
SOM Chapter 5 - Page 1
State Operations Manual
Chapter 5 - Complaint Procedures
Table of Contents
(Rev. 50, 07-10-09)
Transmittals for Chapter 5
Crosswalk to Old Chapter 5
Sections 5000 to 5080.1 relate to all Medicare/Medicaid-certified
provider/supplier types.
................................................................................................ 6
5000 - Management of Complaints and Incidents .......................................................................... 6
5000.1 – Purpose of the Complaint/Incident Process ......................................................... 6
5000.2 - Overview .............................................................................................................. 7
5010 - General Intake Process ........................................................................................................ 7
5010.1 - Information to Collect From Complainant ........................................................... 8
5010.2 - Information to Provide to Complainant ................................................................ 9
5010.3 –Notification to the RO ........................................................................................... 9
5050 - CMS Regional Office Responsibility for Monitoring SA Management of
Complaints and Incidents .................................................................................................. 11
5060 – ASPEN Complaints/Incidents Tracking System (ACTS)................................................. 11
5070 - Priority Assignment for Nursing Homes, Deemed and Non-Deemed
Providers/Suppliers, and EMTALA.................................................................................. 13
5075 - Priority Definitions for Nursing Homes, Deemed and Non-Deemed
Providers/Suppliers, and EMTALA.................................................................................. 14
5075.1 - Immediate Jeopardy (for Nursing Homes, Deemed and Non-Deemed
Providers/Suppliers, and EMTALA) .................................................................... 14
5075.2 - Non-Immediate Jeopardy - High (for Nursing Homes, Deemed and Non-
Deemed Providers/Suppliers, and EMTALA) ...................................................... 15
5075.3 - Non-Immediate Jeopardy - Medium (for Nursing Homes, Deemed and
Non-Deemed Providers/Suppliers, and EMTALA) .............................................. 16
5075.4 - Non-Immediate Jeopardy – Low (for Nursing Homes, Deemed and Non-
Deemed Providers/Suppliers, and EMTALA) ...................................................... 16
5075.5 - Administrative Review/Offsite Investigation (for Nursing Homes,
Deemed and Non-Deemed Providers/Suppliers, and EMTALA) ......................... 16
SOM Chapter 5 - Page 2
5075.6 - Referral – Immediate (for Nursing Homes, Deemed and Non-Deemed
Providers/Suppliers, and EMTALA) .................................................................... 17
5075.7 - Referral – Other (for Nursing Homes, Deemed and Non-Deemed
Providers/Suppliers, and EMTALA) .................................................................... 17
5075.8 - No Action Necessary (for Nursing Homes, Deemed and Non-Deemed
Providers/Suppliers, and EMTALA) .................................................................... 17
5075.9- Maximum Timeframes Related to the Federal Onsite Investigation of
Complaints/Incidents ............................................................................................ 19
5077- State Monitoring Visits ....................................................................................................... 20
5080 - Investigation Findings and Reports ................................................................................... 20
5080.1-Report to the Complainant .................................................................................... 20
5080.2- Survey Exit Conference and Report to the Provider/Supplier ............................. 21
Sections 5100 to 5170 relate to deemed providers/suppliers. ....................................... 21
5100 - Investigation of Complaints for Deemed Providers/Suppliers .......................................... 21
5100.1 - Basis for Investigation ........................................................................................ 21
5100.2- Post-Survey Procedures ...................................................................................... 23
5120 - Life Safety Code Guidance for Deemed Providers/Suppliers ........................................... 26
5130 – Provider/ Supplier Hospital Refusal of Complaint Investigation Surveys ....................... 26
5140 - Hospital Restraints/Seclusion Death Reporting and Investigation .................................... 26
5140.1 - Background ......................................................................................................... 26
5140.2 - Reserved.............................................................................................................. 27
5140.3 - Responsibilities ................................................................................................... 27
5140.4 - Process ................................................................................................................ 28
5150 - Complaints Involving HIV-Infected Individuals ............................................................... 31
5160 - Investigating Complaints Involving ESRD Services Provided by Deemed
Hospitals ........................................................................................................................... 31
5170 – Investigating Complaints Against ESRD Suppliers ......................................................... 31
Sections 5200 to 5240 relate to all non-deemed provider/supplier types,
excluding nursing homes (SNFs/NFs).
................................................................ 33
5200 - Investigating Complaints for Non-Deemed Providers/Suppliers, Excluding
Nursing Homes (SNFs/NFs) ............................................................................................. 33
SOM Chapter 5 - Page 3
5200.1 - General Procedures ............................................................................................. 33
5200.2 - Special Procedures for Psychiatric Hospitals ..................................................... 33
5210- Processing of Complaints Originating with or Investigated by the RO ............................. 34
5220- Investigation Conducted Directly by the RO ..................................................................... 34
5230- Special RO Processing........................................................................................................ 34
5240 - Complaints - HHA Hotline ................................................................................................ 35
Sections 5300 to 5390 relate to nursing homes. ................................................... 35
5300 - Investigation of Complaints for Nursing Homes ............................................................... 35
5300.1 - Task 1: Offsite Survey Preparation ................................................................... 37
5300.2 - Task 2: Entrance Conference/Onsite Preparatory Activities ............................. 37
5300.3 - Task 5: Information Gathering .......................................................................... 37
5300.4 - Task 6: Information Analysis ............................................................................. 40
5300.5 - Task 7: Exit Conference .................................................................................... 40
5310 - Action on Complaints of Resident Neglect and Abuse, and Misappropriation of
Resident Property .............................................................................................................. 41
5310.1 - Written Procedures ............................................................................................. 41
5310.2 - Review of Allegation .......................................................................................... 41
5310.3 - Investigating Allegations .................................................................................... 41
5310.4 - Factors Beyond the Control of the Individual .................................................... 41
5320 – Reporting Findings of Abuse, Neglect, or Misappropriation of Property to the
Nurse Aide Registry .......................................................................................................... 42
5320.1 - Notification Procedures- Preliminary Determinations ....................................... 42
5320.2 - Conduct of Hearing for Nurse Aides .................................................................. 43
5320.3 - Reporting Findings ............................................................................................. 43
5330 - Reporting Abuse to Law Enforcement and the Medicaid Fraud Control Unit .................. 44
5340 - Post-Survey Certification Actions for Nursing Homes ..................................................... 44
5350 – Data Entry ......................................................................................................................... 44
5360 - Processing of Complaints Originating with or Investigated by the CMS RO ................... 45
5370 - Pre-Investigation Actions on Allegations Originating Through the RO ........................... 45
5380 - RO Processing of RO Investigated Complaints ................................................................ 45
5390 – RO Oversight of Complaint-Related Processes ................................................................ 46
SOM Chapter 5 - Page 4
Sections 5400 to 5480.2 relate to alleged EMTALA violations. ............................ 46
5400 - Investigations Involving Alleged EMTALA Violations ................................................... 47
5410 – EMTALA and Born-Alive Infants Protection Act of 2002 .............................................. 49
5410.1 Interaction of the Born-Alive Infant Protection Act and EMTALA..................... 49
5410.3 Conduct of Investigations ..................................................................................... 50
5420 - Basis for Investigation ....................................................................................................... 50
5430 - RO Direction of Investigation ........................................................................................... 50
5430.1 - Evaluation of Allegation ..................................................................................... 50
5430.2 - Request for Investigation of Allegations ............................................................ 51
5440 - Conducting an Investigation .............................................................................................. 51
5440.1 - Selecting the Team ............................................................................................. 51
5440.2 - Scheduling the Investigation .............................................................................. 51
5440.3 - Guidelines for Surveyors Conducting Investigations ......................................... 51
5440.4 - Conducting the Investigation .............................................................................. 52
5440.5 - Exit Conference .................................................................................................. 54
5450 - Forwarding Report of Investigation to the RO .................................................................. 54
5460 - RO Review of Investigation .............................................................................................. 56
5460.1 - Hospital Is In Compliance - No Past Violation .................................................. 56
5460.2 - Hospital Is In Compliance - Past Violation, No Termination ............................ 56
5460.3 - Hospital Is Not in Compliance - Immediate Jeopardy to Patient Health
and Safety.............................................................................................................. 56
5460.4 - Hospital Is Not in Compliance - Situation Does Not Pose an Immediate
Jeopardy to Patient Health and Safety .................................................................. 57
5465 - Procedures for the 5-day QIO Review of Alleged Violations of 42 CFR 489.24 ............. 57
5470 -Termination Procedures for EMTALA Violations ............................................................. 58
5470.1 - Procedures for Termination when the EMTALA Violation is an
Immediate Jeopardy to Patient Health and Safety ................................................ 58
5470.2 - Procedures for Termination When the EMTALA Violation is Not
Immediate Jeopardy to Patient Health and Safety ................................................ 60
5480 - Procedures for QIO Review of Confirmed EMTALA Violation ...................................... 60
5480.1 - Procedures for Coordinating 60 day QIO Review.............................................. 60
5480.2- EMTALA Case Referral to OIG ......................................................................... 62
SOM Chapter 5 - Page 5
5480.3 - Releasing QIO Assessment ................................................................................ 63
Sections 5500 to 5590 relate CLIA. ........................................................................ 63
5500 - Complaints Involving Unaccredited Laboratories ............................................................. 63
5500.1 - Control ................................................................................................................ 64
5500.2 - Acknowledgment ................................................................................................ 64
5500.3 - Evaluation ........................................................................................................... 64
5500.4 - Scheduling Investigations ................................................................................... 65
5500.5 - Conducting Investigations .................................................................................. 65
5500.6 - Conducting Investigations in a Laboratory with a Certificate of Waiver ........... 65
5500.7 - Conducting Investigations in a Laboratory with a Certificate for PPM
Procedures ............................................................................................................. 66
5500.8 - Post Investigation Actions .................................................................................. 66
5500.9 - Resolution/Closeout........................................................................................... 67
5510 - CLIA-Exempt Laboratory Complaint Investigations - General ........................................ 67
5520 - Review of CLIA-Exempt Laboratory Complaints ............................................................ 68
5530 - Conducting Complaint Investigations and Surveys for CLIA-Exempt Laboratories........ 69
5540 - Complaint Investigations and Surveys of Accredited Laboratories Under CLIA ............. 70
5550 - RO Direction of Complaint Investigation of an Accredited Laboratory ........................... 71
5560 - Conducting Complaint Survey of an Accredited Laboratory ............................................ 73
5570 – Forwarding Investigation Report to RO ........................................................................... 73
5580 - Accredited Laboratory Found in Compliance Following a Complaint Survey ................. 74
5590 - Accredited Laboratory Found Not in Condition-level Compliance Following a
Complaint Survey ............................................................................................................. 74
SOM Chapter 5 - Page 6
NOTE: Sections 5000 to 5080A relate to all Medicare/Medicaid-
certified provider/supplier types.
5000 - Management of Complaints and Incidents
(Rev. 18, Issued: 03-17-06; Effective/Implementation Dates: 03-17-06)
5000.1 – Purpose of the Complaint/Incident Process
Mission: To protect Medicare/Medicaid beneficiaries from abuse, neglect, exploitation,
inadequate care or supervision.
The goal of the Federal complaint/incident process is to establish a system that will assist
in promoting and protecting the health, safety, and welfare of residents, patients, and
clients receiving health care services. The complaint/incident management system has
three objectives.
1. The first objective and priority for the complaint/incident management
system is protective oversight. This is accomplished by analyzing the
complaint allegations and reported incidents received to identify and
respond to those that appear to pose the greatest potential for harming
beneficiaries (has caused or is likely to cause, serious injury, harm,
impairment or death). Complaints/incidents of this type that allege an
immediate threat to the health, safety or welfare of individuals are
investigated immediately.
2. The second objective is prevention. Complaints/incidents that do not allege
a threat of serious harm are investigated to determine if a problem exists that
could have a negative impact on the healthcare services provided. The
investigation of these complaints/incidents is designed to identify and
correct less serious complaints/incident to prevent the escalation of these
problems into more serious situations that would threaten the health, safety
and welfare of the individuals receiving the service. These
complaints/incidents are also prioritized and investigated based on the
seriousness of the allegations.
Numerous or more frequent complaints/incidents may indicate systemic problems
and therefore may be assigned a higher priority for investigation.
3. The third objective is to promote efficiency and quality within the health
care delivery system. Complaints/incidents that are not directly related to
Federal requirements are forwarded to the appropriate agency(ies) for
follow-up and investigation. Complaints/incidents in this category may
include but are not limited to Medicare/Medicaid fraud, complaints against
individual licensed practitioners, and billing issues.
SOM Chapter 5 - Page 7
5000.2 – Overview
(Rev. 18, Issued: 03-17-06; Effective/Implementation Dates: 03-17-06)
All the procedures in this chapter are followed when complaints and reported incidents,
including referrals from public entities, involve Medicare-certified providers/suppliers,
Medicaid-certified providers/suppliers, or CLIA-certified laboratories. The investigation
and resolution of complaints are critical certification activities. The CMS, the State
Medicaid Agency (SMA), and the State survey agency (SA) are responsible for ensuring
that participating providers/suppliers of health care services continually meet Federal
requirements. This requires that the SA promptly reviews complaints/incidents, conducts
unannounced onsite investigations of reports alleging noncompliance, and informs the
CMS Regional Office (RO) and/or the SMA any time certification requirements are
found to be out of compliance.
Since there are multiple activities associated with the management of complaints and
incidents, responsibilities often cut across organizational lines. Thus, the SA must
demonstrate clear-cut accountability for each step of the process and a focal
coordinating/controlling responsibility to assure timely and appropriate action. The SA’s
responsibilities cannot be delegated.
5010 - General Intake Process
(Rev. 18, Issued: 03-17-06; Effective/Implementation Dates: 03-17-06)
A complaint is an allegation of noncompliance with Federal and/or State requirements. If
the SA determines that the allegation(s) falls within the authority of the SA, the SA
determines the severity and urgency of the allegations, so that appropriate and timely
action can be pursued. Each SA is expected to have written policies and procedures to
ensure that the appropriate response is taken for each complaint. This structure needs to
include response timelines and a process to document actions taken by the SA in response
to complaints. If a State’s time frames for the investigation of a complaint/incident are
more stringent than the Federal time frames, the intake is prioritized using the State’s
timeframes. The SA is expected to be able to share the logic and rationale that was
utilized in prioritizing the complaint for investigation. The SA response must be
designed to protect the health and safety of all residents, patients, and clients.
Besides the SA, other public entities receive information and/or perform investigations.
These entities include the office of the coroner or medical examiner, end-stage renal
disease (ESRD) networks, quality improvement organizations (QIOs), law enforcement,
the ombudsman’s office, and protection and advocacy systems. At times, these public
entities will forward information to the SA if there are concerns about the health and
safety of residents, patients, and clients. The SAs are required to manage and investigate
these referrals as complaints.

SOM Chapter 5 - Page 8
An allegation is an assertion of improper care or treatment that could result in the citation
of a Federal deficiency. The point of receipt of the allegation is a critical fact-finding and
decision-making point. The SA ensures that its complaint telephone number is listed in
local directories. Information regarding the care, treatment and services provided to
beneficiaries can come from a variety of sources, including beneficiaries themselves,
beneficiaries’ family members, health care providers, concerned citizens, public agencies,
or media reports. Report sources may be verbal or written. In some instances, the
complainant may request anonymity.
The SA and RO ensure the privacy and anonymity of every complainant. Generally, the
SA follows the disclosure procedures under chapter 3, §3308. The SA discloses the
complainant’s identity only to those individuals with a need to know who are acting in an
official capacity to investigate the complaint.
In addition to these Federal requirements, the SA abides by any State procedures not in
direct conflict with CMS instructions. The SA notifies the RO if State regulations
conflict directly with any part of these complaint procedures.
5010.1 - Information to Collect From Complainant
(Rev. 18, Issued: 03-17-06; Effective/Implementation Dates: 03-17-06)
The SA collects information necessary to make important decisions about the allegations.
In instances where written or verbal allegations are received, subsequent communication
may be necessary to obtain additional information.
Comprehensive information should be collected during the intake process to allow for
proper prioritization, including the following:
• Information about the complainant (e.g., name, address, telephone, etc.);
• Individuals involved and affected;
• Narrative/specifics of the complainant’s concerns including the date, and time of
the allegation;
• The complainant’s views about the frequency and pervasiveness of the allegation;
• Name of the provider/supplier including location (e.g., unit, room, floor) of the
allegation, if applicable;
• How/why the complainant believes the alleged event occurred;
SOM Chapter 5 - Page 9
• Whether the complainant initiated other courses of action, such as reporting to
other agencies, discussing issues with the provider, and obtaining a
response/resolution; and
• The complainant’s expectation/desire for resolution/remedy, if appropriate.
5010.2 - Information to Provide to Complainant
(Rev. 18, Issued: 03-17-06; Effective/Implementation Dates: 03-17-06)
The complaint intake process assists the complainant in resolving his/her conflicts. As
part of the intake process the SA provides the following:
• Policies and procedures for handling intakes including the scope of the SA’s
regulatory authority and any considerations pertaining to confidentiality;
• The course of action that the SA or RO will take and the anticipated time frames;
• Information about other appropriate agencies that could provide assistance
including the name and telephone number of a contact person, if available; and
• A SA contact name and number for follow-up by the complainant.
NOTE FOR DEEMED PROVIDERS/SUPPLIERS: If a complaint does not allege
condition-level noncompliance, the SA may: 1) advise the complainant to file the
complaint to the accrediting organization (AO), or 2) ask for the complainant's
permission to release the information to the AO.
5010.3 – Notification to the RO
(Rev. 18, Issued: 03-17-06; Effective/Implementation Dates: 03-17-06)
1 – Notification to the RO
The SA immediately forwards allegations involving the following to the RO:
• Deemed providers/suppliers;
• Hospital and psychiatric residential treatment facility (PRTF) restraint/seclusion-
related deaths;
• EMTALA complaints;
• Fires resulting in serious injury or death in a Medicare/Medicaid-certified facility;

SOM Chapter 5 - Page 10
• Federal facilities;
• Religious Non-medical Health Care Institutions (RNHCIs)(evaluation performed
by Region I, Boston, only);
• CLIA-certified laboratories holding a certificate of accreditation. (See Chapter 6).
• CLIA-exempt laboratory. (See Chapter 6);
• Blood transfusion-related fatalities (See Chapter 6 and Appendix C);
• Over-utilization or inappropriate utilization of services within the QIO’s
jurisdiction;
• Civil rights violations; or
• Medicare or Medicaid fraud
2 – Special Cases
The SA considers whether notification to the RO is appropriate. If a complaint is
especially significant, sensitive, or attracting broad public or media attention, the SA
informs the RO immediately. Additionally, the SA needs to consider any other early
notice requirements prescribed by other State or Federal policies or interagency
agreements.
SOM Chapter 5 - Page 11
5050 - CMS Regional Office Responsibility for Monitoring SA
Management of Complaints and Incidents
(Rev. 18, Issued: 03-17-06; Effective/Implementation Dates: 03-17-06)
CMS ROs are responsible for monitoring the SAs’ management of complaints and
incidents to assure that the SAs are complying with the provisions set forth in Federal
regulations, the SOM, and CMS policy memoranda. As part of the monitoring process,
the SAs will be evaluated in accordance with the criteria set forth by the State
Performance Standard Review. Many States have State laws and regulations that specify
how to manage complaints and incidents. Whenever possible, State and Federal
requirements should be integrated to avoid unnecessary duplication. CMS ROs should
accept State requirements that meet or exceed the intent of the Federal requirements. At
a minimum, it is expected that noncompliance with Federal requirements resulting from a
complaint or reported incident will receive follow-up and be documented in the Aspen
Complaints Tracking System (ACTS).
5060 – ASPEN Complaints/Incidents Tracking System (ACTS)
(Rev. 18, Issued: 03-17-06; Effective/Implementation Dates: 03-17-06)
The ASPEN Complaints/Incidents Tracking System (ACTS) is designed to track,
process, and report on complaints and incidents reported against health care providers
and suppliers regulated by CMS. It is designed to manage all operations associated with
complaint/incident processing, from initial intake and investigation through the final
disposition.
The ACTS must be used for the intake of all allegations against Medicare/Medicaid-
certified providers/suppliers and CLIA. The ACTS is a Federal system and data entered
into ACTS is subject to Federal laws governing disclosure and the protection of an
individual’s right to privacy.
A complaint/incident record is created in ACTS based on how the allegation is received
by the SA or RO. For example, if one person calls with ten allegations about one
provider/supplier, this is counted as one complaint record. If six people call with the
same allegation, this is counted as six telephone calls and is counted as six complaint
records. If one letter is received with one or many allegations and is signed by 20 people,
this is counted as one complaint record.
1 - Data Entry
The SAs and ROs are required to enter into ACTS:
• All complaint information gathered as part of Federal survey and certification
responsibilities, regardless if an onsite survey is conducted; and

