
Back To Chiropractic Continuing Education Seminars
Ethics & Law: SOAP Notes ~ 2 Hours
Welcome to Back To Chiropractic Online CE exams:
This course counts toward your California Board of Chiropractic Examiners CE.
(also accepted in other states, check our website or with your Chiropractic State Board)
The California Board requires that you complete all of your CE hours BEFORE the end of your
Birthday month. We recommend that you send your chiropractic license renewal form and fee in
early to avoid any issues.
COPYRIGHT WARNING The copyright law of the United States (Title 17, United States Code) governs the
making of photocopies or other reproductions of copyrighted material. Under certain conditions specified in the law,
libraries and archives are authorized to furnish a photocopy or other reproduction. One of these specified conditions
is that the photocopy or reproduction is not to be "used for any purpose other than private study, scholarship, or
research." If a user makes a request for, or later uses, a photocopy or reproduction for purposes in excess of "fair
use," that user may be liable for copyright infringement. This site reserves the right to refuse to accept a copying
order if, in its judgment, fulfillment of the order would involve violation of the copyright law.
Exam Process: Please read all instructions before starting!
1. You must register/pay first. If you haven't, please return to: backtochiropractic.net
2. Open a new window or a new internet tab & drag it so it's side-by-side next to this page.
3. On the new window or new tab you just opened, go to: backtochiropractic.net website.
4. Go directly to the Online section. DON'T register again.
5. Click on the Exam for the course you want to take. No passwords needed.
6. Follow the Exam instructions.
7. Upon passing the exam you’ll be able to immediately download your certificate,
and it’ll also be emailed to you. If you don’t pass, you can repeat the exam at no charge.
Please retain the certificate for 4 years.
If you get audited and lose your records, I’ll have a copy.
I’m always a phone call away... 707.972.0047 or email: [email protected]
Marcus Strutz, DC
Back To Chiropractic CE Seminars

Ethics & Law –
Stop Wasting Time Writing Daily SOAP Notes – 2 Hours
Presented by Steven C Eggleston, DC, Esq.
Stop Wasting Time Writing Daily SOAP Notes
In this class I answer the question, “How can I save time on each patient visit with SOAP
notes?” It turns out that daily SOAP notes are NOT required on every visit by the California
Board of Chiropractic Examiners. There are no state or federal laws that require them on
each and every visit either (except MediCare patients.) Medical Doctors don’t do them
“daily” because they only see the patient once a month and the Physical Therapist does the
“daily” treatment in between those M.D. examinations. As it turns out, SOAP notes only need to
be done during examinations and the California State Board only requires monthly examinations.
It is important that Chiropractors keeps excellent SOAP notes during the monthly examination
because, if you do that, you can refer to those SOAP notes in the daily notes and they are
automatically “incorporated by reference” into your daily notes as if you had copied and
pasted them in every time.
Chiropractors have gotten confused because we wear both the doctor hat AND the treatment
deliverer hat. Back in the 1980s, some Chiropractors went around trying to get us to keep better
patient records. They taught us to do SOAP notes just like the MDs do. What they failed to
grasp (and what has cost our profession millions of wasted hours) is that MDs only do SOAP
notes once a month. We started doing them 12 times a month. Back in the 1980s, the health
insurance companies were paying us for doing an exam each time and we billed and were paid
for a 99211, 99212, or 99213 re-examcode on every visit in addition to the 98940, 98941 or
98942 adjustment code.
In the 1990s, health insurance companies stopped paying Chiropractors for the 99211, 99212 and
99213 codes (technically called "Evaluation & Management” or E & M codes.) We just kept on
keeping daily SOAP notes even though we were not being paid for them. It is absolutely NOT
required by the California Board of Chiropractic Examiners (check with your state’s rules &
regulations) that Chiropractors keep daily SOAP notes.
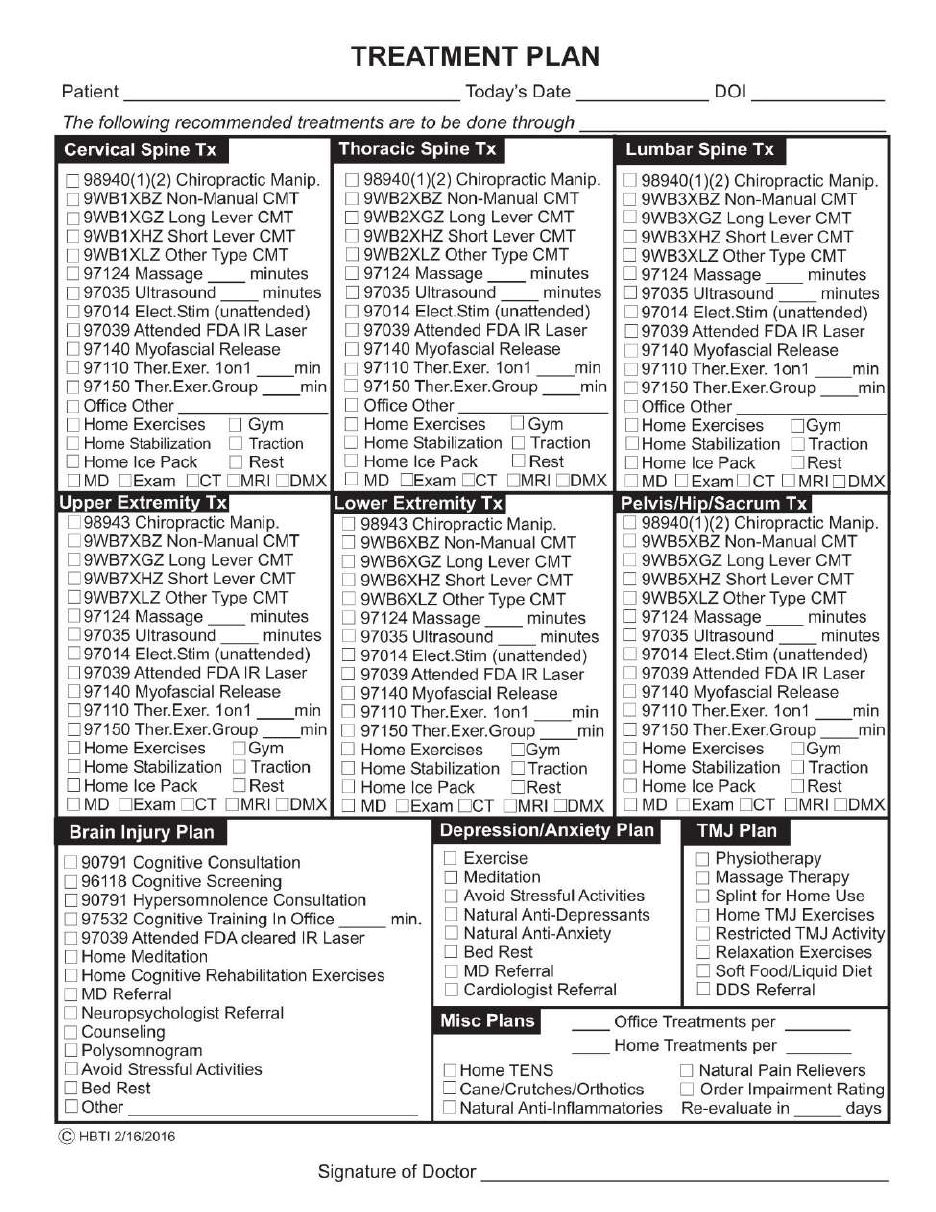
California Board of Chiropractic Examiners Rules & Regulations Section 312 (Illegal Practice)
states in 312(c)(2), “The doctor shall initially examine and prepare a written treatment
program for a patient prior to the providing of physical therapy treatment by (any) unlicensed
individual.” Your first ethical consideration is that you absolutely MUST have a written Treatment
Plan in the patient’s file that YOU have personally filled out BEFORE any of your assistants or
massage therapists can perform any therapy whatsoever. For example, turning on the spinalator is
illegal if your assistant does this BEFORE you have placed a written Treatment Plan in the patient’s
chart. This makes sense since the written treatment plan is your specific instructions to your
unlicensed assistants as to exactly what you want them to do for the patient on each and every patient
visit.
Likewise Section 312(c)(3) states, “The doctor shall provide periodic reevaluation of the
treatment program and of the individual's performance in relation to the patient. ‘Periodic
reevaluation’ shall mean at least once every thirty days the patient is under active care.” You are
absolutely required to perform a re-exam on every chiropractic patient in the state of California
(check your state’s rules) at least every 30 days. If you do not do this, it is completely illegal for you
to allow any chiropractic assistant or massage therapist to do any therapy on your patients. Since
symptoms wax and wane from day to day, recording the patients full SOAP notes three to five days a
week can give you a false understanding of whether the patient is actually improving under your
care. When you only do SOAP notes once a month during the monthly progress exam, you
really get a better understanding of your patient’s response to treatment.
