KATHY HOCHUL
Governor
CHINAZO CUNNINGHAM, MD
Commissioner
501 7
th
Avenue | N ew Yo rk, New Yo rk 10018 -5903 | o as as.ny.gov | 646 -728- 47 6 0
1450 Wes tern Avenue | Albany, N ew Yo rk 12203 -3526 | o asas.ny .gov | 5 18-473- 3460
Updated June 15, 2023
Guidance for Health Care Personnel (HCP) in Clinical and Direct Care Settings to
Return to Work (RTW) Following COVID-19 Exposure or Infection or
Travel
This guidance applies to all facilities and services operated, licensed, or otherwise authorized by OASAS.
OASAS facilities should follow CDC guidance as follows:
o Follow CDC guidance (found here and here) on management strategies for return-to-work for HCP
with COVID-19 or potentially with COVID-19.
Healthcare personnel (HCP) refers to all paid and unpaid persons serving in healthcare settings who
have the potential for direct or indirect exposure to patients or infectious materials, including body
substances (e.g., blood, tissue, and specific body fluids); contaminated medical supplies, devices,
and equipment; contaminated environmental surfaces; or contaminated air. HCPs include, but are
not limited to, emergency medical service personnel, nurses, nursing assistants, home healthcare
personnel, physicians, technicians, therapists, phlebotomists, pharmacists, students and trainees,
contractual staff not employed by the healthcare facility, and persons not directly involved in patient
care, but who could be exposed to infectious agents that can be transmitted in the healthcare setting
(e.g., clerical, dietary, environmental services, laundry, security, engineering and facilities
management, administrative, billing, and volunteer personnel).
Managing HCP with SARS-CoV-2 Infection or Exposure to SARS-CoV-2
All healthcare facilities should follow appropriate Centers for Medicare & Medicaid Services (CMS) and CDC
guidance regarding HCP return to work after SARS-CoV-2 infection or after exposure to SARS-CoV-2, as
found at https://www.cdc.gov/coronavirus/2019-ncov/hcp/guidance-riskassesment-hcp.html and
https://www.cdc.gov/coronavirus/2019-ncov/hcp/mitigating-staffshortages.html.
Transition from conventional to contingency to crisis strategies should be based on ability to provide
essential services, as determined by the facility. Facilities should notify the OASAS Regional Office (RO) if
“crisis” strategies are required, as below.
Crisis Strategies to Mitigate Current or Imminent Staffing Shortages that Threaten Provision of
Essential Patient Services Updated Advisory on Return-to-Work Protocols for Healthcare Personnel
with SARS-CoV-2 Infection or Exposure to SARS-CoV-2
Administrators, Medical Directors, and Nursing Directors of non-hospital-based programs with an actual or
anticipated inability to provide essential patient services despite instituting contingency strategies according
to the guidance above should notify the OASAS RO of the need to follow CDC crisis capacity strategies. The
OASAS RO should be notified of the need to move to “crisis” strategies with a description of mitigation
strategies already employed (Strategies to Mitigate Healthcare Personnel Staffing Shortages), a description
501 7
th
Avenue | N ew Yo rk, New Yo rk 10018 - 5903 | oasas.ny.go v | 646 - 728-4760
1450 Wes tern Avenue | Albany, N ew Yo rk 12203 -3526 | o asas.ny .gov | 5 18-473- 3460
of crisis strategies regarding HCP return-to-work which they intend to implement, and their planned
prioritization strategy.
Before moving to crisis strategies:
• Healthcare entities must ensure that they have strategies in place to mitigate HCP staffing shortages,
including appropriate contingency strategies as outlined in CDC’s Strategies to Mitigate Healthcare
Personnel Staffing Shortages.
• Facilities should ensure that the criteria for identifying higher risk HCP exposures in healthcare settings are
applied properly according to CDC guidance (e.g., missing PPE or inappropriate wearing of PPE while
caring for a patient with suspected or confirmed COVID-19 or during aerosol-generating procedures).
General Recommendations for all Asymptomatic HCP Exposed to COVID-19
From CDC guidance updated 9/23/22 (see here):
• In most circumstances, asymptomatic HCP with higher-risk exposures do not require work restriction.
• Updated recommendations for testing frequency to detect potential for variants with shorter incubation
periods and to address the risk for false negative antigen tests in people without symptoms.
Key Points
• In general, asymptomatic HCP who have had a higher-risk exposure do not require work restriction,
regardless of vaccination status, if they do not develop symptoms or test positive for SARS-CoV-2.
Return to Work Criteria for HCP Who Were Exposed to Individuals with Confirmed SARS-CoV-2
Infection
Exposures that might require testing and/or restriction from work can occur both while at work and in the
community. Higher-risk exposures generally involve exposure of HCP’s eyes, nose, or mouth to material
potentially containing SARS-CoV-2, particularly if these HCP were present in the room for an aerosol-
generating procedure.
