
Minnesota Guidelines for Medication Administration in Schools
Revised June 2015
If you require this document in another format, such as large print, Braille or cassette tape, call:
Division of Community and Family Health
P.O. Box 64882
St. Paul, MN 55164-0882
Phone: 651-215-8960
https://www.health.state.mn.us
This document was written in collaboration with:
Minnesota Board of Nursing
2829 University Ave. SE, #200
Minneapolis, MN 55414-3253
Minnesota Department of Education
1500 Highway 36 West
Roseville, MN 55113
Minnesota Department of Human Services
444 Lafayette Road North
St. Paul, MN 55155-3865
Printed on recycled paper.
TABLE OF CONTENTS
Preface ....................................................................................................................................................1
Guidelines...............................................................................................................................................3
Guideline #1: Legal Considerations .................................................................................................4
1.1 Relevant Laws .............................................................................................................................4
1.2 School District Policies ...............................................................................................................6
1.3 Data Privacy ................................................................................................................................8
1.4 Licensed Medication Prescribers .................................................................................................8
Guidelines #2: Roles .......................................................................................................................10
2.1 Responsibilities ..........................................................................................................................10
2.2 Collaboration ..............................................................................................................................10
2.3 Communication ..........................................................................................................................10
2.4 Planning ......................................................................................................................................11
2.5 Duties .........................................................................................................................................12
Guideline #3: Staffing ....................................................................................................................17
3.1 Student-Focused Staffing ..........................................................................................................17
3.2 Health Services Staffing Options ..............................................................................................17
3.3 Preparing for Emergencies ........................................................................................................18
Guideline #4: Responsibilities of Medication Administration ..........................................................20
4.1 Definition of Delegation by the Licensed School Nurse/Registered Nurse ...............................20
4.2 Definition of Assignment ..........................................................................................................21
4.3 The Responsibilities of Licensed School Nurse/Registered Nursing Delegation ......................21
4.34 The Medication Administration Decision-Making Charts .......................................................22
Guideline #5: Procedures for Medication Administration .................................................................23
5.1 Principles That Influence Medication Administration Procedures .............................................23
5.2 Step-by-Step Procedures ............................................................................................................23
5.3 The Six Rights of Medication Administration ..........................................................................25
5.4 Field Trips ..................................................................................................................................26
5.5 Before-School, After-School, and Summer-School Activities ..................................................27
Guideline #6: Education and Training ..............................................................................................29
6.1 Content and Competencies .........................................................................................................29
6.2 LSN/RN Medication Training for Delegation ...........................................................................29
6.3 Education and Training Needs ..................................................................................................30
Guideline #7: Policies and Procedures ..............................................................................................33
7.1 Health Policies as Legal Responsibilities ..................................................................................33
7.2 Characteristics of Sound Policies ..............................................................................................33
7.3 Contents of Policy and Procedures ............................................................................................33
7.4 Requests to Administer Medications in Schools .......................................................................34
7.5 Medication Types ......................................................................................................................35
7.6 Self-Carrying and Self-Administration of Prescription Medication ..........................................35
7.7 Self-Carrying and Self-Administration of Non-Prescription Medication .................................37
7.8 Handling, Storage, and Disposal of Medications ......................................................................38
7.9 Planning and Standardized Forms .............................................................................................39
7.10 Record Keeping .......................................................................................................................39
7.11 Procedures for Emergency Medications in Schools ................................................................40
7.12 Investigational Drugs ...............................................................................................................41
7.13 Complementary and Alternative Medicines (CAMs) ..............................................................41
Guideline #8: Quality, Assurance, Monitoring, and Assessment ......................................................43
8.1 Definitions ..................................................................................................................................43
8.2 Procedures to Follow in Case of Medication Errors ...................................................................43
8.3 Refusal to Take Medication .......................................................................................................44
8.4 Reducing Errors and Omissions .................................................................................................44
8.5 A High Quality School Health Program .....................................................................................44
Guideline #9: School and Family Relationships ............................................................................45
9.1 Communication and Collaboration ...........................................................................................45
9.2 Documentation ..........................................................................................................................45
Guideline #10: Finances ..................................................................................................................47
10.1 Funding Sources ......................................................................................................................47
REFERENCES .....................................................................................................................................48
APPENDICES ......................................................................................................................................50
Appendix A: LSN/RN Delegation ....................................................................................................51
Appendix B: LPN Assignment .........................................................................................................53
Appendix C: Frequently Asked Questions .......................................................................................54
Appendix D: State of Minnesota Office of the Attorney General Letter..........................................61
Appendix E: Information about the 2005 Guidelines Development ................................................65

Minnesota Guidelines for Medication Administration in Schools
1
Revised June 2015
PREFACE
The comprehensive process for creating this guideline involved a broad search and
rigorous evaluation of pertinent literature, including numerous states’ standards and
guidelines, and analysis of key concepts.
As the number of Minnesota students taking medication during the school day grows, it becomes
increasingly important to address this issue thoroughly to help students maintain an optimal state of
health enhancing their education. The issue has become more complex due to factors, such as federal
and state laws that protect children who require medications to fully benefit from free and
appropriate public education, new pharmaceutical and medical technologies, evolving mental and
medical health practices, and changes in school nurse staffing patterns.
The goal of the Minnesota Guidelines for Medication Administration in Schools (Minnesota Guide-
lines) is to increase the safe and efficacious administration of medications to students in schools by
providing crucial information. As the Centers for Disease Control note (Wheeler, 2004, p. 1), the
benefits of meeting the needs of students with chronic health conditions include “better attendance,
improved alertness and physical stamina, fewer symptoms, fewer restrictions on participation in
physical activities and special activities, such as field trips, and fewer medical emergencies.”
According to the American Academy of Pediatrics, American Public Health Association, and
National Resource Center for Health and Safety in Child Care (2002), a guideline is “a statement of
advice or instruction pertaining to practice…it originates in an organization with acknowledged
professional standing…a guideline is developed in response to a stated request or perceived need for
such advice or instruction.” The Minnesota Guidelines define student-centered goals of medication
administration that are evidence-supported and draw from best practice throughout the nation,
including those recognized by the National Association of School Nurses and the National Council
of State Boards of Nursing, and in accordance with federal and state laws. The Minnesota Guidelines
address both student-specific needs and the school health system.
The study originally requested by the Minnesota Legislature (Minnesota Department of Health,
2002) led to a collaborative process and publication of the guidelines by four state
agencies−Minnesota Department of Health, Minnesota Board of Nursing, Minnesota Department of
Education, and Minnesota Department of Human Services. In addition, a statewide multidisciplinary
work group was established and met regularly to provide direction to and discuss the details of this
project. The Minnesota Guidelines offer advice on what ultimately needs to be in place for students
to be safe in Minnesota schools.
Members of the four state agencies and the state-wide work group brought multiple perspectives to
their invaluable contributions to the guidelines’ development and review processes. Thus the final
document does not represent a consensus, but reflects diverse input from a large number of
individuals in a variety of agencies and organizations.

Minnesota Guidelines for Medication Administration in Schools
2
Revised June 2015
The 2015 guidelines are based upon the 2005 guidelines developed and serve as a continual update
to the Minnesota Legislature on the study recommendations discussed in the Report to the Minnesota
Legislature: Medications dispensed in schools study completed by the Minnesota Department of
Health. Key intended users are health and education organizations across the state that are
developing and updating medication administration policies and procedures.
Special thanks for the 2015 revision go to the Minnesota Department of Health: Kathy Wick and
Cheryl Smoot; the Minnesota Department of Education: Ruth Ellen Luehr; the Minnesota Board of
Nursing: Mariclaire England; and the School Nurse Organization of Minnesota: Cynthia Hiltz and
Mary Heiman.
Minnesota Guidelines for Medication Administration in Schools
3
Revised June 2015
GUIDELINES
Medication administration in schools is a complex issue in part because it intersects health
laws and education laws.
The extensive literature review and discussion processes revealed 10 thematic categories which were
subsequently used to organize the Minnesota Guidelines for Medication Administration Guidelines:
1. Legal Considerations
2. Roles
3. Staffing
4. Responsibilities of Medication Administration by the Licensed School Nurse/Registered
Nurse
5. General Procedures for Medication Administration
6. Education and Training
7. Policies and Procedures
8. Quality Assurance, Monitoring, and Assessment
9. School and Family Relationships
10. Finances
The Minnesota Guidelines provide systems development guidance to manage safe medication
administration including logistics of medication administration request from parents and care givers,
staff training in medication administration, documentation and storage and communication with the
family and health care provider. Both the system and the individual levels are interwoven in the 10
sections of the Minnesota Guidelines.

Minnesota Guidelines for Medication Administration in Schools
4
Revised June 2015
GUIDELINE #1: LEGAL CONSIDERATIONS
1.1 Relevant Laws
The legal basis for the Minnesota Guidelines for Medication Administration in Schools is a set of
federal and state laws.
Medication administration in schools is a complex issue in part because it intersects health laws and
education laws. The laws give guidance and set a foundation for the process that local school
districts use to develop, staff, and maintain a safe system for medication administration.
Federal Laws
Federal laws emphasize (1) the rights of students with special needs, medical or otherwise, to have
access to and to be educated in public schools, and (2) the sensitive topic of records, including
family access to education and health records in schools.
• Americans with Disabilities Act as amended (ADA) (42 U.S.C. § 12101 et seq.) and
regulations promulgated by the Department of Justice
• Drug and Alcohol Treatment Records (D&A) (42 USCS § 290dd, 42 CFR 2.1 et seq.)
• Family Educational Right to Privacy Act (FERPA) (20 U.S.C. § 1232g; 34 C.F.R. Part
99)
• Health Insurance Portability and Accountability Act (HIPAA), and regulations adopted
under it (45 C.F.R. chapters 160 and 164)
• IDEA is the Individuals with Disabilities Education Improvement Act (IDEIA), (Public
Law 108-446) previously IDEA
• Individuals with Disabilities Education Act (IDEA) (20 U.S.C. § 1400 et seq.)
• OSHA Blood-borne Pathogen Standard 29 of C.F.R. 1930.1030
• Proposed New Drug, Antibiotic, and Bio- logical Drug Product Regulations (21 C.F.R.
312.3 (b))
• Section 504 of the Rehabilitation Act of 1973 (29 U.S.C. § 794)
• Prohibition of Mandatory Medication (Child Medication Safety Act 34 CFR 300.174 (20
U.S.C.: 1412 (a)(25))

Minnesota Guidelines for Medication Administration in Schools
5
Revised June 2015
State Laws
State laws pertain to school systems, health care practice, records, and individual rights. In
particular, they focus on access to education and data; the provision of school health services; the
establishment of local school district medication policies; the rights of students; regulation of health
care providers, such as nurses, physicians, and pharma- cists; access to care by students; emergency
care; and protection of children.
• Administration of Drugs and Medicine (Minnesota Statutes §§ Chapters 121A.22,
121A.221, 121A.2205, 121A.2207, and 121A.222)
• Children with a Disability (Minnesota Administrative Rules, Chapter 3525)
• Children with a Disability (Minnesota Statutes § Chapter 125A)
• Emergency Treatment of Minors Act (Minnesota Statutes § Chapter144.344)
• Hazardous Substances, Employee Right-to- Know (Minnesota Administrative Rules,
Chapter 5206)
• Health Care Bill of Rights (Minnesota Statute § Chapter 144.651)
• Health Standards; immunizations; school children (Minnesota Statute § Chapter 121A.15,
Subd. 7.) File on Immunization Records
• Health Records; Children of School Age (Minnesota Statute § Chapter 144.29
• Minnesota Statutes § Chapter 120A.22, Subd. 7. (Compulsory Instruction, Education
Records.)
• Minnesota Statute. § Chapter151.37 Subd. 7 (Legend Drugs, Who May Prescribe,
Possess
• Minnesota Board of Teaching Personnel Licensing (Minnesota Administrative Rules,
Chapter 8710.6100, School Nurse)
• Minnesota Children’s Mental Health Act (Minnesota Statute § Chapter 245.4876, Subd.
5)
• Minnesota Medical Practice Act (Minnesota Statutes, § Chapter 147)

Minnesota Guidelines for Medication Administration in Schools
6
Revised June 2015
• Minnesota Mental Health Act (MMHA) Quality of Services (Minnesota Statutes §
Chapter 245.467)
• Minnesota Nurse Practice Act (Minnesota Statutes §§ Chapters148.171 to 148.285) and
Minnesota Administrative Rules, Chapters 6301 through 6321
• Minnesota Pharmacy Act (Minnesota Statutes § Chapter 151 and Minnesota
Administrative Rules Chapter 6800)
• Minnesota Government Data Practices Act (Minnesota Statutes § Chapter 13; § 13.32,
Subd. 2, 3)
• Records upon school district transfer. (Minnesota Statute § Chapter 123B.08, Sub 3)
• School Health Services (Minnesota Statutes § Chapter 121A.21)
•
Therapeutic Research Act; Medical Cannabis (Minnesota Statutes §§ Chapters 152.21 to
152.37)
• Vulnerable Adult Act (Minnesota Statutes §§ Chapters 626.557 to 626.5573), and
Maltreatment of Minors Act (Minnesota Statutes §§ Chapters 626.556 to 626.5563)
1.2 School District Policies
Within the framework of existing federal and state laws and these Minnesota Guidelines for
Medication Administration in Schools, school districts’ medication administration policies should
reflect recommended practice and be developed in collaboration with the licensed school
nurse/registered nurse (LSN/RN), licensed health care provider, physician, and others, as listed in
Minnesota Guideline 7.2.
Local policies and procedures can be individualized based on the evaluation of the student
population (e.g., individualized student health needs, speakers of English as second language
learners, free and reduced lunch price meal numbers, and student mobility) and based on school
district personnel and resources.
The various pertinent laws and the Minnesota Guidelines offer a foundation upon which to develop
and maintain individual local district policies.
The role of the school board is outlined in Minnesota Statutes §§ Chapters121A.22, Subd. 4: and
121A.2207.

Minnesota Guidelines for Medication Administration in Schools
7
Revised June 2015
Drugs and medicine subject to this section must be administered in a manner consistent with
instructions on the label. Drugs and medicine subject to this section must be administered, to the
extent possible, according to school board procedures that must be developed in consultation:
(1)
with a school nurse, in a district that employs a school nurse;
(2)
with a licensed school nurse, in a district that employs a licensed school nurse;
(3)
with a public or private health or health-related organization, in a district that contracts
with a public or private health or health-related organization, according to Minnesota
Statutes § Chapter 121A.21; or
(4)
with the appropriate party, in a district that has an arrangement approved by the
commissioner of education, according to Minnesota Statutes § Chapter 121A.21.
The authors of this document would like to acknowledge that the ideal system for health and safety
in Minnesota schools is to have a Licensed School Nurse (LSN) manage the health services program
that includes aiding school administration in developing the system for medication administration
and directing specific procedures. An LSN with a bachelor’s degree in nursing and a certificate in
public health is an expert in nursing assessments and plans based on knowledge of the student,
school, home, and community (see National Association of School Nurses, 2011 and the American
Academy of Pediatrics 2009). Using the nursing process, school nurses develop individual health
plans for students. Delegation of nursing tasks can be a safe and effective way to perform some of
the nursing interventions identified in the individual health plan (see National Association of
Schools Nurses, 2004/2014).
In school districts without Licensed School Nurses/Registered Nurses (LSNs/RNs) on staff,
educational administrators working with school boards are responsible to set up a system through
which:
• medication administration policies are developed,
• acceptable LSN/RN/ licensed health care provider coverage for medication
administration oversight via contract or other arrangements is found,
• people are assigned and trained,
• the procedures are done safely and consistently, and
• all necessary documentation is completed.
Educational administrators are also responsible to find appropriate resources and medical expertise
to address their students’ medication administration needs. School administrators cannot legally
fulfill the role of LSNs/RNs. Training for medication administration is beyond the role of education
administrators.

