
Revised 02/26/2024
PUBLIC HEALTH DIVISION, Center for Health Protection
Health Care Regulation and Quality Improvement Section
Health Facility Licensing and Certification Program
Tina Kotek, Governor
Nurse Staffing Plan
Facility: Sky Lakes Medical Center
Received Date: June 3, 2024
Posting Date: June 6, 2024
DISCLAIMER: Oregon’s hospital staffing law directs OHA to post hospital
staffing plans received by OHA. OHA does not review or approve the staffing
plans prior to posting. OHA does not endorse staffing plans nor can OHA
provide advice or guidance about the application or enforcement of any
staffing plan.
It is the hospital’s responsibility to submit plans to OHA that are current,
compliant with applicable laws, and address all units where services covered
by the staffing plan are provided.
If you need this information in an alternate format,
please call our office at (971) 673-0540 or TTY 711
Survey and Certification Unit
800 NE Oregon Street, Suite 465
Portland, OR 97232
Voice: (971) 673-0540
Fax: (971) 673-0556
TTY: 711
http://www.healthoregon.org/nursestaffing
[email protected]on.gov
1
Sky Lakes Medical Center Nurse Staffing Plan
Department: ACD
Approval Date: 05/22/2024
Effective Date: 06/01/2024
UNIT DETAILS
STAFFING
STANDARDS
Unit Description
The Ambulatory Care Department (ACD) is
open Monday through Friday 0545-1815.
ACD is a 10-bed outpatient unit that primarily
provides pre and post procedural care for
Interventional Radiology and Cardiology
patients, however, does care for outpatients
that need infusions, foley catheter exchanges,
trach changes, etc. The 10-bed unit includes
the following room types: 10 private rooms.
There is one negative pressure room. Refer
to Ambulatory Care Department Structure
Standards.
Patient Population/Diagnoses
• Alcoholic cirrhosis
• Thyroid nodule
• Atherosclerotic heart disease
• Other ascites
• Pleural effusion
• Nontoxic multinodular goiter
• Vascular device insertion
• Aortic stenosis
• Small B cell lymphoma
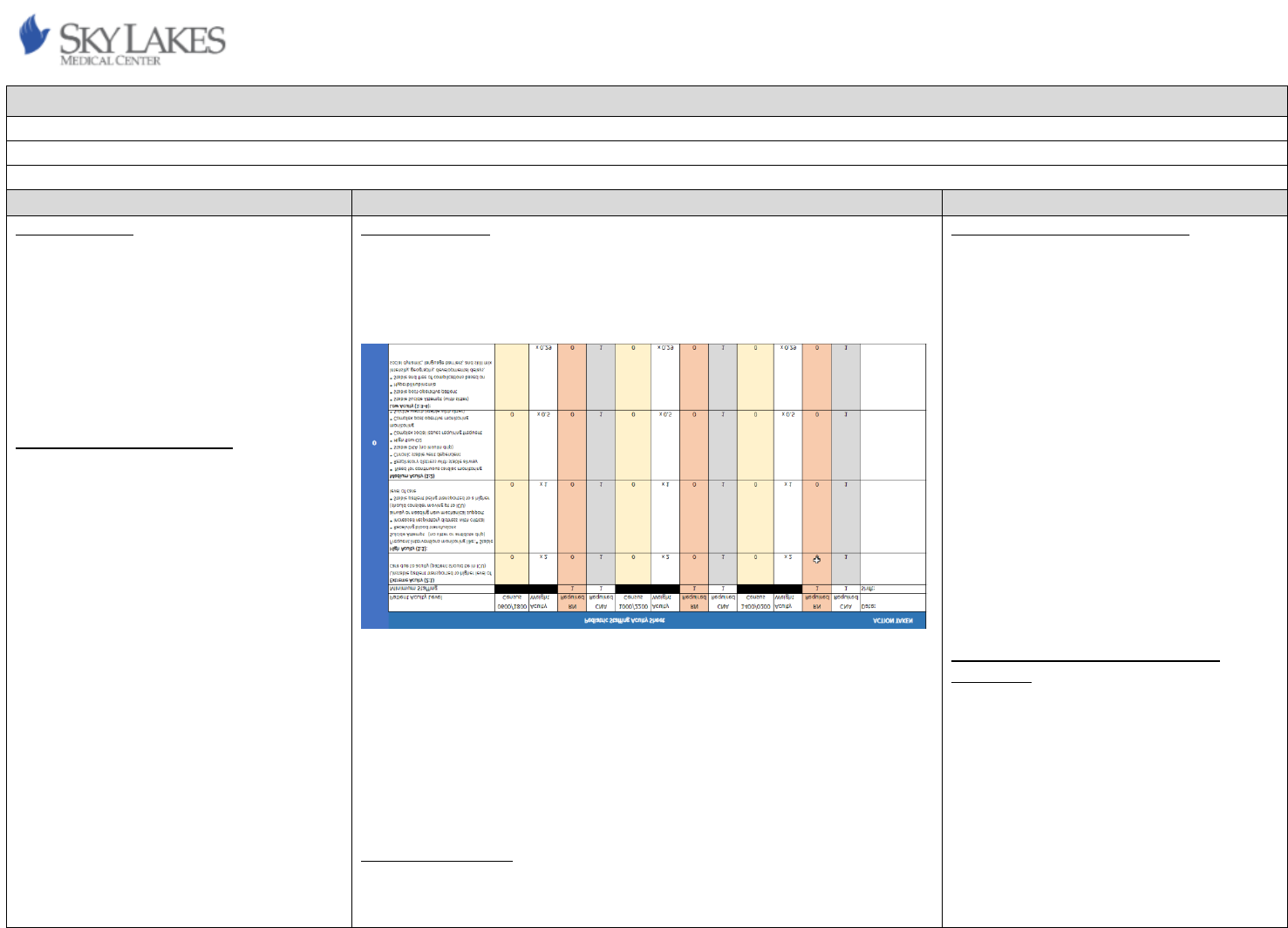
Staffing Summary
Please see attached staffing grid. If CNA staffing is not available per the staffing
grid, assignments shall be adjusted, and additional RN resources shall be made
available. Patient acuity and intensity shall be taken into consideration. The
charge nurse is counted in core staffing and shall take patients per the staffing
grid.
The charge nurse shall determine the number of staff needed for the oncoming
shift and throughout the shift to ensure the number of staff and appropriate
skill mix are available to ensure safe patient care. Charge nurses, in
collaboration with Hospital Supervisor/Bed Coordinator, track ADT data
throughout the shift and this data is used to plan for adequate staff to care for
expected admissions, transfers, and discharges.
Census and acuity fluctuations are managed by bringing in nursing staff to care
for the number of patients present and expected. These staff can be core ACD
nursing staff, nursing staff from other departments who are cross-trained
and/or otherwise qualified, or Flex Team staff.
ACD RN’s admit patients for same-day discharge procedures, including IV starts,
admissions, assessments, telemetry monitoring and pre-procedure medication
administration. When recovering patients post procedure, RNs assess/monitor
every 15-30 minutes until discharge as well as provide education to patients and
family. RN’s for ACD can also be used to monitor MRI pacemaker patients and
support general anesthesia cases in diagnostic imaging department if staffing
allows.
The ACD staff will have a plan for staffing and bed capacity for the first and
second shift admission.
Minimum Staffing
ACD must be staffed with at least one RN and one other licensed nursing
personnel when one or more patients are present.
Qualifications and Competencies
Please refer to the Ambulatory Care
Department Unit Qualifications and
Competencies spreadsheet for details.
Orientation and Annual Competency
All nurses in the Ambulatory Care
Department are oriented and trained upon
hire to the unit to demonstrate competency
in direct care of the aggregate patient
population served.
Skills checklists, continuing education and
competencies are documented in the
organization’s electronic learning
management system (LMS). Each nursing
staff member receives annual skills training
and competency validation through the
organization’s electronic learning
management system, Skills Fairs, online
courses, classroom education, direct
education, and policy review. This ensures
the skill mix of the nursing staff in the
Ambulatory Care Unit is consistent among the
individual nursing staff members. Please refer
to the Ambulatory Care Unit Qualifications
and Competencies spreadsheet for additional
details.
Nationally Recognized Standards and
Guidelines
American Academy of Ambulatory Care
Nursing. (2023). Scope and standards of

2
If CNA staffing is not available per the attached grid, assignments will be
adjusted, and additional RN resources will be made available to provide total
patient care. Total patient care assignments will consist of no more than 3 low
to medium acuity patients.
Direct care registered nurse-to-patient ratio for an individual patient shall be
based on a licensed independent practitioner’s classification of the patient, as
indicated in the patient’s medical record, regardless of the unit where the
patient is being cared for.
Charge Nurse
The charge nurse may take a patient assignment, including for the purpose of
covering staff on meal and rest breaks. The charge nurse may take a partial
assignment or no assignment dependent on the staff skill mix, acuities,
intensities, and other factors that may be relevant at the time.
The charge nurse shall have a plan for staffing and bed capacity for the first and
second admissions.
Acuity and Intensity
Staffing for patient care on ACD considers acuity and intensity using the
following criteria:
• Patient volume
• Nursing intensity
• Complexity of patient’s condition, assessment and required nursing
care
• Knowledge and skills required of nursing staff to provide care
• Degree of supervision required of nursing staff members
• Type of technology involved in patient care
• Infection control and safety issues
• Continuity of patient care
• Patient conditions that may contribute to a higher level of intensity on
the ACD Department include but are not limited to:
• Active chest pain not responding to treatment
• Combative/agitated patients
• IV cardiac med titration
• Respiratory distress; trach care
• Medications or treatments every 1 hour or more frequently
• Frequent VS or CBG monitoring
practice for professional ambulatory care
nursing (10
th
ed.).
3
• Unstable patient: assessing every 15-60 minutes to monitor condition
and responses/Unstable COBRA transfer/physiologically unstable with
treatment or Rapid Response
• CIWA patient with high score
• Complex patient/family dynamics and communication needs
• Comfort care with hourly intervention and family support
• Complicated wound care
• Dementia/delirium
• Bariatric patient
• Post procedural sedation patients
Policy specific patient care that shall contribute to a higher level of acuity on the
ACD Unit and require adjusted ratios:
• Insulin infusion
Call
The ACD does not participate in mandatory call. However, the ACD nurses cross-
trained in Diagnostic Imaging must participate in mandatory call for Diagnostic
Imaging. Call is assigned at the beginning of the year and rotates every 5
th
or 6
th
weekend. Nursing staff can sign up for call shifts voluntarily as mutually
beneficial to the staff member and the ACD Department.
Meal and Break Relief:
Meal and break relief shall be approached in a collaborative manner between
staff and Hospital Supervisor/Manager/Director. The goal is to provide a
resource that ensures that caregivers receive uninterrupted rest and meal
breaks while maintaining safe patient care that continues through the meal and
rest periods.
Meal and break coverage resources may be provided by:
• Core ACD staff
• Flex team coverage
• Resource nurse coverage
• Hospital Supervisor/Manager
Meal break planning shall be initiated at the beginning of the shift in
collaboration with the Hospital Supervisor/Manager/Director. The Charge Nurse
Shift Report Form shall be used as the meal break planning tool. The charge
nurse to the Hospital Supervisor/Manager/Director as soon as possible shall
4
communicate any identified external meal coverage needs to help facilitate
coverage. Minimum numbers of nursing staff shall be maintained during meal
and rest breaks.
If ACD can “flex down”, the Hospital Supervisor/Manager/Director shall assess
lunch coverage and needs that can be provided prior to sending the staff
member home.
5
Sky Lakes Medical Center Nurse Staffing Plan
Department: Cath Lab
Approval Date: 05/22/2024
Effective Date: 06/01/2024
UNIT DETAILS
STAFFING
STANDARDS
Unit Description
The Cardiac Cath Lab is a 2-room Diagnostic
and Therapeutic Unit, which is staffed 5 days
a week from 0730-1800 on Tuesday through
Thursday and from 0800-1630 on Mondays,
but is available 24 hours a day, 7 days a week.
The 2-room unit includes the following:
• 1 Large Philips FD10 room used primarily
for cardiac procedures.
• 1 Small Philips Azurion 7 hybrid room
used for cardiac, peripheral and IR
procedures.
Patient Population/Diagnoses
Cath Lab provides both emergency and
diagnostic care for patients requiring invasive
cardiovascular procedures. Our most
common patient diagnoses are as follows:
1. Myocardial Infarction
2. Acute Coronary Syndromes
3. Valvular Diseases
4. Heart Blocks and/or other Electrical
disease processes
5. Pulmonary Hypertension/Diseases
6. Pulmonary Embolus
Staffing Summary
The Cath Lab will be staffed with a minimum of 1 RN and 1 RT(R), per operating
room, during all operational hours, Monday through Friday 0800 0800-1630
(minus holidays) and will always have at least 1 RN and 1 RT(R) on call, with a
minimum of 4 people on call at all times. In the event the Cath Lab manager is
unavailable or absent, a charge nurse or tech will be assigned. The charge
nurse/coordinator does not scrub cases if possible so they can be available to
facilitate unit needs as needed. If there are no scheduled procedures or if
scheduled procedures are completed for the day, MRO may be asked of the
staff, but the minimum amount of staffing required to operate would remain on
call (per the assignment of the Cath Lab manager) to cover the remainder of the
shift, in order to care for emergent procedures that may arise prior to the start
of the call shift.
Staffing for patients in the Cath Lab will be based on collaboration between Cath
Lab Manager, Nurse Supervisor/ICU Clinical Manager and/or Director of
Interventional Services/Diagnostic Imaging and will take into consideration staff
skill mix/experience and patient acuity.
In general, the only occurrence when staffing needs to be adjusted in the Cath
Lab is when a STEMI, or at times, 2 STEMIs come into the ER at once. During
which time, if staffing allows, STEMIs will always take precedence over other
procedures. There are times in which the room that is not being occupied may
also be prepped for the incoming STEMI while the other room is occupied. In the
event of 2 STEMIs coming in at the same time, if there are enough staff to
operate two rooms and another physician present, then we can treat 2 STEMIs
at the same time, however if there aren’t enough staff that particular day or no
other physician is available, it is up to the discretion of the physician which
STEMI needs to be seen first and/or if a patient should be diverted for more
urgent treatment.
All STEMIs are being tracked in a physical logbook in the Cath Lab. Procedures
such as interventions, IR, as well as STEMIs are color coded. Times in and out of
Qualifications and Competencies
Please refer to Cath lab Qualifications and
Competencies spreadsheet for details.
• BLS (obtained within 2 months of
hire date)
• ACLS (obtained within 6 months of
hire date)
• Moderate Sedation (obtained within
6 months of hire date)
• Basic EKG (obtained within 6 months
of hire date)
• Suturing competency, if applicable
• Arterial Access competency, if
applicable
Nationally Recognized Standards and
Guidelines
Academy of Medical-Surgical Nurses-AMSN.
(Updated 10/2020). Staffing Standards for
Patient Care https://www.amsn.org
American Nurses Association. Code of Ethics
for Nurses (2015)
https://www.nursingworld.org
American Nurses Association. Optimal Nurse
Staffing to Improve Quality of Care and
Patient Outcomes: Executive Summary
(September 2015)
https://www.nursingworld.org/~4ae116/glob
alassets/practiceandpolicy/advocacy/ana_opt
6
the lab are also recorded along with comments to show representation of acuity
and intensity.
Call
The Cath Lab is a 24-hour, seven-day department and so requires that RNs and
RT(R)’s be on call a set amount of time. Currently, that requires each staff
member in the Cath Lab to take call two days per week for two weeks and one
weekend every 3rd week. Call begins at 1630 Monday through Friday and ends
at 0800 the following morning during the week and is 24 hours per day on
weekends. This can result in mandatory overtime, based on the fact that Stand-
by is a requirement of the position. Each call team is comprised of four
individuals, with at least one RN and one RT(R), and a combination of the two to
round out the team.
Assignments:
The Cath Lab Manager or acting lead will determine room and role
assignments for each procedure for the day, assuring that each
procedure consists of at least one RN and one RT(R).
All invasive procedures in which moderate sedation is being administered
requires that a circulator has no additional duties other than administering
medications and monitoring the patient. In the instance that other duties are
required to complete the procedure an additional circulator is assigned to the
procedure along with a scrub tech and monitor tech. These procedures require a
4 staff member team, and roles are assigned based on staff qualifications,
experience, and where the best fit is to provide the best and safest care
possible.
