DentaQuest USA Insurance Company, Inc. February 1, 2024
Current Dental Terminology © American Dental Association. All Rights Reserved.
DentaQuest USA Insurance Company, Inc.
DentaQuest Provider Office Reference Manual
TX HHSC Dental Services‐ Medicaid and CHIP
Provider Manual
1-800-896-2374
www.dentaquest.com/texas
This document contains proprietary and confidential information and
may not be disclosed to others without written permission
©Copyright 2024. All rights reserved.
Version 9.2
DentaQuest USA Insurance Company, Inc. February 1, 2024
Current Dental Terminology © American Dental Association. All Rights Reserved.
DentaQuest USA Insurance Company, Inc. February 1, 2024
Current Dental Terminology © American Dental Association. All Rights Reserved.
2
TABLE OF CONTENTS
TX HHSC Dental Services‐ Medicaid and CHIP .......................................................................................................... 1
Provider Manual ...................................................................................................................................................... 1
TABLE OF CONTENTS ............................................................................................................................................... 2
Introduction to DentaQuest ................................................................................................................................. 8
Quick Reference Phone List ..................................................................................................................................... 8
Program Objectives.................................................................................................................................................. 9
Role of Main Dental Home ...................................................................................................................................... 9
Are you building a “Dental Home” for your Members? ....................................................................................... 9
Role of First Dental Home Initiative for Medicaid Members ................................................................................... 9
Covered Services .................................................................................................................................................... 10
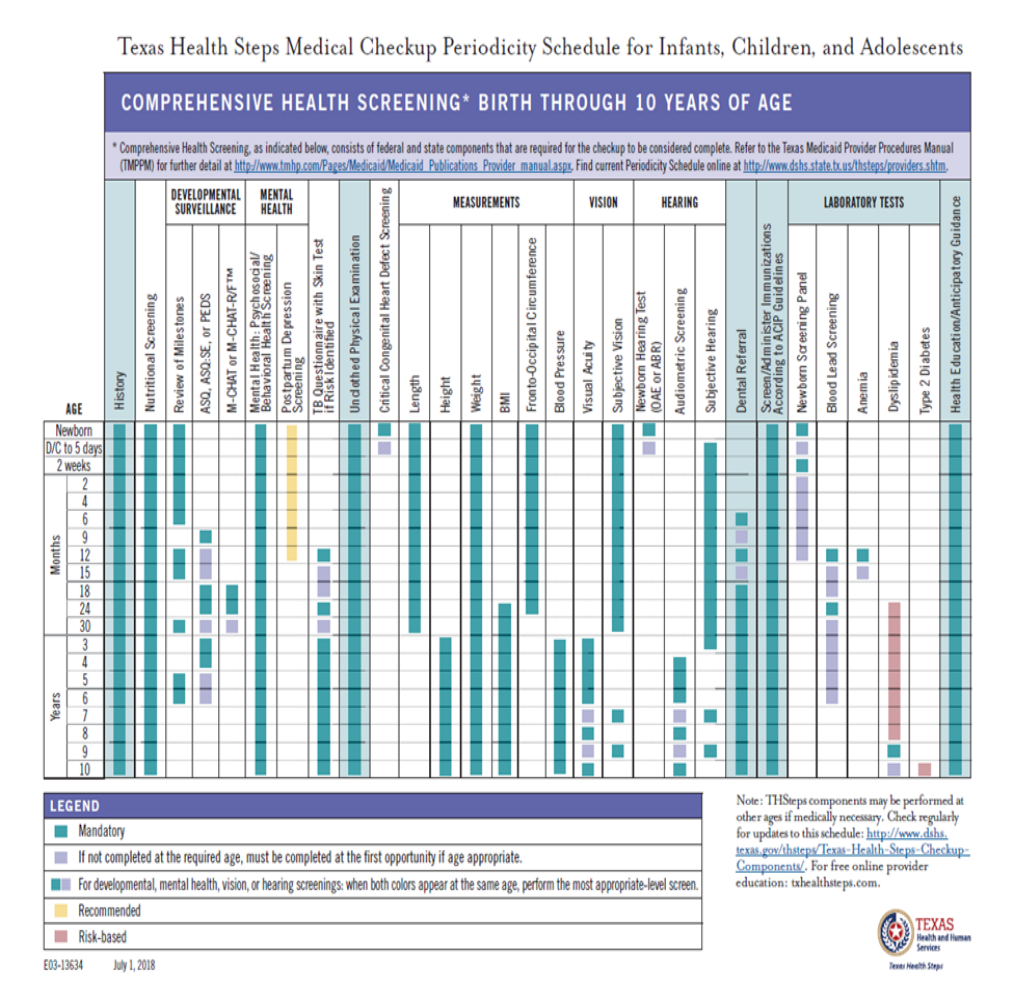
Texas Health Steps Dental Services (Medicaid Only) ............................................................................................. 10
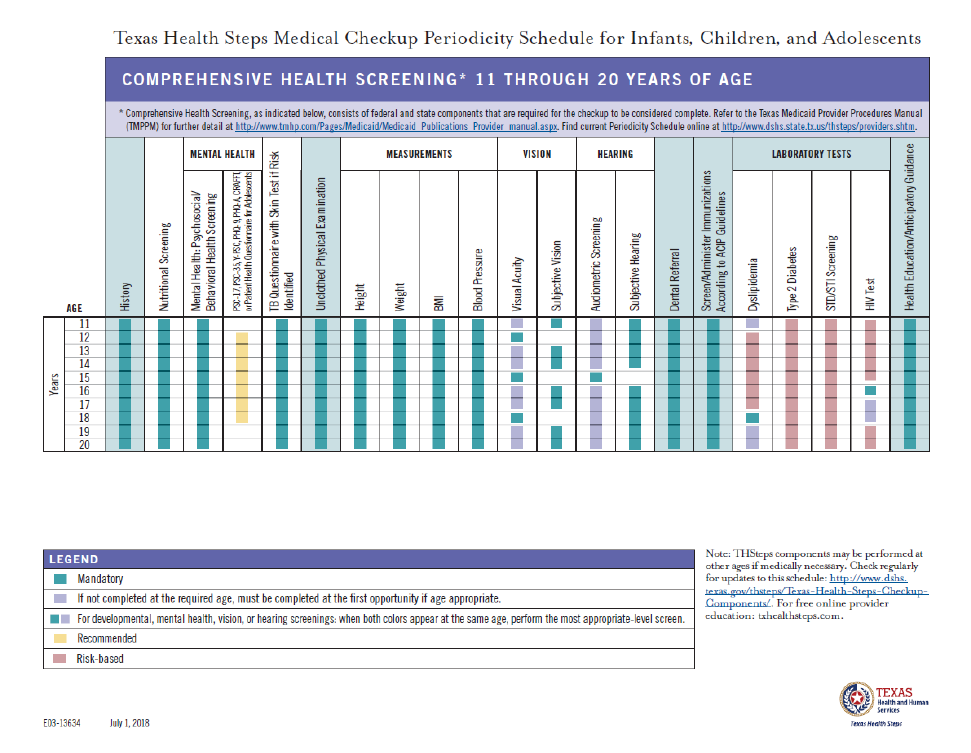
Texas Health Steps Medical Checkup Periodicity Schedule for Infant, Children,
and Adolescents .......................... 10
Exception to Periodicity Oral Evaluation, Dental Checkup, and Emergency or Trauma Related Services for Texas
Health Steps Dental Procedures ............................................................................................................................ 12
Exception-to-Periodicity Oral Evaluation ............................................................................................................... 12
Exception-to-Periodicity Dental Checkup .............................................................................................................. 13
Exception-to-Periodicity Emergency or Trauma Related Oral Evaluation ............................................................. 13
Adjunctive General Services .................................................................................................................................. 13
Children of Migrant Farmworkers ......................................................................................................................... 13
Children’s Medicaid Dental Covered Services .......................................................................................................... 14
Texas Medicaid Dental Program Covered Services include the following Medically Necessary services. ........ 14
CHIP Dental Covered Services .................................................................................................................................. 14
Texas CHIP Dental Program Covered Services include the following Medically Necessary services. ................ 15
C. Quality Management ......................................................................................................................................... 15
Quality Improvement Program (Policies 200 Series) ............................................................................................. 15
Utilization Management Program ......................................................................................................................... 16
Introduction: ...................................................................................................................................................... 16
Community Practice Patterns: ........................................................................................................................... 16
Evaluation: ......................................................................................................................................................... 17
Results: ............................................................................................................................................................... 17
Network Management Program ............................................................................................................................ 17
NETWORK MANAGEMENT PROCEDURES .......................................................................................................... 17
D. Provider Responsibilities ................................................................................................................................... 19
General Responsibilities......................................................................................................................................... 19
Availability and Accessibility .............................................................................................................................. 20
Main Dental Home Responsibilities ................................................................................................................... 20
First Dental Home Initiative Responsibilities ..................................................................................................... 21
Updates to Contact Information ........................................................................................................................ 22
Plan Termination ................................................................................................................................................ 22
Referral to Specialists Process............................................................................................................................ 22
Referrals to Specialists .............................................................................................................................................. 22
Verify Member Eligibility and/or Authorizations for Service ............................................................................. 23
Member Eligibility .............................................................................................................................................. 23
Access to eligibility information via the Provider Web Portal............................................................................ 24
Access to eligibility information via the IVR line ................................................................................................ 25
Authorizations of Service ................................................................................................................................... 25
Submitting Authorization or Claims with X‐Rays ............................................................................................... 26
Electronic Attachments ...................................................................................................................................... 27
Continuity of Care .............................................................................................................................................. 28
DentaQuest USA Insurance Company, Inc. February 1, 2024
Current Dental Terminology © American Dental Association. All Rights Reserved.
3
Dental Records ................................................................................................................................................... 28
Organization ............................................................................................................................................................. 28
Compliance ............................................................................................................................................................... 32
Health Insurance Portability and Accountability Act (HIPAA) ............................................................................ 32
Access to Second Opinion .................................................................................................................................. 33
Justification Regarding Out‐of‐Network Referrals ............................................................................................. 34
Informed Consent for Utilization of Papoose Boards ........................................................................................ 34
Routine, Therapeutic/Diagnostic, and Urgent Care Dental Services ..................................................................... 35
Definitions .......................................................................................................................................................... 35
EMERGENCY Treatments and Authorizations .................................................................................................... 36
Requirements for Scheduling of Appointments ................................................................................................. 36
Coordination of Non‐Capitated Services ............................................................................................................... 36
Medicaid Services Not Covered by DentaQuest ................................................................................................ 36
MEDICAL TRANSPORTATION PROGRAM (MTP) ................................................................................................. 37
CHIP Services Not Covered by DentaQuest ........................................................................................................ 37
Effective January 1, 2019 - Retro eligibility Recoupment Process ..................................................................... 38
Provider Appeal Process to HHSC (related to claim recoupment due to Member disenrollment) .......................... 38
E. Medicaid Dental Services Provider Complaint and Appeal Process .................................................................... 38
Medicaid Provider Complaints ............................................................................................................................... 39
Medicaid Provider Appeals .................................................................................................................................... 39
Peer to Peer Reviews ............................................................................................................................................. 40
F. Medicaid Dental Services Member Complaint and Appeal Process .................................................................... 40
Medicaid Member Complaint ................................................................................................................................ 40
What should I do if I have a complaint? ............................................................................................................. 40
If the Member is not satisfied with the outcome, who else can they call? ....................................................... 41
MDCP/DBMD ESCALATION HELP LINE .................................................................................................................... 41
What is the MDCP/DBMD Escalation Help Line? ................................................................................................... 41
When should I call the escalation help line? ......................................................................................................... 41
Is the escalation help line the same as the HHS Office of the Ombudsman? ........................................................ 41
Who can call the help line? .................................................................................................................................... 42
Medicaid Member Appeals .................................................................................................................................... 42
What can I do if DentaQuest denies or limits my Member’s request for a covered service? ............................. 42
How will I find out if services are denied? .......................................................................................................... 42
Timeframes for the Appeal Process ................................................................................................................... 42
When does the Member have the right to ask for an appeal? ........................................................................... 43
Can someone from DentaQuest help a Member file an appeal? ....................................................................... 43
Medicaid Member Expedited Appeals ................................................................................................................... 43
How to Request an Emergency Appeal .............................................................................................................. 43
Timeframes for Emergency Appeals .................................................................................................................. 43
What happens if DentaQuest denies the request for an Emergency Appeal? ................................................... 43
Who can help me file an Emergency Appeal? .................................................................................................... 44
State Fair Hearing Information .............................................................................................................................. 44
Can a Member ask for a State Fair Hearing? ...................................................................................................... 44
External Medical Review Information .................................................................................................................... 44
Can a Member ask for an External Medical Review? ............................................................................................ 44
Can a Member ask for an emergency External Medical Review? .......................................................................... 45
G. CHIP Provider Complaints and Appeals .............................................................................................................. 46
CHIP Provider Complaints ...................................................................................................................................... 46
CHIP Provider Appeals ........................................................................................................................................... 46
Peer to Peer Reviews ............................................................................................................................................. 47
“Like Specialty” Peer to Peer Reviews ................................................................................................................... 47
DentaQuest USA Insurance Company, Inc. February 1, 2024
Current Dental Terminology © American Dental Association. All Rights Reserved.
4
Procedure ........................................................................................................................................................... 47
CHIP Member Complaints and Appeals ................................................................................................................. 48
CHIP Member Complaint ................................................................................................................................... 48
What should I do if I have a complaint? ............................................................................................................. 49
Who do I call? ..................................................................................................................................................... 49
Can someone from DentaQuest help a Member file a complaint? .................................................................... 49
How long will it take to investigate and resolve my complaint? ........................................................................ 49
If I am not satisfied with the outcome, who else can I call? .............................................................................. 50
CHIP Member Appeal ............................................................................................................................................ 50
What can I do if DentaQuest denies or limits my patient’s request for a covered service? ............................... 50
How will I find out if the appeal is denied? ........................................................................................................ 51
Timeframes for the Appeal Process ................................................................................................................... 52
When does a Member have the right to request an appeal? ............................................................................. 52
Can someone from DentaQuest help the Member file an appeal? .................................................................... 53
CHIP Member Expedited Appeals .......................................................................................................................... 53
How to Request an Expedited Appeal ................................................................................................................ 53
Timeframes for Expedited Appeals .................................................................................................................... 53
What happens if DentaQuest denies the request for an Expedited Appeal? ..................................................... 53
Who can help me file an Expedited Appeal? ...................................................................................................... 53
Independent Review Organization (IRO) for External CHIP Appeal Reviews ......................................................... 54
What is an Independent Review Organization? ................................................................................................. 54
How do I request a review by an Independent Review Organization? ............................................................... 54
HHS‐Administered Federal External Review Request Form ............................................................................... 54
HHS Federal External Review Process Appointment of Representative Form ................................................... 54
How long will it take to investigate and resolve my external appeal? ............................................................... 55
Standard External Review requests: .................................................................................................................. 55
Expedited Independent Review Organization request ...................................................................................... 55
How long will it take to investigate and resolve my expedited external appeal? .............................................. 56
For an expedited External Review request: ....................................................................................................... 56
HHSC Oversight ...................................................................................................................................................... 56
H. Medicaid Member Eligibility and Added Benefits .............................................................................................. 56
Eligibility ................................................................................................................................................................. 56
Verifying Eligibility ................................................................................................................................................. 56
Main Dental Home Verification ......................................................................................................................... 56
DentaQuest Member Identification Card .......................................................................................................... 57
Call DentaQuest ................................................................................................................................................. 57
Automated Inquiry System line/TXMedConnect ............................................................................................... 57
Automatic Re‐enrollment ...................................................................................................................................... 58
Disenrollment ........................................................................................................................................................ 58
Can DentaQuest ask that my child get dropped from their dental plan? .......................................................... 58
Medicaid Plan Changes .......................................................................................................................................... 58
Medicaid Added Benefits ....................................................................................................................................... 59
Medicaid Member Value Added Services .............................................................................................................. 59
Additional value‐added services: .............................................................................................................................. 59
I. CHIP Member Eligibility and Added Benefits ....................................................................................................... 60
Eligibility ................................................................................................................................................................. 60
Verifying Eligibility ................................................................................................................................................. 60
DentaQuest CHIP Identification Card ................................................................................................................. 60
Re‐enrollment ........................................................................................................................................................ 61
Disenrollment ........................................................................................................................................................ 61
Can DentaQuest ask that my child get dropped from their dental plan? .......................................................... 61
CHIP Plan Changes ................................................................................................................................................. 61
DentaQuest USA Insurance Company, Inc. February 1, 2024
Current Dental Terminology © American Dental Association. All Rights Reserved.
5
CHIP Added Benefits .............................................................................................................................................. 62
CHIP Member Value Added Services ...................................................................................................................... 62
Member Rights and Responsibilities ...................................................................................................................... 63
MEMBER RIGHTS ................................................................................................................................................... 63
Medicaid Member Responsibilities ....................................................................................................................... 65
CHIP DENTAL SERVICES MEMBER RIGHTS AND RESPONSIBILITIES........................................................................ 66
CHIP Member Rights .............................................................................................................................................. 66
CHIP Member Responsibilities ............................................................................................................................... 68
Fraud and Abuse Reporting ................................................................................................................................... 68
Do you want to report Waste, Abuse, or Fraud? ............................................................................................... 68
To report waste, abuse, or fraud, choose one of the following: ........................................................................ 69
To report waste, abuse or fraud, gather as much information as possible. ...................................................... 69
J. Medicaid and CHIP Encounter Data, Billing, and Claims Administration ............................................................. 69
Where to Send Claims/Encounter Data ................................................................................................................. 69
Electronic Claim Submission Utilizing DentaQuest’s Internet Website ............................................................. 70
Electronic Authorization Submission Utilizing DentaQuest's Internet Website ................................................ 70
Electronic Claim Submission via Clearinghouse ................................................................................................. 71
HIPAA Compliant 837D File ................................................................................................................................ 71
NPI Requirements for Submission of Electronic Claims ..................................................................................... 71
Paper Claim Submission ..................................................................................................................................... 71
Coordination of Benefits (COB) .......................................................................................................................... 72
Receipt and Audit of Claims ............................................................................................................................... 73
Second Opinion Reviews and Regional Screening ............................................................................................. 73
Form to Use ........................................................................................................................................................... 73
CHIP Cost Sharing Schedule ................................................................................................................................... 73
No Co‐Payments for Medicaid Members .............................................................................................................. 75
Billing Members ..................................................................................................................................................... 75
Member Acknowledgement Statement ............................................................................................................. 75
Private Pay Form Agreement ............................................................................................................................. 75
Time Limit for Submission of Claims/Claims Appeals ............................................................................................ 75
Claims Payment ..................................................................................................................................................... 76
K. Medicaid and CHIP Special Access Requirements ............................................................................................... 76
Interpreter/Translation Services ............................................................................................................................ 76
Dental Contractor/Provider Coordination ............................................................................................................. 77
Reading/Grade Level Consideration ...................................................................................................................... 77
Cultural Sensitivity ................................................................................................................................................. 77
Knowledge .......................................................................................................................................................... 78
Skills.................................................................................................................................................................... 78
Attitudes............................................................................................................................................................. 78
Specialty Health Care Needs .................................................................................................................................. 79
L. DentaQuest Information .................................................................................................................................... 79
Standard of Care .................................................................................................................................................... 79
Identical Restoration: (same tooth, exact same service), same provider or location (Prior Authorization or Pre-
Payment Review) ............................................................................................................................................... 79
Similar Restoration: (same tooth, at least one surface repeated), same provider or location (Prior
Authorization or Pre-Payment Review) ............................................................................................................. 80
Provider Preventable Conditions ........................................................................................................................... 81
Professional Conduct ............................................................................................................................................. 81
Credentialing (Policies PEC Series) ......................................................................................................................... 81
Credentials Committee Denials (Policy PEC01)...................................................................................................... 82
Recredentialing (Policy PEC01) .............................................................................................................................. 82
Disciplinary Actions, Corrective Action Plans & Provider Appeals (Policy PEC05) ................................................. 82
Appeal of Credentials Committee Termination (Policy PEC05) ............................................................................. 82
DentaQuest USA Insurance Company, Inc. February 1, 2024
Current Dental Terminology © American Dental Association. All Rights Reserved.
6
Broken Appointments – Best Practices .................................................................................................................. 82
Logging Broken Appointments in the Provider Web Portal ................................................................................... 83
Direct Deposit ........................................................................................................................................................ 84
Advance Directives ................................................................................................................................................ 85
Clinical Criteria ....................................................................................................................................................... 86
Criteria for Dental Extractions ............................................................................................................................ 87
Documentation needed for authorization procedure: ...................................................................................... 87
Criteria................................................................................................................................................................ 87
Criteria for Cast Crowns ..................................................................................................................................... 87
Documentation needed for authorization of procedure: .................................................................................. 87
Criteria................................................................................................................................................................ 88
Criteria for Endodontics ..................................................................................................................................... 88
Documentation needed for authorization of procedure: .................................................................................. 89
Criteria................................................................................................................................................................ 89
Criteria for Stainless Steel Crowns ..................................................................................................................... 90
Documentation needed for authorization of procedure: .................................................................................. 90
Criteria................................................................................................................................................................ 90
Criteria for Authorization of Operating Room (OR) Cases Documentation needed for authorization of
procedure: .......................................................................................................................................................... 91
Criteria................................................................................................................................................................ 91
Criteria for Removable Prosthodontics (Full and Partial Dentures) ................................................................... 92
Documentation needed for authorization of procedure: .................................................................................. 92
Criteria................................................................................................................................................................ 92
Criteria................................................................................................................................................................ 93
Criteria for the Excision of Bone Tissue .............................................................................................................. 94
Criteria for the Determination of a Non‐Restorable Tooth ............................................................................... 94
Criteria for General Anesthesia and Intravenous (IV) Sedation
Documentation needed for authorization of
procedure: .......................................................................................................................................................... 95
Criteria................................................................................................................................................................ 95
For Members Ages Six and Under ...................................................................................................................... 96
Dental Anesthesiologist ..................................................................................................................................... 97
Treating Dentist.................................................................................................................................................. 97
Medical Anesthesiologist ................................................................................................................................... 98
Treating Dentist.................................................................................................................................................. 98
Medical Anesthesiologist and / or Facility ......................................................................................................... 99
Treating Dentist.................................................................................................................................................. 99
Criteria for Periodontal Treatment .................................................................................................................... 99
Criteria.............................................................................................................................................................. 100
Appendix A
Definitions ........................................................................................................................................ 101
Appendix B Forms to Use ..................................................................................................................................... 103
Non‐Covered Service Disclosure Form ................................................................................................................. 106
OrthoCAD Submission Form ................................................................................................................................. 107
Continuation of Care Submission Form ................................................................................................................ 108
Children’s Medicaid Dental Services Managed Care Orthodontia Review Policy and Procedure‐ Texas ............... 109
Purpose ................................................................................................................................................................ 109
Definitions ............................................................................................................................................................ 109
Policy .................................................................................................................................................................... 109
RECALL EXAMINATION ......................................................................................................................................... 120
RECALL EXAMINATION ......................................................................................................................................... 120
Authorization for Dental Treatment .................................................................................................................... 121
MEDICAL AND DENTAL HISTORY .......................................................................................................................... 122
AUTHORIZATION TO HONOR DIRECT AUTOMATED CLEARING HOUSE (ACH) CREDITS DISBURSED BY DENTAQUEST
USA‐TX HHSC Dental Services Program ................................................................................................................ 124
DentaQuest USA Insurance Company, Inc. February 1, 2024
Current Dental Terminology © American Dental Association. All Rights Reserved.
7
INSTRUCTIONS ..................................................................................................................................................... 124
MAINTENANCE TYPE: ........................................................................................................................................... 124
ACCOUNT HOLDER INFORMATION: ..................................................................................................................... 124
APPENDIX C ......................................................................................................................................................... 125
Covered Benefits (See Exhibits) ........................................................................................................................... 125
800.896.2374, press option 2 .......................................................................................................................... 125
DentaQuest Authorization Process ...................................................................................................................... 127
IMPORTANT ......................................................................................................................................................... 127
Exhibit A Benefits Covered for TX Medicaid Child (Under 21)............................................................................... 128
DentaQuest USA Insurance Company, Inc. February 1, 2024
Current Dental Terminology © American Dental Association. All Rights Reserved.
8
___________________________________________________________________________________________________________
Introduction to DentaQuest
Quick Reference Phone List
Provider Services‐Medicaid and CHIP
1‐800‐896‐2374
Monday – Friday; 8 a.m. – 6 p.m.
Fax numbers:
Claims/payment issues: 262‐241‐7379
Claims to be processed: 262‐834‐3589
All other: 262‐834‐3450
Claims Questions:
Medicaid Member Services
1‐800‐516‐0165
Monday – Friday; 8 a.m. – 6 p.m.
CHIP Member Services
1‐800‐508‐6775
Monday – Friday; 8 a.m. – 6 p.m.
TTY Service
Federal Relay Service 7‐1‐1
TMHP Contact Center/Automated Inquiry
System (AIS)
1‐800‐925‐9126 or 512‐335‐5986
www.tmhp.com
*For interpretation/translation services,
please contact the Provider Services
Department at:
1‐800‐896‐2374
Authorizations should be sent to:
TX HHSC Dental Program‐ Authorization
P.O. Box 2906 Milwaukee,
WI 53201‐2906
Fax: 262‐241‐7150 or 888‐313‐2883
Credentialing applications should be sent
to:
TX HHSC Dental Program‐ Credentialing
P.O. Box 2906 Milwaukee,
WI 53201‐2906
Credentialing Hotline: 800.233.1468
Fax: 262‐241‐4077
Claims should be sent to:
TX HHSC Dental Program –Claims
Box 2906 Milwaukee, WI 53201‐2906
Electronic Claims should be sent:
Direct entry on the web –
www.dentaquest.com
Or,
Via Clearinghouse – Payer ID CX014
Include address on electronic claims –
DentalQuest, LLC
PO Box 2906
Milwaukee, WI 53201-2906

DentaQuest USA Insurance Company, Inc. February 1, 2024
Current Dental Terminology © American Dental Association. All Rights Reserved.
9
Program Objectives
The primary objective of Texas Medicaid and CHIP Dental Services programs are to create a
comprehensive dental care system offering quality dental services to those eligible Texas
residents. We emphasize early intervention and promote access to care, thereby improving
health outcomes for Texas residents.
Role of Main Dental Home
Are you building a “Dental Home” for your Members?
Effective March 1, 2012, DentaQuest USA Insurance Company, Inc. (DentaQuest) implemented
the Dental Home program in Texas for Medicaid and CHIP Members.
The Main Dental Home is a place where a child’s oral health care is delivered in a complete,
accessible and family‐centered manner by a licensed dentist. This concept has been
successfully
employed by primary care physicians in developing a “Medical Home” for their Members, and
the “Dental Home” concept mirrors the “Medical Home” for primary dental and oral health care.
If expanded or specialty dental services are required, the dentist is not
expected to deliver the
services, but to coordinate the referral and to monitor the outcome.
Provider support is essential to effectively employ the Dental Home program for Medicaid and
CHIP Dental Program Members. With assistance and support from dental professionals, a system
for improving the overall health of children in the Medicaid and CHIP Programs can be
achieved.
Main Dental Home assignment must be verified on the DentaQuest Provider Web Portal (located
in the “Providers Only” section of DentaQuest’s website at www.dentaquest.com. You may also
contact DentaQuest’s Customer Service Department at 1‐800‐896‐2374 to verify
Main Dental
Home assignment.
Role of First Dental Home Initiative for Medicaid Members
Medicaid Members from six (6) through 35 months of age may be seen for dental checkups by a
certified First Dental Home Initiative provider as frequently as every sixty (60) days if medically
necessary.
Providers must be certified to be a Texas Health Steps Dentist. To become a First Dental Home
Initiative Provider (Texas Health Steps), the dentist must complete the online module and submit
both the training certificate and the First Dental Home certification application form.
DentaQuest USA Insurance Company, Inc. February 1, 2024
Current Dental Terminology © American Dental Association. All Rights Reserved.
10
The Texas Health Steps online First Dental Home Module is available at
www.txhealthsteps.com.
Go to “Start a free course now” and choose “First Dental Home” from
the drop down menu.
For additional information regarding the Dental Home program, please connect to the
DentaQuest Provider Web Portal www.dentaquest.com under Related Documents – Dental
Home.
Only certified, participating First Dental Home Providers may bill a D0145 for a first dental home
oral evaluation. The member is only allowed one of D0120 or D0150 in a six month period.
D1330, D1206, and D1208 will be denied when billed on the same date of service as D0145.
Covered Services
Texas Health Steps Dental Services (Medicaid Only)
Texas Health Steps is the Texas version of the Medicaid program known as Early and Periodic
Screening, Diagnosis, and Treatment (EPSDT). Texas Health Steps dental services are mandated
by Medicaid to provide for the early detection and treatment of dental health problems for
Medicaid‐eligible members who are from birth through 20 years of age. Texas Health Steps
dental service standards are designed to meet federal regulations and incorporate the
recommendations of representatives of national and state dental professional organizations.
Texas Health Steps’ designated staff (Texas Department of State Health Services [DSHS],
Department of Assistive and Disability Services [DADS], or contractor), through outreach and
informing, encourage eligible children to use Texas Health Steps dental checkups and services
when children first become eligible for Medicaid, and each time children are periodically due for
their next dental checkup.
Please refer to the Texas Medicaid Provider Procedures Manual for more information regarding
Texas Health Steps dental services:
Go to www.tmhp.com. Click on “Providers” at the top of the screen, then “Reference Material”
on the left hand side.
Texas Health Steps Medical Checkup Periodicity Schedule for Infant, Children,
and Adolescents
DentaQuest USA Insurance Company, Inc. February 1, 2024
Current Dental Terminology © American Dental Association. All Rights Reserved.
11
DentaQuest USA Insurance Company
___
I
DentaQuest USA Insurance Company, Inc. February 1, 2024
Current Dental Terminology © American Dental Association. All Rights Reserved.
12
DentaQuest USA Insurance Company
___
Exception to Periodicity Oral Evaluation, Dental Checkup, and Emergency or
Trauma Related Services for Texas Health Steps Dental Procedures
Oral evaluations and dental checkups allow for the early diagnosis and treatment of dental
problems. They might be needed at more frequent intervals than noted in the periodicity
schedule.
If needed, a dental checkup or oral evaluation can still be reimbursed when the service falls
outside the periodicity schedule. The rules for such exceptions are outlined below.
Exception-to-Periodicity Oral Evaluation
A Texas Health Steps exception-to-periodicity oral evaluation is limited to
dental procedure code D0120.
An exception-to-periodicity oral evaluation is allowed when the service is:
• Medically necessary and based on risk factors and health needs for members birth
through 6 months of age.
• Mandated service required to meet federal or state exam requirements for Head Start,
daycare, foster care or preadoption.
DentaQuest USA Insurance Company, Inc. February 1, 2024
Current Dental Terminology © American Dental Association. All Rights Reserved.
13
DentaQuest USA Insurance Company
___
Providers must include all appropriate procedure codes on the dental claim submission form.
Providers would need to include a narrative and comment in box 35.
Exception-to-Periodicity Dental Checkup
A Texas Health Steps exception-to-periodicity dental checkup is allowed
when:
• The member will not be available for the next periodically due dental checkup. This
includes members whose parents are migrant or seasonal workers.
• For members whose parents are migrant or seasonal workers and need the accelerated
services, include “Exception” in block 35, “Remark” field.
Providers must include all appropriate procedure codes on the dental claim
submission form.
Exception-to-Periodicity Emergency or Trauma Related Oral Evaluation
A Texas Health Steps exception-to-periodicity emergency or trauma related oral evaluation is
limited to dental procedure code D0140.
Procedure code D0140 is limited to once per day for the same provider and twice per day for any
provider.
A Texas Health Steps exception-to-periodicity emergency or trauma related dental service will be
allowed when the service is:
• Required for immediate treatment and any follow-up treatment.
• Required for therapeutic services needed to complete a case for members, 5 months of
age and younger, when initiated as emergency services, trauma, or early childhood caries.
When submitting a claim for emergency or trauma related dental services, the provider must
include:
• “Trauma” or “Emergency” in Block 35, “Remark” field
• The original date of treatment or incident in Block 35, “Remark” field
Providers must include all appropriate procedure codes on the dental claim submission form.
Adjunctive General Services
When submitting a claim for an unclassified treatment procedure code D9110
the provider must include:
• “Trauma” or “Emergency” in Block 35, “Remark” field
• The original date of treatment or incident in Block 35, “Remark” field
Providers must include all appropriate procedure codes on the dental claim submission form.
Children of Migrant Farmworkers

DentaQuest USA Insurance Company, Inc. February 1, 2024
Current Dental Terminology © American Dental Association. All Rights Reserved.
14
DentaQuest USA Insurance Company
___
Children of Migrant Farm workers due for a Texas Health Steps medical checkup can receive
their
periodic checkup on an accelerated basis prior to leaving the area. A checkup performed under
this circumstance is an accelerated service but should be billed as a checkup.
Providers must include all appropriate procedure codes on the dental claim along with
“Exception” & “FWC or Farm Worker Child” in Block 35, “Remark” field.
Performing a make‐up exam for a late Texas Health Steps medical checkup previously missed
under the periodicity schedule is not considered an exception to periodicity nor an accelerated
service. It is considered a late checkup.
Children’s Medicaid Dental Covered Services
Texas Medicaid Dental Program benefits are subject to the same benefit limits and exclusions
that apply to Traditional Medicaid, but are not subject to the maximum fees imposed under
Traditional Medicaid. For a complete list of the limitations and exclusions that apply to each
Medicaid benefit category, refer to the current Texas Medicaid Provider Procedures Manual
(TMPPM), which can be accessed online at: http://www.tmhp.com For informational purposes
only, the maximum fees for Traditional Medicaid are located in the Texas Medicaid Fee
Schedule
in the TMPPM and online at http://public.tmhp.com/FeeSchedules/Default.aspx
The following is a non‐exhaustive, high‐level list of Covered Services in the Texas Medicaid
Dental Program. Covered Services are subject to modification based on changes in federal and
state laws, rules, regulations, and policies.
Texas Medicaid Dental Program Covered Services include the following Medically Necessary
services.
• Diagnostic and preventive
• Therapeutic
• Restorative
• Endodontic
• Periodontal
• Prosthodontic (removable and fixed)
• Implant and oral and maxillofacial surgery
• Orthodontic
• Adjunctive general
CHIP Dental Covered Services
Covered Dental Services are subject to a $564 annual benefit limit unless an exception applies. In
addition, some of the benefits identified in the schedule below are subject to annual limits.
Limitations are based on a 12‐month coverage period.
DentaQuest USA Insurance Company, Inc. February 1, 2024
Current Dental Terminology © American Dental Association. All Rights Reserved.
15
DentaQuest USA Insurance Company
___
CHIP Members who have exhausted the $564 annual benefit limit continue to receive the
following Covered Dental Services in excess of the $564 annual benefit maximum:
(1) The diagnostic and preventive services due under the 2009 American Academy of
Pediatric Dentistry periodicity schedule; and
(2) Other Medically Necessary Covered Dental Services approved by the Dental Contractor
through a prior authorization process. These services must be necessary to allow a CHIP
Member to return to normal, pain and infection‐free oral functioning. Typically, this
includes:
• Services related to the relief of significant pain or to eliminate acute infection;
• Services that allow the CHIP Member to attain the basic human functions (e.g., eating,
speech); and
• Services that prevent a condition from seriously jeopardizing the CHIP Member’s
health/functioning or deteriorating in an imminent timeframe to a more serious and
costly dental problem.
Texas CHIP Dental Program Covered Services include the following Medically Necessary
services.
• Diagnostic and preventive
• Therapeutic
• Restorative
• Endodontic
• Periodontal
• Prosthodontic
• Oral and maxillofacial surgery
Note: If a Member is undergoing a course of treatment, the Covered Services terminate on the
Date of Disenrollment.
Refer to the most recent version of the Code on Dental Procedures and Nomenclature for coding
that applies to Covered Dental Services.
C. Quality Management
Quality Improvement Program (Policies 200 Series)
DentaQuest currently administers a Quality Improvement Program modeled after National
Committee for Quality Assurance (NCQA) standards. The NCQA standards are adhered to as
practice guidelines to dental managed care. The Quality Improvement Program includes but is
not limited to:
• Provider credentialing and re‐credentialing.
DentaQuest USA Insurance Company, Inc. February 1, 2024
Current Dental Terminology © American Dental Association. All Rights Reserved.
16
DentaQuest USA Insurance Company
___
• Member satisfaction surveys.
• Provider satisfaction surveys.
• Random Chart Audits.
• Complaint Monitoring and Trending.
• Peer Review Process.
• Utilization Management and practice patterns.
• Initial Site Reviews and Dental Record Reviews.
• Quarterly Quality Indicator tracking (i.e. complaint rate, appointment waiting
time, access to care, etc.)
A copy of DentaQuest’s Quality Improvement Program is available upon request by contacting
DentaQuest’s Customer Service department at 1‐800‐896‐2374
Utilization Management Program
Introduction:
Reimbursement to dentists for dental treatment rendered can come from any number of sources
such as individuals, employers, insurance companies and local, state or federal
government. The
source of dollars varies depending on the particular program. For example,
in traditional
insurance, the dentist reimbursement is composed of an insurance payment and a patient
coinsurance payment. In State Medical Assistance Dental Programs (Medicaid), the
State
Legislature annually appropriates or “budgets” the amount of dollars available for
reimbursement to the dentists as well as the fees for each procedure. Since there is usually no
patient co‐payment, these dollars represent all the reimbursement available to the dentist.
These “budgeted” dollars, being limited in nature, make the fair and appropriate distribution to
the dentists of crucial importance.
Community Practice Patterns:
DentaQuest has developed a philosophy of Utilization Management that recognizes the fact
that
there exists, as in all healthcare services, a relationship between the dentist’s treatment
planning, treatment costs and treatment outcomes. The dynamics of these relationships, in any
region, are reflected by the “community practice patterns” of local dentists and their peers.
With
this in mind, DentaQuest’s Utilization Management Programs are designed to ensure the
fair and
appropriate distribution of healthcare dollars as defined by the regionally based community
practice patterns of local dentists and their peers.
All utilization management analysis, evaluations and outcomes are related to these patterns.
DentaQuest’s Utilization Management Programs recognize that there exists a normal individual
dentist variance within these patterns among a community of dentists and accounts for such
variance. Also, specialty dentists are evaluated as a separate group and not with general
dentists
since the types and nature of treatment may differ.
DentaQuest USA Insurance Company, Inc. February 1, 2024
Current Dental Terminology © American Dental Association. All Rights Reserved.
17
DentaQuest USA Insurance Company
___
Evaluation:
DentaQuest’s Utilization Management Programs evaluate claims submissions in such areas as:
• Diagnostic and preventive treatment.
• Patient treatment planning and sequencing.
• Types of treatment.
• Treatment outcomes.
• Treatment cost effectiveness.
Results:
With the objective of ensuring the fair and appropriate distribution of these budgeted Medicaid
Dental Program dollars to dentists, DentaQuest’s Utilization Management Programs will help
identify those dentists whose patterns show significant deviation from the normal practice
patterns of the community of their peer dentists (typically less than 5% of all dentists). When
presented with such information, dentists will implement slight modification of their diagnosis
and treatment processes that bring their practices back within the normal range. However, in
some isolated instances, it may be necessary to recover reimbursement.
Network Management Program
DentaQuest maintains a program of ongoing monitoring efforts, specific quality and claim
reviews, and other network management initiatives to ensure that its professional service
providers deliver appropriate services within the standard of care and adhere to appropriate cost
and efficiency standards as developed through applicable laws, regulations, contracts, policies,
and procedures. DentaQuest evaluates, among other items, quality, cost, efficiency standards,
claims data, and provider behavioral patterns.
NETWORK MANAGEMENT PROCEDURES
The Network Management Team, Peer Review Committee, Credentialing Committee, Utilization
Oversight Program (UOP), Fraud, Prevention and Recovery team, or other DentaQuest staff may
use DentaQuest’ s data to identify those providers that may be candidates for one or more
network management actions. Each provider may be reviewed further, as appropriate, to
evaluate the quality of care and claim history of that provider.
1. DentaQuest may conduct monitoring, targeted reviews, educational sessions or invoke other
network management initiatives as described in more detail below, including without
limitation, intermediate sanctions or terminations upon determining, in its sole discretion,
that one or more of the following has occurred:
a. Failure to maintain a safe environment for Members and/or DentaQuest provider
representatives
DentaQuest USA Insurance Company, Inc. February 1, 2024
Current Dental Terminology © American Dental Association. All Rights Reserved.
18
DentaQuest USA Insurance Company
___
b. Harassment, discrimination, abuse, inappropriate or unprofessional conduct of or
against a member or a DentaQuest staff member or employee
c. Dental board actions, indictment, or misdemeanor complaint related to the practice
of dentistry
d. More than three (3) substantiated member complaints or grievances within a one-
year period
e. Initiation of one or more clinical audits conducted by Fraud, Prevention and Recovery
that results in Fraud, Waste or Abuse (FWA) findings
f. Referral of the provider to Fraud Prevention and Recovery for a full clinical review
that results in FWA findings
g. Failure to behavior modify after receiving a UOP letter from Fraud Prevention and
Recovery
h. Failure to behavior modify after investigation by Fraud Prevention and Recovery
i. More than three (3) alerts issued to provider under DentaQuest’s UOP within a six-
month period
j. Provision of services by any provider that are determined by DentaQuest in its sole
discretion to be excessive, unnecessary, contraindicated, or indicative of prior failed
services
k. Failure to satisfy established pay for quality (P4Q) metrics
l. More than seventy percent (70%) percent of claims for the same or similar service
denied or adjusted downward within a six-month period
m. Multiple submissions of authorization requests for the same service, same provider or
location on the same day
n. Multiple submissions of authorization requests for the same service, same provider,
same location without providing new supporting information
o. Failure to submit appropriate documentation with authorization requests after being
informed by DentaQuest of the supporting documentation requirements
p. Conviction of any crime of moral turpitude, with conviction defined in accordance
with 42 C.F.R. § 455.2
q. Occurrence of any event set forth in 42 C.F.R. Part 1001, Subparts B or C
r. Noncompliance with terms of the Dental Provider Service Agreement
DentaQuest USA Insurance Company, Inc. February 1, 2024
Current Dental Terminology © American Dental Association. All Rights Reserved.
19
DentaQuest USA Insurance Company
___
s. Noncompliance with terms of the Office Reference Manual (ORM)
2. DentaQuest will initiate mandatory educational sessions upon determining that any of the
events identified in Section 1(j) through 1(o) has occurred and may, in its sole discretion,
offer the provider an opportunity to cure before imposing further intermediate sanctions.
3. Upon determining that any of the events in Section 1 have occurred, DentaQuest, in its sole
and absolute discretion may take any one or more of the following network management
actions:
a. Adjust or recoup future payments to correct overpayments
b. Require refunds to correct overpayments
c. Require a Corrective Action Plan
d. Invoke targeted prior authorizations
e. Invoke utilization oversight periods
f. Require mandatory training or education
g. Place restrictions on network participation
h. Place restrictions or suspensions of Member assignments to dental home
i. Require advanced monitoring by DentaQuest
j. Require the use of an independent auditor at the provider’s expense
k. Suspension or Termination from a DentaQuest network
4. DentaQuest’s determination to initiate corrective action, intermediate sanctions or any
network management initiative is within its sole discretion. A determination not to invoke
network management initiatives or corrective action after an event or violation described in
Section 1 is not and should not be construed as a waiver of DentaQuest’s rights or remedies.
DentaQuest retains its right to employ network management initiatives and impose
corrective actions at any time.
D. Provider Responsibilities
General Responsibilities
DentaQuest USA Insurance Company, Inc. February 1, 2024
Current Dental Terminology © American Dental Association. All Rights Reserved.
20
DentaQuest USA Insurance Company
___
Availability and Accessibility
Each participating DentaQuest office is required to maintain and document a formal system for
patient recall. The system can utilize either written or phone contact. Any system should
encompass routine patient check‐ups, cleaning appointments, follow‐up treatment
appointments, and missed appointments for any health plan Member that has sought dental
treatment.
If a written process is utilized, the following language is suggested for missed appointments:
• “We missed you when you did not come for your dental appointment on month/date.
Regular check‐ups are needed to keep your teeth healthy.”
• “Please call to reschedule another appointment. Call us ahead of time if you cannot keep
the appointment. Missed appointments are very costly to us. Thank you for your help.”
Dental offices indicate that Medicaid Members sometimes fail to show up for appointments.
DentaQuest offers the following suggestions to decrease the “no show” rate.
• Contact the Member by phone or postcard prior to the appointment to remind the
individual of the time and place of the appointment.
• If the appointment is made through a government supported screening program,
contact
staff from these programs to ensure that scheduled appointments are kept.
Members should have the ability to receive direction from their provider on how to obtain
emergency services 24 hours a day, 7 days per week, including holidays and vacations.
Emergency appointments should be scheduled within 24 hours. The patient should be informed
that only the emergent condition will be treated at that time.
Members should not wait for more than fifteen (15) to thirty (30) minutes beyond their
appointment time to begin their dental care. If the wait time goes beyond this period, an
explanation for the delay should be given to the Member and/or Member’s representative,
with
the option to reschedule the appointment.
Main Dental Home Responsibilities
Texas defines a Main Dental Home as the dental provider who supports an ongoing relationship
with the member that includes all aspects of oral health care delivered in a comprehensive,
continuously accessible, coordinated, and family‐centered way. Establishment of a member’s
Main Dental Home, begins no later than 6 months of age and includes referrals to dental
specialists when appropriate.
The Dental Contractor must develop a network of Main Dental Home Providers, consisting of
Federally Qualified Health Centers and individuals who are general dentists and pediatric
dentists, who will provide preventative care and refer Members for specialty care as needed.
In accordance with standards of practice and policy guidelines set forth by the American
DentaQuest USA Insurance Company, Inc. February 1, 2024
Current Dental Terminology © American Dental Association. All Rights Reserved.
21
DentaQuest USA Insurance Company
___
Academy of Pediatric Dentistry, Main Dental Home Providers must perform a caries risk
assessment as part of the comprehensive oral examination. Main Dental Home Providers must
bill one of the following caries risk assessment codes: D0601, D0602, or D0603 with every
comprehensive oral examination (D0150), oral examination for a patient under 3 years of age
(D0145), or periodic dental evaluation (D0120). These risk codes will be included as part of an
informational component of the D0150, D0145 or D0120 billing code and do not have a separate
rate attached to them. Claim will reject when any of the following codes D0150, D0145 or D0120
are submitted without a caries risk assessment code. Providers will be given the standard 120-
day appeal period for the denied claim to submit proof of performing a caries risk assessment.
The TMPPM and the MMC‐CHIP Dental Provider Manual is effective with this change as of
October 1, 2015.
First Dental Home Initiative Responsibilities
In addition to establishing a Network of Main Dental Home Providers, the Dental Contractor
must implement a “First Dental Home Initiative” for Medicaid Members. This initiative will
enhance dental providers’ ability to assist Members and their primary caregivers in obtaining
optimum oral health care through First Dental Home visits. The First Dental Home visit can be
initiated as early as 6 months of age and must include the following:
• Comprehensive oral examination;
• Oral hygiene instruction with primary caregiver;
• Dental prophylaxis, if appropriate;
• Topical fluoride varnish application when teeth are present;
• Caries risk assessment; and
• Dental anticipatory guidance as defined in the Texas Medicaid Provider Procedures
Manual (TMPPM), Volume 2, Children's Services Handbook and requires documentation
of the specific information conveyed to the parent/guardian for at least 3 of the 8
anticipatory guidance topics found in the handbook.
Medicaid Members from 6 through 35 months of age may be seen for dental checkups by a
certified First Dental Home Initiative provider as frequently as every sixty (60) days if Medically
Necessary.
Only certified, participating First Dental Home Providers may bill a D0145 for a first dental home
oral evaluation. The member is only allowed one of D0120 or D0150 in a six month period.
D1330, D1206, and D1208 will be denied when billed on the same date of service as D0145.
Providers must be certified to be a Texas Health Steps Dentist. If you are a dentist and wish to be
certified to bill Medicaid for First Dental Home Services, you must complete the following
requirements:
• Complete this First Dental Home training and download the Continuing Education (CE)
certificate.

DentaQuest USA Insurance Company, Inc. February 1, 2024
Current Dental Terminology © American Dental Association. All Rights Reserved.
22
DentaQuest USA Insurance Company
___
• Submit a First Dental Home Certification Application, Form 1091 (fillable PDF) to be
certified as a First Dental Home provider.
The completed application form and CE certificate should be emailed to:
Alternatively, the completed form and CE certificate can be faxed to 512-483-3979.
Updates to Contact Information
DentaQuest publishes a provider directory to Members. The directory is updated periodically and
includes: provider name, practice name (if applicable), office addresses(s), telephone number(s),
provider specialty, panel status (for example, providers limiting their practice to existing
Members only), office hours, and any other panel limitations that DentaQuest is aware
of, such
as patient age minimum and maximum, etc. The online provider directory reflects the
most
current information.
It is very important that you notify DentaQuest of any change in your practice information.
Please complete the Provider Change Form, fax it to DentaQuest at 262.241.4077 or call us at
1‐800‐896‐2374 to report any changes. Please also contact TMHP to update your Medicaid
enrollment profile.
Plan Termination
Provider shall render to Members all Covered Services and continue to provide Covered
Services
to Members. After the date of termination from participation, upon the request of DentaQuest,
Provider shall continue to provide Covered Services to Members for a period not to exceed
ninety (90) days during which time payment will be made pursuant to the
DentaQuest Provider
Contract.
Please refer to the DentaQuest TX Provider Contract for more information regarding
termination.
Referral to Specialists Process
Referrals to Specialists
Main Dental Home Providers must assess the dental needs of Members for referral
to specialty care providers and provide referrals as needed. Main Dental Home
Providers must coordinate Member’s care with specialty care providers after
referral.
Routine preventative care referrals must be provided within 30 days of request.
Texas Medicaid and CHIP Dental Services Members do not require authorization to
see a dental specialist. However, only services provided by a Contracting Dentist are
covered by DentaQuest, therefore a Texas Medicaid or CHIP Dental Services
DentaQuest USA Insurance Company, Inc. February 1, 2024
Current Dental Terminology © American Dental Association. All Rights Reserved.
23
DentaQuest USA Insurance Company
___
Member must be treated by a dentist enrolled in the Texas Medicaid or
CHIP Dental
Services. In the event it is necessary to refer a Member to a specialist for treatment,
please be sure to refer the Member to a contracted
Texas Medicaid or CHIP Dental
Services dentist. You may look at the DentaQuest website to locate a dental
specialist in the area.
Members with Special Health Care Needs may have direct access to Specialists as
appropriate for the Member’s condition and identified needs.
If you cannot locate a specialist in your area, you may call DentaQuest’s Provider
Call Center’s toll‐free telephone number at 1‐800‐896‐2374 to facilitate a Member
referral to a Specialist.
Referrals from a Main Dentist to General Dentist/Pedodontist for Interim Care Also
known as the “Texas Interim Care Transfer (ICT) Process”
This process is to be utilized when a Main Dentist Dental Home Provider (Main
Dentist) determines that it is necessary for another Main Dentist (general or
pediatric dentist) to provide interim care to a Member; yet the Main Dentist
assignment should be maintained. The Interim Care Transfer Form will need to be
filled out only if other Main Dentist is at a location different than Main Dentist
Dental Home Provider.
A. Main Dentist identifies the need for interim care for a Member.
B. Main Dentist completes the Interim Care Transfer Form (which is available
via the web portal and in A‐23) with the interim Transfer Provider’s (general
or pediatric dentist) information and the need for the Member to have
services rendered outside the Main Dental Home. Transfer Provider must be
in network for claims to be paid.
C. Main Dentist completes the Interim Care Transfer on the portal
(provideraccess.dentaquest.com).
D. The approval is valid for 270 days. Both Main Dental Home Provider and
Transfer Provider may review the status of the submitted Interim Care
Transfer on the portal.
E. Transfer Provider renders services within 270 days (otherwise an extension is
required) and submits claim.
F. DentaQuest processes the claim and pays the Transfer Provider.
G. As the Main Dentist, any follow‐up and coordination of care is the
responsibility of the Main Dentist initiating the Interim Care Transfer.
Verify Member Eligibility and/or Authorizations for Service
Member Eligibility
Participating Providers may access Member eligibility information through DentaQuest’s
DentaQuest USA Insurance Company, Inc. February 1, 2024
Current Dental Terminology © American Dental Association. All Rights Reserved.
24
DentaQuest USA Insurance Company
___
Interactive Voice Response (IVR) system or through the Provider Web Portal (located in the
“Providers Only” section of DentaQuest’s website at www.dentaquest.com.) The eligibility
information received from either system will be the same information you would receive by
calling DentaQuest’s Customer Service department; however, by utilizing either system you can
get information 24 hours a day, 7 days a week without having to wait for an available Customer
Service Representative. A provider must verify Member eligibility and/or authorizations for
service.
If you are having difficulty accessing either the IVR or the Provider Web Portal, please contact
the
Customer Service department at 1‐800‐896‐2374. They will be able to assist you in utilizing
either system.
Access to eligibility information via the Provider Web Portal
DentaQuest’s Provider Web Portal currently allows Providers to verify a Member’s eligibility as
well as submit claims directly to DentaQuest. You can verify the Member’s eligibility on‐line by
entering the Member’s date of birth, the date of service and the Member’s identification number
or last name and first initial. To access the eligibility information via DentaQuest’s
website,
simply log on to the website at www.dentaquest.com. Once you have entered the
website, click
on “Dentist”. From there choose your ‘State” and press go. You will then be able to log in using
your password and ID. First time users will have to register by utilizing TIN and State. If you have
not received instruction on how to complete Provider Self Registration, you can access the guide
at http://www.dentaquest.com/getattachment/State-Plans/Regions/texas/Dentists-Page/New-
Provider-Registration-Tip-Sheet.pdf. If you need further assistance, please contact DentaQuest’s
Customer Service Department at 1‐800‐896‐2374.
Once logged in, select patient from the portal menus then choose Member eligibility search.
You
are able to check on an unlimited number of Members and can print off the summary of
eligibility given by the system for your records. Be sure to verify eligibility on the date of service.
Directions for using DentaQuest’s IVR to verify eligibility:
Entering system with Tax and Location ID’s
1. Call DentaQuest Customer Service at 1-800-896-2374.
2. After the greeting, stay on the line for English or press 1 for Spanish.
3. Enter or state your NPI number.
4. Enter or state your last 4 digits of your Tax ID.
5. The system will read back the NPI entered. If correct, press (1); if it needs to be re-entered, press (2).
6. Enter Member ID – contains only numbers, press (1) or say “number”; contains numbers and letters,
press (2) or say “letter”.
7. Enter Member DOB.
8. The system will read back the DOB entered. If correct, press (1); if it needs to be re-entered, press (2).
9. Multiple options will be given –press the option number that corresponds to the reason for the call.
10. Upon system verification of the Member’s eligibility, you will be prompted to repeat the information
given, verify the eligibility of another Member, get benefit in formation, get limited claim history on this
Member, or get fax confirmation of this call.
11. If you choose to verify the eligibility of an additional Member(s), you will be asked to repeat step 5
above for each Member.
DentaQuest USA Insurance Company, Inc. February 1, 2024
Current Dental Terminology © American Dental Association. All Rights Reserved.
25
DentaQuest USA Insurance Company
___
Access to eligibility information via the IVR line
To access the IVR, simply call DentaQuest’s Customer Service department at 1‐800‐896‐2374
and
press 2 for eligibility. The IVR system will be able to answer all of your eligibility questions for as
many Members as you wish to check. Once you have completed your eligibility checks,
you will
have the option to check benefit history and/or transfer to a Customer Service
Representative to
answer any additional questions. Using your telephone keypad, you can request eligibility
information on a Medicaid or CHIP Member by entering the Member’s
recipient identification
number and a date of service. If the system is unable to verify the
Member information you
entered, you will be transferred to a Customer Service
Representative.
If eligibility is verified, the dentist may not treat the Member as a private‐pay patient to avoid
Texas Medicaid or CHIP Dental Services billing, obtaining prior authorization (when necessary)
or
complying with any other program requirement. In addition, upon obtaining eligibility
verification, the dentist cannot bill the Texas Medicaid Dental Services Member for any covered
service.
Once eligibility verification has been established, a dentist can decline to treat a Member only
under the following circumstances:
• The dentist is unable to provide the particular service(s) that the Member requires.
• The Member is not eligible for dental services.
• The Member is unable to present satisfactory identification.
A dentist who declines to accept a Member must do so before accessing eligibility information
except in the above circumstances. If the dentist is unwilling to accept an individual as a patient,
the dentist has no authority to access the individual’s confidential eligibility
information.
Please note that due to possible eligibility status changes, the information provided by either
system does not guarantee payment. Eligibility is determined by HHSC or its designee(s). The
eligibility information provided by DentaQuest to contracting offices reflects the eligibility
information received. The Medicaid Member will be covered until his/her name no longer
appears on the eligibility information provided to DentaQuest. Therefore, it is vital that
providers verify eligibility before initiating treatment to a patient.
Authorizations of Service
Authorizations are utilization tools that require Participating Providers to submit
“documentation” associated with certain dental services for a Member. Participating Providers
will not be paid if this “documentation” is not provided to DentaQuest. Participating Providers
must hold the Member, DentaQuest, and HHSC harmless as set forth in the Provider
Participation Agreement if coverage is denied for failure to submit documentation for review
after the service is rendered. Authorization can be made through prior approval or by
prepayment review. Approved authorizations expire after 180 days and Orthodontic
authorizations expire after 3 years. Prior authorization is optional for all covered procedures with
the
exception of all Orthodontic codes (see Review Requirements identified in Exhibits A and B).
Non-urgent specialty care should be provided within 60 Days of authorization.
DentaQuest USA Insurance Company, Inc. February 1, 2024
Current Dental Terminology © American Dental Association. All Rights Reserved.
26
DentaQuest USA Insurance Company
___
Providers must note that "PA Not Required" is not equivalent to "Medically Necessary". It is not
to be assumed that payment will be dispensed for a service that does not require Prior
Authorization. Approval of prior authorization does not guarantee payment. The service will still
be subject to retrospective review to confirm medical necessity.
DentaQuest utilizes specific dental utilization criteria as well as an authorization process to
manage utilization of services. DentaQuest’s operational focus is to assure compliance with its
utilization criteria. The criteria are included in this manual. Please review these criteria as well as
the benefits covered (Exhibit A and B) to understand the decision making process used to
determine payment for services rendered.
A. Prior Authorization‐ Dental services or treatment locations that require review
by DentaQuest for determination of medical necessity and approval before
delivery are subject to prior authorization. Proper documentation must be
submitted with requests for prior authorization.
B. Pre‐Payment Review‐ Dental procedures that require review by DentaQuest
for determination of medical necessity prior to reimbursement for the
procedures. These procedures can be administered before determination of
medical necessity is rendered but require submission of proper documentation
for approval to process the claim.
Your submission of “documentation” should include:
1) Radiographs, narrative, or other information where requested (see
Exhibits A and B for specifics by code).
2) CDT codes on the ADA claim form.
Your submission should be sent on a 2018, 2019, or later ADA approved claim form. The tables of
Covered Services (Exhibits A and B) contain a column marked “Review Required.” A “Yes” in this
column indicates that the service listed requires that documentation be submitted with the
claim
for pre‐payment review in order to be considered for reimbursement. The “Documentation
Required” column will describe what information is necessary for pre‐payment
review.
Submitting Authorization or Claims with X‐Rays
• Electronic submission using the web portal
• Electronic submission using National Electronic Attachment (NEA) is recommended.
For more information, please visit www.nea‐fast.com and click the “Learn More”
button. To register, click the “Provider Registration” button in the middle of the home
page.
• Submission of duplicate radiographs (which we will recycle and not return)
• Submission of original radiographs with a self‐addressed stamped envelope (SASE) so
that we may return the original radiographs. Note that determinations will be sent
separately and any radiographs received without a SASE will not be returned to the
sender.

DentaQuest USA Insurance Company, Inc. February 1, 2024
Current Dental Terminology © American Dental Association. All Rights Reserved.
27
DentaQuest USA Insurance Company
___
Please note we also require radiographs be mounted when there are 4 or more radiographs
submitted at one time. If four (4) or more radiographs are submitted and not mounted, they
will
be returned to you and your request for prior authorization and/or claims will not be
processed.
You will need to resubmit a copy of the 2018, 2019, or newer ADA form that was originally
submitted, along with mounted radiographs so that we may process the claim correctly.
Acceptable methods of mounted radiographs are:
• Radiographs duplicated and displayed in proper order on a piece of duplicating
film.
• Radiographs mounted in a radiograph holder or mount designed for this
purpose.
Unacceptable methods of mounted radiographs are:
• Cut out radiographs taped or stapled together.
• Cut out radiographs placed in a coin envelope.
• Multiple radiographs placed in the same slot of a radiograph holder or
mount.
All radiographs, must be of good diagnostic quality, include member’s full name, date films
taken, and identify the patients left and right side
It is important not to submit original x‐rays especially if they are the only diagnostic record for
your patient. Duplicate films and x‐ray copies of diagnostic quality, including paper copies of
digitized images are acceptable. DentaQuest does not generally return x‐rays and other
supporting documentation. However, if you wish to have your x‐rays returned, they must be
submitted with a self‐addressed stamped envelope.
Electronic Attachments
FastAttach™ DentaQuest accepts dental radiographs electronically via FastAttach™ for
authorization requests and claims submissions. DentaQuest, in conjunction with National
Electronic Attachment, Inc. (NEA), allows Enrolled Participating Providers the opportunity to
submit all claims electronically, even those that require attachments. This program allows
transmissions via secure Internet lines for radiographs, periodontic charts, intraoral pictures,
narratives and EOBs.
FastAttach™ is inexpensive and easy to use, reduces administrative costs, eliminates lost or
damaged attachments and accelerates claims and prior authorization processing. It is compatible
with most claims clearinghouses or practice management systems.
For more information or to sign up for FastAttach go to https://fastattachweb.nea-fast.com/ or

DentaQuest USA Insurance Company, Inc. February 1, 2024
Current Dental Terminology © American Dental Association. All Rights Reserved.
28
DentaQuest USA Insurance Company
___
call NEA at
1‐800‐782‐5150.
OrthoCAD™ DentaQuest accepts orthodontic models electronically via OrthoCAD™ for
authorization requests. Submissions using OrthoCAD™ also require the submission of the form
found on page B‐5. DentaQuest allows Enrolled Participating Providers the opportunity to submit
all orthodontic models electronically. This program allows transmissions via secure
Internet lines
for orthodontic models. OrthoCAD™ is inexpensive and easy to use, reduces
administrative costs,
eliminates lost or damaged models and accelerates claims and prior authorization processing. It
is compatible with most claims clearinghouse or practice
management systems.
For more information or to sign up for OrthoCAD™ go to www.cadentinc.com or call OrthoCAD™
at 1‐800‐577‐8767.
Continuity of Care
Subject to compliance with applicable federal and state laws and professional standards
regarding the confidentiality of dental records, participating dentists must assist DentaQuest in
achieving continuity of care for Texas Medicaid and CHIP Dental Services Members through the
maximum sharing of Members’ dental records. Within thirty (30) days of a written request by a
Texas Medicaid or CHIP Dental Services Member, you must be able to provide copies of the
patient’s dental records to any other dentist treating such Member.
Texas Medicaid and CHIP Dental Services Members are not subject to limitations or exclusions of
covered dental benefits due to a pre‐existing condition.
Dental Records
Organization
1. The record must have areas for documentation of the following information:
a. Registration data including a complete health history.
b. Medical alert predominantly displayed inside chart jacket.
c. Initial examination data.
d. Radiographs.
e. Periodontal and Occlusal status.
f. Treatment plan/Alternative treatment plan.
g. Progress notes to include diagnosis, preventive services, treatment
rendered, and medical/dental consultations.
h. Miscellaneous items (correspondence, referrals, and clinical laboratory
reports).
2. The design of the record must provide the capability or periodic update, without
DentaQuest USA Insurance Company, Inc. February 1, 2024
Current Dental Terminology © American Dental Association. All Rights Reserved.
29
DentaQuest USA Insurance Company
___
the loss of documentation of the previous status, of the following information.
a. Health history.
b. Medical alert.
c. Examination/Recall data.
d. Periodontal status.
e. Treatment plan.
3. The design of the record must ensure that all permanent components of the
record are attached or secured within the record.
4. The design of the record must ensure that all components must be readily
identified to the patient, (i.e., patient name, and identification number on each
page).
5. The organization of the record system must require that individual records be
assigned to each patient.
Content ‐ The patient record must contain the following:
1. Adequate documentation of registration information which requires entry of
these items:
a. Patient’s first and last name.
b. Date of birth.
c. Sex.
d. Address.
e. Telephone number.
f. Name and telephone number of the person to contact in case of
emergency.
2. Adequate health history that requires documentation of these items:
a. Current medical treatment.
b. Significant past illnesses.
c. Current medications.
d. Drug allergies.
e. Hematologic disorders.
f. Cardiovascular disorders.
g. Respiratory disorders.
h. Endocrine disorders.
i. Communicable diseases.
j. Neurologic disorders.
DentaQuest USA Insurance Company, Inc. February 1, 2024
Current Dental Terminology © American Dental Association. All Rights Reserved.
30
DentaQuest USA Insurance Company
___
k. Signature and date by patient.
l. Signature and date by reviewing dentist.
m. History of alcohol and/or tobacco usage including smokeless tobacco.
3. Adequate update of health history at subsequent recall examinations which
requires documentation of these items:
a. Significant changes in health status.
b. Current medical treatment.
c. Current medications.
d. Dental problems/concerns.
e. Signature and date by reviewing dentist.
4. A conspicuously placed medical alert inside the chart jacket that documents highly
significant terms from health history. These items are:
a. Health problems which contraindicate certain types of dental treatment.
b. Health problems that require precautions or pre‐medication prior to
dental treatment.
c. Current medications that may contraindicate the use of certain types of
drugs or dental treatment.
d. Drug sensitivities.
e. Infectious diseases that may endanger personnel or other Members.
5. Adequate documentation of the initial clinical examination which is dated and
requires descriptions of findings in these items:
a. Blood pressure. (Recommended)
b. Head/neck examination.
c. Soft tissue examination.
d. Periodontal assessment.
e. Occlusal classification.
f. Dentition charting.
6. Adequate documentation of the patient’s status at subsequent Periodic/Recall
examinations which is dated and requires descriptions of changes/new findings in
these items:
a. Blood pressure. (Recommended)
b. Head/neck examination.
c. Soft tissue examination.
d. Periodontal assessment.
DentaQuest USA Insurance Company, Inc. February 1, 2024
Current Dental Terminology © American Dental Association. All Rights Reserved.
31
DentaQuest USA Insurance Company
___
e. Dentition charting.
7. Radiographs which are:
a. Identified by patient name.
b. Dated.
c. Designated by patient’s left and right side.
d. Mounted (if intraoral films).
8. Indication of the patient’s clinical problems/diagnosis.
9. Adequate documentation of the treatment plan (including any alternate
treatment options) that specifically describes all the services planned for the
patient by entry of these items:
a. Procedure.
b. Localization (area of mouth, tooth number, surface).
10. Adequate documentation of the periodontal status, if necessary, which is dated
and requires charting of the location and severity of these items:
a. Periodontal pocket depth.
b. Furcation involvement.
c. Mobility.
d. Recession.
e. Adequacy of attached gingiva.
f. Missing teeth.
11. Adequate documentation of the patient’s oral hygiene status and preventive
efforts which requires entry of these items:
a. Gingival status.
b. Amount of plaque.
c. Amount of calculus.
d. Education provided to the patient.
e. Patient receptiveness/compliance.
f. Recall interval.
g. Date.
12. Adequate documentation of medical and dental consultations within and outside
the practice which requires entry of these items:
a. Provider to whom consultation is directed.
b. Information/services requested.
DentaQuest USA Insurance Company, Inc. February 1, 2024
Current Dental Terminology © American Dental Association. All Rights Reserved.
32
DentaQuest USA Insurance Company
___
c. Consultant’s response.
13. Adequate documentation of treatment rendered which requires entry of these
items:
a. Date of service/procedure.
b. Description of service, procedure and observation. Documentation in
treatment record must contain documentation to support the level of
American Dental Association Current Dental Terminology code billed as
detailed in the nomenclature and descriptors. Documentation must be
written on a tooth by tooth basis for a per tooth code, on a quadrant basis
for a quadrant code, and on a per arch basis for an arch code.
c. Type and dosage of anesthetics and medications given or prescribed.
d. Localization of procedure/observation. (tooth #, surface, quadrant etc.)
e. Signature of the Provider who rendered the service.
14. Adequate documentation of the specialty care performed by another dentist that
includes:
a. Patient examination.
b. Treatment plan.
c. Treatment status.
Compliance
1. The patient record has one explicitly defined format that is currently in use.
2. There is consistent use of each component of the patient record by all staff.
3. The components of the record that are required for complete documentation of
each patient’s status and care are present.
4. Entries in the records are legible.
5. Entries of symbols and abbreviations in the records are uniform, easily interpreted
and are commonly understood in the practice.
Health Insurance Portability and Accountability Act (HIPAA)
As a healthcare provider, your office is required to comply with all aspects of the HIPAA
regulations that have gone/will go into effect as indicated in the final publications of the various
rules covered by HIPAA.
DentaQuest has implemented various operational policies and procedures to ensure that it is
compliant with the Privacy Standards as well. DentaQuest also intends to comply with all
Administrative Simplification and Security Standards by their compliance dates. One aspect of
our compliance plan will be working cooperatively with our providers to comply with the HIPAA
regulations. In relation to the Privacy Standards, DentaQuest has/will be modifying its provider
contracts to reflect the appropriate HIPAA compliance language. The contractual updates include
DentaQuest USA Insurance Company, Inc. February 1, 2024
Current Dental Terminology © American Dental Association. All Rights Reserved.
33
DentaQuest USA Insurance Company
___
the following in regard to record handling and HIPAA requirements:
• Maintenance of adequate dental/medical, financial and administrative records
related
to covered dental services rendered by Provider in accordance with federal
and state
law.
• Safeguarding of all information about Members according to applicable state and
federal laws and regulations. All material and information, in particular information
relating to Members or potential Members, which is provided to or obtained by or
through a Provider, whether verbal, written, tape, or otherwise, shall be reported as
confidential information to the extent confidential treatment is provided under state
and federal laws.
• Neither DentaQuest nor Provider shall share confidential information with a
Member’s employer absent the Member’s consent for such disclosure.
• Provider agrees to comply with the requirements of the Health Insurance Portability
and Accountability Act (“HIPAA”) relating to the exchange of information and shall
cooperate with DentaQuest in its efforts to ensure compliance with the privacy
regulations promulgated under HIPAA and other related privacy laws.
Provider and DentaQuest agree to conduct their respective activities in accordance with the
applicable provisions of HIPAA and such implementing regulations.
In relation to the Administrative Simplification Standards, you will note that the benefit tables
included in this ORM reflect the most current coding standards (CDT 2009‐2010) recognized by
the ADA. Effective the date of this manual, DentaQuest will require providers to submit all claims
with the proper CDT 2009‐2010 codes listed in this manual. In addition, all paper claims
must be
submitted on a 2018, 2019, or later approved ADA claim form.
Note: Copies of DentaQuest’s HIPAA policies are available upon request by contacting
DentaQuest’s Customer Service department at 1‐800‐896‐2374
Access to Second Opinion
DentaQuest may request a clinical evaluation by a regional dental consultant who conducts
clinical examinations, prepares objective reports of dental conditions and evaluates treatment
that is proposed or has been provided for the purpose of providing DentaQuest with a second
opinion.
A second opinion may be required prior to treatment when necessary to make a benefit
determination. Authorization for second opinions after treatment can be made if a Member has
a complaint regarding the quality of care provided. The Member and the treating dentist will be
notified when a second opinion is necessary and appropriate. When a second opinion is
authorized through a regional dental consultant, all charges will be paid by DentaQuest.
Members may otherwise obtain a second opinion about treatment from any contracting dentist
they choose, and claims for the examination or consultation may be submitted for payment.
DentaQuest USA Insurance Company, Inc. February 1, 2024
Current Dental Terminology © American Dental Association. All Rights Reserved.
34
DentaQuest USA Insurance Company
___
Such claims will be paid in accordance with the benefits of the program.
Justification Regarding Out‐of‐Network Referrals
Out of network referrals are covered only if:
• The service is medically necessary and the covered service is not available through an in‐
network provider.
• The existing (in‐network) provider requests that the work be done by an OON provider
(referral).
• Reimbursement for Medicaid OON providers is 95% of the fee‐for‐service rate in effect
on the date‐of‐service unless a different reimbursement amount is agreed upon.
Please contact Provider Services for assistance in locating an in‐network provider.
Informed Consent for Utilization of Papoose Boards
Written and informed consent from a legal guardian must be obtained and documented in the
patient record prior to protective stabilization. The patient’s record must include:
• Informed consent (should occur on a day separate from the treatment, if possible)
• Type of stabilization used
• Indication for stabilization
• Behavior during stabilization
• Any untoward outcomes, i.e. skin markings
• The duration of the application
Indications*
• A previously cooperative patient quickly becomes uncooperative during the
appointment
in order to protect the patient’s safety and expedite completion of the
treatment
Contradictions**
• Patient’s with a history of psychological trauma due to restraint (unless no other
alternatives are available)
A parent has the right to terminate restraint at any time. If termination is requested, the
practitioner should complete the necessary steps to bring the procedure to a safe conclusion
before ending the appointment.
Goals of Behavior Management
• Establish communication.
• Alleviate fear and anxiety.
DentaQuest USA Insurance Company, Inc. February 1, 2024
Current Dental Terminology © American Dental Association. All Rights Reserved.
35
DentaQuest USA Insurance Company
___
• Deliver quality dental care.
• Build a trusting relationship between dentist and child.
• Promote the child’s positive attitude towards oral/dental health.
Routine use of restraining devices to stabilize young children in order to complete their dental
care is not acceptable practice, violates the standard of care and will result in termination of the
provider from the network.
Dentists must not restrain children without formal training in protective stabilization.
General Dentists should consider referring to dental specialists those Members who they
consider to be candidates for protective stabilization.
Dental auxiliaries must not use restraining devices to stabilize children.
1. Routine use of restraining devices to stabilize young children in order to complete
their dental care is not acceptable practice, violates the standard of care, and will
result in termination of the provider from the network.
2. Dentists must not restrain children without formal training in protective stabilization.
3. General dentists should consider referring to dental specialists those Members who
they consider to be candidates for protective stabilization.
4. Dental auxiliaries must not use restraining devices to immobilize children.
*American Academy of Pediatric Dentistry. Guideline on behavior management.
Reference
Manual 2002‐2003.
2013 AAPD Clinical Guidelines on Protective Stabilization for Pediatric Dental Patients
**Tennessee Board of Dentistry Newsletter. Spring 2004
Routine, Therapeutic/Diagnostic, and Urgent Care Dental Services
Definitions
• Routine dental services include diagnostic and preventive visits.
• Therapeutic services are those such as fillings, crowns, root canals and/or extractions.
• Emergency dental services are limited to the following:
• Procedures necessary to control bleeding, relieve pain, and eliminate acute
infection.
• Operative procedures required to prevent imminent loss of teeth.
• Treatment of injuries to the teeth and supporting structures.
Routine restorative procedures and root canal therapy are not emergency services.
Emergency
services must be justified with documentation. The dentist’s narrative
documentation should
describe the nature of the emergency, including relevant clinical information about the patient’s
condition and stating why the emergency services rendered
were considered to be immediately
DentaQuest USA Insurance Company, Inc. February 1, 2024
Current Dental Terminology © American Dental Association. All Rights Reserved.
36
DentaQuest USA Insurance Company
___
necessary.
EMERGENCY Treatments and Authorizations
If a patient presents with an emergency condition that requires immediate treatment or
intervention, you should always take necessary clinical steps to mitigate pain, swelling,
or other symptoms that might put the members overall health at risk and completely
document your findings. After treatment, please complete the appropriate authorization
request, and enter EMERGENCY/ URGENT in box 35, and the appropriate narrative or descriptor
of the patient’s conditions, including all supporting documentation.
Please FAX this to 262-241-7150.
DentaQuest will process emergency authorization requests as high priority. After you receive the
authorization number, then and only then should you submit the claim. Our system will link the
authorization number and the claim, and payment should be processed.
Requirements for Scheduling of Appointments
DentaQuest Dentists are expected to meet minimum standards with regards to appointment
availability. Dental appointments are to be made during normal business hours and within a
reasonable time from the date of the Member’s request. Appointment Standards are:
• Preventive – 14 calendar days.
• Therapeutic/diagnostic‐ 14 calendar days.
• Urgent‐ 24 hours.
Coordination of Non‐Capitated Services
Medicaid Services Not Covered by DentaQuest
The following Texas Medicaid programs and services are paid for by HHSC’s claims administrator
instead of DentaQuest. Medicaid Members can get these services from Texas Medicaid
providers.
1. Early Childhood Intervention (ECI) case management/service coordination;
2. DSHS case management for Children and Pregnant Women;
3. Texas School Health and Related Services (SHARS); and
Either the Member’s medical plan or HHSC’s claims administrator will pay for treatment and
devices for craniofacial anomalies, and for emergency dental services that a Member gets in a
hospital or ambulatory surgical center. This includes hospital, physician, and related medical
services (e.g., anesthesia and drugs) for:
• Treatment of a dislocated jaw, traumatic damage to teeth, and removal of cysts;
DentaQuest USA Insurance Company, Inc. February 1, 2024
Current Dental Terminology © American Dental Association. All Rights Reserved.
37
DentaQuest USA Insurance Company
___
• Treatment of oral abscess of tooth or gum origin; and
• Treatment of craniofacial anomalies.
Nonemergency medical transportation (NEMT) services may be used to access Covered Dental
Services provided by the Dental Contractor. NEMT Services are coordinated by the member’s
Medicaid medical plan.
If a Member is in need of assistance in coordinating any non‐capitated services, a Member
Advocate may be contacted to assist. Please contact our Member or Provider Service Line and
ask to be referred to a Member Advocate.
MEDICAL TRANSPORTATION PROGRAM (MTP)
What is MTP?
MTP is a state administered program that provides Non‐Emergency Medical Transportation
(NEMT) services statewide for eligible Medicaid members who have no other means of
transportation to attend their covered healthcare appointments. MTP can help with rides to the
doctor, dentist, hospital, drug store, and any other place you get Medicaid services.
What services are offered by MTP?
• Passes or tickets for transportation such as mass transit within and between cities or
states, to include rail, bus, or commercial air
• Curb to curb service provided by taxi, wheelchair van, and other transportation vehicles
• Mileage reimbursement for a registered individual transportation participant (ITP) or a
covered healthcare event. The ITP can be the responsible party, family member, friend,
neighbor, or member.
• Meals and lodging allowance when treatment requires an overnight stay outside the
county of residence
• Attendant services (a responsible adult who accompanies a minor or an attendant
needed for mobility assistance or due to medical necessity, who accompanies the
member to a healthcare service)
• Advanced funds to cover authorized transportation services prior to travel
Call MTP:
For more information about services offered by MTP, members, advocates and providers can call
the toll free line at 1‐877‐633‐8747. In order to be transferred to the appropriate transportation
provider, members are asked to have either their Medicaid ID# or zip code available at the time
of the call.
CHIP Services Not Covered by DentaQuest
DentaQuest USA Insurance Company, Inc. February 1, 2024
Current Dental Terminology © American Dental Association. All Rights Reserved.
38
DentaQuest USA Insurance Company
___
Some services are paid by CHIP medical plans instead of DentaQuest. These services include
treatment and devices for craniofacial anomalies, and emergency dental services that a Member
gets in a hospital or ambulatory surgical center. This includes hospital, physician, and related
medical services (e.g., anesthesia and drugs) for:
• Treatment of a dislocated jaw, traumatic damage to teeth, and removal of cysts;
• Treatment of oral abscess of tooth or gum origin; and
• Treatment of craniofacial anomalies.
If a Member is in need of assistance in coordinating any non‐capitated services, a Member
Advocate may be contacted to assist. Please contact our Member or Provider Service Line and
ask to be referred to a Member Advocate.
Effective January 1, 2019 - Retro eligibility Recoupment Process
Funds will be recouped from paid claims with dates of service on or after January 1, 2019 where the
member’s eligibility has been retro-actively terminated. All decisions with regards to payment are subject
to appeal. You may appeal our handling of payment by submitting a written request for review to HHSC.
Provider Appeal Process to HHSC (related to claim recoupment due to Member
disenrollment)
Provider may appeal claim recoupment by submitting the following information to HHSC:
• A letter indicating that the appeal is related to a managed care disenrollment/recoupment and
that the provider is requesting an Exception Request.
• The Explanation of Benefits (EOB) showing the original payment. Note: This is also used when
issuing the retro-authorization as HHSC will only authorize the Texas Medicaid and Healthcare
Partnership (TMHP) to grant an authorization for the exact items that were approved by the
plan.
• The EOB showing the recoupment and/or the plan's "demand" letter for recoupment. If
sending the demand letter, it must identify the member name, identification number, DOS, and
recoupment amount. The information should match the payment EOB.
• Completed clean claim. All paper claims must include both the valid NPI and TPI number. Note:
In cases where issuance of a prior authorization (PA) is needed, the provider will be contacted
with the authorization number and the provider will need to submit a corrected claim that
contains the valid authorization number.
Mail appeal requests to:
Texas Health and Human Services Commission HHSC Claims Administrator Contract Management
Mail Code-91X P.O. Box 204077
Austin, Texas 78720-4077
E. Medicaid Dental Services Provider Complaint and Appeal
Process

DentaQuest USA Insurance Company, Inc. February 1, 2024
Current Dental Terminology © American Dental Association. All Rights Reserved.
39
DentaQuest USA Insurance Company
___
Medicaid Provider Complaints
Procedures governing the provider complaints process are designed to identify and resolve
provider complaints in a timely and satisfactory manner. Complaints must be resolved within
thirty (30) calendar days. If a complaint cannot be resolved within thirty (30) days, the provider
will be notified in writing the status of the complaint. The submitted documentation must specify
the relevant subject (i.e. Appeal/Complaint). All documentation regarding an appeal/complaint
must be submitted for processing. Submission copies must be retained for the provider's record.
Complaints to DentaQuest may be submitted using the following methods:
(Non‐claim related) • By telephone at 1‐800‐896‐2374
(Claim related) • In writing to:
DentaQuest‐ TX Dental Services
Complaints & Grievances
P.O. Box 2906 Milwaukee,
WI 53201‐2906
If a provider is not satisfied after completing the DentaQuest Complaint Process or feels that
they did not receive due process, providers may file a complaint with HHSC. A provider must
exhaust the DentaQuest Complaint Process before filing with HHSC.
Medicaid complaint requests may be mailed to the following address:
Texas Health and Human Services Commission
Provider Complaints
Health Plan Operations, H‐320
PO Box 85200
Austin, Texas 78708
Or e‐mail complaint requests to: [email protected]
Medicaid Provider Appeals
For appealed claims, Providers must submit all appeals of denied claims and requests for
adjustments on paid claims within one hundred and twenty (120) days from the date of
disposition of the Explanation of Benefits (EOB) on which that claim appeared. The submitted
documentation must specify the relevant subject (i.e. Appeal/Complaint). All documentation
regarding an appeal/complaint must be submitted for processing. Submission copies must be
retained for the provider's record. Appeals should be mailed to:
DentaQuest TX HHSC Dental Services
DentaQuest USA Insurance Company, Inc. February 1, 2024
Current Dental Terminology © American Dental Association. All Rights Reserved.
40
DentaQuest USA Insurance Company
___
Complaints & Grievances - Appeals
P.O. Box 2906 Milwaukee,
WI 53201‐2906
We will respond to the appeal within thirty (30) calendar days after we receive the request with
any necessary supporting documentation.
Peer to Peer Reviews
If you have a question or concern regarding any determination, you may speak with a dental
director during regular business hours, by calling the Provider Services line at 1‐800‐896‐2374.
Clinical review guidelines used in all determinations will be provided in writing, upon request.
F. Medicaid Dental Services Member Complaint and Appeal
Process
Medicaid Member Complaint
The Member receives the following information as it pertains to Medicaid Member Complaints:
A Medicaid Member Complaint is an expression of dissatisfaction expressed by a Member,
orally
or in writing to DentaQuest, about any matter other than an Action. As provided by 42 C.F.R.
§438.400, possible subjects for Complaints include, but are not limited to, the quality of care of
services provided, and aspects of interpersonal relationships such as rudeness of a provider or
employee, or failure to respect the Medicaid Member’s rights.
What should I do if I have a complaint?
We want to help. If you have a complaint, please call us toll‐free at 1‐800‐516‐0165 to tell us
about your problem. A DentaQuest Member Advocate can help you file a complaint. Just call 1‐
800‐516‐0165. Most of the time, we can help you right away or at the most within a few days.
You can also send your complaint in writing to:
DentaQuest‐ TX HHSC Dental Services
Complaints & Grievances
P.O. Box 2906 Milwaukee,
WI 53201‐2906
Once we receive your complaint, DentaQuest will acknowledge your complaint within five (5)
business days of receipt. We will respond within thirty (30) calendar days of receipt of your
complaint.
The resolution letter will:
1. Explain the resolution of the complaint.

