
Merit-Based Incentive Payment System (MIPS):
Total Per Capita Cost (TPCC) Measure
Measure Information Form
2023 P
erformance Period
2
Total Per Capita Cost Measure Information Form (MIF)
Table of Contents
1.0 Introduction 3 .....................................................................................................................
1.1 Measure Name 3 ........................................................................................................
1.2 Measure Description 3 ................................................................................................
1.3 Measure Rationale 3 ..................................................................................................
1.4 Patient Exclusion Criteria 4 .........................................................................................
1.5 Measure Numerator 4 .................................................................................................
1.6 Measure Denominator 4 .............................................................................................
1.7 Data Sources 4 ...........................................................................................................
2.0 Methodology Steps 5 .........................................................................................................
3.0 Measure Specifications Quick Reference 6
......................................................................
Appendix A. Detailed Measure Calculation Methodology 8 .....................................................
A.1 Measure Attribution 8 .................................................................................................
Step 1: Identify Candidate Events 8 ............................................................................
Step 2: Apply Service Category and Specialty Exclusions 9 .......................................
Step 3: Construct Risk Windows 10 .............................................................................
Step 4: Attribute Beneficiary Months to TINs and TIN-NPIs 10
....................................
A.2 Measure Calculation 11 ...............................................................................................
Step 5: Calculate Payment-Standardized Monthly Observed Costs 11 ........................
Step 6: Risk-Adjust Monthly Costs 11 ..........................................................................
Step 7: Specialty Adjust Monthly Costs 13 ..................................................................
Step 8: Calculate the TPCC Measure Score 14 ...........................................................
Appendix B. Evaluation and Management “Primary Care” Services List 15 ...........................
Appendix C. Illustration of Overlapping Risk Windows Triggered by a TIN for the Same
Patient 17
.............................................................................................................................
Appendix D. Illustration of Attribution of Beneficiary Months for the TPCC Measure 19 .......
Appendix E. Example of Specialty Adjustment 21
....................................................................
3
Total Per Capita Cost Measure Information Form (MIF)
1.0 Introduction
This document details the methodology for the Total Per Capita Cost (TPCC) measure. The
methodology should be reviewed along with the Measure Codes List file, which contains the
medical codes used in constructing the measure.
1.1 Measure Name
Total Per Capita Cost (TPCC)
1.2 Measure Description
The TPCC measures the overall cost of care delivered to a patient with a focus on the primary
care they receive from their provider(s). The measure is a payment-standardized, risk-adjusted,
and specialty-adjusted measure. The measure is attributed to clinicians, who are identified by
their unique Taxpayer Identification Number and National Provider Identifier pair (TIN-NPI) and
clinician groups, identified by their TIN number. The TPCC measure can be attributed at the TIN
or TIN-NPI level. In all supplemental documentation, the term “cost” generally means the
standardized
1
Medicare allowed amount.
2
1.3 Measure Rationale
The TPCC measure is an important means of measuring Medicare spending, as health
expenditures continue to increase in the United States. Total health care spending is estimated
to have increased by 4.6% in 2017, reaching $3.5 trillion.
3
Spending for Medicare, which is still
predominantly paid on a fee-for-service (FFS) basis, grew by 3.6%, reaching $672.1 billion.
Spending on services for physicians and other health professionals totaled $69.9 billion and
accounted for 15% of Medicare FFS spending in 2016.
4
The TPCC measure specifically
focuses on the importance of successful payment models for primary care management.
Effective primary care management can support Medicare savings in a number of ways,
including through improvements in the treatment of chronic conditions by obviating the need for
high-cost hospital or emergency department services. More effective primary care management
can also direct a greater proportion of patients to lower hospital costs for the inpatient services.
Given the potential for decreasing spending through improvements in primary care delivery, the
TPCC measure allows for a savings opportunity by capturing the broader healthcare costs
influenced by primary care.
A TPCC measure was originally used in the Physician Value-Based Payment Modifier (VM)
Progr
am and reported in the annual Quality and Resource Use Reports (QRURs). With the
introduction of the Quality Payment Program, a version of the TPCC measure was finalized with
minor adaptations from VM and added to MIPS. The TPCC measure has undergone re-
1
Claim payments are standardized to account for differences in Medicare payments for the same
service(s) across Medicare providers. Payment standardized costs remove the effect of differences in
Medicare payment among health care providers that are the result of differences in regional health care
provider expenses measured by hospital wage indexes and geographic price cost indexes (GPCIs) or
other payment adjustments such as those for teaching hospitals. For more information, please refer to the
“CMS Price (Payment) Standardization - Basics" and “CMS Part A and Part Price (Payment)
Standardization - Detailed Methods” documents posted on the
CMS Price (Payment) Standard
ization
Overview page (htt
ps://www.resdac.org/articles/cms-price-payment-standardizationo
verview)
2
Cost is defined by allowed amounts on Medicare claims data, which include both Medicare trust fund
payments and any applicable beneficiary deductible and coinsurance amounts.
3
“National Health Expenditure Projections, 2017-2026.” US Centers for Medicare & Medicaid Services,
2018.
4
“Report to the Congress: Medicare Payment Policy.” MedPAC, 2018.
4
Total Per Capita Cost Measure Information Form (MIF)
evaluation to address stakeholder feedback received from prior public comment periods and
was finalized for 2020 MIPS performance period.
1.4 Patient Exclusion Criteria
Patients are excluded from the measure population if they meet any of the following conditions:
• They were not enrolled in both Medicare Part A and Part B for every month during the
perf
ormance period, unless part year enrollment was the result of new enrollment or
death.
• They were enrol
led in a private Medicare health plan (e.g., a Medicare Advantage or a
Medicare private FFS plan) for any month during the performance period.
• They resided
outside the United States or its territories during any month of the
performance period.
• They are cov
ered by the Railroad Retirement Board.
1.5 Measure Numerator
The numerator for the measure is the sum of the risk-adjusted, payment-standardized, and
specialty-adjusted Medicare Parts A and B costs across all beneficiary months attributed to a
TIN or TIN-NPI during the performance period.
1.6 Measure Denominator
The denominator for the measure is the number of beneficiary months attributed to a TIN or
TIN-NPI during the performance period.
1.7 Data Sources
The TPCC measure uses the following data sources:
• Medicare Parts A and B claims data from the Common Working File (CWF)
• Enroll
ment Data Base (EDB)
• Common
Medicare Environment (CME)
• Long Term
Care Minimum Data Set (LTC MDS)
5
Total Per Capita Cost Measure Information Form (MIF)
2.0 Methodology Steps
There are 2 parts to the TPCC measure calculation: attribution (Steps 1-4) and measure
calculation (Steps 5-8). This section provides a brief summary of these processes, and
Appendix A describes them in detail.
1. Identify candidate events. A candidate event identifies the start of a primary care
relationship between a clinician and patient. A candidate event is defined using select
evaluation and management (E&M) Current Procedural Terminology / Healthcare Common
Procedure Coding System (CPT/HCPCS) codes for outpatient physician visit, termed E&M
“primary care” service, paired with one or more additional service(s) indicative of general
primary care that together trigger the opening of a risk window.