Meal and Break Relief:
Meal and break relief shall be approached in a collaborative manner between
staff and Cath Lab Manager. The goal is for each staff member to receive two
15-minute breaks, and a 30-minute lunch, depending on the acuity of
our patients at the time. Staff members are responsible for relieving
teammates for lunch, assuring that at least one RN and one RT(R) are
involved in a procedure at any given time.
Meal and Break coverage resources may be provided by:
• Teammates free of any direct duties
imal-nurse-staffing_white-paper-
es_2015sep.pdf
Responsibilities of a Cath Lab RN by Luanne
Kelchner, updated by Dr. Kelly S. Meier
(September 10, 2020)
http://work.chron.com/responsibilities-cath-
lab-rn-18933.html
STEMI Interventions: Searching for the Key to
D2B by Dan Scharbach, Regional Director,
Invasive Cardiovascular Services Providence
Health System, Portland Service Area,
Portland, Oregon (January 2008)
https://www.hmpgloballearningnetwork.com
/site/cathlab/articles/stemi-interventions-
searching-key-d2b
7
• Cath Lab Manager
• A break between cases, which the physicians are aware of
All staff are responsible for the following:
• Be prepared to take break when coverage is available
• Give a brief report to the staff member relieving you for break or lunch.
• Highlight the list of tasks that need to be completed during break;
being mindful of the tasks that can reasonably be completed during the
break period. The patient’s experience should be seamless.
• Return punctually
In the event of a missed meal break, the staff member should promptly report it
on their paper timecard with reason, so it can be reflected in Kronos and the
staff member paid for their missed time.

8
Sky Lakes Medical Center Nurse Staffing Plan
Department: Diagnostic Imaging
Approval Date: 05/22/2024
Effective Date: 06/01/2024
UNIT DETAILS
STAFFING
STANDARDS
Unit Description
The Interventional Services/Diagnostic
Imaging (DI) nursing staff provide care to
patients receiving interventional radiological
evaluation in the Sky Lakes Medical Center
Interventional services/DI Department.
Diagnostic Imaging is open 830-1700 Monday
through Friday.
The DI Nurse provides care for patients in the
following rooms: 1-MRI Suite, 2-CT-Suites, 2-
Ultrasound Suite, 1-Mammography Suite, and
2-Special Procedures Suites
The DI nurse can provide moderate sedation
throughout the hospital.
Patient Population/Diagnoses
DI patients include patients needing
interventional radiological procedures
required for assessment, diagnosis, and
treatment of many disease processes.
Diagnostic imaging interventional radiology
patients include but are not limited to
biopsies, drain placements, paracentesis,
abscess drainages, lumbar punctures, port-a-
cath placements, thoracenteses, myelograms
and other I.R. procedures.
Call
On-call DI Nurse coverage is mandatory for DI
procedures from 0700-1900 on weekends
Staffing Summary
There is one full-time RN, one part-time RN and one supplemental RN who
share a workspace.
Staffing will be adjusted by the charge nurse when there is an emergent add-on
patient, sudden staff illness, etc., by requesting help from the Clinical Manager,
hospital supervisor or the resource nurse. The DI nurse skill mix is equal among
all DI nurses.
Nurse Staffing Ratios
1:1 Regardless of acuity
Minimum staffing is 1-RN and one additional staff member classified as a
Radiology Tech, EKG Tech, Respiratory Therapist, Ultrasound Tech or a CT Tech
per patient procedure.
CNA Staffing Ratios
There are no CNA’s in Diagnostic Imaging
Total Patient Care
DI nurses provide total patient care during the procedure. Post procedure,
patients return to ACD nursing unit.
Charge Nurse
At the beginning of shift the charge nurse assigns patients to themselves and
the second nurse. This is a collaborative effort between nurses to ensure
teamwork.
Assignments:
Assignments are based on scheduled procedures. The DI Nurse can review
patient records prior to patient presentation. In the event an emergency
procedure is required during business hours the nurse will have an appropriate
amount of time to review the medical record. Assignments are shared among
Qualifications and Competencies
All nurses in the Interventional
Services/Diagnostic Imaging are oriented and
trained upon hire to the unit to demonstrate
competence in direct care of the aggregate
patient population served. Upon hire to the
organization, the DI nurse will complete the
SLMC Initial RN Checklist and the Diagnostic
Imaging RN Checklist. The skills checklist will
be validated by the precepting nurse and the
unit Director, Unit Manager or other qualified
designer within the first 90 days of
employment in the unit.
Skill’s checklists, continuing education and
competencies are documented in the
organization ‘s electronic Learning
Management System (LMS). Each nursing
staff member receives continuing education,
annual skills training and competency
validation through a variety of platforms
including but not limited to the organization’s
electronic LMS, Skills Fairs, online courses,
classroom courses, and direct observation.
This ensures the skill mix of the nursing staff
in Diagnostic Imaging is consistent among the
individual nursing staff members.
Nationally Recognized Standards and
Guidelines
• Association For Radiological &
Imaging Nurses, (Association & Ana,
2013).
9
and holidays. Call coverage is assigned at the
beginning of the year rotated on every 5
th
weekend.
If there is a vacant weekend, the Clinical
Nurse Manager will assign call or be on call.
On-call tracking is achieved by the call
calendar located in the DI nurse office and is
evaluated monthly to determine
appropriateness of nurse coverage.
both nurses, each taking turns working in all modalities.
Meal and Break Relief:
Meal and break planning are done at the beginning of the shift with both nurses
evaluating the day's schedule and making plans for meals and breaks. In the
event a patient requires an emergent procedure during the dedicated mealtime
notification of the DI Nurse Manager/Director will be utilized to provide
additional staffing resources to ensure meal breaks.
• www.arinursing.org/ARIN/assets/Fil
e/public/practice-
guidelines/2018_10_28_Staffing_Pa
per_Position_Statement.pdf
10
Sky Lakes Medical Center Nurse Staffing Plan
Department: ED
Approval Date: 05/30/2024
Effective Date: 06/01/2024
UNIT DETAILS
STAFFING
STANDARDS
Unit Description
The Emergency Department (ED) is a 24-hour,
7 days a week, 26 bed unit that provides
emergency nursing care for any person
regardless of age. The 26 bed unit is defined
as the following room types: 18 private
rooms, which include one negative pressure
room, five fast track rooms and one
obstetrics and gynecology room; two
psychiatric hold rooms; one ear/nose/throat
room and one large bay with
accommodations for up to five patients.
Patient Population/Diagnoses
The ED delivers care to patients ranging from
non-urgent to life threatening and includes,
but not limited to medical illness, trauma
care, pediatric care, gerontological care,
injury prevention, women’s health, mental
health issues, and life and limb-saving
measures.
Unique to ED nursing practice is the
application of the nursing process to health
care consumers with a variety of illnesses or
injuries in all ages and populations requiring
triage and prioritization, stabilization,
resuscitation, crisis intervention, and/or
emergency preparedness. In addition, all
care is delivered in accordance with the
Emergency Medical Treatment and Active
Labor Act (EMTALA).
Staffing Summary
The Emergency Department provides direct care registered nurses, along with
Emergency Medical Technicians as support staff to deliver patient care and carry
out unit operations.
Nurse Staffing Ratio
• A direct care registered nurse is assigned to no more than one full-
activation trauma patient. The ratio for trauma patients is based on
full-trauma activations only.
• The ratio of direct care registered nurses to patients averages no more
than one to four over a 12-hour shift, and a single direct care registered
nurse may not be assigned more than five patients at one time. With
the exception to fast-track patients of Emergency Severity Index levels
4 and 5 a direct care registered nurse may not be assigned to more
than six patients at one time.
Charge Nurse
The charge nurse may take assignments, including patient assignments for the
purpose of covering staff who are on meal breaks or rest breaks. The charge
nurse shall use the Charge Nurse Shift Report Form as the meal and rest break
planning tool or other hospital approved form.
Assignments:
The charge nurse will determine assignments based on staff skill mix, acuities,
intensities, and bed availability. The charge nurse will collaborate with the
Hospital Supervisor to monitor Admission/Discharge/Transfer (ADT).
Meal and Break Relief:
A “meal” is defined by the Medical Center as one thirty-minute unpaid break
given when a staff member is working more than six hours during which they
should be relieved of all work duties. A “break” refers to a period of not less
than fifteen minutes of paid time for every four hours worked; three breaks per
Qualifications and Competencies
All nurses in the ED are oriented and trained
upon hire to the unit to demonstrate
competency in direct care of the aggregate
patient population served.
Skills checklists, continuing education and
competencies are documented in the
organization’s electronic learning
management system (LMS). Each nursing
staff member receives continuing education,
annual skills training and competency
validation through a variety of platforms
including but not limited to the organization’s
electronic learning management system, skills
Fairs, online courses, classroom courses,
policy review, and direct observation. This
ensures the skill mix of the nursing staff in the
Emergency Department is consistent among
the individual nursing staff members.
Nationally Recognized Standards and
Guidelines
Standards or guidelines used to develop the
Emergency Department’s staffing plan are
defined by the Emergency Nurses Association
(ENA). http://www.ena.org 2023
Board of Certification for Emergency Nursing
(BCEN) available and encouraged through
ENA.
11
12-hour shift.
The Charge Nurse Shift Report Form shall be used as the meal and rest break
planning tool. Any identified external meal coverage needs shall be
communicated by the charge nurse to the Hospital Supervisor/Resource
Nurse/Manager/Director as soon as possible to help facilitate coverage.
External meal coverage resources must have the minimum qualifications and
competencies to provide safe, effective and seamless patient care.
12
Sky Lakes Medical Center Nurse Staffing Plan
Department: FBC
Approval Date: 05/22/2024
Effective Date: 06/01/2024
UNIT DETAILS
STAFFING
STANDARDS
Unit Description
The Family Birth Center (FBC) is a 24-hour, 7
day a week, 20 bed acute care unit that
provides direct nursing care for obstetric and
neonate patients. The unit is comprised of
the following room types: 12 birthing suites, 1
semi-private obstetric triage room (2 beds), 2
private antepartum/gynecologic rooms, one
free standing operating suite for cesarean
sections, and 3 special care nursery (SCN)
beds for ill/transitioning infants (one private
nursery room for infants who require
isolation). Refer to Scope of Service /
Structure Standards, Maternal Child Health.
Patient Population/Diagnoses
FBC patients include obstetric (antepartum,
intrapartum, and postpartum), neonate,
stable non-infectious pediatric patients,
including pediatric surgical patients and
gynecological patients. Refer to FBC
Qualifications and Competencies attachment
for list of most common patient diagnoses.
Staffing Summary
The FBC provides RNs to deliver patient care and carry out unit operations.
Certified Nursing Assistants (CNAs) are not routinely staffed but at times, they
may be used to. LPNs may work as OB Techs. LPNs take postpartum or
gynecological patient assignments and perform direct patient care as assigned
and supervised by RNs.
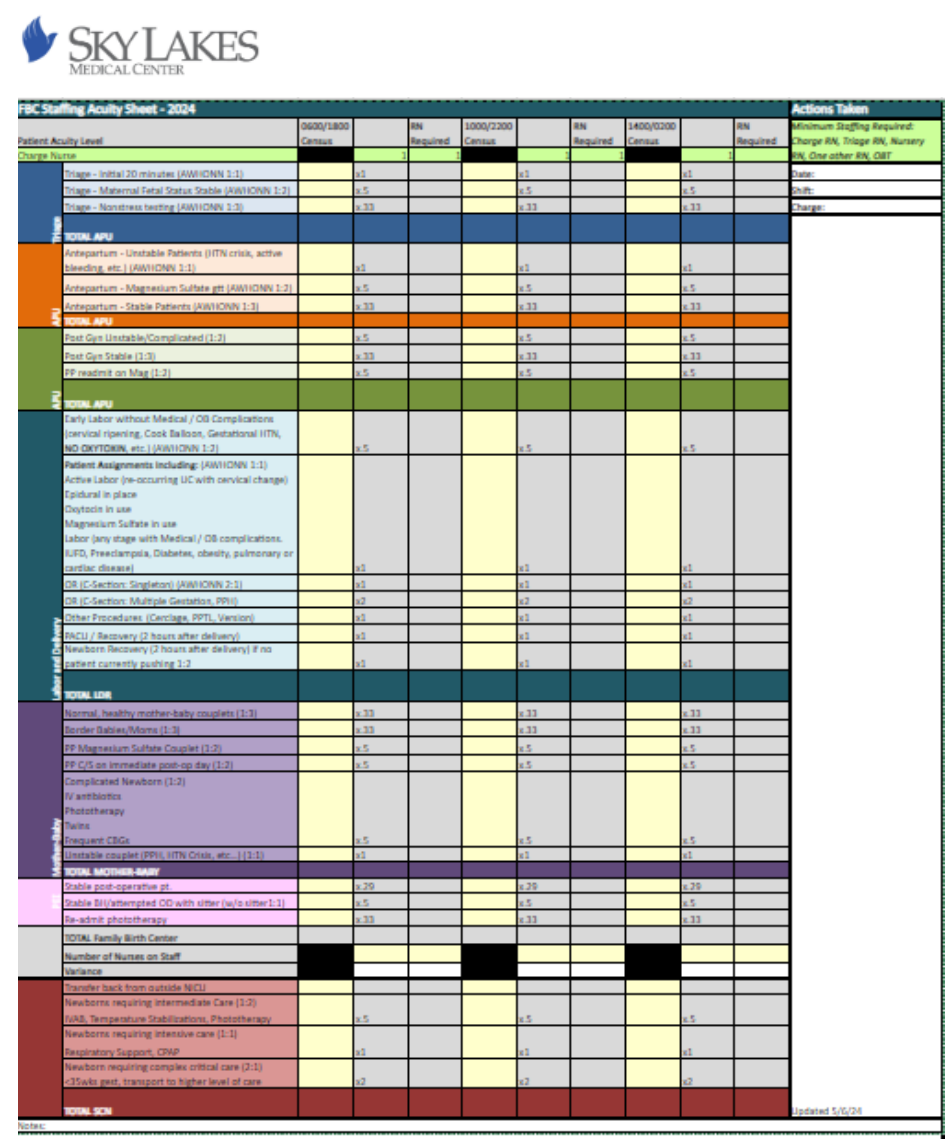
The FBC charge RN utilizes the Staffing Acuity Sheet (see attachment) to assess
patient acuity and intensity every four hours and as needed. Nursing daily
staffing shall be adjusted based on changes in patient acuity/intensity.
Assignments shall be based on staff skill mix, patient acuity/ intensity, and bed
availability.
Minimum Staffing
The Family Birth Center shall be staffed with a minimum of four RNs (two of
whom are labor experienced as defined in Scope of Service/ Structure
Standards, Maternal Child Health) for each shift. Of these four, two core RNs
should be on FBC for each shift to be able to open SCN at any moment
necessary. The two core RNs can be charge and one other core RN or if travel
nurse is charge must have 2 other core staff on unit. OB Tech is also to be
scheduled for every shift. If OB tech only available in house and not working on
the floor and no secretary is scheduled for that shift then 1 extra RN or a CNA
should be added to minimum staffing to help with phones, doors, turning over
triage, stocking rooms, and running Quality Controls.
Nursing Intensity
Patient conditions that may contribute to a higher level of intensity in the FBC
include but are not limited to:
• Family social dynamics
• Complications of pregnancy requiring increased observation/intervention
• Complications of newborn status requiring increased observation/intervention
• Complications related to surgical procedures
• Lack of maternal support system
Qualifications and Competencies
All FBC RNs are oriented and trained upon
hire to the unit to demonstrate competence
in direct care of the aggregate patient
population served. Each nursing staff
member receives continuing education,
annual skills training and competency
validation through a variety of platforms
including but not limited to the organization’s
LMS, Skills Fairs, online courses, classroom
courses, direct observation and policy review.
This ensures the skill mix of the nursing staff
on FBC is consistent among the individual
nursing staff members. Please refer to the
FBC Qualifications and Competencies
attachment for additional details.
