
NATIONAL COMMISSION ON RECOGNITION OF DENTAL
SPECIALTIES AND CERTIFYING BOARDS
2021 PERIODIC REVIEW
OF DENTAL SPECIALTY EDUCATION AND PRACTICE
April 2021
2
Through the Periodic Review of Dental Specialty Education and Practice, the National Commission on Recognition of
Dental Specialties and Certifying Boards hoped to gather strategic information that will be of value to the National
Commission, the recognized specialty sponsoring organizations, the recognized certifying boards, the profession and
the public. The review focuses on changes occurring within the advanced dental education programs, specialty
practice environments, board certification, disease trends, technology, and scope of practice. The review also looks
at the current environment as well as potential trends for the future and how these trends could impact the public and
the profession.
Background: In 1992, the American Dental Association (ADA) House of Delegates adopted Resolution 144H-1992
directing the Periodic Review of Dental Specialty Education and Practice be conducted every ten (10) years
beginning in 2001. In 2001 and 2011, the Council on Dental Education and Licensure conducted the review. With the
establishment of the National Commission in 2017, the Periodic Review became the responsibility of the National
Commission who adopted policy to continue the practice of conducting the review every ten (10) years.
For the 2021 Periodic Review of Dental Specialty Education and Practice, the following specialty sponsoring
organizations submitted reports: American Academy of Oral and Maxillofacial Pathology (AAOMP), American
Academy of Oral and Maxillofacial Radiology (AAOMR), American Academy of Pediatric Dentistry (AAPD), American
Academy of Periodontology (AAP), American Association of Endodontists (AAE), American Association of
Orthodontists (AAO), American Association of Public Health Dentistry (ABDPH), American College of Prosthodontists
(ACP) and American Society of Dentist Anesthesiologists (ASDA).
This summary report is divided into four sections:
I. General Information and Demographic Data of the Specialties
II. Major Research Changes and Technology Advances
III. Trends in Specialty Education
IV. Changes in Scope of Practice
I. GENERAL INFORMATION AND DEMOGRAPHIC DATA OF THE SPECIALTIES
History of Dental Specialties: As noted in Table 1, in 1947, the ADA formally recognized five (5) dental specialties,
oral and maxillofacial surgery, orthodontics (now known as orthodontics and dentofacial orthopedics), pedodontics
(now known as pediatric dentistry) periodontics and prosthodontics. Further, the ADA formally recognized oral and
maxillofacial pathology in 1949; dental public health in 1950; endodontics in 1963 and oral and maxillofacial radiology
in 1999.
The National Commission formally recognized dental anesthesiology in 2019 and oral medicine and orofacial pain in
2020 as dental specialties. Because oral medicine and orofacial pain were recognized during the year the Periodic
Review was being conducted, the organizations were exempt from participating.
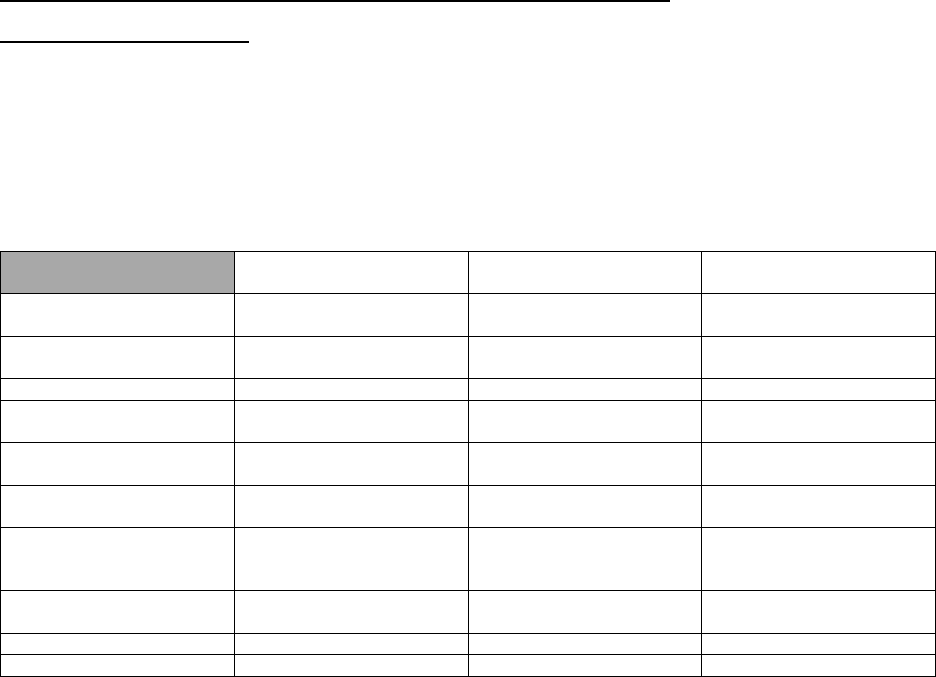
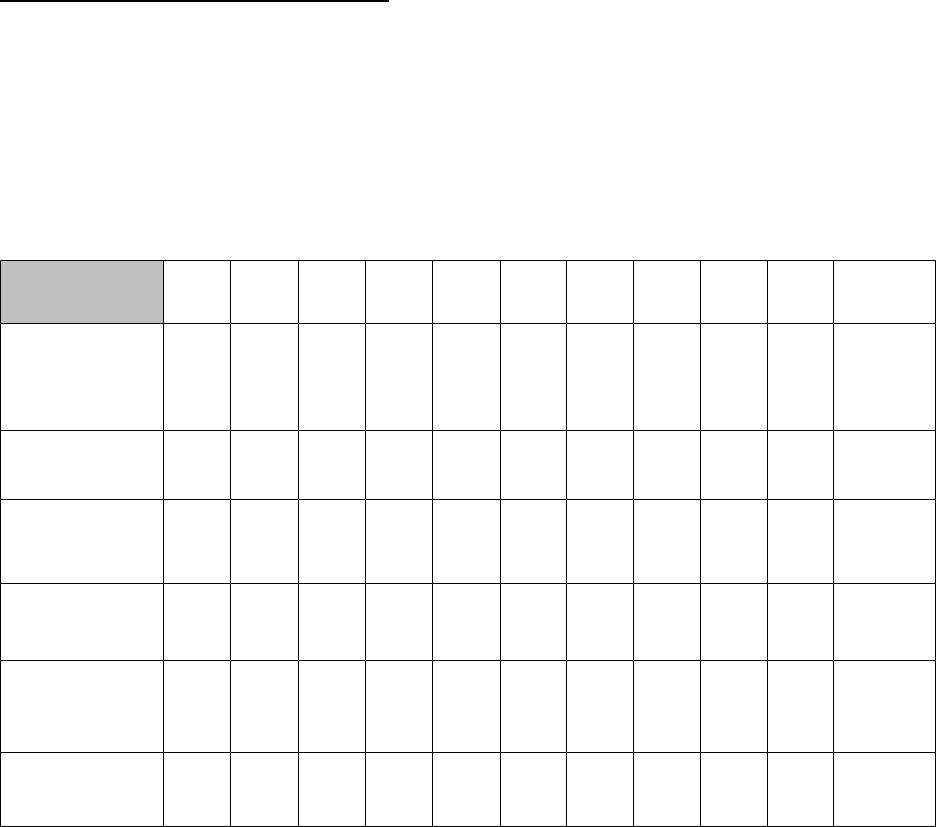
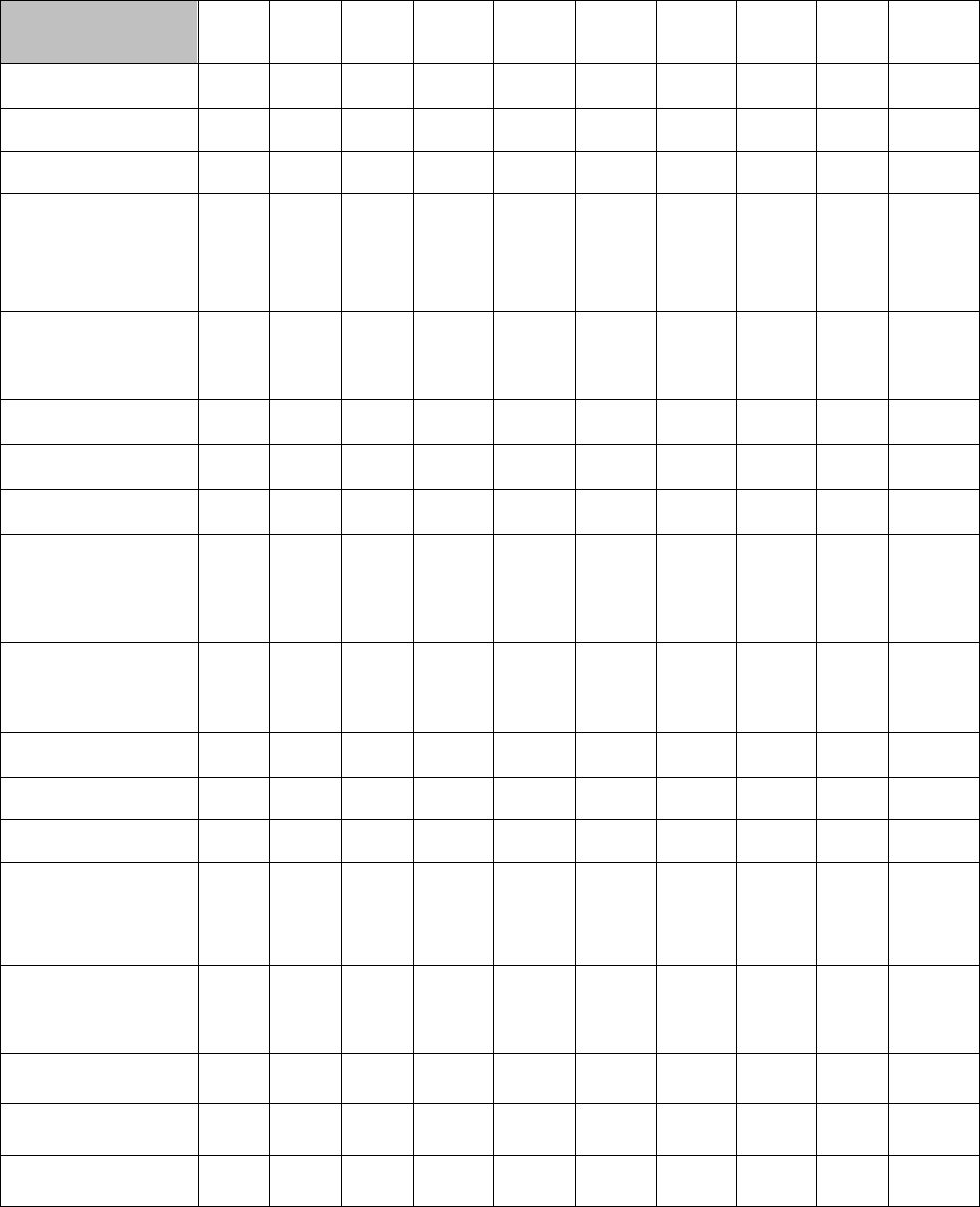
Table 1. History of the Recognized Dental Specialties and Dental Specialty Certifying Boards
Year Specialty
Recognized
Year Specialty Certifying
Board Recognized
Founding Date of
Certifying Board
Dental Anesthesiology
(ASDA)
2019
2020
1994
Dental Public Health
(AADPH)
1950
1951
1950
Endodontics (AAE)
1963
1964
1956
Oral and Maxillofacial
Pathology (AAOMP)
1949
1950
1948
Oral and Maxillofacial
Radiology (AAOMR)
1999
2000
1979
Oral and Maxillofacial
Surgery (AAOMS)
1947
1947
1946
Orthodontics and
Dentofacial Orthopedics
(AAO)
1947
1950
1929
Pediatric Dentistry
(AAPD)
1947
1948
1940
Periodontics (AAP)
1947
1948
1940
Prosthodontics (ACP)
1947
1948
1946

3
Compliance with the Requirements for Recognition of Dental Specialties: The National Commission requested
each of the recognized specialty sponsoring organizations to provide documentation exhibiting that the six (6)
Requirements for Recognition of Dental Specialties are being met.
American Association of Public Health Dentistry
Requirement 1
• Full membership is for dentists who have either completed a Commission on Dental Accreditation (CODA)
accredited advanced education program in dental public health, advanced training in public health (an MPH
degree) without formal dental specialty training or who have sufficiently demonstrated experience or interest
in dental public health as assessed by the AAPHD and the American Board of Dental Public Health
(ABDPH). Only full members are allowed to hold office or vote on issues related to the specialty. The
ABDPH was established in 1950 and recognized as the national certifying board in 1951.
Requirement 2
• Educational preparation for dental public health (DPH) includes successful completion of graduate-level
coursework in public health, including masters or doctoral level courses in epidemiology, biostatistics, health
care policy and management, environmental health, and behavioral sciences. These courses are generally
not included in predoctoral dental curricula.
Requirement 3
• Dental Public Health is the only specialty focused on population health. The body of knowledge and skillsets
are distinct from those involved in all other dental specialties.
Requirement 4
• A large proportion of DPH specialists are employed in academic or research institutions and are active
researchers in the field. DPH specialists were heavily represented among the editors and authors of the
upcoming 2021 Surgeon’s General Report on Oral Health. The Journal of Public Health Dentistry is among
the world’s most widely known and recognized peer-reviewed scientific journals in its field. The National Oral
Health Conference is the largest and most widely recognized scientific conference that focuses on DPH.
Requirement 5
• Dental Public Health is not a clinical specialty and advanced training does not provide training on specific
clinical procedures; however, the specialty directly benefits many aspects of clinical patient care through
research, health promotion, surveillance, and policy development. Dental Public Health specialists are
leaders in promoting oral health and providing care in underserved populations, thereby reducing the
burdens of oral disease in vulnerable populations who face challenges in accessing the oral health care
system.
Requirement 6
• Advanced education programs in Dental Public Health are accredited by CODA and are of at least two years
in length.
American Association of Endodontists
Requirement 1
• Membership is reflective of the specialty of endodontics. Voting members have completed a CODA-
accredited advanced education program in endodontics or were in good standing prior to January 1, 1985.
American Board of Endodontics (ABE) is the recognized certifying board for the specialty and has a close
working relationship with the American Association of Endodontists (AAE).
Requirement 2
•
Endodontics is the only specialty focused on diagnosis, prevention and treatment of pulpal and periradicular
diseases.
Requirement 3
• The scope of endodontics requires advanced knowledge and skills separate and distinct from other dental
specialties and cannot be accommodated through minimal modification of an existing recognized dental
specialty.
Requirement 4
• Endodontics continues to contribute to new knowledge in the field, professional education, research needs
and provision of oral health services.
Requirement 5
• The focus of endodontics is saving the natural tooth in a healthy, functional state that can be predictably
accomplished with appropriate diagnosis and treatment using all clinical approaches to endodontic care.
Requirement 6
• Currently, 56 CODA-accredited 2-3 year endodontic advanced education programs exist in the United
States and there are two (2) programs in Canada.
4
American Academy of Oral and Maxillofacial Pathology
Requirement 1
• Membership consists of practitioners, educators, residents, dental students, and other individuals holding a
professional or doctoral degree in a healthcare discipline or a student enrolled in a biomedical or healthcare
program. Only dentists who have completed a CODA-accredited advanced education program in oral and
maxillofacial pathology (OMP) and who have achieved Fellowship status in the American Academy of Oral
and Maxillofacial Pathology (AAOMP) either by passing the fellowship examination of the American Board of
Oral and Maxillofacial Pathology (ABOMP) certifying examination have the privilege of holding office and of
voting rights. The ABOMP and the AAOMP work in concert to ensure the continuing competency of oral
pathologists through continuing education and certification maintenance
Requirement 2
• The practice of oral and maxillofacial pathology includes research, diagnosis of diseases using clinical,
radiographic, microscopic, biochemical or other examinations, and evidence-based management of patients,
which is not included or taught at the predoctoral level.
Requirement 3
• Oral and Maxillofacial Pathology is the specialty of dentistry which deals with the nature, identification and
management of diseases affecting the oral and maxillofacial region and requires advanced knowledge and
skills that are unique, and well beyond those required of any other dental specialty. Such skills and knowledge
cannot be achieved through modification, minimal or otherwise, of any other recognized specialty.
Requirement 4
• The field of oral and maxillofacial pathology contains individuals who are recognized worldwide for their
expertise in oral and head and neck cancer diagnosis and pathogenesis, medication-related osteonecrosis
of the jaw, immune-mediated mucocutaneous diseases, and other pathologic processes and conditions,
local and systemic, with influence on the oral-maxillofacial complex. Oral pathologists (including residents)
contribute to advances in research that have implications for diagnosis and improved clinical practice.
Requirement 5
• Oral pathologists’ training and practice emphasize microscopic interpretation and diagnosis of tissue biopsy
specimens submitted by various healthcare providers in dentistry, medicine and surgical specialties. Oral
pathologists further bring their unique qualifications into the clinical setting, seeing patients referred by other
practitioners of dentistry, medicine and surgery, for diagnosis and management of local and systemic
disease processes and lesions manifesting in the oral mucosa and jawbones.
Requirement 6
• Oral and Maxillofacial Pathology has 14 CODA-accredited programs that are a minimum of three (3) years in
length.
American Academy of Oral and Maxillofacial Radiology
Requirement 1
• American Academy of Oral and Maxillofacial Radiology (AAOMR) bylaws limits voting privileges and the
ability to hold office to members who have completed a CODA-accredited Oral and Maxillofacial Radiology
(OMR) advanced education program. The AAOMR has a close working relationship with the American Board
of Oral and Maxillofacial Radiology (ABOMR) and both organizations collaborate closely on matters related to
education, certification and practice.
Requirement 2
• Oral and Maxillofacial Radiology practice requires in-depth knowledge of all imaging modalities used in
healthcare, including CT, MRI, ultrasound and nuclear medicine. It further requires knowledge of radiation
physics, biology and safety, and dento-maxillofacial disease pathogenesis that are beyond the education
provided in the predoctoral curriculum.
Requirement 3
• The depth and breadth of knowledge of imaging technology and interpretation provided by OMR programs
are well beyond that provided by other advanced education programs.
Requirement 4
• Oral and maxillofacial radiologists contribute significantly to multi-disciplinary teams and publish in diverse
areas including diagnostic imaging, radiation biology and technology development. Actively educates the
dental profession via CE, position statements and national conferences and is involved in promoting safe
and effective use of x-rays via collaborations with other organizations.
Requirement 5
• Patient care occurs through diagnostic imaging acquisition and interpretation services. With expanded use
of CBCT imaging in dentistry, demand for services has increased.
Requirement 6
• Advanced education programs accredited by CODA are a minimum of two (2) years in length.
5
American Association of Oral and Maxillofacial Surgeons
Requirement 1
• Governed by an 11-member Board of Trustees composed of five officers, including the president, president-
elect, vice president, treasurer and immediate past president, and six trustees, each of whom represents a
geographic membership district. Members must complete a CODA-accredited advanced education program
to be eligible for membership.