Other exposures not classified as higher risk, including having body contact with the patient (e.g., rolling the
patient) without gown or gloves, may impart some risk for transmission, particularly if hand hygiene is not
performed and HCP then touch their eyes, nose, or mouth. When classifying potential exposures, specific
factors associated with these exposures (e.g., quality of ventilation, use of PPE, and source control) should be
evaluated on a case-by-case basis. These factors might raise or lower the level of risk; interventions, including
restriction from work, can be adjusted based on the estimated risk for transmission.
For the purposes of this guidance, higher-risk exposures are classified as HCP who had prolonged
1
close
contact
2
with a patient, visitor, or HCP with confirmed SARS-CoV-2 infection
3
and:
• HCP was not wearing a respirator (or if wearing a facemask, the person with SARS-CoV-2 infection
was not wearing a cloth mask or facemask)
4
• HCP was not wearing eye protection if the person with SARS-CoV-2 infection was not wearing a cloth
mask or facemask
• HCP was not wearing all recommended PPE (i.e., gown, gloves, eye protection, respirator) while
present in the room for an aerosol-generating procedure
Following a higher-risk exposure, HCP should:
• Have a series of three viral tests for SARS-CoV-2 infection.
501 7
th
Avenue | N ew Yo rk, New Yo rk 10018 - 5903 | oasas.ny.go v | 646 - 728-4760
1450 Wes tern Avenue | Albany, N ew Yo rk 12203 -3526 | o asas.ny .gov | 5 18-473- 3460
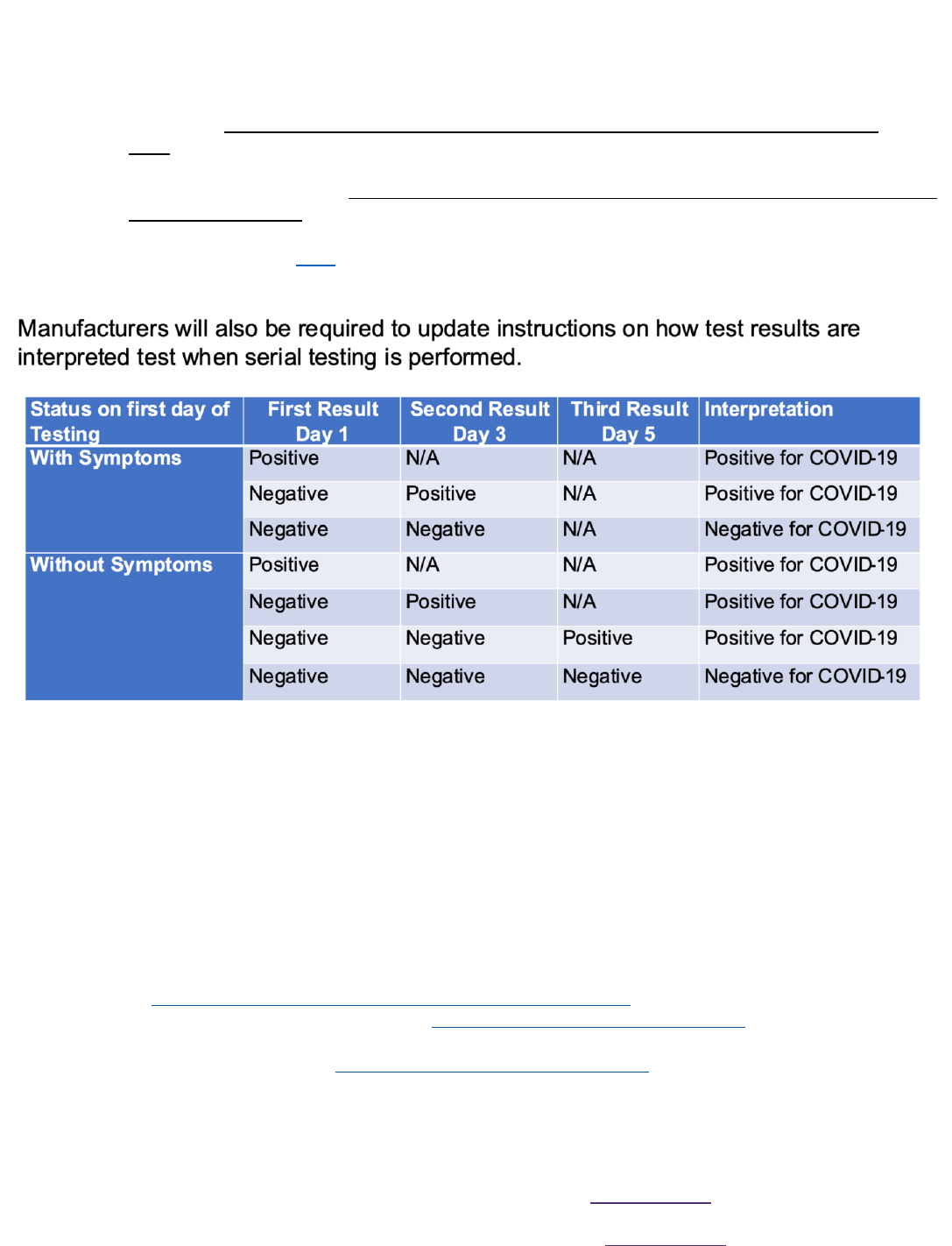
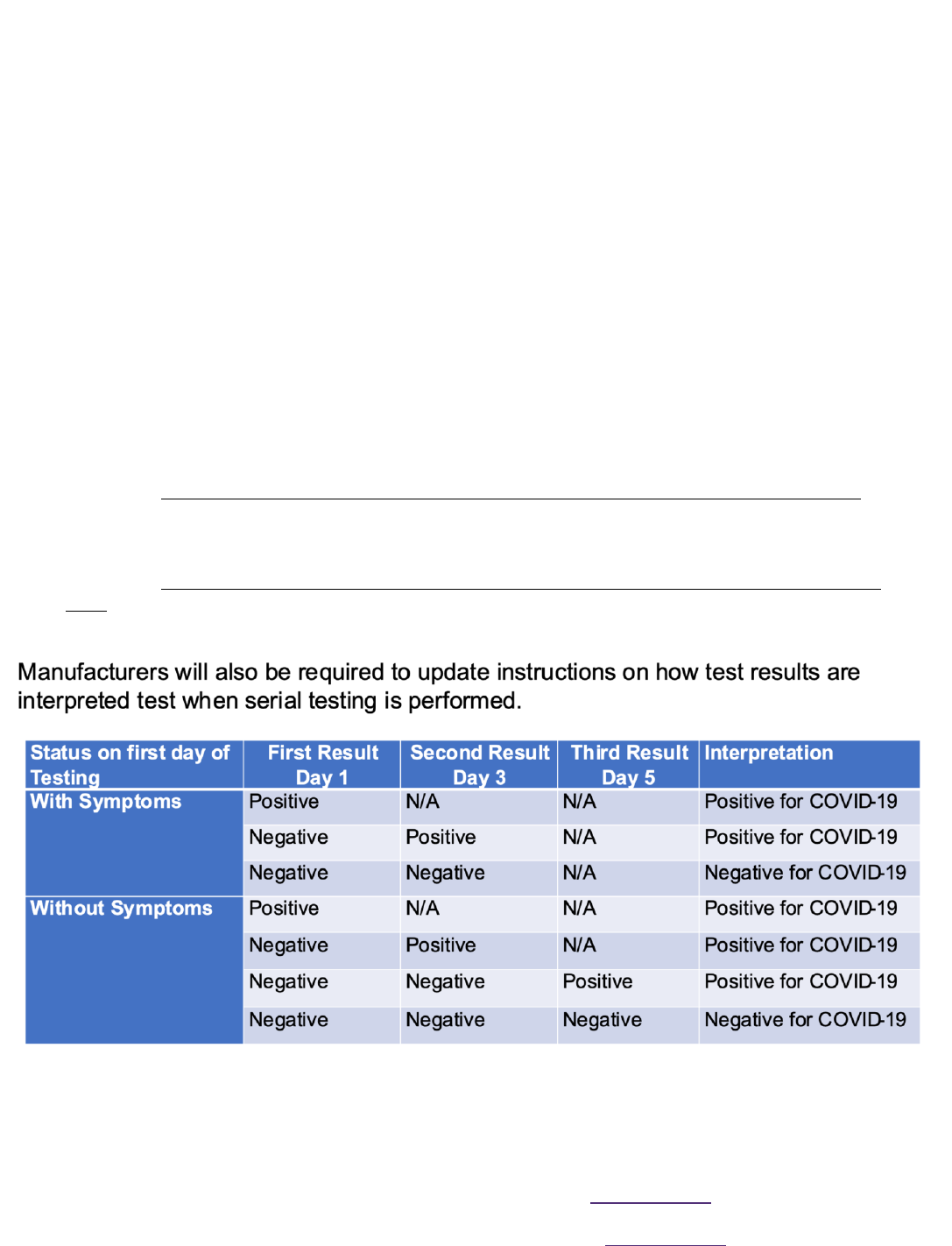
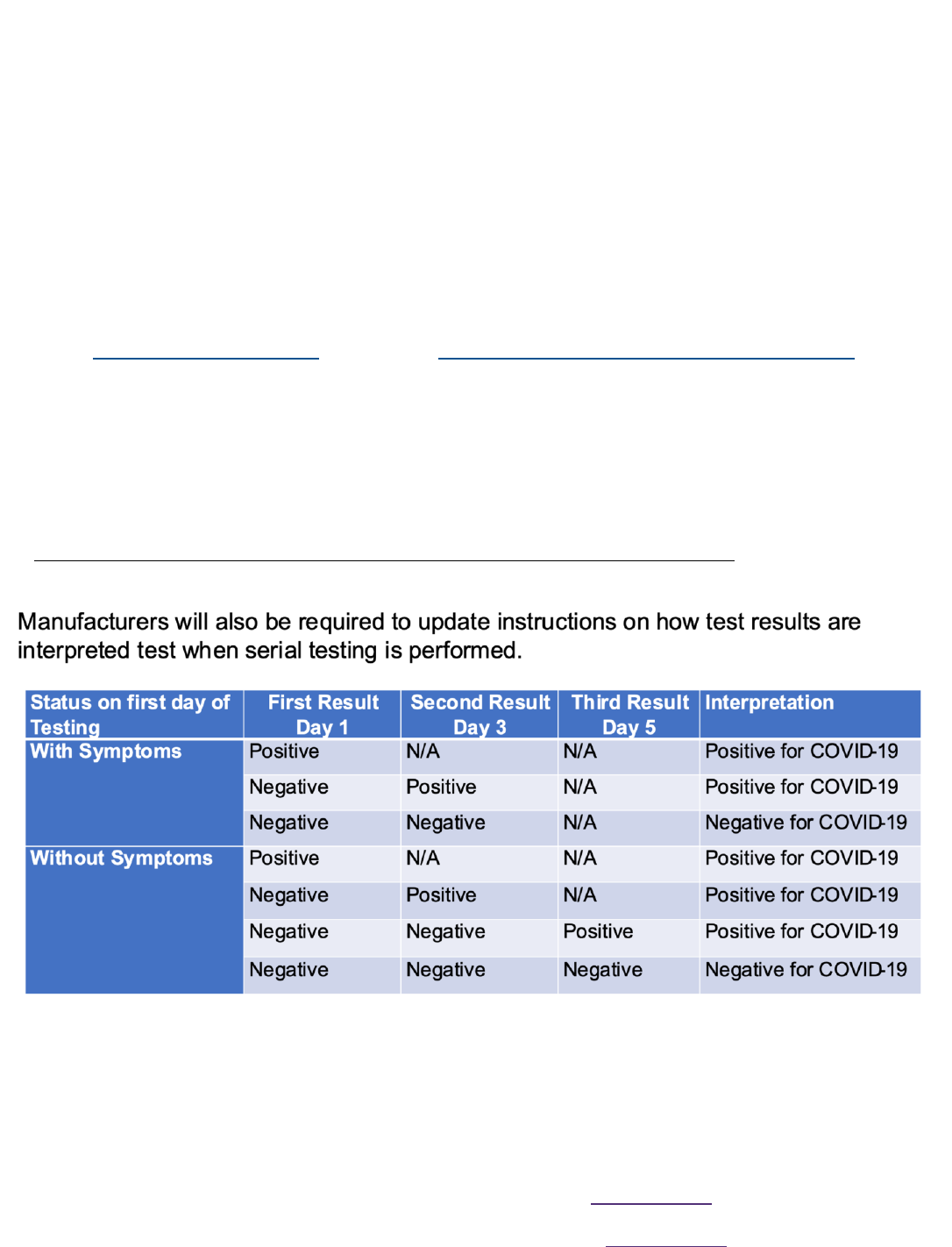
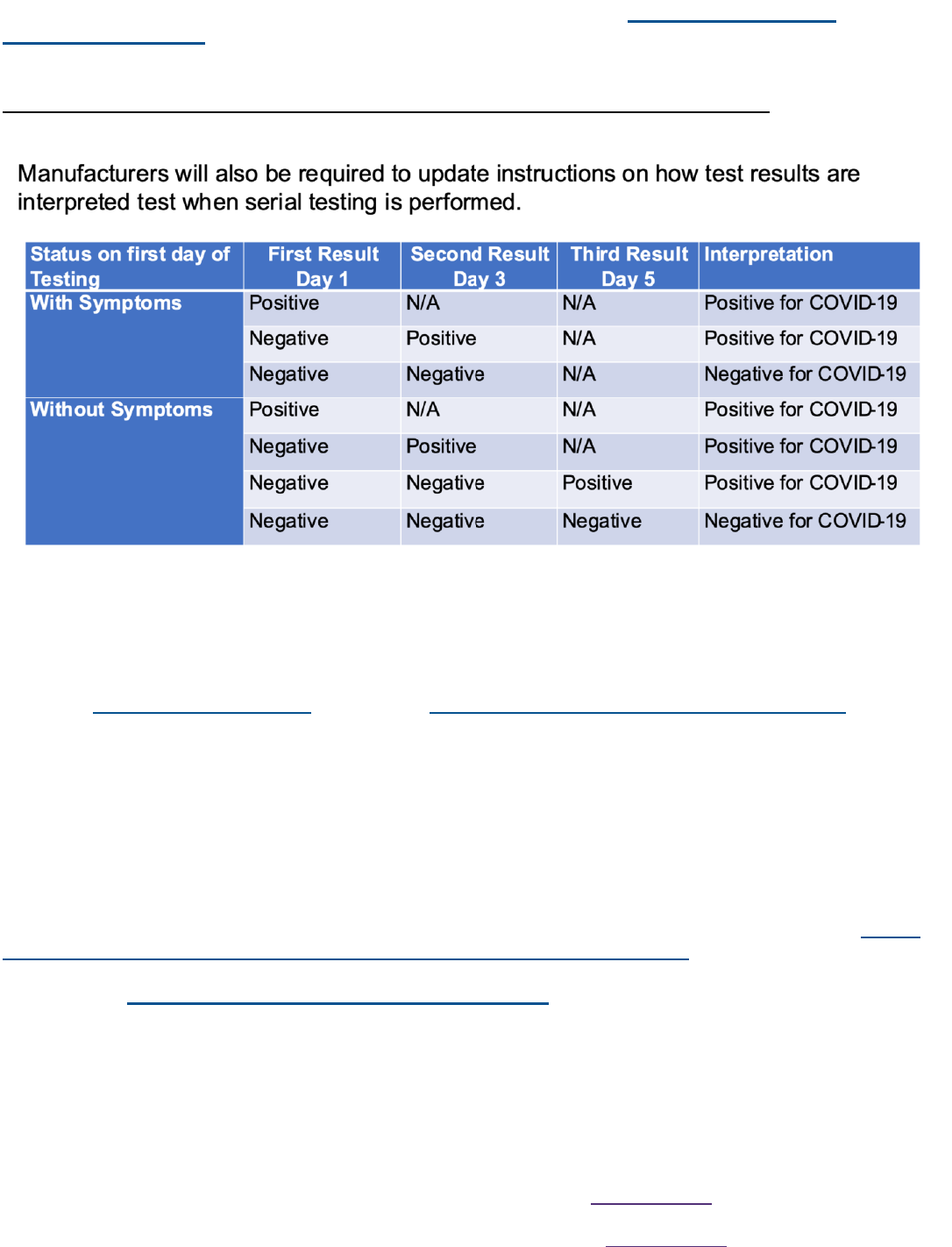
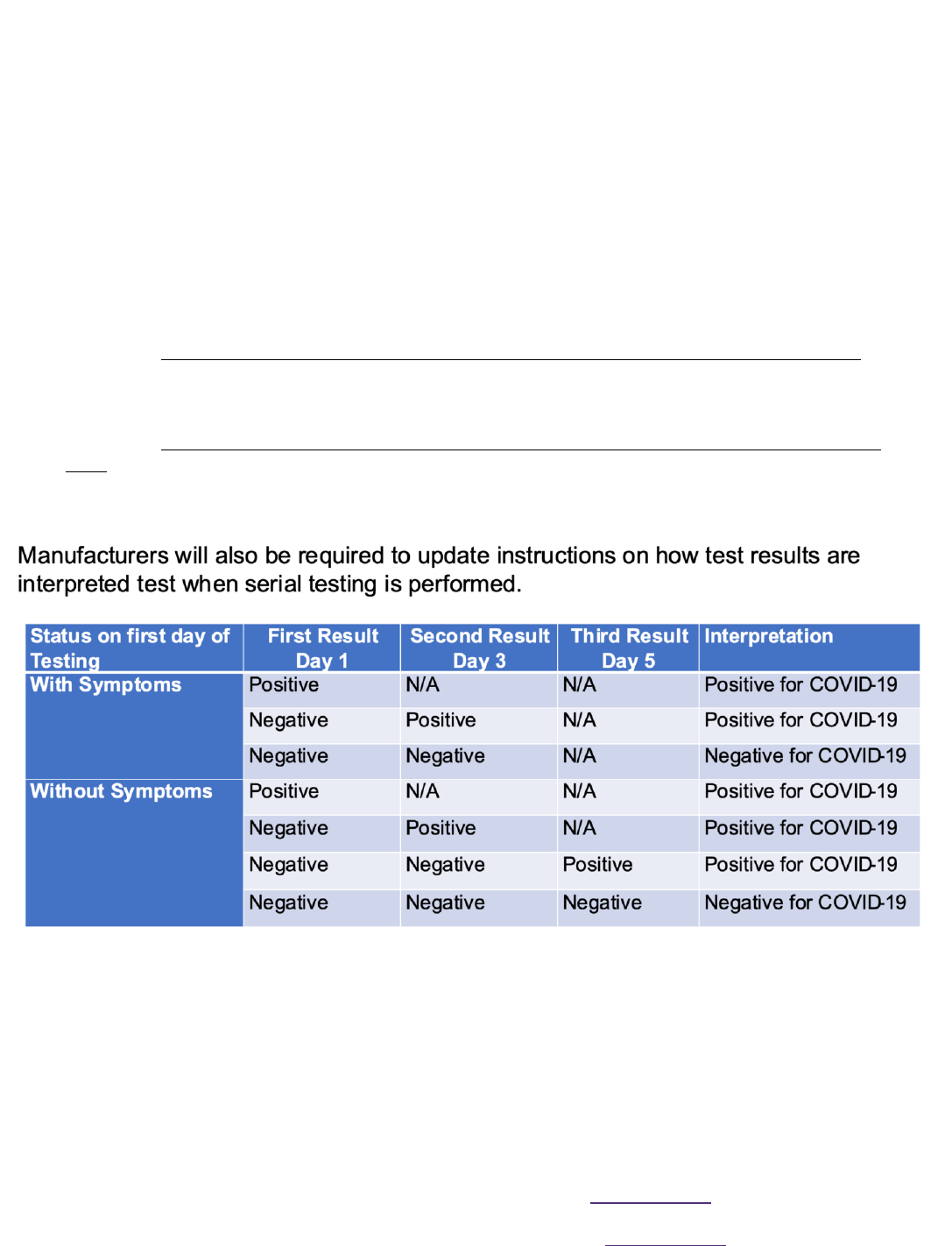
o On November 1, 2022, the U.S. Food and Drug Administration (FDA) informed developers of
SARS-CoV-2 antigen tests that they are revising the authorized use of SARS-CoV-2 antigen
tests. Serial testing is required when testing both symptomatic and asymptomatic
individuals.
o For symptomatic individuals, SARS-CoV-2 antigen tests are authorized for use on symptomatic