2.
Apply service category and specialty exclusions. Clinicians are excluded from attribution
if they meet the criteria for one or more service exclusions in the following categories: global
surgery, anesthesia, therapeutic radiation, and chemotherapy. Clinicians are also excluded
based on their Health Care Finance Administration (HCFA) Specialty designation, if they
identify as one or more of the 56 specialties in the specialty exclusion list.
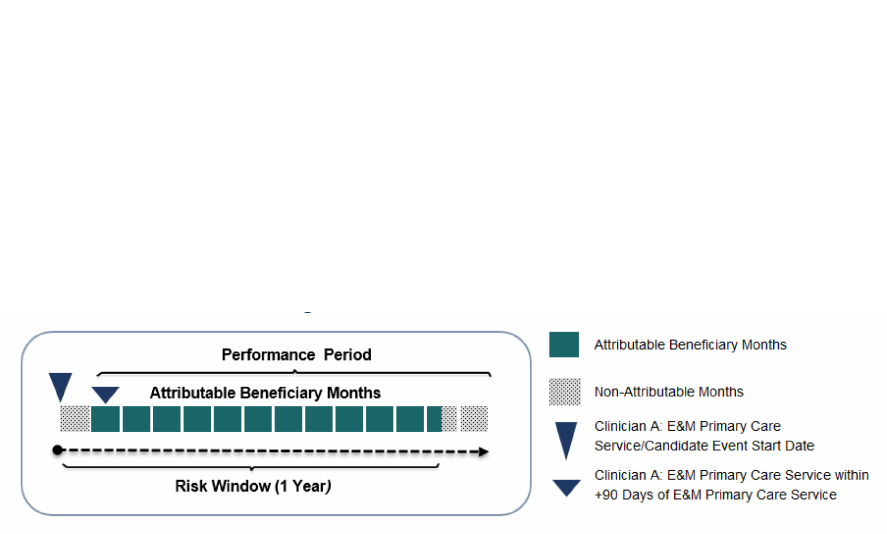
3. Construct risk windows. The risk window begins on the date of the candidate event and
c
ontinues until one year after that date. A patient’s costs are attributable to a clinician during
months where the risk window and performance period overlap.
4. Attribute months to TINs and TIN-NPIs. After service category and specialty exclusions
ar
e applied, all costs occurring during the covered months are attributed to the remaining
eligible TINs. For TIN-NPI attribution, only the TIN-NPI responsible for the majority share, or
plurality, of candidate events provided to the patient within the TIN is attributed that patient’s
costs for their respective candidate events.
Figure 1. TPCC Measure Framework
5. Calculate payment-standardized monthly observed costs. Monthly observed costs are
payment standardized to account for differences in Medicare payments for the same
service(s) across Medicare providers. All standardized cost from services starting in a
beneficiary month are assigned.
6. Calculate risk-adjusted monthly costs. Risk adjustment accounts for patient-level risk
factors that can affect medical costs, regardless of the care provided. After costs are risk-
adjusted, winsorization is applied to reduce the effect of outliers.
7. Apply specialty adjustment to risk-adjusted costs. A specialty adjustment is applied to
m
onthly risk-adjusted costs to account for the fact that costs vary across specialties and
across TINs with varying specialty compositions.
8. Calculate the measure score. Calculate the average payment-standardized, risk-adjusted,
and specialty-adjusted monthly costs across all beneficiary months in the performance
period attributed to a TIN or TIN-NPI for the measure score.
6
Total Per Capita Cost Measure Information Form (MIF)
3.0 Measure Specifications Quick Reference
This page provides a quick, at-a-glance reference for the TPCC measure specifications. The full
list of codes and logic used to define each component can be found within the Measure Codes
List file.
Candidate Event: Which patients are included in the measure?
A candidate event is defined as a pair of services billed by the clinician to the patient within a short period
of time. A candidate event marks the start of a primary care relationship between a patient and a clinician.
Risk Window: When is a clinician responsible for the patient’s costs?
Risk window is a year-long period that begins on the date of the candidate event.
Beneficiary Months Attribution: How is the TPCC measure attributed?
The performance period is a static calendar year that is divided into 13 4-week blocks called beneficiary
months. Beneficiary months that occur during a risk window and the performance period are counted
towards a clinician’s (or clinician group’s) measure scores. These beneficiary months are attributed to the
TIN billing the initial E&M “primary care” service. For TIN-NPI-level attribution, only the TIN-NPI
responsible for the plurality (largest share) of candidate events provided to the patient within the TIN is
attributed the beneficiary months.
Service Assignment: Which services are included in the measure?
TPCC is an all-cost measure.
Risk Adjustors: How does TPCC adjust for patient-level risk factors that can affect medical
costs?
Patient risk score is calculated using CMS-ESRD V21 2022 models (Dialysis New Enrollee Model,
Dialysis Continuing Enrollee Model, Community Functioning Graft Model, Institutional Functioning Graft
Model, and New Enrollee Functioning Graft Model) and CMS-HCC V24 2022 models (New Enrollee
Model, Community Model, Institutional Model).
Risk adjustors included in the CMS-HCC V24 and CMS-ESRD V21 risk adjustment models include the
following:
• Patient comorbidi
ties captured by 86 Hierarchical Condition Category (HCC) codes and 87 HCC
codes in the CMS-HCC and CMS-ESRD risk adjustment models, respectively
• Total number of patient comorbidities captured by HCCs
• Interaction variables accounting for a range of patient comorbidities
• Patient gender
• Patient dual status
• Pat
ient original reason for Medicare enrollment: age, disability and LTI status
• Patient dialysis/End-St
age Renal Disease (ESRD) status, kidney transplant and functioning graft
duration
Exclusions: Which populations are excluded from the measure?
• The patient has a primary payer other than Medicare for any month during the performance period.
•
The patient was not enrolled in Medicare Parts A and B for every month during the performance
period, unless part year enrollment was the result of new enrollment or death.
• The patient’s date of birth is missing.
• The patient’s death dat
e occurred before the performance period.
• The patient resided outside the United States or its territories during any month of the performance
per
iod.
• The patient was cov
ered by the Railroad Retirement Board.
• The clinician met the billing threshold for one or more of the following service category exclusions:
gl
obal surgery, anesthesia, therapeutic radiation, and chemotherapy.
7
Total Per Capita Cost Measure Information Form (MIF)
• The clinician identified as one or more of the 56 specialties in the specialty exclusions list, based on
their HCFA Specialty designation.
8
Total Per Capita Cost Measure Information Form (MIF)
Appendix A. Detailed Measure Calculation
Methodology
This section describes the construction of the TPCC measure in more detail: Section A.1
outlines the construction and attribution of beneficiary months to clinicians and Section A.2
outlines measure calculation.