DentaQuest USA Insurance Company, Inc. February 1, 2024
Current Dental Terminology © American Dental Association. All Rights Reserved.
41
DentaQuest USA Insurance Company
___
2. State the specific dental and contractual reasons for the resolution.
3. State the specialization of any dentist or other Provider consulted.
4. Include a complete description of the process for appeal, including the
deadlines for
the appeals process and the deadlines for the final decision on the appeal.
If the Member is not satisfied with the outcome, who else can they call?
Once you have gone through the DentaQuest complaint process, you can complain to the
Health
and Human Services Commission (HHSC) by calling toll‐free 1‐866‐566‐8989, 8 A.M. – 5P.M.,
Monday - Friday. If you have a hearing disability, call the toll-free Relay Texas service at 7-1-1 or
1-800-735-2389. If you would like to make your complaint in writing, please send it to the
following address:
Mail: Texas Health and Human Services Commission
Ombudsman for Managed Care
P.O. Box 13247
Austin, TX 78711-3247
Fax: 888-780-8099
If you can get on the Internet, you can access more information here:
Online: https://hhs.texas.gov/about-hhs/your-rights/office-ombudsman/hhs-ombudsman-
managed-care-help
MDCP/DBMD ESCALATION HELP LINE
What is the MDCP/DBMD Escalation Help Line?
The MDMDCP/DBMD Escalation Help Line assists people with Medicaid who get benefits through
the Medically Dependent Children Program (MDCP) or the Deaf Blind with Multiple Disabilities
(DBMD) program.
The escalation help line can help solve issues related to the STAR Kids managed care program.
Help can include answering questions about Medicaid fair hearings and continuing services while
appealing.
When should I call the escalation help line?
Call when you have tried to get help but have not been able to get the help you need. If you
don’t know who to call, you can call 844-999-9543 and they will work to connect you with the
right people.
Is the escalation help line the same as the HHS Office of the Ombudsman?
DentaQuest USA Insurance Company, Inc. February 1, 2024
Current Dental Terminology © American Dental Association. All Rights Reserved.
42
DentaQuest USA Insurance Company
___
No. The MDCP/DBMD escalation help line is part of the Medicaid program. The Ombudsman
offers an independent review of concerns and can be reached at 866-566-8989 or go on the
Internet (hhs.texas.gov/managed-care-help). The MDCP/DBMD escalation help line is dedicated
to individuals and families that receive benefits from the MDCP or DBMD program.
Who can call the help line?
The escalation line is available Monday through Friday from 8 a.m.–8 p.m. After these hours,
please leave a message and one of our trained on-call staff will call you back.
Can I call any time?
The escalation line is available Monday through Friday from 8 a.m.-8 p.m. After these hours,
please leave a message and one of our trained on-call staff will call you back.
Medicaid Member Appeals
The Member receives the following information as it pertains to Medicaid Member Appeals:
A Medicaid Member Appeal is the formal process by which a Member or his or her
representative requests a review of DentaQuest’s Action.
If a Member, or Member’s representative, disagrees with a decision made to deny a covered
service, they have the right to appeal. To do this, the appeal must be made within sixty (60) days
from the date of receipt of the notice of action. DentaQuest will acknowledge the receipt
of the
appeal within five (5) business days and complete the appeal within thirty (30) days.
What can I do if DentaQuest denies or limits my Member’s request for a covered service?
You, with the Member’s consent, can ask for an appeal in writing, or you can call and ask
DentaQuest for an appeal. We will send you and the Member a one‐page appeal form that you,
the Member, or someone else representing the Member can fill out and return to us. Every oral
Appeal received must be confirmed by a written, signed Appeal by the Member or his or her
representative, unless an Expedited Appeal is requested.
How will I find out if services are denied?
We will send you a Provider Determination Letter and the Member will receive a Notice of Action
Letter.
Timeframes for the Appeal Process
DentaQuest must complete the entire standard Appeal process within 30 days after receipt of
the initial written or oral request for Appeal.
DentaQuest USA Insurance Company, Inc. February 1, 2024
Current Dental Terminology © American Dental Association. All Rights Reserved.
43
DentaQuest USA Insurance Company
___
You or DentaQuest can ask for an extension of up to fourteen (14) Days if there is a need for
more information in order to make a decision in the best interest of the Member.
DentaQuest
will send you a written notice explaining the reason for the delay.
When does the Member have the right to ask for an appeal?
The Member has the right to request an appeal if he/she is not satisfied or disagrees with the
action. An appeal is the process by which you and/or the Member request a review of the
action.
The Member has the right to request an appeal for denial of payment for service in whole or in
part.
To ensure continuation of currently authorized services, the Member must file the appeal on or
before the later of: ten (10) Days following DentaQuest’s mailing of the notice of the
action or
the intended effective date of the proposed action. The Member may be required to pay the cost
of services furnished while the appeal is pending, if the final decision is adverse to the Member.
Appeals must be accepted orally or in writing.
Can someone from DentaQuest help a Member file an appeal?
Yes. However,
• Member’s option to request an External Medical Review and State Fair Hearing must be no
later than 120 Days after DentaQuest mails the appeal decision notice.
• Member’s option to request only a State Fair Hearing must be no later than 120 Days after
DentaQuest mails the appeal decision notice.
A DentaQuest Member Advocate can help the Member file an appeal. Just call 1‐800‐516‐ 0165.
Medicaid Member Expedited Appeals
The Member receives the following information as it pertains to Medicaid Member Expedited
Appeals:
How to Request an Emergency Appeal
If you have an emergency appeal, you can call us at 1‐800‐516‐0165. Call and tell us you need
an
expedited appeal. A request for an expedited appeal can be made orally or in writing.
Timeframes for Emergency Appeals
We will respond within three (3) business days from the day we receive your request for appeal.
What happens if DentaQuest denies the request for an Emergency Appeal?
DentaQuest USA Insurance Company, Inc. February 1, 2024
Current Dental Terminology © American Dental Association. All Rights Reserved.
44
DentaQuest USA Insurance Company
___
If DentaQuest does not think the appeal is life‐threatening, the Member will be notified the
same
day that the decision is made. The appeal will still be worked on, but the decision may
take up to
thirty (30) days.
Who can help me file an Emergency Appeal?
If you need help filing an expedited appeal, call us toll‐free at 1‐800‐516‐0165, and a DentaQuest
Member Advocate will help you.
State Fair Hearing Information
Can a Member ask for a State Fair Hearing?
If a member, as a member of DentaQuest, disagrees with DentaQuest’s decision, the member
has the right to ask for a State Fair Hearing. The Member may name someone to represent him
or her by writing a letter to DentaQuest telling them the name of the person you want
representing you. A provider may be your representative. You or your representative must ask
for the State Fair Hearing within one‐hundred and twenty (120) days of the date on the
DentaQuest letter that tells of the decision you are challenging. If you do not ask for the State
Fair Hearing within 120 days, you may lose your right to a State Fair Hearing. To ask for a State
Fair Hearing, you or your representative should either send a letter to DentaQuest at:
DentaQuest‐TX Dental Program
Attn: Fair Hearing Coordinator
P.O. Box 2906 Milwaukee,
WI 53201‐2906
Or call: 1‐800‐516‐0165
If you ask for a State Fair Hearing within 10 Days from the time the hearing notice is received
from DentaQuest, you have the right to keep getting any service DentaQuest denied, at least
until the final hearing decision is made. If you do not request a State Fair Hearing within 10 days
from the time the hearing notice is received, the service DentaQuest denied will be
stopped.
If you or your representative requests a State Fair Hearing, you will get a packet of information
with the date, time, and location of the hearing. Most State Fair Hearings are held by telephone.
At that time, you or your representative can tell why you need the service DentaQuest denied.
HHSC will give the Member a final decision within 90 Days from the date you
asked for the
hearing.
External Medical Review Information
Can a Member ask for an External Medical Review?
DentaQuest USA Insurance Company, Inc. February 1, 2024
Current Dental Terminology © American Dental Association. All Rights Reserved.
45
DentaQuest USA Insurance Company
___
If a Member, as a member of the dental plan, disagrees with the dental plan’s decision, the
Member has the right to ask for an External Medical Review. An External Medical Review is an
optional, extra step the Member can take to get the case reviewed for free before the State Fair
Hearing. The Member may name someone to represent him or her by writing a letter to the
dental plan telling the Dental Contractor the name of the person the Member wants to represent
him or her. A provider may be the Member’s representative. The Member or the Member’s
representative must ask for the External Medical Review within 120 days of the date the dental
plan mails the letter with the internal appeal decision. If the Member does not ask for the
External Medical Review within 120 days, the Member may lose his or her right to an External
Medical Review. To ask for an External Medical Review, the Member or the Member’s
representative should either:
• Fill out the ‘State Fair Hearing and External Medical Review Request Form’ provided as an
attachment to the Member Notice of Dental Contractor Internal Appeal Decision letter and mail
or fax it to DentaQuest by using the address or fax number at the top of the form.
• Cal DentaQuest at 1‐800‐516‐0165
• Email DentaQuest at [email protected]
If the Member asks for an External Medical Review within 10 days from the time the Member
gets the appeal decision from the dental plan, the Member has the right to keep getting any
service the dental plan denied, at least until the final State Fair Hearing decision is made. If the
Member does not request an External Medical Review within 10 days from the time the Member
gets the appeal decision from the dental plan, the service the dental plan denied will be stopped.
The Member may withdraw the Member’s request for an External Medical Review before it is
assigned to an Independent Review Organization or while the Independent Review Organization
is reviewing the Member’s External Medical Review request. An External Medical Review cannot
be withdrawn if an Independent Review Organization has already completed the review and
made a decision.
Once the External Medical Review decision is received, the Member has the right to withdraw
the State Fair Hearing request. If the Member continues with the State Fair Hearing, the Member
can also request the Independent Review Organization be present at the State Fair Hearing. The
Member can make both of these requests by contacting the Dental Contractor at
[email protected] or the HHSC Intake Team at [email protected].
Can a Member ask for an emergency External Medical Review?
If a Member believes that waiting for a standard External Medical Review will seriously
jeopardize the Member’s life or health, or the Member’s ability to attain, maintain, or regain
maximum function, the Member or Member’s representative may ask for an emergency External
Medical Review and emergency State Fair Hearing by writing or calling DentaQuest. To qualify for
an emergency External Medical Review and emergency State Fair Hearing review through HHSC,
the Member must first complete DentaQuest’s internal appeals process.
DentaQuest USA Insurance Company, Inc. February 1, 2024
Current Dental Terminology © American Dental Association. All Rights Reserved.
46
DentaQuest USA Insurance Company
___
G. CHIP Provider Complaints and Appeals
CHIP Provider Complaints
Procedures governing the provider complaints process are designed to identify and resolve
provider complaints in a timely and satisfactory manner. Complaints must be resolved within
thirty (30) calendar days. If a complaint cannot be resolved within thirty (30) days, the provider
will be notified in writing the status of the complaint.
The submitted documentation must specify the relevant subject (i.e. Appeal/Complaint). All
documentation regarding an appeal/complaint must be submitted for processing. Submission
copies must be retained for the provider's record.
Complaints to DentaQuest may be submitted using the following methods:
(Non‐claim related) • By telephone at 1‐800‐896‐2374
(Claim related) • In writing to:
DentaQuest‐ TX Dental Services
Complaints & Grievance
P.O. Box 2906 Milwaukee,
WI 53201‐2906
If a provider is not satisfied after completing the DentaQuest Complaint Process or feels that
they did not receive due process, providers may file a complaint with the Texas Department of
Insurance. A provider must exhaust the DentaQuest Complaint Process before filing with TDI.
CHIP complaint requests may be mailed to the following address:
Office Address
Mailing Address
1601 Congress Avenue
Austin, TX 78701
PO Box 12030
Austin, TX 78711-2030
Or e‐mail complaint requests to: HPM [email protected]
CHIP Provider Appeals
For appealed claims, Providers must submit all appeals of denied claims and requests for
adjustments on paid claims within one hundred and twenty (120) days from the date of

DentaQuest USA Insurance Company, Inc. February 1, 2024
Current Dental Terminology © American Dental Association. All Rights Reserved.
47
DentaQuest USA Insurance Company
___
disposition of the Explanation of Benefits (EOB) on which that claim appeared.
The submitted documentation must specify the relevant subject (i.e. Appeal/Complaint). All
documentation regarding an appeal/complaint must be submitted for processing. Submission
copies must be retained for the provider's record.
Appeals should be mailed to:
DentaQuest TX HHSC Dental Services
Complaints & Grievances - Appeals
P.O. Box 2906 Milwaukee,
WI 53201‐2906
We will respond to the appeal within thirty (30) calendar days after we receive the request with
any necessary supporting documentation.
Peer to Peer Reviews
If you have a question or concern regarding any determination, you may speak with a dental
director during regular business hours, by calling the Provider Services line at 1‐800‐896‐2374.
Clinical review guidelines used in all determinations will be provided in writing, upon request.
“Like Specialty” Peer to Peer Reviews
Like Specialty Peer‐to‐Peer Process: DentaQuest’s internal process where the Provider
disagrees
with DentaQuest’s claim appeal’s decision based on Medical Necessity and requests a “like
specialty” Peer‐to‐Peer discussion with a Dental Director. The Dental Director resolving the
dispute must hold the same specialty or a related specialty as the appealing Provider and is not
the Dental Director that was involved in any previous determinations. The Dental Director
completing the “like specialty” peer to peer discussions is a non‐network provider.
Procedure
Requesting a “like specialty” Peer‐to‐Peer discussion
1. Upon completion of an appeal relating to claims payment, if the appealing Provider
disagrees with the appeal decision; they have the right to request a “like specialty”
peer‐to‐peer discussion with a Specialist within 30 days from the
appeal disposition
of an adverse determination. This process applies only when:
a. The services in question have already been rendered;
b. The Provider dispute is related to denial on the basis of Medical Necessity;
and
c. The Provider has completed the appeal process and received the
appeal
determination.
2. Peer‐to‐Peer like‐specialty meeting requests can be submitted verbally or in

DentaQuest USA Insurance Company, Inc. February 1, 2024
Current Dental Terminology © American Dental Association. All Rights Reserved.
48
DentaQuest USA Insurance Company
___
writing. The Provider may contact DentaQuest’s Provider Call Center’s toll free
number at 800.896.2374 or may submit a written request to DentaQuest’s
Complaints & Appeals Department at the following address:
DentaQuest‐ TX HHSC Dental Services
Peer Review Request
P.O. Box 2906 Milwaukee,
WI 53201‐2906
3. Peer‐to‐Peer requests are handled by the Complaint and Appeals Specialist (C&G
Specialist) and the resolution coordinated with Dental Directors and other areas
within DentaQuest. Non‐participating Consultants of a similar specialty as the
Provider will be contracted by DentaQuest to resolve claim disputes related to
denial on the basis of Medical Necessity that remain unresolved subsequent to a
provider appeal.
4. Upon the receipt of the Peer‐to‐Peer request, the Complaints and Grievance
Specialist contacts the Provider within five (5) days from the receipt. The provider
will be contacted via email or phone, based on the provider’s
preference.
5. The C&G Specialists will schedule a conference between the Provider and the
Consultant within two weeks, or as soon as the Provider and Consultant’s schedules
permit.
6. The C&G Specialist will provide all records related to the case to the Consultant in
advance to the scheduled conference. DentaQuest’s Clinical Guidelines which
incorporates the guidelines from: American Dental Association, the American
Pediatric Dental Association, the Medicaid Program and any contract specific
related items will be included. These guidelines are used as a reference and taken
into consideration for each individual case. These guidelines are available upon
request.
Resolution of “like‐specialty” peer‐to‐peer discussion
1. Upon completion of the like‐specialty peer‐to‐peer conference, the Consultant will
communicate the decision via fax or e‐mail to the C&G Specialist.
2. The C&G Specialists will document the Consultant’s decision and relevant
information in the C&G Module.
3. The Consultant’s decision is binding on DentaQuest and the Provider.
4. A resolution to the Provider will be rendered and written communication is sent to
the Provider within two business days from completion of the like‐specialty
discussion.
CHIP Member Complaints and Appeals
CHIP Member Complaint
DentaQuest USA Insurance Company, Inc. February 1, 2024
Current Dental Terminology © American Dental Association. All Rights Reserved.
49
DentaQuest USA Insurance Company
___
The Member receives the following information as it pertains to CHIP Member Complaints:
A CHIP Member Complaint is any dissatisfaction, expressed by a Complainant, orally or in writing,
to DentaQuest, with any aspect of DentaQuest’s operation, including, but not limited to,
dissatisfaction with plan administration, procedures related to review or appeal of an Adverse
Determination, as defined in Texas Insurance Code, Chapter 843, Subchapter G; the
denial,
reduction, or termination of a service for reasons not related to Medical Necessity; and the way a
service is provided. The term does not include misinformation that is resolved
promptly by
supplying the appropriate information or clearing up the misunderstanding to the
satisfaction of
the CHIP Member.
What should I do if I have a complaint?
We want to help. If you have a complaint, please call us toll‐free at 1‐800‐508‐6775 to tell us
about your problem. A DentaQuest Member Services Advocate can help you file a complaint.
You can also send your complaint in writing to:
DentaQuest‐ TX HHSC Dental Services
Complaints & Grievance
P.O. Box 2906 Milwaukee,
WI 53201‐2906
Who do I call?
Just call 1‐800‐508‐6775. Most of the time, we can help you right away or at the most within a
few days.
Can someone from DentaQuest help a Member file a complaint?
Yes. A DentaQuest Member Advocate can help the Member file a complaint. Just call 1‐800‐ 508‐
6775.
How long will it take to investigate and resolve my complaint?
Once we receive your complaint, DentaQuest will acknowledge your complaint within five (5)
business days of receipt. We will respond within thirty (30) calendar days of receipt of your
complaint.
The resolution letter will:
1. Explain the resolution of the complaint.
2. State the specific dental and contractual reasons for the resolution.
DentaQuest USA Insurance Company, Inc. February 1, 2024
Current Dental Terminology © American Dental Association. All Rights Reserved.
50
DentaQuest USA Insurance Company
___
3. State the specialization of any dentist or other Provider consulted.
4. Include a complete description of the process for appeal, including the deadlines for the
appeals process and the deadlines for the final decision on the appeal.
If I am not satisfied with the outcome, who else can I call?
Any Member, including a Member who has attempted to resolve a complaint through the
complaint process described above, may file a complaint with the Texas Department of
Insurance:
Office Address
Mailing Address
1601 Congress Avenue
Austin, TX 78701
PO Box 12030
Austin, TX 78711-2030
The Department’s toll‐free telephone number is 1‐800‐252‐3439.
The commissioner will investigate a complaint against us to determine our compliance with the
insurance laws within sixty (60) days after the Department receives the complaint and all
information necessary for the Department to determine compliance. The commissioner may
extend the time necessary to complete an investigation in the event any of the following
circumstances occur:
a. Additional information is needed.
b. An on‐site review is necessary.
c. We, the Provider, or the complainant do not provide all documentation
necessary to complete the investigation.
d. Other circumstances beyond the control of the Department occur.
We will not engage in any retaliatory action (including termination or refusal to renew a
Contract) against a Member or a dentist (on behalf of a Member) for filing a complaint or
appealing a decision.
CHIP Member Appeal
The Member receives the following information as it pertains to CHIP Member Appeals:
A CHIP Member Appeal is the formal process by which DentaQuest addresses Adverse
Determinations.
What can I do if DentaQuest denies or limits my patient’s request for a covered service?
You, with the Member’s consent, can ask for an appeal in writing, or you can call and ask
DentaQuest for an appeal. We will send you and the Member a one‐page appeal form that you,
DentaQuest USA Insurance Company, Inc. February 1, 2024
Current Dental Terminology © American Dental Association. All Rights Reserved.
51
DentaQuest USA Insurance Company
___
the Member, or someone else representing the Member can fill out and return to us.
How will I find out if the appeal is denied?
We will send a written resolution of the appeal within thirty (30) calendar days after receipt of an
appeal. Investigation and resolution of appeals involving ongoing Emergency Dental Services
will
be concluded in accordance with the dental immediacy of the case, but no later than 24
hours
after receipt of request for appeal. At the request of the Member, we will provide,
instead of an
appeal panel, a Provider who has not previously reviewed the case and who is of the same or
similar specialty as ordinarily manages the procedure or treatment under appeal.
52
DentaQuest USA Insurance Company
DentaQuest USA Insurance Company, Inc February 1, 2024
Current Dental Terminology © American Dental Association. All Rights Reserved.
The Provider reviewing the appeal may interview the Member or the Member’s designated
representative and will make a decision on the appeal. Initial notice of decision of the appeal
may be delivered orally, but will be followed by a written notice of the determination within
three days.
Notice of our final decision will include a statement of the specific clinical and/or Contract
provision(s) on which the decision was based, and the toll‐free telephone number and address
for MAXIMUS.
Timeframes for the Appeal Process
Non‐emergency appeals will be processed within thirty (30) calendar days from the day we
receive it.
You or DentaQuest can ask for an extension of up to fourteen (14) calendar days if there is a
need for more information in order to make a decision. DentaQuest will send you a written
notice explaining the reason for the delay.
When does a Member have the right to request an appeal?
In the event a Member is not satisfied with our resolution of a complaint, other than issues
relating to a Member’s annual maximum or eligibility information provided to DentaQuest by
Texas HHSC or its designee, he/she will have the right to appeal the decision. A Member also has
the right to appeal any adverse decision including denial of payment for services in whole or in
part. A Member may be required to pay the cost of services furnished while the appeal is
pending if the final decision is adverse to the Member.
A Member may call DentaQuest to request an appeal. Within five (5) business days after the
Member calls, we will send them an appeal form. We must receive the Member’s completed,
signed appeal form to confirm their appeal request, unless an expedited appeal is requested.
Every oral appeal received must be confirmed by a written, signed appeal by the Member or his
or her representative, unless an expedited appeal is requested. (If the appeal request is related
to a dental emergency, we do not need a completed, signed form to process the appeal.)
After we receive the written request for an appeal, we will send the Member a letter within five
(5) business days. The letter will explain the Member’s right to:
• Submit a written appeal to an appeal panel or appear before an appeal panel in person.
• Present information to help the Member’s.
• Ask questions about the decision we made regarding the complaint.
No later than five (5) business days before the appeal panel meets, we will send the Member:
• Copies of any documents that the appeal panel will review.
• The specialty field of any dentists who helped us review your case.
53
DentaQuest USA Insurance Company
DentaQuest USA Insurance Company, Inc February 1, 2024
Current Dental Terminology © American Dental Association. All Rights Reserved.
• Information about the Members of the appeal panel.
We may tell you the outcome of your appeal right away. We will always send you a written
letter
of the decision within three (3) business days.
The letter will include:
• Our decision about your appeal.
• The reasons for our decision.
• Contact information for MAXIMUS.
Appeals must be accepted orally or in writing.
Can someone from DentaQuest help the Member file an appeal?
Please have the Member call our Member Call Center toll‐free at 1‐800‐508‐6775 for help in
filing an appeal.
CHIP Member Expedited Appeals
The Member receives the following information as it pertains to CHIP Member Expedited
Appeals:
How to Request an Expedited Appeal
If you have an emergency appeal, you can call us at 1‐800‐516‐0165. Call and tell us you need
an
expedited appeal. A request for an expedited appeal can be made orally or in writing.
Timeframes for Expedited Appeals
We will respond within three (3) business days from the day we receive your request for appeal.
What happens if DentaQuest denies the request for an Expedited Appeal?
If DentaQuest does not think the appeal is life‐threatening, the Member will be notified the
same
day that the decision is made. The appeal will still be worked on, but the decision may
take up to
thirty (30) days.
Who can help me file an Expedited Appeal?
If you need help filing an expedited appeal, call us toll‐free at 1‐800‐516‐0165, and a DentaQuest
Member Advocate will help you.
54
DentaQuest USA Insurance Company
DentaQuest USA Insurance Company, Inc February 1, 2024
Current Dental Terminology © American Dental Association. All Rights Reserved.
Independent Review Organization (IRO) for External CHIP Appeal Reviews
What is an Independent Review Organization?
The purpose of an Independent Review Organization (IRO) is to provide an independent review
of health care services that are denied by certain entities, on the basis that the services are not
medically necessary or appropriate, or are experimental, or investigational. These entities
include Utilization Review Agents, Health Maintenance Organizations, Insurance Carriers, and
Certified Workers' Compensation Networks.
How do I request a review by an Independent Review Organization?
If a CHIP Member, a representative designated by a Member, or their Dentist has sent an appeal
request to DentaQuest and it was denied, they may be able to have their request for medically
necessary services evaluated by DentaQuest’s contracted IRO, MAXIMUS, as part of an External
Review. This evaluation is processed by MAXIMUS at no cost to the Member.
MAXIMUS must receive the completed HHS‐Administered Federal External Review Request Form
within four months of the date that DentaQuest sent you a final decision denying your services
or your claim for payment. You will be asked to describe the dental services that were denied by
DentaQuest and state the reason that you believe DentaQuest’s decision was not correct.
HHS‐Administered Federal External Review Request Form
HHS-Administered Federal External Review Request Form
HHS Federal External Review Process Appointment of Representative Form
Appointment of Representative Form
MAXIMUS Federal Services will use the information you provide on this form to get the relevant
information and documents from DentaQuest. You may add supporting information and
documents you think DentaQuest may not be able to provide.
For example, you may choose to provide MAXIMUS with:
• Documents to support the claim, such as dentist’s letters, reports, bills,
medical records, and Explanation of Benefits (EOB) forms
• Letters you sent to DentaQuest about the claim
• Letters that DentaQuest sent to you about the claim
You do not have to give MAXIMUS this additional information. However, if you do not provide
any additional information, MAXIMUS Federal Services may decide your case based only on the
information DentaQuest gives us.
You can give MAXIMUS additional information for your external review by sending it with this

55
DentaQuest USA Insurance Company
DentaQuest USA Insurance Company, Inc February 1, 2024
Current Dental Terminology © American Dental Association. All Rights Reserved.
form in the below options.
Mail to: HHS Federal External Review Request, MAXIMUS
Federal Services,
3750 Monroe Avenue, Suite 705,
Pittsford, NY 14534.
Fax to: 1-888-866-6190
If you have questions about your external review, call MAXIMUS at 1-888-866-6205.
How long will it take to investigate and resolve my external appeal?
DentaQuest will immediately be contacted by MAXIMUS after receiving the request for an
External Review. DentaQuest will give MAXIMUS all documents and information used to make
the internal appeal decision within five (5) business days.
Standard External Review requests:
The Member or Member’s representative will receive written notice of the final External Review
decision no later than 45 days after MAXIMUS receives the request for an External Review or as
soon as the review has been completed.
Expedited Independent Review Organization request
In most cases, Members, their representative, or Dentist must complete any mandatory appeals
or opportunities for reconsideration offered by DentaQuest before MAXIMUS can do an external
review. In urgent situations, MAXIMUS may be able to do a review even if the Member,
Member’s designated representative, or Dentist have not made all appeals and reconsiderations.
If you believe your situation is urgent, you may ask for an expedited (fast) review. An urgent care
situation is one in which the Member’s health may be in serious jeopardy or, the Member may
have pain that cannot be controlled while awaiting the external review decision.
To ask for an expedited external review:
Submit an online request at https://externalappeal.com
OR Fax this form to 1-888-866-6190
OR Mail this form to:
HHS Federal External Review Request,
MAXIMUS Federal Services,
3750 Monroe Avenue, Suite 705,
Pittsford, NY 14534.
In urgent care situations, MAXIMUS Federal Services will accept a request for external review
from a medical professional who knows about the Member’s condition. The medical professional

56
DentaQuest USA Insurance Company
DentaQuest USA Insurance Company, Inc February 1, 2024
Current Dental Terminology © American Dental Association. All Rights Reserved.
will not be required to submit proof of authorization.
If you have questions about your external review, call MAXIMUS at 1-888-866-6205.
How long will it take to investigate and resolve my expedited external appeal?
For an expedited External Review request:
MAXIMUS will give DentaQuest and the Member or Member’s representative the External
Review decision no later than within 72 hours of receiving the request.
MAXIMUS will contact the Member or Member’s representative by phone and will also send a
written version of the decision within 48 hours of that phone call. DentaQuest must take action
on the notice if the ruling is in favor of the Member, and provide authorization, or coordinate the
services after receiving the External Review decision notice. DentaQuest is bound to comply with
the decision of the External Review.
HHSC Oversight
HHSC reserves the right and retains the authority to make reasonable inquiry and to conduct
investigations into Provider and Texas CHIP Dental Services Member complaints. The dentist
must cooperate in all such HHSC inquiries/investigations.
H. Medicaid Member Eligibility and Added Benefits
Eligibility
The Texas HHSC Medicaid Dental Programs provide dental coverage for children enrolled.
Eligibility is determined by the HHSC.
Verifying Eligibility
To verify Member eligibility providers may contact:
https://www.yourtexasbenefits.com/
*This site is only to verify Member eligibility, not Main Dental Home assignment.
If Members have questions regarding enrolling in the program or their loss of eligibility, they
should be referred to the Enrollment Broker at 1‐800‐964‐2777.
Main Dental Home Verification
Main Dental Home assignment must be verified on the DentaQuest Provider Web Portal (located
in the “Providers Only” section of DentaQuest’s website at www.dentaquest.com. You may also
contact DentaQuest’s Customer Service Department at 1‐800‐896‐2374 to verify
Main Dental
Home assignment.

57
DentaQuest USA Insurance Company
DentaQuest USA Insurance Company, Inc February 1, 2024
Current Dental Terminology © American Dental Association. All Rights Reserved.
DentaQuest Member Identification Card
Members will receive a DentaQuest TX Medicaid ID Card. Participating Providers are
responsible
for verifying that Members are eligible at the time services are rendered and to determine if
Members have other health insurance.
Please note that due to possible eligibility status changes, this information does not guarantee
payment and is subject to change without notice.
Sample of the DentaQuest USA Medicaid Dental Program ID card:
DentaQuest recommends that each dental office make a photocopy of the Member’s
identification card each time treatment is provided. It is important to note that the
identification
card is not dated, and it does not need to be returned should a Member lose eligibility.
Therefore, an identification card in itself does not guarantee that a person is
currently enrolled
in the Texas Medicaid Dental Program.
DentaQuest recommends that providers verify Main Dental Home assignment on the Provider
Web Portal prior to treatment, as the Member’s assignment may have changed, or the
Member may be using an old card.
Call DentaQuest
Participating Providers may access Member eligibility information through DentaQuest’s
Interactive Voice Response (IVR) system or through the Provider Web Portal (“Providers Only”
section of DentaQuest’s website at www.dentaquest.com.
To access the IVR, simply call DentaQuest’s Customer Service department at 1‐800‐896‐2374
and
press 2 for eligibility. The IVR system will be able to answer all of your eligibility questions for as
many Members as you wish to check.
Automated Inquiry System line/TXMedConnect
This is a provider line responsible for assisting with issues not addressed by other available

58
DentaQuest USA Insurance Company
DentaQuest USA Insurance Company, Inc February 1, 2024
Current Dental Terminology © American Dental Association. All Rights Reserved.
provider lines. The Contact Center Representative provides general information concerning the
Texas Medicaid Program. The Contact Center is open from 7 a.m. to 7 p.m. Central Time and can
be reached at the number listed below:
TMHP Contact Center/Automated Inquiry System (AIS)
1‐800‐925‐9126 or 512‐335‐5986
www.tmhp.com
Automatic Re‐enrollment
If a Member loses Medicaid eligibility and then regains eligibility within six (6) months, the
Member is automatically reassigned his previous plan. The Member may choose to switch plans,
please see Medicaid Plan Changes below.
Disenrollment
Can DentaQuest ask that my child get dropped from their dental plan?
DentaQuest can ask that a child be removed from their plan for the following reasons:
• The child or the child’s caregiver misuses the child’s Membership card or
loans it
to another person,
• The child or the child’s caregiver is disruptive, unruly, or uncooperative at the
dentist’s office, or
• The child or the child’s caregiver refuses to follow the dental plan’s rules and
restrictions.
Neither DentaQuest nor a provider m ay request a disenrollment based on an adverse change in
the Member’s health or the utilization of services which are medically necessary for the
treatment of a Member’s condition. A provider cannot take retaliatory action against a Member.
Medicaid Plan Changes
You can change your child’s dental plan to another by contacting the Medicaid Enrollment
Broker’s toll‐free telephone number at 1‐800‐647‐6558. During the first 90 Days after you are
enrolled in a dental plan, you can change to another plan for any reason. After 90 Days, with a
dental plan, you can change to another plan once for any reason. If you show good cause, you
can also change dental plans at any time. An example of good cause is that you can’t get the
care
that you need through the dental plan.
If you call to change dental plans on or before the 15th of the month, the change will take place
on the first day of the next month. If you call after the 15th of the month, the change will take
place the first day of the second month after that. For example:
• If you ask to change plans on or before April 15, the change will take place on May 1.
59
DentaQuest USA Insurance Company
DentaQuest USA Insurance Company, Inc February 1, 2024
Current Dental Terminology © American Dental Association. All Rights Reserved.
• If you ask to change plans after April 15, the change will take place on June 1.
Medicaid Added Benefits
Medicaid Member Value Added Services
Free Dental Care Kit for Child and Parent
Get off to the right start by receiving a preventative dental service within 180 days of when you sign up
with us. When you do, you can get one zippered backpack and a dental kit that includes a toothbrush,
a tube of toothpaste and a brushing chart and stickers. We will also include a spinning toothbrush, a
timer and floss for the parent. That way, you can brush along with your child! One reward per eligible
member, per lifetime.
Walmart Gift Card for Preventive Visit
You can also get a $25 OTC Network Rewards gift card when your child gets a qualifying Texas Health
Steps dental checkup. OTC Network is the gift card vendor. The OTC Network rewards gift card allows
you to buy eligible products with your rewards card at thousands of participating stores. You can use
the OTC Rewards gift card to buy items such as healthy foods, baby care items and over the counter
health products. For a full list of eligible items and participating retailers, visit
SpeakBenefits.com/Dental. One gift card per eligible member, per lifetime.
Additional value‐added services:
Members 6 months – 6 years
There is treatment that can fix some cavities with no
drilling. This treatment is not normally covered under
the Medicaid & CHIP programs. If your dentist says you
need it to protect you from cavities, you can get it at no
cost. Must be prescribed by Main Dentist.
Other limitations may apply, please discuss with your
Main Dentist.
Members who have follow-up
care with their Main Dentist after
visiting the ER for dental care.
Eligible Members may receive one $10 OTC Network
rewards gift card for taking the following steps if they
have had to visit a hospital emergency room for dental
care.
• Have a follow-up visit with their Main Dentist
within 30 days of visiting the emergency room
for a dental related issue.
• Complete the quiz and submit to DentaQuest.
Redemption form & quiz is available on pages
40 and 41 of the Member Handbook, the secure
Member Website at
MemberAccess.DentaQuest.com and online at
www.DentaQuest.com/TXMember.
Here’s what you need to do to get your $25 OTC Network Rewards gift card and/or dental kit:
1. Fill out your information on the Extra Benefits redemption form.
2. You can make copies of the Extra Benefits redemption form if you need more than one.
60
DentaQuest USA Insurance Company
DentaQuest USA Insurance Company, Inc February 1, 2024
Current Dental Terminology © American Dental Association. All Rights Reserved.
3. Mail the signed form to DentaQuest. You can use the postage-paid envelope included with this
Member Handbook: DentaQuest
P.O. Box 2906
Milwaukee, WI 53201-2906
If you have questions on the Extra Benefits, call DentaQuest customer service at 1-800-508-6775.
You can also visit us online at www.DentaQuest.com/TXMember.
I. CHIP Member Eligibility and Added Benefits
Eligibility
The Texas HHSC CHIP Dental Programs provide dental coverage for twelve (12) continuous
months for children enrolled.
Verifying Eligibility
Providers may contact: https://www.yourtexasbenefits.com/
Eligibility is determined by the HHSC. CHIP Children who enroll in Texas CHIP Dental Services
receive twelve (12) months of continuous coverage. Families must re‐enroll their children every
twelve (12) months.
*This site is only to verify Member eligibility, not Main Dental Home assignment.
If Members have questions regarding enrolling in the program or their loss of eligibility, they
should be referred to the Enrollment Broker at 1‐800‐964‐2777.
Main Dental Home Verification
Main Dental Home assignment must be verified on the DentaQuest Provider Web Portal (located
in the “Providers Only” section of DentaQuest’s website at www.dentaquest.com). You may also
contact DentaQuest’s Customer Service Department at 1‐800‐896‐2374 to verify
Main Dental
Home assignment.
DentaQuest CHIP Identification Card
Members will receive a DentaQuest TX CHIP ID Card. Participating Providers are responsible for
verifying that Members are eligible at the time services are rendered and to determine if
Members have other health insurance.
Please note that due to possible eligibility status changes, this information does not guarantee
payment and is subject to change without notice.
Sample of the DentaQuest USA CHIP Dental Program ID card:
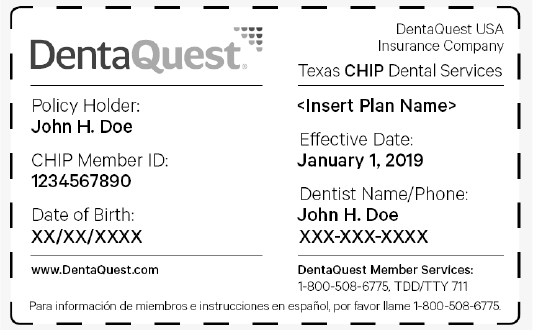
61
DentaQuest USA Insurance Company
DentaQuest USA Insurance Company, Inc February 1, 2024
Current Dental Terminology © American Dental Association. All Rights Reserved.
DentaQuest recommends that each dental office make a photocopy of the Member’s
identification card each time treatment is provided. It is important to note that the
identification
card is not dated and it does not need to be returned should a Member lose eligibility. Therefore,
an identification card in itself does not guarantee that a person is
currently enrolled in the
Texas CHIP Dental Program.
DentaQuest recommends that providers verify Main Dental Home assignment on the Provider
Web Portal prior to treatment, as the Member’s assignment may have changed or the Member
may be using an old card.
Re‐enrollment
Families must re‐enroll their children in the CHIP Dental Program every twelve (12) months.
Disenrollment
Can DentaQuest ask that my child get dropped from their dental plan?
DentaQuest can ask that a child be removed from their plan for the following reasons:
• The child or the child’s caregiver misuses the child’s Membership card or loans
it to another person.
• The child or the child’s caregiver is disruptive, unruly, or uncooperative at the
dentist’s office.
• The child or the child’s caregiver refuses to follow the dental plan’s rules and
restrictions.
Neither DentaQuest nor a provider may request a disenrollment based on an adverse change in
the Member’s health or the utilization of services which are medically necessary for the
treatment of a Member’s condition.
A provider cannot take retaliatory action against a Member.
CHIP Plan Changes
62
DentaQuest USA Insurance Company
DentaQuest USA Insurance Company, Inc February 1, 2024
Current Dental Terminology © American Dental Association. All Rights Reserved.
If the child has been in a CHIP dental plan less than 90 days, they can change dental plans. Call
CHIP toll‐free at 1‐800‐647‐6558.
Members are allowed to make plan changes under the following circumstances:
• For any reason within 90 Days of enrollment in CHIP;
• For cause at any time; and
• During the annual re‐enrollment period.
The Member’s child cannot change dental plans after being in the plan ninety (90) days unless
their child is granted an exception for a “good cause.” The Member also cannot change dental
plans if their child has reached his or her annual dental benefit limit. HHSC will make the final
decision.
CHIP Added Benefits
CHIP Member Value Added Services
Free Dental Care Kit for Child and Parent
Get off to the right start by receiving a preventative dental service within 180 days of when you sign up
with us. When you do, you can get one zippered backpack and a dental kit that includes a toothbrush,
a tube of toothpaste and a brushing chart and stickers. We will also include a spinning toothbrush, a
timer and floss for the parent. That way, you can brush along with your child! One reward per eligible
member, per lifetime.
Walmart Gift Card for Preventive Visit
You can also get a $25 OTC Network Rewards gift card when your child gets a qualifying Texas Health
Steps dental checkup. OTC Network is the gift card vendor. The OTC Network rewards gift card allows
you to buy eligible products with your rewards card at thousands of participating stores. You can use
the OTC Rewards gift card to buy items such as healthy foods, baby care items and over the counter
health products. For a full list of eligible items and participating retailers, visit
SpeakBenefits.com/Dental. One gift card per eligible member, per lifetime.
Additional value‐added services:
Members
6 months – 6 years
There is treatment that can fix some cavities with no drilling.
This treatment is not normally covered under the Medicaid &
CHIP programs. If your dentist says you need it to protect you
from cavities, you can get it at no cost. Must be prescribed by
Main Dentist.
Other limitations may apply, please discuss with your
Main Dentist.
Members who have follow-up care
with their Main Dentist after
visiting the ER for dental care.
Eligible Members may receive one $10 OTC Network rewards
gift card for taking the following steps if they have had to visit a
hospital emergency room for dental care.
• Have a follow-up visit with their Main Dentist within
30 days of visiting the emergency room for a dental
related issue.
63
DentaQuest USA Insurance Company
DentaQuest USA Insurance Company, Inc February 1, 2024
Current Dental Terminology © American Dental Association. All Rights Reserved.
• Complete the quiz and submit to DentaQuest.
Redemption form & quiz is available on pages 37, 38
and 41 of the Member Handbook, the secure
Member Website at MemberAccess.DentaQuest.com
and online at www.DentaQuest.com/TXMember.
* One dental care kit per eligible member, per lifetime.
Here’s what you need to do to get your $25 OTC Network Rewards gift card and/or dental kit:
1. Fill out your information on the Extra Benefits redemption form.
2. You can make copies of the Extra Benefits redemption form if you need more than one.
3. Mail the signed form to DentaQuest. You can use the postage-paid envelope included with
the Member Handbook:
DentaQuest
P.O. Box 2906
Milwaukee, WI 53201-2906
If you have questions on the Extra Benefits, call DentaQuest customer service at 1-800-508-6775.
You can also visit us online at www.DentaQuest.com/TXMember.
Member Rights and Responsibilities
**The Member receives the following information as it pertains to Member Rights and
Responsibilities:
CHILDREN’S MEDICAID DENTAL SERVICES MEMBER RIGHTS AND RESPONSIBILITES
MEMBER RIGHTS
1. You have the right to respect, dignity, privacy, confidentiality and nondiscrimination. That
includes the right to:
a. Be treated fairly and with respect.
b. Know that your dental records and discussions with your dentists will be kept
private and confidential.
2. You have the right to a reasonable opportunity to choose a dental plan and dentist. You
have the right to change to another plan or dentist in a reasonably easy manner. That
includes the right to:
a. Be told how to choose and change your dental plan and dentist.
b. Choose any dental plan you want that is available in their area and choose your
dentist from that plan.
c. Change your dentist.
64
DentaQuest USA Insurance Company
DentaQuest USA Insurance Company, Inc February 1, 2024
Current Dental Terminology © American Dental Association. All Rights Reserved.
d. Change your dental plan without penalty.
e. Be told how to change your dental plan or your dentist.
3. You have the right to ask questions and get answers about anything that you do not
understand. That includes the right to:
a. Have your dentist explain your dental care needs to you and talk to the dentist
about the different ways your dental care problems can be treated.
b. Be told why care or services were denied and not given.
4. You have the right to agree to or refuse treatment and actively participate in treatment
decisions. That includes the right to:
a. Work as part of a team with your dentist in deciding what dental care is best for
you.
b. Say yes or no to the care recommended by your dentist.
5. You have the right to use each available complaint and appeal process through
DentaQuest and through Medicaid, and get a timely response to complaints, appeals,
External Medical Reviews and State Fair Hearings. That includes the right to:
a. Make a complaint to DentaQuest or to the state Medicaid program about your
dental care, your dentist or your dental plan.
b. MDCP/DBMD escalation help line for Members receiving Waiver services via the
Medically Dependent Children Program or Deaf/Blind Multi-Disability Program
c. Get a timely answer to your complaint.
d. Use DentaQuest’s appeal process and be told how to use it.
e. Ask for an External Medical Review and State Fair Hearing from the state Medicaid
program and get information about how that process works.
f. Ask for a State Fair Hearing without an External Medical Review from the state
Medicaid and receive information about how that process works.
6. You have the right to timely access to care that does not have any communication or
physical access barriers. That includes the right to:
a. Have telephone access to a dental professional 24 hours a day, 7 days a week to
get any emergency or urgent care that you need.
b. Get dental care in a timely manner.
c. Be able to get in and out of a dental care provider’s office. This includes barrier‐
free access for people with disabilities or other conditions that limit mobility, in
accordance with the Americans with Disabilities Act.
d. Have interpreters, if needed, during appointments with your dentist and when
talking to your dental plan. Interpreters include people who can speak in your
native language, help someone with a disability, or help you understand the
information.
65
DentaQuest USA Insurance Company
DentaQuest USA Insurance Company, Inc February 1, 2024
Current Dental Terminology © American Dental Association. All Rights Reserved.
e. Be given information you can understand about DentaQuest plan rules, including
the dental care services that you can get and how to get them.
7. You have the right to not be restrained or secluded when it is for someone else’s
convenience, or is meant to force you to do something that you do not want to do, or is
to punish you.
8. You have a right to know that dentists, hospitals, and others who care for you can advise
you about your health status, dental care, and treatment. Before any medically necessary
dental services and treatment begin, the services and treatment must be fully explained
to you and you must give permission in writing (informed consent). DentaQuest cannot
prevent
the dentists, hospitals, and others who care for you from giving you this
information,
even if the care or treatment is not a covered service.
9. You have a right to know that you are not responsible for paying for covered services.
Dentists, hospitals, and others cannot require you to pay copayments or any other
amounts for covered services.
Medicaid Member Responsibilities
1. You must learn and understand each right you have under the Medicaid program. That
includes the responsibility to:
a. Learn and understand your rights under the Medicaid program.
b. Ask questions if you do not understand your rights.
c. Learn what choices of dental plans are available in your area.
2. You must abide by DentaQuest’s and Medicaid’s policies and procedures. That includes
the responsibility to:
a. Learn and follow DentaQuest’s rules and Medicaid rules.
b. Choose your dental plan and a dentist quickly.
c. Make any changes in your dental plan and dentist in the ways established by
Medicaid and by DentaQuest.
d. Keep your scheduled appointments.
e. Cancel appointments in advance when you cannot keep them.
f. Always contact your dentist first for your non‐emergency dental needs.
g. Be sure that you have approval from your dentist before going to a specialist.
h. Understand when you should and should not go to the emergency room.
3. You must share information about your health with your dentist and learn about service
and treatment options. That includes the responsibility to:
a. Tell your dentist about your health.
b. Talk to your dentist about your dental care needs and ask questions about the
different ways your dental care problems can be treated.
66
DentaQuest USA Insurance Company
DentaQuest USA Insurance Company, Inc February 1, 2024
Current Dental Terminology © American Dental Association. All Rights Reserved.
c. Help your dentist get your dental records.
4. You must be involved in decisions relating to service and treatment options, make
personal choices, and take action to maintain your health. That includes the
responsibility to:
a. Work as a team with your provider in deciding what dental care is best for you.
b. Understand how the things that you do can affect your dental health.
c. Do the best that you can to stay healthy.
d. Treat dentists and staff with respect.
Additional Member Responsibilities while using NEMT Services
1. When requesting NEMT Services, you must provide the information requested by the
person arranging or verifying your transportation.
2. You must follow all rules and regulations affecting your NEMT services.
3. You must return unused advanced funds. You must provide proof that you kept your dental
appointment prior to receiving future advanced funds.
4. You must not verbally, sexually, or physically abuse or harass anyone while requesting or
receiving NEMT services.
5. You must not lose bus tickets or tokens and must return any bus tickets or tokens that you
do not use. You must use the bus tickets o tokens only to go to your dental appointment.
6. You must only use NEMT Services to travel to and from your dental appointments.
7. If you have arranged for an NEMT service but something changes, and you no longer need
the service, you must contact the person who helped you arrange your transportation as
soon as possible.
CHIP DENTAL SERVICES MEMBER RIGHTS AND RESPONSIBILITIES
CHIP Member Rights
1. You have a right to get accurate, easy‐to‐understand information to help you make good
choices about your dentists and other providers.
2. You have a right to know how your dentists are paid. You have a right to know about
what those payments are and how they work.
3. You have a right to know how DentaQuest decides whether a service is covered and/or
medically necessary. You have the right to know about the people at DentaQuest who
decide those things.
4. You have a right to know the names of the dentists and other providers enrolled with
DentaQuest and their addresses.
5. You have a right to pick from a list of dentists that is large enough so that your child can
get the right kind of care when your child needs it.
6. You have the right to take part in all the choices about your child's dental care.
67
DentaQuest USA Insurance Company
DentaQuest USA Insurance Company, Inc February 1, 2024
Current Dental Terminology © American Dental Association. All Rights Reserved.
7. You have the right to speak for your child in all treatment choices.
8. You have the right to get a second opinion from another dentist enrolled with
DentaQuest about what kind of treatment your child needs.
9. You have the right to be treated fairly by DentaQuest, dentists, and other providers.
10. You have the right to talk to your child's dentist and other providers in private, and to
have your child's dental records kept private. You have the right to look over and copy
your child's dental records and to ask for changes to those records.
11. You have a right to know that dentists, hospitals, and others who care for your child can
advise you about your child’s health status, medical care, and treatment. DentaQuest
cannot prevent dentists, hospitals, and others who care for your child from giving you this
information, even if the care or treatment is not a covered service.
12. You have a right to know that you are only responsible for paying allowable copayments
for covered services, up to benefit maximum limits. Dentists, hospitals, and others cannot
require you to pay any other amounts for covered services.

68
DentaQuest USA Insurance Company
DentaQuest USA Insurance Company, Inc February 1, 2024
Current Dental Terminology © American Dental Association. All Rights Reserved.
CHIP Member Responsibilities
The Member and DentaQuest both have an interest in seeing their child's dental health improve.
The Member can help by assuming these responsibilities.
1. The Member must try to follow healthy habits. Encourage their child to stay away from
tobacco, and to eat a healthy diet.
2. The Member must become involved in the dentist’s decisions about their child's
treatments.
3. The Member must work together with DentaQuest’s dentists and other providers to pick
treatments for their child that they have all agreed upon.
4. If the Member has a disagreement with DentaQuest, they must try first to resolve it using
DentaQuest’s complaint process.
5. The Member must learn about what DentaQuest does and does not cover. The Member
must read the Member Handbook to understand how the rules work.
6. If the Member makes an appointment for their child, they must try to get to the dentist's
office on time. If they cannot keep the appointment, they must be sure to call and cancel
it.
7. The Member must report misuse of CHIP by dental and health care providers, other CHIP
Members, DentaQuest, or other CHIP plans.
If you think that you have been treated unfairly or discriminated against, call the U.S.
Department of Health and Human Services (HHS) toll‐free at 1‐800‐368‐1019. The Member can
also view information concerning the HHS Office of Civil Rights online at www.hhs.gov/ocr.
Fraud and Abuse Reporting
Do you want to report Waste, Abuse, or Fraud?
Let us know if you think a doctor, dentist, pharmacist at a drug store, other health care
providers,
or a person getting benefits is doing something wrong. Doing something wrong could be waste,
abuse or fraud, which is against the law. For example, tell us if you think someone is:
• Getting paid for Medicaid and CHIP services that weren’t given or necessary.
• Not telling the truth about a medical condition to get medical treatment.
• Letting someone else use a Medicaid or CHIP Dental ID.
• Using someone else’s Medicaid or CHIP Dental ID.
• Not telling the truth about the amount of money or resources he or she has to get
benefits.

69
DentaQuest USA Insurance Company
DentaQuest USA Insurance Company, Inc February 1, 2024
Current Dental Terminology © American Dental Association. All Rights Reserved.
To report waste, abuse, or fraud, choose one of the following:
• Call the OIG Hotline at 1‐800‐436‐6184 or
• Visit https://oig.hhsc.state.tx.us/ Under the box labeled “I WANT TO” click “Report
Waste, Abuse, and Fraud” to complete the online form.
• You can also report fraud directly to DentaQuest:
DentaQuest‐TX HHSC Dental Services
Attention: Utilization Review Department
P.O. Box 2906
Milwaukee, WI 53201‐2906
Toll‐free at 1‐800‐237‐9139
Providers may also send a fax to: 262‐241‐7366
To report waste, abuse or fraud, gather as much information as possible.
• When reporting about a provider (a doctor, dentist, counselor, etc.) include:
o Name, address, and phone number of provider.
o Name and address of the facility (hospital, nursing home, home health
agency, etc.)
o Medicaid number of the provider and facility, if you have it.
o Type of provider (doctor, dentist, therapist, pharmacist, etc.)
o Names and phone numbers of other witnesses who can help in the
investigation.
o Dates of events.
o Summary of what happened.
• When reporting about someone who gets benefits include:
o The person’s name.
o The person’s date of birth, Social Security number, or case number if you
have it.
o The city where the person lives.
o Specific details about the waste, abuse, or fraud.
J. Medicaid and CHIP Encounter Data, Billing, and Claims
Administration
Where to Send Claims/Encounter Data
DentaQuest receives dental claims in four possible formats. These formats include:
70
DentaQuest USA Insurance Company
DentaQuest USA Insurance Company, Inc February 1, 2024
Current Dental Terminology © American Dental Association. All Rights Reserved.
• Electronic claims via DentaQuest’s website (www.dentaquest.com).
• Electronic submission via clearinghouses.
• HIPAA Compliant 837D File.
• Paper claims (ADA Claim Form 2018, 2019, or newer)
Electronic Claim Submission Utilizing DentaQuest’s Internet Website
Participating Providers may submit claims directly to DentaQuest by utilizing the “Dentist”
section of our website. Submitting claims via the website is very quick and easy. It is especially
easy if you have already accessed the site to check a Member’s eligibility prior to providing the
service.
To submit claims via the website, simply log on to www.dentaquest.com. Once you have
entered
the website, click on the “Dentist” icon. From there choose your “State” and press
“Go”. You will
then be able to log in using your password and ID. First time users will have to register by
utilizing the Business’s TIN, State and Zip Code. DentaQuest should have contacted your office in
regards on how to perform Provider Self Registration Once logged in, select
“Claims/Pre‐
Authorizations” and then “Dental Claim Entry“. The Dentist Portal allows you to attach
electronic files (such as x‐rays in jpeg format, reports and charts) to the claim.
If you have not received instruction on how to complete Provider Self Registration, you can
access the guide at http://www.dentaquest.com/getattachment/State-
Plans/Regions/texas/Dentists-Page/New-Provider-Registration-Tip-Sheet.pdf. If you need further
assistance, please contact DentaQuest’s Customer Service Department at 1‐800‐896‐2374.
For Providers who are unable to submit electronically via the Internet or a clearinghouse,
DentaQuest will work with the Provider to receive their claims electronically via a HIPAA
compliant 837D or 837P file from the Provider’s practice management system. Please contact the
Systems Operations Department at 800‐417‐7140 or via e‐mail at
[email protected] to inquire about this option for electronic claim submission.
Electronic Authorization Submission Utilizing DentaQuest's Internet Website
Participating Providers may submit Pre‐Authorizations directly to DentaQuest by utilizing the
“Dentist” section of our website. Submitting Pre‐Authorizations via the website is very quick and
easy. It is especially easy if you have already accessed the site to check a Member’s
eligibility
prior to providing the service.
To submit pre‐authorizations via the website, simply log on to www.dentaquest.com. Once you
have entered the website, click on the “Dentist” icon. From there choose your ‘State” and press
“Go”. You will then be able to log in using your password and ID. First time users will have to
register by utilizing the Business’s TIN, State and Zip Code. If you have not received instruction on
how to complete Provider Self Registration contact DentaQuest’s Customer Service
Department
at 1‐800‐896‐2374. Once logged in, select “Claims/Pre‐Authorizations” and then “Dental Pre‐
Auth Entry“.
71
DentaQuest USA Insurance Company
DentaQuest USA Insurance Company, Inc February 1, 2024
Current Dental Terminology © American Dental Association. All Rights Reserved.
The Dentist Portal also allows you to attach electronic files (such as x‐rays in jpeg format,
reports
and charts) to the pre‐authorization. Please submit to:
Electronic Claim Submission via Clearinghouse
DentaQuest works directly with Emdeon (1‐888‐255‐7293), Tesia 1‐800‐724‐7240, EDI Health
Group 1‐800‐576‐6412, Secure EDI 1‐877‐466‐9656 and Mercury Data Exchange 1‐866‐633‐
1090, for claim submissions to DentaQuest.
You can contact your software vendor and make certain that they have DentaQuest listed as the
payer and claim mailing address on your electronic claim. Your software vendor will be able
to
provide you with any information you may need to ensure that submitted claims are
forwarded
to DentaQuest. DentaQuest’s Payor ID is CX014.
HIPAA Compliant 837D File
For Providers who are unable to submit electronically via the Internet or a clearinghouse,
DentaQuest will work directly with the Provider to receive their claims electronically via a HIPAA
compliant 837D or 837P file from the Provider’s practice management system. Please
email
[email protected] to inquire about this option for electronic claim submission.
NPI Requirements for Submission of Electronic Claims
In accordance with the HIPAA guidelines, DentaQuest has adopted the following NPI standards in
order to simplify the submission of claims from all of our providers, conform to industry required
standards and increase the accuracy and efficiency of claims administered by DentaQuest.
• Providers must register for the appropriate NPI classification at the following website
https://nppes.cms.hhs.gov/#/ and provide this information to DentaQuest in its
entirety.
• All providers must register for an Individual NPI. You may also be required to register
for a group NPI (or as part of a group) dependant upon your designation.
• When submitting claims to DentaQuest you must submit all forms of NPI properly and
in their entirety for claims to be accepted and processed accurately. If you registered
as part of a group, your claims must be submitted with both the Group and Individual
NPI’s. These numbers are not interchangeable and could cause your claims to be
returned to you as non‐compliant.
• If you are presently submitting claims to DentaQuest through a clearinghouse or
through a direct integration, you need to review your integration to assure that it is in
compliance with the revised HIPAA compliant 837D format. This information can be
found on the 837D Companion Guide located on the Provider Web Portal.
Paper Claim Submission
• Claims must be submitted on 2018, 2019, or later ADA approved claim forms.
72
DentaQuest USA Insurance Company
DentaQuest USA Insurance Company, Inc February 1, 2024
Current Dental Terminology © American Dental Association. All Rights Reserved.
• Member name, identification number, and date of birth must be listed on all claims
submitted. If the Member identification number is missing or miscoded on the claim
form, the patient cannot be identified. This could result in the claim being returned to
the submitting Provider office, causing a delay in payment.
• The paper claim must contain an acceptable Provider signature.
• The Provider and office location information must be clearly identified on the claim.
Frequently, if only the dentist signature is used for identification, the dentist’s name
cannot be clearly identified. Please include either a typed dentist (practice) name or the
DentaQuest Provider identification number.
• The paper claim form must contain a valid provider NPI (National Provider
Identification)
number. In the event of not having this box on the claim form, the NPI
must still be
included on the form. The ADA claim form only supplies two (2) fields to enter NPI. On
paper claims, the Type 2 NPI identifies the payee, and may be submitted in conjunction
with a Type 1 NPI to identify the dentist who provided the treatment. For example, on a
standard ADA Dental Claim Form, the treating dentist’s NPI is entered in field 54 and the
billing entity’s NPI is entered in field 49.
• The date of service must be provided on the claim form for each service line submitted.
• Approved ADA dental codes as published in the current CDT book or as defined in this
manual must be used to define all services.
• List all quadrants, tooth numbers and surfaces for dental codes that necessitate
identification (extractions, root canals, amalgams and resin fillings). Missing tooth and
surface identification codes can result in the delay or denial of claim payment.
• Affix the proper postage when mailing bulk documentation. DentaQuest does not accept
postage due mail. This mail will be returned to the sender and will result in delay of
payment.
Claims should be mailed to the following address:
DentaQuest‐ TX HHSC Dental Program
P.O. Box 2906
Milwaukee, WI 53201‐2906
For questions, providers may contact DentaQuest Provider Services at 1‐800‐896‐2374.
Coordination of Benefits (COB)
The TX HHSC Medicaid/CHIP Dental Program/DentaQuest is the payer of last resort. Providers
should ask Members if they have other dental insurance coverage at the time of their
appointment. When TX HHSC Medicaid/CHIP Dental Program/DentaQuest is the secondary
insurance carrier, a copy of the primary carrier's Explanation of Benefits (EOB) must be
submitted with the claim. For electronic claim submissions, the payment made by the primary
73
DentaQuest USA Insurance Company
DentaQuest USA Insurance Company, Inc February 1, 2024
Current Dental Terminology © American Dental Association. All Rights Reserved.
carrier must be indicated in the appropriate COB field. When a primary carrier's payment meets
or exceeds the HHSC Dental Services Program’s fee schedule, DentaQuest will consider the
claim
paid in full and no further payment will be made on the claim.
Receipt and Audit of Claims
In order to ensure timely, accurate remittances to each participating Provider, DentaQuest
performs an audit of all claims upon receipt. This audit validates Member eligibility, procedure
codes and dentist identifying information. A DentaQuest Customer Contact Center
Representative analyzes any claim conditions that would result in non‐payment. When
potential
problems are identified, your office may be contacted and asked to assist in resolving this
problem. Please contact our Customer Service department at 1‐800‐896‐2374 with any
questions you may have regarding claim submission or your remittance.
Each DentaQuest Provider office receives an “Explanation of Benefit” report with their
remittance. This report includes patient information and an allowable fee by date of service for
each service rendered.
Second Opinion Reviews and Regional Screening
DentaQuest may request a clinical evaluation by a regional dental consultant who conducts
clinical examinations, prepares objective reports of dental conditions and evaluates treatment
that is proposed or has been provided for the purpose of providing DentaQuest with a second
opinion.
A second opinion may be required prior to treatment when necessary to make a benefit
determination. Authorization for second opinions after treatment can be made if a Member has
a complaint regarding the quality of care provided. The Member and the treating dentist will be
notified when a second opinion is necessary and appropriate. When a second opinion is
authorized through a regional dental consultant, all charges will be paid by DentaQuest.
Members may otherwise obtain a second opinion about treatment from any contracting dentist
they choose, and claims for the examination or consultation may be submitted for payment.
Such claims will be paid in accordance with the benefits of the program.
Form to Use
Claims must be submitted on a 2018, 2019, or later approved ADA claim form. Please see
Appendix B
Forms to Use for an ADA claim form.
CHIP Cost Sharing Schedule
CHIP Members are subject to cost sharing and are charged co‐pay for each non‐preventive
office
visit (Medicaid Members are not required to pay a co‐payment). DentaQuest will deduct the
required co‐pay from the claim payment. It is the responsibility of the provider to collect the co‐
pay from the Member at the time of visit.
74
DentaQuest USA Insurance Company
DentaQuest USA Insurance Company, Inc February 1, 2024
Current Dental Terminology © American Dental Association. All Rights Reserved.
CHIP Cost Sharing
blank
Effective January
1,
2014**
Enrollment Fees (for 12 month enrollment
period):
Charge
At of Below 151% of FPL*
$0
Above 151% up to and including 186% of FPL
$35
Above 186% up to and including 201% of FPL
$50
Co‐Pays (per visit):
At or below 151% FPL
Charge
Office Visit (non‐preventive)
$5
Non‐Emergency ER
$5
Generic Drug
$0
Brand Drug
$5
Facility Co‐pay, Inpatient (per admission)
$35
Cost‐sharing Cap
5% (of family's
income)**
Above 151% up to and including 186% FPL
Charge
Office Visit (non‐preventative)
$20
Non‐Emergency ER
$75
Generic Drug
$10
Brand Drug
$35
Facility Co‐pay, Inpatient (per admission)
$75
Cost‐sharing Cap
5% (of family's
income)**
Above 186% up to and including 201% FPL
Charge
Office Visit (non‐preventative)
$25
Non‐Emergency ER
$75
Generic Drug
$10
Brand Drug
$35
Facility Co‐pay, Inpatient (per admission)
$125
Cost‐sharing Cap
5% (of family's
income)**
*The federal poverty level (FPL) refers to income guidelines established annually by the federal
government.
** Per 12‐month term of coverage.
Provider shall render to Members all Covered Services and continue to provide Covered
Services
to Members. After the date of termination from participation, upon the request of DentaQuest,
Provider shall continue to provide Covered Services to Members for a period not to exceed
ninety (90) days during which time payment will be made pursuant to the
DentaQuest Provider
Contract.
75
DentaQuest USA Insurance Company
DentaQuest USA Insurance Company, Inc February 1, 2024
Current Dental Terminology © American Dental Association. All Rights Reserved.
Please refer to the DentaQuest TX Provider Contract for more information regarding
termination.
No Co‐Payments for Medicaid Members
Medicaid Members are not to be charged a co‐payment for dental services.
Billing Members
Member Acknowledgement Statement
Participating Providers shall hold Members, DentaQuest, and HHSC harmless for the payment
of
non‐Covered Services except as provided in this paragraph. A provider may charge an eligible
Medicaid/CHIP HHSC Dental Program Member for dental services which are non‐covered
services. These services must be identifiable by specific CDT code. A provider may bill a Member
for non‐Covered Services if the Provider obtains a written waiver from the Member
prior to
rendering such service that indicates:
• The services to be provided.
• DentaQuest and HHSC will not pay for or be liable for said services.
• Member will be financially liable for such services.
Please note that prior authorization may be requested for non‐covered services for eligible
Medicaid Members under age 21. Documentation of medical necessity must be submitted with
this request. This documentation may include radiographs, treatment plan, and/or a narrative
from the provider.
Private Pay Form Agreement
Please use the Non‐Covered Service Disclosure form located in the Appendix.
Time Limit for Submission of Claims/Claims Appeals
DentaQuest must receive your claim requesting payment of services within ninety‐five (95) days
from the date of service.
Any claim submitted beyond the timely filing limit will be denied for "untimely filing." If a claim is
denied for "untimely filing" the Member cannot be billed. If TX HHSC Dental
Program/DentaQuest is the secondary carrier, the timely filing limit begins with the date of
payment or denial from the primary carrier.
For appealed claims, Providers must submit all appeals of denied claims and requests for
adjustments on paid claims within one hundred and twenty (120) days from the date of
disposition of the Explanation of Benefits (EOB) on which that claim appeared.

