
MI Care Team Handbook
Version 2.6
Michigan Department of Health & Human Services
Medical Services Administration
August 14, 2017
The purpose of this handbook is to provide Medicaid policy and billing guidance to providers
participating in Michigan’s MI Care Team Program.
Note: The information included in this handbook is subject to change.
www.michigan.gov/micareteam
V2.6
1
Table of Contents
Preface ....................................................................................................................................................................... 2
Section I: Introduction to the Health Home Service Model .................................................................... 3
1.1 Overview of the MI Care Team ..................................................................................................... 3
1.2 MI Care Team Population Criteria ................................................................................................ 3
1.3 MI Care Team Services .................................................................................................................. 3
1.4 MI Care Team Provider Qualification Standards .......................................................................... 5
1.4a Geographic Area ........................................................................................................................ 5
1.4b Credentials ................................................................................................................................. 6
1.5 MI Care Team Required Provider Infrastructure .......................................................................... 6
Section II: Provider Requirements for MI Care Team Participation ................................................ 10
2.1 MI Care Team Invitation-to-Bid (ITB) ................................................................................................. 10
2.2 MI Care Team Provider Enrollment ................................................................................................... 10
2.3 MI Care Team Provider Termination ................................................................................................. 10
2.4 Training and Technical Assistance ..................................................................................................... 10
Section III: Beneficiary Enrollment and Disenrollment ....................................................................... 13
3.1 Beneficiary Identification and Assignment ........................................................................................ 13
3.2 MI Care Team ICD Codes for Beneficiary Identification and Assignment ......................................... 13
3.3 MI Care Team Benefit Plan Assignment ............................................................................................ 13
3.4 Beneficiary Consent ........................................................................................................................... 13
3.5 Beneficiary Enrollment Letters .......................................................................................................... 14
3.6 Beneficiary Disenrollment ................................................................................................................. 14
3.7 Beneficiary Changing MI Care Team Providers.................................................................................. 14
Section IV: MI Care Team Payment .............................................................................................................. 16
4.1 MI Care Team Provider Enrollment ................................................................................................... 16
4.2 General Provisions for MI Care Team Payment ................................................................................. 16
4.3 Health Action Plan (Care Plan) Requirements ................................................................................... 17
4.4 MI Care Team Service Encounter Codes ............................................................................................ 19
4.5 Encounter Submission ....................................................................................................................... 20
4.6 Payment Schedule ............................................................................................................................. 20
4.7 Recoupment of Payment ................................................................................................................... 20
Section V: MI Care Team and Managed Care ............................................................................................. 22
5.1 MI Care Team Enrollment for Health Plan Beneficiaries ................................................................... 22
5.2 MI Care Team Coordination & Health Plans ...................................................................................... 22
Section VI: Health Information Technology .............................................................................................. 23
6.1 Waiver Support Application (WSA) and the MI Care Team ............................................................... 23
6.2 CareConnect360 and the MI Care Team ........................................................................................... 23
6.3 Electronic Health Records .................................................................................................................. 23
6.4 File Transfer Service (FTS) .................................................................................................................. 23
Section VII: MI Care Team Monitoring and Evaluation ......................................................................... 24
7.1 Monitoring & Evaluation Requirements ............................................................................................ 24
7.2 Federal (CMS) Monitoring & Evaluation Requirements .................................................................... 24
7.3 State Monitoring & Evaluation Requirements .................................................................................. 24
Appendix A: MI Care Team ICD-10 Codes .................................................................................................. 25

V2.6
2
Preface
The Michigan Department of Health & Human Services (MDHHS) created the MI Care Team Handbook
to provide Medicaid policy and billing guidance to providers participating in Michigan’s MI Care Team
Program – an optional service under the Michigan Medicaid State Plan. Most broadly, this handbook will
provide detailed instructions that will help providers complete and submit documentation necessary for
policy adherence and billing completion. The handbook will also provide links to additional information
where necessary. It should be noted the MI Care Team is Michigan’s name for this Health Home
program, and the terms may be used interchangeably throughout the document.
MDHHS requires that all providers participating in the MI Care Team Program are familiar with all
Medicaid policies and procedures prior to rendering services to beneficiaries. This includes policies and
procedure currently in effect in addition to those issued in the future. MI Care Team providers must
adhere to these policies and all provisions of the MDHHS Medicaid Provider Manual.
While it is the intent of MDHHS to keep this handbook as updated as possible, the information provided
throughout is subject to change. All current and future policies and procedures will be maintained on
the MDHHS MI Care Team website listed below. Finally, this handbook should not be construed as policy
for the MI Care Team program.
The handbook will be maintained on the MI Care Team website here: www.michigan.gov/micareteam
V2.6
3
Section I: Introduction to the Health Home Service Model
1.1 Overview of the MI Care Team
Under Section 2703 of the Patient Protection and Affordable Care Act of 2010 (ACA), the Health
Home service model is meant to help chronically ill Medicaid and Healthy Michigan Plan
beneficiaries manage their conditions through an intimate level of care management and
coordination. The MI Care Team Model builds on the philosophies of the IMPACT and Nuka Care
Models, which are centered in whole-person, team-based care. As such, the MI Care Team will
utilize an interdisciplinary team of providers who will operate in a highly behavioral health
integrated primary care setting. To achieve this, the team will include the presence of a nurse care
manager and community health worker. The care team will help ensure seamless transitions of care
and help connect the beneficiary with needed clinical and social services. Currently, eligible provider
types are Federally Qualified Health Centers (FQHC) and Tribal Health Centers (THC). With the
beneficiary’s consent, health information technology will be used to bolster care management and
coordination through data collection and information sharing. Together, the model will address all
facets of a beneficiary’s health status, including clinical needs and the social determinants of health.
It is expected that the model will boost self-management of chronic conditions, reduce health care
costs, and raise quality of life for participating beneficiaries.
1.2 MI Care Team Population Criteria
MI Care Team services are intended for a subset of the Medicaid and Healthy Michigan Plan
population that have multiple complex chronic conditions. Derived from Federal statute and the
recommendation from the state’s Mental Health & Wellness Commission, the MI Care Team target
population will include Medicaid beneficiaries with depression and/or anxiety plus one or more of
the following chronic conditions (see Appendix A for applicable ICD-10 Codes):
1. Heart Disease
2. Chronic Obstructive Pulmonary Disease
3. Hypertension
4. Diabetes
5. Asthma
1.3 MI Care Team Services
The following are required MI Care Team services consistent with Section 2703 of the Affordable
Care Act:
• Comprehensive Care Management, including but not limited to:
o Assessment of each beneficiary, including behavioral and physical health care needs;
o Assessment of beneficiary readiness to change;
o Development of an individualized care plan;
o Documentation of assessment and care plan in the Electronic Health Record; and
o Periodic reassessment of each beneficiary's treatment, outcomes, goals, self-
management, health status, and service utilization.
• Care Coordination and Health Promotion, including but not limited to:
o Organization of all aspects of a beneficiary's care;

V2.6
4
o Management of all integrated primary and specialty medical services, behavioral health
services, physical health services, and social, educational, vocational, housing, and
community services;
o Information sharing between providers, patient, authorized representative(s), and
family;
o Resource management and advocacy;
o Maintaining beneficiary contact, with an emphasis on in-person contact (although
telephonic contact may be used for lower-risk beneficiaries who require less frequent
face-to-face contact);
o Appointment making assistance, including coordinating transportation;
o Development and implementation of care plan;
o Medication adherence and monitoring;
o Referral tracking;
o Use of facility liaisons;
o Use of patient care team huddles;
o Use of case conferences;
o Tracking of test results;
o Requiring discharge summaries;
o Providing patient and family activation and education;
o Providing patient-centered training (i.e., diabetes education, nutrition education, etc.);
and
o Connection of beneficiary to resources (i.e., smoking cessation, substance use disorder
treatment, nutritional counseling, obesity reduction and prevention, disease-specific
education, etc.).