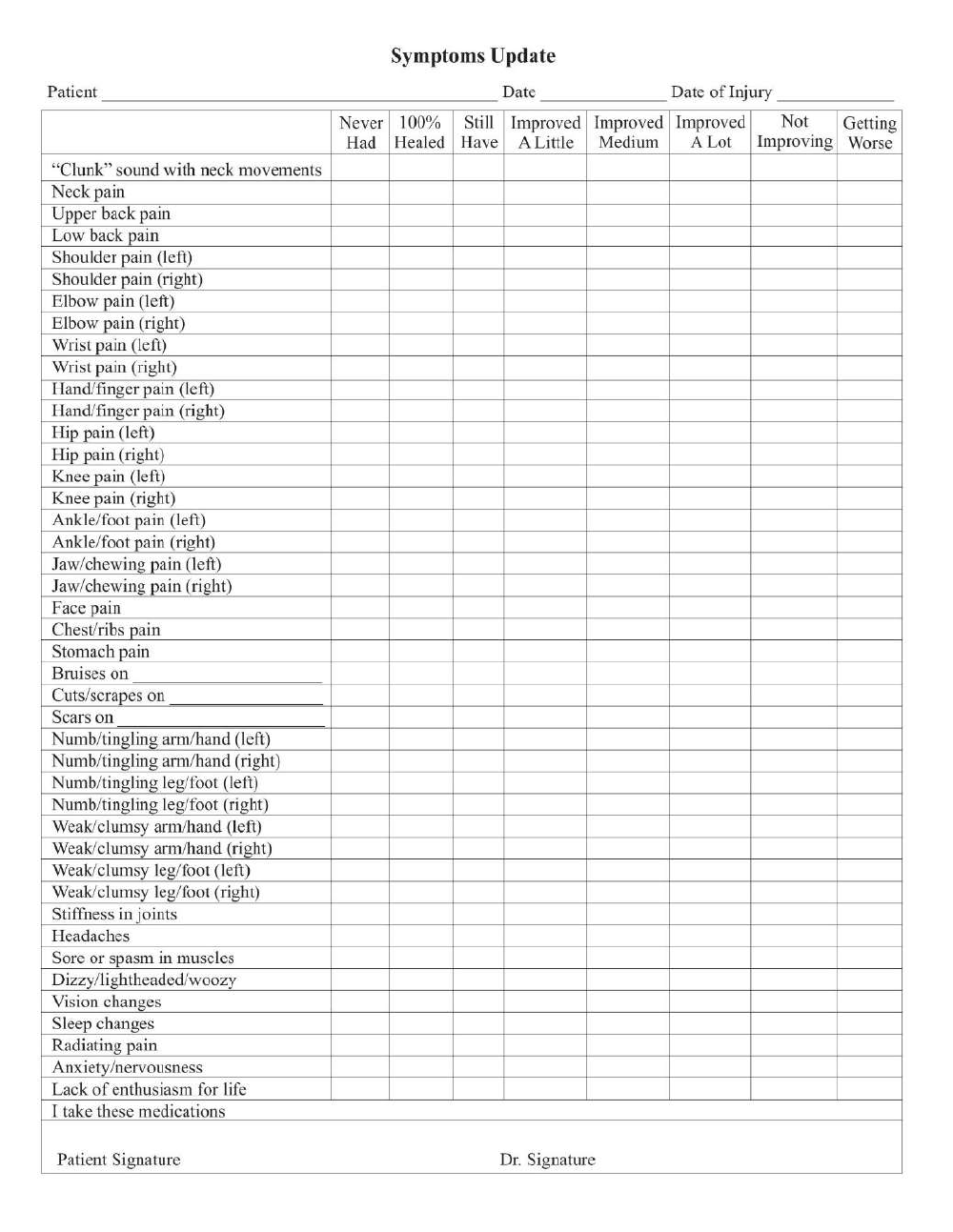
Since you are required to have a written Treatment Plan AND do a re-exam every 30 days under
California Board Rules (check your state’s rules), I suggest we use this to our advantage and do our
SOAP notes every 30 days. That means you will fill out a written Treatment Plan (the “P” in SOAP)
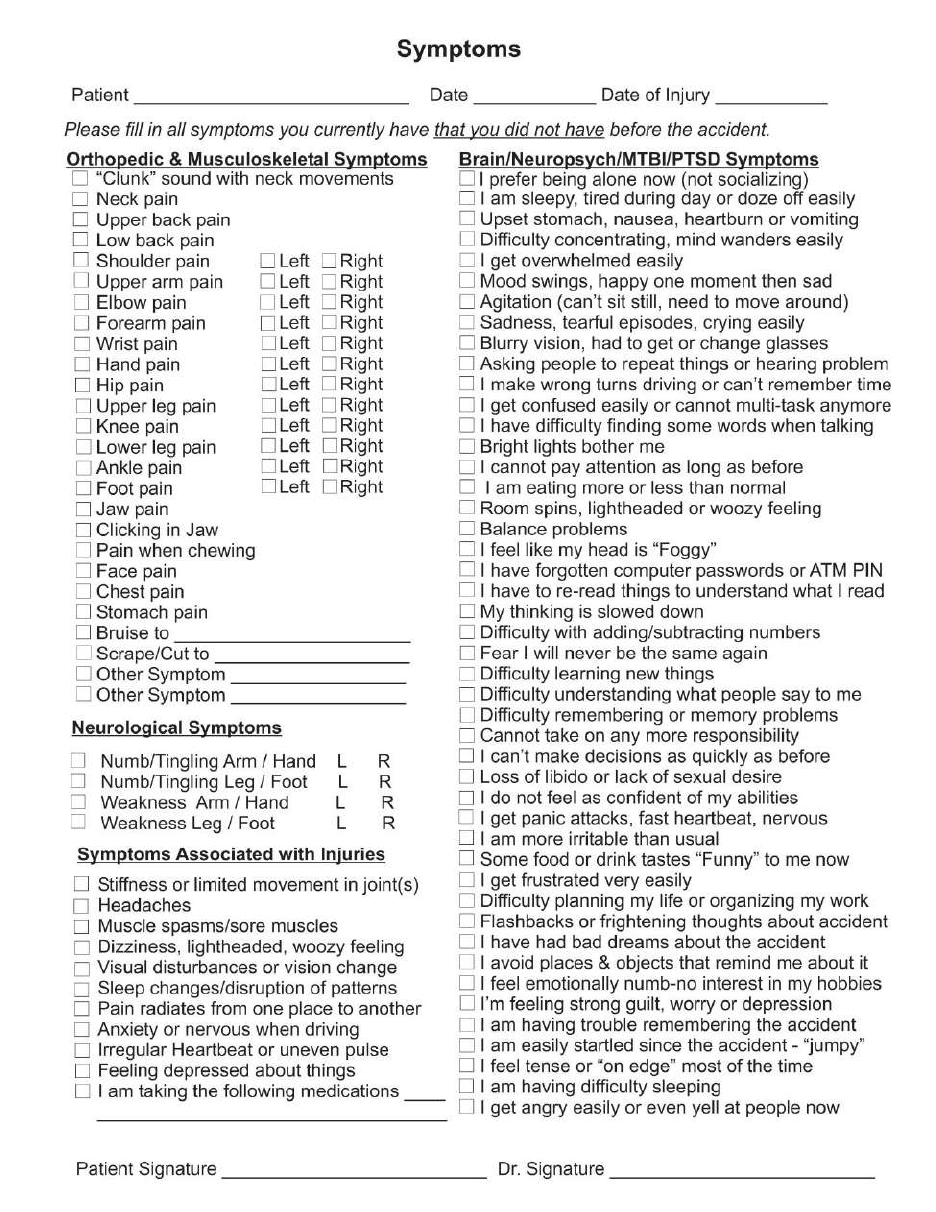
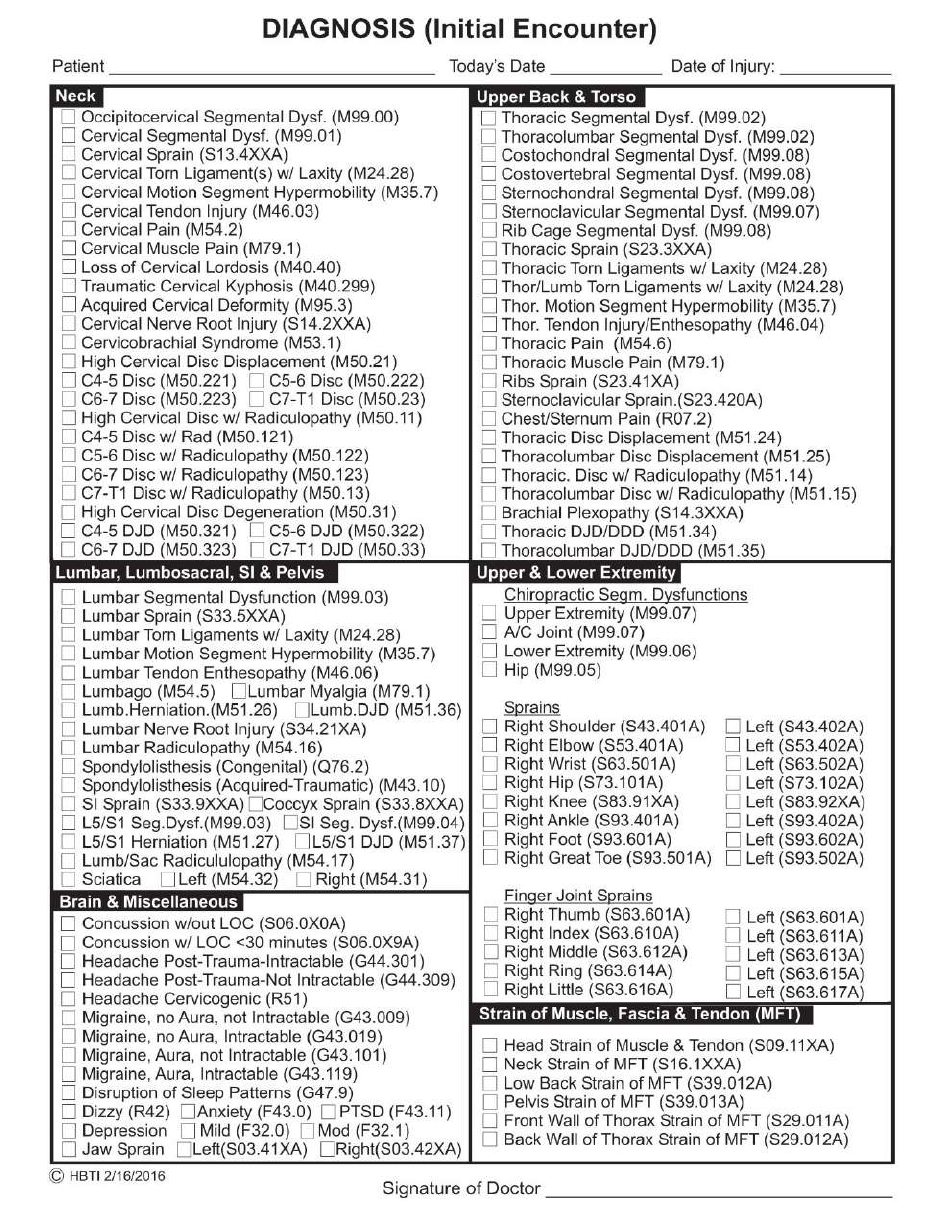
once a month, a written Diagnosis form (the “A” in Soap) and in order to know what to diagnose and
how to treat it, have the patient fill out a Symptoms Form (the “S” in SOAP) once a month and you
examine (the “O” in SOAP) those symptoms. These 4 forms, Symptoms, Examination, Diagnosis
and Treatment Plan are all 4 elements in the acronym SOAP and filling them out once a month keeps
you in compliance with California’s Board Rules & Regulations. (Check your state’s rules.)
You may ask, “But what about all the treatments in between the monthly examination when I fill out
the SOAP notes? Don’t I have to write something down on those visits?” Yes, you do. In
California, you are required to write the date of each and every patient visit. That’s all (in
California at least.)
Now you are wondering, “Is this too good to be true?” I have researched this carefully and it is
absolutely true BUT ONLY if you comply with the monthly SOAP note requirement. You cannot
skip over the monthly reevaluation and then not do any SOAP notes on treatment days. Then you
would have no records at all. You must keep good records and you can do so monthly just like the
MDs do. Then you only have to write the date the patient came in and whether or not you followed
your written Treatment Plan. For example:
May 5, 2017 – I followed the SOAP notes from my most recent reevaluation.
May 7, 2017 – I followed the SOAP notes from my most recent reevaluation except that massage
was not done today.
May 9, 2017 – I followed the SOAP notes from my most recent reevaluation.
May 13, 2017, I followed the SOAP notes from my most recent reevaluation. In addition, today the
patient complained of right great toe pain. He stubbed it on the leg of a table. I observed swelling
and discoloration. Right great toe sprain. I applied ice, ultrasound under water, and advised the
patient to rest it for 3 weeks.
May 15, 2017 – I followed the SOAP notes from my most recent reevaluation.
May 16, 2017 - I followed the SOAP notes from my most recent reevaluation.
May 18, 2017 - I followed the SOAP notes from my most recent reevaluation.
These examples show all you need to write on your daily chart notes (you must initial and/or
sign it either by handwriting or electronically each date) and also shows how you write your
daily notes if you deviate from your written Treatment Plain on file. This satisfies all
California Board Rules but (again, I emphasize) only if you have completed the Symptoms,
Exam, Diagnosis and Treatment Plan forms every month while the patient is under active care.
Check your state’s rules.
Here is how I came up with this idea. I practiced Chiropractic for 15 years and then went to law
school (while continuing to maintain my Chiropractic practice.) During law school, I took a
class on Wills and Trusts in law school. I learned during this class how doctors (especially
chiropractors) can avoid writing SOAP notes in general and save hours every week in
unnecessary writing or typing.
The doctrine of Incorporation by Reference is important in Probate law because a person can
modify his or her will quickly, easily and as many times as she wants using this legal doctrine.
Modifying a will can be expensive and time-consuming and require that the will be re-typed and
witnessed by two people. However, this doctrine of Incorporation by Reference is wonderfully
helpful in this scenario and with chiropractic SOAP notes as well.
A person with a will may place a statement into the will such as, “Please distribute the contents
of my safe deposit box at Wells Fargo Bank according to the note in the safe deposit box after I
die.” Without making any change to the actual will, that person can go to Wells Fargo Bank as
often as she likes and put items into the box or remove items from the box. All she has to do is
cross out whatever she removed and write in what she added to the box and who gets it after she
dies.
For example, suppose there is a Babe Ruth rookie baseball card in the safe deposit box and a
note that reads, “Babe Ruth card to nephew Charles.” If she died while that note was in the box,
her will would give the Babe Ruth rookie card to her nephew Charles. Suppose, however, that
she gets mad at Charles one day and goes to the bank, crosses out “Charles” and writes in
“David.” If she dies the next day then her will (which wasn’t physically re-written) will give the
Babe Ruth rookie card to David. She changed her will without actually re-writing it.
