
*This document is subject to further comments and may therefore be subject to change.
ACCESS TO
HEALTH AND
SOCIAL CARE
GUIDANCE
November 2021

2 | P a g e
Welcome to Northern Ireland
Arriving in a different country can be an
overwhelming experience. We have put
together some information which you might
find useful. This booklet will inform you
about health and social care services and
how to access them. We want to ensure that
you receive a service which meets your
individual needs. Health and Social Care
Services in Northern Ireland are generally
free of charge at the point of delivery for people who are considered to
be ordinarily resident. This will depend on your individual circumstances
and therefore some people may have to pay for anything other than
emergency Health and Social Care.
We have provided details of the Health and Social Care Service in
Northern Ireland and how to appropriately access it.
Alternative Formats
This document is available in a range of alternative
formats and languages and can be made available on
request e.g. Minority Ethnic languages, braille, easy-
read, MP3. Please contact the Equality Lead in your
Trust area if you need the document in a different
language or format (please see 1.3 for contact details).
3 | P a g e
Contents
Page
1
Introduction
6
1.1
Health & Social Care (HSC)
6
1.2
HSC Trust Areas
6
1.3
HSC Trust Equality Leads
7
1.4
Interpreters
8
1.5
Eligibility for Free Treatment
10
1.6
How do you access HSC - Your Medical Card
12
2
What are the options in terms of looking after
your Health?
13
2.1
Self-care
13
2.2
About your General Practitioner (GP or Family
Doctor)
14
2.3
GP Services
14
2.4
How to find a GP Practice
15
2.5
How to be assessed by a GP
15
2.6
Home Visits
15
2.7
Medication / Prescription
15
3
Out of Hours Services
15
3.1
Urgent Care or Minor Injuries Unit
16
3.2
Hospitals
16
3.3
NI New Entrants Service
17
3.4
Urgent and Emergency Care Services
18
4 | P a g e
3.5
Serious accident or emergency
21
3.6
What if English is not your first language?
21
3.7
How are you prioritised?
22
3.8
What can you do while waiting for the ambulance?
22
3.9
What if an ambulance is not the best option for you?
22
3.10
Who will be sent to you?
22
3.11
What happens after the arrival of the Paramedic
23
4
All Other Services
4.1
Maternity Services
24
4.2
Health Visitors
24
4.3
Family Planning Services
25
4.4
Other Sexual Health Services
25
4.5
Social Workers
26
4.6
Child & Adult Protection Services
26
4.7
Mental Health Services
27
4.8
Services for people with a disability
27
4.9
Allied Health Professionals
28
4.10
School Nurse
29
4.11
Childhood Immunisation Programme
29
4.12
Pharmacy Services (The Chemist)
30
4.13
Dentists
30
4.14
Optometrist (The Optician)
30
5
What if you are unhappy with the Service you
receive?
31
5 | P a g e
5.1
Complaints Procedure
31
5.2
How to complain
31
5.3
How to make a complaint
31
5.4
What will happen next?
34
5.5
What happens if you are still not happy after the
Trust has investigated your complaint?
34
6
Where else can you get Advice and Information?
35
6.1
Helplines Network NI
35