• Comprehensive Transitional Care, including but not limited to:
o Connecting the beneficiary to health services;
o Coordinating and tracking the beneficiary’s use of health services;
o Providing and receiving notification of admissions and discharges;
o Receiving and reviewing care records, continuity of care documents, and discharge
summaries;
o Post-discharge outreach to assure appropriate follow up services;
o Medication reconciliation;
o Pharmacy coordination;
o Proactive care (versus reactive care);
o Specialized transitions when necessary (i.e., age, corrections); and
o Home visits.
• Patient and Family Support, including but not limited to:
o Reducing barriers to the beneficiary’s care coordination;
o Increasing patient and family skills and engagement;
o Use of community supports (i.e., Community Health Workers, peer supports, support
groups, self-care programs, etc.);
o Facilitating improved adherence to treatment;
o Advocating for individual and family needs;
o Assessing and increase individual and family health literacy;
o Use of of advance directives;
o Providing assistance with maximizing beneficiary’s level of functioning; and
V2.6
5
o Providing assistance with development of social networks.
• Referral to Community and Social Support Services, including but not limited to:
o Providing beneficiaries with referrals to support services;
o Collaborating/Coordinating with community-based organizations and key community
stakeholders;
o Emphasizing resources closest to the beneficiary’s home
o Emphasizing resources which present the fewest barriers;
o Identifying community-based resources;
o Providing resource materials pertinent to patient needs;
o Assisting in attaining other resources, including benefit acquisition;
o Providing referral to housing resources; and
o Providing referral tracking and follow up.
• Use of Health Information Technology to link services, including but not limited to:
o Use of an Electronic Health Record with meaningful use attainment;
o Use of CareConnect360 for care coordination, transition and planning; and
o Use of telemedicine as needed.
1.4 MI Care Team Provider Qualification Standards
Given the need to coordinate and manage complex clinical conditions and address the social
determinants of health, MI Care Team providers will be held to high standards in order to qualify
and remain as eligible providers. MDHHS will closely monitor MI Care Team providers to ensure that
standards are being met. The qualification standards are described below:
1.4a Geographic Area
In accordance with the Michigan Medicaid State Plan, MI Care Team services will be available in
select counties throughout the state. The geographic area limitation is based on the county that
the enrolled MI Care Team provider is located within. The state has identified MI Care Team
providers within the following counties:
• Bay
• Genesee
• Houghton
• Huron
• Iron
• Kalamazoo
• Kent
• Lapeer
• Lenawee
• Macomb
• Marquette
• Menominee
• Monroe
• Montcalm
• Montmorency
• Oakland

V2.6
6
• Ontonagon
• Presque Isle
• Saginaw
• Shiawassee
• Wayne
1.4b Credentials
In order to serve as a MI Care Team Health Home provider, a FQHC or THC must:
1. Be enrolled as a Michigan Medicaid provider, and be in compliance with all applicable
program policies;
2. Be a Public Health Service Act Section 330 Health Center program grantee of any type, a
Federally Qualified Health Center Look-Alike, a Tribal 638 facility, or an Urban Indian
Organization located in Michigan;
3. Meet and maintain all federal requirements to ensure its designation as a FQHC is in
good standing (FQHCs only);
4. Meet and maintain all federal requirements of the Indian Health Service (THCs only);
5. Meet and maintain all state requirements for participation, along with all standard
provider policies for participation with Medicaid;
6. Adhere to all federal and state laws in regard to Health Home recognition / certification,
including the capacity to perform all core services specified by the Centers for Medicare
& Medicaid Services (CMS);
7. Achieve Patient Centered Medical Home (PCMH) recognition and/or accreditation from
a national recognizing/accrediting body (NCQA, AAAHC, or Joint Commission) before the
Health Home program becomes operational. (PCMH application may be pending, but
must be resolved within 6 months of the entity beginning to provide Health Home
services);
8. Adhere to all provider requirements and all program requirements, and participate in
initial Health Home program orientation and subsequent training(s);
9. Assure that the entity’s medical staff acts as the designated provider for each enrollee,
and maintains ultimate responsibility for providing Health Home services;
10. Use an Office of the National Coordinator for Health Information Technology -certified
Electronic Health Record (EHR) capable of integrating behavioral health and physical
health information;
11. Have achieved Meaningful Use Stage 1, as defined by CMS;
12. Have policies and procedures in place to operate with open access scheduling;
13. Provide on-site behavioral health services;
14. Communicate with Medicaid Health Plans to ensure the health plans are aware of which
members are enrolled in a Health Home;
15. Participate in a readiness assessment that includes a gap analysis and mitigation plan.
1.5 MI Care Team Required Provider Infrastructure
In order to serve as a Health Home provider, each FQHC and THC must provide each Health Home
beneficiary with access to an interdisciplinary care team capable of meeting the beneficiary’s
behavioral and physical health needs. The beneficiary’s specific needs will dictate the size and scope
of provider involvement. At a minimum, each FQHC and THC must provide the following on-site
care team members who are qualified to perform functions including, but not limited to. a primary
care provider, behavioral health consultant, nurse care manager, community health worker, health
V2.6
7
home coordinator, and access to a psychiatrist/psychologist for consultation purposes. Details of
these providers and their role on the MI Care Team are below:
1. Primary Care Provider (i.e., primary care physician, physician assistant, or nurse
practitioner):
• Lead the care team in providing medical care services;
• Lead in selecting strategies to implement evidence based wellness and prevention
initiatives;
• Lead care plan development, including development of specific goals for all
enrollees;
• Lead communication with medical providers, subspecialty providers (including
mental health and substance abuse service providers), long term care providers and
hospital providers regarding patient care and records including
admission/discharge;
• Lead in providing health education, treatment recommendations, medications, and
strategies to implement care plan goals including both clinical and non-clinical
needs;
• Lead in monitoring assessments and screenings to assure findings are integrated in
the care plan;
• Use the EHR and other Health Information Technology (HIT) to link services,
facilitate communication among team members, and provide feedback;
• Lead in meeting regularly with the care team to plan care, review cases, and
exchange information with team members as part of the daily routine of the clinic.
2. Behavioral Health Consultant (i.e., LMSW):
• Screen/evaluate individuals for mental health and substance abuse disorders;
• Refer to licensed mental health provider and/or SUD therapist as necessary;
• Provide brief intervention for individuals with behavioral health problems;
• Meet regularly with the care team to plan care and discuss cases, and exchange
information with team members as part of the daily routine of the clinic;
• Support primary care providers in identifying and providing behavioral
interventions;
• Focus on managing a population of patients versus providing specialty care;
• Work with patients to identify chronic behavior, discuss impact, develop
improvement strategies and specific goal-directed interventions;
• Develop and maintain relationships with community based mental health and
substance abuse providers;
• Identify community resources (i.e. support groups, workshops, etc.) for patient to
use to maximize wellness;
• Provide patient education.