Nationally Recognized Standards and
Guidelines
The 2010 Association of Women’s Health,
Obstetric, and Neonatal Nurses (AWHONN)
Guidelines for Professional Registered Nurse
Staffing for Perinatal Units and the Academy
of Medical-Surgical Nurses (AMSN) Staffing
Standards for Patient Care were used to
develop the FBC’s staffing plan.
13
• Maternal developmental status
Nurse Staffing Ratios
In FBC, a direct care registered nurse is assigned to no more than:
• Two patients if the patients are not in active labor or experiencing
complications; or
• One patient if the patient is in active labor or if the patient is at any
stage of labor and is experiencing complications.
• No more than six patients, counting mother and baby each as separate
patients; postpartum, antepartum and wellbaby nursery.
• No more than eight patients, counting mother and baby each as
separate patients, In a mother-baby unit with a Certified nurse
assistant.
CNA Staffing Ratios
A CNA may not be assigned to more than seven patients at a time during a day
shift or to more than 11 patients during a night shift. (441.768)
Charge Nurse
The charge nurse may take assignments; including patient assignments for the
purpose of covering staff who are on meal breaks or rest breaks. The charge
nurse is responsible for determining patient assignments, number of staff
needed and assisting with breaks when able.
Assignments:
The FBC charge nurse shall determine assignments based on staff skill mix,
acuities, and intensities.
Meal and Break Relief:
Meal and rest break relief shall be approached in a collaborative manner
between the Charge nurse, Hospital Supervisor, and Resource Nurse. Meal
break planning shall be initiated at the beginning of the shift to allow for
proactive planning and resource allocation.
Meal and rest break coverage may be provided by the following:
• Charge nurse, assuming that staffing ratios are maintained
• Core unit staff on shift, assuming that staffing ratios are
maintained
• Core unit staff who voluntarily sign up to provide meal and rest
14
break coverage
• Break nurse
• Flex nurse
• Resource nurse
• Hospital Supervisor/Manager
Nursing staff are responsible for the following:
• Sign up for and know scheduled break periods
• Be prepared to take break when coverage is available
• Give a brief report, understanding that most information can be
obtained
from EMR
• Highlight the list of tasks that need to be completed during break;
being mindful of the tasks that can reasonably be completed
during the break period. The patient’s experience should be
seamless.
• Return punctually
15
16
Sky Lakes Medical Center Nurse Staffing Plan
Department: ICU
Approval Date: 05/22/2024
Effective Date: 06/01/2024
UNIT DETAILS
STAFFING
STANDARDS
Unit Description
The Intensive Care Unit (ICU) is a 24-hour, 7
day a week mixed acuity unit with 10 ICU and
4 Progressive Care (PCU) overflow beds. The
ICU specializes in caring for critically ill
medical and surgical patients and provides
step-down care. The fourteen-bed unit
includes the following room types: Ten
private ICU rooms (including one negative
pressure room with anteroom) and four
private overflow rooms. During times of high
critical care census, the 4 PCU overflow beds
may be used for to care for ICU patients.
Patient Population/Diagnoses
Critical Care patients include but are not
limited to cardiac care, general surgery,
gastroenterology, urology, respiratory,
stroke, and palliative.
Staffing Summary
The Intensive Care Unit provides registered nurses to deliver patient care and
carry out unit operations. Certified Nursing Assistants (CNA) are staffed
dependent on the intensity of nursing care and number of overflow patients.
Staffing for patient care on the Intensive Care Unit considers acuity and intensity
using the following criteria:
• Patient Volume
• Nursing Intensity
• Complexity of patient’s condition, assessment and required nursing
care
• Knowledge and skills required of nursing staff members
• Type of technology involved in patient care
• Infection Control and Safety issues
• Continuity of patient care
Pediatric Care
Staffing for pediatric patients in the ICU shall be based on collaboration
between Hospital Supervisor, ICU Charge Nurse, ICU leadership, PEDS Charge
Nurse and Peds leadership, and will consider staff skill mix/experience and
patient acuity. In the event a pediatric patient needs intensive care support,
please refer to the PEDS Patient to Higher Level of Care Flow Diagram (Rev
2.11.22).
Nurse Staffing Ratios
In the intensive care unit, a direct care registered nurse is assigned to no more
than two ICU patients at any one time.
Overflow Patient Care
ICU may provide care for overflow PCU and Medical/Surgical patients.
Patient acuity and nursing intensity in the mixed assignment are evaluated and
assigned by the charge nurse with consideration for skill mix, acuities,
Qualifications and Competencies
All ICU RNs are oriented and trained upon
hire to the unit to demonstrate competence
in direct care of the aggregate patient
population served.
Skills checklists, continuing education, and
competencies are documented in the
organization’s electronic learning
management system (LMS). Each nursing
staff member receives continuing education,
annual skills training, and competency
validation through a variety of platforms
including but not limited to the organization’s
LMS, Skills Fairs, online courses, classroom
courses, direct observation, and policy
review. Please refer to the Pediatric Unit
Qualifications and Competencies attachment
for additional details.
Nationally Recognized Standards and
Guidelines
Standards or guidelines used to develop the
Intensive Care Unit’s staffing plan include:
• AACN Procedure Manual for High
Acuity, Progressive Care, and Critical
Care. 7
th
edition: 2016.
• American Association of Critical Care
Nurses http://www.aacn.org 2023
17
intensities, bed availability and continuity as appropriate.
An ICU nurse with a mixed assignment (ICU/PCU/MS) will be as follows:
• 1 ICU patient + 2 PCU/MS mix, requires a CNA to be staffed in the unit
• 1 ICU patient and 1 PCU/MS mix, if no CNA is staffed in the unit
• 0 ICU patient + 3 PCU/MS mix, if no CNA is staffed in the unit
• 0 ICU patient + 4 PCU/MS mix, requires a CNA to be staffed in the unit
CNA Staffing Ratios
Certified Nursing Assistants (CNA) are not routinely staffed in the ICU. A CNA
may be staffed dependent on the intensity of nursing care and number of
overflow patients in the unit. When a CNA is present in the unit, they may not
be assigned to more than seven patients at a time during a day shift or to more
than 11 patients during a night shift.
A CNA shall be provided in the following scenarios:
• When there are more than 5 non-ICU patients in the unit
• When any one nurse has 4 or more patients
• When determined necessary by the charge nurse based on staffing
skills set, patient acuity, nursing intensity and other relevant factors.
Charge Nurse
The charge nurse may take a patient assignment, including for the purpose of
covering staff on meal and rest breaks. The charge nurse may take a partial
assignment or no assignment dependent on the staff skill mix, acuities,
intensities, and other factors that may be relevant at the time.
The need for a dedicated charge nurse for the next shift will be decided each
shift by the off going charge nurse. The need for a designated charge will be
based on staffing skill set, patient acuity, nursing intensity, patient procedures
and need for off floor imaging. The charge nurse will communicate needs and
collaborate with the hospital supervisor to prepare for the oncoming shift.
The need for a CNA for the next shift will be decided each shift by the off going
charge nurse. The need for a CNA will be based on staffing skill set, patient
acuity, nursing intensity, and other relevant factors.
The charge nurse shall determine the number of staff needed for the oncoming
shift and throughout the shift to ensure the number of staff and appropriate
18
skill mix are available to ensure safe patient care, including the need for a
dedicated charge and/or CNA. The charge nurse, in collaboration with Hospital
Supervisor, track ADT data throughout the shift and this data is used to plan for
adequate staff to care for expected admissions, transfers, and discharges.
The charge nurse shall have a plan for staffing and bed capacity for the first and
second admissions, transfers, and downgrades.
Assignments:
The charge nurse shall determine assignments based on staff skill mix, acuities,
intensities, bed availability, and continuity as appropriate. In the case of
overflow patients and the need for mixed assignments, the charge nurse shall
make assignments in consideration of available resources and the need to plan
for first and second admissions, transfers and downgrades. The charge nurse
shall collaborate with the Hospital Supervisor to monitor
Admission/Discharge/Transfer (ADT).
Meal and Break Relief:
Meal break planning shall be initiated at the beginning of the shift in
collaboration with the Hospital Supervisor/Manager/Director/Designee. Any
identified external meal coverage needs shall be communicated by the charge
nurse to the Hospital Supervisor/Manager/Director/Designee as soon as
possible to help facilitate coverage. External meal and rest break coverage
resources must possess the minimum qualifications and competencies to
provide safe, effective, and seamless patient care.
Meal and break coverage resources may be provided by the following:
• Charge nurse, assuming that minimum staffing is maintained
• Core unit staff on shift, assuming that minimum staffing is maintained
• Core unit staff who voluntarily sign up to provide meal coverage
• Flex team nurse
• Resource nurse
Nursing Staff are responsible for the following:
• Be prepared to take break when coverage is available
• Give a brief report, understanding that most information can be
obtained from EMR
• Highlight list of tasks that need to be completed during break; being
mindful of the tasks that can reasonably be completed during the break
period
• Return punctually
19
Sky Lakes Medical Center Nurse Staffing Plan
Department: Infusion Clinic
Approval Date: 05/22/2024
Effective Date: 06/01/2024
UNIT DETAILS
STAFFING
STANDARDS
Unit Description
The Sky Lakes Infusion Clinic (SLIC) is an
outpatient department that provides vascular
access services to all Sky Lakes Medical
Center outpatients on an appointment and
insurance approval basis. Providers are
responsible for obtaining prior authorization.
Depending on individual patient
circumstances, inpatient services can be
provided.
The department is staffed seven days per
week for 10 hours daily 0730-1800.
SLIC includes one semi-private bay with 2
chairs; one non-private 5 chair bay; two
private rooms with 1 chair each; and one
private bedroom with one hospital bed and
chair.
Depending on patient appointments and
scheduling, nursing can MRO after 1700 on
weekdays and when all patients have been
seen on holidays and weekends.
Patient Population
The SLIC provides nursing care to patients of
all ages who are in need of vascular access
services including, but not limited to:
• Peripherally Inserted Central Line
Staffing Summary
Typical RN staffing includes 3-4 RNs during weekdays and 2-3 RNs during
weekends and holidays. RN staff will flex up and down depending on census and
patient care needs. RN staff may MRO as needed throughout a shift, at 1700 on
weekdays, and when patient care is completed on weekends and holidays.
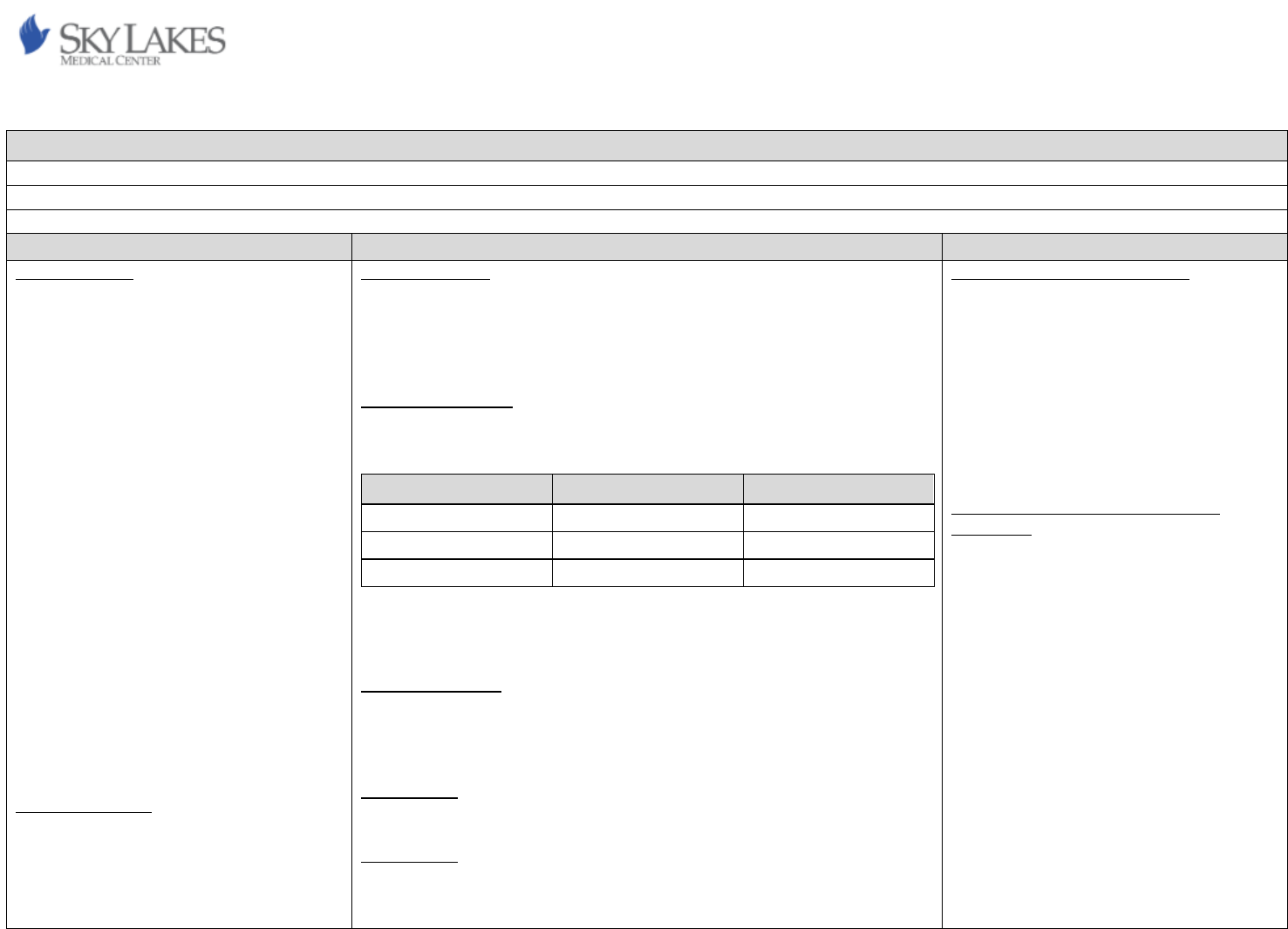
Nurse Staffing Ratios
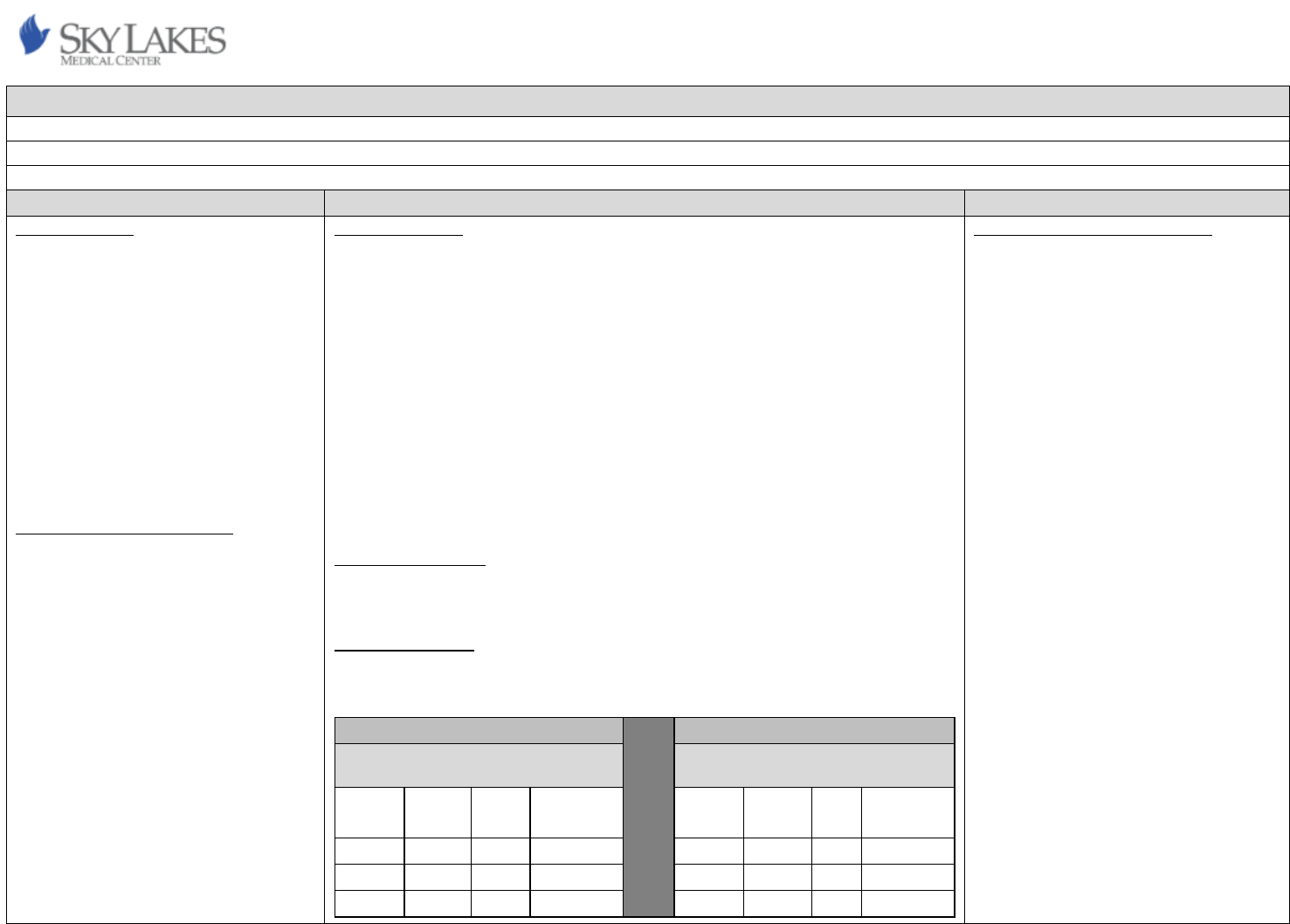
Staffing grid below provides typical ratios but are subject to change based on
census and staff availability.