individuals when tested at least twice over three (3) days with at least 48 hours between
tests. Serial (repeat) testing on symptomatic individuals is a requirement.
o For asymptomatic individuals, SARS-CoV-2 antigen tests are authorized for use on
asymptomatic individuals when tested at least three (3) times over five (5) days with at least 48
hours between tests. Performing serial (repeat) testing 3 times is a requirement.
o Manufacturers will be updating instructions to reflect these serial testing requirements.
o See FDA guidance here.
o Due to challenges in interpreting the result, testing is generally not recommended for
asymptomatic people who have recovered from SARS-CoV-2 infection in the prior 30
days. Testing should be considered for those who have recovered in the prior 31-90 days;
however, an antigen test instead of NAAT is recommended. This is because some people may
remain NAAT positive but not be infectious during this period.
• Follow all recommended infection prevention and control practices, including wearing well-fitting source
control, monitoring themselves for fever or symptoms consistent with COVID-19, and not reporting to
work when ill or if testing positive for SARS-CoV-2 infection.
• Any HCP who develop fever or symptoms consistent with COVID-19 should immediately self-isolate
and contact their established point of contact (e.g., supervisor, occupational health program) to arrange
for medical evaluation and testing.

501 7
th
Avenue | N ew Yo rk, New Yo rk 10018 - 5903 | oasas.ny.go v | 646 - 728-4760
1450 Wes tern Avenue | Albany, N ew Yo rk 12203 -3526 | o asas.ny .gov | 5 18-473- 3460
Work restriction is not necessary for most asymptomatic HCP following a higher-risk exposure,
regardless of vaccination status.
Examples of when work restriction may be considered include:
• HCP is unable to be tested or wear source control as recommended for the 10 days following their
exposure;
• HCP is moderately to severely immunocompromised;
• HCP cares for or works on a unit with patients who are moderately to severely immunocompromised;
• HCP works on a unit experiencing ongoing SARS-CoV-2 transmission that is not controlled with initial
interventions;
If work restriction is recommended, HCP could return to work after either of the following time periods:
• HCP can return to work after day 7 following the exposure (day 0) if they do not develop symptoms and
all viral testing as described for asymptomatic HCP following a higher-risk exposure is negative.
• If viral testing is not performed, HCP can return to work after day 10 following the exposure (day 0) if
they do not develop symptoms.
In addition to above:
• HCP should follow all recommended infection prevention and control practices, including wearing well-
fitting source control, monitoring themselves for fever or symptoms consistent with COVID-19, and not
reporting to work when ill or if testing positive for SARS-CoV-2 infection.
• Any HCP who develop fever or symptoms consistent with COVID-19 should immediately contact their
established point of contact (e.g., supervisor, occupational health program) to arrange for medical
evaluation and testing.