3. Nurse Care Manager (i.e., RN):
• Participate in selecting strategies to implement evidence based wellness and
prevention initiatives;
• Participate in initial care plan development including specific goals for all enrollees;
V2.6
8
• Communicate with medical providers, subspecialty providers including mental
health and SUD service providers, long term care and hospitals regarding patient
care and records including admission/discharge/transfer;
• Provide education in health conditions, treatment recommendations, medications,
and strategies to implement care plan goals including both clinical and non-clinical
needs;
• Monitor assessments and screenings to assure findings are integrated in the care
plan;
• Facilitate the use of the EHR and other HIT to link services, facilitate communication
among team members, and provide feedback;
• Monitor and report performance measures and outcomes;
• Meet regularly with the care team to plan care and discuss cases, and exchange
information with team members as part of the daily routine of the clinic.
4. Community Health Worker (appropriate certificate program and/or curriculum-based
educational modules recommended):
• Coordinate and provide access to individual and family supports, including referral
to community social supports;
• Meet regularly with the care team to plan care and discuss cases, and exchange
information with team members as part of the daily routine of the clinic;
• Identify community resources (i.e. social services, workshops, etc.) for patient to use
to maximize wellness;
• Referral tracking;
• Coordinate and provide access to chronic disease management including self-
management support;
• Implement wellness and prevention initiatives;
• Facilitate health education groups;
• Provide education on health conditions and strategies to implement care plan goals
including both clinical and non-clinical needs.
5. Health Homes Coordinator (i.e., administrative staff):
• Provide leadership to implement and coordinate Health Home activities;
• Serve as the liaison between MDHHS Health Home staff and its contractors;
• Champion practice transformation based on Health Home principles;
• Develop and maintain working relationships with primary and specialty care
providers including Community Mental Health Service Providers (CMHSPs) and
inpatient facilities;
• Collect and report on data that permits an evaluation of increased coordination of
care and chronic disease management;
• Monitor Health Home performance and lead improvement efforts;
• Lead in monitoring and reporting performance measures and outcomes;
• Design and develop prevention and wellness initiatives;
• Referral tracking;
• Provide training and technical assistance;
• Perform data management and reporting.
6. (Access to) a Psychologist and/or Psychiatrist:

V2.6
9
• The care team must have access to a doctoral-level psychologist and/or psychiatrist
for consultation purposes;
• Communicate treatment methods, advice, and recommendations to the Behavioral
Health Provider for inclusion.
Optional Provider Infrastructure: In addition to the above Required Provider Infrastructure,
FQHCs and THCs are encouraged to coordinate care with the following professions:
1. Dentist;
2. Dietician/Nutritionist;
3. Pharmacist;
4. Peer support specialist;
5. Diabetes educator;
6. School personnel;
7. Others as appropriate.
V2.6
10
Section II: Provider Requirements for MI Care Team Participation
2.1 MI Care Team Invitation-to-Bid (ITB)
MDHHS utilized an ITB process to select and award designated MI Care Team Providers. All
applications were reviewed and scored by an MDHHS appointed review team. Award
recommendations were made to the bidders who offer the best value to the state of Michigan.
Best value was determined by the bidders who met the minimum point threshold, who best fit
the bid criteria, and who offered the best combination of service, capability, and quality, as
demonstrated by bid response and other principal factors. Selected MI Care Team Providers
were notified of their awards on January 15, 2016.
2.2 MI Care Team Provider Enrollment
In addition to the award letter, MDHHS will inform selected providers of any contingencies to
their award status. Selected providers will also be required to sign a Memorandum of
Agreement (MOA) to be officially deemed as a MI Care Team Provider.
Should a provider elect to discontinue MI Care Team services, it must notify MDHHS at least six
months in advance of ceasing operations. MI Care Team services may not be discontinued
without MDHHS approval of a provider created cessation plan and protocols for beneficiary
transition.
2.3 MI Care Team Provider Termination
Failure to abide by the terms of the MI Care Team policy, state plan amendment, and the MOA
may result in disciplinary action, including placing the provider in a probationary period and, to
the fullest degree, termination as a MI Care Team provider.
2.4 Training and Technical Assistance
MDHHS is also requiring MI Care Team providers to actively participate in state-sponsored
activities related to training and technical assistance, and will also impose additional functional
provider requirements to optimize care management, coordination, and behavioral health
integration. Those requirements are below:
1. Participate in state-sponsored activities designed to support Health Home providers in
transforming service delivery. This includes a mandatory Health Home orientation for
providers and clinical support staff before the program is implemented;
2. Participate in ongoing technical assistance (including but not limited to trainings and
webinars);
3. Participate in ongoing individual assistance (including but not limited to audits, site
visits, trainings, etc., provided by State and/or State contractual staff);
4. Support Health Home team participation in all related activities and trainings, including
coverage of travel costs associated with attending Health Home activities;
5. Provide each beneficiary, at a minimum, with access to a care team comprised of the
providers mentioned in Section 1.5;
6. Assign a personal care team to each beneficiary;
7. Ensure each patient has an ongoing relationship with a personal member of their care
team who is trained to provide first contact and support continuous and comprehensive
care, where the patient and care team recognize each other as partners;
8. Embed behavioral health care services into primary health care services, with real-time
behavioral health consultation available to each primary care provider;
V2.6
11
9. Provide behavioral and physical health care to beneficiaries using a whole-person
orientation and with an emphasis on quality and safety;
10. Provide care, or arrange for care to be provided by other qualified professionals. This
includes but is not limited to care for all stages of life, acute care, chronic care,
preventive services, long term care, and end of life care;
11. Engage in meaningful use of technology for patient communication;
12. Develop a person-centered care plan for each beneficiary that coordinates and
integrates all clinical and non-clinical health care related needs and services;
13. Coordinate and integrate each beneficiaries’ behavioral health care;
14. Designate for each beneficiary a care coordinator who is responsible for assisting the
beneficiary with follow-up, test results, referrals, understanding health insurance
coverage, reminders, transition of care, wellness education, health support and/or
lifestyle modification, and behavior changes and communication with external
specialists;
15. Communicate with each beneficiary (and authorized representative(s), family and
caregivers) in a culturally and linguistically appropriate manner;
16. Monitor, arrange, and evaluate appropriate evidence-based and/or evidence-informed
preventive services and health promotion;
17. Directly provide, or contract to provide, the following services for each beneficiary:
• Mental health/behavioral health and SUD services;
• Oral health services;
• Chronic disease management;
• Coordinated access to long term care supports and services;
• Recovery services and social health services (available in the community);
• Behavior modification interventions aimed at supporting health management
(Including but not limited to, obesity counseling, tobacco treatment/cessation, and
health coaching);
18. Conduct Health Home outreach to local health systems;
19. Provide comprehensive transitional care from inpatient to other settings, including
appropriate follow-up;
20. Review and reconcile beneficiary medications;
21. Perform assessment of each beneficiary’s social, educational, housing, transportation,
and vocational needs that may contribute to disease and/or present barriers to self-
management;
22. Maintain a reliable system, including written standards/protocols, for tracking patient
referrals;
23. Adhere to all to all applicable privacy, consent, and data security statutes;
24. Demonstrate use of clinical decision support within the practice workflow specific to the
conditions identified in the Health Home project;
25. Demonstrate use of a population management tool such as a patient registry and the
ability to evaluate results and implement interventions that improve outcomes;
26. Implement evidence-based screening tools such as SBIRT, PHQ9, GAD, diabetes and
asthma risk tests to assess treatment needs;
27. Establish a continuous quality improvement program, and collect and report on data
that permit an evaluation of increased coordination of care and chronic disease
management on individual-level clinical outcomes, experience of care outcomes, and
quality of care outcomes at the population level;
V2.6
12
28. Enhance beneficiary access to behavioral and physical health care;
29. Provide each beneficiary with 24/7 access to the care team including, but not limited to
a telephone triage system with after-hours scheduling to avoid unnecessary emergency
room visits and hospitalizations;
30. Monitor access outcomes including but not limited to the average 3rd next available
appointment and same day scheduling availability;
31. Implement policies and procedures to operate with open access scheduling and
available same day appointments;
32. Use HIT, including but not limited to an EHR capable of integrating behavioral and
physical health care information;
33. Use HIT to link services, facilitate communication among team members as well as
between the health team and individual and family caregivers, and provide feedback to
providers;
34. Possess the capacity to electronically report to the State and/or its contracted affiliates
information regarding service provision and outcome measures;
35. Work collaboratively with MDHHS and contractors to adapt and adopt program
processes for Health Home care team use in the participating sites(s);
36. Engage in Health Home process and outcome achievement activities including ongoing
coaching, data feedback and customized improvement plans to meet initiative goals;
37. Commit a management staff member (such as the Health Home Coordinator) and a
clinician champion serving on the care team(s) at the participating site(s) to contribute
actively to and support the project;
38. Commit a staff member to serve as the liaison to the beneficiary’s assigned managed
care health plan;
39. Submit evidence of active care plan development or active care plan
maintenance/management to the state’s Medicaid Management Information System
known as the Community Health Automated Medicaid Processing System (CHAMPS);
40. Practice in accordance with accepted standards and guidelines, and comply with all
applicable policies published in the Michigan Medicaid Provider Manual.