Minnesota Guidelines for Medication Administration in Schools
8
Revised June 2015
Districts with LSNs/RNs on staff or on contract will be able to take the lead on developing school
district policies and procedures which include medication program: supervision, delegation,
assignment, administration, documentation, etc.
Those districts with LSNs/RNs on staff or on contract will be able to call on staff to take the lead on
these responsibilities.
1.3 Data Privacy
State and federal requirements ensure privacy of student education, health, and medication records,
and restrict the sharing of that information. These laws specify how information about medication is
handled, including procedures for health records and the documentation of health information, ad-
ministration of medication, and medication errors. The state laws influencing data privacy are the
Minnesota Government Data Practices Act, the Minnesota Medical Practice Act, the Minnesota
Medical Records Act, and the Minnesota Mental Health Act, and on the federal level, Drug and
Alcohol Treatment Records, FERPA, HIPAA, and IDEA.
Once a parent/legal guardian disclose health information to the school, it becomes private
educational data (but still health information); it is the school district’s responsibility to protect the
data, make sure that school employees who need the health information have it, and guarantee that
staff are trained in and follow appropriate data privacy practices.
School personnel should be cautious about easily overheard verbal communications as well as
visible and easily obtained written/electronic documents. There need to be password protections for
personal/private student health information stored on computers or when accessed and used
remotely. Student information given to school health services should only be disclosed to other third
parties with a “legitimate educational interest.”
Educators should have access to health information on a “need to know” basis for “legitimate
educational interests” as defined in FERPA (see 34 C.F.R. § 99.31 and Health in Schools, 2003).
Schools should rely on the privacy requirements of FERPA to meet the need to protect student
privacy and the need to provide school staff with relevant information about students (e.g., when
students have medical conditions that affect their learning and safety, such as students who have
hearing or vision problems, are subject to seizures, or have asthma or allergies). For school staff to
remain current on this topic and use student data appropriately, training must be provided, per
FERPA, HIPAA, and IDEA on a regular/recurring basis. Parent/legal guardians should be
knowledgeable of who has their child’s private health information.
1.4 Licensed Medication Prescribers
All states, including Minnesota, have professional practice laws that govern who are authorized to
prescribe medications.

Minnesota Guidelines for Medication Administration in Schools
9
Revised June 2015
Who is a licensed authorized prescribing practitioner in Minnesota?
• Physician
• Advanced practice registered nurse (APRN) with prescriptive authority (includes clinical
nurse specialist practice, nurse-midwife practice, nurse practitioner practice, or registered
nurse anesthetist practice)
• Physician’s assistant (PA) who has direction from a physician or written protocol
• Dentist
• Podiatrist
• Osteopath
• Psychiatrist
Who is not a licensed authorized prescribing practitioner in Minnesota?
• Licensed school nurse (LSN)
• Registered nurse (RN)
• Licensed practical nurse (LPN)
• Medical assistant
• Nutritionist
• Psychologist
• Naturopathic provider
• Chiropractor
Under Minnesota Law LSNs/RNs, LPNs (Minnesota Statutes §Chapter 148.235) and Registered
Dieticians (Minnesota Statutes § Chapter148.634) may implement condition-specific protocols
consistent with their scope of practice. Naturopaths may order non-prescription drugs and non-
invasive diagnostic therapeutic procedures (Minnesota Statutes § Chapter 147E.05).
In addition, laws address who can delegate medication administration. Licensed School
Nurse/Registered Nurse delegation allows flexible planning to meet individual student needs and
best utilize staff available in the schools. Delegation of medication administration by LSNs/RNs is
allowed in Minnesota schools. For schools, this is a balance between safety standards and
reasonableness, given limited resources in schools, rights and needs of students and parents/legal
guardians, and the assumption that students constitute a healthy population. Whether or not an
LSN/RN is on school staff or contracted by the school, Minnesota law requires that school boards
are responsible for policy and procedure development leading to safe medication management, but
not without consultation from a from a professional that is knowledgeable about medication
administration. (Minnesota Statute § Chapter 121A.22 Subd 4.).
Minnesota Guidelines for Medication Administration in Schools
10
Revised June 2015
GUIDELINES #2: ROLES
Guidelines should include safe, coordinated practices (as age and skill level appropriate) that
enable the student to successfully manage his or her health in the classroom and at all school-
related activities.
2.1 Responsibilities
Accountability and responsibility for linking systems of student health needs and educational success
is shared among LSNs/RNs, licensed prescribers, pharmacists, the school board and administrators,
unlicensed assistive personnel (UAPs), school staff, parents, and students. The contribution of
persons in each of these roles is important to student success and the safe administration of
medication within the framework of district policies. No employee may be coerced into
compromising student safety by being required to delegate, assign, or administer medication if that
person determines that it is inappropriate to do so.
2.2 Collaboration
Each person shares and depends upon the responsibility of others to contribute to maintaining a safe
system of medication administration. Examples include:
• a student who wears a medical alert bracelet and carries emergency medication per school
district policies,
• a person administering medication who in a timely manner reported any irregularities to the
LSN/RN, and
• a parent/legal guardian who keeps track of medication expiration dates and sends
replacements to school without being reminded.
This involvement sets a community norm with shared expectations and knowledge.
Education personnel and parents/legal guardians have varying levels of understanding and ability to
comply with school district health policies. Factors could include socioeconomic, physical, or
psychosocial status, and cultural understanding and practices (e.g., the school might need a translator
for verbal and written information related to medication administration). School administration will
need to work with staff members and families to ensure understanding and compliance with policy.
2.3 Communication
The school administration should establish procedures and tools for communication among persons
in various roles (e.g., parents’/legal guardian’ and school staff members’ need for interpreters and
translated materials).

Minnesota Guidelines for Medication Administration in Schools
11
Revised June 2015
Three channels of communication—among staff members, with students and their families, and with
the community—clarify expectations, provide education, and facilitate discussion related to student
medication administration issues.
Encompassed in communication of policy and procedures are a handbook, health advisory
committee, newsletter, web site, posters, and job descriptions. Translators, translated materials, and
advocates should be made available when needed. With ongoing open communication between the
parent/legal guardian and LSN/RN, changes in medication can be quickly communicated by the
parent/legal guardian to the LSN/RN, and the parent/legal guardian can receive student medication
updates from the LSN/RN in a timely manner. The LSN/RN can also, with parent/legal guardian
permission, contract the student’s licensed health care provider to ensure continuity of care and
changing medications over time. This is especially critical for students with chronic health problems
and/or special needs.
All communications need to be tailored to the diverse populations served in the school district and
done in a manner consistent with data privacy regulations in IDEA, FERPA, HIPAA, IDEA, the
Minnesota Government Data Practices Act (Chapter 13), and MMHA.
2.4 Planning
In response to requests from parents/legal guardians and students for medication administration in
school, the LSN/RN will assess and create with the family and students a means for safe
administration of medication, utilizing district policy and procedures. The LSN/RN provides a
comprehensive assessment when developing a more formal plan based upon individual student
health needs (e.g., an individualized health care plan(IHP)* and/or emergency care plan(ECP)**)
and participate as appropriate in an Individualized Education Program plan (IEP)*** and/or 504
plan****.
*The Individual Health Plan (IHP) is a written document detailing the required special health services for
general and special education students. The IHP documents health needs that affect a student’s daily
function and impact education or the educational environment, and includes medications.
**The Emergency Care Plan (ECP)is a plan initiated by the LSN/RN that outlines (clearly and completely) in
concise steps how to respond to a student who is experiencing a potentially critical situation; “If you see
this…do this.” The ECP is developed for those students with emergency medications.
***Individualized Education Program, an IEP is the legal document that defines a child's special education
program. An IEP includes the disability category under which the child qualifies for Special Education Services
(developed, reviewed and revised in a meeting), the services the team has determined the school will
provide, the child’s yearly goals and objectives (special education and related services) and any
accommodations that must be made to assist his/her academic achievement and functional performance.
****504 plan refers to Section 504 of the Rehabilitation Act and the Americans with Disabilities Act, which
specifies that no one with a disability can be excluded from participating in federally funded programs or

Minnesota Guidelines for Medication Administration in Schools
12
Revised June 2015
activities, including elementary, secondary or postsecondary schooling. "Disability" in this context refers to a
"physical or mental impairment which substantially limits one or more major life activities." This can include
physical impairments; illnesses or injuries; communicable diseases; chronic conditions like asthma, allergies
and diabetes; and learning problems.
In addition, it is important that community resources be utilized to support a system of safe
medication administration. A health advisory committee can help achieve this goal; see further
discussion in Minnesota Guideline 2.5.
2.5 Duties
School boards are responsible for policy and procedures leading to safe medication management.
School board members, school administrators, parents, students, LSNs/RNs, licensed practical
nurses (LPNs), paraprofessionals, unlicensed assistive personnel (UAPs), and teachers are expected
to comply with school district medication policy regarding prescription, over-the-counter (OTC),
complementary and alternative medicines (CAMs), and/or emergency medicines.
According to Minnesota Statutes § Chapter 121A.22, Subd. 4; the school board is to develop
procedures for their school district. Ways in which the school board ensures the procedures are
carried out include: periodically reviewing aggregate data on the health of district students (e.g.,
analysis of the number of students taking medications, changes over time, and medication
administration procedures that need changing); allocating funding from the district budget for health-
related resources (personnel, materials, space, etc.); being accountable for enforcement of the
medication administration policy; reviewing medication policy annually and updating it as
necessary; ensuring school staff training that includes administration of medication; planning for
improved access to specialty support, which is especially important for school districts without full-
time LSNs/RNs on staff; and setting up an agreement for school health consultation with an
individual physician, an LSN/RN, local community clinic, hospital, or public health agency.
To ensure optimal student safety regarding medication administration, the school district needs to
have an LSN/RN to administer the health services of the district. Whether the school district has its
own school nurse staff, a nurse hired under contract, or no school nurse, the law (Minnesota Statutes
§ Chapter 121A.21) states that schools need to develop and use district policy in conjunction with a
knowledgeable LSN/RN or public/private health providers or health related organizations.
Under Minnesota Statutes § Chapter 121A.2205 under Subd. 2. Plan for use of epinephrine auto-
injectors. (f) The school board of the school district must define instructional day.
In addition, according to Minnesota Statutes § Chapter 121A.2207 notwithstanding pharmacy
Minnesota Statute § Chapter 151.37, districts and schools may obtain and possess epinephrine auto-
injectors to be maintained and administered by school personnel to a student or other individual if, in

Minnesota Guidelines for Medication Administration in Schools
13
Revised June 2015
good faith, it is determined that person is experiencing anaphylaxis regardless of whether the student
or other individual has a prescription for an epinephrine auto-injector.
School administrators are accountable for implementing the medication administration policy;
guiding the planning, gathering, and periodic board review of aggregate student health information,
in conjunction with the LSN/RN; providing the needed staff, financial, and material resources for
safe medication administration; drawing on the advice of other medication experts in the com-
munity when making decisions; assist the LSN/RN in arranging for staff development; and studying
demonstration projects on medication administration for information to enrich local policies and
procedures.
The Emergency Treatment for Minors Act (Minnesota Statutes § Chapter 144.344) allows schools to
make emergency decisions about sensitive health issues and concerns and physicians to provide
immediate care while parents/legal guardians are being contacted.
A health advisory committee can provide input to school policy and procedures. It should reflect a
balance of the internal school community and external community at-large––such as LSNs/RNs,
paraprofessionals, unlicensed assistive personnel (UAP), teachers, parents/legal guardians, school
board members, public health agency representatives, licensed prescribers, pharmacists, and non-
public school members––who counsel the school board and school administration.
The role of parents/legal guardians, along with their children, is to follow and support the school
district policy and procedures regarding medication administration; provide representation on the
health advisory committee and advocate for safe administration of medication; and communicate
with the school about their children’s medication needs in schools. Communication might focus on
getting medications to school; participating in development and use of an IHP or other plan; signing
the parent/legal guardian authorization form; obtaining a licensed prescriber’s order for medications;
transferring medication self- carrying requests; and discussing student self-administration of
medications, refusal, or non-compliance with medication administration.
The roles of students vary, depending on their age and developmental stage. Students at every age
are learning about their health conditions and the role that medications have in managing or curing
the problems. In the early years, the emphasis might be on students as recipients of medication, but
even at young ages, students can take increasing responsibility for their medications. As students
develop, it is important for them to learn to make decisions regarding their medication
administration and skills in self-administration.
The students’ responsibilities are to be knowledgeable about their medications, take their
medications correctly, and communicate any medication issues or concerns to parents/legal
guardians, LSNs/RNs, LPNs, teachers, paraprofessionals, or UAPs, as appropriate. For example,
younger students with diabetes using insulin will know about their medications but might need

Minnesota Guidelines for Medication Administration in Schools
14
Revised June 2015
assistance administering sliding-scale insulin amounts, carbohydrate counting, and glucose
monitoring; older students are likely to be able to do these activities themselves. One option is a
written self-administration contract agreed to by the school, licensed prescriber, LSN/RN,
parent/legal guardian, and individual student.
As employees who bring extensive knowledge of health services, medical systems, and best
practices to the school setting, the LSNs or RNs take the lead in policy and procedure development
for the district and assess the health needs of students, including those taking medications
(prescription, over-the-counter (OTC), complementary alternative medications (CAMs), and/or
emergency medications) as necessary. The practice of each nurse (salaried, contracted, or volunteer)
is regulated by Minnesota Statutes §§ Chapter 148.171-148.285 and Minnesota Administrative
Rules, Chapter 6301 through 6321, commonly referred to as the Minnesota Nurse Practice Act.
Practice of Professional Nursing for LSN/RN
(Taken from the Minnesota Nurse Practice Act)
The "practice of professional nursing" means the performance, with or without compensation, of
those services that incorporates caring for all patients in all settings through nursing standards
recognized by the board and includes, but is not limited to:
(1)
providing a comprehensive assessment of the health status of a patient through the
collection, analysis, and synthesis of data used to establish a health status baseline and
plan of care, and address changes in a patient's condition;
(2)
collaborating with the health care team to develop and coordinate an integrated plan of
care;
(3)
developing nursing interventions to be integrated with the plan of care;
(4)
implementing nursing care through the execution of independent nursing interventions;
(5)
implementing interventions that are delegated, ordered, or prescribed by a licensed health
care provider;
(6)
delegating nursing tasks or assigning nursing activities to implement the plan of care;
(7)
providing safe and effective nursing care;
(8)
promoting a safe and therapeutic environment;
(9)
advocating for the best interests of individual patients;
(10)
evaluating responses to interventions and the effectiveness of the plan of care;
(11)
collaborating and coordinating with other health care professionals in the management
and implementation of care within and across care settings and communities;
(12)
providing health promotion, disease prevention, care coordination, and case finding;
(13)
designing and implementing teaching plans based on patient need, and evaluating their
effectiveness;
(14)
participating in the development of health care policies, procedures, and systems;
(15)
managing, supervising, and evaluating the practice of nursing;
(16)
teaching the theory and practice of nursing; and

