
The Royal College of Pathologists
6 Alie Street
London E1 8QT
T: 020 7451 6700
F: 020 7451 6701
www.rcpath.org
Registered charity in England and Wales, no. 261035
© 2020 The Royal College of Pathologists Unique document reference number: G199
Cause of death list
June 2020
Author: Dr Suzy Lishman, Chair of the RCPath Medical Examiners Committee.
Contents
Foreword ............................................................................................................................................. 2
Introduction ........................................................................................................................................ 3
Registrars ........................................................................................................................................... 3
Referral to the coroner ...................................................................................................................... 4
Notes on the cause of death list ...................................................................................................... 4
Key considerations for registrars of births and deaths ........................................................................ 4
The Medical Certificate of Cause of Death.......................................................................................... 5
Causes of death ................................................................................................................................. 8
A ..................................................................... 8
B ..................................................................... 9
C ................................................................... 10
D ................................................................... 12
E ................................................................... 13
F ................................................................... 14
G ................................................................... 14
H ................................................................... 15
I ..................................................................... 16
J .................................................................... 17
K ................................................................... 17
L ................................................................... 17
M .................................................................. 18
N ................................................................... 19
O ................................................................... 19
P ................................................................... 19
R ................................................................... 20
S ................................................................... 21
T ................................................................... 22
U ................................................................... 23
V ................................................................... 23
W .................................................................. 23

2
Foreword
Achieving accuracy of Medical Certificates of Cause of Death is vital to the health of the nation and
is core to medical examiner work. The Cause of death list has an important part to play, also
helping remind which deaths must be notified to a senior coroner. Publication enables all involved;
registrars, doctors, coroners and coroners’ officers to speak from the same page. This is very
welcome, and I am delighted the Royal College of Pathologists brings medical expertise leading
the Cause of Death List to greater prominence.
Dr Alan Fletcher
National Medical Examiner

3
Introduction
The Royal College of Pathologists is the lead medical royal college for medical examiners,
providing training, guidance and continuing professional development for this important new
medical specialty. Medical examiners will scrutinise all deaths not reported to the coroner, ensuring
appropriate coronial referral and accurate certification and speaking to bereaved families, in
particular answering any questions they might have.
The College has worked closely with the Department of Health and Social Care, National Medical
Examiner, Chief Coroner, General Register Office (GRO), medical royal colleges and patient and
faith groups to support implementation of the medical examiner system, initially in acute trusts and
shared services partnerships and then to cover all deaths in England and Wales. The College is
grateful to these stakeholders for their contribution to updating this important document and their
support of medical examiner implementation in general. We hope that this guide will be helpful for
doctors completing death certificates, medical examiners supporting them and registrars
registering deaths, ultimately for the benefit of the bereaved.
This Cause of death list replaces the 2016 document issued to registrars by the GRO and
intentionally retains the same name and format as that document. It is not intended to be an
exhaustive list of all possible causes of death, but deals with conditions that have previously
prompted discussion between certifying doctors, registrars and coroners. It includes clarification
about common conditions, such as pneumonia and heart failure, and less common ones, such as
ankylostomiasis and spirochaetal jaundice. The list has grown organically and reflects previous
areas of contention rather than a systematic approach. This version seeks to provide consistent
guidance for all stakeholders, removing ambiguity and improving consistency. The College will be
responsible for updating the content as required and welcomes feedback.
The document offers guidance for those completing death certificates and those registering deaths.
In the current non-statutory medical examiner system, registrars will continue to refer deaths to the
coroner in line with the Notification of Deaths Regulations 2019.
The Cause of death list details some of the conditions that may be included on the Medical
Certificate of Cause of Death (MCCD). The MCCD is completed by the certifying doctor in line with
current legislation, which can be found at: www.gov.uk/government/publications/guidance-notes-
for-completing-a-medical-certificate-of-cause-of-death
This document is being published during the emergency legislation of the Coronavirus Act 2020.
Under the Act, several processes relating to the certification and registration of death have
changed temporarily. The changes to the process of death certification do not affect the acceptable
causes of death that can be registered without coronial referral. This guidance will remain current
after the Coronavirus Act 2020 has been repealed.
Registrars
Registrars should use this guide in the first instance if they have a query about the acceptability
of a cause of death.
If a query is not covered in this guide, or if you have additional concerns, please call the GRO
on 0300 123 1837 (select option 2).
To provide feedback on this document, please contact the Royal College of Pathologists.
4
Referral to the coroner
The Notifications of Deaths Regulations came into force in October 2019. These made it a legal
requirement for certain deaths to be reported to the coroner. Briefly, a registered medical
practitioner has a duty to notify the coroner if any of the following circumstances apply:
• poisoning
• exposure to a toxic substance
• use of a medicinal product, controlled drug or psychoactive substance
• violence
• trauma or injury
• self-harm
• neglect, including self-neglect
• the person undergoing a treatment or procedure of a medical or similar nature
• an injury or disease attributable to any employment held by the person during the person’s
lifetime
• the registered medical practitioner suspects that the person’s death was unnatural but does
not fall within any of the circumstances above
• the cause of death is unknown
• the person died in custody
• there is no attending medical practitioner to sign the death certificate
• the deceased cannot be identified.
The regulations can be accessed at: www.legislation.gov.uk/uksi/2019/1112/made
The Ministry of Justice has issued guidance to medical practitioners on the Notifications of Deaths
Regulations:
https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/
851972/registered-medical-practitioners-notification-deaths-regulations-guidance.pdf
Notes on the cause of death list
Key considerations for registrars of births and deaths
This list is not exhaustive and needs to be used in conjunction with the Registrars Handbook,
particularly D2 and D4. The fact that a cause if death does not appear in this list does not
necessarily mean that it is, or is not, acceptable.
Each MCCD should be looked at on its own merits and consideration should be given to all
conditions recorded on the certificate and the order in which they are recorded.
5
The Medical Certificate of Cause of Death
The certifying doctor will complete an MCCD. It is the registrar’s legal responsibility to report
certain deaths to the coroner. Information about which deaths need referring to the coroner are at
D2 and D4 of the Registrar’s Handbook. Consideration should also be given to the expected
statutory provisions by medical practitioners.
The cause of death must be copied precisely from the MCCD – the registrar cannot amend the
cause of death and cannot correct any spelling mistakes. Please take care when completing the
MCCD and write clearly. If the death needs to be referred to the coroner, the registrar should refer
without discussing the cause with the certifying doctor. Under the current non-statutory scheme,
there is no obligation for the registrar to discuss the cause of death with a medical examiner. If in
doubt, the medical examiner may wish to discuss the acceptability of a cause of death with their
local registrar.
Information in the Medical Certificate of Cause of Death
Please note: This section is intended to provide a broad understanding of the type of information
shown in a MCCD. It is not intended to provide definitive definitions or guidance.
The MCCD is divided into two parts, the functions of which are described in more detail below.
When considering the information in Parts I and II, registrars should be alert to whether modes of
death have been recorded and whether a given cause of death appears to be unnatural.
Part I
This is the sequence of causes, conditions or events directly leading to the death and is split into
three parts: a, b and c. There must be an acceptable cause of death in Part I (either in a, b or c). A
condition which is not acceptable as a casue on its own may become acceptable when
accompanised by another condition. However, an acceptable condition does not remain
acceptable if another cause of death in a, b, or c requires referral to the coroner.
Part II
Causes in Part II are other significant conditions contributing to the death, but not directly related to
the disease or the condition causing it.
If there is not an acceptable cause of death in Part I, an acceptable cause of death in Part II does
not mean a registration can be concluded.
Even if there are acceptable causes of death in Part I, Part II can still lead to referral to the coroner,
if it suggests the death might have been unnatural (please see list below).
Remember: Part II cannot make Part I better but it can make it worse.
Modes of dying
A ‘mode’ of dying is one which does not explain ‘why’. For example, ‘coma’ does not explain the
underlying condition leading to death. Examples of modes of death (not a complete list) include:
• cardiac arrest
• coma
• exhaustion
• renal/kidney failure
• respiratory arrest
6
• syncope.
Terms such as ‘acute’, ‘chronic’, ‘acute on chronic’ or ‘multiple’ do not turn modes of dying into
acceptable causes.
The exception to this rule is ‘heart failure’, which is acceptable on its own, although ideally further
supporting information should be provided.
It is acceptable for a mode of dying to be supported/explained by an acceptable disease or
condition beneath it in Part I.
The terms ‘possible’, ‘probable’ and ‘suspected’ should not be used on the MCCD.
‘Unnatural’ causes of death
If there appears to be an unnatural cause of death in either Part I or II, the death must be referred
to the coroner.
Referral to the coroner
Deaths should be referred to the coroner in the usual way for your office.
Infections
The name of the organism responsible for an infection should be included on the MCCD where
known.
Malignancies
The specific type of malignancy should be included where known, e.g. squamous cell carcinoma of
the bronchus, rather than lung cancer.
Use of abbreviations
Abbreviations must not be used on the MCCD (but can be used on the counterfoil).
Unknown
In general, the term ‘unknown’ should be avoided on the MCCD. However, it is acceptable in
certain circumstances, such as metastatic malignancy of unknown primary, and septicaemia/sepsis
of unknown aetiology.
Possible/probable
‘Possible’ and ‘probable’ should not be used on the MCCD. The certifying doctor states the cause
of death to the best of their knowledge and belief. If they do not know the cause of death, they
must notify the coroner.
Industrial disease
Some conditions are commonly associated with occupational exposure to hazardous substances.
Mesothelioma, for example, is often due to occupational exposure to asbestos. In such conditions,
the death must be referred to the coroner unless the doctor states that the disease was
non-industrial or non-occupational. There are also some diseases that are occasionally related to
the deceased’s occupation, such as lung cancer or emphysema, but which also occur commonly in
the general population. In these conditions, the doctor completing the MCCD should check
carefully that they were not related to an occupation, but does not need to state ‘non-occupational’
on the MCCD. If the condition may have been related to the deceased’s occupation, the case must
be referred to the coroner.
7
Definition of terms
Acceptable – This cause of death does not need to be referred to the coroner, however if it is
used in conjunction with another cause that does need to be referred, the death should still be
referred to the coroner.
Some causes of death are acceptable only if further information is provided, for example:
• acceptable if noted to be spontaneous
• acceptable if supported by another acceptable cause of death
• acceptable over a certain age.
Mode of dying – refer to coroner unless supported by an acceptable cause of death. A mode of
dying has to be supported by another cause of death which is acceptable in Part I of the MCCD.
Refer to coroner unless doctor states non-industrial – doctor should write ‘non-industrial’ after
the cause. The informant should not be asked whether the condition was caused by the
deceased’s occupation.
