
HMO
vs
Fee-for-Service
Care
of
Older
Persons
with
Acute
Myocardial
Infarction
David
M.
Carlisle,
MD,
PhD,
Albert
L.
Siu,
MD,
MSPH,
Emmett
B.
Keeler,
PhD,
Elizabeth
A.
McGlynn,
PhD,
Katherine
L.
Kahn,
MD,
Lisa
V.
Rubenstein,
MD,
MSPH,
and
Robert
H.
Brook,
MD,
ScD
Introduction
Methods
Enhanced
competition
within
the
health
care
delivery
system
has
been
en-
couraged
as
a
strategy
to
control
health
care
costs.
One
result
of
this
strategy
has
been
the
rapid
growth
in
the
number
of
individuals
enrolled
in
health
maintenance
organizations
(HMOs).
The
Health
Care
Financing
Administration
(HCFA)
of
the
US
Department
of
Health
and
Human
Services
has
succeeded
in
increasing
the
number
of
elderly
Medicare
beneficiaries
enrolled
in
HMOs
from
521
894
in
1979
to
1.5
million
in
1989.'
Historically,
the
competition
that
has
developed
among
health
plans
has
been
based
on
differences
in
premiums
and
benefit
packages
and
on
public
percep-
tions
about
differences
in
quality.
Al-
though
it
may
be
desirable
for
competition
to
be
based
on
quality,
the
lack
of
objec-
tive
measures
of
quality
of
health
care
has
hindered
the
development
of
such
com-
petition.
Previous
research
has
shown
that
the
quality
of
the
care
delivered
by
HMOs
is
generally
better
than
or
comparable
to
fee-for-service
(FFS)
care.2
However,
only
limited
data
exist
on
the
quality
of
care
received
by
elderly
individuals
en-
rolled
in
HMOs
or
on
the
differences
in
quality
among
individual
health
plans.3,4
This
study
compares
the
quality
of
medical
care
received
by
HMO
and
FFS
elderly
persons
who
had
been
hospitalized
with
an
acute
myocardial
infarction.
How
does
the
quality
of
care
received
by
pa-
tients
from
three
different
HMOs
compare
with
that
received
by
a
nationally
repre-
sentative
sample
of
FFS
patients?
How
does
the
quality
of
care
differ
among
HMOs?
Do
outcome
and
process
mea-
sures
of
quality
of
care
lead
to
similar
con-
clusions?
To
evaluate
the
quality
of
care
re-
ceived
by
Medicare
patients,
we
reviewed
medical
records
of
HMO
and
FFS
pa-
tients
65
years
of
age
or
older
admitted
between
July
1,
1985,
and
June
30,
1986,
with
a
principal
diagnosis
of
acute
myo-
cardial
infarction
(ICD-9-CM5
codes
410.0
through
410.9)
and
signs
or
symptoms
of
a
suspected
acute
myocardial
infarction
at
the
time
of
admission.
We
selected
three
HMOs
from
a
national
consortium
of
12
HMOs
that
had
been
organized
to
evalu-
ate
the
feasibility,
reliability,
and
validity
of
producing
clinically
meaningful
mea-
sures
that
could
be
used
to
compare
qual-
ity
among
health
plans.
The
three
plans
operated
in
separate
states
and
differed
in
size,
geographic
region
served,
and
se-
lected
organizational
characteristics.
We
identified
1469
HMO
admissions
(distributed
among
a
total
of
27
hospitals)
that
met
the
criteria
for
initial
inclusion
in
the
study.
For
each
of
the
three
HMOs,
medical
records
were
stratified
according
to
the
admitting
hospital
and
then
ran-
domly
sampled.
After
oversampling
rec-
ords
from
the
two
smaller
HMOs,
we
se-
lected
459
medical
records
for
review.
Of
these,
90
records
were
excluded
for
the
following
reasons:
39
patients
received
their
initial
care
at
and
were
transferred
The
authors
are
with
the
RAND
Health
Pro-
gram,
Santa
Monica,
Calif.
Drs.
Carlisle,
Siu,
Kahn,
Rubenstein,
and
Brook
are
also
with
the
University
of
California-Los
Angeles.
Requests
for
reprints
should
be
sent
to
David
M.
Carlisle,
MD,
PhD,
RAND,
1700
Main
St,
PO
Box
2138,
Santa
Monica,
CA
90407-2138.
This
paper
was
submitted
to
the
Journal
January
29,
1992,
and
accepted
with
revisions
August
12,
1992.
December
1992,
Vol.
82,
No.
12

EMO
vs
Fee-for-Service
Care
from
a
FFS
hospital
(medical
records
for
these
patients
were
iconsistently
avail-
able);
2
patients
died
in
emergency
depart-
ments;
2
patients
had
incomplete
records;
the
records
of
38
patients
did
not
demon-
strate
signs
or
symptoms
that
were
con-
sistent
with
acute
myocardial
infarction
at
the
time
of
hospital
admission;
and
12
pa-
tients,
upon
detailed
review,
were
deter-
mined
to
have
admission
dates
falling
out-
side
the
sampling
time
frame.
Three
patients
had
more
than
one
reason
for
be-
ing
excluded.