SOM Chapter 5 - Page 12
• All self-reported incidents that require a Federal onsite survey.
The information recorded in ACTS reflects the allegation furnished by the complainant at
the time of the intake. At a minimum, if the intake information requires an onsite survey
and the allegation may involve both Federal and State licensure requirements, a Federal
onsite survey is completed and entered into ACTS.
If an investigation finds one or more violations of Federal requirements, the findings
must be cited under the appropriate tags and entered into the Federal system even if the
information is entered into a State licensure data system. Since this information is
essential to the effective management of the survey and certification program, it is
important that SAs complete the required fields in ACTS in a timely manner.
Exhibit 23 defines the required fields in ACTS.
Tracking of Referrals in ACTS
The SAs are required to enter into ACTS all referrals from public entities that allege
noncompliance with the Federal requirements. For reporting purposes, the SAs should
enter these cases as complaints (i.e., Intake Type=Complaint, Intake Subtype=Federal
COPs, CFCs, RFPs, EMTALA). In order to more quickly identify which of these cases
stem from a referral, the SAs are expected to check the appropriate category under the
“Source” field. For example, for referrals from the coroner’s office, states would check
“Coroner” under the “Source” field for the intake.
Tracking of State Monitoring Visits (See Section 5077) in ACTS
When a State Monitoring Visit results in a Federal deficiency, the SA will identify the
survey in ASPEN as “complaint” and create an intake and survey record in ACTS. The
data should be entered into ACTS as follows:
• Intake Type = Complaint;
• Intake Subtype = Federal COPs, CFCs, RFPs, EMTALA;
• Source = State SA;
• Priority = can vary; and
• Allegation Type = State Monitoring.
2 - Reports
The ACTS produces a variety of reports that may be used for analysis and evaluation of
provider/supplier performance. Complaint/incident reports are generated and displayed
through menus that can be accessed in ACTS. Reports may be produced for one
SOM Chapter 5 - Page 13
provider/supplier, or reports may be combined and present information for multiple
providers/suppliers. Report filtering criteria is available through the Report
Customization window, which allows the user to select criteria for the report to meet the
user’s specifications. Refer to the ACTS Procedures Guide for a list and description of
the reports available in ACTS.
________________________________________________________________________
NOTE:
FOR ADDITIONAL INFORMATION ON SPECIFIC POLICIES RELATED TO:
• DEEMED PROVIDERS AND SUPPLIERS, EXCLUDING CLIA, SEE
SECTION 5100
• NON-DEEMED PROVIDERS AND SUPPLIERS, SEE SECTION 5200
• NURSING HOMES, SEE SECTION 5300
• EMTALA, SEE SECTION 5400
• CLIA LABORATORIES, SEE SECTION 5500
• ESRD, SEE SECTION 5160 AND SECTION 5170
________________________________________________________________________
5070 - Priority Assignment for Nursing Homes, Deemed and Non-
Deemed Providers/Suppliers, and EMTALA
(Rev. 18, Issued: 03-17-06; Effective/Implementation Dates: 03-17-06)
An assessment of each intake must be made by an individual who is professionally
qualified to evaluate the nature of the problem based upon his/her knowledge and/or
experience of current clinical standards of practice and Federal requirements. In
situations where a determination is made that immediate jeopardy may be present and
ongoing, the SA is required to investigate within two working days of receipt of the
information. For all non-immediate jeopardy situations, the complaint/incident is
prioritized within two working days of its receipt, unless there are extenuating
circumstances that impede the collection of relevant information.
An investigation determines if a deficient practice is or was present, and assesses the
degree of harm. To assist in planning the investigation, the SA may review the
provider’s compliance history, quality indicators, ESRD Outcome List and Data or
supporting information received from other programs such as the ombudsman program or
protection and advocacy program. This process may require additional contact with the

SOM Chapter 5 - Page 14
complainant. CMS expects the SA to investigate allegations of non-compliance with the
Federal requirements.
For deemed providers and suppliers, the SA must obtain RO approval to conduct a
complaint validation survey.
For certain provider/supplier types, there are circumstances which require self-reporting
to the SA. This is defined as an incident - an official notification to the SA or RO from a
self-reporting nursing home (i.e., the administrator or authorized official for the provider
or supplier). The reported incident intake is prioritized after information is gathered and
evaluated. The SA response is expected to protect the health and safety of all residents,
patients and clients.
Generally, an alleged event occurring more than 12 months prior to the intake date may
not require the SA to conduct an investigation. However, the SA is not precluded from
conducting a Federal investigation to determine current compliance status based on
identified concerns. For nursing homes, an onsite survey may not be required if there is
sufficient evidence that the facility does not have continuing noncompliance and the
alleged event occurred before the last standard survey.
5075 - Priority Definitions for Nursing Homes, Deemed and Non-
Deemed Providers/Suppliers, and EMTALA
(Rev. 18, Issued: 03-17-06; Effective/Implementation Dates: 03-17-06)
5075.1 - Immediate Jeopardy (for Nursing Homes, Deemed and Non-
Deemed Providers/Suppliers, and EMTALA)
General Provisions
The regulations at 42 CFR 489.3 define immediate jeopardy as, “A situation in which the
provider’s noncompliance with one or more requirements of participation has caused, or
is likely to cause, serious injury, harm, impairment, or death to a resident.” Appendix Q
contains the Guidelines for Determining Immediate Jeopardy. Intakes are assigned this
priority if the alleged noncompliance indicates immediate corrective action is necessary.
When the SA makes the determination that immediate jeopardy may be present and
ongoing, the investigation is to be initiated in accordance with 5075.9.
Fires Resulting in Serious Injury or Death
Fires resulting in serious injury or death are prioritized as “immediate jeopardy”. The
following actions are taken when a report of a fire resulting in serious injury or death in a
Medicare/Medicaid certified facility is received from any source:
The SA
SOM Chapter 5 - Page 15
• Enters the complaint or self-reported incident into ACTS (Priority = IJ,
Allegation Category = Life Safety Code);
• Informs the appropriate RO of fire resulting in serious injury or death
within one working day;
• Compiles information as needed to present a comprehensive picture of the
situation surrounding the fire;
• Takes appropriate action necessary to assist the Medicare/Medicaid-
certified provider/supplier to protect and/or relocate residents or patients
from further harm; and
• Performs the Life Safety Code investigation.
The RO
• Informs CMS Central Office (CO) of the fire and planned actions, sending
a copy of the alert to the Life Safety Code specialist;
• Consults with the CO to determine whether there is an indication for CO
participation in the survey for program evaluation purposes;
• Reports any findings and actions taken by the SA to the CO at the end of
the on-site survey; and
• At its discretion, may accompany the SA during the on-site survey.
The CO
• Consults with the RO to determine whether or not issues are present that
indicate further investigation to determine the adequacy of current
standards and their application; and
• In certain cases CO staff may accompany regional and/or state personnel
on the on-site survey.
5075.2 - Non-Immediate Jeopardy - High (for Nursing Homes)
(Rev. 18, Issued: 03-17-06; Effective/Implementation Dates: 03-17-06)
Intakes are assigned this priority if the alleged noncompliance with one or more
requirements or conditions may have caused harm that negatively impacts the
individual’s mental, physical and/or psychosocial status and are of such consequence to
the person’s well being that a rapid response by the SA is indicated. Usually, specific

SOM Chapter 5 - Page 16
rather than general information (such as, descriptive identifiers, individual names,
date/time/location of occurrence, description of harm, etc.) factors into the assignment of
this level of priority.
When the SA makes the determination that a higher level of actual harm may be present,
the investigation is to be initiated in accordance with 5075.9. The initiation of these
types of investigations is generally defined as the SA beginning an onsite survey.
NOTE: Exhibit 22 provides additional guidance to distinguish between the priorities of
“immediate jeopardy” and “non-immediate jeopardy - high” for nursing home
complaints/incidents.
5075.3 - Non-Immediate Jeopardy - Medium (for Nursing Homes,
Deemed and Non-Deemed Providers/Suppliers, and EMTALA)
(Rev. 18, Issued: 03-17-06; Effective/Implementation Dates: 03-17-06)
Intakes are assigned this priority if the alleged noncompliance with one or more
requirements or conditions caused or may cause harm that is of limited consequence and
does not significantly impair the individual’s mental, physical and/or psychosocial status
or function. An onsite survey should be scheduled to review these intakes.
Non-EMTALA complaints for providers/suppliers with deemed status require an onsite
survey within 45 calendar days after approval by the RO.
5075.4 - Non-Immediate Jeopardy – Low (for Nursing Homes, Deemed
and Non-Deemed Providers/Suppliers, and EMTALA)
(Rev. 18, Issued: 03-17-06; Effective/Implementation Dates: 03-17-06)
Intakes are assigned this priority if the alleged noncompliance with one or more
requirements or conditions may have caused physical, mental and/or psychosocial
discomfort that does not constitute injury or damage. In most cases, an investigation of
the allegation can wait until the next onsite survey.
5075.5 - Administrative Review/Offsite Investigation (for Nursing
Homes, Deemed and Non-Deemed Providers/Suppliers, and EMTALA)
(Rev. 18, Issued: 03-17-06; Effective/Implementation Dates: 03-17-06)
Intakes are assigned this priority if an onsite investigation is not necessary. However, the
SA or RO conducts an offsite administrative review (e.g., written/verbal communication
or documentation) to determine if further action is necessary. The SA may review the
information at the next onsite survey.
SOM Chapter 5 - Page 17
NOTE: For deemed providers/suppliers, SAs should not utilize this prioritization
category for allegations of substantial noncompliance.
5075.6 - Referral – Immediate (for Nursing Homes, Deemed and Non-
Deemed Providers/Suppliers, and EMTALA)
(Rev. 18, Issued: 03-17-06; Effective/Implementation Dates: 03-17-06)
Intakes are assigned this priority if the seriousness of a complaint/incident and/or State
procedures requires referral or reporting to another agency, board, or ESRD network
without delay for investigation.
When the SA refers the complaint to another agency or entity (e.g., law enforcement,
Ombudsman, licensure agency, etc.) for action, the SA must request a written report on
the results of the investigation. Regardless of who conducts the investigation, the SA has
the responsibility to assess compliance with Federal conditions or requirements. The
timeframes for investigation are not altered by the referral to another agency. (Expressed
requests by law enforcement that the SA defer an onsite investigation should be discussed
with the CMS RO, as appropriate.)
5075.7 - Referral – Other (for Nursing Homes, Deemed and Non-
Deemed Providers/Suppliers, and EMTALA)
(Rev. 18, Issued: 03-17-06; Effective/Implementation Dates: 03-17-06)
Intakes are assigned this priority when referred to another agency, board, or ESRD
network for investigation or for informational purposes.
When the SA refers the complaint to another agency or entity (e.g., law enforcement,
Ombudsman, licensure agency, etc.) for action, the SA must request a written report on
the results of the investigation. Regardless of who conducts the investigation, the SA has
the responsibility to assess compliance with Federal conditions or requirements. The time
frames for investigation are not altered by the referral to another agency. (Expressed
requests by law enforcement that the SA defer an onsite investigation should be discussed
with the CMS RO, as appropriate.)
5075.8 - No Action Necessary (for Nursing Homes, Deemed and Non-
Deemed Providers/Suppliers, and EMTALA)
(Rev. 18, Issued: 03-17-06; Effective/Implementation Dates: 03-17-06)
Intakes are assigned this priority if the SA or RO determines with certainty that no further
investigation, analysis, or action is necessary.
For example, no action is necessary if all of the following are met:
SOM Chapter 5 - Page 18
• There is no allegation of immediate jeopardy
• A previous survey investigated the same events
• A previous survey evaluated the appropriate individuals, including those
identified in the intake; and
• The situation did not worsen.
SOM Chapter 5 - Page 19
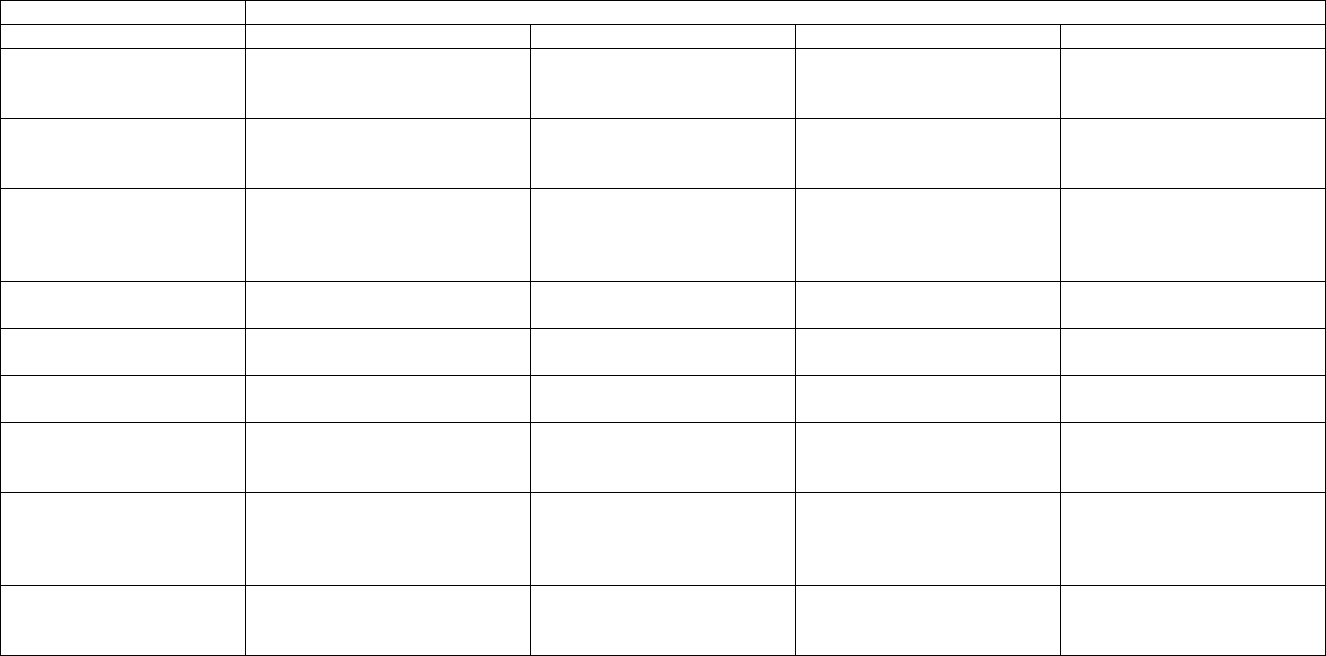
5075.9 - Maximum Time Frames Related to the Federal Onsite Investigation of Complaints/Incidents
(Rev. 18, Issued: 03-17-06; Effective/Implementation Dates: 03-17-06)
Intake Prioritization
Provider Type
Immediate Jeopardy (IJ)
Non-IJ High
Non-IJ Medium
Non-IJ Low
Nursing homes
SA must initiate an onsite
survey within 2 working days of
receipt.
SA must initiate an onsite
survey within 10 working
days of prioritization.
No timeframe specified, but
an onsite survey should be
scheduled.
SA should investigate during
the next onsite survey.
Non-deemed
providers/suppliers, other
than nursing homes
SA must initiate an onsite
survey within 2 working days of
receipt.
N/A
SA must initiate an onsite
survey within 45 calendar
days of prioritization
SA should investigate during
the next onsite survey.
Deemed
providers/suppliers
SA must initiate an onsite
survey within 2 working days of
receipt of RO authorization
N/A
SA must initiate an onsite
survey within 45 calendar
days of receipt of RO
authorization.
SA should investigate during
the next onsite survey.
CLIA, non-exempt, non-
accredited
SA investigates within 2
working days of receipt
N/A
N/A
N/A
CLIA, exempt
SA notifies RO within 10
calendar days
N/A
N/A
N/A
CLIA, accredited
SA submits information to RO
within 2 calendar days
N/A
N/A
N/A
EMTALA
SA must complete investigation
within 5 days of receipt of RO
authorization.
N/A
N/A
N/A
Death related to
restraint/seclusion used for
behavior management-
Hospitals
SA must complete an onsite
investigation within 5 working
days of telephone authorization
from the RO.
N/A
N/A
N/A
Fires resulting in serious
injury or death
SA must initiate an onsite
survey within 2 working days of
receipt.
N/A
N/A
N/A
SOM Chapter 5 - Page 20
5077 - State Monitoring Visits
(Rev. 18, Issued: 03-17-06; Effective/Implementation Dates: 03-17-06)
“State monitoring visits” refers to visits by the SA to oversee a provider’s/supplier’s
compliance status:
• During bankruptcy, in those cases in which CMS has authorized such visits.
• After a change of ownership, as authorized by the CMS RO.
• During or shortly after removal of immediate jeopardy when the purpose of the
visit is to ensure the welfare of the residents/clients/patients by providing an
oversight presence, rather than to perform a structured follow-up visit.
• In other circumstances, as authorized by the CMS RO.
See Section 5060 for data entry requirements for this type of visit.
5080 - Investigation Findings and Reports
(Rev. 18, Issued: 03-17-06; Effective/Implementation Dates: 03-17-06)
Each SA establishes reporting policies, procedures and formats including report language
targeted to specific audiences.
5080.1 - Report to the Complainant
(Rev. 18, Issued: 03-17-06; Effective/Implementation Dates: 03-17-06)
The SA/RO provides the complainant a written report of the investigation findings as a
summary record of the investigation.
The following principles guide preparation of the report to the complainant:
• Acknowledge the complainant’s concern(s);
• Identify the SA’s regulatory authority to investigate the complaint/incident and
any statutory or regulatory limits that may bear on the authority to conduct an
investigation;
• Provide a summary of investigation methods (e.g., on-site visit, written
correspondence, telephone inquiries, etc.);
• Provide date(s) of investigation;
SOM Chapter 5 - Page 21
• Provide an explanation of your SA’s decision-making process including
definitions of terms used (i.e., substantiated or validated, unsubstantiated or not
validated, etc.);
• Provide a summary of your SA’s finding. (NOTE: To the extent possible, the
summary should not compromise the anonymity of individuals, or include
specific situations that may be used to identify individuals, when anonymity has
been requested or is appropriate in the judgment of the SA;
• Identify follow-up action, if any, to be taken by your agency (i.e., follow-up visit,
plan of correction review, no further action, etc.); and
• Identify appropriate referral information (i.e., other agencies that may be
involved).
5080.2 - Survey Exit Conference and Report to the Provider/Supplier
(Rev. 18, Issued: 03-17-06; Effective/Implementation Dates: 03-17-06)
Generally, the SA conducts an exit conference with the provider/supplier at the
completion of the complaint investigation survey. The SA informs the provider/supplier
of the survey findings including deficiencies found. The SA informs the
provider/supplier that survey findings will be documented on Form CMS-2567, which
will be made available to the public under the disclosure of survey information
provisions.
The SA/RO sends to the provider/supplier a written report of the investigation findings as
a summary record of the investigation. At a minimum, this would include the Form CMS-
2567 and applicable notices.
NOTE: For deemed providers/suppliers, the SA informs the provider/supplier that the
RO will inform the hospital of the disposition of the survey investigation.
Sections 5100 to 5170 relate to deemed providers/suppliers.
5100 - Investigation of Complaints for Deemed Providers/Suppliers
(Rev. 18, Issued: 03-17-06; Effective/Implementation Dates: 03-17-06)
5100.1 - Basis for Investigation
(Rev. 18, Issued: 03-17-06; Effective/Implementation Dates: 03-17-06)
SOM Chapter 5 - Page 22
Sections 1864(c) and 1865 of the Social Security Act (the Act) provide the basis for
conducting complaint surveys of deemed providers/suppliers. The SAs should report
poor quality of care or other indications of noncompliance with the Conditions of
Participation (COP)/Conditions for Coverage (CfC) for deemed providers/suppliers to the
RO. The SA refers to the CMS Regional Office (RO) all allegations for deemed
providers/suppliers and all EMTALA allegations for Medicare-participating hospitals.
The RO may authorize the SA to investigate specific areas of the hospital’s operation
related to EMTALA requirements for alleged noncompliance with 42 CFR 489.24 and
the related requirements at 42 CFR 489.20. The SA has responsibility to investigate
whether the conditions are met. Entities and facilities that are subject to the Clinical
Laboratory Improvement Amendments of 1988 (CLIA) are responsible for meeting CLIA
requirements under 42 CFR Part 493.
A substantial allegation of noncompliance refers to a complaint from any of a variety of
sources, including complaints submitted in person, by telephone, through written
correspondence, or in news media articles, that, if substantiated, would have an impact on
the health and safety of patients, and that raises doubts as to a provider’s or supplier’s
compliance with one or more of the COP or CfC.
If the RO learns of a substantial allegation of noncompliance concerning a deemed
provider/supplier, it will review the complaint, to determine if the complaint identifies the
provider/supplier noncompliance with Medicare conditions. If the RO identifies potential
noncompliance, it refers the complaint to the SA for investigation or conducts its own
investigation. If the RO directly receives the allegation , it is responsible for sending the
complainant a letter, which acknowledges the receipt of the complaint and advises the
complainant that an investigation will be initiated. In addition, the RO is responsible for
sending the complainant follow-up letters. These letters may include information
regarding the results of the complaint investigation.
If the SA receives a substantial allegation of noncompliance directly from a complainant
regarding a deemed provider/supplier, it acknowledges receipt of the complaint, and
advises the complainant that an investigation will be initiated when warranted. In this
instance, the RO is not responsible for sending the complainant a letter. The SA forwards
a copy of the acknowledgment letter and the complaint to the RO through the ACTS
system. The SA may not conduct a complaint survey for a deemed provider/supplier
unless it is authorized by the RO. The RO is responsible for determining whether the
complaint identifies an allegation of Medicare noncompliance. If the RO determines that
the complaint does not warrant an investigation by the SA, it sends a copy of the
complaint allegation to the appropriate accreditation organization (AO).
There may be occasions during the course of a state-only activity in a deemed
provider/supplier that state surveyors observe a situation they believe may constitute IJ or
noncompliance with a Medicare condition. In such circumstances, the state should
contact the RO by telephone, explain the situation, and request permission to convert the
survey into a Medicare complaint validation survey. CMS authorizes the investigation as