Refer to coroner – death needs to be referred to the coroner wherever this condition appears on
the MCCD, regardless of any other conditions recorded or where on the MCCD it is written.
Refer to coroner if not accompanied by another acceptable condition – the acceptable
condition must be in part 1.
8
Causes of death
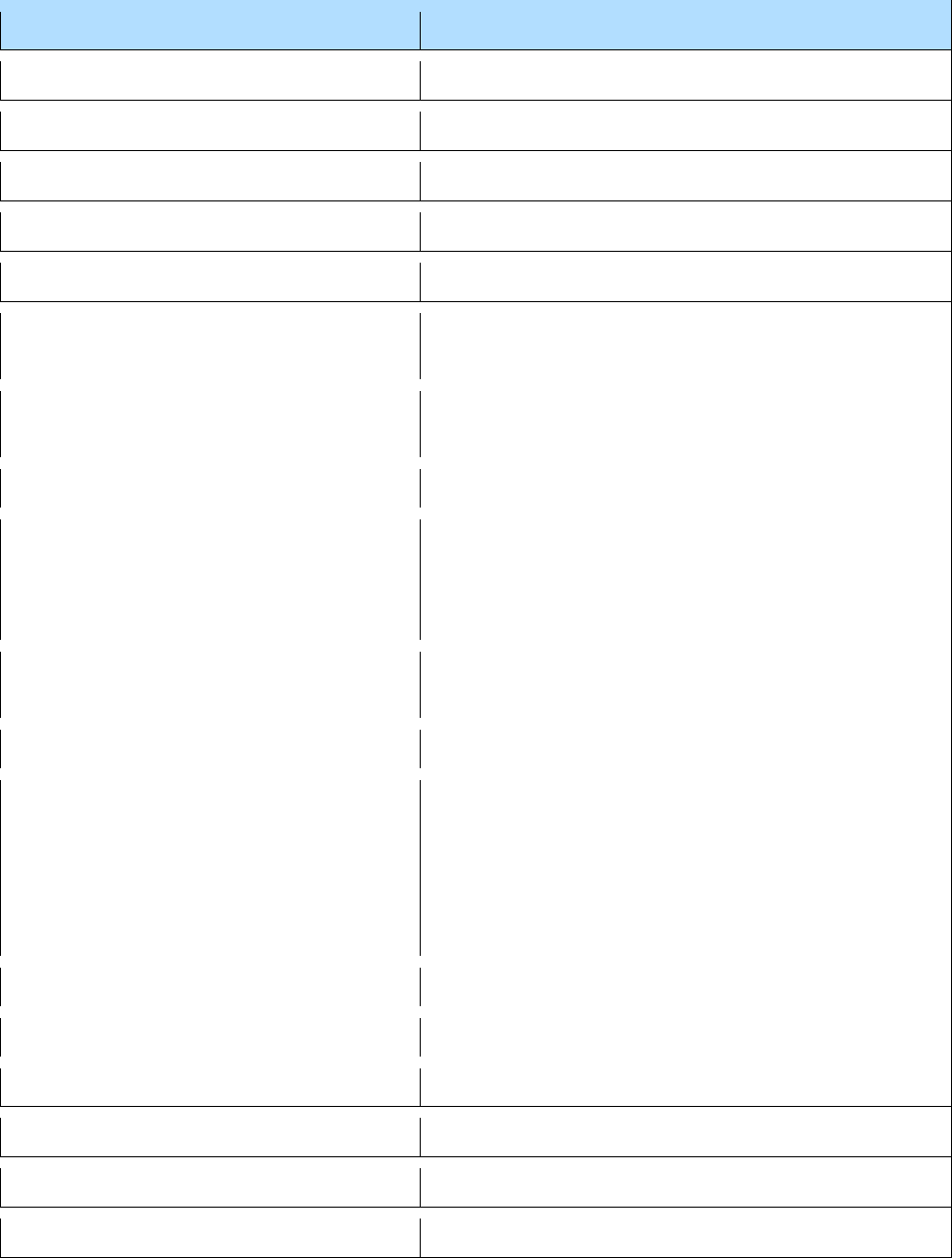
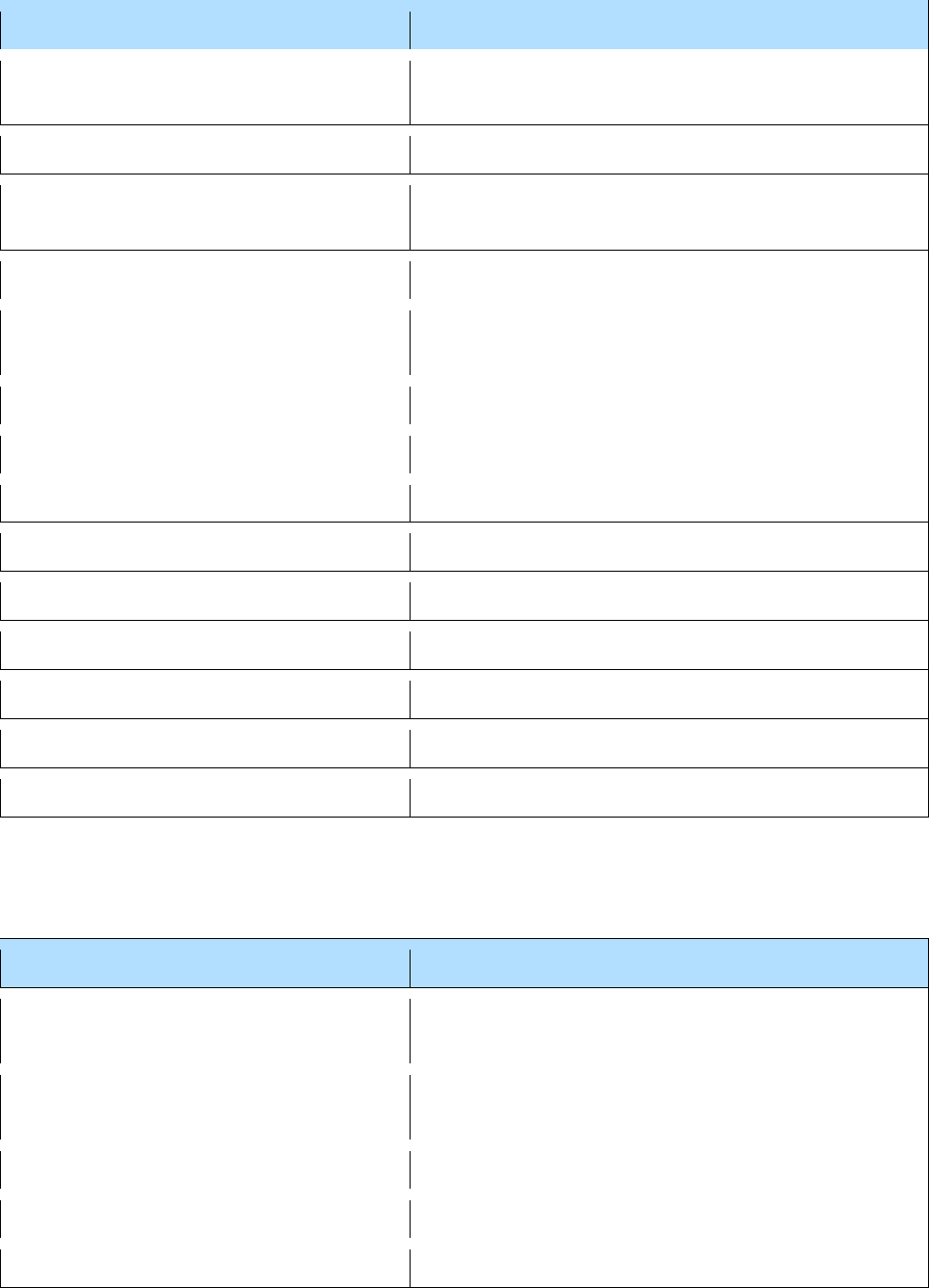
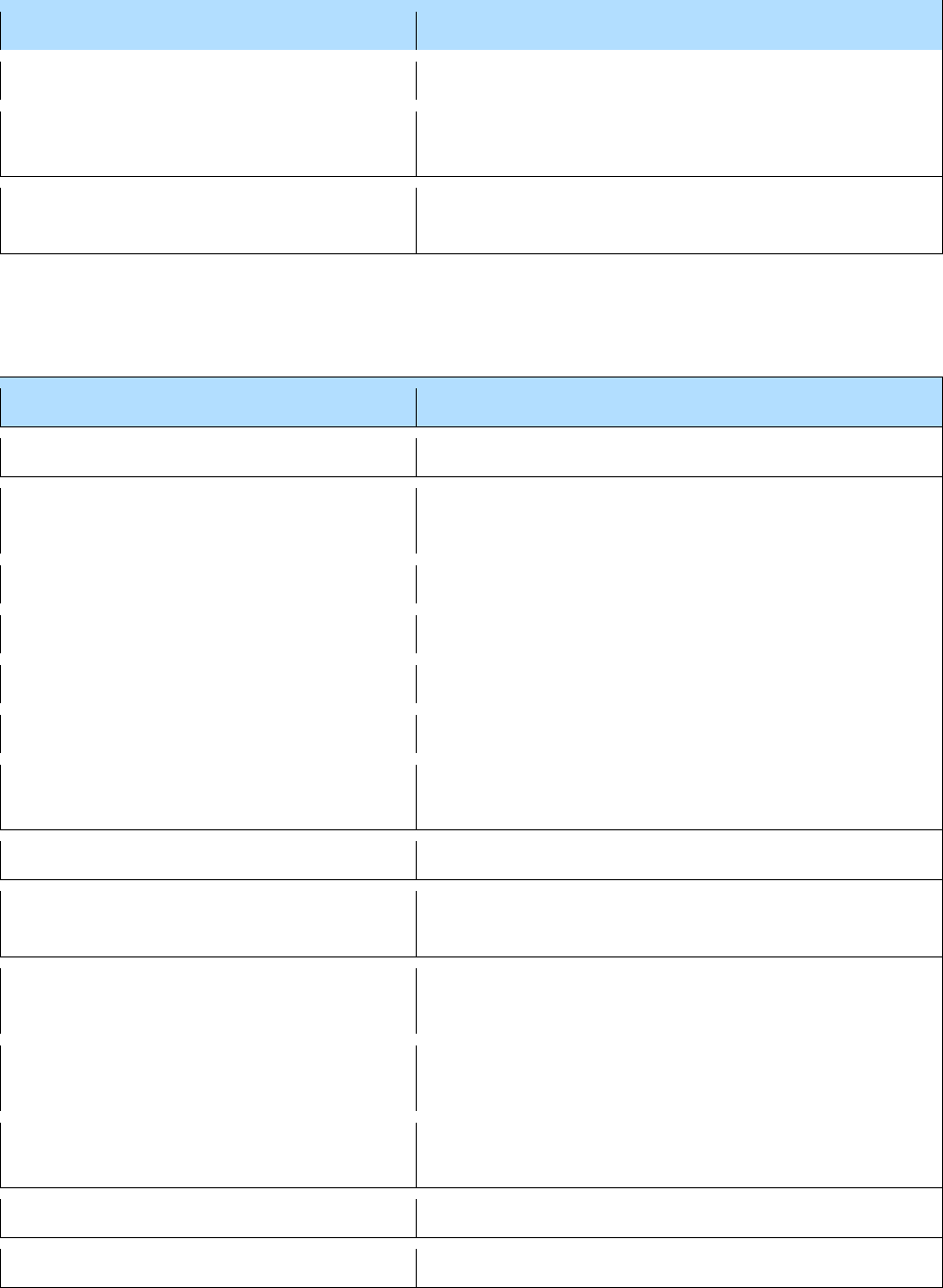
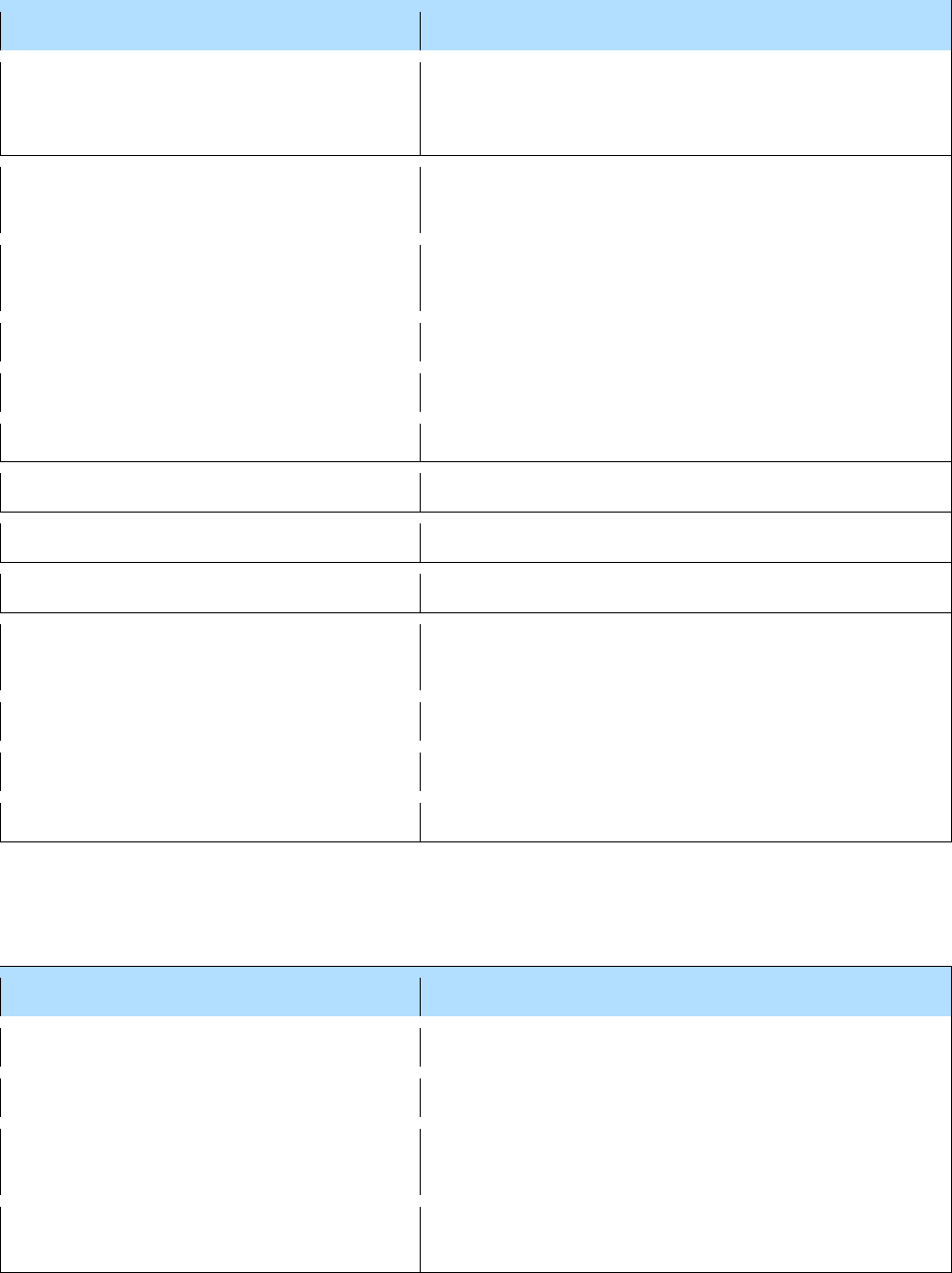
A
Cause of death
Action
Abdominal aortic aneurysm
Acceptable
Acute alcoholism
Refer to coroner
Acute dehydration
Refer to coroner
Acute left/right ventricular failure
Acceptable
Acute aortic syndrome
Acceptable
Acute respiratory distress syndrome
Refer to coroner unless supported by another
acceptable condition
Adult respiratory distress syndrome
Refer to coroner unless supported by another
acceptable condition
Advancing years – old age
Acceptable if deceased was aged 80 or over
Acquired Immunodeficiency Syndrome
Acceptable, unless the informant or MCCD states
due to contaminated blood products or needles
drugs etc.; do not ask question – only if this
information is volunteered
Alcohol abuse
Acceptable if long standing (chronic), refer to
coroner if sudden (acute)
Alzheimer’s disease
Acceptable
Anaemia
Acceptable if deceased is over 70 years old (it
should be possible to give an underlying cause or at
least categorise it as e.g. iron deficiency or
megaloblastic); refer to coroner if deceased is under
70 years old and not supported by another
acceptable condition
Anaphylaxis
Refer to coroner
Ankylostomiasis
Refer to coroner unless doctor states non-industrial
Angiosarcoma of the liver
Refer to coroner unless doctor states non-industrial
Anorexia nervosa
Acceptable
Anthracosis, Anthracosilicosis
Refer to coroner unless doctor states non-industrial
Anthrax
Refer to coroner unless doctor states non-industrial
9
Cause of death
Action
Arrhythmia/Cardiac arrhythmia
Refer to coroner unless supported by an acceptable
cause of death
Arteriosclerosis/Atherosclerosis
Acceptable
Asbestosis
Refer to coroner unless doctor states non-industrial
Aspergillosis
Acceptable
Asphyxia
Refer to coroner
Aspiration pneumonia