76
DentaQuest USA Insurance Company
DentaQuest USA Insurance Company, Inc February 1, 2024
Current Dental Terminology © American Dental Association. All Rights Reserved.
Claims Payment
• Clean Claim payment must be made by DentaQuest within thirty (30) days.
• DentaQuest must receive your claim requesting payment of services within ninety‐five
(95) days from the date of service.
• Claims must be submitted on a 2018, 2019, or later approved ADA claim form.
• For Claims Questions, please send an email to: [email protected]
Or call our Provider Hotline at:
1‐800‐896‐2374
Or Fax Claims/payment issues to:
262‐241‐7379
• For Claims Appeals, please send to:
DentaQuest TX HHSC Dental Services
Complaints and Grievances - Appeals
P.O. Box 2906 Milwaukee,
WI 53201‐2906
• For Peer to Peer Review, please call our Provider Services line during regular business
hours:
1‐800‐896‐2374
K. Medicaid and CHIP Special Access Requirements
Interpreter/Translation Services
DentaQuest is committed to ensuring that staff and subcontractors are educated about, remain
aware of, and are sensitive to the linguistic needs and cultural differences of its Members. In
order to meet this need, DentaQuest provides or coordinates the following:
• Member Services and our Member Advocate department are staffed with Spanish and
English bilingual specialists.
• A Member may request a telephonic interpreter or a face‐to‐face interpreter through
our Member Services Department
TDD access for Members who are hearing impaired: 7-1-1
DentaQuest Member Services and health education materials are available in English and
Spanish.
77
DentaQuest USA Insurance Company
DentaQuest USA Insurance Company, Inc February 1, 2024
Current Dental Terminology © American Dental Association. All Rights Reserved.
Dental Contractor/Provider Coordination
DentaQuest is committed to ongoing coordination with Texas Medicaid and CHIP Dental Services
providers and Members to ensure high quality dental care. We refer Members to contracted
dentists for covered services and provide coordination of non‐capitated services.
Coordination of care includes:
• Identifying providers of medically necessary dental services.
• Assisting Members in accessing medically necessary dental services.
DentaQuest is available for ongoing coordination with providers via our Provider Hotline, on‐
going provider training, Provider Relations Representatives, and Case Management staff. Also,
our Member Advocates are available to coordinate care with providers to ensure Members
with
special health care needs receive services.
Reading/Grade Level Consideration
An estimated 40–44 million Americans are functionally illiterate and another 50 million are only
marginally literate. Nearly half of the functionally illiterate live in poverty and one‐fourth report
physical, mental or health conditions that prevent them from participating fully in work, school
or housework. A study of Members at two public hospitals found that 35 percent of the English‐
speaking and 62 percent of the Spanish‐speaking Members had inadequate or marginal
functional health literacy, with more than 81 percent of the elderly groups having limited health
literacy. Because of this, DentaQuest understands that many of our Members may have limited
ability to understand and read instructions. Yet, most people with literacy problems are
ashamed
and will try to hide them from Providers. Low literacy can mean that your patient may
not be
able to comply with your medical advice and course of treatment because they do not
understand your instructions. Member materials should be written at a fourth to sixth grade
reading level. The guidelines provided for communication with interpreters are also good
guidelines for communicating with Members with limited literacy, especially asking the
Member
to repeat your instructions. Do not assume that the Member will be able to read
instructions or a
drawing/diagram for taking prescription medicines or understanding of treatment. Above all
else, be sensitive to the embarrassment the Member may feel about limited literacy. Please
contact us for interpretation services should there be a language barrier.
Cultural Sensitivity
DentaQuest places great emphasis on the wellness of its Members. A large part of quality health
care delivery is treating the whole patient and not just the medical condition. Sensitivity to
differing cultural influences, beliefs and backgrounds, can improve a Provider’s relationship with
Members and in the long run the health and wellness of the Members themselves.
Following is a list of principles for health care Providers, to include knowledge, skills and
attitudes, related to cultural competency in the delivery of health care services to DentaQuest
Members:
78
DentaQuest USA Insurance Company
DentaQuest USA Insurance Company, Inc February 1, 2024
Current Dental Terminology © American Dental Association. All Rights Reserved.
Knowledge
• Provider’s self‐understanding of race, ethnicity and influence.
• Understanding of the historical factors which impact the health of minority populations,
such as racism and immigration patterns.
• Understanding of the particular psycho‐social stressors relevant to minority Members
including war trauma, migration, acculturation stress, socioeconomic status.
• Understanding of the cultural differences within minority groups.
• Understanding of the minority patient within a family life cycle and intergenerational
conceptual framework in addition to a personal developmental network.
• Understanding of the differences between "culturally acceptable" behavior of psycho‐
pathological characteristics of different minority groups.
• Understanding indigenous healing practices and the role of religion in the treatment of
minority Members.
• Understanding of the cultural beliefs of health and help seeking patterns of minority
Members.
• Understanding of the health service resources for minority Members.
• Understanding of the public health policies and its impact on minority Members and
communities.
Skills
• Ability to interview and assess minority Members based on a psychological/social/
biological/ cultural/ political/ spiritual model.
• Ability to communicate effectively with the use of cross cultural interpreters.
• Ability to diagnose minority Members with an understanding of cultural differences in
pathology.
• Ability to avoid under diagnosis or over diagnosis.
• Ability to formulate treatment plans that are culturally sensitive to the patient and
family's concept of health and illness.
• Ability to utilize community resources (church, community‐based organizations (CBOs),
self‐help groups).
• Ability to ask for consultation.
Attitudes
• Respect the "survival merits" of immigrants and refugees.
• Respect the importance of cultural forces.
• Respect the holistic view of health and illness.

79
DentaQuest USA Insurance Company
DentaQuest USA Insurance Company, Inc February 1, 2024
Current Dental Terminology © American Dental Association. All Rights Reserved.
• Respect the importance of spiritual beliefs.
• Respect and appreciate the skills and contributions of other professional and
paraprofessional disciplines.
• Be aware of transference and counter transference issues.
DentaQuest encourages and advocates for providers to provide culturally competent care for its
Members. Providers are also encouraged to participate in training provided by other
organizations. You can visit Physician's Site (hhs.gov) for an online training course developed by
the U.S. Department of Health & Human Services and earn CEU and/or CME credits.
Specialty Health Care Needs
Special Health Care Needs are defined as any medically compromising condition that may affect
the provision of dental treatment. DentaQuest’s Member Advocates serve as a liaison between
Members with special health care needs, their dental providers, and when needed, their
medical
providers. A DentaQuest contracted provider may contact our Member or Provider
Hotline to
facilitate services for Texas Medicaid and CHIP Members whose medical conditions classify them
as special needs Members. The Member Advocates will ensure that Members
with special health
care needs have direct access to specialist providers as appropriate to their condition and
identified health needs (e.g., a standing referral to a specialty physician).
L. DentaQuest Information
Standard of Care
All covered dental services shall be provided according to generally accepted standards of
dentistry prevailing in the professional community at the time of treatment. Contracting dentists
are required to integrate specialty care into the Member’s course of dental treatment
by making
timely referrals to a specialist when necessary or appropriate. Contracting dentists may not
impose any limitations on the acceptance or treatment of Texas Medicaid or CHIP
Dental
Services Members not imposed on other Members. The dentist is required to maintain the
dentist/patient relationship with the Texas Medicaid or CHIP Dental Services Member and shall
be solely responsible to the Member for dental advice and treatment.
DentaQuest communicated information on October 29, 2018 regarding the standard of care
review that will be effective February 1, 2019 for restorations repeated within 36 months. As a
follow-up, DentaQuest would like to provide the process steps that providers must take to
ensure services are reviewed and considered for reimbursement.
Any restoration that meets the criteria below will be reviewed for standard of care to ensure the
services are medically necessary for the member. Please follow one of the processes outlined
below for consideration of the service:
Identical Restoration: (same tooth, exact same service), same provider or location (Prior
Authorization or Pre-Payment Review)
80
DentaQuest USA Insurance Company
DentaQuest USA Insurance Company, Inc February 1, 2024
Current Dental Terminology © American Dental Association. All Rights Reserved.
Codes: D2140, D2150, D2160, D2161, D2330, D2331, D2332, D2335, D2391, D2392, D2393,
D2394
Prior Authorization
1. Prior Authorization must be submitted for review prior to service being performed
2. Documentation must clearly support medical necessity (x-rays, narrative, photos…etc.)
3. Any claim submitted that does not have an approved Prior Authorization and does not
have Exception written in Box 35 (comments) will be denied
Pre-Payment Review
1. Services may be submitted using the pre-payment review process. This means that all
documentation must be submitted with the claim
2. Documentation must clearly support medical necessity (x-rays, narrative, photos…etc.)
3. The word “Exception” must be placed in Box 35 (comments) section of the claim
4. Any claim submitted that does not meet the pre-payment review requirements listed in
#2 and #3 will not be reviewed for consideration.
Similar Restoration: (same tooth, at least one surface repeated), same provider or location
(Prior Authorization or Pre-Payment Review)
Codes: D2140, D2150, D2160, D2161, D2330, D2331, D2332, D2335, D2391, D2392, D2393,
D2394
Prior Authorization
1. Prior Authorization may be submitted for review prior to service being performed
2. Documentation must clearly support medical necessity (x-rays, narrative, photos…etc.)
3. If Prior Authorization is approved, claim may be submitted for reimbursement
consideration
Pre-Payment Review
1. Services may be submitted using the pre-payment review process. This means that all
documentation must be submitted with the claim
2. Documentation must clearly support medical necessity (x-rays, narrative, photos…etc.)
3. The word “Exception” must be placed in Box 35 (comments) section of the claim
4. Any claim submitted that does not meet the pre-payment review requirements listed in
#2 and #3 will not be reviewed for consideration
Numerous studies on restorations, including appropriateness, materials and longevity have been
researched. For your review, the following may be of interest.
https://jada.ada.org/article/S0002-8177(14)62395-3/abstract

81
DentaQuest USA Insurance Company
DentaQuest USA Insurance Company, Inc February 1, 2024
Current Dental Terminology © American Dental Association. All Rights Reserved.
http://www.aapd.org/media/Policies_Guidelines/G_Restorative.pdf
If you have any questions or need assistance, please contact your Regional Provider Relations
Representative.
Provider Preventable Conditions
Provider-preventable condition” has the same meaning as “provider-preventable condition”
provided in 42 C.F.R. 447.26 and includes the following events: the wrong surgical or other
invasive procedure performed on a Dental Member; surgical or other invasive procedure
performed on the wrong tooth; or surgical or other invasive procedure performed on the wrong
patient. For purposes of this term, most dental procedures, other than preventative procedures,
will be considered “invasive.
DentaQuest must not pay for Provider-preventable conditions. DentaQuest must ensure its
Provider Contracts contain language requiring Providers to report to DentaQuest the following
events: the wrong surgical or other invasive procedure performed on a Dental Member; surgical
or other invasive procedure performed on the wrong tooth; or surgical or other invasive
procedure performed on the wrong patient. DentaQuest must also submit quarterly reports of
Provider-preventable conditions to the HHSC health plan monitoring team and the HHSC Dental
Director.
Professional Conduct
While performing the services described in the Network Provider contract, the network
Provider agrees to:
• Comply with applicable state laws, rules, and regulations and HHSC’s requests regarding
personal and professional conduct generally applicable to the service locations.
• Otherwise conduct themselves in a businesslike and professional manner.
Credentialing (Policies PEC Series)
Every plan requires that DentaQuest credential providers. DentaQuest’s credentialing
process adheres to National Committee for Quality Assurance (NCQA), Utilization Review
Accreditation Commission (URAC), and program requirements.
DentaQuest, in conjunction with the program, has the sole right to determine which dentists (DDS
or DMD); it shall accept and continue as Participating Providers. The purpose of DentaQuest’s
credentialing policies and procedures is to provide a general guide for the acceptance, discipline,
and termination of Participating Providers. DentaQuest reviews each Participating Provider’s
practice history including, but not limited to, license actions, quality of care issues, and any history
of criminal conduct, when making credentialing decisions.

82
DentaQuest USA Insurance Company
DentaQuest USA Insurance Company, Inc February 1, 2024
Current Dental Terminology © American Dental Association. All Rights Reserved.
Nothing in this Office Reference Manual or DentaQuest’s credentialing policies and procedures
limits DentaQuest’s sole discretion to accept and discipline Participating Providers, including the
right to restrict or suspend a Participating Provider’s network participation.
Credentials Committee Denials (Policy PEC01)
If a provider’s application to be a Participating Provider has been denied by DentaQuest’s
Credentials Committee, the provider must wait twelve (12) months from the date of his or her
denial letter to reapply for participation in the network.
Recredentialing (Policy PEC01)
All actively participating providers must be reviewed every thirty-six (36) months from the date of
their previous credentialing actions.
Disciplinary Actions, Corrective Action Plans & Provider Appeals (Policy PEC05)
This policy includes actions which may be taken by DentaQuest in the event of quality of care
issues, noncompliance with program requirements, or failure to adhere to DentaQuest’s policies
and procedures by Participating Providers.
Appeal of Credentials Committee Termination (Policy PEC05)
If the Credentials Committee terminates a Participating Provider from network participation, the
Committee will offer the provider an opportunity to appeal the termination. The provider must
request an appeal in writing and the request must be received by DentaQuest within thirty (30)
days of the date the Committee gave notice of its decision to the provider. If the Credentials
Committee decides to uphold a Participating Provider’s termination on appeal, the Participating
Provider must wait twelve (12) months from the date of his or her decision letter to reapply for
participation in the network.
Note: The aforementioned policies are available upon request by emailing
Broken Appointments – Best Practices
Broken appointments are a concern for the Texas HHSC Medicaid and CHIP Dental Program and
DentaQuest. We recognize that broken appointments are a costly and unnecessary expense for
Providers. Our goal is to remove any barriers that prevent dentists from participating in the HHSC
Medicaid and CHIP Dental Program as well as barriers that prevent our Members from
utilizing
83
DentaQuest USA Insurance Company
DentaQuest USA Insurance Company, Inc February 1, 2024
Current Dental Terminology © American Dental Association. All Rights Reserved.
their benefits.
As a result of feedback, we have received from dentists in the community, we have developed
several Broken Appointment Best Practice guidelines. We encourage you to implement these
practices in your office.
The following list contains office policies which have helped to reduce broken appointments
and the effects of broken appointments in other dental practices.
• Confirm appointments after hours when the patient is likely to be home to answer
the
call.
• Confirm all appointments, including recall and hygiene appointments, the day before
the
appointment.
• Consider telling Members they must confirm their own appointment the day before
the
visit, or their appointment slot will be lost.
• Continuing care appointments made for three (3) to six (6) months ahead should be
reserved for Members of record with no history of broken appointments.
• Members with a history of broken appointments or Members that did not schedule a
continuing care appointment, should receive a postcard asking them to call to schedule
an appointment.
• Many emergency Members will not keep future appointments if scheduled on the
day of
emergency treatment. These Members should be called later during the week
to
schedule follow‐up treatment.
• When a procedure needs to be completed at a subsequent appointment, send
information home with Members about that next appointment. The information should
stress the importance of such a procedure and indicate possible outcomes if it is not
completed within the designated timeframe.
• Maintain a list of Members that can be contacted to come in on short notice; this will
allow you to fill gaps when late notice cancellations occur.
• Many Members cite daytime obligations such as work or childcare as significant
contributing factors to missing appointments. Having extended hours on selected
days of
the week or occasional weekend hours can alleviate this barrier to accessing dental care.
Logging Broken Appointments in the Provider Web Portal
Entering a Member’s broken appointment is an easy alternative to faxing broken appointment
information to DentaQuest. By using the Broken Appointment tool, providers and office staff can
enter the date and reason for the broken appointments or view a list of missed appointments.
The Broken Appointment page is comprised of 2 sections:
• Add Broken Appointment: This is where you add a Member’s broken (missed)
appointment.

84
DentaQuest USA Insurance Company
DentaQuest USA Insurance Company, Inc February 1, 2024
Current Dental Terminology © American Dental Association. All Rights Reserved.
• Broken Appointment History: In this section, you can view a list of all missed
appointments of a specific Member.
Direct Deposit
As a benefit to participating Providers, DentaQuest offers Electronic Funds Transfer (Direct
Deposit) for claims payments. This process improves payment turnaround times as funds are
directly deposited into the Provider’s banking account.
To receive claims payments through the Direct Deposit Program, Providers must:
• Complete and sign the Direct Deposit Authorization Form (see Attachment A‐22)
• Attach a voided check to the form. The authorization cannot be processed without a
voided check.
• Return the Direct Deposit Authorization Form and voided check to DentaQuest.
▪ Via Fax – 262‐241‐4077
▪ Via Mail – DentaQuest TX HHSC Dental Program
P.O. Box 2906
Milwaukee, WI 53201‐2906
ATTN: Provider Enrollment Department
The Direct Deposit Authorization Form must be legible to prevent delays in processing. Providers
should allow up to six weeks for the Direct Deposit Program to be implemented after
the receipt
of completed paperwork. Providers will receive a bank note one check cycle prior to the first
Direct Deposit payment.
Providers enrolled in the Direct Deposit process must notify DentaQuest of any changes to bank
accounts such as: changes in routing or account numbers, or a switch to a different bank. All
changes must be submitted via the Direct Deposit Authorization Form. Changes to bank accounts
or banking information typically take 2 ‐3 weeks. DentaQuest is not responsible for delays in
funding if Providers do not properly notify DentaQuest in writing of any banking changes.
Providers enrolled in the Direct Deposit Program are required to access their remittance
statements online and will no longer receive paper remittance statements. Electronic remittance
statements are located on DentaQuest’s Provider Web Portal (PWP). Providers may
access their
remittance statements by following these steps:
1. Login to the Provider Web Portal at www.dentaquest.com
2. Once you have entered the website, click on the “Dentist” icon. From there choose your
“State” and press “Go”.
3. Log in using your password and ID
4. Once logged in, select “Claims/Pre‐Authorizations” and then “Remittance Advice
Search“.
5. The remittance will display on the screen.
85
DentaQuest USA Insurance Company
DentaQuest USA Insurance Company, Inc February 1, 2024
Current Dental Terminology © American Dental Association. All Rights Reserved.
Advance Directives
Federal and state law require providers to maintain written policies and procedures for
informing and providing written information to all adult members who are 18 years of age and
older about their rights under state and federal law, in advance of their receiving care (Social
Security Act §§1902[a][57] and 1903[m][1][A]). The written policies and procedures must contain
procedures for providing written information regarding the member’s right to refuse,
withhold,
or withdraw medical treatment advance directives.
These policies and procedures must comply with provisions contained in 42 Code of Federal
Regulations (CFR) §§434.28 and 489, SubPart I, relating to the following state laws and rules:
• A member’s right to self‐determination in making health‐care decisions.
• The Advance Directives Act, Chapter 166, Texas Health and Safety Code, which includes:
o A member’s right to execute an advance written directive to physicians and family
or surrogates, or to make a non‐written directive to administer, withhold or
withdraw life‐sustaining treatment in the event of a terminal or irreversible
condition.
o A member’s right to make written and non‐written Out‐of‐Hospital Do‐Not‐
Resuscitate Orders.
o A member’s right to execute a Medical Power of Attorney to appoint an agent to
make health‐care decisions on the member’s behalf if the member becomes
incompetent.
The Declaration for Mental Health Treatment, Chapter 137, Texas Civil Practice and Remedies
Code, which includes a Member’s right to execute a Declaration for Mental Health Treatment in a
document making a declaration of preferences or instructions regarding mental health
treatment.
These policies can include a clear and precise statement of limitation if a participating provider
cannot or will not implement a member’s advance directive. A statement of limitation on
implementing a member’s advance directive should include at least the following information:
• A clarification of the provider’s conscience objections.
• Identification of the state legal authority permitting a provider’s conscience objections to
carrying out an advance directive.
• A description of the range of medical conditions or procedures affected by the
conscience
objection.
• A provider cannot require a member to execute or issue an advance directive as a
condition for receiving health‐care services.
• A provider cannot discriminate against a member based on whether or not the member
has executed or issued an advance directive.
• A provider’s policies and procedures must require the provider to comply with the
requirements of state and federal law relating to advance directives.
86
DentaQuest USA Insurance Company
DentaQuest USA Insurance Company, Inc February 1, 2024
Current Dental Terminology © American Dental Association. All Rights Reserved.
Clinical Criteria
The criteria outlined in DentaQuest’s Provider Office Reference Manual are based around
procedure codes as defined in the American Dental Association’s Code Manuals.
Documentation requests for information regarding treatment using these codes are
determined
by generally accepted dental standards for authorization, such as radiographs, periodontal
charting, treatment plans, or descriptive narratives. In some instances, the State
legislature will
define the requirements for dental procedures.
These criteria were formulated from information gathered from practicing dentists, dental
schools, ADA clinical articles and guidelines, insurance companies, as well as other dental related
organizations. These criteria and policies must meet and satisfy specific State and Program
requirements as well. They are designed as guidelines for authorization and payment
decisions
and are not intended to be all
‐
inclusive or absolute. Additional narrative information is
appreciated when there may be a special situation.
For all procedures, every Provider in the DentaQuest program is subject to random chart audits.
Providers are required to comply with any request for records. These Audits may occur in the
Provider’s office as well as in the office of DentaQuest. The Provider will be notified in writing of
the results and findings of the audit.
DentaQuest Providers are required to maintain comprehensive treatment records that meet
professional standards for risk management. Please refer to the “Patient Record” section for
additional detail.
Documentation in the treatment record must justify the need for the procedure performed due
to medical necessity, for all procedures rendered. Appropriate diagnostic pre‐operative
radiographs clearly showing the adjacent and opposing teeth and substantiating any pathology
of caries present are required. Post‐operative radiographs are required for endodontic
procedures and permanent crown placement to confirm quality of care. In the event that
radiographs are not available or cannot be obtained, diagnostic quality intraoral photographs
must substantiate the need for procedures rendered.
Multistage procedures are reported and may be reimbursed upon completion. The completion
date is the date of insertion for removable prosthetic appliances. The completion date for
immediate dentures is the date that the remaining teeth are removed and the denture is
inserted. The completion date for fixed partial dentures and crowns, onlays, and inlays is the
cementation date regardless of the type of cement utilized. The completion date for endodontic
treatment is the date the canals are permanently filled.
Failure to provide the required documentation, adverse audit findings, or the failure to maintain
acceptable practice standards may result in sanctions including, but not limited to,
recoupment
of benefits on paid claims, follow‐up audits, or removal of the Provider from the
DentaQuest
Provider Panel.
We hope that the enclosed criteria will provide a better understanding of the decision‐making
87
DentaQuest USA Insurance Company
DentaQuest USA Insurance Company, Inc February 1, 2024
Current Dental Terminology © American Dental Association. All Rights Reserved.
process for reviews. We also recognize that “local community standards of care” may vary from
region to region and will continue our goal of incorporating generally accepted criteria that will
be consistent with both the concept of local community standards and the current ADA concept
of national community standards. Your feedback and input regarding the constant evolution of
these criteria is both essential and welcome. DentaQuest shares your commitment and belief to
provide quality care to Members and we appreciate your participation in the program.
Please remember these are generalized criteria. Services described may not be covered in your
particular program. In addition, there may be additional program specific criteria regarding
treatment. Therefore, it is essential you review the Benefits Covered Section before providing
any treatment.
Criteria for Dental Extractions
Not all procedures require authorization.
Documentation needed for authorization procedure:
• Appropriate radiographs showing clearly the adjacent and opposing teeth should be
submitted for authorization review: bitewings, periapicals or panorex.
• Treatment rendered under emergency conditions, when authorization is not possible,
will
still require that appropriate radiographs showing clearly the adjacent and opposing
teeth be submitted with the claim for review for payment.
• Narrative demonstrating medical necessity.
Criteria
The prophylactic removal of asymptomatic teeth (i.e. third molars) or teeth exhibiting no overt
clinical pathology is covered subject to consultant review.
• The removal of primary teeth whose exfoliation is imminent does not meet criteria.
• Alveoloplasty (code D7310) in conjunction with four or more extractions in the same
quadrant will be covered subject to consultant review.
• An unerupted third molar must demonstrate, by radiographic evidence, both an aberrant
tooth position beyond normal variations and substantial (> 50%) root formation.
Criteria for Cast Crowns
Documentation needed for authorization of procedure:
• Appropriate radiographs showing clearly the adjacent and opposing teeth should be
submitted for authorization review: bitewings, periapicals or panorex.
• Treatment rendered without necessary authorization will still require that sufficient and
88
DentaQuest USA Insurance Company
DentaQuest USA Insurance Company, Inc February 1, 2024
Current Dental Terminology © American Dental Association. All Rights Reserved.
appropriate radiographs showing clearly the adjacent and opposing teeth be submitted
with the claim for review for payment.
• Narrative demonstrating medical necessity is required if radiographs are not available.
Criteria
• In general, criteria for crowns will be met only for permanent teeth needing multi‐
surface restorations where other restorative materials have a poor prognosis.
• Permanent molar teeth must have pathologic destruction to the tooth by caries or
trauma, and should involve four or more surfaces and two or more cusps.
• Permanent bicuspid teeth must have pathologic destruction to the tooth by caries or
trauma, and should involve three or more surfaces and at least one cusp.
• Permanent anterior teeth must have pathologic destruction to the tooth by caries or
trauma, and must involve four or more surfaces and at least 50% of the incisal edge.
A request for a crown following root canal therapy must meet the following criteria:
• Request should include a dated post‐endodontic periapical radiograph.
• Tooth should be filled sufficiently close to the radiological apex to ensure that an apical
seal is achieved.
• The filling must be properly condensed/obturated. Filling material does not extend
excessively beyond the apex.
To meet criteria, a crown must be opposed by a tooth or denture in the opposite arch or be an
abutment for a partial denture.
• The patient must be free from active and advanced periodontal disease.
• The fee for crowns includes the temporary crown that is placed on the prepared tooth
and worn while the permanent crown is being fabricated for permanent teeth.
• Cast Crowns on permanent teeth are expected to last, at a minimum, five years.
Authorizations for Crowns will not meet criteria if:
• A lesser means of restoration is possible.
• Tooth has subosseous and/or furcation caries.
• Tooth has advanced periodontal disease.
• Tooth is a primary tooth.
• Crowns are being planned to alter vertical dimension.
Criteria for Endodontics
89
DentaQuest USA Insurance Company
DentaQuest USA Insurance Company, Inc February 1, 2024
Current Dental Terminology © American Dental Association. All Rights Reserved.
Not all procedures require authorization.
Documentation needed for authorization of procedure:
• Sufficient and appropriate radiographs showing clearly the adjacent and opposing teeth
and a pre‐operative radiograph of the tooth to be treated; bitewings, periapicals or
panorex. A dated post‐operative radiograph must be submitted for review for payment.
• Treatment rendered under emergency conditions, when authorization is not possible,
will
still require that appropriate radiographs showing clearly the adjacent and opposing
teeth, pre‐operative radiograph and dated post‐operative radiograph of the tooth
treated with the claim for retrospective review for payment. In cases where pathology is
not apparent, a written narrative justifying treatment is required.
Criteria
Root canal therapy is performed in order to maintain teeth that have been damaged through
trauma or carious exposure.
Root canal therapy must meet the following criteria:
• Fill should be sufficiently close to the radiological apex to ensure that an apical seal is
achieved.
• Fill must be properly condensed/obturated. Filling material does not extend excessively
beyond the apex.
Authorizations for Root Canal therapy will not meet criteria if:
• Gross periapical or periodontal pathosis is demonstrated radiographically (caries
subcrestal or to the furcation, deeming the tooth non‐restorable).
• The general oral condition does not justify root canal therapy due to loss of arch
integrity.
• Root canal therapy is for third molars, unless they are an abutment for a partial denture.
• Tooth does not demonstrate 50% bone support.
• Root canal therapy is in anticipation of placement of an overdenture.
• A filling material not accepted by the Federal Food and Drug Administration (e.g. Sargenti
filling material) is used.
Other Considerations:
• Root canal therapy for permanent teeth includes diagnosis, extirpation of the pulp,
shaping and enlarging the canals, temporary fillings, filling and obliteration of root
90
DentaQuest USA Insurance Company
DentaQuest USA Insurance Company, Inc February 1, 2024
Current Dental Terminology © American Dental Association. All Rights Reserved.
canal(s), and progress radiographs, including a root canal fill radiograph.
• In cases where the root canal filling does not meet DentaQuest’s treatment standards,
DentaQuest can require the procedure to be redone at no additional cost. Any
reimbursement already made for an inadequate service may be recouped after
DentaQuest reviews the circumstances.
Criteria for Stainless Steel Crowns
In most cases, authorization is not required. Where authorization is required for primary or
permanent teeth, the following criteria apply:
Documentation needed for authorization of procedure:
• Appropriate radiographs showing clearly the adjacent and opposing teeth should be
submitted for authorization review: bitewings, periapicals or panorex.
• Treatment rendered under emergency conditions, when authorization is not possible,
will
still require that appropriate radiographs showing clearly the adjacent and opposing
teeth be submitted with the claim for review for payment.
• Narrative demonstrating medical necessity if radiographs are not available.
Criteria
• In general, criteria for stainless steel crowns will be met only for teeth needing multi‐
surface restorations where amalgams and other materials have a poor prognosis.
• Permanent molar teeth must have pathologic destruction to the tooth by caries or
trauma, and should involve four or more surfaces and two or more cusps.
• Permanent bicuspid teeth must have pathologic destruction to the tooth by caries or
trauma, and should involve three or more surfaces and at least one cusp.
• Permanent anterior teeth must have pathologic destruction to the tooth by caries or
trauma, and should involve four or more surfaces and at least 50% of the incisal edge.
• Primary molars must have pathologic destruction to the tooth by caries or trauma, and
should involve two or more surfaces or substantial occlusal decay resulting in an enamel
shell.
An authorization for a crown on a permanent tooth following root canal therapy must meet the
following criteria:
• Request should include a dated post‐endodontic periapical radiograph.
• Tooth should be filled sufficiently close to the radiological apex to ensure that an apical
seal is achieved, unless there is a curvature or calcification of the canal that limits the
dentist’s ability to fill the canal to the apex.
91
DentaQuest USA Insurance Company
DentaQuest USA Insurance Company, Inc February 1, 2024
Current Dental Terminology © American Dental Association. All Rights Reserved.
• The filling must be properly condensed/obturated. Filling material does not extend
excessively beyond the apex.
To meet criteria, a crown must be opposed by a tooth or dentures in the opposite arch or be an
abutment for a partial denture.
• The patient must be free from active and advanced periodontal disease.
• The permanent tooth must be at least 50% supported in bone.
• Stainless steel crowns on permanent teeth are expected to last five years.
Authorization and treatment using stainless steel crowns will not meet criteria if:
• A lesser means of restoration is possible.
• Tooth has subosseous and/or furcation caries.
• Tooth has advanced periodontal disease.
• Tooth is a primary tooth with exfoliation imminent.
• Crowns are being planned to alter vertical dimension.
• Treatment Plan (prior‐authorized, if necessary).
• Narrative describing medical necessity for OR.
Criteria for Authorization of Operating Room (OR) Cases
Documentation needed for authorization of procedure:
• Treatment Plan (prior‐authorized, if necessary).
• Narrative describing medical necessity for OR.
Criteria
In most cases, OR will be authorized (for procedures covered by health plan) if the following is
(are) involved:
• Young children requiring extensive operative procedures such as multiple restorations,
treatment of multiple abscesses, and/or oral surgical procedures if authorization
documentation indicates that in‐office treatment (nitrous oxide or IV sedation) is not
appropriate and hospitalization is not solely based upon reducing, avoiding or
controlling
apprehension, or upon Provider or Member convenience.
• Patients requiring extensive dental procedures and classified as American Society of
Anesthesiologists (ASA) class III and ASA class IV (Class III – patients with uncontrolled
92
DentaQuest USA Insurance Company
DentaQuest USA Insurance Company, Inc February 1, 2024
Current Dental Terminology © American Dental Association. All Rights Reserved.
disease or significant systemic disease; for recent MI, resent stroke, new chest pain, etc.
Class IV – patient with severe systemic disease that is a constant threat to life).
• Medically compromised patients whose medical history indicates that the monitoring of
vital signs or the availability of resuscitative equipment is necessary during extensive
dental procedures.
• Patients requiring extensive dental procedures with a medical history of uncontrolled
bleeding, severe cerebral palsy, or other medical condition that renders in‐office
treatment not medically appropriate.
• Patients requiring extensive dental procedures who have documentation of
psychosomatic disorders that require special treatment.
• Cognitively disabled individuals requiring extensive dental procedures whose prior history
indicates hospitalization is appropriate.
Criteria for Removable Prosthodontics (Full and Partial Dentures)
Documentation needed for authorization of procedure:
• Treatment plan.
• Appropriate radiographs showing clearly the adjacent and opposing teeth must be
submitted for authorization review: bitewings, periapicals or panorex.
• Treatment rendered without necessary authorization will still require appropriate
radiographs showing clearly the adjacent and opposing teeth be submitted with the
claim
for review for payment.
Criteria
Prosthetic services are intended to restore oral form and function due to premature loss of
permanent teeth that would result in significant occlusal dysfunction.
• A denture is determined to be an initial placement if the patient has never worn a
prosthesis. This does not refer to just the time a patient has been receiving treatment
from a certain Provider.
• Partial dentures are covered only for recipients with good oral health and hygiene, good
periodontal health (AAP Type I or II), and a favorable prognosis where continuous
deterioration is not expected.
• Radiographs must show no untreated cavities or active periodontal disease in the
abutment teeth, and abutments must be at least 50% supported in bone.
• As part of any removable prosthetic service, dentists are expected to instruct the
patient
in the proper care of the prosthesis.
93
DentaQuest USA Insurance Company
DentaQuest USA Insurance Company, Inc February 1, 2024
Current Dental Terminology © American Dental Association. All Rights Reserved.
• In general, if there is a pre‐existing removable prosthesis (includes partial and full
dentures), it must be at least 5 years old and unserviceable to qualify for replacement.
• Fabrication of a removable prosthetic includes multiple steps(appointments) these
multiple steps (impressions, try‐in appointments, delivery etc.) are inclusive in the fee
for
the removable prosthetic and as such not eligible for additional compensation.
In general, a partial denture will be approved for benefits for if it replaces one or more anterior
teeth, or replaces two or more posterior teeth unilaterally or replaces three or more posterior
teeth bilaterally, excluding third molars, and it can be demonstrated that masticatory function
has been severely impaired. The replacement teeth should be anatomically full sized teeth.
Authorizations for removable prosthesis will not meet criteria:
• If there is a pre‐existing prosthesis which is not at least 5 years old and unserviceable.
• If good oral health and hygiene, good periodontal health, and a favorable prognosis are
not present.
• If there are untreated cavities or active periodontal disease in the abutment teeth.
• If abutment teeth are less than 50% supported in bone.
• If the recipient cannot accommodate and properly maintain the prosthesis (i.e. Gag
reflex, potential for swallowing the prosthesis, severely handicapped).
• If the recipient has a history or an inability to wear a prosthesis due to psychological or
physiological reasons.
• If a partial denture, less than five years old, is converted to a temporary or permanent
complete denture.
• If extensive repairs are performed on marginally functional partial dentures, or when a
new partial denture would be better for the health of the recipient. However, adding
teeth and/or a clasp to a partial denture is a covered benefit if the addition makes the
denture functional.
Criteria
• If there is a pre‐existing prosthesis, it must be at least 5 years old and unserviceable to
qualify for replacement.
• Adjustments, repairs and relines are included with the denture fee within the first 12
months after insertion. After 12 months of denture placement.
• A new prosthesis will not be reimbursed for within 24 months of reline or repair of the
existing prosthesis unless adequate documentation has been presented that all
procedures to render the denture serviceable have been exhausted.
94
DentaQuest USA Insurance Company
DentaQuest USA Insurance Company, Inc February 1, 2024
Current Dental Terminology © American Dental Association. All Rights Reserved.
• Adjustments will be reimbursed at one per calendar year per denture.
• Repairs will be reimbursed at two repairs per denture per year, with five total denture
repairs per 5 years.
• Relines will be reimbursed once per denture every 36 months.
• Replacement of lost, stolen, or broken dentures less than 5 years of age usually will not
meet criteria for pre‐authorization of a new denture.
• The use of preformed dentures with teeth already mounted (that is, teeth set in acrylic
before the initial impression) cannot be used for the fabrication of a new denture.
• All prosthetic appliances shall be inserted in the mouth and adjusted before a claim is
submitted for payment.
• When billing for partial and complete dentures, dentists must list the date that the
dentures or partials were inserted as the date of service. Recipients must be eligible on
that date in order for the denture service to be covered.
Criteria for the Excision of Bone Tissue
To ensure the proper seating of a removable prosthetic (partial or full denture) some treatment
plans may require the removal of excess bone tissue prior to the fabrication of the prosthesis.
Clinical guidelines have been formulated for the dental consultant to ensure that the removal
of
tori (mandibular and palatal) is an appropriate course of treatment prior to prosthetic
treatment.
Code D7471 (CDT–4) is related to the removal of the lateral exostosis. This code is subject to
authorization and may be reimbursed for when submitted in conjunction with a treatment plan
that includes removable prosthetics. These determinations will be made by the appropriate
dental specialist/consultant.
Authorization requirements:
• Appropriate radiographs and/or intraoral photographs/bone scans which clearly identify
the lateral exostosis must be submitted for authorization review; bitewings, periapicals or
panorex.
• Treatment plan – includes prosthetic plan.
• Narrative of medical necessity, if appropriate.
• Study model or photo clearly identifying the lateral exostosis (es) to be removed.
Criteria for the Determination of a Non‐Restorable Tooth
In the application of clinical criteria for benefit determination, dental consultants must consider
the overall dental health. A tooth that is determined to be non‐restorable may be subject to an
95
DentaQuest USA Insurance Company
DentaQuest USA Insurance Company, Inc February 1, 2024
Current Dental Terminology © American Dental Association. All Rights Reserved.
alternative treatment plan.
A tooth may be deemed non‐restorable if one or more of the following criteria are present:
• The tooth presents with greater than a 75% loss of the clinical crown.
• The tooth has less than 50% bone support.
• The tooth has subosseous and/or furcation caries.
• The tooth is a primary tooth with exfoliation imminent.
• The tooth apex is surrounded by severe pathologic destruction of the bone.
• The overall dental condition (i.e. periodontal) of the patient is such that an alternative
treatment plan would be better suited to meet the patient’s needs.
Criteria for General Anesthesia and Intravenous (IV) Sedation
Documentation needed for authorization of procedure:
• Treatment plan (authorized if necessary).
• Narrative describing medical necessity for general anesthesia or IV sedation.
• Treatment rendered under emergency conditions, when authorization is not possible,
will
still require submission of treatment plan and narrative of medical necessity with the
claim for review for payment.
Criteria
Requests for general anesthesia or IV sedation will be authorized (for procedures
Covered by
health plan) if any of the following criteria are met:
Extensive or complex oral surgical procedures such as:
• Impacted wisdom teeth.
• Surgical root recovery from maxillary antrum.
• Surgical exposure of impacted or unerupted cuspids.
• Radical excision of lesions in excess of 1.25 cm.
And/or one of the following medical conditions:
• Medical condition(s) which require monitoring (e.g. cardiac problems, severe
hypertension).

96
DentaQuest USA Insurance Company
DentaQuest USA Insurance Company, Inc February 1, 2024
Current Dental Terminology © American Dental Association. All Rights Reserved.
• Underlying hazardous medical condition (cerebral palsy, epilepsy, mental retardation,
including Down’s syndrome) which would render patient noncompliant.
• Documented failed sedation or a condition where severe periapical infection would
render local anesthesia ineffective.
• Patients 6 years old and younger with extensive procedures to be accomplished.
For Members Ages Six and Under
Prior Authorization Criteria
Requests for prior authorization must include, but are not limited to, the following member-
specific documents and information:
• A completed Criteria for Dental Therapy Under General Anesthesia form
• A completed Prior Authorization Claim Form. This must include CDT code (s) for all
procedures to be performed and D9222/D9223 or D9500 (a DentaQuest specific code that
indicates Medical Anesthesia Services) based on place of service and anesthesiologist type
• Location where the procedure(s) will be performed (office or outpatient)
• Tentative date of service if outpatient request or in office using a medical anesthesiologist
• Narrative unique to the member, detailing reasons for the proposed level of anesthesia
(indicate procedure code D9222/D9223 or D9500). The narrative must include history of prior
treatment, failed attempts at other levels of sedation, behavior in the dental chair, proposed
restorative treatment (tooth ID and surfaces), urgent need to provide comprehensive dental
treatment based on extent of diagnosed dental caries, and any relevant medical condition(s).
• Diagnostic quality radiographs or photographs
• When appropriate radiographs or photographs cannot be taken prior to general anesthesia,
the narrative must support the reasons for an inability to perform diagnostic services. For
these special cases that receive authorization, diagnostic quality labeled radiographs or
photographs will be required for payment and will be reviewed by the DentaQuest Dental
Director.
The current process of scoring 22 points on the Criteria for Dental Therapy Under General
Anesthesia form does not guarantee authorization or re imbursement for members who are six
years of age and younger.
Note: In cases of an emergency medical condition, accident, or trauma, prior authorization is not
necessary. However, a narrative and appropriate pre- and post-treatment radiographs or
photographs must be submitted with the claim, which will be reviewed by the DentaQuest
Dental Director.
A copy of the Criteria for Dental Therapy under General Anesthesia form must be maintained in
the member’s dental record. The member’s dent al record must be available for review by
representatives of the Health and Human Services Commission (HHSC) or its designee.
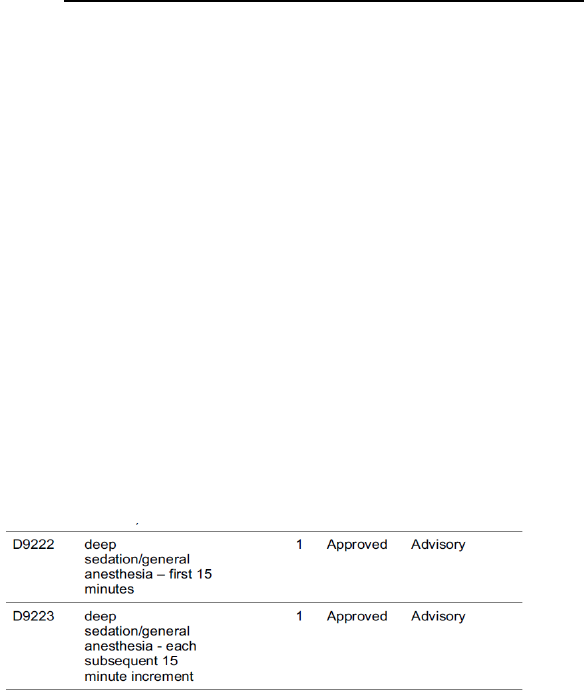
97
DentaQuest USA Insurance Company
DentaQuest USA Insurance Company, Inc February 1, 2024
Current Dental Terminology © American Dental Association. All Rights Reserved.
The following outlines the process based on place of service (in office / outpatient) and
anesthesiologist type (dental / medical).
Dental Therapy under General Anesthesia - In Office
Treating Dentist using Dental Anesthesiologist
• Is responsible for obtaining prior authorization from DentaQuest and is responsible for
providing the anesthesia prior authorization information to the dental anesthesiologist
• Submits one D9222, appropriate units of D9223, and CDT code(s) that will be performed under
general anesthesia for prior authorization DentaQuest will determine medical necessity of the
general anesthesia based on the submitted treatment plan and required documentation
• DentaQuest will notify the treating dentist of the determination via a Provider Determination
Letter (PDL). For services that are approved, the treating dentist would then provide a copy of
the PDL to the dental anesthesiologist. Code D9223 will indicate the DentaQuest
determination and will be either approved or denied. While we are reviewing the necessity of
the general anesthesia on the overall treatment plan, certain services on the PDL will indicate
Service Not Reviewed if they do not typically require authorization under DentaQuest policy.
Failure to submit per Prior Authorization Criteria as outlined above will result in a denial. See
example below, indicating the anesthesia service (D92 22 /D9223) has been approved.
Dental Anesthesiologist
• Upon completion of the approved services, the dental anesthesiologist will submit claims to
DentaQuest
• The DentaQuest approved authorization number from treating dentist must be in “Box 35” of
the claims form or in the notes section of the portal
• Must submit one D9222 and appropriate units of D9223 with supporting documentation
• Must have a current level 4 permit
Treating Dentist
• Upon completion of the approved services, the treating dentist will submit therapeutic
services rendered to DentaQuest
Treating Dentist using Medical Anesthesiologist
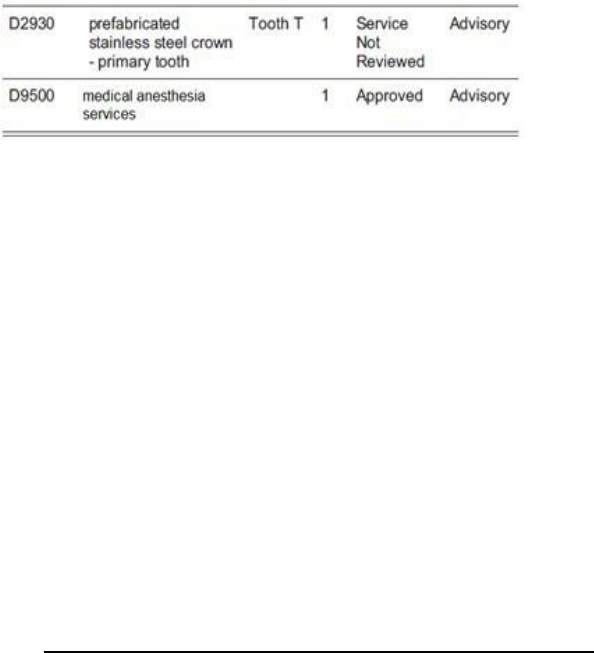
98
DentaQuest USA Insurance Company
DentaQuest USA Insurance Company, Inc February 1, 2024
Current Dental Terminology © American Dental Association. All Rights Reserved.
• Is responsible for obtaining prior authorization from DentaQuest and is responsible for
providing the anesthesia prior authorization information to the medical anesthesiologist
• Submits D9500 and CDT code(s) that will be performed under general anesthesia for prior
authorization
• DentaQuest will determine medical necessity of the general anesthesia based on the
submitted treatment plan and required documentation.
• DentaQuest will notify the treating dentist of the determination via a Provider Determination
Letter (PDL). For anesthesia that is approved, the treating dentist would then provide a copy of
the PDL to the medical anesthesiologist. Code D9500 will indicate the DentaQuest
determination and will be either approved or denied. While we are re viewing the necessity of
the general anesthesia on the overall treatment plan, certain services on the PDL will indicate
Service Not Reviewed if they do not typically require authorization under DentaQuest policy.
Failure to submit per Prior Authorization Criteria as outlined above will result in a denial. See
example bel ow, indicating the medical anesthesia service (D9500) has been approved.
Medical Anesthesiologist
• Is responsible for submitting a separate prior authorization request to the member’s MCO
along with the approved DentaQuest PDL
• The MCO reviews submitted documentation from DentaQuest to determine whether medical
anesthesia is approved or denied
• Upon completion of the approved services, the medical anesthesiologist will submit claim s
to the member’s MCO using the appropriate CPT code(s)
• Treating Dentist
• Upon completion of the approved services, the treating dentist will submit therapeutic
services rendered to DentaQuest
Dental Therapy under General Anesthesia – Outpatient
Treating Dentist
• Is responsible for obtaining prior authorization from DentaQuest and is responsible for
providing the anesthesia prior authorization information to the medical anesthesiologist and
/ or facility
• Submits code D9500 and CDT code(s) that will be performed under general anesthesia for
prior authorization
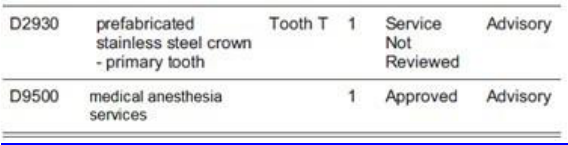
99
DentaQuest USA Insurance Company
DentaQuest USA Insurance Company, Inc February 1, 2024
Current Dental Terminology © American Dental Association. All Rights Reserved.
• The prior authorization request must indicate tentative procedure date(s) of service and
facility name in “Box 35” (remarks) of the ADA claim form
• Place of service must also be indicated in “Box 38” of the ADA claim form.
• DentaQuest will determine medical necessity of the general anesthesia based on the
submitted treatment plan and required documentation
• DentaQuest will notify the treating dentist of the determination via a Provider Determination
Letter (PDL). For anesthesia that is approved, the treating dentist would then provide a copy
of the PDL to the medical anesthesiologist and / or facility. Code D9500 will indicate the
DentaQuest determination for Medical Anesthesia Services
Medical Anesthesiologist and / or Facility
• Is responsible for submitting a separate prior authorization request to the member’s MCO
along with the approved DentaQuest PDL
• The MCO reviews submitted documentation from DentaQuest to determine whether medical
anesthesia and/or facility is approved or denied
• Upon completion of the approved services, the medical anesthesiologist and / or facility will
submit claims to the member’s MCO using the appropriate CPT code(s)
Treating Dentist
• Upon completion of the approved services, the treating dentist will submit therapeutic
services rendered to DentaQuest
Please remember that the provider who submits the authorization for the dental therapeutic
services must be the provider that performs the services. If the authorized provider does not
perform the service, claims will deny. In the event the authorized provider is un able to perform
the services, DentaQuest must be notified to update the authorization prior to the services
being performed. This is not applicable to the anesthesiologist.
Criteria for Periodontal Treatment
Documentation needed for authorization of procedure:
• Radiographs – periapicals or bitewings preferred.
• Complete periodontal charting with AAP Case Type.
• Treatment plan.
100
DentaQuest USA Insurance Company
DentaQuest USA Insurance Company, Inc February 1, 2024
Current Dental Terminology © American Dental Association. All Rights Reserved.
Periodontal scaling and root planing, per quadrant involves instrumentation of the crown and
root surfaces of the teeth to remove plaque and calculus from these surfaces. It is indicated for
patients with periodontal disease and is therapeutic, not prophylactic in nature. Root planing is
the definitive procedure designed for the removal of cementum and dentin that is rough,
and/or
permeated by calculus or contaminated with toxins or microorganisms. Some soft tissue removal
occurs. This procedure may be used as a definitive treatment in some stages of periodontal
disease and as a part of pre‐surgical procedures in others.
It is anticipated that this procedure would be requested in cases of severe periodontal conditions
(i.e. late Type II, III, IV periodontitis) where definitive comprehensive root planing requiring
local/regional block anesthesia and several appointments would be indicated.
From the American Academy of Periodontology (AAP) Policy on Scaling and Root Planing:
“Periodontal scaling is a treatment procedure involving instrumentation of the crown and root
surfaces of the teeth to remove plaque, calculus, and stains from these surfaces. It is performed
on patients with periodontal disease and is therapeutic, not prophylactic, in nature. Periodontal
scaling may precede root planing, which is the definitive, meticulous treatment procedure to
remove cementum and/or dentin that is rough and may be permeated by calculus, or
contaminated with toxins or microorganisms. Periodontal scaling and root planing are arduous
and time consuming. They may need to be repeated and may require local anesthetic.”
Criteria
• A minimum of four (4) teeth affected in the quadrant.
• Periodontal charting indicating abnormal pocket depths in multiple sites.
• Additionally at least one of the following must be present:
1. Radiographic evidence of root surface calculus.
2. Radiographic evidence of significant loss of bone support.

DentaQuest USA Insurance Company, Inc February 1, 2024
Current Dental Terminology © American Dental Association. All Rights Reserved.
101
DentaQuest USA Insurance Company
Appendix A
Definitions
Attachments
General Definitions
The following definitions apply to this Office Reference Manual:
A. “Contract” means the document specifying the services provided by DentaQuest to:
• a Medicaid or CHIP beneficiary, directly or on behalf of TX HHSC, as agreed upon
between the State of Texas and or its regulatory agencies and DentaQuest (a “Medicaid
Contract”);
B. “Covered Services” is a dental service or supply , including those services covered through the Texas
Health Steps Program that satisfies all of the following criteria:
• Is medically necessary;
• Is covered under the Texas HHSC Medicaid Dental Program;
• Is provided to an enrolled Member by a Participating Provider; and
• Is authorized by DentaQuest in accordance with the program guidelines.
C. “HHSC” means the Texas Health and Human Services Commission
D. “DentaQuest” shall refer to DentaQuest USA Insurance Company, Inc.
E. "DentaQuest Service Area" shall be defined as the State of Texas.
F. “Medically Necessary” is a service or benefit that is:
• Directly related to diagnostic, preventative, curative, palliative, rehabilitative, or
ameliorative treatment of an illness, injury, disability, or health condition;
• Consistent with currently accepted standards of good medical practice;
• The most cost effective service that can be provided without sacrificing effectiveness
or access to care; and
• Not primarily for the convenience of the consumer, family or provider.
G. “Member” means any individual who is eligible to receive Covered Services pursuant to a Contract and the
eligible dependents of such individuals. A Member enrolled pursuant to a Medicaid or CHIP Contract is
referred to as a “Medicaid or CHIP Member.”
H. “Participating Provider” is a dental professional or facility or other entity, including a Provider that has
entered into a written agreement with DentaQuest, directly or through another entity, to provide dental
services to selected groups of Members
A-1

DentaQuest USA Insurance Company, Inc February 1, 2024
Current Dental Terminology © American Dental Association. All Rights Reserved.
102
DentaQuest USA Insurance Company
I. "Provider" means the undersigned health professional or any other entity that has entered into a written
agreement with DentaQuest to provide certain health services to Members. Each Provider shall have its
own distinct tax identification number.
J. “Provider Dentist” is a Doctor of Dentistry, duly licensed and qualified under the applicable laws, who
practices as a shareholder, partner, or employee of Provider, and who has executed a Provider Dentist
Participation Addendum.
A-1
DentaQuest USA Insurance Company February 1, 2024
Current Dental Terminology © American Dental Association. All Rights Reserved.
103
DentaQuest USA Insurance Company
Appendix B
Forms to Use
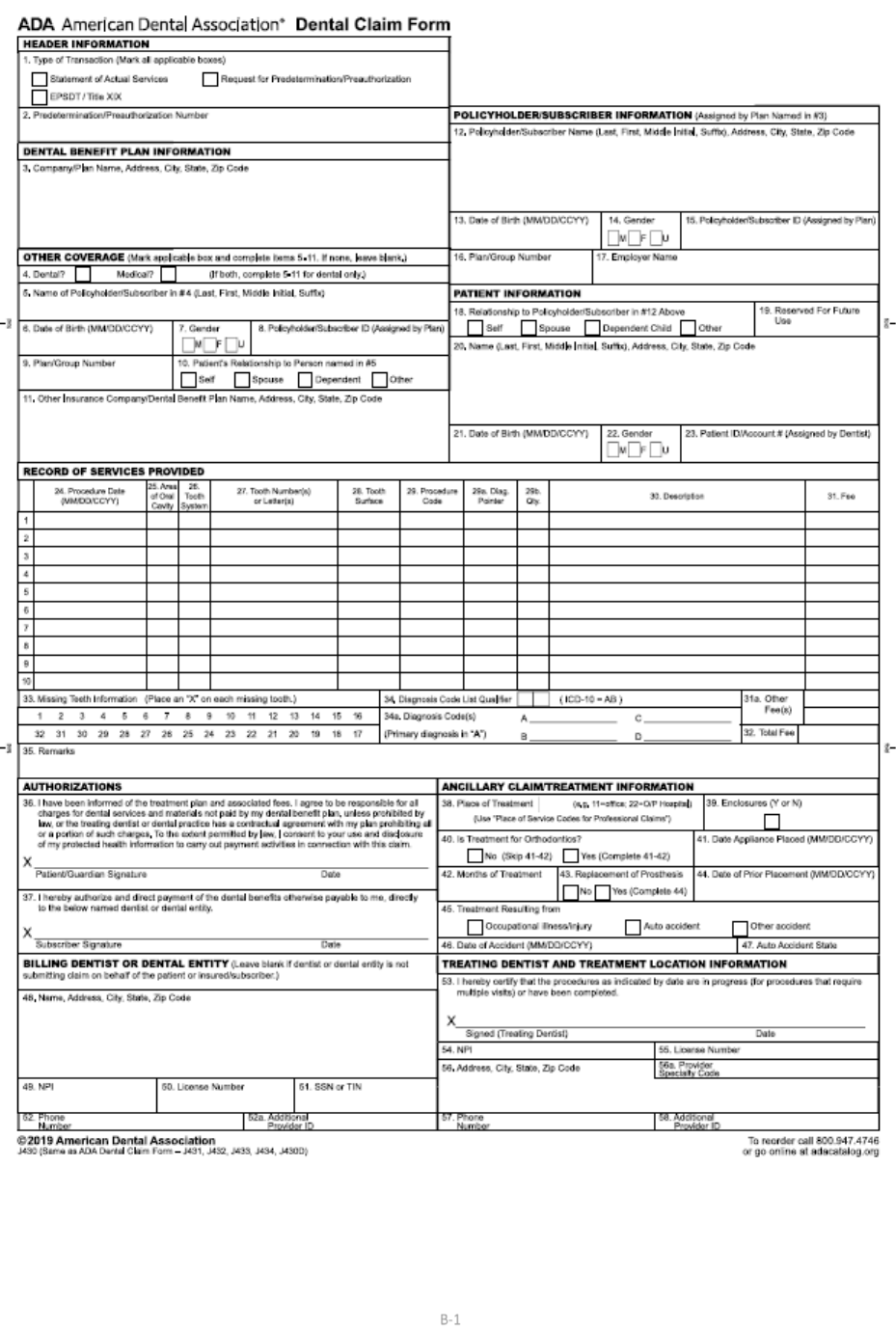
DentaQuest USA Insurance Company, February 1, 2024
Current Dental Terminology © American Dental Association. All Rights Reserved.
104
DentaQuest USA Insurance Company
B-1
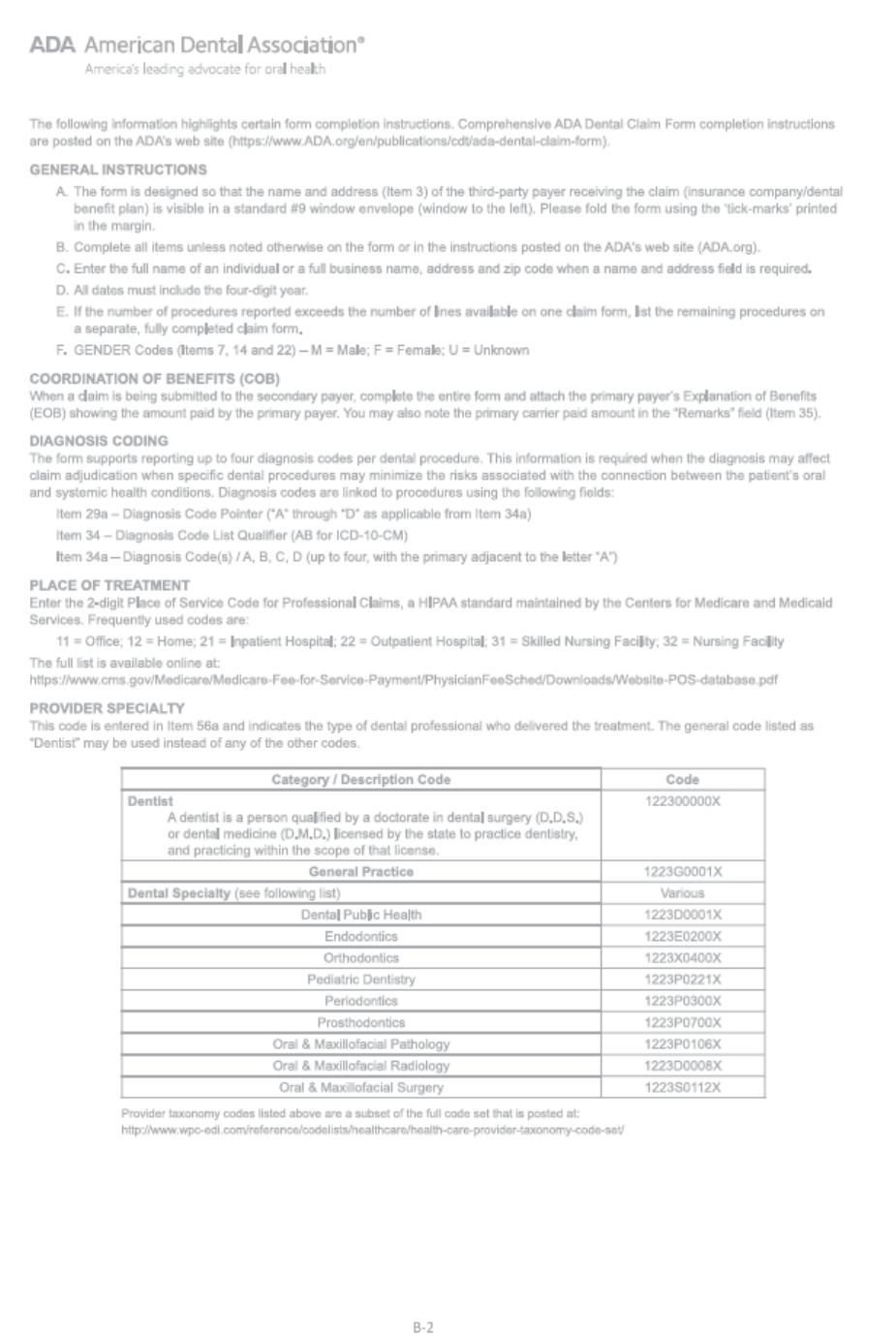
DentaQuest USA Insurance Company, Inc February 1, 2024
Current Dental Terminology © American Dental Association. All Rights Reserved.
105
DentaQuest USA Insurance Company
B-2
DentaQuest USA Insurance Company, Inc February 1, 2024
Current Dental Terminology © American Dental Association. All Rights Reserved.
106
DentaQuest USA Insurance Company
Non‐Covered Service Disclosure Form
The Member may purchase additional services as a non‐covered procedure/s or treatment/s for an additional charge.
DentaQuest requires that you (the provider) and the Member complete the Non‐Covered Services Disclosure Form
prior to rendering these services. A copy of this form must be kept in the Member’s treatment record. If the Member
elects to receive the non‐covered procedure/s or treatment/s the Member would pay a fee not to exceed the
maximum rate of your usual and customary fees as payment in full for the agreed procedure/s or treatment/s.
The Member is financially responsible for such services. If the Member will be subject to collection action upon failure
to make the required payment, the terms of the action must be kept in the Member’s treatment record. Failure to
comply with this procedure will subject the provider to sanctions up to and including termination.
This section to be completed by dentist rendering care
I am recommending that___________________________________receive
(Member Name and Medicaid Number)
services that are not covered by the DentaQuest Covered Benefits and Fee Schedule. The following procedure codes
are recommended: FEES NOT TO EXCEED PROVIDER’S UCF (usual and customary fee).
Code
Description
Fee
Blankcell
Blankcell
Blankcell
Blankcell
Blankcell
Blankcell
Blankcell
Blankcell
Blankcell
Blankcell
Blankcell
Blankcell
The total amount for service(s) to be rendered is $______________________.
________________________________________________________________________
Dentist’s Signature Date
This section to be completed by Member
I_____________, have been told that I require
(Print Name)
services or have requested services that are not covered by the DentaQuest Covered Benefits and Fee Schedule. Read
the following statements and check either Yes or No:
Question
Yes
No
My dentist has assured me that there are no other covered benefits.
Blankcell
Blankcell
I am willing to receive services not covered by DentaQuest.
Blankcell
Blankcell
I am aware that I am financially responsible for paying for these services.
Blankcell
Blankcell
I am aware that DentaQuest is not paying for these services.
blank
blank
I agree to pay $ per month. If I fail to make this payment I may be subject
to collection action by the dentist.
_______________________________________________________________
Parent or Guardian Signature
B-3
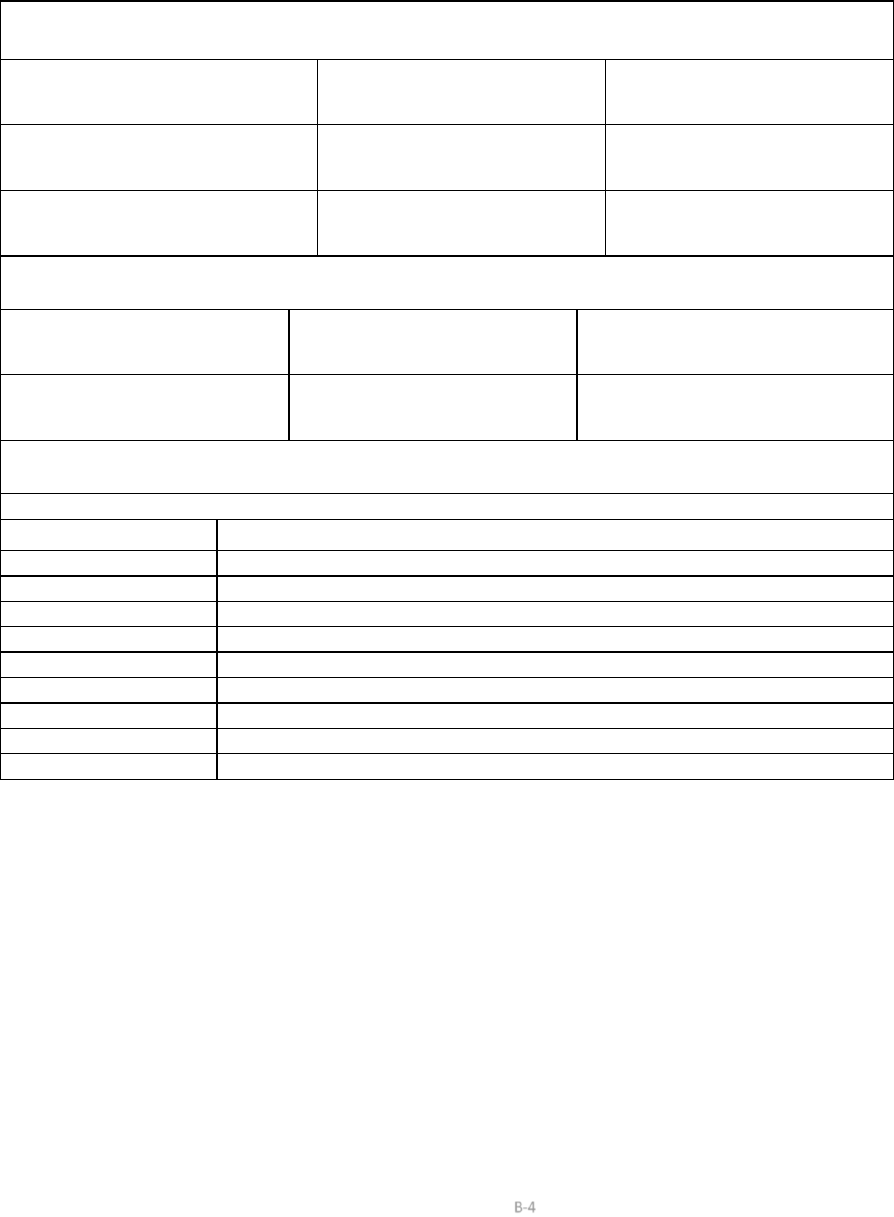
DentaQuest USA Insurance Company, Inc February 1, 2024
Current Dental Terminology © American Dental Association. All Rights Reserved.
107
DentaQuest USA Insurance Company
OrthoCAD Submission Form
Date:_________
Patient Information
Name (First & Last)
Date of Birth:
SS or ID#
Address:
City, State, Zip
Area code & Phone number:
Group Name:
Plan Type:
Provider Information
Dentist Name:
Provider NPI #
Location ID #
Address:
City, State, Zip
Area code & Phone number:
Treatment Requested
Code:
Description of request:
Blankcell
Blankcell
Blankcell
Blankcell
Blankcell
Blankcell
Blankcell
Blankcell
Blankcell
Blankcell
Blankcell
Blankcell
Blankcell
Blankcell
Blankcell
Blankcell
Blankcell
Blankcell
B-4
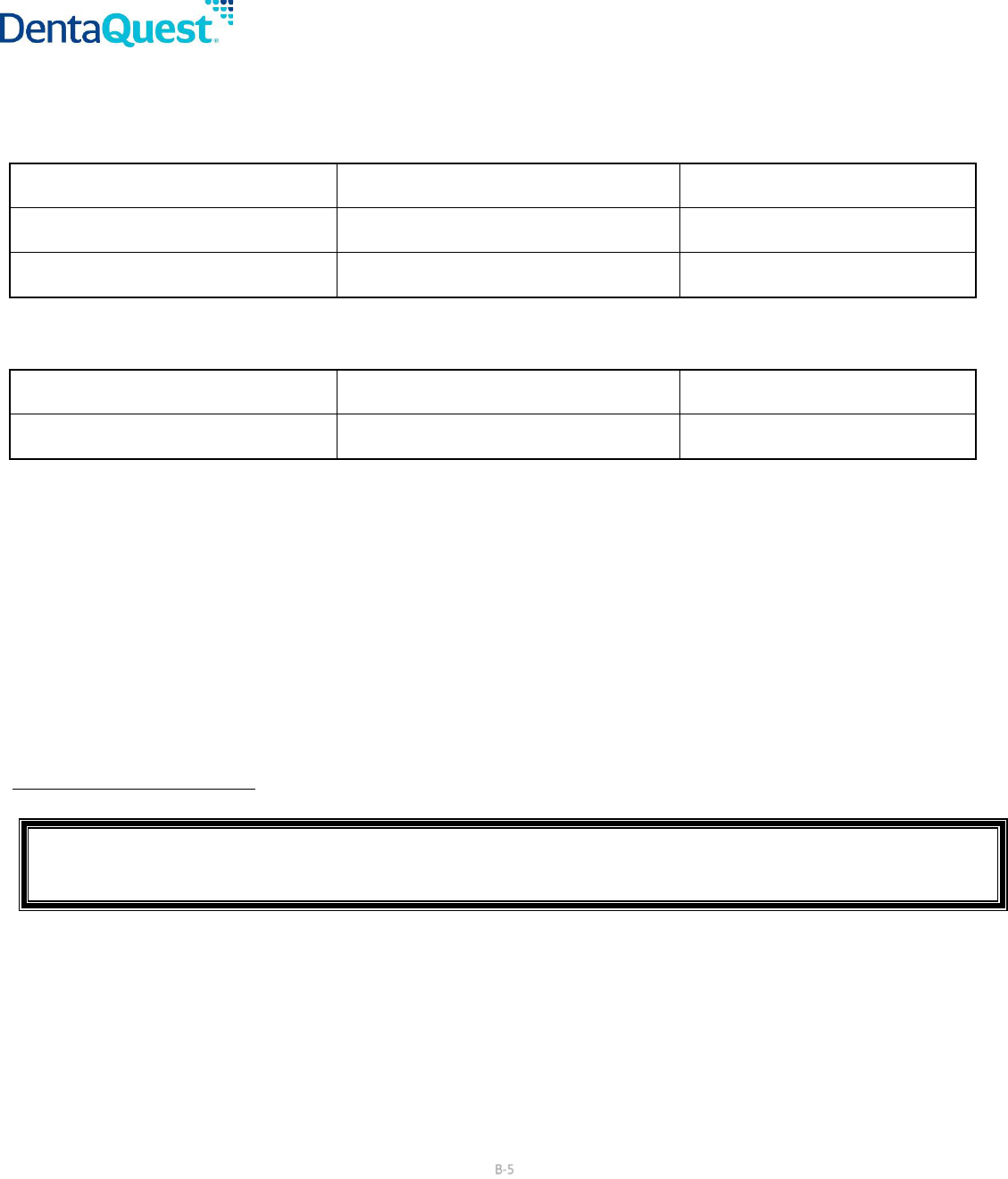
DentaQuest USA Insurance Company, February 1, 2024
Current Dental Terminology © American Dental Association. All RBi-g6hts Reserved.
108
DentaQuest USA Insurance Company
Continuation of Care Submission Form
Date: ___________________
Patient Information
Name (First & Last)
Date of Birth:
SS or ID#
Address:
City, State, Zip
Area code & Phone number:
Group Name:
Plan Type:
Provider Information
Dentist Name:
Provider NPI #
Location ID #
Address:
City, State, Zip
Area code & Phone number:
Name of Previous Vendor that issued original approval:______________________________________________________________
Banding Date: _______________________ Case Rate Approved By Previous Vendor: ______________________________________
Amount Paid for Dates of Service That Occurred Prior to DentaQuest: __________________________________________________
Amount Owed for Dates of Service That Occurred Prior to DentaQuest: _________________________________________________
Balance Expected for Future Dates of Service: _____________________________________________________________________
Numbers of Adjustments Remaining: ____________________________________________________________________________
Additional information required:
• If the Member is transferring from an existing Medicaid program: A copy of the original orthodontic approval.
• If the Member is private pay or transferring from a commercial insurance program Original diagnostic photos or models (or
OrthoCad equivalent), radiographs (optional).
Mail to:
DentaQuest, LLC Attn: Continuation Of Care
P.O. Box 2906
Milwaukee, WI 53201‐2906
B-5
DentaQuest USA Insurance Company, Inc February 1, 2024
Current Dental Terminology © American Dental Association. All Rights Reserved.
109
DentaQuest USA Insurance Company
Children’s Medicaid Dental Services
Managed Care Orthodontia Review Policy and Procedure‐ Texas
Subject:
Orthodontia Review Policy and Procedure
Effective Date: March 1, 2012
Date Last Revised: December 20, 2011; January 18, 2012; January 30, 2012
__________________________________________________________
Purpose
The Dental Contractors established a managed care policy and process to ensure consistent
and equitable determination of orthodontic coverage for the children’s Medicaid and CHIP
dental services. Comprehensive medically necessary orthodontic services are a covered benefit
for Texas Medicaid Members who have a severe handicapping malocclusion or special medical
conditions including cleft palate, post‐head trauma injury involving the oral cavity, and/or
skeletal anomalies involving the oral cavity.
Orthodontic services are covered for Texas CHIP Members for pre‐and postsurgical cases related
to cleft palate, post‐head trauma injury involving the oral cavity, and/or skeletal
anomalies
involving the oral cavity.
Definitions
Severe handicapping malocclusion is defined as an occlusion that is severely functionally
compromised and is described in detail in Levels I, II, III, and IV.
Orthodontic terminology and extent of orthodontic services are based on the American Dental
Association’s Current Dental Terminology (CDT) definitions and explanations of the orthodontic
codes utilized within this policy. The following definitions of dentition established by the CDT
manual are recognized by the Children’s Medicaid dental services:
Primary Dentition: Teeth developed and erupted first in order of time.
Transitional Dentition: The final phase of the transition from primary to adult teeth, in which the
deciduous molars and canines are in the process of shedding and the permanent successors are
emerging.
Adolescent Dentition: The dentition that is present after the normal loss of primary teeth and
prior to cessation of growth that would affect orthodontic treatment.
Adult Dentition: The dentition that is present after the cessation of growth that would affect
orthodontic treatment.
Policy
B-6
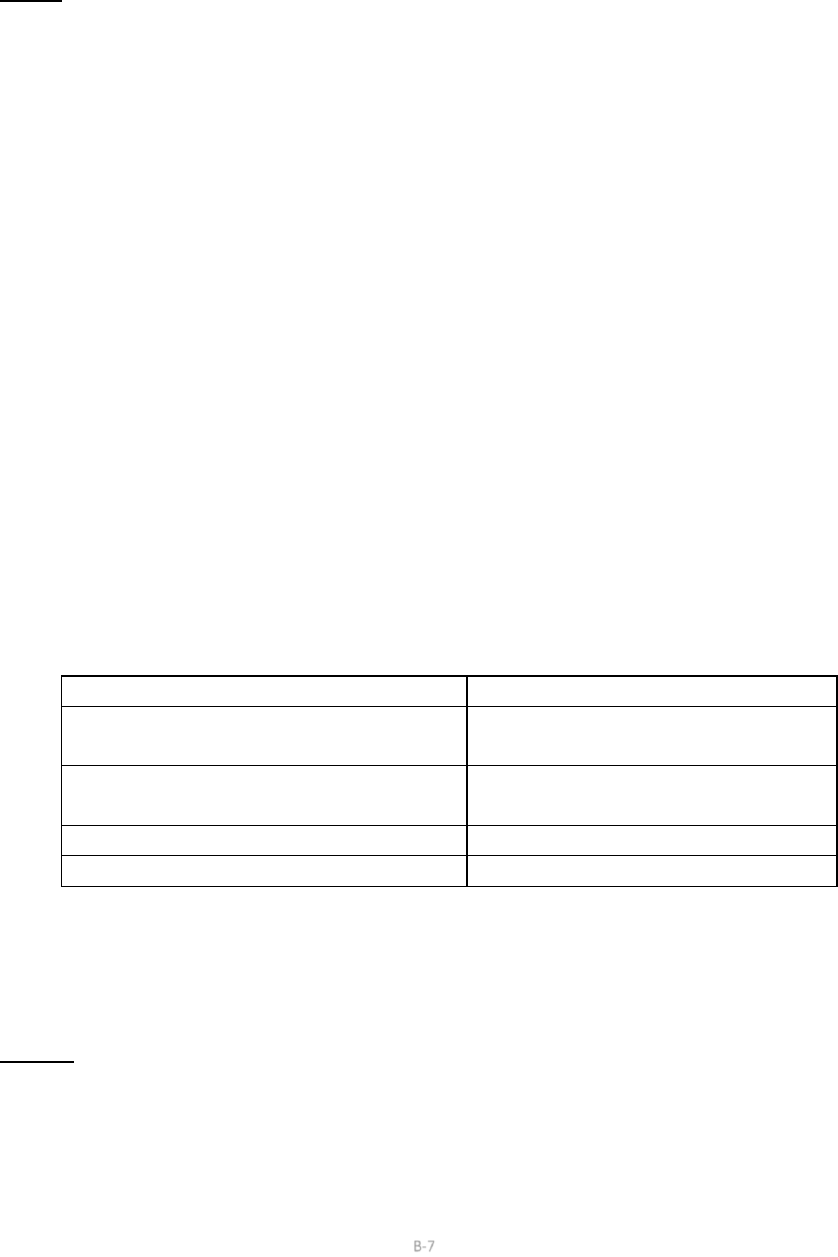
DentaQuest USA Insurance Company, Inc February 1, 2024
Current Dental Terminology © American Dental Association. All Rights Reserved.
110
DentaQuest USA Insurance Company
The Dental Contractors recognize four orthodontic service levels for severe handicapping
malocclusion, and each requires a different amount of time for treatment. These levels require
different levels of skill, orthodontic procedures, and time for completion of the treatment plan.
1.1 Level I: Dedicated to resolution of early signs of handicapping malocclusion in the early
mixed dentition which may significantly impact the health of the developing dentition,
alveolar bone, and symmetrical growth of the skeletal framework. (Presence of the
maxillary and mandibular permanent molars, and the maxillary and mandibular incisors
fully erupted, and deciduous teeth shall constitute the early mixed dentition.)
• Anterior crossbite that is associated with clinically apparent severe
gingival inflammation and/or gingival recession, or severe enamel wear.
• Posterior crossbite with an associated midline deviation and asymmetric
closure pattern.
• Dental cross bites, other than the above described shall not be eligible for
treatment in Level I.
1.2 Level I orthodontic services must be completed within 12 months unless an
exception is granted by DentaQuest upon approval of a prior authorization request
submitted by the provider.
1.3 Exceptions to the expected treatment time may allow for additional treatment
months for one of the following circumstances:
• The Member is the child of a migrant farm worker
• The Member’s orthodontic services were delayed as a result of
temporarily being in state custodial care (foster care).
1.4 Providers may submit the following procedure codes for Level I review:
Procedure Code
Description
D8010
Limited orthodontic treatment of
the primary dentition.
D8020
Limited orthodontic treatment of
the transitional dentition.
D8210
Removable appliance therapy
D8220
Fixed appliance therapy
1.5 Providers may prior authorize for additional services that may be deemed
medically necessary due to overall health of the patient or extenuating
circumstances. Each case will be reviewed and evaluated on a case by case basis
for medical necessity.
2.1 Level II:
2.2 Qualification for treatment at Level II requires submission of documentation to
support the classification of handicapping malocclusion. FOUR of the following
conditions must be clearly apparent in the supporting documentation:
B-7
DentaQuest USA Insurance Company, Inc February 1, 2024
Current Dental Terminology © American Dental Association. All Rights Reserved.
111
DentaQuest USA Insurance Company
A. Full cusp Class II malocclusion with the distal buccal cusp of the maxillary first
molar occluding in the mesial buccal groove of the mandibular first molar.
B. Full cusp Class III malocclusion with the maxillary first molar occluding in the
embrasure distal to the mandibular first molar or on the distal incline of
mandibular molar distal buccal cusp.
C. Overbite measurement shall be in excess of 5 mm.
D. Overjet measurement shall be in excess of 8 mm.
E. More than four congenitally absent teeth, one or more of which shall include
an anterior tooth/ or teeth.
F. Anterior crowding shall be in excess of 6 mm. in the mandibular arch.
G. Anterior cross bite of more than two of the four maxillary incisors.
H. Generalized spacing in both arches of greater than 6 mm. in each arch.
I. Recognition of early impacted maxillary canine or canines. Radiographs shall
support the diagnosis demonstrating a severe mesial angulation of the
erupting canine and the crown of the canine superimposed and crossing the
image of the maxillary lateral incisor.
2.3 Level II orthodontic services must be completed within 24 months unless an
exception is granted.
2.4 Exceptions to the expected treatment time may allow for additional treatment
months for one of the following circumstances:
• The Member is the child of a migrant farm worker
• The Member’s orthodontic services were delayed as a result of temporarily
being in state custodial care (foster care).
2.5 Providers must use the appropriate procedure code that is applicable for banding:
Procedure Code
Description
D8070
Comprehensive
orthodontic
treatment of the transitional
dentition. (1 of D8070, D8080 or
D8090 per lifetime)
D8080
Comprehensive
orthodontic
treatment of the adolescent
dentition. (1 of D8070, D8080 or
D8090 per lifetime)
D8090
Comprehensive
orthodontic
treatment of the adult dentition. (1
of D8070, D8080 or D8090 per
lifetime)
2.6 Interceptive orthodontic treatment is not covered in conjunction with
B-8
DentaQuest USA Insurance Company, Inc February 1, 2024
Current Dental Terminology © American Dental Association. All Rights Reserved.
112
DentaQuest USA Insurance Company
comprehensive orthodontic treatment. In addition, interceptive orthodontic
treatment is not allowed when comprehensive orthodontic treatment is indicated
unless there are extenuating circumstances.
2.7 Providers may prior authorize for additional services that may be deemed
medically necessary due to overall health of the patient or extenuating
circumstances. Each case will be reviewed and evaluated on a case by case basis
for medical necessity.
3.1 Additional Services: There may be extenuating circumstances that warrant additional
treatment, including but not limited to craniofacial anomalies and cleft palate. In the
event that the Member requires additional treatment, the Provider may prior authorize
for additional services that may be deemed medically necessary due to overall health of
the patient or extenuating circumstances. Each case will be reviewed and evaluated on a
case by case basis for medical necessity. Level III and Level IV described below are the
clinical criteria that must be met in order to qualify for additional services.
3.2 To submit for additional services, the provider must complete the following:
A. Submit a prior authorization on a 2018, 2019, or greater ADA claim form with
the appropriate code(s) being requested
B. If the provider is requesting additional monthly adjustments, the code D8670
must be utilized
C. Recent radiographs (x‐rays) showing the progress made to current
D. Photographs
E. Treatment plan
4.1 Level III: Dedicated to resolution of handicapping malocclusion in the adolescent or
adult
dentition.
4.2 Qualification for treatment at Level III requires submission of documentation to
support the classification of handicapping malocclusion. FOUR of the following
conditions must be clearly apparent in the supporting documentation.
A. Full cusp Class II molar malocclusion as described in Level II.
B. Full cusp Class III molar malocclusion as described in Level II.
C. Anterior tooth impaction; unerupted with radiographic evidence to support a
diagnosis of impaction (lack of eruptive space, angularly
malposed, totally
imbedded in the bone) as compared to ectopically erupted anterior teeth
which may be malposed but has erupted into the
oral cavity and is not a
qualifying element.
D. Anterior crowding shall be in excess of 6mm in the mandibular arch.
E. Anterior open bite shall demonstrate that all maxillary and mandibular
incisors have no occlual contact and are separated by a measurement in
B-9
DentaQuest USA Insurance Company, Inc February 1, 2024
Current Dental Terminology © American Dental Association. All Rights Reserved.
113
DentaQuest USA Insurance Company
excess of 6 mm.
F. Posterior open bite shall demonstrate a vertical separation by a measurement
in excess of 5 mm. of several posterior teeth and not be
confused with the
delayed natural eruption of a few teeth.
G. Posterior cross bite with an associated midline deviation and mandibular shift,
a Brodie bite with a mandibular arch totally encumbered by an overlapping
buccally occluding maxillary arch, or a posterior maxillary arch totally lingually
malpositioned to the mandibular arch shall qualify.
H. Anterior cross bite shall include more than two incisors in cross bite and
demonstrate gingival inflammation, gingival recession, or severe enamel wear.
I. Over bite shall be in excess of 5 mm.
J. Overjet shall be in excess of 8 mm.
4.3 Level III orthodontic services must be completed within 36 months unless an
exception is granted.
4.4 Exceptions to the expected treatment time may allow for additional treatment
months for one of the following circumstances:
• The Member is the child of a migrant farm worker
• The Member’s orthodontic services were delayed as a result of temporarily
being in state custodial care (foster care).
5.1 Level IV: Dedicated to resolution of handicapping malocclusion in the adult dentition;
complete eruption of the permanent dentition.
5.2 Qualification for treatment at level IV requires submission of documentation to
support the classification of handicapping malocclusion. Documentation shall be
submitted by an Oral Surgeon justifying the medical necessity of a surgical
approach to treatment.
A. Non‐functional Class II malocclusion.
B. Non‐functional Class III malocclusion
5.3 Models, panorex, Cephalogram, and photos shall be submitted with the above
requested documentation for review. The correction of the malocclusion shall be
beyond that of orthodontics alone and shall require pre‐orthodontic and post‐
orthodontic procedures in conjunction with orthognathic surgery. The patient’s
medical needs shall be based on function and not esthetics.
5.4 Level IV orthodontic services must be completed within 48 months unless an
exception is granted.
5.5 Exceptions to the expected treatment time may allow for additional treatment
months for one of the following circumstances:
• The Member is the child of a migrant farm worker
• The Member’s orthodontic services were delayed as a result of temporarily
B-10
DentaQuest USA Insurance Company, Inc February 1, 2024
Current Dental Terminology © American Dental Association. All Rights Reserved.
114
DentaQuest USA Insurance Company
being in state custodial care (foster care).
6.1 Other Orthodontic Services:
6.2 The following procedure codes are used to bill for other orthodontic services:
Procedure Code
Description
D8670
Periodic orthodontic treatment
visit
‐ the number of monthly
adjustments will vary based on
which level was approved.
D8680
Debanding‐ Orthodontic retention
(removal
of appliances,
construction and
placement
of
retainers).
7.1 Provider Requirements:
7.2 All dental providers must comply with the rules and regulations of the Texas State
Board of Dental Examiners (TSBDE), including the standards for documentation
and record maintenance that are stated in the TSBDE Rules 108.7
Minimum
Standards of Care, General and 108.8 Records of Dentist.
7.3 Dentists (DDS, DMD) who want to provide any of the four levels of orthodontic
services addressed in this policy must be enrolled as a dentist or orthodontist in
Texas Health Steps and must have the qualifications listed below for the relevant
level of service:
Level of Orthodontic Service
Qualifications
Level I or II
Completion of pediatric dental
residency; or a minimum of 200 hours
of continuing dental education in
orthodontics.
Level I, II, III, or IV
Dentists who are orthodontic board
certified or orthodontic board eligible.
7.4 Provider Type 90 – Orthodontist: Board eligible or board certified by an ADA
recognized orthodontic specialty board. This provider type is eligible to provide
Level I‐IV.
7.5 Provider Type 48 – Texas Health Steps – Dental: In order to perform and be
reimbursed for Level I and II, provider must attest to either:
A. Completion of pediatric specialty residency.
B. Minimum of 200 hours of continuing dental education in orthodontics within
the last ten years.
B-11
DentaQuest USA Insurance Company, Inc February 1, 2024
Current Dental Terminology © American Dental Association. All Rights Reserved.
115
DentaQuest USA Insurance Company
8.1 Orthodontic Prior Authorization Requirements
8.2 The following documentation must be submitted with the request for prior
authorization:
A. ADA 2018, 2019, or newer claim form with service codes noted
B. Duplicate diagnostic models or a complete set of diagnostic photographs
C. Radiographs (x‐rays)
D. Cephalometric x‐ray with tracings
E. Photographs (if plaster models are submitted)
F. Treatment plan
G. For CHIP Members Only – a copy of the medical prior authorization approval
letter for surgery
9.1 Completion of Comprehensive Orthodontic Services
9.2 Prior authorization is required for completion of services (last payment) and must
be reviewed for proof of completion of case.
9.3 The following documentation must be submitted with the request for prior
authorization:
A. Post treatment panorex film
B. Photographs
C. A signed statement from the treating Provider indicating that treatment
is
complete
9.4 Providers must use the following procedure code for debanding:
Procedure Code
Description
D8680
Orthodontic Retention (removal of
appliances, construction and
placement of retainer(s))
10.1 Transfer of Comprehensive Orthodontic Services
10.2 Prior authorization issued to a provider for orthodontic services is not
transferable to another provider. The new provider must request a new prior
authorization to complete the treatment initiated by the original provider.
10.3 The new provider must obtain his/her own records. The following supporting
documentation of medical necessity must be submitted with the request for
transfer of services:
A. All of the documentation that is required for the original request,
B. The reason the Member left the previous provider,
C. Narrative noting the treatment status.
B-12
DentaQuest USA Insurance Company, Inc February 1, 2024
Current Dental Terminology © American Dental Association. All Rights Reserved.
116
DentaQuest USA Insurance Company
11.1 Continuation of Orthodontic Case Initiated through a Private Arrangement
11.2 Continuation of a case for a Member that began treatment through a private
arrangement will be considered for prior authorization if the Member began
treatment prior to becoming Medicaid eligible.
11.3 Continuation of a case for a Member that began treatment through a private
arrangement will not be considered for prior authorization if the Member began
treatment while Medicaid eligible and will be denied.
11.4 The following information is required for consideration of payment for
continuation of care cases:
A. A completed Orthodontic Continuation of Care Form
B. A completed 2018, 2019, or greater ADA claim form listing the services to be
rendered
C. A copy of the Member’s prior approval including the total approved case
fee
and payment structure
D. Detailed payment history
11.5 If the Member is private pay, fee for service or transferring from a commercial
insurance and now is Medicaid or CHIP eligible; the following information is
required:
A. A completed Orthodontic Continuation of Care Form
B. A completed 2018, 2019, or greater ADA claim form listing the services to be
rendered
C. A copy of the Member’s prior approval including the total approved case fee
and payment structure
D. Detailed payment history
E. A copy of the original study models prior to the patient being banded
F. Panorex film
12.1 Orthodontic Services authorized by TMHP prior to March 1, 2012
12.2 The Dental Contractor has the option to re‐review any and/or all orthodontic
cases authorized by TMHP prior to March 1, 2012 for medical necessity.
12.3 The following information is required for review and consideration of payment
for
continuation of care:
A. A completed Orthodontic Continuation of Care Form
B. A completed 2018, 2019, or greater ADA claim form listing the services to be
rendered
C. A copy of the Member’s prior approval including the total approved case fee
and payment structure
D. Detailed payment history
B-13

