
1
Title: There is limited evidence supporting the use of the SOS approach to feeding with mixed
results on the effectiveness to improve eating.
Prepared by: Holly Freeman, OTS [email protected]
Alisa Reedy, OTS reedy.alis@uwlax.edu
Ashley Schalow, OTS [email protected]
Date: December 10th, 2015
CLINICAL SCENARIO:
Condition/Problem:
A feeding disorder is characterized by the failure of an infant or child less than six years
of age to eat enough food to gain weight and grow normally over a period of one month or more.
Feeding disorders are more prevalent in infants or children who are born prematurely, had a low
birth weight, or who are developmentally delayed. Some causes for feeding difficulties include:
diseases of the central nervous system, metabolic diseases, sensory defects, anatomical
abnormalities, muscular disorders, heart disease, and gastrointestinal diseases (Encyclopedia of
Mental Health, 2015). Some residual problems that are seen with this condition are dehydration,
poor nutrition, aspiration, pneumonia, repeated upper respiratory infections, and embarrassment
or isolation in social situations involving eating. Due to poor nutrition that may lead to failure to
meet normal weight and growth recommendations, children may be required to have
gastrointestinal tube (g-tube) feedings in order to supplement nutrition (ASHA, 2015). Although
a specific link has not yet been identified, children with Autism seem to be at increased risk for
developing feeding disorders/problems and it is estimated to be as high as 85% (Peterson, 2013).
Incidence/Prevalence:
● “It has been reported that 25%-45% of typically developing children demonstrate feeding
and swallowing problems.”
● “Prevalence is estimated to be 30%-80% for children with developmental disorders.”
● “Significant feeding problems resulting in severe consequences (e.g., growth failure,
susceptibility to chronic illness) have been reported to occur in 3%-10% of children, with
a higher prevalence found in children with physical disabilities” (26%-90%) and medical
illness and prematurity (10%-49%).”
● “It is reported that the prevalence of pediatric dysphasia is increasing due to improved
survival rates of children born prematurely, with low birth weight, and with complex
medical conditions.” (ASHA, 2015)
Impact of the Problem on Occupational Performance:
Areas of occupational performance that may be affected are swallowing/eating because
the child is unable to keep food in the mouth long enough for process of swallowing to take
place. Another area of occupation that is impacted is feeding, meaning that the child is not
interested in eating the food presented to them, and therefore, they will not attempt to bring the
Prepared by Holly Freeman, Alisa Reedy and Ashley Schalow (12/10/2015). Available at
www.UWLAX.EDU/OT
2
item to their mouth. The child may lose their energy and drive to participate in mealtimes due to
emotional mental functions that become associated with eating including tension and anxiety.
The social interactions with family at mealtimes may be problematic due to the child’s
unwillingness to partake in normal feeding/eating habits and the struggle for parents to get child
to eat. There may also be an element of embarrassment for the parents when eating in social
situations because eating problems with the child occur. (American Occupational Therapy
Association, 2014).
Intervention:
The Sequential Oral Sensory (SOS) Approach to feeding is a protocol involving sensory
integrative components developed by Dr. Kay Toomey, a pediatric psychologist (Toomey &
Associates, 2015). The protocol for SOS intervention is available only to therapists who have
completed a 5-day training conference. This approach to feeding is considered a transdisciplinary
approach to feeding difficulties because it involves assessing the whole child on the basis of
physical barriers to eating and proper medical treatment, nutritional issues, developmental,
sensory, motor, oral-motor, and cognitive skills that are all involved and needed in the process of
feeding. The SOS protocol is used as an intervention for feeding difficulties over a twelve week
period that uses progression and gradual introduction of foods based on a desensitization
hierarchy that includes aversive and non-aversive foods (Benson et al., 2013). Each therapy
session can last an hour or a few hours.
This SOS approach to feeding is similar to a common behavioral intervention of
systematic desensitization in which the fear of aversive stimuli is replaced with feelings of
relaxation (McLeod, 2008). In systematic desensitization, the aversive or anxiety-provoking
stimuli are presented to the client through a gradual process which begins with less aversive to
more aversive (McLeod, 2008). Children with feeding disorders might find certain textures,
colors, sizes, and temperatures of food as aversive and anxiety-provoking. Even being near the
food could cause a child to cry, engage in inappropriate mealtime behaviors, gag, choke or
vomit. Therefore, the objective of the SOS protocol is increase the child’s willingness and
acceptance to try a variety of foods through a more calm and inviting environment. The child is
led through multiple steps of the protocol starting with selective sensory input that is child-
directed, stomping to the therapy room, participating in pre-meal setup, interacting with the food
in a gradual sequence, and finishing with a clean up routine. This protocol includes gradually
guiding the child through a hierarchy of aversive stimuli, continuous interaction with various
foods, and incorporation of sensory integrative components to help the child become more
comfortable and prepared for trying different foods (Peterson, 2013). See Appendix A for more
details about SOS protocol intervention.
OT Theoretical Basis:
The SOS approach to feeding incorporates several theories and assumptions that can be
closely related to occupational therapy frames of references and theories. These theories include
behavioral approaches and sensory integration (SI).
Prepared by Holly Freeman, Alisa Reedy and Ashley Schalow (12/10/2015). Available at
www.UWLAX.EDU/OT

3
The behavioral theories assume that behavior is learned, and therefore, behavior can be
altered or reshaped when it is reinforced. If reinforced, a desired behavior will be more likely to
be performed again (Cole et al, 2008). In the SOS approach, the therapist primarily demonstrates
role-modeling, positive reinforcement, and encouragement of learning through behavioral
approaches (Peterson, 2013). The therapist prompts the child to engage in interaction with the
food by using verbal praise when the child performs a positive behavior with the food. An
example of verbal positive reinforcement that the therapist can say is, “Good job taking a bite.”
Additionally, the therapist also demonstrates modeling of behavior during the SOS
protocol. Each step including sensory preparation, transition to the feeding therapy room, pre-
meal set-up, exposure to food, and clean-up routine includes specific behaviors that the therapist
would need to perform and try to encourage the child to model. For example, during the
transition to the feeding therapy room, the therapist marches and sings, and the child is
encouraged to model the behavior. Lastly, the therapist encourages the child at each food
hierarchy step when the child performs a positive interaction or tolerance for the food. The child
is praised for smelling, touching, or eating the aversive food item and can continue up the
hierarchy if the step is completed (Peterson, 2013).
