Electronic Health Record Usability
Vendor Practices and Perspectives
Prepared for:
Agency for Healthcare Research and Quality
U.S. Department of Health and Human Services
540 Gaither Road
Rockville, Maryland 20850
http://www.ahrq.gov
Prepared by:
James Bell Associates
The Altarum Institute
Writers:
Cheryl McDonnell
Kristen Werner
Lauren Wendel
AHRQ Publication No. 09(10)-0091-3-EF
May 2010
HEALTH IT

ii
This document is in the public domain and may be used and reprinted without special
permission. Citation of the source is appreciated.
Suggested Citation:
McDonnell C, Werner K, Wendel L. Electronic Health Record Usability: Vendor Practices and
Perspectives. AHRQ Publication No. 09(10)-0091-3-EF. Rockville, MD: Agency for Healthcare
Research and Quality. May 2010.
This project was funded by the Agency for Healthcare Research and Quality (AHRQ), U.S.
Department of Health and Human Services. The opinions expressed in this document are those
of the authors and do not reflect the official position of AHRQ or the U.S. Department of Health
and Human Services.
iii
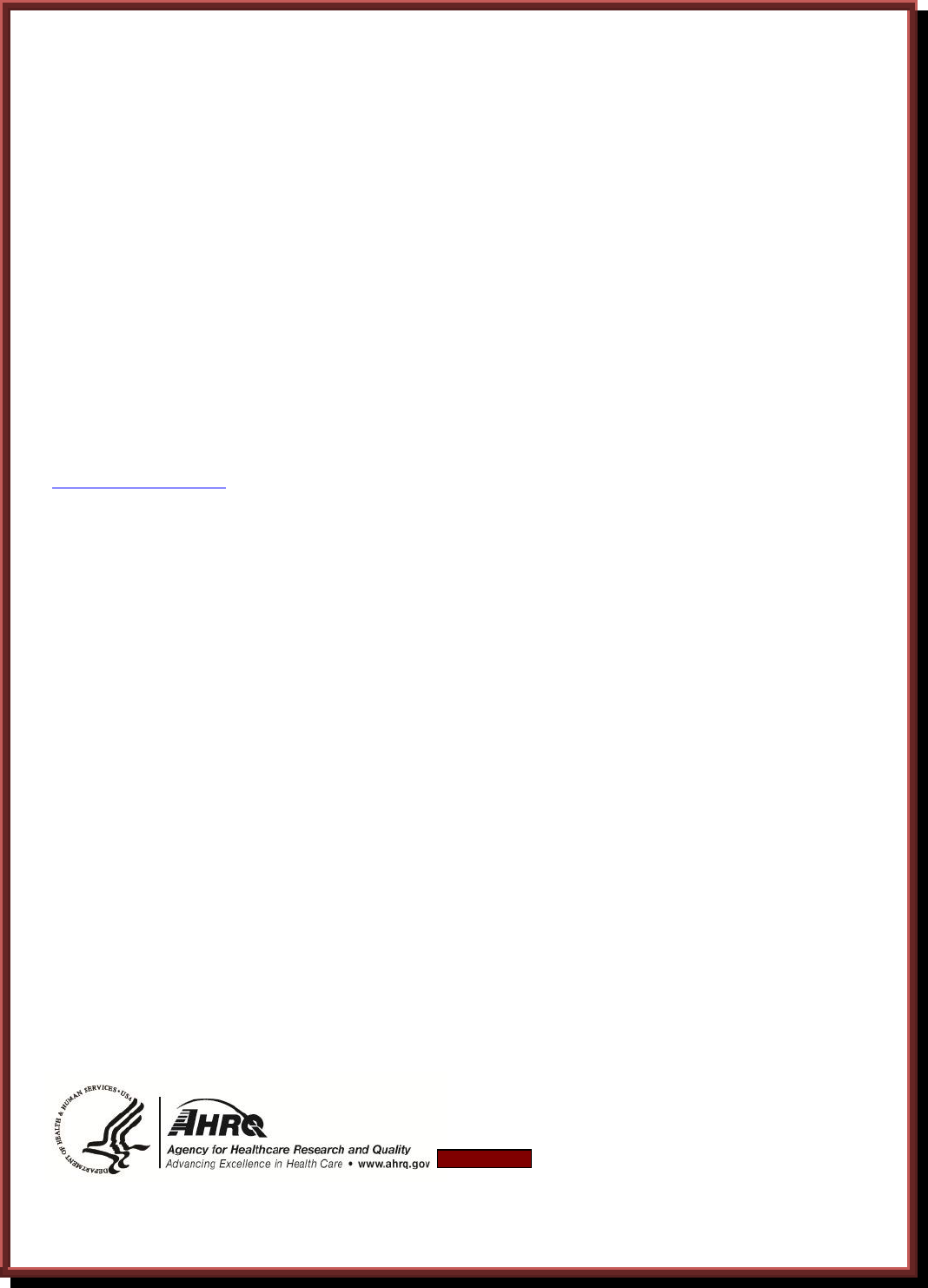
Expert Panel Members
Name
Affiliation
Mark Ackerman, PhD
Associate Professor, School of Information; Associate Professor,
Department of Electrical Engineering and Computer Science,
University of Michigan
Daniel Armijo, MHSA
Practice Area Leader, Information & Technology Strategies,
Altarum Institute
Clifford Goldsmith, MD
Health Plan Strategist, Microsoft, Eastern U.S.
Lee Green, MD, MPH
Professor & Associate Chair of Information Management,
Department of Family Medicine, University of Michigan; Director,
Great Lakes Research Into Practice Network; Co-Director,
Clinical Translation Science Program in the Michigan Institute for
Clinical and Health Research (MICHR)
Michael Klinkman, MD, MS
Associate Professor, Department of Family Medicine, University
of Michigan; Director of Primary Care Programs, University of
Michigan Depression Center
Ross Koppel, PhD
Professor, University of Pennsylvania Sociology Department;
Affiliate Faculty Member, University of Pennsylvania School of
Medicine; President, Social Research Corporation
David Kreda
Independent Computer Software Consultant
Svetlana Lowry
National Institute of Standards and Technology
Donald T. Mon, PhD
Vice President of Practice Leadership, American Health
Information Management Association; Co-Chair, Health Level
Seven (HL7) EHR Technical Committee
Catherine Plaisant, PhD
University of Maryland, Human Computer Interaction Laboratory,
Institute for Advanced Computer Studies, Associate Director
Ben Shneiderman, PhD
Professor, Department of Computer Science; Founding Director,
Human-Computer Interaction Laboratory, Institute for Advanced
Computer Studies, University of Maryland
Andrew Ury, MD
Chief Medical Officer, McKesson Provider Technologies
James Walker, MD
Chief Health Information Officer, Geisinger Health System
Andrew M. Wiesenthal, MD, SM
Associate Executive Director for Clinical Information Support,
Kaiser Permanente Federation
Kai Zheng, PhD
Assistant Professor, University of Michigan School of Public
Health; Assistant Professor, University of Michigan School of
Information; Medical School’s Center for Computational Medicine
and Biology (CCMB); Michigan Institute for Clinical and Health
Research (MICHR)
Michael Zaroukian MD, PhD
Professor and Chief Medical Information Officer, Michigan State
University; Director of Clinical Informatics and Care
Transformation, Sparrow Health System; Medical Director, EMR
Project
iv
Contents
Executive Summary ................................................................................................................... 1
Background ................................................................................................................................ 3
Vendor Profiles .......................................................................................................................... 4
Standards in Design and Development ...................................................................................... 4
End-User Involvement ................................................................................................... 4
Design Standards and Best Practices ............................................................................. 4
Industry Collaboration ................................................................................................... 5
Customization ................................................................................................................ 5
Usability Testing and Evaluation ............................................................................................... 6
Informal Usability Assessments .................................................................................... 6
Measurement .................................................................................................................. 6
Observation .................................................................................................................... 7
Changing Landscape ...................................................................................................... 7
Postdeployment Monitoring and Patient Safety ........................................................................ 7
Feedback Solicitation ..................................................................................................... 7
Review and Response .................................................................................................... 8
Patient Safety ................................................................................................................. 8
Role of Certification in Evaluating Usability ............................................................................ 9
Current Certification Strategies ..................................................................................... 9
Subjectivity .................................................................................................................... 9
Innovation ...................................................................................................................... 9
Recognized Need ........................................................................................................... 10
Conclusion ................................................................................................................................. 10
Implications................................................................................................................................ 11
Standards in Design and Development .......................................................................... 11
Usability Testing and Evaluation ................................................................................... 12
Postdeployment Monitoring and Patient Safety ............................................................ 12
Role of Certification in Evaluating Usability ................................................................ 13
References .................................................................................................................................. 14
Appendixes
Appendix I: Summary of Interviewed Vendors ......................................................................... A-1
Appendix II: Description of Electronic Health Record Products .............................................. B-1
1
Executive Summary
One of the key factors driving the adoption and appropriate utilization of electronic
health record (EHR) systems is their usability.
