REPORT TO CONGRESS
REDUCING BARRIERS TO FURNISHING SUBSTANCE USE DISORDER (SUD)
SERVICES USING TELEHEALTH AND REMOTE PATIENT MONITORING FOR
PEDIATRIC POPULATIONS UNDER MEDICAID
FINAL REPORT
As Required by section 1009(d) of the
Substance Use-Disorder Prevention that Promotes Opioid Recovery and Treatment
for Patients and Communities Act (Pub. L. 115-271)
May 15, 2020
Section 1009(d) of the SUPPORT for Patients and Communities Act required the Secretary of
Health and Human Services (HHS), acting through the Administrator of the Centers for
Medicare & Medicaid Services (CMS), to issue this final report. The Office of the Assistant
Secretary for Planning and Evaluation (ASPE) and their contractor RTI International prepared
this final report in consultation with CMS. While this report includes programs and cites to laws
administered by federal agencies, it is not a federal endorsement of specific programs. All
research included in this report was completed in 2019 prior to the COVID-19 national public
health emergency.

Reducing Barriers to Using Telehealth for Pediatric Populations
Final Report
CONTENTS
Section Page
EXECUTIVE SUMMARY...........................................................................................................ES-1
Background ..................................................................................................................................1
Purpose and Scope ......................................................................................................................2
Data and Methods .......................................................................................................................5
Data Collection .....................................................................................................................5
Environmental Scan ................................................................................................... 5
Case Studies ............................................................................................................... 8
Data Analysis ......................................................................................................................10
Results .......................................................................................................................................12
Overview of Environmental Scan Results ..........................................................................12
Environmental Scan and Discussion Results by Question .................................................14
What Are the Best Practices, Barriers and Potential Solutions for Using
Services Delivered Via Telehealth to Diagnose and Provide Services
and Treatment for Children With SUD, Including OUD? (Research
Question #1) ................................................................................................ 14
What Are the Differences, If Any, in Furnishing Services and Treatment for
Children With SUD Using Services Delivered Via Telehealth and
Using Services Delivered in Person? (Research Question #2) ..................... 18
Delivery of Pediatric Behavioral Health Treatment via Telehealth ...................................23
Program Examples ................................................................................................... 23
Policy and Reimbursement Considerations .......................................................................26
Telehealth Policies that Influence Delivery of SUD Treatment ............................... 26
Medicare and Medicaid Coverage ........................................................................... 29
Federal Models and Programs to Support Telehealth ............................................ 33
Privacy and Confidentiality Considerations ............................................................. 35
Key Informant Discussions ........................................................................................................38
Overview of Key Informant Discussion Results .................................................................38
What Are the Best Practices, Common Barriers and Potential Solutions for Using
Services Delivered via Telehealth to Diagnose and Provide Services and
Treatment for Children with SUD, Including OUD (Research Question 1)? .............38
Best Practices ........................................................................................................... 38
Detailed Best Practices Emphasized by Key Informants.......................................... 41

Reducing Barriers to Using Telehealth for Pediatric Populations
Final Report
Barriers and Solutions .............................................................................................. 43
What Are the Differences, If Any, in Furnishing Services and Treatment for
Children with SUD Using Services Delivered via Telehealth and Using
Services Delivered in Person? (Research Question 2) ..............................................48
Utilization rates, costs and avoidable inpatient admissions and
readmissions ................................................................................................ 48
Quality and Satisfaction ........................................................................................... 49
Case Studies ...............................................................................................................................52
Case Study Programs .........................................................................................................52
Case Study 1: The Medical University of South Carolina’s Telehealth
Outreach Program ....................................................................................... 52
Case Study 2: University of Kansas Medical Center’s Telehealth ROCKS
Schools, Rural Outreach for Children of Kansas .......................................... 55
Case Study Results by Question .........................................................................................62
What Are the Best Practices, Barriers and Potential Solutions for Using
Services Delivered Via Telehealth to Diagnose and Provide Services
and Treatment for Children With SUD, Including OUD? (Research
Question #1) ................................................................................................ 62
What Are the Differences, If Any, in Furnishing Services and Treatment for
Children With SUD Using Services Delivered Via Telehealth and
Using Services Delivered in Person? (Research Question #2) ..................... 64
Discussion ..................................................................................................................................67
Best Practices: ....................................................................................................................67
Videoconferencing ................................................................................................... 67
Support Staff ............................................................................................................ 68
School-based Models ............................................................................................... 68
Barriers, Solutions and Information Gaps..........................................................................68
Quality and Fidelity .................................................................................................. 68
Patient Safety ........................................................................................................... 69
Acceptance of a Telehealth Program....................................................................... 69
Financing .................................................................................................................. 69
Consent for Services ................................................................................................ 70
Cost Studies ............................................................................................................. 70
Summary ............................................................................................................................70
References ...............................................................................................................................R-1

Reducing Barriers to Using Telehealth for Pediatric Populations
Final Report
APPENDIXES
Key Informant Interview Guide ............................................................................................. A-1
Case Study Interview Guides ..................................................................................................B-1
EXHIBITS
Summary of Evidence from Available Literature .................................................................................. 12

Reducing Barriers to Using Telehealth for Pediatric Populations
Final Report
ES-1
EXECUTIVE SUMMARY
Introduction
Section 1009(d) of the SUPPORT Act requires the Secretary of the Department of Health and
Human Services, acting through the Administrator of the Centers for Medicare & Medicaid
Services (CMS), to provide a report to Congress identifying best practices and potential solutions
for reducing barriers to using services delivered via telehealth to furnish services and treatment
for substance use disorder (SUDs) among pediatric populations under Medicaid. The Office of
the Assistant Secretary for Planning and Evaluation (ASPE) and their contractor Research
Triangle Institute (RTI) International drafted this final report in consultation with CMS.
Although generally telehealth has become more prevalent in the last decade, uptake is not yet
widespread (Bashshur, Shannon, Bashshur, & Yellowlees, 2016; Benavides-Vaello, Strode, &
Sheeran, 2013; Dorsey & Topol, 2016), particularly among pediatric populations with SUD.
Understanding the barriers to the use of telehealth and best practices to overcome these barriers
among the pediatric population is critical to increasing access to SUD services for this
population.
Methods
RTI conducted an environmental scan, interviewed key researchers, clinicians, and healthcare
administrator informants via phone, and conducted two in-person case studies to identify best
practices, barriers and potential solutions for using services delivered via telehealth to diagnose
and provide services for pediatric patients with SUD. Differences in service provision for
children with SUD using services delivered via telehealth and using services delivered in person
were also explored with respect to utilization rates; costs; avoidable inpatient admissions and
readmissions; quality of care; and patient, family, and provider satisfaction.
Results
Best Practices
Best practices are still evolving and emerging; however, there are a few general principles for
telehealth applicable to behavioral health, including the need for organizational readiness,
engagement of clinical and administrative staff, investment in technology, efforts to increase

Reducing Barriers to Using Telehealth for Pediatric Populations
Final Report
ES-2
technology acceptance, and support of ongoing service delivery. Key informants also mentioned
workforce shortages, balancing face-to-face and telehealth sessions, having a designated
telehealth coordinator, and engagement of families, specifically.
Barriers
The environmental scan revealed that the lack of technology investment and technology
acceptance are barriers to the provision of services via telehealth. Ongoing service delivery,
capacity issues, licensing and credentialing requirements can also be challenging. Key
informants added that barriers often exist due to state limits and restrictions on reimbursement
for telehealth services. They also noted workforce shortages and concerns about the loss of non-
verbal cues or other SUD-related cues are barriers (e.g., the patient’s smell, hygiene, or visual
indicators of self-harm). A specific barrier that emerged in the case studies were state laws that
prohibited prescribing any controlled substances for students in a school-based clinic other than
attention-deficit/hyperactivity disorder (ADHD) medications.
Potential Solutions
Identification of systems and processes to support coordination within and across organizations
may help address the barriers associated with capacity and ongoing service development. The
key informants stressed the value of having a dedicated telehealth program coordinator to
facilitate solutions to common barriers, and the importance of site-based staff to support
telehealth programs was emphasized in the case studies. Initiatives to increase technology access
(e.g., broadband internet) and decrease technology costs may help address barriers to service
delivery. Training of clinical and administrative staff and patients may also improve technology
acceptance.
Utilization Rates
The environmental scan showed that utilization rates may be higher at schools with versus
without services delivered via telehealth for students with special health care needs and in rural
areas versus urban areas. The case studies showed that the telehealth program representatives
feel that their patients are much more likely to persist in treatment than face-to-face patients,
with one program reporting a 90% completion rate. Further study is needed to obtain more robust

Reducing Barriers to Using Telehealth for Pediatric Populations
Final Report
ES-3
estimates of the net changes in health care utilization associated with telehealth-delivered mental
health or substance use disorder (MH/SUD) services.
Costs
Information specific to the total cost of care and treatment was limited. Few studies provided any
quantifiable results on the costs of telehealth models. While case study participants also did not
have formal economic data available, they noted that payers and other providers had not reported
excess costs or use of other services among their patients. They also noted that, beyond near-
term health care cost savings, they felt strongly that their programs would ultimately save society
resources by reducing inefficient use of misapplied community resources (e.g., teacher time) and
reducing the long-term costs associated with untreated pediatric disorders. On average, the
program representatives believe that the cost of their services delivered via telehealth was equal
to that of in-person services, even including some fixed technology costs.
Avoidable Inpatient Admissions and Readmissions
There was limited information in the environmental scan about how telehealth for pediatric
patients with SUD impacts avoidable inpatient admissions and readmissions. Results are varied
with respect to whether telehealth interventions increase or decrease use of urgent or emergency
care.
Quality of Care
Overall, the quality of telehealth care is similar to that of face-to-face care, both generally and in
behavioral health, specifically. Case study participants felt that the quality of their programs was
as good as or better than face-to-face delivery.
Patient, Family and Provider Satisfaction
Telehealth use and satisfaction is influenced by both pediatric patients’ and their caregivers’
access to technology, knowledge of available resources, and willingness to interact with the
technology, all factors that may be influenced by the potential user’s educational,
socioeconomic, health, and other personal characteristics. Key informants agreed that telehealth
as a modality for pediatric SUDs is often preferred by patients over traditional encounters.

Reducing Barriers to Using Telehealth for Pediatric Populations
Final Report
ES-4
Telehealth satisfaction and uptake is also influenced by provider factors such as training and
technology acceptance.
The environmental scan also yielded examples of programs that demonstrate the potential
advantages of providing services via telehealth, including the reduction of unnecessary patient
transfers, improved access to services through school-based care, and provision of training,
expertise, and/or certification opportunities to providers in areas that are relevant to the patients
they are treating.
Many of the resources reviewed in the environmental scan called for regulatory changes to
promote the uptake of telehealth delivery methods to treat SUDs. The scan identified a number
of policies, many of which support the use of telehealth more generally and were not unique to
pediatric patients with SUD. Those policies that did specifically address telehealth service
delivery methods emphasized the treatment of opioid use disorder (OUD) and medication
assisted treatment (MAT). Policies governing privacy and protection of personal data influence
telehealth models, particularly for pediatric patients and their parents and for sensitive care areas
like SUD and mental health.
Medicaid coverage for services delivered via telehealth varies by state according to factors such
as the setting where the patient is located, types of services, provider type, and whether the
service was delivered synchronously or asynchronously. Some states restrict reimbursement for
services delivered via telehealth for behavioral health issues. All states providing Medicaid-
covered services delivered via telehealth include some form of coverage and reimbursement for
certain mental health services.
Discussion/Conclusion
Much of the evidence base for the use of telehealth with pediatric patients comes from treatment
of mental disorders, which provides valuable lessons learned and next steps forward. Overall,
programs are successfully providing quality services to patients who may not otherwise have
access. Many questions remain, however, around best practices in different settings with
different pediatric patient disorders, optimal staffing and financial viability.

Reducing Barriers to Using Telehealth for Pediatric Populations
Final Report
ES-5
[This page intentionally left blank]

Reducing Barriers to Using Telehealth for Pediatric Populations
Final Report
1
BACKGROUND
Substance use disorder (SUD) among the pediatric population (ages up to 21) has been
identified as a significant public health concern. As of 2018, an estimated 3.7 percent of
adolescents aged 12 to 17, and 12.9 percent of young adults aged 18 to 20, had an SUD
(SAMHSA, 2019). Substance use during adolescence is associated with short- and long-term
negative effects on functioning and well-being. Brain development may be delayed or altered
with consequences that can persist throughout adulthood (Chassin et al., 2010; Eiden et al., 2016;
Squeglia, Jacobus, & Tapert, 2009; Tapert, Caldwell, & Burke, 2004). Substance using
adolescents are more likely to experience worse mental health and have behavioral problems (Ali
et al., 2015; Bouvier et al., 2019; Poon, Turpyn, Hansen, Jacangelo, & Chaplin, 2016; Schuler,
Vasilenko, & Lanza, 2015; Trim, Meehan, King, & Chassin, 2007; Volkow, Baler, Compton, &
Weiss, 2014) and to have poorer academic outcomes (Heradstveit, Skogen, Hetland, & Hysing,
2017; Kelly et al., 2015). Adolescents with early onset heavy substance use are most likely to
remain heavy users as they transition into adulthood (Derefinko et al., 2016; Winters et al.,
2018). Despite evidence for the effectiveness of many different treatment modalities for
adolescents (Nelson, Ryzin, & Dishion, 2015; Wu, Zhu, & Swartz, 2016), only 14.1 percent
received any form of SUD treatment. Among all adolescents with an SUD, those with opioid use
disorder (OUD) are the least likely to receive treatment (Winters et al., 2018; Wu et al., 2016).
Adolescents face many barriers to accessing treatment, including stigma, which may prevent
adolescents or their guardians from seeking help; logistical limitations, such as a lack of
transportation or locally available specialty treatment providers; and financial limitations, such as
being uninsured or underinsured. Among many strategies to reduce barriers to treatment access,
telehealth models of service delivery have the promise of expanding access, improving treatment
engagement and retention, enhancing the clinical outcomes of evidence-based services, and
reducing costs (Bashshur et al., 2016; Benavides-Vaello et al., 2013; Wu et al., 2016).
Although generally telehealth has become more prevalent in the last decade, its it has not
been adopted widely across all patient groups (Bashshur et al., 2016; Benavides-Vaello et al.,
2013; Dorsey & Topol, 2016), particularly pediatric patients. Much of the existing work on
barriers and facilitators to telehealth to support SUD treatment focuses on the adult population.
Common barriers to telehealth implementation for a general patient population include staff and
patient acceptance; cost and reimbursement; workflow challenges; and technology

Reducing Barriers to Using Telehealth for Pediatric Populations
Final Report
2
availability/connectivity (Myers et al., 2017). Additionally, providers often experience barriers
related to ensuring privacy, confidentiality, and security; initial setup costs; and other technical
difficulties that can potentially compromise confidentiality.
While many telehealth considerations apply equally to adult and pediatric populations,
there are some potential differences. For example, pediatric patients may be more likely to
embrace technology. Recent surveys from the Pew Foundation have pointed to adult technology
and social media use remaining stagnant and teen use increasing (Pew Research Center, 2018,
2019a). Meanwhile, privacy while living with family or roommates can be a concern for
pediatric patients. In contrast, stigma about receiving mental health or substance use disorder
(MH/SUD) services may be lessened when delivered via telehealth. However, there is some
evidence that parents’ willingness to access mental health services is more influenced by stigma
when the services are delivered via telehealth (Polaha, Williams, Heflinger, & Studts, 2015).
Financing is another potential barrier to telehealth for the pediatric population. While Medicaid
and the Children’s Health Insurance Program are the main coverage sources for behavioral
health coverage and treatment of SUD for the pediatric population (Centers for Medicare &
Medicaid Services, n.d.-a), Medicaid-covered services delivered via telehealth vary by state.
Although variation in coverage across states is also a challenge for providers serving adults, it
can exacerbate the existing workforce challenges for pediatric patients with MH/SUD who need
services from providers with specialized training. Understanding the barriers to the use of
telehealth and best practices to overcome these barriers among the pediatric population is critical
to increasing access to SUD services delivered via telehealth for this group.
PURPOSE AND SCOPE
The goal of this work is to gain a greater understanding of contextual factors influencing
the use of telehealth for SUD services for pediatric populations, with a focus on services funded
by Medicaid. For the purposes of this work, the term pediatric refers to individuals up to the age
of 21. Telehealth refers to synchronous and asynchronous provider-to-provider and provider-to-
patient services (RTI International, 2017, September 15). However, only provider-to-patient
services are eligible for Medicaid coverage. The literature on telehealth for SUD among pediatric
populations is limited and varied in scope and quality. This report includes relevant findings for

Reducing Barriers to Using Telehealth for Pediatric Populations
Final Report
3
telehealth for SUD among adult populations where appropriate, as well as information on mental
health services delivered via telehealth for pediatric patients.
This study will support fulfillment of the requirements of section 1009(d) of the
Substance Use–Disorder Prevention that Promotes Opioid Recovery and Treatment for Patients
and Communities Act (SUPPORT for Patients and Communities Act), Public Law No. 115-271,
which requires the Secretary of the Department of Health and Human Services to provide a
report “identifying best practices and potential solutions for reducing barriers to using services
delivered via telehealth to furnish services and treatment for SUDs among pediatric populations
under Medicaid.”
Pursuant to section 1009(d) of the SUPPORT for Patients and Communities Act, the
research questions guiding this work are:
1. What are the best practices, barriers and potential solutions for using services
delivered via telehealth to diagnose and provide services and treatment for children
with SUD, including OUD?
2. What are the differences, if any, in furnishing services and treatment for children with
SUD using services delivered via telehealth and using services delivered in person
with respect to:
• utilization rates;
• costs;
• avoidable inpatient admissions and readmissions;
• quality of care; and
• patient, family, and provider satisfaction.
To answer these questions, RTI conducted an environmental scan, met with key
informants via phone, and conducted two in-person case studies. RTI used qualitative analysis
methods to analyze the data and identify themes. This report presents the findings from each
component of the study.

Reducing Barriers to Using Telehealth for Pediatric Populations
Final Report
4
[This page intentionally left blank]

Reducing Barriers to Using Telehealth for Pediatric Populations
Final Report
5
DATA AND METHODS
DATA COLLECTION
Data collection includes findings from the environmental scan, discussions with key
informants, and case studies. The objective of the environmental scan was to assess the current
state of the literature on SUD services delivered via telehealth to help answer our research
questions and inform the discussions with key informants and with case study participants. Key
informant interviews supplemented the environmental scan by ensuring that we identified newer
information and programs, provided the opportunity for more in-depth discussion of key topics,
and helped to identify possible case study sites. The objective of the case studies was to learn
from on-the-ground experiences of those who administer and use telehealth in the field. Even
when literature or documented guidance exists for key topics, firsthand accounts and
explanations add clarity and provide a broader context for the published information, address
emerging issues, and provide concrete examples of challenges and solutions.
Environmental Scan
The scan included a literature review that identified and synthesized findings from peer-
reviewed journals; gray literature; issue briefs; Federal, state, and local government reports; and,
conference proceedings and presentations. Where possible, we focused on publications from
2012 through May 2019. Earlier publications were included if they provided key insights not
available in the more recent literature. To conduct the literature review, we developed a list of
keywords from the research questions. MLS-trained librarians provided input on the keywords
and assisted in searches. We then obtained relevant articles for review and analysis using the
following process.
Search Parameters
We performed a literature search of the four major databases listed below for peer-
reviewed and gray literature published from 2012 to date:
• PubMed
• Web of Science (includes Science Citation Index Expanded, Social Sciences Citation
Index, Conference Proceedings Citation Index-Science, and Conference Proceedings
Citation Index-Social Science & Humanities)

Reducing Barriers to Using Telehealth for Pediatric Populations
Final Report
6
• PsycINFO
• New York Academy of Medicine Grey Literature Database (to 2016)
Each database was queried for the intersection of:
• telehealth AND pediatric populations
• telehealth AND opioids OR substance abuse OR behavioral health
• telehealth AND other terms.
Below are the search parameters.
• Telehealth: telehealth OR "tele-health" OR telemental OR "tele-mental" OR
telemedicine OR "tele-medicine" OR telerehabilitation OR "tele-rehabilitation" OR
teleconsultation* OR "tele-consultation*" OR "remote consultation*"
• Pediatric population: pediatric* OR pediatrician* OR child* OR youth* OR
adolescent* OR teen* OR school* OR college* OR university* OR "young adult*"
OR "transition age"
• Opioids, substance abuse, behavioral health: opioid* OR opiate* OR heroin OR
fentanyl OR OxyContin OR Vicodin OR hydrocodone OR oxycodone OR narcotic*
OR behavioral OR "substance us*" OR "substance abuse*" OR "drug abuse*" OR
"drug us*" OR addiction OR “mental health” OR alcohol
• Other terms: Medicaid OR barrier* OR quality OR utilization OR cost OR costs OR
economic* OR financial* OR finance* OR financing OR satisfaction OR
readmission* OR admission* OR "best practice*"
In addition to the searches listed above, we conducted targeted Google searches to
identify changes in policies around telehealth for this population, relevant Medicaid policies, and
specific telehealth applications such as school-based health.
All publications were downloaded to an EndNote database. We identified 215
unduplicated articles. Two analysts from the research team reviewed abstracts for each and
identified 189 articles for full review. Each member of the team participated in reviewing a
selection of the articles which included reading the entire article and extracting information to be
recorded into a tracking form.

Reducing Barriers to Using Telehealth for Pediatric Populations
Final Report
7
Discussions with Key Informants
To supplement the findings from the environmental scan, we conducted semi-structured
discussions via telephone with nine key informants and categorized findings based on themes
and research questions. Specifically, the results are presented by the best practices, barriers and
solutions, and differences in in-person versus telehealth service delivery for SUD treatment in
pediatric patient populations.
Potential key informants were identified based on the findings of the environmental scan
and a review of professional organizations. From this potential list, informants were categorized
based on several criteria, including the following:
• Experience with telehealth for behavioral health services
• Geography
• Type of behavioral health services provided
• Diversity of role at organization
A discussion guide was developed to support the interview and included probing sub-
questions to prompt the informant to provide their unique perspective on different topics
(Appendix A). The perspectives represented included the following:
• Researchers
• Clinicians
• Health care administrators
The key informant discussions were conducted to help us gain a better understanding of
policies that influence treatment of the pediatric population with SUD via telehealth and
reimbursement aspects, such as coverage by Medicaid and private payers. The RTI team
developed a semi-structured discussion guide to support the discussions that covered the key
research questions. The guide was designed to take advantage of the unique perspectives of each
selected informant.
Key Informant and Program Characteristics
Discussions were held with nine key informants covering a variety of perspectives,
including the following non-mutually exclusive categories:

Reducing Barriers to Using Telehealth for Pediatric Populations
Final Report
8
• five physicians, three of whom were psychiatrists
• three nurses
• three researchers with university faculty appointments
• three government officials
• three acting as administrators in a provider organization
Three university medical centers were represented as well as two private provider organizations.
Two separate state governments were represented. At least one respondent was also associated
with each of the following:
• Indian Health Service
• Telehealth Resource Center funded by the Health Resources & Services
Administration
• American Telemedicine Association
The key informants’ backgrounds in telehealth were varied, ranging from only very
recent experience to more than 20 years of experience with telehealth. One clinician worked for
20+ years in pediatric care and then transitioned into the role of clinical information technology
liaison where they have been developing and running the telemedicine program for the past 7
years. Another stakeholder reported using telehealth for pediatric behavioral health services for
more than 20 years and provided a unique perspective on how telehealth has evolved in their
state. One administrator had worked for more than 24 years within their current state’s
department of public health and has been the point of contact for all telehealth-related activities
since the department established an office dedicated to telehealth. One administrator wrote their
provider organization’s first policy on telehealth and has since continued to expand it.
Four of the key informants had experience providing clinical pediatric MH/SUD services
face-to-face and using telehealth, including one in a school-based telehealth program. The rest
were either administrators associated with such programs or had related policy roles.
Case Studies
In order to gain additional perspective from providers in the field, we conducted in-
person discussions with staff from selected provider organizations. These visits helped to address

Reducing Barriers to Using Telehealth for Pediatric Populations
Final Report
9
gaps and supplement findings from the literature and the key informant interviews. Based on
results from the environmental scan and key informant interviews, we developed an interview
guide for providers, administrators and community partners/stakeholders (Appendix B).
We identified potential provider sites based on several criteria, including:
• Experience with telehealth for pediatric populations
• Experience with telehealth for delivering MH/SUD treatment services
• Geography (rural vs. urban and U.S. regions)
• Setting (e.g., outpatient clinic, Federally Qualified Health Center)
• Type of telehealth in use (provider-to-provider or provider-to-patient)
Sites were contacted by phone or email to discuss the possibility of a site visit following a
script explaining the purpose of the visit and what they might expect during the visit. During the
site visit, we spoke with different stakeholders involved in the telehealth program(s). These
included providers, administrators, and other representatives of the organization delivering the
telehealth services. When feasible, we also met with stakeholders from partner organizations
who may have been directly or indirectly involved with the telehealth program. In addition, we
briefly reviewed the telehealth technology and setting firsthand. We recognized that
organizations’ time was very limited and that meeting with us could have been disruptive;
therefore, we worked with each site to plan a visit that would minimize any burden. We were on-
site for no longer than one day during regular business hours, and our team consisted of two staff
and a representative from ASPE.
The two case study sites that we visited are university medical centers with Health
Resources and Services Administration (HRSA)-funded Telehealth Resource Centers. Both sites
have a broad portfolio of telehealth activities, including programs that provide services to
pediatric patients with mental disorders. Descriptions of the two case study sites are provided in
Appendix B.