A.1 Measure Attribution
This section outlines in detail the following steps in measure attribution:
Step 1: Identify Candidate Events
Step 2: Apply Service Category and Specialty Exclusions
Step 3: Construct Risk Windows
Step 4: Attribute Beneficiary Months to TINs and TIN-NPIs
Step 1: Identify Candidate Events
A candidate event is used to indicate the start of a primary care relationship between a clinician
and patient and is identified by the occurrence of 2 Part B Physician/Supplier (Carrier) claims
with particular CPT/HCPCS services billed in close proximity. There are 2 different sets of
CPT/HCPCS codes used: E&M “primary care” services and primary care services.
E&M “primary care” services are a specific set of evaluation and management codes for
physician visits in the outpatient setting, physician office, nursing facility, or assisted living.
5
Primary care services are a broader list of services related to routine primary care and generally
fall into the following categories
6
:
• Durable Medical Equipment (DME) and Supplies
• Electrocardiogram
• Laboratory - Che
mistry and Hematology
• Other Diagnostic Procedures (I
nterview, Evaluation, Consultation)
• Other Diagnostic Radiology and Related
Techniques
• Prophylactic Vaccinations and Inoculati
ons
• Routine Chest X-ray
• Clinical Labs
7
• Preventive Services
8
5
Appendix B contains the list of evaluation and management “primary care” codes used in construction of
a candidate event.
6
The following primary care service categories are defined using the Clinical Classifications Software
(CCS) (https://www.hcup-us.ahrq.gov/toolssoftware/ccs10/ccs10.jsp) c
ategories developed by the Agency
for Healthcare Research and Quality (AHRQ): DME and supplies, Electrocardiogram, Laboratory -
Chemistry and Hematology, Other diagnostic procedures (interview, evaluation, and consultation), other
diagnostic radiology and related techniques, and Prophylactic vaccinations and inoculations.
7
The Clinical Labs primary care service category is defined using a subset of services included in the
Clinical Laboratory Fee Schedule (htt
ps://www.cms.gov/Medicare/Medicare-Fee-for-Service-
Pay
ment/ClinicalLabFeeSched/index ).
8
The Preventive Services primary care service category is defined using the set of services CMS
considers to be part of the primary care service benefit
(https://www.cms.gov/Medicare/Prevention/PrevntionGenInfo/medicare-preventive-services/MPS-
QuickReferenceChart-1.html
).

9
Total Per Capita Cost Measure Information Form (MIF)
To identify a candidate event, firstly, an initial E&M “primary care” service billed on Part B
Physician/Supplier (Carrier) claim is identified. This E&M “primary care” service isn’t considered
if it occurs during a patient’s stay at a Critical Access Hospital (CAH), Inpatient Facility, or
Skilled Nursing Facility (SNF). Secondly, in addition to the initial E&M “primary care” service, at
least one of the following services should be billed to confirm the candidate event:
• From any TIN within +/- 3 days: Another primary care service
•
From the same TIN within + 90 days: A second E&M “primary care” service OR
anot
her primary care servic
e
See the “E&M_Prim_Care” and the “Prim_Care_Services” tabs of the TPCC Measure Codes
List file for the list of the CPT/HCPCS codes that identify E&M “primary care” services and
primary care services, respectively.
Step 2: Apply Service Category and Specialty Exclusions
Once candidate events are identified, TIN-NPIs
9
can be attributed based on their involvement in
the candidate event. The TIN-NPI responsible for a candidate event is found on the initial E&M
“primary care” service claim of the candidate event. Some TIN-NPIs are excluded from
attribution if they meet 1 of 2 types of exclusions: service category exclusions and specialty
exclusions. Candidate events belonging to TIN-NPIs who meet any of these exclusions are
removed from attribution and measure calculation for both the TIN-NPI and their respective TIN.
Step 2.1: Exclude Clinicians Based on Service Category Exclusions
A TI
N-NPI and their candidate events are removed from attribution if a clinician meets any of the
following 4 service category thresholds:
•
The TIN-NPI billed 10-day or 90-day global surgery services during 15% or more of
their candidate events.
•
The TIN-NPI billed anesthesia services during 5% or more of their candidate events.
•
The TIN-NPI billed therapeutic radiation services during 5% or more of their candidate
events.
•
The TIN-NPI billed chemotherapy services during 10% or more of their candidate
ev
ents.
The steps to determine whether a TIN-NPI qualifies for the service category exclusion are as
f
ollows:
•
Determine the total number of candidate events that are initiated by the TIN-NPI (see
S
tep 1 above on how to identify candidate events).
•
For each candidate event initiated by the TIN-NPI, determine if the TIN-NPI billed an
ex
clusion service (from the list of global surgery, anesthesia, therapeutic radiation, or
chemotherapy services) within +/-180 days of the initial E&M “primary care” service of
the candidate event to the same patient.
• Sum up the number of the candidate events identified in the step above with the
exclusion service of the same type (e.g., sum up the number of candidate events wit
h
t
he anesthesia services separately from the candidate events with the chemotherapy
services), and determine the share of those candidate events out of the total number of
candidate events.
o
If the share meets the threshold listed above (e.g., if more than 5% of the TIN-
NPI’s candidate events have an anesthesia service billed within +/-180 days of
9
Only MIPS eligible clinicians can be attributed the TPCC measure. For more information on MIPS
eligible clinicians, please see “About MIPS Participation” on the QPP website:
https://qpp.cms.gov/participation-lookup/about

10
Total Per Capita Cost Measure Information Form (MIF)
the initial E&M “primary care” service to the same patient), then the TIN-NPI
meets the service category exclusion and thus all candidate events belonging to
that TIN-NPI will be removed from attribution and measure calculation for both
the TIN-NPI and their respective TIN.
The list of CPT/HCPCS codes used for each of the service exclusions can be found in the tabs
of the TPCC
Measure Codes List file labelled: “HCPCS_Surgery,” “HCPCS_Anesthesia,”
“HCPCS_Ther_Rad,” and “HCPCS_Chemo.”
Step 2.2: Exclude Clin
icians Based on Specialty Exclusions
After service category exclusions are applied, clinicians who would not reasonably be
responsible f
or providing primary care are excluded from attribution of the TPCC measure. This
exclusion aims to keep primary care specialists and internal medicine sub-specialists who
frequently manage patients with chronic conditions falling in their areas of specialty. The
excluded specialties list contains 56 specialties that fall into the following broad categories:
• Surgical sub-specialt
ies
• Non-physicians without c
hronic management of significant medical conditions
• Internal medicine sub-specialt
ies with additional highly procedural sub-specialization
• Internal medicine specialties that practice primarily inpatient care without chronic care
management
• Pedi
atricians who do not typic
ally practice adult medicine
The list of HCFA Specialty codes that identify clinicians that are included or excluded from the
measure attr
ibution can be found in the “Eligible_Clinicians” tab of the TPCC Measure Codes
List.
