
February 2004
Centers for Medicare
P o w e r W h e e l c h a i r C
&
o v e r a g e O
Medicaid Services
v e r v i e w
Medicare Coverage of Power Wheelchairs and Other Power Operated Vehicles
Medicare classifies power (motorized) wheelchairs as Durable Medical Equipment (DME), which is covered
under Medicare Part B insurance. DME is equipment that can withstand repeated use, is primarily used for a
medical purpose, and is generally not used in the absence of illness or injury. Power Operated Vehicles (POVs),
commonly known as “scooters”, that may be appropriately used as wheelchairs are also covered under the DME
provision.
To qualify for Medicare reimbursement for a power wheelchair or a POV, the physician must certify the need for
the device, and that it is reasonable and medically necessary for the treatment of illness or injury, or to improve
the functioning of a malformed body part. Durable Medical Equipment Regional Carriers (DMERCs) process
Medicare claims for wheelchairs and other DME.
Prerequisites for Medicare Coverage
Power (Motorized) Wheelchairs: Most patients who require power wheelchairs are totally nonambulatory and
have severe weakness of the upper extremities due to a neurologic or muscular condition.
The following criteria must be met to qualify for Medicare coverage of a power wheelchair:
• The patient is bed or chair-bound without the use of a wheelchair (Note: An individual may qualify
for a wheelchair and still be considered bed-confined);
• The patient’s condition makes a wheelchair medically necessary, and they are unable to manually
operate a wheelchair; and
• The patient is capable of safely operating the controls of a power wheelchair.
All three conditions must be satisfied for Medicare to cover a power wheelchair. Special options or accessories to
power wheelchairs may require additional criteria be met to justify the medical necessity of the modifications.
Medicare will not cover the cost of a power wheelchair if the use of the power wheelchair primarily benefits the
patient in their pursuit of leisure or recreational activities. Additionally, payment is made for only one wheelchair
at a time.
If the patient qualifies for a power wheelchair, a written physician’s order and a Certificate of Medical Necessity
(CMN) must be completed before it can be billed.*
Power Operated Vehicles (POVs): These vehicles have been appropriately used in the home setting for
vocational rehabilitation and to improve the ability of chronically disabled persons to cope with normal
domestic, vocational, and social activities. They may be covered if a wheelchair is medically necessary and the
1

P o w e r W h e e l c h a i r C o v e r a g e O v e r v i e wP o w e r W h e e l c h a i r C o v e r a g e O v e r v i e w
patient is unable to operate a wheelchair manually. Slightly different criteria must be met for Medicare coverage
of these “scooter” devices. They are:
• The patient’s condition is such that without the use of a wheelchair, the patient would not be able to
move around their residence;
• The patient is unable to operate a manual wheelchair;
• The patient is capable of safely operating the controls of the POV;
• The patient can transfer safely in and out of the POV; and
• The POV is ordered by one of the following specialists: Physical Medicine; Orthopedic Surgery;
Neurology; or Rheumatology.
• Exceptions: When a specialist is not reasonably accessible (e.g., more than a day’s round trip
travel from the patient’s home or the patient’s condition precludes travel to a specialist), an
order from the patient’s physician may be acceptable.
All five conditions must be satisfied for Medicare to cover a POV. Special options or accessories for POVs may
require that additional criteria be met to justify the medical necessity of the modifications.
If a POV is covered, a second wheelchair provided at the same time, or subsequently, could be denied coverage
as not medically necessary. Medicare will not cover the cost of a POV if the use of the POV is only needed for
use outside the home, or if it primarily benefits the patient in their pursuit of leisure or recreational activities.
Additionally, large size POVs could be denied coverage as not medically necessary if they cannot be used in the
home and/or have features generally intended for outdoor use.