1
However, a recent study funded by the Agency
for Healthcare Research and Quality (AHRQ) identified information about current EHR vendor
usability processes and practices during the different phases of product development and
deployment as a key research gap.
2
To address this gap and identify actionable recommendations to move the field forward,
AHRQ contracted with James Bell Associates and the Altarum Institute to conduct a series of
structured discussions with selected certified EHR vendors and to solicit recommendations based
on these findings from a panel of multidisciplinary experts in this area.
The objectives of the project were to understand processes and practices by these vendors
with regard to:
The existence and use of standards and “best practices” in designing, developing, and
deploying products.
Testing and evaluating usability throughout the product life cycle.
Supporting postdeployment monitoring to ensure patient safety and effective use.
In addition, the project solicited the perspectives of certified EHR vendors with regard to the role
of certification in evaluating and improving usability.
The key findings from the interviews are summarized below.
All vendors expressed a deep commitment to the development and provision of usable
EHR product(s) to the market.
Although vendors described an array of usability engineering processes and the use of
end users throughout the product life cycle, practices such as formal usability testing, the
use of user-centered design processes, and specific resource personnel with expertise in
usability engineering are not common.
Specific best practices and standards of design, testing, and monitoring of the usability of
EHR products are not readily available. Vendors reported use of general (software) and
proprietary industry guidelines and best practices to support usability. Reported
perspectives on critical issues such as allowable level of customization by customers
varied dramatically.
Many vendors did not initially address potential negative impacts of their products as a
priority design issue. Vendors reported a variety of formal and informal processes for
2
identifying, tracking, and addressing patient safety issues related to the usability of their
products.
Most vendors reported that they collect, but do not share, lists of incidents related to
usability as a subset of user-reported “bugs” and product-enhancement requests. While all
vendors described a process, procedures to classify and report usability issues of EHR
products are not standardized across the industry.
No vendors reported placing specific contractual restrictions on disclosures by system
users of patient safety incidents that were potentially related to their products.
Disagreement exists among vendors as to the ideal method for ensuring usability
standards, and best practices are evaluated and communicated across the industry as well
as to customers. Many view the inclusion of usability as part of product certification as
part of a larger “game” for staying competitive, but also as potentially too complex or
something that will “stifle innovation” in this area.
Because nearly all vendors view usability as their chief competitive differentiator,
collaboration among vendors with regard to usability is almost nonexistent.
To overcome competitive pressures, many vendors expressed interest in an independent
body guiding the development of voluntary usability standards for EHRs. This body
could build on existing models of vendor collaboration, which are currently focused
predominantly on issues of interoperability.
Based on the feedback gained from the interviews and from their experience with
usability best practices in health care and other industries, the project expert panel made the
following recommendations:
Encourage vendors to address key shortcomings that exist in current processes and
practices related to the usability of their products. Most critical among these are lack of
adherence to formal user-design processes and a lack of diversity in end users involved in
the testing and evaluation process.
Include in the design and testing process, and collect feedback from, a variety of end-user
contingents throughout the product life cycle. Potentially undersampled populations
include end users from nonacademic backgrounds with limited past experience with
health information technology and those with disabilities.
Support an independent body for vendor collaboration and standards development to
overcome market forces that discourage collaboration, development of best practices, and
standards harmonization in this area.
Develop standards and best practices in use of customization during EHR deployment.
Encourage formal usability testing early in the design and development phase as a best
practice, and discourage dependence on postdeployment review supporting usability
assessments.
3
Support research and development of tools that evaluate and report EHR ease of learning,
effectiveness, and satisfaction both qualitatively and quantitatively.
Increase research and development of best practices supporting designing for patient
safety.
Design certification programs for EHR usability in a way that focuses on objective and
important aspects of system usability.
Background
Encouraged by Federal leadership, significant investments in health information
technology (IT) are being made across the country. While the influx of capital into the electronic
health record (EHR)/health information exchange (HIE) market will undoubtedly stimulate
innovation, there is the corresponding recognition that this may present an exceptional
opportunity to guide that innovation in ways that benefit a significant majority of potential health
IT users.
One of the key factors driving the adoption and appropriate utilization of EHR systems is
their usability.
1
While recognized as critical, usability has not historically received the same level
of attention as software features, functions, and technical standards. A recent analysis funded by
the Agency for Healthcare Research and Quality (AHRQ) found that very little systematic
evidence has been gathered on the usability of EHRs in practice. Further review established a
foundation of EHR user-interface design considerations, and an action agenda was proposed for
the application of information design principles to the use of health IT in primary care settings.
2,3
In response to these recommendations, AHRQ contracted with James Bell Associates and
the Altarum Institute to evaluate current vendor-based practices for integrating usability during
the entire life cycle of the product, including the design, testing, and postdeployment phases of
EHR development. A selected group of EHR vendors, identified through the support of the
Certification Commission for Health Information Technology (CCHIT) and AHRQ, participated
in semistructured interviews. The discussions explored current standards and practices for
ensuring the usability and safety of EHR products and assessed the vendors’ perspectives on how
EHR usability and information design should be certified, measured, and addressed by the
government, the EHR industry, and its customers. Summary interview findings were then
distributed to experts in the field to gather implications and recommendations resulting from
these discussions.
Vendor Profiles
The vendors interviewed were specifically chosen to represent a wide distribution of
providers of ambulatory EHR products. There was a representation of small-sized businesses
(less than 100 employees), medium-sized businesses (100-500 employees), and large-sized
businesses (greater than 500 employees). The number of clinician users per company varied from
1,000 to over 7,000, and revenue ranged from $1 million to over $10 billion per year. The EHR
products discussed came on the market in some form in the time period from the mid-1990s to
2007. All vendors except one had developed their EHR internally from the ground up, with the

4
remaining one internally developing major enhancements for an acquired product. Many of these
products were initially designed and developed based on a founding physician’s practice and/or
established clinical processes. All companies reported that they are currently engaged in ground-
up development of new products and/or enhancements of their existing ambulatory products.
Many enhancements of ambulatory products center on updates or improvements in usability.
Examples of new developments include changes in products from client-based to Web-based
EHRs; general changes to improve the overall usability and look and feel of the product; and the
integration of new technologies such as patient portals, personal health records, and tablet
devices.
The full list of vendors interviewed and a description of their key ambulatory EHR
products are provided in Appendixes I and II. The following discussion provides a summary of
the themes encountered in these interviews.
Standards in Design and Development
End-User Involvement
All vendors reported actively involving their intended end users throughout the entire
design and development process. Many vendors also have a staff member with clinical
experience involved in the design and development process; for some companies the clinician
was a founding member of the organization.
