i
iii
Table of Contents
Abstract Page IV
1. Background and Model Overview Page 1
2. Scope of the Proposed APM Page 6
3. Quality and Cost Page 8
4. Payment Methodology Page 9
5. Value over volume Page 10
6. Flexibility Page 13
7. Ability to be evaluated Page 13
8. Integration and Care Coordination Page 15
9. Patient Choice Page 16
10. Patient Safety Page 17
11. Health Information Technology Page 18
12. Supplemental Information Page 20
Appendices
I. Abstract: Validation of American Gastroenterological Association’s Crohn’s
Disease Care Pathway
II. Abstract: Project Sonar: Improvement in Patient Engagement Rates Using a
Mobile Application Platform
III. Abstract: Project Sonar: Validating a Cost Normalization Methodology in a
Community-based Registry
IV. Project Sonar Abstract of Distinction: Digestive Disease Week 2016
V. Guide to the use of Crohn’s CDS Tool
VI. AGA Crohn’s Disease Care Pathway Risk Assessment
VII. SonarMD Nurse Care Manager Dashboard
VIII. SonarMD Patient Survey
IX. Examples of SonarMD Ping Reports
X. SonarMD Cost Report - Graphic
iv
Project Sonar Abstract
Project Sonar (PS) is a care management program developed by community-based physicians in
partnership with a major payer to improve the management of patients with chronic disease.
The key to the success of PS is the combined use of evidence based medicine coordinated with
proactive patient engagement. The goal of PS is to move physicians from a dependency on fee
for service medicine into value based practice. The initial chronic disease category chosen by
PS was Inflammatory Bowel Disease (IBD), a family of disorders that are high cost and high risk
with a frequency that has been increasing over the past few decades.
In addition to high cost and high risk, CD is also associated with a high variability in outcome
and cost. We term this combination of factors as “High Beta”
and believe that chronic illnesses
can be stratified into high beta and low beta based upon an analogy from the financial industry.
The essential features of PS for the management of patients with chronic conditions, a PFPM,
are:
Evidence Based Guidelines are used to direct the course of care. These are embedded
into the EMR through use of CDS tools
All patients are risk assessed using a set of biopsychosocial measures
All patients are enrolled in a web-based communication platform; if not web- or smart-
phone enabled, they are engaged by phone calls from the NCM
Every patient is proactively ‘touched’ at least once a month; more frequently as needed
A team based care model has been incorporated into the practice
Clinical and financial data are analyzed
The care pathway is continually refined through the development of care management
algorithms
We intervene before patients even realize they need care

1
PTAC Proposal – Project Sonar
1. Background and Model Overview
In the United States, chronic diseases accounts for an estimated 83% of total U.S. health
spending and virtually all (99%) of Medicare’s expenditures are for beneficiaries with at least
one chronic condition.
12
Project Sonar (PS) is a care management program developed by community-based physicians to
improve the management of patients with chronic disease, using evidence based medicine
coordinated with proactive patient engagement. Project Sonar was initially deployed in 2012 by
the Illinois Gastroenterology Group (IGG), a 50-physician practice with locations in Cook, Lake,
Kane, and DuPage counties. IGG is the largest single-specialty, non-academic, Gastroenterology
practice in Illinois. As envisioned by the leadership of IGG, the goal of PS was to move
physicians from a dependency on fee for service medicine into value based practice. As part of
this exercise, IGG analyzed their practice demographics by conditions / diagnoses, procedures,
age, payor mix, etc. and confirmed that the most significant chronic disease in a community-
based Gastroenterology (GI) practice is Inflammatory Bowel Disease (IBD), which includes
Crohn’s Disease and Ulcerative Colitis. When factoring in the costs of pharmaceuticals,
whether physician or patient administered, IBD is responsible for almost 25% of the services
generated by IGG and likely most other community-based GI Groups. IBD disorders are high
cost (due to hospitalizations for complications and use of biologic medications) and high risk
(loss of intestine, infections, development of cancers and extra-intestinal manifestations) with a
frequency that has been increasing over the past few decades. After evaluating other chronic
conditions managed by a community-based GI practice, such as GERD / Barrett’s esophagus,
celiac disease, and chronic pancreatitis, the group determined that Crohn’s Disease (CD) was
most appropriate for the development of a chronic care management program.
In addition to high cost and high risk, CD is also associated with a high variability in outcome
and cost. We term this combination of factors as “High Beta”
3
and believe that chronic illnesses
can be stratified into high beta and low beta based upon an analogy from the financial industry.
In finance, “beta” is a measure of a stock's volatility in relation to the market
4
. The market has a
beta of 1.0, and individual stocks are ranked according to how much they deviate from the
market. A stock that swings more than the market over time has a beta above 1.0. As beta is a
measure of risk, a beta greater than one generally means that the asset is volatile.
1
Gerteis J, Izrael D, Deitz D, et al. Multiple Chronic Conditions Chartbook. AHRQ Publications No, Q14-0038.
Rockville, MD: Agency for Healthcare Research and Quality; 2014.
2
Partnership for Solutions. Chronic Care: Making the Case for Ongoing Care (2010 Update). February 2010.
3
Kosinski L, Brill J. The Promise of Patient Self-Monitoring: An App a Day Won’t Necessarily Keep the Doctor Away.
Clinical Gastroenterology and Hepatology, December 2016; 1751-1752
4
Sharpe W. Portfolio Theory and Capital Markets. June 1970, McGraw Hill, New York NY

2
This same analogy can be applied to most chronic illnesses. Examples of other high beta
illnesses include asthma, chronic obstructive pulmonary disease, heart failure, end-stage liver
disease, and type 1 diabetes, while examples of low beta illnesses include hypertension,
diabetes, and hyperlipidemia. There are high beta periods in low beta illnesses.
IGG is contracted with every major commercial payor operating in Northeast Illinois, including
Aetna, Blue Cross Blue Shield of Illinois (BCBSIL), Cigna, Humana, and United. Based on their
own internal analysis of data, IGG met with all the payors, and BCBSIL was willing to work with
the group to analyze this issue. A review of commercial claims for 21,000 patients with a ICD-9
diagnosis consistent with CD for the years of 2010 and 2011 revealed:
The annual cost per patient with a diagnosis of CD was $11,000 (2011 data)
The overall hospitalization rate for patients with CD was 17%
Over 50% of the expenditures incurred were for inpatient care for the treatment of
complications of CD
Although 1/3 of the total spend was for physician services, only 3.5% of the total spend
was for gastroenterology care.
Over 2/3 of the patients who were admitted to a hospital for a complication related to
CD had no identifiable contact (based on claims data) with a provider in the 30 days
prior to the admission
Based on this data, we asked the following questions:
Is there a way to decrease the cost of care of patients with CD by decreasing the
complication rate through better medical management?
Is there a way to identify the high-risk patient with CD before complications ensue?
Is there a way to channel the care of these patients to those healthcare professionals
who have the most knowledge, experience and expertise?
Is there a better way to engage our patients so that their early warning signs can be
assessed even before they realize they need intervention?
While IGG was analyzing and researching these questions, the American Gastroenterological
Association developed and published a care pathway for the management of Crohn’s Disease.
AGACDCP
5
. The recommendations in the pathway are as follows:
5
Sandborn WJ. Crohn's Disease Evaluation and Treatment: Clinical Decision Tool. Gastroenterology 2014;147:702-
705.
3
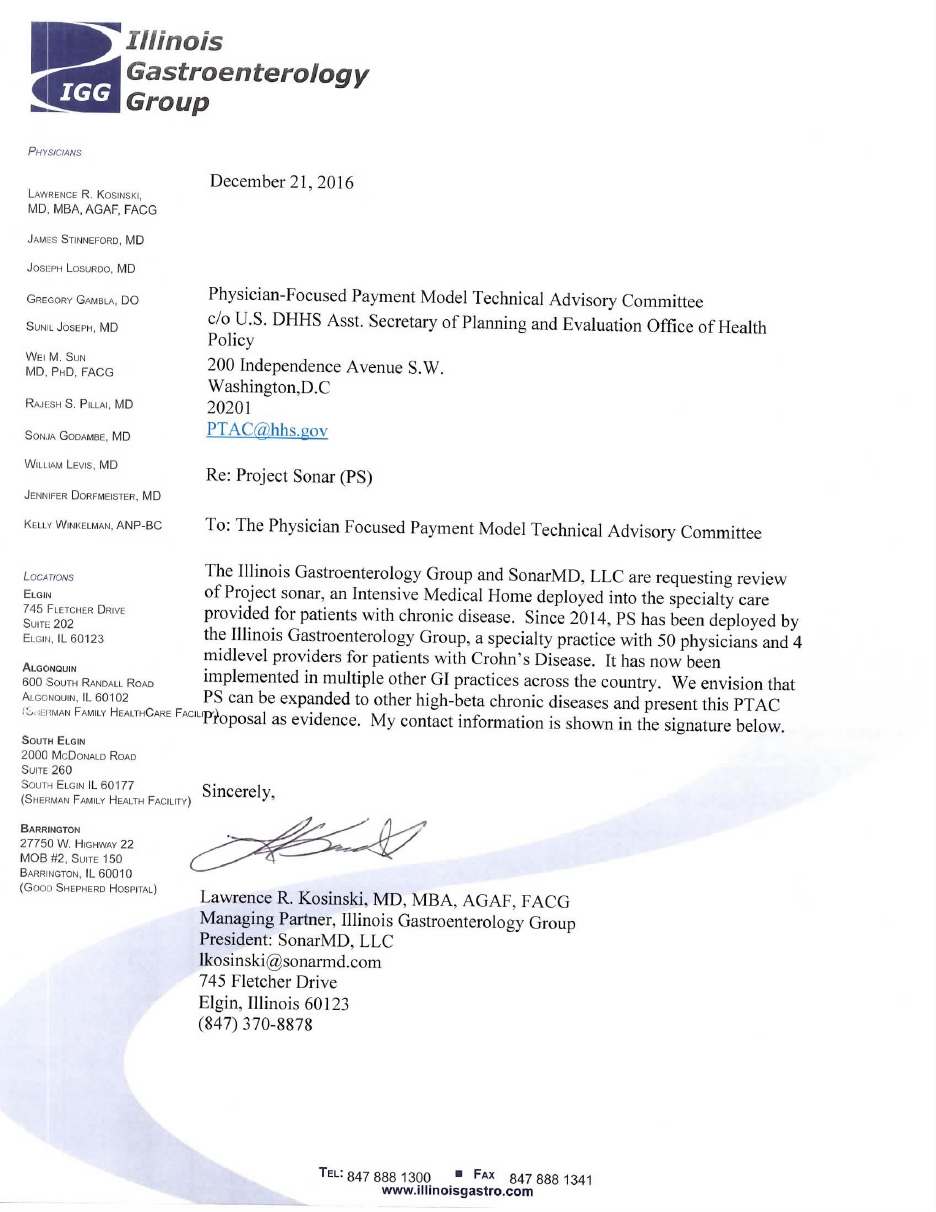
To reduce potentially avoidable hospitalizations and to control the expense of those who are
hospitalized, physicians must work with patients to control complications, which requires
physicians to identify the high-risk patient and control their inflammation. This includes a
biopsychosocial risk assessment that will identify the biological markers of risk and assess the
patient for anxiety/depression along with their social environment.
