NAIC Model Laws, Regulations, Guidelines and Other Resources—1
st
Quarter 2018
© 2018 National Association of Insurance Commissioners 520-1
LIFE AND HEALTH INSURANCE GUARANTY ASSOCIATION MODEL ACT
Table of Contents
Section 1. Title
Section 2. Purpose
Section 3. Coverage and Limitations
Section 4. Construction
Section 5. Definitions
Section 6. Creation of the Association
Section 7. Board of Directors
Section 8. Powers and Duties of the Association
Section 9. Assessments
Section 10. Plan of Operation
Section 11. Duties and Powers of the Commissioner
Section 12. Prevention of Insolvencies
Section 13. Credits for Assessments Paid (Tax Offsets)—OPTIONAL
Section 14. Miscellaneous Provisions
Section 15. Examination of the Association; Annual Report
Section 16. Tax Exemptions
Section 17. Immunity
Section 18. Stay of Proceedings; Reopening Default Judgments
Section 19. Prohibited Advertisement of Insurance Guaranty Association Act in Insurance Sales; Notice to Policy
Owners
Section 20. Prospective Application
Appendix Alternative Provisions
Section 1. Title
This Act shall be known and may be cited as the [State] Life and Health Insurance Guaranty Association Act.
Section 2. Purpose
A. The purpose of this Act is to protect, subject to certain limitations, the persons specified in Section 3A
against failure in the performance of contractual obligations, under life, health, and annuity policies, plans,
or contracts specified in Section 3B, because of the impairment or insolvency of the member insurer that
issued the policies, plans, or contracts.
B. To provide this protection, an association of member insurers is created to pay benefits and to continue
coverages as limited by this Act, and members of the Association are subject to assessment to provide
funds to carry out the purpose of this Act.
Drafting Note: The primary purpose of this model act is to protect policy or contract owners, insureds, beneficiaries, health care providers, annuitants,
payees and assignees against losses (both in terms of paying claims and continuing coverage) which might otherwise occur due to an impairment or
insolvency of an insurer. Unlike the property and liability lines of business, life and annuity contracts in particular are long-term arrangements for security.
An insured may have impaired health or be at an advanced age so as to be unable to obtain new and similar coverage from other insurers. The payment of
cash values alone does not adequately meet such needs. Thus it is essential that coverage be continued. It is also essential that the guaranty association
assesses insurers in a fair and reasonable manner and that the guaranty association has sufficient assessment capacity for all insolvencies.
Section 3. Coverage and Limitations
A. This Act shall provide coverage for the policies and contracts specified in Subsection B:
(1) To persons who, regardless of where they reside (except for nonresident certificate holders under
group policies or contracts), are the beneficiaries, assignees or payees, including health care
providers rendering services covered under health insurance policies or certificates, of the persons
covered under Paragraph (2);
Life and Health Insurance Guaranty Association Model Act
520-2
© 2018 National Association of Insurance Commissioners
(2) To persons who are owners of or certificate holders or enrollees under the policies or contracts
(other than unallocated annuity contracts, and structured settlement annuities) and in each case
who:
(a) Are residents; or
(b) Are not residents, but only under all of the following conditions:
(i) The member insurer that issued the policies or contracts is domiciled in this
State;
(ii) The States in which the persons reside have associations similar to the
association created by this Act;
(iii) The persons are not eligible for coverage by an association in any other State
due to the fact that the insurer or the health maintenance organization was not
licensed in the State at the time specified in the State’s guaranty association law.
(3) For unallocated annuity contracts specified in Subsection B; Paragraphs (1) and (2) of this
subsection shall not apply, and this Act shall (except as provided in Paragraphs (5) and (6) of this
subsection) provide coverage to:
(a) Persons who are the owners of the unallocated annuity contracts if the contracts are
issued to or in connection with a specific benefit plan whose plan sponsor has its
principal place of business in this State; and
(b) Persons who are owners of unallocated annuity contracts issued to or in connection with
government lotteries if the owners are residents.
Drafting Note: It is believed that coverage of unallocated annuities is a policy decision that should be made by each individual State. Attached as an
Appendix are alternative Sections 3, 5 and 6, which specifically exclude all unallocated annuities from coverage.
(4) For structured settlement annuities specified in Subsection B; Paragraphs (1) and (2) of this
subsection shall not apply, and this Act shall (except as provided in Paragraphs (5) and (6) of this
subsection) provide coverage to a person who is a payee under a structured settlement annuity (or
beneficiary of a payee if the payee is deceased), if the payee:
(a) Is a resident, regardless of where the contract owner resides; or
(b) Is not a resident, but only under both of the following conditions:
(i) (I) The contract owner of the structured settlement annuity is a resident; or
(II) The contract owner of the structured settlement annuity is not a
resident; but
a. The insurer that issued the structured settlement annuity is
domiciled in this State; and
b. The State in which the contract owner resides has an
association similar to the association created by this Act; and
(ii) Neither the payee (or beneficiary) nor the contract owner is eligible for coverage
by the association of the State in which the payee or contract owner resides.
NAIC Model Laws, Regulations, Guidelines and Other Resources—1
st
Quarter 2018
© 2018 National Association of Insurance Commissioners 520-3
(5) This Act shall not provide coverage to:
(a) A person who is a payee (or beneficiary) of a contract owner resident of this State, if the
payee (or beneficiary) is afforded any coverage by the association of another State; or
(b) A person covered under Paragraph (3) of this subsection, if any coverage is provided by
the association of another State to the person; or
(c) A person who acquires rights to receive payments through a structured settlement
factoring transaction as defined in 26 U.S.C. 5891(c)(3)(A), regardless of whether the
transaction occurred before or after such section became effective.
(6) This Act is intended to provide coverage to a person who is a resident of this State and, in special
circumstances, to a nonresident. In order to avoid duplicate coverage, if a person who would
otherwise receive coverage under this Act is provided coverage under the laws of any other State,
the person shall not be provided coverage under this Act. In determining the application of the
provisions of this paragraph in situations where a person could be covered by the association of
more than one State, whether as an owner, payee, enrollee, beneficiary or assignee, this Act shall
be construed in conjunction with other State laws to result in coverage by only one association.
Drafting Note: The exclusion from coverage in Section 3A(5)(c) of any person who has purchased from an original structured settlement annuity payee his
or her rights to receive structured settlement annuity benefits and the exclusion of such benefits from covered benefits under Section 3B(2)(n) recognize that
the protections afforded by guaranty associations are intended for insurance consumers, such as the original payees of structured settlement annuities.
Guaranty association protection does not extend to sophisticated investors who acquire rights to receive structured settlement annuity benefits in the
secondary market. These exclusions, however, do not apply to structured settlement annuity benefits that are transferred to children, present or former
spouses or
other dependents as part of domestic relations settlements or orders, or to other transferees (including donees) who acquire rights to receive
structured settlement annuity benefits without providing any monetary consideration. Thus, Section
3A(5)(c) and Section 3B(2)(n) clarify that guaranty
association coverage protects structured settlement annuity benefits to which the original payee and his or her family members retain the rights.
B. (1) This Act shall provide coverage to the persons specified in Subsection A for policies or contracts
of direct, non-group life insurance, health insurance (which for the purposes of this Act includes
health maintenance organization subscriber contracts and certificates), or annuities, and
supplemental contracts to any of these, for certificates under direct group policies and contracts,
and for unallocated annuity contracts issued by member insurers, except as limited by this Act.
Annuity contracts and certificates under group annuity contracts include but are not limited to
guaranteed investment contracts, deposit administration contracts, unallocated funding
agreements, allocated funding agreements, structured settlement annuities, annuities issued to or
in connection with government lotteries and any immediate or deferred annuity contracts.
(2) Except as otherwise provided in Paragraph (3) of this subsection, this Act shall not provide
coverage for:
(a) A portion of a policy or contract not guaranteed by the member insurer, or under which
the risk is borne by the policy or contract owner;
(b) A policy or contract of reinsurance, unless assumption certificates have been issued
pursuant to the reinsurance policy or contract;
(c) A portion of a policy or contract to the extent that the rate of interest on which it is based,
or the interest rate, crediting rate or similar factor determined by use of an index or other
external reference stated in the policy or contract employed in calculating returns or
changes in value;
Life and Health Insurance Guaranty Association Model Act
520-4
© 2018 National Association of Insurance Commissioners
(i) Averaged over the period of four (4) years prior to the date on which the
member insurer becomes an impaired or insolvent insurer under this Act,
whichever is earlier, exceeds the rate of interest determined by subtracting two
(2) percentage points from Moody’s Corporate Bond Yield Average averaged
for that same four-year period or for such lesser period if the policy or contract
was issued less than four (4) years before the member insurer becomes an
impaired or insolvent insurer under this Act, whichever is earlier; and
(ii) On and after the date on which the member insurer becomes an impaired or
insolvent insurer under this Act, whichever is earlier, exceeds the rate of interest
determined by subtracting three (3) percentage points from Moody’s Corporate
Bond Yield Average as most recently available;
(d) A portion of a policy or contract issued to a plan or program of an employer, association
or other person to provide life, health or annuity benefits to its employees, members or
others, to the extent that the plan or program is self-funded or uninsured, including but
not limited to benefits payable by an employer, association or other person under;
(i) A multiple employer welfare arrangement as defined in 29 U.S.C. § 1144;
(ii) A minimum premium group insurance plan;
(iii) A stop-loss group insurance plan; or
(iv) An administrative services only contract;
(e) A portion of a policy or contract to the extent that it provides for
(i) Dividends or experience rating credits;
(ii) Voting rights; or
(iii) Payment of any fees or allowances to any person, including the policy or
contract owner, in connection with the service to or administration of the policy
or contract;
(f) A policy or contract issued in this State by a member insurer at a time when it was not
licensed or did not have a certificate of authority to issue the policy or contract in this
State;
(g) An unallocated annuity contract issued to or in connection with a benefit plan protected
under the federal Pension Benefit Guaranty Corporation, regardless of whether the
federal Pension Benefit Guaranty Corporation has yet become liable to make any
payments with respect to the benefit plan;
(h) A portion of an unallocated annuity contract that is not issued to or in connection with a
specific employee, union or association of natural persons benefit plan or a government
lottery;
(i) A portion of a policy or contract to the extent that the assessments required by Section 9
with respect to the policy or contract are preempted by federal or State law;
(j) An obligation that does not arise under the express written terms of the policy or contract
issued by the member insurer to the enrollee, certificate holder, contract owner or policy
owner, including without limitation:
NAIC Model Laws, Regulations, Guidelines and Other Resources—1
st
Quarter 2018
© 2018 National Association of Insurance Commissioners 520-5
(i) Claims based on marketing materials;
(ii) Claims based on side letters, riders or other documents that were issued by the
member insurer without meeting applicable policy or contract form filing or
approval requirements;
(iii) Misrepresentations of or regarding policy or contract benefits;
(iv) Extra-contractual claims; or
(v) A claim for penalties or consequential or incidental damages;
(k) A contractual agreement that establishes the member insurer’s obligations to provide a
book value accounting guaranty for defined contribution benefit plan participants by
reference to a portfolio of assets that is owned by the benefit plan or its trustee, which in
each case is not an affiliate of the member insurer;
(l) A portion of a policy or contract to the extent it provides for interest or other changes in
value to be determined by the use of an index or other external reference stated in the
policy or contract, but which have not been credited to the policy or contract, or as to
which the policy or contract owner’s rights are subject to forfeiture, as of the date the
member insurer becomes an impaired or insolvent insurer under this Act, whichever is
earlier. If a policy’s or contract’s interest or changes in value are credited less frequently
than annually, then for purposes of determining the values that have been credited and
are not subject to forfeiture under Section 3B(2)(l), the interest or change in value
determined by using the procedures defined in the policy or contract will be credited as if
the contractual date of crediting interest or changing values was the date of impairment
or insolvency, whichever is earlier, and will not be subject to forfeiture;
(m) A policy or contract providing any hospital, medical, prescription drug or other health
care benefits pursuant to Part C or Part D of Subchapter XVIII, Chapter 7 of Title 42 of
the United States Code (commonly known as Medicare Part C& D), or Subchapter XIX,
Chapter 7 of Title 42 of the United States Code (commonly known as Medicaid), or any
regulations issued pursuant thereto; or
(n) Structured settlement annuity benefits to which a payee (or beneficiary) has transferred
his or her rights in a structured settlement factoring transaction as defined in 26 U.S.C.
5891(c)(3)(A), regardless of whether the transaction occurred before or after such section
became effective.
(3) The exclusion from coverage referenced in Paragraph (2)(c) of this subsection shall not apply to
any portion of a policy or contract, including a rider, that provides long-term care or any other
health insurance benefits.
Drafting Note: Some life insurance policies and annuity contracts covered by this Act provide for interest or other changes in value to be determined by the
use of an index or other external reference stated in the policy or contract. Sections 3B(2)(c) and 3B(2)(l) clarify the treatment of such policies or contracts in
order to limit increases in interest in a manner that parallels the treatment provided other policies and contracts under this Act. Section 3B(2)(c) explicitly
states that the application of the limit on “rate of interest” includes returns and changes in value determined by equity index or other reference. Section
3B(2)(l) excludes from coverage any interest or change in value that, as of the date the member insurer becomes an impaired or insolvent insurer under this
Act, whichever is earlier, has not been credited to the policy or contract. It excludes from coverage any interest or change in value as to which the right of the
policy or contract owner is subject to forfeiture on the date the member insurer becomes an impaired or insolvent insurer under this Act, whichever is earlier.
However, for policies or contracts that credit interest or changes in value less than annually, Section 3B(2)(1) clarifies that crediting will be done according
to the procedures set forth in the
policy or contract except that the date of impairment or insolvency under this Act, whichever is earlier, will be deemed the
final date for crediting interest of changes in value. Section 3B(3) is added to clarify that the interest limitation in Section 3B(2)(c) does not apply to long-
term care or any other health insurance benefits.
Life and Health Insurance Guaranty Association Model Act
520-6
© 2018 National Association of Insurance Commissioners
C. The benefits that the Association may become obligated to cover shall in no event exceed the lesser of:
(1) The contractual obligations for which the member insurer is liable or would have been liable if it
were not an impaired or insolvent insurer; or
(2) (a) With respect to one life, regardless of the number of policies or contracts:
(i) $300,000 in life insurance death benefits, but not more than $100,000 in net
cash surrender and net cash withdrawal values for life insurance;
(ii) For health insurance benefits:
(I) $100,000 for coverages not defined as disability income insurance or
health benefit plans or long-term care insurance as defined in [section
of State law dealing with health insurance/disability income
insurance/long-term care insurance] including any net cash surrender
and net cash withdrawal values;
(II) $300,000 for disability income insurance as defined in [section of State
law dealing with health insurance/ disability income insurance], and
$300,000 for long-term care insurance as defined in [section of State
law dealing with health insurance/ long-term care insurance];
(III) $500,000 for health benefit plans;
(iii) $250,000 in the present value of annuity benefits, including net cash surrender
and net cash withdrawal values; or
(b) With respect to each individual participating in a governmental retirement benefit plan
established under Section 401, 403(b) or 457 of the U.S. Internal Revenue Code covered
by an unallocated annuity contract or the beneficiaries of each such individual if
deceased, in the aggregate, $250,000 in present value annuity benefits, including net cash
surrender and net cash withdrawal values;
(c) With respect to each payee of a structured settlement annuity (or beneficiary or
beneficiaries of the payee if deceased), $250,000 in present value annuity benefits, in the
aggregate, including net cash surrender and net cash withdrawal values, if any;
(d) However, in no event shall the Association be obligated to cover more than (i) an
aggregate of $300,000 in benefits with respect to any one life under Paragraphs 2(a), 2(b)
and 2(c) of this subsection except with respect to benefits for health benefit plans under
Paragraph 2(a)(ii) of this subsection, in which case the aggregate liability of the
Association shall not exceed $500,000 with respect to any one individual, or (ii) with
respect to one owner of multiple non-group policies of life insurance, whether the policy
or contract owner is an individual, firm, corporation or other person, and whether the
persons insured are officers, managers, employees or other persons, more than
$5,000,000 in benefits, regardless of the number of policies and contracts held by the
owner;

