Patient Experience Journal Patient Experience Journal
Volume 8 Issue 3 Article 12
2021
The effect of service excellence training: Examining providers' The effect of service excellence training: Examining providers'
patient experience scores patient experience scores
Katelyn J. Cavanaugh
UT MD Anderson Cancer Center
Monica A. Johnson
UT MD Anderson Cancer Center
Courtney L. Holladay
UT MD Anderson Cancer Center
Follow this and additional works at: https://pxjournal.org/journal
Part of the Medicine and Health Sciences Commons, and the Training and Development Commons
Recommended Citation Recommended Citation
Cavanaugh KJ, Johnson MA, Holladay CL. The effect of service excellence training: Examining providers'
patient experience scores.
Patient Experience Journal
. 2021; 8(3):109-116. doi: 10.35680/
2372-0247.1564.
This Research is brought to you for free and open access by Patient Experience Journal. It has been accepted for
inclusion in Patient Experience Journal by an authorized editor of Patient Experience Journal.

The effect of service excellence training: Examining providers' patient experience The effect of service excellence training: Examining providers' patient experience
scores scores
Cover Page Footnote Cover Page Footnote
We would like to acknowledge Elizabeth Garcia and Dr. Randal Weber for reviewing this paper. This article
is associated with the Policy & Measurement lens of The Beryl Institute Experience Framework
(https://www.theberylinstitute.org/ExperienceFramework). You can access other resources related to this
lens including additional PXJ articles here: http://bit.ly/PX_PolicyMeasure
This research is available in Patient Experience Journal: https://pxjournal.org/journal/vol8/iss3/12
Patient Experience Journal
Volume 8, Issue 3 – 2021, pp. 109-116
Patient Experience Journal, Volume 8, Issue 3
© The Author(s), 2021. Published in association with The Beryl Institute.
Downloaded from www.pxjournal.org 109
Research
The effect of service excellence training: Examining providers' patient
experience scores
Katelyn J. Cavanaugh, UT MD Anderson Cancer Center, kjcavanaugh@mdanderson.org
Monica A. Johnson, UT MD Anderson Cancer Center, MAJohnson@mdanderson.org
Courtney L. Holladay, UT MD Anderson Cancer Center, clhollada[email protected]
Abstract
Previous research and applied work has shown that communication-based training has the potential to impact important
outcomes for healthcare organizations. Our institution developed and deployed Service Excellence, a communications-
focused training, in our large academic cancer-focused healthcare system. In this study, we investigated whether patient
experience improved for those with care providers who completed Service Excellence, as measured by Press Ganey
Provider Experience surveys, and whether the effect of Service Excellence training depends on employee engagement.
Results indicated that participating in Service Excellence training positively impacts perceptions of patient experience,
and that the impact of the training is stronger for providers with low engagement as compared to providers with high
engagement. Findings suggest that communications-based training can be an effective mitigation strategy to assist even
those low engaged physicians with displaying the expected behaviors for positive patient interactions. Implications for
healthcare organizations are discussed, including the rationale for motivating providers to attend such training.
Keywords
Engagement, patient experience, patient-centered, provider communication, communication skills, Press Ganey
Introduction
Communication is the thread that pulls healthcare
providers together with their colleagues and patients. As
Gallup identified, employees want to make these
connections within their work environment. However, the
quality of these relationships and the communication
occurring within them can lack substance and purpose.
1
Training has been acknowledged for decades as an
effective and necessary tool for building communication
skills
2
within the medical community.
3,4
Communication is especially important and complex within
the healthcare environment. The National Cancer Institute
identifies the emotions, including denial, fear, and anger,
that can surface when patients are diagnosed with cancer.
5
Providers’ capability to communicate responsively and
empathetically toward patients is critical in this context.
Furthermore, providers’ ability to communicate directly
impacts patient safety. Some organizations have created
training to increase providers’ communication skills and
positively impact safety and the patient experience. For
example, TeamSTEPPS (Strategies and Tools to Enhance
Performance and Patient Safety) is a set of evidence-based
teamwork tools specifically developed as an approach to
increase patient safety as part of the patient experience.
The tools focus on leadership and communication among
team members.
6
The Centers for Medicare and Medicaid Services (CMS)
requires that physicians report patient experience scores in
the Hospital Consumer Assessment of Healthcare
Providers and Systems (HCAHPS) for inpatient care and
in the Clinician and Group Consumer Assessment of
Healthcare Providers and Systems (CGCAHPS) for
outpatient care. A major driver of these scores is provider
communication. Both providers and hospitals have turned
to methods to increase these skills with an eye toward
impacting the patient experience. As one example, the
Cleveland Clinic implemented their REDE model
(Relationship Establishment, Development, and
Engagement) which focuses on improving the patient
experience through patient-physician communication
7
.
Other organizations have shown communications training
can have a positive impact on providers’ skill
demonstration. What is less clear is whether there are
boundary conditions for communications training
effectiveness. The purpose of this investigation is to
describe a communications-based training program and
report the results of our investigation into the potential
impact of this training on the patient experience.

Service excellence training and the patient experience, Cavanaugh et al.
110 Patient Experience Journal, Volume 8, Issue 3 – 2021
Service Excellence Program Purpose and
Development
Our organization, a cancer-focused academic healthcare
institution, developed a Service Excellence program to
provide employees with communication strategies and
decision-making tools to deliver an excellent experience to
patients. The content was based on research of best
practices, such as the service standard strategies of the
Disney Institute and findings published by Press Ganey in
the healthcare industry.
