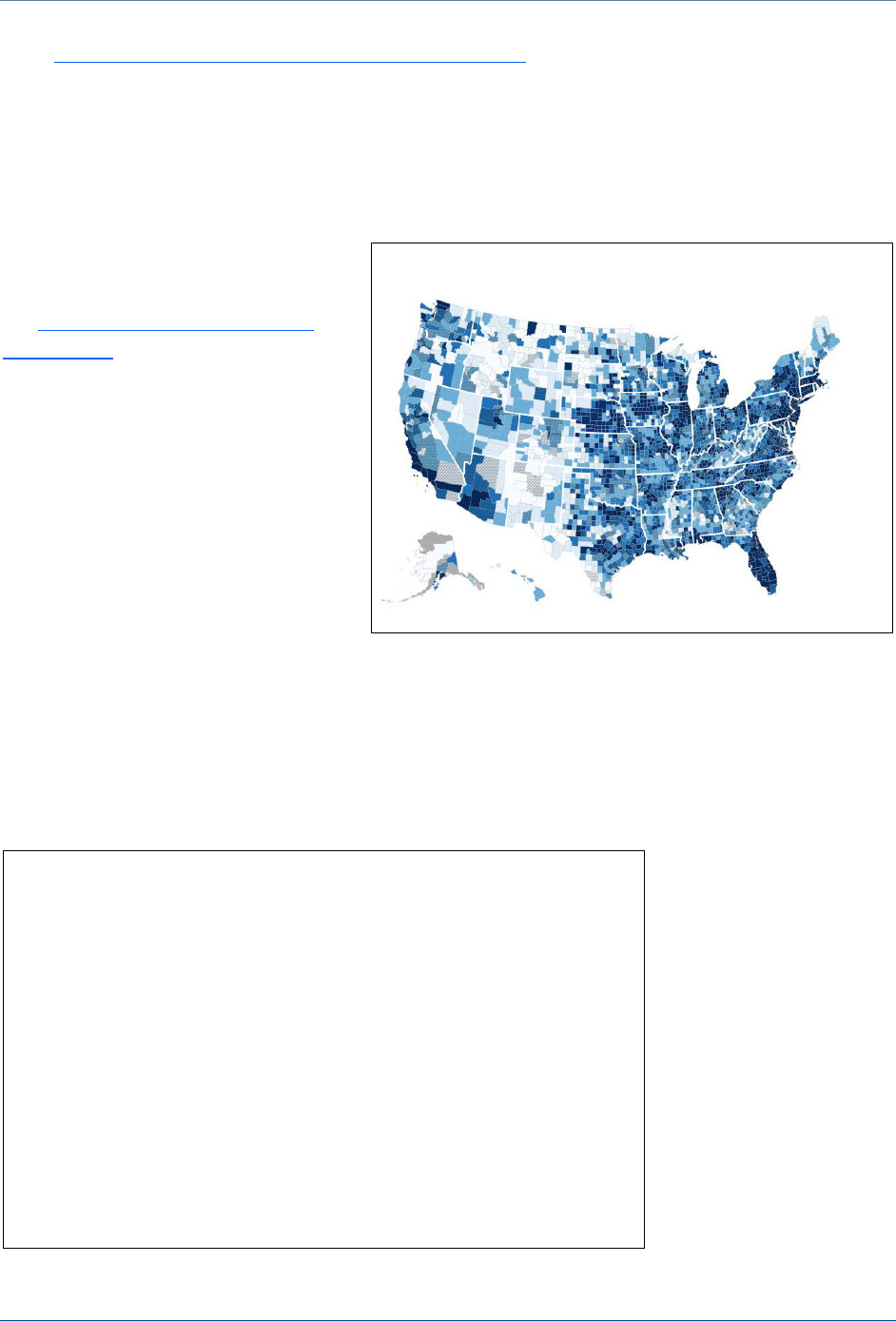
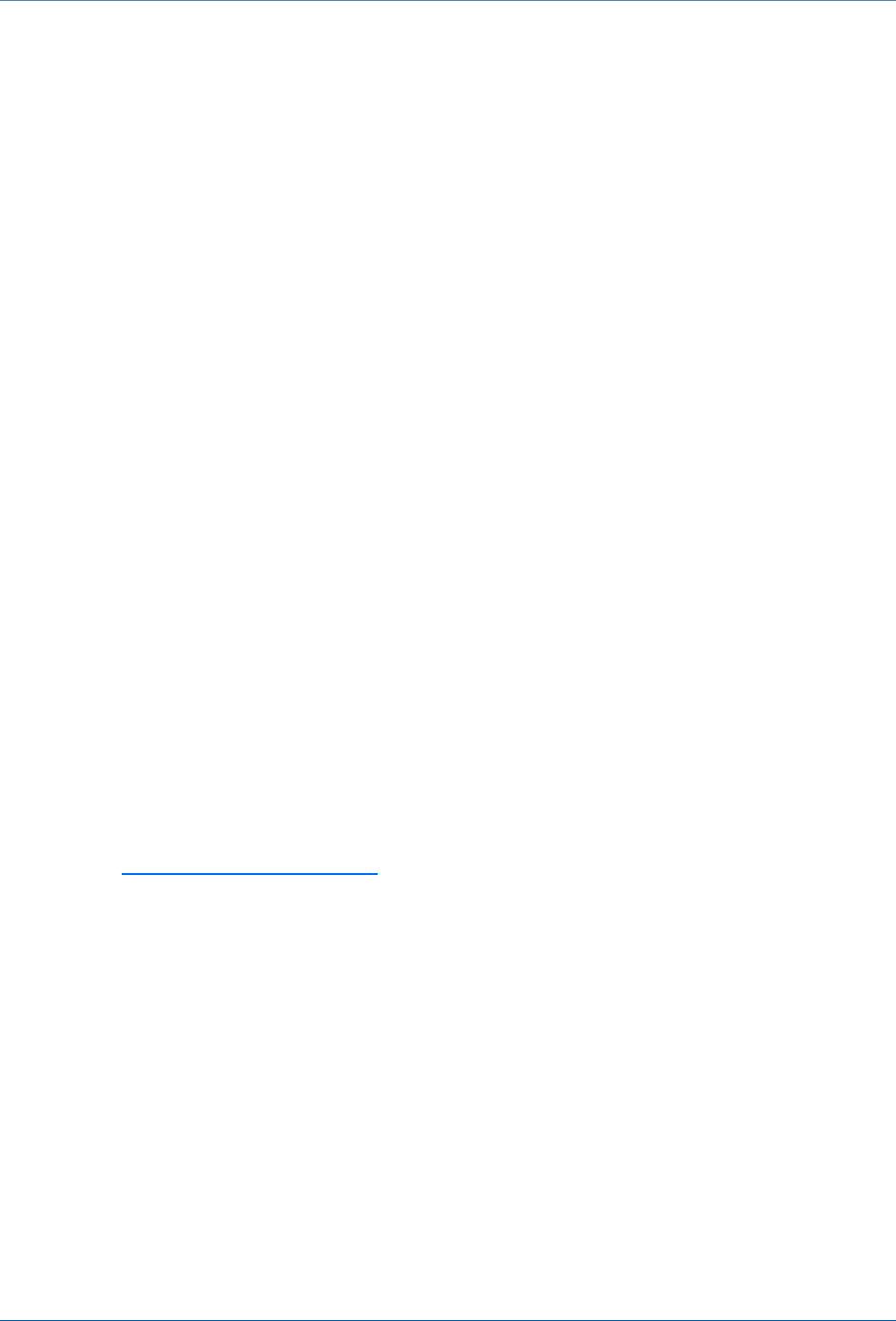
Another important way CMS has
improved the accessibility of existing
data is through the development of
the Mapping Medicare Disparities
(MMD) Tool, an interactive data
visualization tool used to identify
areas of disparities between
subgroups of Medicare beneficiaries
(e.g., racial and ethnic groups) in
health outcomes, utilization, and
spending. The MMD Tool includes
both a Population and Hospital View.
The Population View uses Medicare
FFS data to show the prevalence of
60 chronic conditions, health care
utilization, and health care costs by race, ethnicity, sex, urban/rural location, dual-eligibility
status, and age. The Hospital View includes data from the Hospital Compare website and allows
comparisons of hospitals on quality and cost of care measures. The MMD Tool’s interactive web
interface allows users to visualize disparities in chronic diseases and health care utilization in
their communities, which enables them to target specific interventions where they are needed
most (see
Figure 3
).
CMS released the first
version of the MMD Tool
in 2016. Since then,
CMS has incorporated
multiple enhancements
and data updates based
on user feedback to
provide a broader range
of measures for
identifying and
understanding health
disparities. These
enhancements involved
integrating data on:
additional chronic
Figure 3. Mapping Medicare Disparities (MMD) Tool
Stakeholder Feedback on the
MMD Tool
• “We are going to download the data to understand how the data can
support research in radiology. [The MMD Tool] has great potential to
provide additional insight on disparities in preventive services.” –
Comment from providers, March 2019
• “[We] will be a strong partner in using this tool and would like to
provide bi-directional feedback and expand use of the tool in rural
areas and around screenings and other preventive service disparities.”
