
Walgreens Voluntary
Disability Plan for Hourly
Team Members
Summary Plan Description
Prepared by the Walgreen Human
Resources Department for eligible
hourly-paid team members of
Walgreens
TABLE OF CONTENTS
Voluntary Disability Plan Checklist ....................................................................................................................................... 1
Voluntary Disability Plan Resource Guide ............................................................................................................................. 2
Introduction ......................................................................................................................................................................... 3
Eligibility .............................................................................................................................................................................. 3
Enrollment ........................................................................................................................................................................... 3
Plan Options ........................................................................................................................................................................ 4
Plan Costs and Benefits ........................................................................................................................................................ 5
Responsible Parties .............................................................................................................................................................. 5
Plan Features ....................................................................................................................................................................... 5
Deductible Sources of Income .............................................................................................................................................. 6
Definition & Plan Details ...............................................................................................................................................................7
Benefit Maximums ........................................................................................................................................................................8
Benefit Minimums ............................................................................................................................................................... 8
Restrictions Applying to Benefits ......................................................................................................................................... 8
Right to Recover Overpayments ........................................................................................................................................... 8
Recurrent Disabilities ........................................................................................................................................................... 9
Leaves of Absence................................................................................................................................................................ 9
Partial Disability Benefits .................................................................................................................................................... 9
Indexed Monthly Earnings .................................................................................................................................................... 9
Special Return to Work Benefit ...........................................................................................................................................10
Normal Partial Disability Benefits ....................................................................................................................................... 11
Other Benefits .....................................................................................................................................................................11
Filing a Claim .......................................................................................................................................................................12
Procedures for Reviewing Claims .........................................................................................................................................13
Claim Denials ......................................................................................................................................................................13
Appealing a Denied Claim ....................................................................................................................................................14
Prudential’s Review of Appeal.............................................................................................................................................14
Potential Review of Appeal by the Plan Administrator .........................................................................................................14
Notice of Decision on Appeal ...............................................................................................................................................14
General Claims/Appeals Information ...................................................................................................................................15
Plan Limitations ..................................................................................................................................................................15
Pre-existing Conditions ........................................................................................................................................................15
Psychiatric Conditions, Alcohol, Drug, Substance Abuse or Dependency ..............................................................................16
Exclusions and Discontinuation of Benefits ................................................................................................................................ 16
When Coverage Ends...........................................................................................................................................................17
ERISA Rights ........................................................................................................................................................................17
Plan Amendment & Termination Rights ...............................................................................................................................18
Administrative Facts .......................................................................................................................................................... 19

Walgreen Co. (“Walgreens” or the “Company”) is pleased to provide its team members with a comprehensive package of
health and welfare benefit options as described in the Walgreen Health and Welfare Plan (the “Plan”). To assist you in
better understanding the disability benefits available to Walgreens team members covered by the Voluntary Disability
Plan for Hourly Team Members, as in effect as of January 1, 2018 we have prepared this Summary Plan Description
(“SPD”) booklet. The complete Plan includes contracts and agreements with insurance carriers (“Insurer[s]”) and third-
party administrators who provide and administer benefits, this SPD, including any Summary of Material Modifications,
and summary plan descriptions covering other benefits that are not covered by this SPD. You should read the
information provided in this booklet so that you will have a full understanding of the benefits provided and the other
relevant terms and conditions of the Plan. Throughout this document the term “Company” means Walgreen Co. and its
subsidiaries and affiliates whose team members are eligible to participate in the Plan, unless the context is limited to a
particular subsidiary or business unit. See “Administrative Facts” at the end of this booklet for the name of the legal entity
of the Company that is the official plan sponsor of the Plan, and therefore the Company for purposes of formal approvals
and governmental filings.
The benefits of this Plan are governed by the terms of the insurance policy providing the benefits in effect at the time of a
claim. This Summary Plan Description is meant to provide details on the important features of the Plan. Copies of these
Plan documents can be obtained by contacting the Plan Administrator listed at the end of this booklet. In the event of any
discrepancy between this booklet and the provisions of the insurance policies, the provisions of the insurance policies
will govern.
Please understand that the Company reserves the right to amend, modify or terminate this Plan, including any benefits
provided under this Plan or the amount of any required contributions, if any, at any time, and for any reason. You will be
notified of any changes to the Plan within a reasonable amount of time, but not always prior to the time the change goes
into effect. To determine the proper benefits at any given time, it is necessary to consult the Summary Plan Description
booklet, the Plan, and insurance policies that are in effect at the relevant time.
In the event that any term or provision in the SPD is in conflict with any of the terms or provisions of the Plan, the terms
or provisions in the Plan document will govern. The Plan or the Voluntary Disability Plan as used hereinafter refers to
this SPD.
Important Notice
This booklet contains information in English of your Plan rights and benefits under this Plan. If you have difficulty
understanding any part of this booklet, contact the Benefits Support Center at 855-564-6153.
Noticia Importante
Este boletín contiene informacion, escrito en inglés, de sus derechos y beneficios bajo este Plan. Si es difícil comprender
cualquiera parte de este boletín, por favor de ponerse en contacto Benefits Support Center 855-564-6153.
Kung kailangan ninyo ang tulong sa Tagalog tumawag sa Walgreens Human Resources Department at 800-825-5467
如果需要中文的帮助,请拨打这个号码 Walgreens Human Resources Department at 800-825-5467
Dinek'ehgo shika at'ohwol ninisingo, kwiijigo holne' Walgreens Human Resources Department at 800-825-5467
1
Voluntary Disability Plan Checklist
If you need to be off work for an extended period of time due to a disabling condition (illness, injury or pregnancy), you must file a
claim to be considered for a disability benefit under this Plan. Use this checklist as a guide to make sure you take all the necessary
steps for filing a disability claim.
In most cases, you will file a claim for disability benefits under the Walgreens Company-Paid Disability Plan, after a disabling
condition requires you to be off work for more than seven calendar days. If you file a claim for Company-Paid disability benefits, are
approved for benefits, and are nearing the end of the elimination period for benefits under this Plan - the Company-Paid Disability
Plan Administrator, Sedgwick CMS, will forward your disability claim under this Voluntary Disability Plan to the insurance Carrier,
Prudential, for processing.
You may also file a claim directly with Prudential under this Voluntary Disability Plan:
Call Prudential, the voluntary disability insurance carrier, directly at 800-842-1718, between 8 am and 11 pm Eastern Time,
Monday-Friday. You may speak to a trained disability specialist or follow the prompts to record your disability information.
Or, you may log in to www.prudential.com/mybenefits. Click on “Report Time out of Work” and follow the instructions to
complete the Interactive Claimant Submission form.
Please have the following information ready when filing your claim:
o Company name and Control number: Walgreens #42097;
o Your name, address, telephone number, Social Security number, Employee ID number, job title and date of birth;
o Your treating physician's name, telephone number and fax number;
o Your last day worked, first day of absence due to the condition and date you expect to return to work; and
o If your absence is work-related.
Once you are off work, and you are near the end of the elimination period for benefits under this Voluntary Disability Plan,
Sedgwick will forward your claim information to Prudential Insurance. Prudential will process your claim, and contact you to
verify your benefits.
To process your claim for disability, Prudential needs statements from you, your doctor and Walgreens. When you speak to a
Prudential specialist, they will obtain your information. Prudential will request information from your doctor and from
Walgreens, and a decision will be made after review of all the information.
To get information on your claim status or payments, call 800-842-1718 or log in to www.prudential.com/mybenefits.
You should notify Prudential if you have any updated information on your return to work date, your delivery date or if you’d
like to request any forms.
IMPORTANT INFORMATION FOR RESIDENTS OF CERTAIN STATES: There are state-specific requirements that may change the provisions
under the Coverage(s) described in the Group Insurance Certificate provided by Prudential. If you live in a state that has such
requirements, those requirements will apply to your Coverage(s) and are made a part of your Group Insurance Certificate. Prudential has
a website that describes these state-specific requirements. You may access the website at www.prudential.com/etonline. When you
access the website, you will be asked to enter your state of residence and your Access Code. Your Access Code is 42097.