Sensory integration (SI) is a primary focus of the SOS feeding approach. According to SI,
sensory-motor experiences help a child learn, and if those abilities are impaired, the child cannot
optimally function. Therefore, a child must control the input of sensory stimuli to help the child
modulate and balance the amount of input they are receiving (Case-Smith, 2005). Sensory
integration in the context of the SOS approach to feeding requires that the child practice
appropriate and adaptive responses to food through controlled sensory input before feeding
sessions. It is proposed that the child be an active participant during the therapy process in order
to process the sensory stimuli of the different types of food (Peterson, 2013).
In order to help the child prepare for sensory stimuli and to decrease a child’s sensitivity,
the SOS protocol has the child engage in preparatory activities. These include gross motor
exercises, firm rubbing, vibration, and deep pressure. In the SOS approach, SI is used by
performing gross motor activities on the jungle gym, such as pushing, jumping, running,
swinging or bouncing, singing and marching to help promote vibration in the mouth,
continuation of gross motor exercises, and desensitization of the mouth such as wiping a warm
washcloth around the mouth, blowing bubbles, and hand washing. It is suggested that engaging
in these activities will allow the child to regulate their sensory input and help desensitize the oral
area to increase acceptance and tolerance of a variety of foods (Peterson, 2013).
Science behind the intervention:
The SOS protocol is intended to help address the problem behaviors associated with
eating (Toomey & Associates, 2015). These problem behaviors may emerge as the result of
medical/oral conditions, sensory integration sensitivities, or negative behaviors that are
reinforced during mealtimes (Peterson, 2013). The SOS protocol addresses the child as a whole,
incorporating the child’s organ functioning, muscles, sensory development, behavior, oral-motor
sensations, cognitive level, overall nutrition, and environmental factors (Toomey & Associates,
Prepared by Holly Freeman, Alisa Reedy and Ashley Schalow (12/10/2015). Available at
www.UWLAX.EDU/OT
4
2015). The therapist prepares the child for feedings through participation in a play activity,
which is intended to calm a hypersensitive child or alert and improve tone in a hyposensitive
child through heavy work, deep pressure, or oral stimulation by reducing his/her anxious feelings
about food and decrease sensitivity (Peterson, 2013). In addition, the therapist facilitates oral
