
Hearing Hardware
1
Washington Apple Health (Medicaid)
Hearing Hardware
Billing Guide
January 1, 2019
Every effort has been made to ensure this guide’s accuracy. If an actual or apparent conflict between this
document and an agency rule arises, the agency rules apply.
Hearing Hardware
2
About this guide
∗
This publication takes effect January 1, 2019, and supersedes earlier billing guides to this
program.
The Health Care Authority (agency) is committed to providing equal access to our services. If
you need an accommodation or require documents in another format, please call 1-800-562-
3022. People who have hearing or speech disabilities, please call 711 for relay services.
Washington Apple Health means the public health insurance programs for eligible
Washington residents. Washington Apple Health is the name used in Washington
State for Medicaid, the children's health insurance program (CHIP), and state-
only funded health care programs. Washington Apple Health is administered by
the Washington State Health Care Authority.
Refer also to the agency’s ProviderOne billing and resource guide for valuable information to
help you conduct business with the agency.
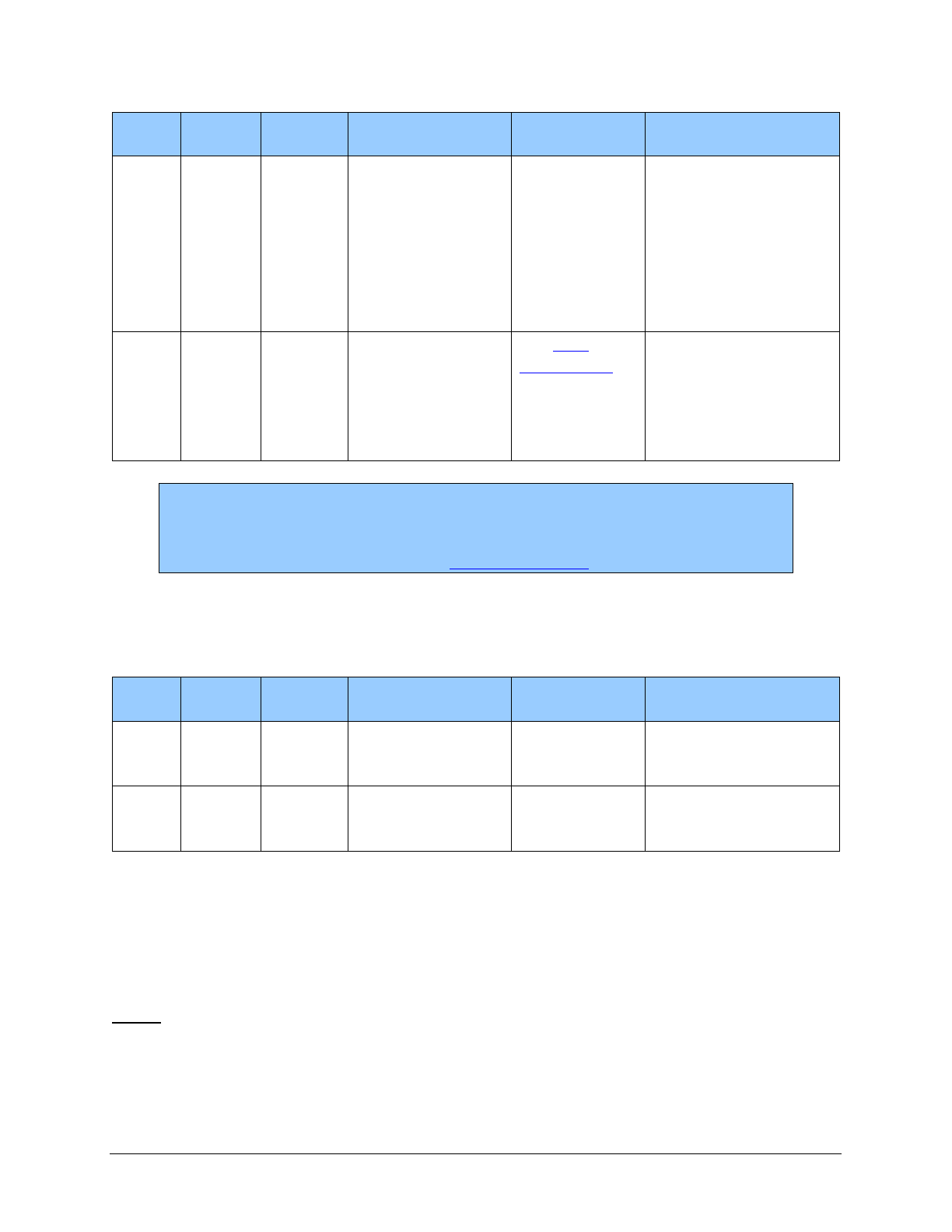
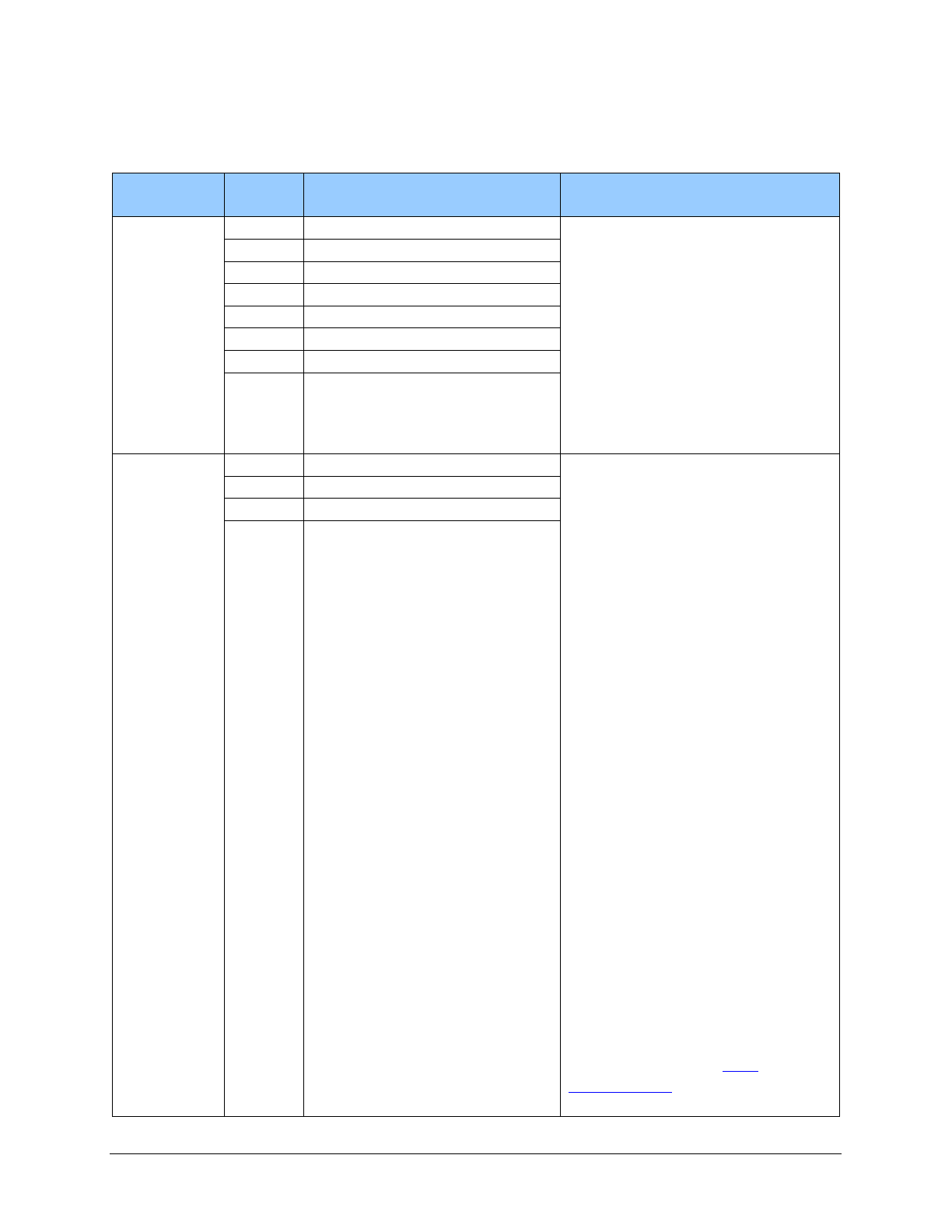
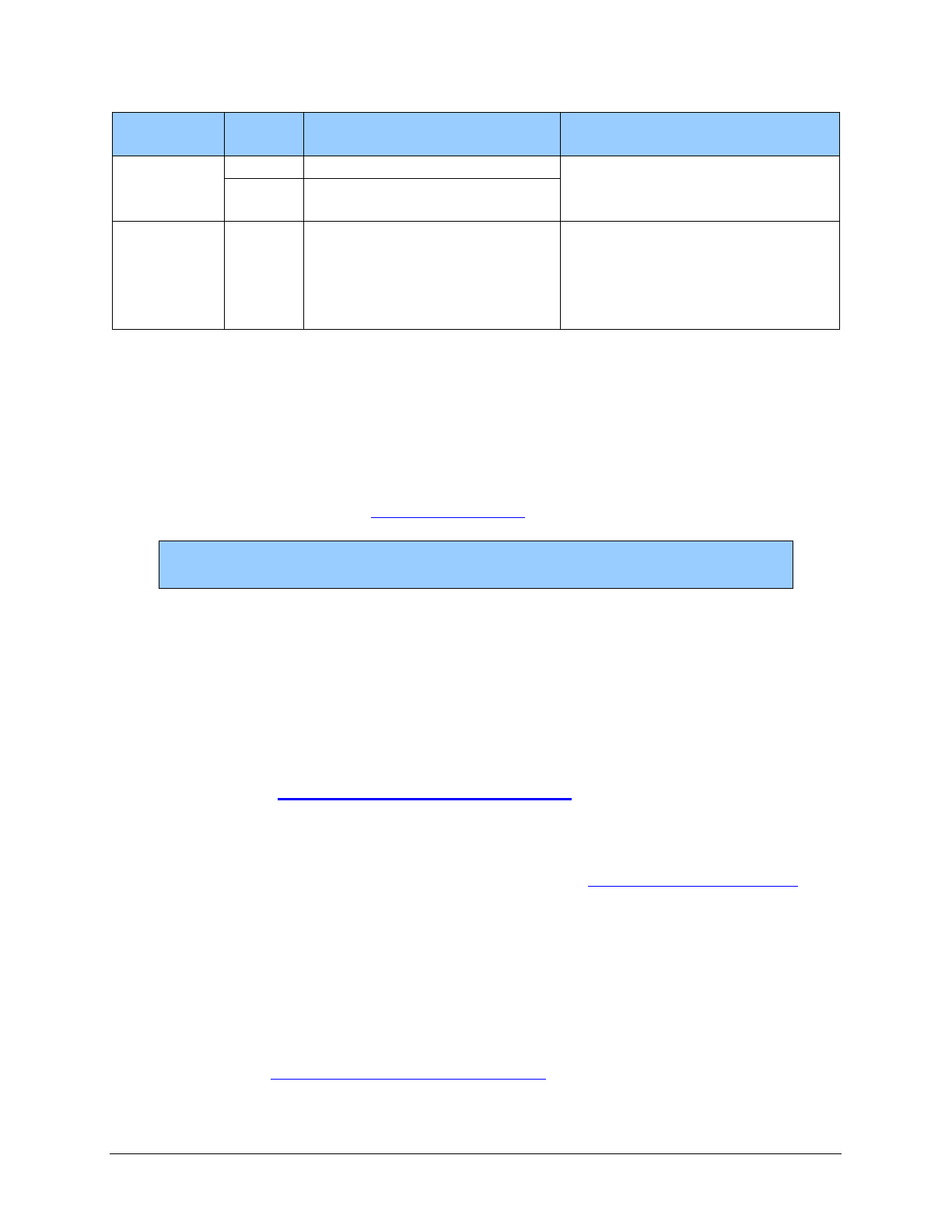
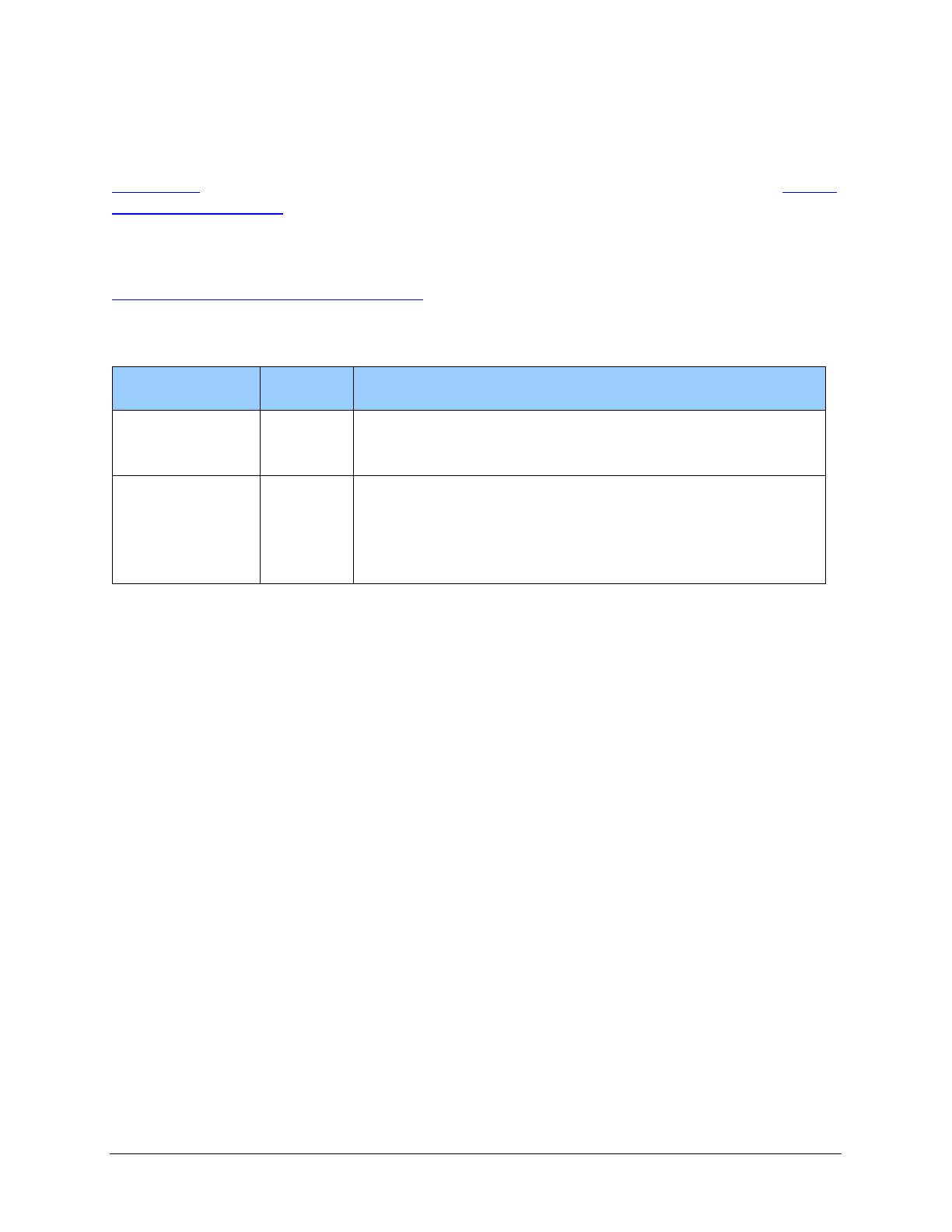
What has changed?