The ensuing management requires a team-based approach deploying Clinical Decision Support
(CDS) tools to guide healthcare professionals on optimal care, appropriate use of anti-tumor
necrosis factor (TNF) and other biologic medications, and incorporation of Nurse Care
Managers (NCMs) as the focal point in the team that was engaging with and managing the
patient. Importantly it requires the engagement of the patients with the use of “hovering
tools” to non-intrusively monitor the patient’s symptoms, in effect creating a “sonar system” to
ping them in their usual environment on a periodic basis. Collectively, the goal of PS was to
engage those patients who might otherwise minimize the severity of their disease, identify
patients who were depressed and/or at risk of decompensation, and optimize patients on
appropriate pharmaceutical treatment as early as possible, with the objectives of improving
patient quality of life and decreasing costs through reducing potentially avoidable
complications, emergency department (ED) visits, and inpatient (IP) admissions.
PS was deployed in IGG in 2013, initially in a pilot study population of 50 patients with CD. CDS
tools designed around the AGACDCP and a hovering tool using the Crohn’s Disease Activity
Index (CDAI) were deployed into IGG’s NextGen electronic medical record (EMR) system. Using
the EMR practice portal, patients were sent a subset of questions derived from the CDAI at the
beginning of each month. This subset of the CDAI returned a score (Sonar Score) that applied a
numeric value to the patient. At the end of the first year, the hospitalization rate for these
patients decreased from 17% to 5%.
4
IGG presented the data from this pilot to BCBSIL. Based on the findings from the pilot, BCBSIL
partnered with IGG to create its first specialty-based Intensive Medical Home (IMH). Using a
model similar to what it had deployed in its primary care PCMH, BCBSIL attributed 303 patients
with CD to IGG of which 185 were enrolled, and the IMH project, which went live on Dec. 1,
2014 was based on the clinical structure described above. The practice receives a supplemental
per member per month (PMPM) payment to cover the infrastructure for participating in PS.
The PMPM payment is additional to fee for service payment and varies on an annual basis,
adjusted based upon mutually agreed-upon goals for the clinical and financial performance of
the patients enrolled. The practice receives one year of historical claims data on its attributed
patients and quarterly medical and pharmacy claims data going forward. The practice is
responsible for calculating the performance of physicians at an individual, strategic business
unit (SBU), and practice level, including comparison of BCBSIL patients depending on their level
of engagement (‘pinger’ vs. ‘nonpinger’) and comparison to patients enrolled in other
commercial and government (Medicare, Medicaid, Tricare) programs.
Early on, it became clear that the EMR patient portal would not sustain the level of patient
engagement required for adequate care. It was replaced with a web and mobile-based
platform which includes interactive text messages to patients, and patient response data which
drops directly into the EMR using a HIPAA-compliant HL7 interface. Patient engagement
increased from 27% to 75-80% which has now been sustained for over 20 months.
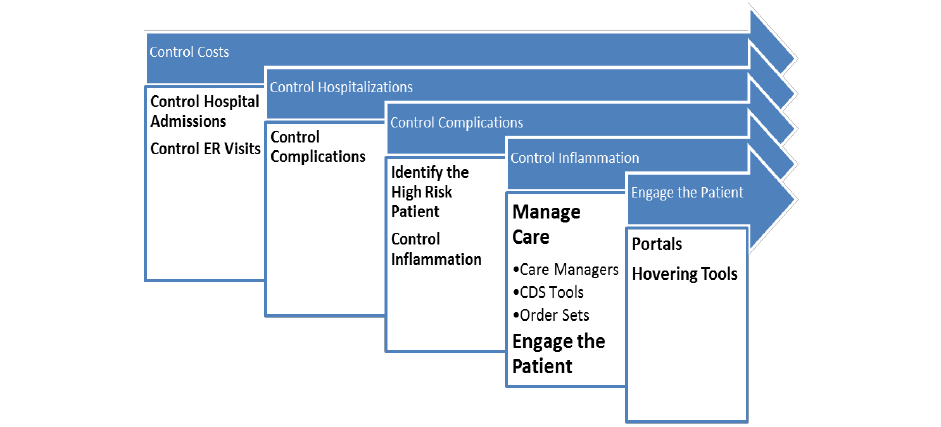
The initial first full year of clinical, financial, and patient engagement data for PS are shown in
the graphic below which was presented as a Distinguished Abstract at Digestive Disease Week
2016:
The data below are normalized to
Medicare payment to emphasize true
utilization rates. They show:
A net decrease in cost of 9.87%
even with an 8.97% increase in
infusible biologics and Net of
PMPM payments to the practices
A 57.14% decline in inpatient costs
driven by an equivalent decline in
admissions/complications
5
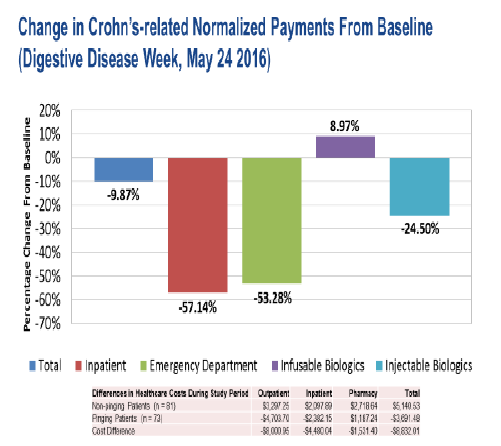
These financial results are highly dependent
upon the patient engagement. When we
filter our patient population by those who
respond to at least 50% of their monthly
surveys (pingers) vs. those who do not
respond (nonpingers), the cost differential of
care falls 18% in the Pinger group whereas it
rises 23% in the nonpinger group. This 41%
difference in cost is shown in the figure
below.
Thus, the cost savings is highly correlated to patient engagement, as it is derived from those
patients who respond. Patient engagement is key to the success of PS and for the care of
patients with chronic disease. Our results, which we believe are generalizable to other high-
beta chronic conditions and to high beta periods in low beta conditions, lead to a model that
must incorporate the use of evidence based medicine and, more importantly, must provide for
ongoing patient engagement which is integrated into the workflow of care.
Key to the success of a management program for a chronic condition must be the use of
appropriate risk measures. Every patient in PS is initially assessed using the risk assessment
tool embedded in the AGACDCP, which includes 26 biopsychosocial risk metrics in three
categories: Inflammation Risk, Disease Burden Risk and Comorbidity Risk. Multiple linear
regression analyses of each risk measure against the Crohn’s Related Cost of Care has helped us
to identify which measures hold predictive value. This has led to further refinement of the
processes within PS.
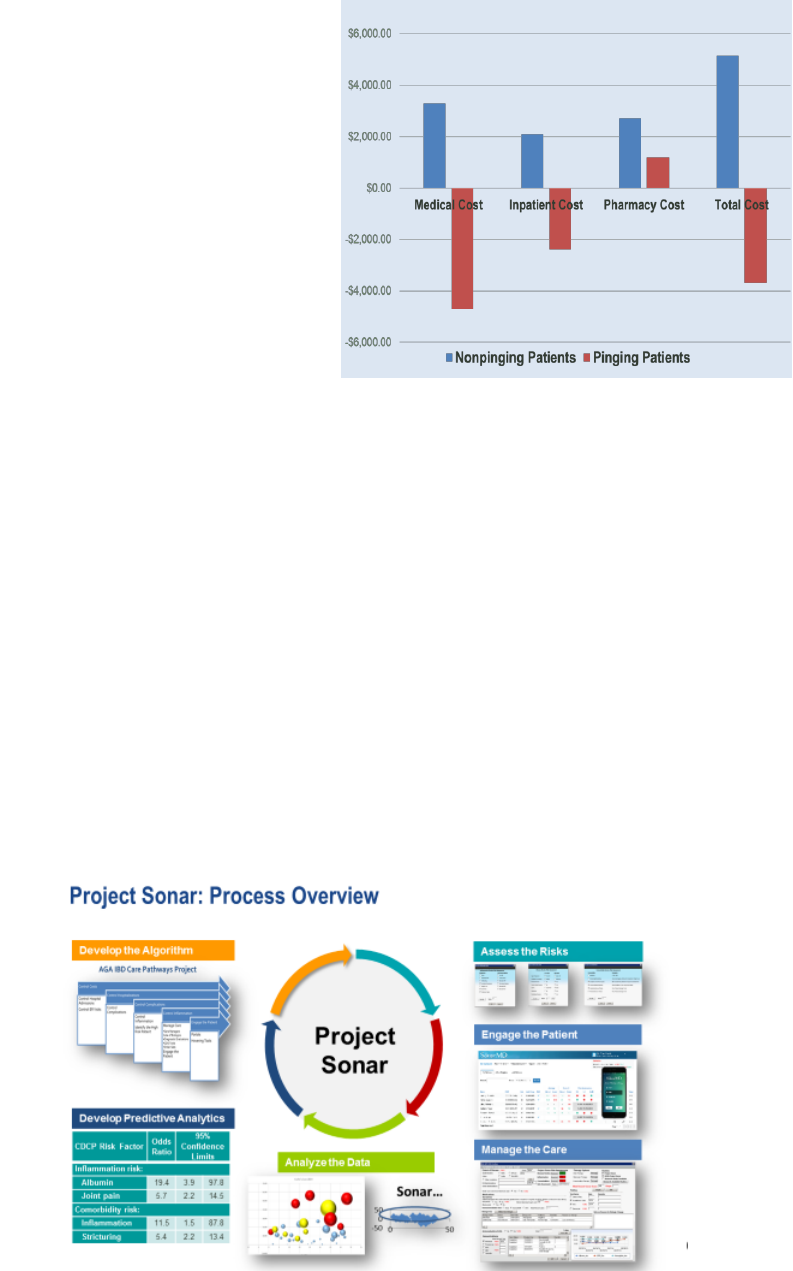
A process overview of PS is shown below:
6
The essential features of PS for the management of patients with chronic conditions, an APM,
are:
Evidence Based Guidelines are used to direct the course of care. These are embedded
into the EMR through use of CDS tools
All patients are risk assessed using a set of biopsychosocial measures
All patients are enrolled in a web-based communication platform; if not web- or smart-
phone enabled, they are engaged by phone calls from the NCM
Every patient is proactively ‘touched’ at least once a month; more frequently as needed
A team based care model has been incorporated into the practice
Clinical and financial data are analyzed
The care pathway is continually refined through the development of care management
algorithms
We intervene before patients even realize they need care
2. Scope of Proposed APM
This proposal to the PTAC will expand CMS’s APM Portfolio in the following ways:
It will move providers, especially specialists, from fee for service to reimbursement
based on value based payment methodologies. It is addressing an issue in payment
policy in several ways:
o Moves patient care from reactive to proactive.
o Focuses on early identification of potential problems and complications,
encouraging ‘preventive’ management
o Rewards physicians and other qualified healthcare professionals for ‘doing the
right thing’ in a team-based manner, as opposed to reimbursement solely on an
RVU-based methodology.
It will promote “cost sensitivity” in specialist providers who are currently almost
exclusively paid on a fee for service basis. This will promote the inclusion of APM
entities for specialists whose opportunities to participate in APMs has been limited.
It will link payment for specialist services to clinical, financial, and patient reported
outcomes.
It will allow specialists to participate in value based care outside of an ACO / MSSP /
CRC+ model.
It will allow physicians to participate in value based care for chronic conditions that are
not triggered by a surgical procedure on an inpatient or outpatient basis.
Specialists want to be part of the value based solution but have not been fully able to exert the
powerful force they have on cost containment and care improvement. The majority of CMS /
CMMI initiatives to date have focused on ACOs, primary care based models, or conditions

7
triggered by a hospital procedure (orthopedic, cardiac). This has left the specialist out of the
solution and kept them as part of the problem.
