
National Health Statistics Reports
Number 129 October 9, 2019
U.S. DEPARTMENT OF HEALTH AND HUMAN SERVICES
Centers for Disease Control and Prevention
National Center for Health Statistics
Breast Cancer Screening Among Women by Nativity,
Birthplace, and Length of Time in the United States
by Tainya C. Clarke, Ph.D., M.P.H., National Center for Health Statistics; and Meheret Endeshaw, M.P.H., Denise Duran,
M.P.H., and Mona Saraiya, M.D., M.P.H., National Center for Chronic Disease Prevention and Health Promotion
Abstract
Objective—The U.S. Preventive Services Task Force (USPSTF) recommends
biennial mammography screening for women aged 50–74 to reduce mortality from
breast cancer. In the United States, foreign-born women have historically had higher
breast cancer mortality rates than their U.S.-born peers. This report presents national
estimates of mammography screening among women by nativity, birthplace, and
percentage of lifetime living in the United States.
Methods—Combined data were analyzed from 29,951 women aged 50–74 years
who participated in the 2005, 2008, 2010, 2013, and 2015 National Health Interview
Survey. The percentage of these women who ever had a mammogram and met the
USPSTF recommendations for screening by nativity, birthplace, and percentage of
lifetime in the United States was generated. Estimates were adjusted for selected
demographic, socioeconomic, and health care access and utilization factors and
presented as predictive margins.
Results—Overall, foreign-born women were less likely than U.S.-born women
to have ever had a mammogram (88.3% compared with 94.1%). Foreign-born
women living in the United States for less than 25% of their lifetime were less likely
to have ever had a mammogram (76.4%) or meet the USPSTF recommendations
(55.0%) compared with U.S.-born women. Foreign-born women living in the
United States for 25% or more of their lifetime were also less likely to have ever had a
mammogram (90.9%) compared with U.S.-born women. After adjustment for selected
sociodemographic characteristics, the percentage of foreign-born women who ever
received a mammogram increased but was still lower than that of U.S.-born women.
Foreign-born women residing in the United States for less than 25% of their lifetime
were as likely as U.S.-born women to have met the USPSTF recommendations (72.1%
and 72.4%, respectively), while those residing in the United States for 25% or more of
their lifetime (75.1%) were more likely to do so than U.S.-born women. Dierences
by birthplace were also observed.
Keywords: mammography • acculturation • health disparities • National Health
Interview Survey
Introduction
In the United States, breast cancer
is the most common cancer in women
(excluding nonmelanoma skin cancer)
(1). Although morbidity and mortality
have remained stable, in 2016, the
latest year for which incidence data
are available, 245,299 new cases of
breast cancer were reported among
women, and 41,487 women died of
breast cancer in the United States (2).
For every 100,000 women, 124 cases
of breast cancer were reported, and 20
died of cancer (2). Breast cancer is the
leading cause of cancer-related death
among Hispanic women, and the second-
leading cause among white, black,
Asian or Pacic Islander, and American
Indian or Alaska Native women in
the United States (1). Breast cancer
incidence and mammography receipt
are associated with race and ethnicity,
income or poverty status, education,
health insurance status, and foreign-born
status (3,4). These correlates often lead to
the observed race and ethnicity disparities
in breast cancer-related morbidity and
mortality. Research on breast cancer
screening by birthplace among foreign-
born women residing in the United States
is scarce.
NCHS reports can be downloaded from: https://www.cdc.gov/nchs/products/index.htm.

Page 2 National Health Statistics Reports Number 129 October 9, 2019
More than 43.7 million persons,
accounting for 13.5% of the U.S.
population, are foreign born. This
proportion is expected to grow to about
70 million, or 20% of the population, in
the next 40 years (5,6). Approximately
51% of the foreign-born population in the
United States is female (5,6). Compared
with their U.S.-born counterparts,
foreign-born women often experience an
elevated cancer risk because of lifestyle
changes associated with living in the
United States (7–9). Understanding the
screening experience of foreign-born
women compared with U.S.-born women
is important because immigrant women
may not be exposed to the same level
of public health messaging or screening
opportunities in their home countries
(10–13).
Past studies of breast cancer
screening among foreign-born women
living in the United States have focused
on specic population subgroups (14,15).
Some have looked at language barriers,
and others have looked at adaptation
to western culture (16–18). However,
few have examined the relationship
between mammography receipt and the
birthplace of ethnically diverse foreign-
born women, and none have examined
the percentage of time living in the
United States, as factors aecting the
likelihood of having a mammogram.
Cervical cancer research has shown that
whether a woman is likely to ever be
screened, as well as adhere to screening
recommendations, varies by birthplace
(19).
Although mammography does not
detect all tumors of the breast, it can
often detect breast cancer at an early
stage when treatment is more eective
(20,21). The reduction and stability of
breast cancer mortality and morbidity
rates in North American and European
countries over the past 2 decades have
been attributed to early detection through
mammography and improved treatment
(2–4). The U.S. Preventive Services Task
Force (USPSTF) recommends biennial
mammography screening for women
aged 50–74 who have an average risk of
breast cancer (22).
Using the National Health Interview
Survey (NHIS), this report examines
the percentage of women aged 50–74
who have ever received a mammogram
as well as those who met the USPSTF
recommendations for screening according
to nativity status (U.S. or foreign
born) and percentage of time in the
United States. Compliance with screening
recommendations among foreign-born
women is also described according to
birthplace.
Methods
Data source
Data in this report are from the
combined 2005, 2008, 2010, 2013, and
2015 NHIS. NHIS is a multipurpose,
cross-sectional health survey of the U.S.
civilian noninstitutionalized population,
based on a stratied multistage sample
of U.S. households (23,24). Data are
collected in person at the respondent’s
home using computer-assisted personal
interviewing, but follow-ups for
completing interviews may be conducted
over the telephone if needed. The survey
consists of both a core set of questions
that remain relatively unchanged from
year to year as well as supplemental
questions that are asked periodically.
Within each household, information
is collected at the family level, then
a sample adult is selected to answer
additional questions about his or her
individual health and health behaviors
such as cancer screening.
Data selected for this study were
restricted to years in which NHIS
elded a cancer supplement. Based on
USPSTF recommendations for breast
cancer screening applicable to the study
period (22,25,26), the analysis was
further restricted to women aged 50–74
at interview (n = 29,951). Final sample
adult response rates varied across survey
years: 69.0% in 2005, 62.6% in 2008,
60.8% in 2010, 61.2% in 2013, and
55.2% in 2015 (27).
Mammography receipt
In NHIS, women aged 30 and
over were asked, “Have you ever
had a mammogram?” Those who
responded “no” were categorized as
never having had a mammogram. Those
who responded “yes” were then asked,
“When did you have your most recent
mammogram?” Current age and time
of most recent screening were used to
calculate the proportion of women who
had a mammogram in the past 2 years for
breast cancer screening out of all women
reporting ever having had a mammogram.
Women who have had a mammogram but
did not have one in the past 2 years, and
those who had never had a mammogram
in their lifetime, were categorized as not
meeting USPSTF recommendations.
Nativity, birthplace, and
percentage of lifetime in
United States
Nativity
Data from the restricted-use NHIS
le, which contains information on the
respondent’s country of birth, were used
to determine nativity and birthplace.
Women who were born in one of the 50
states, the District of Columbia (D.C.),
or Puerto Rico or another U.S. territory
(American Samoa, Guam, Northern
Mariana Islands, and U.S. Virgin
Islands), as well as those born outside
the United States to parents with U.S.
citizenship, were considered to be U.S.-
born. Women not in these categories were
considered foreign born.
Birthplace
Among foreign-born women,
country of birth, geographic proximity,
cultural commonalities, socioeconomic
dierences and similarities, and sample
size guided the creation of the variable
of regional birthplace categories used
for analysis. Mexico was placed in its
own category due to the large number of
foreign-born Mexican persons living in
the United States. Central America and
the Caribbean islands were also presented
separately due to sample size.
Africa and the Middle East were
combined for this analysis due to small
sample size as well as geographic
proximity. Europe (Western Europe) and
Russia (as well as former Union of Soviet
Socialist Republics areas) were combined
due to small sample sizes, some cultural
similarities, and geographic proximity.
The remaining birthplace categories used
in this analysis were South America,
Central Asia (labeled Asia), Southeast

National Health Statistics Reports Number 129 October 9, 2019 Page 3
Asia, South Asia (Indian subcontinent),
and Other. Note that, because of small
sample sizes, foreign-born women from
Canada (0.32%) and Oceana and other
unspecied countries or regions (0.08%)
were placed in the Other category.
However, due to their vast socioeconomic
and cultural dierences, this group is
not discussed in statistical comparisons.
The birthplace variable is a geographic
measure of region of birth and is not
intended to indicate legal status or
citizenship.
Percentage of lifetime in United
States
The length of stay or residence in the
United States was calculated by using the
year from the response to the question,
“In what year did {person} come to the
United States to stay?” and subtracting
it from the year of interview. Length of
stay was then divided by the respondent’s
age and multiplied by 100 to determine
the percentage of lifetime living in the
United States. This measure was divided
into two categories: less than 25% and
25% or more of lifetime residing in the
United States. Categorization was based
on previous research on the health-related
behaviors of foreign-born persons living
in the United States (19,28–32). These
studies revealed that persons who spent
less of their life in the United States
showed similar health behaviors and
access and utilization of health care
services compared with non-English-
speaking immigrants.
Sociodemographic variables
Sociodemographic characteristics
of U.S. women presented in this report
include sex, age group, educational
attainment, poverty status, marital status,
Hispanic or Latino origin, and race. All
characteristics were measured at the time
of the interview. Detailed information on
the categories used for these variables
can be found in Endeshaw et al. (19) and
other sources (33).
Health status and health care
access and utilization
Health status was based on the
question, “Would you say your health
in general is excellent, very good, good,
fair, or poor?” “Excellent” and “very
good” were combined in this analysis, as
were “fair” and “poor.”
Health insurance coverage was
presented as a four-category variable:
private, public, Medicare, and uninsured.