Workgroups and advisory panels are the most
common sources of feedback, with some vendors
utilizing a more comprehensive participatory
design approach, incorporating feedback from all
stakeholders throughout the design process. Vendors seek this information to develop initial
product requirements, as well as to define workflows, evaluate wireframes and prototypes, and
participate in initial beta testing. When identifying users for workgroups, advisory panels, or beta
sites, vendors look for clinicians who have a strong interest in technology, the ability to evaluate
usability, and the patience to provide regular feedback. Clinicians meeting these requirements are
most often found in academic medical centers. When the design concerns an enhancement to the
current product, vendors often look toward users familiar with the existing EHR to provide this
feedback.
Design Standards and Best Practices
A reliance on end-user input and observation for ground-up development is seen as a
requirement in the area of EHR design, where specific design standards and best practices are not
yet well defined. Vendors indicated that appropriate
and comprehensive standards were lacking for EHR-
specific functionalities, and therefore they rely on
general software design best practices to inform
design, development, and usability. While these
software design principles help to guide their
processes, they must be adjusted to fit specific end-
“We want to engage with leadership-level
partners as well as end users from all venues
that may be impacted by our product.”
“There are no standards most of the time,
and when there are standards, there is no
enforcement of them. The software
industry has plenty of guidelines and good
best practices, but in health IT, there are
none.”
5
user needs within a health care setting. In addition to following existing general design
guidelines such as Microsoft Common User Access, Windows User Interface, Nielsen Norman
Group, human factors best practices, and releases from user interface (UI) and usability
professional organizations, many vendors consult with Web sites, blogs, and professional
organizations related to health IT to keep up to date with specific industry trends. Supplementing
these outside resources, many vendors are actively developing internal documentation as their
products grow and mature, with several reporting organized efforts to create internal
documentation supporting product-specific standards and best practices that can be applied
through future product updates and releases.
Industry Collaboration
As these standards and best practices are being developed, they are not being
disseminated throughout the industry. Vendors receive some information through professional
organizations and conferences, but they would like to see a stronger push toward an independent
body, either governmental or research based, to establish some of these standards. The
independent body would be required, as all
vendors reported usability as a key
competitive differentiator for their product;
this creates a strong disincentive for industry-
wide collaboration. While all were eager to
take advantage of any resources commonly
applied across the industry, few were
comfortable with sharing their internally developed designs or best practices for fear of losing a
major component of their product’s competitiveness. Some vendors did report they collaborate
informally within the health IT industry, particularly through professional societies, trade
conferences, and serving on committees. For example, several vendors mentioned participation
in the Electronic Health Record Association (EHRA), sponsored by the Healthcare Information
and Management Systems Society (HIMSS), but noted that the focus of this group is on clinical
vocabulary modeling rather than the usability of EHRs. Some interviewees expressed a desire to
collaborate on standards issues that impact usability and patient safety through independent
venues such as government or research agencies.
Customization
In addition to the initial design and development process, vendors commonly work with
end users to customize or configure specific parts of the EHR. Vendors differed in the extent to
which they allowed and facilitated customization and noted the potential for introducing errors
when customization is pursued. Most customizations involve setting security rules based on roles
within a clinic and the creation of document
templates that fit a clinic’s specific workflow. Many
vendors view this process as a critical step toward a
successful implementation and try to assist users to
an extent in developing these items. While some
vendors track these customizations as insight for
future product design, they do not view the customizations as something that can be generalized
to their entire user base, as so many are context specific. The level of customization varies
“The field is competitive so there is little sharing of
best practices in the community. The industry
should not look toward vendors to create these best
practices. Other entities must step up and define
[them] and let the industry adapt.”
“You cannot possibly adapt technology to
everyone’s workflow. You must provide the
most optimum way of doing something
which [users] can adapt.”
6
according to vendor since vendors have different views about the extent to which their product
can or should be customized. Vendors do not routinely make changes to the code or underlying
interface based on a user request; however, the level to which end users can modify templates,
workflows, and other interface-related characteristics varies greatly by vendor offering.
Usability Testing and Evaluation
Informal Usability Assessments
Formal usability assessments, such as task-centered user tests, heuristic evaluations,
cognitive walkthroughs, and card sorts, are not a common activity during the design and
development process for the majority of vendors. Lack of time, personnel, and budget resources
were cited as reasons for this absence; however, the
majority expressed a desire to increase these types of
formal assessments. There was a common perception
among the vendors that usability assessments are
expensive and time consuming to implement during the
design and development phase. The level of formal
usability testing appeared to vary by vendor size, with larger companies having more staff and
resources dedicated to usability testing while smaller vendors relied heavily on informal methods
(e.g., observations, interviews), which were more integrated into the general development
process. Although some reported that they conduct a full gamut of both formal and informal
usability assessments for some parts of the design process, most reported restricting their use of
formal methods to key points in the process (e.g., during the final design phase or for evaluation
of specific critical features during development).
Measurement
Functions are selected for usability testing according to several criteria: frequency of use,
task criticality and complexity, customer feedback, difficult design areas, risk and liability,
effects on revenue, compliance issues (e.g., Military Health
System HIPAA [Health Insurance Portability and
Accountability Act], and the American Recovery and
Reinvestment Act) and potential impacts on patient safety.
The most common or frequent tasks and tasks identified as
inherently complex are specifically prioritized for usability testing. Neither benchmarks and
standards for performance nor formalized measurements of these tasks are common in the
industry. While some vendors do measure number of clicks and amount of time to complete a
task, as well as error rates, most do not collect data on factors directly related to the usability of
the product, such as ease of learning, effectiveness, and satisfaction. Many vendors reported that
the amount of data collected does not allow for quantitative analysis, so instead they rely on
more anecdotal and informal methods to ensure that their product works more effectively than
paper-based methods and to inform their continuous improvements with upgrades and releases.
“Due to time and resource constraints,
we do not do as much as we would like
to do. It is an area in which we are
looking to do more.”
“Testing is focused more on
functionality rather than
usability.”

7
Observation
Observation is the “gold standard” among all vendors for learning how users interact with
their EHR. These observations usually take place within the user’s own medical practice, either
in person or with software such as TechSmith’s
Morae.
4
Vendors will occasionally solicit feedback on
prototypes from user conferences in an informal lab-
like setting. These observations are typically used to
gather information on clinical workflows or process
flows, which are incorporated into the product design,
particularly if the vendor is developing a new
enhancement or entire product.
Changing Landscape
While informal methods of usability testing seem to be common across most vendors, the
landscape appears to be changing toward increasing the importance of usability as a design
necessity. Multiple vendors reported the current or recent development of formal in-house
observation laboratories where usability testing could be more effectively conducted. Others
reported the recent completion of policies and standards directly related to integrating usability
more formally into the design process, and one reported a current contract with a third-party
vendor to improve usability practices. While it is yet to be seen if these changes will materialize,
it appeared that most respondents recognized the value of usability testing in the design process
and were taking active steps to improve their practices.
Postdeployment Monitoring and Patient Safety
Feedback Solicitation
Vendors are beginning to incorporate more user feedback into earlier stages of product
design and development; however, most of this feedback comes during the postdeployment
phase. As all vendors interviewed are currently engaged in either the development of
enhancements of current products or the creation of new products, the focus on incorporating
feedback from intended end users at all stages of
development has increased. Many of the EHRs have
been on the market for over 10 years; as a result,
many vendors rely heavily on this postdeployment
feedback to evaluate product use and inform future
product enhancements and designs. Maintaining contact with current users is of high priority to
all EHR vendors interviewed and in many ways appeared to represent the most important source
of product evaluation and improvement. Feedback is gathered through a variety of sources,
including informal comments received by product staff, help desk support calls, training and
implementation staff, sales personnel, online user communities, beta clients, advisory panels, and
user conferences. With all of these avenues established, vendors appear to attempt to make it as
easy as possible for current users to report potential issues as well as seek guidance from other
users and the vendor alike.
