Despite AWP
Inflation Near 10%
CVS Health Kept
Drug Price Growth
Nearly Flat at 0.2%
and Adherence Improved
Drug Trend
Report
2017

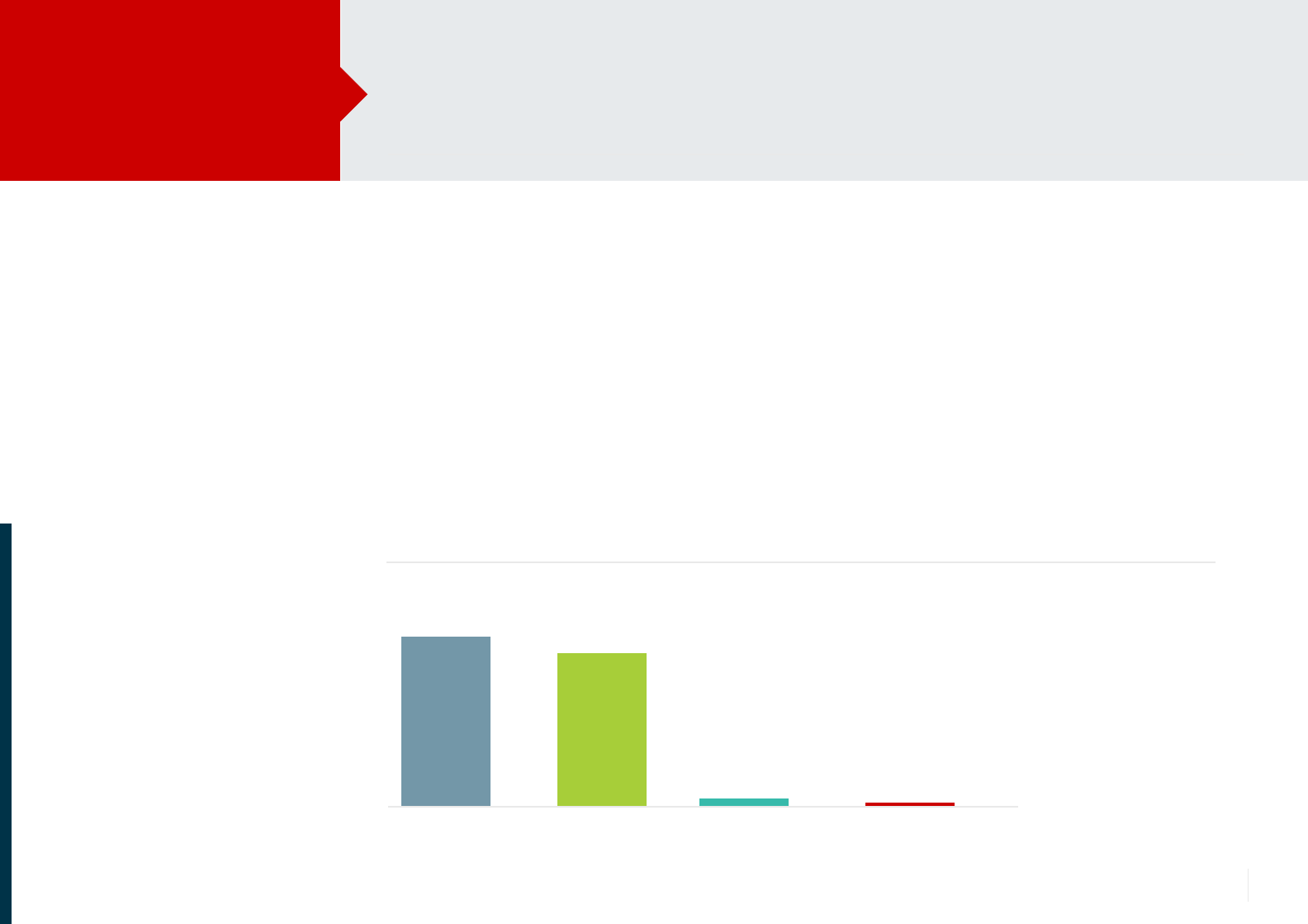
Hyperlipidemia 1.8
Hypertension 1.2
Diabetes 1.2
Out-of-pocket cost
PMPM declined
$11.99
$11.89
2016 2017
In 2018 we are doing even more
to help patients save money.
AWP (Average wholesale price). PMPM (Per member per month).
*Percentage point increase in the number of optimally adherent members.
