UCLA
UCLA Previously Published Works
Title
Racial Disparities in Developmental Delay Diagnosis and Services Received in Early
Childhood
Permalink
https://escholarship.org/uc/item/7g60302v
Journal
Academic Pediatrics, 21(7)
ISSN
1876-2859
Authors
Gallegos, Abraham
Dudovitz, Rebecca
Biely, Christopher
et al.
Publication Date
2021-09-01
DOI
10.1016/j.acap.2021.05.008
Peer reviewed
eScholarship.org Powered by the California Digital Library
University of California
Racial Disparities in Developmental Delay Diagnosis and
Services Received in Early Childhood
Abraham Gallegos, MD, MSHS
a,b
, Rebecca Dudovitz, MD, MSHS
a
, Christopher Biely, MS
a
,
Paul J. Chung, MD, MSHS
a,c,d
, Tumaini R. Coker, MD, MBA
e
, Elizabeth Barnert, MD, MPH,
MS
a
, Alma D. Guerrero, MD, MPH
a
, Peter G. Szilagyi, MD, MPH
a,b
, Bergen B. Nelson, MD,
MS
f
A.
Department of Pediatrics, UCLA Mattel Children’s Hospital and Children’s Discovery &
Innovation Institute, David Geffen School of Medicine at University of California, Los Angeles,
Los Angeles, California
B.
UCLA NRSA T32 Primary Care Research Fellowship, University of California, Los Angeles, Los
Angeles, California
C.
Kaiser Permanente Bernard J. Tyson School of Medicine, Pasadena, CA, USA
D.
Department of Health Policy and Management, Fielding School of Public Health, University of
California, Los Angeles, Los Angeles, California
E.
Department of Pediatrics, University of Washington and Seattle Children’s Research Institute,
Seattle, Washington
F.
Children’s Hospital of Richmond at Virginia Commonwealth University, Richmond, Virginia
Abstract
Background and objectives: Racial disparities in diagnosis and receipt of services for
early childhood developmental delay (DD) are well known but studies have had difficulties
distinguishing contributing patient, healthcare system and physician factors from underlying
prevalence. We examine rates of physician diagnoses of DD by preschool and kindergarten entry
controlling for a child’s objective development via scoring on validated developmental assessment
along with other child characteristics.
Methods: We used data from the preschool and kindergarten entry waves of the Early Childhood
Longitudinal Study, Birth Cohort. Dependent variables included being diagnosed with DD by
a medical provider and receipt of developmental services. Logistic regression models tested
whether a child’s race was associated with both outcomes during preschool and kindergarten while
controlling for the developmental assessments, as well as other contextual factors.
Results: Among 7,950 children, 6.6% of preschoolers and 7.5% of kindergarteners were
diagnosed with DD. Of preschool children with DD, 66.5% were receiving developmental
Corresponding author: Abraham Gallegos; Department of Pediatrics, Mattel Children’s Hospital and Children’s Discovery &
Innovation Institute, David Geffen School of Medicine at University of California, Los Angeles, Los Angeles, California;
Conflict of interest statement: The authors have no financial relationships relevant to this article to disclose. It should be noted Dr.
Peter Szilagyi, Editor-in-Chief of Academic Pediatrics, is part of the authorship group.
HHS Public Access
Author manuscript
Acad Pediatr
. Author manuscript; available in PMC 2022 June 06.
Published in final edited form as:
Acad Pediatr
. 2021 ; 21(7): 1230–1238. doi:10.1016/j.acap.2021.05.008.
Author Manuscript Author Manuscript Author Manuscript Author Manuscript
services, while 69.1% of kindergarten children with DD were receiving services. Children who
were Black, Asian, spoke a primary language other than English and had no health insurance were
less likely to be diagnosed with DD despite accounting for cognitive ability. Black and Latinx
children were less likely to receive services.
Conclusion: Racial minority children are less likely to be diagnosed by their pediatric
provider with DD and less likely to receive services despite accounting for a child’s objective
developmental assessment. The pediatric primary care system is an important target for
interventions to reduce these disparities.
Keywords
developmental delay disparities; Early Childhood Longitudinal Study Birth cohort; Early
intervention
Background
Developmental disabilities affect approximately 16% of children and early identification
of delay and participation in developmental services is associated with individual and
societal benefits.
[1 2]
The pediatric primary care system plays an important role in caring for
children with developmental delay (DD), including providing developmental screening and
surveillance, facilitating a timely diagnoses, addressing any associated medical conditions
and linking families to services
[3]
. This is particularly true prior to school entry, as
pediatricians are often the only trained provider routinely assessing young children’s
development.
There exist multiple racial and ethnic disparities along the continuum of DD diagnosis
and management. These disparities likely represent the culmination of interconnecting
variables, including patient factors, health care system factors, and clinical encounter factors.
[4]
Minority children are less likely to be diagnosed with any form of DD as well as a
number of specific DD conditions.
[1 5]
For example, Latinx, Black and Asian children with
autism spectrum disorder and attention deficit hyperactivity disorder are diagnosed at a later
age and with more severe symptoms than white children.
[6–8]
Additionally, racial/ethnic
minority children are more likely to face disparities in the processes leading to a potential
diagnosis, as they are less likely to access high quality primary care services and their
parents are less likely to be asked about developmental concerns.
[9 10]
Finally, these children
are less likely to receive developmental services and less likely to be placed into special
education.
[11 12]
Many of the studies that have described disparities in DD diagnosis and
use of services have difficulty distinguishing whether these differences are driven by true
epidemiologic differences in prevalence of developmental delay versus health care system
or clinical encounter factors leading to under-recognition or poor management of existing
delays.
[13–15]
We take a unique analytic approach that allows us to more closely examine this distinction.
By accounting for objective measures of a child’s development (via score on validated
developmental assessment tool), access to well child care, and other contextual factors,
we test whether differences in parental report of receiving a DD diagnosis by a doctor
Gallegos et al.
Page 2
Acad Pediatr
. Author manuscript; available in PMC 2022 June 06.
Author Manuscript Author Manuscript Author Manuscript Author Manuscript

across racial and ethnic groups, are largely driven by differences in the prevalence DD
versus patient, health care system, clinical encounter factors. Identifying the factors driving
these racial and ethnic disparities is critical to developing interventions to eliminate those
disparities moving forward.
METHODS
Data Source and Analytic Sample
We utilized the Early Childhood Longitudinal Study, Birth Cohort (ECLS-B) database, a
nationally representative sample of children born in the United States in 2001 followed
longitudinally through kindergarten entry in 2006–2008. The analytic sample included
7,950 children with complete data on the primary outcome (diagnosis by preschool),
developmental trajectory (preschool models), and preschool sampling weight. Data were
collected from birth certificates, parent and guardian interviews, direct child assessments,
and reports from childcare providers and teachers when children were approximately 9
months, 2 years, 4 years (preschool wave), and 5–6 years old (kindergarten entry waves).
Approximately 14,000 births were sampled for the study and yielded 10,688 cases in the
first wave, for a response rate of 76%. Response rates in subsequent waves were 91%−93%.
There was a planned 15% reduction in the sample prior to the kindergarten entry waves;
6,900 children in the kindergarten entry waves completed direct assessments.
Measures
Outcomes—Diagnosis of DD by preschool and diagnosis of DD by kindergarten entry
were assessed with items from the 2-year, preschool, and kindergarten entry parent
interviews. During each interview, parents were asked “Has a doctor ever told you that
(child) has the following conditions?” Delay in learning to talk, another DD, and mental
retardation were listed among the possible conditions in the 2-year interview. In addition,
another DD, mental retardation, and autism or pervasive developmental disorders (PDD)
were listed among the possible conditions in the preschool interview and kindergarten entry
interviews. Children were considered to have a diagnosis by preschool if parents answered
yes to at least one of the above conditions from the 2-year interview or preschool interview.
Children were considered to have a diagnosis by kindergarten entry if parents answered
yes to at least one of the conditions from the 2-year interview, preschool interview, or
kindergarten entry interviews.
Services by preschool and services by kindergarten entry were assessed with items from the
2-year, preschool, and kindergarten entry parent interviews. During each interview, parents
were asked “For each service, please tell me if (child) or your family received this service
to help with (child’s) special needs. Has anyone in your household ever received…” Speech
or language therapy and special classes with other children were listed among the possible
services in the interviews. In addition, parents were asked, “Is (child) currently participating
in an early intervention program or regularly receiving any services for (his/her) conditions
from…” The local school district, a state or local health or social service agency, a doctor,
clinic, or other health care provider, and other sources were listed as the possible services in
the interviews. Children were considered to have services by preschool if parents answered
Gallegos et al.
