
Information Note
Malaria
Allocation Period 2023-2025
Date published: 29 July 2022
Date updated: 2 December 2022
Page 1 of 34
Table of Contents
Introduction 2
Investment Approach 3
Prioritized Interventions to be Funded by the Global Fund 6
1. Evidence-based decision making 6
1.1. Sub-national Tailoring (SNT) of the malaria response 6
1.2. Malaria surveillance 7
2. Prevention 9
2.1. Vector control 9
2.2. Preventive therapies 15
3. Case management 18
3.1. Diagnosis 18
3.2. Treatment 19
3.3. Tailored service delivery across all sectors 21
4. Elimination 23
5. Cross-cutting Areas 24
5.1 Equity, human rights, and gender equality 24
5.2 Community leadership and engagement 25
5.3 Social and Behaviour Change (SBC) 26
5.4 Pandemic Preparedness and Response (PPR) 27
5.5 Environment and climate change 27
5.6. Urban malaria 28
5.7. Challenging Operating Environments (COE) 28
5.8 Malaria emergencies 29
5.9 Program management 29
5.10. Sustainability of malaria response 29
List of Abbreviations 31
Annex 1: Key Data 34
Page 2 of 34
Introduction
The Global Fund has developed a new Strategy for the period 2023-2028. The malaria
component of the Strategy aims to end the disease by funding the development,
implementation, and monitoring of national malaria programs that are tailored to local
contexts. It intends to ensure optimal and effective vector control coverage; make best use
of chemoprevention; expand equitable access to quality early diagnosis and treatment of
malaria; and drive towards malaria elimination and prevent the re-establishment of malaria.
This Information Note supplements the applicant guidance , provides information to prepare
a malaria funding request, makes recommendations on priority interventions and
encourages strategic investments to achieve impact. The document also adheres with and
complements normative technical guidance
1
from the World Health Organization (WHO) and
other partners.
To enable the Technical Review Panel (TRP) evaluation of the funding request within the
country-specific context, this note provides an outline of both the process and information
that are expected from applicants. Applicants are required to:
1. Hold a robust and inclusive country dialogue involving all relevant partners
engaged in the national malaria response and health system strengthening,
including communities, civil society, community-based organizations, and private
sector.
2. Ensure the program split and prioritization decisions are informed by a
comprehensive gap analysis to achieve value for money. Applicants may use the
RBM Country Regional Support Partnership Committee (CRSPC) gap analysis tool
2
to inform the Global Fund gap analysis.
3. Use WHO’s guidance on sub-national tailoring of malaria to inform the decisions
on intervention mixes and delivery strategies.
4. Include a brief overview of the national malaria response and the program
performance at national and sub-national level in the funding request. This includes
the epidemiology of malaria, relevant contextual factors, health system components,
health financing data and progress and challenges towards achievement of strategic
plan goals. Key data points should be included in the funding request (either in the
Essential Data Table or in the narrative) - for details, please see Annex 1.
1
World Health Organization Guidelines for malaria https://www.who.int/publications/i/item/guidelines-for-malaria
2
The RBM partnership CRSPC guidance note on malaria gap analysis tools
Page 3 of 34
Investment Approach
The Global Fund incorporates Program Essentials within all aspects of its investment. They
are derived from normative and technical guidance and are considered critical to meet the
Global Fund’s malaria strategy and the Global Technical Strategy (GTS) targets. Program
Essentials, which include criteria for services (Table-1) and a framework of processes,
standards and requirements that apply to pharmaceuticals and diagnostic products, should
be applied consistently for all interventions funded by the Global Fund.
Applicants are expected to consider the Program Essentials during the country dialogue,
funding request development, grant making, implementation and performance monitoring.
While not all national programs will be able to achieve every Program Essential, the funding
request should clearly demonstrate the program’s plans to achieve these standards,
progress, and challenges and how their achievement is prioritized with the available
resources. As for malaria, the Program Essentials are well aligned with the evolution of
malaria programs and may already be within the National Strategic Plans (NSPs) or other
standard documents which should be annexed as relevant.
Table 1. Malaria program essentials
Objective
Program Essentials
(a) Implement malaria interventions,
tailored to sub-national level using granular
data and capacitating decision-making and
action.
• Build in-country capacity for sub-national
tailoring and evidence-based prioritization of
tailored malaria interventions.
• Build capacity for quality data generation,
analysis & use at national and sub-national
levels.
• Ensure sub-nationally tailored planning
considers factors beyond malaria epidemiology
such as health systems, access to services,
equity, human rights, gender equality (EHRGE),
cultural, geographic, climatic, etc.
• Ensure quality of all commodities and monitor
effectiveness.
• Deliver all interventions in a timely, people-
centered manner
3
.
(b) Ensure optimal vector control coverage.
• Evidence-based prioritization for product
selection, implementation modality and timing,
and frequency of delivery with a focus on
ensuring sustained high coverage among the
highest risk populations.
• Expand entomological surveillance.
• Address barriers hampering the rapid scale-up
of new products.
• Evolve indicators to improve the tracking of
effective vector control coverage.
3
For example, in a migrant community, a community health worker from the migrant population targeted may be more appropriate;
adjusting service hours to address population/patient availability (SMC or ITN delivery early morning or in the evenings), etc.
Page 4 of 34
(c) Expand equitable access to quality,
early diagnosis, and treatment of malaria
through health facilities, at the public
sector and community level, and in the
private sector.
• Understand and address key barriers to access.
• Engage private sector providers to drive
parasitological testing before treatment.
• Expand community platforms where access is
low.
• Improve and evolve surveillance and data
collection tools and processes to enable
continuous quality improvement (CQI) and
accurate surveillance.
• Use of quality of care (QoC) stratification to
tailor support to case management across
sectors.
• Strengthening coordination and linkages
between public, private and community systems
for service provision.
(d) Optimize chemoprevention.
• Support data driven intervention selection and
implementation modality.
• Support flexibility on implementation strategies
including integration within primary healthcare
(PHC) as relevant.
(e) Drive toward elimination and facilitate
prevention of re-establishment.
• Enhance and optimize vector control and case
management.
• Increase the sensitivity and specificity of
surveillance.
• Accelerate transmission reduction.
One of the key program essentials is Sub-national Tailoring (SNT) of malaria
interventions, which is defined as the use of local data and contextual information
4
to
determine the appropriate intervention mixes, and in some cases deliver strategies for
optimum impact on transmission and burden of disease for a given area, such as a district,
health facility catchment or village. Funding requests are expected to demonstrate the use
of SNT strategies and plans where they have been conducted and/or future planning for
such efforts,
5
but also to be aligned with national priorities and normative guidance.
Applicants are strongly encouraged to prioritize interventions based on sub-national data to
the extent possible. Malaria funding requests should be strategically focused on delivering
optimal intervention mixes that are cost-effective and affordable in the context of a country's
own epidemiological, programmatic, financial, and health system contexts.
Value for money (VfM) aims to guide applicants to make sure investments maximize and
sustain equitable and quality health outputs, outcomes and impact for a given level of
resources. VfM is defined through five dimensions: economy, efficiency, effectiveness,
equity, and sustainability. For more information, please refer to the Value for Money
Technical Brief.
Grant implementation arrangements shall be bespoken on the needed capacities to
implement and coordinate the malaria interventions at sub-national level. Integrated risk
management is essential to achieve impact.
4
Contextual information includes health systems, access to service, EHRGE and climatic information,
5
At time of publication, the WHO manual on sub-national tailoring of interventions was not yet published. Please check the WHO
website for update. https://www.who.int/teams/global-malaria-programme
Page 5 of 34
Applicants are also recommended to consider the Protection from Sexual Exploitation,
Abuse and Harassment (PSEAH), as well as child protection in the planning and design of
program interventions. Program related risks of sexual exploitation, abuse and harassment
to beneficiaries, community workers and others (as relevant) need to be identified in the
proposed interventions, which should also include the necessary mitigation measures to
ensure that services are provided to, and accessed by, beneficiaries in a safe way. It is also
recommended to include PSEAH in community awareness activities like outreach
strategies, communication campaigns, trainings or other activities which target grant
beneficiaries.
Effective, integrated, quality, people-centered malaria services are dependent on functional
health system and primary health care (PHC). The required Resilient and Sustainable
Systems for Health (RSSH) interventions, including community systems strengthening,
designed to ensure achievement of malaria outcomes should be discussed during country
dialogue, and the identified priorities should be included for funding. It is critical that malaria
program managers participate in the country dialogue on RSSH investments and vice versa
to prioritize the key RSSH functions required for malaria service delivery. Key considerations
for investments in RSSH for national malaria control programs include:
1. Investments to identify and address quality gaps in key services at primary health
care level, such as quality improvement for acute febrile illness, community health
packages and antenatal care (ANC). Opportunities to integrate activities such as training,
referral networks and support supervision can be considered to improve quality and
efficiency of PHC, of which malaria is a part.
2. Investments to strengthen the health workforce, including both facility-based health
workers (public and private) and community health workers (CHWs). Applicants are
encouraged to prioritize support to workforce planning and optimize available skills mix
through improved deployment of the available personnel. This may include support to
analyses related to human resources for health (HRH), such as workload analyses;
governance and planning, such as data systems and strategic planning; and capacity for
HRH planning and management at national and/or sub-national level.