6 | P a g e
1. Introduction
1.1 Health and Social Care (HSC)
In Northern Ireland the National Health Service (NHS) is referred to as
Health and Social Care or HSC. HSC in Northern Ireland provides
Acute Services in critical and emergency care and also provides social
care services like home care services, family and children's services,
day care services and social work services.
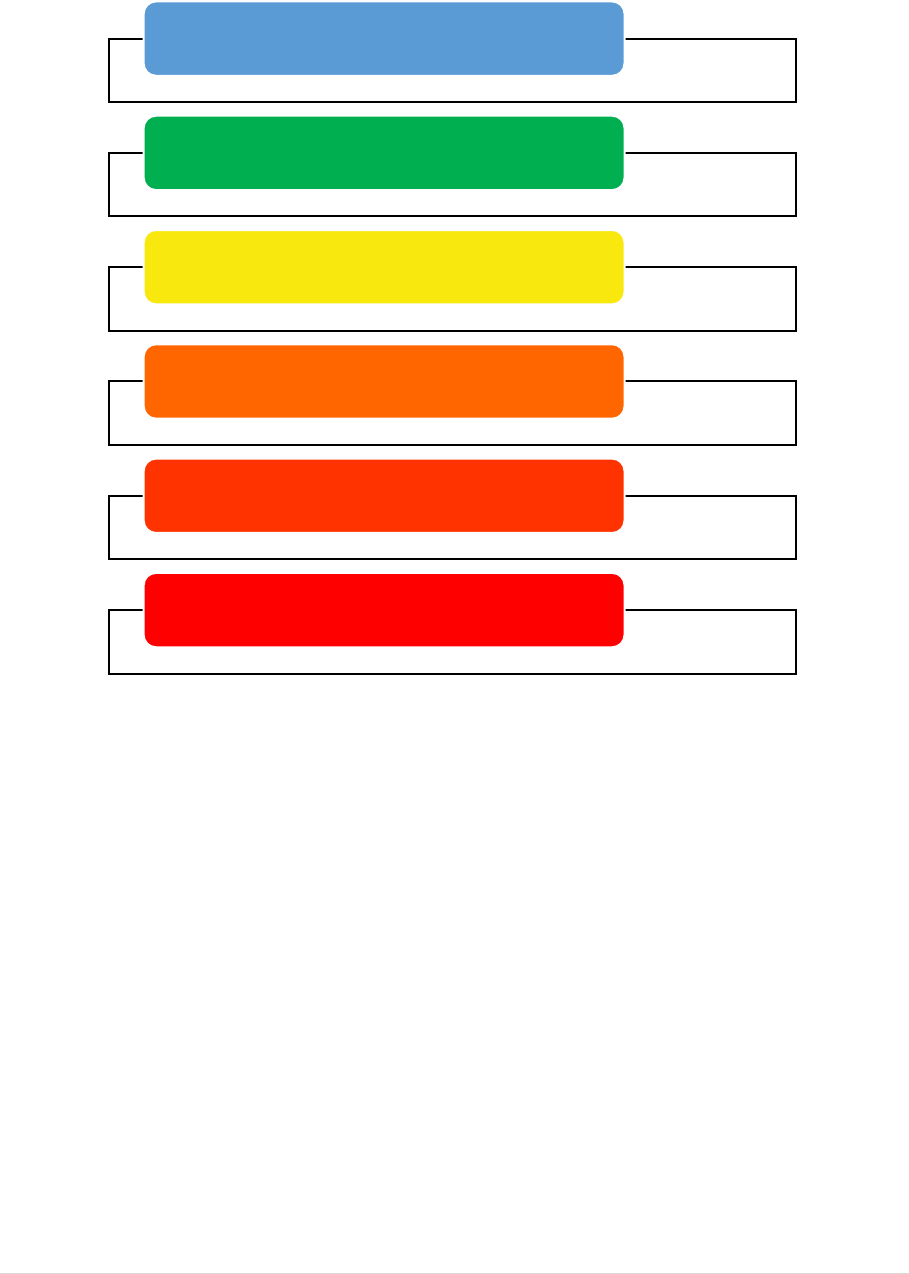
There are 6 Health and Social Care Trusts in Northern Ireland, providing
health and social care services.
The map below shows five regions within Northern Ireland. These
regions are called Health and Social Care Trust areas. The Northern
Ireland Ambulance Service Trust covers all five regions of Northern
Ireland.
1.2 HSC Trust Areas
7 | P a g e
1.3 Health & Social Care Trust Equality Leads:
Belfast
Health
& Social
Care
Trust
Orla Barron
Planning and Equality
Lead
1st Floor, Admin
Building
Knockbracken
Healthcare Park
Saintfield Road
BELFAST BT8 8BH
Telephone: 028 95046567
Mobile: 07825 146432
orla.barron@belfasttrust.hscni.net
Southern
Health &
Social Care
Trust
Cathy Lavery
Head of Equality Unit
1
st
Floor
Hill Building
St Luke’s Hospital
Loughgall Rd
ARMAGH
BT61 7NQ
Telephone: 02837 564 151
Mobile: 07552271620
cathy.lavery@southerntrust.hscni.net
South
Eastern
Health &
Social
Care Trust
Susan Thompson
Equality Manager
2
nd
Floor
Lough House
Ards Hospital
Newtownards
BT23 4AS
Western
Health
& Social
Care
Trust
Jennifer Mayse Equality
Manager
Tyrone & Fermanagh
Hospital
Donaghanie Road
Omagh
Co Tyrone
8 | P a g e
BT79 ONS
Northern
Health &
Social Care
Trust
Alison Irwin
Head of Equality
Route Complex
8e Coleraine Road
Ballymoney
Co Antrim
BT53 6BP
Telephone: 028 2766 1377
Mobile/Textphone: 07825667154
alison.irwin@northerntrust.hscni.net
equality.unit@northerntrust.hscni.net
Northern
Ireland
Ambulance
Service
Trust
John Gow
Equality and Public
Involvement Officer
Ambulance
Headquarters
Site 30, Knockbracken
Healthcare Park
Saintfield Road
BELFAST
BT8 8SG
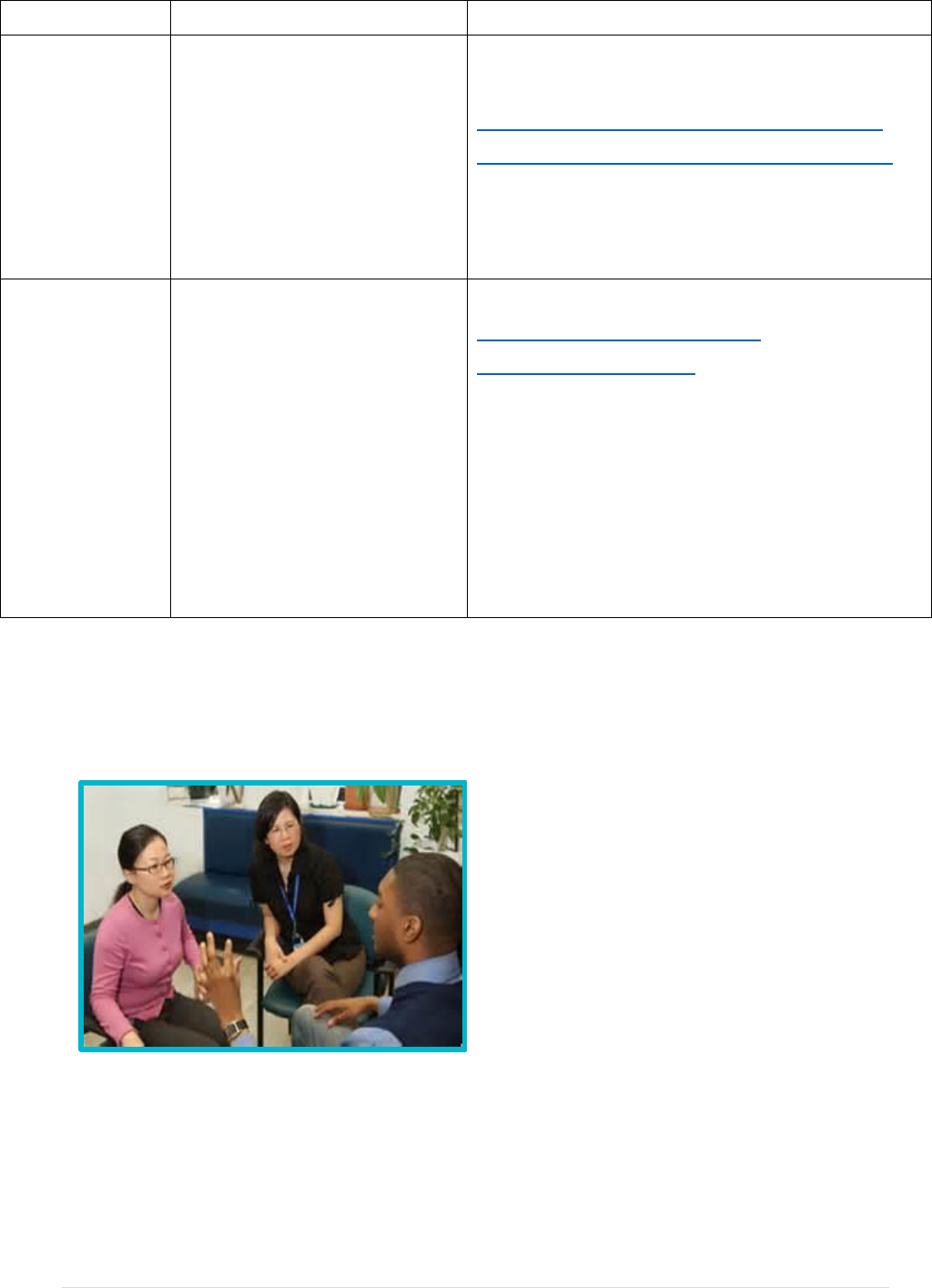
1.4 Interpreters
The Business Services
Organisation (BSO) Health and
Social Care Interpreting Service
strives to make accessing health
and social care services easier for
patients who do not speak English
as a first or competent second
language. The BSO Interpreting
Service provides face to face
interpreters, which means that an
interpreter will be physically present during your appointment. The
service is free-of-charge and legally, it is your right to have professional
language assistance.
The Service operates 24 hours, 7days per week.