Page 3
Acad Pediatr
. Author manuscript; available in PMC 2022 June 06.
Author Manuscript Author Manuscript Author Manuscript Author Manuscript

yes to at least one of these services from the 2-year interview or preschool interview.
Children were considered to have services by kindergarten entry if parents answered yes to
at least one of these services from the 2-year interview, preschool interview, or kindergarten
entry interviews.
Child Characteristics—We identified child characteristics likely associated with the
diagnosis of a DD and receipt of services. Measures included child’s race/ethnicity
(non-Hispanic White, African American, Hispanic or Latino, Asian, other, multiracial),
highest level of parental education (less than high school diploma, high school diploma
or vocational degree, some college, bachelor’s degree or higher), child’s sex, household
income and poverty status, urbanicity (rural, urban), primary home language (English,
non-English), health insurance (yes, no), number of well-child visits between interviews,
center-based child care attendance (yes, no) and developmental trajectory. Health insurance
at the 9-month interview, 2-year interview, and preschool interview were included in the
preschool models and the kindergarten entry models. The kindergarten entry models also
included health insurance at the kindergarten 2006–2007 interview. The number of well-
child visits between the 9-month interview and 2-year interview (less than two, at least two)
and the number of well-child visits between the 2-year interview and preschool interview
(zero, at least one) were included in the preschool models and kindergarten entry models.
The kindergarten entry models also included the number of well-child visits between the
preschool interview and kindergarten entry interview (one, at least one). Center-based child
care attendance at the 9-month interview, 2-year interview, and preschool interview were
included in the preschool models and the kindergarten entry models.
We created a 4-category variable capturing if children scored in the lowest decile on
developmental assessments over time, allowing us to account for both their developmental
status at the time of each assessment, as well as their developmental trajectory over time.
For the preschool models, developmental trajectory was based on the Bayley Short Form-
Research Edition (BSF-R) mental scale score at the 9-month and 2-year interviews with
scoring as follows: 0 = both scores > 10th percentile, 1 = 9-month score ≤10th percentile and
2-year score > 10th percentile, 2 = 9-month score > 10th percentile and 2-year score≤10th
percentile, and 3 = both scores ≤10th percentile. For the kindergarten models, developmental
trajectory was based on the BSF-R mental scale score at the 2-year interview and early
reading and math item response theory (IRT) scale scores at the preschool interview. We
created a 4-category variable to assess whether a child had DD between preschool and
kindergarten as follows: 0 = 2-year BSF-R mental scale score > 10th percentile and 4-year
old preschool early reading and math scale scores > 10th percentile, 1 = 2-year BSF-R
mental scale score ≤10th percentile and 4-year-old preschool early reading and math scale
scores > 10th percentile, 2 = 2-year BSF-R mental scale score > 10th percentile and
4-year-old preschool early reading or math scale score ≤10th percentile, and 3 = 2-year
BSF-R mental scale score ≤10th percentile and preschool early reading or math scale score
≤10th percentile. This variable distinguished children consistently scoring above the bottom
decile from children scoring in the bottom decile.
Gallegos et al.
Page 4
Acad Pediatr
. Author manuscript; available in PMC 2022 June 06.
Author Manuscript Author Manuscript Author Manuscript Author Manuscript

Analytic Approach—To identify child characteristics associated with the likelihood of
receiving a DD diagnosis at both the Preschool wave and Kindergarten wave, we conducted
a weighted multivariable logistic regression model of diagnosis by preschool and diagnosis
by kindergarten on child characteristics, respectively. To identify child characteristics
associated with receipt of developmental support services after a diagnosis has been made,
we conducted weighted multivariate logistic regression models of receipt of services by
preschool and receipt of services by kindergarten on the sample of children who had a
diagnosis of DD by preschool and by kindergarten, respectively. Both models included all
of the child characteristics described above, and controlled for the child’s developmental
status. Unweighted sample sizes were rounded to the nearest 50, as required by the National
Center for Education Statistics. Analyses were conducted using the “svy” suite of commands
in Stata 14.0 (StataCorp LP, College Station, TX) to account for the ECLS-B survey design
elements of stratification, clustering, and weighting.
Results
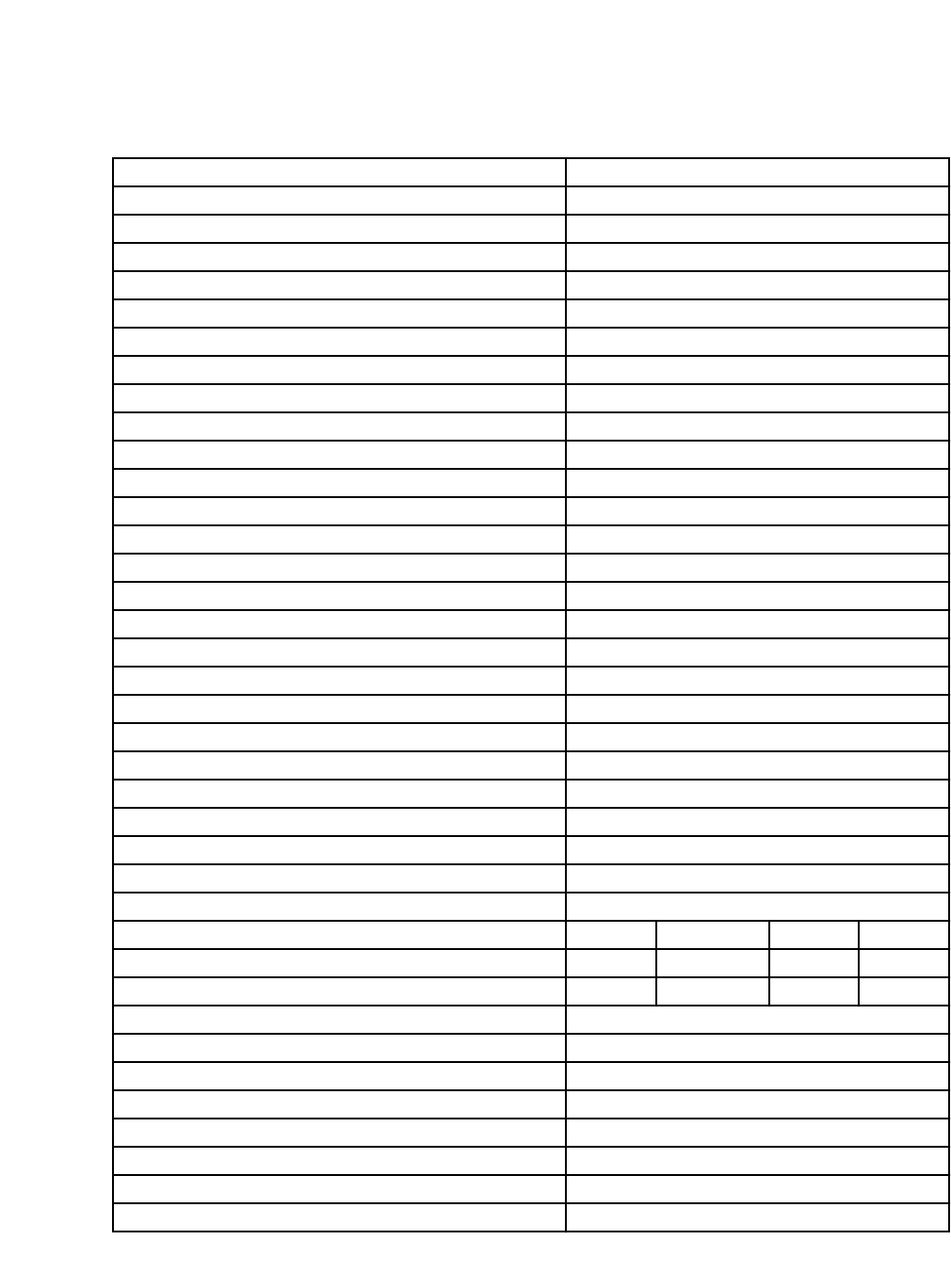
Table 1 displays the characteristics of our analytic sample. Among the 7,950 preschool and
kindergarten children in the analytic sample, 750 (6.6%) preschool children and 600 (7.5%)
kindergarten children were told by their physicians of a DD diagnosis. Of those preschool
children with a DD diagnosis, 500 (66.5%) were receiving developmental services, while
450 (69.1%) kindergarten children with a diagnosis of DD were receiving developmental
services.