The patient has also been left out of the solution. Few value based models built around ACOs
maintain a focus on patient engagement as a value-added solution. This is exacerbated by
initiatives based on hospitalization triggers which do not have an outpatient focus on chronic
management.
Most serious chronic illnesses are managed by specialists who are still paid under fee for
service. PS shows how a specialty group in partnership with a major payer can move from FFS
to value-based care and demonstrate cost-savings with improved patient quality of life. We
believe this model, which has been proven in patients with IBD, is applicable to other
conditions.
Although PS focused on CD, this model can be applied to other chronic illnesses. As noted
earlier, we believe that chronic illnesses can be stratified into high beta and low beta. Some
chronic diseases, like diabetes mellitus, hypercholesterolemia and hypertension, can be slow
and indolent in the expression of their symptoms and morbidities, which we term as “low-beta”
diseases. Other conditions, such as inflammatory bowel disease (IBD) are “high-beta”
conditions that are not as forgiving in their disease progression
67
. There are several high-beta
conditions including asthma, heart failure, chronic obstructive pulmonary disease, end-stage
liver disease, rheumatoid and psoriatic arthritis, cancers, malnutrition and other conditions
where patients are at risk for frequent, potentially avoidable, emergency department visits and
hospitalizations
8
. Even diseases like diabetes may have high beta periods, such as the period
following an admission for diabetic ketoacidosis or when patients have poor control of / high
fluctuations in blood sugar / hemoglobin A1c levels. Although most of the chronic care of
patients with low beta diseases can safely be provided by PCPs, the intervening high beta
periods most often require the care of a specialist. The PS platform can be applied to high beta
illnesses as well as the high beta periods embedded in the management of low beta chronic
diseases.
We believe that PS has applicability to many patients with chronic disease and would be
appropriate for use by primary care and specialist physicians and qualified healthcare
professionals, both cognitive and procedural.
6
Natarajan Y, Kanwal F. Pay for Performance in Chronic Liver Disease. Clin Gastroenterol Hepatol. 2015
Nov;13(12):2042-7.
7
Fortune BE, Golus A, Barsky CL, et al. Linking a Hepatology Clinical Service Line to Quality Improvement. Clin
Gastroenterol Hepatol. 2015 Aug;13(8):1391-5
8
Kosinski L, Brill JV. The Promise of Patient Self-Monitoring: An App a Day Won’t Necessarily Keep the Doctor
Away. Clinical Gastroenterology and Hepatology 2016; 14: 1751 - 2
8
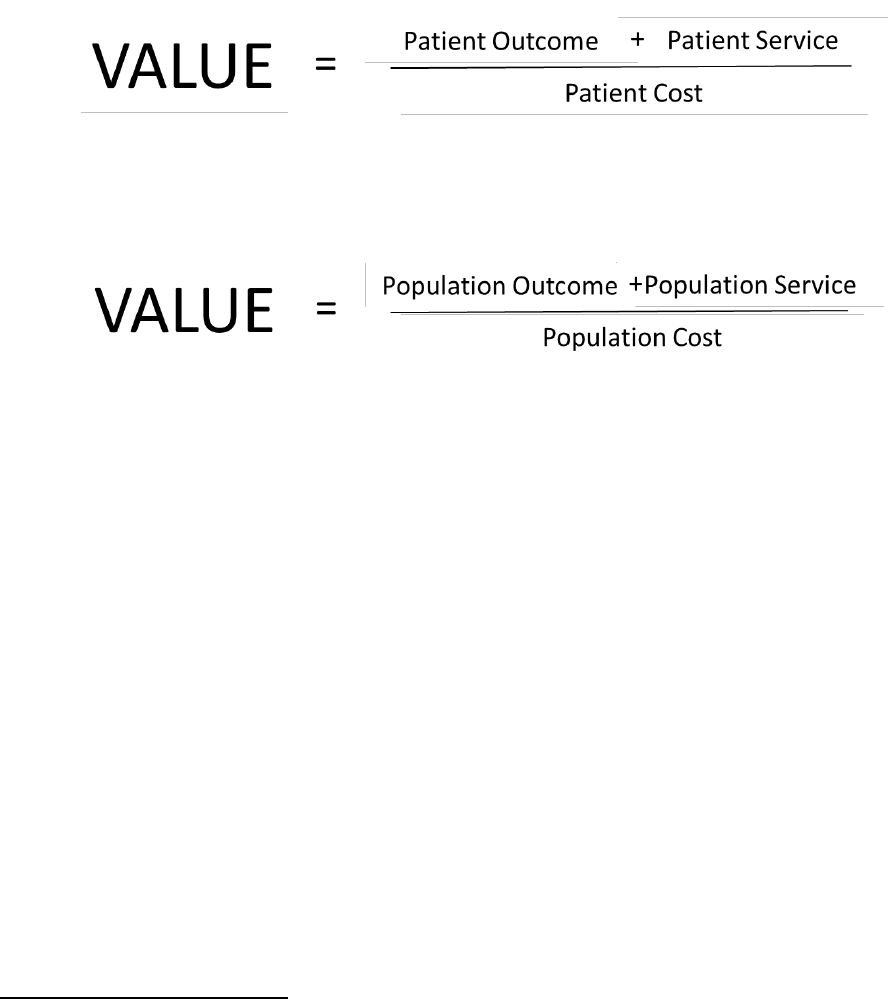
3. Quality and Cost
Value can be defined as Quality/Cost. Since Quality = Outcome, value can be further defined as
Outcome/Cost. The perception of care is essential to the measure of value, so the most
appropriate definition of value is: Value = (Patient Outcome + Patient Satisfaction)/ Patient
Cost.
The triple aim’s value today has refocused us on Population Health. So, the previous patient
based equation applied to a population would be:
PS applied to patients with chronic disease can provide this value through improving quality
and lowering cost. Quality can be improved through:
Use of Evidence Based Guidelines to support a focus on outcomes.
o PS has demonstrated a significant decrease in complications, hospital admissions
and emergency department visits using a model which is applicable to other
chronic conditions.
Improved Patient Satisfaction through targeted patient engagement.
o Patients engaged through PS maintain a very high level of satisfaction with the
program. They are benefitting from “Concierge Medicine” without the extra
expense.
Proactive Patient Engagement
Proactive patient engagement coupled with clinical surveillance and intervention is critical to
the successful management of patients with chronic disease. Patients with chronic disease
often surface only when they recognize they are in trouble and realize they cannot repair their
situation themselves. Patients with high-beta diseases can rapidly deteriorate, resulting in
hospitalization and complications
910
. Patients with CD frequently minimize their own
9
American Hospital Association. Examining the Drivers of Readmissions and Reducing Unnecessary Readmissions
for Better Patient Care. September 2011. Washington, DC
10
Hines AL, Barrett ML, Jiang HJ, et al. Conditions With the Largest Number of Adult Hospital Readmissions by
Payer, 2011. HCUP Statistical Brief #172. April 2014. Agency for Healthcare Research and Quality, Rockville, MD.
9
deteriorating symptoms; they may present too late at which time morbidity has occurred and
significant medical and/or surgical care must be provided. PS has demonstrated that patient
engagement is critical to avoiding these occurrences.
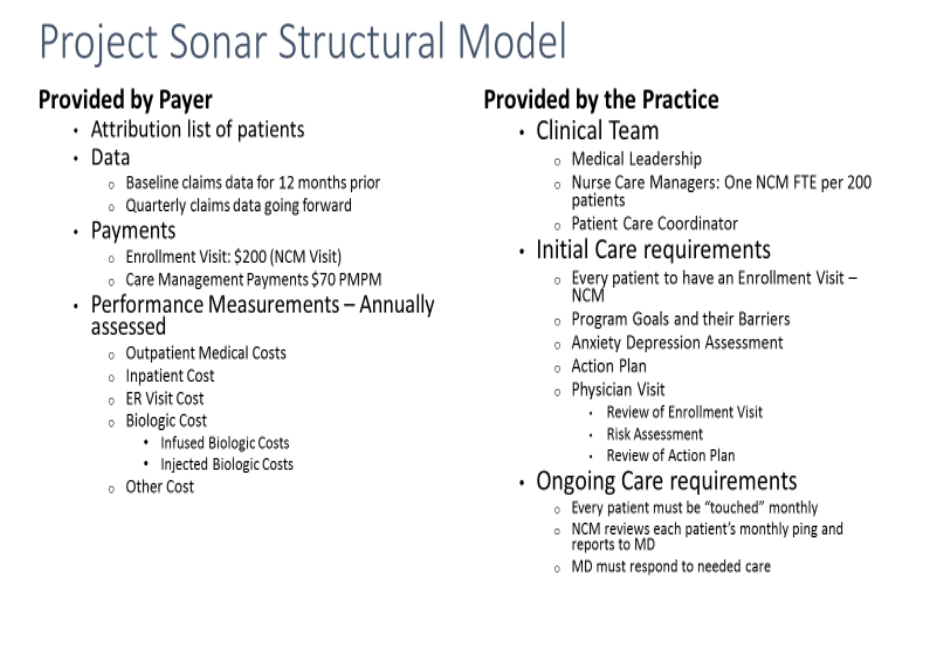
4. Payment Methodology
The payment model of PS represents negotiation of a transition from fee-for-service to fee-for-
value for physicians who may not ready or able to take on full risk, but are capable and should
be ready to accept accountability for the care they provide. PS will facilitate the development
of accountability for the care of the patient with chronic disease and will promote a decline in
the variability in the cost of care of these patients.
The Structural Model of PS is detailed below:
In the PS APM we are proposing a prospective payment model with retrospective
reconciliation. PS is based upon a chronic care management (CCM) model combined with
proactive patient engagement. Physicians who voluntarily choose to participate with the model
would continue to have their services reimbursed through the MPFS. Target prices are
compared to the actual cost of the care provided. Payment adjustments are based on quality
and financial performance. In the case of cost savings, the shared savings component of the
payment would be paid to the physician entity. In a situation where the physician’s attributed

10
costs overrun the expected target, the physician would be required to repay losses up to the
agreed upon limit in its contract with CMS. To protect against catastrophic losses, the model
will build in stop-loss provisions and outlier protections.
Participating providers would also be required to contribute based upon their agreement with
PS as the APM entity. A monthly payment for non ‘face-to-face’ services by clinical staff,
overseen by the physician, is essential for the successful deployment of the model to cover the
infrastructure costs required.
There are initial and ongoing costs for dedicated NCMs and ping coordinators (clinical staff), IT
expenses for incorporation of CDS tools into the EMR workflow and deployment of the patient
engagement platform and data management. These are detailed below:
NCM Cost: $25 PMPM
Ping Coordinator $12 PMPM
IT Platform $20 PMPM
Medical Director $2.50 PMPM
Total Cost $59.50 PMPM
The CCM payment is designed to cover the cost of deployment of the care management
infrastructure not to provide supplemental income to the practice. Incentives to the practice
will be generated by the sharing of cost savings derived from a retrospective adjust. A
Performance Based Adjustment (PBA) is made based upon this retrospective cost reconciliation.
If savings are favorable, the PBA will represent a supplemental payment to the practice. This
will be capped at 10%. If performance is poor and costs are excessive based on risk adjusted
norms, then the PBA would be negative up to a cap of 5%.
This payment structure should be viewed as one designed to promote a continuous process of
value generation over time. We anticipate that going forward many more value-based
initiatives will be necessary to continue to move the cost curve down. Episode and procedural
bundled payments will be necessary as well as consolidation in NCM functions. The goal will be
to gradually push cost down until a convergence to an ideal mean can be accomplished.