Chiropractors can to the same thing with SOAP notes as you are about to learn and not have to
re-write all those notes all the time by simply using the same legal doctrine of Incorporation by
Reference used by this woman who changed her with without re-writing it at all.
Suppose a week later she has somebody offer her $1,000 for the Babe Ruth rookie card. She
goes to Wells Fargo, gets the baseball card out of the safe deposit box, sells it and goes on a
Caribbean cruise with the money. She puts a line through the note in the safe deposit box that
states, “Babe Ruth card to nephew David.” Then she falls overboard somewhere in the
Caribbean and her will effectively disinherits David and he doesn’t get the baseball card. She
did all that without re-writing her will.
Suppose she didn’t really fall overboard in the Caribbean but came home safely. She purchased
two gold coins in Grand Caymen that were part of a shipwreck of gold that was discovered,
brought up and salvaged. The coins are worth $25,000 each. She takes them to the safe deposit
box when she gets home, puts them in and writes a note at the bottom of the page, “One gold
shipwreck coin to my daughter Mary and the other to my son Ricardo.” If she dies the next day,
her will gives the coins to Mary and Ricardo. Neither Charles nor David get the baseball card
that was sold to pay for the cruse. David lost his baseball card to pay for the cruise which was
when she bought some very expensive coins for other people. Yes, wills can be changed in this
way in California.
As I listened to my professor explain this doctrine, a light bulb went off in my head and I had
this idea. If the law allows a person to reference (refer to) another document and to incorporate
the contents of that other document into the will, why can’t I refer to my most recent progress
examination notes in my daily SOAP notes and simply not have to re-write all those Symptoms,
Objective signs, Assessment/Diagnoses and Plans for treatment?
I began doing just that and recommend it for your consideration. Here is what needs to be done.
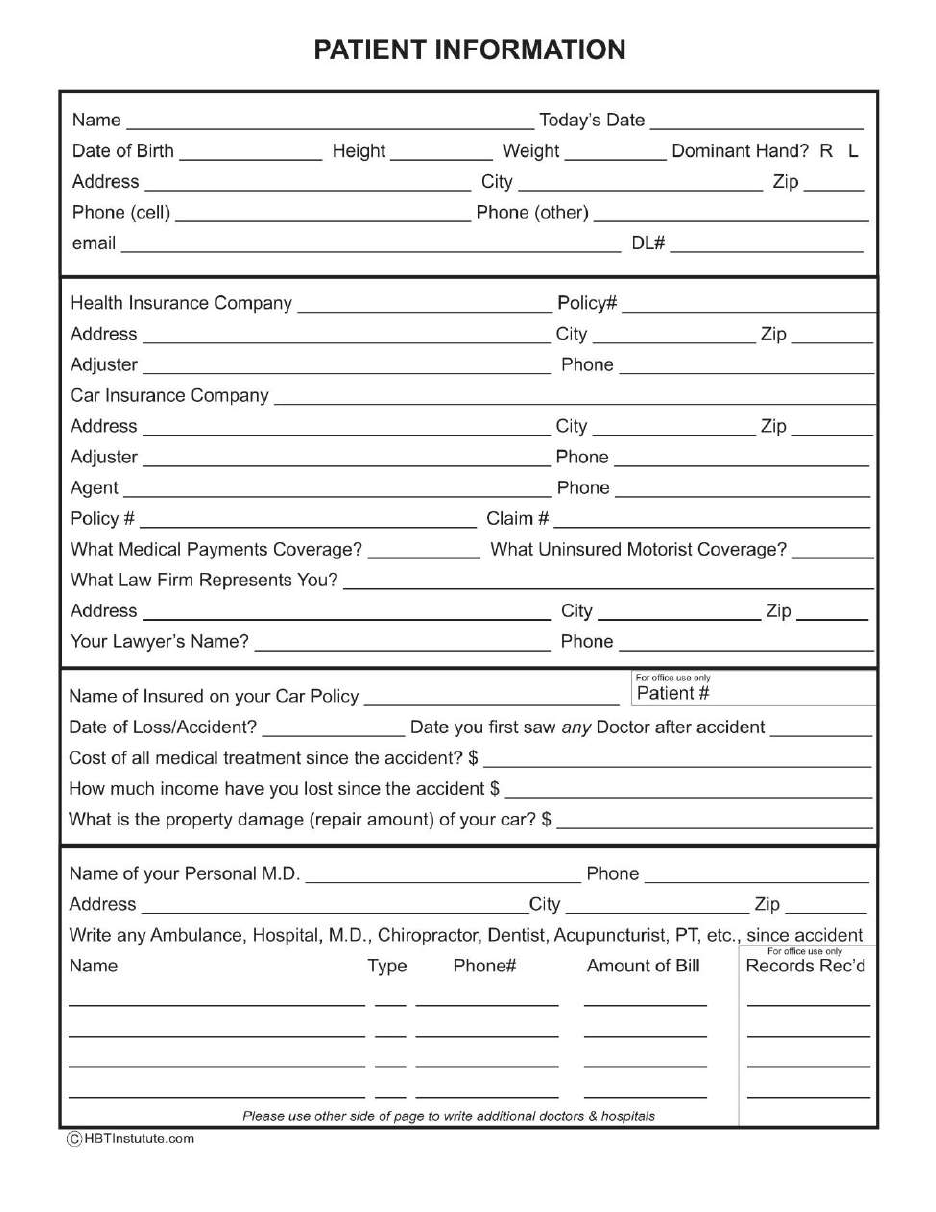
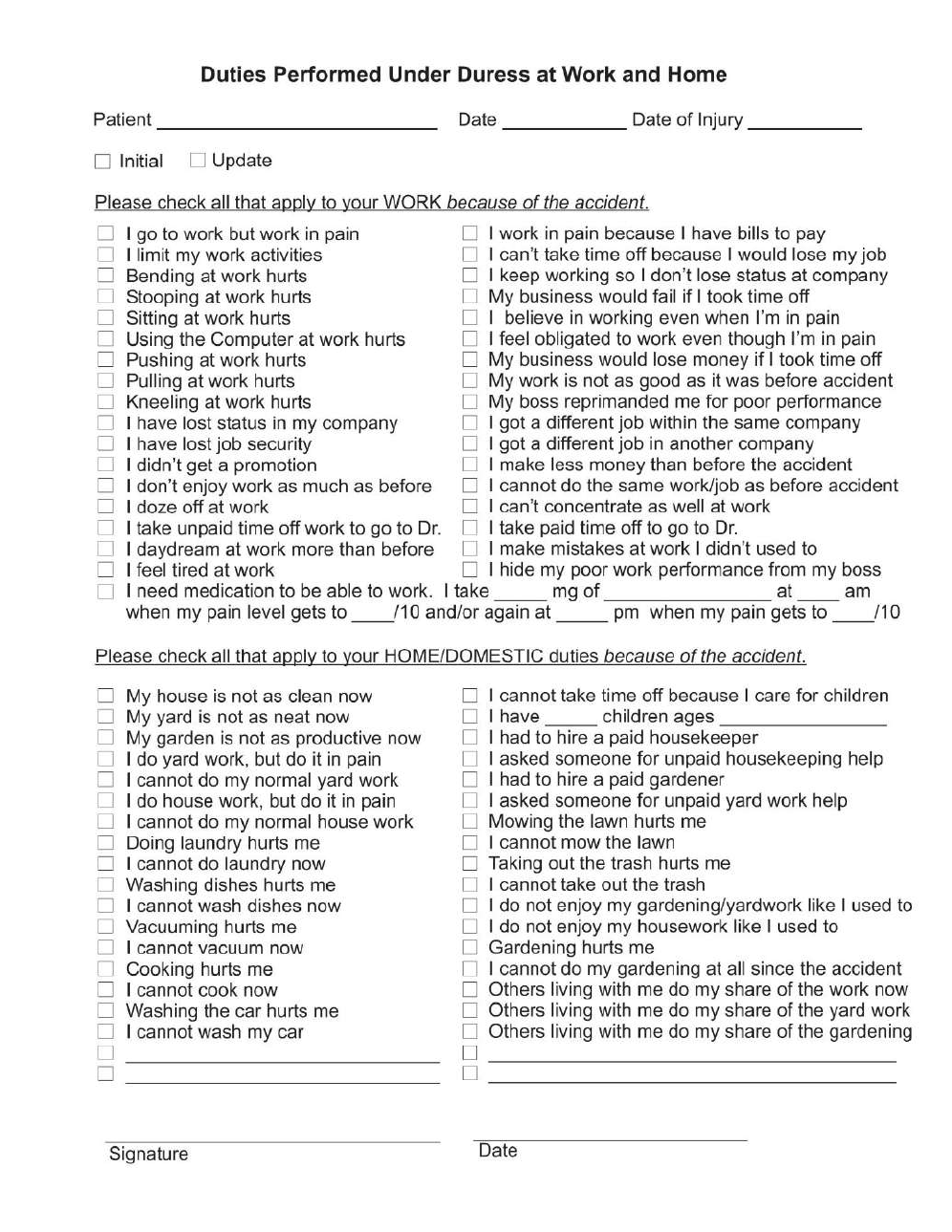
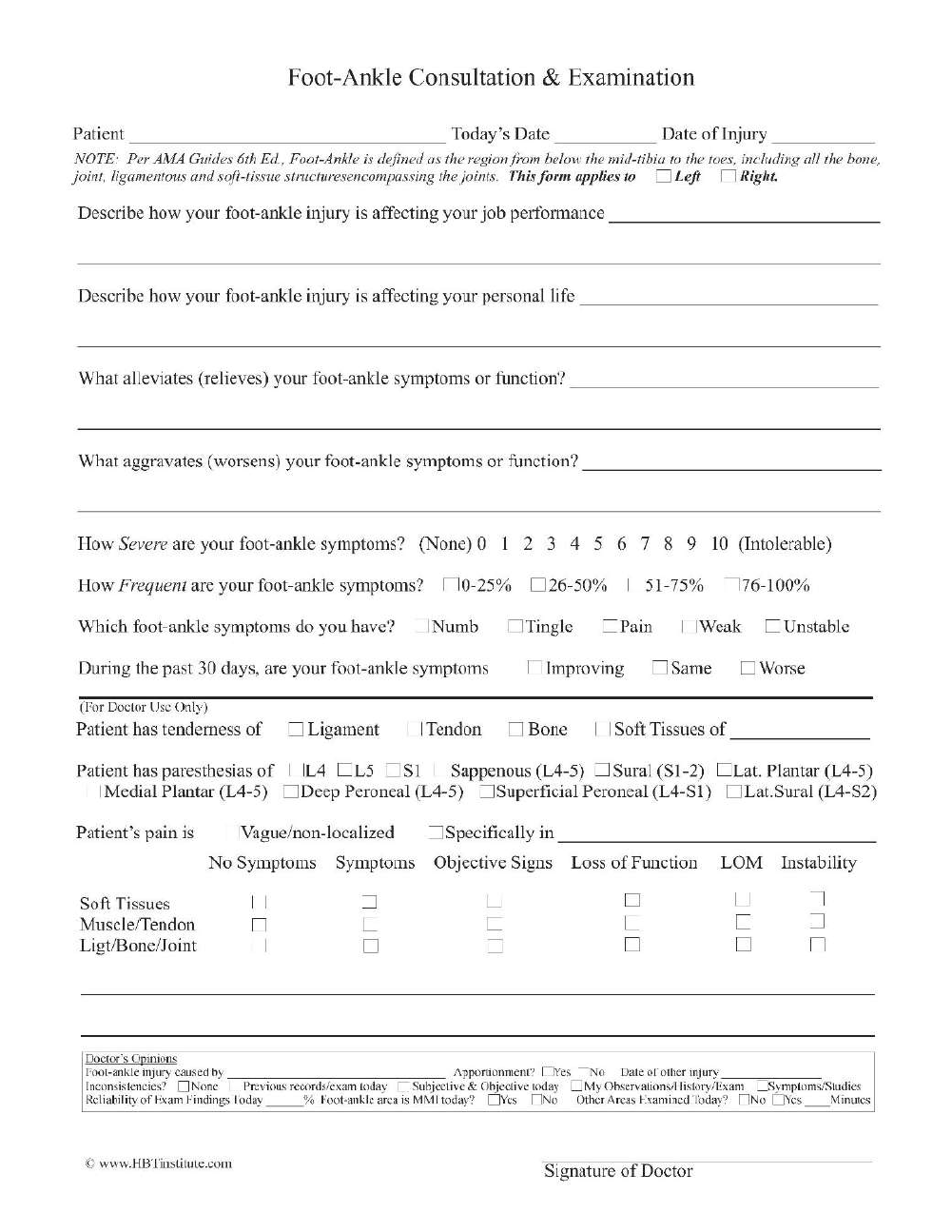