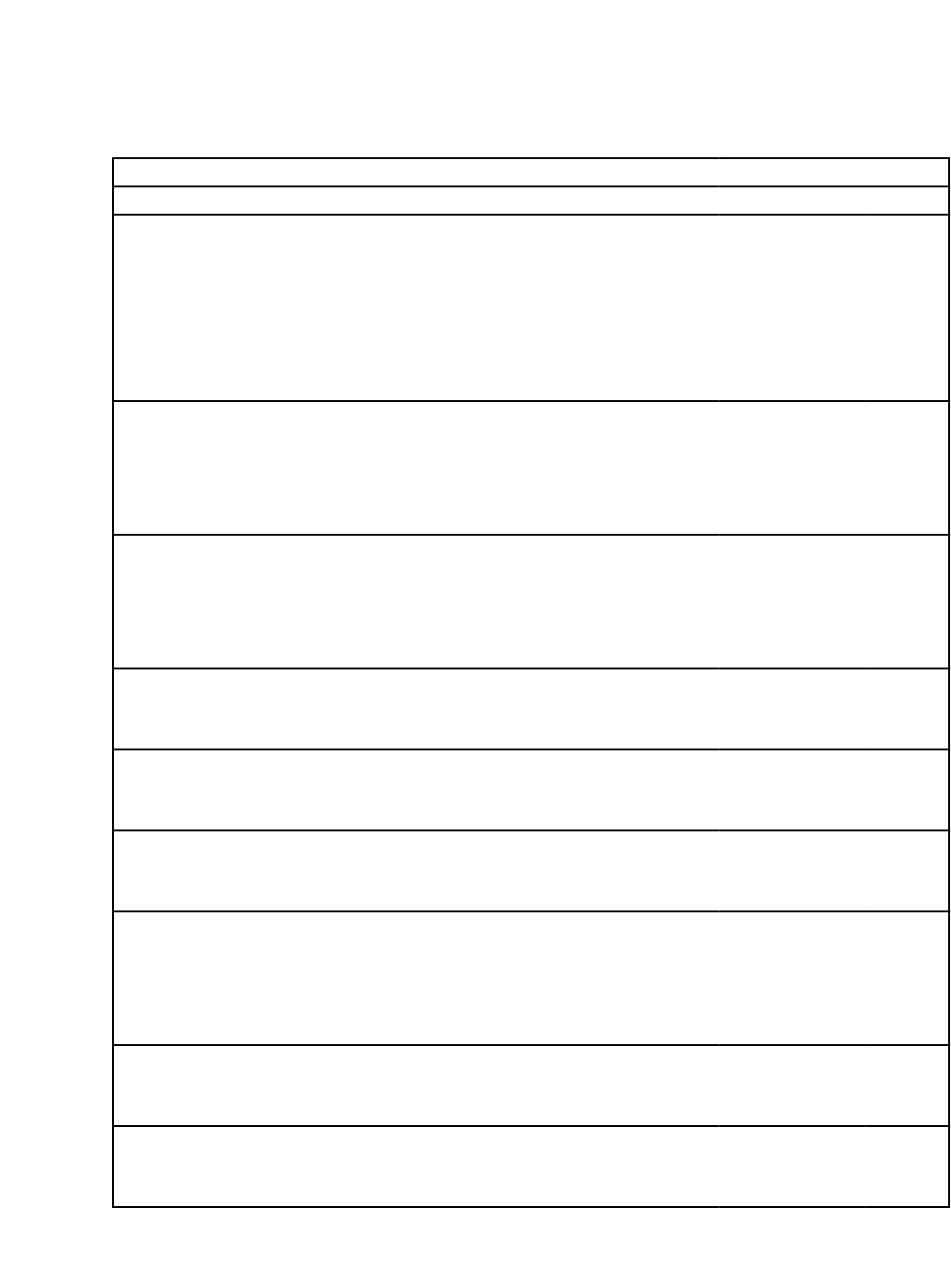
Multiple child characteristics were associated with receiving a DD diagnosis by preschool
(Table 2). Children scoring in the bottom decile on standardized developmental assessment
at any time prior to preschool were more likely to be diagnosed. A child who scored below
the bottom decile on both the 9-month and 2-year assessments had the highest odds of being
diagnosed, with an aOR of 9.53 (95% CI 6.46–14.06). Male children were also more likely
to be diagnosed with DD (aOR 2.27, 95% CI 1.83– 2.81). Black children had the lowest
regression coefficient of other racial/ethnic groups to be diagnosed with DD (aOR 0.42,
95% CI 0.29–0.61). Asian children were also less likely to be diagnosed (aOR 0.56, 95%
CI 0.33–0.97), as were those whose primary language was not English (aOR 0.54, 95%
CI 0.32–0.93) and those who lacked health insurance at 2-years old (aOR 0.43, 95% CI
0.22–0.83). Conversely, children attending center-based child care during preschool were
more likely to obtain a diagnosis than those who did not attend (aOR 1.52, 95% CI 1.17 –
1.97).
Analyses examining child characteristics associated with receipt of developmental services
by preschool amongst those with a diagnosis of DD revealed that race/ethnicity,
developmental status, participation in center-based child care were significantly associated
with receiving services. Black and Latinx children had decreased odds of receiving services
by preschool (Table 2) (aOR 0.31, 95% CI 0.13 – 0.71 and aOR 0.35, 95% CI 0.15 – 0.
86, respectively). Children scoring in the bottom decile on both the 9-month and 2-year
assessments or those with downward trending developmental trajectory (scoring in the
lowest decile at 24-months) and children attending center-based child care during preschool
were more likely to receive developmental services (aOR 2.26, 95% CI 1.19 – 4.30).
Gallegos et al.
Page 5
Acad Pediatr
. Author manuscript; available in PMC 2022 June 06.
Author Manuscript Author Manuscript Author Manuscript Author Manuscript

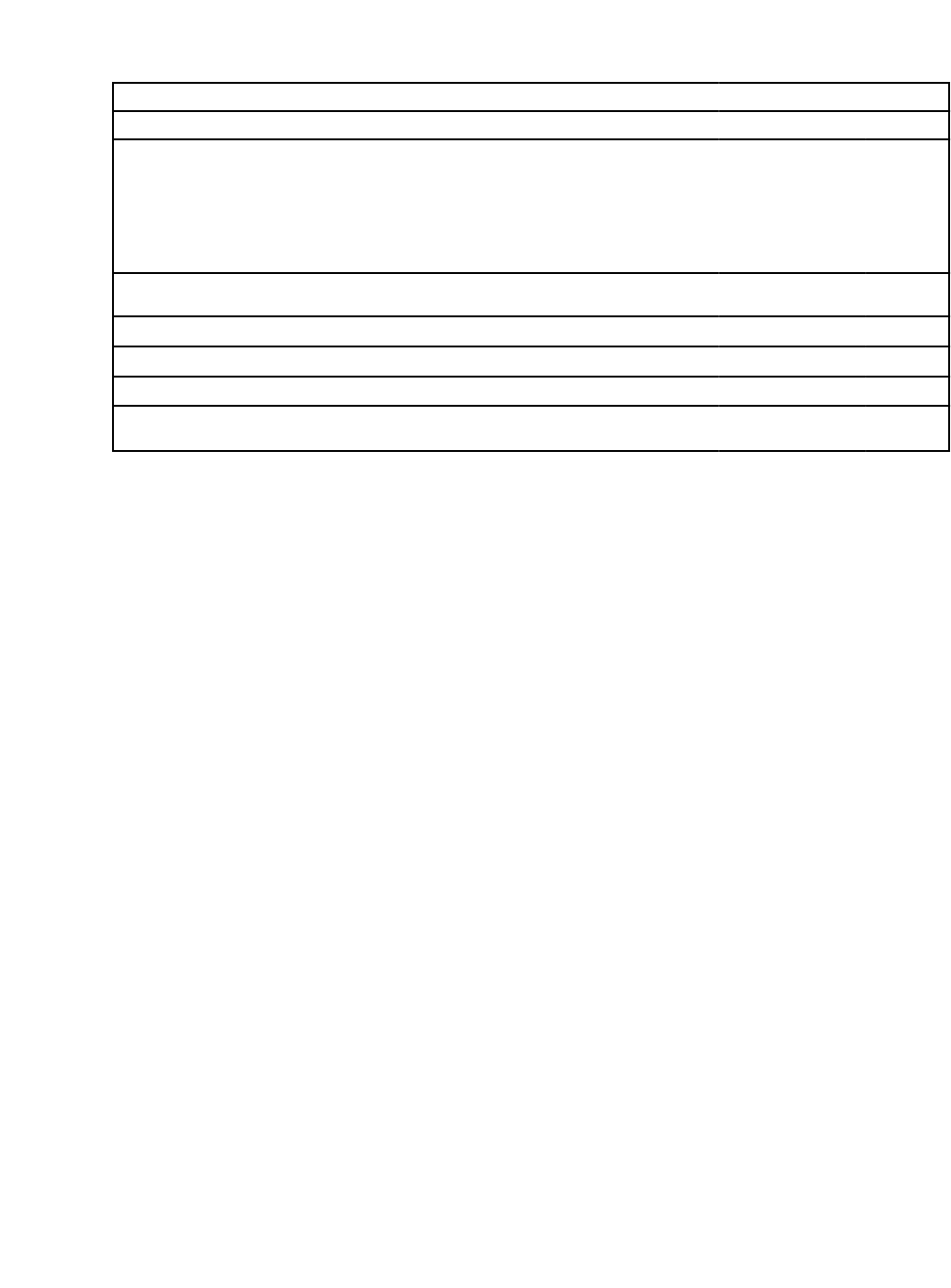
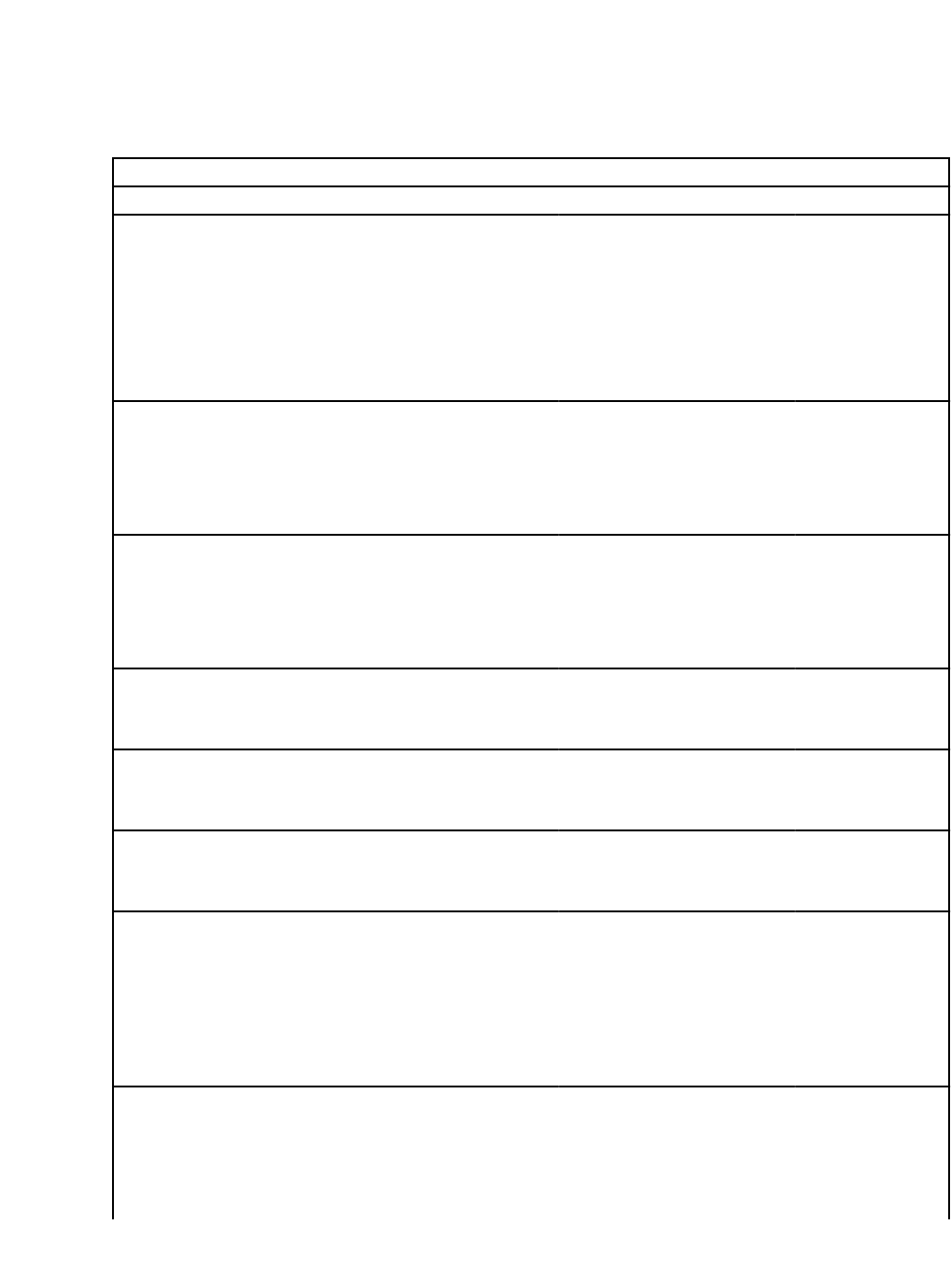
Similar characteristics were associated with the likelihood of receiving a diagnosis by
kindergarten to those associated with receiving a diagnosis in preschool (Table 3). Black
and Asian children had decreased odds of being diagnosed (aOR 0.49, 95% CI 0.28 –
0.87 and aOR 0.53, 95% CI 0.28 – 0.98, respectively). Once again scoring in the lowest
decile on either/both the 2-year and preschool developmental assessment was associated
with increased odds of receiving a diagnosis. Scoring in the lowest decile on both the 2-year
and the preschool assessments was associated with the highest odds of receiving a diagnosis,
with an aOR 13.05 (95% CI 8.18 – 20.82). Children with a non-English primary language
also had lower odds of receiving a diagnosis (aOR 0.47, 95% CI 0.27 – 0.84). Lastly,
children without insurance during the kindergarten wave were less likely to be diagnosed
(aOR 0.35, 95% CI 0.13 – 0.95). Characteristics associated with receiving developmental
support services by kindergarten included race, economic status and parental education.
Black children with a diagnosis had lower odds of receiving services (aOR 0.29, 95% CI
0.11–0.78), as were children living in homes with income 100% - below 130% of the federal
poverty limit (aOR 0.27, 95% CI 0.09 - .85) when compared to children living in homes
with income at or above 185% of the federal poverty limit (Table 3).
Discussion