Minnesota Guidelines for Medication Administration in Schools
15
Revised June 2015
(17)
accountability for the quality of care delivered, recognizing the limits of knowledge and
experience; addressing situations beyond the nurse's competency; and performing to the
level of education, knowledge, and skill ordinarily expected of an individual who has
completed an approved professional nursing education program as described in
Minnesota Statute § Chapter 148.211, Subd. 1.
To oversee and keep medications secure, the LSN/ RN sets up the school’s medication system,
recommends the purchase of supplies, sets up a double- lock storage system, decides where keys are
kept, refrigerates medication as needed, and purchases medication resource documents, such as the
drug formulary and training materials. The LSN/RN sets up, maintains, and secures private
medication and health records, which include medication documentation, medication counts,
authorizations, and prescription orders.
The LSN/RN has input into choosing current staff members for delegation of medication
administration and hiring of new health services staff. The LSN/RN trains and supervises staff
members to whom the LSN/RN is delegating medication ad- ministration, communicates the
delegation plan to delegatees, assesses their competencies, and provides sufficient oversight and
supervision.
The LSN/RN also assesses the medication needs of the aggregate student population. In this way,
the LSN/RN can see patterns of population-based health problems that call for further investigation
or reporting.
Practice of Nursing for Licensed Practical Nurse (LPN) taken from the Minnesota Nurse
Practice Act
The "practice of practical nursing" means the performance, with or without compensation, of those
services that incorporates caring for individual patients in all settings through nursing standards
recognized by the board at the direction of a registered nurse, advanced practice registered nurse, or
other licensed health care provider and includes, but is not limited to:
(1)
conducting a focused assessment of the health status of an individual patient through the
collection and comparison of data to normal findings and the individual patient's current
health status, and reporting changes and responses to interventions in an ongoing manner
to a registered nurse or the appropriate licensed health care provider for delegated or
assigned tasks or activities;
(2)
participating with other health care providers in the development and modification of a
plan of care;
(3)
determining and implementing appropriate interventions within a nursing plan of care or
when delegated or assigned by a registered nurse;
(4)
implementing interventions that are delegated, ordered, or prescribed by a licensed health
care provider;
(5)
assigning nursing activities or tasks to other licensed practical nurses (LPNs);

Minnesota Guidelines for Medication Administration in Schools
16
Revised June 2015
(6)
assigning and monitoring nursing tasks or activities to unlicensed assistive personnel;
(7)
providing safe and effective nursing care delivery;
(8)
promoting a safe and therapeutic environment;
(9)
advocating for the best interests of individual patients;
(10)
assisting in the evaluation of responses to interventions;
(11)
collaborating and communicating with other health care providers;
(12)
providing health care information to individual patients;
(13)
providing input into the development of policies and procedures; and
(14)
accountability for the quality of care delivered, recognizing the limits of knowledge and
experience; addressing situations beyond the nurse's competency; and performing to the
level of education, knowledge, and skill ordinarily expected of an individual who has
completed an approved practical nursing education program described in Minnesota
Statute § Chapter 148.211, Subd. 1.
LPNs can administer medications to students under the delegation of a physician or LSNs/RNs. An
LPN is able to monitors students’ responses to medication administration. LPNs are expected to
communicate significant information to physicians/prescribers, LSNs/RNs, and parents/legal
guardians regarding students’ health. Responsibility for delegation to other nursing personnel and
supervision of the nursing personnel is within the scope of practice of LSNs/RNs. If a physician
licensed health care prescriber or LSN/RN delegates medication administration to a UAP, it is within
the scope of an LPN to assign nursing tasks or medication activities and monitor that individual’s
performance of these activities.
Unlicensed Assistive Personnel (UAP)
Anyone designated, willing, and trained can serve as a UAP in schools (e.g., a health assistant,
teacher, school administrator, or student services staff member); they are “unlicensed” in terms of
providing health services. Under the delegation and supervision of an LSN/RN, UAPs can perform
medication administration based on school district policy and procedures. Anyone designated,
willing, and trained can serve as a UAP in schools (e.g., a health assistant, educational assistant,
teacher, school administrator, or student services staff member); they are “unlicensed” in terms of
providing health services. In order to perform medication administration functions, the UAP needs to
have appropriate training to perform these functions, written documentation, and annual evaluation
of this individual’s competency; knowledge of policy and procedure; and be willing to communicate
to the LSN/RN/LPN his or her own ability to perform medication administration, document
medications administered, and report to the LSN/RN/LPN any inconsistencies or deviations from
expected procedures. If uncomfortable with performing medication administration, a staff member
has the right and responsibility to ask for education and additional supervision about medication
administration.
Minnesota Guidelines for Medication Administration in Schools
17
Revised June 2015
GUIDELINE #3: STAFFING
Clarify the roles and obligations of specific school staff, and provide education and
communication systems necessary to ensure that students’ health and educational needs are met
in a safe and coordinated manner.
3.1 Student-Focused Staffing
The number of health personnel needs to be in proportion to student numbers and the breadth and
severity of health issues. The overall needs of the total population of students should drive the health
program, rather than current staffing, existing funding, or available supervision for medication
administration.
Health services staffing should enable students to successfully manage their medication needs in the
classroom and at all school-related activities. If a student is moving towards self-administration, the
LSN/RN needs to be available to assist the student through health assessment and planning; teach
about medication administration; and supervise changes for medication administration.
3.2 Health Services Staffing Options
Healthy People 2010 (U.S. Department of Health and Human Services, 2000) recommends a school
nurse: student ratio of 1:750. In schools with a significant number of special needs students, the ratio
should be adjusted accordingly. (Minnesota Statutes § Chapter121A for Minnesota requirements)
The National Association of School Nurses has recently published a position document looking at
workload as the driving force behind staffing models. In their position they indicate school nurse
workloads should be determined annually, using student and community specific health data.”
Although the involvement of an LSN/RN in each school’s provision of health services to students is
crucial and a legal requirement, resources are uneven throughout the state, so alternative staffing
options can secure participation of an LSN/ RN. These options include sharing an LSN/RN or
substitute with another school district or hiring health services staff or contract staff through a local
community’s best available resources, such as an education cooperative, public health agency,
hospital, clinic, or home-care agency.
Whether or not an LSN/RN is physically at the school during all school hours, nursing coverage and
availability needs to must be arranged for student safety. Therefore, when medication administration
is delegated, the delegatee must be able to communicate during that time with an LSN/RN or other
health professional with medication administration knowledge and expertise.

Minnesota Guidelines for Medication Administration in Schools
18
Revised June 2015
Each school district should consider having a part-time medical advisor working with its health
services program. The physician or provider could review policies, develop model policies, and
provide individual medical consultation.
3.3 Preparing for Emergencies
When developing school health staff positions, keep in mind that emergencies will inevitably take
place and sometimes involve medication administration. Three types of emergencies can arise:
• those involving individual students receiving medications;
• unknown individual student of staff emergencies (e.g., respiratory events, heart attacks,
anaphylactic reactions, etc.); and
• system-wide emergencies (e.g., violence, threat, or natural disaster).
School staff should be trained and available to ad minister first aid and CPR/AED any time
students/other individuals are in school. It is also important that for times when an LSN/RN is not
available during health emergencies, each school has a plan in place that delineates the roles and
responsibilities of staff members, including communication channels. School policy and procedures
need to include guidelines for intervention in an emergency or crisis and for debriefing following it.
Schools request emergency information from parents/legal guardians each school year. This
information may necessitate the development of emergency care plans (ECPs) or individualized
health plans (IHPs) to ensure student safety. These plans are best developed as soon as the
information is collected/received.
The Emergency Information Form for Children With Special Health Care Needs (EIF) is a tool to
transfer critical information to physicians, parents, emergency medical service (EMS) professionals,
and nurses when dealing with a student’s acute illness or injury (American Academy of Pediatrics,
1999, and American College of Emergency Physicians, 1998). The EIF, also called a safety plan,
concisely summarizes the child’s complicated medical history and makes it available when the
child’s parents and pediatrician are not immediately available.
If parents/legal guardians are don’t provide emergency information and or emergency medications, it
is important that the district have a procedure for communication and follow-up with the parent/legal
guardian. The procedure should document the number of times and type of attempts completed to
obtain information and medication, plus all and any parent/legal guardian response. This
documentation by the district and its staff (LSN/RN) validates due diligence in getting the
appropriate emergency medication and the development of an appropriate emergency plan for this
student. If all efforts are unsuccessful considerations should be given to involving school legal
counsel and or protective services.

Minnesota Guidelines for Medication Administration in Schools
19
Revised June 2015
Access to emergency medications is a high priority. Emergencies may include conditions such as:
anaphylaxis, hypoglycemia, hyperglycemia, seizures, and asthma episodes.
Immediate access to emergency medications is a high priority and is crucial to the effectiveness of
any life-saving interventions. To maintain medication security and safety and provide for timely
medication access and treatment, local procedures must specify where emergency medications are
stored, who is responsible for the emergency medication, who regularly reviews and replaces
outdated emergency medication, and who is responsible for the emergency medication on field trips.

Minnesota Guidelines for Medication Administration in Schools
20
Revised June 2015
GUIDELINE #4: RESPONSIBILITIES OF MEDICATION ADMINISTRATION
4.1 Definition of Delegation by the Licensed School Nurse/Registered Nurse
This section is specific to schools with RNs on staff or contract.
According to the Minnesota Board of Nursing, delegation is the:
“transfer of authority to another nurse or competent, unlicensed assistive person to
perform a specific nursing task or activity in a specific situation.”
According to the Nurse Practice Law according to Minnesota Statute § Chapter148.171, Subd. 7,
delegation is important to:
“provide safe and effective nursing care.”
The dictionary meanings of delegation––direction and prescription––each contain the same
elements:
• a giver,
• a recipient, and
• a degree of authority.
The concept of delegation includes authoritative instruction and the acts of empowering one person
to act for another. The nurse retains accountability for the delegation. Accountability is part of the
scope of practice of the Minnesota Register Nurse and the Minnesota Licensed Practical Nurse. The
nurse is accountable for the quality of care delivered, recognize the limits of knowledge and
experience, addresses situations beyond their own competency, and perform to the level of
education, knowledge, and skill ordinarily expected of an individual who has completed their level
of approved nursing educational program as described in Minnesota Statutes § Chapter
148.221.Subd.1. Accountability (according to ANA 2005) is the state of being responsible or
answerable.
The Nurse Practice Act (Minnesota Statutes § Chapter sections 148.171 to 148.285 and Minnesota
Rules, chapters 6301 to 633021) says that both professional (LSN/RN) and practical nursing (LPN)
include, but are not limited to the performance of acts or functions that are delegated to the nurse by
another health care professional. However, only the LSN/ RN has the direct statutory authority to
delegate to others (see also National Association of School Nurses, 1994/2002), and the UAP may
carry out only those nursing acts or functions that have been delegated by an LSN/RN or assigned by
the LSN/RN/LPN.
Minnesota Guidelines for Medication Administration in Schools
21
Revised June 2015
4.2 Definition of Assignment
This section discusses assignment related to the roles of LSNs/RNs/LPNs. According to the
Minnesota Board of Nursing, “assignment” is: the designation of nursing tasks or activities to be
performed by another nurse or unlicensed assistive person. Medication administration is a nursing
task. According to the law, the nurse retains the accountability for the assignment.
4.3 The Responsibilities of Licensed School Nurse/Registered Nursing Delegation
In Minnesota, LSNs/RNs can delegate medication administration as a delegated medical function as
authorized by state regulation and within their legal scope of practice. The LSN/RN uses
professional judgment to decide what is delegated and to whom if anyone. The LSN/RN may choose
to not delegate some medication administration activities. It is the judgment of the LSN/RN whether
the delegated functions can be properly and safely performed by the person without jeopardizing the
student’s welfare. Some activities that require specialized nursing knowledge and skill may be
delegated to LPNs, but not to UAPs. Some activities that do not require specialized nursing
knowledge may be delegated to UAPs by LSNs/RNs. It is the responsibility of the LPN and/or UAP
to perform the delegated activities correctly. The LSN/RN is accountable to verify that the delegatee
can perform the activity and do so safely. Delegation to UAPs is determined on a case-by-case basis
and is most appropriate when they are caring for students with routine, repetitive, ongoing
medication administration. When medication administration is not routine and the student’s response
to medication is less predictable, nursing delegation should be carefully considered.
When LSNs/RNs have responsibility for medication administration, they are the only ones who can
make delegatory decisions.
The LPN may be involved in the assignment and monitoring of nursing tasks or activities. LPNs
may also implement interventions that are delegated, ordered or prescribed by a licensed health care
provider.
When delegating medication administration to UAPs, the LSN/RN shall assess the situation and
consider the following nursing delegation principles:
Nursing Delegation Principles
Principle 1: The delegating LSN/RN must assess student needs prior to delegating.
Principle 2: The LSN/RN must provide adequate oversight of the medication
administration activities.
Principle 3: The LSN/RN must keep written documentation of the UAP’s initial and
ongoing competency.
Principle 4: The medication administration function must be one in which:

Minnesota Guidelines for Medication Administration in Schools
22
Revised June 2015
• The nursing care needs of the student are stable.
• Performance of the function does not pose potential harm to the student.
• The function involves little or no modification.
• The function has a predictable outcome.
• The function does not inherently involve ongoing assessment,
interpretation, or decision making.
• The UAP has appropriate skills and competency levels.
• Supervision is available.
If medication administration is delegated, those accepting delegation cannot re-delegate those
nursing functions to anyone else without the involvement of and supervision by an LSN/RN. As an
essential component of delegation, appropriate training must be conducted. See section 2 of the
Minnesota Guidelines for further information about delegation of medication administration by the
registered nurse.
4.34 The Medication Administration Decision-Making Charts
The decision-making charts are tools developed to assist LSNs/RNs/LPNs in making delegation and
assignment decisions. Each chart offers a series of questions for the nurse to ask with a specific
student, caregiver, and nursing activity in mind. If any questions are answered with a final “yes,”
the medication administration may be delegated or assigned.
Minnesota Guidelines for Medication Administration in Schools
23
Revised June 2015
GUIDELINE #5: PROCEDURES FOR MEDICATION ADMINISTRATION
5.1 Principles That Influence Medication Administration Procedures
It is important that these principles of medication administration be known and followed by anyone
(nursing and non-nursing personnel) who is administering medications.
Principle 1: Guarantee that medication administration is a clean procedure by washing hands.
Principle 2: Give medication exactly as ordered by the health care provider or indicated on
manufacturer’s instructions.
Principle 3: Everything should be done to avoid “no-shows,” especially for seizure
medications and antibiotics.
Principle 4: Prevent errors! Do not allow yourself to be distracted. Do not use one student’s
medication for another.
Principle 5: Keep individual student information private.
Principle 6: Apply child development principles when working with students (e.g., students
do not want to be considered unique.)
Principle 7: If there is an error or medication incident, it must be reported. Follow district
procedure for notifying your school nurse, administration (within 24 hours), the student’s
parent/legal guardian, and physician/licensed health care provider. Complete documentation.
It is important to act as soon as the error is discovered. The school administrator or
supervisor should evaluate errors/incidents by all persons administering medications.
Note: For detailed information about what to do in the case of medication administration errors, see
Guideline #9: Quality Assurance, Monitoring, and Assessment.
5.2 Step-by-Step Procedures
When medications are administered by any school personnel, procedures such as the following
should be in place:
Procedure 1: Wash hands. Administration of medication is a clean (not sterile) procedure,
unless otherwise specified.
Minnesota Guidelines for Medication Administration in Schools
24
Revised June 2015
Procedure 2: Verify authorization from parent and/or prescriber; check the label and/or
manufacturer’s instructions. Seek help when questions arise.
Procedure 3: Gather necessary items.
Procedure 4: Prepare and give medications in a well-lit, dedicated area. Remove medication
from locked cabinet.
Procedure 5: Check the label for name, time, medication, dose, and route. Use current
resources (e.g., medical pharmacopoeia) to verify the accuracy of the physician’s order.
Procedure 6: Prepare the correct dosage of medication without touching medication, if
possible.
Procedure 7: Check the label and/or manufacturer’s instructions for name, time, medication,
dose, and route while preparing the correct dose.
Procedure 8: Check the label and/or manufacturer’s instructions for name, time, medication,
dose, and route before returning the container to the locked cabinet.
Procedure 9: Do not leave medication unattended.
Procedure 10: Provide equipment and supplies (e.g., medication cups and alcohol wipes) as
needed.
Procedure 11: Identify the student. Ask the student to say his or her name. Nonverbal
students may need third party assistance with identification. Take measures to maintain data
privacy.
Procedure 12: Verify the student’s allergies verbally by asking the student and by checking
the student health records. Also verify contraindications to medicine. Watch for typical
adverse medication reactions. If an adverse reaction is evident, contact the supervisor,
parent/legal guardian, or licensed prescriber, according to school policy.
Procedure 13: If the student questions whether it is the right medication, stop and verify the
medication against records, with parent/legal guardian, or with registered pharmacist.
Procedure 14: Explain procedure to student.
Procedure 15: Position the student properly for medication administration.
Minnesota Guidelines for Medication Administration in Schools
25
Revised June 2015
Procedure 16: Administer medication according to the six rights (right student, right time,
right medicine, right dose, right route, and right documentation).
Procedure 17: Discuss administration procedure and carefully observe the student as
medication is administered.
Procedure 18: Record name, time, medication, dose, route, person administering the
medication, and any unusual observations.
Procedure 19: Ensure accurate documentation of all medications, including the witnessed
disposal of medications.
Procedure 20: Clean, return, and/or dispose of equipment as appropriate.
Procedure 21: Wash hands.
This set of medication administration procedures is modified as needed, based on routine or
emergency administration and the route of administration: oral, inhaled, topical, rectal, intravenous,
pumps, gastrostomy-tube, intramuscular, subcutaneous, or ear and eye.
5.3 The Six Rights of Medication Administration
The Six Rights of Medication Administration:
• Right Student
• Right Time
• Right Medicine
• Right Dose
• Right Route
• Right Documentation
The six rights can be used as a mental checklist to assist those administering medication to
remember and clarify the critical elements of the process. They are the:
• Right student. Properly identify the student (e.g., rather than asking the student, “Are
you Jane Doe?” before administering the medication, ask the student to state his or her
name). If available check the student’s photo.
• Right time. Administer medication at the prescribed time. This can usually be within
30 minutes earlier or later than the designated time unless otherwise specified by the
provider or the pharmacist.
• Right medicine. Administer the correct medication. Check three times, prior to
administration.
• Right dose. Administer the right amount of medication.
Minnesota Guidelines for Medication Administration in Schools
26
Revised June 2015
• Right route. Use the prescribed method of medication administration.
• Right documentation. Promptly and accurately document the medication administration.
5.4 Field Trips
School children on medication(s) have to be accommodated on field trips.
Each school district’s medication administration policy and procedures should address medication
administration on school-sponsored field trips. In most schools, health or education staff is assigned
responsibility for handling and administration of medications. Parents/legal guardians may choose,
but are not required, to accompany their students and administer medications.
One option is to take the medication in its original container and put it in a small, zip-lock bag along
with a copy of the prescriber’s orders and a copy of the parent/legal guardian authorization form.
Pharmacy law allows medications to be administered if in the original container. (Minn. Stat. §
Chapter 151.37 Subd 7 (Legend Drugs, Who May Prescribe, Possess) Send that package with the
person who is delegated or assigned/designated to administer medications on the field trip. The
school district should establish a document and process for check-in and check-out of medications
for field trips.
A second option is that the parent/legal guardian provide the required amount of medication
(depending on the length of the trip) in a separate pharmacy container with an original label (i.e., an
extra from the provider or pharmacist), with a copy of the prescriber’s orders and a copy of the
parental authorization form specific to the event or trip. This may be useful for any trips that exceed
one day in length.
A third option is that the policies may allow the preparation of a supply of medications by the
LSN/RN or parent/legal guardian, not to exceed the duration of the trip, in paper envelopes or other
more suitable containers for use by a student temporarily off-campus. A container may hold
only one medication. A label on the container must include the date, the student’s name, the school,
the name of the medication, its strength, dose, and time of administration, pharmacy, pharmacy
phone number, prescription number, and the initials of the person preparing the medication and
label. Accompanying the envelope will be a copy of the physician/licensed health care prescriber’s
orders and the parental/legal guardian authorization form. Note that the additional steps involved in
transferring medication to an envelope present another opportunity for medication error.
Some schools provide a designated volunteer with appropriate health information on students
requiring medication administration, medication in properly labeled bottles, and forms on which to
document medication administration. The school should provide a job description for the
medication administration volunteer, make sure the volunteer has the education and training
necessary to safely administer the medication, verify and document his or her competencies, and
Minnesota Guidelines for Medication Administration in Schools
27
Revised June 2015
provide procedures for how medication administration is handled on field trips. The volunteer needs
to follow the procedures.
When a volunteer is used, parents/legal guardian must be informed and sign a health data privacy
release form. Some experts (Schwab, 2001) recommend the volunteer be paid, even nominally, as a
school employee, perhaps as a substitute. In so doing, the volunteer becomes a school employee and
is bound by policies on medication administration including documentation and data practices.
Although parents/legal guardians can accompany students on field trips, it is not a requirement for
students with medication needs. Staff designated the responsibility for medication administration
should be trained and accompany the student and ensure that all the medical supplies are brought
along and appropriate documentation is completed.
The plan for coverage and care during extracurricular activities sponsored by the school that take
place outside of school hours should be carefully set out in the student’s health/education plan (504,
ECP, IEP, or IHP).
5.5 Before-School, After-School, and Summer-School Activities
School staff (e.g., educational assistants, bus drivers, and lunchroom staff) will be
designated medication administration or monitoring activities on a case-by-case basis.
Medication administration during these school-based times are based on whether they are school
sponsored programs and activities (e.g., extended day programs and sporting practice and events)
and then should follow district policy for school staff who administer medications and for students
who self-carry and self-administer. School staff (e.g., educational assistants, bus drivers, and
lunchroom staff) will be designated medication administration or monitoring activities on a case-by-
case basis. The school staff members who are assigned/designated delegated responsibility for
medication administration will must have been trained and be supervised related to their
responsibilities and have immediate access to the health offices student health plans, student
medication, and school resources (e.g., student health records/emergency information, high school
league physical examinations, and emergency equipment). Training and supervision will be
documented in the staff personnel file. If these programs are not school sponsored, they are often run
by contracted groups, not the school.
For information on emergency medication administration, see Guideline #7.11. Student needs for
emergency medications needs to be assessed at the initiation of any program activity (e.g., field trip).
Parents/legal guardians need to be informed of the school district’s emergency medication policies
and procedures for these programs as well as the programs of the regular school year.

Minnesota Guidelines for Medication Administration in Schools
28
Revised June 2015
When specific health information is known about a student and her or his potential for a health
emergency, the school should have a plan for medication administration, including information that
enables the student to possess emergency medication and/ or have immediate access to it at all times.
The plan for coverage and care during extracurricular activities sponsored by the school that take
place outside of school hours should be carefully set out in the student’s health/education plan (504,
ECP, IEP, or IHP).

Minnesota Guidelines for Medication Administration in Schools
29
Revised June 2015
GUIDELINE #6: EDUCATION AND TRAINING
6.1 Content and Competencies
Education and training on medication administration needs to be conducted by the LSN/RN on an
ongoing basis to keep students safe and to ensure ongoing competency of staff members.
Coordination of training of other school staff about medication administration is an essential part of
the job descriptions of LSNs/ RNs. The LSN/RN determines what training is needed, for whom, the
content, and available and appropriate training resources (e.g., medication training course through a
local college). Education and training can range in format from formal classroom lectures to one-on-
one discussions, and in content to be student, disease, or procedure, specific, competency-based;
technical; and/or theoretical.
After training, medication administration procedures should be demonstrated by the person being
taught, and that person’s competencies need to be documented in writing.
LSN/RN shall communicate completion of staff medication competencies enabling the LPN to
assign and monitor medication tasks and activities.
Topics to include in initial training, periodic training and refresher training about medication
administration include district policies, directions and time of ad- ministration for all medications,
verification procedures for setting up medications for administration, proper documentation, data
privacy, individualized student health information, emergency protocols, equipment, the six rights of
medication administration, and infection control procedures (e.g., hand-washing). Demonstrations of
medication administration are an excellent method of testing competencies.
It is especially important that staff members be sensitive to changing community and school
populations and their diverse characteristics. All education and training needs to have a component
that addresses the diverse needs of the communities and cultures within which the school is situated.
6.2 LSN/RN Medication Training for Delegation
All individuals (primary and substitute) responsible for medication administration must be trained.
When planning the training for delegation medication administration, the LSN/RN must keep the
following questions in mind:
• Who is being trained?
• What is the content of the training?
• How much time is there for training?
• Where is the training location?
• What are the roles and responsibilities?
• Why is the training necessary?

Minnesota Guidelines for Medication Administration in Schools
30
Revised June 2015
• How will competencies be evaluated and documented?
These questions must be asked and answered to determine if delegation of medication administration
training can occur.
6.3 Education and Training Needs
Different participants in students’ health care have varying needs for information, as outlined below.
Documentation and evaluation of training must follow the training.
Training needs to be done before medication administration is performed. It is important that four
types of staff training be conducted. The supervisor informs the trainee of
(1)
school policies and availability of resources,
(2)
available written criteria that indicate when to contact a supervising LSN/ RN,
monitoring LPN, or call 911,
(3)
student-specific information, and
(4)
procedures for safe medication administration.
The first, second, and fourth are best done before students begin their school year (e.g., during work-
shop week) and the third before delegatee staff work with specific students.
Although there are a variety of curriculum resources available, Minnesota has no required materials
at this time. A training program should have the following:
(1)
a general medication overview that includes the purposes of medications and the
various medication administration routes;
(2)
information on medication handling and administration techniques that includes
cleanliness, care, storage, the six rights of medication administration, preparing
medications, administration procedures, guidance for field trips, proper medical
abbreviations, student plans, and emergency information;
(3)
need for authorizations and record keeping that includes legal requirements, policy
and procedure review, record keeping, errors and omissions, and forms; and
(4)
rights and responsibilities that include delegation, assignment, and reporting, data
privacy, and Minnesota statutes, rules, and guidelines.
Well-designed education of members of the community-at-large will draw on the expertise of
local health care and health education professionals, and advocacy organizations. These individuals,
who may be members of the district’s health advisory committee, will ideally work with the school
district to proactively address medication administration issues, including an understanding of
staffing, expectations, compliance, and resources/financing. To be able to make good decisions
about district health services, school board members must receive information about financial needs
(health care staff and resources) and the health of their student population. The latter can be done
through periodic statistical reports from lead health personnel regarding medication administration in
schools, such as the number of students taking medications, who is giving those medications, and the

Minnesota Guidelines for Medication Administration in Schools
31
Revised June 2015
training needed. Parents/legal guardians have a responsibility to convey the following student-
specific health information about their children to appropriate school staff: their children’s health
conditions, medications, allergies, medication side effects, level of knowledge about their
medications, and any issues with student ability or willingness to take medication.
Parents/legal guardians should be informed of the district policy and be as involved as possible in
their children’s health care, including training of staff on specifics such as their student’s response to
medication administration (e.g., Glucagon™, Diastat™, or epinephrine auto injectors or Epi-pen™).
When parents/legal guardians provide this information to schools, they have a right to legal
protections of data privacy under IDEA, FERPA, HIPAA, IDEA, the Minnesota Government Data
Practices Act (Chapter 13), and Minnesota Mental Health Act (MMHA).
Education of students is geared to their knowledge, skill, and developmental levels which may
range from:
• students who have no knowledge about their medications and administration,
• students with limited knowledge who need to know more,
• students who need observing as they self-administer their medication competently, and
• students who are completely experienced in self-administration of medication and self-
monitoring of their health conditions and do not need assistance.
School district policies and staff members should enable students to grow in their self-care abilities
as part of their life-long learning and educational experiences. In turn, students need to take an active
and responsible role in their health care, self-administer according to the six rights, and learn to
become their own health advocates. Students should be assured that their health information is kept
private.
Both the Minnesota Board of Nursing and Minnesota Board of Teaching require continuing
education units for licensure renewal for RNs and LSNs nurses. These continuing education units are
necessary to stay up to date on nursing practice, medical conditions, medication use, and student
health needs. All health services staff should have an evaluation of their skills and knowledge-based
competencies. Refresher courses, online training, skills based texts, and school nursing texts can be
used to fill any gaps in skills or competencies, such as information about new medications, pediatric
care, and school nursing procedures.
School staff who serve as UAPs working with medications need to be knowledgeable about
medication administration procedures on campus and during extended day experiences (e.g., field
trips and sporting events). The training content should include:
(1)
hands-on student care that is specifically related to the assigned medication
administration,
(2)
school district policy and procedures, such as safety measures, general emergency
procedures, and how and when to contact the LSN/RN, and
(3)
federal, state, and local regulations.

Minnesota Guidelines for Medication Administration in Schools
32
Revised June 2015
In Minnesota, there are at present no specific training requirements for UAPs who are assisting with
medical functions in the school. However, it is recommended by national and state nursing
organizations that UAPs who administer medication be trained to:
• Recognize the student’s right to privacy
• Recognize the student’s skills and abilities.
• Follow facility policies and procedures regarding medication administration, control
substances, facilities, requirements, storage and handling of medications, use of multi dose
vials and syringes, medication expiration dates, documentation, and disposal of medication,
and similar policies and procedures implemented in the facility to safeguard medication
provision to students.
• Demonstrate safe medication administration procedures.
• Understand the relationship between the LSN/RN/LPN and UAP and the importance of
communication.
• Recognize the limits and conditions by which a UAP may administer medications.
• Recognize the student’s property rights and physical boundaries.
• Recognize the responsibility to report and the mechanisms for communicating such to the
appropriate authorities if reasonable cause exists to believe that a child or adolescent has
been subjected to maltreatment or neglect.