HCP with travel or community exposures should consult their supervisor or occupational health program for
guidance on need for work restrictions. In general, HCP who have had prolonged close contact with someone
with SARS-CoV-2 in the community (e.g., household contacts) should be managed as described for higher-risk
occupational exposures above.
Footnotes:
1. For this guidance an exposure of 15 minutes or more is considered prolonged. This could refer to a
single 15-minute exposure to one infected individual or several briefer exposures to one or more
infected individuals adding up to at least 15 minutes during a 24-hour period. However, the presence of
extenuating factors (e.g., exposure in a confined space, performance of aerosol-generating procedure)
could warrant more aggressive actions even if the cumulative duration is less than 15 minutes. For
example, any duration should be considered prolonged if the exposure occurred during performance
of an aerosol generating procedure.
2. For this guidance it is defined as: a) being within 6 feet of a person with confirmed SARS-CoV-2
infection or b) having unprotected direct contact with infectious secretions or excretions of the person
with confirmed SARS-CoV-2 infection. Distances of more than 6 feet might also be of concern,
particularly when exposures occur over long periods of time in indoor areas with poor ventilation.
3. Determining the time period when the patient, visitor, or HCP with confirmed SARS-CoV-2 infection
could have been infectious:
a. For individuals with confirmed COVID-19 who developed symptoms, consider the exposure
window to be 2 days before symptom onset through the time period when the individual meets
criteria for discontinuation of transmission-based precautions criteria for discontinuation of
501 7
th
Avenue | N ew Yo rk, New Yo rk 10018 - 5903 | oasas.ny.go v | 646 - 728-4760
1450 Wes tern Avenue | Albany, N ew Yo rk 12203 -3526 | o asas.ny .gov | 5 18-473- 3460
b. For individuals with confirmed SARS-CoV-2 infection who never developed symptoms,
determining the infectious period can be challenging. In these situations, collecting information
about when the asymptomatic individual with SARS-CoV-2 infection may have been exposed
could help inform the period when they were infectious.
i. If the date of exposure cannot be determined, although the infectious period could be
longer, it is reasonable to use a starting point of 2 days prior to the positive test through
the time period when the individual meets criteria for discontinuation of transmission-
based precautions for contact tracing.
4. While respirators confer a higher level of protection than facemasks and are recommended when
caring for patients with SARS-CoV-2 infection, facemasks still confer some level of protection to HCP,
which was factored into this risk assessment if the patient was also wearing a cloth mask or facemask
Evaluating Healthcare Personnel with Symptoms of SARS-CoV-2 Infection
HCP with even mild symptoms of COVID-19 should be prioritized for viral testing with nucleic acid or antigen
detection assays.
On November 1, 2022, the U.S. Food and Drug Administration (FDA) informed developers of SARS-CoV-2
antigen tests that they are revising the authorized use of SARS-CoV-2 antigen tests. Serial testing is
required when testing both symptomatic and asymptomatic individuals.
• For symptomatic individuals, SARS-CoV-2 antigen tests are authorized for use on symptomatic
individuals when tested at least twice over three (3) days with at least 48 hours between tests. Serial
(repeat) testing on symptomatic individuals is a requirement.
• For asymptomatic individuals, SARS-CoV-2 antigen tests are authorized for use on asymptomatic
individuals when tested at least three (3) times over five (5) days with at least 48 hours between
tests. Performing serial (repeat) testing 3 times is a requirement.
Manufacturers will be updating instructions to reflect these serial testing requirements.
501 7
th
Avenue | N ew Yo rk, New Yo rk 10018 - 5903 | oasas.ny.go v | 646 - 728-4760
1450 Wes tern Avenue | Albany, N ew Yo rk 12203 -3526 | o asas.ny .gov | 5 18-473- 3460
For HCP who were initially suspected of having COVID-19 but, following evaluation, another diagnosis is
suspected or confirmed, return-to-work decisions should be based on their other suspected or confirmed
diagnoses.
Return to Work Criteria for HCP with SARS-CoV-2 Infection
The following are criteria to determine when HCP with SARS-CoV-2 infection could return to work and are
influenced by severity of symptoms and presence of immunocompromising conditions. After returning to work,
HCP should self-monitor for symptoms and seek re-evaluation from their medical provider or occupational
health if symptoms recur or worsen. If symptoms recur (e.g., rebound) these HCP should be restricted from
work and follow recommended practices to prevent transmission to others (e.g., use of well-fitting source
control) until they again meet the healthcare criteria below to return to work unless an alternative diagnosis is
identified.
HCP with mild to moderate illness who are not moderately to severely immunocompromised could
return to work after the following criteria have been met:
• At least 7 days have passed since symptoms first appeared if 3 negative viral tests* are obtained within
48 hours prior to returning to work (or 10 days if testing is not performed or if a positive test at day 5-
7), and
• At least 24 hours have passed since last fever without the use of fever-reducing medications, and
• Symptoms (e.g., cough, shortness of breath) have improved.
