
United States Government Accountability Office
Washington, DC 20548
September 9, 2005
The Honorable Charles E. Grassley
Chairman
The Honorable Max Baucus
Ranking Minority Member
Committee on Finance
United States Senate
The Honorable John D. Rockefeller, IV
United States Senate
Subject:
Overview of the Long-Term Care Par nership Program
t
In 2003, the most recent year for which data are available, national spending on long-
term care totaled $183 billion,
1
and nearly half of that was paid for by the Medicaid
program, the joint federal-state health care financing program that covers basic
health and long-term care services for certain low-income individuals. Private
insurance paid a small portion of long-term care expenditures—about $16 billion or
9 percent in 2003. With the aging of the baby boom generation, long-term care
expenditures are anticipated to increase sharply in coming decades. The projected
spending on long-term care presents a looming fiscal challenge for federal and state
governments. As a result, some policymakers are looking for ways to reduce the
proportion of long-term care spending financed by Medicaid and promote private
insurance as a larger funding source.
The Long-Term Care Partnership Program is a public-private partnership between
states and private insurance companies, designed to reduce Medicaid expenditures
by delaying or eliminating the need for some people to rely on Medicaid to pay for
long-term care services. Individuals, who buy select private long-term care insurance
policies that are designated by a state as partnership policies and eventually need
long-term care services, first rely on benefits from their private long-term care
insurance policy to cover long-term care costs before they access Medicaid. To
qualify for Medicaid, applicants must meet certain eligibility requirements, including
income and asset requirements. Traditionally, applicants cannot have assets that
exceed certain thresholds and must “spend down” or deplete as much of their assets
as is required to meet financial eligibility thresholds. To encourage the purchase of
private partnership policies, long-term care insurance policyholders are allowed to
1
Long-term care includes nursing home services, home health, personal care services, assisted living,
and noninstitutional group living arrangements.
GAO-05-1021R Long-Term Care Partnership Program

protect some or all of their assets from Medicaid spend-down requirements during
the eligibility determination process, but they still must meet income requirements.
2
You asked that we provide summary information about the Long-Term Care
Partnership Program. As agreed with your staff, we examined the demographics of
program participants, the types of policies purchased, and the benefits accessed by
policyholders. On August 18, 2005, we briefed your staff on this information, and this
letter formally conveys our findings. Enclosure I contains the slides we provided
during our briefing with some revisions to incorporate updated information.
To do our work, we interviewed officials from the four states that offer Long-Term
Care Partnership Programs—California, Connecticut, Indiana, and New York—and
reviewed their quarterly reports and other official documents. While all four of the
states with partnership programs collect some information on their programs, the
states do not all collect the same information. The programs began in different years
and data reported by the states are based on different time periods. Therefore, in
some cases, we report information only for those states that had available data.
Based on discussions with state officials and reviewing documentation on uniformly
collected insurer data and surveys of policyholders, we determined that the
information we report was sufficiently reliable for our purposes. We also examined
reports on the program from the Congressional Budget Office, the Congressional
Research Service, and other research organizations. We provided a draft of the
enclosure to officials in the four partnership states for their review. They provided us
with technical comments that we incorporated as appropriate. We conducted our
work from July through September 2005 in accordance with generally accepted
government auditing standards.
Background
The Long-Term Care Partnership Program began in 1987 as a demonstration project
funded through the Robert Wood Johnson Foundation. As part of the demonstration
project, four states—California, Connecticut, Indiana, and New York—developed
partnership programs.
3
These programs are designed to encourage the purchase of
private long-term care insurance, especially among moderate income individuals,
thereby potentially reducing future reliance on Medicaid as a funding source for long-
term care services. Based on the most recently available data, there are over 172,000
active partnership policies in the four states.
2
The definition of assets differs between the Long-Term Care Partnership Program and Medicaid. The
Long-Term Care Partnership Program uses the term assets to denote savings and investments, and
excludes income. For purposes of Medicaid eligibility, assets include both income, which is anything
received during a calendar month that is used or could be used to meet food, clothing, or shelter
needs, and resources, which are anything owned, such as savings accounts, stocks, or property.
3
In general, federal statute limits most states from implementing new partnership programs. To
protect assets under the Long-Term Care Partnership Program, participating states exempt some or all
assets from Medicaid’s estate recovery requirement, which generally requires adjustment or recovery
from an individual’s estate for the costs of medical assistance provided. With the enactment of the
Omnibus Budget Reconciliation Act of 1993, states were no longer allowed to disregard estate assets
from recovery unless the practice had been approved as of May 14, 1993.
GAO-05-1021R Long-Term Care Partnership Program
2

The four states vary in how their partnership programs protect policyholders’ assets.
The programs in California and Connecticut have dollar-for-dollar models, in which
the dollar amount of protected assets is equivalent to the dollar value of the benefits
paid by the long-term care insurance policy. For example, a person purchasing a
long-term care insurance policy with $300,000 total coverage would have $300,000 of
assets protected if she were to exhaust the long-term care insurance benefits and
apply for Medicaid. New York’s program requires the purchase of a comprehensive
long-term care insurance policy, covering a minimum of 3 years of nursing home care
and 6 years of home and community-based care, but offers total asset protection for
all of the purchaser’s assets at the time of Medicaid eligibility determination.
Indiana’s program uses a hybrid model that allows purchasers to obtain
dollar-for-dollar protection up to a certain benefit level as defined by the state; all
policies with benefits above that threshold provide total asset protection for the
purchaser.
Demographics of Program Participants
The average age of partnership policyholders at the time of purchase ranged from 58
to 63 in Connecticut, Indiana, and New York. The median age of partnership
policyholders in California was 60. Most partnership policyholders were female,
married, and purchasing long-term care insurance for the first time. In California and
Connecticut surveys of persons who purchased a partnership policy, most
policyholders reported being in good or very good health. In the three states that
surveyed a sample of partnership policyholders—California, Connecticut, and
Indiana—the majority of policyholders in each of these states reported that their total
assets were greater than $350,000.
4
About half or more of the policyholders in each of
these three states also reported average monthly household incomes of greater than
$5,000.
Policies Purchased
In 2004, the number of partnership policies purchased ranged from about 4,000 in
Indiana to nearly 10,000 in California. The number of partnership policies purchased
each year has increased significantly since the programs began in the early 1990s,
though there has been a decline or leveling off in the number of policies purchased in
recent years. State partnership officials from two states reported that the reason for
the decline in sales of partnership policies in recent years is not specific to
partnership policies but is reflective of overall trends in the long-term care insurance
market. Most partnership policies are comprehensive, covering both nursing home
care and home and community-based care, and are bought individually rather than
through group or organization-sponsored programs. While most applications for
partnership policies were approved, approximately 16 percent were denied.
4
In a policyholder survey, California and Connecticut instructed policyholders to exclude the value of
homes and cars when reporting their assets. Indiana instructed policyholders to include the value of
their homes.
GAO-05-1021R Long-Term Care Partnership Program
3

The amount of coverage purchased by partnership policyholders varies across the
four states. The average daily benefit amount for nursing home care in Connecticut
was approximately $188 per day. The most common daily benefit amounts purchased
for nursing home care in Indiana were $110 and $120 per day. These amounts were
calculated using the daily benefit amounts at the time of purchase and are not
adjusted for inflation.
5
Average premiums for partnership policies differ across states and are based on age
and benefits purchased. For example, in Connecticut average annual premiums for a
comprehensive policy covering 1 year of care with a $200 daily benefit amount range
from $1,500 for a 55-year-old purchaser to $3,400 for a 70-year-old. If the 55-year-old
purchased the same policy with a 3-year benefit period rather than a 1-year benefit
period, the annual premiums would have been $2,500.
Data from Indiana suggest that when consumers are given the incentive of total asset
protection, they are likely to purchase more insurance coverage. Prior to 1998, when
Indiana introduced total asset protection as an option in addition to dollar-for-dollar
asset protection policies, only 29 percent of policies purchased had total coverage
amounts large enough to trigger total asset protection. In contrast, in the first quarter
of 2005, 87 percent of policies purchased were large enough to trigger total asset
protection.
Benefits Accessed by Policyholders
Less than 1 percent of active partnership policyholders are currently accessing their
long-term care insurance benefits. Since the programs began, 251 policyholders in all
four states have exhausted their long-term care insurance benefits. Of those 251
policyholders, 119 (47 percent) have accessed Medicaid. The remaining 53 percent
have not accessed Medicaid. According to interviews with state officials, this may be
because they are spending down income or unprotected assets, their health has
improved, or their families provide informal care. More policyholders have died
while receiving long-term care insurance benefits (899 policyholders) than have
exhausted their long-term care insurance benefits (251 policyholders), which could
suggest that the Long-Term Care Partnership Program may be succeeding in
eliminating some participants’ need to access Medicaid. However, it is difficult to
determine whether and to what extent the Long-Term Care Partnership Program has
resulted in cost savings to the Medicaid program because there are insufficient data
to determine if those individuals who have purchased partnership policies would
have accessed Medicaid had they not purchased long-term care insurance benefits.
Comments from Partnership States
We provided a draft of the enclosure to officials in the four partnership states for
their review. They provided us with technical comments that we incorporated as
appropriate.
5
Most partnership policies are required to have inflation protection. For example, New York generally
requires inflation protection; however, purchasers age 80 or older are not required to have inflation
protection as part of their policies.
GAO-05-1021R Long-Term Care Partnership Program
4
- - - - -
As agreed with your offices, unless you publicly announce the contents earlier, we
plan no further distribution of this report until 30 days after its date. We will then
provide copies of this report upon request. In addition, the report will be available at
no charge on the GAO Web site at
http://www.gao.gov.
If you or your staff have any questions about this report please contact me at (202)
512-7119 or dickenj@gao.gov. Contact points for our Offices of Congressional
Relations and Public Affairs may be found on the last page of this report. GAO staff
who made major contributions to this report are Krister Friday, Clare Mamerow, and
Anna Theisen-Olson.