Subject
Change
Reason for Change
Entire Document
General housekeeping
To improve clarity and
usability
Client Eligibility:
BHO, Changes for
January 1, 2019,
IMC, and Integrated
Apple Health Foster
Care
Effective January 1, 2019, some existing
integrated managed care regions have new
counties, and many new regions and counties
will be implemented.
Apple Health managed
care organizations
(MCOs) in certain
RSAs will expand their
coverage of behavioral
health services (mental
health and substance
use disorder treatment),
along with continuing
to cover physical health
services.
Coverage table –
Children
Added HCPCS codes
To reflect current
policy
∗
This publication is a billing instruction.
Hearing Hardware
3
Subject
Change
Reason for Change
Coverage - Adults
Added entire section
To reflect the
restoration of coverage
of hearing instruments
for adults per
Engrossed Second
Substitute Bill (E2SSB)
5179
Coverage Table -
Adults
Added entire section
To reflect the
restoration of coverage
of hearing instruments
for adults per
Engrossed Second
Substitute Bill (E2SSB)
5179
Prior Authorization
- Adults
Added entire section
To reflect the
restoration of coverage
of hearing instruments
for adults per
Engrossed Second
Substitute Bill (E2SSB)
5179
Payment
Removed the Payment section. Moved
“Where can I find the Fee Schedule?” to the
Coverage section. Moved the blue note box to
What records must be kept in the client’s file?
To remove redundancy
and improve usability
Payment (DDA
Clients)
Removed the Payment (DDA Clients) section.
Moved “Where can I find the Fee Schedule?”
to the Coverage (DDA Clients) section.
Moved the blue note box to “What records
must be kept in the client’s file?”
To remove redundancy
and improve usability
How can I get agency provider documents?
To access provider alerts, go to the agency’s provider alerts webpage.
To access provider documents, go to the agency’s provider billing guides and fee schedules
webpage.
Hearing Hardware
4
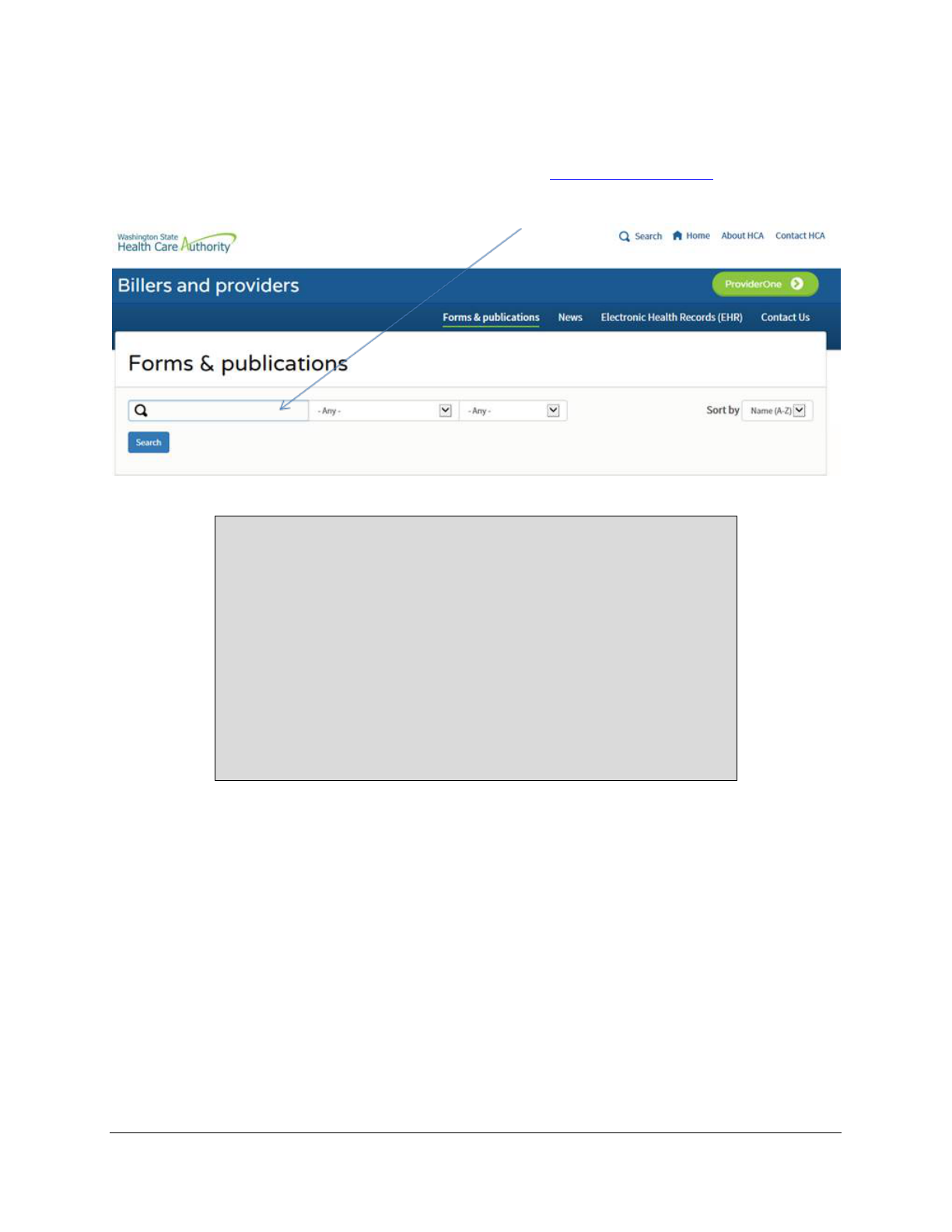
Where can I download agency forms?
To download an agency provider form, go to the agency’s Forms & publications webpage. Type
the agency’s form number into the Search box as shown below (Example: 13-835).
Copyright disclosure
Current Procedural Terminology (CPT) copyright 2018 American
Medical Association (AMA). All rights reserved. CPT is a
registered trademark of the AMA.
Fee schedules, relative value units, conversion factors and/or
related components are not assigned by the AMA, are not part of
CPT, and the AMA is not recommending their use. The AMA does
not directly or indirectly practice medicine or dispense medical
services. The AMA assumes no liability for data contained or not
contained herein.

Hearing Hardware
Alert! This Table of Contents is automated. Click on a page number to go directly to the page.
5
Table of Contents
About this guide .........................................................................................................................2
What has changed? ....................................................................................................................2
How can I get agency provider documents? ..............................................................................3
Where can I download agency forms? .......................................................................................4
Definitions .......................................................................................................................................8
About the Program ......................................................................................................................10
When does the agency pay for hearing aids? ...........................................................................10
Client Eligibility ...........................................................................................................................11
How do I verify a client’s eligibility? ......................................................................................11
Are clients enrolled in managed care eligible? ........................................................................12
Managed care enrollment ...................................................................................................12
Behavioral Health Organization (BHO) ............................................................................13
Apple Health – Changes for January 1, 2019 ....................................................................13
Integrated managed care ....................................................................................................14
Integrated managed care regions .......................................................................................15
Integrated Apple Health Foster Care (AHFC) ...................................................................15
Fee-for-service Apple Health Foster Care .........................................................................16
Coverage (for Children) ..............................................................................................................17
What is covered? ......................................................................................................................17
Monaural or binaural hearing aids .....................................................................................17
Cochlear implant – replacement parts ................................................................................18
What is not covered? ................................................................................................................19
Coverage Table (for Children) ...................................................................................................20
Coverage (for Adults) ..................................................................................................................22
What is covered? ......................................................................................................................22
Replacement .......................................................................................................................22
Repair of hearing aids ........................................................................................................22
Repair or replacement of external parts of cochlear devices and bone-anchored
hearing aids (BAHAs)..................................................................................................23
Rental of hearing aids ........................................................................................................23
Second hearing aid .............................................................................................................23
What is not covered? ................................................................................................................23
Coverage Table (for Adults) .......................................................................................................25
Monaural ..................................................................................................................................25
Binaural ....................................................................................................................................26
CROS/BiCROS ........................................................................................................................27
Other ........................................................................................................................................27

Hearing Hardware
Alert! This Table of Contents is automated. Click on a page number to go directly to the page.
6
Where can I find the fee schedule? ..........................................................................................29
Authorization (for Children) ......................................................................................................30
What is prior authorization (PA)? ............................................................................................30
Does the agency require prior authorization for hearing hardware? ........................................30
What is expedited prior authorization (EPA)? .........................................................................30
Replacement parts - EPA criteria .......................................................................................31
What documentation is required when requesting PA or ETR? ..............................................31
Prior Authorization (for Adults) ................................................................................................32
What is prior authorization (PA)? ............................................................................................32
What hearing hardware does the agency require prior authorization for? ...............................32
What is expedited prior authorization (EPA)? .........................................................................32
What documentation is required when requesting PA or ETR? ..............................................33
EPA criteria table .....................................................................................................................34
What are limitation extensions? ...............................................................................................35
How do I request a limitation extension? ................................................................................35
Billing ............................................................................................................................................36
What are the general billing requirements? .............................................................................36
What records must be kept in the client’s file? ........................................................................36
How do I bill claims electronically? ........................................................................................37
About the Program (for DDA Clients) .......................................................................................38
When does the Division of Developmental Disabilities (DDA) pay for hearing aids? ...........38
Client Eligibility (for DDA Clients) ............................................................................................39
How can I verify a client’s eligibility? ....................................................................................39
Coverage (for DDA Clients) ........................................................................................................40
What is covered? ......................................................................................................................40
Monaural or binaural hearing aids .....................................................................................40
Cochlear implant – replacement parts ................................................................................41
What is not covered? ................................................................................................................42
Coverage Table (for DDA clients) ...........................................................................................42
Where can I find the fee schedule? ..........................................................................................42
Authorization (for DDA Clients) ................................................................................................43
What is a social services authorization? ..................................................................................43
How do I request a social services authorization? ...................................................................43
How do I view a social services authorization? .......................................................................44
What happens after the social services authorization is approved? .........................................44
Billing (for DDA Clients) .............................................................................................................45
What are the general billing requirements? .............................................................................45

Hearing Hardware
Alert! This Table of Contents is automated. Click on a page number to go directly to the page.
