Ozlem Kazan Kizilkurt
1
, Taha Kizilkurt
2
, Medine Yazici Gulec
3
, Ferzan Ergun Giynas
3
,
Gokhan Polat
2
, Onder Ismet Kilicoglu
2
, Huseyin Gulec
3
DOI: 10.14744/DAJPNS.2020.00070
Dusunen Adam The Journal of Psychiatry and
Neurological Sciences 2020;33:109-119
How to cite this article: Kizilkurt OK, Kizilkurt T, Yazici Gulec M, Ergun Giynas F, Polat G, Kilicoglu OI, Gulec H. Quality of life after lower extremity
amputation due to diabetic foot ulcer: the role of prosthesis-related factors, body image, self-esteem, and coping styles. Dusunen Adam The
Journal of Psychiatry and Neurological Sciences 2020;33:109-119.
Quality of life after lower extremity amputation due
to diabetic foot ulcer: the role of prosthesis-related
factors, body image, self-esteem, and coping styles
1
Uskudar University, Department of Psychiatry, NPIstanbul Neuropsychiatry Hospital, Istanbul - Turkey
2
Istanbul University, Istanbul Faculty of Medicine, Department of Orthopedics and Traumatology, Istanbul - Turkey
3
University of Health, Sciences Erenkoy Mental Research and Training Hospital, Istanbul - Turkey
Correspondence: Ozlem Kazan Kizilkurt, Ahmet Tevfik Ileri Street No:18, 34768 Umraniye/Istanbul - Turkey
E-mail: [email protected]
Received: December 19, 2019; Revised: February 03, 2020; Accepted: March 30, 2020
ABSTRACT
Objective: The purpose of this study was to identify clinical and psychosocial factors that predict an individual’s subjective
quality of life after having undergone a lower limb amputation secondary to diabetic foot ulcer.
Method: The study sample comprised 65 patients who underwent amputation because of an infected diabetic foot ulcer. Short
Form 36, The Trinity Amputation and Prosthesis Experience Scale, Coping Attitudes Evaluation Scale, Multidimensional Scale of
Perceived Social Support, Rosenberg Self-Esteem Scale, and Amputee Body Image Scale were administered as questionnaires.
Stepwise linear regression analysis was conducted to assess the factors predicting quality of life.
Results: Quality of life was negatively correlated with depression, anxiety, body image, activity limitation, and dysfunctional
coping strategies and positively correlated with perceived social support, satisfaction with prosthesis, self-esteem, and
problem-focused coping style. Regression analysis showed satisfaction with prosthesis and body perception, problem-focused
coping strategies, dysfunctional coping strategies, and self-esteem to be the factors with the highest predictive power for the
physical component of quality of life, while body perception, problem-focused, and dysfunctional coping strategies were the
strongest predictors for the mental component of quality of life.
Conclusion: Impaired body image and self-esteem, less usage of problem-focused and high usage of dysfunctional coping
strategies, in addition to low satisfaction with the prosthesis were the strongest predictors for poor quality of life. Factors
associated with better quality of life after the amputation were investigated in this study, which may support future
development of post-amputation rehabilitation strategies for lower limb amputees.
Keywords: Amputation, body image, coping strategies, diabetes, self-esteem
RESEARCH ARTICLE
INTRODUCTION
Diabetic foot ulcers are often considered complications
requiring long periods of challenging treatment;
additionally, they may cause anxiety due to the potential
necessity of amputation (1). Although the psychological
status of mobile amputees is known to be better than
that of diabetic foot ulcer patients, extremity amputation

Dusunen Adam The Journal of Psychiatry and Neurological Sciences 2020;33:109-119110
remains an important medical issue and the
psychosocial adaptation of individuals after extremity
amputation involves significant difficulties (2). It is
generally accepted that lower extremity complications
due to diabetic foot ulcer negatively affect a person’s
quality of life, predisposing the patient to psychiatric
symptoms (1,3,4). Depression and anxiety symptoms
that emerge after amputation have been reported to
make significant contributions to a reduced quality of
life (5). In addition, it is reported that although
depression and anxiety are relatively high in a period of
up to 2 years post-amputation, they appear to decline
thereafter to general population norms (6).
After amputation, patients can experience a distorted
body image, decreased self-esteem, social isolation, and
increased dependency on others (7). During the post-
amputation period, perceived social support, adaptation
to the prosthesis, amputation type, presence of phantom
and stump pain, self-esteem, and body image issues are
among the factors reported to affect quality of life and
psychosocial functionality significantly (8,9). Different
coping strategies have been shown to have different
outcomes on adaptation after amputation. Problem-
focused strategies are associated with positive
psychosocial adaptation (10), while emotion-focused
and passive strategies are associated with negative
psychosocial outcomes (11).
We believe that evaluating and detecting the
conditions negatively affecting individuals’ quality of
life after amputation are important in ensuring
appropriate rehabilitation practices. Our first
hypothesis was that the presence of stump and
phantom pain or additional medical disease and the
level and type of prosthesis would have an impact on
quality of life. Secondly, we assumed that depression
and anxiety scores, body image, self-esteem, coping
methods, perceived social support, as well as post-
prosthetic activity restriction and satisfaction with
prosthesis will be factors associated with quality of life.
According to this hypothesis, we predicted that people
with high depression and anxiety scores, distorted
body image, low self-esteem, and poor perceived social
support would have lower quality of life. In addition,
we thought that the quality of life of patients with
activity restriction after receiving the prosthesis who
were not satisfied with the device would be worse off.
We hypothesized that the use of problem-focused
coping methods would affect the quality of life
positively and the use of emotion-focused and
dysfunctional coping methods would have a negative
impact. A number of studies published in the past
evaluated difficulties incurred in the post-amputation
period. These studies typically included individuals
who underwent amputation for various reasons.
Considering the fact that individuals with diabetic foot
ulcers are a homogeneous group with similar
characteristics and a quality of life that is lower than in
the normal population due to the nature of the disease,
we aimed to evaluate the factors affecting the quality
of life of individuals undergoing lower extremity
amputation due to diabetic foot ulcer. We investigated
the effects of clinical variables, perceived social
support, coping attitudes, self-esteem, body image,
and prosthesis adaptation on the quality of life of these
patients.
METHOD
Participants
Patients being followed up at the prosthesis clinics were
invited to participate in the study with a consecutive
approach for 6 months. In total, 65 patients who had
undergone amputation because of an infected diabetic
foot ulcer were included in the study and face-to-face
interviews were performed by the psychiatrists who
conducted the study and orthopedic specialists who
performed clinical follow-up. Measurements were
administered 1-8 years (median 3 years) after fitting the
prosthesis. All prostheses used by patients were of the
socket type. Exclusion criteria were mental retardation,
serious mental conditions that would prevent
participants from being interviewed and completing the
scales (e.g., serious psychotic disorder, bipolar disorder,
organic mental disorder), and physical illnesses at level
IV and above according to the American Society of
Anesthesiologists Physical Status Classification System
(12). The sample size was calculated using the G-power
3.1 program by Heinrich Heine University, Dusseldorf.
A total of 64 participants were needed for a large effect
size of 0.30, a significance level of 0.05, a verification
power (1-β) of 0.8, and 10 predictive variables
(depression, anxiety, body image, self-esteem, perceived
social support, problem focused-emotional focused and
dysfunctional coping mechanisms, activity restriction,
satisfaction with prosthesis). Ten independent variables
predicted to have an impact on quality of life were
determined in the light of the earlier literature
investigating factors affecting quality of life.