In this nationally representative cohort of children, we found that a child’s race/ethnicity,
sex, primary-language spoken at home, insurance status, child care attendance and
objectively measured developmental trajectory were all associated with parents reporting
having being told by a doctor that their child have a DD diagnosis. Children scoring in
the bottom decile of a validated developmental assessment (BSF-R) at either the preschool
and/or kindergarten wave were more likely to have parents who reported their child had a
DD diagnosis and more likely to receive EI services. Notably, parents of children who were
racial/ethnic minorities and those who lived in non-English primary language households
were less likely to report being told by a doctor of a DD diagnosis despite taking into
account multiple patient and healthcare system factors on multivariable logistic regression.
The persistence of decreased odds of receiving a DD diagnosis even after controlling
for access to well child care visits, socioeconomic status, child’s sex, geographical
residential area, insurance status, child care attendance, and scores on formal developmental
assessments over time, suggest that lower likelihood of receiving a DD diagnosis among
racial/ethnic and non-English speaking children are not explained by differences in the
underlying prevalence of DD nor are they explained by the multiple patient and health care
system variables we accounted for.
There are multiple potential sources of this disparity. There are patient factors we were
unable to account for including parental understanding of normal development. Parents
of minority, non-English primary language children may have a different understanding
of normal pediatric development and developmental disorders that may lead to different
help-seeking behavior.
[16 17]
There are healthcare system factors we were unable to account
for, notably access to validated developmental screening, provider availability or quality
of care. Ethnic minority children and children in a non-English primary language home
have been shown to have poorer primary care quality, less access to family-centered care
Gallegos et al.
Page 6
Acad Pediatr
. Author manuscript; available in PMC 2022 June 06.
Author Manuscript Author Manuscript Author Manuscript Author Manuscript

and receive poorer anticipatory guidance.
[18–20]
These children also have decreased access
to formal developmental assessment by being less able to see developmental behavioral
specialists and less likely to receive a formal developmental assessment by EI, though some
of these differences may be driven, in part, by decreased EI referral rates by primary care
providers.
[21–24]
Physician and clinical encounter factors were also largely unexplored. Ethnic minority
children and children in a non-English primary language home are more likely to have
ineffective physician interactions due to difficulties in communication.
[25]
Physicians may
also be under the influence of implicit bias which may impact the encounter by contributing
to difficulties in communication and by impacting the medical decision making process.
[26 27]
In our specific study, our outcome variable was defined as “being told by a doctor”
of a DD diagnosis. It is possible some of our disparities described are a result of physicians
inadequately explaining a diagnosis. Both families and physicians may also lack knowledge
of the EI referral process, which has been recognized to be a barrier to EI referrals
and follow-up.