stimulation through providing pressure to the chest and symmetrical pressure to the face and
mouth, which provides proprioceptive input through oral stimulation (Case-Smith, 1989).
A desensitization approach helps to improve the child’s level of comfort through learning
and exploration of food, where the child begins the intervention through interaction with the
food, in a stress-free environment (Toomey & Associates, 2015). The child progresses through
the intervention from being in the same room as the food to touching/kissing food and finally
tasting/eating food (Toomey & Associates, 2015). The child is presented with foods of various
sizes, color, texture, taste, and temperature throughout the SOS intervention to help reduce the
child’s sensitivity and fear associated with feeding times (Peterson, 2013). It is important that
the child plays a critical role in the feeding intervention, allowing therapy to revolve around a
child’s needs and improving the therapeutic relationship (Peterson, 2013). The aim for the child
at the end of the SOS feeding program is to decrease the level of sensitivity towards foods and
increase the amount of acceptance of new foods (Peterson, 2013).
Why is the intervention appropriate for OT:
The SOS protocol is appropriate for occupational therapy because it falls under the
occupations of swallowing/eating and feeding in the framework (The American Journal of
Occupational Therapy, 2014). Through preparatory methods, such as play and oral stimulation,
occupational therapists are able to prepare a child for the feeding interventions by providing the
child with the necessary stimulation and input that he/she may need (The American Journal of
Occupational Therapy, 2014). The SOS intervention is an occupation-based intervention
because it focuses on increasing a child’s independence during mealtimes by reducing
inappropriate behaviors through desensitization.
The areas under the international classification of function and disability that the SOS
protocol applies to include the health condition, body function and structures, activity,
participation, environmental factors, and personal factors (WHO, 2015). The SOS intervention
applies to the health condition because it addresses a child’s feeding difficulties during
mealtimes. Furthermore, the SOS intervention applies to body function and structures because it
incorporates the child’s oral and swallowing behaviors that may be impeding his/her ability to
swallow food properly. In addition, the SOS protocol is applicable to the area of activity because
it is a feeding intervention that focuses on the child’s occupation of swallowing/eating and