Ethical considerations
All participants gave written informed consent to be
included in the research. Ethical approval for this study

Kazan Kizilkurt et al. Quality of life after lower extremity amputation due to diabetic foot ulcer: the role of prosthesis-related factors, body image... 111
was obtained from the Regional Ethics Committee of
the University of Health Sciences’ Erenkoy Mental
Research and Training Hospital, Istanbul, Turkey.
Measures
Sociodemographic variables were evaluated with a data
form prepared specifically for this study.
Short Form 36 (SF-36): SF-36 was used to assess the
patients’ quality of life and to measure an individual’s
state of health based on 8 dimensions: physical function,
pain, role limitations due to physical problems, general
perception of health, role limitations due to emotional
problems, social function, energy/vitality, and mental
health. For each parameter, higher scores indicate a
better health state (13). Two summary measures were
further calculated from the item scores using the
procedures recommended by the developers: a Physical
Component (PCS) and a Mental Component (MCS)
score (14). The first four dimensions of the scale form
part of the PCS score and the last four dimensions
comprise the MCS score (15). The reliability and validity
of the scale in the Turkish population were confirmed
by Kocyigit et al. (16).
The Trinity Amputation and Prosthesis
Experience Scales (TAPES): TAPES is a multifactorial
assessment tool for lower limb amputees fitted with
prosthesis developed by Gallagher and MacLachlan
(17). It is a 54-item self-report questionnaire comprising
nine factor-analytically derived subscales assessing
three dimensions of psychosocial adjustment (general
adjustment, social adjustment, and adjustment to
limitation), three dimensions of activity restriction
(functional restriction, social restriction, and athletic
activity restriction), and three dimensions of prosthesis
satisfaction (weight satisfaction, functional satisfaction,
and esthetic satisfaction). In addition, phantom and
residual limb pain experiences and other medical
problems unrelated to the amputation are assessed. In
this study, TAPES was used to evaluate the activity
restriction after prosthesis fitting, satisfaction with the
prosthesis, and residual stump and phantom pain. The
reliability and validity of the TAPES in the Turkish
population were studied by Topuz et al. (18).
Coping Attitudes Evaluation Scale (COPE): COPE,
used to assess patients’ coping attitudes, was developed
by Carver et al. (19). Reliability and validity of the
COPE scale in the Turkish population were assessed by
Agargun et al. (20). COPE is a 60-item scale with 15
subscales. Five of these 15 subscales represent problem-
focused attitudes: active coping, planning, suppression
of competing activities, restraint coping, and seeking of
instrumental social support; 5 represent emotion-
focused coping attitudes: seeking of emotional social
support, positive reinterpretation, acceptance, humor,
and turning to religion; and the remaining five subscales
represent dysfunctional coping attitudes: focus on and
venting of emotions, behavioral disregard, substance
use, denial, and mental disregard (19,21). Carver et al.
(19) stated that it is not appropriate to divide coping
strategies into only problem-focused and emotion-
focused. They criticized researchers for viewing factors
other than problem-focused coping as variations on
emotion-focused coping, stating that the “nature of this
diversity would seem to deserve further scrutiny.” In
addition, while developing the COPE scale, they pointed
out that some of the strategies that had been included in
emotion-focused coping strategies so far were more
incompatible, making it appropriate to consider them as
dysfunctional coping methods (19). Therefore, in our
study we evaluated coping methods under three
headings as problem-focused, emotion-focused, and
dysfunctional coping strategies (22,23).
Multidimensional Scale of Perceived Social
Support (MSPSS): The MSPSS is a 12-item scale
measuring three sources of perceived support, namely,
family, friends, and significant other. It is a brief, easy-
to-administer self-report questionnaire containing
twelve items rated on a seven-point Likert-type scale
with scores ranging from ‘very strongly disagree’ (1) to
‘very strongly agree’ (7). The MSPSS has proven to be
psychometrically sound in diverse samples and to have
good internal and test-retest reliability and robust
factorial validity (24). A reliability and validity study of
the MSPSS in the Turkish population was conducted by
Eker (25).
Rosenberg Self-Esteem Scale (RSES): The RSES
scale developed by Rosenberg (26) consists of 12
subcategories. Only the first subscale including 10 items
was used in this study to assess general personal self-
esteem. Each item is rated on a four-point Likert scale
from 0 (strongly agree) to 3 (strongly disagree), producing
a cumulative score from 0 to 30, whereby high mean
scores (computed) indicate high self-esteem (26). The
reliability and validity of the scale in the Turkish
population was examined by Cuhadaroglu et al. (27).
Amputee Body Image Scale (ABIS): The ABIS is a
5-point Likert-type self-assessment scale that contains
20 questions. Items in the scale query an individual’s
perceptions and experiences regarding her/his own
body. High scores represent a distortion of body image
(28). The reliability and validity of the ABIS in the
Turkish population was confirmed by Safaz et al. (29).
Dusunen Adam The Journal of Psychiatry and Neurological Sciences 2020;33:109-119112
Patient Health Questionnaire-Somatic, Anxiety,
and Depressive Symptoms (PHQ-SADS): Patients’
somatic, anxiety, and depressive symptoms were
assessed with the PHQ-SADS evaluation form. The
PHQ-SADS is a self-report questionnaire, consisting of
a Patient Health Questionnaire (PHQ-9) subscale that
assesses nine domains of major depressive disorder and
a General Anxiety Disorder-7 (GAD-7) subscale that
rates seven basic symptoms of anxiety (30). The
reliability and validity of the PHQ-SADS in the Turkish
population was studied by Yazici Gulec et al. (31).
Statistical Analysis
Mean, standard deviation, median, and the lowest and
highest frequency and percentage values were used for
descriptive statistics and the distribution of the variables
was analyzed with the Kolmogorov-Smirnov test.
Factors affecting quality of life after having undergone a
lower limb amputation were collected from the literature
and examined in this study. The Mann-Whitney U test
was performed to analyze the differences in quality of
life for categorical independent variables including
stump pain, phantom pain, level of the prosthesis used,
and comorbid medical diseases. Spearman correlation
analysis was carried out to assess the relationship
between qualitative independent data. Stepwise linear
regression analysis was conducted to assess the factors
predicting the quality of life. In all models where the
MCS and PCS scores were treated as dependent
variables, factors correlated with quality of life were
treated as independent variables. The analyses were
performed using SPSS version 22.0.