2
Voluntary Disability Plan for Hourly Team Members
Resource Guide
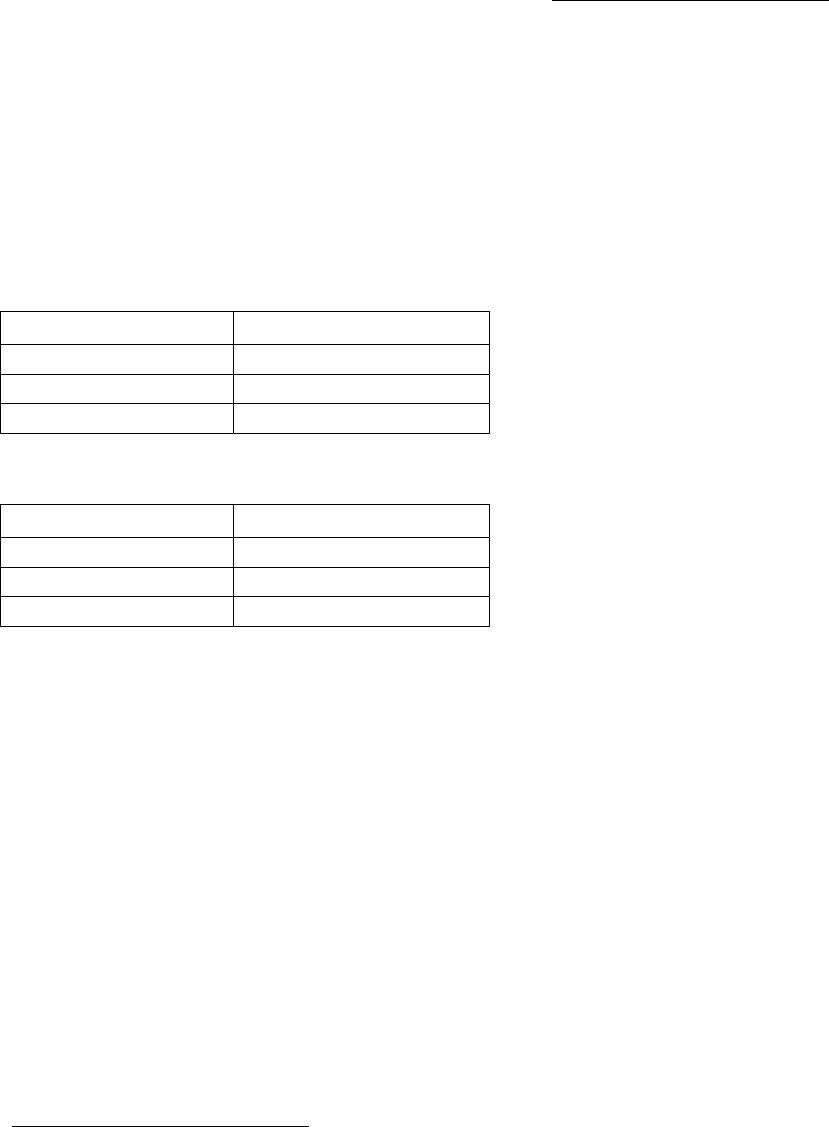
If you have a question about:
Resource
Contact Info
Filing a disability claim under the company-paid plan
and whether it has been forwarded to the Prudential
Voluntary Disability Plan
Sedgwick CMS Disability Center
877-872-0911
TTY: 901-531-4554
Questions about benefit payments after your
v
oluntary disability claim has been approved
Prudential
800-842-1718
Questions on eligibility for coverage under the
Voluntary
Disability Plan
Walgreens Human Resources
Leave Department
800-825-5467
Survivor benefits
Prudential
800-842-1718
Filing an appeal (following a disability claim denial)
Prudential
800-842-1718
Unpaid leave of absence
Walgreens Human Resources
Leave Department
800-825-5467
Medical benefits and/or COBRA
Benefits Support Center
855-564-6153

3
Introduction
Walgreens provides the Voluntary Disability Plan for
Hourly team Members (the “Plan”) to help protect your
financial security if you are unable to earn a full income
due to a covered injury, pregnancy or sickness. This Plan
provides additional income after company-paid disability
benefits under the Walgreens Company-Paid Disability
Plan are exhausted. Coverage is only available to eligible
Walgreen Co. team members – there is no coverage
option for dependents.
This Voluntary Disability Plan has two available options for
providing financial benefits to a covered team member, in
the event the individual is unable to work due to a
disability. These options both provide a benefit of 60% of
covered pay, as long as you qualify – for up to a two year
or five year period. Effective January 1, 2019, these
options both provide a benefit of 50% of covered pay, as
long as you qualify – for up to a two year or five year
period. Eligible team members may enroll in either the
two year or five year option, and pay for the coverage
through after-tax paycheck deductions.
The Plan is meant to provide a disability benefit to
covered team members, once the Company-Paid Disability
Plan benefit ends. The Plan is coordinated with the
Company-Paid Disability Plan, but these are separate plans
with different rules governing qualification for disability
benefits.
There is a 13-week elimination period before disability
benefits begin under this Plan, but that elimination period
may be reduced, so that benefits under this Voluntary
Disability Plan begin as soon as benefits under the
Company-paid plan end.
The Plan is an insured disability benefits program offered
by the Prudential Insurance Company of America.
Prudential reviews and approves your disability claims and
pays disability benefits. The Benefits Support Center is
also involved in the administration of the Plan, as is
Sedgwick CMS for purposes of coordinating claims under
this Plan and the Company-Paid Disability Plan.
Eligibility
To be eligible for coverage under the Voluntary
Disability
Plan for Hourly Team Members, you must:
■
Be an active employee, working in the United States,
excluding Puerto Rico locations;
■
Be paid on an hourly-basis (excluding hourly-paid
pharmacists or registered nurses and hourly-paid
team members who have a Benefit Indicator (BI) of
20 (Assistant Store Managers), 510 (Coordination
Pay Band Team Members) or 511 (Analysis Pay Band
Team Members, who are eligible under a different
plan);
■
Work an average of 30 or more hours per week for
the most recent 52 weeks (or since your start date if
less than 52 weeks);
■
Have at least 181 days of continuous service; and
■
Be actively at work or on approved paid time off or a
regularly scheduled day off on your initial date of
coverage or when the illness or injury occurs. If you
do not meet this requirement on your date of initial
eligibility or onset of illness or injury, that coverage
will be deferred until you return for one full day.
You are not eligible for coverage if you are:
■
A team member of Healthcare Clinics (HCC)
whose payroll is not processed from Walgreens
payroll system.
■
A team member who is covered by a collective
bargaining agreement, unless that agreement
specifically provides for your right to coverage by
this Plan.
■
On a personal leave of absence when the illness or
injury occurs.
A temporary or seasonal team member.
Enrollment
When to Enroll
Evidence of Insurability
If you meet the eligibility requirements, you can enroll in,
cancel or change coverage in the Plan at any time.
However, any enrollment or increase in coverage at any
time other than within 62 days of initial eligibility is subject
to passing Evidence of Insurability (EOI, or proof of good
health). If your EOI is approved, your new coverage will be
effective on the first day of the month, after EOI is
approved.
How to Enroll
To enroll in the Voluntary Disability Plan, go to Your
Benefits Support Center website at
www.BenefitsSupportCenter.com to apply online, or call
the Benefits Support Center at 855-564-6153. If you enroll
online, you will be linked to the Prudential enrollment
website to answer health questions that will assist
Prudential in determining your Evidence of Insurability (EOI
or proof of good health). You will be notified by Prudential
if additional documents are required (such as physician
statements), along with how and when those documents
should be submitted.
When Coverage Begins
Your new coverage or increase in coverage will be effective
the first day of the month following the date your
4
application is received, reviewed and approved, as long as
you are working on the date your coverage would begin (if
not, coverage is deferred until you return to work for one
full day).
Verifying Coverage
Once your coverage begins, the Company will start after-
tax payroll deductions. It is your responsibility to make
sure your premium is deducted from your paycheck. Your
coverage is not in effect if there are no premium
deductions taken from your paycheck. If your deductions
do not begin within two pay periods from your effective
date of coverage, or if your deduction amount is incorrect,
contact the Benefits Support Center by calling 855-564-
6153 to verify your coverage effective date. Payment of
premiums does not activate coverage for any period
during which you do not meet the actively working
requirement.
Your Insurance Certificate
You can obtain a copy of the insurance certificate for your
coverage on Your Benefits Support Center website
www.BenefitsSupportCenter.com, or by calling the
Benefits Support Center at 855-564-6153 to request a
copy. If there are any discrepancies between the
insurance certificate and this Summary Plan Description,
the terms of the certificate will apply.
Changing Your Coverage
You can change your coverage options, add or cancel
coverage at any time, on Your Benefits Support Center
website www.BenefitsSupportCenter.com, or by calling
the Benefits Support Center at 855-564-6153. Please note
that any new coverage or increase in coverage you elect
more than 62 days after your initial eligibility date is
subject to passing Evidence of Insurability (EOI or proof of
good health). You will be notified by the Benefits Support
Center if additional documents are required (such as
physician statements), along with how and when those
documents should be submitted.
Regaining Eligibility
If you lose eligibility for this coverage but remain actively
employed or on an approved leave of absence, and then
you later
become eligible, you will regain eligibility for this
Disability Plan. If your break in coverage is less than six
months, your coverage in this Plan will automatically be
reinstated, and paycheck deductions for premiums will
resume. If you believe your coverage should be reinstated,
but you do not see premium deductions from your
paycheck, contact the Benefits Support Center at 855-564-
6153. If your break in coverage is six months or longer,
you must reapply for coverage, and be subject to passing
Evidence of Insurability (EOI or proof of good health) to be
covered by this Plan again.
Plan Options
Voluntary Disability Plan Benefits
Dates of Disability Prior to 1/1/2019
Option
Benefit Amount
Length of Benefit
Payments
2-Year
Option
60% of monthly
earnings
Until no longer disabled or
24 months from the date
of first payment under the
Voluntary Disability Plan
5-Year
Option
60% of monthly
earnings
Until no longer disabled or
60 months from the date
of first payment under the
Voluntary Disability Plan
Voluntary Disability Plan Benefits
Dates of Disability After 1/1/2019
Option
Benefit Amount
Length of Benefit
Payments
2-Year
Option
50% of monthly
earnings
Until no longer disabled or
24 months from the date
of first payment under the
Voluntary Disability Plan
5-Year
Option
50% of monthly
earnings
Until no longer disabled or
60 months from the date
of first payment under the
Voluntary Disability Plan
Monthly Earnings
Your monthly earnings is determined by multiplying your
hourly rate times your 52-week average weekly work hours
(or your average since date of hire, if less than 52 weeks)
multiplying by 52, and dividing by 12. For purposes of
determining both your premiums for coverage and your
disability benefit payments, your monthly earnings is
generally measured as of a set date prior to initial
enrollment, and then is reset annually, with potential
exceptions for certain types of mid-year changes, as
determined by Walgreens.