Applicants are also encouraged to develop context-specific interventions to improve
health worker performance. CHWs are an essential part of HRH and broader community
systems strengthening (CSS) and recruitment, training, supervision, and reimbursement
of CHWs could be included in any analyses, strategy, planning and performance
improvement efforts. Integrated supportive supervision or quality improvement activities
are evidence-based interventions that can be scaled up through RSSH investments
including CSS.
3. Investments to strengthen generation and use of data, strengthen national supply
chain management and improve routine primary care services.
4. Adaptations to foster people- and population-centered service delivery, including
equity, cultural and gender-relevant issues to improve access and uptake of services;
community-based service delivery; community-led monitoring; CHWs for service in
migrant/refugee/indigenous populations, where such populations are at risk of malaria.
Page 6 of 34
Prioritized Interventions to be Funded by the Global
Fund
1. Evidence-based decision making
1.1. Sub-national Tailoring (SNT) of the malaria response
A sub-national tailored response is based on the use of malaria-specific, health system,
geographic, equity, human rights, gender equality (EHRGE), climatic, political, and other
relevant data as well as intervention quality and performance data at the lowest level
possible. The aim is to provide quality, people-centered care that maximizes resources and
impact. An SNT response requires the gathering, storing and analysis of sub-national data,
the use of this data for decisions on mixes and delivery of interventions, as well as the
continual use of this information for sub-national planning. The Program Essentials outlined
in Table 1 are built around this framework: therefore, funding requests should be based on
an SNT analysis and plan and, when feasible, funding should be included to strengthen data
generation, quality, and use.
The Global Fund can support the different components needed to facilitate a sub nationally
tailored malaria response, which include:
1. Creation, maintenance, and use of malaria data repositories (MDRs) and required
staffing and equipment, in alignment with WHO guidance.
6
MDRs should draw from
routine surveillance (health management information system, surveys, etc.),
retrospective data on the malaria burden and response, as well as human resource
information, health workforce accounts, climate, commodities, etc. They should be
interoperable with existing information systems (laboratory and logistics management
information systems).
2. Introduction of additional relevant data sets into MDRs – such as geospatial mapping,
meteorologic data sets, EHRGE analyses, etc. This includes facilitation for the
required adaptations of data to align with the operational framework of a malaria
program’s MDR.
3. Mapping of sub-national Continuous Quality Improvement (CQI) activities and results
to address quality issues in a targeted and timely manner.
4. Addressing data gaps such as understanding barriers to access, in order to adapt
intervention choice and implementation methodology.
5. Short- and long-term capacity building of national and district malaria programs to
use available data to develop (and update) sub- nationally tailored strategies and
plans (including the associated modelling) with the vision of programs being able to
conduct these exercises independently.
6
WHO guidance for evidence-informed decision-making
Page 7 of 34
1.2. Malaria surveillance
Malaria surveillance is a key intervention in all malaria-endemic countries. It is especially
important in areas approaching elimination or those which have eliminated malaria. A
malaria surveillance system comprises the people, procedures, tools, structures, and
processes necessary to gather and interpret information on when, where and at what level
malaria cases are occurring. An effective national surveillance system allows programs to
monitor and evaluate interventions and to make sub-national tailored, prioritized decisions
on investments.
Malaria programs need to work towards robust surveillance systems and build monitoring
and evaluation (M&E) staff capabilities to: (a) Identify sub-national areas and population
groups most affected by malaria; (b) Assess quality and effectiveness of necessary
interventions through a holistic review of surveillance information with sufficient granularity
to guide the response; (c) Review progress and decide whether adjustments to interventions
or combinations of interventions are required; (d) Detect and respond to epidemics in a
timely way; and (e) Perform case-based surveillance, provide relevant information for
certification and monitor whether the re-establishment of transmission has occurred in
elimination settings.
1.2.1. Health Management Information System (HMIS)
One important aspect of a malaria surveillance system is a strong routine Health
Management Information System (HMIS). Investment in HMIS will also contribute to building
the national SNT capacities. Applicants are strongly encouraged to consider interventions
that better link HMIS to broader national efforts (e.g., District Health Information Software-
2, (DHIS2) roll out) and surveillance, monitoring and evaluation plans. Applicants should
also consider interventions that support the digitization of HMIS and data collection and the
integration with National MIS (e.g., DHIS2) as they contribute to broader national plans and
systems. In countries nearing, elimination surveillance systems should support active case
detection and notification.
The Global Fund supports the people, procedures, tools, training and supervision for routine
data collection and analysis (HMIS). This includes the various components of the routine
data system (public, private, community) and different administrative levels. Robust, quality
assured HMIS data are critical to a sub-national tailored malaria response and should be
supported with quality assurance activities. Actions and decisions based on this data can
only be as strong as the data itself.
Register revisions need to be considered to align with disease categorization across the
case management cascade (for details, see WHO Surveillance Manual
7
), including reasons
for care seeking, test performed, test result, diagnosis and treatment. Activities to support
quality registration of cases can include training and supervision on recording, compilation
7
Malaria surveillance, monitoring & evaluation: a reference manual
Page 8 of 34
and record submission as well as data entry, quality assurance reviews and follow up.
Applicants are strongly encouraged to detail how interventions that support health
information systems will use/analyze data and assess/improve data quality.
The WHO malaria surveillance assessment toolkit
8
can be used to support countries in the
assessment of surveillance systems and data quality. Technical assistance needs in
strengthening the HMIS system and in using the surveillance assessment toolkit can be
budgeted in the funding request.
1.2.2. Other surveillance data collection
The Global Fund also supports the collection and analysis of data through household and
health facility surveys. Such surveys can provide robust estimates of intervention coverage
and access to services at the population level. These results are critical to ensure that
interventions are reaching the intended target population at desired levels. National
household surveys can be supported with appropriate justification of the timing and utility of
the modules. Other survey methodology, potentially useful for program management
evaluation such as lot quality assurance sampling (LQAS) and ANC surveillance, can be
considered when appropriate justification and methodology are presented.
Entomological surveillance, ITN durability studies (see Vector Control section below) and
therapeutic efficacy studies (see Case Management section on page 21) should be included
in the budget. In addition, targeted behavioural surveys, and specific, targeted operations
research to inform access and delivery bottlenecks can be considered. Please see the
respective sections of this Information Note for more information on funding for these data
collection activities.
Malaria programs should also strengthen financial data intelligence and management
system. Possible activities to be funded included to: (1) Assess the funding landscape
including program expenditure by key program areas and source; (2) Understand the unit
costs of key interventions, main cost drivers and variation across regions and delivery
platforms; (3) Compare what types of intervention may be more cost-effective for a given
area, taking into account service accessibility and program feasibility; and (4) Delineate
potential resource needs to implement sub-nationally tailored response or intervention
mixes given the disease burden and program reality.
8
Malaria Surveillance Assessment Toolkit
Page 9 of 34
2. Prevention
2.1. Vector control
All requests for vector control need to be grounded in a national vector control strategy
based on up-to-date entomologic and epidemiologic data and follow the WHO Guidelines
for Malaria
9
. Insecticide resistance management principles, as outlined in the WHO Global
Plan for Insecticide Resistance Management
10
, are expected to be followed. Intervention
choices should be guided by the manual
11
for monitoring insecticide resistance in mosquito
vectors and selecting appropriate interventions.
Applicants should describe:
1. Their target populations for vector control and planned Intervention mixes, as
appropriate; and
2. The rationale for the choice of vector control tools, such as Insecticide Treated
Nets (ITN) or Indoor Residual Spraying (IRS), epidemiological, entomological and
user behaviour context, alongside any other criteria considered relevant by the
program.
Please refer to the relevant Program Essentials in Table 1 to ensure the funding request
includes the relevant information on progress, challenges and plans to address any gaps
and to achieve optimal vector control coverage.
It is assumed populations at risk of malaria will be targeted with at least either ITNs or IRS
(where the main vectors and context make these tools appropriate). If scale back of vector
control is proposed, the chosen approach should be robustly justified: it should demonstrate
how it is part of a sub-nationally tailored malaria control plan that responds to the
epidemiological, entomological and user context, and include a detailed examination of the
potential for resurgence given malaria burden prior to any recent vector control. Any such
scale back should also be accompanied by sufficient surveillance and response capacity in
order to detect and respond to any potential resurgence and be initially moderate in scale
with a plan to assess impact.
2.1.1. Insecticide Treated Nets (ITN)
Expression of full need and rationale for request:
As with all interventions, it is important for the Global Fund and partners to understand the
full need for a country program. While the NSP and tools such as the RBM CRSPC gap
analysis tool
12
cover all interventions, the Global Fund is specifically asking for the full
9
WHO Guidelines on Vector Control
10
Global plan for insecticide resistance management in malaria vectors
11
Manual for monitoring insecticide resistance
12
RBM Country/Regional Support Partner Committee (CRSPC) Gap Analysis
Page 10 of 34
expression of need for ITNs to ensure a clear understanding of a national program’s plans
based on the recent introduction of new ITN products, global reviews on attrition/durability
and widespread piloting of new distribution strategies.