John E. Dicken
Director, Health Care
Enclosure – 1
GAO-05-1021R Long-Term Care Partnership Program
5
1
The Long-Term Care Partnership Program:
An Overview
Briefing to Congressional Staff
Enclosure 1
6 GAO-05-1021R Long-Term Care Partnership Program
2
Enclosure 1
Briefing contents
• This briefing provides information about the Long-Term Care
Partnership Program:
• Background and overview
• Demographics of program participants
• Policies purchased
• Benefits accessed by policyholders
Enclosure 1
GAO-05-1021R Long-Term Care Partnership Program
7
3
Enclosure 1
Background and overview
• The Long-Term Care Partnership Program is a public-private partnership designed
to encourage persons with moderate income to purchase private long-term care
insurance to fund their long-term care needs rather than relying on Medicaid
• Individuals who buy a partnership policy and eventually need long-term care
services first rely on benefits from their private long-term care insurance policy
to cover long-term care costs
• If the policyholders exhaust private long-term care insurance benefits and need
assistance from Medicaid to fund long-term care, they may protect some or all
of their assets
1
from Medicaid spend-down requirements during the eligibility
determination process;
2
however, they are still subject to Medicaid income
requirements
• One goal of the Long-Term Care Partnership Program is to save money for Medicaid
by delaying or eliminating the need for participants to access Medicaid for long-term
care services
1
The Long-Term Care Partnership Program uses the term assets to denote savings and investments, and excludes
income. For purposes of Medicaid eligibility, assets include both income, which is anything received during a
calendar month that is used or could be used to meet food, clothing, or shelter needs, and resources, which are
anything owned, such as savings accounts, stocks, or property.
2
In some cases, policyholders can access Medicaid before exhausting their private insurance benefits if their actual
assets are less than or equal to the amount of insurance benefits paid.
GAO-05-1021R Long-Term Care Partnership Program
8
4
Enclosure 1
Background and overview (continued)
• As a result of a Robert Wood Johnson Foundation
demonstration project, four states have operated
partnership programs since the early 1990s (California,
Connecticut, Indiana, and New York)
• Over 172,000 partnership policies are active in the four
states
• The Omnibus Budget Reconciliation Act of 1993 limits
most states from implementing partnership programs
GAO-05-1021R Long-Term Care Partnership Program
9
5
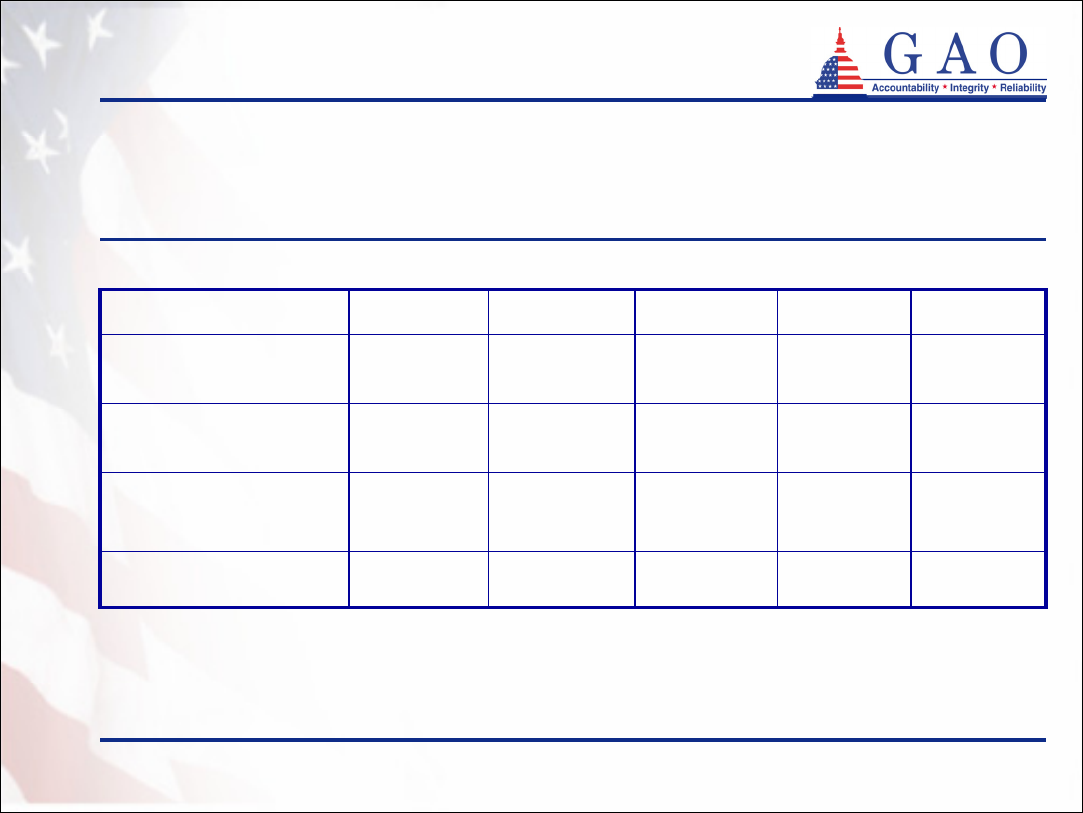
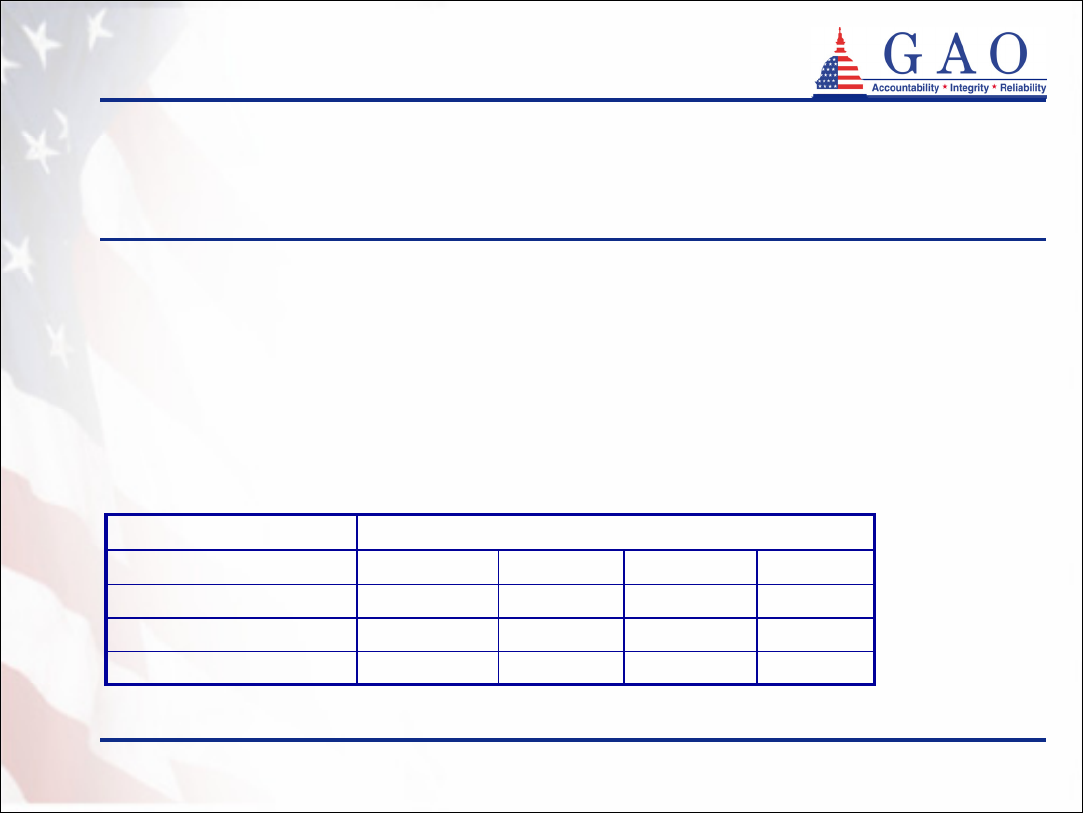
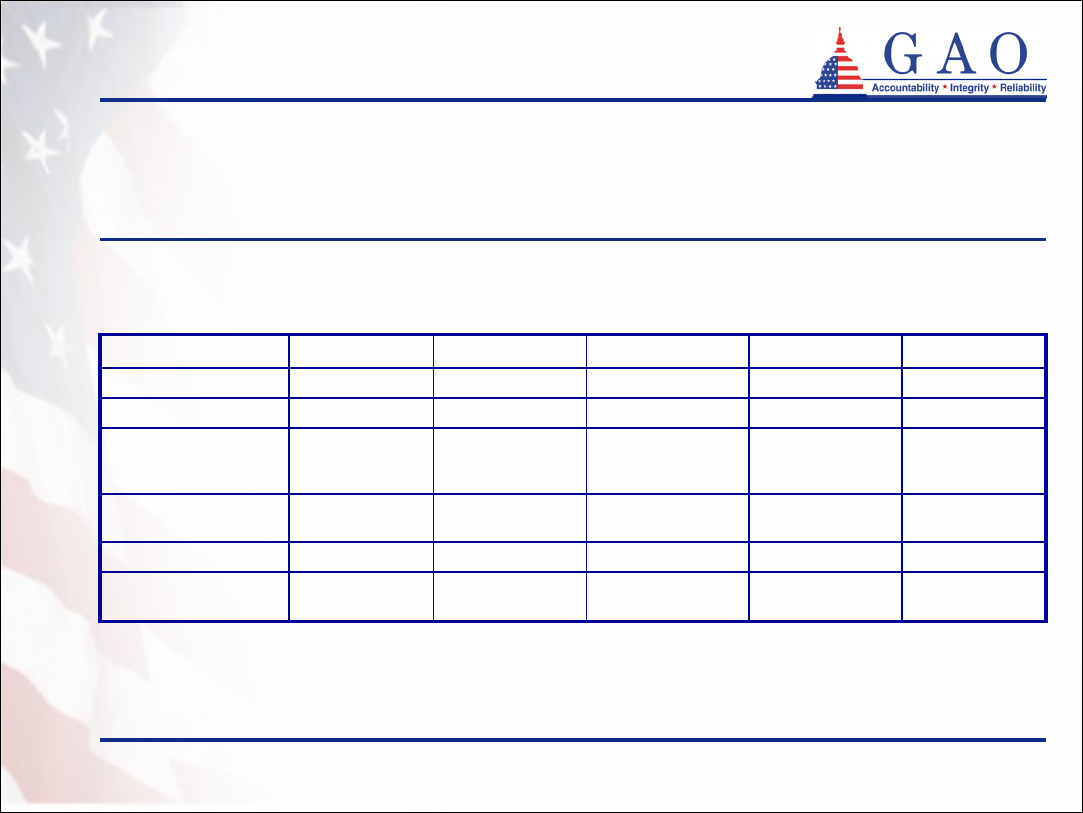
Enclosure 1
Background and overview (continued)
• The four states with partnership programs offer one of three program
models (see table 1). These models exempt different levels of assets from
Medicaid spend-down requirements
• Dollar-for-dollar: Assets are protected up to the amount of the private
insurance benefit paid
• Total asset protection: All assets are protected when a state-defined
minimum benefit package is paid
• Hybrid: Program offers both dollar-for-dollar and total asset protection.