Requirement 2
• Oral and Maxillofacial Surgery (OMS) is the surgical specialty of dentistry with advanced education in
diagnosis, surgical intervention and adjunctive treatment of diseases, injuries and defects, involving
functional and esthetic aspects of hard and soft tissues of the OMS region that is beyond the education
provided in the pre-doctoral curriculum. Oral and Maxillofacial Surgeons are licensed to perform procedures
that are also performed by physicians.
Requirement 3
• Oral and maxillofacial surgeons provide a critical component of the contemporary scope of the profession
that includes: evaluation, diagnosis, prevention and/or treatment (nonsurgical, surgical or related
procedures) of diseased, disordered and/or conditions of the oral cavity, maxillofacial area and/or the
adjacent and associated structures and their impact on the human body. Oral and maxillofacial surgeons
treat such conditions as problem wisdom teeth (dentoalveolar surgery), facial pain (diagnosis and
management of craniofacial disorders), dentofacial/craniofacial abnormalities (correction of skeletal
deformities), severe facial injuries (trauma management and esthetic/cosmetic surgery), oral cancer
(management of malignant disease in the head and neck), and cleft lip/palate (reconstructive and
craniofacial surgery).
Requirement 4
• Through the various research conferences, committee work and research, American Association of Oral and
Maxillofacial Surgeons (AAOMS) has collaborated in the development of relationships between oral and
maxillofacial surgeons and researchers to bridge the gap between clinical and basic science. AAOMS has
researched medication-related osteonecrosis of the jaw (MRONJ) and developed a position paper to inform
practitioners, patients and other interested parties on the diagnosis, staging, and management strategies
regarding risks and benefits of medications related to osteonecrosis of the jaw. Advances in technology
have allowed certified OMSs to utilize an upper airway stimulation device for patients who suffer from
obstructive sleep apnea (OSA) and cannot tolerate positive airway pressure treatments.
Requirement 5
• Oral and maxillofacial surgeons are respected and valued members of the health care team. They maintain
active staff privileges with local and regional hospitals in their community and practice in a variety of settings
including private clinical practice, ambulatory surgical centers and hospitals. OMSs may also be found
contributing their talents in academia, military service, or in dental research and industry.
Requirement 6
• Oral and Maxillofacial Surgery advanced education programs are accredited by CODA and are a minimum
of four (4) years in length. In addition to their OMS training, whether residents are in an MD-integrated or a
single-degree-training program, all residents are required to complete the same surgical training, including
the core surgical year.
American Association of Orthodontists
Requirement 1
• Only active American Association of Orthodontists (AAO) members in good standing are eligible to seek or
hold office or other elective or appointive positions in the association, or to vote or otherwise participate in
the selection of Association officials or the establishment of policies. Membership is reflective of the
specialty who complete a CODA-accredited advanced education orthodontic program, pass the National
Dental Specialty Examination administered by The Royal College of Dentists of Canada, or successfully
complete the educational requirements established by the AAO.
Requirement 2
• The skills and knowledge acquired in an advanced dental education program include the diagnosis,
prevention, interception and correction of malocclusion, as well as neuromuscular and skeletal abnormalities
of the developing or mature orofacial structures that are beyond the education provided in the predoctoral
curriculum.
Requirement 3
• Orthodontics and Dentofacial Orthopedics is the only specialty whose definition specifically addresses the
diagnosis, prevention, interception, and correction of malocclusion as well as neuromuscular and skeletal
abnormalities of the developing or mature orofacial structures.
6
Requirement 4
• The AAO Foundation provides support to orthodontic education programs and orthodontic research and has
award programs for contributing new knowledge and educational research. The AAO’s Practice-Based
Research Network Committee works with the National Dental Practice-Based Research Network. The
committee conducted an Anterior Open Bite Study in 2016-2018, and from this study, three articles were
published in nationally recognized orthodontic journals. Currently, the committee is submitting three studies
for the Network’s current funding cycle: a Class II study, a cleft palate study and an aligner study.
Requirement 5
• The AAO’s Clinical Practice Guideline Review Committee maintains guidelines of clinical care.
Requirement 6
• Orthodontics and Dentofacial Orthopedics has advanced education programs accredited by CODA that are
at least 2 years in duration.
American Academy of Pediatric Dentistry
Requirement 1
• The American Academy of Pediatric Dentistry (AAPD) is made up of specialists with CODA-accredited
advanced education training and represents pediatric dentistry. Affiliate membership is specified in AAPD
Bylaws. The AAPD maintains a close working relationship with the American Board of Pediatric Dentistry
(ABPD).
Requirement 2
• Pediatric dentistry is well-defined, requiring knowledge/skills beyond those possessed by dental school
graduates.
Requirement 3
• Pediatric dentistry is an age-defined specialty that provides both primary and comprehensive preventive and
therapeutic oral care for infants, children and adolescents, including those with special health care needs
and to populations not seen by other specialists/general dentists. Like pediatricians and internists in
medicine, it provides treatment and health supervision. Application of knowledge and skills is in a
developmental, parent-engaged and socially-relevant context.
Requirement 4
• AAPD supports new knowledge and research supported through AAPD journals, the AAPD EBD process
and newly-organized IADR Pediatric Dentistry Section, AAPD Reference Manual triennial review process
and quinquennial update of the Handbook of Pediatric Dentistry. Presentations at annual sessions, support
of fellowship research and symposia support research by the specialty and profession.
Requirement 5
• Pediatric dentistry provides comprehensive surgical and primary health supervision for children including
diagnostic, preventive, surgical, restorative care and true primary prevention and developmental supervision
from age one through adolescence and for children with and without special health care needs.
Requirement 6
• Pediatric dentistry has advanced education programs accredited by the Commission on Dental Accreditation
that are at least two (2) years in length.
American Academy of Periodontology
Requirement 1
• The American Academy of Periodontology (AAP) maintains a membership that is representative of over
90% of periodontists in the United States as well as a significant number of international periodontists. The
right to vote and/or hold office is reserved to Active and Life Active members. The Bylaws define Active and
Life Active members; both membership categories require the individual to have completed an advanced
education program in periodontics that is accredited by CODA. The AAP has a close working relationship
with the American Board of Periodontology (ABP).
Requirement 2
• Periodontics is well-defined, requiring knowledge/skills beyond those possessed by dental school graduates.
Requirement 3
• The skills and knowledge required of a periodontist are specific, unique, and well established. The field of
periodontology has been advanced through rigorous, empirical research, continuing education, and
continuous evolution of training and study.
Requirement 4
• AAP supports rigorous scientific evaluation and studies that regularly contribute new knowledge to the field
and regularly supports consumer awareness about the importance of oral health and the role of the
periodontist in maintaining oral health and treating disease. The continuing education program supported by
AAP is robust and expansive.
7
Requirement 5
• The advanced training, study, research, education, and collaboration that the AAP engages in is focused on
advancing clinical care of patients and improving the understanding of periodontal disease.
Requirement 6
• There are 56 U.S. based CODA-accredited advanced education periodontal programs. Periodontal
postdoctoral education programs are all required to be a minimum of 30 months, with virtually all programs
now 36 months.
American College of Prosthodontists
Requirement 1
• American College of Prosthodontists (ACP) Members/Fellows are required to complete a CODA-accredited
advanced education program in prosthodontics. Members/Fellows have the privilege to hold office and vote.
Resident Members are eligible to vote, but not hold office. The ACP has a close working relationship with
the American Board of Prosthodontics (ABP).
Requirement 2
• The knowledge and skills acquired in the advanced dental education programs are related to treatment
planning, occlusion, fixed and removable prosthodontics, dental implant placement and rehabilitation,
maxillofacial prosthetics, biomaterials and patient management are beyond those possessed by dental
school graduates.
Requirement 3
• The scope of prosthodontics requires advanced knowledge and skills, separate and distinct from the other
recognized specialties in the restoration of oral/orofacial defects. Minimal modification of any other
recognized specialty would not provide the necessary advanced training to treat complex prosthodontic
patient needs.
Requirement 4
• Research designed and directed by prosthodontists positively impacts oral health services for the public.
Prosthodontic journals, such as the Journal of Prosthodontics, publish original research devoted to dental
materials, dental technology, diagnosis, advances in the design and use of dental implants and treatment of
unique patient conditions. Annual education programs showcase how technological advances in digital
dentistry aid diagnosis, prosthesis design and fabrication.
Requirement 5
• Prosthodontists provide health services, including diagnosis, treatment planning, rehabilitation and
maintenance of oral health, improved appearance and function of worn, diseased, mutilated or missing teeth
and/or orofacial structure in a variety of clinical settings for multiple patient populations.
Requirement 6
• There are currently 48 CODA-accredited prosthodontic programs in the United States and 3 CDAC-
accredited prosthodontic programs in Canada. All programs are a minimum of 33 months.
American Society of Dentist Anesthesiologists
Requirement 1
• ASDA membership has increased since 2018 when >60% of dentist anesthesiologists were ASDA
members. Active members may vote and are eligible to hold office. The American Dental Board of
Anesthesiology was recognized as the certifying board of Dental Anesthesiology in 2020.
Requirement 2
• Deep sedation and general anesthesia are beyond the scope of predoctoral training.
Requirement 3
• Dentist anesthesiologists’ advanced knowledge and skills are separate and distinct from those of other
recognized dental specialties and cannot be accommodated through minimal modification or combination of
currently recognized dental specialties.
Requirement 4
• Dentist anesthesiologists have significantly contributed to the creation and dissemination of new knowledge
related to clinical anesthesia care for dental patients including the very young and elderly, and those with
special healthcare needs, chronic pain, inability to receive local anesthesia and those undergoing invasive
procedures requiring additional anesthesia support. Patient safety and access to care for these often
underserved patient populations continue to be focal points. Dentist anesthesiologists also actively
participate in the development of guidelines and regulatory initiatives for dental office sedation and
anesthesia care.
Requirement 5
• Dentist anesthesiologists provide the full scope of pain and anxiety control for all areas of dental practice, in
offices, surgicenters, hospitals and educational institutions, increasing access to care for patients unable to
obtain medically necessary dental treatment without advanced anesthesia care.
8
Requirement 6
• CODA-accredited advanced education programs are three (3) years in duration.
Strategic Planning: In order to understand what each of the recognized specialties envisions as its future role in
improving and providing oral health services to the public; each of the recognized specialty sponsoring organizations
was requested to provide its organization’s mission statement, goals and strategic plan. The organizations were also
requested to include a brief summary highlighting the specific areas and efforts undertaken to promote quality in the
discipline over the last ten (10) years.
The National Commission found that not all of the recognized specialty sponsoring organizations had developed a
formal strategic plan. The recognized specialty sponsoring organizations that did have formal strategic plans provided
direction for continued growth and development.
Efforts to Promote Quality in the Discipline: The National Commission requested that each of the recognized
specialty sponsoring organizations provide information on the efforts the specialty has undertaken over the past ten
(10) years to promote quality in the discipline.
American Association of Public Health Dentistry
Over the past ten (10) years, the AAPHD has worked to improve and promote the quality of public health
dentistry by focusing on the application of knowledge and critical thinking in the Dental Public Health curriculum,
board examination and continuing education to ensure continued growth of the specialty.
• In 2015, the AAPHD and the American Board of Dental Public Health (ABPHD) convened a working
group to review the Dental Public Health competencies, which had been last updated in 1998.
• In 2017, the AAPHD began the process of updating Burt and Eklund’s Dentistry, Dental Practice, and
the Community, which is a major textbook in dental public health.
• AAPHD has provided multiple opportunities for continuing education through the annual National Oral
Health Conference, which has been jointly sponsored by AAPHD and the Association for State and
Territorial Dental Directors for over 20 years. An annual symposium is organized by ABDPH. Through a
collaboration with AIDPH, the annual colloquium which discusses cutting-edge topics in dental public
health. AAPHD also provides several online courses.
• AAPHD’s recertification program of diplomates ensures competency with the DPH standards and
current areas of dental
public health
• The Journal of Public Health Dentistry (JPHD), AAPHD’s official scientific journal, continues to be a
leading peer-reviewed journal on public health dentistry, promoting the quality of the discipline.
American Association of Endodontists
Over the past ten (10) years, AAE sought to establish and uphold a single standard of care for endodontic
treatment, with all root canals completed to the standard of the specialist.
• AAE defined competency in endodontic diagnosis, treatment planning, treatment, and prognosis and developed
treatment standards for imaging, access, disinfection, canal preparation, obturation, retreatment, restoration
• AAE developed a mobile case assessment application
• AAE biannually publishes ENDODONTICS: Colleagues for Excellence, provides education on current
clinical topics to educate dental students and general practitioners and enables assessment of
requirements for quality patient care at the standard of practice.
• AAEF provides care to underserved patients domestically and internationally, and in 2020 will surpass
a total of 7,000 patients served and 500 endodontic treatments performed.
Through the efforts of the AAE, AAEF, ABE, and College of Diplomates (COD), quality in the discipline is further
promoted via:
• Providing clinical resources: Guide to Clinical Endodontics, Glossary of Endodontic Terms, Guidelines
and Position Statements
• Being the premier resource for endodontic continuing education.
• Evaluating board certification protocol, maintaining integrity while streamlining processes,
resulting in increased certification rates and providing mentorship and courses to assist
endodontists in achieving board certification.
• Supporting endodontic educators’ professional development through grants, fellowships, CE, and
educator-specific communications and resources
• Advancing the quality of care through clinical research by standardizing a core set of desired patient-
and clinician-based outcomes that are intended to drive clinical research and establish an evidence base.
9
American Academy of Oral and Maxillofacial Pathology
Lifelong learning is a cornerstone of the profession of Oral and Maxillofacial Pathology, especially since a majority
of the members serve as dental faculty, actively contributing to professional education by providing foundational
and continuing education courses and performing health services as oral pathologists. AAOMP is invested in
informing dental and other health care professionals about best practices concerning diseases affecting the oral and
maxillofacial region.
The AAOMP:
• Defined the parameters of care through position papers on bisphosphonates and osteonecrosis of the
jaw, diagnostic aids used in the detection of oral cancer, policies on excised tissue, oral lichen planus,
and is currently tackling diagnostic guidelines for proliferative verrucous leukoplakia.
• Promoted quality within the discipline by surveying the needs of members related to Continuing Education (CE)
courses at its annual meetings.
• Invited a diverse array of expert pathologists and respected clinicians to present courses to the
Academy with the focus on keeping members abreast of emerging oral/general health issues,
innovative methodologies in pathology, and ensuring a broad range of both clinical and surgical
pathology.
• Through its Education Committee annually assembles a Continued Competency Assurance examination
with challenging clinical, radiographic and microscopy-based cases.
• Maintains a slide-based continued competency program. Members must participate in at least one of these
programs annually and take 40 hours of pathology-based CE every two (2) years to maintain board
certification.
American Academy of Oral and Maxillofacial Radiology
Over the last several years, AAOMR has invested considerable effort toward enriching the educational content
provided at the Annual AAOMR Session, aimed to enhance the level of OMR patient care provided in dentistry.
• Newly incorporated content areas include contemporary head and neck and maxillofacial imaging
delivered by world leaders in education and clinical care, Interdisciplinary clinical care in endodontics,
TMJ and facial pain, craniofacial imaging and biology, implant treatment planning, orthodontic evaluation
and sleep apnea workshops on the role of OMRs in implementing emerging technologies such as CAD-
CAM and 3D printing
• Parameters of care: AAOMR provided financial support for drafting of NCRP Report 177: Radiation
protection in dentistry and oral and maxillofacial imaging, as well as initiatives to develop and
update guidelines for imaging in dentistry. It published position statements on CBCT imaging in
implant dentistry, endodontics, and orthodontics, and teleradiology in dentistry, participated on ADA
committees to provide recommendations on radiologic equipment and quality control and was a voting
member of the Standards Committee on Dental Informatics, an ADA-ANSI committee that develops
standards for imaging and health informatics.
American Association of Oral and Maxillofacial Surgeons
AAOMS has developed and implemented high quality professional educational meetings and resources as well as
opportunities for lifelong learning to improve and expand the educational continuum through clinical and practice
management skills and competencies in a diverse and evolving specialty.
• Published the Parameters of Care, which provides a means for assessing the appropriateness and
quality of a selected treatment modality applied to an identified clinical condition in patients treated by
oral and maxillofacial surgeons.
• Developed the Dental Anesthesia Incident Reporting System (DAIRS)
• Established the Oral and Maxillofacial Surgery Quality Outcomes Registry (OMSQOR)
• Released a white paper on opioid prescribing recommendations during the national opioid epidemic
• Developed the National Simulation Program to create practical simulation-based training courses and
assessments that will measurably increase the safety of sedation administration in oral surgery and
dentistry and built a state of the art 2.5 million dollar education and innovation center
at its headquarters
building.
• Established the Practice Base Research Network, a resource that has allowed oral and maxillofacial
surgeons to participate in relevant clinical research projects in their offices, provide data to support the
specialty and improve patient outcomes.
• Through various standing committees, conducted literature reviews and developed guidelines
highlighting the research conducted and expressing the association’s position on various issues such as:
Head and Neck Cancer Screening Prevention; Human Papillomavirus Vaccination; Tobacco and Electronic
Cigarettes; and Evaluation and Management of Obstructive Sleep Apnea.
10
American Association of Orthodontists
• AAO’s Clinical Practice Guidelines are reviewed and revised every three (3) years to incorporate current
evidence-based orthodontics research.
• The AAO Library has a qualified library staff to meet the information needs of AAO members. Over
the past 10 years, the library staff has conducted over 12,600 mediated searches for
members and
sent over 22,000 journal articles to members.
• The ABO sets the standard for the highest level of patient
care, promotes excellence in orthodontics
for all of its certified orthodontists, serves to protect the orthodontic specialty and encourages
orthodontists to achieve certification.
• The AAO is a participant in ADA’s Dental Quality Alliance (DQA) that uses a collaborative approach to
advance performance measurement as a means to improve oral
health, patient care and safety
through a consensus building approach.
• The AAO offers a wide variety of educational opportunities including live webinars, recorded webinars,
and AJO-DO tests. Approximately 2,066 courses have been uploaded to our site since 2011. The
number of views has been approximately 106,495. Since January 2019, 562 courses have been
added
with 81,019 views. All CE courses meet the ADA’s CERP guidelines.
American Academy of Pediatric Dentistry
• The AAPD Reference Manual has been in existence for three decades and contains policies, guidelines
and best practices that are updated on a triennial cycle. AAPD guidelines are used by most state
Medicaid programs and are a part of Bright Futures, the national health supervision guidelines for
children. It has been listed on the national quality assurance health guideline repository.
• In 2013, the Evidence-Based Dentistry (EBD) initiative was launched to refine AAPD’s commitment to
standard setting with evidence per federal requirements. Three (3) EBD clinical practice documents
have been published and three (3) more are in development.
• The AAPD provides regular continuing education programs in person and on-line. Members can create a
vital educational passport. An annual update on pediatric dentistry assists in making practice EBD-based
and contemporary.
• The ABPD assesses continued competency and the AAPD courses and CODA accreditation standards
support board certification.
• The majority of pediatric dentists hold hospital staff positions and are required to maintain qualifications.
• AAPD has a standing committee to advance the culture of safety in care of children, most recently
creating on-line COVID-19 advice and information. AAPD has partnered with certifying organizations
AAASF and the American Academy of Pediatrics to improve sedation safety and OSAP to advance
office safety.