As with service category exclusions described in Step 2.1, candidate events for clinicians in
excluded speci
alties are removed from attribution and measure calculation for both the TIN-NPI
and their respective TIN.
Step 3: Construct Risk Windows
Candidate events that are not excluded initiate the opening of a risk window, a year-long period
that begins on the date of the initial E&M “primary care” service of the candidate event. The
performance period
10
is divided into 13 4-week blocks called beneficiary months. Beneficiary
months during the risk window are considered attributable if they occur during the performance
period. In the event that a risk window begins or ends with a partially covered month, only the
portion during the risk window and the performance period is considered for attribution.
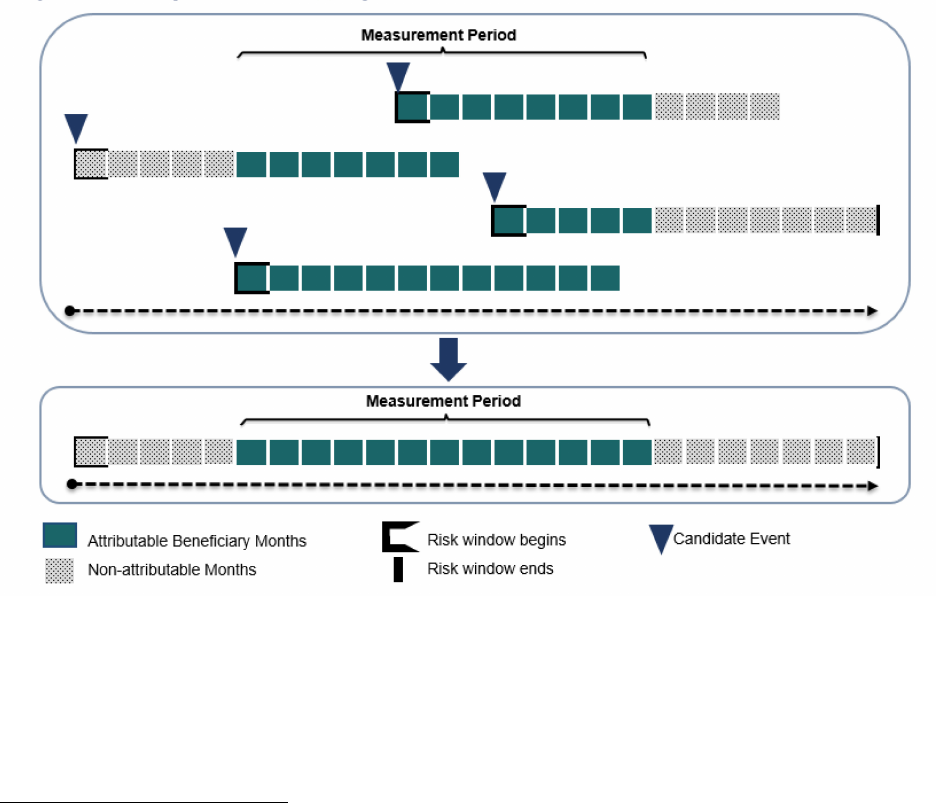
Appendix C contains examples of overlapping risk windows initiated by one or multiple TINs for
the same patient and explains how this overlap is addressed.
Step 4: Attribute Beneficiary Months to TINs and TIN-NPIs
Beneficiary months for a single patient are attributed to a TIN or TIN-NPI according to the
following steps:
• For attribution at the TIN level:
o Identify t
he TIN billing the initia
l E&M “primary care” service claim of each candidate
event.
10
The performance period is a pre-defined and static calendar year performance period.
11
Total Per Capita Cost Measure Information Form (MIF)
o Determine beneficiary months that fall within the risk windows of the candidate
events that were initiated by the TIN and overlap the performance period and
attribute those beneficiary months to the TIN.
• For attribution at the TIN-NPI level:
o Identify the TIN-NPI billing the initial E&M “primar
y care” service claim of each
candidate events.
o Determine beneficiary months that fall within the risk windows of t
he candidate
events that were initiated by the TIN-NPI and that overlap the performance period.
o Identify the TIN-NPI within an attributed TIN
that is responsible for the plurality of
candidate events provided to the patient. If 2 or more TIN-NPIs under a TIN provide
the same proportion of candidate events to a patient, attribute the patient to the TIN-
NPI that provided the earliest candidate event.
o Attribute only the beneficiary months fr
om candidate events that the TIN-NPI is
responsible for initiating, which is not necessarily all candidate events attributed to
the TIN for that patient.
All attributed beneficiary months for all beneficiaries are used for the measure calculation fo
r
each TIN and TIN-NPI.
A.2 Measure Calculation
This section outlines the following steps in measure calculation:
Step 5: Calculate Payment-Standardized Monthly Observed Costs
Step 6: Risk-Adjust Monthly Costs
Step 7: Specialty Adjust Monthly Costs
Step 8: Calculate the TPCC Measure
Step 5: Calculate Payment-Standardized Monthly Observed Costs
Monthly observed cost for attributed beneficiary months is the sum of all service costs billed for
a particular patient during a beneficiary month. Monthly observed costs are standardized to
account for differences in Medicare payments for the same service(s) across Medicare
providers. Payment standardization accounts for differences in Medicare payment unrelated to
the care provided, such as those from payment adjustments supporting larger Medicare
program goals (e.g. indirect medical education add-on payments) or variation in regional
healthcare expenses as measured by hospital wage indexes and geographic price cost indexes
(GPCIs).
11
Standardized costs that occur during partially covered months are pro-rated, based
on the portion of the month covered by the risk window.
Step 6: Risk-Adjust Monthly Costs
Risk adjustment accounts for patient-level risk factors that can affect medical costs, regardless
of the care provided. To ensure that the model measures the influence of health status (as
measured by diagnoses) on the treatment provided (costs incurred) rather than capturing the
influence of treatment on a patient’s health status, the risk adjustment model uses risk factors
from the year prior to a beneficiary month. Separate CMS-HCC models exist for new enrollees,
continuing enrollees, enrollees in long-term institutional settings, and enrollees with ESRD.
11
For more information, please refer to the “CMS Part A and Part B Price (Payment) Standardization -
Basics" and “CMS Part A and Part B Price (Payment) Standardization - Detailed Methods” documents
posted on the
CMS Price (Payment) Standardization Overview
page
(
https://www.resdac.org/articles/cms-price-payment-standardization-overview)
12
Total Per Capita Cost Measure Information Form (MIF)
Risk Adjustment Models
The CMS Hierarchical Condition Category Version 24 (CMS-HCC V24) 2022 Risk Adjustment
models are used for beneficiaries without ESRD. Specifically,
• The new enrollee model is used for beneficiaries that have fewer than 12 months of
M
edicare medical history. The model accounts for each patient’s age, sex, disability
status, original reason for Medicare entitlement (age or disability), and Medicaid
eligibility.