9 | P a g e
Interpreters are professionally trained and accredited with a
Community Interpreting qualification.
Interpreters are required to wear their HSC ID badge at all times.
Interpreters are bound by confidentiality.
Interpreters will only contact the patient/client prior to the
appointment when asked to do so by the HSC
practitioner in order to confirm attendance, or to
relay any specific appointment instructions.
Interpreters should always obtain consent for
interpreting as part of their introduction.
The operational team who deal with requests
will, if asked, try to provide the same interpreter
for continuity purposes.
What your Interpreter can do
Be bilingual and know how to interpret, facilitating communication.
Interpret accurately (not always word by word interpreting, but the
full meaning of the conversation being conveyed).
Be impartial and maintain confidentially.
Clarify cultural nuances and be aware of other cultural or
circumstantial issues.
Signpost clients or patients to other services when possible.
What your Interpreter cannot do
Written translation of a long document.
Client’s advice work (bilingual advocacy).
Speak instead of you – they will only interpret your words.
Look after children.
Provide counselling or transport.
Give out your telephone number or contact details.
To request an Interpreter
You need to let the booking office or the receptionist know if you need
language support. It is best to let them know in advance so that they can
10 | P a g e
try to access an interpreter in your preferred language. The staff or
receptionist will book an interpreter on your behalf.
Telephone Interpreting
At times it may be more appropriate to provide a telephone interpreter or
indeed if a face to face interpreter is not available. Health and Social
Care practitioners can use telephone interpreting via the Big Word
Telephone Interpreting Service. Big Word provides interpreters via
telephone link for Health and Social Care appointments in Northern
Ireland. These interpreters are professional, qualified interpreters and
are bound by a similar code of conduct as those who work for the BSO
Health and Social Care Interpreting Service.
1.5 Eligibility for Healthcare Treatment
Health and Social Care Services in Northern Ireland are
generally free at the point of delivery for people who are
considered to be ordinarily resident, which means that you do
not have to pay to see a doctor nor do you need your own
health insurance. Depending on your circumstances, you may have to
pay for some health services like dental treatment and eye care.
In principle, whether or not you have to pay for your treatment depends
on the type of treatment and on whether you are living in Northern
Ireland or just visiting. If the treatment is emergency and is provided in
an emergency department, walk in clinic or minor injuries unit, it is
provided for free of charge. Once emergency treatment has been
provided, after-care as in inpatient (admitted to hospital), or as an
outpatient (not admitted to hospital) etc. may be chargeable if you are
not “ordinarily” resident in Northern Ireland or are not deemed to fulfil
one of the exemption criteria.
Access to Health Care Teams Contact Details
Belfast Health &
Social Care Trust
Eileen Murphy, Access to Health and Social
11 | P a g e
Care Manager
Phone 02895048408
eileenm.murphy@belfasttrust.hscni.net
accesshealth[email protected].net
Sarah Craig, Access to Health and Social
Care Manager
Phone 02896155436
sarah.craig@belfasttrust.hscni.net
accesshealth[email protected].net
Southern Health &
Social Care Trust
Brigid Quinn, Access to Health & Social Care
Team Manager, SHSCT, Finance
Department, Daisy Hill Hospital
Phone: 02837565296
access.healthcar[email protected]scni.net
South Eastern Health
& Social Care Trust
Financial Assessment Team
Phone: 028 44 513857
Western Health &
Social Care Trust
The Access to Health Care Team
Altnagelvin Hospital
Phone: 02871 345171 Ext 214959, 213052,
214436, 214960 or
Southwest Acute Hospital
Phone: 028 6638 2000 Ext 255502
Northern Health &
Social Care Trust
Melanie Sloan, Access to Health & Social
Care Manager
Antrim Hospital
Phone: 028 9442 4000 Ext 334271

12 | P a g e
1.6 How Do You Access HSC?
Your Medical Card
To get access to services you should register with a
General Practitioner (GP) Practice.
The family doctor, also known as the General Practitioner or GP, is the
entry point for a whole range of services. Some GPs work individually,
others work together with other GPs in a GP Practice or Health and Care
Centre.
You should register with a GP Practice straight away when you arrive in
Northern Ireland rather than wait until you need to access health or
social care services.
To become registered, you will need to fill in an application form. This
form is called an HSCR-1. It is available in a range of other languages.
Click on the link to access the form -
http://www.hscbusiness.hscni.net/1814.htm
The HSCR-1 form and the translated versions are also available from
any GP Practice or from the Business Services Organisation (BSO),
which look after your registration. Their contact details are:
Business Services Organisation
Headquarters
2 Franklin Street
Belfast BT2 8DQ
Phone: (028) 9032 4431
Textphone: (028) 9053 5575
Complaints: Com[email protected]
Website: http://www.hscbusiness.hscni.net
You should get an application form, fill it in and then take it along with
any proof of identification and eligibility requested to your chosen GP
Practice. Your documentation will be sent to BSO who will then assign
you a GP practice. You will then receive a medical card issued by the
BSO. This may take up to eight weeks. You do not have to pay for your
medical card. Your medical card is an important document; it entitles you
to receive a range of services.
13 | P a g e
2. What are the options in terms of looking after your Health?
Remember to Choose Well!
2.1 Self-care
Self-care is the best choice to treat minor illnesses, ailments and
injuries. A range of common illnesses and complaints, such as aches
and pains, coughs, colds, upset stomachs and sore throats can be
treated with over the counter medicines and plenty of rest. Remember,
whether treated or not, most of these will get better. Some self-care
essentials - the following are available to buy over the counter:
Paracetamol, Aspirin, Ibuprofen, rehydration mixtures, indigestion
remedies, plasters and thermometer. (Always follow the instructions on
the pack.)
If you are still feeling unwell you should contact your Local Doctor or
General Practitioner (GP).
Self-Care
Pharmacy
GP
Minor Injuries Unit
Emergency Care
999