7
What records must be kept in the client’s file? ........................................................................45
How do I bill claims electronically? ........................................................................................46
Hearing Hardware
8
Definitions
This section defines terms and abbreviations, including acronyms, used in this billing guide.
Refer to Chapter 182-500 WAC for a complete list of definitions for Washington Apple Health.
Bone-anchored hearing aid (BAHA) or
bone conduction hearing device – A type of
hearing aid that transmits sound vibrations
through bones in the head. The inner ear
translates the vibrations the same way a
normal ear translates sound waves. These
devices can be surgically implanted or worn
on headbands. (WAC 182-547-0200)
Cochlear implants – An electronic hearing
device designed to produce useful hearing
sensations to a person with severe to
profound deafness by electrically stimulating
nerves inside the inner ear. A cochlear
implant has a surgically implanted receiver
and electrode system in the inner ear and an
external microphone, sound processor, and
transmitter system. The external system may
be worn entirely behind the ear or its parts
may be worn in a pocket, belt pouch, or
harness. (WAC 182-547-0200)
Developmental Disabilities Administration
(DDA) – A division administration within the
Department of Social and Health Services.
DDA provides services to children and adults
with developmental disabilities.
Digital hearing aids – Wearable sound-
amplifying devices that use a digital circuit to
analyze and process sound.
(WAC 182-547-0200)
Hearing aids - Wearable sound-amplifying
devices that are intended to compensate for
hearing loss. Hearing aids are described by
where they are worn in the ear as in-the-ear
(ITE), behind-the-ear (BTE), etc. Hearing
aids can also be described by how they
process the amplified signal. This would
include analog conventional, analog
programmable, digital conventional, and
digital programmable. (WAC 182-547-0200)
Hearing health care professional – An
audiologist or hearing aid fitter/dispenser
licensed under Chapter 18.35 RCW, or an
otorhinolaryngologist or otologist licensed
under Chapter 18.71 RCW.
(WAC 182-547-0200)
Maximum allowable fee - The maximum
dollar amount that the agency will pay a
provider for specific services, supplies, and
equipment. (WAC 182-547-0200)
Prior authorization – A form of
authorization used by the provider to obtain
approval for a specific hearing aid and
service(s). The approval is based on medical
necessity and must be received before
service(s) are provided to clients as a
precondition for payment.
(WAC 182-547-0200)
Programmable hearing aids – Hearing
aids that can be “programmed” digitally by a
computer. All digital hearing aids are
programmable, but not all programmable
hearing aids are digital.
Hearing Hardware
9
Social Services Authorization – A form of
authorization used by the Department of
Social and Health Services to preauthorize
services. The approval is based on medical
necessity and client eligibility for the
program or service. A Social Services
Authorization can be viewed in
ProviderOne.
Usual & customary fee - The rate that may
be billed to the agency for a certain service
or equipment. This rate may not exceed
either of the following:
1) The usual and customary charge that you
bill the general public for the same
services
2) If the general public is not served, the
rate normally offered to other
contractors for the same services
Hearing Hardware
10
About the Program
When does the agency pay for hearing aids?
(WAC 182-547-0100)
The agency pays for hearing aids when they are:
• Covered.
• Within the scope of an eligible client's Benefit Package.
• Medically necessary.
• Authorized as required within this billing guide and Chapters 182-501 and 182-502
WAC.
• Billed according to this billing guide and Chapters 182-501 and 182-502 WAC.
• Provided to clients when all of the following are true. The clients:
Are eligible. (See Client Eligibility.)
Have received a hearing evaluation, including an audiogram or developmentally
appropriate diagnostic physiologic test, that is administered by and the results
interpreted by a hearing health care professional.
Received a recommendation by a licensed audiologist, hearing aid specialist,
otorhinolaryngologist, or otologist.
Meet the coverage criteria found in WAC 182-547-0850.
Note: For clients of the Developmental Disabilities Administration (DDA), refer
to the DDA section of this billing guide.
Hearing Hardware
11
Client Eligibility
Most Apple Health clients are enrolled in an agency-contracted managed care organization
(MCO). This means that Apple Health pays a monthly premium to an MCO for providing
preventative, primary, specialty, and other health services to Apple Health clients. Clients in
managed care must see only providers who are in their MCO’s provider network, unless prior
authorized or to treat urgent or emergent care. See the agency’s Apple Health managed care page
for further details.
It is important to always check a client’s eligibility prior to
providing any services because it affects who will pay for the services.
How do I verify a client’s eligibility?
Check the client’s Services Card or follow the two-step process below to verify that a client has
Apple Health coverage for the date of service and that the client’s benefit package covers the
applicable service. This helps prevent delivering a service the agency will not pay for.
Is the client enrolled in an agency-contracted managed care organization (MCO), in a behavioral
health organization (BHO), or is the client receiving services through fee-for-service (FFS)
Apple Health?
Verifying eligibility is a two-step process:
Step 1. Verify the patient’s eligibility for Apple Health. For detailed instructions on
verifying a patient’s eligibility for Apple Health, see the Client Eligibility, Benefit
Packages, and Coverage Limits section in the agency’s ProviderOne billing and
resource guide.
If the patient is eligible for Apple Health, proceed to Step 2. If the patient is not
eligible, see the note box below.
Step 2. Verify service coverage under the Apple Health client’s benefit package. To
determine if the requested service is a covered benefit under the Apple Health client’s
benefit package, see the agency’s Program benefit packages and scope of services
webpage.
Hearing Hardware
12
Note: Patients who are not Apple Health clients may submit an application for
health care coverage in one of the following ways:
1. By visiting the Washington Healthplanfinder’s website at:
www.wahealthplanfinder.org
2. By calling the Customer Support Center toll-free at: 855-WAFINDER
(855-923-4633) or 855-627-9604 (TTY)
3. By mailing the application to:
Washington Healthplanfinder
PO Box 946
Olympia, WA 98507
In-person application assistance is also available. To get information about in-
person application assistance available in their area, people may visit
www.wahealthplanfinder.org or call the Customer Support Center.
Are clients enrolled in managed care eligible?
(WAC 182-547-0700(2) and WAC 182-547-0750 (2))
Hearing aids are covered under agency-contracted managed care organizations (MCO).
Clients who are enrolled in an agency-contracted MCO are eligible for covered hearing aids. Bill
the MCO directly for these services. Additionally, clients enrolled in an agency-contracted MCO
must obtain replacement parts for cochlear implants and bone anchored hearing aids (Baha®),
including batteries, through their MCO.
Managed care enrollment
Apple Health (Medicaid) places clients into an agency-contracted MCO the same month they are
determined eligible for managed care as a new or renewing client. This eliminates a person being
placed temporarily in FFS while they are waiting to be enrolled in an MCO or reconnected with
a prior MCO. This enrollment policy also applies to clients in FFS who have a change in the
program they are eligible for.
New clients are those initially applying for benefits or those with changes in their existing
eligibility program that consequently make them eligible for Apple Health managed care.
Renewing clients are those who have been enrolled with an MCO but have had a break in
enrollment and have subsequently renewed their eligibility.

Hearing Hardware
13
Checking eligibility
• Providers must check eligibility and know when a client is enrolled and with which
MCO. For help with enrolling, clients can refer to the Washington Healthplanfinder’s Get
help enrolling page.
• MCOs have retroactive authorization and notification policies in place. The provider
must know the MCO’s requirements and be compliant with the MCO’s policies.
Behavioral Health Organization (BHO)
The Health Care Authority (agency) manages the contracts for behavioral health services (mental
health and substance use disorder) for the following four Regional Service Areas (RSAs):
• Great Rivers: Includes Cowlitz, Grays Harbor, Lewis, Pacific, and Wahkiakum counties
• North Sound: Includes Island, San Juan, Skagit, Snohomish, and Whatcom counties
• Salish: Includes Clallam, Jefferson, and Kitsap counties
• Thurston-Mason: Includes Thurston and Mason counties
To view a map and table of the integrated managed care plans available within each region,
please see Changes coming to Washington Apple Health. You may also refer to the agency’s
Apple Health managed care webpage.
See the agency’s Mental health services billing guide for details.
Apple Health – Changes for January 1, 2019
Effective January 1, 2019, agency-contracted managed care organizations (MCOs) in certain
Regional Services Areas (RSAs) will expand their coverage of behavioral health services (mental
health and substance use disorder treatment), along with continuing to cover physical health
services. The RSAs are outlined in the Integrated managed care regions section.
Apple Health clients who are not enrolled in an agency-contracted MCO for their physical health
services (e.g., dual-eligible Medicare-Medicaid clients) will still receive their behavioral health
services through one of the agency-contracted MCOs. The MCO will provide only behavioral
health services for the client.
Most clients will remain with the same health plan, except in regions where client’s plan will no
longer be available. The agency will auto-enroll these clients to one of the offered plans.
Hearing Hardware
14
Clients can change their plan at any time by:
• Visiting the ProviderOne client portal.
• Calling Apple Health Customer Service toll-free at 1-800-562-3022. This automated
system is available 24 hours a day, 7 days a week.
• Requesting a change online through our secure Contact us – Apple Health (Medicaid)
client web form. Select the topic “Enroll/Change Health Plans.”
• Visiting the Washington Healthplanfinder (only for clients with a Washington
Healthplanfinder account).
Integrated managed care
For clients who live in an integrated managed care region, all physical health services, mental
health services, and drug and alcohol treatment are covered and coordinated by the client’s
agency-contracted MCO. The BHO will not provide behavioral health services in these regions.
Clients living in an integrated managed care region will enroll with an MCO of their choice that
is available in that region. If the client does not choose an MCO, the client will be automatically
enrolled into one of the available MCOs, unless the client is American Indian/Alaska Native
(AI/AN). Clients currently enrolled in one of the available MCOs in their region may keep their
enrollment when the behavioral health services are added.
American Indian/Alaska Native (AI/AN) clients living in an integrated
managed care region of Washington may choose to enroll in one of the agency-
contracted MCOs available in that region or they may choose to receive all these
services through Apple Health fee-for-service (FFS). If they do not choose an
MCO, they will be automatically enrolled into Apple Health FFS for all their
health care services, including comprehensive behavioral health services. See the
agency’s American Indian/Alaska Native webpage.
For more information about the services available under the FFS program, see the
agency’s Mental health services billing guide and the Substance use disorder
billing guide.
For full details on integrated managed care, see the agency’s Changes to Apple Health managed
care webpage.
Hearing Hardware
15
Integrated managed care regions
Clients who reside in the following integrated managed care regions and who are eligible for
managed care enrollment must choose an available MCO in their region. Details, including
information about mental health crisis services, are located on the agency’s Apple Health
managed care webpage.
Existing integrated managed care regions – Expanding January 1, 2019
• North Central (Chelan, Douglas, Grant, and Okanogan counties)
The agency expanded this region to include Okanogan County
• Southwest Washington (Clark, Klickitat, and Skamania counties)
The agency expanded this region to include Klickitat County
New integrated managed care regions – Effective January 1, 2019
The following new regions are implemented for integrated managed care:
• Greater Columbia (Asotin, Benton, Columbia, Franklin, Garfield, Kittitas, Walla
Walla, Yakima, and Whitman counties)
• King (King County)
• Pierce (Pierce County)
• Spokane (Adams, Ferry, Lincoln, Pend Oreille, Spokane, and Stevens counties)
Integrated Apple Health Foster Care (AHFC)
Effective January 1, 2019, children and young adults in the Foster Care, Adoption Support and
Alumni programs who are enrolled in Coordinated Care of Washington’s (CCW) Apple Health
Foster Care program will receive both medical and behavioral health services from CCW.
Clients under this program are:
• Under the age of 21 who are in foster care (out of home placement).
• Under the age of 21 who are receiving adoption support.
• Age 18-21 years old in extended foster care.
• Age 18 to 26 years old who aged out of foster care on or after their 18
th
birthday (alumni).