It is expected that the ITNs program will be sub-nationally tailored, as appropriate to
variations in epidemiology, vector profile (including insecticide resistance), historical ITN
durability and/or attrition, population behaviors etc. Sub-national variations may include type
of ITN, ITN distribution approach, frequency of ITN distribution, social and behavior change
activities (SBC), or other relevant program areas.
Applicants should therefore:
1. Describe the ITN strategy (including ITN types, volumes, delivery approaches) as
an expression of the full need to maintain optimal effective ITN coverage of the target
populations. The full volume need should be based on local data on durability,
attrition, and coverage at different post-distribution time points; the rational for the
ITN strategy and the data sources should be described.
2. After accounting for all partner contributions, if the funding request does not cover
the full need, applicants should explain the prioritization process that was followed to
balance the need across the three-years grant, cost, effectiveness, coverage, and
potential for impact.
ITN types: Applicants are required to align selection of ITN types with WHO
recommendations. ITN types effective against the local vector population are expected to
be proposed and sub-nationally varied as appropriate. Note that WHO has an updated
conditional recommendation for deployment of pyrethroid-PBO ITNs
13
advising:
• Deployment in areas of pyrethroid resistance should be based on a resource
prioritization exercise due to their higher cost; and
• Prioritization of areas for deployment could be based on data demonstrating
metabolically based resistance.
If additional ITN types are recommended by WHO for use in areas of pyrethroid resistance
by the time of the funding request submission, these will also be considered within a
resource prioritization exercise. Countries who have previously deployed non-pyrethroid-
only ITNs (i.e., pyrethroid-PBO ITNs or dual active ingredient ITNs under the Strategic
Initiative projects) should not revert to pyrethroid-only ITNs for these geographic areas in
their future funding requests.
13
WHO Guidelines for malaria Pyrethroid-PBO nets .
Page 11 of 34
Operational considerations. Distribution may be through:
1. Intermittent campaigns, which need to be accompanied (including during campaign
years) by continuous distribution through proven channels such as ANC, EPI, and/or
school- or community-based distribution; or
2. Higher through-put continuous distribution channels instead of campaigns (e.g.,
annual school distribution).
Sub-national variation in distribution approaches may be appropriate to target the specific
needs and vulnerabilities of the (sub)populations most affected. Applicants are encouraged
to demonstrate how the proposed distribution approaches are based on considerations of
cost per net delivered/used, equity of access, ability to maintain coverage or other
considerations. Using NetCalc can help with the assessment of different options
14
.
Evaluation plans will include assessment of these criteria to inform future planning.
The Alliance for Malaria Prevention (AMP) guidelines
15
for campaign planning should be
followed. It is essential that quantification for campaigns: (1) Assume no capping of ITNs by
household size; (2) Consider whether any quantification factors would be appropriately
tailored sub-nationally; and (3) Include a 10% contingency stock if the population data are
older than five years. A plan for sound waste management should be included in the funding
request, including efforts to limit waste. While retrieval of old nets from households is not
recommended (nor historically funded by the Global Fund), there are recycling pilots
underway for old ITNs. If successful, these could be considered for future fundings.
If a program requires technical assistance for ITN distribution planning, the Global Fund
strongly encourages prioritization of this assistance within the funding request (e.g., AMP
TA). Support for digitization of campaigns can also be included; the Global Fund encourages
an integrated, multi-purpose digital platform that can be used for malaria campaigns as well
as other campaigns and activities (e.g., vaccination campaigns).
ITN use and care: Applicants are required to include data on ITN use where there is access
(at national and sub-national level, if available) and describe how a high use given access
will be achieved/maintained. The scope and scale of social and behaviour change (SBC)
activities should be appropriate to the local profile of use given access (i.e., if a population
has high use given access, funding will focus on access rather than on additional SBC
activities around hang up and use). SBC activities to promote proper net care may be
warranted.
Exclusions: The Global Fund does not invest in ITN container storage, mop-up or hang-up
campaigns, or non-essential data collection required by other partners.
14
Choosing a continuous distribution channel
15
Alliance for Malaria Prevention resources
Page 12 of 34
ITN procurement: The Global Fund guidance on ITN specifications is available here. Only
WHO prequalified and recommended products can be procured. ITNs need to be
rectangular and one of the standard sizes listed here. Color (white, green, or blue) can be
specified as part of the product specifications. Material preference can be indicated, but
applicants cannot restrict their specifications to one single material.
If applicants request procurement of ITNs outside of the standard sizes, shapes or fabrics,
these requests need to be supported by local evidence of significant impact on differential
ITN use and/or durability. If necessary, funding for this evidence generation can be
supported. ITNs can be procured with or without hooks and strings, considering local
understanding of their importance, or otherwise, to encouraging hang-up. Applicants can
consider the unit cost savings on the size of ITN or included accessories (i.e., hooks and
strings) to support the procurement of more ITNs or more expensive, but more effective,
ITNs. When budgeting, applicants are required to use the appropriate Global Fund Standard
Reference Price. In line with WHO recommendations, the Global Fund does not allow
applicants to specify the type of pyrethroid on an ITN.
All products will undergo pre-shipment testing in accordance with Global Fund’s policy on
sourcing and procurement of health products. ITN durability monitoring, using standard
protocols, should be planned for, and are strongly encouraged to be included in the funding
request. Applicants are expected to explain how this data will be used to increase program
efficiency.
2.1.2. Indoor Residual Spraying (IRS)
Given its high cost, IRS in malaria endemic areas shall only be initiated if sustainable
financing is assured. If IRS is requested within the funding request for the 2023-2025
allocation period, applicants are strongly encouraged to include a description of long-term
IRS financing.
When a country maintains an existing IRS program, a sound insecticide-resistance
management strategy must be in place, in line with the Global Plan for Insecticide
Resistance Management
16
, and with the operational guidance in the IRS Operational
Manual
17
, as well as routine monitoring of the quality and coverage of IRS.
Comprehensive health and environmental compliance safeguards need to be implemented
for all IRS programs supported by the Global Fund. Applicants are strongly encouraged to
include and budget the following items/activities for every IRS program: appropriate
environmental contamination containment measures, waste management and disposal, and
personal protective equipment (PPE). A description of how these safety aspects will be
maintained must be included in the funding request if Global Fund resources are used to
support IRS.
16
Global plan for insecticide resistance management in malaria vectors
17
Operational manual for IRS for malaria transmission, control and elimination
Page 13 of 34
2.1.3. Combining ITNs and IRS
The Global Fund supports deployment of ITNs and IRS in the same geographic area if all
the following points are true, which should be made explicit in the funding request:
1. The first method of vector control is funded at optimal coverage and delivered to a
high standard in the area of proposed co-deployment.
2. The combination is proposed for the management of insecticide resistance and as
part of a national insecticide resistance monitoring and management plan.
3. The proposal is part of a comprehensive malaria control plan which:
a. Is adapted at sub-national level.
b. Is supported by a prioritization process that includes cost-effectiveness
considerations, and
c. Leaves no gaps in other high or moderate burden areas.
2.1.4. Supplementary interventions
Larval source management
Larviciding can be supported as a supplementary intervention if applicants include the
following information in their funding request for the 2023-2025 allocation period:
i. Justification by the vector profile based on robust entomological data.
ii. Mapping of areas where optimal coverage with ITNs or IRS either has been achieved
or is inappropriate due to context such as vector or community behavior (justification
must be included); and
iii. Evidence that aquatic habitats are few, fixed and findable, and where its application
is both feasible and cost-effective
18
.
Habitat modification or manipulation is not recommended by WHO unless An. stephensi has
been detected and if this intervention is considered feasible as part of an appropriate,
multisectoral, An. stephensi response.
Larvivorous fish are not recommended by WHO and will not be funded.
House screening
House screening is conditionally recommended by WHO. Applicants proposing to include
this intervention should assess the feasibility, acceptability, impact on equity and resources
needed for screening houses within each context in order to determine whether such an
intervention would be appropriate for their setting. They are strongly advised to review the
18
WHO guidance on Larval source management
Page 14 of 34
detailed recommendation including rationale and practical guidance to determine if a strong
justification for inclusion can be provided. If prioritizing Global Fund resources for house
screening, applicants should detail how this intervention meets the following criteria:
1. Is part of an integrated vector management (IVM) approach.
2. Is proposed as a component of a wider strategy and follows the deployment of
interventions recommended for large-scale deployment (ITN or IRS); and
3. Is accompanied by an evaluation plan.
The proposed deployment approach should be well described and consider the practical
guidance included in the relevant section of the WHO Guidelines for Malaria
19
.
Interventions currently not eligible for funding
Other interventions recently assessed by WHO, and not recommended due to limited
evidence for additional public health impact at the time of writing of this note, include topical
repellents, space spraying, insecticide treated clothing and plastic sheeting, and spatial
repellents. These will not be considered for funding unless a WHO recommendation is made
in the future.
2.1.5 Anopheles Stephensi
An. stephensi is an emerging threat to the control of malaria in Sub-Saharan Africa.