Prudential will determine monthly earnings based on the
set covered pay amount reported by Walgreens prior to
your date of disability. Monthly earnings includes base pay
for all hours worked (including base pay for any overtime
hours worked for hourly team members) but does not
include income received from commissions, bonuses,
overtime premium pay, any other extra compensation or
income received from sources other than Walgreens.
If you become disabled while you are on a covered leave
5
of absence, monthly earnings will be determined as
described above.
Premiums will most likely change each calendar year,
based on changes to your age and salary and any other
relevant factors.
Plan Costs and Benefits
Once enrolled, team members pay for the cost of coverage
through after-tax payroll deductions. Walgreens does not
pay any portion of the cost for this Voluntary Disability
Plan. If you receive disability benefits from Prudential
through this Plan, no premiums are due while you are
receiving disability payments.
The cost of coverage depends on your age, your monthly
earnings (calculated once per year to determine your
premium and disability benefit amount), and the plan you
choose (2-year or 5-year option). If you continue coverage
from year to year, your premiums will be recalculated each
year, and your new coverage amount will begin on January
1 (based on your new monthly earnings calculation and
age). Your age is calculated as of January 1
st
of the year you
will move into a higher age bracket (so if you move to a
higher age bracket in June, you will pay the higher rate
beginning in January of that year).
The rates for both options are available on the enrollment
site, www.Benefits SupportCenter.com
These rates are subject to change –so you should check
for any updated information before enrolling in this Plan.
Responsible Parties
All benefits under this Plan are paid directly from
the
insurance carrier, The Prudential Insurance Company of
America, and Prudential is directly
responsible for the final
adjudication of your disability
claim under this Plan.
Sedgwick CMS may forward information on your disability
to Prudential, to aid in determining your benefits.
No deductions will be taken for taxes or benefits from any
disability payments received from this Voluntary Disability
Plan.
Plan Features
Elimination Period
The Voluntary Disability Plan is intended to coordinate
with any benefits available through the Walgreens
Company-Paid Disability Plan. In all cases, there is a
Benefit Elimination Period before the Voluntary
Disability Plan will begin payments. This Benefit
Elimination Period is the earlier of the end of your
Company-Paid Disability Plan benefit, or 13 weeks (91
days), per the following chart.
Benefits under the Voluntary Disability Plan may begin
earlier than 13 weeks after the onset of your disability, if
your benefits under the Company-Paid Disability Plan end
sooner than 13 weeks. For example, if you were disabled
for six weeks earlier in the calendar year, and received
five weeks of disability plan benefits from the Company-
Paid Disability Benefit Plan for Hourly-Paid Team
Members, some of your calendar year benefits would be
used. If you were later disabled from a different condition
in the same calendar year, your benefit under the
company-paid plan would only last six weeks, so you would
have a shorter Benefit Elimination period before your
Voluntary Disability Plan benefits would begin.
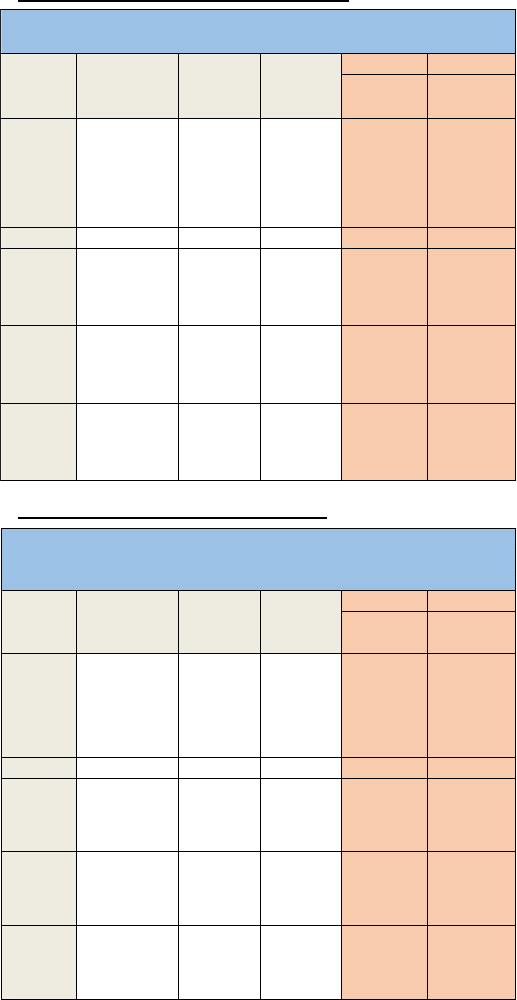
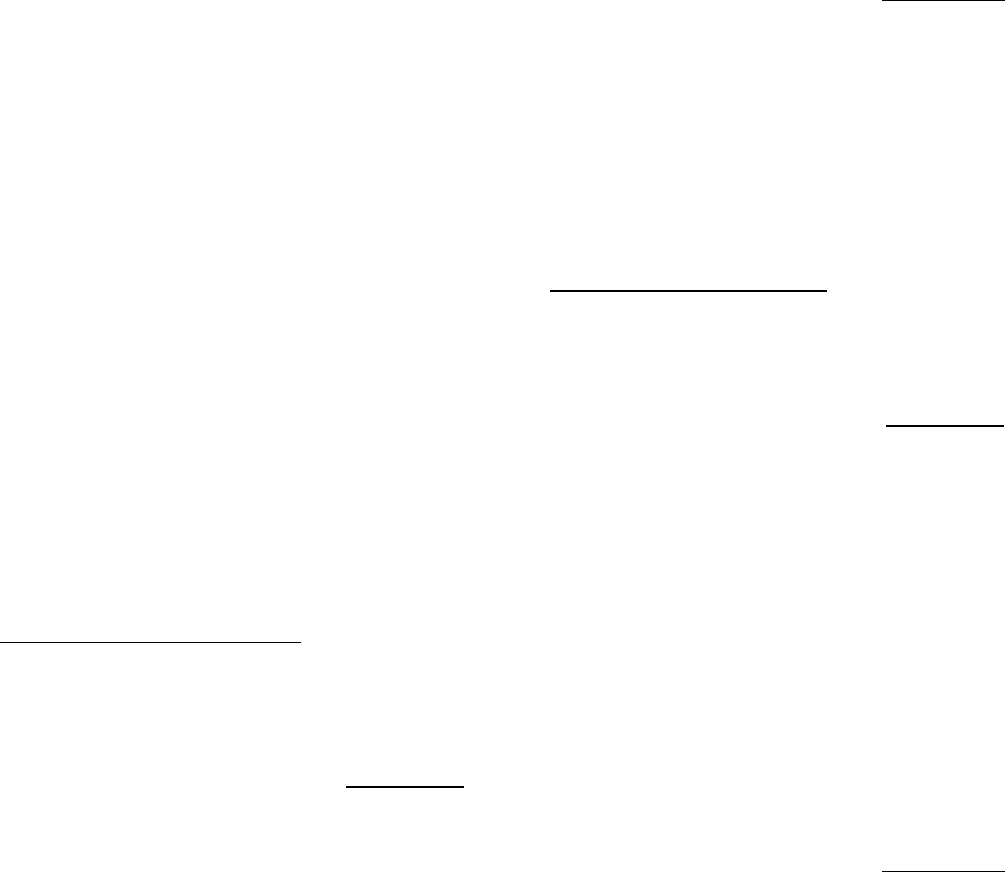
Dates of Disability Prior to 1/1/2019
Dates of Disability After 1/1/2019
VOLUNTARY VOLUNTARY
2-Yea r Income
Re pl a ce Pl a n
Option Pays
5-Yea r Income
Re pl a ce Pl a n
Option Pays
1 week
waiting
period
7 day waiting
period (Full pay to
supplement from
PTO, sick or
vacation time, if
available)
2 – 7 Full Pay
8 – 13
50% of Pay
(PTO, sick or
vacation, if
available to
supplement)
14 – 117
50% of Covered
Pay (PTO, sick
or vacation, if
available to
supplment)
50% of Covered
Pay (PTO, sick
or vacation, if
available to
supplment)
118 – 273
50% of Covered
Pay (PTO, sick
or vacation, if
available to
supplment)
Hourly Team Members
Disability Pay Coordination
Effective 1/1/2019
Week of
Disa bili ty
Avail a ble PTO from
Wa l gree ns
Wa l gree ns
Ful l -Pa y
Disa bili ty
Be nefit
Wa l gree ns
Ha lf-Pay
Disa bili ty
Be nefit
VOLUNTARY VOLUNTARY
2-Yea r Income
Re place Plan
Option Pays
5-Yea r Income
Re place Plan
Option Pays
1 week
waiting
period
7 day waiting
period (Full pay to
supplement from
PTO, sick or
vacation time, if
available)
2 – 7 Full Pay
8 – 13
50% of Pay
(PTO, sick or
vacation, if
available to
supplement)
14 – 117
60% of Covered
Pay (PTO, sick
or vacation, if
available to
supplment)
60% of Covered
Pay (PTO, sick
or vacation, if
available to
supplment)
118 – 273
60% of Covered
Pay (PTO, sick
or vacation, if
available to
supplment)
Hourly Team Members
Disability Pay Coordination
Week of
Disa bil ity
Avail able PTO from
Wa lgreens
Wa lgreens
Ful l-Pay
Disa bil ity
Be nefit
Wa lgreens
Ha l f-Pay
Disa bil ity
Be nefit
6
Taxes
Because you pay for this benefit with after-tax dollars,
any benefit you receive from this Voluntary Disability
Plan, should you become disabled, is income tax-free.