SOM Chapter 5 - Page 23
a complaint validation survey if it determines such action is necessary. The complaint is
entered into ACTS at the earliest possible opportunity.
Before the SA conducts a complaint investigation survey at a deemed provider/supplier,
it must receive authorization from the RO. It is the RO’s responsibility to determine
whether the complaint alleges Condition-level noncompliance. If the complaint identifies
Condition-level noncompliance, the RO authorizes the complaint investigation by
completing the applicable Form CMS-2802 (See Exhibit 33). The RO completes Item 7
of Form CMS-2802 to identify the Conditions to be investigated by the SA. The RO
may, in addition, identify other related areas for SA review during the survey. If the RO
does not authorize the complaint investigation, the SA may investigate the deemed
provider/supplier under its State regulations and/or licensure authority. RO authorization
is not required when the SA’s basis for conducting the complaint investigation is related
to State requirements.
The RO completes the Form CMS-2802 in ACTS even if the SA received an initial
verbal authorization from the RO to initiate the complaint validation survey of a deemed
provider/supplier. Since ACTS allows the RO to authorize a complaint validation survey
electronically by completing the RO Signature box on the Deemed tab, it is not required
to send a signed hard copy of the Form CMS-2802 to the SA via fax or U.S. Postal
Service. Once the SA receives the authorization through ACTS, it may begin its
complaint investigation of a deemed provider/supplier. Whether the survey is of one or
all Medicare conditions, it will be treated as a complaint survey under ACTS rather than a
re-certification survey, since the complaint is the basis for the survey.
5100.2 - Post-Survey Procedures
(Rev. 18, Issued: 03-17-06; Effective/Implementation Dates: 03-17-06)
Condition-Level, IJ
If condition level deficiencies pose an IJ, the SA forwards the survey packet to the RO
within 2 working days after the completion of the survey. If the RO concurs with the
SA’s findings, the provider/supplier is placed on the 23-day termination track. The RO
notifies the provider/supplier of the proposed termination action and requests an
acceptable plan of correction. The notice also contains a statement that removes the
“deemed status” of the provider/supplier and places it under SA jurisdiction. When the
RO receives an acceptable plan of correction, it directs the SA to conduct a full survey of
all Medicare conditions before the scheduled termination date.
The termination action is rescinded if the IJ has been removed, and compliance is
achieved and documented through the onsite verification. The SA will certify to the RO
its findings and recommend that the termination action be rescinded. The RO will notify
the provider/supplier of its compliance status and that it is no longer under the SA survey
jurisdiction. A copy of the letter is forwarded to the SA and the accrediting organization
(AO).

SOM Chapter 5 - Page 24
However, if the IJ has been removed but condition-level deficiencies remain, the SA
gives the provider/supplier up to 67 additional calendar days or 90 calendar days total (23
plus 67) to achieve compliance. The SA certifies to the RO that the IJ has been removed
and recommends rescission of the IJ termination action. The RO places the
provider/supplier on a non-IJ termination track, notifies the provider/supplier of the new
termination date, and requests that an acceptable POC be provided to the SA. The SA
conducts the revisit by the 60th calendar day without approval from the RO.
If substantial compliance is verified during the second revisit, the SA certifies its findings
to the RO and recommends the rescission of the termination action. The RO notifies the
provider/supplier that it has achieved substantial compliance and is no longer under the
SA jurisdiction. A copy of the letter is forwarded to the SA and the AO.
However, if the provider/supplier fails to come into substantial compliance, the SA
forwards the complete survey packet to the RO within 10 working days from the exit date
of the investigation. After review of the survey packet, the RO sends the
provider/supplier a final termination letter and publishes a public notice. The
provider/supplier is terminated from the Medicare program.
Condition-Level, Non-IJ
If condition level deficiencies do not pose an IJ, the SA forwards the survey packet to the
RO within 10 working days after the completion of the survey. If the RO concurs with
the SA’s findings, the RO notifies the provider/supplier of the removal of its deemed
status; sends a copy of the Form CMS-2567 and places the provider/supplier under SA
jurisdiction. No POC is required at this time. The deemed provider/supplier must be
placed first under SA jurisdiction before further enforcement action is initiated. The RO
requests the SA to conduct a full survey of all Medicare conditions within 60 calendar
days from the date of the deemed status removal.
If the SA confirms during the full survey that the provider/supplier is in compliance with
the Medicare conditions, the SA forwards the survey packet to the RO within 30 calendar
days after the completion of the survey. Since no condition-level deficiencies are cited,
the provider/supplier is in substantial compliance. There may or may not be Standard
level deficiencies cited. If the RO concurs that the provider/supplier is in substantial
compliance; it notifies the provider/supplier and forwards a copy of the letter to the SA
and the AO. A revisit is not conducted on standard level deficiencies. Deemed status of
the provider/supplier is restored.
If the SA confirms during the full survey that the provider/supplier is not in compliance
with one or more Medicare conditions, the SA follows the 90-day termination track. The
SA notifies the provider/supplier of the termination action and timelines. If an acceptable
POC is received, the SA conducts the first revisit within 45 calendar days from the date
of the full survey. No revisit is necessary if the provider/supplier fails to submit
SOM Chapter 5 - Page 25
acceptable POCs. CMS will terminate a provider/supplier if it does not submit an
acceptable POC. See SOM 3254F.
If substantial compliance with the Medicare conditions is achieved during the first revisit
to the full survey, the SA certifies its findings to the RO and recommends the rescission
of the termination action. The SA forwards the survey packet to the RO within 10
working days. The RO notifies the provider/supplier that it has achieved substantial
compliance and is no longer under the SA jurisdiction. Deemed status is restored. A
copy of the letter is forwarded to the SA and the AO.
If the provider/supplier remains out of compliance with the Medicare conditions during
the revisit to the full survey, the SA certifies its findings to the RO, notifies the
provider/supplier that the termination action continues, and requests an acceptable POC.
When the SA receives an acceptable POC, the SA requests RO authorization to conduct a
second revisit by the 60th calendar day. Only the second revisit is subject to RO
approval.
If substantial compliance with the Medicare conditions is achieved by the
provider/supplier during the second revisit, the SA certifies its findings to the RO and
recommends the rescission of the termination action. The SA forwards the complete
survey packet to the RO within 10 working days. The RO notifies the provider/supplier
that it has achieved substantial compliance and is no longer under the SA jurisdiction.
Deemed status is restored. A copy of the letter is forwarded to the SA and the AO.
However, if the provider/supplier fails to come into substantial compliance by the second
revisit, the SA forwards the complete survey packet to the RO within 10 working days.
After review of the survey packet, the RO sends the provider/supplier a final termination
letter and publishes a public notice. The provider/supplier is terminated from the
Medicare program.
Substantial Compliance
If condition level deficiencies were not cited, the provider/supplier is substantially in
compliance. There may or may not be Standard level deficiencies cited. A follow-up
survey is not required for any Standard level deficiencies cited. The provider/supplier is
not required to submit a POC, but may choose to do so because the Form CMS-2567 will
be made available to the public. The SA forwards the survey packet to the RO within 30
calendar days after the completion of the survey including POC if the provider chooses to
submit for public disclosure. If the RO determines the deemed provider/supplier is
substantially in compliance with the Medicare conditions, the RO notifies the
provider/supplier and forwards a copy of the letter to the SA and the AO.
SOM Chapter 5 - Page 26
5120 - Life Safety Code Guidance for Deemed Providers/Suppliers
(Rev. 18, Issued: 03-17-06; Effective/Implementation Dates: 03-17-06)
In most States, an engineer or other fire safety specialist surveys for compliance with the
Life Safety Code (LSC) standard and others survey the remaining standards in the
Physical Environment Condition. If the allegation pertains only to LSC requirements, it
is not necessary to survey the remainder of the Physical Environment Medicare
condition.
5130 – Provider/ Supplier Hospital Refusal of Complaint Investigation
Surveys
(Rev. 18, Issued: 03-17-06; Effective/Implementation Dates: 03-17-06)
The SA informs the provider/supplier that refusal to allow a complaint investigation
survey is a basis for termination from the Medicare program, in accordance with Section
1128(b)(12) of the Social Security Act. The SA notifies the RO immediately.
A hospital found out of compliance because of its refusal to allow a survey is returned to
the AO’s jurisdiction when:
• The provider or supplier permits the validation survey to be conducted; and
• The provider or supplier withdraws any prior refusal to authorize its accreditation
organization to release a copy of its current accreditation survey.
5140 - Hospital Restraints/Seclusion Death Reporting and Investigation
(Rev. 18, Issued: 03-17-06; Effective/Implementation Dates: 03-17-06)
5140.1 - Background
(Rev. 50; Issued: 07-10-09; Effective/Implementation Date: 07-10-09)
The Centers for Medicare & Medicaid Services (CMS) hospital restraint and seclusion
requirements are found in the Hospital COP, Patients’ Rights at 42 CFR 482.13,
Standards (e),(f) and (g). (See also 71 FR 71378, December 6, 2006)
The hospital’s reporting requirement for deaths associated with the use of restraint or
seclusion is located at 42 CFR 482.13(g) and states:
“Standard: Death reporting requirements: Hospitals must report deaths
associated with the use of seclusion or restraint.
(1) The hospital must report the following information to CMS:
SOM Chapter 5 - Page 27
(i) Each death that occurs while a patient is in restraint or seclusion.
(ii) Each death that occurs within 24 hours after the patient has been
removed from restraint or seclusion.
(iii) Each death known to the hospital that occurs within 1 week after
restraint or seclusion where it is reasonable to assume that use of
restraint or placement in seclusion contributed directly or
indirectly to a patient's death. “Reasonable to assume” in this
context includes, but is not limited to, deaths related to restrictions
of movement for prolonged periods of time, or death related to
chest compression, restriction of breathing or asphyxiation.
(2) Each death referenced in this paragraph must be reported to CMS by
telephone no later than the close of business the next business day
following knowledge of the patient's death.
(3) Staff must document in the patient's medical record the date and time the
death was reported to CMS.”
Hospitals are required to report a restraint/seclusion death via telephone to their CMS
RO.
The interpretive guidelines found in the Hospital Appendix A at 42 CFR
482.13(e) – (g) discuss in detail what is considered a restraint or seclusion, the
requirements governing hospital use of restraint or seclusion, and these
reporting requirements.
5140.2 - [Reserved]
(Rev. 50; Issued: 07-10-09; Effective/Implementation Date: 07-10-09)
5140.3 - Responsibilities
(Rev. 50; Issued: 07-10-09; Effective/Implementation Date: 07-10-09)
Regional Offices (ROs)
The RO maintains a Hospital Restraint/Seclusion Death Report Worksheet for each case
reported.
The RO is also responsible for data entry into the Automated Survey Processing
Environment (ASPEN) Complaint Tracking System (ACTS) Restraint/Seclusion Death
Module and for maintenance of Data Use Agreement files related to disclosures to
Protection and Advocacy Agencies. (See Process discussion below.)
SOM Chapter 5 - Page 28
Each RO designates one contact person and a backup person who serves as the point of
contact, coordination, and communication regarding reporting, investigation, and follow-
up for the death-reporting requirement under Patients’ Rights.
State Agencies (SAs)
Hospitals report patient deaths associated with restraint or seclusion, as previously
discussed, to their CMS RO, not to the SA. Any hospital patient restraint or seclusion
death report received by a SA directly from a hospital (or other source) must be
forwarded immediately by the SA to its RO.
The SA conducts a complaint investigation related to a patient death associated with a
hospital’s use of restraints or seclusion only when the RO authorizes the investigation.
The SAs are to assist ROs in educating the hospitals in their State about their obligation
to report to their RO any death that meets the reporting requirements found at 42 CFR
482.13(g). State Agencies are to provide hospitals with their RO contact name and
telephone number, as well as the hospital reporting procedures contained in this policy.
The SAs respond to requests from Protection and Advocacy (P&A)
organizations, or any other parties, for information on survey findings related to
specific cases identified by the requestor. The SAs handle these requests in
accordance with the SA’s Data Use Agreement (DUA) with CMS.
5140.4 - Process
(Rev. 50; Issued: 07-10-09; Effective/Implementation Date: 07-10-09)
The RO evaluates the information required to be reported by the hospital under 42 CFR
482.13(g) to determine whether the situation warrants an on-site investigation. The RO
uses the Hospital Restraint/Seclusion Death Report Worksheet when recording the
hospital’s telephonic report. The RO may not require any hospital to complete and
submit a hard copy of the worksheet. However, a hospital may volunteer to submit a
completed worksheet in lieu of providing the requested information telephonically. The
RO may provide a template worksheet to hospitals that volunteer to submit their reports
via a completed worksheet.
Using the worksheet detail provided by the hospital, the RO evaluates whether the case
might involve a violation of 42 CFR 482.13(e) through 42 CFR 482.13(g) and authorizes
an on-site investigation if there appears to be a possible violation. It is likely that the
majority of hospital reports of deaths associated with the use of seclusion or restraint will
not require an on-site investigation. If the RO determines that the restraint/seclusion
death report requires on-site investigation, within 2 working days of receiving the report,
the RO enters the reported information into the ACTS restraint/seclusion module and
immediately notifies the SA to authorize a complaint survey to investigate the hospital’s
compliance with the Patient’s Rights CoP at 42 CFR 482.13(e), (f), or (g), including the
SOM Chapter 5 - Page 29
reported case. The SA accesses the ACTS restraint/seclusion module to see the details of
the reported case prior to conducting the on-site investigation. The SA should complete
the investigation within 5 working days of receipt of survey authorization from the RO.
In addition to completing the ACTS Restraint/Seclusion module for all cases that are
authorized for on-site investigation, the RO also completes this module for all cases
reported by hospitals to the RO during the months of April, October, and January,
regardless of whether an on-site investigation was authorized, in order to provide a
detailed and representative data base that supports analysis of deaths associated with
hospital use of restraint and seclusion.
Notice to Protection and Advocacy Organizations
At the same time that the RO notifies the SA and authorizes the on-site survey, the RO
also provides written notification, by mail or email, to the appropriate Protection and
Advocacy (P&A) Organization within the State where the hospital is located.
Notification is provided only in those cases for which an on-site survey is authorized.
The RO provides the following information to the P&A: hospital’s name, hospital’s
address, date the restraint/seclusion-associated death occurred, patient’s diagnosis, and
type(s) of restraint/seclusion used. THIS IS THE ONLY INFORMATION TO BE
SUPPLIED TO P&A ORGANIZATIONS ON AN UNSOLICITED BASIS. No individual
identifiers are to be provided. The names and addresses for each State’s P&A can be
located at the following website, and at the drop down menu entitled “Get Help in Your
State:” www.ndrn.org .
After reviewing the summary provided by the RO, consistent with the ACTS Notice of a
Modified or Altered System of Records (SOR), published May 23, 2006, in the Federal
Register (SOR 09-70-0565), the P&A may request more detailed information relating to
that case, including the name of the deceased contained in the ACTS restraint/seclusion
module and the worksheet for the case. The P&A must have an approved CMS Data Use
Agreement (DUA), Form CMS-R-0235, (Exhibit 292) in place before the RO may release
a copy of the worksheet and/or information from the ACTS restraint/seclusion module.
Form CMS-R-0235 may be submitted by a P&A to CMS in advance of any specific
request for person-identifiable data. Once the P&A has an approved DUA and has
submitted a copy of it to the RO, that DUA applies to all subsequent disclosures to the
P&A of person-identifiable data in response to requests for hospital restraint/seclusion
death information to the RO. It is not necessary for the P&A to submit a DUA update for
each individual request.
In order to get an approved DUA, the P&A must complete and submit a signed CMS
DUA, Form CMS-R-0235, including an initialed DUA ACTS SOR- P&A Attachment
(Exhibit 293) to the
Director, Division of Privacy Compliance, Centers for Medicare and Medicaid Services,
Mailstop N2-04-27, 7500 Security Boulevard, Baltimore, MD 21244-1850. That Division
SOM Chapter 5 - Page 30
will review the DUA, assign a unique DUA identifier to it, and return a signed copy to
the P&A. When completing the Form, P&As must note the following in particular:
• Line 5 of the DUA must state “Restraint/Seclusion Hospital Death Reports.” The
“Years” and “System of Record” columns should be left blank;
• Line 12 must state “CMS DUA: ACTS SOR Attachment – P&A;”
• The DUA must be signed by the P&A official whom the P&A designates as
“Custodian,” i.e., the individual who will have actual possession of and
responsibility for the data released under the DUA; and
• A P&A may designate more than one Custodian, but if it does so, each individual
must complete and sign a Multi-Signature Addendum Form (Exhibit 294).
For each disclosure of personally identifiable data to a P&A that has an approved DUA,
the RO must complete the DUA Tracking Addendum (Exhibit 295), sequentially listing
each case file disclosed. Disclosure of person-identifiable data is permitted only for
those cases where the:
• RO has previously notified the P&A, without providing person-identifiable data,
of a hospital restraint/seclusion death report for which a SA survey has been
authorized; or
• P&A identifies in its request an individual and hospital by name and requests
restraint/seclusion death report information that may have been submitted by that
hospital with respect to that individual.
The DUA Tracking Addendum must show the DUA number of the primary P&A DUA.
The RO must enter the ACTS Intake Number, Requestor’s Name and Title, Name of the
P&A, Address, Telephone Number and E-Mail Address, (if applicable). Because the RO
is responsible for tracking all disclosures made, the RO must sign the Addendum for each
disclosure. ROs must ensure that the responsibilities related to processing hospital
restraint/seclusion death reports are clearly articulated and implemented within the RO.
Custodians may be added or deleted over the life of the primary DUA. To add a new
Custodian under an existing DUA, the P&A must submit the following to the RO: a letter
from the P&A describing the activities planned for the new Custodian and the length of
time over which the Custodian will serve, and a Multi-Signature Addendum signed by the
appropriate official from the P&A. The Multi-Signature Addendum must show the DUA
number of the existing primary P&A DUA. The P&A must assign a case number to all
Multi-Signature Addendums beginning with “1” and adding consecutively thereafter.
CMS will use this number to track the number of Custodians in each P&A. When a P&A
seeks to delete an existing Custodian, it must send the RO a letter to this effect. The RO
will strike out the name of the deleted Custodian from the DUA or Multi-Signature
SOM Chapter 5 - Page 31
Addendum that added that Custodian, dating and initialing the deletion. The letter from
the P&A removing the Custodian must be kept on file.
Any P&A requests for information about the on-site survey should be submitted to the SA
and handled by the SA in accordance with the SA’s ACTS DUA agreement with CMS.
5150 - Complaints Involving HIV-Infected Individuals
(Rev. 18, Issued: 03-17-06; Effective/Implementation Dates: 03-17-06)
As direct recipients of Federal funds, providers and suppliers are subject to provisions of
Section 504 of the Federal Rehabilitation Act of 1973. Symptomatic and asymptomatic
individuals who are infected with the human immunodeficiency virus (HIV), or “AIDS
virus,” are protected by the Rehabilitation Act as “individuals with handicaps.”
Therefore, HIV-infected individuals who are provided services, are employed, or are to
be employed by providers and suppliers in Federally-conducted or financed programs or
activities would be treated like anyone else in the workforce, so long as these individuals
do not, on a case-by-case basis, pose a substantial health and safety risk to others, or pose
a performance problem, and are “otherwise qualified.”
A provider participating in the Medicare or Medicaid programs cannot discriminate
against individuals who are HIV-infected so long as these individuals do not, on a case-
by-case basis, pose a substantial health and safety risk to others and so long as the
provider provides comparable services and care to non HIV-infected individuals.
The SA or the RO refers discrimination complaints to the Office of Civil Rights (OCR),
which is the authority to determine whether Medicare or Medicaid providers and
suppliers comply with this non-discrimination statute.
5160 - Investigating Complaints Involving ESRD Services Provided by
Deemed Hospitals
(Rev. 18, Issued: 03-17-06; Effective/Implementation Dates: 03-17-06)
Most of the hospitals participating in the ESRD program are deemed by JCAHO or AOA.
“Deemed status” applies only to the hospital’s approval as a provider, not to its status as a
supplier of ESRD transplantation or dialysis services. The SA investigates all complaints
and allegations related solely to ESRD services since ESRD services fall outside the
purview of accreditation.
5170 – Investigating Complaints Against ESRD Suppliers
(Rev. 18, Issued: 03-17-06; Effective/Implementation Dates: 03-17-06)
1. General