RESULTS
Sixty-five patients were included in the study, of whom
41.5% were women, 9.2% were single, 78.5% were
married, 12.3% were either divorced or widowed. Of
the patients, 38.5% were primary school graduates,
35.4% had completed middle school and 26.2% had a
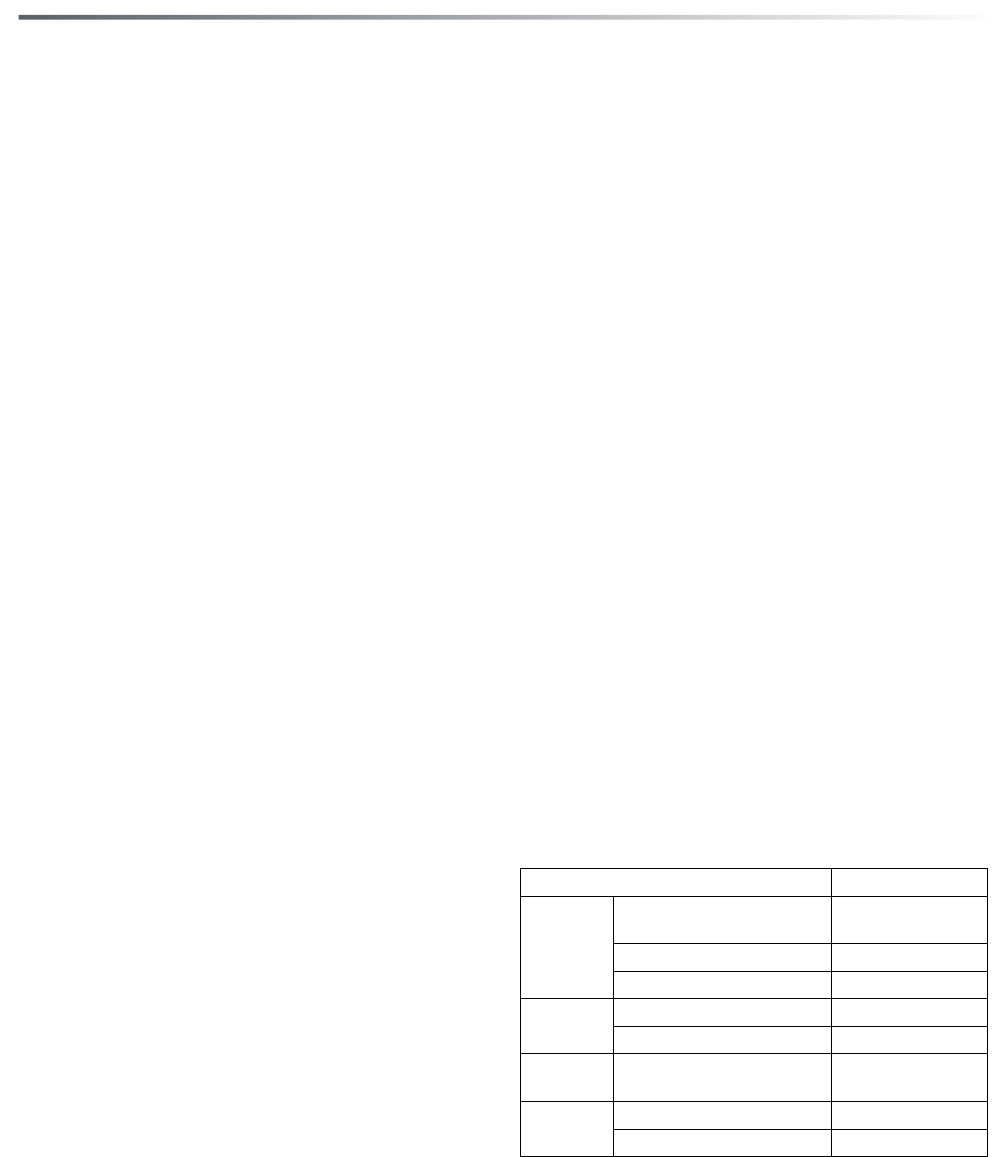
high school degree. Tables 1 and 2 report clinical data
and descriptive statistics for the quality of life
assessments. When the norm values in the quality of
life domains were evaluated for the Turkish population
(32), all domains in our study were below the average
(Table 2).
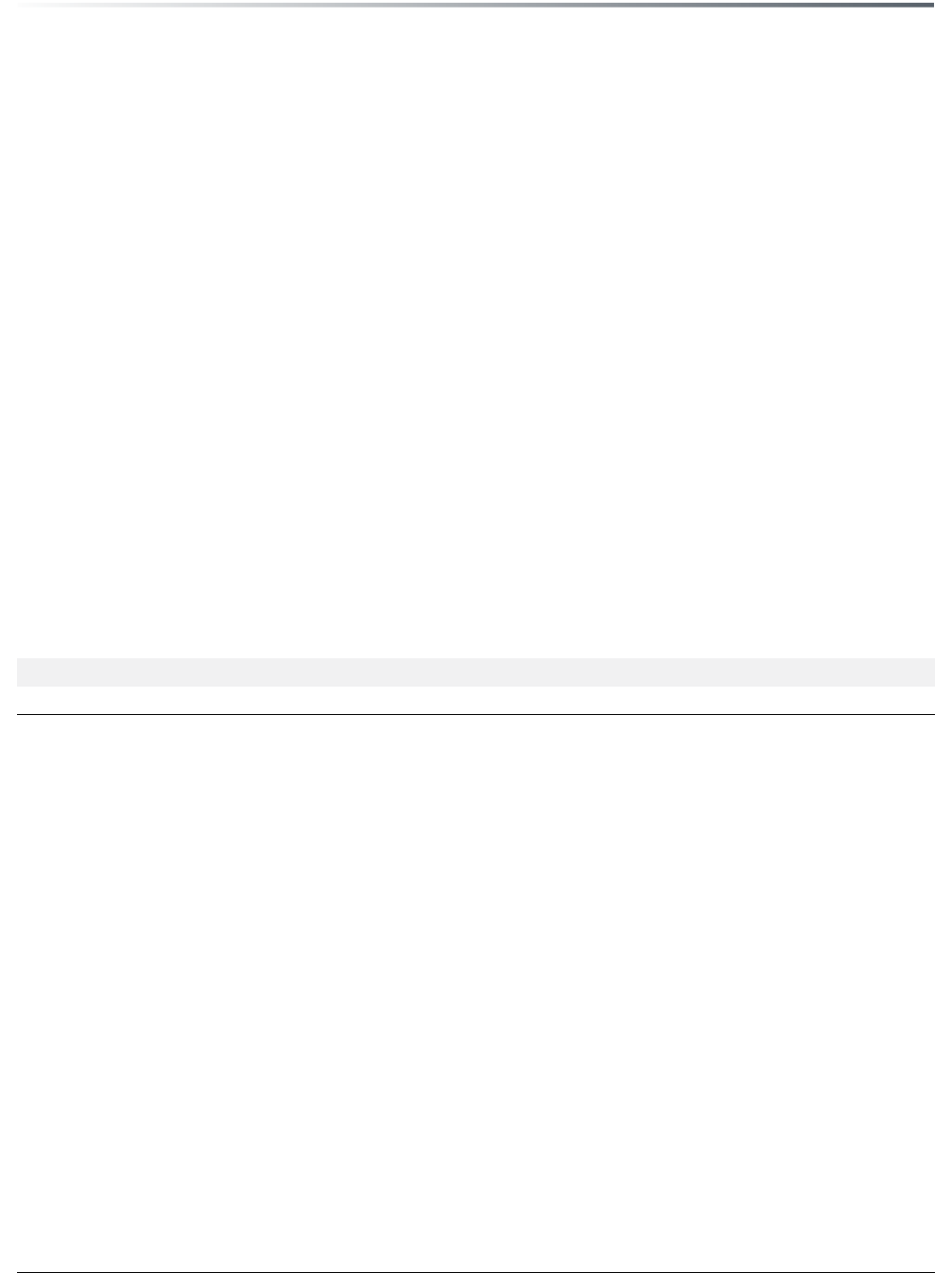
Table 1: Descrptve statstcs of clncal features, RSES, ABIS, MSPSS, GAD-7, PHQ-9, and TAPES scores (n=65)
Median Mean SD n %
Age 58.0 57.8 7.6
DM duration (Years) 8.0 9.4 4.9
GAD-7 (Anxiety) 6.0 6.0 4.7
PHQ-9 (Depression) 8.0 8.7 6.8
RSES (Self-esteem) 18.0 18.7 5.4
ABIS (Body image) 56.0 56.2 12.1
MSPSS
MSPSS family 22.0 21.1 6.1
MSPSS friends 19.0 18.2 6.8
MSPSS others 16.0 16.9 6.6
MSPSS total 58.0 56.2 17.6
Prosthetic duration (Years) 3.0 3.6 2.04
Prosthesis type
Below the knee 48 73.8
Above the knee 17 26.2
Having stump pain 16 24.6
Having phantom pain 17 26.2
TAPES Part 1
Activity restriction 24.0 23.3 5.9
Satisfaction with the prosthesis 35.0 33.3 8.4
SD: Standard deviation, DM: Diabetes mellitus, PHQ-9: Patient Health Questionnaire-9, GAD-7: General Anxiety Disorder-7, ABIS: Amputee Body Image Scale,
RSES: Rosenberg Self Esteem Scale, MSPSS: Multidimensional Scale of Perceived Social Support, TAPES: Trinity Amputation and Prosthesis Experience Scales,
PCS: Physical component summary, MCS: Mental component summary
Kazan Kizilkurt et al. Quality of life after lower extremity amputation due to diabetic foot ulcer: the role of prosthesis-related factors, body image... 113
Comparative analysis (Mann-Whitney U test) was
first established statistically. The patient group was
divided into two subgroups according to the presence or
not of phantom and stump pain. A significant difference
in the PCS and MSC scores was found between groups:
PCS and MCS scores in the subgroup suffering from
stump and phantom pain were significantly lower than
those in the patient group without such pain (p<0.01).