14 | P a g e
2.2 About your General Practitioner (GP) or Family
Doctor
Local or Family doctors, also known as General Practitioners (GPs), look
after the health of people in their local community and deal with a whole
range of health problems. There are over 330 GP Practices throughout
Northern Ireland.
2.3 GP or Family Doctor Services
GPs provide a range of services including:
Medical advice on a range of issues
Physical examinations
Diagnosis of symptoms
Prescribing of medication
Health education and health screening
Giving vaccinations
Carrying out simple surgical operations.
Providing ongoing care for more longstanding or chronic conditions
Some GP Practices provide an online Appointments Booking or
Repeat Prescription service (via their Practice websites).
The GP or family doctor is responsible for helping you to look after your
health needs. They will decide whether you should see any other health
specialist and, if so, will make all necessary arrangements. Your GP will
also decide what medicines you need and can give you a prescription.
You are entitled to treatment from one of the GPs at the practice where
you are registered. You have no automatic right to see a particular GP.
When you register with a GP practice, you may be assessed by any GP
within the practice and may not always deal with the same GP, however
you will have continuity of care from within that practice.

15 | P a g e
2.4 How to find a GP Practice
There are over 330 GP Practices in Northern Ireland. Search
for a GP Practice in your area - Find a GP practice | nidirect.
It is important that you are aware of your basic rights:
You have the right to ask to be treated by a doctor of your own
gender
You should note that you have the right to change your GP
practice at any time.
2.5 How to be assessed by a GP
Due to the COVID-19 Pandemic GP practices have changed how they
operate. If you need to contact a GP, do not go to the surgery in person.
Instead phone first - telephone call your GP surgery and request to
speak to a GP. The phone calls will be triaged to decide the order of
treatment of patients. GP appointments are then likely to be virtual, by
phone or video call. The GP may also decide they need to see you in
person.
2.6 Home Visits
If you feel too unwell to attend the practice, you may be entitled to a
home visit by a GP. You should contact your GP Practice to request this.
You cannot, however, insist that a GP visits you at home. A GP will only
visit you at home if they think your medical condition requires it.
2.7 Medication/Prescription
If a GP decides you need medication, they will write you a prescription,
which you should then collect from the GP practice and take to any
pharmacy / chemist to collect the medication. See Section on ‘Pharmacy
Services’.
3. Out of Hours Services
GP Practices are usually open Monday to Friday, at times advertised in
the Practice. For nights, weekends and public holidays services are
provided by Out of Hours services. Practices will have information about
16 | P a g e
how to contact Out of Hours services if you need a doctor. There should
be a recorded message on the Practice telephone as well as notices on
the door which provide further details.
All Out of Hours Centres will provide urgent medical care for problems
that cannot wait until your own GP practice opens again. They also
provide services even if you are not registered with a local Practice.
GP Out of Hours is available if you require urgent medical care when
your GP surgery is closed. GP Out of Hours services operate from 6pm
each weekday evening until your GP surgery opens the next morning
and 24 hours on Saturdays, Sundays and public holidays. Remember to
telephone the service first. The doctor or nurse will give you advice over
the telephone, decide if you need to be seen by a doctor or will refer you
to another service if required. Your GP surgery will have the contact
details for your area.
Urgent GP Out of Hours care can be found by contacting your local GP
Practice and also online at https://www.nidirect.gov.uk/articles/gp-out-
hours-service
3.1 Urgent Care or Minor Injuries Unit
An Urgent Care or Minor Injuries Unit can treat injuries that are not
critical or life threatening, such as:
Injuries to upper and lower limbs
Broken bones, sprains, bruises and wounds
Bites – human, animal and insect
Burns and scalds
Abscesses and wound infections
Minor head injuries
Broken noses and nosebleeds
Foreign bodies in the eyes and nose.
If you or a child over 5 years old suffers a minor injury you can go to one
of the Minor Injuries Units. Children under 5 years must be brought to
the Emergency Department in your area.
3.2 Hospitals
17 | P a g e
Your GP may refer you to a specialist doctor at a hospital or you may
need to go to hospital if you require emergency treatment.
If your GP cannot deal with a problem then you’ll usually be referred to a
hospital for tests, treatment, or to see a consultant with specialist
knowledge.
If your GP arranges for a referral this means they have arranged for you
to see a Consultant or a Specialist regarding tests or treatment. You will
receive a letter from the hospital or clinic with details of an appointment
which has been made for you to see a Specialist Doctor. For most
Specialists, there might be waiting times involved. If you are unable to
attend you need to cancel your appointment. You will then be given a
new date.
The Specialist will see you and discuss your health issue with you. If
necessary, they will arrange for tests to be carried out. In this case, you
will receive a further letter from your hospital with information regarding
the date and time when you need to go back for your tests.
3.3 Northern Ireland New Entrants Service
(NINES)
Belfast and Southern Health and Social Care Trusts in
collaboration with the Public Health Agency and the Health and Social
Care Board, has established a Nurse-led service for new entrants to
Belfast Health and Social Care Trust and Southern Health and Social
Care Trust areas.
The service provides a variety of clinics to support the health and well-
being of new immigrants, asylum seekers, refugees and targeted
children 0-16 years for Tuberculosis screening.
This unique service aims to support all new entrants by offering
screening, health education and sign posting to other services. A range
of clinics can be accessed to address the health and well-being needs of
the client group to include health assessment and health promotion
clinics, BBV bloods and IGRA/Quantiferon testing for Tuberculosis ,
Mantoux/BCG clinics for the under 16 years of age.