Minnesota Guidelines for Medication Administration in Schools
33
Revised June 2015
GUIDELINE #7: POLICIES AND PROCEDURES
7.1 Health Policies as Legal Responsibilities
It is the legal responsibility of school boards to put health policies in place. According to Minnesota
Statutes § Chapter 121A.22, Subd. 4, school board health procedures must be developed in
consultation with health specialists (e.g., licensed school nurse, public health nurse, licensed health
care providers, medical advisor, etc.
It is also the responsibility of the school board of the local school district under Minnesota Statutes §
Chapter 121A.2205 to define the instructional day. See additional information in Minnesota
Guideline 1.2.
7.2 Characteristics of Sound Policies
Local district policies and procedures on medication administration should be balanced, consistent,
periodically updated according to school district directives for policy review, adaptable, based on the
needs and ages of the student population at-large, consider community resources, and are aligned
with professional practice standards and guidelines.
Decisions made at the school district level will impact how students are ultimately served. The best
policies are developed collaboratively, with the advice and assistance of the following: school board
members, medical advisors, licensed health care providers, families, school staff (LSN/RN, LPN,
UAPs, principal, etc.), local partners (pharmacists, public health workers, social workers, health care
administrators), and other community members (see National Association of School Nurses,
1993/1997/2003). These individuals might already be serving on a school health advisory
committee. School staff, students, and parents/legal guardians all need to be aware of, understand,
comply with, and aid in successful implementation of district policy and procedures. Parents/legal
guardian should be advised annually of the district’s medication policy and procedures.
7.3 Contents of Policy and Procedures
A policy is a framework for operational decisions, which specifies a recommended course of
direction consistent with the intent of the organization. It is an understanding by members of a group
that make the actions of each person more predictable. Procedures are specific steps outlining how to
implement policy, a way of telling how to perform activities or tasks (e.g., who does what and
when).
District policies and procedures on medication administration should address the following: types of
medications administered (see glossary for definitions of prescribed, OTC, CAMs, insulin,
emergency, investigational, and controlled substances); required information and authorization for

Minnesota Guidelines for Medication Administration in Schools
34
Revised June 2015
initiating medication administration; desired medication administration outcomes; delegation of
medication administration; training and supervision; procedures for medication administration;
secure handling, storage, infection control, and disposal of medications; self-carrying of medications
and self-administration; summer school, extended-day activities; emergency protocols;
documentation and record keeping; and errors and omissions. School District policy and procedures
also need to address students’ individual health needs (short-term to long-term medication
requirements), which might or might not involve a health/education plan.
7.4 Requests to Administer Medications in Schools
When medication administration in a school is requested by a parent/legal guardian, the policy will
specify: (1) who will give the medications (LSNs/ RNs, LPNs or in their temporary absence,
delegation or assignment to paraprofessionals/UAPs, and in schools with no LSNs/RNs on staff,
individuals trained and qualified to administer medication and assigned by school principals) and (2)
whether and under what conditions self-medication by students is allowed.
No prescription medication may be administered without: (1) the written order of a
physician/licensed health care prescriber and (2) the written or oral authorization of the student’s
parent/legal guardian. If the parent’s/ legal guardian’s authorization is oral, then the oral
authorization must be reduced to writing within two school days. Prescribed medication shall be
administered to and taken by only the person for whom the prescription has been written.
The school district board and school personnel need to carefully consider Federal Drug
Administration (FDA) warnings and the student safety ramifications for allowing OTC medication
administration without a prescription. If a decision is made to administer OTC medication without
orders from a licensed prescriber, directions should be taken from the official container’s
manufacturer’s label.
When queried, the State of Minnesota Office of the Attorney General concluded in a letter dated
February 14, 2000, that, “school nurses do have the authority to provide over-the-counter
medications to students upon a parent’s request, even without a physician’s order. It is important to
note, however, that the school nurse has the ultimate authority and responsibility to reject a parent’s
request and to decline to administer an over-the-counter medication [our emphasis] if the nurse
believes that such medication is unnecessary, inappropriate, or could lead to patient harm. Further,
school districts retain independent authority to implement policies that govern the administration of
non-prescription drugs by school nurses. A school district, or an individual nurse LSN/RN, could
choose to adopt a policy that requires a licensed prescriber order before a school nurse administers a
non-prescription medication to a student.” (The full letter from the Attorney General’s Office is in
the appendices)

Minnesota Guidelines for Medication Administration in Schools
35
Revised June 2015
7.5 Medication Types
A number of different types of medications may be requested to be administered in schools:
prescribed, OTC, CAMs, emergency, investigational, and/or controlled substances. These are not
exclusive categories. For example, Ritalin™ is a prescription medicine and also a controlled
substance, and ibuprofen is an OTC, but if this OTC medication drug is prescribed it is can also be a
prescription medication. Responses to requests should be based on school district policies, the
judgment of the LSN/RN, staff capabilities and training, and the school district administration’s
level of support for established health policies.
Schools and school staff should not purchase or have a supply of any OTC medications or distribute
them to students.
7.6 Self-Carrying and Self-Administration of Prescription Medication
An authorization form completed and renewed annually by the parent/legal guardian and physician
licensed health care prescriber and on file in the school will allow a student to responsibly carry
medications for self-administration (see Minnesota Statutes §§ Chapters 121A.22, 121A.2205,
121A.221 and 121A.222, and Wheeler, 2004). This authorization is renewed each school year.
Documentation from the prescriber should include all of the following:
• records verifying that the student is capable of and has received training on administering
the prescribed medication,
• name and purpose of the medication,
• effective date of medication,
• prescribed dosage of the medication,
• times at which or circumstances under which the medication may be given,
• period for which the medication is pre- scribed,
• route of administration,
• potential side effects, and
• duration of time the student can self-administer.
In the case of a disagreement regarding a student’s self-carrying and self-administration of
medication, a meeting should be held among all those involved to sort out differences of opinion and
develop a plan, keeping as a priority the student’s educational goals and health safety. If the meeting
is unsuccessful and the situation is related to special education, a number of organizations can be
reached for advice, such as PACER, Children’s Disability Law Center, or the Minnesota Department
of Education or the Special Education, Compliance, and Assistance unit.
The LSN/RN, in consultation with the parent/legal guardian and physician/licensed health care
prescriber, needs to evaluate the student’s health status and abilities for safe self-administration of
prescription and non-prescription medications, observe the student’s first self-administration at
school, and communicate regularly with the parent/legal guardian about any medication

Minnesota Guidelines for Medication Administration in Schools
36
Revised June 2015
administration difficulties or successes. Two ways for an LSN/RN to assess student competence are
to have the student come to the health office to self-administer, where the LSN/RN can periodically
observe the procedure, or by written documentation from a physician/licensed health care prescriber
stating that the student is administering appropriately. A student self-administering medications may
document it on a personal daily medication form.
When the request for self-carrying includes controlled substances, the individual request and
privilege needs to be examined and a plan made for keeping the student as independent as possible
but in compliance with drug laws and safe storage. (e.g., medications could be self-administered, but
stored in the health office).
When students are self-carrying and self-administering medications, the student teaching team and
other appropriate staff can be informed on a need-to-know basis for legitimate educational interests,
as specified by FERPA. The student and his or her parent/legal guardian are informed of how and to
whom this information is shared. If there are difficulties with the student’s ability to safely self-
administer, including medication security issues, the building administrator discusses with the
student and parent/legal guardian the possible discontinuance of the student’s self-administration.
This privilege can also be discontinued if medications are shared with other students or not taken as
authorized by parents/legal guardians.
In school districts without LSNs/RNs on staff, educational administrators under the direction of
school boards are responsible to set up a system through which:
• policies are developed in consultation with LSNs/RNs,
• people are assigned and trained to do health services,
• the procedures are done safely and consistently, and
• all necessary documentation is completed.
They are also responsible to find appropriate resources and medical expertise to address their
students’ medication administration needs. School administrators cannot legally fulfill the role of
RNs.
Those districts with LSNs/RNs on staff or on contract will be able to call on staff to take the lead on
these responsibilities.
According to the National Standards of School Nursing Practice , the LSN/RN/LPN has the
authority and responsibility to reject a request if the LSN/RN/LPN believes the request is
unnecessary, inappropriate, or could lead to harm. It is required that nurses are expected to clarify
the orders that are unclear or unsafe. (IOM Future of Nursing Report).
For further information on the duties of students, see Guidelines 2.5.
Minnesota Guidelines for Medication Administration in Schools
37
Revised June 2015
7.7 Self-Carrying and Self-Administration of Non-Prescription Medication
No request for self-carrying or self-administration will be honored if dosage exceeds the
recommendations on the manufacturer’s label.
According to MS Chapter 121A.222 , a secondary student may possess and use non-prescription
pain relief in a manner consistent with the labeling if the district has written parental or legal
guardian authorization. However, this law does not apply to the possession or use of any drug or
product containing ephedrine or pseudoephedrine as its sole active ingredient or as one of its active
ingredients.
The FDA states there are two categories of over- the-counter pain reliever/fever reducers:
acetaminophen and nonsteroidal anti-inflammatory drugs (NSAID).
Acetaminophen is used to relieve headaches, muscle aches and fever. It is also found in
many other medicines, such as cough syrup and cold and sinus medicines. OTC NSAIDs
are used to help relieve pain and reduce fever. NSAIDs include aspirin, naproxen,
ketoprofen and ibuprofen, and are also found in many medicines taken for colds, sinus
pressure and allergies.
It is important that students are not taking medications with aspirin, unless prescribed, as research
has established a link between Reyes Syndrome and the use of aspirin and other salicylate containing
medications.
If a student happens to take two medications that contain the same active ingredients, they might be
taking two times the normal dose and not realize it. It is best practice for the LSN/RN to have
knowledge of over-the-counter medications. To avoid multiple dosing, it is best practice if the school
health staff (e.g., school nurse) LSN/RN is informed and is available to provide education and
guidance related to student’s self-administration of OTC medications. In addition, a student self-
administration agreement should be in place.
School districts can offer the following two options.
1. As was required for prescription medications, one option for schools is to have an
authorization form completed by the parent/legal guardian and physician/licensed health care
provider on file in the school or a temporary oral authorization will allow a student to
responsibly carry non-prescription medications for self-administration.
No request for self-carrying or self-administration will be honored if dosage exceeds the
recommendations on the manufacturer’s label. Physician/licensed health care prescriber
authorization is especially important when there is no LSN/RN available to the school
district.
2. A second option for schools is to have written parental/legal guardian authorization, a student
contract, and LSN’s/RN’s assessment. If the LSN/RN assesses that it is appropriate, a request

Minnesota Guidelines for Medication Administration in Schools
38
Revised June 2015
would be made for a physician’s licensed health care prescriber’s order. If the student is
allowed by school policy to carry medication, the LSN/RN performs an assessment and
works with the parent/legal guardian and student to draw up a written contract. This privilege
can be discontinued if medications are shared with other students or not taken as authorized
by parents/legal guardians.
In school districts without LSNs/RNs on staff, educational administrators under the direction of
school boards are responsible to set up a system through which: policies are developed in
consultation with LSNs/RNs, people are assigned and trained to do health services, the procedures
are done safely and consistently, and all necessary documentation is completed. They are also
responsible to find appropriate resources and medical expertise to address their students’ medication
administration needs. School administrators cannot legally fulfill the role of LSNs/RNs.
Those districts with RNs on staff or on contract will be able to call on staff to take the lead on these
responsibilities.
For further information on the duties of students, see Guideline #2.5.
7.8 Handling, Storage, and Disposal of Medications
Although ideally parents/legal guardians deliver their students’ medications to the LSN/RN/LPN as-
signed to the school, this is most often done by students. The LSN/RN/LPN should be notified in
advance when students will be bringing medication. This is the first step in student accountability for
medication administration.
It should be made clear in advance where emergency medications such as rescue inhalers, Diastat™,
epinephrine auto injectors, and Glucagon™ are stored and who is responsible for supplying or
administering them. District policy or procedures should specify that emergency medications should
be accessible to staff or students who might need them, but are inaccessible to others.
The LSN/RN must examine on-site any new medication, medication order, and permission form and
assess the appropriateness of delegating medication administration to any other school personnel.
Schools should consider counting all medications brought to school and mandate counting on all
controlled substances. Documentation should include person bringing the medication, date received,
type and amount of medication received.
All medications should be stored on school property, in a locked drawer or cabinet used exclusively
for medications and kept no longer than the medication expiration date or end of the school year,
whichever is sooner. Cabinets should not contain glass doors and should be anchored securely to a
solid surface. Access to stored medication and medication cabinet keys must be limited to school
personnel authorized to administer medications. Medication requiring refrigeration should be stored

Minnesota Guidelines for Medication Administration in Schools
39
Revised June 2015
in a locked refrigerator or in a locked container in the refrigerator specifically for medications.
Medications should not be stored in individual classrooms unless all of the above standards can be
met and the individuals responsible for administration have been properly trained. Each medication
should be stored in the original pharmacy- or manufacturer-labeled container with the student’s
name on it.
Expiration dates should be checked, medications disposed of upon expiration, and parents/legal
guardians notified. All unused, discontinued, or outdated medications shall be returned to the
parent/legal guardian and the return appropriately documented. With parent/legal guardian consent,
such medications may be destroyed by the school when two individuals are present to witness and
document the disposal.
Needles and syringes should be disposed of in a manner consistent with the following guidelines
(see OSHA Blood-borne Pathogen Standard 29 of C.F.R. 1930.1030 and Minnesota Rules, chapter
5206):
• Needles should not be recapped and should not be purposely bent or broken.
• Disposable syringes and needles (and other sharp items) should be placed in approved
sharps containers and labeled “biohazard.”
• Custodial staff or other agents must be given directions for disposing of containers
according to established procedures for regulated medical waste.
7.9 Planning and Standardized Forms
The school district should establish standardized record-keeping forms that are uniform and
consistent across the district and make them available in a variety of ways (e.g., district web site and
handbook).
Medication management plans include overall district plans and individual student plans, which give
contingency directions for when the LSN/RN or designee is not available. Plans need to be flexible
for the number of staff who interacts with the students on medication regimes in school.
Parents/legal guardians and appropriate school staff all give input into the medication administration
plan for individual students.
7.10 Record Keeping
School health records should be kept in a central location with a locked system to assure
record security.
School health personnel should maintain accurate written or electronic records specific for each
student receiving medications, including parental consent forms, authorization from licensed
prescribers, individual documentation, immunization, and emergency procedures.
Minnesota Guidelines for Medication Administration in Schools
40
Revised June 2015
A picture of the student attached to the medication log or the medication authorization form can help
ensure that the proper student gets the proper medication. Documentation must contain student
name and identification number; room; name of medication; purpose, dosage; route; date and time
given; beginning and end dates; any special circumstances related to the procedure, the student’s
unusual reactions or responses, omissions, absences, or refusals, name of the individuals giving the
medication, count of controlled substances, and medication disposal. Documentation must be done
in unalterable ink (no erasing, no deleting/white out) and should include significant reactions. These
are legal documents and provide protection to those who administer medications in schools.
School districts are required to have a record retention policy and procedures. Typically, health room
documents/logs should be retained by the school district for six years after student graduation or
leaving the district (State of Minnesota School District General Record Retention Schedule, 2000).
Health and immunization information should be retained for at least five years after the student
attains the age of majority (18), so until the age of 23 (Minnesota Statutes § 121A.15, Subd. 7).
More information is available from the local district retention policy, which is filed in school
administration files, and from the following Region 1 website:
http://www.region1.k12.mn.us/main/Portals/0/SMARTFIN/docs/DistrictGeneralRecordsRetention.pdf
Additional information regarding Minnesota Department of Education record retention is available
at: http://education.state.mn.us/MDE/SchSup/ComplAssist/QA/DueProcRight/055464
A summary of individual student medication records (paper or electronic) should be transcribed
(e.g., 9/15/00 – 5/1/01 – Ritalin™ 20 mg. at lunch time) to a student’s cumulative health record
(electronic or paper). Logs should not be destroyed if summary information has not been transferred
to the cumulative health record. Student privacy must be protected as outlined in A&D, FERPA,
HIPAA, IDEA, Minnesota Government Data Practices (Chapter 13), and MMHA.
School health records (paper or electronic) should be reviewed annually and kept in a central
location with a locked/secured system to assure record security safety. All files should be
locked/secured at the end of each day. Policy and procedures must define who has responsibility for
maintaining files, entrance and exit of records, tracking, security, and when files are pulled and sent
to another school.
It is important to note that a school district, a charter school or a non-public school that receives
services or aids under Minnesota Statutes §§ Chapters 123B.40 to 123B.48 must under law make a
reasonable effort to find, locate and transfer a students’ educational record when no longer attending
that student transfers to another location. This includes medications records as they are part of the
educational record under FERPA.
7.11 Procedures for Emergency Medications in Schools
Students with known chronic health conditions sometimes need emergency medications to prevent
or treat anaphylaxis, respiratory distress, diabetic hypoglycemia, seizures, cardiac incidents, and