SOM Chapter 5 - Page 32
Refer to the guidance for investigation of complaints against non-deemed providers and
suppliers. See SOM §5200.
The ESRD Networks are required to have a complaint /grievance resolution system.
Networks (NW) and the SA are frequently contacted by the same complainant with the
same or similar allegations. If the allegations require an onsite investigation or allege
potential risk to patient health or safety, the SA is responsible for the investigation. If the
allegations are primarily focused on relationship or communication issues, the NW may
assume primary responsibility for the investigation. If the focus of the allegations is a
medical practice issue, the SA and NW may need to collaborate on the investigation. The
NWs and SA are encouraged to communicate and collaborate to reduce or prevent
redundant investigations.
2. Conducting the Investigation
The SA surveyors should use the ESRD survey protocol in Appendix H to investigate
complaints. The allegations of the complaint will determine the tasks needed. For
example, an allegation of inadequate patient care staffing would require use of the
following tasks, at a minimum:
• Pre survey activities;
• Entrance Conference: Provide an overview of the complaint allegations and the
planned agenda for your survey time;
• Tour and observations;
• Patient interviews;
• Staff interviews;
• Record reviews;
• Review of quality management materials; and
• Exit conference.
Conduct each of the identified survey tasks in Appendix H, “Guidance to Surveyors:
End-Stage Renal Disease Facilities.”
3. Pre-survey Task for Complaint Investigations
Review the allegations of the complaint to identify needed survey tasks. Review the
State Outcomes List and the Dialysis Facility Report to determine if there are data
outliers related to the allegations. For example, if the complaint alleges staff members do
SOM Chapter 5 - Page 33
not wash their hands, the surveyor should review the facility’s rate of hospitalization and
hospitalizations related to septicemia, and consider this information in the survey process.
To facilitate meeting the requirement of surveying each ESRD facility every 3 years, the
SA evaluates all available information (outcome list rank, Dialysis Facility Report, time
since last survey, complaint history, NW information, etc.) to determine whether a
recertification survey should be conducted at the time of the complaint investigation.
NOTE: Sections 5200 to 5240 relate to all non-deemed
provider/supplier types, excluding nursing homes (SNFs/NFs).
5200 - Investigating Complaints for Non-Deemed Providers/Suppliers,
Excluding Nursing Homes (SNFs/NFs)
(Rev. 18, Issued: 03-17-06; Effective/Implementation Dates: 03-17-06)
5200.1 - General Procedures
(Rev. 18, Issued: 03-17-06; Effective/Implementation Dates: 03-17-06)
For complaint surveys on non-deemed providers/suppliers, the SA uses the appropriate
survey protocol and interpretive guidelines. A focus survey is conducted on the specific
regulatory requirements related to the allegation. Based on an initial assessment or other
observations, if significant problems are identified, the SA expands the scope of review
as necessary to determine compliance or noncompliance. The SA does not refer
complaints regarding non-deemed providers/suppliers to the RO.
If deficiencies are cited, the SA documents the deficiencies on Form CMS-2567 and
obtains an acceptable POC. If non-compliance with the Medicare conditions is identified,
the SA will follow the appropriate termination procedures and document and report as
required. (See SOM Chapter 3, §§3010-3028 for termination procedures.)
5200.2 - Special Procedures for Psychiatric Hospitals
(Rev. 18, Issued: 03-17-06; Effective/Implementation Dates: 03-17-06)
The special conditions for psychiatric hospitals cannot be deemed to meet the Medicare
requirements. The remaining conditions for hospitals apply to psychiatric hospitals, and
a hospital may be deemed to meet those conditions.
When the SA receives a complaint allegation against a psychiatric hospital under the
general conditions of participation, it must determine whether or not the hospital is
deemed. If the hospital is deemed, the SA follows the appropriate survey protocol for

SOM Chapter 5 - Page 34
deemed facilities. If the hospital is not deemed, the SA investigates the complaint if
appropriate under these procedures listed above in §5200.1.
If the complaint allegation concerns the special conditions for psychiatric hospitals, the
SA may conduct an investigation if it has appropriate qualified personnel or refer it to the
RO. If the complaint is referred to the RO, the RO will evaluate and refer it to the CO as
required.
5210- Processing of Complaints Originating with or Investigated by the
RO
(Rev. 18, Issued: 03-17-06; Effective/Implementation Dates: 03-17-06)
The RO establishes procedures and clear organizational accountability to ensure that
complaints are properly evaluated, documented, acknowledged, and handled timely and
appropriately. The RO uses ACTS to ensure timely and appropriate action on all
allegations originating with or investigated by the RO. The extent and nature of the RO
involvement with a given complaint varies depending on the nature of the allegation and
the receiving organization.
Most complaints originate through the SA and are recorded and controlled by the SA.
When a complaint is filed directly with the RO, the RO assumes those initial SA
responsibilities.
5220- Investigation Conducted Directly by the RO
(Rev. 18, Issued: 03-17-06; Effective/Implementation Dates: 03-17-06)
This less frequent class of complaints includes allegations retained by the RO or
forwarded to the RO by the SA for investigation. The RO’s responsibilities vary based
on the type of complaint.
The RO uses the appropriate survey protocol and interpretive guidelines for the
provider/supplier. These procedures apply when a direct RO investigation is conducted,
such as for Federal facilities, Religious Non-Medical Health Care Institutions (RNHCIs),
or special situations. When directly investigating, the RO begins by ensuring that it or
the SA has met all initial data collection and acknowledgement requirements.
If the allegation involves an IJ, the RO investigates within two working days. Otherwise,
the RO schedules the investigation based on the severity of the allegation. (See §5075.9
for time frames related to Federal onsite investigations.)
5230 - Special RO Processing
(Rev. 18, Issued: 03-17-06; Effective/Implementation Dates: 03-17-06)

SOM Chapter 5 - Page 35
The following types of allegations are subject to special RO handling:
1. Over-Utilization or Inappropriate Utilization of Services- The RO refers to the
local QIO for investigation, and documents the provider’s files as for other
allegations. The RO acts, as necessary, on any findings returned by the QIO;
2. Civil Rights Violations- The RO refers to the regional OCR for investigation.
The RO documents the provider’s files as for other allegations. The RO acts as
necessary on any findings returned by OCR; and
3. Medicare/Medicaid/CLIA fraud- The RO refers to the RO of the Inspector
General/DHHS for investigation. The RO documents the provider’s files as for
other allegations.
In each of the above instances, the RO ensures that the complainant and SA are notified
of any findings.
5240 - Complaints - HHA Hotline
(Rev. 18, Issued: 03-17-06; Effective/Implementation Dates: 03-17-06)
Each State has a Medicare home health hotline that can be called by patients who are
dissatisfied with the home health services they are receiving or by other individuals with
a complaint about a specific HHA. Under the Medicare COPs for Patient Rights at 42
CFR 484.10, HHAs are required to provide their patients with the hotline number for
their state. Concerns about an HHA not complying with the COPs, or reports that an
HHA is misinforming beneficiaries or inappropriately terminating care for patients, can
be referred to the SA for investigation via the home health hotline. Concerned consumers
may also call the SA directly. A violation of the COPs or the provider agreement could
lead to termination of the HHA from the Medicare program.
As part of the patient rights COPs, the HHA is required to investigate complaints made
by a patient or the patient’s family or guardian regarding treatment or care that is, or fails
to be, furnished, and to document both the existence of the complaint and resolution of
the complaint.
Surveyors, as part of their investigation of the HHA’s compliance of the COPs, may ask
to review complaints received by the HHA and the resolution of these complaints. The
HHA must permit examination of these records by or on behalf of CMS, or risk
termination from the Medicare program.
NOTE: Sections 5300 to 5390 relate to nursing homes.
5300 - Investigation of Complaints for Nursing Homes

SOM Chapter 5 - Page 36
(Rev. 18, Issued: 03-17-06; Effective/Implementation Dates: 03-17-06)
Section 42 CFR 488.332 provides the Federal regulatory basis for the investigation of
complaints about nursing homes.
The survey agency must review all complaint allegations and conduct a standard or an
abbreviated standard survey to investigate complaints of violations of requirements if its
review of the allegation concludes that:
• A deficiency in one or more of the requirements may have occurred; and
• Only a survey can determine whether a deficiency or deficiencies exist.
The survey agency does not conduct a survey if the complaint raises issues that are
outside the purview of Federal participation requirements.
Complaint investigations follow, as appropriate, the pertinent survey tasks, and
information gathered is recorded on the appropriate survey worksheets. However, if the
documentation required is minimal, use Form CMS-807 to record information during the
complaint investigation. Record deficiencies on Form CMS-2567 and/or, the “Statement
of Isolated Deficiencies Which Cause No Harm with Only a Potential for Minimal Harm
for SNFs and NFs” . The completed Form CMS-2567 must be made a part of the
complaint record.
If necessary, a specialized team may be used to investigate complaints. Team members
may include, but are not limited to, an attorney, auditor, and appropriate health
professionals. The specialized team is not necessarily composed of qualified surveyors.
However, specialized team members provide unique talents and expertise that assist at
least one qualified surveyor in identifying, gathering, and preserving documented
evidence. Further information regarding the composition of the survey team is provided
in Chapter 7
.
The timing, scope, duration and conduct of a complaint investigation are at the discretion
of the SA, except when a determination is made that immediate jeopardy may be present
and ongoing or a higher level of actual harm may be present. If the complaint concerns
conditions on a certain day (e.g., on weekends), or on a certain shift (e.g., 11 p.m. - 7
a.m.), the SA should make an attempt to investigate it at the relevant time. In most cases,
the following tasks, or portion of tasks, should be performed during a complaint
investigation.

SOM Chapter 5 - Page 37
5300.1 - Task 1: Offsite Survey Preparation
(Rev. 18, Issued: 03-17-06; Effective/Implementation Dates: 03-17-06)
Review any information about the facility that would be helpful to know in planning the
investigation. Contact the ombudsman to discuss the nature of the complaint and whether
there have been any similar complaints reported to and substantiated by the ombudsman.
Review the related regulatory requirements or standards that pertain to the complaint.
For example, if it is a complaint about abuse, review the requirements at 42 CFR 483.13.
Plan the investigation. Before going to the nursing home, plan what information to
obtain during the complaint investigation based on the information already acquired.
Consider practical methods to obtain that information.
5300.2 - Task 2: Entrance Conference/Onsite Preparatory Activities
(Rev. 18, Issued: 03-17-06; Effective/Implementation Dates: 03-17-06)
Onsite complaint investigations should always be unannounced. Upon entrance, advise
the facility’s Administrator of the general purpose of the visit. The SA explains the
reason for the survey and avoids any impression that a predetermination has been made
as to the validity of the allegation. It is important to let the facility know why you are
there, but protect the confidentiality of those involved in the complaint. Do not release
information that will cause opportunities to be lost for pertinent observations, interviews,
and record reviews required for a thorough investigation. For example, if the complaint
is that food that is intended to be served hot is always served cold, do not tell the facility
the exact complaint. Rather, tell them it is a situation related to dietary requirements.
5300.3 - Task 5: Information Gathering
(Rev. 18, Issued: 03-17-06; Effective/Implementation Dates: 03-17-06)
The order and manner in which information is gathered depends on the type of complaint
that is being investigated. Conduct comprehensive, focused, and/or closed record
reviews as appropriate for the type of complaint. Generally, it is not necessary to review
records and information from more than one year ago. However, the SA is not precluded
from doing so if concerns identified during the investigation indicate it is necessary in
order to determine current compliance. It is very important to remember that the
determination of whether the complaint happened is not enough. The surveyor needs to
determine noncompliant facility practices related to the complaint situation and which, if
any, requirements are not met by the facility.
Perform information gathering in order of priorities, i.e., obtain the most critical
information first. Based on this critical information about the incident, determine what
other information to obtain in the investigation.
SOM Chapter 5 - Page 38
Observations, record review and interviews can be done in any order necessary. As
information is obtained, use what has been learned to determine what needs to be
clarified or verified as the investigation continues.
Observe the physical environment, situations, procedures, patterns of care, delivery of
services to residents, and interactions related to the complaint. Also, if necessary,
observe other residents with the same care need. After determining what occurred, i.e.,
what happened to the resident and the outcome, investigate what facility practice(s) or
procedures affected the occurrence of the incident.
EXAMPLE
It was verified through the investigation that a resident developed a pressure sore/ulcer
which progressed to a Stage IV, became infected and resulted in the resident requiring
hospitalization for aggressive antibiotic therapy. Observe as appropriate: dressing
changes, especially to any other residents with Stage III or IV pressure sores; infection
control techniques such as hand washing, linen handling, and care of residents with
infections; care given to prevent development of pressure sores (e.g., turning and
repositioning, use of specialized bedding when appropriate, treatments done when
ordered, keeping residents dry, and provision of adequate nutritional support for wound
healing).
Record Review: If a specific resident is involved, focus on the condition of the resident
before and after the incident. If there are care issues, determine whether the appropriate
assessments, care planning, implementation of care, and evaluations of the outcome of
care have been done as specified by the regulatory requirements.
EXAMPLE
For a complaint of verbal and physical abuse, review the record to determine the
resident’s mood and demeanor before and after the alleged abuse. Determine if there are
any other reasons for the change in the resident’s demeanor and behavior. Determine
whether an assessment has been done to determine the reason for the change in mood and
behavior. Does the record document any unexplained bruises and/or complaints of pain,
and whether they occurred in relation to the alleged incident?
Interviews: Interview the person who made the complaint. If the complainant is not at
the facility at the time of the survey, he/she should be interviewed by telephone, if
possible. Also, interview the person the complaint is about. Then, interview any other
witnesses or staff involved. In order to maintain the confidentiality of witnesses, change
the order of interviews if necessary. It may not always be desirable to interview the
person who made the complaint first, as that may identify the person as the complainant
to the facility. Interview residents with similar care needs at their convenience.
SOM Chapter 5 - Page 39
As interviews proceed, prepare outlines needed for other identified witnesses and revise
outlines as new information is obtained.
During information gathering to investigate a complaint about the care and services
provided to residents in a nursing home, findings of past noncompliance may be
identified. Before considering a citation of past noncompliance with a specific regulatory
tag, surveyors must determine if current compliance with the specific regulatory tag
exists. Similar to verifying correction of current noncompliance on a revisit, surveyors
should use a variety of methods to determine whether correction of the past
noncompliance occurred and continues. This may include, but is not limited to, the
following:
• Interviews with facility staff, such as the administrator, nursing staff, social
services staff, medical director, quality assessment and assurance committee
members, and/or other facility staff, as indicated, to determine what procedures,
systems, structures, and processes have been changed.
• Reviewing through observation, interview and record review, how the facility
identified and implemented interventions to address the noncompliance.
Examples of interventions may include, but are not limited to:
o The facility’s review, revision, or development of policies and/or
procedures to address the areas of concerns;
o The provision and use of new equipment, as necessary;
o The provision of staff training required to assure ongoing compliance for
the implementation and use of new and/or revised policies, procedures,
and/or equipment, especially with new and/or temporary staff;
o The provision of additional staffing, changes in assignments or
deployment of staff, as needed; and
o The provision of a monitoring mechanism to assure that the changes made
are being supervised, evaluated, and reinforced by responsible facility
staff.
• Evaluating whether the facility has a functioning quality assessment and
assurance committee whose responsibilities include the identification of quality
issues; providing timely response to ascertain the cause; implementing corrective
action; implementing monitoring mechanisms in place to assure continued
correction and revision of approaches, as necessary, to eliminate the potential risk
of occurrence to other residents and to assure continued compliance.
A citation of past noncompliance must meet all of the criteria described in Task 6 below.