– Comment from providers, March 2019
• “[The MMD Tool] map and included data are very interesting. The Tool
will help reduce provider burden.” – Comment from a Medicare
Administrative Contractor (MAC), April 2019
Paving the Way to Equity: A Progress Report (2015-2021)
14
diseases; the utilization of preventive services; opioid use disorders; certain cancer diagnoses;
emergency department visits; the prevalence of disabilities; and behavioral health. The MMD
Tool also now includes county social-risk profiles based on American Community Survey (ACS)
data regarding the proportion of the county’s population with limited English proficiency, average
household income, unemployment rate, percent of vacant homes, average household size, and
poverty rate. The ACS profile is also available at the state and national level. Additionally, a new
trend analysis feature allows users to view changes over time (2012-2018) and compare
differences by race and ethnicity, gender, age, urban/rural location, or Medicare and Medicaid
eligibility within or by county and/or state. To further increase the accessibility of this data, CMS
created a Spanish-language version of the tool for MMD’s Population View along with
accompanying documentation, including end user guidance. As of October 2020, the MMD Tool
had received more than 39,800 views.
CMS increased and improved the collection of standardized data
While evidence-based guidelines and practices exist for improving the collection of data on
race, ethnicity, and language in health care settings, these guidelines may not be known nor
implemented, resulting in wide variations in data collection that negatively impact the accuracy
and reliability of the data. To improve standardized data collection among stakeholders, CMS
developed the Inventory of Resources for Standardized Demographic and Language Data
Collection (updated March 2020). The inventory combines data collection best practices from
reports, toolkits, webinars, and training tools into a single resource that can be used by health
care organizations of all types. Stakeholders can use these resources to improve the collection
of standardized data, which can help them identify and address health disparities. Each year,
the inventory is updated to ensure it reflects the most up-to-date guidance available. Between
its initial publication in 2016 and October 2020, this inventory was downloaded over 1,200
unique times and it has been used and shared by CMS quality improvement partners among
their members and providers to improve local and regional data collection.
To improve federal data collection, in 2016, CMS conducted cognitive testing around modified
Spanish language for a question about sexual orientation for the National Health Interview
Survey (NHIS). The NHIS has been conducted for more than 50 years through household
telephone interviews to assess the health of the nation. This survey collects data on important
health topics, such as health status, health care access, and progress toward achieving national
health objectives. The research showed that the updated language, while not a direct translation
of the English question, is better understood by Spanish speakers, which could lead to lower
rates of non-response. As a direct result of this work, the Bureau of Justice Statistics adopted
the revised sexual orientation question in the Spanish version of the 2016 National Crime
Victimization Survey, and in 2017, the Centers for Disease Control and Prevention (CDC) began
using the modified language for the
Error! Hyperlink reference not valid.
. These changes will
enable surveys to capture a more accurate picture of health disparities among Spanish-
speaking sexual minorities.
CMS has also been instrumental in improving the availability and use of standardized Medicare
data through the Medicare Current Beneficiary Survey (MCBS). The MCBS is a continuous, in-
Paving the Way to Equity: A Progress Report (2015-2021)
15
person, longitudinal survey of a representative national sample of the Medicare population.
CMS supported the development of the MCBS Public Use File, which allows individuals to
assess and monitor the impact of the Medicare program on beneficiaries’ health. This public
data file lets users sort beneficiaries by age, race, ethnicity, and gender. Users can view
information about health conditions, access to and satisfaction with care, type of insurance
coverage, and information on utilization, including the number of fee-for-service claims per
beneficiary for certain health care event types. The MCBS data is designed to represent the
Medicare population as a whole and CMS has supported oversampling of certain smaller, but
critically important populations. This method ensures that researchers and other users can
examine the health status of elderly beneficiaries (age 85 and over), beneficiaries with
disabilities, beneficiaries in Accountable Care Organizations (ACOs), and Hispanic beneficiaries
to see health changes over time. The release of the public use file, or PUF, of the MCBS data
makes this information more accessible and usable for anyone interested in understanding
outcomes and disparities among Medicare beneficiaries over time, regardless of whether they
are a researcher with a formal data use agreement with the government.
2
CMS DEVELOPED RESOURCES TO INCREASE THE HEALTH CARE
WORKFORCE’S UNDERSTANDING OF DISPARITIES
CMS has worked to achieve health equity by supporting the health care workforce’s ability to
provide patients with more culturally appropriate and person-centered care. The agency has
focused on giving providers tools to better understand and meet patients’ needs by sharing
research, information, and best practices that providers can easily find and use in their everyday
practice.
CMS disseminated research findings on disparities and their drivers to increase
the health care workforce’s understanding of disparities
CMS analyzes Medicare beneficiary data to identify and better understand the drivers of
disparities among target populations, including racial and ethnic minorities, sexual and gender
minorities, people with disabilities, and individuals living in rural areas. For example, CMS
analyzed data for transgender beneficiaries, which resulted in three published
manuscripts.
xxxiv,xxxv,xxxvi
CMS routinely disseminates reports, briefs, maps, and guidance to stakeholders through its
website. Data highlights, infographics, and research reports on topics related to health
disparities
across a number of vulnerable Medicare populations are available on the CMS OMH
website. A small subset of the products published between 2015 – 2021 are noted on the
following page.
2
The MCBS sample frame includes all aged individuals, but only individuals 18 and over are interviewed and
included in the LDS files.
Paving the Way to Equity: A Progress Report (2015-2021)
16
In addition, CMS has supported
innovation in telehealth by
exploring trends of the effect and
utility of expanded telehealth
services for vulnerable Medicare
beneficiaries. This analysis
informs the Agency’s
understanding of this mode of
health care delivery. CMS
analyzed claims data from 2014
through 2016 to quantify the
current extent of telehealth
services provided to Medicare
beneficiaries, the demographic
and diagnostic characteristics of
beneficiaries who receive them,
and high-volume services
provided to Medicare
beneficiaries. Results of this work
showed that telehealth services
can increase access to critically
important care for older, rural, and
low-income beneficiaries as well
as those with disabilities.
xxxvii
CMS
shared these results with
Congress, federal colleagues,
public health professionals, health
care providers, and policy
experts.
CMS worked to increase the health care workforce’s understanding of disparities
by disseminating best practices on providing culturally and linguistically
appropriate services
Providing culturally and linguistically appropriate services (CLAS) and consistently monitoring
health care quality among at-risk populations are effective tactics to address persistent
disparities among vulnerable communities.
xxxviii
,
xxxix
,
xl
,
xli
However, there is little national data
available to characterize the provision of CLAS services, nor are there relevant quality
measures that can be used to monitor and engage the health care system to drive
improvement. To address this need, CMS examined the current state of health quality measures
related to CLAS and disparities. CMS assessed gaps in existing measures and their
implementation. CMS then identified measurement opportunities to address these gaps among
racial and ethnic minorities, people with limited English proficiency, people with low health
literacy, people with disabilities, and sexual and gender minorities. In 2016, CMS released A
Practical Guide to Implementing the National CLAS Standards: For Racial, Ethnic and Linguistic
Selection of CMS Products to Increase
Understanding of Disparities
• Racial and Ethnic Disparities in Diabetes Prevalence, Self-
Management, and Health Outcomes among Medicare
Beneficiaries (March 2017)
• Does Disability Affect Receipt of Preventive Care Services
among Older Medicare Beneficiaries? (July 2017)
• Medicare Fee-For-Service Beneficiaries with Disabilities, by
End Stage Renal Disease Status, 2014 (July 2017)
• Understanding the Health Needs of Diverse Groups of Asian
and Native Hawaiian or Other Pacific Islander Medicare
Beneficiaries (August 2017)
• Toward the Creation of a Patient-Reported Disability Index
(September 2018)
• Understanding the Health Needs of Diverse Groups of
Hispanic Medicare Beneficiaries (November 2018)
• Putting Patients First: Special Issue of Health Services
Research Journal (January 2019)
• Opioid Prescription in Medicare Beneficiaries: Prescription
Opioid Policies and Implications for Beneficiaries with Sickle
Cell Disease (June 2019)
• How Does Disability Affect Access to Health Care for Dual
Eligible Beneficiaries (July 2019)
• Z Codes Utilization among Medicare Fee-for-Service (FFS)
Beneficiaries in 2017 (January 2020)
• Understanding Rural Hospital Bypass Among Medicare Fee-
for-Service (FFS) Beneficiaries in 2018 (September 2020)
• Chronic Kidney Disease Often Undiagnosed in Medicare
Beneficiaries (October 2020)
Paving the Way to Equity: A Progress Report (2015-2021)
17
Minorities, People with Disabilities and Sexual and Gender Minorities to support hospitals,
health plans, and other health care organizations in improving health equity and implementing
the National CLAS Standards. This toolkit presents best practices for implementing the national
CLAS standards to address disparities in clinical practice, for example: organizational policies
focused on the provision of CLAS; practical tools for use by organizations and providers;
training and educational resources for organizational governance, leadership, and providers;
assessment tools to gauge cultural competence; and examples of programs designed to provide
culturally competent and person-centered care.