The type of asset protection depends on the initial amount of coverage
purchased. Total asset protection is available for policies with initial
coverage amounts greater than or equal to a coverage level defined by
the state
GAO-05-1021R Long-Term Care Partnership Program
10
6
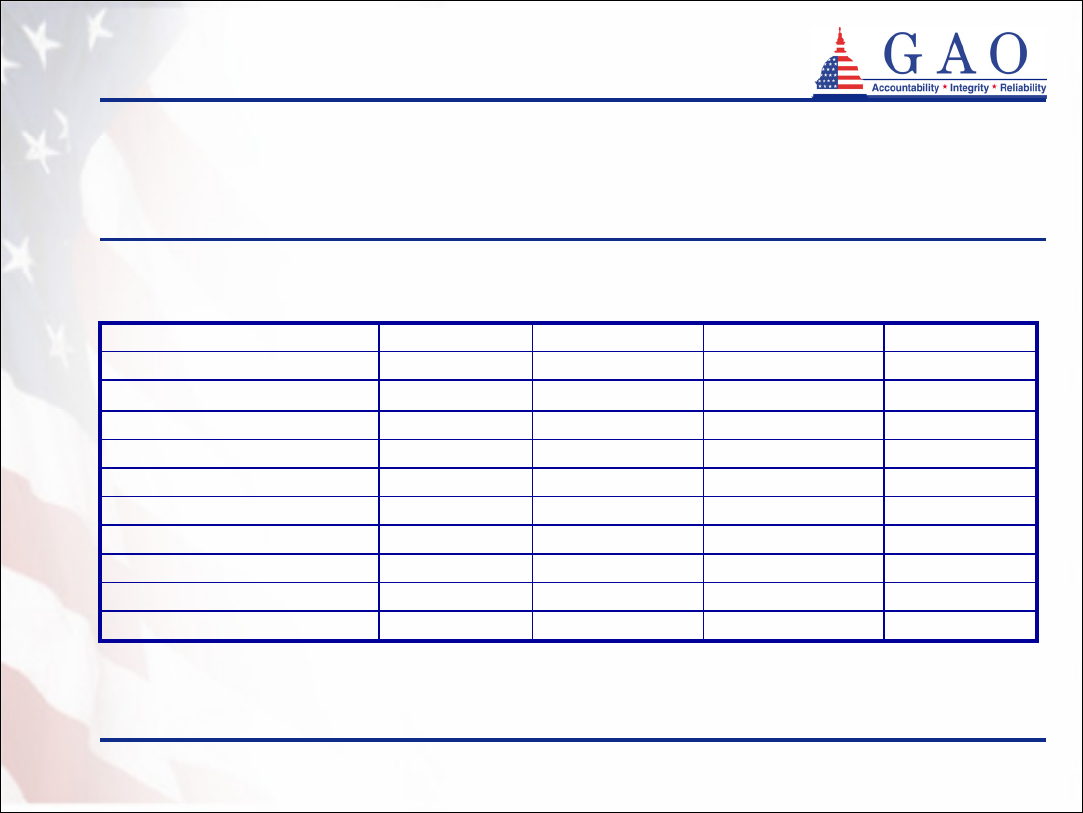
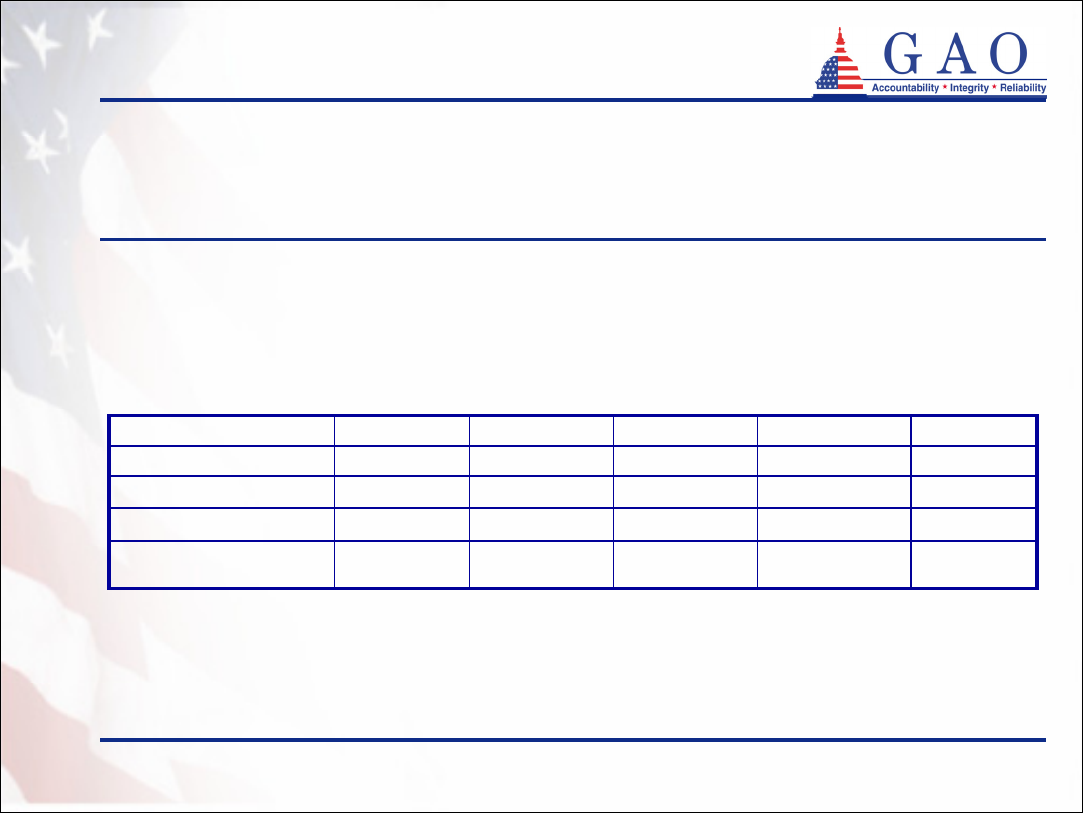
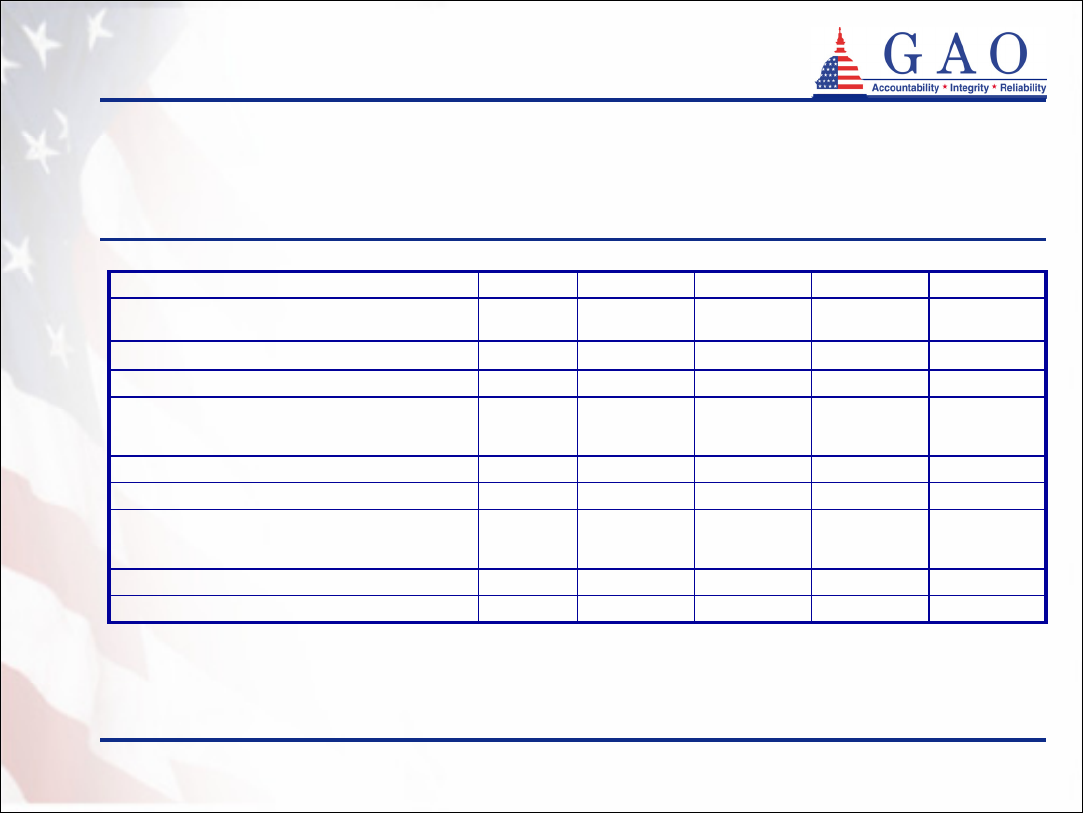
Enclosure 1
Background and overview (continued)
17
c
81385Number of
participating insurance
companies
172,47747,53929,18930,83464,915Number of active
partnership policies
-Total asset
protection
HybridDollar-for-
dollar
Dollar-for-
dollar
Partnership model
-1993199319921994Year implemented
TotalNew York
b
Indiana
a
Connecticut
a
California
a
Table 1: Overview of Partnership Programs
Sources: GAO analysis of data from
Robert Wood Johnson Foundation
California Partnership for Long-Term Care
Connecticut Partnership for Long-Term Care
Indiana Long-Term Care Insurance Program
New York State Partnership for Long-Term Care
a
Based on data through March 2005
b
Based on data through December 2004
c
Some insurers participate in more than one state
GAO-05-1021R Long-Term Care Partnership Program
11
7
Enclosure 1
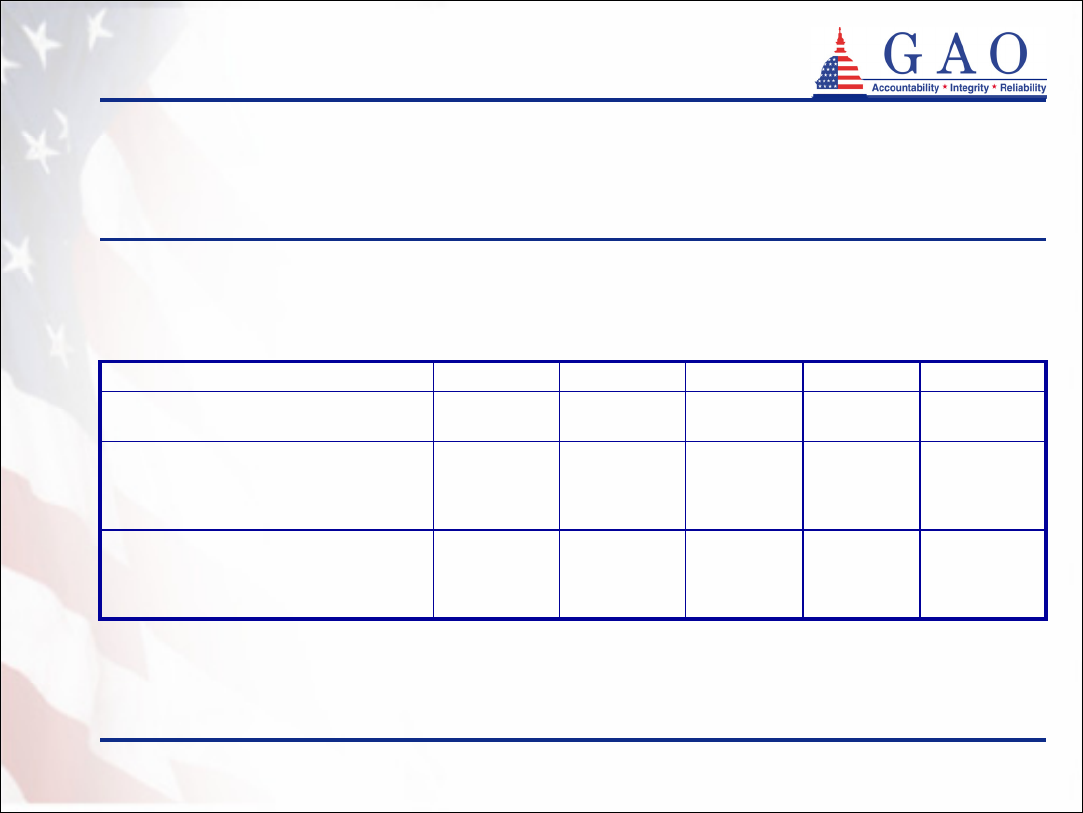
Demographics of program participants
• Average age of partnership policyholders at time of purchase
ranges from 58 to 63 in Connecticut, Indiana, and New York.