DentaQuest USA Insurance Company, Inc February 1, 2024
Current Dental Terminology © American Dental Association. All Rights Reserved.
117
DentaQuest USA Insurance Company
E. A copy of the original study models prior to the patient being banded (only if
requested)
F. Panorex film (only if requested)
12.4 The clinical criteria used in making the qualifying decision will be the criteria
stated in this document (Level I, II, III and IV).
12.5 Should the request for continuation of payment be denied due to lack of medical
necessity under the new clinical criteria; the Dental Contractor will authorize a
treatment plan to deband the Member.
13.1 Premature Termination of Comprehensive Orthodontic Services
13.2 Premature termination of comprehensive orthodontic treatment by the
originally
treating provider is included in the comprehensive services.
13.3 Premature termination of orthodontic services includes all of the following:
A. Removal of brackets and arch wires
B. Other special orthodontic appliances
C. Fabrication of special orthodontic appliances
D. Delivery of orthodontic retainers
13.4 Premature removal of an orthodontic appliance must be prior authorized. A
release form must be signed by the parent or legal guardian, or by the Member if
he/she is 18 years of age or older or an emancipated minor. A copy of the signed
release form and a completed prior authorization request form must be
submitted, and one of the following must be documented on the prior
authorization request:
A. The Member is uncooperative or is non‐compliant
B. The Member requested the removal of the orthodontic appliance(s)
C. The Member has requested the removal due to extenuating circumstances to
include, but not limited to:
1. Incarceration
2. Mental health complications with a recommendation from the treating
physician
3. Foster Care placement
4. Child of a Migrant Farm Worker, with the intent to complete treatment at
a later date if Medicaid eligibility for orthodontic services continues
NOTE: A Member for whom removal of an appliance has been authorized due to
the above, will be eligible for completion of their Medicaid orthodontic services if
the services are re
‐
initiated while Medicaid eligible. Should the Member choose
to
have the appliances removed for reasons other than those listed under “C”,
the
Member may not be eligible for any additional Medicaid orthodontic services.
B-14
DentaQuest USA Insurance Company, Inc February 1, 2024
Current Dental Terminology © American Dental Association. All Rights Reserved.
118
DentaQuest USA Insurance Company
13.5 The requesting provider is responsible for removal of the orthodontic appliances,
final records and x‐rays at the time of termination.
13.6 Providers must use the following procedure code for premature debanding:
Procedure Code
Description
D8680
Orthodontic Retention (removal of
appliances, construction and
placement of retainer(s))
14.1 Reimbursement:
14.2 An initial payment is payable when bands are placed. Providers must bill with the
appropriate prior authorized procedure code.
14.3 Providers must bill the appropriate monthly adjustment code (D8670). The total
number of monthly adjustments allowed will vary by level.
14.4 The last payment is payable when the treatment is complete. Providers must bill
with the appropriate prior authorized procedure code (D8680).
15.1 General Information:
15.2 Providers may prior authorize for additional services that may be deemed
medically necessary due to overall health of the patient or extenuating
circumstances. Each case will be reviewed and evaluated on a case by case basis
for medical necessity. For example, debanding in regular treatment would limit
retainers and appliance removal to a single episode however in the case of cleft
palate, craniofacial and head trauma with dental consequences; the case may
involve multiple courses of treatment and would gain additional consideration
based on the circumstances.
15.3 Orthodontic services that are performed solely for cosmetic purposes are not a
benefit of Texas Medicaid.
15.4 Members enrolled in the Dental Contractor’s plan for at least one month and are
receiving orthodontic treatment and either ages out or loses eligibility; the
Dental
Contractor is responsible for completion of payment for the course of treatment.
The only exception is if the Member is disenrolled with cause, but is still Medicaid
eligible.
15.5 There will be no payment for denied cases.
15.6 Payment for banding includes the initial work up.
15.7 Study models submitted with the request will not be returned to the provider
unless a self-addressed postage paid box is included.
B-15
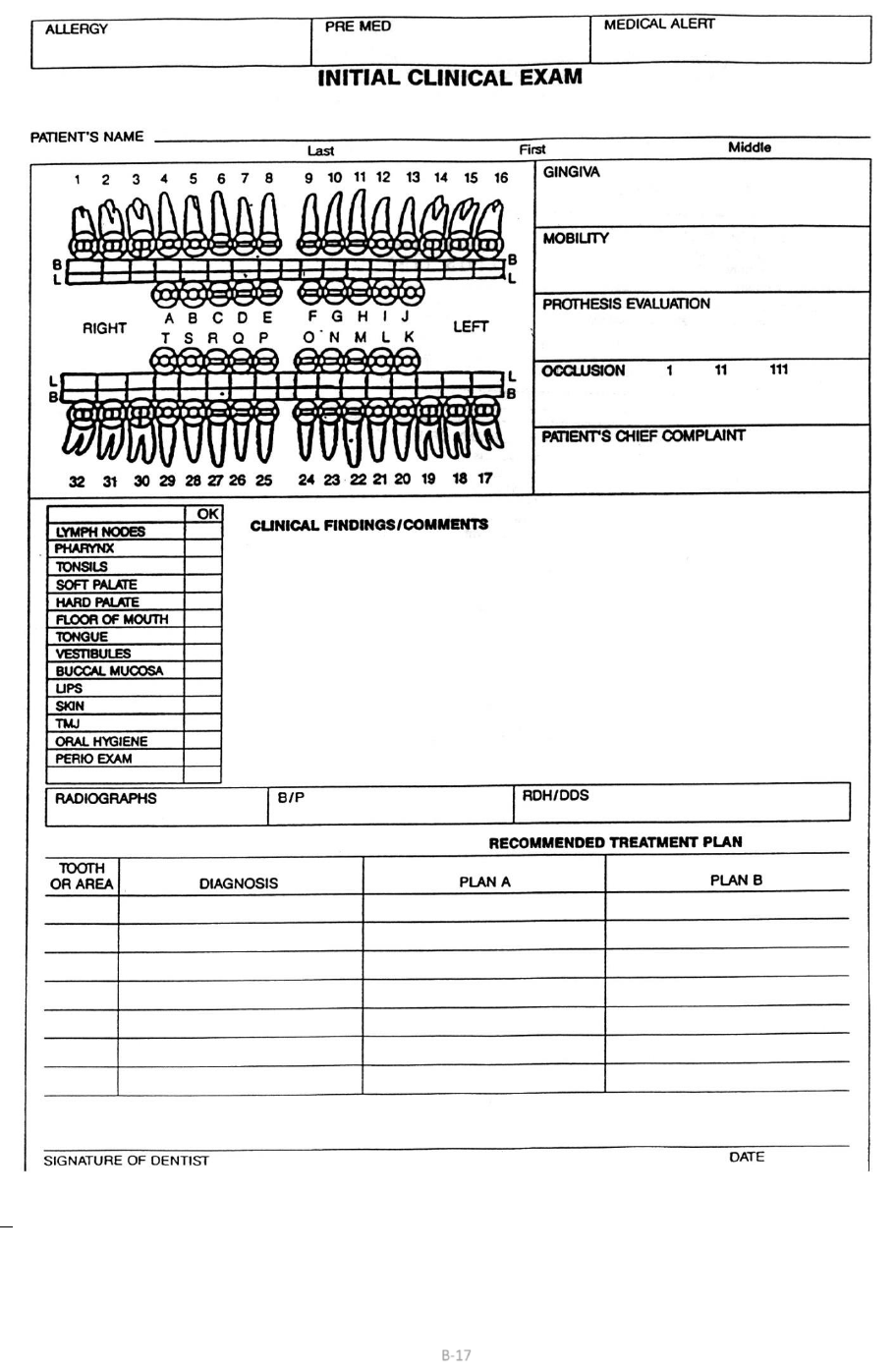
DentaQuest USA Insurance Company, Inc February 1, 2024
Current Dental Terminology © American Dental Association. All Rights Reserved.
119
DentaQuest USA Insurance Company
NOTE: The above form is intended to be a sample. DentaQuest is not mandating the use of this form. Please refer
to State statutes for specific State requirements and guidelines.
B-17
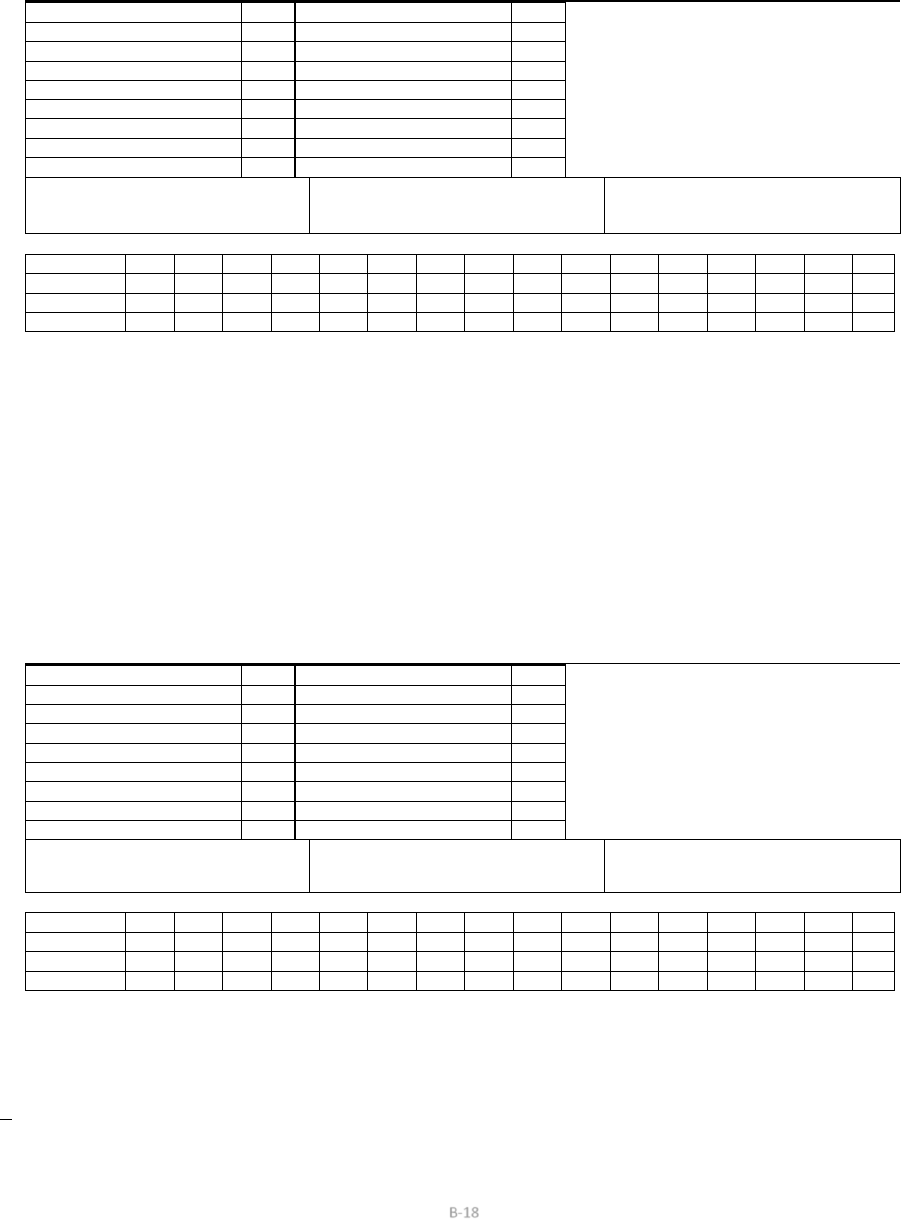
DentaQuest USA Insurance Company, Inc October 24, 2023, 2023
Current Dental Terminology © American Dental Association. All Rights Reserved.
120
DentaQuest USA Insurance Company
RECALL EXAMINATION
PATIENT’S NAME _________________________________________________________________________________________________________________
CHANGES IN HEALTH STATUS/MEDICAL HISTORY __________________________________________________________________________________
Blank cell
OK
Blank cell
OK
CLINICAL FINDINGS/COMMENTS
LYMPH NODES
Blank cell
TMJ
Blank cell
PHARYNX
Blank cell
TONGUE
Blank cell
TONSILS
Blank cell
VESTIBULES
Blank cell
SOFT PALATE
Blank cell
BUCCAL MUCOSA
Blank cell
HARD PALATE
Blank cell
GINGIVA
Blank cell
FLOOR OF MOUTH
Blank cell
PROSTHESIS
Blank cell
LIPS
Blank cell
PERIO EXAM
Blank cell
SKIN
Blank cell
ORAL HYGIENE
Blank cell
RADIOGRAPHS
B/P
RDH/DDS
R WORK NECESSARY L
TOOTH
1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
SERVICE
Blank cell
Blank cell
Blank cell
Blank cell
Blank cell
Blank cell
Blank cell
Blank cell
Blank cell
Blank cell
Blank cell
Blank cell
Blank cell
Blank cell
Blank cell
Blank cell
TOOTH
32
31
30
29
28
27
26
25
24
23
22
21
20
19
18
17
SERVICE
Blank cell
Blank cell
Blank cell
Blank cell
Blank cell
Blank cell
Blank cell
Blank cell
Blank cell
Blank cell
Blank cell
Blank cell
Blank cell
Blank cell
Blank cell
Blank cell
COMMENTS: ___________________________________________________________________________________________________
______________________________________________________________________________________________________________
______________________________________________________________________________________________________________
RECALL EXAMINATION
PATIENT’S NAME ___________________________________________________________________________________________________________________
CHANGES IN HEALTH STATUS/MEDICAL HISTORY ____________________________________________________________________________________
Blank cell
OK
Blank cell
OK
CLINICAL FINDINGS/COMMENTS
LYMPH NODES
Blank cell
TMJ
Blank cell
PHARYNX
Blank cell
TONGUE
Blank cell
TONSILS
Blank cell
VESTIBULES
Blank cell
SOFT PALATE
Blank cell
BUCCAL MUCOSA
Blank cell
HARD PALATE
Blank cell
GINGIVA
Blank cell
FLOOR OF MOUTH
Blank cell
PROSTHESIS
Blank cell
LIPS
Blank cell
PERIO EXAM
Blank cell
SKIN
Blank cell
ORAL HYGIENE
Blank cell
RADIOGRAPHS
B/P
RDH/DDS
R WORK NECESSARY L
TOOTH
1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
SERVICE
Blank cell
Blank cell
Blank cell
Blank cell
Blank cell
Blank cell
Blank cell
Blank cell
Blank cell
Blank cell
Blank cell
Blank cell
Blank cell
Blank cell
Blank cell
Blank cell
TOOTH
32
31
30
29
28
27
26
25
24
23
22
21
20
19
18
17
SERVICE
Blank cell
Blank cell
Blank cell
Blank cell
Blank cell
Blank cell
Blank cell
Blank cell
Blank cell
Blank cell
Blank cell
Blank cell
Blank cell
Blank cell
Blank cell
Blank cell
COMMENTS: __________________________________________________________________________________________________
_____________________________________________________________________________________________________________
_____________________________________________________________________________________________________________
NOTE: The above form is intended to be a sample. DentaQuest is not mandating the use of this form. Please refer to State
statutes for specific State requirements and guidelines.
B-18

DentaQuest USA Insurance Company, February 1, 2024
Current Dental Terminology © American Dental Association. All Rights Reserved.
121
DentaQuest USA Insurance Company
Authorization for Dental Treatment
I hereby authorize Dr. ______________ and his/her associates to provide dental services,
prescribe, dispense and/or administer any drugs, medicaments, antibiotics, and local
anesthetics that he/she or his/her associates deem, in their professional judgment,
necessary or
appropriate in my care.
I am informed and fully understand that there are inherent risks involved in the administration
of any drug, medicament, antibiotic, or local anesthetic. I am informed and fully understand
that there are inherent risks involved in any dental treatment and extractions (tooth removal).
The most common risks can include, but are not limited to:
Bleeding, swelling, bruising, discomfort, stiff jaws, infection, aspiration, paresthesia, nerve
disturbance or damage either temporary or permanent, adverse drug response, allergic
reaction, and cardiac arrest.
I realize that it is mandatory that I follow any instructions given by the dentist and/or his/her
associates and take any medication as directed.
Alternative treatment options, including no treatment, have been discussed and understood.
No guarantees have been made as to the results of treatment. A full explanation of all
complications is available to me upon request from the dentist.
Procedure(s): _______________________________________________________________
Tooth Number(s): ____________________________________________________________
Date: ______________________________________________________________________
Dentist: ____________________________________________________________________
Patient Name: _______________________________________________________________
Legal Guardian/
Patient Signature: ____________________________________________________________
Witness: ____________________________________________________________________
Note: The above form is intended to be a sample. DentaQuest is not mandating the use of this form. Please refer
to State statutes for specific State requirements and guidelines.
B-19

DentaQuest USA Insurance Company, February 1, 2024
Current Dental Terminology © American Dental Association. All Rights Reserved.
122
DentaQuest USA Insurance Company
MEDICAL AND DENTAL HISTORY
Patient Name:_________________________Date of Birth: ___________________
Address: _________________________________________________________________________
Why are you here today? ___________________________________________________________
Are you having pain or discomfort at this time?
Yes
/
No ___
If yes,
what type and where?
_______________________________________________________
Have you been under the care of a medical doctor during the past two years?
Yes
/
No ___
Medical
Doctor’s Name: _____________________________________________________________
Address: ____________________________________________________________________
Telephone: _________________________________________________________________
Have you taken any medication or drugs during the past two years?
Yes
/
No ___
No Are you
now taking any medication, drugs, or pills?
Yes
/
No ___
If yes, please list medications: _________________________________________________
Are you aware of being allergic to or have you ever reacted badly to any medication or substance?
Yes
/
No ___
If yes, please list: ___________________________________________________________
When you walk up stairs or take a walk, do you ever have to stop because of pain in your chest, shortness or
breath, or because you are very tired?
Yes
/
No ___
Do your ankles swell during the day?
Yes
/
No ___
Do you use more than two pillows to sleep?
Yes
/
No ___
Have you lost or gained more than 10 pounds in the past year?
Yes
/
No ___
Do you ever wake up from sleep and feel short of breath?
Yes
/
No ___
Are you on a special diet?
Yes
/
No ___
Has your medical doctor ever said you have cancer or a tumor?
Yes
/
No ___
If yes, where? ___________________________________________________________________
Do you use tobacco products (smoke or chew tobacco)?
Yes
/
No ___
If yes, how often and how much?
___________________________________________________
Do you drink alcoholic beverages (beer, wine, whiskey, etc.)?
Yes
/
No ___
Do
you have or have you had any disease, or condition not listed?
Yes
/
No ___
N
o If yes, please list:
_____________________________________________________
B-20
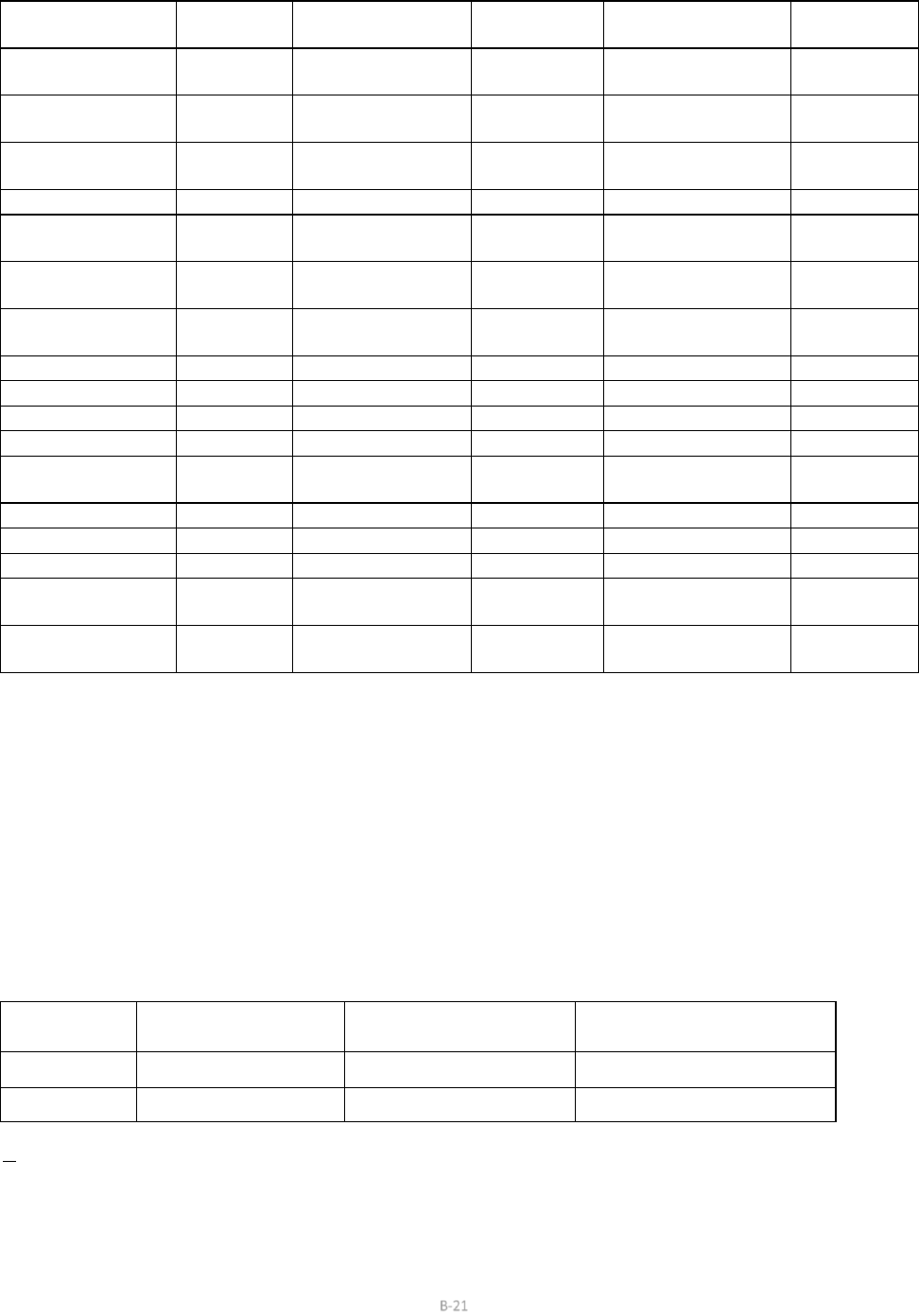
DentaQuest USA Insurance Company, February 1, 2024
Current Dental Terminology © American Dental Association. All Rights Reserved.
123
DentaQuest USA Insurance Company
Indicate which of the following you have had, or have at present. Circle “Yes” or “No” for each item.
Heart Disease or
Attack
Yes/No ___
Stroke
Yes/No ___
Hepatitis C
Yes/No ___
Heart Failure
Yes/No ___
Kidney Trouble
Yes/No ___
Arteriosclerosis
(hardening of
arteries)
Yes/No ___
Angina Pectoris
Yes/No ___
High Blood
Pressure
Yes/No ___
Ulcers
Yes/No ___
Congenital Heart
Disease
Yes/No ___
Venereal Disease
Yes/No ___
AIDS
Yes/No ___
Diabetes
Yes/No ___
Heart Murmur
Yes/No ___
Blood Transfusion
Yes/No ___
HIV Positive
Yes/No ___
Glaucoma
Yes/No ___
Cold
sores/Fever
blisters/
Herpes
Yes/No ___
High Blood
Pressure
Yes/No ___
Cortisone
Medication
Yes/No ___
Artificial Heart Valve
Yes/No ___
Mitral Valve
Prolapse
Yes/No ___
Cosmetic Surgery
Yes/No ___
Heart Pacemaker
Yes/No ___
Emphysema
Yes/No ___
Anemia
Yes/No ___
Sickle Cell Disease
Yes/No ___
Chronic Cough
Yes/No ___
Heart Surgery
Yes/No ___
Asthma
Yes/No ___
Tuberculosis
Yes/No ___
Bruise Easily
Yes/No ___
Yellow Jaundice
Yes/No ___
Liver Disease
Yes/No ___
Rheumatic fever
Yes/No ___
Rheumatism
Yes/No ___
Arthritis
Yes/No ___
Epilepsy or
Seizures
Yes/No ___
Fainting or Dizzy Spells
Yes/No ___
Allergies or Hives
Yes/No ___
Nervousness
Yes/No ___
Chemotherapy
Yes/No ___
Sinus Trouble
Yes/No ___
Radiation Therapy
Yes/No ___
Drug Addiction
Yes/No ___
Pain in Jaw Joints
Yes/No ___
Thyroid Problems
Yes/No ___
Psychiatric Treatment
Yes/No ___
Hay Fever
Yes/No ___
Hepatitis A
(infectious)
Yes/No ___
Blank cell
Blank cell
Artificial Joints
(Hip, Knee, etc.)
Yes/No ___
Hepatitis B (serum)
Yes/No ___
Blank cell
Blank cell
For Women Only:
Are you pregnant?
Yes/No___
If yes, what month? __________________________________________________
Are you nursing?
Yes/No___
Are you taking birth control pills?
Yes/No___
I understand the above information is necessary to provide me with dental care in a safe and efficient
manner. I have answered all questions truthfully.
Patient Signature:______________________Date: ________________________________
Dentist’s Signature:____________________Date: _________________________________
Review Date
Changes in Health
Status
Patient’s signature
Dentist’s signature
Blank cell
Blank cell
Blank cell
Blank cell
Blank cell
Blank cell
Blank cell
Blank cell
Note: The above form is intended to be a sample. DentaQuest is not mandating the use of this form. Please refer to State
statutes for specific State requirements and guidelines.
B-21
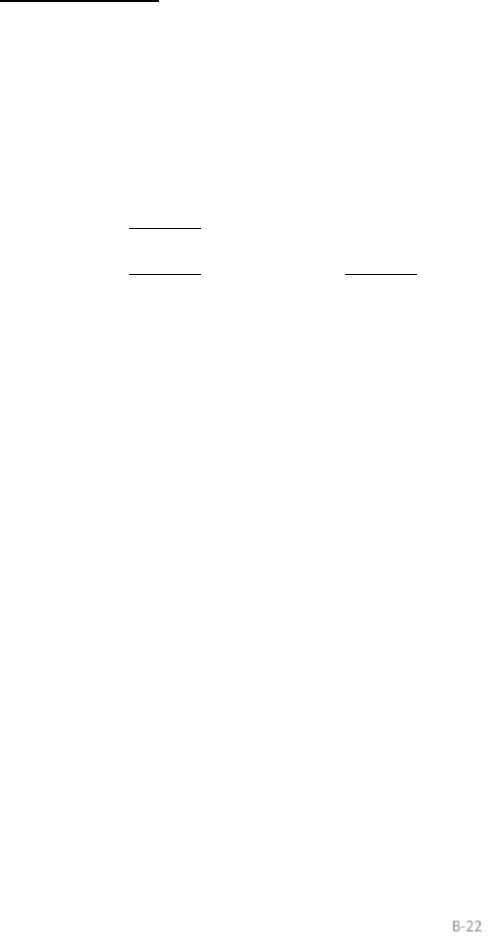
DentaQuest USA Insurance Company, February 1, 2024
Current Dental Terminology © American Dental Association. All Rights Reserved.
124
DentaQuest USA Insurance Company
AUTHORIZATION TO HONOR DIRECT AUTOMATED CLEARING HOUSE (ACH)
CREDITS
DISBURSED BY DENTAQUEST USA‐TX HHSC Dental Services Program
INSTRUCTIONS
1. Complete all parts of this form.
2. Execute all signatures where indicated. If account requires counter signatures, both signatures must appear on this form.
3. IMPORTANT: Attach voided check from checking account.
MAINTENANCE TYPE:
_______ Add
_______
Change
(Existing Set Up)
_______
Delete
(Existing Set Up)
ACCOUNT HOLDER INFORMATION:
Account Number: _____________________________________________________________________________
Account Type: Checking
Personal
Business (choose one)
Bank Routing Number: ___ ___ ___ ___ ___ ___ ___ ___ ___
Bank Name: ____________________________________________________________________________________
Account Holder Name: ____________________________________________________________________________
Effective Start Date: ______________________________________________________________________________
As a convenience to me, for payment of services or goods due me, I hereby request and authorize DentaQuest USA Insurance Company, Inc. to
credit my bank account via Direct Deposit for the (agreed upon dollar amounts and dates.) I also agree to accept my remittance statements online
and understand paper remittance statements will no longer be processed.
This authorization will remain in effect until revoked by me in writing. I agree you shall be fully protected in honoring any such credit entry.
I understand in endorsing or depositing this check that payment will be from Federal and State funds and that any falsification,
or concealment of
a material fact, may be prosecuted under Federal and State laws.
I agree that your treatment of each such credit entry, and your rights in respect to it, shall be the same as if it were signed by me. I fully agree that
if any such credit entry be dishonored, whether with or without cause, you shall be under no liability
whatsoever.
_______________________________________ ____________________________________________________
Date
Print Name
_______________________________________ ____________________________________________________
Phone Number Signature of Depositor (s) (As shown on Bank records
for the account, which
this authorization applicable.)
______________________________________________
Legal Business/Entity Name (As appears on W‐9 submitted to
DentaQuest)
_____________________________________________
Tax Id (As appears on W‐9 submitted to
DentaQuest)
B-22

DentaQuest USA Insurance Company, February 1, 2024
Current Dental Terminology © American Dental Association. All Rights Reserved.
125
DentaQuest USA Insurance Company
APPENDIX C
Covered Benefits (See Exhibits)
This section identifies covered benefits, provides specific criteria for coverage
and defines
individual age and benefit limitations for Medicaid Members under the age of 21 and CHIP
Members under the age 19. Providers with benefit
questions should contact
DentaQuest’s Customer Service department directly
at:
800.896.2374, press option 2
Dental offices are not allowed to charge Members for missed appointments. Program
Members are to be allowed the same access to dental treatment, as any other patient in
the dental practice. Private reimbursement arrangements
may be made only for non‐
covered services.
DentaQuest recognizes tooth letters “A” through “T” for primary teeth and tooth numbers
“1” to “32” for permanent teeth. Supernumerary teeth should be
designated by “AS
through TS” for primary teeth and tooth numbers “51” to “82” for permanent teeth and.
These codes must be referenced in the patient’s file for record retention and review. All
dental services performed must be recorded in the patient record, which must be
available as required by your
Participating Provider Agreement.
For reimbursement, DentaQuest Providers should bill only per unique surface
regardless
of location. For example, when a dentist places separate fillings in both occlusal pits on an
upper permanent first molar, the billing should state a one surface occlusal amalgam ADA
code D2140. Furthermore, DentaQuest will reimburse for the total number of surfaces
restored per tooth, per day; (i.e. a separate occlusal and buccal restoration on tooth 30
will be reimbursed as 1
(OB) two surface restoration).
The DentaQuest claim system can only recognize dental services described using the current
American Dental Association CDT code list or those as defined as a Covered Benefit. All other
service codes not contained in the following tables will be rejected when submitted for
payment. A complete, copy of the CDT book can be purchased from the American Dental
Association at the following address:
American Dental Association
211 East Chicago Avenue
Chicago, IL 60611
800.947.4746
C-1
DentaQuest USA Insurance Company, February 1, 2024
Current Dental Terminology © American Dental Association. All Rights Reserved.
126
DentaQuest USA Insurance Company
Furthermore, DentaQuest subscribes to the definition of services performed as described in the
CDT manual.
The benefit tables (Exhibits) are all inclusive for covered services. Each category of service is
contained in a separate table and lists:
1. the ADA approved service code to submit when billing,
2. brief description of the covered service,
3. any age limits imposed on coverage,
4. a description of documentation, in addition to a completed ADA claim form,
that
must be submitted when a claim or request for prior authorization is submitted,
and
5. an indicator of whether or not the service is subject to prior authorization, any
other applicable benefit limitations
C-2
127
DentaQuest USA Insurance Company
127
DentaQuest Authorization Process
IMPORTANT
For procedures where “Authorization Required” fields indicate “yes”.
Please review the information below on when to submit documentation to DentaQuest. The
information refers to the “Documentation Required” field in the Benefits Covered section (Exhibits).
In this section, documentation may be requested to be sent prior to beginning treatment or “with
claim” after completion of treatment.
When documentation is requested:
“Review
Required” Field
“Documentation
Required”
Field
Treatment
Condition
When to Submit
Documentation
Yes
Documentation Requested
Non‐emergency
(routine)
Send
documentation
prior to beginning
treatment
Yes
Documentation Requested
Emergency
Send
documentation with
claim after
treatment
When documentation is requested “with claim:”
“Review
Required” Field
“Documentation
Required”
Field
Treatment
Condition
When to Submit
Documentation
Yes
Documentation Requested
with Claim
Non
‐
emergency
(routine) or
emergency
Send
documentation with
claim after
treatment
Exhibit A Benefits Covered for TX
Medicaid Child (Under 21)
This document contains proprietary and confidential information and may not be disclosed to others
without written permission. ©Copyright 2024. All rights reserved.
128
Exhibit A Benefits Covered for TX Medicaid Child (Under 21)
Diagnostic services include the oral examinations, and selected radiographs needed to assess the oral health, diagnose oral pathology, and develop an adequate treatment
plan for the member's oral health.
Reimbursement for some or multiple x-rays of the same tooth or area may be denied if DentaQuest determines the number to be redundant, excessive or not in keeping
with the federal guidelines relating to radiation exposure. The maximum amount paid for individual radiographs taken on the same day will be limited to the allowance for a
full mouth series. Reimbursement for radiographs is limited to when required for proper treatment and/or diagnosis.
DentaQuest utilizes the guidelines published by the Department of Health and Human Services Center for Devices and Radiological Health. However, please consult the
following benefit tables for benefit limitations. All radiographs, must be of good diagnostic quality, include member's full name, date films taken, and identify the patients
left and right side. Substandard radiographs will not be reimbursed for, or if already paid for, DentaQuest will recoup the funds previously paid.
Covered dental services that indicate “Yes” in the “Review Required” column require documentation of medical necessity and will be subject to retrospective pre-payment
review. These procedures can be rendered before determination of medical necessity but require submission of proper documentation (as indicated in the “Documentation
Required” column) with the claim form.
Under 1 TAC §353.409(b) and §353.1001(b) EPSDT regulations, DentaQuest is required to provide the services in an amount, duration, and scope that is no less than the
amount, duration, and scope for the same services furnished to Members under FFS Medicaid. Please refer to the TMPPM for the FFS Medicaid language. However, all
requests to exceed listed benefit limitations in this provider manual, must be prior authorized with documentation supporting medical necessity for an increased benefit.
When the need for an exception is established, a narrative explaining the reason for the exception of limitations must be documented in the member's file and on the
claim submission. In order to submit a claim with an exception, the claim must have the key word “EXCEPTION” in Block 35 of the ADA claim form. If the key word
“EXCEPTION” is missing from Box 35, the claim may deny for exceeding benefit limitations.
Services Submitted with D9222 and, D9223, and D9500 for ages 1-6 will require prior authorization. Please reference ‘Criteria for General Anesthesia and Intravenous (IV)
Sedation’ in the Clinical Criteria section of this ORM
Any reimbursement already made for an inadequate service may be recouped after the DentaQuest Consultant reviews the circumstances.
Clinical Oral Evaluations/Diagnostics
Code
Brief Description
Age
Limitation
Teeth Covered
Review
Required
Benefit Limitations
Documentation
Required
D0120
periodic oral evaluation -
established patient
0-20
blank
No
Limited to one every six months by the same
provider OR location. Denied when submitted for the
same DOS as procedure codes D0120, D0140, D0145,
D0150, D0160, D0170, D0180 by the same provider.
Codes D0120, D0145, and D0150 must be performed
on same date as D0601, D0602, or D0603 to receive
reimbursement.
blank
Exhibit A Benefits Covered for TX
Medicaid Child (Under 21)
This document contains proprietary and confidential information and may not be disclosed to others
without written permission. ©Copyright 2024. All rights reserved.
129
Clinical Oral Evaluations/Diagnostics
Code
Brief Description
Age
Limitation
Teeth Covered
Review
Required
Benefit Limitations
Documentation
Required
D0140
limited oral evaluation-
problem focused
0-20
blank
No
Limited to one service per day by the same provider
OR location or two services per day per patient by
different providers. Denied when submitted for the
same DOS as procedure codes D0120, D0140, D0145,
D0150, D0160, D0170, D0180 by the same provider.
Limited emergency exam for an emergency situation
that is medically necessary to treat pain, infection,
swelling, uncontrolled bleeding or traumatic injury.
Not allowed with routine dental services. Document
of Medical Necessity must be indicated on the claim.
narrative of medical
necessity
D0145
first dental home oral
evaluation
6-35
months
blank
No
Providers must be certified by Texas Health Steps
staff to perform this procedure as a First Dental
Home (FDH) Provider. Members are limited to one
D0145 per day with a maximum of 10 services
allowed per member’s lifetime with at least 60 days
between dates of service per provider. Cannot be
billed within a 6-month period of a (D0120 or
D0150). Codes D1330, D1206, D1120, and D1208 will
be denied when billed on the same date of service as
a D0145. D0145 must be performed on same date as
D0601, D0602, or D0603 to receive reimbursement.
blank
D0150
comprehensive oral
evaluation - new or
established patient
0-20
blank
No
Limited to one service every three years by the same
provider or location. Denied when submitted for the
same DOS as D0145 by any provider. One of (D0120,
D0150) per 6 Month(s) Per Provider OR Location.
Codes D0120, D0145, and D0150 must be performed
on same date as D0601, D0602, or D0603 to receive
reimbursement.
blank
D0160
detailed and extensive oral
eval-problem focused, by
report
1 - 20
blank
No
Limited to one service per day by the same provider
OR location. Not payable for routine postoperative
follow-up. Denied when submitted for the same DOS
as procedure codes D0120, D0140, D0145, D0150,
D0160, D0170, D0180 by the same provider.
narrative of medical
necessity
Exhibit A Benefits Covered for TX
Medicaid Child (Under 21)
This document contains proprietary and confidential information and may not be disclosed to others
without written permission. ©Copyright 2024. All rights reserved.
130
Clinical Oral Evaluations/Diagnostics
Code
Brief Description
Age
Limitation
Teeth Covered
Review
Required
Benefit Limitations
Documentation
Required
D0170
re-evaluation, limited
problem focused
0-20
blank
No
Limited to one service per day by the same provider
OR location. Denied when submitted for the same
DOS as procedure codes D0120, D0140, D0145,
D0150, D0160, D0170, D0180 by the same provider.
narrative of medical
necessity
D0180
comprehensive periodontal
evaluation - new or
established patient
13 - 20
blank
No
Limited to one service per day by the same provider
OR location. Denied when submitted for the same
DOS as procedure codes D0120, D0140, D0145,
D0150, D0160, D0170, D0180 by the same provider.
narrative of medical
necessity
D0210
intraoral - complete series
of radiographic images
2-5
blank
Yes
Limited to one service of D0210 or D0330 every
three years by the same provider OR location.
Narrative of medical necessity and x-ray.
narr. of med.
necessity, pre-op x-
ray(s)
D0210
intraoral - complete series
of radiographic images
6 - 20
blank
No
Limited to one service of D0210 or D0330 every
three years by the same provider OR location.
D0220
intraoral - periapical first
radiographic image
1 - 20
blank
No
Limited to one service per day by the same provider
OR location.
blank
D0230
intraoral - periapical each
additional radiographic
image
1 - 20
blank
No
blank
blank
D0240
intraoral - occlusal
radiographic image
0-20
blank
No
Limited to two services per day by the same provider
OR location.
blank
D0250
extra-oral – 2D projection
radiographic image created
using a stationary radiation
source, and detector
1 - 20
blank
No
Limited to one service per day by the same provider
OR location.
blank
D0270
bitewing - single
radiographic image
1
blank
Yes
Limited to one service of D0270, D0272, D0273,
D0274 per day by the same provider OR location.
Narrative of medical necessity and x-ray showing
fully erupted primary first molar.
narr. of med.
necessity, pre-op x-
ray(s)
D0270
bitewing - single
radiographic image
2-20
blank
No
Limited to one service of D0270, D0272, D0273,
D0274 per day by the same provider OR location.
D0272
bitewings - two
radiographic images
1
blank
Yes
Limited to one service of D0270, D0272, D0273,
D0274 per day by the same provider OR location.
Narrative of medical necessity and x-ray showing
fully erupted primary first molar.
narr. of med.
necessity, pre-op x-
ray(s)
Exhibit A Benefits Covered for TX
Medicaid Child (Under 21)
This document contains proprietary and confidential information and may not be disclosed to others
without written permission. ©Copyright 2024. All rights reserved.
131
Clinical Oral Evaluations/Diagnostics
Code
Brief Description
Age
Limitation
Teeth Covered
Review
Required
Benefit Limitations
Documentation
Required
D0272
bitewings - two
radiographic images
2-20
blank
No
Limited to one service of D0270, D0272, D0273,
D0274 per day by the same provider OR location.
One service of D0210, D0272 per day per patient.
D0273
bitewings - three
radiographic images
1-9
blank
Yes
Limited to one service of D0270, D0272, D0273,
D0274 per day by the same provider OR location.
One service of D0210, D0272 per day per patient.
Narrative of medical necessity and x-rays showing
fully erupted left and right second permanent
molars.
narr. of med.
necessity, pre-op x-
ray(s)
D0273
bitewings - three
radiographic images
10 - 20
blank
No
Limited to one service of D0270, D0272, D0273,
D0274 per day by the same provider OR location.
One service of D0210, D0272 per day per patient.
blank
D0274
bitewings - four
radiographic images
1-9
blank
Yes
Limited to one service of D0270, D0272, D0273,
D0274 per day by the same provider OR location.
One service of D0210, D0272 per day per patient.
Narrative of medical necessity and x-rays showing
fully erupted left and right second permanent
molars.
narr. of med.
necessity, pre-op x-
ray(s)
D0274
bitewings - four
radiographic images
10 - 20
blank
No
Limited to one service of D0270, D0272, D0273,
D0274 per day by the same provider OR location.
One service of D0210, D0272 per day per patient.
blank
D0277
vertical bitewings - 7 to 8
films
2 - 20
blank
No
Limited to one service per day by the same provider
OR location. One service of D0210, D0277 per day
per patient.
blank
D0310
sialography
1 - 20
blank
No
blank
blank
D0320
temporomandibular joint
arthrogram, including
injection
1 - 20
blank
No
blank
blank
D0321
other temporomandibular
joint films, by report
1 - 20
blank
No
blank
blank
D0322
tomographic survey
1 - 20
blank
No
blank
blank
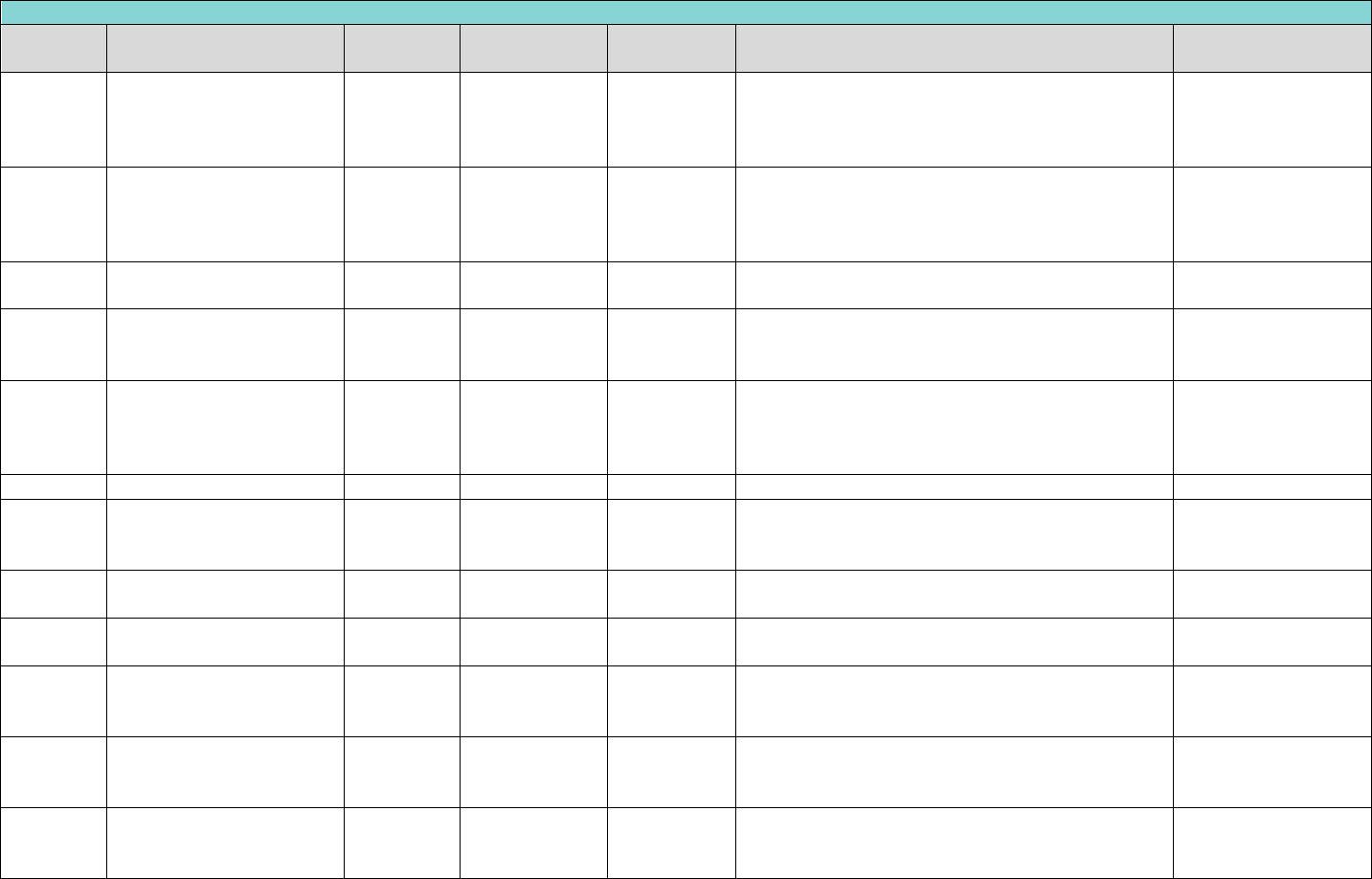
Exhibit A Benefits Covered for TX
Medicaid Child (Under 21)
This document contains proprietary and confidential information and may not be disclosed to others
without written permission. ©Copyright 2024. All rights reserved.
132
Clinical Oral Evaluations/Diagnostics
Code
Brief Description
Age
Limitation
Teeth Covered
Review
Required
Benefit Limitations
Documentation
Required
D0330
panoramic radiographic
image
3-5
blank
Yes
Limited to one service of D0210 or D0330 every
three years by the same provider OR location. One
service of D0210, D0277, D0330 per day per
provider. Narrative of medical necessity and x-ray.
narr. of med.
necessity, pre-op x-
ray(s)
D0330
panoramic radiographic
image
6 - 20
blank
No
Limited to one service of D0210 or D0330 every
three years by the same provider OR location. One
service of D0210, D0277, D0330 per day per
provider.
blank
D0340
cephalometric radiographic
image
1 - 20
blank
No
Limited to one service per day by the same provider
OR location. Not billable with orthodontic work up.
blank
D0350
2D oral/facial photographic
image obtained intra-orally
or extra-orally
0-20
blank
No
Limited to one service per day by the same provider
OR location. Not billable with orthodontic work up.
blank
D0367
Cone beam CT capture and
interpretation with field of
view of both jaws, with or
without cranium
0-20
blank
Yes
Limited to a combined maximum of three services
per year, per patient.
narrative of medical
necessity
D0415
bacteriologic studies
1 - 20
blank
No
blank
blank
D0460
pulp vitality tests
1 - 20
blank
No
Limited to one service per day by the same provider
OR location. Not allowed on primary teeth. Not
billable with endodontic procedures.
blank
D0470
diagnostic casts
1 - 20
blank
No
Not billable with crowns, prosthodontics (fixed or
removable) orthodontics, or diagnostic work up.
blank
D0502
other oral pathology
procedures, by report
1 - 20
blank
No
blank
blank
D0601
Caries risk assessment and
documentation, with a
finding of low risk
0-20
blank
No
Codes D0120, D0145, and D0150 must be performed
on same date as D0601, D0602, or D0603 to receive
reimbursement.
blank
D0602
Caries risk assessment and
documentation, with a
finding of moderate risk
0-20
blank
No
Codes D0120, D0145, and D0150 must be performed
on same date as D0601, D0602, or D0603 to receive
reimbursement.
blank
D0603
Caries risk assessment and
documentation, with a
finding of high risk
0-20
blank
No
Codes D0120, D0145, and D0150 must be performed
on same date as D0601, D0602, or D0603 to receive
reimbursement.
blank
Exhibit A Benefits Covered for TX
Medicaid Child (Under 21)
This document contains proprietary and confidential information and may not be disclosed to others
without written permission. ©Copyright 2024. All rights reserved.
133
Clinical Oral Evaluations/Diagnostics
Code
Brief Description
Age
Limitation
Teeth Covered
Review
Required
Benefit Limitations
Documentation
Required
D0999
unspecified diagnostic
procedure, by report
1 - 20
blank
Yes
blank
narrative of medical
necessity
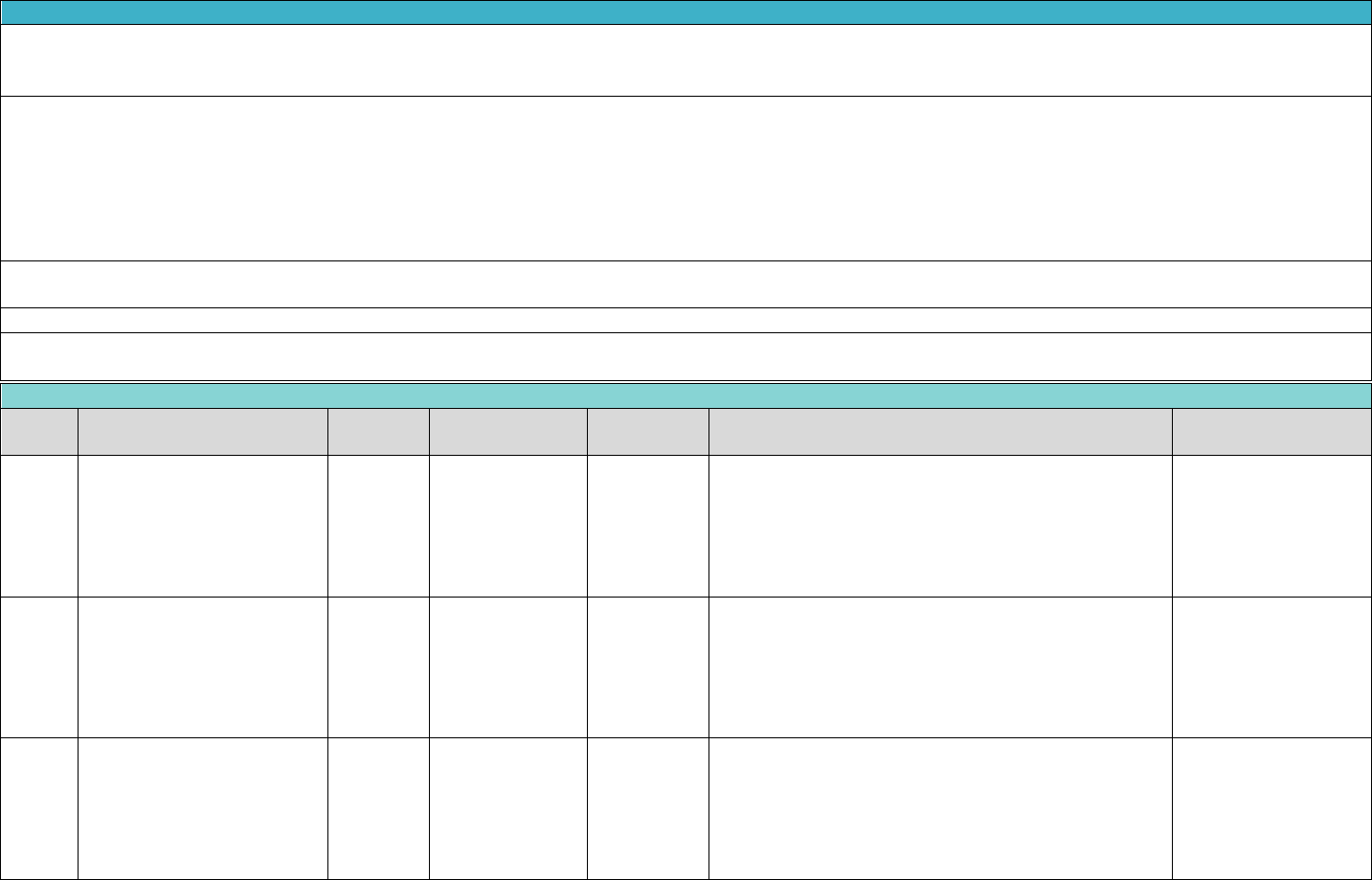
Exhibit A Benefits Covered for TX
Medicaid Child (Under 21)
This document contains proprietary and confidential information and may not be disclosed to others
without written permission. ©Copyright 2024. All rights reserved.
134
Exhibit A Benefits Covered for TX Medicaid Child (Under 21)
Covered dental services that indicate “Yes” in the “Review Required” column require documentation of medical necessity and will be subject to retrospective pre-payment
review. These procedures can be rendered before determination of medical necessity but require submission of proper documentation (as indicated in the “Documentation
Required” column) with the claim form.
Under 1 TAC §353.409(b) and §353.1001(b) EPSDT regulations, DentaQuest is required to provide the services in an amount, duration, and scope that is no less than the
amount, duration, and scope for the same services furnished to Members under FFS Medicaid. Please refer to the TMPPM for the FFS Medicaid language. However, all
requests to exceed listed benefit limitations in this provider manual, must be prior authorized with documentation supporting medical necessity for an increased benefit.
When the need for an exception is established, a narrative explaining the reason for the exception of limitations must be documented in the member's file and on the
claim submission. In order to submit a claim with an exception, the claim must have the key word “EXCEPTION” in Block 35 of the ADA claim form. If the key word
“EXCEPTION” is missing from Box 35, the claim may deny for exceeding benefit limitations.
Services Submitted with D9222 and, D9223, and D9500 for ages 1-6 will require prior authorization. Please reference ‘Criteria for General Anesthesia and Intravenous (IV)
Sedation’ in the Clinical Criteria section of this ORM.
Any reimbursement already made for an inadequate service may be recouped after the DentaQuest Consultant reviews the circumstances.
Tobacco counseling (procedure code D1320) is considered a part of all dental procedures and may not be billed separately. Oral hygiene instruction procedure code D1330 is
limited to services rendered in the office setting.
Preventative
Code
Brief Description
Age
Limitation
Teeth Covered
Review
Required
Benefit Limitations
Documentation
Required
D1110
prophylaxis - adult
13 - 20
blank
No
Limited to one D1110, D1120 per patient, any provider,
per six-month period. Denied when submitted for the
same DOS as any D4000 series periodontal procedure
code. Denied when billed with emergency treatment.
Cannot be billed by Orthodontist or Maxillofacial Surgery
Specialist.
blank
D1120
prophylaxis - child
0-12
blank
No
Limited to one D1110, D1120 per patient, any provider,
per six-month period. Denied when submitted for the
same DOS as any D4000 series periodontal procedure
code. Denied when billed with emergency treatment.
Cannot be billed by Orthodontist or Maxillofacial Surgery
Specialist.
blank
D1206
topical application of fluoride
varnish
0-20
blank
No
One service of D1206, D1208 per patient, any provider,
per six-month period. Denied when submitted for the
same DOS as any D4000 series periodontal procedure
code or with procedure code D0145. If submitted on
emergency claim, D1206 will be denied. Cannot be billed
by Orthodontist or Maxillofacial Surgery Specialist.
blank
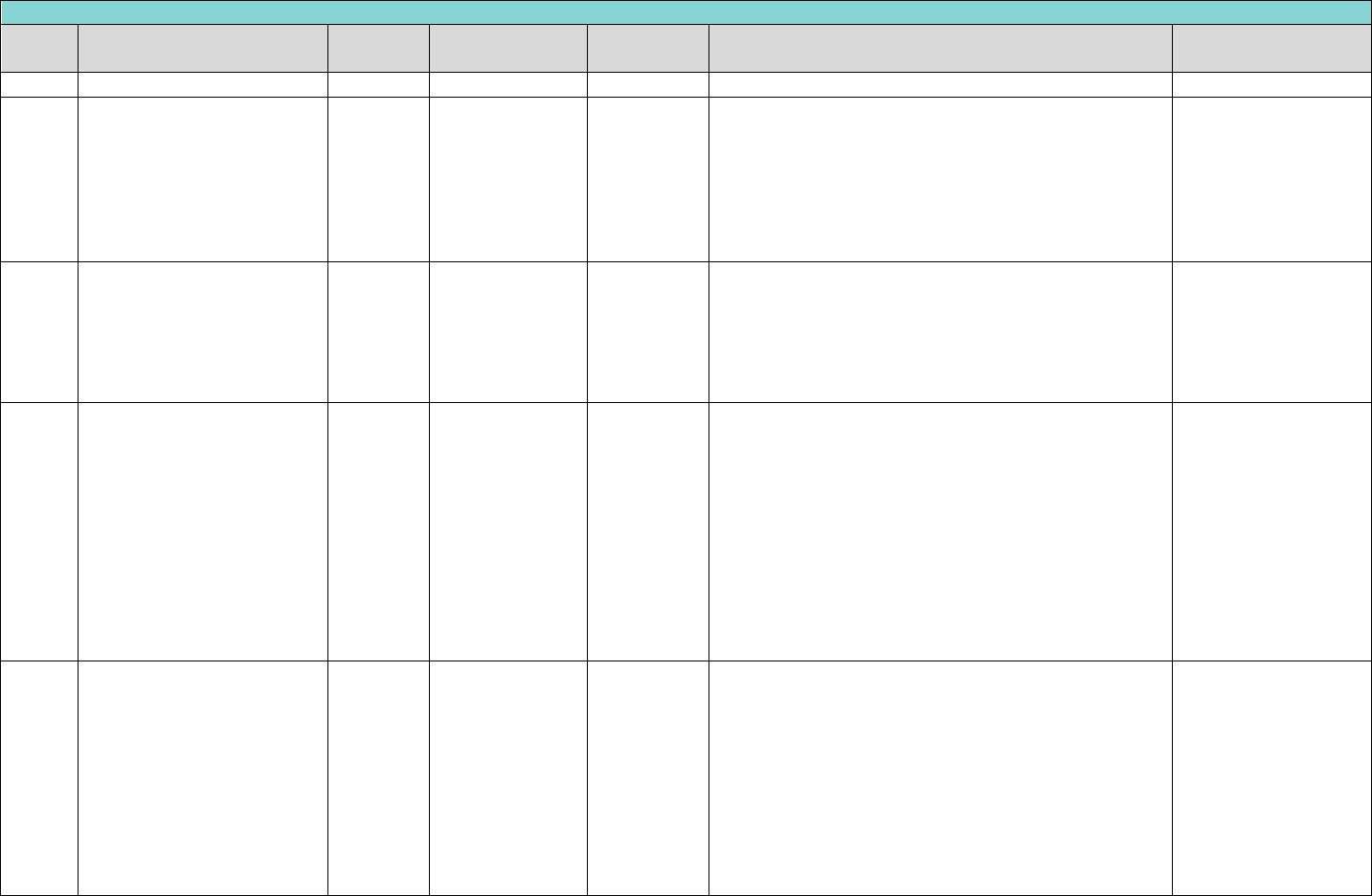
Exhibit A Benefits Covered for TX
Medicaid Child (Under 21)
This document contains proprietary and confidential information and may not be disclosed to others
without written permission. ©Copyright 2024. All rights reserved.
135
Preventative
Code
Brief Description
Age
Limitation
Teeth Covered
Review
Required
Benefit Limitations
Documentation
Required
Includes oral health instructions.
D1208
topical application of fluoride
- excluding varnish
0-20
blank
No
One service of D1206, D1208 per patient, any provider,
per six-month period. Denied when submitted for the
same DOS as any D4000 series periodontal procedure
code or with procedure code D0145. If submitted on
emergency claim, D1206 will be denied. Cannot be billed
by Orthodontist or Maxillofacial Surgery Specialist.
Includes oral health instructions.
blank
D1330
oral hygiene instructions
0-20
blank
No
One service of D1330 per year, per patient, any
provider. Denied when billed for the same DOS as oral
hygiene instructions (D1330), prophylaxis (D1110 or
D1120), or topical fluoride treatments (D1206 or
D1208), by any provider. Limited to services performed
in an office setting.
blank
D1351
sealant - per tooth
1-5
Teeth 2 - 5, 12 -
15, 18 - 21, 28 -
31
Yes
Limited to one service of (D1351, D1352) per tooth, per
lifetime. D1351 will be denied when submitted for the
same date of service as any D4000 Series periodontal
procedure code. For those members without a history
of caries or restorations within the past year, such
narrative should describe the tooth anatomy of the area
to be sealed to support that the tooth is at risk for
dental caries and the affectivity of placing a sealant
outside of the 6-14 age band. If submitted on emergency
claim, D1351 will be denied. Not billable by Orthodontist
or Oral Surgeon.
Narrative of medical
necessity
D1351
sealant - per tooth
17-20
Teeth 2 - 5, 12 -
15, 18 - 21, 28 -
31
Yes
Limited to one service of (D1351, D1352) per tooth, per
lifetime. D1351 will be denied when submitted for the
same date of service as any D4000 Series periodontal
procedure code. For those members without a history
of caries or restorations within the past year, such
narrative should describe the tooth anatomy of the area
to be sealed to support that the tooth is at risk for
dental caries and the affectivity of placing a sealant
outside of the 6-14 age band. If submitted on emergency
claim, D1351 will be denied. Not billable by Orthodontist
blank
Exhibit A Benefits Covered for TX
Medicaid Child (Under 21)
This document contains proprietary and confidential information and may not be disclosed to others
without written permission. ©Copyright 2024. All rights reserved.
136
Preventative
Code
Brief Description
Age
Limitation
Teeth Covered
Review
Required
Benefit Limitations
Documentation
Required
or Oral Surgeon.
D1351
sealant - per tooth
1-20
Teeth 1, 6 - 11,
16, 17, 22 - 27,
32, 51 - 82, C - H,
M - R, AS, BS, CS,
DS, ES, FS, GS,
HS, IS, JS, KS, LS,
MS, NS, OS, PS,
QS, RS, SS, TS
Yes
Limited to one service of (D1351, D1352) per tooth, per
lifetime. D1351 will be denied when submitted for the
same date of service as any D4000 Series periodontal
procedure code. For those members without a history
of caries or restorations within the past year, such
narrative should describe the tooth anatomy of the area
to be sealed to support that the tooth is at risk for
dental caries and the affectivity of placing a sealant
outside of the 6-14 age band. If submitted on emergency
claim, D1351 will be denied. Not billable by Orthodontist
or Oral Surgeon.
Narrative of medical
necessity and photos
D1351
sealant - per tooth
1-5
Teeth A, B, I - L,
S, T
Yes
Limited to one service of (D1351, D1352) per tooth, per
lifetime. D1351 will be denied when submitted for the
same date of service as any D4000 Series periodontal
procedure code. If submitted on emergency claim,
D1351 will be denied. Not billable by Orthodontist or
Oral Surgeon.
blank
D1351
sealant - per tooth
15-16
Teeth 2 - 5, 12 -
15, 18 - 21, 28 -
31
Yes
Limited to one service of (D1351, D1352) per tooth, per
lifetime. D1351 will be denied when submitted for the
same date of service as any D4000 Series periodontal
procedure code. If submitted on emergency claim,
D1351 will be denied. Not billable by Orthodontist or
Oral Surgeon.
Narrative of medical
necessity
D1351
sealant - per tooth
7-14
Teeth 2 - 5, 12 -
15, 18 - 21, 28 -
31
No
Limited to one service of (D1351, D1352) per tooth, per
lifetime. D1351 will be denied when submitted for the
same date of service as any D4000 Series periodontal
procedure code. If submitted on emergency claim,
D1351 will be denied. Not billable by Orthodontist or
Oral Surgeon.
blank
D1351
sealant - per tooth
7-20
Teeth A, B, I - L,
S, T
No
Limited to one service of (D1351, D1352) per tooth, per
lifetime. D1351 will be denied when submitted for the
same date of service as any D4000 Series periodontal
procedure code. If submitted on emergency claim,
Exhibit A Benefits Covered for TX
Medicaid Child (Under 21)
This document contains proprietary and confidential information and may not be disclosed to others
without written permission. ©Copyright 2024. All rights reserved.
137
Preventative
Code
Brief Description
Age
Limitation
Teeth Covered
Review
Required
Benefit Limitations
Documentation
Required
D1351 will be denied. Not billable by Orthodontist or
Oral Surgeon.
D1351
sealant - per tooth
6
(72
nd
month –
83
rd
month)
Teeth 2 - 5, 12 -
15, 18 - 21, 28 –
31,
A, B, I - L, S, T
Yes
Limited to one service of (D1351, D1352) per tooth, per
lifetime. D1351 will be denied when submitted for the
same date of service as any D4000 Series periodontal
procedure code. If submitted on emergency claim,
D1351 will be denied. Not billable by Orthodontist or
Oral Surgeon.
D1352
Preventive resin restoration
is a mod. to high caries risk
patient perm tooth
conservative rest of an active
cavitated lesion in a pit or
fissure that doesn't extend
into dentin: includes
placement of a sealant in
radiating non-carious fissure
or pits.
5-6
Teeth 2 - 5, 12 -
15, 18 - 21, 28 -
31
Yes
Limited to one service of (D1351, D1352) per tooth, per
lifetime. D1352 will be denied when submitted for the
same date of service as any D4000 Series periodontal
procedure code. Denied if a caries risk assessment
(procedure code D0602 or D0603) has not been
submitted, by any provider, within 180 days prior.
D1352
Preventive resin restoration
is a mod. to high caries risk
patient perm tooth
conservative rest of an active
cavitated lesion in a pit or
fissure that doesn't extend
into dentin: includes
placement of a sealant in
radiating non-carious fissure
or pits.
7-14
Teeth 2 - 5, 12 -
15, 18 - 21, 28 -
31
No
Limited to one service of (D1351, D1352) per tooth, per
lifetime. D1352 will be denied when submitted for the
same date of service as any D4000 Series periodontal
procedure code. Denied if a caries risk assessment
(procedure code D0602 or D0603) has not been
submitted, by any provider, within 180 days prior.
D1352
Preventive resin restoration
is a mod. to high caries risk
patient perm tooth
conservative rest of an active
cavitated lesion in a pit or
fissure that doesn't extend
into dentin: includes
5-20
Teeth 1, 16, 17,
32
Yes
Limited to one service of (D1351, D1352) per tooth, per
lifetime. D1352 will be denied when submitted for the
same date of service as any D4000 Series periodontal
procedure code. For members without a history of
caries or restorations within the past year, such
narrative should describe the tooth anatomy of the area
to be sealed to support that the tooth is at risk for
Narrative of medical
necessity and photos
Exhibit A Benefits Covered for TX
Medicaid Child (Under 21)
This document contains proprietary and confidential information and may not be disclosed to others
without written permission. ©Copyright 2024. All rights reserved.
138
Preventative
Code
Brief Description
Age
Limitation
Teeth Covered
Review
Required
Benefit Limitations
Documentation
Required
placement of a sealant in
radiating non-carious fissure
or pits.
dental caries and the affectivity of placing a sealant
outside of the 5-14 age band. Documentation can also
include patient-centric risk factors that may exist.
Denied if a caries risk assessment (procedure code
D0602 or D0603) has not been submitted, by any
provider within 180 days prior.
D1352
Preventive resin restoration
is a mod. to high caries risk
patient perm tooth
conservative rest of an active
cavitated lesion in a pit or
fissure that doesn't extend
into dentin: includes
placement of a sealant in
radiating non-carious fissure
or pits.
15-20
Teeth 2 - 5, 12 -
15, 18 - 21, 28 -
31
Y
Limited to one service of (D1351, D1352) per tooth, per
lifetime. D1352 will be denied when submitted for the
same date of service as any D4000 Series periodontal
procedure code. Denied if a caries risk assessment
(procedure code D0602 or D0603) has not been
submitted, by any provider, within 180 days prior.
Narrative of medical
necessity
D1354
interim caries arresting
medicament application –
per tooth
6 months-
6 years
Teeth 1 ‐ 32, 51 ‐
82, A ‐ T, AS, BS,
CS, DS, ES, FS,
GS, HS, IS, JS, KS,
LS, MS, NS, OS,
PS, QS, RS, SS, TS
No
D1354 is limited to one application per lifetime of tooth.
Not allowed on the same date of service as D1351 or
D1352 on the same tooth. D1354 must be deemed
medically necessary by Main Dental Home provider.
Silver Diamine Fluoride is the only materials that may be
used for D1354.
D1510
space maintainer-fixed-
unilateral – Per Quadrant
1 - 6
Per Quadrant
(10, 20, 30, 40,
LL, LR, UL, UR)
Yes
Limit to one service of (D1510, D1520) per lifetime, per
patient, per quadrant. After premature loss of a
deciduous/primary first and/or second molar for clients
who are 1 through 12 years of age (procedure codes
D1510 and D1516 and D1517)
blank
D1510
space maintainer-fixed-
unilateral – Per Quadrant
7 - 12
Per Quadrant
(10, 20, 30, 40,
LL, LR, UL, UR)
No
Limit to one service of (D1510, D1520) per lifetime, per
patient, per quadrant. After premature loss of a
deciduous/primary first and/or second molar for clients
who are 1 through 12 years of age (procedure codes
D1510 and D1516 and D1517)