Applicants are strongly encouraged to review the WHO GMP documents
20
advising on
surveillance and control approaches and include associated activities in their applications.
2.1.6. Entomologic surveillance
Applicants are strongly encouraged to put in place an insecticide resistance and
management plan, based on the WHO framework
21
and manual for monitoring insecticide
resistance
22
. Entomological surveillance should be prioritized in their funding request for the
2023-2025 allocation period if other sources of funding are not available. The surveillance
plan should cover data needs to inform planning and evaluation, including insecticide
susceptibility testing, at least annually. This data is important for supporting procurement
requests and shall therefore be prioritized.
2.1.7. Vector control capacity building
The Global Fund fully supports WHO’s recommendation in the Global Vector Control
Response that vector control needs assessments
23
be conducted via an inter-sectoral
process, to cover both vector control operational capacity and entomological surveillance
capacity. The funding request can include financial resources required to support the needs
assessment, as well as capacity building activities.
19
WHO guidelines for Supplementary interventions
20
WHO initiative to stop the spread of Anopheles stephensi in Africa
21
Framework for a national plan for monitoring and management of insecticide resistance in malaria vectors
22
Manual for monitoring insecticide resistance in mosquito vectors and selecting appropriate interventions
23
Framework for a National Vector Control Needs Assessment
Page 15 of 34
2.2. Preventive therapies
2.2.1. Drug-based therapies
Decision-making on type of chemoprevention. With growing evidence on the impact of
different types of drug-based prevention tools, national programs can explore what needs
to be prioritized based on the local epidemiology, transmission intensity, seasonality, access
to services, and interaction of multiple chemoprevention strategies where applicable. Note
that people living with HIV and receiving Cotrimoxazole preventive treatment are not eligible
for malaria chemoprevention using Sulfadoxine-pyrimethamine (SP). In June 2022, WHO
updated a guidance on chemoprevention strategies
24
.
Refer to the relevant Program Essentials in Table 1 to ensure the funding request includes
the relevant information on progress, challenges and plans to address any gaps and meet
these standards.
Seasonal Malaria Chemoprevention (SMC)
25
WHO guidance has broadened the flexibility around targeting SMC to consider regions with
highly seasonal transmission outside of the Sahel region, different age groups, transmission
intensity and duration, and drug choice. Therefore, applicants should: (1) Provide the
relevant information and analysis on these factors when requesting resources for SMC (e.g.,
local age pattern of severe malaria admissions, duration of high transmission season, etc.);
(2) Provide an overview of the implementation plan containing a strong monitoring and
evaluation component that includes pharmacovigilance and drug resistance monitoring; (3)
Describe strategies to improve efficiency and quality of service delivery, including but not
limited to (nor required) digitalization and/or integration with other interventions (such as
malnutrition screening or Vitamin A supplementation); and (4) Consider the cost-
effectiveness of SMC i.e. accounting for the burden of disease in the targeted geographic
area as well as the age group(s).
Intermittent Preventive Treatment of Malaria in Pregnancy (IPTp)
26
Strategies to increase uptake of IPTp need to consider improving Antenatal Care (ANC)
attendance as well as improving quality of ANC, as low quality of service can affect
attendance. New methods of delivering IPTp such as community IPTp (cIPTp) require an
integrated systems approach in which the continuum of care for pregnant women is
reinforced. Intermittent screening and treatment of pregnant women is not supported by the
Global Fund as it has been found to be less effective than IPTp.
Integration of IPTp with other activities targeting pregnant women within reproductive,
maternal, newborn, child, and adolescent health (RMNCAH) services, sexual and
reproductive health and rights (SRHR) and activities such as HIV services for pregnant
24
WHO guidance on preventive chemotherapies
25
WHO guidance on SMC
26
WHO guidance on IPTp
Page 16 of 34
women will be encouraged as ANC is the usual entry point into the health care system for
women of reproductive age. Applicants are encouraged to think comprehensively about a
pregnant woman’s overall health and invest to strengthen antenatal and postnatal care
(ANC-PNC), including through training of CHWs who can deliver RMNCAH and malaria
interventions as part of a comprehensive package of care. Women, children and newborns
still have limited access to quality of care, and there are opportunities to invest in the health
system building blocks such as HRH, data systems, procurement and supply chain systems
and laboratory systems to strengthen IPTp as part of ANC-PNC. All Global Fund malaria
grants supporting Malaria in Pregnancy (MIP) services should include an indicator on IPTp3
and monitor ANC attendance.
Perennial Malaria Chemoprevention (PMC)
27
The Global Fund will continue to support Intermittent Preventive Treatment for infants (IPTi)
and its updated nomenclature with a broadened spectrum, PMC, to reach a larger number
of children with this preventive intervention. Countries introducing IPTi/PMC or modifying
the delivery mechanisms or target age groups need to closely monitor coverage and, where
possible, impact on malaria. PMC should be integrated with other strategies targeting the
same age group populations, such as EPI or deworming. Note that new evidence from the
several ongoing projects on IPTi will be generated in the coming years and may have
implications for the guidance. Where IPTi/PMC are implemented, monitoring of SP
resistance is advised.
Mass Drug Administration (MDA)
28
Mass drug administration (MDA) can be used with two different objectives: burden reduction
or transmission reduction. WHO recommends that MDA for burden reduction can be
considered in areas with moderate to high P. falciparum transmission for short-term burden
reduction (evidence of 1-3 months post-MDA). The Global Fund will support MDA for
emergency burden reduction (including malaria outbreaks and malaria control in emergency
settings, section 5.8) and will require strong justification given the short duration of the effect.
MDA for transmission reduction will continue to be supported by The Global Fund in the
context of intensified elimination efforts targeting all or specific vulnerable populations.
Plasmodium Vivax elimination is currently not included in the MDA elimination guidance.
Funding for MDA implementation needs to be balanced against funding for other
interventions with longer-term effects on malaria burden or transmission and on the overall
health system. Countries are expected to monitor susceptibility to the drug deployed, as well
as interaction with first line Artemisinin-based combination therapies (ACTs).
27
WHO guidance on Perennial Malaria Chemoprevention
28
WHO MDA guidelines
Page 17 of 34
Other chemoprevention strategies
The funding request can include the two new chemoprevention strategies, Intermittent
Preventive Treatment for school children
29
(IPTsc) and Post Discharge Malaria
Chemoprevention
30
(PDMC). Introduction of IPTsc should not compromise
chemoprevention interventions for those carrying the highest burden of severe disease (e.g.,
children under 5 years old). PDMC provides a full therapeutic course of an antimalarial at
predetermined times following hospital discharge to reduce re-admission and death, and
targets children admitted with severe anaemia not due to blood loss following trauma,
surgery, malignancy, or a bleeding disorder. Applicants are requested to justify the selection
of the strategy at national or sub-national level and include methods to ensure equitable
access to preventive strategies.
2.2.2. Malaria vaccine
The Malaria Vaccine implementation program
31
will be funded until 2023 by the Global
Fund's Malaria Strategic Initiative, in collaboration with Gavi and Unitaid, in order to generate
more evidence on the vaccine's impact, safety, and feasibility.
The Global Fund will continue to support implementing countries' efforts to develop
evidence-based, costed national malaria plans and determine the best malaria intervention
mixes based on national context. Malaria vaccine RTS,S/AS01 (RTSS) introduction requires
a strong coordination between the national immunization program and the malaria control
program and has to consider several factors such as: levels of malaria transmission at sub-
national level, pattern of severe malaria, structure and function of the health system, use
and coverage of existing malaria control interventions, and the context where the vaccine
could best complement other tools as part of a package of interventions.
The WHO recommendation and position on the RTSS vaccine is now published in
an updated WHO position paper as well as in the WHO guidelines
32
for the prevention of P.
falciparum malaria for children living in regions with moderate to high transmission. Gavi has
approved an investment
33
to support the introduction, procurement and delivery of RTSS in
Gavi-eligible countries in sub-Saharan Africa in 2022-2025. To facilitate the distribution of
the limited supply, WHO has led the development of an “allocation framework”
34
that
provides guidance on the allocation of RTSS between countries, and priority criteria for
vaccination of certain countries’ areas until supply constraints are resolved.
A recent modelling analysis commissioned by the Global Fund in consultation with partners
showed that the optimal intervention mixes for a given country or subnational area is highly
dependent on its epidemiological and programmatic setting (e.g., parasite prevalence,
malaria seasonality, programmatic coverage achieved, cost of intervention including
29
WHO guidance IPTsc
30
WHO guidance PDMC
31
Malaria vaccine implementation program
32
WHO guidelines for the malaria vaccine
33
Gavi application window
34
Malaria Vaccine Allocation Framework
Page 18 of 34
products and service delivery, others). Countries are highly encouraged to carry out
intervention prioritization analysis with latest data, both epidemiological and financial, to
identify the optimal intervention mix given the resource envelope and considering
programmatic feasibility and other key factors.
While the Global Fund will not support the vaccine procurement and introduction, the funding
request can include technical support for SNT or for the National Strategic Plans (NSP)
update and Malaria Program Reviews (MPR) including the vaccine.