If the patient clinically qualifies for a POV, it will only be covered if the physician provides a
written signed and dated order to the DME supplier
before the POV is delivered to the patient. In
addition, a CMN must be completed and sent to the supplier
before it can be billed.*
heelchair Options/A
ccessories
If a patient qualifies for a power wheelchair or POV, they may need
additional accessories to maximize the benefit of the device. Such
devices include, but are not limited to: adjustable arm height;
reinforced back upholstery; headrest extensions; fully reclining back;
solid seat; various leg rest types; batteries; and custom parts. In addition
to meeting the requirements for the power wheelchair or POV, the
following criteria must be met:
If the patient clinically qualifies for a POV, it will only be covered if the physician provides a
written signed and dated order to the DME supplier
addition, a CMN must be completed and sent to the supplier
Wheelchair Options/Accessories
If a patient qualifies for a power wheelchair or POV, they may need
additional accessories to maximize the benefit of the device. Such
devices include, but are not limited to: adjustable arm height;
reinforced back upholstery; headrest extensions; fully reclining back;
solid seat; various leg rest types; batteries; and custom parts. In addition
to meeting the requirements for the power wheelchair or POV, the
following criteria must be met:
•
The options/accessories are necessary for the patient to perform
one or more of the following activities:
• Function in the home; or
• Perform instrumental activities of daily living.
Note: Medicare will not cover the cost of an option/accessory
if it primarily benefits thepatient in their pursuit of
leisure or recreational activities.
2
P o w e r W h e e l c h a i r C o v e r a g e O v e r v i e w P o w e r W h e e l c h a i r C o v e r a g e O v e r v i e w
If the patient clinically qualifies for a wheelchair or POV option/accessory, a written physician’s order must be
sent to the supplier before it can be billed.* Some options/accessories will also require that a CMN be completed
and sent to the supplier before it can be billed.
*For items that require a CMN (and for related accessories, supplies, and drugs requiring a CMN), the CMN may serve as the written order
if the narrative description in Section C of the CMN is sufficiently detailed.
Patient Costs for Power Wheelchairs and POVs
Medicare pays for power wheelchairs and POVs differently:
POVs:
Beneficiaries may rent or purchase a POV. If the rental option is selected, the supplier retains ownership of the