5. Value over Volume
Volume based drivers have dominated physician practices for the last 50 years. Since “every
system is perfectly designed to get the results it gets”
11
, medical practices are designed to “do
more”. In primary care practices this correlates to the metric: patients seen and RVU generated
per hour. The obvious challenge is to maintain quality of care when the physician or qualified
healthcare professional is seeing 4 or more patients per hour, especially if the patient has
multiple co-morbid conditions, complex medication regimens, psychosocial issues, etc. There is
11
Conway E, Bataiden P. Institute for Healthcare Improvement; August 21
st
, 2015
11
a limit to the productivity of a practice, whether primary care or specialist, which cannot be
solved through use of qualified healthcare professionals.
While specialists may be more procedural, they are equally as volume driven. Data from IGG
shows that over 54% of the revenue of a community-based GI practice comes from screening
(G0105, G0121), diagnostic (45378), and procedural colonoscopy (45380, 45384, 45385),
primarily related to colorectal cancer (CRC) screening, diagnosis, and surveillance. Many
Gastroenterologists have developed a very efficient focused-factory model for performing this
procedure.
Why should a GI move from this model to one based on value? Colonoscopy is a mature
service; CMS has adjusted procedure wRVU downwards in CY 2016 and 2017, revenue is
declining and costs are rising, compressing margins. Alternative methods for CRC screening are
available which, in a population based environment, might lead to a shift from procedural to
diagnostic colonoscopy with a corresponding decline in the volume of colonoscopy.
Anticipating this trend, Project Sonar was developed to provide GI physicians with an option to
improve care based on value based chronic disease management, rather than attempting to
perform more procedures.
In our initial review of commercial payer claim data from 2010 and 2011, the average
cost/patient with CD was $11,000, which includes professional, laboratory, imaging, hospital /
facility, and pharmaceutical costs. The average yearly reimbursement to a GI for managing
these patients was $385, which includes only professional fees for office visits, procedures, and
supervision of physician-administered infusions. Similar to oncology, physician administered
infusions represent an additional source of revenue to the practice, while prescribing a patient
self-administered drug would not generate any practice revenue.
The problems in today’s FFS model are obvious and include:
Physicians are compensated more to do more. Physicians are incented to perform more
procedures where the revenue per RVU is higher. By revising the 2017 fee schedule to
pay a facility more for colonoscopy procedures (e.g. 45380, 45385) and less for
screening / diagnostic procedures (e.g. G0105, G0121, 45378), CMS has potentially
created an incentive for physicians who own an ASC to perform more procedural
services.
As the per-minute compensation for cognitive services is less per RVU compared to
procedural services, many of these visits have been relegated to qualified healthcare
professionals (nurse practitioners, physician assistants) in the practice who might not
detect early signs of deterioration in a patient. This creates a paradoxical situation
where the most knowledgeable member of the healthcare team is busy performing the
most repetitive and least cognitive task (procedures) while the more complex cognitive
services are performed by less-trained professionals.
Prescribing infused biologics to increase practice revenue.
12
o The patient is seen every 6-8 weeks when they come in for their infusion. If that
infusion is performed in an office setting where the physician sees the patient,
our data suggests that the hospitalization rate is much lower than if the infusion
is performed in a setting (hospital outpatient or, for commercial patient, free-
standing infusion center) where the patient is not seen by their provider involved
in the ongoing management of their condition.
o Patients do not want to disrupt their lives every six to eight weeks to come in for
an infusion. This results in lost productivity at work, use of PTO days and time
away from family. For these and other reasons, patients may prefer self-
administered drugs, which creates a potential management issue as the patient
is not being monitored as they would if they were coming in for an infusion.
o On a total cost basis when looking at the cost of drug and infusion, the cost of
infusible biologics is higher than the cost of self-administered agent, which does
not consider the lost productivity cost. This must be balanced by the higher
hospitalization rate with self-administered agents due to a loss of ongoing
communication with the provider.
PS was developed to address these issues. How does PS move this to value?
The provider in PS is compensated a prospective payment fee in addition to their usual
FFS compensation. In our commercial model, this represents approximately $600 per
year to the provider, which is not significantly different from the approximately $490
per year were the physician to bill CPT code 99490 (chronic care management). The
physician is encouraged to continue office visits for the patient, and to provide
procedural services when clinically indicated, such as for CRC screening / surveillance.
The physician practice is responsible for paying the NCM and ping coordinator and data
management out of the monthly CCM payment.
Expenses for all procedures are paid under a bundled payment methodology.
Physicians are encouraged to utilize anti-TNF and other biologics based upon the most
efficacious agent, not the one that generates the most revenue to the practice. The PS
system facilitates patient engagement and communication regardless of the site of
service.
Performance data using PS in a commercial population has shown a “Net” 9.87% savings.
Based upon the $11,000 cost per patient, this amounts to a savings of over $1,000 per patient.
This is net of the monthly CCM payments and is a normalized savings based upon Medicare
Payment Rates. The combination of prospective CCM payments which support care
infrastructure of NCMs combined with the use of the Sonar Platform facilitate this overall
savings and its improvement in the quality of life of its patients.
13
6. Flexibility
PS represents a flexible and scalable platform upon which to expand its use to most all
practices. To date, we have installed the common PS platform in 20 GI practices across the
country representing approximately 600 physicians in 12 states, including community and
academic practices.
The “glue” that binds the PS practices is the use of the web and mobile-based platform, which
represents a single database of provider driven and patient driven metrics. A web-based
platform which is both EMR and smartphone device agnostic allows PS to apply changes
centrally and distribute automatically to all sites. The results of Sonar Scores are pushed into
EMRs as lab data using a HL7 interface.
The PS platform has been used for research on clinical and pharmacological outcomes and
effectiveness. For example, the network of PS practices has been leveraged to study the effects
of oral therapies for irritable bowel syndrome as well as IBD, and to assess whether assessment
of small bowel mucosa correlates with clinical and CDAI findings.
PS requires the practice to change its focus from ‘passive-reactive’ to proactive population
health. Instead of a “one patient at a time” passive focus, waiting for the patient to contact the
physician with new or intensifying symptoms, the PS practice is focused on the population of
patients. The practice, and the patients with a disease process, are actively engaged to improve
the care of the patient. This requires infrastructure changes such as the incorporation of NCMs
and the ping coordinator.
We believe that a similar care management infrastructure is applicable to other illnesses. We
further believe that PS is agnostic to the specialty and is applicable to other chronic illnesses,
and can be used by primary care and specialist physicians involved in the care of patients with
high beta chronic disease or the high beta periods in patients with low beta conditions.
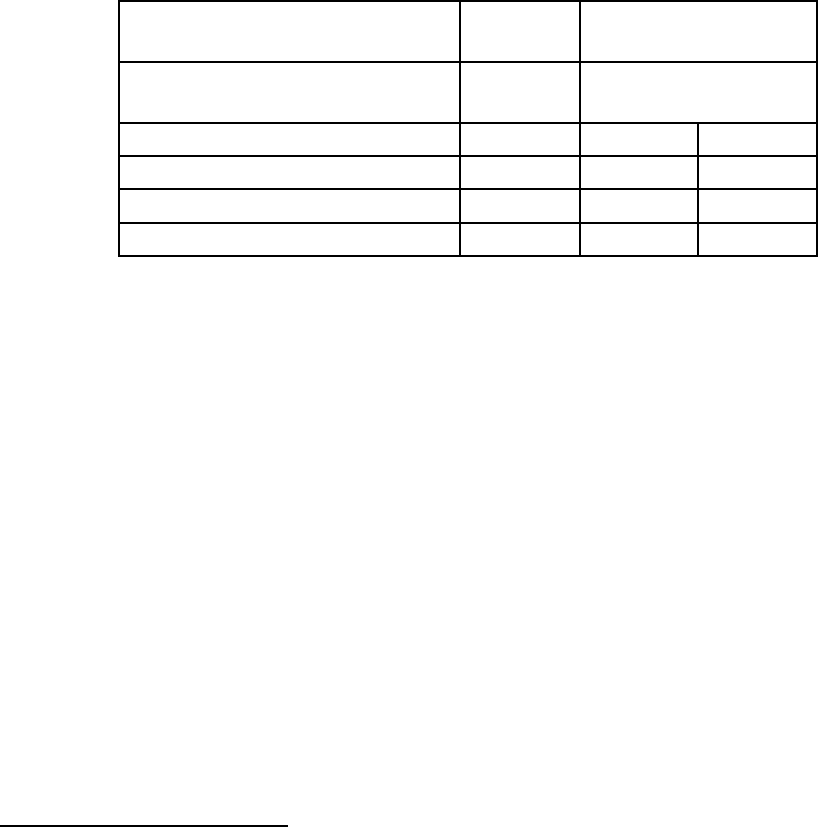
7. Ability to be evaluated
Evaluation of any new care model is essential to validate its value. PS has been under
evaluation since its inception. The following financial metrics are monitored on a regular basis:
Average total cost/patient
Average inpatient cost/patient
Average Emergency Room cost/patient
Average biologic cost/patient – both infused vs injected
Total cost from a commercial plan is a misleading metric as it must be normalized to Medicare
Payment Rates to minimize the site of service differential. That is not to say the site of service
is not important, it must be minimized as well. By using a single payment methodology,
utilization can be better assessed.
14
Ultimately the most important outcome is the improvement in the quality of life of the patients
with the disease in question. Financial measures alone may not reveal the entire patient
benefit. We must always place higher value on the costs incurred for disease morbidity. An
example is the cost of inpatient care vs the cost of biologic therapy. Despite the expense of the
latter, it does not come with the suffering of the morbidity of disease.
Outcomes driven quality metrics, difficult to develop, have slowed the movement from volume
to value. Since PS has a unique access to both quality as well as claims data it has been able to
develop predictive models based on how changes in quality metrics effect cost. Utilizing the 26
risk assessment metrics in the AGACDCP, PS ran multiple linear regressions of each metric
against the Crohn’s Disease Cost of Care. This has allowed for the development of a
mathematical model which assigns a relative strength to each metric with respect to its ability
to control the cost of care.
CDCP Risk Factor
Odds
Ratio
95% Confidence
Limits
Lower
Limit
Upper
Limit
Inflammation risk: Albumin
19.4
3.9
97.8
Inflammation risk: Joint pain
5.7
2.2
14.5
Comorbidity risk: Inflammation
11.5
1.5
87.8
Comorbidity Risk: Stricturing
5.4
2.2
13.4
Each risk assessment metric has a relative value. Patients can be profiled with this scoring
methodology and placed accurately in risk categories. An example would be the use of serum
albumin levels as a predictive value for risk. We have shown that changes in serum albumin are
predictive of 19.4% of the variation in cost of care for CD
12
. Patients are monitored quarterly
for serum albumin level changes.
We continue to refine this mathematical model, which will benefit from a larger “n” of patients.
This model enables rating of each physician and NCM performance on a risk adjusted basis.
Ping response rate is critical to the outcome of PS; provider and NCM specific ping response
rates can be used as a metric for performance.
We have developed an upside risk revenue share model which creates the proper incentives for
physician behavior. Working with physician groups in a variety of practice and geographic
settings, we have arrived at the following formula:
33%: based on number of patients followed
33%: based on the ping response rate
34%: based on the risk adjusted cost of care
12
Kosinski L, et al. Validation of AGA Crohn’s Disease Care Pathway Risk Assessment Metrics Against Crohn’s
Related Cost. Abstract. Inflammatory Bowel Diseases 22 S23-24 March 2016

15
With additional data and additional participating practices, we believe this formula can and will
be adjusted in the future to promote optimal value-based behaviors.