“[Methods with] low time and resource
efforts are the best [to gather feedback];
wherever users are present, we will gather
data.”
“A lot of feedback and questions are often
turned into enhancements, as they speak to
the user experience of the product.”
8
Review and Response
Once the vendors receive both internal and external feedback, they organize it through a
formal escalation process that ranks the severity of the issue based on factors such as number of
users impacted, type of functionality involved, patient
safety implications, effects on workflow, financial
impact to client, regulation compliance, and the
source of the problem, either implementation based or
product based. In general, safety issues are given a
high-priority tag. Based on this escalation process, priorities are set, resources within the
organization are assigned, and timelines are created for directly addressing the reported issue.
Multiple responses are possible depending on the problem. Responses can include additional
user training, software updates included in the next product release, or the creation and release of
immediate software patches to correct high-priority issues throughout the customer base.
Patient Safety
Adoption of health IT has the potential for introducing beneficial outcomes along many
dimensions. It is well recognized, however, that the actual results achieved vary from setting to
setting,
5
and numerous studies have reported health IT implementations that introduced
unintended adverse consequences detrimental to patient care practice.
6
Surprisingly, in many
interviews patient safety was not initially verbalized as a priority issue. Initial comments focused
on creating a useful, usable EHR product, not one that addresses potential negative impacts on
patient safety. Vendors rely heavily on physicians to notice
potential hazards and report these hazards to them through their
initial design and development advisory panels and
postdeployment feedback mechanisms. After further questioning
specific to adverse events, however, most vendors did describe
having processes in place for monitoring potential safety issues
on a variety of fronts. Some vendors become aware of patient safety issues through user
feedback collected from patient safety offices and field visits; others educate support staff as well
as users on how to identify potential patient safety risks and properly notify those who can
address the issue. Once patient safety issues are identified, vendors address them in various
ways, including tracking and reporting potential issues online, using patient safety review boards
to quantify risk, and engaging cognitive engineers to uncover root causes.
When asked about client contracts, no vendors reported placing specific contractual
restrictions on disclosures by system users of patient safety incidents that were potentially related
to the EHR products, sharing patient safety incidents with other customers or other clinicians, or
publishing research on how the EHR system affects patient safety or their clinical operations.
“Every suggestion is not a good suggestion;
some things do not help all users because
not all workflows are the same.”
“Physicians are very acutely
aware of how technology is
going to impact patient safety;
that’s their focus and
motivation.”
9
Role of Certification in Evaluating Usability
Current Certification Strategies
The issue of certification is one that elicited strong opinions from most vendors.
Certification of any type represents an investment of time and money to meet standards
originating outside the organization. For many vendors, particularly the smaller ones, this
investment was seen as burdensome. Vendors commonly described the current CCHIT
certification process as part of a larger “game” they
must play in order to remain viable in the
marketplace, not as a way to improve their
product(s). Accounts of functions added
specifically for certification but not used by
customers were common, as well as specific
instances where vendors felt meeting certification guidelines actually reduced aspects of their
product’s quality. As one vendor noted, sometimes providing the functionality for “checking the
box” to meet a certification requirement involves a backward step and a lowering of a potentially
innovative internal standard. As meaningful use has entered the picture, however, vendors are
striving to provide their customers with products that will comply with this definition and plan to
participate in any associated certifications.
Subjectivity
Interviewees held mixed opinions on whether the certification process can effectively
evaluate the usability aspect of EHR performance. Without exception, participating vendors had
concerns about the inherent subjectivity of
evaluation of usability, which can be strongly
affected by the past EHR experience of the user,
the context in which the product is used, and even
the education and background of the evaluator.
Methods for overcoming these types of bias issues
included suggestions such as certifying workflows
rather than attempting to measure usability, comparing objective product performance (time and
error rates) for specific tasks, or measuring usability based on end-user surveys instead of juror
analysis.
Innovation
Several interviewees also expressed
concern about the effect of usability certification
on innovation within the EHR marketplace. This
seemed to stem from experience with CCHIT’s
feature- and function-based criteria. It was noted
that in the developing EHR marketplace, current
systems are striving to make significant changes
in the way physicians practice care, which has inherent negative implications for perceived
“We don’t want to get dinged for an
innovative standard that we’ve developed
and [that] tested well with users because it
doesn’t fit the criteria.”
“Some products may be strong, but due to the
familiarity of jurors of a product or technology,
some products may be overrated or
underrated.”
“Products are picked on the amount of
things they do, not how well they do them.
CCHIT perpetuates this cycle; if a product
contains certain functions, it is placed among
the elite. That has nothing to do with
usability.”

10
usability early in the product’s release. Guidelines or ratings that are too prescriptive may have
the effect of forcing vendors to create technologies that more directly mirror current practices, a
strategy that could limit innovation and the overall effectiveness of EHRs.
Recognized Need
Despite these concerns, vendors recognized the role certification could play both as an
indicator to support customers in selecting EHRs and as a method through which established
standards could be disseminated across the industry.
While there is unease about the details of the conduct
of certification, many vendors thought that some form
of certification or evaluation had the potential to serve
as a complement to what is now a predominantly
market-driven issue. While each vendor viewed itself as a leader in the development of usable
EHR systems and supported the role of consumer demand in continuing to improve product
usability, vendors recognized that there could be utility to more standardized testing that could
be evenly applied throughout the industry.
Conclusion
All vendors interviewed expressed a deep commitment to the continued development and
provision of usable EHR product(s) to the market. Vendors believe that as features and functions
become more standardized across the industry, industry leaders will begin to differentiate
themselves from the rest of the market based on usability. Current best practices and standards of
design, testing, and monitoring EHR product(s), particularly for usability, are varied and not well
disseminated. While models for vendor collaboration for issues such as interoperability currently
exist through EHRA and IHE (Integrating the Healthcare Enterprise), collaboration among
vendors with regard to usability is almost nonexistent. Given the current move toward the
adoption and meaningful use of health IT, and the role usability plays in realizing intended
benefits, a transition from the current environment seems likely. This could be driven by many
sources, including standards developed by academic research, certification required by
government entities, collaboration through a nonprofit association such as EHRA or IHE, or
simply market pressures demanding more usable offerings.
Vendors recognize these pressures and the importance of usability to the continued
success of their products. Disagreement exists as to the ideal method for ensuring that usability is
evaluated and communicated across the industry as well as to customers. This disagreement
exists even within companies, as well as across vendors. Regardless of this uncertainty, there is
agreement that end users need to remain a central component within the development process,
innovation needs to be encouraged, and usability needs to be a critical driver of efficient,
effective, and safe EHRs.
“Being aware of standards and guidelines is
very important, but we also want to make
sure we are not hamstrung by them.”
11
Implications and Recommendations
The summary interview findings were distributed to selected experts in the field, who
provided additional thoughts on the implications of these discussions and developed
recommendations based on the discussions. A summary of these suggestions follows.
Standards in Design and Development
Increase diversity of users surveyed for pre-deployment feedback. While the use of
subject-matter experts and inclusion of end-user feedback in the design and development process
are beneficial and important approaches, the end-user selection process currently in use has a
potential for bias. Vendors noted extensive use of volunteered feedback. Clinicians with a strong
interest in technology, the ability to evaluate usability, and the patience to provide regular
feedback are not indicative of the typical end user. Additionally, as these types of clinicians are
commonly found in academic medical centers, they may rely on residents or other trainees to do
most of the work involving the EHR. Similar issues exist when soliciting input from users
familiar with the existing EHR; these users have potentially learned, sometimes unconsciously,
to work around or ignore many of the usability problems of the current system. To some extent,
vendors must utilize this “coalition of the willing” to gather feedback, given the extremely busy
schedules of most practicing clinicians. However, steps must be taken both in the vendor
community and by independent bodies to encourage inclusion of a more diverse range of users in
all stages of the design process. This more inclusive approach will ultimately support a more
usable end product.