Exhibit A Benefits Covered for TX
Medicaid Child (Under 21)
This document contains proprietary and confidential information and may not be disclosed to others
without written permission. ©Copyright 2024. All rights reserved.
139
Preventative
Code
Brief Description
Age
Limitation
Teeth Covered
Review
Required
Benefit Limitations
Documentation
Required
D1516
space maintainer – fixed –
bilateral, maxillary
1 - 6
Per Arch (01, UA)
Yes
Limit to one service of (D1516, D1526) per lifetime, per
patient, per arch. After premature loss of a
deciduous/primary first and/or second molar (TID A, B, I,
and J) for clients who are 1 through 12 years of age
(procedure codes D1510 and D1516)
blank
D1516
space maintainer – fixed –
bilateral, maxillary
7 - 12
Per Arch (01, UA)
No
Limit to one service of (D1516, D1526) per lifetime, per
patient, per arch. After premature loss of a
deciduous/primary first and/or second molar (TID A, B, I,
and J) for clients who are 1 through 12 years of age
(procedure codes D1510 and D1516)
D1517
space maintainer – fixed –
bilateral, mandibular
1 - 6
Per Arch (02, LA)
Yes
One of (D1517, D1527) per 24 Month(s) Per patient, per
lifetime, same arch. After premature loss of a
deciduous/primary first and/or second molar (TID K, L, S,
and T) for clients who are 1 through 12 years of age
(procedure codes D1510 and D1517)
blank
D1517
space maintainer – fixed –
bilateral, mandibular
7 - 12
Per Arch (02, LA)
No
One of (D1517, D1527) per 24 Month(s) Per patient, per
lifetime, same arch. After premature loss of a
deciduous/primary first and/or second molar (TID K, L, S,
and T) for clients who are 1 through 12 years of age
(procedure codes D1510 and D1517)
D1520
Space maintainer-
removable-unilateral
1 - 6
Per Quadrant
(10, 20, 30, 40,
LL, LR, UL, UR)
Yes
Limit to one service of (D1510 or D1520) per lifetime,
per patient, per quadrant.
blank
D1520
Space maintainer-
removable-unilateral
7 - 12
Per Quadrant
(10, 20, 30, 40,
LL, LR, UL, UR)
No
Limit to one service of (D1510 or D1520) per lifetime,
per patient, per quadrant.
D1526
space maintainer –
removable – bilateral,
maxillary
1 - 6
Per Arch (01, UA)
Yes
Limit to one service of (D1516, D1526) per lifetime, per
patient, per arch. After premature loss of a
deciduous/primary first and/or second molar (TID A, B, I,
and J) for clients who are 1 through 12 years of age
(procedure codes D1510 and D1516)
blank
D1526
space maintainer –
removable – bilateral,
maxillary
7 - 12
Per Arch (01, UA)
No
Limit to one service of (D1516, D1526) per lifetime, per
patient, arch. After premature loss of a
deciduous/primary first and/or second molar (TID A, B, I,
Exhibit A Benefits Covered for TX
Medicaid Child (Under 21)
This document contains proprietary and confidential information and may not be disclosed to others
without written permission. ©Copyright 2024. All rights reserved.
140
Preventative
Code
Brief Description
Age
Limitation
Teeth Covered
Review
Required
Benefit Limitations
Documentation
Required
and J) for clients who are 1 through 12 years of age
D1527
space maintainer –
removable – bilateral,
mandibular
1 - 6
Per Arch (02, LA)
Yes
Limit to one service of (D1517 or D1527) per lifetime,
per patient, per arch. After premature loss of a
deciduous/primary first and/or second molar (TID K, L, S,
and T) for clients who are 1 through 12 years of age
(procedure codes D1510 and D1517). Removal of a fixed
space maintainer is not payable to the provider or
provider group that originally placed the device.
blank
D1527
space maintainer –
removable – bilateral,
mandibular
7 - 12
Per Arch (02, LA)
No
Limit to one service of (D1517 or D1527) per lifetime,
per patient, per arch. After premature loss of a
deciduous/primary first and/or second molar (TID K, L, S,
and T) for clients who are 1 through 12 years of age
(procedure codes D1510 and D1517). Removal of a fixed
space maintainer is not payable to the provider or
provider group that originally placed the device.
D1551
re-cement or re-bond
bilateral space maintainer -
maxillary
1 ‐ 6
Per Arch (01, UA)
Yes
Not allowed within 12 months of initial placement. The
recementation of space maintainers (procedure code
D1551, D1552, or D1553) may be considered for
reimbursement to either the same or different Texas
Health Steps dental provider when procedure code
D1510, D1516, or D1517 has been previously
reimbursed.
blank
D1551
re-cement or re-bond
bilateral space maintainer -
maxillary
7 ‐ 12
Per Arch (01, UA)
No
Not allowed within 12 months of initial placement. The
recementation of space maintainers (procedure code
D1551, D1552, or D1553) may be considered for
reimbursement to either the same or different Texas
Health Steps dental provider when procedure code
D1510, D1516, or D1517 has been previously
reimbursed.
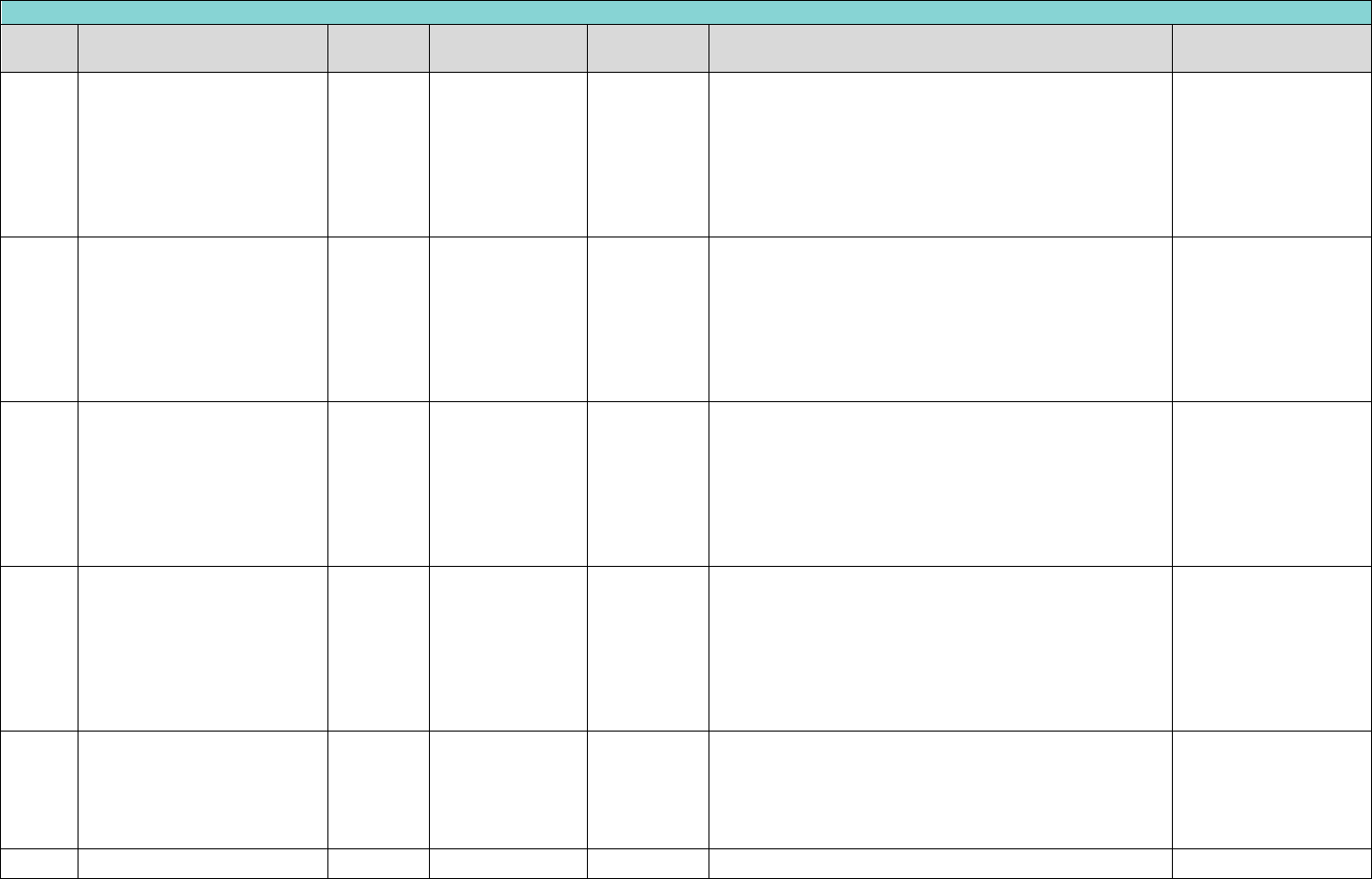
Exhibit A Benefits Covered for TX
Medicaid Child (Under 21)
This document contains proprietary and confidential information and may not be disclosed to others
without written permission. ©Copyright 2024. All rights reserved.
141
Preventative
Code
Brief Description
Age
Limitation
Teeth Covered
Review
Required
Benefit Limitations
Documentation
Required
D1552
re-cement or re-bond
bilateral space maintainer -
mandibular
1 ‐ 6
Per Arch (02, LA)
Yes
Not allowed within 12 months of initial placement. The
recementation of space maintainers (procedure code
D1551, D1552, or D1553) may be considered for
reimbursement to either the same or different Texas
Health Steps dental provider when procedure code
D1510, D1516, or D1517 has been previously
reimbursed.
blank
D1552
re-cement or re-bond
bilateral space maintainer -
mandibular
7 ‐ 12
Per Arch (02, LA)
No
Not allowed within 12 months of initial placement. The
recementation of space maintainers (procedure code
D1551, D1552, or D1553) may be considered for
reimbursement to either the same or different Texas
Health Steps dental provider when procedure code
D1510, D1516, or D1517 has been previously
reimbursed.
D1553
re-cement or re-bond
unilateral space maintainer -
per quadrant
1 ‐ 6
Per Quadrant
(10, 20, 30, 40,
LL, LR, UL, UR)
Yes
Not allowed within 12 months of initial placement. The
recementation of space maintainers (procedure code
D1551, D1552, or D1553) may be considered for
reimbursement to either the same or different Texas
Health Steps dental provider when procedure code
D1510, D1516, or D1517 has been previously
reimbursed.
blank
D1553
re-cement or re-bond
unilateral space maintainer -
per quadrant
7 ‐ 12
Per Quadrant
(10, 20, 30, 40,
LL, LR, UL, UR)
No
Not allowed within 12 months of initial placement. The
recementation of space maintainers (procedure code
D1551, D1552, or D1553) may be considered for
reimbursement to either the same or different Texas
Health Steps dental provider when procedure code
D1510, D1516, or D1517 has been previously
reimbursed.
D1556
removal of fixed unilateral
space maintainer - per
quadrant
1 ‐ 6
Per Quadrant
(10, 20, 30, 40,
LL, LR, UL, UR)
Yes
Not allowed by same provider OR location that placed
appliance. Removal of a space maintainer (procedure
code D1556, D1557, or D1558) is not payable to the
provider or dental group practice that originally placed
the device.
blank
D1556
removal of fixed unilateral
7 ‐ 12
Per Quadrant
No
Not allowed by same provider OR location that placed
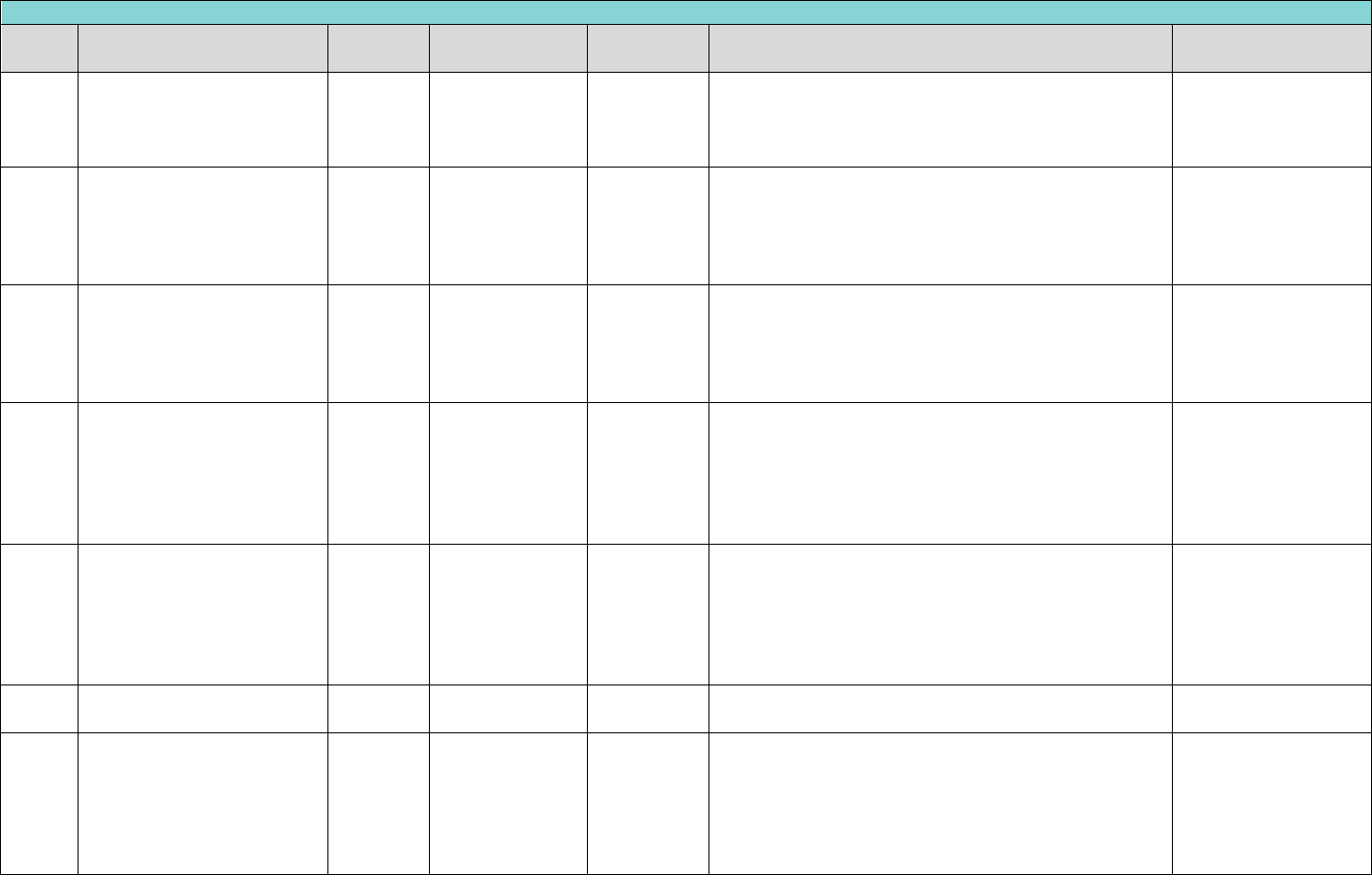
Exhibit A Benefits Covered for TX
Medicaid Child (Under 21)
This document contains proprietary and confidential information and may not be disclosed to others
without written permission. ©Copyright 2024. All rights reserved.
142
Preventative
Code
Brief Description
Age
Limitation
Teeth Covered
Review
Required
Benefit Limitations
Documentation
Required
space maintainer - per
quadrant
(10, 20, 30, 40,
LL, LR, UL, UR)
appliance. Removal of a space maintainer (procedure
code D1556, D1557, or D1558) is not payable to the
provider or dental group practice that originally placed
the device.
D1557
removal of fixed bilateral
space maintainer - maxillary
1 ‐ 6
Per Arch (01, UA)
Yes
Not allowed by same provider OR location that placed
appliance. Removal of a space maintainer (procedure
code D1556, D1557, or D1558) is not payable to the
provider or dental group practice that originally placed
the device.
blank
D1557
removal of fixed bilateral
space maintainer - maxillary
7 ‐ 12
Per Arch (01, UA)
No
Not allowed by same provider OR location that placed
appliance. Removal of a space maintainer (procedure
code D1556, D1557, or D1558) is not payable to the
provider or dental group practice that originally placed
the device.
D1558
removal of fixed bilateral
space maintainer -
mandibular
1 ‐ 6
Per Arch (02, LA)
Yes
Not allowed by same provider OR location that placed
appliance. Procedure codes D1553 and D1556 are
limited to once per quadrant, per day, same provider.
Removal of a space maintainer (procedure code D1556,
D1557, or D1558) is not payable to the provider or
dental group practice that originally placed the device.
blank
D1558
removal of fixed bilateral
space maintainer -
mandibular
7 ‐ 12
Per Arch (02, LA)
No
Not allowed by same provider OR location that placed
appliance. Procedure codes D1553 and D1556 are
limited to once per quadrant, per day, same provider.
Removal of a space maintainer (procedure code D1556,
D1557, or D1558) is not payable to the provider or
dental group practice that originally placed the device.
D1575
distal shoe space maintainer
– fixed - unilateral
3 - 6
Teeth A, J, K, T
Yes
Limit to one service of (D1575) per lifetime, per patient,
per tooth.
blank
D1575
distal shoe space maintainer
– fixed - unilateral
84
th
month
through
the 95
th
month
birthday
Teeth A, J, K, T
No
Limit to one service of (D1575) per lifetime, per patient,
per tooth.
Exhibit A Benefits Covered for TX
Medicaid Child (Under 21)
This document contains proprietary and confidential information and may not be disclosed to others
without written permission. ©Copyright 2024. All rights reserved.
143
Preventative
Code
Brief Description
Age
Limitation
Teeth Covered
Review
Required
Benefit Limitations
Documentation
Required
Exhibit A Benefits Covered for TX
Medicaid Child (Under 21)
This document contains proprietary and confidential information and may not be disclosed to others
without written permission. ©Copyright 2024. All rights reserved.
144
Exhibit A Benefits Covered for TX Medicaid Child (Under 21)
Reimbursement includes local anesthesia.
Generally, once a particular restoration is placed in a tooth, a similar restoration will not be covered for at least twelve months. It is DentaQuest’s expectation that
replacement prior to published frequency remain the responsibility of the treating provider.
A replacement of an identical restorative service in less than 36 months by the same provider is not considered the standard of care for quality by DentaQuest. If there
are special circumstances requiring this repeat service, please send in a prior authorization request along with a narrative establishing medical necessity.
When restorations involving multiple surfaces are requested or performed, that are outside the usual anatomical expectation, the allowance is limited to that of a one-
surface restoration. Any fee charged in excess of the allowance for the one-surface restoration is DISALLOWED.
Payment is made for restorative services based on the number of surfaces restored, not on the number of restorations per surface, or per tooth, per day. A restoration is
considered a two or more surface restoration only when two or more actual tooth surfaces are involved, whether they are connected or not. Tooth preparation, all
adhesives (including amalgam and resin bonding agents), acid etching, copalite, liners, bases, direct and indirect pulp caps, curing, and polishing are included as part of
the fee for the restoration.
Direct restoration of a primary tooth through the use of a prefabricated crown is considered to be a once in a lifetime restoration, same tooth, any provider. Exceptions
may be considered when pre‐treatment x‐ray images, intra‐oral photos, and narrative documentation clearly support the medical necessity for the replacement of the
prefabricated crown (procedure codes D2930, D2932, D2933, D2934, during pre‐payment review.
BILLING AND REIMBURSEMENT FOR CAST CROWNS AND POST & CORES OR REMOVABLE PROSTHETICS SHALL BE BASED ON THE
CEMENTATION OR INSERTION DATE.
The fee for crowns includes the temporary crown that is placed on the prepared tooth and worn while the permanent crown is being fabricated for permanent teeth.
Covered dental services that indicate “Yes” in the “Review Required” column require documentation of medical necessity and will be subject to retrospective pre-
payment review. These procedures can be rendered before determination of medical necessity but require submission of proper documentation (as indicated in the
“Documentation Required” column) with the claim form.
Under 1 TAC §353.409(b) and §353.1001(b) EPSDT regulations, DentaQuest is required to provide the services in an amount, duration, and scope that is no less than
the amount, duration, and scope for the same services furnished to Members under FFS Medicaid. Please refer to the TMPPM for the FFS Medicaid language.
However, all requests to exceed listed benefit limitations in this provider manual, must be prior authorized with documentation supporting medical necessity for an
increased benefit.
When the need for an exception is established, a narrative explaining the reason for the exception of limitations must be documented in the member's file and on the
claim submission. In order to submit a claim with an exception, the claim must have the key word “EXCEPTION” in Block 35 of the ADA claim form. If the key word
“EXCEPTION” is missing from Box 35, the claim may deny for exceeding benefit limitations.
Services Submitted with D9222 and, D9223, and D9500 for ages 1-6 will require prior authorization. Please reference ‘Criteria for General Anesthesia and Intravenous (IV)
Sedation’ in the Clinical Criteria section of this ORM.
The following codes require prior authorization for all ages: D2710, D2720, D2721, D2722, D2740, D2750, D2751, D2752, D2780, D2781, D2790, D2791, D2792, and
D2794.
Any reimbursement already made for an inadequate service may be recouped after the DentaQuest Consultant reviews the circumstances.
Exhibit A Benefits Covered for TX
Medicaid Child (Under 21)
This document contains proprietary and confidential information and may not be disclosed to others
without written permission. ©Copyright 2024. All rights reserved.
145
Restorative
Code
Brief Description
Age
Limitation
Teeth Covered
Review
Required
Benefit Limitations
Documentation
Required
D2140
Amalgam - one surface,
primary or permanent
0-20
Teeth 1 - 32, A -
T
No
Limit to one service of (D2140, D2150, D2160, D2161,
D2330, D2331, D2332, D2335, D2390, D2391, D2392,
D2393, D2394), per year, per provider, per tooth.
blank
D2150
Amalgam - two surfaces,
primary or permanent
0-20
Teeth 1 - 32, A -
T
No
Limit to one service of (D2140, D2150, D2160, D2161,
D2330, D2331, D2332, D2335, D2390, D2391, D2392,
D2393, D2394), per year, per provider, per tooth.
blank
D2160
amalgam - three surfaces,
primary or permanent
1 - 20
Teeth 1 - 32, A -
T
No
Limit to one service of (D2140, D2150, D2160, D2161,
D2330, D2331, D2332, D2335, D2390, D2391, D2392,
D2393, D2394), per year, per provider, per tooth.
blank
D2161
amalgam - four or more
surfaces, primary or
permanent
1 - 20
Teeth 1 - 32, A -
T
No
Limit to one service of (D2140, D2150, D2160, D2161,
D2330, D2331, D2332, D2335, D2390, D2391, D2392,
D2393, D2394), per year, per provider, per tooth.
blank
D2330
resin-based composite - one
surface, anterior
0-20
Teeth 6 - 11, 22 -
27, C - H, M - R
No
Limit to one service of (D2140, D2150, D2160, D2161,
D2330, D2331, D2332, D2335, D2390, D2391, D2392,
D2393, D2394), per year, per provider, per tooth.
blank
D2331
resin-based composite – two
surfaces, anterior
0-20
Teeth 6 - 11, 22 -
27, C - H, M - R
No
Limit to one service of (D2140, D2150, D2160, D2161,
D2330, D2331, D2332, D2335, D2390, D2391, D2392,
D2393, D2394), per year, per provider, per tooth.
blank
D2332
resin-based composite -
three surfaces, anterior
1 - 20
Teeth 6 - 11, 22 -
27, C - H, M - R
No
Limit to one service of (D2140, D2150, D2160, D2161,
D2330, D2331, D2332, D2335, D2390, D2391, D2392,
D2393, D2394), per year, per provider, per tooth.
blank
D2335
resin-based composite - four
or more surfaces or involving
incisal angle (anterior)
1 - 20
Teeth C ‐ H, M ‐
R
No
D2335 and D2390 will deny if any of the following
restorations have been paid on the same tooth within
last 12 months: D2140, D2150, D2160, D2161, D2330,
D2331, D2332, D2335, and D2390, D2930, D2931,
D2932, D2933, and D2934. D2335 and D2390 when
provided to primary teeth are limited to once per
lifetime, per tooth, any provider.
blank
D2335
resin-based composite - four
or more surfaces or involving
incisal angle (anterior)
1 - 20
Teeth 6 ‐ 11, 22 ‐
27
No
D2335 and D2390 will deny if any of the following
restorations have been paid on the same tooth within
last 12 months: D2140, D2150, D2160, D2161, D2330,
D2331, D2332, D2335, and D2390, D2930, D2931,
D2932, D2933, and D2934.
blank
Exhibit A Benefits Covered for TX
Medicaid Child (Under 21)
This document contains proprietary and confidential information and may not be disclosed to others
without written permission. ©Copyright 2024. All rights reserved.
146
Restorative
Code
Brief Description
Age
Limitation
Teeth Covered
Review
Required
Benefit Limitations
Documentation
Required
D2390
resin-based composite
crown, anterior
0-20
Teeth C ‐ H, M ‐
R
No
D2335 and D2390 will deny if any of the following
restorations have been paid on the same tooth within
last 12 months: D2140, D2150, D2160, D2161, D2330,
D2331, D2332, D2335, and D2390, D2930, D2931,
D2932, D2933, and D2934. D2335 and D2390 when
provided to primary teeth are limited to once per
lifetime, per tooth, any provider.
blank
D2390
resin-based composite
crown, anterior
0-20
Teeth 6 - 11, 22 -
27
No
D2335 and D2390 will deny if any of the following
restorations have been paid on the same tooth within
last 12 months: D2140, D2150, D2160, D2161, D2330,
D2331, D2332, D2335, and D2390, D2930, D2931,
D2932, D2933, and D2934.
blank
D2391
resin-based composite - one
surface, posterior
0-20
Teeth 1 - 5, 12 -
21, 28 - 32, A, B,
I - L, S, T
No
Limit to one service of (D2140, D2150, D2160, D2161,
D2330, D2331, D2332, D2335, D2390, D2391, D2392,
D2393, D2394), per year, per provider, per tooth.
blank
D2392
resin-based composite - two
surfaces, posterior
0-20
Teeth 1 - 5, 12 -
21, 28 - 32, A, B,
I - L, S, T
No
Limit to one service of (D2140, D2150, D2160, D2161,
D2330, D2331, D2332, D2335, D2390, D2391, D2392,
D2393, D2394), per year, per provider, per tooth.
blank
D2393
resin-based composite -
three surfaces, posterior
1 - 20
Teeth 1 - 5, 12 -
21, 28 - 32, A, B,
I - L, S, T
No
Limit to one service of (D2140, D2150, D2160, D2161,
D2330, D2331, D2332, D2335, D2390, D2391, D2392,
D2393, D2394), per year, per provider, per tooth.
blank
D2394
resin-based composite - four
or more surfaces, posterior
1 - 20
Teeth 1 - 5, 12 -
21, 28 - 32, A, B,
I - L, S, T
No
Limit to one service of (D2140, D2150, D2160, D2161,
D2330, D2331, D2332, D2335, D2390, D2391, D2392,
D2393, D2394), per year, per provider, per tooth.
blank
D2510
inlay - metallic -1 surface
13 - 20
Teeth 1 - 32
Yes
Limit to one service of (D2510, D2520, D2530, D2542,
D2543, D2544, D2650, D2651, D2652, D2662, D2663,
D2664, D2710, D2720, D2721, D2722, D2740, D2750,
D2751, D2752, D2780, D2781, D2782, D2783, D2790,
D2791, D2792, D2794) every ten years, per patient, per
tooth.
narr. of med.
necessity, pre and
post-op x-ray(s)
Exhibit A Benefits Covered for TX
Medicaid Child (Under 21)
This document contains proprietary and confidential information and may not be disclosed to others
without written permission. ©Copyright 2024. All rights reserved.
147
Restorative
Code
Brief Description
Age
Limitation
Teeth Covered
Review
Required
Benefit Limitations
Documentation
Required
D2520
inlay-metallic-2 surfaces
13 - 20
Teeth 1 - 32
Yes
Limit to one service of (D2510, D2520, D2530, D2542,
D2543, D2544, D2650, D2651, D2652, D2662, D2663,
D2664, D2710, D2720, D2721, D2722, D2740, D2750,
D2751, D2752, D2780, D2781, D2782, D2783, D2790,
D2791, D2792, D2794) every ten years, per patient, per
tooth.
narr. of med.
necessity, pre and
post-op x-ray(s)
D2530
inlay-metallic-3+ surfaces
13 - 20
Teeth 1 - 32
Yes
Limit to one service of (D2510, D2520, D2530, D2542,
D2543, D2544, D2650, D2651, D2652, D2662, D2663,
D2664, D2710, D2720, D2721, D2722, D2740, D2750,
D2751, D2752, D2780, D2781, D2782, D2783, D2790,
D2791, D2792, D2794) every ten years, per patient, per
tooth.
narr. of med.
necessity, pre and
post-op x-ray(s)
D2542
onlay - metallic - two
surfaces
13 - 20
Teeth 1 - 32
Yes
Limit to one service of (D2510, D2520, D2530, D2542,
D2543, D2544, D2650, D2651, D2652, D2662, D2663,
D2664, D2710, D2720, D2721, D2722, D2740, D2750,
D2751, D2752, D2780, D2781, D2782, D2783, D2790,
D2791, D2792, D2794) every ten years, per patient, per
tooth.
narr. of med.
necessity, pre and
post-op x-ray(s)
D2543
onlay-metallic-3 surfaces
13 - 20
Teeth 1 - 32
Yes
Limit to one service of (D2510, D2520, D2530, D2542,
D2543, D2544, D2650, D2651, D2652, D2662, D2663,
D2664, D2710, D2720, D2721, D2722, D2740, D2750,
D2751, D2752, D2780, D2781, D2782, D2783, D2790,
D2791, D2792, D2794) every ten years, per patient, per
tooth.
narr. of med.
necessity, pre and
post-op x-ray(s)
D2544
onlay-metallic-4+ surfaces
13 - 20
Teeth 1 - 32
Yes
Limit to one service of (D2510, D2520, D2530, D2542,
D2543, D2544, D2650, D2651, D2652, D2662, D2663,
D2664, D2710, D2720, D2721, D2722, D2740, D2750,
D2751, D2752, D2780, D2781, D2782, D2783, D2790,
D2791, D2792, D2794) every ten years, per patient, per
tooth.
narr. of med.
necessity, pre and
post-op x-ray(s)
Exhibit A Benefits Covered for TX
Medicaid Child (Under 21)
This document contains proprietary and confidential information and may not be disclosed to others
without written permission. ©Copyright 2024. All rights reserved.
148
Restorative
Code
Brief Description
Age
Limitation
Teeth Covered
Review
Required
Benefit Limitations
Documentation
Required
D2650
inlay-composite/resin
1surface
13 - 20
Teeth 1 - 32
Yes
Limit to one service of (D2510, D2520, D2530, D2542,
D2543, D2544, D2650, D2651, D2652, D2662, D2663,
D2664, D2710, D2720, D2721, D2722, D2740, D2750,
D2751, D2752, D2780, D2781, D2782, D2783, D2790,
D2791, D2792, D2794) every ten years, per patient, per
tooth.
narr. of med.
necessity, pre and
post-op x-ray(s)
D2651
inlay-composite/resin-2
surfaces
13 - 20
Teeth 1 - 32
Yes
Limit to one service of (D2510, D2520, D2530, D2542,
D2543, D2544, D2650, D2651, D2652, D2662, D2663,
D2664, D2710, D2720, D2721, D2722, D2740, D2750,
D2751, D2752, D2780, D2781, D2782, D2783, D2790,
D2791, D2792, D2794) every ten years, per patient, per
tooth.
narr. of med.
necessity, pre and
post-op x-ray(s)
D2652
inlay-composite/resin-3+
surfaces
13 - 20
Teeth 1 - 32
Yes
Limit to one service of (D2510, D2520, D2530, D2542,
D2543, D2544, D2650, D2651, D2652, D2662, D2663,
D2664, D2710, D2720, D2721, D2722, D2740, D2750,
D2751, D2752, D2780, D2781, D2782, D2783, D2790,
D2791, D2792, D2794) every ten years, per patient, per
tooth.
narr. of med.
necessity, pre and
post-op x-ray(s)
D2662
onlay-composite/resin-2
surfaces
13 - 20
Teeth 1 - 32
Yes
Limit to one service of (D2510, D2520, D2530, D2542,
D2543, D2544, D2650, D2651, D2652, D2662, D2663,
D2664, D2710, D2720, D2721, D2722, D2740, D2750,
D2751, D2752, D2780, D2781, D2782, D2783, D2790,
D2791, D2792, D2794) every ten years, per patient, per
tooth.
narr. of med.
necessity, pre and
post-op x-ray(s)
D2663
onlay-composite/resin-3
surfaces
13 - 20
Teeth 1 - 32
Yes
Limit to one service of (D2510, D2520, D2530, D2542,
D2543, D2544, D2650, D2651, D2652, D2662, D2663,
D2664, D2710, D2720, D2721, D2722, D2740, D2750,
D2751, D2752, D2780, D2781, D2782, D2783, D2790,
D2791, D2792, D2794) every ten years, per patient, per
tooth.
narr. of med.
necessity, pre and
post-op x-ray(s)
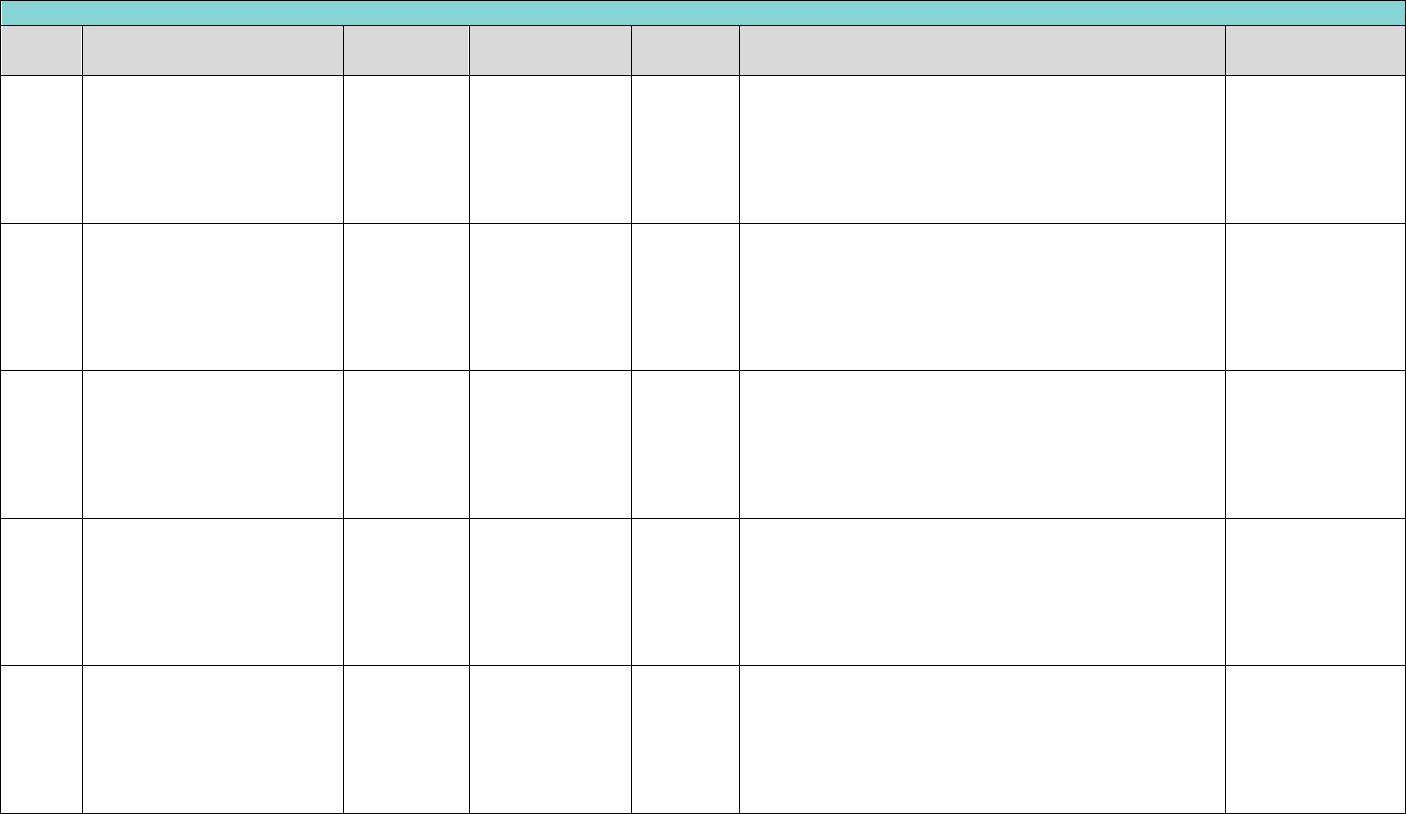
Exhibit A Benefits Covered for TX
Medicaid Child (Under 21)
This document contains proprietary and confidential information and may not be disclosed to others
without written permission. ©Copyright 2024. All rights reserved.
149
Restorative
Code
Brief Description
Age
Limitation
Teeth Covered
Review
Required
Benefit Limitations
Documentation
Required
D2664
onlay-composite/resin-4+
surfaces
13 - 20
Teeth 1 - 32
Yes
Limit to one service of (D2510, D2520, D2530, D2542,
D2543, D2544, D2650, D2651, D2652, D2662, D2663,
D2664, D2710, D2720, D2721, D2722, D2740, D2750,
D2751, D2752, D2780, D2781, D2782, D2783, D2790,
D2791, D2792, D2794) every ten years, per patient, per
tooth.
narr. of med.
necessity, pre and
post-op x-ray(s)
D2710
crown - resin-based
composite (indirect)
13 - 20
Teeth 1 - 32
Yes
Limit to one service of (D2510, D2520, D2530, D2542,
D2543, D2544, D2650, D2651, D2652, D2662, D2663,
D2664, D2710, D2720, D2721, D2722, D2740, D2750,
D2751, D2752, D2780, D2781, D2782, D2783, D2790,
D2791, D2792, D2794) every ten years, per patient, per
tooth.
narr. of med.
necessity, pre-op x-
ray(s)
D2720
crown-resin with high noble
metal
13 - 20
Teeth 1 - 32
Yes
Limit to one service of (D2510, D2520, D2530, D2542,
D2543, D2544, D2650, D2651, D2652, D2662, D2663,
D2664, D2710, D2720, D2721, D2722, D2740, D2750,
D2751, D2752, D2780, D2781, D2782, D2783, D2790,
D2791, D2792, D2794) every ten years, per patient, per
tooth.
narr. of med.
necessity, pre-op x-
ray(s)
D2721
crown - resin with
predominantly base metal
13 - 20
Teeth 1 - 32
Yes
Limit to one service of (D2510, D2520, D2530, D2542,
D2543, D2544, D2650, D2651, D2652, D2662, D2663,
D2664, D2710, D2720, D2721, D2722, D2740, D2750,
D2751, D2752, D2780, D2781, D2782, D2783, D2790,
D2791, D2792, D2794) every ten years, per patient, per
tooth.
narr. of med.
necessity, pre-op x-
ray(s)
D2722
crown - resin with noble
metal
13 - 20
Teeth 1 - 32
Yes
Limit to one service of (D2510, D2520, D2530, D2542,
D2543, D2544, D2650, D2651, D2652, D2662, D2663,
D2664, D2710, D2720, D2721, D2722, D2740, D2750,
D2751, D2752, D2780, D2781, D2782, D2783, D2790,
D2791, D2792, D2794) every ten years, per patient, per
tooth.
narr. of med.
necessity, pre-op x-
ray(s)
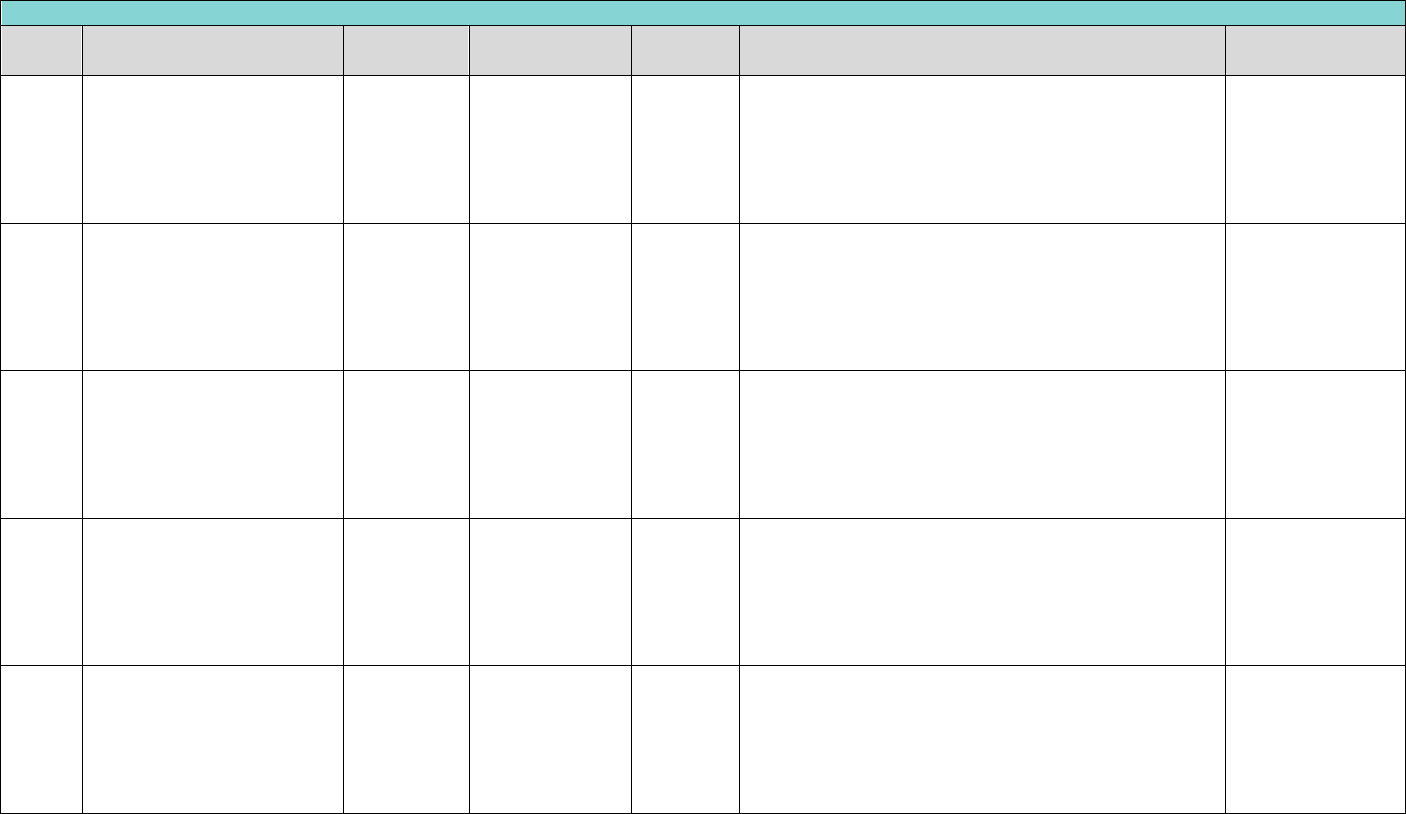
Exhibit A Benefits Covered for TX
Medicaid Child (Under 21)
This document contains proprietary and confidential information and may not be disclosed to others
without written permission. ©Copyright 2024. All rights reserved.
150
Restorative
Code
Brief Description
Age
Limitation
Teeth Covered
Review
Required
Benefit Limitations
Documentation
Required
D2740
crown - porcelain/ceramic
13 - 20
Teeth 4-13, 20-
29
Yes
Limit to one service of (D2510, D2520, D2530, D2542,
D2543, D2544, D2650, D2651, D2652, D2662, D2663,
D2664, D2710, D2720, D2721, D2722, D2740, D2750,
D2751, D2752, D2780, D2781, D2782, D2783, D2790,
D2791, D2792, D2794) every ten years, per patient, per
tooth.
narr. of med.
necessity, pre-op x-
ray(s)
D2750
crown - porcelain fused to
high noble metal
13 - 20
Teeth 4-13, 20-
29
Yes
Limit to one service of (D2510, D2520, D2530, D2542,
D2543, D2544, D2650, D2651, D2652, D2662, D2663,
D2664, D2710, D2720, D2721, D2722, D2740, D2750,
D2751, D2752, D2780, D2781, D2782, D2783, D2790,
D2791, D2792, D2794) every ten years, per patient, per
tooth.
narr. of med.
necessity, pre-op x-
ray(s)
D2751
crown - porcelain fused to
predominantly base metal
13 - 20
Teeth 4-13, 20-
29
Yes
Limit to one service of (D2510, D2520, D2530, D2542,
D2543, D2544, D2650, D2651, D2652, D2662, D2663,
D2664, D2710, D2720, D2721, D2722, D2740, D2750,
D2751, D2752, D2780, D2781, D2782, D2783, D2790,
D2791, D2792, D2794) every ten years, per patient, per
tooth.
narr. of med.
necessity, pre-op x-
ray(s)
D2752
crown - porcelain fused to
noble metal
13 - 20
Teeth 4-13, 20-
29
Yes
Limit to one service of (D2510, D2520, D2530, D2542,
D2543, D2544, D2650, D2651, D2652, D2662, D2663,
D2664, D2710, D2720, D2721, D2722, D2740, D2750,
D2751, D2752, D2780, D2781, D2782, D2783, D2790,
D2791, D2792, D2794) every ten years, per patient, per
tooth.
narr. of med.
necessity, pre-op x-
ray(s)
D2780
crown - ¾ cast high noble
metal
13 - 20
Teeth 1 - 32
Yes
Limit to one service of (D2510, D2520, D2530, D2542,
D2543, D2544, D2650, D2651, D2652, D2662, D2663,
D2664, D2710, D2720, D2721, D2722, D2740, D2750,
D2751, D2752, D2780, D2781, D2782, D2783, D2790,
D2791, D2792, D2794) every ten years, per patient, per
tooth.
narr. of med.
necessity, pre-op x-
ray(s)