AAPD is working with the AAOMS on its DAIRS surveillance registry.
American Academy of Periodontology
The AAP is committed to promoting quality in the profession through a multi-faceted approach utilizing scientific
innovation, robust continuing education, collaborative efforts among periodontal organizations, and rigorous
educational standards and practices.
• The AAP regularly partners with global periodontal organizations to strengthen scientific understanding of
the disease. The AAP has held joint workshops with the European Federation of Periodontology (EFP)
and collaborates regularly with the Japanese Society of Periodontology and Japanese Academy of
Clinical Periodontology.
• AAP continues to support scientific innovation through collaborative work with US partners. The AAP
collaborated with the US Centers for Disease Control and Prevention on the NHANES Periodontal
Disease Prevalence Study, released a joint statement in 2012 with the American Heart Association and
is participating the Surgeon General’s Report on Oral Health (2020).
• The Journal of Periodontology and Clinical Advances in Periodontics (CAP) are standard-bearers for the
profession. These publications continue to innovate, including moving to a large publishing house,
evaluating editorial positions and securing CAP’s indexing in MEDLINE.
• AAP’s CE offerings remain a centerpiece of periodontal scientific advancement. CE-based meetings and
conferences highlight cutting-edge science for members. CE programming is supplemented by ongoing
scientific projects such as the 2011 statement on comprehensive periodontal therapy; position papers
and statements on lasers, peri-implant disease, and moderate sedation; and development of Best
Evidence Consensus statements that are designed to provide consensus-based guidance on clinical
scenarios that may have limited existing evidence.
• AAP maintains a multi-faceted mechanism to ensure the profession is evolving and keeping pace through
integrated work with the education community, CODA and the American Board of Periodontology.

11
American College of Prosthodontists
The ACP continues to host vital CE to address the specialist’s needs and provide the latest updates on
prosthodontic patient management, techniques, treatments, digital dentistry, implant surgery, private practice
management, and the
latest evidence-based practices.
• Within the past 10 years, the ACP has created new CE courses such as the Practice Management
Course and Digital Dentistry Symposium to address the additional needs of practitioners and help them
stay informed of new and emerging trends.
• ACP Position Statements helps guide prosthodontists and the public by clarifying the specialty’s
position on various topics within dentistry.
• The Prosthodontic Parameters of Care have been updated, reflecting the evolution of the specialty over
the past 10 years.
• The ACP offers research grants to prosthodontic students/residents to advance basic scientific and
applied clinical knowledge in the specialty. The Sharry Research Competition provides the opportunity
for students/residents to be recognized for their completed research during training.
• The ACP assisted with major revisions to the CODA Standards for Prosthodontics that resulted in the
addition of competency standards for implant surgery and digital technology. Curriculum and additional
resources were developed around competencies, well-defined learning objectives, and an assessment
plan with measurable outcomes to help programs effectively implement digital technology into their
curriculum and ensure the quality of education.
American Society of Dentist Anesthesiologists
• In 2015, the CODA-accredited advanced education programs increased their complexity. The
duration of the programs increased to 36 months.
• In 2018, the ASDA Parameters of Care were revised and ASA Practice Guidelines for
Procedural Moderate Sedation and Analgesia were updated. Professional and educational
relationships were created with ASA and SAMBA.
• In 2019, ASDA supported AAPD/AAP Guidelines for Monitoring and Management of
Pediatric Patients Before, During and After Sedation for Diagnostic and Therapeutic
Procedures.
• The ASDA participates in the AASA NACOR database, which is the largest national anesthesia database
• Supports the ASA Anesthesia Patient Safety Foundation and established ASDA Dental Anesthesia
Patient Safety Foundation.
• The ASDA participated on the Council for Dental Education and Licensure Committee on
Anesthesia for the development of ADA Guidelines for Sedation and Anesthesia education and
training
• ASDA provided Interim Guidance For Dentist Anesthesiologists Practicing In The Office-Based Setting
During The COVID-19 Pandemic
• The ASDA Education and Research Foundation was established.
• ASDA’s Annual Scientific Session offer high-quality CE specific to Dental Anesthesiology
• ASDA’s IMPA-Partnership with the AGD provides continuing education in sedation, anesthesia, and pain control
• The ASDA provided continuing education in sedation, anesthesia and pain control for local,
national and international organizations, including state component dental societies and
dental schools.
• The ASDA initiated model legislation reform, a collaborative effort with a goal of developing safe
and fair sedation and anesthesia regulations
• The ASDA is an affiliate sponsor and expert content contribution for the peer-reviewed journal
dedicated to pain and anxiety control in dentistry-Anesthesia Progress
Specialty Membership and Certification: The National Commission requested that the recognized specialty
sponsoring organizations provide data and overview comments related to membership trends over the past ten (10)
years. The National Commission further requested overview comments on future membership trend forecasts for the
next ten (10) years.
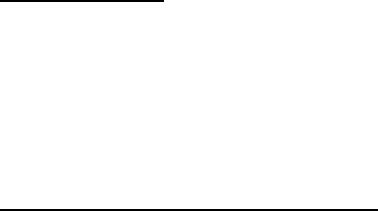
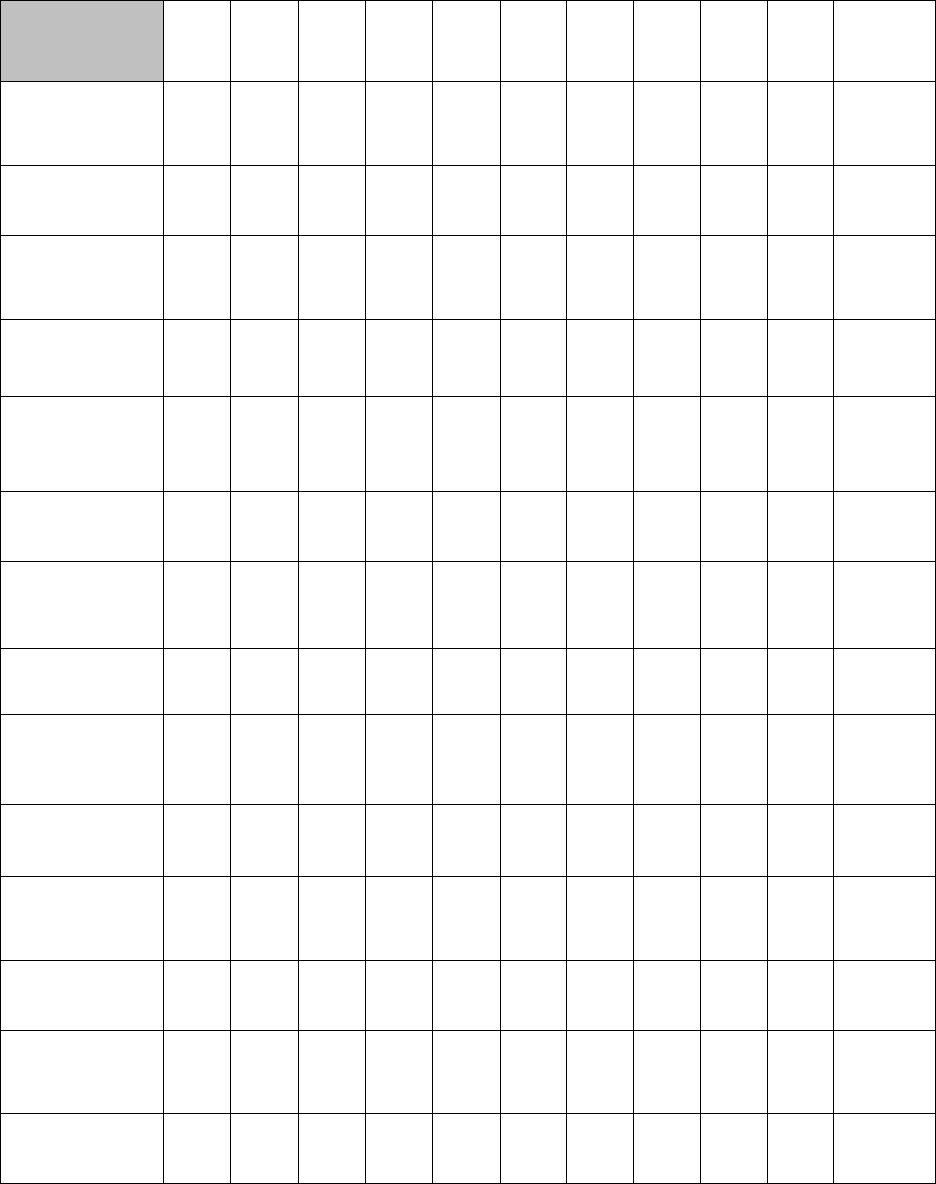
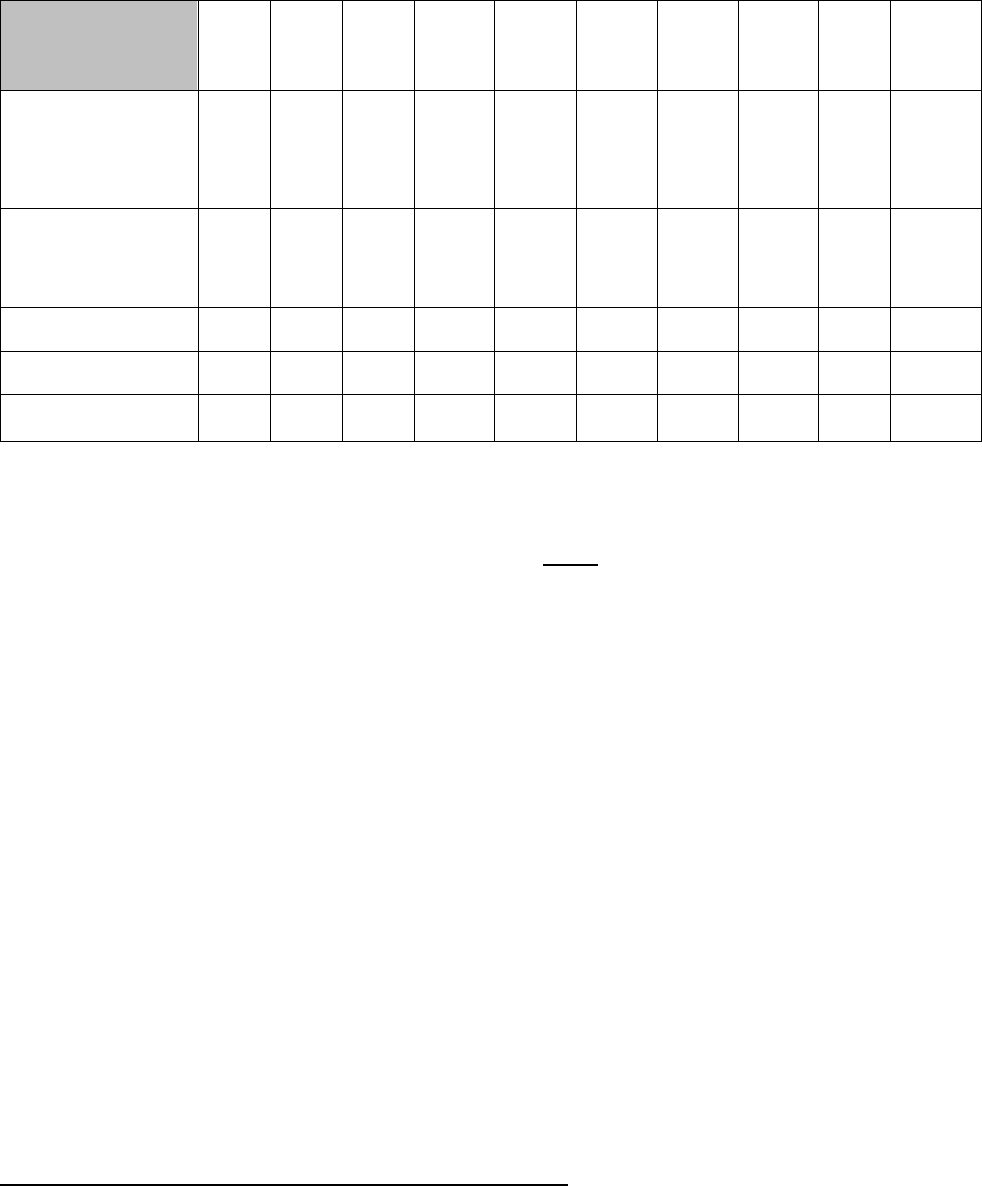
Table 2 reflects the recognized specialty sponsoring organization’s total membership figures over the last ten (10)
years, as reported by the organizations.
12
Table 2. Total Specialty Membership in All Membership Categories 2010-2019
2010
2011
2012
2013
2014
2015
2016
2017
2018
2019
2010-2019
%
Increase/
Decrease
AAPHD
0*
790
841
897
795
876
935
973
727
654
-17%*
AAE
7,219
7,386
7,520
7,692
7,650
7,889
8,015
8,013
8,055
8,099
+12%
AAOMP
580
563
560
573
542
545
560
569
534
531
-8%
AAOMR
291
N/A*
N/A*
397
399
441
298
351
349
377
+30%
AAOMS
7,348
7,429
7,498
7,606
7,737
7,783
7,801
7,849
7,973
8,034
+9%
AAO
16,357
16,643
17,096
17,281
17,758
18,089
18,946
19,014
18,955
19,332
+18%
AAPD
7,686
8,080
8,401
9,062
9,304
9,462
9,737
10,189
10,454
10,598
+38%
AAP
7,028
7,171
7,106
7,143
7,280
7,382
7,114
7,206
7,199
7,363
+5%
ACP
3,383
3,457
3,472
3,703
3,881
3,751
3,898
3,995
4,071
4,124
+22%
ASDA
274
267
261
328
370
384
387
393
356
391
+43%
*AAOMR was unable to retrieve the data for 2011 and 2012
*AAPDH was unable to retrieve data for 2010.
The National Commission noted that while some of the recognized specialty sponsoring organizations had minor
fluctuations in total membership over the course of ten (10) years, all but two (2) organizations had an overall
increase in membership. Overall, total membership across all the recognized specialty sponsoring organizations
increased from 50,166 members in 2010 to 59,503 members in 2019.
With regard to future trends:
• AAE projected a steady and modest growth rate of 0.5% to 2% annually over the next ten (10) years. While
roughly 100 members per year transition to Life and Retired membership annually, almost 200 newly
graduated endodontists convert to Active membership. Expansion in the International membership category
is expected to show the most significant growth in the next decade.
• AAOMR has devoted considerable effort toward membership retention by providing high-quality CE
programs and increasing member benefits. It is confident that recruitment and retention efforts will
continue to increase the membership numbers.
• AAOMS anticipates continued growth in total membership over the next ten years, as the incoming
members from graduating residents will exceed inactivated members.
• AAO noted that consistent, gradual growth is attainable and expected over the next ten (10) years as
more orthodontists are entering the market than are exiting.
• AAPD estimated that with current programs training pediatric dentists, there will be 10,600 pediatric dentists in
2030. The pediatric dentist to population ratio, currently 9 FTE/100,000 children, will increase to 14FTE/100,000,
but not in all U.S. regions.
• AAP noted that as the advanced education program periodontics see an increase in the number of international
students, the diversity of younger membership segments has evolved; however, as these students/residents return
to their home countries following graduation, the potential to maintain them as International members is growing.
• ACP noted that as experienced practitioners continue to retire, the ACP is committed to engaging the
next generation of prosthodontists as members of the organization, and leaders within the dental
community.
• ASDA anticipates an increase in its membership, related to increased interest in the discipline, an
increasing number of training programs, and retention of graduates from the training programs.
Membership Based on Gender and Ethnicity 2010-2019: The National Commission requested information on the
gender and ethnicity of the membership for each of the recognized specialty sponsoring organizations. Five (5) of the
ten (10) recognized specialty sponsoring organizations provided gender information. Further, with relation to ethnicity,
one (1) recognized specialty sponsoring organization started tracking the ethnicity of its membership in 2016, one (1)
recognized specialty sponsoring organization started tracking the ethnicity of its membership in 2019 and eight (8) of
the recognized specialty sponsoring organizations did not track ethnicity. Because very little data was available
related to gender and ethnicity from the recognized specialty sponsoring organizations, the data is excluded from this
report. The National Commission strongly encourages the recognized specialty sponsoring organizations to start
routinely tracking and gender and ethnicity data.
Active Diplomates: The National Commission monitors the recognized dental specialty certifying boards’
compliance with the Requirements for Recognition of National Certifying Boards for Dental Specialists through annual
13
reports provided by each of the recognized certifying boards. The National Commission provided each specialty
sponsoring organization with certification trend data collected via these annual reports. The National Commission
requested that each recognized specialty sponsoring organization review the certification data in collaboration with
their respective recognized certifying board and provide comments on significant trends.
The recognized specialty certifying boards are committed to the highest standards of practice including recertification
of diplomates, which provides a mechanism to assure these standards are maintained throughout the specialist’s
career. All of the recognized certifying boards require recertification with each of them determining their process.