Support an independent body for vendor collaboration and standards development.
Lack of vendor collaboration resulting from attempts to protect intellectual property and uphold
a competitive edge is understandable. However, with the accelerated adoption timeframe
encouraged by recent legislation and increasing demand, letting the market act as a primary
driver to dictate usability standards may not ensure that appropriate standards are adopted. The
user base currently has relatively limited abilities to accurately determine product usability
before purchase and, if dissatisfied after purchase, may incur significant expense to explore more
usable products. Simply deeming an EHR usable or not usable does not create or disseminate
standards and best practices for design. The market can provide direction, but more must be done
to document trends and best practices, create new standards for design, and regulate
implementation across the industry.
Develop standards and best practices in use of customization during EHR deployment.
Customization is often a key to successful implementation within a site, as it can enable users to
document the clinical visit in a way that accommodates their usual methods and existing
workflow. However, customization may also serve to hide existing usability issues within an
EHR, prevent users from interacting with advanced functions, or even create unintended
consequences that negatively impact patient safety. There is an additional concern that
customization may negatively impact future interoperability and consistency in design across the
industry. Customer demand for customization exists and some level of customization can be
beneficial to supporting individual workflows; however, more work must be done to evaluate the
level of customization that maximizes the EHR’s benefits and limits its risks.
12
Usability Testing and Evaluation
Encourage formal usability testing early in the design and development phase as a best
practice. Usability assessments can be resource intensive; however, it has been demonstrated that
including them in the design and development phase is more effective and less expensive than
responding to and correcting items after market release.
7
Identifying and correcting issues before
release also reduce help desk support and training costs. Vendors indicated an awareness of this
tradeoff and a move toward investment in usability assessment up front. Further monitoring will
be required to evaluate how the vendor community incorporates formal usability testing within
future design and development practices.
Evaluate ease of learning, effectiveness, and satisfaction qualitatively and
quantitatively. Observations are an important component of usability testing but are insufficient
for assessment of the root cause of usability issues. Alternatively, quantitative data such as
number of clicks, time to complete tasks, and error rates can help the vendor identify tasks that
may present usability issues but must be further explored to identify underlying issues. A mix of
structured qualitative and quantitative approaches, incorporating at minimum an assessment of
the three basic factors directly contributing to product usability—ease of learning, effectiveness,
and satisfaction—will serve to broaden the impact of usability assessments beyond the informal
methods commonly employed today.
Postdeployment Monitoring and Patient Safety
Decrease dependence on postdeployment review supporting usability assessments.
Usability issues are usually not simple, one-function problems, but tend to be pervasive
throughout the EHR. So while small-scale issues are often reported and corrected after
deployment, the identified issue may not be the primary determinant of a product’s usability. It
is chiefly within the main displays of information that are omnipresent, such as menu listings,
use of pop-up boxes, and the interaction between screens, that the EHR’s usability is determined.
Even with the best of intentions, it is unlikely that vendors will be able to resolve major usability
issues after release. By not identifying critical usability issues through a wide range of user
testing during design and development, vendors are opening the door to potential patient safety
incidents and costly postrelease fixes.
Increase research and development of best practices supporting designing for patient
safety. Monitoring and designing for patient safety, like usability testing, appear to be most
prevalent late in the design of the product or during its release cycle. Vendors’ heavy reliance on
end users or advisory panels to point out patient safety issues in many ways mirrors the informal
methods used to advance usability of their products. While patient safety similarly lacks specific
standards for vendors to follow, vendors are currently collaborating on patient safety issues.
These collaborations appear to be in their early stages, but they provide an opportunity to
enhance vendor awareness and vendor response to potential patient safety issues within their
products and improve their ability to incorporate patient safety much earlier in the design
process. Further work must be done to directly connect design to patient safety and ensure that
standards are created and disseminated throughout the industry.
13
Role of Certification in Evaluating Usability
Certification programs should be carefully designed and valid. Any certification or
outside evaluation will be initially approached with questions as to its validity, and the concept
of usability certification is no exception. Usability is a complex multifaceted system
characteristic, and usability certification must reflect that complexity. Further complicating this
issue is the fact that vendors have already participated in a certification process that most did not
find particularly valuable in enhancing their product. Driving the EHR market toward creation of
usable products requires development of a process that accurately identifies usable products,
establishes and disseminates standards, and encourages innovation.

14
References
1. Belden J, Grayson R, Barnes J. Defining and
Testing EMR Usability: Principles and
Proposed Methods of EMR Usability
Evaluation and Rating. Healthcare
Information Management and Systems
Society Electronic Health Record Usability
Task Force. Available at:
http://www.himss.org/content/files/HIMSS_
DefiningandTestingEMRUsability.pdf.
Accessed June 2009.
2. Armijo D, McDonnell C, Werner K.
Electronic Health Record Usability:
Interface Design Considerations. AHRQ
Publication No. 09(10)-0091-2-EF.
Rockville, MD: Agency for Healthcare
Research and Quality. October 2009.
3. Armijo D, McDonnell C, Werner K.
Electronic Health Record Usability:
Evaluation and Use Case Framework.
AHRQ Publication No. 09(10)-0091-1-EF.
Rockville, MD: Agency for Healthcare
Research and Quality. October 2009.
4. TechSmith. Morae: usability testing and
market research software. Available at:
http://www.techsmith.com/morae.asp.
5. Ammenwerth E, Talmon J, Ash JS, et al.
Impact of CPOE on mortality rates—
contradictory findings, important messages.
Methods Inf Med 2006;45:586-93.
6. Koppel R, Metlay JP, Cohen A, et al. Role
of computerized physician order entry
systems in facilitating medication errors.
JAMA 2005;293:1197-203.
7. Gilb T, Finzi S. Principles of software
engineering management. Reading, MA:
Addison-Wesley Pub. Co.; 1988.