The median age of partnership policyholders in California is
60 (see table 2)
• More partnership policyholders are female than male
• Most partnership policyholders are married
• Most partnership policy purchasers are buying long-term care
insurance for the first time
GAO-05-1021R Long-Term Care Partnership Program
12
8
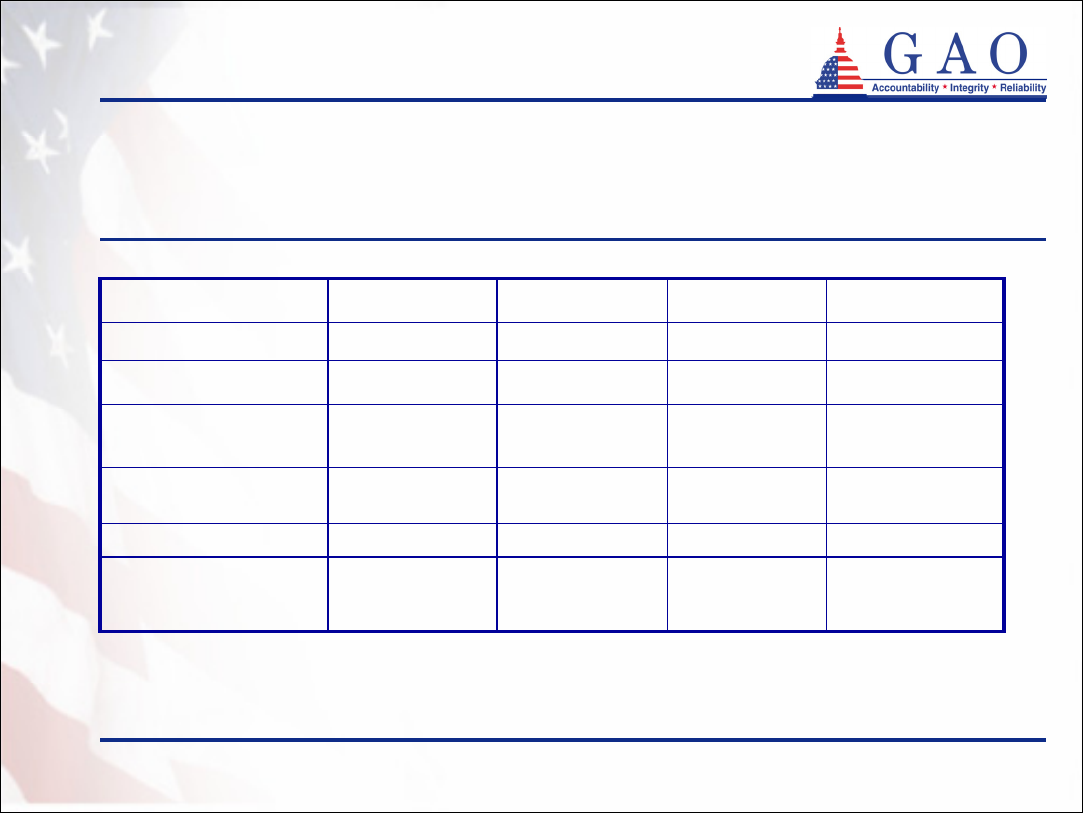
Enclosure 1
Demographics of program participants
(continued)
Average age: 63Average age: 62Average age: 58Median age: 60Age
19 – 9619 – 9020 – 8918 – 92Age range
95%94%92%94%First time purchasers
3%1%0%
c
1%
Unknown
25%21%23%
c
29%
Not married
72%78%76%
c
70%
Married
Marital status
41%43%44%41%
Male
59%57%56%59%
Female
Sex
New York
b
Indiana
a
Connecticut
a
California
a
Table 2: Demographics of Partnership Policyholders at Time of
Purchase
Sources: California Partnership for Long-Term Care
Connecticut Partnership for Long-Term Care
Indiana Long-Term Care Insurance Program
New York State Partnership for Long-Term Care
a
Based on data through March 2005
b
Based on data through December 2004
c
Based on data through June 2004
Note: Percentages may not add to 100 due to rounding
GAO-05-1021R Long-Term Care Partnership Program
13
9
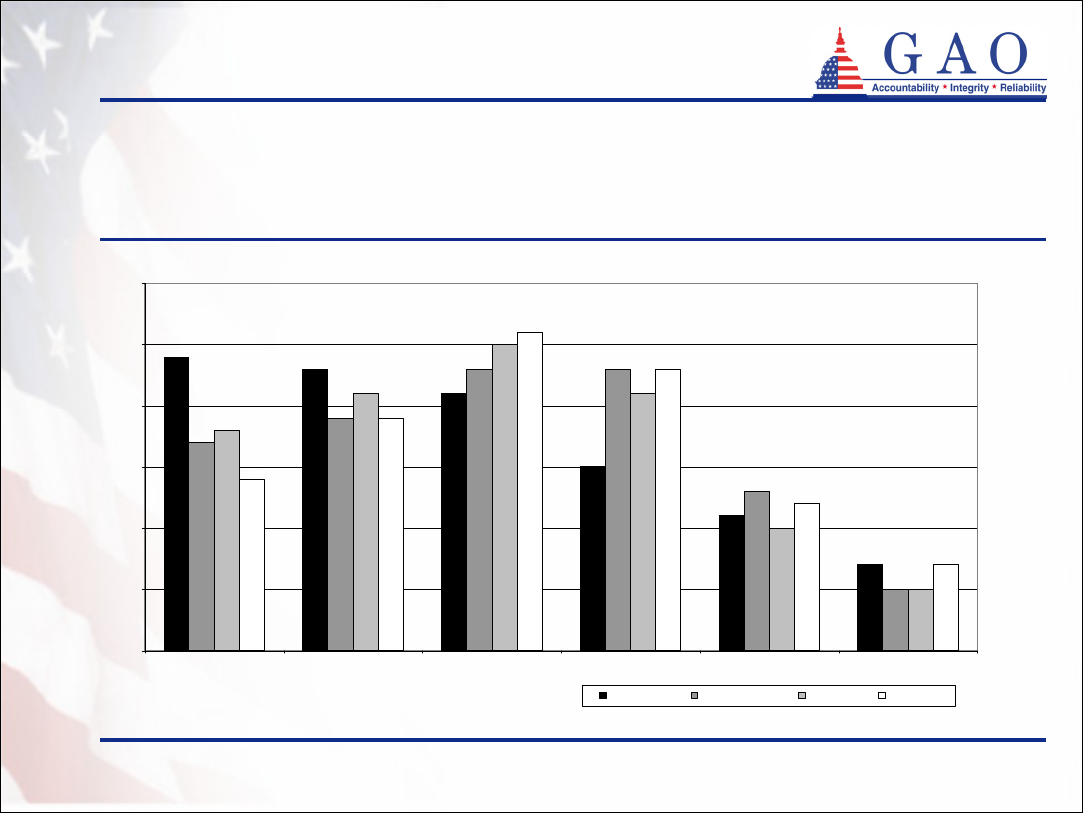
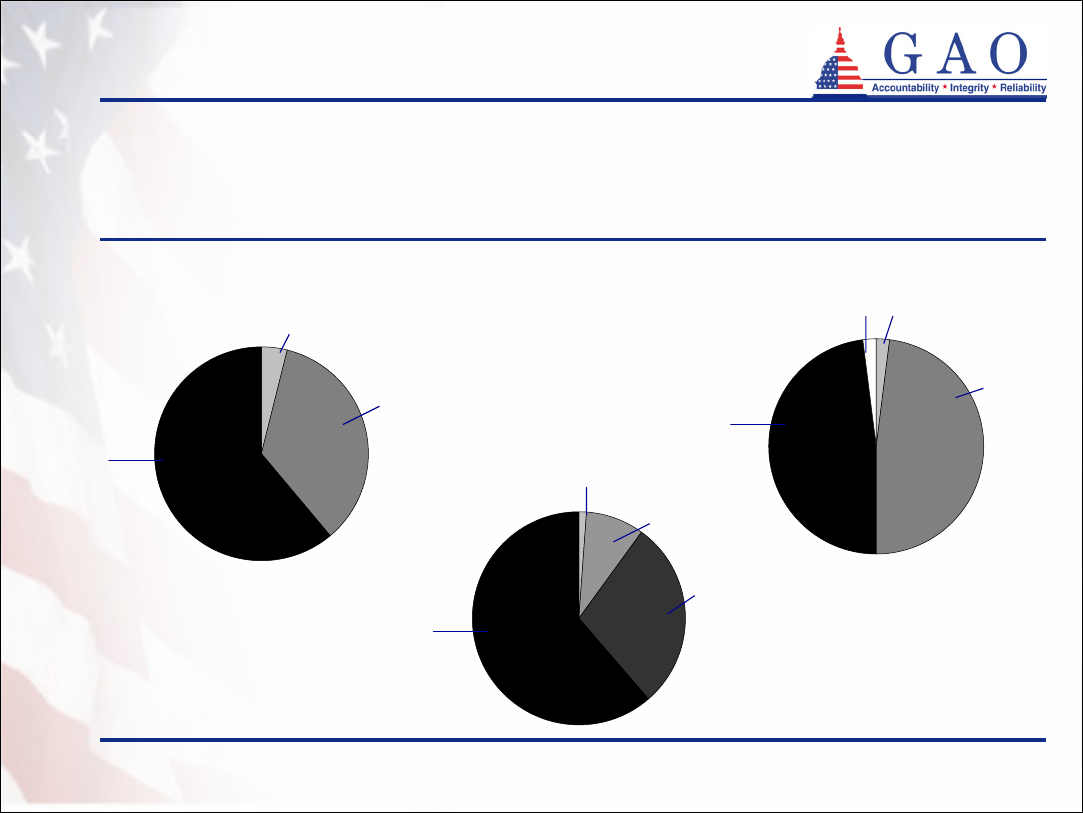
Enclosure 1
23%
21%
15%
11%
7%
23%
13%
5%
25%
10%
5%
26%
23%
12%
7%
24%
23%
19%
17%
21%
21%
18%
19%
14%
0%