POV and Medicare limits its total rental payments to the purchase price. Therefore, if the beneficiary needs the
POV for an extended period, purchase is a preferable option.
Power Wheelchairs:
Beneficiaries may elect to purchase a power wheelchair when it is furnished. If the beneficiary declines the
purchase option, Medicare will pay on a rental basis for ten months. After the 10th rental payment, the
beneficiary may again elect to purchase the wheelchair. If the beneficiary elects the purchase option, Medicare
will make three additional monthly rental payments and then the beneficiary owns the wheelchair. If the
beneficiary declines this purchase option, Medicare will make five additional monthly rental payments and the
supplier, not the beneficiary, owns the wheelchair.
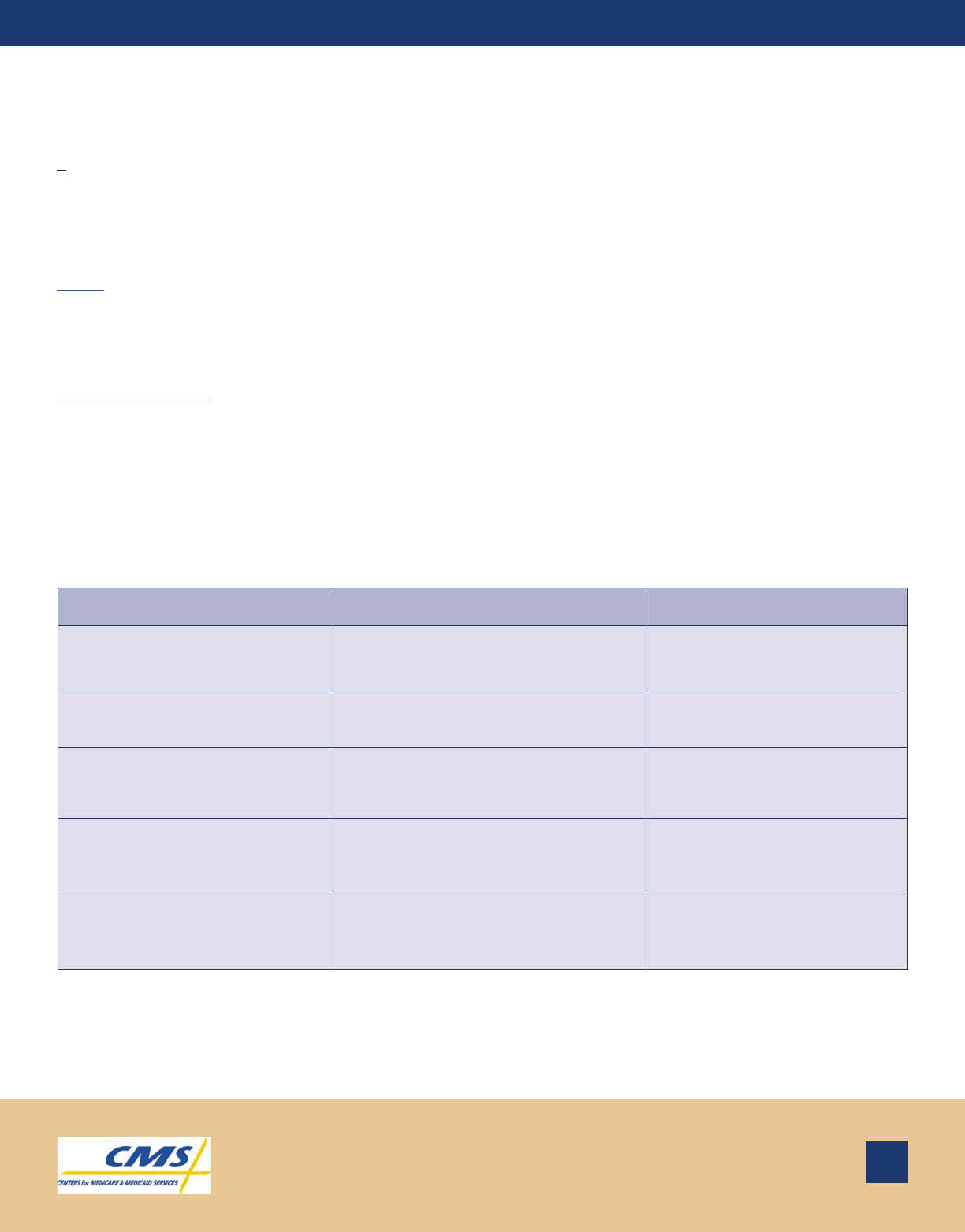
Summary of Patient Costs
If the patient… Then Medicare Part B will pay… And the patient will pay…**
Chooses to purchase the power
wheelchair or POV…
80% of the allowed purchase price in
one lump sum payment.
20% of the allowed purchase
price.
Chooses to rent the power
wheelchair…
80% of the allowed rental price for
months 1 - 10.
20% of the allowed rental
charge.
Chooses purchase option for the
power wheelchair after ten rental
months…
80% of the allowed rental price for
months 11 - 13.
20% of the allowed rental
charge.
Chooses rental option for the
power wheelchair after ten rental
months…
80% of the allowed rental price for
months 11 - 15.
20% of the allowed rental
charge.
Chooses to rent the POV…
80% of the allowed rental price. Total
Medicare payments cannot exceed
80% of the allowed purchase price.
20% of the allowed rental
charge as their co-insurance.
**Patient payment responsibility is based upon receiving equipment from a provider that accepts assignment. Patient costs are higher
when obtaining wheelchairs from suppliers that do not accept assignment. If the patient is enrolled in a Medicare Managed Care Plan, the
patient will need to contact the plan to determine their costs. In addition, the managed care plan may require preauthorization and have a
limited number of participating DME suppliers.
3
P o w e r W h e e l c h a i r C o v e r a g e O v e r v i e wP o w e r W h e e l c h a i r C o v e r a g e O v e r v i e w
Note: If the power wheelchair is rented, Medicare will pay 80% of the allowable service and maintenance charge
once every six months, whether or not the equipment is actually serviced, to the extent that the charges
are not covered under a supplier or manufacturer warranty. Therefore, the patient must pay 20% of the
allowed service charge as their co-insurance once every six months.