Minnesota Guidelines for Medication Administration in Schools
41
Revised June 2015
social/emotional crises. In an emergency, if two or more people are available, one can administer the
emergency medication while the other calls 911. If only one person is available, that person should
first administer the medication and then call 911.
Some students will have individual emergency care plans and parental/legal guardian and
physician’s authorization forms and instructions that need to be accessed and adhered to.
See Guideline 3.3 for further information on preparing for emergencies.
7.12 Investigational Drugs
Medication administration policies should address the specific requirements for administering
research medication in school, including providing the LSN/RN with information regarding the
protocol or a study summary from the research organization, signed parental/legal guardian
permission, reporting requirements, and any follow-up nursing actions to be taken. The National
Association of School Nurses recommends that a parent’s/legal guardian’s requests to have
investigational drugs administered at school should be evaluated on a case-by-case basis with the
parent/legal guardian, the licensed prescriber or provider, and the LSN/RN. It must be done in
accordance with federal and state laws regarding investigational drugs. Pediatric experimental or
investigational drugs are those medications currently involved in clinical trials and are undergoing
formal study to determine the efficacy and safety of pediatric dosing, but they do not have FDA
approval.
7.13 Complementary and Alternative Medicines (CAMs)
The National Center for Complementary and Alternative Medicine (NCCAM) defines
Complementary and Alternative Medicine (CAM) as:
A group of diverse medical and health care systems, practices, and products that are
not generally considered part of conventional medicine. (NCCAM, 2011).
Medication administration policies should reflect local and state policies related to the administration
of alternative medications and treatments. No substance should be administered to any child or
adolescent without the express written request of the parent or legal guardian. Schools should
exercise caution about CAMs administration in school, and the LSN/RN should assess the necessity
of administering CAMs in school. Such products should be provided by the parent/legal guardian (as
with all medications administered at school) and in an original container with proper labeling (name
of student, date, name of medication, dose, time of administration, pre- scriber as appropriate, and
expiration date) and manufacturer’s indications and contraindications. CAMs can frequently interact
with other prescribed and non-prescribed medications, enhancing or inhibiting effects, so
parents/legal guardians should seek guidance from their licensed prescribers about drug interactions.
7.14 Medical Cannabis

Minnesota Guidelines for Medication Administration in Schools
42
Revised June 2015
Minnesota Code Ann. § 152.32 Subd. 3 provides that unless an exception applies, an individual’s
status as a registered medical marijuana patient may not be used: 1) by schools as a reason to refuse
enrollment; 2) by landlords as reason to refuse to lease to the person ; 3) by employers as a reason to
refuse to hire or as a reason to terminate employment; or 4) as a reason to deny custody or visitation
rights. An employer generally cannot discriminate against a patient based on a failed drug test for
marijuana. The law does not require accommodation if it would violate federal law or regulations, or
cause the entity to lose a federal licensing or monetary benefit. Employers may punish patients if
they are impaired at work or possess marijuana at work. In addition, Minn. Code Ann. § 152.23
provides that patients may face civil penalties for undertaking a task under the influence of
marijuana that would constitute negligence or professional malpractice.
At the present time the Minnesota Law for Medical Cannabis allows for Medical Cannabis to be
administered by a registered designated caregiver. The law sets forth limitations in 152.23 for
Medical Cannabis Possessing or engaging in the use of medical cannabis on a school bus or van or
on the grounds of any preschool or primary or secondary school …and other settings. There are still
discussions that are happening between the federal and state authority related to the legality of
marijuana substances. Parents and legal guardians are urged to discuss with their licensed prescriber
how to best handled the administer Medical Cannabis away from the school setting.
Minnesota Guidelines for Medication Administration in Schools
43
Revised June 2015
GUIDELINE #8: QUALITY, ASSURANCE, MONITORING, AND
ASSESSMENT
School administrators and/or the LSN/RN should review medication error reports and take
steps to develop a correction plan to avoid future problems.
8.1 Definitions
If a medication error occurs, districts are best protected from liability when policies and procedures
are established collaboratively with input from school nursing personnel, district administrators, and
parents/legal guardians.
Medication errors include any failure to administer a medication as prescribed for a particular
student and may include not administering to the right student, at the right time, the right medicine,
the right dose, by the right route, or with the right documentation.
8.2 Procedures to Follow in Case of Medication Errors
If an error in medication administration occurs, the following steps should be initiated:
• Identify the nature of the error.
• Keep the student in the health office. If the student has already returned to class when the
error is determined, have the student accompanied to the health office.
• Monitor the student’s behavior and physical symptoms. If the student’s symptoms are life-
threatening, call 911 prior to calling parents.
• Notify parents/legal guardians, supervising LSN/RN, principal/designee, and student’s
physician.
• If unable to contact the physician or licensed prescriber, contact the Poison Control Center
for instructions. Give the name and dose of the medication given in error; the age and
approximate weight of the student; and the name, dose, other medications being taken by the
student, and time of last dose of other medication, if possible.
• Carefully record in the student’s health re- cord all circumstances and actions taken.
• Submit an occurrence report to the principal or program administrator within 24 hours.
Include the name of the student, the parent/legal guardian’s name and phone number, and a
specific statement of what the medication error was, who was notified, and what remedial
actions were taken.

Minnesota Guidelines for Medication Administration in Schools
44
Revised June 2015
8.3 Refusal to Take Medication
Schools should have consistent policies to address handling situations with students who do not
appear or who refuse to take ordered medications. It is best to address these situations on an
individual basis depending upon what the medication is and how often the student fails to take the
medication. If a medication is not given, policies should address the extent to which school
personnel will attempt to administer the medication, as well as procedures for notifying a
parent/legal guardian and licensed prescriber and completing an occurrence report.
Health services staff should monitor student noncompliance with medication administration. Action
or issues of medication administration refusal or noncompliance should be reported by the LSN/RN
or designated school health personnel to the licensed prescriber, parent/legal guardian, and student.
8.4 Reducing Errors and Omissions
The LSN/RN or designated school health personnel should review reports of medication errors,
analyze patterns, and take necessary steps to avoid future problems. The purpose of monitoring
medication errors is for system correction rather than individual blame. Eliminating distractions
and/or other responsibilities during periods of concentrated medication administration can increase
safety and decrease the potential for errors. School administration and/or the LSN/RN should review
medication error reports and take steps to develop a correction plan to avoid future problems.
8.5 A High Quality School Health Program
The following are significant actions leading to a high quality school health program (for additional
information, see National Heart, Lung, and Blood Institute, National Asthma Education and
Prevention Program, National Association of School Nurses, American School Health Association,
American Academy of Pediatrics, Institute of Medicine, the Centers for Disease Control, and many
others.in their publications related to asthma, obesity, suggests that: et al., 2003):
• The school would identify students with conditions that require IHPs and utilize use
applicable and current health information to develop IHPs.
• Schools would have highly qualified staff members who have access to an LSN/RN and are
trained in student health issues, first aid, emergency medication issues, AED, and CPR;
teachers should be informed of their students’ health needs.
• All students who need IHPs or ECPs would have them implemented in a timely manner.
Minnesota Guidelines for Medication Administration in Schools
45
Revised June 2015
GUIDELINE #9: SCHOOL AND FAMILY RELATIONSHIPS
All communication, even phone contacts, should be documented.
9.1 Communication and Collaboration
The best student educational and medication administration outcomes will result from
communication and collaboration among all involved—students, parents/legal guardians,
physicians/licensed health care providers, school health office personnel, teachers, pharmacists,
health advisory committee members, school board members, and school administrators. Together,
with everyone contributing his or her own part, the quality of health care decision-making and
actions can be maximized.
A variety of communication methods—such as telephone, electronic, and in-person—can facilitate
prompt and accurate transmittal of information. All communication, even phone contacts, should be
documented. All communication with the school is subject to federal and state data privacy laws.
These laws are not barriers to communication, but can be used to enhance communication by
developing trust in the sharing of health and educational information. See Guideline 1.3 for
additional details.
Schools need to reach out to families and develop a standard mechanism for two-way
communication, with language translation as needed, between parents and school personnel
regarding students’ health. Examples include when medication is needed at school; when students
receive medications in school, or when a scheduled medication is missed at school, or there are
changes in students’ medication needs; when issues arise about reactions to new medications or
medication effectiveness (e.g., a student’s educational performance changes based on a new dosage
of Ritalin™); and what the alternative plans are for medication administration. Medications given
outside of the school day may still affect student performance at school.
Student health plans (504 plans, ECPs, IEPs, and IHPs) can better address specific health and
educational needs and can serve as the mechanism to bring everyone together for efficient planning
and collaboration.
9.2 Documentation
Student health documents related to communication include written, telephone, and verbal orders for
medication, parents’/legal guardian’s written and oral authorizations for medication,
medication administration records (medication, date, time, who administered it, etc.), controlled
substance records, and medication error notations. The LSN/RN is ultimately responsible for
maintaining and securing documentation of medication administration in students’ private health

Minnesota Guidelines for Medication Administration in Schools
46
Revised June 2015
records, but anyone who gives medication (LSN/RN, LPN, paraprofessional, UAP, or student) needs
to chart his or her activities on student records, be knowledgeable about records, and keep them
updated. The school district can standardize forms for all of its students’ health records and make
blank forms available through web sites or as hard copies.
All medication administration records need to be kept secure, so when someone views a record or
takes a record out of the file, it must be noted or signed out specific to that individual noting time
and date.

Minnesota Guidelines for Medication Administration in Schools
47
Revised June 2015
GUIDELINE #10: FINANCES
10.1 Funding Sources
The school board’s responsibility is to ensure resources to support its school health program. The
school board can also raise and successfully package funds from a variety of other sources, such as
general funds, state and federal special education funds, third- party reimbursement for IEP health
related services, the federal Free Care Rule, and grants.
Some students need medication to benefit from special education. The time spent by eligible staff,
such as nurses, can be eligible for state aide if accurately documented and reported in the district’s
Electronic Data Reporting System (EDRS). In addition, the district is able to bill third parties such as
the Minnesota Health Care Programs (includes Medical Assistance (MA or MinnesotaCare) for
those students with IEPs.
Under the direction of the board, people from within the system, such as members of the health
advisory committee, can identify financial sources and write grant applications to strengthen their
district’s health services program. Some grants will pay for equipment and some will pay for pilot
programs, allowing the district to try out different levels of staffing.

Minnesota Guidelines for Medication Administration in Schools
48
Revised June 2015
REFERENCES
American Academy of Pediatrics, American Public Health Association, & National Resource Center
for Health and Safety in Child Care and Early Education. Caring for our Children. 3
rd
ed. Author.
Health in Schools. (2003, June). The impact of FERPA and HIPAA on privacy protections for health
information at school: Questions from readers. Health and Health Care in Schools: A Report on the
Policies, Politics and Financing of Health Programming in Schools [On-line serial], 4(4).
Joint Committee on National Health Education Standards. (January 2007). National health education
standards: Achieving health literacy. Atlanta, GA: Centers for Disease Control and Prevention and
American Cancer Society; ISBN 9780944235737.
Minnesota Department of Administration, Information Policy Analysis Division. (2000). St. Paul,
MN: Author.
Minnesota Department of Health. (2002). Report to the Minnesota Legislature: Medications
dispensed in schools study. St. Paul, MN: Author.
Minnesota Department of Health. (2005). Medication administration in schools annotated
bibliography. [Available on request].
2005 • MDH - Minnesota Guidelines for Medication Administration in Schools
Available on request.
National Association of School Nurses, Inc. (1993/1997/2003/2010/2012). Medication
Administration in the School Setting (Amended January 2012) [Online].
National Association of School Nurses, Inc. (1994/1995/2002/2014). Delegation, Nursing
Delegation to Unlicensed Assistive Personnel in the School Setting (Revised June 2014) [Online]
National Association of School Nurses, Inc. Role of the School Nurse (Revised 2011) [On-line].
National Association of School Nurses, Inc. School Nurse Workload: Staffing for Safe Care
(Adopted January 2015) [Online].
National Council of State Boards of Nursing (©2005) Working with Others: A Position Paper.
Chicago: Author.
“Joint Statement on Delegation.” American Nurses Association (ANA) and the National Council of
State Boards of Nursing (NCSBN).
Minnesota Guidelines for Medication Administration in Schools
49
Revised June 2015
National Heart, Lung, and Blood Institute; National Asthma Education and Prevention Program;
School Education Subcommittee; National School Boards Association; American School Health
Association; Food Allergy and Anaphylaxis Network; American Diabetes Association; and Epilepsy
Foundation of America. (2003). “Students with chronic illnesses: Guidance for families, schools, and
students”. [On-line], 1-2.
Selekman, Janice DNSc, RN, Editor. School Nursing: A Comprehensive Text, 2nd Edition. ISBN-
13: 978-0-8036-2209-8. FA Davis Company, PA. (2012).
Schwab, N. (Ed.). (2001). Legal issues in school health services: A resource for school
administrators, school attorneys, school nurses. North Branch, MN: Sunrise River Press.
Scope and Standards of Practice, School Nursing, 2
nd
ed. American Nurses Association and the
National Association of School Nurses, July 2011. ANA Silver Spring, MD 20910.
Out-of-Hospital Medication Errors among Young Children in the United States, (Pediatrics,
American Academy of Pediatrics, Smith et al, 2014).
U.S. Department of Health and Human Services. “Healthy People 2010” and “Healthy People
2020.” Rockville, MD: Author.
Wheeler, L. (2004). “Guidance for health care providers who prescribe life-saving medications for
students with asthma or allergies to self-carry and administer at school.