These clients are identified in ProviderOne as
“Coordinated Care Healthy Options Foster Care.”
Hearing Hardware
16
Fee-for-service Apple Health Foster Care
Children and young adults in the fee-for-service Apple Health Foster Care, Adoption Support and
Alumni programs receive behavioral health services through the regional Behavioral Health
Administrative Services Organization (BH-ASO). For details, see the agency’s Mental health
services billing guide, under How do providers identify the correct payer?
Hearing Hardware
17
Coverage (for Children)
What is covered?
(WAC 182-547-0800)
Monaural or binaural hearing aids
The agency covers new, nonrefurbished, monaural or binaural hearing aid(s), which includes the
ear mold and batteries, for eligible clients age 20 and younger. In order for the provider to
receive payment, the hearing aid must meet the client's specific hearing needs and be under
warranty for a minimum of one year.
See the Social service blanket codes for specific procedure codes.
Replacement
The agency pays for the following replacements as long as the need for replacements is not due
to the client’s carelessness, negligence, recklessness, or misuse in accordance with WAC 182-
501-0050(8):
• Hearing aid(s), which includes the ear mold, when all warranties are expired and the
hearing aid(s) are one of the following:
Lost
Beyond repair
Not sufficient for the client's hearing loss
• Ear mold(s) when the client's existing ear mold is damaged or no longer fits the client's
ear
• Batteries with a valid prescription from an audiologist
Repair
The agency pays for a maximum of two repairs, per hearing aid, per year, when the repair is less
than 50% of the cost of a new hearing aid. To receive payment, all the following must be met:
• All warranties are expired.
• The repair is under warranty for a minimum of 90 days.
Hearing Hardware
18
Rental
The agency pays for a rental hearing aid(s) for up to two months while the client's own hearing
aid is being repaired. In the case of a rental hearing aid(s), the agency pays separately for an ear
mold(s).
Cochlear implant – replacement parts
(WAC 182-547-0800 (3))
The agency covers:
• Cochlear implant external speech processors, including maintenance, repair, and
batteries.
• Baha® speech processors, including maintenance, repair, and batteries.
See the Coverage Table for specific procedure codes.
The agency pays for cochlear implant and Baha® replacement parts when:
• The manufacturer's warranty has expired.
• The part is for immediate use, not a back-up part.
• The part needs to be replaced due to normal wear and tear and is not related to misuse or
abuse of the item (see WAC 182-502-0160).
The client must pay for repairs to additional speech processors and parts.
When reimbursing for battery packs, the agency covers the least costly, equally effective
product.
Note: The agency does not pay providers for repairs or replacements that are
covered under the manufacturer’s warranty.
The agency will reimburse only those vendors with a current Core Provider Agreement. If the
cochlear implant device is provided by a vendor without a current Core Provider Agreement,
replacement parts, accessories, and repairs for these devices may or may not be covered. See
WAC 182-502-0005.
See What is expedited prior authorization (EPA)? for EPA codes and clinical criteria for billing
for replacement parts using the EPA process.
Hearing Hardware
19
What is not covered?
(WAC 182-547-0900)
The agency does not cover the following hearing and hearing aid-related items and services for
clients age 20 and younger:
• Tinnitus maskers
• Group screenings for hearing loss, except as provided under the Early and Periodic
Screening, Diagnosis and Treatment (EPSDT) program (refer to the agency’s Early and
periodic screening, diagnosis and treatment (EPSDT) program billing guide)
• FM systems, including the computer-aided hearing devices for FM systems
When EPSDT applies, the agency evaluates a noncovered service, equipment, or supply
according to the process in WAC 182-501-0165 to determine if it is medically necessary, safe,
effective, and not experimental. See WAC 182-534-0100 for EPSDT rules.
Exception to Rule (ETR)
The agency evaluates a request for medical services, equipment, and/or supplies that are listed as
noncovered under the provisions of WAC 182-501-0160 that relates to noncovered services. The
request for a noncovered medical service, equipment, or supply is called a “request for an
exception to rule.” See WAC 182-501-0160 for information about exception to rule (ETR).
To request an ETR, see What documentation is required when requesting a PA or ETR?
Hearing Hardware
20
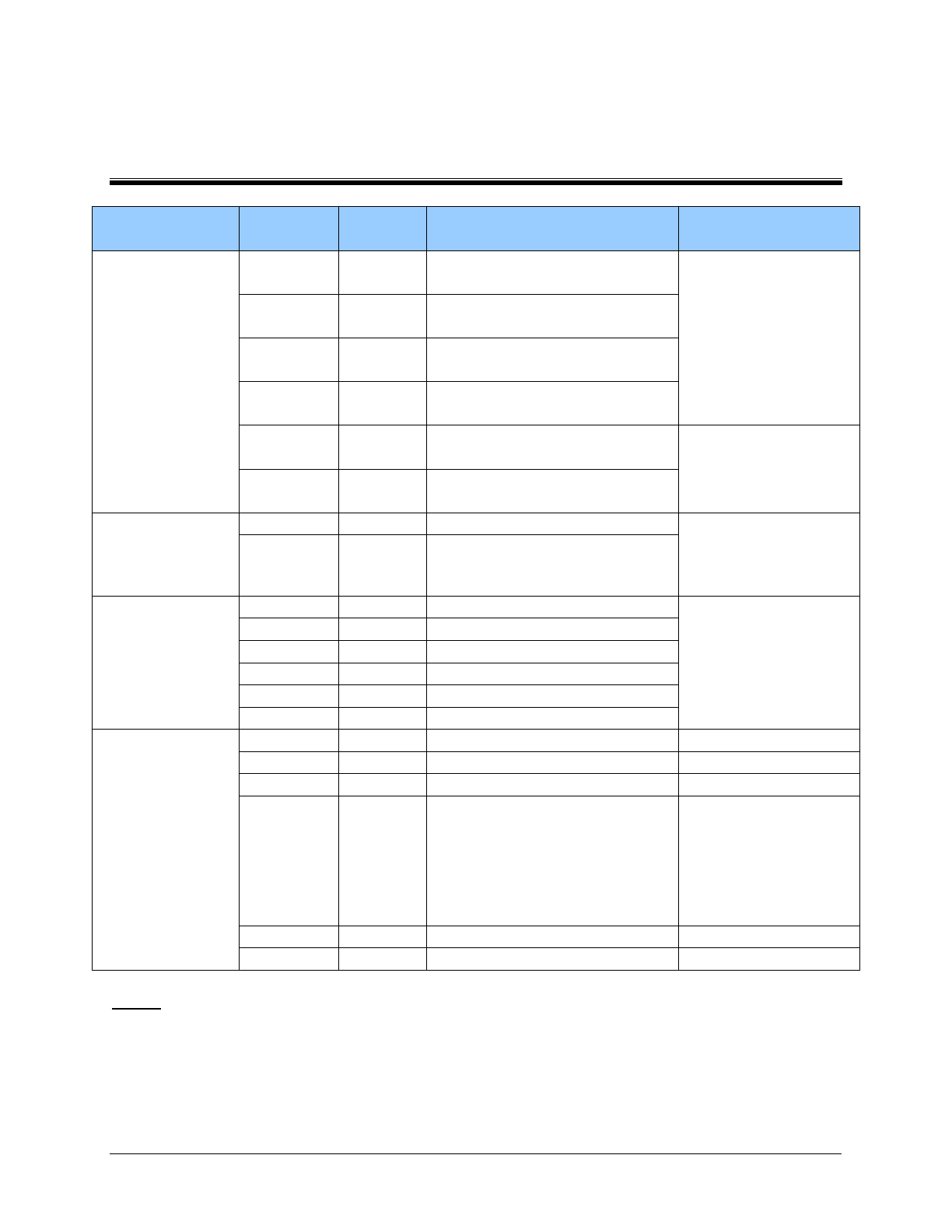
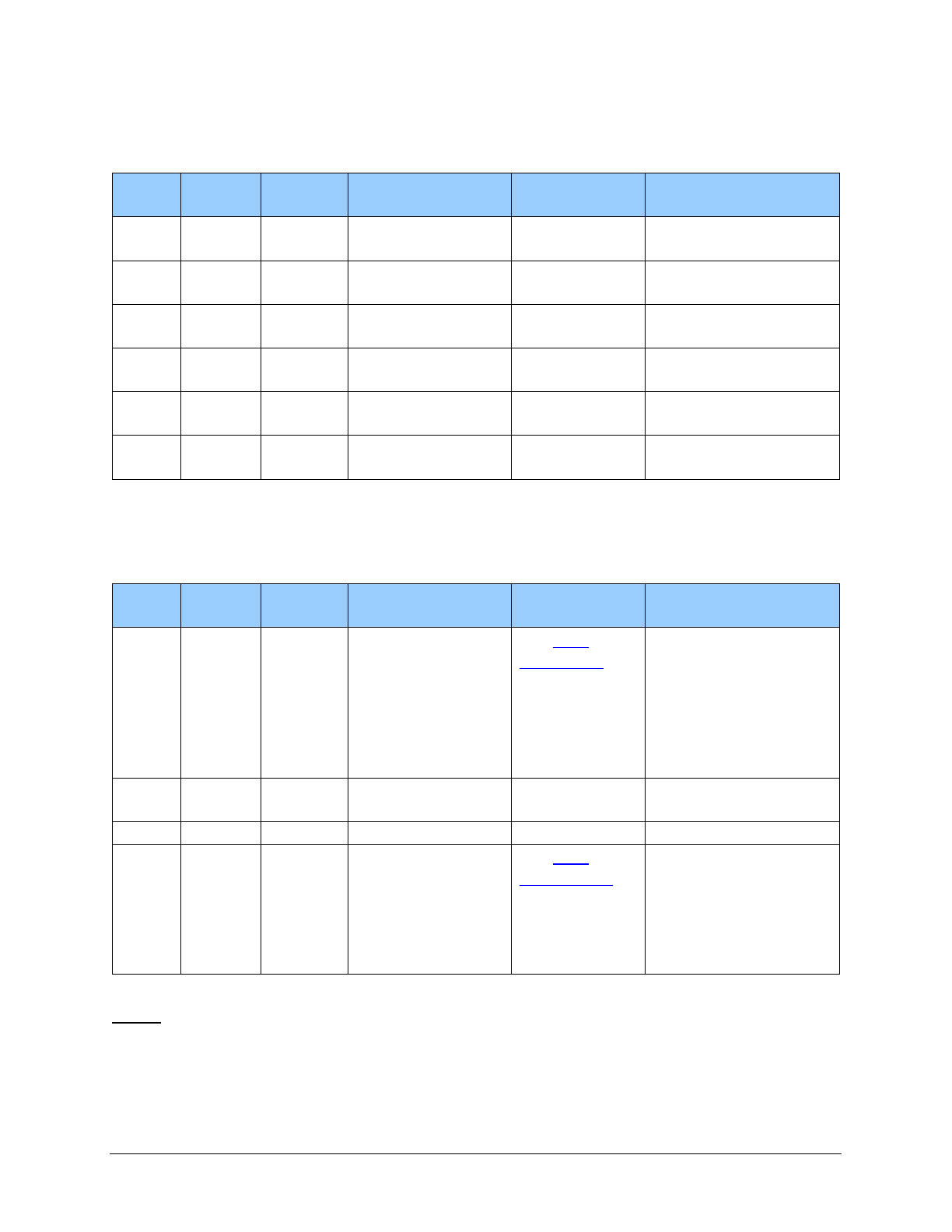
Coverage Table (for Children)
Procedure
Code
Modifier Short Description Policy Comments
Monaural
V5246
LT, RT,
RA
Hearing aid, prog, mon, ite
Includes a prefitting
evaluation, an ear
mold and at least 3
follow-up
appointments.
V5247
LT, RT,
RA
Hearing aid, prog, mon, bte
V5256
LT, RT,
RA
Hearing aid, digit, mon, ite
V5257
LT, RT,
RA
Hearing aid, digit, mon, bte
V5050
LT, RT,
RA, RR
Hearing aid monaural in ear
Invoice required.
V5060
LT, RT,
RA, RR
Behind ear hearing aid
Binaural
V5260
RA
Hearing aid, digit, bin, ite
Do not bill in
conjunction with a
monaural hearing aid.
V5261 RA Hearing aid, digit, bin, bte
CROS/BiCROS
V5171
Hearing aid monaural ite
Invoice required.
V5181
Hearing aid monaural bte
V5211
Hearing aid binaural ite/ite
V5213
Hearing aid binaural ite/bte
V5215
Hearing aid binaural itc/bte
V5221
Hearing aid binaural bte/bte
Other
V5040
Body-worn hearing aid bone
V5264
RA
Ear mold/insert
Replacement only.