SOM Chapter 5 - Page 40
5300.4 - Task 6: Information Analysis
(Rev. 18, Issued: 03-17-06; Effective/Implementation Dates: 03-17-06)
Review all information collected. If there are inconsistencies, do additional data
collection as needed, to resolve the inconsistencies. Determine if there is any other
information still needed.
Determine whether:
• The allegations are substantiated or unsubstantiated;
• The facility failed to meet any of the regulatory requirements; and
• The facility practice or procedure that contributed to the complaint has been
changed to achieve and/or maintain compliance.
To cite past noncompliance with a specific survey data tag (F-tag or K-tag), all of the
following three criteria must be met:
1) The facility was not in compliance with the specific regulatory requirement(s) (as
referenced by the specific F-tag or K-tag) at the time the situation occurred;
2) The noncompliance occurred after the exit date of the last standard recertification
survey and before the survey (standard, complaint, or revisit) currently being
conducted; and
3) There is sufficient evidence that the facility corrected the noncompliance and is in
substantial compliance at the time of the current survey for the specific
regulatory requirement(s), as referenced by the specific F-tag or K-tag.
A nursing home does not provide a plan of correction for a deficiency cited as past
noncompliance as the deficiency is already corrected; however, the survey team
documents the facility’s corrective actions on Form CMS-2567.
5300.5 - Task 7: Exit Conference
(Rev. 18, Issued: 03-17-06; Effective/Implementation Dates: 03-17-06)
Advice the Administrator of the complaint investigation findings and any deficiencies
identified. Do not inform him/her of confidential information unless the individual who
provided the information specifically authorizes you to do so.
If a deficiency is not present now, but was present and has been corrected, notify the
facility orally and in writing that the complaint was substantiated because deficiencies
existed at the time that the complaint situation occurred. (See SOM Chapter 7, Survey
SOM Chapter 5 - Page 41
and Enforcement Process for Skilled Nursing Facilities and Nursing Facilities, for
specific information about citing past noncompliance.)
If the complaint is unsubstantiated, i.e., the surveyor(s) cannot determine that it occurred
and there is no indication of deficient practice, notify the facility of this decision.
5310 - Action on Complaints of Resident Neglect and Abuse, and
Misappropriation of Resident Property
(Rev. 18, Issued: 03-17-06; Effective/Implementation Dates: 03-17-06)
5310.1 - Written Procedures
(Rev. 18, Issued: 03-17-06; Effective/Implementation Dates: 03-17-06)
The State must have written procedures for the timely review and investigation of
allegations of resident abuse and neglect, and misappropriation of resident property.
5310.2 - Review of Allegation
(Rev. 18, Issued: 03-17-06; Effective/Implementation Dates: 03-17-06)
The State Reviews all allegations of resident neglect and abuse and misappropriation of
resident property regardless of the source of the complaint.
5310.3 - Investigating Allegations
(Rev. 18, Issued: 03-17-06; Effective/Implementation Dates: 03-17-06)
If there is reason to believe, either through oral or written evidence, that an individual
used by a facility to provide services to residents could have abused or neglected a
resident or misappropriated a resident's property, the State must investigate the allegation.
During the investigation, the SA should evaluate how the facility developed policies and
procedures to prevent the abuse, and after the abuse occurred, how the facility took action
to report and investigate the allegations while ensuring the safety of the residents.
5310.4 - Factors Beyond the Control of the Individual
(Rev. 18, Issued: 03-17-06; Effective/Implementation Dates: 03-17-06)
The State must not make a finding that an individual neglected a resident if the individual
demonstrates that such neglect was caused by factors beyond the control of the
individual.
SOM Chapter 5 - Page 42
EXAMPLE: A nurse aide could not be found negligent for not providing clean bed and
bath linens to a resident if the facility had no clean bed and bath linens available.
However, the facility is responsible for providing clean bed and bath linens to residents.
5320 – Reporting Findings of Abuse, Neglect, or Misappropriation of
Property to the Nurse Aide Registry
(Rev. 18, Issued: 03-17-06; Effective/Implementation Dates: 03-17-06)
5320.1 - Notification Procedures - Preliminary Determinations
(Rev. 18, Issued: 03-17-06; Effective/Implementation Dates: 03-17-06)
If the State makes a preliminary determination, based on oral or written evidence and its
investigation, that resident neglect, abuse, or misappropriation of property has occurred,
the State completes the following notification procedures:
1. Individuals Notified - The State notifies the following individuals in writing
within 10 working days of the investigation:
a. Individual(s) implicated in the investigation; and
b. The current administrator of the facility in which the incident occurred.
2. Notice Information - The following information is included in the notice:
a. Nature of the allegation (specific facts);
b. Date and time of the occurrence;
c. A statement that the individual implicated in the investigation has a right to a
hearing and must request the hearing within 30 days from the date of the
notice. Provide the individual with the specific information needed to request
a hearing, such as the name and address of a contact in the State to request a
hearing;
d. Statement that if the individual fails to request a hearing, in writing, within 30
days from the date of the notice, the presumed substantiated findings is
reported to the nurse aide registry or the appropriate licensure authority;
e. The intent to report findings substantiated by a hearing in writing to the nurse
aide registry and/or to the appropriate licensure authority;
f. Consequences of waiving the right to a hearing;

SOM Chapter 5 - Page 43
g. Consequences of a finding through the hearing process that the resident abuse
or neglect, or misappropriation of property did occur; and
h. Right of the accused individual to be represented by an attorney at the
individual’s own expense.
5320.2 - Conduct of Hearing for Nurse Aides
1- Time frame to Complete the Hearing
The State must complete the hearing and the hearing record within 120 days from the day
it receives the request for a hearing.
2 - Hearing Location
The State must hold the hearing in a manner consistent with State practice at a reasonable
place and time convenient for the individual.
5320.3 - Reporting Findings
1 - Reporting to Entities
If the individual waives the right to a hearing or the time to request a hearing has expired,
or if the hearing finding is that the individual neglected or abused a resident or
misappropriated a resident’s property, the substantiated findings must be reported in
writing within 10 working days to:
a. The individual;
b. Current administrator of the facility in which the incident occurred;
c. The administrator of the facility that currently employs the individual, if it is not
the same facility in which the incident occurred;
d. Applicable licensing authorities; and
e. The nurse aide registry for nurse aides as specified in 42 CFR 483.156(c) and
discussed in §4141. Section 4141 discusses the function of the registry, the
information contained in the registry, and responsibility for the registry.
2 - Information Submitted to the Nurse Aide Registry
The following information must be included and remain in the registry permanently,
unless the finding was made in error, the individual was found not guilty in a court of
law, or the State is notified of the individual’s death. See §4141.B.

SOM Chapter 5 - Page 44
a. Documentation of the investigation, including the nature of the allegation and the
evidence that led to the conclusion that the allegation was valid;
b. The date of the hearing, if the individual chose to have one, and its outcome; and
c. A statement by the individual disputing the allegation if the individual chose to
make one.
3 - Information Retained in the Nurse Aide Registry Permanently
The registry must remove entries for individuals who have performed no nursing or
nursing-related services for 24 consecutive months, unless the individual’s registry entry
includes documented findings of abuse, neglect, or misappropriation of property.
5330 - Reporting Abuse to Law Enforcement and the Medicaid Fraud
Control Unit
When the SA or RO substantiates a finding of abuse, the SA or RO must report the
substantiated findings to local law enforcement and, if appropriate, the Medicaid Fraud
Control Unit.
5340 - Post-Survey Certification Actions for Nursing Homes
Following the investigation, the SA records any findings on Form CMS-2567 and sends
the provider a copy of Form CMS-2567. The SA requests a POC for any uncorrected
deficiencies. See §2728.
When Federal deficiencies are identified, the SA initiates certification actions as follows:
1. Noncompliance that Constitutes Immediate Jeopardy to Resident Health
and Safety - The SA initiates procedures in accordance with §§7307 to 7309.
2. Noncompliance that Does Not Constitute Immediate Jeopardy to Resident
Health and Safety - The SA initiates procedures in accordance with §§7311 to
7316.
3. In Substantial Compliance - The SA initiates procedures in accordance with
§7319.
5350 – Data Entry
(Rev. 18, Issued: 03-17-06; Effective/Implementation Dates: 03-17-06)
The SA enters survey information into the ASPEN system (via ASPEN Central Office or
ACTS), including Forms CMS-670 and CMS-2567.
SOM Chapter 5 - Page 45
5360 - Processing of Complaints Originating with or Investigated by the
CMS RO
(Rev. 18, Issued: 03-17-06; Effective/Implementation Dates: 03-17-06)
The RO establishes procedures and clear organizational accountability to ensure that any
complaint is properly evaluated, documented, acknowledged, and handled timely and
appropriately. The RO uses ACTS to ensure timely and appropriated action on all
allegations originating with or investigated by the RO.
The extent and nature of RO involvement with a given complaint varies depending on the
nature of the allegation and the receiving organization. The following procedures address
the major variants of RO involvement.
5370 - Pre-Investigation Actions on Allegations Originating Through
the RO
(Rev. 18, Issued: 03-17-06; Effective/Implementation Dates: 03-17-06)
Most complaints originate through the SA and are recorded and controlled by the SA.
When a complaint is filed directly with the RO, however, the RO assumes those initial
SA responsibilities.
5380 - RO Processing of RO Investigated Complaints
(Rev. 18, Issued: 03-17-06; Effective/Implementation Dates: 03-17-06)
This less frequent class of complaints includes allegations retained by the RO or
forwarded to the RO by the SA for investigation or special processing. The RO
responsibilities vary based on the type of complaint.
1 - Direct RO Investigation
These procedures apply when a direct RO investigation is conducted. When directly
investigating, the RO begins by ensuring that it or the SA has met all intake,
acknowledgment, and priority assignment requirements in §5010 to §5020.
2 - Conducting the Investigation
The RO follows the procedures for investigation in §5300.

SOM Chapter 5 - Page 46
3 – RO Certification Actions
When Federal deficiencies are identified, the RO initiates certification actions as follows:
a. Noncompliance that Constitutes Immediate Jeopardy to Resident Health and
Safety - The RO initiates procedures in accordance with §§7307 to 7309. The RO
performs the SA responsibilities described in these sections.
b. Noncompliance that Does Not Constitute Immediate Jeopardy to Resident Health
and Safety - The RO initiates procedures in accordance with §§7311 to 7316.
c. In Substantial Compliance - The RO initiates procedures in accordance with
§7319.
4 - Reporting
The RO should report survey information into the ASPEN system (via ASPEN Central
Office or ACTS), including Forms CMS-670 and CMS-2567.
5390 – RO Oversight of Complaint-Related Processes
(Rev. 18, Issued: 03-17-06; Effective/Implementation Dates: 03-17-06)
1. The RO considers any complaint data in targeting look-behind surveys or reviews.
2. The RO monitors data in summary form - either through a log or data system. See
§5060.
These records should include:
• Identification of region or State-wide patterns;
• Pinpointing of problem providers or States;
• Evaluation of SA processing times, workloads, performance, etc.; and
• Identification of overall SA workloads, including unsubstantiated and Medicaid-
only complaint volumes.
3. Based on needs identified from oversight activities, the RO provides SA training and
technical assistance.
NOTE: Sections 5400 to 5480.2 relate to alleged EMTALA violations.
SOM Chapter 5 - Page 47
5400 - Investigations Involving Alleged Emergency Medical Treatment
and Labor Act (EMTALA) Violations
(Rev. 18, Issued: 03-17-06; Effective/Implementation Dates: 03-17-06)
Section 1866 of the Act, Agreements with Providers of Services, specifies that for a
hospital, or any provider of services, to qualify for participation in the Medicare program,
it must enter into an agreement with the Secretary of HHS. Effective August 1, 1986,
participating hospitals with emergency departments must comply with the requirements
of §1867 of the Act as a condition of their provider agreement.
The following Medicare provider agreement requirements, which closely parallel
provisions contained in §1866of the Act, must be met by Medicare participating hospitals
with emergency departments:
• 42 CFR 489.20(l) requires a hospital to comply with the requirements of 42 CFR
489.24. Section 1866(a)(1)(I) of the Act requires a hospital to have and enforce
policies to ensure compliance with the requirements of §1867;
• 42 CFR 489.20(m) requires a hospital to report to CMS or the SA any time it has
reason to believe it may have received an individual who has been transferred in
an unstable emergency medical condition (EMC) from another hospital in
violation of the requirements of 42 CFR 489.24(e);
• 42 CFR 489.20(q) requires a hospital to post conspicuously a sign(s) specifying
the rights of individuals, under §1867 of the Act, with respect to examination and
treatment for emergency medical conditions and women in labor and to indicate
whether or not the hospital participates in the Medicaid program. The letters
within the signs must be clearly readable at a distance of at least 20 feet or the
expected vantage point of the emergency department clients. The wording of the
sign(s) must be clear and in simple terms and language(s) that are understandable
by the population served by the hospital;
• 42 CFR 489.20(r)(1) requires a hospital to maintain medical and other records
related to individuals transferred, including discharges, to or from the hospital for
a period of five years from the date of transfer;
• 42 CFR 489.20(r)(2) requires a hospital to maintain a list of physicians who are
on call to provide treatment necessary to stabilize an individual with an
emergency medical condition;
• 42 CFR 489.20(r)(3) requires a hospital to maintain a central log on each
individual who comes seeking assistance and whether he or she refused treatment,
was refused treatment, or whether the individual was transferred, admitted and
treated, stabilized and transferred, or discharged.
SOM Chapter 5 - Page 48
When hospitals do not conform to the requirements of §1867 of the Act, the practice is
commonly called “dumping.” A hospital with a dedicated emergency department is
defined in 42 CFR 489.24(b) as a hospital that offers services for emergency medical
conditions within its capacity to do so. The regulations at 42 CFR 489.24 parallel the
provisions of §1867 of the Act and contain the following requirements that a hospital
with a dedicated emergency department must meet:
• 42 CFR §489.24(a) General. Applicability of provisions of this section.
• 42 CFR §489.24(b) Definitions. As used in this section.
• 42 CFR §489.24(c) Use of dedicated emergency department for non-emergency
services.
• 42 CFR §489.24(d) Necessary stabilizing treatment for emergency medical
conditions.
• 42 CFR §489.24(d)(1) General. Subject to the provisions of paragraph (d)(2).
• 42 CFR §489.24(d)(2) Exception: Application to inpatients.
• 42 CFR §489.24(d)(3) Refusal to consent to treatment.
• 42 CFR §489.24(d)(4) Delay in examination or treatment.
• 42 CFR §489.24(d)(5) Refusal to consent to transfer.
• 42 CFR §489.24(e) Restricting transfer until the individual is stabilized.
• 42 CFR §489.24(e)(1) General.
• 42 CFR §489.24(e)(2) Appropriate transfer to another medical facility.
• 42 CFR §489.24(e)(3) Provides whistleblower protection to physicians and
qualified medical personnel.
• 42 CFR §489.24(f) Recipient hospital responsibilities.
• 42 CFR §489.24(g) Termination of provider agreement.
• 42 CFR §489.24(h) Consultation with Quality Improvement Organization (QIO).
• 42 CFR §489.24(i) Release of QIO Assessment.
• 42 CFR §489.24(j) Availability of on-call physicians.
SOM Chapter 5 - Page 49
• 42 CFR §489.24 (j)(1) On-call list.
• 42 CFR §489.24 (j)(2) Hospital on-call policy and procedures.
If a hospital fails to meet these requirements, CMS may terminate the provider agreement
in accordance with 42 CFR 489.53. The Office of the Inspector General (OIG) has the
responsibility and authority to assess civil monetary penalties (CMPs) or to exclude
physicians from the Medicare program when a hospital or physician violates these
requirements. Additionally, individuals suffering personal harm and medical facilities
suffering financial loss as a result of a violation of these provisions can bring civil action
against the offending hospital and physicians. Filing for such civil action is limited to a
period of 2 years after the date of the alleged violation. This legislation does not preempt
any State or local laws, except to the extent that State or local requirements directly
conflict with a requirement of this legislation.
5410 – EMTALA and Born-Alive Infants Protection Act of 2002
(Rev. 18, Issued: 03-17-06; Effective/Implementation Dates: 03-17-06)
5410.1 - Interaction of the Born-Alive Infant Protection Act and
EMTALA
(Rev. 18, Issued: 03-17-06; Effective/Implementation Dates: 03-17-06)
With the definition of the terms “person” and “individual” codified at 1 U.S.C. §8, it is
clear that there are circumstances where EMTALA protections are applicable to an infant
who is born alive, as that term is defined in 1 U.S.C. §8(b).
For example, assume that a hospital’s labor and delivery department meets the definition
of a “dedicated emergency department.” If an infant was born alive in that dedicated
emergency department, and a request was made on that infant’s behalf for screening for a
medical condition, (or if a prudent layperson would conclude, based on the infant’s
appearance or behavior, that the infant needed examination or treatment for an
emergency medical condition and that a request would have been made for screening) the
hospital and physician could be liable for violating EMTALA for failure to provide such
a screening examination. The born-alive infant is a “person” and an “individual” under 1
U.S.C. § 8(a) and the screening requirement of EMTALA applies to “any individual”
who comes to the emergency department.
Another example is a case of an infant born alive elsewhere on the hospital’s campus
(i.e., not in the hospital’s dedicated emergency department) and a prudent layperson
observer concluded, based on the born-alive infant’s appearance or behavior, that the
infant was suffering from an emergency medical condition. In such a circumstance, the
hospital and its medical staff are required to perform a medical screening examination on
that infant to determine whether or not an emergency medical condition existed. If the