Then, the patient group was divided into two subgroups
according to the level of the prosthesis. PCS and MCS
scores in the group having a prosthesis fitted above the
knee were found to be significantly lower than scores in
the group with a prosthesis fitted below the knee
(transtibial amputation) (p<0.01). In addition, 40% of
patients had comorbid medical diseases. PCS (p=0.011)
and MCS (p=0.006) scores showed significant
differences between groups with and without a
comorbid disease, and the life quality scores in the
group with comorbid medical diseases were lower.
After comparative analysis, correlation analysis
(Spearman analysis) was used for numerical variables.
No significant correlations were found between age,
duration of diabetes diagnosis, years of using prosthesis,
and PCS and MCS scores (p>0.05). A negative
correlation was observed between PHQ-9 and also
GAD-7 scores and PCS and MCS scores separately.
Higher depression scores were associated with lower
PCS and MCS scores (p<0.001). Similarly, PCS and
MCS scores showed a decrease as anxiety scores
increased (p<0.001). A negative correlation was
observed between body image and quality of life, and
higher ABIS scores were associated with lower PCS and
MCS scores (p<0.001). In addition, it was found that
perceived social support and self-esteem scores
correlated positively with quality of life scores. Higher
MSPSS scores (p<0.001) and RSES scores (p<0.001)
were associated with higher PCS and MCS scores. In
addition, as activity limitation increased, quality of life
was negatively affected. A significant positive correlation
was noted between the total score for prosthesis
satisfaction and quality of life (p<0.001). No significant
correlations were found between the emotion-focused
coping score and the quality-of-life subscales (p>0.05).
In contrast, it was observed that quality of life scores
were positively correlated with problem-focused coping
strategies scores (p<0.001) and negatively related with
dysfunctional coping strategies scores (p<0.001). The
quality of life was better with increasing use of problem-
focused coping strategies, while greater use of
dysfunctional coping strategies was associated with
poor quality of life (Table 3).
Independent effects of the predictors associated with
quality of life according to correlation analysis were
examined using a multivariate regression model. In two
separate analyses with PCS and MCS scores as
dependent variables, PHQ-9, GAD-7, MSPSS, ABIS,
RSES, problem-focused and dysfunctional coping
strategies, activity restriction, and satisfaction with
prosthesis were taken as independent variables.
Regression analysis showed that patients’ PCS scores
Table 2: Descrptve statstcs of COPE and SF-36 scores (n=65)
Median Mean SD
COPE
Problem-focused coping 57.0 56.2 8.5
Emotion-focused coping 56.0 56.6 7.4
Dysfunctional coping 56.0 53.3 10.9
SF-36
Physical functioning 50.0 45.3 33.1
Role limitations (physical problems) 25.0 38.5 40.3
Role limitations (emotional problems) 33.3 36.9 41.7
Energy 50.0 49.6 17.5
Mental health 52.0 51.4 16.1
Social functioning 62.5 59.8 20.3
Pain 67.5 65.7 20.3
General health status 45.0 47.8 5.5
PCS 39.1 39.3 9.1
MCS 39.6 39.8 8.9
SD: Standard deviation, COPE: Coping Attitudes Evaluation Scale, SF-36: Short Form-36, PCS: Physical component summary, MCS: Mental component summary
Dusunen Adam The Journal of Psychiatry and Neurological Sciences 2020;33:109-119114
were significantly correlated negatively with ABIS
scores (β=−0.34, p=0.01) and dysfunctional coping
strategies (β=−0.43, p<0.001), positively with
satisfaction with the prosthesis (β=0.27, p=0.01), RSES
scores (β=0.27, p<0.001), and problem-focused coping
strategies (β=0.23, p=0.01), and the combination of
these factors explained 78% of the variability of the
patients’ PCS scores. The regression model for the MCS
scores correlated negatively with ABIS scores (β=−0.32,
p=0.01) and dysfunctional coping strategies (β=−0.47,
p<0.001) and positively with problem-focused coping
strategies (β=0.31, p<0.001). These three significant
variables explained 80% of the variance observed in the
patients’ MCS scores (Tables 4,5).
DISCUSSION
The present study was designed to investigate the
factors affecting the quality of life of patients
undergoing amputation of a lower extremity following
complications arising from diabetes mellitus. Our
results were consistent with those of previous studies
conducted in this field (33) and revealed that both the
physical and mental quality of life after lower limb
amputation were reduced compared to the normal
population (32). The results of our study supported our
first hypothesis: The presence of stump and phantom
pain, additional medical diseases, and the level of
prosthetics were found to be factors related to quality
of life. With regard to our second hypothesis, we have
seen that many aspects are supported by the results of
our study. It was observed that depression and anxiety
scores, body perception, self-esteem, perceived social
support, problem-focused and dysfunctional coping
strategies, post-prosthetic activity restriction, and
prosthetic satisfaction were related to quality of life.
