
SPD280509-3 1023 (Approved 11-10-23)
UNIVERSITY OF CALIFORNIA
Effective January 1, 2024
UC Health Savings Plan
Plan ID#280509
Benefit Booklet

This Benefit Booklet provides a complete explanation of your Benefits, limitations and other Plan provisions
that apply to you. Your Plan is a Preferred Provider Medical Plan. Be sure you understand the Benefits
offered under this Plan before receiving services.
Benefits of this Plan are available only for Covered Services and supplies furnished during the term the
Plan is in effect and while the Individual claiming Benefits is actually covered by this Plan.
Benefits may be modified during the term of this Plan as specifically provided under the terms of the Plan
or upon renewal. If Benefits are modified, the revised Benefits (including any reduction in Benefits or the
elimination of Benefits) apply for the Covered Services or supplies furnished on or after the Effective Date
of modification. There is no vested right to receive the Benefits of this Plan.
Many words used in this Benefit Booklet have special meanings (e.g., Covered Services and Medically
Necessary). These words are capitalized and are defined in the "DEFINITIONS" section. See these
definitions for the best understanding of what is being stated. Throughout this Benefit Booklet you may also
Claims Administrator. The Plan Administrator is the University of California Executive Steering Committee
on Health Benefits Programs, which has delegated certain duties to Anthem Blue Cross Life and Health
Insurance Company (Anthem). This booklet explains the plan's provisions and the policies and rules that
govern them. The Plan Administrator has the authority to interpret disputed provisions.
All capitalized words in this benefit
booklet are in the DEFINITIONS section starting at page 89.
Please read this Benefit Booklet carefully so that you understand all the Benefits your Plan offers. Keep this
Benefit Booklet handy in case you have any questions about your coverage. This booklet, the University of
California Group Insurance Regulations (Medical-related portions), and applicable fact sheets, constitute
both the Plan document and summary for the Plan.
Prescription Drug Benefits are provided separately, visit www.UChealthplans.com for details.
Important: The Regents of the University of California is the Employer and may change or terminate the
Plan by action of the Plan Administrator. Anthem Blue Cross Life and Health Insurance Company (Anthem)
has been appointed the Claims Administrator. On behalf of Anthem Blue Cross Life and Health Insurance
Company, Anthem Blue Cross processes and reviews the claims submitted under this Plan. This is not an
insured benefit plan. The Benefits described in this Benefit Booklet or any rider or amendments are funded
by, and paid out of the assets of, the Employer who is responsible for their payment and employee
contributions. Anthem Blue Cross Life and Health Insurance Company provides administrative claims
payment services only and does not assume any financial risk or obligation with respect to claims.
Anthem Blue Cross Life and Health Insurance Company is an independent licensee of the Blue Cross
Association.
COMPLAINT NOTICE
All complaints and disputes relating to coverage under this Plan must be resolved in accordance
with the Plan’s grievance procedures. Grievances may be made by telephone (please call the
Member Services number on your Identification Card) or in writing (write to Anthem Blue Cross Life
and Health Insurance Company, 21215 Burbank Blvd., Woodland Hills, CA 91367). If you wish,
Accolade will provide a Complaint Form which you may use to explain the matter.
All grievances received under the Plan will be acknowledged in writing, together with a description
of how the Plan proposes to resolve the grievance. Grievances that cannot be resolved by this
procedure shall be submitted to arbitration.
TABLE OF CONTENTS
SUMMARY OF BENEFITS ........................................................................................................................... 1
Medical Benefit Summary Notes ......................................................................................................... 21
INTRODUCTION ......................................................................................................................................... 23
TYPES OF PROVIDERS ............................................................................................................................ 25
YOUR MEDICAL BENEFITS ...................................................................................................................... 28
Maximum Allowed Amount ................................................................................................................. 28
Deductibles, Copayments, Out-of-Pocket Amounts and Medical Benefit Maximums ................... 32
Crediting Prior Plan Coverage ............................................................................................................ 34
Conditions of Coverage ....................................................................................................................... 34
Medical Care That Is Covered ............................................................................................................. 35
Abortion Services................................................................................................................................. 35
Acupuncture Benefits........................................................................................................................... 35
Advanced Imaging Procedure Benefits ............................................................................................... 35
Allergy Testing and Treatment Benefits ............................................................................................... 35
Ambulance Benefits ............................................................................................................................. 35
Ambulatory Surgery Center Benefits ................................................................................................... 36
Bariatric Surgery Benefits .................................................................................................................... 36
Bariatric Travel Expense Benefits ........................................................................................................ 36
Blood Benefits ..................................................................................................................................... 37
Breast Cancer Benefits ........................................................................................................................ 37
Chemotherapy Benefits ....................................................................................................................... 38
Chiropractic Benefits ............................................................................................................................ 38
Clinical Trial of Cancer and Other Life Threatening Conditions Benefits ............................................. 38
Contraceptive Benefits ......................................................................................................................... 39
Dental Care Benefits............................................................................................................................ 39
Diabetes Care Benefits ........................................................................................................................ 41
Diagnostic Services ............................................................................................................................. 41
Durable Medical Equipment Benefits ................................................................................................... 41
Emergency Room ................................................................................................................................ 42
Family Planning Benefits ..................................................................................................................... 42
Hearing Aid Benefits ............................................................................................................................ 42
Hemodialysis Treatment Benefits ........................................................................................................ 42
Home Health Care Benefits ................................................................................................................. 42
Hospice Care Benefits ......................................................................................................................... 43
Hospital Benefits .................................................................................................................................. 44
Infertility Treatment Benefits ................................................................................................................ 44
Infusion / Injectable Therapy Benefits .................................................................................................. 45
Jaw Joint Disorder Benefits ................................................................................................................. 45
Mental Health and Substance Use Disorder Benefits .......................................................................... 45
Online Visits ......................................................................................................................................... 47
Osteoporosis Benefits.......................................................................................................................... 47
Pediatric Asthma Equipment and Supplies Benefits ............................................................................ 47
Phenylketonuria (PKU) Benefits .......................................................................................................... 47
Physical Therapy, Physical Medicine and Occupational Therapy Benefits ......................................... 48
Pregnancy and Maternity Care Benefits .............................................................................................. 48
Prescription Drug for Abortion Benefits................................................................................................ 49
Prescription Drugs Obtained From Or Administered By a Medical Provider ....................................... 49
Preventive Care Benefits ..................................................................................................................... 49
Preventive Care Benefits for Chronic Conditions (per IRS guidelines) ................................................ 49
Professional Services Benefit .............................................................................................................. 50
Prosthetic Devices Benefits ................................................................................................................. 51
Radiation Therapy Benefits ................................................................................................................. 51
Reconstructive Surgery Benefits ......................................................................................................... 51
Retail Health Clinic Benefits ................................................................................................................ 51
Skilled Nursing Facility Benefits ........................................................................................................... 51
Speech Therapy and Speech-language pathology (SLP) Benefits...................................................... 52
Sterilization Benefits ............................................................................................................................ 52
Transgender Benefits .......................................................................................................................... 52
Transgender Travel Expense Benefits ................................................................................................ 52
Transplant Benefits .............................................................................................................................. 53
Transplant Travel Expense Benefits .................................................................................................... 54
Travel Immunization Benefits .............................................................................................................. 56
Urgent Care Benefits ........................................................................................................................... 56
Medical Care That Is NOT Covered ..................................................................................................... 57
Acupuncture ........................................................................................................................................ 57
Air Conditioners ................................................................................................................................... 57
Clinical Trials ....................................................................................................................................... 57
Commercial Weight Loss Programs .................................................................................................... 57
Contraceptive Devices ......................................................................................................................... 57
Cosmetic Surgery ................................................................................................................................ 57
Crime or Nuclear Energy ..................................................................................................................... 57
Custodial Care or Rest Cures .............................................................................................................. 57
Dental Services or Supplies ................................................................................................................. 57
Educational or Academic Services ...................................................................................................... 58
Excess Amounts .................................................................................................................................. 58
Experimental or Investigative ............................................................................................................... 58
Eye Surgery for Refractive Defects ..................................................................................................... 58
Food or Dietary Supplements .............................................................................................................. 58
Fraud, Waste, Abuse, and Other Inappropriate Billing ........................................................................ 58
Gene Therapy ...................................................................................................................................... 58
Government Treatment........................................................................................................................ 58
Health Club Memberships ................................................................................................................... 58
Hearing Aids or Tests .......................................................................................................................... 58
Infertility Treatment .............................................................................................................................. 59
Inpatient Diagnostic Tests ................................................................................................................... 59
Lifestyle Programs ............................................................................................................................... 59
Massage Therapy ................................................................................................................................ 59
Medical Equipment, Devices and Supplies .......................................................................................... 59
Non-Licensed Providers ...................................................................................................................... 59
Not Medically Necessary ..................................................................................................................... 59
Optometric Services or Supplies ......................................................................................................... 59
Orthodontia .......................................................................................................................................... 59
Orthopedic Supplies ............................................................................................................................ 59
Outpatient Occupational Therapy ........................................................................................................ 59
Outpatient Prescription Drugs and Medications .................................................................................. 59
Personal Items ..................................................................................................................................... 60
Physical Therapy or Physical Medicine ............................................................................................... 60
Private Contracts ................................................................................................................................. 60
Private Duty Nursing ............................................................................................................................ 60
Residential accommodations ............................................................................................................... 60
Routine Exams or Tests ...................................................................................................................... 60
Scalp hair prostheses .......................................................................................................................... 60
Services of Relatives ........................................................................................................................... 60
Speech Therapy .................................................................................................................................. 60
Sterilization Reversal ........................................................................................................................... 60
Surrogate Mother Services .................................................................................................................. 60
Telephone, Facsimile Machine, and Electronic Mail Consultations ..................................................... 60
Varicose Vein Treatment ..................................................................................................................... 60
Voluntary Payment .............................................................................................................................. 60
Waived Cost-Shares Out-of-Network Provider .................................................................................... 61
Work-Related ....................................................................................................................................... 61
BENEFITS FOR AUTISM SPECTRUM DISORDERS ................................................................................ 62
SUBROGATION AND REIMBURSEMENT ................................................................................................ 64
COORDINATION OF BENEFITS................................................................................................................ 68
BENEFITS FOR MEDICARE ELIGIBLE MEMBERS ................................................................................. 71
UTILIZATION REVIEW PROGRAM ........................................................................................................... 72
UNIVERSITY OF CALIFORNIA ELIGIBILITY, ENROLLMENT, TERMINATION AND PLAN
ADMINISTRATION PROVISIONS .............................................................................................................. 77
CONTINUATION OF COVERAGE ............................................................................................................. 78
GENERAL PROVISIONS ........................................................................................................................... 82
BINDING ARBITRATION............................................................................................................................ 91
DEFINITIONS .............................................................................................................................................. 92
YOUR RIGHT TO APPEALS .................................................................................................................... 102
FOR YOUR INFORMATION ..................................................................................................................... 108
CONSOLIDATED APPROPRIATIONS ACT OF 2021 NOTICE .............................................................. 111
No Surprises Act Requirements ....................................................................................................... 111
Provider Directories ........................................................................................................................... 112
Transparency Requirements ............................................................................................................. 112
1
SUMMARY OF BENEFITS
Note: The following SUMMARY OF BENEFITS contains the Benefits and applicable Copayments of your
medical Plan only. The SUMMARY OF BENEFITS represents only a brief description of the Benefits.
Please read this booklet carefully for a complete description of Covered Services and exclusions of the
Plan. Your prescription drug benefits are administered by a different plan administrator. For further
information, refer to www.UChealthplans.com.
See the end of this SUMMARY OF BENEFITS for important Benefit information.
In-Network Providers: Services by any combination of Anthem Prudent Buyer PPO Providers and Other
Health Care Providers
Many words or phrases in this Benefit Booklet have special meanings. Whenever any key terms are shown,
the first letter of each word will be capitalized. When you see these capitalized words, you should refer to
DEFINITIONSsection starting at page 89.
Health Savings Plan
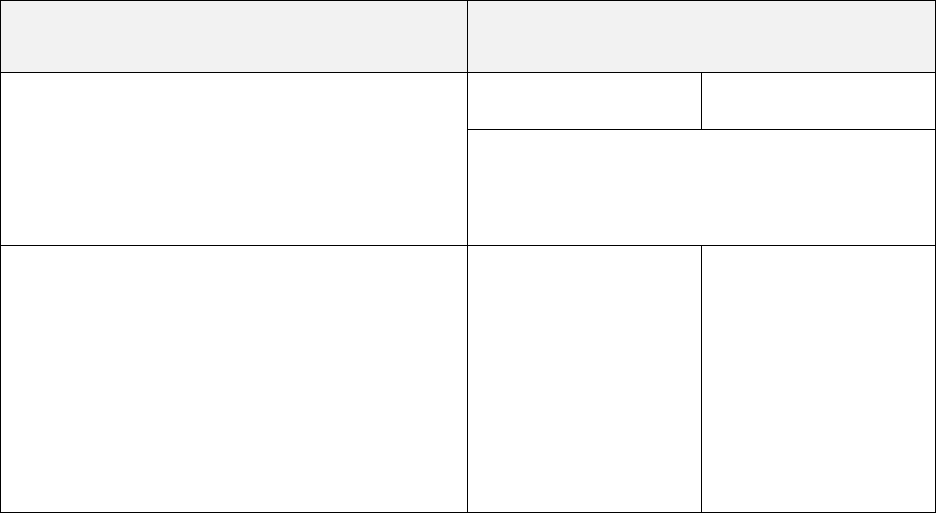
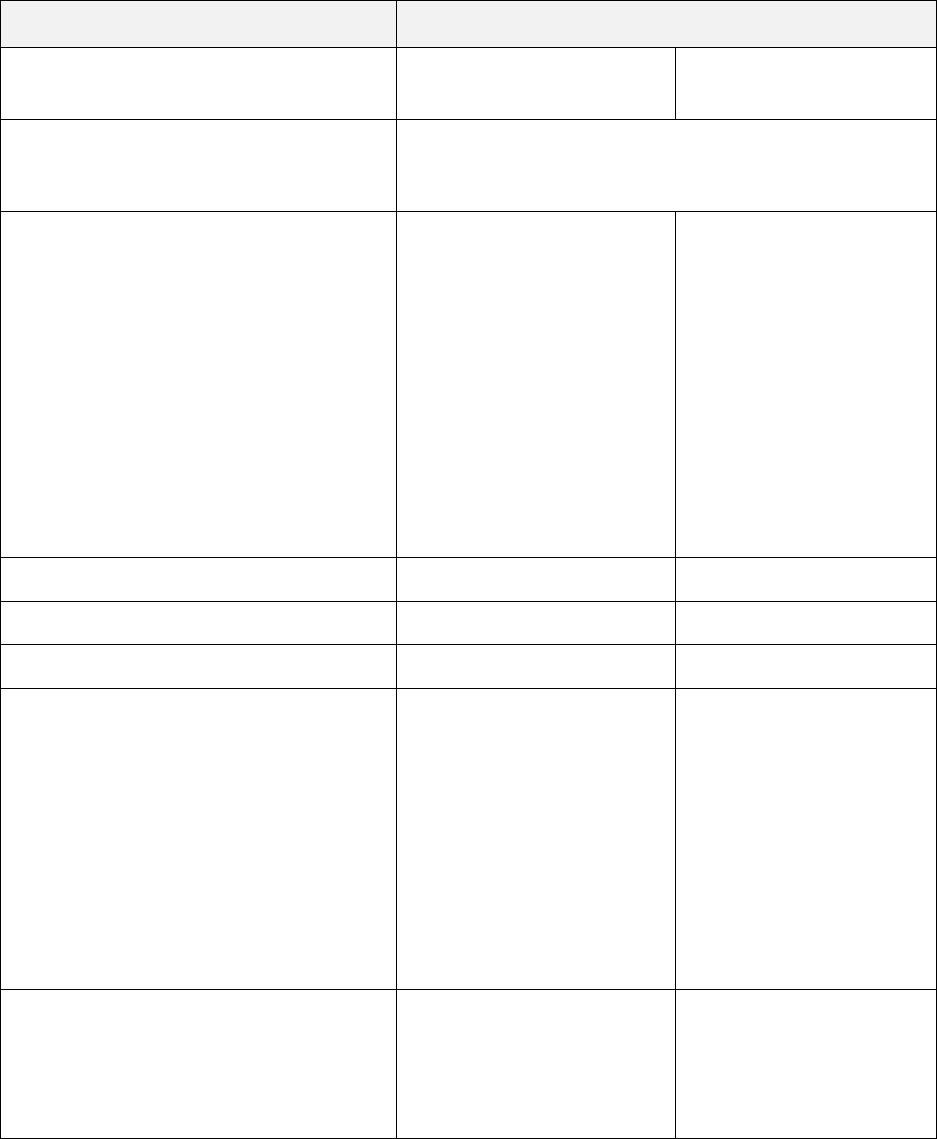
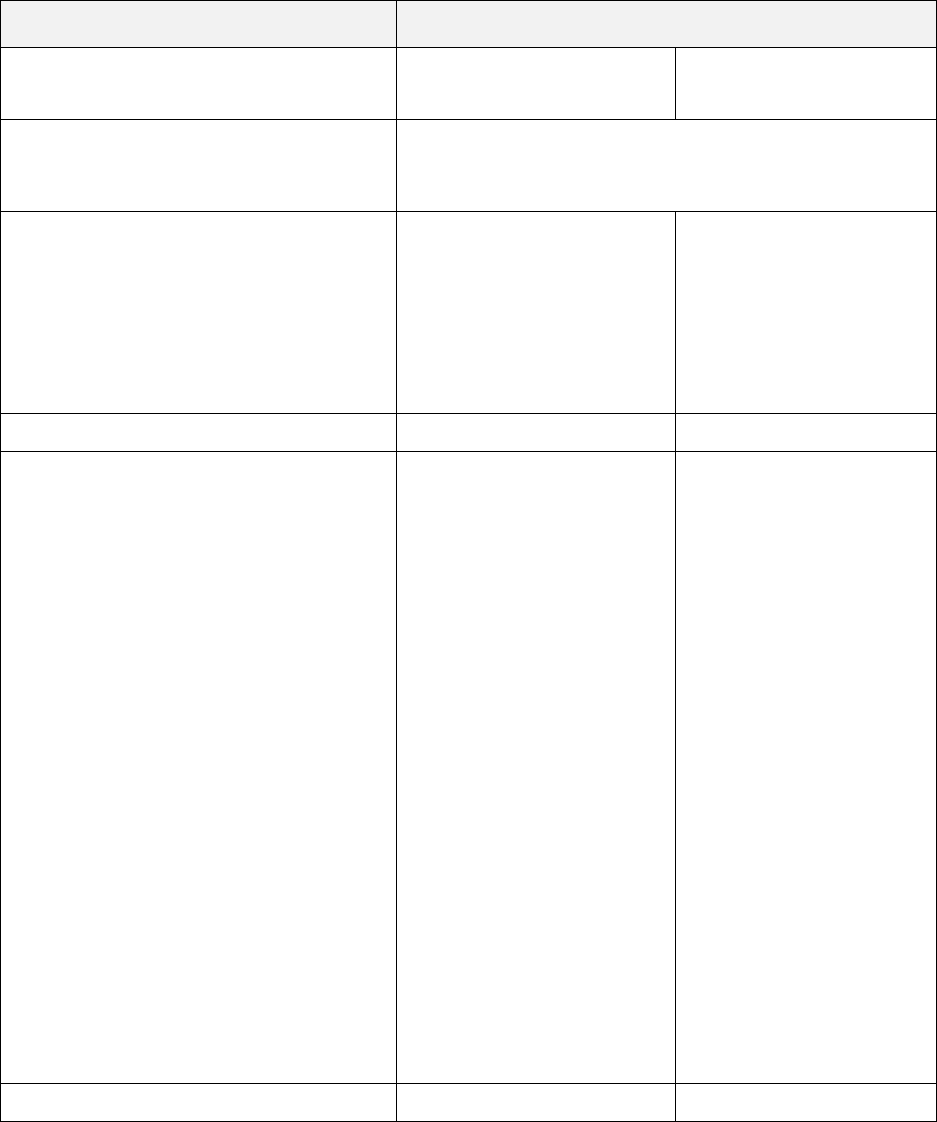
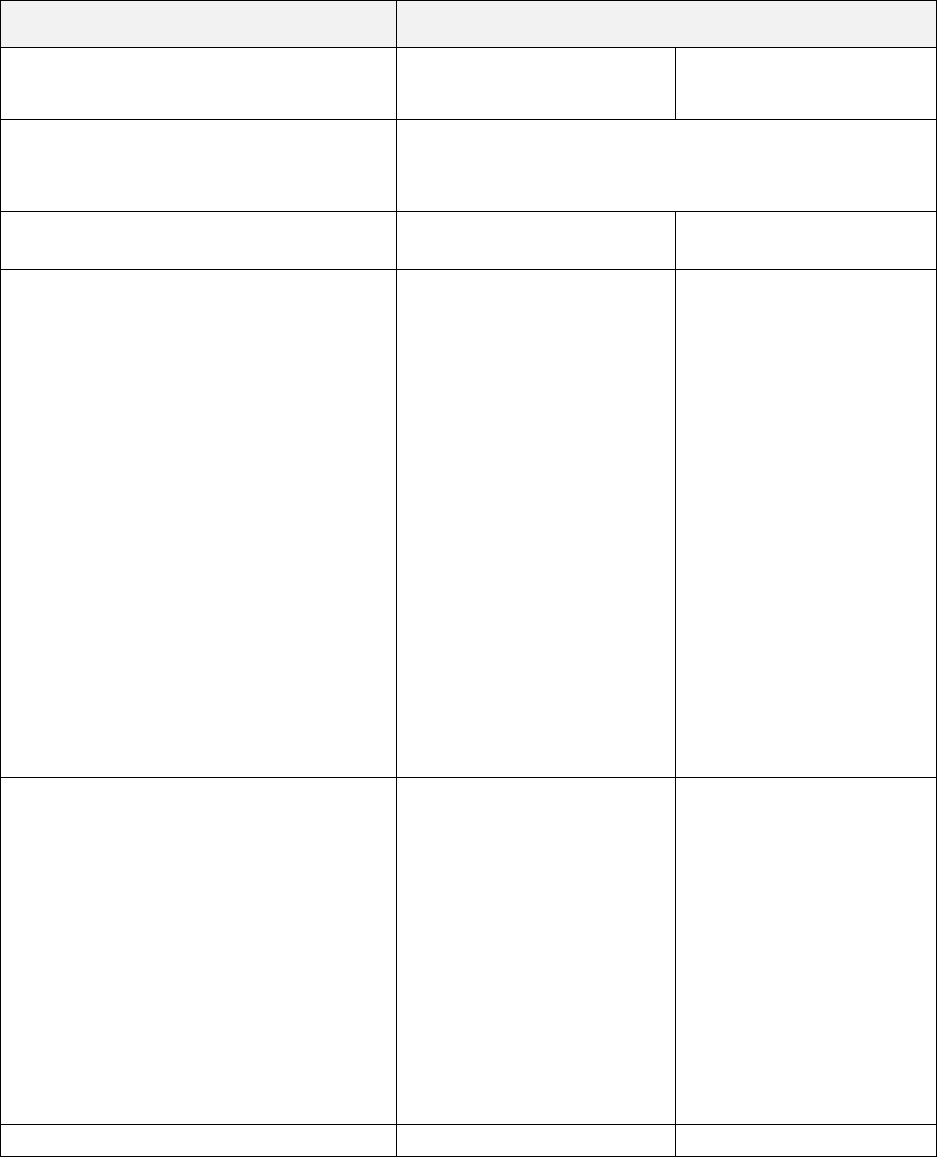
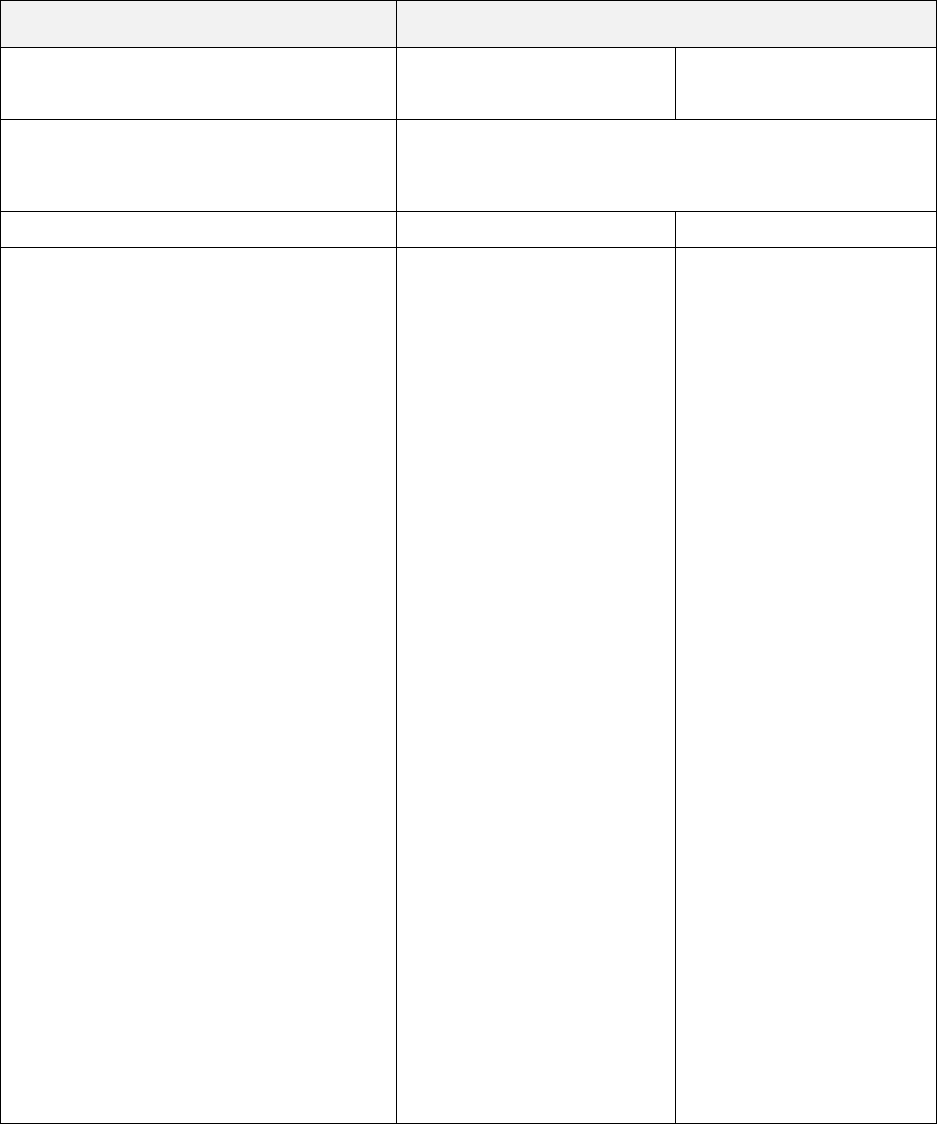
Member Calendar Year Deductible
Responsibility
Deductible Amount
Services by In-Network
Providers
Services by Out-of-
Network Providers*
*For Covered Services from Out-of-Network
Providers, you are responsible for any Deductible,
Copayment and all charges above the Maximum
Allowed Amount, except for Surprise Billing
Claims*.
Calendar Year Deductible
$1,600 Individual /
$3,200 family
$2,600 Individual /
$5,200 family
Please refer to the Member Deductible in the
information on how your Calendar Year Deductible
works.
For additional details about how your non-
embedded Deductibles work, please refer to the
-of-Pocket Amounts
* Surprise Billing Claims are described in the
this Booklet. Please refer to that section for further details.
2
Member Calendar Year Out-of-Pocket
Responsibility
Out-of-Pocket Amount
Services by In-Network
Providers
Services by Out-of-
Network Providers*
*For Covered Services from Out-of-Network
Providers, you are responsible for any Deductible,
Copayment and all charges above the Maximum
Allowed Amount, except for Surprise Billing
Claims*.
Calendar Year Out-of-Pocket Maximum
When you meet your Out-of-Pocket Maximum
amount, you will no longer have to pay the cost
shares during the remainder of your Calendar Year.
Your Deductible is included in your Out-of-Pocket
Maximum.
Pharmacy Copayments will apply towards your
Out-of-Pocket Maximum, unless otherwise noted.
Please refer to the Member Out-of-Pocket
section for information on how your Out-of-Pocket
Maximum works.
For additional details about how non-embedded
Out-of-Pocket Maximums work, please refer to the
-of-Pocket Amounts
$4,000 Individual /
$6,400 family
$8,000 Individual /
$16,000 family
* Surprise Billing Claims are
this Booklet. Please refer to that section for further details.
Member Maximum Lifetime Benefits
Maximum Anthem Payment
Services by In-Network
Providers
Services by Out-of-
Network Providers
Lifetime Benefit Maximum
No maximum
3
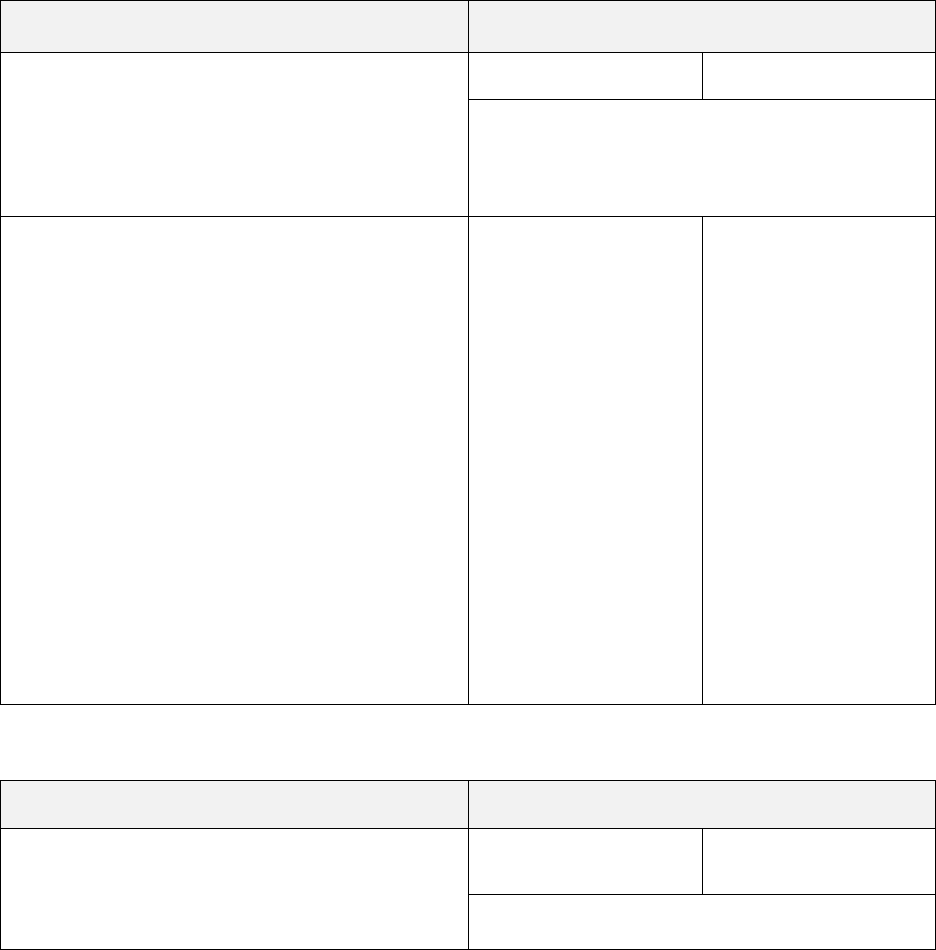
Note: Please refer to the section Medical Care That Is Covered for additional details regarding your Benefits.