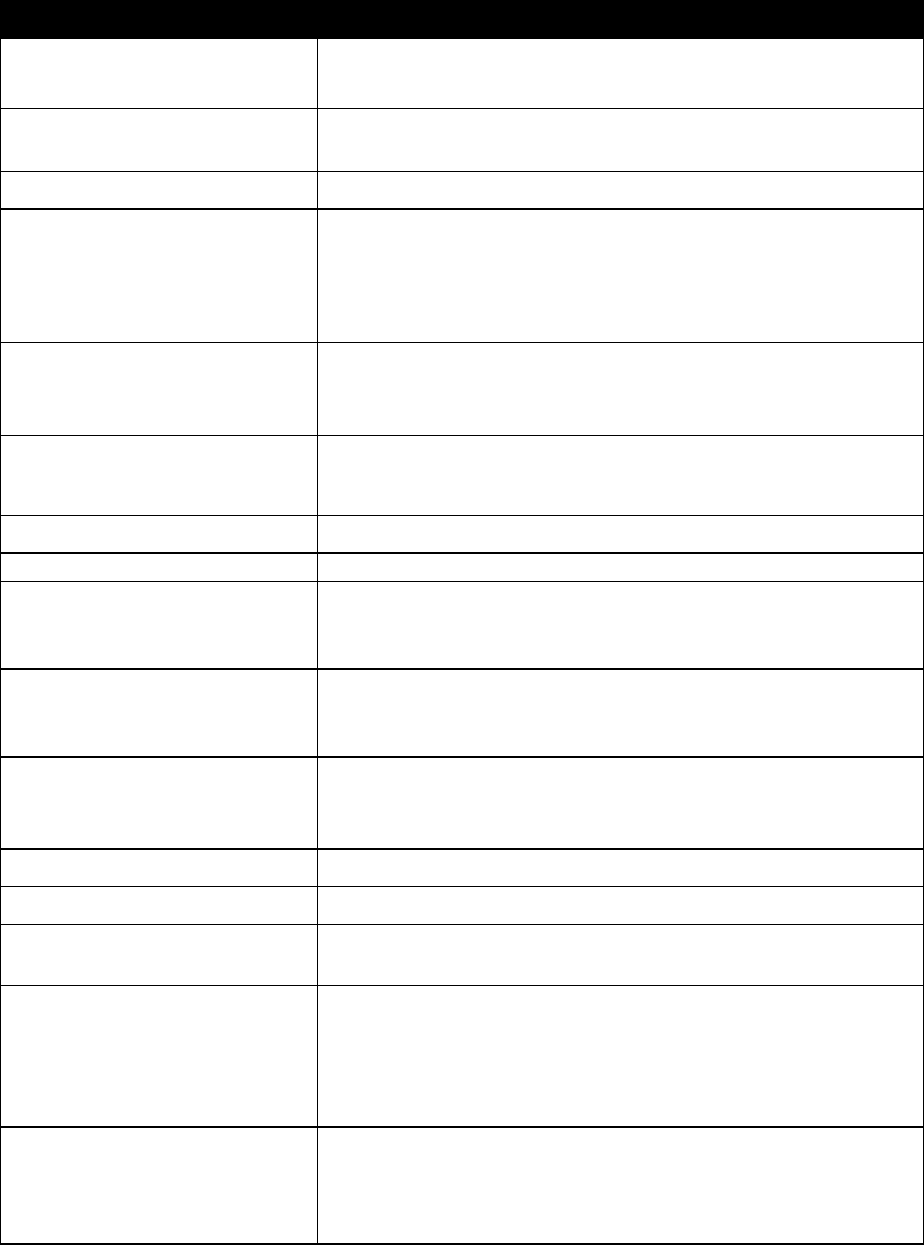
A-1
Appendix I: Summary of Interviewed
Vendors
Interviewed companies with disclosed company information that had CCHIT-certified
ambulatory electronic health records: 2008
Company
Product(s)
Core
markets
No.
employees
No. live
sites (all
versions)
No. users
Years in
business
Company Web site
athenahealth, Inc.
athenaClinicals 9.15.1
Multiple
101– 1,000
101-500
1,001–5,000
>10
http://www.athenahealth.com/
Cerner
Corporation
Cerner Millennium
Powerchart/PowerWorks EMR
2007.19
Multiple
101–1,000
>500
>5,000
>10
http://www.cerner.com
Criterions, LLC
Criterions 1.0.0
Multiple
11-100
>500
>5,000
>10
http://www.criterions.com
e-MDs
e-MDs Solution Series 6.3
Multiple
101–1,000
>500
>5,000
>10
http://www.e-MDs.com
EHS
CareRevolution 5.3
Multiple
101-1,000
> 500
>5,000
>10
http://www.ehsmed.com
GE Healthcare
Centricity Electronic Medical
Record 9.2
Multiple
101–1,000
>500
>5,000
>10
http://www.gehealthcare.com
NextGen
NextGen EMR 5.5
http://www.nextgen.com
Veterans
Administration
VISTA
Federal
Govt.
http://www4.va.gov/VISTA_MONOGRAPH/
B-1
Appendix II: Description of Electronic Health Record
Products
This appendix gives background information on select ambulatory electronic health
record (EHR) systems. Selected system characteristics are shown in Table 1.
A. athenahealth, Inc.: athenaClinicals
SM
9.15.1
athenaHealth, Inc., produces four integrated software systems for ambulatory
clinics/practices: (1) athenaClinicals, an EHR system; (2) athenaCollector, a physician billing
and practice management system; (3) athenaCommunicator, an automated patient
communications system; and (4) PayerView, a system that contains payer rankings and identifies
payers that provide high or low percentages of billed fees and charges. athenaClinicals is a Web-
based EHR system that requires only a computer with Internet access on the part of the
physician.
athenaClinicals incorporates tools such as Clinical Inbox, Workflow Dashboard, and
Intuitive Reporting Wizard that allow the physician to have visibility into practice management
processes and performance, including comparative benchmarks and metrics for compliance,
preventive guidelines, workflow lag times, and followthrough on clinical tasks. The system
receives incoming electronic documents and scans faxes, which are then matched to existing
patients and patient orders, routed to appropriate staff members, and stored for later access.
Through Clinical Inbox, physicians automatically see the documents that require attention, such
as lab results and prescription renewal requests.
The system’s advanced features are based on the athenaHealth Rules Database, which
brings together a compilation of industry data sources, including a real-time database of
insurance company rules and regulations, a list of billing codes, drug formulary rules, Pay for
Performance (P4P) quality program rules, and clinical guidelines and protocols. The information
in the Rules Database gets updated continuously by athenaHealth staff and embedded into the
patient encounters, providing drug interaction alerts, drug allergy alerts, and information required
for reporting. If the practice also has the athenaCollector software, the clinical information then
generates billing information for the patient’s visit.
The system’s updated database and reporting functions support compliance with
government mandates, such as P4P, the Physician Quality Reporting Initiative (PQRI), and the
Health Information Technology for Economic and Clinical Health (HITECH) Act, making it
easier for smaller practices to participate. Data required for participation in these incentive
programs are presented at the time of the patient’s visit.
athenaHealth offers a Federal Stimulus Bonus Payment Guarantee Program to its
athenaClinicals clients. The company guarantees that physicians using their software will
receive their HITECH Act payment from Medicare for “meaningful use” of an EHR. Under the
guarantee program, practices’ total liabilities are capped at 6 months of their revenue.
B-2
B. Cerner Corporation: PowerWorks EMR
Cerner Corporation provides a comprehensive set of clinical and business application
systems to ambulatory care practices, small hospitals, and surgery centers encompassing more
than 3,300 clients and 30,000 physicians. Cerner’s Center Millennium system provides
comprehensive clinical and management systems for small hospitals, while their PowerWorks
Surgery Center system suite is tailored to the data needs of ambulatory surgery centers and
outpatient surgical hospitals. Cerner’s products for ambulatory clinics/practices are contained in
their PowerWorks EMR suite, which includes the following three options:
1. PowerWorks EMR—The full-function system that contains all of the suite’s features.
2. PowerWorks EMR Lite—A scaled-down version of the full-function system for practices
that want a user-friendly and affordable entry into EHR systems without comprehensive
physician documentation, E&M (evaluation and management) coding, and clinical
reporting capabilities.
3. PowerWorks ePrescribe—A stand-alone electronic prescription system without
comprehensive health records and reporting capabilities.
PowerWorks EMR is a Web-based system. Cerner hosts the data, and a computer with a
high-speed Internet connection is all that is required by the practitioner. The system’s EMR
functions include: Since Last Time, which offers a concise picture of any updates with the
patient; This Visit, which gives a quick summary of why the patient is there; Sticky Notes, which
incorporates personal patient information on the chart; and Key Notifications, which triages
results and orders by critical, abnormal, and due. In addition to basic electronic medical record
(EMR) functions, PowerWorks EMR includes electronic prescription, intra-office messaging,
staff/task management, diagnosis lists, decision support, immunization schedules, health
maintenance, nursing and physician documentation, E&M coding assistance, and clinical
reporting capabilities. Two additional modules are available for the PowerWorks EMR system:
(1) Patient Education provides the latest medical findings on disease management, procedures,
and aftercare instructions and (2) PowerWorks Advanced Reporting increases reporting
flexibility.