[28 29]
Decreased use of developmental screening and overreliance on the
generally less sensitive practice of developmental surveillance may also contribute.
Whether the factors contributing to the observed disparities are occurring inside or
outside of the pediatric primary care clinic, pediatric primary care providers manage the
culmination of potentially inadequate care and bear a large responsibility for identifying DD,
communicating that diagnosis, and connecting a child with developmental services. Hence,
it is critical to that pediatricians have the resources necessary to delivery care in a way that
advances health equity.
Potential interventions to reduce the disparities observed in this study include integrating
developmental and primary care services with the use of developmental specialist,
parent coaches or developmental programs focused around strengthening the parent-child
relationship via videotaping parental-patient interactions.
[30–32]
These programs work to
both educate parents and facilitate communication between parents and the pediatric team.
Improving reimbursement rates for developmental screening can serve to increase their
use. Building an infrastructure within the pediatric clinic, with case managers and social
workers to improve screening completion and follow up of DD referrals. Physicians need
training in cross-cultural communication and strategies to mitigate implicit bias. Finally,
we must recognize the role of systemic racism in contributing to and perpetuating these
disparities.
[33]
As child health providers, we should advocate for policy changes that can
improve child health equity, including, advocating for improved quality of pediatric primary
care, combatting childhood poverty, increased rates of reimbursement for developmental
screening, improved quality and access to public preschool and child care, increased
administrative workers dedicated to assuring equal utilization of EI services and improving
cultural competency and cross cultural communication training.
This present study has several limitations. We used the ECLS-B, and while it is a nationally
representative cohort, we were limited by the available variables. Diagnosis was determined
by parental report, which may under-estimate the true rate of diagnosis for DD. We also
recognize that our outcome variable is dependent entirely on parental report and it is largely
Gallegos et al.
Page 7
Acad Pediatr
. Author manuscript; available in PMC 2022 June 06.
Author Manuscript Author Manuscript Author Manuscript Author Manuscript

reliant on parental recall and it is possible differences in recall may be contributing to
disparities described; however, studies demonstrate parental recall of medical diagnosis
correlate well with pediatricians’ records, even for specific DD diagnoses and even while
accounting for parental education.
[34 35]
Additionally, data collection concluded in 2007, and
the prevalence of DD has increased in recent years, which may impact the generalizability
of our findings to the current era. However, we believe that many of the barriers and
facilitators to diagnosis and management of DD are unlikely to have significantly. Despite
these limitations we feel this study has important implications for pediatricians and child
health advocates.
Conclusion
The study is the first to demonstrate racial and ethnic disparities in parental reports’ of DD
diagnoses, accounting for children’s developmental status. Specifically, Black and Asian
children, as well as children from non-English speaking households were less likely to
receive a DD diagnosis and/or receive services for DD. This finding points to a critical
need to develop and test interventions to reduce these disparities, including those delivered
in clinical settings. Primary care providers have the potential to play a critical role in
developing and implementing interventions to reduce disparities in access to developmental
support services, as they are often the only professional with developmental training who
regularly see children and families prior to starting school. As both direct providers and
child health advocates, pediatricians are well poised to ensure that all children receive
regular developmental screening, which supports timely diagnosis of delays, and the
necessary care coordination to access services to ultimately maximize their developmental
potential and reduce health disparities starting from a young age.
Funding source:
UCLA NRSA T32 Primary Care Research Fellowship, UL1TR000124 and KL2TR000122 from the National
Institutes of Health/National Center for Advancing Translational Science, through the UCLA Clinical and
Translational Sciences Institute
Role of Funder/Sponsor:
The funder/sponsor did not participate in the work.
References:
1. Zablotsky B, Black LI, Maenner MJ, et al. Prevalence and Trends of Developmental
Disabilities among Children in the United States: 2009–2017. Pediatrics 2019;144(4) doi: 10.1542/
peds.2019-0811[published Online First: Epub Date]|.
2. Anderson LM, Shinn C, Fullilove MT, et al. The effectiveness of early childhood development
programs. A systematic review. Am J Prev Med 2003;24(3 Suppl):32–46 doi: 10.1016/
s0749-3797(02)00655-4[published Online First: Epub Date]|. [PubMed: 12668197]
3. The Pediatrician’s Role in Development and Implementation of an Individual Education Plan (IEP)
and/or an Individual Family Service Plan (IFSP). Pediatrics 1999;104(1):124–27 doi: 10.1542/
peds.104.1.124[published Online First: Epub Date]|. [PubMed: 10390275]
4. Institute of Medicine Committee on U, Eliminating R, Ethnic Disparities in Health C. In: Smedley
BD, Stith AY, Nelson AR, eds. Unequal Treatment: Confronting Racial and Ethnic Disparities in
Health Care. Washington (DC): National Academies Press (US) Copyright 2002 by the National
Academy of Sciences. All rights reserved., 2003.
Gallegos et al.
Page 8
Acad Pediatr
. Author manuscript; available in PMC 2022 June 06.
Author Manuscript Author Manuscript Author Manuscript Author Manuscript

5. Rosenberg SA, Zhang D, Robinson CC. Prevalence of developmental delays and participation
in early intervention services for young children. Pediatrics 2008;121(6):e1503–9 doi: 10.1542/
peds.2007-1680[published Online First: Epub Date]|. [PubMed: 18504295]
6. Mandell DS, Wiggins LD, Carpenter LA, et al. Racial/ethnic disparities in the identification of
children with autism spectrum disorders. Am J Public Health 2009;99(3):493–98 doi: 10.2105/
AJPH.2007.131243[published Online First: Epub Date]|. [PubMed: 19106426]
7. Mandell DS, Listerud J, Levy SE, Pinto-Martin JA. Race differences in the age at diagnosis among
medicaid-eligible children with autism. J Am Acad Child Adolesc Psychiatry 2002;41(12):1447–
53 doi: 10.1097/00004583-200212000-00016[published Online First: Epub Date]|. [PubMed:
12447031]
8. Stevens J, Harman JS, Kelleher KJ. Race/ethnicity and insurance status as factors associated
with ADHD treatment patterns. J Child Adolesc Psychopharmacol 2005;15(1):88–96 doi: 10.1089/
cap.2005.15.88[published Online First: Epub Date]|. [PubMed: 15741790]
9. Stevens GD, Seid M, Mistry R, Halfon N. Disparities in primary care for vulnerable
children: the influence of multiple risk factors. Health Serv Res 2006;41(2):507–31 doi: 10.1111/
j.1475-6773.2005.00498.x[published Online First: Epub Date]|. [PubMed: 16584462]
10. Guerrero AD, Rodriguez MA, Flores G. Disparities in provider elicitation of parents’
developmental concerns for US children. Pediatrics 2011;128(5):901–9 doi: 10.1542/
peds.2011-0030[published Online First: Epub Date]|. [PubMed: 22007017]
11. Morgan PL, Farkas G, Hillemeier MM, et al. Minorities Are Disproportionately Underrepresented
in Special Education: Longitudinal Evidence Across Five Disability Conditions. Educational
Researcher 2015;44(5):278–92 doi: 10.3102/0013189X15591157[published Online First: Epub
Date]|. [PubMed: 27445414]
12. Morgan PL, Farkas G, Hillemeier MM, Maczuga S. Are minority children disproportionately
represented in early intervention and early childhood special education? Educational Researcher
2012;41(9):339–51 [PubMed: 24683265]
13. Boyle CA, Boulet S, Schieve LA, et al. Trends in the Prevalence of Developmental Disabilities in
US Children, 1997–2008. Pediatrics 2011;127(6):1034–42 doi: 10.1542/peds.2010-2989[published
Online First: Epub Date]|. [PubMed: 21606152]
14. Rosenberg SA, Robinson CC, Shaw EF, Ellison MC. Part C early intervention for infants
and toddlers: percentage eligible versus served. Pediatrics 2013;131(1):38–46 doi: 10.1542/
peds.2012-1662[published Online First: Epub Date]|. [PubMed: 23266922]
15. McManus BM, Robinson CC, Rosenberg SA. Identifying Infants and Toddlers at
High Risk for Persistent Delays. Matern Child Health J 2016;20(3):639–45 doi: 10.1007/
s10995-015-1863-2[published Online First: Epub Date]|. [PubMed: 26518005]
16. Keels M. Ethnic group differences in early head start parents’ parenting beliefs and practices
and links to children’s early cognitive development. Early Childhood Research Quarterly
2009;24(4):381–97 doi: 10.1016/j.ecresq.2009.08.002[published Online First: Epub Date]|.