Minnesota Guidelines for Medication Administration in Schools
50
Revised June 2015
APPENDICES
Minnesota Guidelines for Medication Administration in Schools
51
Revised June 2015
Appendix A: LSN/RN Delegation
Medication Administration Licensed School Nurse/Registered Nurse (LSN/RN) delegation chart
when medication nursing tasks or activities are delegated by the LSN/RN
Medication Administration and Delegation is within the scope of
practice of LSN/RN Nurses in Minnesota
Column 1
Column 2
1. Are there laws or rules in place that
support medication administration
delegation? If yes, continue to # 2,
Column 1.
If no, go to A, Column 2.
A. The Minnesota Nurse Practice Act;
Minnesota Statutes 148.171 to 148.285
allows LSNs/RNs to delegate nursing
tasks and activities, one of which is
medication administration.
Go to Column 1, #2.
2. Is the LSN/RN competent to make
medication administration delegation
decisions (e.g., knowledge of the
medication & side effects)?
If yes, continue to #3,
Column 1. If no, go to B,
Column 2.
B. No, Do Not Delegate
Obtain and document education and
training. When complete…Go to Column
1, #3.
3. Has there been a comprehensive
assessment of the patient’s (student’s)
need for medication administration in the
school?
If yes continue to #4,
Column 1. If no go to C,
Column 2.
C. No, Do Not Delegate
Assess and then proceed with consideration
of delegation
Go to Column 1, #4.
4. Does the Unlicensed Assistive
Personnel (UAP)/Licensed Practical
Nurse (LPN) possess the knowledge
and skills consistent with the
complexity of medication
administration or assistance with self-
administration of medication?
If yes, continue to #5,
Column 1. If no, go to D,
Column 2.
D. No, Do Not Delegate
Provide and document
training/education/skills to the LPN/UAP.
Go to Column 1, #5.
Minnesota Guidelines for Medication Administration in Schools
52
Revised June 2015
Column 1
Column 2
5. Can medication administration be
performed without requiring
comprehensive nursing patient
(student) assessment?
If yes, continue to #6, Column 1. If no, go
to E, Column 2.
E. No, Do Not Delegate
Seek alternative options to provide the
needed assessment and medication e.g.,
refer to home care agency or public health
agency, or provide special needs
assessment and request scheduling changes
and/or hire/contract for additional qualified
staff.
Go to Column 1, #6.
6. Are the effect of the medication being
administered reasonably predictable?
If yes, continue to #7, Column 1. If no,
go to F, Column 2.
F. No, Do Not Delegate
First dose of medication could be supervised
by LSN/RN or have available a list of
specific and potential side effects of the
medication being administered.
Go to Column 1, #7.
7. Can the administration of medication(s)
be safely performed according to exact,
unchanging directions and according to
established procedures?
If yes, continue to #8, Column 1. If no, go
to G, Column 2.
G. No, Do Not Delegate.
8.
Can the medication be safely
administered without comprehensive
assessments?
If yes, continue to #9, Column 1. If no, go
to H, Column 2.
H. No, Do Not Delegate
Seek other nursing and/or licensed health
care provider and supervision.
9. Is supervision and monitoring available? If
yes, continue to #10, Column 1.
If no, go to I, Column 2.
I. No, Do Not Delegate.
10. DELEGATE MEDICATION
ADMINISTRATION
Left blank
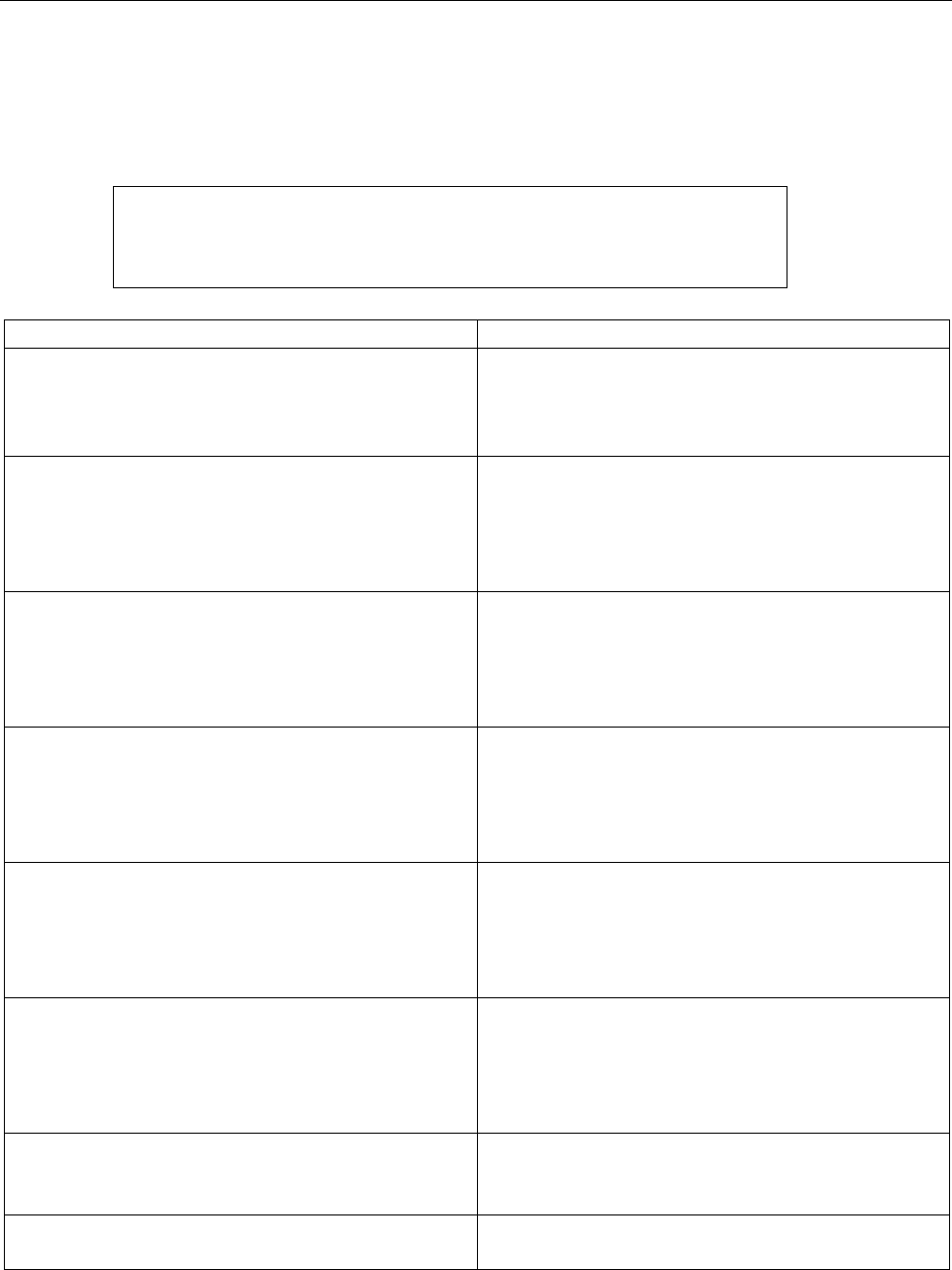
Minnesota Guidelines for Medication Administration in Schools
53
Revised June 2015
Appendix B: LPN Assignment
Medication Administration Licensed Practical Nurse (LPN) assignment chart when nursing tasks or
activities may be assigned
Medication Administration and Assignment is within the scope of
practice of LPNs in Minnesota at the direction of an Advanced Practice
Registered Nurse/Licensed School Nurse/Registered Nurse or other
Licensed Health Care Professional
Column 1
Column 2
1. Are there laws or rules in place that
support medication administration
assignment? If yes continue on in Column
1, #2. If not go to Column 2, A.
A. No, Do Not Assign.
Obtain training and document training. Go to
Column 1, #2.
2. Has there been a patient (student) focused
assessment of the patient’s (student’s)
need for medication administration?
If yes continue to Column 1, #3. If no go
to B, Column 2.
B. No, Do Not Assign.
Provide focused assessment with a call to
the
LSN/RN or licensed health care provider.
Go to Column 1, #3.
3. The UAP or LPN has been trained. If
yes continue to Column 1, #4
If no go to C, Column 2.
C. No, Do Not Assign
Refer to LSN/RN. Have LSN/RN document
education & training necessary. When
complete…
Go to Column 1,#4.
4. Are the effects of the individual
medication being administered
reasonably predictable?
If yes continue to Column 1, #5 If no
go to D, Column 2.
D. No, Do Not Assign
Collaborate and communicate with LSN/RN
on how to proceed.
5. Does the LPN/UAP how have both the
validated training and skills in medication
administration?
If yes continue to Column 1, #6 If no go to
E, Column 2.
E. No, Do Not Assign.
6. Can the medications be safely administered
without further focused assessment?
If yes continue to Column 1, #7 If
no go to F,
Column 2.
F. No, Do Not Assign.
7. Is appropriate monitoring available? If
yes continue to Column 1, #8
If no go to G, Column 2.
G. No, Do Not Assign.
8. ASSIGN

Minnesota Guidelines for Medication Administration in Schools
54
Revised June 2015
Appendix C: Frequently Asked Questions
1. Who is authorized to administer medication in schools?
A variety of individuals can administer medication in school (e.g., licensed school
nurses/registered nurses, licensed practical nurses, unlicensed assistive personnel, secretaries,
teachers, and principals). Parents/legal guardians should be aware of the medication process at
the school their student attends and are to provide the school with written authorization for
school personnel to provide medication to their students.
2. What is nursing delegation?
According to the Minnesota Nurse Practice Act (Minnesota Statutes § Chapter 148.171 Subd. 7b,
delegation means the transfer of authority to another nurse or competent, unlicensed assistive
person to perform a specific nursing task or activity in a specific situation.
3. What is nursing assignment?
According to the Minnesota Nurse Practice Act (Minnesota Statutes § Chapter148.171 Subd. 3a)
assignment means the designation of nursing tasks or activities to be performed by another nurse
or unlicensed assistive person.
4. Is every school system required to employ a school nurse?
No. Minnesota Statutes § Chapter121A.21 specifies that all schools need to provide services to
promote the health of their students. Minnesota Statutes § Chapter121A.21 states that school
districts “with 1,000 pupils or more in average daily membership in early childhood family
education, preschool handicapped, elementary, and secondary programs” are required to have a
school nurse. This is a minimum requirement by state statute. Workload should be looked at and
reviewed when considering school nurse staffing/health services models.
5. Does a school board have to approve a policy regarding medication administration?
Yes; Minnesota Statute § Chapter 121A.22, Subd. 4, specifies that drugs and medicine must be
administered according to the directions on the label and, to the extent possible, in accordance
with policies and rules of local boards of education and developed with health expertise.
6. May a school district apply for a variance from the requirements of the Nurse Practice Act?

Minnesota Guidelines for Medication Administration in Schools
55
Revised June 2015
No. School districts should examine existing policies, procedures, and practices to ensure
compliance with the Nurse Practice Act. Questions regarding compliance with the act can be
directed to the Minnesota State Board of Nursing.
7. Can parents/legal guardians authorize school personnel to give medications to their child?
Yes. According to Minnesota Statutes § Chapter 121A.22, Subd. 1, school personnel can
administer prescription drugs or medicine to a child at the request of the parent. The request can
be either oral or in writing, but an oral request must be provided in writing within two school
days.
8. Is it permissible for parents/legal guardians to come to school to give medication?
Yes, but only for their child. However, parents/legal guardians cannot be required to come to
school to perform the child’s procedure.
9. Can an LSN/RN provide OTC medication to students upon a parent’s request, according to
labeling but without a prescriber’s authorization?
Yes, according to the Minnesota Attorney General’s Office. It is important to note, however, that
the school nurse has the ultimate authority and responsibility to reject a parent’s request and to
decline to administer an OTC medication if the nurse believes that such medication is
unnecessary, inappropriate, or could lead to patient harm. Alternatively, the school nurse and/or
school policy could require a physician’s order to administer the OTC medication.
10. Can parents/legal guardians train school staff on medications related to their child’s specific
diagnosis (e.g., diabetes, epilepsy, asthma, or allergies)?
Parents/legal guardians can be a great source of knowledge regarding their individual child’s
health condition and when the student needs and how the student takes his or her own
medications. Parents/legal guardians have received information and education when their child
was diagnosed and prescribed the medication; they live with and provide for the child at home;
and they might have attended workshops or belong to advocacy organizations. It is appropriate
for the schools to listen to and utilize parents’ knowledge to help accommodate their child in the
school setting. A school nurse will fulfill this training for staff needs when part of the education
team.
11. Can a teaching assistant or secretary administer medication?
Yes. A secretary or other school personnel can administer medication or assist a child in the self-
administration of medication when an LSN/RN has delegated medication administration to that
person and guidelines are followed, including receipt of oral or written permission from a

Minnesota Guidelines for Medication Administration in Schools
56
Revised June 2015
parent/legal guardian. A parent permission form should include the student name, date,
medication name, amount, and instructions on dose, route, and when to take the medication (see
sample form in appendices). If the school has no nurse on staff, school policies and sound
medical procedures must be developed to comply with Minnesota Statutes § Chapter 121A.22,
Subd. 4. See #1 Legal Considerations 1.2 School District Policies for details.
12. Can a teacher or other personnel administer epinephrine in an emergency if a child has an
allergic reaction to a bee sting?
Yes, with or without delegation and with appropriate training and supervision. Minnesota
Statutes § Chapter 144.344 allows health services “to be rendered to minors of any age without
the consent of a parent or legal guardian when, in the professional’s judgment, the risk to the
minor’s life or health is of such a nature that treatment should be given without delay and the
requirement of consent would result in delay or denial of treatment.”
Under Minnesota Statute § Chapter 121A.2207 “districts and schools may obtain and possess
epinephrine auto injectors to be maintained and administered by school personnel to a student
other individual if, in good faith it is determined that person is experiencing anaphylaxis
regardless of whether the student or other individual has a prescription for an epinephrine auto-
injector.”
13. What is the principal’s/administrator’s role in medication administration?
The principal’s/administrator’s responsibility is to assist the school board with development of
the health policy according to Minnesota Statutes § Chapter 121.A22, Subd. 4; hire appropriate
staff members; and supervise the policy’s implementation in the school, ensuring the safety of
students.
Under Minnesota Statutes § Chapter 121A.2205 Subd 2. (f) assist the school board in a definition
of the instructional day for the purposes of the emergency epinephrine auto injector policy.
14. How do you determine if a child is competent to self-administer medications?
Things to be considered include a physician’s/licensed health care provider evaluation and/or
nursing assessment, parent/legal guardian authorization, and the student’s physical and mental
development and age.
To assist in determining if a student is competent to self-administer medication, it might be
useful to list criteria in Minnesota Administrative Rules 9505.0335, Subp. 1(A): “Capable of
directing his or her own care” refers to a recipient’s functional impairment status as determined
by the recipient’s ability to communicate: (1) orientation to person, place, and time; (2) an
understanding of the recipient’s plan of care, including medications and medication schedule; (3)
needs; and (4) an understanding of safety issues, including how to access emergency assistance.

Minnesota Guidelines for Medication Administration in Schools
57
Revised June 2015
15. Is training required for persons assisting with self-administration of medications?
Yes; training must be considered when a registered nurse delegates such assistance. Training is
an essential part of delegation. Training ensures consistent and safe care of students. It is
recommended that back-up personnel be trained at each school site. Training must be provided
for school personnel who administer emergency medications such as rescue inhalers, Diastat™,
epinephrine auto injectors, and Glucagon™.
16. Must the delegating nurse provide all the training of the UAP?
No. Some educational institutions and community colleges provide in-service or orientation
programs that include the information and skills training needed to perform medication
administration. The delegating nurse should ensure the competency of the individual trained;
documentation of training and competencies should be in the delegatee’s personnel file.
17. Can a student who has diabetes perform his/her own glucose monitoring and insulin
administration, either by syringe or pump?
Yes. If not done by the student, it may be performed by an LSN/RN or delegated to others who
are trained to assist in the procedure. Consider the development of an IHP to better communicate
actions and expectations.
18. As an LSN/RN, am I accountable for the acts of a UAP when I delegate medication
administration to that individual?
Delegation standards require LSNs/RNs, in keeping with their nursing scope of practice, to
assess the student, determine the care needs of the student, determine whether the particular
function is appropriate to delegate, determine whether the trained UAP has the skills needed to
safely perform the task, and determine whether the appropriate supervision is available.
The trained UAP is responsible for performing the activity according to the delegation of the
LSN/RN. If the UAP deviates from proper procedure and it is determined that the LSN/RN has
appropriately delegated and trained the medication administration activity, the LSN/RN has
fulfilled the duties of proper delegation.
19. May an LPN supervise or direct the nursing practice of LSNs/RNs?
No. Supervision of nursing personnel is not within the legal scope of practice of the LPN.