SOM Chapter 5 - Page 50
hospital or its medical staff determined that the infant was suffering from an emergency
medical condition, the hospital has an obligation to admit the infant, or to comply with
either the stabilization requirement or the transfer requirement of EMTALA. The born-
alive infant is a “person” and an “individual,” as described above, and the stabilization
and transfer requirements of EMTALA apply to “any individual” who comes to the
hospital.
Finally, a third example is when the hospital admits a born-alive infant. EMTALA does
not apply to inpatients. If a born–alive infant is admitted to the hospital, EMTALA would
not apply to protect the infant in most circumstances. However, the Medicare COPs
would apply to the infant once he or she was admitted to the hospital as an inpatient.
5410.2 - Conduct of Investigations
(Rev. 18, Issued: 03-17-06; Effective/Implementation Dates: 03-17-06)
If a complaint indicates that a born-alive infant has been denied a screening examination,
stabilizing treatment, or an appropriate transfer, the complaint is prioritized as an alleged
EMTALA violation. It is not necessary to determine that the hospital acted with an
improper motive in any failure to provide a screening examination, stabilizing treatment,
or an appropriate transfer in order to conclude that an EMTALA violation has occurred.
The Supreme Court of the United States has held that a finding of improper motive is not
required to conclude that an EMTALA violation has occurred.
5420 - Basis for Investigation
(Rev. 18, Issued: 03-17-06; Effective/Implementation Dates: 03-17-06)
The SA enters alleged EMTALA violations into ACTS. The RO approves or disapproves
requests for EMTALA investigations in ACTS.
5430 - RO Direction of Investigation
(Rev. 18, Issued: 03-17-06; Effective/Implementation Dates: 03-17-06)
5430.1 - Evaluation of Allegation
(Rev. 18, Issued: 03-17-06; Effective/Implementation Dates: 03-17-06)
The RO evaluates all complaints and refers to the SA those that warrant SA investigation.
The SA or the RO sends a letter to the complainant acknowledging the complaint and
informing the complainant of whether an investigation is warranted. The SA’s
responsibility is to verify whether a violation of 42 CFR 489.24 and/or the related
requirements at 42 CFR 489.20 occurred, and if there were other violations.
SOM Chapter 5 - Page 51
5430.2 - Request for Investigation of Allegations
(Rev. 18, Issued: 03-17-06; Effective/Implementation Dates: 03-17-06)
The RO gives an initial verbal authorization to the SA to investigate the EMTALA
allegation, and then completes Form CMS-1541A in ACTS. If the RO identifies
Medicare conditions or standards it wants the SA to survey, related to the EMTALA
allegation at a deemed hospital, the RO completes Form CMS-2802 in ACTS. If the RO
identifies conditions or standards it wants the SA to survey related to the EMTALA
allegation at a non-deemed hospital, it directs the SA to conduct a survey by completing
Form CMS-1541A in ACTS.
5440 - Conducting an Investigation
(Rev. 18, Issued: 03-17-06; Effective/Implementation Dates: 03-17-06)
5440.1 - Selecting the Team
(Rev. 18, Issued: 03-17-06; Effective/Implementation Dates: 03-17-06)
The SA selects surveyors with a background in the profession or area to be investigated.
Preferably, the surveyors should have acute care training and experience. All surveyors
must be adequately trained in the evaluation of 42 CFR 489.24 cases. Physicians should
have experience in peer review.
5440.2 - Scheduling the Investigation
(Rev. 18, Issued: 03-17-06; Effective/Implementation Dates: 03-17-06)
Allegations of EMTALA violation against a non-deemed or deemed hospital represent a
probable immediate jeopardy to the next individual who comes to the hospital requesting
examination and treatment for an emergency medical condition. Therefore, complete the
investigation within five working days after receipt of the telephone authorization from
the RO. The onsite investigation must be conducted on consecutive working days. The
survey must be completed promptly and is not to be interrupted by other activities. DO
NOT ANNOUNCE ANY INVESTIGATIONS.
5440.3 - Guidelines for Surveyors Conducting Investigations
(Rev. 18, Issued: 03-17-06; Effective/Implementation Dates: 03-17-06)
Attention to Procedures
The purpose of conducting the investigation is to ascertain whether or not the hospital
violated the EMTALA requirements. The survey must be in accordance with applicable
SOM Chapter 5 - Page 52
survey procedures and policies. Review instructions in Appendix V, before beginning
the investigation. The guidelines provide a detailed interpretation of the regulations.
Involvement of Complainants
Complainants, if known, receive a letter of acknowledgment from the SA or RO. Do not
disclose the identity of complainants. When information obtained during the
investigation appears to be in conflict with the information supplied by the complainant,
consult with the complainant, if this can be done without disclosing the person’s identity.
5440.4 - Conducting the Investigation
(Rev. 18, Issued: 03-17-06; Effective/Implementation Dates: 03-17-06)
A complete investigation consists of assessment of the following components:
• Completeness, adequacy and enforcement of policies and procedures which
address the provisions of 42 CFR 489.24;
• Prompt reports to the SA or CMS of receipt of an improperly transferred
individual by the receiving hospital;
• Presence and completeness of signs posted in emergency departments specifying
the rights of individuals under 42 CFR 489.24, and information indicating
whether the hospital participates in the Medicaid program;
• Maintenance of medical and other records related to individuals transferred to or
from the hospital for a period of five years from the date of transfer, including
discharged patients;
• Maintenance of a list of physicians who are on call to provide necessary
stabilizing treatment;
• Maintenance of a central log on each individual who comes to the hospital
seeking emergency services;
• Provision of an appropriate medical screening examination sufficient to determine
the presence of an emergency medical condition;
• Provision of necessary stabilizing treatment;
• Provision of no delay in examination or treatment in order to inquire about
insurance status or capability for payment;
• Provision of an appropriate transfer to another medical facility/provider;
SOM Chapter 5 - Page 53
• Provision of whistleblower protections; and
• Adequacy of responsibilities of the recipient hospital with specialized capabilities
(nondiscrimination).
The survey tasks are listed below for easy reference. See Appendix V for detailed
guidance.
• Task 1: Entrance Conference;
• Task 2: Case Selection Methodology;
• Task 3: Record review;
• Task 4: Interviews;
• Task 5: Exit Conference;
• Task 6: Professional Medical Review; and
• Task 7: Assessment of Compliance and Completion of the Deficiency Report.
After the investigation is concluded, complete a Form CMS-1541B (Exhibit 137). If one
or more of the provisions of EMTALA are not met, complete Form CMS-2567, using
“Principles of Documentation.” Describe in detail the facts of each individual case. In
addition, specify whether the hospital was aware of the problem and took steps to remedy
it prior to the survey. If a SA physician was a member of the investigation team, include
the medical review of the case. Use the “Physician Review Outline for Emergency Care
Obligations of Medicare Hospitals,”
(Exhibit 138) for this purpose. In addition, complete
Form CMS-562. All the forms must be signed, showing the professional titles of all
participating surveyors, and dated.
A hospital may have multiple sites listed under its Medicare provider number. These sites
may not be in close proximity of each other and each site may have its own dedicated
emergency department (DED). In cases where the alleged EMTALA violation is against
a specific site of the hospital, the surveyors should focus their survey investigation at the
hospital site mentioned in the complaint intake. However, the surveyors should review
all EMTALA related Policies and Procedures of all sites of the hospital. The surveyors
need to survey the other sites of the hospital if the survey findings indicate that the
potential EMTALA violation maybe widespread.

SOM Chapter 5 - Page 54
5440.5 - Exit Conference
(Rev. 18, Issued: 03-17-06; Effective/Implementation Dates: 03-17-06)
It is usually desirable and appropriate to conduct an exit conference. The surveyor(s) may
outline the basic facts uncovered during the onsite investigation. However, the
surveyor(s) must inform the hospital that the RO makes the final compliance
determination, and the determination is often made with information obtained after the
onsite investigation. Do not reveal the complainant and do not venture an opinion on
what determination the RO might make. The exit conference should include a
description of the process that is followed if the RO determines that a violation has
occurred.
5450 - Forwarding Report of Investigation to the RO
(Rev. 18, Issued: 03-17-06; Effective/Implementation Dates: 03-17-06)
Transmit the results of the investigation and your recommendations to the RO through
ACTS within 10 working days following completion of the onsite survey, if it appears
there may be an EMTALA violation. If there appears to be no violation, this time frame
may be extended to 15 working days, in order to allow the SA additional processing time.
Transmit the following materials to the RO through ACTS:
• Form CMS-562,”Medicare/Medicaid/CLIA Complaint Form;”
• Form CMS-1541B, “Responsibilities of Medicare Participating Hospitals in
Emergency Cases Investigation Report.” Recommend one or more of the actions
below on the form:
o None - This means the complaint was not substantiated;
o In Compliance, but Previously Out of Compliance - This means that the
hospital identified the problem on its own and took effective corrective
action prior to the investigation. In addition to this recommendation,
document on the Form CMS-2567 when the hospital identified the
violation or a similar problem, the corrective action taken, and the date of
such action. Also, document that the hospital has had no violations or
similar problems for at least the past 6 months;
o Recommend Termination (23 calendar day track) - This means that the
hospital is out of compliance with 42 CFR 489.24 or the related
requirements at 42 CFR 489.20(l), (m), (q) or (r) and the violation presents
an immediate jeopardy to patient health and safety;

SOM Chapter 5 - Page 55
o Recommend Termination (90 calendar day track) - This means that the
hospital is out of compliance with 42 CFR 489.24 or the related
requirements at 42 CFR 489.20(l), (m), (q) or (r), but the violation does
not present an immediate jeopardy to patient health and safety;
o Request Physician Review. This means that it is recommended that the
RO obtain a medical review of the case;
o Possible Discrimination. This means that it is believed that
discrimination occurred based on financial status, race, color, nationality,
handicap, or diagnosis.
• Form CMS-670, “Survey Team Composition and Workload Report;”
• Form CMS-2567, “Statement of Deficiencies and POC;”
NOTE: If the hospital had identified the deficiency and took corrective action
prior to the investigation, indicate on the Form CMS-2567 that the
requirement was not met. However, indicate on the Form CMS-2567
and the narrative report that the hospital took corrective action prior to
the investigation, what action was taken, and for how long the hospital
has been in compliance.
• Physician Review Outline for Emergency Care Obligations of Medicare Hospital
(if physician review was done by SA);
• Complaint investigation narrative;
• Copies of pertinent hospital policies and procedures that relate to the identified
deficiencies;
• Summary listing of all patients comprising the sample, including an explanation
of how and why the cases were selected for review;
• Summary of interviews.
Transmit the following to the RO by overnight mail:
• Copies of medical records for substantiated cases, medical records of individuals
named in the complaints, and other medical records for which a QIO review is
requested;
• Certification of benefits versus risks of the transfer, if this is a transfer case.

SOM Chapter 5 - Page 56
5460 - RO Review of Investigation
(Rev. 18, Issued: 03-17-06; Effective/Implementation Dates: 03-17-06)
Upon receiving the case from the SA, the RO has 10 working days to review the
investigation findings. The RO requests a 5-day advisory medical review of the case by
the QIO to determine if there is an EMTALA violation. The RO has 5 working days to
review the case upon return from the QIO. With this information, and any other
additional information, the RO determines whether the hospital complied with the
EMTALA requirements and determines whether the violation constitutes an immediate
jeopardy to patient health and safety.
Prior to determining compliance or noncompliance, the RO is encouraged to confer with
the State Agency, and may confer with the hospital’s representatives. The RO shares as
much data as possible in accordance with current Privacy Act requirements.
5460.1 - Hospital Is In Compliance - No Past Violation
(Rev. 18, Issued: 03-17-06; Effective/Implementation Dates: 03-17-06)
If the RO determines that the allegation is not substantiated and that the hospital is in
compliance with 42 CFR 489.24 and/or the related requirements at 42 CFR 489.20, the
RO notifies the hospital and forwards a copy of the letter to the SA. If the SA received
the complaint, it notifies the complainant that the complaint was not substantiated. If the
RO received the complaint, the RO notifies the complainant.
5460.2 - Hospital Is In Compliance - Past Violation, No Termination
(Rev. 18, Issued: 03-17-06; Effective/Implementation Dates: 03-17-06)
If the RO determines that the allegation was substantiated, but the hospital had identified
the violation on its own, took effective corrective action prior to the investigation, and
has had no EMTALA violations for at least the past 6 months, termination action is not
initiated. The RO notifies the hospital via a “Past Violation - No Termination Letter.”
The SA receives a copy of the letter through ACTS. The RO or SA sends a letter to the
complainant regarding the outcome of the investigation. Although no termination action
is taken, the RO refers past violations of 42 CFR 489.24 to the OIG for assessment of
civil monetary penalties (CMPs) if warranted.
5460.3 - Hospital Is Not in Compliance - Immediate Jeopardy to Patient
Health and Safety
(Rev. 18, Issued: 03-17-06; Effective/Implementation Dates: 03-17-06)
If the RO determines that the hospital is not in compliance and the violation represents an
immediate jeopardy to patient health and safety, the RO follows a 23 calendar-day

SOM Chapter 5 - Page 57
termination process. The termination procedures in §3010 are followed. Uncorrected
deficiencies that resulted in a violation of 42 CFR 489.24 may pose an immediate
jeopardy to people seeking emergency care. The RO notifies the complainant that the
complaint was substantiated. It also informs the hospital in writing of the specific
violations via a preliminary determination letter, and sends the hospital a copy of Form
CMS-2567. The SA receives a copy of the letter through ACTS.
5460.4 - Hospital Is Not in Compliance - Situation Does Not Pose an
Immediate Jeopardy to Patient Health and Safety
(Rev. 18, Issued: 03-17-06; Effective/Implementation Dates: 03-17-06)
If the RO determines that the hospital is not in compliance with the EMTALA
requirements, but the violation does not pose an immediate jeopardy to patient’s health
and safety, or the hospital took corrective action after the investigation to remove the
immediate jeopardy, the RO follows a 90 calendar-day termination process. The
termination procedures in §3012 are followed. The RO notifies the complainant that the
complaint was substantiated. The RO informs the hospital, in writing, of the specific
violations via a preliminary determination letter and sends the hospital a copy of Form
CMS-2567. The SA receives a copy of the letter through ACTS.
Examples of noncompliance that usually do not pose an immediate jeopardy:
1. A transfer which was appropriate, but not signed or dated by the physicians;
2. An appropriate, functioning, central log that on one particular day is not fully
completed; and
3. A written hospital policy that is missing, but is nonetheless being implemented.
The fact that the hospital has completed a POC should not be interpreted to mean that the
hospital admits violating the EMTALA requirements. However, the hospital is included
on the log of facilities with EMTALA violations, with the notation that an acceptable
POC was received by CMS, and termination action was stopped.
5465 - Procedures for the 5-day QIO Review of Alleged Violations of 42
CFR 489.24
(Rev. 18, Issued: 03-17-06; Effective/Implementation Dates: 03-17-06)
Prior to terminating a hospital from the Medicare program because of possible
violation(s) of EMTALA, the RO requests the QIO to assess whether the individual
involved was provided an appropriate medical screening examination, stabilizing
treatment, or an appropriate transfer as required by EMTALA.

SOM Chapter 5 - Page 58
The QIO 5-day review is mandatory if the RO determines that a case involves a possible
violation of 42 CFR 489.24 to support possible termination action against a hospital if in
fact it violated EMTALA. The RO is responsible for providing the QIO with all
information relevant to the case that is within its possession and control. The RO sends
the “Physician Review Outline for Emergency Care Obligations of Medicare Hospitals,”
(Exhibit 138) to capture this information. The QIO completes the review within 5
working days upon the receipt of RO’s request. The QIO sends the case file back to the
RO including a copy of the review report. It is not required that the physician reviewer
give the hospital and/or the physician an opportunity to respond to the allegations at this
time. If the affected physician and/or hospitals have questions concerning the case, they
are to consult with the RO.
The QIO Review is not required in cases where a delay in effecting a sanction would
jeopardize the health and safety of individuals or in situations where medical review is
inappropriate (e.g., cases where the individual was denied a medical screening
examination). The QIO 5-day review is required to seek medical expertise on whether
the individual was adequately screened, examined and treated.
The RO shall release upon request the 5 day QIO review to the affected physician and/or
hospital, after the RO has made a determination as to whether the hospital violated or is
in compliance with EMTALA. In addition, the RO may release the QIO review to the
complainant or his/her representative upon request. The physician reviewer’s identity is
confidential, therefore, when releasing the QIO report the physician’s identity is not to be
disclosed unless he or she consents to the release of their identity in accordance with the
disclosure regulations at 42 CFR 480.132 and 480.133.
The cases in which the RO determined that the hospital was in compliance with
42 CFR
489.24 but in violation of 42 CFR 489.20 of the EMTALA regulation do not need to be
forwarded to the QIO for review. The RO takes action as warranted.
5470 - Termination Procedures for EMTALA Violations
(Rev. 18, Issued: 03-17-06; Effective/Implementation Dates: 03-17-06)
5470.1 - Procedures for Termination when the EMTALA Violation is an
Immediate Jeopardy to Patient Health and Safety
(Rev. 18, Issued: 03-17-06; Effective/Implementation Dates: 03-17-06)
In cases where the RO determined that an immediate jeopardy existed, after a 5-day QIO
advisory review has been completed, the RO follows the termination procedures in
§3010. The processing timeframes are the maximum allowed. The termination
procedures are not postponed or stopped unless evidence of correction of the deficiencies
or proof that the violation did not exist is provided by the hospital to the RO. The RO
forwards the supporting documents to the QIO (for a 60 day QIO review) in order to
provide a medical opinion on the case. The RO refers the case to the OIG that has the