3. Case management
Effective diagnosis and treatment
Interventions included for malaria case management are required to support the expansion
and equitable access to quality, early diagnosis, and treatment of malaria, throughout the
continuum of care regardless of the sector, (e.g., public sector, community level and private
sector) and to address biologic threats such as drug resistance and parasite gene deletions
through generation of country-specific data and targeted implementation of mitigating
measures.
Refer to the relevant Program Essentials in Table1 to ensure the funding request includes
the relevant information on progress, challenges and plans to address any gaps in order to
meet these standards.
3.1. Diagnosis
The Global Fund supports early diagnosis of malaria through testing of suspected cases
with microscopy or Rapid Diagnostic Tests (RDTs). Achieving universal coverage of testing
and confirmation of parasitological diagnosis of malaria before treatment requires availability
of testing capacity, reinforced by training, supervision, agile supply chain and quality
assurance at all levels of the health system. In the case of microscopy, consider efficiencies
across disease programs when funding external quality assurance (EQA), procurement and
lab technicians’ capacity.
Current evidence is still limited on the individual and public health cost-benefits of detecting
and treating low density malaria infections contribution to malaria transmission reduction.
As a result, for routine case management, the Global Fund does not support more sensitive
diagnostic tools targeting low density parasite infections such as polymerase chain reaction,
highly sensitive RDTs, and loop-mediated isothermal application (LAMP). If additional
evidence and related WHO policy guidance are developed, the Global Fund will reassess
support for these tools.
Key considerations for RDTs selection and procurement:
• Procurement of malaria RDTs needs to be in accordance with Global Fund’s Quality
Assurance Policy for Diagnostic Products and procurement policies.
Page 19 of 34
• Technical considerations for selection need to be based on plasmodium species
prevalence.
• RDTs within species categories are considered interchangeable, therefore brand
preference is not a criterion for selection. Continued supervision and training are
required to ensure quality of diagnosis, but brand-specific training is not necessary
based on RDT use and experience across many countries.
3.1.1. Addressing biologic threats: Pfhrp2/3 Gene Deletions
A critical biologic threat is the emergence of pfhrp2/3 gene deletions that evade detection of
the most used malaria RDTs. P. falciparum with deletions of pfhrp2/3 genes can cause false-
negative RDT results with standard Hrp2 based RDTs, resulting in patients going untreated
and potentially progressing to severe disease, while also perpetuating transmission.
First identified in Latin America, parasite gene deletions have been confirmed in the Horn of
Africa with signals of emergence in neighboring countries, posing a wider risk in all of Africa.
Depending on the country specific context, the Global Fund can support baseline and
periodic surveys
35
to determine whether local prevalence of mutations in the pfhrp2/3 genes
causing false negative RDTs has reached a threshold that might require a change in the
local or national diagnostic policy. Alternative RDTs appropriate for pfhrp2/3 gene deletion
settings can be procured with The Global Fund support in consultation with the technical
and sourcing operations teams and in accordance with product eligibility requirements.
3.2. Treatment
There are currently six WHO recommended and pre-qualified Artemisinin-based
combination therapies (ACTs)
36
which, in the absence of resistance, have all been shown
to be safe and result in parasitological cure rates above 95%. The selection
37
of first line
ACTs should be in line with country treatment guidelines, and informed by in-country drug
resistance surveillance, adherence, cost and usage in other settings, such as private sector
and chemoprevention interventions.
Quantification and forecasting for antimalarials are expected to consider trends on burden,
current access to care and any potential increases in access (e.g., scale-up of community
services), and/or removal of barriers to access to care (e.g., removal of user fees or inclusion
of people-centered care service delivery that improves access).
38
3.2.1. Management of severe malaria
At the health facility level, the Global Fund continues to support parenteral artesunate as
the first-line treatment for severe malaria in children and adults, including pregnant women
35
Protocol for surveillance surveys to monitor HRP2 gene deletion
36
Artemisinin-based combination therapies (ACTs)
37
For further details see WHO guidelines Artemisinin-based combination therapy
38
For further details please see the RBM CRSPC guidance note on malaria gap analysis tools

Page 20 of 34
in all trimesters. If artesunate is not available, then parenteral artemether is the second line
choice.
For community case management, the Global Fund supports pre-referral treatment with
rectal artesunate (RAS) for children under 6 years of age. However, recent implementation
evaluation results from CARAMAL project (Community Access to Rectal Artesunate for
Malaria), a three-year operational research project (2018–2020), highlighted significant
challenges to the effective delivery and expected impact of pre-referral treatment in part due
to weak or non-functional referrals systems and incomplete post-referral treatment. If the
funding request includes procurement of RAS, it has to elaborate on the ongoing and
planned activities in order to ensure effective training of CHWs and CHW supervisors,
education of caregivers, operation of the referral systems, 3-day treatment with ACTs
following initial parenteral treatment and other related aspects of the full continuum of care.
The funding request can include support for these activities.
3.2.2. Management of Plasmodium vivax
When requesting funding for primaquine (PQ) for radical cure, we recommend that countries
demonstrate having an adequate monitoring system for detecting and managing hemolysis
(irrespective of whether a country employs glucose-6-phosphate dehydrogenase (G6PD)
deficiency testing or not). This includes a pharmacovigilance system consisting of significant
patient education, appropriate follow-up and referrals. The Global Fund can support testing
for G6PD deficiency through diagnostics which are WHO pre-qualified or approved by
Expert Review Panel for Diagnostics (ERPD). This includes the laboratory-based
fluorescent spot tests and G6PD RDTs. Appropriate monitoring of relapses should also be
included in these contexts to follow up the efficacy of radical cure.
Single-dose treatment with tafenoquine for radical cure has received approval from two
stringent regulatory agencies with a follow-up label change: they state that tafenoquine
should be co-administered with chloroquine only and no other antimalarials (e.g., ACTs).
Tafenoquine does not currently have WHO prequalification pending development of
guidance around the use of tafenoquine in conjunction with approved G6PD point-of-care
quantitative tests. As confirming G6PD status is a critical safety component of tafenoquine
use, and has important operational challenges, procurement of tafenoquine through the
Global Fund will require consultations with the technical teams on a case-by-case basis until
such guidance is available.
Page 21 of 34
3.2.4 Addressing biologic threats: Antimalarial Drug Resistance
In addition to efforts to address drug resistance in the Great Mekong Subregion, the
emergence of artemisinin partial resistance and reduced efficacy of partner drugs in Africa
require a coordinated and proactive response
39
. The Global Fund supports routine
surveillance for drug resistance through Therapeutic Efficacy Studies (TES) which need to
be conducted at least once every two years. The U.S. President’s Malaria Initiative (PMI)
will provide funding and support implementation of TES to the countries they are supporting.
Therefore, these interventions do not need to be included in the funding request. If funding
is not available through other sources, TES will then need to be prioritized within the funding
request. The funding request can include surveillance for molecular markers of drug
resistance which can be integrated in ongoing TES, surveys or surveillance activities and
support for the in-country capacity to do so.
Transitions of first line ACTs are expected to be based on results from TESs, documented
signals of drug failure/delayed parasite clearance, evidence of low adherence to a current
treatment and need to consider cost implications. As further guidance on strategies to
address antimalarial drug resistance is developed in collaboration with WHO and other
partners, the Global Fund may support proactive mitigation measures including the
introduction of multiple first lines or rotation of ACTs. Programs that have already developed
antimalarial resistance mitigation strategies should elaborate their plans within the funding
request within a summary or as an annex. The Global Fund programmatic gap table includes
a request for information on the different ACTs planned for use (for first and second line
and/or alternative first line treatment). Applicants are encouraged to express any gaps, in
particular antimalarial molecules due to the significant differences in price between
molecules and prioritization of resources across all malaria interventions.
3.3. Tailored service delivery across all sectors
The Global Fund continues to support all channels of service delivery (public, private and
community level) and encourages people-centered approaches, with a focus on the
continuum of care, integration within PHC and other programs and levels of care. Service
delivery needs to be tailored according to the context in order to ensure that all suspected
malaria cases are tested, malaria infections are treated, timely referrals are done, and all
cases are reported. Stratification and programming should follow sub-national tailoring
guidance at the lowest sub-national level feasible and include a robust analysis of the
following: care seeking behaviors; community perception and values; provider adherence to
guidelines; EHRGE-related and other barriers to access and use of malaria case
management services; challenges and funding gaps to inform targeted, sector specific,
interventions. This will help justify any needs for prioritization and coordination of support
across sectors.
39
The Strategy to respond to antimalarial drug resistance in Africa
Page 22 of 34
3.4.1. Additional considerations: public sector health facilities
Interventions to strengthen service delivery of malaria case management should focus on
testing and confirmation of malaria prior to treatment, and accurate recording and reporting
of the clinical encounter. Stratification of key indicators for case management need to be
performed by districts on a routine basis to assess performance, to guide quality of care
interventions in low performing facilities and systematically document the root causes of
district challenges in meeting targets. In addition, as further elaborated in the RSSH
Information Note, the Global Fund strongly encourages applicants to invest in locally defined
intervention packages to improve the quality of people-centered, integrated care. These
packages, including supervision, training, and quality improvement approaches, can often
be combined across programs in an integrated manner.