8,9
To customize the content to our
organization, we held workshops with more than 100 staff
and faculty to discuss stakeholder groups – their needs,
wants, stereotypes, and emotions – and to establish the
Service Standards needed in our organization. The service
standards and preliminary training content were evaluated
by a cross-sectional group of institutional leaders and
piloted within one division prior to organization-wide
implementation. The Service Standards identified were: 1.
Safety, 2. Courtesy, 3. Accountability, 4. Efficiency and 5.
Innovation. They are prioritized in that order in instances
when employees need to make a service decision.
Employees should deliver on all service standards in every
interaction when possible, however, employees know
which standard takes priority if a choice must be made.
Figure 1 contains our Service Standards and their full
definitions.
Service Excellence Training Program
The curriculum is modular in nature to address the
multiple components of Service Excellence. The online
prerequisite showcases leaders from across the institution
voicing their support for a culture in which “we care while
we provide care.” The remaining six hours of training are
divided into two-hour sequential modules of experiential
learning, each containing both discussion and hands-on
activities. Module 1 evokes discussions around the
importance of engagement and walks through the service
standards. Module 2 focuses on communication tools to
enhance the patient experience and to enable
empowerment among employees. Module 3 encourages
employees to anticipate the needs of their stakeholders and
provides the tools for Service Recovery when expectations
are not met (see Table 1 for summary). The three modules
are designed for a facilitator and co-facilitator to lead the
sessions. This format allows for a wide variety of examples
to be shared with employees, helping them to connect to
the content and understand how to apply it in their roles.
Both facilitator roles participate in at least three hours of
train-the-trainer training prior to leading the sessions.
Our Study
We recognized that committing to the patient experience
through Service Excellence means committing to building
relationships in an environment of open communication.
One available method to measure our success of this
commitment is the Press Ganey survey, which measures
patient perceptions of their interactions with our care
providers.
10
Press Ganey is a company external to our
institution that develops and distributes patient satisfaction
surveys for the majority of US hospitals.
11
Patients
automatically receive and complete the Press Ganey survey
after their appointments. One portion of this survey asks
patients to rate their interaction with their care provider on
five dimensions.
12
We also recognize that important individual factors may
affect care providers’ ability to enact what they have
Figure 1. Service Excellence Standards
Service excellence training and the patient experience, Cavanaugh et al.
Patient Experience Journal, Volume 8, Issue 3 – 2021 111
learned in Service Excellence training. One factor that has
been shown to influence interactions and relationships,
including those between providers and patients, is
employee engagement.
13,14
Employee engagement has been
defined as “involvement and satisfaction with as well as
enthusiasm for work”.
15
We measure employee
engagement through our biennial employee engagement
survey which invites all employees to complete a
confidential online survey to gather their perspectives on
their work environment.
The purpose of this study was two-fold. First, we wanted
to investigate whether completing Service Excellence
training influences patients’ experiences with their
providers. To do so, we compared the Press Ganey Patient
Experience scores of our providers prior to and post
training. Second, we wanted to investigate whether the
impact of the training depends on the engagement levels
of the participating providers. Specifically, we sought to
identify the influence of Service Excellence training on
Press Ganey scores at different levels of provider
engagement. By doing so, we provide evidence to
determine whether communications training such as
Service Excellence (i.e., providing communication tools
and establishing cultural expectations) can help providers’
develop skills to better connect with their patients during
their interactions.
Method
Participants
Participants included 360 providers at a cancer-focused
academic research institution. Demographics including
provider type, gender, and ethnicity can be found in Table
2.
Measures
Service Excellence Course Completion.
During a two-
year time period from March 2017 through February 2019,
109 providers completed Service Excellence training.
During that same period, there were 251 providers that did
not complete Service Excellence.
Engagement
. All providers completed the biennial online
engagement survey sent to all employees in the institution
in February 2019. Three engagement items comprised the
mean composite engagement score; these items were
created specifically for this engagement survey by an
external consulting company for benchmarking purposes.
Responses were indicated on a 5-point Likert scale ranging
from 1 (Strongly Disagree) to 5 (Strongly Agree). Thus, higher
scores indicate higher engagement (i.e., more positive
attitudes towards employees’ jobs and the organization).
The full text items, along with descriptive statistics for the
participants’ responses, can be found in Table 3. Together,
the items exhibited acceptable internal consistency
reliability (Cronbach’s α = 0.87).