Refer to coroner unless supported by an acceptable
cause of death
Asystole
Refer to coroner unless supported by an acceptable
cause of death
Atrial fibrillation
Acceptable
B
Cause of death
Action
Bacterial meningitis
Acceptable
Bagassosis
Refer to coroner unless doctor states non-industrial
Barotrauma
Refer to coroner
Berylliosis
Refer to coroner unless doctor states non-industrial
Biliary (biliary tract) infection/sepsis
Acceptable
Bilateral pleural thickening
Refer to coroner unless doctor states non-industrial
Birth asphyxia
Refer to coroner
Birth injury
Refer to coroner
Biventricular failure
Acceptable
Bladder – Cancer of the bladder or renal
pelvis or urethra or ureter
Refer to coroner if deceased’s occupation took them
into contact with industrial chemical or dyestuff
preparations or process; otherwise acceptable
Bleeding peptic ulcer
Acceptable
Blood Poisoning/septicaemia
Refer to coroner if on its own or in association with
an injury
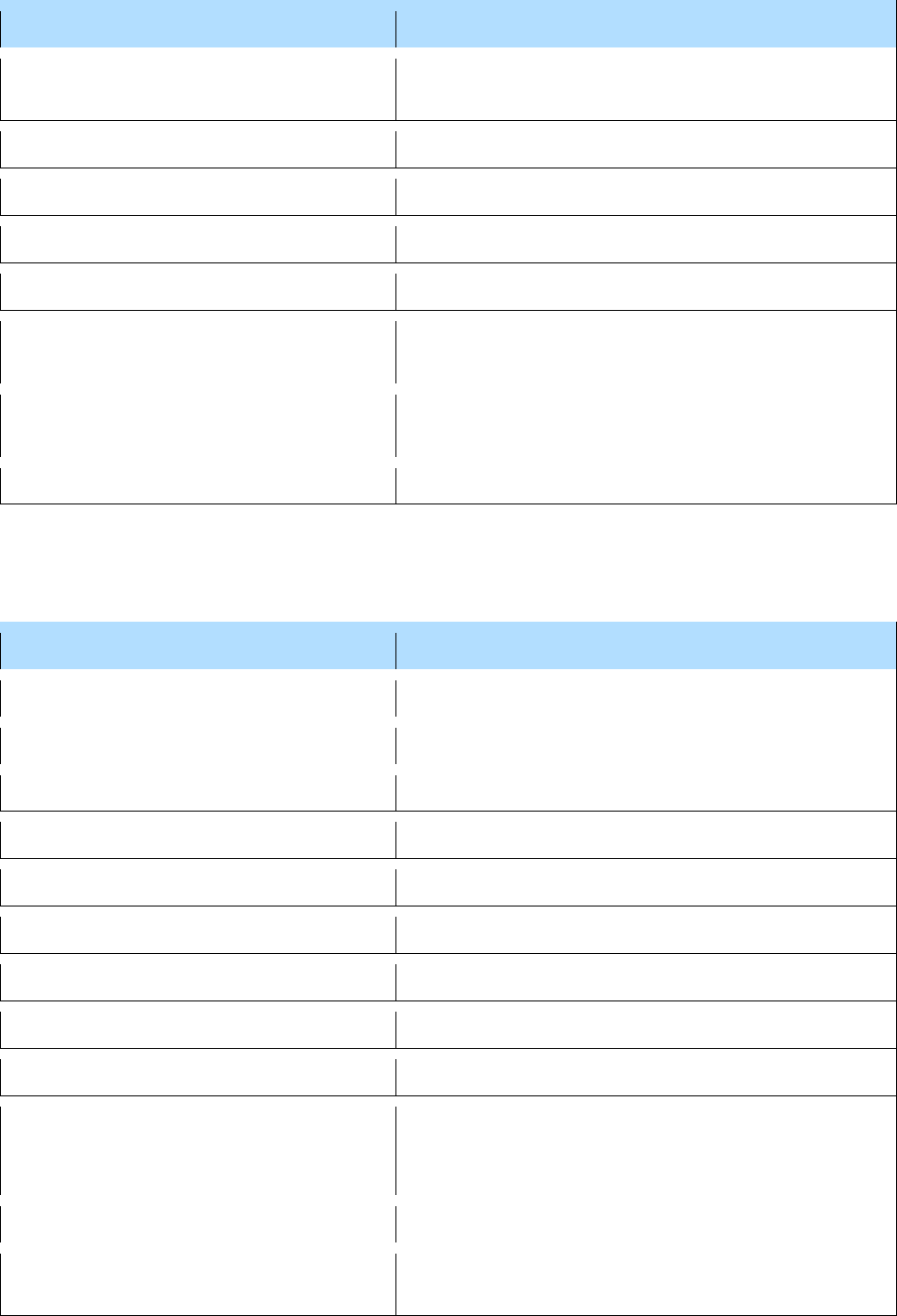
10
Cause of death
Action
Bone marrow failure
Refer to coroner unless supported by an acceptable
cause of death, e.g. myelodysplasia or old age
Bowel obstruction
Acceptable if qualified as spontaneous or with an
acceptable underlying cause
Brain failure
Mode of dying – refer to coroner unless supported by
an acceptable cause of death
Bronchial or bronchus cancer
Refer to coroner if deceased’s occupation took them
into contact with nickel fumes or vapour or
associated with fibre board or wooden goods;
otherwise acceptable
Bronchopneumonia
Acceptable
Bronchospasm
Refer to coroner if not supported by another
acceptable condition
Brucella/Brucellosis
Refer to coroner unless doctor states non-industrial
Byssinosis
Refer to coroner unless doctor states non-industrial
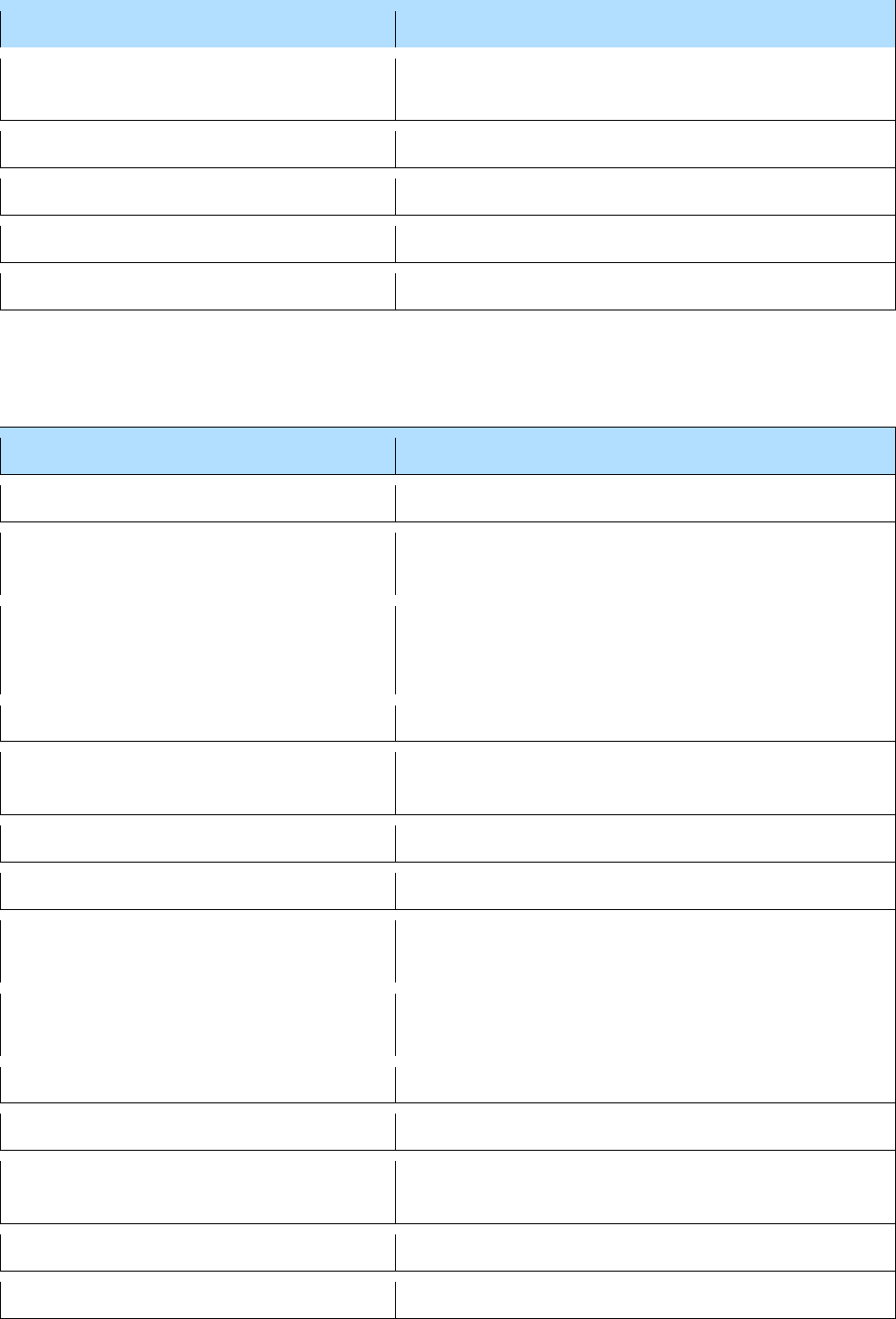
C
Cause of death
Action
Cachexia
Mode of dying – refer to coroner unless supported by
an acceptable cause of death
Caisson disease
Refer to coroner
Cancer of the bladder or renal pelvis or
urethra or ureter
Refer to coroner if deceased’s occupation took them
into contact with industrial chemical or dyestuff
preparations or process; otherwise acceptable
Cancer of the lung/bronchus
Refer to coroner if deceased’s occupation took them