feeding. Throughout the feeding intervention, the SOS protocol requires the child’s participation
during therapy sessions to help decrease sensitivity and increase appropriate mealtime behaviors.
Lastly, the SOS protocol addresses a child’s environmental and personal factors because it
identifies limitations within or surrounding a child that may be affecting a child’s ability to
participate fully throughout mealtime.
Prepared by Holly Freeman, Alisa Reedy and Ashley Schalow (12/10/2015). Available at
www.UWLAX.EDU/OT
5
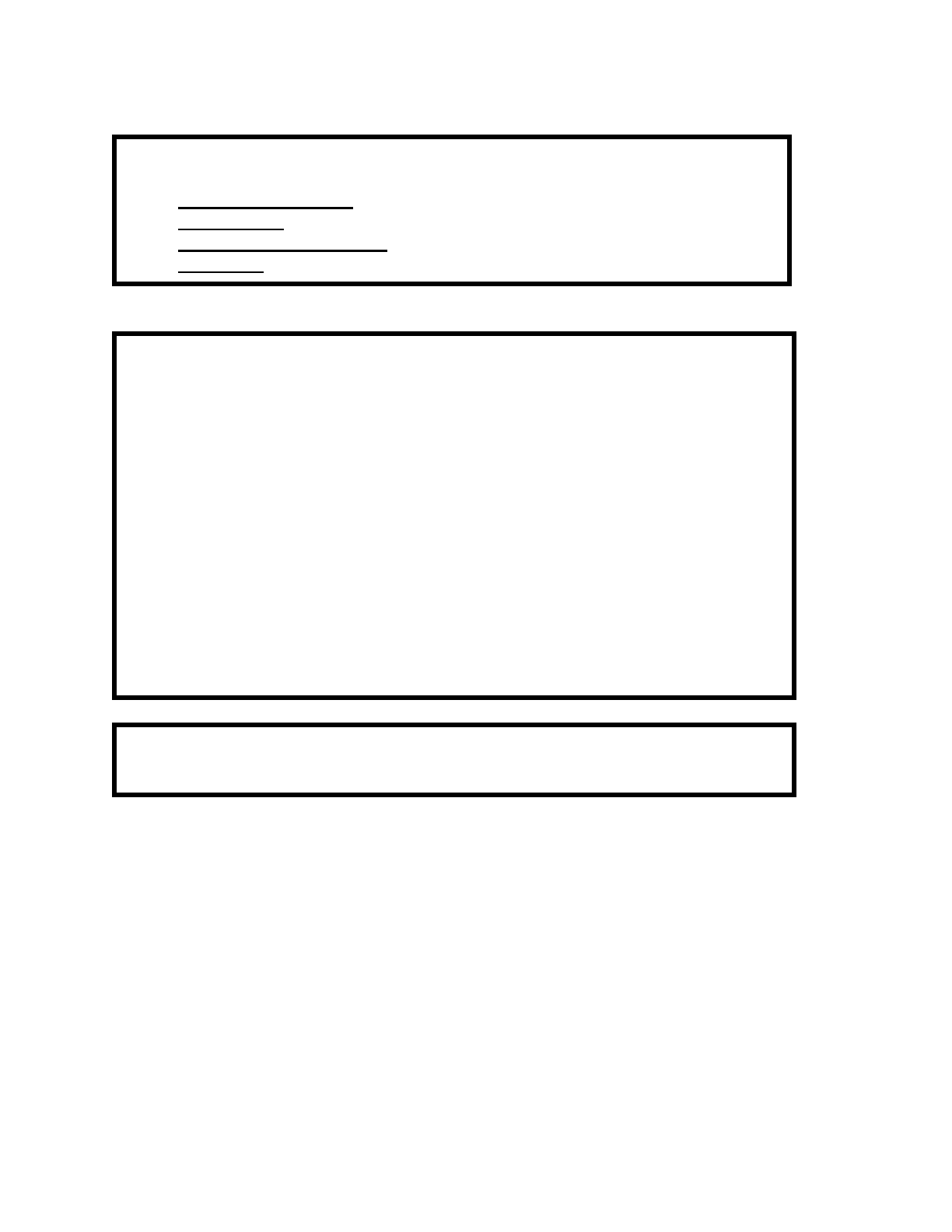
Focused Clinical Question:
● Patient/Client Group: Children 8 months to 8 years with feeding difficulties
● Intervention: SOS approach to feeding
● Comparison Intervention: Applied Behavioral Approach (ABA)
● Outcomes: To increase the number and variety of foods that a child eats
Summary:
● Summarize clinical question: This CAT investigates the effectiveness of the
SOS protocol for improving feeding behaviors in children with feeding
difficulties.
● Search: We searched six databases and located nine articles related to feeding
disorders in children. Of those, we selected and review three articles that were
all case-studies. One article had a strength of 3B and a high rigor. The other two
articles had a strength of 4. However, one article was medium rigor and the other
was high rigor. We selected the three articles reviewed because each of the
studies included the SOS protocol in the intervention and involved children that
were under the age of eight with a feeding difficulty.
● Summary of findings: There is limited and inconclusive information for or
against the SOS protocol.
CLINICAL BOTTOM LINE: There is limited evidence supporting the use of the
SOS approach to feeding with mixed results on the effectiveness to improve eating.
Limitation of this CAT: This critically appraised paper (or topic) has been reviewed by
occupational therapy graduate students and the course instructor.
Prepared by Holly Freeman, Alisa Reedy and Ashley Schalow (12/10/2015). Available at
www.UWLAX.EDU/OT
6
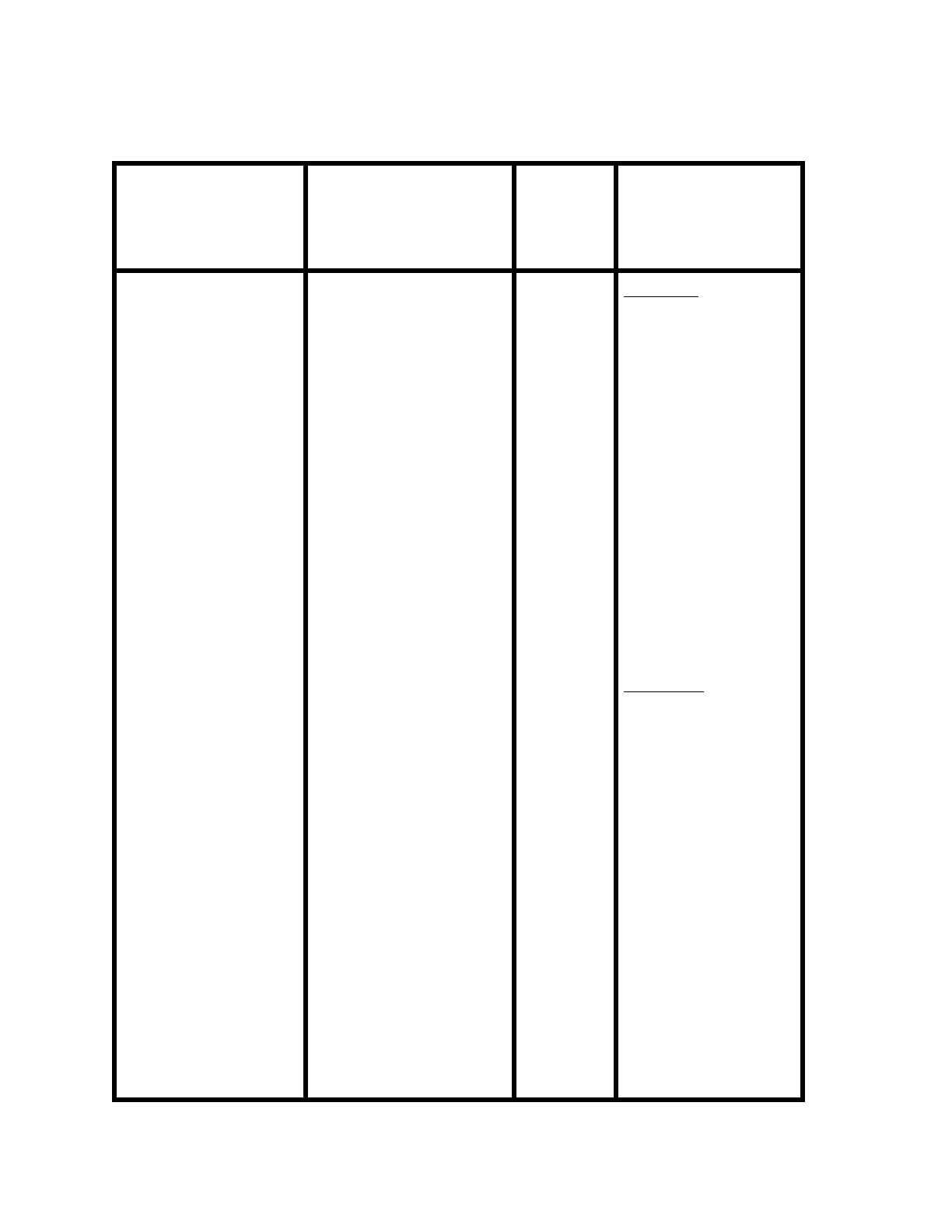
SEARCH STRATEGY:
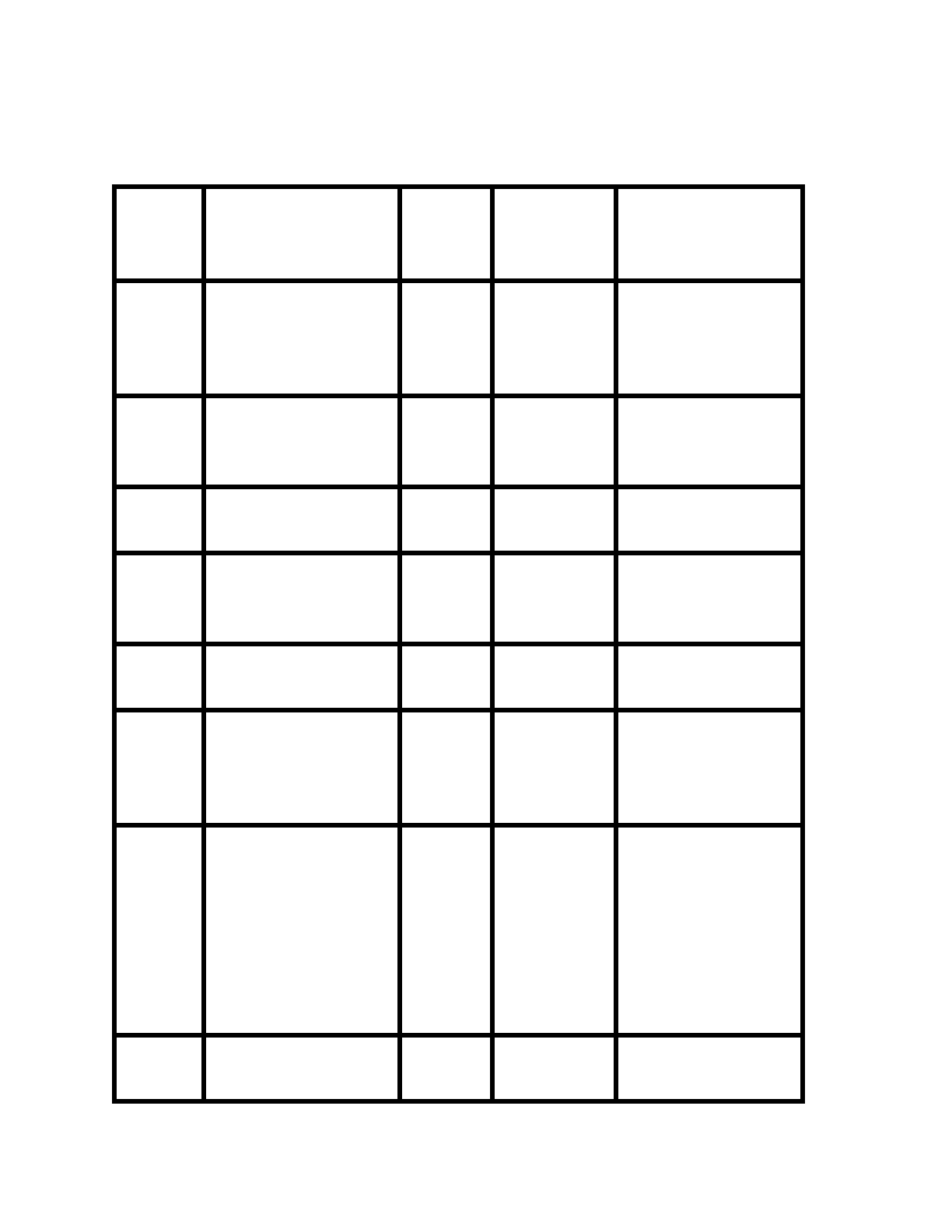
Table 1: Search Strategy
Databases Searched Search Terms Limits
used
Inclusion and
Exclusion Criteria
● Cochrane
● Health
Professions
Data Base via
EBSCO Host
● OT Search
● OT Seeker
● AOTA
● OVID Data
Base
● feeding
● desensitization
● sequential oral
sensory approach
● oral aversion
● feeding therapy
● feeding
difficulties
● problematic
feeding
● premature birth
● sensation
disorders
● pediatric
● eating
● eating behavior
● oral sensory
● intervention
● children
● oral sensory
therapy