Reducing Barriers to Using Telehealth for Pediatric Populations
Final Report
10
DATA ANALYSIS
All study data were analyzed using qualitative analytic methods. Results from the
literature review were analyzed by identifying themes relevant to the research questions.
Qualitative data from key informant and in-person discussions were also analyzed thematically.
The results of each of the three data sources are organized by primary research question.
The key informant and in-person case studies reflect on the environmental scan results when
appropriate. We also highlight innovative programs and approaches to the use of telehealth
identified in the literature and in discussions with key stakeholders and providers.

Reducing Barriers to Using Telehealth for Pediatric Populations
Final Report
11
[This page intentionally left blank]
Reducing Barriers to Using Telehealth for Pediatric Populations
Final Report
12
RESULTS
OVERVIEW OF ENVIRONMENTAL SCAN RESULTS
Overall, the environmental scan highlighted the knowledge gaps in the field about the use
of telehealth for SUD services for the pediatric population. Much of the evidence base for the use
of telehealth with pediatric patients comes from treatment of mental disorders. Most of the
evidence found regarding use of telehealth for SUD services is based on adult populations, and it
is unclear the extent to which these experiences would be similar among a pediatric population.
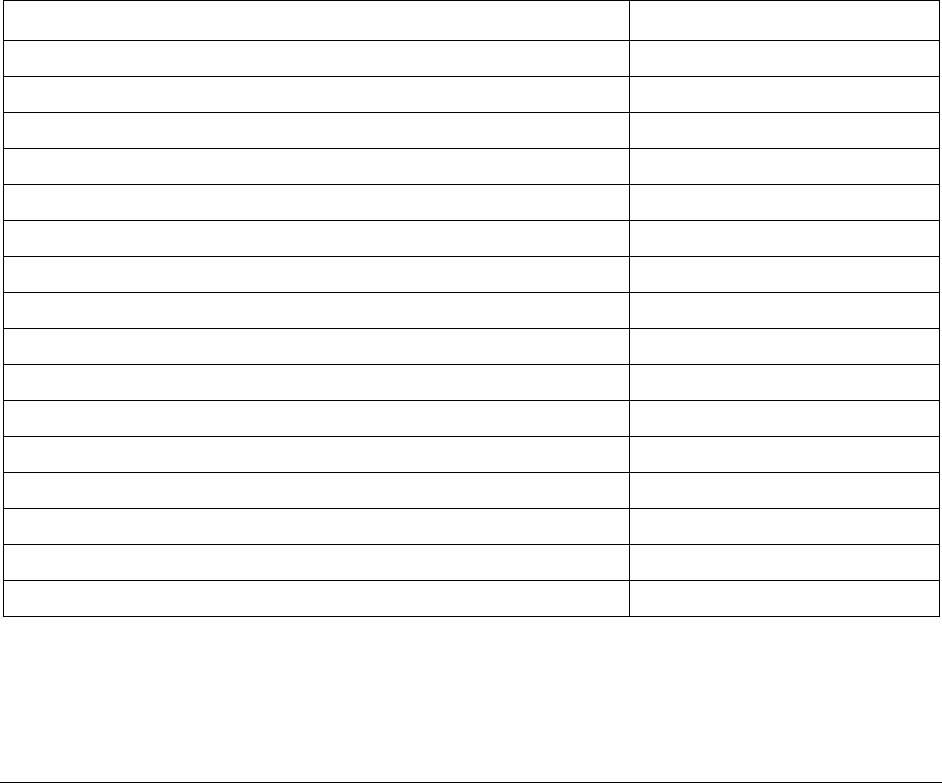
Exhibit 1 summarizes differences in the evidence base by modality, funding sources,
barriers and facilitators. We have categorized the strength of evidence as scant (very little or no
information about this topic), emerging (several resources about the topic, but not enough to gain
a consensus) or strong (many resources about this topic over a period of time).
Exhibit 1. Summary of Evidence from Available Literature
Category State of Evidence
Research Question 1. Best practices, barriers and solutions
Telehealth best practices
SUD treatment with pediatric populations
Scant
SUD treatment with adult populations
Emerging
Other treatment focus with pediatric populations
Scant
Barriers/issues for using telehealth treatment/services for SUD
SUD treatment with pediatric populations
Emerging
SUD treatment with adult populations
Strong
Other treatment focus with pediatric populations
Emerging
Facilitators to address barriers
SUD treatment with pediatric populations
Emerging
SUD treatment with adult populations
Strong
Other treatment focus with pediatric populations
Emerging
Research Question #2: Telehealth vs. in-person
Utilization rates
Utilization rates for adult or pediatric populations with SUD
Scant

Reducing Barriers to Using Telehealth for Pediatric Populations
Final Report
13
Exhibit 1. Summary of Evidence from Available Literature (continued)
Category State of Evidence
Costs
Costs for treatment of adult or pediatric populations with SUD
Scant
Avoidable inpatient admissions and readmissions
Avoidable inpatient admissions and Readmissions for adult or
pediatric SUD
Scant
Quality of care
SUD treatment for pediatric populations
Scant
SUD treatment for adult populations with SUD
Scant
Other treatment focus with pediatric populations
Emerging
Patient and family satisfaction
SUD treatment with pediatric populations
Scant
SUD treatment with adult populations
Emerging
Other treatment focus with adult or pediatric populations
Strong
Provider satisfaction
SUD treatment with pediatric populations
Scant
SUD treatment with adult populations
Scant
Other treatment focus with pediatric populations
Emerging
Examples of programs
Telehealth in schools
SUD treatment with pediatric populations
Emerging
SUD treatment with adult populations
Emerging
Other treatment focus with pediatric populations
Emerging
Teleconsultations in the emergency department
SUD treatment with pediatric populations
Scant
SUD treatment with adult populations
Scant
Other treatment focus with pediatric populations
Emerging
Family-based treatment approaches
SUD treatment with pediatric populations
Strong
Other treatment focus with pediatric populations
Emerging
Provider to provider use of telehealth to augment face-to-face care
SUD treatment with pediatric populations
Scant
SUD treatment with adult populations
Emerging
Other treatment focus with pediatric populations
Scant

Reducing Barriers to Using Telehealth for Pediatric Populations
Final Report
14
ENVIRONMENTAL SCAN AND DISCUSSION RESULTS BY QUESTION
What Are the Best Practices, Barriers and Potential Solutions for Using Services Delivered
Via Telehealth to Diagnose and Provide Services and Treatment for Children With SUD,
Including OUD? (Research Question #1)
Best Practices
As telehealth use has grown, some best practices have been formalized and disseminated
in the form of handbooks or guidelines. These are not specific to SUD for pediatric populations
and apply to telehealth generally or to pediatric telehealth generally (American Academy of
Pediatrics, 2017). Some of these resources offer broad guidance—for example, the United
Kingdom’s National Health Service released a guide on telehealth capabilities aimed at
demonstrating value to public officials (National Health Services, 2016). Other telehealth best
practices are tailored to specific treatment programs, such as enhancing access to medication
assisted treatment (MAT) and frequent contact with support systems for OUD treatment (Knopf,
2013). Although best practices are still evolving and emerging, there are a few general principles
for telehealth that will apply to telehealth for behavioral health.
Organizational Readiness
One of the best practices frequently noted in the literature involves ensuring
organizational readiness. These activities include planning, understanding the current state of the
organization’s culture and infrastructure and its particular needs. Planning should begin with an
early assessment of the needs of the community and the capability of telehealth to address any
gaps or issues (California Telehealth Resource Center, 2014). Factors such as the existing
technology available, how technology might be adapted for future programs, and quality
assurance should all be considered and addressed early on (Molfenter, Brown, O'Neill,
Kopetsky, & Toy, 2018; V. Perry, 2016). In addition, planning should include how telehealth
will be integrated into clinical and administrative workflows (Molfenter et al., 2018). This
includes identifying how care will be scheduled, coordinated and delivered (Gagnon, Duplantie,
Fortin, & Landry, 2006). This also includes mechanisms for identifying emergency and non-
emergency communications (Tofighi, Grossman, Sherman, Nunes, & Lee, 2016).

Reducing Barriers to Using Telehealth for Pediatric Populations
Final Report
15
Engagement
Involving clinical and administrative staff in the decision to implement telehealth and
develop related policies and protocols can improve their engagement and perceptions of
telehealth. Often, administrative staff such as telehealth coordinators at originating and distant
sites maintain communication and work together closely on tasks such as coordinating
scheduling, relaying laboratory results, and following up with providers and patients. In addition,
administrative engagement at the leadership level can help facilitate buy-in and engagement.
Provider engagement and buy-in are needed to support telehealth uptake. One way to do
that is to get provider involvement in identifying and developing clinical practice guidelines and
outlining the ways in which telehealth is appropriate (Myers et al., 2017). Initiatives are more
likely to have an impact on care outcomes and facilitate access to care when providers champion
telehealth use. In rural Alabama, for example, a community organized a child telepsychiatry
program using distance learning equipment available at the county technical high school. To
accomplish this, providers in the community had to work with state Medicaid officials to
understand reimbursement policies, as well as arrange for services from the University of
Alabama Department of Psychiatry to be furnished. Their program now provides weekly services
to children with a range of diagnoses (Merrell & Doarn, 2013).
Barriers and Solutions to Overcome Them
The literature includes discussion of several barriers to telehealth use, including the need
for technology investment, technology acceptance, and challenges associated with ongoing
service delivery.
Technology Investment
Barriers.
Although specific equipment needs vary across telehealth programs, all programs need
internet connectivity. Broadband gaps throughout the United States mean that some areas are
more likely than others to have sufficient connectivity to support telehealth (Federal
Communications Commission, n.d.-a). Applications such as videoconferencing require more
bandwidth and a faster connection than what is consistently available throughout the country
(California Telehealth Resource Center, 2014; McGinty, Saeed, Simmons, & Yildirim, 2006). A

Reducing Barriers to Using Telehealth for Pediatric Populations
Final Report
16
strong internet connection is needed to prevent quality issues such as lagging or skipping while
providing services. In addition, high network use by a telehealth application may interfere with
other staff members' work, particularly if the organization uses cloud-based services. Current
industry standards recommend that small physician practices and rural health clinics have
internet capability in line with U.S. Federal Communications Commission (FCC) broadband
internet benchmarks. Broadband download speeds are generally 25 Mbps for streaming ultra HD
4k video. Accounting for at least that capacity would allow for EHRs, videoconferencing, and
other uses of technology (Federal Communications Commission, 2019a; HealthIT.gov, 2019a).
This is in line with the bandwidth needed to stream high-quality video generally.
Solutions.
There are a number of initiatives aimed at increasing broadband capability throughout the
country which may ameliorate these concerns (Federal Communication Commission, 2010). For
example, the FCC has allocated funds to expand broadband access (Federal Communications
Commission, 2019b) and 4G access throughout the country (Federal Communications
Commission, n.d.-b). In addition, efforts have been made to support broadband adoption through
launching the Broadband Deployment Advisory Committee (Federal Communications
Commission, 2019c) and developing, reviewing and revising rules to promote streamlining the
process to transition to modern broadband networks. These initiatives may reduce the cost of
increasing the bandwidth necessary for telehealth interventions.
Technology Acceptance
Barriers.
Lack of access to technology and low technology competency across providers and
patients are barriers to telehealth (Muench, n.d.; K. Perry, Gold, & Shearer, 2019). In addition,
interruptions, technological complexity or other challenges in the visit can reduce technology
acceptance for both providers and patients (Boudreaux, Haskins, Harralson, & Bernstein, 2015;
Tofighi et al., 2016).
Solutions.
Organizations can help promote technology acceptance and combat issues by providing
initial training and technical support for both patients and providers (Batastini, King, Morgan, &
McDaniel, 2016).

Reducing Barriers to Using Telehealth for Pediatric Populations
Final Report
17
Some provider associations have started being proactive to encourage technology use and
assuage concerns. For example, the American Telemedicine Association maintains directories of
their members, allowing practitioners the opportunity to communicate with their peers (Becevic,
Boren, Mutrux, Shah, & Banerjee, 2015). The National Frontier and Rural—Addiction
Technology Transfer Center holds an annual summit for telehealth training during which
providers can interact in person (Reynolds & Maughan, 2015).
Telehealth can greatly reduce initial visit wait times for patients seeking mental health
services in rural clinics by making additional providers available, which can influence patient
acceptance. Thorough planning for integration into provider workflow (organizational readiness)
can help support efficiency and reduce interruption to workflow, both of which are critical to
physician buy-in and the ultimate success of initiatives (Gagnon et al., 2006).
Supporting Ongoing Service Delivery
Barriers.
Ongoing service delivery can be challenging due to workforce shortages and capacity
issues and the need for coordination. In the past, telehealth educational services were scheduled
as far a year in advance because of demand (HealthIT.gov, 2019b; Kraetschmer, Deber, Dick, &
Jennett, 2009). In addition, telehealth services across organizations require coordination and
information sharing, which may be difficult due to interoperability concerns.
Solutions.
Identification of systems and processes to support coordination within and across
organizations may help address the barriers associated with capacity (Luxton, Pruitt, &
Osenbach, 2014). In one model, remote providers can more quickly perform initial diagnostic
assessments and help plan for ongoing medication maintenance (Johnston & Yellowlees, 2016).
The Office of the National Coordinator is embarking on efforts to improve interoperability to
enhance data sharing across organizations, including for technologies to enable services
delivered via telehealth (The Office of the National Coordinator for Health Information
Technology, 2015).

Reducing Barriers to Using Telehealth for Pediatric Populations
Final Report
18
What Are the Differences, If Any, in Furnishing Services and Treatment for Children With
SUD Using Services Delivered Via Telehealth and Using Services Delivered in Person?
(Research Question #2)
For the general population, the literature indicates no significant difference between
services delivered via telehealth and face-to-face services. Limited information is available about
telehealth use for pediatrics, particularly for those patients with SUD.
Utilization Rates
Although there were no studies comparing the rates of service utilization for SUDs for a
pediatric population between telehealth and face-to-face encounters, a few studies analyzed
service utilization rates for broader health care services. In a systematic review of school-based
telehealth studies for acute and chronic illness, utilization was equal or higher in schools with
telehealth for students with special health care needs or medical complexities (Sanchez, Reiner,
Sadlon, Price, & Long, 2019). In another national study of Medicaid beneficiaries of all ages,
rural patients used telehealth more than urban patients, particularly for psychotropic medication
management (Talbot et al., 2018).
Costs
Although there was information available about financing, information specific to the
total cost of care and treatment was limited. Some publications mentioned that telehealth reduced
transfers to other facilities and reduced the use of transportation overall, but few showed
quantifiable results on the costs of telehealth models.
There are a number of business models to support telehealth, depending on the specific
application used (Chen, Cheng, & Mehta, 2013). However, there is no clearly established best
practice approach to compare cost between services delivered via telehealth and face-to-face
care. For example, the cost of equipment (e.g., computers or higher-speed internet) should be
included in any comparison if that equipment is only used for the telehealth intervention.
However, its inclusion in a cost assessment is less clear if the equipment is used for non-
telehealth purposes (Bounthavong et al., 2016).

Reducing Barriers to Using Telehealth for Pediatric Populations
Final Report
19
Avoidable Inpatient Admissions and Readmissions
There was limited information available about how telehealth for pediatric patients with
SUD impacts avoidable inpatient admissions and readmissions. Some studies show decreases in
urgent care or emergency room settings with use of telehealth interventions. In one study, 67
percent of parents of patients with varying acute health concerns would have visited an urgent
care center, emergency room, or retail clinic had the telehealth intervention not been available
(Vyas, Murren-Boezem, & Solo-Josephson, 2018). However, in a claims data analysis for a large
national health plan, use of direct-to-consumer telehealth by pediatric patients was associated
with greater use of both urgent care and emergency department visits (Ray, Shi, Poon, Uscher-
Pines, & Mehrotra, 2019; Talbot et al., 2018). One current program estimates a reduction in
downstream costs (Williams & Vance, 2019).
Quality of Care
Overall, the quality of telehealth care is similar to that of face-to-face care. This appears
to be true, both generally and in behavioral health, specifically (Lin et al., 2019). In one
retrospective review study, telehealth was associated with similar MAT outcomes in comparison
to face-to-face care (Zheng et al., 2017). In another, telehealth was associated with similar
treatment retention rates compared to face-to-face care (Fleischman et al., 2016).
With respect to quality as a process (Hanefield, Powell-Jackson, & Balabanova, 2017),
telehealth can help overcome issues of distant providers not being able to engage with local
resources or conduct assessments. An effectiveness review of telemental health in 2013 by Hilty
and colleagues found that telehealth is effective for behavioral health diagnosis and assessment
across many populations (adult, pediatric, geriatric, and minority) and for disorders in many
settings (e.g., emergency, home health), and appears to be comparable with in-person care (Hilty
et al., 2013). A recent review by the Agency for Healthcare Research and Quality (AHRQ) found
a large volume of research reporting that telehealth interventions produced positive results when
used in the clinical areas of chronic conditions and behavioral health, and when used for
providing communication or counseling and monitoring or management (Totten et al., 2016).
These review articles suggest that using telehealth for behavioral health services provides quality
similar to in-person services.

Reducing Barriers to Using Telehealth for Pediatric Populations
Final Report
20
Telehealth does create new challenges for quality of service delivery. Some areas lack
access to broadband, high-speed internet with stable connectivity (Bashir, 2018). Poor
connectivity can cause poor quality audio and video, disconnections, and slowed information
exchange (Celio et al., 2017; Cunningham, Connors, Lever, & Stephan, 2013). For pediatric
patients, it is important to ensure that they can see and be seen on the computer screen; this
entails making sure that webcams are set to the appropriate height, and that a staff member is
present to provide flexible or moveable technology (Goldschmidt, 2016; Stiles-Shields, Corden,
Kwasny, Schueller, & Mohr, 2015). For home-based services, some patients and families may
not have access to technology to participate in telehealth (Fischer et al., 2017).
Additional quality of care measures related to patient and family satisfaction are
discussed below.
Patient, Family, and Provider Satisfaction
Patients and Families
Telehealth use and satisfaction is influenced by individuals’ access to technology,
knowledge of available resources, and willingness to interact with the technology. For pediatric
patients, this includes both the patient and their caregiver. Some patients and their families may
face digital and cultural barriers (Bashir, 2018), and it may be difficult for those with limited
technology skills to adopt treatment approaches delivered via telehealth (Batastini et al., 2016).
Patient and family experiences may vary across demographics. For example, Schmeida
and McNeal (2007) found that older, low-income individuals were likely to search for Medicare
and Medicaid information online and young, highly-educated, and wealthy individuals were
more likely to use the internet in general. College graduates, young adults and those from high-
income households have extremely high levels of internet use and 80 percent of users have
searched for health information online in general (Pew Research Center, 2019b). Patients with
more than a high school education were more likely to use services delivered via telehealth than
those without a high school education (Lowery, Bronstein, Benton, & Fletcher, 2014).
Computer-based treatments for OUD have been shown to be more effective for patients
who are employed, suffering from anxiety, or are ambivalent about continuing substance use
than for other populations (Kim, 2015). Goldschmidt (2016) found that patients and families

Reducing Barriers to Using Telehealth for Pediatric Populations
Final Report
21
using telehealth for cognitive behavioral therapy needed support to ensure that they knew how to
use the technology, that they were aware of camera placement, and that they removed
distractions during therapy.
Beyond patient demographics, other factors may influence use and effectiveness of
telehealth. In a clinical trial of a remote Screening, Brief Intervention and Referral to Treatment
(SBIRT) program implemented in an emergency department setting, researchers found several
factors that could hinder use, including complications with provider engagement, delays in warm
handoffs to other remote behavioral health interventions, and disruptions from other medical
staff during the encounter, as well as family members and friends. Overall, the evidence
indicates that patients and caregivers had positive perceptions about telehealth. Despite the
challenges with SBIRT, the feedback and acceptance ratings from participants were generally
favorable, and the study ultimately concluded that a remote SBIRT application held great
promise. In addition, in a regional survey of patients across specialties, the majority found that
lack of physical touch was not a barrier and they were satisfied with the care received via
telehealth (Becevic et al., 2015; Vyas et al., 2018). Two additional studies—one of patients
diagnosed with attention-deficit/hyperactivity disorder (ADHD) and their caregivers and one of
parents with children with varying acute health concerns—reported a high degree of satisfaction
with care via telehealth (McCarty, Stoep, Violette, & Myers, 2015). Several other treatment
studies were found where patients with complex psychological problems (e.g., adult substance
use, PTSD), reported high rates of client satisfaction (Frueh, Henderson, & Myrick, 2005; King,
Brooner, Peirce, Kolodner, & Kidorf, 2014; Luxton, Pruitt, O'Brien, & Kramer, 2015; Martinez
et al., 2018; McKellar et al., 2012).
Providers
Telehealth satisfaction and uptake is also influenced by provider factors such as training
and technology acceptance. In a comprehensive survey study across provider types, providers
indicated that they were able to treat patients with telehealth and were satisfied with care
delivery via this mode (Becevic et al., 2015). However, from a long-term perspective, another
pilot study found that after 10 months, only two of 12 rural providers were using the telehealth
methods for which they trained. The physicians cited difficulty with the infrastructure needed to
implement telehealth as a key barrier (SAMHSA, 2016). Providers may also be wary of

Reducing Barriers to Using Telehealth for Pediatric Populations
Final Report
22
becoming credentialed (a process that involves a facility’s acceptance of a remote providers
medical credentials) at facilities they plan to serve only through telehealth.
A state-wide telepsychiatry intervention in Wyoming found that telehealth produced
noticeable results only when a range of providers were included and involved (Hilt et al., 2015).
Hilt (2017) found that ensuring that providers understand how to use technology is key to
provider engagement and satisfaction (Hilt, 2017).
Provider Organizations.
Telehealth also necessitates changes within the organizations through which care is delivered.
Provider organizations vary in size, complexity and resources. Thus, the ability to accommodate a
change in care delivery such as telehealth varies. Some organizational challenges include
credentialing, billing, technical barriers, and workflow.
Care delivery across organizations has implications for credentialing (McSwain &
Marcin, 2014). Facilities require that providers delivering services in their locations be
credentialed to ensure that services are within their scope of practice. Although the use of
delegated credentialing has increased, providers may not wish to undertake the credentialing
process for multiple organizations. And while there have been some strides to streamline
credentialing for telehealth purposes, it remains an issue (LeRouge & Garfield, 2013).
Although Medicaid, Medicare, and private payers have expanded payment for services
delivered via telehealth over time, the variability of requirements between states related to
coverage and payment remain a barrier. States vary with respect to policies around
reimbursement for telehealth and the conditions under which telehealth encounters are
reimbursable (Center for Connected Health Policy, n.d.-a). In addition, recent legislation, as
discussed in the next section, has changed certain payment policies for Medicare telehealth
services, such as what is considered a permissible originating site (site at which the beneficiary is
located) for certain services, which CMS implemented in 2019 (Centers for Medicare &
Medicaid Services, 2019). Members from provider organizations perceive that billing for
services delivered via telehealth in general is a challenge (N. M. Antoniotti, Drude, & Rowe,
2014). This is, in part, due to lack of training on how to manage these claims, perceptions that
these claims may be audited more frequently, and changes in billing codes and modifiers (N. M.
Antoniotti et al., 2016).

Reducing Barriers to Using Telehealth for Pediatric Populations
Final Report
23
Although patient visits are largely similar regardless of modality, there are a few
workflow differences between services delivered via telehealth and face-to-face visits that
organizations must accommodate. These include identifying when to refer and schedule
telehealth visits (Lambert, Gale, Hartley, Croll, & Hansen, 2016). Other workflow considerations
include streamlining data entry to save time and promote information sharing (Langkamp,
McManus, & Blakemore, 2015). Identifying staff and processes to manage telehealth visits is an
important part of telehealth uptake and use.
DELIVERY OF PEDIATRIC BEHAVIORAL HEALTH TREATMENT VIA
TELEHEALTH
Program Examples
Telehealth in the Emergency Department: Reducing Transfers
Telehealth delivery methods in emergency departments can be used to bring expertise
quickly and prevent unnecessary transfers to different institutions. The literature search did not
yield resources addressing SUD in pediatric patients specifically; however, just as services
delivered via telehealth can be used for diagnosis and treatment planning for other areas (Burke
& Hall, 2015), it can also be used for this application. Some potential outcomes include patient
and provider satisfaction and reducing transfers without degradation of care (Burke & Hall,
2015). Telehealth has been successful in reducing or eliminating the time psychiatric patients
wait in an emergency department for an inpatient bed by facilitating the development of a
tailored treatment plan (Deslich, Thistlethwaite, & Coustasse, 2013).
Telehealth Supplementing in-Person Visits: Enhancing Care
Telehealth delivery methods can supplement in-person visits by establishing links
between providers and pediatric patients when ongoing in-person care is infeasible. This is of
particular importance for those who might not be able to travel due to their location in a
childcare center, preschool, school, or juvenile detention facility (Burke & Hall, 2015). When
used as part of an enhanced medical home, some reported advantages of this model for the
pediatric population include fewer school absences for the children; less money spent by parents
on travel; less time away from employment for parents; and less crowding in emergency
departments where there may be a lack of pediatric expertise.