Exhibit A Benefits Covered for TX
Medicaid Child (Under 21)
This document contains proprietary and confidential information and may not be disclosed to others
without written permission. ©Copyright 2024. All rights reserved.
151
Restorative
Code
Brief Description
Age
Limitation
Teeth Covered
Review
Required
Benefit Limitations
Documentation
Required
D2781
crown - ¾ cast
predominantly base metal
13 - 20
Teeth 1 - 32
Yes
Limit to one service of (D2510, D2520, D2530, D2542,
D2543, D2544, D2650, D2651, D2652, D2662, D2663,
D2664, D2710, D2720, D2721, D2722, D2740, D2750,
D2751, D2752, D2780, D2781, D2782, D2783, D2790,
D2791, D2792, D2794) every ten years, per patient, per
tooth.
narr. of med.
necessity, pre-op x-
ray(s)
D2782
crown - ¾ cast noble metal
13 - 20
Teeth 1 - 32
Yes
Limit to one service of (D2510, D2520, D2530, D2542,
D2543, D2544, D2650, D2651, D2652, D2662, D2663,
D2664, D2710, D2720, D2721, D2722, D2740, D2750,
D2751, D2752, D2780, D2781, D2782, D2783, D2790,
D2791, D2792, D2794) every ten years, per patient, per
tooth.
narr. of med.
necessity, pre and
post-op x-ray(s)
D2783
crown - ¾ porcelain/ceramic
13 - 20
Teeth 6 - 11, 22 -
27
Yes
Limit to one service of (D2510, D2520, D2530, D2542,
D2543, D2544, D2650, D2651, D2652, D2662, D2663,
D2664, D2710, D2720, D2721, D2722, D2740, D2750,
D2751, D2752, D2780, D2781, D2782, D2783, D2790,
D2791, D2792, D2794) every ten years, per patient, per
tooth.
narr. of med.
necessity, pre and
post-op x-ray(s)
D2790
crown - full cast high noble
metal
13 - 20
Teeth 1–5, 12–
21, 28–32
Yes
Limit to one service of (D2510, D2520, D2530, D2542,
D2543, D2544, D2650, D2651, D2652, D2662, D2663,
D2664, D2710, D2720, D2721, D2722, D2740, D2750,
D2751, D2752, D2780, D2781, D2782, D2783, D2790,
D2791, D2792, D2794) every ten years, per patient, per
tooth.
narr. of med.
necessity, pre-op x-
ray(s)
D2791
crown - full cast
predominantly base metal
13 - 20
Teeth 1–5, 12–
21, 28–32
Yes
Limit to one service of (D2510, D2520, D2530, D2542,
D2543, D2544, D2650, D2651, D2652, D2662, D2663,
D2664, D2710, D2720, D2721, D2722, D2740, D2750,
D2751, D2752, D2780, D2781, D2782, D2783, D2790,
D2791, D2792, D2794) every ten years, per patient, per
tooth.
narr. of med.
necessity, pre-op x-
ray(s)
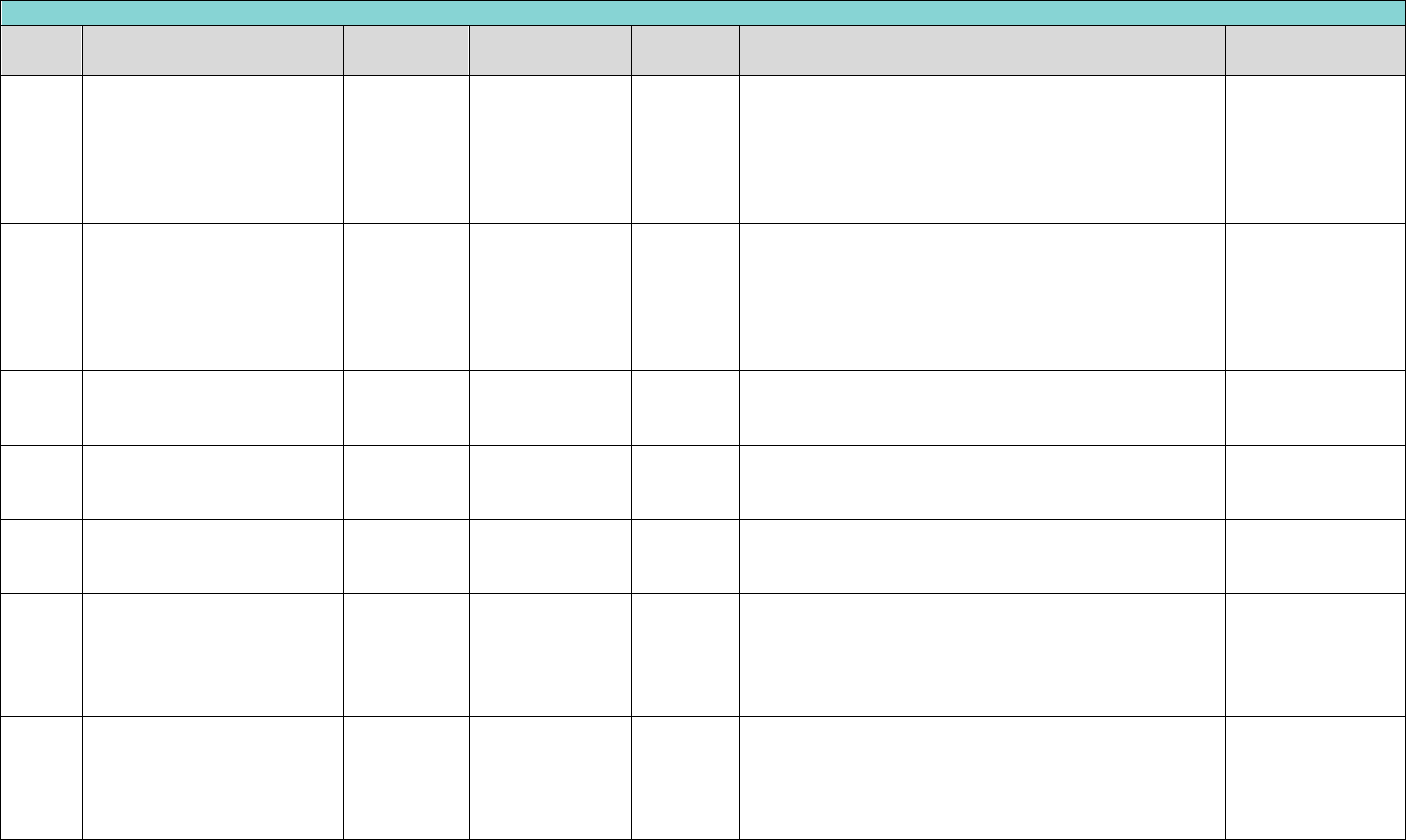
Exhibit A Benefits Covered for TX
Medicaid Child (Under 21)
This document contains proprietary and confidential information and may not be disclosed to others
without written permission. ©Copyright 2024. All rights reserved.
152
Restorative
Code
Brief Description
Age
Limitation
Teeth Covered
Review
Required
Benefit Limitations
Documentation
Required
D2792
crown - full cast noble metal
13 - 20
Teeth 1–5, 12–
21, 28–32
Yes
Limit to one service of (D2510, D2520, D2530, D2542,
D2543, D2544, D2650, D2651, D2652, D2662, D2663,
D2664, D2710, D2720, D2721, D2722, D2740, D2750,
D2751, D2752, D2780, D2781, D2782, D2783, D2790,
D2791, D2792, D2794) every ten years, per patient, per
tooth.
narr. of med.
necessity, pre-op x-
ray(s)
D2794
crown – titanium and
titanium alloys
13 - 20
Teeth 1 - 32
Yes
Limit to one service of (D2510, D2520, D2530, D2542,
D2543, D2544, D2650, D2651, D2652, D2662, D2663,
D2664, D2710, D2720, D2721, D2722, D2740, D2750,
D2751, D2752, D2780, D2781, D2782, D2783, D2790,
D2791, D2792, D2794) every ten years, per patient, per
tooth.
narr. of med.
necessity, pre-op x-
ray(s)
D2910
re-cement or re-bond inlay,
onlay, veneer or partial
coverage restoration
13 - 20
Teeth 1 - 32
No
Limit to one service every six months, per patient, per
tooth. Not allowed within 6 months of initial placement
or previous re-cement.
blank
D2915
re-cement or re-bond
indirectly fabricated or
prefabricated post and core
4 - 20
Teeth 1 - 32
No
Limit to one service every six months, per patient, per
tooth. Not allowed within 6 months of initial placement
or previous re-cement.
blank
D2920
re-cement or re-bond crown
1 - 20
Teeth 1 - 32, A -
T
No
Limit to one service every six months, per patient, per
tooth. Not allowed within 6 months of initial placement
or previous re-cement.
blank
D2930
prefabricated stainless steel
crown - primary tooth
0-20
Teeth A - T
No
Limit to one service per lifetime, per patient, per tooth.
D2930 will deny if the following procedure codes have
been billed within last 12 months, same tooth, same
provider: D2140, D2150, D2160, D2161, D2330, D2331,
D2332, D2335, D2390, D2391, D2392, D2393 or D2394.
blank
D2931
prefabricated stainless steel
crown-permanent tooth
1 - 20
Teeth 1 -32
No
D2931 will deny if the following procedure codes have
been billed within last 12 months, same tooth, same
provider: D2140, D2150, D2160, D2161, D2330, D2331,
D2332, D2335, D2390, D2391, D2392, D2393, D2394,
D2931, or D2932.
blank
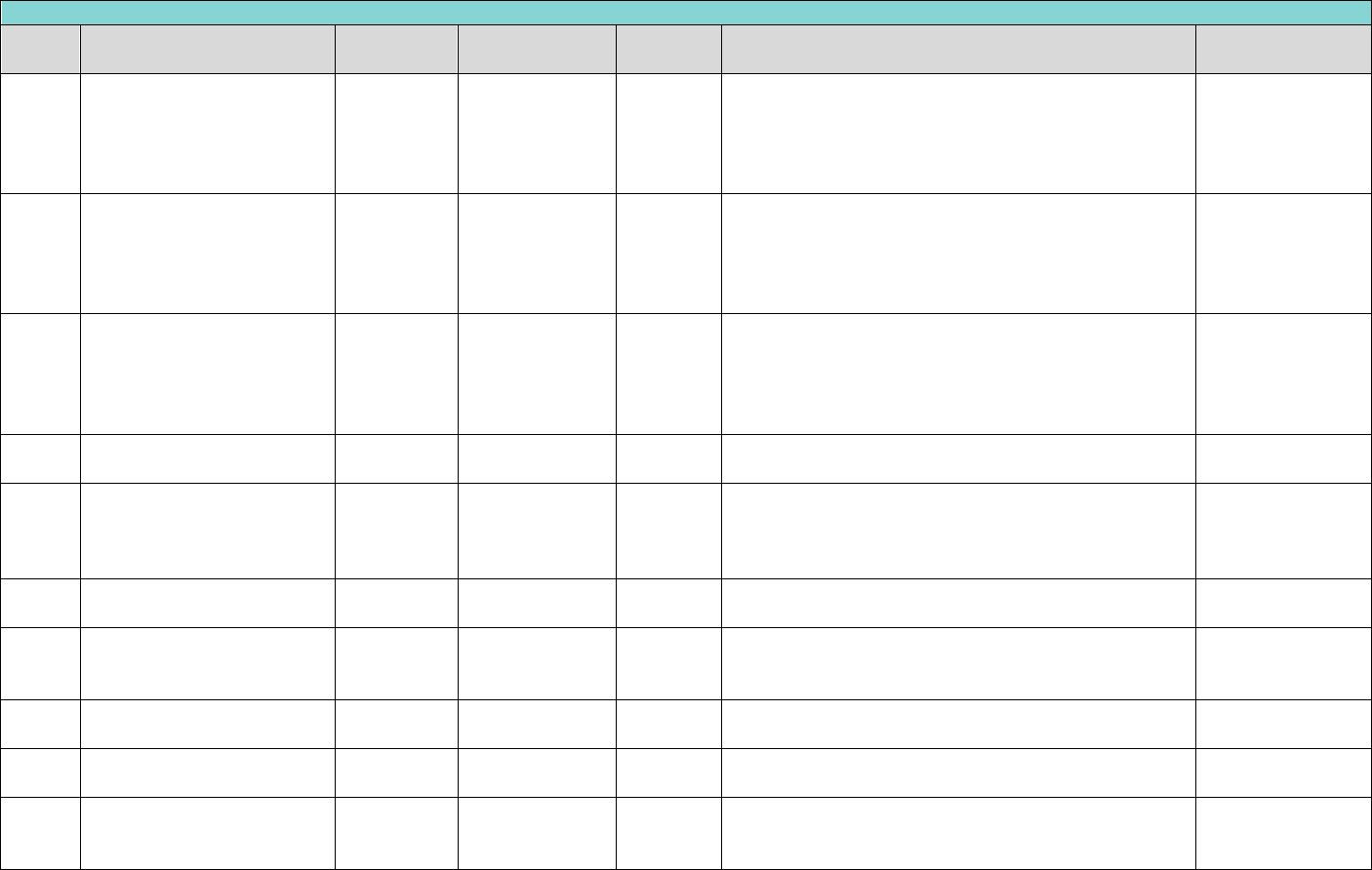
Exhibit A Benefits Covered for TX
Medicaid Child (Under 21)
This document contains proprietary and confidential information and may not be disclosed to others
without written permission. ©Copyright 2024. All rights reserved.
153
Restorative
Code
Brief Description
Age
Limitation
Teeth Covered
Review
Required
Benefit Limitations
Documentation
Required
D2932
prefabricated resin crown
1 - 20
Teeth 1-32, C-H,
M-R
No
D2932 will deny if the following procedure codes have
been billed within last 12 months, same tooth, same
provider: D2140, D2150, D2160, D2161, D2330, D2331,
D2332, D2335, D2390, D2391, D2392, D2393, D2394,
D2931, or D2932.
blank
D2933
prefabricated stainless steel
crown with resin window
0-20
Teeth C - H, M -
R
No
Limit to one service per lifetime, per patient, per tooth.
D2933, D2934 will deny if the following procedure codes
have been billed within last 12 months, same tooth,
same provider: D2140, D2150, D2160, D2161, D2330,
D2331, D2332, D2335 or D2390.
blank
D2934
prefabricated esthetic
coated stainless steel crown
– primary tooth
0-20
Teeth C - H, M -
R
No
Limit to one service per lifetime, per patient, per tooth.
D2933, D2934 will deny if the following procedure codes
have been billed within last 12 months, same tooth,
same provider: D2140, D2150, D2160, D2161, D2330,
D2331, D2332, D2335 or D2390.
blank
D2940
protective restoration
0-20
Teeth 1 - 32, A -
T
No
Not allowed with any other D2000, D3000, or D6000
series code, but is allowed with D3110 and D3120.
blank
D2950
core buildup, including any
pins when required
4 - 20
Teeth 1 - 32
No
Limited to one service of D2950 per year, per patient,
per tooth. Limit to one service of (D2950, D2952, D2954)
per day, per patient, per tooth. Not allowed on primary
teeth.
blank
D2951
pin retention - per tooth, in
addition to restoration
4 - 20
Teeth 1 - 32
No
Limited to two (D2951) per lifetime, per patient, per
tooth. Not allowed on primary teeth.
blank
D2952
cast post and core in
addition to crown
13 - 20
Teeth 1 - 32
No
Limited to one service every five years, per patient, per
tooth. Not allowed on primary teeth. Not payable with
D2950.
blank
D2953
each additional cast post –
same tooth
13 - 20
Teeth 1 - 32
No
Not allowed on primary teeth. Must be billed with
D2952.
blank
D2954
prefabricated post and core
in addition to crown
13 - 20
Teeth 1 - 32
No
Limited to one service of (D2952, D3950) per day, per
patient, per tooth. Not allowed on primary teeth.
blank
D2955
post removal (not in
conjunction with endodontic
therapy)
4 - 20
Teeth 1 - 32
No
Limited to one service of (D3346, D3347, D3348) per
day, per patient, per tooth. Not allowed on primary
teeth.
blank
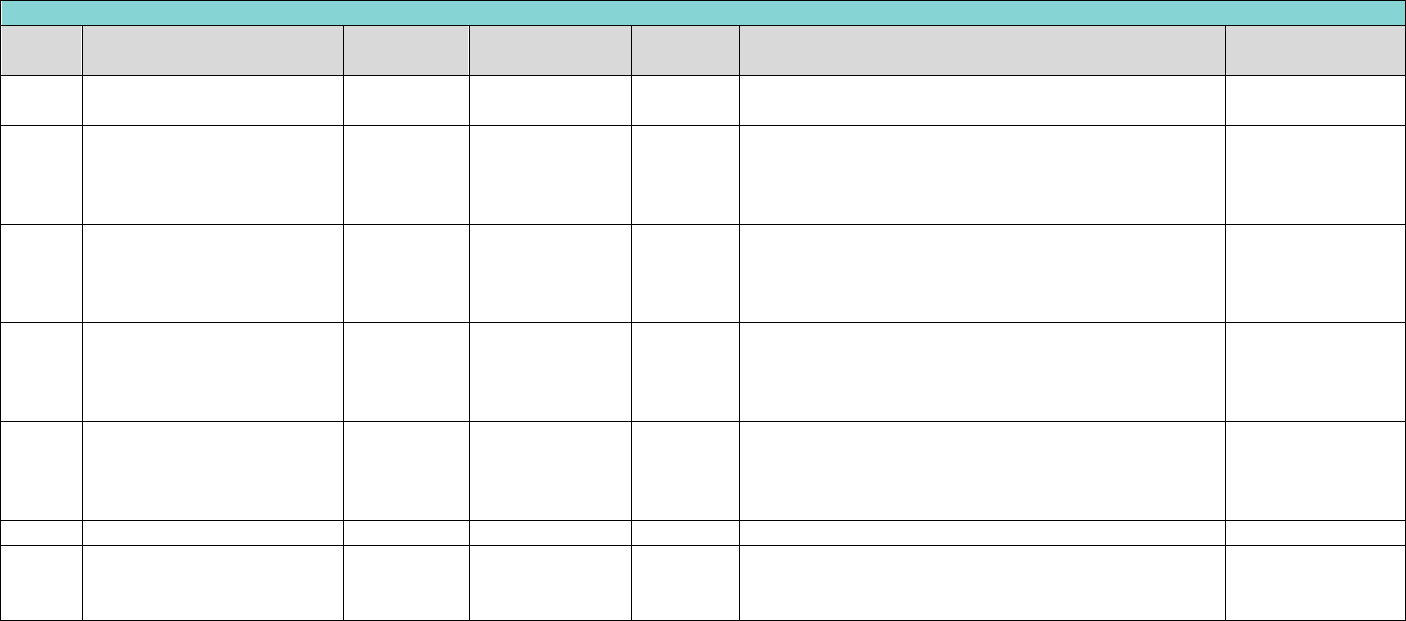
Exhibit A Benefits Covered for TX
Medicaid Child (Under 21)
This document contains proprietary and confidential information and may not be disclosed to others
without written permission. ©Copyright 2024. All rights reserved.
154
Restorative
Code
Brief Description
Age
Limitation
Teeth Covered
Review
Required
Benefit Limitations
Documentation
Required
D2957
each additional prefabricated
post - same tooth
13 - 20
Teeth 1 - 32
No
Not allowed on primary teeth. Must be billed with
D2954.
blank
D2960
labial veneer (laminate)-chair
13 - 20
Teeth 1 - 32
Yes
Limited to one service of (D2710, D2720, D2721, D2722,
D2740, D2750, D2751, D2752, D2780, D2781, D2782,
D2783, D2790, D2791, D2792, D2794) every ten years,
per patient, per tooth.
narr. of med.
necessity, pre and
post-op x-ray(s)
D2961
labial veneer (resin laminate)
- laboratory
13 - 20
Teeth 1 - 32
Yes
Limited to one service of (D2710, D2720, D2721, D2722,
D2740, D2750, D2751, D2752, D2780, D2781, D2782,
D2783, D2790, D2791, D2792, D2794) every ten years,
per patient, per tooth.
narr. of med.
necessity, pre and
post-op x-ray(s)
D2962
labial veneer (porc laminate)
- laboratory
13 - 20
Teeth 1 - 32
Yes
Limited to one service of (D2710, D2720, D2721, D2722,
D2740, D2750, D2751, D2752, D2780, D2781, D2782,
D2783, D2790, D2791, D2792, D2794) every ten years,
per patient, per tooth.
narr. of med.
necessity, pre and
post-op x-ray(s)
D2971
additional procedures to
construct new crown under
partial denture framework
13 - 20
Teeth 1 - 32
Yes
Limited to four services per Lifetime, Per patient, per
tooth. Allowed only to the same provider that
performed the cementation in conjunction with the
crown.
narrative of
medical necessity
D2980
crown repair, by report
1 - 20
Teeth 1 - 32
No
blank
D2999
unspecified restorative
procedure, by report
1 - 20
Teeth 1 - 32, A -
T
Yes
blank
narr. of med.
necessity, pre-op x-
ray(s)
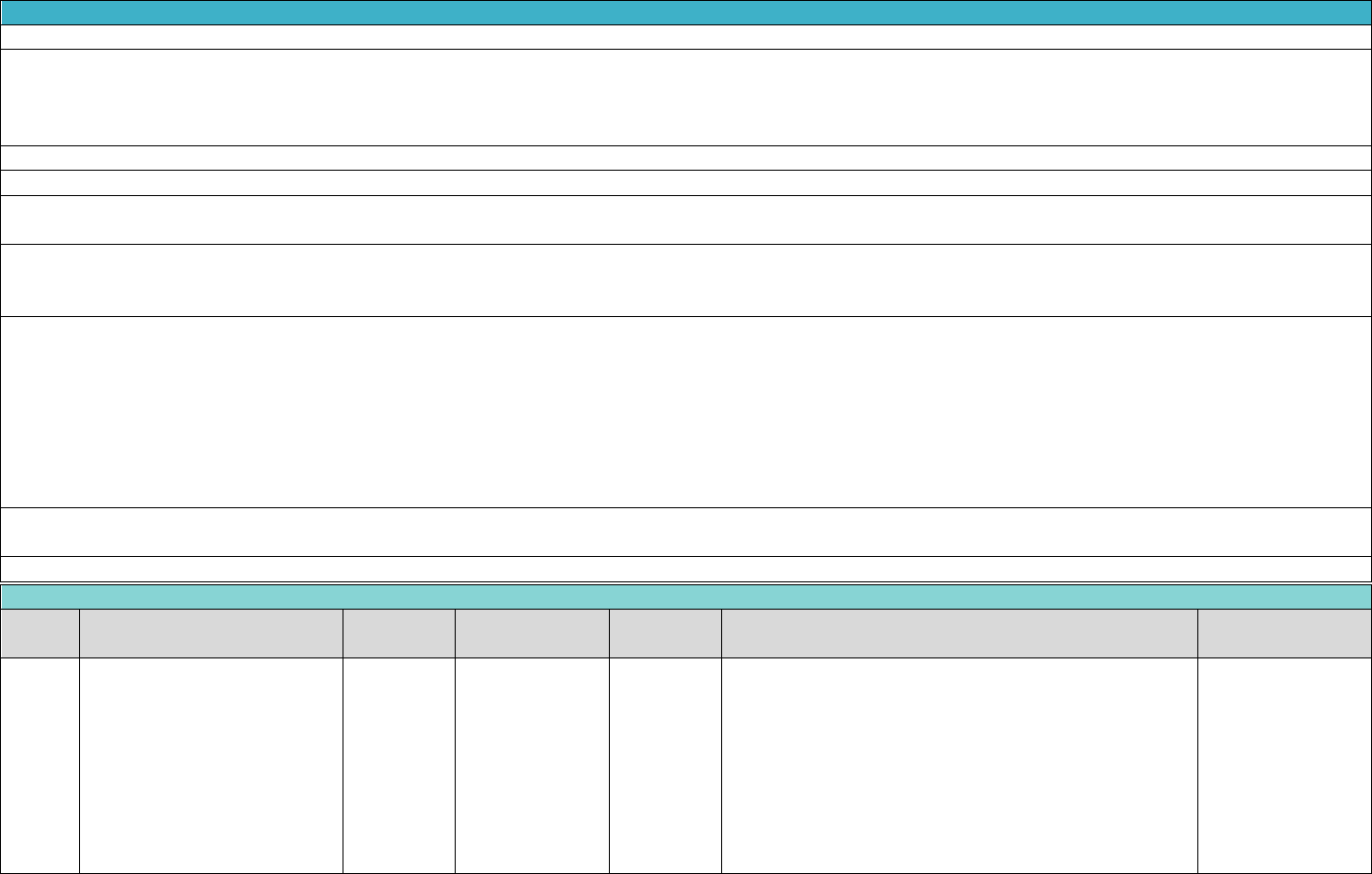
Exhibit A Benefits Covered for TX
Medicaid Child (Under 21)
This document contains proprietary and confidential information and may not be disclosed to others
without written permission. ©Copyright 2024. All rights reserved.
155
Exhibit A Benefits Covered for TX Medicaid Child (Under 21)
"Payment for conventional root canal treatment is limited to treatment of permanent teeth.
The standard of acceptability employed for endodontic procedures requires that the canal(s) be completely filled apically and laterally. In cases where the root canal
filling does not meet DentaQuest's treatment standards, DentaQuest can require the procedure to be redone at no additional cost. Any reimbursement already made for
an inadequate service may be recouped after any post payment review by the DentaQuest Consultants. A pulpotomy or palliative treatment is not to be billed in
conjunction with a root canal treatment.
Filling material not accepted by the Federal Food and Drug Administration (FDA) (e.g. Sargenti filling material) is not covered.
Pulpotomies will be limited to primary teeth or permanent teeth with incomplete root development.
The fee for root canal therapy for permanent teeth includes diagnosis, extirpation treatment, temporary fillings, filling and obturation of root canals, and progress
radiographs. A completed fill radiograph is also included.
Covered dental services that indicate “Yes” in the “Review Required” column require documentation of medical necessity and will be subject to retrospective pre-
payment review. These procedures can be rendered before determination of medical necessity but require submission of proper documentation (as indicated in the
“Documentation Required” column) with the claim form.
Under 1 TAC §353.409(b) and §353.1001(b) EPSDT regulations, DentaQuest is required to provide the services in an amount, duration, and scope that is no less than
the amount, duration, and scope for the same services furnished to Members under FFS Medicaid. Please refer to the TMPPM for the FFS Medicaid language.
However, all requests to exceed listed benefit limitations in this provider manual, must be prior authorized with documentation supporting medical necessity for an
increased benefit.
When the need for an exception is established, a narrative explaining the reason for the exception of limitations must be documented in the member's file and on the
claim submission. In order to submit a claim with an exception, the claim must have the key word “EXCEPTION” in Block 35 of the ADA claim form. If the key word
“EXCEPTION” is missing from Box 35, the claim may deny for exceeding benefit limitations.
Services Submitted with D9222 and, D9223, and D9500 for ages 1-6 will require prior authorization. Please reference ‘Criteria for General Anesthesia and Intravenous (IV)
Sedation’ in the Clinical Criteria section of this ORM.
Any reimbursement already made for an inadequate service may be recouped after the DentaQuest Consultant reviews the circumstances."
Endodontics
Code
Brief Description
Age
Limitation
Teeth Covered
Review
Required
Benefit Limitations
Documentation
Required
D3110
pulp cap - direct (excluding
final restoration)
1 - 20
Teeth 1 - 32
No
(D3110) may be reimbursed for the same tooth, on the
same date of service, by the same provider or location
when billed with D2140, D2150, D2160, D2161, D2330,
D2331, D2332, D2335, D2390, D2391, D2392, D2393,
D2394, D2510, D2520, D2530, D2542, D2543, D2544,
D2650, D2651, D2652, D2662, D2663, D2664, D2410,
D2720, D2721, D2722, D2740, D2750, D2751, D2752,
D2780, D2781, D2782, D2783, D2790, D2791, D2792,
D2794, D2931, D2932.
blank
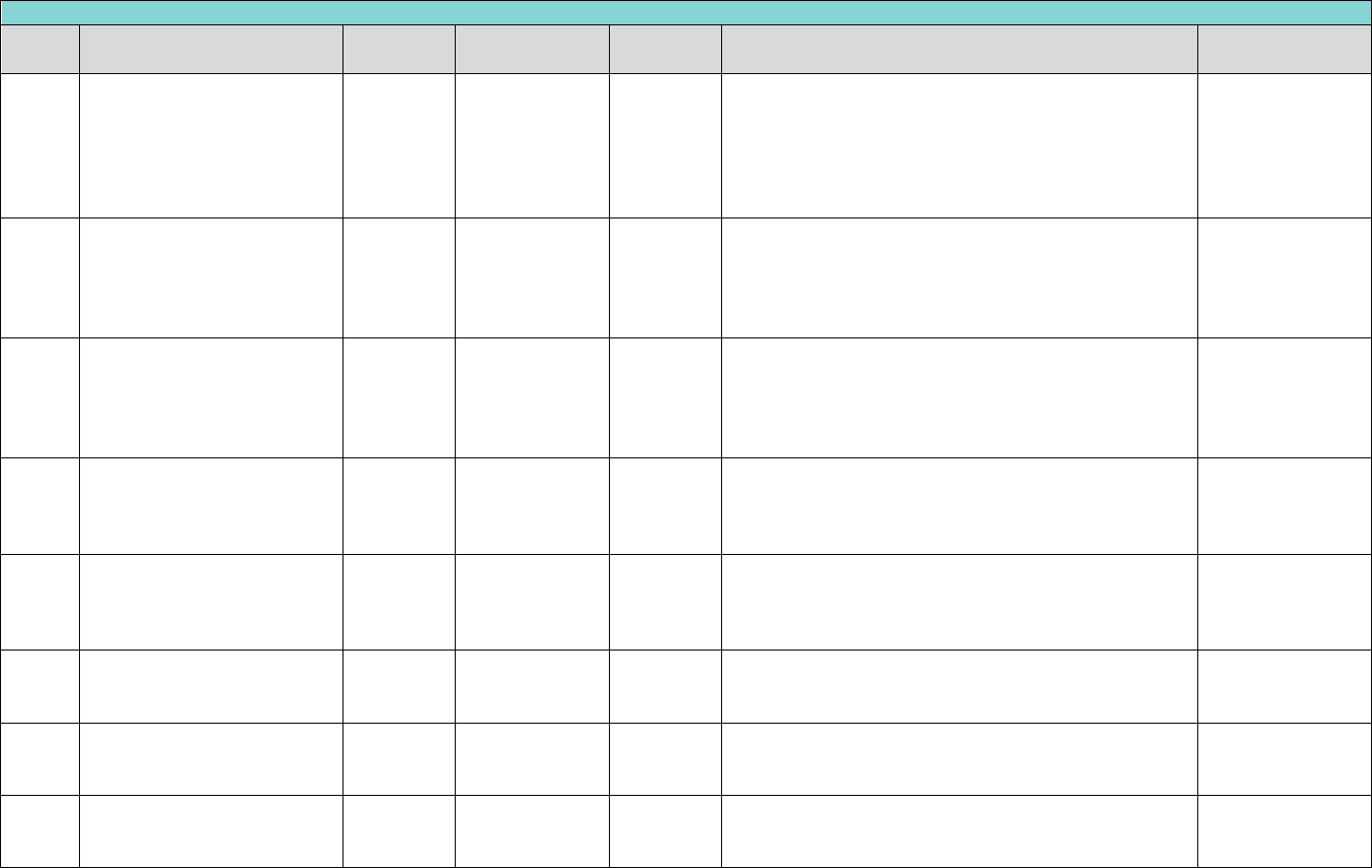
Exhibit A Benefits Covered for TX
Medicaid Child (Under 21)
This document contains proprietary and confidential information and may not be disclosed to others
without written permission. ©Copyright 2024. All rights reserved.
156
Endodontics
Code
Brief Description
Age
Limitation
Teeth Covered
Review
Required
Benefit Limitations
Documentation
Required
D3120
pulp cap - indirect (excluding
final restoration)
1 - 20
Teeth 1 - 32
No
(D3120) will only be reimbursed when submitted with
D2940 for the same TID, on the same date of service, by
the same provider or location. Any indirect pulp caps
placed with routine restorations are considered inclusive
of the final restoration and are not separately
reimbursable.
blank
D3220
therapeutic pulpotomy
(excluding final restoration) -
removal of pulp coronal to the
dentinocemental junction and
application of medicament
0-20
Teeth 2 - 15, 18
- 31
No
Limited to one service of (D3220, D3230, D3240, D3310,
D3320, D3330) per six months, per patient, per tooth.
blank
D3220
therapeutic pulpotomy
(excluding final restoration) -
removal of pulp coronal to the
dentinocemental junction and
application of medicament
0-20
Teeth A - T
No
One service of (D3220, D3230, D3240, D3310, D3320,
D3330) per lifetime, per patient, per tooth for primary
Teeth.
blank
D3230
pulpal therapy (resorbable
filling) - anterior, primary
tooth (excluding final
restoration)
1 - 20
Teeth C - H, M -
R
No
Limit to one service per lifetime, per patient, per tooth.
blank
D3240
pulpal therapy (resorbable
filling) - posterior, primary
tooth (excluding final
restoration)
1 - 20
Teeth A, B, I - L,
S, T
No
Limit to one service per lifetime, per patient, per tooth.
blank
D3310
endodontic therapy, anterior
tooth (excluding final
restoration)
6 - 20
Teeth 6 - 11, 22
- 27
No
Limit to one service per lifetime, per patient, per tooth.
blank
D3320
endodontic therapy, premolar
tooth (excluding final
restoration)
6 - 20
Teeth 4, 5, 12,
13, 20, 21, 28,
29
No
Limit to one service per lifetime, per patient, per tooth.
blank
D3330
endodontic therapy, molar
tooth (excluding final
restoration)
6 - 20
Teeth 2, 3, 14,
15, 18, 19, 30,
31
No
Limit to one service per lifetime, per patient, per tooth.
blank
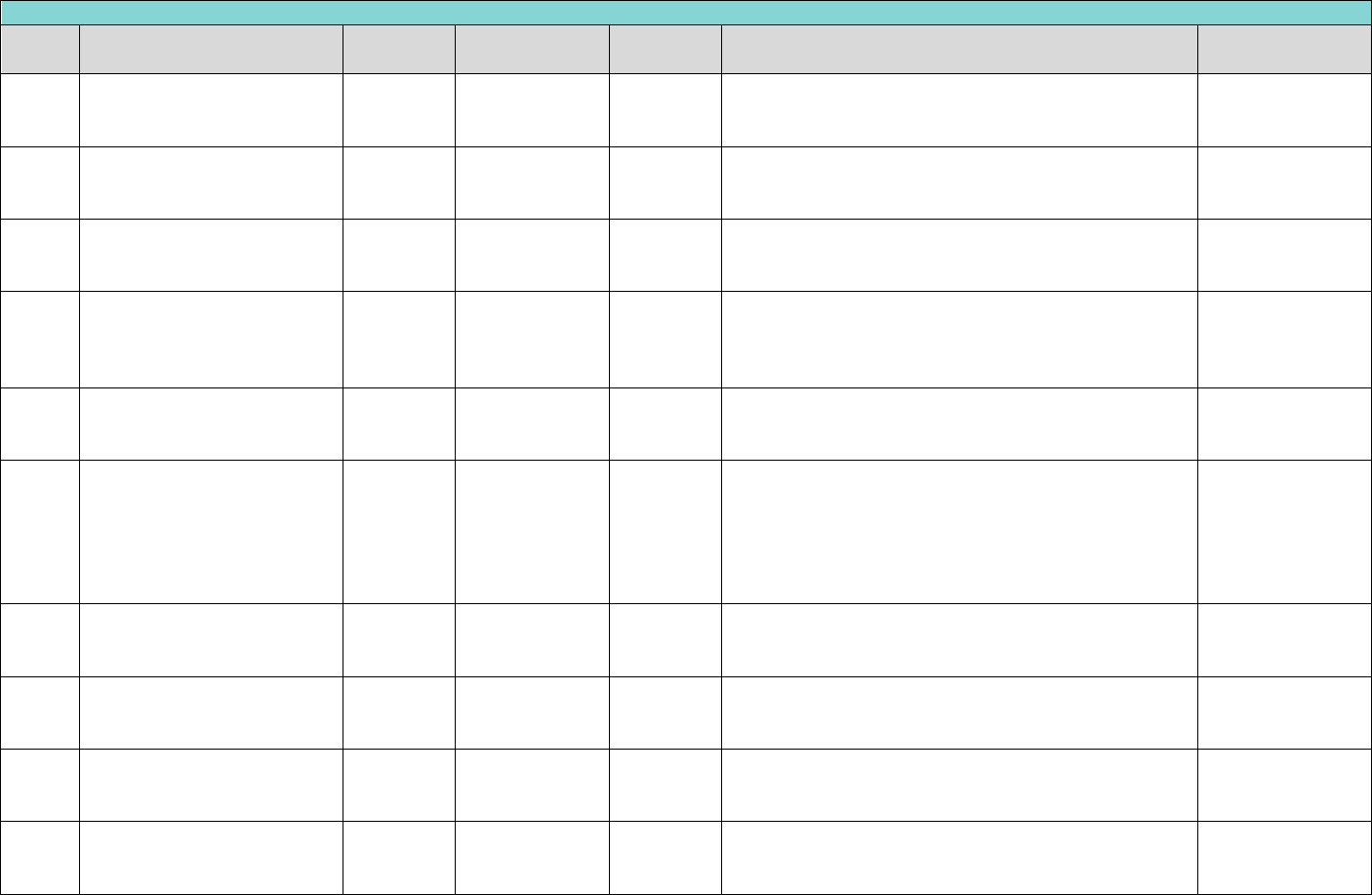
Exhibit A Benefits Covered for TX
Medicaid Child (Under 21)
This document contains proprietary and confidential information and may not be disclosed to others
without written permission. ©Copyright 2024. All rights reserved.
157
Endodontics
Code
Brief Description
Age
Limitation
Teeth Covered
Review
Required
Benefit Limitations
Documentation
Required
D3346
retreatment of previous root
canal therapy-anterior
6 - 20
Teeth 6 - 11, 22
- 27
Yes
blankFcred
narr. of med.
necessity, pre and
post-op x-ray(s)
D3347
retreatment of previous root
canal therapy - premolar
6 - 20
Teeth 4, 5, 12,
13, 20, 21, 28,
29
Yes
Limit to one service per lifetime, per patient, per tooth.
narr. of med.
necessity, pre and
post-op x-ray(s)
D3348
retreatment of previous root
canal therapy-molar
6 - 20
Teeth 1 - 3, 14 -
19, 30 - 32
Yes
Limit to one service per lifetime, per patient, per tooth.
narr. of med.
necessity, pre and
post-op x-ray(s)
D3351
apexification/recalcification –
initial visit (apical closure /
calcific repair of perforations,
root resorption, etc.)
6 - 20
Teeth 1 - 32
No
blank
blank
D3352
apexification/recalcification –
interim medication
replacement
6 - 20
Teeth 1 - 32
No
blank
blank
D3353
apexification/recalcification –
final visit (includes completed
root canal therapy - apical
closure/calcific repair of
perforations, root resorption,
etc.)
6 - 20
Teeth 1 - 32
No
blank
blank
D3410
apicoectomy - anterior
6 - 20
Teeth 6 - 11, 22
- 27
Yes
blank
narr. of med.
necessity, pre and
post-op x-ray(s)
D3421
apicoectomy - premolar (first
root)
6 - 20
Teeth 4, 5, 12,
13, 20, 21, 28,
29
Yes
blank
narr. of med.
necessity, pre and
post-op x-ray(s)
D3425
apicoectomy - molar (first
root)
6 - 20
Teeth 1 - 3, 14 -
19, 30 - 32
Yes
blank
narr. of med.
necessity, pre and
post-op x-ray(s)
D3426
apicoectomy (each additional
root)
6 - 20
Teeth 1 - 5, 12 -
21, 28 - 32
Yes
blank
narr. of med.
necessity, post-op
x-ray(s)
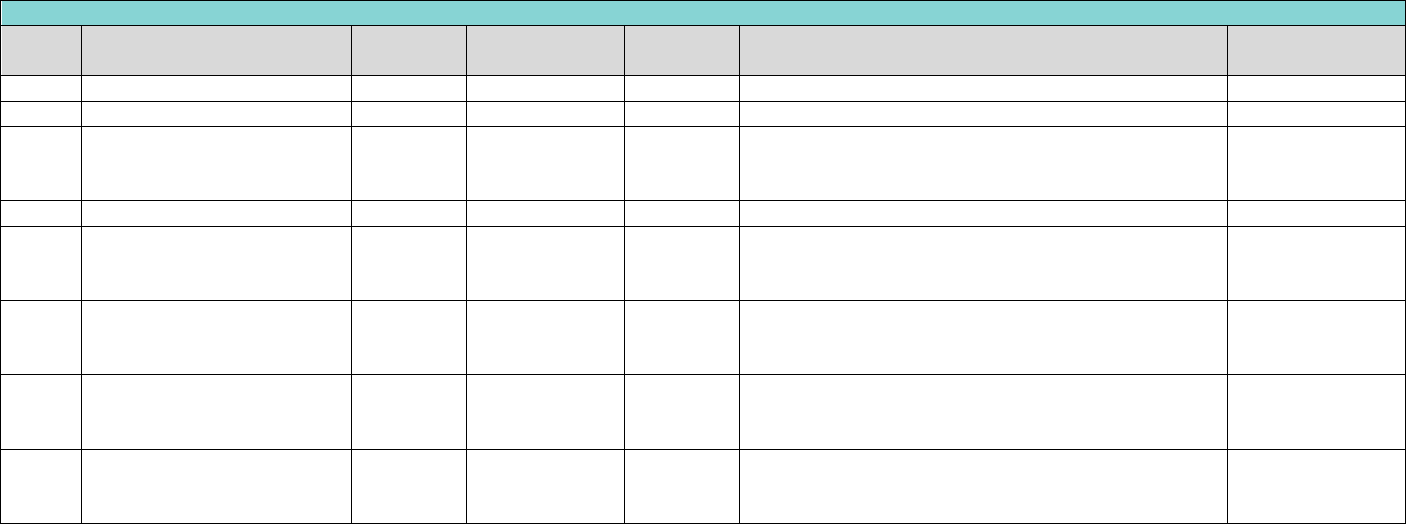
Exhibit A Benefits Covered for TX
Medicaid Child (Under 21)
This document contains proprietary and confidential information and may not be disclosed to others
without written permission. ©Copyright 2024. All rights reserved.
158
Endodontics
Code
Brief Description
Age
Limitation
Teeth Covered
Review
Required
Benefit Limitations
Documentation
Required
D3430
retrograde filling - per root
6 - 20
Teeth 1 - 32
No
blank
blank
D3450
root amputation - per root
6 - 20
Teeth 1 - 32
No
blank
blank
D3460
endodontic end osseous
implant
16 - 20
Teeth 1 - 32
Yes
blank
narr. of med.
necessity, pre and
post-op x-ray(s)
D3470
intentional reimplantation
6 - 20
Teeth 1 - 32
No
blank
blank
D3910
surgical procedure for
isolation of tooth with rubber
dam
1 - 20
Teeth 1 - 32
No
blank
blank
D3920
hemi section (including any
root removal), not incl root
canal therapy
6 - 20
Teeth 1 - 3, 14 -
19, 30 - 32
No
blank
blank
D3950
canal preparation and fitting
of preformed dowel or post
6 - 20
Teeth 1 - 32
No
blank
narr. of med.
necessity, post-op
x-ray(s)
D3999
unspecified endodontic
procedure, by report
1 - 20
Teeth 1 - 32, A -
T
Yes
blank
narr. of med.
necessity, post-op
x-ray(s)
Exhibit A Benefits Covered for TX
Medicaid Child (Under 21)
This document contains proprietary and confidential information and may not be disclosed to others
without written permission. ©Copyright 2024. All rights reserved.
159
Exhibit A Benefits Covered for TX Medicaid Child (Under 21)
"Claims for preventive dental procedure codes D1110, D1120, D1206, D1208, D1351, and D1352 will be denied when submitted for the same DOS as any D4000 series
periodontal procedure codes, any provider.
Covered dental services that indicate “Yes” in the “Review Required” column require documentation of medical necessity and will be subject to retrospective pre-payment
review. These procedures can be rendered before determination of medical necessity but require submission of proper documentation (as indicated in the
“Documentation Required” column) with the claim form.
Under 1 TAC §353.409(b) and §353.1001(b) EPSDT regulations, DentaQuest is required to provide the services in an amount, duration, and scope that is no less than the
amount, duration, and scope for the same services furnished to Members under FFS Medicaid. Please refer to the TMPPM for the FFS Medicaid language. However, all
requests to exceed listed benefit limitations in this provider manual, must be prior authorized with documentation supporting medical necessity for an increased
benefit.
When the need for an exception is established, a narrative explaining the reason for the exception of limitations must be documented in the member's file and on the
claim submission. In order to submit a claim with an exception, the claim must have the key word “EXCEPTION” in Block 35 of the ADA claim form. If the key word
“EXCEPTION” is missing from Box 35, the claim may deny for exceeding benefit limitations.
Services Submitted with D9222 and, D9223, and D9500 for ages 1-6 will require prior authorization. Please reference ‘Criteria for General Anesthesia and Intravenous (IV)
Sedation’ in the Clinical Criteria section of this ORM.
Any reimbursement already made for an inadequate service may be recouped after the DentaQuest Consultant reviews the circumstances."
Periodontics
Code
Brief Description
Age
Limitation
Teeth Covered
Review
Required
Benefit Limitations
Documentation
Required
D4210
gingivectomy or
gingivoplasty – four or more
contiguous teeth or tooth
bounded spaces per
quadrant
13 - 20
Per Quadrant (10,
20, 30, 40, LL, LR,
UL, UR)
Yes
Limit to one service of ( D4210, D4211 ) every two years,
per patient, per quadrant.
narr. of med.
necessity, pre and
post-op x-ray(s)
D4211
gingivectomy or
gingivoplasty – one to three
contiguous teeth or tooth
bounded spaces per
quadrant
13 - 20
Per Quadrant (10,
20, 30, 40, LL, LR,
UL, UR)
Yes
Limit to one service of ( D4210, D4211 ) every two years,
per patient, per quadrant.
narr. of med.
necessity, pre-op x-
ray(s)
D4230
anatomical crown exposure
- four or more contiguous
teeth or bounded tooth
spaces per quadrant
13 - 20
blank
Yes
Limit to one service of (D4230, D4231) every two years,
per patient, per quadrant.
narr. of med.
necessity, pre-op x-
ray(s)
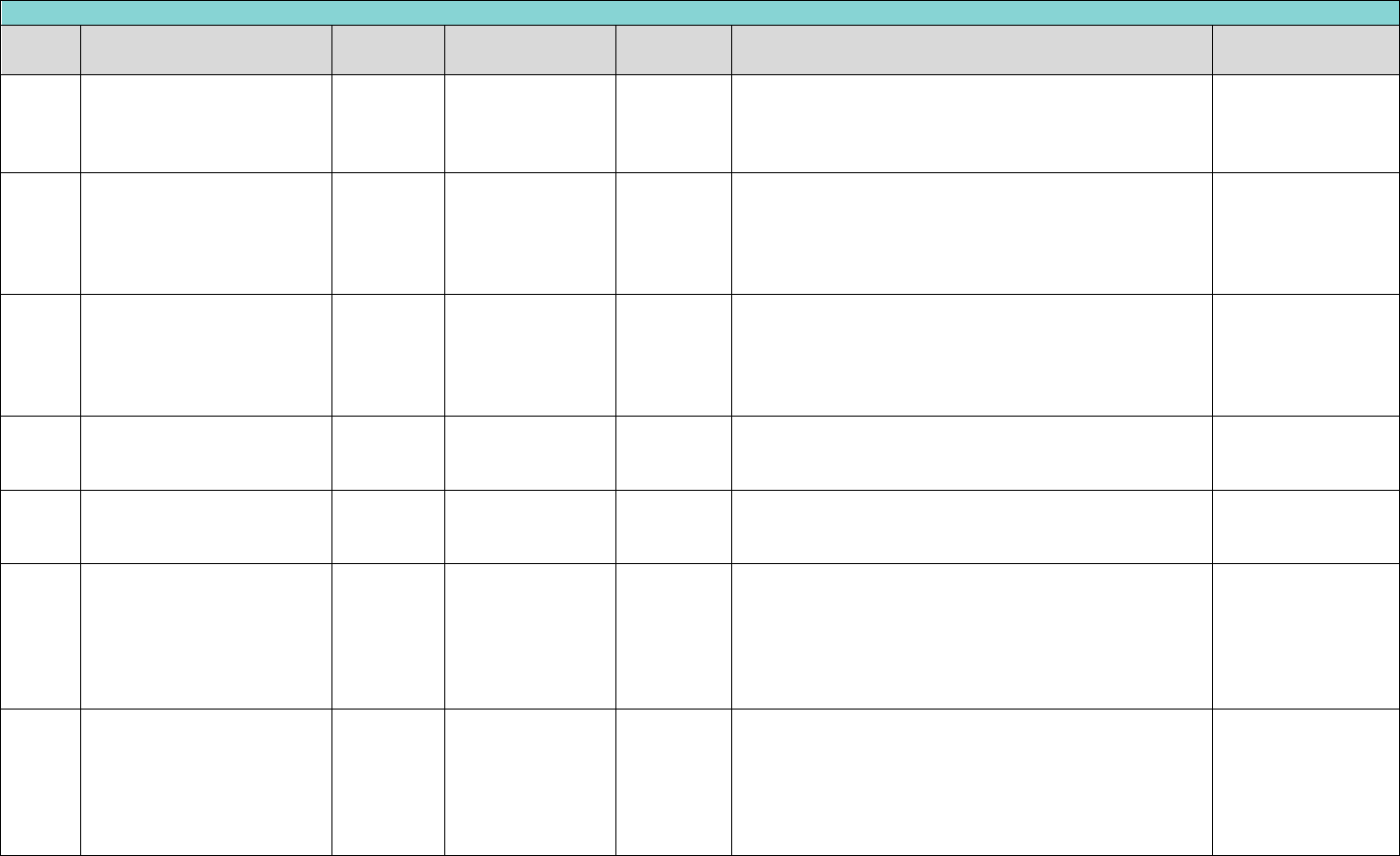
Exhibit A Benefits Covered for TX
Medicaid Child (Under 21)
This document contains proprietary and confidential information and may not be disclosed to others
without written permission. ©Copyright 2024. All rights reserved.
160
Periodontics
Code
Brief Description
Age
Limitation
Teeth Covered
Review
Required
Benefit Limitations
Documentation
Required
D4231
anatomical crown exposure
- one to three teeth or
bounded tooth spaces per
quadrant
13 - 20
blank
Yes
Limit to one service of (D4230, D4231) every two years,
per patient, per quadrant.
narr. of med.
necessity, pre-op x-
ray(s)
D4240
gingival flap procedure,
including root planning -
four or more contiguous
teeth or tooth bounded
spaces per quadrant
13 - 20
Per Quadrant (10,
20, 30, 40, LL, LR,
UL, UR)
Yes
Limit to one service of (D4240, D4241) every two years,
per patient, per quadrant.
narr of med
necessity & full
mouth xrays
D4241
gingival flap procedure,
including root planning -
one to three contiguous
teeth or tooth bounded
spaces per quadrant
13 - 20
Per Quadrant (10,
20, 30, 40, LL, LR,
UL, UR)
Yes
Limit to one service of (D4240, D4241) every two years,
per patient, per quadrant.
narr of med
necessity & full
mouth x-rays
D4245
apically positioned flap
13 - 20
Per Quadrant (10,
20, 30, 40, LL, LR,
UL, UR)
Yes
Limit to one service per two years, per patient, per
quadrant.
narr. of med.
necessity, pre-op x-
ray(s)
D4249
clinical crown lengthening –
hard tissue
13 - 20
Teeth 1 - 32
Yes
Limit to one service per lifetime, per patient, per tooth.
narr. of med.
necessity, pre and
post-op x-ray(s)
D4260
osseous surgery (including
elevation of a full thickness
flap and closure) - four or
more contiguous teeth or
tooth bounded spaces per
quadrant
13 - 20
Per Quadrant (10,
20, 30, 40, LL, LR,
UL, UR)
Yes
Limit to one service of (D4260, D4261) per year, per
patient, per quadrant.
full mouth x-rays,
perio charting &
narrative
D4261
osseous surgery (including
elevation of a full thickness
flap and closure) - one to
three contiguous teeth or
tooth bounded spaces per
quadrant
13 - 20
Per Quadrant (10,
20, 30, 40, LL, LR,
UL, UR)
Yes
Limit to one service of (D4260, D4261) per year, per
patient, per quadrant.
full mouth x-rays,
perio charting &
narrative
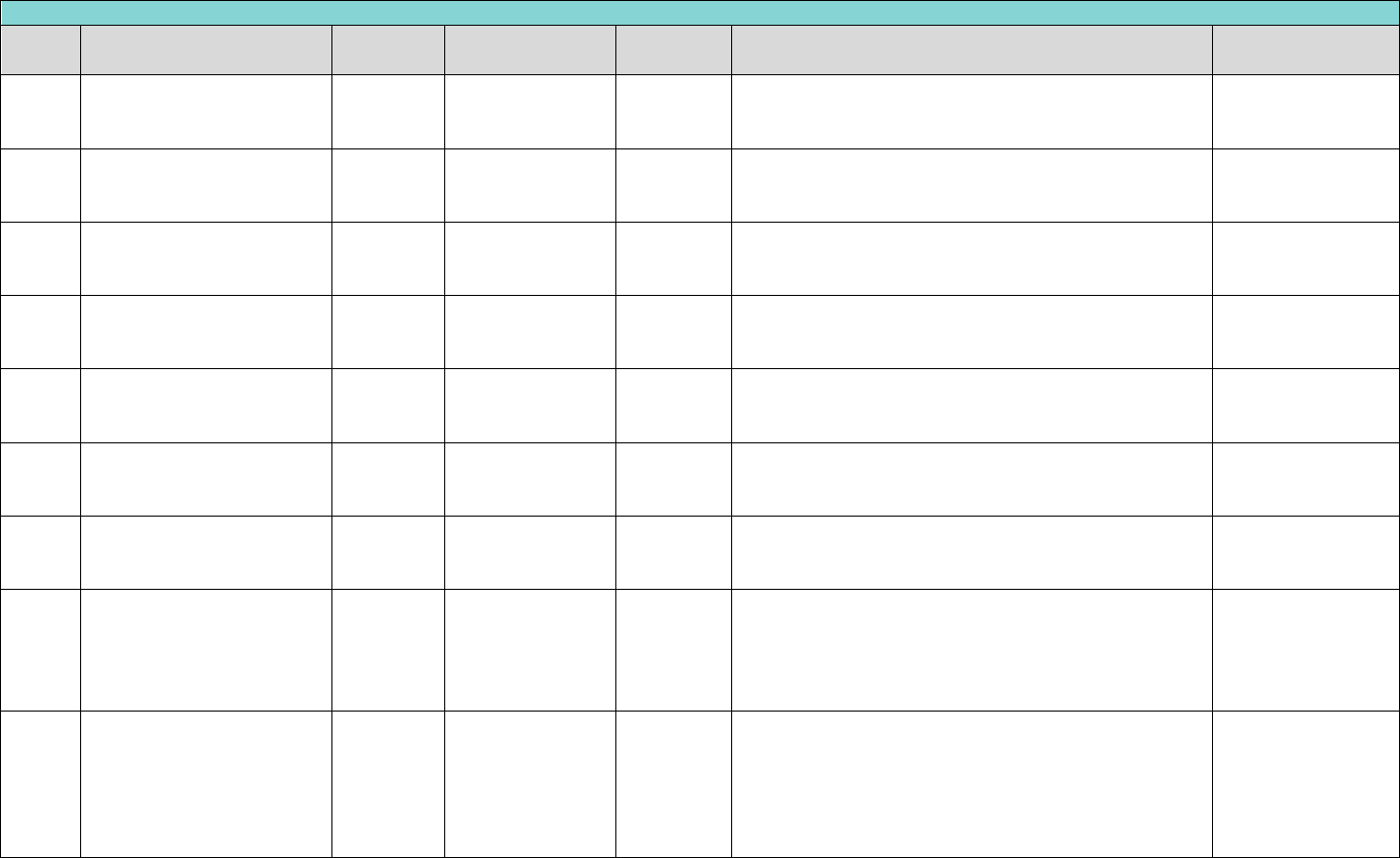
Exhibit A Benefits Covered for TX
Medicaid Child (Under 21)
This document contains proprietary and confidential information and may not be disclosed to others
without written permission. ©Copyright 2024. All rights reserved.
161
Periodontics
Code
Brief Description
Age
Limitation
Teeth Covered
Review
Required
Benefit Limitations
Documentation
Required
D4266
guided tissue regenerate-
resorbable barrier, per site,
per tooth
13 - 20
Teeth 1 - 32
Yes
Limit to one service per two years, per patient, per
tooth.
narr. of med.
necessity, pre-op x-
ray(s)
D4267
guided tissue regeneration
– non-resorbable barrier,
per site, per tooth
13 - 20
Teeth 1 - 32
Yes
Limit to one service per two years, per patient, per
tooth.
narr. of med.
necessity, pre-op x-
ray(s)
D4270
pedicle soft tissue graft
procedure
13 - 20
Teeth 1 - 32
Yes
Limit to one service per two years, per patient, per
tooth.
narr. of med.
necessity, pre-op x-
ray(s)
D4273
subepithelial connective
tissue graft procedure
13 - 20
Teeth 1 - 32
Yes
Limit to one service per two years, per patient, per
tooth.
narr. of med.
necessity, pre-op x-
ray(s)
D4274
distal or proximal wedge
procedure
13 - 20
Teeth 1 - 32
Yes
Limit to one service per two years, per patient, per
tooth.
narr. of med.
necessity, pre-op x-
ray(s)
D4275
soft tissue allograft
13 - 20
Teeth 1 - 32
Yes
Limit to one service per day, per patient, per tooth.
narr. of med.
necessity, pre-op x-
ray(s)
D4276
combined connective tissue
and double pedicle graft
13 - 20
Teeth 1 - 32
Yes
Limit to one service per two years, per patient, per
tooth. Not payable in addition to D4273 and D4276 for
the same date of service.
narr. of med.
necessity, pre-op x-
ray(s)
D4277
Free soft tissue graft
procedure (including donor
site surgery), first tooth or
edentulous tooth position in
graft
13 - 20
Teeth 1 - 32, 51 -
82
Yes
Limit to one service per two years, per patient, per
tooth.
narr. of med.
necessity, pre-op x-
ray(s)
D4278
Free soft tissue graft
procedure (including donor
site surgery), each
additional contiguous tooth
or edentulous tooth
position in same graft site
13 - 20
Teeth 1 - 32, 51 -
82
Yes
Must be billed on the same DOS as D4277.
narr. of med.
necessity, pre-op x-
ray(s)
Exhibit A Benefits Covered for TX
Medicaid Child (Under 21)
This document contains proprietary and confidential information and may not be disclosed to others
without written permission. ©Copyright 2024. All rights reserved.
162
Periodontics
Code
Brief Description
Age
Limitation
Teeth Covered
Review
Required
Benefit Limitations
Documentation
Required
D4283
autogenous connective
tissue graft procedure
(including donor and
recipient surgical sites) –
each additional contiguous
tooth, implant or
edentulous tooth position in
same graft site
13 - 20
Teeth 1 - 32
Yes
Limited to three services of (D4283, D4285) per day, per
provider, per tooth. D4283 is an add-on code and must
be billed along with procedure code D4273.
narr. of med.
necessity, pre-op x-
ray(s)
D4285
non-autogenous connective
tissue graft procedure
(including recipient surgical
site and donor material) –
each additional contiguous
tooth, implant or
edentulous tooth position in
same graft site
13 - 20
Teeth 1 - 32
Yes
Limited to three services of (D4283, D4285) per day, per
provider, per tooth. D4283 is an add-on code and must
be billed along with procedure code D4273.
narr. of med.
necessity, pre-op x-
ray(s)
D4341
periodontal scaling and root
planning - four or more
teeth per quadrant
13 - 20
Per Quadrant (10,
20, 30, 40, LL, LR,
UL, UR)
Yes
D4341 is denied if provided within 21 days of D4355.
D4341 and D4342 are denied when submitted for the
same DOS as other D4000 series codes, except D4341
and D4342, or with D1110, D1120, D1206, D1208,
D1351, D1510, D1515, D1520, or D1525, Any Provider.
full mouth x-rays,
perio charting &
narrative
D4342
periodontal scaling and root
planning - one to three
teeth per quadrant
13 - 20
Per Quadrant (10,
20, 30, 40, LL, LR,
UL, UR)
Yes
D4342 and D4341 are denied when submitted for the
same DOS as other D4000 series codes, except D4341
and D4342, or with D1110, D1120, D1206, D1208,
D1351, D1510, D1515, D1520, or D1525, Any Provider.
full mouth x-rays,
perio charting &
narrative
D4355
full mouth debridement to
enable a comprehensive
oral evaluation and
diagnosis on a subsequent
visit
13 - 20
blank
Yes
D4355 is not payable if provided within 21 days of
D4341. Denied when submitted for the same DOS as
other D4000 series codes (D4210, D4211, D4230, D4231,
D4240, D4241, D4245, D4249, D4260, D4266, D4267,
D4270, D4273, D4274, D4275, D4276, D4278, D4283,
D4285, D4320, D4321, D4381, D4910, D4920, D4999) or
with D0150, D0160, D0180, D1110, D1120, D1206,
D1208, D1351, D1510, D1515, D1520, or D1525.
narr. of med.
necessity, pre and
post-op x-ray(s)
Exhibit A Benefits Covered for TX
Medicaid Child (Under 21)
This document contains proprietary and confidential information and may not be disclosed to others
without written permission. ©Copyright 2024. All rights reserved.
163
Periodontics
Code
Brief Description
Age
Limitation
Teeth Covered
Review
Required
Benefit Limitations
Documentation
Required
D4381
localized delivery of
antimicrobial agents
13 - 20
Teeth 1 - 32
Yes
Limit one service every two years, per patient, per tooth.
narr. of med.
necessity, pre-op x-
ray(s)
D4910
periodontal maintenance
procedures
13 - 20
blank
Yes
Limit of two services per year, per patient. Once a D4910
is used, then only a D4910 can be used. Cannot be used
in conjunction with D4341 on the same date of service.
Only allowed in conjunction with a history of periodontal
pre-surgical or surgical treatment, excluding D4355.
Limit is 2 times per year either code D1110 or D4910 but
not both.
narr. of med.
necessity, pre-op x-
ray(s)
D4920
unscheduled dressing
change (by someone other
than treating dentist or
their staff)
13 - 20
blank
No
blank
blank
D4999
unspecified periodontal
procedure, by report
13 - 20
blank
Yes
blank
narr. of med.
necessity, pre-op x-
ray(s)
Exhibit A Benefits Covered for TX
Medicaid Child (Under 21)
This document contains proprietary and confidential information and may not be disclosed to others
without written permission. ©Copyright 2024. All rights reserved.
164
Exhibit A Benefits Covered for TX Medicaid Child (Under 21)
Provision for removable prostheses when masticatory function is impaired, or when existing prostheses is unserviceable and when evidence is submitted that indicates
that the masticatory insufficiencies are likely to impair the general health of the member.
Authorization for partial dentures to replace posterior teeth will not be allowed if there are in each quadrant at least three (3) peridontially sound posterior teeth in fairly
good position and occlusion with opposing dentition.
Authorization for cast partial dentures for anterior teeth generally will not be given unless one or more anterior teeth in the same arch are missing. Partial dentures are
not a covered benefit when 8 or more posterior teeth are in occlusion.
Dentures will not be preauthorized when: Dental history reveals that any or all dentures made in recent years have been unsatisfactory for reasons that are not
remediable because of physiological or psychological reasons, or repair, relining or rebasing of the patient's present dentures will make them serviceable.
A preformed denture with teeth already mounted forming a denture module is not a covered service.
BILLING AND REIMBURSEMENT FOR CAST CROWNS AND POST & CORES OR REMOVABLE PROSTHETICS SHALL BE BASED ON THE CEMENTATION OR INSERTION DATE.
Fabrication of a removable prosthetic includes multiple steps(appointments) these multiple steps (impressions, try-in appointments, delivery etc.) are inclusive in the fee
for the removable prosthetic and as such not eligible for additional compensation.
Covered dental services that indicate “Yes” in the “Review Required” column require documentation of medical necessity and will be subject to retrospective pre-payment
review. These procedures can be rendered before determination of medical necessity but require submission of proper documentation (as indicated in the
“Documentation Required” column) with the claim form.
Under 1 TAC §353.409(b) and §353.1001(b) EPSDT regulations, DentaQuest is required to provide the services in an amount, duration, and scope that is no less than the
amount, duration, and scope for the same services furnished to Members under FFS Medicaid. Please refer to the TMPPM for the FFS Medicaid language. However, all
requests to exceed listed benefit limitations in this provider manual, must be prior authorized with documentation supporting medical necessity for an increased
benefit.
When the need for an exception is established, a narrative explaining the reason for the exception of limitations must be documented in the member's file and on the
claim submission. In order to submit a claim with an exception, the claim must have the key word “EXCEPTION” in Block 35 of the ADA claim form. If the key word
“EXCEPTION” is missing from Box 35, the claim may deny for exceeding benefit limitations.
Services Submitted with D9222 and, D9223, and D9500 for ages 1-6 will require prior authorization. Please reference ‘Criteria for General Anesthesia and Intravenous (IV)
Sedation’ in the Clinical Criteria section of this ORM.
Any reimbursement already made for an inadequate service may be recouped after the DentaQuest Consultant reviews the circumstances.
Prosthodontics, removable
Code
Brief Description
Age
Limitation
Teeth Covered
Review
Required
Benefit Limitations
Documentation
Required
D5110
complete denture -
maxillary
3 - 20
Per Arch (01, UA)
Yes
Limit one service of (D5110, D5130, D5863) every five years,
per patient.
pre-operative x-
ray(s)
D5120
complete denture -
mandibular
3 - 20
Per Arch (02, LA)
Yes
Limit one service of (D5120, D5140, D5865) every five years,
per patient.
pre-operative x-
ray(s)
Exhibit A Benefits Covered for TX
Medicaid Child (Under 21)
This document contains proprietary and confidential information and may not be disclosed to others
without written permission. ©Copyright 2024. All rights reserved.
165
Prosthodontics, removable
Code
Brief Description
Age
Limitation
Teeth Covered
Review
Required
Benefit Limitations
Documentation
Required
D5130
immediate denture -
maxillary
13 - 20
Per Arch (01, UA)
Yes
Limit one service of (D5110, D5130, D5863) every five years,
per patient. One of (D5130) per 1 Lifetime Per patient.
narr. of med.
necessity, pre-op x-
ray(s)
D5140
immediate denture -
mandibular
13 - 20
Per Arch (02, LA)
Yes
Limit one service of (D5120, D5140, D5865) every five years,
per patient. One of (D5140) per 1 Lifetime Per patient.
narr. of med.
necessity, pre-op x-
ray(s)
D5211
maxillary partial denture –
resin base (including any
conventional clasps, rests
and teeth)
6 - 20
blank
Yes
Limit one service of (D5211, D5213, D5864) every five years,
per patient.
pre-operative x-
ray(s)
D5212
mandibular partial denture
- resin base (including any
conventional clasps, rests
and teeth)
6 - 20
blank
Yes
Limit one service of (D5212, D5214, D5866) every five years,
per patient.
pre-operative x-
ray(s)
D5213
maxillary partial denture -
cast metal framework with
resin denture bases
(including
retentive/clasping
materials, rests and teeth)
9 - 20
blank
Yes
Limit one service of (D5211, D5213, D5866) every five years,
per patient.
narr. of med.
necessity, pre-op x-
ray(s)
D5214
mandibular partial denture
- cast metal framework with
resin denture bases
(including
retentive/clasping
materials, rests and teeth)
9 - 20
blank
Yes
Limit one service of (D5212, D5214, D5866) every five years,
per patient.
narr. of med.
necessity, pre-op x-
ray(s)
D5410
adjust complete denture -
maxillary
3 - 20
blank
No
Limit one service per year, per patient. Not covered within 6
months of placement.
blank
D5411
adjust complete denture -
mandibular
3 - 20
blank
No
Limit one service per year, per patient. Not covered within 6
months of placement.
blank
D5421
adjust partial denture -
maxillary
6 - 20
blank
No
Limit one service per year, per patient. Not covered within 6
months of placement.
blank
D5422
adjust partial denture -
mandibular
6 - 20
blank
No
Limit one service per year, per patient. Not covered within 6
months of placement.
blank
Exhibit A Benefits Covered for TX
Medicaid Child (Under 21)
This document contains proprietary and confidential information and may not be disclosed to others
without written permission. ©Copyright 2024. All rights reserved.
166
Prosthodontics, removable
Code
Brief Description
Age
Limitation
Teeth Covered
Review
Required
Benefit Limitations
Documentation
Required
D5511
repair broken complete
denture base, mandibular
3 - 20
Per Arch (02, LA)
No
Cost of repairs cannot exceed replacement costs.
blank
D5512
repair broken complete
denture base, maxillary
3 - 20
Per Arch (01, UA)
No
Cost of repairs cannot exceed replacement costs.
blank
D5520
replace missing or broken
teeth - complete denture
(each tooth)
3 - 20
Teeth 1 - 32
No
Cost of repairs cannot exceed replacement costs.
blank
D5611
repair resin partial denture
base, mandibular
3 - 20
Teeth 17 - 32
No
Cost of repairs cannot exceed replacement costs.
The laboratory
portion of the claim
must be submitted.
D5612
repair resin partial denture
base, maxillary
3 - 20
Teeth 1 - 16
No
Cost of repairs cannot exceed replacement costs.
The laboratory
portion of the claim
must be submitted.
D5630
repair or replace broken
clasp
6 - 20
Teeth 1 - 32
No
Cost of repairs cannot exceed replacement costs.
The laboratory
portion of the claim
must be submitted.
D5640
replace broken teeth-per
tooth
6 - 20
Teeth 1 - 32
No
Cost of repairs cannot exceed replacement costs.
The laboratory
portion of the claim
must be submitted.
D5650
add tooth to existing partial
denture
6 - 20
Teeth 1 - 32
No
Cost of repairs cannot exceed replacement costs.
The laboratory
portion of the claim
must be submitted.
D5660
add clasp to existing partial
denture
6 - 20
blank
No
Cost of repairs cannot exceed replacement costs.
The laboratory
portion of the claim
must be submitted.
D5670
replace all teeth and acrylic
on cast metal framework
(maxillary)
6 - 20
blank
No
Limit one service every three years, per patient. Not covered
within 6 months of placement. Denied with D5211, D5213,
D5281, D5640.
blank
D5671
replace all teeth and acrylic
on cast metal framework
(mandibular)
6 - 20
blank
No
Limit one service every three years, per patient. Not covered
within 6 months of placement. Denied with D5211, D5213,
D5281, D5640.
blank
Exhibit A Benefits Covered for TX
Medicaid Child (Under 21)
This document contains proprietary and confidential information and may not be disclosed to others
without written permission. ©Copyright 2024. All rights reserved.
167
Prosthodontics, removable
Code
Brief Description
Age
Limitation
Teeth Covered
Review
Required
Benefit Limitations
Documentation
Required
D5710
rebase complete maxillary
denture
4 - 20
blank
No
Limit one service of (D5710, D5720, D5730, D5740, D5750,
and D5760) every 36 months, per provider. D5710 placement
not covered within 12 months of D5110, D5130, D5211, or
D5213, any provider.
blank
D5711
rebase complete
mandibular denture
4 - 20
blank
No
Limit one service of (D5711, D5721, D5731, D5741, D5751,
and D5761) every 36 months, per provider. D5711 placement
not covered within 12 months of D5120, D5140, D5212, or
D5214 any provider.
blank
D5720
rebase maxillary partial
denture
7 - 20
blank
No
Limit one service of ( D5710, D5720, D5730, D5740, D5750,
and D5760) every 36 months, per provider. D5710 placement
not covered within 12 months of D5110, D5130, D5211, or
D5213, any provider.
blank
D5721
rebase mandibular partial
denture
7 - 20
blank
No
Limit one service of (D5711, D5721, D5731, D5741, D5751,
and D5761) every 36 months, per provider. D5711
placement not covered within 12 months of D5120, D5140,
D5212, or D5214 any provider.
blank
D5730
reline complete maxillary
denture (chairside)
4 - 20
blank
No
Limit one service of (D5710, D5720, D5730, D5740, D5750,
and D5760) every 36 months, per provider. D5710 placement
not covered within 12 months of D5110, D5130, D5211, or
D5213, any provider.
blank
D5731
reline complete mandibular
denture (chairside)
4 - 20
blank
No
Limit one service of (D5711, D5721, D5731, D5741, D5751,
and D5761) every 36 months, per provider. D5711
placement not covered within 12 months of D5120, D5140,
D5212, or D5214 any provider.
blank
D5740
reline maxillary partial
denture (chairside)
7 - 20
blank
No
Limit one service of (D5710, D5720, D5730, D5740, D5750,
and D5760) every 36 months, per provider. D5710
placement not covered within 12 months of D5110, D5130,
D5211, or D5213, any provider.
blank
D5741
reline mandibular partial
denture (chairside)
7 - 20
blank
No
Limit one service of (D5711, D5721, D5731, D5741, D5751,
and D5761) every 36 months, per provider. D5711
placement not covered within 12 months of D5120, D5140,
D5212, or D5214 any provider.
blank
Exhibit A Benefits Covered for TX
Medicaid Child (Under 21)
This document contains proprietary and confidential information and may not be disclosed to others
without written permission. ©Copyright 2024. All rights reserved.
168
Prosthodontics, removable
Code
Brief Description
Age
Limitation
Teeth Covered
Review
Required
Benefit Limitations
Documentation
Required
D5750
reline complete maxillary
denture (laboratory)
4 - 20
blank
No
Limit one service of (D5710, D5720, D5730, D5740, D5750,
and D5760) every 36 months, per provider. D5710 placement
not covered within 12 months of D5110, D5130, D5211, or
D5213, any provider.
blank
D5751
reline complete mandibular
denture (laboratory)
4 - 20
blank
No
Limit one service of (D5711, D5721, D5731, D5741, D5751,
and D5761) every 36 months, per provider. D5711 placement
not covered within 12 months of D5120, D5140, D5212, or
D5214 any provider.
blank
D5760
reline maxillary partial
denture (laboratory)
7 - 20
blank
No
Limit one service of (D5710, D5720, D5730, D5740, D5750,
and D5760) every 36 months, per provider. D5710 placement
not covered within 12 months of D5110, D5130, D5211, or
D5213, any provider.
blank
D5761
reline mandibular partial
denture (laboratory)
7 - 20
blank
No
Limit one service of (D5711, D5721, D5731, D5741, D5751,
and D5761) every 36 months, per provider. D5711 placement
not covered within 12 months of D5120, D5140, D5212, or
D5214 any provider..
blank
D5810
interim complete denture-
maxillary
3 - 20
blank
Yes
Limit to one service per lifetime, per patient.
narr. of med.
necessity, pre-op x-
ray(s)
D5811
interim complete denture-