If the power wheelchair or POV is purchased, Medicare will pay 80% of the allowable service and
maintenance charge each time the equipment is actually serviced.
Frequently Asked Questions
Q: Why does a physician have to certify the need for a power wheelchair or POV?
A: The Medicare program only pays for health care services that are medically necessary. In determining
what services meet these criteria, Medicare primarily relies on the professional judgment of the patient’s
treating physician, since he or she knows the patient’s history. Under Medicare, physicians play a key role
in determining the medical need for DME billed by other providers and suppliers. Therefore, Medicare
requires physicians to certify the medical necessity for a power wheelchair or POV and some related options/
accessories.
Q: How does a physician certify the medical necessity of a power wheelchair or POV?
A: The Centers for Medicare & Medicaid Services (CMS) has developed a Certificate of Medical Necessity (CMN)
Form for Motorized Wheelchairs (Form HCFA 843) and POVs (Form HCFA 850). These forms require
information to be completed by the patient’s physician, the supplier, and any other non-physician clinician
involved in the assessment of the patient related to this certification.
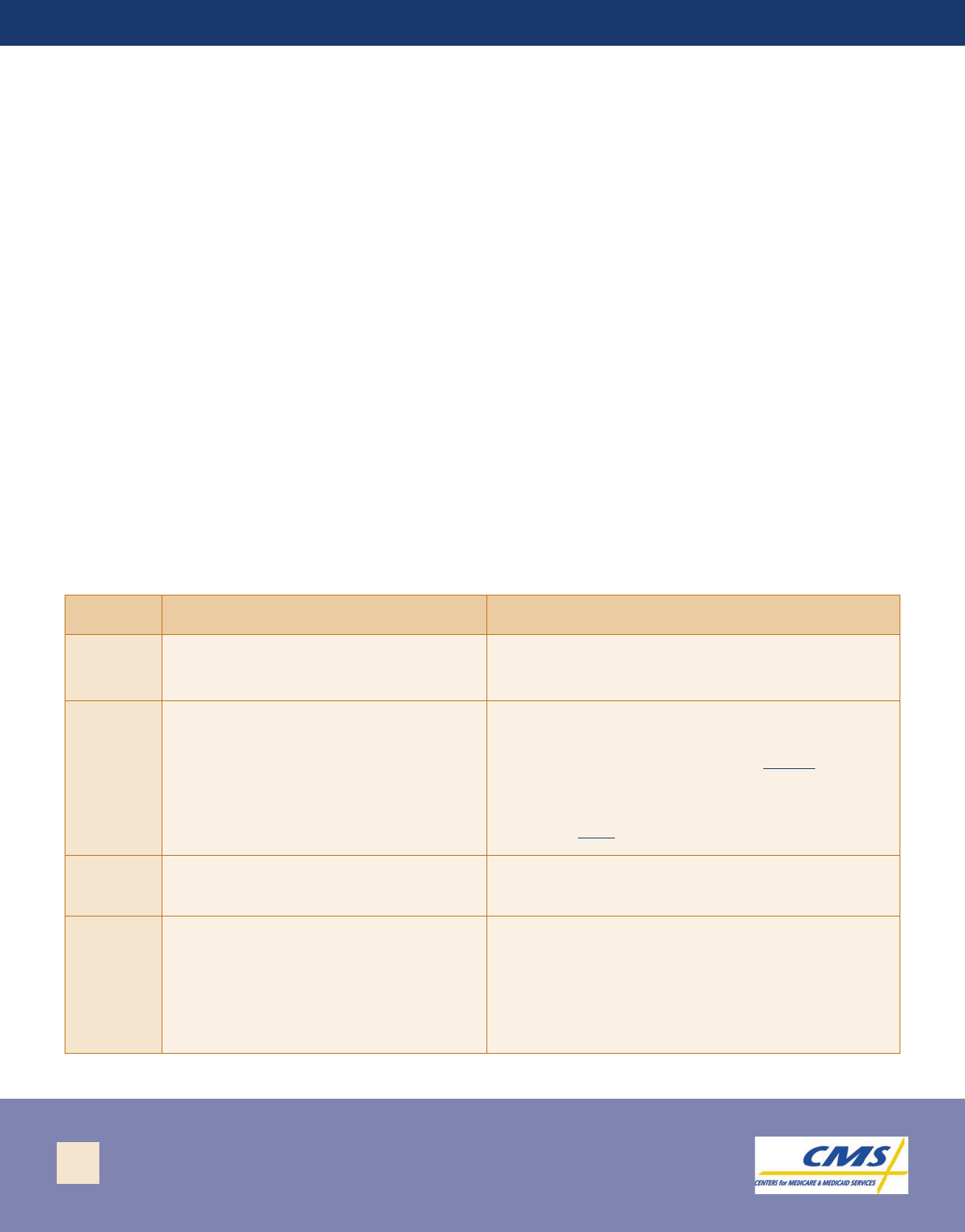
Generally, a CMN has four sections:
Section Contains… Is Completed…
Section A
General information regarding the
patient, supplier, and physician.