8. Integration and Care Coordination
The success of PS rests on the deployment of a team-based care infrastructure. MD can no
longer stand for “My Decision”. To successfully manage the patient with a chronic condition,
physicians and qualified healthcare professionals, NCMs, Ping Coordinators and ancillary
personnel such as behavioral health and pharmacists are required.
At present, the current care management model for PS centers around the NCM, who is the
most important component of the team. Based on data from the Case Management Society of
America, each FTE NCM should be able to follow 150-200 patients
13
. Our data shows that using
PS’s web and mobile patient engagement platform, this number can be safely increased to 250
patients per FTE NCM. Practice management data indicates that one NCM can provide support
to multiple physicians and qualified healthcare professionals in the practice. For solo and
smaller practices that might not have the patient volume to support a dedicated NCM, we
believe that a shared-service model could support such practices.
The NCM relationship begins at enrollment when the patient comes in for a “Supervisit”. At
this visit, patients are introduced to the NCM and queried as to their personal goals for the
program. Barriers to accomplishing these goals are identified and an action plan generated.
Patients are rated with respect to depression/anxiety using a PHQ-2 tool as these components
affect all chronic diseases. Diet histories are generated with action plans for nutritional
support. At the conclusion of the initial visit, the patient is seen by the physician or qualified
healthcare professional who reviews the details of the Supervisit and all parties sign off on the
action plan.
After the initial Supervisit, ongoing management begins. The PS platform provides a desktop to
the NCMs where their patients can be monitored together as a population. The NCM follows
the Sonar scores of the patients and contacts all patients whose scores fall out of standards, or
who does not respond to their ‘ping’ within a predetermined amount of time. Based on the
patient responses, if required the NCM goes into the practice EMR and initiates a
communication with the physician or qualified healthcare professional. Patients whose scores
indicate that they are deteriorating are contacted and engaged with the physician or qualified
healthcare professional, either in-person or telephonically. Precision care is being managed
proactively and constantly. Patients are engaged and physician services are initiated as needed
by the NCM.
13
Case Management Society of America and National Association of Social Workers. Case Management Caseload
Concept Paper: Proceedings of the Caseload Work Group. October 30, 2008. Available at
http://www.cmsa.org/portals/0/pdf/CaseloadCalc.pdf
16
All care, from the Supervisit through the ongoing care, is contained in the same relational
database. Reports can be generated from queries developed by the PS leadership team.
Interactions between the members of the team can be monitored and rated. The platform
provides the ability to rate NCMs separately from providers.
Each practice should have a clinical staff member who functions as a “ping coordinator”,
monitoring the ping process on a regular basis. This person monitors who is entering and
exiting the program.
The issue of integration with PCPs and other specialists needs to be discussed. We see this
model as being integrated into the structure of the entire care team. In pure high beta illnesses
like CD, the specialist may be the only member of the team that receives the PMPM payment.
In high beta periods of low beta conditions, the specialist will receive the PMPM only during the
high beta period. The bottom line is that the provider managing the care of the chronic illness
in question receives the payment. When comorbidities exist which require management by
multiple specialists, then multiple management fees may be necessary.
9. Patient Choice
PS is focused around the needs of the patient. In fact, the focus of PS is the patient. Our data
and results have shown that the patients prefer the engaged infrastructure of PS - their NCM
functions as their own personal care coordinator, or “concierge care within a managed
environment.” Patient satisfaction is high; PS has maintained a 75-80% sustained patient ping
response rate over 2 years.
We learned this that hard way. In the first six months of PS, we used a patient portal for our
patient communication. This was not ideal and the patients did not like logging in to the portal
to obtain their surveys. The EMR portals are cumbersome, inflexible, and slow to align with
advancements in technology (e.g. new smartphones and devices used by consumers). In June
2015, we switched to a web and mobile-based platform developed by PS that utilizes smart
phone technology, which has been very well received by the patients and is clearly their choice
of communication.
For the 20-25% of the patients who either do not have a smart phone or choose not to use one,
we use more conventional means of communication. A small number of patients prefer the
portal. Telephone calls from the NCM asking the patients the questions in the survey are used
when other means are not possible. As we serve a population in whom English might not be
the primary language for some patients, PS is in process of translating the questions into
Spanish and using ATT Language Line for others. In the end, we “touch” every patient every
month.
Approximately 24% of patients are deemed depressed or anxious at enrollment. These patients
require a higher level of service which can be provided through PS. As our data shows that
17
patients with behavioral health issues is associated with a 13% higher cost of care, they are a
major focus for the NCM. These patients may receive multiple calls and touches during the
calendar month. In the end, PS is the patient’s choice. High levels of patient satisfaction exist.
10. Patient Safety
PS must be considered a Sonar System for patients with chronic disease. It is like looking out at
the ocean. Think of the patients as submarines, submerged and running silent and deep. They
only surface when they are in trouble which means two things will need to happen for them to
surface: they recognize they are in trouble, and realize they can’t get out of trouble on their
own. Unfortunately, patients make mistakes on both issues and their safety can be
compromised. In high beta diseases like Crohn’s Disease or end-stage liver disease, there is not
much room for error. They surface in deep trouble and must be brought in to port (the
emergency department) which usually results in hospitalization.
Our data shows a significant improvement in patient safety with implementation of PS, as
demonstrated by the significant decrease in emergency department use and hospitalization
rate. The close patient engagement built into PS minimizes patient safety issues.
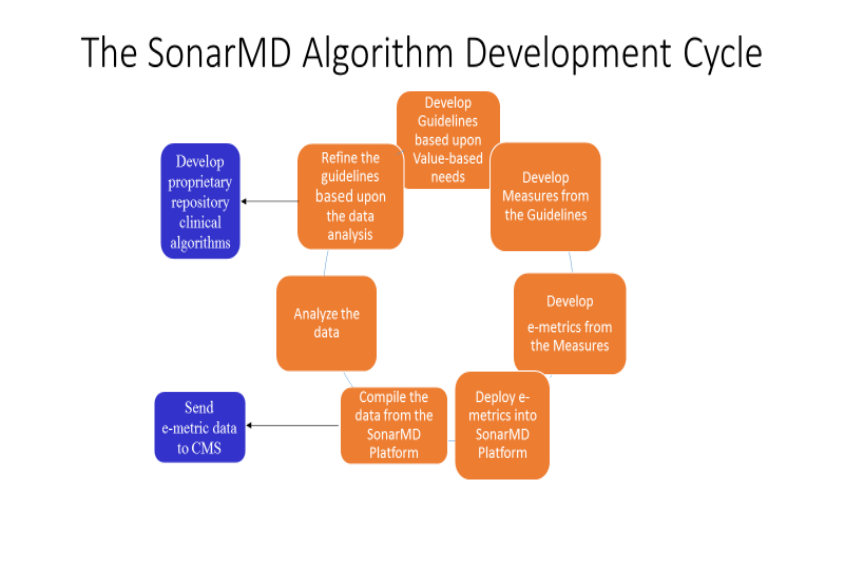
The algorithms which are built into PS are a key component of our success. The NCM desktop is
alerted when a patient’s Sonar Scores fall out of safety ranges. These ranges are based upon a
continuous process of refinement / development of algorithms:
18
11. Health Information Technology
PS is built on an HIT platform which utilizes both web and mobile-based technology to
communicate with providers, their staffs and their patients. It is cloud-based and agnostic to
the operating system of the handheld device as well as the practice EMR. Although not an
EMR, the PS platform integrates with all EMRs by pushing sonar scores through to the EMR as
lab data using an HL7 Interface.
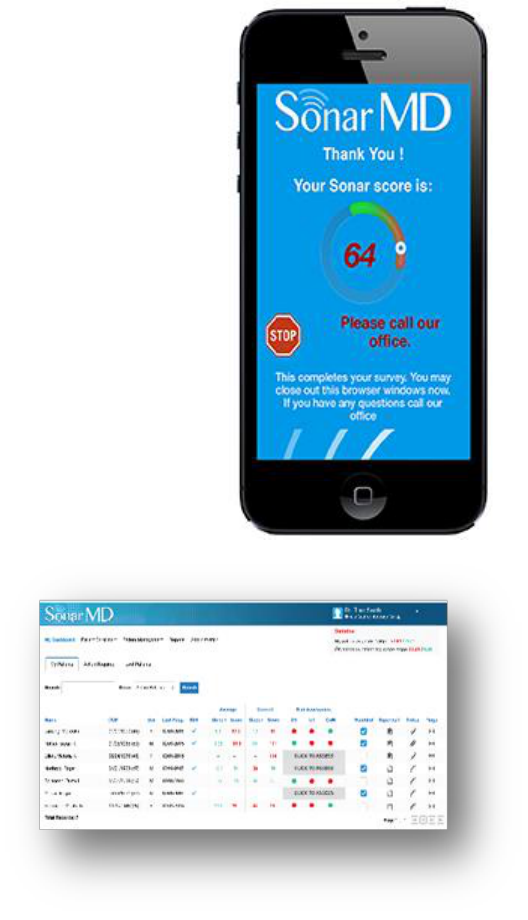
Patients using the PS platform receive monthly “pings” on the
device of their choice: smartphone, tablet, PC, etc. Some
patients who do not have access to this technology receive
their communication via telephone.
The strength of the mobile platform lies in its ability to provide
immediate feedback to the patient. Since it is a web-based
platform communicating to a SQL database, algorithmically
generated responses can provide patients with immediate
feedback. If the patient’s Sonar Score triggers one of the
algorithms, the patient is instructed to contact the office of the
practice. Concurrently, the NCM in the practice receives the
same notification and most often contacts the patient before
the patient does. This provides not only an excellent
communication tool, it provides the patient with a sense of
security that someone is constantly monitoring their condition.
On the practice side, the NCMs utilize a set of desktop
templates where they can monitor the
performance of each of their patients as
well as their assigned patients in
aggregate. Sonar Scores are color coded
based on algorithmic rules. See
Appendix VII for full images. Unlike an
EMR where patient charts are opened
one patient at a time, the Sonar
Platform is designed for population
health providing the NCM and the
physician with the ability to see all of
their PS patients in a user-friendly
interface.
Each practice participating in PS has its own sub-platform, thus they cannot comingle data from
other practices. At a central level, PS’s “Sonar Central” can pull data into a central repository
for query creation and reporting. The ability to aggregate and analyze data from practices
19
across the United States has in effect created a GI Registry for IBD. PS is able to monitor trends
across the population, study clinical factors related to outcomes, and provide guidance and
recommendations back to the practices. It is also our vision to use these capabilities to further
drive clinical decision support at the time of engagement and evidences based medicine across
the specific disease state(s).