18 | P a g e
Clients are offered a holistic health assessment; screening for
communicable diseases such as TB, Hepatitis B and C, HIV for clients
from high risk countries. Assistance/advice is given with registration for
General Practitioner and dental services; signposting to other services
and onward referral as appropriate.
Service Delivery:
In Belfast Trust the service can be delivered in the clinical setting
or in the individual’s place of residence. In the Southern Trust the
service is delivered in the clinical setting
A new client held passport has been piloted by the BHSCT
(currently on hold due to Covid-19) which is sent with the GP
registration form to encourage a smoother process.
Delivery of mantoux/BCG
[1]
programme for children 0-16 years.
Support in registering with General Practitioners/Dentist/Opticians.
Health Screening.
BBV Blood screening tests.
Direct referral pathways have been established to specialist
services i.e. Genito-urinary medicine clinic, Maternity Services,
Hepatology, Chest Clinic, Paediatric Infectious Diseases.
Fast tracking for chest x-rays allows early detection of
Tuberculosis and onward referral to chest clinic for investigations
and treatment if required.
Client advocacy.
Confidential help and advice
For further information on the services available, clinic time or to make a
referral, the Northern Ireland New Entrant Service can be contacted:
Belfast Trust – Monday to Friday (028) 95042830
Southern Trust – Monday to Friday (028) 37561370
3.4 Urgent and Emergency Care Services
[1]
BCG is a vaccination used to help prevent Tuberculosis. BCG stands for "Bacille
Calmette-Guerin" and is named after Dr Calmette and Dr Guerin who developed the
vaccine
19 | P a g e
Urgent and Emergency Care services in Northern Ireland perform critical
roles in responding to patient needs. While closely related, it is important
to understand the differences between urgent and emergency care.
Urgent Care or Minor Injuries Unit:
An illness or injury that requires urgent attention but is not a life-
threatening situation. Urgent care in Northern Ireland includes: General
Practice during weekdays; GP Out of Hours (GP OOH) Services at night
and weekends; pharmacies; minor injury units; an urgent treatment
centre; Emergency Departments (EDs); and, the Northern Ireland
Ambulance Service (NIAS).
Phone First Service - Some of the Health and
Social Care Trusts in Northern Ireland operate a
Phone First service. This is designed for patients,
including children, who are feeling unwell and
considering travelling to an Emergency
Department or Urgent Care Treatment Centre
with an injury or illness which requires urgent
treatment but is not immediately life
threatening.
When you call the Phone First service your condition, or that of the
person you are calling on behalf of, will be clinically assessed and
arrangements made for you to access the most appropriate service to
your needs.
You may receive telephone advice on self-care, be directed to a
scheduled appointment at the Urgent Care Treatment Centre or Minor
Injuries Unit, Emergency Department or recommended to see your own
GP.
In a serious accident or emergency, you should attend the Emergency
Department or you can telephone 999 or 112
Accessing Urgent Care or Minor Injuries Care Services in your Area
Belfast Health &
Social Care Trust
If you attend the Emergency Department you will
be guided to either Urgent Care or Emergency
Care services depending on your needs.
20 | P a g e
Link:
Emergency Departments | Belfast Health & Social
Care Trust (hscni.net)
Southern Health &
Social Care Trust
Phone First servicer operates between 9am and
6pm Monday to Friday
Phone: 0300 123 3 111
Text Relay: 18001 0300 123 3 111
Outside of these hours you should attend the
Minor Injuries Unit.
Link: https://southerntrust.hscni.net/phone-first-
for-urgent-care/
South Eastern
Health & Social
Care Trust
The three hospital in the South Eastern Trust
have varying ways to access Urgent Care and
Minor Injuries – please see the links below for
each hospital:
Lagan Valley - https://setrust.hscni.net/our-
hospitals/hospital-3/emergency-department-
lagan-valley-hospital/
Ulster - https://setrust.hscni.net/our-
hospitals/ulsterhospital/
Downe - https://setrust.hscni.net/our-
hospitals/downehospital/
Western Health &
Social Care Trust
Phone First Service
Phone: 0300 020 6000
Text relay: 0870 240 5152
Link:
https://westerntrust.hscni.net/services/emergency-
department-and-urgent-care-services/phone-first/
Northern Health &
Social Care Trust
Phone First Service
Phone: 0300 123 1 123
Text relay: 18001 0300 123 1 123
It is also available through the Interpreter Now
App.
Link:
New ‘Phone First’ service for Emergency
21 | P a g e
Departments and Minor Injuries Units - Northern
Health and Social Care Trust (hscni.net)
All of the above is subject to change, always check the website, if in
doubt and in need of urgent care, attend ED.
Emergency Care:
Life threatening illnesses or accidents which require
immediate intensive treatment. Emergency Care is
currently provided in hospitals with Type 1 and Type
2 Emergency Departments and by Northern Ireland
Ambulance Service.
3.5 Serious accident or emergency
In a serious accident or emergency, you should attend the Emergency
Department or you can telephone 999 or 112 for Emergency Services -
Emergency ambulances should be kept for real emergencies where
lives are at risk. If you genuinely need ambulance assistance, you or
someone on your behalf should call 999 or 112 and when asked by the
operator which service you require you should answer “ambulance”.
You will then be connected to ambulance control who will ask questions
regarding:
Telephone number of caller
Location of incident
Nature of incident.
An ambulance will be sent to you as soon as possible, if appropriate.
3.6 What if English is not your first language?
If English is not your first language, the Ambulance
Service can quickly bring a qualified interpreter into the