V5275
RA
Ear impression, each
Replacement only.
V5014
RT, LT,
RB (for
casing)
Hearing aid repair/modifying
Used when billing for
repair of a hearing
aid. Maximum of 2
repairs in 1 year.
(Includes parts and
labor)
V5266
Battery for hearing device
V5298
Hearing aid noc
PA/invoice required.
Legend
Modifiers: RA = Replacement of DME Item
RB = Replacement Part of DME Item
LT = Left
RT = Right
RR = Rental
Hearing Hardware
21
Note: Reimbursement for all hearing instruments dispensed includes all of the
following:
• A prefitting evaluation
• An ear mold
• A minimum of three post-fitting consultations
HCPCS
Code
Short Description
PA?
Policy
L7510
Prosthetic device repair rep
PA
L8615
Coch implant headset replace
Use EPA #870000001.
If client does not meet
EPA clinical criteria,
PA is required.
L8616
Coch implant microphone repl
L8617
Coch implant trans coil repl
L8618
Coch implant tran cable repl
L8619
Coch imp ext proc/contr rplc
PA
PA
L8621
Repl zinc air battery
Use EPA #870000001.
If client does not meet
EPA clinical criteria,
PA is required.
L8622
Repl alkaline battery
L8623
Lith ion batt CID,non-earlvl
L8624
Lith ion batt CID, ear level
L8625
Charger coch impl/aoi battry
PA
Replacement
only, each
L8627
CID ext speech process repl
PA
L8628
CID ext controller repl
PA
L8629
CID transmit coil and cable
PA
L8691
Osseointegrated snd proc rpl
PA
L8692
Non-osseointegrated snd proc
PA
L8693
Aud osseo dev, abutment
PA
Replacement
only, each
L8694
Aoi transducer/actuator repl
PA
Replacement
only, each
L9900
O&P supply/accessory/service
PA
Legend
EPA: Expedited Prior Authorization
PA: Prior Authorization required
Hearing Hardware
22
Coverage (for Adults)
To receive payment from the Health Care Authority (agency) for providing hearing hardware to
clients age 21 and older, clients must meet the eligibility and criteria stated in this billing guide.
What is covered? (WAC 182-547-0850)
For clients age 21 and older, the agency covers the following:
• Nonrefurbished, monaural hearing aids. The agency covers one new nonrefurbished
monaural hearing aid, which includes the ear mold, every 5 years. The client must have
an average decibel loss of 45 or greater in the better ear, based on a pure-tone
audiometric evaluation by a licensed audiologist or a licensed hearing aid specialist at
1000, 2000, 3000, and 4000 Hertz (Hz) with effective masking as indicated. The hearing
aid must meet the client’s specific hearing needs and carry a manufacturer’s warranty for
a minimum of one year.
• Binaural hearing aids. The agency covers binaural hearing aids. Prior authorization
(PA) is required. See Prior Authorization - Adults for more details.
Replacement
The agency covers the following replacements only if the need for the replacement is not due to
the client’s carelessness, negligence, recklessness, deliberate intent, or misuse under WAC 182-
501-0050:
• One replacement hearing aid, including the ear mold, in a 5-year period when the client’s
hearing aid(s) is lost or broken and cannot be repaired, and the warranty is expired
• One replacement ear mold, per year when the client’s existing ear mold is damaged or no
longer fits the client’s ear
Repair of hearing aids
The agency covers two repairs, per hearing aid, per year, when the cost of the repair is less than
50% of the cost of a new hearing aid. To receive payment, all warranties must have expired and
the repair is under warranty for a minimum of 90 days.
Hearing Hardware
23
Repair or replacement of external parts of cochlear devices
and bone-anchored hearing aids (BAHAs)
The agency covers the following:
• Repair or replacement of external parts of cochlear devices. If the client has bilateral
cochlear devices, both devices are eligible for repair and replacement of external parts.
• Repair or replacement of external parts of BAHAs, whether implanted or worn with a
headband. If the client has bilateral BAHAs, both devices are eligible for repair and
replacement of external parts.
PA is required. See the Coverage Table for specific procedure codes.
Rental of hearing aids
The agency covers the rental of hearing aid(s) for up to 2 months while the client’s own hearing
aid(s) is being repaired. For rental hearing aid(s) only, the agency pays separately for an ear mold(s).
Second hearing aid
The agency covers a second hearing aid. PA is required. When the client meets the specific
clinical criteria, providers may use the EPA process. If the client does not meet the specific
clinical criteria, but a second hearing aid is medically necessary, providers may request PA.
Note: Auditory rehabilitation may be covered under other programs. Clients may
be referred to an audiologist or speech language pathologist to determine the
medical necessity of auditory rehabilitation. See the Physician-related services
billing guide and the Outpatient rehabilitation billing guide for details.
What is not covered? (WAC 182-547-0950)
The agency does not cover the following items for clients age 21 and older:
• Batteries
• Tinnitus maskers
• Frequency Modulation (FM) systems, including the computer-aided hearing devices for
FM systems
Hearing Hardware
24
• Nonprescription hearing aids or similar devices including, but not limited to, the
following:
Personal sound amplification products (PSAPs)
Hearables
Pocket talkers or similar devices
Exception to Rule (ETR)
The agency evaluates a request for medical services, equipment, and supplies that are listed as
noncovered under the provisions of WAC 182-501-0160 that relates to noncovered services. The
request for a noncovered medical service, equipment, or supply is called a “request for an
exception to rule.” See WAC 182-501-0160 for information about exception to rule.
See What documentation is required when requesting PA or ETR? for details on submitting
requests for ETR.
(See Where can I download agency forms?)
Hearing Hardware
Legend
Modifiers: RA = Replacement of DME Item
RB = Replacement Part of DME Item
LT = Left
RT = Right
RR = Rental
25
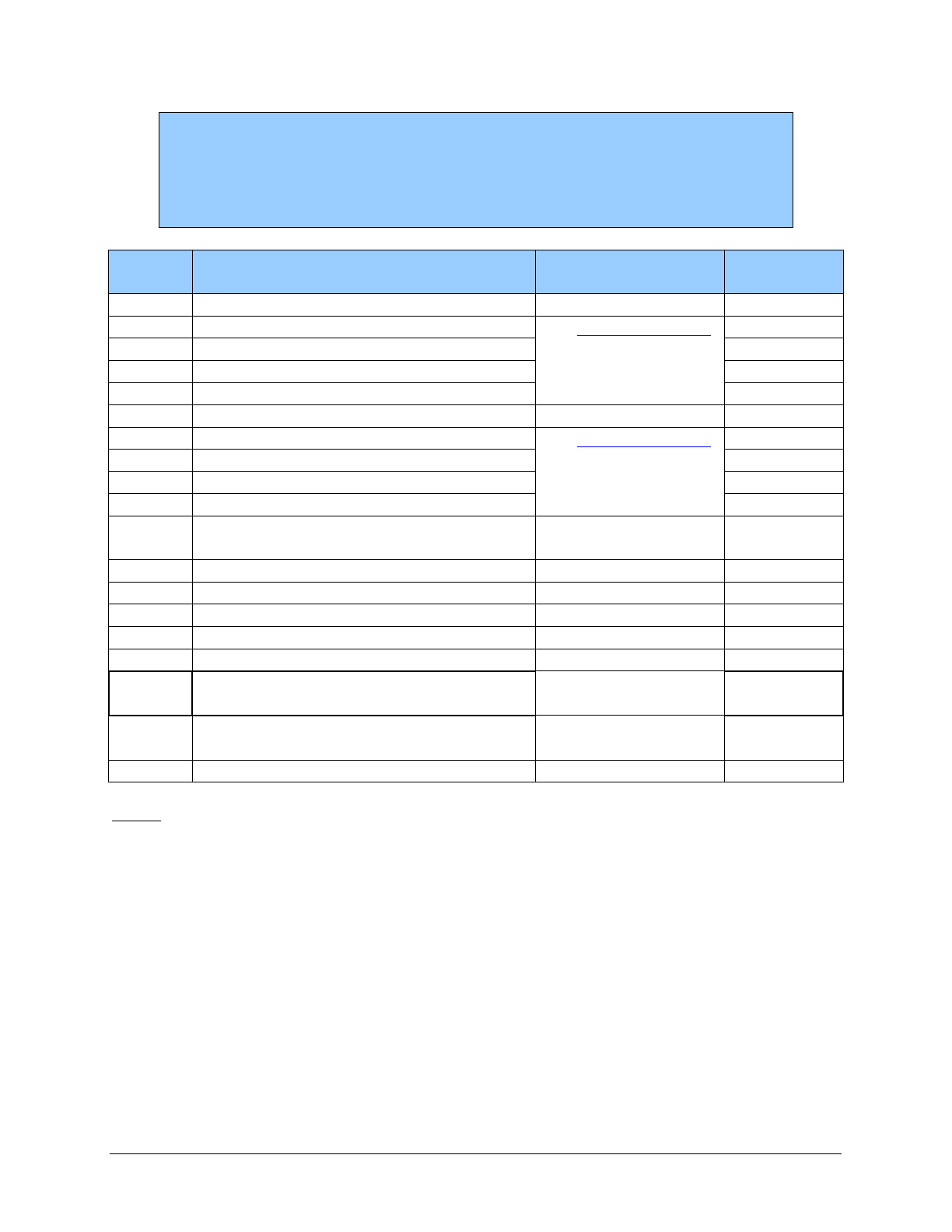
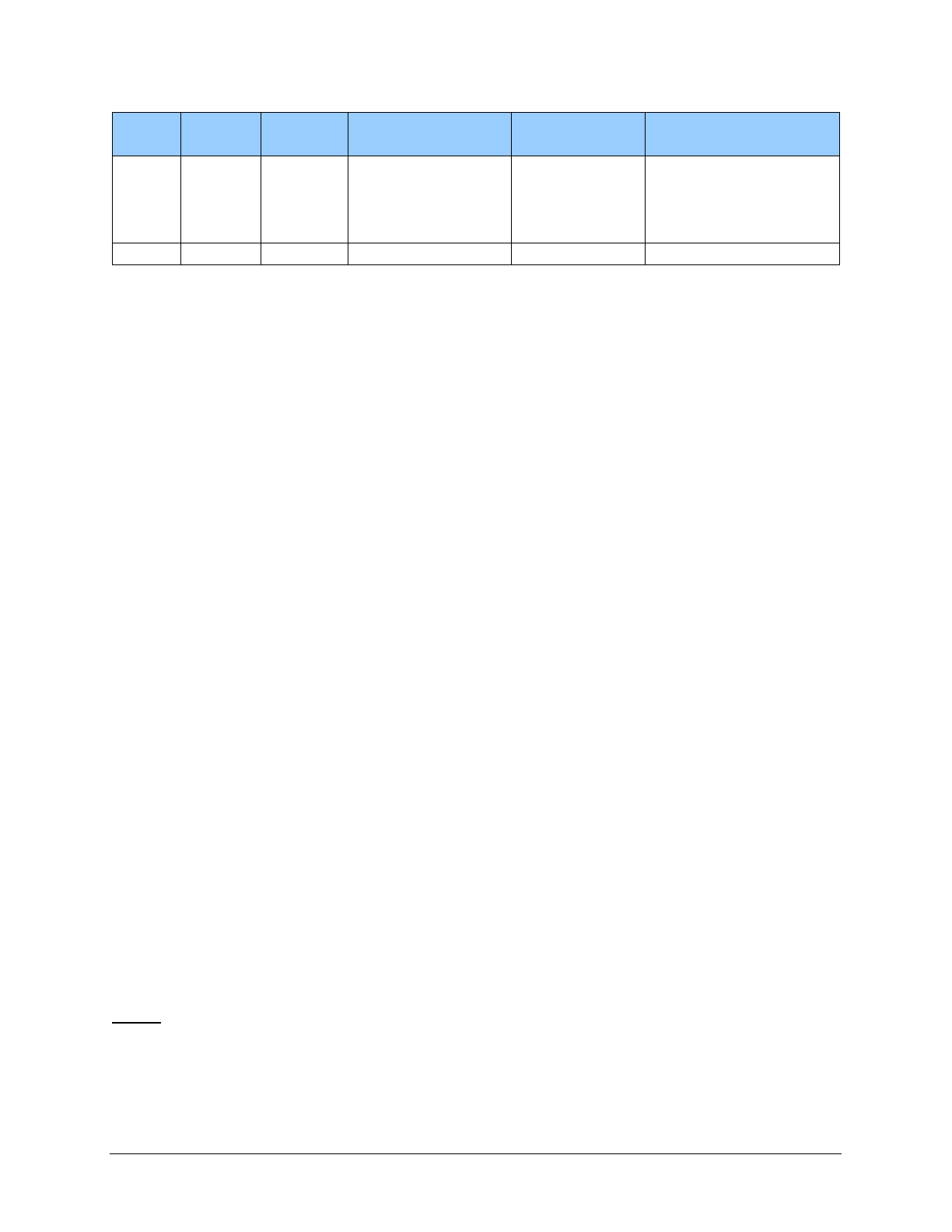
Coverage Table (for Adults)
The following procedure codes are the only procedure codes the agency pays for under the
Hearing Hardware program. Bill your usual and customary charge. Payment will be the lesser of
the billed charge or the maximum allowable fee.