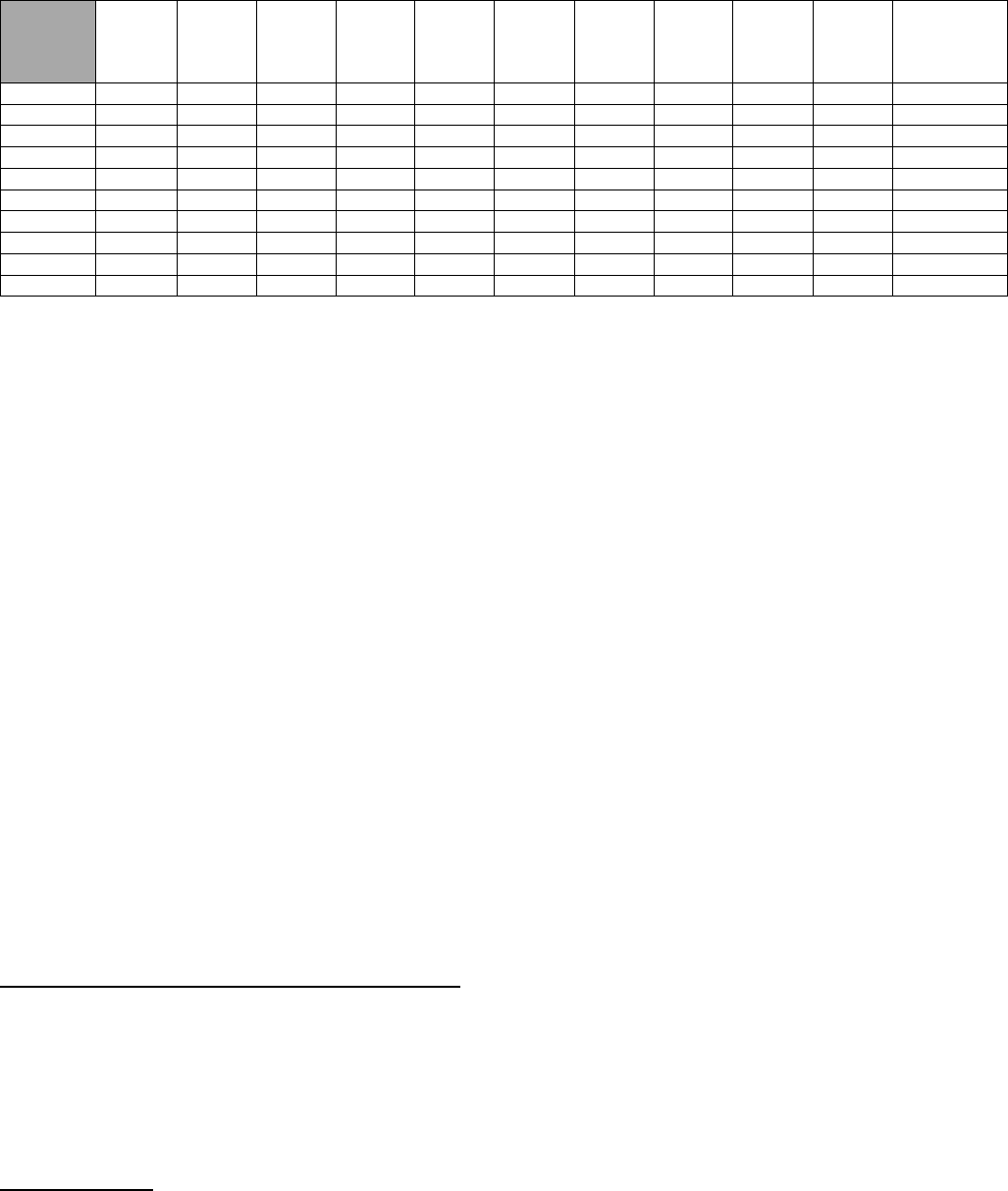
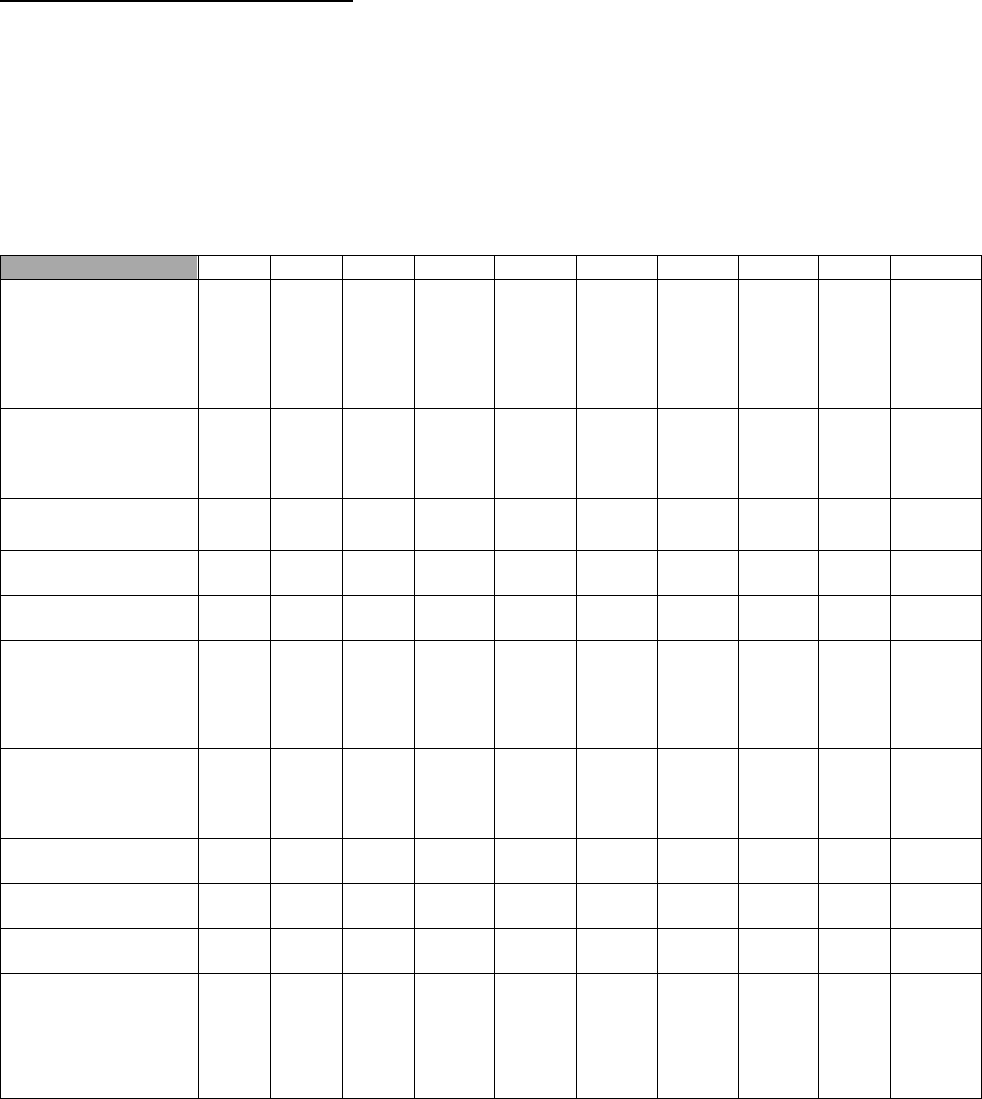
Table 3 reflects the number of active diplomates over the last ten (10) years, as reported by the respective certifying
boards.
Table 3. Active Diplomates 2009-2018
2009
2010
2011
2012
2013
2014
2015
2016
2017
2018
2009-2018
%
Increase/
Decrease
AAPHD
157
160
159
159
158
146
151
144
164
171
+9%
AAE
815
831
846
904
959
985
1075
1131
1189
1261
+55%
AAOMP
302
306
313
323
328
332
338
344
357
367
+22%
AAOMR
106
113
124
121
131
146
156
174
181
184
+74%
AAOMS
4616
4904
4983
5186
5096
5167
5219
5305
5305
5342
+16%
AAO
5164
5034
4858
4436
3163
3134
3266
3364
3504
3488
-32%
AAPD
2383
2726
3100
3509
4019
4323
4605
5011
5169
5880
+147%
AAP
2381
2506
2544
2648
2766
2598
2687
2782
2926
3047
+28%
ACP
1085
1141
1147
1176
1195
933
970
1011
1026
1058
-2%
ASDA*
N/A
N/A
N/A
N/A
N/A
N/A
N/A
N/A
N/A
N/A
N/A
*The National Commission did not recognize a certifying board for dental anesthesiology until 2020; therefore, no data was
available.
In general, eligibility for board certification is based on the completion of an advanced dental education program
accredited by CODA and experience in the field. To achieve diplomate status, all certifying boards require successful
completion of a written examination; all but the American Board of Oral and Maxillofacial Pathology (ABOMP) and the
American Board of Oral and Maxillofacial Radiology (ABOMR) require successful completion of an oral examination,
and five (5) of the nine (9) recognized certifying boards require either a case history presentation or clinical
examination.
While not all specialists seek board certification, overall the number of active diplomates increased for all but two (2)
of the specialties. The National Commission noted that the number of active diplomates increased from 16,405 in
2009 to 20,798 in 2018, representing a 27% increase.
The National Commission noted a 32% decrease in active diplomats for orthodontics. In March 2005, the ABO
announced a one-time offering that ended in July 2007, which allowed all practicing orthodontists who successfully
passed the ABO Written Examination to receive an ABO certificate that was valid for 5 years. Within these 5 years,
these orthodontists were required to pass the ABO Clinical Examination to remain a Board Certified Diplomate past
the 5-year expiration. Many orthodontists signed up for the offer which is why there was a dramatic increase in
diplomates from 2005-2007. Unfortunately, many did not follow through; therefore, there was a large decrease in
diplomates at the end of 2012.
The National Commission further noted a 2% decrease in active diplomates for prosthodontics. The ACP reported
several discrepancies occurred in their active diplomates category, including a philosophical and managerial shift in
2014 which resulted in only active diplomates being reported, where previously the life diplomates were included
(2009-2013).
Future trends:
• The AAPHD noted the upward trend in the number of certified, active diplomates, and applications received.
This is encouraging and speaks well for the future of the specialty. With changes in the healthcare systems
and the need for continued surveillance of oral health diseases and conditions, the types of skills and
expertise it will require suggest an increased demand for Public Health Dentists.
14
• The AAOMR noted the number of active diplomates has increased significantly since 2009 and the
Academy expects this trend to continue for the foreseeable future, as the number of advanced education
programs continues to increase.
• As of January 2020, the ABOMS Certification Maintenance (CM) has changed to a continuous process of
learning, self-assessment and testing that occurs over a 10-year period, during which Diplomates must fulfill
specified requirements in certain years of the cycle. It is designed to affirm a surgeon’s continued
competency after certification and contains four areas of assessment.
• The AAO
noted that the number of orthodontic specialists seeking and qualifying for board certification has
steadily increased over the cited 10-year period and this trend is expected to continue for the foreseeable
future. It is anticipated that the majority of orthodontic specialists in North America will have become board
certified within the next few years.
• The AAPD supports the ABPD examination process with test-preparation continuing education which is
monitored by the ABPD. The trends in certification in terms of numbers bode well for the availability of
pediatric dentists who can qualify for the ever-increasing demand for board-certified clinicians in hospitals
and third-party programs. The growth in certified pediatric dentists who demonstrate continued competency
bodes well for the quality of health care provided to children and persons with SHCN as well as equitable
health care to underserved communities.
Certification and Examination Data 2009-2018: The National Commission monitors the recognized dental specialty
certifying boards’ compliance with the Requirements for Recognition of National Certifying Boards for Dental
Specialists through annual reports provided by each of the recognized certifying boards. The National Commission
provided each recognized specialty sponsoring organization with certification and examination trend data collected
via these annual reports. The National Commission requested that each recognized specialty sponsoring
organization review the certification and examination data in collaboration with their respective recognized certifying
board and provide comments on significant trends.
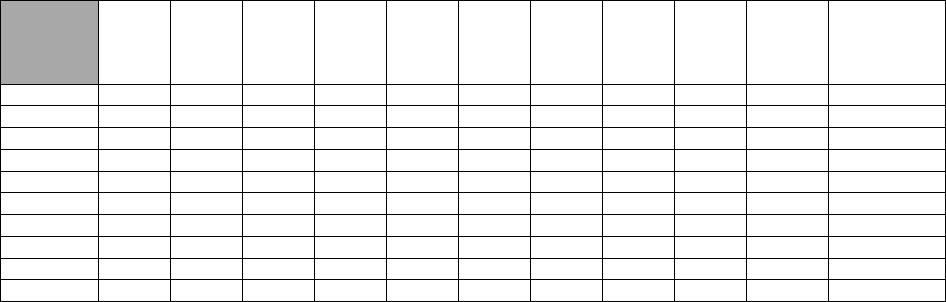
Table 4 reflects the certification and examination trend data over the last ten (10) years, as reported by the respective
recognized certifying boards.
Table 4. Certification and Examination Data 2009-2018
2009
2010
2011
2012
2013
2014
2015
2016
2017
2018
%
Increase/
Decrease
Dental
Anesthesiology*
Total Number
Certified By
Examination
N/A
N/A
N/A
N/A
N/A
N/A
N/A
N/A
N/A
N/A
N/A
Number of
Acceptable
Applications
N/A
N/A
N/A
N/A
N/A
N/A
N/A
N/A
N/A
N/A
N/A
DPH
Total Number
Certified By
Examination
292
297
299
299
306
317
325
333
345
354
+21%
Number of
Acceptable
Applications
8
9
10
9
16
12
9
11
14
15
+88%
ENDO
Total Number
Certified by
Examination
1,339
1,378
1,420
1,486
1,572
1,621
1,740
1,820
1,905
2,012
+50%
Number of
Acceptable
Applications
278
248
230
239
232
260
277
305
298
303
+9%
15
2009
2010
2011
2012
2013
2014
2015
2016
2017
2018
%
Increase/
Decrease
OMP
Total Number
Certified by
Examination
433
437
449
461
471
485
499
508
526
541
+25%
Number of
Acceptable
Applications
9
7
9
14
12
19
19
13
17
20
+122%
OMR
Total Number
Certified by
Examination
99
105
112
123
127
137
152
162
180
187
+89%
Number of
Acceptable
Applications
9
10
23
29
26
32
31
38
32
44
+389%
OMS
Total Number
Certified by
Examination
6,811
6,983
6,983
7,340
7,496
7,678
7,869
8,086
8,293
8,472
+24%
Number of
Acceptable
Applications
530
634
485
751
730
781
949
850
780
832
+57%
ORTHO
Total Number
Certified by
Examination
6,930
7,022
7,294
7,610
7,977
7,325
7,528
7,743
7,972
8,187
+18%
Number of
Acceptable
Applications
387
373
354
397
365
362
391
391
390
384
-0.8%
PEDO
Total Number
Certified by
Examination
2,501
2,908
3,322
3,750
4,178
4,532
4,879
5,275
5,761
6,217
+149%
Number of
Acceptable
Applications
336
377
355
365
333
394
371
467
446
475
+41%
PERIO
Total Number
Certified by
Examination
2,705
2,864
2,951
3,112
3,279
3,448
3,609
3,766
3,935
4,809
+78%
Number of
Acceptable
Applications
383
392
311
415
377
399
385
309
420
424
+11%
PROS
Total Number
Certified by
Examination
1,644
1,693
1,728
1,778
1,831
1,896
1,957
2,062
2,097
2,160
+31%
Number of
Acceptable
Applications
208
253
294
303
298
420
443
455
334
360
+73%
*The National Commission did not recognize a certifying board for dental anesthesiology until 2020; therefore, no data was
available.
The National Commission noted that the recognized certifying boards reported some minor fluctuations in the total
number of diplomates certified by examination and the number of acceptable applications over the ten (10) period;
16
however, overall all of the certifying boards showed some significant increases in the total number certified and the
number of acceptable applications. The National Commission did note a 0.8% decrease for Orthodontics in the
number of acceptable applications over the period but the overall number of acceptable applications remained
relatively stable over the ten (10) year period.
Board Eligibility Requirements 2009-2018: The National Commission monitors the recognized dental specialty
certifying boards’ compliance with the Requirements for Recognition of National Certifying Boards for Dental
Specialists through annual reports provided by each of the recognized certifying boards. The National Commission
provided each recognized specialty sponsoring organization with board eligibility requirement trend data collected via
these annual reports. The National Commission requested that each recognized specialty sponsoring organization
review the board eligibility data in collaboration with their respective certifying board and provide comments on
significant trends.
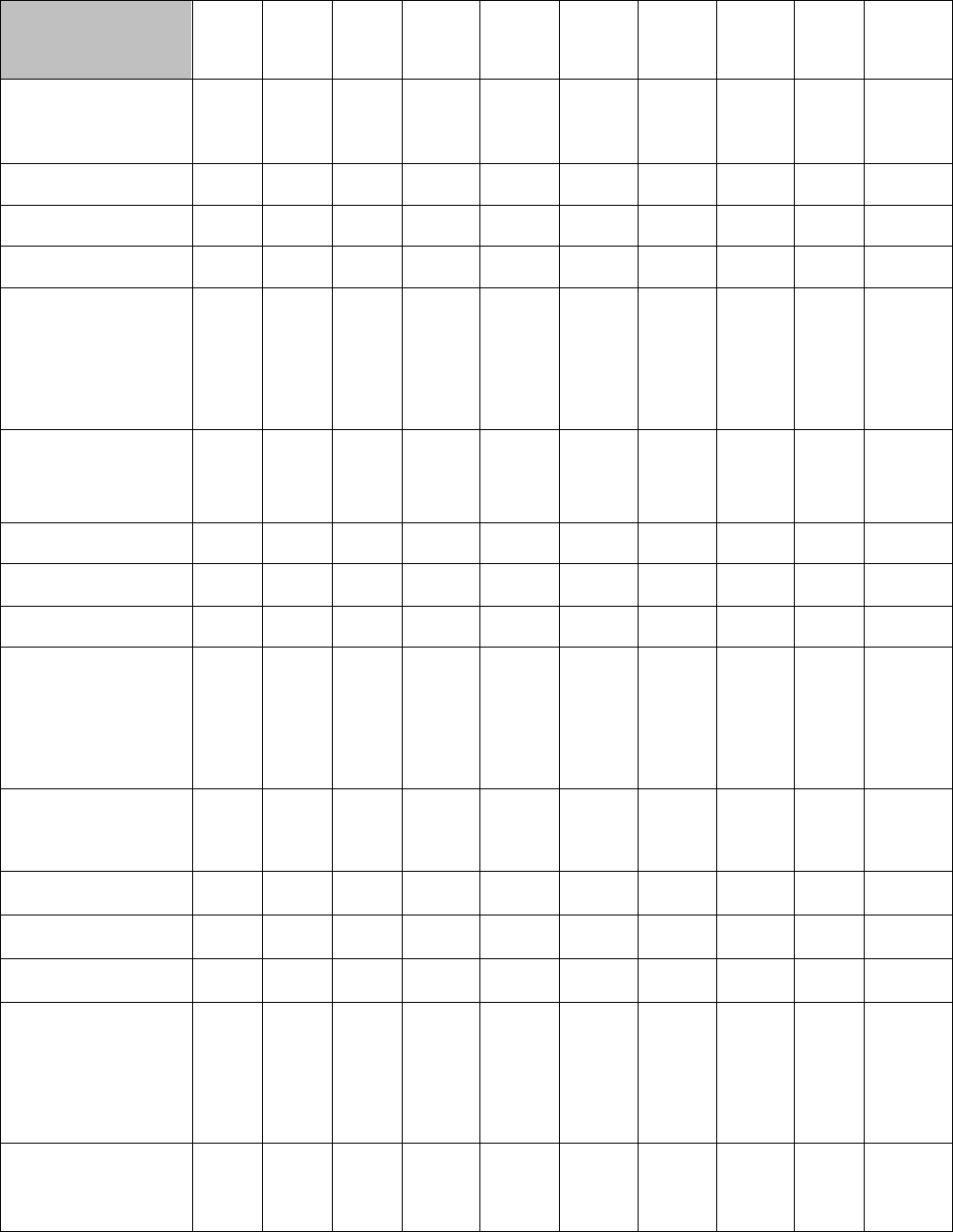
Table 5 reflects the certification and examination trend data over the last ten (10) years, as reported by the respective
certifying boards.