22 | P a g e
telephone call to enable communication.
Telephone interpreters are:
Available 24 hours, 7days per week, 365 days per year
Professionally trained and qualified
Provided under contract by The Big Word.
The interpreter will:
Be bilingual and know how to interpret, facilitating communication
Interpret accurately
Be impartial and maintain confidentially
Not speak instead of you – they will only interpret your words.
3.7 How are you prioritised?
The person on the phone will ask you more questions to determine the
seriousness of your situation and the urgency of response required.
Calls in Ambulance Control are prioritised based on clinical need with
the most immediate response sent to those whose clinical need is
greatest.
3.8 What can you do while waiting for the ambulance?
Depending on the situation, the call-taker may stay on the line with you
to give you practical advice while you wait for the ambulance to arrive.
This advice may include actions to take to:
Position the patient
Clear the patient’s airway
Stem blood loss
Perform CPR (Cardiopulmonary Resuscitation).
3.9 What if an ambulance is not the best option for you?
It may become evident from the information provided that an emergency
ambulance is not actually required immediately to deal with your
situation. In such circumstances, Ambulance Control may pass you

23 | P a g e
through to a clinician in the Control Centre who will give you advice
relating to the treatment of your condition.
On occasions, Ambulance Control may signpost you to a more
appropriate service within Health and Social Care to deal with your need
as an alternative to attending the Emergency Department.
3.10 Who will be sent to you?
In life threatening emergencies, people in Northern Ireland tend to
expect an ambulance crew of two people to arrive. However NIAS
makes effective use of Rapid Response Paramedics who will arrive in a
car. These vehicles are equipped with the vital life-saving equipment
that may be needed in an emergency. The car can get to the scene
more quickly and allow the Paramedic to deliver treatment in a timelier
manner.
An ambulance will also be sent to provide further support to the
Paramedic and to transport the patient to the Emergency Department.
You will be asked details regarding your name, your location and the
nature of the medical problem. An ambulance will be sent to you as
soon as possible. There is no charge for this service.
The ambulance will take you to the Emergency Department (ED) at the
hospital where a doctor will examine you. Again, this treatment is free of
charge.
The following is a list of hospital services:
Emergency Departments - providing 24 hour emergency
treatment
In-patient Services - perform operations or provide treatment,
patients stay in hospital for one night or more.
Day Services - perform small operations and investigations and
discharge patients home on the same day.
Out-patients Services - appointments with specialist doctors or
care professionals (such as Nurses or Allied Health Professionals)
in a range of clinical specialties.

24 | P a g e
3.11 What happens after the arrival of the Paramedic?
After assessing, and possibly providing treatment to, the patient, the
Paramedic may decide that:
Further treatment is required at the Emergency Department and
that ambulance transport is required
Further treatment is required at the Emergency Department but
that ambulance transport is not required
No further treatment is required and the patient may remain at
home
The patient may be referred to another healthcare professional
within Health and Social Care e.g. GP or District Nurse
The patient may be referred to a specialist and more appropriate
treatment centre within Health and Social Care.
REMEMBER – KEEP AMBULANCES FOR REAL EMERGENCIES
4. All Other Services
4.1 Maternity Services
If you are planning to have a baby or think you might be pregnant, you
should contact your family doctor as soon as possible. Your family
doctor can confirm your pregnancy, refer you to maternity services and
offer health advice. Alternatively you can self-refer to maternity services
by calling or emailing the hospital and requesting a referral form or
completing a form online.
Midwives have specialist training to care for you and your newborn baby
and they can help you decide where and how you wish to give birth.
They work in both hospitals and the community. They will care for you
and help you prepare for the birth when you are pregnant, at the birth of
your baby and up to 28 days after the birth. The community midwife will
call to see you and your new baby after birth to make sure that all is well.
The midwife will see you in your own home after you come home from
hospital. You do not need to make any arrangements yourself - the
hospital will do this for you.

25 | P a g e
4.2 Health Visitors
Health Visitors are specialist community public health nurses trained to
support families and children in all aspects of health and well-being.
They will visit you at home just before and 10 to 14 days after your baby
is born. The level of visiting after this will be determined on the outcome
of a family health assessment. The Health Visitor will check your baby’s
health and development up until they are ready for school. They will
also provide support and help to families on all aspects of health e.g.
post-natal depression, sleeping, feeding, immunisations and behaviour
management. If your child has a health problem the Health Visitor will
refer the child for further tests and treatment.
4.3 Family Planning Services
Family Planning Services offer free advice on contraception and cervical
screening as well as sexual health screening, advice and treatment.
These services are provided by local Family Planning Clinics and by
some family doctors.
You can get details of Family Planning Clinics from your GP Practice
(family doctor), Midwife or Health Visitor. Family Planning Services are
free and totally confidential.
The Family Planning Association (FPA) provides a confidential local rate
telephone service (0845 122 8687) from 9.00 am to 5.00 pm, Monday to
Friday, offering information and advice on a range of sexual health
issues.
4.4 Other Sexual Health Services
Clinics that specialise in sexually transmitted infections are called
genitourinary medicine (GUM) and sexual health clinics. You can get
the number of a clinic in your area from the phone book under GUM
(genitourinary medicine), Sexually Transmitted Diseases (STD), special
clinic or sexual health clinic. You can refer yourself to these clinics,
which are also:

26 | P a g e
Free and confidential - they will not contact anyone, not even your
GP without your permission and are open to everyone (regardless
of age, sexual orientation etc.)
To find your local GUM or Sexual Health Clinic please click on the link:
https://www.sexualhealthni.info/gum-clinics-northern-ireland
4.5 Social Workers
Social Workers give advice and support to people with a variety of social
needs. This would include relationships, alcohol or domestic problems,
disability, general health and mental health issues and child protection.
The service covers all ages from children to older people. Social
Workers who work in Adult services assess the needs of older people,
people with a physical or a learning disability, or mental health needs.
They will work with individuals to support them to achieve their lifestyle
choices and with their family and community to achieve their desired
outcome. The Social Worker may assist with accessing services or
resources as part of the outcome of assessed need, such as care and
support at home, day care, respite breaks or residential or nursing home
care. Social workers assist people to find ways forward after a traumatic
event in their lives and support them to determine their own solutions.
4.6 Child and Adult Protection Services
There are circumstances where Social Workers may have to intervene to
protect children or adults from harm or abuse. Social services in
Northern Ireland have a legal duty to protect those who are at risk of or
who have experienced abuse or ill-treatment within our society.
If you have any concerns about the safety or well-being of a child, or you
think they may be at risk of harm, please contact the child care Gateway
Team using the numbers below:
Belfast Trust: 028 9050 7000
Northern Trust: 0300 1234333
Western Trust: 028 7131 4090
South Eastern Trust: 0300 1000300
Southern Trust: 0800 7837745