Monaural
Code
Status
HCPCS
Code
Modifier
Short Description
PA?
Policy Comments
V5050 RR
Hearing aid
monaural in ear
No
Billed as a rental only
V5060 RR
Behind ear hearing
aid
No
Billed as a rental only
V5246
LT, RT,
RA
Hearing aid, prog,
mon, ite
No
For average hearing
loss 45 dBHLs or
greater.
When billing for a
second hearing aid, use
EPA #870001552. If
client does not meet
EPA clinical criteria,
PA is required.
Includes all of the
following:
• An audiometric
evaluation
• An impression for
an ear mold
• An ear mold
• The dispensing fee
• A conformity
evaluation, if done
V5247
LT, RT,
RA
Hearing aid, prog,
mon, bte
No
V5256
LT, RT,
RA
Hearing aid, digit,
mon, ite
No
Hearing Hardware
Legend
Modifiers: RA = Replacement of DME Item
RB = Replacement Part of DME Item
LT = Left
RT = Right
RR = Rental
26
Code
Status
HCPCS
Code
Modifier
Short Description
PA?
Policy Comments
• Three batteries
• At least three
follow-up visits for
the fitting,
orientation, and
checking of the
hearing aid
V5257
LT, RT,
RA
Hearing aid, digit,
mon, bte
Use EPA
#870001599. If
client does not
meet EPA
clinical criteria,
PA is required.
For annual ear
impression, per hearing
aid if needed.
Note: If a client has been using one hearing aid for 6 months and the agency
authorizes a second hearing aid, bill for the second hearing aid using a monaural
procedure code. Billing a binaural code in conjunction with a monaural code
within 5 years is not allowed without prior authorization.
Binaural
Code
Status
HCPCS
Code
Modifier
Short Description
PA?
Policy Comments
V5260 RA
Hearing aid, digit,
bin, ite
Yes
Do not bill in
conjunction with a
monaural hearing aid.
V5261 RA
Hearing aid, digit,
bin, bte
Yes
Do not bill in
conjunction with a
monaural hearing aid.
Hearing Hardware
Legend
Modifiers: RA = Replacement of DME Item
RB = Replacement Part of DME Item
LT = Left
RT = Right
RR = Rental
27
CROS/BiCROS
Code
Status
HCPCS
Code
Modifier
Short Description
PA?
Policy Comments
V5171
Hearing aid
monaural ite
Yes
Invoice required
V5181
Hearing aid
monaural bte
Yes
Invoice required
V5211
Hearing aid
binaural ite/ite
Yes
Invoice required
V5213
Hearing aid
binaural ite/bte
Yes
Invoice required
V5215
Hearing aid
binaural itc/bte
Yes
Invoice required
V5221
Hearing aid
binaural bte/bte
Yes
Invoice required
Other
Code
Status
HCPCS
Code
Modifier
Short Description
PA?
Policy Comments
V5011
Hearing aid
fitting/checking
Use EPA
#87001600. If
client does not
meet EPA
clinical criteria,
PA is required.
Allowed up to three
times per year for
additional follow-up
visits only after the
initial three visits
bundled with each new
hearing aid are used
V5040
Body-worn hearing
aid bone
V5264
RA
Ear mold/insert
V5275
Ear impression
Use EPA
#870001599. If
client does not
meet EPA
clinical criteria,
PA is required.
For annual ear
impression, per hearing
aid if needed.
Hearing Hardware
Legend
Modifiers: RA = Replacement of DME Item
RB = Replacement Part of DME Item
LT = Left
RT = Right
RR = Rental
28
Code
Status
HCPCS
Code
Modifier
Short Description
PA?
Policy Comments
V5014
RT, LT,
RB (for
casing
only)
Hearing aid
repair/modifying
V5298
Hearing aid noc
Hearing Hardware
29
HCPCS
Code
Short Description
PA?
Policy
L7510
Prosthetic device repair rep
PA
L8615
Coch implant headset replace
Use EPA #870000001.
If client does not meet
EPA clinical criteria,
PA is required.
L8616
Coch implant microphone repl
L8617
Coch implant trans coil repl
L8618
Coch implant tran cable repl
L8619
Coch imp ext proc/contr rplc
PA
PA
L8621
Repl zinc air battery
Use EPA #870000001.
If client does not meet
EPA clinical criteria,
PA is required.
L8622
Repl alkaline battery
L8623
Lith ion batt CID,non-earlvl
L8624
Lith ion batt CID, ear level
L8625
Charger coch impl/aoi battry
PA
Replacement
only, each
L8627
CID ext speech process repl
PA
L8628
CID ext controller repl
PA
L8629
CID transmit coil and cable
PA
L8691
Osseointegrated snd proc rpl
PA
L8692
Non-osseointegrated snd proc
PA
L8693
Aud osseo dev, abutment
PA
Replacement
only, each
L8694
Aoi transducer/actuator repl
PA
Replacement
only, each
L9900
O&P supply/accessory/service
PA
Legend
EPA: Expedited Prior Authorization
PA: Prior Authorization required
Where can I find the fee schedule?
See the agency’s Hearing hardware fee schedule webpage.
Hearing Hardware
30
Authorization (for Children)
What is prior authorization (PA)?
PA is agency approval for certain medical services, equipment, or supplies, before the services
are provided to clients, as a precondition for provider payment.
Does the agency require prior authorization for
hearing hardware?
(WAC 182-547-1000)
No. Except for certain services specified in the Coverage table, PA is not required for
clients age 20 and younger for hearing aids and services. Providers must send claims for
clients age 20 and younger directly to the agency. Providers do not need to obtain
authorization from the local Children with Special Health Care Needs (CSHCN)
Coordinator.
Note: The agency evaluates requests for covered services that are subject to
limitations or other restrictions and approves such services beyond those
limitations or restrictions as described in WAC 182-501-0169.
(WAC 182-547-1000 (2))
What is expedited prior authorization (EPA)?
The EPA process is designed to eliminate the need for written authorization. The agency
establishes authorization criteria and identifies these criteria with specific codes, enabling
providers to create an EPA number using those codes.
The agency denies claims submitted without the appropriate diagnosis, procedure code, or
service as indicated by the last three digits of the EPA number. The billing provider must
document in the client’s file how the EPA criteria were met and make this information available
to the agency upon request.
Note: When billing electronically, enter the EPA number in the Prior
Authorization section.
Hearing Hardware
31
Replacement parts - EPA criteria
The following EPA criteria must be met:
• The cochlear implant or bone conduction (Baha®) is unilateral (bilateral requires PA).
• The manufacturer’s warranty has expired.
• The part is for immediate use (not a back-up part).
Note: If the client does not meet the EPA criteria, then PA is required.
Use EPA 870000001 with HCPCS codes L8615-L8618, L8621-L8624 when billing for
cochlear implant and bone conduction (Baha®) replacement parts.
What documentation is required when requesting
PA or ETR?
Providers may submit requests for prior authorization online through direct entry into
ProviderOne (see the agency’s prior authorization webpage for details), or by faxing the
following to 1-866-668-1214:
A completed, TYPED General Information for Authorization form, HCA 13-835. This
request form MUST be the initial page when you submit your request.
A completed Hearing Aid Authorization Request form, HCA 13-772, and all the
documentation listed on this form and any other medical justification.
To access forms, see Where can I download agency forms?

Hearing Hardware
32
Prior Authorization (for Adults)
What is prior authorization (PA)?
PA is agency approval for certain medical services, equipment, or supplies, before the services
are provided to clients, as a precondition for provider payment.
What hearing hardware does the agency require
prior authorization for?
(WAC 182-547-0850 (2))
The agency requires PA for binaural hearing aids for eligible clients age 21 and older.
Note: The agency evaluates requests for covered services that are subject to
limitations or other restrictions and approves such services beyond those
limitations or restrictions as described in WAC 182-501-0169.
(WAC 182-547-1000 (2))
What is expedited prior authorization (EPA)?
The EPA process is designed to eliminate the need for written authorization. The agency
establishes authorization criteria and identifies these criteria with specific codes, enabling
providers to create an EPA number using those codes.
The agency denies claims submitted without the appropriate diagnosis, procedure code, or
service as indicated by the last three digits of the EPA number. The billing provider must
document in the client’s file how the EPA criteria were met and make this information available
to the agency upon request.
Note: When billing electronically, enter the EPA number in the Prior
Authorization section.
Hearing Hardware
33
What documentation is required when requesting
PA or ETR?
Providers may submit requests for PA online through direct entry into ProviderOne (see the
agency’s prior authorization webpage for details). Providers must complete the Hearing Aid
Authorization Request form, HCA 13-772, attach all documentation listed on the form, and
provide medical justification.
Providers may also submit their requests for PA by faxing the following to 1-866-668-1214:
A completed, TYPED General Information for Authorization form, HCA 13-835. This
request form MUST be the initial page when you submit your request.
A completed Hearing Aid Authorization Request form, HCA 13-772, and all the
documentation listed on this form and any other medical justification.
To access forms, see Where can I download agency forms?
Note: When the agency authorizes hearing hardware, the PA indicates only that
the specific hardware is medically necessary; it is not a guarantee of
payment. The client must be eligible for covered hardware at the time the
hardware is provided.