In-Network Providers: Services by any combination of Anthem Prudent Buyer PPO and Other Health Care
Providers
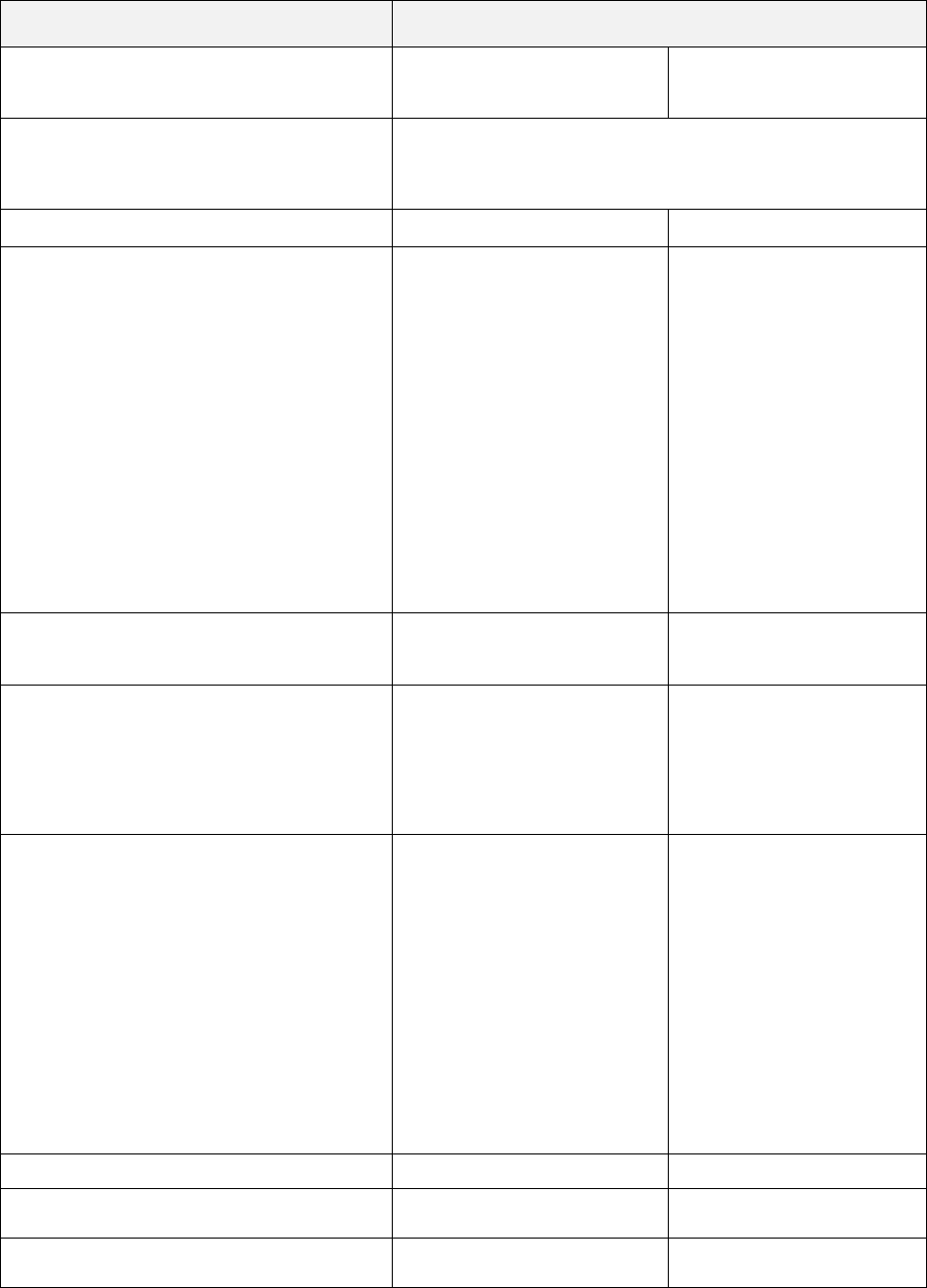
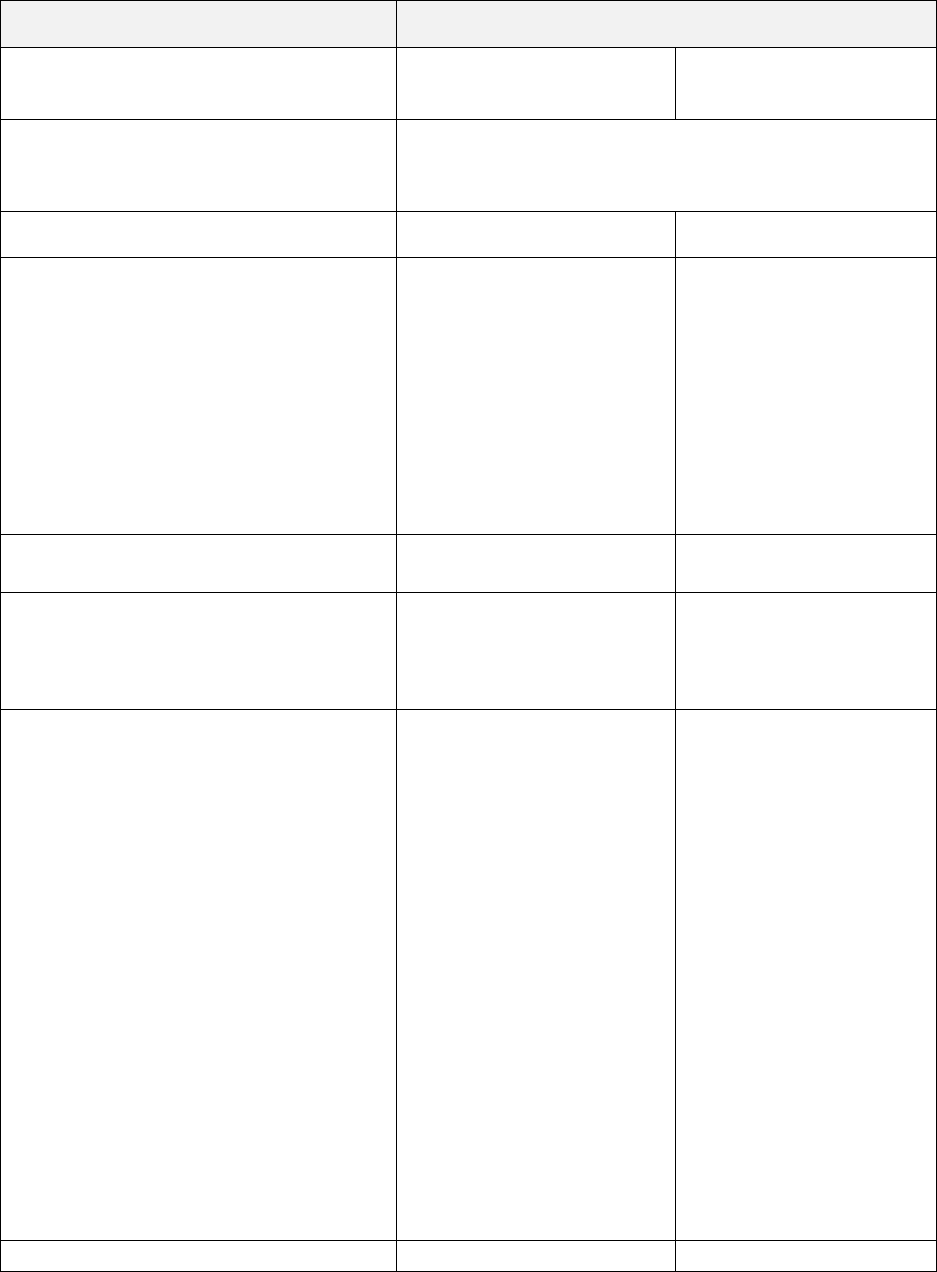
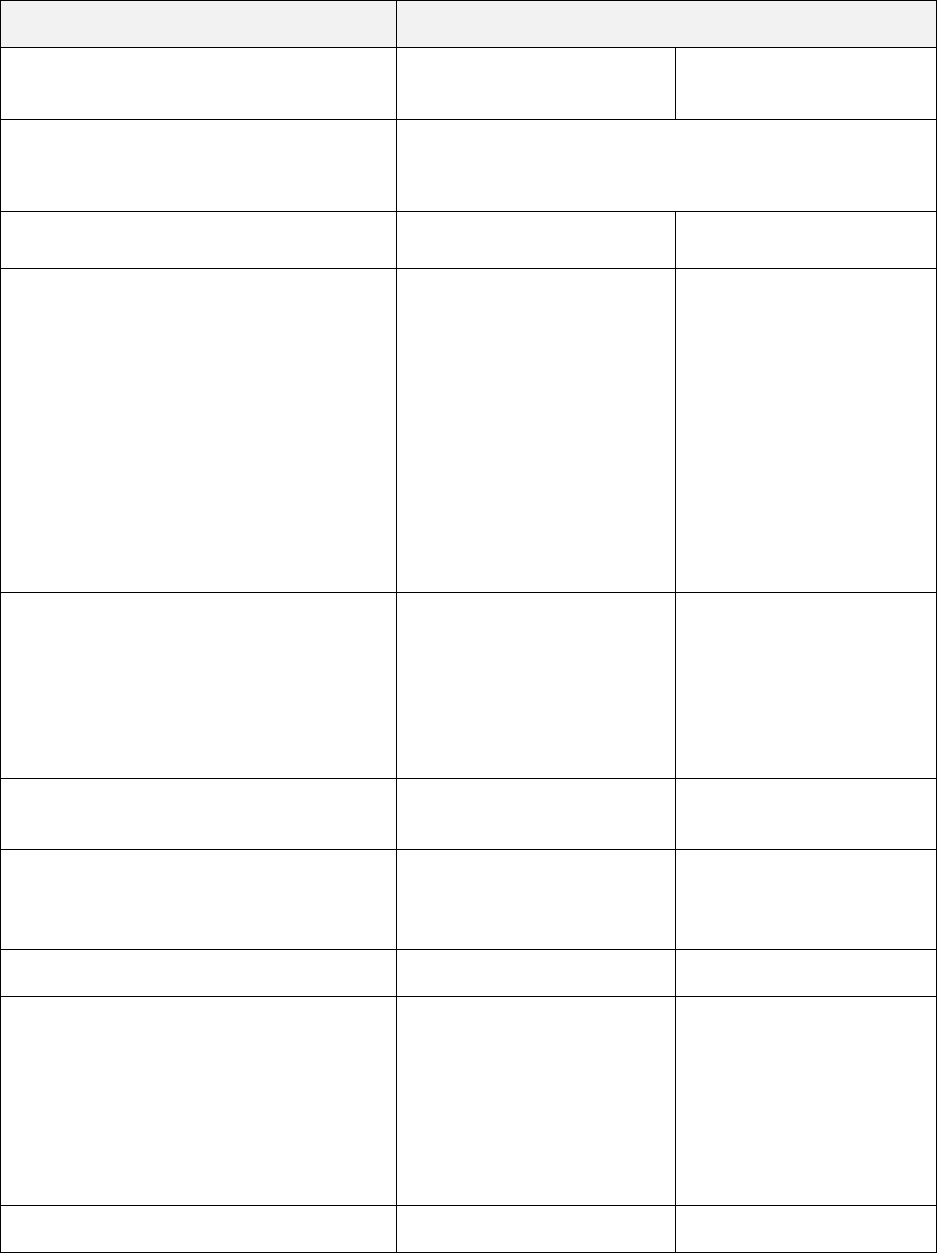
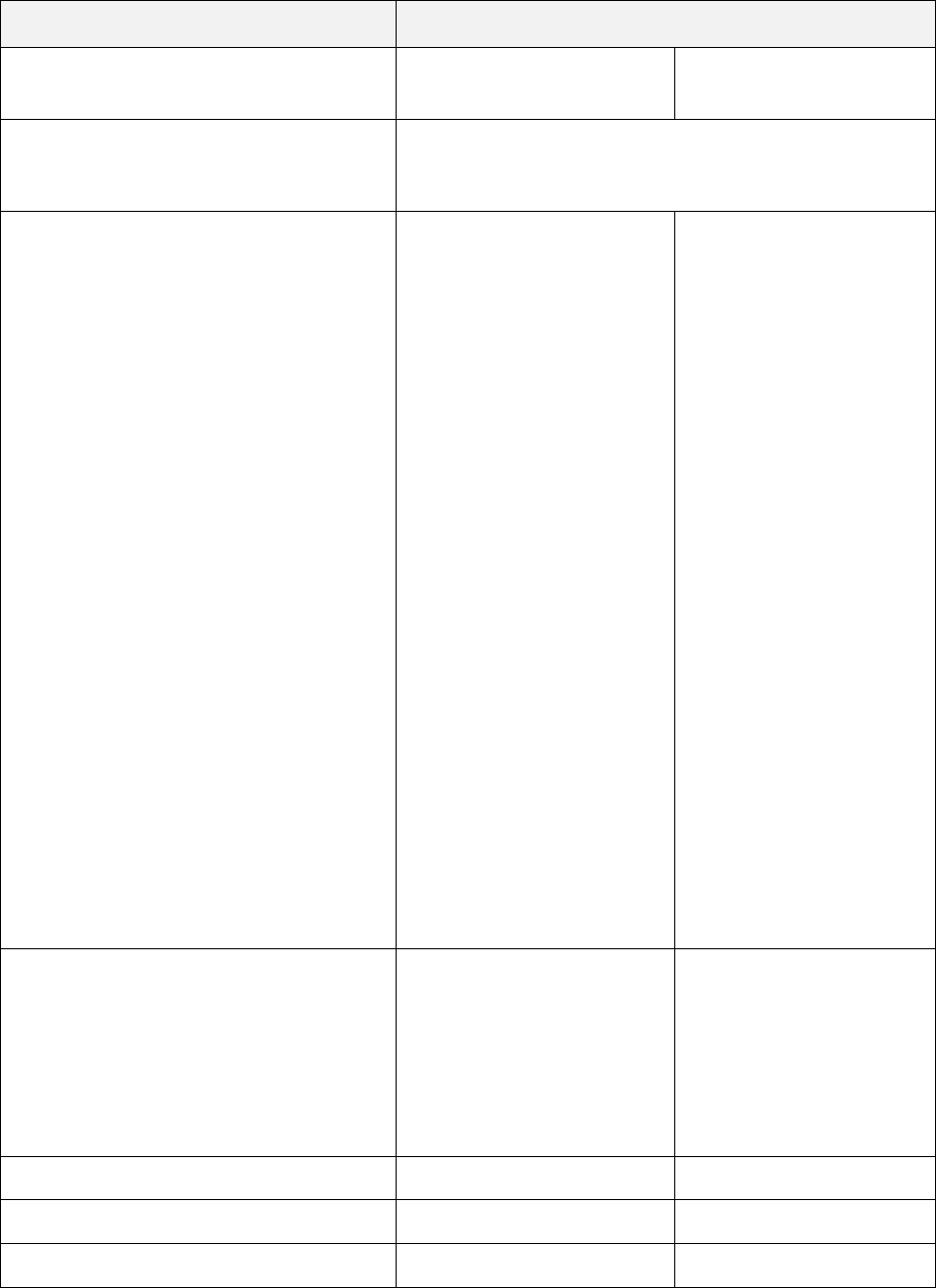
Benefit
Member Copayment/Coinsurance
Services by In-Network
Providers
Services by Out-of-
Network Providers*
* For Covered Services from Out-of-Network Providers,
you are responsible for any Deductible, Copayment and all
charges above the Maximum Allowed Amount, except for
Surprise Billing Claims*.
Acupuncture Benefits
• Acupuncture services office location
The Plan will pay for up to 24 visits per
Member during a Calendar Year (visits
lease refer to Medical Benefit
Maximums in the Medical Benefit
Summary Notes section for maximums
that apply to your Plan. Office visit
Benefits will apply to an office visit when
billed along with the services.
Since your Plan has a Calendar Year
Deductible, the number of visits will start
counting toward the maximum when
services are first provided even if the
Calendar Year Deductible has not been
met.
20%
20%
Advanced Imaging Procedure Benefits
Advanced imaging procedure services are
subject to pre-service review to determine
whether Medically Necessary. Please
refer to the section UTILIZATION REVIEW
PROGRAM for information on how to
obtain the proper reviews.
• Physician services office location
20%
40%
• Freestanding facility
20%
40%
• Outpatient Hospital
Advanced imaging procedures, when
performed by an Out-of-Network Provider,
will have a maximum payment of $210 per
visit. Please refer to Medical Benefit
Maximums in the Medical Benefit
Summary Notes section for maximums
that apply to your Plan.
20%
40%
4
Benefit
Member Copayment/Coinsurance
Services by In-Network
Providers
Services by Out-of-
Network Providers*
* For Covered Services from Out-of-Network Providers,
you are responsible for any Deductible, Copayment and all
charges above the Maximum Allowed Amount, except for
Surprise Billing Claims*.
Allergy Testing and Treatment Benefits
• Testing and treatment, includes serum
and serum injections
20%
40%
• Allergy serum purchased separately for
treatment
20%
40%
Ambulance Benefits
• Emergency or authorized transport
(ground, air or water) by In-Network or
Out-of-Network Providers will apply to
the In-Network Deductible and Out-of-
Pocket Maximum
20%
20%
Ambulatory Surgery Center Benefits
Ambulatory Surgical Center services are
subject to pre-service review to determine
whether Medically Necessary. Please
refer to the section UTILIZATION REVIEW
PROGRAM for information on how to
obtain the proper reviews.
• Outpatient services (Hospital or
freestanding surgical center)
For the services of an Out-of-Network
Provider, the maximum payment is
limited to $210 per visit. Please refer to
Medical Benefit Maximums in the Medical
Benefit Summary Notes section for
maximums that apply to your Plan.
20%
40%
• Physician services
20%
40%
5
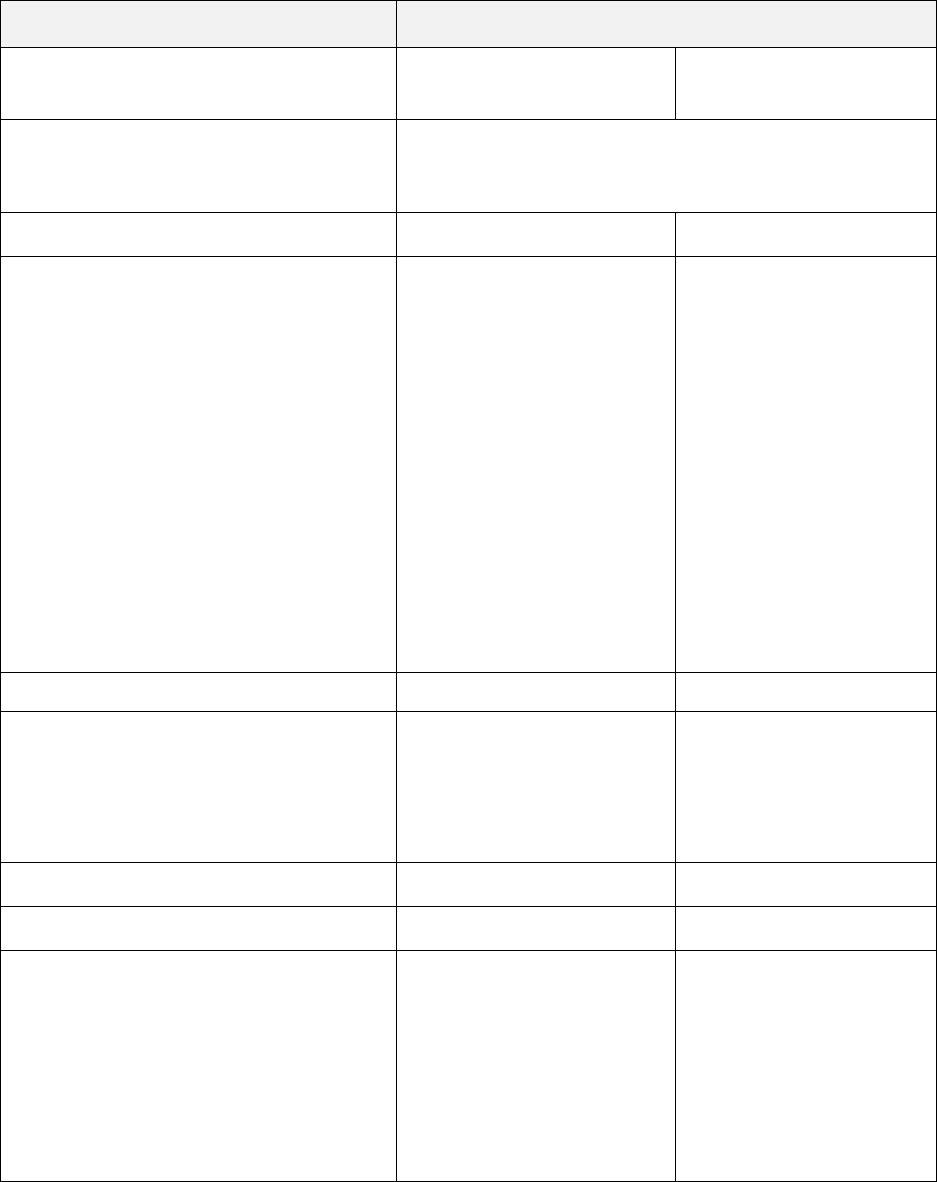
Benefit
Member Copayment/Coinsurance
Services by In-Network
Providers
Services by Out-of-
Network Providers*
* For Covered Services from Out-of-Network Providers,
you are responsible for any Deductible, Copayment and all
charges above the Maximum Allowed Amount, except for
Surprise Billing Claims*.
Bariatric Surgery Benefits
Services and supplies in connection with
Medically Necessary surgery for weight
loss,
only for morbid obesity. These
procedures are covered only when
performed at a BDCSC. See page 35
under Medical Care That Is Covered for
details.
You must obtain pre-service review for all
bariatric surgical procedures. Please refer
to the section UTILIZATION REVIEW
PROGRAM for information on how to
obtain the proper reviews.
• Hospital inpatient services
20%
Not covered
• Hospital outpatient surgery services
20%
Not covered
• Physician inpatient services
20%
Not covered
• Bariatric Travel Expenses
The Plans maximum payment will not
exceed $5,000 per surgery. Please refer to
Medical Benefit Maximums in the Medical
Benefit Summary Notes section for
maximums that apply to your Plan.
**No Copayment will be required for
bariatric travel expenses authorized by
Anthem once your Calendar Year
Deductible is met.
No charge**
Not covered
Cardiac Rehabilitation
If rendered in Outpatient Hospital setting,
for services of an Out-of-Network
Provider, the maximum payment is
limited to $210 per visit.
20%
40%
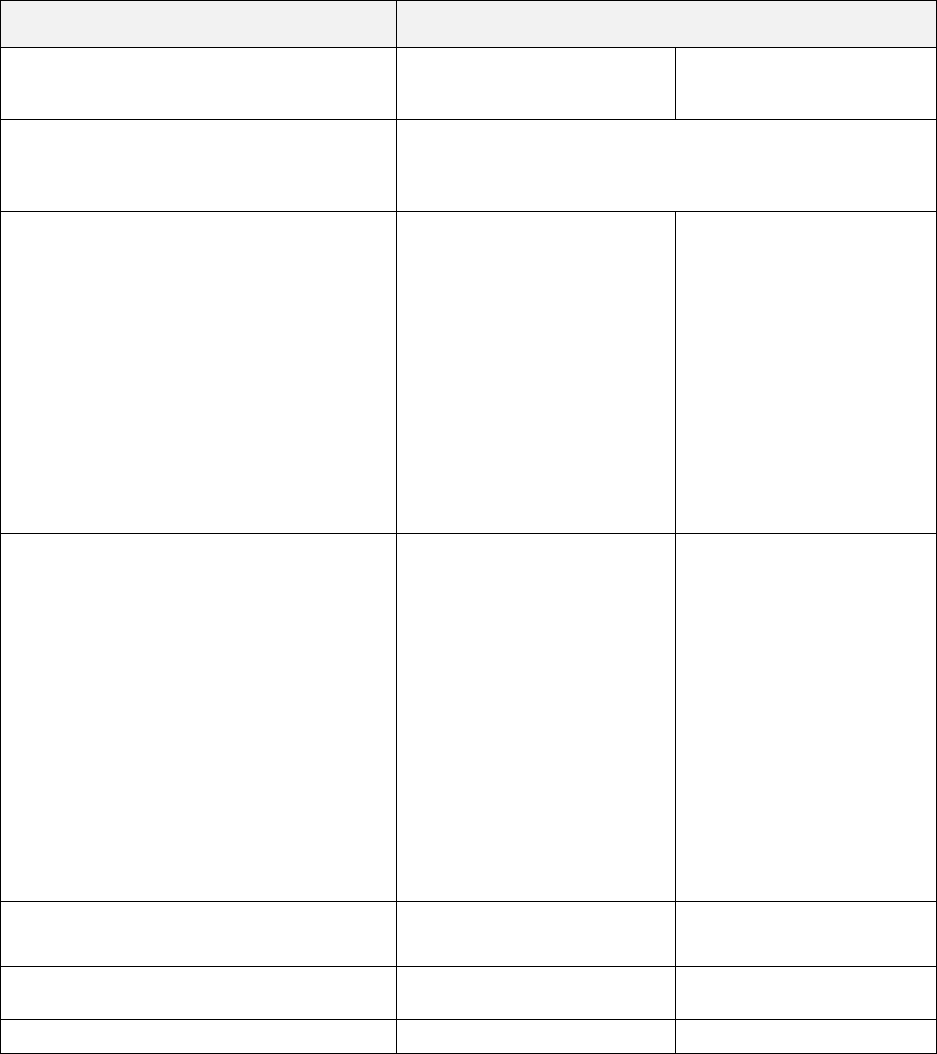
6
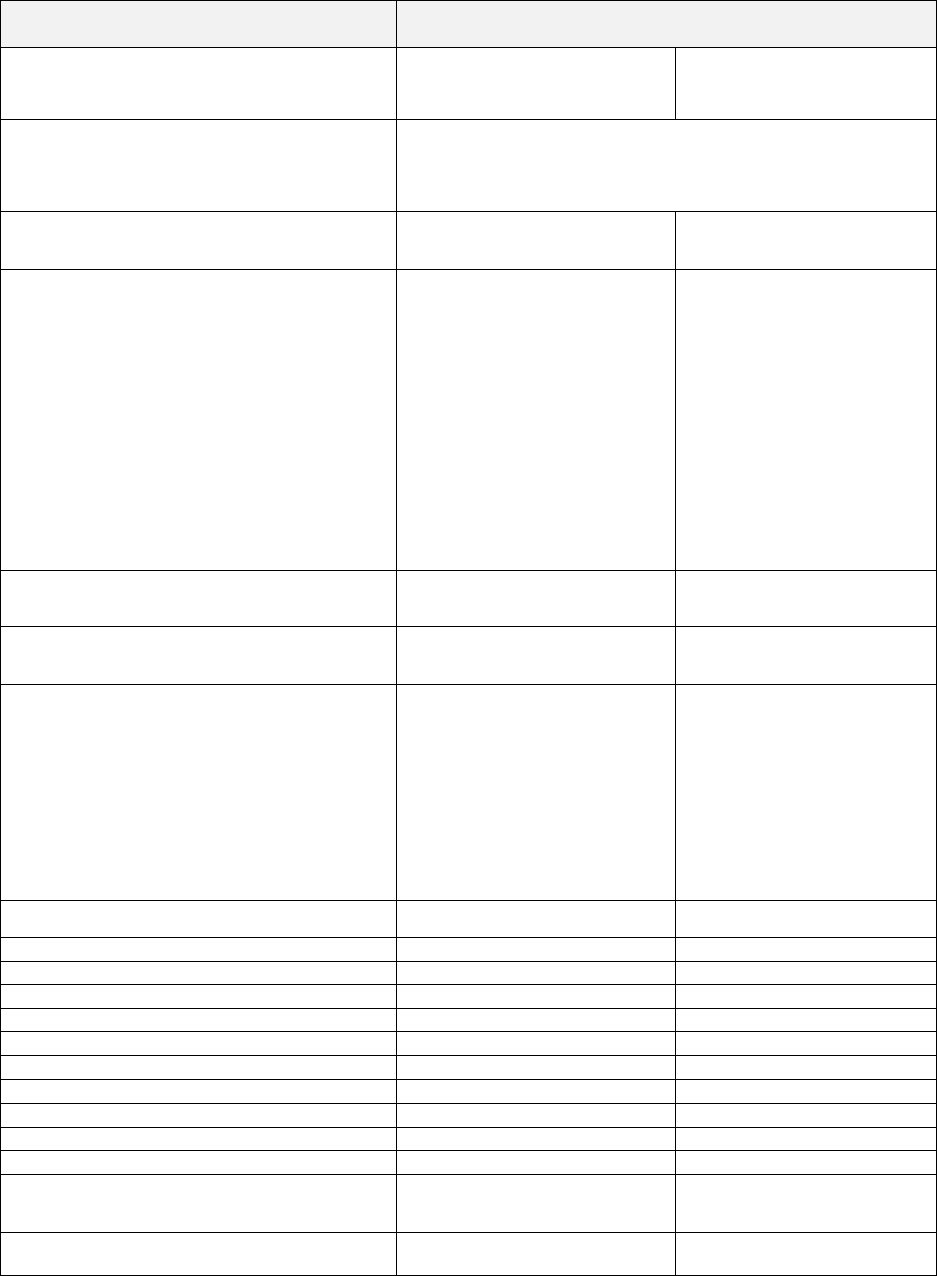
Benefit
Member Copayment/Coinsurance
Services by In-Network
Providers
Services by Out-of-
Network Providers*
* For Covered Services from Out-of-Network Providers,
you are responsible for any Deductible, Copayment and all
charges above the Maximum Allowed Amount, except for
Surprise Billing Claims*.
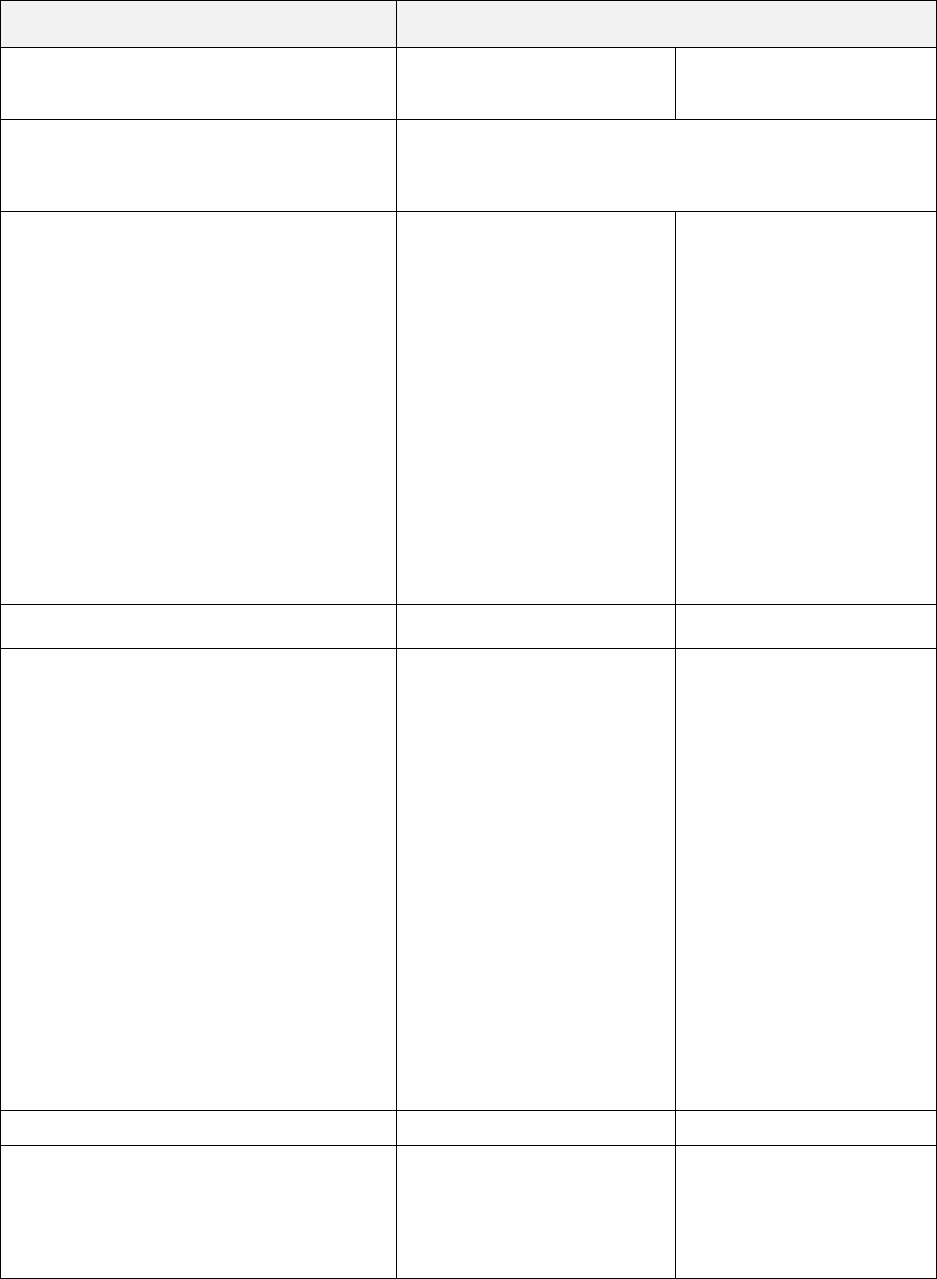
Chiropractic Benefits
• Chiropractic Services office location
The Plan will pay for up to 24 visits per
Member during a Calendar Year (visits
lease refer to Medical Benefit
Maximums in the Medical Benefit
Summary Notes section for maximums
that apply to your Plan.
Since your Plan has a Calendar Year
Deductible, the number of visits will start
counting toward the maximum when
services are first provided even if the
Calendar Year Deductible has not been
met.
20%
40%
Clinical Trial of Cancer and Other Life
Threatening Conditions Benefits
Coverage is provided for routine patient
costs you receive as a Member in an
approved clinical trial. The services must
be those that are listed as covered by
this Plan for Members
who are not
enrolled in a clinical trial.
20%
40%
Contraceptive Benefits
Certain contraceptives are covered under
that provision for further details.
The Calendar Year Deductible will not
apply to services provided by Anthem
Preferred Providers.
See page 38 under Medical Care That Is
Covered for details for information about
• Diaphragm fitting procedure
No charge
40%
• Implantable and injectable
contraceptives
No charge
40%
• Insertion and/or removal of
intrauterine device (IUD)
No charge
40%
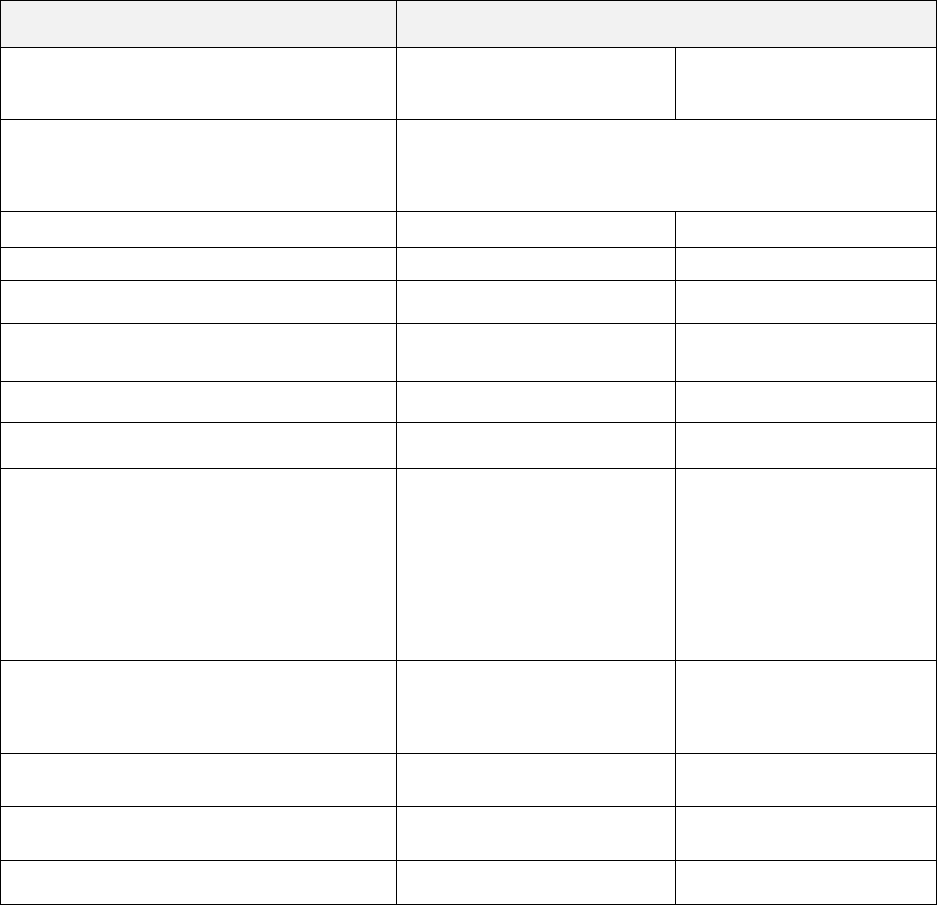
7
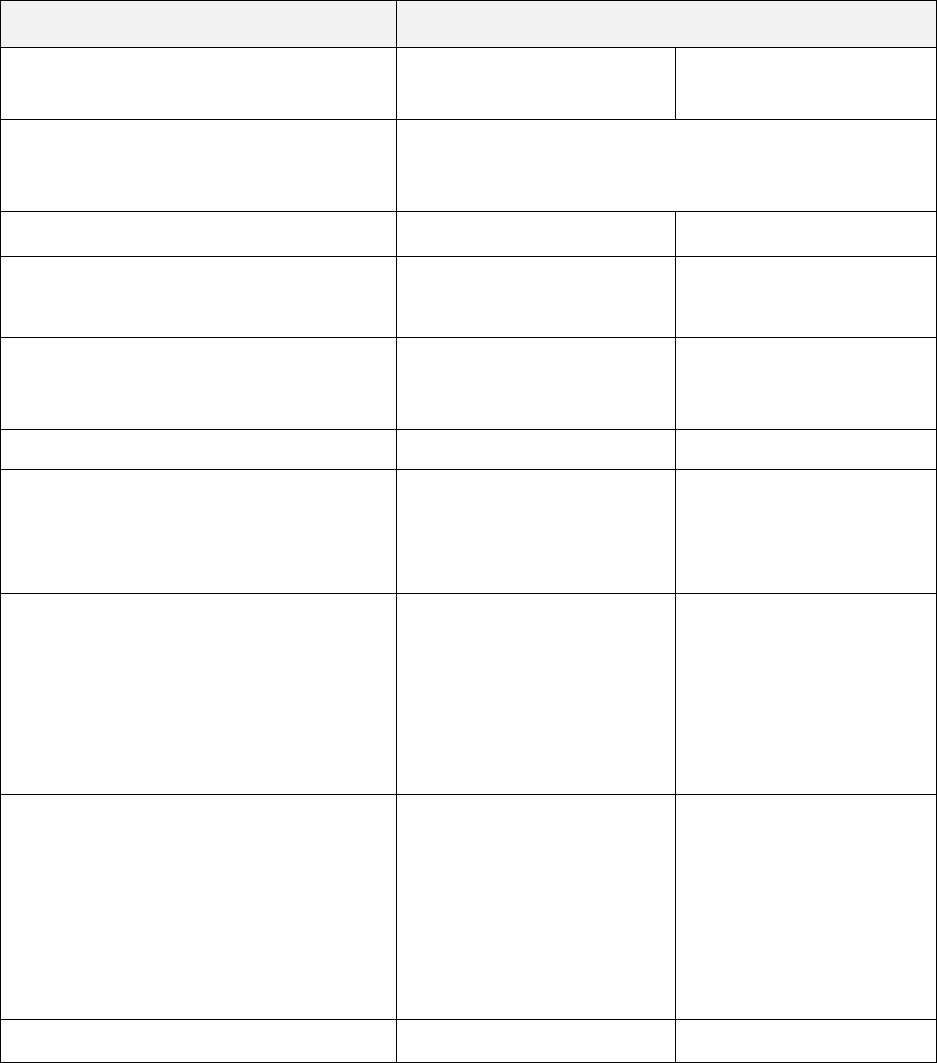
Benefit
Member Copayment/Coinsurance
Services by In-Network
Providers
Services by Out-of-
Network Providers*
* For Covered Services from Out-of-Network Providers,
you are responsible for any Deductible, Copayment and all
charges above the Maximum Allowed Amount, except for
Surprise Billing Claims*.
• Intrauterine device (IUD)
No charge
40%
Diabetes Care Benefits
• Devices, equipment and supplies
20%
40%
• Diabetes self-management training
office location
20%
40%
Durable Medical Equipment Benefits
• Breast Pump
No charge
Not covered
• Other Durable Medical Equipment
Specific durable medical equipment is
subject to pre-service review to determine
whether Medically Necessary. Please
refer to the section UTILIZATION REVIEW
PROGRAM for information on how to
obtain the proper reviews.
20%
40%
Emergency Room Benefits
Services by In-Network or Out-of-Network
Providers will apply to the In-Network
Deductible and Out-of-Pocket Maximum
• Emergency room facility services not
resulting in an admission
20%
20%
• Emergency room facility services
resulting in an admission
20%
20%
• Physician services
20%
20%
8
Benefit
Member Copayment/Coinsurance
Services by In-Network
Providers
Services by Out-of-
Network Providers*
* For Covered Services from Out-of-Network Providers,
you are responsible for any Deductible, Copayment and all
charges above the Maximum Allowed Amount, except for
Surprise Billing Claims*.
Family Planning Benefits
Certain contraceptives are covered under
that provision for further details.
The Calendar Year Deductible will not
apply to contraceptive or tubal ligation
services provided by Anthem Prudent
Buyer Providers.
See page 40 under Medical Care That Is
Covered for details for information about
• Counseling and consulting (including
Physician office visits for diaphragm
fitting, injectable contraceptives, or
implantable contraceptives)
No charge
40%
• Tubal ligation
No charge
40%
• Vasectomy
No charge
after deductible is met
40%
Abortion/ Abortion Related Services
No charge
after deductible is met
No charge
after deductible is met
Hearing Aid Benefits
• Hearing aids and ancillary equipment up
to a maximum of $2,000 every 36
months. Please refer to Medical Benefit
Maximums in the Medical Benefit
Summary Notes section for maximums
that apply to your Plan.
50%
50%
Hemodialysis Benefits
• Hemodialysis services
For the services of an Out-of-Network
Provider, the maximum payment is
limited to $210 per visit. Please refer to
Medical Benefit Maximums in the Medical
Benefit Summary Notes section for
maximums that apply to your Plan.