This
resulted
in
a
final
sam-
ple
of
369
admissions
to
a
total
of
27
hos-
pitals
in
the
HMO
group.
The
FFS
sample
was
obtained
from
a
previously
reported
study.6,7
In
that
study
a
sample
of
Medicare
FFS
admissions
was
drawn
from
297
hospitals
(in
five
states)
that
were
selected
to
closely
match
the
nation
in
terms
of
urban-rural
mix,
size,
teaching
status,
ownership,
patient
demo-
graphics,
and
Medicare
and
Medicaid
dis-
tribution.
FFS
patients
from
rural
hospi-
tals
were
excluded
from
this
analysis
because
none
of
our
HMOs
were
in
pri-
marily
rural
areas.
After
we
excluded
these
patients,
1119
patients
remained.
Additional
information
about
the
FFS
sample
is
available
in
an
earlier
publica-
tion.8
We
collected
data
from
hospital
med-
ical
records
using
an
abstraction
tool
de-
veloped
to
collect
process
and
outcome
data
for
patients
with
acute
myocardial
in-
farction.9
For
the
FFS
group,
contracted
peer-review
organizations
in
each
of
the
five
states
received
photocopies
of
each
of
the
admission
records.
Nurses
and
medi-
cal-record
abstractors
specifically
trained
in
the
use
of
this
abstraction
tool
then
ab-
stracted
each
of
the
admission
records.
For
the
HMO
sample,
medical
records
were
photocopied
by
each
HMO
and
sent
to
a
nurse
who
had
previously
abstracted
FFS
records
but
was
unaware
of
the
pur-
pose
of
this
study.
For
both
HMO
and
FFS
samples,
a
nonphysician
reviewer
checked
all
abstraction
forms
for
com-
pleteness,
legibility,
and
internal
consist-
ency.
A
physician
reviewer
then
evalu-
ated
them
to
confirm
the
diagnosis
of
acute
myocardial
infarction.
Abstracted
information
was
used
to
generate
sickness-at-admission
and
quali-
ty-of-care
scales
that
were
designed
to
predict
mortality
at
30
and
180
days
after
admission,
respectively.
Previously
de-
veloped
and
validated
from
the
pooled
FFS
samples,10
the
sickness-at-admission
scales
incorporated
items
from
the
KilliplI
and
Norris12
measures
of
the
severity
of
acute
myocardial
infarction,
the
APACHE
II13
severity-of-illness
scale,
and
measures
of
comorbidity.
(The
Killip,
Norris,
and
APACHE
II
scales
are
based
on
information
obtained
at
the
time
of
hos-
pital
admission,
including
patient
vital
signs,
laboratory
values,
and
components
of
initial
history
and
physical
examina-
tions.)
Measures
such
as
patient
age
and
the
presence
of
chronic
conditions
were
important
predictors
of
long-term
mortal-
ity
and
received
greater
weight
when
in-
corporated
into
our
quality-of-care
index
predicting
mortality
at
180
days.
For
the
HMO
group,
postdischarge
death
data
(30
and
180
days
after
admis-
sion)
were
obtained
from
the
National
Death
Index
maintained
by
the
National
Center
for
Health
Statistics.
For
the
FFS
sample,
similar
data
were
obtained
from
HCFA's
Health
Insurance
Master
File.
Mortality
was
adjusted
for
sickness
at
ad-
mission.
The
quality
of
the
process
of
in-hos-
pital
care
was
assessed
by
a
recently
de-
veloped
and
validated
process-of-care
al-
gorithm14
that
incorporated
93
specific
process-of-care
criteria.
To
generate
these
criteria,
process
measures
were
identified
by
literature
review
and
by
expert
consul-
tation.
These
criteria
were
then
reviewed
by
an
expert
panel
(including
academi-
cians
and
FFS
practitioners)
to
see
if
they
were
clinically
acceptable
and
to
deter-
mine
if
they
were
reliably
recorded
in
the
medical
record.
Internists
and
cardiolo-
gists
from
each
of
the
participating
HMOs
also
reviewed
the
criteria
to
ensure
that
they
remained
valid
within
the
HMO
set-
ting.
No
criteria
were
eliminated
by
HMO
physicians.
Criteria
were
grouped
by
clinical
opinion
and
tested
by
psychometric
anal-
ysis.
This
resulted
in
an
overall
process-
of-care
scale
and
five
process
subscales:
(1)
the
MD
Cognitive
subscale,
which
measures
the
physician's
performance
of
the
patient's
initial
history,
physical
ex-
amination,
and
repeated
clinical
assess-
ment
during
the
hospital
stay;
(2)
the
RN
Cognitive
subscale,
which
measures
the
nurse's
clinical
assessment
of
the
patient;
(3)
the
Technical
Diagnostic
subscale,
which
evaluates
the
use
of
diagnostic
tests
and
procedures
in
the
care
of
the
patient;
(4)
the
Technical
Therapeutic
subscale,
which
evaluates
the
use
of
medications
and
therapeutic
procedures;
and
(5)
the
ICU/Telemetry
subscale,
which
measures
the
appropriate
use
of
the
intensive-care
unit
or
telemetry
monitoring.
Because
pa-
tients
differ
in
terms
of
the
level
of
services
they
need,
each
scale
contains
criteria
that
are
not
applicable
to
all
patients
with
a
myocardial
infarction.