● sensory
● Kay Toomey
● Peterson
“+”
“and”
“author”
Inclusion:
● English
● Within the last
10 years
● Includes SOS
protocol or SI
or ABA
interventions
related to
feeding
difficulties
● Population
consisting of
children with
feeding
difficulties
Exclusion:
● Other language
that was not
English
● Article older
than 2005
● Not related to
SOS or ABA
treatment for
feeding
difficulties
● Population that
did not include
children with
feeding
difficulties
Prepared by Holly Freeman, Alisa Reedy and Ashley Schalow (12/10/2015). Available at
www.UWLAX.EDU/OT
7
RESULTS OF SEARCH:
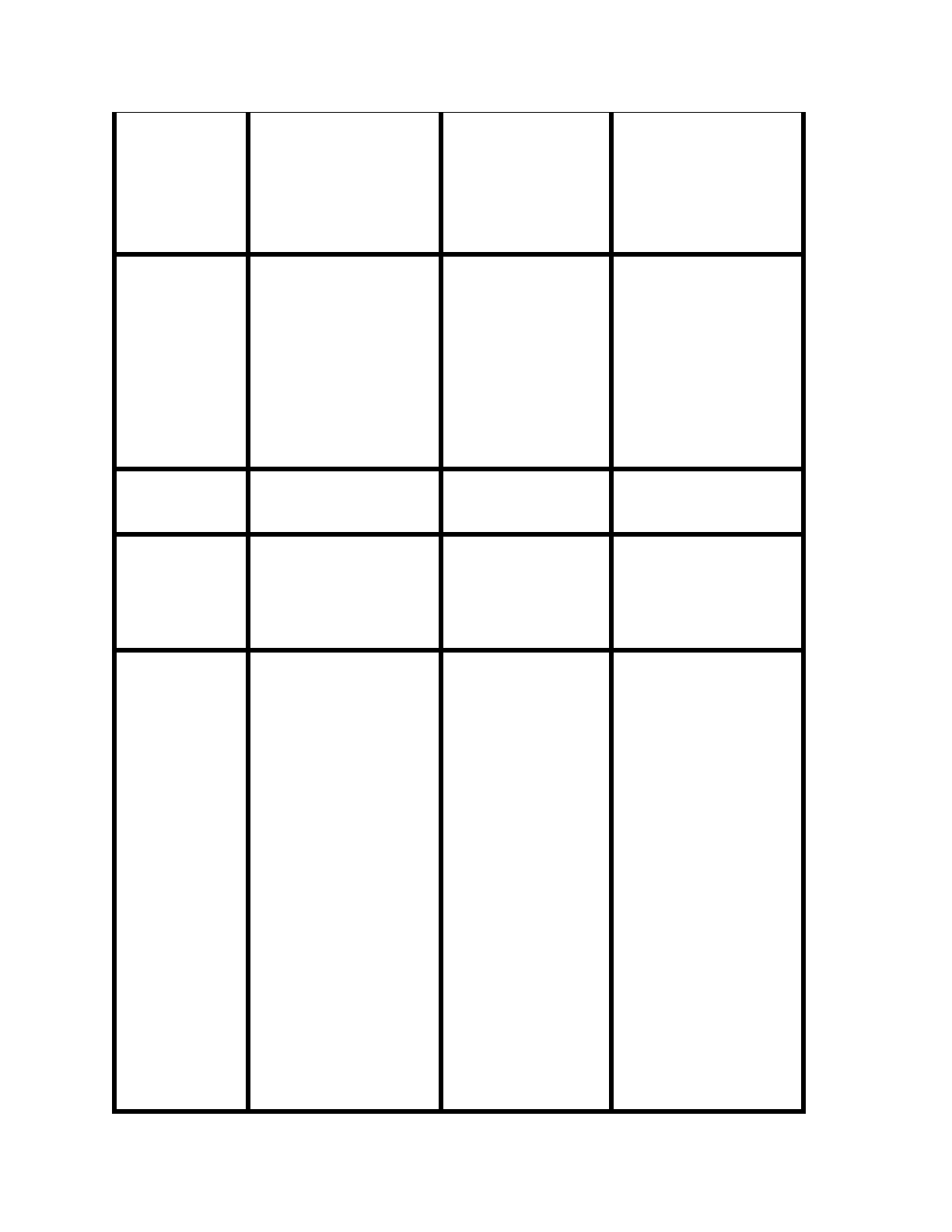
Table 2: Summary of Study Designs of Articles Retrieved
Level
Study Design/
Methodology of
Articles Retrieved
Total
Number
Located
Data Base
Source
Citation (Name, Year)
Level 1a
Systematic Reviews or
Meta-analysis of
Randomized Control
Trials
Level 1b
Individualized
Randomized Control
Trials
Level 2a
Systematic reviews of
cohort studies
Level 2b
Individualized cohort
studies and low quality
RCT’s (PEDro < 6)
Level 3a
Systematic review of
case-control studies
Level
3b
Case-control studies
and non-randomized
controlled trials
I
ProQuest
Dissertations
& Theses
(PQDT)
(Boyd, 2007)
Level 4
Case-series and poor
quality cohort and case-
control studies
III
PUBMED
EBSCOhost
ProQuest
Dissertations
& Theses
(PQDT)
(Addison, 2012)
(Benson, 2013)
(Peterson, 2013)
Level 5
Expert Opinion,
qualitative research,
V
EBSCOhost
(Dobbelsteyn, 2005)
Prepared by Holly Freeman, Alisa Reedy and Ashley Schalow (12/10/2015). Available at
www.UWLAX.EDU/OT

8
program descriptions
EBSCOhost
EBSCOhost
EBSCOhost
EBSCOhost
Geggie, 1999)
(Gisel, 1994)
(Ghanizadeh, 2013)
(Toomey, 2011)
STUDIES INCLUDED:
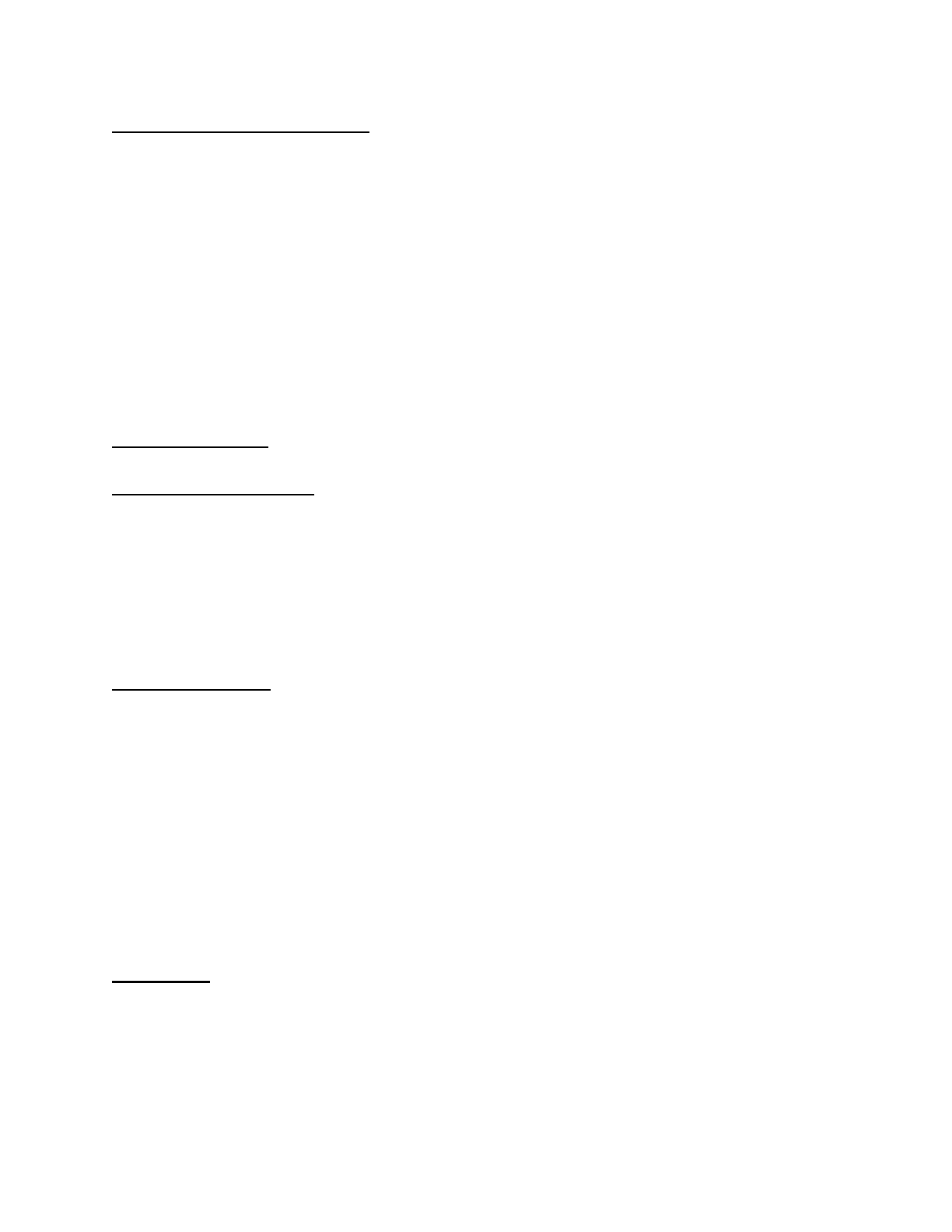
Table 3: Summary of Included Studies
Study 1
Benson, 2013
Study 2
Peterson, K., 2013
Study 3
Boyd, K.L., 2007
Design
Case-series
retrospective repeated-
measures within
subject design
Random control
trial
Quasi-experimental
design
Level of
Evidence
Strength: 4
Strength: 4
Strength: 3B
Rigor Score
SCED: 5/11
SCED: 8/11
SNS:6/8
Population
-34 children (56% M,
44% F) ages 30-92
months
-Mean age= 57.2
months
-Autism (38%), CP
(12%), neurological
impairments (38%),
and no specific
diagnosis (12%)
-6 male, school-
aged children ages
4-6
-Mean age = not
provided
-Issues consuming a
variety of foods and
a diagnosis of ASD
-37 children ages 8-61
months (21 M, 16 F)
-Mean age= 37.23
months
-7 children had GI
feeding tubes
-Other diagnoses
included
gastroesophageal
reflux, oral motor
delays, low tone,
sensory difficulties,
anxiety or trauma
related to food, heart
issues, autism, and
developmental delays.