27 | P a g e
If you have any concerns about the safety or well-being of an adult, or
you think they may be at risk of harm, please contact the Adult
Protection service using the numbers below:
Belfast Trust: 028 95041744
Northern Trust: 028 9441 3659
Western Trust: 028 71611366/ 028 82835960
South Eastern Trust: 028 92501227
Southern Trust: 028 3756 4423
Outside of office hours an Emergency Social Work Service for adults or
children can be contacted using: 028 9504 9999
In an emergency the Police Service of Northern Ireland (PSNI) can also
contacted using: 999.
4.7 Mental Health Services
If you have a mental health problem you should see your family doctor
first. They will assess the problem and may either provide medication
and monitor your condition or may refer you to a specialist, for example
psychiatrist, psychologist or counsellor, if necessary. Your family doctor
may be able to recommend a support group for the particular issue.
Where others are involved in your care, such as a psychiatrist, social
worker or family members, your family doctor may liaise with them in
order to provide you with the best overall treatment, care and support.
4.8 Services for People with a Disability
Throughout Northern Ireland, a range of health and social care services
are provided to meet the needs of people with a disability (including
learning, mental, physical, and sensory disabilities), and their family or
carers. This includes assessments, counselling, help with daily living
and the provision of specialist equipment, as well as rehabilitation,
advocacy and respite care services.
Your family doctor will be able to provide you with further information on
the services that are available.

28 | P a g e
4.9 Allied Health Professionals
Allied Health Professionals (AHPs) is the collective title given to 12
professional groups:
Dietetics
Occupational Therapy
Speech and Language Therapy
Physiotherapy
Podiatry
Prosthetics and Orthotics
Orthoptics
Paramedics
Radiography
Art Therapy
Drama Therapy
Music Therapy
AHPs work with all age groups and within all specialities. Their particular
skills and expertise can be the most significant factor in helping people to:
recover movement or mobility
overcome visual problems
improve nutritional status
develop communication skills
restore confidence in everyday living skills
AHPs work in a range of surroundings including hospitals, people’s homes,
clinics, surgeries and schools.
They work in partnership with health and social care colleagues across
primary, secondary and social care, as well as in the independent and
voluntary sectors.
4.10 School Nurse
School Nurses will provide a general health assessments in the
school for all children in their first year in primary school and in
29 | P a g e
first year in secondary school. You will normally be invited to attend
these sessions with the nurse to discuss your child’s health and
development. This will include immunisations and vaccinations,
screening of vision, hearing, height, and body mass index. If your child
has a health need, the School Nurse will discuss this with parents or
guardians and may refer the child for further tests and treatment.
If you need to contact the School nurse you can ask for their details at
your child’s school.
4.11 Childhood Immunisation Programme
Immunisation is the best and safest way to stop your baby or child
becoming sick from various infectious diseases for example measles.
A baby usually has its first vaccination at 8 weeks old. This will be given
at your GP practice (family doctor). It takes a number of injections to
fully protect your child so it is important to complete the course.
If vaccinations have been missed your child can still catch up, even after
a long gap. They do not have to start the course again. Some diseases
can be serious in older children so it is also important that they receive
their booster injections. In Northern Ireland, the diseases for which
immunisation is offered include: Polio, Diphtheria, Tetanus, Whooping
Cough (Pertussis), Hib, Meningococcal Group C, Measles, Mumps, and
Rubella (German measles). You do not need to pay for these
immunisations.
Information on Tuberculosis otherwise known as (TB) and BCG
infectious diseases can be found in various languages on the Public
Health Agency website. http://www.publichealth.hscni.net/
The information leaflets provide detail on symptoms, preventions and
treatments.
Your GP, Health Visitor, School Nurse or a Nurse at your GP Practice
will be able to help with any questions about immunisations.
4.12 Pharmacy Services (The Chemist)
30 | P a g e
Pharmacists (sometimes called Chemists) are experts in medicines and
how they work. Your family doctor is the person who decides what
medicines you need. They will give you a form called a prescription
giving you permission to collect the medicine in a pharmacy. Without it
your pharmacist cannot give you medicines, except for some very simple
medicines such as painkillers, which you can also get in supermarkets
and other stores. Medicines dispensed with a prescription are currently
free within Northern Ireland.
Pharmacists also provide a range of services related to specific health
issues - such as emergency contraception, pregnancy testing, needle
exchange, oxygen or incontinence supplies - and can offer advice on
healthy living and minor ailments - such as bugs and viruses, allergies,
women’s health or aches and pains.
Details of pharmacy rotas in your local area are published online at
http://www.hscbusiness.hscni.net/services/pharmacyrota.htm.
4.13 Dentists
If you are looking for dental treatment you have to register with a Dentist
first. To register with a Dentist you must have a Medical Card. If you
are a visitor you will also be able to access some treatments. You
should check that the Dentist you contact will treat you as a health
service patient (HSC). You may or may not have to pay for some dental
services, depending on your circumstances, such as if you are aged
under 16, you are aged under 19 and are in full-time education and if
you are pregnant.
Find a Dentist in Northern Ireland
http://www.hscbusiness.hscni.net/services/2070.htm
4.14 Optometrists (The Optician)
If you need to have your eyes tested, contact a registered Optometrist.
You may or may not have to pay for some ophthalmic services,
depending on your circumstances, such as if you aged under 16, you
are aged under 19 and are in full-time education, if you have certain
conditions or are in receipt of an eligible benefit. If you are entitled to the
treatment, you will also need your medical card to access free HSC
31 | P a g e
treatment. Many Optometry practices now also offer a service for people
who have a new and sudden onset of an eye problem or e.g. a ‘sore
eye’. More information on how to access eye care services is found at
the following link -
Optometry Services: Information for Patients (hscni.net)
5. What if you are unhappy with the Service you
receive?
5.1 Complaints Procedure
Making a complaint does not affect your rights and will not result in the
loss of any service you have been assessed as needing.
5.2 How to Complain
You can make your complaint in the way, format or language that best
suits you. This can be face to face, on the telephone, in a letter or by
email. You should try to provide the Complaints Department with details
of:
How to contact you
Who or what you are complaining about
Where and when the event that caused your complaint happened
Where possible, what action you would like taken.
Ideally you should try to complain as soon as possible, usually within six
months of you becoming aware that you have a cause for complaint and
normally no longer than 12 months after the event.
5.3 How to make a Complaint about a Health Care
Provider
If you want an apology, an explanation or a review of your treatment,
you should first contact the place where you received care. The
32 | P a g e
Hospital, GP Practice, Private Hospital or Clinic where you received care
has its own complaints procedures. Please contact them for details.
You can find details of the Northern Ireland health service complaints
procedures on the NI Direct website at http://www.nidirect.gov.uk/make-
a-complaint-against-the-health-service
You can also contact the Patient and Client Council by email
complaints.pcc@hscni.net or freephone 0800 917 0222.
Below are the contact details for each Trust Complaints
Department:
Belfast Health and Social Care Trust:
Complaints Department for the Belfast Health and Social Care Trust:
Level 7, McKinney House
Musgrave Park Hospital
Belfast BT9 7JB
Tel: (028) 9504 8000
Email: complaint[email protected]
Online: https://belfasttrust.hscni.net/contact-us/compliments-and-
complaints/compliments-complaints-form/
Northern Health and Social Care Trust:
Service User Feedback Department,
Bush House,
45 Bush Road, Antrim,
BT41 2Q3
Telephone (028) 9442 4655.
Email: user.feedba[email protected]scni.net
Online: http://www.northerntrust.hscni.net/contact-us/service-user-
feedback-form/
You can also complete and submit the Service User Feedback Form
South Eastern Health and Social Care Trust:
Complaints Department
South Eastern HSC Trust
Lough House
Ards Community Hospital
Church Street
33 | P a g e
Newtownards
BT23 4AS
Tel: (028) 9056 1427
Fax: (028) 9056 4815
Email: complaint[email protected]
Online: https://setrust.hscni.net/contact-us/complaints/
Southern Health and Social Care Trust:
Service User Feedback Team
Southern Health and Social Care Trust
Beechfield House
Craigavon Area Hospital
68 Lurgan Road
Portadown
BT63 5QQ
Phone: (028) 37564600
Email: serviceuserfeedback@southerntrust.hscni.net
Online: https://southerntrust.hscni.net/get-in-touch/service-user-
feedback-form/
Western Health and Social Care Trust:
Complaints Department
Trust Headquarters
Altnagelvin Area Hospital
Londonderry
BT47 6SB
Tel: 028 7134 5171 – extension: 214142
Or Direct Dial No. 028 7161 1226
SMS Text Facility: 077 8094 9796
Email: complaints.department@westerntrust.hscni.net
Northern Ireland Ambulance Service (NIAS)
Administrative and Complaints Manager
Northern Ireland Ambulance Service HSC Trust Headquarters,
Site 30
Knockbracken Healthcare Park
Saintfield Road
BELFAST