20%
40%
9
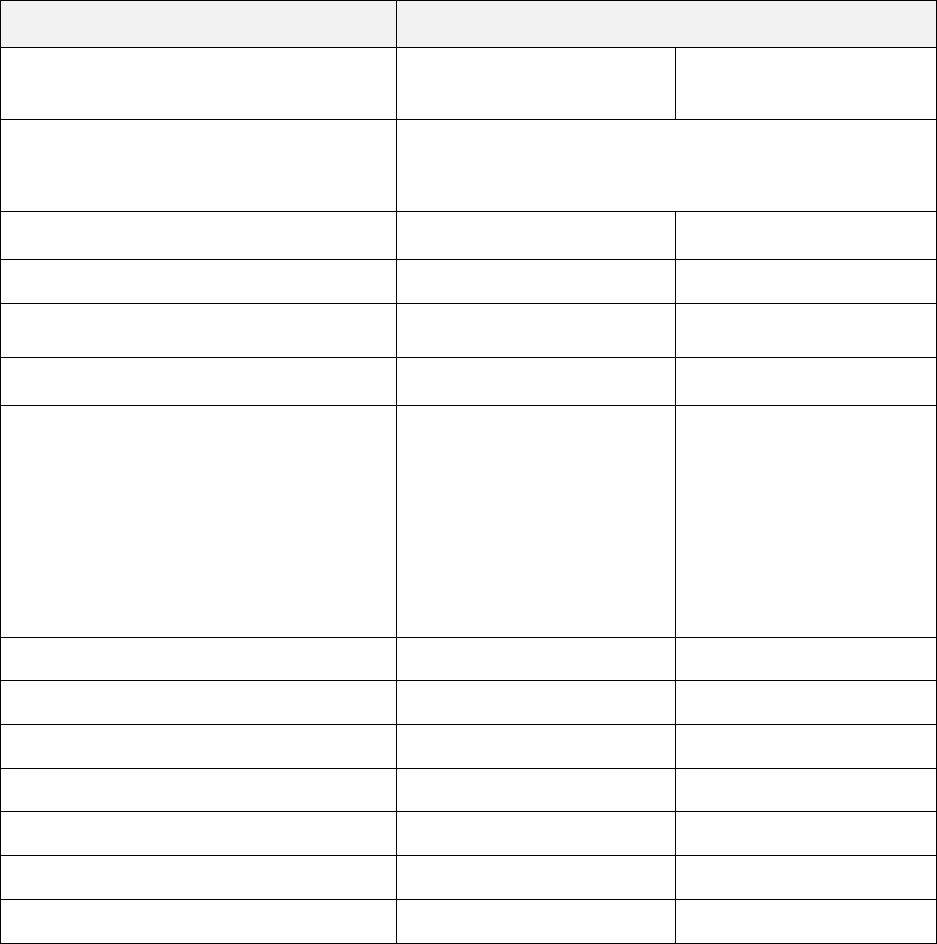
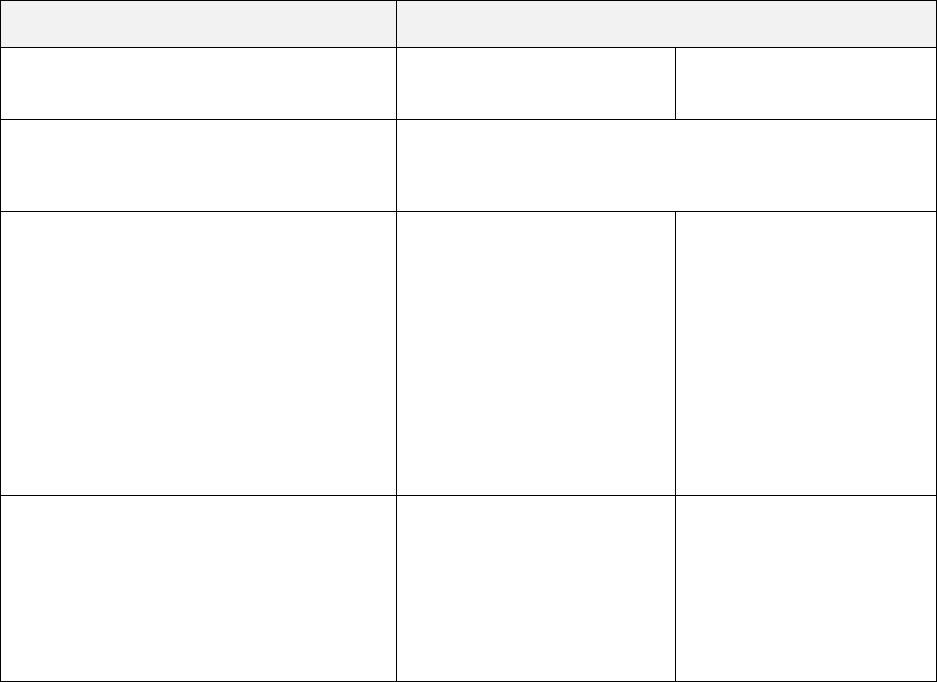
Benefit
Member Copayment/Coinsurance
Services by In-Network
Providers
Services by Out-of-
Network Providers*
* For Covered Services from Out-of-Network Providers,
you are responsible for any Deductible, Copayment and all
charges above the Maximum Allowed Amount, except for
Surprise Billing Claims*.
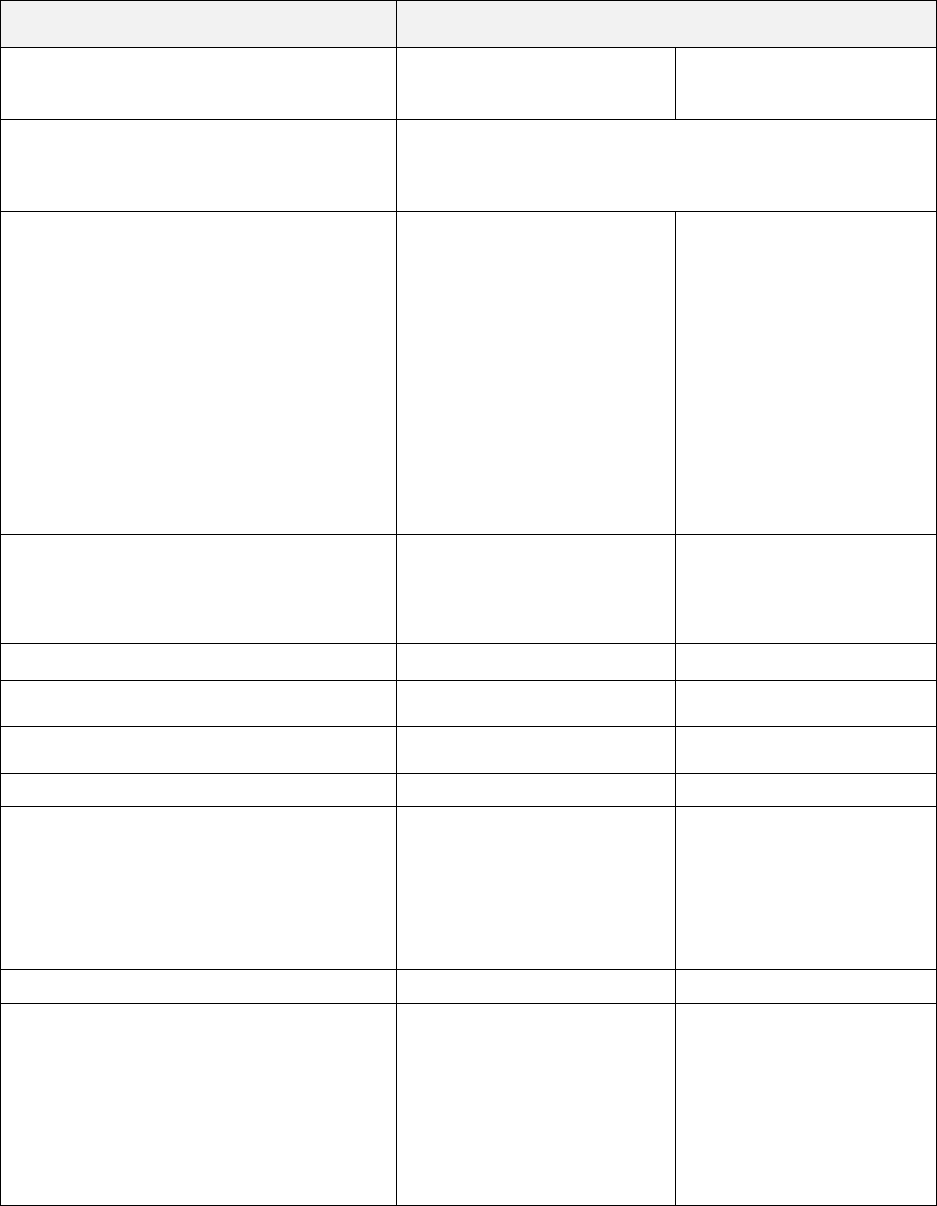
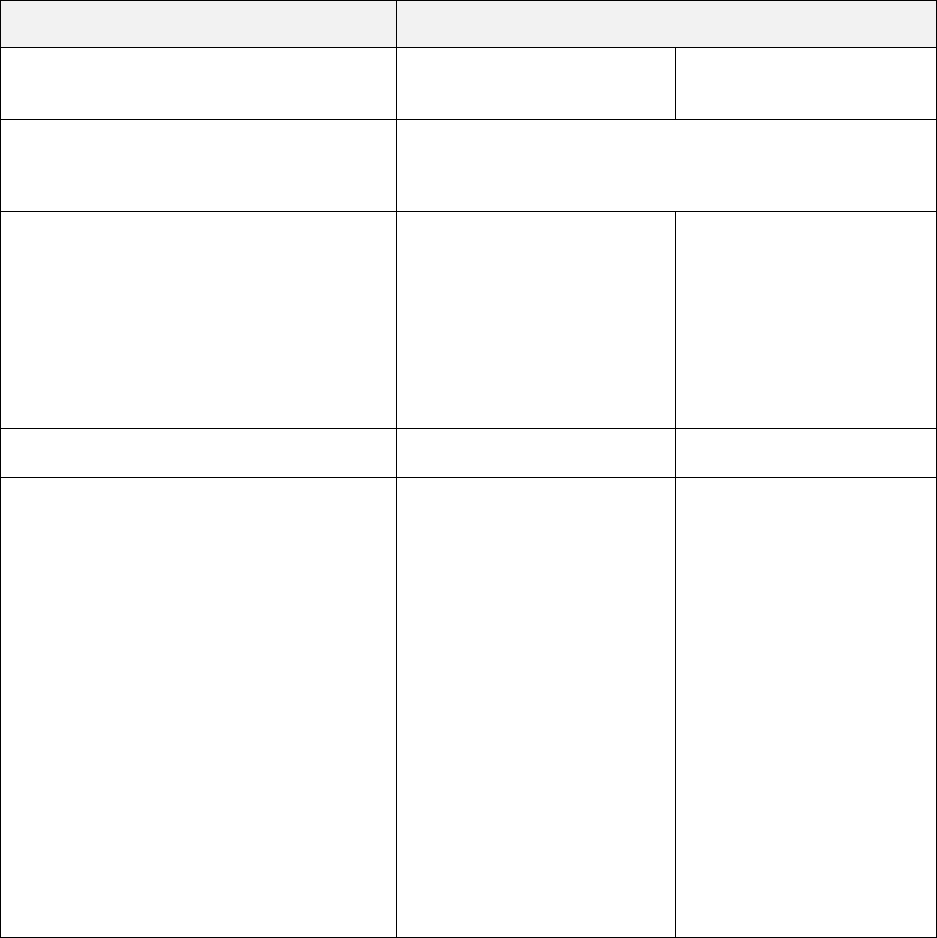
• Outpatient services
For the services of an Out-of-Network
Provider, the maximum payment is
limited to $210 per visit. Please refer to
Medical Benefit Maximums in the Medical
Benefit Summary Notes section for
maximums that apply to your Plan.
20%
40%
Home Health Care Benefits
• Home health care agency services
Benefits are provided for up to a maximum
of 100 visits per Calendar Year. Please
refer to Medical Benefit Maximums in the
Medical Benefit Summary Notes section
for maximums that apply to your Plan.
Since your Plan has a Calendar Year
Deductible, the number of visits will start
counting toward the maximum when
services are first provided even if the
Calendar Year Deductible has not been
met.
** For an Out-of-Network Provider,
services may be covered if preauthorized.
Please refer to Copayments in the Medical
Benefit Summary Notes section for
additional Benefit information.
Home health care services are subject to
pre-service review to determine whether
Medically Necessary. Please refer to the
section UTILIZATION REVIEW
PROGRAM for information on how to
obtain the proper reviews.
20%
Not covered**
• Medical supplies
20%
Not covered**
10
Benefit
Member Copayment/Coinsurance
Services by In-Network
Providers
Services by Out-of-
Network Providers*
* For Covered Services from Out-of-Network Providers,
you are responsible for any Deductible, Copayment and all
charges above the Maximum Allowed Amount, except for
Surprise Billing Claims*.
Hospice Care Benefits
The services and supplies are covered
when provided by a Hospice for the
palliative treatment of pain and other
symptoms associated with a terminal
disease.
** For an Out-of-Network Provider,
services may be covered if preauthorized.
Please refer to Copayments in the Medical
Benefit Summary Notes section for
additional Benefit information.
20%
Not covered**
Hospital Benefits
• Inpatient services resulting from an
Emergency
Services by In-Network or Out-of-Network
Providers will apply to the In-Network
Deductible and Out-of-Pocket Maximum
20%
20%
• Inpatient services and supplies,
provided by a Hospital, including
services in Special Care Units.
For the services of an Out-of-Network
Provider, there is an additional $250
Copayment if prior authorization is not
obtained
For the services of an Out-of-Network
Provider, the maximum payment is
limited to $360 per day. Please refer to
Medical Benefit Maximums in the Medical
Benefit Summary Notes section for
maximums that apply to your Plan.
Hospital services are subject to pre-
service review to determine whether
Medically Necessary. Please refer to the
section UTILIZATION REVIEW
PROGRAM for information on how to
obtain the proper reviews.
20%
40%
• Inpatient Physician services
20%
40%
11
Benefit
Member Copayment/Coinsurance
Services by In-Network
Providers
Services by Out-of-
Network Providers*
* For Covered Services from Out-of-Network Providers,
you are responsible for any Deductible, Copayment and all
charges above the Maximum Allowed Amount, except for
Surprise Billing Claims*.
• Outpatient surgery including
freestanding facilities
For the services of an Out-of-Network
Provider, the maximum payment is
limited to $210 per visit. Please refer to
Medical Benefit Maximums in the Medical
Benefit Summary Notes section for
maximums that apply to your Plan.
Hospital services are subject to pre-
service review to determine whether
Medically Necessary. Please refer to the
section UTILIZATION REVIEW
PROGRAM for information on how to
obtain the proper reviews.
20%
40%
• Outpatient Physician services
20%
40%
• Outpatient diagnostic services including
freestanding facilities
For the services of an Out-of-Network
Provider, the maximum payment is
limited to $210 per visit. Please refer to
Medical Benefit Maximums in the Medical
Benefit Summary Notes section for
maximums that apply to your Plan.
Note: Professional (Physician) reading
charge may apply.
Hospital services are subject to pre-
service review to determine whether
Medically Necessary. Please refer to the
section UTILIZATION REVIEW
PROGRAM for information on how to
obtain the proper reviews.
20%
40%
Infertility Benefits
• Diagnosis of cause of Infertility
provided you are under the direct
care and treatment of a Physician.
• IVF, ZIFT, and/or GIFT
20%
50%
40%
50%
12
Benefit
Member Copayment/Coinsurance
Services by In-Network
Providers
Services by Out-of-
Network Providers*
* For Covered Services from Out-of-Network Providers,
you are responsible for any Deductible, Copayment and all
charges above the Maximum Allowed Amount, except for
Surprise Billing Claims*.
Limited to 2 cycles per lifetime.
Coinsurance for these services does not
apply towards Calendar Year Out-of-
Pocket Limit.
Prior Authorization is required. Please
refer to the section UTILIZATION REVIEW
PROGRAM for information on how to
obtain the proper reviews.
Infusion / Injectable Therapy Benefits
Services and supplies when provided by
an Infusion Therapy Provider/Injectable
Therapy Provider in your home or in any
other outpatient setting by a qualified
health care provider
* For an Out-of-Network Provider,
services may be covered if preauthorized.
Please refer to Copayments in the
Medical Benefit Summary Notes section
for additional Benefit information.
Oncology and transplant related Infusion /
Injection therapy services are subject to
pre-service review to determine whether
Medically Necessary. Please refer to the
section UTILIZATION REVIEW
PROGRAM for information on how to
obtain the proper reviews.
20%
Not covered*
13
Benefit
Member Copayment/Coinsurance
Services by In-Network
Providers
Services by Out-of-
Network Providers*
* For Covered Services from Out-of-Network Providers,
you are responsible for any Deductible, Copayment and all
charges above the Maximum Allowed Amount, except for
Surprise Billing Claims*.
Jaw Joint Disorder Benefits
• Inpatient Hospital services
For the services of an Out-of-Network
Provider, there is an additional $250
Copayment if prior authorization is not
obtained
For the services of an Out-of-Network
Provider, the maximum payment is
limited to $360 per day. Please refer to
Medical Benefit Maximums in the Medical
Benefit Summary Notes section for
maximums that apply to your Plan
Hospital services are subject to pre-
service review to determine whether
Medically Necessary. Please refer to the
section UTILIZATION REVIEW
PROGRAM for information on how to
obtain the proper reviews.
20%
40%
• Outpatient surgery facility services
For the services of an Out-of-Network
Provider, the maximum payment is
limited to $210 per visit. Please refer to
Medical Benefit Maximums in the Medical
Benefit Summary Notes section for
maximums that apply to your Plan.
Hospital services are subject to pre-
service review to determine whether
Medically Necessary. Please refer to the
section UTILIZATION REVIEW
PROGRAM for information on how to
obtain the proper reviews.
20%
40%
• Physician services
20%
40%
14
Benefit
Member Copayment/Coinsurance
Services by In-Network
Providers
Services by Out-of-
Network Providers*
* For Covered Services from Out-of-Network Providers,
you are responsible for any Deductible, Copayment and all
charges above the Maximum Allowed Amount, except for
Surprise Billing Claims*.
Mental Health and Substance Use
Disorder
• Inpatient Hospital services
For the services of an Out-of-Network
Provider, there is an additional $250
Copayment if prior authorization is not
obtained
Hospital services are subject to pre-
service review to determine whether
Medically Necessary. Please refer to the
section UTILIZATION REVIEW
PROGRAM for information on how to
obtain the proper reviews.
20%
40%
• Outpatient facility services
Hospital services are subject to whether
Medically Necessary necessity. Please
refer to the section UTILIZATION REVIEW
PROGRAM for information on how to
obtain the proper reviews.
20%
40%
• Physician services including
psychiatrists, psychologists, MFTs,
MFCCs, etc. office visit or telehealth visit
20%
40%
Physical Therapy, Physical Medicine,
Occupational and Speech Therapy
Services, including Habilitation and
Rehabilitation
• Physician services office location
20%
40%
• Outpatient Hospital
For the services of an Out-of-Network
Provider, the maximum payment is
limited to $210 per visit. Please refer to
Medical Benefit Maximums in the Medical
Benefit Summary Notes section for
maximums that apply to your Plan.
20%
40%
• Speech therapy-office location
20%
20%
15
Benefit
Member Copayment/Coinsurance
Services by In-Network
Providers
Services by Out-of-
Network Providers*
* For Covered Services from Out-of-Network Providers,
you are responsible for any Deductible, Copayment and all
charges above the Maximum Allowed Amount, except for
Surprise Billing Claims*.
Pregnancy and Maternity Care Benefits
• Inpatient Hospital services
For the services of an Out-of-Network
Provider, the maximum payment is
limited to $360 per day. Please refer to
Medical Benefit Maximums in the Medical
Benefit Summary Notes section for
maximums that apply to your Plan.
Please refer to the section UTILIZATION
REVIEW PROGRAM for information on
how to obtain the proper reviews.
20%
40%
• Prenatal and postnatal Physician office
visits
20%
40%
Preventive Care Benefits
• Preventive care services
See page 47 under Medical Care That Is
Covered for details for information about
your Preventive Care Services.
The Calendar Year Deductible will not
apply to services provided by Anthem
Prudent Buyer Providers.
No charge
40%
• Travel Immunizations Benefits
ACA Travel Vaccinations
Hepatitis A
No charge
40%
Hepatitis B
No charge
40%
Meningitis
No charge
40%
Polio
No charge
40%
• Other Travel Vaccinations
Japanese Encephalitis
20%
40%
Rabies
20%
40%
Typhoid
20%
40%
Yellow Fever
20%
40%
Professional (Physician) Benefits
• Inpatient Physician services
20%
40%
16
Benefit
Member Copayment/Coinsurance
Services by In-Network
Providers
Services by Out-of-
Network Providers*
* For Covered Services from Out-of-Network Providers,
you are responsible for any Deductible, Copayment and all
charges above the Maximum Allowed Amount, except for
Surprise Billing Claims*.
• Outpatient Physician services, other
than an office setting
20%
40%
• Physician home visits
20%
40%
• Physician office visit or telehealth visit
20%
40%
• Online visits (LiveHealth Online)
20%
Not covered
• Chemotherapy and radiation therapy
services
Chemotherapy and radiation therapy
services are subject to pre-service review
to determine whether Medically
Necessary. Please refer to the section
UTILIZATION REVIEW PROGRAM for
information on how to obtain the proper
reviews.
20%
40%
• Hemodialysis services
20%
40%
• Office based injectable service
20%
40%
• Retail Health Clinic
20%
40%
• Urgent Care services
20%
40%
Prosthetic Devices Benefits
• Physician services
20%
40%
• Prosthetic Devices
20%
40%
17
Benefit
Member Copayment/Coinsurance
Services by In-Network
Providers
Services by Out-of-
Network Providers*
* For Covered Services from Out-of-Network Providers,
you are responsible for any Deductible, Copayment and all
charges above the Maximum Allowed Amount, except for
Surprise Billing Claims*.
Skilled Nursing Facility Benefits
• Inpatient Hospital services
Benefits are provided for up to a maximum
of 100 visits per Calendar Year. Please
refer to Medical Benefit Maximums in the
Medical Benefit Summary Notes section
for maximums that apply to your Plan.
For the services of an Out-of-Network
Provider, there is an additional $250
Copayment if prior authorization is not
obtained
For the services of an Out-of-Network
Provider, the maximum payment is
limited to $360 per day. Please refer to
Medical Benefit Maximums in the Medical
Benefit Summary Notes section for
maximums that apply to your Plan.
Since your Plan has a Calendar Year
Deductible, the number of visits will start
counting toward the maximum when
Services are first provided even if the
Calendar Year Deductible has not been
met.
Please refer to Copayments in the Medical
Benefit Summary Notes section for
additional Benefit information.
Skilled Nursing Facility services are
subject to pre-service review to determine
whether Medically Necessary. Please
refer to the section UTILIZATION REVIEW
PROGRAM for information on how to
obtain the proper reviews.
20%
40%
18
Benefit
Member Copayment/Coinsurance
Services by In-Network
Providers
Services by Out-of-
Network Providers*
* For Covered Services from Out-of-Network Providers,
you are responsible for any Deductible, Copayment and all
charges above the Maximum Allowed Amount, except for
Surprise Billing Claims*.
• Services by a free-standing Skilled
Nursing Facility
Benefits are provided for up to a maximum
of 100 visits per Calendar Year. Please
refer to Medical Benefit Maximums in the
Medical Benefit Summary Notes section
for maximums that apply to your Plan.
For the services of an Out-of-Network
Provider, there is an additional $250
Copayment if prior authorization is not
obtained
Since your Plan has a Calendar Year
Deductible, the number of visits will start
counting toward the maximum when
Services are first provided even if the
Calendar Year Deductible has not been
met.
Please refer to Copayments in the Medical
Benefit Summary Notes section for
additional Benefit information.
Skilled nursing facility services are subject
to pre-service review to determine whether
Medically Necessary. Please refer to the
section UTILIZATION REVIEW
PROGRAM for information on how to
obtain the proper reviews.
20%
20%
Transgender Benefits
Transgender services are subject to prior
authorization in order for coverage to be
provided. Please refer to the section
UTILIZATION REVIEW PROGRAM for
information on how to obtain the proper
reviews.
• Hospital inpatient services
20%
40%
• Hospital outpatient surgery services
20%
40%
• Physician services
20%
40%
19
Benefit
Member Copayment/Coinsurance
Services by In-Network
Providers
Services by Out-of-
Network Providers*
* For Covered Services from Out-of-Network Providers,
you are responsible for any Deductible, Copayment and all
charges above the Maximum Allowed Amount, except for
Surprise Billing Claims*.
• Transgender Travel Expenses
The Plan's maximum payment will not
exceed $10,000 per surgery or series of
surgeries. Please refer to Medical Benefit
Maximums in the Medical Benefit
Summary Notes section for maximums
that apply to your Plan.
*No Copayment will be required for
transgender travel expenses authorized by
Anthem once your Calendar Year
Deductible is met.
Transplant Benefits
Services and supplies provided in
connection with a non-Investigative organ
or
tissue transplant. These procedures
are covered only when performed at a
CME or BDCSC. See page 50 under
Medical Care That Is Covered for details.
Transplant services, excluding cornea
transplant, are subject to pre-service
review to determine whether Medically
Necessary. Please refer to the section
UTILIZATION REVIEW PROGRAM for
information on how to obtain the proper
reviews.
• Hospital inpatient services
20%
Not covered
• Hospital outpatient surgery services
20%
Not covered
• Physician services
20%
Not covered
20
Benefit
Member Copayment/Coinsurance
Services by In-Network
Providers
Services by Out-of-
Network Providers*
* For Covered Services from Out-of-Network Providers,
you are responsible for any Deductible, Copayment and all
charges above the Maximum Allowed Amount, except for
Surprise Billing Claims*.
• Transplant Travel Expenses
The Plan's maximum payment will not
exceed $10,000 per surgery. Please refer
to Medical Benefit Maximums in the
Medical Benefit Summary Notes section
for maximums that apply to your Pan.
*No Copayment will be required for
transplant travel expenses authorized by
Anthem once your Calendar Year
Deductible is met.
No charge
Not covered
• Unrelated Donor Search service
The Plan's maximum payment will not
exceed $30,000 per transplant. Please
refer to Medical Benefit Maximums in the
Medical Benefit Summary Notes section
for maximums that apply to your Plan.
* Surprise Billing Claims are described in the
this Booklet. Please refer to that section for further details.
21
Medical Benefit Summary Notes
Member Deductible
The Calendar Year Deductible per Individual is shown on the SUMMARY OF BENEFITS. Each year, you
will be responsible for satisfying the Member Calendar Year Deductible amount before the Plan begins to
pay Benefits. The family Deductible is non-embedded meaning the cost shares of all Family Members apply
to one shared family Deductible. The Individual Deductible only applies to Individuals enrolled under single
coverage. If Members of an enrolled family pay Deductible expense in a year equal to the family Deductible,
the Calendar Year Deductible for all Family Members will be considered to have been met. For additional
information about Deductibles please see the Deductibles, Copayments, Out-of-Pocket Amounts and
Medical Benefit Maximums section of this booklet.
Member Out-of-Pocket Maximum
1. The per Individual and per family Out-of-Pocket Maximum responsibility each Calendar Year for
Covered Services rendered by an Anthem Prudent Buyer Providers and Other Healthcare Providers is
shown on the SUMMARY OF BENEFITS.
2. The per Individual and per family Out-of-Pocket Maximum responsibility each Calendar Year for
Covered Services rendered by Out-of-Network Providers is shown on the SUMMARY OF BENEFITS.
After a Member has made the total out-of-pocket payments for covered medical and prescription drug
services and supplies during a Calendar Year, the Member will no longer be required to pay a Copayment
for the remainder of that Year, unless otherwise stated, but will remain responsible for costs in excess of the
Maximum Allowed Amount. The family Out-of-Pocket Maximum is non-embedded meaning the cost shares
of all Family Members apply to one shared family Out-of-Pocket Maximum. The Individual Out-of-Pocket
Maximum only applies to Individuals enrolled under single coverage.
Note: Expenses and Copayments you make for Infertility Treatment, non-Covered Services or supplies or
which is in excess of the maximum allowable amount provided by an Out-of-Network Provider will not be
applied to your Out-of-Pocket Maximum. For additional information about Out-of-Pocket Maximums please
see the Deductibles, Copayments, Out-of-Pocket Amounts and Medical Benefit Maximums section of this
booklet.
Copayments
The Member Copayment amounts for Covered Services are shown in the SUMMARY OF BENEFITS.
The SUMMARY OF BENEFITS also contains information on Benefit and Copayment maximums and
restrictions. In addition to your Copayment, you will be required to pay any amount in excess of the Maximum
Allowed Amount for the services of Other Health Care Provider or Out-of-Network Provider.
Your Copayment for the following services for Out-of-Network Providers will be the same as for Anthem
Prudent Buyer Providers if services are authorized. You may be responsible for charges which exceed
the Maximum Allowed Amount. See UTILIZATION REVIEW PROGRAM.
a. Home health care
b. Infusion/Injection therapy
c. Hospice
d. Skilled Nursing Facility
- Skilled Nursing Facility day limit does not apply to Mental Health and Substance Use Disorder.
22
Medical Benefit Maximum. The Plan will pay for Covered Services and supplies, up to the maximum
amounts, or for the maximum number of days or visits as shown on the SUMMARY OF BENEFITS. The
Plan will not make Benefit payments for any Member in excess of any of the Medical Benefit Maximums.
Complete Benefit descriptions may be found in the Medical Care That Is Covered section. Plan exclusions
and limitations may be found in the Medical Care That Is NOT Covered section.
23
INTRODUCTION
Your Employer
may include pre-service review and utilization management requirements, coordination of Benefits, timely
filing limits, and other requirements to administer the Benefits under this Plan.
The Benefits of this Plan are provided only for those services that are considered to be Medically Necessary.
The fact that a Physician prescribes or orders a service does not, in itself, mean that the services is Medically
Necessary or that the service is covered under this Plan. Consult this Benefit Booklet or contact the Member
Services number on the back of the identification card if you have any questions regarding whether services
are covered.
This Plan contains many important terms (such as “Medically Necessary” and “Maximum Allowed
Amount”) that are defined in the DEFINITIONS section starting at page 89. When reading through
this booklet, consult the DEFINITIONS section to be sure that you understand the meaning of these
words.
This Plan is designed to reduce the cost of health care to you, the Member. In order to reduce your costs, much
greater responsibility is placed on you.
If you have questions about your Benefits, contact the Member Services number on the back of the
identification card before Hospital or medical services are received.
You should read your Benefit Booklet carefully. Your booklet tells you which services are covered by your
health Plan and which are excluded. It also lists your Copayment and Deductible responsibilities.
When you need health care, present your identification card to your Physician, Hospital, or other licensed
healthcare provider. Your identification card has your participant and group numbers on it. Be sure to include
these numbers on all claims you submit to Anthem.
In order to receive the highest level of Benefits, you should assure that your Provider is an In-Network
Provider.
You are responsible for following the provisions as described in the UTILIZATION REVIEW section of this
booklet, including:
1. You or your Physician must obtain approval at least 48 hours before Hospital or Skilled
Nursing Facility admissions for all non-Emergency inpatient Hospital or Skilled Nursing Facility services.
2. You or your Physician must notify Accolade within 48 hours or by the end of the first business day
following Emergency admissions, or as soon as it is reasonably possible to do so.
3. You or your Physician must obtain prior authorization in order to determine if contemplated services are
UTILIZATION REVIEW section for a listing of services requiring
prior authorization.
Failure to meet these responsibilities may result in your incurring a substantial financial liability. Some services
may not be covered unless prior review and other requirements are met.
Note: Accolade will render a decision on all requests for prior authorization within 5 business days from
receipt of the request. The treating Provider will be notified of the decision within 24 hours followed by written
notice to the Provider, Member, and Facility within 2 business days of the decision. For urgent services in
situations in which the routine decision making process might seriously jeopardize the life or health of a
Member or when the Member is experiencing severe pain, Accolade will respond as soon as possible to
accommodate the Member
Mental Health Parity and Addiction Equity Act. The Mental Health Parity and Addiction Equity Act
provides for parity in the application of aggregate treatment limitations (day or visit limits) on mental health
and substance use disorder Benefits with day or visit limits on medical and surgical benefits. In general,
24
group health plans offering mental health and substance use disorder benefits cannot set day/visit limits on
mental health or substance use disorder benefits that are lower than any such day or visit limits for medical
and surgical benefits. A plan that does not impose day or visit limits on medical and surgical benefits may
not impose such day or visit limits on mental health and substance use disorder benefits offered under the
plan.
The Mental Health Parity and Addiction Equity Act also provides for parity in the application of non-
quantitative treatment limitations (NQTL). An example of a non-quantitative treatment limitation is a
precertification requirement.
Also, the Plan may not impose Deductibles, Copayments and out of pocket expenses on mental health and
substance use disorder benefits that are more restrictive than Deductibles, Copayments and out of pocket
expenses applicable to other medical and surgical benefits.
Medical Necessity criteria and other plan documents showing comparative criteria, as well as the processes,
strategies, evidentiary standards, and other factors used to apply an NQTL are available upon request.
You may also refer to the following website for more information, The Mental Health Parity and Addiction
Equity Act (MHPAEA) - CMS.gov.
Second Opinions. If you have a question about your condition or about a plan of treatment which your
Physician has recommended, you may receive a second medical opinion from another Physician. This
second opinion visit will be provided according to the Benefits, limitations, and exclusions of this Plan. If you
wish to receive a second medical opinion, remember that greater Benefits are provided when you choose
an Anthem Prudent Buyer Provider. You may also ask your Physician to refer you to an Anthem Prudent
Buyer Provider to receive a second opinion.
After Hours Care. After hours care is provided by your Physician who may have a variety of ways of
addressing your needs. You should call your Physician for instructions on how to receive medical care after
their normal business hours, on weekends and holidays, or to receive non-Emergency care and non-Urgent
Care within the service area for a condition that is not life threatening but that requires prompt medical
attention. If you have an Emergency, call 911 or go to the nearest emergency room.
All benefits are subject to coordination with benefits. Please refer to the COORDINATION OF
BENEFITS section of this booklet for details.
The Benefits of this Plan are subject to the SUBROGATION AND REIMBURSEMENT section.
25
TYPES OF PROVIDERS
PLEASE READ THE FOLLOWING INFORMATION SO YOU WILL KNOW FROM WHOM OR WHAT
GROUP OF PROVIDERS HEALTH CARE MAY BE OBTAINED. THE MEANINGS OF WORDS AND
PHRASES IN CAPITALIZATION ARE DESCRIBED IN THE SECTION OF THIS BOOKLET ENTITLED
DEFINITIONS.
Introduction
Your Plan is a PPO plan. The Plan has two sets of Benefits: In-Network and Out-of-Network. If you choose
an In-Network Provider as described below, you will pay less in out-of-pocket costs, such as Copayments
and Deductibles. If you use an Out-of-Network Provider, you will have to pay more out-of-pocket costs. Cost
sharing for services with Copayments is the lesser of the Copayment amount or the Maximum Allowed
Amount.
Anthem Prudent Buyer Providers in California. Anthem has made available to Members a network of
various types of In-Network Providers. Anthem Prudent Buyer Providers because
they have agreed to participate in preferred provider organization program (PPO), called the
Prudent Buyer Plan. Anthem Prudent Buyer Providers have agreed
to a rate they will accept as
reimbursement for Covered Services. The amount of Benefits payable under
this Plan will be different for
Out-of-Network Providers than for Anthem Prudent Buyer Providers. See the definition of
"Anthem Prudent
Buyer Providers" in the DEFINITIONS section starting at page 89, for a complete list of the types of
Providers which may be participating providers.
A directory of Anthem Prudent Buyer Providers is available upon request. The directories list In-
Network Providers in your area, including health care facilities such as Hospitals and Skilled Nursing
Facilities, Physicians, laboratories, and diagnostic x-ray and imaging providers. You may call the Member
Services number on the back of the identification card and request for a directory to be sent to you. A
member services representative will be able to assist you with locating a provider online.
If you need details about a ProviderPhysician who is right for you,
call the Member Services number on the back of the identification card.
How to Access Primary and Specialty Care Services
Your health Plan covers care provided by primary care physicians and specialty care providers. To see a
primary care physician, simply visit any Anthem Prudent Buyer Provider Physician who is a general or family
practitioner, internist or pediatrician. Your health Plan also covers care provided by any Anthem Prudent
Buyer Provider specialty care provider
. Referrals are never
needed to visit any Anthem Prudent Buyer Provider specialty care provider including a behavioral health
care provider.
To make an appointment call your office:
• Tell them you are a Prudent Buyer Plan Member.
• Have your Member identification card handy. They may ask you for your group number, Member ID
number, or office visit Copayment.
• Tell them the reason for your visit.
When you go for your appointment, bring your Member identification card.
After hours care is provided by your Physician who may have a variety of ways of addressing your needs.
Call your Physician for instructions on how to receive medical care after their normal business hours, on
weekends and holidays. This includes information about how to receive non-Emergency care and non-

26
Urgent Care within the service area for a condition that is not life threatening, but that requires prompt medical
attention. If you have an Emergency, call 911 or go to the nearest emergency room.