A person was dened as uninsured
if he or she did not have any private
health insurance, Medicare, Medicaid,
state-sponsored or other government-
sponsored health plan, or military plan at
the time of interview. A person was also
dened as uninsured if he or she had only
Indian Health Service coverage or had
only a private plan that paid for one type
of service, such as accidents or dental
care. Public health insurance included
persons on Medicaid, persons with dual
Medicare and Medicaid enrollment, and
persons with military coverage or other
government health insurance coverage.
Persons aged 65 and over with Medicare
coverage only, including Medicare
Advantage plans, were placed in a
separate category.
Usual place of care was based on
a survey question, “Is there a place that
you usually go to when you are sick or
need advice about your health?” For
number of visits to a health care provider,
respondents were asked, “During the
past 12 months, how many times have
you seen a doctor or other health care
professional about your own health at a
doctor’s oce, a clinic, or some other
place?” Respondents were instructed
to exclude overnight hospitalizations,
visits to hospital emergency rooms, home
visits, dental visits, and telephone calls.
U.S. region of current
residence
For region of current U.S. residence,
the 50 states and D.C. were categorized
into nine regions:
● New England—Connecticut, Maine,
Massachusetts, New Hampshire,
Rhode Island, Vermont
● Mid-Atlantic—Delaware, D.C.,
Maryland, New Jersey, New York,
Pennsylvania
● East North Central—Illinois,
Indiana, Michigan, Ohio, Wisconsin
● West North Central—Iowa, Kansas,
Minnesota, Missouri, Nebraska,
North Dakota, South Dakota
● South Atlantic—Florida, Georgia,
North Carolina, South Carolina,
Virginia, West Virginia
● East South Central—Alabama,
Kentucky, Mississippi, Tennessee
● West South Central—Arkansas,
Louisiana, Oklahoma, Texas
● Mountain—Arizona, Colorado,
Idaho, Nevada, New Mexico,
Montana, Utah, Wyoming
● Pacic—Alaska, California, Hawaii,
Oregon, Washington
Statistical analyses
Estimates in this report were
calculated using the sample adult
sampling weights and are representative
of the civilian noninstitutionalized
population of U.S. women aged 50–74.
Weights were adjusted to account for
combined survey years. Data weighting
procedures are described in more detail
elsewhere (23,24). Point estimates,
and estimates of their variances, were
calculated using SAS-callable SUDAAN
version 11.0.0 (34,35), a software
package that accounts for the complex
sample design of NHIS. Unless otherwise
specied, the denominator used was
women aged 50–74. Calculations
excluded persons with unknown
information on the variables examined.
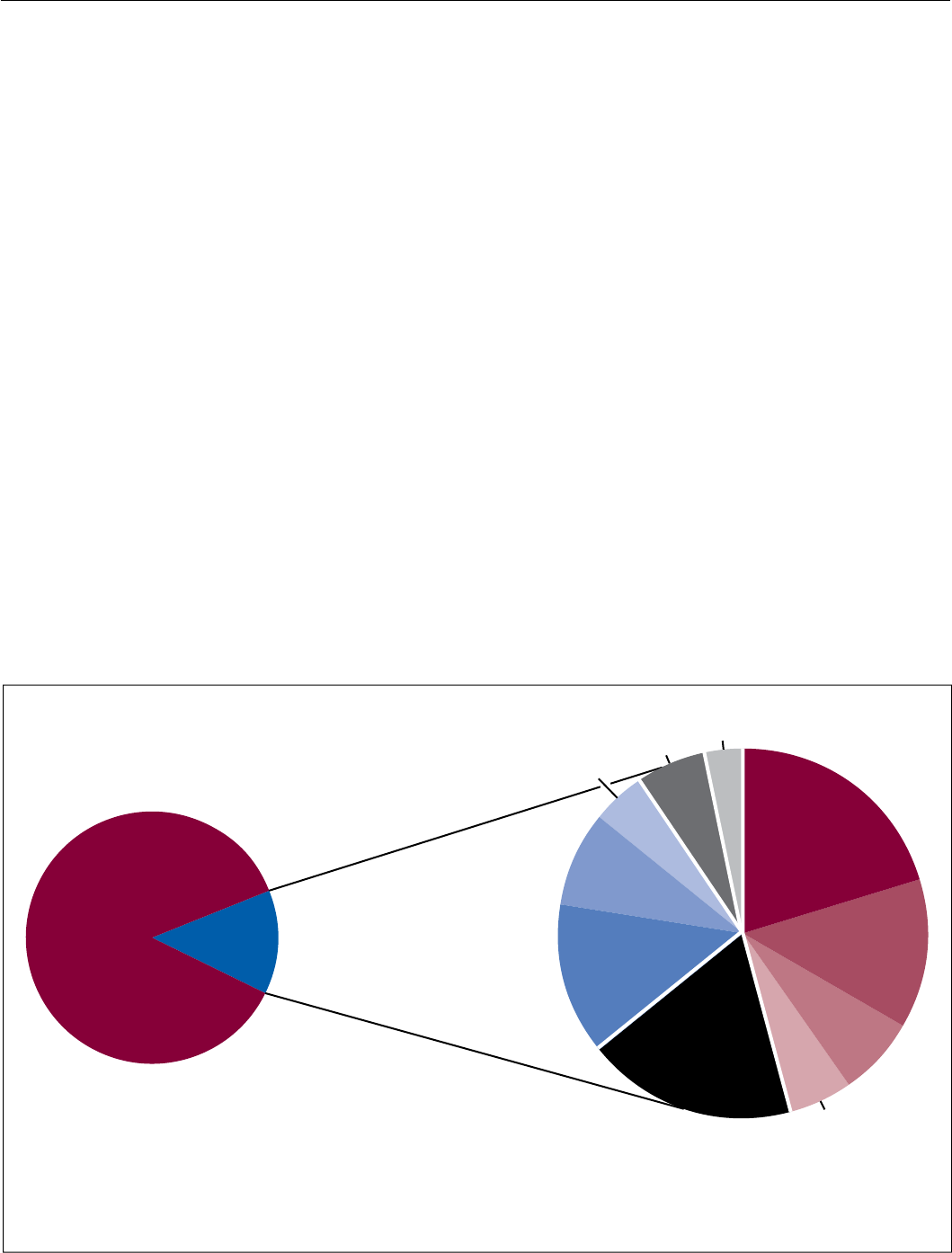
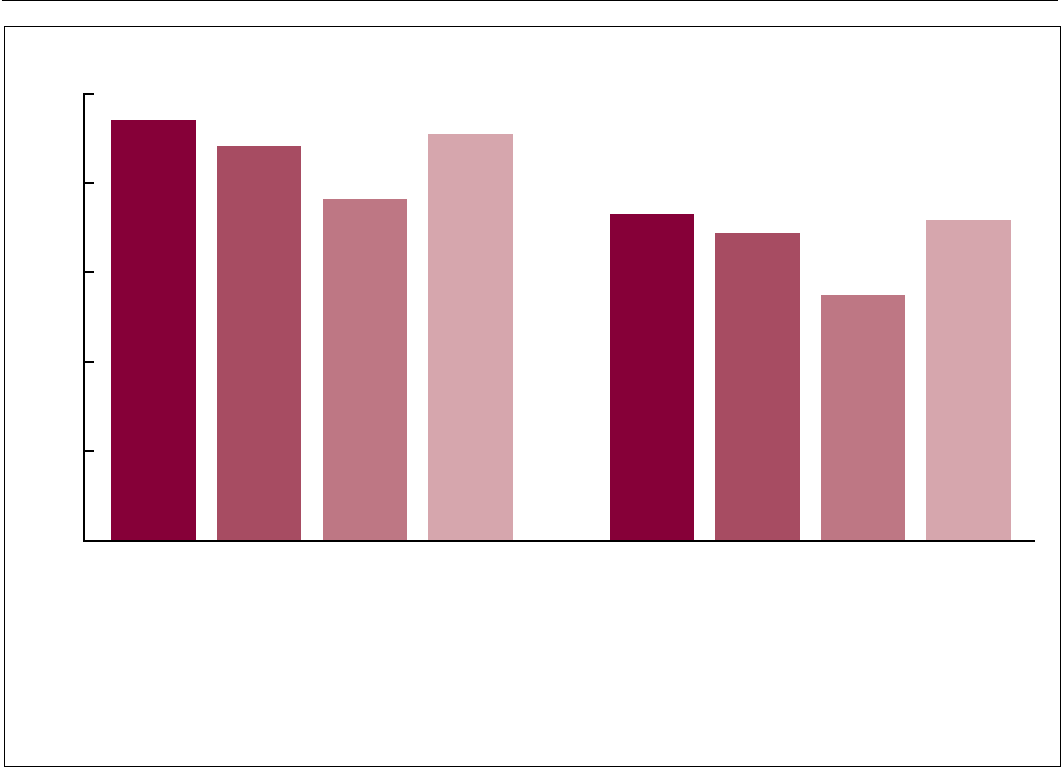
Descriptive statistics of the
population (Figure 1, Table 1)
and estimates of ever receiving a
mammogram and meeting the USPSTF
recommendations for screening
(Figure 2) by nativity and percentage
of lifetime in the United States are
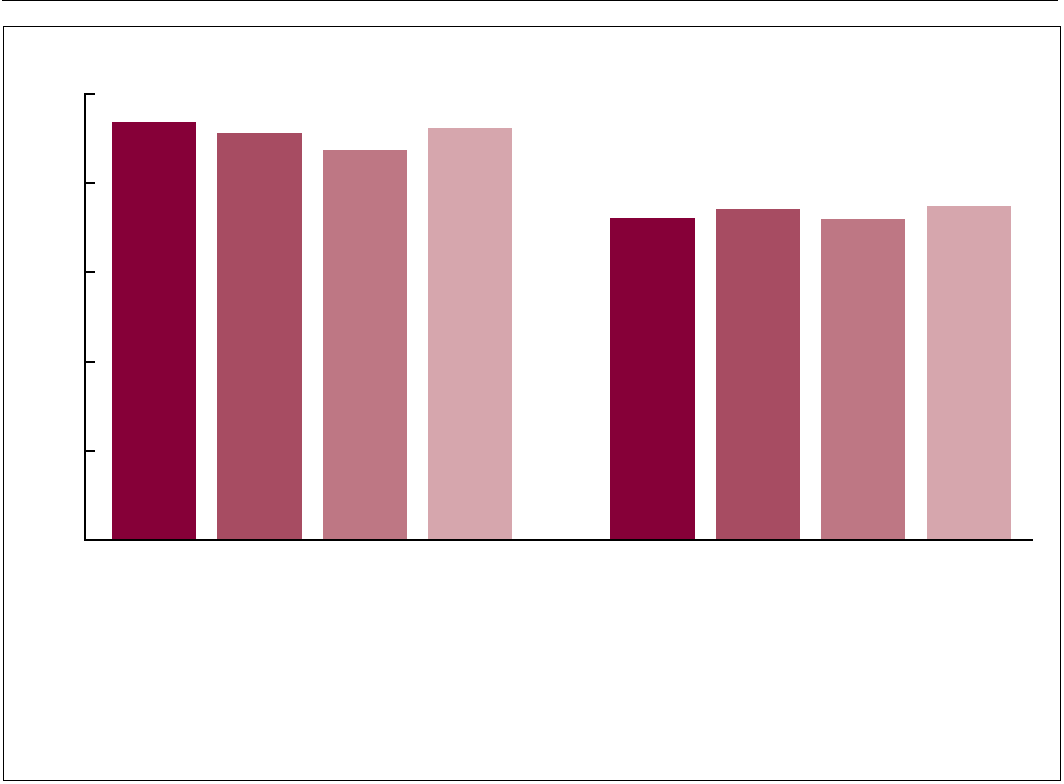
unadjusted. Figure 3 and Table 2 present
estimates of mammography receipt
adjusted for age, marital status, poverty
status, U.S. region of current residence,
educational attainment, health status,
health insurance coverage, usual place
for medical care, and number of doctor
visits in the past 12 months; these
are presented as predictive margins
from logistic regression models. The
predictive marginal approach is a
regression-based equivalent of the
common epidemiological technique of
Page 4 National Health Statistics Reports Number 129 October 9, 2019
standardization, in which the estimates
are proportionally adjusted according to a
weight for each level of the confounding
factors. The marginal probabilities
obtained reect a weighted average over
the distribution of the confounders and
are equivalent to estimates obtained by
standardizing to the total population
(36). This means that comparisons of
mammography receipt by birthplace
and percentage of lifetime in the
United States were made as though
women in those population subgroups
had the same sociodemographic
characteristics, health status, and selected
indicators of health care access and
utilization. Thus, resulting estimates
should largely reect dierences by
birthplace and percentage of lifetime in
the United States. Because correlation
analyses showed that race and ethnicity
were highly correlated with birthplace,
they were not included in the group of
sociodemographic variables used for
standardization.