NAIC Model Laws, Regulations, Guidelines and Other Resources—1
st
Quarter 2018
© 2018 National Association of Insurance Commissioners 520-7
(e) With respect to either (i) one contract owner provided coverage under Subsection
A(3)(b) of this section; or (ii) one plan sponsor whose plans own directly or in trust one
or more unallocated annuity contracts not included in Paragraph (2)(b) of this subsection,
$5,000,000 in benefits, irrespective of the number of contracts with respect to the
contract owner or plan sponsor. However, in the case where one or more unallocated
annuity contracts are covered contracts under this Act and are owned by a trust or other
entity for the benefit of two (2) or more plan sponsors, coverage shall be afforded by the
Association if the largest interest in the trust or entity owning the contract or contracts is
held by a plan sponsor whose principal place of business is in this State and in no event
shall the Association be obligated to cover more than $5,000,000 in benefits with respect
to all these unallocated contracts.
(f) The limitations set forth in this subsection are limitations on the benefits for which the
Association is obligated before taking into account either its subrogation and assignment
rights or the extent to which those benefits could be provided out of the assets of the
impaired or insolvent insurer attributable to covered policies. The costs of the
Association’s obligations under this Act may be met by the use of assets attributable to
covered policies or reimbursed to the Association pursuant to its subrogation and
assignment rights.
(g) For purposes of this Act, benefits provided by a long-term care rider to a life insurance
policy or annuity contract shall be considered the same type of benefits as the base life
insurance policy or annuity contract to which it relates.
D. In performing its obligations to provide coverage under Section 8 of this Act, the Association shall not be
required to guarantee, assume, reinsure, reissue or perform, or cause to be guaranteed, assumed, reinsured,
or reissued or performed, the contractual obligations of the insolvent or impaired insurer under a covered
policy or contract that do not materially affect the economic values or economic benefits of the covered
policy or contract.
Drafting Note: This section and Section 8 are key sections of the Act. Section 3 identifies who and what are covered and not covered by the Act. Section 8
specifies the responsibilities of the Association toward covered persons with covered policies.
Protection of this Act is primarily extended to resident persons but certain nonresidents under specific circumstances will be protected by this Act if the
insolvent insurer was domiciled in this State.
This model does not apply to reinsurance unless assumption certificates were issued to the direct insureds or enrollees. Furthermore, it applies only to direct
individual or group certificate insurance issued or written by member insurers licensed to transact business in this State at any time.
Persons to whom coverage is typically provided are resident enrollees, policy or contract owners, or their beneficiaries, assignees or payees. For group
contracts or policies, coverage is provided to resident enrollees, and certificate holders and not to the owners of the group contracts or policies; this avoids
the possibility of double coverage and indirect coverage of nonresident enrollees, and certificate holders through resident group policy or contract owners.
However, for unallocated annuities, coverage is provided under Subsection A(3) to plan sponsors whose principal place of business is in this State, rather
than to contract owners. No coverage is provided to individuals who have or might have an interest in the plan or unallocated annuity contract because there
is no contractual guaranty by the insurer to individuals under those contracts. Subsection A(4) provides coverage for structured settlement annuities to
resident payees rather than to the contract owners.
Subsection A(3) providing unallocated annuity contract coverage to plan sponsors whose principal place of business is in the State and Subsection A(4)
providing structured settlement annuity coverage to resident payees are significant changes from previous versions of this Model Act intended to place the
coverage in the State of the resident persons to be protected rather than in the State where the nominal owner of the contract resides. Subsections A(5) and
(6) avoid the possibility of double coverage due to differing approaches for determining the covered persons in different State statutes and provide
mechanisms for resolving which State’s statutes will be used to determine the existence and limits of coverage.
Policies and contracts covered by the model act are life insurance, health insurance and annuity policies and contracts, and policies or contracts supplemental
thereto. The use of the term health insurance is intended to include “accident and health” insurance, “sickness and accident” insurance, “disability income”
insurance, health maintenance organization contracts, etc. The use of the term disability income insurance is intended to include insurance policies and
contracts that cover the loss of income due to a disability. The individual State may want to adjust this language to fit its particular terminology.
Subsection B(2) identifies certain types of contracts or policies or portions of contracts or policies that are specifically not covered by this Act. If a portion of
a contract or policy is not covered, the remainder of the contract or policy is covered unless excluded otherwise. Subsection B(2) also provides a ready means
by which an individual State can exempt from the Act those policies and contracts issued by member insurers or similar organizations deemed appropriate
for exemption by the State.
Subsection B(2)(h) excludes coverage for any unallocated annuity contract not used to fund a benefit plan for natural persons or governmental lottery.
Life and Health Insurance Guaranty Association Model Act
520-8
© 2018 National Association of Insurance Commissioners
Subsection B(2)(k) is intended to exclude from coverage those products commonly referred to as “financial guaranty” products.
Subsection C provides the maximum limitations of the Association’s liability by type of contract or policy or line of business and overall per one life, plan
sponsor or owner. The limits may be reached through cash surrender payments, benefit payments, or continuing coverage or a combination thereof. The
maximum limits for each type of coverage should be set at an appropriate level after review by each State.
Section 4. Construction
This Act shall be construed to effect the purpose under Section 2.
Section 5. Definitions
As used in this Act:
A. “Account” means either of the two accounts created under Section 6.
B. “Association” means the [State] Life and Health Insurance Guaranty Association created under Section 6.
C. “Authorized assessment” or the term “authorized” when used in the context of assessments means a
resolution by the Board of Directors has been passed whereby an assessment will be called immediately or
in the future from member insurers for a specified amount. An assessment is authorized when the
resolution is passed.
D. “Benefit plan” means a specific employee, union or association of natural persons benefit plan.
E. “Called assessment” or the term “called” when used in the context of assessments means that a notice has
been issued by the Association to member insurers requiring that an authorized assessment be paid within
the time frame set forth within the notice. An authorized assessment becomes a called assessment when
notice is mailed by the Association to member insurers.
F. “Commissioner” means the Commissioner of Insurance of this State.
Drafting Note: Insert the title of the chief insurance regulatory official whenever the term “commissioner” appears.
G. “Contractual obligation” means an obligation under a policy or contract or certificate under a group policy
or contract, or portion thereof for which coverage is provided under Section 3.
H. “Covered contract” or “covered policy” means a policy or contract or portion of a policy or contract for
which coverage is provided under Section 3.
I. “Extra-contractual claims” shall include, for example, claims relating to bad faith in the payment of claims,
punitive or exemplary damages or attorneys’ fees and costs.
J. “Health benefit plan” means any hospital or medical expense policy or certificate, or health maintenance
organization subscriber contract or any other similar health contract. “Health benefit plan” does not
include:
(1) Accident only insurance:
(2) Credit insurance;
(3) Dental only insurance;
(4) Vision only insurance;
(5) Medicare Supplement insurance;
(6) Benefits for long-term care, home health care, community-based care, or any combination thereof;
NAIC Model Laws, Regulations, Guidelines and Other Resources—1
st
Quarter 2018
© 2018 National Association of Insurance Commissioners 520-9
(7) Disability income insurance;
(8) Coverage for on-site medical clinics; or
(9) Specified disease, hospital confinement indemnity, or limited benefit health insurance if the types
of coverage do not provide coordination of benefits and are provided under separate policies or
certificates.
K. “Impaired insurer” means a member insurer which, after the effective date of this Act, is not an insolvent
insurer, and is placed under an order of rehabilitation or conservation by a court of competent jurisdiction.
L. “Insolvent insurer” means a member insurer which after the effective date of this Act, is placed under an
order of liquidation by a court of competent jurisdiction with a finding of insolvency.
M. “Member insurer” means an insurer or health maintenance organization licensed or that holds a certificate
of authority to transact in this State any kind of insurance or health maintenance organization business for
which coverage is provided under Section 3, and includes an insurer or health maintenance organization
whose license or certificate of authority in this State may have been suspended, revoked, not renewed or
voluntarily withdrawn, but does not include:
(1) A hospital or medical service organization, whether profit or non-profit;
(2) A fraternal benefit society;
(3) A mandatory State pooling plan;
(4) A mutual assessment company or other person that operates on an assessment basis;
(5) An insurance exchange;
(6) An organization that has a certificate or license limited to the issuance of charitable gift annuities
under [insert the appropriate section of the State code]; or
(7) An entity similar to any of the above.
Drafting Note: States that license Health Care Service Corporations or similar organizations that undertake to provide basic health care services may want to
address these entities in this Act.
N. “Moody’s Corporate Bond Yield Average” means the Monthly Average Corporates as published by
Moody’s Investors Service, Inc., or any successor thereto.
O. “Owner” of a policy or contract and “policyholder,” “policy owner” and “contract owner” mean the person
who is identified as the legal owner under the terms of the policy or contract or who is otherwise vested
with legal title to the policy or contract through a valid assignment completed in accordance with the terms
of the policy or contract and properly recorded as the owner on the books of the member insurer. The terms
owner, contract owner, policyholder and policy owner do not include persons with a mere beneficial
interest in a policy or contract.
P. “Person” means an individual, corporation, limited liability company, partnership, association,
governmental body or entity or voluntary organization.
Q. “Plan sponsor” means:
(1) The employer in the case of a benefit plan established or maintained by a single employer;
(2) The employee organization in the case of a benefit plan established or maintained by an employee
organization; or
Life and Health Insurance Guaranty Association Model Act
520-10
© 2018 National Association of Insurance Commissioners
(3) In a case of a benefit plan established or maintained by two (2) or more employers or jointly by
one or more employers and one or more employee organizations, the association, committee, joint
board of trustees, or other similar group of representatives of the parties who establish or maintain
the benefit plan.
R. “Premiums” means amounts or considerations (by whatever name called) received on covered policies or
contracts less returned premiums, considerations and deposits and less dividends and experience credits.
“Premiums” does not include amounts or considerations received for policies or contracts or for the
portions of policies or contracts for which coverage is not provided under Section 3B except that
assessable premium shall not be reduced on account of Sections 3B(2)(c) relating to interest limitations and
3C(2) relating to limitations with respect to one individual, one participant and one policy or contract
owner. “Premiums” shall not include:
(1) Premiums in excess of $5,000,000 on an unallocated annuity contract not issued under a
governmental retirement benefit plan (or its trustee) established under Section 401, 403(b) or 457
of the United States Internal Revenue Code, or
(2) With respect to multiple non-group policies of life insurance owned by one owner, whether the
policy or contract owner is an individual, firm, corporation or other person, and whether the
persons insured are officers, managers, employees or other persons, premiums in excess of
$5,000,000 with respect to these policies or contracts, regardless of the number of policies or
contracts held by the owner.
S. (1) “Principal place of business” of a plan sponsor or a person other than a natural person means the
single State in which the natural persons who establish policy for the direction, control and
coordination of the operations of the entity as a whole primarily exercise that function, determined
by the Association in its reasonable judgment by considering the following factors:
(a) The State in which the primary executive and administrative headquarters of the entity is
located;
(b) The State in which the principal office of the chief executive officer of the entity is
located;
(c) The State in which the board of directors (or similar governing person or persons) of the
entity conducts the majority of its meetings;
(d) The State in which the executive or management committee of the board of directors (or
similar governing person or persons) of the entity conducts the majority of its meetings;
(e) The State from which the management of the overall operations of the entity is directed;
and
(f) In the case of a benefit plan sponsored by affiliated companies comprising a consolidated
corporation, the State in which the holding company or controlling affiliate has its
principal place of business as determined using the above factors.
However, in the case of a plan sponsor, if more than fifty percent (50%) of the participants in the
benefit plan are employed in a single State, that State shall be deemed to be the principal place of
business of the plan sponsor.
(2) The principal place of business of a plan sponsor of a benefit plan described in Subsection Q(3) of
this section shall be deemed to be the principal place of business of the association, committee,
joint board of trustees or other similar group of representatives of the parties who establish or
maintain the benefit plan that, in lieu of a specific or clear designation of a principal place of
business, shall be deemed to be the principal place of business of the employer or employee
organization that has the largest investment in the benefit plan in question.
NAIC Model Laws, Regulations, Guidelines and Other Resources—1
st
Quarter 2018
© 2018 National Association of Insurance Commissioners 520-11
T. “Receivership court” means the court in the insolvent or impaired insurer’s State having jurisdiction over
the conservation, rehabilitation or liquidation of the member insurer.
U. “Resident” means a person to whom a contractual obligation is owed and who resides in this State on the
date of entry of a court order that determines a member insurer to be an impaired insurer or a court order
that determines a member insurer to be an insolvent insurer, whichever occurs first. A person may be a
resident of only one State, which in the case of a person other than a natural person shall be its principal
place of business. Citizens of the United States that are either (i) residents of foreign countries, or (ii)
residents of United States possessions, territories or protectorates that do not have an association similar to
the Association created by this Act, shall be deemed residents of the State of domicile of the member
insurer that issued the policies or contracts.
V. “Structured settlement annuity” means an annuity purchased in order to fund periodic payments for a
plaintiff or other claimant in payment for or with respect to personal injury suffered by the plaintiff or other
claimant.
W “State” means a State, the District of Columbia, Puerto Rico, and a United States possession, territory or
protectorate.
X. “Supplemental contract” means a written agreement entered into for the distribution of proceeds under a
life, health or annuity policy or contract.
Y. “Unallocated annuity contract” means an annuity contract or group annuity certificate which is not issued
to and owned by an individual, except to the extent of any annuity benefits guaranteed to an individual by
an insurer under the contract or certificate.
Drafting Note: Each State will wish to examine its own statutes to determine whether these definitions are applicable and to determine whether some should
be deleted and others added.
Section 6. Creation of the Association
A. There is created a nonprofit legal entity to be known as the [State] Life and Health Insurance Guaranty
Association. All member insurers shall be and remain members of the Association as a condition of their
authority to transact insurance or a health maintenance organization business in this State. The Association
shall perform its functions under the plan of operation established and approved under Section 10 and shall
exercise its powers through a board of directors established under Section 7. For purposes of
administration and assessment, the Association shall maintain two (2) accounts:
(1) The life insurance and annuity account which includes the following subaccounts:
(a) Life insurance account;
(b) Annuity account which shall include annuity contracts owned by a governmental
retirement plan (or its trustee) established under Section 401, 403(b) or 457 of the United
States Internal Revenue Code, but shall otherwise exclude unallocated annuities; and
(c) Unallocated annuity account, which shall exclude contracts owned by a governmental
retirement benefit plan (or its trustee) established under Section 401, 403(b) or 457 of the
United States Internal Revenue Code.
(2) The health account.
B. The Association shall come under the immediate supervision of the commissioner and shall be subject to
the applicable provisions of the insurance laws of this State. Meetings or records of the Association may be
opened to the public upon majority vote of the board of directors of the Association.
Life and Health Insurance Guaranty Association Model Act
520-12
© 2018 National Association of Insurance Commissioners
Section 7. Board of Directors
A. The board of directors of the Association shall consist of not less than seven (7) nor more than eleven (11)
member insurers serving terms as established in the plan of operation. The insurer members of the board
shall be selected by member insurers subject to the approval of the commissioner. In addition, two (2)
persons who must be public representatives shall be appointed by the commissioner to the board of
directors. A “public representative” may not be an officer, director or employee of an insurance company
or a health maintenance organization or any person engaged in the business of insurance.
Vacancies on the board shall be filled for the remaining period of the term by a majority vote of the
remaining board members, for member insurers subject to the approval of the commissioner, and by the
commissioner for public representatives. To select the initial board of directors, and initially organize the
Association, the commissioner shall give notice to all member insurers of the time and place of the
organizational meeting. In determining voting rights at the organizational meeting each member insurer
shall be entitled to one vote in person or by proxy. If the board of directors is not selected within sixty (60)
days after notice of the organizational meeting, the commissioner may appoint the initial insurer members
in addition to the public representatives.
B. In approving selections or in appointing members to the board, the commissioner shall consider, among
other things, whether all member insurers are fairly represented.
C. Members of the board may be reimbursed from the assets of the Association for expenses incurred by them
as members of the board of directors but members of the board shall not otherwise be compensated by the
Association for their services.
Drafting Note: Subsection A provides that the number and term of the members of the board of directors shall be determined in the plan of operation. To
avoid problems in initially selecting the board, this section includes a provision for a start-up meeting which will be called by the commissioner. To
determine voting rights at the organizational meeting each member would have one vote. Thereafter the plan of operation will establish the voting
procedures, by-laws, etc. governing the conduct of the Association. States that are amending an existing statute should provide for a continuation of the
board.
States may consider including language in Subsection B to effectuate the fair representation of guaranty association members.
Section 8. Powers and Duties of the Association
A. If a member insurer is an impaired insurer, the Association may, in its discretion, and subject to any
conditions imposed by the Association that do not impair the contractual obligations of the impaired
insurer and that are approved by the commissioner:
(1) Guarantee, assume, reissue, or reinsure, or cause to be guaranteed, assumed, reissued, or
reinsured, any or all of the policies or contracts of the impaired insurer; or
(2) Provide such monies, pledges, loans, notes, guarantees or other means as are proper to effectuate
Paragraph (1) and assure payment of the contractual obligations of the impaired insurer pending
action under Paragraph (1).
B. If a member insurer is an insolvent insurer, the Association shall, in its discretion, either:
(1) (a) (i) Guaranty, assume, reissue, or reinsure, or cause to be guaranteed, assumed,
reissued, or reinsured, the policies or contracts of the insolvent insurer; or
(ii) Assure payment of the contractual obligations of the insolvent insurer; and
(b) Provide monies, pledges, loans, notes, guarantees, or other means reasonably necessary
to discharge the Association’s duties; or
NAIC Model Laws, Regulations, Guidelines and Other Resources—1
st
Quarter 2018
© 2018 National Association of Insurance Commissioners 520-13
(2) Provide benefits and coverages in accordance with the following provisions:
(a) With respect to policies and contracts, assure payment of benefits that would have been
payable under the policies or contracts of the insolvent insurer, for claims incurred:
(i) With respect to group policies and contracts, not later than the earlier of the next
renewal date under those policies or contracts or forty-five (45) days, but in no
event less than thirty (30) days, after the date on which the Association becomes
obligated with respect to the policies and contracts;
(ii) With respect to non-group policies, contracts, and annuities not later than the
earlier of the next renewal date (if any) under the policies or contracts or one
year, but in no event less than thirty (30) days, from the date on which the
Association becomes obligated with respect to the policies or contracts;
(b) Make diligent efforts to provide all known insureds, enrollees or annuitants (for non-
group policies and contracts), or group policy or contract owners with respect to group
policies and contracts, thirty (30) days notice of the termination (pursuant to
Subparagraph (a) of this paragraph) of the benefits provided;
(c) With respect to non-group policies and contracts covered by the Association, make
available to each known insured, enrollee, or annuitant, or owner if other than the
insured or annuitant, and with respect to an individual formerly an insured, enrollee or
annuitant under a group policy or contract who is not eligible for replacement group
coverage, make available substitute coverage on an individual basis in accordance with
the provisions of Subparagraph (d), if the insureds, enrollees or annuitants had a right
under law or the terminated policy, contract, or annuity to convert coverage to individual
coverage or to continue an individual policy, contract, or annuity in force until a
specified age or for a specified time, during which the insurer or health maintenance
organization had no right unilaterally to make changes in any provision of the policy,
contract, or annuity or had a right only to make changes in premium by class:
(d) (i) In providing the substitute coverage required under Subparagraph (c), the
Association may offer either to reissue the terminated coverage or to issue an
alternative policy or contract at actuarially justified rates[, subject to the prior
approval of the commissioner];
(ii) Alternative or reissued policies or contracts shall be offered without requiring
evidence of insurability, and shall not provide for any waiting period or
exclusion that would not have applied under the terminated policy or contract;
(iii) The Association may reinsure any alternative or reissued policy or contract.
(e) (i) Alternative policies or contracts adopted by the Association shall be subject to
the approval of the commissioner. The Association may adopt alternative
policies or contracts of various types for future issuance without regard to any
particular impairment or insolvency.
(ii) Alternative policies or contracts shall contain at least the minimum statutory
provisions required in this State and provide benefits that shall not be
unreasonable in relation to the premium charged. The Association shall set the
premium in accordance with a table of rates that it shall adopt
. The premium
shall reflect the amount of insurance to be provided and the age and class of risk
of each insured, but shall not reflect any changes in the health of the insured
after the original policy or contract was last underwritten.
Life and Health Insurance Guaranty Association Model Act
520-14
© 2018 National Association of Insurance Commissioners
(iii) Any alternative policy or contract issued by the Association shall provide
coverage of a type similar to that of the policy or contract issued by the impaired
or insolvent insurer, as determined by the Association.
(f) If the Association elects to reissue terminated coverage at a premium rate different from
that charged under the terminated policy or contract, the premium shall be actuarially
justified and set by the Association in accordance with the amount of insurance or
coverage provided and the age and class of risk[, subject to prior approval of the
commissioner ];
(g) The Association’s obligations with respect to coverage under any policy or contract of
the impaired or insolvent insurer or under any reissued or alternative policy or contract
shall cease on the date the coverage or policy or contract is replaced by another similar
policy or contract by the policy or contract owner, the insured, the enrollee, or the
Association;
(h) When proceeding under this Subsection B(2) with respect to a policy or contract carrying
guaranteed minimum interest rates, the Association shall assure the payment or crediting
of a rate of interest consistent with Section 3B(2)(c).
C. Nonpayment of premiums within thirty-one (31) days after the date required under the terms of any
guaranteed, assumed, alternative or reissued policy or contract or substitute coverage shall terminate the
Association’s obligations under the policy, contract, or coverage under this Act with respect to the policy,
contract, or coverage, except with respect to any claims incurred or any net cash surrender value which
may be due in accordance with the provisions of this Act.
D. Premiums due for coverage after entry of an order of liquidation of an insolvent insurer shall belong to and
be payable at the direction of the Association. If the liquidator of an insolvent insurer requests, the
Association shall provide a report to the liquidator regarding such premium collected by the Association.
The Association shall be liable for unearned premiums due to policy or contract owners arising after the
entry of the order.
E. The protection provided by this Act shall not apply where any guaranty protection is provided to residents
of this State by the laws of the domiciliary State or jurisdiction of the impaired or insolvent insurer other
than this State.
F. In carrying out its duties under Subsection B, the Association may:
(1) Subject to approval by a court in this State, impose permanent policy or contract liens in
connection with a guarantee, assumption or reinsurance agreement, if the Association finds that
the amounts which can be assessed under this Act are less than the amounts needed to assure full
and prompt performance of the Association’s duties under this Act, or that the economic or
financial conditions as they affect member insurers are sufficiently adverse to render the
imposition of such permanent policy or contract liens, to be in the public interest;
(2) Subject to approval by a court in this State, impose temporary moratoriums or liens on payments
of cash values and policy loans, or any other right to withdraw funds held in conjunction with
policies or contracts, in addition to any contractual provisions for deferral of cash or policy loan
value. In addition, in the event of a temporary moratorium or moratorium charge imposed by the
receivership court on payment of cash values or policy loans, or on any other right to withdraw
funds held in conjunction with policies or contracts, out of the assets of the impaired or insolvent
insurer, the Association may defer the payment of cash values, policy loans or other rights by the
Association for the period of the moratorium or moratorium charge imposed by the receivership
court, except for claims covered by the Association to be paid in accordance with a hardship
procedure established by the liquidator or rehabilitator and ap
proved by the receivership court.
NAIC Model Laws, Regulations, Guidelines and Other Resources—1
st
Quarter 2018
© 2018 National Association of Insurance Commissioners 520-15
G. A deposit in this State, held pursuant to law or required by the commissioner for the benefit of creditors,
including policy or contract owners, not turned over to the domiciliary liquidator upon the entry of a final
order of liquidation or order approving a rehabilitation plan of a member insurer domiciled in this State or
in a reciprocal State, pursuant to [insert citation to this State’s law dealing with the handling of special
deposits] shall be promptly paid to the Association. The Association shall be entitled to retain a portion of
any amount so paid to it equal to the percentage determined by dividing the aggregate amount of policy or
contract owners’ claims related to that insolvency for which the Association has provided statutory benefits
by the aggregate amount of all policy or contract owners’ claims in this State related to that insolvency and
shall remit to the domiciliary receiver the amount so paid to the Association less the amount retained
pursuant to this subsection. Any amount so paid to the Association and retained by it shall be treated as a
distribution of estate assets pursuant to applicable State receivership law dealing with early access
disbursements.
H. If the Association fails to act within a reasonable period of time with respect to an insolvent insurer, as
provided in Subsection B of this section, the commissioner shall have the powers and duties of the
Association under this Act with respect to the insolvent insurer.
I. The Association may render assistance and advice to the commissioner, upon the commissioner’s request,
concerning rehabilitation, payment of claims, continuance of coverage, or the performance of other
contractual obligations of an impaired or insolvent insurer.
J. The Association shall have standing to appear or intervene before a court or agency in this State with
jurisdiction over an impaired or insolvent insurer concerning which the Association is or may become
obligated under this Act or with jurisdiction over any person or property against which the Association
may have rights through subrogation or otherwise. Standing shall extend to all matters germane to the
powers and duties of the Association, including, but not limited to, proposals for reinsuring, reissuing,
modifying or guaranteeing the policies or contracts of the impaired or insolvent insurer and the
determination of the policies or contracts and contractual obligations. The Association shall also have the
right to appear or intervene before a court or agency in another State with jurisdiction over an impaired or
insolvent insurer for which the Association is or may become obligated or with jurisdiction over any
person or property against whom the Association may have rights through subrogation or otherwise.
K. (1) A person receiving benefits under this Act shall be deemed to have assigned the rights under, and
any causes of action against any person for losses arising under, resulting from or otherwise
relating to, the covered policy or contract to the Association to the extent of the benefits received
because of this Act, whether the benefits are payments of or on account of contractual obligations,
continuation of coverage or provision of substitute or alternative policies, contracts, or coverages.
The Association may require an assignment to it of such rights and cause of action by any
enrollee, payee, policy or contract owner, beneficiary, insured or annuitant as a condition
precedent to the receipt of any right or benefits conferred by this Act upon the person.
(2) The subrogation rights of the Association under this subsection shall have the same priority
against the assets of the impaired or insolvent insurer as that possessed by the person entitled to
receive benefits under this Act.
(3) In addition to Paragraphs (1) and (2) above, the Association shall have all common law rights of
subrogation and any other equitable or legal remedy that would have been available to the
impaired or insolvent insurer or owner, beneficiary, enrollee, or payee of a policy or contract with
respect to the policy or contracts (including without limitation, in the case of a structured
settlement annuity, any rights of the owner, beneficiary or payee of the annuity, to the extent of
benefits received pursuant to this Act, against a person originally or by succession responsible for
the losses arising from the personal injury relating to the annuity or payment therefore), excepting
any such person responsible solely by reason of serving as an assignee in respect of a qualified
assignment under Internal Revenue Code Section 130).
Life and Health Insurance Guaranty Association Model Act
520-16
© 2018 National Association of Insurance Commissioners
(4) If the preceding provisions of this subsection are invalid or ineffective with respect to any person
or claim for any reason, the amount payable by the Association with respect to the related covered
obligations shall be reduced by the amount realized by any other person with respect to the person
or claim that is attributable to the policies or contracts (or portion thereof) covered by the
Association.
(5) If the Association has provided benefits with respect to a covered obligation and a person recovers
amounts as to which the Association has rights as described in the preceding paragraphs of this
subsection, the person shall pay to the Association the portion of the recovery attributable to the
policies or contracts (or portion thereof) covered by the Association.
L. In addition to the rights and powers elsewhere in this Act, the Association may:
(1) Enter into such contracts as are necessary or proper to carry out the provisions and purposes of
this Act;
(2) Sue or be sued, including taking any legal actions necessary or proper to recover any unpaid
assessments under Section 9 and to settle claims or potential claims against it;
(3) Borrow money to effect the purposes of this Act; any notes or other evidence of indebtedness of
the Association not in default shall be legal investments for domestic member insurers and may be
carried as admitted assets;
(4) Employ or retain such persons as are necessary or appropriate to handle the financial transactions
of the Association, and to perform such other functions as become necessary or proper under this
Act;
(5) Take such legal action as may be necessary or appropriate to avoid or recover payment of
improper claims;
(6) Exercise, for the purposes of this Act and to the extent approved by the commissioner, the powers
of a domestic life insurer, health insurer, or health maintenance organization, but in no case may
the Association issue policies or contracts other than those issued to perform its obligations under
this Act;
(7) Organize itself as a corporation or in other legal form permitted by the laws of the State;
(8) Request information from a person seeking coverage from the Association in order to aid the
Association in determining its obligations under this Act with respect to the person, and the
person shall promptly comply with the request;
(9) Unless prohibited by law, in accordance with the terms and conditions of the policy or contract,
file for actuarially justified rate or premium increases for any policy or contract for which it
provides coverage under this Act; and
(10) Take other necessary or appropriate action to discharge its duties and obligations under this Act or
to exercise its powers under this Act.
M. The Association may join an organization of one or more other State associations of similar purposes, to
further the purposes and administer the powers and duties of the Association.
NAIC Model Laws, Regulations, Guidelines and Other Resources—1
st
Quarter 2018
© 2018 National Association of Insurance Commissioners 520-17
N. (1) (a) At any time within one hundred eighty (180) days of the date of the order of liquidation,
the Association may elect to succeed to the rights and obligations of the ceding member
insurer that relate to policies, contracts, or annuities covered, in whole or in part, by the
Association, in each case under any one or more reinsurance contracts entered into by the
insolvent insurer and its reinsurers and selected by the Association. Any such assumption
shall be effective as of the date of the order of liquidation. The election shall be effected
by the Association or the National Organization of Life and Health Insurance Guaranty
Associations (NOLHGA) on its behalf sending written notice, return receipt requested, to
the affected reinsurers.
(b) To facilitate the earliest practicable decision about whether to assume any of the
contracts of reinsurance, and in order to protect the financial position of the estate, the
receiver and each reinsurer of the ceding member insurer shall make available upon
request to the Association or to NOLHGA on its behalf as soon as possible after
commencement of formal delinquency proceedings (i) copies of in-force contracts of
reinsurance and all related files and records relevant to the determination of whether such
contracts should be assumed, and (ii) notices of any defaults under the reinsurance
contacts or any known event or condition which with the passage of time could become a
default under the reinsurance contracts.
(c) The following Subparagraphs (i) through (iv) shall apply to reinsurance contracts so
assumed by the Association:
(i) The Association shall be responsible for all unpaid premiums due under the
reinsurance contracts for periods both before and after the date of the order of
liquidation, and shall be responsible for the performance of all other obligations
to be performed after the date of the order of liquidation, in each case which
relate to policies, contracts, or annuities covered, in whole or in part, by the
Association. The Association may charge policies, contracts, or annuities
covered in part by the Association, through reasonable allocation methods, the
costs for reinsurance in excess of the obligations of the Association and shall
provide notice and an accounting of these charges to the liquidator;
(ii) The Association shall be entitled to any amounts payable by the reinsurer under
the reinsurance contracts with respect to losses or events that occur in periods
after the date of the order of liquidation and that relate to policies, contracts, or
annuities covered, in whole or in part, by the Association, provided that, upon
receipt of any such amounts, the Association shall be obliged to pay to the
beneficiary under the policy, contracts, or annuity on account of which the
amounts were paid a portion of the amount equal to the lesser of:
(I) The amount received by the Association; and
(II) The excess of the amount received by the Association over the amount
equal to the benefits paid by the Association on account of the policy,
contracts, or annuity less the retention of the insurer applicable to the
loss or event.