In-Network Providers Outside of California
The Blue Cross and Blue Shield Association, of which Anthem is a member, has a program (called the
Members to have the reciprocal use of In-Network Providers
Plan).
If you are outside of the California service areas, please call the toll free BlueCard Provider Access
number on your identification card to find an In-Network Provider in the area you are in visit the
website www.provider.bcbs.com. A directory of PPO Providers for outside of California is available
upon request.
Certain categories of Providers defined in this Benefit Booklet as In-Network Providers may not be available
in the Blue Cross and/or Blue Shield Plan in the service area where you receive services. See Medical
Benefit Summary Notes YOUR MEDICAL BENEFITS section
for additional information on how health care services you obtain from such Providers are covered.
Out-of-Network Providers. Out-of-network Providers are Providers which have not agreed to participate
in the Prudent Buyer Plan network or the Blue Cross and/or Blue Shield Plan. They have not agreed to the
reimbursement rates and other provisions of a Prudent Buyer Plan contract nor the Blue Cross and/or Blue
Shield Plan.
Anthem has processes to review claims before and after payment to detect fraud, waste, abuse and other
inappropriate activity. Members seeking services from Out-of-Network Providers could be Balance Billed by
the Out-of-Network Providers for those services that are determined to be not payable as a result of these
review processes and meets the criteria set forth in any applicable state regulations adopted pursuant to
state law. A claim may also be determined to be not payable due to a provider's failure to submit medical
records with the claims that are under review in these processes.
Physicians. "Physician" means more than an M.D. Certain other practitioners are included in this term as
it is used throughout the Plan. This doesn't mean they can provide every service that a medical doctor could;
it just means that the Plan will cover expense you incur from them when they're practicing within their
specialty the same as if the care were provided by a medical doctor. As with the other terms, be sure to
read the definition of "Physician" to determine which providers' services will be covered. Only Providers
listed in the definition are covered as Physicians
covered only upon referral of an M.D. (medical doctor) or D.O. (doctor of osteopathy). Providers for whom
Physician
Other Health Care Providers. "Other Health Care Providers" are neither Physicians nor Hospitals. They
are mostly free-standing facilities or service organizations, such as a certified registered nurse anesthetist
or a blood bank. See the definition of "Other Health Care Providers" in the DEFINITIONS section starting at
page 89, for a complete list of those providers. Other Health Care Providers are not part of the Prudent
Buyer Plan Provider network or the Blue Cross and/or Blue Shield Plan.
Reproductive Health Care Services. Some Hospitals and other Providers do not provide one or more of
the following services that may be covered under your Plan and that you or your Family Member might need:
family planning; contraceptive services, including emergency contraception; sterilization, including tubal
ligation at the time of labor and delivery; Infertility treatments; or abortion. You should obtain more
information before you enroll. Call your prospective Physician or clinic, or call the Member Services number
on the back of the identification card to ensure that you can obtain the health care services that you need.
27
Centers of Medical Excellence and Blue Distinction Centers. Anthem is providing access to Centers of
Medical Excellence (CME) networks and Blue Distinction Centers for Specialty Care (BDCSC). The facilities
included in each of these networks are selected to provide the following specified medical services:
• Transplant Facilities. Transplant facilities have been organized to provide services for the following
specified transplants: heart, liver, lung, combination heart-lung, kidney, pancreas, simultaneous
pancreas-kidney, or bone marrow/stem cell and similar procedures. Subject to any applicable
Copayments or Deductibles, CME and BDCSC have agreed to a rate they will accept as payment in full
for Covered Services. These procedures are covered only when performed at a CME or BDCSC.
• Bariatric Facilities. Hospital facilities have been organized to provide services for bariatric surgical
procedures, such as gastric bypass and other surgical procedures for weight loss programs. These
procedures are covered only when performed at a BDCSC.
An Anthem Prudent Buyer Provider in the Prudent Buyer Plan or the Blue Cross and/or Blue Shield Plan
network is not necessarily a CME or BDCSC Facility. For additional information, please see the
DEFINITIONS section of this book or call the Member Services number on the back of the identification card.
28
YOUR MEDICAL BENEFITS
Maximum Allowed Amount
General
This section describes the term Maximum Allowed Amount as used in this Benefit Booklet, and what the
term means to you when obtaining Covered Services under this Plan. The Maximum Allowed Amount is the
total reimbursement payable under your Plan for Covered Services you receive from Anthem Prudent Buyer
Providers and Out-of-Network Providers. It is the Plan
Provider combined with any Deductible or Copayment owed by you. In some cases, you may be required
to pay the entire Maximum Allowed Amount. For instance, if you have not met your Calendar Year
Deductible under this Plan, then you could be responsible for paying the entire Maximum Allowed Amount
for Covered Services. Except for Surprise Billing Claims, when you receive services from an Out-of-Network
Provider, you may be responsible for paying any difference between its charges and the Maximum Allowed
Amount . In many situations, this difference could be significant.
Surprise Billing Claims are described in the “Consolidated Appropriations Act of 2021 Notice” at the end of
this booklet. Please refer to that section for further details.
Below are two examples, which illustrate how the Maximum Allowed Amount works. These examples are
for illustration purposes only.
Example: The Plan has a Member Copayment of 20% for Anthem Prudent Buyer Provider services after
the Calendar Year Deductible has been met.
• The Member receives services from a participating surgeon. The charge is $2,000. The Maximum
Allowed Amount under the Plan for the surgery is $1,000. The MemberCopayment responsibility when
a participating surgeon is used is 20% of $1,000, or $200. This is what the Member pays. The Plan
pays 80% of $1,000, or $800. The participating surgeon accepts the total of $1,000 as payment for the
surgery regardless of the charges.
Example: The Plan has a Member Copayment of 40% for Out-of-Network Provider services after the
Calendar Year Deductible has been met.
• The Member receives services from an out-of-network surgeon. The charge is $2,000. The Maximum
Allowed Amount under the Plan for the surgery is $1,000. The Copayment responsibility when
an out-of-network surgeon is used is 40% of $1,000, or $400. The Plan pays the remaining 60% of
$1,000, or $600. In addition, the out-of-network surgeon could bill the Member the difference between
$2,000 and $1,000. So the total out-of-pocket charge would be $400 plus an additional
$1,000, for a total of $1,400.
When you receive Covered Services, Anthem will, to the extent applicable, apply claim processing rules to
the claim submitted. Anthem uses these rules to evaluate the claim information and determine the accuracy
and appropriateness of the procedure and diagnosis codes included in the submitted claim. Applying these
rules may affect the Maximum Allowed Amount if Anthem determines that the procedure and/or diagnosis
codes used were inconsistent with procedure coding rules and/or reimbursement policies. For example, if
your Provider submits a claim using several procedure codes when there is a single procedure code that
includes all of the procedures that were performed, the Maximum Allowed Amount will be based on the single
procedure code.
Provider Network Status
The Maximum Allowed Amount may vary depending upon whether the Provider is an Anthem Prudent Buyer
Provider, an Out-of-Network Provider or Other Health Care Provider.
Anthem Prudent Buyer Providers. For Covered Services performed by an Anthem Prudent Buyer
Provider, the Maximum Allowed Amount for this Plan will be the rate the Anthem Prudent Buyer Provider
has agreed with Anthem to accept as reimbursement for the Covered Services. Because Anthem Prudent
Buyer Providers have agreed to accept the Maximum Allowed Amount as payment in full for those Covered
29
Services, they should not send you a bill or collect for amounts above the Maximum Allowed Amount.
However, you may receive a bill or be asked to pay all or a portion of the Maximum Allowed Amount to the
extent you have not met your Calendar Year Deductible or have a Copayment. Please call the Member
Services number on the back of the identification card for help in finding an Anthem Prudent Buyer Provider.
If you go to a Hospital which is an Anthem Prudent Buyer Provider, you should not assume all Providers in
that Hospital are also Anthem Prudent Buyer Providers. To receive the greater Benefits afforded when
Covered Services are provided by an Anthem Prudent Buyer Provider, you should request that all your
Provider services (such as services by an anesthesiologist) be performed by Anthem Prudent Buyer
Providers whenever you enter a Hospital.
If you are planning to have outpatient surgery, you should first find out if the Facility where the surgery is to
be performed is an Ambulatory Surgical Center. An Ambulatory Surgical Center is licensed as a separate
Facility even though it may be located on the same grounds as a Hospital (although this is not always the
case). If the center is licensed separately, you should find out if the Facility is an Anthem Prudent Buyer
Provider before undergoing the surgery.
Note: If an Other Health Care Provider is participating in a Blue Cross and/or Blue Shield Plan at the time
you receive services, such Provider will be considered an Anthem Prudent Buyer Provider for the purposes
of determining the Maximum Allowed Amount.
If a Provider defined in this Benefit Booklet as an Anthem Prudent Buyer Provider is of a type not represented
in the local Blue Cross and/or Blue Shield Plan at the time you receive services, such Provider will be
considered an Out-of-Network Provider for the purposes of determining the Maximum Allowed Amount.
Out-of-Network Providers and Other Health Care Providers.*
Providers who are not in the Prudent Buyer network are Out-of-Network Providers or Other Health Care
Providers, subject to Blue Cross Blue Shield Association rules governing claims filed by certain ancillary
providers. Except for Surprise Billing Claims, for Covered Services you receive from an Out-of-Network
Provider or Other Health Care Provider the Maximum Allowed Amount will be based on the applicable Out-
of-Network Provider rate or fee schedule for this Plan, an amount negotiated by Anthem or a third party
vendor which has been agreed to by the Out-of-Network Provider, an amount derived from the total charges
billed by the Out-of-Network Provider, or an amount based on information provided by a third party vendor,
or an amount based on reimbursement or cost information from the Centers for Medicare and Medicaid
Maximum Allowed Amount upon the level or method of reimbursement
used by CMS, Anthem will update such information, which is unadjusted for geographic locality, no less than
annually.
Providers who are not contracted for this product, but are contracted for other products, are also considered
Out-of-Network Providers. For this Plan, the Maximum Allowed Amount for services from these Providers
or if your
claim involves a Surprise Billing Claim.
For Covered Services rendered outside the Anthem Blue Cross service area by Out-of-Network Providers,
-of-Network Provider fee schedule /
rate or the pricing arrangements required by applicable state or federal law. In certain situations, the Maximum
Allowed Amount for out of area claims may be based on billed charges, the pricing we would use if the healthcare
services had been obtained within the Anthem Blue Cross service area, or a special negotiated price.
Unlike an Anthem Prudent Buyer Provider, Out-of-Network Providers and Other Health Care Providers may
send you a bill and collect for the amount of the Out-of-
charge that exceeds the Maximum Allowed Amount under this Plan. You may be responsible for paying the
difference between the Maximum Allowed Amount and the amount the Out-of-Network Provider or Other
Health Care Provider charges. This amount can be significant. Choosing an Anthem Prudent Buyer Provider
will likely result in lower out of pocket costs to you. Please call the Member Services number on the back of
the identification card for help in finding an Anthem Prudent Buyer Provider. Member Services is also
available to assist you in determining this PlanMaximum Allowed Amount for a particular Covered Service
from an Out-of-Network Provider or Other Health Care Provider.
30
- GENERAL PROVISIONS for
additional information.
*Exceptions:
Clinical Trials of Cancer and Other Life Threatening Conditions Benefits. The Maximum Allowed
Amount for services and supplies provided in connection with clinical trials will be the lesser of the billed
charge or the amount that ordinarily applies when services are provided by an Anthem Prudent Buyer
Provider.
If Medicare is the primary payor, the Maximum Allowed Amount does not include any charge:
1. By a Hospital, in excess of the approved amount as determined by Medicare; or
2. By a Physician who is an Anthem Prudent Buyer Provider who accepts Medicare assignment, in
excess of the approved amount as determined by Medicare; or
3. By a Physician who is an Out-of-Network Provider or Other Health Care Provider who accepts
Medicare assignment, in excess of the lesser of Maximum Allowed Amount stated above, or the
approved amount as determined by Medicare; or
4. By a Physician or Other Health Care Provider who does not accept Medicare assignment, in excess
of the lesser of the Maximum Allowed Amount stated above, or the limiting charge as determined by
Medicare.
Surprise Billing Claims.
You will always be responsible for expense Incurred which is not covered under this Plan.
Member Cost Share
For certain Covered Services, and depending on your plan design, you may be required to pay all or a part
of the Maximum Allowed Amount as your cost share amount (Deductibles or Copayments). Your cost share
amount and the Out-Of-Pocket Amounts may be different depending on whether you received Covered
Services from an Anthem Prudent Buyer Provider or Out-of-Network Provider. Specifically, you may be
required to pay higher cost-sharing amounts or may have limits on your Benefits when using Out-of-Network
Providers. Please see the SUMMARY OF BENEFITS section for your cost share responsibilities and
limitations, or call the member Services number on the back of the identification card to learn how this
Benefits or cost share amount may vary by the type of Provider you use. For additional details about
Deductibles or Copayments please refer to the -of-Pocket Amounts and
section.
Anthem will not provide any reimbursement for non-Covered Services. You may be responsible for the total
amount billed by your Provider for non-Covered Services, regardless of whether such services are performed
by an Anthem Prudent Buyer Provider or Out-of-Network Provider. Non-Covered Services include services
specifically excluded from coverage by the terms of your Plan and services received after Benefits have
been exhausted. Benefits may be exhausted by exceeding, for example, Medical Benefit Maximums or
day/visit limits.
31
Authorized Referrals
In some circumstances Accolade may authorize Anthem Prudent Buyer Provider cost share amounts
(Deductibles or Copayments) to apply to a claim for a Covered Service you receive from an Out-of-Network
Provider. In such circumstance, you or your Physician must contact Accolade in advance of obtaining the
Covered Service. It is your responsibility to ensure that Accolade has been contacted. If Accolade
authorizes an Anthem Prudent Buyer Provider cost share amount to apply to a Covered Service received
from an Out-of-Network Provider, you also may still be liable for the difference between the Maximum
Allowed Amount and the Out-of--of-
Network Provider due to network adequacy issues, you will not be responsible for the difference between
the Out-of-Maximum Allowed Amount. Please call the Member Services
number on the back of the identification card for Authorized Referral information or to request authorization.
32
Deductibles, Copayments, Out-of-Pocket
Amounts and Medical Benefit Maximums
After any applicable Deductible and your Copayment are subtracted, the Plan will pay Benefits up to the
Maximum Allowed Amount, not to exceed any applicable Medical Benefit Maximum. The Deductible
amounts, Copayments, Out-Of-Pocket Amounts and Medical Benefit Maximums are set forth in the
SUMMARY OF BENEFITS.
Deductibles
The In-Network and Out-of-Network Deductibles under this Plan are separate and distinct from the other.
Only the covered charges that make up the Maximum Allowed Amount will apply toward the satisfaction of
any Deductible except as specifically indicated in this booklet.
Calendar Year Deductible. Each Year, you will be responsible for satisfying the Calendar Year
Deductible before Benefits are paid. The family Deductible is non-embedded meaning the cost shares of all
Family Members apply to one shared family Deductible. The Individual Deductible only applies to Individuals
enrolled under single coverage. If Members of an enrolled family pay Deductible expense in a Year equal
to the family Deductible, the Calendar Year Deductible for all Family Members will be considered to have
been met.
Anthem Preferred Providers, In-Network Pharmacies, Home Delivery Pharmacies and Other Health
Care Providers. Only covered charges up to the Maximum Allowed Amount for the services of Anthem
Preferred Providers, In-Network Pharmacies, Home Delivery Pharmacies and Other Health Care Providers
will be applied to the Anthem Preferred Provider, In-Network Pharmacy, Home Delivery Pharmacy and Other
Health Care Provider Calendar Year Deductibles. When these Deductibles are met, the Plan will pay
Benefits only for the services of Anthem Preferred Providers, In-Network Pharmacies, Home Delivery
Pharmacies and Other Health Care Providers. The Plan will not pay any Benefits for Out-of-Network
Providers and Out-of-Network Pharmacies unless the separate Out-of-Network Provider and Out-of-Network
Pharmacies Calendar Year Deductibles (as applicable) are met.
Out-of-Network Providers and Out-of-Network Pharmacies. Covered charges up to the Maximum
Allowed Amount for the services of any combination of Providers will be applied to the Out-of-Network
Provider and Out-of-Network Pharmacy Calendar Year Deductibles. The Plan will pay Benefits for the
services of Out-of-Network Providers and Out-of-Network Pharmacies only when the applicable Out-of-
Network Provider Deductibles and Out-of-Network Pharmacies are met.
Prior Plan Calendar Year Deductibles. If you were covered under the Prior Plan any amount paid during
the same Calendar Year toward your Calendar Year Deductible under the Prior Plan, will be applied toward
your Calendar Year Deductible under this Plan; provided that, such payments were for charges that would
be covered under this Plan.
Copayments
After you have satisfied any applicable Deductible, your Copayment will be subtracted from the remaining
Maximum Allowed Amount.
Depending on the type of service rendered, your Copayment will either be a percentage or a set-dollar
Copayment. If your Copayment is a percentage, the Plan will apply the applicable percentage to the
Maximum Allowed Amount remaining after any Deductible has been met. If your Copayment is a set-dollar
Copayment, the Plan will apply the applicable set-dollar Copayment, such as an office visit or emergency
room visit.
33
Anthem Prudent Buyer Provider and Out-of-Network Provider Out-of-Pocket-Amounts
Satisfaction of the Anthem Prudent Buyer Provider Out-Of-Pocket Amount. If, after you have met your
Calendar Year Deductibles and you pay Copayments equal to your Out-of-Pocket Amount per Member
during a Calendar Year, you will no longer be required to make Copayments for any additional Covered
Services or supplies during the remainder of that year, except as specifically stated below under Charges
Which Do Not Apply Toward the Out-of-Pocket Amount.
The family Out-of-Pocket Maximum is non-embedded meaning the cost shares of all Family Members apply
to one shared family Out-of-Pocket Maximum. The Individual Out-of-Pocket Maximum only applies to
Individuals enrolled under single coverage. If enrolled Members of a family pay Copayments in a year equal
to the Out-of-Pocket Amount per family, the Out-of-Pocket Amount for all Family Members will be considered
to have been met. Once the family Out-of-Pocket Amount is satisfied, no Family Member will be required to
make Copayments for any additional Covered Services or supplies during the remainder of that year, except
as specifically stated under Charges Which Do Not Apply Toward the Out-of-Pocket Amount below.
However, any expense previously applied to the Out-of-Pocket Amount per Member in the same year will
not be credited for any other Family Member.
Anthem Prudent Buyer Provider, In-Network Pharmacies, Home Delivery Pharmacies and Other
Health Care Providers. Only covered charges up to the Maximum Allowed Amount for the services of an
Anthem Prudent Buyer Provider, In-Network Pharmacy, Home Delivery Pharmacy or Other Health Care
Provider will be applied to the Anthem Prudent Buyer Provider, In-Network Pharmacy, Home Delivery
Pharmacy and Other Health Care Provider Out-of-Pocket Amount.
After this Out-of-Pocket Amount per Member or family has been satisfied during a Calendar Year, you will
no longer be required to make any Copayment for the Covered Services provided by an Anthem Prudent
Buyer Provider, In-Network Pharmacy, Home Delivery Pharmacy and Other Health Care Provider for the
remainder of that year. You will continue to be required to make Copayments for the Covered Services of
an Out-of-Network Provider until the Out-of-Network Provider Out-of-Pocket Amount has been met.
Out-of-Network Providers and Out-of-Network Pharmacies. Covered charges up to the Maximum
Allowed Amount for the services of any combination of Providers will be applied to the Out-of-Network
Provider and Out-of-Network Pharmacy Out-of-Pocket Amount. After this Out-of-Pocket Amount per
Member has been satisfied during a Calendar Year, you will no longer be required to make any Copayment
for the Covered Services provided by an Out-of-Network Provider and Out-of-Network Pharmacy for the
remainder of that year.
Note: Any covered expense applied to any Deductible or Copayments for Prescription Drugs will apply
towards your Out-of-Pocket Amount, unless otherwise stated.
Charges Which Do Not Apply Toward the Out-Of-Pocket Amount. The following charges will not be
applied toward satisfaction of an Out-Of-Pocket Amount:
• Charges for services or supplies not covered under this Plan.
• Charges which exceed the Maximum Allowed Amount.
• Charges which exceed the Prescription Drug Maximum Allowed Amount.
• Coinsurance paid for Infertility Treatment
Medical Benefit Maximums
The Plan does not make Benefit payments for any Member in excess of any of the Medical Benefit
Maximums.
Prior Plan Maximum Benefits. If you were covered under the Prior Plan, any Benefits paid to you under
the Prior Plan will reduce any maximum amounts you are eligible for under this Plan which apply to the same
Benefit for the remainder of the calendar year.
34
Crediting Prior Plan Coverage
If you were covered by Prior Plan immediately before UC signs up with Anthem, with no lapse in
coverage, then you will get credit for any accrued Calendar Year Deductible and, if applicable and approved
by UC, out-of-pocket amounts under the Prior Plan. This does not apply to Individuals who were not covered
by the Prior Plan on the day before coverage with Anthem began, or who join UC later. Credits are
applied to the same Individual only.
If UC moves from one of plans to another, (for example, changes its coverage from HMO to PPO),
and you were covered by the other product immediately before enrolling in this product with no break in
coverage, then you may get credit for any accrued Calendar Year Deductible and out-of-pocket amounts, if
applicable and approved by UC. Credits are applied to the same Individual only. Any maximums, when
applicable, will be carried over and charged against the Medical Benefit Maximums under this Plan.
If UC offers more than one of products, and you change from one product to another with no break
in coverage, you will get credit for any accrued Calendar Year Deductible and, if applicable, out-of-pocket
amounts and any maximums will be carried over and charged against Medical Benefit Maximums under this
Plan. Credits are applied to the same Individual only.
If UC offers coverage through other products or carriers in addition to , and you change products
or carriers to enroll in this product with no break in coverage, you will get credit for any accrued Calendar
Year Deductible, out-of-pocket amount, and any Medical Benefit Maximums under this Plan, if applicable
and approved by UC. Credits are applied to the same Individual only.
This Section Does Not Apply To You If:
• UC moves to this Plan at the beginning of a Calendar Year;
• You change from one of individual policies to plan;
• You change Employers; or
• You are a new Member of UC who joins after initial enrollment with Anthem.
Conditions of Coverage
The following conditions of coverage must be met for expense Incurred for services or supplies to be covered
under this Plan.
1. You must incur this expense while you are covered under this Plan. Expense is Incurred on the date
you receive the service or supply for which the charge is made.
2. The expense must be for a medical service or supply furnished to you as a result of illness or injury or
pregnancy, unless a specific exception is made.
3. The expense must be for a medical service or supply included in Medical Care That Is Covered.
Additional limits on covered charges are included under specific Benefits and in the SUMMARY OF
BENEFITS.
4. The expense must not be for a medical service or supply listed in Medical Care That Is NOT Covered.
If the service or supply is partially excluded, then only that portion which is not excluded will be covered
under this Plan.
5. The expense must not exceed any of the maximum Benefits or limitations of this Plan.
6. Any services received must be those which are regularly provided and billed by the provider. In addition,
those services must be consistent with the illness, injury, degree of disability and your medical needs.
Benefits are provided only for the number of days required to treat your illness or injury.
7. All services and supplies must be ordered by a Physician.
Contact the Member Services number on the back of the identification card if you have any questions.
35
Medical Care That Is Covered
Subject to the Medical Benefit Maximums in the SUMMARY OF BENEFITS, the requirements set forth under
Conditions of Coverage and the exclusions or limitations listed under Medical Care That Is NOT Covered,
the Plan will provide Benefits for the following services and supplies:
Abortion Services. Benefits include all abortion and abortion-related services, including pre-abortion and
follow-up services. For outpatient abortion services, precertification is not required.
purpose of producing a live birth.
Acupuncture Benefits. The services of a Physician for acupuncture treatment to treat a disease, illness or
injury, including a patient history visit, physical examination, treatment planning and treatment evaluation,
electroacupuncture, cupping and moxibustion. The Plan will pay for up to 24 visits (combined with
Chiropractic ) during a Calendar Year.
Since your Plan has a Calendar Year Deductible, the number of visits will start counting toward the
maximum when services are first provided even if the Calendar Year Deductible has not been met.
Advanced Imaging Procedure Benefits. Imaging procedures, including, but not limited to, Magnetic
Resonance Imaging (MRI), Positron Emission Tomography (PET scan), and Magnetic Resonance
Angiogram (MRA scan) are subject to pre-service review to determine whether Medically Necessary. You
may call the Member Services number on the back of the identification card to find out if an imaging
procedure requires pre-service review. See UTILIZATION REVIEW PROGRAM for details.
Advanced imaging procedures, when performed by an Out-of-Network Provider, will have a maximum
payment of $210 per visit.
Allergy Testing and Treatment Benefits. Allergy testing and treatment, including serum and serum
injections.
Ambulance Benefits. Ambulance services are covered when you are transported by a state licensed
vehicle that is designed, equipped, and used to transport the sick and injured and is staffed by Emergency
Medical Technicians (EMTs), paramedics, or other licensed or certified medical professionals. Ambulance
services are covered when one or more of the following criteria are met:
• For ground ambulance, you are transported:
- From your home, or from the scene of an accident or medical Emergency, to a Hospital,
- Between Hospitals, including when you are required to move from a Hospital that does not contract
with Anthem to one that does, or
- Between a Hospital and a Skilled Nursing Facility or other approved Facility.
• For air or water ambulance, you are transported:
- From the scene of an accident or medical Emergency to a Hospital,
- Between Hospitals, including when you are required to move from a Hospital that does not contract
with Anthem to one that does, or
- Between a Hospital and another approved Facility.
Emergency ground ambulance services do not require pre-service review. Pre-service review is required
for air ambulance in a non-medical Emergency. When using an air ambulance in a non-Emergency situation,
Accolade reserves the right to select the air ambulance provider. If you do not use the air ambulance
Accolade selects in a non-Emergency situation, no coverage will be provided by the Plan and Members will
be responsible for the entire cost of transport.
36
You must be taken to the nearest Facility that can provide care for your condition. In certain cases, coverage
may be approved for transportation to a Facility that is not the nearest Facility.
Coverage includes Medically Necessary treatment of an illness or injury by medical professionals from an
ambulance service, even if you are not transported to a Hospital. Ambulance services are not covered when
another type of transportation can be used without endangering your health. Ambulance services for your
convenience or the convenience of your Family Members or Physician are not a Covered Service.
Other non-covered ambulance services include, but are not limited to, trips to:
• A Physician's office or clinic;
• A morgue or funeral home.
If provided through the 911 emergency response system*, ambulance services are covered if you reasonably
believed that a medical Emergency existed even if you are not transported to a Hospital.
Important information about air ambulance coverage. Coverage is only provided for air ambulance
services when it is not appropriate to use a ground or water ambulance. For example, if using a ground
ambulance would endanger your health and your medical condition requires a more rapid transport to a
Hospital than the ground ambulance can provide, this Plan will cover the air ambulance. Air ambulance will
also be covered if you are in a location that a ground or water ambulance cannot reach.
Air ambulance will not be covered if you are taken to a Hospital that is not an acute care Hospital (such as
a Skilled Nursing Facility), or if you are taken to a office or to your home.
Hospital to Hospital transport: If you are being transported from one Hospital to another, air ambulance
will only be covered if using a ground ambulance would endanger your health and if the Hospital that first
treats you cannot give you the medical services you need. Certain specialized services are not available at
all Hospitals. For example, burn care, cardiac care, trauma care, and critical care are only available at certain
Hospitals. For services to be covered, you must be taken to the closest Hospital that can treat you. Coverage
is not provided for air ambulance transfers because you, your family, or your Physician prefers a specific
Hospital or Physician.
If you have an Emergency
emergency response system if you are in an area where the system is established and operating. At your
earliest opportunity, call the Member Services number on the back of the identification card to discuss plan
benefits for Ambulance services.
Ambulatory Surgery Center Benefits. Services and supplies provided by an Ambulatory Surgical Center
in connection with outpatient surgery.
For the services of an Out-of-Network Provider Facility only, the maximum payment is limited to $210
per visit each time you have outpatient surgery at an Ambulatory Surgical Center.
Ambulatory Surgical Center services are subject to pre-service review to determine whether Medically
Necessary. Please refer to UTILIZATION REVIEW PROGRAM for information on how to obtain the proper
reviews.
Bariatric Surgery Benefits. Services and supplies in connection with Medically Necessary surgery for
weight loss, only for morbid obesity and only when performed at a designated BDCSC Facility. See
UTILIZATION REVIEW PROGRAM for details.
You must obtain pre-service review for all bariatric surgical procedures. Charges for services provided
for or in connection with a bariatric surgical procedure performed at a Facility other than a BDCSC
will not be covered.
Bariatric Travel Expense Benefits. Certain travel expenses Incurred in connection with an approved,
specified bariatric surgery, performed at a designated BDCSC that is fifty (50) miles or more from the
place of residence, are covered, provided the expenses are authorized by Accolade in advance.
The fifty (50) mile radius around the BDCSC will be determined by the Bariatric BDCSC Coverage Area (See
37
DEFINITIONS). The Plan's maximum payment will not exceed $5,000 per surgery for the following travel
expenses Incurred by the Member and/or one companion:
• Transportation for the Member and/or one companion to and from the BDCSC.
• Mileage is reimbursed equal to one round trip to the medical care facility. Mileage is reimbursed per
Internal Revenue Service (IRS) Guidelines for medical related mileage. See http:///www.irs.gov/ for
details on the mileage rate applicable to the year of service on the claim. Additional commuting to
and from the medical care facility is not a reimbursable expense. Fees for parking, tolls, gas, car
maintenance, repairs, or the like are not covered.
• Coach airfare to and from the Hospital when it is 300 miles or more from your residence.
•
city airport is a reimbursable expense. Mileage to
and from the airport nearest to the medical care facility and the medical care facility is a reimbursable
expense. Coverage can be provided for alternate sources of transportation from the airport to the
medical care facility and back to the airport after treatment has been completed. These can include
taxi, shuttle, and car rental. This benefit is only for arrival and departure days.
• Lodging, limited to one room, double occupancy.
• Lodging is reimbursed at the lesser of the actual lodging charges or $50 for the member and $50 for
each covered caregiver for a maximum of $100 per night. Minor patients are eligible to have two
caregivers. In this situation a maximum of $150 per night would be reimbursable. Lodging can be in
the form of a hotel, motel, Airbnb, or short-term apartment rental. Service and cleaning charges are
not covered. Receipts must be itemized and contain the number of guests listed. Short term
apartment rental must include a copy of the signed lease. Credit card receipts are not an acceptable
form of documentation or proof of payment.
• Other reasonable expenses. Tobacco, alcohol, drug expenses, and meals are excluded from coverage.
is available in connection with access
to the selected bariatric BDCSC. Details regarding reimbursement can be obtained by calling the Member
Services number on the back of the identification card. A travel reimbursement form will be provided and
will include instructions for submission of legible copies of all applicable receipts in order to obtain
reimbursement.
Blood Benefits. Blood transfusions, including blood processing and the cost of unreplaced blood and blood
products. Charges for the collection, processing and storage of self-donated blood are covered, but only
when specifically collected for a planned and covered surgical procedure.
Breast Cancer Benefits. Services and supplies provided in connection with the screening for, diagnosis of,
and treatment for breast cancer whether due to illness or injury, including:
1. Diagnostic mammogram examinations in connection with the treatment of a diagnosed illness or injury.
Routine mammograms will be covered initially under the Preventive Care Benefits. A follow-up
mammogram may be considered diagnostic or treatment of a diagnosed illness or injury. Please talk
with your treating Physician to understand what care is being provided so you will know which coverage
applies.
2. Breast cancer (BRCA) testing, if appropriate, in conjunction with genetic counseling and evaluation.
When done as a preventive care service, BRCA testing will be covered under the Preventive Care
Benefits.
3. Mastectomy and lymph node dissection; complications from a mastectomy including lymphedema.

38
4. Reconstructive surgery of both breasts performed to restore and achieve symmetry following a Medically
Necessary mastectomy.
5. Benefits
This coverage is provided according to the terms and conditions of this Plan that apply to all other medical
conditions.
Breast Health Screening (Athena). Covered Members who receive mammography screening are eligible
to complete a breast health screening tool which provides additional information on the risk of developing
breast cancer. High risk individuals may receive telephonic or in person counseling from an Athena breast
health specialist. For further information on the Athena program, please go to the following website:
www.wisdomstudy.org.
Chemotherapy Benefits. This includes the treatment of disease using chemical or antineoplastic agents
and the cost of such agents in a professional or Facility setting. Chemotherapy services are subject to pre-
service review to determine whether Medically Necessary, please refer to UTILIZATION REVIEW
PROGRAM for details.
Chiropractic Benefits. Chiropractic Services for manual manipulation of the spine to correct subluxation
demonstrated by Physician-read x-ray. The Plan will pay for up to 24 visits (combined with Acupuncture
) during a Calendar Year.
Since your Plan has a Calendar Year Deductible, the number of visits will start counting toward the
maximum when services are first provided even if the Calendar Year Deductible has not been met.
Clinical Trial of Cancer and Other Life Threatening Conditions Benefits. Coverage is provided for
routine patient costs you receive as a voluntary participant in an approved clinical trial. The services must
be those that are listed as covered by this Plan for Members who are not enrolled in a clinical trial.
Routine patient care costs include items, services, and drugs provided to you in connection with an approved
clinical trial that would otherwise be covered by the Plan.
detection, or treatment of cancer or another life-threatening disease or condition, from which death is likely
unless the disease or condition is treated. Coverage is limited to the following clinical trials:
1. Federally funded trials approved or funded by one or more of the following:
a. The National Institutes of Health,
b. The Centers for Disease Control and Prevention,
c. The Agency for Healthcare Research and Quality,
d. The Centers for Medicare and Medicaid Services,
e. A cooperative group or center of any of the four entities listed above or the Department of Defense
or the Department of Veterans Affairs,
f. A qualified non-governmental research entity identified in the guidelines issued by the National
Institutes of Health for center support grants, or
g. Any of the following departments if the study or investigation has been reviewed and approved
through a system of peer review that the Secretary of Health and Human Services determines (1)
to be comparable to the system of peer review of investigations and studies used by the National
Institutes of Health, and (2) assures unbiased review of the highest scientific standards by qualified
Individuals who have no interest in the outcome of the review:
i. The Department of Veterans Affairs,

39
ii. The Department of Defense, or
iii. The Department of Energy.
2. Studies or investigations done as part of an investigational new drug application reviewed by the Food
and Drug Administration.
3. Studies or investigations done for drug trials that are exempt from the investigational new drug
application.
Participation in the clinical trial must be recommended by your Physician after determining participation has
a meaningful potential to benefit you. All requests for clinical trials services, including requests that are not
part of approved clinical trials, will be reviewed according to the PlanClinical Coverage Guidelines, related
policies and procedures. If you have any questions about the information in this section, please refer to the
Member Services number on the back of the identification card.
Routine patient costs do not include the costs associated with any of the following:
1. The investigational item, device, or service.
2. Any item or service provided solely to satisfy data collection and analysis needs and that is not used in
the clinical management of the patient.
3. Any service that is clearly inconsistent with widely accepted and established standards of care for a
particular diagnosis.
4. Any item, device, or service that is paid for, by the sponsor of the trial or is customarily provided by the
sponsor free of charge for any enrollee in the trial.
Note: You will be financially responsible for the costs associated with non-Covered Services.
Contraceptive Benefits
Services and supplies provided in connection with the following methods of contraception:
• Injectable drugs and implants for birth control, administered in a P Medically
Necessary.
• Intrauterine contraceptive devices (IUDs) and diaphragms, dispensed by a Physician if Medically
Necessary.
• Professional services of a Physician in connection with the prescribing, fitting, and insertion of
intrauterine contraceptive devices or diaphragms.
Contraceptive supplies prescribed by a Physician for reasons other than contraceptive purposes for
Medically Necessary treatment such as decreasing the risk of ovarian cancer, eliminating symptoms of
menopause or for contraception that is necessary to preserve life or health may also be covered.
If your Physician determines that none of these contraceptive methods are appropriate for you based on
your medical or personal history, coverage will be provided for another prescription contraceptive method
that is approved by the Food and Drug Administration (FDA) and prescribed by your Physician.
for further details.
Dental Care Benefits
1. Admissions for Dental Care. Listed inpatient Hospital services for up to three days during a Hospital
Stay, when such Stay is required for dental treatment and has been ordered by a Physician (M.D.) and
a dentist (D.D.S. or D.M.D.). Anthem will make the final determination as to whether the dental treatment
could have been safely rendered in another setting due to the nature of the procedure or your medical
40
condition. Hospital Stays for the purpose of administering general anesthesia are not considered
necessary and are not covered except as specified in #2, below.
2. General Anesthesia. General anesthesia and associated Facility charges when your clinical status or
underlying medical condition requires that dental procedures be rendered in a Hospital or Ambulatory
Surgical Center. This applies only if (a) the Member is less than seven years old, (b) the Member is
developmentally disabled, or (c) the Member
Medically Necessary. Charges for the dental procedure itself, including professional fees of a dentist,
may not be covered.
3. Dental Injury. Services of a Physician (M.D.) or dentist (D.D.S. or D.M.D.) solely to treat an Accidental
Injury to natural teeth. Coverage shall be limited to only such services that are Medically Necessary to
repair the damage done by Accidental Injury and/or restore function lost as a direct result of the
Accidental Injury. Damage to natural teeth due to chewing or biting is not Accidental Injury unless the
chewing or biting results from a medical or mental condition.