Prepared by Holly Freeman, Alisa Reedy and Ashley Schalow (12/10/2015). Available at
www.UWLAX.EDU/OT
9
-All children were
given therapy in a
group setting at
Toomey and
Associates Inc.
Intervention
Investigated
Effectiveness of the
SOS protocol
intervention leading to
positive trend in
feeding scores in
children with feeding
difficulties.
To determine
whether the SOS
protocol or ABA
behavioral approach
is more effective for
the treatment of
sensory-based
feeding disorders
To examine the
effectiveness of the
SOS protocol with
feeding disorders, as
developed by Dr. Kay
Toomey
Comparison
Intervention
N/A
ABA behavioral
intervention
N/A
Dependent
Variables
-Level of interaction
with the food (25-step
scale)
-Food type
-Food acceptance
-Clean mouth
-Food (gram) intake
-Number of foods
consumed
Outcome
Measures
-25 step scale
developed by Toomey
(feeding score from 1-
25)
-Food (characterized
by hard munchable,
meltable, solid, puree,
or drink)
-Acceptance was
defined as the child
picking up an eating
utensil or using his
fingers to pick up
the bite of food and
placing the entire
bite of food into
mouth within 8
seconds after food
presentation.
-Mouth clean was
defined as the child
having a bite of
food no larger than
a grain of rice in his
mouth 30 seconds
after placing the
-3 day diet histories
done by parents (prior
to and after treatment)
-Initiation of tasting
new food 80-90% of
time
-30 different foods in
food preferences (10
protein, 10 starches, 10
fruits/vegetables)
-Height/weight must
consistently increase
over a 6-12 week
period and following
growth curves
appropriate for age and
condition
-Able to handle age
Prepared by Holly Freeman, Alisa Reedy and Ashley Schalow (12/10/2015). Available at
www.UWLAX.EDU/OT

10
food into his mouth.
If the child spit the
food out, this was
not included.
-To measure amount
of food intake, the
therapist measured
the weight of the
food on a scale
before and after the
therapy sessions.
appropriate foods
without negative
behaviors during
mealtimes
-Able to consume
appropriate amount of
fluid for age group
Results
-5 patterns in feeding
scores were found.
- Patterns 1 & 2
showed no positive
trends in feeding scores
(16 children).
-Pattern 3 had 1 or
more food types with a
positive trend in the
last few sessions of the
intervention (7
children).
-Pattern 4 was positive
trend for 1 or more
food
types (5 children).
-Pattern 5 was positive
trend for all food types
(6 children).
-High levels of food
acceptance, clean
mouth, and food
intake were
observed after half
of the participants
received ABA
treatment.
-However, the other
half of the
participants who
received the SOS
treatment did not
achieve any change
throughout
participation in the
program.
-After participants
switched over to the
ABA treatment, it
was observed that
high levels of
acceptance began to
occur across all
areas.
-Children who received
one 12-week SOS
intervention had an
increase in the number
of foods consumed,
which was assessed
with the 3-day diet
history.
-Children who attended
two 12-week
interventions improved
the number of foods
consumed
significantly.
-Children who went on
to attend three or four
12-week sessions did
not have a significant
increase in the number
of foods consumed.
Prepared by Holly Freeman, Alisa Reedy and Ashley Schalow (12/10/2015). Available at
www.UWLAX.EDU/OT

11
Effect Size
N/A
N/A
-Group 1: 46% (17/37)
of participants
improved after first 12-
week session.
-Group 2: Additional
22% (8/37) improved
after second 12-week
session.
-After third 12-week
session of SOS
protocol, no significant
improvement was
observed.
Conclusion
The results of this
study were
inconclusive as to
whether the SOS
protocol was an
effective intervention
for improving eating in
children with
neurological disorders.
It was concluded
that the ABA
treatment was
effective at
increasing food
acceptance and
consumption in all 6
of the children,
whereas the SOS
intervention was
not.
It was concluded that
children who attended
one or two 12-week
SOS feeding sessions
significantly improved
the number of foods
consumed. However,
it was found that
children that attended
three or more 12-week
feeding sessions did
not continue to see
significant
improvements in
number of foods
consumed.
IMPLICATIONS FOR PRACTICE, EDUCATION and FUTURE RESEARCH:
PICO Question:
What is the effectiveness of the Sequential Oral Sensory (SOS) approach in occupational therapy
for improving eating in children ages 8 months-8 years with feeding difficulties compared to
ABA or no treatment?
Prepared by Holly Freeman, Alisa Reedy and Ashley Schalow (12/10/2015). Available at
www.UWLAX.EDU/OT
12
Operational Definition of Terms:
SOS: Sequential Oral Sensory approach is a desensitization therapy intervention developed by
Dr. Kay Toomey to address issues with feeding difficulties in children.
ABA: Applied Behavioral Analytic approaches are based on applied behavioral theories which
assume that behavior is learned, and therefore, behavior can be altered or reshaped when it is
reinforced.