Life and Health Insurance Guaranty Association Model Act
520-18
© 2018 National Association of Insurance Commissioners
(iii) Within thirty (30) days following the Association’s election (the “election
date”), the Association and each reinsurer under contracts assumed by the
Association shall calculate the net balance due to or from the Association under
each reinsurance contract as of the election date with respect to policies,
contracts, or annuities covered, in whole or in part, by the Association, which
calculation shall give full credit to all items paid by either the member insurer or
its receiver or the reinsurer prior to the election date. The reinsurer shall pay the
receiver any amounts due for losses or events prior to the date of the order of
liquidation, subject to any set-off for premiums unpaid for periods prior to the
date, and the Association or reinsurer shall pay any remaining balance due the
other, in each case within five (5) days of the completion of the aforementioned
calculation. Any disputes over the amounts due to either the Association or the
reinsurer shall be resolved by arbitration pursuant to the terms of the affected
reinsurance contracts or, if the contract contains no arbitration clause, as
otherwise provided by law. If the receiver has received any amounts due the
Association pursuant to Subparagraph (c)(ii) of this Paragraph (1), the receiver
shall remit the same to the Association as promptly as practicable.
(iv) If the Association or receiver, on the Association’s behalf, within sixty (60)
days of the election date, pays the unpaid premiums due for periods both before
and after the election date that relate to policies, contracts, or annuities covered,
in whole or in part, by the Association, the reinsurer shall not be entitled to
terminate the reinsurance contracts for failure to pay premium insofar as the
reinsurance contracts relate to policies, contracts, or annuities covered, in whole
or in part, by the Association, and shall not be entitled to set off any unpaid
amounts due under other contracts, or unpaid amounts due from parties other
than the Association, against amounts due the Association.
(2) During the period from the date of the order of liquidation until the election date (or, if the
election date does not occur, until one hundred eighty (180) days after the date of the order of
liquidation),
(a) (i) Neither the Association nor the reinsurer shall have any rights or obligations
under reinsurance contracts that the Association has the right to assume under
Subsection (1), whether for periods prior to or after the date of the order of
liquidation; and
(ii) The reinsurer, the receiver and the Association shall, to the extent practicable,
provide each other data and records reasonably requested;
(b) Provided that once the Association has elected to assume a reinsurance contract, the
parties’ rights and obligations shall be governed by Subsection (1).
(3) If the Association does not elect to assume a reinsurance contract by the election date pursuant to
Subsection (1), the Association shall have no rights or obligations, in each case for periods both
before and after the date of the order of liquidation, with respect to the reinsurance contract.
(4) When policies, contracts, or annuities, or covered obligations with respect thereto, are transferred
to an assuming insurer, reinsurance on the policies, contracts, or annuities may also be transferred
by the Association, in the case of contracts assumed under Subsection (1), subject to the
following:
(a) Unless the reinsurer and the assuming insurer agree otherwi
se, the reinsurance contract
transferred shall not cover any new policies of insurance, contracts, or annuities in
addition to those transferred;
(b) The obligations described in Subsection (1) of this Section shall no longer apply with
respect to matters arising after the effective date of the transfer; and
NAIC Model Laws, Regulations, Guidelines and Other Resources—1
st
Quarter 2018
© 2018 National Association of Insurance Commissioners 520-19
(c) Notice shall be given in writing, return receipt requested, by the transferring party to the
affected reinsurer not less than thirty (30) days prior to the effective date of the transfer.
(5) The provisions of this Section N shall supersede the provisions of any State law or of any affected
reinsurance contract that provides for or requires any payment of reinsurance proceeds, on
account of losses or events that occur in periods after the date of the order of liquidation, to the
receiver of the insolvent insurer or any other person. The receiver shall remain entitled to any
amounts payable by the reinsurer under the reinsurance contracts with respect to losses or events
that occur in periods prior to the date of the order of liquidation, subject to applicable setoff
provisions.
(6) Except as otherwise provided in this section, nothing in this Section N shall alter or modify the
terms and conditions of any reinsurance contract. Nothing in this section shall abrogate or limit
any rights of any reinsurer to claim that it is entitled to rescind a reinsurance contract. Nothing in
this section shall give a policyholder, contract owner, enrollee, certificate holder, or beneficiary an
independent cause of action against a reinsurer that is not otherwise set forth in the reinsurance
contract. Nothing in this section shall limit or affect the Association’s rights as a creditor of the
estate against the assets of the estate. Nothing in this section shall apply to reinsurance agreements
covering property or casualty risks.
O. The Board of Directors of the Association shall have discretion and may exercise reasonable business
judgment to determine the means by which the Association is to provide the benefits of this Act in an
economical and efficient manner.
P. Where the Association has arranged or offered to provide the benefits of this Act to a covered person under
a plan or arrangement that fulfills the Association’s obligations under this Act, the person shall not be
entitled to benefits from the Association in addition to or other than those provided under the plan or
arrangement.
Q. Venue in a suit against the Association arising under the Act shall be in [insert name of county] County.
The Association shall not be required to give an appeal bond in an appeal that relates to a cause of action
arising under this Act.
Drafting Note: Along with Section 3, this section is a key to the specific responsibilities of the Association toward covered persons. That responsibility
varies by type of policy or contract involved.
The Association is primarily intended to act after the entry of an order of liquidation with the finding of insolvency against a member insurer. However, the
Association may act (Section 8A) in the case of an impaired insurer to guarantee, assume, reissue, or reinsure any or all policies or contracts or otherwise
provide money to the member insurer.
Subsection B details the main role of the Association in the instance of an order of liquidation against an insolvent insurer. The responsibilities of the
Association vary depending on the kind of coverage and type of policy or contract—group or individual. The Association may offer alternative policies or
contracts or change the premiums or benefits of existing policies or contracts. “New contracts or policies” shall be offered without new underwriting and
with coverage for existing conditions. This subsection also details that any rate changes, including rates for new or replacement contracts or policies, must be
actuarially justified and, if specified by the State, the commissioner must approve the rates prior to the rates becoming effective. In order to facilitate the sale
of blocks of business for which the Association is responsible, the cooperation of the domestic receiver may be necessary.
Subsection F relates to the imposition of policy and contract liens, moratoriums, etc. These are devices which have been used in the past in connection with
continuation of the insolvent insurer’s coverage. Since, by definition, the assets of the insolvent insurer were not adequate to support its contractual
obligations, liens were used to reduce those obligations to a level where the assets would be adequate. However, in the past there was no means to infuse
additional funds where needed to make whole policy or contract owners, insureds, enrollees, and beneficiaries. The purpose of the model act is to provide
timely payment and protect against losses due to an insolvency, by providing prompt fulfillment of insurance or health maintenance organization benefits to
the extent of the Association’s obligations under this Act. To the extent that liens and moratoriums are sanctioned, the model act retreats from this principle.
On the one hand, it can be argued that if liens and moratoriums cannot be used, there will be a run on the assets of the impaired or insolvent company. In the
past this seems to have been true. However, unlike the past, the performance of the member insurer’s contractual obligations would be guaranteed.
Also, the standard nonforfeiture laws provide that an insurer in its policies shall reserve the right to defer the payment of cash values for a period of six
months after demand therefor with surrender of the policy. Similarly, it is common to require an insurer to reserve for a period of six months the right to
defer the granting of any policy loan (other than to pay premiums). For those various reasons, the model act does not encourage the use of liens and
moratoriums in ordinary situations.
Life and Health Insurance Guaranty Association Model Act
520-20
© 2018 National Association of Insurance Commissioners
On the other hand, in periods of severe liquidity problems and economic stress, perhaps of even catastrophic proportions, such devices may become essential.
While the model act concentrates on the protection of those to whom the impaired or insolvent insurer has a contractual obligation, the impact of assessments
on the policyholders, contract owners, certificate holders, or enrollees of assessed companies is also an important consideration (e.g., significant sales of
depressed value assets in a tight money market). Consequently Subsection F(1) authorizes the Association to cause to be imposed liens and moratoriums (or
other similar means):
1. If the Court finds that the amounts assessable are less than what is needed, or that the economic or financial conditions as they affect member
insurers are sufficiently adverse to render the use of such tools in the public interest; and
2. The Court approves the use of the specific lien, moratorium, etc.
This provides a highly flexible mechanism while at the same time it avoids impairing the contractual obligations of the impaired or insolvent insurer as a
routine matter under ordinary economic and financial conditions. The provision also recognizes that while contractual rights of policy owners, contract
owners, certificate holders, or enrollees may not constitutionally be impaired, when the impaired or insolvent insurer’s obligation under the contract is
assumed by another insurer the policy owner, contract owners, certificate holders, or enrollees has two options. The policy owner, contract owners,
certificate holders, or enrollees may accept the new contract with such liens or moratoriums as permitted by the court, or accept such pro rata payment as is
available from the estate of the insolvent insurer.
Furthermore, to provide added flexibility in a temporary situation (e.g., run on assets), Subsection F(2) provides for temporary moratoriums or liens on
payment of cash values and policy loans, but not on the payment of other benefits, with the Court’s approval.
Subsection J, to enable the Association to protect its interest and the best interests of the policyholders, contract owners, certificate holders, or enrollees in
the handling of an impairment or insolvency, provides that the Association shall have standing to appear in courts with jurisdiction over an insolvent insurer
and such standing will extend to any matters concerning the duties of the Association.
Subsection L(9) was added to clarify that the Association has the authority to request rate increases under Section 8 in accordance with the terms of the
policies or contracts, unless prohibited by law. States should determine whether it would be consistent with other provisions of State law to make this power
of the Association subject to prior approval of the commissioner. States that have adopted long-term care insurance laws and regulations similar to the
NAIC’s Long-Term Care Insurance Model Act and Long-Term Care Insurance Model Regulation should consider whether this language should be changed
to conform to any applicable notice and approval requirements for premium rate schedule increases for long-term care insurance policies.
Subsection M explicitly recognizes that prompt and efficient discharge of the Association’s obligations will be greatly facilitated, especially in multistate
insolvencies by acting in concert through the National Organization of Life and Health Insurance Guaranty Associations (NOLHGA) to develop and, where
appropriate, carry out coordinated plans.
Subsection N has been revised to conform to the provisions of Section 612 of the Insurer Receivership Model Act. Section 612 represents a compromise
among receivers, reinsurers and guaranty associations regarding reinsurance of life and health insurance contracts. The revisions of Section 8N are intended
to preserve that compromise in this Act insofar as the Association is concerned.
R. In carrying out its duties in connection with guaranteeing, assuming, reissuing, or reinsuring policies or
contracts under Subsections A or B, the Association may issue substitute coverage for a policy or contract
that provides an interest rate, crediting rate or similar factor determined by use of an index or other external
reference stated in the policy or contract employed in calculating returns or changes in value by issuing an
alternative policy or contract in accordance with the following provisions:
(1) In lieu of the index or other external reference provided for in the original policy or contract, the
alternative policy or contract provides for (i) a fixed interest rate or (ii) payment of dividends with
minimum guarantees or (iii) a different method for calculating interest or changes in value;
(2) There is no requirement for evidence of insurability, waiting period or other exclusion that would
not have applied under the replaced policy or contract, and;
(3) The alternative policy or contract is substantially similar to the replaced policy or contract in all
other material terms
Section 9. Assessments
A. For the purpose of providing the funds necessary to carry out the powers and duties of the Association, the
board of directors shall assess the member insurers, separately for each account, at such time and for such
amounts as the board finds necessary. Assessments shall be due not less than thirty (30) days after prior
written notice to the member insurers and shall accrue interest at [insert amount] percent per annum on and
after the due date.
NAIC Model Laws, Regulations, Guidelines and Other Resources—1
st
Quarter 2018
© 2018 National Association of Insurance Commissioners 520-21
B. There shall be two (2) classes of assessments, as follows:
(1) Class A assessments shall be authorized and called for the purpose of meeting administrative and
legal costs and other expenses. Class A assessments may be authorized and called whether or not
related to a particular impaired or insolvent insurer.
(2) Class B assessments shall be authorized and called to the extent necessary to carry out the powers
and duties of the Association under Section 8 with regard to an impaired or an insolvent insurer.
C. (1) The amount of a Class A assessment shall be determined by the board and may be authorized and
called on a pro rata or non-pro rata basis. If pro rata, the board may provide that it be credited
against future Class B assessments.
(2) The amount of a Class B assessment, except for assessments related to long-term care insurance,
shall be allocated for assessment purposes between the accounts and among the subaccounts of
the life insurance and annuity account, pursuant to an allocation formula which may be based on
the premiums or reserves of the impaired or insolvent insurer or any other standard deemed by the
board in its sole discretion as being fair and reasonable under the circumstances.
(3) The amount of the Class B assessment for long-term care insurance written by the impaired or
insolvent insurer shall be allocated according to a methodology included in the Plan of Operation
and approved by the Commissioner. The methodology shall provide for 50% of the assessment to
be allocated to accident and health member insurers and 50% to be allocated to life and annuity
member insurers.
Drafting Note: The purpose of Subsection C(3) is to allocate the responsibility for an insolvency of a long-term care member insurer evenly between
member insurers in the health industry and member insurers in the life and annuity industries. As it is likely that life and annuity member insurers will be
subject to assessments from the health account, and accident and health member insurers will be subject to assessments from the life account, the formula
below should be utilized by guaranty associations so that member insurers in the health industry pay 50% of the assessment and member insurers in the life
and annuity industries pay 50% of the assessment.
In determining the shares that shall be allocated to the life and annuity account pursuant to Subsection C(3), guaranty associations should use the following
formula:
(.50 - Life and annuity member insurers’ share of HA) / (Life and annuity member insurers’ share of LIAA - Life and annuity member insurers’ share of HA)
For the purposes of the formula above and Subsection C(3) only, a “life and annuity member insurer” means a member insurer for which (i) the sum of its
assessable life insurance premiums and annuity premiums is greater than or equal to (ii) its assessable health insurance premiums, which shall include its
assessable health maintenance organization premiums but shall exclude its assessable premiums written for disability income and long-term care insurance.
For purposes of this definition, assessable premiums shall be measured within the state. An “accident and health member insurer” means any member insurer
not defined as a “life and annuity member insurer.” HA represents the guaranty association Health Account and LIAA represents the guaranty association
Life Insurance and Annuity Account.
(4) Class B assessments against member insurers for each account and subaccount shall be in the
proportion that the premiums received on business in this State by each assessed member insurer
on policies or contracts covered by each account for the three (3) most recent calendar years for
which information is available preceding the year in which the member insurer became insolvent
(or, in the case of an assessment with respect to an impaired insurer, the three (3) most recent
calendar years for which information is available preceding the year in which the member insurer
became impaired) bears to premiums received on business in this State for those calendar years by
all assessed member insurers.
(5) Assessments for funds to meet the requirements of the Association with respect to an impaired or
insolvent insurer shall not be authorized or called until necessary to implement the purposes of
this Act. Classification of assessments under Subsection B and computation of assessments under
this subsection shall be made with a reasonable degree of accuracy, recognizing that exact
determinations may not always be possible. The Association shall notify each member insurer of
its anticipated pro rata share of an authorized assessment not yet called within one hundred eighty
(180) days after the assessment is authorized.
Life and Health Insurance Guaranty Association Model Act
520-22
© 2018 National Association of Insurance Commissioners
D. The Association may abate or defer, in whole or in part, the assessment of a member insurer if, in the
opinion of the board, payment of the assessment would endanger the ability of the member insurer to fulfill
its contractual obligations. In the event an assessment against a member insurer is abated, or deferred in
whole or in part, the amount by which the assessment is abated or deferred may be assessed against the
other member insurers in a manner consistent with the basis for assessments set forth in this section. Once
the conditions that caused a deferral have been removed or rectified, the member insurer shall pay all
assessments that were deferred pursuant to a repayment plan approved by the Association.
E. (1) (a) Subject to the provisions of Subparagraph (b) of this paragraph, the total of all
assessments authorized by the Association with respect to a member insurer for each
subaccount of the life insurance and annuity account and for the health account shall not
in one calendar year exceed two percent (2%) of that member insurer’s average annual
premiums received in this State on the policies and contracts covered by the subaccount
or account during the three (3) calendar years preceding the year in which the member
insurer became an impaired or insolvent insurer.
(b) If two (2) or more assessments are authorized in one calendar year with respect to
member insurers that become impaired or insolvent in different calendar years, the
average annual premiums for purposes of the aggregate assessment percentage limitation
referenced in Subparagraph (a) of this paragraph shall be equal and limited to the higher
of the three-year average annual premiums for the applicable subaccount or account as
calculated pursuant to this section.
(c) If the maximum assessment, together with the other assets of the Association in an
account, does not provide in one year in either account an amount sufficient to carry out
the responsibilities of the Association, the necessary additional funds shall be assessed as
soon thereafter as permitted by this Act.
(2) The board may provide in the plan of operation a method of allocating funds among claims,
whether relating to one or more impaired or insolvent insurers, when the maximum assessment
will be insufficient to cover anticipated claims.
(3) If the maximum assessment for a subaccount of the life and annuity account in one year does not
provide an amount sufficient to carry out the responsibilities of the Association, then pursuant to
Subsection C(2), the board shall access the other subaccounts of the life and annuity account for
the necessary additional amount, subject to the maximum stated in Paragraph (1) above.
F. The board may, by an equitable method as established in the plan of operation, refund to member insurers,
in proportion to the contribution of each member insurer to that account, the amount by which the assets of
the account exceed the amount the board finds is necessary to carry out during the coming year the
obligations of the Association with regard to that account, including assets accruing from assignment,
subrogation, net realized gains and income from investments. A reasonable amount may be retained in any
account to provide funds for the continuing expenses of the Association and for future losses claims.
G. It shall be proper for any member insurer, in determining its premium rates and policy owner dividends as
to any kind of insurance or health maintenance organization business within the scope of this Act, to
consider the amount reasonably necessary to meet its assessment obligations under this Act.
H. The Association shall issue to each member insurer paying an assessment under this Act, other than a Class
A assessment, a certificate of contribution, in a form prescrib
ed by the commissioner, for the amount of the
assessment so paid. All outstanding certificates shall be of equal dignity and priority without reference to
amounts or dates of issue. A certificate of contribution may be shown by the member insurer in its financial
statement as an asset in such form and for such amount, if any, and period of time as the commissioner may
approve.