Press Ganey Scores
. Five items from the Care Provider
section of the Press Ganey survey comprised the mean
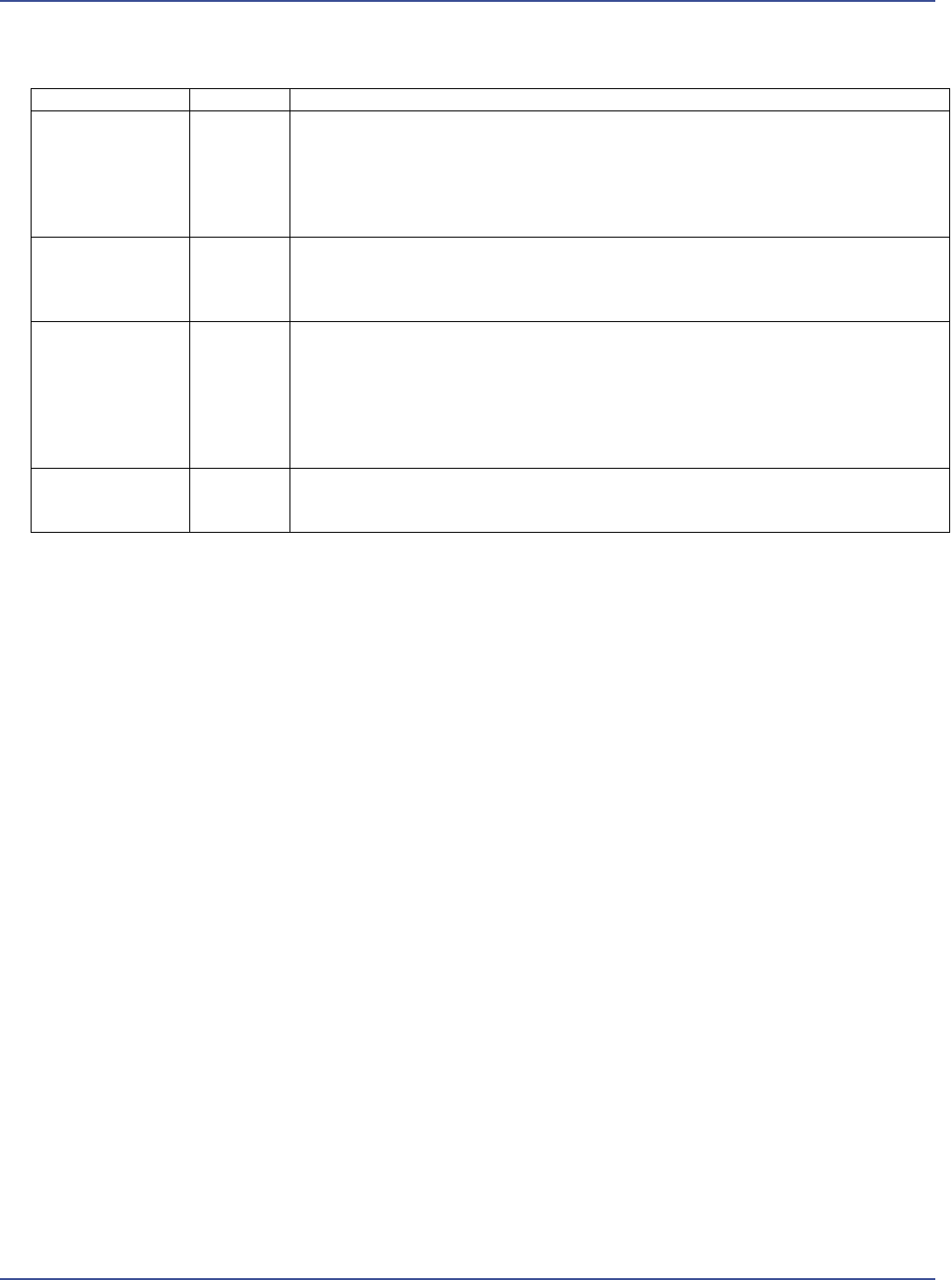
Table 1. Service Excellence Curriculum Overview
Course
Timing
Topics
Online
Prerequisite
45 minutes
History – Create an emotional connection to our organization’s purpose and how each
employee fits into our institution and its history
The Why – Understand why patients, caregivers, and colleagues choose to come to our
institution and the choice they have among competitors
Service Foundations – Recognize the Service Standards as a tool to empower each
employee to deliver on Service Excellence
Module 1
2 hours
Engagement – Create awareness of how engagement can impact the environment and
interactions with stakeholders
Service Standards – Establish the standards of service and use them as a decision-making
tool
Module 2
2 hours
Communication – Increase awareness of the need to convey feelings and rationale when
motivating others, and use communication tools, such as AIDET (Acknowledge,
Introduce, Duration, Explanation, and Thank You), to improve interactions
Patient Experience – Understand the patient perspective and how direct and indirect
patient-facing positions affect the patient experience
Empowerment – Define the boundaries to allow each employee to deliver on their role
with purpose
Module 3
2 hours
Anticipating Needs – Promote behaviors that create moments of hope for stakeholders
Service Recovery – Build stakeholder loyalty and trust when service is less than what is
set by standards
Service excellence training and the patient experience, Cavanaugh et al.
112 Patient Experience Journal, Volume 8, Issue 3 – 2021
composite scores for patient experience. These items were
selected because they most directly asked patients about
their interaction with their care provider. Previous research
evaluating the psychometric properties of Press Ganey
items have found “acceptable” levels of internal
consistency reliability, factor structure, and convergent and
discriminant validity.
16
The Press Ganey surveys were
completed by patients during two time periods; pre Service
Excellence from December 2016-February 2017 (n =
15,002 patient respondents, with an average of 34
respondents per provider) and post Service Excellence
from March-May 2019 (n = 13,717 patient respondents,
with an average of 33 respondents per provider). Year-
over-year, the average patient response rate to the surveys
is 20%, and the response rate is mirrored within gender
and ethnic subpopulations, ranging from 15-20% response
rates year-over-year.
Patients rated their provider on a 5-point Likert scale
ranging from 1 (Very Poor) to 5 (Very Good), in which
higher scores indicate more positive perceptions of patient
experience. Press Ganey automatically converts all
responses to a score ranging from 0 to 100 in increments
of 25 because “most people find it easier to interpret
scores from 0-100.”
12
This is an automatic conversion and
the raw responses are not available at the individual level;
thus, Press Ganey item responses are reported on the 0-
100 scale, although the response scale is not continuous.