CMS also shared knowledge and promising practices to address disparities among Medicare
beneficiaries with limited English proficiency and those with sensory disabilities who need
additional communication services during health care visits. CMS analyzed 2014 American
Community Survey data to improve understanding of the communication and language needs of
Medicare beneficiaries at the national, state, and local levels. Findings indicated that local
beneficiary needs are not always the same as needs at a state or national level. This
emphasizes the need for providers to understand communication and language trends in the
smallest geography relevant to their service areas. This analysis led to Understanding
Communication and Language Needs of Medicare Beneficiaries (April 2017), an issue brief with
recommendations and promising practices for providers, CMS quality improvement partners,
and other health care stakeholders. From its initial publication through October 2020, the issue
brief has been downloaded more than 1,400 times. CMS also conducted interviews with a
variety of health care organizations across the country (i.e., community health centers,
hospitals, health systems, and health plans) about the innovative approaches to provide
language assistance services to persons with limited English proficiency. Key findings from this
work are highlighted in Providing Language Services to Diverse Populations: Lessons from the
Field (February 2018). This resource describes language assistance approaches suited to
different settings, populations served, and resource availability.
GAPS, NEEDS, AND NEXT STEPS TO INCREASE UNDERSTANDING
AND
AWARENESS OF DISPARITIES
Moving forward, CMS will continue working to achieve health equity by increasing
understanding and awareness of disparities in Medicare, and will explore new opportunities
across all of its programs and policies. For example, consistent with the CMS Rural Health
Strategy and Rethinking Rural Health initiative, the agency will continue to increase
understanding around disparities in rural communities’ health care access, outcomes, and
quality. As the number of individuals with chronic conditions continues to grow, CMS will build
on its ongoing work understanding disparities in diabetes and chronic kidney disease. As
increasing numbers of older adults seek long term care, CMS also recognizes that a growing
proportion of these individuals are racial, ethnic, sexual and gender minorities, individuals with
disabilities, and those living in rural areas.
xlii
,
xliii
CMS will also continue to improve understanding
around disparities related to, and emerging from, our experience with COVID-19. This includes
disparities related to access, quality, and outcomes for those in post-acute care and other
settings. In addition, CMS will continue to work with federal and private partners to collect and
leverage data on social determinants of health to improve our understanding of how social risk
Paving the Way to Equity: A Progress Report (2015-2021)
18
factors can be addressed to reduce disparities. Finally, and of critical importance, CMS will build
on its commitment to the standardization of data and will continue to release public data that are
standardized and stratified to reveal and monitor disparities among the individuals and
communities CMS serves.
Developing and Disseminating Solutions to
Achieve Health Equity
The second step along the Path to Equity is developing
and disseminating solutions to achieve health equity. CMS’
activities in this area respond to the research question:
How are the activities in the CMS Equity Plan for Medicare
developing and disseminating solutions to achieve health
equity in Medicare quality?
In this section, we explore two major areas of progress: 1)
evaluating disparities impacts and integrating equity
solutions across CMS programs, and 2) developing and
disseminating promising approaches to support the health
care workforce in addressing health disparities.
CMS EVALUATED DISPARITIES IMPACTS AND
INTEGRATED EQUITY SOLUTIONS ACROSS CMS PROGRAMS
CMS has focused on results and unleashing innovation, creating solutions for evaluating the
impacts of disparities and embedding new resources and tools within CMS programs and
partner organizations to help quantify disparities and close gaps. CMS’ goals are two-fold: 1)
enhancing providers’ and other stakeholders’ ability to easily identify disparities and
opportunities for improvement among those they serve, and 2) relieving the burden on providers
and planning for creating and testing new solutions that can produce measurable results and
improve outcomes among vulnerable populations.
CMS developed and embedded Disparities Impact Statements and other
evaluation mechanisms across CMS programs and partner organizations
CMS has worked to ensure its programs, policies, and stakeholders are equipped to identify
disparities. This allows stakeholders to prioritize efforts where gaps are greatest, take actions to
improve care, and monitor changes over time. To support this effort, CMS developed and
piloted the CMS Disparities Impact Statement. The CMS Disparities Impact Statement is a
quality improvement tool that enables CMS and its stakeholders to systematically evaluate the
impacts of a policy or program on health disparities. CMS has facilitated organizations’ quality
improvement efforts to reduce disparities through targeted interventions. For example, the HIIN
Paving the Way to Equity
through Solutions involves:
• Creating new solutions based on
our understanding of disparities
and the unique health care
needs of individuals and
communities;
• Testing promising strategies and
interventions; and
• Sharing flexible tools that CMS
stakeholders can use to improve
the health care experience and
health outcomes for those they
serve.

Paving the Way to Equity: A Progress Report (2015-2021)
19
11
th
Statement of Work incorporated provisions
around the Disparities Impact Statement to facilitate
ongoing monitoring and reporting on disparities
reduction. At the close of the 11
th
Statement of Work
in 2019, more than 4,000 hospitals across 16 HIINs
nationwide participated in the Partnership for Patients
(PfP), a program that focuses on reducing inpatient
harms and readmissions. HIINs were charged to
develop strategic plans to identify, address, and
monitor progress on reducing disparities across harm
areas among their aligned hospitals. Additionally,
within the Accountable Health Communities (AHC)
program, CMS used an instrument called a Health
Equity Resource Statement, a variation on the CMS Disparities Impact Statement, as part of the
scored evaluation criteria for grant awards. The CMS Disparities Impact Statement has been
promoted and used by various organizations, including QIOs, Health Care Innovation
Awardees, health plans, hospital systems, and provider networks.
Further, through internal partnerships across Centers and Offices, CMS has strengthened the
evaluation and reporting elements for the QIO program, Medicare, Medicare Advantage, and
other programs. This yields a more informed understanding of how the agency and its partners
are structuring disparities reduction efforts and helps identify gaps, challenges, and future
opportunities. For example, the recent reports and data highlights focused on Sickle Cell
Disease and the use of opioids among Medicare beneficiaries mentioned in the “Understanding”
section of this report pave the way to “Solutions,” helping drive decisions and quality
improvement work related to pain management in the Medicare program. In addition, annual
reporting of stratified HEDIS and CAHPS scores is now part of the agency’s ongoing monitoring
and CMS Medicare Advantage Organizations are leveraging this data to identify areas of
opportunity to enhance patient experience, access, quality, and outcomes among MA and dual
beneficiaries. Moving forward, CMS will continue to strengthen monitoring and reporting of
disparities across QIOs and other quality improvement contractors. This supports CMS and its
partners in tailored interventions and focuses improvement on our most vulnerable Medicare
beneficiaries.
CMS embedded equity solutions across CMS programs and partners
Through our work with partners and stakeholders, we found that many organizations and federal
partners recognize that disparities exist. However, stakeholders expressed that they do not
know how to evaluate the impact of their program on disparities, nor what steps they should
take to achieve health equity among the individuals they serve. To address this need, in 2016,
CMS formed the Health Equity Technical Assistance program. Health Equity Technical
Assistance provides direct, flexible, on-demand technical assistance to internal CMS partners
and external stakeholders, including quality improvement partners, providers, health systems,
federal partners, health plans, state Medicaid agencies, health care organizations, local
agencies, and community associations. As of October 2020, through the Health Equity
Feedback on the
Disparities Impact Statement
“The Disparities Impact Statement is a
really nice tool. I like that it used the
PDSA approach and helps you think
about what you are doing, identify why
this is a need, what the data show, [and]
who you can partner with to impact
change and develop interventions. What
a great way to get health care
professionals to think about disparities in
a QI framework! This is a thoughtful tool.”
- HIIN, February 2019
Paving the Way to Equity: A Progress Report (2015-2021)
20
Technical Assistance Program, CMS health equity subject matter experts have responded to
over 278 technical assistance requests from stakeholders in 39 states as well as Washington,
DC, and Puerto Rico. Requests for technical assistance have come from internal CMS staff as
well as partner organizations, including health plans, health departments, universities, hospitals
and health systems, associations, quality improvement contractors, individual providers,
community organizations, researchers, and other stakeholders.
Recognizing the growing numbers of individuals enrolled in Medicare Advantage and managed
care, CMS continues to embed equity solutions to support health plans’ actions to reduce
disparities. For example, CMS began a series of strategic conversations to gather input from
Medicare Advantage Organizations (MAOs) and Medicare-Medicaid Plans (MMPs) focused on
what they are doing to reduce disparities and how CMS could support their progress. This led to
the development of a cross-agency work group focused on learning from plans and generating
program and policy solutions to address disparities among Medicare Advantage enrollees. CMS
continues to engage with MAOs and MMPs to identify and address areas of opportunity where
plans and CMS can work together to improve care for Medicare Advantage and dual-eligible
beneficiaries.
CMS DEVELOPED AND DISSEMINATED PROMISING APPROACHES TO
SUPPORT THE HEALTH CARE WORKFORCE IN ADDRESSING HEALTH
DISPARITIES
CMS has promoted innovative solutions through trainings and resources for health care
professionals and Medicare beneficiaries to reduce disparities and improve the patient
experience among vulnerable populations. Expanding care teams to incorporate a diverse
group of providers and enhancing providers’ skills and cultural competence can help reduce
burden on the workforce as they improve the health of vulnerable communities.
CMS developed and enhanced trainings and resources for health care
professionals to include health equity solutions
Through the Medicare Learning Network (MLN), CMS’s primary mechanism for engaging and
educating Medicare providers on how to work with CMS programs and beneficiaries, the agency
developed and enhanced trainings for the health care workforce. These trainings are quality-
improvement focused. They help organizations and health care providers understand why and
how to improve the care they provide to vulnerable populations, including racial and ethnic
minorities, sexual and gender minorities, individuals with disabilities, and individuals living in
rural areas. CMS quality improvement contractors and providers can use these trainings to
reduce disparities and improve patient experience across multiple settings, while earning
continuing education credits. Recent trainings have focused on improving the quality of care and
data collection for sexual and gender minorities, and developing and strengthening strategic
responses to reducing disparities among beneficiaries. In addition, CMS has embedded content
related to disparities and practical solutions to achieve health equity in practice settings into
existing MLN trainings. This reduces burden on providers and minimizes the number of
individual training courses the workforce would need to take to feel well-equipped to care for all
patients. By incorporating a health equity lens into existing training content, CMS is efficiently
Paving the Way to Equity: A Progress Report (2015-2021)
21
enhancing providers’ cultural competency and reinforcing the importance of including health
equity approaches among professionals in all health care settings.
To illustrate CMS’ reach, between its release in January 2017 and October 2020, over 3,700
individuals from all 50 U.S. states, the District of Columbia and U.S. territories, and other
countries completed the training on improving the quality of care and data collection for sexual
and gender minorities. Participants included clinical providers, such as physicians, nurses, and
pharmacists; non-clinical support staff, such as medical billers and coders, front office staff, and
office managers; and others, including researchers. Although the Medicare Learning Network is
tailored to providers serving Medicare beneficiaries, individuals who take this training may be
serving populations that include Medicare, Medicare Advantage, Medicaid, Marketplace and
individuals with other private coverage.
As a complement to accredited training modules, CMS has created a number of provider-
focused resources to help drive solutions to reducing disparities. For example, to address
disparities in diabetes, a key focus area for CMS quality improvement contractors and partners,
CMS created a Culturally and Linguistically Tailored for Type 2 Diabetes Prevention Resources
Inventory for CDC-managed Diabetes Prevention Program (DPP) suppliers. This inventory
includes fully translated curricula and supplemental materials tailored to various minority
populations. The inventory meets the need for culturally and linguistically tailored resources to
support organizations delivering lifestyle-change programs to minority populations. As of
October 2020, it includes links to 11 sets of culturally and linguistically tailored materials
developed for organizations that may work with minorities seeking to prevent type 2 diabetes
and improve overall health and wellness. The materials presented in this inventory can support
organizations offering the National DPP lifestyle-change program and lifestyle-change program
curricula recognized by the CDC’s DPP, including the Medicare Diabetes Prevention Program
(DPP) Expanded Model. The inventory is available to all Diabetes Prevention Program providers
and other aligned stakeholders to help enhance DPP programming and will be updated
regularly to reflect improved and new training resources as they become available.
CMS also created a
Directory of Provider Resources for Diabetes Management, which compiles
existing guidelines and clinical recommendations; toolkits and clinical reference tools; continuing
education courses; and diabetes care, e-prescribing, and formulary management apps. The
directory is designed to facilitate the effective management of type 2 diabetes by primary care
teams. It is tailored to meet the needs of providers working with Medicare beneficiaries and
vulnerable populations who experience a higher prevalence of type 2 diabetes and its
complications. As with the DPP Resource Inventory, this directory will be routinely updated to
equip providers with timely tools to help patients manage their health. These two resources
were both released at the end of 2019. As of October 2020, together they have been
downloaded from the CMS website more than 2,700 times.
To support hospital-based practices and hospital networks, CMS has spread solutions for
reducing disparities among vulnerable populations through the Guide to Reducing Disparities in
Readmissions (revised August 2018). Hospital admissions and readmissions for chronic
illnesses generate significant costs for Medicare, and research has shown that minority and
Paving the Way to Equity: A Progress Report (2015-2021)
22
other vulnerable populations are more likely to be readmitted to the hospital within 30 days of
discharge for chronic conditions.
xliv
,
xlv
,
xlvi
CMS developed this guide as a tool for hospital leaders
to reduce avoidable readmissions for their diverse Medicare beneficiary populations. It provides
leaders of all types of hospitals (e.g., rural, urban, private, and nonprofit), and quality
improvement organizations that provide support to hospitals, with: 1) an overview of key issues
related to disparities in readmissions; 2) a set of activities that can help hospital leaders address
readmissions in these populations; and 3) strategies aimed at reducing readmissions in diverse
populations. From its initial release in August 2016 through October 2020, the guide was
downloaded from the CMS website more than 5,300 times and was shared widely by CMS
quality improvement contractors to address key drivers of readmission rates at hospitals
nationwide.
CMS developed Modernizing Health Care to Improve Physical Accessibility, to educate health
care providers across all practice settings on strategies to increase physical accessibility of
health care facilities and services. This resource was downloaded more than 1,900 times
between its release in July 2019 and October 2020. In addition, CMS collaborated with the
Department of Justice (DOJ), the HHS Office of Civil Rights (OCR), and the Administration for
Community Living (ACL) on Increasing the Physical Accessibility of Health Care Facilities (May
2017). This issue brief provides an overview of the importance of physical accessibility of health
care facilities, laws to promote accessibility, and examples of federal and state-level efforts to
better understand patient needs and support improvements in accessibility. The brief has been
downloaded more than 1,400 times since its publication through October 2020. These
resources educate stakeholders about the complexity of issues related to Medicare beneficiary
access and highlight opportunities for CMS and other federal agencies to work together in
addressing the need for more accessible facilities. They also close a gap in research and
practice by focusing explicitly on improving care for members of the Medicare population with
mobility-related disabilities. Each provides examples of mechanisms that have increased the
accessibility of facilities and real-world strategies and tools providers can access to make
improvements in their practice for individuals they serve.
Further, because effective communication is critical to ensuring mutual provider-patient
understanding, empowering patients, and providing high-quality care across all patient care
settings and provider types, CMS developed a practical tool to improve how providers and plans
communicate with individuals and communities. The Guide to Developing a Language Access
Plan (February 2018) helps organizations go through the steps they can take to provide high-
quality, appropriate language assistance services to all individuals they serve. Following a
Language Access Plan helps ensure that staff members are aware of what to do when an
individual with limited English proficiency needs assistance. CMS also developed two resources
(November 2020) to support providers serving those with sensory disabilities. When serving a
patient who is blind or has low vision or who is deaf or hard of hearing, it is important for an
organization to plan how they will provide effective, accessible communication. These resources
describe how to assess practices, develop communication plans, and be prepared to implement
accessible services.
Paving the Way to Equity: A Progress Report (2015-2021)
23
During the public health emergency, CMS is working to support providers and partners in our
most vulnerable communities. To assist administrators and providers in rural communities
during COVID-19, CMS OMH developed a Rural Crosswalk: CMS Flexibilities to Fight COVID-
19. The crosswalk is intended to assist rural providers in accessing information on key
provisions CMS has issued during the public health emergency. Rural providers including those
in Rural Health Clinics, Federally Qualified Health Centers, Critical Access Hospitals, rural
hospitals, and long term care facilities face numerous challenges while trying to serve their
patients. This document brings together key information that CMS has released to date in one
location to improve provider access to this crucial information and allowing them time to better
serve their patients. In addition, the CMS OMH website now includes a site with COVID-19-
related federal resources for vulnerable populations to help consumers, health care
professionals, community organizations, and other CMS stakeholders find trusted resources in
one place, including resources in languages other than English.
CMS designed, pilot-tested, and continuously enhances these provider tools and other
resources through engagement with health care professionals and disparities experts. This
ensures organizations have relevant, applicable tools and solutions to improve the quality of
care provided to vulnerable populations and create inclusive clinical practice environments.
CMS developed beneficiary-facing resources to improve care in vulnerable
communities
In addition to developing trainings and resources for health care professionals, CMS has also
developed individual and family-facing resources for Medicare beneficiaries. For example, CMS
developed the consumer-facing Getting the Care You Need: A Guide for People with Disabilities
to help raise awareness among individuals with disabilities about working with their providers to
ask for needed accommodations. An accompanying checklist highlights steps individuals and
family members can take before, during, and after appointments with health care providers to
ensure individuals with access challenges can get the care they need. From their publication in
July 2019 through October 2020, the handout and accompanying checklist have been
downloaded from the CMS website over 2,900 times. CMS’ release of these resources included
a Braille translation, and based on user feedback they are translated into multiple languages.
CMS also produced a suite of videos featuring the personal experiences of individuals with
disabilities navigating care, called Navigating Health Care with a Disability: Our Stories. One
video is aimed at a provider audience while the other is intended for individuals with disabilities.
As of October 2020, together these videos had been viewed on YouTube 5,000 times.
Further, to address the growing number of Medicare beneficiaries managing chronic conditions,
CMS partnered with HRSA’s Federal Office of Rural Health Policy to launch the Connected
Care campaign. This campaign was designed to raise beneficiary and provider awareness for
the services now available for chronic care management (CCM).
3
Medicare beneficiaries with
two or more chronic conditions may be eligible for CCM services. CCM services can be
3
The CCM campaign was specifically mandated by Congress to focus on racial and ethnic minorities, and rural
populations, and a Report to Congress was prepared and delivered to address the Connected Care campaign.
Paving the Way to Equity: A Progress Report (2015-2021)
24
delivered by several provider types and bring significant benefits to individuals in rural areas and
other vulnerable communities. CMS has released a number of beneficiary- and provider-facing
Connected Care resources to ensure that all eligible Medicare-covered individuals can get
services to help them manage their multiple chronic conditions. The campaign focused on
ensuring that individuals and providers in underserved communities were aware of these
reimbursable services. Connected Care resources include patient education resources such as
a poster, postcard, and video that can be used in clinical and community settings, and a toolkit
for healthcare professionals and community partners. CMS recognizes that CCM services take
providers’ time and effort. These resources help individuals with asking the right questions so
they can get help managing their care. These support tools also help providers account for the
additional time and resources they spend to provide help between appointments. Since the
campaign’s launch at the end of 2016, the Connected Care website has more than 108,000
unique pageviews, and resources have been downloaded by tens of thousands of users. Many
Medicare and dual eligible patients, including those in underserved communities, depend on this
extra effort to help them stay on track with their treatments and plan for health.
To address the public health emergency, CMS looked for ways to assist local communities and
our partners who work with those most vulnerable—such as older adults, those with underlying
medical conditions, racial and ethnic minorities, rural communities, and people with disabilities.
CMS sought feedback through a series of calls and listening sessions to find out what partners
needed to better serve vulnerable populations, specifically racial and ethnic minority
populations. Based off of this feedback, the From Coverage to Care (C2C) initiative created two
new consumer-facing resources to encourage people to stay healthy during COVID-19, receive
needed care, and understand how their health coverage would work during the public health
emergency. The first resource Coronavirus and Your Health Coverage: Get the Basics
helps
consumers learn how to protect themselves and their family during COVID-19 with tips for
staying healthy. This resource also has information about what health services are typically
covered under Medicare and Marketplace plans and additional resources. Second, C2C
released Stay Safe: Getting the Care You Need, at Home which offers tips for how to stay
healthy during COVID-19 with information about scheduling health appointments from home
and planning ahead for prescriptions. Both resources were originally posted in English and
Spanish with additional languages in development. To further assist partners in their work with
local communities, social tiles and graphics with key messages were also created.
Recognizing the interaction between chronic conditions and COVID-19 outcomes, and the
disproportionate number of racial and ethnic minorities with diagnosed Type 2 diabetes, CMS
created Managing Diabetes: Medicare Coverage and Resources. This two-page resource is
available in English and Spanish and pools CDC and CMS resources from over 20 websites into
a single, easy-to-navigate document. With one click on Medicare.gov, Medicare beneficiaries
can find links to help live with diabetes, how to find diabetes self-management education and a
provider to help them manage their care, how to get coverage for diabetes services, and how to
get help with costs. CMS and CDC’s collaboration on this product aims to help individuals,
particularly members of vulnerable communities who bear a high burden of Type 2 diabetes,
improve their management of diabetes and their overall health to decrease the risk of the severe
and adverse effects of COVID-19.
Paving the Way to Equity: A Progress Report (2015-2021)
25
GAPS, NEEDS, NEXT STEPS TO ACHIEVE HEALTH EQUITY BY DEVELOPING
AND DISSEMINATING SOLUTIONS
Moving forward, CMS will continue working to achieve health equity by developing and sharing
solutions and tools to eliminate disparities in Medicare, and will explore new opportunities
across all of its programs and policies. CMS will remain focused on developing resources for
beneficiaries and providers to improve vulnerable communities’ understanding and
management of their chronic conditions. This includes paying deliberate attention to conditions
that heavily impact minority and rural communities, such as diabetes, cancer, and heart
disease. Each of these conditions, among many others, place beneficiaries at increased risk for
severe illness from the virus that causes COVID-19. If current data trends hold, COVID-19
related disparities will continue to deepen across CMS OMH’s priority populations.
xlvii
Based on ongoing stakeholder feedback, the agency will also prioritize resources that help
providers and partners reduce avoidable readmissions, address social determinants of health in
various care settings, and manage patient safety concerns across settings from hospitals to
primary and post-acute care and as individuals transition between settings. Consistent with the
agency’s overarching priorities, CMS will continue to focus efforts on ensuring rural communities
have resources and tools to improve access, quality, and outcomes, and will work to develop
and share innovative solutions to address the opioid epidemic for vulnerable communities
nationwide. Finally, CMS will continue to build on its ongoing commitment to results through the
evaluation and monitoring of disparities among those we serve by embedding tools including the
CMS Disparities Impact Statement and monitoring and reporting on disparities across our
programs.
Implementing Sustainable Actions to Achieve
Health Equity
The third step along the Path to Equity is
implementing sustainable actions to achieve health
equity. CMS’ activities under this area inform the
following research question: How are the activities in
the CMS Equity Plan for Medicare leading to
sustainable actions that achieve equity in Medicare
quality?
In this section, we explore two major areas of
progress: 1) taking action to improve CMS programs
and policies to reduce disparities, and 2) mobilizing
partners to take action to reduce disparities.
Paving the Way to Equity through
Actions involves:
• Bringing stakeholders together and
spurring collective and individual
action among partners;
• Supporting stakeholders in their efforts
to achieve health equity;
• Making adjustments for continuous
quality improvement; and
• Ensuring actions are sustained over
time.
Paving the Way to Equity: A Progress Report (2015-2021)
26
CMS LEVERAGED QUALITATIVE AND QUANTITATIVE RESEARCH FINDINGS TO
IMPROVE PROGRAMS AND POLICIES TO REDUCE DISPARITIES
CMS has driven results across the nation and the agency, promoting action among CMS
components and external stakeholders through new partnerships and focused efforts to
measure, monitor, and eliminate disparities.
CMS programs are measuring and monitoring progress to eliminate disparities
The QIO program is one of the largest federal programs dedicated to improving health and
health care quality at the local level for Medicare beneficiaries. The program’s 11
th
Statement of
Work focused on five primary functions: 1) excellence in operations; 2) better health; 3) better
care; 4) lower costs; and 5) technical assistance. Under this program, CMS specifically aimed to
reduce disparities in diabetes and cardiac health. QIOs routinely updated CMS on their activities
related to vulnerable communities across all tasks, for example those targeting racial and ethnic
minorities, sexual and gender minorities, individuals with disabilities, and individuals living in
rural areas. CMS tracked QIO progress, as well as progress made by HIINs, CMS’ hospital-
focused quality improvement contractors. This helped ensure that the agency was aware of, and
able to encourage, our partners and stakeholders to continue to move the needle on health
disparities. As CMS and partners support the 12
th
Statement of Work, the agency will continue
to support the network of quality improvement and innovation contractors’ strong focus on
health equity so that together we can demonstrate results. In particular, CMS will work with
quality improvement contractors and individual providers to drive improvements in nursing
homes and hospitals as they navigate the current public health emergency. The Agency and our
partners will seek opportunities for improvement in health care quality, outcomes, and access
for vulnerable and rural communities – particularly those hardest hit by COVID-19.
CMS has also focused on testing approaches to reducing disparities through our models and
demonstrations. For example, health equity monitoring and measurement was embedded into
the scored grant selection criteria for the Accountable Health Communities (AHC) model. As
mentioned above, the AHC model required a Health Resource Equity Statement, a form of the
CMS disparities impact statement, to be included with each application and monitored over
time. CMS’ grant application with embedded equity statement ensured that selected awardees
were demonstrating a commitment and awareness of local health disparities and the
communities they serve. This was the first time a scored element related to health equity was
included in CMS’ grant application process and represents a significant step along the Path to
Equity for the agency.
CMS has increased internal collaboration to reduce disparities
Over the last several years, CMS has worked to increase collaboration and communication
across teams to ensure that beneficiaries and providers benefit from the most streamlined and
intelligently designed programs and policies. For example, CMS collaborated across Centers
and Offices to gather feedback from Medicare beneficiaries, providers, advocates, and health
care suppliers that would inform changes to Medicare payment policy to improve access to care
of people with disabilities. As a result of this work, CMS implemented a change to the Medicare

Paving the Way to Equity: A Progress Report (2015-2021)
27
Physician Fee Schedule (PFS) to support providers in spending additional time providing
preventive care to their patients. Beginning January 1, 2018, using a new provider billing code,
providers can bill for services that extend beyond the typical time assumed for eligible
preventive services. This change recognizes the increased resource costs associated with
providing care to some patients, including the medically necessary use of specialized mobility-
assistive technology during an office visit, such as adjustable height chairs or tables, patient
lifts, and adjustable padded leg supports.
CMS also recommended that beneficiaries with sickle cell disease be excluded from the opioid
safety edits starting in 2020. Previously, the CDC Guideline for Prescribing Opioids for Chronic
Pain stated that “given the challenges of managing the painful complications of sickle cell
disease, readers are referred to the NIH National Heart, Lung, and Blood Institute’s Evidence
Based Management of Sickle Cell Disease Expert Panel Report for management of sickle cell
disease.”
xlviii
In 2018, CMS released a report on the challenges of pain management for
beneficiaries with sickle cell disease titled “The Invisible Crisis: Understanding Pain
Management in Medicare Beneficiaries with Sickle Cell Disease” (September 2018), which
provided supporting evidence for this change. CMS encouraged its partners to work with their
pharmacy and therapeutics (P&T) committees to identify other vulnerable patient populations for
exclusion from the opioid safety edits. To further support these efforts, CMS released
comprehensive guidance for sponsors and educational materials for providers, beneficiaries,
and other partners, such as pharmacies, professional organizations, and advocacy groups,
which are available on the Improving Drug Utilization Review Controls in Part D webpage.
In addition, in 2019, CMS identified and developed standardized patient assessment data
elements (SPADEs) to assess social determinants of health and embedded these data
elements into the Post-Acute Care Quality Reporting Programs, to be collected starting in 2020.
Although data collection is delayed due to the public health emergency, this policy change in
Medicare’s prospective payment system makes collection of social determinants of health data
part of the required standardized patient assessments administered in post-acute care settings.
This extends to long-term care hospitals, skilled nursing facilities, intermediate rehabilitation
facilities, and home health agencies. The additional SPADEs include race, ethnicity, preferred
language/interpreter services, health literacy, transportation, and social isolation. Collecting
these data elements will allow CMS to inform provider understanding, facilitate coordinated care
and care planning, reduce readmissions, and improve quality of care and outcomes for
beneficiaries. While CMS acknowledges that there are other important social determinants
worth measuring, CMS also aims to balance the value of capturing data with the burden of
reporting for post-acute care providers. CMS strategically identified these specific demographics
and determinants of health because of their relevance to patients and residents receiving post-
acute care. Post-acute care settings have an opportunity to address SDOH. For example, they
may connect patients and residents to transportation programs, certified interpreters, or social
support programs. Collecting these data elements will provide the basis for CMS’ periodic
analyses of the relationship between an individual’s health status and demographic and social
risk factors that can inform efforts to promote health equity. To support post-acute care
providers in meeting this new requirement, CMS continues to refine our guidance on how to
collect these additional data with minimal burden.
Paving the Way to Equity: A Progress Report (2015-2021)
28
CMS leveraged internal partnerships to identify and mitigate challenges beneficiaries face in
identifying providers with accessible office locations and equipment. To help prospective
enrollees identify providers with accessible offices, CMS worked with states and plans
participating in the Financial Alignment Initiative (FAI) to improve Medicare-Medicaid Plan
(MMP) provider and pharmacy directories. CMS is seeing improvements in these directories,
which now indicate if a provider location is on a public transportation route. Some MMPs have
made progress in indicating which providers have completed cultural competency training. CMS
continues to work with plans about indicating the specific accommodations available at provider
locations for individuals with physical disabilities.
In support of Medicare’s evolving payment systems in 2019, CMS strengthened the validation
criteria for Quality Payment Program Merit-Based Incentive Payment System (QPP MIPS)
Improvement Activities to align with our goal of achieving health equity. Providers participating
in the Merit-Based Incentive Payment System, or MIPS, may participate in Improvement
Activities to improve their score, and therefore their reimbursement, under this new Medicare
payment system. Improvement Activities are structured to improve care for beneficiaries, and
CMS’ cross-component collaboration helps reduce burden on providers as they engage in – and
are recognized for – meaningful, impactful disparities reduction efforts as a part of their
participation in the Medicare program.
This progress report has highlighted a number of examples of internal CMS collaboration to
reduce disparities among priority populations. However, there are many more partnerships that
help inform and advance health equity work across the agency each day. CMS has
strengthened its internal operations to improve our work across components, paving the way for
the agency to address new and emerging equity issues and continually improve CMS programs
and policies.
CMS CONVENED AND MOBILIZED PARTNERS TO TAKE ACTION ON
DISPARITIES
CMS mobilized communities, partners, and providers to take action on reducing disparities and
implementing innovative, self-directed health equity activities.
CMS inspired action and sharing among providers and external partners
In an effort to spur ongoing, sustainable health equity actions among health care providers and
others, CMS announced the CMS Health Equity Award in 2018. From 2018-2020, this
recognition highlighted organizations demonstrating an exceptional commitment to health equity
by reducing disparities among the CMS beneficiaries they serve, particularly among racial and
ethnic minorities, individuals with disabilities, sexual and gender minorities, and those living in
rural areas. CMS used a rigorous, peer-reviewed selection process to select and recognize
organizations who can demonstrate results in reducing disparities in health care quality, access,
or outcomes for a priority population. This award helped mobilize CMS stakeholders, spurring
CMS’ partners to share and spread innovative best practices that measurably reduce

Paving the Way to Equity: A Progress Report (2015-2021)
29
disparities, and lifting up organizations who are successfully closing gaps among those they
serve.
4
For example, in 2018, CMS recognized Kaiser Permanente for reducing disparities in
hypertension control, closing the Black/White gap to dramatically improve hypertension control
for African Americans through a targeted intervention. CMS also recognized Novant Health for
identifying and reducing a disparity in pneumonia readmission rates, improving pneumonia-
related readmissions for African Americans over less than one year to close the gap between
this population and other patients served. In 2019, CMS recognized HealthPartners for their
organization-wide approach which helped them reduce health disparities and close or eliminate
gaps between racial and ethnic minority enrollees and white enrollees for multiple health
outcomes across the clinic, health plan, and hospital settings. CMS also recognized Centene
Corporation for their national initiative to increase the accessibility of provider offices and
services for people with disabilities by providing grant funding directly to providers to make
improvements. In 2020, CMS presented the award to UnitedHealthcare, which used home
visits, local primary care and obstetric nurse partnerships, and care coordination to improve the
delivery of timely, comprehensive postpartum care among Black women in Michigan and Ohio
as well as rural women in Hawaii. CMS also presented the award to Atrium Health, which
improved their collection of demographic data, created an analytic tool that stratifies health-
related data by key demographic variables, and used the results to design and implement
culturally appropriate interventions in communities and primary care practices. This effectively
closed the gap in colorectal cancer screenings for Hispanic males.
Further, in 2018, inspired by CMS’ work to reduce disparities, the HIIN community initiated a
self-driven effort to develop, test, and implement a Health Equity Organizational Assessment.
This assessment was completed by enrolled hospitals and helped HIINs, hospitals, and CMS to
refine our understanding of where hospitals are on their journeys to eliminating disparities and
how to meet their members’ needs. The elements that HIINs identified and measured in their
hospital assessment bring health equity to the forefront of the program. Coupled with CMS
Disparities Impact Statements and the robust self-governed HIIN Health Equity Affinity Group,
CMS and HIINs gained insight on a broad swath of hospitals and could track health equity
progress nationwide.
Another example of how CMS has generated self-directed health equity activities is through
engagement with federal stakeholders to identify actions to improve accessibility in health care
and other facilities for people with disabilities. CMS has engaged more than 40 federal
stakeholders representing 11 federal agencies on a regular basis to identify solutions that will
4
The receipt of a CMS Health Equity Award should not be interpreted as a release of or a statement made on a recipient’s
compliance with its specific legal or regulatory obligations, or the merit, existence or lack of existence of any investigation, lawsuit, or
other matter relating to compliance or law enforcement. The CMS Health Equity Award solely represents recognition for specific
efforts to improve health equity, as evaluated based on the information reviewed by CMS’s selection committee.
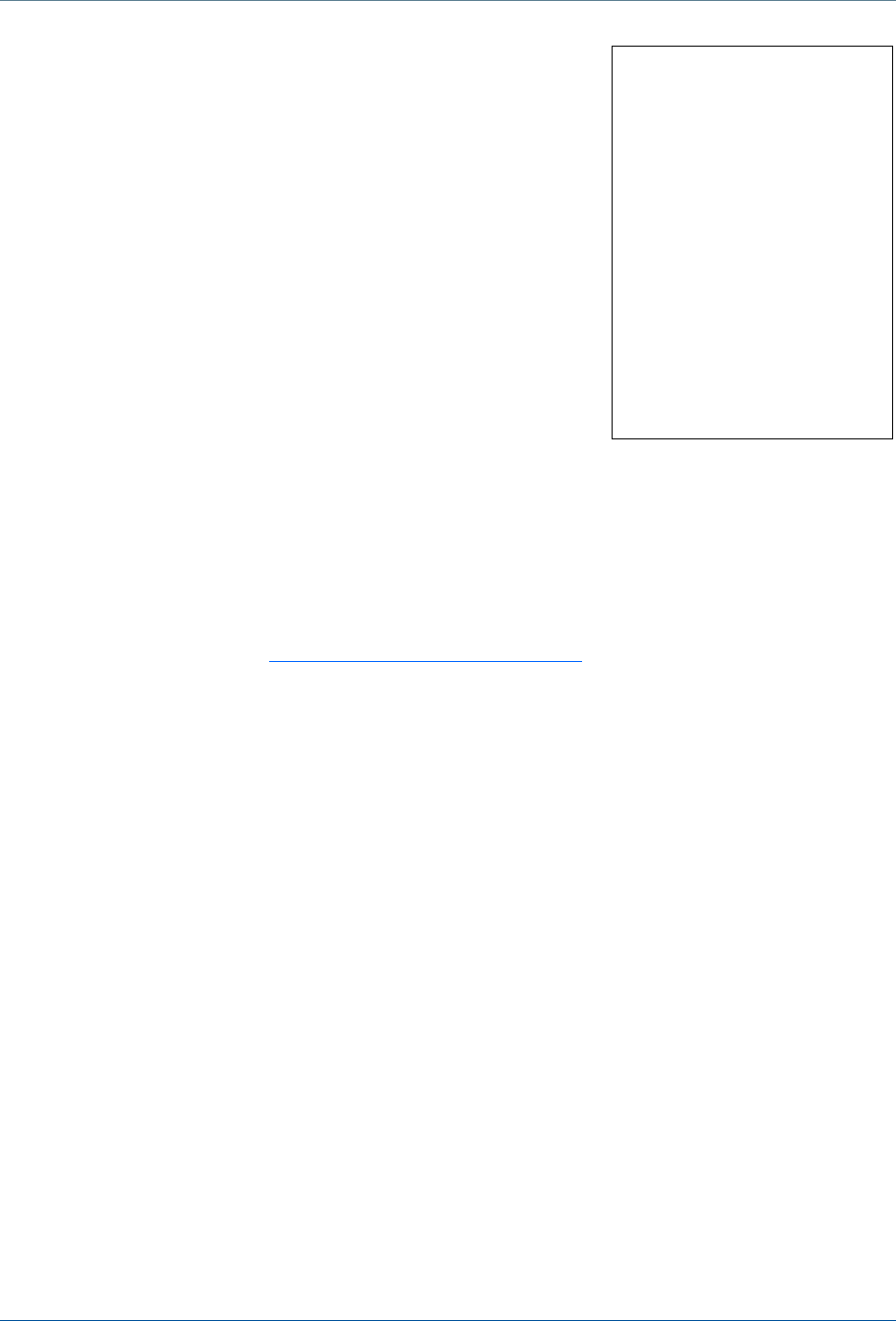
Paving the Way to Equity: A Progress Report (2015-2021)
30
ensure health care and other facilities are physically accessible
to individuals with mobility impairment. This work created a
robust network of disability experts who are now pursuing and
generating opportunities to eliminate disparities for beneficiaries
with disabilities. For example, this group collaborated to inform
CMS’ most recently released provider accessibility resources,
ensuring providers and beneficiaries get the most well-rounded
and well-informed perspective. Throughout the public health
emergency, this group has engaged in regular discussions to
assess the unique challenges and barriers that individuals with
disabilities face related to COVID-19. Each agency has shared
their perspectives, assets, and the challenges they face to
collectively identify solutions and improve quality, access, and
outcomes for individuals with disabilities in the public health
emergency.
Understanding that many of the office’s populations were being hit the hardest by the COVID-19
public health emergency, CMS hosted three listening sessions focusing on racial and ethnic
minority populations and COVID-19. The feedback received in these sessions was shared
within the Agency to inform next steps to continue addressing the unique needs minority
communities face during the public health emergency.
Lastly, CMS administers the Minority Research Grant Program (MRGP) to support researchers
at minority-serving institutions who are exploring how CMS can better meet the health care
needs of racial and ethnic minorities, people with disabilities, sexual gender minorities, and
individuals living in rural areas. Minority-serving institutions include Historically Black Colleges
and Universities, Hispanic-Serving Institutions, Tribal Colleges and Universities, and Asian
American and Native American Pacific Islander-Serving Institutions. CMS supports recipients of
the MRGP by providing research funding for 24 months along with technical assistance, one-on-
one support, and progress reports. Between 2005 – 2020, the MRGP has funded 48 grantees
resulting in expanded health-related knowledge, attitudes, behaviors, and outcomes as evident
by more than 40 published manuscripts, 55+ abstracts and presentations, book publications,
and over 190 citations in subsequent research. This work has increased the agency’s and
external partners’ knowledge of new and emerging research to support health equity through
the expertise and technical mastery of research faculty at minority-serving institutions.
GAPS, NEEDS, AND NEXT STEPS TO IMPLEMENT SUSTAINABLE ACTIONS
In the future, CMS will continue to implement sustainable actions across its programs and
policies to achieve health equity among Medicare beneficiaries, and will explore new
opportunities across all of its programs and policies. CMS will promote and expand upon its
current efforts to support providers in small practices, and those in rural and underserved areas,
through the Quality Payment Program as they transition to Advanced Alternative Payment
Methodologies and the Merit-Based Incentive Payment System, as well as through other CMS
payment systems and models. In addition, CMS, in collaboration with the Office of the Assistant
Feedback from Listening
Session Participant:
“Thanks very much for
providing an opportunity for
those of us who have been
working for many years on
health equity for people with
disabilities to participate in
today's listening session on
increasing physical
accessibility of health care
facilities. We appreciate the
leadership of [CMS] OMH on
this issue and look forward to
continued discussions.”

Paving the Way to Equity: A Progress Report (2015-2021)
31
Secretary for Planning and Evaluation (ASPE) and other HHS partners, will continue to consider
ways to standardize data collection of social determinants of health and demographic
information. CMS and HHS partners will continue to collaborate on ways to leverage this data
collection to add value to federal agencies, providers, and local communities.
CMS will continue convening partners and consumers to understand where action is needed,
and what actions will be most impactful. The Agency will maintain their focus on continuous,
system-wide, sustainable quality improvement. CMS will continue to engage on ways to
encourage providers to address the needs of the whole person and link individuals with the
services they need to achieve their highest level of health. CMS will also continue to explore
how best to encourage providers to eliminate disparities through Medicare and other value
based payment systems and model tests. The agency will maintain a focus on vulnerable
communities hit hardest by the public health emergency, considering barriers and solutions
specific populations face during the COVID-19 crises and other emerging diseases. Finally,
CMS will build on its current work embedding health equity and standardized data into its rules,
regulations, and guidance across health care settings. This work, and all of the work of the CMS
Equity Plan, will maintain a focus on ensuring that CMS programs and policies are designed to
help organizations across the health care continuum work together to reduce disparities and
achieve health equity for CMS beneficiaries nationwide.
Paving the Way to Equity: A Progress Report (2015-2021)
32
SUGGESTED CITATION
Centers for Medicare & Medicaid Services, “Paving the Way to Equity: A Progress Report
(2015-2021),” (2021).
CMS OFFICE OF MINORITY HEALTH
7500 Security Blvd.
MS S2-12-17
Baltimore, MD 21244
HealthEquityTA@cms.hhs.gov
go.cms.gov/omh
Paid for by the US Department of Health & Human Services.
January 2021
Paving the Way to Equity: A Progress Report (2015-2021)
33
References
i
2017 National Healthcare Quality and Disparities Report. Agency for Healthcare Research and Quality. 2018.
http://www.ahrq.gov/research/findings/nhqrdr/nhqdr17/index.html
ii
Fredriksen-Goldsen KI, Hoy-Ellis CP, Muraco A, Goldsen J, Kim H-J. The health and well-being of LGBT older adults: Disparities,
risks, and resilience across the life course. The lives of LGBT older adults: Understanding challenges and resilience. Washington,
DC, US: American Psychological Association; 2015:25-53.
iii
Health, United States, 2015: With special feature on racial and ethnic health disparities. National Center for Health Statistics.
“2016. https://www.cdc.gov/nchs/data/hus/hus15.pdf
iv
Krahn GL, Walker DK, Correa-De-Araujo R. Persons with disabilities as an unrecognized health disparity population. Am J Public
Health. 2015;105 Suppl 2(Suppl 2):S198-S206. doi:10.2105/AJPH.2014.302182
v
Douthit N, Kiv S, Dwolatzky T, Biswas S. Exposing some important barriers to health care access in the rural USA. Public Health.
2015;129(6):611-620. doi:10.1016/j.puhe.2015.04.001
vi
Mapping Medicare Disparities (MMD) Tool. Centers for Medicare & Medicaid Services. Updated 2019.
https://data.cms.gov/mapping-medicare-disparities
vii
Stratified Reporting: Part C and D Performance Data Stratified by Race, Ethnicity, and Gender. Centers for Medicare & Medicaid
Services. Updated 2019. https://www.cms.gov/About-CMS/Agency-Information/OMH/research-and-data/statistics-and-
data/stratified-reporting.html
viii
Disparities in Health Care and Health Outcomes in Selected Conditions. National Quality Forum, “January 15, 2017.
https://www.qualityforum.org/Projects/c-d/Disparities/Final_Report.aspx
ix
HHS Action Plan to Reduce Racial and Ethnic Health Disparities. US Dept. of Health & Human Services; April
2011. http://minorityhealth.hhs.gov/npa/files/plans/hhs/hhs_plan_complete.pdf
x
Frieden TR; Centers for Disease Control and Prevention (CDC). Forward: CDC Health Disparities and Inequalities Report - United
States, 2011. MMWR Suppl. 2011;60(1):1-2.
xi
Carter-Pokras O, Baquet C. What is a "health disparity"?. Public Health Rep. 2002;117(5):426-434. doi:10.1093/phr/117.5.426
xii
NCHHSTP Social Determinants of Health: Frequently Asked Questions. Centers for Disease Control and Prevention. Accessed
December 2019. https://www.cdc.gov/nchhstp/socialdeterminants/faq.html
xiii
HHS Action Plan to Reduce Racial and Ethnic Health Disparities. US Dept. of Health & Human Services; April
2011. http://minorityhealth.hhs.gov/npa/files/plans/hhs/hhs_plan_complete.pdf.
xiv
Frieden TR; Centers for Disease Control and Prevention (CDC). Forward: CDC Health Disparities and Inequalities Report - United
States, 2011. MMWR Suppl. 2011;60(1):1-2.
xv
Carter-Pokras O, Baquet C. What is a "health disparity"?. Public Health Rep. 2002;117(5):426-434. doi:10.1093/phr/117.5.426
xvi
Agency for Healthcare Research and Quality: Division of Priority Populations. Agency for Healthcare Research and Quality., April
2016. http://www.ahrq.gov/sites/default/files/wysiwyg/research/findings/factsheets/priority-
populations/prioritypopulations_factsheet.pdf
xvii
Chapter Eight: Focusing on Vulnerable Populations. Agency for Healthcare Research and Quality. March
1998. http://archive.ahrq.gov/hcqual/meetings/mar12/chap08.html
xviii
Disparities in Health Care and Health Outcomes in Selected Conditions. National Quality Forum. January 15, 2017.
https://www.qualityforum.org/Projects/c-d/Disparities/Final_Report.aspx
xix
National Healthcare Quality and Disparities Reports. Agency for Healthcare Research and Quality, Rockville, MD. Updated June
2020. https://www.ahrq.gov/research/findings/nhqrdr/index.html
xx
Braveman P. What are Health Disparities and Health Equity? We Need to Be Clear. Public Health Rep. 2014;129(1_suppl2):5-8.
doi:10.1177/00333549141291S203
xxi
Mapping Medicare Disparities (MMD) Tool. Centers for Medicare & Medicaid Services. Updated 2019.
https://data.cms.gov/mapping-medicare-disparities
xxii
American Heart Association News. LGBT health disparities the ‘next frontier’. June 2015. https://news.heart.org/lgbt-health-
disparities/.
xxiii
Kates J, Ranji U, Beamesderfer A, Salganicoff A, Dawson L. Health and Access to Care and Coverage for Lesbian, Gay,
Bisexual, and Transgender Individuals in the U.S. Kaiser Family Foundation. May 2018. https://www.kff.org/disparities-policy/issue-
brief/health-and-access-to-care-and-coverage-for-lesbian-gay-bisexual-and-transgender-individuals-in-the-u-s/.
xxiv
Havercamp SM, Scott HM, National health surveillance of adults with disabilities, adults with intellectual and developmental
disabilities, and adults with no disabilities. Disabil Health J. 2015;8(2):165-172. doi:10.1016/j.dhjo.2014.11.002
xxv
Wisdom JP, McGee MG, Horner-Johnson W, et al. Health disparities between women with and without disabilities: a review of
the research. Soc Work Public Health. 2010;25(3):368-386. doi:10.1080/19371910903240969
xxvi
Skrepnek GH, Mills JL Sr, Armstrong DG. A diabetic emergency one million feet long: disparities and burdens of illness among
diabetic foot ulcer cases within emergency departments in the United States, 2006-2010. PLOS One. 2015;10(8):e0134914.
doi:10.1371/journal.pone.0134914
Paving the Way to Equity: A Progress Report (2015-2021)
34
xxvii
Institute of Medicine (US). How Far Have We Come in Reducing Health Disparities? Progress Since 2000: Workshop Summary.
Washington (DC): National Academies Press (US); 2012. 2, What Progress in Reducing Health Disparities Has Been Made? A
Historical Perspective. https://www.ncbi.nlm.nih.gov/books/NBK114236/.
xxviii
2018 National Healthcare Quality and Disparities Report. Rockville, MD: Agency for Healthcare Research and Quality;
September 2019. AHRQ Pub. No. 19-0070-EF. https://www.ahrq.gov/sites/default/files/wysiwyg/research/findings/nhqrdr/2018qdr-
final.pdf.
xxix
Ferdows NB, Aranda MP, Baldwin JA, Baghban Ferdows S, Ahluwalia JS, Kumar A. Assessment of Racial Disparities in Mortality
Rates Among Older Adults Living in US Rural vs Urban Counties From 1968 to 2016. JAMA Netw Open. 2020; 3(8):e2012241.
doi:10.1001/jamanetworkopen.2020.12241.
xxxi
National Academies of Sciences, Engineering, and Medicine; Health and Medicine Division; Board on Population Health and
Public Health Practice; Baciu A, Negussie Y, Geller A, et al., eds. Communities in Action: Pathways to Health Equity. Washington
(DC): National Academies Press (US); January 11, 2017. https://www.ncbi.nlm.nih.gov/books/NBK425844/
xxxii
5. Improving Data Collection across the Health Care System. Agency for Healthcare Research and Quality. Updated May 2018.
https://www.ahrq.gov/research/findings/final-reports/iomracereport/reldata5.html.
xxxiii
Bhalla R, Yongue BG, Currie BP. Standardizing race, ethnicity, and preferred language data collection in hospital information
systems: results and implications for healthcare delivery and policy. J Healthc Qual. 2012;34(2):44-52. doi:10.1111/j.1945-
1474.2011.00180.x
xxxiv
Proctor K, Haffer SC, Ewald E, Hodge C, James CV. Identifying the Transgender Population in the Medicare Program.
Transgender Health. 2016;1(1):250-265. doi:10.1089/trgh.2016.0031
xxxv
Dragon CN, Guerino P, Ewald E, Laffan AM. Transgender Medicare Beneficiaries and Chronic Conditions: Exploring Fee-for-
Service Claims Data. LGBT Health. 2017;4(6):404-411. doi:10.1089/lgbt.2016.0208
xxxvi
Ewald E, Guerino P, Dragon C, Laffan AM, Goldstein Z, Streed C. Identifying Medicare Beneficiaries Accessing Transgender
Related Care in the Era of ICD-10. LGBT Health 2019;6(4):166-173. doi:10.1089/lgbt.2018.0175
xxxvii
Information on Medicare Telehealth. Centers for Medicare & Medicaid Services. November 2018. https://www.cms.gov/About-
CMS/Agency-Information/OMH/Downloads/Information-on-Medicare-Telehealth-Report.pdf
xxxviii
National Standards for CLAS in Health and Health Care: A Blueprint for Advancing and Sustaining CLAS Policy and Practice.
US Dept. of Health & Human Services, Office of Minority Health. April 2013.
https://thinkculturalhealth.hhs.gov/assets/pdfs/EnhancedCLASStandardsBlueprint.pdf
xxxix
Weech-Maldonado R, Elliott M, Pradhan R, Schiller C, Hall A, Hays RD. Can hospital cultural competency reduce disparities in
patient experiences with care?. Med Care. 2012;50 Suppl(0):S48-S55. doi:10.1097/MLR.0b013e3182610ad1
xl
Betancourt JR, Green AR, Carrillo JE, Ananeh-Firempong O 2nd. Defining cultural competence: a practical framework for
addressing racial/ethnic disparities in health and health care. Public Health Rep. 2003;118(4):293-302. doi:10.1093/phr/118.4.293
xli
Institute of Medicine (US) Committee on Understanding and Eliminating Racial and Ethnic Disparities in Health Care, Smedley
BD, Stith AY, Nelson AR, eds. Unequal Treatment: Confronting Racial and Ethnic Disparities in Health Care. Washington (DC):
National Academies Press (US); 2003.
xlii
Feng Z, Fennell ML, Tyler DA, Clark M, Mor V. The Care Span: Growth of racial and ethnic minorities in US nursing homes
driven by demographics and possible disparities in options. Health Aff (Millwood). 2011;30(7):1358-1365.
doi:10.1377/hlthaff.2011.0126
xliii
Rivera-Hernandez M, Rahman M, Mukamel DB, Mor V, Trivedi AN. Quality of Post-Acute Care in Skilled Nursing Facilities That
Disproportionately Serve Black and Hispanic Patients. J Gerontol A Biol Sci Med Sci. 2019;74(5):689-697.
doi:10.1093/gerona/gly089
xliv
Ash M, Brandt S. Disparities in Asthma Hospitalization in Massachusetts. Am J Public Health. Feb 2006;96(2):358-362.
xlv
Jiang HJ, Andrews R, Stryer D, Friedman B. Racial/Ethnic Disparities in Potentially Preventable Readmissions: The case of
diabetes. Am J Public Health. Sep 2005;95(9):1561-1567. doi:10.2105/AJPH.2004.044222
xlvi
Rathore SS, Foody JM, Wang Y, et al. Race, Quality of Care, and Outcomes of Elderly Patients Hospitalized with Heart Failure.
JAMA. May 21 2003;289(19):2517-2524. doi:10.1001/jama.289.19.2517
xlvii
Your Health: People With Certain Medical Conditions. Centers for Disease Control. 2020. https://www.cdc.gov/coronavirus/2019-
ncov/need-extra-precautions/people-with-medical-
conditions.html#:~:text=Having%20COPD%20(including%20emphysema%20and,severe%20illness%20from%20COVID%2D19.
xlviii
National Heart Lung and Blood Institute. Evidence-based management of sickle cell disease. Expert Panel report. Washington,
DC: National Institutes of Health; 2014.