NAIC Model Laws, Regulations, Guidelines and Other Resources—1
st
Quarter 2018
© 2018 National Association of Insurance Commissioners 520-23
I. (1) A member insurer that wishes to protest all or part of an assessment shall pay when due the full
amount of the assessment as set forth in the notice provided by the Association. The payment shall
be available to meet Association obligations during the pendency of the protest or any subsequent
appeal. Payment shall be accompanied by a statement in writing that the payment is made under
protest and setting forth a brief statement of the grounds for the protest.
(2) Within sixty (60) days following the payment of an assessment under protest by a member insurer,
the Association shall notify the member insurer in writing of its determination with respect to the
protest unless the Association notifies the member insurer that additional time is required to
resolve the issues raised by the protest.
(3) Within thirty (30) days after a final decision has been made, the Association shall notify the
protesting member insurer in writing of that final decision. Within sixty (60) days of receipt of
notice of the final decision, the protesting member insurer may appeal that final action to the
commissioner.
(4) In the alternative to rendering a final decision with respect to a protest based on a question
regarding the assessment base, the Association may refer protests to the commissioner for a final
decision, with or without a recommendation from the Association.
(5) If the protest or appeal on the assessment is upheld, the amount paid in error or excess shall be
returned to the member insurer. Interest on a refund due a protesting member insurer shall be paid
at the rate actually earned by the Association.
J. The Association may request information of member insurers in order to aid in the exercise of its power
under this section and member insurers shall promptly comply with a request.
Drafting Note: The Association is authorized to raise funds to fulfill its obligations under this Model Act with respect to an impaired or insolvent insurer by
assessing the member insurers on the basis of the premiums they write in the State. This corresponds to the Association’s liability which, in most cases, is
limited to covered policies of residents. This assessment system provides a base broad enough to meet fairly large demands on the Association. Equally
important, since it reflects the market share of each member insurer in the State including health maintenance organizations, it is an equitable method of
apportioning the burden of the assessments.
Subsection E provides some limitations on the amounts that can be assessed in a given year. The maximum assessment per year may be varied from State to
State depending on the size of the base and the concentration of the business. The two percent (2%) maximum assessment per year should produce an
adequate amount while at the same time not impose an undue strain in any given year on the assessed member insurers and their policy owners, contract
owners, certificate holders, or enrollees. The maximum is applied to the amount of assessments authorized in a given year, and not the amount called; this
allows the Association the flexibility to utilize current capacity for future obligations without collecting assessments from the member insurers until required.
The Model Act provides additional discretion and flexibility for the Association in fulfilling its responsibilities by authorizing it to borrow funds that later
can be paid out of future assessments.
Subsection G provides that a member insurer may consider in its premium rates and dividend scale an amount reasonably necessary to meet its assessment
obligations. This makes it clear that the cost can be ultimately passed on to the policy owners, contract owners, certificate holders, or enrollees—i.e., to
persons who enjoy the protection provided by the Act. Subsection H provides that the Association shall issue to assessed member insurers certificates of
contribution in the amount levied. The certificates may be carried by a member insurer in its annual statement as an asset in such form, amount and period as
may be approved by the commissioner. By permitting the member insurers to carry these certificates as an asset, to the extent of their estimated value, the
impact on member insurers will be lessened.
States may consider establishing a pre-funding arrangement for both insurance companies and health maintenance organizations that write health benefit
plans to meet their assessment obligations to the Association. To pre-fund, member insurers writing health benefit plans would collect a set amount per
member or per certificate per month and remit that amount directly to the Association. The pre-funded amounts would be utilized by the member insurers to
satisfy Class B assessment obligations for future insolvencies. When the fund reaches a statutory cap, the pre-funding would stop. In the event of a depletion
of the fund below the statutory cap, the pre-funding assessment would be reinstated.
Establishing a pre-funding arrangement allows for the use of interest and investment income to lessen the impact of insolvencies on State taxpayers. Pre-
funding also spreads the assessment obligations amongst policyholders prior to an insolvency and does not require the member health insurers or health
maintenance organizations to look to the State taxpayers for recoupment. In addition, member insurers in the health industry that do not pay income or
premium taxes would be offered a recoupment methodology that is the same as other member insurers in their markets. If a pre-funding arrangement is
established, the funds should be legally insulated to avoid diversion for any other purposes, and ensure that they are held exclusively for the Association’s
obligations.
Life and Health Insurance Guaranty Association Model Act
520-24
© 2018 National Association of Insurance Commissioners
Section 10. Plan of Operation
A. (1) The Association shall submit to the commissioner a plan of operation and any amendments thereto
necessary or suitable to assure the fair, reasonable and equitable administration of the Association.
The plan of operation and any amendments thereto shall become effective upon the
commissioner’s written approval or unless it has not been disapproved within thirty (30) days.
(2) If the Association fails to submit a suitable plan of operation within 120 days following the
effective date of this Act or if at any time thereafter the Association fails to submit suitable
amendments to the plan, the commissioner shall, after notice and hearing, adopt and promulgate
such reasonable rules as are necessary or advisable to effectuate the provisions of this Act. The
rules shall continue in force until modified by the commissioner or superseded by a plan
submitted by the Association and approved by the commissioner.
B. All member insurers shall comply with the plan of operation.
C. The plan of operation shall, in addition to requirements enumerated elsewhere in this Act:
(1) Establish procedures for handling the assets of the Association;
(2) Establish the amount and method of reimbursing members of the board of directors under Section
7;
(3) Establish regular places and times for meetings including telephone conference calls of the board
of directors;
(4) Establish procedures for records to be kept of all financial transactions of the Association, its
agents, and the board of directors;
(5) Establish the procedures whereby selections for the board of directors will be made and submitted
to the commissioner;
(6) Establish any additional procedures for assessments under Section 9;
(7) Contain additional provisions necessary or proper for the execution of the powers and duties of
the Association;
(8) Establish procedures whereby a director may be removed for cause, including in the case where a
member insurer director becomes an impaired or insolvent insurer;
(9) Require the Board of Directors to establish a policy and procedures for addressing conflicts of
interests.
D. The plan of operation may provide that any or all powers and duties of the Association, except those under
Section 8L(3) and Section 9, are delegated to a corporation, association or other organization which
performs or will perform functions similar to those of this Association, or its equivalent, in two (2) or more
States. Such a corporation, association, or organization shall be reimbursed for any payments made on
behalf of the Association and shall be paid for its performance of any function of the Association. A
delegation under this subsection shall take effect only with the approval of both the board of directors and
the commissioner, and may be made only to a corporation, association, or organization which extends
protection not substantially less favorable and effective than that provided by this Act.
NAIC Model Laws, Regulations, Guidelines and Other Resources—1
st
Quarter 2018
© 2018 National Association of Insurance Commissioners 520-25
Section 11. Duties and Powers of the Commissioner
In addition to the duties and powers enumerated elsewhere in this Act,
A. The commissioner shall:
(1) Upon request of the board of directors, provide the Association with a statement of the premiums
in this and any other appropriate States for each member insurer;
(2) When an impairment is declared and the amount of the impairment is determined, serve a demand
upon the impaired insurer to make good the impairment within a reasonable time; notice to the
impaired insurer shall constitute notice to its shareholders, if any; the failure of the impaired
insurer to promptly comply with such demand shall not excuse the Association from the
performance of its powers and duties under this Act.
B. The commissioner may suspend or revoke, after notice and hearing, the certificate of authority to transact
business in this State of any member insurer which fails to pay an assessment when due or fails to comply
with the plan of operation. As an alternative the commissioner may levy a forfeiture on any member insurer
that fails to pay an assessment when due. The forfeiture shall not exceed five percent (5%) of the unpaid
assessment per month, but no forfeiture shall be less than $100 per month.
C. A final action of the board of directors or the Association may be appealed to the commissioner by a
member insurer if the appeal is taken within sixty (60) days of its receipt of notice of the final action being
appealed. A final action or order of the commissioner shall be subject to judicial review in a court of
competent jurisdiction in accordance with the laws of this State that apply to the actions or orders of the
commissioner.
D. The liquidator, rehabilitator or conservator of an impaired or insolvent insurer may notify all interested
persons of the effect of this Act.
Drafting Note: Subsection A(2) requires that the commissioner give notice of an impairment to the impaired insurer, and hence to its stockholders, and serve
a demand that the impairment be made good. If the company and stockholders fail to raise the necessary funds, this will be a factor bearing upon the
stockholder’s ownership rights under Section 14E.
State Proceedings for the liquidation, rehabilitation or conservation of member insurers present several difficulties that both acts seek to solve. Briefly, the
difficulties have two sources. First, in some States the liquidator, rehabilitator or ancillary receiver may be a person unfamiliar with insurance or health
benefit plan regulation. Inefficient administration of the proceedings may result.
Second, the laws of more than one State may be applied to the proceedings, particularly regarding ownership of assets and preferences for payment. The
result is confusion and inequity in the collection and distribution of the assets. The Insurers Rehabilitation and Liquidation Model Act and the Uniform
Insurers Liquidation Act meet the first source of problems by designating the insurance commissioner as the receiver of a domestic insurer or the ancillary
receiver of a foreign insurer. To solve the problem of multiple laws and marshaling of assets, both acts give the receiver title to the assets. The ancillary
receiver is then required to forward all assets to the receiver. Both acts also detail the laws under which preferences in the distribution of assets will be
determined.
In drafting this model guaranty act, particular effort was made to avoid (to the extent possible) disrupting existing State liquidation and rehabilitation laws.
However, each individual State may want to consider adopting the Insurers Rehabilitation and Liquidation Model Act or the Uniform Insurers Liquidation
Act, if it has not already done so.
Section 12. Prevention of Insolvencies
To aid in the detection and prevention of member insurer insolvencies or impairments,
A. It shall be the duty of the commissioner:
(1) To notify the commissioners of all the other States, territories of the United States and the District
of Columbia within thirty (30) days following the action taken or the date the action occurs, when
the commissioner takes any of the following actions against a member insurer:
Life and Health Insurance Guaranty Association Model Act
520-26
© 2018 National Association of Insurance Commissioners
(a) Revocation of license;
(b) Suspension of license; or
(c) Makes a formal order that the member insurer restrict its premium writing, obtain
additional contributions to surplus, withdraw from the State, reinsure all or any part of its
business, or increase capital, surplus, or any other account for the security of policy
owners, contract owners, certificate holders, or creditors.
(2) To report to the board of directors when the commissioner has taken any of the actions set forth in
Paragraph (1) or has received a report from any other commissioner indicating that any such
action has been taken in another State. The report to the board of directors shall contain all
significant details of the action taken or the report received from another commissioner.
(3) To report to the board of directors when the commissioner has reasonable cause to believe from
an examination, whether completed or in process, of any member insurer that the insurer may be
an impaired or insolvent insurer.
(4) To furnish to the board of directors the NAIC Insurance Regulatory Information System (IRIS)
ratios and listings of companies not included in the ratios developed by the National Association
of Insurance commissioners, and the board may use the information contained therein in carrying
out its duties and responsibilities under this section. The report and the information contained
therein shall be kept confidential by the board of directors until such time as made public by the
commissioner or other lawful authority.
B. The commissioner may seek the advice and recommendations of the board of directors concerning any
matter affecting the duties and responsibilities of the commissioner regarding the financial condition of
member insurers and insurers or health maintenance organizations seeking admission to transact business
in this State.
C. The board of directors may, upon majority vote, make reports and recommendations to the commissioner
upon any matter germane to the solvency, liquidation, rehabilitation or conservation of any member insurer
or germane to the solvency of any insurer or health maintenance organization seeking to do business in this
State. The reports and recommendations shall not be considered public documents.
D. The board of directors may, upon majority vote, notify the commissioner of any information indicating a
member insurer may be an impaired or insolvent insurer.
E. The board of directors may, upon majority vote, make recommendations to the commissioner for the
detection and prevention of member insurer insolvencies.
[Section 13. Credits for Assessments Paid (Tax Offsets)—OPTIONAL
A. A member insurer may offset against its [premium, franchise or income] tax liability to this State an
assessment described in Section 9H to the extent of twenty percent (20%) of the amount of the assessment
for each of the five (5) calendar years following the year in which the assessment was paid. In the event a
member insurer should cease doing business, all uncredited assessments may be credited against its
[premium, franchise, or income] tax liability for the year it ceases doing business.
B. A member insurer that is exempt from taxes referenced in Subsection A above may recoup its assessments
by a surcharge on its premiums in a sum reasonably calculated to recoup the assessments over a reasonable
period of time, as approved by the commissioner. Amounts recouped shall not be considered premiums for
any other purpose, including the computation of gross premium tax, the medical loss ratio, or agent
commission. If a member insurer collects excess surcharges, the insurer shall remit the excess amount to
the association, and the excess amount shall be applied to reduce future assessments in the appropriate
account.
NAIC Model Laws, Regulations, Guidelines and Other Resources—1
st
Quarter 2018
© 2018 National Association of Insurance Commissioners 520-27
C. Any sums that are acquired by refund, pursuant to Section 9F, from the Association by member insurers,
and that have been offset against [premium, franchise or income] taxes as provided in Subsection A above,
shall be paid by the member insurers to this State in such manner as the tax authorities may require. The
Association shall notify the commissioner that refunds have been made.]
Drafting Note: Subsection A provides an offset against future premium, franchise or income taxes of assessments, over a five-year period. The timing of the
credit is dependent on the year the assessment is paid. It also allows the member insurer to select the applicable tax (premium, franchise or income) against
which the credit may be applied and it permits member insurers going out of business to make use of the credit in their final year of operations.
Life insurance premiums, and premiums for certain forms of health insurance, cannot be changed on existing policyholders. Thus, a suitable and practical
method of recoupment available to companies writing life and health insurance lies in offsets against premium or other taxes on such companies. The method
suggested in this section is not only equitable to the companies involved but also reduces the impact on State revenue by the partial offset over a period of
years. To the extent the recovery from the insolvent company exceeds the tax credit received, the State would be the ultimate beneficiary. The equitable
treatment of assessments for tax purposes would have additional positive effects: (1) the State legislature would have an additional incentive for providing
adequate funds for insurance department personnel and administration, and (2) participation in the economic loss would be shared, to some degree, by the
general public rather than solely by insureds, thus minimizing what might otherwise be a penalty on thrift and savings. It may be advisable in some
jurisdictions to provide a cross-reference to the premium or other tax statutes to avoid questions of conflicting statutory provisions.
Subsection B provides an alternative mechanism for tax-exempt member insurers to recoup funds paid for assessments, and is intended to avoid
disadvantaging tax-exempt or non-profit member insurers that are not subject to a [premium, franchise or income] tax liability, and thus would not benefit
from a premium tax offset. The amount and duration of a surcharge is subject to approval by the commissioner, and any such surcharge cannot be considered
premium for any purpose. Building assessments into surcharges for future policyholders or contract owners has proven to be an effective way for insurers to
recoup funds, and a surcharge mechanism is necessary to provide tax-exempt and non-profit member insurers with a meaningful opportunity to recoup funds
paid for assessments.
This section is optional, and the NAIC neither endorses nor rejects the tax credit or the surcharge concept. Each State will wish to consider this provision in
the light of its own regulatory experience.
Section 14. Miscellaneous Provisions
A. This Act shall not be construed to reduce the liability for unpaid assessments of the insureds of an impaired
or insolvent insurer operating under a plan with assessment liability.
B. Records shall be kept of all meetings of the board of directors to discuss the activities of the Association in
carrying out its powers and duties under Section 8. The records of the Association with respect to an
impaired or insolvent insurer shall not be disclosed prior to the termination of a liquidation, rehabilitation
or conservation proceeding involving the impaired or insolvent insurer, except (i) upon the termination of
the impairment or insolvency of the member insurer, or (ii) upon the order of a court of competent
jurisdiction. Nothing in this subsection shall limit the duty of the Association to render a report of its
activities under Section 15.
C. For the purpose of carrying out its obligations under this Act, the Association shall be deemed to be a
creditor of the impaired or insolvent insurer to the extent of assets attributable to covered policies reduced
by any amounts to which the Association is entitled as subrogee pursuant to Section 8K. Assets of the
impaired or insolvent insurer attributable to covered policies shall be used to continue all covered policies
and pay all contractual obligations of the impaired or insolvent insurer as required by this Act. Assets
attributable to covered policies or contracts, as used in this subsection, are that proportion of the assets
which the reserves that should have been established for such policies or contracts bear to the reserves that
should have been established for all policies of insurance or health benefit plans written by the impaired or
insolvent insurer.
D. As a creditor of the impaired or insolvent insurer as established in Subsection C of this section and
consistent with [insert cite of applicable State receivership law provision dealing with early access
disbursements], the Association and other similar associations shall be entitled to receive a disbursement of
assets out of the marshaled assets, from time to time as the assets become available to reimburse it, as a
credit against contractual obligations under this Act. If the liquidator has not, within 120 days of a final
determination of insolvency of a member insurer by the receivership court, made an application to the court
for the approval of a proposal to disburse assets out of marshaled assets to guaranty associations having
obligations because of the insolvency, then the Association shall be entitled to make application to the
receivership court for approval of its own proposal to disburse these assets.
Life and Health Insurance Guaranty Association Model Act
520-28
© 2018 National Association of Insurance Commissioners
E. (1) Prior to the termination of any liquidation, rehabilitation or conservation proceeding, the court
may take into consideration the contributions of the respective parties, including the Association,
the shareholders, contract owners, certificate holders, enrollees and policy owners of the insolvent
insurer, and any other party with a bona fide interest, in making an equitable distribution of the
ownership rights of the insolvent insurer. In such a determination, consideration shall be given to
the welfare of the policy owners, contract owners, certificate holders, and enrollees of the
continuing or successor member insurer.
(2) No distribution to stockholders, if any, of an impaired or insolvent insurer shall be made until and
unless the total amount of valid claims of the Association with interest thereon for funds expended
in carrying out its powers and duties under Section 8 with respect to the member insurer have
been fully recovered by the Association.
[F. (1) If an order for liquidation or rehabilitation of a member insurer domiciled in this State has been
entered, the receiver appointed under the order shall have a right to recover on behalf of the
member insurer, from any affiliate that controlled it, the amount of distributions, other than stock
dividends paid by the member insurer on its capital stock, made at any time during the five (5)
years preceding the petition for liquidation or rehabilitation subject to the limitations of
Paragraphs (2) to (4).
(2) No such distribution shall be recoverable if the member insurer shows that when paid the
distribution was lawful and reasonable, and that the member insurer did not know and could not
reasonably have known that the distribution might adversely affect the ability of the member
insurer to fulfill its contractual obligations.
(3) Any person who was an affiliate that controlled the member insurer at the time the distributions
were paid shall be liable up to the amount of distributions received. Any person, who was an
affiliate that controlled the member insurer at the time the distributions were declared, shall be
liable up to the amount of distributions which would have been received if they had been paid
immediately. If two (2) or more persons are liable with respect to the same distributions, they shall
be jointly and severally liable.
(4) The maximum amount recoverable under this subsection shall be the amount needed in excess of
all other available assets of the insolvent insurer to pay the contractual obligations of the insolvent
insurer.
(5) If any person liable under Paragraph (3) is insolvent, all its affiliates that controlled it at the time
the distribution was paid, shall be jointly and severally liable for any resulting deficiency in the
amount recovered from the insolvent affiliate.]
Drafting Note: Subsection A is intended to preserve the assessment liability of the insureds of assessment mutuals.
Subsection B addresses record-keeping by the Association. The Association should be held publicly accountable for its actions. On the other hand, effective
handling of the rehabilitation or liquidation effort requires minimum publicity. Thus, such records will be made public only after the liquidation,
rehabilitation or conservation proceeding is terminated, the impairment or insolvency is terminated or there is a prior order by a court of competent
jurisdiction.
Since this Act imposes the obligation upon the Association to continue coverage for policyholders, contract owners, certificate holders, or enrollees of
insolvent insurers, the assets of the insolvent insurer ought to be used, to the extent available, for the purpose of continuing such coverage. Subsections C
and D are designed to accomplish this purpose.
Subsection E, in conjunction with Section 11A(2), is intended to prevent the shareholders of an impaired or insolvent insurer from sitting back and doing
nothing and then reaping the benefits of funds put up by the Association. These stockholders should not obtain a more advantageous position than they
would have occupied in the absence of this Act. The court is empowered to modify and distribute the ownership rights of an impaired or insolvent insurer in
order to do equity as between the interested parties.
NAIC Model Laws, Regulations, Guidelines and Other Resources—1
st
Quarter 2018
© 2018 National Association of Insurance Commissioners 520-29
Subsection F, which should be deleted if the State has adopted Section 602 of the NAIC Insurers Receivership Model Act dealing with affiliated
transactions, is designed to recapture excessive dividend payments to affiliates that exercised control over the impaired or insolvent insurer. The NAIC
Insurance Holding Company System Regulatory Model Act in large measure prevents improper distribution of dividends by an insurer to its holding
company since extraordinary dividends are subject to the prior approval of the commissioner, and ordinary dividends are required to be reported to the
commissioner. If, however, dividends are paid under circumstances that the member insurer should have reasonably known that such payment could
reasonably be expected to affect its ability to perform its contractual obligation to its policyholders, contract owners, certificate holders, or enrollees the
holding company and affiliates should be required to repay such dividends subject to certain reasonable limitations.
If a State has the NAIC Insurance Holding Company System Regulatory Model Act, the definitions therein could be referred to by this subsection. States
without the Model Act could incorporate the relevant definitions in this subsection.
Section 15. Examination of the Association; Annual Report
The Association shall be subject to examination and regulation by the commissioner. The board of directors shall submit to
the commissioner each year, not later than 120 days after the Association’s fiscal year, a financial report in a form approved
by the commissioner and a report of its activities during the preceding fiscal year. Upon the request of a member insurer, the
Association shall provide the member insurer with a copy of the report.
Section 16. Tax Exemptions
The Association shall be exempt from payment of all fees and all taxes levied by this State or any of its subdivisions, except
taxes levied on real property.
Section 17. Immunity
There shall be no liability on the part of and no cause of action of any nature shall arise against any member insurer or its
agents or employees, the Association or its agents or employees, members of the board of directors, or the commissioner or
the commissioner’s representatives, for any action or omission by them in the performance of their powers and duties under
this Act. This immunity shall extend to the participation in any organization of one or more other State associations of
similar purposes and to any such organization and its agents or employees.
Drafting Note: This drafting note is for the purpose of clarifying the intent of the drafters of Section 17. As the courts have indicated, this provision was
never intended to protect the Association from actions seeking to enforce its statutory obligations to pay covered claims. See, e.g., Mendes v. Hawaii
Insurance Guaranty Association, 950 P.2d 1214, 1218 (Haw. Sup. Ct. 1998), (“HIGA is amenable to suit for the limited purpose of compelling it to perform
its statutory duty to deal with the covered claims of insolvent insurers”); PIE Mutual Insurance Company v. Ohio Insurance Guaranty Association, 611 N.E.
2d. 313, 317 (Ohio Sup. Ct. 1993) (“ … insured or third-party claimant is entitled to judicial relief to force OIGA to perform its statutory duties”).
Nor was the provision ever intended to protect the Association from contract actions to enforce express obligations of the Association under contracts
entered into by the Association.
Each State may wish to review its own statutes to determine whether its Tort Claims Act, if it has one, could be used as an alternative to this section insofar
as it applies to the commissioner or his representative.
Section 18. Stay of Proceedings; Reopening Default Judgments
All proceedings in which the insolvent insurer is a party in any court in this State shall be stayed one hundred eighty (180)
days from the date an order of liquidation, rehabilitation or conservation is final to permit proper legal action by the
Association on any matters germane to its powers or duties. As to judgment under any decision, order, verdict or finding
based on default the Association may apply to have such judgment set aside by the same court that made such judgment and
shall be permitted to defend against such suit on the merits.
Life and Health Insurance Guaranty Association Model Act
520-30
© 2018 National Association of Insurance Commissioners
Section 19. Prohibited Advertisement of Insurance Guaranty Association Act in Insurance Sales; Notice to
Policy Owners
A. No person, including a member insurer, agent or affiliate of a member insurer shall make, publish,
disseminate, circulate or place before the public, or cause directly or indirectly, to be made, published,
disseminated, circulated or placed before the public, in any newspaper, magazine or other publication, or in
the form of a notice, circular, pamphlet, letter or poster, or over any radio station or television station, or in
any other way, any advertisement, announcement or statement, written or oral, which uses the existence of
the Insurance Guaranty Association of this State for the purpose of sales, solicitation or inducement to
purchase any form of insurance or other coverage covered by the [State] Life and Health Insurance
Guaranty Association Act. However, this section shall not apply to the [State] Life and Health Insurance
Guaranty Association or any other entity which does not sell or solicit insurance or coverage by a health
maintenance organization.
B. Within one hundred eighty (180) days of the effective date of this Act, the Association shall prepare a
summary document describing the general purposes and current limitations of the Act and complying with
Subsection C of this section. This document shall be submitted to the commissioner for approval. At the
expiration of the sixtieth day after the date on which the commissioner approves the document, a member
insurer may not deliver a policy or contract to a policy owner, contract owner, certificate holder, or
enrollee unless the summary document is delivered to the policy owner, contract owner, certificate holder,
or enrollee at the time of delivery of the policy or contract. The document shall also be available upon
request by a policy owner, contract owner, certificate holder, or enrollee. The distribution, delivery or
contents or interpretation of this document does not guarantee that either the policy or the contract or the
policy owner, contract owner, certificate holder, or enrollee is covered in the event of the impairment or
insolvency of a member insurer. The description document shall be revised by the Association as
amendments to the Act may require. Failure to receive this document does not give the policy owner,
contract owner, certificate holder, enrollee, or insured any greater rights than those stated in this Act.
C. The document prepared under Subsection B shall contain a clear and conspicuous disclaimer on its face.
The commissioner shall establish the form and content of the disclaimer. The disclaimer shall:
(1) State the name and address of the Life and Health Insurance Guaranty Association and insurance
department;
(2) Prominently warn the policy owner, contract owner, certificate holder, or enrollee that the Life
and Health Insurance Guaranty Association may not cover the policy or contract or, if coverage is
available, it will be subject to substantial limitations and exclusions and conditioned on continued
residence in this State;
(3) State the types of policies or contracts for which guaranty funds will provide coverage;
(4) State that the member insurer and its agents are prohibited by law from using the existence of the
Life and Health Insurance Guaranty Association for the purpose of sales, solicitation or
inducement to purchase any form of insurance or health maintenance organization coverage;
(5) State that the policy owner, contract owner, certificate holder, or enrollee should not rely on
coverage under the Life and Health Insurance Guaranty Association when selecting an insurer or
health maintenance organization;
(6) Explain rights available and procedures for filing a complaint to allege a violation of any
provisions of this Act; and
(7) Provide other information as directed by the commissioner i
ncluding but not limited to, sources
for information about the financial condition of insurers provided that the information is not
proprietary and is subject to disclosure under that State’s public records law.
NAIC Model Laws, Regulations, Guidelines and Other Resources—1
st
Quarter 2018
© 2018 National Association of Insurance Commissioners 520-31
D. A member insurer shall retain evidence of compliance with Subsection B for so long as the policy or
contract for which the notice is given remains in effect.
Drafting Note: Subsection A continues the prohibition of using the existence of the Association in the inducement of sale of insurance or health
maintenance organization coverage. However, Subsection B requires notification to new policyholders concerning the general parameters of the association
law and responsibility thereunder.
The following form for the disclaimer notice is suggested:
LIFE AND HEALTH INSURANCE GUARANTY ASSOCIATION DISCLAIMER
The [insert name of the Life and Health Insurance Guaranty Association] provides coverage of claims under some
types of policies or contracts if the insurer or health maintenance organization becomes impaired or insolvent.
COVERAGE MAY NOT BE AVAILABLE FOR YOUR POLICY. Even if coverage is provided, there are
significant limits and exclusions. Coverage is always conditioned on residence in this State. Other conditions may
also preclude coverage.
The Life and Health Insurance Guaranty Association will respond to any questions you may have which are not
answered by this document. Your insurer or health maintenance organization and agent are prohibited by law from
using the existence of the association or its coverage to sell you an insurance policy or health maintenance
organization coverage.
You should not rely on availability of coverage under the Life and Health Insurance Guaranty Association when
selecting an insurer or a health maintenance organization.
[Insert addresses of the Association and department.]
Insurers, health maintenance organizations and agents should be required to deliver the document and disclaimer described
under Subsections B and C when a customer is solicited if a “free look” period is not required by State law.
Computer programs or other evidence of established procedures for including the notice required under Subsection 19B in
the policy or contract in the printing, assembly or issue process would be considered evidence of the compliance required
under Subsection 19D.
Section 20. Prospective Application
This Act shall not apply to any member insurer that is insolvent or unable to fulfill its contractual obligations on the effective
date of this Act.

Life and Health Insurance Guaranty Association Model Act
520-32
© 2018 National Association of Insurance Commissioners
APPENDIX
ALTERNATIVE PROVISIONS
Drafting Note: The underlining and overstrikes in the following provisions show the necessary changes from the model if a State decides to eliminate
coverage for unallocated annuities.
Alternative Section 3. Coverage and Limitations
A. This Act shall provide coverage for the policies and contracts specified in Subsection B:
(1) To persons who, regardless of where they reside (except for nonresident certificate holders under
group policies or contracts), are the beneficiaries, assignees or payees including health care
providers rendering services covered under health insurance policies or certificates, of the persons
covered under Paragraph (2);
(2) To persons who are owners of or certificate holders or enrollees under the policies or contracts
(other than structured settlement annuities) and in each case who
(a) Are residents; or
(b) Are not residents, but only under all of the following conditions:
(i) The member insurer that issued the policies or contracts is domiciled in this
State;
(ii) The States in which the persons reside have associations similar to the
association created by this Act;
(iii) The persons are not eligible for coverage by an association in any other State
due to the fact that the insurer or the health maintenance organization was not
licensed in the State at the time specified in the State’s guaranty association law.
(3) For structured settlement annuities specified in Subsection B; Paragraphs (1) and (2) of this
subsection shall not apply, and this Act shall (except as provided in Paragraphs (5) and (6) of this
subsection) provide coverage to a person who is a payee under a structured settlement annuity (or
beneficiary of a payee if the payee is deceased), if the payee:
(a) Is a resident, regardless of where the contract owner resides; or
(b) Is not a resident, but only under both of the following conditions;
(i) (I) The contract owner of the structured settlement annuity is a resident; or
(II) The contract owner of the structured settlement annuity is not a
resident; but
a. The insurer that issued the structured settlement annuity is
domiciled in this State; and
b. The State in which the contract owner resides has an
association similar to the association created by this Act; and
(ii) Neither the payee (or beneficiary) nor the contract owner is eligible for coverage
by the association of the State in which the payee or contract owner resides.
(4) This Act shall not provide coverage to a person who is a payee (or beneficiary) of a contract
owner resident of this State, if the payee (or beneficiary) is afforded any coverage by the
association of another State.
NAIC Model Laws, Regulations, Guidelines and Other Resources—1
st
Quarter 2018
© 2018 National Association of Insurance Commissioners 520-33
(5) This Act is intended to provide coverage to a person who is a resident of this State and, in special
circumstances, to a nonresident. In order to avoid duplicate coverage, if a person who would
otherwise receive coverage under this Act is provided coverage under the laws of any other State,
the person shall not be provided coverage under this Act. In determining the application of the
provisions of this paragraph in situations where a person could be covered by the association of
more than one State, whether as an owner, payee, enrollee, beneficiary or assignee, this Act shall
be construed in conjunction with other State laws to result in coverage by only one association.
B. (1) This Act shall provide coverage to the persons specified in Subsection A for policies or contracts
of direct, non-group life insurance, health insurance (which for the purposes of this Act includes
health maintenance organization subscriber contracts and certificates), or annuities and
supplemental contracts to any of these and for certificates under direct group policies and
contracts, except as limited by this Act. Annuity contracts and certificates under group annuity
contracts include allocated funding agreements, structured settlement annuities and any immediate
or deferred annuity contracts.
(2) Except as otherwise provided in Paragraph (3) of this subsection, this Act shall not provide
coverage for:
(a) A portion of a policy or contract not guaranteed by the member insurer, or under which
the risk is borne by the policy or contract owner;
(b) A policy or contract of reinsurance, unless assumption certificates have been issued
pursuant to the reinsurance policy or contract;
(c) A portion of a policy or contract to the extent that the rate of interest on which it is based
(i) Averaged over the period of four (4) years prior to the date on which the
Association becomes obligated with respect to the policy or contract, exceeds a
rate of interest determined by subtracting two (2) percentage points from
Moody’s Corporate Bond Yield Average averaged for that same four-year
period or for such lesser period if the policy or contract was issued less than
four (4) years before the Association became obligated; and
(ii) On and after the date on which the Association becomes obligated with respect
to the policy or contract, exceeds the rate of interest determined by subtracting
three (3) percentage points from Moody’s Corporate Bond Yield Average as
most recently available;
(d) A portion of a policy or contract issued to a plan or program of an employer, association
or other person to provide life, health or annuity benefits to its employees, members or
others, to the extent that the plan or program is self-funded or uninsured, including but
not limited to benefits payable by an employer, association or other person under:
(i) A multiple employer welfare arrangement as defined in 29 U.S.C. § 1144;
(ii) A minimum premium group insurance plan;
(iii) A stop-loss group insurance plan; or
(iv) An administrative services only contract;
(e) A portion of a policy or contract to the extent that it provides for
(i) Dividends or experience rating credits;
Life and Health Insurance Guaranty Association Model Act
520-34
© 2018 National Association of Insurance Commissioners
(ii) Voting rights; or
(iii) Payment of any fees or allowances to any person, including the policy or
contract owner, in connection with the service to or administration of the policy
or contract;
(f) A policy or contract issued in this State by a member insurer at a time when it was not
licensed or did not have a certificate of authority to issue the policy or contract in this
State;
(g) A portion of a policy or contract to the extent that the assessments required by Section 9
with respect to the policy or contract are preempted by federal or State law;
(h) An obligation that does not arise under the express written terms of the policy or contract
issued by the member insurer to the enrollee, contract holder, contract owner or policy
owner, including without limitation:
(i) Claims based on marketing materials;
(ii) Claims based on side letters, riders or other documents that were issued by the
member insurer without meeting applicable policy or contract form filing or
approval requirements;
(iii) Misrepresentations of or regarding policy or contract benefits;
(iv) Extra-contractual claims; or
(v) A claim for penalties or consequential or incidental damages;
(i) A contractual agreement that establishes the member insurer’s obligations to provide a
book value accounting guaranty for defined contribution benefit plan participants by
reference to a portfolio of assets that is owned by the benefit plan or its trustee, which in
each case is not an affiliate of the member insurer;
(j) An unallocated annuity contract; and
(k) A policy or contract providing any hospital, medical, prescription drug or other health
care benefits pursuant to Part C or Part D of Subchapter XVIII, Chapter 7 of Title 42 of
the United States Code (commonly known as Medicare Part C & D), or Subchapter XIX,
Chapter 7 of Title 42 of the United States Code (commonly known as Medicaid), or any
regulations issued pursuant thereto.
(3) The exclusion from coverage referenced in Paragraph (2)(c) of this subsection shall not apply to
any portion of a policy or contract, including a rider, that provides long-term care or any other
health insurance benefits.
C. The benefits that the Association may become obligated to cover shall in no event exceed the lesser of:
(1) The contractual obligations for which the member insurer is liable or would have been liable if it
were not an impaired or insolvent insurer, or
(2) (a) With respect to one life, regardless of the number of policies or contracts:
(i) $300,000 in life insurance death benefits, but not more than $100,000 in net
cash surrender and net cash withdrawal values for life insurance;
NAIC Model Laws, Regulations, Guidelines and Other Resources—1
st
Quarter 2018
© 2018 National Association of Insurance Commissioners 520-35
(ii) For health insurance benefits:
(I) $100,000 for coverages not defined as disability income insurance or
health benefit plans or long-term care insurance as defined in [section
of State law dealing with health insurance/disability income
insurance/long-term care insurance] including any net cash surrender
and net cash withdrawal values;
(II) $300,000 for disability income insurance as defined in [section of State
law dealing with health insurance/disability income insurance] and
$300,000 for long-term care insurance as defined in [section of State
law dealing with health insurance/long-term care insurance];
(III) $500,000 for health benefit plans;
(iii) $250,000 in the present value of annuity benefits, including net cash surrender
and net cash withdrawal values; or
(b) With respect to each payee of a structured settlement annuity (or beneficiary or
beneficiaries of the payee if deceased), $250,000 in present value annuity benefits, in the
aggregate, including net cash surrender and net cash withdrawal values;
(c) However, in no event shall the Association be obligated to cover more than (i) an
aggregate of $300,000 in benefits with respect to any one life under Paragraphs 2(a), 2(b)
and 2(c) of this subsection except with respect to benefits for health benefit plans under
Paragraph 2(a)(ii) of this subsection, in which case the aggregate liability of the
Association shall not exceed $500,000 with respect to any one individual, or (ii) with
respect to one owner of multiple non-group policies of life insurance, whether the policy
owner is an individual, firm, corporation or other person, and whether the persons
insured are officers, managers, employees or other persons, more than $5,000,000 in
benefits, regardless of the number of policies and contracts held by the owner;
(d) The limitations set forth in this subsection are limitations on the benefits for which the
Association is obligated before taking into account either its subrogation and assignment
rights or the extent to which those benefits could be provided out of the assets of the
impaired or insolvent insurer attributable to covered policies. The costs of the
Association’s obligations under this Act may be met by the use of assets attributable to
covered policies or reimbursed to the Association pursuant to its subrogation and
assignment rights.
(e) For purposes of this Act, benefits provided by a long-term care rider to a life insurance
policy or annuity contract shall be considered the same type of benefits as the base life
insurance policy or annuity contract to which it relates.
D. In performing its obligations to provide coverage under Section 8 of this Act, the Association shall not be
required to guarantee, assume, reinsure, reissue or perform, or cause to be guaranteed, assumed, reinsured
reissued or performed, the contractual obligations of the insolvent or impaired insurer under a covered
policy or contract that do not materially affect the economic values or economic benefits of the covered
policy or contract.
Drafting Note: This section and Section 8 are key sections of the Act. Section 3 identifies who and what are covered and not covered by the Act. Section 8
specifies the responsibilities of the Association toward covered persons with covered policies.
Protection of this Act is primarily extended to resident persons but certain nonresidents under specific circumstances will be protected by this Act if the
insolvent insurer was domiciled in this State.
This model does not apply to reinsurance unless assumption certificates were issued to the direct insureds or enrollees. Furthermore, it applies only to direct
individual or group certificate insurance issued or written by member insurers licensed to transact business in this State at any time.