Usually by the supplier.
Section B
The medical necessity justification for
the DME.
By the physician, a non-physician clinician
involved in the care of the patient, or a
physician employee. The supplier cannot fill out
this section. If the physician did not personally
complete Section B, the name of the person who
did complete Section B and their title and
employer must be specified.
Section C
A description of the equipment and its
cost.
By the supplier.
Section D
The treating physician's attestation
and signature, which certify that the
physician has reviewed Sections A, B,
and C of the CMN and that the
information in Section B is true,
accurate, and complete.
By the treating physician. Signature stamps and
date stamps are not acceptable.
4
P o w e r W h e e l c h a i r C o v e r a g e O v e r v i e w P o w e r W h e e l c h a i r C o v e r a g e O v e r v i e w
By signing the CMN, the physician represents that:
•
•
and
• The information in Section B relating to medical
the physician’s knowledge.
• Form HCFA 843 may be downloaded from:
http://www.cms.hhs.gov/forms/cms843.pdf
• Form HCFA 854 is a continuation of Form 843 and
may be downloaded from: http://www.cms.hhs.gov/
forms/cms854.pdf
• Form HCFA 850 may be downloaded from:
http://www.cms.hhs.gov/forms/cms850.pdf
The physician is the patient’s treating physician and the
information regarding the physician’s address and Unique
Physician Identification Number (UPIN) is correct;
The entire CMN, including the sections filled out by the
supplier, was completed prior
necessity is true, accurate, and complete to the best of
to the physician’s signature;
Q: Who qualifies as a non-physician clinician that may complete Section B of the
Motorized Wheelchairs CMN?
A: Section B contains information representing a clinical assessment of the patient’s current condition. The
non-physician completing this section must be an employee of the physician or a qualified Medicare provider
practicing within their scope of practice. For example, physical and occupational therapists meet these
standards. The supplier cannot complete Section B.
Q: Is a physician prescription for a power wheelchair or POV needed in addition to the
completed CMN Form?
A: Yes. Medicare will only cover DME that has been ordered or prescribed by a physician. The order or
prescription must be personally signed and dated by the patient’s treating physician [stamped signatures are
not permitted unless the physician qualifies for an Americans with Disabilities Act (ADA) exclusion]. For
POVs, the written, signed, and dated order must be furnished to the supplier prior to delivery of the device to
the patient. In limited situations, DMERCs may accept a CMN as a substitute for a written order if it contains
all the required elements of the order.
The physician’s order or prescription for a power wheelchair or POV must include:
• The patient’s name and full address;
• The physician’s signature;
• The date the physician signed the prescription (or order);
• A description of the item needed;
• A diagnosis supporting the medical necessity of the equipment; and
• A realistic estimate of the total length of time the equipment will be needed (in months or years).