Table 5. Board Eligibility Requirements 2009-2018
2009
2010
2011
2012
2013
2014
2015
2016
2017
2018
Dental
Anesthesiology
Education-Years of
Advanced Education
in Addition to
DDS/DMD Degree
N/A*
N/A*
N/A*
N/A*
N/A*
N/A*
N/A*
N/A*
N/A*
N/A*
Experience-Total
Years of Specialty
Experience including
Advanced Education
N/A*
N/A*
N/A*
N/A*
N/A*
N/A*
N/A*
N/A*
N/A*
N/A*
Citizenship
Requirement
N/A*
N/A*
N/A*
N/A*
N/A*
N/A*
N/A*
N/A*
N/A*
N/A*
State Licensure
Requirement
N/A*
N/A*
N/A*
N/A*
N/A*
N/A*
N/A*
N/A*
N/A*
N/A*
Alternate Pathways to
Certification
N/A*
N/A*
N/A*
N/A*
N/A*
N/A*
N/A*
N/A*
N/A*
N/A*
Dental Public Health
Education-Years of
Advanced Education
in Addition to
DDS/DMD Degree
2
2
2
2-3
2-3
2-3
2-3
2-3
2-3
2
Experience-Total
Years of Specialty
Experience including
Advanced Education
4
4
4
3-4
3-4
3-4
3-4
3-4
3-4
3
Citizenship
Requirement
Any
Any
Any
Any
Any
Any
Any
Any
Any
No
State Licensure
Requirement
No
No
No
No
No
No
No
No
No
No
Alternate Pathways to
Certification
Yes
Yes
Yes
Yes
Yes
Yes
Yes
Yes
Yes
Yes
Endodontics
Education-Years of
Advanced Education
in Addition to
DDS/DMD Degree
2-3
2-3
2-3
2-3
2-3
2-3
2-3
2-3
2-3
2-3
17
Endodontics cont:
2009
2010
2011
2012
2013
2014
2015
2016
2017
2018
Experience-Total
Years of Specialty
Experience including
Advanced Education
4
2-3
2-3
2-3
2-3
2-3
2-3
2-3
2-3
2-3
Citizenship
Requirement
Any
Any
Any
Any
Any
Any
Any
Any
Any
Any
State Licensure
Requirement
No
No
No
No
No
Yes
No
No
No
No
Alternate Pathways to
Certification
No
No
No
No
Yes
Yes
Yes
Yes
Yes
Yes
Oral and
Maxillofacial
Pathology
Education-Years of
Advanced Education
in Addition to
DDS/DMD Degree
3
3
3
3
3
3
3
3
3
3
Experience-Total
Years of Specialty
Experience including
Advanced Education
3
3
3
3
3
3
3
3
3
3
Citizenship
Requirement
Any
Any
Any
Any
Any
Any
Any
Any
Any
Any
State Licensure
Requirement
No
No
No
No
No
No
No
No
No
No
Alternate Pathways to
Certification
Yes
Yes
Yes
Yes
Yes
No
Yes
Yes
No
Data
Yes
Oral and
Maxillofacial
Radiology
Education-Years of
Advanced Education
in Addition to
DDS/DMD Degree
2-3
2-3
2-3
2-3
2-3
2-3
2-3
2-3
2-3
2-3
Experience-Total
Years of Specialty
Experience including
Advanced Education
2-3
2-3
2-3
2-3
2-3
2-3
2-3
2-3
2-3
2-3
Citizenship
Requirement
Any
Any
Any
Any
Any
Any
Any
Any
Any
Any
State Licensure
Requirement
No
No
No
No
No
No
No
No
No
No
Alternate Pathways to
Certification
No
No
No
No
No
No
No
No
No
No
Oral and
Maxillofacial
Surgery
Education-Years of
Advanced Education
in Addition to
DDS/DMD Degree
4
4
4
4
4
4
4
4
4
4-6
Experience-Total
Years of Specialty
Experience including
Advanced Education
5
5
5
5
5
5
5
5
5
5
18
Oral and
Maxillofacial
Surgery cont:
2009
2010
2011
2012
2013
2014
2015
2016
2017
2018
Citizenship
Requirement
Any
Any
Any
Any
Any
Any
Any
Any
Any
Any
State Licensure
Requirement
No
Yes
Yes
Yes
Yes
Yes
Yes
Yes
Yes
Yes
Alternate Pathways to
Certification
No
Yes
Yes
Yes
Yes
Yes
Yes
Yes
Yes
Yes
Orthodontics
Education-Years of
Advanced Education
in Addition to
DDS/DMD Degree
2-3
2-3
2-3
2-3
2-3
2-3
2-3
2-3
2-3
2-3
Experience-Total
Years of Specialty
Experience including
Advanced Education
2-3
2-3
2-3
2-3
2-3
2-3
2-3
2-3
2-3
2-3
Citizenship
Requirement
Any
Any
Any
Any
Any
Any
Any
Any
Any
Any
State Licensure
Requirement
No
No
No
No
No
No
No
No
N/A
N/A
Alternate Pathways to
Certification
No
No
No
No
No
No
No
No
No
No
Pediatric Dentistry
Education-Years of
Advanced Education
in Addition to
DDS/DMD Degree
2-3
2-3
2-3
2-3
2-3
2-3
2-3
2-3
2-3
2-3
Experience-Total
Years of Specialty
Experience including
Advanced Education
2-3
2-3
2-3
2-3
2-3
2-3
2-3
2-3
2-3
2-3
Citizenship
Requirement
Any
Any
Any
Any
Any
Any
Any
Any
Any
Any
State Licensure
Requirement
No
Yes
Yes
Yes
Yes
Yes
Yes
Yes
Yes
Yes
Alternate Pathways to
Certification
Yes
Yes
Yes
Yes
Yes
Yes
Yes
Yes
Yes
Yes
Periodontics
Education-Years of
Advanced Education
in Addition to
DDS/DMD Degree
3
3
3
3
3
3
3
3
3
3
Experience-Total
Years of Specialty
Experience including
Advanced Education
3
3
3
3
3
3
3
3
3
3
Citizenship
Requirement
Any
Any
Any
Any
Any
Any
Any
Any
Any
No
State Licensure
Requirement
No
No
No
No
No
No
No
No
No
No
Alternative Pathways
to Certification
No
No
No
No
No
No
No
No
No
No
19
2009
2010
2011
2012
2013
2014
2015
2016
2017
2018
Prosthodontics
Education-Years of
Advanced Education
in Addition to
DDS/DMD Degree
3
3
3
3
3
3
3
3
3
3
Experience-Total
Years of Specialty
Experience including
Advanced Education
3
3
3
3
3
3
3
3
3
3
Citizenship
Requirement
Any
Any
Any
Any
Any
Any
No
No
No
N/A
State Licensure
Requirement
No
No
No
No
No
No
No
No
No
N/A
Alternate Pathways to
Certification
No
No
No
No
No
No
No
No
No
N/A
The National Commission noted that overall the board eligibility requirements have remained fairly consistent over
the past ten (10) years. The recognized specialty certifying boards are committed to increasing the number of board-
certified specialists and have created eligibility pathways to assist specialists who have practiced for many years and
internationally trained specialists who are not graduates of CODA-accredited advanced education programs to
pursue diplomate status. The following recognized certifying boards do not have alternative pathways to certification
oral and maxillofacial radiology, oral and maxillofacial surgery, periodontics and prosthodontics.
Trends:
• The ABE collaborates at least annually with other specialty certifying boards to ensure that they are on track
for an equitable application, examination and recertification process. Over the past decade, these processes
created improvements for both policies and exams and have helped them to increase our overall number of
Board-certified endodontists.
• The ABOMR continues to improve the quality of their exam items based on psychometric data analysis and
to strengthen the calibration and intra-and interrater reliability during the grading process. The exams are
updated yearly to incorporate new imaging guidelines and technology.
• The AAO’s Board Eligibility Requirements remain the same and it is expected that this condition will remain
the same over the next few years. Internationally educated specialists must still meet the specified
requirements for certification by the ABO.
• The ABPD and the AAPD work collaboratively to address issues/concerns that may be reported. Monitoring
and quality measurement ensure that changes in practice and education will continue to be evaluated in the
future. Psychometric analysis and feedback in both formal and informal channels support that the
requirements are supporting the specialty’s ability to address oral health needs of the public effectively,
using evidence-based guidelines and maximizing quality care
.
• Eligibility requirements for periodontists to pursue Board certification have not changed in recent years, and
no future changes are anticipated by the ABP. Although not specific to eligible candidates, beginning in
2017, the ABP implemented a new pathway for diplomates certified prior to 2003 to obtain an updated
certificate that references certification in periodontology and dental implant surgery.
• A recent change was made to the ABPROS examination eligibility criteria to increase candidate applications
by allowing students/residents to challenge two parts of the current four-part examination process upon
entering the 3rd year of the program compared to six months before graduation. The ABPROS closely
monitors the examination process and pathways to reflect current knowledge, skills and values in the
practice of prosthodontics and the approved curricula and standards for postdoctoral education.
II. MAJOR RESEARCH CHANGES AND TECHNOLOGY ADVANCES
The National Commission requested that each recognized specialty organization examine the impact of major dental
research and new technology in the specialty over the last decade. Specifically, each organization was requested to
list major research changes and technology advances over the last ten (10) years and provide an overview comment
on how these changes and advances have affected the practice of the specialty.
20
American Association of Public Health Dentistry
Major Areas of Research:
• Oral health disparities including social determinants of health and health inequality
• Relationships among oral health and other health conditions
• Interdisciplinary (dental-medical) workforce models to improve the oral health of the community
• Continued research in preventative and alternative approaches to prevention and care
Technology Advances:
• Teledentistry
• Mobile health in the delivery of preventative strategies and management of chronic diseases
• Informatics and data in genomics and precision oral health based on DNA
• Integration of medical and dental Electronic Health Records
Research in oral health disparities and inequities has shifted towards understanding social determinants of health as
risk factors for chronic disease and adverse oral health outcomes to gain a better understanding of the forces (such
as oral health literacy and cultural competence) at both the community and individual levels. Research and
knowledge about the relationships between oral health and other health conditions have been important in integrating
oral health and primary care, exploring workforce models incorporating interprofessional collaboration and integration
of dental care into primary care. This greater emphasis on dental-medical integration, such as integrating electronic
medical and dental records, has led to better management of health for patients and improved access to dental
services.
American Association of Endodontists
Major Areas of Research:
• Dental materials specifically bioceramics and nanoparticles
• Pain management with a focus on non-opioid approaches and head and neck pain classifications
• Endodontic microbiology
• Regenerative endodontics and revascularization
• Genetic influences, including host factors (systemic disorders, DNA polymorphisms and epigenetic events),
predisposition to pulpal and periapical disease and effect on treatment, and associations between
endodontic disease and systemic conditions.
• Dental trauma
• Diagnostic imaging techniques including cone beam CT (CBCT) and magnetic resonance imaging (MRI) for
guided surgery and endodontic access
• Vital pulp therapy
Technology Advances:
• Rotary files to facilitate safer and more predictable debridement of the root canal system, superflexible rotary
and reciprocating root canal preparation systems based on enhanced properties to improve the outcome of
non-surgical root canal therapy and retreatments with emphasis on anatomical canal preparation and dentin
preservation
• Canal obturation materials and techniques such as bioceramic sealers and single cone techniques
• Active canal irrigation using sonic energy, negative pressure and lasers
• Imaging modalities including small field CBCT and MR
• Surgical planning and guided endodontics using 3-D printing
• Computer software adapted to orient the operator during access of calcified canals or during surgery to
locate and treat the root end in a conservative and precise manner
Research has impacted the specialty by providing more predictable endodontic clinical procedures, better outcomes
for surgical and reparative procedures, better management of pain during and following treatment, improved
understanding of traumatic dental injuries, enhanced treatment options related to a better understanding of pulp
revascularization and endodontic regeneration and improved diagnostic and treatment modalities. These technological
advances have prompted the integration of state-of-the-art basic, clinical and translational research approaches to further
advance knowledge of the underlying mechanisms and treatment outcomes of endodontic disease. These integrated
approaches have the potential to contribute to the development of more effective, patient-centered treatment strategies.
American Academy of Oral and Maxillofacial Pathology
Major Areas of Research:
• Identifying molecular changes predictive of the biologic behavior of OCSCCa and its precursor lesions
• Osteonecrosis of the jaws (ONJ) related to bisphosphonate and anti-metabolic agents used in the
management of osteoporosis and certain metastatic malignant neoplasms
Technology Advances:
21
• Next-generation sequencing (NGS) approaches
• Advanced microscopic techniques
• Novel methods to improve analysis of hematoxylin and eosin (H&E) stained slides
• Virtual microscopy
• Application of artificial intelligence in the interpretation of biopsied tissues
Through NGS technology, new tumor types and subtypes have been identified and new genetic mutations have been
characterized that have improved not only diagnostics but also the disciplines understanding of the underlying
molecular mechanisms related to disease etiopathogenesis.
NGS approaches are now used routinely in basic
research laboratories and are likely to be used more commonly in clinical settings as they continue to become more
affordable. Advanced microscopic techniques, such as super-resolution confocal microscopy, allow for the imaging of
tissue in incredible detail
. Many technologies have led to an enhanced analysis of H&E-stained tissue biopsies. For
example, dual-mode emission and transmission microscopy (DUET) and multispectral analysis tools improve image
quality and reduce costs. Together, these improved technologies will continue to revolutionize the development of
diagnostics. A tangible example of this is the development of a “simple” device that utilizes florescence-based
technology to distinguish benign mucosa from cancerous and precancerous lesions. Virtual microscopy is the ability
to digitize glass slides and the accompanying improvements in image viewing software, data storage, and sharing of
large files
. Technologies related to slide digitization have enhanced our ability to share slides of biopsy tissues in a
virtual forum.
American Academy of Oral and Maxillofacial Radiology
Major Areas of Research:
• Clinical research using CBCT
• Developing MRI and ultrasound for dental use
Technology Advances:
• As darkrooms have phased out, newer CCD, CMOS and PSP sensors with better diagnostic capabilities are
exploiting remote, Bluetooth, or Wi-Fi technologies
• Advancement in panoramic radiography allowing better resolution, automatic selection of the ideal focal
troughs and superior extraoral bitewing radiographs
• Developing artificial intelligence to streamline the diagnosis of common dental diseases (caries, periodontal
bone loss, and periapical lesions)
• Teleradiology
In the last decade, major changes have taken place in the delivery of dental care due to progress in oral and
maxillofacial radiology. Widespread availability of CBCT units has changed the way oral and maxillofacial radiologists
interact with other practitioners and how all branches of dentistry function and deliver care. CBCT units are now
essential equipment in oral surgery, endodontics, implant dentistry and orthodontic offices. In the last decade, several
dental PACS systems were introduced to facilitate academic, armed forces, and corporate dental practices. PACS
and HIPAA compliant file transfer services have significantly reduced consultation time.
Teleradiology is now widely
practiced where a dental practitioner can quickly consult with a radiologist.
American Association of Oral and Maxillofacial Surgeons
Major Areas of Research:
• Patient Safety and Surgery Quality, Personalized and Precision Medicine in Pain Management
• Precision Medicine in Head and Neck Oncology
• Business of Innovation in Oral and Maxillofacial Surgery
• Regenerative Medicine for Dentoalveolar Reconstruction
• Medication-related osteonecrosis of the jaw
Technology Advances:
• Upper airway stimulation device for patients who suffer from obstructive sleep apnea (OSA) and for those
whom cannot tolerate positive airway pressure treatments
• National Simulation Program to create practical simulation-based training courses and assessments to
increase the safety of sedation administration in oral surgery and dentistry
Through the various research conferences, committee work and research, the AAOMS has collaborated in the development
of relationships between oral and maxillofacial surgeons and researchers to bridge the gap between clinical and basic
science. The goal is to improve the care of oral and maxillofacial surgical patients through the advancement of translational
and clinical research. TMD research will identify multidisciplinary approaches necessary to the development and
implementation of safe and effective clinical treatments for TMD, as well as strategies to advance TMD research and
education. Advances in technology have allowed certified oral and maxillofacial surgeons to utilize upper airway stimulation
devices for patients who suffer from obstructive sleep apnea (OSA) and cannot tolerate positive airway pressure treatments.
22
American Association of Orthodontists
Major Areas of Research:
• Improvements in study design to provide stronger evidence, including more cohort studies and
randomized
control trials (RCTs)
• Genetic influences on orthodontic tooth movement and facial growth
• Potential methods for accelerating orthodontic tooth movement, including vibration, micro-osteoperforation,
and photobiomodulation
• Sleep Disordered Breathing and the effects of orthodontic treatment on airway
Technology Advances:
• Intraoral scanning, 3-D Printing, and fabrication of In-House Aligners
• CBCT Scanners – updating norms and treatment goals using 3-dimensional imaging
• Customized appliances and treatment outcomes, including customized fixed appliances and aligners due to
the rapid developments in 3-D scanning and printing
• Teledentistry – utilizing modern technology to remotely monitor treatment and communicate with patients
• Cloud Computing and Network Security
Improved study designs have provided a higher weight of evidence validating multiple orthodontic treatment
techniques. The advent of cost-effective, efficient, and patient-friendly intra-oral scanners has revolutionized
how practices can acquire 3D data. Combined with the reduced cost of 3-D printing many practices are
moving towards customized aligner therapy and customized fixed
appliances to truly individualize care to each
patient.
American Academy of Pediatric Dentistry
Major Areas of Research:
• Moved from a largely surgical to a comprehensive care model based on research over the last decade
• Evidence-based dentistry
• Created the first pediatric-specific evidence-based clinical guidelines in areas of vital pulp therapy in primary
teeth, use of pits and fissure sealants and use of silver diamine fluoride and fluoride varnish for the
management of dental caries in children
• Prevention, care compliance, motivational interviewing, and non-surgical address of dental caries
• Integrating patient and provider safety
• Interdisciplinary research to develop standards for practice
• Offering on-line information
• Workforce research to assess the effect of future care models, provider distribution and workforce trends on
children’s oral health.
Technology Advances:
• Zirconia technology
• New generation composites
• Advanced sedation medications
• Advanced pulpal agents for primary teeth
• Telehealth
AAPD’s policies, guidelines and best practices derived from research and its translation are incorporated into most
state Medicaid periodicity schedules driving oral health for the underserved. The policies and scientific care
recommendations are incorporated into Bright Futures, national guidelines directing health supervision of all children
in the U.S. Workforce studies and translation through advocacy into public training of pediatric dentists have helped
alter the DMFT distribution positively in children under 5 years of age and encouraged the rational placement of both
pediatric dentistry practitioners and faculty. The AAPD Pediatric Oral Health Research and Policy Center is nationally
recognized with its focus on access, equity, safety and is a resource for pediatric dental providers along with general
dentists, safety-net providers, insurers, and government for pediatric oral health data and the compilation of research
and technical briefs.
American Academy of Periodontology
Major Areas of Research:
• In 2017, the AAP adopted a new classification for periodontal and peri-implant diseases and conditions
based
on new evidence to more reliably diagnose and treat patients. This classification is also expected to enable
researchers to investigate etiology, pathogenesis, natural history, and treatment of the diseases and conditions
utilizing unified terminology
23
• Evidenced-based personalized/precision medicine as well as patient-centered therapeutic outcome assessment
using patient stratification
• The link between systemic diseases and periodontal and peri-implant diseases and conditions
• Novel anti-inflammatory therapeutics (resolvins) for the treatment of periodontal and peri-implant diseases
• Regenerative medicine and tissue engineering
Technology Advances:
• Advanced diagnostic tools (ultrasound technology, optical coherence tomography)
• Sequencing and artificial intelligence/machine learning technologies for analysis of immunology and microbiology
data
The new classification of periodontitis has been a major collective effort at the global scale to support the widespread
adoption of personalized medicine in Periodontics. Advances in microbiology and immunology have led to a better
understanding of the pathogenesis of periodontal and peri-implant diseases. This knowledge has been harnessed by
practitioners to optimize patient care in both diagnosis and therapeutic developments. Analytic technology using
computing capabilities has allowed the analysis of massive data sets. Developments in this line of research are
expected to enable a more comprehensive understanding of what causes dysbiosis and the relationships between
different systemic diseases and oral inflammatory diseases. Periodontal and peri-implant plastic reconstructive
procedures have greatly benefited from the introduction of new techniques and materials over the past decade
.