There will be no deductions for taxes or Walgreen
benefit plan premiums taken from any monthly benefit
payments you receive from Prudential. If you receive
benefits from Prudential through this plan, you should
receive a year end W2 for informational purposes only.
Voluntary Disability Coverage
If you are disabled but not yet receiving benefits from this
Voluntary Disability Plan, because you have not yet met
the elimination period for benefits, you must continue to
pay premiums for this Plan to keep your coverage in force.
If, due to a leave of absence or other circumstances, the
amount of your pay from the Company is not sufficient for
the Company to deduct full premiums for your voluntary
coverage under this Plan, you must contact the Benefits
Support Center at 855-564-6153 to make arrangements to
pay directly for your Plan coverage. If you fail to do so,
your coverage will terminate after a period of 60 days of
unpaid or partial-paid coverage.
Deductible Sources of Income
If you receive disability related benefits from other
sources and/or Social Security disability or retirement-
related income,
your benefits under this Plan will be
reduced, or offset,
by the total amount(s) received from
these sources as
their primary benefit. The “Primary
Offset Benefit” amount
is the total amount you, the
covered team member, receive from
other sources.
Your benefits under this Plan will be reduced by the
amount of benefits you are eligible to receive from other
sources, such as (but not limited to):
Social Security disability and/or retirement
benefits,
Workers' Compensation,
state-mandated or Commonwealth-mandated
disability plans,
any other disability plan to which Walgreens or any
other employer
sponsors or contributes,
disability benefits from any employer-
sponsored retirement or pension plan,
wages received under maritime doctrine of
maintenance, wages and cure,
amounts received from a partnership,
proprietorship or any similar draws, and
Unemployment insurance.
For example, suppose your pre-disability monthly
earnings are $3,000 per month and you receive $500 per
month
from Social Security with an additional Social
Security
dependent benefit amount of $500. Your benefit
from
this Voluntary Disability Plan would be calculated as
follows:
Dates of Disability Prior to 1/1/2019
Base salary $3,000/month
Disability benefit (60%) $1,800/month
Social Security benefit - $1,000/month
Benefit after offset $800/month
Dates of Disability After 1/1/2019
Base salary $3,000/month
Disability benefit (50%) $1,500/month
Social Security benefit - $1,000/month
Benefit after offset $500/month
Any benefit you receive from this Voluntary Disability
Plan
is not taxable to you because you paid the premium
for this benefit with after-tax dollars.
You are required to promptly apply for all other income
benefits for which you are potentially eligible and to
promptly appeal any other income claim denial. If you
fail to do so, your benefits under this Voluntary Disability
Plan will be reduced by the estimated amount of the
Primary Offset Benefit you could have received if your
claim had been approved. Your benefits may be withheld
entirely until you do apply for the offset benefit,
including appeals of these claims. If you receive benefits
under this Voluntary Disability Plan, and are later
awarded benefits from one or
more of the sources
listed, you must reimburse the Plan
for any
overpayment the award causes. Plan benefits may also
be delayed while Primary Offset Benefits are pending.
If you receive other income benefits in a lump sum
instead of in monthly payments, you must provide to
Prudential, satisfactory proof of the
breakdown for the
lump sum amount attributable to lost
income, and the
time period for which the lump sum is
applicable. If you
do not provide this information, your
monthly benefit
will be reduced by an amount equal to
the total lump
sum. In that case, Prudential will withhold your
benefit
each month until the calculated lump sum has
been
exhausted. However, if Prudential is
given proof of the
time period and amount attributable
to lost income, any
appropriate adjustments will be
made.
In the event any benefits eligible as offsets are denied
because a claim was not filed in the required time
frame, benefits from this Voluntary Disability Plan will
be reduced by assuming that plan’s maximum disability
benefit would have been awarded.

7
Definitions & Plan Details
What it means to be disabled
You must be considered “disabled”
to receive Plan benefits.
For purposes of the Voluntary Disability Plan, “Disability” is
defined as follows:
Option 1 (2 Year Plan):
You are disabled when Prudential determines that:
you are unable to perform the material and
substantial duties of your regular occupation due
to your sickness or injury;
you are under the regular care of a doctor; and
you have a 20% or more loss in your monthly
earnings due to that sickness or injury.
Option 2 (5 Year Plan):
Regular Occupation Period. You are disabled when
Prudential determines that:
you are unable to perform the material and
substantial duties of your regular occupation due
to your sickness or injury;
you are under the regular care of a doctor; and
you have a 20% or more loss in your monthly
earnings due to that sickness or injury.
Gainful Occupation Period. After 24 months of
payments, you are disabled when Prudential determines
that due to the same sickness or injury:
you are unable to perform the duties of any
gainful occupation including self-employment,
that is or can be expected to provide you with an
income within 12 months of your return to work
that exceeds 60% of your monthly earnings, for
which you are reasonably fitted by education,
training or experience; and
you are under the regular care of a doctor.
While working during Regular Occupation Period
disability earnings cannot exceed 80% of indexed pre-
disability earnings. During the Gainful Occupation Period
disability earnings cannot exceed 60% of indexed pre-
disability earnings.
Your loss of earnings must be a direct result of your
illness, pregnancy or injury. Economic factors such as, but
not limited to, recession, job obsolescence, pay cuts and
job-sharing will not be considered in determining
whether you meet the loss of earnings test.
For an employee whose occupation requires a license,
"loss of license" or inability to qualify for a license for any
reason does not constitute disability.
You may be required to submit to an independent
medical
examination (IME), sign a written authorization
to release
medical records and furnish medical records. If
you fail to
complete a requested IME, furnish requested
medical
records or provide a written authorization for
release of
medical records, each in a timely fashion,
disability
benefits will cease.
In some cases, you will be required to give Prudential
authorization to obtain additional medical information,
and to provide non-medical information (e.g., copies of
your IRS federal income tax return, W-2s and 1099s) as
part of your proof of claim, or proof of continuing
disability. This proof, provided at your expense, must be
received within 30 days of a request by Prudential.
"Regular care" means:
one personally visits a doctor as frequently as is
medically required, according to generally
accepted medical standards, to effective manage
and treat one’s disabling condition(s); and
one is receiving the most appropriate treatment
and care, which conforms with generally
accepted medical standards, for one’s disabling
condition(s) by a doctor whose specialty or
experience is the most appropriate for one’s
disabling condition(s), according to generally
accepted medical standards.
"Regular occupation" means the occupation you are
routinely performing when your disability begins. Prudential
will look at your occupation as it is normally performed
instead of how the work tasks are performed for a specific
employer or at a specific location.
“Material and substantial duties” means duties that:
are normally required for the performance of your
regular occupation; and
cannot be reasonably omitted or modified.
“Sickness” means any disorder of your body or mind, but
not an injury; pregnancy including abortion, miscarriage
or childbirth. A disability must begin while you are
covered under the plan.
“Injury” means a bodily injury that:
is the direct result of an accident;
is independent of sickness;
occurs while you are covered under the Plan;
and
results in immediate disability. Disability must
begin while you are covered under the Plan.
8
Benefit Maximums
The maximum benefit this plan will pay is $10,000 per
month.
Benefits under this Plan reduce or end if you are
released to return to work on a regular, full-time or
part-time basis, or you are no longer disabled as
defined
by this Plan. This requirement is modified by
the terms of
the Residual Benefit section, discussed
later in this
document.
If you remain disabled as defined by the Plan, benefits
may continue according to the following maximum
benefit period schedule:
2-Year Option
Disability begins at age
Maximum benefit period:
Under age 68
63 or 64
24 months
36 months
Age 68
To age 70
Age 69 or older
12 months
5-Year Option
Maximum benefit period:
Under age 68
63 or 64
24 months
36 months
Age 68
To age 70
Age 69 or older
12 months
Disability begins at age
Maximum benefit period:
Under age 65
63 or 64
60 months
36 months
Age 65 - 68
To age 70
Age 69 or older
12 months
The benefit period may be shorter for certain disabling
conditions. (See the "Plan Limitations" section.)
Benefit Minimums
Should your benefit under this voluntary disability plan
be reduced under the Residual Disability, Return to Work
or Deductible Sources of Income features of the Plan
your actual monthly
benefit from this Plan will be at
least 10%
of your benefit before reductions for other
income,
or $100 (whichever is greater).
For example, if your base rate of pay is $2,000 per
month, your normal disability benefit (60%) is $1,200 per
month, and
you are receiving $1,300 per month from
primary and family Social Security benefits, your
monthly benefit from
this Plan will be calculated as
follows:
Dates of Disability Prior to 1/1/2019
Base salary $2,000/mo
Normal Plan Benefit 60% $1,200/mo
SS Disability Benefit $1,300/mo
Benefit after offset $0
Minimum Plan benefit paid $120/mo*
*The greater of 10% of $1,200 ($120) or $100.
Dates of Disability After 1/1/2019
If your base rate of pay is $2,000 per month, your normal
disability benefit (50%) is $1,000 per month, and
you are
receiving $1,300 per month from primary and family Social
Security benefits, your monthly benefit from
this Plan will
be calculated as follows:
Base salary $2,000/mo
Normal Plan Benefit 50% $1,000/mo
SS Disability Benefit $1,300/mo
Benefit after offset $0
Minimum Plan benefit paid $100/mo*
*The greater of 10% of $1,000 ($100) or $100.