Reducing Barriers to Using Telehealth for Pediatric Populations
Final Report
24
Telehealth in the School Setting: Meeting the Population in the Community
Delivering services via telehealth while school-aged patients are at school allows patients
to receive care where they are during the day. In addition, school-based telehealth can help
connect patients and families with community resources that can help them manage their health
(Reynolds & Maughan, 2015). School-based services delivered via telehealth have shown
promising results to improve social, emotional, and behavioral outcomes among school-aged
children in need of a school psychologist, especially in rural settings where psychologist travel
time is a real concern (Bice-Urbach & Kratochwill, 2016). Teachers, students, and counselors
had favorable perceptions of telehealth. This mirrors an experience of using telehealth delivery
methods to address behavioral problems in the schools, where teachers had positive impressions
and there was a notable decrease in on-task behavior after implementation (Fischer et al., 2017).
Other school-based health clinics served as a medical home for patients who received a
variety of services delivered via telehealth for specialty care, including psychiatric care (RTI
International, 2016). In order for school-based interventions to be successful, communication and
coordination with school administration and teachers is important (Bice-Urbach & Kratochwill,
2016). One school-based telepsychiatry intervention emphasized the importance of
communication and coordination between different providers, staff, and parents (Cunningham et
al., 2013). Students had positive perceptions of telehealth used in this way. Similarly, in a
telehealth intervention designed for pediatric obesity, the importance of coordination was
identified as a key factor for success (Slusser, Whitley, Izadpanah, Kim, & Ponturo, 2016).
Telehealth to Support Family-Based Treatment Approaches
Family-based treatment approaches view SUD as a disease that includes the entire family
system. Thus, therapeutic approaches involve treating the individual and his or her family system
in tandem (Center for Substance Abuse Treatment, 2004; Kuhn & Laird, 2014; Lammers et al.,
2019; Sherr, 2018). Family-based treatment has been shown to be more effective than
approaches that focus on the patient alone (Crum & Comer, 2016). These approaches are often
used in face-to-face care (Allen et al., 2016; Donelan et al., 2019; Kaslow, Broth, Smith, &
Collins, 2012). In studies of the use of telehealth for substance use treatment and prevention,
interventions via telehealth demonstrated equal or better outcomes to face-to-face interventions
(Danaher et al., 2018; Donelan et al., 2019). Some considerations with this approach include

Reducing Barriers to Using Telehealth for Pediatric Populations
Final Report
25
ensuring the entire family is engaged with technology and ensuring connectivity at home for
home-based interventions (Crum & Comer, 2016). In another study of non-pediatric patients
with chronic disease at the Veterans Administration, patients found that incorporating family
members in care planning with telehealth had similar satisfaction rates as incorporating them
using face-to-face interaction (Bashir, 2018).
In a family-based approach using telehealth for a behavioral intervention focused on diabetes
management, outcomes were similar between telehealth and face-to-face cohorts, but patients
reported greater satisfaction with their provider in the telehealth cohort (Freeman, Duke, &
Harris, 2013). Project ECHO: Supporting Provider to Provider Education
The primary focus of telehealth financing has been on reimbursing direct services from
remote providers to patients. Provider to provider training is not covered by most payers,
including under Medicare and Medicaid. However, one of the most promising telehealth
approaches is the use of telehealth to connect providers with training, expertise, and/or
certification in areas that are relevant to the patients they are treating. This is of particular
importance for pediatric SUD, where there is a dearth of providers.
Project ECHO (Extension for Community Healthcare Outcomes) is a telehealth program
focused on building capacity at the local level. This effort virtually links specialists at an
academic “hub” to providers in local communities—the “spokes” of the model. Connections
occur by providing remote training and specialist consultations. Specifically, the spokes
participate in weekly teleECHO clinics, which are virtual grand rounds, combined with
mentoring and patient case presentations facilitated by the hub. As of 2017, this model is in use
in more than 130 hubs across the United States, as well as 23 other countries (Lewiecki et al.,
2017). Many of the studies we reviewed were based on the ECHO model or were working
directly with the model, and reported an increase in the number of MAT-prescribing providers in
rural communities. Some communities integrated support for the Drug Addiction Treatment Act
(DATA 2000) waiver for prescribing medications for OUD with training to further support spoke
providers (Quest, Merrill, Roll, Saxon, & Rosenblatt, 2012).
One of the challenges affecting provider participation is the lack of funding for the time
providers spend attending and participating in these types of telehealth activities. Project ECHO
has addressed this concern by holding TeleECHO clinics at or near lunchtimes for the local

Reducing Barriers to Using Telehealth for Pediatric Populations
Final Report
26
providers and by offering Continuing Education Units as an incentive (American Medical
Association, 2016; University of New Mexico, 2016). In some cases, Project ECHO participation
is covered by grant funding or included as time to be covered by the provider organization under
employment contracts. Although these efforts may be effective in some cases, some providers
may still choose not to take advantage of telehealth training in the absence of specific
reimbursement for their time.
In one study, sites noted that funding for TeleECHO is a challenge. Payers including
Medicaid do not reimburse for provider to provider communication and training. Often, such
programs have been initiated with grant funding and face a sustainability challenge after the
grant ends (Dunlap et al., 2018).
POLICY AND REIMBURSEMENT CONSIDERATIONS
Many of the resources we reviewed called for regulatory changes to promote the uptake
of telehealth delivery methods to treat SUDs. Policies supporting the use of telehealth more
generally were not unique to pediatric patients. Some articles examined regulatory issues as a
component of payment policy, for example focusing on variation in licensure requirement.
Telehealth Policies that Influence Delivery of SUD Treatment
Our environmental scan found that many of the policies explicitly focused on telehealth
delivery methods for SUD treatment emphasized the treatment of OUD and MAT in particular.
The majority of resources describing these policies either reflected adult populations or did not
make any age distinctions. Telehealth-delivered MAT for OUD is not as prevalent as the use of
telehealth in other behavioral health services due to some unique considerations. Methadone is
only available from federally designated opioid treatment providers who typically require in-
person visits. Naltrexone requires a 7- to 10-day period of abstinence prior to start, which is often
a challenge without local provider support. Limitations on prescribing controlled substances is
recognized as a barrier for the provision of MAT via telehealth. For pediatric patients, MAT is
uncommon. Methadone and naltrexone are not approved for patients under age 18 (although an
exception can be made for methadone if the patient has had two documented unsuccessful
attempts at detoxification and has parental consent). Buprenorphine products are allowed for
patients 16 or older.

Reducing Barriers to Using Telehealth for Pediatric Populations
Final Report
27
Regardless, many of the policies are likely to have a similar influence on treatment for
pediatric patient populations delivered via telehealth. Other policies we describe below do apply
specifically to services delivered via telehealth for pediatric populations. Finally, some policies
apply similarly to all medical conditions while others are particular to both mental and substance
use disorders.
The Agriculture Improvement Act of 2018 (Pub. L. No. 115-334), commonly known as
the Farm Bill, includes key provisions for the use of telehealth to address SUD in rural
communities. These include increasing the annual budget for U.S. Department of Agriculture
Distance Learning and Telemedicine grants from $75 million to $82 million, and requiring 20
percent of all financial assistance for telehealth projects to be set aside for programs that address
SUD. In addition, this Act addresses connectivity concerns by increasing Federal resources for
broadband expansion projects in rural parts of the country. This includes creating a Federal
advisory committee to study opportunities for and barriers to rural broadband expansion.
The Substance Use-Disorder Prevention that Promotes Opioid Recovery and Treatment
for Patients and Communities Act of 2018 (“SUPPORT for Patients and Communities Act”, Pub.
L. 115-271) includes a number of provisions to support services delivered via telehealth. For
example, the SUPPORT for Patients and Communities Act amended section 1834(m) of the
Social Security Act (Pub. L. 74-271) to change certain payment policies for Medicare telehealth
services, as described in section 3.4.2.
The Ryan Haight Online Pharmacy Consumer Protection Act of 2008 (“Ryan Haight
Act”, Pub. L. 110-425) modified the Controlled Substances Act (CSA, Pub. L. 91-513), placing
challenges on the ability of telehealth providers to prescribe controlled substances. The Ryan
Haight Act requires providers to conduct at least one in-person medical evaluation prior to
prescribing controlled substances via telemedicine, with limited exceptions. However, there was
a clarification of the Ryan Haight Act which allowed MAT prescribers to be exempted from a
required in-person medical evaluation (U.S. Department of Justice, n.d.). States, however, still
vary in their own provisions around telehealth delivery methods for MAT; for example,
Connecticut recently joined the minority of states who make a specific exception for MAT for
OUD (Dizon, 2018).

Reducing Barriers to Using Telehealth for Pediatric Populations
Final Report
28
Credentialing
Credentialing requirements remain a general barrier to telehealth delivery of services.
Hospitals require providers to be credentialed per Joint Commission Standards (Joint
Commission on Accreditation of Healthcare Organizations, 2012, January). Hospitals may need
the services of numerous telehealth providers such as psychiatrists and counselors to meet the
needs of their patients. In turn, those providers may serve patients across numerous hospital
systems in which they must be separately credentialed. Depending on the model being used for
telehealth, credentialing can be a very expensive and burdensome activity for hospitals and
telehealth providers (Zeller & Mao, 2016).
Privacy Laws and Regulations
Policies around privacy and protection of private data influence telehealth models,
particularly for pediatric patients and for sensitive care areas like SUD and mental health. The
Privacy Rule, issued pursuant to Title II of the Health Insurance Portability and Accountability
Act of 1996 (Pub. L. No. 104-191) (HIPAA) addresses patient privacy generally and 42 CFR
Part 2, implementing 42 U.S.C. § 290dd-2, specifically governs the confidentiality of substance
use disorder patient records of federally-assisted SUD treatment programs. The Family
Educational Rights and Privacy Act (FERPA) (20 U.S.C. § 1232g; 34 CFR Part 99) provides
privacy protections for student education records maintained by educational agencies (for, e.g.,
school districts) and institutions (i.e., schools) that receive funds under any program
administered by the U.S. Department of Education. Further, the Individuals with Disabilities
Education Act (IDEA) contains confidentiality provisions that are similar to, but broader than,
FERPA. IDEA Part B protects the privacy of personally identifiable information in education
records of children with disabilities ages 3 through 21, while IDEA Part C protects the privacy of
personally identifiable information in early intervention records of children with disabilities
under the age of 3 (20 U.S.C. 1417(c) and 1442; 34 CFR 300.610 through 300.626; 34 CFR
303.401 through 303.417).
Compliance with these federal laws and rules presents some burden to telehealth provider
organizations, especially smaller ones (Mountain-Pacific Quality Health, 2017, Sept 27). And the
complexities of HIPAA, FERPA, and the IDEA together can complicate how student health
information is shared, which can create a particular challenge to telehealth providers for students

Reducing Barriers to Using Telehealth for Pediatric Populations
Final Report
29
in school-based settings (Boling & Company, 2016). See section 3.4.4 of this report for further
discussion of how these federal privacy laws influence telehealth models. It is also important to
note that state privacy laws, which may be more protective of, or contain different provisions
regarding, privacy than federal law, and should be reviewed to determine how student health
information is shared.
Consent for Services
Most states and the District of Columbia require informed consent for telehealth service
delivery for general and behavioral health care (Center for Connected Health Policy, n.d.-b).
Telehealth service delivery for pediatric patients can be particularly challenging for providers
because they must follow laws regarding age of consent. The ages at which a child is able to
offer consent on their own behalf, without requiring involvement of a parent or legal guardian,
vary not only by state but also by specific conditions (Hoffman, 2019; McSwain et al., 2017).
McSwain et al. reported an example of a state in which a 12-year old may provide consent to
treatment for a sexually transmitted disease, and may consent to treatment for substance abuse at
age 14 (2017).
This means that telehealth providers of care for MH/SUD must develop and enforce
complex policies around patient interaction and clinical care that may lead to re-consent, new
consent, or the need for parent/guardian involvement at any point over the course of treatment.
Medicare and Medicaid Coverage
Medicare Coverage
The health care community uses the term “telehealth” broadly to refer to medical services
furnished via communication technology. Although all of these kinds of services might be called
“telehealth” by patients, other payers and health care providers, CMS has generally used the term
“Medicare telehealth services” to refer to the subset of services defined in section 1834(m) of the
Social Security Act (the Act). Section 1834(m) of the Act defines Medicare telehealth services
and specifies the payment amounts and circumstances under which Medicare makes payment for
a discrete set of services, all of which must ordinarily be furnished in-person, when they are
instead furnished using interactive, real-time telecommunication technology. Section 1834(m) of
the Act limits the scope of Medicare telehealth services for which payment may be made to those

Reducing Barriers to Using Telehealth for Pediatric Populations
Final Report
30
furnished to a beneficiary who is located in certain types of originating sites in certain, mostly
rural, areas and permits only physicians and certain other types of practitioners to furnish and be
paid for Medicare telehealth services.
For CY 2019, CMS aimed to increase access for Medicare beneficiaries to physicians'
services that are routinely furnished using communication technology, but are not Medicare
telehealth services. CMS established a discrete set of separately billable services that are defined
by and inherently involve the use of communication technology. Accordingly, in the CY 2019
Physician Fee Schedule (PFS) final rule, CMS finalized several proposals for modernizing
Medicare physician payment for communication technology-based services. These included two
newly defined physicians’ services that are furnished using communication technology: the brief
communication technology-based service (i.e. a virtual check-in) and the remote evaluation of
recorded video and/or images submitted by an established patient. Additionally, CMS finalized
policies to pay separately for new coding describing chronic care remote physiologic monitoring
and interprofessional internet consultation. Because these services are not considered Medicare
telehealth services, they are not subject to the geographic and other limitations in section
1834(m) of the Act.
Although section 1834(m) of the Act grants the Secretary the authority to add services to,
and delete services from, the list of Medicare telehealth services based on the established annual
process, it does not provide any authority to change the limitations relating to geography, patient
setting, or type of furnishing practitioner because these requirements are specified in statute.
However, we note that sections 50302, 50324, and 50325 of the Bipartisan Budget Act of 2018
(BBA of 2018) (Pub. L. 115-123) have amended section 1834(m) and certain other provisions of
the Act to modify or remove the limitations relating to geography and patient setting for certain
telehealth services, including for certain home dialysis end-stage renal disease-related services,
services furnished by physicians and other practitioners in certain Medicare Shared Savings
Program Accountable Care Organizations (ACOs), and acute stroke-related services,
respectively. Additionally, in accordance with the BBA of 2018, CMS finalized changes that
would allow Medicare Advantage plans to cover certain Part B benefits on a telehealth basis as
“additional telehealth benefits,” starting in plan year 2020. These additional telehealth benefits
offer patients the option to receive these health care services from places like their homes, rather
than requiring them to go to a healthcare facility.

Reducing Barriers to Using Telehealth for Pediatric Populations
Final Report
31
The SUPPORT for Patients and Communities Act amended section 1834(m) of the Act to
change certain payment policies for Medicare telehealth services. Specifically, the SUPPORT for
Patients and Communities Act removed the originating site geographic requirements and added
the home of an individual as a permissible originating site for telehealth services furnished for
purposes of treatment of a substance use disorder or a co-occurring mental health disorder for
services furnished on or after July 1, 2019.
Additionally, the SUPPORT for Patients and Communities Act established a new
Medicare Part B benefit for opioid use disorder (OUD) treatment services, including medications
for medication- assisted treatment (MAT), furnished by opioid treatment programs (OTPs). To
support the use of telehealth technology in the provision of OUD treatment services, CMS
finalized a policy to allow OTPs to furnish the substance use counseling, individual therapy, and
group therapy included in the OTP bundled payment via two-way interactive audio-video
communication technology, as clinically appropriate, in order to increase access to care for
beneficiaries. This includes allowing these services to be furnished via telecommunications
technology in a beneficiary’s home. By allowing use of communication technology in furnishing
these services, OTPs in rural communities or federally-designated geographic health professional
shortage areas would be able to facilitate treatment through virtual care coming from an urban or
other external site, subject to applicable requirements relating to professional licensing and scope
of practice. To further increase access to OUD treatment, CMS established new bundled
payments under the Medicare Physician Fee Schedule beginning in 2020 for OUD treatment
services furnished by clinicians in an office or outpatient setting. These services were also added
to the Medicare telehealth services list beginning in CY 2020.
Although these Medicare policies do not directly affect Medicaid programs, Medicaid
program policies are often informed by Medicare policy (Olson, McSwain, Curfman, & Chuo,
2018).
Medicaid Coverage
Forty-nine states and the District of Columbia have formal definitions of telehealth, but
those definitions vary by state (Center for Connected Health Policy, 2019a). This variation is
reflected in coverage by Medicaid, which is not consistent across states (Thomas & Capistrant,
2015). All 50 states and the District of Columbia provide Medicaid reimbursement for some
form of live video for telehealth (Center for Connected Health Policy, n.d.-a). However,

Reducing Barriers to Using Telehealth for Pediatric Populations
Final Report
32
Medicaid reimbursement varies across states in several ways including the setting where the
patient is located (often restricted to hospitals or clinics), types of services that are reimbursable,
and type of health care provider providing services (Center for Connected Health Policy, n.d.-c).
The District of Columbia and 24 states do not restrict the location and setting in which patients
receive services delivered via telehealth. Fifteen of these states do not restrict the type of health
care provider delivering services via telehealth. Overall, we did not find evidence of any explicit
restrictions for pediatric patients whose services are reimbursed by Medicaid.
Finally, CMS issued a guidance document to State Medicaid directors in June of 2018
outlining ways that technology can be used to support identification, management and treatment
of SUD, specifically focused on OUD (Centers for Medicare & Medicaid Services, 2018a). In
this document, CMS suggested integrating telehealth delivery methods into treatment programs,
and specifically suggested “telehealth optimized Medication Assisted Treatment.” In later
guidance to State Medicaid directors, CMS described the possibility of financial matching for
state development of telehealth-enabling technology for Medicaid providers to use for better care
coordination for patients with serious mental illness or serious emotional disturbance (Centers
for Medicare & Medicaid Services, 2018b; Medicaid.gov, n.d.).
1
State Medicaid Variations
All state Medicaid programs include some form of coverage and reimbursement for
mental health services delivered via telehealth (Center for Connected Health Policy, 2019b). In
addition, they all require providers to be licensed in the state in which the patient is located
(Centers for Medicare & Medicaid Services, n.d.-b). Nine states have special licenses to allow
out-of-state providers to deliver services via telehealth (Center for Connected Health Policy,
2019a), and compacts between states and licensing agencies are becoming more common. For
example, 29 states and the District of Columbia belong to the Interstate Licensing Compact
(Interstate Medical Licensure Compact, 2019), and compacts also exist for other professional
designations.
1
Under MITA 3.0, implementation of new technologies may qualify for enhanced match of 90 percent federal match for establishing the
technology and 75 percent match for operational support. See CMS State Medicaid Director Letter # 18-006, “Leveraging Medicaid
Technology to Address the Opioid Crisis” (June 2018): https://www.medicaid.gov/federal-policy-guidance/downloads/smd18006.pdf

Reducing Barriers to Using Telehealth for Pediatric Populations
Final Report
33
There are other reimbursement considerations that vary by state (Federation of State
Medical Boards, n.d.). Reimbursement may depend on whether the service was delivered
synchronously or asynchronously. Some states restrict reimbursement for services delivered via
telehealth for behavioral health issues to physicians who are psychiatrists, advanced practice
nurses with clinical specialties, and psychologists. Other states also allow licensed clinical social
workers or licensed professional counselors to provide services. However, only a few states
specify coverage for telehealth when provided by an SUD or addiction specialist (Thomas &
Capistrant, 2015).
State Medicaid policies around services delivered via telehealth for MH/SUD are also
continuing to evolve: California passed legislation allowing Medicaid reimbursement for
services delivered via telehealth provided by licensed or certified SUD counselors (Dizon, 2018);
Illinois is requiring Medicaid to reimburse for telehealth-delivered mental health services; and,
Kentucky has eliminated the requirements that a physician be present and prior authorization be
given for telehealth reimbursement for any type of care. We found no indication that these policy
changes are applied differentially to pediatric patients.
The American Telemedicine Association’s Telemental Health and Business and Finance
Special Interest Groups conducted a survey to study private payer reimbursement of services
delivered via telehealth (N. M. Antoniotti et al., 2014). Of the respondents 65 percent indicated
they did not provide services delivered via telehealth because of perceived lack of
reimbursement. Some respondents did indicate that they continued to provide services delivered
via telehealth even when they were not reimbursed.
Federal Models and Programs to Support Telehealth
Federal agencies are supporting several new efforts to include telehealth in opioid use
disorder treatment and behavioral health care. For example, AHRQ is supporting three
demonstrations in Colorado, Oklahoma, and Pennsylvania that will attempt to train rural primary
care providers in OUD treatment. Their model includes collaboration with Project ECHO for
specialty training (Whitman, 2016).
The Health Resources and Services Administration (HRSA) supports the Pediatric
Mental Health Care Access (PMHCA) Program to promote the integration of behavioral health
into pediatric primary care by supporting the development of new, or the improvement of

Reducing Barriers to Using Telehealth for Pediatric Populations
Final Report
34
existing, statewide or regional pediatric mental health care telehealth access programs. These
programs provide tele-consultation, training, technical assistance, and care coordination for
pediatric primary care providers to diagnose, treat and refer children with behavioral health
conditions. HRSA supports 21 PMHCA programs, which are authorized by the 21
st
Century
CURES Act.
In addition, the CMS Center for Medicare and Medicaid Innovation (Innovation Center)
develops new payment and service delivery models in accordance with the requirements of
section 1115A of the Social Security Act. For example, in August 2018, the Innovation Center
announced the Integrated Care for Kids (InCK) Model, which seeks to reduce expenditures and
improve quality of care for children enrolled in Medicaid and CHIP (Center for Medicare and
Medicaid Innovation, 2019). Awardees have developed state-specific pediatric alternative
payment models and service delivery infrastructure to coordinate and integrate health care
services for children with significant health needs, including those with behavioral health
challenges. The use of telehealth is identified as a possible strategy to increase capacity to deliver
services.
In addition, CMS also uses its waiver authority under the Innovation Center statute to
waive certain Medicare requirements solely for purposes of testing models, including waiving
Medicare telehealth requirements. For example, the Next Generation ACO Model’s benefit
enhancements include the option to use telehealth in circumstances not otherwise permitted
under Medicare, including providing coverage for teledermatology and teleophthalmology
services furnished using asynchronous store and forward technologies.
CMS has also established regulations that govern the payment for certain telehealth
services furnished by ACO participants in Medicare Shared Savings Program ACOs
participating under performance-based risk, in accordance with section 50324 of the Bipartisan
Budget Act of 2018. This policy allows for payment for telehealth services furnished by
physicians and other practitioners to prospectively assigned beneficiaries in non-rural areas, and
allows beneficiaries to receive certain telehealth services at their home, to support care
coordination across settings.

Reducing Barriers to Using Telehealth for Pediatric Populations
Final Report
35
Privacy and Confidentiality Considerations
Resources reviewed highlight the need for provider organizations to establish
mechanisms to protect patient privacy when using telehealth delivery methods. Privacy for
patients receiving SUD services is generally protected through the HIPAA Privacy Rule and 42
CFR Part 2, which applies to substance use disorder patient records. The former protects patient
privacy and security for all types of health care services. The latter provides specific, stronger
protections for the privacy of patients who receive treatment at federally-assisted SUD treatment
programs (SAMHSA.gov, n.d.). With few exceptions, providers covered by 42 CFR Part 2 are
prohibited from sharing patient information without patient consent, even to law enforcement or
other health care providers.
Telehealth services provided in a school-based setting or by educational agencies and
institutions may implicate FERPA. FERPA addresses how and to whom educational agencies
and institutions can share, both internally and externally, personally identifiable information
from student education records, without the prior written consent of the parent or the eligible
student. An eligible student is a student who is aged 18 years or older or attending an institution
of postsecondary education. For example, FERPA protects student health and health care records
maintained by an educational agency or institution or by a person acting for such agency or
institution in the process of a student receiving health care services, such as from a school nurse.
None of these three laws and regulations specifically address telehealth services, which are often
delivered through outside vendors. Many organizations rely on their vendors to address technical
aspects of legal compliance.
School-based telehealth programs generally need to comply with the HIPAA Privacy
Rule or FERPA (both standards may apply in the limited instance that a program serves students
and non-students). While the HIPAA Privacy Rule specifically excludes FERPA-protected
education records and “treatment records” from its coverage, a key ambiguity is whether a
telehealth provider from an external organization is considered to be “acting on behalf” of the
school, in which case FERPA would apply to students’ health records maintained by the
telehealth provider (note: a narrow exception to FERPA’s applicability exists under 20 U.S.C. §
1232g(a)(4)(B)(iv) for “treatment records” of students aged 18 years or older attending
institutions of postsecondary education; however, of note, among other things, this exception

Reducing Barriers to Using Telehealth for Pediatric Populations
Final Report
36
generally does not apply to records made available to anyone other than persons providing
treatment to the students). Whether the HIPAA Privacy Rule or FERPA applies would impact
the telehealth provider’s flexibility in sharing, without prior written consent, protected health
information for purposes of payment, treatment, and operations. Meanwhile, FERPA would
allow school staff to share, without prior written consent, a student’s health records maintained
by the school or by a person acting for the school with other school employees who constitute
“school officials” and who have a “legitimate educational interest” in the records for purposes
unrelated to health care, provided they meet the school official requirements under FERPA.
Federal guidance issued jointly clarified the HIPAA-FERPA interaction in 2008 and
more recently in 2019, but did not anticipate telehealth provision (U.S. Department of Health and
Human Services & U.S. Department of Education, 2008, November). Given the remaining
uncertainty, providers for school-based programs continue to carefully tailor their policies and
procedures in cooperation with each school or district, often under consultation with legal
counsel. Of note, some providers ensure compliance by requiring their partner schools to sign a
business associate agreement that contractually commits them to follow HIPAA rules (Boling &
Company, 2016). Provider organizations can address operational aspects of compliance by
incorporating telehealth delivery methods into their privacy plans when considering aspects such
as ensuring privacy during a consultation, obtaining and sharing consent virtually, coordinating
care, and exchanging data. In addition, patients may have concerns about privacy. One study
recommended that organizations develop patient education materials to assuage those concerns
(Adkins et al., 2017). In a study of adults using tablet computers to support methadone treatment,
participants were taught how to use the tablet, how to select a private space for the intervention,
and how to use secure connections to preserve privacy (Brusoski & Rosen, 2015).
Other operational aspects include measures to ensure that patients know with whom they
are communicating. To address this, some practices have policies in place to limit the number of
people communicating with a patient; some place a limit on one provider at a practice who can
communicate with a patient via text messaging. Other ways to protect patient privacy mirror
face-to-face considerations, such as ensuring that only individuals who are involved with the
patient's care are involved in visits (Paing et al., 2009). Organizations must take both technical
and process factors into account when planning and implementing telehealth delivery methods to
protect patient privacy.