4. Cleft Palate. Medically Necessary dental or orthodontic services that are an integral part of
Reconstructive Surgery
cleft palate, cleft lip, or other craniofacial anomalies associated with cleft palate.
5. Orthognathic Surgery. Orthognathic surgery for a physical abnormality that prevents normal function
of the upper or lower jaw and is Medically Necessary to attain functional capacity of the affected part.
Important: If you decide to receive dental services that are not covered under this Plan, an Anthem Prudent
Buyer Provider who is a dentist may charge you his or her usual and customary rate for those services. Prior
to providing you with dental services that are not a covered benefit, the dentist should provide a treatment
plan that includes each anticipated service to be provided and the estimated cost of each service. If you
would like more information about the dental services that are covered under this Plan, please call the
Member Services number on the back of the identification card. To fully understand your coverage under
this Plan, please carefully review this Benefit Booklet document.
Designated Pharmacy Provider Benefits
Anthem may establish one or more Designated Pharmacy Provider programs which provide specific
pharmacy services (including shipment of Prescription Drugs) to Members. A participating provider is not
necessarily a Designated Pharmacy Provider. To be a Designated Pharmacy Provider, the participating
provider must have signed a Designated Pharmacy Provider agreement with the Plan. You or your Physician
can contact the Member Services number on the back of the identification card to learn which Pharmacy or
pharmacies are part of a Designated Pharmacy Provider program.
For Prescription Drugs that are shipped to you or your Physician and administered in your office,
you and your Physician are required to order from a Designated Pharmacy Provider. A patient care
coordinator will work with you and your Physician to obtain precertification and to assist shipment to your
office.
Anthem may also require you to use a Designated Pharmacy Provider to obtain Prescription Drugs for
treatment of certain clinical conditions such as hemophilia. Anthem reserves the right to modify the list of
Prescription Drugs as well as the setting and/or level of care in which the care is provided to you. Anthem
may, from time to time, change with or without advance notice, the Designated Pharmacy Provider for a
Drug. Such change can help provide cost effective, value based and/or quality services.
If you are required to use a Designated Pharmacy Provider and you choose not to obtain your Prescription
Drug from a Designated Pharmacy Provider, coverage will be the same as for an Out-of-Network Provider.
You can get the list of the Prescription Drugs covered under this section by calling the Member Services
number on the back of the identification card.
41
Diabetes Care Benefits. Services and supplies provided for the treatment of diabetes, including:
1. The following equipment and supplies:
a. Blood glucose monitors, including monitors designed to assist the visually impaired, and blood
glucose testing strips.
b. Insulin pumps.
c. Pen delivery systems for insulin administration (non-disposable).
d. Visual aids (but not eyeglasses) to help the visually impaired to properly dose insulin.
e. Podiatric devices, such as therapeutic shoes and shoe inserts, to treat diabetes-related
complications.
Items a. through d. above are covered under your Benefits for durable medical equipment (see
e. above is covered under your Plan's Benefits for
Prosthetic Devices (see "Prosthetic Devices Benefit").
2. Diabetes education program which:
a. Is designed to teach a Member who is a patient and covered Members of the patient's family about
the disease process and the daily management of diabetic therapy;
b. Includes self-management training, education, and medical nutrition therapy to enable the Member
to properly use the equipment, supplies, and medications necessary to manage the disease; and
c. Is supervised by a Physician.
Diabetes education services are covered under Plan Benefits for office visits to Physicians.
3. The following items are covered as medical supplies:
a. Insulin syringes, disposable pen delivery systems for insulin administration. Charges for insulin and
other prescriptive medications are not covered.
b. Testing strips, lancets, and alcohol swabs.
4. Screenings for gestational diabetes are covered under your Preventive Care Benefits. Please see that
provision for further details.
Diagnostic Services. Outpatient diagnostic imaging and laboratory services. This does not include
services covered under the "Advanced Imaging Procedure Benefits" provision of this section.
Durable Medical Equipment Benefits. Rental or purchase of dialysis equipment; dialysis supplies. Rental
or purchase of other medical equipment and supplies which are:
1. Of no further use when medical needs end;
2. For the exclusive use of the patient;
3. Not primarily for comfort or hygiene;
4. Not for environmental control or for exercise; and
5. Manufactured specifically for medical use.
Specific durable medical equipment is subject to pre-service review to determine whether Medically
Necessary. Please refer to UTILIZATION REVIEW PROGRAM for information on how to obtain the proper
reviews.
42
Emergency Room. Benefits are provided for Medically Necessary services provided in the Emergency
room of a Hospital.
Family Planning Benefits. Family planning services, counseling and planning for problems of fertility and
Infertility, as Medically Necessary. Artificial insemination, in vitro fertilization, and any related laboratory
procedures are not covered.
Fertility Preservation Services. Fertility preservation services to prevent iatrogenic infertility when
medically necessary are covered. Iatrogenic infertility means infertility caused directly or indirectly, as a
possible side effect, by surgery, chemotherapy, radiation, or other covered medical treatment.
American Society of Clinical Oncology or the American Society for Reproductive Medicine. Note that this
benefit covers fertility preservation services only, as described. Fertility preservation services under this
section do not include testing or treatment of infertility.
Hearing Aid Benefits. The following hearing aid services are covered when provided by or purchased as
a result of a written recommendation from an otolaryngologist or a state-certified audiologist. The
payment will not exceed of $2,000 every 36 months.
1. Audiological evaluations to measure the extent of hearing loss and determine the most appropriate make
and model of hearing aid. These evaluations will be covered under Plan Benefits for office visits to
Physicians.
2. Hearing aids (monaural or binaural) including ear mold(s), the hearing aid instrument, batteries, cords
and other ancillary equipment.
3. Visits for fitting, counseling, adjustments and repairs for a one Year period after receiving the covered
hearing aid.
No Benefits will be provided for the following:
1. Charges for a hearing aid which exceeds specifications prescribed for the correction of hearing loss, or
for more than $2000 every 36 months.
2. Surgically implanted hearing devices (i.e., cochlear implants, audient bone conduction devices).
Medically necessary surgically implanted hearing devices may be covered under your Benefits
Hemodialysis Treatment Benefits. This includes services related to renal failure and chronic (end-stage)
renal disease, including hemodialysis, home intermittent peritoneal dialysis home continuous cycling
peritoneal dialysis and home continuous ambulatory peritoneal dialysis.
The following renal dialysis services are covered:
• Outpatient maintenance dialysis treatments in an outpatient dialysis Facility;
• Home dialysis; and
• Training for self-dialysis at home including the instructions for a person who will assist with self-dialysis
done at a home setting.
Treatment provided by a freestanding outpatient hemodialysis center which is an Out-of-Network Provider
is limited to $210 per visit.
Home Health Care Benefits. The following services provided by a Home Health Agency:
1. Services of a registered nurse or licensed vocational nurse under the supervision of a registered nurse
or a Physician.
2. Services of a licensed therapist for physical therapy, occupational therapy, speech therapy, or respiratory
therapy.
3. Services of a medical social service worker.
43
4. Services of a health aide who is employed by (or who contracts with) a Home Health Agency. Services
must be ordered and supervised by a registered nurse employed by the Home Health Agency as
professional coordinator. These services are covered only if you are also receiving the services listed
in 1 or 2 above.
5. Medically Necessary supplies provided by the Home Health Agency.
Benefits are also available for Intensive In-Home Behavioral Health Services. These do not require
Mental Health and Substance Use Disorder
this coverage.
In no event will Benefits exceed 100 visits during a Calendar Year. A visit of four hours or less by a home
health aide shall be considered as one home health visit.
Since your Plan has a Calendar Year Deductible, the number of visits will start counting toward the maximum
when services are first provided even if the Calendar Year Deductible has not been met.
Home health care services are subject to pre-service review to determine whether Medically Necessary.
Please refer to UTILIZATION REVIEW PROGRAM for information on how to obtain the proper reviews.
Home health care services are not covered if received while you are receiving Benefits under the "Hospice
Care Benefits" provision of this section.
Hospice Care Benefits. The services and supplies listed below are covered when provided by a Hospice
for the palliative treatment of pain and other symptoms associated with a terminal disease. Palliative care is
care that controls pain and relieves symptoms but is not intended to cure the illness. You must be suffering
from a terminal illness for which the prognosis of life expectancy is one year or less, as certified by your
Physician and submitted to Anthem. Covered Services are available on a 24-hour basis for the management
of your condition.
1. Interdisciplinary team care with the development and maintenance of an appropriate plan of care.
2. Short-term inpatient Hospital care when required in periods of crisis or as respite care. Coverage of
inpatient respite care is provided on an occasional basis and is limited to a maximum of five consecutive
days per admission.
3. Skilled nursing services provided by or under the supervision of a registered nurse. Certified home
health aide services and homemaker services provided under the supervision of a registered nurse.
4. Social services and counseling services provided by a qualified social worker.
5. Dietary and nutritional guidance. Nutritional support such as intravenous feeding or hyperalimentation.
6. Physical therapy, occupational therapy, speech therapy, and respiratory therapy provided by a licensed
therapist.
7. Volunteer services provided by trained Hospice volunteers under the direction of a Hospice staff
member.
8. Pharmaceuticals, medical equipment, and supplies necessary for the management of your condition.
Oxygen and related respiratory therapy supplies.
9. Bereavement services, including assessment of the needs of the bereaved family and development of
a care plan to meet those needs, both prior to and following the or the death.
Bereavement services are available to surviving Members of the immediate family for a period of one
year after the death. Your immediate family means your Spouse, children, step-children, parents, and
siblings.
10. Palliative care (care which controls pain and relieves symptoms, but does not cure) which is appropriate
for the illness.
44
Your Physician must consent to your care by the Hospice and must be consulted in the development of your
treatment plan. The Hospice must submit a written treatment plan to Anthem every 30 days.
This P Hospice benefit will meet or exceed Hospice benefit. If you use an Out-of-Network,
that pHospice benefit unless your claim involves
a Surprise Billing Claim.
Hospital Benefits
1. Inpatient services and supplies, provided by a Hospital. The Maximum Allowed Amount will not include
charges in excess of the Hospital-bed room rate unless there is a negotiated per diem
rate between Anthem and the Hospital, or unless your Physician orders, and Anthem authorizes, a
private room as Medically Necessary. For inpatient services and supplies provided by an Out-of-Network
Provider Facility, the maximum payment is limited to $360* per day.
2. Services in Special Care Units.
3. Outpatient services and supplies provided by a Hospital, including outpatient surgery. For outpatient
services and supplies provided by an Out-of-Network Provider, the maximum payment is limited
to $210* per day.
*The Out-of-Network Provider Facility maximums do not apply to Emergency Services or Mental Health
or Substance Use Disorder services.
Hospital services are subject to pre-service review to determine whether medical necessity.
Please refer to the section UTILIZATION REVIEW PROGRAM for information on how to obtain the proper
reviews. For inpatient services at an Out-of-Network Provider, there is an additional $250 Copayment if prior
authorization is not obtained.
Infertility Treatment Benefits. Diagnosis of cause of Infertility, provided you are under the direct care and
treatment of a Physician.
Additional Covered Services include in-vitro fertilization, GIFT (gamete intrafallopian transfer), ZIFT (zygote
intra-
ligible Covered Members.
Eligible Covered Members, with a diagnosis of infertility, in need of medical services to achieve pregnancy
Program is required prior to initiation of medical treatment for family building. Failure to initiate
preauthorization of services for each service will result in a denial of benefits. Coverage is subject to available
benefits at time of claim submission. Out of pocket cost shares are applicable and should be verified prior to
initiating services.
Included Subject to medical necessity and prior authorization, the following are covered under this benefit:
timed intercourse and intrauterine insemination (IUI) cycles, assisted reproductive technologies (ART)
(lifetime maximum of two in vitro fertilization (IVF) oocyte retrievals), and ART related services.
Exclusions: The following services are not covered:
a. Gonadotropin or menotropin stimulated ovulation induction cycles including monitoring of timed
intercourse and IUI cycles unless member has a diagnosis of hypogonadotropic anovulatory disorders
or hypopituitarism, or after member has not ovulated or conceived after a prior trial of 3 cycles or
clomiphene citrate or letrozole.
b. If a member or the member's partner has undergone an elective sterilization procedure, they are not
eligible for benefits unless they undergo a successful reversal and thereafter meet DOI; Or WIN's
consulting medical director determines that the reversal of the elective sterilization procedure is not
medically indicated or will not improve the likelihood of conception due to multifactorial causes of
infertility. Reversal of a sterilization procedure is not covered.
45
c. Experimental or Investigational medical and surgical procedures.
d. Services which are not medically appropriate.
e. Expenses for Surrogacy and fees associated with surrogacy.
f. Expenses for procuring Donated Oocytes or Sperm, including all medical expenses, travel
expenses, agency, laboratory and donor fees, psychological screening, FDA testing for the donor and
partner, genetics screening and all medications for the donor (e.g., suppression medications, stimulation
medications)
g. Services which are not listed as covered in this benefit.
For more information or to initiate prior authorization, contact WINFertility at (877) 451-3077.
Infusion / Injectable Therapy Benefits. The following services and supplies, when provided in your home
by an Infusion / Injectable Therapy Provider or in any other outpatient setting by a qualified health care
provider, for the intravenous administration of your total daily nutritional intake or fluid requirements, including
but not limited to Parenteral Therapy and Total Parenteral Nutrition (TPN), medication related to illness or
injury, chemotherapy, antibiotic therapy, aerosol therapy, tocolytic therapy, special therapy, intravenous
hydration, or pain management:
1. Medication, ancillary medical supplies and supply delivery, (not to exceed a 14-day supply); however,
medication which is delivered but not administered is not covered;
2. Pharmacy compounding and dispensing services (including pharmacy support) for intravenous solutions
and medications (if outpatient prescription drug benefits are provided under this Plan, Compound
Medications must be obtained from an In-Network Pharmacy);
3. Hospital and home clinical visits related to the administration of infusion therapy, including skilled nursing
services including those provided for: (a) patient or alternative caregiver training; and (b) visits to monitor
the therapy;
4. Rental and purchase charges for durable medical equipment; maintenance and repair charges for such
equipment;
5.
6. Total Parenteral Nutrition (TPN), Enteral Nutrition Therapy, antibiotic therapy, pain management,
chemotherapy, and may also include injections (intra-muscular, subcutaneous, or continuous
subcutaneous).
Oncology and Transplant related infusion / injectable therapy services are subject to pre-service review to
determine whether Medically Necessary. (See UTILIZATION REVIEW PROGRAM.)
Jaw Joint Disorder Benefits. The Plan will pay for splint therapy or surgical treatment for disorders or
conditions directly affecting the upper or lower jawbone or the joints linking the jawbones and the skull (the
temporomandibular joints), including the complex of muscles, nerves and other tissues related to those joints.
Mental Health and Substance Use Disorder Benefits. This Plan provides coverage for the Medically
Necessary treatment of Mental Health and Substance Use Disorder. This coverage is provided according
to the terms and conditions of this Plan that apply to all other medical conditions, except as specifically stated
in this section. Medically Necessary services are a Benefit only when the procedure is in accordance with
Medical Policy. (See UTILIZATION REVIEW PROGRAM)
Services for the treatment of Mental Health and Substance Use Disorder covered under this Plan are subject
to the same Deductible and Copayments that apply to services provided for other covered medical conditions
and prescription drugs.
46
Covered Services shown below for the Medically Necessary treatment of Mental Health and Substance Use
Disorder, or to prevent the deterioration of chronic conditions.
1. Inpatient Hospital services and short term services from a Residential Treatment Center (including
crisis residential treatment) as stated in the "Hospital Benefits" provision of this section, for
inpatient services and supplies, and Physician visits during a covered inpatient Stay.
2. Outpatient Office Visits for the following:
- individual and group mental health evaluation and treatment,
- nutritional counseling for the treatment of eating disorders such as anorexia nervosa and bulimia
nervosa,
- drug therapy monitoring,
- individual and group chemical dependency counseling,
- medical treatment for withdrawal symptoms,
- methadone maintenance treatment,
- Behavioral health treatment for autism spectrum disorders delivered in an office setting.
• Other Outpatient Items and Services:
- Partial hospitalization, including Intensive Outpatient Programs and visits to a Day Treatment
Center Benefits
section, for outpatient services and supplies.
- Psychological testing,
- Multidisciplinary treatment in an intensive outpatient psychiatric treatment program,
- Behavioral health treatment for autism spectrum disorders delivered at home.
3. Behavioral health treatment for autism spectrum disorders. Inpatient services, office visits, and other
outpatient items and services are covered under this section. See the section BENEFITS FOR
AUTISM SPECTRUM DISORDERS for a description of the services that are covered by this Plan
(see UTILIZATION REVIEW PROGRAM for details).
Treatment for substance use disorder does not include smoking cessation programs, nor treatment for
s
Please see that provision for further details.
Examples of providers from whom you can receive covered services include the following:
• Psychiatrist,
• Psychologist,
• Registered psychological assistant, as described in the CA Business and Professions Code,
• Psychology trainee or person supervised as set forth in the CA Business and Professions Code,
• Licensed clinical social worker (L.C.S.W.),
• Associate clinical social worker functioning pursuant to the CA Business and Professions Code,
• Mental health clinical nurse specialist,
• Licensed marriage and family therapist (L.M.F.T.),

47
• Associate marriage and family therapist or marriage and family therapist trainee functioning pursuant to
the CA Business and Professions Code,
• Licensed professional counselor (L.P.C.),
• Associate professional clinical counselor or professional clinical counselor trainee functioning pursuant
to the CA Business and Professions Code, and
Qualified Autism Service Providers, Qualified Autism Service Professionals, and Qualified Autism Service
below.
Online Visits. When available in your area, your coverage will include visits from a LiveHealth Online
Provider. Covered services include medical consultations using the internet via webcam, chat, or voice.
Online visits are covered under Plan only from Providers who contract with LiveHealth Online.
Non-Covered Services include, but are not limited to, the following:
• Reporting normal lab or other test results.
• Office visit appointment requests or changes.
• Billing, insurance coverage, or payment questions.
• Requests for referrals to other Physicians or healthcare practitioners.
• Benefit precertification.
• Consultations between Physicians.
• Consultations provided by telephone, electronic mail, or facsimile machines.
Note: You will be financially responsible for the costs associated with non-Covered Services.
For Mental Health or substance use disorder online care visits, please see the SUMMARY OF BENEFITS
under Online visits (LiveHealth Online)
Osteoporosis Benefits. Coverage for services related to diagnosis, treatment, and appropriate
management of osteoporosis including, but not limited to, all Food and Drug Administration approved
technologies, including bone mass measurement technologies as deemed Medically Necessary.
Pediatric Asthma Equipment and Supplies Benefits. The following items and services when required for
the Medically Necessary treatment of asthma in a Dependent child:
1. Nebulizers, including face masks and tubing, inhaler spacers, and peak flow meters. These items are
covered under the Plan's medical Benefits and are not subject to any limitations or maximums that apply
to coverage for durable medical equipment (see "Durable Medical Equipment Benefits").
2. Education for pediatric asthma, including education to enable the child to properly use the items listed
above. This education will be covered under the Plan's Benefits for office visits to a Physician.
Phenylketonuria (PKU) Benefits. Benefits for the testing and treatment of phenylketonuria (PKU) are paid
on the same basis as any other medical condition. Coverage for treatment of PKU shall include those
formulas and special food products that are part of a diet prescribed by a licensed Physician and managed
by a health care professional in consultation with a Physician who specializes in the treatment of metabolic
disease and who participates in or is authorized by the Plan. The diet must be deemed Medically Necessary
to avert the development of serious physical or mental disabilities or to promote normal development or
function as a consequence of PKU.
The cost of the necessary formulas and special food products is covered only as it exceeds the cost of a
prescribed by a Physician or nurse practitioner, or ordered by a registered dietician upon referral by a health

48
care Provider authorized to prescribe dietary treatments, and is Medically Necessary for the treatment of
PKU. Formulas and special food products used in the treatment of PKU that are obtained from a Pharmacy
are covered as Prescription Drugs. Formulas and special food products that are not obtained from a
pharmacy are covered under this Benefit.
• Prescribed by a Physician or nurse practitioner for the treatment of PKU, and
• Consistent with the recommendations and best practices of qualified Physicians with expertise in the
treatment and care of PKU, and
• Used in place of normal food products, such as grocery store foods, used by the general population.
Note: It does not include a food that is naturally low in protein, but may include a food product that is specially
formulated to have less than one gram of protein per serving.
Physical Therapy, Physical Medicine and Occupational Therapy Benefits. The following services
provided by a Physician under a treatment plan:
1. Physical therapy and physical medicine provided on an outpatient basis for the treatment of illness or
injury including the therapeutic use of heat, cold, exercise, electricity, ultra violet radiation, manipulation
of the spine, or massage for the purpose of improving circulation, strengthening muscles, or encouraging
the return of motion. (This includes many types of care which are customarily provided by chiropractors,
physical therapists and osteopaths. It does not include massage therapy services at spas, health clubs
or by standalone massage therapists.)
2. Occupational therapy provided on an outpatient basis when the ability to perform daily life tasks has
been lost or reduced by, or has not been developed due to, illness or injury including programs which
are designed to rehabilitate mentally, physically or emotionally handicapped persons. Occupational
therapy programs are designed to maximize or improve a patient's upper extremity function, perceptual
motor skills and ability to function in daily living activities.
Benefits are not payable for care provided to relieve general soreness or for conditions that may be expected
to improve without treatment. For the purposes of this Benefit, the term "visit" shall include any visit by a
Physician in that office, or in any other outpatient setting, during which one or more of the
services covered under this limited Benefit are rendered, even if other services are provided during the same
visit.
Pregnancy and Maternity Care Benefits
1. All medical Benefits for an enrolled Member when provided for pregnancy or maternity care, including
the following services:
a. Prenatal, postnatal and postpartum care;
b. Ambulatory care services (including ultrasounds, fetal non-stress tests, Physician office visits, and
other Medically Necessary maternity services performed outside of a Hospital);
c. Involuntary complications of pregnancy;
d. Diagnosis of genetic disorders in cases of high-risk pregnancy; and
e. Inpatient Hospital care including labor and delivery.
Inpatient Hospital Benefits in connection with childbirth will be provided for at least 48 hours following a
normal delivery or 96 hours following a cesarean section, unless the mother and her Physician decide
on an earlier discharge. Please see the section entitled FOR YOUR INFORMATION for a statement of your
rights under federal law regarding these services.
49
2. Medical Hospital Benefits for routine nursery care of a newborn child
enrolled Member. Routine nursery care of a newborn child includes screening of a newborn for genetic
diseases, congenital conditions, and other health conditions provided through a program established by
law or regulation.
3. Benefits
details.
Prescription Drug for Abortion Benefits. Mifepristone is covered when provided under the Food and Drug
Administration (FDA) approved treatment regimen.
Prescription Drugs Obtained From Or Administered By a Medical Provider. Your Plan includes Benefits
for Prescription Drugs, including specialty drugs that must be administered to you as part of a Physician visit,
services from a Home Health Agency, or at an outpatient Hospital when they are Covered Services. This
may include drugs for infusion therapy / injectable therapy, chemotherapy, blood products, certain injectables
and any drug that must be administered by a Physician. These may require Prior Authorization. This section
describes your Benefits when your Physician orders the medication and administers it to you.
Benefits for drugs that you inject or get at a retail pharmacy (i.e., self-administered drugs) are not covered
under this section. Benefits for these and other covered drugs are administered by a different plan
administrator. For further information, refer to www.UChealthplans.com.
Non-duplication of Benefits applies to pharmacy drugs under this Plan. When Benefits are provided for
pharmacy drugs under the PlanBenefits, they will not be provided under your prescription drug
Benefits, if included. Conversely, if Benefits are provided for pharmacy drugs under your prescription drug
Benefits, if included, they will not be provided under the medical Benefits.
Preventive Care Benefits. Preventive care includes screenings and other services for adults and children.
All recommended preventive services will be covered as required by the Affordable Care Act (ACA) and
applicable state law. This means for Preventive Care Services, the Calendar Year Deductible will not apply
to these services or supplies when they are provided by an Anthem Prudent Buyer Provider. No Copayment
will apply to these services or supplies when they are provided by an Anthem Prudent Buyer Provider. The
claim must be billed with a procedure code and diagnosis code combination that is identified or listed as
preventive by the ACA.
Certain Benefits for Members who have current symptoms or a diagnosed health problem may be covered
under a different Benefit instead of this benefit, if the coverage does not fall within the state or ACA-
recommended Preventive Care Services.
1. A Physician's services for routine physical examinations.
2. Immunizations prescribed by the examining Physician.
3. Radiology and laboratory services and tests ordered by the examining Physician in connection with a
routine physical examination, excluding any such tests related to an illness or injury. Those radiology
and laboratory services and tests related to an illness or injury will be covered as any other medical
service available under th Benefit
4. Health screenings as ordered by the examining Physician for the following: breast cancer, including
BRCA testing if appropriate (in conjunction with genetic counseling and evaluation), cervical cancer,
including human papillomavirus (HPV), prostate cancer, colorectal cancer, and other medically accepted
cancer screening tests, blood lead levels, high blood pressure, type 2 diabetes mellitus, cholesterol,
obesity, and screening for iron deficiency anemia in pregnant women.
5. Human immunodeficiency virus (HIV) testing, regardless of whether the testing is related to a primary
diagnosis, including screenings for preexposure prophylaxis (PrEP) for prevention of HIV infection.
6. Counseling and risk factor reduction intervention services for sexually transmitted infections, human
immunodeficiency virus (HIV), contraception, tobacco use, and tobacco use-related diseases.

50
7. Additional preventive care and screening for women provided for in the guidelines supported by the
Health Resources and Services Administration, including the following:
a. All FDA-approved contraceptive drugs, devices and other products for women, including over-the-
counter items, if prescribed by a Physician. This includes contraceptive drugs as well as other
contraceptive medications such as injectable contraceptives and patches and devices such as
diaphragms, intra uterine devices (IUDs) and implants, as well as voluntary sterilization procedures,
contraceptive education and counseling. It also includes follow-up services related to the drugs,
devices, products and procedures, including but not limited to management of side effects,
counseling for continued adherence, and device insertion and removal.
will be covered as preventive care under this section. If there is only one form of contraception in a
given method, or if a form of contraception is deemed not medically advisable by a Physician, the
prescribed FDA-approved form of contraception will be covered as preventive care under this
section.
In order to be covered as preventive care, contraceptive prescription drugs must be either a generic
or Single-Source Brand Name Drug (those without a generic equivalent). Multi-Source Brand Name
Drugs (those with a generic equivalent) will be covered as Preventive Care Services when Medically
Necessary according to your attending doctor, otherwise they will be covered under your
prescription drug Benefits.
b. Breast feeding support, supplies, and counseling. One breast pump will be covered per pregnancy
under this benefit.
c. Gestational diabetes screening.
d. Preventive prenatal care.
8. Preventive services for certain high-risk populations as determined by your Physician, based on clinical
expertise.
This list of preventive care services is not exhaustive. Preventive tests and screenings with a rating of A or
B in the current recommendations of the United States Preventive Services Task Force (USPSTF), or those
supported by the Health Resources and Services Administration (HRSA) will be covered with no Copayment
and will not apply to the Calendar Year Deductible.
Preventive Care ServicesDEFINITIONS section starting at page 89, for more
information about services that are covered by this Plan.
Preventive Care for Chronic Conditions (per IRS guidelines)
Members with certain chronic health conditions may be able to receive preventive care for those conditions
prior to meeting their Deductible when services are provided by an In-Network Provider. These benefits are
available if the care qualifies under guidelines provided by the Treasury Department, Internal Revenue
Details
on those guidelines can
https://www.irs.gov/newsroom/irs-expands-list-of-preventive-care-for-hsa-participants-to-include-certain-
care-for-chronic-conditions
The agencies will periodically review the list of preventive care services and items to determine whether
additional services or items should be added or if any should be removed from the list. You will be notified
if updates are incorporated into your Plan.
Professional Services Benefit
1. Services of a Physician.
51
2. Services of an anesthetist (M.D. or C.R.N.A.).
Prosthetic Devices Benefits
1. Breast prostheses following a mastectomy.
2. Prosthetic devices to restore a method of speaking when required as a result of a covered Medically
Necessary laryngectomy.
3. The Plan will pay for other Medically Necessary prosthetic devices, including:
a. Surgical implants;
b. Artificial limbs or eyes;
c. Therapeutic shoes and inserts only for the prevention and treatment of diabetes-related foot
complications;
d. Benefits are available for certain types of orthotics (braces, boots, splints). Covered services include
the initial purchase, fitting, and repair of a custom made rigid or semi-rigid supportive device used
to support, align, prevent, or correct deformities, or to improve the function of movable parts of the
body, or which limits or stops motion of a weak or diseased body part; and
e. Cochlear implants.
Radiation Therapy Benefits. This includes treatment of disease using x-ray, radium or radioactive
isotopes, other treatment methods (such as teletherapy, brachytherapy, intra operative radiation, photon or
high energy particle sources), material and supplies used in the therapy process and treatment planning.
These services can be provided in a Facility or professional setting. Radiation therapy services are subject
to pre-service review to determine whether Medically Necessary. Please refer to UTILIZATION REVIEW
PROGRAM for details.
Reconstructive Surgery Benefits. Reconstructive surgery performed to correct or repair abnormal
structures of the body caused by congenital defects, developmental abnormalities, trauma, infection, tumors,
or disease to do either of the following: (a) improve function; or (b) create a normal appearance, to the extent
possible. This includes surgery performed to restore and achieve symmetry following a Medically Necessary
mastectomy. This also includes Medically Necessary dental or orthodontic services that are an integral part
of Reconstructive Surgery
palate, cleft lip, or other craniofacial anomalies associated with cleft palate.
Benefits
of this service.
Retail Health Clinic Benefits. Services and supplies provided by medical professionals who provide basic
medical services in a Retail Health Clinic including, but not limited to:
1. Exams for minor illnesses and injuries.
2. Preventive services and vaccinations.
3. Health condition monitoring and testing.
Skilled Nursing Facility Benefits. Inpatient services and supplies provided by a Skilled Nursing Facility,
for up to 100 days per Calendar Year. The amount by which your room charge exceeds the prevailing two-
bed room rate of the Skilled Nursing Facility is not considered covered under this plan.
Skilled nursing facility services and supplies are subject to pre-service review to determine whether Medically
Necessary. Please refer to UTILIZATION REVIEW PROGRAM for information on how to obtain the proper
reviews.
If covered charges are applied toward the Calendar Year Deductible and payment is not provided, those
days will be included in the 100 days for that year.
52
Speech Therapy and Speech-language pathology (SLP) Benefits. Services to identify, assess, and treat
speech, language, and swallowing disorders in children and adults. Therapy that will develop or treat
communication or swallowing skills to correct a speech impairment.
Sterilization Benefits. Benefits include sterilization services and services to reverse a non-elective
sterilization that resulted from an illness or injury. Reversals of elective sterilizations are not covered.
Benefits. Please see that provision
for further details.
Transgender Benefits. Services and supplies provided in connection with gender transition when you have
been diagnosed with gender identity disorder or gender dysphoria by a Physician. This coverage is provided
according to the terms and conditions of the Plan that apply to all other covered medical conditions, including
medical necessity requirements, utilization management, and exclusions for cosmetic services. Coverage
includes, but is not limited to, Medically Necessary services related to gender transition such as transgender
surgery, hormone therapy, psychotherapy, and vocal training.
Coverage is provided for specific services according to Plan Benefits that apply to that type of service
generally, if the Plan includes coverage for the service in question. If a specific coverage is not included, the
service will not be covered. For example, transgender surgery would be covered on the same basis as any
other covered, Medically Necessary surgery; hormone therapy would be covered under the
prescription drug Benefits (if such Benefits are included).
Transgender services are subject to prior authorization in order for coverage to be provided. Please refer to
UTILIZATION REVIEW PROGRAM for information on how to obtain the proper reviews.
Transgender Travel Expense Benefits. Certain travel expenses Incurred in connection with an approved
transgender surgery, when the Hospital at which the surgery is performed is 75 miles or more from your
place of residence, provided the expenses are authorized in advance by Accolade. The maximum
payment will not exceed $10,000 per transgender surgery, or series of surgeries (if multiple surgical
procedures are performed), for the following travel expenses Incurred by the Member and one companion:
• Ground transportation to and from the Hospital when it is 75 miles or more from your place of residence.
• Mileage is reimbursed equal to one round trip to the medical care facility. Mileage is reimbursed
per Internal Revenue Service (IRS) Guidelines for medical related mileage. See
http:///www.irs.gov/ for details on the mileage rate applicable to the year of service on the claim.
Additional commuting to and from the medical care facility is not a reimbursable expense. Fees
for parking, tolls, gas, car maintenance, repairs, or the like are not covered.
• Coach airfare to and from the Hospital when it is 300 miles or more from your residence.
• Charges for baggage are reimbursable if a receipt is provided. Mileage to and from the
Mileage to and from the airport nearest to the medical care facility and the medical care facility
is a reimbursable expense. Coverage can be provided for alternate sources of transportation
from the airport to the medical care facility and back to the airport after treatment has been
completed. These can include taxi, shuttle, and car rental. This benefit is only for arrival and
departure days.
• Lodging, limited to one room, double occupancy.
• Lodging is reimbursed at the lesser of the actual lodging charges or $50 for the member and
$50 for each covered caregiver for a maximum of $100 per night. Minor patients are eligible to
have two caregivers. In this situation a maximum of $150 per night would be reimbursable.
Lodging can be in the form of a hotel, motel, Airbnb, or short-term apartment rental. Service and
cleaning charges are not covered. Receipts must be itemized and contain the number of guests
listed. Short term apartment rental must include a copy of the signed lease. Credit card receipts
are not an acceptable form of documentation or proof of payment.
53
• Other reasonable expenses. Tobacco, alcohol, drug, and meal expenses are excluded.
No Copayments will be required for transgender travel expenses authorized in advance by Anthem. Benefits
will be provided for lodging and transportation up to the current limits set forth in the Internal Revenue Code,
not to exceed the maximum amount specified above. This travel expense Benefit is not available for non-
surgical transgender services.
Details regarding reimbursement can be obtained by calling the Member Services number on the back of
the identification card. A travel reimbursement form will be provided for submission of legible copies of all
applicable receipts in order to obtain reimbursement.
Transplant Benefits. Services and supplies provided in connection with a non-Investigative organ or tissue
transplant, if you are:
1. The recipient; or
2. The donor.
Benefits for an organ donor are as follows:
• When both the person donating the organ and the person getting the organ are covered Members under
this Plan, each will get Benefits under their plans.
• When the person getting the organ is a Member under this Plan, but the person donating the organ is
not, Benefits under this Plan are limited to Benefits not available to the donor from any other source.
This includes, but is not limited to, other insurance, grants, foundations, and government programs.
• If a Member covered under this Plan is donating the organ to someone who is not a Member, Benefits
are not available under this Plan.
The Maximum Allowed Amount for a donor, including donor testing and donor search, is limited to expense
Incurred for Medically Necessary medical services only. The Maximum Allowed Amount for services incident
to obtaining the transplanted material from a living donor or a human organ transplant bank will be covered.
Such charges, including complications from the donor procedure for up to six weeks from the date of
procurement, are covered. Services for treatment of a condition that is not directly related to, or a direct
result of, the transplant are not covered.
An unrelated donor search may be required when the patient has a disease for which a transplant is needed
and a suitable donor within the family is not available. The payment for unrelated donor searches
from an authorized, licensed registry for bone marrow/stem cell transplants will not exceed $30,000 per
transplant.
Covered Services are subject to any applicable Deductibles, Copayments and medical Benefit maximums
set forth in the SUMMARY OF BENEFITS. The Maximum Allowed Amount does not include charges for
services received without first obtaining prior authorization or which are provided at a Facility
other than an approved transplant center. See UTILIZATION REVIEW PROGRAM for details.
To maximize your Benefits, you should call Accolade as soon as you think you may need a transplant to talk
about your Benefit options. You must do this before you have an evaluation or work-up for a transplant.
Accolade will help you maximize your Benefits by giving you coverage information, including details on what
is covered and if any clinical coverage guidelines, medical policies, Centers of Medical Excellence (CME) or
Blue Distinction Centers for Specialty Care (BDCSC) rules, or exclusions apply. Call the Member Services
number on the back of the identification card.
You or your Physician must call Accolade for pre-service review prior to the transplant, whether it is
performed in an inpatient or outpatient setting. Prior authorization is required before Benefits for a transplant
will be provided. Your Physician must certify, and Accolade must agree, that the transplant is Medically
Necessary. Your Physician should contact Accolade as soon as possible to start this process. Not getting
prior authorization will result in a denial of Benefits.

54
Please note that your Physician may ask for approval for HLA (human leukocyte antigen) testing, donor
searches, or collection and storage of stem cells prior to the final decision as to what transplant procedure
will be needed. In these cases, the HLA testing and donor search charges will be covered as routine
diagnostic tests. The collection and storage request will be reviewed for medical necessity and may be
approved. However, such an approval for HLA testing, donor search, or collection and storage is NOT an
approval for the later transplant. A separate medical necessity decision will be needed for the transplant
itself.
Specified Transplant Benefits
You must obtain prior authorization for all services including, but not limited to, preoperative tests
and postoperative care related to the following specified transplants: heart, liver, lung, combination heart-
lung, kidney, pancreas, simultaneous pancreas-kidney, or bone marrow/stem cell and similar procedures.