Tissue engineering-based applications for regenerative purposes have also advanced significantly, with the
continuous development of minimally invasive procedures; novel grafting biomaterials, scaffolds, and matrices;
molecular-based biologics; and cell-based therapy approaches.
American College of Prosthodontists
Major Areas of Research:
• Dental Materials
o FDA-approved resins for use in surgical guides and digital dentures
o Translucent zirconia
o Nanotechnology/nanoparticles to strengthen acrylic/composites resins
• Genetic and Tissue Engineering
o Tissue-engineered scaffolds for regeneration of oral tissues
o Alloplastic grafts (block bone and skin)
o Growth factors to stimulate bone formation
• Dental Implants
o Implant design and primary stability
o Influence of medications and systemic conditions on implant success
o Utility, survival rates, and complications of CAD/CAM abutments and Ti bases
o Angled screw channel abutments, loading and torqueing protocol
• Clinical Research
o Survival rates and complications of all-ceramic crowns
o Clinical behavior of monolithic zirconia full-arch restorations
o Immediate loading of implants
o Definition, etiology, and prevalence of peri-implantitis/mucositis
o Efficacy of the CAMBRA protocol
Technology Advances:
• Intraoral digital surface scans/intraoral scanners and desktop digital scanners, superimposition of digital
surface scans with CBCT facilitating implant surgical planning and placement, and scan bodies Implant
impressions
• Additive and subtractive manufacturing of dental prostheses with improved accuracy
• CAD software for virtual restoration design and implant placement
• CAD/CAM titanium bars and abutments
• In-office printing and milling prostheses, and printing frameworks for RPD’s
• Fabrication of complete dentures using additive and subtractive technologies, and fabrication of ceramic
crowns using additive technology
• Improved smile design software
New and improved dental materials, research, and major technological advances have positively influenced clinical
practice and applications in fixed, removable, implant and maxillofacial prosthodontics. Improvements in dental
materials have contributed to the longevity and esthetics of restorations. Genetics and tissue engineering research on
bone formation, and advances in implant surfaces, designs and clinical techniques, have improved surgical and
restorative outcomes. Dental implant-related research has focused on the influence of systemic conditions and
medications on implant success, improving surgical techniques/applications, restoration designs, biomechanics and
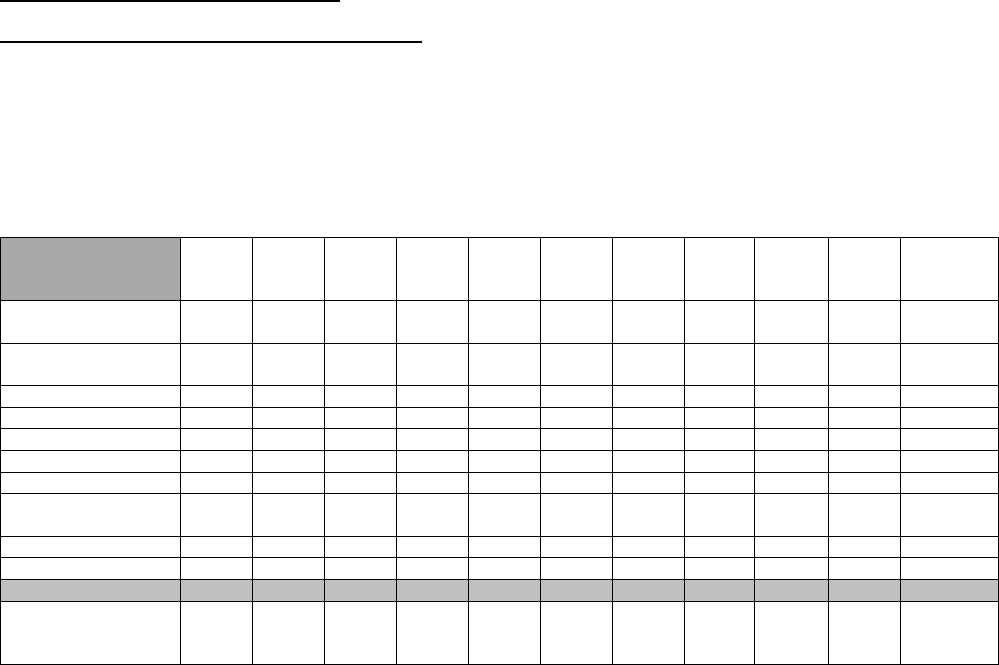
24
implant assessment tools. Clinical research on prevention, prostheses survival and complications has influenced
treatment decisions and improved longevity. Advances in digital technologies have had the greatest impact on the
practice of prosthodontics, enhancing diagnosis, treatment planning, presentation, workflow, execution and
techniques, interdisciplinary collaboration, patient awareness/education, and the efficient transfer of information.
American Society of Dentist Anesthesiologists
Major Areas of Research:
• New drugs, including Dexmedetomidine, for anesthesia and sedation
• Investigations into the prevalence, incidence, mechanisms and prevention of intraoral fires
• Written guidance for identifying and managing known and suspected COVID dental anesthesia patients
• Local anesthetic liposomes to improve the quality and duration of postoperative dental pain control
• The evaluation of both standard and new local anesthetic delivery systems
Technology Advances:
• Use of high-fidelity simulation training and cognitive aids to enhance the predictability and safety of office-
based anesthesia
Dental Anesthesiology is at the forefront of Office Based Anesthesia (OBA) with many of the techniques used and
described by dentist anesthesiologists having been adopted by physician anesthesiologists. Modern medications
such as dexmedetomidine, liposomal bupivacaine and remifentanil have aided in the concept of opioid-free
anesthesia and enhanced recovery after surgery (ERAS), both of which increase safety and patient satisfaction in
OBA. The improvements in high-fidelity simulation have aided in the training and the maintenance of skills and
knowledge of emergency situations.
The National Commission was impressed with the extensive, innovative and ground-breaking research the
recognized dental specialty sponsoring organizations have undertaken in the past ten (10) years. Without exception,
each recognized dental specialty is creating new knowledge and new ways to apply this knowledge, resulting in
better patient care.
III. TRENDS IN SPECIALTY EDUCATION
Number of Advanced Dental Education Programs: The National Commission requested that each recognized
specialty sponsoring organization review summary data collected over the last ten (10) years regarding the number of
advanced education programs, program enrollments and faculty and provide overview comments on past or future
education trends.
Table 6 reflects the number of advanced dental education programs, as reported by the American Dental
Association’s Health Policy Institute.
Table 6. Number of Advanced Dental Education Programs 2009-2019
2009
-
2010
2010
-
2011
2011
-
2012
2012
-
2013
2013
-
2014
2014
-
2015
2015
-
2016
2016
-
2017
2017
-
2018
2018
-
2019
Range
Dental
Anesthesiology
6
9
10
10
9
9
9
9
9
9
6-10
Dental Public
Health
10
10
12
12
13
15
15
15
15
15
10-15
Endodontics
54
54
55
55
56
56
56
56
56
55
54-56
Pathology
14
15
14
14
15
16
16
16
14
14
14-16
Radiology
5
4
5
6
7
8
8
8
9
9
4-9
Oral Surgery
102
103
102
102
101
101
101
102
102
101
101-103
Orthodontics
64
65
66
66
66
66
67
68
67
67
64-68
Pediatric
Dentistry
74
77
77
77
77
77
77
78
80
82
74-82
Periodontics
54
54
54
55
55
56
57
58
58
58
54-58
Prosthodontics
47
47
47
48
49
49
49
49
50
50
47-50
Total Number of
Programs
by Year
430
438
442
445
448
453
455
459
460
460
430-460
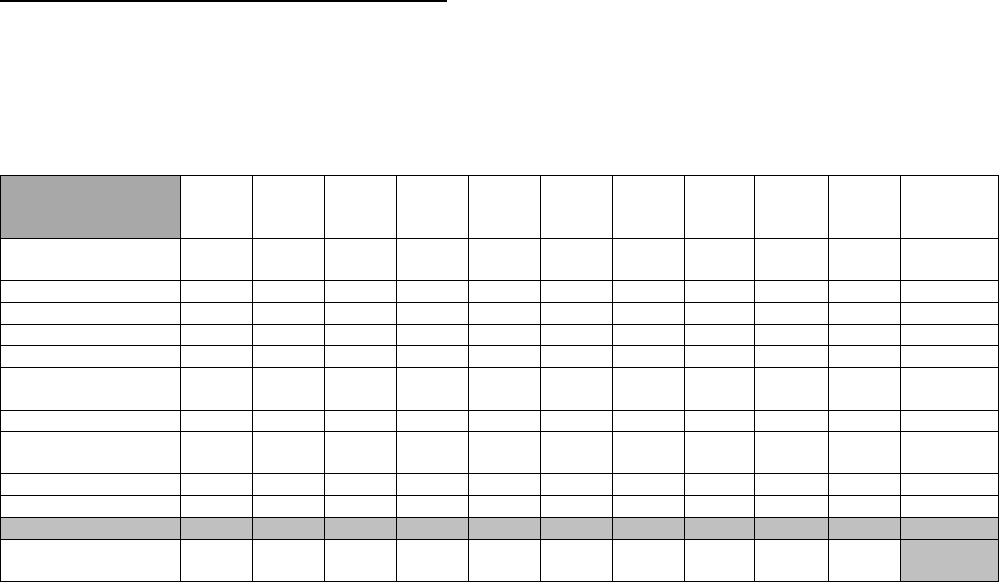
25
The National Commission noted that while there were minor fluctuations in the number of educational programs for
some of the disciplines, there was a steady increase in the number of advanced education programs across all of the
disciplines. Overall, the number of advanced education programs increased 7% between 2009-2019 from 430 to 460.
Trends:
• Dental Anesthesiology - From 2009 to 2011, the number of programs has held steady. Future growth in the
number of programs is anticipated following specialty recognition.
• Dental Public Health - In the past ten (10) years, four (4) new Dental Public Health advanced education
programs were accredited.
• Endodontics -
Numbers over the last decade indicate a healthy stabilization in the growth in the number of
programs. From 2000-2018, the number of programs increased by 17%.
• Oral and Maxillofacial Pathology - As with any specialty dominated by an academic role at dental schools,
the report shows a very slight fluctuation in the number of programs across the country.
This trend reflects
dental deans’ and dental schools’ desire for the continuation of existing programs and only minor increases
in additional training programs throughout the country.
• Oral and Maxillofacial Radiology - Since the last reporting period, the number of advanced education
programs has almost doubled.
• Orthodontics -The number of accredited advanced dental education programs in orthodontics increased by
6%.
• Pediatric Dentistry - Continues to grow to meet the demands of the oral health needs of children. Since
2008, the number of pediatric dental training programs increased 11%.
• Periodontics -
There was a 7% increase in the number of advanced dental education programs.
• Prosthodontics- The number of accredited advanced education programs increased by 6%.
Enrollment in Advanced Dental Education Programs: The National Commission requested that each recognized
specialty sponsoring organization review summary data collected over the last ten (10) years regarding enrollment in
the advanced education programs and provide overview comments on past or future education trends.
Table 7 reflects the enrollment in advanced dental education programs over the last ten (10) years, as reported by
the American Dental Association’s Health Policy Institute.
Table 7. Enrollment in Advanced Dental Education Programs 2009-2019
2009
-
2010
2010
-
2011
2011
-
2012
2012
-
2013
2013
-
2014
2014
-
2015
2015
-
2016
2016
-
2017
2017
-
2018
2018
-
2019
Range
Dental
Anesthesiology
25
35
43
63
66
69
81
76
87
79
25-79
Public Health
44
32
42
46
48
59
64
62
65
62
44-65
Endodontics
433
448
446
455
454
472
464
473
472
477
433-477
Pathology
40
42
47
52
53
48
48
44
52
56
40-56
Radiology
31
31
32
41
42
43
47
48
50
55
31-55
Oral Surgery
1040
1081
1081
1118
1131
1150
1170
1195
1199
1208
1040-
1208
Orthodontics
931
949
974
991
1010
1008
1023
1043
1064
1080
931-1080
Pediatric
Dentistry
733
763
803
823
844
879
900
921
940
955
733-955
Periodontics
541
544
541
550
556
563
551
565
568
575
541-575
Prosthodontics
455
455
453
467
459
463
463
467
477
496
455-496
Total Enrollment
Per Year
4273
4380
4462
4606
4663
4754
4811
4894
4974
5043
The National Commission noted that enrollment in all of the advanced education programs increased by 18% from
4,273 to 5,043 total students/residents. Notable is the 216% increase in enrollment in dental anesthesiology
advanced education programs. The National Commission further noted a 17% decrease in enrollment in the oral and
maxillofacial pathology programs from 2013-2017.
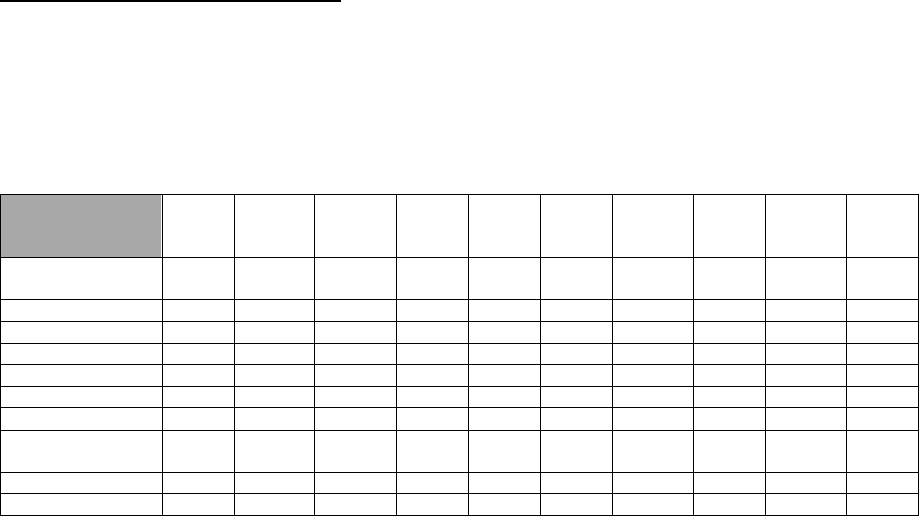
26
Trends:
• Dental Anesthesiology -Total enrollment numbers have steadily increased, due in part to the increased
duration of programs from 2 to 3 years
• Dental Public Health- In the last the past ten years, four (4) new Dental Public Health advanced education
programs were accredited.
• Endodontics - Numbers over the last decade indicate a healthy stabilization in the growth in the number of
enrollments, which increased16%.
• Oral and Maxillofacial Radiology is concerned that financial restrictions at higher education institutions due
to the COVID-19 pandemic may challenge the growth in the number of programs. However, they do not
anticipate a significant negative impact on our increasing numbers of graduates.
• Orthodontics -
The total number of enrolled students/residents per year increased by 20%.
• Pediatric Dentistry found that if current graduation and retirement trends continue, the number of full-time
pediatric dentists is expected to increase from 9 to 14 per 100,000 children by 2030.
• Periodontics -
Overall, the status of advanced education in periodontics remains stable with modest growth
in the number of graduates over the last ten (10) years. This trend is projected to continue in the coming
years.
• Prosthodontics -
Enrollment increased by 10%, while the applicants per program have increased by 60%
per the 2018-19 HPI Survey of Advanced Dental Education.
Advanced Education Program Directors: The National Commission requested that each recognized specialty
sponsoring organization review summary data collected over the last ten (10) years regarding the percentage of
advanced education program directors that are full-time and the number of program directors and provide overview
comments on past or future trends regarding this information.
Table 8 reflects the percentage of full-time program directors in the advanced dental education programs over the last
ten (10) years, as reported by the American Dental Association’s Health Policy Institute.
Table 8. Percentage of Program Directors That Are Full-Time 2009-2010
2009
-
2010
2010
-
2011
2011
-
2012
2012
-
2013
2013
-
2014
2014
-
2015
2015
-
2016
2016
-
2017
2017
-
2018
2018
-
2019
Dental
Anesthesiology
67%
67%
40%
50%
44%
56%
56%
56%
44%
67%
Public Health
100%
90%
92%
83%
85%
87%
87%
87%
80%
80%
Endodontics
98%
98%
98%
100%
100%
100%
98%
98%
98%
100%
Pathology
100%
100%
100%
100%
100%
100%
93%
93%
86%
93%
Radiology
100%
100%
100%
100%
100%
100%
100%
100%
100%
89%
Oral Surgery
99%
100%
100%
99%
100%
100%
100%
100%
100%
100%
Orthodontics
92%
89%
89%
88%
88%
88%
91%
93%
91%
91%
Pediatric
Dentistry
89%
86%
83%
86%
87%
84%
90%
91%
89%
87%
Periodontics
98%
98%
98%
96%
96%
98%
96%
98%
100%
98%
Prosthodontics
94%
96%
94%
96%
96%
94%
94%
96%
96%
96%
The National Commission is aware of concerns in the dental community related to faculty shortages and the need for
full-time program directors. Existing and projected faculty shortages have and will continue to plague all of the
advanced dental education programs. With the continued growth of new dental schools across the nation, the number
of advanced dental education programs is expected to grow, increasing the projected shortage of qualified faculty.
Trends:
• Endodontics - Challenges in recruitment and retention of qualified educators continue and the AAE has
continued to prioritize this issue by supporting legislation that incentivizes specialists to return to academia.
• Oral and Maxillofacial Radiology - The number of ABOMR-certified radiologists has increased, and it is
anticipated that the trend for an increase in the number of programs and/or enrollees will continue.
• Oral and Maxillofacial Surgery -
Over the last several years, some of the oral and maxillofacial surgery
residency programs have promoted junior faculty, who have recently obtained board certification, to the role
of the program director. AAOMS anticipates, with junior faculty acquiring leadership and administrative roles
within oral and maxillofacial surgery programs, the specialty will have a strong future of remaining compliant
with the accreditation standards that all programs be administrated by a board-certified program director.
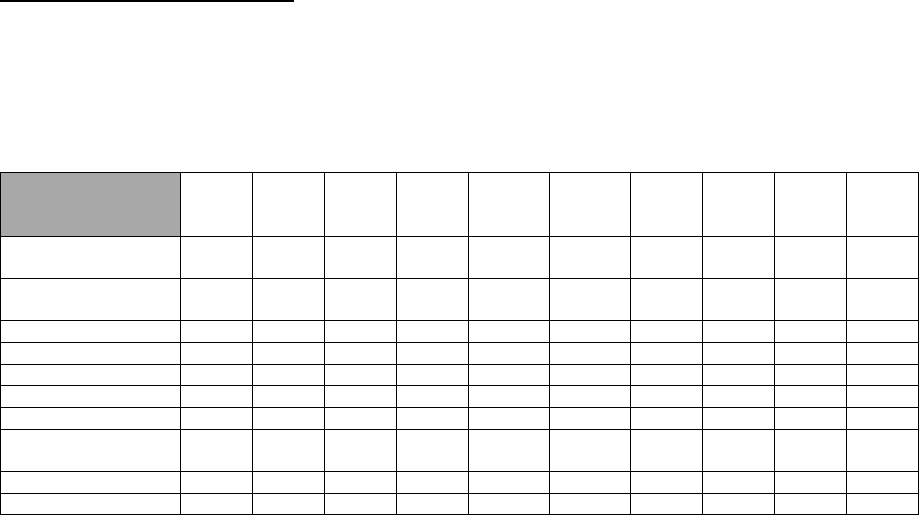
27
• Orthodontics – There is a growing trend is retired private practitioners starting second careers as full-time
faculty.