5
P o w e r W h e e l c h a i r C o v e r a g e O v e r v i e wP o w e r W h e e l c h a i r C o v e r a g e O v e r v i e w
Q: What documentation should be furnished to the DME supplier to support payment for power
wheelchairs or POVs?
A: A supplier must have a faxed or copied, original signed order or CMN in their records before they can submit a claim
for payment to Medicare. The CMN can serve as the physician's order if the narrative description is sufficiently
detailed.
Q: Are there local policies that may apply to motorized wheelchairs or POVs?
A: Yes. The four regional DMERCs have local coverage policies that contain more detailed criteria than national
coverage requirements. Local coverage policy is described in the DMERCs’ Local Medical Review Policies
(LMRPs) and should also be reviewed when ordering DME for patients. The most common LMRP titles
described in this article are:
• Motorized/Power Wheelchair Bases
• Power Operated Vehicles
• Wheelchair Options/Accessories
Access to Local Medical Review Policies and links to DMERC Web pages are available at:
http://www.cms.hhs.gov/mcd/search.asp?.
Q: What are some examples of inappropriate practices regarding the certification of power wheelchairs
or POVs?
A: The Health and Human Services (HHS) Office of Inspector General (OIG) discovered the following instances
of inappropriate certifications in the course of its investigations of fraud:
• At the prompting of a DME supplier, a physician signs a stack of blank CMNs. The CMNs are later
completed with false information in support of fraudulent claims for the equipment. The false
certified the medical necessity for the equipment.
• A physician signs CMNs for equipment, falsely
representing that the equipment was medically
necessary.
• A physician signs CMNs for wheelchairs without
seeing the patients, then falsifies the medical
records to indicate that the physician treated the
patients.
• A physician accepts money from a DME supplier
for each prescription he or she signs.
• A non-physician completes Section B of CMNs
falsely (without seeing the patient or by accepting
money from a DME supplier).
please contact the HHS OIG at 1-800-HHS-TIPS (1-800-447-8477).
If you have concerns or questions regarding fraudulent behavior,
information purports to show that the physician ordered and
6
P o w e r W h e e l c h a i r C o v e r a g e O v e r v i e w P o w e r W h e e l c h a i r C o v e r a g e O v e r v i e w
Q: Where can I find additional information regarding power wheelchairs and POVs?
A: For more information about power wheelchairs, DME, or Medicare, please visit one of the following
online references:
• The Medlearn Home Page
http://www.cms.hhs.gov/medlearn/
The Medlearn Home Page helps providers locate regulations, educational materials, and mailing lists
regarding various Medicare-related topics.
• The Medlearn Provider Toll-Free Customer Service Telephone Numbers Listing
http://www.cms.hhs.gov/medlearn/tollnums.asp
This Web page features an interactive map to help providers locate toll-free numbers for DMERCs,
Provider Services, and other organizations.
• Medicare Program Integrity Manual
Chapter 5 – Items and Services Having Special DMERC Review Considerations
http://www.cms.hhs.gov/manuals/108_pim/pim83c05.pdf
This chapter provides instructions to providers and medical review specialists regarding DME claims.
It focuses on the documentation required to support that the proper referral, certification, and
justification of medical necessity has been met for equipment such as powered wheelchairs and POVs.
• Medicare Coverage Issues Manual: Durable Medical Equipment
http://www.cms.hhs.gov/manuals/06_cim/ci60.asp
The Coverage Issues Manual describes the following official national coverage policies related to
power wheelchairs and POVs:
Section Title
60-5 Power-operated vehicles that may be used as wheelchairs
60-6 Specially sized wheelchairs
60-9 Durable medical equipment reference list
• National Coverage Determinations (NCDs) Home Page
http://www.cms.hhs.gov/ncd/default.asp
The NCD Database contains information regarding current and pending national coverage policy.
This feature provides easy access to information about what items and services are covered, or not
covered, by Medicare.
• Medicare Certificates of Medical Necessity (CMN) Home Page
http://www.cms.hhs.gov/providers/mr/cmn.asp
This Web site provides links to all current Medicare CMN forms, including instructions for
completion.
7