Together, the items exhibited acceptable internal
consistency reliability (Cronbach’s α for 2017 = 0.95;
Cronbach’s α for 2019 = 0.87). Full items and descriptive
statistics can be found in Table 4.
IRB approval was received for the analysis of these data
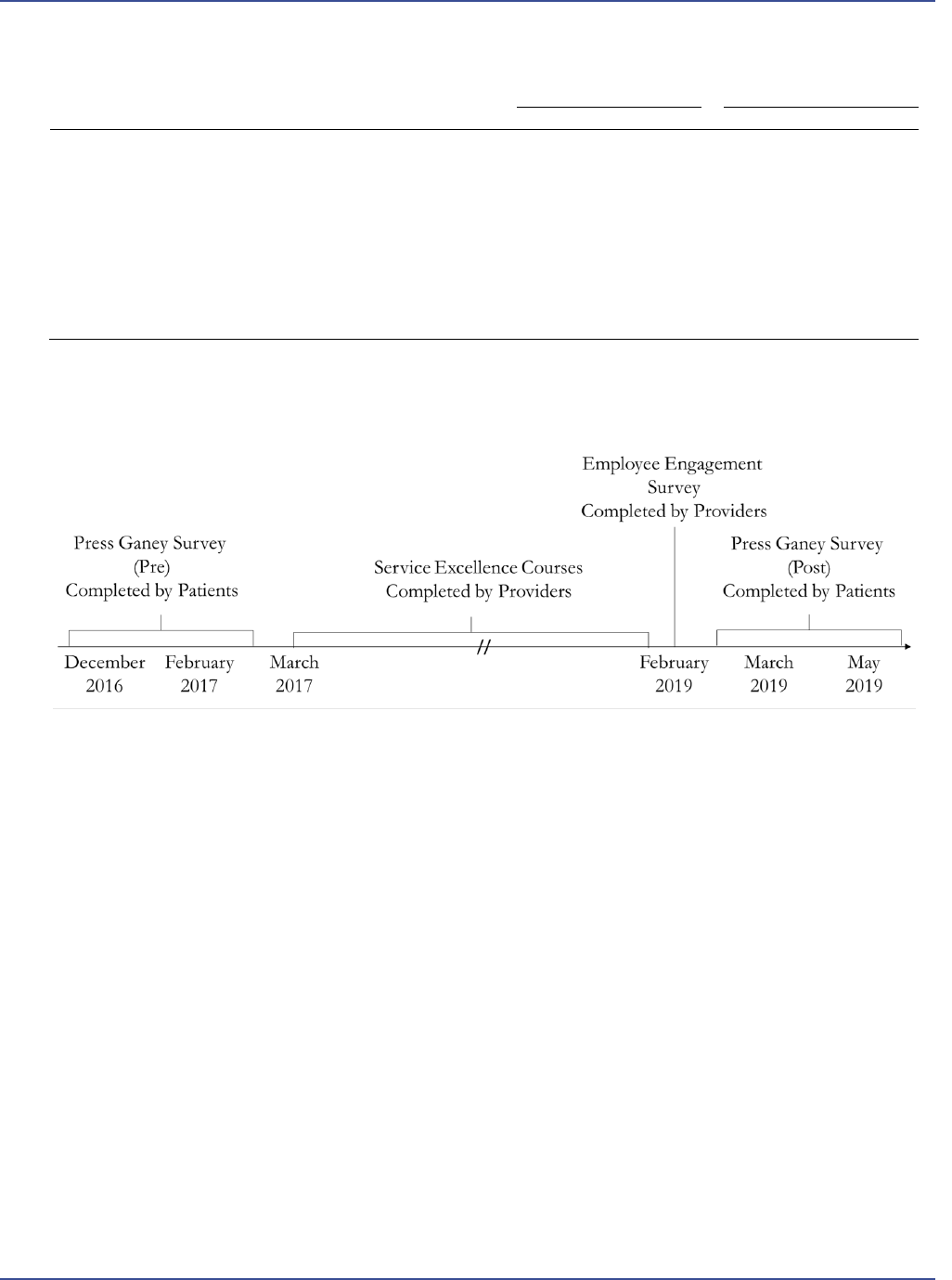
(IRB Protocol number # 2020-1323). Figure 2 depicts the
timing of the Service Excellence training, the employee
engagement survey, and Press Ganey survey completion.
Data Analysis
The engagement composite appeared bimodal based on
visual inspection of the data, indicating the existence of
two groups of providers based on their responses to
engagement items. Thus, engagement was split into two
groups; 142 providers with low engagement (ranging from
1.33 to 4.00) and 141 providers with high engagement
(ranging from 4.33 to 5.00).
In order to investigate the effects of Service Excellence
training, as well as the role of engagement, two ANOVA
models were conducted. First, a Repeated Measures
ANOVA was conducted to investigate the effects of
Service Excellence training on Press Ganey Care Provider
Table 2. Participant Demographic Characteristics
N
%
Provider Type
Doctor of Medicine (MD)
290
80.6
Advanced Practice Registered Nurse (APRN)
47
13.1
Certified Physician Assistant (PA-C)
14
3.9
Doctor of Osteopathic Medicine (DO)
1
0.3
Gender
Male
185
51.4
Female
175
48.6
Ethnicity
Caucasian
210
58.3
Asian
96
26.7
Hispanic
27
7.5
African American
21
5.8
Two or more races
3
0.8
Native American
2
0.6
Pacific Islander
1
0.3
Table 3. Descriptive Statistics for Employee Engagement Items
Item
N
Mean
SD
1. My job provides me with a sense of personal accomplishment
283
4.35
0.69
2. I feel like I really belong in this institution
283
4.06
0.91
3. I would recommend [this institution] to others as a great place
to work
283
4.15
0.83
Service excellence training and the patient experience, Cavanaugh et al.