• The community model is used for beneficiaries that have at least 12 months of Medicare
medical history. The model includes the same demographic information as the new
enrollee model but also accounts for clinical conditions as measured by HCCs, and
various interaction terms. The community model is further broken down as follows: non-
dual aged, non-dual disabled, full-dual aged, full-dual disabled, partial-dual aged, and
partial-dual disabled.
• The institutional model is used for beneficiaries who were in long-term institutional
settings. The model includes demographic variables, clinical conditions as measured by
HCCs, and various interaction terms.
The CMS-ESRD Version 21 (CMS-ESRD V21) 2022 Risk Adjustment models are used for
ESRD beneficiaries receiving dialysis, transplant and beneficiaries with a functioning graft.
Specifically,
• The dia
lysis new enrollee model is used for ESRD beneficiaries that have fewer than 12
months of Medicare medical history. The model accounts for each patient’s age, sex,
disability status, original reason for Medicare entitlement (age or disability), Medicaid
eligibility, and ESRD.
• The dialysis continuing enrollee model is used for ESRD beneficiaries that have at least
12 months of Medicare medical history. The model includes the same demographic
information as the new enrollee model but also accounts for clinical conditions as
measured by HCCs.
• The functioning graft model, which is based on the model for the general population,
excludes HCCs for kidney transplant status and dialysis status but accounts for the
months after the transplant is received. Specifically, if a beneficiary receives a kidney
transplant, the score is calculated using the transplant model for the month of the
transplant and the two subsequent months, regardless of whether the beneficiary returns
to dialysis status during that time period. The model is further broken down into the
following:
o The new enrollee for functioning graft model is used for beneficiaries that have
fewer than 12 months of Medicare medical history. The model accounts for each
patient’s age, sex, disability status, original reason for Medicare entitlement (age
or disability), Medicaid eligibility and duration of functioning graft.
o The community for functioning graft model is used for beneficiaries that have at
least 12 months of Medicare medical history. The model includes the same
demographic information as the new enrollee model, but also accounts for
clinical conditions as measured by HCCs, various interaction terms, and duration
of functioning graft.
o The institutional for functioning graft model is used for beneficiaries who were in
long-term institutional settings. The model includes demographic variables,
clinical conditions as measured by HCCs, various interaction terms, and duration
of functioning graft.

13
Total Per Capita Cost Measure Information Form (MIF)
The “HCC_Risk_Adjust” tab of the Measure Codes List file lists all variables included in the
CMS-ESRD V21 and the CMS-HCC V24 risk adjustment models.
Risk Score Calculation
The CMS-ESRD V21 and CMS-HCC V24 models generate a risk score for each patient that
summarizes the patient’s expected cost of care relative to other beneficiaries. Risk scores for
patients using the CMS-ESRD V21 models are normalized to be on a comparable scale with the
HCC V24 risk scores.
• A risk score equal to one indicates risk associated with expenditures for the average
patient nationwide.
• A risk score greater than
one indicates above average risk.
• A risk score les
s than one indicates below average risk.
The risk-adjusted total for each covered month at the TIN or TIN-NPI level is calculated
accordi
ng to the following steps:
• Calculate CMS ri
sk score for each beneficiary month using diagnostic data from the
year prior to the month. This risk score is normalized by dividing by the average risk
score for all beneficiary months.
• Divide observed cos
ts for each beneficiary month by the normalized risk score to obtain
risk-adjusted monthly costs.
• Winsorize risk-adjusted monthly costs at the 99
th
percentile by assigning the 99
th
percentile of monthly costs to all attributable beneficiary months with costs above the
99
th
percentile.
• Normalize mon
thly costs to account for differences in expected costs based on the
number of clinician groups to which a patient is attributed in a given month.
12
Step 7: Specialty Adjust Monthly Costs
The specialty adjustment for the TPCC measure is a cost adjustment applied to account for the
fact that costs vary across specialties and across TINs with varying specialty compositions. An
example of the specialty adjustment calculation is available in Appendix E. The specialty
adjustment at the TIN and TIN-NPI levels is calculated as follows:
1. Calculate the average risk-adjusted monthly cost for each TIN and TIN-NPI by averaging
isk-adjusted monthly cost across all attributed beneficiary months. r
2. Calculate the national sp
ecialty-specific expected cost for each specialty as the weighted
average of TIN/TIN-NPI’s risk-adjusted monthly cost.
a. Define the weight for each TIN/TIN-NPI as the percentage of clinicians with that
special
ty multiplied by the total number of beneficiary months attributed to the
TIN/TIN-NPI multiplied by the number of clinicians with that specialty.
b. There will only be one specialty designation for a TIN-NPI. Therefore, the
percentage of clinicians with a specialty and number of clinicians with a specialty
will always be equal to one.
3. Calculate the specialty-adjustment factor for each TIN or TIN-NPI as follows:
a. Multiply the national specialty-specific expected cost for each specialty by the
respective specialty’s share of Part B payment within a TIN or TIN-NPI.
b. Sum the weighted s
hare of national specialty-specific expected cost calculated in
the previous step across all the specialties under a given TIN or TIN-NPI.
12
Specifically, monthly costs are divided by the cube root of the number of clinician groups (TINs) to
which a patient is attributed for a month.
14
Total Per Capita Cost Measure Information Form (MIF)
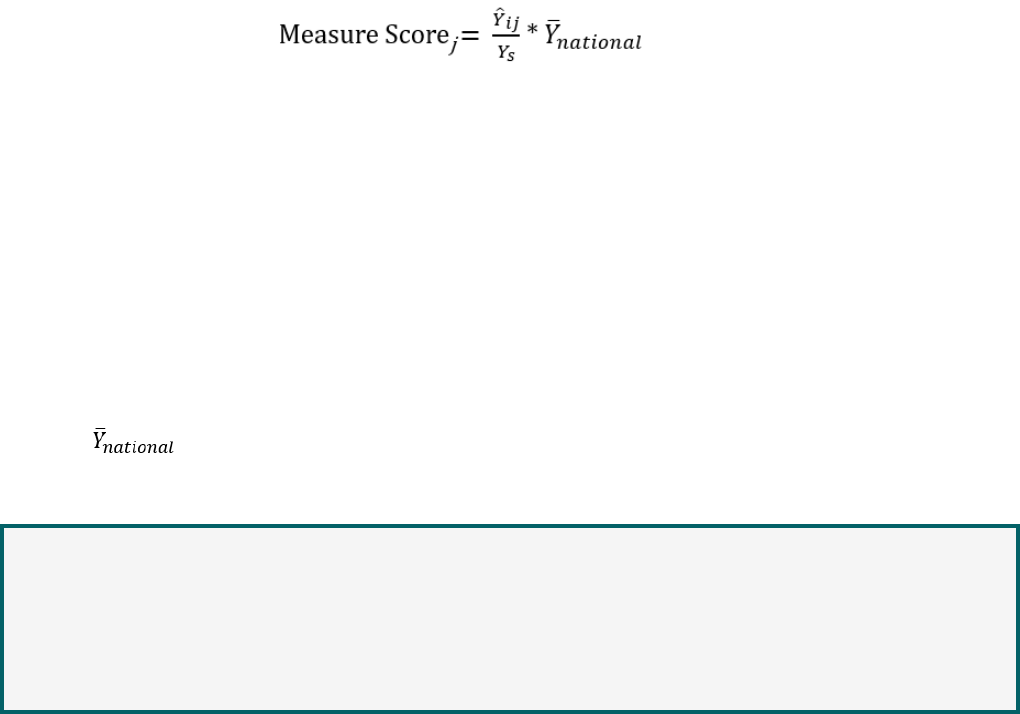
Step 8: Calculate the TPCC Measure Score
Calculate final risk-adjusted, specialty-adjusted cost measure by dividing each TIN and TIN-
NPI’s average risk-adjusted monthly cost by their specialty-adjustment factor and multiply this
ratio by the average non-risk-adjusted, winsorized observed cost across the total population of
attributed beneficiary months.