Life and Health Insurance Guaranty Association Model Act
520-36
© 2018 National Association of Insurance Commissioners
Persons to whom coverage is typically provided are resident enrollees, policy or contract owners, or their beneficiaries, assignees or payees. For group
contracts or policies, coverage is provided to resident enrollees, and certificate holders and not to the owners of the group contracts or policies; this avoids
the possibility of double coverage and indirect coverage of nonresident enrollees, and certificate holders through resident group policy or contract owners.
Subsection A(3) provides coverage for structured settlement annuities to resident payees rather than to the contract owners.
Subsection A(3) providing structured settlement annuity coverage to resident payees is a significant change from previous versions of this Model Act
intended to place the coverage in the State of the resident persons to be protected rather than in the State where the nominal owner of the contract resides.
Subsections A(4) and (5) avoid the possibility of double coverage due to differing approaches for determining the covered persons in different State statutes
and provide mechanisms for resolving which State’s statutes will be used to determine the existence and limits of coverage.
Policies and contracts covered by the model act are life insurance, health insurance and annuity policies and contracts and policies or contracts supplemental
thereto. The use of the term health insurance is intended to include “accident and health” insurance, “sickness and accident” insurance, “disability income”
insurance, health maintenance organization contracts, etc. The use of the term disability income insurance is intended to include insurance policies and
contracts that cover the loss of income due to a disability. The individual State may want to adjust this language to fit its particular terminology.
Subsection B(2) identifies certain types of contracts or policies or portions of contracts or policies that are specifically not covered by this Act. If a portion of
a contract or policy is not covered, the remainder of the contract or policy is covered unless excluded otherwise. Subsection B(2) also provides a ready means
by which an individual State can exempt from the Act those policies and contracts issued by member insurers or similar organizations deemed appropriate
for exemption by the State.
Subsection B(2)(i) is intended to exclude from coverage those products commonly referred to as “financial guaranty” products.
Subsection C provides the maximum limitations of the Association’s liability by type of contract or policy or line of business and overall per one life, plan
sponsor or owner. The limits may be reached through cash surrender payments, benefit payments, or continuing coverage or a combination thereof. The
maximum limits for each type of coverage should be set at an appropriate level after review by each State.
Alternative Section 5. Definitions
As used in this Act:
A. “Account” means either of the two accounts created under Section 6.
B. “Association” means the [State] Life and Health Insurance Guaranty Association created under Section 6.
C. “Authorized assessment” or the term “authorized” when used in the context of assessments means a
resolution by the Board of Directors has been passed whereby an assessment will be called immediately or
in the future from member insurers for a specified amount. An assessment is authorized when the
resolution is passed.
D. “Benefit plan” means a specific employee, union or association of natural persons benefit plan.
E. “Called assessment” or the term “called” when used in the context of assessments means that a notice has
been issued by the Association to member insurers requiring that an authorized assessment be paid within
the time frame set forth within the notice. An authorized assessment becomes a called assessment when
notice is mailed by the Association to member insurers.
F. “Commissioner” means the Commissioner of Insurance of this State.
Drafting Note: Insert the title of the chief insurance regulatory official whenever the term “commissioner” appears.
G. “Contractual obligation” means an obligation under a policy or contract or certificate under a group policy
or contract, or portion thereof for which coverage is provided under Section 3.
H. “Covered contract” or “covered policy” means a policy or contract or portion of a policy or contract for
which coverage is provided under Section 3.
I. “Extra-contractual claims” shall include, for example, claims relating to bad faith in the payment of claims,
punitive or exemplary damages or attorneys’ fees and costs.
J. “Health benefit plan” means any hospital or medical expense policy or certificate, or health maintenance
organization subscriber contract or any other similar health contract. “Health benefit plan” does not
include:
NAIC Model Laws, Regulations, Guidelines and Other Resources—1
st
Quarter 2018
© 2018 National Association of Insurance Commissioners 520-37
(1) Accident only insurance:
(2) Credit insurance;
(3) Dental only insurance;
(4) Vision only insurance;
(5) Medicare Supplement insurance;
(6) Benefits for long-term care, home health care, community-based care, or any combination thereof;
(7) Disability income insurance;
(8) Coverage for on-site medical clinics; or
(9) Specified disease, hospital confinement indemnity, or limited benefit health insurance if the types
of coverage do not provide coordination of benefits and are provided under separate policies or
certificates.
K. “Impaired insurer” means a member insurer which, after the effective date of this Act, is not an insolvent
insurer, and is placed under an order of rehabilitation or conservation by a court of competent jurisdiction.
L. “Insolvent insurer” means a member insurer which after the effective date of this Act, is placed under an
order of liquidation by a court of competent jurisdiction with a finding of insolvency.
M. “Member insurer” means an insurer or health maintenance organization licensed or that holds a certificate
of authority to transact in this State any kind of insurance or health maintenance organization business for
which coverage is provided under Section 3, and includes an insurer or health maintenance organization
whose license or certificate of authority in this State may have been suspended, revoked, not renewed or
voluntarily withdrawn, but does not include:
(1) A hospital or medical service organization, whether profit or non-profit;
(2) A fraternal benefit society;
(3) A mandatory State pooling plan;
(4) A mutual assessment company or other person that operates on an assessment basis;
(5) An insurance exchange;
(6) An organization that has a certificate or license limited to the issuance of charitable gift annuities
under [insert the appropriate section of the State code]; or
(7) An entity similar to any of the above.
Drafting Note: States that license Health Care Service Corporations or similar organizations that undertake to provide basic health care services may want to
address these entities in this Act.
N. “Moody’s Corporate Bond Yield Average” means the Monthly Average Corporates as published by
Moody’s Investors Service, Inc., or any successor thereto.
Life and Health Insurance Guaranty Association Model Act
520-38
© 2018 National Association of Insurance Commissioners
O. “Owner” of a policy or contract and “policyholder, “policy owner” and “contract owner” mean the person
who is identified as the legal owner under the terms of the policy or contract or who is otherwise vested
with legal title to the policy or contract through a valid assignment completed in accordance with the terms
of the policy or contract and properly recorded as the owner on the books of the member insurer. The terms
owner, contract owner, policyholders and policy owner do not include persons with a mere beneficial
interest in a policy or contract.
P. “Person” means an individual, corporation, limited liability company, partnership, association,
governmental body or entity or voluntary organization.
Q. “Premiums” means amounts or considerations (by whatever name called) received on covered policies or
contracts less returned premiums, considerations and deposits and less dividends and experience credits.
“Premiums” does not include amounts or considerations received for policies or contracts or for the
portions of policies or contracts for which coverage is not provided under Section 3B except that
assessable premium shall not be reduced on account of Sections 3B(2)(c) relating to interest limitations and
3C(2) relating to limitations with respect to one individual, one participant and one policy or contract
owner. “Premiums” shall not include:
(1) Premiums on an unallocated annuity contract State; or
(2) With respect to multiple non-group policies of life insurance owned by one owner, whether the
policy or contract owner is an individual, firm, corporation or other person, and whether the
persons insured are officers, managers, employees or other persons, premiums in excess of
$5,000,000 with respect to these policies or contracts, regardless of the number of policies or
contracts held by the owner.
R. (1) “Principal place of business” of a plan sponsor or a person other than a natural person means the
single State in which the natural persons who establish policy or contract for the direction, control
and coordination of the operations of the entity as a whole primarily exercise that function,
determined by the Association in its reasonable judgment by considering the following factors:
(a) The State in which the primary executive and administrative headquarters of the entity is
located;
(b) The State in which the principal office of the chief executive officer of the entity is
located;
(c) The State in which the board of directors (or similar governing person or persons) of the
entity conducts the majority of its meetings;
(d) The State in which the executive or management committee of the board of directors (or
similar governing person or persons) of the entity conducts the majority of its meetings;
(e) The State from which the management of the overall operations of the entity is directed;
and
(f) In the case of a benefit plan sponsored by affiliated companies comprising a consolidated
corporation, the State in which the holding company or controlling affiliate has its
principal place of business as determined using the above factors.
However, in the case of a plan sponsor, if more than fifty percent (50%) of the participants in the
benefit plan are employed in a single State, that State shall be deemed to be the principal place of
business of the plan sponsor.

NAIC Model Laws, Regulations, Guidelines and Other Resources—1
st
Quarter 2018
© 2018 National Association of Insurance Commissioners 520-39
(2) The principal place of business of a plan sponsor of a benefit plan shall be deemed to be the
principal place of business of the association, committee, joint board of trustees or other similar
group of representatives of the parties who establish or maintain the benefit plan that, in lieu of a
specific or clear designation of a principal place of business, shall be deemed to be the principal
place of business of the employer or employee organization that has the largest investment in the
benefit plan in question.
S. “Receivership court” means the court in the insolvent or impaired insurer’s State having jurisdiction over
the conservation, rehabilitation or liquidation of the member insurer.
T. “Resident” means a person to whom a contractual obligation is owed and who resides in this State on the
date of entry of a court order that determines a member insurer to be an impaired insurer or a court order
that determines a member insurer to be an insolvent insurer, whichever occurs first. A person may be a
resident of only one State, which in the case of a person other than a natural person shall be its principal
place of business. Citizens of the United States that are either (i) residents of foreign countries, or (ii)
residents of United States possessions, territories or protectorates that do not have an association similar to
the Association created by this Act, shall be deemed residents of the State of domicile of the member
insurer that issued the policies or contracts.
U. “Structured settlement annuity” means an annuity purchased in order to fund periodic payments for a
plaintiff or other claimant in payment for or with respect to personal injury suffered by the plaintiff or other
claimant.
V. “State” means a State, the District of Columbia, Puerto Rico, and a United States possession, territory or
protectorate.
W. “Supplemental contract” means a written agreement entered into for the distribution of proceeds under a
life, health or annuity policy or contract.
X. “Unallocated annuity contract” means an annuity contract or group annuity certificate which is not issued
to and owned by an individual, except to the extent of any annuity benefits guaranteed to an individual by
an insurer under the contract or certificate.
Drafting Note: Each State will wish to examine its own statutes to determine whether these definitions are applicable and to determine whether some should
be deleted and others added.
Alternative Section 6. Creation of the Association
A. There is created a nonprofit legal entity to be known as the [State] Life and Health Insurance Guaranty
Association. All member insurers shall be and remain members of the Association as a condition of their
authority to transact insurance or a health maintenance organization business in this State. The Association
shall perform its functions under the plan of operation established and approved under Section 10 and shall
exercise its powers through a board of directors established under Section 7. For purposes of
administration and assessment, the Association shall maintain two (2) accounts:
(1) The life insurance and annuity account which includes the following subaccounts:
(a) Life insurance account; and
(b) Annuity account which shall include annuity contracts owned by a governmental
retirement plan (or its trustee) established under Section 401, 403(b) or 457 of the United
States Internal Revenue Code.
(2) The health account.
B. The Association shall come under the immediate supervision of the commissioner and shall be subject to
the applicable provisions of the insurance laws of this State. Meetings or records of the Association may be
opened to the public upon majority vote of the board of directors of the Association.