5%
10%
15%
20%
25%
30%
<55 55-59 60-64 65-69 70-74 75+
California
Connecticut
Indiana
New York
Demographics of program participants
(continued)
Figure 1: Age Distribution of Partnership Policyholders at Time of Purchase
Sources: GAO analysis of data from
California Partnership for Long-Term Care, data through March 2005
Connecticut Partnership for Long-Term Care, data through June 2004
Indiana Long-Term Care Insurance Program, data through March 2005
New York State Partnership for Long-Term Care, data through December 2004
Age Range
Note: Percentages may not add to 100 due to rounding
GAO-05-1021R Long-Term Care Partnership Program
14
10
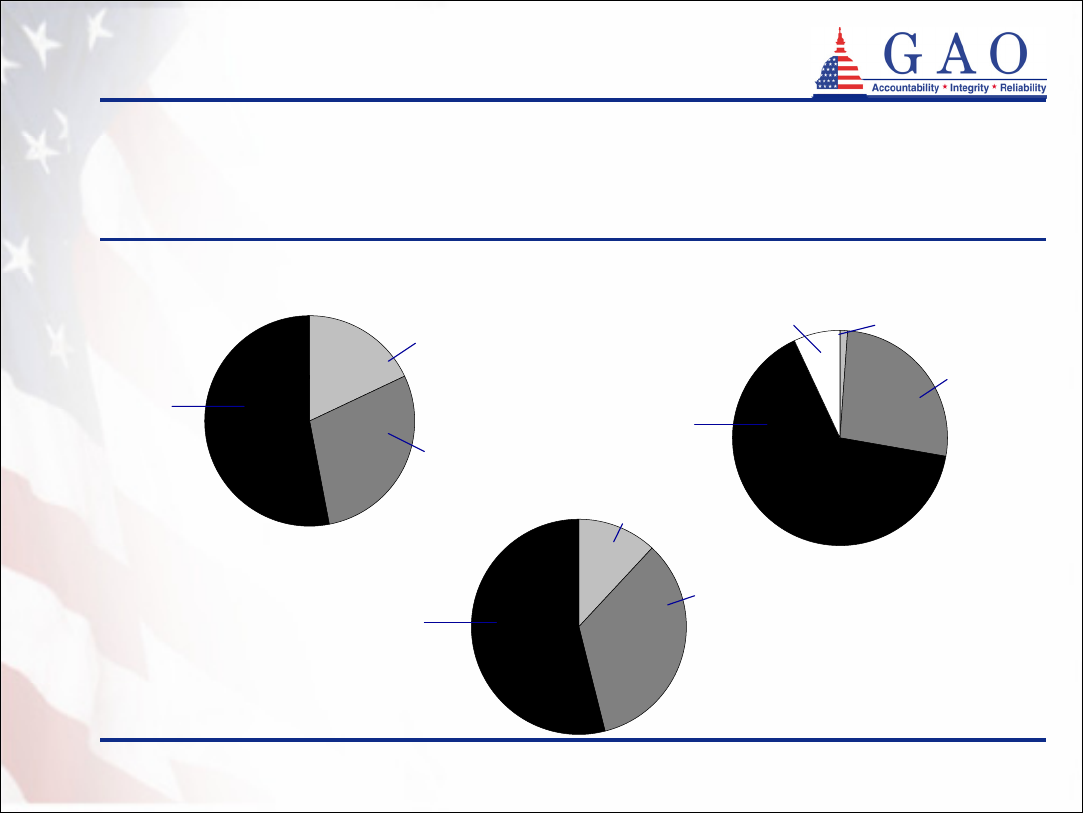
Enclosure 1
Demographics of program participants
(continued)
• California, Connecticut, and Indiana surveyed a sample of
policyholders at the time they purchased their policies
1
• The majority of policyholders in each of the three states
reported having total assets greater than $350,000 (see
figure 2)
2
• About half or more of policyholders in each of the three states
reported average monthly household incomes of greater than
$5,000 (see figure 3)
1
Recent income and asset information is not available from New York
2
California and Connecticut instructed policyholders to exclude the value of homes and cars when reporting their
assets. Indiana instructed policyholders to include the value of their homes.