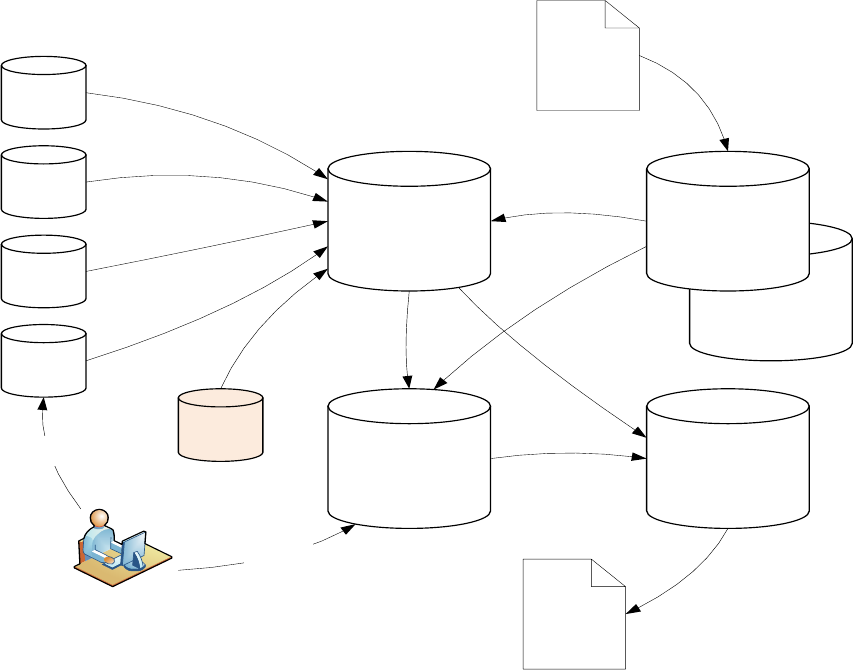
Safety and security are maintained through the appropriate use of encryption and use of
firewalls. This is shown in the diagram below.
Payer_XXX
Practice
Database
Practice
Database
Practice
Database
Practice
Database
Data Landing
Area
Claims Data
Practice Analytics
De-identified
Research
Analytics
Payer Database
Practice Users
(Nurses/Physicians/Administrators)
SonarMD
Application
Analytics &
Dashboards
Research
Extracts
Sonar
Central
The PS’ IT infrastructure lends itself to being expanded and scaled as necessary to
accommodate multiple practices and disorders. Safety and security are maintained through the
appropriate use of encryption and use of firewalls. Sonar has a full HIPAA compliance program
in place to safeguard access and use of the PS data.
There are currently over 600 in 20 large GI practices across the country who have implemented
the SonarMD platform. All of the data from these practices is contained in the above structure
in a safe/secure environment. This infrastructure is perfectly positioned to be expanded to
other disease processes and practices in other specialties.
20
12. Supplemental Information
The expansion of Project Sonar beyond the Illinois Gastroenterology Group necessitated the
formation of an entity to provide the necessary structure for a national project. SonarMD, LLC
is a Delaware LLC founded in 2014 by physicians dedicated to the development of chronic care
management tools. Through development of its provider focused CDS tools and its patient
engagement digital platform SonarMD provides medical practices with a patient friendly
infrastructure for population health.
The medical practices currently using the SonarMD digital platform constitute the SonarMD
Medical Group (SMG). Each practice is contracted with SonarMD under identical contractual
arrangements, and nominates a member to the SMG advisory board. We anticipate that as PS
grows, advisory groups will be organized around specialty and condition.
We have considered whether SonarMD, LLC could be the APM entity that contracts directly
with CMS. In this scenario, the risk arrangement for the APM entity including, total risk and
stop-loss provisions would be agreed upon in the APM entity’s contract with CMS.
Infrastructure expenses would include:
Development of a CCM payment designed to cover the infrastructure necessary to
implement the PS platform: NCMs, Ping coordination, IT Platform
Mechanisms for claims processing under prospective bundled vs. retrospective
payments.
Claims data reporting
Quality reporting based upon mutually agreed upon measures and metrics. These
measures will include MIPS measures as well as PS derived measures. An example for
IBD would be as follows:
Financial reporting measures as previously addressed
Category
Description
NQF 128
Preventive Care and Screening: Body Mass Index (BMI) Screening and Follow-Up Plan
NQF 226
Preventive Care and Screening: Tobacco Use: Screening and Cessation Intervention
NQF 271
Inflammatory Bowel Disease (IBD): Preventive Care: Corticosteroid Related Iatrogenic Injury
– Bone Loss Assessment:
NQF 275
Inflammatory Bowel Disease (IBD): Assessment of Hepatitis B Virus (HBV) Status Before
Initiating Anti-TNF (Tumor Necrosis Factor) Therapy
PHQ 2 Q1
Little Interest or Pleasure in doing things?
PHQ 2 Q2
Feeling Down Depressed or Hopeless
Lab
Serum Albumin
Lab
Serum Hb
Lab
Fecal Calprotectin
Lab
C-reactive protein
Lab
Endoscopic Assessment of Disease Activity
Sonar
Ping Response Rate
Sonar
Average Sonar Score

21
Appendices
I. Abstract: Validation of American Gastroenterological Association’s Crohn’s Disease Care
Pathway
Project Sonar: Validating Predictive Algorithms and Risk Scores for IBD Outcomes Using a
Community-Based Registry and Patient Engagement Data
Background
Project Sonar is a community-based registry and disease management program developed to
improve clinical and economic outcomes in Inflammatory Bowel Disease (IBD). This cloud-
based program integrates monthly patient-reported symptoms and health-related quality of life
(HRQoL) information with clinical data delivered through electronic medical record derived
Clinical Decision Support tools (CDS). These fields are then combined with payer provided-
claims data to provide comprehensive, real-time information to physicians and patients on
current symptoms and health status, as well as composite ‘Sonar’ scores. The CDS tools were
developed using the American Gastroenterological Association’s Crohn’s Disease Care
Pathway (CDCP), and Ulcerative Colitis Care Pathway, both of which determine treatment
guidelines for Crohn’s Disease and Ulcerative colitis (UC), respectively. The objective of this
project was to verify and measure the variation of data within Project Sonar, validate the CDCP
and UCCP guidelines, and Sonar risk scores using the real world data collected via Project
Sonar and healthcare claims of a subset of patients. The objective of this presentation is to
detail the methods used in this process.
Methods
The verification and validation project consisted of three major steps: (1) verification and
comprehensive quality check of all Project Sonar data to assure its quality mirrors that of
commercially available patient databases; (2) creation of an analytic dataset that merges
disparate patient level data from electronic medical records, healthcare claims data, and patient
reported outcomes; and (3) validation of CD and UC algorithms and Sonar risk scores.
Assignment of patients into correct risk category was confirmed by verifying the elements of the
three sub-scores (i.e., burden categories) that were important to the treatment algorithm and
development of the overall risk score, and assuring that each element and sub-score were
weighted appropriately. Then, the drivers for risk categorization were identified (i.e. the variables
most commonly associated with patients moving to a higher risk category). Finally, convergent
validity was assessed for the three sub-scores, risk categories, and Sonar scores by assessing
the correlations between risk categories and other indicators of disease severity (e.g.,
healthcare resource use, health-related quality of life).
Results/Conclusions
Project Sonar provides a unique opportunity to combine electronic medical records, healthcare
claims/resource utilization data, and patient reported outcomes to predict treatment failure and
target appropriate therapy in a community-based setting. With the completion of this
22
comprehensive verification and validation process, the Project Sonar database provides a rich
source of IBD patient data for understanding the natural course of IBD, identifying practice
patterns, comparing treatment options and outcomes, and identifying potential therapeutic cost
savings.
II. Project Sonar: Improvement in Patient Engagement Rates Using a Mobile Application
Platform
Project Sonar: Improvement in Patient Engagement Rates Using a Cloud-based Platform
Background
Project Sonar (PS) is a community-based registry and disease management program
developed by the Illinois Gastroenterology Group (IGG) to improve clinical and economic
outcomes in patients with Inflammatory Bowel Disease (IBD). PS integrates monthly patient-
reported health-related quality of life (HRQoL) information using a subset of questions from the
Crohn’s Disease Activity Index (CDAI) sent via a Patient Portal (PP) producing a monthly ‘Sonar
Score’. These scores are then joined by clinical data fields delivered through electronic medical
record derived Clinical Decision Support tools (CDS). This combined data is analyzed against
payer provided-claims data to provide comprehensive, real-time information to physicians and
patients on current symptoms and health status, as well as composite ‘Sonar’ scores. In an
effort to improve portal-based patient response rates PS deployed the SonarMD Platform
(SMDP), a cloud based platform developed by SonarMD, LLC which uses smartphone
technology to improve patient engagement instead of a PP.
Methods
Patient surveys were developed using five questions derived from the Crohn’s Disease Activity
Index in an effort to obtain HRQoL scores. The sum of the values on these questions results in
a Sonar Score (SS) which produces a quantifiable assessment of HRQoL. SSs are monitored
for individual scores as well as the slope of change over time, which allows for the development
of care management algorithms that drive interventions. The PP was used to send these
surveys from January 2014 through May 2015. Due to an unacceptable PP response rate, the
SMDP was deployed in June 2015. Patient response rates were compared for each of the two
methods.
Results
The patient response rate for the PP averaged 27.6% over the 17 months of its use. Due to the
structure of the PP, SSs needed to be individually calculated upon their receipt resulting in
significant staff expense and a delay in patient feedback. The patient response rate for the
SMDP was 66.27% for the three months it has been deployed, far exceeding the rate of the PP.
Since the SMDP platform automatically calculates the SS at the time the patient answers the
survey, patients receive immediate algorithm derived responses. Staff time is significantly
reduced as a result.
23
Conclusion
Project Sonar provides a unique opportunity to combine electronic medical records, healthcare
claims/resource utilization data, and patient reported outcomes to predict treatment failure and
target appropriate therapy in a community-based setting. Since patient participation is critical to
the success of PS, the cloud-based SMDP’s superior performance improved the patient
response rate over the patient portal from 27.6% to 60%. It also resulted in significant savings
in staff time. More time of deployment will be necessary to confirm that these findings will stand
the test of time.
III. Project Sonar: Validating a Cost Normalization Methodology in a Community-based
Registry
TITLE: Project Sonar: Validating a Cost Normalization Methodology in a Community-Based Registry
AUTHORS: Kosinski, Lawrence
1, 2
; Sorensen, Michael
2
; Brill, Joel
2, 3
; Landsman-Blumberg, Pamela
4
;
Turpin, Robin
5
; Baum, Charles
5
INSTITUTIONS (ALL):
1. Illinois Gastroenterology Group, Elgin, IL, United States.
2. SonarMD, LLC, Elgin, IL, United States.
3. Predictive Health, Paradise Valley, AZ, United States.
4. Xcenda, LLC, Palm Harbor, FL, United States.
5. Takeda Pharmaceuticals USA, Inc, Deerfield, IL, United States.
BACKGROUND
Project Sonar, a community-based registry and disease management program developed to
improve clinical and economic outcomes in Inflammatory Bowel Disease.
Project Sonar, uses a cloud-based platform combining health-related quality of life (HRQoL)
information with clinical data delivered through electronic medical record derived Clinical
Decision Support tools.
These data fields are then combined with payer provided-claims data obtained from the
Intensive Medical Home with Blue Cross Blue Shield of Illinois (BCBS-IL) database.
OBJECTIVES
Develop and validate a normalization methodology to mitigate the variation of cost data
between actual payments made vs a normalized payment structure derived from Medicare
Payment information to allow for meaningful assessment of Project Sonar’s economic impact.
METHODS
Patient Sample
Patients participating in Project Sonar and continuously enrolled in BCBS-IL from January 1, 2014
through September 30, 2015.
Costing Method
24
Crohn’s related claims-based payments were identified for each patient in the BCBS-IL medical
claims with ICD-9-CM 555.X or select ICD-9-CM symptom codes.
Claims-based payments were calculated and presented as total Crohn’s-related payments and
by type of service (i.e., infusible injection, diagnostic services, inpatient services, and physician
services).