Reducing Barriers to Using Telehealth for Pediatric Populations
Final Report
37
For some uses, patients preferred telehealth delivery methods because they felt it gave
them privacy. In a feasibility study for a home-based telehealth intervention for service personnel
with post-traumatic stress, service members reported that they preferred telehealth because it
afforded them privacy that they would not have by going to a Veterans Health Administration
facility (Luxton et al., 2015). Similarly, those in small communities may feel that telehealth
delivery methods afford privacy so that they don’t feel the stigma of being seen in a behavioral
health setting (Dunlap et al., 2018).

Reducing Barriers to Using Telehealth for Pediatric Populations
Final Report
38
KEY INFORMANT DISCUSSIONS
OVERVIEW OF KEY INFORMANT DISCUSSION RESULTS
To supplement the findings from the environmental scan, we conducted semi-structured
discussions via telephone with nine key informants and categorized findings in similar fashion to
the environmental scan. Specifically, the results are presented by the primary research topics,
barriers and solutions, and differences in service deliver for in-person versus telehealth for SUD
treatment in pediatric patient populations.
For several areas in both research questions, the key informant interviews supported the
results from the environmental scan around barriers and enhanced our understanding of potential
solutions and important next steps. In some areas such as utilization, costs, and avoidable
inpatient admissions, key information discussion yielded limited information. Much of the key
informant information below applies to serving pediatric patients with a MH/SUD via telehealth,
as well as to other patient populations. Where appropriate, we explain the rationale for why a
general consideration applies specifically to our study’s target population. We also make
clarifying notes in cases in which information may apply differently for a mental health disorder
service rather than a SUD service, applies to pediatric patients generally or applies to a subset of
our study’s target population, such as for younger patients or patients with less stability.
WHAT ARE THE BEST PRACTICES, COMMON BARRIERS AND POTENTIAL
SOLUTIONS FOR USING SERVICES DELIVERED VIA TELEHEALTH TO
DIAGNOSE AND PROVIDE SERVICES AND TREATMENT FOR CHILDREN WITH
SUD, INCLUDING OUD (RESEARCH QUESTION 1)?
Best Practices
Several of the best practices frequently mentioned in the environmental scan were also
mentioned by the key informants. Their suggestions included: organizational readiness and
provider engagement; addressing workforce shortages; balancing face-to-face and telehealth
sessions; and engaging families. Key informants noted that available resources often determine
what best practices can be implemented and what barriers a program could face during
implementation. Resources include reliable technology with appropriate assurances for privacy
and staff with capacity for both treating pediatric SUDs and for using the technology.

Reducing Barriers to Using Telehealth for Pediatric Populations
Final Report
39
Clinical Practice
The most common telehealth-delivered MH/SUD services provided for pediatric patients
were in the form of traditional counseling with sessions lasting an hour or less. Models based on
motivational interviewing and cognitive behavioral therapy were the most common clinical
approaches. Family-based therapy or informal family involvement were a common variant in
these counseling programs. Medication management by a psychiatrist or other provider with
prescribing privileges was also referred to in some programs described by the key informants.
However, medication management was specific to mental health and the informants did not
know of any programs focused on MAT for OUD or alcohol use disorder. For young adult
patients (age 18 to 20) seeking MAT in conventional settings, there was no discussion of
particular telehealth barriers outside of what is typical for all adults as described in the
environmental scan results.
Only one key informant described using telehealth for MH/SUD assessments in school-
based settings and noted several challenges. The established models for pediatric patients with
which they were most familiar were based on MH/SUD treatment providers serving patients in
their originating location after some screening and assessment had already occurred. There was
difficulty making linkages with MH/SUD treatment providers (either in the community or via
telehealth) in general. In his state, Medicaid Accountable Care Organizations (ACOs) could not
bill for initial assessments and thus focused on assessing a smaller number of referral patients
who were most likely to become a patient following assessment (and thus making the model
more sustainable).
Telehealth Modality
The key informants all agreed that patient-provider videoconferencing is the only
prominent telehealth modality for MH/SUD patients. Five of the nine key informants currently
provide such services. Asynchronous methods were not used by many known programs and were
considered less relevant than synchronous methods by several key informants. Asynchronous
video for direct counseling has less of an evidence base and there are concerns about rapport,
therapeutic alliance and the overall clinical impact of using it to conduct current evidence-based
in-person practices. One consideration is that asynchronous video may become more prominent
for medication management, in stable, well-established patients.

Reducing Barriers to Using Telehealth for Pediatric Populations
Final Report
40
Several key informants did describe some emerging direct-to-consumer telehealth for
pediatric MH/SUD patients in which the patient could access a clinician via videoconferencing at
certain times of the day using a personal device with a secure interface. The services were not
limited to MH/SUD services although managing crises in real time was a major goal. In one
model, the pediatric patients to whom the direct-to-consumer option was being made available
were primarily MH/SUD patients who were most likely to overuse emergency care.
Several informants were hopeful about the use of texting to support treatment. Texting
was seen as an additional tool for keeping patients engaged in treatment, appointment reminders
and other types of care coordination. The ability to prompt or interact with patients at different
times of the day has potential to keep patients mindful of their moods, risk factors and the
exercises they need to continue to practice as part of their recovery. Informants posited that
texting could be an evidence-based clinical strategy.
Finally, all informants were very positive about the use of provider-to-provider
consultation and training to enhance care for patients. All were familiar with Project ECHO and
similar models but noted that many health systems were also developing their own internal
practices. Although not unique to pediatric patients with MH/SUD, Project ECHO type models
should be considered relevant because of concerns about too few providers having such narrow
clinical expertise.
Financing
The specific programs described by key informants were based within health systems,
specialty behavioral health providers that focused on MH/SUD, and school-based clinics. All
such settings could bill Medicaid and other payers. However, billing Medicaid was less common
for school-based programs. Current programs in the health systems were likely to be sustained
and continue to expand. Often, health system programs had been built to enhance or expand care
for a currently-covered population and the business case for using telehealth had been carefully
made at each step to ensure that revenue from payers would sufficiently maintain the model.
Conversely, several informants noted that programs based in specialty behavioral health
providers and schools were heavily dependent on other funding sources such as grants and direct
funding for certain necessary infrastructure (e.g., telehealth equipment, school nurse salaries).

Reducing Barriers to Using Telehealth for Pediatric Populations
Final Report
41
Detailed Best Practices Emphasized by Key Informants
Videoconferencing
For several reasons, the most common telehealth modality being used to deliver
MH/SUD services to pediatric patients is videoconferencing between a provider and a patient.
Videoconferencing is well-established and has been well-studied for general health and adult
populations. Pediatric MH/SUD programs have taken advantage of past successes in health care
around overcoming videoconferencing technology and workflow challenges and obtaining
institutional support within health systems. For MH/SUD services, the technology needs are even
simpler than for other telehealth-delivered services. Only a device with a video camera and an
internet connection are needed. The devices are usually common technology that both providers
and patients are familiar with, typically laptops or tablets. Videoconferencing provides services
to patients who would otherwise have no access due to location or other barriers. Finally, when
videoconferencing is used to reproduce the same service unit as an existing in-person service
(e.g., a session of counseling), it has a clear potential revenue source under conventional health
care payment models.
A major feature of videoconferencing with pediatric patients with a MH/SUD is being
able to flexibly incorporate family members. This was done through three-way
videoconferencing, patient and family together at home or in a clinic site, or meeting with
parents separately from the child in order to accommodate work and school schedules. Several
key informants noted how in face-to-face settings, getting patients and their families to a clinic
location is very challenging.
Support Staff
The value of staff supporting telehealth programs was a clear message from five of the
key informants. This is succinctly emphasized by the statement made by a clinical provider that
“telehealth is more than a counselor and a screen.” The most common support staff discussed
were telehealth coordinators, nurses, and guidance counselors. Their roles included outreach,
intake processing, screening and assessments, technical support for the use of technology,
scheduling and planning, coordinating with other systems like the school administration or other
health care providers, and case management—all of which make the program efficient, increase
Reducing Barriers to Using Telehealth for Pediatric Populations
Final Report
42
treatment engagement and help provide integrated care for pediatric MH/SUD patients who often
have broader health care needs.
While support staff are also ideal for adult patients, there are two reasons that they are
potentially more important for pediatric patients with MH/SUDs. As noted earlier, pediatric
patients have less agency and autonomy than adult patients. They rely heavily on their caregivers
for transportation, financial access, and administrative tasks like making appointments and
completing intake paperwork. Yet the patients who need telehealth to have access to care are
most often in the areas with more poverty, more single-parent families, and fewer community
resources. Moreover, pediatric patients with MH/SUD are more likely to have a parent who also
has a MH/SUD (Moreira-Almeida & de Souza, 2016; Pearson et al., 2013; Sawyer, Zunszain,
Dazzan, & Pariante, 2019; Smith, Wilson, & Committee on Substance Use and Prevention, 2016;
Weissman, Warner, Wickramaratne, Moreau, & Olfson, 1997), which may decrease their support
of their child’s non-emergency care (Alston, Bennett, & Rochani, 2019; Gopalan et al., 2010;
Sills, Shetterly, Xu, Magid, & Kempe, 2007). Several informants noted that pediatric patients’
traumatic experiences may be associated with the same caregivers they rely on to access care.
Local support staff are an effective strategy for overcoming the challenge of pediatric patients
relying on caregivers to access treatment. The support staff help by coordinating community
resources, reducing the administrative barriers to participating in treatment and by doing
effective outreach to help a pediatric patient engage in and complete treatment. In many
programs, these staff are the in-person, “warm, friendly face” that the patient first interacts with
prior to building rapport with the direct service provider. They are a key component to providing
a consistent “safe space” for the patients.
The second reason support staff are crucial is ensuring the safety of pediatric patients
receiving telehealth-delivered MH/SUD services. Outside of a home-based setting, these staff are
“One of the things we found is that having people connected to the
community involved in the program and supporting the program helps in
uptake in acceptance. In every county we have a program director who is
from there and they handle relationships with school nurses and schools
and they’re at PTA meetings and that presence is really important for
success. It’s all about relationships and how the system operates that needs
the most effort.”

Reducing Barriers to Using Telehealth for Pediatric Populations
Final Report
43
the first line of defense for patients who may be a danger to themselves or others, and are key to
implementing safety protocols. The best practices around these safety protocols are described
later in this report.
School-based Programs
When delivering telehealth in school settings for pediatric MH/SUD, access is perhaps
the biggest challenge. Access to behavioral, developmental specialists and psychiatrists is a
major problem. In order to keep pediatric patients with MH/SUD treatment-compliant, they need
consistency in appointment attendance and medication monitoring. School is an ideal setting for
this as it is difficult to miss appointments when patients are receiving care in a place they
regularly attend. Discussants mentioned how difficult it is to get enough specialized care (e.g.,
MH/SUD services) in schools and telehealth approaches lent themselves perfectly for this.
“If the patient has the option to join remotely, you
are increasing the likelihood of appointment being
kept and therefore outcomes are going to be better. I
think the school needs to be a place of service in all
states.”
Barriers and Solutions
Key informants discussed seven barriers to using telehealth for pediatric populations. One
common theme that emerged from discussion was that barriers often exist due to limits and
restrictions states place on reimbursement.
Technology investment and performance
Similar to what was reported in the environmental scan, internet connectivity is critical
with more bandwidth and faster connections being essential. One key informant noted that it is
also important to prioritize bandwidth for telehealth services and limit other network clinic use
during telehealth service delivery. One solution mentioned by key informants was the use of
cellular networks and data-enabled devices.
Another technology-related barrier that was raised was incompatibility of EHR systems.
This challenge emerges in two ways. First, telehealth services often need a tailored EHR that

Reducing Barriers to Using Telehealth for Pediatric Populations
Final Report
44
does not always integrate well with the provider organization’s main EHR. Second, as telehealth
providers often serve patients across different health systems, they have to deal with more than
one EHRs. One key informant noted that getting providers to use their EHR was already a barrier
for face-to face service provision but was amplified when delivering telehealth services.
Although these issues also affect adult patients and general health care delivery, they can be
particularly frustrating for pediatric patients and their providers. Disruptions for these patients
can lead to a larger amount of distraction time than for adult patients or more stable patients.
Having on-site staff to intervene when technology leads to a disruption was a recommended
solution. The key informants offered no current solutions for EHR incompatibility.
“Promising Practice: Have a telehealth checklist at
each site that providers can have in case they need
help troubleshooting. Also, bandwidth isn’t always
what you need. You can have a lot and it be taken up
by other clinic or site activities. Make sure traffic is
low and telehealth is prioritized.”
Technology Acceptance
Obtaining provider buy-in to use technology was mentioned as a challenge by several key
informants. One reason was adaptation; key informants noted that telehealth adoption is often
more challenging for older providers. One key informant referred to this as the “real digital
divide” in that providers who are more hesitant to use new technology may also be resistant to
telehealth service provision. Still, anecdotal reports from key informants suggest that many
providers learn to adapt quickly within the first 15 minutes of the session. Another concern
related to loss of non-verbal cues and other substance use relevant cues. Such clues might
include the client’s smell (indicating, for example, hygiene or recent smoking) or evidence of
self-harm such as cutting. Overall, rapport development and engagement were viewed to be the
same by the key informants between face-to-face and telehealth, and in some cases, telehealth
was superior for the pediatric population. Non-verbal communication can still be observed, and
some providers felt that videoconferencing actually made the patient more relaxed and thus more
likely to manifest non-verbal cues.

Reducing Barriers to Using Telehealth for Pediatric Populations
Final Report
45
Workforce shortages
Workforce shortages were noted by all key informants and include multiple practitioner
types: psychiatrists, nurse practitioners, psychologists, and counselors with pediatric experience
and MH/SUD expertise. Shortages are more acute in remote or rural areas. Two key informants
were particularly worried about the lack of expertise for working with younger pediatric patients
(e.g., age 12 and under).
Licensure and Credentialing
Contributing to the workforce shortage were barriers around licensure and credentialing.
The principal licensing issue is the state-to-state variability in requirements to practice and be
reimbursed. Thus, servicing multiple states is a challenge due to state-specific licensing
regulations. One key informant also expressed concern in the state allowing training and
licensing companies to drive the conversation around licensure and credentialing regulatory
requirements. Another key informant noted that providers themselves are also concerned about
conducting unallowable services because it can affect their licensure. Although these challenges
are not unique to providers serving pediatric patients with a MH/SUD, it exacerbates the already
major workforce shortage.
Overall, credentialing was noted to be a major challenge. For credentialing, providers
must have privileges at the site (school, clinic hospital, city) where the patient is located. The
credentialing process can take a substantial amount of time to complete. This can be a major
hindrance to providers being available to a broad range of locations. If the potential number of
patients in a remote site is too small, a telehealth-based provider may decide not to invest in
credentialing with their organization. Adding to the problem is the fact that provider
organizations may have their own practices and requirements for credentialing. As an example of
this almost ubiquitous issue, one discussant noted that there could be eight or nine different
credentialing practices if they work with eight or nine sites.
Some states have licensure policies in place to specifically address workforce shortages.
For example, in Wisconsin, if a provider has a practice license, they can work from any other
state. One key informant described a provider living in Maryland with a Wisconsin license who
was currently providing services via telehealth to patients in Wisconsin. This is not the case in
many other states. Hybrid models exist where pediatric specialists at one site can consult with

Reducing Barriers to Using Telehealth for Pediatric Populations
Final Report
46
providers who primarily serve adults on mild to moderate cases but use telehealth for more
severe cases. Several discussants advocated for an eventual move towards national interstate
licensure agreements as the best way to address many of the licensure. While interstate licensing
compacts are somewhat reducing the licensing barrier, credentialing remains a challenge for
providers of pediatric MH/SUD services. The key informants knew of no programs taking
advantage of credentialing by proxy or any other practical solution.
Consent for Services
Issues around consent vary by the age of the child across state. Consent in some states
can be gathered in children as young as 12 years old. One discussant noted that for pediatric
SUDs and related mental health issues, consent should be obtained with adolescents. When
working with younger patients with MH/SUD, family involvement is preferred in any treatment
modality and gathering consent from a parent/guardian with the child is ideal. However, as noted
above, some of these patients may have parents and caregivers who can be a barrier to care.
Thus, programs need to be careful in how they balance compliance with their state’s laws and
patient safety and access to care. The key informants felt that this was an area for more research.
Privacy
Key informants noted that privacy issues should be attended to early in the program
planning process, especially when considering equipment and platform. This is a particular
challenge in school-based settings in which FERPA, the HIPAA Privacy Rule, and State privacy
laws may apply. Successful programs have developed solutions tailored to their state and setting.
These are based on a technology platform and detailed processes that control how information is
stored in separate systems, and limits who can access and share different records. During the
development phase for these solutions, attorneys with relevant privacy law expertise were
consulted. On a positive note, once a solution was developed, implementing it in new settings
within the same state was much simpler. As mentioned above one key informant suggested
having a telehealth coordinator that could assist the patient with telehealth related service
delivery (e.g., set up and troubleshooting technological challenges).

Reducing Barriers to Using Telehealth for Pediatric Populations
Final Report
47
Patient Safety
Concerns about crisis support and important recommendations were provided by some
key informants. These are important for all telehealth service provision but are especially
relevant for providers working with pediatric MH/SUD patients. One key informant speculated
that provider resistance to telehealth with this population might be around concerns with safety
and crisis management when at a distance. Many safety concerns could be assuaged with crisis
policies and procedures, which should address technology troubleshooting, general emergencies,
behavioral health-specific emergencies, self-harm, and interpersonal violence. Specific
guidelines for attending to situations when patient is at danger to him/herself and/or others is
crucial. Clear definitions to determine risk levels for involuntary commitment and other
decisions are also critical. Again, the role of on-site staff was cited as a solution to this problem.
Financing Services
Many programs rely on grant or other state funding in order to operate, even if their
patients are covered by insurance. Grants and state funding pay not only for telehealth equipment
and support staff and other administrative costs, but also support the providers themselves.
Limits on what providers can be reimbursed for specific services delivered by telehealth is a
major problem that varies across states. Providers trained and licensed to provide MH/SUD
services to pediatric patients often command higher wages. School-based programs face
challenges depending on how the onsite staff are funded. For example, if a school nurse is
funded by an independent source, such as the local school district, the financial viability of a
program is substantially improved.
Potential solutions are focused on changing state Medicaid policies and exploring APMs.
For state Medicaid policies, the emphasis varies by state but includes better coverage and
reimbursement for telehealth services and increasing the types of providers eligible for
reimbursement. One key informant from a provider serving patients in multiple states described
how one state mandated coverage parity and reimbursement parity for telehealth services with
face-to-face services while their home state on mandated only coverage parity.
Both shared savings and value-based models have potential to sustain telehealth-
delivered pediatric MH/SUD services. However, much more research is needed to understand the
viability of such models. For value-based models, programs are optimistic about the viability of

Reducing Barriers to Using Telehealth for Pediatric Populations
Final Report
48
quality-based payments around pediatric access and treatment completion. However, such
models are still in an exploration stage with many policy hurdles yet to be overcome.
WHAT ARE THE DIFFERENCES, IF ANY, IN FURNISHING SERVICES AND
TREATMENT FOR CHILDREN WITH SUD USING SERVICES DELIVERED VIA
TELEHEALTH AND USING SERVICES DELIVERED IN PERSON? (RESEARCH
QUESTION 2)
Utilization rates, costs and avoidable inpatient admissions and readmissions
Key informants could cite little evidence on rates of general health care utilization of
patients receiving pediatric MH/SUD services via telehealth. Most felt that more MH/SUD
assessments were happening due to telehealth access or to related programs targeting the
pediatric population. Several informants also believed strongly that the amount of MH/SUD
treatment services being provided per patient was higher via telehealth than for patients who
traveled to receive equivalent care in-person simply because they lacked easy access to services
locally. In addition, the informants believed that patients in underserved areas were more likely
to complete their treatment program when delivered via telehealth. However, despite the greater
amount of MH/SUD services being provided overall, informants did not believe that patients
receiving services via telehealth had higher total health care utilization than those receiving
services in-person from a local provider on a per patient basis. All noted that there are many
communities that would have no access to any of the services without telehealth.
Most of the key informants felt that telehealth-delivered services had, on average,
comparable costs to face-to-face services and thus could be profitable under conventional fee-
for-service reimbursement if coverage were available and reimbursement rates were comparable
to those for in-person services. The main exception to this was around how to support on-site or
in-community staff support.
More evidence is needed on the possible cost savings to payers of providing such
services, but these studies face several challenges. First, it is difficult to obtain rigorous, accurate
estimates of cost savings in programs that do not have comparison groups who received no
services. Second, for pediatric patients with these disorders, a large portion of preventable costs
may occur years or decades later. The possible solution to this second challenge is to focus on
avoidable near-term, high-cost care such as emergency department visits and inpatient stays. The

Reducing Barriers to Using Telehealth for Pediatric Populations
Final Report
49
one caveat with that approach is that such findings apply may apply more to a higher risk, higher
severity patient group at the expense of a larger, less severe patient group. Nonetheless, multiple
key informants believed that telehealth could reduce avoidable emergency and inpatient care
among a certain portion of the patient population. As noted above, at least one direct-to-
consumer telehealth access program was being implemented specifically for those patients.
Quality and Satisfaction
Some providers have been concerned that videoconferencing reduces the quality of a
service and reduces fidelity to evidence-based practice. The concern for MH/SUD for pediatric
patients is that the therapeutic relationship will not develop and that the providers will not be
able to observe non-verbal communication which they find particularly important for pediatric
patients. However, the key informants, overall, did not feel that this was a major issue. Providers
and patients feel good about the relationship and some providers even believe videoconferencing
helps patients engage more easily. Non-verbal communication was still being observed and,
again, some providers felt that videoconferencing actually made the patient more relaxed and
thus more likely to manifest non-verbal cues.
Key informants consistently emphasized that telehealth approaches have an important
edge when compared to face-to-face therapy with pediatric populations. This is the case
regardless of the actual treatment approach used (e.g., cognitive behavioral therapy). Telehealth
counseling and family therapy allow for enhanced engagement, especially with pediatric
populations. Because pediatric populations today are more connected than ever, this assists in
engagement. One key informant noted that pediatric patients are not bothered by technology and
services using telehealth modalities. Providers can develop rapport with pediatric patients
quicker than face-to-face particularly for pediatric patients with anxiety or shyness. One key
informant shared anecdotal experiences where pediatric patients communicate more openly
between one and two sessions earlier than they would in a similar face-to-face encounter.