Life and Health Insurance Guaranty Association Model Act
520-40
© 2018 National Association of Insurance Commissioners
_________________________________
Chronological Summary of Action (all references are to the Proceedings of the NAIC).
1971 Proc. I 54, 58, 134, 159, 160-173 (adopted).
1976 Proc. I 2, 9, 270, 296-297, 298-312 (amended and reprinted).
1977 Proc. II 19, 21, 355, 363 (amended).
1978 Proc. I 13, 15, 211, 241 (corrected).
1986 Proc. I 9-10, 22, 149, 294-295, 306-322 (amended and reprinted).
1987 Proc. II 15, 22, 160, 320 (decertification of 4-account approach).
1988 Proc. I 9, 18-19, 157-159, 337-338, 339-354 (amended to create 2 accounts and reprinted).
1993 Proc. 2
nd
Quarter 12, 33, 227, 600, 602, 620-621 (amended).
1993 Proc. 3
rd
Quarter 7, 30, 333-334, 341-343, 350-352 (amended).
1995 Proc. 1
st
Quarter 7, 10, 461, 466 (amended).
1995 Proc. 3
rd
Quarter 4, 18, 582, 585-586 (amended).
1996 Proc. 4
th
Quarter 11, 45-46, 938, 956, 959-981 (amended and reprinted).
1997 Proc. 4
th
Quarter 25, 27-28, 645, 646-647 (amended).
1998 Proc. 1
st
Quarter 15, 17, 598, 602, 603-616 (amended to add appendix).
1999 Proc. 1
st
Quarter 8, 9, 443, 445-446 (amended).
1999 Proc. 2
nd
Quarter 10, 11, 435, 436-438 (amended).
2009 Proc. 1
st
Quarter, Vol. I 111, 135, 139, 188, 240-287, 293, 821-835 (amended).
2016 Proc. 4
th
Quarter (amended).
2017 Proc. 4
th
Quarter (amended)
NAIC Model Laws, Regulations, Guidelines and Other Resources—Summer 2020
LIFE AND HEALTH INSURANCE GUARANTY ASSOCIATION MODEL ACT
© 2020 National Association of Insurance Commissioners ST-520-1
This chart is intended to provide readers with additional information to more easily access state statutes, regulations,
bulletins or administrative rulings related to the NAIC model. Such guidance provides readers with a starting point
from which they may review how each state has addressed the model and the topic being covered. The NAIC Legal
Division has reviewed each state’s activity in this area and has determined whether the citation most appropriately
fits in the Model Adoption column or Related State Activity column based on the definitions listed below. The NAIC’s
interpretation may or may not be shared by the individual states or by interested readers.
This chart does not constitute a formal legal opinion by the NAIC staff on the provisions of state law and should not
be relied upon as such. Nor does this state page reflect a determination as to whether a state meets any applicable
accreditation standards. Every effort has been made to provide correct and accurate summaries to assist readers in
locating useful information. Readers should consult state law for further details and for the most current information.
NAIC Model Laws, Regulations, Guidelines and Other Resources—Summer 2020
LIFE AND HEALTH INSURANCE GUARANTY ASSOCIATION MODEL ACT
ST-520-2
© 2020 National Association of Insurance Commissioners
This page is intentionally left blank
NAIC Model Laws, Regulations, Guidelines and Other Resources—Summer 2020
LIFE AND HEALTH INSURANCE GUARANTY ASSOCIATION MODEL ACT
© 2020 National Association of Insurance Commissioners ST-520-3
KEY:
MODEL ADOPTION: States that have citations identified in this column adopted the most recent version of the NAIC
model in a substantially similar manner. This requires states to adopt the model in its entirety but does allow for variations
in style and format. States that have adopted portions of the current NAIC model will be included in this column with an
explanatory note.
RELATED STATE ACTIVITY: Examples of Related State Activity include but are not limited to: older versions of the
NAIC model, statutes or regulations addressing the same subject matter, or other administrative guidance such as bulletins
and notices. States that have citations identified in this column only (and nothing listed in the Model Adoption column) have
not adopted the most recent version of the NAIC model in a substantially similar manner.
NO CURRENT ACTIVITY: No state activity on the topic as of the date of the most recent update. This includes states that
have repealed legislation as well as states that have never adopted legislation.
NAIC MEMBER
MODEL ADOPTION RELATED STATE ACTIVITY
Alabama
A
LA
.
C
ODE
§§ 27-44-1 to 27-44-21
(1982/2014) (3 accounts) (previous version of
model).
Alaska
A
LASKA
S
TAT
. §§ 21.79.010 to 21.79.990
(1990/2018).
B
ULLETIN
2006-14 (2006); O
RDER
R2018-3
(2018).
American Samoa
NO CURRENT ACTIVITY
Arizona
A
RIZ
.
R
EV
.
S
TAT
.
A
NN
.
§§
20-681
to 20-695
(1977/2018).
Arkansas
A
RK
.
C
ODE
A
NN
. §§ 23-96-101 to 23-96-121
(1989/2019).
054.00.49 A
RK
.
C
ODE
R.
§§
1
to
6
(1992/1999)
(notice to policyholders); BULLETIN 16-2013
(2013).
California
C
AL
.
I
NS
.
C
ODE
§§ 1067 to 1067.19
(1993/2019) (3 accounts) (previous version of
model).
Colorado
C
OLO
.
R
EV
.
S
TAT
. §§ 10-20-101 to 10-20-120
(1991/2013) (3 accounts) (previous version of
model).
Connecticut
C
ONN
.
G
EN
.
S
TAT
. §§ 38a-858 to 38a-879
(1972/2019).
NAIC Model Laws, Regulations, Guidelines and Other Resources—Summer 2020
LIFE AND HEALTH INSURANCE GUARANTY ASSOCIATION MODEL ACT
ST-520-4
© 2020 National Association of Insurance Commissioners
NAIC MEMBER
MODEL ADOPTION RELATED STATE ACTIVITY
Delaware
D
EL
.
C
ODE
A
NN
.
tit. 18 §§ 4401 to 4419
(1982/2019).
District of Columbia
D.C.
C
ODE
§§
31-5401
to
31-5416
(1992/2015)
(previous version of model);
BULLETIN 04-003-IB (2006).
Florida
F
LA
.
S
TAT
. §§ 631.711 to 631.735 (1979/2019).
Georgia
H.B. 1050 (2020).
G
A
.
C
ODE
A
NN
. §§ 33-38-1 to 33-38-22
(1981/2019) (2 accounts with subaccounts)
(previous version of model).
Guam
NO CURRENT ACTIVITY
Hawaii
H
AW
.
R
EV
.
S
TAT
.
§§
431:16-201
to 431:16-219
(1987/2012) (3 accounts) (previous version of
model);
HAW. CODE R. §§ 16-18-1 to 16-18-4
(1992) (notice to policyholders).
Idaho
I
DAHO
C
ODE
A
NN
. §§ 41-4301 to 41-4320
(1977/2018).
Illinois
215 I
LL
.
C
OMP
.
S
TAT
. 5/531.01 to 5/531.20
(1981/2018) (2 accounts with subaccounts).
I
LL
.
ADMIN
.
CODE
tit.
50,
§§
3401.10
to
3401.40;
Illus. A (2014/2019); BULLETIN 2010-7 (2010).
Indiana
I
ND
.
C
ODE
§§
27-8-8-2
to 27-8-8-18
(1978/2019).
B
ULLETIN
249
(2019).
Iowa
I
OWA
C
ODE
§§ 508C.1 to 508C.19
(1987/2019).
B
ULLETIN
2012-2 (2012); B
ULLETIN
2012-3
(2012).
Kansas
K
AN
.
S
TAT
.
A
NN
. §§ 40-3001 to 40-3018
(1972/2011) (3 accounts) (portions of previous
version of model).
Kentucky
K
Y
.
R
EV
.
S
TAT
.
A
NN
. §§ 304.42-010 to
304.42-190 (1978/2019).
NAIC Model Laws, Regulations, Guidelines and Other Resources—Summer 2020
LIFE AND HEALTH INSURANCE GUARANTY ASSOCIATION MODEL ACT
© 2020 National Association of Insurance Commissioners ST-520-5
NAIC MEMBER
MODEL ADOPTION RELATED STATE ACTIVITY
Louisiana
L
A
.
R
EV
.
S
TAT
.
A
NN
.
§§
22:2081
to
22:2099
(2008/2018).
L
A
.
A
DMIN
.
C
ODE
tit. 37, §§ XIII.901 to
XIII.909 (Regulation 40) (4 accounts)
(1992/2016) (notice to policyholders).
Maine
M
E
.
R
EV
.
S
TAT
.
A
NN
. tit. 24-A, §§ 4601 to
4621 (1984/2018) (3 accounts).
Maryland
2020 M
D
.
L
AWS
, Ch. 74 (S.B. 186) (2020).
M
D
.
A
NN
.
C
ODE
I
NS
.
§§
9-401
to
9-419
(1971/2018) (3 accounts) (previous version of
model);
MD. CODE REGS. 31.04.14.03
(2010/2015); BULLETIN 2012-13 (2012).
Massachusetts
S.B.
2227
(2020).
M
ASS
.
G
EN
.
L
AWS
ch. 175, § 146B
(1985/2014) (3 accounts) (previous version of
model).
Michigan
M
ICH
.
C
OMP
.
L
AWS
§§
500.7701
to 500.7780
(1982/2016) (2 accounts with subaccounts)
(previous version of model);
BULLETIN 2013-13-INS (2013).
Minnesota
S.F.
4091
(2020).
M
INN
.
S
TAT
. §§ 61B.18 to 61B.32
(1993/2009) (2 accounts with subaccounts)
(previous version of model); § 60C.21 (2012).
Mississippi
S.B.
2227
(2020).
M
ISS
.
C
ODE
A
NN
. §§ 83-23-205 to 83-23-237
(1985/2014) (2 accounts with subaccounts)
(previous version of model).
Missouri
M
O
.
R
EV
.
S
TAT
.
§§
376.715
to 376.758
(1988/2018).
M
O
.
C
ODE
R
EGS
.
A
NN
. tit. 20, § 400-5.600
(1988/2016).
Montana
M
ONT
.
C
ODE
A
NN
. §§ 33-10-201 to
33-10-236 (1974/2019).
Nebraska
N
EB
.
R
EV
.
S
TAT
. §§ 44-2701 to 44-2720
(1975/2019).
Nevada
N
EV
.
R
EV
.
S
TAT
. §§ 686C.010 to 686C.390
(1973/2019).
B
ULLETIN
2011-009 (2011).
NAIC Model Laws, Regulations, Guidelines and Other Resources—Summer 2020
LIFE AND HEALTH INSURANCE GUARANTY ASSOCIATION MODEL ACT
ST-520-6
© 2020 National Association of Insurance Commissioners
NAIC MEMBER
MODEL ADOPTION RELATED STATE ACTIVITY
New Hampshire
S.B.
No. 251 (2019).
N.H. R
EV
.
S
TAT
.
A
NN
.
§§ 408-B:1 to
408-B:20 (1995/2015) (2 accounts with
subaccounts) (previous version of model).
New Jersey
N.J. S
TAT
.
A
NN
. §§ 17B:32A-1 to
17B-32A-19 (1991) (2 accounts with
subaccounts) (previous version of model).
New Mexico
N.M. S
TAT
.
A
NN
. §§ 59A-42-1 to
59A-42-17 (1985/2014) (2 accounts)
(previous version of model).
New York
N.Y.
I
NS
.
L
AW
§§ 7701 to 7719 (1985/2014)
(2 accounts) (previous version of model);
N.Y. I
NS. LAW §§ 7501 to 7507 (1984/2014).
North Carolina
N.C. G
EN
.
S
TAT
. §§ 58-62-2 to 58-62-86
(1991/2018).
B
ULLETIN
2009-B-3 (2009);
BULLETIN 2010-B-5 (2010).
North Dakota
N.D. C
ENT
.
C
ODE
§§ 26.1-38.1-01 to
26.1-38.1-16 (1989/2019).
N.D. A
DMIN
.
C
ODE
§ 45-11-01-01
(1990/2012) (advertising rules).
Northern Marianas
NO CURRENT ACTIVITY
Ohio
O
HIO
R
EV
.
C
ODE
A
NN
.
§§ 3956.01 to 3956.20
(1989/2015) (2 accounts with subaccounts)
(previous version of model).
Oklahoma
O
KLA
.
S
TAT
. tit. 36, §§ 2021 to 2044
(1981/2019).
O
KLA
.
A
DMIN
.
C
ODE
§
365:10-1-6 (2011);
BULLETIN 2010-03 (#2) (2010).
Oregon
O
R
.
R
EV
.
S
TAT
.
§§
734.750
to 734.890
(1975/2011) (3 accounts) (previous version of
model).
Pennsylvania
40 P
A
.
C
ONS
.
S
TAT
.
A
NN
. §§ 991.1701 to
991.1718 (1992/2007) (2 accounts with
subaccounts) (previous version of model).
Puerto Rico
P.R. L
AWS
A
NN
. tit. 26, §§ 3901 to 3918
(1974/2009) (3 accounts) (previous version of
model).
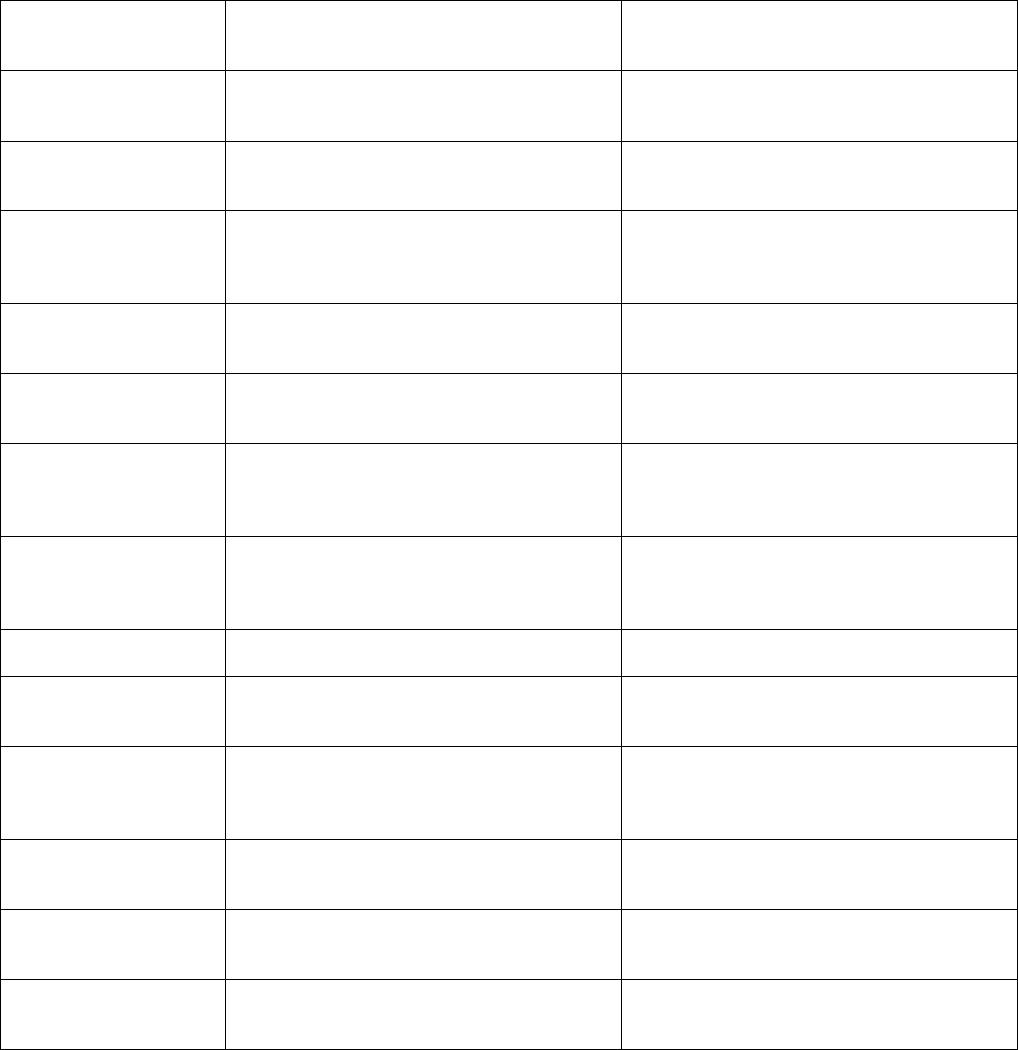
NAIC Model Laws, Regulations, Guidelines and Other Resources—Summer 2020
LIFE AND HEALTH INSURANCE GUARANTY ASSOCIATION MODEL ACT
© 2020 National Association of Insurance Commissioners ST-520-7
NAIC MEMBER
MODEL ADOPTION RELATED STATE ACTIVITY
Rhode Island
R.I.
G
EN
.
L
AWS
§§
27-34.3-1
to 27-34.3-20
(1995/2012) (previous version of model).
South Carolina
S.C. C
ODE
A
NN
. §§ 38-29-10 to 38-29-210
(1988/2020).
South Dakota
S.D. C
ODIFIED
L
AWS
§§ 58-29C-44
to 58-29C-62 (1989/2013) (3 accounts)
(previous version of model).
Tennessee
T
ENN
.
C
ODE
A
NN
. §§ 56-12-201 to 56-12-220
(1989/2019).
B
ULLETIN
6-7-2010
(2010).
Texas
T
EX
.
I
NS
.
C
ODE
A
NN
. §§ 463.001 to 463.206
(1985/2019).
Utah
U
TAH
C
ODE
A
NN
.
§§
31A-28-101
to
31A-28-120 (1986/2018) (2 accounts with
subaccounts).
U
TAH
A
DMIN
.
C
ODE
r. R590-155 (2010/2019).
Vermont
V
T
.
S
TAT
.
A
NN
. tit. 8, §§ 4151 to 4169
(1972/2015) (3 accounts) (previous version of
model).
Virgin Islands
NO CURRENT ACTIVITY
Virginia
V
A
.
C
ODE
A
NN
. §§ 38.2-1700 to 38.2-1721
(1986/2018) (2 accounts).
A
DMINISTRATIVE
L
ETTER
2018-2 (2018).
Washington
W
ASH
.
R
EV
.
C
ODE
§§ 48.32A.005 to
48.32A.901 (2001/2005) (2 accounts with
subaccounts) (previous version of model).
West Virginia
W. V
A
.
C
ODE
§§ 33-26A-1 to 33-26A-19
(1977/2018) (2 accounts).
Wisconsin
W
IS
.
S
TAT
. §§ 646.01 to 646.61 (1979/2017)
(“Insurance Security Fund”).
Wyoming
W
YO
.
S
TAT
.
A
NN
. §§ 26-42-101 to 26-42-118
(1990/2019).
NAIC Model Laws, Regulations, Guidelines and Other Resources—Summer 2020
LIFE AND HEALTH INSURANCE GUARANTY ASSOCIATION MODEL ACT
ST-520-8
© 2020 National Association of Insurance Commissioners
This page is intentionally left blank

NAIC Model Laws, Regulations, Guidelines and Other Resources—October 2010
LIFE AND HEALTH INSURANCE GUARANTY ASSOCIATION MODEL ACT
Proceedings Citations
Cited to the Proceedings of the NAIC
© 2010 National Association of Insurance Commissioners PC-520-1
The Financial Condition (E) Committee adopted amendments to this model. The Committee summarized the more significant
changes to the model including the changes to the coverage limits as well as the disposition on Medicare Parts C & D. 2008
Proc. 4
th
Quarter Vol. II 10-5.
The joint Executive Committee/Plenary adopted amendments to this model. These amendments received broad support that
was attributed to significant improvements in coverage limits and the treatment of Stranger-Owned Life Insurance/Investor-
Owned Life Insurance, structured settlements and Medicare Part C & D. 2009 Proc. 1
st
Quarter Vol. I 3-5.
Section 1. Title
Amendments to the model proposed first in early 1996 included deletion of a comment that had been in the model since its
adoption in 1970. The comment highlighted the difference between the property/casualty and life/health guaranty funds.
The set of proposed amendments included both substantive and technical revisions and reflected changes in the life insurance
industry and the products offered by insurers as well as lessons learned in connection with major life insurance insolvencies
in recent years. 1996 Proc. 1
st
Quarter 570; 1996 Proc. 4
th
Quarter 959.
Those presenting suggestions on behalf of the life insurance industry suggested that large insurance insolvencies in the early
1990s demonstrated that some parts of the model act worked well and others did not. The intent of the drafters of the
amendments was to make the act more workable and clarify the authority of the guaranty associations with respect to multi-
state rehabilitation plans. Among the issues addressed in the 1996 amendments were (1) the need for a different method of
covering guaranteed investment contracts and structured settlement annuities to avoid concentration of coverage in a few
guaranty associations and the concomitant capacity problems; (2) the need to change the assessment process to allow
assessments to be called in one year and collected in another and to delete the current 1% spillover requirement; and (3)
implementation of national rehabilitation and reinsurance plans. 1996 Proc. 2
nd
Quarter 594.
Section 2. Purpose
After development of the guaranty association for property and casualty insurance, it was questioned whether there was need
to develop legislation specifically to deal with insolvencies of life and health insurers. However, industry representatives
cautioned that the approaches and solutions developed for property and casualty insurers were not only inadequate, but
inappropriate for the life and health insurance business. 1970 Proc. II 1072.
Industry organizations maintained the position that the NAIC should be concentrating on legislation for solvency rather than
insolvency. The primary purpose of state regulation is not fulfilled if a preventable insolvency occurs. They cited an NAIC
study prepared when the property and casualty guaranty association model was adopted (1969 Proc. II 564-593) which stated
insolvencies of life insurance companies had been relatively insignificant. They also argued that policyholders of one
company should not be protected at the expense of policyholders of other companies. They asserted the property and
casualty guaranty association model had been adopted because of the imminence of federal legislation. The same urgency
did not exist with respect to life and health insurance. 1971 Proc. I 174-177.
When the model was being considered, the insurance company representative expressed the opinion that the guaranty fund
encouraged improvident management and the creation of marginally financed companies, which would hurt the industry.
Potential policyholders would no longer need to be concerned with the financial condition of the company from which they
would consider purchase of coverage. The public would be lulled into overlooking the need for dealing with sound
companies. 1971 Proc. I 179.

NAIC Model Laws, Regulations, Guidelines and Other Resources—October 2010
LIFE AND HEALTH INSURANCE GUARANTY ASSOCIATION MODEL ACT
Proceedings Citations
Cited to the Proceedings of the NAIC
PC-520-2 © 2010 National Association of Insurance Commissioners
Section 3. Coverage and Limitations
A. The model as originally enacted had a Section 3 entitled “Scope.” As urged by the industry spokespersons, it
extended to all policyholders, wherever located, of a domestic company in the state of enactment. Also, they urged, in order
for an insurance department to carry out its responsibility to residents of its state who hold policies of foreign and alien
companies, a guaranty measure should apply to resident policyholders of such companies. 1970 Proc. II 1073. The model
as originally adopted covered any policies or contracts issued by persons authorized to transact insurance in the state at any
time. 1971 Proc. I 161.
A memo from an insurance industry organization included a proposal that the guaranty association be responsible for
covering only residents of its own state. The major purpose for the suggested change was to increase the assessment capacity
of the system. Other important purposes were to encourage the states that did not have statutes providing for guaranty
associations to enact them, to protect insureds who did not reside in the insolvent insurer’s state with an association in their
own state, to avoid litigation over the issue of whether the protection provided by the association in the insolvent insurer’s
state of domicile is “substantially similar” to that of non-domiciliary states’ associations, and to eliminate any justification for
failing to provide a tax offset in the law. 1984 Proc. II 461.
The system provided that the domestic guaranty association should assess its members on the basis of premiums they receive
on business in each of the states where they and the insolvent insurer did business. However, because of the two percent
limitation, situations arose in which the guaranty association was unable to assess a sufficient amount to cover all
policyholders. The proposed system of providing coverage only to residents would remedy the assessment capacity problem
in all but the largest cases of insolvency. 1984 Proc. II 462.
The approach suggested in 1984 also minimized the need to have all the state laws virtually identical. Under the model
originally adopted the guaranty association of a non-domiciliary state did not cover its own residents if the domiciliary state
provided them “substantially similar” protection. 1984 Proc. II 462.
A system of covering residents only would show a direct benefit from the tax offset to the residents of the state providing the
offset, and not to residents of other states. 1984 Proc. II 462.
The working group draft considered during 1985 contained a provision that each guaranty association would cover residents
only, except in some limited instances. Nonresidents may be entitled to coverage by the guaranty association where the
insurer was domiciled. This exception was aimed primarily to cover persons who move into a state where their insurer was
not admitted, and therefore, not a member of that guaranty association. Individuals with group insurance will be covered in
states where the individual certificate holder resides. The situs of the group will be irrelevant. 1985 Proc. I 205.
The focus of the amendments proposed in 1996 was to shift the situs of coverage of guaranteed investment contracts issued to
pension plans and of structured settlement annuities. For structured settlement annuities, the situs of coverage was shifted to
the state of residence of the beneficiary rather than the owner. For tax reasons, ownership of the contracts must be in one
entity. If the situs of coverage is the state of residence of the owner, there is a potential for concentration of guaranty
association liability in one or a few states. A similar situation exists with respect to unallocated contracts issued to pension
plans. The amendments proposed to shift coverage to the state of residence of the plan sponsor rather than the owner. This
would avoid an arbitrary concentration of liability in a few state guaranty associations and discourage forum shopping for the
state offering the most generous coverage. 1996 Proc. 2
nd
Quarter 594.
In 1997 the NAIC began a discussion of whether it was appropriate to exclude coverage of unallocated annuity contracts.
The ultimate result of the discussion was amendments to the model, including the drafting note following Section 3A(3).
1997 Proc. 1
st
Quarter 619, 1998 Proc 1
st
Quarter 603.

NAIC Model Laws, Regulations, Guidelines and Other Resources—October 2010
LIFE AND HEALTH INSURANCE GUARANTY ASSOCIATION MODEL ACT
Proceedings Citations
Cited to the Proceedings of the NAIC
© 2010 National Association of Insurance Commissioners PC-520-3
Section 3 (cont.)
B. Revisions to the model were made necessary by the nature of new products now being sold by life insurance
companies. The current practice of marketing products which are tied to external interest rates has increased their volatility.
In drafting the original model, it does not appear that consideration was given to whether such products should be covered by
the act, and if so, to what extent. The committee felt it was especially important to clarify the coverage of annuities under the
act. Group investment annuities and deposit administration accounts were more like deposit accounts than insurance risks so
might be considered for exclusion from coverage, since they are purchased by sophisticated buyers who have the ability to
investigate the seller. 1985 Proc. I 204-205.
The NAIC struggled for several years with the role the guaranty association should play in recovery of losses under
guaranteed investment contracts (GICs) and deposit administration accounts (DACs). A “fact sheet” prepared by an
industry representative suggested that these unallocated annuities should be covered like life and health contracts. In 1984
half of all the annuity premiums received were on GICs. In addition to questions of fairness, the NAIC attempted to
determine if the capacity existed to place unallocated annuities in a separate account. 1986 Proc. I 340, 354.
The last sentence of B(1), added in 1987, made it explicitly clear that coverage is provided for all types of contracts issued by
insurance companies which are used as a funding arrangement for retirement benefits or savings vehicles and the like for
individuals. This amendment should result in easier administration of assessments in that there has been some experience in
the past that individual companies have deemed some of these types of contracts not to be covered; therefore they have not
included premiums on such contracts in their reports in regard to assessable premiums. 1988 Proc. I 355.
The list of exceptions in B(2) was expanded to include some aspects of variable life contracts in Subparagraph (a). The
purpose of this exception was to exclude the portion of the contract where the risk was borne by the policyholder. However,
the obligations of the insurer (e.g. mortality and expense guarantees) are covered. 1976 Proc. I 299.
It was suggested that the exception be expanded to clarify that certain types of contractual relationships are not covered by
the Act. Clearly excluded would be self-funded and uninsured plans, multiple employer welfare arrangements, stop-loss
plans, and administrative services only contracts. 1984 Proc. II 462.
The exclusions list in B(2) was modified to add (g) and (h). The task force believed that the guaranty association should be
viewed as an extraordinary and last resort mechanism to provide benefits only when insureds or beneficiaries may suffer an
extreme financial hardship if benefits were not paid. 1988 Proc. I 356.
When considering amendments in 1996, the working group expressed concern about whether the exclusion in Paragraph
(2)(g) was appropriate, considering the difficulty an employee might have in obtaining benefits from the Pension Benefit
Guaranty Corporation (PBGC). An interested party responded that the employer should be able to meet the obligation to the
employee in most cases, and if not, the Pension Benefit Guaranty Corporation would become liable. He suggested that the
guaranty association should not provide what amounts to a third safety net for the employee. 1996 Proc. 2
nd
Quarter 594.
While considering this amendment further at a subsequent meeting, one regulator expressed concern about the effect of the
exclusion on smaller employers and their employees. He said the prerequisites for the triggering of PBGC coverage are
onerous, and that, in his experience, the PBGC does not pay benefits to plan participants until three to eight years after the
plan becomes insolvent. Industry representatives who spoke in favor of the exclusion said the unallocated annuity contract
issued by the insolvent insurer would be just one of many assets of the plan and over time the plan should be able to
compensate for the loss with the earnings on other investments. It was also pointed out that smaller employers generally do
not participate in the PBGC. 1996 Proc. 4
th
Quarter 984.

NAIC Model Laws, Regulations, Guidelines and Other Resources—October 2010
LIFE AND HEALTH INSURANCE GUARANTY ASSOCIATION MODEL ACT
Proceedings Citations
Cited to the Proceedings of the NAIC
PC-520-4 © 2010 National Association of Insurance Commissioners
Section 3B (cont.)
An amendment to Paragraph (2)(h) was suggested by interested parties in 1996. It had the effect of excluding unallocated
annuity contracts issued to a collective investment trust or similar pooled fund. The working group chair questioned whether
the participants and trustees of these funds are sophisticated investors. One of the drafters explained that the exclusion was
proposed because guaranty associations would otherwise be providing protections for fiduciaries. He pointed out that
individuals participating in these funds could look to their plan fiduciary, the trust or pooled fund fiduciary, and possibly the
Pension Benefit Guaranty Corporation for protection. 1996 Proc. 3
rd
Quarter 838.
At a public hearing on the proposed amendments, an interested party disputed the notion that participants in a collective
investment trust or pooled fund are large, sophisticated investors. He argued that the majority of pension plans participating
in pooled funds are smaller plans. He said the model act lacked a uniform standard for a sophisticated buyer and the
proposed amendment ignored the fact that losses due to the insolvency of the insurer that issued a guaranteed investment
contract to a plan would ultimately be borne by the individual plan participants. Another interested party responded that
pooled funds are not covered under then-existing model and the proposed amendment was meant to clarify the issue and
prevent litigation. Some regulators suggested that guaranty fund coverage for pooled funds might be appropriate. An
interested party suggested the treatment of plan participants under the model act should be consistent for plan participants
regardless of whether the plan sponsor purchases a contract directly or through a pooled fund. 1996 Proc. 3
rd
Quarter 816-
817.
A regulator reminded the working group that the model act is based on the principle that guaranty association protection is a
limited resource and that some coverage exclusions are necessary and appropriate. 1996 Proc. 3
rd
Quarter 817.
At the next working group meeting, discussion continued on the exclusion of pooled funds from guaranty fund coverage.
Some interested parties spoke against the proposal because it would create a disparity of coverage solely based on form. An
insurer representative said the current model excludes such contracts from coverage because the contracts are not issued to a
specific plan sponsor or trustee. The working group raised the question of how insurers that sell guaranteed investment
contracts to pooled funds report the consideration received for purposes of guaranty association assessments. The insurance
industry representatives were unable to answer the question. 1996 Proc. 4
th
Quarter 956.
The working group agreed to adopt the model without the exclusion of coverage for unallocated annuity contracts issued to
collective investment trusts or pooled funds and then consider during 1997 whether coverage should be provided for any
unallocated annuity contracts. 1996 Proc. 4
th
Quarter 956.
In 1997 discussion again took place on whether the model should be amended to exclude coverage of unallocated annuity
contracts. A trade association representative noted that changes in the marketplace and a trend toward investment products
were reasons not to cover unallocated annuities. An insurer representative said purchasers of these products are generally
sophisticated purchasers and often utilize the services of skilled financial advisors. 1997 Proc. 1
st
Quarter 619.
A representative from the life insurance guaranty association said that, when the issue was last discussed by the NAIC, the
focus was on capacity concerns. Companies that sold individual annuities were concerned there would be insufficient
capacity in the guaranty association system if unallocated annuities were not included in the assessment base. 1997 Proc. 1
st
Quarter 619.
At the Summer National Meeting regulators scheduled a hearing so they could hear reasons why they should consider
excluding unallocated annuities from the models. One interested party listed six reasons to exclude unallocated annuities:
(1) they are more in the nature of investments than insurance policies; (2) purchasers are sophisticated buyers capable of
protecting their own interests; (3) the trustee of a qualified benefit plan has fiduciary duties under ERISA; (4) similar
protection is not provided for any other funding vehicle used by benefit plans; (5) the purpose of the model is to provide
protection for individuals, not sophisticated fiduciaries; and (6) unallocated annuities have presented significant difficulties to
receivers and guaranty associations in recent insolvencies. 1997 Proc. 2
nd
Quarter 537-538.