Specified transplants must be performed at Centers of Medical Excellence (CME) or Blue Distinction Centers
for Specialty Care (BDCSC). Charges for services provided for or in connection with a specified
transplant performed at a Facility other than a CME or BDCSC will not be considered covered. Call
the Member Services number on the back of the identification card if your Physician recommends a specified
transplant for your medical care. A case manager transplant coordinator will assist in facilitating your access
to a CME or BDCSC. See UTILIZATION REVIEW PROGRAM for details.
Transplant Travel Expense Benefits
Certain travel expenses Incurred in connection with an approved, specified transplant (heart, liver, lung,
combination heart-lung, kidney, pancreas, simultaneous pancreas-kidney, or bone marrow/stem cell and
similar procedures) performed at a designated CME, BDCSC, or other approved facility that is 75 miles or
by Accolade in advance.
Evaluations: Reimbursement of travel expenses associated with one round trip to the medical facility for
transplant evaluation. This benefit does not apply to services related to the treatment of the disease leading
to the need for a transplant. However, if the member is required to travel a distance for the evaluation and is
advised to remain at the medical transplant facility for the treatment of the disease prior to the transplant,
this will be considered on a case by case basis and determined by Accolade.
Transplant: Reimbursement of travel expenses associated with one round trip for the actual transplant
procedure for the member and the caregiver(s).
Post-Transplant Follow-up: Reimbursement of travel expenses associated with medically necessary post-
transplant visit(s) when the member is required to remain within close proximity of the medical facility for a
short period of time. This is considered on a case by case basis.
Outpatient Post Transplant Follow-up visits: Reimbursement of travel expenses associated with medically
necessary post-transplant visit(s) for the member when the member commutes from their permanent
residence to an approved medical facility for follow-up visits.
The maximum payment will not exceed $10,000 per transplant for the following travel expenses
Incurred by the recipient and one companion* or the donor:
• Ground transportation to and from the CME, BDCSC, or other approved facility when the facility is 75
• Mileage is reimbursed equal to one round trip to the medical care facility. Mileage is reimbursed
per Internal Revenue Service (IRS) Guidelines for medical related mileage. See
http:///www.irs.gov/ for details on the mileage rate applicable to the year of service on the claim.
Additional commuting to and from the medical care facility is not a reimbursable expense. Fees
for parking, tolls, gas, car maintenance, repairs, or the like are not covered.
55
• Coach airfare to and from the CME or BDCSC when the designated CME or BDCSC is 300 miles or
• Charges for baggage are reimbursable if a receipt is provided. Mileage to and from the
Mileage to and from the airport nearest to the medical care facility and the medical care facility
is a reimbursable expense. Coverage can be provided for alternate sources of transportation
from the airport to the medical care facility and back to the airport after treatment has been
completed. These can include taxi, shuttle, and car rental. This benefit is only for arrival and
departure days.
• Lodging, limited to one room, double occupancy
• Lodging is reimbursed at the lesser of the actual lodging charges or $50 for the member and
$50 for each covered caregiver for a maximum of $100 per night. Minor donor recipients are
eligible to have two caregivers. In this situation a maximum of $150 per night would be
reimbursable. Lodging can be in the form of a hotel, motel, Airbnb, or short-term apartment
rental. Service and cleaning charges are not covered. Receipts must be itemized and contain
the number of guests listed. Short term apartment rental must include a copy of the signed lease.
Credit card receipts are not an acceptable form of documentation or proof of payment.
• Other reasonable expenses. Tobacco, alcohol, drug expenses, and meals are excluded.
*Note: When the Member recipient is under 18 years of age, this Benefit will apply to the recipient and two
companions or caregivers.
No Copayments will be required for transplant travel expenses authorized in advance by Accolade.
Expense Incurred for the following is not covered: interim visits to a medical care Facility while waiting for
the actual transplant procedure; travel expenses for a companion and/or caregiver for a transplant donor;
return visits for a transplant donor for treatment of a condition found during the evaluation; rental cars, buses,
taxis or shuttle services; and mileage within the city in which the medical transplant Facility is located.
Details regarding reimbursement can be obtained by calling the Member Services number on the back of
the identification card. A travel reimbursement form will be provided for submission of legible copies of all
applicable receipts in order to obtain reimbursement.
Living Donor Benefits
The following benefits apply to living donors:
Evaluations: Benefits for travel expenses associated with one round trip for the medical donor evaluation
is covered. This benefit applies to the donor only.
Actual Donor Organ Acquisition: Benefits for travel expenses associated with one round trip for the actual
donor organ acquisition procedure is covered. This benefit applies to the donor only.
Post-Donor Organ Acquisition: Benefits for travel expenses for donor for post organ acquisition
procedure is covered for a maximum of up to six weeks after the organ acquisition.
Stem Cell Donor
Stem cell donor charges for travel are reimbursable if a written letter stating the medically necessity from
Accolade for travel expenses is provided and pre-approved.
56
Travel Immunization Benefits
1. ACA Travel Vaccinations:
a. Hepatitis A
b. Hepatitis B
c. Meningitis
d. Polio
2. Other Travel Vaccinations:
a. Japanese Encephalitis
b. Rabies
c. Typhoid
d. Yellow Fever
Urgent Care Benefits. Services and supplies received to prevent serious deterioration of your health or, in
the case of pregnancy, the health of the unborn child, resulting from an unforeseen illness, medical condition,
or complication of an existing condition, including pregnancy, for which treatment cannot be delayed. Urgent
Care services are not Emergency Services. Services for Urgent Care are typically provided by an Urgent
Care Center or other Facility such as a office. Urgent Care can be obtained from Anthem Prudent
Buyer Providers or Out-of-Network Providers. For Covered Services from Out-of-Network Providers you
may be required to pay higher cost-sharing amounts or may have limits on your Benefits.
57
Medical Care That Is NOT Covered
No payment will be made under this Plan for services or supplies that are not Medically Necessary or that
were Incurred before the or after a coverage has ended in connection
with any of the items below. (The titles given to these exclusions and limitations are for ease of reference
only; they are not meant to be an integral part of the exclusions and limitations and do not modify their
meaning.)
Acupuncture. Acupuncture treatment except as specifically stated in the "Acupuncture Benefits" provision
of Medical Care That Is Covered. Acupressure, or massage to control pain, treat illness or promote health
by applying pressure to one or more specific areas of the body based on dermatomes or acupuncture points.
Air Conditioners. Air purifiers, air conditioners, or humidifiers.
Clinical Trials. Services and supplies in connection with clinical trials, except as specifically stated in the
of Cancer and Other Life Threatening Conditions BenefitsMedical
Care That Is Covered.
Commercial Weight Loss Programs. Weight loss programs, whether or not they are pursued under
medical or Physician supervision, unless specifically listed as covered in this Plan.
This exclusion includes, but is not limited to, commercial weight loss programs (Weight Watchers, Jenny
Craig, LA Weight Loss) and fasting programs.
This exclusion does not apply to Medically Necessary treatments for morbid obesity or dietary evaluations
and counseling, and behavioral modification programs for the treatment of anorexia nervosa or bulimia
Benefits
provision of Medical Care That Is Covered.
Contraceptive Devices. Contraceptive devices prescribed for birth control except as specifically stated in
BenefitsMedical Care That Is Covered.
Cosmetic Surgery. Cosmetic surgery or other services performed to alter or reshape normal (including
aged) structures or tissues of the body to improve appearance.
Crime or Nuclear Energy. Conditions that result from: (1) your commission of or attempt to commit a
felony, as long as any injuries are not a result of a medical condition or an act of domestic violence; or (2)
any release of nuclear energy, whether or not the result of war, when government funds are available for
treatment of illness or injury arising from such release of nuclear energy.
Custodial Care or Rest Cures. Inpatient room and board charges in connection with a Hospital Stay
primarily for environmental change or physical therapy. Custodial Care, rest cures, except as specifically
provided under the "Hospice Care Benefits" or "Infusion Therapy / Injectable Therapy" provision of Medical
Care That Is Covered. Services provided by a rest home, a home for the aged, a nursing home or any similar
Facility. Services provided by a Skilled Nursing Facility, except as specifically stated in the "Skilled Nursing
Facility Benefits" provision of Medical Care That Is Covered.
Dental Services or Supplies. For dental treatment, regardless of origin or cause, except as specified below.
supplies, appliances, dental implants and all associated expenses; diagnosis and treatment related to the
teeth, jawbones or gums, including but not limited to:
• Extraction, restoration, and replacement of teeth;
• Services to improve dental clinical outcomes.
This exclusion does not apply to the following:
• Services which are required by law to be covered;
• Services specified as covered in this Benefit Booklet;
• Dental services to prepare the mouth for radiation therapy to treat head and/or neck cancer.
58
Educational or Academic Services. This Plan does not cover:
1. Educational or academic counseling, remediation, or other services that are designed to increase
academic knowledge or skills.
2. Educational or academic counseling, remediation, or other services that are designed to increase
socialization, adaptive, or communication skills.
3. Academic or educational testing.
4. Teaching skills for employment or vocational purposes.
5. Teaching art, dance, horseback riding, music, play, swimming, or any similar activities.
6. Teaching manners and etiquette or any other social skills.
7. Teaching and support services to develop planning and organizational skills such as daily activity
planning and project or task planning.
This exclusion does not apply to the Medically Necessary treatment of autism spectrum disorders, to the
extent stated in the section BENEFITS FOR AUTISM SPECTRUM DISORDERS.
Excess Amounts. Any amounts in excess of Maximum Allowed Amounts, except for Surprise Billing Claims
, or any Medical
Benefit Maximum.
Experimental or Investigative. Any Experimental or Investigative procedure or medication. But, if you are
denied Benefits because it is determined that the requested treatment is Experimental or Investigative, you
may request that the denial be reviewed.
Eye Surgery for Refractive Defects. Any eye surgery solely or primarily for the purpose of correcting
refractive defects of the eye such as nearsightedness (myopia) and/or astigmatism. Contact lenses and
eyeglasses required as a result of this surgery.
Food or Dietary Supplements. Nutritional and/or dietary supplements and counseling, except as provided
in this Plan or as required by law. This exclusion includes, but is not limited to, those nutritional formulas
and dietary supplements that can be purchased over the counter, which by law do not require either a written
prescription or dispensing by a licensed pharmacist.
Fraud, Waste, Abuse, and Other Inappropriate Billing. Services from a non-participating provider that
are determined to be not payable as a result of fraud, waste, abuse or inappropriate billing activities. This
includes a non-participating provider's failure to submit medical records required to determine the
appropriateness of a claim.
Gene Therapy. Gene therapy as well as any drugs, procedures, health care services related to it that
introduce or is related to the introduction of genetic material into a person intended to replace or correct
faulty or missing genetic material.
Government Treatment. Any services you actually received that were provided by a local, state, or federal
government agency, or by a public school system or school district, except when payment under this Plan is
expressly required by federal or state law. The Plan will not cover payment for these services if you are not
required to pay for them or they are given to you for free. You are not required to seek any such services
prior to receiving Medically Necessary health care services that are covered by this Plan.
Health Club Memberships. Health club memberships, exercise equipment, charges from a physical fitness
instructor or personal trainer, or any other charges for activities, equipment or facilities used for developing
or maintaining physical fitness, even if ordered by a Physician. This exclusion also applies to health spas.
Hearing Aids or Tests. Benefits
of Medical Care That Is Covered. Routine hearing tests, except as specifically provided as part of a routine
BenefitsMedical Care That Is Covered.
59
Infertility Treatment. Services or supplies furnished in connection with the treatment of Infertility, except
as specifically stated in the "Infertility Treatment" provision of Medical Care That Is Covered.
Inpatient Diagnostic Tests. Inpatient room and board charges in connection with a Hospital Stay primarily
for diagnostic tests which could have been performed safely on an outpatient basis.
Lifestyle Programs.
imagery or nutrition. This exclusion will not apply to cardiac rehabilitation programs approved by Accolade.
Massage Therapy.
.
Medical Equipment, Devices and Supplies. This Plan does not cover the following:
• Replacement or repair of purchased or rental equipment because of misuse, abuse, or loss/theft.
• Surgical supports, corsets, or articles of clothing unless needed to recover from surgery or injury.
• Enhancements to standard equipment and devices that is not Medically Necessary.
• Supplies, equipment and appliances that include comfort, luxury, or convenience items or features that
exceed what is Medically Necessary in your situation.
This exclusion does not apply to the Medically Necessary
Equipment BenefitsMedical Care That Is Covered.
Non-Licensed Providers. Treatment or services rendered by non-licensed health care providers and
treatment or services for which the Provider of services is not required to be licensed. This includes treatment
or services from a non-licensed Provider under the supervision of a licensed Physician, except as specifically
provided or arranged by Anthem. This exclusion does not apply to the Medically Necessary treatment of
autism spectrum disorders, to the extent stated in the section BENEFITS FOR AUTISM SPECTRUM
DISORDERS.
Not Medically Necessary. Services or supplies that are not Medically Necessary, as defined. This includes
See pages
92-93 in the DEFINITIONS section for more information.
Optometric Services or Supplies. Optometric services, eye exercises including orthoptics. Routine eye
Care Benefits Medical Care That Is Covered. Eyeglasses or contact lenses, except as
specifically stated in the "Prosthetic Devices Benefits" provision of Medical Care That Is Covered.
Orthodontia. Braces and other orthodontic appliances or services, except as specifically stated in the
Benefits BenefitsMedical Care That Is Covered.
Orthopedic Supplies. Orthopedic shoes and shoe inserts. This exclusion does not apply to orthopedic
footwear used as an integral part of a brace, shoe inserts that are custom molded to the patient, or
therapeutic shoes and inserts designed to treat foot complications due to diabetes, as specifically stated in
BenefitsMedical Care That Is Covered.
Outpatient Occupational Therapy. Outpatient occupational therapy, except as specifically stated in the
"Infusion Therapy / Injectable Therapy Benefits" provision of Medical Care That Is Covered, or when provided
by a Home Health Agency or Hospice, as specifically stated in the "Home Health Care Benefits", "Hospice
Care Benefits" or "Physical Therapy, Physical Medicine and Occupational Therapy Benefits" provisions of
that section. This exclusion also does not apply to the Medically Necessary treatment of Mental Health and
Substance Use Disorder, or to the Medically Necessary treatment of autism spectrum disorders, to the extent
stated in the section BENEFITS FOR AUTISM SPECTRUM DISORDERS.
Outpatient Prescription Drugs and Medications. Outpatient prescription drugs or medications and
/ Injectable Therapy Benefits
Drug for Abortion Benefits Benefits Medical Care That Is Covered.
60
Cosmetics, health or beauty aids. However, health aids that are Medically Necessary and meet the
Benefits
provision of Medical Care That Is Covered, are covered, subject to all terms of this Plan that apply to that
benefit. Your benefits for prescription drug coverage are administered by a different plan administrator. For
further information, refer to www.UChealthplans.com.
Personal Items. Any supplies for comfort, hygiene or beautification.
Physical Therapy or Physical Medicine. Services of a Physician for physical therapy or physical medicine,
except when provided during a covered inpatient confinement, or as specifically stated in the "Home Health
Care Benefits", "Hospice Care Benefits", "Infusion Therapy / Injectable Therapy" or "Physical Therapy,
Physical Medicine and Occupational Therapy Benefits" provisions of Medical Care That Is Covered. This
exclusion also does not apply to the Medically Necessary treatment of autism spectrum disorders, to the
extent stated in the section BENEFITS FOR AUTISM SPECTRUM DISORDERS.
Private Contracts. Services or supplies provided pursuant to a private contract between the Member and
a provider, for which reimbursement under the Medicare program is prohibited, as specified in Section 1802
(42 U.S.C. 1395a) of Title XVIII of the Social Security Act.
Private Duty Nursing. Private duty nursing services of a registered nurse or licensed vocational nurse under
the supervision of a registered nurse
or a Physician.
Residential accommodations. Residential accommodations to treat medical or behavioral health
conditions, except when provided in a Hospital, Hospice, Skilled Nursing Facility or short term services in a
Residential Treatment Center.
Routine Exams or Tests. Routine physical exams or tests which do not directly treat an actual illness,
injury or condition, including those required by employment or government authority, except as specifically
stated in the "Preventive Care Benefits" provision of Medical Care That Is Covered.
Scalp hair prostheses. Scalp hair prostheses including wigs or any form of hair replacement.
Services of Relatives. Professional services received from a person who lives in your home or who is
related to you by blood or marriage, except as specifically stated in the "Infusion Therapy / Injectable Therapy
Benefits" provision of Medical Care That Is Covered.
Speech Therapy. Speech therapy except as stated in the "Speech Therapy and Speech language
pathology (SLP) Benefits" provision of Medical Care That Is Covered. This exclusion also does not apply the
Medically Necessary treatment of autism spectrum disorders, to the extent stated in the section BENEFITS
FOR AUTISM SPECTRUM DISORDERS.
Sterilization Reversal. Reversal of an elective sterilization.
Surrogate Mother Services. For any services or supplies provided to a person not covered under the Plan
in connection with a surrogate pregnancy (including, but not limited to, the bearing of a child by another
woman for an infertile couple).
Telephone, Facsimile Machine, and Electronic Mail Consultations. Consultations provided using
telephone, facsimile machine, or electronic mail.
Varicose Vein Treatment. Treatment of varicose veins or telangiectatic dermal veins (spider veins) by any
method (including sclerotherapy or other surgeries) when services are rendered for cosmetic purposes.
Voluntary Payment. Services for which you have no legal obligation to pay, or for which no charge would
be made in the absence of insurance coverage or other health plan coverage, except services received at a
non-governmental charitable research Hospital. Such a Hospital must meet the following guidelines:
1. It must be internationally known as being devoted mainly to medical research;
2. At least 10% of its yearly budget must be spent on research not directly related to patient care;
61
3. At least one-third of its gross income must come from donations or grants other than gifts or payments
for patient care;
4. It must accept patients who are unable to pay; and
5. Two-thirds of its patients must have conditions directly related to the Hospital
Waived Cost-Shares Out-of-Network Provider. For any service for which you are responsible under the
terms of this Plan to pay a Copayment or Deductible, and the Copayment or Deductible is waived by an Out-
of-Network Provider.
Work-Related. Work-related conditions if benefits are recovered or can be recovered, either by adjudication,
settlement or otherwise, under any workers' compensation, employer's liability law or occupational disease
law, even if you do not claim those benefits.
62
BENEFITS FOR AUTISM SPECTRUM DISORDERS
This Plan provides coverage for behavioral health treatment for autism spectrum disorders. This coverage
is provided according to the terms and conditions of this Plan that apply to all other medical conditions,
except as specifically stated in this section.
Behavioral health treatment services covered under this Plan are subject to the same Deductibles and
Copayments that apply to services provided for other covered medical conditions. Services provided by
Qualified Autism Service Providers, Qualified Autism Service Professionals, and Qualified Autism Service
vered under Plan Benefits that apply for outpatient
office visits or other outpatient items and services. Services provided in a Facility, such as the outpatient
department of a Hospital, will be covered under Plan Benefits that apply to such facilities. See also the
Use Disorder Medical Care That Is Covered.
The meanings of key terms used in this section are shown below. Whenever any of the key terms shown
below appear in this section, the first letter of each word will be capitalized. When you see these capitalized
DEFINITIONS
Autism Spectrum Disorders means one or more of disorders defined in the most recent edition of the
Diagnostic and Statistical Manual of Mental Disorders.
Applied Behavior Analysis (ABA) means the design, implementation, and evaluation of systematic
instructional and environmental modifications to promote positive social behaviors and reduce or ameliorate
behaviors which interfere with learning and social interaction.
Intensive Behavioral Intervention means any form of Applied Behavioral Analysis that is comprehensive,
designed to address all domains of functioning, and provided in multiple settings, across all settings,
depending on the individual's needs and progress. Interventions can be delivered in a one-to-one ratio or
small group format, as appropriate.
Qualified Autism Service Provider is either of the following:
• A person, entity, or group that is certified by a national entity, such as the Behavior Analyst Certification
Board, that is accredited by the National Commission for Certifying Agencies, and who designs,
supervises, or provides treatment for autism spectrum disorders, provided the services are within the
experience and competence of the person, entity, or group that is nationally certified; or
• A person licensed as a Physician and surgeon (M.D. or D.O.), physical therapist, occupational therapist,
psychologist, marriage and family therapist, educational psychologist, clinical social worker, professional
clinical counselor, speech-language pathologist, or audiologist pursuant to state law, who designs,
supervises, or provides treatment for autism spectrum disorders, provided the services are within the
experience and competence of the licensee.
Anthem's network of Anthem Prudent Buyer Providers is limited to licensed Qualified Autism Service
Providers who contract with Anthem or a Blue Cross and/or Blue Shield Plan and who may supervise and
employ Qualified Autism Service Professionals or Qualified Autism Service Paraprofessionals who provide
and administer Behavioral Health Treatment.
Qualified Autism Service Professional is a Provider who meets all of the following requirements:
• Provides behavioral health treatment,
• Is employed and supervised by a Qualified Autism Service Provider,
• Provides treatment according to a treatment plan developed and approved by the Qualified Autism
Service Provider,
• Is a behavioral service Provider approved as a vendor by a California regional center to provide services
as an associate behavior analyst, behavior analyst, behavior management assistant, behavior
63
management consultant, or behavior management program as defined in state regulation or who meets
equivalent criteria in the state in which he or she practices if not providing services in California, and
• Has training and experience in providing services for autism spectrum disorders pursuant to applicable
state law.
Qualified Autism Service Paraprofessional is an unlicensed and uncertified individual who meets all of
the following requirements:
• Is employed and supervised by a Qualified Autism Service Provider,
• Provides treatment and implements services pursuant to a treatment plan developed and approved by
the Qualified Autism Service Provider,
• Meets the criteria set forth in any applicable state regulations adopted pursuant to state law concerning
the use of paraprofessionals in group practice provider behavioral intervention services, and
• Has adequate education, training, and experience, as certified by a Qualified Autism Service Provider.
BEHAVIORAL HEALTH TREATMENT SERVICES COVERED
The behavioral health treatment services covered by this Plan for the treatment of autism spectrum disorders
are limited to those professional services and treatment programs, including Applied Behavior Analysis and
evidence-based behavior intervention programs, that develop or restore, to the maximum extent practicable,
the functioning of an individual with autism spectrum disorders and that meet all of the following
requirements:
• The treatment must be prescribed by a licensed Physician and surgeon (an M.D. or D.O.) or developed
by a licensed psychologist,
• The treatment must be provided under a treatment plan prescribed by a Qualified Autism Service
Provider and administered by one of the following: (a) Qualified Autism Service Provider, (b) Qualified
Autism Service Professional supervised and employed by the Qualified Autism Service Provider, or (c)
Qualified Autism Service Paraprofessional supervised and employed by a Qualified Autism Service
provider, and
• The treatment plan must have measurable goals over a specific timeline and be developed and approved
by the Qualified Autism Service Provider for the specific patient being treated. The treatment plan must
be reviewed no less than once every six months by the Qualified Autism Service Provider and modified
whenever appropriate, and must be consistent with applicable state law that imposes requirements on
the provision of Applied Behavioral Analysis services and Intensive Behavioral Intervention services to
certain persons pursuant to which the Qualified Autism Service Provider does all of the following:
Describes the patient's behavioral health impairments to be treated,
Designs an intervention plan that includes the service type, number of hours, and parent participation
needed to achieve the intervention plan's goal and objectives, and the frequency at which the
patient's progress is evaluated and reported,
Provides intervention plans that utilize evidence-based practices, with demonstrated clinical efficacy
in treating autism spectrum disorders,
Discontinues Intensive Behavioral Intervention services when the treatment goals and objectives
are achieved or no longer appropriate, and
The treatment plan is not used for purposes of providing or for the reimbursement of respite care,
day care, or educational services, and is not used to reimburse a parent for participating in the
treatment program.
64
SUBROGATION AND REIMBURSEMENT
These Subrogation and Reimbursement provisions apply when the Plan pays benefits as a result of injuries
or illnesses You sustained, and You have a right to a Recovery or have received a Recovery from any
source. Consequently, a third Party may be liable, or legally or equitably responsible, for payment of charges
incurred in connection with Your injury or illness. If so, You may have a claim against that third party for
payment of the medical or other charges. In that event, the Plan will be secondary payer, not primary, and
the Plan will be subrogated (i.e., substituted in to, or put in, your place as to) to all rights You may have
against that third party.
Definitions
behalf the plan pays benefits. These Subrogation and Reimbursement provisions apply to all current or
former plan participants and plan beneficiaries. The provisions also apply to the parents, guardian, or other
rights under these provisions shall also apply to the personal representative or administrator of Your estate,
Your heirs or beneficiaries, minors, and legally incompetent or disabled persons. If the covered person is a
shall be subject to these
relatives, heirs, and/or assignees make any Recovery because of injuries sustained by the covered person,
or because of the death of the covered person, that Recovery shall be subject to this provision, regardless
of how any Recovery is allocated or characterized.
motorist coverage, underinsured motorist covera
-
protection insurance and/or automobile medical payments coverage, or any other first or third party
insurance coverage, whether by lawsuit, settlement or otherwise. Regardless of how You or Your
representative or any agreements allocate or characterize the money You receive as a Recovery, it shall be
subject to these provisions.
Subrogation
Immediately upon paying or providing any benefit under the Plan, the Plan shall be subrogated to, or stand
in the place of, all of Your rights of recovery with respect to any claim or potential claim against any party,
due to an injury, illness or condition to the full extent of benefits provided or to be provided by the Plan. The
Plan has the right to recover payments it makes on Your behalf from any party or insurer responsible for
compensating You for Your illnesses or injuries. The Plan has the right to take whatever legal action it sees
fit against any person, party, or entity to recover the benefits paid under the Plan. The Plan may assert a
claim or file suit in Your name and take appropriate action to assert its subrogation claim, with or without
Your consent. The Plan is not required to pay You part of any recovery it may obtain, even if it files suit in
Your name.
The Plan Administrator may, in its discretion, designate a third party service provider or other person or entity
to exercise the rights described in these Subrogation and Reimbursement provisions on behalf of the Plan.
Reimbursement
If You receive any payment as a result of an injury, illness or condition, You agree to reimburse the Plan first
from such payment for all amounts the Plan has paid and will pay as a result of that injury, illness or condition,
up to and including the full amount of Your recovery. If You obtain a Recovery and the Plan has not been
repaid for the benefits the Plan paid on Your behalf, the Plan shall have a right to be repaid from the Recovery
in the amount of the benefits paid on Your behalf. You must promptly reimburse the Plan from any Recovery
65
to the extent of benefits the Plan paid on Your behalf regardless of whether the payments You receive make
You whole for Your losses, illnesses and/or injuries.
Secondary to Other Coverage
The Plan shall be secondary in coverage to any medical payments provision, no-fault automobile insurance
policy, or personal injury protection policy regardless of any election made by You to the contrary. The Plan
shall also be secondary to any excess insurance policy, including, but not limited to, school and/or athletic
policies. This provision applies notwithstanding any coordination of benefits term to the contrary.
Assignment
assign to the Plan any benefits or claims or rights of recovery You have under any automobile policy or other
subrogation and reimbursement claims. This assignment allows the
Plan to pursue any claim You may have regardless of whether You choose to pursue the claim.
Applicability to All Settlements and Judgments
Notwithstanding any allocation or designation of Your Recovery made in any settlement agreement,
judgment, verdict, release, or court order, the Plan shall have a right of full recovery, in first priority, against
any Recovery You make. Furthermore, the Pl
provisions will not be reduced due to Your own negligence. The terms of these Subrogation and
Reimbursement provisions shall apply and the Plan is entitled to full recovery regardless of whether any
liability for payment is admitted and regardless of whether the terms of any settlement, judgment, or verdict
pertaining to Your Recovery identify the medical benefits the Plan provided or purport to allocate any portion
of such Recovery to payment of expenses other than medical expenses. The Plan is entitled to recover from
any Recovery, even those designated as being for pain and suffering, non-economic damages, and/or
general damages only.
Constructive Trust
By accepting benefits from the Plan, You agree that if You receive any payment as a result of an injury,
illness or condition, You will serve as a constructive trustee over those funds. You and Your legal
representative must hold in trust for the Plan the full amount of the Recovery to be paid to the Plan
immediately upon receipt. Failure to hold such funds in trust will be deemed a breach of your fiduciary duty
to the Plan. Any Recovery You obtain must not be dissipated or disbursed until such time as the Plan has
been repaid in accordance with these Subrogation and Reimbursement provisions.
Lien Rights
You hereby automatically grant an equitable lien to the Plan to be imposed upon and against all rights of
Recovery with respect to Third Parties, as described as follows. The Plan will automatically have a lien to
the extent of benefits paid by the Plan for the treatment of Your illness, injury or condition upon any Recovery
related to treatment for any illness, injury or condition for which the Plan paid benefits. The lien may be
enforced against any party who possesses funds or proceeds from Your Recovery including, but not limited
to, you, your representative or agent, and/or any other source possessing funds from Your Recovery. You
lien applies is a Plan asset. The Plan shall be entitled to equitable relief, including without limitation restitution,
the imposition of a constru
to obtain (or preclude the transfer, dissipation or disbursement of) such portion of any Recovery in which the
Plan may have a right or interest.
First-Priority Claim
66
By accepting benefits
are a first priority claim and are to be repaid to the Plan before You receive any Recovery for your damages.
The Plan shall be entitled to full reimbursement on a first-dollar basis from any Recovery, even if such
payment to the Plan will result in a Recovery which is insufficient to make You whole or to compensate You
in part or in whole for the losses, injuries, or ill-
To the extent that the total assets from which a Recovery is available are insufficient to satisfy in full the
Plan's subrogation claim and any claim held by You, the Plan's subrogation claim shall be first satisfied
before any part of a Recovery is applied to Your claim, Your attorney fees, other expenses or costs. The
Plan is not responsible for any attorney fees, attorney liens, other expenses or costs You incur. In other
any reason, including Your
is not responsible for Your legal fees and costs, is not required to share in any way for any payment of such
fees and costs, and its equitable lien will not be reduced by any such fees and costs. The ''common fund''
doctrine does not apply to any funds recovered by any attorney You hire regardless of whether funds
recovered are used to repay benefits paid by the Plan.
Cooperation
but is not limited, to the following:
• You must authorize the Plan to sue, compromise and settle in Your name to the extent of the amount
of medical or other benefits paid for Your injury or illness under the Plan and the expenses incurred
by the Plan in collecting this amount, and assign to the Plan Your rights to Recovery when the
provisions of these Subrogation and Reimbursement provisions apply.
• You must promptly notify the Plan of how, when and where an accident or incident resulting in
personal injury or illness to You occurred, all information regarding the parties involved and any
other information requested by the Plan.
• You must notify the plan within 30 days of the date when any notice is given to any party, including
an insurance company or attorney, of Your intention to pursue or investigate a claim to recover
damages or obtain compensation due to Your injury, illness or condition.
• You must cooperate with the Plan in the investigation, settlement and protection of the Plan's rights.
In the event that You or Your legal representative fails to do whatever is necessary to enable the
Plan to exercise its subrogation or reimbursement rights, the Plan shall be entitled to deduct the
amount the Plan paid from any future benefits under the Plan.
• You and your agents shall provide all information requested by the Plan, the Claims Administrator
or its representative including, but not limited to, completing and submitting any applications or other
forms or statements as the Plan may reasonably request and all documents related to or filed in
personal injury litigation.
• You recognize that to the extent that the Plan paid or will pay benefits under a capitated agreement,
the value of those benefits for purposes of these provisions will be the reasonable value of those
payments or the actual paid amount, whichever is higher.
• You must not do anything to prejudice the Plan's rights under these Subrogation and
Reimbursement provisions. This includes, but is not limited to, refraining from making any settlement
or recovery that attempts to reduce or exclude the full cost of all benefits provided by the Plan.
• You must send the Plan copies of all police reports, notices or other papers received in connection
with the accident or incident resulting in personal injury or illness to You.
67
• You must promptly notify the Plan if You retain an attorney or if a lawsuit is filed on Your behalf.
• You must authorize the Plan to join or intervene into any action by You against a third party.
• You must immediately notify the Plan if a trial is commenced, if a settlement occurs or if potentially
dispositive motions are filed in a case.
In the event that You or Your legal representative fails to do whatever is necessary to enable the Plan to
exercise its rights under these Subrogation and Reimbursement provisions, the Plan shall be entitled to
deduct the amount the Plan paid from any future benefits under the Plan.
If You fail to repay the Plan, the Plan shall be entitled to deduct any of the unsatisfied portion of the amount
of benefits the Plan has paid or the amount of Your Recovery whichever is less, from any future benefit under
the Plan if:
1. The amount the Plan paid on Your behalf is not repaid or otherwise recovered by the Plan; or
2. You fail to cooperate.
In the event You fail to disclose the amount of Your settlement to the Plan, the Plan shall be entitled to deduct
The Plan shall also be entitled to recover any of the unsatisfied portion of the amount the Plan has paid or
the amount of Your Recovery, whichever is less, directly from the Providers to whom the Plan has made
payments on Your behalf. In such a circumstance, it may then be Your obligation to pay the Provider the full
billed amount, and the Plan will not have any obligation to pay the Provider or reimburse You.
You are hereby notified that the Plan Administrator will have the power and authority, in its sole discretion,
to (i) deny payment of any claims for benefits by or on behalf of the Participant and (ii) deny or reduce future
benefits payable (including payment of future benefits for the same or other injuries or illnesses) under the
Plan by the amount due as reimbursement to the Plan. The Plan Administrator may also, in its sole discretion,
deny or reduce future benefits (including future benefits for the same or other injuries or illnesses) under any
other group benefits plan maintained by the Plan Sponsor. The reductions will equal the amount of the
required reimbursement. If the Plan must bring an action against You to enforce the provisions of these
Subro
You acknowledge the Plan has the right to conduct an investigation regarding the injury, illness or condition
to identify potential sources of recovery. The Plan reserves the right to notify all parties and their agents of
its lien. Agents include, but are not limited to, insurance companies and attorneys.
You acknowledge the Plan has notified you that it has the right pursuant to the Health Insurance Portability
et seq, to share Your personal health information in
exercising these Subrogation and Reimbursement provisions.
Subrogation and Reimbursement provisions.
Discretion
The Plan Administrator has sole discretion to interpret the terms of the Subrogation and Reimbursement
provisions of this Plan in its entirety and reserves the right to make changes as it deems necessary.
68
COORDINATION OF BENEFITS
If you are covered by more than one group medical plan, your benefits under this Plan
coordination provisions apply separately to each member, per calendar year, and are largely determined by
California law. Any coverage you have for medical or dental benefits will be coordinated as shown below.
DEFINITIONS
The meanings of key terms used in this section are shown below. Whenever any of the key terms shown
below appear in these provisions, the first letter of each word will be capitalized. When you see these
Allowable Expense is any necessary, reasonable and customary item of expense which is at least partially
covered by any plan covering the person for whom claim is made. When a plan provides benefits in the form
of services rather than cash payments, the reasonable cash value of each service rendered will be deemed
to be both an Allowable Expense and a benefit paid. An expense that is not covered by any plan covering
the person for whom a claim is made is not Allowable Expense.
The following are not Allowable Expense:
1. Use of a private hospital room is not an Allowable Expense unless the patient's stay in a private hospital
room is medically necessary in terms of generally accepted medical practice, or one of the plans routinely
provides coverage for hospital private rooms.
2. If you are covered by two plans that calculate benefits or services on the basis of a reasonable and
customary amount or relative value schedule reimbursement method or some other similar
reimbursement method, any amount in excess of the higher of the reasonable and customary amounts.
3. If a person is covered by two plans that provide benefits or services on the basis of negotiated rates or
fees, an amount in excess of the lower of the negotiated rates.
4. If a person is covered by one plan that calculates its benefits or services on the basis of a reasonable
and customary amount or relative value schedule reimbursement method or some other similar
reimbursement method and another plan provides its benefits or services on the basis of negotiated
rates or fees, any amount in excess of the negotiated rate.
5.
provisions is not an Allowable Expense. Examples of these types of provisions include second surgical
opinions, utilization review requirements, and network provider arrangements.
6. If you advise us that all plans covering you are high deductible health plans as defined by Section 223
of the Internal Revenue Code, and you intend to contribute to a health savings account established in
accordance with Section 223 of the Internal Revenue Code, any amount that is subject to the primary
Other Plan is any of the following:
1. Group, blanket or franchise insurance coverage;
2. Group service plan contract, group practice, group individual practice and other group prepayment
coverages;
3. Group coverage under labor-management trusteed plans, union benefit organization plans, employer
organization plans, employee benefit organization plans or self-insured employee benefit plans.
4. Medicare. This does not include Medicare when, by law, its benefits are secondary to those of any
private insurance program or other non-governmental program.
69
The term "Other Plan" refers separately to each agreement, policy, contract, or other arrangement for
services and benefits, and only to that portion of such agreement, policy, contract, or arrangement which
reserves the right to take the services or benefits of other plans into consideration in determining benefits.
Principal Plan is the plan which will have its benefits determined first.
This Plan is that portion of this plan which provides benefits subject to this provision.
EFFECT ON BENEFITS
benefits under This Plan and any Other Plans, exceed the Allowable Expenses for that calendar year.
1. If This Plan is the Principal Plan, then its benefits will be determined first without taking into account the
benefits or services of any Other Plan.