3.4.2. Additional considerations: private sector
The Global Fund strongly encourages a costed strategy for the delivery of quality malaria
case management in countries where private sector care offers the potential to expand the
reach of services. Priorities include efforts to expand parasitological diagnosis for
confirmation of malaria prior to treatment, support regulatory framework to allow testing and
availability of quality drugs, to reduce cost barriers to quality diagnosis and treatment and to
ensure reporting of malaria cases to national systems.
Governments can use various pathways to engage systematically with the private sector,
such as: 1) Policy and strategic level dialogue, 2) Two-way information sharing, 3) Inclusive
balanced regulations (across service sectors), 4) Capacity building for the private sector;
and 5) Financing the private sector (e.g., performance-based contracting, subsidies, etc.).
The funding request can include supporting activities. The private sector technical brief and
RSSH Information Note elaborate further on private sector engagement strategies.
As part of setting and implementing standards for service delivery requirements, the Global
Fund will only support the ACT co-payment mechanism for the private sector in settings
offering the full test and treat pathway, including confirmation of malaria with a diagnostic
test before treatment, recording and reporting into national information systems.
3.4.3. Additional considerations: integrated community case management
As part of broader PHC, CHWs play a critical role in the fight against malaria. They make
malaria interventions closer and more accessible to populations at greatest risk and increase
access to malaria case management, typically as part of integrated community case
management (iCCM) for children under-five and increasingly as malaria case management
for older children and adults. They also play an essential role in the delivery and promotion
of vector control interventions (e.g., ITNs) and drug-based malaria prevention services (e.g.,
SMC, IPTp, PMC). Building effective, strong, resilient, and sustainable CHWs programs with
the capacity to surge and scale is necessary for expanding access to quality malaria case
Page 23 of 34
management whether within the malaria epidemic and pandemic preparedness at
community level, or the broader context of strengthening PHC services and community
systems.
The Global Fund will invest in the systems components of CHWs programs,
40
including
where CHWs provide malaria case management services (i.e., iCCM and case management
for malaria among older children and adults). Detailed information on the CHW investments
eligible for Global Fund support are provided in the table Investments in health policy and
systems support to optimize CHWs in Section 4.5 Human Resources for Health and Quality
of Care of the RSSH Information Note. Use the CHW programmatic gap table to facilitate
planning for funding requests. They can also refer to the Global Fund Budgeting Guidance
regarding remuneration (i.e., salaries, allowances, and benefits).
Strengthening community health systems also requires emphasis on improving bidirectional
referrals between community and facility care. A detailed intervention approach on referrals
is outlined in Annex 2 of the RSSH Information Note. Applicants should outline the needs
and sources of funding for CHW commodities not provided by the Global Fund. Funding of
non-malaria commodities for iCCM can be considered co-financing in most countries (please
consult the Global Fund Co-Financing Policy). Note that the Global Fund will now support
non-malaria medications for iCCM (e.g., for pneumonia and diarrhea) where CHWs provide
malaria case management, where iCCM is part of the package of services CHWs are
allowed to provide, and where the criteria in Annex 3 of the RSSH Information Note are met.
If resources and/or supplies for non-malaria illness included in the iCCM package are not
available simultaneously during implementation, the malaria component should continue as
planned, though efforts should be made to identify additional sources of funding to deliver
the complete package.
4. Elimination
Malaria elimination requires country ownership, with strong political commitment, reaching
hard-to-reach populations, robust surveillance systems including case-based surveillance
and case investigations-response, addressing cross-border issues and innovation in
products and service delivery. The transition from malaria control to elimination requires a
shift in strategy supported by evidence and the implementation of new activities tailored to
each country’s specific context. Please refer to the relevant Program Essentials in Table 1
to ensure the funding request includes the relevant information on progress, challenges and
plans to address any gaps to meet these standards.
Intervention packages
41
in countries approaching elimination are required to focus on: (1)
Enhancing and optimizing vector control and case management (component A); (2)
Increasing the sensitivity and specificity of surveillance to detect, characterize and monitor
40
WHO guideline on health policy and system support to optimize community health worker programmes
41
WHO guidance on interventions in the final phase of elimination and prevention of reestablishment

Page 24 of 34
all cases (component B); (3) Accelerating transmission reduction (component C); and (4)
Investigating and clearing individual cases, managing foci, and following up (component D).
This could be achieved through the following interventions:
i. Local stratification by malaria transmission intensity and other key
characteristics. This is essential for effective targeting of interventions and needs
be specific, ideally at the level of localities or health facility catchment areas. The
funding request would benefit from describing how intervention strategies have been
tailored to the different strata.
ii. Enhancing and optimizing vector control. Vector control is expected to target
remaining foci and areas of on-going transmission.
iii. Enhancing and optimizing case detection and case management including
support for quality assurance and reference laboratories. Case management
needs to focus on 100 percent parasite-based, quality-assured diagnosis, and
universal access to appropriate treatment including gametocytocidal primaquine
where deemed effective. The Global Fund will also continue to support approaches
to promptly investigate and respond to cases or foci detected such as case
investigations and focus investigation and responses (CIFIR) or Diagnostic,
Treatment, Investigation, Response (DTIR) and encourages applicants to
decentralize these wherever possible to shorten the time from detection to response.
iv. Strengthening surveillance systems to detect symptomatic and asymptomatic
cases; notify, report, and investigate all malaria infections. Routine surveillance,
active case detection and foci investigation are recommended, as well as response
planning and epidemic preparedness. Outbreak preparedness should include clear
alert mechanisms as well as systems to enable rapid access to malaria commodities.
v. Other activities aimed at accelerating malaria elimination (e.g., community
engagement and communication campaigns to promote awareness and avoid
reintroduction).
vi. Applicants are also asked to include a description of programs addressing
prevention of re-establishment of the disease.
5. Cross-cutting Areas
5.1 Equity, human rights, and gender equality
Equity, human rights, and gender equality considerations are essential for inclusion in the
sub-national tailoring analysis. Therefore, they should be incorporated into the
implementation approach to ensure people- and population-centred service delivery.
Page 25 of 34
While certain populations may have more health-related vulnerabilities than others,
prioritization on malaria prevention and control activities need to be based on malaria-
specific vulnerability. For example, children under five years of age and pregnant women in
areas with on-going malaria transmission are more at risk of suffering serious consequences
of and death from the disease. As such, malaria programs should focus interventions
accordingly. Migrants, internally displaced people (IDPs) and refugees can also be more
vulnerable, particularly if coming from an area with limited/no transmission into an area with
high transmission. Disaggregation of data (e.g., gender, age, other equity-related variables)
should be considered when needed to guide decision-making. For example, gender and
socioeconomic variables collected through community-based surveys such as the Malaria
Indicators Survey and Demographic and Health Surveys should be analyzed to better
understand potential inequalities or barriers to access and uptake to guide appropriate
tailoring of interventions.
If not already in the National Strategic Plan (NSP) or other document, the funding request
should include an analysis of the data available to demonstrate any known barriers to access
and uptake of malaria services. Funding for implementation of the Malaria Matchbox or other
similar tools can be included where EHRGE analyses have not been undertaken and/or
information gaps exist, or to improve understanding of how to address identified issues.
Additional disaggregated information and analysis on workforce composition to deliver
malaria services may provide additional insights on increasing equity and access.
Interventions informed by such data, aimed at addressing EHRGE barriers, can be included
under the respective modules. RBM has developed an e-learning training
42
for national
programs for the assessment of human rights and gender-related barriers to equitable
access to malaria services. For further information please refer to the technical brief on
Equity, Human Rights and Gender Equality and Malaria.
5.2 Community leadership and engagement
Community Systems Strengthening (CSS) are useful to improve and monitor access to
malaria services for most affected, marginalized, and underserved populations in endemic
areas. This includes empowering and supporting communities, especially the most
vulnerable, to participate in national and local structures, platforms, and processes, including
in country coordination mechanisms (CCMs) and ensuring that communities and civil society
are key partners and play a meaningful role in the Global Fund grant application, decision-
making and implementation. Community leadership and engagement have been and
continue to be key to supporting strong responses to malaria: they should be at the heart of
future efforts to address novel health threats.
There is no “one size fits all” strategy; it is crucial for community-based and community-led
organizations to play a meaningful role in determining the elements of effective, equitable
and sustainable malaria responses.
42
Community, Human Rights and Gender in malaria programming for Malaria Program Managers
Page 26 of 34
Strengthening community participation may be especially important in elimination settings
43
.
Elimination strategies represent an opportunity for rights-based action to reach traditionally
excluded and geographically marginalized populations with malaria services.
Applicants are encouraged to explore the potential of community-led monitoring (CLM) as
part of efforts to improve availability, accessibility, responsiveness, and quality of services.
CLM can focus on general health, disease-specific or intervention-specific services (e.g.,
monitoring of correct usage of ITN, stock/workforce availability at health facilities or
geographic and other structural, and human rights and gender-related barriers).