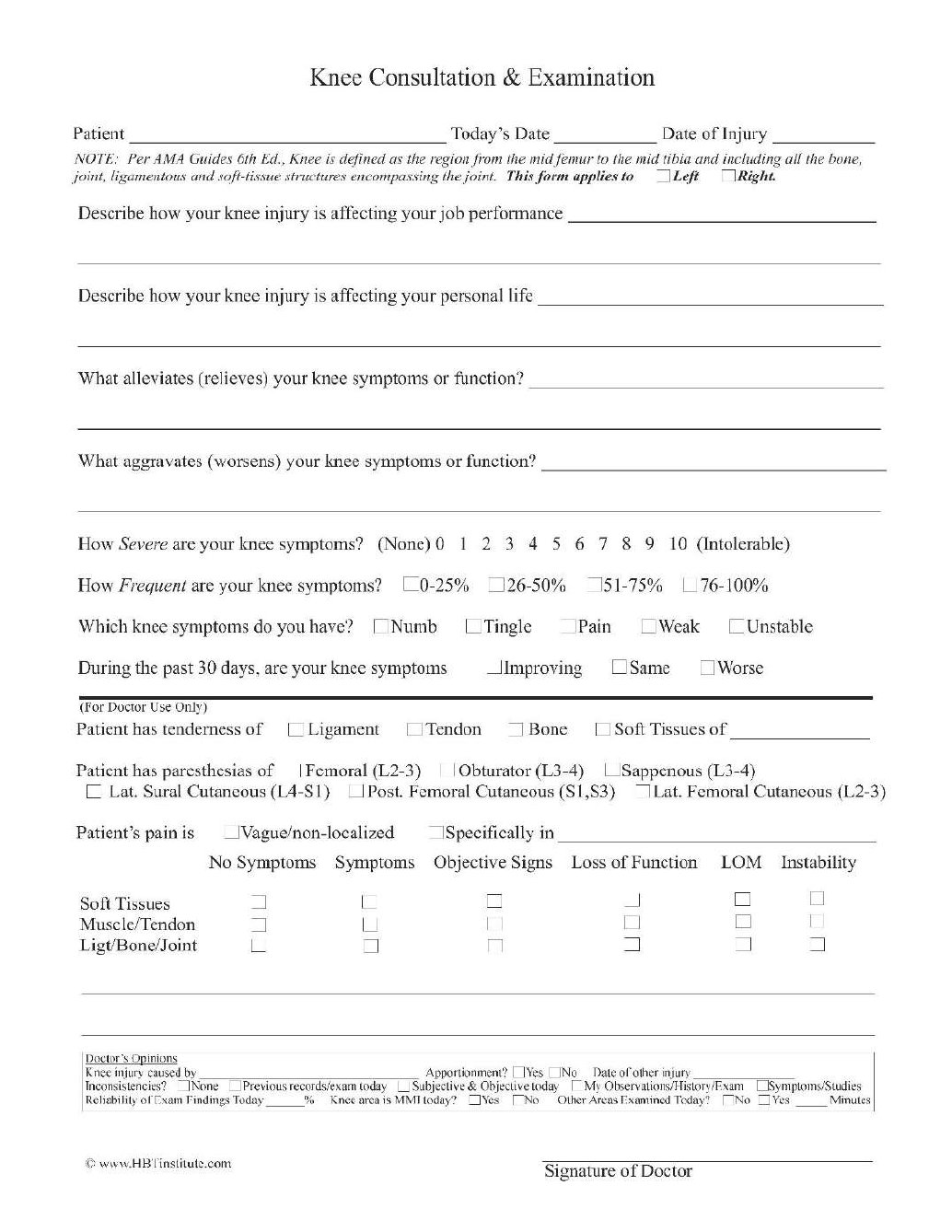
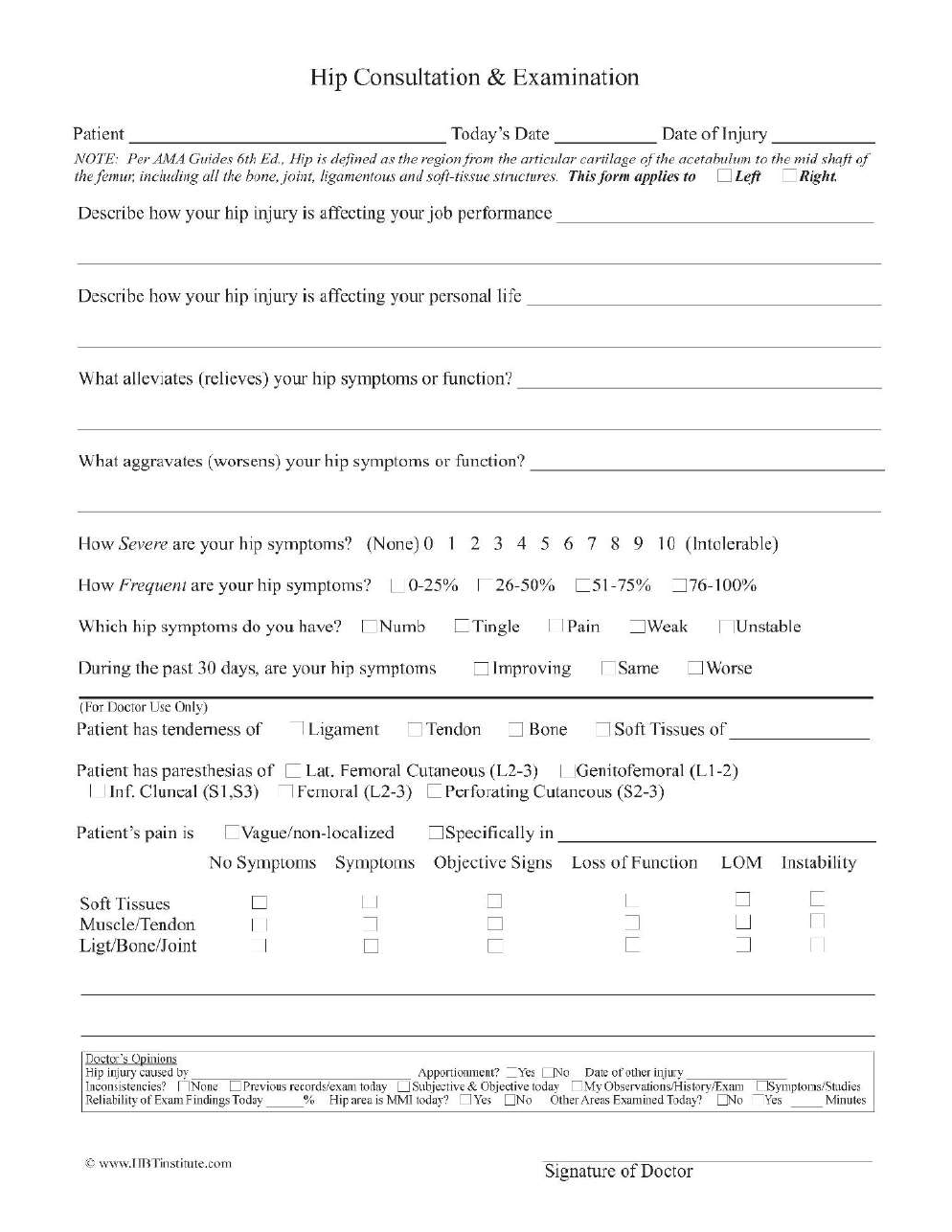
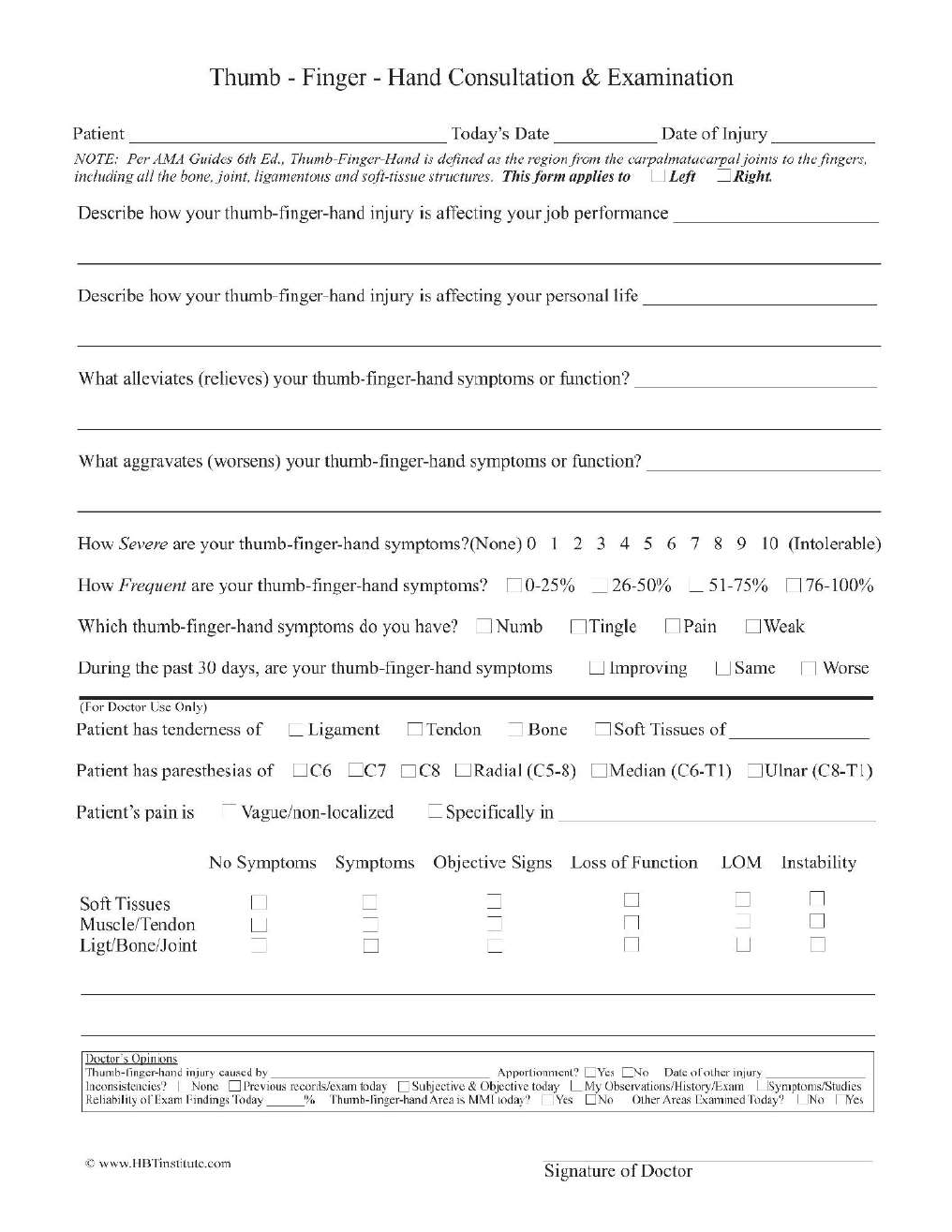
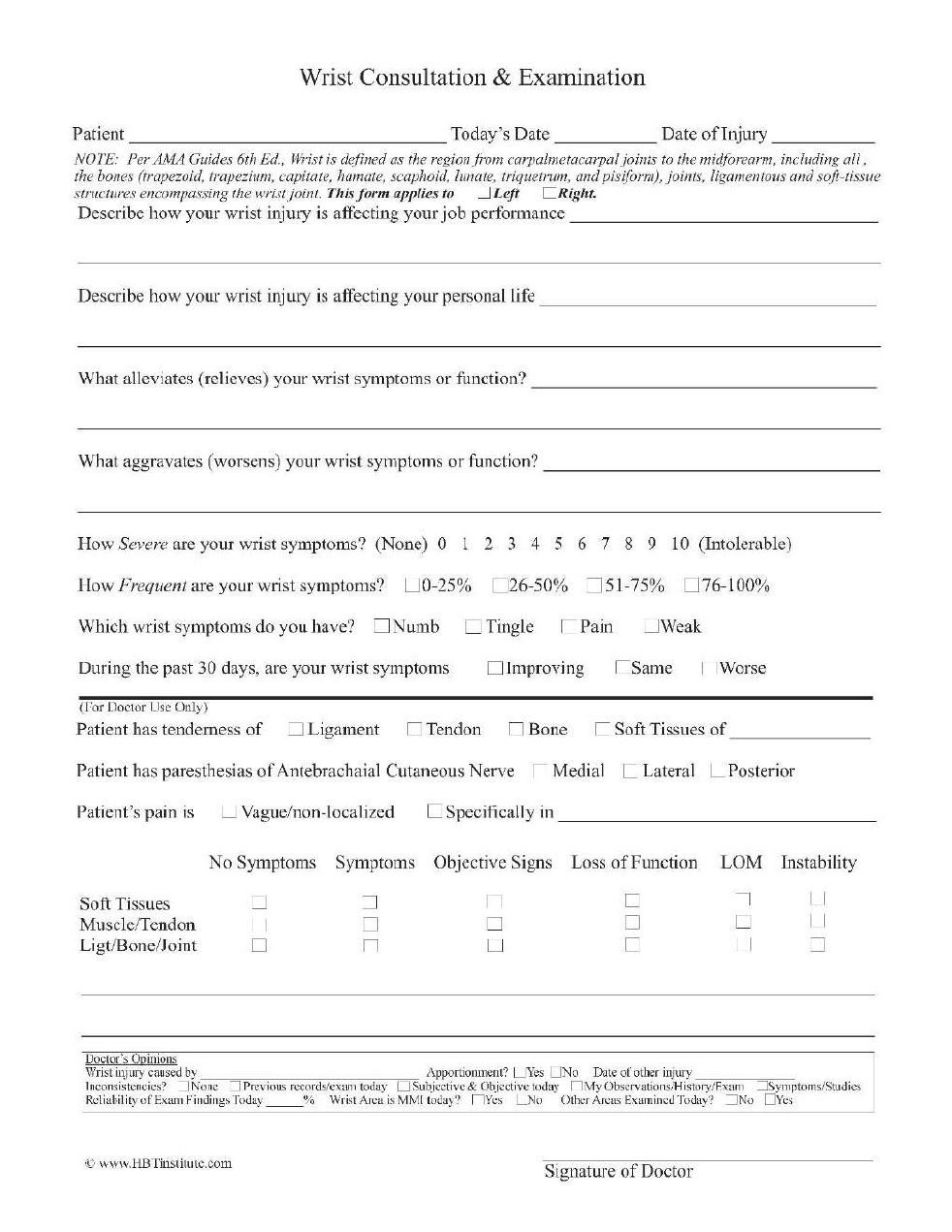
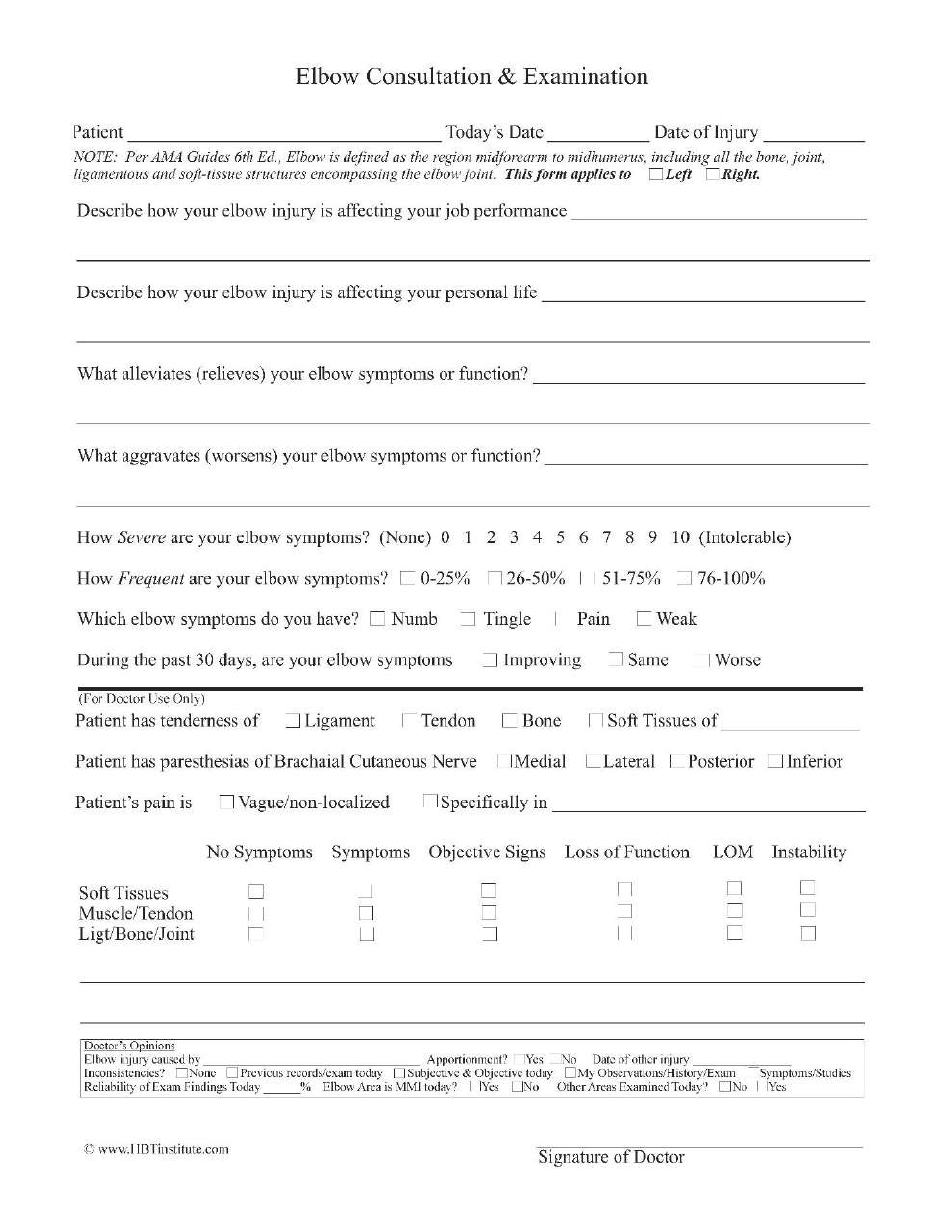
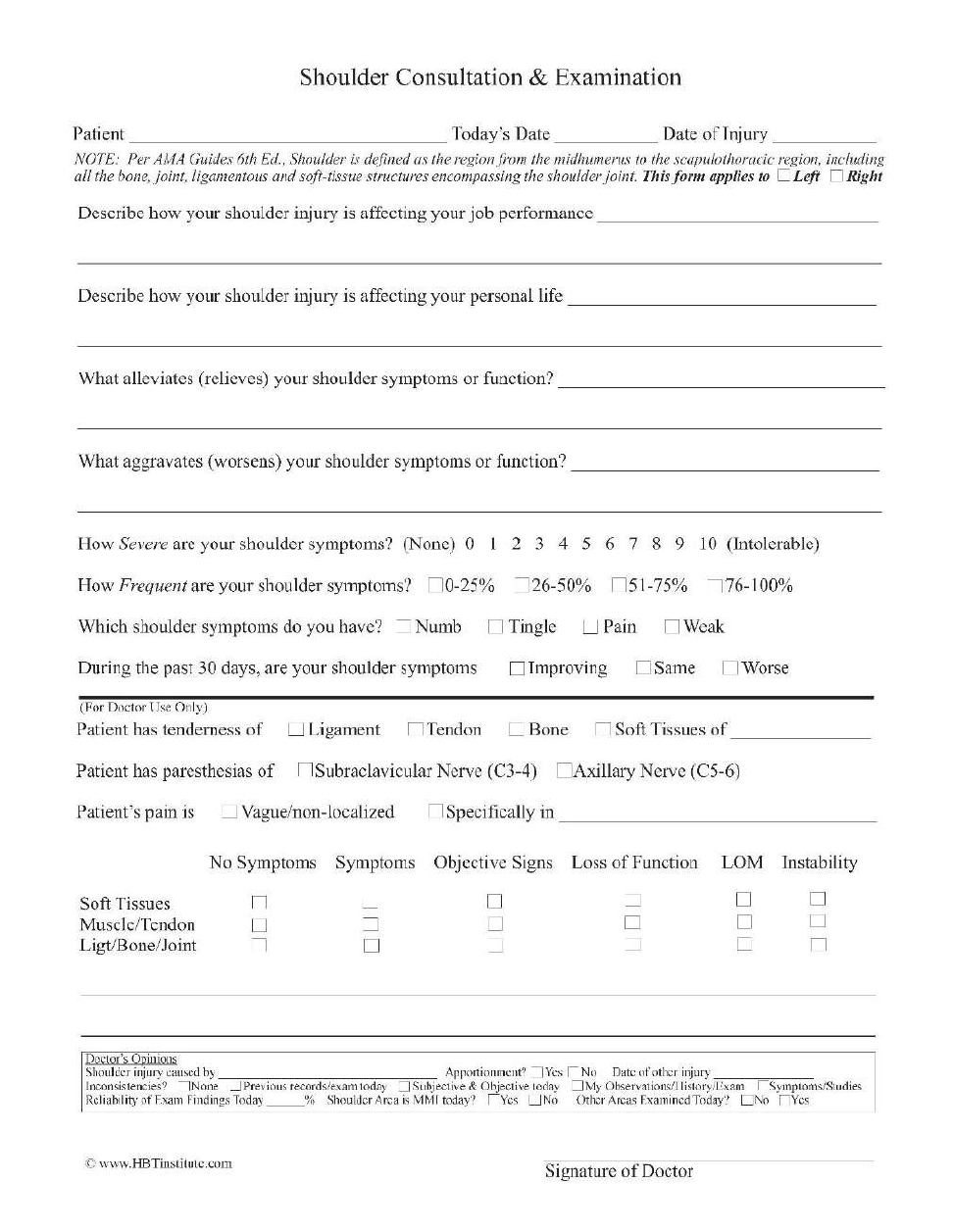
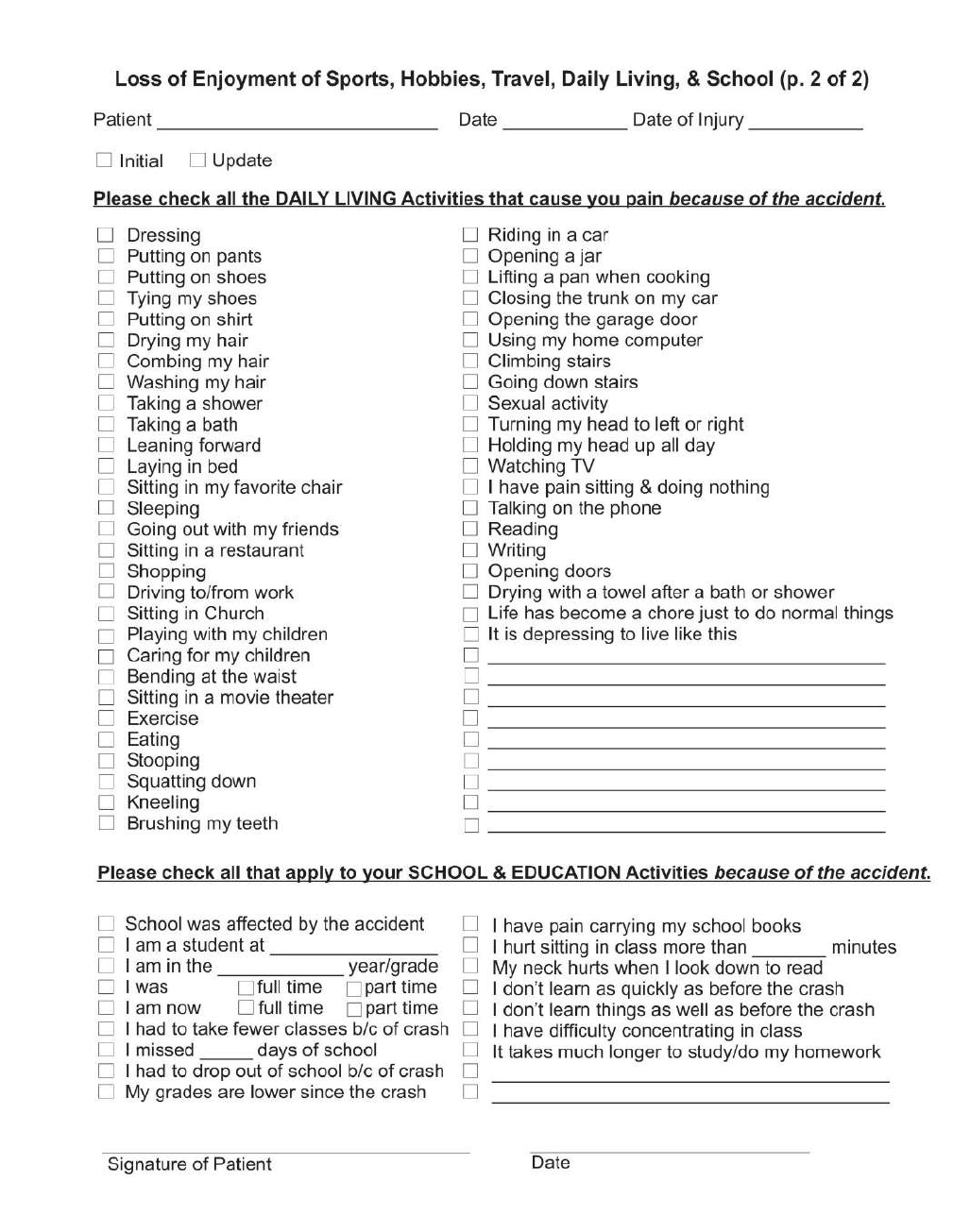
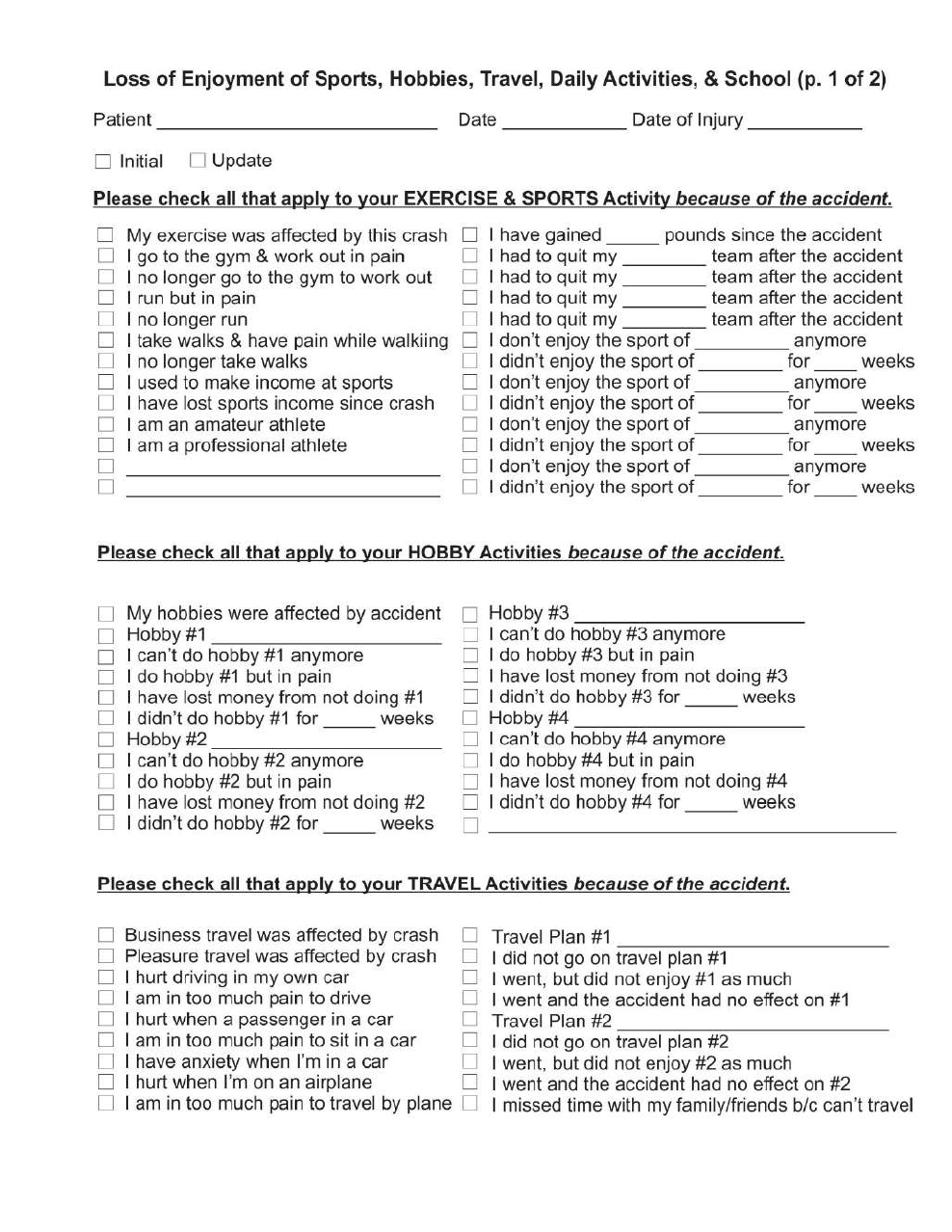
I designed a comprehensive Symptoms form, exam forms for all seven peripheral joints,
Diagnosis form and Treatment plan form. They are simple to use (boxes to check) and thorough
at the same time. They are easily understood by non-doctors so claim adjusters can easily
understand what is wrong with the patient with no need to write a narrative report. A copy of
each of these forms is in the appendix that comes with these class materials.
How Do You Get Paid For Doing Progress Exams?
Once a doctor has these forms, he or she can use them during any examination or re-examination
of the patient. CPT code 99213 is for 15 minutes of the doctor’s time doing consultation,
examination, decision making and coordination of care for an existing patient. Use 99203 for 30
minutes of consultation, examination, decision making and coordination of care for a new
patient. CPT code 99354 is for billing an “extra 30 minutes” when it takes 45 minutes or longer
to do a progress examination for an existing patient or it takes me longer than 60 minutes for a
new patient.
The beauty of knowing these billing codes and using them properly is that the doctor can
perform progress exams whenever needed (at least monthly for California “Active” patients as
mandated by State Board Rules) then then incorporate my (or any equally good) Symptoms,
Exam, Diagnosis and Treatment Plan forms directly into their daily SOAP notes simply by
referencing them. Viola! The doctor no longer has to keep writing everything on every visit.
Doctors know that the symptoms do not change that much from day to day so a once a month
complete Symptoms analysis is what the doctor treats that patient for during a period of 30 days.
All the doctor has to do to incorporate each and every one of the patient’s symptoms into the
daily SOAP notes is refer to the most recent Symptoms form in the daily SOAP notes like this:
“S: See most recent Symptoms form on file.”
Exam findings do not change in one or two days so the doctor can treat the patient for a month
using the same objective findings until the next progress exam. All the doctor has to do to
include all the latest exam results into the daily SOAP notes is reference them in the SOAP notes
like this: “O: See most recent exam results on file.”
The patient’s diagnosis does not change from day to day so the doctor can use the same
diagnosis to treat the patient for 30 days until the next progress exam. All the doctor needs to do
to incorporate each and every one of the patient’s current diagnoses into the daily SOAP notes is
to refer to them in the daily SOAP notes like this: “A: See most recent Diagnosis form on file.”
The patient’s treatment typically does not change from day to day. The doctor decides to do a
month of treatments and does them for 30 days and then evaluates the results of those treatments
at the next progress exam. All the doctor needs to do to incorporate the entire treatment plan into
the daily SOAP notes is to refer to it in the daily SOAP notes like this: “P: See most recent
Treatment Plan on file.”
For the doctors reading these class notes (and weeping for joy right now) the secret to all of this
is to do high quality and thorough progress examinations. A lot of chiropractors do not like
doing progress examination because they do not get paid reasonably for doing them. However,
here is where it gets interesting. Assume that a doctor’s hourly billing rate is $100 (that would
be too low in reality since the doctor has to pay all his employees, electricity, rent and other
business costs out of his or her “hourly rate”.) Using this example of $100, that doctor would
charge $25 for the billing code 99213 (1/4 hour of time face to face with patient doing
consultation, exam, decision making and coordination of care.) If it took the doctor 45 minutes
or more to do the progress exam, he or she would bill code 99354 in addition to the 99213 code
($50) to indicate that it took at least another half hour to complete the progress exam.