Signicant dierences in
demographic characteristics and
mammography receipt among U.S.
women by nativity, birthplace, and
percentage of lifetime living in the
United States were compared using
two-sided t tests at the 0.05 level and
assuming consistency, asymptotic
normality, and asymptotic independence
of the estimates (37). Terms such as
“more likely” and “less likely” indicate a
statistically signicant dierence. Terms
such as “not signicantly dierent”
indicate that no statistically detectable
dierences were found between the
estimates being compared. In this report,
estimates that do not meet National
Center for Health Statistics standards of
reliability as specied in the “National
Center for Health Statistics Data
Presentation Standards for Proportions”
(38) are denoted by an asterisk (*).
Results
Birthplace
Among women aged 50–74, the
majority were born in one of the 50
states, D.C., or a U.S. territory, or
abroad to parents who were U.S. citizens
(86.9%); 13.1% were born in other
countries (Figure 1). Among foreign-born
women, 20.4% were born in Mexico,
18.3% in Europe, 13.5% in Southeast
Asia, 13.1% in the Caribbean, and the
remainder in other specied regions
(Table 1).
Sociodemographic
characteristics
The distribution of selected
sociodemographic characteristics
examined in this study diered by
nativity and percentage of lifetime in the
United States (Table 2). The percentage
of foreign-born Hispanic women (38.9%)
was more than eight times that of U.S.-
born Hispanic women (4.8%). Hispanic
women also constituted the largest
proportion of foreign-born women,
regardless of the length of time in the
United States (43.5% for less than 25% of
their lifetime and 37.8% for 25% or more
of lifetime). More non-Hispanic black
women were born in the United States
(11.8%) than abroad (7.9%). The
percentage of foreign-born Asian women
(26.5%) was more than twentyfold higher
than the percentage of U.S.-born Asian
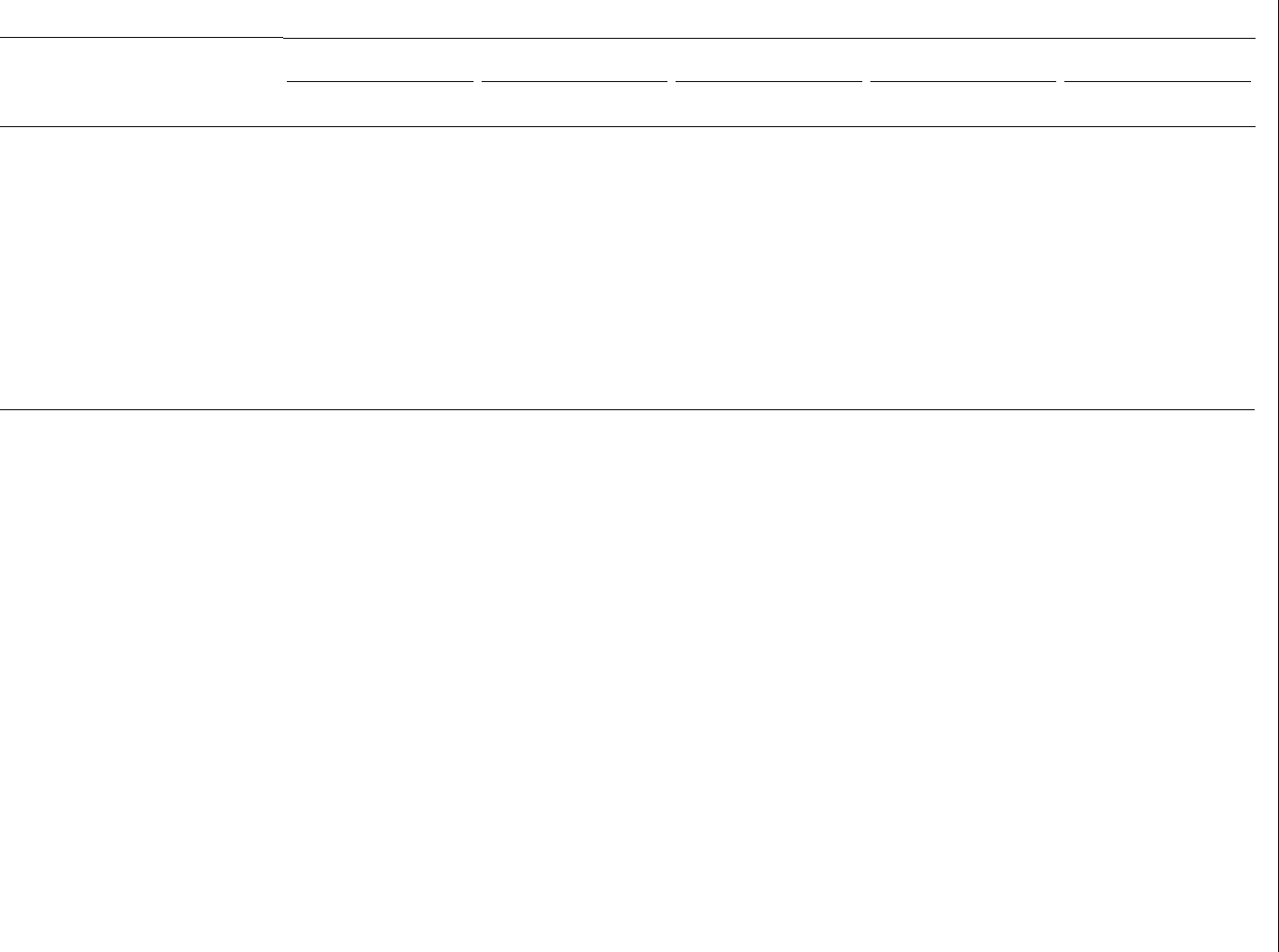
Figure 1. Percent distribution of women aged 50–74, by birthplace: United States, 2005, 2008, 2010, 2013, and 2015
13.1
U.S. born
86.9
NOTES: The denominator used for analysis is the number of U.S. women aged 50–74. Women born in the United States or born abroad to parents who were U.S. citizens are categorized
as U.S. born. If born abroad to parents who were non-U.S. citizens, country of birth, geographic proximity, cultural commonalities, socioeconomic differences and similarities, and sample
size are used to categorize participants by birthplace. South Asia, also known as the Indian subcontinent, includes Afghanistan, Bangladesh, Bhutan, India, Maldives, Nepal, Pakistan, and
Sri Lanka. Europe includes Russia and former Union of Soviet Socialist Republics areas. Percentages may not add to 100 due to rounding.
SOURCE: NCHS, National Health Interview Survey, 2005, 2008, 2010, 2013, and 2015.
Other
3.3
Europe
18.3
Mexico
20.4
Caribbean
13.1
South
America
7.1
Central
America
5.4
Africa and
Middle East
5.9
Other
3.3
Southeast
Asia
13.5
Central Asia
8.3
South Asia
4.9

National Health Statistics Reports Number 129 October 9, 2019 Page 5
women (0.8%). Compared with U.S.-
born women, foreign-born women were
more likely to be currently married or
living with a partner (66.7% compared
with 62.9%), have less than a high school
education (30.2% compared with 11.1%),
and live below the federal poverty level
(16.7% compared with 9.2%).
Foreign-born women residing in the
United States for less than 25% of their
lifetime were more likely to have less
than a high school education (38.3%) and
less likely to have some college education
(13.7%) compared with U.S.-born
women (11.1% and 31.2%, respectively).
Foreign-born women living in the
United States for less than 25% of their
lifetime were more likely to be living
below the federal poverty level (24.1%)
and at 100%–199% of the federal poverty
level (28.5%), but less likely to live at
400% or more of the federal poverty
level (17.6%) compared with U.S.-born
women.