The clinician-level or clinician group practice-level measure score for any attributed clinician (or
cl
inician group practice) “j” can be represented mathematically as:
Figure 2: TPCC Measure Score Formula
where:
Item
Description
i
is the beneficiary month attributed to a clinician or clinician group
practice
j
is the clinician or clinician group practice
s
is the TIN-NPI’s specialty or TIN’s specialty composition
�
is the average winsorized, normalized risk-adjusted costs across all
beneficiary months i attributed to clinician (or clinician group practice) j
Y
s
is the specialty-adjustment factor for the attributed clinician (or clinician
group practice) j
is the national average per capita cost (used to convert the ratio to a
dollar amount)
A lower measure score indicates that the observed beneficiary month costs are lower than the
expected costs for the care provided by the given specialist for the particular patients and beneficiary
months included in the calculation.
A higher measure score indicates that the observed beneficiary month costs are higher than the
expected costs for the care provided by the given specialist for the particular patients and beneficiary
months included in the calculation.
0
15
Total Per Capita Cost Measure Information Form (MIF)
Appendix B. Evaluation and Management
“Primary Care” Services List
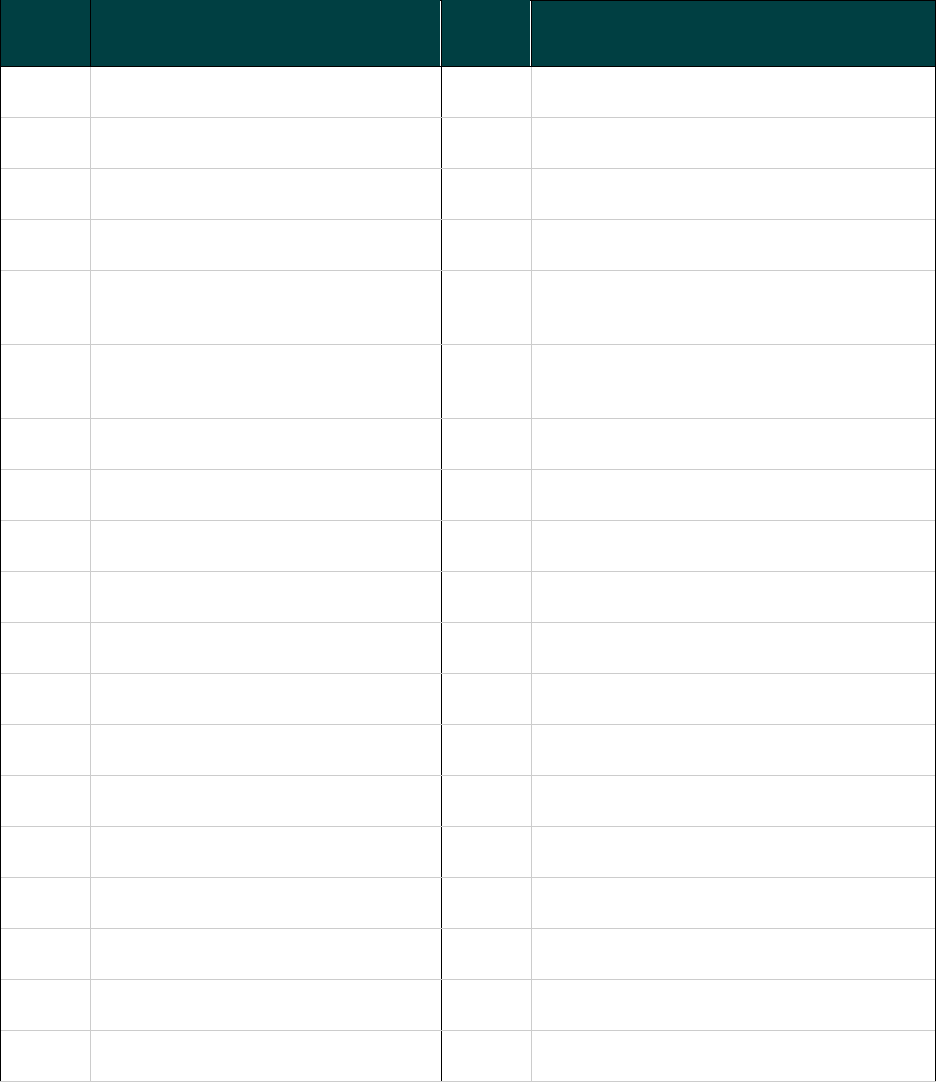
Table B below contains a list of select codes that identify E&M “primary care” services.