Likewise, a doctor would properly bill the code 99203 for thirty minutes of time to consult with,
examine, make all the clinical decisions and coordinate care with other doctors. At the hourly
rate of $100, this doctor would charge $50 for one-half hour of time allotted to that CPT code. If
it took the doctor more than an hour with the new patient to go over the Symptoms form and
discuss it with the patient (consultation), fill out the examination form(s) for the spine and every
injured joint (examine), fill out the Diagnosis and Treatment Plan forms (decision making) and
ordering an MRI (coordination of care) then the doctor should properly bill code 99354 for the
extra 30 minutes it took to do all that work while face to face with the patient. If the hourly rate
for this doctor is $100 per hour then the extra 30 minutes code should be billed at $50.
Each doctor determines his or her own hourly rate depending on the doctor’s experience,
knowledge and factors such as the cost of office space in that neighborhood. These codes can be
applied to the doctor’s hourly rate in any situation. For example, if the doctor’s hourly rate is
$200 per hour then he or she would bill $100 for the first half hour of the new patient exam
(99203) and another $100 for the second half hour of the new patient exam (99354.) Progress
exams would be properly billed as $50 for the fifteen minutes (99213) and $100 for the next
thirty minutes (99354) assuming the progress exam took at least forty-five minutes. I suggest the
doctor or staff member write down the number of minutes in the chart somewhere to document
the amount of face to face time with the patients in case an insurance company ever questions the
billing of these timed codes.
Suppose the doctor practices in a very nice neighborhood and has a lovely office. His or her
hourly rate might be $400 an hour. In that case, he or she would bill $200 for the first half hour
of the new patient exam (99203) and another $200 for the second half hour of the new patient
exam (99354). Progress exams would be properly billed as $100 for the fifteen minutes (99213)
and $200 for the next thirty minutes (99354) assuming the progress exam took at least forty-five
minutes.