into contact with nickel fumes, vapour or associated
with fibre board or wooden goods; otherwise
acceptable
Cancer of the nose/nasopharynx/nasal
sinuses
Refer to coroner if deceased’s occupation took them
into contact with nickel fumes, vapour or associated
with fibre board or wooden goods; otherwise
acceptable
Cancer of the skin/squamous-cell
carcinoma
Refer to coroner if deceased’s occupation took them
in contact with tar, mineral, oil, pitch, bitumen, soot,
etc.; otherwise acceptable

11
Cause of death
Action
Cardiac arrest
Mode of dying – refer to coroner unless supported by
an acceptable cause of death
Cardiac tamponade
Refer to corner unless supported by an acceptable
cause of death
Cardiogenic shock
Mode of dying – refer to coroner unless supported by
an acceptable cause of death
Cardiorespiratory arrest
Mode of dying – refer to coroner unless supported by
an acceptable cause of death
Cardiovascular accident/event/incident
Refer to coroner unless supported by an acceptable
cause of death
Cellulitis
Acceptable
Cerebral/intracerebral haemorrhage
Not acceptable on its own unless it is qualified as
spontaneous* or primary; otherwise needs an
acceptable underlying disease as it can be caused
by trauma
Cerebral palsy
Refer to coroner (may be as result of birth injury)
Cerebellar ataxia
Acceptable
Cerebrovascular
accident/event/haemorrhage
Acceptable (but ‘accident’ should be avoided if
possible)
Chest infection
Acceptable
Cholecystitis
Acceptable
Chronic airflow limitation
Refer to coroner if deceased’s occupation was an
underground coal miner; otherwise acceptable
Chronic bronchitis
Refer to coroner if deceased’s occupation was an
underground coal miner; otherwise acceptable
Chronic obstructive airways disease
(COAD)
Refer to coroner if deceased’s occupation was an
underground coal miner; otherwise acceptable
Chronic obstructive pulmonary disease
(COPD)
Refer to coroner if deceased’s occupation was an
underground coal miner; otherwise acceptable
Chronic alcoholism†
Acceptable
Circulatory failure
Mode of dying – refer to coroner unless supported by
an acceptable cause of death
*
A spontaneous cerebral haemorrhage is natural and the same as a haemorrhagic stroke.
†
Or Alcohol dependence syndrome.