Table B: Evaluation and Management “Primary Care” Services List
CPT /
HCPCS
Code
CPT/HCPCS Code Description
CPT /
HCPCS
Code
CPT/HCPCS Code Description
99201
New patient office or other outpatient
visit, typically 10 minutes
99202
New patient office or other outpatient
visit, typically 20 minutes
99203
New patient office or other outpatient
v
isit, typically 30 minutes
99204
New patient office or other outpatient
v
isit, typically 45 minutes
99205
New patient office or other outpatient
visit, typically 60 minutes
99211
Established patient office or other
outpatient visit, typically 5 minutes
99212
Established patient office or other
outpatient visit, typically 10 minutes
99213
Established patient office or other
outpatient visit, typically 15 minutes
99214
Established patient office or other
outpatient, visit typically 25 minutes
99215
Established patient office or other
outpatient, visit typically 40 minutes
99304
Initial nursing facility visit, typically 25
minutes per day
99305
Initial nursing facility visit, typically 35
minutes per day
99306
Initial nursing facility visit, typically 45
minutes per day
99307
Subsequent nursing facility visit,
t
ypically 10 minutes per day
99308
Subsequent nursing facility visit,
ypically 15 minutes per day
t
99309
Subsequent nursing facility visit,
typically 25 minutes per day
99310
Subsequent nursing facility visit,
t
y
pically 35 minutes per day
99315
Nursing facility discharge day
management, 30 minutes or less
99316
Nursing facility discharge
m
anagement, more than 30 minutes
99334
Established patient assisted living visit,
typically 15 minutes
99335
Established patient assisted living visit,
typically 25 minutes
99336
Established patient assisted living visit,
typically 40 minutes
99337
Established patient assisted living visit,
typically 60 minutes
99339
Physician supervision of patient care at
home or assisted living facility, 15-29
minutes in one month
99340
Physician supervision of patient care at
home or assisted living facility, 30 minutes
or more in one month
99341
New patient home visit, typically 20
minutes
99342
New patient home visit, typically 30
minutes
99343
New patient home visit, typically 45
minutes
99344
New patient home visit, typically 60
minutes
99345
New patient home visit, typically 75
minutes
99347
Established patient home visit, typically 15
minutes
99348
Established patient home visit, typically 25
minutes
99349
Established patient home visit, typically 40
minutes
99350
Established patient home visit, typically 60
minutes
99441
Physician telephone patient service, 5-10
minutes of medical discussion
99442
Physician telephone patient service, 11-20
minutes of medical discussion
99443
Physician telephone patient service, 21-30
minutes of medical discussion
99490
Chronic care management services at
l
east 20 minutes per calendar month
CPT /
HCPCS
Code
CPT/HCPCS Code Description
16
Total Per Capita Cost Measure Information Form (MIF)
CPT /
HCPCS
Code
CPT/HCPCS Code Description
99318
Nursing facility annual assessment,
ty
pically 30 minutes
99324
New patient assisted living visit,
typically 20 minutes
99325
New patient assisted living visit,
typically 30 minutes
99326
New patient assisted living visit,
ty
pically 45 minutes
99327
New patient assisted living visit
,
typically 60 minutes
99328
New patient assisted living visit,
typically 75 minutes
99495
Transitional care management services,
m
oderately complexity, requiring face-to-
face visits within 14 days of discharge
99496
Transitional care management services,
highly complexity, requiring face-to-face
visits within 7 days of discharge
G0402
Initial preventive physical examination;
face-to-face visit, services limited to new
beneficiary during the first 12 months of
Medicare enrollment
G0438
Annual wellness visit; includes a
per
sonalized prevention plan of service
(pps), initial visit
G0439
Annual wellness visit, includes a
per
sonalized prevention plan of service
(pps), subsequent visit
No
Data
No Data
AMA CPT Code Description Licensing: Codes and descriptions included are from the Current Procedural Terminology (CPT®)
Copyright 2019 American Medical Association. All rights reserved.
17
Total Per Capita Cost Measure Information Form (MIF)
Appendix C. Illustration of Overlapping Risk
Windows Triggered by a TIN for the Same Patient
Due to the nature of primary care, it’s possible for multiple risk windows to be initiated if one or
several TINs see the patient multiple times during the year. This appendix provides further
information on how potentially attributable beneficiary months are determined when the patient
is seen by the TIN(s) multiple times before or during the performance period.
13
Overlapping Risk Windows Initiated by One TIN for the Same Patient
Figure C-1 below provides an example of the interactions of multiple risk windows initiated by
the
same TIN for one patient.
Figure C- 1. Diagram of overlapping risk windows initiated for the same patient under 1 TIN
The first part of the diagram shows multiple candidate events between a TIN and a patient that
trigger the opening of overlapping risk windows. For each risk window, the months that overlap
with the performance period are attributable (indicated by a teal fill). The second part of the
diagram shows the resulting collapsed months for which the TIN will be held accountable. In this
example, all 13 beneficiary months in the performance period will be attributed to the TIN
because together, the 5 risk windows cover the entirety of the performance period. Provided
that the TIN-NPIs responsible for any of these candidate events don’t meet the service category
13
The attributable months identified in figures C-1 and C-2 will only be attributed to the TIN provided that
the TIN-NPI on the initial E&M “primary care” service of the candidate event doesn’t meet the service
category or specialty exclusions for this measure. If a TIN-NPI meets at least one of the service category
or specialty exclusions, the candidate events and associated beneficiary months for which they’re
considered responsible are removed from both TIN and TIN-NPI attribution
.
18
Total Per Capita Cost Measure Information Form (MIF)
or specialty exclusions, the costs assigned to these 13 beneficiary months for this patient will be
attributed to the TIN.
Overlapping Risk Windows Initiated by Multiple TINs for the Same Patient
Figure
C-2 below shows the interactions of multiple risk windows initiated by multiple TINs for
one patient, illustrating multiple attribution.
14
Figure C - 2. Diagram of overlapping risk window initiated by multiple TINs for the same
patient
The top part of the diagram shows multiple candidate events, each triggering the opening of a
risk w
indow. For each risk window, the months that overlap with the performance period are
attributable and are represented by teal rectangles. The bottom part of the diagram shows how
the beneficiary months will get attributed to different TINs, depending on the risk windows that
they triggered.
In the example illustrated in figure C-2, all 13 beneficiary months in the performance period are
attri
butable because together, the 4 risk windows cover the entirety of the performance period.
Since different TINs initiated the risk windows, the beneficiary months will be attributed to the
corresponding TINs in the following manner:
• TIN A initiated 2 overlapping risk window
s for the patient.
o Together these 2 risk windows
overlap with each of the 13 beneficiary months
in the performance period and, therefore, all of these 13 beneficiary months will
be attributed to TIN A.
• TIN B initiated 2 non-overlapping risk windows that partially overlap with the
perfor
mance period.
o 3 beneficiary months from the first risk window and 2 beneficiary months from
the second
risk window overlapping the performance period will get attributed to
TIN B.
14
Multiple attribution is intended to reflect the team-based nature of primary care, and allows attribution to
reflect changes in a patient’s primary care provider. Since the measure calculation compares each
clinician’s expected costs among their peers for patients with the same observable characteristics, rather
than to a pre-defined standard, no costs are double-counted.
19
Total Per Capita Cost Measure Information Form (MIF)
Appendix D. Illustration of Attribution of
Beneficiary Months for the TPCC Measure
This appendix provides further details and examples of attribution for the TPCC measure
beneficiary months.