The system’s PowerWorks ePrescribe function allows the physician to electronically
order prescriptions and automate renewals. Functionalities include electronic decision support at
the time of order entry (the Multum® expert database checks against patient allergies and current
medication list) and the support of regulatory compliance. PowerWorks ePrescribe partners with
SuperScripts®, a third-party provider with access to 95 percent of the pharmacies throughout the
country. If the pharmacy is not a SuperScripts® partner, the system converts the prescription to a
fax.
PowerWorks EMR does not include a practice management function. The clinical practice
system does, however, interface with other PowerWorks business systems from Cerner,
including PowerWorks PM and PowerWorks Business Office Services.
B-3
C. Criterions LLC: The Criterions Medical Suite (TCMS) 1.0.0
Criterions provides a single product system that integrates medical practice management
and EHR functionalities for over 2,000 providers. TCMS is a client-server-based system.
Criterions’ system runs on a client-provided server and internal practice computing
communication system.
TCMS is an open-architecture system that employs a Health Level Seven (HL7) standard
communications interface. The system is HIPAA ready, and it supports real-time, live data
backups. The system’s clinical functions include:
Medical charting.
EHR HandRight, which captures handwritten progress notes.
e-Prescriptions, including formulary checking, drug-diagnosis warnings, and patient
pharmacy suggestions.
Total Recall, which offers physician-specific learning of problem treatment.
Validation reports.
Electronic remittance notification.
User tracking and auditing.
Electronic superbill.
Automated payment posting.
Workflow management.
Online system updates.
The TCMS system includes integrated practice management capabilities. The system’s
business functions include:
Accounts receivable management.
Automated collections.
Recall procedures.
Customized coding.
Eligibility checking.
Automated payment processing.
Recall procedures.
The system supports communication between mobile devices, including TCMS Mobile
and most PDAs (personal digital assistants). TCMS also has a number of document-management
functions, including scanning and imaging.
D. e-MDs: e-MDs Solution Series 6.3
The e-MDs Solution Series is a client-server-based system (Web-based version under
development) with an integrated suite of clinical and practice management modules that are
purchased separately in order to customize the system to the needs of the practice. The e-MDs
Solution Series is currently in use by over 1,350 ambulatory practices in the United States and
contains the following modules:
B-4
e-MDs Chart for electronic medical records.
e-MDs Bill for billing and filing claims.
e-MDs Schedule for staff scheduling.
e-MDs Tracking Board for enterprise workflow management.
e-MDs Rounds for mobile scheduling and charge capture.
e-MDS Patient Portal for scheduling and other patient communication.
e-MDs DocMan for electronic document management.
e-MDs Search ICD-9 for billing codes.
Medicapaedia for sharing data across providers and care settings.
The e-MDs Chart module facilitates point-of-care electronic documentation of clinical
data. The module’s features include:
Customizable point-and-click templates.
Automated E&M coding for calculating optimal codes.
Lab tracking for overdue tests and procedures.
Coding database that includes all ICD-9 (Ninth Revision International Classification of
Diseases) and HCPCS (Healthcare Common Procedure Coding System) codes.
ScriptWriter, a database of over 35,000 drugs with informative consults.
Rules engine that tracks overdue preventive care.
Best-practice guidelines to guide optimal clinical treatment.
Immunization function that retains and reuses lot numbers and expiration date.
Customizable patient education handouts.
The e-MDs Bill module incorporates a number of integrated practice management
functions. The module’s features include:
Automated charge entry from e-MDs Chart.
Automated billing, including secondary and tertiary insurance billing.
In-office e-mail and task management to assign and track work.
On-screen work lists to schedule routine tasks.
Indepth and flexible reporting.
Referral management that creates a history of inbound and outbound referrals.
Electronic remittance for accounts receivable management.
Recall reporting that generates letters, envelopes, and other reminders for patient
followup.
The e-MDs DocMan module produces, stores, and retrieves electronic documents. The
module supports scanning of paper documents and then categorizing in customizable patient
and/or specialty folders. e-DocMan supports multiple document formats, including lab results,
color images, referral letters, images of insurance cards, and video with sound for reference
purposes.
B-5
E. GE Healthcare: Centricity Electronic Medical Record 9.2
GE Centricity represents a brand of 31 software systems from GE Healthcare. Introduced
in 1994 as Logician, Centricity Electronic Medical Record (EMR) is GE Healthcare’s clinical
data system designed for ambulatory clinics/practices and in use by over 30,000 clinicians.
Centricity EMR is a client-server-based system by GE Healthcare that can exchange data with
Centricity Enterprise, the company’s clinical data system for hospitals. In addition, Centricity®
Practice Solution from GE Healthcare is a completely integrated clinical and financial
management system that helps take care of the whole patient from first visit to final
reimbursement and every point in between. It is a singular approach to a more efficient, high-
quality practice.
Centricity EMR includes workflow, order management, electronic prescribing, and
clinical decision support functionalities. The system brings nationally accepted, evidence-based
guidelines to the patient encounter. Through the GE Medical Quality Improvement Consortium,
patient outcomes can be benchmarked by comparisons with those of other practices and/or
against nationally published standards by the American Medical Association, the American
Diabetes Association, and other professional organizations. Automatic reminders can alert the
clinician to needed tests or procedures required to proactively manage potential problems. The
system also includes an E&M advisor that assists with coding accuracy and reporting capabilities
that facilitate application for pay-for-performance and other incentives.
Centricity EMR’s e-Prescribing function can connect to over 95 percent of the country’s
pharmacies through its partnership with SuperScripts®. Centricity EMR has a formulary
eligibility-checking capability to ascertain patients’ eligibility status through their insurer.
Patients’ medication fill history can also be obtained. e-Prescribe communications are
bidirectional, allowing the pharmacy to submit renewal requests electronically.
Centricity EMR does not include billing or other practice management functions. The
system does, however, integrate with all of GE Centricity’s five practice management systems:
Centricity Business.
Centricity Group Management.
Centricity Practice Management.
Centricity Practice Solution.
Centricity Solutions.
All of the Centricity practice management systems provide patient and financial
management, document management, decision support, and connectivity capabilities. The
functional specifics of each system are tailored to best suit the business needs of different
practice types.
F. EHS Inc.: EHS CareRevolution 5.3
EHS CareRevolution is an integrated practice management and EHR system for
ambulatory clinics/practices. EHS is a single-product firm. EHS provides the system in three
configurations:
B-6
Application Service Provider (ASP) is a Web-based system that is completely hosted by
the EHS DataCenter. The clinic/practice is responsible only for the computer and Internet
connection. The ASP system includes the software license, servers, backup, maintenance,
and upgrades for a monthly fee.
Turnkey is a client-server-based system in which the clinic/practice purchases the
software license and hardware from EHS and the system is installed by EHS at the
clinic/practice. After installation, EHS provides only system support.
Hosted Turnkey combines the service advantages of the hosted ASP system with the
potential tax advantages for business equipment expenditure of the Turnkey system. The
clinic/practice purchases the hardware and software license. The software is installed,
operated, and maintained by EHS in their data center. The clinician then accesses the
system through a computer with an Internet connection.
EHS CareRevolution is designed around the clinical encounter. The system has a number
of customizable features that support the clinician before, during, and after the encounter to
facilitate optimal health outcomes for patients. The system’s clinical features include:
The option of using SpeechMagic® voice recognition by Phillips to populate data and
note fields in the chart through dictation.
Use of the Medcin® knowledge database for intelligent prompting, differential diagnoses,
and an E&M code advisor.
Interoffice communication to review orders, lab results, or phone messages.
Patient tracking to know where patients are located, how long they have been waiting, or
the next steps in the patient encounter.
e-RX to send prescriptions to the pharmacy and refill prescriptions electronically.
Order tracking and management for an order audit trail that automatically queues orders
for patient followup.