mandibular
3 - 20
blank
Yes
Limit to one service per lifetime, per patient.
narr. of med.
necessity, pre-op x-
ray(s)
D5820
interim partial denture
(maxillary)
3 - 20
blank
Yes
Limit to one service per lifetime, per patient.
narr. of med.
necessity, pre-op x-
ray(s)
D5821
interim partial denture-
mandibular
3 - 20
blank
Yes
Limit to one service per lifetime, per patient.
narr. of med.
necessity, pre-op x-
ray(s)
D5850
tissue conditioning,
maxillary
3 - 20
blank
No
blank
blank
D5851
tissue conditioning,
mandibular
3 - 20
blank
No
blank
blank
D5862
precision attachment, by
report
4 - 20
Teeth 1 - 32
No
blank
blank
Exhibit A Benefits Covered for TX
Medicaid Child (Under 21)
This document contains proprietary and confidential information and may not be disclosed to others
without written permission. ©Copyright 2024. All rights reserved.
169
Prosthodontics, removable
Code
Brief Description
Age
Limitation
Teeth Covered
Review
Required
Benefit Limitations
Documentation
Required
D5863
Overdenture - complete
maxillary
4 - 20
Per Arch (01, UA)
Yes
Limit one service of (D5110, D5130, D5863) every five years,
per patient.
narr. of med.
necessity, pre-op x-
ray(s)
D5864
Overdenture - partial
maxillary
4 - 20
Yes
Limit one service of (D5211, D5213, D5864) every five years,
per patient.
narr. of med.
necessity, pre-op x-
ray(s)
D5865
Overdenture - complete
mandibular
4 - 20
Per Arch (02, LA)
Yes
Limit one service of (D5120, D5140, D5865) every five years,
per patient.
narr. of med.
necessity, pre-op x-
ray(s)
D5866
unspecified removable
prosthodontic procedure,
by report
4 - 20
blank
Yes
Limit one service of (D5212, D5214, D5866) every five years,
per patient.
narr. of med.
necessity, pre-op x-
ray(s)
D5899
unspecified removable
prosthodontic procedure,
by report
1 - 20
blank
Yes
blank
narr. of med.
necessity, pre-op x-
ray(s)
D5911
facial moulage (sectional)
1 - 20
blank
Yes
blank
narr. of med.
necessity, pre-op x-
ray(s)
D5912
facial moulage (complete)
1 - 20
blank
Yes
blank
narr. of med.
necessity, pre-op x-
ray(s)
D5913
nasal prosthesis
1 - 20
blank
Yes
blank
narr. of med.
necessity, pre-op x-
ray(s)
D5914
auricular prosthesis
1 - 20
blank
Yes
blank
narr. of med.
necessity, pre-op x-
ray(s)
D5915
orbital prosthesis
1 - 20
blank
Yes
blank
narr. of med.
necessity, pre-op x-
ray(s)
D5916
ocular prosthesis
1 - 20
blank
Yes
blank
narr. of med.
necessity, pre-op x-
ray(s)
D5919
facial prosthesis
1 - 20
blank
Yes
blank
narr. of med.
Exhibit A Benefits Covered for TX
Medicaid Child (Under 21)
This document contains proprietary and confidential information and may not be disclosed to others
without written permission. ©Copyright 2024. All rights reserved.
170
Prosthodontics, removable
Code
Brief Description
Age
Limitation
Teeth Covered
Review
Required
Benefit Limitations
Documentation
Required
necessity, pre-op x-
ray(s)
D5922
nasal septal prosthesis
1 - 20
blank
Yes
blank
narr. of med.
necessity, pre-op x-
ray(s)
D5923
ocular prosthesis, interim
1 - 20
blank
Yes
blank
narr. of med.
necessity, pre-op x-
ray(s)
D5924
cranial prosthesis
1 - 20
blank
Yes
blank
narr. of med.
necessity, pre-op x-
ray(s)
D5925
facial augment implant
prosthesis
1 - 20
blank
Yes
blank
narr. of med.
necessity, pre-op x-
ray(s)
D5926
nasal prosthesis,
replacement
1 - 20
blank
Yes
blank
narr. of med.
necessity, pre-op x-
ray(s)
D5927
auricular prosthesis, replace
1 - 20
blank
Yes
blank
narr. of med.
necessity, pre-op x-
ray(s)
D5928
orbital prosthesis, replace
1 - 20
blank
Yes
blank
narr. of med.
necessity, pre-op x-
ray(s)
D5929
facial prosthesis,
replacement
1 - 20
blank
Yes
blank
narr. of med.
necessity, pre-op x-
ray(s)
D5931
obturator prosthesis,
surgical
1 - 20
blank
Yes
blank
narr. of med.
necessity, pre-op x-
ray(s)
D5932
obturator prosthesis,
definitive
1 - 20
blank
Yes
blank
narr. of med.
necessity, pre-op x-
ray(s)
D5933
obturator prosthesis,
modification
1 - 20
blank
Yes
blank
narr. of med.
necessity, pre-op x-
Exhibit A Benefits Covered for TX
Medicaid Child (Under 21)
This document contains proprietary and confidential information and may not be disclosed to others
without written permission. ©Copyright 2024. All rights reserved.
171
Prosthodontics, removable
Code
Brief Description
Age
Limitation
Teeth Covered
Review
Required
Benefit Limitations
Documentation
Required
ray(s)
D5934
mandibular resection
prosthesis with guide flange
1 - 20
blank
Yes
blank
narr. of med.
necessity, pre-op x-
ray(s)
D5935
mandibular resection
prosthesis without guide
flange
1 - 20
blank
Yes
blank
narr. of med.
necessity, pre-op x-
ray(s)
D5936
obturator prosthesis,
interim
1 - 20
blank
Yes
blank
narr. of med.
necessity, pre-op x-
ray(s)
D5937
trismus appliance (not for
TMD treatment)
1 - 20
blank
Yes
blank
narr. of med.
necessity, pre-op x-
ray(s)
D5951
feeding aid
0-20
blank
Yes
blank
narr. of med.
necessity, pre-op x-
ray(s)
D5952
speech aid prosthesis,
pediatric
0-20
blank
Yes
blank
narr. of med.
necessity, pre-op x-
ray(s)
D5953
speech aid prosthesis, adult
13 - 20
blank
Yes
blank
narr. of med.
necessity, pre-op x-
ray(s)
D5954
palatal augment prosthesis
0-20
blank
Yes
blank
narr. of med.
necessity, pre-op x-
ray(s)
D5955
palatal lift prosthesis,
definitive
0-20
blank
Yes
blank
narr. of med.
necessity, pre-op x-
ray(s)
D5958
palatal lift prosthesis,
interim
0-20
blank
Yes
blank
narr. of med.
necessity, pre-op x-
ray(s)
D5959
palatal lift prosthesis,
modification
0-20
blank
Yes
blank
narrative of medical
necessity
D5960
speech aid prosthesis,
0-20
blank
Yes
blank
narrative of medical
Exhibit A Benefits Covered for TX
Medicaid Child (Under 21)
This document contains proprietary and confidential information and may not be disclosed to others
without written permission. ©Copyright 2024. All rights reserved.
172
Prosthodontics, removable
Code
Brief Description
Age
Limitation
Teeth Covered
Review
Required
Benefit Limitations
Documentation
Required
modification
necessity
D5982
surgical stent
1 - 20
blank
Yes
blank
narr. of med.
necessity, pre-op x-
ray(s)
D5983
radiation carrier
1 - 20
blank
Yes
blank
narr. of med.
necessity, pre-op x-
ray(s)
D5984
radiation shield
1 - 20
blank
Yes
blank
narr. of med.
necessity, pre-op x-
ray(s)
D5985
radiation cone locator
1 - 20
blank
Yes
blank
narr. of med.
necessity, pre and
post-op x-ray(s)
D5986
fluoride gel carrier
1 - 20
blank
Yes
blank
narr. of med.
necessity, pre-op x-
ray(s)
D5987
commissure splint
1 - 20
blank
Yes
blank
narr. of med.
necessity, pre-op x-
ray(s)
D5988
surgical splint
1 - 20
blank
Yes
Not allowed within 6 months of delivery.
narr. of med.
necessity, pre-op x-
ray(s)
D5992
Adjust maxillofacial
prosthetic appliance, by
report
0-20
blank
No
Limit one service every five years, per patient.
blank
D5993
Maintenance and cleaning
of a maxillofacial prosthesis
(extra or intraoral) other
than required adjustments.
0-20
blank
No
blank
blank
D5999
unspecified maxillofacial
prosthesis, by report
1 - 20
blank
Yes
blank
narr. of med.
necessity, pre-op x-
ray(s)
Exhibit A Benefits Covered for TX
Medicaid Child (Under 21)
This document contains proprietary and confidential information and may not be disclosed to others
without written permission. ©Copyright 2024. All rights reserved.
173
Exhibit A Benefits Covered for TX Medicaid Child (Under 21)
BILLING AND REIMBURSEMENT FOR CROWNS AND POST & CORES OR ANY OTHER FIXED PROSTHETIC SHALL BE BASED UPON THE CEMENTATION DATE. Periapical
radiographs are required for each tooth involved in the authorization request. The criteria used by DentaQuest is noted below:
ꞏ At least one abutment tooth requires a crown (based on traditional requirements of medical necessity and dental disease).
ꞏ The space cannot be filled with a removable partial denture.
ꞏ The purpose is to prevent the drifting of teeth in all dimensions (anterior, posterior, lateral, and the opposing arch).
ꞏ Each abutment or each pontic constitutes a unit in a bridge.
ꞏ Porcelain is allowed on all teeth.
The fee for crowns includes the temporary crown that is placed on the prepared tooth and worn while the permanent crown is being fabricated for permanent teeth.
Covered dental services that indicate “Yes” in the “Review Required” column require documentation of medical necessity and will be subject to retrospective pre-payment
review. These procedures can be rendered before determination of medical necessity but require submission of proper documentation (as indicated in the
“Documentation Required” column) with the claim form.
Under 1 TAC §353.409(b) and §353.1001(b) EPSDT regulations, DentaQuest is required to provide the services in an amount, duration, and scope that is no less than the
amount, duration, and scope for the same services furnished to Members under FFS Medicaid. Please refer to the TMPPM for the FFS Medicaid language. However, all
requests to exceed listed benefit limitations in this provider manual, must be prior authorized with documentation supporting medical necessity for an increased
benefit.
When the need for an exception is established, a narrative explaining the reason for the exception of limitations must be documented in the member's file and on the
claim submission. In order to submit a claim with an exception, the claim must have the key word “EXCEPTION” in Block 35 of the ADA claim form. If the key word
“EXCEPTION” is missing from Box 35, the claim may deny for exceeding benefit limitations.
Services Submitted with D9222 and, D9223, and D9500 for ages 1-6 will require prior authorization. Please reference ‘Criteria for General Anesthesia and Intravenous (IV)
Sedation’ in the Clinical Criteria section of this ORM.
Any reimbursement already made for an inadequate service may be recouped after the DentaQuest Consultant reviews the circumstances.
Prosthodontics, fixed
Code
Brief Description
Age
Limitation
Teeth Covered
Review
Required
Benefit Limitations
Documentation
Required
D6210
pontic - cast high noble
metal
16 - 20
Teeth 1 - 32
Yes
Limit one service of the following (D6210, D6211, D6212,
D6240, D6241, D6242, D6245, D6250, D6251, D6252,
D6545, D6548, D6720, D6721, D6722, D6740, D6750,
D6751, D6752, D6780, D6781, D6782, D6783, D6790,
D6791, D6792) every five years, per patient, per tooth.
narr. of med.
necessity, pre and
post-op x-ray(s)
D6211
pontic-cast base metal
16 - 20
Teeth 1 - 32
Yes
Limit one service of the following (D6210, D6211, D6212,
D6240, D6241, D6242, D6245, D6250, D6251, D6252,
D6545, D6548, D6720, D6721, D6722, D6740, D6750,
D6751, D6752, D6780, D6781, D6782, D6783, D6790,
D6791, D6792) every five years, per patient, per tooth.
narr. of med.
necessity, pre and
post-op x-ray(s)
Exhibit A Benefits Covered for TX
Medicaid Child (Under 21)
This document contains proprietary and confidential information and may not be disclosed to others
without written permission. ©Copyright 2024. All rights reserved.
174
Prosthodontics, fixed
Code
Brief Description
Age
Limitation
Teeth Covered
Review
Required
Benefit Limitations
Documentation
Required
D6212
pontic - cast noble metal
16 - 20
Teeth 1 - 32
Yes
Limit one service of the following (D6210, D6211, D6212,
D6240, D6241, D6242, D6245, D6250, D6251, D6252,
D6545, D6548, D6720, D6721, D6722, D6740, D6750,
D6751, D6752, D6780, D6781, D6782, D6783, D6790,
D6791, D6792) every five years, per patient, per tooth.
narr. of med.
necessity, pre and
post-op x-ray(s)
D6240
pontic-porcelain fused-high
noble
16 - 20
Teeth 1 - 32
Yes
Limit one service of the following (D6210, D6211, D6212,
D6240, D6241, D6242, D6245, D6250, D6251, D6252,
D6545, D6548, D6720, D6721, D6722, D6740, D6750,
D6751, D6752, D6780, D6781, D6782, D6783, D6790,
D6791, D6792) every five years, per patient, per tooth.
narr. of med.
necessity, pre and
post-op x-ray(s)
D6241
pontic-porcelain fused to
base metal
16 - 20
Teeth 1 - 32
Yes
Limit one service of the following (D6210, D6211, D6212,
D6240, D6241, D6242, D6245, D6250, D6251, D6252,
D6545, D6548, D6720, D6721, D6722, D6740, D6750,
D6751, D6752, D6780, D6781, D6782, D6783, D6790,
D6791, D6792) every five years, per patient, per tooth.
narr. of med.
necessity, pre and
post-op x-ray(s)
D6242
pontic-porcelain fused-
noble metal
16 - 20
Teeth 1 - 32
Yes
Limit one service of the following (D6210, D6211, D6212,
D6240, D6241, D6242, D6245, D6250, D6251, D6252,
D6545, D6548, D6720, D6721, D6722, D6740, D6750,
D6751, D6752, D6780, D6781, D6782, D6783, D6790,
D6791, D6792) every five years, per patient, per tooth.
narr. of med.
necessity, pre and
post-op x-ray(s)
D6245
prosthodontics fixed, pontic
- porcelain/ceramic
16 - 20
Teeth 1 - 32
Yes
Limit one service of the following (D6210, D6211, D6212,
D6240, D6241, D6242, D6245, D6250, D6251, D6252,
D6545, D6548, D6720, D6721, D6722, D6740, D6750,
D6751, D6752, D6780, D6781, D6782, D6783, D6790,
D6791, D6792) every five years, per patient, per tooth.
narr. of med.
necessity, pre and
post-op x-ray(s)
D6250
pontic-resin with high noble
metal
16 - 20
Teeth 1 - 32
Yes
Limit one service of the following (D6210, D6211, D6212,
D6240, D6241, D6242, D6245, D6250, D6251, D6252,
D6545, D6548, D6720, D6721, D6722, D6740, D6750,
D6751, D6752, D6780, D6781, D6782, D6783, D6790,
D6791, D6792) every five years, per patient, per tooth.
narr. of med.
necessity, pre and
post-op x-ray(s)
Exhibit A Benefits Covered for TX
Medicaid Child (Under 21)
This document contains proprietary and confidential information and may not be disclosed to others
without written permission. ©Copyright 2024. All rights reserved.
175
Prosthodontics, fixed
Code
Brief Description
Age
Limitation
Teeth Covered
Review
Required
Benefit Limitations
Documentation
Required
D6251
pontic-resin with base
metal
16 - 20
Teeth 1 - 32
Yes
Limit one service of the following (D6210, D6211, D6212,
D6240, D6241, D6242, D6245, D6250, D6251, D6252,
D6545, D6548, D6720, D6721, D6722, D6740, D6750,
D6751, D6752, D6780, D6781, D6782, D6783, D6790,
D6791, D6792) every five years, per patient, per tooth.
narr. of med.
necessity, pre and
post-op x-ray(s)
D6252
pontic-resin with noble
metal
16 - 20
Teeth 1 - 32
Yes
Limit one service of the following (D6210, D6211, D6212,
D6240, D6241, D6242, D6245, D6250, D6251, D6252,
D6545, D6548, D6720, D6721, D6722, D6740, D6750,
D6751, D6752, D6780, D6781, D6782, D6783, D6790,
D6791, D6792) every five years, per patient, per tooth.
narr. of med.
necessity, pre and
post-op x-ray(s)
D6545
retainer - cast metal fixed
16 - 20
Teeth 1 - 32
Yes
Limit one service of the following (D6210, D6211, D6212,
D6240, D6241, D6242, D6245, D6250, D6251, D6252,
D6545, D6548, D6720, D6721, D6722, D6740, D6750,
D6751, D6752, D6780, D6781, D6782, D6783, D6790,
D6791, D6792) every five years, per patient, per tooth.
narr. of med.
necessity, pre and
post-op x-ray(s)
D6548
prosthodontics fixed,
retainer - porcelain/ceramic
for resin bonded fixed
prosthodontic
16 - 20
Teeth 1 - 32
Yes
Limit one service of the following (D6210, D6211, D6212,
D6240, D6241, D6242, D6245, D6250, D6251, D6252,
D6545, D6548, D6720, D6721, D6722, D6740, D6750,
D6751, D6752, D6780, D6781, D6782, D6783, D6790,
D6791, D6792) every five years, per patient, per tooth.
narr. of med.
necessity, pre and
post-op x-ray(s)
D6549
Resin retainer-For resin
bonded fixed prosthesis
16 - 20
Teeth 1 - 32
No
Limit one service every five years, per patient.
D6720
crown-resin with high noble
metal
16 - 20
Teeth 1 - 32
Yes
Limit one service of the following (D6210, D6211, D6212,
D6240, D6241, D6242, D6245, D6250, D6251, D6252,
D6545, D6548, D6720, D6721, D6722, D6740, D6750,
D6751, D6752, D6780, D6781, D6782, D6783, D6790,
D6791, D6792) every five years, per patient, per tooth.
narr. of med.
necessity, pre and
post-op x-ray(s)
D6721
crown-resin with base
metal
16 - 20
Teeth 1 - 32
Yes
Limit one service of the following (D6210, D6211, D6212,
D6240, D6241, D6242, D6245, D6250, D6251, D6252,
D6545, D6548, D6720, D6721, D6722, D6740, D6750,
D6751, D6752, D6780, D6781, D6782, D6783, D6790,
D6791, D6792) every five years, per patient, per tooth.
narr. of med.
necessity, pre and
post-op x-ray(s)
Exhibit A Benefits Covered for TX
Medicaid Child (Under 21)
This document contains proprietary and confidential information and may not be disclosed to others
without written permission. ©Copyright 2024. All rights reserved.
176
Prosthodontics, fixed
Code
Brief Description
Age
Limitation
Teeth Covered
Review
Required
Benefit Limitations
Documentation
Required
D6722
crown-resin with noble
metal
16 - 20
Teeth 1 - 32
Yes
Limit one service of the following (D6210, D6211, D6212,
D6240, D6241, D6242, D6245, D6250, D6251, D6252,
D6545, D6548, D6720, D6721, D6722, D6740, D6750,
D6751, D6752, D6780, D6781, D6782, D6783, D6790,
D6791, D6792) every five years, per patient, per tooth.
narr. of med.
necessity, pre and
post-op x-ray(s)
D6740
retainer crown –
porcelain/ceramic
16 - 20
Teeth 1 - 32
Yes
Limit one service of the following (D6210, D6211, D6212,
D6240, D6241, D6242, D6245, D6250, D6251, D6252,
D6545, D6548, D6720, D6721, D6722, D6740, D6750,
D6751, D6752, D6780, D6781, D6782, D6783, D6790,
D6791, D6792) every five years, per patient, per tooth.
narr. of med.
necessity, pre and
post-op x-ray(s)
D6750
crown-porcelain fused high
noble
16 - 20
Teeth 1 - 32
Yes
Limit one service of the following (D6210, D6211, D6212,
D6240, D6241, D6242, D6245, D6250, D6251, D6252,
D6545, D6548, D6720, D6721, D6722, D6740, D6750,
D6751, D6752, D6780, D6781, D6782, D6783, D6790,
D6791, D6792) every five years, per patient, per tooth.
narr. of med.
necessity, pre and
post-op x-ray(s)
D6751
crown-porcelain fused to
base metal
16 - 20
Teeth 1 - 32
Yes
Limit one service of the following (D6210, D6211, D6212,
D6240, D6241, D6242, D6245, D6250, D6251, D6252,
D6545, D6548, D6720, D6721, D6722, D6740, D6750,
D6751, D6752, D6780, D6781, D6782, D6783, D6790,
D6791, D6792) every five years, per patient, per tooth.
narr. of med.
necessity, pre and
post-op x-ray(s)
D6752
crown-porcelain fused
noble metal
16 - 20
Teeth 1 - 32
Yes
Limit one service of the following (D6210, D6211, D6212,
D6240, D6241, D6242, D6245, D6250, D6251, D6252,
D6545, D6548, D6720, D6721, D6722, D6740, D6750,
D6751, D6752, D6780, D6781, D6782, D6783, D6790,
D6791, D6792) every five years, per patient, per tooth.
narr. of med.
necessity, pre and
post-op x-ray(s)
D6780
crown-3/4 cst high noble
metal
16 - 20
Teeth 1 - 32
Yes
Limit one service of the following (D6210, D6211, D6212,
D6240, D6241, D6242, D6245, D6250, D6251, D6252,
D6545, D6548, D6720, D6721, D6722, D6740, D6750,
D6751, D6752, D6780, D6781, D6782, D6783, D6790,
D6791, D6792) every five years, per patient, per tooth.
narr. of med.
necessity, pre and
post-op x-ray(s)
Exhibit A Benefits Covered for TX
Medicaid Child (Under 21)
This document contains proprietary and confidential information and may not be disclosed to others
without written permission. ©Copyright 2024. All rights reserved.
177
Prosthodontics, fixed
Code
Brief Description
Age
Limitation
Teeth Covered
Review
Required
Benefit Limitations
Documentation
Required
D6781
prosthodontics fixed, crown
¾ cast predominantly based
metal
16 - 20
Teeth 1 - 32
Yes
Limit one service of the following (D6210, D6211, D6212,
D6240, D6241, D6242, D6245, D6250, D6251, D6252,
D6545, D6548, D6720, D6721, D6722, D6740, D6750,
D6751, D6752, D6780, D6781, D6782, D6783, D6790,
D6791, D6792) every five years, per patient, per tooth.
narr. of med.
necessity, pre and
post-op x-ray(s)
D6782
prosthodontics fixed, crown
¾ cast noble metal
16 - 20
Teeth 1 - 32
Yes
Limit one service of the following (D6210, D6211, D6212,
D6240, D6241, D6242, D6245, D6250, D6251, D6252,
D6545, D6548, D6720, D6721, D6722, D6740, D6750,
D6751, D6752, D6780, D6781, D6782, D6783, D6790,
D6791, D6792) every five years, per patient, per tooth.
narr. of med.
necessity, pre and
post-op x-ray(s)
D6783
prosthodontics fixed, crown
¾ porcelain/ceramic
16 - 20
Teeth 1 - 32
Yes
Limit one service of the following (D6210, D6211, D6212,
D6240, D6241, D6242, D6245, D6250, D6251, D6252,
D6545, D6548, D6720, D6721, D6722, D6740, D6750,
D6751, D6752, D6780, D6781, D6782, D6783, D6790,
D6791, D6792) every five years, per patient, per tooth.
narr. of med.
necessity, pre and
post-op x-ray(s)
D6790
crown-full cast high noble
16 - 20
Teeth 1 - 5, 12 -
21, 28 - 32
Yes
Limit one service of the following (D6210, D6211, D6212,
D6240, D6241, D6242, D6245, D6250, D6251, D6252,
D6545, D6548, D6720, D6721, D6722, D6740, D6750,
D6751, D6752, D6780, D6781, D6782, D6783, D6790,
D6791, D6792) every five years, per patient, per tooth.
narr. of med.
necessity, pre and
post-op x-ray(s)
D6791
crown - full cast base metal
16 - 20
Teeth 1 - 5, 12 -
21, 28 - 32
Yes
Limit one service of the following (D6210, D6211, D6212,
D6240, D6241, D6242, D6245, D6250, D6251, D6252,
D6545, D6548, D6720, D6721, D6722, D6740, D6750,
D6751, D6752, D6780, D6781, D6782, D6783, D6790,
D6791, D6792) every five years, per patient, per tooth.
narr. of med.
necessity, pre and
post-op x-ray(s)
D6792
crown - full cast noble
metal
16 - 20
Teeth 1 - 5, 12 -
21, 28 - 32
Yes
Limit one service of the following (D6210, D6211, D6212,
D6240, D6241, D6242, D6245, D6250, D6251, D6252,
D6545, D6548, D6720, D6721, D6722, D6740, D6750,
D6751, D6752, D6780, D6781, D6782, D6783, D6790,
D6791, D6792) every five years, per patient, per tooth.
narr. of med.
necessity, pre and
post-op x-ray(s)
D6920
connector bar
16 - 20
Per Arch (01, 02,
LA, UA)
Yes
Limit one service every five years, per patient, per tooth.
pre-operative x-
ray(s)
D6930
re-cement or re-bond fixed
partial denture
16 - 20
No
Not allowed within 6 months of initial placement.
blank
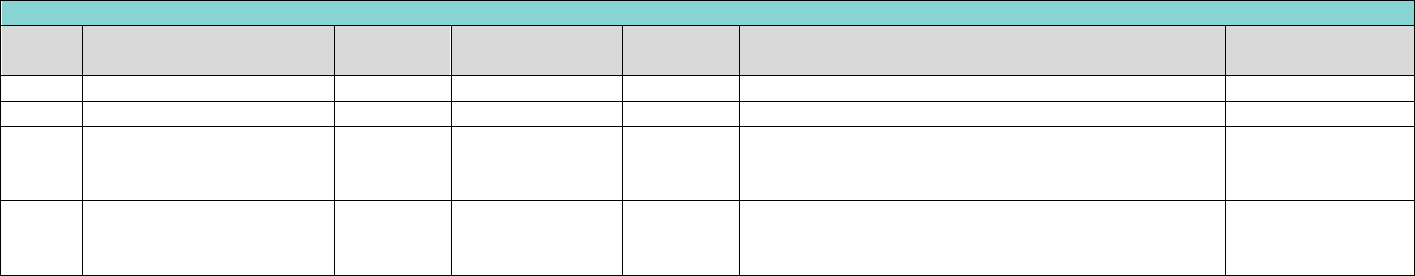
Exhibit A Benefits Covered for TX
Medicaid Child (Under 21)
This document contains proprietary and confidential information and may not be disclosed to others
without written permission. ©Copyright 2024. All rights reserved.
178
Prosthodontics, fixed
Code
Brief Description
Age
Limitation
Teeth Covered
Review
Required
Benefit Limitations
Documentation
Required
D6940
stress breaker
16 - 20
Teeth 1 - 32
No
Limit one service every five years, per patient, per tooth.
blank
D6950
precision attachment
16 - 20
Teeth 1 - 32
No
Limit one service every five years, per patient, per tooth.
blank
D6980
fixed partial denture repair
16 - 20
Per Quadrant (10,
20, 30, 40, LL, LR,
UL, UR)
No
blank
blank
D6999
fixed prosthodontic
procedure
16 - 20
Teeth 1 - 32
Yes
blank
narr. of med.
necessity, pre-op x-
ray(s)
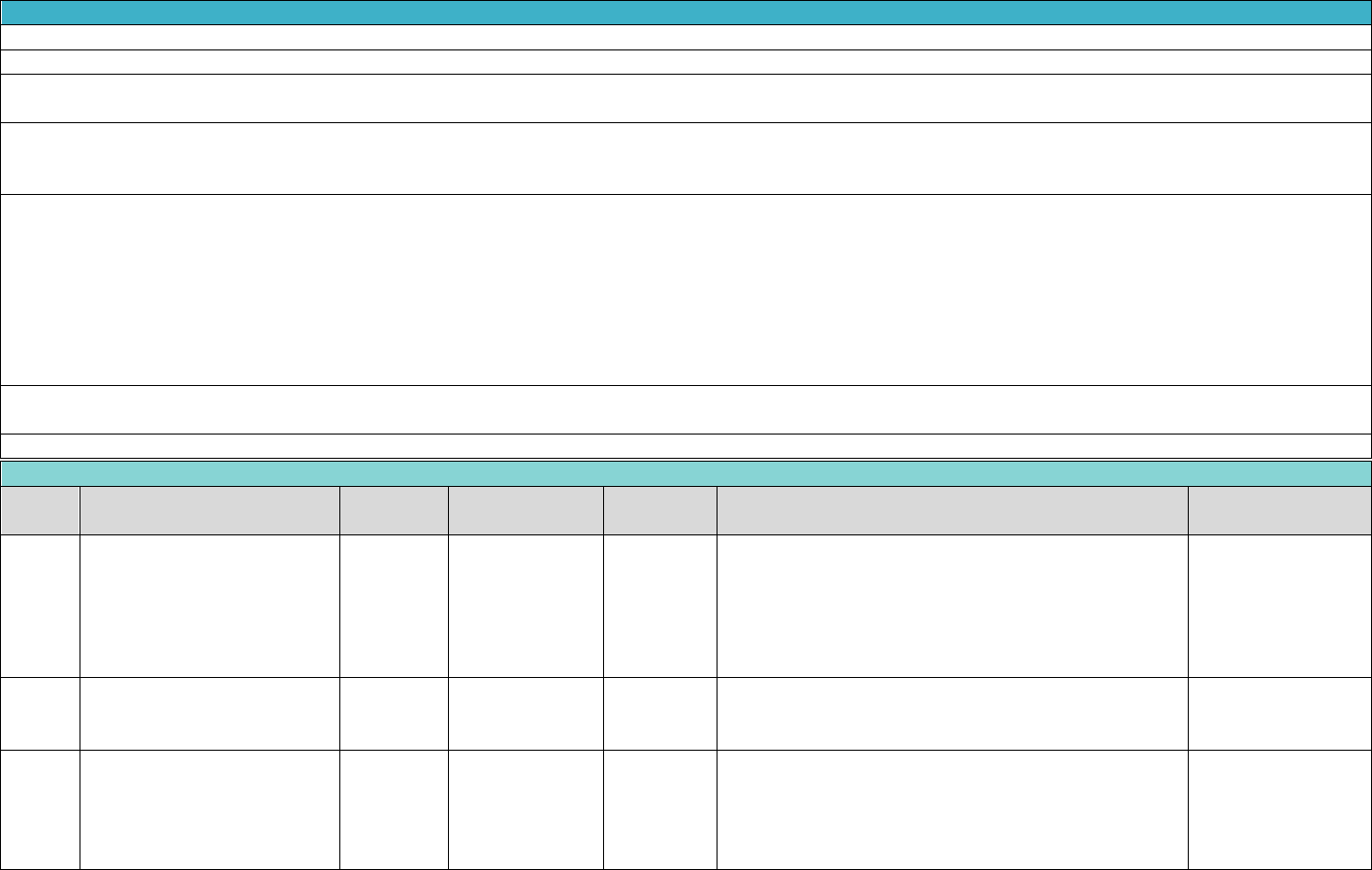
Exhibit A Benefits Covered for TX
Medicaid Child (Under 21)
This document contains proprietary and confidential information and may not be disclosed to others
without written permission. ©Copyright 2024. All rights reserved.
DentaQuest USA Insurance Company, Inc October 24, 2023, 2023
179
Exhibit A Benefits Covered for TX Medicaid Child (Under 21)
Reimbursement includes local anesthesia and routine post-operative care.
The extraction of asymptomatic impacted teeth is not a covered benefit. Symptomatic conditions would include pain and/or infection.
The incidental removal of a cyst or lesion attached to the root(s) of an extraction is considered part of the extraction or surgical fee and should not be billed as a separate
procedure.
Covered dental services that indicate “Yes” in the “Review Required” column require documentation of medical necessity and will be subject to retrospective pre-payment
review. These procedures can be rendered before determination of medical necessity but require submission of proper documentation (as indicated in the
“Documentation Required” column) with the claim form.
Under 1 TAC §353.409(b) and §353.1001(b) EPSDT regulations, DentaQuest is required to provide the services in an amount, duration, and scope that is no less than the
amount, duration, and scope for the same services furnished to Members under FFS Medicaid. Please refer to the TMPPM for the FFS Medicaid language. However, all
requests to exceed listed benefit limitations in this provider manual, must be prior authorized with documentation supporting medical necessity for an increased
benefit.
When the need for an exception is established, a narrative explaining the reason for the exception of limitations must be documented in the member's file and on the
claim submission. In order to submit a claim with an exception, the claim must have the key word “EXCEPTION” in Block 35 of the ADA claim form. If the key word
“EXCEPTION” is missing from Box 35, the claim may deny for exceeding benefit limitations.
Services Submitted with D9222 and, D9223, and D9500 for ages 1-6 will require prior authorization. Please reference ‘Criteria for General Anesthesia and Intravenous (IV)
Sedation’ in the Clinical Criteria section of this ORM.
Any reimbursement already made for an inadequate service may be recouped after the DentaQuest Consultant reviews the circumstances.
Oral and Maxillofacial Surgery
Code
Brief Description
Age
Limitation
Teeth Covered
Review
Required
Benefit Limitations
Documentation
Required
D7111
extraction, coronal remnants -
primary tooth
0-20
Teeth A - T, AS,
BS, CS, DS, ES,
FS, GS, HS, IS, JS,
KS, LS, MS, NS,
OS, PS, QS, RS,
SS, TS
No
blank
blank
D7140
extraction, erupted tooth or
exposed root (elevation
and/or forceps removal)
0-4
Teeth D - G, N -
Q, DS, ES, FS, GS,
NS, OS, PS, QS
No
blank
blank
D7140
extraction, erupted tooth or
exposed root (elevation
and/or forceps removal)
0-9
Teeth A - C, H -
M, R - T, AS, BS,
CS, HS, IS, JS, KS,
LS, MS, RS, SS,
TS
No
blank
blank
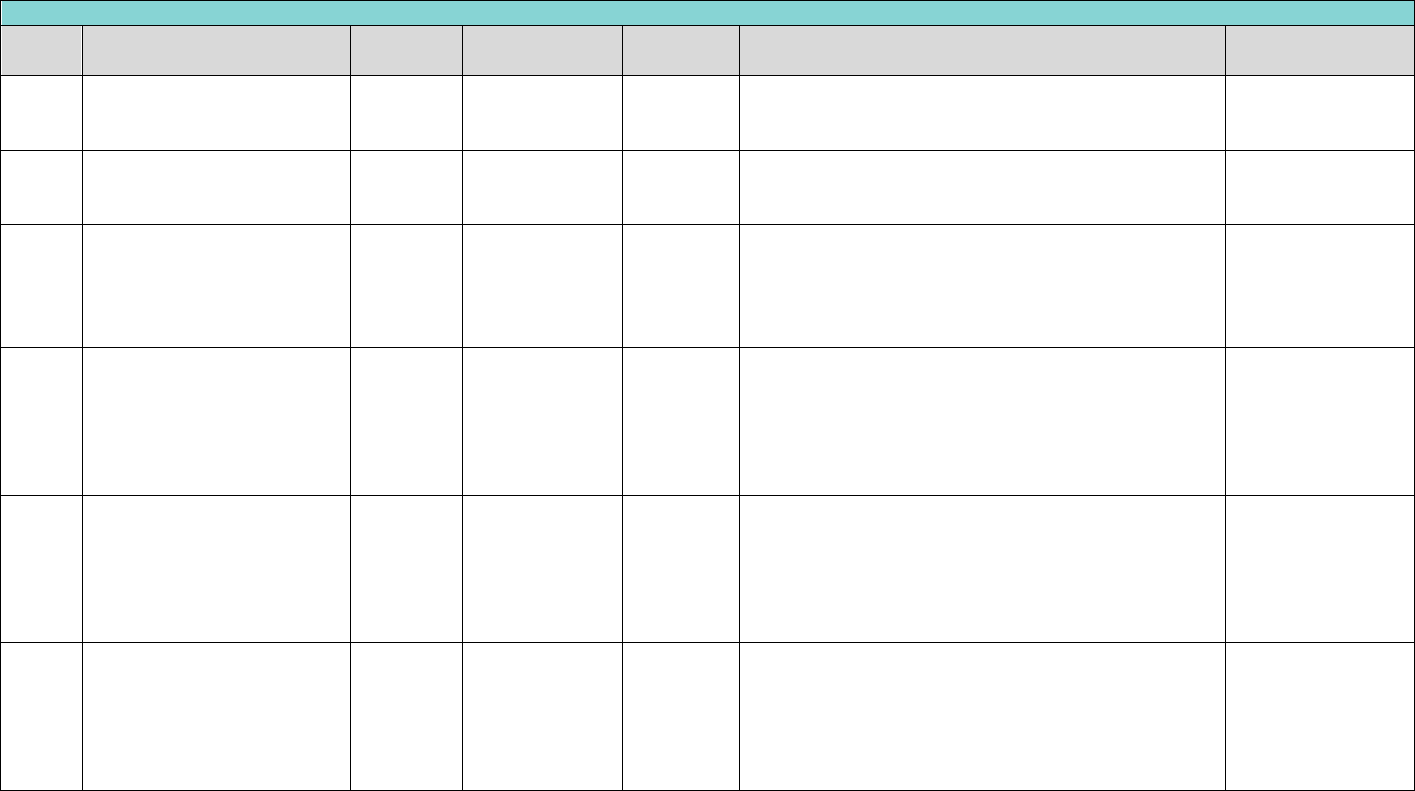
Exhibit A Benefits Covered for TX
Medicaid Child (Under 21)
This document contains proprietary and confidential information and may not be disclosed to others
without written permission. ©Copyright 2024. All rights reserved.
DentaQuest USA Insurance Company, Inc October 24, 2023, 2023
180
Oral and Maxillofacial Surgery
Code
Brief Description
Age
Limitation
Teeth Covered
Review
Required
Benefit Limitations
Documentation
Required
D7140
extraction, erupted tooth or
exposed root (elevation
and/or forceps removal)
0-20
Teeth 1 - 32, 51 -
82
No
blank
blank
D7140
extraction, erupted tooth or
exposed root (elevation
and/or forceps removal)
5 - 20
Teeth D - G, N -
Q, DS, ES, FS, GS,
NS, OS, PS, QS
Yes
blank
narr. of med.
necessity, pre-op x-
ray(s)
D7140
extraction, erupted tooth or
exposed root (elevation
and/or forceps removal)
10 - 20
Teeth A - C, H -
M, R - T, AS, BS,
CS, HS, IS, JS, KS,
LS, MS, RS, SS,
TS
Yes
blank
narr. of med.
necessity, pre-op x-
ray(s)
D7210
surgical removal of erupted
tooth requiring removal of
bone and/or sectioning of
tooth, and including elevation
of mucoperiosteal flap if
indicated
1 - 20
Teeth 1 - 32, 51 -
82, A - T, AS, BS,
CS, DS, ES, FS,
GS, HS, IS, JS, KS,
LS, MS, NS, OS,
PS, QS, RS, SS, TS
Yes
blank
narr. of med.
necessity, pre-op x-
ray(s)
D7220
removal of impacted tooth-
soft tissue
1 - 20
Teeth 1 - 32, 51 -
82, A - T, AS, BS,
CS, DS, ES, FS,
GS, HS, IS, JS, KS,
LS, MS, NS, OS,
PS, QS, RS, SS, TS
Yes
blank
narr. of med.
necessity, pre-op x-
ray(s)
D7230
removal of impacted tooth-
partially bony
1 - 20
Teeth 1 - 32, 51 -
82, A - T, AS, BS,
CS, DS, ES, FS,
GS, HS, IS, JS, KS,
LS, MS, NS, OS,
PS, QS, RS, SS, TS
Yes
blank
narr. of med.
necessity, pre-op x-
ray(s)
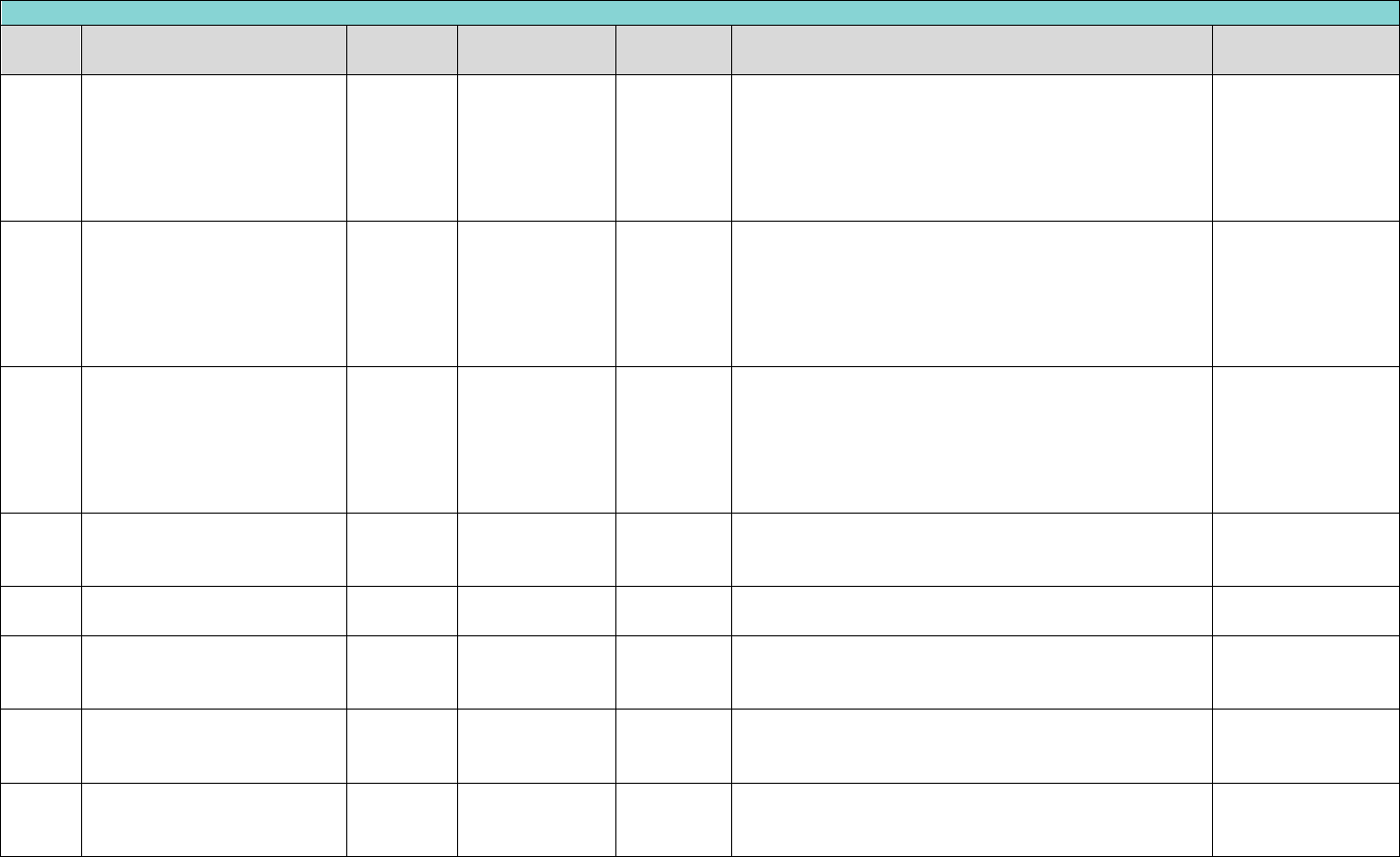
Exhibit A Benefits Covered for TX
Medicaid Child (Under 21)
This document contains proprietary and confidential information and may not be disclosed to others
without written permission. ©Copyright 2024. All rights reserved.
DentaQuest USA Insurance Company, Inc October 24, 2023, 2023
181
Oral and Maxillofacial Surgery
Code
Brief Description
Age
Limitation
Teeth Covered
Review
Required
Benefit Limitations
Documentation
Required
D7240
removal of impacted tooth-
completely bony
1 - 20
Teeth 1 - 32, 51 -
82, A - T, AS, BS,
CS, DS, ES, FS,
GS, HS, IS, JS, KS,
LS, MS, NS, OS,
PS, QS, RS, SS, TS
Yes
blank
narr. of med.
necessity, pre-op x-
ray(s)
D7241
removal of impacted tooth-
completely bony, with
unusual surgical
complications
1 - 20
Teeth 1 - 32, 51 -
82, A - T, AS, BS,
CS, DS, ES, FS,
GS, HS, IS, JS, KS,
LS, MS, NS, OS,
PS, QS, RS, SS, TS
Yes
blank
narr. of med.
necessity, pre-op x-
ray(s)
D7250
surgical removal of residual
tooth roots (cutting
procedure)
1 - 20
Teeth 1 - 32, 51 -
82, A - T, AS, BS,
CS, DS, ES, FS,
GS, HS, IS, JS, KS,
LS, MS, NS, OS,
PS, QS, RS, SS, TS
No
blank
blank
D7260
oroantral fistula closure
1 - 20
Teeth 1 - 16
Yes
blank
narr. of med.
necessity, pre-op x-
ray(s)
D7261
primary closure of a sinus
perforation
1 - 20
Teeth 1 - 16
Yes
May not be paid for the same date of service as D7260.
blank
D7270
tooth reimplantation and/or
stabilization of accidentally
evulsed or displaced tooth
1 - 20
Teeth 1 - 32
No
blank
D7272
tooth transplantation
(includes reimplantation from
one site to another)
1 - 20
Teeth 1 - 32
Yes
narr. of med.
necessity, pre-op x-
ray(s)
D7280
Surgical access of an
unerupted tooth
1 - 20
Teeth 2-15, 18-
31
Yes
D7280 will be denied unless billed with an authorized
procedure code D7283, for the same tooth, on the same
day, by the same provider.
narr. of med.
necessity, full
mouth x-ray(s)
Exhibit A Benefits Covered for TX
Medicaid Child (Under 21)
This document contains proprietary and confidential information and may not be disclosed to others
without written permission. ©Copyright 2024. All rights reserved.
DentaQuest USA Insurance Company, Inc October 24, 2023, 2023
182
Oral and Maxillofacial Surgery
Code
Brief Description
Age
Limitation
Teeth Covered
Review
Required
Benefit Limitations
Documentation
Required
D7282
mobilization of erupted or
malpositioned tooth to aid
eruption
4 - 20
Teeth 1 - 32
No
May not be paid for the same date of service as D7280.
blank
D7283
placement of device to
facilitate eruption of
impacted tooth
1 - 20
Teeth 2-15, 18-
31
Yes
blank
narr. of med.
necessity, full
mouth x-ray(s)
D7285
incisional biopsy of oral
tissue-hard (bone, tooth)
1 - 20
No
blank
blank
D7286
incisional biopsy of oral
tissue-soft
1 - 20
No
blank
blank
D7290
surgical repositioning of teeth
1 - 20
Teeth 1 - 32
No
blank
blank
D7291
transseptal fiberotomy, by
report
4 - 20
Teeth 1 - 32
No
blank
blank
D7310
alveoloplasty in conjunction
with extractions - four or
more teeth or tooth spaces,
per quadrant
1 - 20
Per Quadrant
(10, 20, 30, 40,
LL, LR, UL, UR)
Yes
Limit one service per lifetime, per patient, per quadrant.
narr. of med.
necessity, pre-op x-
ray(s)
D7320
alveoloplasty not in
conjunction with extractions -
four or more teeth or tooth
spaces, per quadrant
1 - 20
Per Quadrant
(10, 20, 30, 40,
LL, LR, UL, UR)
Yes
Limit one service per lifetime, per patient, per quadrant.
narr. of med.
necessity, pre-op x-
ray(s)
D7340
vestibuloplasty - ridge
extension (secondary
epithelialization)
1 - 20
Per Quadrant
(10, 20, 30, 40,
LL, LR, UL, UR)
Yes
Limit one service per lifetime, per patient, per quadrant.
narr. of med.
necessity, pre-op x-
ray(s)
D7350
vestibuloplasty - ridge
extension
1 - 20
Per Arch (01, 02,
LA, UA)
Yes
Limit one service per lifetime, per patient, per quadrant.
narr. of med.
necessity, pre-op x-
ray(s)
D7410
radical excision - lesion
diameter up to 1.25cm
1 - 20
blank
No
blank
blank
D7411
excision of benign lesion
greater than 1.25 cm
1 - 20
blank
No
blank
blank
D7413
excision of malignant lesion
up to 1.25 cm
1 - 20
blank
No
blank
blank
Exhibit A Benefits Covered for TX
Medicaid Child (Under 21)
This document contains proprietary and confidential information and may not be disclosed to others
without written permission. ©Copyright 2024. All rights reserved.
DentaQuest USA Insurance Company, Inc October 24, 2023, 2023
183
Oral and Maxillofacial Surgery
Code
Brief Description
Age
Limitation
Teeth Covered
Review
Required
Benefit Limitations
Documentation
Required
D7414
excision of malignant lesion
greater than 1.25 cm
1 - 20
blank
No
blank
blank
D7440
excision of malignant tumor -
lesion diameter up to 1.25cm
1 - 20
blank
No
The incidental removal of cysts/lesions attached to the
root(s) of an extracted tooth is considered part of the
extraction or surgical fee.
blank
D7441
excision of malignant tumor –
lesion diameter greater than
1.25cm
1 - 20
blank
No
The incidental removal of cysts/lesions attached to the
root(s) of an extracted tooth is considered part of the
extraction or surgical fee.
blank
D7450
removal of odontogenic cyst
or tumor - lesion diameter up
to 1.25cm
1 - 20
blank
No
The incidental removal of cysts/lesions attached to the
root(s) of an extracted tooth is considered part of the
extraction or surgical fee
blank
D7451
removal of odontogenic cyst
or tumor - lesion greater than
1.25cm
1 - 20
blank
No
The incidental removal of cysts/lesions attached to the
root(s) of an extracted tooth is considered part of the
extraction or surgical fee
blank
D7460
removal of nonodontogenic
cyst or tumor - lesion
diameter up to 1.25cm
0-20
blank
No
The incidental removal of cysts/lesions attached to the
root(s) of an extracted tooth is considered part of the
extraction or surgical fee
blank
D7461
removal of nonodontogenic
cyst or tumor - lesion greater
than 1.25cm
0-20
blank
No
The incidental removal of cysts/lesions attached to the
root(s) of an extracted tooth is considered part of the
extraction or surgical fee
blank
D7465
destruction of lesion(s) by
physical or chemical method,
by report
1 - 20
blank
No
The incidental removal of cysts/lesions attached to the
root(s) of an extracted tooth is considered part of the
extraction or surgical fee
blank
D7472
removal of torus palatinus
1 - 20
blank
Yes
blank
narrative of medical
necessity
D7510
incision and drainage of
abscess - intraoral soft tissue
1 - 20
Teeth 1 - 32, 51 -
82, A - T, AS, BS,
CS, DS, ES, FS,
GS, HS, IS, JS, KS,
LS, MS, NS, OS,
PS, QS, RS, SS, TS
No
Not allowed on same day as extraction.
blank
D7520
incision and drainage of
abscess - extraoral soft tissue
1 - 20
blank
No
blank
blank
Exhibit A Benefits Covered for TX
Medicaid Child (Under 21)
This document contains proprietary and confidential information and may not be disclosed to others
without written permission. ©Copyright 2024. All rights reserved.
DentaQuest USA Insurance Company, Inc October 24, 2023, 2023
184
Oral and Maxillofacial Surgery
Code
Brief Description
Age
Limitation
Teeth Covered
Review
Required
Benefit Limitations
Documentation
Required
D7530
Removal of foreign body from
mucosa, skin, or
subcutaneous alveolar tissue
1 - 20
blank
No
blank
blank
D7540
removal of reaction-
producing foreign bodies,
musculoskeletal system
1 - 20
blank
No
blank
blank
D7550
Partial
ostectomy/sequestrectomy
for removal of non-vital bone
1 - 20
Per Quadrant
(10, 20, 30, 40,
LL, LR, UL, UR)
No
blank
blank
D7560
maxillary sinusotomy for
removal of tooth fragment or
foreign body
1 - 20
blank
No
blank
blank
D7670
alveolus stabilization of teeth,
closed reduction splinting
1 - 20
blank
No
blank
blank
D7820
closed reduction dislocation
1 - 20
blank
No
blank
blank
D7880
occlusal orthotic device, by
report
1 - 20
blank
Yes
Limit one service every five years, per patient.
narrative of medical
necessity
D7899
unspecified TMD therapy, by
report
1 - 20
blank
Yes
narrative of medical
necessity
D7910
suture small wounds up to 5
cm
1 - 20
blank
No
D7910, D7911, and D7912 will deny if billed on the same
date of service with any other D7000 series code.
D7911
complicated suture-up to 5
cm
1 - 20
blank
Yes
D7911, D7910, and D7912 will deny if billed on the same
date of service with any other D7000 series code.
narrative of medical
necessity
D7912
complex suture - greater than
5cm
1 - 20
blank
Yes
D7912, D7910, and D7911 will deny if billed on the same
date of service with any other D7000 series code.
narr. of med.
necessity, pre-op x-
ray(s)
D7955
repair of maxillofacial soft
and/or hard tissue defect
1 - 20
blank
Yes
blank
narrative of medical
necessity
D7961
buccal / labial frenectomy
(frenulectomy) - separate
procedure not incidental to
another procedure
12 - 20
blank
Yes
blank
Pre-Operative
Radiographs,
narrative/
treatment plan,
photos optional
Exhibit A Benefits Covered for TX
Medicaid Child (Under 21)
This document contains proprietary and confidential information and may not be disclosed to others
without written permission. ©Copyright 2024. All rights reserved.
DentaQuest USA Insurance Company, Inc October 24, 2023, 2023
185
Oral and Maxillofacial Surgery
Code
Brief Description
Age
Limitation
Teeth Covered
Review
Required
Benefit Limitations
Documentation
Required
D7962
lingual frenectomy
(frenulectomy) – separate
procedure not incidental to
another procedure
1 - 20
blank
Yes
blank
Pre-Op and Post-Op
X-rays, narrative/
treatment plan,
photos optional
D7970
excision of hyperplastic tissue
– per arch
1 - 20
Per Arch (01, 02,
LA, UA)
Yes
Limit one service per lifetime, per patient, per arch.
narr. of med.
necessity, pre-op x-
ray(s)
D7971
excision of pericoronal gingiva
1 - 20
Teeth 1 - 32
No
Limit one service per lifetime, per patient, per arch.
D7972
surgical reduction of fibrous
tuberosity
13 - 20
Teeth 1, 16, 17,
32
No
Limit of two services per lifetime, per patient. Not
allowed with extraction of 1, 16, 17, or 32 on the same
date of service. May not be paid in addition to D7971 for
the same date of service.
narrative of medical
necessity
D7980
surgical sialolithotomy
1 - 20
blank
No
blank
blank
D7983
closure of salivary fistula
1 - 20
blank
No
blank
blank
D7997
appliance removal (not by
dentist who placed
appliance), includes removal
of archbar
1 - 20
blank
Yes
Limit one service per lifetime, per patient. Not allowed
by provider or office that placed the appliance.
narrative of medical
necessity
D7999
unspecified oral surgery
procedure, by report
1 - 20
blank
Yes
blank
narr. of med.
necessity, pre-op x-
ray(s)
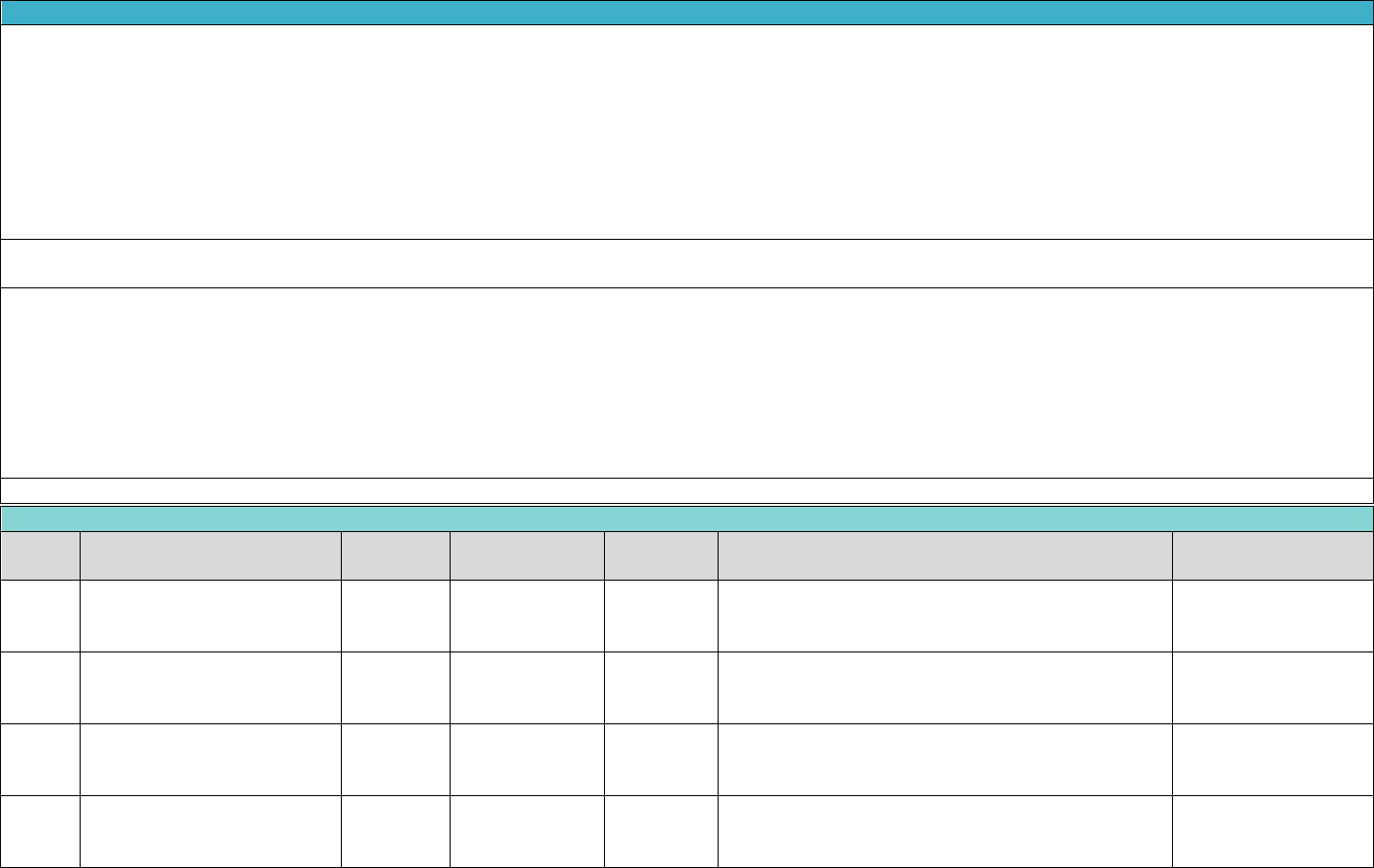
Exhibit A Benefits Covered for TX
Medicaid Child (Under 21)
This document contains proprietary and confidential information and may not be disclosed to others
without written permission. ©Copyright 2024. All rights reserved.
DentaQuest USA Insurance Company, Inc October 24, 2023, 2023
186
Exhibit A Benefits Covered for TX Medicaid Child (Under 21)
Please see Appendix A-7 for the Texas Orthodontia Review Policy for additional information on definitions, case levels, criteria and requirements for submission.
Comprehensive orthodontic services include all of the following:
• Diagnostic workups
• Banding
• Initial brackets
• Replacement brackets
• Monthly visits
• Initial retainers
• Special orthodontic treatment appliance(s)”
Services Submitted with D9222 and, D9223, and D9500 for ages 1-6 will require prior authorization. Please reference ‘Criteria for General Anesthesia and Intravenous (IV)
Sedation’ in the Clinical Criteria section of this ORM.
Under 1 TAC §353.409(b) and §353.1001(b) EPSDT regulations, DentaQuest is required to provide the services in an amount, duration, and scope that is no less than the
amount, duration, and scope for the same services furnished to Members under FFS Medicaid. Please refer to the TMPPM for the FFS Medicaid language. However, all
requests to exceed listed benefit limitations in this provider manual, must be prior authorized with documentation supporting medical necessity for an increased
benefit.
When the need for an exception is established, a narrative explaining the reason for the exception of limitations must be documented in the member's file and on the
claim submission. In order to submit a claim with an exception, the claim must have the key word “EXCEPTION” in Block 35 of the ADA claim form. If the key word
“EXCEPTION” is missing from Box 35, the claim may deny for exceeding benefit limitations.
Any reimbursement already made for an inadequate service may be recouped after the DentaQuest Consultant reviews the circumstances.
Orthodontics
Code
Brief Description
Age
Limitation
Teeth Covered
Review
Required
Benefit Limitations
Documentation
Required
D8010
limited orthodontic treatment
of the primary dentition
0-20
blank
Yes
Limit one service of (D8010, D8020) per lifetime, per
patient. No more than 10 adjustments (D8670)
allowed. Pre-authorization is required.
models, pano,
cephalo, photos
D8020
limited orthodontic treatment
of the transitional dentition
0-20
blank
Yes
Limit one service of (D8010, D8020) per lifetime, per
patient. No more than 10 adjustments (D8670)
allowed. Pre-authorization is required.
models, pano,
cephalo, photos
D8070
comprehensive orthodontic
treatment of the transitional
dentition
10-12
blank
Yes
Limit one service of (D8070, D8080, D8090) per
lifetime, per patient. No more than 22 adjustments
(D8670) allowed. Pre-authorization is required.
models, pano,
cephalo, photos
D8080
comprehensive orthodontic
treatment of the adolescent
dentition
12-20
blank
Yes
Limit one service of (D8070, D8080, D8090) per
lifetime, per patient. No more than 22 adjustments
(D8670) allowed. Pre-authorization is required.
models, pano,
cephalo, photos
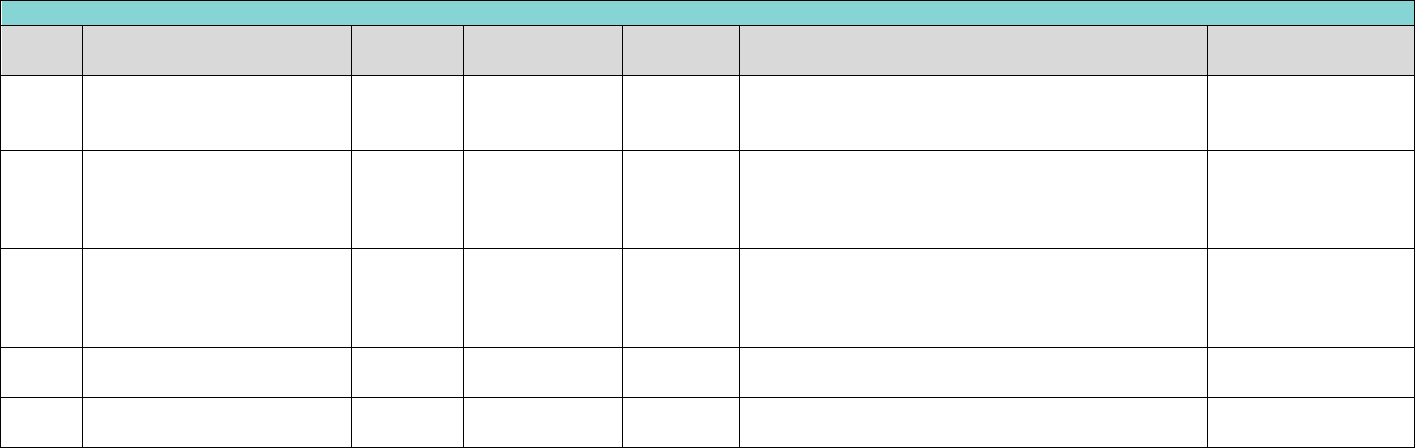
Exhibit A Benefits Covered for TX
Medicaid Child (Under 21)
This document contains proprietary and confidential information and may not be disclosed to others
without written permission. ©Copyright 2024. All rights reserved.
DentaQuest USA Insurance Company, Inc October 24, 2023, 2023
187
Orthodontics
Code
Brief Description
Age
Limitation
Teeth Covered
Review
Required
Benefit Limitations
Documentation
Required
D8090
comprehensive orthodontic
treatment of the adult
dentition
12-20
blank
Yes
Limit one service of (D8070, D8080, D8090) per
lifetime, per patient. No more than 22 adjustments
(D8670) allowed. Pre-authorization is required.
models, pano,
cephalo, photos
D8210
removable appliance therapy
(includes appliances for
thumb sucking and tongue
thrusting)
0-12
blank
Yes
Limit two services of (D8210, D8220) per lifetime, per
patient. One per arch. Pre-authorization is required.
narrative of medical
necessity
D8220
fixed appliance therapy
(includes appliances for
thumb sucking and tongue
thrusting)
0-12
blank
Yes
Limit two services of (D8210, D8220) per lifetime, per
patient. One per arch. Pre-authorization is required.
narrative of medical
necessity
D8670
periodic orthodontic
treatment visit
0-20
blank
Yes
Limit one service per 21 days, per patient. Pre-
authorization is required.
models, pano,
cephalo, photos
D8680
orthodontic retention
(removal of appliances)
0-20
blank
Yes
Limit one service per lifetime, per patient. Pre-
authorization is required.
models, pano,
cephalo, photos