17. Bornstein MH, Cote LR. “Who is sitting across from me?” Immigrant mothers’ knowledge
of parenting and children’s development. Pediatrics 2004;114(5):e557–64 doi: 10.1542/
peds.2004-0713[published Online First: Epub Date]|. [PubMed: 15520089]
18. Bethell C, Reuland C, Halfon N, Schor E. Measuring the quality of preventive and developmental
services for young children: National estimates and patterns of clinicians’ performance. Pediatrics
2004;113:1973–83 [PubMed: 15173469]
19. Guerrero AD, Chen J, Inkelas M, Rodriguez HP, Ortega AN. Racial and Ethnic Disparities in
Pediatric Experiences of Family-Centered Care. Medical Care 2010;48(4)
20. Schuster MA, Duan N, Regalado M, Klein DJ. Anticipatory guidance: what information do
parents receive? What information do they want? Archives of pediatrics & adolescent medicine
2000;154(12):1191–98 [PubMed: 11115301]
21. Liptak GS, Benzoni LB, Mruzek DW, et al. Disparities in diagnosis and access to health
services for children with autism: data from the National Survey of Children’s Health. Journal
of Developmental & Behavioral Pediatrics 2008;29(3):152–60 [PubMed: 18349708]
22. Mandell DS, Novak MM, Zubritsky CD. Factors associated with age of diagnosis among children
with autism spectrum disorders. Pediatrics 2005;116(6):1480–86 [PubMed: 16322174]
Gallegos et al.
Page 9
Acad Pediatr
. Author manuscript; available in PMC 2022 June 06.
Author Manuscript Author Manuscript Author Manuscript Author Manuscript

23. Delgado CE, Scott KG. Comparison of referral rates for preschool children at risk for disabilities
using information obtained from birth certificate records. The Journal of Special Education
2006;40(1):28–35
24. Barfield WD, Clements KM, Lee KG, Kotelchuck M, Wilber N, Wise PH. Using linked data to
assess patterns of early intervention (EI) referral among very low birth weight infants. Matern
Child Health J 2008;12(1):24–33 [PubMed: 17562149]
25. Cooper LA, Roter DL, Carson KA, et al. The associations of clinicians’ implicit attitudes about
race with medical visit communication and patient ratings of interpersonal care. Am J Public
Health 2012;102(5):979–87 doi: 10.2105/AJPH.2011.300558[published Online First: Epub Date]|.
[PubMed: 22420787]
26. Green AR, Carney DR, Pallin DJ, et al. Implicit bias among physicians and its prediction of
thrombolysis decisions for black and white patients. J Gen Intern Med 2007;22(9):1231–8 doi:
10.1007/s11606-007-0258-5[published Online First: Epub Date]|. [PubMed: 17594129]
27. Sabin JA, Greenwald AG. The influence of implicit bias on treatment recommendations for 4
common pediatric conditions: pain, urinary tract infection, attention deficit hyperactivity disorder,
and asthma. Am J Public Health 2012;102(5):988–95 doi: 10.2105/AJPH.2011.300621[published
Online First: Epub Date]|. [PubMed: 22420817]
28. Pediatrics AAo. Periodic survey of fellows# 53: Identification of children< 36 months at risk
for developmental problems and referral to early identification programs. Retrieved November
2003;11:2007
29. Jimenez ME, Barg FK, Guevara JP, Gerdes M, Fiks AG. Barriers to evaluation for early
intervention services: parent and early intervention employee perspectives. Acad Pediatr
2012;12(6):551–7 doi: 10.1016/j.acap.2012.08.006[published Online First: Epub Date]|. [PubMed:
23159037]
30. Minkovitz CS, Strobino D, Mistry KB, et al. Healthy Steps for Young Children: sustained results at
5.5 years. Pediatrics 2007;120(3):e658–e68 [PubMed: 17766506]
31. Coker T, Chacon S, Elliot M, Bruno Y, Chavis T, Biely C. A parent coach model for well-child
care among low-income children: a randomized controlled trial. Pediatr [Internet]. 2016 [cited
2017 Mai 23]; 137 (3): e201553013.
32. Mendelsohn AL, Dreyer BP, Flynn V, et al. Use of videotaped interactions during pediatric well-
child care to promote child development: a randomized, controlled trial. Journal of developmental
and behavioral pediatrics : JDBP 2005;26(1):34–41 [PubMed: 15718881]
33. Trent M, Dooley DG, Dougé J. The impact of racism on child and adolescent health. Pediatrics
2019;144(2):e20191765 [PubMed: 31358665]
34. Lee H, Marvin AR, Watson T, et al. Accuracy of phenotyping of autistic children based on Internet
implemented parent report. Am J Med Genet B Neuropsychiatr Genet 2010;153b(6):1119–26 doi:
10.1002/ajmg.b.31103[published Online First: Epub Date]|. [PubMed: 20552678]
35. Pless CE, Pless IB. How well they remember. The accuracy of parent reports. Arch Pediatr
Adolesc Med 1995;149(5):553–8 doi: 10.1001/archpedi.1995.02170180083016[published Online
First: Epub Date]|. [PubMed: 7735412]
Gallegos et al. Page 10
Acad Pediatr
. Author manuscript; available in PMC 2022 June 06.
Author Manuscript Author Manuscript Author Manuscript Author Manuscript
Author Manuscript Author Manuscript Author Manuscript Author Manuscript
Gallegos et al. Page 11
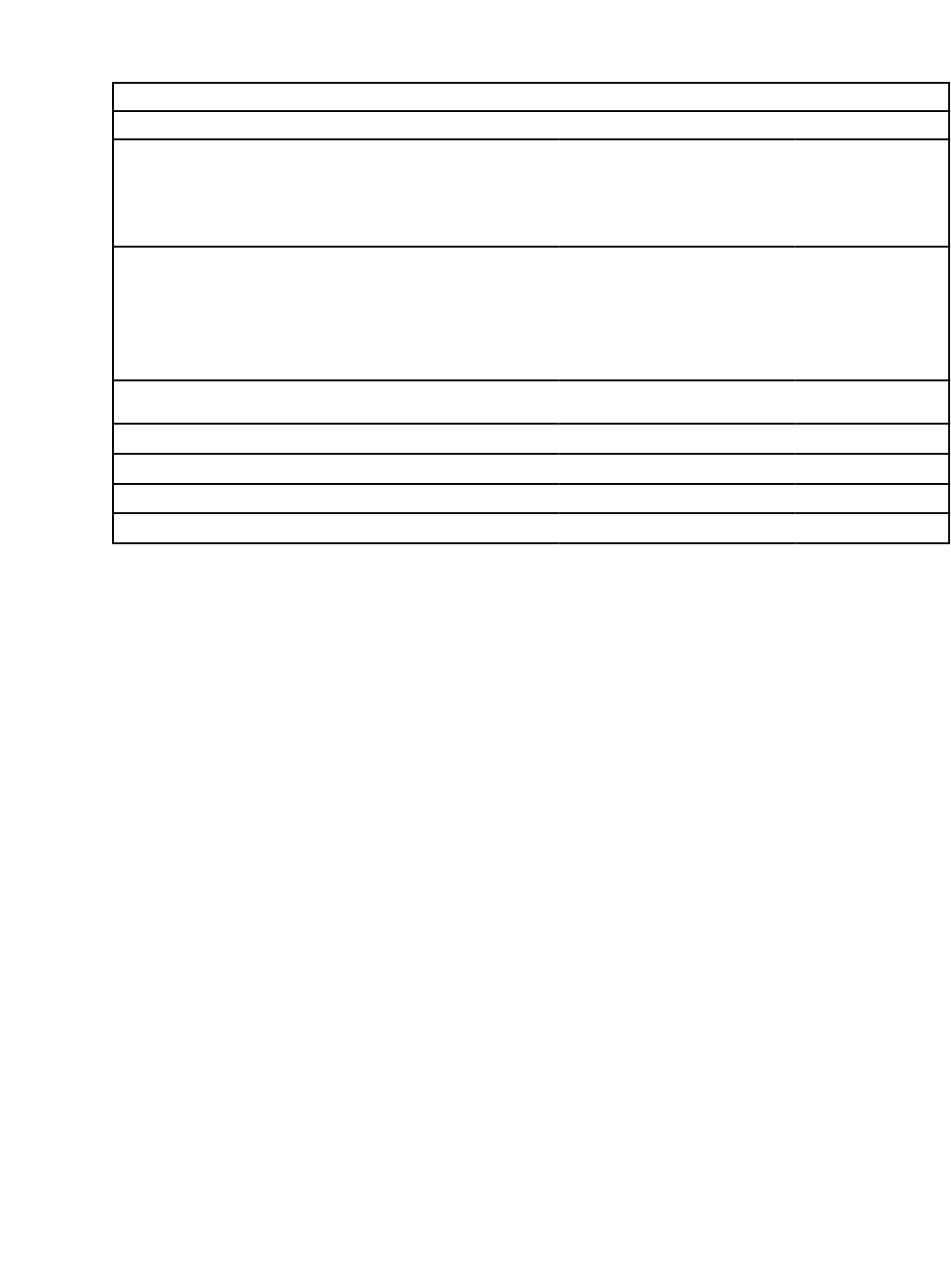
Table 1:
Characteristics of sample population (weighted sample)
N = 7,950 Percentage (N)
Race
White 53.8 (3,500)
Black 13.8 (1,250)
Hispanic 25.2 (1,550)
Asian 2.6 (750)
Other 0.7 (250)
Multiracial 3.9 (650)
Annual Household Income
≥ 185% of FPL 53.7 (4,300)
130% - below 185% of FPL 12.6 (1,000)
100% - below 130% of FPL 9.9 (750)
< 100% of FPL 23.8 (1,900)
Highest Parental Education
≥ Bachelor’s 31.5 (2,850)
Some college 25.9 (2,000)
High school diploma/vocational 29.7 (2,150)
< High school diploma 12.9 (950)
Child Sex
Female 48.8 (3,900)
Male 51.2 (4,050)
Urbanicity
Rural 15.2 (1,300)
Urban 84.9 (6,700)
Primary Language Spoken at Home
English 81.0 (6,400)
Non-English 19.0 (1,550)
Health Insurance
9-months 2-years Preschool Kinder
Yes 95.9 (7,700) 95.7 (7,650) 95.2 (7,600) 95.6 (5,900)
No 4.1 (250) 4.3 (300) 4.8 (350) 4.4 (250)
Well-child Visit in the past year (2 years old)
≥2 88.9 (7,050)
<2 11.1 (850)
Well-child Visit in the past year (Preschool)
≥1 96.3 (7,650)
0 3.7 (250)
Well-child Visit in the past year (Kindergarten)
≥1 95.8 (5,850)
Acad Pediatr
. Author manuscript; available in PMC 2022 June 06.