Restrictions Applying to Benefits
In no case will disability benefits be payable after the
earliest of the following events:
you are able to return to work on a regular,
full-
time basis,
you are no longer disabled
as defined by this
Plan,
you are no longer under the regular care of
a
physician,
you fail to furnish proof of continuing
disability
when requested by Prudential,
you do not participate in an approved
rehabilitation program as described in
"Mandatory Rehabilitation Requirements",
or
you die.
Right to Recover Overpayments
The Prudential Insurance Company of America or its
designated
agent has the right to recover from you any
amount
determined to be an overpayment. You have the
obligation to repay Prudential any such amount. Rights
and obligations in this regard are set forth in the
reimbursement agreement you are required to sign
when
you submit a claim for benefits under this Plan. The
agreement confirms you will repay all overpayments and
authorizes Prudential, or its designated agent, to
obtain
any information relating to other income benefits.
An
overpayment occurs when it is determined that the
total
amount paid on your claim is more than the total of
the
benefits due under this Plan.
The overpayment equals the amount paid in excess of
the amount that should have been paid under this Plan.
9
An overpayment also occurs when payment is made
that
should have been made under another group
plan. In
that case, Prudential, or its designated agent,
may
recover the payment from one or more of the
following:
any other organization; or
any person to or for whom payment was
made.
Prudential may recover the overpayment by:
offsetting against any future benefits payable
to
you or your survivors, and/or
demanding an immediate refund of the
overpayment from you, and/or,
taking civil actions to recover any Plan
overpayments.
As part of your
claims/appeals rights described in this
booklet, you have
the right to appeal any overpayment
recovery or
demand.
Recurrent Disabilities
If you return to work after a disability (and are not
eligible for residual disability benefits), meet the Plan's
eligibility requirements, and then become disabled again,
the following rules apply to the way your benefits are
paid.
Your benefit under this Voluntary Disability Plan may be
treated as part of your prior claim, so that you will not
need to complete another elimination period provided:
The recurrent disability occurs within six months of
the end of the prior claim; and
You are continuously insured under this voluntary
disability plan, with paid premiums between the
prior claim and the new disability.
Your new disability will not be considered a
continuation of your original disability if your
new
disability starts more than six months after
your return
to full-time employment, or if you have not been
continuously insured under this Plan. In this
situation,
you must meet the eligibility
requirements for a new
disability, and must meet a new elimination period.
A ”recurrent disability” is defined as a disability which
is:
caused by a worsening in your condition; and
due to the same cause(s) as your prior disability
for which Prudential made a disability payment.
Leaves of Absence
Walgreens policies regarding leaves of absence and
employment status are independent of your rights to
disability benefits under this Plan. The duration of your
disability benefit is based solely on the terms and
conditions of this Plan, while the duration of any leave of
absence (and your continued employment status) is
based on separate policies and legal rules. At the time
your disability leave commences, Walgreens or its
agent,
Sedgwick, will provide you with information regarding
leaves
of absence and employment status.
If you are not receiving paid disability benefits from the
Walgreens Company-Paid Disability Plan for Hourly Team
Members you must apply for an Unpaid Medical Leave of
Absence while you are not working due to disability, to
maintain your employment status with Walgreens.
Partial Disability Benefits
If your disability is such that you can work — but are not
able to earn more than 80% of your
indexed prior
earnings, as defined below — you may be eligible for a
reduced benefit,
called a Partial Disability Benefit. This
feature
encourages you to return to work when physically
able.
A partial disability is any disability that prevents you
from
performing on a normal full-time basis, one or more
of the
essential duties of your regular occupation, but allows you
to work at your regular or any occupation, on less than a
normal full-time basis. The wages you earn
while on a
partial disability are called your partial
disability wages.
Partial disability benefits are only available from this
Voluntary Disability Plan when you have met all other Plan
requirements.
Indexed Monthly Earnings
In determining your eligibility for a partial benefit
amount, the Plan uses a special definition of your
monthly earnings called indexed monthly earnings.
Indexed monthly earnings means your monthly
earnings as adjusted on each July 1 provided you were
disabled for all of the 12 months before that date.
Your monthly earnings will be adjusted on that date
by the lesser of 10% or the current annual percentage
increase in the Consumer Price Index. Your indexed
monthly earnings may increase or remain the same,
but will never decrease.
The Consumer Price Index (CPI-W) is published by the
U.S. Department of Labor. Prudential reserves the
right to use some other similar measurement if the
Department of Labor changes or stops publishing the
10
CPI–W. Indexing is only used to determine your
percentage of lost earnings while you are disabled
and working.
While working during Regular Occupation period,
disability earnings cannot exceed 80% of indexed
monthly earnings. After the Regular Occupation period,
disability earnings cannot exceed 60% of indexed
monthly earnings.
Special Return-to-Work Benefit
The Special Return-to-Work Benefit is designed to
encourage you to return to work as soon as you are
able.
If you return to work on a partial disability basis,
your payments under this Voluntary Disability Plan will
not be reduced by any earnings you receive provided:
You are within the first 12 months of working
part-time and receiving benefits from this Plan,
and
The total of your disability benefit under this
Plan and your disability earnings do not exceed
100% of your pre-disability earnings.
If you continue to work on a partial disability basis after
the maximum 12 month Return to Work Period, your
benefit under this Plan will be based on a percentage of
your lost income.
For example, suppose you’re covered under the 2-year
option, and your monthly earnings are $3,000 a
month,
and your
partial disability wages are $1,000 a month.
Your
return-to-work benefit would be calculated as
follows:
Dates of Disability Prior to 1/1/2019
Example A
Monthly earnings $3,000/month
Disability normal benefit
(60% of monthly earnings) $1,800/month
Partial disability wages + $1,000/month
Total income from all sources $2,800/month
Return-to-work benefit $1,800/month
In Example A, your return-to-work benefit equals your
disability normal benefit, since your total income
from all
sources ($2,800) does not exceed your monthly earnings
of $3,000.
Example B
If using the same example, your monthly earnings are the
same, but you earn partial disability wages of $2,000 a
month. In this case, your return-to-work benefit would
be
calculated as follows:
Monthly earnings $3,000/month
Disability normal benefit
(60% of monthly earnings) $1,800/month
Partial disability wages + $2,000/month
Total income from all sources $3,800/month
Excess benefit ($3,800-$3,000) $800/month
Return-to-work benefit
($1,800-$800)
$1,000/month
In Example B, the return-to-work benefit is $800 less
than
the disability normal benefit, since your total
income from
all sources cannot be greater than your
monthly earnings
(in this case $3,000).
Dates of Disability After 1/1/2019
Example A
Monthly earnings $3,000/month
Disability normal benefit
(50% of monthly earnings) $1,500/month
Partial disability wages + $1,000/month
Total income from all sources $2,500/month
Return-to-work benefit $1,500/month
In Example A, your return-to-work benefit equals your
disability normal benefit, since your total income
from all
sources ($2,500) does not exceed your monthly earnings
of $3,000.
Example B
If using the same example, your monthly earnings are the
same, but you earn partial disability wages of $2,000 a
month. In this case, your return-to-work benefit would
be
calculated as follows:
Monthly earnings $3,000/month
Disability normal benefit
(50% of monthly earnings) $1,500/month
Partial disability wages + $2,000/month
Total income from all sources $3,500/month
Excess benefit ($3,500-$3,000) $500/month
Return-to-work benefit
($1,500-$500)
$1,000/month
In Example B, the return-to-work benefit is $500 less
than
the disability normal benefit, since your total
income from
all sources cannot be greater than your
monthly earnings
(in this case $3,000).
11
Normal Partial Disability
Benefits
If you are still partially disabled after 12 months of
receiving benefits under this Voluntary Disability Plan,
the Plan will apply a Partial Disability Earnings Test to
determine if your benefits under this plan will be
reduced for any Partial Disability Wages.
2-Year Plan
While receiving benefits under this Plan during
months 12-24, your Plan benefits will be
calculated based on the percentage of income
you are losing due to your disability as long as
your disability wages are between 20% and 80%
of your indexed prior earnings.
5-Year Plan
During months 12-24 of receiving benefits under
this Plan, your Plan benefits will be calculated
based on the percentage of income you are
losing due to your disability as long as your
disability wages are between 20% and 80% of
your indexed prior earnings.
After 24 months of receiving benefits under this
Plan, your Plan benefits will be calculated based
on the percentage of income you are losing due
to your disability as long as your disability wages
are between 20% and 60% of your indexed prior
earnings.
Example C
Suppose you’re enrolled in the 5-year option, and
before you became disabled your monthly earnings
were $3,000 a month and after 24 months of receiving
benefits under this Voluntary Disability Plan, your partial
disability wages
are $1,500/month. Your indexed prior
earnings are
calculated according to the Consumer
Price Index for the
most recent 12-month period (not
to exceed a 10%
maximum change per 12-month
period). Your normal
partial disability benefit amount
would be calculated as
follows:
Dates of Disability Prior to 1/1/2019
Monthly earnings $3,000
Indexed prior earnings $3,200
Indexed benefit @ 60%
$1,920
Partial Disability Wages
$1,500
% of income lost
53%
$3,420
Partial benefit payable
1017.60
$1,700
In this example, the percentage of income lost is
calculated by subtracting your Partial Disability Wages
(1,500) from your indexed prior earnings (3,200) and then
dividing that answer by your indexed prior earnings (3,200).
Your benefit under this Plan would be the percentage of
income lost multiplied by the indexed benefit (1,920 x .53).