GAO-05-1021R Long-Term Care Partnership Program
15
11
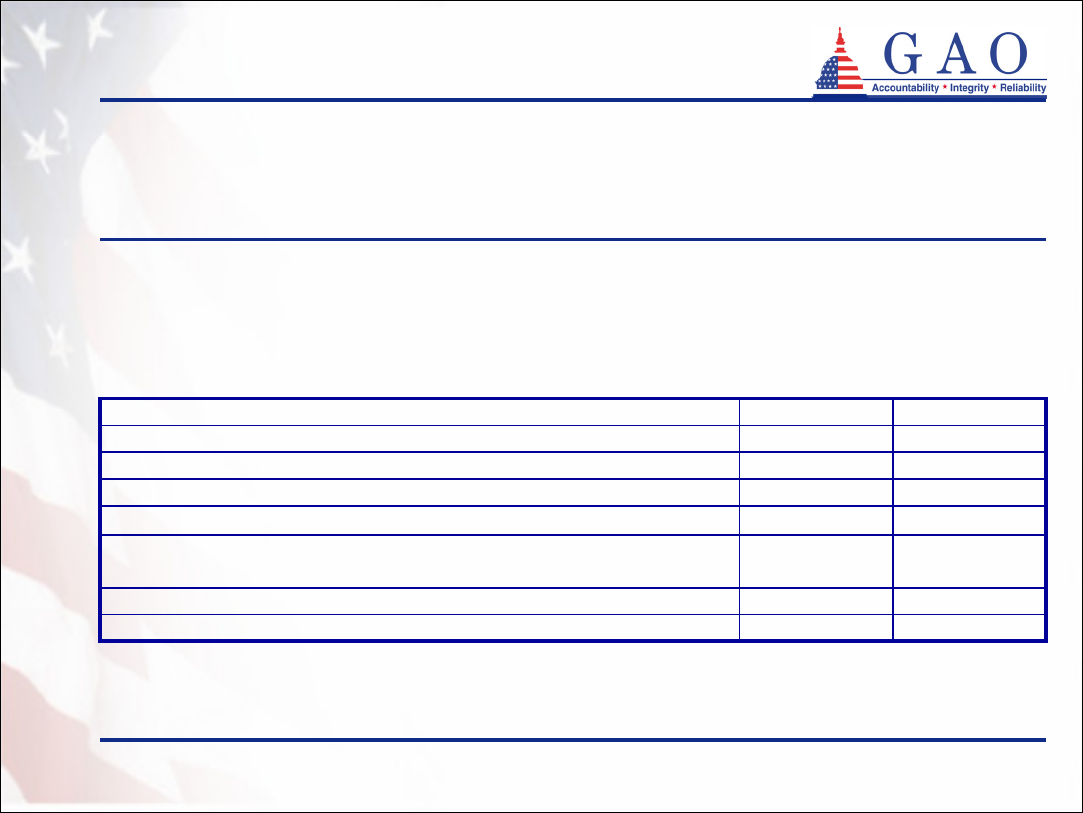
Enclosure 1
Demographics of program participants
(continued)
Connecticut
d
Figure 2: Distribution of Policyholders’ Reported Assets in Three
Partnership States
a
Indiana
c
Sources: GAO analysis of survey data from
California Partnership for Long-Term Care
Connecticut Partnership for Long-Term Care
Indiana Long-Term Care Insurance Program
a
California and Connecticut exclude the value of homes and cars
b
Based on survey data from calendar year 2003
c
Based on survey data from calendar year 2004
d
Based on survey data from July 2003 to June 2004
Less than $100,000
$100,000 - $349,999
Less than $100,000
$100,000 -
$349,999
Unknown
12%
34%
7% 1%
27%
Less than $100,000
California
b
18%
29%
Greater than
$350,000
53%
$100,000 - $350,000
$350,000
or greater
54%
$350,000
or greater
66%
Note: Percentages may not add to 100 due to rounding
GAO-05-1021R Long-Term Care Partnership Program
16
12
Enclosure 1
Demographics of program participants
(continued)
California
a
Connecticut
c
Figure 3: Distribution of Policyholders’ Reported Monthly Household
Income in Three Partnership States
Indiana
b
Greater than
$5,000
$5,000 or
greater
$5,000 or
greater
Less than $2,000
$2,000 - $4,999
Less than $1,000
$1,000 - $2,499
$2,500 - $4,999
Less than $2,000
$2,000 –
$4,999
Unknown
4%
35%
61%
1%
9%
29%
2%
49%
49%
2%
Note: Percentages may not add to 100 due to rounding
Sources: GAO analysis of survey data from
California Partnership for Long-Term Care
Connecticut Partnership for Long-Term Care
Indiana Long-Term Care Insurance Program
62%
a
Based on survey data from calendar year 2003
b
Based on survey data from calendar year 2004
c
Based on survey data from July 2003 to June 2004
GAO-05-1021R Long-Term Care Partnership Program
17
13
Enclosure 1
Demographics of program participants
(continued)
• In California and Connecticut surveys of persons who purchased a
partnership policy, most policyholders reported being relatively healthy (see
table 3)
0%0.3%Activities of daily living
d
Respondents who reported needing assistance with one or
more:
0.6%1.4%Instrumental activities of daily living
e
36%37%Good
63%61%Excellent
Respondents who reported health status as:
5958Average age of respondents
Connecticut
c
California
b
Table 3: Reported Health Status of Partnership Policyholders in California
and Connecticut
a
a
Comparable data are not publicly available from Indiana and New York
b
Based on survey data from calendar year 2003
c
Based on survey data from July 2003 through June 2004
d
Activities of daily living include such activities as dressing, bathing, transferring, toileting, and eating
e
Instrumental activities of daily living include such activities as preparing meals, shopping for groceries, managing money, doing laundry, and taking medications
Sources: California Partnership for Long-Term Care
Connecticut Partnership for Long-Term Care
GAO-05-1021R Long-Term Care Partnership Program
18
14
Enclosure 1
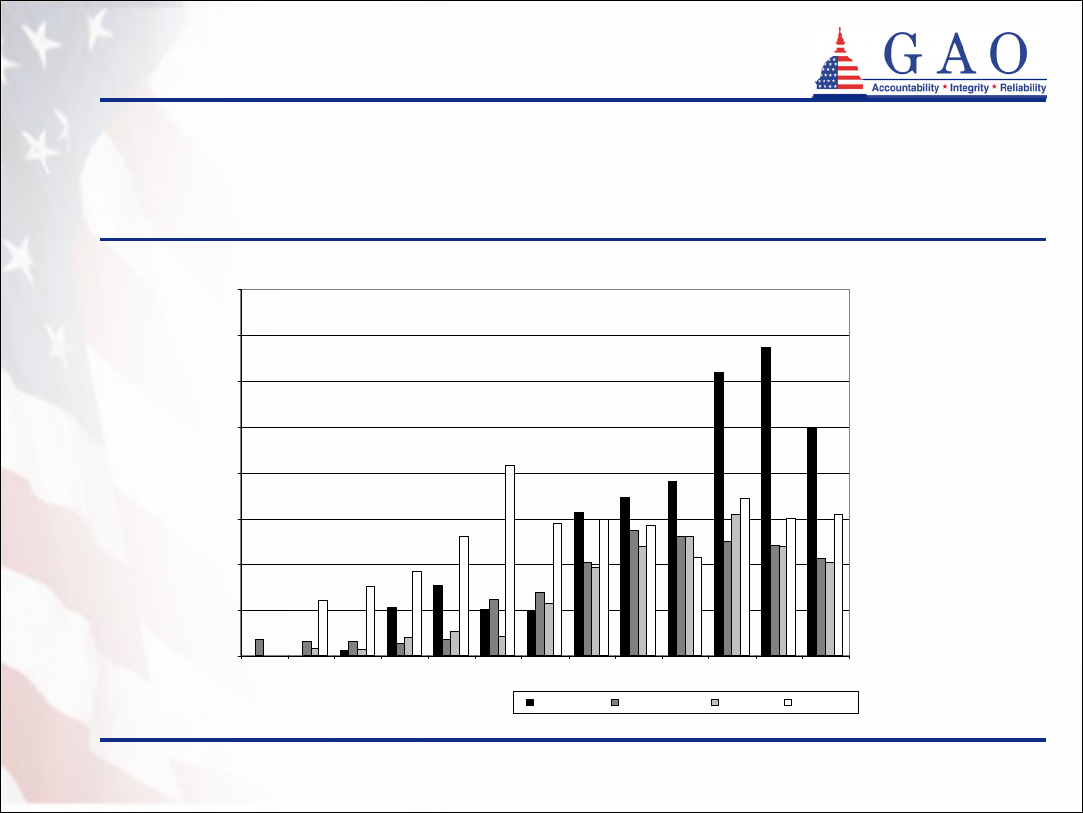
Policies purchased
• The purchase of partnership policies has increased
significantly since the programs began (see figure 4)
• However, the partnership states have seen a decline or
leveling off in the number of policies purchased in recent
years
• State partnership officials from two states reported that
the reason for the decline in sales of partnership policies
in recent years is not specific to partnership policies but is
reflective of overall trends in the long-term care insurance
market
GAO-05-1021R Long-Term Care Partnership Program
19
15
Enclosure 1
0
2,000
4,000
6,000
8,000
10,000
12,000
14,000
16,000
1992 1993 1994 1995 1996 1997 1998 1999 2000 2001 2002 2003 2004
California Connecticut Indiana New York
Policies purchased (continued)
Figure 4: Number of Partnership Policies Purchased by State
Sources: California Partnership for Long-Term Care
Connecticut Partnership for Long-Term Care
Indiana Long-Term Care Insurance Program
New York State Partnership for Long-Term Care
Policies purchased
GAO-05-1021R Long-Term Care Partnership Program
20
16
Enclosure 1
Policies purchased (continued)
11,326 (4%)8,519 (10%)202 (0.5%)2,605 (6%)0 (0%)
Number pending or
withdrawn
42,311 (16%)14,096 (17%)6,324 (15%)5,815 (12%)16,076 (17%)
Number denied
265,60983,97341,49546,56493,577
Number received
Applications
TotalNew York
b
Indiana
a
Connecticut
a
California
a
Table 4: Status of Partnership Applications
Sources: GAO analysis of data from
California Partnership for Long-Term Care
Connecticut Partnership for Long-Term Care
Indiana Long-Term Care Insurance Program
New York State Partnership for Long-Term Care
• Like other long-term care insurance, partnership policies are
subject to medical underwriting
1
• While most applications for partnership policies were
approved, approximately 16 percent were denied (see table 4)
a
Based on data through March 2005
b
Based on data through December 2004
1
Insurance companies evaluate applicants’ health status and possibly deny coverage, offer more limited benefits, or
charge higher premiums to applicants with certain health conditions. However, in some cases, such as with a large
group offering, medical underwriting requirements may be relaxed or eliminated completely.