Feeding difficulties: Behaviors or medical conditions that lead to a child’s decreased ability to
eat the adequate amount of food to gain weight and grow normally.
Improved eating: Improved eating includes level of interaction with and acceptance of food,
amount of food taken in (gram intake), mouth clean (no packing of food), number of foods
consumed (number and types of food the child eats), and decrease negative behaviors (outbursts,
gagging, crying, and spitting out food).
Overall conclusions:
Results: Similar Findings
● All three studies were single case studies, measuring various aspects of feeding and
eating during the intervention period.
● Each study included children with feeding issues, however, autism was the most common
diagnosis between all studies.
● All studies were similar amongst the intervention (SOS protocol), which measured some
aspect how of children are eating throughout the intervention.
Results: Differences
● The SOS protocol resulted in 46% of participants improving after 12 weeks in the Boyd
study. After 24 weeks, an additional 22% improved from the SOS protocol, but after the
third session (36 weeks) no further improvement was found.
● No other studies saw improvement with SOS even with a variety of measures including
mouth clean, level of acceptance, gram intake, and number of foods consumed.
● In the study conducted by Peterson, it was found that the ABA treatment had more
positive results on feeding difficulties for all of the children involved in the study.
Overall, the findings of these studies reveal inconclusive and limited results as to whether the
SOS protocol is effective for improving eating with children who have eating difficulties.
Boundaries:
There was a total of 77 participants ages 8 months to 8 years in all 3 articles together with
a mean of 4.3 years. Diagnoses differed between studies and included autism, cerebral palsy,
neurological impairments, GI feeding tubes, gastroesophageal reflux, oral motor delays, low
tone, sensory difficulties, anxiety or trauma related to food, heart issues, developmental delays,
and no specific diagnoses. All children displayed some form of feeding difficulty during
Prepared by Holly Freeman, Alisa Reedy and Ashley Schalow (12/10/2015). Available at
www.UWLAX.EDU/OT
13
mealtimes. Exclusion criteria varied across studies, when you combine studies, the exclusion
criteria included severe medical issues, failure to thrive, insufficient caloric intake, and any child
who did not fit the diet history criteria.
Implications for practice:
All three articles showed limited evidence of the use of SOS in practice. The SOS
protocol developer, Kay Toomey, has shown minimal support for this intervention. In the study
done by Boyd, the only article that supported the use of SOS, participants were gathered from
Toomey and Associates, Inc. This company was developed by Kay Toomey. Therefore, the
Boyd study may have been influenced by experimenter effects which could be the reason that it
was the only study to show positive results of the SOS protocol. Toomey suggests that there be a
minimum of 12 weeks of SOS therapy before successful results were shown to be effective, and
in the study done by Boyd, the results showed similar findings. Based on the literature reviewed,
ABA has been shown to be more effective for feeding difficulties in children, and one study that
was found provided ABA treatment to every child in the study after effectiveness was
demonstrated. Overall, there is limited research and evidence to determine effectiveness or
ineffectiveness of the SOS protocol. In summary, without a randomized control trial, the
evidence is inconclusive as to whether this treatment approach is a practical use of clinician’s
money and time.
Clinical Bottom Line:
There is limited evidence supporting the use of the SOS approach to feeding with mixed
results on the effectiveness to improve eating.
Prepared by Holly Freeman, Alisa Reedy and Ashley Schalow (12/10/2015). Available at
www.UWLAX.EDU/OT

14
APPENDIX A.
The SOS protocol involves a series of steps to help the child become more comfortable
and prepared for trying different foods. Because one of the assumptions to development of eating
difficulties is based on hypersensitivity, the first step in the SOS protocol is to prepare the child
with sensory integrative approaches. According to the protocol, this initial preparation is to
promote organization of the senses and to increase body awareness. The sensory preparation
routine involves playing on jungle gym equipment or an obstacle course to engage the child in
gross motor activities such as running, lifting, pushing, and jumping. The therapist models these
behaviors for the child and praises the child when he or she engages in the modeled behaviors.
However, the therapist allows the child to perform other activities on the jungle gym to enable
the child to create his or her own sensory preparation routine and promote child-directed therapy
(Peterson, 2013).
After about 10 minutes, the sensory preparation period is complete, and the therapist
guides the child into the therapy room or area of intervention. The child is prompted to sing and
march while on the way to the room where eating will take place. The therapist uses modeling to
do so, but if the child does not choose to sing or march, the child may choose to do as they wish.
As the child enters the feeding therapy room, the therapist guides or helps the child sit in his or
her seat in order to engage the child in the pre-meal setup step (Peterson, 2013).
During this stage and throughout the rest of the SOS approach, the therapist sequentially
encourages the child by giving the child positive, non-directive statements, using behavior
modeling, using light physical prompts, and using full physical guidance. An example of a non-
directive statement that the therapist could say is, “Cleaning up is fun!” If the child did not do
what was asked in 10 seconds, the therapist would give the next sequential prompt. Meal time
setup included washing face, washing hands, blowing bubbles with the remainder of the soap,
washing the table, and setting the table. The therapist again modeled the behavior even if the
child did not do meal time setup (Peterson, 2013).
Once the pre-meal setup step is complete, the therapist then introduces the food, in a
hierarchical and gradual manner. Therefore, if twelve foods are to be presented to the child in
each session, the first exposure would include one aversive food, and eleven non-aversive foods.
The preferences of aversive and non-aversive foods of the child would be determined by
interview with the caregiver. The non-aversive foods always included pureed, meltable hard
solids and hard munchable solids. The first food that was presented to the child was a non-
aversive food that was available for the child to interact with for four minutes and then placed on
the food plate within arm’s reach. Each food item after the first presented food contained one
similar property, such as color, taste, texture or size. The therapist encouraged the child to
interact with each food item based on the steps-to-eating hierarchy. For example, food in front of
the child would be lower on the hierarchy than the child touching the food to his or her lips. The
major steps involved in the hierarchy incorporate visual tolerance, indirect interaction, smelling,
touching, tasting, and consuming the food (Peterson, 2013).
Prepared by Holly Freeman, Alisa Reedy and Ashley Schalow (12/10/2015). Available at
www.UWLAX.EDU/OT

15
Visual tolerance gradually introduces the child to the food at varying distances in relation
to the child. Indirect interaction encompasses promoting the child to help prepare the food, use
utensils to serve or touch the food, and to touch the food through other objects, such as a napkin.