All claims-based payments were adjusted to 2015 US dollars using the medical component of
the Consumer Price Index
Normalization Method
Normalized Crohn’s-related payments were calculated using standardized provider payments as
displayed in Table 1.
Table 1. Factors to Normalize
Service Type
Factors to Normalize
Physician Services
CPT Code Payment on 2015 Outpatient Prospective Payment System
Diagnostic Services
2015 Clinical Diagnostic Laboratory Fee Schedule
Infusible Biologics
2015 office based payment rates
Inpatient Hospital Payments
DRG Payment
To remove bias from site of service all infusible biologics were normalized to office based
infusion rate of $85/unit compared to $158/unit
For inpatient Hospital Payments:
o The DRG Payment was calculated using a base rate derived as the sum of the Operating
Base Payment and the Capital Base Payment.
o The base rate was then multiplied by the DRG Weight derived from the Medicare
Severity Diagnosis-Related Groups Relative Weighting Factors.
Analysis
We examined the absolute difference and percentage difference between actual and
standardized payments for total Crohn’s-related payments and by type of service.
RESULTS
Sample Description
185 patients participating in Project Sonar and continuously enrolled in BCBS-IL were included in
the analysis
Figure 1. Crohn’s-Related Payments, Total and by Type of Service
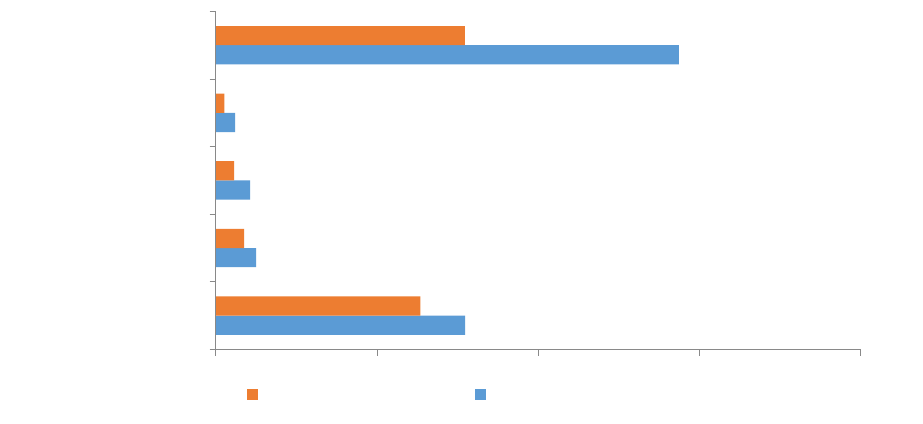
25
Normalized Crohn’s –related payments are consistently lower than claims-based payments (see
Figure 1), although the percentage difference varies by service type
o Total: - 18%
o Physician services: - 30%
o Inpatient services: - 47%
o Diagnostic services: - 56%
o Infusible biologics: - 46%
Diagnostic
Inpatient
Physician
X% of infusions were administered in the hospital outpatient department which may contribute
to the large difference in normalized payments compared to claims based payments
LIMITATIONS
ICD-9-CM codes for Crohn’s related symptoms were selected based on clinical opinion after
review of a sample of medical claims for BCBS-IL Crohn's patients enrolled in Project Sonar and
the published literature. Therefore, costs could be underestimated if relevant ICD-9-CM codes
were omitted and overestimated if symptom claims included were related to alternative
diagnoses.
Claims data are collected for the purpose of billing, not research. Therefore, diagnoses may be
coded incorrectly or under-coded, possibly introducing measurement error.
CONCLUSIONS
Project Sonar represents a unique opportunity to manage care using the AGA Crohn’s Care
Pathway and analyze the results on payments.
For meaningful comparison, it is essential that payments are normalized against Medicare
Payments in order to mitigate the site of service differential in payment reporting.
The normalization methodology presented has broad applicability for those seeking to analyze
complex real-world clinical practice data and cost.
$1,546,899
$248,877
$210,967
$118,211
$2,872,914
$1,270,337
$173,776
$111,612
$52,028
$1,545,555
$0 $1,000,000 $2,000,000 $3,000,000 $4,000,000
Total Crohn's Payments
Physician Services
Inpatient Payments
Diagnostic Payments
Infusible Biologics
Normalized Payments Claims-Based Payments
26
IV. Project Sonar Abstract of Distinction: Digestive Disease Week 2016
Project Sonar: Reduction in Cost of Care in an attributed cohort of patients with Crohn’s
Disease.
Lawrence Kosinski,
1
Michael Sorensen,
1
Joel V. Brill,
2
Pamela B Landsman-Blumberg,
3
Robin Turpin,
4
Charles Baum
4
1. Sonar MD, LLC, Elgin, Illinois; 2. Predictive Health, LLC, Paradise Valley, Arizona; 3. Xcenda, LLC,
Palm Harbor, Florida; 4. Takeda Pharmaceuticals U.S.A., Inc., Deerfield, Illinois.
Background: Project Sonar (PS), a joint venture between Illinois Gastroenterology Group and Blue Cross
Blue Shield Illinois, is a community-based registry and disease management program developed to
improve clinical and economic outcomes in Inflammatory Bowel Disease (IBD). PS integrates patient-
reported symptoms and health-related quality of life information with clinical data delivered through
electronic medical record derived Clinical Decision Support tools (CDS) using a cloud-based program
developed by SonarMD, LLC. CDS tools are based on the American Gastroenterological Association’s
Crohn’s Disease Care Pathway (CDCP) to determine treatment guidelines for Crohn’s Disease (CD).
Clinical data is combined with payer claims data to provide comprehensive, real-time information to
physicians and patients on current symptoms and health status, as well as composite ‘Sonar’ scores.
This study reports performance of Project Sonar in a subset of continuously enrolled CD patients.
Methods: 152 attributed patients with CD were continuously enrolled in PS between Jan 1, 2014 and Sept
30, 2015. The baseline period was Jan 1 through Nov 30, 2014, and the study period was the PS go-live
of Dec 1, 2014 through Sept 30, 2015. Total Costs were corrected for the difference in time periods. CD -
based claims were identified using ICD-9 555 codes plus additional codes identified as Crohn’s-based
due to their relationship with CD. Payments for physician and diagnostic services were normalized using
a methodology based on Medicare payment rates; DRG payments for inpatient stays were adjusted to
eliminate site of service differentials in payment rates.
Results
Findings: Total payments for PS patients with CD declined by 11.03% driven by > 50% declines in
hospital and emergency room payments. Utilization of physician administered biologics rose 8.97% but
total biologic costs declined 3.95% driven by a 24.5% reduction in the use of injectable biologics.
Normalization of payments to eliminate site of service payment differentials resulted in a 9.87% savings
in payments.
Conclusions: PS demonstrates value-based improvement in care for CD patients in a community-based
setting through integration of clinical data, patient reported outcomes and healthcare claims/resource
utilization data. Over 50% declines in hospital admissions and emergency room visits were achieved
through CDS tools promoting adherence to AGA CDCP combined with intense patient engagement. PS
represents an innovative model of population health likely applicable to other chronic conditions.
Crohn's Payments
Total Crohn's
Payments
Average Per
Patient
Payment
Total Normalized
Crohn's
Payments
Normalization
Difference
Inpatient
Payments
Emergency
Room
Payments
Infusable
Biologics
Injectable
Biologics
Total Biologics
Pre-Period 2,118,308.65$ 13,936.24$ 1,932,069.37$ (186,239.28)$ 210,967.47$ 52,363.19$ 892,443.30$ 560,980.84$ 1,453,424.14$
Study Period 1,884,758.63$ 12,399.73$ 1,741,326.02$ (143,432.62)$ 90,410.85$ 24,465.00$ 972,485.87$ 423,561.72$ 1,396,047.59$
Difference (233,550.02)$ (1,536.51)$ (190,743.36)$ 42,806.66$ (120,556.62)$ (27,898.19)$ 80,042.57$ (137,419.12)$ (57,376.55)$
Percentage Difference -11.03% -11.03% -9.87% -22.98% -57.14% -53.28% 8.97% -24.50% -3.95%
27
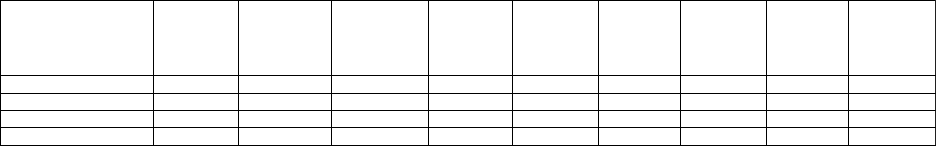
V. Guide to the Use of the Crohn’s Disease CDS Tool
The use of CDS tools is critical to our success in the management of our patients with chronic
disease. They also provide us an opportunity to bring together our PQRS requirements and
serve as a platform for participation in research studies. Accordingly, the Project Sonar
Physician Advisory Board, with the approval of the IGG Board of Managers, has decided to make
the use of these CDS tools mandatory. This document will provide you clarity in how to enter
data into this template.
The Crohn’s Disease CDS Tool is a “Demographic” template and therefore only has to be
populated only once. It will remain in its populated state from visit to visit and only requires
updates. It will be launched automatically when you enter a chief complaint of Crohn’s Disease.
The template has several sections as shown below:
28
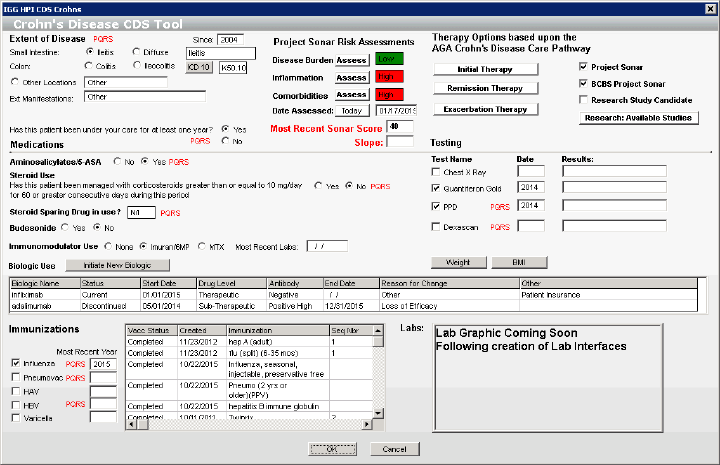
VI. AGA Crohn’s Disease Care Pathway Risk Assessment
25 metrics are captured in three categories: Disease Burden, Inflammation Burden, and
Comorbidity Burden. This assessment is updated annually on each patient. SonarMD is
developing a mathematical model behind the relative strengths of each metric.
Currently due to the size of our sample population, we are not able to reach statistical
significance. The implementation of this APM on a national basis would provide the
necessary patient population.