NAIC Model Laws, Regulations, Guidelines and Other Resources—October 2010
LIFE AND HEALTH INSURANCE GUARANTY ASSOCIATION MODEL ACT
Proceedings Citations
Cited to the Proceedings of the NAIC
© 2010 National Association of Insurance Commissioners PC-520-5
Section 3B (cont.)
Another interested party testified that those who favor exclusion are focusing on the form of the contracts over their
substance. He said pension plan participants are not sophisticated investors and need the protection of guaranty association
coverage. He said excluding unallocated products from coverage would shrink assessment capacity to a level at which
capacity might be insufficient in the event of a large insolvency. 1997 Proc. 2
nd
Quarter 538.
A consumer representative questioned whether the majority of persons who purchase unallocated annuities are sophisticated
in their understanding of insurance products or the risk that the issuing insurer may become insolvent. He suggested
consumers have an expectation that contracts purchased from insurers are more secure than other investments. 1997 Proc.
3
rd
Quarter 1126.
A regulator asked whether the issue might be addressed with a “net worth exclusion” similar to that contained in the property
and casualty insurance guaranty fund model. An insurer representative opined that a net worth exclusion would complicate
the assessment process. 1997 Proc. 3
rd
Quarter 1126.
A representative for the National Organization of Life and Health Insurance Guaranty Associations reported that the prior
year assessments for life insurance decreased by 50 percent and assessments for unallocated annuities increased by 100
percent. 1997 Proc. 3
rd
Quarter 1077.
At the next working group meeting a regulator submitted an extensive drafting note prepared by a trade association
suggesting that coverage should be optional at the election of each state. He said the question of coverage of unallocated
annuities is a difficult one and there are good arguments on each side of the issue. 1997 Proc. 4
th
Quarter 645.
A regulator took exception to the statement in the draft comment that purchasers of unallocated annuities are sophisticated
and very capable of protecting their own interests. He cited examples to illustrate the opposite. 1997 Proc. 4
th
Quarter 645.
The working group discussed amending the model to present two options to states on the controversial issue of guaranty
association coverage of unallocated annuities. A working group member noted that 26 states currently provide guaranty
association coverage for unallocated annuities, 19 states exclude coverage, and the rest are silent on the issue. He said the
proposal reflects the reality that each state makes its own decision on the matter. 1998 Proc. 1
st
Quarter 601-602.
An additional exception was added in 1993 to exclude coverage for any policy or contract where assessments were
preempted by federal or state law. 1993 Proc. 2
nd
Quarter 602.
The proposal was adopted as Subparagraph (i) by the working group without further discussion. 1993 Proc. 3
rd
Quarter
350-352.
Paragraph (2)(j) was added with the 1996 amendments. The working group asked whether the guaranty association should
provide coverage for the promises made by the insurer to policyholders, even if the promise is contained in marketing
materials or documents other than the policy. An interested party responded that the guaranty association should not be
expected to provide coverage for an extra-contractual promise, especially if there was no regulatory approval of the side
agreement. 1996 Proc. 2
nd
Quarter 595.
Paragraph (2)(k) was part of the 1996 amendments, added to provide an exclusion for synthetic guaranteed investment
contracts. An industry spokesperson justified this exemption by saying these contracts are purchased by ultra-sophisticated
investors and the plan sponsor was assured that the assets it invested in were fully insulated from the insolvency of the
issuing insurer. 1996 Proc. 2
nd
Quarter 595.

NAIC Model Laws, Regulations, Guidelines and Other Resources—October 2010
LIFE AND HEALTH INSURANCE GUARANTY ASSOCIATION MODEL ACT
Proceedings Citations
Cited to the Proceedings of the NAIC
PC-520-6 © 2010 National Association of Insurance Commissioners
Section 3B (cont.)
The draft provided to the working group also suggested an exclusion for a structured settlement annuity where the liability
insurer or other person liable for the personal injury remains able to pay any remaining amounts due. The working group
decided that would not be an appropriate exclusion because its effect was to put the injured person in the position of having
to reinitiate litigation to protect his or her right to payment. 1996 Proc. 2
nd
Quarter 595.
At the beginning of 1998, a working group began to consider the issue of guaranty coverage for equity-indexed products.
1998 Proc. 1
st
Quarter 602.
The Life Insurance and Annuities Committee concluded that equity-indexed products are fixed products and therefore would
be afforded guaranty association coverage. The problem was determining the extent of coverage, given the unique features
of equity-indexed products. One regulator suggested the contract values are entirely fixed; however, the guaranteed account
value may not be determinable until some time after the date of the insolvency. 1998 Proc. 2
nd
Quarter I 578.
An industry committee concluded that equity-indexed products are covered to the extent that the account value is guaranteed
by the issuing insurer, that any risk borne by the insured is excluded from coverage, and that the interest rate rollback
provisions apply. The committee also concluded that coverage would be limited to the account value on the date of
insolvency. 1998 Proc. 2
nd
Quarter I 578.
The chair asked about the value or potential earnings that had not yet vested at the date of insolvency and whether there was
guaranty association coverage for these amounts. If not, he wondered if the policyholder would have a claim for these
amounts against the receivership estate. The industry committee was of the opinion that it would not be practical to wait until
the end of the term of the contract to determine the contract value. That was why the committee recommended that the value
of the contract be determined at the date of insolvency for purposes of guaranty association coverage. 1998 Proc. 3
rd
Quarter 475.
Another regulator said that equity-indexed products with “ratchet” provisions did not present significant problems regarding
guaranty association coverage, but that “point to point” contracts did present problems. Such contracts could not be valued
as provided in the contract because the end of the term could be several years in the future. An interested party opined that
litigation over guaranty association coverage might be prevented if the model and provisions were clarified. 1998 Proc. 3
rd
Quarter 475.
The working group discussed what disclosures should be made to consumers concerning what would occur in the event of an
insolvency of an insurer that issued equity-indexed products. 1998 Proc. 4
th
Quarter I 533.
When the working group reviewed a draft of suggested amendments to address issues related to equity-indexed products, one
regulator suggested the amendments did not provide adequate protection to holders of point-to-point contracts in that the
potential existed for them to lose all gains in the reference index if the insolvency occurs before the end of the contract term.
He noted that an actuarial group suggested that the value of the reference index should be fixed at the date of insolvency for
purposes of determining account value. This value would also be rolled into any replacement contract issued by a guaranty
association. The regulator suggested that unless the value of the index and, consequently, the account value were fixed at the
date of insolvency, the contract holder was subjected to investment risk. 1999 Proc. 1
st
Quarter 445.
The revised draft addressed the concerns raised about the treatment of point-to-point contracts. The value would be
determined on the date the insurer became an impaired or insolvent insurer. Any earnings or losses determined by use of an
index or other external reference as of the date of impairment or insolvency would be credited to the policy or contract. 1999
Proc. 2
nd
Quarter 435.

NAIC Model Laws, Regulations, Guidelines and Other Resources—October 2010
LIFE AND HEALTH INSURANCE GUARANTY ASSOCIATION MODEL ACT
Proceedings Citations
Cited to the Proceedings of the NAIC
© 2010 National Association of Insurance Commissioners PC-520-7
Section 3 (cont.)
C. An industry draft prepared in 1984 suggested this section be changed by adding limitations to terminate the guaranty
associations obligation by the next renewal date or 180 days, whichever is earlier. The committee did not look favorably
upon this suggestion, indicating that it put life and health company insolvencies in the same mode as property and casualty
insolvencies. 1984 Proc. II 445.
The original model contained the limits of the guaranty association liabilities in Section 8, but it was moved to Section 3
when that section was amended in 1985. 1976 Proc. I 302, 1986 Proc. I 307. The original language simply limited the
aggregate liability of the association to $100,000 in cash values or $300,000 for all benefits on one life. The industry draft
submitted in 1984 suggested a different approach with percentages to be paid on a sliding scale. 1984 Proc. II 465-466. A
regulator commenting on the industry proposal found it to be unreasonable and unfair. He found a 75% limitation on health
insurance recoveries, regardless of the size of the claim, to be particularly offensive. 1984 Proc. II 476.
The revised model adopted in 1985 contained limitations on liability quite different from the industry suggestion. The
$100,000/$300,000 of the original model had been retained, with clarifications and expanded provisions. The adopted
version now limited health insurance benefits to $100,000 and present value of annuity benefits to $100,000. During the task
force meeting the coverage maximum for unallocated annuities was raised to $5 million from the $2 million in the draft.
1986 Proc. I 294-295.
In 1993 a discussion was held on whether to increase the $100,000 limit for health insurance coverage, or to eliminate the cap
completely. The working group acknowledged that national health care reform and the effect of long-term disability
coverage should be considered further before a recommendation was made. 1993 Proc. 4
th
Quarter 569.
In the fall of 1994 a working group considered a proposal to increase to the coverage for medical expense and disability
benefits. The draft contained a $300,000 limit for disability benefits and paid medical expense payments up to the limit of
the policy. 1994 Proc. 3
rd
Quarter 418, 431.
An insurance trade association submitted comments on the proposal. It said that the inclusion of a cap on medical expense
benefits would make the association subject to enormous anti-selective pressures. It also noted that the inclusion of a dollar
cap would not have a significant effect on those currently under care. 1994 Proc. 4
th
Quarter 590.
Another trade association also expressed concern about the unlimited coverage and suggested a cap of $300,000. The
association pointed out that $100,000 of benefits had been considered quite broad when the model was first adopted in 1970,
but medical cost have increased considerably since then. A recent study showed, however, that only .06 percent of the
reviewed claims exceeded $100,000. 1994 Proc. 4
th
Quarter 590.
The trade association noted that the terminology used in the amendment was not clear. It suggested clarifying the meaning of
“health insurance,” “medical insurance” and “disability insurance.” The recommendation was to make the meanings
consistent with the terminology used in the NAIC Health Insurance Shoppers’ Guide. 1994 Proc. 4
th
Quarter 590.
A regulator explained the intent of the removal of the cap on health insurance benefits was to benefit insureds suffering from
catastrophic illnesses. An insurer responded that a cap served to protect the guaranty associations from irresponsible insurers
that sold policies without contractual limits.
Another regulator suggested the limit on coverage should be the contractual limits of the policy or $1,000,000, whichever
was less. 1994 Proc. 4
th
Quarter 575-576.
In December 1994 the working group recommended to the subcommittee that a proposed amendment be adopted that would
provide for $100,000 net cash surrender value, $300,000 for disability income insurance, and $1,000,000 on benefits for
medical expenses. The subcommittee adopted that provision. 1994 Proc. 4
th
Quarter 565-566.

NAIC Model Laws, Regulations, Guidelines and Other Resources—October 2010
LIFE AND HEALTH INSURANCE GUARANTY ASSOCIATION MODEL ACT
Proceedings Citations
Cited to the Proceedings of the NAIC
PC-520-8 © 2010 National Association of Insurance Commissioners
Section 3C (cont.)
When the Executive Committee was to consider this amendment for final adoption, the chair of the Insolvency Committee
asked that the proposal be returned to the drafters for further work. He noted that, in making the recommendation, the
subcommittee had not considered the effect of these increases on the aggregate limits. 1994 Proc. 4
th
Quarter 26.
When the document was referred back to the subcommittee, an association representative asked the subcommittee to
reconsider whether increasing the limit of guaranty association coverage from $100,000 to $1,000,000 was appropriate. The
working group was instructed to reconsider the coverage limits. 1995 Proc. 1
st
Quarter 461.
As a compromise, the working group decided to recommend the coverage for medical expense be set at $500,000. 1995
Proc. 3
rd
Quarter 585.
Subsection C(2)(c) was added in December of 1993. When the draft was first exposed, it was explained that this amendment
was needed to clarify that, for purposes of structured settlement annuity benefits, the limitations in guaranty fund benefits
applied per payee or beneficiary with an aggregate limitation. 1993 Proc. 2
nd
Quarter 602.
The amendment was adopted by the working group in September without further discussion. 1993 Proc. 3
rd
Quarter 350-
351.
When regulators were considering technical amendments to Paragraph (2)(c), an interested party suggested adding the phrase,
“if any” after the reference to cash surrender and net cash withdrawal values. She said her organization was not aware of
structured settlement annuity contracts being issued that contained these features, but the language would address the
products if developed in the future. 1997 Proc. 4
th
Quarter 645.
When considering amendments to the model in 1996, changes to Paragraph (2)(d) were considered. One regulator pointed
out that the current policy of limiting coverage of unallocated products to $5 million per policy owner may prove to be
inadequate in the case of a large employer with multiple union contracts. 1996 Proc. 2
nd
Quarter 595.
The amendments to Subparagraph (e) of Subsection C(2) were made when the NAIC clarified its position on coverage of
unallocated annuities. The task force believed that the nature of most unallocated annuity contracts required a different
approach due to the problems that could result. The task force adopted a “per participant” approach for government plans and
a “contract holders” approach for non-governmental plans. Even though the Proceedings indicate governmental plans under
Section 401(k) are included, the original document indicates the (k) was deleted and the section includes all plans authorized
under I.R.C. Section 401. 1988 Proc. I 356.
Further amendments to Paragraph (2)(e) were made in 1996. Subparagraph (f) was added. 1996 Proc. 4
th
Quarter 963.
D. When considering amendments to the model in 1996, Subsection D was added. An industry spokesperson explained
that large companies that assume business from smaller insolvent insurers object to incurring the costs associated with
modifying their systems to accommodate the forms of small insurers. 1996 Proc. 2
nd
Quarter 595.
In conjunction with the development of the 1996 amendments, several new paragraphs were added to the comments
following Subsection D. Some language was deleted also. 1996 Proc. 4
th
Quarter 963.
Section 4. Construction
When the model was amended in 1996 this provision was modified so that it no longer said the act “shall be liberally
construed . . . .” The working group chair opined that deleting the word “liberally” would restrict interpretation of the act by
the courts. An interested party disagreed, saying the purpose of the proposal was to discourage the courts from finding
coverage where it was not intended. 1996 Proc. 2
nd
Quarter 595.

NAIC Model Laws, Regulations, Guidelines and Other Resources—October 2010
LIFE AND HEALTH INSURANCE GUARANTY ASSOCIATION MODEL ACT
Proceedings Citations
Cited to the Proceedings of the NAIC
© 2010 National Association of Insurance Commissioners PC-520-9
Section 5. Definitions
C. Subsection C was added with the 1996 revisions. It was proposed to allow guaranty associations to fully utilize
available capacity. An interested party noted that insurers are already in the practice of establishing reserves for assessments.
It was also noted that some state guaranty associations have taken the position that the association may not authorize an
assessment but defer calling the assessment under existing law. 1996 Proc. 2
nd
Quarter 595.
D. Subsections D and E were added with the amendments considered in 1996. 1996 Proc. 4
th
Quarter 964.
I. Subsection I was an addition included with the 1996 amendments. 1996 Proc. 4
th
Quarter 964.
J. When the model was revised in 1975 the definition of impaired insurer was modified and a definition of insolvent
insurer added. At that time “insolvent insurer” was defined to include an insurer under an order of liquidation and an
“impaired insurer” was defined as one unable or potentially unable to fulfill its contractual obligations. The changes in
definition were accompanied by changes in Section 8 allowing the association to get involved prior to an actual court order.
1976 Proc. I 300.
In 1996 amendments were proposed that eliminated the discretionary triggering of a guaranty association absent entry of an
order of conservation or rehabilitation. The suggestion was made because the drafters felt the previous language was
ambiguous and that a more objective standard was needed to determine whether guaranty associations are triggered. 1996
Proc. 2
nd
Quarter 595.
L. A suggestion was made in 1984 to expand the definition of member insurer to include entities whose license may
have been suspended or revoked. Insureds should not lose guaranty association coverage because of enforcement actions
against an insurer. The suggestion included a list of who is NOT a member insurer. The entities suggested were those not
required to adhere to the same laws and regulations designed to assure solvency, proper market conduct and competitive
equality. 1984 Proc II 462. Changes to the model were made during the extensive revisions adopted in December, 1985.
1986 Proc. I 309.
While considering amendments to the model in 1996, the working group discussed insolvency protection for all health care
consumers, including those utilizing health maintenance organizations. One commissioner suggested three objections should
be considered: (1) correlation with other efforts of regulators in the health care area, specifically the effort to include all risk-
bearing entities in the regulatory process, including risk-based capital standards for health organizations; (2) the creation of a
consistent regulatory framework for health organizations, regardless of the type of entity from which the consumer purchased
health care; and (3) a consistent sharing of the costs of consumer protection among the various types of health organizations.
1996 Proc. 3
rd
Quarter 816.
An insurer representative took issue with the commissioner’s suggestion that all health organizations should be included
under one insolvency protection mechanism. He said each type of entity presents different problems and calls for different
solutions. The commissioner predicted that the differences between health organizations would become less distinct in the
future. He challenged the working group to develop a single model to address insolvency protection for health care
consumers. 1996 Proc. 3
rd
Quarter 816.
In March 1998 a working group briefly discussed guaranty coverage of charitable gift annuities. Staff reported that the Life
Insurance and Annuities (A) Committee was discussing the issue and asked the Insolvency Subcommittee to determine
whether there was guaranty association coverage for charitable gift annuities. 1998 Proc. 1
st
Quarter 602.
The working group questioned whether licensed insurance companies could, in some instances, issue contracts that might be
considered charitable gift annuities. A charitable organization might, in effect, reinsure its obligation to the donor by
purchasing an annuity from an insurance company. 1998 Proc. 2
nd
Quarter I 578.

NAIC Model Laws, Regulations, Guidelines and Other Resources—October 2010
LIFE AND HEALTH INSURANCE GUARANTY ASSOCIATION MODEL ACT
Proceedings Citations
Cited to the Proceedings of the NAIC
PC-520-10 © 2010 National Association of Insurance Commissioners
Section 5L (cont.)
The chair of the life group drafting the Charitable Gift Annuities Model Act [#240] said the purpose of that model law was to
allow charitable gift annuities to be regulated without requiring that the contracts be issued by insurance companies. 1998
Proc. 2
nd
Quarter I 578.
An NAIC staff memo noted that one important aspect of a charitable gift annuity is that it is an unsecured promise of the
charitable organization to pay the annuitant the agreed upon amount. If the promise to pay is secured, the annuitant may lose
the tax advantage of the transaction. Consequently, many states have begun to concern themselves with charitable gift
annuities and the issue of default by the charitable organization. 1998 Proc. 2
nd
Quarter I 578.
The working group decided to consider an amendment to Subsection L to add a new Paragraph (7) to exclude charitable gift
annuities. 1998 Proc. 3
rd
Quarter 475.
The group adopted the model law amendment. 1999 Proc. 1
st
Quarter 445.
N. The working group agreed to add a definition of “owner” when discussing the 1996 proposed amendments. The
group decided the definition was sensible. 1996 Proc. 2
nd
Quarter 595.
P. The definition of “plan sponsor” was included in the amendments discussed in 1996. The working group agreed it
was sensible to add the definition. 1996 Proc. 2
nd
Quarter 595.
Q. The subsection was modified to eliminate premiums from the assessment base for unallocated annuities when
coverage is not provided. Even though the Proceedings indicate governmental plans under Section 401(k) are included, the
original document indicates the (k) was deleted and the section includes all plans authorized under I.R.C. Section 401. 1988
Proc. I 357.
When the definition was amended in 1996, it was amplified to be as broad as possible. The revised definition also limits
assessments to conform with the extent of coverage provided for unallocated products and corporate-owned and bank-owned
life insurance contracts. This was accomplished by adding Paragraph (2) to Subsection Q. 1996 Proc. 2
nd
Quarter 595.
R. The definition of “principal place of business” was added to the model in the amendments discussed in 1996. 1996
Proc. 2
nd
Quarter 595.
S. Subsection S was also added in 1996. 1996 Proc. 2
nd
Quarter 603.
T. When considering amendments in 1996, the working group agreed that Subsection T should be amended to provide
coverage for U.S. citizens residing in foreign countries and residents of U.S. possessions, territories and protectorates by the
guaranty association in the state of domicile of the insolvent insurer. 1996 Proc. 2
nd
Quarter 595.
U. This subsection was added as part of the 1996 amendments. 1996 Proc. 2
nd
Quarter 603.
V. This definition was added as part of the 1996 amendments. It was designed to complement Subsection T. 1996
Proc. 2
nd
Quarter 595.
Section 6. Creation of the Association
A. The model originally adopted in 1970 provided for three accounts: the health insurance account, the life insurance
account, and the annuity account. Earlier drafts had lumped life insurance and annuities into one account, but the drafters
heard evidence on the volume of annuity considerations in each state and were urged by the industry to make the two types of
coverage separate. 1971 Proc. I 184.

NAIC Model Laws, Regulations, Guidelines and Other Resources—October 2010
LIFE AND HEALTH INSURANCE GUARANTY ASSOCIATION MODEL ACT
Proceedings Citations
Cited to the Proceedings of the NAIC
© 2010 National Association of Insurance Commissioners PC-520-11
Section 6A (cont.)
In 1985 the drafting committee wrestled with the problem of the new annuity products being developed. For a time they
considered excluding these products (1985 Proc. I 204-205), but by the June 1985 meeting distributed an exposure draft
which established four accounts, dividing the annuity products into two accounts: (1) individual annuities and group products
where benefits are guaranteed to specific individuals, and (2) guaranteed investment contracts. The chair said there was a
clear consensus on the task force about what products should be included under the model bill, but the details of how that
should be accomplished were uncertain. The task force felt it needed more information to determine how to treat guaranteed
investment type products. The task force needed more information on company reporting, premium taxes and market share
by state of those guaranteed interest products so they could make an informed decision. 1985 Proc. II 472.
The draft adopted in December 1985 contained provision for four accounts, but requested a state-by-state study of the
adequacy of coverage and assessment capacity of the allocated and unallocated annuity contracts be completed so that
reconsideration of the merits of the current stated preference could be addressed at the December 1986 meeting of the NAIC.
1986 Proc. I 148, 309.
By June 1987 an extensive annuity survey had been completed and the results reported to the task force. 1987 Proc. II 320-
396. After receipt of the report the task force agreed that a note should be added to the model that the four-account approach
is no longer the preferred methodology. They were not ready at that time to make a decision on what type of account
structure would be preferable. 1987 Proc. II 319-320.
A compromise plan was agreed upon in December 1987. The amendment created two accounts a life and annuity account
and a health account, with subaccounts created under the life account for allocated annuities, unallocated annuities, and for
life insurance. The amendments offered the commissioners a balanced approach from which to pattern their individual state
acts. 1988 Proc. I 337.
When the original model life and health guaranty fund model was adopted it provided for three accounts—life, accident and
health, and annuities. The volume and type of life insurance and annuity contracts being issued then were remarkably
different from those prevalent in the marketplace today. The distinction between products not only within the life insurance
and annuity industry is becoming blurred, but also with products offered by other financial institutions. Today both life and
annuity products have a predominant accumulation feature. In the consumer’s eyes there is very little difference between a
single-premium deferred annuity and a single-premium whole life insurance policy. Therefore, retaining the current
distinction between life and annuity products in the guaranty association model act seems unnecessary and inappropriate.
Also, from a capacity standpoint, combining the life and annuity accounts will result in optimum capacity. 1988
Proc. I 355. The executive committee amended the model to clarify that Section 403(b) plans were unallocated annuities.
1988 Proc. I 18.
Suggestions to revise the model were first presented in June 1994. The proposal was made because regulators saw the
treatment of governmental plans as inconsistent. 1994 Proc. 2
nd
Quarter 535.
Subsection A(1) was revised in 1995 to move Section 403(b) plans and other governmental retirement plans from the
unallocated annuity account to the annuity account. The reason for the amendment was because coverage provided by the
model act for participants in the plan was the same as that for allocated annuities. 1995 Proc. 1
st
Quarter 461.
B. Subsection B was added to the model in 1985. 1986 Proc. I 310.

NAIC Model Laws, Regulations, Guidelines and Other Resources—October 2010
LIFE AND HEALTH INSURANCE GUARANTY ASSOCIATION MODEL ACT
Proceedings Citations
Cited to the Proceedings of the NAIC
PC-520-12 © 2010 National Association of Insurance Commissioners
Section 7. Board of Directors
A. An advisory group was asked to consider the issue of public representation on guaranty association boards in 1992.
The committee report recommended against it, but one member proposed that a drafting note be added to include a provision
for public representation on the board where the state had a premium tax offset. 1993 Proc. IB 703.
One member of the advisory group submitted a minority report explaining her reasons for recommending public
representation on guaranty association boards. The main reasons given by the consumer representative were because the
public ultimately bears the cost of guaranty fund assessments, because a different perspective is needed, and because
accountability is needed. 1993 Proc. I 707.
As a follow-up from that minority report, the working group decided to draft amendments to both the Life and Health
Insurance Guaranty Association Model Act and the Post-Assessment Property and Liability Insurance Guaranty Association
Model Act, which were designed to add two public representatives as members of the board of directors of the guaranty
associations without increasing the overall number of members on the boards. The amendments also addressed potential
conflicts of interest by requiring that the public representatives not be employed or contracted by any entity regulated by the
state insurance department or required to register as a lobbyist in the state, or related to either. 1993 Proc. 2
nd
Quarter 619.
A representative from an association of guaranty funds said an earlier suggestion for public representatives failed to gain
support because of a perception that the commissioner was the representative of the public. Another association
representative said his organization’s position was that it was a public policy question for the legislatures to determine. The
underlying question related to the individual members themselves: their expertise, accountability and responsibility. 1993
Proc. 2
nd
Quarter 619.
The consumer representative who authored the minority report restated her position. She believed that because the public
ultimately bears the burden of insolvencies either through increased taxes or policy surcharges, the public was entitled to
representation on the boards. Any problem experienced with incentive to attend meetings or structure of the board should be
addressed separately from the overall issue of representation and should not result in a denial of representation of the public.
1993 Proc. 2
nd
Quarter 619.
In a letter of comment on the exposure draft providing for public representation, one association said it had developed a
position opposed to public representation when the model was originally drafted. The association’s position was that there
were substantial conflicts of interest in having consumers and other public representatives on the board. The state guaranty
funds stand in the shoes of the insolvent insurer and must pay claims and decide coverage issues as the insolvent insurer
would have done. Had the insolvent insurer remained solvent, it would not have had consumers involved in its internal
claims process. 1993 Proc. 2
nd
Quarter 605.
The consumer representative said insurers also faced a conflict of interest because their interests were not aligned with those
of policyholders either, but rather with the solvent insurers who paid the assessment. 1993 Proc. 2
nd
Quarter 619.
Another insurer association gave conditional support for the amendment. Its experience had been that qualified public
representatives can make a positive contribution to board deliberations. The association expressed some concern about
selecting qualified individuals who should be knowledgeable about the insurance industry. It recommended the draft be
revised to require only one public member, who should not be eligible to serve as the chair of guaranty fund boards. 1993
Proc. 2
nd
Quarter 604.