Shift
# of RNs
Patient load
Weekdays
3
16-28 patients*
Weekdays
4
>28 patients*
Weekends and Holidays
2
1-15 patients*
*Based on # of patients and acuity, additional RNs will be utilized to
accommodate patient needs and safety. For example, 3 RNs on a weekend
CNA Staffing Ratios
When present in the unit, CNAs may not be assigned to no more than seven
patients at a time during a day or evening shift or to more than 11 patients at a
time during a night shift.
Charge Nurse
The charge nurse role is not utilized in SLIC.
Assignments:
Patient acuity, intensity, and appropriateness to receive care at SLIC will be
triaged by SLIC nursing staff over the phone with ordering providers. If nursing
cannot determine appropriateness and/or questions arise, SLIC manager and/or
Qualifications and Competencies
Refer to the Infusion Clinic Qualifications and
Competencies attachment for details.
Annual, biennial, and additional
competencies will be completed and
maintained by hired RNs through courses,
Learning Management System (LMS), SLMC
Skills Fairs, observations/demonstrations,
trainings, and policy review.
Nationally Recognized Standards and
Guidelines
Infusion Nurses Society (INS) standards and
guidelines are implemented at SLIC. The 2016
Policies and Procedures for Infusion Therapy,
5
th
edition provide the current reference.
20
(PICC), port-a-cath, vascath, and
central venous catheter (CVC) care
to include occlusion management
• Laboratory draws via access devices,
IV starts, and peripheral sticks.
• Peripheral IV starts
• Medication, chemotherapy, and
blood product infusion on an
outpatient basis
• Management of home CADD
infusion pumps, including set up,
monitoring, and discontinuation
• SQ/IM injections
• Medtronic pain pump refills,
evaluation, and programming
• Patient/family education.
• Psychosocial care and support
• Coordination of patient care and
collaboration with support services
director will make final decisions on accepting patients.
Appropriateness, acuity, and intensity of patients and the number of nursing
staff required will be reviewed daily by SLIC RNs for the next day’s schedule. If
additional nursing staff are required, SLIC RNs will flex to accommodate staffing
needs while notifying SLIC manager and/or director.
Meal and Break Relief:
Meal break planning shall be initiated at the beginning of the shift in
collaboration with the scheduled RNs present. During meal and rest breaks, a
minimum of 2 RNs will remain present for patient care. Any identified meal
coverage needs shall be communicated by the nursing staff to the
manager/director/ hospital supervisor.
SLIC utilizes appointments which are made in a manner allowing for nursing
meal breaks.
21
Sky Lakes Medical Center Nurse Staffing Plan
Department: MED/SURG
Approval Date: 05/22/2024
Effective Date: 06/01/2024
UNIT DETAILS
STAFFING
STANDARDS
Unit Description
The Medical-Surgical Unit is a 24-hour, 7 day-
a-week, 41-bed acute care unit that provides
direct care nursing for general medical and
surgical patients (15 years and older). The 41-
bed unit includes the following room types:
Twenty-three private rooms (10 in “A-
module”, nine in “B-module” and four in “C-
module”), nine semi-private rooms (18 beds
total with two in A-module, eight in B-module
and eight in C-module). A-module and C-
module both house one positive pressure and
one negative pressure room while B-module
houses one negative pressure room. B-
module is also equipped with two ceiling
lifts—one rated for 600 pounds and one rated
for 1000 pounds. In addition, there are five
private rooms throughout the unit equipped
with 1000-pound capable toilets.
Patient Population/Diagnoses
Medical and surgical patients include
orthopedic, neurologic, gynecologic, urologic,
general surgeries, gastroenterology, medical
w/telemetry, stroke care, end of life, and
other MedSurg entities.
Staffing Summary
The MedSurg Unit provides registered nurses, and CNAs to deliver patient care
and carry out unit operations.
Staffing for patient care on the MedSurg Unit considers acuity and intensity
using the following criteria:
• Patient volume
• Nursing intensity
• Complexity of patient’s condition, assessment and required nursing
care
• Knowledge and skills required of nursing staff to provide care
• Degree of supervision required of nursing staff members
• Type of technology involved in patient care
• Infection control and safety issues
• Continuity of patient care
Patient conditions that may contribute to a higher level of intensity on the
MedSurg Unit include but are not limited to:
• Any surgical patient the day/night of surgery
• Maximum assist or stand lift/Hoyer lift for transfers
• Patients with behavioral disturbances/agitation/uncooperative
• Complex patient/family dynamics, communication barriers and/or
emotional needs currently impacting delivery of care
• End of life patient whose family is not coping, including post-mortem
care
• Complex wound care
• Complex admission, transfer and/or discharge including new diagnosis
and education
Patient care that may contribute to a higher level of acuity on the MedSurg Unit
and require adjusted ratios:
• Allergic reaction with respiratory distress
• Active seizures
Qualifications and Competencies
For RNs:
Obtain and maintain BLS within 2 months of
hire through RQI
Obtain and maintain ACLS within 6 months of
hire through RQI
Total Joint training: New hire and annually
Top unit diagnoses: New hire and biennial
For CNAs:
Obtain and maintain Responder CPR within 2
months of hire
Total Joint training: New hire and annually
Top unit diagnoses (as pertinent to role): New
hire and biennial
Nationally Recognized Standards and
Guidelines
Standards or guidelines used to develop the
MedSurg Unit’s staffing plan are derived from
the following organizations, websites
accessed April 2024:
• Academy of Medical-Surgical Nurses
(AMSN)
• National Association of Orthopedic
Nurse (NAON)
• Oregon Health Authority (OHA)
• National Hospice and Palliative Care
Organization (NHPCO)
• Medical-Surgical Certification
available through AMSN and ANCC
Orthopedic certification available through
NAON
22
• Multiple complex drains requiring frequent interventions
• Non-violent restraints
• Patients requiring multiple staff for basic care interventions
• PCA, epidural, insulin drip and/or heparin drip requiring frequent
adjustments, interventions, and/or assessments
• Sitter indicated but not available
• Uncontrolled pain and/or nausea despite interventions
• Unstable patient requiring STAT medications, tests, etc.
• Combative patients
• Multiple drains/lines/intense wound care management
• Contact precautions requiring a minimum of hourly interventions
• CIWA/RASS with active withdrawals
• Comfort care requiring a minimum of hourly interventions
Policy specific patient care that contributes to a higher level of intensity and/or
acuity and require adjusted ratios include:
• Insulin Infusion
• Violent Restraints
• Moderate Sedation
Nurse Staffing Ratios
A direct care registered nurse is assigned to no more than five patients.
(441.765). RNs will take a maximum of 3 fresh surgeries (surgeries returning on
said shift), one additional surgery may be placed and taken at the staff nurses’
discretion.
Staffing will be based upon current census, acuity and intensities of patient and
surgical admissions whose scheduled OR out time is 10:00 or earlier.
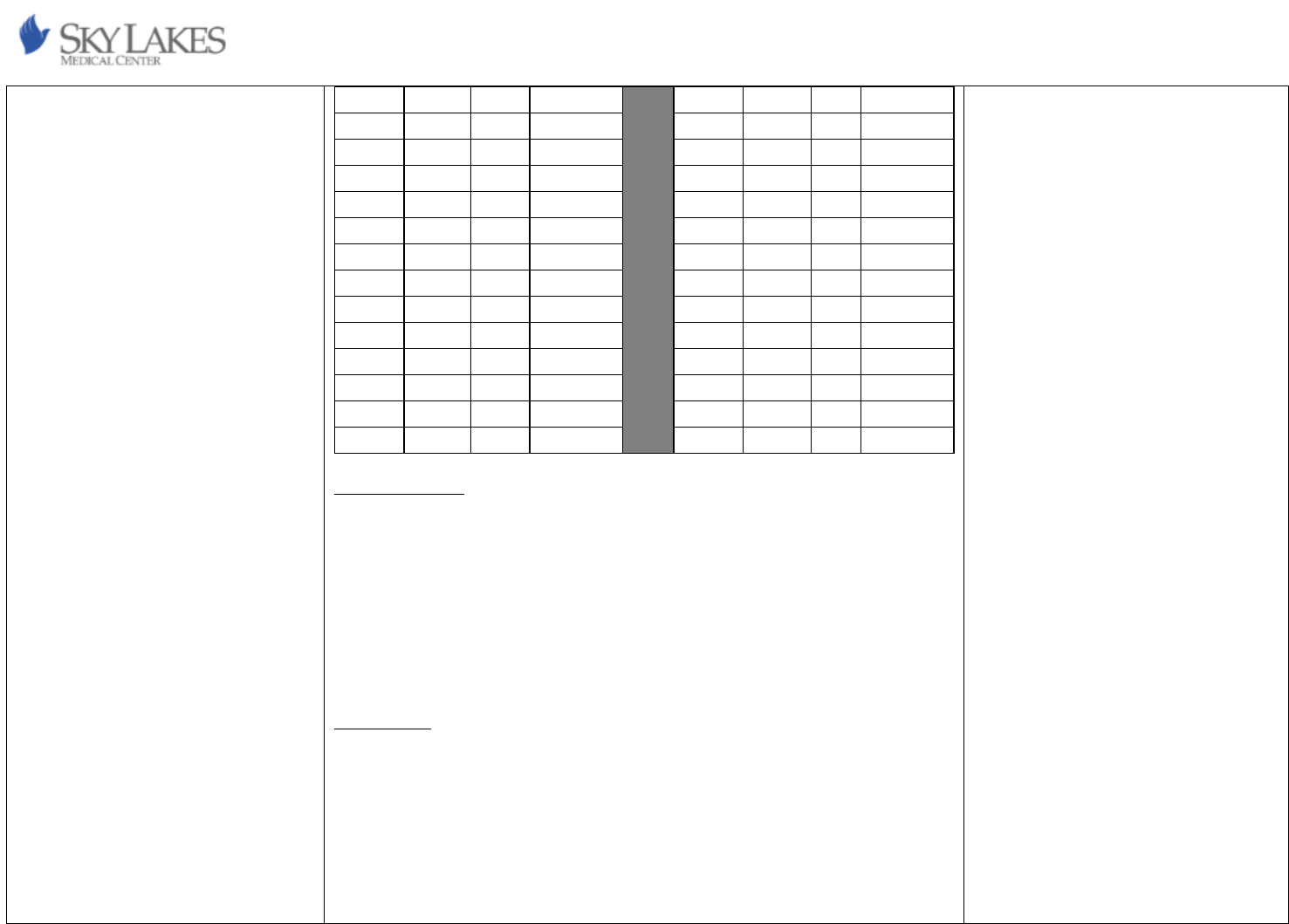
A & B Mod RN Ratios
Patient #
0
1
2
3
4
5
6
7
8
9
10
RN #
0
1
1
1
1
1
2
2
2
2
2
Designated
Charge
0
0
0
0
0
0
0
0
0
0
0
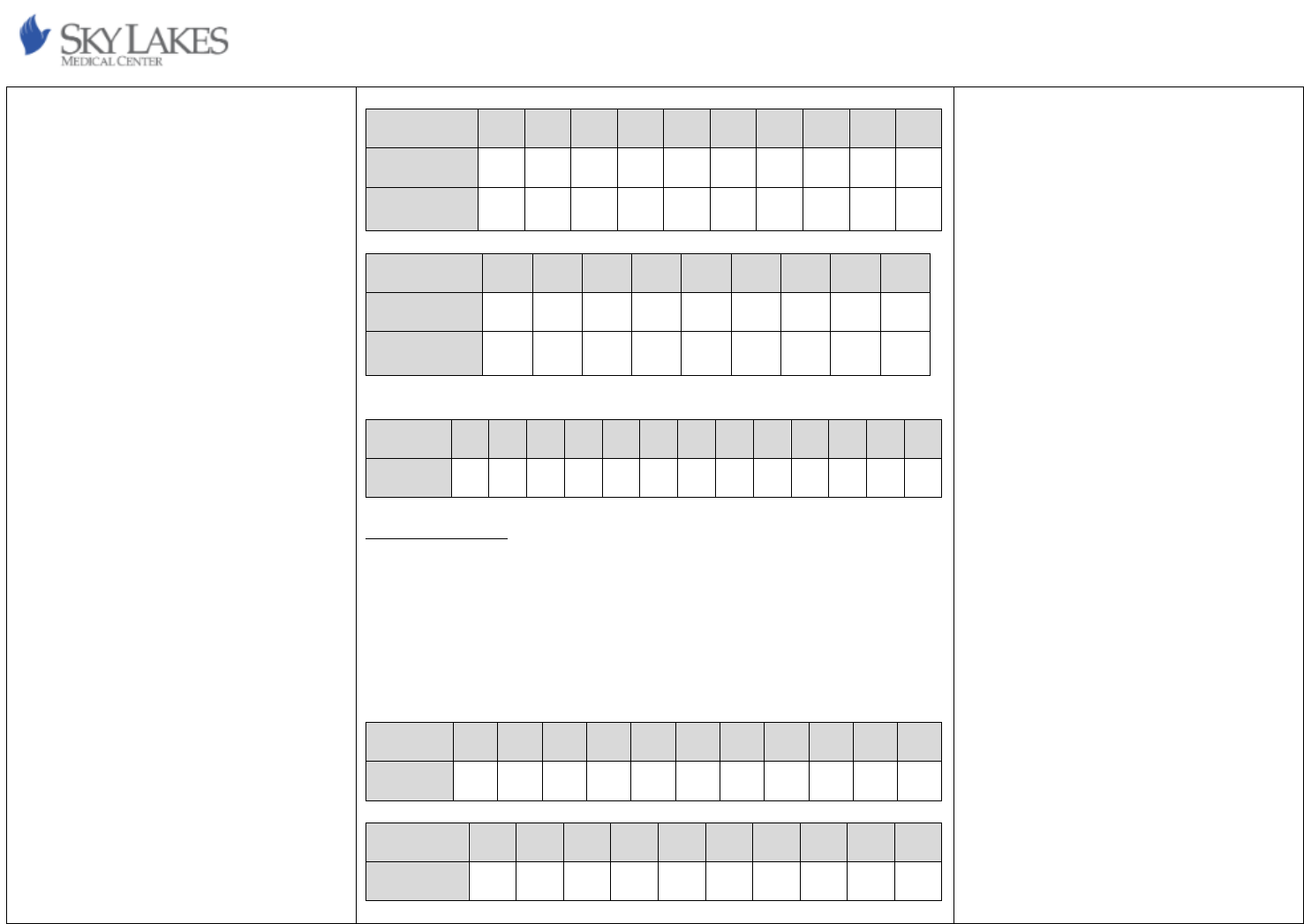
23
Patient #
11
12
13
14
15
16
17
18
19
20
RN #
3
3
3
3
3
4
4
4
4
4
Designated
Charge
0
0
0
1
1
1
1
1
1
1
Patient #
21
22
23
24
25
26
27
28
29
RN #
5
5
5
5
5
6
6
6
6
Designated
Charge
1
1
1
1
1
1
1
1
1
C Mod RN Ratios
Patient #
0
1
2
3
4
5
6
7
8
9
10
11
12
RN #
0
1
1
1
1
1
2
2
2
2
2
3
3
CNA Staffing Ratios
A CNA may not be assigned to more than seven patients at a time during a day
shift or no more than 9 patients during a night shift. (441.768) CNAs will take a
maximum of 5 fresh surgeries (surgeries returning on said shift), one additional
surgery may be placed and taken at the CNA’s discretion.
Secretary is not included in the CNA ratios.
Dayshift A & B Mod CNA Ratios
Patient #
0
1
2
3
4
5
6
7
8
9
10
CNA #
0
1
1
1
1
1
1
1
2
2
2
Patient #
11
12
13
14
15
16
17
18
19
20
CNA #
2
2
2
2
3
3
3
3
3
3
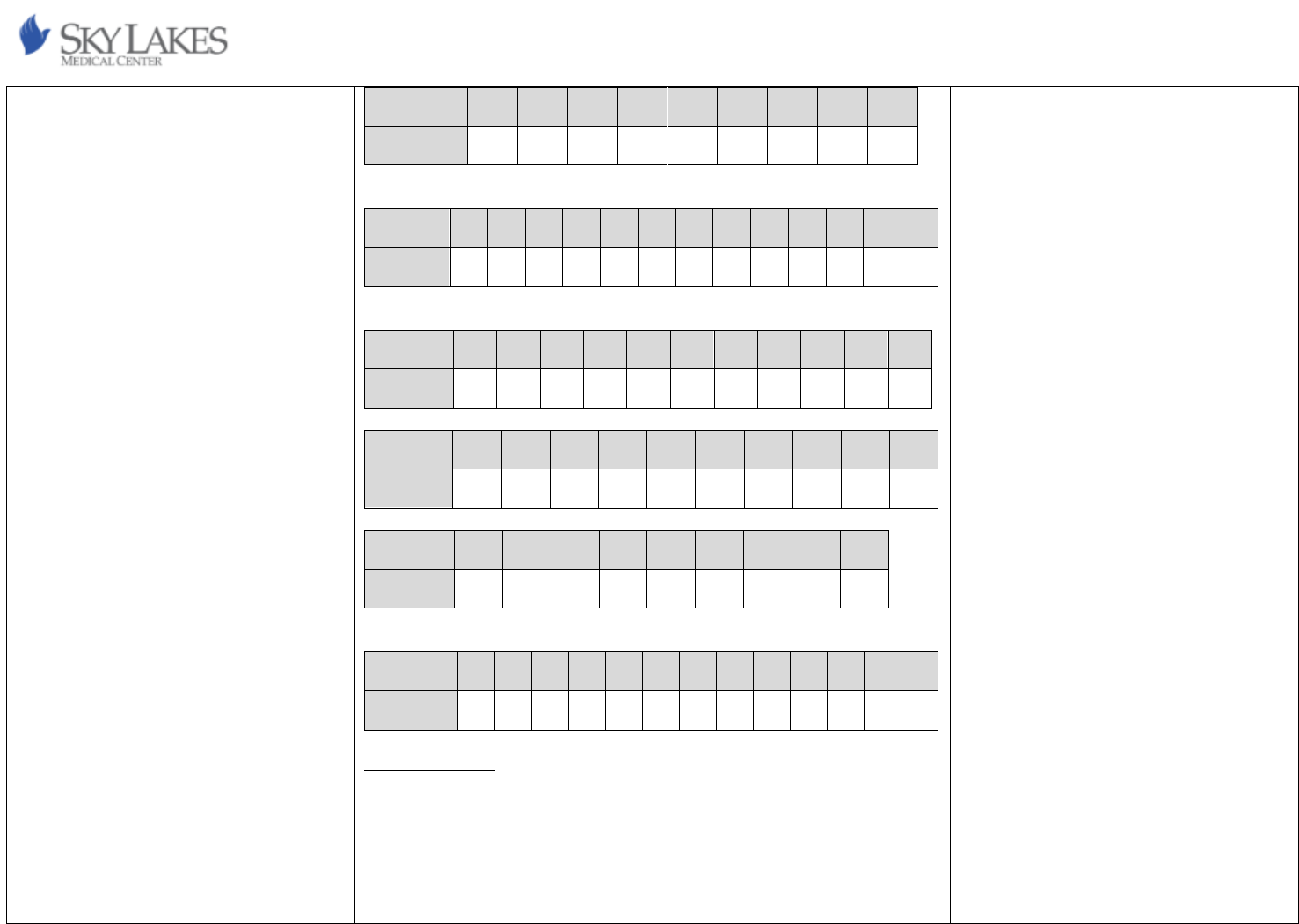
24
Patient #
21
22
23
24
25
26
27
28
29
CNA #
3
4
4
4
4
4
4
4
5
Dayshift C Mod CNA Ratios
Patient #
0
1
2
3
4
5
6
7
8
9
10
11
12
CNA #
0
1
1
1
1
1
1
1
2
2
2
2
2
Nightshift A & B Mod CNA Ratios
Patient #
0
1
2
3
4
5
6
7
8
9
10
CNA #
0
1
1
1
1
1
1
1
1
1
2
Patient #
11
12
13
14
15
16
17
18
19
20
CNA #
2
2
2
2
2
2
2
2
3
3
Patient #
21
22
23
24
25
26
27
28
29
CNA #
3
3
3
3
3
3
3
4
4
Nightshift C Mod CNA Ratios
Patient #
0
1
2
3
4
5
6
7
8
9
10
11
12
CNA #
0
1
1
1
1
1
1
1
1
1
2
2
2
Total Patient Care
If CNA staffing is not available per the above grid, assignments shall be adjusted,
and additional RN resources shall be made available to provide total patient
care. Patient acuity, nurse intensity, staff skill mix, and other relevant factors
shall be taken into consideration when making these assignments.
Total patient care assignments will consist of no more than 3 low to medium
acuity patients with no charge nurse duties.
25
If the charge nurse determines that mixed assignments (TPC and non-TPC) are
necessary, the primary RN will determine which patient (s) are most appropriate
for TPC in the assigned patient group.
The following guidelines are used in determining mixed assignment.
• 3 non-TPC and 1 TPC
• More than 1 TPC in grouping, mixed assignment will be limited to 3
patients.
Charge Nurse
The charge nurse may take patient assignments as follows:
• For the for the purpose of covering staff who are on meal or rest breaks
• For the purpose of covering staff who need to accompany a patient off
the floor for a test or procedure
• When all staffing options have been exhausted and no other qualified
nursing staff are available to take patient assignments
• Under any other circumstances that the charge nurse deems
appropriate
It is with the utmost intent to maintain a charge RN who does not take a patient
assignment as the primary RN. If staffing availability does not allow for such an
assignment, the charge nurse maximum shall be no greater than 3 patients.
The charge nurse shall determine the number of staff needed for the oncoming
shift and throughout the shift to ensure the number of staff and appropriate
skill mix are available to ensure safe patient care. Charge nurses, in
collaboration with Hospital Supervisor, track ADT data throughout the shift and
this data is used to plan for adequate staff to care for expected admissions,
transfers, and discharges.
The charge nurse shall have a plan for staffing and bed capacity for the first and
second shift admission.
Assignments:
The charge nurse shall determine assignments based on staff skill mix, acuities,
intensities, and bed availability. Geographic location assignments shall be a
lower priority than the above criteria. The charge nurse shall collaborate with
the Hospital Supervisor to monitor Admission/Discharge/Transfer (ADT).
26
Sky Lakes Medical Center Nurse Staffing Plan
Department: Operating Room
Approval Date: 05/22/2024
Effective Date: 06/01/2024
UNIT DETAILS
STAFFING
STANDARDS
Unit Description
The Operating Room (OR) is a twenty-four
hour, seven days a week, eight-room unit that
provides surgical care for patients requiring
surgical intervention. Patient populations
served are adults, geriatrics, and pediatrics.
The eight-room unit includes the following
room types:
Six OR suites (currently only staff 4 rooms)
Hours of operation are:
• 0740-1700 for 4 rooms;
o 1 of 4 rooms is the “late room”
and will handle add-on cases
until 1900
o 1 of 4 rooms is the “call room”
and will take call cases 24 hours
a day every day of the year
Two procedural rooms (currently only staff 1
room)
Hours of operation are:
• 0740-1500 for 1 room
Staffing Summary
Weekday staffing is planned around the OR Block schedule allows for one
operating room crew consisting of a RN circulator, a surgical technician, and an
Operating Room Assistant (ORA) per room. ORAs are assigned to no more than
two rooms at a time. Weekday staffing will also include a charge RN, resource
RN and a resource surgical technician. Staff schedules are developed by the OR
clinical manager and cover the surgery blocks created and approved by the
Surgical Services Executive Committee. As surgeon blocks change, staffing
changes shift accordingly.
Nurse Staffing Ratios
Surgical patients are a minimum of one-to-one care with an RN.
Charge Nurse
Charge Nurses (one per shift) manage personnel and flow of the surgery
schedule for the day. Charge nurses may take an assignment and/or take
patients for the purpose of covering meal and rest breaks. They function as
staff in times of high census, high acuity/intensity, and throughput of patients
when necessary. If the Charge RN is moved to staff, the unit manager or
department educator will fill the charge RN role. Nurses who fill this role do not
need any special training concerning patient care, credentialing, or
competencies to hold the position. The only skill necessary is the willingness to
take on additional tasks to include statistical gathering and operating room
staffing assignments.
Meal and Break Relief:
The Charge RN coordinates lunches and breaks with the assistance of resource
staff. If the resource staff are not able to complete these duties due to the high
volume of surgical cases, the surgical educator, charge RN and Clinical manager
Qualifications and Competencies
Refer to Surgical Services Operating Room RN
Qualifications and Competencies for
additional information.
• Current unencumbered Oregon RN
license
• BLS (obtained within two months of hire
date)
• ACLS (obtained within six months of hire
date)
• CNOR (preferred after two years of OR
experience) Two years of OR Nursing is
required prior to the OR RN sitting for
their CNOR Certification Exam.
Because of the specialized nature of OR
Nursing, no staff from outside the OR ever
“float” into the unit.
Nationally Recognized Standards and
Guidelines
Standards or guidelines used to develop the
Operating Room’s staffing plan include:
Association of Perioperative Registered
Nurses (AORN) - 2023 Edition Guidelines
Perioperative Practice (New copy located on
27
Patient Population/Diagnoses
Surgical patients include general surgery,
gastroenterology, orthopedic spine, obstetric,
pulmonary, orthopedic, gynecology, ear, nose
and throat, podiatry, ophthalmic, urology and
oncology.
will ensure breaks and lunches are completed. Minimum numbers of nursing
staff shall be maintained during meal and rest breaks.
the unit for ease of reference.)
28
Sky Lakes Medical Center Nurse Staffing Plan
Department: Progressive Care Unit
Approval Date: 05/22/2024
Effective Date: 06/01/2024
UNIT DETAILS
STAFFING
STANDARDS
Unit Description
The Progressive Care Unit (PCU) is
referred to as a “progressive care” but
does not currently reflect the provided
level of care. PCU provides cardiac
telemetry level nursing care for stable
medical and surgical patients through
direct nursing care. PCU is a 24-hour, 7
day a week, adult acute care unit
consisting of 17 beds. PCU has 9 private
rooms (which include 2 positive pressure
rooms and 1 negative pressure room) and
4 semiprivate rooms (8 beds).
Patient Population/Diagnoses
Progressive Care patients include cardiac
care, general surgery, gastroenterology,
urology, respiratory, stroke, palliative,
and a variety of other Med/Surg
diagnoses.
Overflow patients may be cared for in
PCU and adjacent patient care areas
including 3A (ICU) and 3C.
Staffing Summary
The Progressive Care Unit provides registered nurses and C.N.A.’s, to deliver patient
care and carry out unit operations.
Staffing adjustments are made dynamically to meet the needs of the patient
population using the following:
• Patient volume
• Patient acuity
• Nursing intensity
• Knowledge and skills required of nursing staff to provide care
• Degree of supervision required of nursing staff members
• Type of technology involved in patient care
• Infection control and safety issues
• Continuity of patient care
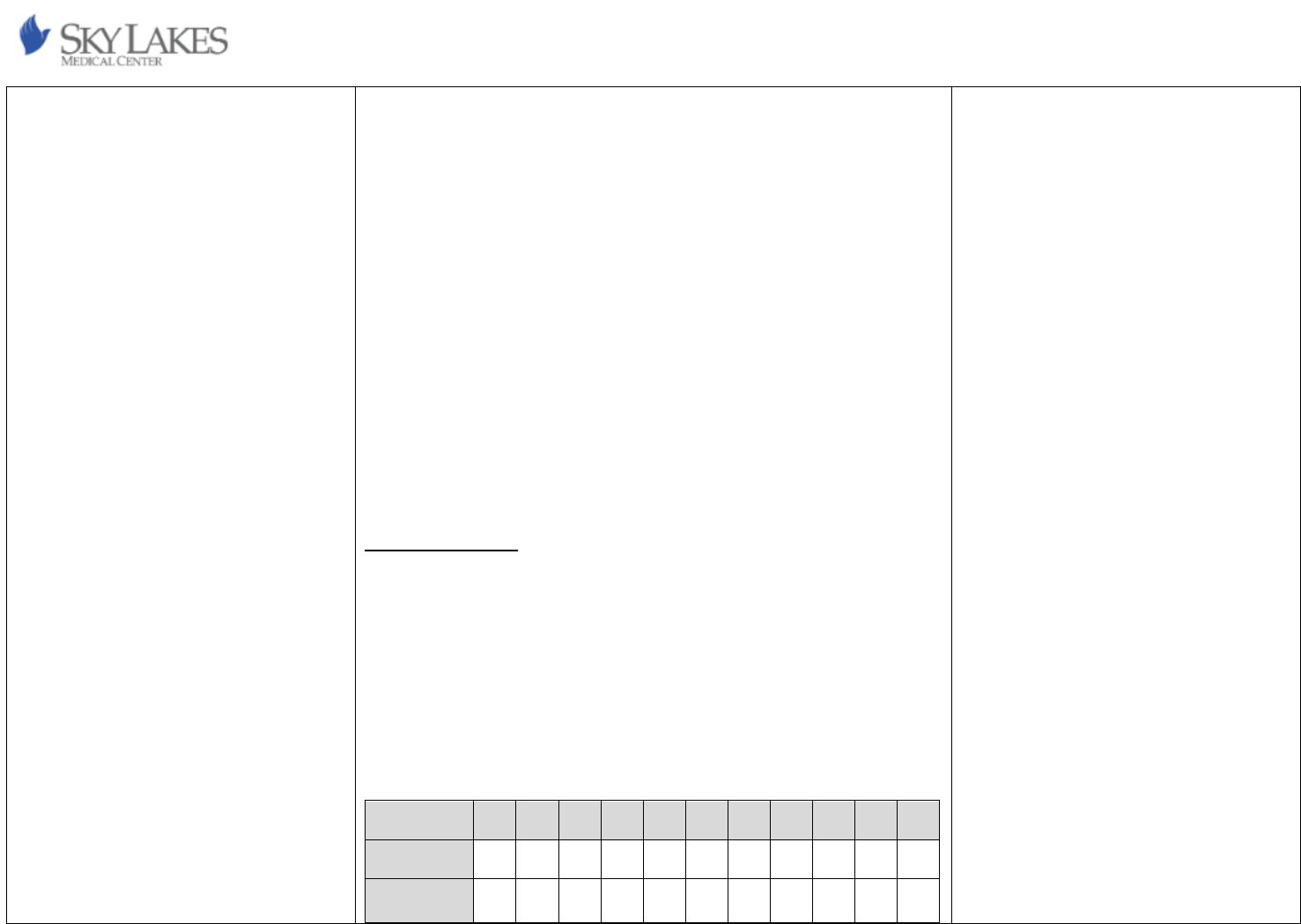
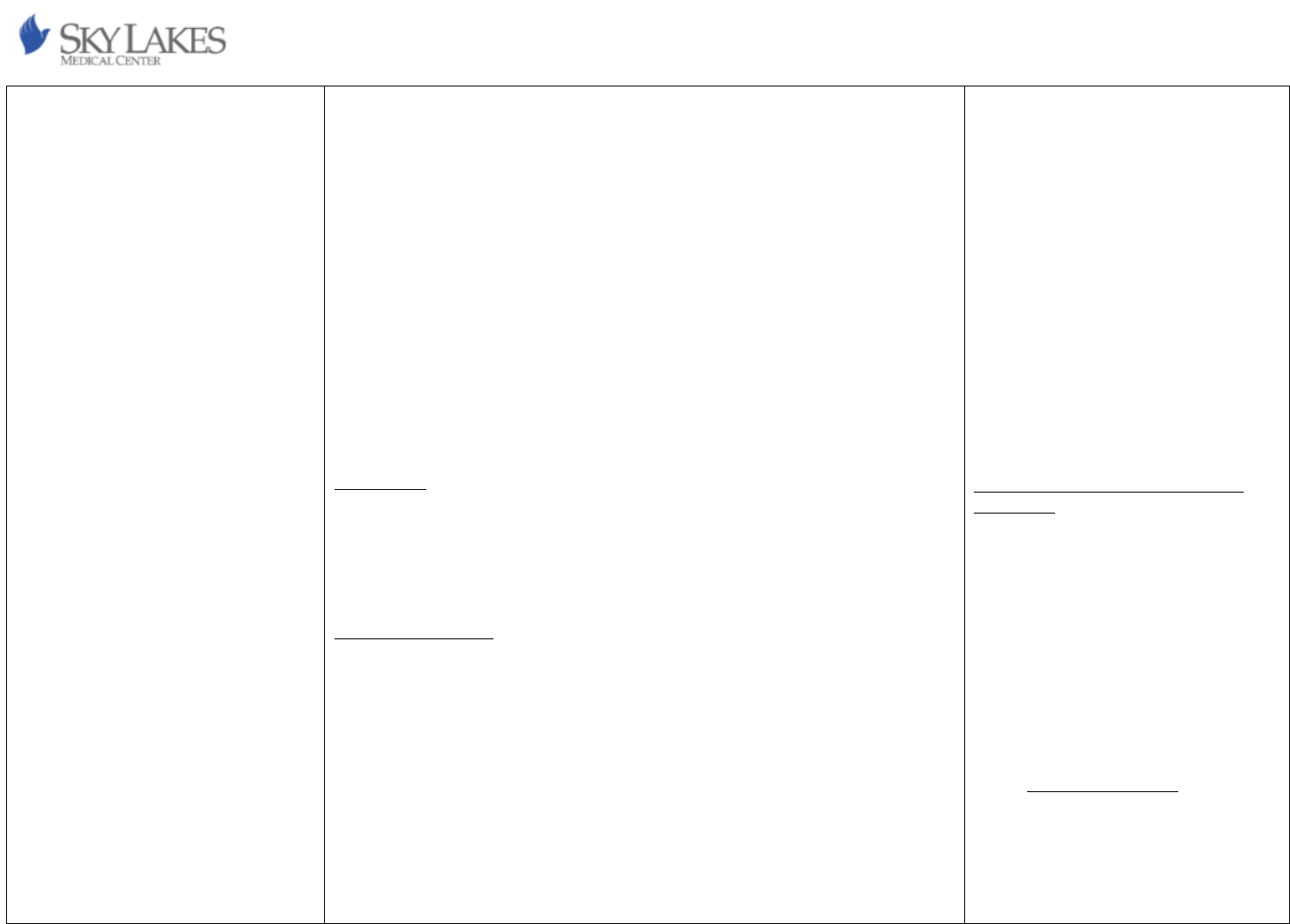
Nurse Staffing Ratios
In the PCU a direct care registered nurse will be assigned to no more than four
patients.
CNA Staffing Ratios
A CNA will be assigned to no more than seven patients during a day shift and to no
more than nine patients during a night shift.
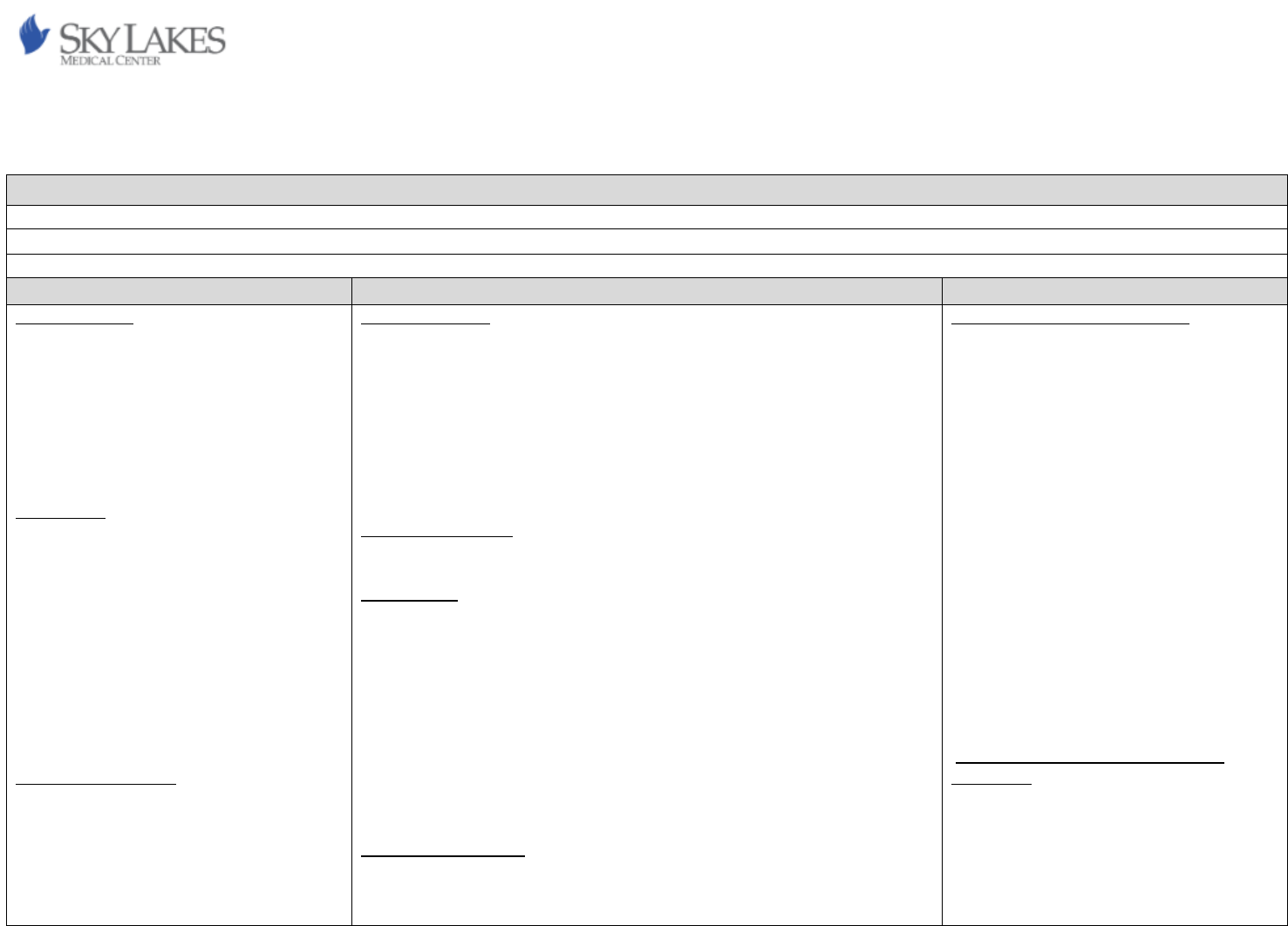
Day Shift
Night Shift
3B
3B
Patient
Direct
Care RN
CNA
Dedicated
Charge RN
Patient
Direct
Care RN
CNA
Dedicated
Charge RN
1
1
1
0
1
1
1
0
2
1
1
0
2
1
1
0
3
1
1
0
3
1
1
0
Qualifications and Competencies
Nursing staff working in the Progressive
Care Unit must maintain qualifications and
competencies that align with the needs of
a complex patient population.
Skills checklists, continuing education and
competencies are documented in the
organization’s electronic learning
management system (LMS). Each nursing
staff member receives annual skills
training and competency validation
through the organization’s electronic
learning management system, Skills Fairs,
online courses, classroom education,
direct education, and policy review.
Critical Thinking and Decision-Making:
• Ability to assess and prioritize
patient needs based on acuity,
vital signs, laboratory results, and
clinical data.
• Proficiency in making rapid and
sound clinical judgments,
especially in emergency situations
or when managing unstable
patients.
Communication Skills:
• Excellent interpersonal and
communication skills to interact
effectively with patients, families,
and interdisciplinary team
members.
29
4
1
1
0
4
1
1
0
5
2
1
0
5
2
1
0
6
2
1
0
6
2
1
0
7
2
1
0
7
2
1
0
8
2
2
1
8
2
1
1
9
3
2
1
9
3
1
1
10
3
2
1
10
3
2
1
11
3
2
1
11
3
2
1
12
3
2
1
12
3
2
1
13
4
2
1
13
4
2
1
14
4
2
1
14
4
2
1
15
4
3
1
15
4
2
1
16
4
3
1
16
4
2
1
17
5
3
1
17
5
2
1
Total Patient Care
In the event that CNA staffing is not available per the above grid, assignments shall be
adjusted, and additional RN resources shall be made available to provide total patient
care (TPC). Patient acuity, nurse intensity, staff skill mixes and other relevant factors
shall be taken into consideration when making these assignments. A direct care
registered nurse will take no more than three patients for TPC if no CNA help is
available on facility wide staffing. The Acuity level of patients taken for TPC is dictated
by Charge nurse. Assignments for TPC will not be mixed with the standard direct care
ratios (ex. having one total patient care and three non-total patient care).
Charge Nurse
The charge nurse will evaluate the available staffing resources, patient acuity, and staff
skill mix to determine the most appropriate patient assignments.
The charge nurse may take patient assignments, including for the purpose of covering
rest and meal breaks. When the charge nurse is in the role as dedicated charge, the
charge nurse will not be a primary nurse to a patient assignment but may take patient
assignments for the purpose of covering staff who are on meal breaks, rest breaks, or
transporting patients to other units or imaging. The dedicated charge nurse may also
take patients assignments for the purpose of covering staff that have been called into
• Ability to convey complex medical
information in a clear and
understandable manner.
Teamwork and Collaboration:
• Demonstrated ability to work
collaboratively as part of a
multidisciplinary team, fostering a
culture of mutual respect and
cooperation.
• Willingness to support colleagues
and share knowledge and
expertise to achieve common
goals.
Technical Proficiency:
• Competency in utilizing electronic
health records (EHR) and clinical
documentation systems to
accurately record patient
assessments, interventions, and
outcomes.
• Familiarity with medical
equipment and technology used
in progressive care settings
Clinical Skills:
• Proficiency in cardiac monitoring
and the interpretation of cardiac
rhythms. Performing advanced
nursing procedures such as
titration of vasoactive
medications and management of
invasive lines. Management of
complex medical conditions.
Continuous Learning and Professional
Development:
• Commitment to ongoing
professional development
through participation in
continuing education programs,
conferences, and advanced
30
shift. Once the direct care registered nurse arrives, they will then assume care from the
charge nurse.
When the unit has seven or less patients, the charge nurse may take a patient
assignment and continue duties of charge. Once the unit reaches eight patients, an
additional direct care registered nurse will be assigned to the unit to assume care of
charge nurse’s patient assignment. The charge nurse will then become dedicated
charge.
The charge nurse shall determine the number of staff needed for the oncoming shift
and throughout the shift to ensure the number of staff and appropriate skill mix are
available to ensure safe patient care. Charge nurses, in collaboration with Hospital
Supervisor/Bed Coordinator, track ADT data throughout the shift and this data is used
to plan for adequate staff to care for expected admissions, transfers, and discharges.
The charge nurse shall have a plan for staffing and bed capacity for the first and second
shift admission.
Assignments
The charge nurse will determine assignments based on staff skill mix, acuities and bed
availability. Geographic location assignments shall be a lower priority than the above
criteria. The charge nurse will collaborate with the Hospital Supervisor/Bed
Coordinator to monitor
ADT.
Meal and Break Relief
Meal break planning shall be initiated at the beginning of the shift to allow for
proactive planning and resource allocation.
Meal and rest break coverage will be predominantly accomplished by the dedicated
charge nurse, assuming staffing ratios are maintained. In the event the dedicated
charge nurse needed assistance with meal and rest break coverage, they may be
provided by the following:
• Resource nurse
• Core unit staff on shift, assuming that staffing ratios are maintained
• Core unit staff who voluntarily sign up to provide meal and rest break
coverage
• Flex team staff
• Hospital Supervisor/Manager
certifications.
• Engagement in evidence-based
practice initiatives to enhance
clinical knowledge and improve
patient outcomes.
Cultural Competence and Patient
Advocacy:
• Sensitivity to cultural, ethnic, and
socioeconomic diversity among
patient populations, with a focus
on providing culturally competent
care.
• Advocacy for patients' rights,
preferences, and needs, ensuring
that care delivery is patient-
centered and respectful of
individual values and beliefs.
Nationally Recognized Standards and
Guidelines
List nationally recognized standards and
guidelines used in the development of the
unit staffing plan and used in the care of
the patient population.
Standards or guidelines used to develop
the Progressive Care Unit’s staffing plan
include:
• AACN Procedure Manual for High
Acuity, Progressive Care, and Critical
Care. 7th edition: 2016
American Association of Critical Care
Nurses http://www.aacn.org 2023

31
Nursing staff are responsible for the following:
• Sign up for and know scheduled break periods
• Be prepared to take break when coverage is available
• Give a brief report, understanding that most information can be obtained
from EMR
• Highlight the list of tasks that need to be completed during break; being
mindful of the tasks that can reasonably be completed during the break
period. The patient’s experience should be seamless.
• Return punctually
32
Sky Lakes Medical Center Nurse Staffing Plan
Department: Pediatrics
Approval Date: 05/22/2024
Effective Date: 06/01/2024
UNIT DETAILS
STAFFING
STANDARDS
Unit Description
The Pediatrics Unit is a 24-hour, 7 day a week,
6-bed acute care unit that provides direct
nursing care for general medical and surgical
patients 17-years of age and younger. The
unit is comprised of six private rooms and
one procedure room. Refer to Scope of
Service / Structure Standards, Maternal Child
Health.
Patient Population/Diagnoses
The Pediatrics Unit patients include general
medical, surgical, and chronically ill children
17-years of age and younger.
Staffing Summary
The Pediatric Unit provides registered nurses, licensed practical nurses, and
certified nursing assistants (CNAs) to deliver patient care and carry out unit
operations. The following Pediatrics Staffing Acuity Sheet shall be utilized to
provide a plan for staffing throughout the shift:
The charge nurse utilizes the Staffing Acuity Sheet to assess patient acuity and
intensity every four hours and as needed. Staffing is adjusted based on nursing
judgement, which supersedes any ‘number’. Acuity is defined as the measure of
how sick a patient is and the associated level of nursing skill required to care for
a particular patient and their associated diagnoses. Intensity is defined as the
measure of how much nursing time and effort is required to provide for the
individual needs of a patient. Nursing daily staffing shall be adjusted based on
changes in patient acuity/intensity.
Nurse Staffing Ratios
The Pediatric Unit shall be staffed with a minimum of two (2) licensed
professions when open; one of which must be a pediatric trained RN and the
other may either be another RN, LPN, or CNA
Qualifications and Competencies
All Pediatric Unit RNs are oriented and
trained upon hire to the unit to demonstrate
competence in direct care of the aggregate
patient population served.
Skills checklists, continuing education, and
competencies are documented in the
organization’s electronic learning
management system (LMS). Each nursing
staff member receives continuing education,
annual skills training, and competency
validation through a variety of platforms
including but not limited to the organization’s
LMS, Skills Fairs, online courses, classroom
courses, direct observation, and policy
review. Please refer to the Pediatric Unit
Qualifications and Competencies attachment
for additional details.