When chiropractors follow the correct billing procedures, use these timed billing codes properly
and apply their own hourly billing rate to these codes then the doctor can be paid for the time
needed to sit face to face with the patient and fill out the Symptoms, Exam, Diagnosis and
Treatment Plan forms. With these forms completely filled out and in the patient file, the doctor
can then use the Incorporation by Reference doctrine, refer to them in the daily SOAP notes and
dramatically reduce the amount of time it takes to write daily chart notes. On top of this
enormous time savings to the treating doctor, she is paid her hourly rate for the time spent filling
out the forms because these “Evaluation & Management” codes include the time that the doctor
spend consulting, examining and making clinical decisions such as “what is the patient’s
diagnoses and what kinds of treatment should I do to help the patient get well.” Filling out these
forms is “decision making” and , if the doctors does it with the patient in the office face to face,
the doctor can charge his/her hourly rate for filling out these forms as decisions are made.
Imagine how happy the chiropractor’s staff would be if all of the patient’s paperwork was filled
out at the time of the patient’s visit before they go back up to the front desk. Imagine how happy
the chiropractor would be knowing that he or she never has to hear the staff say, “Doctor, would
you get the paperwork filled out?”
So How Does This Allow You To Stop Writing SOAP Notes?
Once you have filled out the forms and billed your hourly rate for the proper Evaluation &
Management time spent face to face with the patient, you can take off the “doctor” had where
you “diagnose” the patient and then put on the “treatment” hat for a month without having to
write extensive SOAP notes all the time. Each time the patient comes into the office, you simply
“Incorporate by Reference” all of your most recent Symptoms form, Exam forms, Diagnosis
form and Treatment plan form into your SOAP notes by referring to them in your SOAP notes as
I described above. SOAP notes can look like this:
May 12, 2017
S: See most recent Symptoms form on file
O: See most recent Exam forms on file
A: See most recent Diagnosis form on file
P: Treatment Plan As Outlined in most recent Treatment Plan on file
The can also look like this:
May 12, 2017 – I followed the most recent SOAP notes on file
What If You Deviate From Your Written Treatment Plan?
As I demonstrated earlier during this course, only then do you have to actually write something
in your SOAP notes. For example, you might write:
P: Treatment Plan As Outlined in most recent Treatment Plan on file except 15 minutes of
neck massage substituted for 15 minutes of ultrasound today.
If the patient comes in with new symptoms, simply write, “See most recent Symptoms form
on file. In addition, the patient has the new symptom of right hip pain.”
Try to remember that the medical doctor (who wears the diagnosis hat) sends the patient to the
physical therapist (who wears the treatment hat) and if the patient tells the physical therapist
about some new symptom, the physical therapist would have to send the patient back to the
medical doctor to get a new diagnosis. Since this is a hassle, it is not usually done and the
physical therapist assumes that the medical doctor will figure out any new diagnoses the next
time the patient is examined. If the new symptom or injury is significant (I’m having a heart
attack) then the therapist needs to take care of that right away. If the new symptom is minor or,
as is most common, represents only waxing and waning of the same symptoms from day to day,
there is no need to put on your doctor hat and start making new diagnosis all the time. Trust that
you will be thoroughly examining the patient within the month at the next progress exam and
you can analyze it then, put it into your new diagnosis and treatment plan forms and then change
how you plan to help the patient during the ensuing month.
Does This REALLY Work?
Yes. California Board Rules & Regulations Section 318 states: Active and inactive
chiropractic patient records must include all of the following:
(1) Patient's full name, date of birth, and social security number (if available);
(2) Patient gender, height and weight. An estimated height and weight is acceptable where the
physical condition of the patient prevents actual measurement;
(3) Patient history, complaint, diagnosis/analysis, and treatment must be signed by the primary
treating doctor. Thereafter, any treatment rendered by any other doctor must be signed or initialed by
said doctor;
(4) Signature of patient;
(5) Date of each and every patient visit;
(6) All chiropractic X-rays, or evidence of the transfer of said X-rays;
(7) Signed written informed consent as specified in Section 319.1.
Notice that number 1, 2 and 4 can be accomplished on the patient intake forms the first day the
patient comes into your office. Number 3 is accomplished by doing your SOAP notes during your
initial exam AND once a month during your re-exams. Number 5 is the ONLY thing you are
required to write (in California, check your state’s rules) on the days you perform treatments in
between the monthly re-exams.
The secret is genuine and thorough progress exams. You will note that with my forms, the
patient fills out the Symptoms form and the top two-thirds of every extremity exam form. The
patient with a brain concussion also fills out the Acute Concussion Evaluation, the Epworth
Sleepiness Scale and the Rivermead Post-Concussion Symptoms Questionnaire. Using my
forms means the patient is doing a lot of your work and you are billing your hourly rate for all
the time you spend reviewing those forms with the patient and checking off all the boxes on the
Diagnosis and Treatment Plan forms.
These forms communicate exactly what is wrong with the patient in plain English so that
attorneys and claim adjusters. Your records are bullet-proof. If anyone ever asks, “What were
Mary’s symptoms on May 3?” You reply, “The note I made May 3
rd
refer back to and
incorporate my most recent consultation and Symptoms form with this patient. The most recent
Symptoms form on the patient was filled out April 14
th
. Mary’s symptoms waxed and waned
from day to day but I was still treating Mary on May 3
rd
for the same symptoms she had on April
14
th
. So Mary’s symptoms on May 3
rd
were (list off all the symptoms checked on the April 14
th
Symptoms form in your patient chart.)
What if you are pressed with a question like, “How do you know that is accurate?” You simply
reply, “My standard practice with note keeping is to incorporate by reference forms that are
already in my patient file and to only write an exception when I deviate from what is already on
file. For example, look at the note I made March 28
th
. See how I wrote, See most recent
symptoms form on file. In addition, patient also has the new symptom of left index finger pain.
Since I did not write any deviation or exception on May 3
rd
, I am quite certain that the symptoms
for which I treated Mary on May 3
rd
are accurately reflected in the April 14
th
Symptoms form to
which I referred on May 3
rd
.”
Show Your Work To Get Paid For Doing Progress Exams
I also suggest that the treating chiropractor using my forms follow the advice of their sixth grade
teachers. Show your work. Remember that the teacher would give partial credit on math
problems if you showed your work (even if you did not get the answer correctly.) Claim
adjusters at the medical payments department get claims all the time printed on simple claim
forms and they think, “This is a lot of money. I wonder how much work this chiropractor
actually did?” In a situation involving Medical Payments insurance, faxing the Symptoms,
Exam, Diagnosis and Treatment Plan forms to the medical payments adjuster along with the bill
allows them to see all the work you did. The claim adjuster will see your excellent work, know
that you did all the work you have billed for and will pay the claim (and be far less likely to try
to reduce the bill.) Show your work and get paid like a doctor again.
In the case of group health insurance, there is often no mechanism of showing your work when
you submit a bill (especially electronically.) However, you still have all this thorough and
accurate written documentation in your file in case they ask to see your file or ask you to “send
your SOAP notes.)
In case the State Board receives a complaint about you from any patient, you have a thorough,
accurate, detailed patient chart that describes on paper exactly what is wrong with your patient
and your reasoning for treating the patient in the way you did. Ethical, accurate patient notes
will help you very much in case of a State Board complaint or a malpractice lawsuit.
Doctors Must Stop Leaving Out Important Facts
It is assumed by all the lawyers and insurance company adjusters that ALL the facts that exist are
in the doctor’s records and reports. I can tell you as a doctor that the reality is that 90% of the
material facts surrounding your injuries are in the doctor’s head and are never written down.
Claim adjusters and lawyers do not know what is in the doctor's head. They only know what is
written down in the doctor's notes. Doctors must keep better records than they have been or the
patient will be the victim of the accident a second time.
Some of the worst offenders in the medical community are specialists. Specialists tend to write
down only the facts that are related to their specialty. For example, orthopedic surgeons
routinely fail to assess or report a brain concussion since it is not an “orthopedic” problem.
Brain concussions are neurological so orthopedic surgeons often do not even mention it. Claim
adjusters and lawyers do not understand the way specialists write notes and reports. They think
the specialist included all the facts. The reality is that the orthopedist only included the
orthopedic facts. The neurology, cardiology, urology, proctology, dermatology, and gynecology
facts are generally always left out of an orthopedic report. The claim adjusters and lawyers are
often missing a very large percentage of the material facts about what is wrong with the patient.
Many (if not most) personal injury cases do not have both a neurosurgeon and an orthopedic
surgeon involved. They merely have one or the other. Justice cannot be served where the only
specialist that sees the patient is an orthopedic surgeon who does not report the patient’s brain
concussion because it is not an orthopedic injury. As the saying goes, “If you are a hammer, the
whole world looks like a nail.” Orthopedic surgeons examine the joints and report on the
medical status of the patient’s joints. They may miss or simply do not report many other injuries
from the car accident. Claim adjusters and lawyers may not have all the facts when they make a
decision about your financial fate. The insurance companies have exploited this situation to
prove you are not really injured. The reality is that doctors may have failed the patient by
keeping poor records or being too specialized to report all of the patient’s injuries.
Likewise, emergency rooms are notorious for missing injuries. The specialty of the emergency
room is to make sure you do not die. If you live, they consider that they have done their job.
Insurance adjusters exploit emergency room records all the time and use them incorrectly to
"prove" that the patient did not have certain injuries on the day of the accident. They imply the
patient must have made up a bunch of phony injuries later to try to scam their insurance
company for more money. They tend to get away with it because the patient’s attorney (the
plaintiff attorney) does not understand this specialization of doctors and how it affects the
records they keep.
Lawyers have no idea whether that patient was the only patient in the emergency room at the
time with a team of doctors and nurses working on her/him (as if this were ever true) or whether
that patient was one of many, many patients in the emergency room at the time she/he was there.
The lawyer may not appreciate or understand that patient may have sat there for three hours
while the E.R. doctors went away to take care of a gunshot victim. They didn’t think the patient
in the car accident as going to die so they just left her/him there to go save the life of somebody
else. It is entirely possible that when they returned to help the car accident patient several hours
later, another patient came in with who was gushing blood out of a deeply cut hand or arm. The
car accident patient may have been left alone to wait again while E.R. personnel handled bigger
emergencies.
The emergency room may have been so busy that they never got around to checking the car
accident patient thoroughly. They may have needed the bed for somebody else who might die if
they did not give away the bed. The car accident patient may have been looked at briefly and
sent home. Doctors do not like to admit this occurs (fearing malpractice lawsuits.) I assure you
it happens.
If the E.R. was very busy, the medical team had very little time or resources to examine the car
accident patient. They made sure she/he was not bleeding to death and was likely to live and
sent her/him home. There is frequently a tremendous amount of medical information that is not
written down in the emergency room records. Some of it is left out because they didn't ask all
the questions. Some of it is left out because they do not have time to write it all down because an
ambulance just rolled in with a gunshot victim that will die if they don't stop dealing with the car
accident victim and rush over to treat the gaping hole in the gunshot victim's stomach.
Let me just state for the record, emergency room consultations and examinations are not
thorough. They are not designed to be thorough. They are designed to quickly assess the patient
for life-threatening injuries and prevent death. If the patient lived, the emergency room doctors
and nurses did their job. Claim adjusters mistakenly believe the E.R. records accurately and
thoroughly explain all the patient’s injuries. They most certainly do not.
Don't think that I don't respect and admire emergency room doctors and nurses. They are often
the cream of the crop of doctors and nurses in the world. They are talented and have an
unbelievable constitution to be able to deal with life and death on a daily basis and still remain
sane. If you have a heart attack or your leg was bit off by a shark, the men and women in your
emergency room are the best in the world to save your life. Thoroughly examining every car
accident victim that has no life-threatening injuries is simply not their job.
In addition to your injuries that are overlooked in the E.R. because they are not life-threatening,
E.R. personnel frequently make a serious omission when it comes to the question about whether
the car accident patient was unconscious after a car accident. Most E.R. nurses ask, “Do you
remember being unconscious?” That is the dumbest question in the history of the English
language. It is the same as asking, “Are you asleep?" These are perhaps the only two questions
that can never be answered, "Yes." Do you remember what happened during the eight hours you
were asleep last night?