Drug Trend
Report 2017
By the Numbers
2017 Trend: CVS Health 2
•
Increasing price transparency at all points of care
•
Giving members greater access to more affordable options
By keeping drugs
affordable, we also
helped more members
stay on therapy in
key categories*
We helped make
prescriptions
more affordable
for members
<$100 for their
prescriptions
3 of 4
members spent
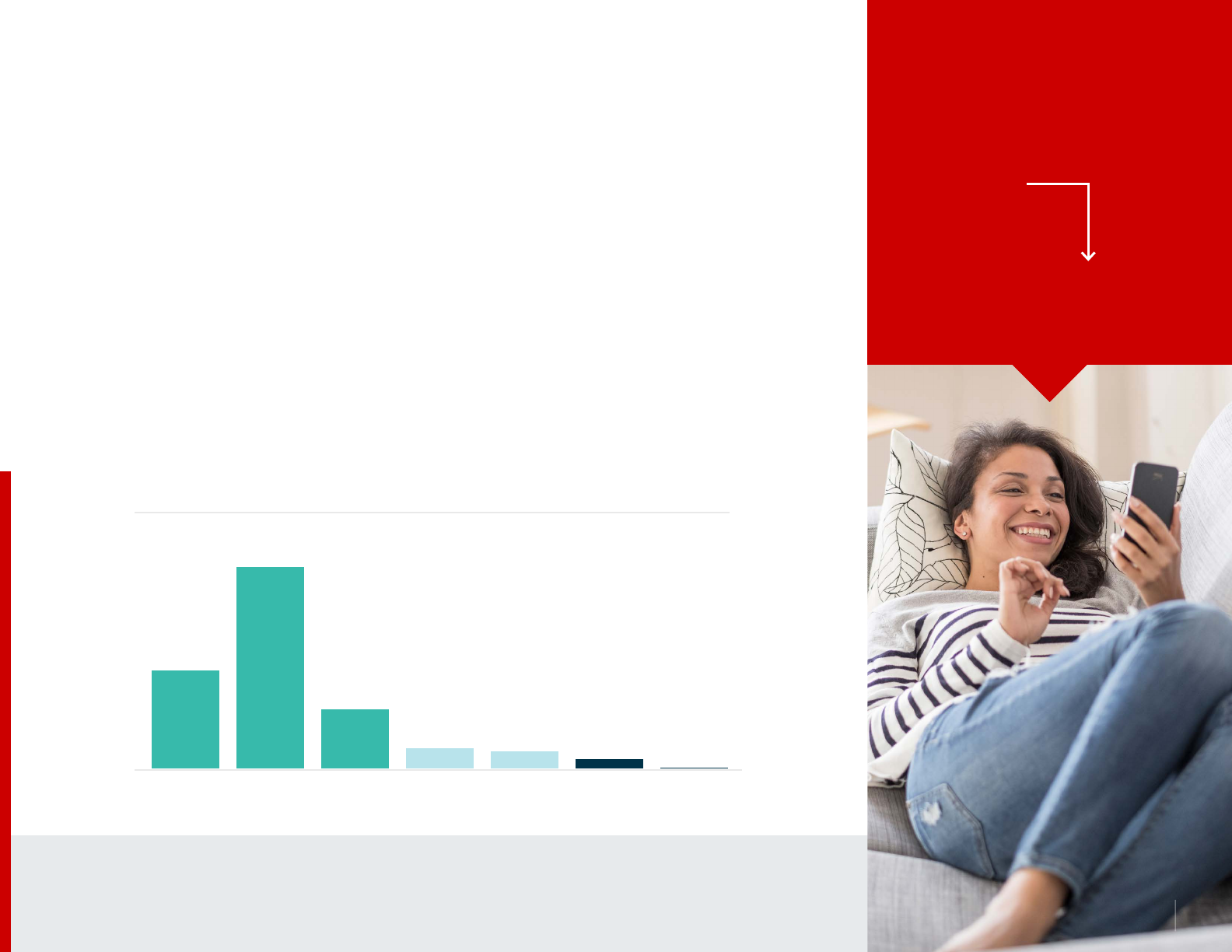
In 2017, despite
AWP ination ~10%
our strategies kept
drug price growth
nearly flat at 0.2%
9.2%
Traditional
Brands
8.3%
Specialty
Brands
0.4% 0.2%
Generics CVS Health
Drug Price Growth

The health care landscape continues to evolve, but the cost of drugs remains a top concern for payors and
consumers, and an area of focus for the government. At CVS Health, our goal is to ensure that clients and
members are getting the most out of their pharmacy benefit plan and that the cost of a drug is aligned with the
value it delivers in terms of patient outcomes. We leverage competition within drug classes where applicable,
develop innovative strategies to keep prescriptions affordable, and help members be more adherent.
In 2017, CVS Health pharmacy benefit management (PBM) strategies reduced trend for commercial clients to
1.9 percent per member per year (PMPY) the lowest in five years. Despite manufacturer price increases of near
10 percent, CVS Health kept drug price growth at a minimal 0.2 percent. Forty-two percent of our payor
clients spent less on their pharmacy benefit plan in 2017 than they had in 2016.