Dates of Disability After 1/1/2019
Monthly earnings $3,000
Indexed prior earnings $3,200
Indexed benefit @ 50%
$1,600
Partial Disability Wages
$1,500
% of lost income
53%
$3,100
Partial benefit payable
$848
$1,700
In this example, the percentage of income lost is calculated
by subtracting your Partial Disability Wages (1,500) from
your indexed prior earnings (3,200) and then dividing that
answer by your indexed prior earnings (3,200). Your benefit
under this Plan would be the percentage of income lost
multiplied by the indexed benefit (1,600 x .53).
Other Benefits
Mandatory Rehabilitation Requirements
Disabled individuals often need to follow a program of
vocational rehabilitation services in order to regain the
ability to work productively. The Prudential Insurance
Company of America will work with you when
appropriate
to develop a work rehabilitation plan. This
will allow you
to return to work on a full- or part-time
basis, in an
occupation for which you are reasonably
qualified, taking
into account your training, education,
experience and
past earnings. This program could
include vocational
training and/or physical therapy. If
you decline to
participate in a Prudential-approved work
rehabilitation plan, you will no longer be eligible for any
benefits from this Plan.
Enhanced Rehabilitation Benefits
While you are receiving benefits under this Plan, and
actively participating in a Prudential approved
rehabilitation program, the Plan will pay enhanced
benefits to you for a maximum of six months. The benefit
enhancement may include:
An additional benefit up to 5% of your monthly
payment. However, the monthly rehabilitation
payment, together with your monthly payment,
will not exceed the maximum monthly payment.
An additional monthly payment up to $500, for
eligible day care expenses for each eligible child.
An additional monthly payment up to $500, for
eligible elder and spouse care expenses for the
care of each eligible family member.
Please contact Prudential at 800-842-1718, for more
information on Rehabilitation Benefits.

12
Survivor Benefit
The Plan will pay a benefit to your eligible survivors if you
die while you are disabled and
receiving voluntary
disability benefits under this Plan at the time of your
death. The
survivor benefit will be paid in a single lump
sum, and
will be equal to three times your most recent
gross
monthly benefit. The benefit is
payable to your
spouse/partner (as defined by Walgreens for its medical
plan qualifications), if living at
the time payment is made.
Otherwise, it is payable by
dividing the benefit amount
equally among your eligible
children. If there is no
eligible survivor, the benefit will be paid to your estate.
Eligible children are your unmarried children, your
eligible spouse/partner's unmarried children, your
unmarried adopted children, and unmarried children
placed for adoption with you prior to legal adoption
being final, and all under age 25.
To file a claim for this benefit, your survivor should
contact Prudential at 800-842-1718.
Please keep this
booklet with your other important
papers so your
beneficiaries will know the correct
procedures to follow.
Filing a Claim
If you file a claim under the Company Paid Disability
Plan for Hourly Team Members through Sedgwick CMS
Disability Claim Center at 877-872-0911 or TTY Line
(Teletypewriter for the hearing
impaired) 901-531-
4554, Sedgwick will forward your claim information to
Prudential, once you are getting close to the end of the
elimination period for benefits under this Plan, so you
may not need to file a separate claim through
Prudential.
If you need to file a claim directly with Prudential for
benefits under this Plan, it's important
to follow the
correct benefit claim procedure.
How to File a Claim
To submit a claim for benefits under this Plan, call
Prudential at 800-842-1718 between 8 am and 11
pm, Eastern Time, Monday – Friday. You can speak
to a trained disability specialist or follow the prompts
to record your disability information. You may also
file a claim online by logging into
www.prudential.com/mybenefits. Click on “Report
Time out of Work” and follow the instructions to
complete the Interactive Claimant Submission form.
You should ensure your claim has been filed with
Prudential within 30 days of the start of your
disability. However, you must give Prudential written
proof of your claim no later than 90 days after your
elimination period ends. If it is not possible to give
proof within 90 days, it must be given no later than 1
year after the time proof is otherwise required except
in the absence of legal capacity.
You should have the following information ready
when you report your claim:
Company Name: Walgreens
Company Control Number: 42097
Your Employee ID or Social Security number
Your address and telephone number
Your date of birth
Your job title
Your doctor’s name, phone number and fax
number
Your last day worked and first day absent due to
the condition
The date you expect to return to work
Whether your absence is work-related.
Prudential will contact you if additional information is
needed.
To process your claim for disability, Prudential will need
a statement from you, your doctor and Walgreens.
When you speak to a Prudential specialist, he or she will
obtain your information. Prudential will then request
the necessary information for your doctor and
Walgreens. A decision will be made after all this
information is reviewed.
Be sure to tell your doctor that he or she will be
contacted by Prudential, to
obtain information
concerning your disability. Your doctor will need
authorization from you to provide Prudential with any
of your medical
information. In most cases, you must
provide each
doctor with a signed authorization to
release medical
information. You may use the
authorization form
provided by the medical provider.
You will also be
required to sign and return an
authorization form for
release of information before any
benefit will be
approved. Prudential will attempt to
work directly with your doctor to obtain the needed
medical history information, but it is your responsibility
to provide these proofs of disability.
If you are unable to personally file your claim, you may
have a friend or relative file it on your behalf, following
the procedures in this section. If you need to designate
someone to authorize the release of any health
information, you will need to appoint a person with
power of attorney to act in your place. This requires a
formal document.
It is your responsibility to pay for any charges by your
medical provider to furnish medical information or
copies of medical records. The company will not
reimburse you or your medical provider for these
13
expenses.
When necessary, Prudential may use the
services of
outside consultants and other sources to aid
in the
evaluation of your disability status. Prudential reserves
the right to determine whether
your disability qualifies
for benefits.
As a condition of receiving benefits, you may be required
to submit to an independent medical examination (IME),
which would be paid for by Prudential. If you do not
complete the requested IME in a timely manner,
disability benefits will cease (or not be approved).
Prudential has the right to request an IME, but is not
obligated to do so.
You should contact Prudential again by phone or online
if:
You have updated information
You are unable to return to work when
planned
You have returned to work or are returning
You want to report your delivery date
You need forms.
If you have questions on the status of your disability
claim or payments, please call Prudential at 800-842-
1718, or log into www.prudential.com/mybenefits.
If you are eligible for state disability
benefits from New
York, Rhode Island, New Jersey,
California or Hawaii,
you are responsible for
filing your separate disability
claim for the
state plan. Upon receipt of the
Explanation of Benefits (EOB) from that plan, you must
provide a copy of the EOB to Prudential before any
voluntary disability benefit payment will be made.
Please Note: If you are eligible for workers' compensation
and/or state disability payments, benefit approval and
payment information for those plans must be submitted
to Prudential in order to receive benefit payments from
this Plan.
Procedures for Reviewing
Claims
The claims procedures described below are prescribed
by
a federal law called the Employee Retirement
Income
Security Act of 1974 (ERISA). The following
disability Claims and Appeals Procedures apply only to
disability claims filed on or after April 1, 2018.
Initial Claims Determinations: All formal benefit claims
under the Plan will be reviewed by Prudential (the
insurance carrier), or any third party engaged by
Prudential for this purpose (collectively, the “Claim
Administrator”), which will make its decision, based
on
the information submitted by you, within 45 days
after
the claim is submitted. By notice to you before this
period ends, the Claim Administrator may extend this
deadline by up to 30 additional days if it determines that
a decision cannot be made during the initial period for
reasons beyond the control of the Plan. An extension
notice will specify the length of the extension and inform
you that a decision cannot be made within the deadline
because of reasons beyond the control of the Claim
Administrator. A second extension of up to an additional
30 days also may be declared. If such an extension is
necessary, the notification will include a description of
the circumstances requiring the extension and an
estimate of the decision date.
Claim Denials
If your claim is denied, the Claim Administrator will send
you a notice that will:
be written in a manner that you should
understand;
include the specific reasons for the adverse
benefit determination;
refer to the provisions of the Plan on which the
determination was based;
describe any additional material or information
necessary to perfect the claim and explain why
the additional material is necessary;
explain the Plan's review procedures including
relevant deadlines;
include a statement of your right to bring a civil
action under ERISA after receiving a final
determination upon appeal. The notice will also
include an explanation of any applicable
contractual limitation period for bringing a civil
action under section 502(a) of ERISA, and a
description of the calendar date on which the
limitations period expires;
identify any internal rule, protocol or
criterion
that was relied on in making the
a d v e r s e
b e n e f i t
determination or, alternatively, a
statement that no such specific rule, guideline,
protocol, standard or criterion exists;
include a language assistance notice in
Chinese, Tagalog, Navajo and Spanish;
if advice is obtained from medical or vocational
experts in connection with an adverse benefit
determination that is inconsistent with its
decision, an explanation as to why the Claims
Administrator disagreed with, or did not
follow, this advice without regard to whether
the advice was relied on in making the
determination; and
an explanation of disagreement with any
14
disability determination made by the Social
Security Administration (SSA), or any view of
health care professionals who are treating
you or vocational experts who are evaluating
your claim to the extent you presented such
determination or views to the Claims
Administrator.