According to our results, the only factor that differed
from our hypothesis was the use of emotion-focused
coping strategies, which was not found not be related to
the quality of life. Regression analysis was performed to
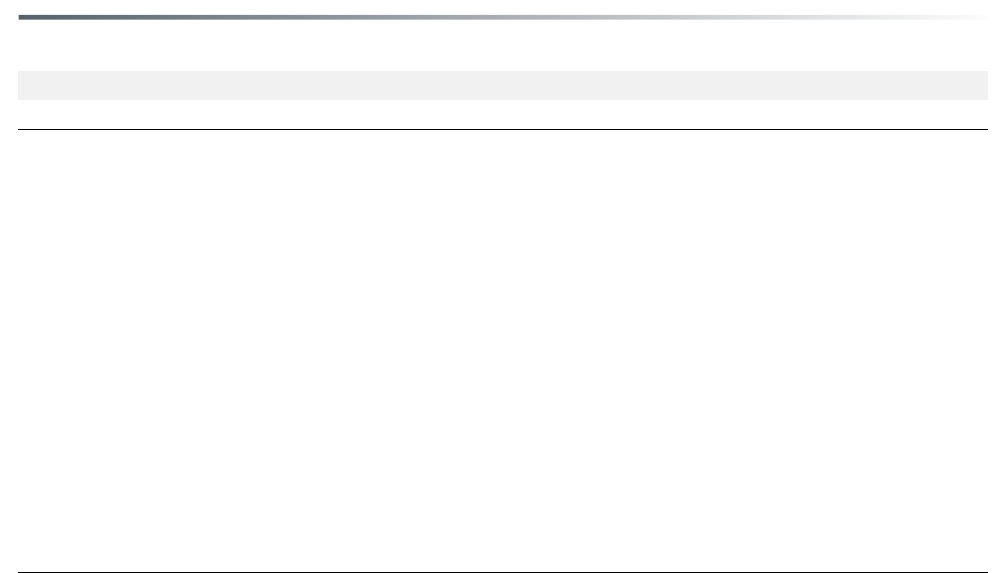
Table 3: Spearman correlaton analyss between PHQ-9, GAD-7, ABIS, RSES, MSPSS, COPE subgroups, Actvty
restrcton, Satsfacton wth the prosthess scores and PCS and MCS scores
PHQ-9 GAD-7 ABIS RSES MSPSS Problem- Emotion- Dysfunctional Activity Satisfaction
total focused focused Coping restriction with the
coping coping prosthesis
PCS
r -0.51 -0.49 -0.72 0.29 0.38 0.43 -0.07 -0.56 -0.69 0.61
p <0.001 <0.001 <0.001 <0.001 <0.001 <0.001 0.53 <0.001 <0.001 <0.001
MCS
r -0.59 -0.49 -0.61 0.53 0.48 0.57 0.04 -0.62 -0.63 0.54
p <0.001 <0.001 <0.001 <0.001 <0.001 <0.001 0.76 <0.001 <0.001 <0.001
Spearman correlation analysis, PHQ-9: Patient Health Questionnaire-9, GAD-7: General Anxiety Disorder-7, ABIS: Amputee Body Image Scale, RSES: Rosenberg Self
Esteem Scale, MSPSS: Multidimensional Scale of Perceived Social Support, PCS: Physical component summary, MCS: Mental component summary
Table 4: Stepwse multple regresson analyss model of the varables that affect MSC scores (p<0.05)
MCS
B t p R² Adjusted R² F
Model 1
ABIS -5.58 -10.36 <0.001 0.63 0.62 107.40
Model 2
ABIS -3.71 -6.23 <0.001 0.73 0.73 85.63
Dysfunctional coping -3.26 -4.92 <0.001
Model 3
ABIS -2.27 -3.67 0.01 0.79 0.79 80.47
Dysfunctional coping -3.67 -6.25 <0.001
Problem focused coping 3.09 4.41 <0.001
Stepwise Multiple Regression Analysis, ABIS: Amputee Body Image Scale, MCS: Mental component summary
Kazan Kizilkurt et al. Quality of life after lower extremity amputation due to diabetic foot ulcer: the role of prosthesis-related factors, body image... 115
observe the predictive effects of these related factors,
and body image, problem-focused and dysfunctional
coping strategies, self-esteem, and satisfaction with the
prosthesis were all observed to have a significant effect
on the physical component of quality of life.
Furthermore, body image and problem-focused and
dysfunctional coping strategies were found to be the
factors with the highest predictive power for the mental
component of quality of life.
Firstly, it was observed that patients with stump and
phantom pain had reduced quality of life. In the
literature, in addition to studies showing that phantom
pain and stump pain are not an important determinant
for the quality of life (34), there are also articles arguing
that these two types of pain have important effects on
both physical and mental quality of life (35,36). It is
known that stump pain causes activity restriction as a
result of negative effects on mobility and rehabilitation
(6). We think that this activity restriction, which is an
important factor for life quality, may explain the
importance of stump pain for quality of life. In addition,
phantom limb pain in some patients may gradually
disappear over the course of a few months or up to one
year even when untreated, but some patients suffer from
phantom limb pain for decades (37). The average period
of prosthesis use in our sample group was three years.
We found no relationship between the duration of
prosthesis use and quality of life. This result suggests
that phantom pain may have an impact on the quality of
life even after years have passed since fitting the
prosthesis. We think that the negative effect of phantom
pain on quality of life in patients with long-term
prosthesis use can be evaluated as an important data
point in the rehabilitation process. In our study, it was
found that the patients who had undergone transtibial
amputation had a better quality of life than others with
higher-level amputations, and this result is compatible
with the data in the literature (38). Patients with
transtibial amputation level are far more mobile than
those with transfemoral amputation, and rates of using
crutches are higher after transfemoral amputation
(39,40). This is probably one of the reasons why the
results of individual domains of the quality of life
displayed significantly higher scores in individuals with
transtibial amputations compared to patients with a
higher level of amputation.
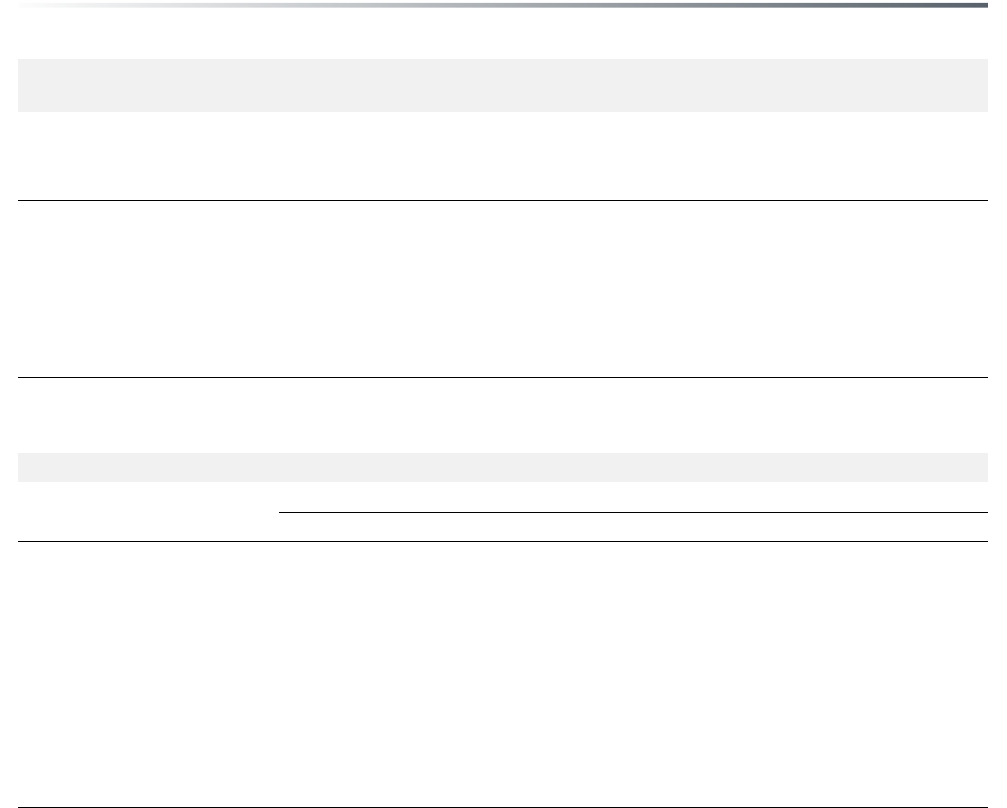
Table 5: Stepwse multple regresson analyss model of the varables that affect PSC scores (p<0.05)
PCS
B t p R² Adjusted R² F
Model 1
ABIS -5.64 -10.07 <0.001 0.62 0.61 101.43
Model 2
ABIS -4.01 -6.13 <0.001 0.69 0.68 69.70
Dysfunctional coping -2.83 -3.89 <0.001
Model 3
ABIS -1.90 -2.17 0.03 0.74 0.73 57.82
Dysfunctional coping -3.35 -4.85 <0.001
Satisfaction with the prosthesis 3.50 3.35 <0.001
Model 4
ABIS -2.46 -2.75 0.01 0.76 0.74 46.68
Dysfunctional coping -3.30 -4.90 <0.001
Satisfaction with the prosthesis 3.81 3.69 <0.001
RSES -2.63 -2.05 0.04
Model 5
ABIS -2.41 -2.81 0.01 0.78 0.76 42.14
Dysfunctional coping -3.42 -5.29 <0.001
Satisfaction with the prosthesis 2.83 2.68 0.01
Self-esteem -4.33 -3.10 <0.001
Problem focused coping 2.39 2.57 0.01
Stepwise Multiple Regression Analysis, ABIS: Amputee Body Image Scale, RSES: Rosenberg Self Esteem Scale, PCS: Physical components summary

Dusunen Adam The Journal of Psychiatry and Neurological Sciences 2020;33:109-119116
One of the most important factors affecting
functional and life quality results of amputee
rehabilitation is compatible with the patient’s
prosthesis satisfaction (41). Patient dissatisfaction with
the artificial limb can create major problems for the
individual on a physical, psychological, and social
level, and can directly impact health-related life quality
(42). Individuals using a suitable prosthesis can regain
their mobility more quickly and are more likely to
adapt to the amputation successfully (43). Their self-
confidence increases as they gain functional
independence and the adaptation to their social
environment and working life are also affected
positively (44). Similar to our work, Matsen et al. (45)
found that quality of life in people with a lower-
extremity amputation correlated with the comfort,
function, and appearance of the prosthesis. In addition,
a positive correlation has been determined in the
literature between prosthesis satisfaction and quality
of life and positive adaptation to extremity loss (6,46).
Asano et al. (5) found that problems with prosthetics
after lower limb amputation are an important
predictive factor for quality of life. In our study,
satisfaction with the prosthesis was measured using
the three subscales functional satisfaction, esthetic
satisfaction, and weight satisfaction. Prosthesis