2. If This Plan is not the Principal Plan, then its benefits may be reduced so that the benefits and services
of all the plans do not exceed Allowable Expense. Benefits of This Plan cannot be determined until the
Principal Plan has completed processing.
3. The benefits of This Plan will never be greater than the sum of the benefits that would have been paid if
you were covered under This Plan only.
ORDER OF BENEFITS DETERMINATION
The first of the following rules which applies will determine the order in which benefits are payable:
1. A plan which has no Coordination of Benefits provision pays before a plan which has a Coordination of
Benefits provision. This would include Medicare in all cases, except when the law requires that This
Plan pays before Medicare.
2. A plan which covers you as a member pays before a plan which covers you as a dependent. But, if you
are retired and eligible for Medicare, Medicare pays (a) after the plan which covers you as a dependent
of an active employee, but (b) before the plan which covers you as a retired employee.
For example: You are covered as a retired employee under This Plan and entitled to Medicare
(Medicare would normally pay first). You are also covered as a dependent of an active employee under
another plan (in which case Medicare would pay second). In this situation, the plan which covers you
as a dependent will pay first, Medicare will pay second, and the plan which covers you as a retired
employee would pay last.
3. For a dependent child covered under plans of two parents, the plan of the parent whose birthday falls
earlier in the calendar year pays before the plan of the parent whose birthday falls later in the calendar
year. But if one plan does not have a birthday rule provision, the provisions of that plan determine the
order of benefits.
Exception to rule 3: For a dependent child of parents who are divorced or separated, the following
rules will be used in place of Rule 3:
a. If the parent with custody of that child for whom a claim has been made has not remarried, then the
plan of the parent with custody that covers that child as a dependent pays first.
b. If the parent with custody of that child for whom a claim has been made has remarried, then the
order in which benefits are paid will be as follows:
i. The plan which covers that child as a dependent of the parent with custody.
ii. The plan which covers that child as a dependent of the stepparent (married to the parent with
custody).
iii. The plan which covers that child as a dependent of the parent without custody.
70
iv. The plan which covers that child as a dependent of the stepparent (married to the parent without
custody).
c. Regardless of a and b above, if there is a court decree which establishes a parent's financial
plan which covers that child as a dependent of
that parent pays first.
4. The plan covering you as a laid-off or retired employee or as a dependent of a laid-off or retired employee
pays after a plan covering you as other than a laid-off or retired employee or the dependent of such a
person. But if either plan does not have a provision regarding laid-off or retired employees, provision 6
applies.
5. The plan covering you under a continuation of coverage provision in accordance with state or federal
law pays after a plan covering you as an employee, a dependent or otherwise, but not under a
continuation of coverage provision in accordance with state or federal law. If the order of benefit
determination provisions of the Other Plan does not agree under these circumstances with the Order of
Benefit Determination provisions of This Plan, this rule will not apply.
6. When the above rules do not establish the order of payment, the plan on which you have been enrolled
the longest pays first unless two of the plans have the same effective date. In this case, Allowable
Expense is split equally between the two plans.
OUR RIGHTS UNDER THIS PROVISION
Responsibility For Timely Notice. UC is not responsible for coordination of benefits unless timely
information has been provided by the requesting party regarding the application of this provision. In addition
to the provisions outlined under Notice of Claim, a copy of the Other Plan Explanation of Benefits is required
for coordination of benefits.
Reasonable Cash Value. If any Other Plan provides benefits in the form of services rather than cash
payment, the reasonable cash value of services provided will be considered Allowable Expense. The
reasonable cash value of such service will be considered a benefit paid, and our liability reduced accordingly.
Facility of Payment. If payments which should have been made under This Plan have been made under
any Other Plan, we have the right to pay that Other Plan any amount we determine to be warranted to satisfy
the intent of this provision. Any such amount will be considered a benefit paid under This Plan, and such
payment will fully satisfy our liability under this provision.
Right of Recovery. If payments made under This Plan exceed the maximum payment necessary to satisfy
the intent of this provision, Anthem or this Plan has the right to recover that excess amount from any persons
or organizations to or for whom those payments were made, or from any insurance company or service plan.
71
BENEFITS FOR MEDICARE ELIGIBLE MEMBERS
If you are entitled to Medicare, you will receive the full Benefits of this Plan, except as listed below:
1. You are receiving treatment for end-stage renal disease following the first 30 months you are entitled to
end-stage renal disease benefits under Medicare; or
2. You are entitled to Medicare benefits as a disabled person, unless you have a current employment status
as determined by Medicare rules through a group of 100 or more employees (according to federal OBRA
legislation).
In cases where exceptions 1 or 2 apply, payment will be determined according to the provisions in the section
entitled COORDINATION OF BENEFITS with
Coordinating Benefits With Medicare. Benefits will not be provided under this Plan that duplicate any
benefits to which you would be entitled under Medicare. This exclusion applies to all parts of Medicare in
which you can enroll without paying additional premium. If you are required to pay additional premium for
any part of Medicare, this exclusion will apply to that part of Medicare only if you are enrolled in that part.
If you are entitled to Medicare, your Medicare coverage will not affect the services covered under this Plan
except as follows:
1. Medicare must provide benefits first to any services covered both by Medicare and under this Plan.
2. For services you receive that are covered both by Medicare and under this Plan, coverage under this
Plan will apply only to Medicare Deductibles and other charges for Covered Services over and above
what Medicare pays.
3. For any given claim, the combination of benefits provided by Medicare and the Benefits provided under
this Plan will not exceed the Maximum Allowed Amount for the Covered Services.
Anthem will apply any charges paid by Medicare for services covered under this Plan toward your Plan
Deductible, if any.
72
UTILIZATION REVIEW PROGRAM
Your Plan includes the process of utilization review to decide when services are Medically Necessary,
Experimental, or Investigative as those terms are defined in this booklet. Utilization review aids the delivery
of cost-effective health care by reviewing the use of treatments and, when proper, level of care and/or the
setting or place of service that they are performed. A service must be Medically Necessary to be a Covered
Service. When level of care, setting or place of service is part of the review, services in a higher level of
care or higher cost setting / place of care will not be Medically Necessary if they can be safely given to you
in a lower level of care or lower cost setting / place of care.
Certain services must be reviewed to determine medical necessity in order for you to get Benefits. Utilization
review criteria will be based on many sources including medical policy and clinical guidelines. Accolade may
decide that a service that was asked for is not Medically Necessary if you have not tried other treatments
that are more cost-effective.
If you have any questions about the information in this section, you may call the Member Services number
on the back of the identification card.
Coverage for or payment of the service or treatment reviewed is not guaranteed. For Benefits to be
covered, on the date you get service:
1. You must be eligible for Benefits;
2. The service or supply must be a Covered Service under your Plan;
3. The service cannot be subject to an exclusion under your Plan (please see Medical Care That Is NOT
Covered for more information); and
4. You must not have exceeded any applicable limits under your Plan.
TYPES OF REVIEWS
• Pre-service Review – A review of a service, treatment or admission for a coverage determination which
is done before the service or treatment begins or admission date.
- Precertification A required pre-service review for a Benefit coverage determination for a service
or treatment. Certain services require precertification in order for you to get Benefits. The Benefit
coverage review will include a review to decide whether the service meets the definition of medical
necessity or is Experimental / Investigative as those terms are defined in this booklet.
For admissions following an Emergency, you, your authorized representative or Physician must tell
the Plan within 48 hours or as soon as it is possible within a reasonable period of time.
For childbirth admissions, precertification is not needed for the first 48 hours for a vaginal delivery
or 96 hours for a cesarean section. Admissions longer than 48/96 hours require precertification.
For inpatient Hospital Stays for mastectomy surgery, including the length of Hospital Stays
associated with mastectomy, precertification is not needed.
• Continued Stay / Concurrent Review – A utilization review of a service, treatment or admission for a
Benefit coverage determination which must be done during an ongoing Stay in a Facility or course of
treatment.
− Both pre-service and continued Stay / concurrent reviews may be considered urgent when, in the
view of the treating Provider or any Physician with knowledge of your medical condition, without
such care or treatment, your life or health or your ability to regain maximum function could be
seriously threatened or you could be subjected to severe pain that cannot be adequately managed
without such care or treatment. Urgent reviews are conducted under a shorter timeframe than
standard reviews.
73
• Post-service Review – A review of a service, treatment or admission for a Benefit coverage that is
conducted after the service has been provided. Post-service reviews are performed when a service,
treatment or admission did not need a precertification, or when a needed precertification was not
obtained. Post-service reviews are done for a service, treatment or admission in which Accolade have
a related clinical coverage guideline and are typically initiated by the Plan.
Services for which precertification is required (i.e., services that need to be reviewed by the Plan to determine
whether they are Medically Necessary) include, but are not limited to, the following:
• Scheduled, non-Emergency inpatient Hospital Stays and Residential Treatment Center admissions,
including detoxification and rehabilitation.
Exceptions: Pre-service review is not required for inpatient Hospital Stays for the following service:
Maternity care of 48 hours or less following a normal delivery or 96 hours or less following a
cesarean section
• Specific non-Emergency outpatient services, including diagnostic treatment and other services.
• Specific outpatient surgeries performed in an outpatient F
• Transplant services, excluding cornea transplant, including transplant travel expense. The following
criteria must be met for certain transplants, as follows:
For bone or skin transplants, if the Physicians on the surgical team and the Facility in which the
transplant is to take place are approved for the transplant requested.
For transplantation of heart, liver, lung, combination heart-lung, kidney, pancreas, simultaneous
pancreas-kidney or bone marrow/stem cell and similar procedures, if the Providers of the related
preoperative and postoperative services are approved and the transplant will be performed at a
Centers of Medical Excellence (CME) or a Blue Distinction Centers for Specialty Care (BDCSC)
Facility.
• Air ambulance in a non-medical Emergency.
• Specific durable medical equipment.
• Oncology and Transplant related infusion therapy / injectable therapy, if the attending Physician has
submitted both a prescription and a plan of treatment before services are rendered.
• Home health care. The following criteria must be met:
The services can be safely provided in your home, as certified by your attending Physician;
Your attending Physician manages and directs your medical care at home; and
Your attending Physician has established a definitive treatment plan which must be consistent
with your medical needs and lists the services to be provided by the Home Health Agency.
• Admissions to a Skilled Nursing Facility if you require daily skilled nursing or rehabilitation, as
certified by your attending Physician.
• Bariatric surgical services, such as gastric bypass and other surgical procedures for weight loss,
including bariatric travel expense, if:
The services are to be performed for the treatment of morbid obesity;
The Physicians on the surgical team and the Facility in which the surgical procedure is to take
place are approved for the surgical procedure requested; and
The bariatric surgical procedure will be performed at a BDCSC Facility.
74
• Advanced imaging procedures, including but not limited to: Magnetic Resonance Imaging (MRI),
Positron Emission Tomography (PET scan), Magnetic Resonance Angiogram (MRA scan). You
may call the Member Services number on the back of the identification card to find out if an imaging
procedure requires pre-service review.
• Partial hospitalization, Intensive Outpatient Programs.
•
Benefits of YOUR MEDICAL BENEFITS - Medical Care That Is Covered. You must be
diagnosed with gender identity disorder or gender dysphoria by a Physician.
For a list of current procedures requiring precertification, please call the Member Services number on
the back of the identification card.
Infertility Treatment - prior authorization by edical Management Program is required prior
to initiation of medical treatment for family building. Contact WINFertility for more information at (877)
451-3077.
75
Who is Responsible for Precertification?
Typically, Anthem Prudent Buyer Providers know which services need precertification and will get any
precertification when needed. Your Physician and other Anthem Prudent Buyer Providers have been given
detailed information about these procedures and are responsible for meeting these requirements. Generally,
the ordering provider, Hospital or attending Physician Plan
to ask for a precertification. However, you may request a precertification or you may choose an authorized
representative to act on your behalf for a specific request. The authorized representative can be anyone
who is 18 years of age or older. The table below outlines who is responsible for precertification and under
what circumstances.
Provider
Network Status
Responsibility to Get
Precertification
Comments
All
Member
• Member must get precertification for Infertility
Treatment regardless of provider network status.
(Call WINFertility at (877) 451-3077)
Anthem Prudent
Buyer Providers
Provider
• The Provider must get precertification when
required.
Out-of-Network
Providers
Member
• Member must get precertification when required.
(Call the Pre-Authorization phone number on the
back of the identification card)
• Member should contact the Pre-Authorization
phone number on the back of the identification
card before seeking care with an Out-of-Network
Provider when outside of the U.S.
• Member may be financially responsible for
charges or costs related to the service and/or
setting in whole or in part if the service and/or
setting is found to not be Medically Necessary.
Blue Card
Provider
Member
(Except for Inpatient
Admissions)
• Member must get precertification when required.
(Call the Pre-Authorization phone number on the
back of the identification card)
• Member may be financially responsible for
charges or costs related to the service and/or
setting in whole or in part if the service and or
setting is found to not be Medically Necessary.
• Blue Card Providers must obtain
precertification for all Inpatient Admissions.
NOTE: For an Emergency admission, precertification is not required. However, you, your
authorized representative or Physician must notify Accolade within 48hours or as soon as it is
possible within a reasonable period of time.
76
How Decisions Are Made
Decisions are based on multiple sources, such as medical policy, clinical guidelines, and other applicable
policies and procedures to help make medical necessity determinations. This includes decisions about
Prescription D
Medical policies and clinical guidelines reflect the standards of practice and medical
interventions identified as proper medical practice. Accolade reserves the right to review and update these
clinical coverage guidelines from time to time.
You are entitled to ask for and get, free of charge, reasonable access to any records concerning your request.
To ask for this information, please call the Member Services number on the back of the identification card.
If you are not satisfied with decision under this section of your BenefitsYOUR
RIGHT TO APPEALS section to see what rights may be available to you.
Decision Notice and Requirements
Accolade will review requests for medical necessity according to the timeframes listed below. The
timeframes and requirements listed are based on state and federal laws. Where state laws are stricter than
federal laws, the Plan will follow state laws. If you live in and/or get services in a state other than the state
where your Plan was issued, other state-specific requirements may apply. You may call the phone number
on the back of your identification card for more details.
Request Category
Timeframe Requirement for Decision
Urgent Pre-Service Review
72 hours from the receipt of the request
Non-Urgent Pre-Service Review
5 business days from the receipt of the request
Urgent Continued Stay / Concurrent Review when
hospitalized at the time of the request and no
previous authorization exists
72 hours from the receipt of the request
Urgent Continued Stay / Concurrent Review when
request is received at least 24 hours before the end
of the previous authorization
72 hours from the receipt of the request
Urgent Continued Stay / Concurrent Review when
request is received less than 24 hours before the
end of the previous authorization
72 hours from the receipt of the request
Non-Urgent Continued Stay / Concurrent Review
5 business days from the receipt of the request
Post-Service Review
30 calendar days from the receipt of the request
If more information is needed to make a decision, Accolade will tell the requesting Physician of the specific
information needed to finish the review. If Accolade does not get the specific information it needs by the
required timeframe identified in the written notice, Accolade will make a decision based upon the information
received.
Accolade will notify you and your Physician of a decision as required by state and federal law. Notice may
be given by one or more of the following methods: verbal, written and/or electronic.
For a copy of the medical necessity review process, please contact the Member Services number on the
back of the identification card.
Revoking or modifying a Precertification Review decision. Accolade will determine in advance whether
certain services (including procedures and admissions) are Medically Necessary and are the appropriate
77
length of Stay, if applicable. These review decisions may be revoked or modified prior to the service being
rendered for reasons including but not limited to the following:
• Your coverage under this Plan ends;
• The agreement with the group terminates;
• You reach a Benefit maximum that applies to the service in question;
• Your Benefits under the Plan change so that the service is no longer covered or is covered in a different
way.
How Accolade Case Management Works
The case management program helps coordinate services for Members with health care needs due to
serious, complex, and/or chronic health conditions. The programs coordinate benefits and educate Members
who agree to take part in the Case Management program to help meet their health-related needs.
The Case Management programs are confidential and voluntary, and are made available at no extra cost to
you. These programs are provided by, or on behalf of and at the request of, your Accolade case
management staff. These Case Management programs are separate from any Covered Services you are
receiving.
If you meet program criteria and agree to take part, then Accolade will help you meet your identified health
care needs. This is reached through contact and team work with you and /or your chosen authorized
representative, treating physicians, and other providers.
In addition, Accolade may assist in coordinating care with existing community-based programs and services
to meet your needs. This may include giving you information about external agencies and community-based
programs and services.
UNIVERSITY OF CALIFORNIA ELIGIBILITY, ENROLLMENT, TERMINATION AND
PLAN ADMINISTRATION PROVISIONS
The University establishes its own medical plan eligibility, enrollment and termination criteria based on the
University of California Group Insurance Regulations and any corresponding Administrative Supplements.
Employees
Information pertaining to your eligibility, enrollment, cancellation or termination of coverage and conversion
options can be found in the . A copy of this booklet is available
in the HR Forms & Publications section of UCnet (ucnet.universityofcalifornia.edu). Additional resources
are also available in the Compensation and Benefits section of UCnet to help you with your health and
welfare plan decisions.
Retirees
Information pertaining to your eligibility, enrollment, cancellation or termination of coverage and conversion
options can be found in the and Eligible Family
Members. A copy of this fact sheet is available in the HR Forms & Publications section of UCnet
(ucnet.universityofcalifornia.edu). Additional resources are also available in the Compensation and
Benefits section of UCnet to help you with your health and welfare plan decisions.
78
CONTINUATION OF COVERAGE
Most employers who employ 20 or more people on a typical business day are subject to The Consolidated
Omnibus Budget Reconciliation Act of 1985 (COBRA). If the employer who provides coverage under the
Plan is subject to the federal law which governs this provision (Title X of P. L. 99-272), you may be entitled
to continuation of coverage. Check with UC for details.
DEFINITIONS
The meanings of key terms used in this section are shown below. Whenever any of the key terms shown
below appear in these provisions, the first letter of each word will appear in capital letters. When you see
these capitalized words, you should refer to
Initial Enrollment Period is the period of time following the original Qualifying Event, as indicated in the
"Terms of COBRA Continuation" provisions below.
Qualified Beneficiary means: (a) a person enrolled for this COBRA continuation coverage who, on the day
before the Qualifying Event, was covered under this Plan as either a Member or Dependent; and (b) a child
who is born to or placed for adoption with the Member during the COBRA continuation period. Qualified
Beneficiary does not include any person who was not enrolled during the Initial Enrollment Period, including
any Dependents acquired during the COBRA continuation period, with the exception of newborns and
adoptees as specified above.
Qualifying Event means any one of the following circumstances which would otherwise result in the
termination of your coverage under the Plan. The events will be referred to throughout this section by
number.
1. For Members and Dependents:
a. The Member termination of employment, for any reason other than gross misconduct; or
b. Loss of coverage under an health plan due to a reduction in the work hours.
2. For Retired Employees and their Dependents. Cancellation or a substantial reduction of retiree
Benefits under the Plan due to the Plan
a. The Plan expressly includes coverage for retirees; and
b. Such cancellation or reduction of Benefits occurs within one Year before or after the filing for
bankruptcy.
3. For Dependents:
a. The death of the Member;
b. The divorce or legal separation from the Member;
c. The end of a partnership with the Member;
d. Dependent child, as defined by the Plan; or
e. The Member
ELIGIBILITY FOR COBRA CONTINUATION
A Member or Dependent may choose to continue coverage under the Plan if his or her coverage would
otherwise end due to a Qualifying Event.
79
TERMS OF COBRA CONTINUATION
Notice. UC will notify either the Member or Dependent of the right to continue coverage under COBRA, as
provided below:
1. For Qualifying Events 1, or 2, UC will notify the Member of the right to continue coverage.
2. For Qualifying Events 3(a) or 3(e) above, a Dependent will be notified of the COBRA continuation right.
3. You must inform UC within 60 days of Qualifying Events 3(b), 3(c), or 3(d) above, if you wish to continue
coverage. UC, in turn, will promptly give you official notice of the COBRA continuation right.
If you choose to continue coverage you must notify UC within 60 days of the date you receive notice of your
COBRA continuation right. The COBRA continuation coverage may be chosen for all Dependents within a
family, or only for selected dependent.
If you fail to elect the COBRA continuation during the Initial Enrollment Period, you may not elect the COBRA
continuation at a later date.
Notice of continued coverage, along with the initial required monthly contribution, must be delivered to us
within 45 days after you elect COBRA continuation coverage.
Additional Dependents. A Spouse, Domestic Partner or child acquired during the COBRA continuation
period is eligible to be enrolled as a Dependent. The standard enrollment provisions of the Plan apply to
enrollees during the COBRA continuation period.
Cost of Coverage. UC may require that you pay the entire cost of your COBRA continuation coverage.
This cost, called the "required monthly contribution", must be remitted to UC each month during the COBRA
continuation period in order to maintain the coverage in force.
Besides applying to the Member, the Member
1. A Spouse whose COBRA continuation began due to divorce, separation or death of the Member;
2. A Domestic Partner whose COBRA continuation began due to the end of the domestic partnership or
death of the Member;
3 A child, if neither the Member nor the Spouse has enrolled for this COBRA continuation coverage (if
more than one child is so enrolled, the required monthly contribution will be the two-party or three-party
rate depending on the number of children enrolled); and
4. A child whose COBRA continuation began due to the person no longer meeting the Dependent child
definition.
Subsequent Qualifying Events. Once covered under the COBRA continuation, it's possible for a second
Qualifying Event to occur. If that happens, a Member or Dependent, who is a Qualified Beneficiary, may be
entitled to an extended COBRA continuation period. This period will in no event continue beyond 36 months
from the date of the first qualifying event.
For example, a child may have been originally eligible for this COBRA continuation due to termination of the
employment, and enrolled for this COBRA continuation as a Qualified Beneficiary. If, during the
COBRA continuation period, the child reaches the upper age limit of the Plan, the child is eligible for an
extended continuation period which would end no later than 36 months from the date of the original Qualifying
Event (the termination of employment).
When COBRA Continuation Coverage Begins. When COBRA continuation coverage is elected during
the Initial Enrollment Period and the required monthly contribution is paid, coverage is reinstated back to the
date of the original Qualifying Event, so that no break in coverage occurs.
For Dependents properly enrolled during the COBRA continuation, coverage begins according to the
enrollment provisions of the Plan.

80
When the COBRA Continuation Ends. This COBRA continuation will end on the earliest of:
1. The end of 18 months from the Qualifying Event, if the Qualifying Event was termination of employment
or reduction in work hours;*
2. The end of 36 months from the Qualifying Event, if the Qualifying Event was the death of the Member,
divorce or legal separation, the end of a domestic partnership, or the end of Dependent child status;*
3. The end of 36 months from the date the Member became entitled to Medicare, if the Qualifying Event
was the entitlement to Medicare. If entitlement to Medicare does not result in coverage
terminating and Qualifying Event 1 occurs within 18 months after Medicare entitlement, coverage for
Qualified Beneficiaries other than the Member will end 36 months from the date the Member became
entitled to Medicare;
4. The date the Plan terminates;
5. The end of the period for which required monthly contributions are last paid;
6. The date, following the election of COBRA, the Member first becomes covered under any other group
health plan; or
7. The date, following the election of COBRA, the Member first becomes entitled to Medicare. However,
entitlement to Medicare will not preclude a person from continuing coverage which the person became
eligible for due to Qualifying Event 2.
Subject to the Plan remaining in effect, a retired employee whose COBRA continuation coverage began due
to Qualifying Event 2 may be covered for the remainder of his or her life; that person's covered Dependents
may continue coverage for 36 months after the death. However, coverage could terminate prior
to such time for either Member or Dependent in accordance with items 4, 5 or 6 above.
Other Coverage Options Besides COBRA Continuation Coverage. Instead of enrolling in COBRA
continuation coverage, there may be other coverage options for you and your family through the Health
Insurance Marketplace, Medicaid, or other group health plan coverage options. Some of these options may
cost less than COBRA continuation coverage. You can learn more about many of these options at
www.healthcare.gov.
EXTENSION OF CONTINUATION DURING TOTAL DISABILITY
If at the time of termination of employment or reduction in hours, or at any time during the first 60 days of the
COBRA continuation, a Qualified Beneficiary is determined to be disabled for Social Security purposes, all
covered Members may be entitled to up to 29 months of continuation coverage after the original Qualifying
Event.
Eligibility for Extension. To continue coverage for up to 29 months from the date of the original Qualifying
Event, the disabled Member must:
1. Satisfy the legal requirements for being totally and permanently disabled under the Social Security Act;
and
2. Be determined and certified to be so disabled by the Social Security Administration.
Notice. The Member must furnish UC with proof of the Social Security Administration's determination of
disability during the first 18 months of the COBRA continuation period and no later than 60 days after the
later of the following events:
1. The date of the Social Security Administration's determination of the disability;
2. The date on which the original Qualifying Event occurs;
3. The date on which the Qualified Beneficiary loses coverage; or
4. The date on which the Qualified Beneficiary is informed of the obligation to provide the disability notice.
81
Cost of Coverage. For the 19th through 29th months that the total disability continues, the cost for the
extended continuation coverage must be remitted to UC or its administrator. This cost (called the "required
monthly contribution") shall be subject to the following conditions:
1. If the disabled Member continues coverage during this extension, this charge shall be 150% of the
applicable rate for the length of time the disabled Member remains covered, depending upon the number
of covered Dependents. If the disabled Member does not continue coverage during this extension, this
charge shall remain at 102% of the applicable rate.
2. The cost for extended continuation coverage must be remitted to UC or its administrator each month
during the period of extended continuation coverage. UC or its administrator must receive timely
payment of the required monthly contribution in order to maintain the extended continuation coverage in
force.
3. You may be required to pay the entire cost of the extended continuation coverage.
If a second Qualifying Event occurs during this extended continuation, the total COBRA continuation may
continue for up to 36 months from the date of the first Qualifying Event. The required monthly contribution
shall then be 150% of the applicable rate for the 19th through 36th months if the disabled Member remains
covered. The charge will be 102% of the applicable rate for any periods of time the disabled Member is not
covered following the 18th month.
When The Extension Ends. This extension will end at the earlier of:
1. The end of the month following a period of 30 days after the Social Security Administration's final
determination that you are no longer totally disabled;
2. The end of 29 months from the Qualifying Event*;
3. The date the Plan terminates;
4. The end of the period for which required monthly contributions are last paid;
5. The date, following the election of COBRA, the Member first becomes covered under any other group
health plan; or
6. The date, following the election of COBRA, the Member first becomes entitled to Medicare. However,
entitlement to Medicare will not preclude a person from continuing coverage which the person became
eligible for due to Qualifying Event 2.
You must inform UC within 30 days of a final determination by the Social Security Administration that you
are no longer totally disabled.
82
GENERAL PROVISIONS
Providing of Care. We are not responsible for providing any type of Hospital, medical or similar care, nor
are we responsible for the quality of any such care received.
Independent Contractors. Anthem Providers is that of an independent contractor.
Physicians, and other health care professionals, Hospitals, Skilled Nursing Facilities and other community
agencies are not agents nor are they, or any of their employees, an employee or agent of any
Hospital, medical group or medical care Provider of any type.
Non-Regulation of Providers. The Benefits of this Plan do not regulate the amounts charged by Providers
of medical care, except to the extent that the rates for Covered Services are regulated with Anthem Prudent
Buyer Providers.
Inter-Plan Arrangements
Out-of-Area Services
Overview. We have a variety of relationships with other Blue Cross and/or Blue Shield Licensees. Generally,
-Plan Arrangements. These Inter-Plan Arrangements work based on
Anthem Blue Cross
the claim for those services may be processed through one of these Inter-Plan Arrangements. The Inter-
Plan Arrangements are described below.
When you receive care outside of the Anthem Blue Cross Service Area, you will receive it from one of two
kinds of providers. Most providers
providers -
contract with the Host Blue. We explain below how we pay both kinds of providers.
Inter-Plan Arrangements Eligibility – Claim Types
Most claim types are eligible to be processed through Inter-Plan Arrangements, as described above.
Examples of claims that are not included are prescription drugs that you obtain from a pharmacy and most
dental or vision benefits.
A. BlueCard® Program
Under the BlueCard® Program, when you receive Covered Services within the geographic area served by
a Host Blue, we will still fulfill our contractual obligations. But, the Host Blue is responsible for: (a) contracting
with its providers; and (b) handling its interactions with those providers.
When you receive Covered Services outside the Anthem Blue Cross Service Area and the claim is processed
through the BlueCard Program, the amount you pay is calculated based on the lower of:
- The billed charges for Covered Services; or
- The negotiated price that the Host Blue makes available to Anthem.
the provider. Sometimes, it is an estimated price that takes into account special arrangements with that
provider. Sometimes, such an arrangement may be an average price, based on a discount that results in
expected average savings for services provided by similar types of providers. Estimated and average pricing
arrangements may also involve types of settlements, incentive payments and/or other credits or charges.
Estimated pricing and average pricing also take into account adjustments to correct for over- or
underestimation of past pricing of claims, as noted above. However, such adjustments will not affect the
price we used for your claim because they will not be applied after a claim has already been paid.
83
B. Negotiated (non–BlueCard Program) Arrangements
With respect to one or more Host Blues, instead of using the BlueCard Program, Anthem Blue Cross may
process your claims for Covered Services through Negotiated Arrangements for National Accounts.
The amount you pay for Covered Services under this arrangement will be calculated based on the lower of
either billed charges for Covered Services or the negotiated price (refer to the description of negotiated price
under Section A. BlueCard Program) made available to Anthem Blue Cross by the Host Blue.
C. Special Cases: Value-Based Programs
BlueCard® Program
If you receive Covered Services under a Value-
not be responsible for paying any of the Provider Incentives, risk-sharing, and/or Care Coordinator Fees that
are a part of such an arrangement, except when a Host Blue passes these fees to Anthem Blue Cross
through average pricing or fee schedule adjustments. Additional information is available upon request.
Value-Based Programs: Negotiated (nonBlueCard Program) Arrangements
If Anthem Blue Cross has entered into a Negotiated Arrangement with a Host Blue to provide Value-Based
Programs to the group on your behalf, Anthem Blue Cross will follow the same procedures for Value-Based
Programs administration and Care Coordinator Fees as noted above for the BlueCard Program.
D. Inter-Plan Programs: Federal/State Taxes/Surcharges/Fees
Federal or state laws or regulations may require a surcharge, tax or other fee. If applicable, we will include
any such surcharge, tax or other fee as part of the claim charge passed on to you.
E. Non-participating Providers Outside Our Service Area
1. Allowed Amounts and Member Liability Calculation
When Covered Services are provided outside of Anthem Blue Cross -
participating providers, we may determine benefits and make payment based on pricing from either
the Host Blue or the pricing arrangements required by applicable state or federal law. In these
situations, the amount you pay for such services as a Deductible or Copayment will be based on that
allowed amount. Also, you may be responsible for the difference between the amount that the non-
participating provider bills and the payment we will make for the Covered Services as set forth in this
paragraph. Federal or state law, as applicable, will govern payments for out-of-network Emergency
Services.
2. Exceptions
In certain situations, we may use other pricing methods, such as billed charges or the pricing we
would use if the healthcare services had been obtained within the Anthem Blue Cross Service Area,
or a special negotiated price to determine the amount we will pay for services provided by non-
participating providers. In these situations, you may be liable for the difference between the amount
that the non-participating provider bills and the payment we make for the Covered Services as set
forth in this paragraph.
F. Blue Cross Blue Shield Global Core® Program
If you plan to travel outside the United States, call the Member Services number on the back of the
identification card to find out your Blue Cross Blue Shield Global Core benefits. Benefits for services received
outside of the United States may be different from services received in the United States. Remember to take
an up to date health identification card with you.
When you are traveling abroad and need medical care, you can call the Blue Cross Blue Shield Global Core
Service Center any time. They are available 24 hours a day, seven days a week. The toll free number is
(800) 810-BLUE (2583). Or you can call them collect at (804) 673-1177.

84
If you need inpatient Hospital care, you or someone on your behalf, should contact Accolade for
preauthorization. Keep in mind, if you need Emergency medical care, go to the nearest Hospital. There is
no need to call before you receive care.
Please refer to the UTILIZATION REVIEW PROGRAM section in this booklet for further information. You
can learn how to get pre-authorization when you need to be admitted to the Hospital for Emergency or non-
Emergency care.
How Claims are Paid with Blue Cross Blue Shield Global Core
In most cases, when you arrange inpatient Hospital care with Blue Cross Blue Shield Global Core, claims
will be filed for you. The only amounts that you may need to pay up front are any Copayment or Deductible
amounts that may apply.
You will typically need to pay for the following services up front:
- Physician services;
- Inpatient Hospital care not arranged through Blue Cross Blue Shield Global Core; and
- Outpatient services.
You will need to file a claim form for any payments made up front.
When you need Blue Cross Blue Shield Global Core claim forms you can get international claims forms in
the following ways:
- Call the Blue Cross Blue Shield Global Core Service Center at the numbers above; or
- Online at www.bcbsglobalcore.com.
You will find the address for mailing the claim on the form. Please also refer to the Notice of Claim section
within this booklet for additional details.
Terms of Coverage
1. In order for you to be entitled to Benefits under the Plan, both the Plan and your coverage under the
Plan must be in effect on the date the expense giving rise to a claim for Benefits is Incurred.
2. The Benefits to which you may be entitled will depend on the terms of coverage in effect on the date the
expense giving rise to a claim for Benefits is Incurred. An expense is Incurred on the date you receive
the service or supply for which the charge is made.
3. The Plan is subject to amendment, modification or termination according to the provisions of the Plan
without your consent or concurrence.
Nondiscrimination. No person who is eligible to enroll will be refused enrollment based on health status,
health care needs, genetic information, previous medical information, disability, sexual orientation or identity,
gender, or age.
Protection of Coverage. UC does not have the right to cancel your coverage under this Plan while: (1)
this Plan is in effect; (2) you are eligible; and (3) your required monthly contributions are paid according to
the terms of the Plan.
Free Choice of Provider. This Plan in no way interferes with your right as a Member entitled to Hospital
Benefits to select a Hospital. You may choose any Physician who holds a valid Physician and surgeon's
certificate and who is a member of, or acceptable to, the attending staff and board of directors of the Hospital
where services are received. You may also choose any other health care professional or Facility which
provides care covered under this Plan, and is properly licensed according to appropriate state and local laws.
However, your choice may affect the Benefits payable according to this Plan.
Provider Reimbursement. Physicians and other professional Providers are paid on a fee-for-service basis,
according to an agreed schedule. A participating Physician may, after notice from Anthem, be subject to a

85
reduced negotiated rate in the event the participating Physician fails to make routine referrals to Anthem
Prudent Buyer Providers, except as otherwise allowed (such as for Emergency Services). Hospitals and
other health care facilities may be paid either a fixed fee or on a discounted fee-for-service basis.
Other forms of payment arrangement are Payment Innovation Programs. These programs may include
financial incentives to help improve quality of care and promote the delivery of health care services in a cost-
efficient manner. The programs may vary in methodology and subject area of focus and may be modified
by UC from time to time, but they will be generally designed to tie a certain portion of an Anthem Prudent
Buyer Provider-defined quality, cost, efficiency or service standards or metrics.
In some instances, Anthem Prudent Buyer Provider may be required to make payment to the Plan under the
program as a consequence of failing to meet these pre-defined standards. The programs are not intended
to affect the access to health care. The program payments are not made as payment for specific
Covered Services provided to the Member, but instead, are based on the Anthem Prudent Buyer s
achievement of these pre-defined standards. The Member is not responsible for any Copayment amounts
related to payments made by the Plan or to the Plan under the programs and the Member does not share in
any payments made by Anthem Prudent Buyer Providers to the Plan under the programs.
Availability of Care. If there is an epidemic or public disaster and you cannot obtain care for Covered
Services, we refund the unearned part of the required monthly contribution paid. A written request for that
refund and satisfactory proof of the need for care must be sent to us within 31 days of date of service. This
payment fulfills our obligation under this Plan.
Medical Necessity. The Benefits of this Plan are provided only for services which Accolade determines to
be Medically Necessary. The services must be ordered by the attending Physician for the direct care and
treatment of a covered condition. They must be standard medical practice where received for the condition
being treated and must be legal in the United States. The process used to authorize or deny health care
services under this Plan is available to you upon request.
Expense in Excess of Benefits. We are not liable for any expense you incur in excess of the Benefits of
this Plan.
Benefits Not Transferable. Only the Member is entitled to receive Benefits under this Plan. The right to
Benefits cannot be transferred.
Notice of Claim. You must send Anthem properly and fully completed claim forms within 90 days of the
date you receive the service or supply for which a claim is made. If it is not reasonably possible to submit
the claim within that time frame, an extension of up to 12 months will be allowed. UC is not liable for the
Benefits of the Plan if you do not file claims within the required time period. UC will not be liable for Benefits
if Anthem does not receive written proof of loss on time.
Services received and charges for the services must be itemized, and clearly and accurately described
including the Tax ID and National Provider Identifier of the provider(s) who rendered each service. Claim
forms must be used; canceled checks or receipts are not acceptable.
To obtain a claim form you or someone on your behalf may call the Member Services number on the back
of the identification card or go to the website at www.anthem.com/ca and download and print one.