Patient Experience Journal, Volume 8, Issue 3 – 2021 113
scores in 2017 and 2019. Second, a two-way ANOVA was
conducted to investigate the effects of engagement and
Service Excellence training on 2019 Press Ganey Care
Provider scores. We had no theoretical reason to believe
that sociodemographic factors would impact these
relationships, thus no specific hypotheses were made
regarding the effects of group membership (provider type,
gender, and ethnicity). However, we tested for the
presence of effects by adding three dichotomous
covariates to the analyses. Dichotomous variables were
used due to sample size constraints (M.D. provider type
versus all others, male versus female, and Caucasian
ethnicity versus all others).
Results
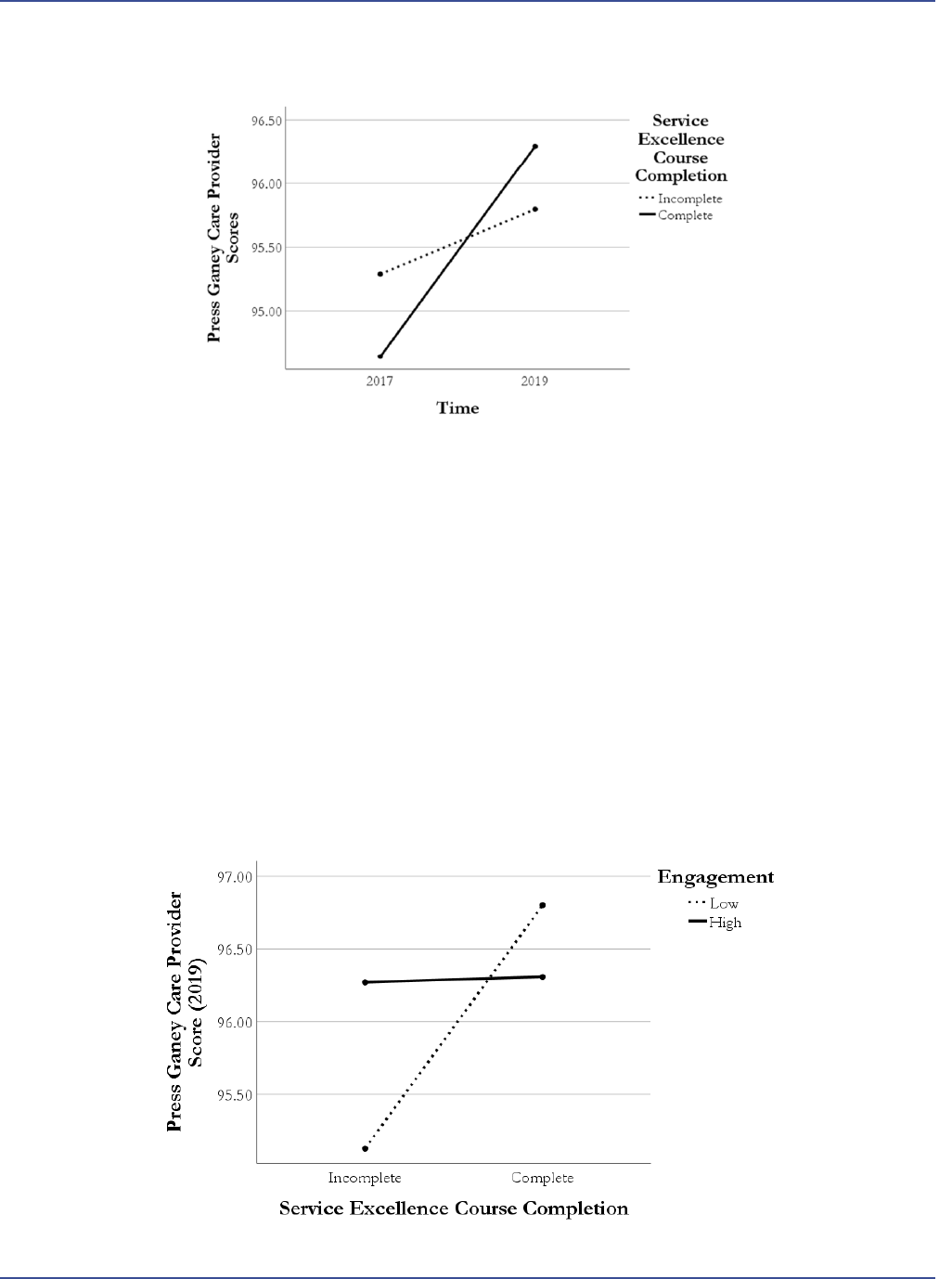
2017-2019 Press Ganey Care Provider Scores
Holding Service Excellence constant, ANOVA results
revealed that providers received higher Press Ganey Care
Provider scores in 2019 than in 2017. This difference was
statistically significant, F(1, 177.038) = 16.28, p < 0.001,
partial η
2
= 0.044. The interaction between time and
Service Excellence training was statistically significant,
indicating that providers who completed Service
Excellence training increased Press Ganey scores to a
greater extent than those who did not, F(1, 49.673) = 4.57,
p = 0.033, partial η
2
= 0.013. A graph of these effects can
be found in Figure 3. No sociodemographic factors were
statistically significant and were removed from the analyses
reported here for ease of interpretation.