NAIC Model Laws, Regulations, Guidelines and Other Resources—October 2010
LIFE AND HEALTH INSURANCE GUARANTY ASSOCIATION MODEL ACT
Proceedings Citations
Cited to the Proceedings of the NAIC
© 2010 National Association of Insurance Commissioners PC-520-13
Section 7A (cont.)
Before the Executive Committee voted on adoption of the amendment regarding public representatives, further discussion
took place. The chair of the Financial Condition Subcommittee said the purpose of the amendment was to improve
communication among regulators, the insurance industry and consumers on guaranty fund and insurer insolvency issues. The
addition of public representatives to the governing boards would provide consumers with access to the guaranty fund process
and a direct means to express concerns. The addition of public representatives also recognizes the impact of insurer
insolvencies on the general revenues of states and taxpayers. 1993 Proc. 2
nd
Quarter 32.
Another commissioner stated that he occupied a position on the guaranty association boards and acted as a public
representative since it was his function to protect the public interest. 1993 Proc. 2
nd
Quarter 32.
A third commissioner said that public input into the guaranty fund process would be valuable, and that even though the
commissioner’s function was protection of the consumers, the issue was one of direct public access. He did not favor
inclusion of this provision in the financial regulation standards for accreditation. The chair of the subcommittee responded
that this was not being recommended. 1993 2
nd
Quarter 32.
Before final adoption the NAIC plenary body considered the matter again. Concern was expressed that the amendment
regarding public representatives would be required for a state to be accredited. After assurance that the amendments were not
being considered, indeed were not even related to financial solvency, the model amendment was adopted. 1993 Proc. 2
nd
Quarter 12.
When amendments to the model were considered in 1996, the working group recommended that the definition of “public
representative” be simplified. 1996 Proc. 2
nd
Quarter 595.
Section 8. Powers and Duties of the Association
A. Industry spokespersons urged adoption of provisions giving more authority to the insurance companies. They made
a series of suggestions for change to this section to accomplish that. Some of them were incorporated into the model adopted
in 1970, but the commissioner still retained much control over the association. 1971 Proc. I 184-186.
As originally adopted, the model contained language specifically allowing the association to act prior to an order of
liquidation or rehabilitation. This language was modified in December 1975 to allow the association to act subject to any
conditions imposed by the association and approved by the commissioner. 1976 Proc. I 301. The language was modified
again to except court-ordered conservation or rehabilitation. 1986 Proc. I 310.
Subsection A’s opening paragraph was modified when the 1985 amendments were adopted. 1986 Proc. I 310.
In 1996 a proposal was made to broaden the application of the model by deletion of a word, so that Subsection A would no
longer begin, “If a member insured is an impaired domestic insurer . . . .” 1996 Proc. 2
nd
Quarter 595.
In 1996 a provision that had been included in the model since its inception was deleted. An interested party said the
provision allowing a guaranty association to lend money to an impaired insurer placed the non-profit status of the guaranty
association in jeopardy. 1996 Proc. 2
nd
Quarter 595.

NAIC Model Laws, Regulations, Guidelines and Other Resources—October 2010
LIFE AND HEALTH INSURANCE GUARANTY ASSOCIATION MODEL ACT
Proceedings Citations
Cited to the Proceedings of the NAIC
PC-520-14 © 2010 National Association of Insurance Commissioners
Section 8 (cont.)
B. A policyholder with a life or health insurance contract in an impaired company is concerned with preserving the full
benefit of his contract. Any plan which is designed to provide only for the payment of outstanding claims falls far short of
meeting this concern. If the policyholder is in impaired health or at an advanced age, he would not be able to obtain
equivalent insurance through a new policy issued by another company. This contrasts with the typical situation under
property and casualty insurance coverages which are short term and under which a policyholder can ordinarily substitute a
new policy. The drafters were urged to take these considerations into account when drafting the model statute. 1970 Proc. II
1072.
Significant changes to Section 8 were included in the redraft adopted in late 1985. 1986 Proc. I 310-315.
In conjunction with the amendments of 1996, what had been Subsection D was incorporated in the subsection above it, which
became Subsection B when the previous Subsection B was deleted. A drafter indicated the changes were being
recommended because the prior arrangement did not lend itself to effectuating a multistate rehabilitation plan. The working
group chair said some insurance regulators might object to authorizing the receivership court to approve substitute policies.
He suggested a revision to provide for approval of substitute policies by the domiciliary insurance commissioner and the
receivership court. 1996 Proc. 2
nd
Quarter 596.
F. The working group suggested that Subsection F be amended to grant the local court jurisdiction over the imposition
of moratoria or policy liens by the guaranty association in that jurisdiction. Paragraph (2) was extensively amended to make
it clear that policyholders cannot expect payment from a guaranty association when a moratorium has been put in place by
the receivership court. 1996 Proc. 2
nd
Quarter 596.
G. As originally written in 1996, the subsection conflicted with Section 56 of the Insurers Rehabilitation and
Liquidation Model Act, which requires that all deposits be returned to the domiciliary receiver. 1996 Proc. 2
nd
Quarter 596.
At its next meeting the working group discussed Subsection G at length. The chair opined that guaranty associations should
not receive a larger share of a deposit than other creditors of the same class. Another working group member suggested that
deposits could be paid over to the guaranty association, but that the guaranty association should not be allowed to retain more
than its appropriate share. Any funds in excess of the guaranty association’s share would be delivered to the receiver of the
insolvent insurer. The working group decided to include language in Subsection G to this effect. 1996 Proc. 3
rd
Quarter
838-839.
H. The working group suggested a nonsubstantive revision to Subsection H to make it clear that the commissioner’s
authority to act for the guaranty association is limited to the insolvent insurer in question. 1996 Proc. 2
nd
Quarter 596.
J. The working group discussed at length a proposal made in 1996 to allow the National Organization of Life and
Health Guaranty Associations (NOLHGA) to intervene in receivership proceedings. The proponents of the amendment
argued that the amendment was necessary because guaranty associations organized as unincorporated associations may not be
allowed to intervene in some jurisdictions. It was also argued that the participation of guaranty associations is critical to the
development and effectuation of a plan of rehabilitation. Those opposing the amendment said that the current provision
granting guaranty associations standing to appeal in receivership proceedings is consistent with the provision of the Insurers
Rehabilitation and Liquidation Model Act and is sufficient. Concern was also expressed about the potential cost to the estate
of intervention by NOLHGA. The extent to which NOLHGA, if allowed to intervene, could bind its member associations to
obey any judgment issued by the court was discussed. 1996 Proc. 2
nd
Quarter 596.
After further discussion the working group agreed that, if NOLGHA is allowed to intervene, it should do so as a
representative of the affected guaranty associations. The amendments were revised to include standing for individual
guaranty associations. 1996 Proc. 3
rd
Quarter 839.

NAIC Model Laws, Regulations, Guidelines and Other Resources—October 2010
LIFE AND HEALTH INSURANCE GUARANTY ASSOCIATION MODEL ACT
Proceedings Citations
Cited to the Proceedings of the NAIC
© 2010 National Association of Insurance Commissioners PC-520-15
Section 8 (cont.)
K. The working group considered an amendment to Subsection 3B to exclude a structured settlement annuity where the
liability insurer or other person remains able to pay any remaining amount due The working group decided this placed an
inappropriate burden on the injured person but did address the issue by adding a subrogation right to Subsection K(3). 1996
Proc. 3
rd
Quarter 838.
A trade association representing structured settlement providers suggested technical amendments to Subsection K. 1997
Proc. 3
rd
Quarter 1126, 1128.
L. Paragraph (7) was added to address recent litigation in which a trial court ruled that a discovery request served upon
a guaranty association as an unincorporated association should be passed through to each member company of the
association. 1996 Proc. 2
nd
Quarter 596.
N. The Subsection N added with the 1996 amendments was proposed to make it clear that a guaranty association may
elect to succeed to the rights of the insolvent insurer regarding any reinsurance agreements. 1996 Proc. 2
nd
Quarter 596.
At the working group’s suggestion, the proposal was amended to provide for payment to the beneficiary by the guaranty
association of an amount specified in Paragraph (1), to preclude termination by the reinsurer of the reinsurance agreement or
any setoff against the amounts due to the guaranty association if the guaranty association pays premium within a specified
time, and to provide for the transfer of rights and obligations of the guaranty association to another insurer. The revised
section also provided for the receiver to remain entitled to any amounts payable by the reinsurer with respect to losses or
events occurring prior to the coverage date and to remain liable for premiums prior to the coverage date. 1996 Proc. 3
rd
Quarter 839.
O. An interested party opined that the new Subsection O proposed in 1996 afforded the board of directors of a guaranty
association the benefit of the “reasonable business judgment” rule, and made it clear that those who opt out of rehabilitation
plans are not entitled to benefits from the guaranty association. 1996 Proc. 2
nd
Quarter 596.
P. Subsections P and Q were added in 1996 without comment. 1996 Proc. 4
th
Quarter 972.
R. When discussion of coverage for equity-indexed products commenced, an industry committee recommended
receivers have the authority to convert equity-indexed products to simpler products because of the complexities of
administering equity-indexed products. 1998 Proc. 2
nd
Quarter I 579.
An interested party said the suggestion was made because of the complicated nature of the product, the difficulty of
administering the products, and the limited universe of companies capable of assuming equity-indexed products. He said
state laws comparable to the Life and Health Guaranty Association Model Act would have to be amended to provide
authority to convert these products in a liquidation proceeding. 1998 Proc. 3
rd
Quarter 475.
Section 9. Assessments
B. Prior to the amendments adopted in 1985, the model provided for three classes of assessments, one for
administrative expenses, one for insolvency of a domestic insurer and one for an insolvency of a foreign or alien insurer. At
the same time as treatment of residents and nonresidents changed, the treatment of domestic versus foreign insurers was
merged into discussions of an insolvent insurer, regardless of domicile. 1986 Proc. I 315.
C. In 1985 the assessment for administrative expenses increased from $50 to $150 per member insurer. 1986 Proc. I
315.

NAIC Model Laws, Regulations, Guidelines and Other Resources—October 2010
LIFE AND HEALTH INSURANCE GUARANTY ASSOCIATION MODEL ACT
Proceedings Citations
Cited to the Proceedings of the NAIC
PC-520-16 © 2010 National Association of Insurance Commissioners
Section 9 (cont.)
E. The model contained a two percent cap on assessments from the beginning. It was revised to create two accounts
with subaccounts, consideration was given to reducing the cap to one percent. 1988 Proc. I 357. After considerable debate,
the model adopted retained the two percent cap on assessments. The proposal adopted was recognized as complex, but
would require the offending account to pay one percent before the act crossed over and assessed the other accounts. 1988
Proc. I 157-158.
To clarify the mechanisms of the amendments to Subsection E(1), the task force adopted the following statement: “If a one
percent assessment of the offending subaccount is insufficient, then all three subaccounts will be assessed one percent. This
would result in the offending subaccount paying two percent at the same time the others are paying one percent. If this is still
insufficient, the other two subaccounts could be assessed to the maximum two percent.” 1988 Proc. II 335. It was also
noted that this was an interpretation, not an amendment to the model. 1988 Proc. II 196.
The amendments proposed in 1996 required that the affected subaccount be assessed up to the 2% limit before spillover to
the other subaccounts. 1996 Proc. 2
nd
Quarter 596.
H. In the first draft of the model prepared, provision was made for the issuance of certificates of contribution, in the
amount of assessments paid by member insurers, which could be carried by member insurers as admitted assets. At a
drafting session it was decided to delete the provision, presumably because of concern that such items ought not be carried as
admitted assets because of their questionable or indefinite value. The drafters were urged to return the provision to the
model, and did so, adding language that they would be “in such form, and for such amount, if any, and period of time as the
commissioner may approve.” The industry put forth the argument that this was different than the property and casualty
guaranty model which merely provided for payment of claims. This model takes into account the fact that insurance
coverage will be continued and that business may very well be profitable in later years. 1971 Proc. I 186.
I. Subsection I was entirely new in the 1996 amendments. It was included without any specific comment. 1996 Proc.
4
th
Quarter 974.
J. Subsection J was new material added with the 1996 amendments. 1996 Proc. 4
th
Quarter 974.
Section 10. Plan of Operation
A model plan of operation to complement this section was adopted. 1973 Proc. I 164-169.
Section 11. Duties and Powers of the Commissioner
C. When the model was amended in 1985, this subsection was revised, including a change in the appeal period from 30
to 60 days. 1986 Proc. I 317.
When revisions to this subsection were considered in 1996, a working group member suggested that the provision might
conflict with the laws of some states regarding administrative procedures. The working group agreed to add “in accordance
with the laws of this state that apply to the actions or orders of the commissioner” to the last sentence of the subsection. 1996
Proc. 3
rd
Quarter 839.
Section 12. Prevention of Insolvencies
When consideration was being given to the adoption of a life and health guaranty association model, those opposed to the
model argued that the real need was prevention of insolvency. They opined state regulation should be designed to maintain
the solvency of companies and to make certain that companies would be able to meet their obligations to shareholders. 1971
Proc. I 175.

NAIC Model Laws, Regulations, Guidelines and Other Resources—October 2010
LIFE AND HEALTH INSURANCE GUARANTY ASSOCIATION MODEL ACT
Proceedings Citations
Cited to the Proceedings of the NAIC
© 2010 National Association of Insurance Commissioners PC-520-17
Section 12 (cont.)
The model amendments adopted in 1975 included revision of this section. In the original model only the duties of the board
of directors now found in Subsections C to G were spelled out. The revised model began by enumerating duties of the
commissioner. 1976 Proc. I 308-309.
The amendments of 1996 deleted two subsections; one that had included the duty of the board of directors to prepare a report
for the commissioner (old Subsection G) and a Subsection E that allowed the board of directors to request the commissioner
to order an examination of any member insurer, and requiring the commissioner to begin the examination within 30 days.
1996 Proc. 4
th
Quarter 977.
Section 13. Credits for Assessments Paid (Tax Offsets)
Industry representatives urged the inclusion of a section providing for tax write-offs for assessments paid. This was in
contrast to the provision in the property and casualty insurance guaranty association model which allowed for rates to include
amounts sufficient to recoup amounts paid to the association. The first drafts of the model allowed insurers to build into their
rate and dividend structure an amount reasonably necessary to meet assessment obligations. Because this assumed insurers
could put a price on what future assessments might be, it was suggested that approach was not valid in either a theoretical or
practical sense. It would in effect require prefunding, a concept which was deemed undesirable by the regulators. 1971
Proc. I 188.
Despite the urging of industry spokespersons, the majority of the subcommittee voted against the inclusion of a premium tax
offset. At the meeting six months after adoption of the model, industry again argued for an offset. The subcommittee instead
adopted a motion recommending that each state consider the question of tax offset in the light of its regulatory experience.
1971 Proc. II 337.
The subcommittee report issued upon adoption of the model explained the reason no tax offset would be part of the model.
They said the insolvency fund legislation provided a “mechanism by which each policyholder, through a slightly increased
cost, purchases protection for himself against the insolvency of his insurer.” Industry argued that this approach overlooked
two fundamental factors:
1. With respect to most life insurance policies and many health insurance policies, the increased cost cannot be passed on
because the premium is fixed. 2. If premiums were raised just for future policyholders, they would bear the cost of present
insolvencies, while present policyholders would not. The representation that each policyholder is buying protection becomes
illusory. 1971 Proc. II 338-339.
A draft incorporating proposed revision to the model to include a section providing for a tax offset was presented in June
1974. 1974 Proc. II 400-401.
The draft was considered and revised over the next two years before being adopted in December 1975. 1976 Proc. I 309. At
the next meeting it was clarified that this is to be an optional provision. 1977 Proc. II 363.
Section 14. Miscellaneous Provisions
C. The industry draft of the new model suggested the addition of this section so that the guaranty association was a
creditor of the impaired insurer. 1971 Proc. I 187.
D. Subsection D was added as part of the 1996 amendments. There was no group discussion recorded on the issue.
1996 Proc. 4
th
Quarter 978.

NAIC Model Laws, Regulations, Guidelines and Other Resources—October 2010
LIFE AND HEALTH INSURANCE GUARANTY ASSOCIATION MODEL ACT
Proceedings Citations
Cited to the Proceedings of the NAIC
PC-520-18 © 2010 National Association of Insurance Commissioners
Section 14 (cont.)
E. This provision was patterned after a section of the Wisconsin law. It was designed to recapture excessive dividend
payments to affiliates that exercise control over an impaired insurer. The NAIC Holding Company Act in large measure
prevents improper distribution of dividends by an insurer to its holding company, but if dividends are paid under
circumstances that the insurer should have reasonably known could affect its ability to perform its contractual obligations, the
holding company should be required to repay the dividends. 1971 Proc. I 187.
Section 15. Examination of the Association; Annual Report
The last sentence, allowing members to request a copy of the report, was added in 1996. 1996 Proc. 4
th
Quarter 979.
Section 16. Tax Exemptions
Section 17. Immunity
Section 18. Stay of Proceedings; Reopening Default Judgments
Section 19. Prohibited Advertising of Insurance
When the drafters were receiving comments on the original model before adoption, one insurance executive put forth the
argument that properly managed companies would suffer because the agents of marginal companies could point to the
guaranty fund as “free reinsurance.” 1971 Proc. I 182-183.
When the property and casualty guaranty association model was adopted, the general comments at the end contained a
suggestion that states might want to add a section specifically prohibiting advertisements referring to the coverage of the
guaranty association. 1970 Proc. I 262. It was suggested that such a provision be included in the life and health guaranty
association model. The industry commentators suggested this was essential to prohibit the unscrupulous from taking
advantage of the guaranty law. They suggested unethical operators would put a lot of business on the books without real
concern for the adequacy of underwriting. They visualized the agent telling his prospects that they need have no concern
since the assets of all other companies in the state would protect them if his company’s rates were inadequate. 1971 Proc. I
187.
The model prohibits mentioning the guaranty association in the sale or inducement to sell insurance policies. To prohibit
misuse of the protections of the system, however, the breadth of the existing provisions has caused great confusion to the
consuming public regarding the purposes and limitations of the guaranty association. That was the reason the working group
considered changes to the section. 1985 Proc. I 204.
A. When the model was originally adopted a sentence in Section 14 stated that it was an unfair trade practice to make
use of the guaranty fund protection in the sale of insurance. 1971 Proc. I 172. This was replaced with what is now Section
19A. It was the conviction of the drafters that the unfair trade practices provision was inadequate because it didn’t
specify any penalty, and in any case should properly be included in that statute instead of here. The new language proposed
was more comprehensive both as to prescribed conduct as well as permitted activity. 1976 Proc. I 312.
The last sentence of Section 19A was added in December 1993. The drafters considered two alternatives. One made the use
of guaranty fund protection in sales solicitation a violation of the general provisions of the state insurance code. The second
alternative, which was exposed in June of 1993, made such use a violation of the unfair trade practices law. 1993 Proc. 2
nd
Quarter 602, 613.

NAIC Model Laws, Regulations, Guidelines and Other Resources—October 2010
LIFE AND HEALTH INSURANCE GUARANTY ASSOCIATION MODEL ACT
Proceedings Citations
Cited to the Proceedings of the NAIC
© 2010 National Association of Insurance Commissioners PC-520-19
Section 19 (cont.)
B. The draft adopted in December 1985 contained an expanded Section 19 in an effort to deal with the recognized
problems. The model as amended contains a description of a document to deliver to policyholders which would inform them
about the availability and limitations of the guaranty fund. 1986 Proc. I 413.
C. More detail was added to the disclosure document to be prepared by the association and provided to the policyholder
prior to or at the time of delivery of the policy or contract. Subsection C(3) and C(6) were new in 1993 and Subsection C(7)
was amplified to specify that certain financial information could be included. 1993 Proc. 2
nd
Quarter 613.
The amendment was adopted by the working group without further comment in September 1993. 1993 Proc. 3
rd
Quarter
350, 352.
D. Subsection D was added to the model in 1995 without specific comment. It required that the insurer or agent give
the policyholder or contract owner a separate written notice, prior to or at the time of delivery, that clearly and conspicuously
disclosed that the policy or contract was not covered by the guaranty association, if that was the case. 1986 Proc. I 321.
When model amendments were being considered in 1996, one regulator said he saw this provision as problematic because it
requires one of two separate notices to be delivered to policyholders and requires the insurer to determine if a product is
covered by the guaranty association. He suggested that Section 19 be redrafted to require one general notice that would
provide policyholders with general information about guaranty fund coverage and exclusions. 1996 Proc. 3
rd
Quarter 839.
The proposed amendment eliminated the requirement that insurers deliver a separate notice to policyholders if the policy in
question is not subject to guaranty association coverage. As amended, Section 19 provides for a single form of notice
alerting the consumer to the existence of the guaranty association, but not stating whether the policy in question is covered or
not covered. An interested party spoke in opposition to the amendment, saying insurers should be required to determine
whether or not a contract is covered to insure that premiums are correctly reported for purposes of calculating assessments.
1996 Proc. 4
th
Quarter 984.
Some insurance industry representatives expressed concern about the amendment to Subsection D to require insurers to retain
evidence of delivery of the required disclosure form. The working group discussed the issue and agreed that the requirement
was not onerous and could be satisfied easily, either by paper or electronic records. The working group considered the
recommendation for a specific penalty for failure to deliver the required disclosure form, but decided to delete the sentence so
the penalty was the same as for any general violation of the insurance code. A comment was added to point out ways to
demonstrate compliance. 1996 Proc. 4
th
Quarter 981, 985.
Section 20. Prospective Application
This section was not in the original model, but was part of a package of suggestions from an industry association adopted in
the extensive revisions of 1985. 1986 Proc. I 322.
Appendix. Alternative Provisions
When the NAIC adopted a suggestion to make guaranty coverage for unallocated annuities optional (see discussion under
Section 3B), the appendix was added to show how the existing model could be altered to exclude unallocated annuities. 1998
Proc. 1
st
Quarter 609-616.

NAIC Model Laws, Regulations, Guidelines and Other Resources—October 2010
LIFE AND HEALTH INSURANCE GUARANTY ASSOCIATION MODEL ACT
Proceedings Citations
Cited to the Proceedings of the NAIC
PC-520-20 © 2010 National Association of Insurance Commissioners
_______________________________
Chronological Summary of Actions
December 1970: Adopted model.
December 1975: Technical amendments made, added section providing for tax offset.
June 1977: Clarified that tax offset is optional.
December 1985: Completely revised model to make applicable to residents only in most cases, to set out more extensively the limits of liability for covered
claims, and to create a four-account approach. It was decided to include unallocated annuities in the guaranty fund protection. The section on advertising
of guaranty funds protection was substantially revised, and Section 20 added.
June 1987: Decertification of four-account approach.
December 1987: Amended to create two accounts with subaccounts. Clarified treatment of Section 403(b) plans and set $5 million limit in benefits from
unallocated annuity contract. Set limits on type of unallocated annuities covered.
September 1993: Adopted amendment to Section 7 to provide for public representatives on the guaranty fund board.
December 1993: Amended Section 3 to clarify the limitation in regard to structured settlements and to exclude coverage for any policy where assessments
are preempted by federal or state law. Amended Section 19 to make use of guaranty coverage in sales solicitations an unfair trade practice.
June 1995: Amended Section 6 to provide for the assessment of governmental retirement plans under the annuity subaccount.
December 1995: Amended Section 3C to increase cap on coverage for health and disability insurance.
June 1997: Made amendments throughout model to update language and eliminate unnecessary comments.
March 1998: Revised Section 3 and 8 relative to structured settlements.
June 1998: Added drafting note to Section 3 suggesting coverage of unallocated annuities is a decision to be made by each state. Added appendix to show
how to revise the model if coverage is not included.
June 1999: Amended Section 5L to exclude charitable gift annuities from guaranty fund coverage.
October 1999: Amended Sections 3 and 8 to address issues related to equity-indexed products.
January 2009: Adopted amendments to clarify and update the model.