GAO-05-1021R Long-Term Care Partnership Program
21
17
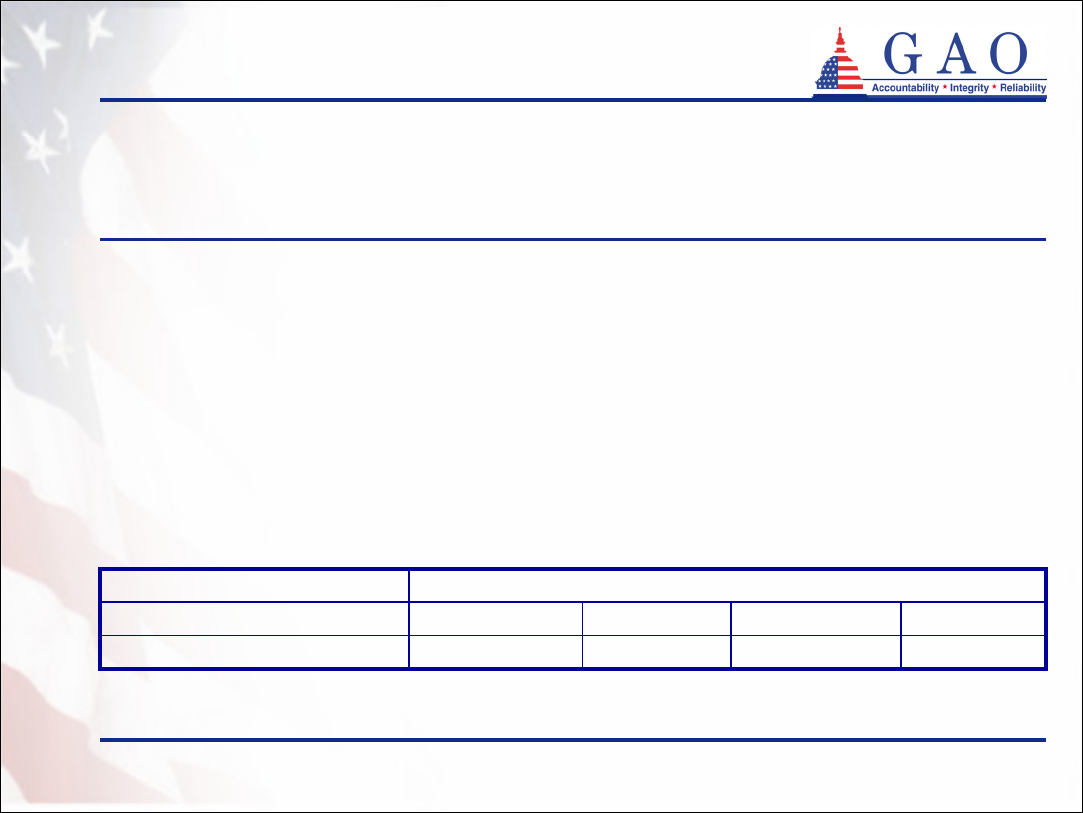
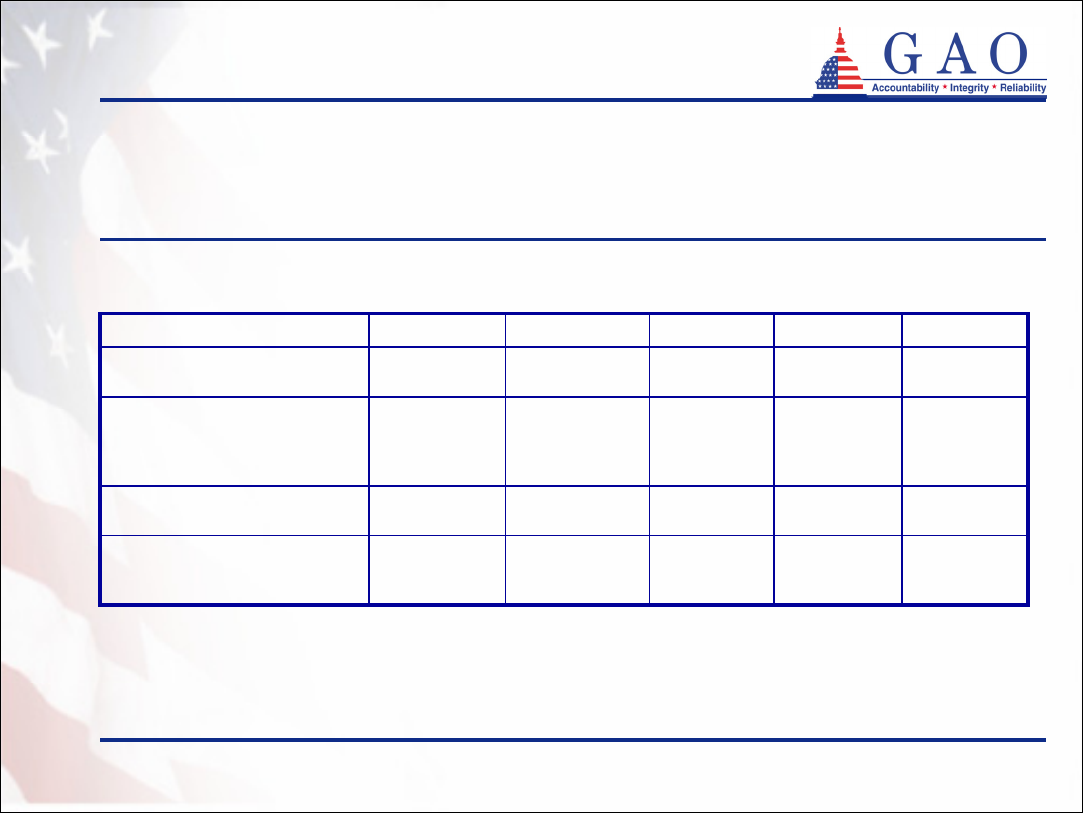
Enclosure 1
Policies purchased (continued)
• Most partnership policies are comprehensive, covering both
nursing home care and home and community-based care
(see table 5)
• Most purchasers buy partnership policies individually
• Few policies are purchased on the group market or
through organization-sponsored programs
GAO-05-1021R Long-Term Care Partnership Program
22
18
Enclosure 1
Policies purchased (continued)
10%4%16%0%
d
Group market or
organization-
sponsored
90%96%84%100%
d
Individual market
Percent of policies
purchased
0%
c
12%1%5%
Nursing home
only
100%
c
88%99%95%
Comprehensive
Type of coverage
New York
b
Indiana
a
Connecticut
a
California
a
Table 5: Types of Policies Purchased
Sources: California Partnership for Long-Term Care
Connecticut Partnership for Long-Term Care
Indiana Long-Term Care Insurance Program
New York State Partnership for Long-Term Care
a
Based on data through March 2005
b
Based on data through December 2004
c
Comprehensive coverage is a requirement of the New York State Partnership for Long-Term Care
d
California partnership policies are only available on the individual market
GAO-05-1021R Long-Term Care Partnership Program
23
19
Enclosure 1
Policies purchased (continued)
• The amount of coverage purchased by partnership policyholders
varies across the four states
• The average daily benefit amount for nursing home care in
Connecticut was approximately $188 per day. The most
common daily benefit amounts purchased for nursing home
care in Indiana were $110 and $120 per day
• The daily and total benefit amounts on the following pages are
calculated using the daily and total benefit amounts at the time of
purchase and are not adjusted for inflation
1
• For example, a $150 per day policy purchased in 1995 with 5
percent inflation protection is worth approximately $244 per day
today
1
Most partnership policies are required to have inflation protection. For example, New York generally requires
inflation protection; however, purchasers age 80 or older are not required to have inflation protection as part of their
policies.
GAO-05-1021R Long-Term Care Partnership Program
24
20
Enclosure 1
Policies purchased (continued)
• California (policies reported in the first quarter of 2005)
• Daily benefit amount: $150 per day most common
• Benefit coverage period: Lifetime coverage most common
• Connecticut (all active policies with fixed daily benefit amounts)
• Average daily benefit amount for nursing home care:
$187.60 per day
• Average daily benefit amount for home and community-
based care: $166.91 per day
• Benefit coverage period: 2 to 3 years of coverage most
common
• Total benefit amount: median of $200,000
GAO-05-1021R Long-Term Care Partnership Program
25
21
Enclosure 1
Policies purchased (continued)
• Indiana (all active policies)
• Nursing home daily benefit amounts: $110 and $120 per day most
common
• Home and community-based care daily benefit amounts: $120 and
$130 per day most common
• Benefit coverage period: 6 years or greater, excluding lifetime
coverage, most common
• New York (policies reported in the last half of 2004)
• Nursing home daily benefit amount: median of $200 per day
• Home and community-based care daily benefit amount: median of
$100 per day
• Benefit coverage period: 3 years of nursing home care, 6 years of
home and community-based care, which is the minimum required
coverage in New York, most common
GAO-05-1021R Long-Term Care Partnership Program
26
22
Enclosure 1
Policies purchased (continued)
• Average annual premiums in Connecticut for long-term care insurance coverage
based on the following coverage options and purchaser age (see table 6)
1
• $200 per day nursing home coverage
• $200 per day home and community-based care coverage
• 90 or 100 days of care paid for by consumer before long-term care insurance
benefits begin (elimination period)
• 5 percent compounded inflation protection
$5,900$4,100$3,100$2,5003 Years
$4,700$3,300$2,400$2,0002 Years
$3,400$2,400$1,800$1,5001 Year
70656055Minimum duration
Purchaser age
Source: Connecticut Partnership for Long-Term Care
Table 6: Average Annual Premiums in Connecticut for Long-Term Care
Insurance Coverage by Age
1
Comparable premium information for California and Indiana is not available
GAO-05-1021R Long-Term Care Partnership Program
27
23
Enclosure 1
• 3 years of nursing home care ($180 daily benefit in 2005)
• 6 years of home and community-based care ($90 daily benefit in 2005)
• 100 days of care paid for by consumer before long-term care insurance benefits
begin (elimination period)
• 5 percent compounded inflation protection
• No nonforfeiture benefit (no refund or coverage if consumer fails to pay
premiums)
Policies purchased (continued)
• Average annual premiums in New York for long-term care insurance coverage
based on the following coverage options and purchaser age (see table 7)1
Source: New York State Partnership for Long-Term Care
$3,817$2,587$1,968$1,531Average premium amount
70656055
Purchaser age
Table 7: 2005 Average Annual Premiums in New York for Basic Long-Term Care Insurance
Coverage by Age
1
Comparable premium information for California and Indiana is not available
GAO-05-1021R Long-Term Care Partnership Program
28
24
Enclosure 1
Policies purchased (continued)
• In Indiana, since the hybrid model was introduced in 1998,
consumers have purchased more long-term care insurance
coverage to get total asset protection rather than less
coverage to get dollar-for-dollar protection
• To trigger total asset protection in 2005, policyholders
must purchase a policy valued at $196,994 or greater
• Prior to 1998, 29 percent of policies purchased had total
coverage amounts large enough to trigger total asset
protection
• In contrast, in the first quarter of 2005, 87 percent of
policies purchased had total coverage amounts large
enough to trigger total asset protection
Source: Indiana Long-Term Care Insurance Program
GAO-05-1021R Long-Term Care Partnership Program
29
25
Enclosure 1
Policies purchased (continued)
22,129
c
6,2363,802
c
3,9998,092
Dropped (after
30 days)
d
81%77%83%81%84%
Policies that remain
active
172,47747,53929,18930,83464,915
Active
15,721
c
5,9172,557
c
2,7894,458
Dropped
(within 30
days)
211,97261,35834,96938,14477,501
Purchased
Number of policies
Total
New York
b
Indiana
a
Connecticut
a
California
a
Table 8: Status of Partnership Policies
Sources: GAO analysis of data from
California Partnership for Long-Term Care
Connecticut Partnership for Long-Term Care
Indiana Long-Term Care Insurance Program
New York State Partnership for Long-Term Care
• Most partnership policies remain active (see table 8)