Health status and health care
access and utilization
Compared with U.S.-born women,
foreign-born women were less likely
to have excellent or very good health
(43.6% compared with 51.7%), more
likely to have fair or poor health (22.3%
compared with 18.6%), more than
twice as likely to be uninsured (17.8%
compared with 7.4%), and more likely
to have public health insurance (19.8%
compared with 13.5%) and Medicare
only or Medicare Advantage (10.6%
compared with 9.3%). This pattern held
true regardless of percentage of lifetime
in the United States. Foreign-born women
were more than twice as likely to not
have a usual place of care compared with
U.S.-born women (11.8% compared with
5.8%). Foreign-born women were more
likely than U.S.-born women to have
had no visit to a health care provider
(14.1% compared with 8.4%) or only one
visit (15.8% compared with 12.5%) in the
past 12 months.
Foreign-born women living in the
United States for less than 25% of their
lifetime were more likely to have fair
or poor health (25.7%) compared with
U.S.-born women (18.6%). Foreign-
born women living in the United States
for less than 25% of their lifetime were
also less likely to have Medicare only
or Medicare Advantage than U.S.-born
women (6.7% compared with 9.3%). On
the contrary, foreign-born women living
in the United States for 25% or more of
their lifetime were more likely to have
Medicare only or Medicare Advantage
(11.5%) compared with U.S.-born
women.
Foreign-born women living in the
United States for less than 25% of their
lifetime were more than four times as
likely to be uninsured (33.5%) compared
with U.S.-born women (7.4%). Foreign-
born women living in the United States
for less than 25% of their lifetime were
more likely to not have a usual place of
care (22.2%) compared with U.S.-born
women (5.8%). They were also more
likely to have no visits to a health care
provider in the past 12 months (23.2%)
compared with U.S.-born women (8.4%).
U.S. region of current
residence
The population distribution of
U.S.-born women diered from foreign-
born women when compared with the
region of current U.S. residence. While
the majority of U.S.-born women were
distributed across ve of the nine regions
examined (Mid-Atlantic [15.2%], East
North Central [17.0%], South Atlantic
[18.1%], West South Central [11.0%],
and Pacic [12.4%]), more than two-
thirds of foreign-born women in the
United States resided in the Mid-Atlantic
(20.8%), South Atlantic (16.2%), and
Pacic (32.1%) regions. No dierence
in distribution was observed among the
nine regions of current U.S. residence for
foreign-born women by percentage of
lifetime in the United States.
Mammography screening
U.S. born compared with foreign
born
Unadjusted estimates—Overall,
foreign-born women were less likely
than U.S.-born women to have ever had
a mammogram (88.3% compared with
94.1%) (Figure 2). Foreign-born women
who resided in the United States for
less than 25% of their lifetime were less
likely to have ever had a mammogram
than U.S.-born women (76.4% compared
with 94.1%). Foreign-born women who
spent more than 25% of their lives living
in the United States were also less likely
to have ever had a mammogram (90.9%)
compared with U.S.-born women.
However, the percentage point dierence
was less than that of foreign-born women
who resided in the United States for less
than 25% of their lifetime.
Foreign-born women were less likely
than U.S.-born women to have met the
USPSTF recommendation of having had
a mammogram in the past 2 years (68.8%
compared with 73.0%). Foreign-born
women who spent less than 25% of their
lifetime living in the United States were
also less likely than U.S.-born women to
have met the USPSTF recommendation
for screening (55.0% compared with
73.0%). No statistically signicant
dierence was found between foreign-
born women who spent 25% or more of
their lifetime living in the United States
(71.8%) and U.S.-born women.
Adjusted estimates—After
adjustment, the dierences in the
percentage of women ever screened were
attenuated. Overall, foreign-born women
(91.4%)—both those who resided in the
United States for less than 25% of their
lifetime (87.6%) and those who lived
in the United States for 25% or more of
their lifetime (92.5%)—remained less
likely than U.S.-born women (93.9%)
to have ever had a mammogram
(Figure 3). However, the percentage point
dierences were smaller. With regard
to meeting USPSTF recommendations
for screening, no signicant dierence
was observed between U.S.-born women
(72.4%) and foreign-born women
(74.4%), particularly those who resided
in the United States for less than 25%
of their lifetime (72.1%). Although the
percentage point dierence was relatively
small, foreign-born women who lived
in the United States for 25% or more of
their lifetime (75.1%) were more likely to
have met the USPSTF recommendations
compared with U.S.-born women.
U.S. born compared with foreign
born by birthplace
Unadjusted estimates—Foreign-
born women from Mexico (85.8%),
the Caribbean (87.3%), South America
Page 6 National Health Statistics Reports Number 129 October 9, 2019
(89.4%), Africa and the Middle East
(86.1%), Central Asia (82.8%), Southeast
Asia (89.2%), and South Asia (83.7%)
were less likely than those born in the
United States (94.1%) to have ever had
a mammogram, while the dierences for
those born in Central America (93.3%)
and Europe (92.4%) were not statistically
signicant (Table 3).
Dierences in meeting the
USPSTF recommendations for breast
cancer screening were also observed
by birthplace. Foreign-born women
from Mexico (65.1%), Central Asia
(59.6%), and South Asia (60.9%) were
less likely to have met the USPSTF
recommendations compared with U.S.-
born women. However, no signicant
dierence was found in the percentage
of those who met the USPSTF
recommendations for screening among
women born in the Caribbean (72.3%),
Central America (72.6%), South America
(67.3%), Africa and the Middle East
(66.2%), Southeast Asia (72.8%), and
Europe (72.9%) compared with U.S.-born
women (73.0%).
Adjusted estimates—After
adjustment, dierences by birthplace
resulted in a change in pattern for some
groups (Table 3). The percentage of
women who had ever had a mammogram
was still lower among those born in
Central Asia (84.1%), Southeast Asia
(88.8%), and South Asia (81.5%)
compared with U.S.-born women
(93.9%). However, there was no longer a
signicant dierence in ever receiving a
mammogram between U.S.-born women
and women from Mexico (93.7%), the
Caribbean (91.8%), South America
(93.3%), and Africa and the Middle East
(88.4%), while women from Central
America (96.6%) were more likely to
have ever been screened compared with
U.S.-born women.
U.S.-born women were less likely to
have met the USPSTF recommendations
compared with foreign-born women from
Mexico (81.4%), the Caribbean (78.6%),
and Central America (82.8%). However,
women born in Central Asia (61.6%)
and South Asia (58.4%) remained
less likely to have met the USPSTF
recommendations compared with U.S.-
born women.
Discussion
In this report, unadjusted estimates
show signicant dierences in
mammography receipt between foreign-
born and U.S.-born women. After
adjusting for several sociodemographic
characteristics—including education,
age, marital status, and usual place of
care, which are usually some of the
most prominent factors associated with
mammography receipt (39–41)—the
dierence in ever having a mammogram
between foreign-born women residing
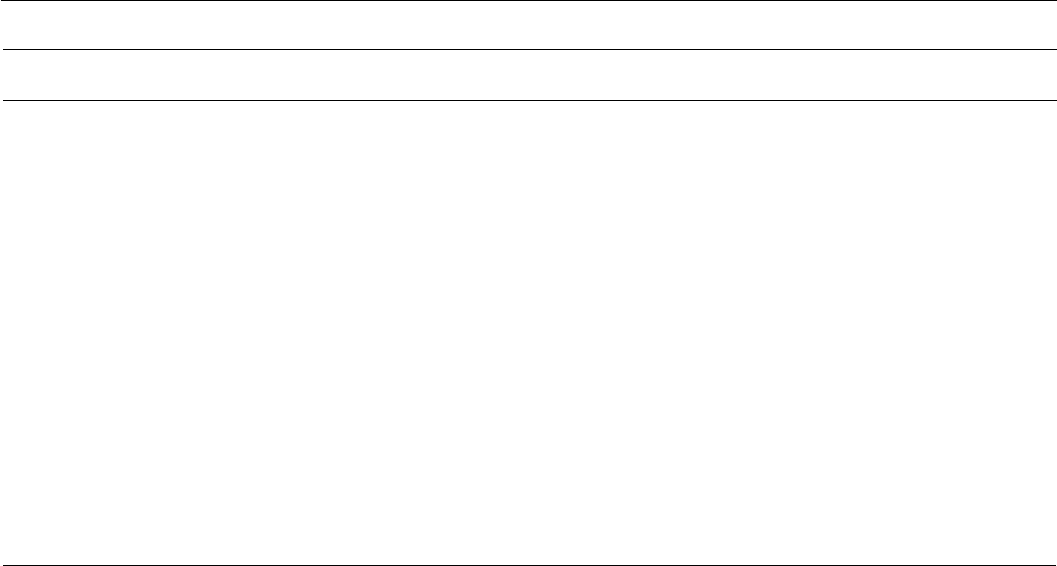
Figure 2. Unadjusted estimates of mammography receipt among women aged 50–74, by nativity and percentage of lifetime in United States:
National Health Interview Survey, 2005, 2008, 2010, 2013, and 2015
0
20
40
60
80
100
Foreign born
with 25% or
more of
lifetime
in U.S.
Foreign born
with less
than 25%
of lifetime
in U.S.
Foreign bornU.S. born Foreign born
with 25% or
more of
lifetime
in U.S.
Foreign born
with less
than 25%
of lifetime
in U.S.
Foreign bornU.S. born
94.1
1
88.3
1
76.4
1
90.9
73.0
1
68.8
1
55.0
71.8
1
Significantly different from U.S. born, p < 0.05.
NOTES: The denominator used for analysis is the number of U.S. women aged 50–74. A mammogram is a radiograph of the breast that can be used to check for breast cancer in
women who have no signs or display no symptoms of the disease. The U.S. Preventive Services Task Force recommends screening for breast cancer with mammography every 2 years
for women aged 50–74. Country of birth, number of years residing in the United States, and current age are used to determine nativity and percentage of time in the United States.
Women born in the United States or born abroad to parents who were U.S. citizens are categorized as U.S. born.
SOURCE: NCHS, National Health Interview Survey, 2005, 2008, 2010, 2013, and 2015.
Percent
Ever had a mammogram
Met U.S. Preventive Services Task Force
recommended mammography screening
National Health Statistics Reports Number 129 October 9, 2019 Page 7
in the United States for less than 25%
of their lifetime and U.S.-born women
was reduced by more than 10 percentage
points (76.4% compared with 94.1%
narrowed to 87.6% compared with
93.9%), although the dierence remained
statistically signicant. A similar pattern
was seen for the likelihood of meeting
the USPSTF recommendations among
foreign-born women who spent less
than 25% of their lifetime compared
with women born in the United States.