V2.6
13
Section III: Beneficiary Enrollment and Disenrollment
3.1 Beneficiary Identification and Assignment
MDHHS expects MI Care Team providers to be primarily responsible for conducting outreach to
eligible beneficiaries. Enrollment for the MI Care Team uses a two-pronged approach, where both
MDHHS and the MI Care Team providers participate. The process is as follows:
1. MDHHS will identify eligible beneficiaries using claims data. MDHHS will also send each
beneficiary a letter notifying them of their eligibility, and notify participating Health Home
providers that have an existing relationship with the beneficiary using the Waiver Support
Application (WSA). The WSA will be updated on a monthly basis to maintain the most
updated list of prospective Medicaid beneficiaries meeting the MI Care Team eligibility
criteria. It is expected that the MI Care Team provider will conduct a necessary level of
outreach to eligible beneficiaries in their service area to facilitate enrollment. Since
enrollment is contingent on beneficiary consent (see Section 3.4 below), beneficiary
assignment will occur only after a beneficiary visits a MI Care Team provider and establishes
an individualized care plan. These steps must be documented in the WSA.
2. To account for beneficiaries who may not be captured in claims data, Health Home
providers are permitted to recommend beneficiaries for enrollment through the WSA. The
WSA will include an option for providers to input new beneficiary information and attest
that all eligibility conditions have been met for enrollment, including presence of qualifying
conditions, consent, and establishment of an individualized care plan. MDHHS will monitor
all provider-initiated enrollments and may audit charts for verification at any time.
The MI Care Team site must complete all the required information for beneficiary enrollment
through the WSA. The enrollment date will be effective on the last date required to be entered in to
the WSA (i.e., the last date entered between the care plan and enrollment/consent). The enrollment
file for the month will be sent to CHAMPS on the 26
th
of the month for processing.
3.2 MI Care Team ICD Codes for Beneficiary Identification and Assignment
[See Appendix A for list of codes]
3.3 MI Care Team Benefit Plan Assignment
Once the steps outlined above are completed, the beneficiary will be assigned a benefit plan of
“HHMICARE” associated to their Medicaid member ID in CHAMPS. It is incumbent upon MI Care
Team providers to verify a beneficiary’s “HHMICARE” assignment prior to rendering services.
Beneficiaries without the benefit plan assignment “HHMICARE” will not be eligible for MI Care Team
payment.
3.4 Beneficiary Consent
In order to be enrolled in the MI Care Team Health Home program, a beneficiary must first consent
to participate. Signed consent forms must be collected and stored in the beneficiary’s health record
at the provider level. The consent form must be signed by the medically eligible individual (when
legally responsible for self) or the person(s) who is legally responsible for the individual. Verification
of court-appointed guardianship may be required. Providers are responsible for verifying receipt of
signed consent and indicating this in the WSA. All documents must be maintained and made
available for MDHHS review.
V2.6
14
The required beneficiary consent form (MSA-1030) can be found here on the MI Care Team website:
www.michigan.gov/micareteam
In addition to beneficiary consent to participate, MI Care Team providers are required to use the
standard State of Michigan “Consent to Share Behavioral Health Information for Care Coordination
Purposes” form (DCH-3297). The use of a standard form will streamline sharing of information
across the health care system for individuals and providers.
The most up-to-date form and supporting resources (including FAQ) can be found on the following
State of Michigan website: www.michigan.gov/bhconsent
3.5 Beneficiary Enrollment Letters
Eligible beneficiaries will receive a letter about the MI Care Team service model with instructions on
how to enroll in the benefit. The letter will emphasize that an existing relationship may exist
between the beneficiary and an eligible MI Care Team provider, and that the provider may have
already reached out to them to discuss the program and enrollment. Additionally, the letter will
instruct beneficiaries to contact their health plan with questions or concerns (if applicable). Health
plans will help explain beneficiary options and may assist with coordinating enrollment into the MI
Care Team program.
A sample letter can be found on the MI Care Team website:
www.michigan.gov/micareteam
3.6 Beneficiary Disenrollment
Beneficiaries may disenroll at any time. Beneficiaries who decline enrollment in the MI Care Team at
the outset may elect to enroll in the MI Care Team at any time contingent on meeting eligibility
requirements. Beneficiaries who decline or disenroll may do so without jeopardizing their access to
other medically necessary services.
With the exception of voluntary disenrollment initiated by the beneficiary, disengaged beneficiaries
will be categorized into the following two groups, which have unique disenrollment processes:
1. Beneficiaries having moved outside of an eligible geographic area or died. Providers may
note this information in the WSA and recommend disenrollment to MDHHS.
2. Beneficiaries who are unresponsive for reasons other than moving or death. Providers must
attempt at least three beneficiary contacts within three consecutive months that are
unsuccessful for MDHHS to deem a beneficiary as unresponsive. Providers will not be
reimbursed for unsuccessful contacts. Providers will indicate unsuccessful contact attempts
in the WSA. After the final unsuccessful attempt, providers may recommend disenrollment
to the State. Providers and the State must maintain a list of disenrolled beneficiaries and
providers must try to re-establish contact with these beneficiaries at least bi-annually, as
applicable.
3.7 Beneficiary Changing MI Care Team Providers
If a beneficiary chooses to switch MI Care Team providers, they should notify their current MI Care
Team provider and health plan (if applicable) immediately. The two MI Care Team providers must
V2.6
15
discuss the timing of the transfer and communicate transition options to the beneficiary. Ideally, the
change would occur on the first day of the next month, but the timing may be limited by a given
provider’s level of access. Only one MI Care Team provider may be paid per beneficiary per month,
so it is imperative that providers coordinate care as efficiently as possible. Moreover, the new
provider will not be eligible for the initial “Access and Health Action Plan” payment if that one-time
payment was already made to the initial MI Care Team provider (please see Section IV for payment
information).