2019 Press Ganey Care Provider Scores
The ANOVA revealed that the main effect of engagement
was not significant, F(1, 279) = 0.63, p = 0.428, partial η
2
= 0.002, but the main effect of Service Excellence training
was statistically significant F(1, 279) = 4.37, p = 0.037,
partial η
2
= 0.015. The interaction between engagement
and training was statistically significant, indicating that the
effect of Service Excellence on Press Ganey Care Provider
scores depends upon the level of employee engagement,
F(1, 279) = 4.01, p = 0.046, partial η
2
= 0.014.
For low engagement employees, the simple effect of
Service Excellence indicated that Press Ganey Care
provider scores were significantly higher for those that
completed training, F(1, 279) = 5.89, p = 0.016, partial η
2
= 0.021. For high engagement employees, the simple
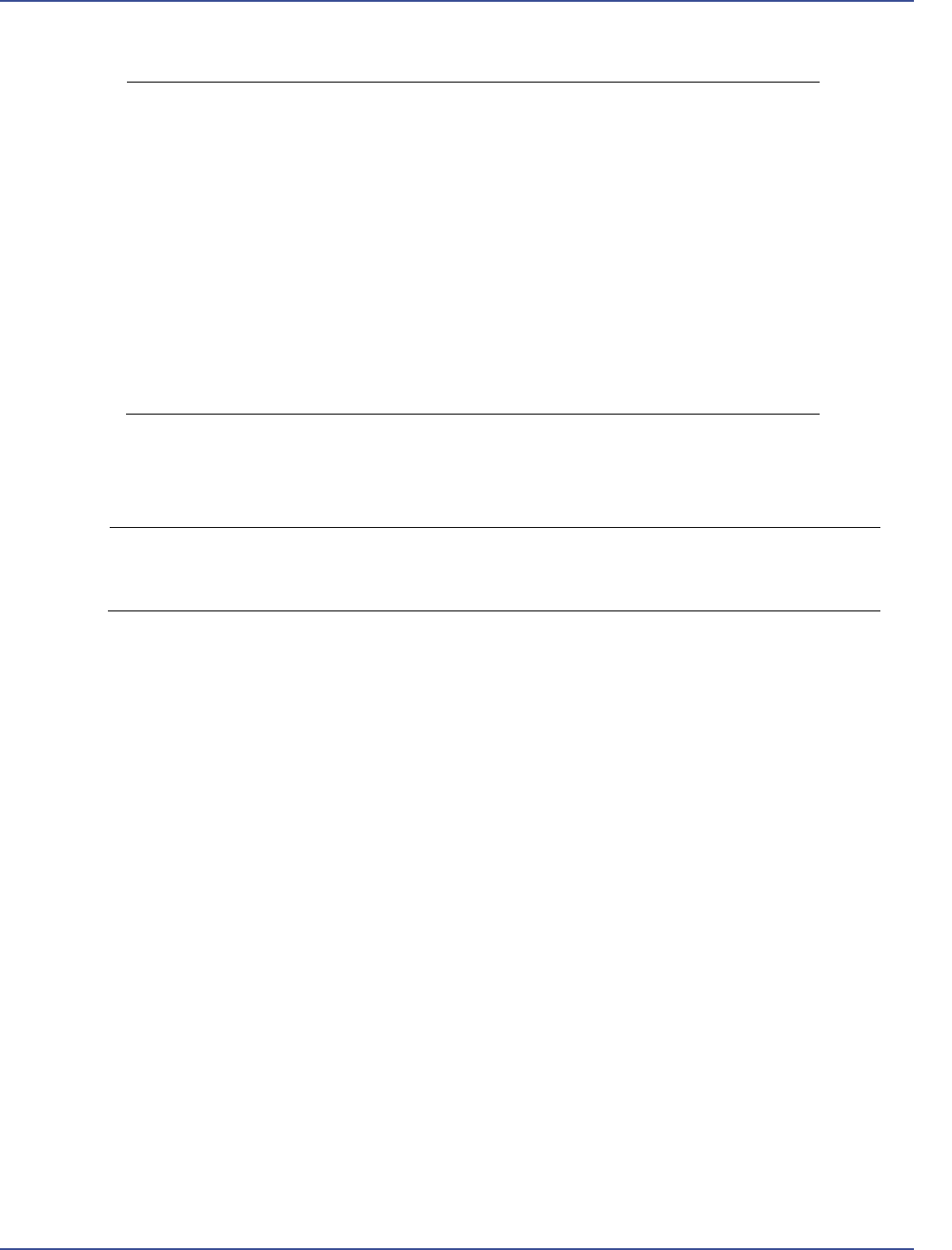
Table 4. Descriptive Statistics for 2017 and 2019 Care Provider Press Ganey Items
2017 (pre)
2019 (post)
Item
N
Mean
SD
N
Mean
SD
1. Concern the care provider showed for your
questions or worries
360
95.19
5.48
360
96.21
3.50
2. Explanations the care provider gave you about your
problem or condition
360
95.44
4.47
360
95.96
3.85
3. Care provider’s efforts to include you in decisions
about your care
360
94.80
4.85
360
95.99
3.57
4. Likelihood of your recommending this care provider
to others
360
95.35
5.80
360
96.18
4.32
5. Extent to which your care provider talked with you
about your pain (if any)
358
94.71
5.04
356
95.35
4.23
Figure 2. Timeline of Press Ganey survey, Service Excellence courses, and Employee Engagement Survey
Service excellence training and the patient experience, Cavanaugh et al.