After adjustment, those who spent 25%
or more of their lifetime in the United
States were slightly more likely than
U.S.-born women to have met the
USPSTF recommendations, although this
dierence was still signicantly dierent.
Adjustment for sociodemographic
characteristics also aected dierences in
mammography receipt by birthplace. The
dierences in lifetime mammography
receipt between U.S.-born women and
foreign-born women from Mexico, the
Caribbean, South America, and Africa
and the Middle East were attenuated and
no longer signicant. Adjustment resulted
in women from some foreign-born
regions being more likely to have met the
USPSTF recommendations for screening
compared with U.S.-born women, while
for others, dierences in receipt of
recommended mammography compared
with U.S.-born women were attenuated
and no longer signicant.
Previous studies have shown that
morbidity and mortality associated
with breast cancer is reduced by
routine screening (12,42). Some studies
have found that in the absence of
cultural barriers, foreign-born women
may be more receptive to physician
recommendations compared with U.S.-
born women (43). However, this analysis
shows that foreign-born women from
predominantly Spanish-speaking regions
such as Mexico and Central America
had a higher prevalence of adherence
to USPSTF recommendations for
mammography compared with U.S.-born
women, while foreign-born women from
other countries did not. The reduced
dierence in foreign-born women
from Spanish-speaking regions after
adjustment may be explained, in part, by
targeted health care and mammography
programs in some states (44–52). The
inability to further assess dierences by
birthplace and percentage of lifetime
in the United States due to sample size
precludes further assumptions related to
mammography screening and birthplace
in this report. However, these ndings
may inform future research.
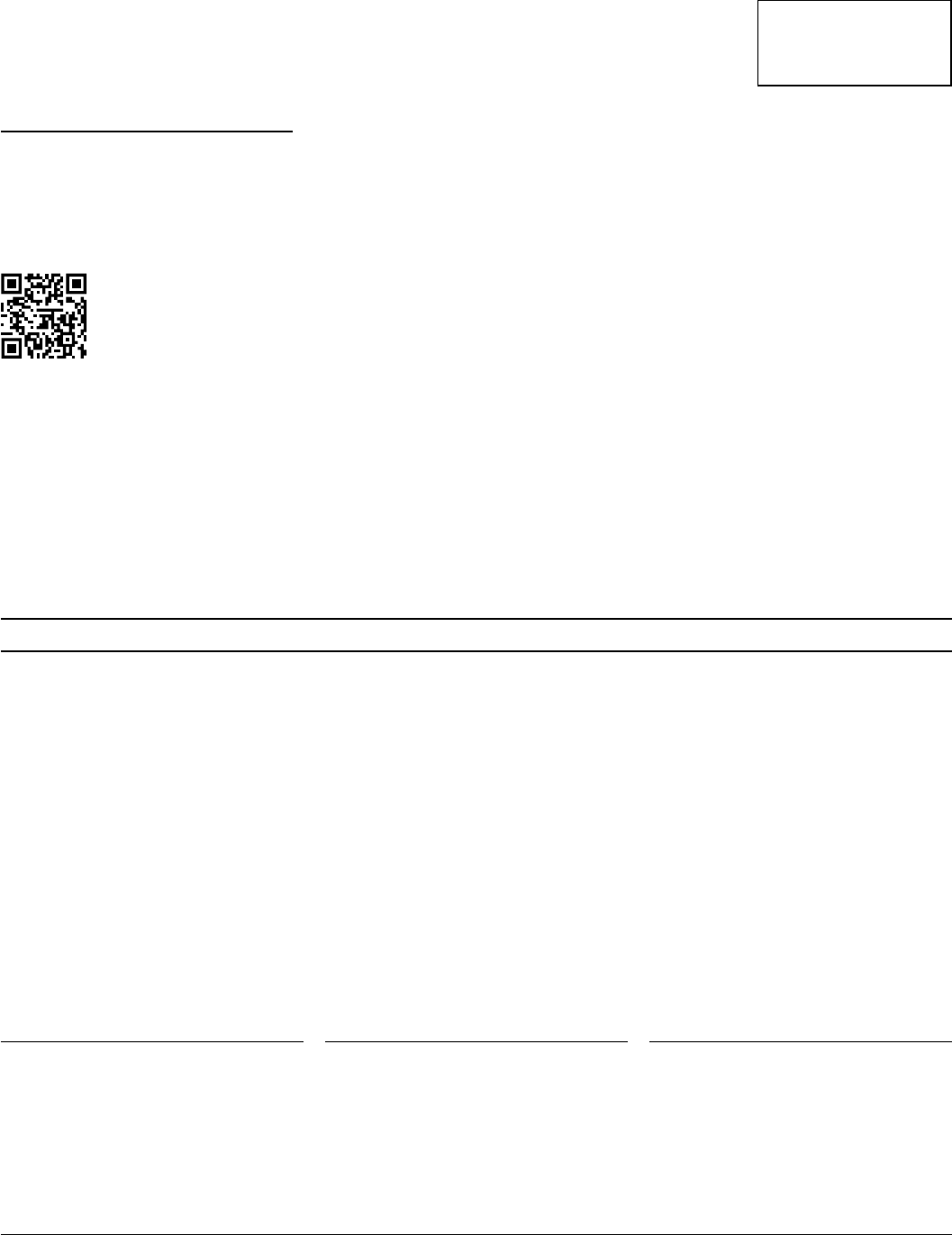
The reduced dierences in having
ever been screened and meeting the
1
Significantly different from U.S. born, p < 0.05.
NOTES: The denominator used for analysis is the number of U.S. women aged 50–74. Estimates are adjusted for age, marital status, income, U.S. region of current residence,
education, health status, health insurance coverage, usual place for medical care, and number of doctor visits in the past 12 months. A mammogram is a radiograph of the breast that
can be used to check for breast cancer in women who have no signs or display no symptoms of the disease. The U.S. Preventive Services Task Force recommends screening for breast
cancer with mammography every 2 years for women aged 50–74. Country of birth, number of years residing in the United States, and current age are used to determine nativity and
percentage of time in the United States. Women born in the United States or born abroad to parents who were U.S. citizens are categorized as U.S. born.
SOURCE: NCHS, National Health Interview Survey, 2005, 2008, 2010, 2013, and 2015.
Percent
Ever had a mammogram
Met U.S. Preventive Services Task Force
recommended mammography screening
Foreign born
with 25% or
more of
lifetime
in U.S.
Foreign born
with less
than 25%
of lifetime
in U.S.
Foreign bornU.S. born Foreign born
with 25% or
more of
lifetime
in U.S.
Foreign born
with less
than 25%
of lifetime
in U.S.
Foreign bornU.S. born
0
20
40
60
80
100
93.9
1
91.4
1
87.6
1
92.5
72.4
74.4
72.1
1
75.1
Figure 3. Predicted marginal distributions of mammography receipt among women aged 50–74, by nativity and percentage of time in
United States: National Health Interview Survey, 2005, 2008, 2010, 2013, and 2015

Page 8 National Health Statistics Reports Number 129 October 9, 2019
USPSTF recommendations among
foreign-born women who have lived
in the United States for 25% or more
of their lifetime after adjustment is
supported by research that suggests
time spent in the United States can be
used as an indirect measure or proxy
of acculturation. In their report titled,
“Assimilation Today,” Myers and Pitkin
suggested that evidence showed the
latest immigrants to the United States
were quickly adapting to their new
home and following in the footsteps of
migrants from early U.S. history (53).
Other research has shown that the length
of time spent in the United States is
highly correlated with English language
adoption (28,29). These studies also
reported that the adoption of English
in everyday communication among
Spanish-speaking persons was shown to
predict breast cancer screening.
In summary, after adjustment for
potential confounders, regardless of
the percentage of lifetime in the United
States, foreign-born women were still
less likely to ever have received a
mammogram. However, this pattern
diered to some extent by birthplace.
After adjustment, foreign-born women
who resided in the United States for less
than 25% of their lifetime were as likely
as U.S.-born women to have met the
USPSTF recommendations for breast
cancer screening. Although the relative
dierence was small, foreign-born
women who resided in the United States
for 25% or more of their lifetime were
more likely than U.S.-born women to
have met the USPSTF recommendations.
This was also true of women from
Mexico, the Caribbean, and Central
America.
The data in this report have some
limitations. Responses are dependent on
participants’ recall of ever receiving, and
recent receipt of, a mammogram, as well
as their willingness to accurately report
information on socioeconomic factors
and health care access and utilization.
Due to small sample size, and to increase
the precision of mammography estimates
at very detailed levels, data were used
from ve periodic cancer supplements
spanning 11 years. While sampling errors
are signicantly reduced by combining
data across years, limitations are also
associated with this estimation procedure
because it only provides an average
across the years. However, preliminary
analysis using Joinpoint software showed
no signicant trend in ever having
received a mammogram across the survey
years within the sample (54,55). Lastly,
despite combining data across years,
small sample sizes prevented some group
dierences from reaching statistical
signicance as well as examining
the interaction between percentage
of lifetime in the United States and
birthplace on mammography receipt.
A major strength of these analyses
is that the data were from a nationally
representative sample of civilian
noninstitutionalized adults living in the
United States, allowing for population
estimates. Although data were pooled
across years, the consistency of the
questions examined from NHIS allows
for a large enough sample size to permit
subgroup analyses. Because both foreign-
and U.S.-born women in this study
received the same survey instrument,
comparisons between these two groups
are more likely to accurately measure the
dierences due to birthplace, compared
with using multiple national surveys
with dierent questions and sampling
methods. Analytically, estimating and
interpreting adjusted predictions and
marginal eects make the results more
tangible and provide a more accurate
picture of relative dierences. Compared
with the direct standardization approach,
the predictive marginal approach permits
the use of a larger number of variables in
the standardization process.
These ndings may inform other
research on the potential relationship
with, and impact of, nativity, percentage
of lifetime in the United States, and
birthplace, and the likelihood of engaging
in recommended preventive cancer
screening.
References
1. Centers for Disease Control and
Prevention. Breast cancer statistics.