• Pediatric Dentistry -
Approximately 13% of program directors are in part-time academic positions. This is
problematic as a full-time, on-site, engaged program director is essential for the adequate training of
pediatric dental students/residents. Challenges in recruiting full-time pediatric dental faculty stem from the
student-loan burden incurred by new graduates and the lower salary earned in academics versus private
practice.
• Periodontics - Potential concerns for the future of advanced education include the number of qualified
faculty, decreases in funding, increases in tuition, and the increased burden on the education system due to
expanded requirements for infection control. The COVID-19 pandemic has exposed challenges in dental
education and the practice of dentistry in general. Stricter personal protective equipment requirements,
patient concerns about the safety of care, the overall priority given to care by patients with decreased
discretionary income, and the increased workload of the faculty have the potential to impact clinical
education. A potential positive from the COVID-19 pandemic is a shift towards smaller student cohorts and
more individualized teaching. While this may not be a permanent change, it currently provides benefits for
student education.
Board-Certified Program Directors: The National Commission requested that each recognized specialty
sponsoring organization review summary data collected over the last ten (10) years regarding the percentage of
board-certified program directors and provide overview comments on past or future trends regarding this information.
Table 9 reflects the percentage of board-certified program directors in the advanced dental education programs over
the last ten (10) years, as reported by the American Dental Association’s Health Policy Institute.
Table 9. Percentage of Program Directors That Are Board-Certified 2009-2018
2009
-
2010
2010
-
2011
2011
-
2012
2012
-
2013
2013
-
2014
2014
-
2015
2015
-
2016
2016
-
2017
2017
-
2018
2018
-
2019
Dental
Anesthesiology
100%
90%
90%
90%
100%
100%
100%
100%
67%
100%
Dental Public
Health
100%
100%
100%
100%
100%
93%
93%
100%
100%
100%
Endodontics
91%
92%
93%
96%
96%
98%
100%
96%
98%
98%
Pathology
100%
100%
100%
100%
100%
100%
100%
100%
100%
100%
Radiology
100%
100%
100%
100%
100%
100%
100%
100%
100%
100%
Oral Surgery
100%
100%
100%
100%
100%
100%
100%
99%
99%
100%
Orthodontics
98%
97%
97%
95%
94%
92%
97%
97%
99%
99%
Pediatric
Dentistry
91%
92%
95%
96%
95%
95%
96%
97%
96%
99%
Periodontics
93%
96%
96%
96%
98%
98%
98%
98%
97%
98%
Prosthodontics
100%
100%
100%
100%
100%
98%
96%
96%
98%
100%
The National Commission noted that overall the number of board-certified program directors in the advanced dental
education programs is close to or at 100%, which shows that the advanced education programs are attracting highly
qualified board-certified program directors. The National Commission recognizes the challenges facing the advanced
dental education programs in meeting faculty shortages.
Trends:
• Dental Public Health - All program directors, full-time and part-time, are required to be board-certified.
• Oral and Maxillofacial Radiology believes that the expanding pool of ABOMR-certified individuals will be
adequate to take on positions of program director created by the opening of new programs as well as by
attrition.
• Oral and Maxillofacial Surgery- The current Accreditation Standards for Advanced Dental Education
Programs in Oral and Maxillofacial Surgery accreditation standards require that the program must be
administered by a director who is board-certified.
• Pediatric Dentistry - The increase in board-certified program directors has been facilitated by changes in the
board-certification process, enacted in 2005, allowing a candidate to achieve certification in approximately
18 months through a written qualifying exam followed by an oral clinical exam.
• Orthodontics - An increasing number of full-time faculty are trained outside of North America who are not
eligible for board certification.
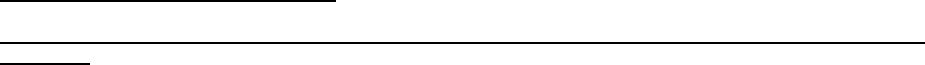
28
• Periodontics - The expectation for the next ten (10) years is that the number of Board-certified program
directors will continue to remain consistently close to 100%.
• Prosthodontics -
The current Accreditation Standards for Advanced Dental Education Programs in
Prosthodontics require program directors appointed after 1997 to be board-certified.
IV. CHANGES IN SCOPE OF PRACTICE
Incidence and/or Prevalence of Major Conditions Routinely Diagnosed and/or Treated by Practitioners in the
Specialty: The National Commission requested that each recognized specialty sponsoring organization highlight
recent epidemiological data or studies that establish the incidence and/or prevalence of major conditions routinely
diagnosed and/or treated by practitioners in the specialty and describe how these changes have affected the practice
of the specialty.
American Association of Public Health Dentistry
The practice of Dental Public Health (DPH) involves thorough knowledge of the epidemiology of all oral and
craniofacial diseases and conditions, their risk factors, indicators, and determinants at the individual and population
levels. The DPH specialist obtains, analyzes, and reports the epidemiologic data all other dental specialties diagnose,
prevent, and treat throughout the life course of an individual. These include dental caries, periodontal diseases, oral
cancer, and craniofacial anomalies. Despite advances in disease prevention, DPH practitioners are needed to
address disparities and social determinants of health to identify strategies, reduce gaps, and move toward oral health
equity. Dental Public Health plays essential roles in the design, implementation, and analysis of national health
surveys, such as NHANES, to advance understandings of health status, interactions between systemic health and
oral health, and access to dental care. The specialty also works with state and local health departments to implement
and improve state- and county-based oral health surveillance systems.
Epidemiological data collected and analyzed provide the basis for expanded roles for dentists, including DPH
specialists, in addressing health problems. For example, the marked increase in oropharyngeal cancer incidence has
led to expanded roles for dentists in promoting and delivering HPV vaccination for their patients. Data showing very
high expenditures for emergency department visits for non-traumatic dental conditions have led DPH practitioners to
work with payers and hospitals to reduce those visits.
American Association of Endodontists
The major conditions routinely diagnosed and/or treated by endodontists continue to be pulpal and periapical
disease. These conditions are the result of caries, dental trauma, periodontal disease, extensive restorations, tooth
fractures, or compromised host factors. Several studies indicate that the prevalence of apical lesions related to at
least one tooth in the adult population varies by country. The incidence of dental injuries has remained stable over the
past 25 years. The most recent study has estimated that up to 30% of all 18-year-old have sustained some type of
injury to their teeth. According to a recent study, one billion people have sustained a dental injury, ranking fifth on the
list of main chronic diseases and injuries, after caries, headache, anemia and hearing loss. Tooth fracture has been
described as a major problem in dentistry. For vertical root fractures in endodontically treated teeth, there is an
overall prevalence of 11%. There is a 6.8% incidence of cracked teeth in an endodontic specialty practice, Another
condition diagnosed and treated by endodontists is maxillary sinusitis of endodontic origin. Odontogenic sinusitis
causes nearly 50% of all unilateral sinus disease with maxillary sinus opacification.
American Academy of Oral and Maxillofacial Pathology
Oral cavity and oropharyngeal squamous cell carcinoma together represent a major cause of morbidity and mortality,
with an estimated 53,260 new cases and 10,750 deaths in the United States in 2020. Age-adjusted rates of new
cases and deaths continue to increase. Oral and maxillofacial pathologists have a unique understanding of the
clinical and histopathologic presentation and its precursor lesions and are responsible for educating dentists, dental
specialists and other health care professionals on the early diagnosis. Through ongoing research aimed at identifying
molecular changes predictive of the biologic behavior, oral and maxillofacial pathologists continue to lead prospective
studies that will guide treatment decisions and inform dental and medical colleagues and the public about the
strengths and limitations of oral cancer screening tools. Oral and Maxillofacial Pathologists continue to play a leading
role in understanding the risk factors, presentation and pathogenesis of osteonecrosis of the jaws (ONJ) related to
bisphosphonate and anti-metabolic agents used in the management of osteoporosis and certain metastatic malignant
neoplasms.
American Academy of Oral and Maxillofacial Radiology
The practice of oral and maxillofacial radiology has markedly changed over the last decade. Oral and Maxillofacial
Radiologists encounter a broad spectrum of diseases and conditions including jaw pathoses, odontogenic
inflammations, TMJ disorders, sleep disorders, dental and craniofacial anomalies and implant treatment planning.
Affordable high-resolution point-of-service CBCT imaging has increased almost 11% per year. The FDA’s NEXT 2017
29
survey estimates that there are approximately 5,500 CBCT units in the US, with more than 4 million examinations
performed annually. Dentists seek radiology consultations to opine on CBCT examinations/scans which often
encompass anatomic areas outside the dentoalveolar region (paranasal sinuses, cranium and cervical spine). The
trending increase in “digital dentistry” will also shape the scope of OMR practice, requiring expertise on the imaging
aspects of such technologies. The emerging field of artificial intelligence and machine-learning will impact the practice
of oral and maxillofacial radiology and increase efficiency and allow better use of imaging data in clinical decision
making.
American Association of Oral and Maxillofacial Surgeons
Advances in technology and virtual planning have been validated to improve patient outcomes and efficiency in the
surgical correction of dentofacial deformities and oncologic defects. Advances in hard and soft tissue regenerative
technology have led to explosive growth in the understanding and development of techniques to reconstruct
congenital and acquired defects of the oral and maxillofacial region that were previously not possible. Personalized
medicine in the era of biotechnology allows for individualized treatment specific to the genotype of both benign and
malignant diseases. Much focus is on pain management and understanding the influence of one enzyme, CYP2D6,
and its significant variability on patient response to opioids, understanding the advantages and disadvantages of
opioid use in temporomandibular joint pain and understanding the potential benefit of personalized pharmacogenetics
pain management. Initial results of a prospective study of subjects undergoing third molar removal revealed
significantly less opioid requirement for those that were extensive metabolizers compared to those that were partial
metabolizers. In addition, partial metabolizers had more adverse opioid effects. The potential to use testing to identify
genetic variations among individuals may provide the opportunity to personalize post-operative pain management to
obtain an optimal patient response and minimize adverse effects.
American Association of Orthodontists
Orthodontists principally diagnose and treat individuals with varying degrees of malocclusion and related skeletal and
structural discrepancies within the jaws. The World Health Organization estimates malocclusions as the third most
prevalent oral health problem, following dental caries and periodontal diseases. Recent surveys have demonstrated
that the prevalence of malocclusion in the general population is approximately: Class I 74%; Class II 21%; and Class
III 5%. Orthodontists have traditionally employed a variety of treatment strategies, appliances, and techniques to treat
these various types of malocclusions. While treatment strategies and techniques will continue to evolve, there is a
need for large orthodontic practice-based studies to help practitioners determine successful treatment options. For
example, in 2013 the AAO, through the National Dental Practice Based Research Network, had a practice-based
study funded on adult anterior open bite. This study highlighted how practitioners treat anterior open bite and what
treatment options were successful. Information was disseminated through journal articles, and a conference
dedicated to the topic was held in February 2020. A similar conference was convened in February 2019 on the topic
of Sleep Apnea and Orthodontics which resulted in the creation of a white paper on the topic.
American Academy of Pediatric Dentistry
Pediatric dentistry remains the specialty addressing oral health and dental caries in infants, children and adolescents.
Pediatric dental populations are skewed to younger ages, as pediatric dentists are willing to see infants and toddlers
and skilled at implementing professionally accepted early childhood oral health measures. A segment of pediatric
practice is creating a dental home, risk assessment, and well-child oral health supervision from the first year of life.
Early oral health care hasn’t been embraced by the general dental or pediatric medical community and likely will
remain a focus of pediatric dentistry. Recent U.S. caries prevalence data confirm its persistence, increase with age,
and disproportionate affliction in poor and minority populations. Early childhood caries plagues U.S. children with 1 in
10 under 5 years experiencing caries-related pain and needing advanced behavioral guidance skills of pediatric
dentists, which will likely continue through the next decade. Pediatric dentists disproportionately see Medicaid
children (>70%), manage their oral conditions and will likely continue to be the main source of care and health equity.
General anesthesia care of children has increased with penetration of caries into younger children. Most pediatric
dentists report hospital care as part of their practice. Sedation has increased due to denial of access to operating
room access; pediatric dentists provide this service by virtue of their training and ability to secure
licensure/certification. The percentage of children with special health care needs is growing with 100% of pediatric
dentists caring for children with special needs as well as many adults with special needs.
American Academy of Periodontology
It has been estimated that ~42% of the US population aged 30 to 70 years exhibit some degree of periodontitis;
34.4% of the population have mild to moderate periodontitis (Stage I and II, Grade A and B); and 7.8% have severe
periodontitis (Stage III and IV, Grade A, B, or C). Further, ~60% of adults aged 65 years and older have periodontitis.
Based on U.S. Census data from 2013-2017 these percentages translate to ~33.4 million and ~6 million people with
mild/moderate and severe periodontitis, respectively. Gingival recession is also highly prevalent in the U.S.
population. Recent investigations have indicated a thin gingival phenotype is associated with diminished thickness of
underlying bone and increased risk of recession and a thick phenotype appears more resistant to recession. Further,

30
the extent and severity of peri-implant diseases are influenced by different etiologic and predisposing factors. The
average prevalence of peri-implant mucositis at the patient level is ~47% and at the implant level ~38%. The
prevalence of peri-implantitis on a patient basis averages ~27% and on an implant basis ~18%. Undiagnosed,
untreated, or inappropriately treated periodontal and peri-implant diseases in the U.S. have become a significant
public health issue, particularly considering various associations of periodontitis on systemic health. There are also
concerns regarding social gradients of disease where economically disadvantaged individuals have limited access to
advanced therapies to treat these diseases. Epidemiologic studies have shown 11% of the world's population is over
60 years of age; this is projected to increase to 22% by 2050. With the aging population comes an increase in root
caries and periodontitis.
American College of Prosthodontists
Prosthodontists diagnose dental diseases, oral manifestations of systemic/autoimmune diseases, and coordinating
with medical/dental specialists to perform complex reconstructions. Edentulism remains a public health problem
worldwide. In the U.S., the number of edentulous individuals is 9 million with 25% of adults over 60 years of age
missing at least one tooth. Tooth loss may be congenital (oligodontia, ED, AI) or acquired (dental diseases, trauma,
cancer, systemic diseases with oral manifestations). Prosthodontists diagnose and plan implant prostheses, place
and restore dental implants and manage related complications. Prosthodontists treat dentate patients who exhibit root
caries secondary to xerostomia, tooth wear, TMJ/TMD, and sleep apnea. The highest prevalence of erosive tooth
wear is found in North America. Prosthodontists have in-depth knowledge in biomaterials and occlusion to diagnose,
treat, and maintain these patients. Oral cancer patient demographics are changing due to the influence of HPV-
related cancers, especially in younger patients. The prevalence is significantly reduced in vaccinated patients, but the
overall effect is modest due to low patient participation. Risk factors still include age, tobacco use, and alcohol
consumption. Prosthodontists are uniquely qualified with their training and expertise to treat the prosthetic needs of
head and neck cancer patients.
American Society of Dentist Anesthesiologists
Dental anxiety continues to be the strongest predictor of patient pain during general dental procedures. A 2018
survey of practice patterns for dentist anesthesiologists identified anesthesia for pediatric dentistry as the most
commonly-provided service, followed by anesthesia for oral surgical procedures and anesthesia for patients with
special health care needs. The provision of office-based anesthesia for pediatric dentistry and patients with special
health care needs is particularly important for increasing access to dental care for underserved populations. In
2012, the Pediatric Oral Health Research and Policy Center declared general anesthesia for the treatment of early
childhood caries an essential health benefit for United States citizens. A 2011 examination of the capacity of the
U.S. dental care system to treat children with special health care needs concluded the capacity to care for this
population is extremely limited. The demand for dentist anesthesiologists to assist dentists in meeting the needs of
these populations is well-documented, and access to care for these individuals continues to be a focus of the
specialty.
Principle Health Services Provided to the Public and Where the Services are Customarily Provided: The
National Commission requested that each specialty sponsoring organization identify the principal health services
provided to the public by individuals in the area of practice and whether this has changed in the past ten (10) years.
Further, the National Commission requested that each specialty sponsoring organization identify the setting(s) in
which these services are customarily provided and whether this has changed in the past ten (10) years.
American Association of Public Health Dentistry
The principal health services provided include research, education, health service administration, policy/program
development and quality assessment services. DPH specialists prevent oral diseases, work to reduce oral health
inequities and provide oral health expertise within the core public health activities of assessment, policy development,
and assurance. DPH specialists are involved in conducting public health surveillance for oral diseases and conditions
and disseminating the findings to policymakers and the public. Such activities result in the development and
evaluation of community-based oral health program, guidance for oral health advocacy (community water fluoridation
and workforce models) and stimulation of research on effective interventions for high-risk populations (Native
Americans, low socioeconomic status families, and nursing home residents). DPH specialists lead the creation of
population-based oral health promotion and prevention strategies that are implemented at the community level.
These include school-based oral health prevention programs (sealants and fluoride varnish); promotion of HPV
vaccine for adolescents to prevent oropharyngeal cancer; development of protocols to improve oral hygiene in long-
term care facilities; development of protocols for mobile dentistry and teledentistry; and development of materials on
the use of tobacco and e-cigarettes, opioid prescribing by dentists, and sugar consumption. DPH plays a critical role
in oral health coalitions and community partnerships to reduce the burden of oral diseases.
31
American Association of Endodontists
The principal health services provided to the public by endodontists continue to be non-surgical root canal treatments
and endodontic retreatments. Additionally, endodontists provide various surgical procedures, including surgical repair
of root resorption (internal and external), apexification, apicoectomies, bone grafts in conjunction with periradicular
surgeries, guided tissue regeneration, root generation, re-implantation (including splinting), auto-transplantation, root
submersion, decoronation, dental implants, hemisections and various associated procedures. With a commitment to
saving natural teeth, the last ten (10) years have seen an increased commitment to maintaining the vitality of as much
of the dental pulp as possible, with pulpotomies and other vital pulp therapies (VPT). Moreover, regenerative
endodontics, or the “idea that one can replace damaged structures and regain functionality in previously necrotic and
infected root canal systems” has seen significant advancements over the last decade. Endodontists also increasingly
provide diagnoses of cracked teeth and non-odontogenic diagnoses, for example, in the event of trigeminal neuralgia,
TMD, and myofascial conditions.