satisfaction covering these three areas was found to be
correlated with both physical and mental quality of life
scores, but it was predictive only for the physical
component. No study in the literature investigated the
predictive power of quality of life for physical and
mental components separately, but the importance of
mobility for physical functioning has been reported in
other studies (5,47). When the important effect of
prosthesis satisfaction on mobilization is taken into
consideration, it is thought that its predictive power
for the physical component may be related to this
situation. Considering that a prosthesis is a means of
replacing a natural limb, the importance of patient
satisfaction with the device is evidently of utmost
importance (7).
The loss of a limb causes emotional stress and
inevitably requires examining the patient’s capacity to
cope with this stressful situation (48). Problem-
focused coping was also found to be a major predictor
of psychological and physical quality of life in our
study. There are results similar to our findings in the
literature. In their study with 63 individuals with lower
limb amputation due to diabetes and peripheral
vascular disease, Pereira et al. (49) showed that
satisfaction with life was positively associated with
active and planning coping. In our study, emotion-
focused coping methods were found to be unrelated to
the quality of life, thus not supporting our hypothesis.
In contrast, a limited number of studies in the literature
showed that emotion-focused and passive strategies
have been associated with poor psychosocial outcomes
(50). We think that the reason may be that the coping
methods used in the literature are problem-oriented
and emotion-oriented, while in our study, the coping
assessment tool used also included dysfunctional
strategies. These dysfunctional coping methods
comprise some of the methods that are routinely
evaluated in emotional coping methods, but are more
incompatible. We think that the negative relationship
of emotion-focused coping in the literature with
psychosocial adjustment and quality of life may be
related to these incompatible coping strategies that we
determined in the dysfunctional coping strategies
group. Desmond and MacLachlan (50), evaluating 3
coping strategies, namely, problem solving, seeking
social support, and avoidance, found avoidance to be
associated with poor psychosocial adaptation to
amputation. Likewise, in our study the use of
dysfunctional coping strategies was similar in effect to
the non-adaptive nature of avoidance-type coping, and
it was found to be a negative predictor for the physical
and mental components of quality of life. The
international literature has already documented that
coping strategies focused on active resolution are more
effective in decreasing the level of restriction in
physical activities and in the adjustment to amputation
(51,52). Coping strategies are important not only to
minimize the negative effects of lower extremity
amputation but also for the amputee’s psychological
well-being (53). In the light of this information, which
is also parallel to our results, we think that evaluating
coping mechanisms as an important parameter
especially in a rehabilitation program may have
positive effects on patients’ quality of life and general
well-being.
Emotions created by breaking up the integrity of the
body cause a distorted body image, leading to
inadequate and negative feelings about the body and
decreased self-esteem (7,54). It is well known that our
way of perceiving our bodies has a major effect on our
social lives, psychological and physical states, and the
overall quality of our lives (55). When individuals’
perceptions of their bodies are distorted after
amputation, they experience greater difficulties carrying
out the bodily movements required for daily activities
and struggle to accept their new body image; this can
Kazan Kizilkurt et al. Quality of life after lower extremity amputation due to diabetic foot ulcer: the role of prosthesis-related factors, body image... 117
lead to rejection of the prosthesis and difficulties in
functional adaptation (56). It has been stated that the
deterioration in the body image perception of the
amputated person may affect their lives physically,
socially, and psychologically, as they do not conform to
the esthetic perception accepted by the majority of
social media users and society (57). Holzer et al. (9)
found that body image was distorted in patients who
had undergone amputation, and the physical and
mental components of their quality of life was negatively
affected. In our study, it was observed that the
perception of body image was an important predictive
factor for both physical and mental quality of life.
Similar to our results, Rybarczyk et al. (8) stated that
body image is an independent predictor of quality of
life. Helping amputees to integrate into society
successfully requires their amputation-associated body
image distortions to be addressed during rehabilitation,
and understanding the impact of body image is critical
for appropriate rehabilitation interventions (8).
Studies have also indicated that self-perception and
evaluating one’s body are a significant source of self-
esteem (58). Although many studies show that self-
esteem decreases after amputation (7,28), few studies
trace the relationship between self-esteem and quality of
life. One study investigating the relationship between
self-esteem and quality of life reported a weak
correlation between these two variables (9). In contrast,
we observed that decreased self-esteem was a significant
predictor of a poor physical component of quality of
life. In a study with patients undergoing mastectomy, a
procedure that similarly leads to the feeling of mutilation
of the body, self-esteem was also reported to be
decreased, which was a significant predictive factor for
impaired health-associated quality of life (59). Cognitive
Behavioral Therapy (CBT) was introduced as a method
to increase individuals’ adaptation to chronic health
states. CBT is advocated in helping patients recognize
and adjust their distorted thinking patterns and non-
productive behaviors by focusing on their emotional,
cognitive, and behavioral responses (60). Studies have
shown that CBT is effective in improving self-esteem,
body image, and quality of life among patients with
chronic diseases (61,62). A recent study examining the
beneficial effect of CBT on self-esteem and quality of
life among elder amputees demonstrated that self-
esteem and life quality significantly improved among
these individuals (60).