We also helped members save money and lower out-of-pocket costs. Three out of four members spent less than
$100 out of pocket in 2017, and nearly 90 percent spent less than $300. Monthly cost per member declined
by 10 cents to $11.89. To further enhance affordability and price transparency, we introduced real-time benefits
enabling prescribers to see the member-specific out-of-pocket costs of a prescribed medication as well as the
costs of clinically appropriate alternatives in real-time. This allows them to make more informed prescribing
decisions and offer members medication options that may be more affordable.
Keeping drugs affordable helped improve adherence to the highest level in seven years. With plan designs
that promoted lower-cost options and targeted adherence interventions, we increased the number of
optimally adherent members in key categories like diabetes, hypertension and hyperlipidemia by as much
as 1.8 percentage points. Better adherence can help reduce overall health care costs and improve quality of life.
In 2018, we are doing even more to help keep drugs affordable with our new Saving Patients Money initiative.
Saving Patients Money is designed to help address the high cost of prescription drugs by providing greater
pricing transparency across all points of care, including at the pharmacy, and directly to members.
CVS Health is delivering value for payors and their members with better
outcomes and cost management. It’s part of how we help people on their
path to better health.
It’s All About ValueDrug Trend
Report 2017
2017 Trend: CVS Health 3
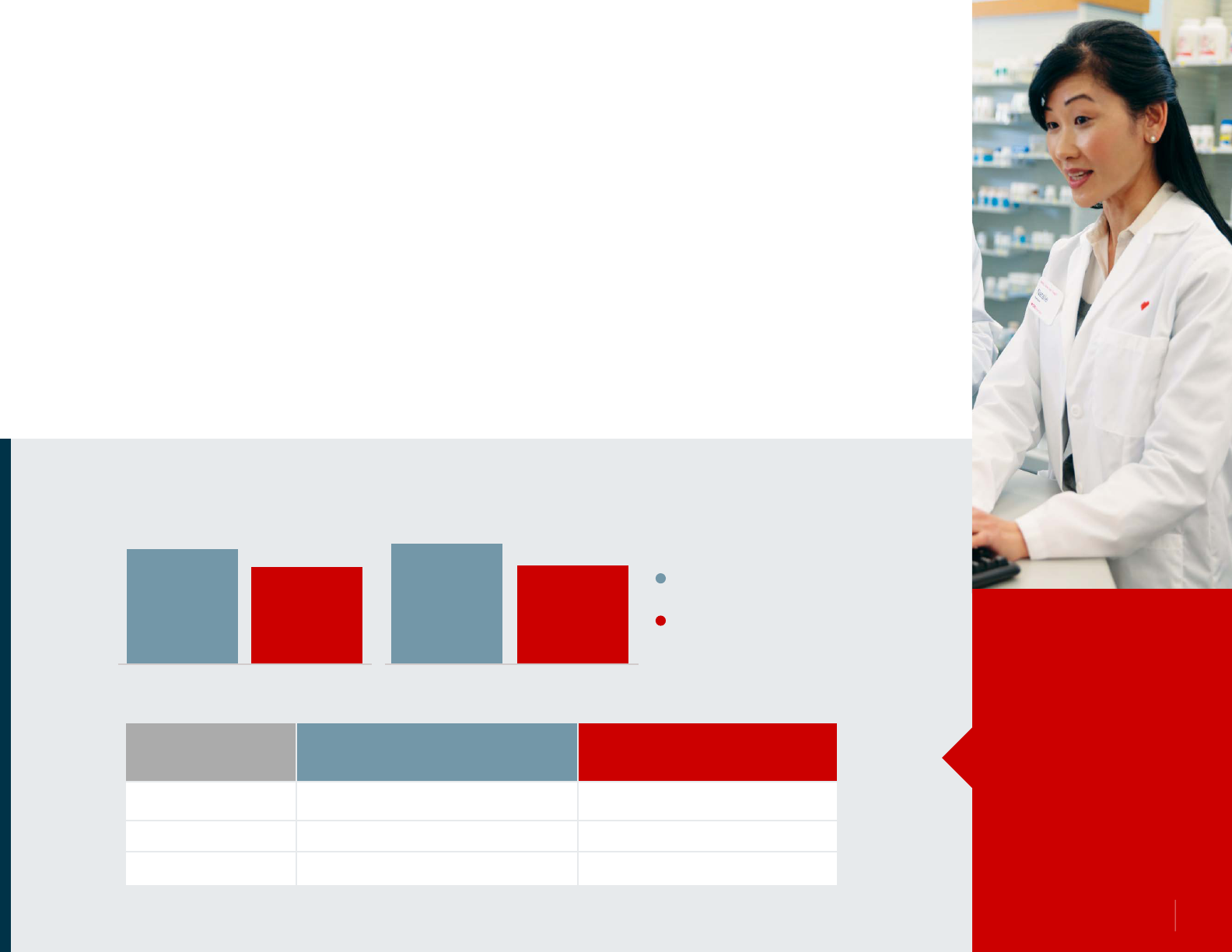
AWP Ination Near 10%, But Minimal Drug Price Growth
9.2%
Traditional
Brands
8.3%
Specialty
Brands
0.4% 0.2%
Generics CVS Health
Drug Price Growth
In 2017, we leveraged market competition, maximized use of low-cost generics, and effectively negotiated discounts and rebates,
all of which helped keep drug price growth nearly flat at 0.2 percent for our payor clients. Our strategies helped protect clients
from manufacturer price increases of almost 10 percent. By minimizing cost growth we were also able to reduce overall trend for
clients to 1.9 percent PMPY — the lowest in five years. Forty-two percent of our clients had negative trend; meaning their benefit
plan spent less in 2017 on prescription drugs than they had in 2016.