Reducing Barriers to Using Telehealth for Pediatric Populations
Final Report
50
Although technology disruptions were considered a problem, the key informants felt that
this was primarily with a minority of patients who are either much younger or are in crisis. One
key informant noted pediatric patients are rarely bothered by technological glitches and often
offer to help.
None of the key informants had concerns about quality of care provided by telehealth for
pediatric MH/SUD treatment. Consistent with what was reported in the environmental scan,
telehealth services can enhance treatment engagement in most therapeutic telehealth contexts.
One key informant did mention safety issues are more challenging when there is a distance
between provider and a patient who is in danger (e.g., of self-harm) but if there are plans in place
to attend to these, quality is not compromised, and may in fact be enhanced.
All key informants had anecdotes for how satisfied patients, their caregivers and
providers are with telehealth services. One key informant noted that, with this population,
telehealth encounters were well received and often preferred to traditional face-to-face
encounters. They added that patients will frequently include comments in their post encounter
surveys that detail their enjoyment of this modality, and that telehealth for pediatric patients with
SUD allows more flexibility for getting families into therapy. Caregivers and providers strongly
note that there would simply be no access to care without telehealth. Caregivers also find the
flexibility of telehealth to be a great benefit relative to traveling to a clinic. Providers describe
their frustration at not being able to provide the services their patients need the most and
telehealth allows them to close the treatment gaps. Although patients themselves volunteer fewer
anecdotal reports on their satisfaction, their providers claim that patients receiving services via
telehealth are as satisfied as those receiving in-person services. Several key informants were
aware of satisfaction surveys delivered to patients and caregivers in certain programs. The survey
results were consistently positive.
“Youth overall prefer using technology and interacting with their
provider on a screen; they prefer this to interacting with providers
in person…youth feel less intimidated even if they are not familiar
with the platform used, they are receptive to it and open to
interacting on it”

Reducing Barriers to Using Telehealth for Pediatric Populations
Final Report
51
[This page intentionally left blank]

Reducing Barriers to Using Telehealth for Pediatric Populations
Final Report
52
CASE STUDIES
CASE STUDY PROGRAMS
To investigate the practices of innovative pediatric MH/SUD services programs delivered
via telehealth, we visited two sites in-person and met with multiple providers, administrators and
experts. Both programs provide services to pediatric patients in schools across their state. The
programs’ providers operate out of university medical centers. They are both embedded in a
larger portfolio of telehealth programs targeting a variety of patient populations.
Case Study 1: The Medical University of South Carolina’s Telehealth Outreach Program
The RTI/ASPE team visited the Medical University of South Carolina (MUSC) in
Charleston, South Carolina and spoke with five individuals including clinicians, administrators,
telehealth specialists and a community partner. Among a variety of adult and pediatric telehealth
programs, the MUSC operates the Telehealth Outreach Program (TOP) which uses telehealth
technology to increase access to mental health services for underserved, trauma-exposed children
across South Carolina. The program began in 2015 and works with students in over 80 schools in
18 counties across the state. Most of the counties being served are rural. The TOP program sees
patients aged 7 to 18.
Organizational Context
The MUSC Center for Telehealth is one of two HRSA-funded National Telehealth
Centers of Excellence. The Center for Telehealth is also the headquarters and fiscal agent of the
state-funded South Carolina Telehealth Alliance (SCTA), a statewide collaboration of
stakeholders dedicated to expanding the use of telehealth. Their innovative programs include
“Tele-ICU” for continuous patient monitoring in remote hospital intensive care units,
telepsychiatry delivering (primarily adult) MH/SUD services including medication for opioid use
disorder (MOUD) and supporting skilled nursing facilities.
Telehealth Outreach Program
TOP is specialized in providing Trauma-Focused Cognitive Behavioral Therapy (TF-
CBT), an evidence-based treatment for individuals aged 3 to 21 who have experienced trauma
ranging from physical or sexual abuse, crime victimization, traumatic grief, disasters and
multiple or other complex traumas (Gillies, Taylor, Gray, O'Brien, & D'Abrew, 2013; Goldbeck,

Reducing Barriers to Using Telehealth for Pediatric Populations
Final Report
53
Muche, Sachser, Tutus, & Rosner, 2016; Lenz & Hollenbaugh, 2015; Weiner, Schneider, &
Lyons, 2009) lasts approximately 12 to 24 sessions. It is on the National Child Traumatic Stress
Network list of recommended treatments (NCTSN, 2019). Recent research has demonstrated the
value of TF-CBT delivered via telehealth pediatric patients (Stewart, Orengo-Aguayo, Cohen,
Mannarino, & de Arellano, 2017a; Stewart, Orengo-Aguayo, Gilmore, & de Arellano, 2017b).
In TOP, most services are school-based with some interactions occurring with the patient
at home or with parents at home when family is included in the therapy. Patients are typically
identified in a school setting by guidance counselors, although a small number of referrals come
from other community organizations, providers or the criminal justice system. They serve
patients aged 7 to 18. Once a patient is referred and assessed they can receive from 12 to 20 TF-
CBT weekly sessions lasting from 30 to 45 minutes. For sessions in the school setting, the
guidance counselor calls the child out of class, checks the telehealth connection with the TOP
provider and leaves the room. The guidance counselor or school staff member is always near the
room and has the child’s emergency contacts accessible. The TOP provider has the cell phone
and landline number of the counselor or other staff person in case of an emergency. At the end of
the session, the guidance counselor gets a call on their cell phone that the session is over and
goes back to the room to bring the child to class.
Cellular data-enabled iPads and laptops are used for video conferencing. The TF-CBT is
currently being provided by PhD-level psychologists. They are supported by case managers who
help coordinate with schools and other referral sources, and support the patients and their
families in linking to other community resources and coordinating their broader health care. TOP
has four hours per week of a child psychiatrist’s time for medication management.
TOP uses telehealth to include family members in treatment. A parent has the option of
coming to the school to participate during a session or video-conference in from a remote
location. TOP providers also do independent sessions with parents at times outside the patient’s
session time. TOP loans the program’s cellular data-enabled iPads to families who have limited
or no internet access at home.
TF-CBT sessions provided to pediatric patients in the home are clinically identical to
school-based sessions. TOP requires that a caregiver over the age of 18 be present in the home
with the child and remain available by phone. TOP providers have the patient periodically step

Reducing Barriers to Using Telehealth for Pediatric Populations
Final Report
54
out and interact with the caregiver to ensure that they are still present. Knowing the location of
the patient is also necessary in case they need to call emergency services.
TOP Challenges
The providers noted that there are some challenges in conducting telehealth visits with
younger children. The children may have issues with being by themselves and they may not stay
in the view of the camera, which can be a safety hazard. Thus, the program has a minimum age
of seven for eligibility. Some children may be too high risk for telehealth, such and those who
engage in self-harm or experience suicidal ideation. These patients are sometimes referred to
other community-based health care providers.
TOP providers face multiple barriers to getting prescriptions for their patients, even with
access to a psychiatrist. Controlled substances are difficult to prescribe via telehealth and the
only controlled substances that can be prescribed in a school-based setting are those for ADHD.
Until recently, paper-based prescriptions were still required and delivering them to parents was a
challenge.
A major concern is the lack of aftercare or ongoing services that are needed for patients
once the TOP intervention is completed. There are a limited number of local providers who offer
related services and there have been few linkages to them. Integrated telehealth-delivered care
would be an ideal strategy to increase access. However, even when available, patients may not be
covered for services by insurance.
When TOP started in 2015, they had difficulties getting buy-in with schools and school
districts. Ultimately, having a champion TOP provider travel to these sites and do outreach was
the key to making meaningful connections with each community.
Finally, it was noted that EHR systems do not all integrate very well together, even when
built by the same vendor. Telehealth programs are often siloed by default as they are based in a
different health system with a different EHR, or the telehealth technology was developed with a
tailored version of an EHR that is not fully compatible with the main EHR.
Policy and Financing
Although TOP does not emphasize prescribing via telehealth, the Ryan Haight Act and
state policies were noted as a barrier to care for pediatric and adult patients with a variety of

Reducing Barriers to Using Telehealth for Pediatric Populations
Final Report
55
conditions. The 2016 South Carolina Telemedicine Act reinforces restrictions around prescribing
Schedule II and Schedule III controlled substances, and certain other medications via telehealth.
It emphasizes the need for in-person diagnosis for related conditions in order to establish the
physician-patient relationship prior to initiating pharmacotherapy. It was noted that changes in
national law and clearer guidance on the Ryan Haight Act would be the best solution for
increasing access equally across all states and eliminating an additional barrier to telehealth
being used to treat patients.
The program is funded mainly through a grant from the Substance Abuse and Mental
Health Services Administration (SAMHSA), which pays for the providers’ time and
administrative costs. Additional support is provided by the MUSC Center for Telehealth, the
South Carolina Telehealth Alliance, and the Duke Endowment. The South Carolina Telehealth
Alliance funds the telehealth equipment. Although over half the patients are covered by
Medicaid, the TOP providers (PhD-level counselors) are not eligible for reimbursement. In South
Carolina, only physicians, physician assistants and nurse practitioners can be reimbursed for
mental health services delivered via telehealth (Center for Connected Health Policy, 2018). Staff
at the Center for Telehealth did not anticipate these restrictions changing until 2021 at the
earliest. Currently, the project is working on other sustainability options as the SAMHSA grant
ends in two years. They will likely depend on additional grants from SAMHSA and foundations
to sustain core project service delivery moving forward.
Case Study 2: University of Kansas Medical Center’s Telehealth ROCKS Schools, Rural
Outreach for Children of Kansas
The RTI/ASPE team visited the University of Kansas Medical Center in Kansas City,
Kansas and spoke with 24 individuals leading and facilitating telehealth projects including the
Telehealth Rural Outreach for the Children of Kentucky (ROCKS) Schools program. These
included providers (physicians, nurses, and counselors), administrators, researchers and other
program stakeholders. Telehealth ROCKS Schools brings “telemedicine into the school setting in
South Central and Southeast Kansas to assist children and families with developmental and
behavioral concerns.” Implemented in 2017, Telehealth ROCKS Schools serves 11 counties and
is present in 19 schools and is continuing to expand. The services supported include behavioral
strategies for autism, psychological strategies for behavioral concerns, trauma and chronic

Reducing Barriers to Using Telehealth for Pediatric Populations
Final Report
56
conditions, behavioral medication management, family-based counseling, and other behavioral
issues such as eating disorders and obesity. More students under the age of 12 are served than
students aged 13 to 18.
Organizational Context
The University of Kansas Medical Center houses the Center for Telemedicine and
Telehealth which was founded in 1992. Its Tele-Behavioral Health Network has more than 100
sites throughout the state and has conducted over 100,000 clinical consultations and educational
events. Since 2006, the Medical Center has also been home to The Heartland Telehealth
Resource Center, a federally designated telehealth resource center providing technical assistance
to developing and existing telehealth programs. Telehealth is integrated throughout the entire
Medical Center.
A major development in the telehealth network was supported by a Health Care
Innovation Award from CMS in 2014 to the University of Kansas Hospital Authority (which has
oversight over the Medical Center’s hospital). The project, the Kansas Heart and Stroke
Collaborative, developed a rural, clinically integrated network of providers to improve
cardiovascular health and acute and chronic stroke care. Telehealth solutions were a key part of
implementing the project. They have been able to improve the network of providers and use
telehealth to improve access to clinical expertise, to improve overall care practice and processes
and to ensure fidelity to evidence-based practices. Coordination of care and patient engagement
are led by local health coaches, a title chosen deliberately to distinguish the role from “care
coordinator” or “patient navigator.” The health coaches have broader expertise around health
care resources, help link between primary care and specialty care and are trained in practices
such as motivational interviewing to improve patient engagement. In addition, the health coaches
are trained on other community resources to help link patients and their families to non-clinical
recovery support services. The project is now a Medicare Shared Savings ACO and is simply
called the Kansas Clinical Improvement Collaborative.
The Medical Center is using the infrastructure and the lessons learned from the Care
Collaborative experience as it develops care systems for other patient populations, including for
pediatric patients and for care for MH/SUD. In support of state Medicaid policymakers, the team
is currently exploring how an APM might work for a Medicaid population, including for

Reducing Barriers to Using Telehealth for Pediatric Populations
Final Report
57
pediatric patients. Their research includes analyses of patient costs and outcomes from a private
payer partner in order to accurately represent populations for which they have less experience
providing services. Overall, the team feels that their Care Collaborative experience is very useful
for helping rural, small providers participate in an APM.
They noted that rural community hospitals, in particular, are reluctant to participate in an
APM. One concern they have is that their patient populations increase downside risk in APMs,
whether using shared savings or quality-based reimbursement. Their patients are often
geographically dispersed, reducing access to specialty care and overall decreasing treatment
adherence. Moreover, their populations lack the volume of care episodes needed to make an
APM actuarially sound. Finally, rural community hospitals have less experience with APMs and
have fewer resources to invest in infrastructure changes that might be needed.
As part of their efforts to reduce SUD treatment gaps, the Medical Center is leveraging a
recent HRSA Rural Communities Opioid Response Program grant to disseminate best MAT
practices around the state. They noted that urban populations have the least access to MAT per
capita. In addition, the Medical Center is using their telehealth network and lessons from the
collaborative to train and ensure fidelity to the Centers for Disease Control and Prevention
(CDC) guideline for the prescribing opioids for chronic pain (Dowell, Haegerich, & Chou,
2016).
Telehealth ROCKS Schools’ Autism Spectrum Disorder Programming
A key strategy for supporting children who may have autism spectrum disorder (ASD) is
early diagnosis. Currently, 40 teams across Kansas have been trained in early diagnosis. A team
may be comprised of psychologists, developmental specialists, and certain school staff. For
children meeting diagnosis, Medical Center experts can provide services via telehealth. HIPAA-
compliant Zoom software is used to provide services and can be used on a typical laptop with a
standard high-speed internet connection. Patients can be located in mental health facilities,
hospitals, and schools. Telehealth ROCKS coordinates with a distant site close to the family so
they do not have to travel far to get care.
The main therapies provided for children meeting ASD diagnostic criteria are based on
Applied Behavioral Analysis (ABA). ABA is a framework designed to understand patterns of
behavior and to promote sustained behavior change through individualized interventions and

Reducing Barriers to Using Telehealth for Pediatric Populations
Final Report
58
positive reinforcement. ABA is an effective therapy to help individuals with autism manage
behaviors and acquire skills. (Roane, Fisher, & Carr, 2016; Steege, Mace, Perry, & Longenecker,
2007; Virues-Ortega, Rodríguez, & Yu, 2013). ABA-based methodologies have also been used
as an adjunct to cognitive behavioral therapy for pediatric and emerging adult patients with ASD
(Kerns, Roux, Connell, & Shattuck, 2016). The theory underlying ABA is similar to that of
contingency management for treating adult SUDs (Petry, 2013).
Telehealth ROCKS Schools also combine direct patient services with parental support
and training via their Online and Applied System for Intervention Skills (OASIS) Training
Program. The OASIS training uses online instruction and training to provide parents with skills
to best teach and care for their child with ASD. Parents can access eight web-based tutorials as
well as connect with coaches to learn specific skills with their child. Some trainings may involve
other family members, such as siblings, grandparents, and extended family. The program enables
parents to implement and evaluate interventions when a service provider is unavailable. OASIS
also empowers the parent to be an equal member of their child’s care team. One goal of this
program is to decrease family separation that may result from the lack of local ASD services.
Children with ASD may need to seek services that are a significant distance away, leading them
to live with another family member who lives closer to services, or for a caregiver to travel with
their child to find services. The OASIS program addresses this issue by increasing access to ASD
services through telehealth. Students, their families, and the partner schools had “very positive
feedback” for services provided via telehealth.
Telehealth ROCKS Schools’ Parent-Child Interaction Therapy
Parent-Child Interaction Therapy (PCIT) is an evidence-based therapy for children with
ADHD (Bussing, Nelson, & Kurtz, 2016) and has also been used to support management of
externalizing disorders among children (Zimmer-Gembeck et al., 2019) and to support pediatric
patients with ASD (Scattone, Sarver, & Cox, 2018). PCIT is conducted in schools and delivered
to the parent and child at the same time. PCIT is a hands-on approach that involves the parent
and child in one room, typically a classroom, and the provider in another room watching the
parent and child via video. The provider communicates with the parent through an earpiece using
Bluetooth technology, which enables multiple people to listen to the provider and parent
interaction without the child knowing.

Reducing Barriers to Using Telehealth for Pediatric Populations
Final Report
59
Telehealth ROCKS Schools: Challenges
One challenge for both pediatric programs is establishing a safe space for the child so
they cannot hurt themselves or others. This challenge was overcome by conducting the therapy
in a school classroom with the classroom door cut horizontally in half to allow viewing and easy
access by staff who could intervene quickly in an emergency.
Not all students do well with the telehealth-delivered ASD services. Students who have
positive experiences generally have obvious indicators of ASD, have strong communication
skills, have attended the school long enough that staff have observed their interactions with
peers, and have received services previously. Comparatively, older, reluctant students or those
who are particularly uncommunicative do not do as well with telehealth-delivered services.
An ongoing challenge for the schools is inadequate internet service, which can cause
lags, delays, or issues with visuals. Nonetheless, the program reported that the connectivity
challenges did not seem to disrupt the overall therapeutic impact. They noted that major
connectivity problems are usually fixed in a timely manner.
One major infrastructure challenge to all its school-based programs is that it has become
difficult to maintain appropriate support staff on-site. Some schools do not have school nurses
and other schools only have a nurse once per week. The nurses are responsible for facilitating the
communication of information about the child from teachers, school psychologists and other
school-based administrative data such as the results of general testing. One school hired a full-
time nurse who used telehealth to prevent and resolve inappropriate placement in special
education. The teachers are also heavily involved in PCIT, which instills a unified approach that
supports the child and improves treatment outcomes.
An initial challenge with PCIT, in particular, was demonstrating its potential value to
parents. Another challenge for PCIT was the parent’s implementation and maintenance of skills
acquired through training. Between the telehealth sessions there is little ability for the program to
monitor parental fidelity to the evidence-based practice. In face-to-face practice, providers are
more likely to have some informal interactions with the parents and the students to observe
whether PCIT-informed parental behaviors are used.

Reducing Barriers to Using Telehealth for Pediatric Populations
Final Report
60
We spoke with the Pediatric Care Coordinator at The Community Health Center of
Southeast Kansas which services three counties in southeast Kansas. A care coordinator is
located in most call centers to connect people with necessary resources and establish a
relationship with the community. Their presence builds trust over time, as patients are more
comfortable with a familiar face. The care coordinator calls patients daily to promote treatment
compliance, address any barriers to care, and support patients in navigating services. The Health
Center noted that one challenge patients and providers face in southeast Kansas is a low literacy
rate. According to the Pediatric Care Coordinator, one in four adults in southeast Kansas cannot
read. Often, when patients are provided their intake summary to take home, it “usually ends up in
the trash on their way out”. To try to address this, the Health Center conducts outreach and
education to their patients, but it is a difficult barrier to overcome. Overall, the Patient Care
Coordinator notes that the availability of telehealth-delivered services increases the likelihood
that pediatric patients and their families will engage in treatment.
Policy and Financing
The governor of Kansas signed into law, the Kansas Telemedicine Act in late 2018, to
take effect January 1
st
, 2019. The act requires private payers to cover telehealth services, though
not necessarily at the same reimbursement rates as in-person services. In addition to physicians,
physician assistants, advance practice registered nurses, behavioral health professionals who are
“registered, certified or otherwise authorized to practice by the Behavioral Sciences Regulatory
Board” were identified as eligible providers for reimbursement. Store-and-forward was
specifically included as a covered telehealth modality beyond videoconferencing. The law allows
for state Medicaid (KanCare) to cover services delivered via telehealth including individual
psychotherapy and mental health assessments. KanCare reimburses for live video and home
telehealth (remote patient monitoring) for certain medical conditions. It is not clear how store-
and-forward services will operate for Medicaid given the KanCare requirement that patients be
present at the originating site for coverage. Private insurance companies must cover telehealth
for mental health services which include any psychological services provided in Kansas. Kansas
is part of the Interstate Medical Licensure Compact, which helps expedite the medical licensing
process across state lines. This makes it easier for out-of-state health care providers to serve
patients in Kansas using telehealth.

Reducing Barriers to Using Telehealth for Pediatric Populations
Final Report
61
The Telehealth ROCKS Schools program is partly funded by insurance (mostly
Medicaid). For children meeting the diagnosis criteria, ABA and PCIT services delivered via
telehealth are billable. A grant from the Children’s Cabinet pays for services when patients are
uninsured, as well as for other support services to help families who struggle financially, such
transportation and accessing food stamps. The grant money is also used to train staff, provide
equipment, and enhance or supplement services (e.g., allowing providers to observe the kids in
their natural setting via telehealth).
A major challenge to sustaining telehealth delivery models for their pediatric patients is
the paying for telehealth coordinators. Telehealth ROCKS Schools noted that good models are
not simply “a provider on one end and patient on the other.” Rather, the support system in place
is what brings the most value, namely: having staff who coordinate schedules, present the
patient, manage workflow, test the equipment, do patient outreach and help patients and their
families find other resources they need that are not directly related to the primary clinical
services being delivered. These services and service supports are not sustainable since they
typically are not billable.
A related staffing challenge is that rural clinics struggle to find qualified staff. The
shortage of “pediatric behavioral health care providers” (speaking of mental health providers,
generally) can only be partially remedied using telehealth delivery because the compensation of
these in-demand providers is too high for the typical reimbursement rates. In another telehealth
program at the Medical Center that serves oncology patients covered by Medicare, they noted
that they were able to take advantage of shared savings (a type of value-based APM) when
billing through the rural health clinics to make up the difference. They do not see a similar path
for telehealth-delivered behavioral health services currently and hope that Medicaid will
eventually adopt similar APMs.
Another consideration in the financial viability of telehealth-delivered services is
equipment costs. For their telehealth-delivered oncology services, they estimated that within five
years of purchase, 50 percent of the telehealth equipment was no longer functioning. However,
they noted that telehealth equipment for oncology services is very complex and niche-specific,
and thus particularly expensive. In contrast, the equipment needed to deliver their pediatric
services via telehealth is minimal, typically only a laptop computer.

Reducing Barriers to Using Telehealth for Pediatric Populations
Final Report
62
CASE STUDY RESULTS BY QUESTION
The case study programs are for pediatric patients with specific mental disorders.
However, almost all the information we collected pertains directly to programs that use
telehealth to provide services to pediatric patients with broader MH/SUD.
What Are the Best Practices, Barriers and Potential Solutions for Using Services Delivered
Via Telehealth to Diagnose and Provide Services and Treatment for Children With
SUD, Including OUD? (Research Question #1)
The models in our case studies provide several insights that pertain to MH/SUD services
delivered via telehealth for pediatric populations. Most importantly, the case studies
demonstrated that existing evidence-based practices for pediatric patients can be provided via
telehealth with virtually no change to clinical components. Providers use the same approaches
via telehealth as they would in person, including therapeutic language, educational content,
worksheets and exercises, roleplaying, tactile activities and games, and developing a therapeutic
alliance. In addition, the inclusion of family members as part of the therapeutic process was more
likely to occur via telehealth than in traditional office-based visits. Prescribing medication,
including MAT for OUD (buprenorphine and naltrexone products) and alcohol use disorder,
remains a problem for one program studied due to the broader policy barriers to prescribing via
telehealth. The one unique pediatric-specific barrier to prescribing was that state law prohibited
prescribing any controlled substances for students in a school-based clinic other than ADHD
medications. This restriction limits the possibility of school-based clinics developing a
buprenorphine-based MAT program.
Second, the technology requirements for the treatments used in two case studies are
minimal. For counseling-based approaches, which comprise the majority of services for
MH/SUD, the main technologies needed are a laptop, phone or tablet and an internet connection.
Pediatric patients, in particular, are very comfortable with these technologies. No providers or
support staff at the case study locations (e.g., school guidance counselors) reported any
challenges using standard videoconferencing on these devices. Connectivity continues to be a
challenge in certain local sites and for disadvantaged families in rural areas, but case study
programs considered it a “periodic challenge” that only disrupted service-delivery rather than

Reducing Barriers to Using Telehealth for Pediatric Populations
Final Report
63
prevented it entirely. Providing cellular-enabled devices on a data plan was one solution to this
challenge.
One unique and contrary concern was raised about the licensure and credentialing
challenges telehealth providers face. Although increasing access to telehealth is a priority,
licensing compacts and easier credentialing have a drawback: they increase the likelihood that
large, for-profit national telehealth provider companies will dominate the market. There is
concern that they may not provide quality services and that they are not carefully evaluating each
new telehealth-delivered service offering for fidelity. The licensing and credentialing barriers
somewhat limit those types of health care providers from dominating the market.
On-site Staff
A prominent feature in both case study programs was the role of on-site staff. Having an
originating site and a local clinician to support telehealth is not limited to pediatric patients with
MH/SUD. However, in the case studies, these staff had some important and unique tasks. In both
programs, local staff conducted initial assessments and determined eligibility for the telehealth-
delivered services. Importantly, this process included more than asking the patients clinical
assessment questions. The local staff informally assessed the maturity and stability of the patient
to determine whether telehealth-delivery would be effective. Patients who were overly
hyperactive, agitated, or potentially a danger to themselves or others were either excluded from
or delayed in program participation. In the case of schools, local provider staff also had other
information from administrative records and feedback from other school staff. Although this
information was not necessarily shared with the providers using telehealth, it could influence the
decision to move forward with the patient. Overall, local staff were uniquely positioned for both
active and passive assessment of the appropriateness of patients receiving services via telehealth.
The second unique role of local staff was for ensuring the safety of the patient while
receiving services via telehealth. A major concern in using telehealth with pediatric patients with
MH/SUD was not being able to respond quickly in case of emergency. In was also noted that, in
contrast to adults, pediatric patients are more likely to overreact to minor disruptions in the
technology. In both programs, reliable communication with a nearby staff person was a requisite
for conducting a telehealth session.

Reducing Barriers to Using Telehealth for Pediatric Populations
Final Report
64
What Are the Differences, If Any, in Furnishing Services and Treatment for Children With
SUD Using Services Delivered Via Telehealth and Using Services Delivered in
Person? (Research Question #2)
Both case study programs believed that using telehealth did not alter the clinical content
of the services delivered. They felt they had the same if not better rapport with patients over
telehealth than face-to-face. Several providers felt that pediatric patients are often more
comfortable and open with providers using videoconferencing rather than being alone and face-
to-face with an adult in a room. Similar to face-to-face services, it is not feasible to simply
dialogue with pediatric patients during an entire session. Both programs’ evidence-based
practices included certain therapy-related activities like games, worksheets and other general,
hands-on activities to help the patient feel comfortable and have more open conversation that
may occur when they are slightly distracted and not being forced to make eye contact. The
providers noted having very little difficulty conducting the same types of activities other than
occasionally reminding a patient to orient the camera correctly. One practical difference from the
providers’ perspective was the greater need to plan ahead for such activities. For example, when
in-person, the provider can quickly print off worksheets or run to the supply closet for a
particular game. For telehealth-delivered session to work similarly, providers need to plan ahead
consistently in order to ship materials or email local staff to print worksheets or have other items
prepared.
Utilization Rates, Costs and Avoidable Inpatient Admissions and Readmissions
Both programs feel that their patients are much more likely to persist in treatment than
face-to-face patients. One program has a 90 percent treatment completion rate. The main reason
noted for this is that telehealth reduces barriers to access. For pediatric patients in particular,
coming to in-person appointments relies on coordinating the schedules of parents and the child
and even when local providers are available, travel time can often double the time required to
attend a session. School-based programs are particularly good for increasing access. In one
school-based program it was noted that the child only misses 30-45 minutes of class time in
school. The provider can also see the parent at the school during the time of the visit, or they can
do a parallel session with the parent at a separate time.

Reducing Barriers to Using Telehealth for Pediatric Populations
Final Report
65
Neither program had conducted an economic analysis of health care utilization, costs and
cost offsets. Respondents from both programs did note several points. First, they have received
no feedback from either the broader health system or their patients’ payers that patients were
using more non-program services nor incurring more charges than normal. Second, both
programs noted that, beyond near-term health care cost savings, they felt strongly that their
programs would ultimately save societal resources by reducing inefficient use of misapplied
community resources (e.g., teacher time) and reducing the long-term costs associated with
untreated pediatric disorders, including avoidable inpatient care. As part of this argument, they
point out that their patients are unlikely to receive any services for their disorders without the
availability of telehealth.
Finally, on average, the programs believe that the cost of their telehealth-delivered
services was equal to that of in person services, even including some fixed technology costs. The
one hesitation they had about claiming equivalent costs was paying for the role of local support
or provider staff. Nonetheless, they stated that such support staff are not completely absent in
traditional settings and that models using staff like patient navigators are becoming more
common.
Quality of Care and Patient, Family and Provider Satisfaction
As noted earlier, both programs felt that the quality of their programs was as good as or
better than face-to-face service delivery. School-based telehealth service delivery was further
described as better than in person because it allows the student patient to receive services in a
non-threatening environment with which they are familiar.