12
Cause of death
Action
Circulatory collapse
Mode of dying – refer to coroner unless supported by
an acceptable cause of death
Clostridium difficile
Acceptable
Coma
Mode of dying – refer to coroner unless supported by
an acceptable cause of death
Compressed air illness
Refer to coroner
Congenital
Acceptable as a generic term qualifying a condition
at any age
Congenital ventricular septal defect
Acceptable
Congestive cardiac failure
Acceptable
Congestive heart failure
Acceptable
Coronavirus infection/disease
Acceptable
Cot death
Refer to coroner
COVID-19
Acceptable
COVID-19 infection/pneumonia
Acceptable
Creutzfeldt Jakob disease
Acceptable
Cryptogenic* fibrosing alveolitis
Refer to coroner
D
Cause of death
Action
Debility
Mode of dying – refer to the coroner unless
supported by an acceptable cause of death
Debility of old age
Acceptable provided the deceased is 80 or over;
otherwise refer to coroner
Dehydration
Refer to coroner
Dementia
Acceptable
Depression
Not acceptable as a standalone cause of death
*
Also Idiopathic
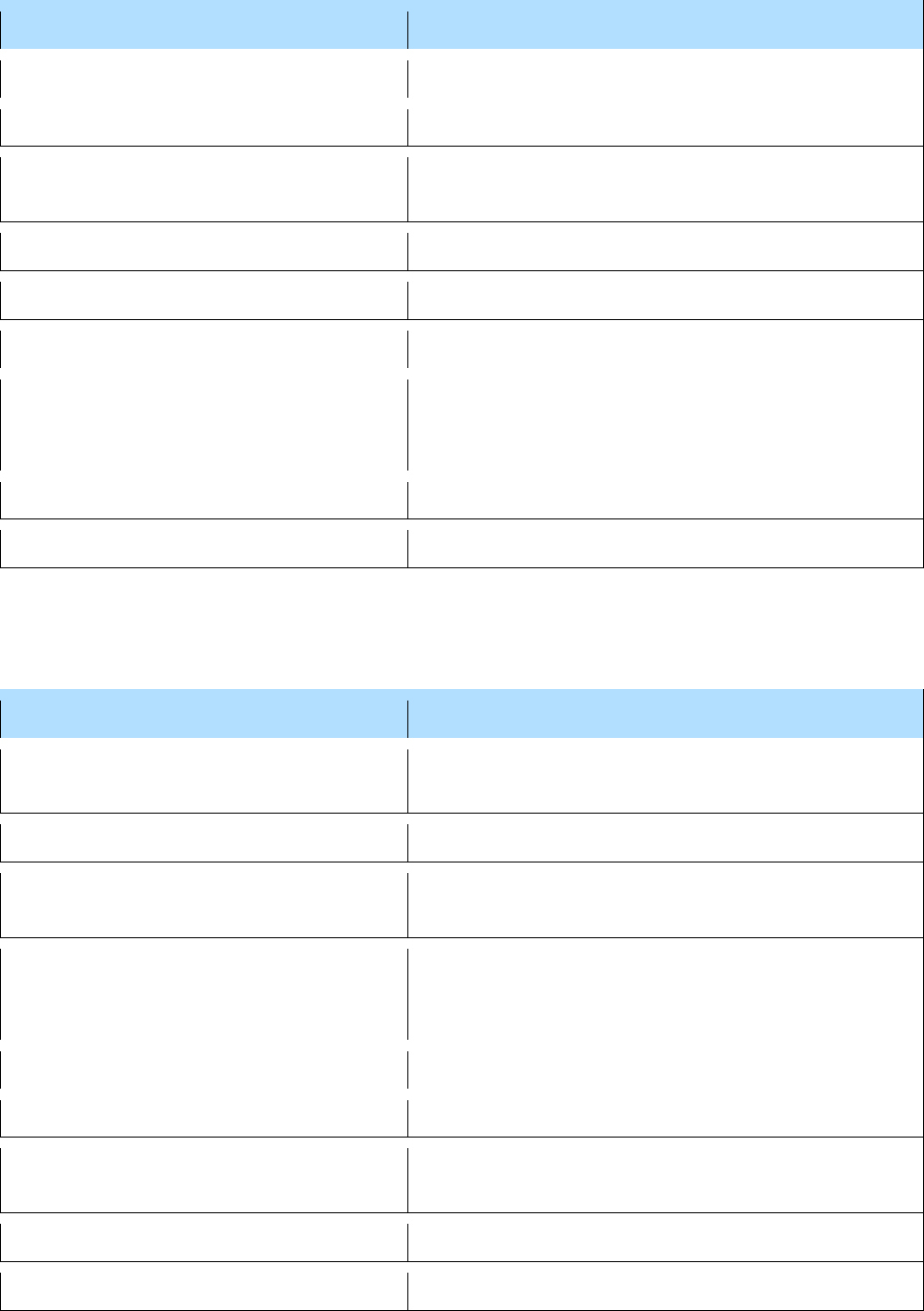
13
Cause of death
Action
Diabetes mellitus
Acceptable
Diabetic foot gangrene
Acceptable
Dissection of thoracic aorta/aortic
aneurysm
Acceptable
Diver’s palsy, Diver’s paralysis
Refer to coroner
Diverticulitis/diverticular abscess
Acceptable
Digoxin toxicity
Refer to coroner if in Part I
Duodenal ulcer
Not acceptable as a standalone cause of death but
acceptable if supporting, e.g. upper gastrointestinal
haemorrhage
Dust reticulation
Refer to coroner unless doctor states non-industrial
Dysbarism
Refer to coroner unless doctor states non-industrial
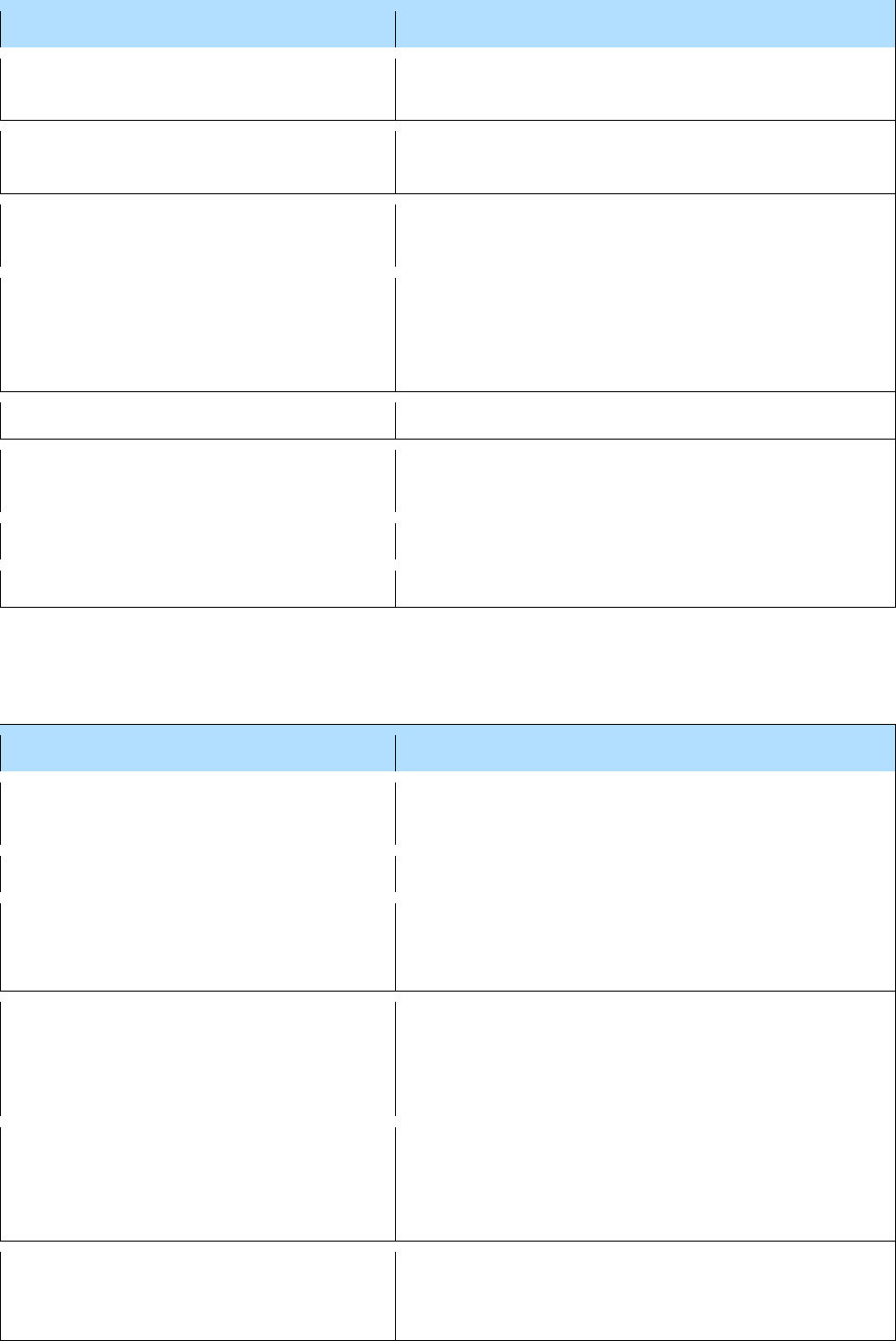
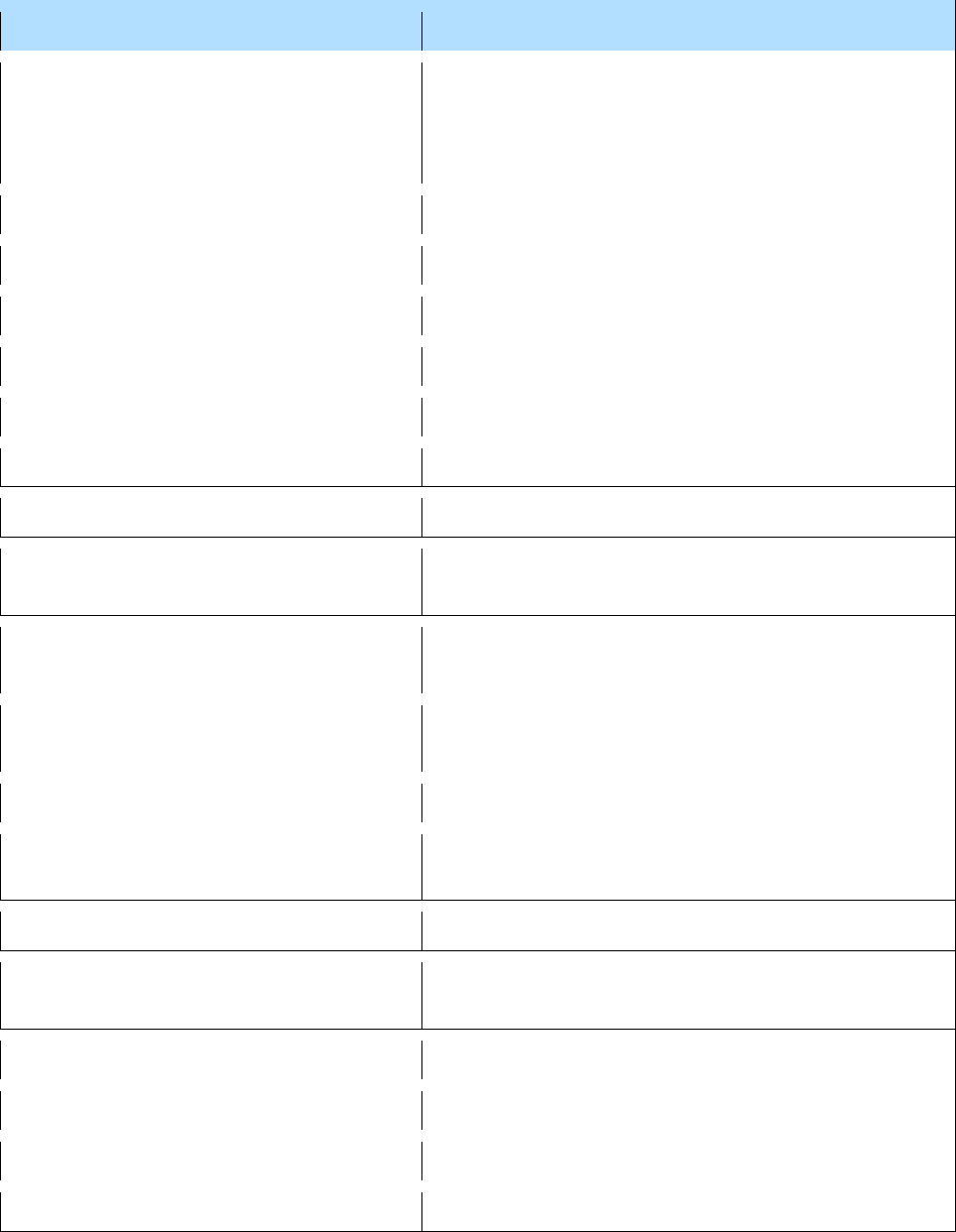
E
Cause of death
Action
Escherichia coli (E-coli)
Refer to coroner if not supported by another
acceptable condition
Escherichia coli (E-coli) septicaemia
Acceptable
Electromechanical dissociation
Refer to coroner if not supported by another
acceptable condition
Emphysema
Refer to coroner if deceased’s occupation was a coal
miner/worker exposed to dust for more than 20
years; otherwise acceptable
Empyema
Acceptable
Encephalitis
Acceptable
Exhaustion
Mode of dying – Refer to coroner unless supported