Appealing a Denied Claim
To appeal a claim denial, you must send your written
appeal to
Prudential within 180 days of receiving
notice
of the claim denial. Your appeal should contain:
Your name, control number (42097), and Social
Security number (or claim number)
The reasons that you disagree with the
determination
Medical evidence or information to support
your position such as:
• Copies of therapy treatment notes
• Any additional treatment records from
physicians
• Actual test results (e.g. EMG, MRI)
Your appeal may also contain written
comments,
documents, records and other pertinent
information. You
will be given reasonable access to, and
copies of, all
documents, records and other information
relevant to the
claim. It is essential that you supply all
information or
opinions that you believe may be relevant
to the claim. To
be assured of a proper response to the
appeal, it must be
directed to Prudential Appeals Review Unit at:
Appeals Review Unit
The Prudential Insurance Company of America
Disability Management Services
PO Box 13480
Philadelphia, PA 19176
Phone: (800) 842-1718
Fax: (877) 889-4885
Prudential’s Review of Appeal
The appeal will be conducted by the Prudential Appeals
Review Unit,
and the reviewer will be a named fiduciary
who is neither
the individual nor a subordinate of the
individual who
made the initial denial. This reviewer will
not give
deference to the initial benefit determination
and will
take into account all comments, documents,
records and
other information that you submit relating
to the claim,
without regard to whether the information
was
submitted or considered in the initial benefit
determination.
If the initial denial was based on a medical judgment, the
reviewer will consult with a health care professional who
has appropriate training and experience in the medical
field. This health care professional will not be an
individual
who was consulted in connection with the
initial benefit
determination or the subordinate of any
such individual.
Potential Review of Appeal by
the Plan Administrator
If Prudential determines that the appeal presents
material issues that are outside the expertise or purview
of the Prudential Appeals Review Unit (such as hours
worked, employment status or new or unique procedural
or Plan
interpretation issues), then the decisions will be
subject to further review by the Plan Administrator. You
will be notified if such a further
review will be performed.
Unless you are instructed that
additional information is
needed for this review, you will
not be required to submit
any further information to the Plan Administrator
(although you may do so if you wish).
The Plan
Administrator’s decision will be based on all
information
submitted by you and any other information
that the Plan
Administrator considers relevant.
Notice of Decision on Appeal
Regardless of whether the Plan Administrator gets
involved in the decision, you will be notified of the
benefit determination within 45 days of the receipt of
the appeal. By notice to you before this period ends,
Prudential may extend this deadline by up to 45
additional days if it determines that a decision cannot
be made during the initial period for reasons beyond the
control of the Plan. If any adverse benefit determination
is anticipated during the appeal review, you will be
provided with the new information or rationale sufficiently
in advance of the appeal decision to allow you a
reasonable opportunity to respond. An extension notice
will specify the
length of the extension and inform you
that a decision
cannot be made within the deadline
because of reasons
beyond the control of Prudential.
If the decision on appeal is denied, the Prudential
Appeals Review Unit will provide
you with a notice of
the denial that will:
be written in a manner that you should
understand;
include the specific reasons for the denial;
refer to the provisions of the Plan on which the
determination was based;
inform you that, upon request and free of
charge, you are entitled to reasonable access to
and copies of all documents, records and other
information relevant to your claim;
explain the Plan's claim review procedures
(including relevant time limits) and your right to
bring legal action under ERISA;
15
include an explanation of any applicable
contractual limitation period for bringing a
civil action under section 502(a) of ERISA, and
a description of the calendar date on which
the limitations period expires for filing any
legal action;
identify any internal rule, guideline,
protocol, standard or criterion that was
relied on in making the adverse benefit
determination or, alternatively, a statement
that no such specific rule, guideline,
protocol, standard or criterion exists;;
if the advice of a health care professional or
vocational expert was obtained, identify
such
person or persons;
if advice is obtained from medical or
vocational experts in connection with an
adverse benefit determination that is
inconsistent with the appeal decision, an
explanation as to why the Claims
Administrator disagreed with, or did not
follow, this advice without regard to
whether the advice was relied on in making
the determination;
an explanation of disagreement with any
disability determination made by the SSA,
or any view of health care professionals
who are treating you or vocational experts
who are evaluating your claim to the extent
you presented such determination or views
to the Claims Administrator;
include a language assistance notice in
Chinese, Tagalog, Navajo and Spanish; and
notify you that you can contact the
Department
of Labor to learn about other
voluntary dispute
resolution options.
General Claims/Appeals
Information
Both in the context of initial claims determination and in
the context of reviewing appeals, there may be situations
where Prudential needs additional information from you
before it can
make its determination. If that is the case,
you will be
notified of the specific information that is
needed and/or
any issues that need to be resolved, and
you will be given
a reasonable period of time to supply
the needed
information (generally 30 days). In such
situations, the
deadlines for responding to the claim or
appeal may be
put on hold while the receipt of this
additional
information is pending.
The claims and appeals reviewers described above will
apply their judgment to claims and appeals in a manner
that they deem to be consistent with the Plan and any
rules, regulations or prior interpretations of the Plan.
Those reviewers will
make their decisions in a manner
that they believe will
apply the Plan consistently to
similarly situated
participants.
The authority granted to these claims and appeals
reviewers to construe and interpret the Plan and make
benefit determinations, including claims and
appeals
determinations, shall be exercised by them (or
persons
acting under their supervision) as they deem
appropriate
in their sole discretion. Benefits under this
Plan will be
paid or provided to you only if these reviewers decide in
their discretion that you are entitled to them.
All such
benefit determinations shall be final and binding
on all
persons, except to the limited extent to which the
Prudential
Appeals Review Unit's decisions are subject to
further
review by the Plan Administrator.
You must first utilize the claim and appeal rights
described
above before you may properly assert any
claims in court.
If you fully exhaust these rights, but
remain dissatisfied
with the outcome of your appeal, you
may challenge the
decision in an ERISA Section 502(a)
benefit claim. No such
legal action may be commenced more than one year, or
later if required by state or federal law, after (i) the date
you are informed of the decision on your appeal, or (ii) the
date you are informed of the last claim decision if you
attempt to file legal action without utilizing all of the
required claim and appeal rights. See venue provision in
the “Enforce Your Rights” section.
If you believe a violation of the Plan rules related to your
claim may have occurred, you may write to the Claims
Administrator for an explanation. The Claims
Administrator has the option of providing a response
within 10 days of your notice.
Plan Limitations
Some situations are not covered by this Plan, or there
may
be limitations imposed by this Plan on coverage or
benefits.
Pre-existing Conditions
In most cases, there is a pre-existing condition limitation
applying to the Voluntary Disability Plan for Hourly Team
Members.
You have a pre-existing condition if both 1. and 2. are
true:
1. (a) You received medical treatment, consultation,
care or services, including diagnostic measures, or took
prescribed drugs or medicines, or followed treatment
recommendation in the three months just prior to your
effective date of coverage or the date an increase in
benefits would otherwise be available; or
16
(b) you had symptoms for which an ordinarily prudent
person would have consulted a health care provider
in the three months just prior to your effective date
of coverage or the date an increase in benefits would
otherwise be available.
2. Your disability begins within 12 months of the date
your coverage under the Plan becomes effective.
If you lose eligibility for coverage under the Plan, and
later regain eligibility, this pre-existing condition
limitation will again apply beginning with your new
coverage effective date.
The pre-existing condition limitation does not apply for
Plan participants who enrolled in the Plan during the
initial enrollment period of March 16 through April 30,
2018, and have been continuously covered by the Plan
within the same coverage option.
Psychiatric Conditions, Alcohol,
Drug, Substance Abuse or
Dependency
Disabilities which, as determined by Prudential, are
due to mental illness have a limited pay period during
your lifetime. The limited pay period for mental illness
is 24 months during your lifetime. Prudential will
continue to send you payments for disabilities due to
mental illness beyond the 24 month period if you meet
one or both of these conditions
1. If you are confined to a hospital or institution at the
end of the 24 month period, Prudential will continue to
send you payments during your confinement. If you
are still disabled when you are discharged, Prudential
will send you payments for a recovery period of up to
90 days. If you become reconfined at any time during
the recovery period and remain confined for at least
14 days in a row, Prudential will send payments during
that additional confinement and for one additional
recovery period up to 90 more days.
2. In addition to item 1, if, after the 24 month period
for which you have received payments, you continue
to be disabled and subsequently become confined to a
hospital or institution for at least 14 days in a row,
Prudential will send payments during the length of the
confinement.
Prudential will not pay beyond the limited pay period
as indicated above, or the maximum period of
payment, whichever occurs first.
Prudential will not apply the mental illness limitation
to dementia if it is a result of:
stroke;
trauma;
viral infection;
Alzheimer’s disease; or
other conditions not listed which are not usually
treated by a mental health provider or other
qualified provider using psychotherapy,
psychotropic drugs or other similar methods of
treatment as standardly accepted in the practice
of medicine.
Mental illness means a psychiatric or psychological
condition regardless of cause. Mental illness includes but
is not limited to schizophrenia, depression, manic
depressive or bipolar illness, anxiety, somatization,
substance related disorders and/or adjustment disorders
or other conditions. These conditions are usually treated
by a mental health provider or other qualified provider
using psychotherapy, psychotropic drugs or other similar
methods of treatment as standardly accepted in the
practice of medicine.
Exclusions & Discontinuation of
Benefits
The Voluntary Disability Plan does not cover any
disabilities caused by, or resulting from employees:
intentionally self-inflicted injuries;
active participation in a riot; or
commission of a crime for which you have been
convicted under state or federal law.
The Plan does not cover a disability due to a pre-existing
condition as defined in the “Pre-existing Conditions”
section above.
The Plan does not cover a disability due to war, declared
or undeclared or any act of war.
Prudential will stop sending you payments while you are
incarcerated as a result of a conviction.