For
example,
using
a
Swan-Ganz
catheter
in
myocardial
in-
farction
patients
with
severe
congestive
heart
failure
and
hypotension
was
consid-
ered
indicated,
but,
in
a
patient
without
these
complications,
invasive
monitoring
was
not
considered
necessary.
As
a
result,
the
number
of
applicable
criteria
varied
from
patient
to
patient.
Performance
on
process
scales
was
scored
by
calculating
compliance
with
applicable
criteria.
Pro-
cess
scores
obtained
in
this
manner
have
been
shown
to
correlate
with
the
proba-
bility
of
death.14
Compliance
with
process
scales
and
the
severity-adjusted
death
rates
for
the
aggregated
HMO
population
of
369
admis-
sions
were
compared
to
the
1119
FFS
ad-
missions.
Intra-HMO
group
comparisons
were
also
performed.
All
scales
were
stan-
dardized
to
have
a
mean
of
0
and
a
stan-
dard
deviation
of
1,
using
as
the
reference
population
the
FFS
sample
that
included
rural
patients.
Thus,
if
a
process
scale
was
reported
as
having
a
value
of
0.54
in
the
HMO
group
and
0.32
in
the
FFS
group,
the
process
score
for
the
HMO
was
0.54
standard
deviations
greater
than
the
ref-
erence
population
(FFS
rural
and
urban
patients)
and
0.22
standard
deviations
greater
than
the
FFS
comparison
used
in
this
analysis.
Differences
in
process
of
care
were
tested
for
significance
using
two-tailed
t
tests.
Resuls
There
was
a
small
difference
between
the
proportions
of
HMO
and
FFS
patients
excluded
from
the
study
(21
and
16%,
re-
spectively,
P
>
.05).
Twenty-six
percent
of
admissions
sampled
from
the
first
HMO
(HM01)
were
excluded,
compared
with
14%
from
HM02
(P
<
.05)
and
20%
from
HM03.
Most
of
the
percentage
difference
between
HM01
and
HM02
was
pro-
duced
by
the
exclusion
of
admitted
pa-
tients
who
had
been
transferred
from
one
hospital
to
the
facility
where
they
received
the
remainder
of
their
care.
HMO
enroll-
ees
were
twice
as
likely
as
their
FFS
coun-
terparts
to
be
transferred
during
the
hos-
pital
admission.
Additionally,
18%
of
admissions
from
HM03
were
excluded
because
they
were
erroneously
coded
with
a
discharge
diagnosis
of
acute
myo-
cardial
infarction.
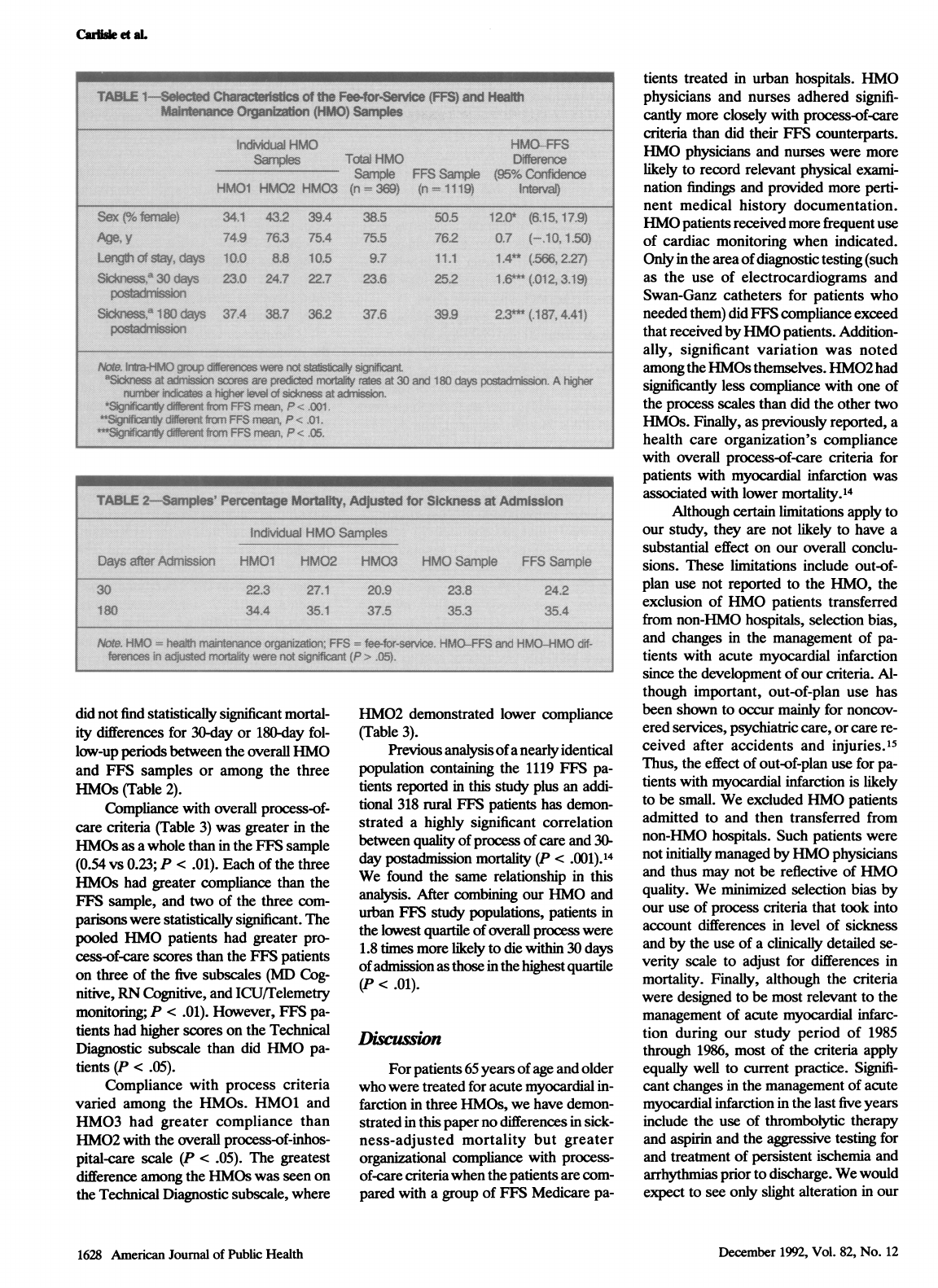
HMO
patients
were
more
likely
to
be
male
(P
<
.001),
were
less
severely
ill
upon
admission
(P
<
.05),
and
were
dis-
charged
from
the
hospital
earlier
(P
<
.01)
than
their
FFS
counterparts
(Table
1).