Exhibit A Benefits Covered for TX
Medicaid Child (Under 21)
This document contains proprietary and confidential information and may not be disclosed to others
without written permission. ©Copyright 2024. All rights reserved.
DentaQuest USA Insurance Company, Inc October 24, 2023, 2023
188
Exhibit A Benefits Covered for TX Medicaid Child (Under 21)
Local anesthesia is considered part of the treatment procedure, and no additional payment will be made for it. Adjunctive general services include: IV sedation and
emergency services provided for relief of dental pain.
Covered dental services that indicate “Yes” in the “Review Required” column require documentation of medical necessity and will be subject to retrospective pre-payment
review. These procedures can be rendered before determination of medical necessity but require submission of proper documentation (as indicated in the
“Documentation Required” column) with the claim form.
Under 1 TAC §353.409(b) and §353.1001(b) EPSDT regulations, DentaQuest is required to provide the services in an amount, duration, and scope that is no less than the
amount, duration, and scope for the same services furnished to Members under FFS Medicaid. Please refer to the TMPPM for the FFS Medicaid language. However, all
requests to exceed listed benefit limitations in this provider manual, must be prior authorized with documentation supporting medical necessity for an increased
benefit.
When the need for an exception is established, a narrative explaining the reason for the exception of limitations must be documented in the member's file and on the
claim submission. In order to submit a claim with an exception, the claim must have the key word “EXCEPTION” in Block 35 of the ADA claim form. If the key word
“EXCEPTION” is missing from Box 35, the claim may deny for exceeding benefit limitations.
Services Submitted with D9222 and, D9223, and D9500 for ages 1-6 will require prior authorization. Please reference ‘Criteria for General Anesthesia and Intravenous (IV)
Sedation’ in the Clinical Criteria section of this ORM.
For D9920: Provider must indicate the client’s medical diagnosis of intellectual disability described as mild, moderate, severe, profound, or unspecified by using the most
appropriate diagnosis code in the diagnosis code field of the claim form, or the provider must indicate that the client is ICF-IID eligible in the Remarks field of the claim
form. Documentation supporting the medical necessity and appropriateness of dental behavior management must be retained in the client’s chart and available to state
agencies upon request, and is subject to retrospective review. Documentation of medical necessity must include: A current physician statement detailing the client’s the
intellectual disability. The statement must be signed and dated within one year prior to the dental behavior management. A description of the service performed
(including the specific problem and the behavior management technique applied). Personnel and supplies required to provide the behavioral management. The duration
of the behavior management (including session start and end times). Dental behavior management is not reimbursed with an evaluation, prophylactic treatment, or
radiographic procedure.
Any reimbursement already made for an inadequate service may be recouped after the DentaQuest Consultant reviews the circumstances.
Adjunctive General Services
Code
Brief Description
Age
Limitation
Teeth Covered
Review
Required
Benefit Limitations
Documentation
Required
D9110
palliative (emergency)
treatment of dental pain -
minor procedure
0-20
blank
No
Emergency service only. The type of treatment
rendered must be indicated. It must be a service other
than a prescription or topical medication. The reason
for emergency and a narrative of the procedure
actually performed must be documented and the
appropriate block for emergency must be checked.
Not allowed for prescriptions or medication.
Narrative of medical
necessity
D9120
fixed partial denture
sectioning
1 - 20
Teeth 1 - 32
No
blank
blank
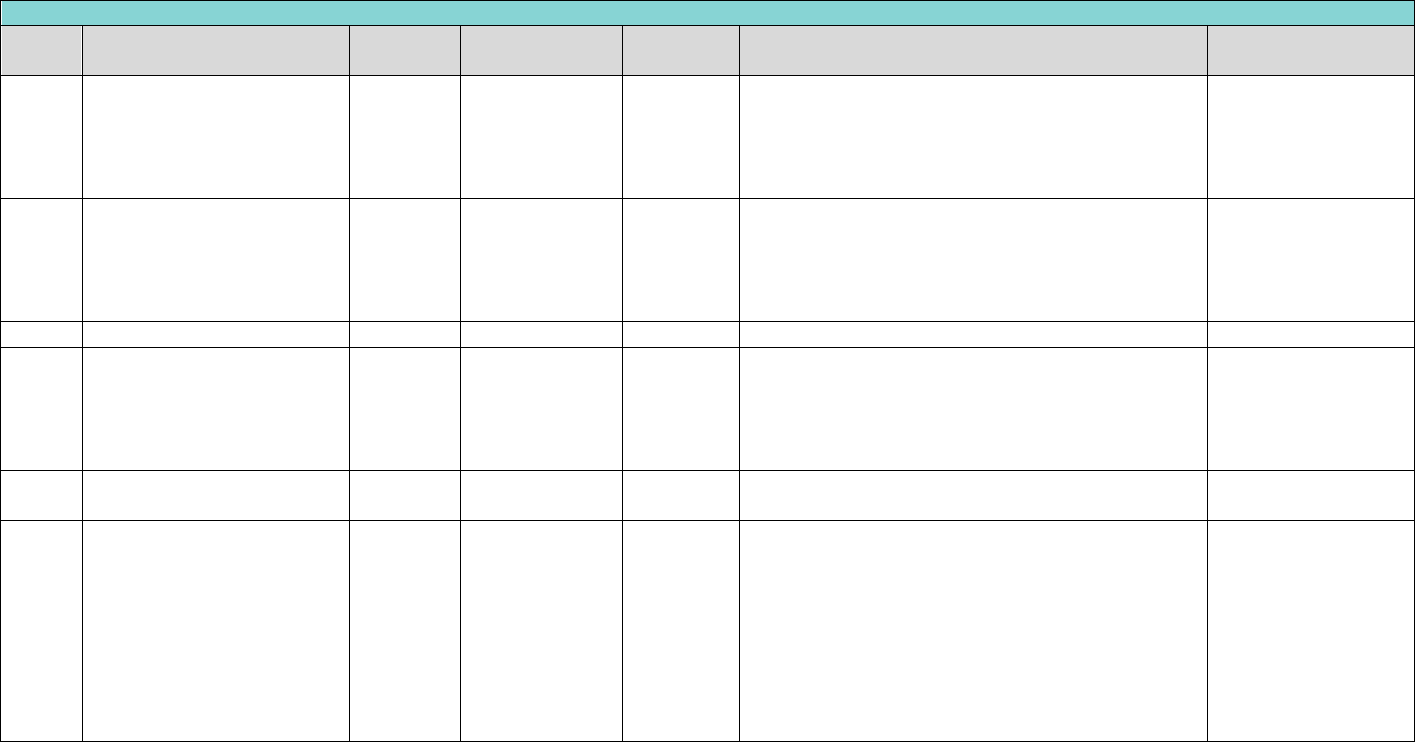
Exhibit A Benefits Covered for TX
Medicaid Child (Under 21)
This document contains proprietary and confidential information and may not be disclosed to others
without written permission. ©Copyright 2024. All rights reserved.
DentaQuest USA Insurance Company, Inc October 24, 2023, 2023
189
Adjunctive General Services
Code
Brief Description
Age
Limitation
Teeth Covered
Review
Required
Benefit Limitations
Documentation
Required
D9210
local anesthesia not in
conjuction with operative or
surgical procedures
1 - 20
blank
Yes
Code D9210 is not to be billed in conjunction with
operative or surgical procedures, the administration of
local anesthetic is inclusive in operative and surgical
procedures. Not allowed with D9248. Pre-payment
review required.
narrative of medical
necessity
D9211
regional block anesthesia
1 - 12
blank
No
Providers must meet TSBDE requirement for Sedation
/Anesthesia of Pediatric Patients (TX Anesthesia Level
3 or 4 – Pediatric, TX Anesthesia Level 3 or 4 – High
Risk) to perform this procedure. Not allowed with
D9248.
blank
D9211
regional block anesthesia
13 - 20
blank
No
Not allowed with D9248.
blank
D9212
trigeminal division block
anesthesia
1 - 12
blank
No
Providers must meet TSBDE requirement for Sedation
/Anesthesia of Pediatric Patients (TX Anesthesia Level
3 or 4 – Pediatric, TX Anesthesia Level 3 or 4 – High
Risk) to perform this procedure. Not allowed with
D9248.
blank
D9212
trigeminal division block
anesthesia
13 - 20
blank
No
Not allowed with D9248.
blank
D9222
deep sedation/general
anesthesia –
first 15 minutes
1-6
blank
Yes
Providers must meet TSBDE requirement for Sedation
/Anesthesia of Pediatric Patients (TX Anesthesia Level
4 – Pediatric, TX Anesthesia Level 4 – High Risk) to
perform this procedure. Limit one service per day, per
patient. Once per six calendar months, any provider. It
is to be billed for one 15-minute increment. Not
allowed on same day as D9230 or D9248. D9222 and
D9223 cannot be billed on the same day as D9239 and
D9243
narr. of med.
necessity, pre-op x-
ray(s)
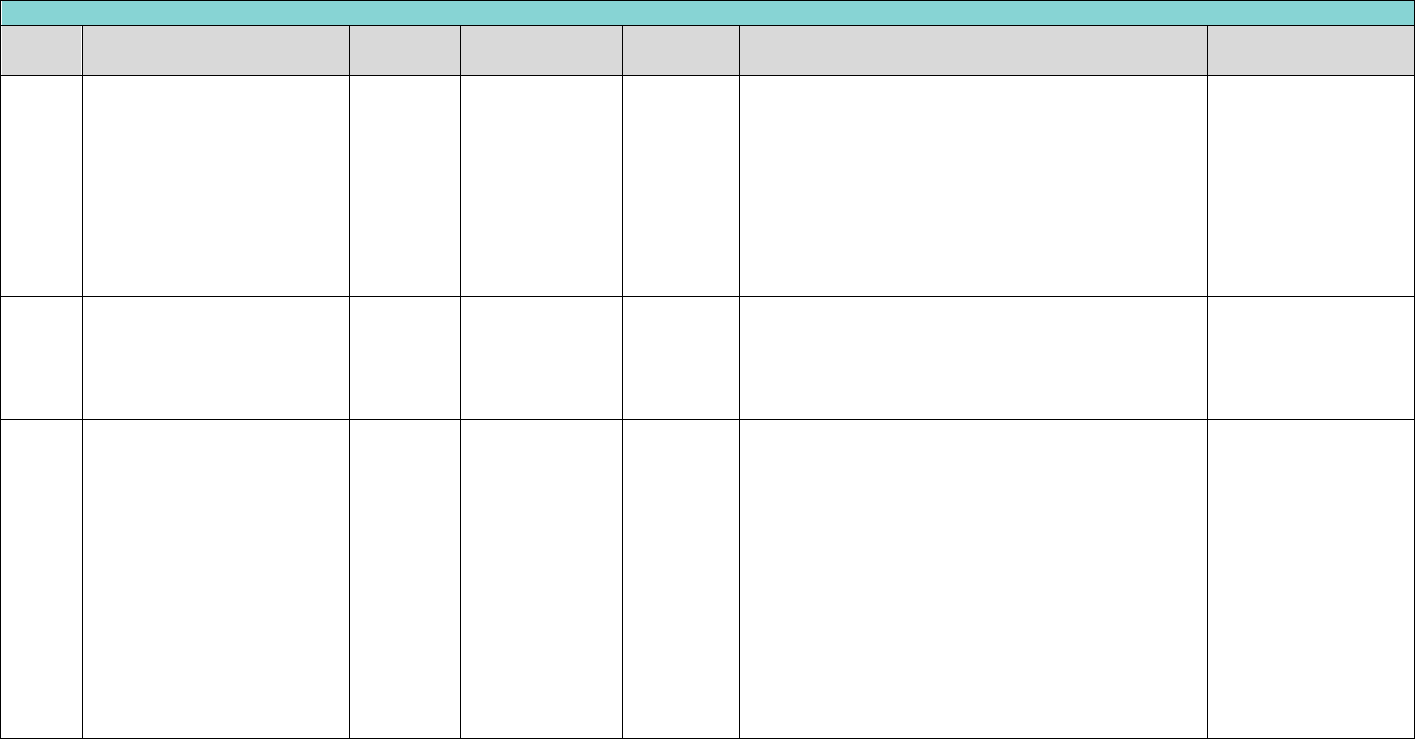
Exhibit A Benefits Covered for TX
Medicaid Child (Under 21)
This document contains proprietary and confidential information and may not be disclosed to others
without written permission. ©Copyright 2024. All rights reserved.
DentaQuest USA Insurance Company, Inc October 24, 2023, 2023
190
Adjunctive General Services
Code
Brief Description
Age
Limitation
Teeth Covered
Review
Required
Benefit Limitations
Documentation
Required
D9222
deep sedation/general
anesthesia – first 15 minutes
7-12
blank
Yes
Providers must meet TSBDE requirement for Sedation
/Anesthesia of Pediatric Patients (TX Anesthesia Level
4 – Pediatric, TX Anesthesia Level 4 – High Risk) to
perform this procedure. Limit one service per day, per
patient. Once per six calendar months, any provider. It
is to be billed for one 15-minute increment. Not
allowed on same day as D9230 or D9248. D9222 and
D9223 cannot be billed on the same day as D9239 and
D9243
narrative of medical
necessity
D9222
deep sedation/general
anesthesia – first 15 minutes
13 - 20
blank
Yes
Limit one service per day, per patient. Once per six
calendar months, any provider. It is to be billed for
one 15-minute increment. Not allowed on same day as
D9230 or D9248. D9222 and D9223 cannot be billed
on the same day as D9239 and D9243
narrative of medical
necessity
D9223
deep sedation/general
anesthesia -
each subsequent 15-minute
increment
1-6
blank
Yes
Providers must meet TSBDE requirement for Sedation
/Anesthesia of Pediatric Patients (TX Anesthesia Level
4 – Pediatric, TX Anesthesia Level 4 – High Risk) to
perform this procedure. Limit eleven services per day,
per patient. Once per six calendar months, any
provider. It is to be billed in 15-minute increments
totaling three hours per day, when billed with
(D9222), for each 15-minute additional increment.
D9223 must be billed by the same provider, same
claim in conjunction with primary procedure code
D9222. Not allowed on same day as D9230 or D9248.
D9222 and D9223 cannot be billed on the same day as
D9239 and D9243.
narr. of med.
necessity, pre-op x-
ray(s)
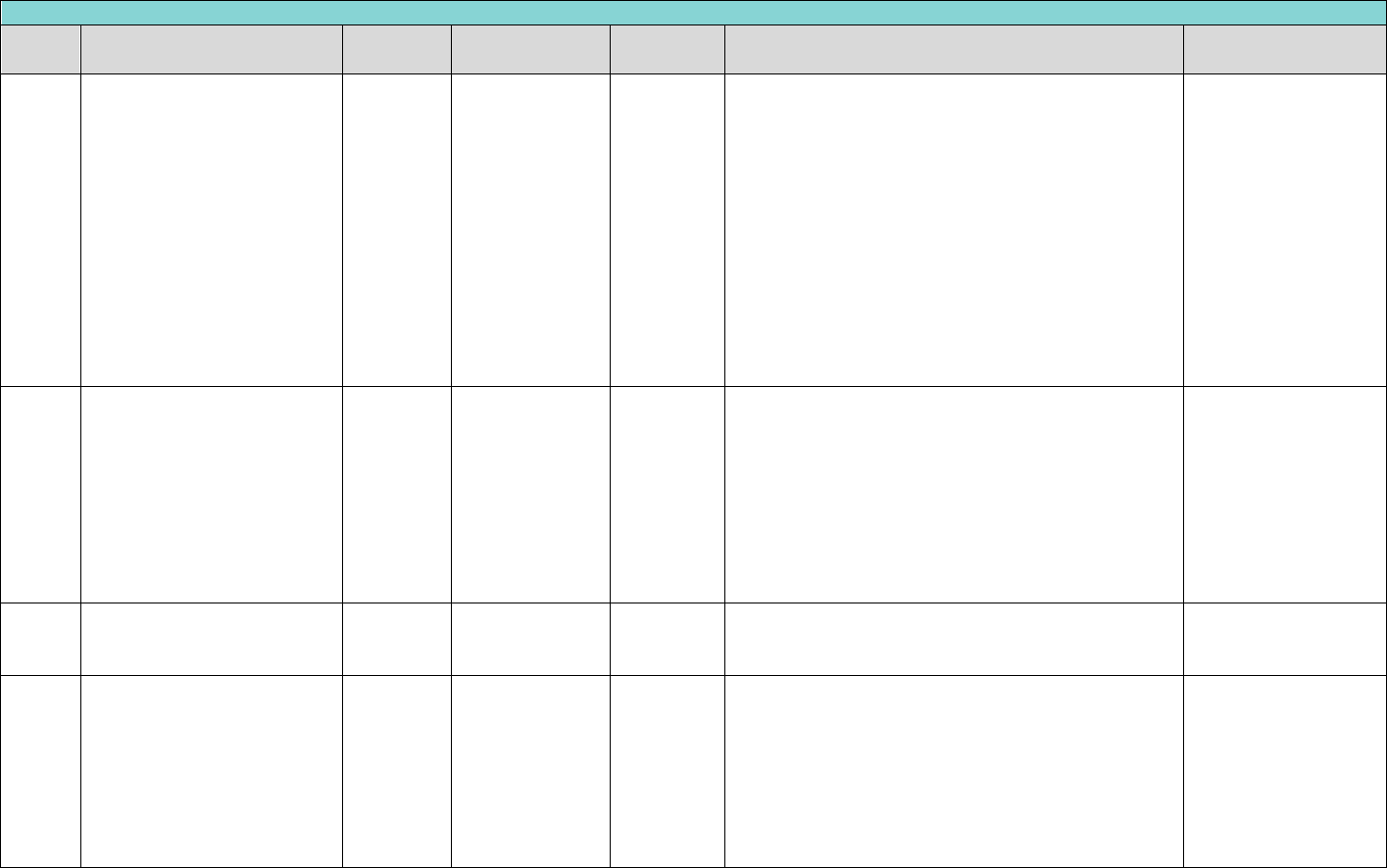
Exhibit A Benefits Covered for TX
Medicaid Child (Under 21)
This document contains proprietary and confidential information and may not be disclosed to others
without written permission. ©Copyright 2024. All rights reserved.
DentaQuest USA Insurance Company, Inc October 24, 2023, 2023
191
Adjunctive General Services
Code
Brief Description
Age
Limitation
Teeth Covered
Review
Required
Benefit Limitations
Documentation
Required
D9223
deep sedation/general
anesthesia - each subsequent
15- minute increment
7 - 12
blank
Yes
Providers must meet TSBDE requirement for Sedation
/Anesthesia of Pediatric Patients (TX Anesthesia Level
4 – Pediatric, TX Anesthesia Level 4 – High Risk) to
perform this procedure. Limit eleven services per day,
per patient. Once per six calendar months, any
provider. It is to be billed in 15-minute increments
totaling three hours per day, when billed with
(D9222), for each 15-minute additional increment.
D9223 must be billed by the same provider, same
claim in conjunction with primary procedure code
D9222. Not allowed on same day as D9230 or D9248.
D9222 and D9223 cannot be billed on the same day as
D9239 and D9243.
narrative of medical
necessity
D9223
deep sedation/general
anesthesia - each subsequent
15 -minute increment
13 - 20
blank
Yes
Limit eleven services per day, per patient. Once per six
calendar months, any provider. It is to be billed in 15-
minute increments totaling three hours per day, when
billed with (D9222), for each 15-minute additional
increment. D9223 must be billed by the same
provider, same claim in conjunction with primary
procedure code D9222. Not allowed on same day as
D9230 or D9248. D9222 and D9223 cannot be billed
on the same day as D9239 and D9243.
narrative of medical
necessity
D9230
inhalation of nitrous
oxide/analgesia, anxiolysis
1 - 20
blank
No
Limit one service per day, per patient. Not allowed
with D9222, D9223, D9239, D9243 and D9248 on
same date of service.
blank
D9239
intravenous moderate
(conscious)
sedation/analgesia- first 15
minutes
1 - 12
blank
Yes
Providers must meet TSBDE requirement for Sedation
/Anesthesia of Pediatric Patients (TX Anesthesia Level
3 or 4 – Pediatric, TX Anesthesia Level 3 or 4 – High
Risk) to perform this procedure. Limit one service per
day, per patient ages 1 and above. It is to be billed for
one 15-minute increment. Not allowed on same day as
D9230 or D9248. D9239 and D9243 cannot be billed
on the same day as D9222 and D9223.
narrative of medical
necessity
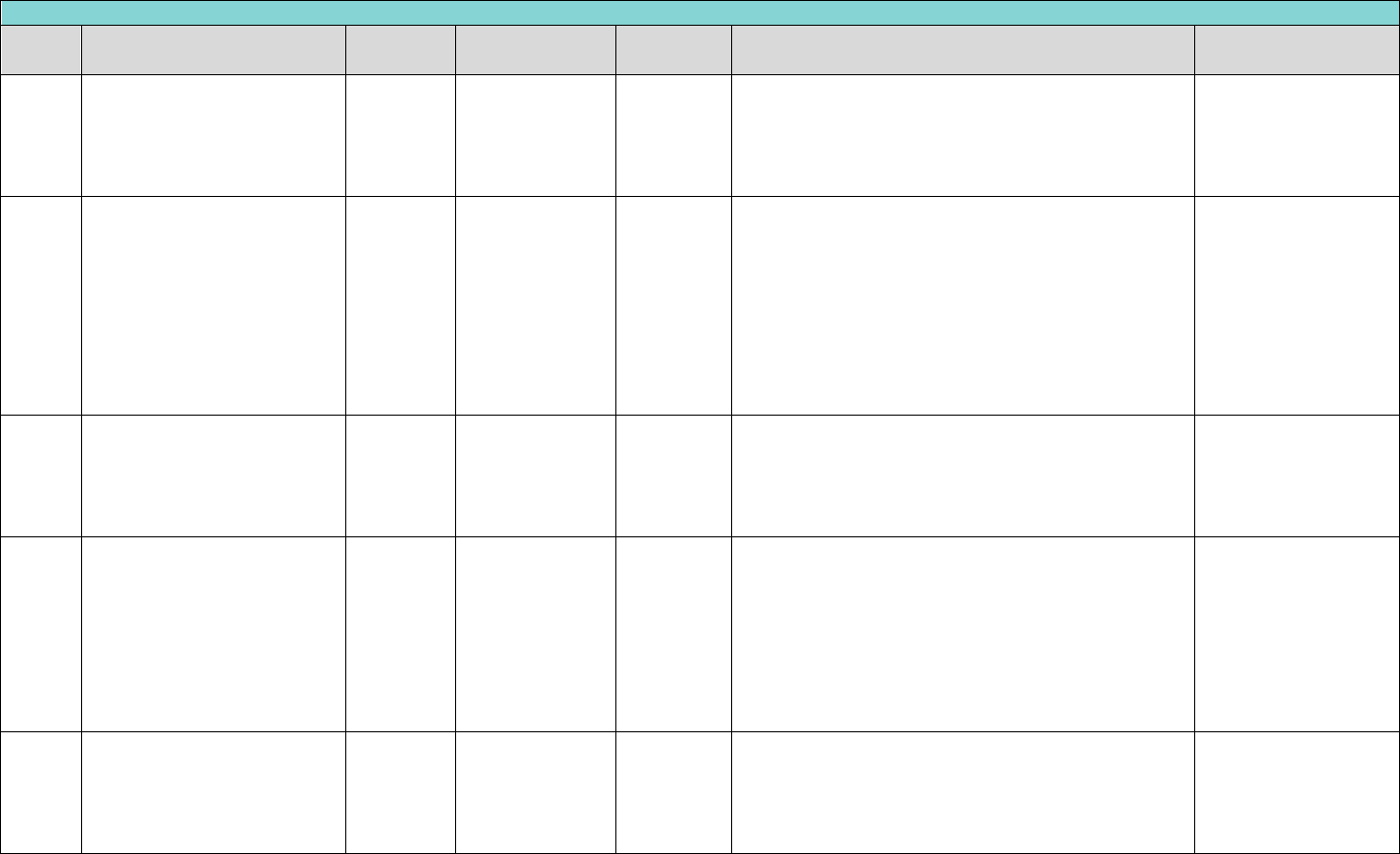
Exhibit A Benefits Covered for TX
Medicaid Child (Under 21)
This document contains proprietary and confidential information and may not be disclosed to others
without written permission. ©Copyright 2024. All rights reserved.
DentaQuest USA Insurance Company, Inc October 24, 2023, 2023
192
Adjunctive General Services
Code
Brief Description
Age
Limitation
Teeth Covered
Review
Required
Benefit Limitations
Documentation
Required
D9239
intravenous moderate
(conscious)
sedation/analgesia- first 15
minutes
13 - 20
blank
Yes
Limit one service per day, per patient ages 1 and
above. It is to be billed for one 15-minute increment.
Not allowed on same day as D9230 or D9248. D9239
and D9243 cannot be billed on the same day as D9222
and D9223.
narrative of medical
necessity
D9243
intravenous moderate
(conscious)
sedation/analgesia – each
subsequent 15- minute
increment
1 - 12
blank
Yes
Providers must meet TSBDE requirement for Sedation
/Anesthesia of Pediatric Patients (TX Anesthesia Level
3 or 4 – Pediatric, TX Anesthesia Level 3 or 4 – High
Risk) to perform this procedure. Limit five services per
day, per patient. It is to be billed in 15-minute
increments totaling one and one-half hours per day.
Not allowed on same day as D9230 or D9248. D9239
and D9243 cannot be billed on the same day as D9222
and D9223.
narrative of medical
necessity
D9243
intravenous moderate
(conscious)
sedation/analgesia – each
subsequent 15- minute
increment
13 - 20
blank
Yes
Limit five services per day, per patient. It is to be billed
in 15-minute increments totaling one and one-half
hours per day. Not allowed on same day as D9230 or
D9248. D9239 and D9243 cannot be billed on the
same day as D9222 and D9223.
narrative of medical
necessity
D9248
non-intravenous moderate
(conscious) sedation
1 - 12
blank
Yes
Providers must meet TSBDE requirement for Sedation
/Anesthesia of Pediatric Patients (TX Anesthesia Level
2, 3, or 4 – Pediatric, TX Anesthesia Level 2, 3, or 4 –
High Risk) to perform this procedure. Limit two
services per year, per patient. Denied when submitted
for the same date of service as procedure code D9420,
any provider. Not allowed with D9222, D9223 D9230,
D9239 and D9243. Pre authorization is required.
narr. of med.
necessity, pre-op x-
ray(s)
D9248
non-intravenous moderate
(conscious) sedation
13 - 20
blank
Yes
Limit two services per year, per patient. Denied when
submitted for the same date of service as procedure
code D9420, any provider. Not allowed with D9222,
D9223 D9230, D9239 and D9243. Pre-authorization is
required.
narr. of med.
necessity, pre-op x-
ray(s)
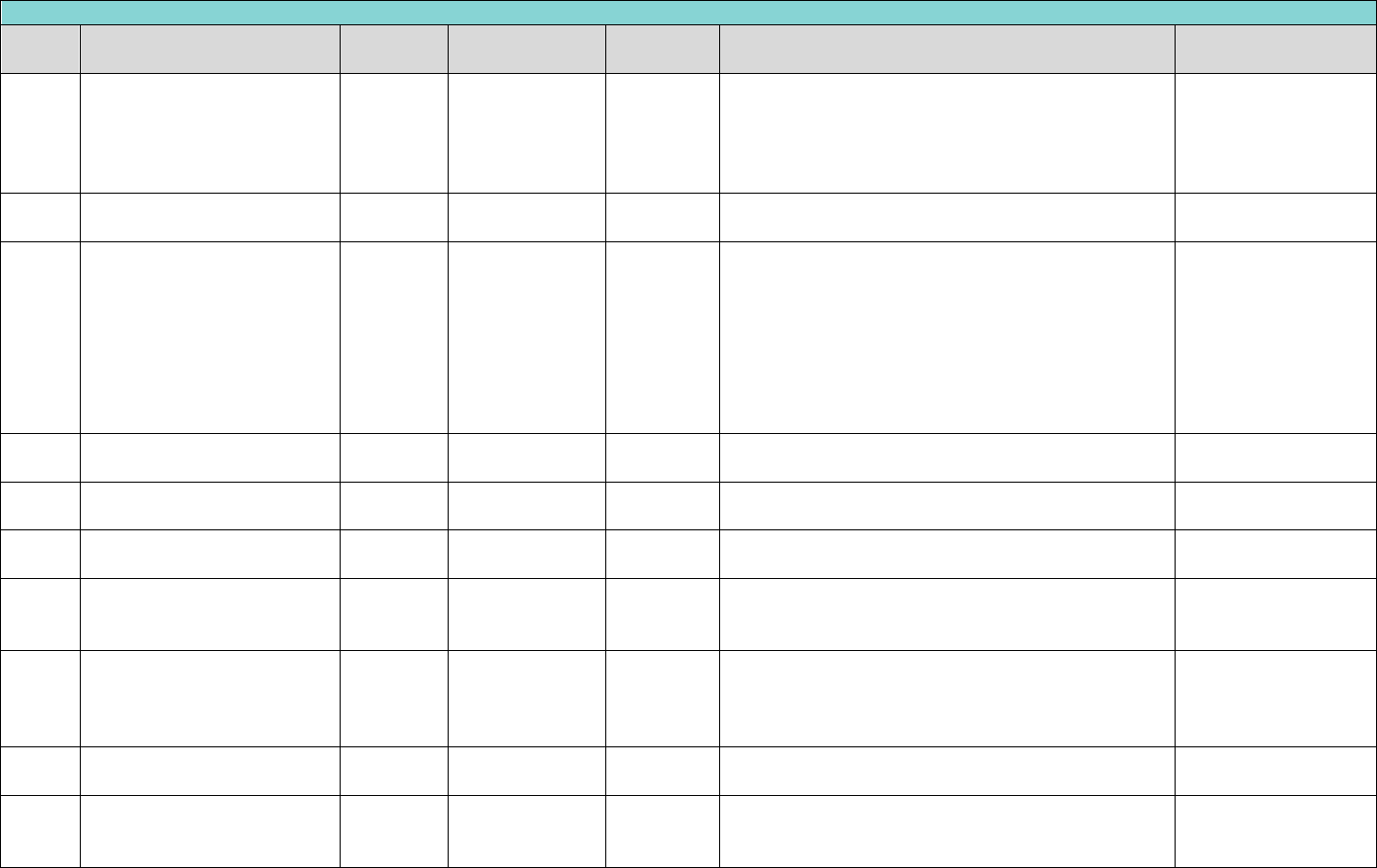
Exhibit A Benefits Covered for TX
Medicaid Child (Under 21)
This document contains proprietary and confidential information and may not be disclosed to others
without written permission. ©Copyright 2024. All rights reserved.
DentaQuest USA Insurance Company, Inc October 24, 2023, 2023
193
Adjunctive General Services
Code
Brief Description
Age
Limitation
Teeth Covered
Review
Required
Benefit Limitations
Documentation
Required
D9310
consultation - diagnostic
service provided by dentist or
physician other than
requesting dentist or
physician
1 - 20
blank
No
An oral evaluation by specialist of any type who is also
providing restorative or surgical services must be
submitted as D0160.
blank
D9410
house/extended care facility
call
1 - 20
blank
No
Should be billed as D0160 for specialist who is
providing treatment.
blank
D9420
hospital or ambulatory
surgical center call
1 - 20
blank
No
Limit two services per year, per patient, per tooth.
Dental hospital calls (procedure code D9420) are
currently limited to twice per rolling year, per
member, any provider. Documentation supporting the
reason that dental services could not be performed in
the office setting must be retained in the member’s
record and may be subject to retrospective review and
recoupment.
narrative of medical
necessity
D9430
office visit for observation -no
other services performed
1 - 20
blank
No
No other services allowed. Not to be used for post-
operative care.
D9440
office visit - after regularly
scheduled hours
1 - 20
blank
No
Not to be used for post-operative care.
narrative of medical
necessity
D9610
therapeutic drug injection, by
report
1 - 20
blank
Yes
Limit one service of (D9610, D9612) per day per
patient. May not be submitted with code D9248.
Description of drugs
with claim
D9612
therapeutic drug injection - 2
or more medications by
report
1 - 20
blank
Yes
Limit one service of (D9610, D9612) per day per
patient.
Description of drugs
with claim
D9630
other drugs and/or
medicaments, by report
1 - 20
blank
Yes
Includes, but is not limited to, oral antibiotics, oral
analgesic, and oral sedatives administered in the
office. Not allowed with D9230, D9241, D9248, D9610
or D9920.
narrative of medical
necessity
D9910
application of desensitizing
medicament
18 - 20
blank
No
Not to be used as a base or a liner.
D9920
behavior management, by
report
0-20
blank
Yes
Limit one service per day, per patient. Denied if billed
with D9248, D0120-D0180, D1110, D1120 or D0210-
D0363.
narrative of medical
necessity
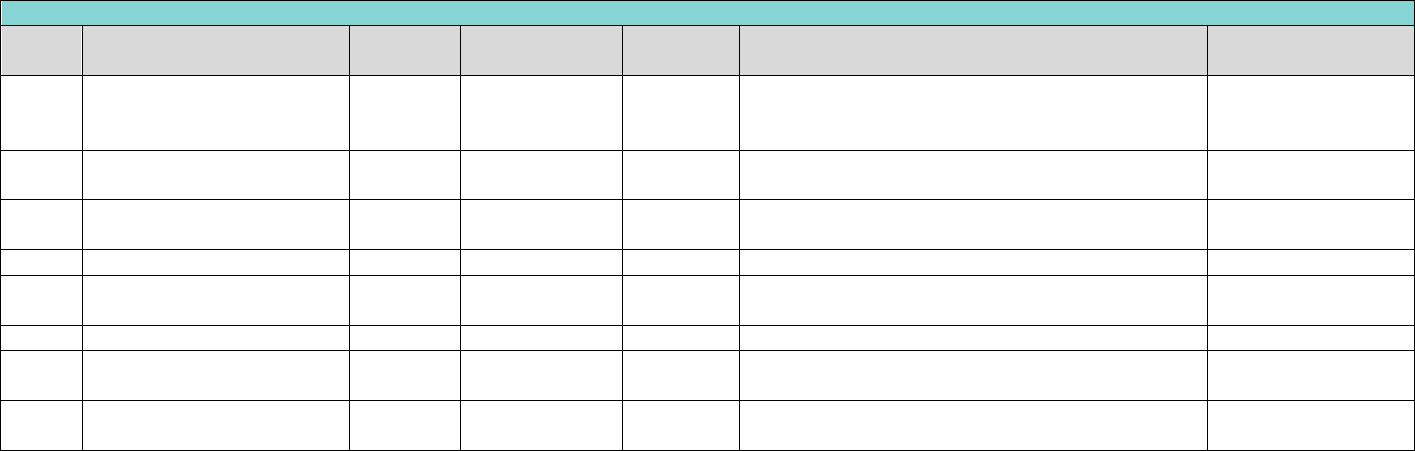
Exhibit A Benefits Covered for TX
Medicaid Child (Under 21)
This document contains proprietary and confidential information and may not be disclosed to others
without written permission. ©Copyright 2024. All rights reserved.
DentaQuest USA Insurance Company, Inc October 24, 2023, 2023
194
Adjunctive General Services
Code
Brief Description
Age
Limitation
Teeth Covered
Review
Required
Benefit Limitations
Documentation
Required
D9930
treatment of complications
(post-surgical) – unusual
circumstances, by report
1 - 20
blank
Yes
blank
narrative of medical
necessity
D9944
occlusal guard – hard
appliance, full arch
16 - 20
LA, UA
Yes
Limit 1 service per lifetime, per member.
narrative of medical
necessity
D9950
occlusion analysis-mounted
case
13 - 20
blank
Yes
blank
narrative of medical
necessity
D9951
occlusal adjustment - limited
13 - 20
blank
No
Limit one service per year, per provider.
blank
D9952
occlusal adjustment -
complete
13 - 20
blank
No
Limit one service per lifetime, per provider.
blank
D9970
enamel micro-abrasion
13 - 20
Teeth 1 - 32
No
Limit One service per day, per provider.
blank
D9974
internal bleaching - per tooth
13 - 20
Teeth 1 - 32
No
Narrative of medical
necessity
D9999
unspecified adjunctive
procedure, by report
1 - 20
Yes
blank
narrative of medical
necessity
Exhibit B Benefits Covered for TX
CHIP (Child Under 19)
This document contains proprietary and confidential information and may not be disclosed to others
without written permission. ©Copyright 2024. All rights reserved.
DentaQuest USA Insurance Company, Inc October 24, 2023, 2023
195
Exhibit B Benefits Covered for TX CHIP (Child Under 19)
Covered Dental Services are subject to a $564 annual benefit limit unless an exception applies. In addition, some of the benefits identified in the schedule below are subject
to annual limits. Limitations are based on a 12-month coverage period.
CHIP Members who have exhausted the $564 annual benefit limit continue to receive the following Covered Dental Services in excess of $564 annual benefit maximum:
(1) the diagnostic and preventive services due under the 2009 American Academy of Pediatric Dentistry periodicity schedule; and
(2) other Medically Necessary Covered Dental Services approved by the Dental Contractor through a prior authorization process. These services must be necessary to allow a
CHIP Member to return to normal, pain and infection-free oral functioning. Typically, this includes:
- Services related to the relief of significant pain or to eliminate acute infection;
- Services related to treat traumatic clinical conditions;
- Services that allow the CHIP Member to attain the basic human functions (e.g. eating, speech, etc.); and
- Services that prevent a condition from seriously jeopardizing the CHIP Member's health/functioning or deteriorating in an imminent timeframe to a more serious and costly
dental problem.
Diagnostic services include the oral examination, and selected radiographs needed to assess the oral health, diagnose oral pathology, and develop an adequate treatment
plan for the member's oral health.
Reimbursement for some or multiple radiographs of the same tooth or area may be denied if DentaQuest determines the number to be redundant, excessive or not in
keeping with the federal guidelines relating to radiation exposure. The maximum amount paid for individual radiographs taken on the same day will be limited to the
allowance for a full mouth series.
Reimbursement for radiographs is limited to those films required for proper treatment and/or diagnosis.
DentaQuest utilizes the guidelines published by the Department of Health and Human Services Center for Devices and Radiological Health. However, please consult the
following benefit tables for benefit limitations.
All radiographs, must be of good diagnostic quality, include member's full name, date films taken, and identify the patients left and right side. Substandard radiographs will
not be reimbursed for, or if already paid for, DentaQuest will recoup the funds previously paid.
Covered dental services that indicate “Yes” in the “Review Required” column require documentation of medical necessity and will be subject to retrospective pre-payment
review. These procedures can be rendered before determination of medical necessity but require submission of proper documentation (as indicated in the “Documentation
Required” column) with the claim form.
Any reimbursement already made for an inadequate service may be recouped after the DentaQuest Consultant reviews the circumstances.
Diagnostic
Code
Brief Description
Age
Limitation
Teeth Covered
Review
Required
Benefit Limitations
Documentation
Required
D0120
periodic oral evaluation -
established patient
0-18
blank
No
Limited to one every six months by the same provider
OR location. Denied when submitted for the same DOS
as procedure codes D0120, D0140, D0150,
by the same provider. Codes D0120, and D0150 must
be performed on same date as D0601, D0602, or D0603
to receive reimbursement.
blank
Exhibit B Benefits Covered for TX
CHIP (Child Under 19)
This document contains proprietary and confidential information and may not be disclosed to others
without written permission. ©Copyright 2024. All rights reserved.
DentaQuest USA Insurance Company, Inc October 24, 2023, 2023
196
Diagnostic
Code
Brief Description
Age
Limitation
Teeth Covered
Review
Required
Benefit Limitations
Documentation
Required
D0140
limited oral evaluation-
problem focused
0-18
blank
No
Limited of one service per day, per provider or two
services per day, per patient. Denied when submitted
for the same DOS as procedure codes D0120, D0140,
D0150 per provider. Limited emergency exam for an
emergency situation that is medically necessary to treat
pain, infection, swelling, uncontrolled bleeding or
traumatic injury. Not allowed with routine dental
services. Document of Medical Necessity must be
indicated on the claim.
blank
D0150
comprehensive oral
evaluation - new or
established patient
0-18
blank
No
Limit of one service per lifetime, per provider. Codes
D0120 and D0150 must be performed on same date as
D0601, D0602, or D0603 to receive reimbursement.
blank
D0210
intraoral - complete series
of radiographic images
2-5
blank
Yes
Limit of one service of (D0210, D0330) every three
years per provider OR location. Narrative of medical
necessity and x-ray.
narr. of med.
necessity, pre-op x-
ray(s)
D0210
intraoral - complete series
of radiographic images
6-18
blank
No
Limit of one service of (D0210, D0330) per three years
per provider OR location
blank
D0220
intraoral - periapical first
radiographic image
1-18
blank
No
Limit of one service per day, per provider OR location.
blank
D0230
intraoral - periapical each
additional radiographic
image
1-18
blank
No
blank
blank
D0270
bitewing - single
radiographic image
1
blank
Yes
Limited to one service of (D0270, D0272, D0274) per
day, per provider OR location. Narrative of medical
necessity and x-ray showing fully erupted primary first
molar.
narr. of med.
necessity, pre-op x-
ray(s)
D0270
bitewing - single
radiographic image
2 - 18
blank
No
Limit one service of (D0270, D0272, D0274) per day, per
provider OR location.
blank
D0272
bitewings - two
radiographic images
1
blank
Yes
Limit one service of (D0270, D0272, D0274) per day, per
provider OR location. Narrative of medical necessity
and x-rays showing fully erupted left and right primary
first molars.
narr. of med.
necessity, pre-op x-
ray(s)
Exhibit B Benefits Covered for TX
CHIP (Child Under 19)
This document contains proprietary and confidential information and may not be disclosed to others
without written permission. ©Copyright 2024. All rights reserved.
DentaQuest USA Insurance Company, Inc October 24, 2023, 2023
197
Diagnostic
Code
Brief Description
Age
Limitation
Teeth Covered
Review
Required
Benefit Limitations
Documentation
Required
D0272
bitewings - two
radiographic images
2 - 18
blank
No
Limit one service of (D0270, D0272, D0274) per day, per
provider OR location. Limit one service of D0210, D0272
per day, per patient.
blank
D0274
bitewings - four
radiographic images
2-9
blank
Yes
Limit one service of (D0270, D0272, D0274) per day, per
provider OR location. Limit one service of D0210, D0274
per day, per patient. Narrative of medical necessity and
x-rays showing fully erupted left and right second
permanent molars.
narr. of med.
necessity, pre-op x-
ray(s)
D0274
bitewings - four
radiographic images
10 - 18
blank
No
Limit one service of (D0270, D0272, D0274) per day, per
provider OR location. Limit one service of D0210, D0274
per day, per patient.
blank
D0330
panoramic radiographic
image
5
blank
Yes
Limit one service of (D0210, D0330) every five years,
per provider OR location. Limit one service of D0210,
D0330 per day, per patient. Narrative of medical
necessity and x-ray.
narr. of med.
necessity, pre-op x-
ray(s)
D0330
panoramic radiographic
image
6 - 18
blank
No
Limit one service of (D0210, D0330) every five years,
per provider OR location. Limit one service of D0210,
D0330 per day, per patient.
blank
D0601
Caries risk assessment and
documentation, with a
finding of low risk
0-18
blank
No
Codes D0120 and D0150 must be performed on same
date as D0601, D0602, or D0603 to receive
reimbursement.
blank
D0602
Caries risk assessment and
documentation, with a
finding of moderate risk
0-18
blank
No
Codes D0120 and D0150 must be performed on same
date as D0601, D0602, or D0603 to receive
reimbursement.
blank
D0603
Caries risk assessment and
documentation, with a
finding of high risk
0-18
blank
No
Codes D0120 and D0150 must be performed on same
date as D0601, D0602, or D0603 to receive
reimbursement.
blank
Exhibit B Benefits Covered for TX
CHIP (Child Under 19)
This document contains proprietary and confidential information and may not be disclosed to others
without written permission. ©Copyright 2024. All rights reserved.
DentaQuest USA Insurance Company, Inc October 24, 2023, 2023
198
Exhibit B Benefits Covered for TX CHIP (Child Under 19)
Covered dental services that indicate “Yes” in the “Review Required” column require documentation of medical necessity and will be subject to retrospective pre-payment
review. These procedures can be rendered before determination of medical necessity but require submission of proper documentation (as indicated in the “Documentation
Required” column) with the claim form.
Any reimbursement already made for an inadequate service may be recouped after the DentaQuest Consultant reviews the circumstances.
Preventative
Code
Brief Description
Age
Limitation
Teeth Covered
Review
Required
Benefit Limitations
Documentation
Required
D1110
prophylaxis - adult
13-18
blank
No
Limit one service of (D1110, D1120) per six months, per
patient. D1110 will be denied when submitted for the
same date of service as any D4000 Series periodontal
procedure code. Any provider. Denied when billed with
emergency treatment. Cannot be billed by Orthodontist
or Maxillofacial Surgery Specialist.
blank
D1120
prophylaxis - child
0-12
blank
No
Limit one service of (D1110, D1120) per six months, per
patient. D1120 will be denied when submitted for the
same date of service as any D4000 Series periodontal
procedure code. Any provider. Denied when billed with
emergency treatment. Cannot be billed by Orthodontist
or Maxillofacial Surgery Specialist.
blank
D1206
topical application of
fluoride varnish
0-18
blank
No
Limit one service of (D1206, D1208) per six months, per
patient. D1206 will be denied when submitted for the
same date of service as any D4000 Series periodontal
procedure code. If submitted on emergency claim,
D1206 will be denied. Denied when billed with
emergency treatment. Cannot be billed by Orthodontist
or Maxillofacial Surgery Specialist.
blank
D1208
topical application of
fluoride - excluding varnish
0-18
blank
No
Limit one service of (D1206, D1208) per six months, per
patient. D1208 will be denied when submitted for the
same date of service as any D4000 Series periodontal
procedure code. Denied when billed with emergency
treatment. Cannot be billed by Orthodontist or
Maxillofacial Surgery Specialist.
blank
D1351
sealant - per tooth
0-18
Teeth 2 - 5, 12 -
15, 18, 19, 30,
31
No
Limit one service per lifetime, per patient, per tooth.
D1351 will be denied when submitted for the same
date of service as any D4000 Series periodontal
procedure code. Not billable by Orthodontist or Oral
blank
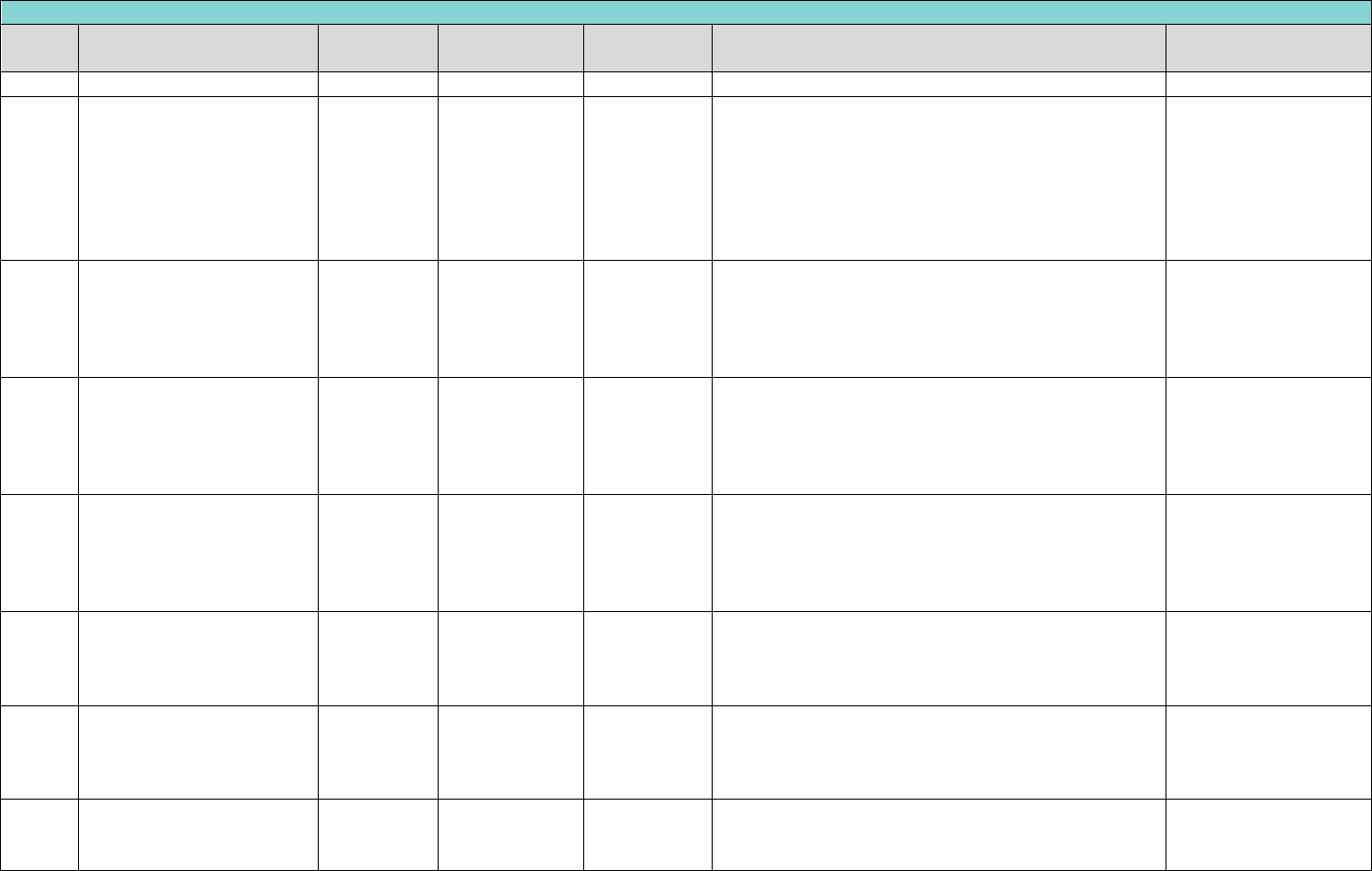
Exhibit B Benefits Covered for TX
CHIP (Child Under 19)
This document contains proprietary and confidential information and may not be disclosed to others
without written permission. ©Copyright 2024. All rights reserved.
DentaQuest USA Insurance Company, Inc October 24, 2023, 2023
199
Preventative
Code
Brief Description
Age
Limitation
Teeth Covered
Review
Required
Benefit Limitations
Documentation
Required
Surgeon.
D1354
interim caries arresting
medicament application –
per tooth
6 months-6
years
Teeth 1 ‐ 32, 51
‐ 82, A ‐ T, AS,
BS, CS, DS, ES,
FS, GS, HS, IS,
JS, KS, LS, MS,
NS, OS, PS, QS,
RS, SS, TS
D1354 is limited to one application per lifetime of
tooth. Not allowed on the same date of service as
D1351 or D1352 on the same tooth. D1354 must be
deemed medically necessary by Main Dental Home
provider. Silver Diamine Fluoride is the only materials
that may be used for D1354.
D1510
space maintainer-fixed-
unilateral – Per quadrant
1 - 12
Per Quadrant
(10, 20, 30, 40,
LL, LR, UL, UR)
No
Limit to one service of (D1510, D1520) per lifetime, per
patient, per quadrant. After premature loss of a
deciduous/primary first and/or second molar for clients
who are 1 through 12 years of age (procedure codes
D1510 and D1516 and D1517)
blank
D1516
space maintainer – fixed –
bilateral, maxillary
1 - 12
Per Arch (01,
UA)
No
Limit to one service of (D1516, D1526) per lifetime, per
patient, per quadrant. After premature loss of a
deciduous/primary first and/or second molar (TID A, B,
I, and J) for clients who are 1 through 12 years of age
(procedure codes D1510 and D1516)
blank
D1517
space maintainer – fixed –
bilateral, mandibular
1 - 12
Per Arch (02,
LA)
No
One of (D1517, D1527) per lifetime, same Arch. After
premature loss of a deciduous/primary first and/or
second molar (TID K, L, S, and T) for clients who are 1
through 12 years of age (procedure codes D1510 and
D1517)
blank
D1520
Space maintainer-
removable-unilateral
1 - 12
Per Quadrant
(10, 20, 30, 40,
LL, LR, UL, UR)
No
Limit to one service of (D1510 or D1520) per lifetime,
per patient, per quadrant. After premature loss of a
deciduous/primary first and/or second molar for clients
who are 1 through 12 years of age
blank
D1526
space maintainer –
removable – bilateral,
maxillary
1 - 12
Per Arch (01,
UA)
No
Limit to one service of (D1516, D1526) per lifetime, per
patient, arch. After premature loss of a
deciduous/primary first and/or second molar (TID A, B,
I, and J) for clients who are 1 through 12 years of age.
blank
D1527
space maintainer –
removable – bilateral,
mandibular
1 - 12
Per Arch (02,
LA)
No
One of (D1517, D1527) per lifetime, same Arch. After
premature loss of a deciduous/primary first and/or
second molar (TID K, L, S, and T) for clients who are 1
blank
Exhibit B Benefits Covered for TX
CHIP (Child Under 19)
This document contains proprietary and confidential information and may not be disclosed to others
without written permission. ©Copyright 2024. All rights reserved.
DentaQuest USA Insurance Company, Inc October 24, 2023, 2023
200
Preventative
Code
Brief Description
Age
Limitation
Teeth Covered
Review
Required
Benefit Limitations
Documentation
Required
through 12 years of age
D1575
distal shoe space
maintainer – fixed -
unilateral
3-7
Teeth A, J, K, T
No
Limit one service of (D1517 or D1527) per Lifetime Per
patient per tooth.
blank
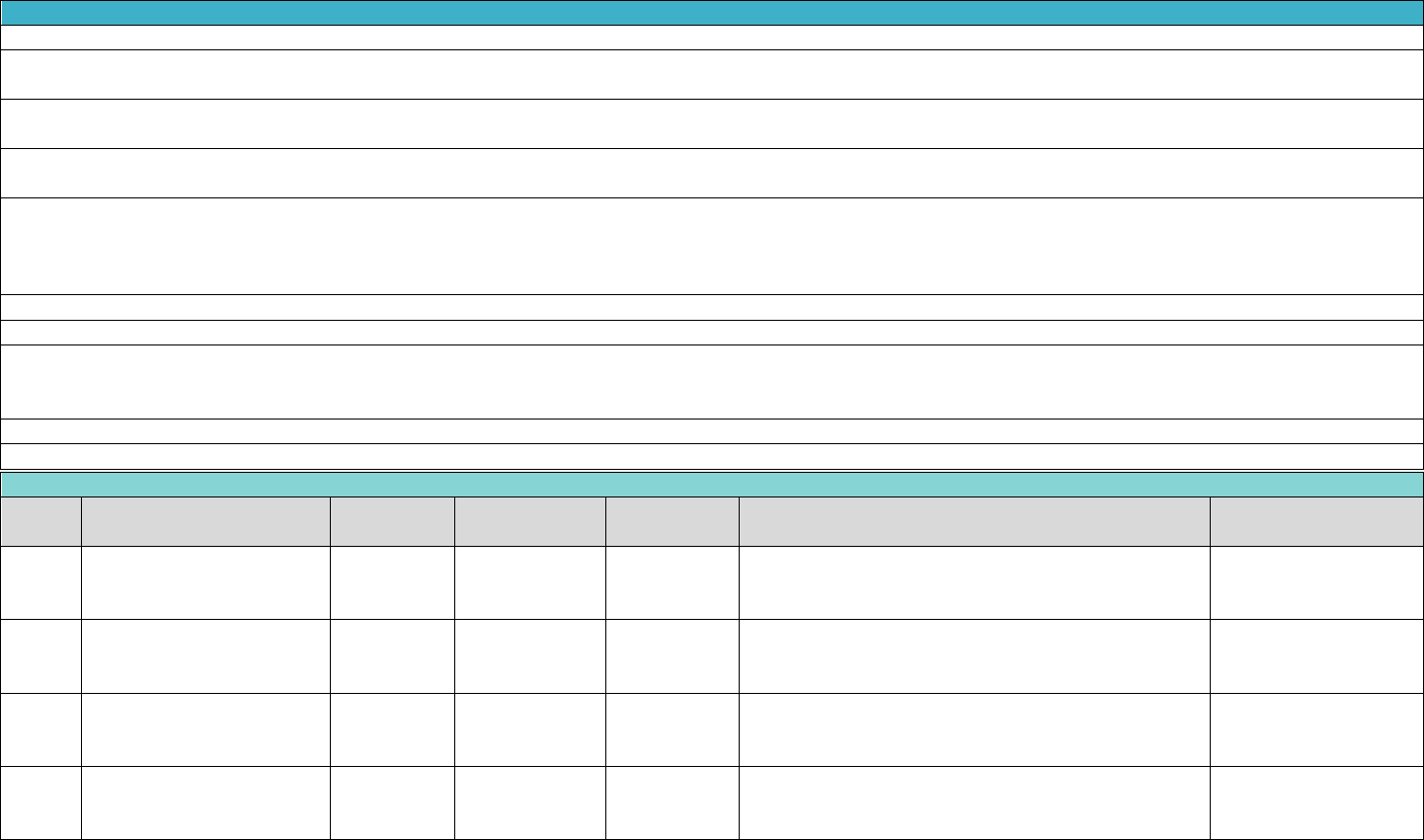
Exhibit B Benefits Covered for TX
CHIP (Child Under 19)
This document contains proprietary and confidential information and may not be disclosed to others
without written permission. ©Copyright 2024. All rights reserved.
DentaQuest USA Insurance Company, Inc October 24, 2023, 2023
201
Exhibit B Benefits Covered for TX CHIP (Child Under 19)
Reimbursement includes local anesthesia.
Generally, once a particular restoration is placed in a tooth, a similar restoration will not be covered for at least twelve months. It is DentaQuest’s expectation that
replacement prior to published frequency remain the responsibility of the treating provider.
A replacement of an identical restorative service in less than 36 months by the same provider is not considered the standard of care for quality by DentaQuest. If there are
special circumstances requiring this repeat service, please send in a prior authorization request along with a narrative establishing medical necessity.
When restorations involving multiple surfaces are requested or performed, that are outside the usual anatomical expectation, the allowance is limited to that of a one-surface
restoration. Any fee charged in excess of the allowance for the one-surface restoration is DISALLOWED.
Payment is made for restorative services based on the number of surfaces restored, not on the number of restorations per surface, or per tooth, per day. A restoration is
considered a two or more surface restoration only when two or more actual tooth surfaces are involved, whether they are connected or not. Tooth preparation, all adhesives
(including amalgam and resin bonding agents), acid etching, copalite, liners, bases, direct and indirect pulp caps, curing, and polishing are included as part of the fee for the
restoration.
BILLING AND REIMBURSEMENT FOR CAST CROWNS AND POST & CORES OR REMOVABLE PROSTHETICS SHALL BE BASED ON THE CEMENTATION OR INSERTION DATE.
The fee for crowns includes the temporary crown that is placed on the prepared tooth and worn while the permanent crown is being fabricated for permanent teeth.
Covered dental services that indicate “Yes” in the “Review Required” column require documentation of medical necessity and will be subject to retrospective pre-payment
review. These procedures can be rendered before determination of medical necessity but require submission of proper documentation (as indicated in the “Documentation
Required” column) with the claim form.
The following codes require prior authorization for all ages: D2710, D2720, D2721, D2722, D2740, D2750, D2751, D2752, D2790, and D2791.
Any reimbursement already made for an inadequate service may be recouped after the DentaQuest Consultant reviews the circumstances.
Restorative
Code
Brief Description
Age
Limitation
Teeth Covered
Review
Required
Benefit Limitations
Documentation
Required
D2140
Amalgam - one surface,
primary or permanent
0-18
Teeth 1 - 32, A -
T
No
Limit one service of (D2140, D2150, D2160, D2161,
D2330, D2331, D2332, D2335, D2391, D2392, D2393,
D2394) per year, per provider, per tooth.
blank
D2150
Amalgam - two surfaces,
primary or permanent
0-18
Teeth 1 - 32, A -
T
No
Limit one service of (D2140, D2150, D2160, D2161,
D2330, D2331, D2332, D2335, D2391, D2392, D2393,
D2394) per year, per provider, per tooth.
blank
D2160
amalgam - three surfaces,
primary or permanent
1-18
Teeth 1 - 32, A -
T
No
Limit one service of (D2140, D2150, D2160, D2161,
D2330, D2331, D2332, D2335, D2391, D2392, D2393,
D2394) per year, per provider, per tooth.
blank
D2161
amalgam - four or more
surfaces, primary or
permanent
1-18
Teeth 1 - 32, A -
T
No
Limit one service of (D2140, D2150, D2160, D2161,
D2330, D2331, D2332, D2335, D2391, D2392, D2393,
D2394) per year, per provider, per tooth.
blank
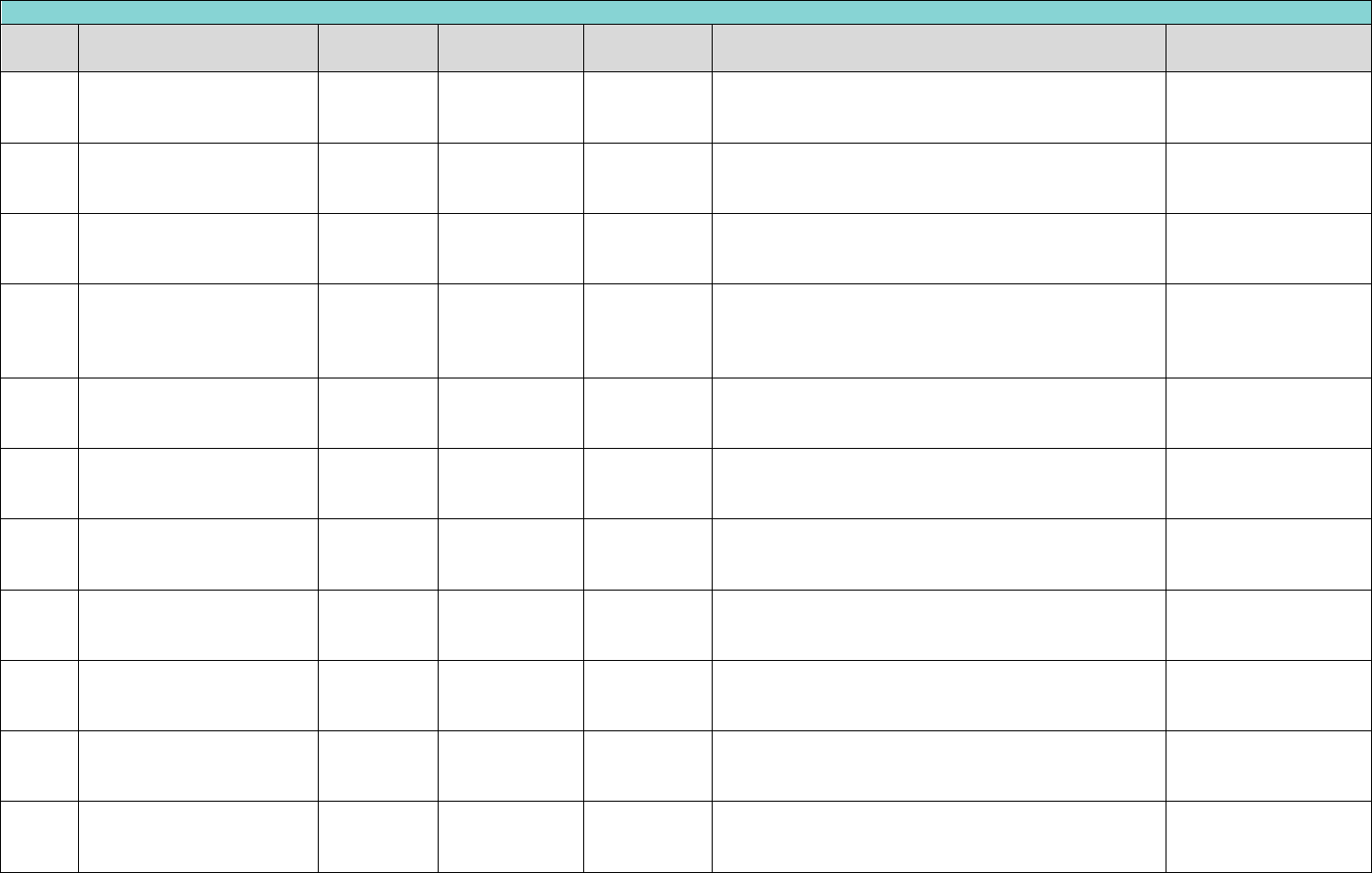
Exhibit B Benefits Covered for TX
CHIP (Child Under 19)
This document contains proprietary and confidential information and may not be disclosed to others
without written permission. ©Copyright 2024. All rights reserved.
DentaQuest USA Insurance Company, Inc October 24, 2023, 2023
202
Restorative
Code
Brief Description
Age
Limitation
Teeth Covered
Review
Required
Benefit Limitations
Documentation
Required
D2330
resin-based composite - one
surface, anterior
0-18
Teeth 6 - 11, 22
- 27, C - H, M - R
No
Limit one service of (D2140, D2150, D2160, D2161,
D2330, D2331, D2332, D2335, D2391, D2392, D2393,
D2394) per year, per provider, per tooth.
blank
D2331
resin-based composite –
two surfaces, anterior
0-18
Teeth 6 - 11, 22
- 27, C - H, M - R
No
Limit one service of (D2140, D2150, D2160, D2161,
D2330, D2331, D2332, D2335, D2391, D2392, D2393,
D2394) per year, per provider, per tooth.
blank
D2332
resin-based composite -
three surfaces, anterior
1-18
Teeth 6 - 11, 22
- 27, C - H, M - R
No
Limit one service of (D2140, D2150, D2160, D2161,
D2330, D2331, D2332, D2335, D2391, D2392, D2393,
D2394) per year, per provider, per tooth.
blank
D2335
resin-based composite -
four or more surfaces or
involving incisal angle
(anterior)
1-18
Teeth 6 - 11, 22
- 27, C - H, M - R
No
Limit one service of (D2140, D2150, D2160, D2161,
D2330, D2331, D2332, D2335, D2391, D2392, D2393,
D2394) per year, per provider, per tooth.
blank
D2391
resin-based composite - one
surface, posterior
0-18
Teeth 1 - 5, 12 -
21, 28 - 32, A,
B, I - L, S, T
No
Limit one service of (D2140, D2150, D2160, D2161,
D2330, D2331, D2332, D2335, D2391, D2392, D2393,
D2394) per year, per provider, per tooth.
blank
D2392
resin-based composite -
two surfaces, posterior
0-18
Teeth 1 - 5, 12 -
21, 28 - 32, A,
B, I - L, S, T
No
Limit one service of (D2140, D2150, D2160, D2161,
D2330, D2331, D2332, D2335, D2391, D2392, D2393,
D2394) per year, per provider, per tooth.
blank
D2393
resin-based composite -
three surfaces, posterior
1 - 18
Teeth 1 - 5, 12 -
21, 28 - 32, A,
B, I - L, S, T
No
Limit one service of (D2140, D2150, D2160, D2161,
D2330, D2331, D2332, D2335, D2391, D2392, D2393,
D2394) per year, per provider, per tooth.
blank
D2394
resin-based composite -
four or more surfaces,
posterior
1 - 18
Teeth 1 - 5, 12 -
21, 28 - 32, A,
B, I - L, S, T
No
Limit one service of (D2140, D2150, D2160, D2161,
D2330, D2331, D2332, D2335, D2391, D2392, D2393,
D2394) per year, per provider, per tooth.
blank
D2710
crown - resin-based
composite (indirect)
13 - 18
Teeth 1 - 32
Yes
Limit one service of (D2710, D2720, D2721, D2722,
D2740, D2750, D2751, D2752, D2790, D2791) every five
years, per patient, per tooth.
pre-operative x-ray(s)
D2720
crown-resin with high noble
metal
13 - 18
Teeth 1 - 32
Yes
Limit one service of (D2710, D2720, D2721, D2722,
D2740, D2750, D2751, D2752, D2790, D2791) every five
years, per patient, per tooth.
narr. of med. necessity,
pre op x-ray(s)
D2721
crown - resin with
predominantly base metal
13 - 18
Teeth 1 - 32
Yes
Limit one service of (D2710, D2720, D2721, D2722,
D2740, D2750, D2751, D2752, D2790, D2791) every five
years, per patient, per tooth.
pre-operative x-ray(s)
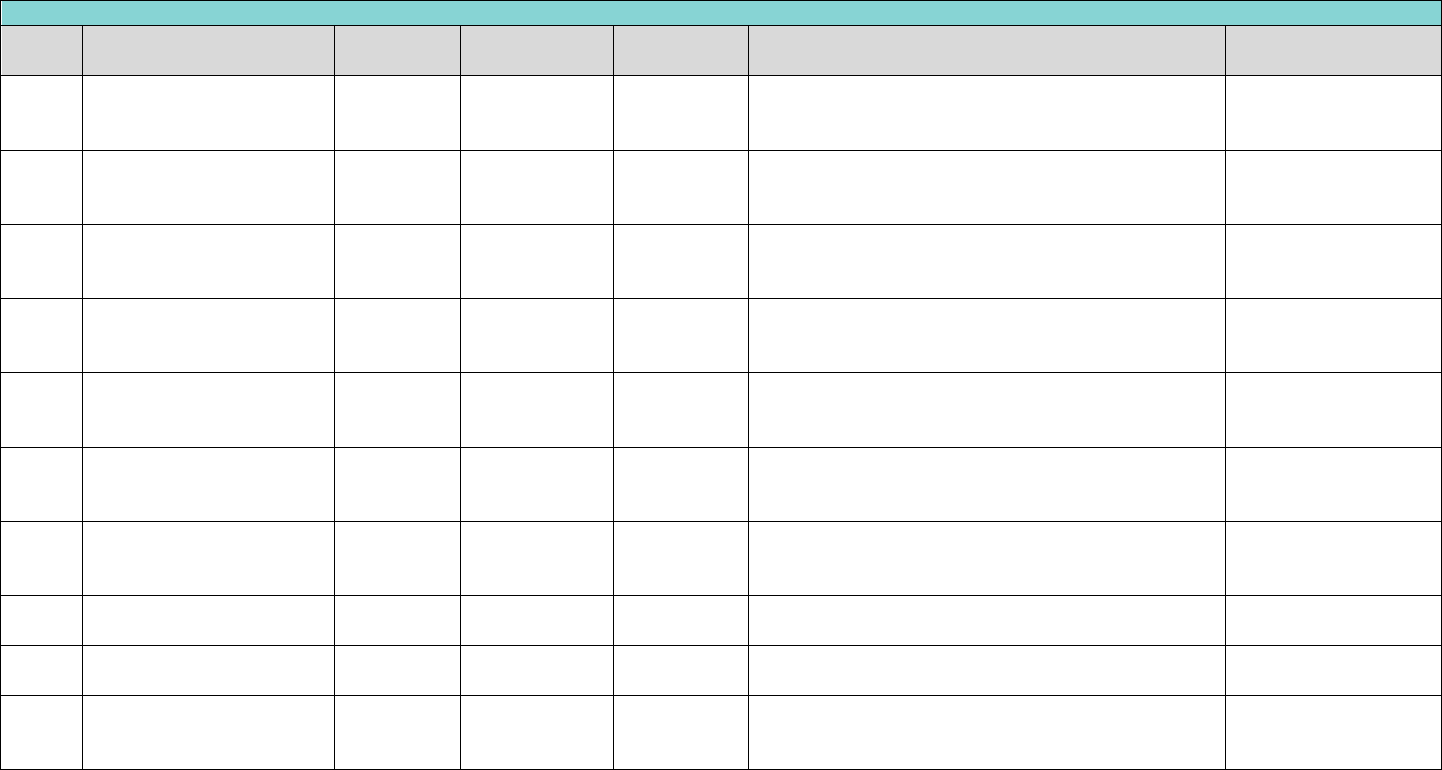
Exhibit B Benefits Covered for TX
CHIP (Child Under 19)
This document contains proprietary and confidential information and may not be disclosed to others
without written permission. ©Copyright 2024. All rights reserved.
DentaQuest USA Insurance Company, Inc October 24, 2023, 2023
203
Restorative
Code
Brief Description
Age
Limitation
Teeth Covered
Review
Required
Benefit Limitations
Documentation
Required
D2722
crown - resin with noble
metal
13 - 18
Teeth 1 - 32
Yes
Limit one service of (D2710, D2720, D2721, D2722,
D2740, D2750, D2751, D2752, D2790, D2791) every five
years, per patient, per tooth.
narr. of med. necessity,
pre op x-ray(s)
D2740
crown - porcelain/ceramic
13 - 18
Teeth 4-13, 20-
29
Yes
Limit one service of (D2710, D2720, D2721, D2722,
D2740, D2750, D2751, D2752, D2790, D2791) every five
years, per patient, per tooth.
narr. of med. necessity,
pre-op x-ray(s)
D2750
crown - porcelain fused to
high noble metal
13 - 18
Teeth 4-13, 20-
29
Yes
Limit one service of (D2710, D2720, D2721, D2722,
D2740, D2750, D2751, D2752, D2790, D2791) every five
years, per patient, per tooth.
narr. of med. necessity,
pre-op x-ray(s)
D2751
crown - porcelain fused to
predominantly base metal
13 - 18
Teeth 4-13, 20-
29
Yes
Limit one service of (D2710, D2720, D2721, D2722,
D2740, D2750, D2751, D2752, D2790, D2791) every five
years, per patient, per tooth.
narr. of med. necessity,
pre-op x-ray(s)
D2752
crown - porcelain fused to
noble metal
13 - 18
Teeth 4-13, 20-
29
Yes
Limit one service of (D2710, D2720, D2721, D2722,
D2740, D2750, D2751, D2752, D2790, D2791) every five
years, per patient, per tooth.
narr. of med. necessity,
pre-op x-ray(s)
D2790
crown - full cast high noble
metal
13 - 18
Teeth 1–5, 12–
21, 28–32
Yes
Limit one service of (D2710, D2720, D2721, D2722,
D2740, D2750, D2751, D2752, D2790, D2791) every five
years, per patient, per tooth.
narr. of med. necessity,
pre-op x-ray(s)
D2791
crown - full cast
predominantly base metal
13 - 18
Teeth 1–5, 12–
21, 28–32
Yes
Limit one service of (D2710, D2720, D2721, D2722,
D2740, D2750, D2751, D2752, D2790, D2791) every five
years, per patient, per tooth.
narr. of med. necessity,
pre-op x-ray(s)
D2930
prefabricated stainless steel
crown - primary tooth
0-18
Teeth A - T
No
Limit to one (D2934 or D2930) per lifetime, per patient,
per tooth.
blank
D2931
prefabricated stainless steel
crown-permanent tooth
1 - 18
Teeth 1–32
No
Limit one service per lifetime, per patient, per tooth.
blank
D2934
Prefabricated esthetic
coated stainless steel crown
– primary tooth
0-18
Teeth C-H, M-R
No
Limit to one (D2934 or D2930) per lifetime, per patient,
per tooth.
blank
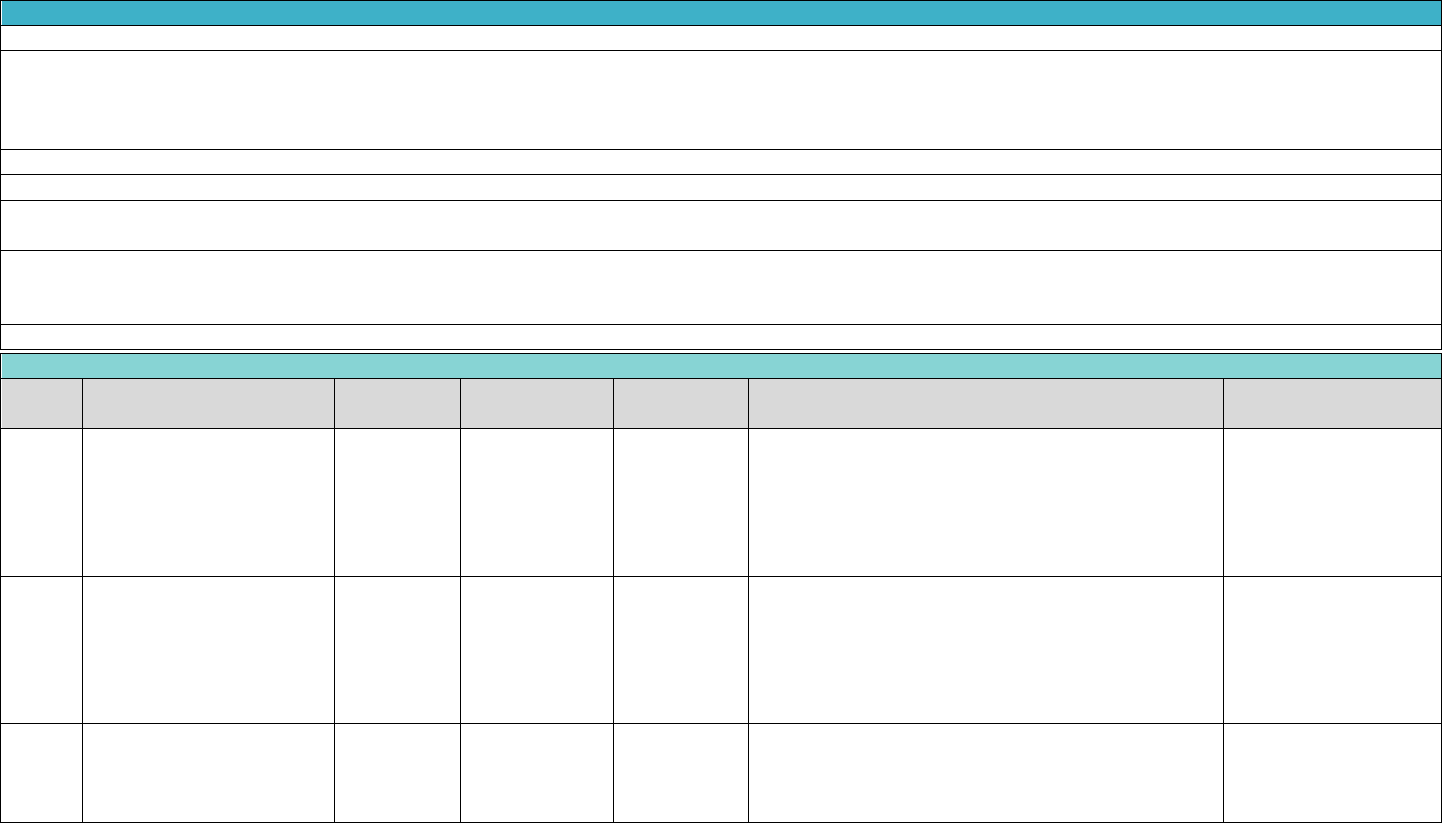
Exhibit B Benefits Covered for TX
CHIP (Child Under 19)
This document contains proprietary and confidential information and may not be disclosed to others
without written permission. ©Copyright 2024. All rights reserved.
DentaQuest USA Insurance Company, Inc October 24, 2023, 2023
204
Exhibit B Benefits Covered for TX CHIP (Child Under 19)
Payment for conventional root canal treatment is limited to treatment of permanent teeth.
The standard of acceptability employed for endodontic procedures requires that the canal(s) be completely filled apically and laterally. In cases where the root canal filling
does not meet DentaQuest's treatment standards, DentaQuest can require the procedure to be redone at no additional cost. Any reimbursement already made for an
inadequate service may be recouped after any post payment review by the DentaQuest Consultants. A pulpotomy or palliative treatment is not to be billed in conjunction
with a root canal treatment.
Filling material not accepted by the Federal Food and Drug Administration (FDA) (e.g. Sargenti filling material) is not covered.
Pulpotomies will be limited to primary teeth or permanent teeth with incomplete root development.
The fee for root canal therapy for permanent teeth includes diagnosis, extirpation treatment, temporary fillings, filling and obturation of root canals, and progress
radiographs. A completed fill radiograph is also included.
Covered dental services that indicate “Yes” in the “Review Required” column require documentation of medical necessity and will be subject to retrospective pre-payment
review. These procedures can be rendered before determination of medical necessity but require submission of proper documentation (as indicated in the “Documentation
Required” column) with the claim form.
Any reimbursement already made for an inadequate service may be recouped after the DentaQuest Consultant reviews the circumstances.
Endodontics
Code
Brief Description
Age
Limitation
Teeth Covered
Review
Required
Benefit Limitations
Documentation
Required
D3220
therapeutic pulpotomy
(excluding final restoration)
- removal of pulp coronal to
the dentinocemental
junction and application of
medicament
0-18
Teeth A - T
No
Limit one service per lifetime, per patient, per tooth.
blank
D3220
therapeutic pulpotomy
(excluding final restoration)
- removal of pulp coronal to
the dentinocemental
junction and application of
medicament
0-18
Teeth 2 - 15, 18
- 31
No
Limit one service of (D3220, D3230, D3240, D3310,
D3320, D3330) every 6 months, per patient, per tooth.
D3230
pulpal therapy (resorbable
filling) - anterior, primary
tooth (excluding final
restoration)
1 - 18
Teeth C - H, M -
R
No
Limit one service per lifetime, per patient, per tooth.
blank
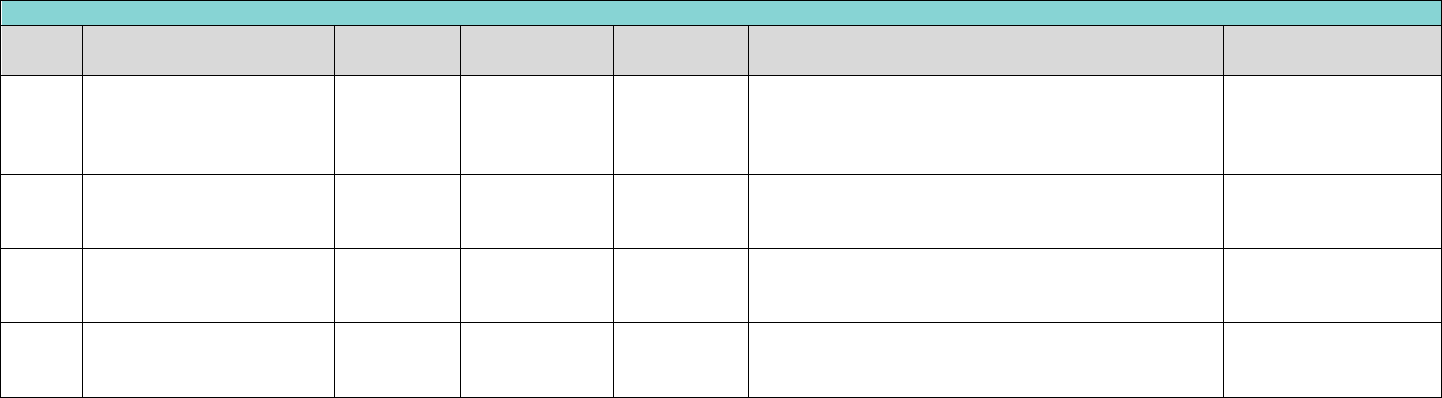
Exhibit B Benefits Covered for TX
CHIP (Child Under 19)
This document contains proprietary and confidential information and may not be disclosed to others
without written permission. ©Copyright 2024. All rights reserved.
DentaQuest USA Insurance Company, Inc October 24, 2023, 2023
205
Endodontics
Code
Brief Description
Age
Limitation
Teeth Covered
Review
Required
Benefit Limitations
Documentation
Required
D3240
pulpal therapy (resorbable
filling) - posterior, primary
tooth (excluding final
restoration)
1 - 18
Teeth A, B, I - L,
S, T
No
Limit one service per lifetime, per patient, per tooth.
blank
D3310
endodontic therapy,
anterior tooth (excluding
final restoration)
6 - 18
Teeth 6 - 11, 22
- 27
No
Limit one service per lifetime, per patient, per tooth.
blank
D3320
endodontic therapy,
premolar tooth (excluding
final restoration)
6 - 18
Teeth 4, 5, 12,
13, 20, 21, 28,
29
No
Limit one service per lifetime, per patient, per tooth.
blank
D3330
endodontic therapy, molar
tooth (excluding final
restoration)
6 - 18
Teeth 2, 3, 14,
15, 18, 19, 30,
31
No
Limit one service per lifetime, per patient, per tooth.
blank
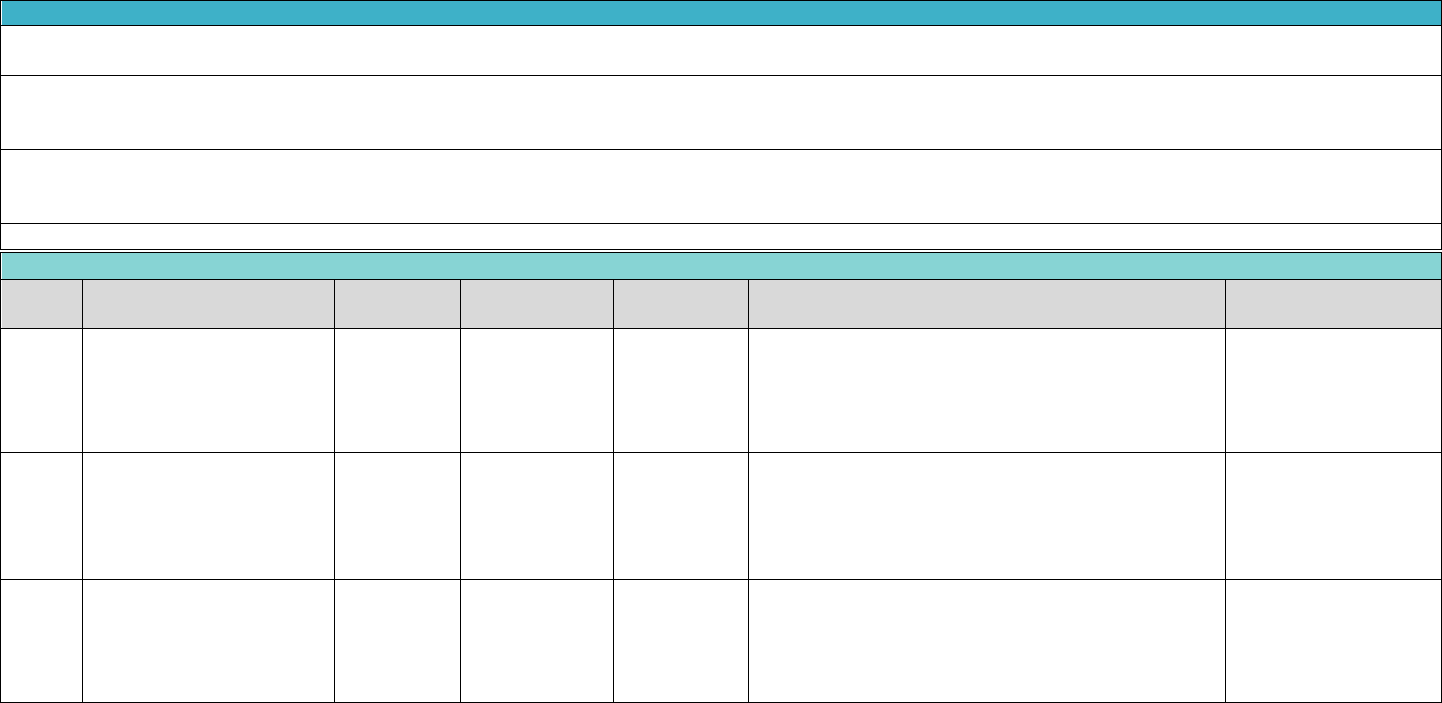
Exhibit B Benefits Covered for TX
CHIP (Child Under 19)
This document contains proprietary and confidential information and may not be disclosed to others
without written permission. ©Copyright 2024. All rights reserved.
DentaQuest USA Insurance Company, Inc October 24, 2023, 2023
206
Exhibit B Benefits Covered for TX CHIP (Child Under 19)
Claims for preventive dental procedure codes D1110, D1120, D1206, D1208, D1351, and D1352 will be denied when submitted for the same DOS as any D4000 series
periodontal procedure codes, any provider.
Covered dental services that indicate “Yes” in the “Review Required” column require documentation of medical necessity and will be subject to retrospective pre-payment
review. These procedures can be rendered before determination of medical necessity but require submission of proper documentation (as indicated in the “Documentation
Required” column) with the claim form.
When the need for an exception to periodicity is established, a narrative explaining the reason for the exception to periodicity limitations must be documented in the
member’s file and on the claim submission. In order to submit a claim with an exception, the claim must have the key word “EXCEPTION” in Block 35 of the ADA claim form. If
the key word “EXCEPTION” is missing from Box 35, the claim may deny for exceeding benefit limitations.
Any reimbursement already made for an inadequate service may be recouped after the DentaQuest Consultant reviews the circumstances.
Periodontics
Code
Brief Description
Age
Limitation
Teeth Covered
Review
Required
Benefit Limitations
Documentation
Required
D4210
gingivectomy or
gingivoplasty – four or more
contiguous
13 - 18
Per Quadrant
(10, 20, 30, 40,
LL, LR, UL, UR)
Yes
Limit one service every two years, per patient, per
quadrant. Limit One service of (D4210, D4355,) per day,
per patient, per quadrant. Limit one service of (D1110,
D1120D1206, D1208, D1351, D1510, D1520,) per day,
per patient, per quadrant.
narr. of med. necessity,
pre-op x-ray(s)
D4341
periodontal scaling and root
planning - four or more
teeth per quadrant
13 - 18
Per Quadrant
(10, 20, 30, 40,
LL, LR, UL, UR)
Yes
D4341 is denied if provided within 21 days of D4355.
D4341 and are denied when submitted for the same
DOS as other D4000 series codes, except with D4341 or
with D1110, D1120, D1206, D1208, D1351, D1510,
D1520, or D1525, Any Provider.
Full mouth xrays, perio
charting & narrative
D4355
full mouth debridement to
enable a comprehensive
oral evaluation and
diagnosis on a subsequent
visit
13 - 18
blank
Yes
D4355 is not payable if provided within 21 days of
D4341. Denied when submitted for the same DOS as
other D4000 series codes D4210, or with D0150, D1110,
D1120, D1206, D1208, D1351, D1510, D1520.
narr. of med. necessity,
pre-op x-ray(s)
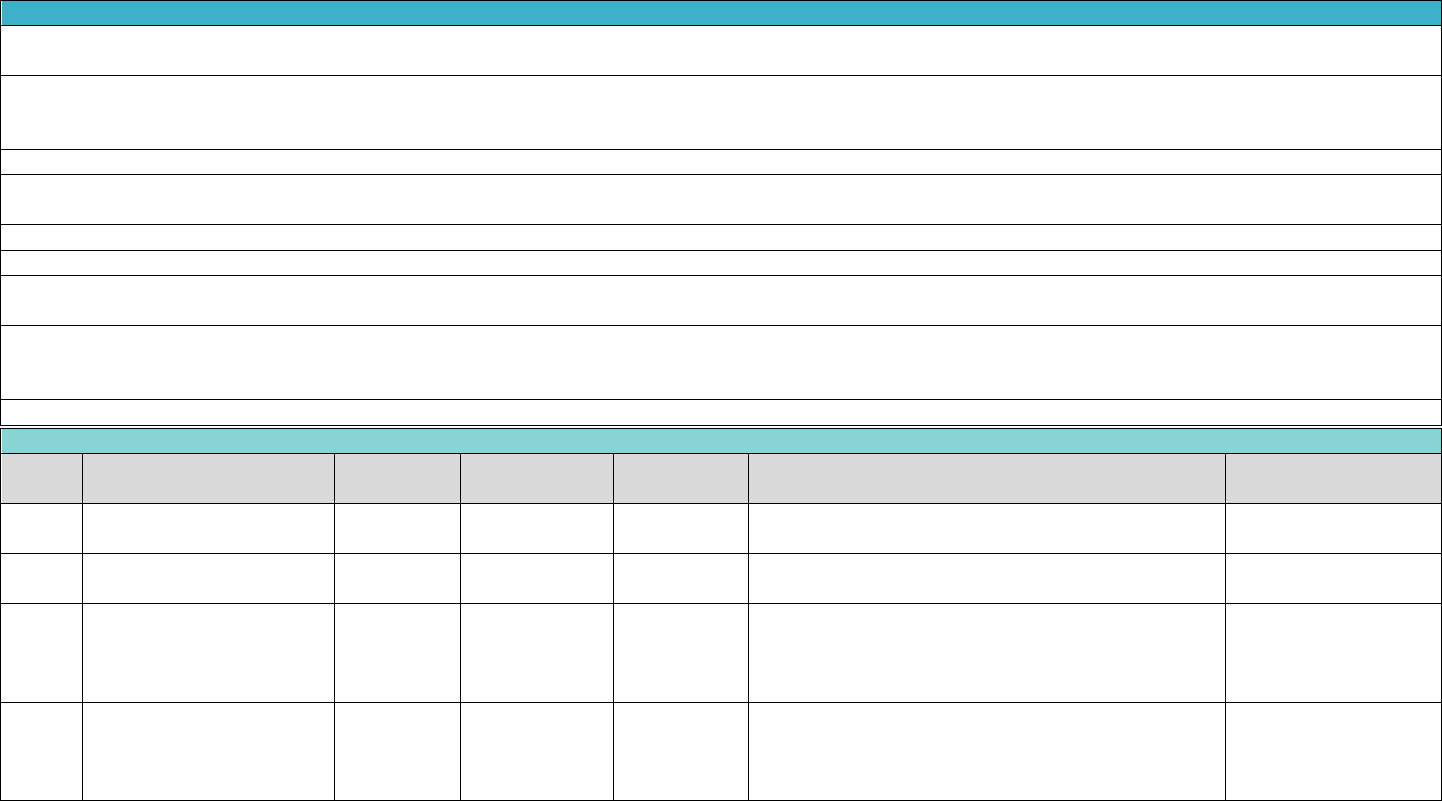
Exhibit B Benefits Covered for TX
CHIP (Child Under 19)
This document contains proprietary and confidential information and may not be disclosed to others
without written permission. ©Copyright 2024. All rights reserved.
DentaQuest USA Insurance Company, Inc October 24, 2023, 2023
207
Exhibit B Benefits Covered for TX CHIP (Child Under 19)
Provision for removable prostheses when masticatory function is impaired, or when existing prostheses is unserviceable and when evidence is submitted that indicates that
the masticatory insufficiencies are likely to impair the general health of the member.
Authorization for partial dentures to replace posterior teeth will not be allowed if there are in each quadrant at least three (3) peridontially sound posterior teeth in fairly
good position and occlusion with opposing dentition. Authorization for cast partial dentures for anterior teeth generally will not be given unless one or more anterior teeth in
the same arch are missing. Partial dentures are not a covered benefit when 8 or more posterior teeth are in occlusion.
Dentures will not be preauthorized when:
Dental history reveals that any or all dentures made in recent years have been unsatisfactory for reasons that are not remediable because of physiological or psychological
reasons, or repair, relining or rebasing of the patient's present dentures will make them serviceable.
A preformed denture with teeth already mounted forming a denture module is not a covered service.
BILLING AND REIMBURSEMENT FOR CAST CROWNS AND POST & CORES OR REMOVABLE PROSTHETICS SHALL BE BASED ON THE CEMENTATION OR INSERTION DATE.
Fabrication of a removable prosthetic includes multiple steps(appointments) these multiple steps (impressions, try-in appointments, delivery etc.) are inclusive in the fee for
the removable prosthetic and as such not eligible for additional compensation.
Covered dental services that indicate “Yes” in the “Review Required” column require documentation of medical necessity and will be subject to retrospective pre-payment
review. These procedures can be rendered before determination of medical necessity but require submission of proper documentation (as indicated in the “Documentation
Required” column) with the claim form.
Any reimbursement already made for an inadequate service may be recouped after the DentaQuest Consultant reviews the circumstances.
Prosthodontics, removable
Code
Brief Description
Age
Limitation
Teeth Covered
Review
Required
Benefit Limitations
Documentation
Required
D5110
complete denture -
maxillary
3 - 18
Per Arch (01,
UA)
Yes
Limit one service every five years, per patient.
pre-operative x-ray(s)
D5120
complete denture -
mandibular
3 - 18
Per Arch (02,
LA)
Yes
Limit one service every five years, per patient.
pre-operative x-ray(s)
D5211
maxillary partial denture –
resin base (including any
conventional clasps, rests
and teeth)
6 - 18
blank
Yes
Limit one service of (D5211, D5213) every five years,
per patient.
pre-operative x-ray(s)
D5212
mandibular partial denture
- resin base (including any
conventional clasps, rests
and teeth)
6 - 18
blank
Yes
Limit one service of (D5212, D5214) every five years,
per patient.
pre-operative x-ray(s)
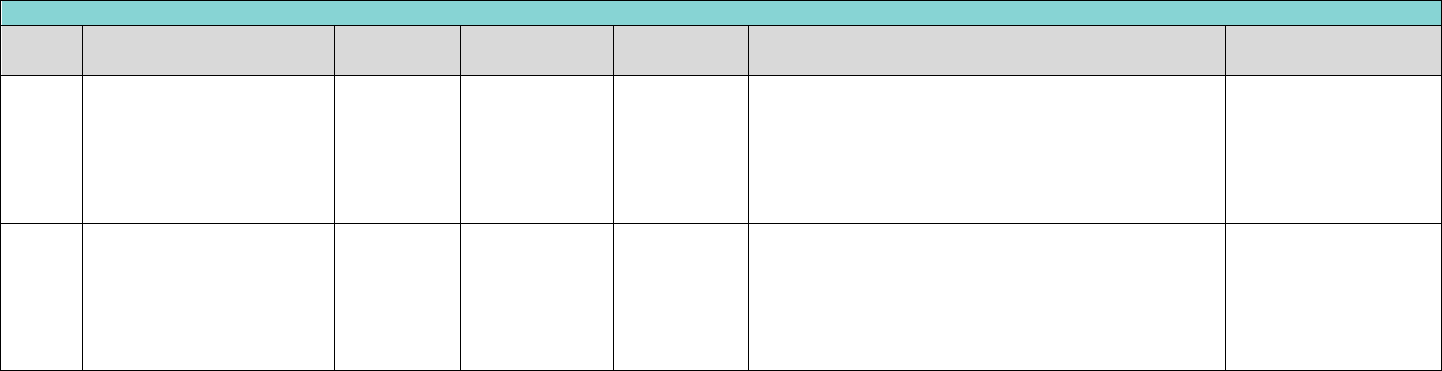
Exhibit B Benefits Covered for TX
CHIP (Child Under 19)
This document contains proprietary and confidential information and may not be disclosed to others
without written permission. ©Copyright 2024. All rights reserved.
DentaQuest USA Insurance Company, Inc October 24, 2023, 2023
208
Prosthodontics, removable
Code
Brief Description
Age
Limitation
Teeth Covered
Review
Required
Benefit Limitations
Documentation
Required
D5213
maxillary partial denture -
cast metal framework with
resin denture bases
(including
retentive/clasping materials
rests and teeth)
9 - 18
blank
Yes
Limit one service of (D5211, D5213) every five years,
per patient.
pre-operative x-ray(s)
D5214
mandibular partial denture
- cast metal framework with
resin denture bases
(including
retentive/clasping
materials, rests and teeth)
9 - 18
blank
Yes
Limit one service of (D5212, D5214) every five years,
per patient.
pre-operative x-ray(s)
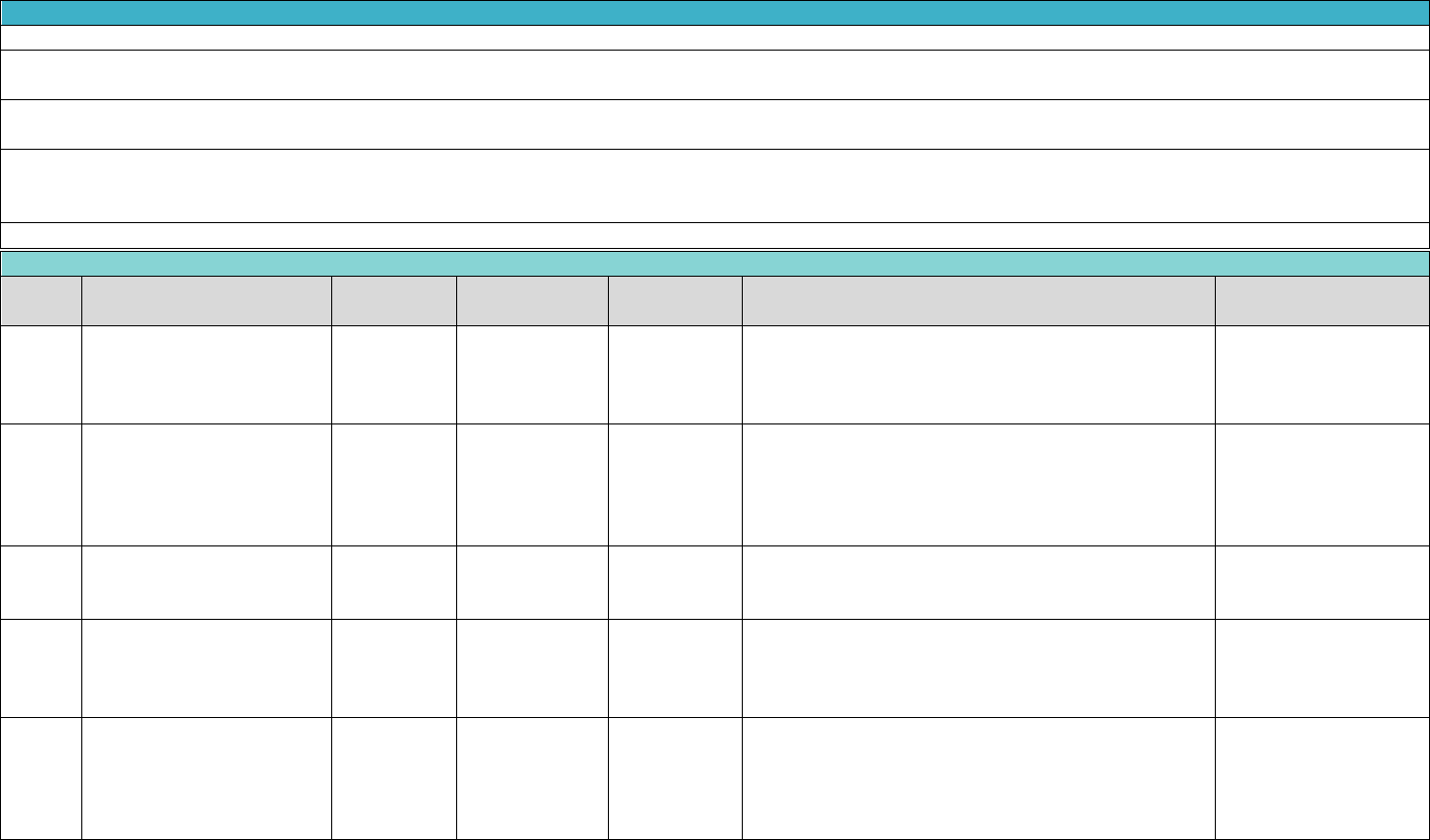
Exhibit B Benefits Covered for TX
CHIP (Child Under 19)
This document contains proprietary and confidential information and may not be disclosed to others
without written permission. ©Copyright 2024. All rights reserved.
DentaQuest USA Insurance Company, Inc October 24, 2023, 2023
209
Exhibit B Benefits Covered for TX CHIP (Child Under 19)
Reimbursement includes local anesthesia and routine post-operative care.
The extraction of asymptomatic impacted teeth is not a covered benefit. Symptomatic conditions would include pain and/or infection or demonstrated malocclusion causing a
shifting of existing dentition.
The incidental removal of a cyst or lesion attached to the root(s) of an extraction is considered part of the extraction or surgical fee and should not be billed as a separate
procedure.
Covered dental services that indicate “Yes” in the “Review Required” column require documentation of medical necessity and will be subject to retrospective pre-payment
review. These procedures can be rendered before determination of medical necessity but require submission of proper documentation (as indicated in the “Documentation
Required” column) with the claim form.
Any reimbursement already made for an inadequate service may be recouped after the DentaQuest Consultant reviews the circumstances.
Oral and Maxillofacial Surgery
Code
Brief Description
Age
Limitation
Teeth Covered
Review
Required
Benefit Limitations
Documentation
Required
D7140
extraction, erupted tooth or
exposed root (elevation
and/or forceps removal)
0-4
Teeth D - G, N -
Q, DS, ES, FS,
GS, NS, OS, PS,
QS
No
blank
blank
D7140
extraction, erupted tooth or
exposed root (elevation
and/or forceps removal)
0-9
Teeth A - C, H -
M, R - T, AS, BS,
CS, HS, IS, JS,
KS, LS, MS, RS,
SS, TS
No
blank
blank
D7140
extraction, erupted tooth or
exposed root (elevation
and/or forceps removal)
0-18
Teeth 1 - 32, 51
- 82
No
blank
blank
D7140
extraction, erupted tooth or
exposed root (elevation
and/or forceps removal)
5 - 18
Teeth D - G, N -
Q, DS, ES, FS,
GS, NS, OS, PS,
QS
Yes
blank
narr. of med. necessity,
pre-op x-ray(s)
D7140
extraction, erupted tooth or
exposed root (elevation
and/or forceps removal)
10 - 18
Teeth A - C, H -
M, R - T, AS, BS,
CS, HS, IS, JS,
KS, LS, MS, RS,
SS, TS
Yes
blank
narr. of med. necessity,
pre-op x-ray(s)
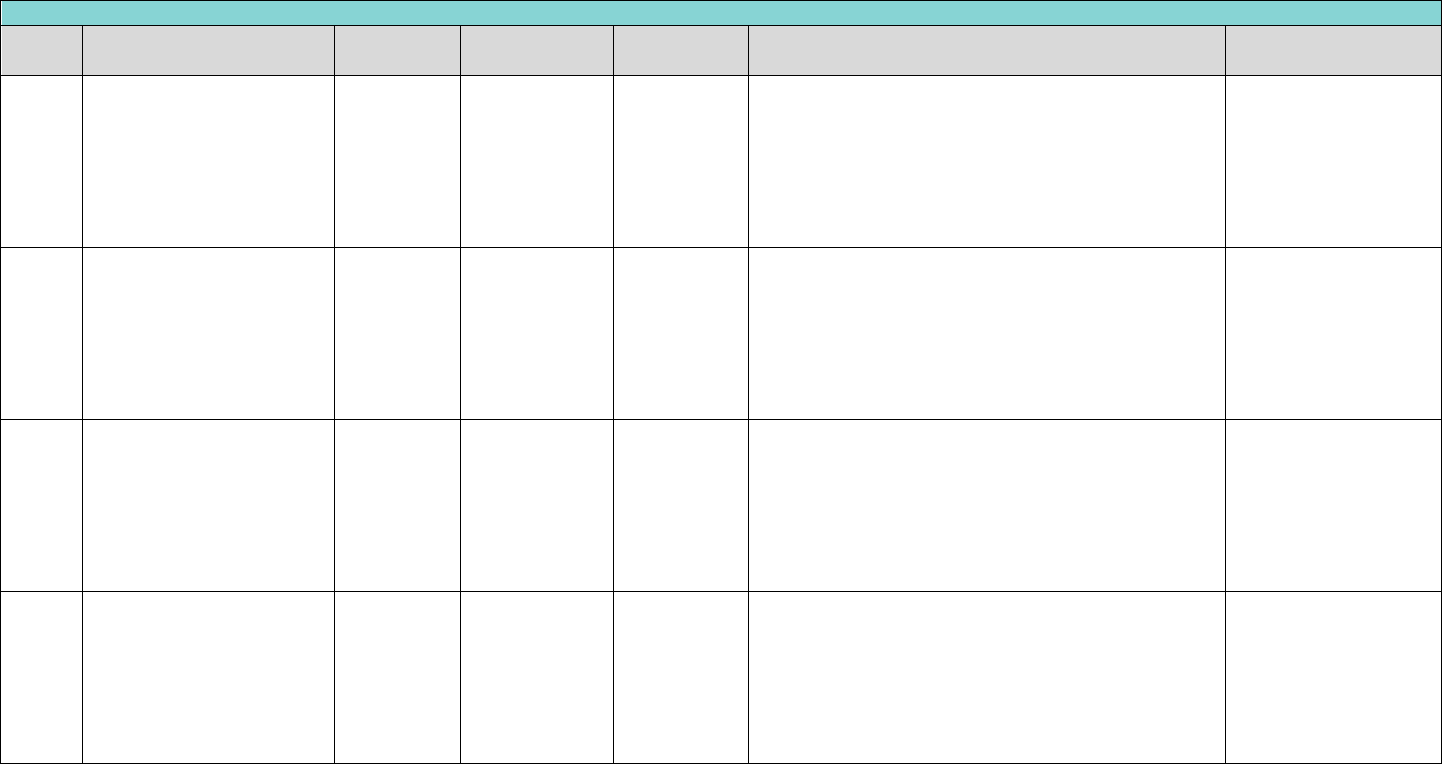
Exhibit B Benefits Covered for TX
CHIP (Child Under 19)
This document contains proprietary and confidential information and may not be disclosed to others
without written permission. ©Copyright 2024. All rights reserved.
DentaQuest USA Insurance Company, Inc October 24, 2023, 2023
210
Oral and Maxillofacial Surgery
Code
Brief Description
Age
Limitation
Teeth Covered
Review
Required
Benefit Limitations
Documentation
Required
D7210
surgical removal of erupted
tooth requiring removal of
bone and/or sectioning of
tooth, and including
elevation of mucoperiosteal
flap if indicated
1 - 18
Teeth 1 - 32, 51
- 82, A - T, AS,
BS, CS, DS, ES,
FS, GS, HS, IS,
JS, KS, LS, MS,
NS, OS, PS, QS,
RS, SS, TS
Yes
blank
narr. of med. necessity,
pre-op x-ray(s)
D7220
removal of impacted tooth-
soft tissue
1 - 18
Teeth 1 - 32, 51
- 82, A - T, AS,
BS, CS, DS, ES,
FS, GS, HS, IS,
JS, KS, LS, MS,
NS, OS, PS, QS,
RS, SS, TS
Yes
blank
narr. of med. necessity,
pre-op x-ray(s)
D7230
removal of impacted tooth-
partially bony
1 - 18
Teeth 1 - 32, 51
- 82, A - T, AS,
BS, CS, DS, ES,
FS, GS, HS, IS,
JS, KS, LS, MS,
NS, OS, PS, QS,
RS, SS, TS
Yes
blank
narr. of med. necessity,
pre-op x-ray(s)
D7240
removal of impacted tooth-
completely bony
1 - 18
Teeth 1 - 32, 51
- 82, A - T, AS,
BS, CS, DS, ES,
FS, GS, HS, IS,
JS, KS, LS, MS,
NS, OS, PS, QS,
RS, SS, TS
Yes
blank
narr. of med. necessity,
pre-op x-ray(s)
Exhibit B Benefits Covered for TX
CHIP (Child Under 19)
This document contains proprietary and confidential information and may not be disclosed to others
without written permission. ©Copyright 2024. All rights reserved.
DentaQuest USA Insurance Company, Inc October 24, 2023, 2023
211
Exhibit B Benefits Covered for TX CHIP (Child Under 19)
"Please see Appendix A-7 for the Texas Orthodontia Review Policy for additional information on definitions, case levels, criteria and requirements for submission.
Any reimbursement already made for an inadequate service may be recouped after the DentaQuest Consultant reviews the circumstances."
Orthodontics
Code
Brief Description
Age
Limitation
Teeth Covered
Review
Required
Benefit Limitations
Documentation
Required
D8010
limited orthodontic
treatment of the primary
dentition
0-18
blank
Yes
Limited to pre- and post-surgical orthodontic services
to treat craniofacial anomalies requiring surgical
intervention.
blank
D8020
limited orthodontic
treatment of the
transitional dentition
0-18
blank
Yes
blank
blank
D8070
comprehensive orthodontic
treatment of the
transitional dentition
10-12
blank
Yes
Limit one service of (D8070, D8080, D8090) per
lifetime, per patient. No more than 22 adjustments
(D8670) allowed. Pre-authorization is required.
Models, pano, Cephalo,
photos
D8080
comprehensive orthodontic
treatment of the adolescent
dentition
12-18
blank
Yes
Limit one service of (D8070, D8080, D8090) per
lifetime, per patient. No more than 22 adjustments
(D8670) allowed. Pre-authorization is required.
Models, pano, Cephalo,
photos
D8090
comprehensive orthodontic
treatment of the adult
dentition
12-18
blank
Yes
Limit one service per lifetime, per patient. No more
than 48 adjustments (D8670) allowed. Pre-
authorization is required.
Models, pano, Cephalo,
photos
D8670
periodic orthodontic
treatment visit
10-18
blank
Yes
Limit one service per 21 days per patient. Pre-
authorization is required.
Models, pano, Cephalo,
photos
D8680
orthodontic retention
(removal of appliances)
10-18
blank
Yes
Limit one service per lifetime, per patient. Pre-
authorization is required.
Models, pano, Cephalo,
photos