a
Based on data through March 2005
b
Based on data through December 2004
c
Some policies may be counted in each of the dropped categories
d
Does not include drops reported as deaths, rescissions, or exhausted benefits
GAO-05-1021R Long-Term Care Partnership Program
30
26
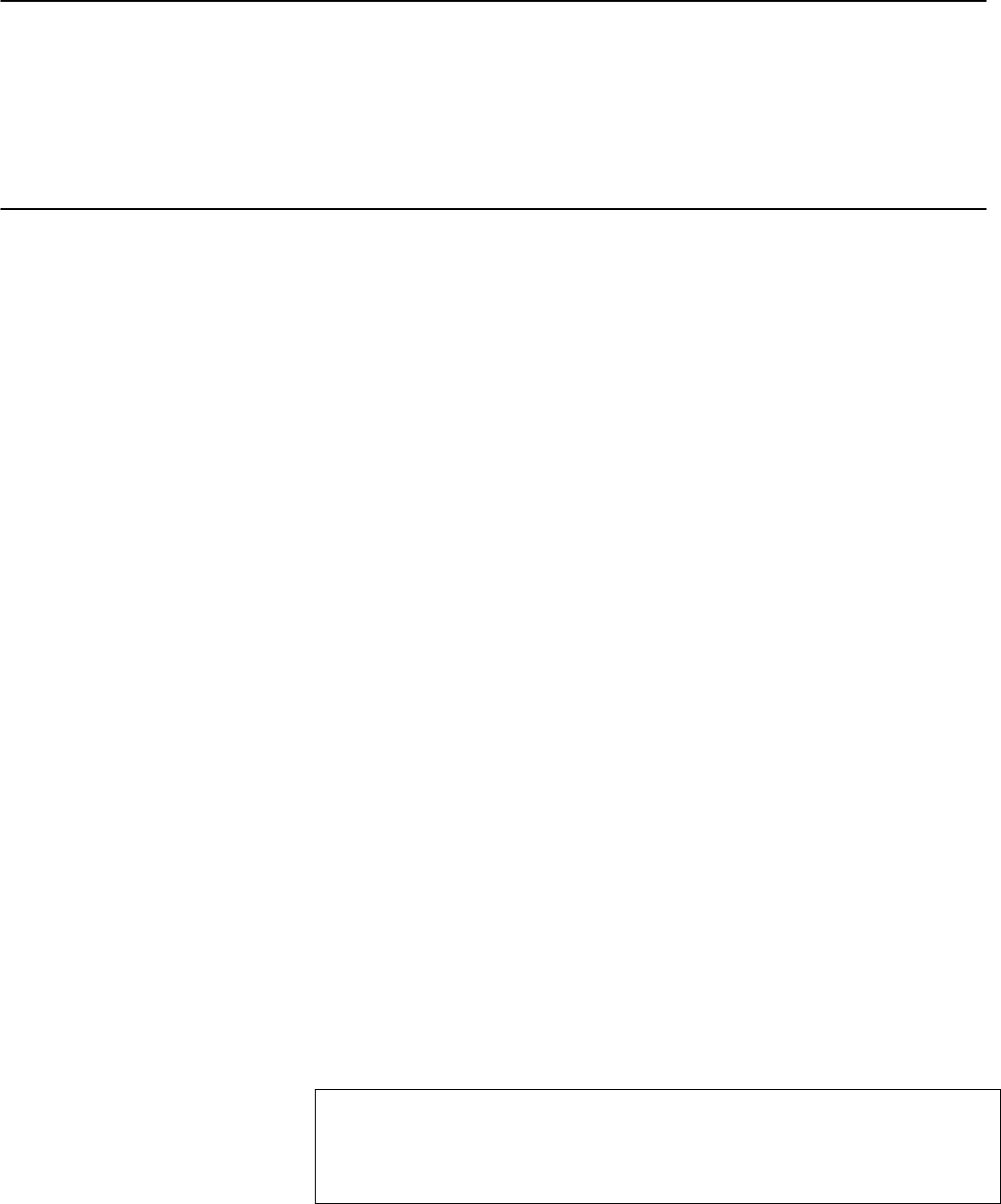
Enclosure 1
• Relatively few partnership policyholders have accessed their
long-term care insurance benefits (see table 9)
Benefits accessed by policyholders
GAO-05-1021R Long-Term Care Partnership Program
31
27
Enclosure 1
Benefits accessed by policyholders
(continued)
172,47747,53929,18930,83464,915
Number of currently active
policies
1,209
(0.7%)
642
(1.4%)
83
(0.3%)
141
(0.5%)
343
(0.5%)
Number of policyholders
currently receiving long-term
care insurance benefits
1,248
(2.0%)
61,358
New York
b
249
(0.7%)
34,969
Indiana
a
211,97238,14477,501
Number of policies ever
purchased
2,761
(1.3%)
351
(0.9%)
913
(1.2%)
Number of policyholders
who have ever received
long-term care insurance
benefits
Total
Connecticut
a
California
a
Table 9: Policies Purchased and Benefits Received in the Partnership
Program
Sources: GAO analysis of data from
California Partnership for Long-Term Care
Connecticut Partnership for Long-Term Care
Indiana Long-Term Care Insurance Program
New York State Partnership for Long-Term Care
a
Based on data through March 2005
b
Based on data through December 2004
GAO-05-1021R Long-Term Care Partnership Program
32
28
Enclosure 1
• Few partnership policyholders have accessed Medicaid (see
table 10)
Benefits accessed by policyholders
(continued)
GAO-05-1021R Long-Term Care Partnership Program
33
29
Enclosure 1
Not available
c
Not available
c
Not available
c
Not available
c
Not available
c
Not available
c
37 (39%)
59 (61%)
96
New York
b
$75,333
d
$69,380
d
$73,028
d
$7,156,597
d
$4,162,812
d
$11,319,409
d
132 (53%)
119 (47%)
251
Total
$83,208
$57,004
$69,683
$1,248,113
$912,067
$2,160,180
15 (48%)
16 (52%)
31
Indiana
a
$2,182,076$3,726,408
Have not accessed Medicaid
$2,018,732$1,232,013
Have accessed Medicaid
$4,200,808$4,958,421
Cumulative asset protection earned by
policyholders who have exhausted long-term
care insurance benefits
$136,380$58,225
Have not accessed Medicaid
$106,249$49,281
Have accessed Medicaid
$120,023$55,713
Per capita asset protection earned by
policyholders who have exhausted long-term
care insurance benefits
16 (46%)64 (72%)
Have not accessed Medicaid
19 (54%)25 (28%)
Have accessed Medicaid
3589
Number of active policyholders who have
exhausted long-term care insurance benefits
Connecticut
a
California
a
Table 10: Medicaid Usage by Partnership Policyholders
Sources: GAO analysis of data from
California Partnership for Long-Term Care
Connecticut Partnership for Long-Term Care
Indiana Long-Term Care Insurance Program
New York State Partnership for Long-Term Care
a
Based on data through March 2005
b
Based on data through December 2004
c
New York does not collect asset protection information
d
Based on data from California, Connecticut, and Indiana
Benefits accessed by policyholders
(continued)
GAO-05-1021R Long-Term Care Partnership Program
34
30
Enclosure 1
Not
available
c
Not
available
c
365
New York
b
$26,685
$1,921,351
72
Indiana
a
$20,355
d
$10,869,369
d
899
Total
$3,699,361$5,248,657
Cumulative asset protection earned
that will not be accessed due to
policyholder dying while receiving
benefits
$30,076$15,483
Per capita asset protection earned
that will not be accessed due to
policyholder dying while receiving
benefits
123339
Number of policyholders who died
while receiving benefits
Connecticut
a
California
a
Table 11: Mortality Statistics for Partnership Policyholders
• 899 partnership policyholders died before exhausting their
long-term care insurance benefits (see table 11)
Sources: GAO analysis of data from
California Partnership for Long-Term Care
Connecticut Partnership for Long-Term Care
Indiana Long-Term Care Insurance Program
New York State Partnership for Long-Term Care
a
Based on data through March 2005
b
Based on data through December 2004
c
New York does not collect asset protection information
d
Based on data from California, Connecticut, and Indiana
Benefits accessed by policyholders
(continued)
(290470)
GAO-05-1021R Long-Term Care Partnership Program
35
This is a work of the U.S. government and is not subject to copyright protection in the
United States. It may be reproduced and distributed in its entirety without further
permission from GAO. However, because this work may contain copyrighted images or
other material, permission from the copyright holder may be necessary if you wish to
reproduce this material separately.
The Government Accountability Office, the audit, evaluation and
investigative arm of Congress, exists to support Congress in meeting its
constitutional responsibilities and to help improve the performance and
accountability of the federal government for the American people. GAO
examines the use of public funds; evaluates federal programs and policies;
and provides analyses, recommendations, and other assistance to help
Congress make informed oversight, policy, and funding decisions. GAO’s
commitment to good government is reflected in its core values of
accountability, integrity, and reliability.
The fastest and easiest way to obtain copies of GAO documents at no cost
is through GAO’s Web site (www.gao.gov). Each weekday, GAO posts
newly released reports, testimony, and correspondence on its Web site. To
have GAO e-mail you a list of newly posted products every afternoon, go
to www.gao.gov and select “Subscribe to Updates.”
The first copy of each printed report is free. Additional copies are $2 each.
A check or money order should be made out to the Superintendent of
Documents. GAO also accepts VISA and Mastercard. Orders for 100 or
more copies mailed to a single address are discounted 25 percent. Orders
should be sent to:
U.S. Government Accountability Office
441 G Street NW, Room LM
Washington, D.C. 20548
To order by Phone: Voice: (202) 512-6000
TDD: (202) 512-2537
Fax: (202) 512-6061
Contact:
Web site: www.gao.gov/fraudnet/fraudnet.htm
E-mail: [email protected]
Automated answering system: (800) 424-5454 or (202) 512-7470
Gloria Jarmon, Managing Director, [email protected] (202) 512-4400
U.S. Government Accountability Office, 441 G Street NW, Room 7125
Washington, D.C. 20548
Paul Anderson, Managing Director, [email protected] (202) 512-4800
U.S. Government Accountability Office, 441 G Street NW, Room 7149
Washington, D.C. 20548
GAO’s Mission
Obtaining Copies of
GAO Reports and
Testimony
Order by Mail or Phone
To Report Fraud,
Waste, and Abuse in
Federal Programs
Congressional
Relations
Public Affairs
PRINTED ON
RECYCLED PAPER