SOM Chapter 5 - Page 59
responsibility for assessment of CMPs against the hospital and/or physician and
physician exclusion provisions for violations of 42 CFR 489.24. The case is also referred
to the Office for Civil Rights (OCR) because OCR may take action under the Hill-Burton
Subpart G Community Services regulations at 42 CFR 124.603(b) (1).
The termination track starts on the date that the RO makes the determination of
noncompliance with 42 CFR 489.24. It is the date of the preliminary determination
letter. The letter is forwarded to the hospital by the fastest method available (fax, e-mail
or telephone). In addition, a written letter follows up by mail. The preliminary
determination letter informs the hospital of:
• The RO’s findings based on the investigation and the results of medical review;
• The projected termination date (the 23rd calendar day from the date of the
preliminary determination letter);
• The date on which the RO issues a Notice of Termination Letter and notifies the
public (at least two calendar days, but no more than four calendar days prior to
the termination date); and
• That the hospital may avoid the termination action and notice to the public by
either providing acceptable POCs for the deficiencies or by successfully showing
that the deficiencies did not exist. In either case, the necessary information must
be furnished to the CMS RO in time for the SA to verify the corrections before
the projected termination date.
If, during the resurvey, the SA finds that the provider had implemented systems and
processes to ensure that the likelihood of further violation is remote and there is adequate
evidence that the provider is in compliance with the requirements, the termination action
is rescinded and the provider is put back in compliance.
If, during the resurvey, the SA finds that the provider has not adequately implemented
systems and processes to ensure compliance, the RO gives the hospital an additional 67
days or a total of 90 days (23 plus 67) to achieve compliance.
This allows the hospital time to prove that the corrective action is good for the long-term
(i.e., the corrective action is adequate to ensure that no further violations will occur). The
RO directs the SA to conduct a second survey by the 60th calendar day. On the resurvey,
the surveyor(s) reviews patients’ emergency department (ED) records and other relevant
documents for the period since the last survey to assess continued compliance. If the
hospital fails to achieve compliance, it is terminated from the Medicare program. The
RO sends the complainant a letter reporting the final results of the investigation.
If the termination takes place and the hospital desires to become re-certified as a
Medicare provider, the hospital must provide reasonable assurance that compliance will
be maintained. The procedures at §2016 are followed.
SOM Chapter 5 - Page 60
5470.2 - Procedures for Termination When the EMTALA Violation is
Not Immediate Jeopardy to Patient Health and Safety
(Rev. 18, Issued: 03-17-06; Effective/Implementation Dates: 03-17-06)
In cases where the RO determined that a violation existed but not an immediate jeopardy,
after a 5-day QIO advisory review has been completed when it was warranted, the RO
follows the termination procedures in §3012 The processing timeframes are the
maximum allowed. The termination procedures are not postponed or stopped unless
evidence of correction of the deficiencies or proof that the violation did not exist is
provided to the RO by the hospital. If warranted, the RO forwards supporting documents
to the QIO (for a 60 day QIO review) in order to provide a medical opinion on the case.
The RO refers the case to the OIG, if warranted, that has the responsibility for assessment
of CMPs against the hospital and/or physician and physician exclusion provisions for
violations of 42 CFR 489.24 The case is also referred to the Office for Civil Rights
(OCR) because OCR may take action under the Hill-Burton Subpart G Community
Services regulations at 42 CFR 124.603(b)(1)
The termination track starts on the date that the RO makes the determination of
noncompliance with
42 CFR 489.24 and/or the related requirements at 42 CFR 489.20. It
is the date of the preliminary determination letter.
5480 - Procedures for QIO Review of Confirmed EMTALA Violation
(Rev. 18, Issued: 03-17-06; Effective/Implementation Dates: 03-17-06)
Before imposing sanctions under §1867 of the Act for violations of 42 CFR 489.24, 42
CFR 489.24(h) requires that CMS obtain consultation from the QIO. The OIG holds the
authority to assess CMPs against the hospital or physicians or to exclude physicians from
the Medicare program for violations of
42 CFR 489.24.
5480.1 - Procedures for Coordinating 60 day QIO Review
(Rev. 18, Issued: 03-17-06; Effective/Implementation Dates: 03-17-06)
The RO requests the QIO to provide a medical opinion on EMTALA violation cases
within 60 calendar days. The cases referred for 60-day QIO review are outlined in
§5480B. The RO uses the “Model Letter Requesting QIO Review of a Confirmed
Violation of 42 CFR 489.24 for Purposes of Assessing Civil Monetary Penalties or
Excluding Physicians,” (Exhibit 212). The QIO provides the physician and the hospital
reasonable notice of its review a reasonable opportunity for discussion, and an
opportunity for the physician and hospital to submit additional information before issuing
its report. (Instructions on notice of review and opportunity for discussion, and
additional information that follow the regulatory requirements in 42 CFR 489.24(h) are
found in §§9100-9150 of the QIO Manual.)
SOM Chapter 5 - Page 61
The RO is responsible for providing the QIO with all information relevant to the case that
is within its possession and control. The RO sends the “Physician Review Outline for
Emergency Care Obligations of Medicare Hospitals,” (Exhibit 138) to capture this
information. This outline is helpful for organizing the review of the medical record. The
specialty of the reviewing physician should be matched to the specialty of the physician
who attended the patient and/or the individual’s medical condition. If the patient was not
seen by a physician, the QIO uses the diagnosis of the patient or the usual physician
assignment practice of the hospital to determine the specialty of the physician reviewer.
Within 60 calendar days of receiving the case, the QIO must submit to the RO a report on
its findings. The report provides an expert medical opinion regarding whether the
individual involved had an emergency medical condition, whether the individual’s
emergency medical condition was stabilized, whether the individual was transferred
appropriately, and whether there are any medical utilization or quality of care issues
involved in the case. Upon request, the RO provides copies of the QIO report to the
affected physician and/or hospital after all investigative activity has been completed.
When there was no screening examination or when a delay would jeopardize the health or
safety of individuals, QIO Review is not required before the OIG may impose CMPs or
exclude a physician from the Medicare program. In addition, if the QIO determines, after
a preliminary review, that there was an appropriate medical screening examination and
the individual did not have an emergency medical condition, the QIO returns the case to
the RO with its documented opinion. The RO will close the case and no referral to OIG is
necessary.
When the RO determines that a hospital was non-compliant with the requirements of
42
CFR 489.24, one of its notice requirements is to notify the OIG that the violation was
confirmed and that termination action was initiated. (See Exhibit 208.) The RO
completes the notification after receipt of the QIO 60-day review report. If the QIO
report does not support an EMTALA violation, the RO closes the case without referring
it to the OIG.
The RO forwards the following documents to the OIG:
• Form CMS-1541B;
• Form CMS-2567;
• Medical record;
• Summary of interviews;
• Explanation of sample selection;
SOM Chapter 5 - Page 62
• Copies of pertinent hospital policies and procedures related to the identified
deficiencies;
• Complaint investigation narrative;
• Certification of benefits versus risks of the transfer (if this is a transfer case);
• Copy of the 5 working-day advisory QIO Review, and
• Copy of the 60 calendar-day advisory QIO Review.
The RO sends the above information and any other pertinent documentation in its
possession to the OIG at the following address:
Office of Inspector General
Office of Counsel to the Inspector General
Department of Health and Human Services
Room 5527, Cohen Building
330 Independence Avenue SW
Washington, D.C. 20201
5480.2 - EMTALA Case Referral to OIG
(Rev. 18, Issued: 03-17-06; Effective/Implementation Dates: 03-17-06)
CMS refers appropriate cases to the OIG for investigation. Periodically, OIG will advise
us of the criteria they would prefer CMS to use in referring cases. Examples of the types
of cases that may be referred include:
1. Financial Screening - The hospital and/or responsible physician refused to
examine or treat a person based on the person’s insurance status or inability to pay
a fee. The financial basis for the decision must be clearly supported by evidence
in the file, e.g., documented policy, interview reports.
2. Patient with Trauma or Acute Emergency Condition - The hospital and/or
responsible physician (including an on-call physician who failed to come to the
hospital) failed to screen, stabilize, or appropriately transfer (or, in the case of a
hospital with specialized capabilities or facilities, refused to accept an appropriate
transfer of) a person with trauma, e.g., a severe head injury, or other acute
emergency condition, e.g., heart attack or stroke, requiring immediate and
substantial medical intervention.
3. High Risk Event (such as Birth) Occurs Prior to Arrival at Another Hospital
- The hospital and/or responsible physician discharged or refused to screen/treat a
SOM Chapter 5 - Page 63
person who gave birth (or is subject to another high risk medical event) prior to
arriving at another hospital (especially if transport is by private vehicle).
4. Death or Serious Harm Results from Dump - The evidence in the file
(including the QIO Review) demonstrates that the dumping violation caused
serious medical harm or death to the victim of the violation.
5. Egregious Violation Prioritized by CMS - CMS concludes that a CMP is
appropriate because of the seriousness of the violation (the person must have had
an emergency medical condition) and other relevant factors, e.g., long history of
noncompliance, hospital policy resulting in violations, pattern of serious
violations, knowing and willful violation. This category is for those cases that
CMS determines are very serious and merit a CMP but do not fit within other
categories identified by OIG.
5480.3 - Releasing QIO Assessment
(Rev. 18, Issued: 03-17-06; Effective/Implementation Dates: 03-17-06)
Upon request, the RO may release QIO assessment(s) to the physician and/or hospital or
the affected individual, or his/her representative. The QIO physician’s identity is
confidential unless he/she consents to its release. The QIO Review may be released
pursuant to the requirements of 42 CFR 480.132 and 480.133.
Sections 5500 to 5590 relate CLIA.
5500 - Complaints Involving Unaccredited Laboratories
(Rev. 18, Issued: 03-17-06; Effective/Implementation Dates: 03-17-06)
NOTE: This section applies to complaints against laboratories that hold a CLIA
certificate of compliance, certificate of waiver (COW), and certificate of PPM
(See §§5540-5590 for complaints regarding accredited laboratories).
A complaint is an allegation that could result in citing noncompliance with CLIA
requirements. A complaint may be substantiated or unsubstantiated as a result of an
investigation or survey. A substantiated complaint is one resulting in a finding of
noncompliance at the time of the investigation, or a finding that noncompliance was
proven to exist, but was corrected prior to the investigation. An unsubstantiated
complaint is an allegation where sufficient evidence could not be found to conclude that
noncompliance with CLIA requirements existed during the investigation or at the time of
the alleged violation. A complaint may be received in either the SA or the RO. The
receiving organization should follow the procedures outlined below.
SOM Chapter 5 - Page 64
The SA obtains the following information for every complaint:
• Complainant’s name, address, and telephone number, unless the complainant
requests anonymity;
• Laboratory’s name and address; and
• Description of problem, (e.g., personnel, places, and dates of occurrence).
5500.1 - Control
(Rev. 18, Issued: 03-17-06; Effective/Implementation Dates: 03-17-06)
The SA establishes a file for the complaint and logs the action in a control system. The
system may be manual or automated, but must facilitate tracking and control of the
complaint.
5500.2 - Acknowledgment
(Rev. 18, Issued: 03-17-06; Effective/Implementation Dates: 03-17-06)
If the complainant is known, the SA promptly issues written acknowledgment that the
complaint is being investigated. The SA should not delay acknowledgment pending an
investigation unless the investigation takes place within three working days. The SA
must take appropriate precautions to protect the complainant’s anonymity and privacy.
The SA maintains a copy or record of the notification with the complaint documentation.
5500.3 - Evaluation
(Rev. 18, Issued: 03-17-06; Effective/Implementation Dates: 03-17-06)
The SA evaluates any complaint to determine whether it should be investigated by the
SA, or whether it should be forwarded to the RO for investigation or referral to the
appropriate authority (e.g., OCR, OSHA, RO). The SA assesses the complaint to
determine if an immediate survey is necessary. While the SA will perform most
complaint surveys, complaints involving State-operated facilities are the responsibility of
the RO. When the SA does not have jurisdiction, it should forward the complaint to the
RO within three working days. If referral is not necessary, the SA considers whether or
not any special notification is appropriate.
If a complaint is especially significant, sensitive, or attracting broad public or media
attention, the SA informs the RO immediately.

SOM Chapter 5 - Page 65
5500.4 - Scheduling Investigations
(Rev. 18, Issued: 03-17-06; Effective/Implementation Dates: 03-17-06)
The SA investigates within two working days of receiving the complaint and focuses on
the specific problem area if the complaint involves possible immediate jeopardy to
patient health and safety. Otherwise, the SA follows procedures for prioritizing and
investigating certification-related complaints. Laboratories with complaints pending are
identified and given priority in scheduling of regular certification surveys.
5500.5 - Conducting Investigations
(Rev. 18, Issued: 03-17-06; Effective/Implementation Dates: 03-17-06)
The SA investigates complaints by means of an onsite survey, by telephone, by electronic
communication, by letter, or by a documentary review. Complaint investigations are
unannounced.
For onsite complaint investigations, the SA performs a full or partial survey based on the
allegations. If a complaint alleges generalized inappropriate laboratory practices, the SA
evaluates compliance with applicable requirements or conducts a full survey, as needed.
If the complaint is of a specific nature, the SA performs a survey focused on areas
relevant to the complaint.
5500.6 - Conducting Investigations in a Laboratory with a Certificate of
Waiver
(Rev. 18, Issued: 03-17-06; Effective/Implementation Dates: 03-17-06)
The RO authorizes an unannounced complaint survey of a laboratory holding a certificate
of waiver only if it is based on a substantial allegation of noncompliance. The fact that a
deficiency is not at the Condition-level does not preclude taking adverse action based on
provisions contained in 42 CFR 493.1840. As with other laboratories, the SA
investigates complaints made against laboratories with a certificate of waiver by means of
an onsite survey, by telephone, letter, or by a review of documents.
The SA performs the onsite investigation based on the allegation and determines whether
a laboratory is performing only waived tests and if the laboratory is following the
manufacturer’s instructions for performing the tests (See Appendix C).
SOM Chapter 5 - Page 66
5500.7 - Conducting Investigations in a Laboratory with a Certificate
for PPM Procedures
(Rev. 18, Issued: 03-17-06; Effective/Implementation Dates: 03-17-06)
The RO authorizes an unannounced complaint survey of a laboratory holding a certificate
for PPM procedures only if based on a substantial allegation of noncompliance. This
survey should not differ from a complaint survey done in any other laboratory performing
non-waived testing, as all requirements for moderate complexity apply except routine
survey.
Substantial indication that a laboratory is performing tests that do not appear on the PPM
procedures test list; e.g., through billing procedures, should prompt a complaint survey of
a certificate for PPM procedures laboratory followed by either proper registration or
appropriate sanctions.
5500.8 - Post Investigation Actions
(Rev. 18, Issued: 03-17-06; Effective/Implementation Dates: 03-17-06)
Following the investigation, the SA records any deficiencies on a Form CMS-2567 and
provides it to the facility using regular procedures. Subsequent actions depend on the
severity and nature of the deficiencies cited and the facility’s willingness or ability to
correct them.
When deficiencies are identified, the SA initiates actions as follows:
1. Condition-Level Deficiencies - Immediate Jeopardy - Certifies noncompliance
and initiates procedures to recommend imposing alternative and principal
sanctions.
2. Condition-Level Deficiencies - No Immediate Jeopardy; Facility Provides an
Acceptable POC - Certifies noncompliance and initiates procedures to
recommend imposing alternative sanctions based on the severity and nature of the
deficiencies found.
3. Lower Level Deficiencies - Facility Provides an Acceptable POC - Certifies
compliance based upon an acceptable POC and assembles documentation for RO
review.
4. Lower Level Deficiencies - Facility Unable or Unwilling to Provide
Acceptable POC - A facility with deficiencies may not participate without an
acceptable POC. The SA recommends sanction action to the RO.
When no deficiencies are identified, no certification action is required.
SOM Chapter 5 - Page 67
5500.9 - Resolution/Closeout
(Rev. 18, Issued: 03-17-06; Effective/Implementation Dates: 03-17-06)
1 - Unsubstantiated
The SA enters the unsubstantiated complaint into ACTS and documents the facility’s
certification file.
2 - Substantiated
The SA reports substantiated complaints using the Form CMS-2567 and any appropriate
supporting documentation. The SA logs summary information in the control system and
files a copy of the complaint documents in the facility’s certification file. The SA enters
complaints into ACTS. The laboratory will be charged a fee to cover the cost of the
survey if noncompliance is documented.
The SA closes out all complaints with a follow-up notice to the complainant with the
findings and disposition of the complaint. The SA should send this notice soon after the
investigation and retains a copy with the complaint record.
The SA provides follow-up reports, as necessary, to any other appropriate parties such as
the State Medicaid agency and/or initial referring agencies. The SA must be sure to
protect the anonymity and privacy of the complainant.
The SA inputs the investigation information into ACTS within 45 days of the completion
of the complaint survey.
5510 - CLIA-Exempt Laboratory Complaint Investigations - General
(Rev. 18, Issued: 03-17-06; Effective/Implementation Dates: 03-17-06)
Complaints may be from any source, including verbal, written, electronic or in the media.
Complaints are investigated if they meet the following criteria:
• If substantiated, would have an impact on the health and safety of the general
public or individuals served by the laboratory, and
• Would raise doubt as to the laboratory's compliance with one or more CLIA
Conditions and/or requirements.
An attempt to maintain the anonymity of the complainant should always be made.
There are a number of entities that must address laboratory complaints including: CMS
Central and Regional Offices, the state agencies (including those with state licensure
SOM Chapter 5 - Page 68
programs), approved states, and accreditation organizations. Each of these entities shares
a strong interest in ensuring the quality of patient care and the services provided by
laboratories. When the complaint involves more than one of these entities, there should
be coordination and communication to ensure an effective and timely resolution of the
issue.
5520 - Review of CLIA-Exempt Laboratory Complaints
(Rev. 18, Issued: 03-17-06; Effective/Implementation Dates: 03-17-06)
If the RO receives a complaint against a CLIA-exempt laboratory, the RO determines
what action is appropriate. The RO may do any of the following:
• Determine the severity of the complaint;
• Send the information to the approved State for their action;
• Conduct a survey (full or partial);
• Investigate the complaint during the course of a validation survey (full survey),
if it is conducted within 45 days of the laboratory’s licensure survey and the
complaint does not present immediate jeopardy concerns.
• If the seriousness of the complaint or the circumstances warrant, the RO should
invoke the Rapid Response Alert Protocol.
NOTE: Transfusion-related fatality investigations must be conducted by the RO. They
may not be delegated to the approved State; however, the approved State may
accompany the RO on the investigation. In either case, there must be
coordination and communication between the RO and the State. Where State
laws apply to transfusion-related incidents, the approved State program should
follow its established procedures and coordinate with the RO.
The RO Reviews the approved State program’s complaint activities as part of the overall
annual review. The RO has the discretion to maintain its own complaint tracking system
for those that have been forwarded to the approved State program. However, this
information should be an integral part of the State’s annual review.
If the approved State program receives a complaint against a CLIA-exempt laboratory,
the approved State program determines what action is appropriate. If the approved State
sanctions a CLIA-exempt laboratory in any way (e.g., licensure is withdrawn), it must
notify the RO within 30 days.
If the laboratory against which the complaint is alleged is accredited, the State must also
notify the accreditation organization.
SOM Chapter 5 - Page 69
5530 - Conducting Complaint Investigations and Surveys for CLIA-
Exempt Laboratories
(Rev. 18, Issued: 03-17-06; Effective/Implementation Dates: 03-17-06)
The RO will complete the “Medicare/Medicaid/CLIA Complaint Form,” Form CMS-562,
for every complaint investigation it performs in a CLIA-exempt laboratory. When an
investigation can be conducted via telephone (e.g., personnel credentials), the RO should
do so. The RO obtains the following information for every allegation:
• Complainant’s name and address, unless complainant requests anonymity. Do not
disclose the identity of the complainant to the laboratory;
• Laboratory’s name and address; and
• Description of problem, involving names, places, and dates.
The RO follows the same procedures for control and acknowledgement indicated in
§5500. Complaints involving potential immediate jeopardy will be investigated by the
RO within 2 working days of receipt. Complaints not involving potential immediate
jeopardy are investigated within 45 days. All complaint surveys are unannounced.
If a laboratory representative refuses to permit a complaint survey, the RO contacts the
State and requests that it contact the laboratory to explain the protocol and, if necessary,
suggest that the State take enforcement action against the CLIA-exempt laboratory. The
RO conducts the complaint survey in accordance with the survey protocol and uses the
appropriate survey forms specified in Exhibit 63 and the outcome-oriented protocol
found in Appendix C.
Initially, the RO focuses the survey only on the Condition(s) or requirement(s) related to
the complaint area(s). If the complaint is substantiated or if additional deficiencies are
found during the course of the investigation, the RO expands the scope of the survey to
include additional standards, conditions, and other CLIA requirements. If the complaint
is not substantiated, the RO notifies the laboratory that it is in compliance with the CLIA
Condition(s) (Exhibit 243). The RO also notifies the approved State program of the
Condition-level compliance (Exhibit 244).
At the exit conference, the RO informs the laboratory of the deficiencies found. If the
deficiencies pose immediate jeopardy to the health and safety of individuals served by a
laboratory or that of the general public, the RO notifies the approved State program and
the laboratory within two working days by overnight mail and includes a copy of the
Form CMS-2567. The RO directs the State program to take the appropriate enforcement
action. (See Exhibits 231 and 228). The RO follows-up with the State program within
15 working days of its notification to the laboratory to verify that the enforcement action
has either been taken against the laboratory or that the laboratory has achieved
compliance with CLIA requirements.
SOM Chapter 5 - Page 70
If the State program fails to take appropriate enforcement action for an immediate
jeopardy case within 23 days of the RO’s notification, and the laboratory has not
achieved Condition-level compliance, the RO may request CO to either contact the State
or attempt other resolution to eliminate the jeopardy.
If the deficiencies do not pose immediate jeopardy to the health and safety of individuals
served by a laboratory or that of the general public, the RO prepares a Form CMS-2567
and forwards a letter along with the Form CMS-2567 to the laboratory and to the State
program within 10 working days of completing the survey. The State program is
responsible for taking any enforcement action, if necessary, monitoring the correction of
the deficiencies, and providing a report to the RO. (See Exhibit 231.)
The RO completes a Survey Team Composition and Workload Report, Form CMS-670,
for all complaint surveys and related activity.
If the approved State program fails to take appropriate enforcement action in non-
immediate jeopardy situations, the RO documents its files accordingly and notifies CO.
Failure to take and document the necessary enforcement action may subsequently
jeopardize current or future approval of the State's laboratory licensure program.
5540 - Complaint Investigations and Surveys of Accredited
Laboratories Under CLIA
(Rev. 18, Issued: 03-17-06; Effective/Implementation Dates: 03-17-06)
There are a number of entities that must address laboratory complaints including: CMS
Central and Regional Offices, the state agencies (including those with state licensure
programs), approved states, and accreditation organizations. Each of these entities shares
a strong interest in ensuring the quality of patient care and the services provided by
laboratories. When the complaint involves more than one of these entities, there should
be coordination and communication to ensure an effective and timely resolution of the
issue.
The statutory basis for conducting surveys of accredited laboratories based on allegations
of noncompliance is found in §353(e)(2)(D) of the Public Health Service Act (PHSA).
Since accreditation organization (AO) requirements are equivalent to CLIA requirements,
a complaint may affect the laboratory’s accreditation status as well.
Complaints are investigated if they meet the following criteria:
• If substantiated, would have an impact on the health and safety of the general
public or individuals served by the laboratory, and
• Would raise doubt as to the laboratory's compliance with one or more CLIA
Conditions and/or requirements.