Reducing Barriers to Using Telehealth for Pediatric Populations
Final Report
66
[This page intentionally left blank]

Reducing Barriers to Using Telehealth for Pediatric Populations
Final Report
67
DISCUSSION
In this study, we assessed contextual factors influencing the use of telehealth for
MH/SUD services for pediatric populations. The study supports the fulfillment of the
requirements of Section 1009(d) of the SUPPORT for Patients and Communities Act, Pub. L.
No. 115-271, which requires the Secretary of the Department of Health and Human Services to
provide a report “identifying best practices and potential solutions for reducing barriers to using
services delivered via telehealth to furnish services and treatment for SUDs among pediatric
populations under Medicaid.” In order to identify current models, best practices, barriers and
facilitators for such programs, we collected data from an environmental scan, key informants and
two case studies.
A primary finding highlighted by the environmental scan and key informants is that
telehealth programs designed specifically for SUD services for pediatric patients are still
emerging, and there is a limited evidence base for them. Most dedicated telehealth programs
targeting any behavioral health condition focus on pediatric mental health services, for which the
evidence base is positive. Literature and stakeholder discussions suggest that many of the
contextual factors that influence pediatric mental health services also pertain to pediatric SUD
services, because many pediatric patients have co-occurring SUD. Thus, our findings on best
practices and barriers relevant to telehealth for SUD for pediatric patients are informed by a
broader range of pediatric programs. When appropriate, we have also referenced telehealth
programs for adult populations.
BEST PRACTICES:
Videoconferencing
For a variety of reasons, videoconferencing is the most common telehealth modality for
providing MH/SUD services to pediatric patients. Videoconferencing provides access to
pediatric patients who may not receive services otherwise because of a lack of local services or
other barriers. Videoconferencing models are working in different clinical and organizational
settings, ranging from large health systems to schools. Overall, there is confidence that
videoconferencing is able to reproduce the face-to-face counseling-based interventions for
pediatric patients. A major feature of programs using videoconferencing is that they can more
effectively involve family members in treatment.

Reducing Barriers to Using Telehealth for Pediatric Populations
Final Report
68
Support Staff
The value of staff supporting telehealth programs for pediatric patients with a MH/SUD
was a clear message from both key informants and the case study programs. These staff include
telehealth coordinators, nurses, and guidance counselors. Increased quality, engagement, and
coordination were all cited as significant benefits to programs. In addition, ensuring patient
safety was a key function of support staff. Funding such support staff outside of grants or other
sources was an open question confronting the models that used them.
School-based Models
School-based programs are successfully using telehealth to provide access to services for
pediatric patients with MH/SUD. Telehealth allows for specialty providers to serve patients
across a large geographic area and in a safe, easy-to-access location. School-based programs do
face some challenges. New programs may have a greater challenge obtaining buy-in from school
boards and individual schools than they would in a health care organization. A school-based
program is often dependent on support from staff who are not associated with the telehealth
provider organization and who must be funded independently. They also face some unique
challenges around privacy and consent, including ensuring compliance with IDEA, and FERPA
privacy and confidentiality requirements, and HIPAA’s rules, if HIPAA applies. There is some
evidence that school-based health clinic patients have increased health care costs. More study is
needed to explore the economic feasibility of school-based models and understand how a variety
of projects have overcome some common challenges.
BARRIERS, SOLUTIONS AND INFORMATION GAPS
Quality and Fidelity
Some providers have been concerned that videoconferencing reduces the quality of a
service and reduces fidelity to evidence-based practice. The concern for MH/SUD for pediatric
patients is that the therapeutic relationship will not develop and that the providers will not be
able to observe non-verbal communication, which they find particularly important in this
population. We found little evidence of either of these concerns being a problem. Providers and
patients feel good about the relationship, and some providers even believe videoconferencing
helps patients engage more easily. Non-verbal communication was still being observed, and

Reducing Barriers to Using Telehealth for Pediatric Populations
Final Report
69
videoconferencing made some patients more relaxed and thus more likely to manifest non-verbal
cues.
Studies to date have not shown problems with clinical fidelity. However, some experts
voiced concerns that this issue was not resolved. Effectiveness and observational studies in real-
world settings need to be conducted to both assess loss to fidelity and develop solutions to
maintain fidelity. One key area in which models still need to be developed and be assessed for
fidelity is group-based counseling.
Patient Safety
Ensuring safety for pediatric patients with a MH/SUD is a particular concern. The
programs and experts all emphasized the vulnerability of this population and the need for
specific safety protocols to be followed. The main strategy is to have staff on-site and on call in
order to intervene immediately in case of an emergency. Sessions did not begin unless the remote
provider had the correct telephone contact information for the local staff. For home-based
delivery, an adult caregiver was required to be present.
Acceptance of a Telehealth Program
Currently, despite some challenges, most clinical providers eventually embrace telehealth
programs when offered. A minority do have reluctance around the quality and fidelity concerns
described above or around using technology. However, receiving training and then using the
technology appear to resolve these concerns. Outreach efforts by champions to providers and
other community stakeholders was noted as another strategy for overcoming acceptance barriers,
particularly for school-based programs.
Financing
The majority of the programs we learned about involved some form of external funding
that did not come from a health care payer. Support staff, training, infrastructure and, in some
cases, the service units were funded by grants or direct funding from states or foundations.
Moreover, limited reimbursement for MH/SUD services delivered by telehealth is a major
problem that varies across states. Potential solutions are focused on increasing reimbursement by
extending coverage to more provider types (e.g., counselors) for telehealth services and receiving
equal reimbursement telehealth services. Of note, these efforts tend to be targeted to individual

Reducing Barriers to Using Telehealth for Pediatric Populations
Final Report
70
states by in-state providers. APMs are also being watched closely. However, such models are
still in an exploration stage with many policy hurdles yet to be overcome.
Consent for Services
Age of consent and caregiver notification varies across and within states. While family
involvement is often preferred by clinicians working with younger patients with MH/SUD,
patient and/or caregiver consent may not be clinically appropriate. Caregiver consent may even
be a barrier to care in some cases. More study is needed to understand the implications of
consent policy and to help clinicians balance legal compliance with patient safety and access
concerns.
Cost Studies
There has been limited rigorous study of whether providing MH/SUD services to
pediatric patients via telehealth is associated with cost savings or reductions in avoidable costs. It
is difficult to design a population-level study that compares telehealth delivery to either in-
person services or to “no services”. However, as programs begin to be implemented on a larger
scale, there may be better opportunities to use health care claims data to take advantage of
variation by communities in access to telehealth to obtain quasi-experimental estimates of cost
savings for broad MH/SUD service bundles delivered via telehealth.
SUMMARY
Key informant interviews from a diverse group of stakeholders and case studies were
used to supplement evidence from the environmental scan about current barriers to using
telehealth for pediatric populations for MH/SUD services. Important factors for delivering better
care and overcoming technological and provider-related barriers were described in the context of
financing and policy challenges. There remain a variety of unresolved questions requiring future
study. Overall, this study highlights that telehealth for pediatric services in the field of MH/SUD
is still an emerging area full of potential (despite the barriers), particularly with respect to
increases in access to services where there are no other options for pediatric patients requiring
MH/SUD services.

Reducing Barriers to Using Telehealth for Pediatric Populations
Final Report
71
[This page intentionally left blank]

Reducing Barriers to Using Telehealth for Pediatric Populations
Final Report
R-1
REFERENCES
Adkins, E. C., Zalta, A. K., Boley, R. A., Glover, A., Karnik, N. S., & Schueller, S. M. (2017).
Exploring the potential of technology-based mental health services for homeless youth: A
qualitative study. Psychol Serv, 14(2), 238-245. doi:10.1037/ser0000120
Ali, M. M., Dean, D., Jr., Lipari, R., Dowd, W. N., Aldridge, A. P., & Novak, S. P. (2015). The
mental health consequences of nonmedical prescription drug use among adolescents. J
Ment Health Policy Econ, 18(1), 3-15. Retrieved from
https://www.ncbi.nlm.nih.gov/pubmed/25862204
Allen, M. L., Garcia-Huidobro, D., Porta, C., Curran, D., Patel, R., Miller, J., & Borowsky, I.
(2016). Effective parenting interventions to reduce youth substance use: A systematic
review. Pediatrics, 138(2), e20154425.
Alston, M., Bennett, C. F., & Rochani, H. (2019). Treatment adherence in youth with first-
episode psychosis: Impact of Family support and telehealth delivery. Issues Ment Health
Nurs, 1-6. doi:10.1080/01612840.2019.1630532
American Academy of Pediatrics. (2017). Operating procedures for pediatric telehealth.
Pediatrics, 140(2), e20171756.
American Medical Association. (2016). Adopting the ECHO model™ (Extension for
Community Healthcare Outcomes)—STEPS Forward. Retrieved from
https://www.stepsforward.org/modules/project-echo
Antoniotti, N. M., Armstrong, A., Bernstein, D., Burdick, A., Edison, K., Goldyne, M., . . .
Kvedar, J. (2016). Teledermatology Practice Guidelines Work Group.
Antoniotti, N. M., Drude, K. P., & Rowe, N. (2014). Private payer telehealth reimbursement in
the United States. Telemed J E Health, 20(6), 539-543. doi:10.1089/tmj.2013.0256
Bashir, A. (2018). Commentary and Reflection Related to the Perspectives of Nurses Toward
Telehealth Efficacy and Quality of Health Care. Health Serv Res Manag Epidemiol, 5,
2333392818800549. doi:10.1177/2333392818800549
Bashshur, R. L., Shannon, G. W., Bashshur, N., & Yellowlees, P. M. (2016). The empirical
evidence for telemedicine interventions in mental disorders. Telemedicine and e-Health,
22(2), 87-113. doi:10.1089/tmj.2015.0206
Batastini, A. B., King, C. M., Morgan, R. D., & McDaniel, B. (2016). Telepsychological services
with criminal justice and substance abuse clients: A systematic review and meta-analysis.
Psychol Serv, 13(1), 20-30. doi:10.1037/ser0000042
Becevic, M., Boren, S., Mutrux, R., Shah, Z., & Banerjee, S. (2015). User satisfaction with
telehealth: Study of patients, providers, and coordinators. The Health Care Manager,
34(4), 337-349. doi:10.1097/hcm.0000000000000081

Reducing Barriers to Using Telehealth for Pediatric Populations
Final Report
R-2
Benavides-Vaello, S., Strode, A., & Sheeran, B. C. (2013). Using technology in the delivery of
mental health and substance abuse treatment in rural communities: a review. J Behav
Health Serv Res, 40(1), 111-120. doi:10.1007/s11414-012-9299-6
Bice-Urbach, B. J., & Kratochwill, T. R. (2016). Teleconsultation: The use of technology to
improve evidence-based practices in rural communities. J Sch Psychol, 56, 27-43.
doi:10.1016/j.jsp.2016.02.001
Boling & Company. (2016). The emerging HIPAA/FERPA conundrum in school-based
telehealth. Retrieved from http://www.bolingandcompany.com/blog/2016/1/11/the-
emerging-hipaaferpa-conundrum-in-school-based-telehealth
Boudreaux, E. D., Haskins, B., Harralson, T., & Bernstein, E. (2015). The remote brief
intervention and referral to treatment model: Development, functionality, acceptability,
and feasibility. Drug and Alcohol Dependence, 155, 236-242.
doi:10.1016/j.drugalcdep.2015.07.014
Bounthavong, M., Pruitt, L. D., Smolenski, D. J., Gahm, G. A., Bansal, A., & Hansen, R. N.
(2016). Economic evaluation of in-home telehealth compared to in-person treatment
delivery for managing depression. Value in Health, 19(3), A189-A189.
doi:10.1016/j.jval.2016.03.1381
Bouvier, B. A., Kinnard, E. N., Yedinak, J. L., Li, Y., Elston, B., Green, T. C., . . . Marshall, B.
D. L. (2019). Prevalence and correlates of depressive symptomology among young adults
who use prescription opioids non-medically. J Psychoactive Drugs, 1-12.
doi:10.1080/02791072.2019.1654151
Brusoski, M., & Rosen, D. (2015). Health promotion using tablet technology with older adult
African American methadone clients: A case study. Journal of Technology in Human
Services, 33(2), 119-132. doi:10.1080/15228835.2014.989297
Burke, B. L., Jr., & Hall, R. W. (2015). Telemedicine: Pediatric Applications. Pediatrics, 136(1),
e293-308. doi:10.1542/peds.2015-1517
Bussing, R., Nelson, M. M., & Kurtz, S. (2016). Parent–child interaction therapy: Treatment
components and evidence-base. Journal of the American Academy of Child & Adolescent
Psychiatry, 55(10), S351.
California Telehealth Resource Center. (2014). The CTRC Telehealth Program Developer Kit.
Retrieved from http://www.telehealthresourcecenter.org/sites/main/files/file-
attachments/complete-program-developer-kit-2014-web1.pdf
Celio, M. A., Mastroleo, N. R., DiGuiseppi, G., Barnett, N. P., Colby, S. M., Kahler, C. W., . . .
Monti, P. M. (2017). Using video conferencing to deliver a brief motivational
intervention for alcohol and sex risk to emergency department patients: A proof-of-
concept pilot study. Addiction Research & Theory, 25(4), 318-325.
doi:10.1080/16066359.2016.1276902

Reducing Barriers to Using Telehealth for Pediatric Populations
Final Report
R-3
Center for Connected Health Policy. (2018). State telehealth laws & reimbursement policies.
Public Health Institute, The National Telehealth Policy Research Center Retrieved from
https://www.cchpca.org/sites/default/files/2018-
10/CCHP_50_State_Report_Fall_2018.pdf
Center for Connected Health Policy. (2019a). State telehealth laws and reimbursement policies:
At a glance. Retrieved from https://www.cchpca.org/sites/default/files/2019-05/50-
State%20Infograph%20Spring%202019%20FINAL.pdf
Center for Connected Health Policy. (2019b). State telehealth laws and reimbursement policies.
Retrieved from https://www.cchpca.org/sites/default/files/2019-
05/cchp_report_MASTER_spring_2019_FINAL.pdf
Center for Connected Health Policy. (n.d.-a). State telehealth laws and reimbursement policies
report: CCHP’s comprehensive assessment and compendium of state Medicaid telehealth
policies and laws covers all fifty states and the District of Columbia. Retrieved from
https://www.cchpca.org/telehealth-policy/state-telehealth-laws-and-reimbursement-
policies-report
Center for Connected Health Policy. (n.d.-b). Is a nonprofit, nonpartisan organization working to
maximize telehealth’s ability to improve health outcomes, care delivery, and cost
effectiveness: Research laws & track regulation. Retrieved from https://www.cchpca.org
Center for Connected Health Policy. (n.d.-c). Is a nonprofit, nonpartisan organization working to
maximize telehealth’s ability to improve health outcomes, care delivery, and cost
effectiveness: Research laws & track regulation. Retrieved from https://www.cchpca.org
Center for Medicare and Medicaid Innovation. (2019). Integrated Care for Kids (InCK) Model
Notice of Funding Opportunity. Centers for Medicare & Medicaid Services Retrieved
from https://www.grants.gov/web/grants/view-opportunity.html?oppId=312759
Center for Substance Abuse Treatment. (2004). Substance abuse treatment and family therapy.
(Treatment Improvement Protocol (TIP) Series, No. 39.). Rockville (MD): Substance
Abuse and Mental Health Services Administration (US) Retrieved from
https://www.ncbi.nlm.nih.gov/books/NBK64269/
Centers for Medicare & Medicaid Services. (2018a). SMD # 18-006: Leveraging Medicaid
technology to address the opioid crisis. Baltimore, MD: Department of Health and
Human Services Retrieved from https://www.medicaid.gov/federal-policy-
guidance/downloads/smd18006.pdf
Centers for Medicare & Medicaid Services. (2018b). SMD # 18--011: Opportunities to design
innovative service delivery systems for adults with a serious mental illness or children
with a serious emotional disturbance. Baltimore, MD: Department of Health & Human
Services Retrieved from https://www.medicaid.gov/federal-policy-
guidance/downloads/smd18011.pdf
Reducing Barriers to Using Telehealth for Pediatric Populations
Final Report
R-4
Centers for Medicare & Medicaid Services. (2019). Telehealth services. Retrieved from
https://www.cms.gov/outreach-and-education/medicare-learning-network-
mln/mlnproducts/downloads/telehealthsrvcsfctsht.pdf
Centers for Medicare & Medicaid Services. (n.d.-a). Behavioral health services. Retrieved from
https://www.medicaid.gov/medicaid/benefits/bhs/index.html
Centers for Medicare & Medicaid Services. (n.d.-b). Telemedicine. Retrieved from
https://www.medicaid.gov/medicaid/benefits/telemed/index.html
Chassin, L., Dmitrieva, J., Modecki, K., Steinberg, L., Cauffman, E., Piquero, A. R., . . . Losoya,
S. H. (2010). Does adolescent alcohol and marijuana use predict suppressed growth in
psychosocial maturity among male juvenile offenders? Psychology of Addictive
Behaviors, 24(1), 48.
Chen, S., Cheng, A., & Mehta, K. (2013). A review of telemedicine business models. Telemed J
E Health, 19(4), 287-297. doi:10.1089/tmj.2012.0172
Crum, K. I., & Comer, J. S. (2016). Using Synchronous Videoconferencing to Deliver Family-
Based Mental Healthcare. Journal of Child and Adolescent Psychopharmacology, 26(3),
229-234. doi:10.1089/cap.2015.0012
Cunningham, D. L., Connors, E. H., Lever, N., & Stephan, S. H. (2013). Providers' perspectives:
Utilizing telepsychiatry in schools. Telemedicine and e-Health, 19(10), 794-799.
doi:10.1089/tmj.2012.0314
Danaher, B. G., Seeley, J. R., Stormshak, E. A., Tyler, M. S., Caruthers, A. S., Moore, K. J., &
Cardenas., L. (2018). The family check-up online program for parents of middle school
students: Protocol for a randomized controlled trial. JMIR Research Protocols, 7(7),
E11106.
Derefinko, K. J., Charnigo, R. J., Peters, J. R., Adams, Z. W., Milich, R., & Lynam, D. R.
(2016). Substance use trajectories from early adolescence through the transition to
college. Journal of Studies on Alcohol and Drugs, 77(6), 924-935.
Deslich, S. A., Thistlethwaite, T., & Coustasse, A. (2013). Telepsychiatry in correctional
facilities: using technology to improve access and decrease costs of mental health care in
underserved populations. Perm J, 17(3), 80-86. doi:10.7812/tpp/12-123
Dizon, R. (2018, 2018, December 18). 2018 in review: State & federal telehealth policy.
Retrieved from https://www.telehealthresourcecenter.org/2018-in-review-state-federal-
telehealth-policy/
Donelan, K., Barreto, E. A., Sossong, S., Michael, C., Estrada, J. J., Cohen, A. B., . . .
Schwamm, L. H. (2019). Patient and clinician experiences with telehealth for patient
follow-up care. Am J Manag Care, 25(1), 40-44. Retrieved from
https://www.ncbi.nlm.nih.gov/pubmed/30667610

Reducing Barriers to Using Telehealth for Pediatric Populations
Final Report
R-5
Dorsey, E. R., & Topol, E. J. (2016). State of Telehealth. N Engl J Med, 375(2), 154-161.
doi:10.1056/NEJMra1601705
Dowell, D., Haegerich, T. M., & Chou, R. (2016). CDC guideline for prescribing opioids for
chronic pain — United States, 2016. MMWR Recomm Rep, 65(No. RR-1), 1-49.
doi:http://dx.doi.org/10.15585/mmwr.rr6501e1
Dunlap, L., Haque, S., Mallonee, E., Dubenitz, J., Fuller, L., & Schwartz, D. (2018). Using
telehealth to support opioid use disorder treatment issue brief. Office of the Assistant
Secretary for Planning and Evaluation (ASPE), U.S. Department of Health & Human
Services Retrieved from https://aspe.hhs.gov/basic-report/using-telehealth-support-
opioid-use-disorder-treatment-issue-brief
Eiden, R. D., Lessard, J., Colder, C. R., Livingston, J., Casey, M., & Leonard, K. E. (2016).
Developmental cascade model for adolescent substance use from infancy to late
adolescence. Dev Psychol, 52(10), 1619-1633. doi:10.1037/dev0000199
Federal Communication Commission. (2010). National Broadband Plan. Retrieved from
https://www.fcc.gov/general/national-broadband-plan
Federal Communications Commission. (2019a). Broadband speed guide. Retrieved from
https://www.fcc.gov/reports-research/guides/broadband-speed-guide
Federal Communications Commission. (2019b). FCC authorizes first wave of funding for rural
broadband from Connect America Fund auction. Retrieved from
https://docs.fcc.gov/public/attachments/DOC-357434A1.pdf
Federal Communications Commission. (2019c). Broadband deployment advisory committee.
Retrieved from https://www.fcc.gov/broadband-deployment-advisory-committee
Federal Communications Commission. (n.d.-a). Mapping broadband health in America 2017.
Retrieved from https://www.fcc.gov/reports-
research/maps/connect2health/#ll=40.055205,-
94.768946&z=4&t=broadband&bbm=fixed_access&dmf=none&zlt=county
Federal Communications Commission. (n.d.-b). Bridging the digital divide for all Americans.
Retrieved from https://www.fcc.gov/about-fcc/fcc-initiatives/bridging-digital-divide-all-
americans
Federation of State Medical Boards. (n.d.). Telemedicine policies: Board by board overview.
Retrieved from http://www.fsmb.org/siteassets/advocacy/key-
issues/telemedicine_policies_by_state.pdf
Fischer, A. J., Dart, E. H., Radley, K. C., Richardson, D., Clark, R., & Wimberly, J. (2017). An
Evaluation of the Effectiveness and Acceptability of Teleconsultation. Journal of
Educational and Psychological Consultation, 27(4), 437-458.
doi:10.1080/10474412.2016.1235978

Reducing Barriers to Using Telehealth for Pediatric Populations
Final Report
R-6
Fleischman, A., Hourigan, S. E., Lyon, H. N., Landry, M. G., Reynolds, J., Steltz, S. K., . . .
Ebbeling, C. B. (2016). Creating an integrated care model for childhood obesity: a
randomized pilot study utilizing telehealth in a community primary care setting. Clin
Obes, 6(6), 380-388. doi:10.1111/cob.12166
Freeman, K. A., Duke, D. C., & Harris, M. A. (2013). Behavioral health care for adolescents
with poorly controlled diabetes via Skype: does working alliance remain intact? J
Diabetes Sci Technol, 7(3), 727-735. doi:10.1177/193229681300700318
Frueh, B. C., Henderson, S., & Myrick, H. (2005). Telehealth service delivery for persons with
alcoholism. Journal of Telemedicine and Telecare, 11(7), 372-375.
Gagnon, M. P., Duplantie, J., Fortin, J. P., & Landry, R. (2006). Implementing telehealth to
support medical practice in rural/remote regions: What are the conditions for success?
Implementation Science, 1(1), 1.
Gillies, D., Taylor, F., Gray, C., O'Brien, L., & D'Abrew, N. (2013). Psychological therapies for
the treatment of post-traumatic stress disorder in children and adolescents (Review). Evid
Based Child Health: A Cochrane Review Journal, 8(3), 1004-1116.
doi:10.1002/ebch.1916
Goldbeck, L., Muche, R., Sachser, C., Tutus, D., & Rosner, R. (2016). Effectiveness of trauma-
focused cognitive behavioral therapy for children and adolescents: A Randomized
controlled trial in eight German mental health clinics. Psychother Psychosom, 85(3), 159-
170. doi:10.1159/000442824
Goldschmidt, K. (2016). Tele-Mental Health for Children: Using Videoconferencing for
Cognitive Behavioral Therapy (CBT). Journal of Pediatric Nursing-Nursing Care of
Children & Families, 31(6), 742-744. doi:10.1016/j.pedn.2016.09.001
Gopalan, G., Goldstein, L., Klingenstein, K., Sicher, C., Blake, C., & McKay, M. (2010).
Engaging families into child mental health treatment: Updates and special considerations.
Journal of the Canadian Academy of Child and Adolescent Psychiatry/Journal de
l'Académie canadienne de psychiatrie de l'enfant et de l'adolescent.
Hanefield, J., Powell-Jackson, T., & Balabanova, D. (2017). Policy & Practice: Understanding
and measuring quality of care: Dealing with complexity. Bulletin of the World Health
Organization, 95, 368-374. doi:http://dx.doi.org/10.2471/BLT.16.179309
HealthIT.gov. (2019a). What is the recommended bandwidth for different types of health care
providers? Retrieved from https://www.healthit.gov/faq/what-recommended-bandwidth-
different-types-health-care-providers
HealthIT.gov. (2019b). Interoperability. Retrieved from
https://www.healthit.gov/topic/interoperability