114 Patient Experience Journal, Volume 8, Issue 3 – 2021
effect of Service Excellence indicated Press Ganey Care
Provider scores was also higher for those that completed
training, though the effect was much weaker, F(1, 279) =
0.55, p = 0.461, partial η
2
= 0.002. Together, these results
indicate that Press Ganey Care Provider scores were
greater for providers that completed Service Excellence
training, and the effect of the training was stronger for low
engagement providers. A graph of these simple effects can
be found in Figure 4. No sociodemographic factors were
statistically significant and were removed from the analyses
reported here for ease of interpretation.
Discussion
Our results showed that providers who completed Service
Excellence training showed a greater improvement over
time in their patient experience scores compared to those
providers who did not complete the training. This finding
helps to establish the efficacy of training as an intervention
to support providers in growing in their communication
skills.
Employee engagement has been touted and repeatedly
reported to be related to patient experience; organizations
with lower employee engagement scores tend to have
lower patient satisfaction.
17, 18
Our results show that
Figure 4. Simple Effects of Service Excellence Training and Engagement on Press Ganey Care Provider Scores
Figure 3. 2017-2019 Press Ganey Care Provider Scores by Service Excellence Training

Service excellence training and the patient experience, Cavanaugh et al.
Patient Experience Journal, Volume 8, Issue 3 – 2021 115
training can potentially have a mitigating effect, such that
providers with low engagement are better able to increase
their patient experience scores following completion of
training. This finding shows that providers can learn new
communication skills and improve their interactions with
patients, and that training may be especially impactful for
providers or organizations with lower levels of
engagement.
The finding further shows that training can be an effective
intervention for organizations seeking to counter the
effects that low engagement can have. Those who are
already actively engaged may already behave in ways that
are aligned with a service culture. Those with low
engagement may benefit from communications training by
applying their new skills, awareness, and tools to foster
more effective and positive communication with their
patients. While this result may appear counterintuitive, the
effect could be due to contrasting behavior, where the
same behavior appears as marked improvement based on
comparison.
19
Patients could be perceiving the interactions
with less engaged physicians following training more
favorably when contextualizing them against their prior
interactions. Overall, this tie to engagement aligns with
recent efforts proposed to improve burnout by focusing
on communication and relationships
20,21
and provides
initial evidence showing the positive effects these efforts
can have on the patient experience.
Implications
Research shows that patients are likely to recommend or
not recommend care providers to others based on their
experiences; in fact, they are more likely to share their
negative reviews.
22
A positive patient experience is
necessary for organizations to not only do the right thing
but also stay competitive with their peer organizations.
Patient experience scores are becoming increasingly
transparent and are being used for decision-making; for
example, payers can now access such scores to determine
reimbursement (e.g., the National Research Corporation
Health Transparency StarCard rating system). While this
could serve as a motivator to attend training, it could also
explain why in our own organization we saw an increase in
scores across both trained and untrained providers. That
is, providers may already have been working to improve
their patient interactions to ensure positive feedback from
patients because of its visibility and its impact on
reimbursement. Supplying providers with resources and
tools to help improve these interactions is ultimately the
responsibility of organizations. These reasons together
provide healthcare organizations with the rationale to
support such training.
Finally, we want to note that less engaged providers are
more likely to cite time away from patient care as a reason
to not attend training, and in fact, time is a precious
resource in their patient interactions.
23
Our findings
provide evidence for rationale at the individual provider
level; training could help improve provider-patient
interactions and improve the quality of provider time
spent with patients. Showing providers the results other
providers achieved following training could serve to
minimize resistance, even from low engaged providers.
Limitations and Future Research Directions
The study described here took place within a single
organization. Future research could explore these same
effects across organizations and across different healthcare
providers to ensure the generalizability. While the findings
show promise for the impact of training on providers’
behaviors in their interactions with patients, more research
is needed to unpack the effects of communication-focused
training on provider behaviors and patient outcomes.
Specifically, research is needed to identify which aspects of
the training are most effective in transferring to patient
interactions and what organizations can do to support
providers in transferring their training to patient
interactions. Additionally, the effects we found on Press
Ganey scores were small. However, given the many factors
that contribute to these scores, even small effects are quite
notable. Examining more detailed information about
provider training beyond completion or participation (e.g.,
knowledge gained or engagement in the training program)
may provide deeper insights into the effects of training.
Conclusion
Healthcare is an especially important setting in which
effective communication facilitates relationships and leads
to a better patient experience. With training, providers may
raise their awareness and skills to positively impact how
they build relationships through more effective
communication, and this impact can be observed for less
engaged providers. The results presented here provide
much-needed evidence that providers can apply what they
learn in training to positively impact the patient
experience.
Acknowledgement
The authors would like to acknowledge Elizabeth Garcia
and Dr. Randal Weber for reviewing this paper.
References
1. State of the American Workplace Report. Gallup,
2017. Retrieved July 07, 2021 from
https://www.gallup.com/workplace/238085/state-
american-workplace-report-2017.aspx
2. Nestel D, Woodward-Kron R, Keating JL. Learning
outcomes for communication skills across the health

Service excellence training and the patient experience, Cavanaugh et al.