Af-
ter
adjusting
for
sickness
at
admission,
we
American
Journal
of
Public
Health
1627
December
1992,
Vol.
82,
No.
12
Caiu
et
aL
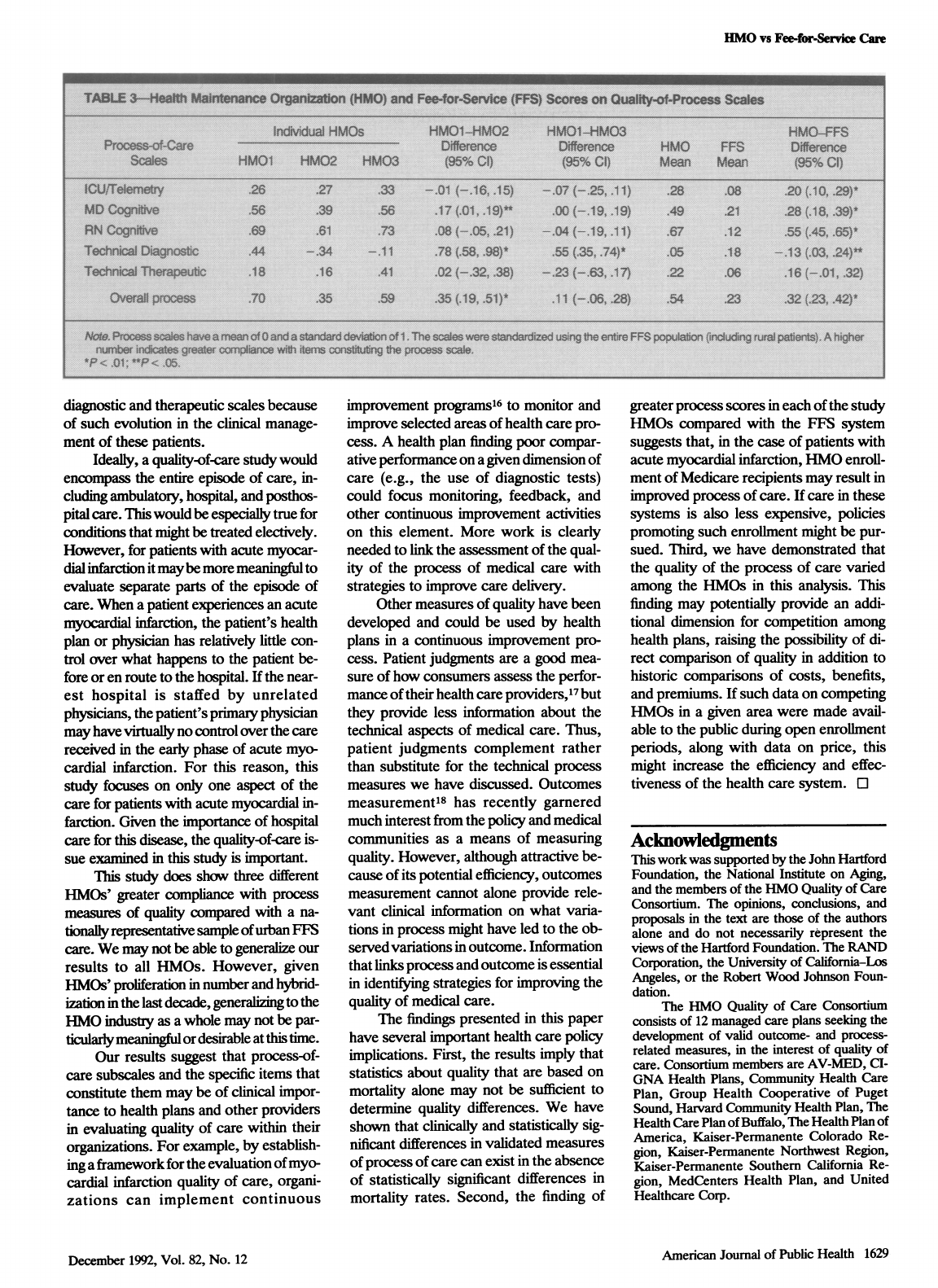
did
not
find
statistically
significant
mortal-
ity
differences
for
30-day
or
180-day
fol-
low-up
periods
between
the
overall
HMO
and
FFS
samples
or
among
the
three
HMOs
(Table
2).