Available from: https://www.cdc.
gov/cancer/breast/statistics/index.
htm.
2. U.S. Cancer Statistics Working
Group. U.S. Cancer Statistics
Data Visualizations Tool, based on
November 2018 submission data
(1999–2016). Centers for Disease
Control and Prevention; National
Cancer Institute. 2019. Available
from: https://gis.cdc.gov/Cancer/
USCS/DataViz.html.
3. White A, Thompson TD, White MC,
Sabatino S, de Moor J, Doria-Rose
PV, et al. Cancer screening test use—
United States, 2015. MMWR Morb
Mortal Wkly Rep. 66(8):201–6. 2017.
4. Clarke TC, Endeshaw M, Duran D,
Saraiya M. QuickStats: Percentage of
U.S. women aged 50–74 years who
never had a mammogram, by place
of birth and length of residence in
the United States—National Health
Interview Survey, 2013 and 2015.
MMWR Morb Mortal Wkly Rep
66(11):309. 2017.
5. Zong J, Batalova J, Hallock J.
Frequently requested statistics
on immigrants and immigration
in the United States. Migration
Policy Institute. 2018. Available
from: https://www.migrationpolicy.
org/article/frequently-requested-
statistics-immigrants-and-
immigration-united-states-7.
6. Migration Policy Institute. U.S.
immigrant population by state and
county. Available from: https://www.
migrationpolicy.org/programs/data-
hub/charts/us-immigrant-population-
state-and-county.
7. Khan F, Ruterbusch JJ, Gomez
SL, Schwartz K. Dierences in the
cancer burden among foreign-born
and US-born Arab Americans living
in metropolitan Detroit. Cancer Causes
Control 24(11):1955–61. 2013.
8. Kato I, Yee CL, Ruterbusch J,
Schwartz K. Patterns of cancer in
rst generation immigrants from the
Arab League and other countries. J
Registry Manag 36(3):71–6; quiz
101–2. 2009.
9. Singh GK, Hiatt RA. Trends and
disparities in socioeconomic and
behavioural characteristics, life
expectancy, and cause-specic
mortality of native-born and
foreign-born populations in the
United States, 1979–2003. Int J
Epidemiol 35(4):903–19. 2006.
10. Bray F, Jemal A, Grey N, Ferlay
J, Forman D. Global cancer
transitions according to the Human
Development Index (2008–2030):

National Health Statistics Reports Number 129 October 9, 2019 Page 9
A population-based study. Lancet
Oncol 13(8):790–801. 2012.
11. Bray F, Ferlay J, Soerjomataram
I, Siegel RL, Torre LA, Jemal
A. Global cancer statistics 2018:
GLOBOCAN estimates of incidence
and mortality worldwide for 36
cancers in 185 countries. CA Cancer
J Clin 68(6):394–424. 2018.
12. Youlden DR, Cramb SM, Dunn
NA, Muller JM, Pyke CM, Baade
PD. The descriptive epidemiology
of female breast cancer: An
international comparison of
screening, incidence, survival
and mortality. Cancer Epidemiol
36(3):237–48. 2012.
13. Torre LA, Bray F, Siegel RL, Ferlay
J, Lortet-Tieulent J, Jemal A. Global
cancer statistics, 2012. CA Cancer J
Clin 65(2):87–108. 2015.
14. John EM, Phipps AI, Davis A, Koo
J. Migration history, acculturation,
and breast cancer risk in Hispanic
women. Cancer Epidemiol
Biomarkers Prev 14(12):2905–13.
2005.
15. Engelman KK, Cupertino AP, Daley
CM, Long T, Cully A, Mayo MS,
et al. Engaging diverse underserved
communities to bridge the
mammography divide. BMC Public
Health 11:47. 2011.
16. Lubetkin EI, Zabor EC, Brennessel
D, Kemeny MM, Hay JL. Beyond
demographics: Dierences in patient
activation across new immigrant,
diverse language subgroups. J
Community Health 39(1):40–9.
2014.
17. Brown WM, Consedine NS, Magai
C. Time spent in the United States
and breast cancer screening
behaviors among ethnically diverse
immigrant women: Evidence for
acculturation? J Immigr Minor
Health 8(4):347–58. 2006.
18. Alexandraki I, Mooradian AD.
Barriers related to mammography
use for breast cancer screening
among minority women. J Natl Med
Assoc 102(3):206–18. 2010.
19. Endeshaw M, Clarke T, Senkomago
V, Saraiya M. Cervical cancer
screening among women by
birthplace and percent of lifetime
living in the United States. J Low
Genit Tract Dis 22(4):280–7 2018.
20. Jemal A, Ward E, Thun MJ.
Recent trends in breast cancer
incidence rates by age and tumor
characteristics among U.S. women.
Breast Cancer Res 9(3):R28. 2007.
21. Wun LM, Feuer EJ, Miller BA.
Are increases in mammographic
screening still a valid explanation
for trends in breast cancer incidence
in the United States? Cancer Causes
Control 6(2):135–44. 1995.
22. U.S. Preventive Services Task Force.
Screening for breast cancer: U.S.
Preventive Services Task Force
Recommendation Statement. Ann
Intern Med 151(10):716–26. 2009.
23. Botman SL, Moore TF, Moriarity
CL, Parsons VL. Design and
estimation for the National Health
Interview Survey, 1995–2004.
National Center for Health Statistics.
Vital Health Stat 2(130). 2000.
24. Parsons VL, Moriarity C, Jonas K,
Moore TF, Davis KE, Tompkins
L. Design and estimation for the
National Health Interview Survey,
2006–2015. National Center for
Health Statistics. Vital Health Stat
2(165). 2014.
25. Nelson HD, Tyne K, Naik A,
Bougatsos C, Chan BK, Humphrey
L. Screening for breast cancer:
An update for the U.S. Preventive
Services Task Force. Ann Intern Med
151(10):727–37. 2009.
26. U.S. Preventive Services Task
Force. Breast cancer: Screening.
2016. Available from: https://www.
uspreventiveservicestaskforce.org/
Page/Document/UpdateSummary
Final/breast-cancer-screening1.
27. National Center for Health Statistics.
2015 National Health Interview
Survey (NHIS) public use data
release: Survey description.
Hyattsville, MD. 2016. Available
from: https://ftp.cdc.gov/pub/
Health_Statistics/NCHS/Dataset_
Documentation/NHIS/2015/
srvydesc.pdf.
28. O’Malley AS, Kerner J, Johnson
AE, Mandelblatt J. Acculturation
and breast cancer screening among
Hispanic women in New York City.
Am J Public Health 89(2):219–27.
1999.
29. Mandelblatt JS, Gold K, O’Malley
AS, Taylor K, Cagney K, Hopkins
JS, Kerner J. Breast and cervix
cancer screening among multiethnic
women: Role of age, health,
and source of care. Prev Med
28(4):418–25. 1999.
30. Gorman BK, Read JG, Krueger PM.
Gender, acculturation, and health
among Mexican Americans. J Health
Soc Behav 51(4):440–57. 2010.
31. Lee S, Nguyen HA, Tsui J. Interview
language: A proxy measure
for acculturation among Asian
Americans in a population-based
survey. J Immigr Minor Health
13(2):244–52. 2011.
32. Samuel PS, Pringle JP, James NW
4th, Fielding SJ, Faireld KM.
Breast, cervical, and colorectal
cancer screening rates amongst
female Cambodian, Somali, and
Vietnamese immigrants in the USA.
Int J Equity Health 8(30). 2009.
33. U.S. Census Bureau. How the
U.S. Census Bureau measures
poverty. 2014. Available from:
https://www.census.gov/library/
visualizations/2014/demo/poverty_
measure-how.html.
34. SAS Institute Inc. SAS/STAT
(version 9.3) [computer software].
2012.
35. RTI International. SUDAAN (release
11.0.0) [computer software]. 2012
36. Sato T, Matsuyama Y. Marginal
structural models as a tool for
standardization. Epidemiology
14(6):680–6. 2003.
37. Schenker N, Gentleman JF.
On judging the signicance of
dierences by examining the overlap
between condence intervals. The
American Statistician 55(3):182–6.
2001.
38. Parker JD, Talih M, Malec DJ,
Beresovsky V, Carroll M, Gonzalez
JF Jr, et al. National Center for
Health Statistics data presentation
standards for proportions. National
Center for Health Statistics. Vital
Health Stat 2(175). 2017.
39. Dallo FJ, Kindratt TB. Disparities in
vaccinations and cancer screening
among U.S.- and foreign-born
Arab and European American
non-Hispanic white women. Womens
Health Issues 25(1):56–62. 2015.
40. Theme Filha MM, Leal MD, Oliveira
EF, Esteves-Pereira AP, Gama SG.

Page 10 National Health Statistics Reports Number 129 October 9, 2019
Regional and social inequalities
in the performance of Pap test and
screening mammography and their
correlation with lifestyle: Brazilian
National Health Survey. Int J Equity
Health 15(1):136. 2016.
41. Sabatino SA, Coates RJ, Uhler
RJ, Breen N, Tangka F, Shaw KM.
Disparities in mammography use
among US women aged 40–64 years,
by race, ethnicity, income, and health
insurance status, 1993 and 2005.
Med Care 46(7):692–700. 2008.
42. Oenger KC, Fontham ET,
Etzioni R, Herzig A, Michaelson
JS, Shih YC, et al. Breast cancer
screening for women at average
risk: 2015 guideline update from the
American Cancer Society. JAMA
314(15):1599–614. 2015.
43. Julliard K, Vivar J, Delgado C, Cruz
E, Kabak J, Sabers H. What Latina
patients don’t tell their doctors: A
qualitative study. Ann Fam Med
6(6):543–9. 2008.
44. Health Resources and Services
Administration, Bureau of Primary
Health Care. Public Health Service
Act [42 USC 254b], Section 330(b).
Available from: https://www.hrsa.
gov/advisorycommittees/shortage/
Meetings/20100922/section330mua.
pdf.
45. Health Resources and Services
Administration, Rural Health
Information Hub. Federally qualied
health centers (FQHCs) and the
Health Center Program. Available
from: https://www.ruralhealthinfo.
org/topics/federally-qualied-health-
centers.