116 Patient Experience Journal, Volume 8, Issue 3 – 2021
professions: a systematic literature review and
qualitative synthesis. BMJ Open. 2017;7:e014570.
doi:10.1136/bmjopen-2016-014570
3. O’Keefe M, Henderson A, Pitt R. Health, medicine
and veterinary science: Learning and teaching
academic standards statement. New South Wales,
Australia: Australian Government Department of
Education, Employment and Workplace Relations,
2011.
4. CanMEDS Physician Competency Framework—
Communicator. Royal College of Physicians and
Surgeons of Canada, 2015.
http://www.royalcollege.ca/portal/page/portal/rc/ca
nmeds/framework/communicator
5. National Cancer Institute. Feelings and Cancer.
Published 2018. Retrieved July 07. 2021 from
https://www.cancer.gov/about-
cancer/coping/feelings
6. Agency for Healthcare Research and
Quality. TeamSTEPPS: National Implementation.
2013 http://teamstepps.ahrq.gov/about-2cl_3.htm.
7. Windover AK, Boissy A, Rice TW, Gilligan T, Velez
VJ, Merlino J. The REDE model of healthcare
communication: optimizing relationship as a
therapeutic agent. Journal of patient experience.
2014;1(1):8-13.
8. Press Ganey. Will Your Patients Return? The
Foundation for Success. Published 2017. Retrieved
July 7. 2021 from
https://helpandtraining.pressganey.com/Documents
_secure/Medical%20Practices/White%20Papers/med
ical-practice_4.pdf
9. Jones B. How Disney Empowers Its Employees to
Deliver Exceptional Customer Service. Harvard
Business Review; 2018. Retrieved July 7, 2021 from
https://hbr.org/sponsored/2018/02/how-disney-
empowers-its-employees-to-deliver-exceptional-
customer-service
10. Press Ganey. Hospital Consumer Assessment of
Healthcare Providers and Systems. Published 2015.
Retrieved December 09, 2020
from https://www.pressganey.com/resources/progr
am-summary/hospital-consumer-assessment-of-
healthcare-providers-and-systems
11. Graham B, Green A, James M, Katz J, Swiontkowski
M. Measuring Patient Satisfaction in Orthopaedic
Surgery. The Journal of Bone and Joint Surgery. 2015;97(1):
80-84. doi: 10.2106/JBJS.N.00811.
12. Press Ganey. Guide to Interpreting. Published 2014.
Retrieved July 7, 2021 from
https://helpandtraining.pressganey.com/lib-
docs/default-source/ip-training-resources/guide-to-
interpreting---part-2.pdf?sfvrsn=2
13. Khan A, Spector ND, Baird JD, Ashland
M, Starmer AJ, Rosenbluth G, et al. Patient safety
after implementation of a coproduced family centered
communication programme: multicenter before and
after intervention study. BMJ 2018;5;363:k4764. doi:
10.1136/bmj.k4764
14. Heath S. Employee Engagement Tied to Higher
Patient Satisfaction Levels. Published 2019. Retrieved
December 12, 2020
from https://patientengagementhit.com/news/emplo
yee-engagement-tied-to-higher-patient-satisfaction-
levels
15. Harter JK, Schmidt FL, Hayes TL. Business-unit-level
relationship between employee satisfaction, employee
engagement, and business outcomes: a meta-analysis.
Journal of Applied Psychology. 2002;87(2); 268-279. doi:
10.1037/0021-9010.87.2.268
16. Presson AP, Zhang C, Abtahi AM, Kean J, Hung M,
Tyser AR. Psychometric properties of the Press
Ganey® Outpatient Medical Practice Survey. Health
Qual Life Outcomes. 2017;15(1):32. doi:10.1186/s12955-
017-0610-3
17. Buhlman NW, Lee TH. When Patient Experience and
Employee Engagement Both Improve, Hospitals’
Ratings and Profits Climb. Harvard Business Review,
2019. Retrieved December 12, 2020, from
https://hbr.org/2019/05/when-patient-experience-
and-employee-engagement-both-improve-hospitals-
ratings-and-profits-climb
18. Heath S. Employee Engagement Tied to Higher
Patient Satisfaction Levels. Published 2019. Retrieved
December 12, 2020,
from https://patientengagementhit.com/news/emplo
yee-engagement-tied-to-higher-patient-satisfaction-
levels
19. Sumer, H C & Knight, P A. Assimilation and contrast
effects in performance ratings: Effects of rating the
previous performance on rating subsequent
performance. Journal of Applied Psychology, 1996; 81.4:
436.
20. Maslach C, Leiter MP. New insights into burnout and
health care: Strategies for improving civility and
alleviating burnout. Med Teach. 2017;39(2):160-163.
doi: 10.1080/0142159X.2016.1248918
21. Parks T. Cleveland Clinic’s approach to burnout
focuses on relationships. AMA. 2016. Retrieved July
07, 2021 from https://www.ama-assn.org/delivering-
care/patient-support-advocacy/cleveland-clinic-s-
approach-burnout-focuses-relationships
22. 75 Customer Service Facts, Quotes & Statistics.
Retrieved December 12, 2020 from
https://www.helpscout.com/75-customer-service-
facts-quotes-statistics/
23. Dugdale DC, Epstein R, Pantilat SZ. Time and the
patient-physician relationship. J Gen Intern Med.
1999;14 Suppl 1(Suppl 1):S34-S40.
doi:10.1046/j.1525-1497.1999.00263.x