29
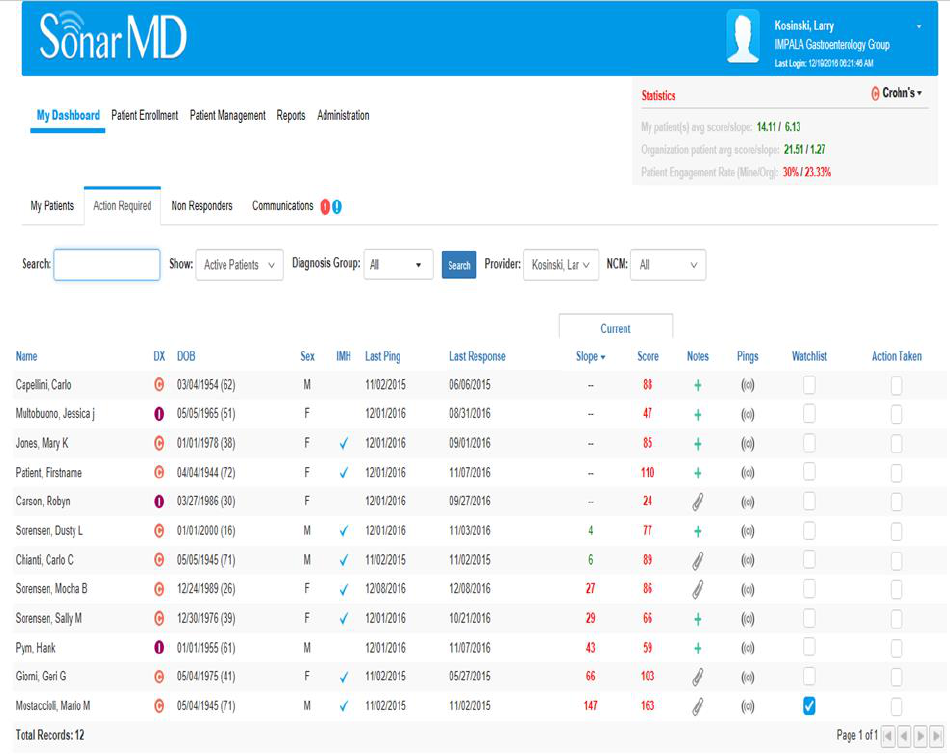
VII. SonarMD Nurse Care Manager Dashboard
The demo site shown below with fictitious patients demonstrates the user interface that the
NCMs and Physicians use each month to monitor their patients. Patients are listed according to
the assigned list of each NCM and Physician. Their raw Sonar Scores as well as the slope of
their scores over time are listed with color coordination based upon algorithmic rules. The
NCM or Physician can drill down on each one for further details. See VIII below.
30
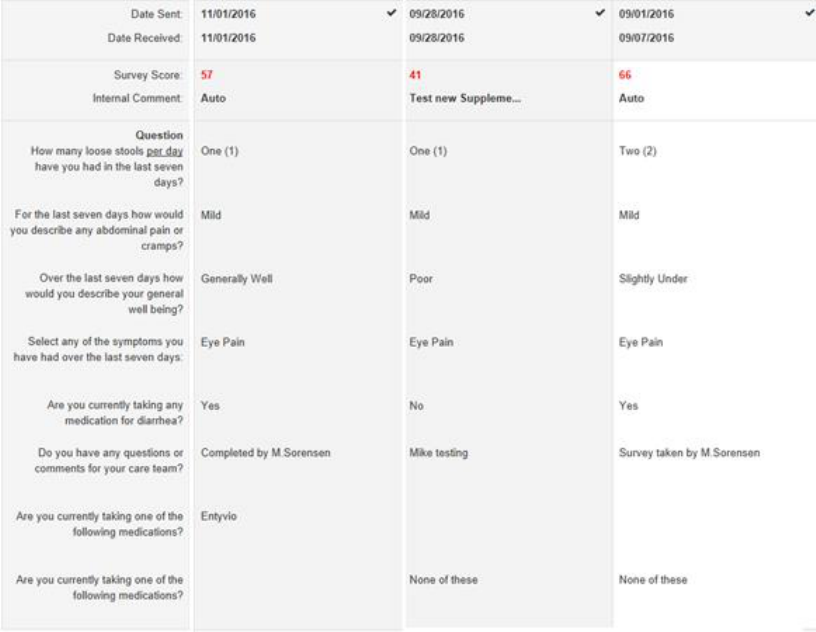
VIII. SonarMD Patient Survey
This template allows the reviewer to drill down on individual surveys. Each patient
receives the following questions every month via their device of choice. This template is
an example of what the NCMs utilize to monitor the answers and scores.
31
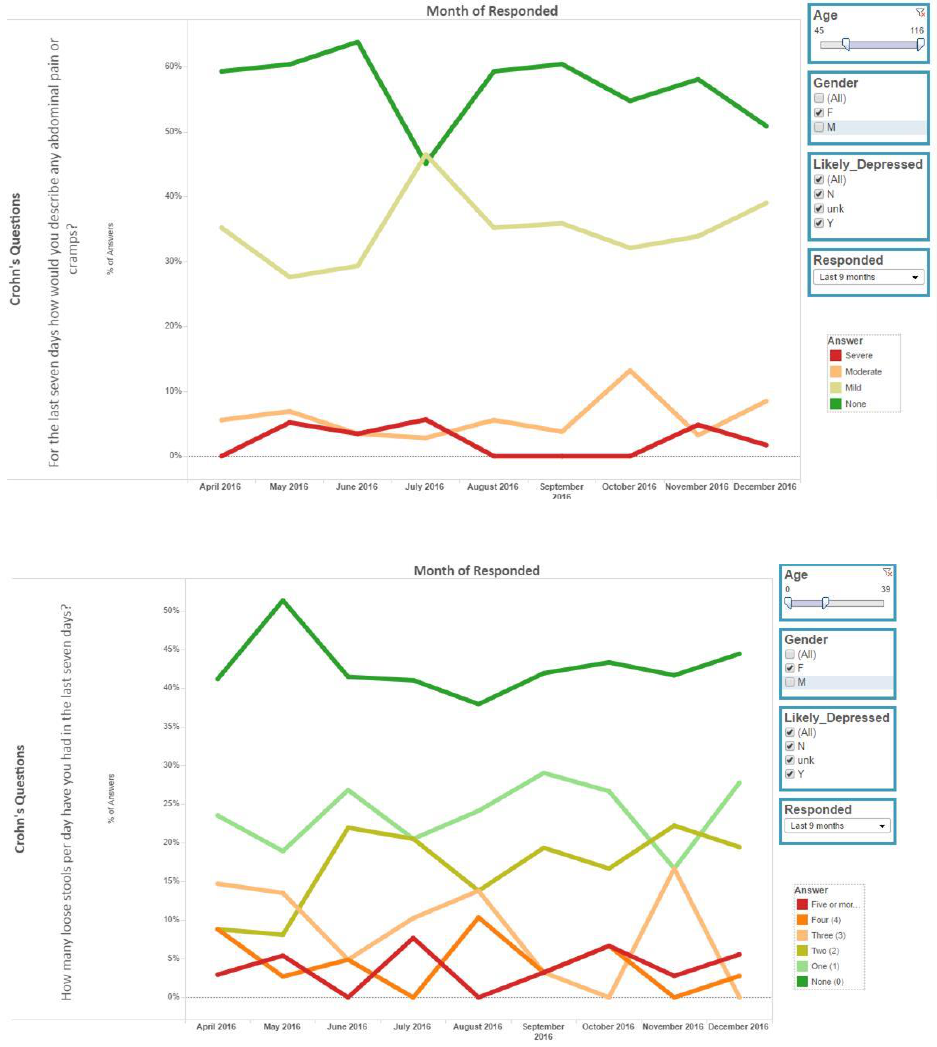
IX. Examples of SonarMD Ping Reports
The report corresponds to the answers for the first question in the survey shown in the
vertical axis. For the last seven days how would you describe any abdominal pain or
cramps? The figure can be filtered by the items shown on the right side: age, gender,
depression rating and by responder percentage.
The following figure demonstrates the same findings for the second question: “How
many loose stools per day have you had in the last seven days”
32
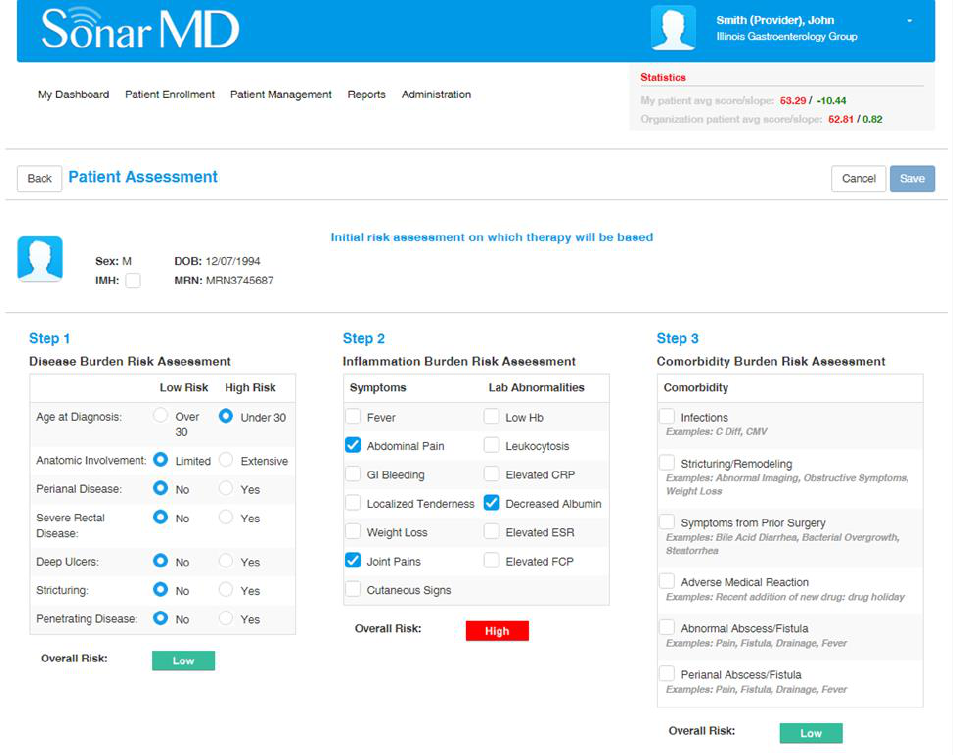
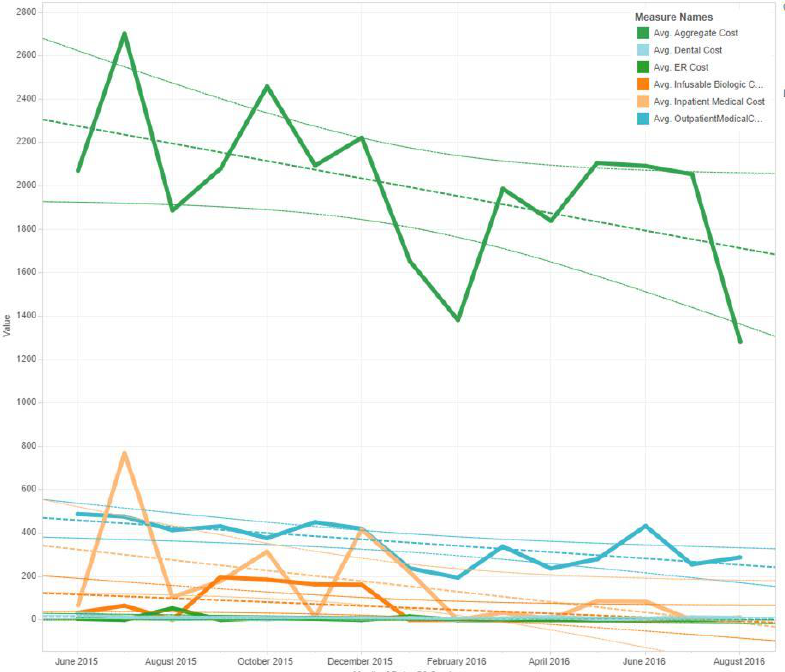
X. SonarMD Cost Report
The following figure shows a stead fall in average aggregate cost of care over the time
period of June 1
st
2015 through August 31
st
2016.