46. United States–Mexico Border Health
Commission. Border lives: Health
status in the United States–Mexico
border region. 2010. Available from:
https://www.ruralhealthinfo.org/assets/
940-3105/health-status-in-the-united-
states-mexico-border-region.pdf.
47. Cleveland Clinic. Three reasons why
we opened a Hispanic clinic: A new
model of patient-centered care. 2015.
Available from: https://consultqd.
clevelandclinic.org/3-reasons-why-
we-opened-a-hispanic-clinic/.
48. Oce of Minority Health. State and
territorial eorts to reduce health
disparities: Findings of a 2016
survey by the U.S. Department of
Health and Human Services Oce
of Minority Health. Washington,
DC: U.S. Department of Health and
Human Services. 2018. Available
from: https://minorityhealth.hhs.
gov/assets/PDF/OMH-Health-
Disparities-Report-State-and-
Territorial-Eorts-October-2018.pdf.
49. Coronado GD, Beresford SA,
McLerran D, Jimenez R, Patrick
DL, Ornelas I, et al. Multilevel
intervention raises Latina
participation in mammography
screening: Findings from ¡Fortaleza
Latina! Cancer Epidemiol
Biomarkers Prev 25(4):584–92.
2016.
50. Lairson DR, Kim J, Byrd T, Salaiz
R, Shokar NK. Cost-eectiveness
of community interventions for
colorectal cancer screening: Low-
income Hispanic population. Health
Promot Pract 19(6):863–72. 2018.
51. Luque JS, Logan A, Soulen G,
Armeson KE, Garrett DM, Davila
CB, Ford ME. Systematic review of
mammography screening educational
interventions for Hispanic women
in the United States. J Cancer Educ
34(3):412–22. 2019.
52. New York State Department of
Public Health. Public health works!
2017. Available from:
https://www.health.ny.gov/
prevention/public_health_works/.
53. Myers D, Pitkin J. Assimilation
today: New evidence shows the
latest immigrants to America are
following in our history’s footsteps.
Washington, DC: Center for
American Progress. 2010. Available
from: https://cdn.americanprogress.
org/wp-content/uploads/
issues/2010/09/pdf/immigrant_
assimilation.pdf.
54. National Cancer Institute. Joinpoint
Regression Program (Version
4.5.0.1) [computer software]. 2017.
55. Kim HJ, Fay MP, Feuer EJ,
Midthune DN. Permutation tests
for joinpoint regression with
applications to cancer rates. Stat Med
19(3):335–51. 2000.
National Health Statistics Reports Number 129 October 9, 2019 Page 11
Table 1. Percent distribution of women aged 50–74, by birthplace: United States, 2005, 2008, 2010, 2013, and 2015
Birthplace Sample size Percent of total population
Relative percent among
foreign-born women
United States . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 25,707 86.9 …
Mexico . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 1,022 2.7 20.4
Caribbean. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 694 1.7 13.1
Central America . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 283 0.7 5.4
South America . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 340 0.9 7.1
Europe . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 577 2.4 18.3
Central Asia . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 328 1.1 8.3
Southeast Asia . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 559 1.8 13.5
South Asia . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 137 0.6 4.9
Africa and Middle East . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 182 0.8 5.9
Other. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 122 0.4 3.3
Total . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 29,951 100.0 100.2
... Category not applicable
NOTES: The denominator used for analysis is the number of U.S. women aged 50–74. Women born in the United States or born abroad to parents who were U.S. citizens are categorized as U.S. born.
If born abroad to parents who were non-U.S. citizens, country of birth, geographic proximity, cultural commonalities, socioeconomic differences and similarities, and sample sizes are used to catego-
rize participants by birthplace. South Asia, also known as the Indian subcontinent, includes Afghanistan, Bangladesh, Bhutan, India, Maldives, Nepal, Pakistan, and Sri Lanka. Europe includes Russia
and former Union of Soviet Socialist Republics areas. Percentages may not add to 100 due to rounding.
SOURCE: NCHS, National Health Interview Survey, 2005, 2008, 2010, 2013, and 2015.

Page 12 National Health Statistics Reports Number 129 October 9, 2019
Table 2. Sociodemographic characteristics and health care access and utilization among women aged 50–74, by nativity and percentage of lifetime in United States: National Health
Interview Survey, 2005, 2008, 2010, 2013, and 2015
Characteristic
Total U.S. born Foreign born
Less than 25% of
lifetime in United States
25% or more of lifetime
in United States
Sample size
Percent
distribution (SE) Sample size
Percent
distribution (SE) Sample size
Percent
distribution (SE) Sample size
Percent
distribution (SE) Sample size
Percent
distribution (SE)
All women. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 29,951 100.0 (0.0) 25,707 86.9 (0.3) 4,244
1
13.1 (0.4) 792
1
2.4 (0.1) 3,452
1
10.7 (0.3)
Age group
50–59 . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 13,945 50.4 (0.4) 11,867 49.9 (0.4) 2,078
1
53.8 (1.0) 400
1
55.2 (2.1) 1,678
1
53.5 (1.1)
60–69 . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 11,620 36.8 (0.4) 10,076 37.2 (0.4) 1,544
1
34.0 (0.9) 297 35.4 (2.0) 1,247
1
33.6 (1.0)
70–74 . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 4,386 12.8 (0.2) 3,764 12.9 (0.3) 622 12.2 (0.6) 95
1
9.4 (1.1) 527 12.9 (0.7)
Race and ethnicity
2
Hispanic . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 3,772 9.3 (0.3) 1,731 4.8 (0.2) 2,041
1
38.9 (1.1) 406
1
43.5 (2.2) 1,635
1
37.8 (1.2)
Non-Hispanic white. . . . . . . . . . . . . . . . . . . . . . . . . 19,679 73.6 (0.5) 18,874 80.8 (0.4) 805
1
26.0 (1.1) 109
1
19.3 (2.1) 696
1
27.5 (1.1)
Non-Hispanic black. . . . . . . . . . . . . . . . . . . . . . . . . 4,644 11.2 (0.3) 4,299 11.8 (0.3) 345
1
7.9 (0.7) 73
1
8.8 (1.2) 272
1
7.7 (0.8)
Non-Hispanic Asian . . . . . . . . . . . . . . . . . . . . . . . . 1,274 4.2 (0.2) 247 0.8 (0.1) 1,027
1
26.5 (1.0) 202
1
27.9 (2.0) 825
1
26.2 (1.1)
Other or mixed race . . . . . . . . . . . . . . . . . . . . . . . . 582 1.6 (0.1) 556 1.8 (0.1) 26
1
0.7 (0.2) * * 24
1
0.8 (0.2)
Marital status
Never married . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 2,816 6.4 (0.2) 2,421 6.4 (0.2) 395 6.4 (0.4) 69 5.8 (0.8) 326 6.5 (0.5)
Currently married or living with partner. . . . . . . . . . 14,420 63.4 (0.4) 12,235 62.9 (0.4) 2,185
1
66.7 (0.9) 401 63.1 (2.0) 1,784
1
67.6 (1.0)
Formerly married . . . . . . . . . . . . . . . . . . . . . . . . . . 12,570 30.2 (0.3) 10,932 30.7 (0.4) 1,638
1
26.9 (0.8) 311 31.1 (1.9) 1,327
1
25.9 (0.9)
Education
Less than high school. . . . . . . . . . . . . . . . . . . . . . . 4,711 13.6 (0.3) 3,228 11.1 (0.3) 1,483
1
30.2 (0.9) 325
1
38.3 (2.1) 1,158
1
28.5 (0.9)
High school graduate or GED. . . . . . . . . . . . . . . . . 8,481 29.2 (0.4) 7,557 30.2 (0.4) 924
1
22.9 (0.9) 165
1
23.2 (1.9) 759
1
22.9 (1.0)
Some college . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 8,879 29.6 (0.3) 8,098 31.2 (0.4) 781
1
18.7 (0.8) 109
1
13.7 (1.5) 672
1
19.8 (0.9)
College degree . . . . . . . . . . . . . . . . . . . . . . . . . . . . 7,695 27.6 (0.4) 6,701 27.5 (0.4) 994 28.2 (0.9) 161 24.8 (2.0) 833 28.9 (1.0)
Poverty status
3
Less than 100% of poverty level. . . . . . . . . . . . . . . 4,328 10.2 (0.2) 3,362 9.2 (0.2) 966
1
16.7 (0.7) 235
1
24.1 (1.9) 731
1
15.0 (0.8)
100%–199% of poverty level . . . . . . . . . . . . . . . . . 5,936 17.1 (0.3) 4,910 16.5 (0.3) 1,026
1
21.1 (0.7) 233
1
28.5 (2.0) 793
1
19.5 (0.8)
200%–399% of poverty level . . . . . . . . . . . . . . . . . 8,758 29.5 (0.4) 7,574 29.4 (0.4) 1,184 29.9 (0.9) 204 29.8 (2.0) 980 29.9 (1.0)
400% or more of poverty level . . . . . . . . . . . . . . . . 10,929 43.2 (0.5) 9,861 44.9 (0.5) 1,068
1
32.3 (1.0) 120
1
17.6 (2.0) 948
1
35.6 (1.1)
Health status
Excellent or very good . . . . . . . . . . . . . . . . . . . . . . 14,465 50.7 (0.4) 12,734 51.7 (0.5) 1,731
1
43.6 (1.0) 296
1
39.9 (2.1) 1,435
1
44.5 (1.1)
Good. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 9,086 30.2 (0.3) 7,650 29.7 (0.4) 1,436
1
34.1 (0.9) 272
1
34.4 (2.0) 1,164
1
34.0 (1.0)
Fair or poor . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 6,386 19.1 (0.3) 5,314 18.6 (0.3) 1,072
1
22.3 (0.8) 224
1
25.7 (1.8) 848
1
21.5 (0.9)
Health insurance coverage
4
Private. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 18,598 67.5 (0.4) 16,704 69.8 (0.4) 1,894
1
51.8 (1.0) 243
1
34.3 (2.2) 1,651
1
55.6 (1.1)
Public . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 5,247 14.3 (0.3) 4,230 13.5 (0.5) 1,017
1
19.8 (0.8) 223
1
25.5 (1.9) 794
1
18.5 (0.8)
Medicare only and Medicare Advantage. . . . . . . . . 3,248 9.5 (0.2) 2,736 9.3 (0.2) 512
1
10.6 (0.6) 55
1
6.7 (0.9) 457
1
11.5 (0.6)
Uninsured . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 2,775 8.7 (0.2) 1,975 7.4 (0.2) 800
1
17.8 (0.8) 264
1
33.5 (2.1) 536
1
14.3 (0.8)
Usual place of care
None. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 2,103 6.6 (0.2) 1,585 5.8 (0.2) 518
1
11.8 (0.6) 174
1
22.2 (1.8) 344
1
9.4 (0.7)
Has a usual place. . . . . . . . . . . . . . . . . . . . . . . . . . 27,587 93.4 (0.2) 23,897 94.2 (0.2) 3,690
1
88.2 (0.6) 613
1
77.8 (1.8) 3,077
1
90.6 (0.7)
See footnotes at end of table.