*For symptomatic individuals, SARS-CoV-2 antigen tests are authorized for use on symptomatic individuals
when tested at least twice over three (3) days with at least 48 hours between tests. Serial (repeat) testing
on symptomatic individuals is a requirement.
501 7
th
Avenue | N ew Yo rk, New Yo rk 10018 - 5903 | oasas.ny.go v | 646 - 728-4760
1450 Wes tern Avenue | Albany, N ew Yo rk 12203 -3526 | o asas.ny .gov | 5 18-473- 3460
HCP who were asymptomatic throughout their infection and are not moderately to severely
immunocompromised could return to work after the following criteria have been met:
*For asymptomatic individuals, SARS-CoV-2 antigen tests are authorized for use on asymptomatic individuals
when tested at least three (3) times over five (5) days with at least 48 hours between tests. Performing serial
(repeat) testing 3 times is a requirement.
HCP with severe to critical illness who are not moderately to severely immunocompromised could
return to work after the following criteria have been met:
• At least 10 days and up to 20 days have passed since symptoms first appeared, and
• At least 24 hours have passed since last fever without the use of fever-reducing medications, and
• Symptoms (e.g., cough, shortness of breath) have improved.
• The test-based strategy as described below for moderately to severely immunocompromised HCP can
be used to inform the duration of work restriction.
The exact criteria that determine which HCP will shed replication-competent virus for longer periods are not
known. Disease severity factors and the presence of immunocompromising conditions should be considered
when determining the appropriate duration for specific HCP. For a summary of the literature, refer to Ending
Isolation and Precautions for People with COVID-19: Interim Guidance (cdc.gov)
HCP who are moderately to severely immunocompromised may produce replication-competent virus
beyond 20 days after symptom onset or, for those who were asymptomatic throughout their infection, the date
of their first positive viral test.
• Use of a test-based strategy (as described below) and consultation with an infectious disease specialist
or other expert and an occupational health specialist is recommended to determine when these HCP
may return to work.
501 7
th
Avenue | N ew Yo rk, New Yo rk 10018 - 5903 | oasas.ny.go v | 646 - 728-4760
1450 Wes tern Avenue | Albany, N ew Yo rk 12203 -3526 | o asas.ny .gov | 5 18-473- 3460
Test-based strategy
HCP who are symptomatic could return to work after the following criteria are met:
• Resolution of fever without the use of fever-reducing medications, and
• Improvement in symptoms (e.g., cough, shortness of breath), and
• Results are negative from at least three consecutive respiratory specimens collected 48 hours apart
(total of three negative specimens) tested using an antigen test or NAAT.
HCP who are not symptomatic could return to work after the following criteria are met:
• Results are negative from at least three consecutive respiratory specimens collected 48 hours apart
(total of three negative specimens) tested using an antigen test or NAAT.
On November 1, 2022, the U.S. Food and Drug Administration (FDA) informed developers of SARS-CoV-2
antigen tests that they are revising the authorized use of SARS-CoV-2 antigen tests. Serial testing is
required when testing both symptomatic and asymptomatic individuals.
• For symptomatic individuals, SARS-CoV-2 antigen tests are authorized for use on symptomatic
individuals when tested at least twice over three (3) days with at least 48 hours between tests. Serial
(repeat) testing on symptomatic individuals is a requirement.
• For asymptomatic individuals, SARS-CoV-2 antigen tests are authorized for use on asymptomatic
individuals when tested at least three (3) times over five (5) days with at least 48 hours between
tests. Performing serial (repeat) testing 3 times is a requirement.
Manufacturers will be updating instructions to reflect these serial testing requirements.
501 7
th
Avenue | N ew Yo rk, New Yo rk 10018 - 5903 | oasas.ny.go v | 646 - 728-4760
1450 Wes tern Avenue | Albany, N ew Yo rk 12203 -3526 | o asas.ny .gov | 5 18-473- 3460
Staff Who Travel
The CDC has updated their travel guidance.
Consider getting a COVID-19 test if you:
• Develop COVID-19 symptoms before, during, or after travel.
• Will be traveling to visit someone who is at higher risk of getting very sick from COVID-19.
• Were in a situation with a greater risk of exposure during travel (e.g., in an indoor, crowded space like
an airport terminal while not wearing a mask).
If you traveled and feel sick, particularly if you have a fever, talk to a healthcare professional, and tell them
about your recent travel.
From the CDC, “Health care personnel (HCP) with travel or community exposures should
consult their occupational health program for guidance on need for work restrictions.” Any
exposure to COVID-19 during travel would warrant following the RTW protocols. Travel
alone, without a known exposure, would not constitute an exposure.
See complete CDC Travel Guidance h ere.
General questions or comments about this guidance can be sent to Add[email protected]