Nobody remembers being unconscious. The correct question is, “What is the first thing you
remember after the accident?”
I recently met with a law client. I had read the E.R. records before the meeting and knew the
nurse had written, “Denies LOC.” This is short for “Denies loss of consciousness.” I first asked
my client if she remembered the E.R. nurse asking her whether she had been unconscious after
the accident. She did not remember being asked the question. There are two possible answers
for that: (1) The nurse never asked the question; or (2) my client had been so stunned or dazed
after the accident that she had anterograde amnesia (cannot remember events after the
concussion.) Something was terribly wrong with the E.R. records. They either missed a
concussion or lied about asking the question about loss of consciousness. I tend to believe the
nurse would not have lied. It is far more likely that the nurse asked the wrong question, “Were
you unconscious?” The dazed patient said, “No.”
I then asked my client the correct question, “What is the first thing you remember after the
accident?” She stared off into space for almost a full minute and then replied, “I remember my
daughter shaking me and when I opened my eyes I saw yellow police tape around my car and a
big red fire truck parked next to us.” It was obvious she had been unconscious long enough for
someone to call 911, for the police and paramedics to drive to the scene, and for police to string
up yellow tape around her car. This E.R. nurse made a critical medical mistake. She failed to
ask the correct question. She missed a significant brain concussion. She did irreparable damage
to my client’s legal case because the insurance company will not let go of her note despite a
respected neurosurgeon that examined her later and wrote an accurate account of my client’s
injuries (including the fact that she was unconscious and had a concussion.) The insurance
adjuster just keeps saying, “But the E.R. records say she was not unconscious.”
Chiropractors Must Be Thorough and Accurate
The time to be thorough and accurate is when you are wearing your doctor hat (during progress
exams when you make all the decision about diagnosis and treatment.) Once you have accurate,
thorough Symptoms, Exam, Diagnosis and Treatment Plan forms filled out during the progress
exam, simply refer to them in the daily SOAP notes and save yourself about 95% of the time you
used to spend writing SOAP notes.
It is not ethical for you to just write down a bunch of canned or computer generated SOAP notes
about the patient. Since you have learned in this class that you do not (generally) even need to
do anything on treatment days except refer to all your most recent Symptoms, Exam, Diagnosis
and Treatment Plan forms in your file, there is no need at all to even use computer generated
canned SOAP notes anymore. Just use the Incorporation by Reference doctrine and eliminate
95% of your SOAP note writing on treatment days.
Doctors must be thorough, accurate and honest in their record-keeping. In personal injury cases,
the doctor’s records are scrutinized very closely. A bunch of obviously canned or computer-
generated SOAP notes is really obvious and destroys your credibility.
Five Body “Parts” In Each Body “Area”
Each body area has five different parts (physical structures with the body area) that the doctor
must examine, diagnosis, and treat. The body “parts” in each area of the body are:
• Nerves
• Ligaments
• Tendons
• Muscles
• Bones
Your neck is not a body part. It is an area of your body that is made up of nerves, ligaments,
tendons, muscles, and bones. Your neck is thrown around violently during a whiplash and many
of the parts in your neck can be injured at the same time. Your doctor must examine each part
and diagnose each injured part. This is a tedious and time-consuming job if it is done correctly.
You may remember from chapters four and five that there are 22 ligaments in your neck. Your
doctor should evaluate and diagnose each of the 22 ligaments in your neck and report accurately
and thoroughly the injuries to each one. My job as your lawyer is very difficult if your doctor
ignores your ligaments and fails to diagnose three torn ligaments.
What is different about the typical motor vehicle collision case is the sheer number of injuries
you may have after a car accident. It is not uncommon for the car accident patient to come in
with 25 or 35 separate injuries to various body parts in several different body areas. For
example, you may have three injured ligaments in your neck, six injured muscles in your neck,
and two injured nerves in your neck for a total of eleven injured parts in your neck. Each of
these injured parts must have its own diagnosis code. You may also have one injured ligament,
three injured muscles, and two injured tendons for a total of six separate injured parts in your
right knee. Each of these must have its own diagnosis code. You may also have a brain
concussion with associated diagnosis of sleep disorder, fatigue, and cognitive dysfunction for a
total of four separate diagnosis codes for your brain.
In this example, eleven neck injuries plus six knee injuries plus four brain injuries make a total of
twenty-one injured parts in three separate areas of your body. The claim adjuster and attorneys
cannot accurately assess your claim if your doctor has failed to write each and every ICD-9
diagnosis code for all twenty-one injuries. Thorough, accurate, and honest is the standard
doctors must follow. Twenty-one total diagnosis codes is the only way a doctor can accurately
and honestly describe your injuries on paper.
If a basketball player sprains her ankle, there is only one injured body area (the ankle) and maybe
only one or two injured parts (e.g. tendons, ligaments.) If a baseball player throws out a runner
at home plate, he might injure his shoulder and, again, there is only one injured body area (the
shoulder) with maybe three injured parts in that shoulder (tendons, ligaments, and muscles.)
However, many or most people in car accidents have three, five, or sometimes seven injured
areas of the body with potentially four or five parts injured in each body area. The medical legal
system needs the facts and only the doctor can provide an accurate list of the facts that describe
your injuries. Use progress exam time to figure all of this out, write it down and get paid for it.
Then simply refer to all that good work in your SOAP notes for the next month until the next
progress exam.
The Symptoms Form
First of all, let me say that you can use any symptoms form in order to accomplish the goal of
reducing the amount of SOAP notes you write by using the Incorporation by Reference doctrine
as long as it is comprehensive and asks all the symptoms that your patient may have. I designed
my form and give it away for free to Chiropractors because it is so easy to use and
comprehensive at the same time.
Go to the Symptoms Form supplied with these notes and class materials now. Read through it
and you notice that it has the Patient’s Name, Today’s Date and the Date of Injury. It is
important that all three pieces of information are on each and every Symptoms Form (again,
whether you are using mine or not) because after four months or more, you will have done a
number of progress exams (aka re-exams) on the patient and people that look at your records
later will want to organize them by dates. It also makes it much easier to put the Exam Forms,
Diagnosis Forms and Treatment Plan forms all together and organize them to chart the patient’s
progress when the date it is filled out is on each form.
The attorney or claim adjuster reviewing your records might want to put all the Symptoms forms
in order and look to see if the patient is having fewer symptoms over time (hopefully because of
your treatments.) They the reviewer might want to reorganize them by date so that the
Symptoms, Exam, Diagnosis and Treatment Plan forms for each date are together. The reviewer
can then see quickly if all the symptoms were examined (by looking at the exam forms), see
quickly if you made a diagnosis for each symptom that was verified by the exam and finally to
see if you ignored any of the patient’s symptoms by never treating it (or putting it on your
treatment plan.)

Not only does this system of accountability work well for anyone reviewing your file but it is
also helpful for you, the Chiropractor, to organize your patient files, find things quickly, and scan
the forms to look for a pattern of improvement in the patient. Use the progress examination time
to review the file with the patient and if you already have several sets of all these forms, it is easy
to tell the patient, “We have been doing ultrasound on your neck for the past month. Now I am
going to change your therapy to _____________ for the next 30 days.”
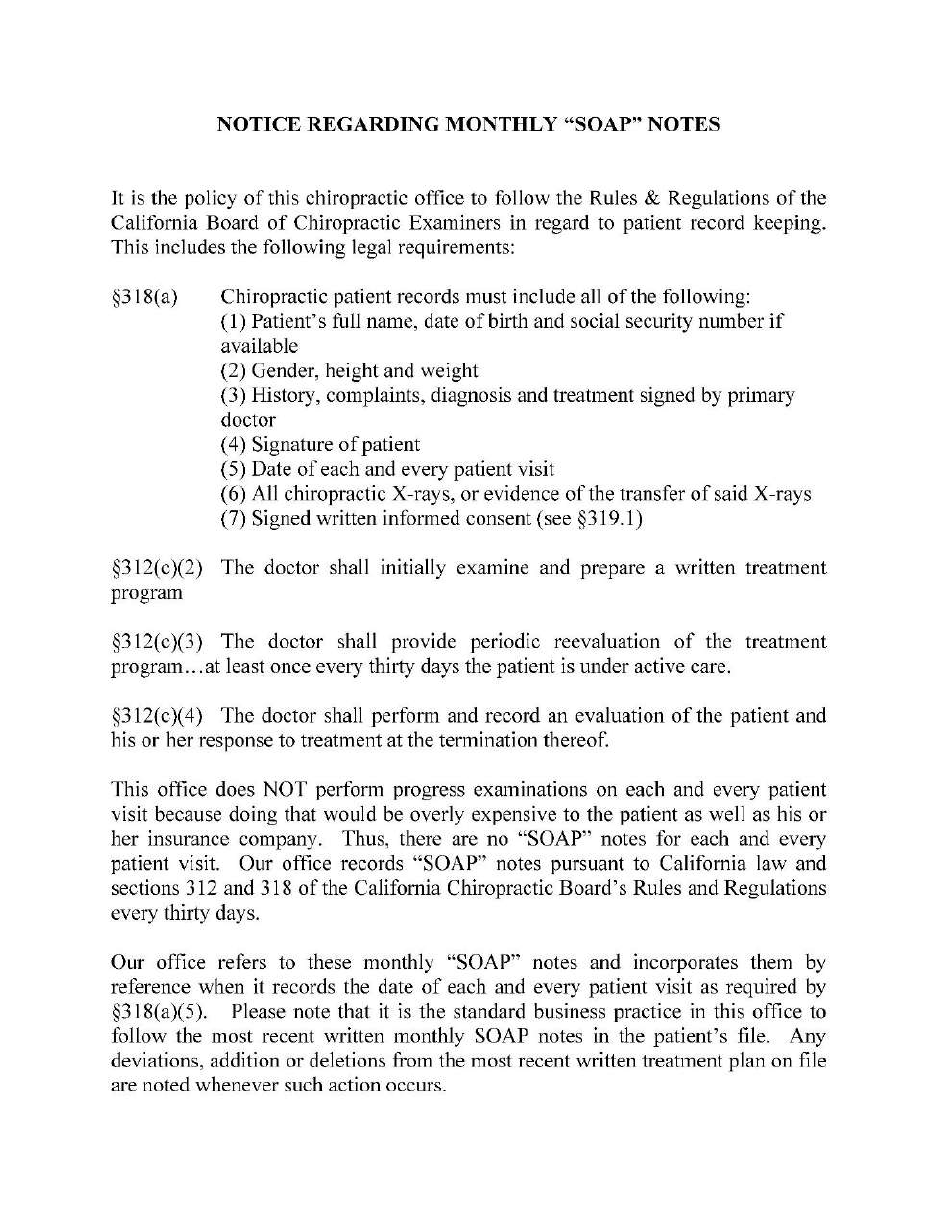
One Final Thought
It will take us some time to train the insurance companies that we have a new system of record
keeping. The reality is that by following my advice, your patient records should be infinitely
more accurate, more detailed and more thorough. Once everybody gets used to our new system,
we will no longer have to keep explaining it. In the mean time, I have included a form titled
“Notice Regarding Monthly SOAP Notes” and I suggest you place a copy of this form in your
patient’s chart so that when the insurance companies copy your records, they will understand
how your records are kept and why they comply with California’s Board Rules and Regulations.
For doctors taking this course in states other than California, I suggest reading your state’s rules
and regulations and modifying this form by quoting your state’s rules.
Below please find samples of the forms
from Steve Eggleston’s website.
To access these forms
click on this link
Doctors Forms Page
User Name: great
Password: Doctor88**
Thanks for taking CE Seminars with Back To Chiropractic.
I hope you enjoyed the course. Please feel free to provide feedback.
Check out: Back To Chiropractic Resources
Free Materials: Notes & Forms hundreds of files ~ posters, newsletters & more
Services & Listings People helping people for free
Marcus Strutz DC
Back To Chiropractic CE Seminars
marcusstrutz[email protected]
707.972.0047