by an acceptable cause of death
Extreme prematurity
Acceptable
Extrinsic allergic alveolitis
Refer to coroner unless doctor states non-industrial
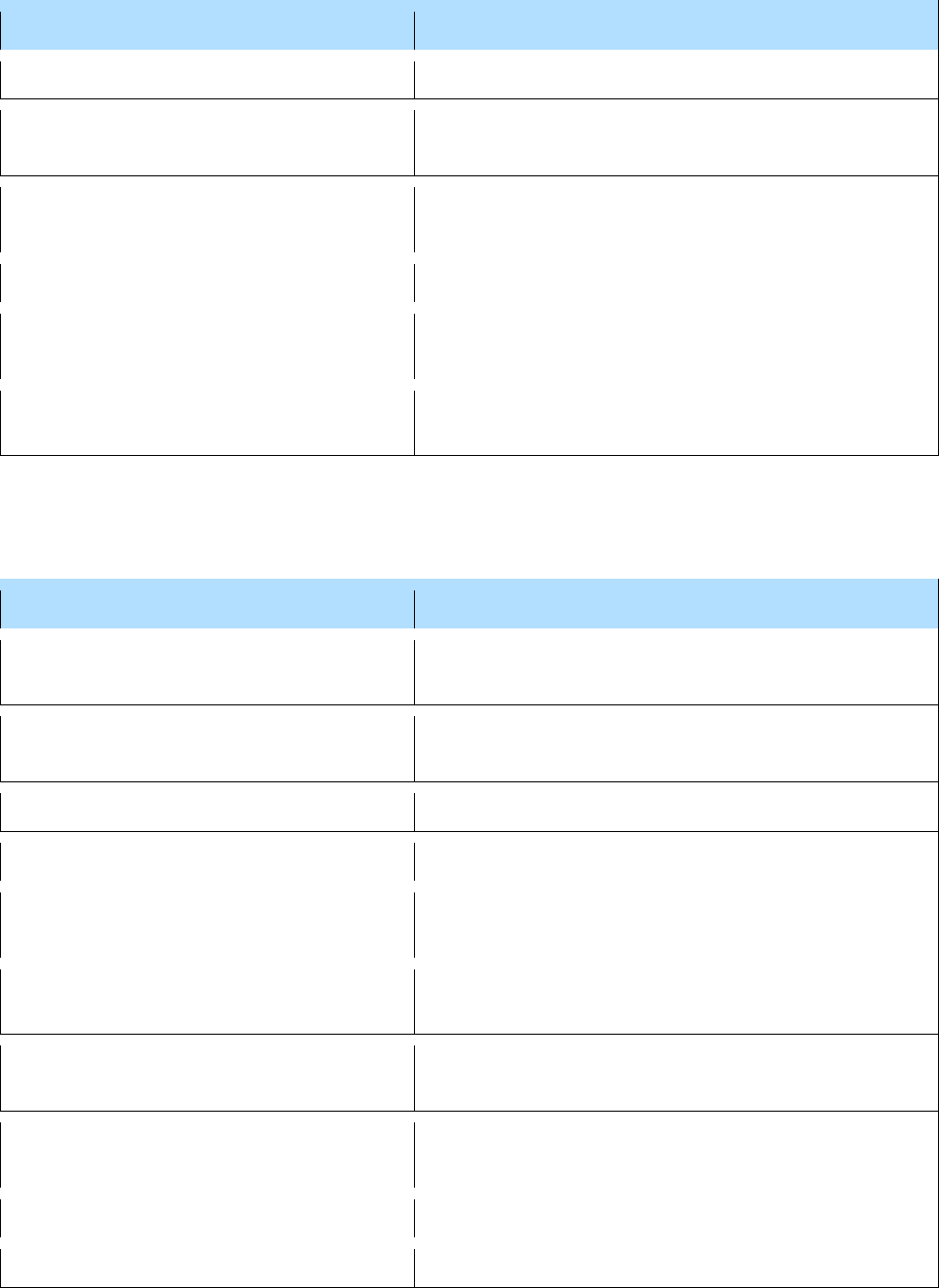
14
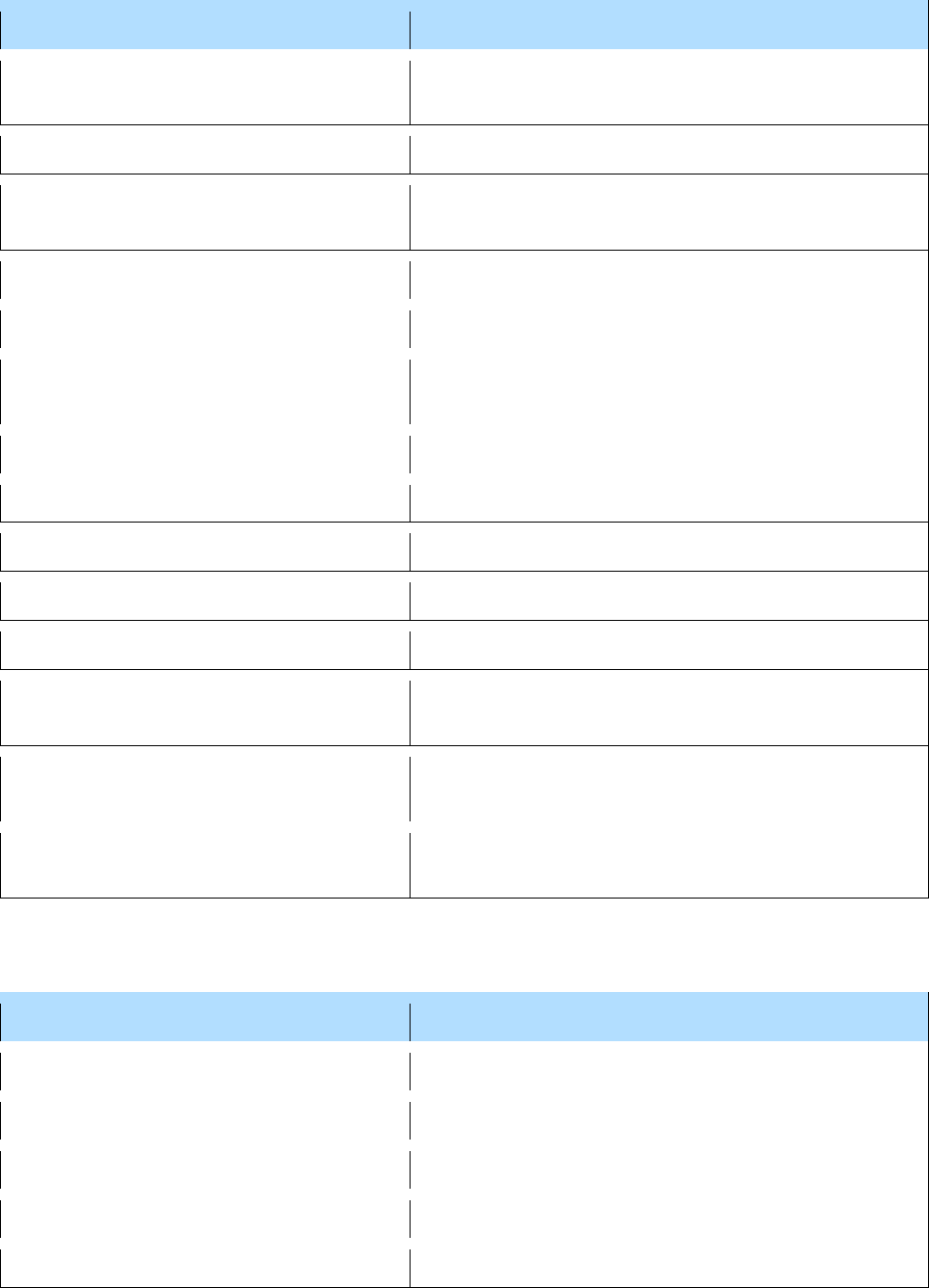
F
Cause of death
Action
Farmer’s lung
Acceptable
Fibrosing alveolitis*
Refer to coroner if deceased’s occupation brought
them in to contact with dust; otherwise acceptable
Fracture
Refer to coroner unless doctor states that it was
caused by a disease (e.g. osteoporosis)
Fracture – pathological
Acceptable if underlying disease stated
Frailty of old age
Acceptable provided the deceased is 80 or over,
otherwise refer to coroner
Frailty syndrome
Refer to corner unless supported by an acceptable
cause of death
G
Cause of death
Action
Gangrene
Refer to coroner if not supported by a circulatory
disease
Gastric aspiration/aspiration of gastric
contents
Refer to coroner if not supported by another
acceptable condition
Gastroenteritis
Acceptable
Gastrointestinal bleed/haemorrhage
Refer to coroner unless stated to be spontaneous
General debility
Mode of dying – refer to coroner if not supported by
an underlying condition
General system failure
Refer to coroner if not supported by another
acceptable condition
Goodpasture’s syndrome/Anti Glomerular
Basement Membrane disease
Acceptable
Gram negative septicaemia
Refer to coroner unless supported by an acceptable
cause of death
Grinder’s asthma
Refer to coroner
Grinder’s phthisis
Refer to coroner
*
Insertion of the word Idiopathic will reassure not industrial or drug-related
15
H
Cause of death
Action
Haematemesis
Refer to coroner if not supported by another
acceptable condition
Haemothorax
Refer to coroner
Haemorrhagic shock
Refer to coroner if not supported by another
acceptable condition
Hartmann’s procedure
Refer to coroner
Heart attack
Refer to coroner
Heart Block (Complete or Möbitz Type 2)
Acceptable (See arrhythmia)
Heart failure
Acceptable
Hepatic failure
Refer to coroner if not supported by another
acceptable condition
Hepatitis
Refer to coroner if deceased was a health or care
worker; otherwise acceptable
Hepatitis Australian antigen
Refer to coroner if deceased was a health or care
worker; otherwise acceptable
Hepatitis B
Refer to coroner if deceased was a health or care
worker; otherwise acceptable
Hepatitis viral
Refer to coroner if deceased was a health or care
worker; otherwise acceptable
Hepatorenal failure
Refer to coroner if not supported by another
acceptable condition
Hernia
Acceptable, if described anatomically and supporting
another acceptable cause of death (e.g. intestinal
obstruction/peritonitis); refer to coroner if
incisional/parastomal (may be related to surgical
procedure)
Huntington’s chorea/disease
Acceptable
Hydrocephalus
Refer to corner unless supported by an acceptable
cause of death (or state congenital)
Hypertension
Not acceptable as a standalone cause of death but
acceptable if supporting, e.g. intracerebral
haemorrhage
Hyperthermia
Refer to coroner
16
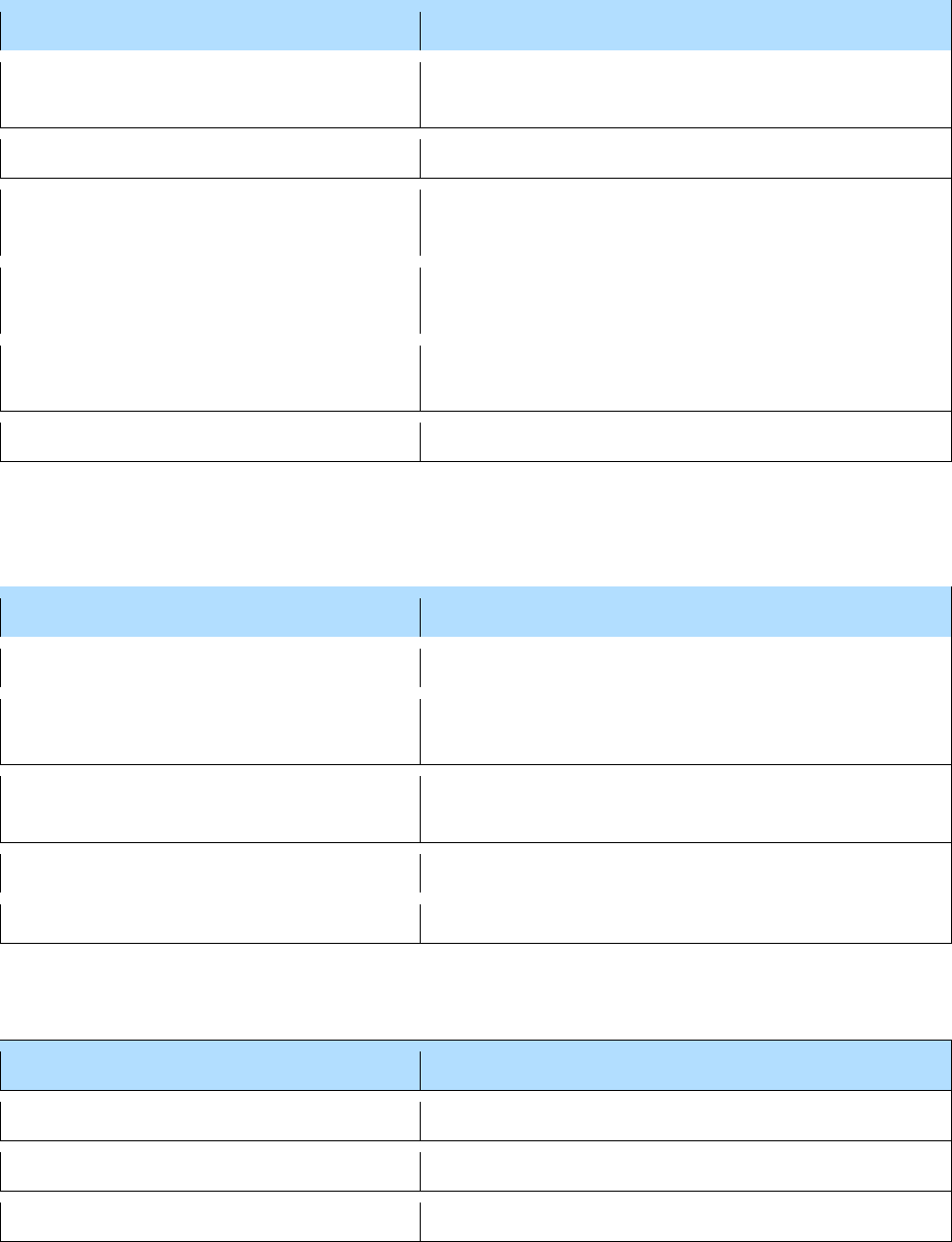
Cause of death
Action
Hypothermia
Refer to coroner
Hypovolaemia/hypovolaemic shock
Refer to coroner, unless supported by an acceptable
cause of death
Hypoxic brain injury
Refer to coroner unless supported by an acceptable
cause of death
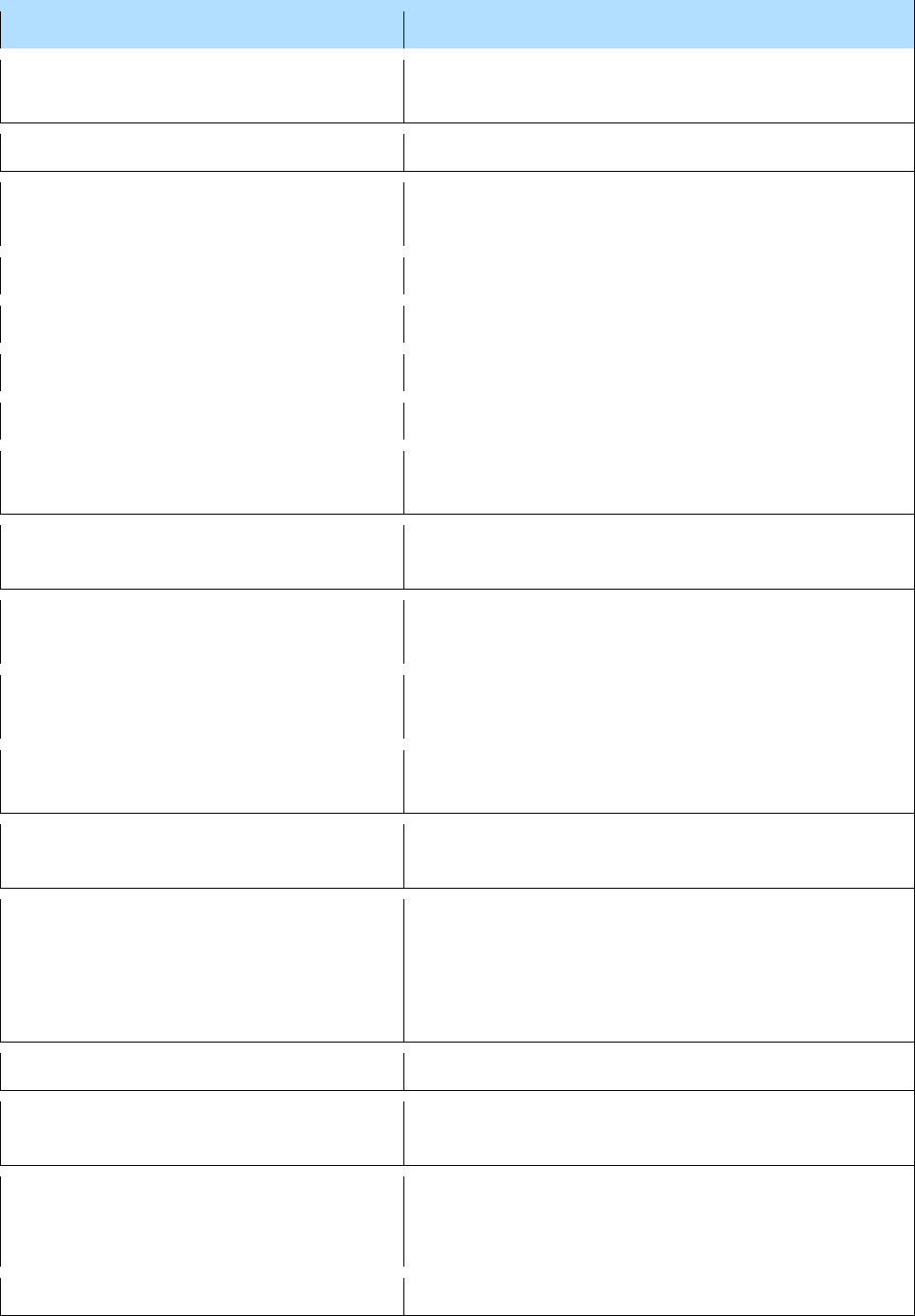
I
Cause of death
Action
Iatrogenic
Refer to coroner if anywhere on the MCCD
Inanition
Refer to coroner unless supported by an acceptable
cause of death
Inflammatory bowel disease
Acceptable
Infective endocarditis
Acceptable
Influenza
Acceptable
Injury*
Refer to coroner
Intestinal bleeding/haemorrhage
Refer to coroner unless supported by an acceptable
cause of death
Intestinal ischaemia
Acceptable
Intestinal obstruction
Refer to coroner unless supported by an acceptable
cause of death (or spontaneous)
Intracerebral haemorrhage (duplication
with cerebral)
Refer to coroner unless supported by an acceptable
cause of death (or spontaneous/primary)
Intracranial haemorrhage (duplication
with cerebral)
Refer to coroner unless supported by an acceptable
cause of death (or spontaneous/primary)
Intraoral squamous-cell carcinoma
Refer to coroner if deceased’s occupation brought
them in to contact with tar; otherwise acceptable
Ischaemic heart disease
Acceptable
Ischaemic bowel
Acceptable
*
Unless as acute kidney injury supported by an acceptable underlying cause of death.
17
J
Cause of death
Action
Jaundice
Refer to coroner unless qualified by an acceptable
underlying cause of death
K
Cause of death
Action
Kidney failure/injury
Refer to coroner if not supported by another
acceptable condition
Kidney stones
Acceptable
L
Cause of death
Action
Leaking aortic aneurysm
Acceptable
Left ventricular failure
Acceptable
Leptospira canicola
Refer to coroner unless doctor states non-industrial
Leptospira icterohaemorrhagiae
Refer to coroner unless doctor states non-industrial
Learning disability/difficulties
Not acceptable as a standalone cause of death; this
non-medical term should be avoided where possible
Lewy body dementia
Acceptable
Linitis plastica
Acceptable
Liver failure
Refer to coroner if not supported by another
acceptable condition
Lower respiratory tract infection
Acceptable
Lung cancer (cancer of the lung,
bronchus or bronchial)
Refer to coroner if deceased’s occupation brought
them into contact with nickel fumes or vapour or
associated with fibreboard or wooden goods;
otherwise acceptable
(Systemic) lupus erythematosus
Acceptable
Lymphoproliferative disorder/disease
Acceptable
18
M
Cause of death
Action
Malignant disease (cancer or sarcoma or
leukaemia or anaemia)
Refer to coroner if deceased’s occupation brought
them into contact with X-rays or radioactive
substances or radiation; acceptable if qualified as of
unknown primary
Malnutrition
Refer to coroner
Medical techniques
Refer to coroner
Meningitis
Acceptable
Meningococcal meningitis
Acceptable
Meningococcal septicaemia
Acceptable
Mesothelioma
Refer to coroner unless doctor states non-industrial
Motor neurone disease
Acceptable
Meticillin Resistant Staphylococcus
Aureus (MRSA)
Refer to coroner if not supported by another
acceptable condition
Meticillin Resistant Staphylococcus
Aureus (MRSA) septicaemia
Refer to coroner if not supported by another
acceptable condition
Mycobacterium avium intracellulare
infection
Acceptable
Multiple sclerosis
Acceptable
Multiple organ failure
Refer to coroner if not supported by another
acceptable condition
Multiple system atrophy
Acceptable
Multiple organ failure/multiple organ
dysfunction syndrome
Refer to coroner if not supported by another
acceptable condition
Myelodysplasia
Acceptable
Myeloma
Acceptable
Myeloproliferative disorder
Acceptable
Myocardial infarction or degeneration
Acceptable
19
N
Cause of death
Action
Natural causes
This is not a cause of death and is not acceptable
anywhere on the MCCD
Nephrotic syndrome
Acceptable
Neurodegenerative disease of unknown
cause
Acceptable
Neutropaenic sepsis
Refer to coroner if not supported by another
acceptable condition
Non-cirrhotic portal fibrosis
Refer to coroner if not supported by another
acceptable condition
Norovirus
Acceptable
O
Cause of death
Action
Occipital lobe infarction
Acceptable
Old age
Acceptable provided the deceased is 80 or over,
otherwise refer to coroner
On chronic renal failure*
Refer to coroner if not supported by another
acceptable condition
Osteomyelitis
Acceptable
Osteonecrosis
Refer to coroner unless doctor states non-industrial
P
Cause of death
Action
Pancreatitis
Acceptable
Parkinsonism, Parkinson’s Disease
Acceptable
Pathological fracture
Acceptable provided cause is included and is natural
*
Chronic kidney disease is acceptable.
20
Cause of death
Action
Peptic ulcer
Not acceptable as a standalone cause of death but
acceptable if supporting, e.g. upper gastrointestinal
haemorrhage
Perforated (perforation of the)
bowel/intestine*
Refer to coroner unless supported by an acceptable
cause of death (or spontaneous)
Perforated intra-abdominal viscus†
Refer to coroner unless supported by an acceptable
cause of death (or spontaneous)
Perinatal asphyxia
Acceptable for a neonatal death
Peripheral vascular disease
Acceptable
Peritonitis
Acceptable
Pleural mesothelioma
Refer to coroner unless doctor states non-industrial
Pneumococcal septicaemia
Acceptable
Pneumoconiosis
Refer to coroner unless doctor states non-industrial
Pneumothorax
Refer to coroner unless supported by an acceptable
cause of death (or spontaneous)
Pseudo-obstruction (of the intestine)
Acceptable
Pulmonary embolism
Acceptable
Pulmonary tuberculosis
Acceptable unless certificate states industrial
R
Cause of death
Action
Radiation colitis
Refer to coroner
Refusal to eat
Refer to coroner
Renal failure
Refer to coroner unless supported by an acceptable
cause of death
Renal/kidney injury‡
Refer to coroner unless supported by an acceptable
cause of death
*
Prefixed with ‘spontaneous’ is acceptable.
†
Prefixed with ‘spontaneous’ is acceptable.
‡
This refers to abnormal renal function, not traumatic injury.
21
Cause of death
Action
Respiratory arrest or failure
Mode of dying – refer to coroner unless supported by
an acceptable cause
Rheumatic heart disease
Acceptable
Rheumatoid arthritis
Acceptable
Right ventricular failure
Acceptable
Ruptured abdominal aortic aneurysm
Acceptable
S
Cause of death
Action
SARS-CoV-2 infection
Acceptable
Schizophrenia/psychosis
Refer to coroner unless supporting an acceptable
cause of death
Senile dementia
Acceptable if deceased was aged 80 or over. Refer
to coroner if deceased under 80 years old and not
supported by another acceptable condition
Senility
Acceptable if deceased was aged 80 or over
Sepsis
Refer to coroner unless supported by an acceptable
cause of death
Sepsis of unknown aetiology
Acceptable
Septic arthritis
Acceptable
Septic shock
Refer to coroner unless supported by an acceptable
cause of death
Septicaemia
Refer to coroner unless supported by an acceptable
cause of death (or unknown aetiology)
Siderosis
Refer to coroner unless doctor states non-industrial
Silicosis
Refer to coroner unless doctor states non-industrial
Smoking
Refer to coroner if not supporting another acceptable
condition
Spinal cord ischaemia
Acceptable
Spirochaetal jaundice
Refer to coroner unless doctor states non-industrial
22
Cause of death
Action
Spontaneous gastrointestinal
bleed/haemorrhage
Acceptable
Spontaneous intracerebral haemorrhage
Acceptable
Staphylococcus (aureus)
Refer to coroner if not supported by another
acceptable condition
Steele Richardson syndrome
Acceptable
Streptococcal septicaemia
Acceptable (See meningococcal septicaemia)
Streptococcus
Refer to coroner unless supported by an acceptable
cause of death
Streptococcus suis
Refer to coroner unless doctor states non-industrial
Stroke
Acceptable provided deceased is not a child
Spontaneous subarachnoid haemorrhage
Acceptable
Stent/stented
Refer to coroner
Subdural haematoma
Refer to coroner
Sudden infant death syndrome
Refer to coroner if not supported by another
acceptable condition
Syncope
Mode of death - Refer to coroner if not supported by
another acceptable condition
(Systemic) mixed connective tissue
disorder
Acceptable
T
Cause of death
Action
Tetanus
Refer to coroner
Toxic anaemia
Refer to coroner
Toxic jaundice
Refer to coroner
Toxicity
Refer to coroner
Tuberculosis
Refer to coroner unless doctor states non-industrial
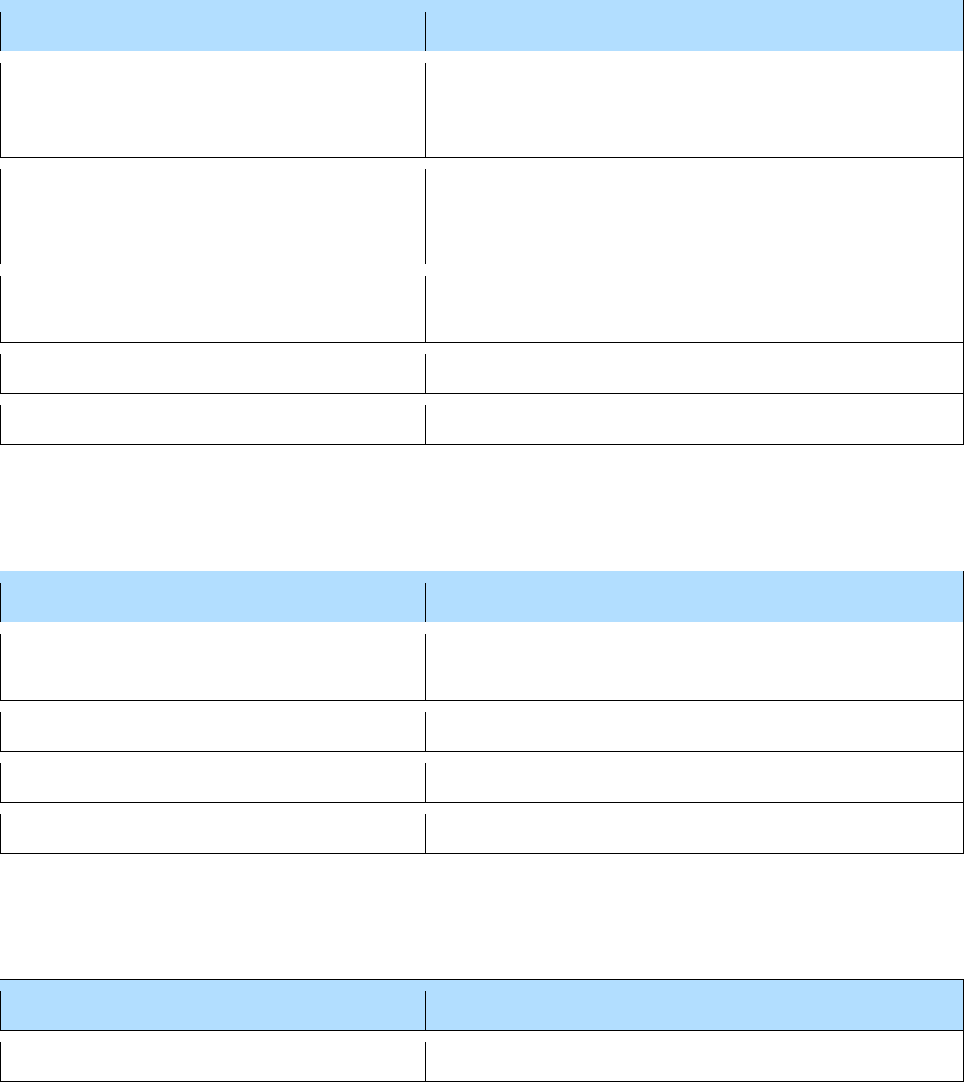
23
U
Cause of death
Action
Ulcer duodenal/gastric/peptic
Not acceptable as a standalone cause of death but
acceptable if supporting, e.g. upper gastrointestinal
haemorrhage
Unknown
Refer to coroner unless cause of death given is a
malignant disease or septicaemia where the
site/cause is unknown.
Uraemia
Refer to coroner if not supported by another
acceptable condition
Urinary tract infection
Acceptable
Urosepsis
Acceptable
V
Cause of death
Action
Vagal inhibition
Refer to coroner if not supported by another
acceptable condition
Vascular dementia
Acceptable
Ventricular failure
Acceptable
Viral hepatitis
Refer to coroner unless doctor states non-industrial
W
Cause of death
Action
Weil’s disease
Refer to coroner unless doctor states non-industrial