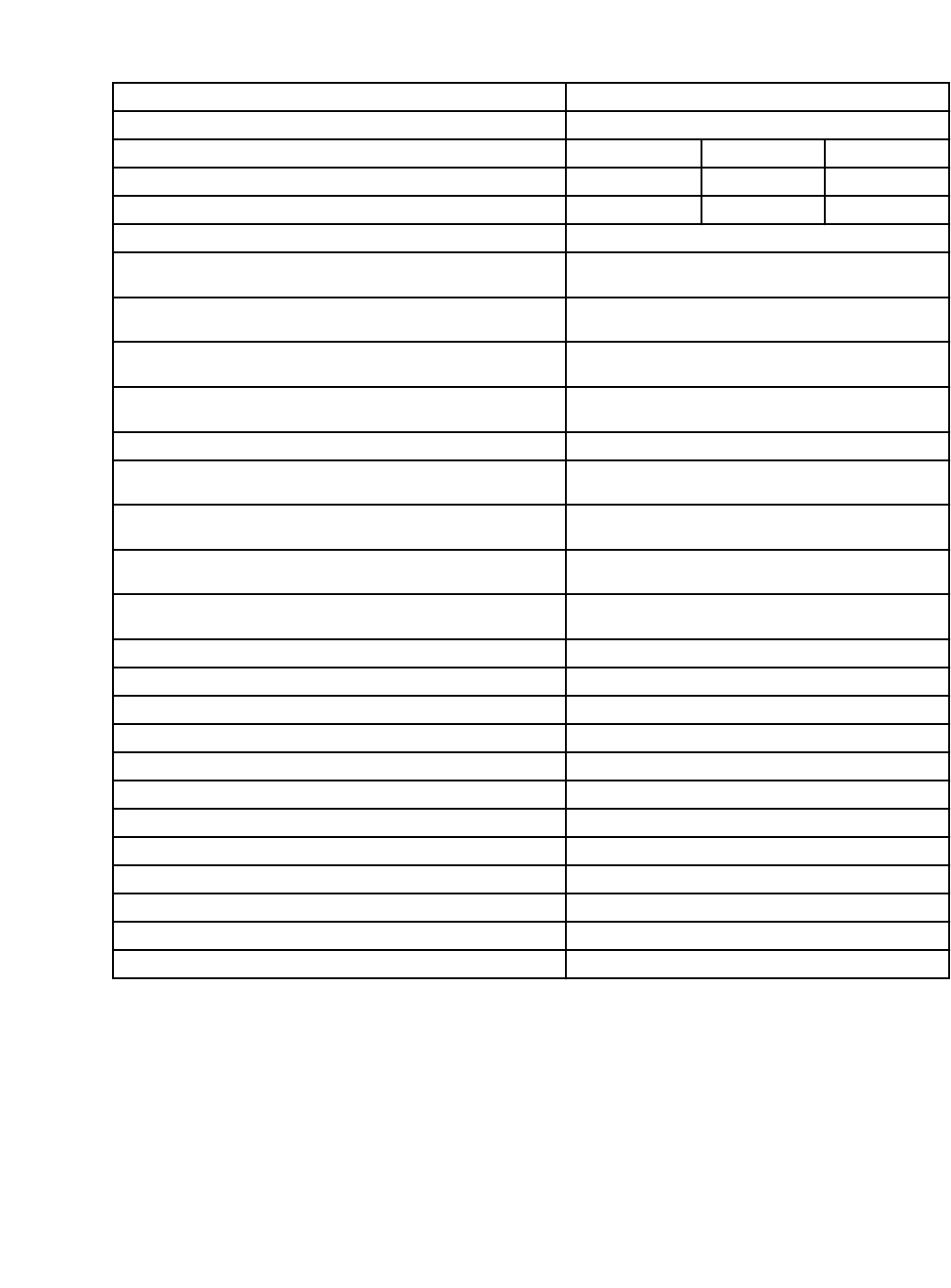
Author Manuscript Author Manuscript Author Manuscript Author Manuscript
Gallegos et al. Page 12
N = 7,950 Percentage (N)
0 4.2 (250)
Center-based Child Care Attendance 9-months 2-years Preschool
Yes 9.1 (700) 17.1 (1,350) 54.6 (4,500)
No 90.9 (7,250) 82.9 (6,650) 45.4 (3,450)
Developmental Trajectory (Preschool models)
>10
th
percentile 9-month BSF-R mental score and >10
th
percentile 2-year
BSF-R mental score
81.8 (6,000)
<=10
th
percentile 9-month BSF-R mental score and >10
th
percentile 2-
year BSF-R mental score
8.3 (900)
>10
th
percentile 9-month BSF-R mental score and <=10
th
percentile 2-
year BSF-R mental score
8.2 (750)
<=10
th
percentile 9-month BSF-R mental score and <=10
th
percentile
2-year BSF-R mental score
1.8 (300)
Developmental Trajectory (Kindergarten models)
>10
th
percentile 2-year BSF-R mental score and >10
th
percentile for both
preschool academic scores
78.1 (5,750)
<=10
th
percentile 2-year BSF-R mental score and >10
th
percentile for
both preschool academic scores
5.5 (600)
>10
th
percentile 2-year BSF-R mental score and <=10
th
percentile at least
one preschool academic score
13.0 (900)
<=10
th
percentile 2-year BSF-R mental score and <=10
th
percentile at
least one preschool academic score
3.4 (350)
Diagnosis (by Preschool)
No 93.4 (7,250)
Yes 6.6 (750)
Diagnosis (by Kindergarten entry)
No 92.5 (5,500)
Yes 7.5 (600)
Services (by Preschool)
No 33.5 (250)
Yes 66.5 (500)
Services (by Kindergarten entry)
No 30.9 (200)
Yes 69.1 (450)
Unweighted sample sizes are rounded to the nearest 50, as required by the National Center for Education Statistics. We used a kindergarten entry
wave sampling weight for the kindergarten entry variables. For the other variables, we used a preschool wave sampling weight. Receipt of services
by preschool and receipt of services by kindergarten entry were restricted to children who had a diagnosis of developmental delay by preschool and
kindergarten entry, respectively.
Acad Pediatr
. Author manuscript; available in PMC 2022 June 06.