There are some limitations of our study. First of all,
due to its cross-sectional design, it was not possible to
establish cause-effect relationships. There was no
longitudinal follow-up before and after amputation and
non-amputee diabetic foot patients were not included in
the study as a comparison group. Secondly, in parallel
with amputation, the effect of diabetes mellitus itself on
the quality of life should be taken into consideration, as
all negative effects on quality of life are unlikely to be
attributable to the amputation. Comorbid medical and
psychiatric disorders were not considered as a
confounding factor on outcome. Eventually, when this
study examined the effect of medical diseases and
psychiatric burdens such as depression, anxiety, and
somatization on the outcome, it was observed that these
burdens had no predictive power on the outcome.
In conclusion, the results of our study emphasize the
significance of multiple physical and psychosocial
aspects in the successful adaptation of patients after
amputation. This study investigated the variables
affecting the quality of life of individuals in orthopedic
practice, applying a biopsychosocial approach. It has
shown that patients’ existing schemas of coping styles,
self-esteem, and body perception have a greater impact
on the outcome than their physical variables and
psychological burdens such as depression and anxiety.
Furthermore, the importance of multidisciplinary
evaluation of patients is evident, both during
amputation, which is a traumatic process, and during
rehabilitation. We suggest that rehabilitation after
amputation should be a multifactorial process including
physical functional adaptation and psychosocial
schemes.
Contribution Categories Author Initials
Category 1
Concept/Design
O.K.K., T.K., M.Y.G., F.E.G.,
G.P., I.O.K., H.G.
Data acquisition T.K., G.P.
Data analysis/Interpretation O.K.K., H.G.
Category 2
Drafting manuscript O.K.K., T.K., F.E.G., G.P.
Critical revision of manuscript M.Y.G., I.O.K., H.G.
Category 3 Final approval and accountability
O.K.K., T.K., M.Y.G., F.E.G.,
G.P., O.I.K., H.G.
Other
Technical or material support N/A
Supervision N/A
Ethics Committee Approval: Ethical approval for this study was
obtained from the Regional Ethics Committee of the University of
Health Sciences’ Erenkoy Mental Research and Training Hospital,
Istanbul, Turkey.
Informed Consent: Written informed consent of all patients was
obtained.
Peer-review: Externally peer-reviewed.
Conflict of Interest: There in no conflict of interest.
Financial Disclosure: There is no any financial support.

Dusunen Adam The Journal of Psychiatry and Neurological Sciences 2020;33:109-119118
REFERENCES
1. Ragnarson Tennvall G, Apelqvist J. Health-related quality of
life in patients with diabetes mellitus and foot ulcers. J Diabetes
Complications 2000; 14:235-241.
2. Carrington AL, Mawdsley SK, Morley M, Kincey J, Boulton AJ.
Psychological status of diabetic people with or without lower
limb disability. Diabetes Res Clin Pract 1996; 32:19-25.
3. Willrich A, Pinzur M, McNeil M, Juknelis D, Lavery L. Health
related quality of life, cognitive function, and depression in
diabetic patients with foot ulcer or amputation. A preliminary
study. Foot Ankle Int 2005; 26:128-134.
4. Boutoille D, Féraille A, Maulaz D, Krempf M. Quality of life with
diabetes-associated foot complications: comparison between
lower-limb amputation and chronic foot ulceration. Foot Ankle
Int 2008; 29:1074-1078.
5. Asano M, Rushton P, Miller WC, Deathe BA. Predictors of quality
of life among individuals who have a lower limb amputation.
Prosthet Orthot Int 2008; 32:231-243.
6. Horgan O, MacLachlan M. Psychosocial adjustment to lower-
limb amputation: a review. Disabil Rehabil 2004; 26:837-850.
7. Grossman EF. The Gestalt approach to people with amputations.
J Appl Rehabil Couns 1990; 21:16-19.
8. Rybarczyk B, Nyenhuis D, Nicholas JJ, Cash SM, Kaiser J. Body
image, perceived social stigma, and the prediction of psychosocial
adjustment to leg amputation. Rehabil Psychol 1995; 40:95-110.
9. Holzer LA, Sevelda F, Fraberger G, Bluder O, Kickinger W,
Holzer G. Body image and self-esteem in lower-limb amputees.
PLoS One 2014; 9:e92943.
10. Dunn DS. Well-being following amputation: Salutary effects of
positive meaning, optimism, and control. Rehabil Psychol 1996;
41:285-302.
11. Livneh H, Antonak RF, Gerhardt J. Psychosocial adaptation to
amputation: the role of sociodemographic variables, disability-
related factors and coping strategies. Int J Rehabil Res 1999;
22:21-31.
12. Daabiss M. American Society of Anaesthesiologists physical
status classification. Indian J Anaesth 2011; 55:111-115.
13. Ware JE Jr, Sherbourne CD. The MOS 36-item short-form health
survey (SF-36). I. Conceptual framework and item selection. Med
Care 1992; 30:473-483.
14. Ware JE, Jr, Kosinski MA, Keller SD. SF-36 physical and mental
health summary scales: a User’s Manual. Fifth ed., Boston: MA
Health Assessment Lab, New England Medical Center, 1994.
15. Ware JE Jr. SF-36 health survey update. Spine (Phila Pa 1976)
2000; 25:3130-3139.
16. Kocyigit H, Aydemir O, Fisek G, Olmez N, Memis AK. Reliability
and validity of the Short Form 36, Turkish version (KF-36). Ilac
ve Tedavi Dergisi 1999; 12:102-106. (Turkish)
17. Gallagher P, MacLachlan M. Development and psychometric
evaluation of the Trinity Amputation and Prosthesis Experience
Scales (TAPES). Rehabil Psychol 2000; 45:130-154.
18. Topuz S, Ulger O, Yakut Y, Gul Sener F. Reliability and construct
validity of the Turkish version of the Trinity Amputation and
Prosthetic Experience Scales (TAPES) in lower limb amputees.
Prosthet Orthot Int 2011;35:201-206.
19. Carver CS, Scheier MF, Weintraub JK. Assessing coping strategies:
a theoretically based approach. J Pers Soc Psychol 1989; 56:267-
283.
20. Agargun MY, Besiroglu L, Kiran UK, Ozer OA, Kara H. The
psychometric properties of the COPE inventory in Turkish
sample: a preliminary research. Anadolu Psikiyatri Derg 2005;
6:221.
21. Carver CS, Scheier MF. Situational coping and coping dispositions
in a stressful transaction. J Pers Soc Psychol 1994; 66:184-195.
22. Cooper C, Katona C, Orrell M, Livingston G. Coping strategies
and anxiety in caregivers of people with Alzheimer’s disease: the
LASER-AD study. J Affect Disord 2006; 90:15-20.
23. Coolidge FL, Segal DL, Hook JN, Stewart S. Personality disorders
and coping among anxious older adults. J Anxiety Disord 2000;
14:157-172.
24. Zimet GD, Dahlem NW, Zimet SG, Farley GK. The
multidimensional scale of perceived social support. J Pers Assess
1988;52:30-41.
25. Eker D, Arkar H, Yaldiz H. Factorial Structure, Validity, and
Reliability of Revised Form of the Multidimensional Scale of
Perceived Social Support. Turk Psikiyatri Derg 2001; 12:17-25.