According to a 2015 report in the Journal of the American Dental Association, 13.5% of dentists worked in small
group practices and 10.2% worked in large group practices. The report further showed that 11.4% of solo
practitioners were oral surgeons, endodontists, or orthodontists. A 2019 survey of AAE members found that the most
common practice settings were private practice/solo (37%) or endodontic group practice (21%), followed by dental
school faculty (15%). Relatively few endodontists practiced in other settings: multi-specialty group practice-private
(5%); military/government practice (3%); independent contractor (2%); multi-specialty group practice-corporate (2%);
or some other setting (4%). Since the 2013 survey of AAE members, changes to practice settings of endodontists
have been small. The proportion who are solo private practice (38% in 2013) has changed only slightly, while fewer
today are in an endodontic group practice (21% in 2013) or are independent contractors (2% now, 5% in 2013), and
more are dental school faculty members (12% in 2013).
American Academy of Oral and Maxillofacial Pathology
Historically, the principal health services oral pathologists have engaged in include practicing clinical oral pathology
primarily in the dental school faculty practice setting, and participation in oral pathology biopsy services, based either
in dental or medical school laboratories, or affiliated hospital settings. However, the settings for these services have
been expanding. During the last ten (10) years, some seasoned dental faculty and some recent graduates of oral
pathology residencies who have been unwilling or unable to secure dental faculty positions have ventured into the
private practice arena either full or part-time, providing clinical oral pathology services. Some oral pathologists set up
their private biopsy services, and a few participate in private pathology laboratory services, including large
multispecialty group pathology laboratories. Increasingly, graduates of oral pathology residencies have opted for
additional training in head and neck pathology and research through fellowships based in hospital pathology
departments.
In a 2018 AAOMP Laboratory Services survey, oral pathologists reported that their services and laboratories were
based in dental schools (51.28%), hospital/medical centers (7.69%), medical schools (5.13%), or private or non-
hospital laboratories (35.90%). Notably, the percentage of pathologists practicing in private or non-hospital
laboratories as independent proprietors or affiliates with private corporations has increased significantly during the
past ten (10) years (14.3% in 2009, 35.90% in 2018). This shift towards the private sector is likely related to several
factors, including changes in insurance reimbursement and increasing constraints associated with practice in
academic and hospital venues. The AAOMP’s Fall 2019 manpower survey of the specialty revealed 73% of oral
pathologists are primarily employed as full- or part-time dental school faculty involved in teaching predoctoral
students and residents. Many also participate in and/or direct school-based biopsy services and clinical oral
pathology faculty practices. Roughly 18% have appointments as medical school faculty, and about 35% of oral
pathologists’ practices are either in hospital-associated, independent non-hospital practices or within corporate
pathology practices. A small but significant percentage of oral pathologists are based in the military (Army, 2%; Navy,
1%, Air Force, 0.35%). About 22% of oral pathologists are based in research facilities.
American Academy of Oral and Maxillofacial Radiology
The welfare of the public is a serious concern and important responsibility for the AAOMR. Ionizing radiation is the
primary tool used by oral and maxillofacial radiologists and the detrimental effects of diagnostic radiation are seen in
the population decades later. Dental offices use ionizing radiation daily, leaving a major footprint on public health. In
the past ten (10) years, OMR specialists and the AAOMR have taken multiple approaches to decrease radiation
exposure and to mitigate the effects on the public. AAOMR promotes education and research on the application of
non-invasive imaging methods, including MRI and ultrasound. Oral and Maxillofacial Radiologists are improving the
health of the public by assisting other dental practitioners with appropriate diagnoses of and management options for
complex diseases.
Patient care is provided in various settings including academic institutions, hospitals and private practices. In general,
practices offer imaging services as well as consultative radiology services, often by teleradiology. OMR services have
32
significantly increased in number and scope, which is in part, reflective of the expanded use of CBCT imaging,
include endodontic diagnosis and treatment planning, implant treatment planning, and TMJ imaging. The workflow
and physical configuration of radiological facilities have changed markedly in the last decade. The increasing
application of digital technologies has eliminated the need for darkrooms and chemical processing, changing the
traditional landscape of radiologic facilities. With handheld x-ray units, radiographic examinations are being done in
operating rooms in hospitals, nursing homes or in areas of disaster. Traditional imaging projections (lateral skull,
Waters’ sinus view, tomography, etc.) have been largely replaced by CBCT. The demand for OMR services has
markedly increased in recent years. For example, radiology reporting services at a leading corporate provider
increased more than 100% between 2015 and 2019.
American Association of Oral and Maxillofacial Surgeons
Oral and Maxillofacial Surgeons are competent to perform a wide variety of diagnostic and surgical procedures for the
comprehensive management of the diseases, injuries and defects involving both the functional and cosmetic aspects
of the hard and soft tissues of the oral, maxillofacial and head and neck regions. Dentoalveolar surgery has not
experienced any significant changes in technique, skills and management. It remains a steady component of oral and
maxillofacial surgery practice. Third molar management has been studied for the past 20 years in a prospective study
relative to the timing of removal. Anesthesia continues to be an important area of oral and maxillofacial surgery
practice. Oral and Maxillofacial Surgeons provide the majority of office-based dental anesthesia care in the country.
During 2018, anesthesia services were delivered to 4,048,697 individuals insured by private dental insurance in the
United States. Of all moderate and deep sedation/general anesthesia (DS/GA) cases performed in 2018 (1,764,588),
80% were delivered by oral and maxillofacial surgeons (1,423,249). Oral and Maxillofacial Surgeons place dental and
craniomaxillofacial implants in the pediatric patient, treat cleft and craniofacial anomalies conditions; provide trauma
patient rehabilitation; use irradiated bone; perform ridge augmentation with the use of absorbable pins and
membrane, place immediate implants and reconstruct severely resorbed maxilla with bone grafting and
osseointegrated implants. Early awareness and early detection reduce the risks associated with oral cancer and an
increasing number of patients are referred to oral and maxillofacial surgeons for treatment. Surgeons also treat
obstructive sleep apnea caused by craniofacial syndromes, complications of pharyngeal flap surgery and obesity.
Oral and maxillofacial surgery services continue to be provided in the inpatient and outpatient facilities. Medically
compromised patients and select OMS procedures continue to be provided in the hospital. Oral and Maxillofacial
Surgeons continue to provide a similar number of services and procedures in the ambulatory and office setting as
that reported in 2011. Technological advancements in the last ten (10) years have dramatically altered the delivery of
health care services. These services may involve several modalities, including the following: live video, store-and-
forward transmission of healthcare information, remote patient monitoring, mobile health and mail-order treatment
through the internet. With judicious application, many patients are now able to receive remote treatment from
healthcare providers, granting access to much-needed care and services previously out of reach.
American Association of Orthodontists
Orthodontists require in-depth knowledge of craniofacial growth and development to provide services to diagnose,
intercept, and correct malocclusions in the developing or mature orofacial structures. Traditionally children and
adolescents have been the focus of orthodontic care, but recently there has been an increase in the number of adults
initiating treatment because much has changed in the way orthodontic needs are identified and services are
delivered. More efficient materials enhanced through technology like 3D digital scanning and printing, aligner therapy,
computer customized lingual brackets and wires, photography, videography and social media have put an ever-
greater emphasis on the importance of facial esthetics. Adults are living longer and appreciate the quality of life
afforded by healthy teeth. Orthodontists are playing an important role in helping them maintain their dentition into their
golden years. The biomechanical predictability of certain tooth and bone movements has also improved over the past
ten (10) years. Techniques such as mini-screw aided maxillary expansion or other mini-screw and bone plate uses
have prevented the need for orthognathic surgery in cases that previously required it. Aligners have improved the
orthodontist’s ease in intruding teeth, useful in closing anterior open bites. Lastly, orthodontists have begun to play a
role in screening patients for signs of airway deficiencies and sleep-disordered breathing.
Historically, most orthodontists worked in single-doctor private practices. However, over the last ten (10) years, there
has been significant growth of large multi-specialty group practices and corporate dental service organizations (DSO).
According to the McGill Advisory, from the years 2011 to 2015, there was almost a 100% increase in the number of
offices belonging to the four largest DSOs; this number grew from 1065 to 1967. A 2010 survey of graduating
orthodontic students/residents showed only 26% were interested in working as an associate. When the same
question was asked in 2018, 68% were looking for opportunities in either a DSO or as a private practice associate.
American Academy of Pediatric Dentistry
Pediatric dentists oversee health supervision as a dental home for children and work with generalists and specialists,
like orthodontists and oral and maxillofacial surgeons, to provide comprehensive care. Scope of practice includes
33
most accepted dental procedures relative to and appropriate for children, provided in a developmental context in
conjunction with other specialists as indicated. Pediatric dentists are often first responders to dental trauma in
children and work with dental specialists to deal with advanced behavior needs that occur with many of these injuries.
This has resulted in better long-term management including identification of systemic co-morbidities and trauma-
preventive interventions.
Most pediatric dentistry occurs in private practices largely in urban and suburban communities. There has been a
trend in having more than one pediatric dentist in a practice, which has: (1) fostered extension of existing practices
into underserved populations; (2) permitted seamless operation of a model of primary care through specialty practice
which creates a dental home for children as well as fosters advanced behavior guidance opportunities, such as
general anesthesia and in-office sedation; (3) supported a critical economic base to allow engagement of families
depending upon governmental coverage; (4) created practices with patient populations sizable enough to support
other community specialists in dentistry; and (5) provided centers for referral in areas where pediatric specialty care
for CSHCN and children with extensive caries requiring advanced behavior guidance cannot find services. Pediatric
dentists are likely to maintain hospital staff membership and provide services in institutional settings, acting as the
oral health component of comprehensive care models for children in major health systems. Pediatric dentistry, like
general dentistry, is being engaged by larger group practices and community health centers to complete a family-
oriented, whole-patient care model which endeavors to provide a full range of services.
American Academy of Periodontology
The principal health services provided by periodontists include: (1) diagnosis, assessment for future risk and
treatment of diseases and conditions that affect the periodontium, including periodontitis, and the peri-implant tissues;
(2) correction of bone and soft tissue defects to achieve and/or enhance esthetic and functional outcomes, often in
the context of multidisciplinary care; (3) implant site development and surgical placement of dental implants to
replace missing teeth or provide anchorage for prosthetic and orthodontic purposes; and (4) promotion of stable long-
term dental, periodontal, peri-implant, and systemic health through personalized preventive maintenance care
programs.
Periodontitis is one of the most prevalent diseases in humans and is currently viewed as an oral inflammatory
disease of microbial origin with biological links to many systemic conditions including diabetes, cardiovascular
disease, adverse pregnancy outcomes, and others. Collaboration with physicians and other health care providers has
grown in the past decade and is expected to continue to increase. Such expansion has allowed periodontists to adopt
an integrated approach to personalized periodontal and peri-implant care, which translates into a direct benefit for
patients’ overall health. Advances in the diagnosis of periodontal and peri-implant diseases and patient risk
assessment have enabled clinicians to communicate efficiently with other health care professionals and patients to
establish personalized treatment plans. Improvements in the armamentarium, biomaterials, and advanced minimally
invasive surgical techniques have expanded the options available to treat patients, which has enhanced the delivery
and quality of patient care. Computer-assisted diagnosis, treatment planning, and surgical interventions have allowed
better quality care with less risk for adverse outcomes in the management of periodontal and peri-implant conditions.
Regenerative therapies have expanded to include novel bioresorbable or image-based scaffolds and materials
derived from autogenous (cell-based therapies) and exogenous sources. Such therapies have been used to treat
inflammation-derived destructive conditions affecting the tissues supporting teeth and dental implants, as well as
edentulous areas for implant site development.
Periodontists have historically provided the majority of their services in a clinical office setting. The Academy's
Practice Profile Survey, published in 2003, shows an overwhelming majority (96.5%) of the procedures performed by
members are done so in the periodontal office. The survey also showed a slight increase since 1998 (0.3% to 1.7%)
in members performing procedures in another professional setting that may be due to members moving towards
group practices or itinerant practice styles. The emergence of dental service organizations in recent years has likely
affected these patterns.
American College of Prosthodontists
The principal health services provided by prosthodontists are the diagnosis, treatment planning, rehabilitation and
maintenance of oral health and improving the appearance of worn, diseased, mutilated and/or missing teeth and
orofacial structures. Prosthodontists use a systematic diagnostic approach to determine appropriate treatment
recommendations for patients exhibiting occlusal disease, bruxism, caries, xerostomia, trauma, edentulism, cancer
and many other oral diseases. During rehabilitation, peri-implant disease assessment and CAMBRA-influenced
treatment protocols may lead to improved patient outcomes. Prosthetically-driven treatment planning often guides
interdisciplinary treatment providing esthetic smile enhancements, full mouth reconstructions, implant rehabilitations
and maxillofacial prosthetic therapies. Dramatic improvements in digital technologies, materials, and techniques have
increased the efficiency and effectiveness of treatment delivery. In-office CBCT, digital radiography and photography,

34
intraoral scanners, tactile force measurement and pressure mapping and CAD/CAM software have streamlined the
diagnostic and planning processes, providing seamless integration to improve treatment presentation (digital smile
design), patient awareness/education as well as improved workflows for interdisciplinary collaboration through the
internet and cloud-based services. Additive and subtractive manufacturing has greatly influenced guided implant
surgery and restoration fabrication by simplifying workflows leading to decreased time to prosthetic rehabilitation
completion. Semi-crystalline polymer esthetic and strength improvements, PEEK utilization and increased zirconia
applications have been witnessed in prosthetic rehabilitations. Zirconia implants provide an esthetic and
biocompatible alternative to titanium. CAD/CAM titanium bars/abutments have improved the accessibility and
interchangeability of components for complex implant reconstructions. Biological growth factors are used to stimulate
bone formation and decrease healing times.
Prosthodontists practice in a variety of settings including solo private practice, group private practice, hospitals,
Dental Service Organizations (DSO), DSO-Managed Group Practices (DMGP), Federal Services,
universities/academic settings and charitable outreach activities. A recent study of private practice prosthodontists
reported that 60.1% of prosthodontists were sole proprietors, 12.2% partners, 20.8% were employees, and 6.9%
independent contractors. This differs from the 2007 publication where it was reported that 75.7% were sole
proprietors, 15.3% partners, 6.3% employees, and 2.8% independent contractors.
American Society of Dentist Anesthesiologists
The principal health services provided by dentist anesthesiologists are anesthesia and sedation care, provided in
collaboration with a dentist or surgeon. Safe, efficient and accessible sedation and anesthesia services have enabled
access to dental care and improved oral health for many patients who could not receive care otherwise. This is
particularly important for the very young, patients with special needs and for patients with high fears and anxiety
related to dental and oral surgical treatment. Without access to anesthesia services, many of these patients would
continue to suffer from untreated dental disease.
Dentist anesthesiologists practice, teach and conduct research in a variety of settings, including dental offices, dental
schools, surgery centers, hospitals and major academic centers. Most dentist anesthesiologists provide office-based,
mobile anesthesia and sedation care. The anesthesiologist transports the necessary equipment and medications to
dental offices for the planned dental or oral surgical treatment. In doing so, the dentist anesthesiologist works
collaboratively with dentist colleagues to provide much-needed care for patients who may otherwise be unable to
receive dental treatment. Interest in office-based anesthesia has been growing and dental office-based
sedation/anesthesia is no exception. It is anticipated that the dental office will continue to be the primary setting for
dentist anesthesiologists.
Conclusions: In reviewing all of the information submitted by each of the recognized specialty sponsoring
organizations for the 2021 Periodic Review of Dental Specialty Education and Practice, the National Commission
concluded that each specialty is unique. However, the information submitted demonstrates that the specialties also
share common concerns.
Faculty Shortage: Unfilled faculty positions, resignations, retirements and projected retirements, and the shortage of
graduating students/residents having an interest in academia as a career poses a threat to the dental workforce in the
coming years. Faculty shortages at dental schools across the country may compromise student/resident learning at a
time when the public need for dentists continues to grow.
Faculty loan repayment is crucial to recruiting and retaining
dental faculty due to the student loan debt burden and income disparity between academic positions and private
practice.
Financial Restrictions due to COVID-19 Pandemic: Potential concerns for the future of advanced education include
the number of qualified faculty, decreased funding, increased tuition and increased burden on the education system
due to expanded requirements for infection control. The COVID-19 pandemic has exposed challenges in dental
education and the practice of dentistry in general. Stricter personal protective equipment requirements, patient
concerns about the safety of care, the overall priority given to care by patients with decreased discretionary income,
and the increased workload of the faculty have the potential to impact clinical education.
Final Comments: The National Commission wishes to acknowledge the cooperation, participation and contributions
of the recognized dental specialty sponsoring organizations and the recognized certifying boards for dental specialists
in providing critical information for the 2021 Periodic Review of Specialty Education and Practice.
The recognized dental specialty sponsoring organizations and recognized certifying boards provided valuable
information that is beneficial to the profession. The format of the 2021 Periodic Review of Specialty Education and
Practice served to facilitate each recognized dental sponsoring organization’s internal review by highlighting specific
areas of growth and accomplishments over the past decade and provided the opportunity for each organization to
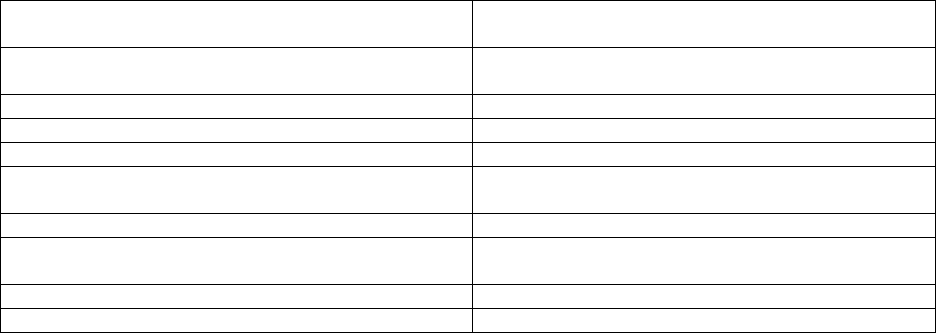
35
note ongoing and future challenges. In broader terms, the format of the review allowed the organizations to note past
and future trends, new research and cross-cutting issues such as faculty shortages, potential membership and
program enrollment increases/decreases and efforts to increase the number of board-certified specialists.
After thoroughly reviewing all of the information submitted by the recognized dental specialty sponsoring
organizations, the National Commission believes that all of the sponsoring organizations have documented evidence
that they continue to be in a healthy and viable state. From the information provided related to each specialty’s scope
of practice, the National Commission concludes that there continues to be a need and demand by the public for the
recognized specialties’ oral health services. The National Commission believes that over the past decade, the
recognized dental specialties have demonstrated ongoing efforts to improve the quality of advanced dental education,
research, practice and oral health care services.
Recognition Status of the Recognized Dental Specialty Sponsoring Organizations
American Academy of Oral and Maxillofacial
Pathology
Recognition
American Academy of Oral and Maxillofacial
Radiology
Recognition
American Academy of Pediatric Dentistry
Recognition
American Academy of Periodontology
Recognition
American Association of Endodontists
Recognition
American Association of Oral and Maxillofacial
Surgeons
Recognition
American Association of Orthodontists
Recognition
American Association of Public Health
Dentistry
Recognition
American College of Prosthodontists
Recognition
American Society of Dentist Anesthesiologists
Recognition