V2.6
16
Section IV: MI Care Team Payment
4.1 MI Care Team Provider Enrollment
Payment for MI Care Team Health Home services is dependent on the organization enrolling as a
billing agent or utilizing an existing relationship with a billing agent and submitting appropriate
service encounter codes (see section 4.3) to MDHHS through the File Transfer Service (FTS) (see
section 6.4). If FQHCs already have a Billing Agent ID under which they submit FFS claims, they do
not need to apply for a new ID. They will submit Encounters with file number 5476 under their
existing Billing Agent ID. Please note that if an outside agency is used as the MI Care Team billing
agent, they will need to submit encounters on behalf of the care team, not a fee-for-service claim. If
the MI Care Team organization chooses to submit their own encounters, they must complete the
billing agent enrollment process.
A billing agent is a business authorized by MDHHS to submit Medicaid Health Insurance Portability
and Accountability Act (HIPAA) compliant transactions. Before an organization can receive a billing
agent identification number (CHAMPS provider ID) they must submit the Billing Agent Enrollment
Application for approval. All new billing agent enrollments must be completed utilizing CHAMPS. The
CHAMPS Web Application resides within the MDHHS Single Sign-On website. All providers who are
associated to a billing agent will not be able complete a new enrollment until the billing agent has
been approved in CHAMPS.
MI Care Team organizations should refer to the billing agent enrollment resources available on the
MDHHS website. Specifically, prospective billing agents should review the electronic submissions
manual, applicable HIPAA companion guides, B2B testing instructions, and Federal TR3
implementation guides. These are essential documents that are necessary for the completion of
clean Michigan Medicaid encounters. Most questions that a MI Care Team organization may have
regarding an electronic claim file should be able to be answered within one of these documents. The
billing agent user guide provides a step-by-step enrollment process for MI Care Team organizations
to follow. Go to www.michigan.gov/medicaidproviders
>> Provider Enrollment >> Billing Agent >>
User Guide. Complete the necessary steps outlined in the user guide and record the billing agent
application number for future reference.
Additional questions or issues with enrolling as a billing agent can be directed to the following email
address: [email protected]
. For questions and issues related to encounters, please
direct those to the following email address: MDHHSEncounterData@michigan.gov.
MDHHS will review the application and complete the CHAMPS enrollment process. Approved MI
Care Team organizations will be provided a 7-digit CHAMPS provider ID and FTS user ID and
password. All providers must associate to the corresponding Billing Agent within the CHAMPS
system. This association provides the Billing Agent with the authorization to submit claims on behalf
of the Provider. If the Provider has not associated the Billing Agent in CHAMPS all testing and
production claims will deny.
4.2 General Provisions for MI Care Team Payment
Payment for MI Care Team Health Home services is contingent on MI Care Team providers meeting
the requirements of the MI Care Team program, as determined by MDHHS. One important
requirement for payment is that MI Care Team beneficiaries must receive a MI Care Team service
(defined in Section 1.3) per calendar month. Failure to meet these requirements may result in
recoupment or denial of payment, loss of Health Home status, and/or termination of payments.
V2.6
17
MI Care Team payment will be a monthly case rate. The monthly payment is contingent upon a MI
Care Team beneficiary receiving a MI Care Team service during the month at issue. The payment for
MI Care Team services is in addition to the existing fee-for-service payments, encounters, or daily
rate payments for direct clinical services. MDHHS’ payment methodology is designed to only
reimburse for the cost of the MI Care Team staff for the delivery of health home services that are
not covered by any other currently available Medicaid reimbursement mechanism. MI Care Team
providers will have their own unique identifier within the Community Health Automated Medicaid
Processing System (CHAMPS) and are required to submit encounters for MI Care Team Services. The
Group (Type 2 - Organization) National Provider Identifier (NPI) number must be used as the billing
provider on all MI Care Team service encounters submitted. Do not use Provider (Type 1 - Individual)
as the billing provider. The billing provider loop or field is mandatory to complete. The Provider
(Type 1 - Individual) NPI number of the provider who performed the service encounter, or the
supervising physician, should be entered as the rendering provider. If the provider who performed
the service is not enrolled in CHAMPS (e.g., CHW), then a supervising primary care provider must be
entered as the rendering provider (i.e., primary care physician, nurse practitioner, physician’s
assistant). Do not enter the Group NPI number as the rendering provider.
Payment for the MI Care Team program uses two rates, which are as follows:
1. The program uses a once-in-a-lifetime-per-beneficiary “Health Action Plan” rate to be paid
only for the first month that a beneficiary participates in the MI Care Team program. This
once-in-a-lifetime-per-beneficiary rate represents reimbursement for certain actions and
services, including, but not limited to, initial care plan development.
2. Additionally, the program uses an “Ongoing Care Coordination” rate, to be paid for MI Care
Team services rendered in all subsequent months of a beneficiary’s participation in the MI
Care Team program (provided the beneficiary remains eligible for the program and received
MI Care Team services during the month at issue).
MDHHS established the monthly payment rate to reflect personnel costs for the required care team
that provides MI Care Team services. The monthly payment rate also reflects related administrative
costs that are necessary for the implementation of MI Care Team services. The MI Care Team service
rate will be assessed and re-based state-wide by MDHHS on an annual basis, as indicated, due to
changes in staffing costs, administrative costs, or other factors determined by MDHHS. MDHHS will
make MI Care Team payments on a monthly schedule. Adjustments to the payment schedule may
occur to accommodate processing around State Holidays. Additional payments may be scheduled as
required. The MI Care Team case rate includes payment for MI Care Team enrolled beneficiaries
who have met eligibility requirements for the current calendar month. In addition, a MI Care Team
payment may be adjusted for:
• Recovery of payments previously made to beneficiaries prior to MDHHS notification of
death;
• Recovery of payments previously made to beneficiaries who, upon retrospective review, did
not meet all MI Care Team enrollment requirements;
• Modifications to any of the MI Care Team rate development factors.
4.3 Health Action Plan (Care Plan) Requirements
V2.6
18
At the time of enrollment beneficiaries will develop a care plan with a member of the care team.
The plan will guide the care and support services to be provided by the care team and the
expectations of the beneficiary and their family toward achieving the goals. The Health Action Plan
is to be updated as needed based on significant changes in health status or as goals are achieved.