34 | P a g e
BT8 8SG
Tele: 028 9040 0999
Fax: 028 9040 0901
www.niamb.co.uk
5.4 What Will Happen Next?
Your complaint will be acknowledged within 2 working days of receipt.
They will aim to respond to your complaint in full within 20 working days.
Some complaints take longer to resolve than others. They will tell you if
it becomes clear that they are unable to respond within these
timescales, and they will explain why.
5.5 What happens if you are still not happy after a
health care provider has investigated your
complaint?
If you remain unhappy, you can refer your complaint to the Northern
Ireland Commissioner for Complaints (the Ombudsman). The
Ombudsman will consider your complaint to determine whether it
warrants investigation by him.
Further information on the services provided by the Ombudsman is
available by contacting:
The Ombudsman
Freepost BEL 1478
Belfast
BT1 6BRFreephone: 0800 34 34 24
Email: mailto:ombudsman@ni-ombudsman.org.uk
www.ni-ombudsman.org.uk
6 Where else can you get key Advice and Information?
Further advice and information can be obtained from:
35 | P a g e
The Health and Social Care Board http://www.hscboard.hscni.net
Your local Health and Social Care Trusts:
http://www.belfasttrust.hscni.net
http://www.northerntrust.hscni.net
http://www.setrust.hscni.net
http://www.southerntrust.hscni.net
http://www.westerntrust.hscni.net
The Public Health Agency http://www.publichealth.hscni.net/
Patient Client Council http://www.patientclientcouncil.hscni.net
Business Services Organisation http://www.hscbusiness.hscni.net
6.1 Helplines Network NI: www.helplinesnetworkni.com
The website www.helplinesnetworkni.com offers a single point of access
to Northern Ireland helpline numbers and websites, where people can
find the right helpline to suit their needs. The easy to navigate website
lists the details of over 20 Northern Ireland helplines run by public,
voluntary and community organisations, all non-profit making. The
website offers a search facility which allows users to search for the right
support by entering a key word, find out information about what the
helpline offers and get up to date contact details and operating times.
The Network members provide a variety of vital support services
including information, advice, counselling, a listening ear and
befriending, covering a wide range of needs and issues.
Your local Elected Representatives
http://www.nidirect.gov.uk/elections-in-northern-ireland
Your local Citizens Advice Bureaux
http://www.citizensadvice.co.uk
Law Centre NI http://www.lawcentreni.org
Northern Ireland Human Rights Commission http://www.nihrc.org
Family Support http://www.familysupportni.gov.uk
South Tyrone Empowerment Programme (STEP)
http://www.stepni.org
The Northern Ireland Council for Ethnic Minorities (NICEM)
http://www.nicem.org.uk
Northern Ireland Council for Voluntary Action (NICVA)
http://www.nicva.org
If you would like any further information about HSC in Northern Ireland
please click on the link provided:

