
CARDIOVASCULAR
DISEASE:
A COSTLY BURDEN
FOR AMERICA
PROJECTIONS
THROUGH 2035
3
CARDIOVASCULAR DISEASE: A COSTLY BURDEN FOR AMERICA — PROJECTIONS THROUGH 2035
american heart association CVD Burden Report
INTRODUCTION ...................................................................................5
ABOUT THIS STUDY ................................................................................................... 6
WHAT IS CVD? ......................................................................................................... 6
Atrial Fibrillation
Congestive Heart Failure
Coronary Heart Disease
High Blood Pressure
Stroke
PROJECTIONS: PREVALENCE OF CVD .............................................................7
Latest Projections
Age, Race, Sex – Differences That Matter
PROJECTIONS: COSTS OF CVD ................................................................. 8-11
The Cost Generators: Aging Baby Boomers
Medical Costs Breakdown
Direct Costs + Indirect Costs
RECOMMENDATIONS .............................................................................13-14
Research
Prevention
Affordable Health Care
table of contents

5
CARDIOVASCULAR DISEASE: A COSTLY BURDEN FOR AMERICA — PROJECTIONS THROUGH 2035
american heart association CVD Burden Report
Introduction
Cardiovascular disease (CVD) has been the leading killer
of Americans for decades. In years past, a heart attack
or stroke almost certainly resulted in death. But advances
in biomedical research, improved emergency response
systems and treatment and prevention efforts have
helped Americans ght back. Between 2000 and 2011,
researchers found the national heart-related mortality
rate declined at an average of 3.7 percent per year, while
stroke mortality declined at 4.5 percent per year.
But in the past few years this remarkable progress
has stalled.
The burden of cardiovascular disease is now growing
faster than our ability to combat it due to the obesity
epidemic, poor diet, high blood pressure and a dramatic
rise in Type 2 diabetes – all major risk factors for heart
disease and stroke. In a frightening reversal, the overall
decline in CVD mortality rates have attened to less
than 1 percent per year since 2011, and rates have even
worsened for our most at-risk populations. In 2015, the
death rate from heart disease actually increased by 1
percent for the rst time since 1969, according to the
Centers for Disease Control and Prevention’s (CDC)
National Center for Health Statistics.
In addition, CVD has become our nation’s costliest chronic
disease. In 2014, stroke and heart failure were the most
expensive chronic conditions in the Medicare fee-for-service
program. Expenses associated with CVD are expected to
soar in the coming years and surpass medical cost estimates
for other chronic diseases, such as diabetes and Alzheimer’s.
Based on prevalence, death rates, disability and cost, CVD
will continue to be the most burdensome disease Americans
will face in the next decades.
Given these developments, it is hard to understand
why federal research funding levels for heart and stroke
research are not commensurate with the number of
Americans aficted with CVD and the toll it exacts.
Even though heart disease and stroke account for 23 percent
and 4 percent of all deaths respectively, the National
Institutes of Health (NIH) invests a meager 4 percent of its
budget on heart disease research, a mere 1 percent on
stroke research and only 2 percent on other CVD research.
We believe this must change and change dramatically. The
stakes are too high.
This comprehensive analysis projects what lies ahead in
CVD prevalence and costs from the present through 2035.
The American Heart Association hopes this tool will help
guide and inform policymakers as to what we must do as
a nation to reduce the heavy toll of CVD on our nation’s
health and economy.
6
CARDIOVASCULAR DISEASE: A COSTLY BURDEN FOR AMERICA — PROJECTIONS THROUGH 2035
american heart association CVD Burden Report
6
CARDIOVASCULAR DISEASE: A COSTLY BURDEN FOR AMERICA — PROJECTIONS THROUGH 2035
american heart association CVD Burden Report
About this Study
The association commissioned this study, and it was
conducted by RTI International. The goal was to project
the prevalence and medical costs of cardiovascular
disease from the present through 2035. These new
projections update similar ones made by the American
Heart Association in 2011.
What is CVD?
Cardiovascular disease represents a number of heart and
blood vessel diseases. Specically, this study incorporates
the prevalence and medical costs of high blood pressure,
coronary heart disease (CHD), congestive heart failure
(CHF), stroke, atrial brillation (AFib) and other heart
diseases from the present through 2035. Below are
denitions of each of these conditions:
Atrial Fibrillation: Atrial brillation is a disorder of the heart’s
internal electrical system affecting heart rate and rhythm.
Also commonly abbreviated as AF or AFib, it occurs when
the heart’s two small, upper chambers (atria) beat in a fast
and irregular manner and empty blood into the heart’s lower
chambers (ventricles) in a disorganized manner instead of
beating effectively. Blood that isn’t pumped completely out
of the atria when the heart beats may pool and clot. If a
piece of a clot enters the bloodstream, it may lodge in the
brain, causing a stroke. Causes of atrial brillation include
dysfunction of the sinus node (the heart’s pace-making area
in the right atrium), coronary artery disease, rheumatic heart
disease, high blood pressure and hyperthyroidism.
Congestive Heart Failure: Also called heart failure,
congestive heart failure is when the heart can’t pump
enough blood to the organs. The heart works, but not as
well as it should. Heart failure is almost always a chronic,
long-term condition. The older you are, the more common
congestive heart failure becomes. Your risk also increases if
you are overweight, diabetic, smoke, abuse alcohol or use
cocaine. When a heart begins to fail, uid can pool in the
body; this manifests as swelling (edema), usually in the lower
legs and ankles. Fluid also may collect in the lungs, causing
shortness of breath.
Coronary Heart Disease: Also called coronary artery
disease, coronary heart disease is the most common type
of heart disease. It occurs when plaque builds up in the
heart’s arteries, a condition called atherosclerosis. As plaque
builds up, the arteries narrow, making it more difcult for
blood to ow to the heart. If blood ow becomes reduced
or blocked, angina (chest pain) or a heart attack may occur.
Over time, coronary artery disease can also lead to heart
failure and arrhythmias.
High Blood Pressure: Blood pressure is the pressure of
the blood against the walls of the arteries. When that
pressure is consistently above the normal range, it is
considered hypertension, or high blood pressure. This
increases the heart’s workload, putting a person at a greater
risk for heart attack, angina, stroke, kidney failure and
peripheral artery disease.
Stroke: A stroke is an interruption of blood ow to the
brain, causing paralysis, slurred speech and/or altered
brain function. About nine of every 10 strokes are caused
by a blockage in a blood vessel that carries blood to the
brain; this is known as an ischemic stroke. The other type
of stroke is known as hemorrhagic, caused by a blood
vessel bursting. Warning signs include sudden numbness
or weakness of the face, arm or leg (especially on one
side); sudden confusion, trouble speaking or understanding
(aphasia); sudden trouble seeing in one or both eyes;
sudden trouble walking, dizziness, loss of balance or
coordination; and sudden, severe headache with no known
cause. Call 9-1-1 if you think you or someone else is having
a stroke.
For more information on CVD, please see the American
Heart Association’s Heart and Stroke Encyclopedia at heart.
org/encyclopedia.
7
CARDIOVASCULAR DISEASE: A COSTLY BURDEN FOR AMERICA — PROJECTIONS THROUGH 2035
american heart association CVD Burden Report
Projections: Prevalence of CVD
Cardiovascular disease has been the No. 1 killer of
Americans since 1920. Your great-grandparents or another
member of your family tree probably died from it. What’s
more disturbing, however, is your great-grandchildren could
die from CVD, too, if we don’t take deliberate and focused
action now.
In our 2011 projections, the American Heart Association
predicted that by 2030, upwards of 40 percent of the
U.S. population – or more than 100 million Americans –
would suffer from some form of CVD. Disturbingly, we
reached that benchmark in 2015 – almost 15 years sooner
than anticipated.
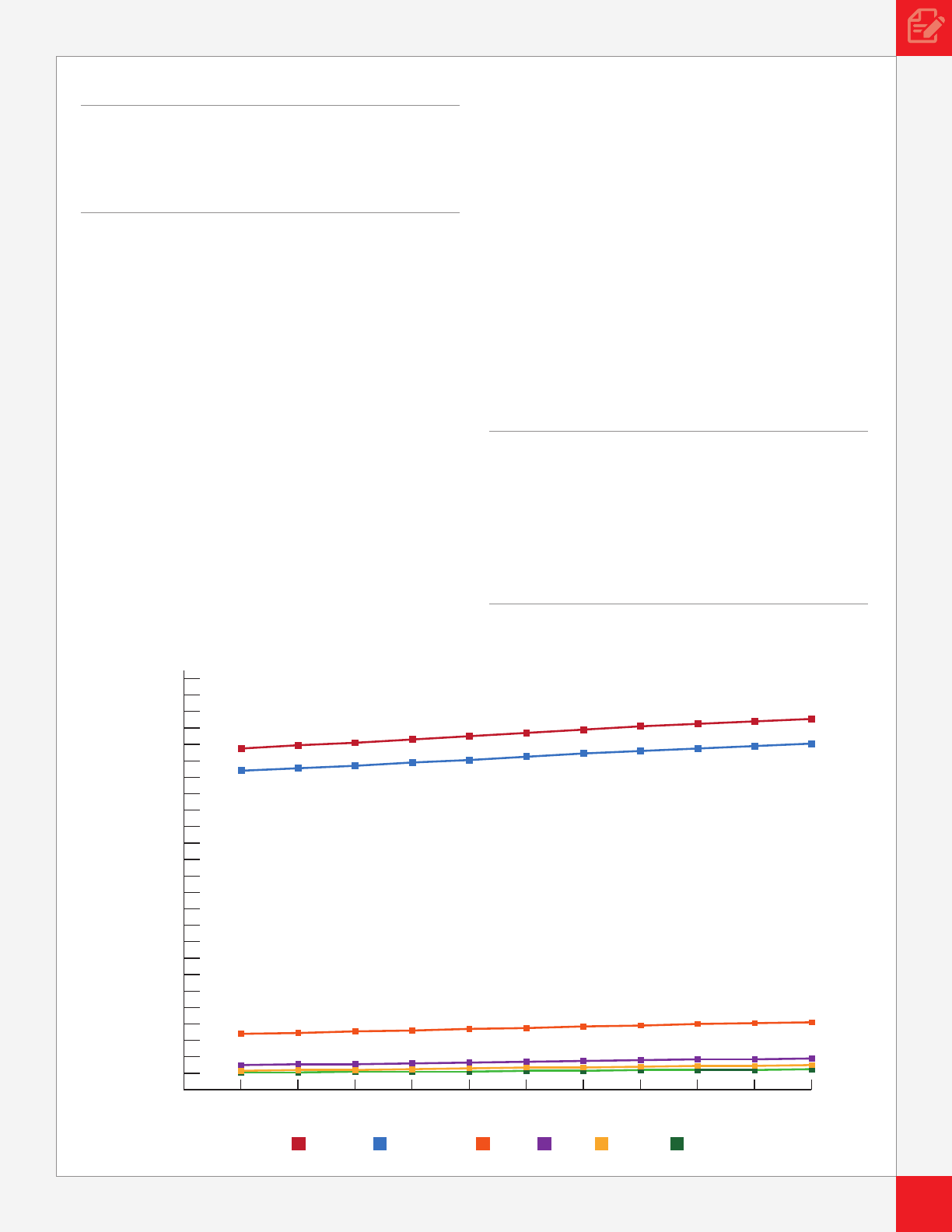
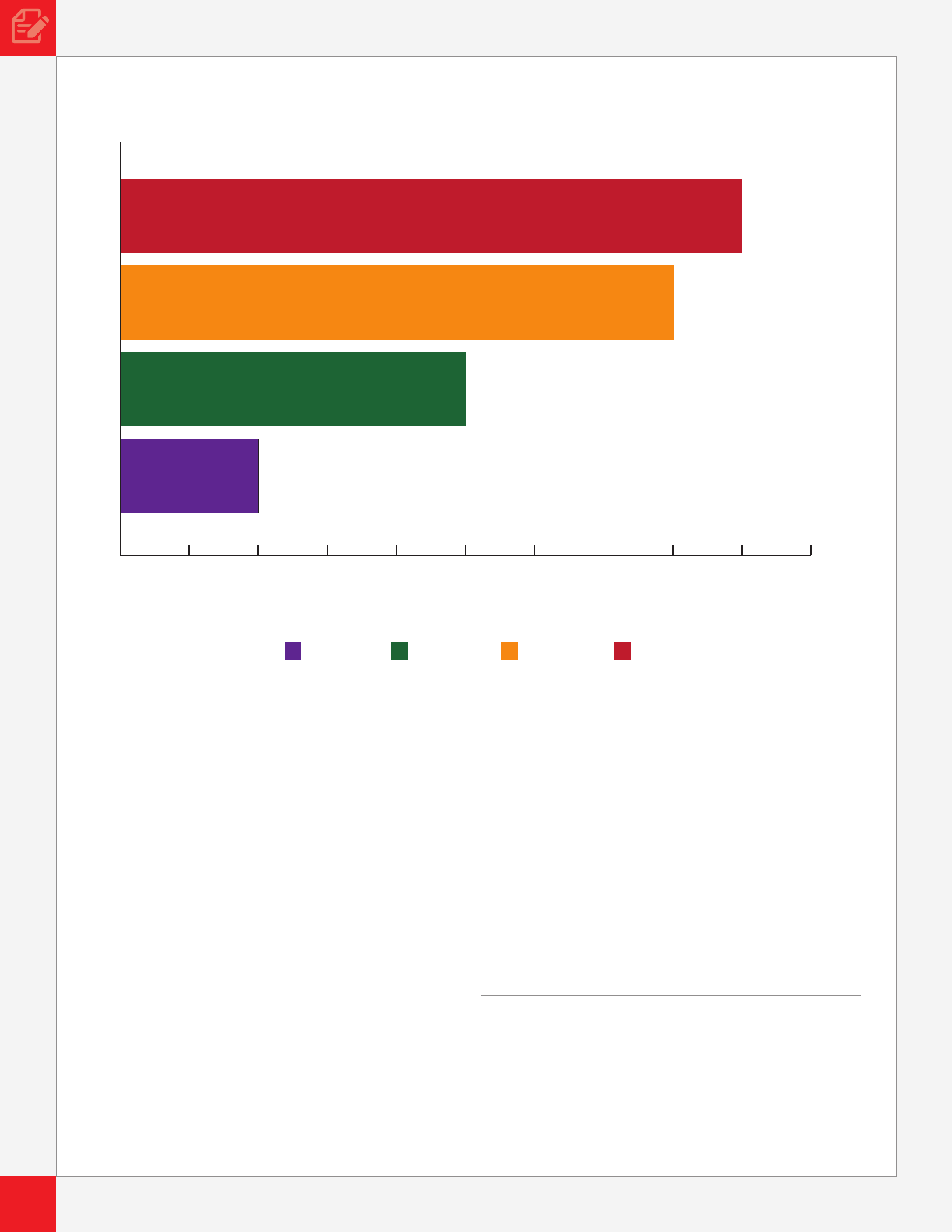
Our Latest Projections on the Prevalence of CVD Reveal:
• In 2015, 41.5 percent (102.7 million) of the U.S. population
had at least one CVD condition:
High Blood Pressure .............................. 96.1 million
Coronary Heart Disease ..........................16.8 million
Stroke .......................................................7.5 million
Congestive Heart Failure ..........................5.8 million
Atrial Fibrillation ........................................5.2 million
• In 2035, the number of Americans with CVD is projected
to rise to 131.2 million – 45 percent of the total U.S.
population. This means additional increases of:
High Blood Pressure ...............................27.1 million
Coronary Heart Disease ............................7.2 million
Stroke .......................................................3.7 million
Congestive Heart Failure ..........................3.0 million
Atrial Fibrillation ........................................2.0 million
Age, Race, Sex – Differences That Matter
Age, race, ethnicity or sex should not put people at a higher
risk for CVD. But unfortunately, each of these factors has
an impact on whether you are likely to experience a heart
attack or stroke. These differences not only affect your
prospects for having CVD, they also help determine your
chance of survival.
Not surprisingly, the prospect of having some form of
cardiovascular disease increases the older you get.
0
2015 2017 2019 2021 2023 2025
Year and Condition
2027 2029 2031 2033 2035
2
4
6
8
10
12
14
16
18
20
22
24
26
28
30
32
34
36
38
40
42
44
46
48
50
Percent of U.S. Population
Projected Prevalence of Stated Disease (2015-2035)
Any CVD Hypertension CHD CHF Stroke AFib
“ At age 24, your risk for CVD is just
20 percent. By age 45, your chances
more than double to 50 percent. Ninety
percent of individuals over the age of
80 have some form of CVD.”
“ By 2035, nearly half of the U.S.
population will have some form of
cardiovascular disease.”
8
CARDIOVASCULAR DISEASE: A COSTLY BURDEN FOR AMERICA — PROJECTIONS THROUGH 2035
american heart association CVD Burden Report
8
CARDIOVASCULAR DISEASE: A COSTLY BURDEN FOR AMERICA — PROJECTIONS THROUGH 2035
american heart association CVD Burden Report
CVD and its associated risk factors exact a disproportionate
toll on many racial and ethnic groups, accounting for nearly
40 percent of the disparity in life expectancy, for example,
between blacks and whites.
Racial and ethnic minority populations also confront more
barriers to CVD diagnosis and care, receive lower quality
treatment and experience worse health outcomes than their
white counterparts.
Such disparities are linked to a number of complex factors,
such as income and education, residential neighborhood
and physical environment, access to care, social support,
culture and communication barriers. To illustrate just one of
these factors – life expectancy for low-income men in the
United States is 14.6 years lower than men in the highest
income category and for women, the difference is 10.1
years. These disparities have tremendous implications for
diminished earnings potential, labor productivity and stress
on our health care system.
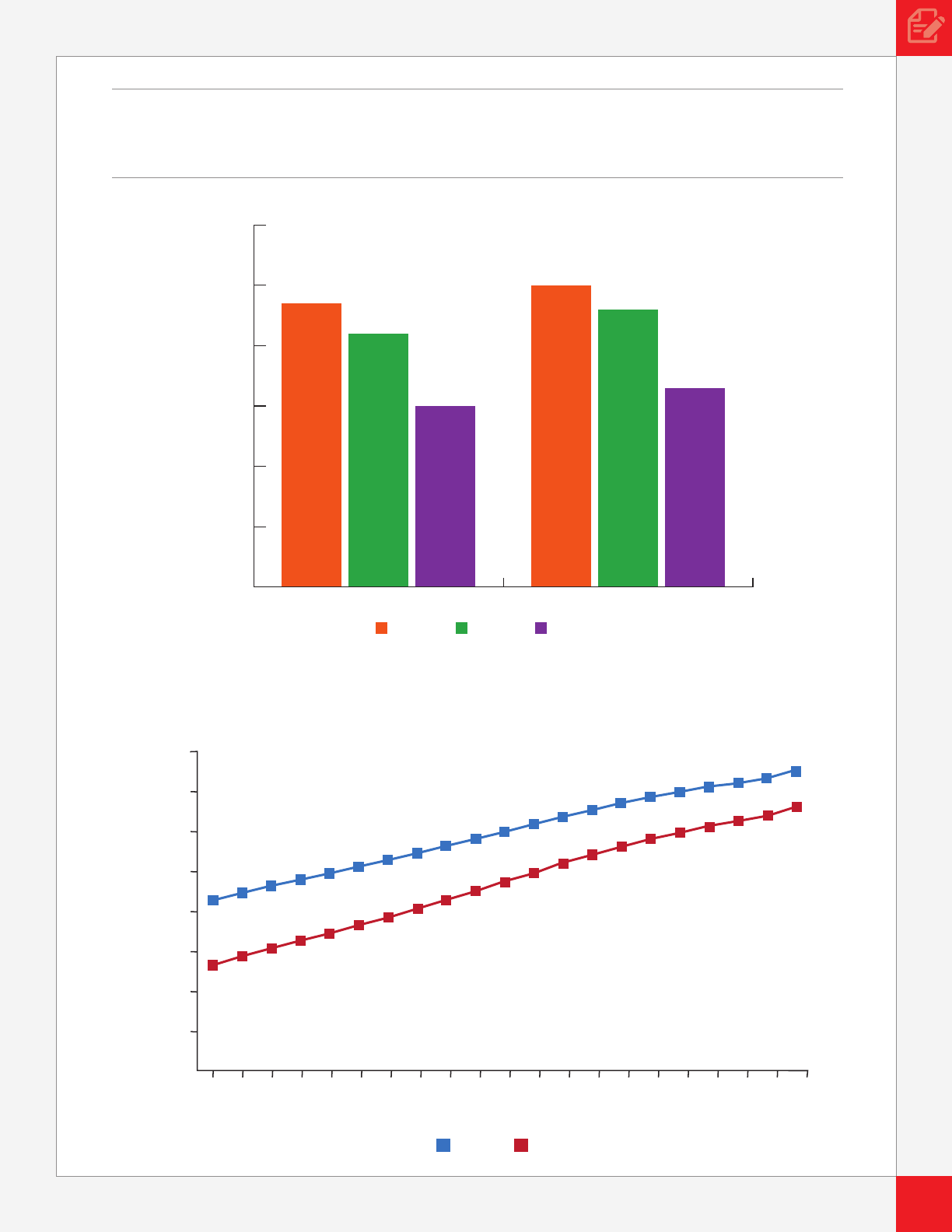
Men are projected to suffer from cardiovascular disease at a
greater rate than women between now and 2035, but women
appear to be catching up. Rates of high blood pressure,
coronary heart disease, congestive heart failure, stroke and
AFib among women are projected to see a huge upsurge.
According to the CDC, heart disease is the leading cause of
death for women in the United States.
Projections: Costs of CVD
Cardiovascular disease not only exacts a heavy toll on the
health of Americans, its economic burden is enormous.
Right now it is America’s costliest disease, and this price tag
will soar in the coming decades.
Prevalence of CVD by Age (2015)
Percent of U.S. Population with CVD
0 10 20 30 40 50 60 70 80 90 100
Age
18-44
45-64 65-79 80+
“ In 2016, CVD cost America
$555 billion. By 2035, the cost will
skyrocket to $1.1 trillion.”
9
CARDIOVASCULAR DISEASE: A COSTLY BURDEN FOR AMERICA — PROJECTIONS THROUGH 2035
american heart association CVD Burden Report
0
2015 2035
10
20
30
40
50
60
Black White Hispanic
Prevalence of CVD by Race
Percent of U.S. Population with CVD
“ In the next two decades, black Americans will have the highest
rates of cardiovascular disease.”
46%
45%
44%
43%
42%
41%
40%
39%
38%
2015 2017 2019 2021 2023 2025
Year
Male Female
Percent of U.S. Population with CVD
2027 2029 2031 2033 2035
Projected Prevalence of CVD by Sex (2015-2035)
10
CARDIOVASCULAR DISEASE: A COSTLY BURDEN FOR AMERICA — PROJECTIONS THROUGH 2035
american heart association CVD Burden Report
10
CARDIOVASCULAR DISEASE: A COSTLY BURDEN FOR AMERICA — PROJECTIONS THROUGH 2035
american heart association CVD Burden Report
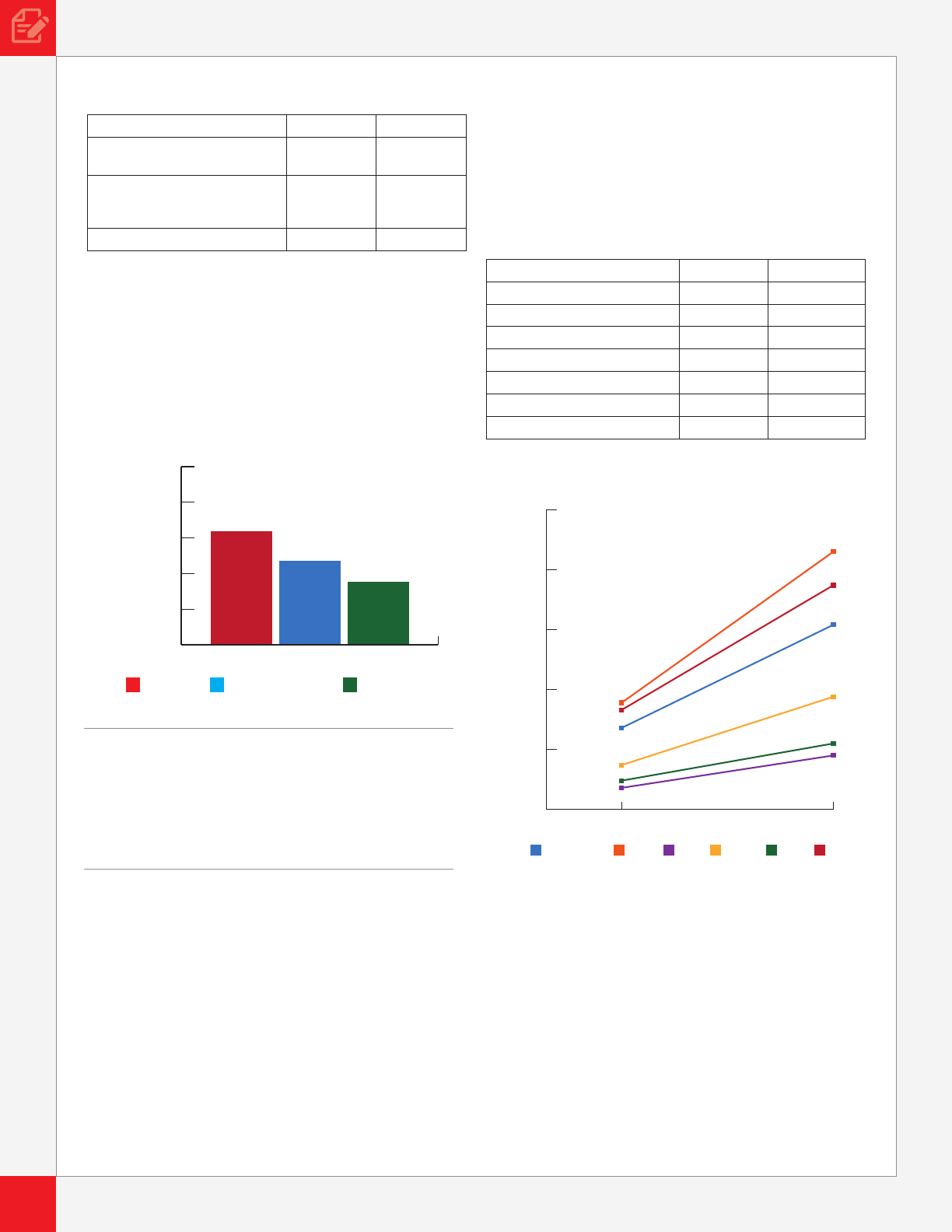
Projections – CVD Total Costs Through 2035
Current 2035
Medical costs up
135 percent
$318 billion $749 billion
Indirect costs up
55 percent
(Lost productivity)
$237 billion $368 billion
TOTAL COSTS $555 billion $1.1 trillion
The Cost Generators: Aging Baby Boomers
As Baby Boomers age, costs for CVD will shift from middle-
aged Americans to individuals ages 65 and over. By 2035,
Boomers who are 80 and older will be the source of the
largest cost increases for CVD.
Medical Costs Breakdown
Direct Costs
Direct medical costs related to CVD are more extensive
than medical costs related to any other disease, including
Alzheimer’s and diabetes.
Such costs include money spent on medical services via a
physician, hospital or health care system, and corresponding
or follow-up costs, such as prescription drugs, home health
or nursing home care.
Direct costs will continue to rise for white, black and Hispanic
Americans with CVD. As the nation’s black and Hispanic
populations increase, costs for both groups over the next two
decades are expected to surpass costs of white Americans.
Regardless of the condition, medical costs will likely triple
over the next 20 years for Hispanics, more than double
among blacks and be higher for women than men.
Projections – CVD Medical Costs Through 2035
Current 2035
High Blood Pressure $68 billion $154 billion
CHD $89 billion $215 billion
CHF $18 billion $45 billion
Stroke $37 billion $94 billion
AFib $24 billion $55 billion
Other $83 billion $187 billion
TOTAL MEDICAL COSTS $318 billion $749 billion
Indirect Costs
Indirect costs of CVD related to lost productivity in
the workplace and at home can also have damaging
consequences.
This study includes projections for two different types of
indirect costs: morbidity and premature mortality.
Costs from morbidity include three components: days
of work lost by employed individuals due to CVD, home
productivity loss (days spent in bed due to CVD and the
need to hire housekeeping services) and work loss among
individuals who are too sick to work.
“ By 2035, across all conditions, total
CVD costs will more than triple
among those age 80+ and more than
double among those age 65-79.”
CVD Alzheimer’s Diabetes
Medical Costs of CVD
Compared to Other Diseases (2015)
$0
$200
$100
$300
$400
$500
Billions of Dollars
OtherHypertension CHD CHF Stroke AFib
$0
$50
2015 2035
$100
$150
$200
$250
Billions of Dollars
Projected CVD Direct Costs Through 2035
by Condition

11
CARDIOVASCULAR DISEASE: A COSTLY BURDEN FOR AMERICA — PROJECTIONS THROUGH 2035
american heart association CVD Burden Report
Costs from mortality include the value of lost earnings and
household productivity from premature death due to CVD.
Individuals age 45-64 face the highest indirect costs due to
CVD. While white Americans face the highest indirect costs,
Hispanics are expected to experience the largest relative
increase over the next 20 years.
Projections – CVD Indirect Costs Through 2035
Current 2035
High Blood Pressure $42 billion $67 billion
CHD $99 billion $151 billion
CHF $11 billion $19 billion
Stroke $30 billion $49 billion
AFib $7 billion $11 billion
Other $48 billion $71 billion
TOTAL COSTS $237 billion $368 billion
$50
$100
$150
$200
$250
$300
$350
$400
$450
$500
$0
2015 2017 2019 2021 2023 2025
Billions of Dollars
Age
Year
2027 2029 2031 2033 2035
Projected Total (Direct + Indirect) Costs
of CVD by Age (2015–2035)
45-64
18-44
65-79
80+
$0
$50
$100
$150
$200
OtherHypertension CHD CHF Stroke AFib
2015 2035
Billions of Dollars
Projected CVD Indirect Costs Through 2035
by Condition

13
CARDIOVASCULAR DISEASE: A COSTLY BURDEN FOR AMERICA — PROJECTIONS THROUGH 2035
american heart association CVD Burden Report
Recommendations
As the oldest and foremost organization dedicated to
improving the cardiovascular health of all Americans,
the American Heart Association advocates for policies
that support a robust research agenda, help prevent
cardiovascular disease and broaden access to affordable,
high quality care. To address the escalating burden of
cardiovascular disease highlighted in this report, the
association recommends the following changes in
federal policies:
• Increasing NIH research funding for heart disease
and stroke.
• Enhancing focus on prevention to improve and
preserve population health from birth to old age.
• Preserving and expanding access to high quality
affordable health care.
Research
Robust NIH-funded heart and stroke research is our
country’s best hope to discover innovative ways to prevent,
treat and ultimately develop cures for heart disease
and stroke. This analysis acknowledges the enormous
progress that has been made in the ght against CVD while
recognizing the signicant challenges that lie ahead.
Now is the time to make meaningful investment in the
NIH and the CDC. NIH-funded biomedical research has
resulted in nearly a 70 percent reduction in the death rate
for coronary disease and stroke over the past century. But,
as this analysis shows, we need to do more if we are to stop
the rising tide of CVD prevalence that is already outpacing
previous predictions.
In addition, the association supports health services,
genomics and population and epidemiological studies
conducted by other federal agencies.
There is no one-size-ts-all answer to the questions of who
gets CVD and why. This analysis clearly points out that age,
race and sex can increase risk and determine survival rates.
Given these ndings, we advocate for addressing disparities,
removing barriers to medical research and increasing
participation of women, racial and ethnic minorities, and
older Americans in clinical research. This forward thinking
is also critical in light of the higher prevalence rates among
black and older Americans, and for certain types of CVD that
disproportionately affect women and Hispanics.
Prevention
Even today, stroke and heart failure top the list of chronic
conditions that account for the most spending in the
Medicare fee-for-service program. This spending pattern
reects how the U.S. health care system often rewards
efforts that treat disease and injury rather than those that
prevent them. Cardiovascular disease is largely preventable,
and prevention programs represent an enormous return on
investment by reducing some costs and promoting patient
well-being, including length and quality of life.
Rather than treating illness when it is far advanced, the
American Heart Association advocates for heart-healthy
habits and wellness throughout a person’s life – and the
earlier the better. Those who follow a lifestyle of regular
exercise, a heart-healthy diet and regular screenings for
blood pressure, cholesterol and diabetes can dramatically
reduce their risk of developing CVD. If we have any chance
of overcoming the burden that heart disease and stroke
impose on our health care costs, our workforce productivity
and our quality of life, we have to commit to policies,
systems and environment changes that can transform
population health.
We must promote access to healthy, affordable foods and
beverages, and provide fully transparent nutrition labeling
to help keep consumers informed about food and beverage
choices and encourage healthy eating. To this end, we
strongly support federal programs that provide nutritious
foods and meals to our most vulnerable populations such
as children, older americans and low-income individuals,
including keeping nutrition standards for school meals
strong and evidenced-based.
To reverse sedentary behavior, the association supports
science-based policies that promote physical activity and
physical education in schools and early care and education;
deliver exercise prescriptions in the clinical environment;
include investments in biking and walking in transportation
infrastructure; increase and improve recreational spaces in
communities; and reduce sedentary work environments.
Prevention and control efforts have contributed to a decline
in U.S. cigarette consumption by more than 24 percent over
the past 10 years. However, new products like e-cigarettes
that are especially enticing to children have entered the
marketplace. We will continue to address CVD risk factors
such as tobacco use by strongly supporting FDA regulation
of these products; advocating for comprehensive clean
indoor air laws and increased tobacco excise taxes;
raising the purchasing age for tobacco to 21; and ensuring
comprehensive coverage of tobacco cessation services in
public and private health care plans.
Finally, a focus on prevention in the workplace is a win for
both employees and employers. Prevention strategies keep
workers healthy and productive and help employers steer
clear of economic losses from morbidity and mortality. A
2012 study conducted by researchers at the University of
Colorado found that each short-term disability claim led
because of a heart attack or hindering chest pain resulted
in nearly $8,000 in lost productivity, while long-term claims
resulted in a more than $52,000 loss to employers.
14
CARDIOVASCULAR DISEASE: A COSTLY BURDEN FOR AMERICA — PROJECTIONS THROUGH 2035
american heart association CVD Burden Report
14
CARDIOVASCULAR DISEASE: A COSTLY BURDEN FOR AMERICA — PROJECTIONS THROUGH 2035
american heart association CVD Burden Report
Affordable Health Care
The American Heart Association has long advocated for
policies that expand access to meaningful and affordable
health care coverage for all Americans. This report makes
clear that if we do not address CVD risks for all Americans,
we will fall short of our goals to eliminate heart disease and
stroke. Building on this evidence, the association supports
policies that remove barriers to affordable and quality health
care and preventive benets, improve the delivery of timely,
quality health care, and eliminate disparities.
Although the future of the Affordable Care Act remains
in ux, it is crucial to the association that lawmakers and
administration ofcials provide Americans with an option
for high quality, affordable health care coverage and protect
programs such as Medicare, Medicaid and CHIP that serve
our must vulnerable populations. In addition, we support
payment models for the use of telehealth and mobile health
technologies and call for an adequate supply of and access
to affordable pharmaceuticals and devices.
This research points to a future where more and more
Americans will likely suffer and die from CVD. It speaks
also to the mission of the American Heart Association
and its more than 30 million volunteers and supporters
who work each day to help everyone in our nation build
healthier lives free of heart disease and stroke.
We dedicate this report to them.
©2017, American Heart Association 1/17DS11775
For More Information, Contact:
The American Heart Association Office of Federal Advocacy
1150 Connecticut Ave., NW, Suite 300, Washington, DC 20036
www.heart.org/advocacy