All members of the team are to have access to view the Health Action Plan and progress notes are to
be kept in the patient file. At minimum the Health Action Plan must contain the following elements:
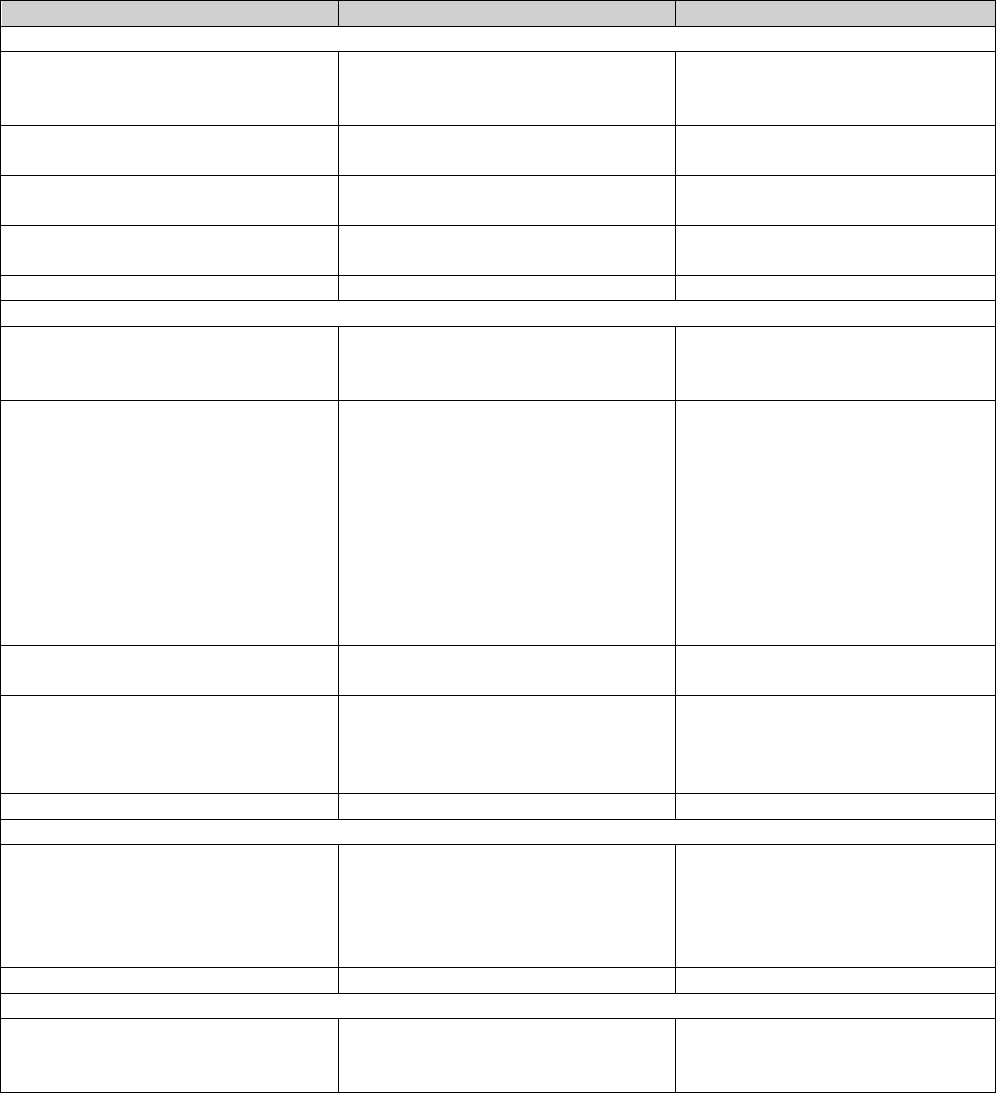
FOCUS AREA
MEASUREMENT/SCORE
TREATMENT/PREVENTION/GOAL
Diagnosis
*Physical
Document every visit (e.g., A1C, blood
pressure, PHQ scores, etc.; monitor
for change)
e.g., medication, exercise (patient
will walk 1 mile 3 times per week)
*Behavioral Health
Document every visit (e.g., GAD score,
PHQ-9)
e.g., medication, counseling as
prescribed
*Risk Factors/Co-morbidities
Document every visit (e.g., smoking,
tobacco use, obesity, alcohol)
e.g., reduce number or cigarettes
smoked to 10 per day
*Specialist
Document referral to specialist and/or
services
e.g., make appointment with social
workers
Patient Engagement
*Readiness to Change
Document on standard scale (i.e.,
Patient Activation Measure or
Readiness to Change)
*Health Literacy
Document understanding of the use of
the health center for urgent care
needs vs ER
e.g., patient know what number to
call after hours to get nurse triage
line and has put number in cell
phone, understanding of treatment
plan and why medication will
support wellness and will refill
prescription monthly, importance of
appointments with providers and
care teams and commitment to
appointments
*Goal Setting and Self-Care Plans
Agreement to notify Care Team of
other providers or hospitalizations
e.g., medication adherence, call
health center before going to ER
*Coaching
Patients goals and priorities, discuss
family/friend/caregiver support,
discuss MI Care Team support, health
education needs
Barriers to Success/Areas of Concern
*Social Determinants of Health
Stable housing, food insecurity, social
support/isolation, education,
employment, safety/violence/trauma,
transportation, language,
family/relationships, reading literacy
Prioritize
Plan Activation
*Support
Signature of patient, signature of care
team representative, signature by
family/caregiver support
e.g., discuss next steps
V2.6
19
The Health Action Plan must also align with the MI Care Team services consistent with Section 2703
of the Affordable Care Act. They include:
1. Comprehensive Care Management
2. Care Coordination and Health Promotion
3. Comprehensive Transitional Care, including appropriate follow-up , from in-patient to other
settings
4. Patient and Family Support
5. Referral to Community and Social Support
6. Use of Health Information Technology
4.4 MI Care Team Service Encounter Codes
Payment for MI Care Team services is dependent on the submission of appropriate service
encounter codes. Valid MI Care Team encounters must be submitted within 90 days of providing a
MI Care Team service in order to assure timely service verification. Both the Health Action Plan rate
and Ongoing Care Coordination rate have specific code requirements, as outlined below:
• Health Action Plan
To receive the Health Action Plan payment, designated MI Care Team providers must submit
the following service encounter code:
Comprehensive Care Management: S0280
• This code must only be used for the Health Action Plan encounter.
• This service must be delivered in-person.
• Ongoing Care Coordination
For all subsequent months following the Health Action Plan payment, the “Ongoing Care
Coordination” will be paid for eligible MI Care Team beneficiaries. To receive Ongoing Care
Coordination payments, designated MI Care Team providers must provide at least one MI
Care Team service per calendar month (as defined in Section 1.3) and bill the S0281 service
encounter code, along with an applicable ICD-10 diagnosis code. Please note that the TS
Modifier should be used on the S0281 code to document non face-to-face encounters
rendered to a beneficiary.
MI Care Team providers are required to track the factors influencing a beneficiary’s health
status being addressed during the monthly contact. ICD-10 diagnosis codes to be used with
the S0281 code include the following groups:
Z55-Z65 (Persons with potential health hazards related to socioeconomic and
psychosocial circumstances)
Z69-Z76 (Persons encountering health services in other circumstances)
Z77-Z99 (Persons with potential health hazards related to family and personal
history and certain conditions influencing health status)
As mentioned above, MI Care Team providers must provide at least one of the services cited
in Section 1.3 per calendar month to continue receiving the Ongoing Care Coordination
payment. These services are intended to provide follow-up care and supports to the initially
created Health Action Plan. As such, it is imperative that MI Care Team providers clearly
document the details of the services provided that support the beneficiary’s Health Action
Plan. This documentation provides the foundation for care coordination and transitions and
allow for optimal tracking of a beneficiary’s condition(s). This tracking can be juxtaposed to

V2.6
20
reassessing the initial Health Action Plan to ensure it is still the best care trajectory for the
beneficiary or if modifications are needed.
4.5 Encounter Submission
MI Care Team providers will use the File Transfer Service (FTS) to submit and retrieve encounter
related files electronically with MDHHS. Refer to section 6.4 of this handbook for additional
information relating to FTS.
MI Care Team providers will need to use the ‘Class ID Filename’ for files that are submitted through
the FTS to MDHHS, and to recognize files that MDHHS returns to the MI Care Team provider billing
agent “mailbox”. When submitting MI Care Team encounters, the Class ID Filename will be 5476.