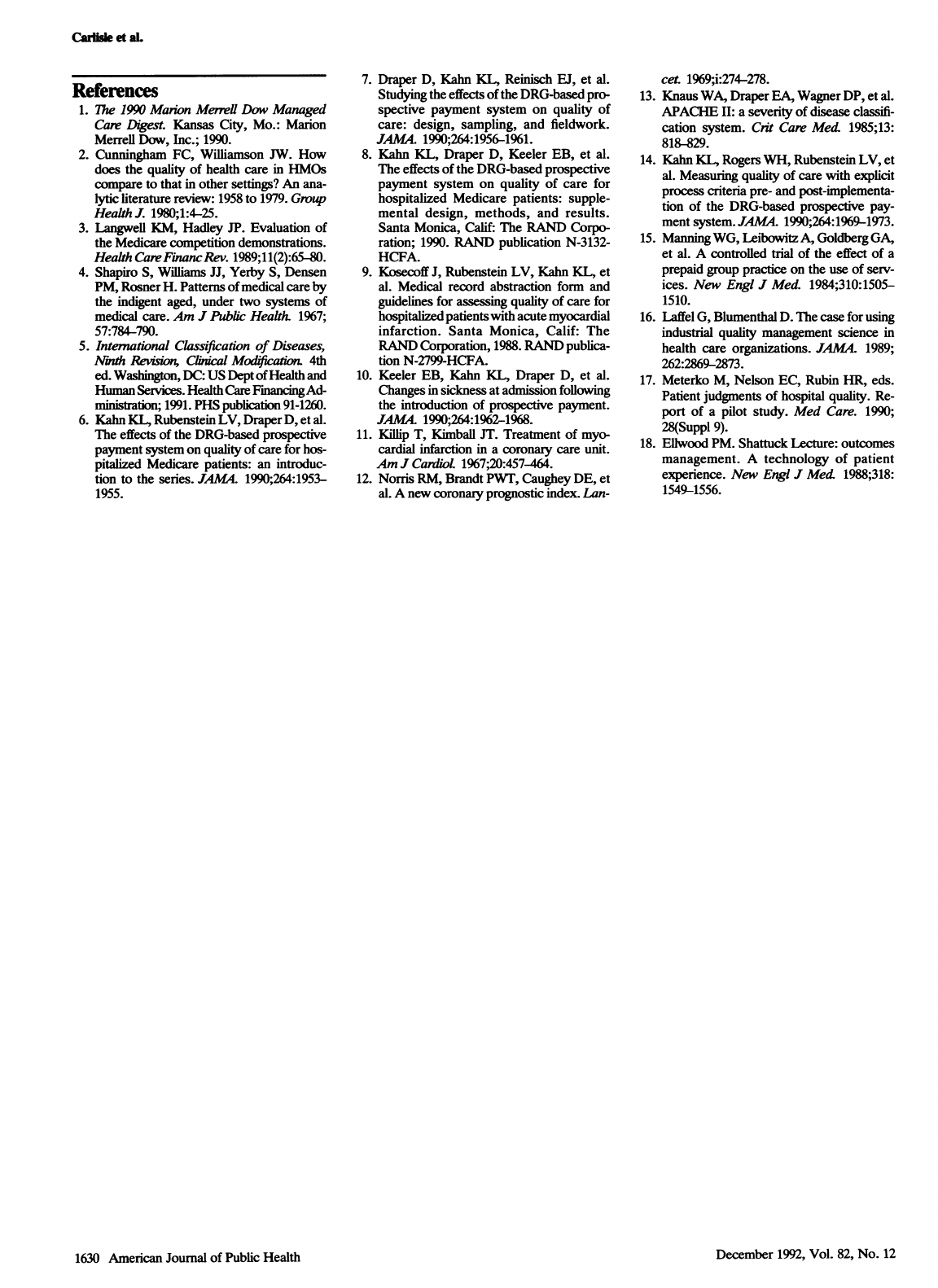
Compliance
with
overall
process-of-
care
criteria
(Table
3)
was
greater
in
the
HMOs
as
a
whole
than
in
the
FFS
sample
(0.54
vs
0.23;
P
<
.01).
Each
of
the
three
HMOs
had
greater
compliance
than
the
FFS
sample,
and
two
of
the
three
com-
parisons
were
statistically
significant.
The
pooled
HMO
patients
had
greater
pro-
cess-of-care
scores
than
the
FFS
patients
on
three
of
the
five
subscales
(MD
Cog-
nitive,
RN
Cognitive,
and
ICU/Telemetry
monitoring;
P
<
.01).
However,
FFS
pa-
tients
had
higher
scores
on
the
Technical
Diagnostic
subscale
than
did
HMO
pa-
tients
(P
<
.05).
Compliance
with
process
criteria
varied
among
the
HMOs.
HM01
and
HM03
had
greater
compliance
than
HM02
with
the
overall
process-of-inhos-
pital-care
scale
(P
<
.05).
The
greatest
difference
among
the
HMOs
was
seen
on
the
Technical
Diagnostic
subscale,
where
HM02
demonstrated
lower
compliance
(Table
3).
Previous
analysis
of
a
nearly
identical
population
containing
the
1119
FFS
pa-
tients
reported
in
this
study
plus
an
addi-
tional
318
rural
FES
patients
has
demon-
strated
a
highly
significant
correlation
between
quality
of
process
of
care
and
30-
day
postadmission
mortality
(P
<
.001).14
We
found
the
same
relationship
in
this
analysis.
After
combining
our
HMO
and
urban
FF5
study
populations,
patients
in
the
lowest
quartile
of
overall
process
were
1.8
times
more
likely
to
die
within
30
days
of
admission
as
those
in
the
highest
quartile
(P
<
.01).
Diwssion
For
patients
65
years
of
age
and
older
who
were
treated
for
acute
myocardial
in-
farction
in
three
HMOs,
we
have
demon-
strated
in
this
paper
no
differences
in
sick-
ness-adjusted
mortality
but
greater
organizational
compliance
with
process-
of-care
criteria
when
the
patients
are
com-
pared
with
a
group
of
FFS
Medicare
pa-
tients
treated
in
urban
hospitals.
HMO
physicians
and
nurses
adhered
signifi-
cantly
more
closely
with
process-of-care
criteria
than
did
their
FFS
counterparts.
HMO
physicians
and
nurses
were
more
likely
to
record
relevant
physical
exami-
nation
findings
and
provided
more
perti-
nent
medical
history
documentation.
HMO
patients
received
more
frequent
use
of
cardiac
monitoring
when
indicated.
Only
in
the
area
of
diagnostic
testing
(such
as
the
use
of
electrocardiograms
and
Swan-Ganz
catheters
for
patients
who
needed
them)
did
FFS
compliance
exceed
that
received
by
HMO
patients.
Addition-
ally,
significant
variation
was
noted
among
the
HMOs
themselves.
HM02
had
significantly
less
compliance
with
one
of
the
process
scales
than
did
the
other
two
HMOs.
Finally,
as
previously
reported,
a
health
care
organization's
compliance
with
overall
process-of-care
criteria
for
patients
with
myocardial
infarction
was
associated
with
lower
mortality.14
Although
certain
limitations
apply
to
our
study,
they
are
not
likely
to
have
a
substantial
effect
on
our
overall
conclu-
sions.
These
limitations
include
out-of-
plan
use
not
reported
to
the
HMO,
the
exclusion
of
HMO
patients
transferred
from
non-HMO
hospitals,
selection
bias,
and
changes
in
the
management
of
pa-
tients
with
acute
myocardial
infarction
since
the
development
of
our
criteria.
Al-
though
important,
out-of-plan
use
has
been
shown
to
occur
mainly
for
noncov-
ered
services,
psychiatric
care,
or
care
re-
ceived
after
accidents
and
injuries.15
Thus,
the
effect
of
out-of-plan
use
for
pa-
tients
with
myocardial
infarction
is
likely
to
be
small.
We
excluded
HMO
patients
admitted
to
and
then
transferred
from
non-HMO
hospitals.
Such
patients
were
not
initially
managed
by
HMO
physicians
and
thus
may
not
be
reflective
of
HMO
quality.
We
minimized
selection
bias
by
our
use
of
process
criteria
that
took
into
account
differences
in
level
of
sickness
and
by
the
use
of
a
clinically
detailed
se-
verity
scale
to
adjust
for
differences
in
mortality.
Finally,
although
the
criteria
were
designed
to
be
most
relevant
to
the
management
of
acute
myocardial
infarc-
tion
during
our
study
period
of
1985
through
1986,
most
of
the
criteria
apply
equally
well
to
current
practice.
Signifi-
cant
changes
in
the
management
of
acute
myocardial
infarction
in
the
last
five
years
include
the
use
of
thrombolytic
therapy
and
aspirin
and
the
aggressive
testing
for
and
treatment
of
persistent
ischemia
and
arrhythmias
prior
to
discharge.
We
would
expect
to
see
only
slight
alteration
in
our
1628
American
Journal
of
Public
Health
December
1992,
Vol.
82,
No.
12
EIMO
vs
Fee-for-Service
Care
diagnostic
and
therapeutic
scales
because
of
such
evolution
in
the
clinical
manage-
ment
of
these
patients.
Ideally,
a
quality-of-care
study
would
encompass
the
entire
episode
of
care,
in-
cluding
ambulatory,
hospital,
and
posthos-
pital
care.
This
would
be
especially
true
for
conditions
that
might
be
treated
electively.
However,
for
patients
with
acute
myocar-
dial
infarction
it
maybe
more
meaningful
to
evaluate
separate
parts
of
the
episode
of
care.
When
a
patient
experiences
an
acute
myocardial
infarction,
the
patient's
health
plan
or
physician
has
relatively
little
con-
trol
over
what
happens
to
the
patient
be-
fore
or
en
route
to
the
hospital.
If
the
near-
est
hospital
is
staffed
by
unrelated
physicians,
the
patient's
primary
physician
may
have
virtualy
no
control
over
the
care
received
in
the
early
phase
of
acute
myo-
cardial
infarction.
For
this
reason,
this
study
focuses
on
only
one
aspect
of
the
care
for
patients
with
acute
myocardial
in-
farction.
Given
the
importance
of
hospital
care
for
this
disease,
the
quality-of-care
is-
sue
examined
in
this
study
is
important.
This
study
does
show
three
different
HMOs'
greater
compliance
with
process
measures
of
quality
compared
with
a
na-
tionally
representative
sample
of
urban
FFS
care.
We
may
not
be
able
to
generalize
our
results
to
all
HMOs.
However,
given
HMOs'
proliferation
in
number
and
hybrid-
ization
in
the
last
decade,
generaizing
to
the
HMO
industry
as
a
whole
may
not
be
par-
ticularly
meanigfl
or
desirable
at
this
time.
Our
results
suggest
that
process-of-
care
subscales
and
the
specific
items
that
constitute
them
may
be
of
clinical
impor-
tance
to
health
plans
and
other
providers
in
evaluating
quality
of
care
within
their
organizations.
For
example,
by
establish-
ing
a
framework
for
the
evaluation
of
myo-
cardial
infarction
quality
of
care,
organi-
zations
can
implement
continuous
improvement
programs16
to
monitor
and
improve
selected
areas
of
health
care
pro-
cess.
A
health
plan
finding
poor
compar-
ative
performance
on
a
given
dimension
of
care
(e.g.,
the
use
of
diagnostic
tests)
could
focus
monitoring,
feedback,
and
other
continuous
improvement
activities
on
this
element.
More
work
is
clearly
needed
to
link
the
assessment
of
the
qual-
ity
of
the
process
of
medical
care
with
strategies
to
improve
care
delivery.
Other
measures
of
quality
have
been
developed
and
could
be
used
by
health
plans
in
a
continuous
improvement
pro-
cess.
Patient
judgments
are
a
good
mea-
sure
of
how
consumers
assess
the
perfor-
mance
of
their
health
care
providers,17
but
they
provide
less
information
about
the
technical
aspects
of
medical
care.
Thus,
patient
judgments
complement
rather
than
substitute
for
the
technical
process
measures
we
have
discussed.
Outcomes
measurement'8
has
recently
garnered
much
interest
from
the
policy
and
medical
communities
as
a
means
of
measuring
quality.
However,
although
attractive
be-
cause
of
its
potential
efficiency,
outcomes
measurement
cannot
alone
provide
rele-
vant
clinical
information
on
what
varia-
tions
in
process
might
have
led
to
the
ob-
servedvariations
in
outcome.
Information
that
links
process
and
outcome
is
essential
in
identifying
strategies
for
improving
the
quality
of
medical
care.
The
findings
presented
in
this
paper
have
several
important
health
care
policy
implications.
First,
the
results
imply
that
statistics
about
quality
that
are
based
on
mortality
alone
may
not
be
sufficient
to
determine
quality
differences.
We
have
shown
that
clinically
and
statistically
sig-
nificant
differences
in
validated
measures
of
process
of
care
can
exist
in
the
absence
of
statistically
significant
differences
in
mortality
rates.
Second,
the
finding
of
greater
process
scores
in
each
of
the
study
HMOs
compared
with
the
FFS
system
suggests
that,
in
the
case
of
patients
with
acute
myocardial
infarction,
HMO
enroll-
ment
of
Medicare
recipients
may
result
in
improved
process
of
care.
If
care
in
these
systems
is
also
less
expensive,
policies
promoting
such
enrollment
might
be
pur-
sued.
Third,
we
have
demonstrated
that
the
quality
of
the
process
of
care
varied
among
the
HMOs
in
this
analysis.
This
finding
may
potentially
provide
an
addi-
tional
dimension
for
competition
among
health
plans,
raising
the
possibility
of
di-
rect
comparison
of
quality
in
addition
to
historic
comparisons
of
costs,
benefits,
and
premiums.
If
such
data
on
competing
HMOs
in
a
given
area
were
made
avail-
able
to
the
public
during
open
enrollment
periods,
along
with
data
on
price,
this
might
increase
the
efficiency
and
effec-
tiveness
of
the
health
care
system.
O
Acknowledgments
This
work
was
supported
by
the
John
Hartford
Foundation,
the
National
Institute
on
Aging,
and
the
members
of
the
HMO
Quality
of
Care
Consortium.
The
opinions,
conclusions,
and
proposals
in
the
text
are
those
of
the
authors
alone
and
do
not
necessarily
represent
the
views
of
the
Hartford
Foundation.
The
RAND
Corporation,
the
University
of
California-Los
Angeles,
or
the
Robert
Wood
Johnson
Foun-
dation.
The
HMO
Quality
of
Care
Consortium
consists
of
12
managed
care
plans
seeking
the
development
of
valid
outcome-
and
process-
related
measures,
in
the
interest
of
quality
of
care.
Consortium
members
are
AV-MED,
CI-
GNA
Health
Plans,
Community
Health
Care
Plan,
Group
Health
Cooperative
of
Puget
Sound,
Haivard
Community
Health
Plan,
The
Health
Care
Plan
of
Buffalo,
The
Health
Plan
of
America,
Kaiser-Permanente
Colorado
Re-
gion,
Kaiser-Permanente
Northwest
Region,
Kaiser-Permanente
Southern
California
Re-
gion,
MedCenters
Health
Plan,
and
United
Healthcare
Corp.
American
Journal
of
Public
Health
1629
December
1992,
Vol.
82,
No.
12
Cailisle
et
aL
References
1.
The
1990
Manon
Merrell
Dow
Managed
Care
Digest.
Kansas
City,
Mo.:
Marion
Meffeil
Dow,
Inc.;
1990.
2.
Cunningham
FC,
Williamson
JW.
How
does
the
quality
of
health
care
in
HMOs
compare
to
that
in
other
settings?
An
ana-
lytic
literature
review:
1958
to
1979.
Group
Health
J.
1980;1:4-25.
3.
Langwell
KM,
Hadley
JP.
Evaluation
of
the
Medicare
competition
demonstrations.
Health
Care
FinancRev.
1989;11(2):65-80.
4.
Shapiro
S,
Williams
JJ,
Yerby
S,
Densen
PM,
Rosner
H.
Patterns
of
medical
care
by
the
indigent
aged,
under
two
systems
of
medical
care.
Am
J
Public
Health.
1967;
57:784-790.
5.
International
Classification
of
Diseases,
Nith
Reision,
Clinical
Modfication.
4th
ed.
Washingto,
DC:
US
Dept
of
Health
and
Human
Services.
Health
Care
FinancingAd-
ministration;
1991.
PHS
publication
91-1260.
6.
Kahn
KL,
Rubenstein
LV,
Draper
D,
et
al.
The
effects
of
the
DRG-based
prospective
payment
system
on
quality
of
care
for
hos-
pitalized
Medicare
patients:
an
introduc-
tion
to
the
series.
JAMA.
1990;264:1953-
1955.
7.
Draper
D,
Kahn
KL,
Reinisch
EJ,
et
al.
Studying
the
effects
of
the
DRG-based
pro-
spective
payment
system
on
quality
of
care:
design,
sampling,
and
fieldwork.
JAMA
1990;264:1956-1961.
8.
Kahn
KL,
Draper
D,
Keeler
EB,
et
al.
The
effects
of
the
DRG-based
prospective
payment
system
on
quality
of
care
for
hospitalized
Medicare
patients:
supple-
mental
design,
methods,
and
results.
Santa
Monica,
Calif:
The
RAND
Corpo-
ration;
1990.
RAND
publication
N-3132-
HCFA.
9.
Kosecoff
J,
Rubenstein
LV,
Kahn
KL,
et
al.
Medical
record
abstraction
form
and
guidelines
for
assessing
quality
of
care
for
hospitalized
patients
with
acute
myocardial
infarction.
Santa
Monica,
Calif:
The
RAND
Corporation,
1988.
RAND
publica-
tion
N-2799-HCFA.
10.
Keeler
EB,
Kahn
KL,
Draper
D,
et
al.
Changes
in
sickness
at
admission
following
the
introduction
of
prospective
payment.
JAMA.
1990;264:1962-1968.
11.
Killip
T,
Kimball
JT.
Treatment
of
myo-
cardial
infarction
in
a
coronary
care
unit.
Am
J
CardioL
1967;20:457-464.
12.
Norris
RM,
Brandt
PWT,
Caughey
DE,
et
al.
A
new
coronary
prognostic
index.
Lan-
cet.
1969;i:274-278.
13.
Knaus
WA,
Draper
EA,
Wagner
DP,
et
al.
APACHE
II:
a
severity
of
disease
classifi-
cation
system.
C,it
Care
Med.
1985;13:
818-829.
14.
Kahn
KL,
Rogers
WH,
Rubenstein
LV,
et
al.
Measuring
quality
of
care
with
explicit
process
criteria
pre-
and
post-implementa-
tion
of
the
DRG-based
prospective
pay-
ment
system.
JAMA.
1990;264:1969-1973.
15.
Manning
WG,
Leibowitz
A,
Goldberg
GA,
et
al.
A
controlled
trial
of
the
effect
of
a
prepaid
group
practice
on
the
use
of
serv-
ices.
New
Engl
J
Med.
1984;310:1505-
1510.
16.
Laffel
G,
Blumenthal
D.
The
case
for
using
industrial
quality
management
science
in
health
care
organizations.
JAMA.
1989;
262:2869-2873.
17.
Meterko
M,
Nelson
EC,
Rubin
HR,
eds.
Patient
judgments
of
hospital
quality.
Re-
port
of
a
pilot
study.
Med
Care.
1990;
28(Suppl
9).
18.
Ellwood
PM.
Shattuck
Lecture:
outcomes
management.
A
technology
of
patient
experience.
New
Engl
J
Med.
1988;318:
1549-1556.
1630
American
Journal
of
Public
Health
December
1992,
Vol.
82,
No.
12