Prudential will stop sending you payments and your claim
will end on the earliest of the following:
1. During the first 24 months of payments, when
you are able to work in your regular occupation
on a part-time basis but you choose not to;
2. After 24 months of payments, when you are able
to work in any gainful occupation on a part-time
basis but you choose not to.
3. The end of the maximum period of payment.
4. The date you are no longer disabled under the
terms of the Plan.
5. The date you fail to submit proof of continuing
17
disability satisfactory to Prudential.
6. The date your disability earnings exceed the
amount allowable under the Plan.
7. The date you die.
8. The date you decline to participate in a
rehabilitation program that Prudential considers
appropriate for your situation and that is
approved by an independent doctor.
Maximum period of payment means the longest period
of time Prudential will make payments to you for any
one period of disability.
Part-time basis means the ability to work and earn 20%
or more of your indexed monthly earnings.
Please Note: Loss, restriction, non-issuance, revocation
or
non-renewal of any license, permit or certification
required to engage in an occupation will not be
considered a disability.
When Coverage Ends
Your coverage under this Plan ends when you no longer
meet the Plan's eligibility requirements.
Loss of Eligibility
Failure to meet the eligibility requirements will result in a
loss of disability coverage under this Plan. You will not be
covered by this Plan when any of the following occur:
your 52-week work average (or average since
your date of first becoming eligible for this
coverage, if less than 52 weeks) is below 30
hours per week on your first day of disability;
you are no longer actively working in a
position
eligible for this Plan (unless you are
receiving
disability benefits from this Plan);
the Company discontinues the Plan;
you are still an active employee of the
Company, but your initial
date of disability is
more than 30 days after the
latest of your last
day worked or the end of a
leave covered by
the Family & Medical Leave
Act, or your last
vacation day;
the end of the month you fail to pay the
required premiums. If, due to a leave of
absence or other circumstances, the amount
of your pay from the Company is not sufficient
for the Company to deduct full premiums for
your voluntary coverage under this Plan, you
must contact the Benefits Support Center at
855-564-6153 to make arrangements to pay
directly for your Plan coverage. If you fail to
do so, your coverage will terminate after a
period of 60 days of unpaid or partial-paid
coverage;
you are on an approved personal leave of
absence;
you are on any type of leave of absence
for six or more months. Your coverage
under this Plan will end 6 months from
your last day worked, unless you are
receiving disability benefits from this Plan.
your employment ends (as determined by
the Company); or
you die.
ERISA Rights
Your rights under the Employee Retirement Income
Security Act of 1974, as amended (ERISA) are explained
here.
As an employee eligible to participate in the Plan, you are
entitled to certain rights and protections under ERISA.
ERISA provides that all Plan participants are entitled to:
Receive Information about Your Plan and Benefits
Examine, without charge, at the Plan
Administrator's office and at other specified
locations, all documents governing the Plan,
including insurance policies/contracts and
collective bargaining agreements (if applicable),
and a copy of the latest annual report (Form
5500 Series) filed by the Plan with the U.S.
Department of Labor and available at the
Public
Disclosure Room of the Employee
Benefits
Security Administration.
Obtain, upon written request to the Plan
Administrator, copies of documents governing
the
operation of the Plan, including insurance
policies/contracts and collective bargaining
agreements (if applicable), and copies of the
latest
annual report (Form 5500 Series) and
updated
Summary Plan Description. The Plan
Administrator
may make a reasonable charge
for the copies and
will inform you in advance of
the cost. To view or
receive a copy of any plan
documents, you should
send a written request
(noting the specific
document(s) of interest) to
the following address:
Health & Welfare Plan Committee
Walgreen Co.
108 Wilmot Road, MS 1825
Deerfield, IL 60015-5143
Receive a summary of the Plan's annual financial
report. The Plan Administrator is required by law to
furnish each participant with a copy of this summary
annual report.
18
Receive information about your Plan and
benefits.
Prudent Actions by Plan Fiduciaries
In addition to creating rights for plan participants, ERISA
imposes duties upon the people who are responsible for
the operation of the plan. The people who operate your
plan, called "fiduciaries" of the plan, have a duty to do
so
prudently and in the interest of you and other plan
participants and beneficiaries. No one, including your
employer, your union (if applicable) or any other person,
may fire you or otherwise discriminate against you in
any
way to prevent you from obtaining a welfare
benefit or
exercising your rights under ERISA.
Enforce Your Rights
If a claim for a welfare benefit is denied or ignored, in
whole or in part, you have a right to know why this was
done, to obtain copies of documents relating to the
decision without charge and to appeal any denial, all
within
certain time schedules.
Under ERISA, there are steps you can take to enforce the
above rights. For instance, if you request a copy of Plan
documents or the latest annual report from the Plan and
do not receive them within 30 days, you may file suit in a
federal court. In such a case, the court may require the
Plan
Administrator to provide the materials and pay you
up to
$110 a day until you receive the materials, unless
the
materials were not sent because of reasons beyond
the
control of the Plan Administrator. If you have a claim
for
benefits which is denied or ignored, in whole or in
part,
you may file suit in a federal court, but only after
you have
exhausted your claims and appeals rights
described above.
In addition, if you disagree with the
Plan's decision or lack
thereof concerning the qualified
status of a domestic
relations order or a medical child
support order, you may
file suit in federal court after you
have exhausted your
claims and appeals rights described
above. If it should
happen that Plan fiduciaries misuse
the Plan's money, or if
you are discriminated against for
asserting your rights, you
may seek assistance from the U.S. Department of Labor, or
you may file suit in a
federal court. The court will decide
who should pay court
costs and legal fees. If you are
successful, the court may
order the person you have sued
to pay these costs and
fees. If you lose, the court may
order you to pay these
costs and fees, for example, if it
finds your claim is
frivolous.
No action at law or in equity shall be brought in
connection with the Plan except in the following venues:
(A) all actions arising under federal law must be filed in
the United States District Court for the Northern District
of Illinois, and (B) all actions arising under state law must
be filed in the Circuit Court of Cook County, Illinois.
Plan Amendment and
Termination Rights
The Company, and as applicable the insurance carrier,
reserves the right to alter, amend or cancel
the Plan at their
sole discretion at any time. Modifications to the Plan,
including amendment and termination, will be implemented
at the written direction of the Chief Executive Officer,
Executive Chairman of the Board or Chief Human Resources
Officer of the Company. In the event of Plan
termination,
claims incurred prior to the date of
termination will be paid
out of any remaining Plan funds.
Participation in this Plan
does not create a contract or a
guarantee of employment or
coverage, nor does it give
any company or person a legal or
equitable right against
the Company, its shareholders,
directors or officers.
This booklet is intended to provide an easy-to-understand
summary of the Walgreens Voluntary Disability Plan for
Hourly Team Members. It simplifies, but does not replace
the legal text of the Walgreen Health and Welfare Plan. In
the case of conflict, the legal text of the Walgreen Health
and Welfare Plan governs.
19
Administrative Facts
The establishment of this Plan, or any modification to it, does not create a contract or guarantee of employment or
coverage, nor does it give any company or person a legal or equitable right against the Company, its shareholders, directors
or officers.
Plan Name
Walgreens Voluntary Disability Plan for Hourly Team Members
Plan Sponsor
Walgreen Co. (The term "Walgreen Co" refers to the Walgreens family of
companies)
Plan Type
Long-Term Disability
Plan Administrator and
Agent for Legal Service
The Plan Administrator is the Health and Welfare Plan Committee, Walgreen Co.,
108 Wilmot Road, MS 1825, Deerfield, IL 60015-5143.
The Company and, except in limited circumstances, the Plan Administrator have no
authority or discretion regarding the payment of or determination of Plan benefits.
This Plan Administrator has delegated authority to the Prudential Insurance
Company of America to provide claim processing, claim investigation, claim control
and the daily administration of the Plan. While an insurance policy is in force, the
Insurance Carrier, Prudential Insurance Company of America is responsible for
processing benefit claims and paying benefits in accordance with the terms of the
insurance policy issued to the insured.
Insurance Carrier / Claims
Administrator
The Prudential Insurance Company of America
751 Broad Street
Newark, NJ 07102
Type of Administration
Insurer Administration
Plan Year
January 1–December 31
Plan Number
501
Employer ID Number
36-1924025
Plan Costs
Benefits are provided by the insurance carrier, the Prudential Insurance Company of
America, and funded by premiums paid by participants.
Administration Office for
Carrier
Benefits Support Center
www.BenefitsSupportCenter.com 855-564-6153
If you have any questions about this Plan, contact the Benefits Support Center at 855-564-6153 or Walgreens Human
Resources Leave Department at 800-825-5467. The Plan Administrator is available to answer your general questions.
However, raising questions or making an inquiry in this fashion will not satisfy the claims procedure requirements (see the
"Claims Procedures" section). If you wish to file a formal claim or
appeal a claim denial, you must follow these formal claims
procedure requirements. If you have any questions about this statement or about your rights under ERISA, or if you need
assistance in obtaining documents from the Plan Administrator,
you should contact the nearest office of the Employee
Benefits Security Administration, U.S. Department of Labor, listed in
your phone directory or the Division of Technical
Assistance and Inquiries, Employee Benefits Security Administration, U.S. Department of Labor, 200 Constitution Avenue
N.W., Washington, D.C. 20210. You may also obtain certain publications
about your rights and responsibilities under ERISA
by calling the publications hotline of the Employee Benefits Security
Administration at 866-444-3272 or at
www.dol.gov/ebsa.

1/1/2018