SOM Chapter 5 - Page 71
The RO should evaluate the complaint and take appropriate investigatory action. If the
seriousness of the complaint or the circumstances warrant, the RO should invoke the
Rapid Response Alert Protocol. Every effort should be made to secure a written form of
the complaint, while maintaining anonymity, if requested.
All complaint surveys are unannounced and conducted according to outcome-oriented
survey principles (See Appendix C). If an investigation can be conducted by letter or
telephone, in lieu of an onsite survey, those means should be utilized.
Upon receipt, all complaints are logged and tracked and the same information as for
CMS certified laboratories is collected, monitored and maintained (see Section
5500).
5550 - RO Direction of Complaint Investigation of an Accredited
Laboratory
(Rev. 18, Issued: 03-17-06; Effective/Implementation Dates: 03-17-06)
The RO has primary responsibility for the coordination of all activities involving
complaints relating to an accredited laboratory.
This includes:
• Ensuring that all pertinent information concerning the complaint is obtained;
• Assessing the level of severity of the complaint;
• Determining actions required for investigation;
• Determining whether multiple AOs may be involved; and
• When warranted (e.g., in cases potentially involving media coverage,
Federal/State Congressional or political interest, legal intervention, etc.),
informing and coordination with all affected parties, including AO's, State
Agencies and Central Office.
Although the RO has the lead role in directing the investigation of complaints involving
accredited laboratories, all affected entities (i.e., State Agencies, AO's, Central Office)
share responsibility in ensuring timely and effective action is taken.
Complaints received by the SA:
If the SA receives a substantial allegation of noncompliance directly from a complainant
about an accredited laboratory, it promptly acknowledges receipt of the complaint and
SOM Chapter 5 - Page 72
advises the complainant that it is being forwarded to the RO for action. The SA forwards
a copy of the acknowledgment letter and the complaint to the RO. This includes SAs
with a State laboratory licensure program.
Complaints received by the RO:
If the complaint is received directly by the RO, the RO will promptly send a letter to the
complainant acknowledging the complaint and advising the complainant of the intended
course of action, and subsequently the results of any investigation, if appropriate, and of
the corrective action taken.
In either case (complaint received by SA or RO), the RO evaluates the complaint and has
the lead in determining the course of action. The RO determines whether the RO, the
SA, or the AO, including multiple AOs if circumstances so warrant, will investigate the
complaint. The RO will also determine whether one or multiple AOs may be impacted
by the complaint and, if so, alert them of the pending action. In certain instances the RO
may enlist CO support to help determine the most effective course of action.
If the RO determines that the SA should investigate the complaint, the RO prepares a
“Request for Complaint Investigation or Validation Survey of Accredited Laboratory,
Form CMS-2802A,” (See Exhibit 107) and a “Medicare/Medicaid/CLIA Complaint,”
Form CMS-562, and forwards them to the SA along with a copy of the complaint and
notifies the AO. If the RO authorizes the SA to perform a full survey (all specialties and
subspecialties covered by the certificate), and the survey can be performed within 90 days
of the AO’s inspection, the survey can be counted in the SA’s validation workload.
If the RO determines that the complaint involves a potential immediate jeopardy to the
individuals served by the laboratory, or to the general public, the SA investigates the
complaint within two working days of receiving it from the RO. Otherwise, the RO will
direct the SA to investigate non-Immediate Jeopardy complaints within 45 days and
report their findings to the RO and AO at the conclusion of the survey.
Complaints investigated by AOs:
If the RO determines that the accreditation organization should carry out its own
investigation, it promptly forwards the complaint to the accreditation organization for
immediate attention. The RO will request to be notified of the results of any investigative
action taken. The RO will then notify the SA and, if warranted, CO.
NOTE: Transfusion-related fatality investigations must be conducted by the RO or
SA. Transfusion-related fatality investigations must not be referred to an
accreditation organization for action. However, the AO or multiple AOs,
as appropriate, should be notified when such an investigation is taking
place.
Complaints received by AOs:
SOM Chapter 5 - Page 73
Complaints received directly by AOs will be investigated under each AOs own
standards and procedures. If multiple AOs are potentially impacted, the AO
receiving the complaint will promptly inform the other AOs and a determination
should be reached regarding the need for coordinated action. In cases potentially
involving media coverage, Federal/State Congressional or political interest, legal
intervention, etc., the SA, RO and CO should be promptly alerted by the AO
receiving the complaint and consulted concerning appropriate action.
5560 - Conducting Complaint Survey of an Accredited Laboratory
(Rev. 18, Issued: 03-17-06; Effective/Implementation Dates: 03-17-06)
If an onsite survey is warranted, the SA will conduct an unannounced survey of an
accredited laboratory based on the substantial allegation of noncompliance. The SA
conducts the complaint survey in accordance with outcome-oriented principles (see
Appendix C). The SA conducts a focused complaint survey, as instructed by the RO on
Form CMS-2802A. If the SA finds additional deficiencies during the course of the
complaint investigation, it may expand the scope of the survey with RO approval.
At the exit conference, the SA informs the laboratory director of the deficiencies found
and the procedures to respond to them. If the deficiencies do not pose an immediate
jeopardy to the health and safety of individuals served by a laboratory, or to the general
public, the SA prepares a Form CMS-2567 and requests that the laboratory submit a POC
for all Condition-level deficiencies. Condition level deficiencies must be corrected;
those at the standard level are optional. The SA informs the laboratory that the Form
CMS-2567 will be made available to the public under the disclosure of survey
information provisions. The SA indicates to the laboratory that the “Statement of
Deficiencies” (Form CMS-2567) will be forwarded to the laboratory within 10 working
days and that the POC must be returned to the SA within 10 calendar days. Upon receipt
of the survey information and POC, the RO makes a determination of whether or not
sanctions will be imposed against the laboratory and notifies the AO.
5570 – Forwarding Investigation Report to RO
(Rev. 18, Issued: 03-17-06; Effective/Implementation Dates: 03-17-06)
If non-immediate jeopardy is found, the SA will submit the appropriate information as
specified in the List of Documents in the Certification Packet (see Exhibit 63) to the RO,
or through an update to ACTS within 45 days of completing the survey and notifies the
RO of the entry. If the laboratory chooses not to submit a POC when deficiencies are
found, the SA reports any known information about the laboratory’s efforts to correct
deficiencies to the RO and AO.
SOM Chapter 5 - Page 74
5580 - Accredited Laboratory Found in Compliance Following a
Complaint Survey
(Rev. 18, Issued: 03-17-06; Effective/Implementation Dates: 03-17-06)
If after review of the documentation the RO determines that the accredited laboratory is
in compliance with all CLIA Condition-level requirements, it officially notifies the
laboratory and forwards a copy of this letter to the SA and the AO. This letter advises
that the accreditation organization may contact the laboratory about correcting any
deficiencies below Condition-level.
5590 - Accredited Laboratory Found Not in Condition-level Compliance
Following a Complaint Survey
(Rev. 18, Issued: 03-17-06; Effective/Implementation Dates: 03-17-06)
If the deficiencies found pose an immediate jeopardy to the health and safety of
individuals, the SA prepares the Form CMS-2567, (which is included as part of the List
of Documents in the Certification Package, See Exhibit 63) and notifies the RO and sends
Form CMS-2576 to the laboratory within 2 working days. RO will notify the AO. Based
on the information forwarded, and the laboratory’s POC, the RO determines if sanctions
are to be imposed against the laboratory. The RO will then notify the AO.
Should the immediate jeopardy situation be corrected before the adverse action is taken
or completed, the SA will advise the laboratory that it will revisit it to inspect all
remaining Conditions not in compliance. The RO will notify the AO.
If non-immediate jeopardy is found, the SA will submit the appropriate information as
specified in the List of Documents in the Certification Packet (See Exhibit 63) to the RO,
or through an update to ACTS within 45 days of completing the survey and notifies the
RO of the entry. The POC should also be forwarded to the RO. If the laboratory chooses
not to submit a POC when deficiencies are found, the SA reports any known information
about the laboratory’s efforts to correct deficiencies to the RO and the RO will notify the
AO and the laboratory that the laboratory is out of compliance and has been placed under
SA monitoring jurisdiction (see Exhibit 241). The laboratory is monitored by the SA, RO,
and/or AO until it reaches Condition-level compliance or its certificate of accreditation is
revoked. A copy of all correspondence is provided to the accreditation organization by
the RO.
For standard only deficiencies, responsibility rests with the AO to follow-up and pursue
corrective action. The laboratory continues to be accredited by its accreditation
organization and retains its CLIA certificate of accreditation during this monitoring
period; however, it becomes subject to the same CLIA requirements, survey and
enforcement procedures as applied to non-accredited laboratories found out of
compliance.
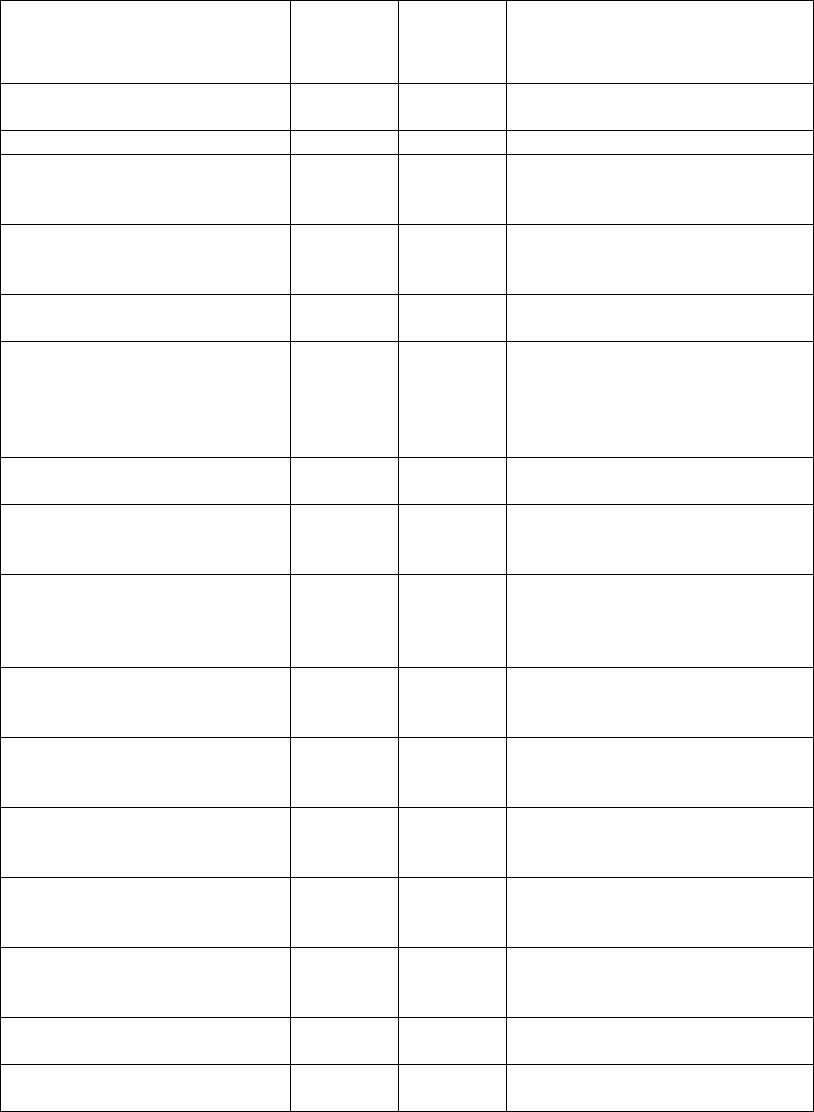
SOM Chapter 5 - Page 75
CROSSWALK TO THE OLD CHAPTER 5
A crosswalk from sections of the State Operations Manual Chapter Five published 5-
21-2004 to the revised chapter five is as follows:
Name of Old Section
Old
Section
Number
New
Section
Number
Name of New Section
Management of Complaints and
Incidents
5000
5000
Management of Complaints and
Incidents
Intake Process
5010
5010
Intake Process
Triage and Priority Assignment
5020
5070
Priority Assessment for Nursing
Homes, Deemed and Non-Deemed
Providers/Suppliers, and EMTALA
Priority Definitions
5030
5075
Priority Definitions for Nursing
Homes, Deemed and Non-Deemed
Providers/Suppliers, and EMTALA
Investigation Findings and
Reports
5040
5080
Investigation Findings and Reports
CMS Regional Office
Responsibility for Monitoring
SA Management of Complaints
and Incidents
5050
5050
CMS Regional Office
Responsibility for Monitoring SA
Management of Complaints and
Incidents
Aspen Complaints/Incidents
Tracking System (ACTS)
5060
5060
ASPEN Complaints/Incidents
Tracking System (ACTS)
Investigation of Complaints
Against Accredited/Deemed
Providers and Suppliers
5100
5100
Investigation of Complaints for
Deemed Providers/Suppliers
Basis for Investigation of
Complaints Against
Accredited/Deemed Providers
and Suppliers
5110
5100.1
Basis for Investigation
RO Direction of Accredited
Hospital Complaint Investigation
5120
5210
Processing of Complaints
Originating with or Investigated by
RO
Conducting an Accredited
Hospital Complaint Validation
Survey
5130
5050
CMS RO Responsibility for
Monitoring SA Management of
Complaints and Incidents
Forwarding Investigation Report
to RO
5140
5050
CMS RO Responsibility for
Monitoring SA Management of
Complaints and Incidents
Accredited Hospital Found in
Compliance Following
Complaint Validation Survey
5150
5100
Investigation of Complaints for
Deemed Providers/Suppliers
Accredited Hospital Found Not
in Compliance Following
Complaint Validation Survey
5160
5100
Investigation of Complaints for
Deemed Providers/Suppliers
Reinstatement to Accreditation
Organization Jurisdiction
5170
5100.2
Post-Survey Procedures
Termination of Accredited
Hospital
5180
5100.2
Post-Survey Procedures
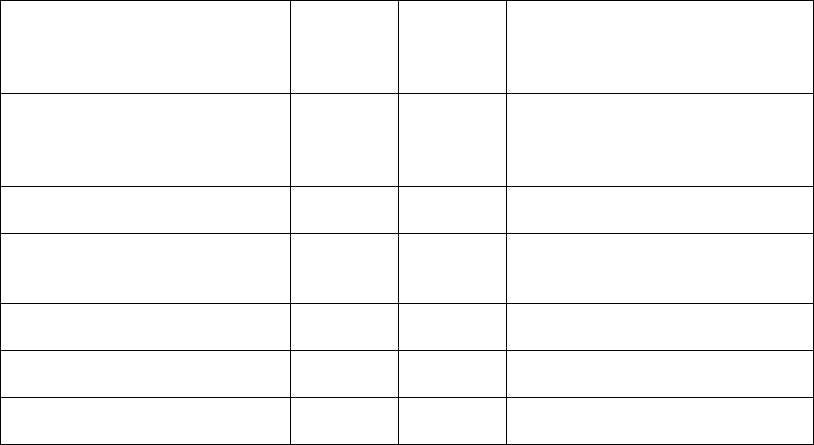
SOM Chapter 5 - Page 76
Investigating Complaints
Involving ESRD Services
Provided by Accredited
Hospitals
5190
5160
Investigating Complaints Involving
ESRD Services Provided by
Deemed Hospitals
Investigation of Complaints
Against Other Than
Accredited/Deemed Providers
and Suppliers
5200
5200
Investigating Complaints for Non-
Deemed Providers/Suppliers,
Excluding Nursing Homes
SA Processing of General,
Certification-Related Complaints
5210
5010
General Intake Process
Hospital Restraints/Seclusion
Death Reporting and
Investigation
5240
5140
Hospital Restraints/Seclusion
Death Reporting and Investigation
Complaints Involving HIV-
Infected Individuals
5250
5150
Complaints Involving HIV-
Infected Individuals
Investigations Involving Alleged
EMTALA Violations
5300-
5400
5400-
5500
Investigations Involving Alleged
EMTALA Violations
Complaints Involving
Unaccredited Laboratories
5500-
5590
5500-
5590
Complaints Involving
Unaccredited Laboratories
SOM Chapter 5 - Page 77
Chapter Five State Operations Manual
Acronyms
(Rev. 18, 03-17-06)
ACTS ASPEN Complaint Tracking System
AIDS Auto-immune deficiency syndrome
AO Accreditation Organization
the ACT Social Security Act
CFC Conditions for Coverage
CFR Code of Federal Regulations
CLIA Clinical Laboratory Improvement Amendments
CMP Civil Monetary Penalties
CMS Center for Medicare and Medicaid Services
CO Central Office
CoP Conditions of Participation
COW Certificate of Waiver
DED Dedicated Emergency Department
DHHS Department of Health and Human Services
EMS Emergency Medical System
EMTALA Emergency Medical Treatment and Labor Act
ESRD End-Stage Renal Disease
FDA Food and Drug Administration
HHA Home Health Agency
SOM Chapter 5 - Page 78
HIV Human Immunodeficiency Virus
IJ Immediate Jeopardy
JCAHO Joint Commission on Accreditation of Healthcare Organizations
LSC Life Safety Code
NF Nursing Facility
NW Networks
OCR Office of Civil Rights
OIG Office of Inspector General
OSHA Occupational Safety and Health Administration
P & A Protection and Advocacy Group
PHSA Public Health Service Act
POC Plan of Correction
PPM Provider Perform Microscopy (PPM) Procedures
PRTF Psychiatric Residential Treatment Facility
QIO Quality Improvement Organization
RFP Requirements for Participation
RNHCI Religious Non-Medical Health Care Institutions
RO Regional Office
SA State Agency
SMA State Medicaid Agency
SNF Skilled Nursing Facility
SOM State Operations Manual
USC United States Code
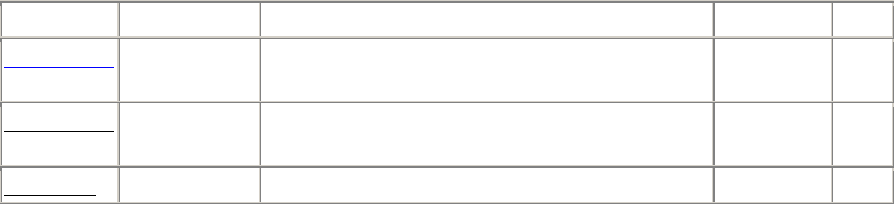
SOM Chapter 5 - Page 79
Transmittals Issued for this Chapter
Rev #
Issue Date
Subject
Impl Date
CR#
R50SOMA
07/10/2009
Revisions to Chapter 5, "Complaint
Procedures"
07/10/2009
N/A
R18SOMA
03/17/2006
Revisions to Chapter 5, "Complaint
Procedures"
03/17/2006
N/A
R01SOM
05/21/2004
Initial Issuance of Pub 100-07
N/A
N/A