Nationally Recognized Standards and
Guidelines
The Society of Pediatric Nurses’ (SPN)
position statement on Safe Staffing for
Pediatric Patients (2020) states, “The
healthcare needs of pediatric patients
present unique challenges due to different
developmental stages, limited
communication skills, and differences in
epidemiology and approaches to treatment
as compared to adults”. Staffing models shall
consider indirect care needs, patient acuity,
patient volume and availability of ancillary
33
Staffing levels reflect differences in patient populations relative to age, severity
of illness, and complexity of care with a maximum nurse to patient ration of
1:4.
CNA Staffing Ratios
A CNA may not be assigned to more than seven patients at a time during a day
shift or to more than 11 patients during a night shift.
Charge Nurse
The charge nurse may take a patient assignment, including for the purpose of
covering staff on meal and rest breaks. The charge nurse, in collaboration with
the Hospital Supervisor, track ADT data throughout the shift and this data is
used to plan for adequate staff to care for expected admissions, discharges and
transfers.
The charge nurse shall have a plan for staffing and bed capacity for the first and
second admissions, transfers, and downgrades.
Assignments:
Assignments shall be based on staff skill mix, patient acuity/ intensity, and bed
availability.
Patient conditions that may contribute to a higher level of intensity in the
Pediatric Unit include but are not limited to:
• Family social dynamics
• Complications requiring increased observation/intervention
• Oxygen titration
• Involvement with investigation/agencies
• Communication barriers or congenital behavior/emotional issues
that impede care delivery
• Parent not at the bedside
In the event when a pediatric patient needs intensive care support, please refer
to the PEDS Patient to Higher Level of Care Flow Diagram (Rev 2.11.22).
Meal and Break Relief:
Meal break planning shall be initiated at the beginning of the shift by the Family
Birthing Center Charge Nurse in collaboration with the Hospital
Supervisor/Manager/Director/Designee. Any identified external meal coverage
services and resources in the development of
staffing models.
34
needs shall be communicated by the charge nurse to the Hospital Supervisor/
Manager/Director/Designee as soon as possible in order to help facilitate
coverage.
Minimum numbers of nursing staff shall be maintained during meal and rest
breaks. Meal and break coverage resources may be provided by:
• Core unit staff that voluntarily provides meal coverage
• Flex team
• Resource nurse
• Hospital Supervisor/Manager/Director
Nursing staff shall be responsible for the following:
• Sign up for and know scheduled break periods
• Be prepared to take break when coverage is made available
• Give a brief report, understanding that most information can
be obtained from EMR
• Highlight the list of tasks that need to be completed during
break; being mindful of the tasks that can reasonably be
completed during the break period. The patient’s experience
should be seamless.
• Return punctually
Call
All nursing staff are required to take mandatory call to provide appropriately
trained core staffing and to maintain safe patient care. For further details
related to the call procedure, refer to Call, Maternal Child Health Policy.
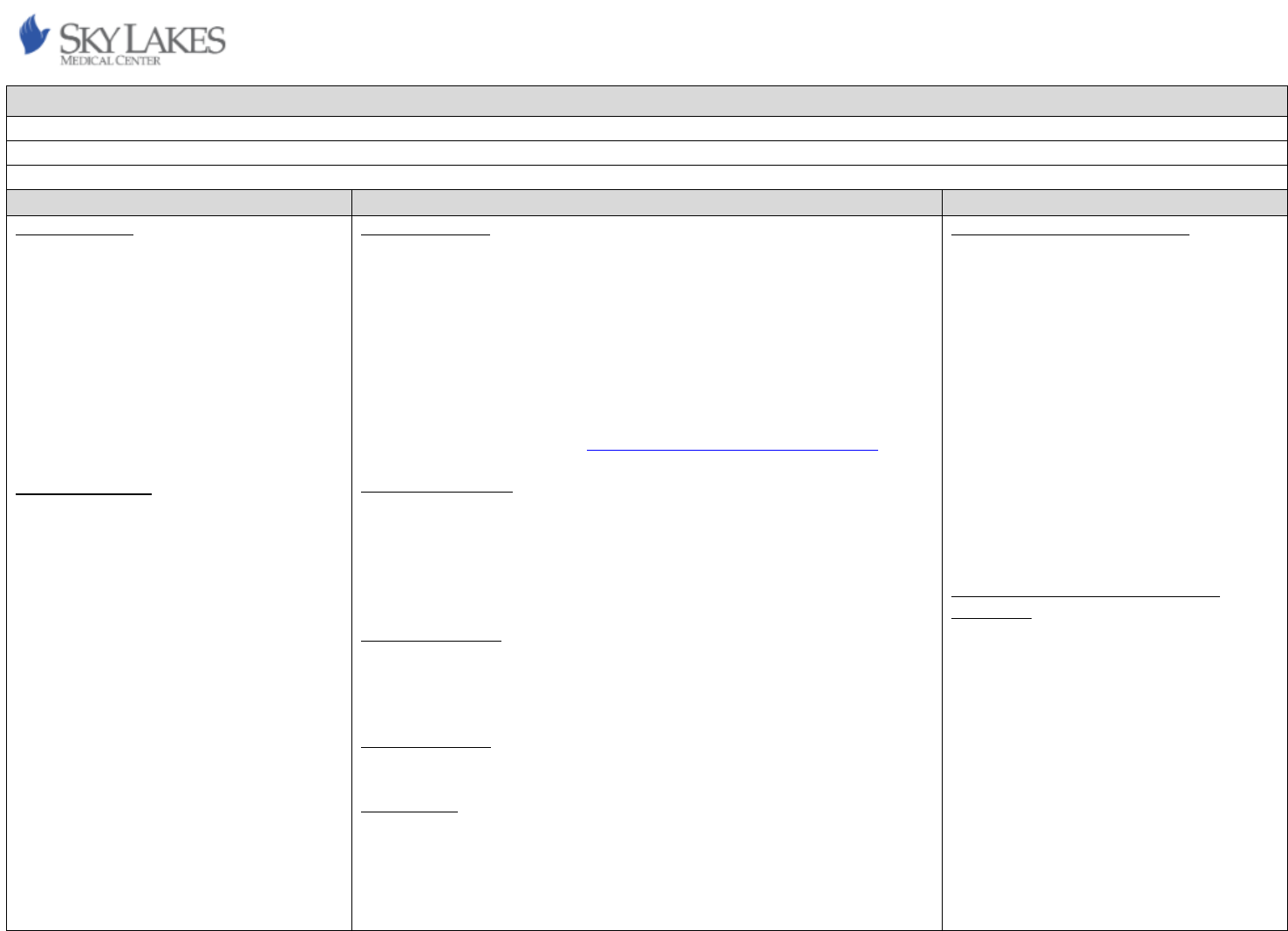
35
Sky Lakes Medical Center Nurse Staffing Plan
Department: Phase 3 Recovery
Approval Date: 05/22/2024
Effective Date: 06/01/2024
UNIT DETAILS
STAFFING
STANDARDS
Unit Description
Phase III is an Outpatient unit.
• Type/level of care:
Outpatient Same Day Surgery/Phase
III Recovery (Extended Care)
• Hours/days of service:
0930-2200 Mon-Thurs
• Number of beds:
Variable 1-9
• Types of beds:
Outpatient
Patient Population
Patient populations include adults and
geriatrics, and occasionally, pediatric patients
over 8 years of age.
Phase III cares for outpatient postsurgical
patients who require extended
observation/intervention after discharge
from Phase I or Phase II. The expectation is
that these patients will discharge home on
the same day as their surgery.
The procedures most seen in Phase III
include:
• Diagnostic Laparoscopy
• Hemithyroidectomy
• Laparoscopic Appendectomy
• Laparoscopic Cholecystectomy
• Laparoscopic Hysterectomy
• Open or Laparoscopic Hernia repair
Staffing Summary
Two competent personnel, one of whom is an RN possessing competence
appropriate to the patient population, are in the same room/unit where the
patient is receiving extended care. (ASPAN, 2022, p. 52). The second staff
member must be BLS certified but is not necessarily an RN. The need for
additional RNs and support staff is dependent on patient acuity, patient census,
and physical facility.
The following tool measures patient acuity and intensity and has been
calibrated to the Phase III unit: Phase III Acuity/Staffing/Guidlelines.docx
Nurse Staffing Ratios
This is an outpatient unit. Staffing patterns reflect ASPAN’s Patient
Classification/Staffing Recommendations for Phase II and extended care.
Generally, a 1:3 nurse patient ratio allows for appropriate assessment, planning,
implementing care and evaluation for discharge and increased efficiency and
flow of patients through the unit (ASPAN, 2022, p. 51).
CNA Staffing Ratios
This is an outpatient unit. Phase III RNs are assigned total patient care. CNAs are
not utilized in the unit except when necessary to meet the requirement that two
staff members be in the same unit where the patient is receiving care.
Total Patient Care
Total patient care is the standard of care in the unit.
Charge Nurse
Though not required, a charge nurse may be utilized. The charge nurse will take
patient assignments. The charge nurse will coordinate patient care
responsibilities among nurses, manage lunch and break schedules, and provide
guidance and support to colleagues. The charge nurse will also perform indirect
care duties as assigned.
Qualifications and Competencies
All nurses working Phase III are required to
maintain their BLS and comply with annual
training requirements for the Orthopedic
Service Line. Core staff also complete
selected PeriAnesthesia competencies which
are maintained via ASPAN guidelines. Proof of
compliance is kept in the Perioperative
Educator’s office, orthopedic service line
records, and approved hospital provided
computer-based training (CBT). CBT provides
additional hospital approved and required
employee training.
Refer to Phase III Recovery RN Qualifications
and Competencies for additional information.
Nationally Recognized Standards and
Guidelines
The Phase III source material is the nationally
recognized American Society of
PeriAnesthesia Nurses (ASPAN). Examples of
the standards can be referenced in the
following document: 2022-2023
PeriAnesthesia Nursing Standards, Practice
Recommendations and Interpretive
Statements kept in Phase II for ease of
reference.
36
• Open Reduction Internal Fixation
• Shoulder Arthroscopy
• Total Shoulder Arthroplasty
Unilateral Mastectomy
Assignments:
Assignments consider staff skill mix, acuities, intensities, and bed availability.
When a charge nurse is being utilized, the charge nurse will make assignments.
If a charge nurse is not being utilized, assignments are made by mutual
agreement of on-duty nurses.
Meal and Break Relief:
A “meal” is defined by the Medical Center as a thirty-minute unpaid break given
when a staff member is working more than six hours during which they should
be relieved of all work duties. A “break” refers to a period of not less than
fifteen minutes of paid time for every four hours worked (BOLI). Meal break
planning shall be initiated at the beginning of the shift in collaboration with the
Manager/Hospital Supervisor/Director/Designee.
The staff nurse(s) on duty shall identify any external meal coverage needs and
communicate that to the Manager/Hospital Supervisor/Director/Designee as
soon as possible to help facilitate coverage.
Meal and break coverage resources may be provided by:
• Periods of downtime without patients which are sufficient in length
(preferred)
• Unit staff who will not be put over the 1:3 ratio (preferred)
• Unit staff who voluntarily sign up to provide meal coverage
• Clinical Manager
• Phase I/Phase II staff
• Resource nurse or flex team coverage
• Hospital Supervisor/Director/Designee
Nursing staff shall be responsible for the following:
• Identify external meal coverage needs and know planned break
periods.
• Be prepared to take a break when coverage is made available.
• Give a brief report, understanding that most information can be
obtained from the electronic medical record.
• Highlight the list of tasks that need to be completed during break. The
patient’s experience should be seamless.
• Return punctually.

37
Phase III Acuity/Intensity Staffing Guidelines
Patients should meet minimum standards for Phase II level of care prior to transfer into Phase III.
Level 1 - (1:3 nurse patient ratio) Patient requires routine post anesthesia care and may experience slight post-anesthesia/post-operative complications
• Standard monitoring of vital signs. Q30 –60 minutes including admit and discharge or per destination unit standard if holding for inpatient bed
• Vital signs stable or returning to baseline
• Routine oxygen administration and pulse oximetry
• Pediatric patient 8-14 years with family present
• Pain or nausea requiring up to 2 medications each
• Bladder scanning/placement of catheter
Level 2 - (1:2)
• Pediatric patient 8-14 years without family present
• Total Joint replacement
• Pain or nausea requiring 3 or more interventions
• Mechanical lift for transfers
• Behavior disturbances/agitation/uncooperative
• Complex patient/family dynamics, communication barriers and/or emotional needs currently impacting delivery of care
• Complex wound care
• Complex discharge including new diagnosis and education
• Blood administration 1 unit
• Fluid bolus for blood pressure x 1
Level 3 - (1:1) Strongly consider returning the patient to Phase I. If return to Phase I indicated, consult Phase I manager or charge nurse. Contact supervisor or manager for
assistance
• Hemodynamic instability requiring any of the following: > 1 unit of blood, more than 1 fluid bolus, or administration of blood pressure medications that the
patient does not take at baseline.
• Uncontrolled pain and/or nausea despite interventions
• Return to OR due to significant/unstable post-op complications
• Significant allergic reaction
• Sitter indicated but not available
• Unstable patient requiring STAT medications, tests, etc.
• Combative patients
Level 4/ Level 5 - (2:1 or greater) Call for rapid response or code blue as indicated. Plan for imminent transfer of patient to higher level of care (Phase I or ICU). Contact
supervisor or Phase I/Phase III managers.
• Loss of airway
• Rapidly deteriorating patient condition (respiratory or cardiac arrest, significant post-op blood loss)
• Malignant Hyperthermia
• Unstable neuro status (for example signs and symptoms of CVA, seizures or withdrawal)
38
Sky Lakes Medical Center Nurse Staffing Plan
Department: Recovery
Approval Date: 05/22/2024
Effective Date: 06/01/2024
UNIT DETAILS
STAFFING
STANDARDS
Unit Description
Monday through Friday 0730-1900, or until
all surgeries are done, then operation of the
Operating Room (OR) changes to the call
schedule and personnel.
Recovery Room Consists of Three Distinct
Environments
Surgical Admissions (SA) Wing. There are nine
patient care areas for pre-anesthesia care and
surgical evaluation only. Each bay is equipped
with a monitor that can be used continuously
when necessary to increase capability.
Phase 1 (PACU). The Phase 1 area is an open
bay with seven patient care areas. Each area
is telemetry equipped, including invasive
monitoring. One of the seven bays is
designed as an isolation room with negative
air flow.
Phase 2 (DSU (Day Surgery Unit)). The Phase 2
area is telemetry equipped with 12 patient
care areas. The Recovery Room team consists
of Certified Nursing Assistants (CNA) and
Nurses (RN). The Clinical Manager acts as
staff in times of high census, high
acuity/intensity and manages personnel and
throughput of patients when necessary. The
manager supports and facilitates the needs of
the Recovery Room team and other
Staffing Summary
The recovery room is made up of the following staff: registered nurses (RN) and
certified nursing assistants (CNA). The recovery room conducts primary nursing
care with 2 CNA who facilitate the primary nursing care by being delegated to
simple tasks and administrative duties. Additionally, the recovery room has
designated charge nurses with relief charge nurses as necessary.
Staffing of Surgical Admissions (SA), PACU & DSU
The staffing schedule is created and managed by the unit’s Charge RN with
significant input from the frontline staff. The schedule is then reviewed and
approved by Management no later than 15 days (about 2 weeks) before the due
date defined in the Nursing Contract. Staffing patterns reflect ASPAN’s Patient
Classification/Recommended Staffing Guidelines.
Staffing of the SA, PACU, and DSU is based on several elements. The number of
OR rooms running dictates the number of SA, PACU and DSU nurses required
each day. In SA, during the initial assessment and interview the patient to nurse
ratio is 1:1. After patient/s initial assessment and interview, the minimum
patient to nurse ratio is changed to no more than 5:1, with two nursing staff in
the unit, with patients, always.
In general, a maximum patient to nurse ratio of 2:1 in PACU allows for
appropriate assessment, planning, implementation of care, and evaluation for
discharge as well as increased efficiency and flow of patients through the PACU
area (American Society of Peri-Anesthesia Nurses, 2020, p. 48-53). Use of the
acuity/intensity tracking found in the Electronic Medical Record (EMR) facilitates
assessment and continued reassessment of patient condition and intensity and
facilitates real-time staffing adjustments (see acuity and intensity).