National Health Statistics Reports Number 129 October 9, 2019 Page 13
Table 2. Sociodemographic characteristics and health care access and utilization among women aged 50–74, by nativity and percentage of lifetime in United States: National Health
Interview Survey, 2005, 2008, 2010, 2013, and 2015—Con.
Characteristic
Total U.S. born Foreign born
Less than 25% of
lifetime in United States
25% or more of lifetime
in United States
Sample size
Percent
distribution (SE) Sample size
Percent
distribution (SE) Sample size
Percent
distribution (SE) Sample size
Percent
distribution (SE) Sample size
Percent
distribution (SE)
Visits to health care provider
None. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 2,829 9.2 (0.2) 2,213 8.4 (0.2) 616
1
14.1 (0.7) 173
1
23.2 (1.9) 443
1
12.0 (0.7)
1 . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 3,796 12.9 (0.3) 3,172 12.5 (0.3) 624
1
15.8 (0.8) 119 14.7 (1.5) 505
1
16.1 (0.8)
2 or 3 . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 7,747 27.0 (0.3) 6,637 26.9 (0.4) 1,110 28.0 (0.9) 187 25.1 (1.9) 923 28.6 (1.0)
4 or more . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 14,984 50.9 (0.4) 13,186 52.2 (0.4) 1,798
1
42.1 (0.9) 293
1
37.0 (2.0) 1,505
1
43.3 (1.1)
U.S. region of current residence
New England . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 2,020 5.5 (0.5) 1,812 5.5 (0.5) 208 5.1 (0.6) 33
1
3.5 (0.8) 175 5.5 (0.7)
Mid-Atlantic. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 4,315 16.0 (1.1) 3,499 15.2 (1.0) 816
1
20.8 (2.1) 138 18.9 (2.8) 678
1
21.3 (2.0)
East North Central . . . . . . . . . . . . . . . . . . . . . . . . . 3,860 15.6 (0.7) 3,613 17.0 (0.7) 247
1
7.0 (0.9) 51
1
8.4 (1.6) 196
1
6.8 (0.9)
West North Central. . . . . . . . . . . . . . . . . . . . . . . . . 2,499 7.2 (0.4) 2,409 7.9 (0.4) 90
1
2.1 (0.3) 24
1
3.1 (0.8) 66
1
1.8 (0.3)
South Atlantic . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 4,958 17.9 (0.7) 4,231 18.1 (0.7) 727 16.2 (1.3) 151 18.0 (2.1) 576
1
5.7 (1.3)
East South Central . . . . . . . . . . . . . . . . . . . . . . . . . 1,868 6.1 (0.3) 1,829 6.9 (0.4) 39
1
1.2 (0.3) * * 30
1
1.2 (0.3)
West South Central. . . . . . . . . . . . . . . . . . . . . . . . . 3,295 10.8 (0.5) 2,858 11.0 (0.5) 437 9.8 (0.6) 102 10.7 (1.6) 335 9.6 (0.7)
Mountain. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 2,538 6.1 (0.3) 2,269 6.2 (0.4) 269 5.6 (0.6) 36 5.3 (1.1) 233 5.7 (0.5)
Pacic . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 4,598 14.9 (0.4) 3,187 12.4 (0.4) 1,411
1
32.1 (2.2) 248
1
30.9 (2.2) 1,163
1
32.4 (1.4)
* Estimate does not meet NCHS standards of reliability.
1
Signicantly different from U.S. born, p < 0.05.
2
Hispanic refers to persons who are of Hispanic or Latino origin and may be of any race or combination of races. Non-Hispanic refers to persons who are not of Hispanic or Latino origin, regardless of race.
3
Based on family income and family size using the U.S. Census Bureau poverty thresholds for 2004, 2007, 2009, 2012, and 2014.
4
A person is dened as uninsured if he or she did not have any private health insurance, Medicare, Medicaid, state-sponsored or other government–sponsored health plan, or military plan at the time of interview. A person is also dened as uninsured if he or she
had only Indian Health Service coverage or had only a private plan that paid for one type of service, such as accidents or dental care. Public health insurance includes persons with Medicaid, dual Medicare and Medicaid enrollment, or military or other government
health insurance coverage. Women aged 65 and over with only Medicare coverage including Medicare Advantage plans were placed in a separate category.
NOTES: Estimates are based on household interviews of a sample of the U.S. civilian noninstitutionalized population. Estimates were weighted using the Sample Adult weight. Unless indicated, unknowns for the columns were not included in the denominators
when calculating percentages, but they were included in the category of All women. Percentages may not add to 100 due to rounding. Country of birth, number of years residing in the United States, and current age are used to determine nativity and percentage of
time in the United States. Women born in the United States or born abroad to parents who were U.S. citizens are categorized as U.S. born. SE is standard error.
SOURCE: NCHS, National Health Interview Survey, 2005, 2008, 2010, 2013, and 2015.
Page 14 National Health Statistics Reports Number 129 October 9, 2019
Table 3. Estimates of mammography receipt among women aged 50–74, by birthplace: United States, 2005, 2008, 2010, 2013, and 2015
Birthplace Ever had a mammogram
Met U.S. Preventive Services Task Force
mammography screening recommendations
Unadjusted estimates Percent (standard error)
United States . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 94.1 (0.2) 73.0 (0.4)
Mexico . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .
1
85.8 (1.5)
1
65.1 (2.0)
Caribbean. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .
1
87.3 (1.4) 72.3 (2.0)
Central America . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 93.3 (1.7) 72.6 (3.5)
South America . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .
1
89.4 (2.0) 67.3 (3.6)
Africa and Middle East . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .
1
86.1 (3.2) 66.2 (4.8)
Central Asia . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .
1
82.8 (2.6)
1
59.6 (3.5)
Southeast Asia . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .
1
89.2 (1.8) 72.8 (2.6)
South Asia
2
. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .
1
83.7 (3.9)
1
60.9 (5.4)
Europe
3
. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 92.4 (1.4) 72.9 (2.4)
Adjusted estimates
4
United States . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 93.9 (0.2) 72.4 (0.4)
Mexico . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 93.7 (0.8)
1
81.4 (1.4)
Caribbean. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 91.8 (1.1)
1
78.6 (2.0)
Central America . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .
1
96.6 (0.9)
1
82.8 (2.3)
South America . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 93.3 (1.5) 74.7 (2.6)
Africa and Middle East . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 88.4 (2.8) 69.6 (4.4)
Central Asia . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .
1
84.1 (2.3)
1
61.6 (3.4)
Southeast Asia . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .
1
88.8 (1.6) 73.6 (2.2)
South Asia
2
. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .
1
81.5 (4.0)
1
58.4 (5.3)
Europe
3
. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 92.3 (1.3) 72.5 (2.3)
1
Signicantly different from U.S.-born women, p < 0.05.
2
Also known as the Indian subcontinent; includes Afghanistan, Bangladesh, Bhutan, India, Maldives, Nepal, Pakistan, and Sri Lanka.
3
Includes Russia and former Union of Soviet Socialist Republics areas.
4
Adjusted for age, marital status, income, U.S. region of current residence, education, health status, health insurance coverage, usual place for medical care, and number of doctor visits in the
past 12 months.
NOTES: The denominator used for analysis is the number of U.S. women aged 50–74. A mammogram is a radiograph of the breast that can be used to check for breast cancer in women who have no
signs or display no symptoms of the disease. The U.S. Preventive Services Task Force recommends screening for breast cancer with mammography every 2 years for women aged 50–74. For women
born abroad to parents who were non-U.S. citizens, country of birth, geographic proximity, cultural commonalities, socioeconomic differences and similarities, and sample size are used to categorize
participants by birthplace.
SOURCE: NCHS, National Health Interview Survey, 2005, 2008, 2010, 2013, and 2015.
National Health Statistics Reports Number 129 October 9, 2019
For more NCHS NHSRs, visit:
https://www.cdc.gov/nchs/products/nhsr.htm.
For e-mail updates on NCHS publication releases, subscribe online at: https://www.cdc.gov/nchs/govdelivery.htm.
For questions or general information about NCHS: Tel: 1–800–CDC–INFO (1–800–232–4636) • TTY: 1–888–232–6348
Internet: https://www.cdc.gov/nchs • Online request form: https://www.cdc.gov/info
DHHS Publication No. 2020–1250 • CS310396
FIRST CLASS MAIL
POSTAGE & FEES PAID
CDC/NCHS
PERMIT NO. G-284
U.S. DEPARTMENT OF
HEALTH & HUMAN SERVICES
Centers for Disease Control and Prevention
National Center for Health Statistics
3311 Toledo Road, Room 4551, MS P08
Hyattsville, MD 20782–2064
OFFICIAL BUSINESS
PENALTY FOR PRIVATE USE, $300
Suggested citation
Clarke TC, Endeshaw M, Duran D, Saraiya M.
Breast cancer screening among women by
nativity, birthplace, and length of time in the
United States. National Health Statistics
Reports; no 129. Hyattsville, MD: National
Center for Health Statistics. 2019.
Copyright information
All material appearing in this report is in
the public domain and may be reproduced
or copied without permission; citation as to
source, however, is appreciated.
National Center for Health Statistics
Jennifer H. Madans, Ph.D., Acting Director
Amy M. Branum, Ph.D., Acting Associate
Director for Science
Division of Health Interview Statistics
Stephen J. Blumberg, Ph.D., Director
Anjel Vahratian, Ph.D., M.P.H., Associate
Director for Science