Hearing Hardware
34
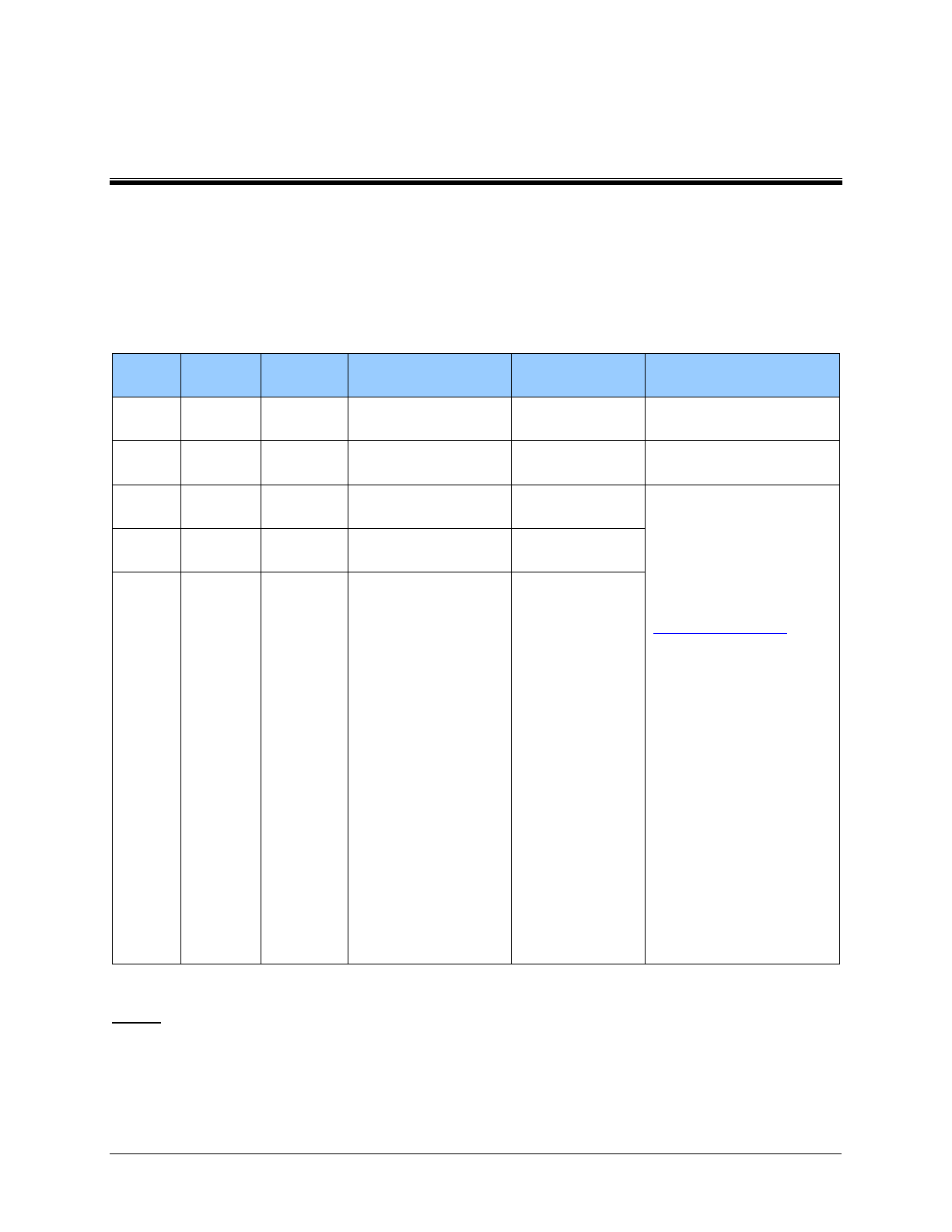
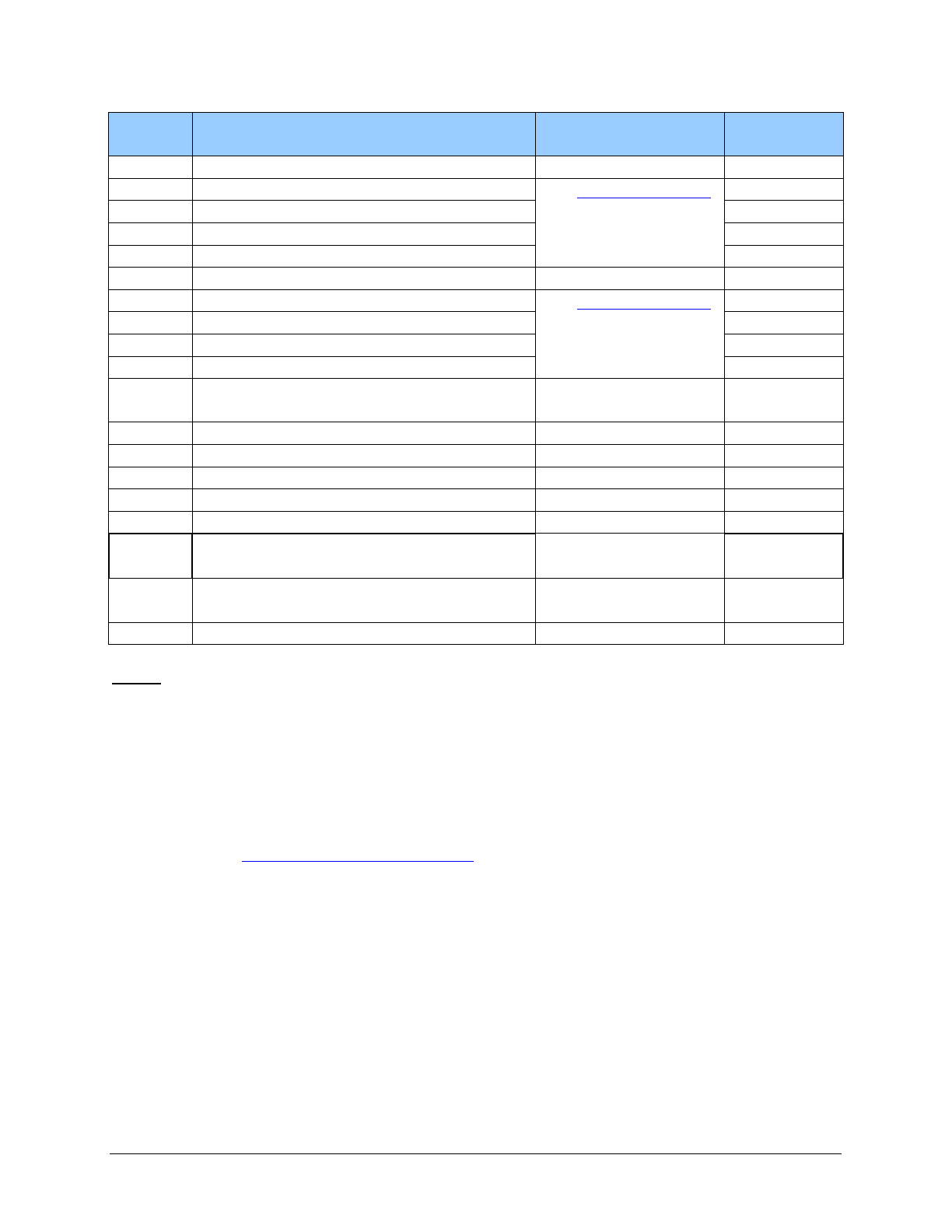
EPA criteria table
EPA code
HCPCS
code
Short description
Clinical criteria
870000001
L8615
Coch implant headset replace
The following must be met:
1. The cochlear implant or bone
conduction (Baha®) is
unilateral (bilateral requires
PA).
2. The manufacturer’s warranty
has expired.
3. The part is for immediate use
(not a back-up part).
L8616
Coch implant microphone repl
L8617
Coch implant trans coil repl
L8618
Coch implant tran cable repl
L8621
Repl zinc air battery
L8622
Repl alkaline battery
L8623
Lith ion batt CID,non-earlvl
L8624
Lith ion batt CID, ear level
870001552
V5246
Hearing aid, prog, mon, ite
Second Hearing Aid for clients
21 years of age and older, who
have tried to adapt with one
hearing aid for a period of 6
months, whose auditory screening
shows an average hearing of 45
dBHL or greater in both ears and
one or more of the following is
documented in the client’s records:
1. Inability to hear has caused
difficulty with job
performance.
2. Inability to hear has caused
difficulty in functioning in the
school environment.
3. The client is legally blind.
If a client has been using one
hearing aid for 6 months, and the
agency authorizes a second
hearing aid, bill for the second
hearing aid using a monaural
procedure code. Billing a binaural
code in conjunction with a
monaural code within 5 years is
not allowed without prior
authorization.
V5247
Hearing aid, prog, mon, bte
V5256
Hearing aid, digit, mon, ite
V5257
Hearing aid, digit, mon, bte
Hearing Hardware
35
EPA code
HCPCS
code
Short description
Clinical criteria
870001599
V5257
Hearing aid, digit, mon, bte
For annual ear impression, per
hearing aid if needed.
V5275
Ear impression
870001600
V5011
Hearing aid fitting/checking
Allowed up to three times per year
for additional follow-up visits only
after the initial three visits bundled
with each new hearing aid are used
What are limitation extensions?
Limitation extensions (LEs) are requests to authorize covered services beyond the limit regarding
scope, amount, duration, or frequency of a covered service. The agency does not approve Les
when prohibited by program rules. When an LE is permissible, the client’s provider must
establish that it satisfies criteria in WAC 182-501-0169, including being medically necessary.
Note: Requests for LEs must be appropriate to the client’s eligibility and/or
program limitations. Not all eligibility groups receive all services.
How do I request a limitation extension?
You may request an LE two ways:
• Providers may be able to obtain authorization for an LE using an EPA number. These
EPA numbers are subject to post payment review as in any other authorization process.
(See: What is Expedited prior authorization (EPA)
• In cases where the client’s situation does not meet the EPA criteria for an LE, but
additional services appear medically necessary, providers may submit LE requests online
through direct entry into ProviderOne (see the agency’s prior authorization webpage for
details), or by faxing the following to 866-668-1214:
A completed, TYPED General Information for Authorization form, HCA 13-835.
This request form MUST be the initial page when you submit your request.
A completed Hearing Aid Authorization Request form, HCA 13-772, and all the
documentation listed on this form and any other medical justification.
To access forms, see Where can I download agency forms?
Hearing Hardware
36
Billing
All claims must be submitted electronically to the agency, except under limited circumstances.
For more information about this policy change, see Paperless Billing at HCA.
For providers approved to bill paper claims, see the agency’s Paper Claim Billing Resource.
What are the general billing requirements?
Providers must follow the agency’s ProviderOne billing and resource guide. These billing
requirements include the following:
• Time limits for submitting and resubmitting claims and adjustments
• How to bill for services provided to primary care case management (PCCM) clients
• How to bill for clients eligible for both Medicare and Medicaid
• How to handle third-party liability claims
• What standards to use for record keeping
Note: For guidance on when a provider may bill a client, see the agency’s ”Billing
a Client” webinar presentation.
What records must be kept in the client’s file?
In addition to the documentation listed in What is included in the agency’s payment for hearing
aids, providers must keep documentation of all hearing tests and results in the complete client’s
chart and record.
This includes, but is not limited to, the following tests:
• Audiogram results/graphs/tracings (including air conduction and bone conduction
comparisons)
• Basic or simple hearing tests or screening, such as is done in many schools
• Tympanogram
A valid prescription from an audiologist for replacement batteries must be kept in the client’s
chart.
Note: To receive payment, the provider must keep documentation in the client's
medical file to support the medical necessity for the specific make and model of
the hearing aid ordered for the client. This documentation must include the record
of the audiology testing providing evidence that the client's hearing loss meets the
eligibility criteria for a hearing aid. (WAC 182-547-1100 (4))
Hearing Hardware
37
How do I bill claims electronically?
Instructions on how to bill Direct Data Entry (DDE) claims can be found on the agency’s Billers,
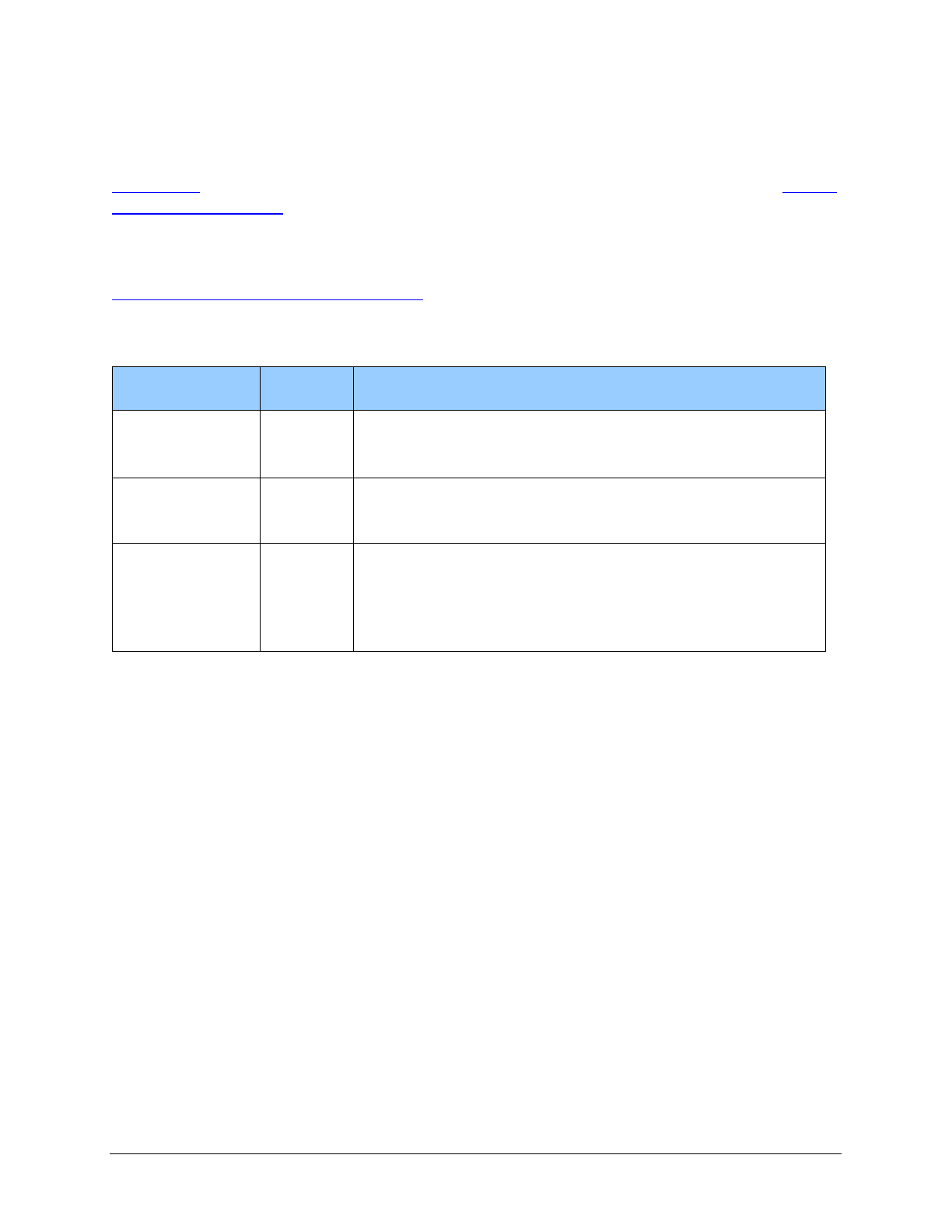
providers, and partners webpage.