Smelling consisted of presenting a food with a prominent stench and having the child be near the
food and picking up the food and smelling it. Touching involves the child touching the food
using any body parts including fingers, arms, chest, neck, or tongue. Tasting the food includes
licking with tip of tongue, full tongue, biting a piece and spitting it out, biting a piece and
keeping it in the mouth, and biting the food, chewing it and expelling the food. Eating the food
consisted of chewing the food and swallowing part and spitting out the rest, chewing,
swallowing, and drinking immediately after, and chewing, swallowing without taking a drink.
Throughout the feeding hierarchy session, the therapist used descriptive, positive, and
neutral comments about the child engaging with the food, such as “Johnny can lick the carrot.”
Additionally, the therapist used playfulness to evoke relaxation such as singing, playing with the
food, squishing the food and painting with the food. The therapist would continue with light
physical prompts or full physical guidance if after 30 seconds the child did not engage with the
food. The child was never forced with comply with the behaviors if the child resisted. The
therapist would attempt to place the food as close as the child would allow. If the child required
full physical guidance, the step was failed, and the subsequent step before that one would be
given (Peterson, 2013).
The intention of the SOS protocol is to allow the child to progress through the hierarchy
of steps in order for the child to bite, chew, and swallow the aversive food. To increase
consumption and tolerance of an aversive food, the therapist would present it through different
manners, such as changing the texture of the food. In addition, the aversive food would be
discontinued and a different aversive food would be presented if the child did not interact or
consume the food within six therapy sessions. The first three sessions included presentation of
the same food items in the same order and the same manner, so that the child can be accustomed
to a routine. However in the fourth session, the therapist changed the properties of the food by
altering the shaped, temperature or texture (Peterson, 2013).
Following the feeding intervention, the therapist facilitated a clean-up routine by saying
“All done, time to clean up.” The therapist then asked the child to “blow or throw away” at the
least one food that was used in the eating session by placing it on the lips and spitting the food
into the trashcan. If the child did not comply, the therapist would encourage the child to touch
the food, with or without a napkin, and throw it in the trash. The child was then asked to help
wash the table, throw away the trash, and wash his or her face and hands (Peterson, 2013).
Once the intervention has been administered, the therapist then provides caregiver
training to continue and facilitate the progress of the child with tolerating and accepting different
types of food. Written material on the instructions of the protocol, modeling behaviors, role-
playing, and feedback should be given to the caregivers to help the child maintain a consistency
when interacting with food at home (Peterson, 2013). Children with a sensory processing deficit
have troubles modulating their sensory input and may not be able to identify all the sensory
Prepared by Holly Freeman, Alisa Reedy and Ashley Schalow (12/10/2015). Available at
www.UWLAX.EDU/OT

16
properties of an object. They may over-react or under-react to these sensory inputs, and this may
lead to sensitivities to food because the child cannot decipher the sensory information that they
are receiving (Peterson, 2013).
Prepared by Holly Freeman, Alisa Reedy and Ashley Schalow (12/10/2015). Available at
www.UWLAX.EDU/OT
17
References
Benson, J. D., Parke, C. S., Gannon, C., & Muñoz, D. (2013). A retrospective analysis of the
sequential oral sensory feeding approach in children with feeding difficulties. Journal of
Occupational Therapy, Schools & Early Intervention, 6(4), 289-300 12p.
doi:10.1080/19411243.2013.860758
Boyd, K. (2007). The effectiveness of the sequential oral sensory approach group feeding
program (Doctoral dissertation). Available from ProQuest Dissertations & Theses (PQDT)
database. Dissertation Abstract International, B 69/01, P. 665 Retrieved October 29th,
2015 from http://search.proquest.com/docview/304762667
Peterson, K.M. (2013) A comparison of the sequential-oral-sensory approach to an applied
behavior analytic approach in the treatment of pediatric feeding disorders (Doctoral
dissertation). Retrieved September 18th, 2015, from ProQuest Dissertations & Theses
(PQDT) database.
Related Articles:
Addison, L.R., Piazza C.C., Patel, M.R., Bachmeyer, M.H., Rivas, K.M., Milnes, S.M. and
Oddo, J. (2012). A comparison of sensory integrative and behavioral therapies as
treatment for pediatric feeding disorders. Journal of Applied Behavioral Analysis, 45, 455-
471 17p. doi:10.1901/jaba.2012.45-455
American Occupational Therapy Association (2014). Occupational therapy practice framework:
Domain and process (3rd ed.). American Journal of Occupational Therapy. 68(suppl. 1),
S1-S48. http://dx.doi.org/10.5014/ajot.2014.682006
American Speech-Language-Hearing Association | ASHA. (2015). Retrieved October 28,
2015, from http://www.asha.org/default.aspx
Prepared by Holly Freeman, Alisa Reedy and Ashley Schalow (12/10/2015). Available at
www.UWLAX.EDU/OT
18
Applied behavioral frames (2008). In M. Cole & E. Tufano (Ed.), Applied theories in
occupational therapy: A practical approach (pp. 125-132). Thorofare, NJ: SLACK,
Incorporated.
Case-Smith, J. (2005). Occupational therapy for children (5th ed.). St Louis: Elsevier.
Dobbelsteyn, C., Marche, D., Blake, K., & Rashid, M. (2005). Early oral sensory experiences and
feeding development in children with CHARGE syndrome: a report of five cases.
Dysphagia (0179051X), 20(2), 89-100 12p.
Geggie, J., Dressler-Mund, D., Creighton, D., & Cormack-Wong, E. (1999). An interdisciplinary
feeding team approach for preterm, high-risk infants and children. Canadian Journal Of
Dietetic Practice & Research,60(2), 72-77 6p.
Ghanizadeh, A. (2013). Parents reported oral sensory sensitivity processing and food preference
in ADHD. Journal Of Psychiatric & Mental Health Nursing, 20(5), 426-432 7p.
doi:10.1111/j.1365-2850.2011.01830.x
Gisel, E. (1994). Oral sensorimotor therapy: assessment, efficacy and future directions.
Occupational Therapy International, 1(4), 209-232 24p.
McLeod, S. A. (2008). Systematic Desensitization. Retrieved from
www.simplypsychology.org/Systematic-Desensitisation.html
SOS Approach to Feeding. Toomey and Associates, 2015. Web. 29 Oct. 2015.
http://www.sosapproach-conferences.com/about-us/sos-approach-to-feeding
Toomey, K. A., & Ross, E. (2011). SOS Approach to Feeding. Perspectives On Swallowing &
Swallowing Disorders (Dysphagia), 20(3), 82-87 6p. doi:10.1044/sasd20.3.82
WHO (2015). International classification of functioning, disability and health (ICF).
Retrieved from http://www.who.int/classifications/icf/en
Prepared by Holly Freeman, Alisa Reedy and Ashley Schalow (12/10/2015). Available at
www.UWLAX.EDU/OT