Reducing Barriers to Using Telehealth for Pediatric Populations
Final Report
R-7
Heradstveit, O., Skogen, J. C., Hetland, J., & Hysing, M. (2017). Alcohol and illicit drug use are
important factors for school-related problems among adolescents. Frontiers in
Psychology, 8, 1023. doi:10.3389/fpsyg.2017.01023
Hilt, R. J. (2017). Telemedicine for Child Collaborative or Integrated Care. Child Adolesc
Psychiatr Clin N Am, 26(4), 637-645. doi:10.1016/j.chc.2017.05.001
Hilt, R. J., Barclay, R. P., Bush, J., Stout, B., Anderson, N., & Wignall, J. R. (2015). A Statewide
Child Telepsychiatry Consult System Yields Desired Health System Changes and
Savings. Telemed J E Health, 21(7), 533-537. doi:10.1089/tmj.2014.0161
Hilty, D. M., Ferrer, D. C., Parish, M. B., Johnston, B., Callahan, E. J., & Yellowlees, P. M.
(2013). The effectiveness of telemental health: A 2013 review. Telemedicine and e-
Health, 19(6), 444-454.ss. doi:10.1089/tmj.2013.0075
Hoffman, L. C. (2019). Telehealth, children, and pediatrics: Should the doctor make house calls
again, digitally? Nova Law Review, 43(3), 321-351.
Interstate Medical Licensure Compact. (2019). Facts about the IMLCC. Retrieved from
https://imlcc.org/facts-about-the-imlcc/
Johnston, B., & Yellowlees, P. (2016). Telepsychiatry consultations in primary care coordinated
by virtual care navigators. Psychiatric Services, 67(1), 142. doi:10.1176/appi.ps.660905
Joint Commission on Accreditation of Healthcare Organizations. (2012, January). Accepted:
Final revisions to telemedicine standards. Joint Commission Perspectives®, 32(1), 4-6.
Retrieved from
https://www.jointcommission.org/assets/1/6/Revisions_telemedicine_standards.pdf
Kaslow, N. J., Broth, M. R., Smith, C. O., & Collins, M. H. (2012). Family-based interventions
for child and adolescent disorders. J Marital Fam Ther, 38(1), 82-100.
doi:10.1111/j.1752-0606.2011.00257.x
Kelly, A. B., Evans-Whipp, T. J., Smith, R., Chan, G. C., Toumbourou, J. W., Patton, G. C., . . .
Catalano, R. F. (2015). A longitudinal study of the association of adolescent polydrug
use, alcohol use and high school non-completion. Addiction, 110(4), 627-635.
doi:10.1111/add.12829
Kerns, C. M., Roux, A. M., Connell, J. E., & Shattuck, T. P. (2016). Adapting cognitive
behavioral techniques to address anxiety and depression in cognitively able emerging
adults on the autism spectrum. Cognitive and Behavioral Practice, 23(3), 329-340.
Kim, S. J., Marsch, L. A., Guarino, H., Acosta, M. C., & Aponte-Melendez, Y. (2015).
Predictors of outcome from computer-based treatment for substance use disorders:
Results from a randomized clinical trial. Drug and Alcohol Dependence, 15(7), 174-178.
doi:10.1016/j.drugalcdep.2015.09.019

Reducing Barriers to Using Telehealth for Pediatric Populations
Final Report
R-8
King, V. L., Brooner, R. K., Peirce, J. M., Kolodner, K., & Kidorf, M. S. (2014). A randomized
trial of Web-based videoconferencing for substance abuse counseling. Journal of
Substance Abuse Treatment, 46(1), 36-42. doi:10.1016/j.jsat.2013.08.009
Knopf, A. (2013). Buprenorphine by telemedicine: Reaching rural West Virginia patients.
Alcoholism & Drug Abuse Weekly, 25(41), 3-4.
Kraetschmer, N. M., Deber, R. B., Dick, P., & Jennett, P. (2009). Telehealth as gatekeeper:
Policy implications for geography and scope of services. Telemedicine and e-Health,
15(7), 655-663. doi:10.1089/tmj.2009.0004
Kuhn, E. S., & Laird, R. D. (2014). Family support programs and adolescent mental health:
review of evidence. Adolescent Health, Medicine and Therapeutics, 5, 127-142.
doi:10.2147/AHMT.S48057
Lambert, D., Gale, J., Hartley, D., Croll, Z., & Hansen, A. (2016). Understanding the business
case for telemental health in rural communities. Journal of Behavioral Health Services
Research, 43(3), 366-379. doi:10.1007/s11414-015-9490-7
Lammers, E. J., Zickafoose, J. S., Peterson, G. G., Blue, L., Stewart, K. A., & Kranker, K.
(2019). Parent partners: Evaluation of a novel peer-support intervention for the caregivers
of children hospitalized for behavioral health conditions. Academic Pediatrics.
doi:10.1016/j.acap.2019.06.001
Langkamp, D. L., McManus, M. D., & Blakemore, S. D. (2015). Telemedicine for children with
developmental disabilities: a more effective clinical process than office-based care.
Telemed J E Health, 21(2), 110-114. doi:10.1089/tmj.2013.0379
Lenz, A. S., & Hollenbaugh, K. M. (2015). Meta-analysis of trauma-focused cognitive
behavioral therapy for treating PTSD and co-occurring depression among children and
adolescents. Counseling Outcome Research and Evaluation, 6(1), 18-32.
LeRouge, C., & Garfield, M. J. (2013). Crossing the telemedicine chasm: have the U.S. barriers
to widespread adoption of telemedicine been significantly reduced? Int J Environ Res
Public Health, 10(12), 6472-6484. doi:10.3390/ijerph10126472
Lewiecki, E. M., Rochelle, R., Bouchonville, M. F., 2nd, Chafey, D. H., Olenginski, T. P., &
Arora, S. (2017). Leveraging Scarce Resources With Bone Health TeleECHO to Improve
the Care of Osteoporosis. J Endocr Soc, 1(12), 1428-1434. doi:10.1210/js.2017-00361
Lin, L. A., Casteel, D., Shigekawa, E., Weyrich, M. S., Roby, D. H., & McMenamin, S. B.
(2019). Telemedicine-delivered treatment interventions for substance use disorders: A
systematic review. J Subst Abuse Treat, 101, 38-49. doi:10.1016/j.jsat.2019.03.007
Lowery, C. L., Bronstein, J. M., Benton, T. L., & Fletcher, D. A. (2014). Distributing medical
expertise: The evolution and impact of telemedicine in Arkansas. Health Affairs, 33(2),
235–243. doi:10.1377/hlthaff.2013.1001

Reducing Barriers to Using Telehealth for Pediatric Populations
Final Report
R-9
Luxton, D. D., Pruitt, L. D., O'Brien, K., & Kramer, G. (2015). An evaluation of the feasibility
and safety of a home-based telemental health treatment for posttraumatic stress in the
U.S. Military. Telemed J E Health, 21(11), 880-886. doi:10.1089/tmj.2014.0235
Luxton, D. D., Pruitt, L. D., & Osenbach, J. E. (2014). Best practices for remote psychological
assessment via telehealth technologies. Professional Psychology-Research and Practice,
45(1), 27-35. doi:10.1037/a0034547
Martinez, K. A., Rood, M., Jhangiani, N., Kou, L., Rose, S., Boissy, A., & Rothberg, M. B.
(2018). Patterns of Use and Correlates of Patient Satisfaction with a Large Nationwide
Direct to Consumer Telemedicine Service. J Gen Intern Med, 33(10), 1768-1773.
doi:10.1007/s11606-018-4621-5
McCarty, C. A., Stoep, A. V., Violette, H., & Myers, K. (2015). Interventions developed for
psychiatric and behavioral treatment in the children’s ADHD Telemental Health
Treatment Study. Journal of Child and Family Studies, 24(6), 1735-1743.
doi:10.1007/s10826-014-9977-5
McGinty, K. L., Saeed, S. A., Simmons, S. C., & Yildirim, Y. (2006). Telepsychiatry and e-
mental health services: Potential for improving access to mental health care. Psychiatric
Quarterly, 77, 335-342.
McKellar, J., Wagner, T., Harris, A., Oehlert, M., Buckley, S., & Moos, R. (2012). One-year
outcomes of telephone case monitoring for patients with substance use disorder.
Addictive Behaviors, 37(10), 1069-1074. doi:10.1016/j.addbeh.2012.03.009
McSwain, S. D., Bernard, J., Burke, B. L., Jr., Cole, S. L., Dharmar, M., Hall-Barrow, J., . . .
Yeager, B. (2017). American Telemedicine Association Operating Procedures for
Pediatric Telehealth. Telemed J E Health, 23(9), 699-706. doi:10.1089/tmj.2017.0176
McSwain, S. D., & Marcin, J. P. (2014). Telemedicine for the care of children in the hospital
setting. Pediatr Ann, 43(2), e44-49. doi:10.3928/00904481-20140127-10
Medicaid.gov. (n.d.). Medicaid information technology architecture. Retrieved from
https://www.medicaid.gov/medicaid/data-and-systems/mita/index.html
Merrell, R. C., & Doarn, C. R. (2013). Tales of telemedicine-telepsychiatry at work.
Telemedicine and e-Health, 19(4), 233-234. doi:10.1089/tmj.2013.9995
Molfenter, T., Brown, R., O'Neill, A., Kopetsky, E., & Toy, A. (2018). Use of Telemedicine in
Addiction Treatment: Current Practices and Organizational Implementation
Characteristics. Int J Telemed Appl, 2018, 3932643. doi:10.1155/2018/3932643
Moreira-Almeida, A., & de Souza, M. J. (2016). Childhood environment and intergenerational
transmission of depression. Br J Psychiatry, 208(2), 198. doi:10.1192/bjp.208.2.198
Mountain-Pacific Quality Health. (2017, Sept 27). HIPAA pass privacy and security solutions:
HIPAA highlights and impact to your telehealth program. Retrieved from

Reducing Barriers to Using Telehealth for Pediatric Populations
Final Report
R-10
https://www.uwyo.edu/wind/_files/docs/wytn-doc/wytn-webinar-doc/wytn-webinar-
sept.pdf
Muench, F. (n.d.). Technology based interventions for substance users: Promises and pitfalls of
integration into clinical care. Retrieved from http://www.nfarattc.org/wp-
content/uploads/2016/08/Frederick-Muench.pdf
Myers, K., Nelson, E. L., Rabinowitz, T., Hilty, D., Baker, D., Barnwell, S. S., . . . Bernard, J.
(2017). American Telemedicine Association Practice Guidelines for Telemental Health
with Children and Adolescents. Telemed J E Health, 23(10), 779-804.
doi:10.1089/tmj.2017.0177
National Health Services. (2016). Technology enabled care services. Retrieved from
https://www.england.nhs.uk/ourwork/qual-clin-lead/tecs/
NCTSN. (2019). Interventions. Retrieved from https://www.nctsn.org/treatments-and-
practices/trauma-treatments/interventions
Nelson, S. E., Ryzin, M. J. V., & Dishion, T. J. (2015). lcohol, marijuana, and tobacco use
trajectories from age 12 to 24 years: Demographic correlates and young adult substance
use problems. Development and Psychopathology, 27(1), 253-277.
Olson, C. A., McSwain, S. D., Curfman, A. L., & Chuo, J. (2018). The Current Pediatric
Telehealth Landscape. Pediatrics, 141(3), e20172334. doi:10.1542/peds.2017-2334
Paing, W. W., Weller, R. A., Welsh, B., Foster, T., Birnkrant, J. M., & Weller, E. B. (2009).
Telemedicine in children and adolescents. Curr Psychiatry Rep, 11, 114-119.
Pearson, R. M., Evans, J., Kounali, D., Lewis, G., Heron, J., Ramchandani, P. G., . . . Stein, A.
(2013). Maternal depression during pregnancy and the postnatal period: risks and
possible mechanisms for offspring depression at age 18 years. JAMA Psychiatry, 70(12),
1312-1319. doi:10.1001/jamapsychiatry.2013.2163
Perry, K., Gold, S., & Shearer, E. M. (2019). Identifying and addressing mental health providers'
perceived barriers to clinical video telehealth utilization. Journal of Clinical Psychology.
doi:10.1002/jclp.22770
Perry, V. (2016, September 2) Recorded Webinar: Telehealth at Intermountain Healthcare |
Sirius Computer Solutions.
Petry, N. M. (2013). Contingency management for substance abuse treatment: A guide to
implementing this evidence-based practice. Routledge.
Pew Research Center. (2018). Teens’ social media habits and experiences. Retrieved from
https://www.pewinternet.org/2018/11/28/teens-social-media-habits-and-experiences/
Pew Research Center. (2019a). Share of U.S. adults using social media, including Facebook, is
mostly unchanged since 2018. Retrieved from https://www.pewresearch.org/fact-
Reducing Barriers to Using Telehealth for Pediatric Populations
Final Report
R-11
tank/2019/04/10/share-of-u-s-adults-using-social-media-including-facebook-is-mostly-
unchanged-since-2018/
Pew Research Center. (2019b). Internet/broadband fact sheet. Retrieved from
https://www.pewinternet.org/fact-sheet/internet-broadband/
Polaha, J., Williams, S. L., Heflinger, C. A., & Studts, C. R. (2015). The perceived stigma of
mental health services among rural parents of children with psychosocial concerns.
Journal of Pediatric Psychology, 40(10), 1095-1104. doi:10.1093/jpepsy/jsv054
Poon, J. A., Turpyn, C. C., Hansen, A., Jacangelo, J., & Chaplin, T. M. (2016). Adolescent
substance use & psychopathology: Interactive effects of cortisol reactivity and emotion
regulation. Cognit Ther Res, 40(3), 368-380. doi:10.1007/s10608-015-9729-x
Quest, T. L., Merrill, J. O., Roll, J., Saxon, A. J., & Rosenblatt, R. A. (2012). Buprenorphine
therapy for opioid addiction in rural Washington: the experience of the early adopters. J
Opioid Manag, 8(1), 29-38. Retrieved from
https://www.ncbi.nlm.nih.gov/pubmed/22479882
Ray, K. N., Shi, Z., Poon, S. J., Uscher-Pines, L., & Mehrotra, A. (2019). Use of commercial
direct-to-consumer telemedicine by children. Academic Pediatrics, 2019 Jan 10 [Epub
ahead of print]. doi:10.1016/j.acap.2018.11.016
Reynolds, C. A., & Maughan, E. D. (2015). Telehealth in the school setting: an integrative
review. J Sch Nurs, 31(1), 44-53. doi:10.1177/1059840514540534
Roane, H. S., Fisher, W. W., & Carr, J. E. (2016). Applied behavior analysis as treatment for
autism spectrum disorder. J Pediatr, 175, 27-32. doi:10.1016/j.jpeds.2016.04.023
RTI International. (2016). Evaluation of the Health Care Innovation Awards: Community
resource planning, prevention, and monitoring, Second annual report. Retrieved from
RTP, NC: https://downloads.cms.gov/files/cmmi/hcia-communityrppm-secondevalrpt.pdf
RTI International. (2017, September 15). Using telehealth to identify and manage health and
substance use disorder conditions in rural areas. Prepared under contract
#HHSP233201600021I between the U.S. Department of Health and Human Services
(HHS), Office of Disability, Aging and Long-Term Care Policy (DALTCP) and Research
Triangle Institute. Retrieved from
SAMHSA. (2016). Rural behavioral health: Telehealth challenges and opportunities. In Brief,
9(2). Retrieved from http://store.samhsa.gov/shin/content/SMA16-4989/SMA16-
4989.pdf
SAMHSA. (2019). Reports and detailed tables from the 2018 National Survey on Drug Use and
Health (NSDUH). Retrieved from https://www.samhsa.gov/data/nsduh/reports-detailed-
tables-2018-NSDUH

Reducing Barriers to Using Telehealth for Pediatric Populations
Final Report
R-12
SAMHSA.gov. (n.d.). Substance abuse confidentiality regulations Retrieved from
https://www.samhsa.gov/about-us/who-we-are/laws-regulations/confidentiality-
regulations-faqs
Sanchez, D., Reiner, J. F., Sadlon, R., Price, O. A., & Long, M. W. (2019). Systematic review of
school telehealth evaluations. The Journal of School Nursing, 35(1), 61-76.
doi:10.1177/1059840518817870
Sawyer, K. M., Zunszain, P. A., Dazzan, P., & Pariante, C. M. (2019). Intergenerational
transmission of depression: clinical observations and molecular mechanisms. Mol
Psychiatry, 24(8), 1157-1177. doi:10.1038/s41380-018-0265-4
Scattone, D., Sarver, D. E., & Cox, A. D. (2018). Parent-child interaction therapy (PCIT):
Autism case study #4. In C. B. McNeil, L. B. Quetsch, & C. M. Andreson (Eds.),
Handbook of parent-child interaction therapy for children on the autism spectrum (pp.
651-664): Springer.
Schmeida, M., & McNeal, R. (2007). The telehealth divide: Disparities in searching public
health information online. Journal of Health Care for the Poor and Underserved, 18(3),
637–647. doi:10.1353/hpu.2007.0068
Schuler, M. S., Vasilenko, S. A., & Lanza, S. T. (2015). Age-varying associations between
substance use behaviors and depressive symptoms during adolescence and young
adulthood. Drug Alcohol Depend, 157, 75-82. doi:10.1016/j.drugalcdep.2015.10.005
Sherr, L. (2018). Mental health challenges and interventions for adolescents. Handbook of
adolescent development research and its impact on global policy. Retrieved from
http://dx.doi.org/10.1093/oso/9780190847128.003.0017
Sills, M. R., Shetterly, S., Xu, S., Magid, D., & Kempe, A. (2007). Association between parental
depression and children's health care use. Pediatrics, 119(4), e829-836.
doi:10.1542/peds.2006-2399
Slusser, W., Whitley, M., Izadpanah, N., Kim, S. L., & Ponturo, D. (2016). Multidisciplinary
Pediatric Obesity Clinic via Telemedicine Within the Los Angeles Metropolitan Area:
Lessons Learned. Clin Pediatr (Phila), 55(3), 251-259. doi:10.1177/0009922815594359
Smith, V. C., Wilson, C. R., & Committee on Substance Use and Prevention. (2016). Families
Affected by Parental Substance Use. Pediatrics, 138(2). doi:10.1542/peds.2016-1575
Squeglia, L. M., Jacobus, J., & Tapert, S. F. (2009). The influence of substance use on
adolescent brain development. Clin EEG Neurosci, 40(1), 31-38.
doi:10.1177/155005940904000110
Steege, M. W., Mace, F. C., Perry, L., & Longenecker, H. (2007). Applied behavior analysis:
Beyond discrete trial teaching. Psychology in the Schools, 44(1), 91-99.

Reducing Barriers to Using Telehealth for Pediatric Populations
Final Report
R-13
Stewart, R. W., Orengo-Aguayo, R. E., Cohen, J. A., Mannarino, A. P., & de Arellano, M. A.
(2017a). A pilot study of trauma-focused cognitive–behavioral therapy delivered via
telehealth technology. Child Maltreatment, 22(4), 324-333.
doi:10.1177/1077559517725403
Stewart, R. W., Orengo-Aguayo, R. E., Gilmore, A. K., & de Arellano, M. (2017b). Addressing
barriers to care among Hispanic youth: Telehealth delivery of trauma-focused cognitive
behavior therapy. the Behavior Therapist, 40(3), 112-118. Retrieved from
http://search.ebscohost.com/login.aspx?direct=true&db=psyh&AN=2017-13135-
012&authtype=shib&site=ehost-
live&scope=site&authtype=ip,shib&custid=s2919029stewartr@musc.edu
Stiles-Shields, C., Corden, M. E., Kwasny, M. J., Schueller, S. M., & Mohr, D. C. (2015).
Predictors of outcome for telephone and face-to-face administered cognitive behavioral
therapy for depression. Psychological Medicine, 45(15), 3205-3215.
doi:10.1017/s0033291715001208
Talbot, J. A., Burgess, A. R., Thayer, D., Parenteau, L., Paluso, N., & Coburn, A. F. (2018).
Patterns of telehealth use among rural Medicaid beneficiaries. Journal of Rural Health,
2018 Oct 4 [Epub ahead of print]. doi:10.1111/jrh.12324
Tapert, S. E., Caldwell, L., & Burke, C. (2004). Alcohol and the adolescent brain: Human
studies. Alcohol Research & Health, 28, 205–213.
The Office of the National Coordinator for Health Information Technology. (2015). Connecting
health and care for the nation. Retrieved from
https://www.healthit.gov/sites/default/files/hie-interoperability/nationwide-
interoperability-roadmap-final-version-1.0.pdf
Thomas, L., & Capistrant, G. (2015). State telemedicine gaps analysis. Retrieved from
http://cdn2.hubspot.net/hubfs/1775981/omada-pdf/50-state-telemedicine-gaps-analysis---
coverage-and-reimbursement.pdf?t=1461875181706
Tofighi, B., Grossman, E., Sherman, S., Nunes, E. V., & Lee, J. D. (2016). Mobile phone
messaging during unobserved "home" induction to buprenorphine. Journal of Addiction
Medicine, 10(5), 309-313. doi:10.1097/ADM.0000000000000198
Totten, A. M., Womack, D. M., Eden, K. B., McDonagh, M. S., Griffin, J. C., Grusing, S., &
Hersh, W. R. (2016, June). Telehealth: Mapping the Evidence for Patient Outcomes From
Systematic Reviews [Internet]. Rockville (MD): Agency for Healthcare Research and
Quality (US). (Technical Briefs, No. 26.) Findings. Retrieved from
https://www.ncbi.nlm.nih.gov/books/NBK379312/
Trim, R. S., Meehan, B. T., King, K. M., & Chassin, L. (2007). The relation between adolescent
substance use and young adult internalizing symptoms: Findings from a high-risk
longitudinal sample. Psychol Addict Behav, 21(1), 97-107. doi:10.1037/0893-
164X.21.1.97

Reducing Barriers to Using Telehealth for Pediatric Populations
Final Report
R-14
U.S. Department of Health and Human Services, & U.S. Department of Education. (2019,
December). Joint guidance on the application of the Family Educational Rights and
Privacy Act (FERPA) and the Health Insurance Portability and Accountability Act of
1996 (HIPAA) to student health records. Retrieved from
https://studentprivacy.ed.gov/resources/joint-guidance-application-ferpa-and-hipaa-
student-health-records
U.S. Department of Justice, Drug Enforcement Administration. (n.d.). Use of telemedicine while
providing Medication Assisted Treatment (MAT). Retrieved from
www.deadiversion.usdoj.gov/GDP/(DEA-DC-
7)%20Use%20of%20Telemedicine%20While%20Providing%20Medication%20Assisted
%20Treatment%20(MAT).pdf
University of New Mexico. (2016). Project ECHO: A revolution in medical education and care
delivery. Retrieved from http://echo.unm.edu/
Virues-Ortega, J., Rodríguez, V., & Yu, C. T. (2013). Prediction of treatment outcomes and
longitudinal analysis in children with autism undergoing intensive behavioral
intervention. International Journal of Clinical and Health Psychology, 13(2), 91-100.
Volkow, N. D., Baler, R. D., Compton, W. M., & Weiss, S. R. (2014). Adverse health effects of
marijuana use. N Engl J Med, 370(23), 2219-2227. doi:10.1056/NEJMra1402309
Vyas, S., Murren-Boezem, J., & Solo-Josephson, P. (2018). Analysis of a pediatric telemedicine
program. Telemedicine and e-Health, 24(12), 993-997.
Weiner, D., Schneider, S., & Lyons, J. S. (2009). Evidence-based treatments for trauma among
culturally diverse foster care youth: Treatment retention and outcomes. Children and
Youth Services Review, 31, 1199-1205.
Weissman, M. M., Warner, V., Wickramaratne, P., Moreau, D., & Olfson, M. (1997). Offspring
of depressed parents. 10 Years later. Arch Gen Psychiatry, 54(10), 932-940.
doi:10.1001/archpsyc.1997.01830220054009
Whitman, E. (2016). Building a lifeline for rural addicts. Modern Healthcare, 46(40), 18.
Williams, J., & Vance, M. (2019, March 28). Using telemedicine for pediatric behavioral health
services. Retrieved from https://www.childrenshospitals.org/Events/2019/03/28/Using-
Telemedicine-for-Pediatric-Behavioral-Health-Services
Winters, K. C., Botzet, A. M., Stinchfield, R., Gonzales-Castaneda, R., Finch, A. J., Piehler, T.
F., . . . Hemze, A. (2018). Adolescent substance abuse treatment: A review of evidence-
based research. In C. G. Leukefeld, T. P. Gullotta, & M. Staton-Tindall (Eds.),
Adolescent substance abuse (pp. 141-171). Cham?: Springer.
Wu, L. T., Zhu, H., & Swartz, M. S. (2016). Treatment utilization among persons with opioid
use disorder in the United States. Drug and Alcohol Dependence, 169, 117-127.
doi:10.1016/j.drugalcdep.2016.10.015

Reducing Barriers to Using Telehealth for Pediatric Populations
Final Report
R-15
Zeller, S., & Mao, R. J. (2016). Telepsychiatry, emergency psychiatric services can reduce
mental health patient boarding. Retrieved from
https://www.acepnow.com/article/telepsychiatry-emergency-psychiatric-services-can-
reduce-mental-health-patient-boarding/?singlepage=1&theme=print-friendly
Zheng, W., Nickasch, M., Lander, L., Wen, S., Xiao, M., Marshalek, P., . . . Sullivan, C. (2017).
Treatment outcome comparison between telepsychiatry and face-to-face buprenorphine
medication-assisted treatment for opioid use disorder: A 2-Year retrospective data
analysis. J Addict Med, 11(2), 138-144. doi:10.1097/adm.0000000000000287
Zimmer-Gembeck, M. J., Kerin, J. L., Webb, H. J., Gardner, A. A., Campbell, S. M., Swan, K.,
& Timmer, S. G. (2019). Improved perceptions of emotion regulation and reflective
functioning in parents: Two additional positive outcomes of parent-child interaction
therapy. Behav Ther, 50(2), 340-352. doi:10.1016/j.beth.2018.07.002

Reducing Barriers to Using Telehealth for Pediatric Populations
Final Report
R-16
[This page intentionally left blank]