Minnesota Guidelines for Medication Administration in Schools
58
Revised June 2015
20. Can an LPN delegate medication administration to a UAP?
Delegation is not within the LPN’s scope of practice.
21. Can an LPN assign medication administration to another LPN and UAP?
Yes. Assignment of nursing tasks and activities are within the LPNs scope of practice. The type
of medication administration must be within the LPNs scope of practice and training. The UAP
must have the appropriate delegation and training from the LSN/RN.
22. Must medication administration be re-delegated each day?
No. When medication administration is delegated, the LSN/RN should periodically assure the
medication administration delegated is completed as directed.
23. Why is documentation stressed related to medication administration?
Documentation can be critical evidence in the event the delegation or delegated services are
challenged legally. Appropriate documentation serves as additional protection for the delegating
nurse, the UAP, and the student receiving the medication.
24. When the health records of students do not impact the students’ education or academic
performance, does being a member of the school staff automatically qualify as “a legitimate need
to know”?
No. The FERPA regulations say student records may be released to school officials “whom the
agency or institution has determined to have legitimate educational interests.” 34 C.F.R. § 99.31
(2004). Not all school staff will have “legitimate education interests” in the information. The
school district must set policy on release of information, within the limits of the FERPA
regulations.
25. Can the task of medication administration by gastrostomy-tube, insulin pump, or injection be
delegated?

Minnesota Guidelines for Medication Administration in Schools
59
Revised June 2015
Yes, by delegation from an LSN/RN and the student’s 504 plan, IEP, or IHP. The LSN/RN will
train and supervise the person to whom the medication administration is delegated. If the school
has no nurse on staff, school policies and sound medical procedures must be developed in
adherence to Minnesota Statutes § Chapter121A.22, Subd. 4.
26. Can a volunteer administer medication on a field trip?
Yes. Each school district should have a set of policies on medication administration that can be
followed on school-sponsored field trips.
One option is to take the medication in its original container and put it in a small, zip-lock bag
along with a copy of the prescriber’s orders and a copy of the parent/legal guardian authorization
form. Pharmacy law allows medications to be administered if in the original container.
(Minnesota Statute. § Chapter 151.37 Subd 7 (Legend Drugs, Who May Prescribe, Possess) Send
that package with the person who is delegated or assigned/designated to administer medications
on the field trip. The school district should establish a document and process for check-in and
check-out of medications for field trips.
A second option is that the parent/legal guardian provide the required amount of medication
(depending on the length of the trip) in a separate pharmacy container with an original label (i.e.,
an extra from the provider or pharmacist), with a copy of the physician’s/licensed health care
providers orders and a copy of the parental/legal guardian authorization form specific to the
event or trip. This may be useful for any trips that exceed one day in length.
A third option is that the policies may allow the preparation of a supply of medications by the
LSN/RN or parent/legal guardian, not to exceed the duration of the trip, in paper envelopes or
other more suitable containers for use by a student temporarily off-campus. A container may
hold only one medication. A label on the container must include the date, the student’s name, the
school, the name of the medication, the purpose, the side effects, its strength, dose, and time of
administration, pharmacy, pharmacy phone number, prescription number, and the initials of the
person preparing the medication and label. Accompanying the envelope will be a copy of the
prescriber’s orders and the parental authorization form. Note that the additional steps involved in
transferring medication to an envelope present an- other opportunity for medication error.
Some schools provide a designated volunteer with appropriate health information on students
requiring medication administration, medication in properly labeled bottles, and forms on which
to document medication administration. The school should provide a job description for the
medication administration volunteer, make sure the volunteer has the education and training
necessary to safely administer the medication, verify and document his or her competencies, and
provide procedures for how medication administration is handled on field trips. The volunteer
needs to follow the procedures.

Minnesota Guidelines for Medication Administration in Schools
60
Revised June 2015
When a volunteer is used, parents must be informed and sign a health data privacy release form.
Some experts (Schwab, 2001) recommend the volunteer be paid, even nominally, as a school
employee, perhaps as a substitute. In so doing, the volunteer becomes a school employee and is
bound by policies on medication administration including documentation and data practices.
Although parents/legal guardians can accompany students on field trips, it is not a requirement
for students with medication needs. Staff designated the responsibility for medication
administration should be trained and accompany the student and ensure that all the medical
supplies are brought along and appropriate documentation is completed.
The plan for coverage and care during extracurricular activities sponsored by the school that take
place outside of school hours should be carefully set out in the student’s health/education plan
(504, ECP, IEP, or IHP).
27. Does the school district medication administration policy apply to summer school?
Yes, unless the school district has a separate policy specific to summer-school activity.
28. Are schools and school systems required to make reasonable accommodations for students who
require medication administration during on-site sporting activities?
Yes. Federal law requires student accommodations for extracurricular and athletic activities
(U.S. Department of Education, Office of Civil Rights, Dear Colleagues letter 01-25-13).

Minnesota Guidelines for Medication Administration in Schools
61
Revised June 2015
Appendix D: State of Minnesota Office of the Attorney General Letter
February 14, 2000
Minnesota Guidelines for Medication Administration in Schools
MIKE HATCH
ATTORNEY GENERAL
STATE OF MINNESOTA
OFFICE OF THE ATTORNEY GENERAL
February 14, 2000
SUITE 1100
445 MINNESOTA STREET ST.
PAUL, MN 55101-2128
TELEPHONE: (651) 282-5700
Mr. Ralph Christofferson
Superintendent
Lake of the Woods ISD #390
P. 0. Box 310 - Highway 11 West
Baudette, MN 56623
Re: Authority of School Nurses to Provide Non-Prescription Medications
Dear Mr. Christofferson:
This opinion is issued under Minn. Stat. § 8.07 (1998) in response to your question
regarding the authority of school nurses to provide non-prescription medications to students upon
a parent's request.
The duties and authority or nurses are set forth in the Minnesota Nurse Practice Act
("MNPA"). The MNPA defines the practice of professional nursing to include both
"independent nursing functions" as well as "delegated medical functions." Minn. Stat. §
148.171(3) (1998). The MNPA makes no reference to any required procedures for nurses to
follow regarding non-prescription medications. Nor does the MNPA address the dispensing of
medications to students by school nurses.
A separate Minnesota statute, Minn. Stat. § 121A.22 (1998), sets the procedures that
school personnel must follow in dispensing prescription medications to students. This statute
states that school personnel must first receive a request from a student's parent to administer
prescription medications. The statute further provides that the medication must be in a container
with a label prepared by a pharmacist, must be administered in a manner consistent with
instructions on the label, and must be administered by a school nurse, a public or private health
related organization, or any other party where an agreement has been approved by the
Commissioner of Children, Families and Learning. The above statute specifically exempts the
administration of medication if it is purchased without a prescription, if it is for a student who is
18 years of age or older, if it is administered off school grounds, if it is used in connection with
athletics or extra-curricular activities, or if it is administered by a public health agency. It is
therefore clear that section 121A.22 provides no restrictions on school personnel administering
non-prescription drugs.
The Minnesota Board of Nursing, however, has taken the position that a school nurse
cannot administer over-the-counter medicine to a student at the parent's request, unless
authorized by a doctor's order. In so doing, the Nursing Board states that under the Medical
Practice Act ("MPA") a person is "practicing medicine" and needs to be licensed as such if the
Facsimile: (651) 282-5382 • TTY: (651) 296-1410 • Toll Free Lines: (800) 657-3787 (Voice), (800) 366-4812 (TTY) • http://www.ag.state.mn.us
An Equal 0pportunity Employer Who Values Diversity
Printed on 50% recycled paper (15% post consumer content)

Mr. Ralph Christofferson
February 14, 2000
Page 2
person "administer[s] any drug or medicine for the use of another." Minn. Stat. § 147.081, subd.
2 (1998). The Nursing Board notes that the term "drug or medicine" is not defined in the MPA
and therefore presumes that it includes both prescription and non-prescription medications.
Accordingly, the Nursing Board concludes that providing non-prescription medications to
another person is a "medical function" that must be delegated to a nurse by a physician. This
office disagrees with the Nursing Board's legal analysis, at least as it applies to situations such as
the one raised by your question.
The Board's position would lead to the conclusion that any parent who gives a child a
1
Tylenol tablet, an antibiotic ointment, or even cough medicine,
would be engaged in the
unauthorized practice of medicine and therefore would be guilty of a gross misdemeanor. Minn.
Stat. § 147.081, subd. 2 (1998). Similarly, under the Nursing Board's interpretation, any caregiver
or person responsible for the well being of a child, elderly parent, or anybody else would need a
physician's order before providing any over-the-counter medications to that person. This
interpretation would mean that millions of Minnesotans have engaged in an unauthorized
practice of medicine if they have entered a drug store and bought over-the-counter medicines for
use by a family member.
It is well settled under Minnesota law that statutes are to be construed to avoid a result
2
that is "absurd, impossible of execution, or unreasonable." Minn. Stat. § 645.17(1).
Indeed, our
laws must be construed in a "sensible" fashion. See Thoresen v. Schmahl, 24 N.W.2d 273, 277
(Minn. 1946). As indicated above, the conclusion that, for example, a parent cannot administer
a non-prescription medication to his or her child, absent a physician's order, leads to an absurd
and nonsensical result. Construing the MPA to require a physician's order for the administration
of non-prescription medications in that and similar situations clearly produces the type of result
that must be avoided in interpreting state laws.
Equally absurd and nonsensical is the proposition that a parent cannot request other
persons temporarily responsible for the care of their children to provide the requested non-
prescription medications. Examples of people that parents may entrust with the care of their
1
Under Minnesota law, a parent, guardian, or caretaker "who willfully deprives a child of necessary food, clothing,
shelter, health care, or supervision" is guilty of "neglect or endangerment." Minn. Stat. § 609.378, subd. 1 (1998).
See also Minn. Stat. § 626.556, subd. 2(c) (1998) (providing that parents, guardians, and other caregivers must
"supply a child with necessary food, clothing, shelter, or medical care when reasonably able to do so").
2
See Wegener v. Commissioner of Revenue, 505 N.W.2d 612, 617 (Minn. 1993) (stating that the courts are
"obliged to reject a construction that leads to absurd results" and "it is necessary to look to the purpose for
which the statute was enacted"); see also Guderian v. Olmsted County, 595 N.W.2d 540, 542 (Minn. Ct. App.
1999) (stating that when faced with an "absurd result, courts must look beyond a statute's literal meaning to
ascertain and fulfill the legislature's intent").

Mr. Ralph Christofferson
February 14, 2000
Page 3
children include other family members, daycare providers, babysitters, and school personnel. It
would be unreasonable to suggest that a parent must obtain a physician's order each time a
parent requests that any of these individuals provide non-prescription medications to a child.
Moreover, in many cases it would be impractical or even logistically impossible for parents to obtain
a physician's order before asking another person taking temporary care of a child to provide a non-
prescription medication to the child. Accordingly, this interpretation of Minnesota law surely does
not reflect legislative intent.
It should also be noted that the Nursing Board's interpretation relies on the definitions of
"drug" and "medicine" in a separate statute that regulates pharmacists. The Pharmacy Act, set forth
as Chapter 151 of Minnesota statutes, specifically states that the definitions utilized in that chapter
apply "for the purposes of this chapter." Minn. Stat. § 151.01, subd. 1 (1998). The definitions in
chapter 151 therefore do not apply to or control the use of the term "drugs" or "medicines" in other
provisions of the Minnesota statutes. Further, other provisions of the Minnesota statutes contain
specific regulations for "prescription" drugs, which establishes that prescription drugs are subject to
more stringent regulation and control than non-prescription drugs. For instance, if non-prescription
drugs were to be treated in the same manner as prescription drugs, there would be no need to have an
exclusion for non-prescription drugs in the statute that sets forth procedures for school nurses to
follow in dispensing prescription medications. Minn. Stat. § 121A.22 (1998). In other words, if non-
prescription and prescription drugs both required a physician's order before a school nurse could
dispense them, then it is difficult to understand why the Legislature excluded non-prescription
drugs from the statute.
For the above reasons, this office concludes that school nurses do have the authority to
provide over-the-counter medications to students upon a parent's request, even without a physician's
order. It is important to note, however, that the school nurse has the ultimate authority and
responsibility to reject a parent's request and to decline to administer an over-the- counter medication
if the nurse believes that such medication is unnecessary, inappropriate, or could lead to patient
harm. Further, school districts retain independent authority to implement policies that govern the
administration of non-prescription drugs by school nurses. A school district, or an individual nurse,
could choose to adopt a policy that requires a physician's order before a school nurse administers a
non-prescription medication to a student.
I thank you for seeking our opinion regarding this issue.
Very truly yours,
AG: 357648.v. 01
Alan Gilbert
Chief Deputy and Solicitor General
Appendix E: Information about the 2005 Guidelines Development
The comprehensive process of developing the Minnesota Medication Administration Guidelines for
Schools involved a broad search and rigorous evaluation of pertinent literature, including numerous
states’ standards and guidelines, and analysis of key concepts. From an initial pool of 686 pieces of
literature published from 1990 to 2004, 475 of the highest quality were selected for evaluation by 16
trained graduate students and Minnesota Department of Health staff members who scored them
using a system of 51 criteria and reported results on an online database. The top-ranking literature
was then examined by expert panels held throughout the state and made up of 193 parents,
educators, school administrators, nurses, other health professionals, paraprofessionals, regulatory
board representatives, and advocacy group members, among others. Expert panelists drew from the
literature a long list of key concepts that they considered most significant for inclusion in the
Minnesota Guidelines. These concepts were sorted into categories that form the 10 content areas in
the final Minnesota Guidelines.
The reviewers also utilized medication guidelines from other states for review. Appreciation goes to
the numerous individuals, ad hoc groups, and multidisciplinary teams of students, health and
education professionals, and parents who contributed across the state. Literature evaluators, who
spent hundreds of hours reading, analyzing, scoring, and reporting on articles and books, and
members of the multidisciplinary work group are listed in the appendices. The initial 2005 work
group, which provided direction for this project, represented 20 statewide agencies and
organizations.
Additional acknowledgement for the 2005 document goes to the core Minnesota Department of
Health team –– Gwen Willems, Kathy Wittnebel, Cheryl Smoot, Nancy Blume, Gretchen Griffin,
Sue Strohschein, Kathy Wick; members of the State Interagency Staff Team –– Joan Lee, Minnesota
Department of Health; Gayle Hallin, formerly Minnesota Department of Health; Shirley Brekken
and Mariclaire England, Minnesota Board of Nursing; Cathy Griffin, Ruth Ellen Luehr, and
Debbykay Peterson, Minnesota Department of Education; Jan Bodnia, formerly Minnesota
Department of Education; Colleen Olson, Minnesota Department of Human Services; and Pat
Brandstaetter, Northeast Service Cooperative.
65
Revised June 2015