After submission, MI Care Team provider billing agents will receive a response in the mailbox via a
999 acknowledgment file. The 999 file does not mean that all encounters submitted were accepted.
Once the 5476 file is processed by MDHHS, MI Care Team provider billing agents will receive a 4950
error report which will provide details on accepted and rejected encounters.
MI Care Team providers are encouraged to review the “Electronic Submissions Manual” (ESM) for
additional information and instructions relating to submitting data electronically and the FTS. The
ESM can be found at www.michigan.gov/tradingpartners >> HIPAA - Companion Guides >>
Electronic Submissions Manual.
The MDHHS Encounter Team will handle all electronic questions related to encounter file
submission and FTS issues for MI Care Team organizations. Questions or issues can be directed to
the following email address: MDHHSEncounterData@michigan.gov
.
4.6 Payment Schedule
The enrollment file for the month will be sent to CHAMPS on the 26
th
of the month for processing.
For illustrative purposes, the July 26
th
enrollment file would include:
• Payment for newly enrolled beneficiaries added to MI Care Team from July 1 through July
25.
• Retroactive payment for beneficiaries enrolled from June 26 to June 30.
• Prospective payment for the month of August (for all enrolled beneficiaries, as of July 26).
Payment will be made on the second pay cycle (the Thursday after the 2
nd
Wednesday of the
month). The payment will be included with any other scheduled payments associated with the MI
Care Team organization’s tax identification number.
4.7 Recoupment of Payment
The monthly payment is contingent upon a MI Care Team beneficiary receiving a MI Care Team
service during the month at issue. The payment is subject to recoupment if the beneficiary does not
receive a MI Care Team service during the calendar month. The recoupment lookback will occur four
months after the monthly payment is made. Thus, four months after the month a payment is made
(for example, in November MDHHS would look back at the month of July’s payment), CHAMPS will
conduct an automatic recoupment process that will look for an approved encounter code (refer to
section 4.3) that documents that the MI Care Team provided at least one of the five core MI Care
Team services (excluding the Health Information Technology core service requirement) during the
calendar month in question. If a core MI Care Team service is not provided during a month, that
month’s payment will be subject to recoupment by MDHHS. Once a recoupment has occurred, there
V2.6
21
shall be no further opportunity to submit a valid MI Care Team encounter code and/or claim for the
month that has a payment recouped.
The recoupment process will run automatically on the 2
nd
of the month. MI Care Team sites must
submit encounters by the end of the month before the scheduled recoupment. To continue with the
example provided above, on November 2
nd
the recoupment will process for the month of July. July’s
encounters would need to be submitted no later than October 31
st
to ensure an accurate
recoupment process. This allows up to 3 months for sites to submit their encounters.
In addition, a recoupment could also occur if the beneficiary is no longer eligible for the MI Care
Team benefit due to a higher priority benefit plan activating. For example, if the beneficiary is
admitted to a skilled nursing facility on July 7
th
and a MI Care Team professional speaks to the
beneficiary via phone on July 29
th
, the month of July’s payment would not be maintained due to the
higher priority benefit plan being assigned. The beneficiary could be discharged from the nursing
facility in August and reenrolled to the MI Care Team benefit.

V2.6
22
Section V: MI Care Team and Managed Care
5.1 MI Care Team Enrollment for Health Plan Beneficiaries
MI Care Team providers and Health Plans will work together to coordinate services for eligible
beneficiaries who wish to enroll in the MI Care Team program. Both the providers and the applicable
health plans will be given a list of their beneficiaries deemed eligible for the MI Care Team program.
MDHHS will require providers and health plans to confer to optimize communication to
beneficiaries. MI Care Team providers will primarily be responsible for conducting outreach to
eligible beneficiaries, while health plans will provide support in addressing beneficiary questions. Bi-
directional communication is imperative throughout the process so that all parties have current
knowledge about a beneficiary. As mentioned previously, MDHHS will also provide beneficiaries
with a letter indicating their eligibility, which will contain benefit information and instructions on
who to contact should there be any questions.
There are different scenarios that MDHHS anticipates could manifest with eligible beneficiaries
enrolled in a health plan who wish to participate in the MI Care Team Program. Those are detailed
below:
A) For health plan beneficiaries whose current primary care provider is a MI Care Team
provider, health plans, upon beneficiary request, will direct beneficiaries to setup an
appointment with their MI Care Team primary care provider and inform the beneficiary that
their provider will help enroll them in the MI Care Team (this may be in addition to the
provider having already conducted outreach). If a health plan beneficiary enrolls directly
with a MI Care Team provider, the MI Care Team provider must ensure that the
beneficiary’s health plan is apprised of this development.
B) For health plan beneficiaries whose current primary care provider is not a MI Care Team
provider, health plans, upon beneficiary request, should change the beneficiary’s primary
care provider to the MI Care Team provider of the beneficiary’s choice that is also within the
health plan’s provider network. If there is no in-network MI Care Team provider in the
eligible county, then the health plan should help the interested beneficiary find an in-
network MI Care Team provider in a nearby eligible contiguous county that is within a
rational service area (if applicable).
5.2 MI Care Team Coordination & Health Plans
Health Plans are contractually obligated to provide a certain level of care coordination and care
management services to their beneficiaries. Moving forward, health plans will also be required to
support embedded care management activities within the primary care construct. To this extent, bi-
directional communication between the MI Care Team provider and health plan is essential to
maximize care coordination, particularly with regard to care transitions and disease management.
MDHHS expects the MI Care Team provider to take the lead in the provision of care management,
spanning health and social supports at the primary care practice level. At the same time, health plan
coordination in terms of supporting enrollment, facilitating access to beneficiary resources, and
maintaining updated information in CareConnect360 will be critical to the success of the MI Care
Team and the beneficiary’s health status.
V2.6
23
Section VI: Health Information Technology
6.1 Waiver Support Application (WSA) and the MI Care Team
The WSA will provide support to MI Care Team providers in the areas of beneficiary enrollment,
including pre-enrollment activities (e.g., maintaining updated list of eligible beneficiaries),
enrollment management including beneficiary disenrollment, and report generation. Every week, a
new batch of eligible beneficiaries will be uploaded to the WSA.
6.2 CareConnect360 and the MI Care Team
CareConnect360 is the HIT-supported care coordination application for the MI Care Team benefit.
Broadly, it is a statewide care management web portal that provides a comprehensive view of
individuals in multiple health care programs and settings based on claims information. This will allow
MI Care Team providers and other entities with access to CareConnect360 the ability to analyze
health data spanning different settings of care. In turn, this will afford MI Care Team providers a
more robust snapshot of a beneficiary and allow smoother transitions of care. It will also allow
providers to make better and faster decisions for the betterment of the beneficiary. Providers will
only have access to individuals that are established as patients of record within their practice.
Finally, with appropriate consent, CareConnect360 facilitates the sharing of cross-system
information, including behavioral health, physical health, and social support services.
6.3 Electronic Health Records
The use of electronic health records and the attainment of Stage 1 Meaningful Use is a pre-requisite
for provider participation in the MI Care Team benefit. It is also essential to the overarching goals of
the MI Care Team in that it allows for the maintenance and transmittal of data necessary to
optimize care coordination and management activities.
6.4 File Transfer Service (FTS)
Michigan’s data-submission portal is the File Transfer Service (FTS); however, it has previously been
referred to as the Data Exchange Gateway (DEG). Some documents may still reference the DEG; be
aware that a reference to the DEG portal is a reference to the FTS.