In general, the patient-to-nurse ratio is 3:1 in DSU, which best allows for
appropriate assessment, planning, implementation of care and evaluation for
discharge and increased efficiency and flow of patients through the unit (ASPAN,
2023, p. 48-53). Use of the AITF facilitates assessment and continued
reassessment of patient condition and intensity and dictates the following
Qualifications and Competencies
Refer to Surgical Services Operating Room
RN’s Qualifications and Competencies for
additional information.
Phase 1 (PACU), Phase 2 (DSU) and Surgical
Admissions
All nurses working PACU, DSU and Surgical
Admissions are required to maintain their
BLS, ACLS and PALS. Peri-Anesthesia
approved competencies are maintained via
ASPAN guidelines. Proof of compliance of
competencies are kept in the Surgery
Department Educator’s office and approved
hospital provided Computer Based Training
(CBT). CBT provides additional hospital
approved and required employee training.
Nationally Recognized Standards and
Guidelines
Recovery Room source material is the
nationally recognized American Society of
Peri-Anesthesia Nurses (ASPAN). Examples of
the standards can be referenced in the
following document: 2023-2024 Peri-
Anesthesia Nursing Standards, Practice
Recommendations and Interpretive
Statements kept in the unit for ease of
reference.
39
management duties as indicated.
Designated Charge Nurses work as staff in
times of high census, high acuity/intensity,
otherwise they control throughput of patients
when necessary and direct duties of staff. The
Charge Nurses also are responsible for
developing the monthly schedule and
providing it to management no later than 15
days (about 2 weeks) before approval and
posting. Nurses who fill this role do not need
any special training, credentialing, or
competencies to hold the position.
The only skill necessary is the willingness to
take on additional tasks as delegated by
management.
All Float Personnel are required to complete
competencies for Peri-Anesthesia care,
complete an orientation to the Recovery
Room environment and have BLS (Basic Life
Support), ACLS (Advanced Cardiac Life
Support) and PALS (Pediatric Advanced Life
Support) credentials. Float Personnel are
called in times of high census and high
acuity/intensity. This resource is accessed
weeks in advance and on occasion as needed,
via the nurse staffing office, or staff
volunteers contacted by Management or
Charge Nurses.
Patient Population/Diagnoses
Any patient recovering from anesthesia and
surgical intervention, including but not
limited to adults, geriatrics, pediatrics,
developmentally delayed adults, children,
pregnant, and post-partum women.
Diagnoses include, but are not limited to
staffing adjustments.
Note. Class I and II patients may fast track directly from the OR. Additionally,
Class III from endoscopy or patients that deteriorate in the Phase 2 area may be
transferred into Phase 1 area, if necessary, to facilitate throughput in the Phase
2 area. Any class IV or V is not suitable for post op care or boarding in Phase 2 as
they require 2 or more nurses per patient and will be transferred into Phase 1
area.
Surgical Admissions
At least one nurse and one other nursing staff member (RN, CNA) on the unit
while patients are present. Staffing is dependent on the number of OR rooms
that are running that day. Staffing also depends on the acuity of the patients
boarded in the admit department. High acuity patients will be boarded in the
PACU secondary to acuity/intensity and the telemetry capabilities of the PACU.
However, they can be boarded in the Admit Department with proper monitoring
capabilities, supplies, and staff. Approximate patient volume per month from
fiscal year, available upon request.
Post Anesthesia Care Unit: Phase 1
Two registered nurses, one of whom is an RN competent in Phase 1 Post-
Anesthesia nursing, are in the same room/unit where the patient is receiving
Phase 1 level of care (ASPAN, 2023, p. 48-53). Staffing reflects patient
acuity/intensity, patient census, and the physical facility. Phase 1 nurses
continuously re-evaluate the patient's acuity and intensity using the Recovery
Room Acuity/Intensity Tracking via EPR. Then utilizing the Resource
Nurse/Charge Nurse/Clinical Manager as needed to maintain proper staffing. In
general, a 1:1, or 2:1 patient-to-nurse ratio allows for appropriate assessment,
planning, implementing care, and evaluation for transfer and increasing
efficiency and flow of patients through the Phase 1 area (ASPAN, 2023, p. 48-
53). The Peri-Anesthesia registered nurse maintains appropriate staffing
recommendations when planning for transport of patients in and out of the
unit. Approximate patient volume per month from fiscal year, available upon
request.
Post Anesthesia Care Unit: Phase 2
Two competent personnel, one of whom is an RN competent in Phase 2 post
anesthesia nursing, are in the same room/ unit where the patient is receiving
Phase 2 level of care. Two RNs are always in the Phase 2 DSU area while a
patient is present (ASPAN, 2023, p. 48-53). Phase 2, or DSU is not utilized “on

40
(ICD 10 Code)
Admission Screening
o Cardiovascular Disorders
(Z13.6)
o Diabetes Mellitus (Z13.1)
o Dental Disorders (Z13.89)
o Behavioral Disorders
(Z13.89)
o Respiratory Disorders
(Z13.83)
o Infections and parasitic
disease, unspecified
(Z11.9)
o Counseling, unspecified
(Z71.9)
o Aftercare following
explanation of
▪ Shoulder joint
prosthesis (Z47.31)
▪ Hip joint prosthesis
(Z47.32)
▪ Knee joint
prosthesis (Z47.33)
o Contact with and
(suspected) exposure to
▪ Unspecified
communicable
disease (Z20.9)
▪ Pediculosis,
ascariasis, and
other infestations
(Z20.7)
Phase 1 and Phase 2
o Aftercare following
surgery: (Z48)
o Surgical aftercare
following, orthopedic (Z47)
▪ Drain (Z48.03)
call”. In a very uncommon instance, the patient is going to be discharged from
the Recovery Room, the Phase 1 RN works in the capacity of a Phase 2 RN.
Staffing reflects patient acuity and the complexity of patient care. In general, a
3:1 patient-to-nurse ratio allows for appropriate assessment, planning,
implementation of care, and evaluation for discharge and increasing efficiency
and flow of patients through the Phase 2 area (ASPAN, 2023, p. 48-53). The
Recovery Room nurses continuously re-evaluate the patient's acuity and
intensity using the Recovery Room Acuity/Intensity Tracking via the EMR.
Approximate patient volume per month from fiscal year, available upon request.
Acuity and Intensity
Acuity is defined as the degree of a patient's "sickness" or "physical state"
before and after surgery. The American Society of Anesthesiologists (ASA)
Physical Status Classification System (American Society of Anesthesiologist,
2023, December 13) will be used to quantify acuity. Staffing is adjusted to
support high or low ASA patients. ASA Rating is used to clarify acuity in the OR
environment.
Intensity is defined as the number of resources, both physical environment and
FTE (staff) count needed to safely care for a patient. In the Recovery Room, the
Recovery Room Acuity /Intensity Tracking tool, via the EMR, is used exclusively
by frontline staff and is being tracked on every patient. The data compiled is
used concordantly with the Analytic Tracking Tool (for example, see Appendix
A).
These tools provide us with the information necessary to predict the
appropriate number of staff effectively and accurately for any given day. This
data is supported by the IBM Action IO benchmarking database. The Recovery
Room Acuity /Intensity Tracking via the EMR, tool is a “living document” and is
reviewed and modified as needed by staff regularly and approved by
management, to better reflect the ever-changing conditions of the patient
populations. Data recorded by staff is entered into Epic via the patient’s EMR.
Acuity/Intensity by Class
Class I. Patients are suitable for a 3:1 patient to nurse ratio. In most of these
cases the patient meets fast tracking criteria. Fast tracking is defined as having a
patient bypass Phase 1 level of care and go directly to Phase 2. The patient must
meet Phase 1 discharge criteria prior to leaving the OR. (ASPAN, 2023, p. 50-53).
Class II. Patients are suitable for a 2:1 patient to nurse ratio. In most of these
cases the patient also meets fast tracking criteria.
Class III. Patients are suitable for a 1:1 patient to nurse ratio. These patients
41
▪ Surgical wound
dressing (Z48.01)
▪ Sutures (Z48.02)
o Surgical aftercare
following, orthopedic (Z47)
o Surgical aftercare following
surgery on the
Genitourinary system
(Z48.816)
o Surgical aftercare following
surgery on the teeth or
oral cavity (Z48.814)
o Surgical aftercare following
surgery on the Respiratory
system (Z48.813)
o Surgical aftercare following
surgery on the Digestive
system (Z48.815)
o Surgical aftercare following
surgery on the Spine
(Z48.89)
o Encounter for Sterilization
(Z30.2)
o Other Acute Post
Procedural Pain (G89.18)
▪ Postoperative pain
▪ Post procedural
pain
o Unspecified Nausea &
Vomiting (R11.2)
o Laryngospasm (J.38.5)
o Insufficient or Poor
Respirations (R06.89)
o Acute post procedural
respiratory failure
(J95.821)
o Post Procedural (Post-
Operative) Delirium (F05)
require additional care and assessment and require an RN to be within a few
steps “present” (ASPAN, 2023, pg. 49) of patient until they have recovered
enough from anesthesia to be downgraded to a lower-level acuity.
Class IV or V. Patients are suitable for 1:2 (1:2 or more) patient to nurse ratio.
These patients require 2 or more nurses at the bedside and need constant
monitoring and/or intervention. They often require significant respiratory,
cardiovascular and/or emotional support for an extended period.
Note. There are two RN at the bedside for every pediatric patient in Phase 1.
CNA Staffing Ratios
CNAs are not assigned a patient load in the Recovery Room.
Charge Nurse Responsibilities: The charge nurse may take patient assignments,
including for the purpose of providing meal and rest breaks. Managing
workflow/Facilitating patient throughput, communicating with the other charge
nurses to help keep flow for the day between Admit -> OR ->
PACU/DSU. Reevaluating staffing and assignments throughout the day based off
the OR board changes. Anticipating schedule challenges/problems and making
the necessary adjustments to keep the day moving forward (I.e., Nuclear Med,
Mag seed placement, IR interventions, etc.)
• Supporting Staff
• Lunch relief
• Break relief
• Random admits or Call cases
• Procedure support (I.e. medication administration, IV placement, lab
collection, etc.)
• Sudden increase in patient acuity
• Communicating with house supervisor and other units about bed admit
needs.
• Product support/expertise
• Managing doctors
• Clarify or get orders
• Present the staff’s concern to MD and work together to create a better
solution for the patient
• Facilitating doctor's workflow
• Administration
• MRO management
• Schedule creation and management
• Assignments
42
o Malignant hyperthermia
due to anesthesia (T88.3)
o Hypothermia following
anesthesia (T88.51)
o Other complications of
anesthesia (T88.59)
▪ Arrhythmia
▪ Hypo/Hypertension
▪ Pseudocholinestera
se Deficiency
o Post-procedural
hemorrhage of a
circulatory system organ or
structure following
procedure (I97.620)
o Infection following a
procedure (T81.44)
o Other intraoperative and
post procedural
complications and
disorders or the digestive
system (K91.8)
o Other intraoperative
complications of
genitourinary system
(N99.81)
• Analytics
• Dealing with complaints/concerns of patients and families
• Deescalating difficult patients/families
• Weekly meetings for unit development and improvement
Relief Charge Nurses do not have any of the administrative duties the
Designated Charge Nurses do.
Assignments:
Staff assignments are made as early as one week in advance and posted in the
units for all staff to reference when they come to work. They can be changed by
the Charge RN, or Management, depending on unit need. They give details on
what environment a staff member is to be assigned to any day.
Recovery Room is one department, made up of three units (Surgical Admissions,
DSU, and PACU). In the DSU and PACU patients are assigned to an available
nurse as they [patient] enter the environment, as opposed to being “assigned” a
patient in the traditional scene of the word. Note that the nurses in the
Recovery room have all been cross-trained and will be moved to different
sections of the unit as needed.
CNA assignments are not managed in the traditional sense. The CNA in
Recovery works in concert with the RN to facilitate patient care (bedding, VS,
turnover, snacks, water, ambulating to and from bathrooms and so on), but are
not “assigned” patients, or a patient load. They are also responsible for some
minor administrative duties as assigned to them by the leadership.
Meal and Break Relief:
Everyone in the Recovery Room works more than 7 hours/day. Because of team
nursing and resource nursing, the nursing staff gets 15 min breaks as expected
and staff takes a 30min break sometime between the 3
rd
and the 6
th
hour, or 9
th
hour if over a 10-hour day. Most days there is a “Resource Nurse,” who is a
Recovery Room RN and is of the same caliber and competency as their
colleagues. This “Resource Nurse” will be responsible for helping the team meet
their lunch and break responsibilities. It should be noted that on most days the
ebb and flow of the OR makes lunches and breaks possible. However, on those
days that this “ebb and flow” does not accommodate lunches and breaks, the
Resource RN, Charge RN and/or the Recovery Room Manager help to cover
patient load so lunches and breaks can be managed.
43
Sky Lakes Medical Center Nurse Staffing Plan
Department: Stress Lab
Approval Date: 05/22/2024
Effective Date: 06/01/2024
UNIT DETAILS
STAFFING
STANDARDS
Unit Description
The Cardiac Stress Lab is an 8 hour per day, 5
days a week (Monday-Friday) outpatient unit
for patients requiring a stress test. The
Cardiac Stress lab is comprised of a single
room with one bed, monitoring equipment,
and a treadmill.
Cardiac stress lab patients include standard
EKG treadmill stress tests, EKG treadmill with
cardiolite, nuclear stress tests, echo stress
treadmill/bike, and echo stress dobutamine
tests.
Patient Population/Diagnoses
The nurse cares for patients across the
lifespan, except pediatric patients. The top
diagnoses are cardiovascular disease and
chest pain.
Call
The cardiac stress lab does not participate in
mandatory call.
Staffing Summary
There is one full time RN scheduled in Stress Lab daily. There is one EKG tech
assigned to work with the RN.
Nurse Staffing Ratios
The RN to patient ratio is 1:1.
The cardiac stress lab is staffed by one RN and an EKG tech. When there are
patients scheduled for a stress test, an RN must be present for the test to take
place. The process for determining the ability for the Cardiac Stress Nurse to
take procedures is initiated with consideration for the current scheduled
procedures. This is determined based on the overall workload of the day with
respect to patient procedures and from the primary Stress Lab nurse’s
judgement on whether they are able to deliver safe patient care.
CNA Staffing Ratios
There are no CNA’s in stress lab.
Total Patient Care
The stress lab RN performs total patient care.
Charge Nurse
The charge nurse is the only RN working in the unit and assumes assignment of
patients in the department.
Assignments:
The cardiac stress lab nurse cares for one patient at a time and is responsible for
all patients scheduled in the stress lab during the weekdays. If a patient
becomes high acuity, the Stress lab RN may cancel and/or postpone cases.
In case of staffing issues that are problematic, the nurse has a chain of
Nationally Recognized Standards and
Guidelines
The Cardiac Stress Lab Staffing Plan will be
reviewed and approved annually by the Nurse
Staffing Committee; and then submitted to
Senior Management Team. See annual
department staffing plan review.
Standards or guidelines used to develop the
Stress Lab’s staffing plan include:
• Alliance of Cardiovascular
Professionals (ACP) Fourth Edition
44
command to follow:
Cath Lab/Stress Lab Manager-- Interventional Services Director--- Hospital
Supervisor → CNO/Admin on call.
The Cardiac Stress Lab works mostly with outpatients and a few inpatients. The
nurse is responsible for looking the patient up the day before to assess for
patient’s ability to complete the scheduled test. For inpatients, the RN calls and
gets a brief report before the patient is brought to the stress lab and then calls
the floor back to give a brief report before sending the patient back to the floor.
Meal and Break Relief:
Meal and break relief shall be approached jointly between staff and Hospital
Supervisor/Manager/Director.
There is a break in the schedule from 12-12:30 where the RN and EKG tech take
their lunch break.
The Cardiac Stress Lab recognizes 12:00-12:30 as a dedicated mealtime for staff.
The Cardiac Stress Lab Nurse will utilize time frame between procedures to
ensure breaks are achieved which, includes but is not limited to, delaying next
procedure start or rescheduling of procedure to another day.