Reducing Barriers to Using Telehealth for Pediatric Populations
Final Report
A-1
APPENDIX A: Key Informant Interview Guide
Reducing Barriers to Using Telehealth for Pediatric Populations
ASPE TELEHEALTH KEY STAKEHOLDER DISCUSSION GUIDE
Discussion Lead: Note Taker:
Key Stakeholder: Organization:
Date/Time of Discussion:
PURPOSE:
The purpose of this discussion is to gather different perspectives on the key issues related to telehealth use
for youth populations with substance use disorder. These discussions will provide each key informant an opportunity
to identify what they believe are the key factors and reimbursement issues.
Thank you for making time to speak with us today. As we explained in our email, we are independent
researchers from RTI International who are contracted with the Office of the Assistant Secretary for Planning and
Evaluation (ASPE) to better understand factors influencing use of telehealth for youth with mental and substance
use disorders. For the purposes of our project, we are defining youth to include individuals under age 21. To
understand this further, we are conducting discussions with key stakeholders to gather different perspectives on the
issues related to telehealth use for behavioral health care. Given your position in the field, we are interested in your
perspectives and there are no right or wrong answers. Also, we recognize that there is currently limited research on
telehealth specifically for youth mental and substance use disorder treatment. With that in mind, we welcome your
perspective based on related programs such as telehealth for adult substance use disorder treatment or telehealth for
adolescent mental health treatment. In addition, we welcome your perspectives whether they are based on your
current involvement in the delivery of telehealth services or based on your general expertise and understanding of
the broader landscape of telehealth.
(Introduce team members and briefly describe qualifications/background and roles during the discussion.)
We expect that our conversation will take less than 1 hour. Participation in this discussion is voluntary. If
you do not wish to participate or answer any specific questions, please let us know.
Finally, we would like to audio-record our conversation to ensure that our notes from today are complete.
Although we are taking detailed notes, the audio recording will help verify our discussion notes. We will not share
the recording outside of this team and it will be deleted when the project is complete.
Do we have your permission to record this discussion?
Do you have any questions about what I have explained?
INTRODUCTION AND CONSENT TO AUDIO RECORD

Reducing Barriers to Using Telehealth for Pediatric Populations
Final Report
A-2
Note to RTI staff:
- If yes, start audio recording.
- Begin discussion.
OVERARCHING QUESTIONS
1. Thanks again for joining us today. Just to start, could you please introduce yourself and tell
us about your background with telehealth (and/or other specific domains as appropriate:
substance use disorder treatment, pediatric populations, policy, financing, mental health
etc.)?
2. How would you describe the current state of telehealth programs for identifying or treating
mental and substance use disorders? (e.g., direct delivery, service support or enhancement,
telephone/video asynchronous video, mobile technology, etc.)
a. What models or practices are common or conventional?
b. What populations are typically served using telehealth?
i. Have the populations served changed since introducing the use of telehealth?
If so, how?
c. What telehealth approaches are still being developed and studied?
d. What new models or uses of telehealth technology are on the horizon?
3. How would you describe any differences in telehealth services for youth versus adults?
a. Service delivery model (e.g., type of technology, setting, provider staff types, etc.)
b. Clinical model/content (e.g., community reinforcement, family involved, MOUD,
etc.)
c. Accessibility (e.g., logistic, financial, etc.)
4. What are your thoughts on differences between face-to-face and telehealth services for youth
mental and substance use disorder treatment in terms of service delivery or clinical
approach?
a. Rapport?
b. Engagement?
c. Compliance?
d. Quality of care?
e. Patient, family, and provider satisfaction

Reducing Barriers to Using Telehealth for Pediatric Populations
Final Report
A-3
5. What barriers do you see in implementing telehealth for mental and substance use
disorders/conditions in youth? What strategies/solutions have been used to overcome those
barriers?
a. Service delivery?
b. Policy barriers?
c. Credentialing?
d. Reimbursement?
e. Operational considerations?
f. Patient/caregiver engagement?
g. Provider/staff engagement?
6. What are your thoughts on the differences between treating youth with substance use
disorders versus mental disorders via telehealth?
7. Are there special considerations in treating youth with co-occurring mental and substance use
disorders via telehealth? If so, please explain?
8. Pharmacotherapy is an increasingly important treatment for mental and substance use
disorders. What barriers are there for prescribing practices for treating substance use
disorders via telehealth?
a. Medications for opioid use disorders?
b. Alcohol use disorders?
c. Mental health?
d. Co-occurring disorders?
BEST PRACTICES
9. What factors facilitate the use of telehealth for mental and substance use disorders in youth?
10. Are there best practices you have identified for telehealth to identify and manage mental and
substance use disorders/conditions in youth? If so, please describe.

Reducing Barriers to Using Telehealth for Pediatric Populations
Final Report
A-4
FINANCING QUESTIONS
11. How are telehealth services reimbursed when used in the treatment of mental and substance
use disorders? Does reimbursement differ between Medicaid and other payers? (e.g., CHIP,
Medicare, private insurance)?
a. Are there any payer-based incentives for using telehealth?
b. Is telehealth part of a payment bundle?
12. What are your thoughts on differences between face-to-face and telehealth services for youth
mental and substance use disorder treatment in terms of financing, utilization and cost?
a. Reimbursement amounts?
b. Different requirements for coverage (e.g., provider credentials, technology etc.)?
c. Utilization rates?
d. Costs?
e. Reductions in other avoidable healthcare use?
13. Does reimbursement for telehealth for behavioral health disorders differ from reimbursement
available for medical/surgical services?
14. Are there any other special considerations with reimbursement for telehealth? If so, please
explain.
WRAP UP AND FUTURE DIRECTIONS
15. When thinking of the future of telehealth service delivery for mental and substance use
disorders among youth, are there any things you think would need to be changed in order to
improve service delivery? If so, what would you change?
16. Is there anything else you think we should know about the use of telehealth for mental and
substance use disorder treatment and related services in youth that we have not asked about
today?

Reducing Barriers to Using Telehealth for Pediatric Populations
Final Report
B-1
APPENDIX B: Case Study Interview Guides
Reducing Barriers to Using Telehealth for Pediatric Populations
ASPE TELEHEALTH CASE STUDY DISCUSSION GUIDE - PROVIDER
Provider Organization:
Discussion Lead:
Note Taker:
Participant(s) (Name and role):
Date/Time of Discussion:
PURPOSE:
The purpose of this discussion is to gain insight into the key issues related to telehealth use for youth
populations with mental and substance use disorders from the perspective of different stakeholders at a provider
organization. These discussions will provide each stakeholder an opportunity to describe (1) what they believe are
the factors associated with successful clinical and service delivery models and (2) the features of the policy and
financing environment in which their program is implemented.
(Depending on how much communication may have occurred prior to or during the site visit, the following
script may not need to be covered in detail)
Thank you for making time to speak with us today. As we explained in our email, we are independent
researchers from RTI International who are contracted with the Office of the Assistant Secretary for Planning and
Evaluation (ASPE) to better understand factors influencing use of telehealth for youth with mental and substance
use disorders. For the purposes of our project, we are defining youth to include individuals under age 21. To
understand this further, we are conducting discussions with providers to gather different perspectives on the issues
related to telehealth use. Given your position and expertise we are interested in learning from your experience. There
are no right or wrong answers. Also, we recognize that there is currently limited research and work to date on
telehealth specifically for youth mental and substance use disorder treatment. With that in mind, we welcome your
perspective based on related programs such as telehealth for adult substance use disorder treatment or telehealth for
adolescent mental health treatment. In addition, we welcome your perspectives whether they are based on your
current involvement in the delivery of telehealth services or based on your general expertise and understanding of
the broader landscape of telehealth.
(Introduce team members and briefly describe qualifications/background and roles during the discussion.)
INTRODUCTION AND CONSENT TO AUDIO RECORD

Reducing Barriers to Using Telehealth for Pediatric Populations
Final Report
B-2
We expect that our conversation will take less than 1 hour. Participation in this discussion is voluntary. If
you do not wish to participate or answer any specific questions, please let us know.
Finally, we would like to audio-record our conversation to ensure that our notes from today are complete.
Although we are taking detailed notes, the audio recording will help verify our discussion notes. We will not share
the recording outside of this team and it will be deleted when the project is complete. If you agree to the audio
recording, you may ask us to stop recording at any time.
Do we have your permission to record this discussion?
(Obtain permission from each participant in the interview.)
Do you have any questions about what I have explained?
Note to RTI staff:
- If yes, start audio recording.
- Begin discussion.
OVERARCHING QUESTIONS
(If there are multiple participants, use plural grammar, inclusive language and guide the
discussion in such a way that all participants contribute)
(Factual answers to some questions may already have been discussed earlier in the day and do
not need to be repeated. For example, the basic description of the organization and telehealth
program may not need to be repeated in each interview.)
(Note: Some questions may not be applicable to the program being visited.)
1. Thanks again taking the time to speak with us today. Just to start, could you please introduce
yourself and tell us about how you use telehealth (and/or other specific domains as
appropriate: substance use disorder treatment, pediatric populations, policy, financing,
mental health etc.)?
a. How long have you been using telehealth in your practice?
b. How did you get started with it?
2. How does your organization use telehealth for identifying or treating mental and substance
use disorders? (e.g., direct delivery, service support or enhancement, telephone/video
asynchronous video, mobile technology, etc.)
a. What populations are you typically serving using telehealth?

Reducing Barriers to Using Telehealth for Pediatric Populations
Final Report
B-3
i. Have the populations served changed since introducing the use of telehealth?
If so, how?
ii. What are the primary mental or substance use disorder service needs of your
patients?
iii. How do patients get referred to you/linked to your program?
iv. Do you also provide similar services face-to-face?
b. What types of telehealth are in use?
i. Provider to provider?
ii. Provider to patient?
iii. Are these services synchronous or asynchronous?
iv. Are they direct-to-consumer?
3. How would you describe any differences in telehealth services for youth versus adults?
a. Service delivery model (e.g., type of technology, setting, provider staff types, etc.)
b. Clinical model/content (e.g., community reinforcement, family involved, MOUD,
etc.)
c. Accessibility (e.g., logistic, financial, etc.)
4. What are your thoughts on the differences between treating youth with substance use
disorders versus mental disorders via telehealth?
5. What are your thoughts on differences between face-to-face and telehealth services for youth
mental and substance use disorder treatment in terms of service delivery or clinical
approach?
a. Rapport?
b. Engagement?
c. Compliance?
d. Quality of care?
e. Patient, family, and provider satisfaction?

Reducing Barriers to Using Telehealth for Pediatric Populations
Final Report
B-4
6. What barriers do you see/have you seen in implementing and using telehealth for mental and
substance use disorders/conditions in youth?
a. Service delivery?
b. Policy barriers?
c. Credentialing?
d. Reimbursement?
e. Operational considerations?
f. Patient/caregiver engagement?
g. Provider/staff engagement?
h. Privacy considerations?
7. Are there special considerations in treating youth with co-occurring mental and substance use
disorders via telehealth? If so, please explain?
8. Pharmacotherapy is an increasingly important treatment for mental and substance use
disorders. What barriers are there for prescribing practices for treating substance use
disorders via telehealth?
a. Medications for opioid use disorders?
b. Alcohol use disorders?
c. Mental health?
d. Co-occurring disorders?
BEST PRACTICES
9. What works well when using telehealth to identify and manage mental and substance use
disorders in youth? What doesn’t work so well?

Reducing Barriers to Using Telehealth for Pediatric Populations
Final Report
B-5
FINANCING QUESTIONS
10. How are your telehealth services for the treatment of mental and substance use disorders with
pediatric patients financed?
a. Are these patients primarily covered by commercial payers or Medicaid?
b. Is this a fee-for-service model, a Managed Care model or other model?
c. Are there any payer-based incentives for using telehealth?
d. Is telehealth part of a payment bundle?
e. Are you aware of any incentives to incorporate telehealth into current care models?
f. Are your services supported by any other sources, e.g., foundation grants, Federal
discretionary grants, etc.?
11. Does the way in which services are financed change how you deliver telehealth services for
the treatment of mental and substance use disorders with pediatric patients?
a. Billing and procedure codes
b. Interactions with other providers, e.g., operating under other providers’ licenses
c. Service location considerations
d. Others?
12. What are your thoughts on differences between face-to-face and telehealth services for youth
mental and substance use disorder treatment in terms of financing, utilization and cost?
a. Reimbursement amounts?
b. Different requirements for coverage (e.g., provider credentials, technology etc.)?
c. Utilization rates?
d. Costs?
e. Reductions in other avoidable healthcare use?
13. Does reimbursement for telehealth for mental and substance use disorders differ from
reimbursement available for medical/surgical services? If so, how?
14. Are there any other special considerations with reimbursement for telehealth? If so, please
explain.

Reducing Barriers to Using Telehealth for Pediatric Populations
Final Report
B-6
WRAP UP AND FUTURE DIRECTIONS
15. When thinking of the future of telehealth service delivery for mental and substance use
disorders among youth, are there any things you think would need to be changed in order to
improve service delivery? If so, what would you change?
16. If you could give advice to another organization implementing telehealth what would it be?
17. Is there anything else you think we should know about the use of telehealth for mental and
substance use disorder treatment and related services in youth that we have not asked about
today?

Reducing Barriers to Using Telehealth for Pediatric Populations
Final Report
B-7
Reducing Barriers to Using Telehealth for Pediatric Populations
ASPE TELEHEALTH CASE STUDY DISCUSSION GUIDE –
DIRECTOR/ADMINISTRATOR
Provider Organization:
Discussion Lead:
Note Taker:
Participant(s) (Name and role):
Date/Time of Discussion:
PURPOSE:
The purpose of this discussion is to gain insight into the key issues related to telehealth use for youth
populations with mental and substance use disorders from the perspective of different stakeholders at a provider
organization. These discussions will provide each stakeholder an opportunity to describe (1) what they believe are
the factors associated with successful clinical and service delivery models and (2) the features of the policy and
financing environment in which their program is implemented.
(Depending on how much communication may have occurred prior to or during the site visit, the following
script may not need to be covered in detail)
Thank you for making time to speak with us today. As we explained in our email, we are independent
researchers from RTI International who are contracted with the Office of the Assistant Secretary for Planning and
Evaluation (ASPE) to better understand factors influencing use of telehealth for youth with mental and substance
use disorders. For the purposes of our project, we are defining youth to include individuals under age 21. To
understand this further, we are conducting discussions with providers to gather different perspectives on the issues
related to telehealth use. Given your position and expertise we are interested in learning from your experience. There
are no right or wrong answers. Also, we recognize that there is currently limited research and work to date on
telehealth specifically for youth mental and substance use disorder treatment. With that in mind, we welcome your
perspective based on related programs such as telehealth for adult substance use disorder treatment or telehealth for
adolescent mental health treatment. In addition, we welcome your perspectives whether they are based on your
current involvement in the delivery of telehealth services or based on your general expertise and understanding of
the broader landscape of telehealth.
(Introduce team members and briefly describe qualifications/background and roles during the discussion.)
INTRODUCTION AND CONSENT TO AUDIO RECORD

Reducing Barriers to Using Telehealth for Pediatric Populations
Final Report
B-8
We expect that our conversation will take less than 1 hour. Participation in this discussion is voluntary. If
you do not wish to participate or answer any specific questions, please let us know.
Finally, we would like to audio-record our conversation to ensure that our notes from today are complete.
Although we are taking detailed notes, the audio recording will help verify our discussion notes. We will not share
the recording outside of this team and it will be deleted when the project is complete. If you agree to the audio
recording, you may ask us to stop recording at any time.
Do we have your permission to record this discussion?
(Obtain permission from each participant in the interview.)
Do you have any questions about what I have explained?
Note to RTI staff:
- If yes, start audio recording.
- Begin discussion.
OVERARCHING QUESTIONS
(If there are multiple participants, use plural grammar, inclusive language and guide the
discussion in such a way that all participants contribute)
(Factual answers to some questions may already have been discussed earlier in the day and do
not need to be repeated. For example, the basic description of the organization and telehealth
program may not need to be repeated in each interview.)
(Note: Some questions may not be applicable to the program being visited.)
1. Thanks again taking the time to speak with us today. Just to start, could you please introduce
yourself and tell us about your organization’s telehealth program(s) (and/or other specific
domains as appropriate: substance use disorder treatment, pediatric populations, policy,
financing, mental health etc.)?
a. How long have you all been using telehealth in your practice?
b. How did your organization get started with it?
2. How does your organization use telehealth for identifying or treating mental and substance
use disorders? (e.g., direct delivery, service support or enhancement, telephone/video
asynchronous video, mobile technology, etc.)
a. What populations are typically being served using telehealth?

Reducing Barriers to Using Telehealth for Pediatric Populations
Final Report
B-9
i. Have the populations served changed since introducing the use of telehealth?
If so, how?
ii. How does the population served using telehealth fit into your organization’s
overall patient population?
iii. What are the primary mental or substance use disorder service needs of your
patients?
iv. How do patients get referred to you/linked to your program?
v. Do you also provide similar services face-to-face?
b. Types of telehealth in use
i. Provider to provider
ii. Provider to patient
iii. Are these services synchronous or asynchronous?
iv. Are they direct-to-consumer?
3. How would you describe any differences in telehealth services for youth versus adults?
a. Service delivery model (e.g., type of technology, setting, provider staff types, etc.)
b. Clinical model/content (e.g., community reinforcement, family involved, MOUD,
etc.)
c. Accessibility (e.g., logistic, financial, etc.)
4. What are your thoughts on the differences between treating youth with substance use
disorders versus mental disorders via telehealth?
5. What are your thoughts on differences between face-to-face and telehealth services for youth
mental and substance use disorder treatment in terms of service delivery or clinical
approach?
a. Rapport?
b. Engagement?
c. Compliance?
d. Quality of care?
e. Patient, family, and provider satisfaction?

Reducing Barriers to Using Telehealth for Pediatric Populations
Final Report
B-10
6. What barriers do you see/have you seen in implementing and using telehealth for mental and
substance use disorders/conditions in youth? What strategies/solutions have been used to
overcome those barriers?
a. Service delivery?
b. Policy barriers?
c. Credentialing?
d. Reimbursement?
e. Operational considerations?
f. Patient/caregiver engagement?
g. Provider/staff engagement?
h. Privacy considerations?
7. Has your organization made changes to policies and procedures, service delivery models, or
other business operations since adopting telehealth? If so, how?
a. Were any changes specific to the pediatric population? If so, please explain?
b. Were any changes specific to treatment for mental and substance use disorders? If so,
please explain?
8. Are there special considerations in treating youth with co-occurring mental and substance use
disorders via telehealth? If so, please explain?
9. Pharmacotherapy is an increasingly important treatment for mental and substance use
disorders. What barriers are there for prescribing practices for treating substance use
disorders via telehealth?
a. Medications for opioid use disorders?
b. Alcohol use disorders?
c. Mental health?
d. Co-occurring disorders?

Reducing Barriers to Using Telehealth for Pediatric Populations
Final Report
B-11
BEST PRACTICES
10. What works well when using telehealth to identify and manage mental and substance use
disorders in youth? What doesn’t work so well?
11. Why did your organization adopt its current program?
a. What alternative telehealth models were considered?
FINANCING QUESTIONS
12. How are your telehealth services for the treatment of mental and substance use disorders with
pediatric patients financed?
a. Are these patients primarily covered by commercial payers or Medicaid?
b. Is this a fee-for-service model, a Managed Care model or other model?
c. Are there any payer-based incentives for using telehealth?
d. Is telehealth part of a payment bundle?
e. Are you aware of any incentives to incorporate telehealth into current care models?
f. Are your services supported by any other sources, e.g., foundation grants, Federal
discretionary grants, etc.?
13. How does telehealth service delivery fit in your organization’s overall business model or
sustainability model?
14. Does the way in which services are financed change how you deliver telehealth services for
the treatment of mental and substance use disorders with pediatric patients?
a. Billing and procedure codes
b. Interactions with other providers, e.g., operating under other providers’ licenses
c. Service location considerations
d. Others?
15. What are your thoughts on differences between face-to-face and telehealth services for youth
mental and substance use disorder treatment in terms of financing, utilization and cost?
a. Reimbursement amounts?

Reducing Barriers to Using Telehealth for Pediatric Populations
Final Report
B-12
b. Different requirements for coverage (e.g., provider credentials, technology etc.)?
c. Utilization rates?
d. Costs?
e. Reductions in other avoidable healthcare use?
16. Does reimbursement for telehealth for mental and substance use disorders differ from
reimbursement available for medical/surgical services? If so, how?
17. Are there any other special considerations with reimbursement for telehealth? If so, please
explain.
WRAP UP AND FUTURE DIRECTIONS
18. When thinking of the future of telehealth service delivery for mental and substance use
disorders among youth, are there any things you think would need to be changed in order to
improve service delivery? If so, what would you change?
19. If you could give advice to another organization implementing telehealth what would it be?
Is there anything else you think we should know about the use of telehealth for mental and
substance use disorder treatment and related services in youth that we have not asked about
today?
Reducing Barriers to Using Telehealth for Pediatric Populations
Final Report
B-13
Reducing Barriers to Using Telehealth for Pediatric Populations
ASPE TELEHEALTH CASE STUDY DISCUSSION GUIDE – PARTNER/COMMUNITY
STAKEHOLDER
Associated Provider Organization:
Community Organization Represented:
Discussion Lead:
Note Taker:
Participant(s) (Name and role):
Date/Time of Discussion:
PURPOSE:
The purpose of this discussion is to gain insight into the key issues related to telehealth use for youth
populations with mental and substance use disorders from the perspective of different stakeholders at a provider
organization. These discussions will provide each stakeholder an opportunity to describe (1) what they believe are
the factors associated with successful clinical and service delivery models and (2) the features of the policy and
financing environment in which their program is implemented.
(Depending on how much communication may have occurred prior to or during the site visit, the following
script may not need to be covered in detail)
Thank you for making time to speak with us today. As we explained in our email, we are independent
researchers from RTI International who are contracted with the Office of the Assistant Secretary for Planning and
Evaluation (ASPE) to better understand factors influencing use of telehealth for youth with mental and substance
use disorders. For the purposes of our project, we are defining youth to include individuals under age 21. To
understand this further, we are conducting discussions with providers to gather different perspectives on the issues
related to telehealth use. Given your position and expertise we are interested in learning from your experience. There
are no right or wrong answers. Also, we recognize that there is currently limited research and work to date on
telehealth specifically for youth mental and substance use disorder treatment. With that in mind, we welcome your
perspective based on related programs such as telehealth for adult substance use disorder treatment or telehealth for
adolescent mental health treatment. In addition, we welcome your perspectives whether they are based on your
current involvement in the delivery of telehealth services or based on your general expertise and understanding of
the broader landscape of telehealth.
(Introduce team members and briefly describe qualifications/background and roles during the discussion.)
INTRODUCTION AND CONSENT TO AUDIO RECORD

Reducing Barriers to Using Telehealth for Pediatric Populations
Final Report
B-14
We expect that our conversation will take less than 1 hour. Participation in this discussion is voluntary. If
you do not wish to participate or answer any specific questions, please let us know.
Finally, we would like to audio-record our conversation to ensure that our notes from today are complete.
Although we are taking detailed notes, the audio recording will help verify our discussion notes. We will not share
the recording outside of this team and it will be deleted when the project is complete. If you agree to the audio
recording, you may ask us to stop recording at any time.
Do we have your permission to record this discussion?
(Obtain permission from each participant in the interview.)
Do you have any questions about what I have explained?
Note to RTI staff:
- If yes, start audio recording.
- Begin discussion.
OVERARCHING QUESTIONS
(If there are multiple participants, use plural grammar, inclusive language and guide the
discussion in such a way that all participants contribute)
(Factual answers to some questions may already have been discussed earlier in the day and do
not need to be repeated. For example, the basic description of the organization and telehealth
program may not need to be repeated in each interview.)
(Note: Some questions may not be applicable to the program being visited.)
1. Thanks again taking the time to speak with us today. Just to start, could you please introduce
yourself and tell us about your organization, how it serves your [patients, students, other
designation for the population represented by a stakeholder organization] and its relationship
with [the telehealth provider organization being studied – hereafter, “the Program”]? (e.g.,
service delivery partner, referral source or recipient, community stakeholder such as county
health department youth services programming, etc.)
a. How long have you been partnering with the Program?
i. [Alternatively] How long have you been aware of the Program and its role in
the community/in the population you represent?
b. How long has the Program been using telehealth services with your [patients,
students, other designation]?
c. How did the partnership form?

Reducing Barriers to Using Telehealth for Pediatric Populations
Final Report
B-15
2. How has the use of telehealth for your [patients, students, other designation] changed the
types of services that you provide?
3. Has the Program’s use of telehealth had any impact on your organization? If so, how?
a. Population served?
b. Increased access?
c. Improved patient population outcomes or satisfaction?
d. Workload?
4. What are your thoughts on the differences between treating youth with substance use
disorders versus mental disorders via telehealth?
5. What are your thoughts on differences between face-to-face and telehealth services for youth
mental and substance use disorder treatment in terms of service delivery or clinical
approach?
a. Rapport?
b. Engagement?
c. Compliance?
d. Quality of care?
e. Patient, family, and provider satisfaction?
6. What barriers do you see/have you seen in service delivery using telehealth for mental and
substance use disorders/conditions in youth? What strategies/solutions have been used to
overcome those barriers?
a. Service delivery?
b. Policy barriers?
c. Credentialing?
d. Reimbursement?
e. Operational considerations?
f. Patient/caregiver engagement?

Reducing Barriers to Using Telehealth for Pediatric Populations
Final Report
B-16
g. Provider/staff engagement?
h. Privacy considerations?
7. Has your organization made changes to policies and procedures, service delivery models, or
other business operations since working with the Program? If so, how?
a. Were any changes specific to the pediatric population? If so, please explain?
b. Were any changes specific to treatment for mental and substance use disorders? If so,
please explain?
WRAP UP AND FUTURE DIRECTIONS
8. When thinking of the future of telehealth service delivery for mental and substance use
disorders among youth, are there any things you think would need to be changed in order to
improve service delivery? If so, what would you change?
9. If you could give advice to another organization implementing telehealth or partnering with a
telehealth provider, what would it be?
10. Is there anything else you think we should know about the use of telehealth for mental and
substance use disorder treatment and related services in youth that we have not asked about
today?