Patient portal to provide a two-way communication with the patient for appointment
requests, updating of demographic information, prescription refill requests, questions for
nursing staff, and automated forms and other correspondence.
Protocol management that employs a clinical event manager to aid the clinician in
monitoring best-practice guidelines and clinical protocols.
EHS CareRevolution includes integrated practice management capabilities. The system’s
business functions include:
Management of accounts receivable, billing, and collections with customizable
procedures and policies.
Insurance followup on delinquent claims that includes the ability to identify and address
the errors that cause payer rejections.
Alpha II CodeWizard, embedded to scrutinize the data from each encounter like a payer
and ensure accurate E&M coding.
Ad hoc query capability and customizable standard reporting formats.
Management of work queues and task assignments.
EHS also offers complete back-office business process outsourcing for clinics/practices.
EHS employees handle billing, claim submission, statement inquiries, collections, delinquent
B-7
claims, errors and rejections, and claim scrubbing based on the client’s data and practice business
preferences.
G. NextGen Healthcare Information Systems, Inc.: NextGen
Ambulatory Electronic Health Records (EHR) 5.6
NextGen Ambulatory Electronic Health Records (EHR) is NextGen’s EHR system for
clinics and practices, with over 1,800 installations nationwide. The system is available in either
client-server or Web-based formats. NextGen EHR is a patient charting and clinical data system.
For business and patient communication functions, NextGen EHR must be combined with one or
both of the following additional systems available from NextGen:
NextGen Enterprise Practice Management provides claims management, denial
management, eligibility verification, billing, collections, appointment scheduling,
accounts receivable, reporting, and workflow management capabilities.
NextMD Patient Portal provides online consulting, downloading and filing of patient
forms, patient messaging, communication of test results, and customized disease and
health management plan capabilities.
In addition to electronic charting, NextGen EHR provides reporting and document
management functions. The system’s specific features include:
Electronic data connectivity through interfaces to a number of lab devices.
Clinical content templates for over 25 specialties with built-in workflow management
capabilities.
E&M calculator for coding optimization and compliance.
Disease management templates for diabetes, hypertension, and other chronic diseases.
Image management to capture and import images into the patient chart.
Referral management to automatically populate treatment forms with authorization and
provider information.
Reporting capabilities that allow patient data to be collected, stored, and reported for
business analysis, outcomes analysis, medication recalls, and filing of P4P and other
incentives.
Health maintenance management that allows providers to create orders, customize
schedules, and determine overdue patient exams, screenings, immunizations, and tests.
e-prescribing that electronically transmits prescriptions to the pharmacy, manages refill
requests, checks formulary eligibility, and checks allergy, drug-to-drug, and disease
interaction alerts.

B-8
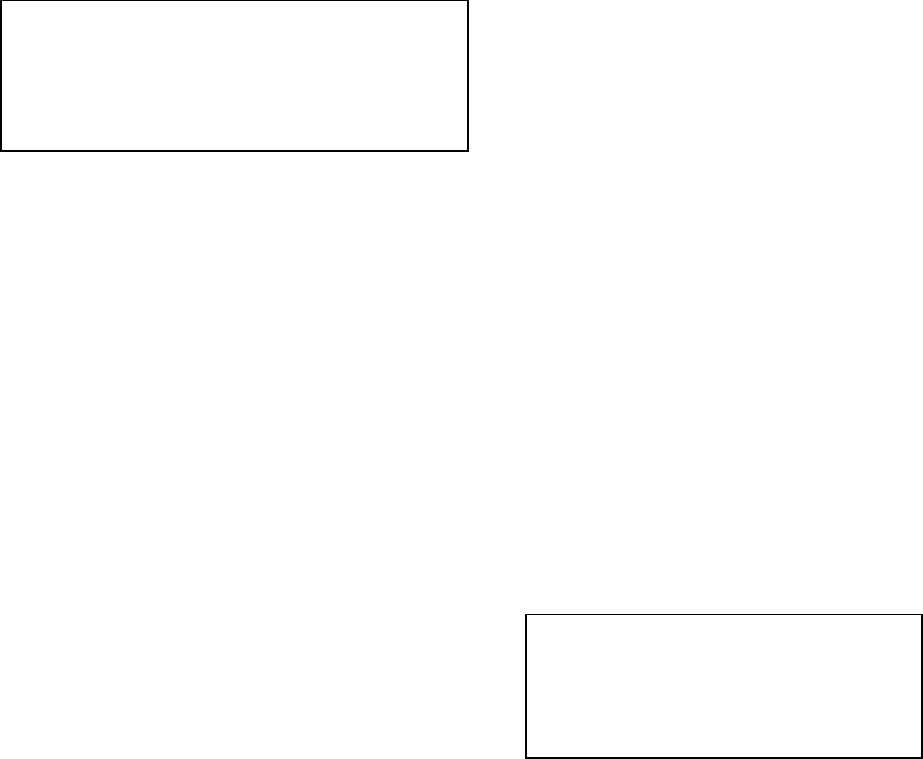
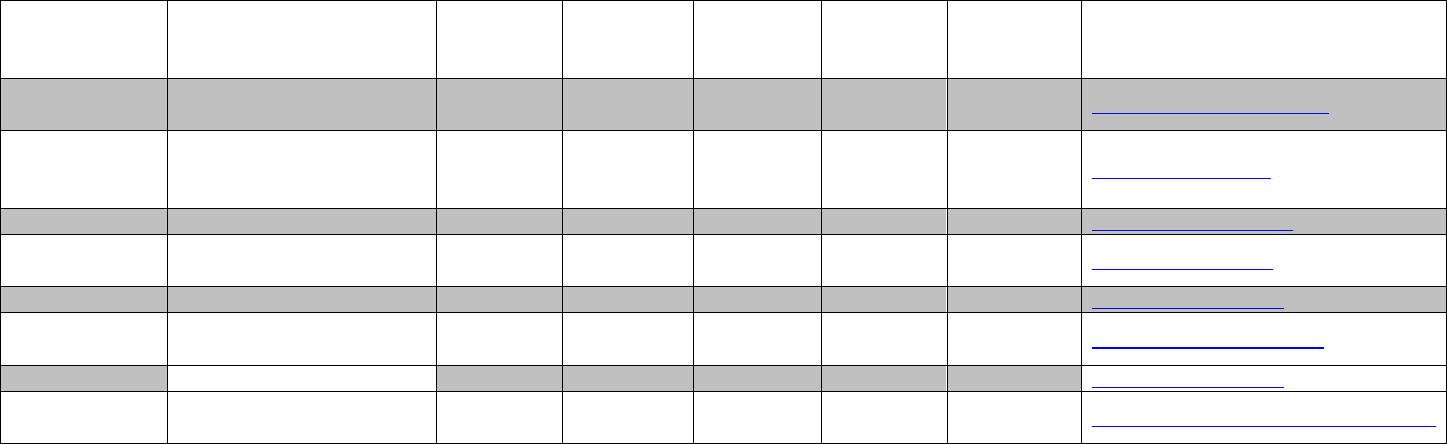
Table 1. Selected system characteristics
EHR system
Practice
management
Patient
comm.
Hardware
format
athenaClinicals
SM
9.15.1
S
S
W
PowerWorks EMR
S
S
W
The Criterions Medical Suite (TCMS) 1.0.0
I
N
C
e-MDs Solution Series 6.3
I/S
I/S
C
Centricity Electronic Medical Record 9.2
S
S
W
EHS CareRevolution 5.3
I
I
W/C
NextGen Ambulatory EHR 5.6
S
S
W/C
EHR=electronic health record.
Practice management and patient communication abbreviations:
I=integrated function within EHR system. I/S=separately purchased module within an integrated EHR system series. N=not
available. S =separately purchased system that integrates with EHR system.
Hardware format abbreviations: C=client server based. W=Web based. W/C=both formats offered.