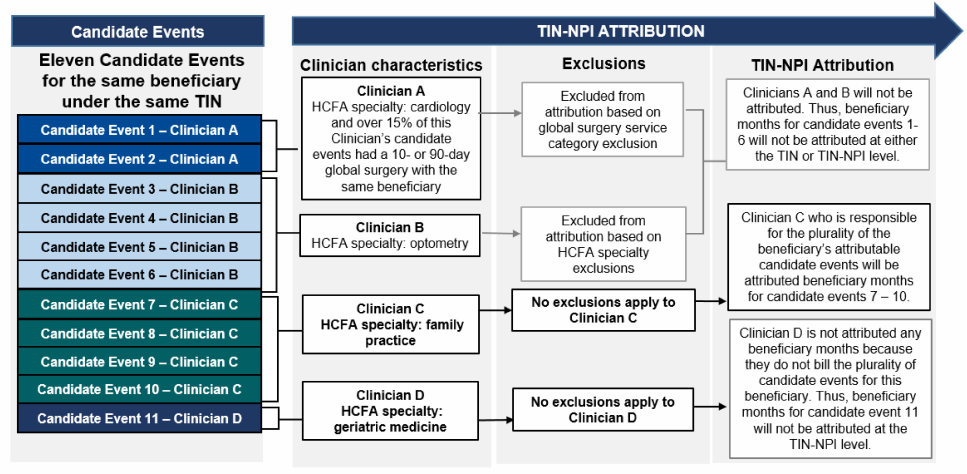
Figure D - 2. Diagram of attribution of beneficiary months at the TIN-NPI level
In the example shown above, the stacked, colored boxes on the left represent 11 candidate
events billed by 4 different clinicians (clinician A through D) practicing under the same TIN. The
next set of boxes to the right of the colored boxes shows the specialties for each clinician and/or
whether they billed any of the services that are part of the service category exclusions at the
threshold needed to qualify for exclusion (10-day and 90-day global surgery, anesthesia,
chemotherapy, and therapeutic radiation). The set of boxes to the far right shows which
clinicians are excluded from attribution based on service category and/or specialty exclusions
and which clinicians are included.
• Clinician A bi
lled over 15% of 10-day or 90-day global surgery codes to his patients.
o Clinician A i
s excluded from attribution based on the global surgery service
category exclusion, and
o Candidate events 1 and 2 are removed from both the TIN and TIN-NPI’s
meas
ure calculation.
• Clinician B had a
n optometry HCFA specialty.
o Clinician B has
a HCFA specialty that is included in the list of 56 specialties that
are excluded from attribution, and
o Candidate events 3 through 6 ar
e removed from both the TIN and TIN-NPI’s
measure calculation.
• Clinician C didn’t meet any of the service category exclusions and had a HCFA specialty
fo
r family practice which isn’t one of the 56 specialties excluded from the TPCC
measure.
o Clinician C i
s attributed beneficiary months overlapping the performance period
and the risk windows initiated by candidate events 7 through 10.
20
Total Per Capita Cost Measure Information Form (MIF)
o The resulting beneficiary months are included in both the TIN and TIN-NPI’s
measure calculation.
• Clinician D
didn’t meet any of the service category exclusions and had a HCFA specialty
for geriatric medicine which isn’t one of the 56 specialties excluded from the TPCC
measure.
o Clinician D
wasn’t attributed any beneficiary months because they didn’t bill the
plurality of candidate events for this patient within the TIN.
o Candidate event 11 will not be attributed at the TIN-NPI level, but will be
attr
ibuted at the TIN level.
21
Appendix E. Example of Specialty Adjustment
This appendix provides some further details and example of specialty adjustment. In this
example numbers have been rounded to the nearest whole integer for simplicity. When
calculating the measure for performance, no such rounding will occur.
1. Suppose the entire population c
onsists of 2 TINs (TIN A and TIN B) with 2 types of
specialists under them, Family Practice and Internal Medicine. Table F below provides
some additional information on the TINs’ characteristics.
Table E. TIN A and TIN B Characteristics
TIN
Average
Risk-
Adju
sted
Monthly
Cost
# of
Benefici
a
ry
Months
# of
Inter
nal
Medicine
Clinicians
% of
Internal
Medicine
Clinicians
% of TIN’s
Part B
Ph
ysician/Sup
plier Cost by
of Internal
M
edici
ne
Clinicians
# Family
Pract
ice
Clinicians
% of
Fami
ly
Practice
Clinicians
% of TIN’s
Part B
P
hysician/S
u
p
plier Cost
by Family
Practice
Clinicians
A $1,000 110 10 20% 15%
40 80% 85%
B $800 122 48 75% 50% 16 25% 50%
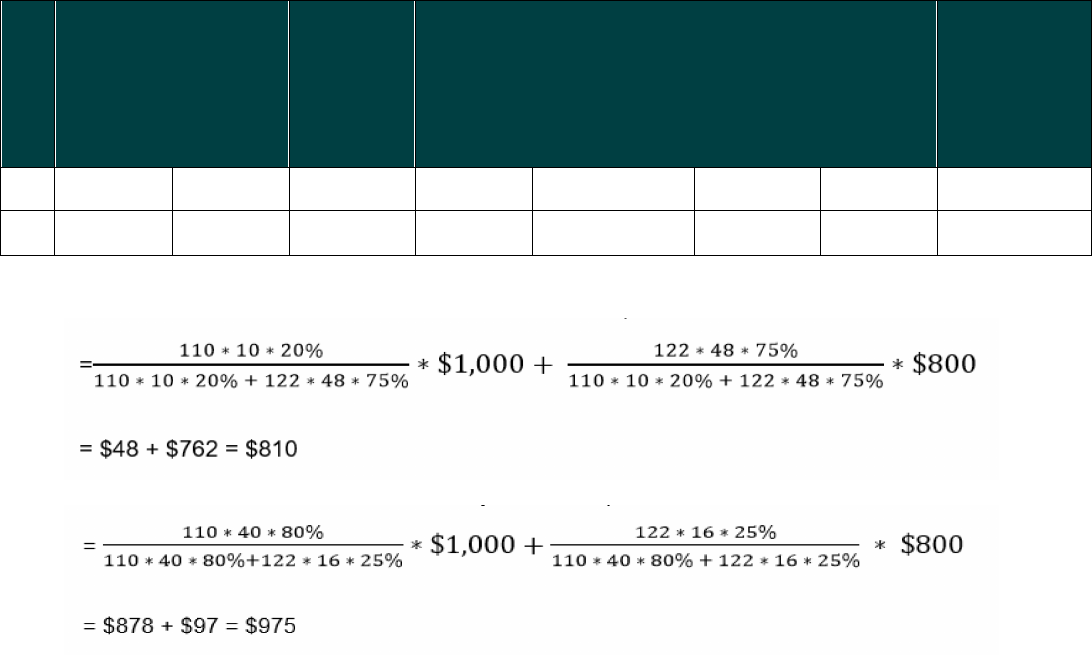
2. Calculate the national specialty-specific expected cost for each specialty
a. Calculate the national Internal Medicine expected cost a
s follows:
b. Calculate the national Family Practice expected cost as follows:
3. Calculate the specialty-adjustment factor for TIN A and TIN B as the weighted average
of the national specialty-specific expected costs. The weight is the TIN’s % of Part B
Physician/Supplier payments for that specialty.
a. TIN A’s specialty-adjustment factor is calculated as follows:
($810 * 15%) + ($975 * 85%) = $950
b. TIN B’s specialty-adjustment fact
or is calculated as follows:
($810 * 50%) + ($975 * 50%) = $893
4. For each TIN, calculate the TPCC measure score (assuming
the national average cost is
$900):
a. TIN A’s measure score is calc
ulated as follows:
(($1,000 / $950) * $900 = $947
b. TIN B’s measure score is calculated as follows:
(($800 / $89
3) * $900) = $806
Total Per Capita Cost Measure Information Form (MIF)