Many plans adopted generics first strategies or preventive drug lists with $0 copays for generics. Our generic dispensing rate
reached 86.1 percent, and played a significant role in keeping drug price growth down. Brand drugs, both traditional and specialty,
accounted for only 14 percent of prescriptions dispensed, but 69 percent of pharmaceutical spend.
1.7%
Utilization
Growth
+
=
0.2%
CVS Health
Drug Price Growth
1.9%
PMPY 2017
Drug Trend
Minimal drug price
growth helped reduce
trend to the lowest
level in five years.
Low Drug Price Growth and Trend Despite AWP Ination
Prescription drug trend is the measure of growth in
prescription spending per member per month. Trend
calculations take into account the effects of drug price,
drug utilization and the mix of branded versus generic
drugs, as well as the positive effect of negotiated rebates on
overall trend. The 2017 trend cohort represents CVS Health
commercial PBM clients—employers and health plans.
Price is measured as cost per days supply.
2017 Trend: CVS Health 4

Most of our post-rebate trend was driven by growth in utilization, trending at 1.7
percent. Generics played a major role in this utilization growth, helping keep overall as
well as member costs low. Generic utilization grew at 3.6 percent, while utilization of
brands dropped substantially — trending at a negative 9.5 percent.
Affordable generics, along with targeted adherence interventions, also helped increase
the percentage of members who were optimally adherent. Key chronic disease
categories, including hyperlipidemia, hypertension and diabetes, saw adherence
improvements. Preventive drug lists with $0 copays for generics, as well as formulary
strategies and plan designs that promoted the use of generics first, helped drive rapid
member transition to newly launched generics, reducing costs for high-utilization
categories such as antihypertensives and cholesterol-reducing drugs.
Utilization Grew, Adherence Improved
Affordable Generics Also
Helped Promote Adherence*
Hyperlipidemia 1.8
Hypertension 1.2
Diabetes 1.2
Generics Were Top Drivers of Utilization Growth
Ranked in order of contribution to 2017 utilization trend.
rosuvastatin calcium
atorvastatin calcium
ezetimibe
olmesartan medoxomil
metformin HCL
amlodipine besylate
losartan potassium
hyperlipidemia
hyperlipidemia
hyperlipidemia
hypertension
diabetes
hypertension
hypertension
Generic Reference Brand Used in Treating
Crestor
Lipitor
Zetia
Benicar
Glucophage, Glumetza
Norvasc
Cozaar
1
2
3
4
5
6
7
*Percentage point increase in number of optimally
adherent members.
2017 Trend: CVS Health 5

Strategic Management Kept Specialty Drug Price
Growth to 3.7% Despite AWP Ination of 8.3%
Specialty pharmaceuticals have expanded beyond the treatment of small populations and rare conditions to treat
conditions that affect millions of patients. Ongoing growth in utilization and manufacturer-driven price increases
continued to drive rapid growth in specialty spending making these therapies a top payor concern.
In 2017, the AWP inflation rate for specialty drugs was 8.3 percent. However, through effective formulary
strategies, indication- and outcomes-based contracting, and cost-cap based rebates we were able to keep
specialty drug cost growth for payors at just 3.7 percent. The specialty drug pipeline continues to be robust,
fueling further strong growth for years to come. Last year alone, the Food and Drug Administration (FDA) approved
67 new specialty drugs — including five biosimilars — and 69 supplemental specialty indications.
1
Hundreds
more new drugs are in development including therapies for conditions such as eczema, asthma, cancer, and
osteoarthritis. Most, if not all, are expected to carry annual price tags in the tens, if not hundreds, of thousands of
dollars. These new drugs, and supplemental indications for existing therapies, will continue to significantly expand
the population of specialty pharmaceutical users.