For information about billing Health Insurance Portability and Accountability Act (HIPAA)
Electronic Data Interchange (EDI) claims, see the ProviderOne 5010 companion guides on the
HIPAA electronic data interchange (EDI) webpage.
The following claim instructions relate to the Hearing Hardware program.
Name
Field
Required
Entry
Reserved for
Local Use
When
applicable
Enter either of the following:
• “SCI=B” (Baby on parent’s ProviderOne Client ID).
• Claim notes.
Prior
Authorization
Number
When
applicable
Use the prior authorization number assigned to you if/when
services have been denied and you are requesting an
exception to rule.
Procedure Code
Yes
Enter the appropriate Current Procedural Terminology
(CPT) or Common Procedure Coding System (HCPCS)
procedure code for the services being billed.
Modifier: When appropriate enter a modifier.
Hearing Hardware
38
About the Program (for DDA
Clients)
When does the Division of Developmental
Disabilities (DDA) pay for hearing aids?
DDA pays for hearing aids when they are:
• Medically necessary.
• Authorized as required within this billing guide and Chapters 182-501, 182-502, and 388-
845 WAC.
• Billed according to this billing guide and Chapters 182-501 and 182-502 WAC.
• Provided to an eligible client. (See How can I verify a patient’s eligibility?).
• Of direct medical or remedial benefit to the client and necessary as a result of the client's
disability.
• Identified in the waiver participant’s DDA assessment and documented in the person-
centered plan.
• Requested for prior approval by the DDA client’s case manager and approved by the
DDA regional administrator or designee.
Hearing Hardware
39
Client Eligibility (for DDA
Clients)
How can I verify a client’s eligibility?
Providers must verify that a patient has a valid social services authorization for the date of
service and that the client’s benefit package covers the applicable service. This helps prevent
delivering a service the administration will not pay for.
Providers can verify that a client has a valid social services authorization in ProviderOne.
(See How do I view a social services authorization?)
Hearing Hardware
40
Coverage (for DDA Clients)
What is covered?
(WAC 388-845-1810)
Monaural or binaural hearing aids
The administration covers new, non-refurbished, monaural or binaural hearing aids, which
includes the ear mold and batteries, for clients eligible for the service. In order for the provider to
receive payment, the hearing aid must meet the client's specific hearing needs necessary as a
result of the individual’s disability and be under warranty for a minimum of one year.
See the Social services blanket code to procedure crosswalk for specific procedure codes.
Replacement
The administration pays for the following replacements when approved with a social services
authorization:
• Hearing aids, which includes the ear mold, when all warranties are expired and the
hearing aids are one of the following:
Lost
Beyond repair
Not sufficient for the client's hearing loss
• Ear molds when the client's existing ear mold is damaged or no longer fits the client's ear
• Batteries with a valid prescription from an audiologist
Repair
The administration pays for repair when approved with a social services authorization. To
receive payment, all the following must be met:
• All warranties are expired.
• The repair is under warranty for a minimum of 90 days.
Hearing Hardware
41
Rental
The administration pays for a rental hearing aid for up to two months while the client's own
hearing aid is being repaired. In the case of a rental hearing aid, the agency pays separately for an
ear mold.
Cochlear implant – replacement parts
(WAC 182-547-0800 (3))
The administration covers:
• Cochlear implant external speech processors, including maintenance, repair, and
batteries.
• Baha® speech processors, including maintenance, repair, and batteries.
See the Social services blanket code to procedure crosswalk for specific procedure codes.
The administration pays for cochlear implant and Baha® replacement parts when:
• The manufacturer's warranty has expired.
• The part is for immediate use, not a back-up part.
• The part needs to be replaced due to normal wear and tear and is not related to misuse or
abuse of the item (see WAC 182-502-0160).
When reimbursing for battery packs, the administration covers the least costly, equally effective
product.
Note: The administration does not pay providers for repairs or replacements that
are covered under the manufacturer’s warranty.
The administration will reimburse only those vendors with a current Core Provider Agreement. If
the cochlear implant device is provided by a vendor without a current Core Provider Agreement,
replacement parts, accessories, and repairs for these devices may or may not be covered. See
WAC 182-502-0005.
Hearing Hardware
42
What is not covered?
(WAC 182-547-0900)
The administration does not cover the following hearing and hearing aid-related items and
services for clients age 21 and older:
• Tinnitus maskers
• Group screenings for hearing loss
Coverage Table (for DDA clients)
See the Social services blanket code to procedure crosswalk for a list of covered services.
Where can I find the fee schedule?
See the agency’s Hearing hardware fee schedule webpage.
Hearing Hardware
43
Authorization (for DDA
Clients)
What is a social services authorization?
A social services authorization is administration approval for certain services, equipment, or
supplies before the services are provided to clients as a precondition for provider payment.
How do I request a social services authorization?
The client or the client’s representative may request authorization of hearing hardware through
the Washington State Developmental Disabilities Administration (DDA) Home and Community
Based waiver benefit by contacting the client’s case manager. The provider can assist the client
or representative in requesting a social services authorization by providing the following
information to the DDA case manager:
• Reason for denial through the client’s Apple Health benefit
• What equipment is necessary, using the names and procedure codes of the equipment
• An exact amount of the total cost of all equipment requested, using the Apple Health
Hearing Hardware Fee Schedule
• How the hearing hardware will assist the client to perceive, control, or communicate with
the environment in which they live or to increase their abilities to perform activities of
daily living
• How the items are of direct medical or remedial benefit to the client and necessary
because of the client’s disability
• How the ancillary supplies or equipment will support proper functioning and continued
use of the equipment, if the needed equipment supports the continued functioning of
equipment the client already uses

Hearing Hardware
44
How do I view a social services authorization?
The social services authorization can be viewed in ProviderOne. If you have questions about the
social services authorization, contact the case manager listed on the authorization.
Providers will receive an alert message when a social services authorization has been created or
changed. To view the social services authorization from the provider portal:
1. Select Social Services View Authorization List. The Provider Authorization List Page
will appear.
2. Enter the authorization number from the alert or search by the Client ID.
What happens after the social services
authorization is approved?
When the prior approval is reviewed and approved, the case manager will enter a social service
authorization for SA893 for one unit and a dollar amount based on the information used to
request a prior approval.
The provider will bill using the appropriate HCPCS codes for the equipment and will be paid no
more than the amount listed in the Hearing hardware fee schedule.
Hearing Hardware
45
Billing (for DDA Clients)
What are the general billing requirements?
Providers must follow the Apple Health ProviderOne billing and resource guide. These billing
requirements include the following:
• Time limits for submitting and resubmitting claims and adjustments
• How to bill for clients eligible for both Medicare and Medicaid
• How to handle third-party liability claims
• What standards to use for record keeping
Note: For information on when a provider may bill a client, see the agency’s
”Billing a Client” webinar presentation.
What records must be kept in the client’s file?
In addition to the documentation listed in What is included in the administration’s payment for
hearing aids, providers must keep documentation of all hearing tests and results in the complete
client’s chart and record.
This includes, but is not limited to, the following tests:
• Audiogram results/graphs/tracings (including air conduction and bone conduction
comparisons)
• Basic or simple hearing tests or screening, such as those done in schools
• Tympanogram
A valid prescription from an audiologist for replacement batteries must be kept in the client’s
chart.
Note: To receive payment, the provider must keep documentation in the client's
medical file to support the medical necessity for the specific make and model of
the hearing aid ordered for the client. This documentation must include the record
of the audiology testing providing evidence that the client's hearing loss meets the
eligibility criteria for a hearing aid. (WAC 182-547-1100 (4))
Hearing Hardware
46
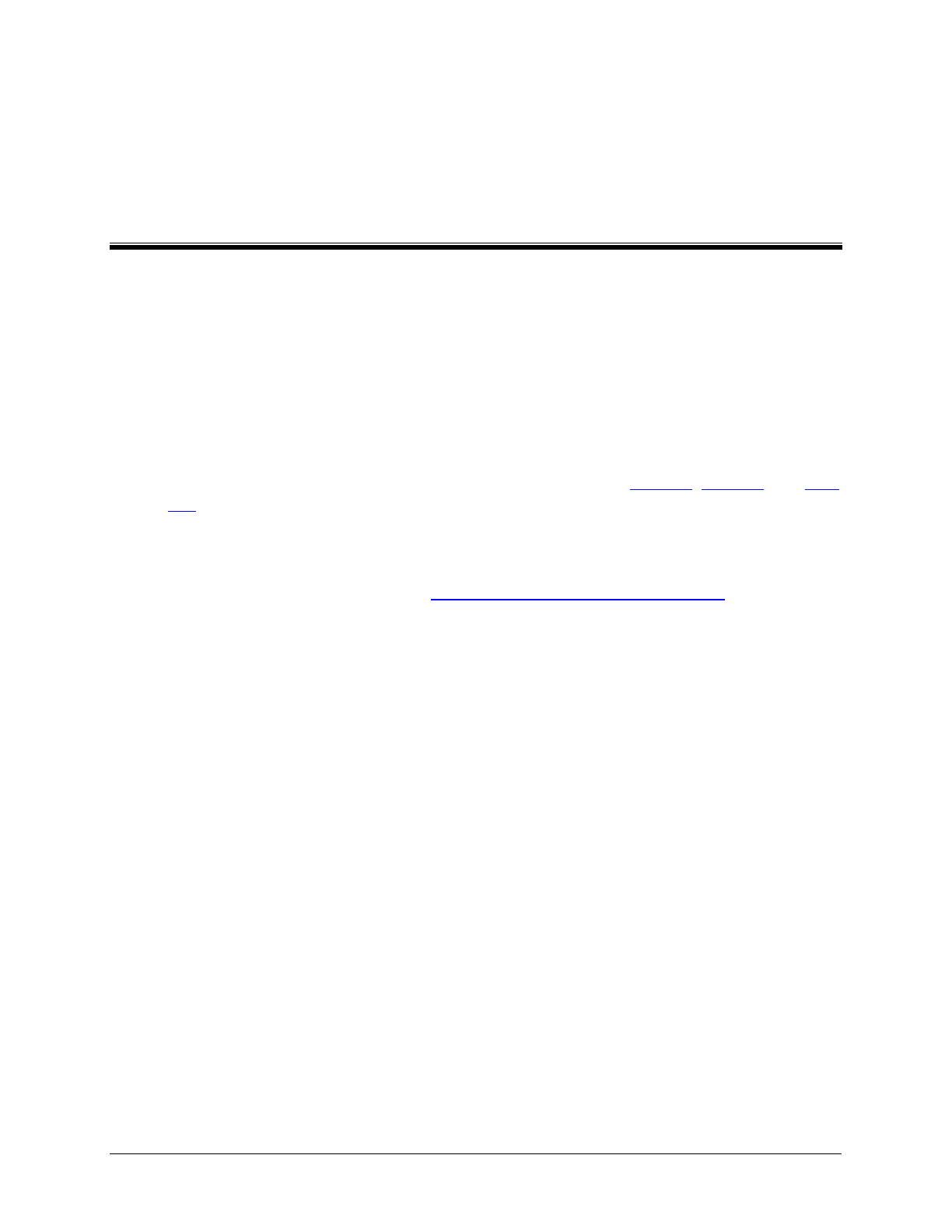
How do I bill claims electronically?
Instructions on how to bill Direct Data Entry (DDE) claims can be found on the agency’s Billers,
providers, and partners webpage.
For information about billing Health Insurance Portability and Accountability Act (HIPAA)
Electronic Data Interchange (EDI) claims, see the ProviderOne 5010 companion guides on the
HIPAA electronic data interchange (EDI) webpage.
The following claim instructions relate to the Hearing Hardware program.
Name
Field
Required
Entry
Prior
Authorization
Number
Yes
Use the social services authorization number assigned to
you.
Procedure Code
Yes
Enter the appropriate Current Procedural Terminology
(CPT) or Common Procedure Coding System (HCPCS)
procedure code for the services being billed.
Modifier: When appropriate enter a modifier.