The community also plays a role in improving services by identifying individuals or groups
of individuals who do not have appropriate access, or who do not understand the barriers
they face. Examples of CLM tools that applicants are expected to consider include
scorecards (like the ALMA community scorecards
44
), complaint mechanisms and monitoring
of human rights and gender-related barriers to services.
Additional information on CSS and CLM are available in the RSSH Information Note.
5.3 Social and Behaviour Change (SBC)
Investments in SBC need to be evidence-based, results-oriented, theory-informed and part
of the national malaria SBC strategy. The strategy and investments need to reflect the
relevant prevention, control and elimination objectives of the national malaria strategy and
include an M&E plan to guide and adapt approaches to improve access to and usage of
malaria interventions. SBC plans and activities should build on existing best-practice and
SBC efforts in other health sectors (e.g., maternal and child health, community systems).
While integration is encouraged, advocacy efforts, such as “Zero Malaria Starts with Me”
campaigns and activities, can also be considered.
SBC activities are required to:
• Account for differences amongst and within populations (e.g., cultural, socio-
economic, geographic, gender, occupational, literacy, race, ethnic and indigenous
backgrounds, and other considerations) that may affect equitable access and
utilization of interventions.
• Address identified barriers, including human rights and gender-related ones, to
uptake and use of malaria interventions (and health services more generally).
• Address issues related to provider behaviours, such as adherence to case
management guidelines, respect of fee policies and compassionate care.
• Address risk perception by communicating changes in the transmission dynamics
and associated risks.
43
The Malaria Free Mekong is an example of network platform of civil society organizations and communities.
44
ALMA Scorecard
Page 27 of 34
5.4 Pandemic Preparedness and Response (PPR)
In malaria endemic countries, components of the health system responding to malaria are
key in early identification of other conditions leading to pandemics. Investments in PPR can
build on already existing systems, including malaria control and surveillance systems for
acute febrile illness. Lessons learned from the COVID-19 pandemic and response should
also be considered, as well as investments to ensure appropriate capacity and expertise,
recognizing that malaria program personnel at national and district level are often engaged
in investigation and response for acute febrile illness outbreaks. In addition, investments in
the PHC service delivery will strengthen the fight against malaria and preparedness for
future pandemics.
Malaria early warning systems (MEWS) are among the potential areas for integration, as
they can strengthen laboratory-based and community-based approaches. Exploring the
overlap between the 7-1-7 approach
45
recommended for PPR and malaria surveillance in
different transmission settings, notably the 1-3-7 approach in elimination contexts.
46
Synergies in HRH (training, remuneration, supportive supervision, and quality improvement)
at national, facility and community levels may exist. CHWs play important roles in PPR,
including risk communication and community engagement (RCCE), dispelling myths,
promoting, and supporting vaccination, behavioural interventions and other relevant
prevention tools, community-based testing and contact tracing, providing support to patients
on treatment, and surveillance.
47
When considering PPR efforts or integration of other activities into CHW’s terms of
reference, analyse the scope and readiness of the existing CHWs and ensure sufficient
resources (e.g., training, support supervision, etc.) for successful service delivery. The
Global Fund encourages countries to consider laboratory system strengthening to further
support malaria control, co-morbidities with other key endemic diseases and emerging
pathogens. See RSSH-Lab module to learn more.
5.5 Environment and climate change
Environmental factors including climate events and climate change disproportionally affect
malaria. Climate data is expected to be routinely incorporated in malaria data repositories
and used as one of the factors to guide program planning, adaptations, and coverage.
Integration of malaria into emergency response plans (epidemic, climate/natural disasters)
should be considered, where relevant. Multisectoral partnerships
48
can help foster
collaboration on improving prediction and response to potential climate events, addressing
the impact of climate change on malaria, other vector-borne diseases, nutrition, etc., as well
45
Frieden et.al, Lancet 2021
46
Zhou et al, Infectious Diseases of Poverty, 2015
47
Bhaumik et al 2020 ; Ballard et al 2022
48
The Comprehensive Multisectoral Action framework - Malaria and Sustainable Development

Page 28 of 34
as provide opportunities to mitigate the impact of malaria interventions on the environment
(WHO Strategic Advisory Group on Malaria Eradication
49
).
Lastly, waste management support needs to be included for the relevant malaria
interventions (e.g., vector control), and applicants are encouraged to include environmental
considerations in this activity (e.g., collaboration with recycling plants during an ITN mass
campaign). Malaria funding requests can include these activities, while the broader waste
management and green technology for facilities (e.g., solar panels) can be considered under
RSSH see RSSH Information Note).
5.6. Urban malaria
The built urban environment, such as urban agriculture, settlement construction, roads and
water drainage systems, and exposed water channels, can have a significant impact on
urban malaria risk and burden. In malaria-endemic countries, large-scale rural-to-urban
migration frequently leads to the expansion of unplanned settlements and an increased
socioeconomic inequity. These changes may lead to vector changes (e.g., Anopheles
gambiae s.l. adapting to polluted waters increased Anopheles stephensi expansion).
A strong example of a sub-nationally tailored approach is an adapted approach to malaria
in urban settings
50
. As malaria transmission in urban areas is usually focal and varies across
short geographic spaces, a response targeting focal areas of transmission is likely more
effective than an urban-wide approach, especially for malaria prevention. The funding
request could include geospatial and epidemiological surveillance and analysis to identify
clusters of malaria transmission, technical assistance for using data to tailor malaria
interventions to urban settings, facilitation of community engagement, delivery of prevention
and health care, and support private sector initiatives to improve quality and reporting (as a
large portion of the population in urban areas seek care in the private sector).
Applicants are encouraged to document current practices and lessons learned on effective
malaria control and elimination interventions in urban settings.
5.7. Challenging Operating Environments (COE)
The Global Fund will continue to support implementation of malaria activities in COEs and
will help adapt the strategies, partnership, and implementation modalities to these difficult
environments in order to ensure optimal access to the whole vulnerable population, including
migrants, refugees, and IDPs.
Some examples of adapted strategies would consist in increasing the frequency of
distributions to refugees, individual ITN distribution to displaced persons, selecting CHWs
amongst mobile or migrant populations, or engaging with humanitarian actors to ensure
delivery of malaria services in conflict-affected zones. Applicants should explore integration
49
Malaria eradication: benefits, future scenarios & feasibility. A report of the Strategic Advisory Group on Malaria Eradication
50
Global framework for the response to malaria in urban areas
Page 29 of 34
of services as much as possible, especially given the often severely limited access such
populations often have. They should also provide holistic, patient-centered services that all
populations deserve. Special attention will be given to include forcibly displaced populations
in grants: refugees are expected to be considered within host country grants, and applicants
are asked to ensure these populations have access to malaria prevention and control.
Flexibilities may be applicable to countries designated COEs by the Global Fund, and are
detailed in the Global Fund operational manual.
5.8 Malaria emergencies
The Global Fund Emergency Fund special initiative is a mechanism to provide urgent
funding for emergencies, including but not limited to, malaria outbreaks, natural disasters,
and population displacement. If needed, the request can be focused on commodities, in
order to respond to urgent needs - see the guidelines on the Emergency Fund for details.
Note that malaria emergencies can also be funded through reprogramming of funds within
the malaria grants.
5.9 Program management
The funding request can include activities related to leadership, coordination, and
management of the malaria program at national, subnational, and cross-border level. The
Malaria Modular framework outlines the specific activities to be included under this module.
Special attention needs to be given to include capacity building for data generation, use and
analysis at sub-national level,
51
in line with the principle of SNT. The Global Fund will provide
short-term support (e.g., specific technical assistance requested by the program), as well as
longer-term support (e.g., program staffing), both of which can be included in the funding
request.
5.10. Sustainability of malaria response
The Global Fund’s approach to sustainability focuses on the ability of a health system to
both maintain and scale up service coverage for continuing control of a public health problem
and support efforts for elimination of the three diseases, even after funding from external
donors comes to an end. As part of the Global Fund 2023-2028 Strategy and the
implementation of the Sustainability, Transition, and Co-Financing (STC) Policy, the Global
Fund strongly encourages all countries to incorporate sustainability considerations into
national planning, funding request development, grant design, co-financing commitments,
and grant implementation, regardless of where a country is on the development continuum
or of their proximity to transition from Global Fund financing. While financial sustainability is
a critical priority, sustainability considerations cut across many thematic areas, including
epidemiological, programmatic, systems-related, governance, and human rights and vary
according to the specific country context.
51
Depending on the scope of the capacity building activity, it can be classified/budgeted/reported under program management or other
intervention specific modules.
Page 30 of 34
Strengthening sustainability is critical to maintaining the gains in the fight against malaria
and moving towards malaria elimination. As external financing reduces or countries seek to
strengthen malaria control, various factors may present sustainability challenges – for
instance, the epidemiology of malaria transmission and/or strength of the national malaria
program and broader health system. Strengthening the national health systems which serve
as the foundation for national malaria responses is critical to sustaining the gains and
supporting successful transitions from Global Fund financing. This is particularly relevant in
the context of the COVID-19 pandemic and preparation for any future pandemics. While not
exhaustive, examples of focus areas to support sustainability of national malaria responses
include:
• Financial: Increasing the overall availability of resource for national malaria
responses, while also addressing dependencies on donor financing for specific
interventions critical to malaria control and elimination.