With the increase in number of specialty drugs, the growing population of patients on specialty therapies, and
ever-rising prices, careful management is required to help manage utilization of these complex therapies to ensure
that the right patient is receiving the right drug at the right time and that reimbursement is related to the value a
drug delivers. Ensuring high-touch, holistic patient support for optimal adherence, and symptom and co-morbidity
management are also key. Now, more than ever, payors need to have the right strategies in place to ensure
appropriate patient access and utilization.
Growth in appropriate utilization drove most of post-rebate specialty trend.
9.2%
Specialty
Utilization
+
=
3.7%
Drug Price
Growth
12.9%
2017 Specialty
Trend
2017 Trend: CVS Health 6

Market Competition Determines Management Approach
At 1.9 percent, our low 2017 trend reflects a strategic approach to the complex dynamics of the pharmaceutical market. We carefully
evaluate the pharmaceutical landscape to identify competitive therapy classes and compare drug efficacy, to determine appropriate
formulary placement for specific drugs for each condition. This enables us to effectively negotiate rebates and offer competitive
pricing to clients, to help keep overall costs in control.
• Categories with multiple brand and generic options
• Market competition limits price increases
• Use formulary, preventive drug lists to maximize utilization
of generics
• PBM management helped to improve adherence in these
categories by 1.8 (for antihyperlipidemics) and 1.2 (for
antihypertensives) percentage points
• Account for nearly 70% of cost and all cost and trend growth
• Specialty drugs tend to face less competition in their categories
• Manage formulary and leverage competition to negotiate for lowest-net cost
• For specialty: indication- and outcomes-based contracting, and cost-cap based rebates;
utilization management
• Gross trend for autoimmune was 25.5%
• Adherence improved by 1.2 (for antidiabetics) and 1.9 (for rheumatoid arthritis)
percentage points
Competitive Brand
Categories
Less Competitive
Categories
More Competitive Categories
Antihyperlipidemics
AWP Inflation:
Example Categories:
Antihypertensives Antidiabetics Autoimmune
1.9% 3% 4.9% 11.7%
-25.8%
-11.6%
1.4%
20.3%
Post-Rebate
Trend by
Category
Rebates and
competitive
pricing help
keep overall
costs in control.
.
More Competitive/Less Competitive
2017 Trend: CVS Health 7
Age-adjusted, post-rebate.
CVS Health Managed Formularies: Include Standard with Opt-In to Drug Removals, Advanced Control Formulary, and Template Value Formulary.
Drug Price Declined for Clients Aligned with
Our Formulary Management Strategy
Across our commercial cohort, management strategies helped keep drug price growth to a low 0.2 percent. For clients aligned with
our managed formularies, drug price actually declined — by 0.1 percent — in 2017. Despite greater utilization, these clients had lower
PMPM costs as well as overall trend.
Formulary is one of the most effective means of leveraging market competition and promoting the use of lower-cost options,
including generics. Our management approach includes a strategic assessment of the marketplace, allowing us to evaluate how
products compete in therapeutic categories and where it may be appropriate to remove specific products in categories with multiple
clinical options. This enables us to effectively negotiate rebates and offer competitive pricing to clients. We also continue to develop and
implement more targeted management approaches such as indication-based formularies, in which prices and rebates for a drug are
negotiated based on its effectiveness to treat a specific diagnosis rather than at a therapy class level.
Formulary Strategy Lowers Cost, Improves Utilization
Formularies with
drug removals did
not reduce utilization
but did cause drug
price to decline.
Utilization Trend
1.6% 1.8%
Drug Price Change
2.6% -0.1%
Overall Trend
4.2%
1.7%
2016-2017
Standard Formulary
without Drug Removals
Managed Formularies
with Drug Removals
$104.10
$108.42
$87.43
$88.94
2016 Gross Cost PMPM 2017 Gross Cost PMPM
Standard Formulary
without Drug Removals
Managed Formularies
with Drug Removals
2017 Trend: CVS Health 8

Lower Cost and Trend for Antidiabetics
Diabetes affects a huge portion of the U.S. population, and accounts for substantial health care as well as pharmacy
spend. Effectively managing diabetes with the appropriate medication regimen can help improve outcomes and
lower overall pharmacy as well as health care costs, but managing this complex drug category can be challenging.
Our formulary and utilization management options helped reduce cost for antidiabetic drugs for clients. Trend for the
category fell to just 1.4 percent.
Metformin, a biguanide, is the cornerstone of oral antidiabetic treatment and is available in various forms, as a
generic as well as a branded drug. Prices for both brand drugs and generics vary widely. Our management approach
focuses on encouraging the utilization of the most cost-effective choices, helping reduce cost per day’s supply for
metformin, and for the biguanide class overall.