Author Manuscript Author Manuscript Author Manuscript Author Manuscript
Gallegos et al. Page 13
Table 2:
Diagnosis and service for preschool
Preschool Diagnosis Preschool Services
Odds ratio p-value 95% CI Odds ratio p-value 95% CI
Race
White Reference Reference
Black 0.42 <0.001 0.29–0.61 0.31 0.01 0.13 – 0.71
Hispanic 0.84 0.47 0.53– 1.34 0.35 0.02 0.15 – 0.86
Asian 0.56 0.04 0.33– 0.97 0.37 0.11 0.11 – 1.26
Other 0.99 0.98 0.50– 1.97 0.61 0.46 0.16 – 2.29
Multiracial 0.52 0.03 0.30– 0.92 0.79 0.69 0.25 – 2.49
Annual household income
At or above 185% of the poverty level Reference Reference
below 100% poverty 1.41 0.07 0.97– 2.07 0.65 0.23 0.33 – 1.31
100% - below 130% poverty 0.96 0.86 0.59 – 1.54 0.43 0.17 0.13 – 1.43
130% - below 185% poverty 1.08 0.72 0.69– 1.70 0.56 0.22 0.22 – 1.42
Highest parental education
≥ Bachelor’s Reference Reference
Some college 0.95 0.79 0.63– 1.43 1.06 0.87 0.56 – 2.00
HS diploma 0.79 0.28 0.51– 1.22 1.87 0.09 0.91 – 3.82
< HS diploma 0.79 0.40 0.46– 1.36 1.79 0.25 0.66 – 4.88
Child Sex
Female Reference Reference
Male 2.27 <0.001 1.83– 2.81 1.39 0.29 0.75 – 2.59
Urbanicity
Rural Reference Reference
Urban 0.89 0.55 0.62– 1.30 1.39 0.42 0.62 – 3.12
Primary Language spoken at home
English Reference Reference
Non-English language 0.54 0.03 0.32– 0.93 0.77 0.55 0.33 – 1.81
Insurance status: 9 months, 2 years, preschool
Yes Reference Reference
9 months: No insurance 1.16 0.75 0.47– 2.87 0.34 0.18 0.07– 1.64
24 months: No insurance 0.43 0.01 0.22– 0.83 0.47 0.38 0.09 – 2.55
Preschool: No insurance 0.90 0.77 0.45– 1.81 0.90 0.89 0.20 – 4.10
Well child visits: 9 months – 2 years
≥ 2 Well child visits from 9 months to 2 years Reference Reference
< 2 Well child visits from 9 months to 2 years 1.19 0.38 0.81– 1.74 0.93 0.87 0.38 – 2.27
Well child visits: 2 years to preschool
≥ 1 Well child visits 2 years to preschool Reference Reference
0 Well child visits 2 years to preschool 0.67 0.31 0.31– 1.47 0.36 0.30 0.05 – 2.54
Acad Pediatr
. Author manuscript; available in PMC 2022 June 06.
Author Manuscript Author Manuscript Author Manuscript Author Manuscript
Gallegos et al. Page 14
Preschool Diagnosis Preschool Services
Odds ratio p-value 95% CI Odds ratio p-value 95% CI
Child is in center-based child care
No Reference Reference
9 months: yes 0.97 0.88 0.61 – 1.54 1.12 0.83 0.39 – 3.24
2 year: yes 1.33 0.09 0.95 – 1.86 1.17 0.61 0.64 – 2.12
Preschool: yes 1.52 0.002 1.17 – 1.97 2.26 0.01 1.19 – 4.30
Developmental trajectory:
9-month BSF-R mental score, 2-year BSF-R mental score
>10
th
% 9-month BSF-R score, >10
th
% 2-year BSF-R score
Reference Reference
<=10
th
% 9-month BSF-R score, >10
th
% 2-year BSF-R score
2.39 <0.001 1.61– 3.54 0.94 0.85 0.50 – 1.77
>10
th
% 9-month BSF-R score, <=10
th
% 2-year BSF-R score
7.16 <0.001 5.13– 10.01 2.84 <0.001 1.63 – 4.94
<=10
th
% 9-month BSF-R score, <=10
th
% 2-year BSF-R
score
9.53 <0.001 6.46– 14.06 3.25 0.04 1.08 – 9.71
We used a preschool wave sampling weight for the preschool models.
Acad Pediatr
. Author manuscript; available in PMC 2022 June 06.
Author Manuscript Author Manuscript Author Manuscript Author Manuscript
Gallegos et al. Page 15
Table 3
Diagnosis and service for kindergarten entry
Kindergarten Diagnosis Kindergarten Services
Odds ratio p-value 95% CI Odds ratio p-value 95% CI
Race
White Reference Reference
Black 0.49 0.02 0.28 – 0.87 0.29 0.02 0.11 – 0.78
Hispanic 0.80 0.40 0.47 – 1.35 0.45 0.12 0.16 – 1.23
Asian 0.53 0.04 0.28 – 0.98 0.39 0.19 0.09 – 1.61
Other 0.94 0.89 0.43 – 2.09 1.19 0.81 0.29 – 4.85
Multiracial 0.58 0.18 0.26 – 1.28 0.58 0.51 0.11 – 3.01
Annual household income
At or above 185% of the poverty level Reference Reference
below 100% poverty 1.29 0.33 0.77 – 2.18 0.81 0.62 0.35 – 1.87
100% - below 130% poverty 1.01 0.98 0.53 – 1.91 0.27 0.03 0.09 – 0.85
130% - below 185% poverty 1.20 0.43 0.79 – 1.91 0.73 0.58 0.24 – 2.23
Highest parental education
≥ Bachelor’s Reference Reference
Some college 0.67 0.11 0.40 – 1.10 1.06 0.88 0.51 – 2.19
HS diploma 0.79 0.40 0.46 – 1.36 3.18 0.02 1.23 – 8.27
< HS diploma 0.64 0.20 0.32 – 1.28 1.43 0.56 0.41 – 4.96
Child sex
Female Reference Reference
Male 2.28 <0.001 1.57 – 3.31 1.12 0.76 0.55 – 2.29
Urbanicity
Rural Reference Reference
Urban 1.06 0.81 0.66 – 1.71 1.23 0.60 0.56 – 2.71
Primary Language spoken at home
English Reference Reference
Non-english language 0.47 0.01 0.27 – 0.84 1.23 0.72 0.39 – 3.81
Insurance status: 9 months, 2 years, preschool,
kindergarten
Yes Reference Reference
9 months: No insurance 0.92 0.89 0.29 – 2.91 2.69 0.27 0.46 – 15.78
24 months: No insurance 0.61 0.33 0.22 – 1.68 0.13 0.14 0.01 – 1.90
Preschool: No insurance 0.63 0.42 0.20 – 1.95 0.67 0.70 0.08 – 5.47
Kindergarten: No insurance 0.35 0.04 0.13 – 0.95 0.70 0.74 0.08 – 5.92
Well child visits: Number of visits, 9 months – 2 years
≥ 2 Well child visits Reference Reference
< 2 Well child visits 0.96 0.86 0.59 – 1.56 0.52 0.28 0.16 – 1.73
Well child visits: Number of visits, 2 years to preschool
≥ 1 Well child visits Reference Reference
Acad Pediatr
. Author manuscript; available in PMC 2022 June 06.
Author Manuscript Author Manuscript Author Manuscript Author Manuscript
Gallegos et al. Page 16
Kindergarten Diagnosis Kindergarten Services
Odds ratio p-value 95% CI Odds ratio p-value 95% CI
0 Well child visits 0.91 0.84 0.34 – 2.43 0.68 0.77 0.05 – 9.22
Well child visits: Number of visits, preschool to kinder
≥ 1 Well child visits Reference Reference
< 0 Well child visits 0.44 0.11 0.16 – 1.21 0.11 0.11 0.01 – 1.71
Child is in center-based child care
No Reference Reference
9 months: yes 0.61 0.10 0.34 – 1.11 1.13 0.85 0.30 – 4.20
2 year: yes 1.37 0.17 0.88 – 2.13 1.95 0.07 0.94 – 4.02
Preschool: yes 1.71 0.002 1.22 – 2.40 2.12 0.06 0.98 – 4.62
Developmental trajectory: 2-year BSF-R mental scale
score, Preschool early reading and math IRT scale scores
>10
th
% 2-year BSF-R score, >10
th
% Preschool score
Reference Reference
<=10
th
% 2-year BSF-R score, >10
th
% Preschool score
6.52 <0.001 4.32 – 9.84 2.37 0.12 0.79 – 7.07
>10
th
% 2-year BSF-R score, <=10
th
% Preschool score
2.83 <0.001 1.86 – 4.32 0.74 0.51 0.30 – 1. 84
<=10
th
% 2-year BSF-R score, <=10
th
% Preschool score
13.05 <0.001 8.18 – 20.82 2.47 0.06 0.95 – 6.42
We used a kindergarten entry wave sampling weight for the kindergarten entry models.
Acad Pediatr
. Author manuscript; available in PMC 2022 June 06.