Billing agents will use the FTS to submit and retrieve files electronically with MDHHS. MDHHS has
established an internet connection to the FTS, which is a Secure Sockets Layer connection. This
connection is independent of the platform used to transmit data. Every billing agent receives a
“mailbox”, which is where their files are stored and maintained. Billing agents can access this
mailbox to send and retrieve files.
MI Care Team organizations are encouraged to review the “Electronic Submissions Manual” (ESM)
for additional information and instructions relating to the FTS. The ESM can be found at
www.michigan.gov/tradingpartners >> HIPAA - Companion Guides >> Electronic Submissions
Manual
V2.6
24
Section VII: MI Care Team Monitoring and Evaluation
7.1 Monitoring & Evaluation Requirements
Both CMS and MDHHS have quality monitoring and evaluation requirements for the Health Home
program. To the extent necessary to fulfill these requirements, providers must agree to share any
and all MI Care Team clinical and cost data with MDHHS. It is the goal of MDHHS to utilize
administrative data as much as possible to avoid administrative burden on providers. The data will
be reported annually by MDHHS to CMS.
7.2 Federal (CMS) Monitoring & Evaluation Requirements
CMS has supplied reporting requirements and guidance for health home programs. There are two
broad sets of requirements – core utilization and core quality measures. It is essential that MI Care
Team providers are aware of these measures and how they are calculated for evaluation purposes
and the program’s longevity. The specific Core Measures and other federal requirements are laid
out below:
1. Core Utilization Measures (reported annually)
a. Ambulatory Care Sensitive Emergency Department Visits
b. Inpatient Utilization
c. Skilled Nursing Facility Utilization
2. Core Quality Measures (reported annually)
a. Adult Body Mass Index (BMI) Assessment
b. Screening for Clinical Depression and Follow-up Plan
c. Plan All-Cause Readmission Rate
d. Follow-up After Hospitalization for Mental Illness
e. Controlling High Blood Pressure
f. Care Transition – Timely Transmission of Transition Record
g. Initiation and Engagement of Alcohol and Other Drug Dependence Treatment
h. Prevention Quality Indicator (PQI) 92: Chronic Conditions Composite
In addition to the CMS Core Measures, CMS also requires participating states to conduct an
independent cost-savings evaluation. MDHHS and its partner have developed an evaluation plan
that will evaluate cost-efficiency of the MI Care Team.
7.3 State Monitoring & Evaluation Requirements
CMS also requires states to define a separate quality monitoring plan specific to the population their
Health Home program will target. It is imperative MI Care Team providers are cognizant of what
MDHHS will be monitoring to help facilitate baseline information and to ensure validity of
measurement. MDHHS will monitor and report on the following data annually:
1. Depression – Antidepressant Medication Management (AMM)
a. Effective Acute Phase Treatment: the percentage of members who remained on an
antidepressant medication for at least 84 days (12 weeks).
b. Effective Continuation Phase Treatment: the percentage of members who remained
on an antidepressant medication for at least 180 days (6 months).
2. Asthma – Medication Management for People with Asthma (MMA)
3. Diabetes – Hemoglobin A1c (HbA1c) Testing

V2.6
25
Appendix A: MI Care Team ICD-10 Codes
The ICD-10 Codes below provide diagnostic eligibility for the MI Care Team. As reference, the applicable
ICD-9 Code cognates were used to initially develop a target population estimate. MI Care Team
providers should use the ICD-10 Codes below to identify eligible beneficiaries.
Depression
• Major Depressive Disorder: Single episode
o F32.0 mild
o F32.1 moderate
o F32.2 severe without psychotic features
o F32.3 severe with psychotic features
o F32.4 single episode partial remission; 32.5 full remission
o F32.8 Other depressive episodes
o F32.9 Single episode, unspecified (Acute)
• Major Depressive Disorder: Recurrent
o F33.0 mild
o F33.1 moderate
o F33.2 severe without psychotic features
o F33.3 severe with psychotic features
o F33.4 recurrent, unspecified remission; 33.41 recurrent, partial remission; 33.42
recurrent, full remission
o F33.8 Other recurrent depressive episodes
o F33.9 recurrent, unspecified
• F34.1 Dysthymic Disorder
• F34.8 Other persistent mood [affective] disorders
• F34.9 Persistent mood [affective] disorder, unspecified
• F43.21 Adjustment disorder with depressed mood
• F43.23 Adjustment disorder with mixed anxiety and depressed mood
Anxiety
• F40.0 – F40.9 Phobic anxiety disorders
• F41.0 Panic disorder without agoraphobia
• F41.1 Generalized anxiety disorder
• F41.3 Other mixed anxiety disorder
• F41.8 Other specified anxiety disorders
• F41.9 Anxiety disorder, unspecified
• F43.22 Adjustment disorder with anxiety
• F43.23 Adjustment disorder with mixed anxiety and depressed mood
Hypertension
• I10 Essential hypertension
• I11.0 Hypertensive heart disease with heart failure
• I11.9 Hypertensive heart disease without heart failure
• I12.0 Hypertensive chronic kidney disease with Stage 5 or ESRD
• I12.9 Hypertensive chronic kidney disease with Stage 1-4 or unspecified chronic kidney disease
V2.6
26
• I13.0 Hypertensive heart and chronic kidney disease with heart failure, Stage 1-4 or unspecified
chronic kidney disease
• I13.10 HTN heart and chronic kidney disease without heart failure, Stage 1-4 or unspecified
• I13.11 HTN heart and chronic kidney disease without heart failure, Stage 5 or ESRD
• I13.20 HTN heart and chronic kidney disease with heart failure and with Stage 5 or ESRD
• I15.0- I15.9 Secondary HTN
• I50.10 Left heart failure
• I50.20 – I50.23 Systolic heart failure
• I50.30 – I50.33 Diastolic heart failure
• I50.40 – I50.43 Combined systolic and diastolic heart failure
• I50.9 Heart failure, unspecified
COPD
• J44.0 COPD with acute lower respiratory infection
• J44.1 COPD with acute exacerbation
• J44.9 COPD unspecified
Emphysema (COPD)
• J43.0 Unilateral
• J43.1 Panlobular
• J43.2 Centrilobular
• J43.8 Other
• J43.9 Unspecified
Asthma
• J45.20 – J47.9
Diabetes
• E08.00 – E13.90
Heart Disease
• I20.0 – I20.90 Angina
• I21 – I23.8 Myocardial infarction codes (acute and subsequent with complications)
• I25.1 – I25.90 Chronic Ischemic Heart Disease
• I27.0 – I27.9 Pulmonary Heart Disease
• I30.0 – I30.9 Pericarditis
• I31.0 – I32 Other Disease of Pericardium
• I33.0 – I33.9 Endocarditis
• I34.0 – I37.9 Nonrheumatic valve disorders
• I38 Endocarditis, valve unspecified
• I39 Endocarditis and heart valve disorders in disease classified elsewhere
• I40.0 – I40.9 Myocarditis
• I41.0 Myocarditis classified elsewhere
• I42.0 – I42.9 Cardiomyopathy
• I43 Cardiomyopathy classified elsewhere
• I44.0 – I44.7 AV blocks
V2.6
27
• I45.0 – I45.9 Other conduction disorders
• I47.0 – I47.9 Paroxysmal ventricular tachycardia
• I48.0 – I48.9 Atrial fib/flutter
• I49.0 – I49.9 Other cardiac arrhythmias