The U.S. Food and Drug Administration approved the biosimilar Basaglar as safe and effective at improving glycemic
control late in 2015, followed by its launch in late 2016.
2
We were ahead of the industry in adopting Basaglar as the
preferred long-acting insulin, removing the branded products Lantus and Toujeo from our managed formularies.
This helped reduce costs for payors and for members. Preferred formulary placement for drugs with lower member
out-of-pocket costs also helped improve the number of optimally adherent members by 1.2 percentage points.
Higher adherence to diabetes medications can help significantly lower the risk for adverse events, and save money in
avoidable, downstream health care costs.
Reducing Cost Per Days Supply
DRUG TYPE 2016 2017 Decline
Biguanides $1.32 $1.05 -20.5%
Long-Acting Insulin $8.53 $6.51 -23.7%
In 2017, the antidiabetic
category trended at
1.4% PMPY despite
AWP inflation of 4.9%.
What’s more, adherence
increased.
2017 Trend: CVS Health 9
Reducing Trend for Autoimmune Therapies Through Targeted Management
The autoimmune category is one of the fastest growing therapy classes. Many autoimmune drugs — including Humira, the top-selling drug in the U.S., as well as
Enbrel, Stelara, and other specialty medications, rank among the highest cost therapies in the market today.
3
However, ensuring patients have access to the drugs they
need to effectively manage their condition helps improve health outcomes. Through our formulary and utilization management strategies, we have been able to ensure
appropriate utilization, while minimizing impact to payors’ overall drug spend.
Effectively managing the autoimmune class is complex. Many of these drugs have multiple indications, including rheumatoid arthritis, psoriasis, and Crohn’s disease.
Supplemental indications, as well as the aging of the population, contribute significantly to the ongoing growth in utilization. Given the serious nature of these
conditions, it is difficult — and potentially risky — to switch a patient who may be stable on a particular drug to a different brand or biosimilar. This means payors
continue to bear the burden of high-cost drugs even when more cost-effective alternatives may be available.
Pre-rebate trend for the category was 25.5 percent. Through targeted management, including indication-based pricing and rebates, we have been able to mitigate the
impact on payors, resulting in an overall trend of 20.3 percent, driven mostly by an 11.0 percent utilization increase.
We helped keep drug price growth under control by encouraging the use of generic drugs as first-line therapy through our utilization management programs.
Research has demonstrated that generics can equal biologics in effectiveness. Our indication-based formulary targets specific conditions and drugs for appropriate
management. That is, drugs that have shown particular efficacy for a specific indication receive preferred placement for that indication, thereby increasing competition
in the category.
By taking a strategic and targeted approach, we helped payors manage their spend for this high-impact category while supporting appropriate utilization and helping
improve member outcomes.
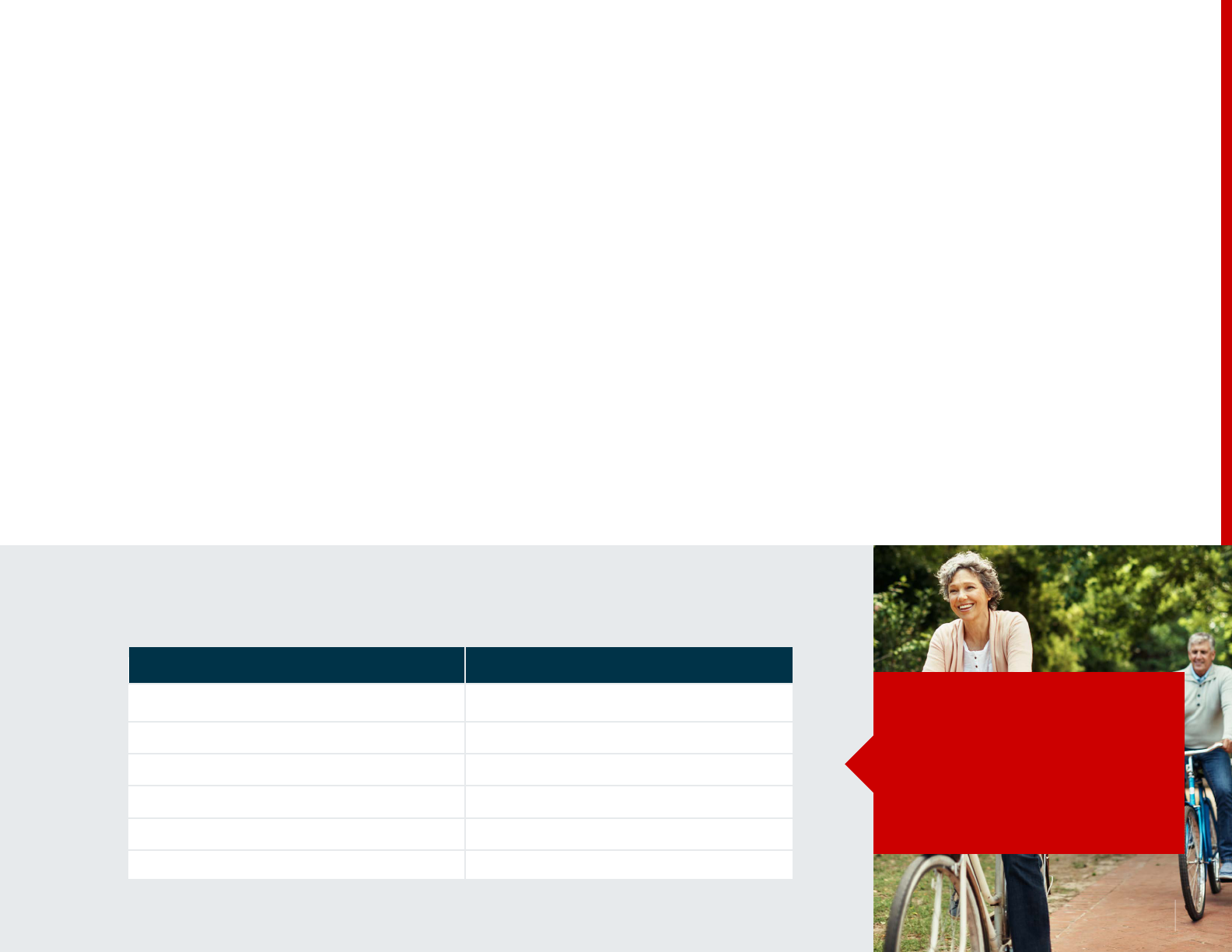
2018 Advanced Control Specialty Formulary:
Indication-Based Approach for Autoimmune Category
*After failure of Humira.
Contracting at the
indication level can
increase competitiveness
and add value for payors.
Ankylosing spondylitis
Crohn’s disease
Psoriasis
Psoriatic arthritis
Rheumatoid arthritis
Humira, Simponi*
Condition Formulary Preferred Products
Cosentyx, Enbrel, Humira
Cimzia*, Humira
Humira, Stelara*, Taltz*
Cosentyx, Enbrel, Humira, Otezia
Enbrel, Humira, Kevzara, Orencia
Ulcerative colitis
2017 Trend: CVS Health 10

Right drug the first time
• Management according to NCCN
regimen guideline vs. managing
the drug
• Incorporation of tumor genomics into
decision trees
Rigorous avoidance of waste
• Split lls for orals
• Partial vials for infused medications
• Site of care management
• Precise claims management
$8M Projected Annual Oncology
Savings per 1M Members
Specialty Management: Keeping Pace
with the Complexity of Oncology
Cancer treatment has changed dramatically. Rather than treating colon cancer or breast
cancer, we tailor treatment to the individual’s tumor and stage of disease. We’re at the
point of defining the cellular abnormalities in a tumor and guiding therapy based on those
abnormalities. This “precision medicine” is advancing rapidly. Guidelines from the National
Comprehensive Cancer Network (NCCN), considered the gold standard, change 500
times a year.
4
There are 60,000 different genetic testing products on the market, with 10
new tests added every day.
5
At CVS Specialty, our focus is to provide support to oncologists and patients ensuring
that all patients have the opportunity to receive the most current recommended regimens
as early as possible. Once the appropriate regimen is in place we diligently eliminate
waste, avoid the use of supportive agents where there is little clinical utility, and whenever
possible drive to the lowest-cost site of care.
The Novologix management platform enables these efforts. By analyzing prescribed
regimens across medical and pharmacy benefits we are able to ensure conformance with
NCCN guidelines and drive appropriate conversations with physicians when care is off-
guideline. The platform enables several approaches to limiting waste, from partial fills in
clinical scenarios where 30-day supplies often go unused, to paying for partial vials under
the medical benefit. The platform can help us ensure that any patient with any cancer,
regardless of how rare, has the opportunity to get the best possible care from the start,
no matter where they are being treated.
The Novologix platform will help ensure that any patient,
with any cancer, can receive the best possible care, no
matter where they are being treated.
2017 Trend: CVS Health 11
Members who spent over $1,000 were more likely to use specialty drugs
or be in high deductible health plans
88% of Members Spent Less Than
$300 Out-of-Pocket
Prescription affordability is an important issue for consumers, and for our nation, but data indicates that high
out-of-pocket costs affect relatively few members. Among our commercial clients, average member out-of-pocket
(OOP) cost declined in 2017. Primary credit for the decline goes to the increasing utilization of generics, spurred by
formulary and plan designs as well as preventive drug lists with $0 copays for generics.