• Governance and political will: Maintaining political will to ensure that the national
malaria program has adequate resources to achieve and maintain impact, especially
as countries re-orient their programs towards elimination and prevention of re-
establishment (POR), or seek to leverage integration, decentralization, and other
health sector reforms.
• Service Delivery: Integrating aspects of malaria programs into the broader health
system, while maintaining sufficient technical expertise and quality.
Given the diversity of potential sustainability challenges facing national malaria responses,
the Sustainability, Transition and Co-financing Guidance Note includes a detailed Annex on
Malaria and Sustainability.

Page 31 of 34
List of Abbreviations
Abbreviation
Definition
ACTs
Artemisinin-based Combination Therapies
AMP
Alliance for Malaria Prevention
ANC
Antenatal Care
CHWs
Community Health Workers
CIFIR
Case Investigation, Focus Investigation and Response
CLM
Community-Led Monitoring
CRSPC
Country Regional Support Partnership Committee
CSS
Community Systems Strengthening
DHIS2
District Health Information Software 2
DTIR
Diagnostic Treatment Investigation and Response
EPI
Essential Program on Immunization
EQA
External Quality Assurance
G6PD
Glucose-6-Phosphate Dehydrogenase
GAVI
Gavi, the Vaccine Alliance
GTS
The Global Technical Strategy for Malaria 2016–2030
HMIS
Health Management and Information Systems

Page 32 of 34
EHRGE
Equity, Human Rights, and Gender Equality
HRH
Human Resources for Health
iCCM
Integrated Community Case Management
IPTp
Intermittent Preventive Treatment of Malaria in Pregnancy
IRS
Indoor Residual Spraying
ITN
Insecticide Treated Net
LQAS
Lot Quality Assurance Sampling
M&E
Monitoring and Evaluation
MDA
Mass Drug Administration
NSP
National Strategic Plan
PDMC
Post Discharge Malaria Chemoprevention
PE
Program Essentials
PMC
Perennial Malaria Chemoprevention
PNC
Postnatal Care
PPR
Pandemic Preparedness and Response
PQ
Primaquine
PSEAH
Protection from Sexual Exploitation, Abuse and Harassment
RAS
Rectal Artesunate
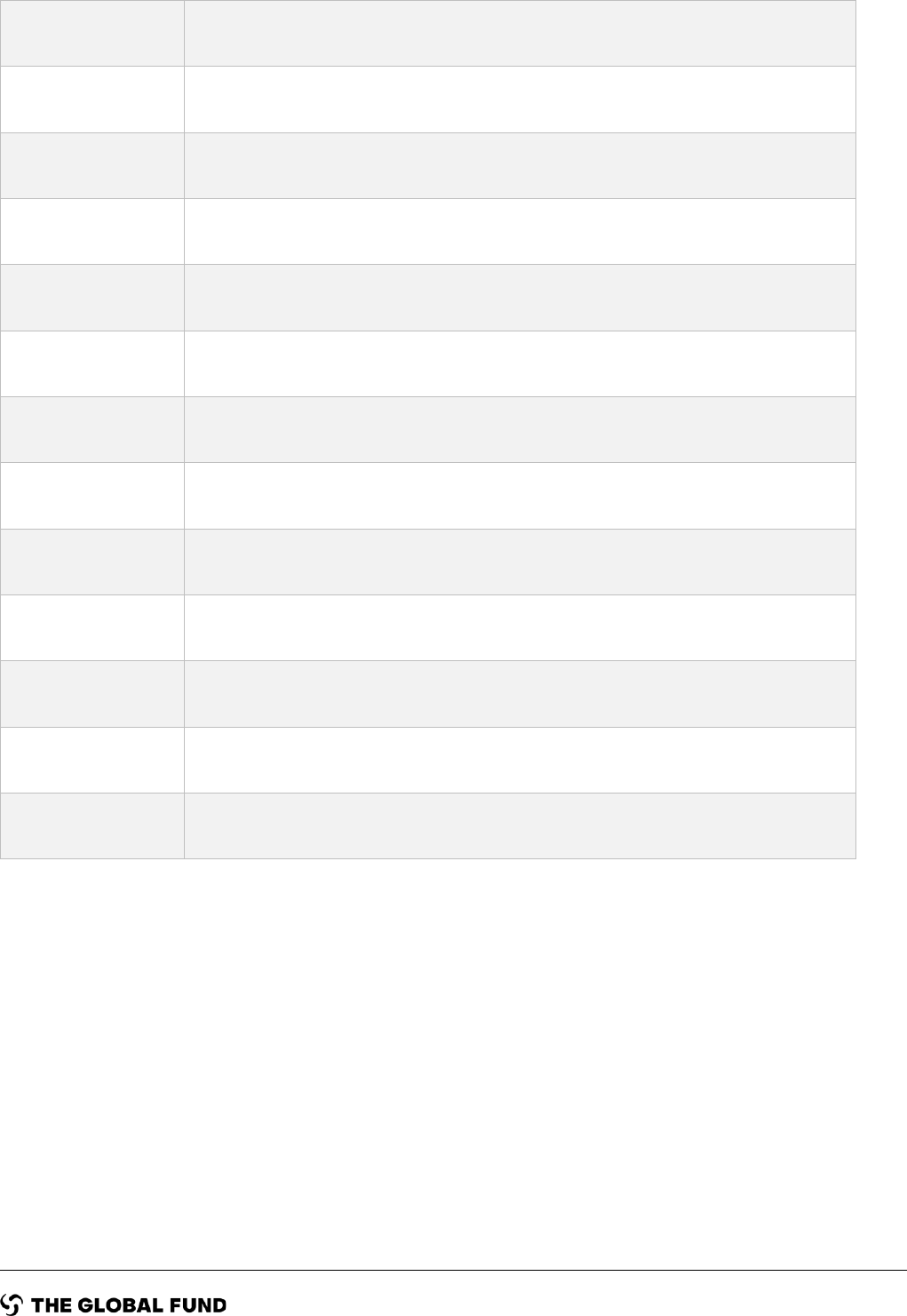
Page 33 of 34
RBM
The RBM Partnership to End Malaria
RDTs
Rapid Diagnostic Tests
RMNCAH
Reproductive, maternal, newborn, child, and adolescent health
RSSH
Resilient and Sustainable Systems for Health
RTSS
Malaria Vaccine (RTS,S/AS01)
SBC
Social and Behavior Change
SMC
Seasonal Malaria Chemoprevention
SNT
Sub-national Tailoring of Malaria Interventions
SP
Sulfadoxine-pyrimethamine
STC
Sustainability, Transition, and Co-Financing
TES
Therapeutic Efficacy Studies
TQ
Tafenoquine
WHO
World Health Organization

Page 34 of 34
Annex 1: Key Data
Key Data to include in funding requests
The information below is essential to include in the funding request – whether within the Essential
Data Table, as an annex or within the narrative.
1) Summary of country context, highlight the epidemiology of malaria including:
• Parasite species present and their relative contribution towards burden.
• Malaria burden, including description of epidemiological trends (incidence, prevalence,
historical burden) and stratification, geographic distribution of cases, as well as other relevant
programmatic data.
• Disaggregated data (by age and gender, as appropriate) and relevant details on vulnerable
and other populations, noting any barriers (including, but not limited to equity, gender, and
human rights-related barriers) to access to prevention and case management service.
• Description and proportions of different channels where people seek care (e.g., public,
private, community, including traditional healers); proportion of population with access to
diagnosis and treatment.
2) Past and current implementation, as well as lessons-learned:
• Brief description of the health system including at the community level.
• Prevention and control implementation challenges encountered to date including, but not
limited to changes in the financial landscape, issues with insecurity, etc.
• Current knowledge gaps.
• Equity assessments and relevant findings (e.g., Malaria Matchbox or other tools).
• Brief overview of current malaria interventions:
• Diagnostic tool(s) in use and current testing coverage (e.g., testing rate).
• First- and second-line antimalarial treatment; treatment for severe malaria.
• Vector control interventions implemented and respective coverage and use. This
should include types of nets deployed (ex. pyrethroid-only, pyrethroid-PBO net) and
insecticides used for IRS.
• Other core interventions e.g., IPTp, SMC, etc. and relevant coverage.
• Monitoring and evaluation (M&E):
• Coverage of key malaria interventions from population-based household
surveys (DHS, MIS, MICS), including the date of last survey and planned
date(s) for upcoming survey(s).
• Date of last therapeutic efficacy study (TES); date of last hrp2/3 gene deletion
study; relevant findings and plans for future studies.
• Dates and findings of recent insecticide resistance studies (including
mechanisms and intensity of resistance) and plans for future studies; date and
findings of ITN durability studies.
• Routine monitoring/HMIS systems (disaggregation metrics, lowest
administrative unit where data analysis is possible, etc.) and malaria-specific
surveillance (particularly for countries approaching elimination).
• Digital platforms.
• Cross border or regional activities/initiatives, as applicable.