(Turkish)
26. Rosenberg M. Society and the Adolescent Self-Image. First ed.,
Princeton, NJ.:Princeton University Press, 1965.
27. Cuhadaroglu F. Self-esteem in Adolescents. Specialization Thesis,
Hacettepe University Medical Faculty Department of Psychiatry,
Ankara. 1986. (Turkish)
28. Breakey JW. Body image: the lower-limb amputee. JPO J
Prosthetics Orthot 1997; 9:58-66.
29. Safaz I, Yilmaz B, Goktepe AS, Yazicioglu K. Turkish version of
the amputee body image scale and relationship with quality of
life. Bulletin Clin Psychopharmacol 2010; 20:79-83.
30. Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of
a brief depression severity measure. J Gen Intern Med 2001;
16:606-613.
31. Yazici Gulec M, Gulec H, Simsek G, Turhan M, Aydin Sunbul
E. Psychometric properties of the Turkish version of the
Patient Health Questionnaire-Somatic, Anxiety, and Depressive
Symptoms. Compr Psychiatry 2012; 53:623-629.
32. Demiral Y, Ergor G, Unal B, Semin S, Akvardar Y, Kivircik B, et
al. Normative data and discriminative properties of short form 36
(SF-36) in Turkish urban population. BMC Public Health 2006;
6:247.
33. Hagberg K, Brånemark R. Consequences of non-vascular trans-
femoral amputation: a survey of quality of life, prosthetic use and
problems. Prosthet Orthot Int 2001; 25:186-194.
34. Sinha R, van den Heuvel WJ, Arokiasamy P. Factors affecting
quality of life in lower limb amputees. Prosthet Orthot Int 2011;
35:90-96.

Kazan Kizilkurt et al. Quality of life after lower extremity amputation due to diabetic foot ulcer: the role of prosthesis-related factors, body image... 119
35. Arena JG, Sherman RA, Bruno GM, Smith JD. The relationship
between situational stress and phantom limb pain: cross-lagged
correlational data from six month pain logs. J Psychosom Res
1990; 34:71-77.
36. van der Schans CP, Geertzen JH, Schoppen T, Dijkstra PU.
Phantom pain and health-related quality of life in lower limb
amputees. J Pain Symptom Manage 2002; 24:429-436.
37. Kaur A, Guan Y. Phantom limb pain: A literature review. Chin J
Traumatol 2018; 21:366-368.
38. Knežević A, Salamon T, Milankov M, Ninković S, Jeremić Knežević
M, Tomašević Todorović S. Assessment of quality of life in patients
after lower limb amputation. Med Pregl 2015; 68:103-108.
39. Burger H, Marincek C, Isakov E. Mobility of persons after
traumatic lower limb amputation. Disabil Rehabil. 1997; 19:272-
277.
40. Raya MA, Gailey RS, Fiebert IM, Roach KE. Impairment
variables predicting activity limitation in individuals with lower
limb amputation. Prosthet Orthot Int 2010; 34:73-84.
41. Schürmann T, Beckerle P, Preller J, Vogt J, Christ O. Theoretical
implementation of prior knowledge in the design of a multi-scale
prosthesis satisfaction questionnaire. Biomed Eng Online 2016;
15:143.
42. Millstein S, Bain D, Hunter GA. A review of employment patterns
of industrial amputees--factors influencing rehabilitation.
Prosthet Orthot Int 1985; 9:69-78.
43. Sansam K, Neumann V, O’Connor R, Bhakta B. Predicting
walking ability following lower limb amputation: a systematic
review of the literature. J Rehabil Med 2009; 41:593-603.
44. Fernández A, Isusi I, Gómez M. Factors conditioning the return
to work of upper limb amputees in Asturias, Spain. Prosthet
Orthot Int 2000; 24:143-147.
45. Matsen SL, Malchow D, Matsen FA 3rd. Correlations with
patients’ perspectives of the result of lower-extremity amputation.
J Bone Joint Surg Am 2000; 82:1089-1095.
46. Akarsu S, Tekin L, Safaz I, Göktepe AS, Yazicioğlu K. Quality of
life and functionality after lower limb amputations: comparison
between uni- vs. bilateral amputee patients. Prosthet Orthot Int
2013; 37:9-13.
47. Deans SA, McFadyen AK, Rowe PJ. Physical activity and quality
of life: A study of a lower-limb amputee population. Prosthet
Orthot Int 2008; 32:186-200.
48. Copuroglu C, Ozcan M, Yilmaz B, Gorgulu Y, Abay E, Yalniz E.
Acute stress disorder and post-traumatic stress disorder following
traumatic amputation. Acta Orthop Belg 2010; 76:90-93.
49. Pereira MG, Ramos C, Lobarinhas A, Machado JC, Pedras S.
Satisfaction with life in individuals with a lower limb amputation:
The importance of active coping and acceptance. Scand J Psychol
2018; 59:414-421.
50. Desmond DM, MacLachlan M. Coping strategies as predictors
of psychosocial adaptation in a sample of elderly veterans with
acquired lower limb amputations. Soc Sci Med 2006; 62:208-216.
51. Andersson M, Deighan F. Coping strategies in conjunction with
amputation: A literature study. Thesis, Division for Health and
Caring Sciences, Karlstads University, Sweden, 2006.
52. Couture M, Desrosiers J, Caron CD. Coping with a lower limb
amputation due to vascular disease in the hospital, rehabilitation,
and home setting. ISRN Rehabil 2012; 179878.
53. Oaksford K, Frude N, Cuddihy R. Positive coping and stress-
related psychological growth following lower limb amputation.
Rehabil Psychol 2005; 50:266-277.
54. Parkes CM. Components of the reaction to loss of a lamb, spouse
or home. J Psychosom Res 1972; 16:343-349.
55. Adamson PA, Doud Galli SK. Modern concepts of beauty. Curr
Opin Otolaryngol Head Neck Surg 2003; 11:295-300.
56. Deusen J Van. Body image of non-clinical and clinical populations
of men: a literature review. Occup Ther Ment Heal 1996; 13:37-
57.
57. Ching S, Thoma A, McCabe RE, Antony MM. Measuring
outcomes in aesthetic surgery: a comprehensive review of the
literature. Plast Reconstr Surg 2003; 111:469-480.
58. Goldenberg JL, McCoy SK, Pyszczynski T, Greenberg J, Solomon
S. The body as a source of self-esteem: the effect of mortality
salience on identification with one’s body, interest in sex, and
appearance monitoring. J Pers Soc Psychol 2000; 79:118-130.
59. Mustian KM, Katula JA, Gill DL, Roscoe JA, Lang D, Murphy
K. Tai Chi Chuan, health-related quality of life and self-esteem:
a randomized trial with breast cancer survivors. Support Care
Cancer 2004; 12:871-876.
60. Alavi M, Molavi H, Molavi R. The impact of cognitive behavioral
therapy on self-esteem and quality of life of hospitalized amputee
elderly patients. Nurs Midwifery Stud 2017; 6:162-167.
61. Didarloo A, Alizadeh M. Health-Related Quality of Life and its
Determinants Among Women With Diabetes Mellitus: A Cross-
Sectional Analysis. Nurs Midwifery Stud. 2016; 5:e28937.
62. Kiani J, Pakizeh A, Ostovar A, Namazi S. Effectiveness of
cognitive behavioral group therapy (CBGT) in increasing the
self esteem & decreasing the hopelessness of β-thalassemic
adolescents. Iran South Med J 2010; 13:241-252. (Persian)