Across our commercial trend cohort, 88 percent of members spent less than $300 out-of-pocket. Only 2.7 percent
spent over $1,000. These higher cost members tended to be older, use specialty drugs or were enrolled in high
deductible health plans (HDHPs). About 20 percent of our cohort members were in HDHPs, but they comprised 30
percent of those spending $1,000 or more.
Over a quarter of the money members spent went to two categories. Antidiabetics accounted for 14.7 percent of
member spend. Autoimmune agents, including specialty drugs such as Humira and Enbrel, accounted for 11.4 percent
of the cohort’s out-of-pocket expense.
Nearly 3 out of 4 Members Spent Less than $100 in 2017
49.4%
14.6%
5%
4.3%
2.4%
0.3%
24%
W/O Claims $0 – $100 $100 – $299 $500 – $999 $1000 – $3000 >$3000$300 – $499
This analysis is based on commercial member OOP spend and percentages are based on average eligible members in 2017.
Out-of-pocket
cost PMPM declined
$11.99
$11.89
2016
2017
2017 Trend: CVS Health 12

CVS Health: Saving Patients Money
In fall 2017, we announced the launch of real-time benefits, giving prescribers transparent access to member-specific
information. In 2018, we are expanding this capability to all points of care with the Savings Patients Money initiative.
During a provider visit: With real-time benefits, all of the information is integrated into the e-prescribing workflow
enabling prescribers to select a clinically appropriate medication that may be more affordable for the member. If the
selected drug has any restrictions, the prescriber can automatically submit an electronic PA (ePA) request, speeding
up the process and helping to avoid a disruption or delay of therapy.
At the pharmacy counter: CVS pharmacists have access to a Rx Savings Finder that lets them quickly and easily
determine the best way members can save money on out-of-pocket costs — with the primary goal of helping find the
lowest cost alternative under their pharmacy benefit. If the member’s prescription is not covered, the pharmacist is
alerted in their workflow and can request a prescription change from the provider at the click of a button.
On the go: Members can also use the Check Drug Cost tool in the CVS Caremark app and on Caremark.com to look
up drug costs, find if there are any lower-cost alternatives available, or learn how they can save by filling a 90-day
prescription rather than a 30-day supply. With this information, they can proactively start a conversation with their
provider or the pharmacist about their prescription options.
Real-time benefits further build on our connections with electronic health records, bringing the system closer to true,
seamless interoperability. It means prescribers, pharmacists and members have transparent access to information at
critical decision points to help members get the medications they need faster and more affordably.
Saving Patients Money at All Points of Care
We’ve made real-time benefit information available to prescribers, CVS pharmacists and to members via the
CVS Caremark app and on Caremark.com. The available information includes:
• Cost of a selected drug based on the member’s plan coverage, deductible, and how much of the deductible
the member has met
• Up to five clinically appropriate, potentially lower-cost therapeutic alternatives, mapped for clinical substitution
and specific to the member’s formulary
• Restrictions on the selected drug such as prior authorization (PA) or step therapy requirement
Today, CVS pharmacists
have access to member-
specific information,
including clinically
appropriate prescription
alternatives, built into
their workflow.
2017 Trend: CVS Health 13

1. New drug count includes new molecular entities, new biologics, biosimilars, new combinations, new formulations, projections by Pipeline Services, data 2017.
2. https://www.mdedge.com/clinicalendocrinologynews/article/105252/diabetes/lantus-competitor-basaglar-wins-fda-approval.
3. https://www.webmd.com/drug-medication/news/20171003/humira-again-top-selling-drug-in-us.
4. https://www.nccn.org/disclosures/transparency.aspx. Accessed February 2, 2018.
5. https://www.concertgenetics.com/resources/current-landscape-of-genetic-testing/. Accessed February 2, 2018.
Trend Methodology
This report provides an overview of performance for CVS Health commercial clients — employers and
health plans. Trend was calculated on a cohort of more than 1,400 clients, covering 24.5 million lives.
The cohort is built only on clients eligible throughout all of 2016 and 2017, removing commercial clients
with eligibility shifts exceeding 20% as well as any clients contractually prohibited from inclusion.
All of the savings and/or trend results discussed in this report will vary for specic populations based on a variety of factors, including demographics, plan design
and programs adopted by the client. Client-specic modeling available upon request.
This document includes references to brand-name prescription drugs that are trademarks of pharmaceutical manufacturers not associated with CVS Health.
Image source: Licensed from Getty Images, 2018.
Data source, unless noted otherwise, CVS Health Enterprise Analytics.
©2018 CVS Health. All rights reserved. 106-45365A 040518
2017 Trend: CVS Health 14