Payment to Providers. The Benefits of this Plan will be paid directly to contracting Hospitals, Anthem
Prudent Buyer Providers and medical transportation providers. If you or one of your Dependents receives
services from non-contracting Hospitals or Out-of-Network Providers, payment may be made directly to the
Member and you will be responsible for payment to the provider. Any assignment of Benefits, even if
Authorized Referral has been
approved by Anthem. The Plan will pay non-contracting Hospitals and other Providers of service directly
when Emergency Services and care are provided to you or one of your Dependents. The Plan will continue
such direct payment until the Emergency care results in stabilization. If you are a MediCal beneficiary and
you assign Benefits in writing to the State Department of Health Services, the Benefits of this Plan will be
paid to the State Department of Health Services. These payments will fulfill the obligation to you for
those Covered Services.
86
Care Coordination. The Plan pays Anthem Prudent Buyer Providers in various ways to provide Covered
Services to you. For example, sometimes Anthem Prudent Buyer Providers are paid a separate amount for
each Covered Service they provide. The Plan may also pay one amount for all Covered Services related to
treatment of a medical condition. Other times, a periodic, fixed pre-determined amount may be paid to cover
the costs of Covered Services. In addition, the Plan may pay Anthem Prudent Buyer Providers financial
incentives or other amounts to help improve quality of care and/or promote the delivery of health care
services in a cost-efficient manner, or compensate Anthem Prudent Buyer Providers for coordination of your
care. In some instances, Anthem Prudent Buyer Providers may be required to make payment to the Plan
because they did not meet certain standards. You do not share in any payments made by Anthem Prudent
Buyer Providers to the Plan under these programs.
Right of Recovery. Whenever payment has been made in error, Anthem will have the right to recover such
payment from you or, if applicable, the provider, in accordance with applicable laws and regulations. In the
event Anthem recovers a payment made in error from the provider, except in cases of fraud or
misrepresentation on the part of the provider, Anthem will only recover such payment from the Provider
within 365 days of the date the payment was made on a claim submitted by the provider. Anthem reserves
the right to deduct or offset any amounts paid in error from any pending or future claim.
Under certain circumstances, if Anthem pays your healthcare Provider amounts that are your responsibility,
such as Deductibles or Copayments Anthem may collect such amounts directly from you. You agree that
Anthem has the right to recover such amounts from you.
Anthem has oversight responsibility for compliance with Provider and vendor and subcontractor contracts.
Anthem may enter into a settlement or compromise regarding enforcement of these contracts and may retain
any recoveries made from a provider, vendor, or subcontractor resulting from these audits if the return of the
overpayment is not feasible.
Anthem has established recovery policies to determine which recoveries are to be pursued, when to incur
costs and expenses, and whether to settle or compromise recovery amounts. Anthem will not pursue
recoveries for overpayments if the cost of collection exceeds the overpayment amount. Anthem may not
provide you with notice of overpayments made by the Plan or you if the recovery method makes providing
such notice administratively burdensome.
Plan Administrator - COBRA. In no event will Anthem be Plan Administrator for the purposes of compliance
with the Consolidated Omnibus Budget Reconciliation Act (COBRA). The term "Plan Administrator" refers
to the University of California Executive Steering Committee on Health Benefits Programs or to a person or
entity other than Anthem, engaged by to perform or assist in performing administrative tasks in connection
with the Plan. In providing notices and otherwise performing under the CONTINUATION OF COVERAGE
section of this Benefit Booklet, UC is fulfilling statutory obligations imposed on it by federal law and, where
applicable, acting as your agent.
Workers’ Compensation Insurance. The Plan
compensation insurance. It also does not replace that insurance.
Prepayment Fees. UC may require that you contribute all or part of the costs of the required monthly
contributions. Please consult UC for details.
Financial Arrangements with Providers. Anthem or an affiliate has contracts with certain health care
providers in this section) for the provision of and
payment for health care services rendered to its members and members entitled to health care benefits
under individual certificates and group policies or contracts to which Anthem or an affiliate is a party, including
all persons covered under the Plan.
87
Under the above-referenced contracts between Providers and Anthem or an affiliate, the negotiated rates
paid for certain medical services provided to persons covered under the Plan may differ from the rates paid
for persons covered by other types of products or programs offered by Anthem or an affiliate for the same
medical services. In negotiating the terms of the Plan, UC was aware that Anthem or its affiliates offer
several types of products and programs. The Members and UC are entitled to receive the Benefits of only
those discounts, payments, settlements, incentives, adjustments and/or allowances specifically set forth in
the Plan.
Also, under arrangements with some Providers certain discounts, payments, rebates, settlements,
incentives, adjustments and/or allowances, including, but not limited to, pharmacy rebates, may be based
on aggregate payments made by Anthem or an affiliate in respect to all health care services rendered to all
persons who have coverage through a program provided or administered by Anthem or an affiliate. They
are not attributed to specific claims or plans and do not inure to the benefit of any covered individual or group,
but may be considered by Anthem or an affiliate in determining its fees or subscription charges or premiums.
Transition Assistance for New Members: Transition Assistance is a process that allows for completion of
Covered Services for new Members receiving services from an Out-of-Network Provider. If you are a new
Member, you may request Transition Assistance if any one of the following conditions applies:
1. An acute condition. An acute condition is a medical condition that involves a sudden onset of symptoms
due to an illness, injury, or other medical problem that requires prompt medical attention and that has a
limited duration. Completion of Covered Services shall be provided for the duration of the acute
condition.
2. A serious chronic condition. A serious chronic condition is a medical condition caused by a disease,
illness, or other medical problem or medical disorder that is serious in nature and that persists without
full cure or worsens over an extended period of time or requires ongoing treatment to maintain remission
or prevent deterioration. Completion of Covered Services shall be provided for a period of time
necessary to complete a course of treatment and to arrange for a safe transfer to another provider, as
determined by Anthem in consultation with you and the Out-of-Network Provider and consistent with
good professional practice. Completion of Covered Services shall not exceed twelve (12) months from
the time you enroll in this Plan.
3. A pregnancy. A pregnancy is the three trimesters of pregnancy and the immediate postpartum period.
Completion of Covered Services shall be provided for the duration of the pregnancy.
4. A terminal illness. A terminal illness is an incurable or irreversible condition that has a high probability
of causing death within one (1) year or less. Completion of Covered Services shall be provided for the
duration of the terminal illness.
5. The care of a newborn child between birth and age thirty-six (36) months. Completion of Covered
Services shall not exceed twelve (12) months from the time the child enrolls in this Plan.
6. Performance of a surgery or other procedure that Accolade has authorized as part of a documented
course of treatment and that has been recommended and documented by the Provider to occur within
180 days of the time you enroll in this Plan.
Please contact the Member Services number on the back of the identification card to request Transition
Assistance or to obtain a copy of the written policy. Eligibility is based on your clinical condition and is not
determined by diagnostic classifications. Transition Assistance does not provide coverage for services not
otherwise covered under the Plan.
You will be notified by telephone, and the Provider by telephone and fax, as to whether or not your request
for Transition Assistance is approved. If approved, you will be financially responsible only for applicable
Deductibles and Copayments under the Plan. Financial arrangements with Out-of-Network Providers are
negotiated on a case-by-case basis. The Out-of-Network Provider will be asked to agree to accept
reimbursement and contractual requirements that apply to Anthem Prudent Buyer Providers, including
payment terms. If the Out-of-Network Provider does not agree to accept said reimbursement and contractual
88
requirements, the Out-of- services will not be continued. If you do not meet the criteria
for Transition Assistance, you are afforded due process including having a Physician review the request.
Continuity of Care after Termination of Provider: Subject to the terms and conditions set forth below,
Benefits will be provided at the Anthem Prudent Buyer Provider level for Covered Services (subject to
applicable Copayments, Deductibles and other terms) received from a Provider at the time the provider's
contract with Anthem terminates (unless the provider's contract terminates for reasons of medical disciplinary
cause or reason, fraud, or other criminal activity). If your Physician leaves our network for any reason other
than termination of cause, or if coverage under this plan ends because your group’s agreement ends, or
because your group changes plans, and you are in active treatment, you may be able to continue seeing
that provider for a limited period of time and still get the In-Network benefits.
You must be under the care of the Anthem Prudent Buyer Provider
terminates. The terminated Provider must agree in writing to provide services to you in accordance with the
terms and conditions of his or her agreement with Anthem prior to termination. The Provider must also agree
in writing to accept the terms and reimbursement rates under his or her agreement with Anthem prior to
termination. If the Provider does not agree with these contractual terms and conditions,
services will not be continued beyond the contract termination date.
Benefits for the completion of Covered Services by a terminated Provider will be provided only for the
following conditions:
1. An acute condition. An acute condition is a medical condition that involves a sudden onset of symptoms
due to an illness, injury, or other medical problem that requires prompt medical attention and that has a
limited duration. Completion of Covered Services shall be provided for the duration of the acute
condition.
2. A serious chronic condition. A serious chronic condition is a medical condition caused by a disease,
illness, or other medical problem or medical disorder that is serious in nature and that persists without
full cure or worsens over an extended period of time or requires ongoing treatment to maintain remission
or prevent deterioration. Completion of Covered Services shall be provided for a period of time
necessary to complete a course of treatment and to arrange for a safe transfer to another provider, as
determined by Anthem in consultation with you and the terminated Provider and consistent with good
professional practice. Completion of Covered Services shall not exceed twelve (12) months from the
date the provider's contract terminates.
3. A pregnancy. A pregnancy is the three trimesters of pregnancy and the immediate postpartum period.
Completion of Covered Services shall be provided for the duration of the pregnancy.
4. A terminal illness. A terminal illness is an incurable or irreversible condition that has a high probability
of causing death within one (1) year or less. Completion of Covered Services shall be provided for the
duration of the terminal illness.
5. The care of a newborn child between birth and age thirty-six (36) months. Completion of Covered
Services shall not exceed twelve (12) months from the date the provider's contract terminates.
6. Performance of a surgery or other procedure that Accolade has authorized as part of a documented
course of treatment and that has been recommended and documented by the Provider to occur within
180 days of the date the provider's contract terminates.
Such Benefits will not apply to Providers who have been terminated due to medical disciplinary cause or
reason, fraud, or other criminal activity.
Please contact the Member Services number on the back of the identification card to request continuity of
care or to obtain a copy of the written policy. Eligibility is based on your clinical condition and is not
determined by diagnostic classifications. Continuity of care does not provide coverage for services not
otherwise covered under the Plan.
You will be notified by telephone, and the Provider by telephone and fax, as to whether or not your request
for continuity of care is approved. If approved, you will be financially responsible only for applicable
89
Deductibles and Copayments under the Plan. Financial arrangements with terminated Providers are
negotiated on a case-by-case basis. The terminated Provider will be asked to agree to accept
reimbursement and contractual requirements that apply to Anthem Prudent Buyer Providers, including
payment terms. If the terminated Provider does not agree to accept the same reimbursement and contractual
continuity of care, you may file complaint as described in the COMPLAINT NOTICE.
Policies, Procedures, and Pilot Programs. We are able to introduce new policies, procedures, rules and
interpretations, as long as they are reasonable. Such changes are introduced to make the plan more orderly
and efficient. Members must follow and accept any new policies, procedures, rules, and interpretations.
Under the terms of the agreement, we have the authority to introduce or terminate from time to time, pilot or
test programs for disease management, care management, case management, clinical quality or wellness
initiatives which may result in the payment of benefits not otherwise specified in this booklet. We reserve
the right to discontinue a pilot or test program at any time.
Program Incentives. UC may offer incentives from time to time at its discretion in order to introduce you to
new programs and services available under this Plan. UC may also offer the ability for you to participate in
certain voluntary health or condition-focused digital applications or use other technology based interactive
tool, or receive educational information in order to help you stay engaged and motivated, manage your
health, and assist in your overall health and well-being. The purpose of these programs and incentives
include, but are not limited to, making you aware of cost effective Benefit options or services, helping you
achieve your best health, and encouraging you to update Member-related information. These incentives
may be offered in various forms such as retailer coupons, gift cards and health-related merchandise.
Acceptance of these incentives is voluntary as long as the Plan offers the incentives program. Motivational
rewards, awards or points for achieving certain milestones may be a feature of the program. UC may
discontinue an incentive for a particular new service or program at any time. If you have any questions about
whether receipt of an incentive or retailer coupon results in taxable income to you, please consult your tax
advisor.

90
Plan Notice of Privacy Practices for Anthem*
Notice of Privacy Practices
The Health Insurance Portability and Accountability Act of 1996 (HIPAA) is a federal law governing the
privacy of individually identifiable health information. Anthem is required by HIPAA to notify you of the
availability of its Notice of Privacy Practices. The notice describes the privacy practices, legal duties and
your rights concerning your Protected Health Information. Anthem must follow the privacy practices
described in the notice while it is in effect (it will remain in effect unless and until Anthem publishes and
issues a new notice).
Anthem may collect, use and share your Protected Health Information (PHI) for the following reasons and
others as allowed or required by law, including the HIPAA Privacy Rule:
For payment: use and share PHI to manage your account or Benefits; or to pay claims for health care you
get through your Plan.
For health care operations: use and share PHI for health care operations.
For treatment activities: do not provide treatment. This is the role of a health care provider, such as your
doctor or a Hospital. Examples of ways Anthem uses your information for payment, treatment and health
care operations:
o keep information about your premium and Deductible payments.
o Benefits.
o may share explanation of benefits (EOB) with the Member of your Plan for payment purposes.
o may share PHI with your health care Provider so that the Provider may treat you.
o may use PHI to review the quality of care and services you get.
o may use PHI to provide you with case management or care coordination services for conditions like
asthma, diabetes or traumatic injury.
o may also use and share PHI directly or indirectly with or through health information exchanges for
payment, health care operations and treatment. If you do not want your PHI to be shared for
payment, health care operations, or treatment purposes in health information exchanges, please
visit https://www.anthem.com/ca/privacy for more information.
Anthem, including our affiliates or vendors, may call or text any telephone numbers provided by you using
an automated telephone dialing system and/or a prerecorded message. Without limitation, these calls may
concern treatment options, other health-related Benefits and services, enrollment, payment, or billing.
You may obtain a full copy of the Notice of Privacy Practices at https://www.anthem.com/ca/privacy or you
may contact the Member Services number on the back of the identification card.
*Business Associate to the UC Health Savings Plan
Notice of Privacy Practice for Plan
A copy of the University of California Healthcare Plan Notice of Privacy Practices- Self-Funded Plans
(Notice) that applies to your Plan can be found at ucal.us/hipaa or you may obtain a paper copy of the UC
Notice by calling the UC Healthcare Plan Privacy Office at 800-888-8267, press 1.
91
BINDING ARBITRATION
A dispute regarding a claim for Benefits, including prescription drug benefits administered as a Covered
Service, must proceed first through the claims process described in YOUR RIGHT TO APPEALS section
before any further legal action can be taken with respect to that claim. Otherwise any dispute or claim, of
whatever nature, including a claim for Benefits that has completed the internal appeals process, that arises
out of, in connection with, or in relation to this Plan, or breach or rescission thereof, or in relation to care or
delivery of care, including any claim based on contract, tort or statute, must be resolved by arbitration if the
amount sought exceeds the jurisdictional limit of the small claims court.
Any dispute regarding a claim for damages within the jurisdictional limits of the small claims court will be
resolved in such court.
The Federal Arbitration Act shall govern the interpretation and enforcement of all proceedings under this
BINDING ARBITRATION provision. To the extent that the Federal Arbitration Act is inapplicable, or is held
not to require arbitration of a particular claim, state law governing agreements to arbitrate shall apply.
The Member and UC agree to be bound by this Binding Arbitration provision and acknowledge that they are
each giving up their right to a trial by court or jury.
The Member and UC agree to give up the right to participate in class arbitration against each other. Even if
applicable law permits class actions or class arbitrations, the Member waives any right to pursue, on a class
basis, any such controversy or claim against UC and UC waives any right to pursue on a class basis any
such controversy or claim against the Member.
The arbitration findings will be final and binding except to the extent that state or Federal law provides for
the judicial review of arbitration proceedings.
The arbitration is begun by the Member making written demand on UC. The arbitration will be conducted by
for any reason, JAMS is unavailable to conduct the arbitration, the arbitration will be conducted by another
neutral arbitration entity, by mutual agreement of the Member and UC, or by order of the court, if the Member
and UC cannot agree that has completed the internal appeals process.
92
DEFINITIONS
The meanings of key terms used in this booklet are shown below. Whenever any of the key terms shown
below appears in these provisions, the first letter of each word will be capitalized. When you see these
capitalized words, you should refer to this section.
Accidental Injury is physical harm or disability which is the result of a specific unexpected incident caused
by an outside force. The physical harm or disability must have occurred at an identifiable time and place.
Accidental Injury does not include illness or infection, except infection of a cut or wound.
Ambulatory surgical center is a Facility licensed as an ambulatory surgery center as required by law that
satisfies our accreditation requirements and is approved by us.
Anthem Prudent Buyer Provider is one of the following Providers or other licensed health care
professionals who have a Prudent Buyer Plan Participating Provider Agreement in effect with Anthem or is
participating in a Blue Cross and/or Blue Shield Plan at the time services are rendered:
• A Hospital
• A Physician
• An Ambulatory Surgical Center
• A Home Health Agency
• A Facility which provides diagnostic imaging services
• A durable medical equipment outlet
• A Skilled Nursing Facility
• A clinical laboratory
• A home infusion/home injection therapy provider
• An Urgent Care Center
• Centers for Medical Excellence (CME)
• Blue Distinction Centers for Specialty Care (BDCSC)
• A Retail Health Clinic
• A Hospice
• A licensed ambulance company
• A licensed qualified autism service provider
Anthem Prudent Buyer Providers agree to accept the Maximum Allowed Amount as payment for Covered
Services. A directory of Anthem Prudent Buyer Provider is available upon request.
Authorized Referral occurs when you, because of your medical needs, require the services of a specialist
who is an Out-of-Network Provider, or require special services or facilities not available at a contracting
Hospital, but only when the referral has been authorized by Accolade before services are rendered and when
the following conditions are met:
1. there is no Anthem Prudent Buyer Provider who practices in the appropriate specialty, or there is no
contracting Hospital which provides the required services or has the necessary facilities;
2. that meets the adequacy and accessibility requirements of state or federal law.
3. the Member is referred to Hospital or Physician that does not have an agreement with Anthem for
a Covered Service by an Anthem Prudent Buyer Provider.
Benefits for Medically Necessary and appropriate Authorized Referral services received from an Out-of-
Network Provider will be payable as shown in the Medical Benefit Summary Notes.
You or your Physician must call the Member Services number on the back of the identification card prior to
scheduling an admission to, or receiving the services of an Out-of-Network Provider.
93
Such Authorized Referrals are not available to bariatric surgical services. These services are only covered
when performed at a designated bariatric BDCSC.
Balance Billed is when a Provider bills you for the difference between the amount they charge and the
amount that the Plan will pay.
Bariatric BDCSC Coverage Area is the area within the 50-mile radius surrounding a designated bariatric
BDCSC.
Benefit is a Benefit provided to eligible Members under the Plan consistent with any terms and conditions
stated in the Plan.
Benefit Booklet is this written description of the Benefits provided under the Plan.
Blue Distinction Centers for Specialty Care (BDCSC) are health care providers designated by Anthem
as a selected Facility for specified medical services. A Provider participating in a BDCSC network has an
agreement in effect with Anthem at the time services are rendered or is available through their affiliate
companies or our relationship with the Blue Cross and Blue Shield Association. BDCSC agree to accept the
Maximum Allowed Amount as payment in full for Covered Services.
An Anthem Prudent Buyer Provider in the Prudent Buyer Plan network or the Blue Cross and/or Blue Shield
Plan is not necessarily a BDCSC Facility.
Centers of Medical Excellence (CME) are health care providers designated by Anthem as a selected
Facility for specified medical services. A Provider participating in a CME network has an agreement in effect
with Anthem at the time services are rendered or is available through their affiliate companies or their
relationship with the Blue Cross and Blue Shield Association. CME agree to accept the Maximum Allowed
Amount as payment in full for Covered Services.
An Anthem Prudent Buyer Provider in the Prudent Buyer Plan network or the Blue Cross and/or Blue Shield
Plan is not necessarily a CME Facility.
Chiropractic Services means Medically Necessary care by means of adjustment of the spine (to correct a
subluxation) performed by a legally licensed chiropractor pursuant to the terms of their license. (Subluxation is
a term used in the chiropractic field to describe what happens when one of the vertebrae in your spine moves
out of position.)
Claims Administrator refers to Anthem Blue Cross Life and Health Insurance Company. On behalf of
Anthem Blue Cross Life and Health Insurance Company, Anthem Blue Cross shall perform all administrative
services in connection with the processing of claims under the Plan.
Consolidated Appropriations Act of 2021 is a federal law described in the
Act of 202ooklet for details.
Covered Service(s) are those Medically Necessary services and supplies associated with a Benefit under
the Plan.
Copayment is the dollar amount or percentage of the Maximum Allowed Amount unless otherwise specified
that a Member is required to pay for specific Covered Services after meeting any applicable Deductible. See
page 31 under YOUR MEDICAL BENEFITS section.
Creditable Coverage is any individual or group plan that provides medical, Hospital and surgical coverage,
including continuation coverage, coverage under Medicare or Medicaid, TRICARE, the Federal Employees
Health Benefits Program, programs of the Indian Health Service or of a tribal organization, a state health
benefits risk pool, coverage through the Peace Corps, the State Children's Health Insurance Program, or a
public health plan established or maintained by a state, the United States government, or a foreign country.
Creditable Coverage does not include accident only, credit, coverage for on-site medical clinics, disability
income, coverage only for a specified disease or condition, hospital indemnity or other fixed indemnity
insurance, Medicare supplement, long-term care insurance, dental, vision, workers' compensation
insurance, automobile insurance, no-fault insurance, or any medical coverage designed to supplement other
94
private or governmental plans. Creditable Coverage is used to set up eligibility rules for children who cannot
get a self-sustaining job due to a physical or mental condition. In addition, eligible children were covered
under one of the above types of health coverage on his or her own and not as a Dependent child.
If your prior coverage was through an employer, you will receive credit for that coverage if it ended because
your employment ended, the availability of medical coverage offered through employment or sponsored by
the employer terminated, or the employer's contribution toward medical coverage terminated, and any lapse
between the date that coverage ended and the date you become eligible under this Plan is no more than
180 days (not including any waiting period imposed under this Plan by the Employer).
If your prior coverage was not through an employer, you will receive credit for that coverage if any lapse
between the date that coverage ended and the date you become eligible under this Plan is no more than 63
days (not including any waiting period imposed under this Plan by the Employer).
Custodial Care is care provided primarily to meet your personal needs. This includes help in walking,
bathing or dressing. It also includes: preparing food or special diets; feeding by utensil, tube or gastrostomy;
suctioning and administration of medicine which is usually self-administered or any other care which does
not require continuing services of medical personnel.
If Medically Necessary, Benefits will be provided for feeding (by tube or gastrostomy) and suctioning.
Day Treatment Center is an outpatient psychiatric Facility which is licensed according to state and local
laws to provide outpatient programs and treatment of Mental Health or substance use disorder under the
supervision of Physicians.
Deductible is the Calendar Year amount which you must pay for specific Covered Services that are a Benefit
of the Plan before you become entitled to receive Benefit payments from the Plan for those services. See
page 31 under YOUR MEDICAL BENEFITS section.
Dependent as used in Eligibility RequirementsUniversity of California
Group Insurance Regulations. A copy of this document is available in the HR Tools and Resources section
of UCnet (ucnet.universityofcalifornia.edu). Additional resources are also available in the Compensation and
Benefits section of UCnet to help you with your health and welfare plan decisions.
Designated Pharmacy Provider is an In-Network Pharmacy that has executed a Designated Pharmacy
Provider Agreement with the Plan or an In-Network Provider that is designated to provide Prescription Drugs,
including Specialty Drugs, to treat certain conditions.
Domestic Partner as defined in Eligibility RequirementsUniversity of
California Group Insurance Regulations. A copy of this document is available in the HR Tools and Resources
section of UCnet (ucnet.universityofcalifornia.edu). Additional resources are also available in the
Compensation and Benefits section of UCnet to help you with your health and welfare plan decisions.
Effective Date is the date your coverage begins under this Plan.
Emergency is a sudden, serious, and unexpected acute illness, injury, or condition (including without
limitation sudden and unexpected severe pain), or a Psychiatric Emergency Medical Condition, which the
Member reasonably perceives, could permanently endanger health if medical treatment is not received
immediately. Final determination as to whether services were rendered in connection with an Emergency
will rest solely with Anthem.
Emergency Services are services provided in connection with the initial treatment of a medical or psychiatric
Emergency or active labor.
Employee is an Individual who meets the eligibility requirements established by the Employer and accepted
by Anthem.
Employer is the Regents of the University of California and its affiliate, UC College of the Law, San
Francisco.
95
Experimental is any medical, surgical and/or other procedures, services, products, Drugs or devices
Clinical Trials of Cancer and
Other Life Threatening Conditions Benefits MEDICAL CARE THAT IS
COVERED.
Facility is a facility including but not limited to, a hospital, freestanding ambulatory surgery center, chemical
dependency treatment Facility, Residential Treatment Center, Skilled Nursing Facility, or Mental Health
Facility, as defined in this booklet. The Facility must be licensed as required by law, satisfy our accreditation
requirements, and be approved by us.
Family Member is the Member and all enrolled Dependents.
Generally Accepted Standards of Mental Health and Substance Use Disorder Care are standards of
care and clinical practice that are generally recognized by health care Providers practicing in relevant clinical
specialties such as psychiatry, psychology, clinical sociology, addiction medicine and counseling, and
behavioral health treatment pursuant to state law. Valid, evidence-based sources establishing Generally
Accepted Standards of Mental Health and Substance Use Disorder Care include peer-reviewed scientific
studies and medical literature, clinical practice guidelines and recommendations of nonprofit health care
Provider professional associations, specialty societies and federal government agencies, and drug labeling
approved by the United States Food and Drug Administration.
Home health agencies are providers, licensed when required by law and approved by us, that:
• Gives skilled nursing and other services on a visiting basis in your home; and
• Supervises the delivery of services under a plan prescribed and approved in writing by the attending
physician.
Hospice is an agency or organization providing a specialized form of interdisciplinary health care that
provides palliative care (pain control and symptom relief) and alleviates the physical, emotional, social, and
spiritual discomforts of a terminally ill person, as well as providing supportive care to the primary caregiver
Hospice must be: currently licensed as a Hospice pursuant to Health and Safety
Code section 1747 or a licensed Home Health Agency with federal Medicare certification pursuant to Health
and Safety Code sections 1726 and 1747.1. A list of hospices meeting these criteria is available upon
request.
Hospital is a facility licensed as a Hospital as required by law that satisfies our accreditation requirements
and is approved by us. The term Hospital does not include a provider, or that part of a provider, used mainly
for:
• Nursing care
• Rest care
• Convalescent care
• Care of the aged
• Custodial Care
• Educational care
• Subacute care
Incurred is a charge that will be considered Incurred on the date the particular services or supply which
gives rise to it is provided or obtained.
Infertility is: (1) the presence of a condition recognized by a Physician as a cause of Infertility; or (2) the
inability to conceive a pregnancy or to carry a pregnancy to a live birth after a year or more of regular sexual
relations without contraception or after 3 cycles of artificial insemination.
Infusion Therapy Provider / Injectable Therapy Provider is a Provider licensed according to state and
local laws as a pharmacy, and must be either certified as a home health care provider by Medicare, or
accredited as a home pharmacy by the Joint Commission on Accreditation of Health Care Organizations.
96
In-Network Provider refers to a Provider who has contracted with Anthem to accept payment, plus any
applicable Member Deductible, Copayment, or amounts in excess of specified Benefit maximums, as
payment in full for Covered Services provided to Members.
Intensive In-Home Behavioral Health Program is a range of therapy services provided in the home to
address symptoms and behaviors that, as the result of a Mental Health or substance use disorder, put the
Members and others at risk of harm.
Intensive Outpatient Program is a short-term behavioral health treatment that provides a combination of
individual, group and family therapy.
Investigative or Investigational procedures, treatments, supplies, devices, equipment, facilities, or drugs
(all services) that do not meet one (1) or more of the following criteria:
• have final approval from the appropriate government regulatory body; or
• have the credible scientific evidence published in peer-reviewed medical literature generally recognized
by the relevant medical community which permits reasonable conclusions concerning the effect of the
procedure, treatment, supply, device, equipment, facility or drug (all services) on health outcomes; or
• be proven materially to improve the net health outcome; or
• be as beneficial as any established alternative; or
• show improvement outside the investigational settings.
Recommendations of national physician specialty societies, nationally recognized professional healthcare
organizations and public health agencies, as well as information from the practicing community, may also be
considered.
Maximum Allowed Amount is the maximum amount of reimbursement Anthem will allow for covered
medical services and supplies under this Plan. See YOUR MEDICAL BENEFITS - Maximum Allowed
Amount.
Medically Necessary procedures, supplies equipment or services are those Accolade determines to be:
1. Appropriate and necessary for the diagnosis or treatment of the medical condition;
2. Clinically appropriate in terms of type, frequency, extent, site and duration and considered effective for
3. Provided for the diagnosis or direct care and treatment of the medical condition;
4. Within standards of good medical practice within the organized medical community;
5. Not primarily for your convenience, or for the convenience of your Physician or another provider;
6. Not more costly than an equivalent service or sequence of services that is medically appropriate and is
likely to produce equivalent therapeutic or diagnostic results in regard to the diagnosis or treatment of
; and
7. The most appropriate procedure, supply, equipment or service which can safely be provided. The most
appropriate procedure, supply, equipment or service must satisfy the following requirements:
a. There must be valid scientific evidence demonstrating that the expected health benefits from the
procedure, supply, equipment or service are clinically significant and produce a greater likelihood of
benefit, without a disproportionately greater risk of harm or complications, for you with the particular
medical condition being treated than other possible alternatives; and
b. Generally accepted forms of treatment that are less invasive have been tried and found to be
ineffective or are otherwise unsuitable.

97
For purposes of treatment of Mental Health and Substance Use Disorder, Medically Necessary means a
service or product addressing the specific needs of that patient, for the purpose of preventing, diagnosing,
or treating an illness, injury, condition, or its symptoms, including minimizing the progression of an illness,
injury, condition, or its symptoms, in a manner that is all of the following:
(i) In accordance with the Generally Accepted Standards of Mental Health and Substance Use Disorder
Care,
(ii) Clinically appropriate in terms of type, frequency, extent, site, and duration, and
(iii) Not primarily for the economic benefit of the Claims Administrator and the Member or for the convenience
of the patient, treating Physician, or other health care Provider.
Member/Individual is the eligible Employee, Spouse, Domestic Partner, or Dependent covered by the Plan.
Mental health and substance use disorder include conditions that are listed in the most current edition of
the Diagnostic and Statistical Manual (DSM) of Mental Disorders.
National Provider Identifier or NPI is a unique identification number for covered health care providers.
Covered health care providers and all health plans and health care clearinghouses must use the NPIs in the
administrative and financial transactions adopted under HIPAA.
Other Health Care Provider is one of the following providers:
• A certified registered nurse anesthetist
• A blood bank
The Provider must be licensed according to state and local laws to provide covered medical services.
Out-of-Network Provider is one of the following Providers which does NOT have a Prudent Buyer Plan
Participating Provider Agreement in effect with Anthem or is NOT participating in a Blue Cross and/or Blue
Shield Plan at the time services are rendered:
• A Hospital
• A Physician
• An Ambulatory Surgical Center
• A Home Health Agency
• A Facility which provides diagnostic imaging services
• A durable medical equipment outlet
• A Skilled Nursing Facility
• A clinical laboratory
• An Infusion Therapy Provider/Injectable Therapy Provider
• An Urgent Care Center
• A Retail Health Clinic
• A Hospice
• A licensed ambulance company
• A licensed qualified autism service provider
These Providers are not Anthem Prudent Buyer Providers. Remember that the Maximum Allowed Amount
may only represent a portion of the amount which an Out-of-Network Provider charges for services. See
YOUR MEDICAL BENEFITS Maximum Allowed Amount.
Out-of-Pocket Maximum is the highest Deductible and Copayment amount an Individual or family is
required to for Covered Services each year as indicated in the SUMMARY OF BENEFITS. Charges for
98
services that are not covered, charges in excess of the Maximum Allowed Amount do not accrue to the
Calendar Year Out-of-Pocket Maximum.
Partial Hospitalization Program is a structured, short-term behavioral health treatment that offers nursing
care and active treatment in a program that operates no less than 6 hours per day, 5 days per week.
Physician means:
1. A doctor of medicine (M.D.) or doctor of osteopathy (D.O.) who is licensed to practice medicine or
osteopathy where the care is provided; or
2. One of the following providers, but only when the Provider is licensed to practice where the care is
provided, is rendering a service within the scope of that license and such license is required to render
that service, and is providing a service for which Benefits are specified in this booklet:
• A dentist (D.D.S. or D.M.D.)
• An optometrist (O.D.)
• A dispensing optician
• A podiatrist or chiropodist (D.P.M., D.S.P. or D.S.C.)
• A licensed clinical psychologist
• A licensed educational psychologist or other Provider permitted by California law to provide
behavioral health treatment services for the treatment of autism spectrum disorders only
• A chiropractor (D.C.)
• An acupuncturist (A.C.)
• A licensed clinical social worker (L.C.S.W.)
• A marriage and family therapist (M.F.T.)
• A licensed professional clinical counselor (L.P.C.C.)*
• A physical therapist (P.T. or R.P.T.)*
• A speech pathologist*
• An audiologist*
• An occupational therapist (O.T.R.)*
• A respiratory care practitioner (R.C.P.)*
• A nurse midwife**
• A nurse practitioner
• A Physician assistant
• A Psychiatric Mental Health Nurse (R.N.)*
• A registered dietitian (R.D.)* or another nutritional professional* with a or higher degree in
a field covering clinical nutrition sciences, from a college or university accredited by a regional
accreditation agency, who is deemed qualified to provide these services by the referring M.D. or
D.O. A registered dietitian or other nutritional professional as described here are covered for the
provision of diabetic medical nutrition therapy and nutritional counseling for the treatment of eating
disorders such as anorexia nervosa and bulimia nervosa only.
• A qualified autism service provider, qualified autism service professional, and a qualified autism
service paraprofessional, as described under the BENEFITS FOR AUTISM SPECTRUM
DISORDERS section.
*Note: The Providers indicated by asterisks (*) are covered only by referral of a Physician as defined in 1
above.

99
**If there is no nurse midwife who is an Anthem Prudent Buyer Provider in your area, you may call the
Member Services number on the back of the identification card for a help finding an OB/GYN.
Plan is the UC Health Savings Plan (Medical and Behavioral Health Benefit Plan for eligible Employees and
Non-Medicare Retirees of the Employer and their covered Dependents).
Plan Administrator is the University of California Executive Steering Committee on Health Benefits
Programs, or its authorized delegate.
Plan Sponsor is The Regents of the University of California, a public corporation and agency of the State
of California, and the constitutional trustee of the public trust known as the University of California.
Preventive Care Services include routine examinations, screenings, tests, education, and immunizations
administered with the intent of preventing future disease, illness, or injury. Services are considered
preventive if you have no current symptoms or prior history of a medical condition associated with that
screening or service. These services shall meet requirements as determined by federal and state law.
Sources for determining which services are recommended include the following:
1.
2. Immunizations recommended by the Advisory Committee on Immunization Practices of the Centers for
Disease Control and Prevention;
3. Preventive care and screenings for infants, children, and adolescents as provided for in the
comprehensive guidelines supported by the Health Resources and Services Administration; and
4. Additional preventive care and screening for women provided for in the guidelines supported by the
Health Resources and Services Administration.
Please call the Member Services number on the back of the identification card for additional information
about services that are covered by this Plan as preventive care services. You may also refer to the following
websites that are maintained by the U.S. Department of Health & Human Services.
http://www.healthcare.gov/what-are-my-preventive-care-benefits
http://www.ahrq.gov
http://www.cdc.gov/vaccines/acip/index.html
Prior Plan is a Plan sponsored by us which was replaced by this Plan within 60 days. You are considered
covered under the Prior Plan if you: (1) were covered under the Prior Plan on the date that plan terminated;
(2) properly enrolled for coverage within 31 days of this Effective Date; and (3) had coverage
terminate solely due to the Prior Plan's termination.
Prosthetic Devices are appliances which replace all or part of a function of a permanently inoperative,
absent or malfunctioning body part. The term "Prosthetic Devices" includes orthotic devices, rigid or semi-
supportive devices which restrict or eliminate motion of a weak or diseased part of the body.
Provider(s) is a professional or Facility licensed by law that gives health care services within the scope of
that license and is approved by the Plan. Providers that deliver Covered Services are described
throughout this Benefit Booklet. If you have a question about a Provider not described in this Plan, please
call the Member Services number on the back of the identification card.
Psychiatric Emergency Medical Condition is a mental disorder that manifests itself by acute symptoms
of sufficient severity that the patient is either (1) an immediate danger to himself or herself or to others, or
(2) immediately unable to provide for or utilize food, shelter, or clothing due to the mental disorder.
Psychiatric Health Facility is an acute 24-hour Facility as defined in California Health and Safety Code
1250.2. It must be:
1. Licensed by the California Department of Health Services;
100
2. Qualified to provide short-term inpatient treatment according to the California Insurance Code;
3. Accredited by the Joint Commission on Accreditation of Health Care Organizations; and
4. Staffed by an organized medical or professional staff which includes a Physician as medical director.
Psychiatric Mental Health Nurse is a registered nurse (R.N.) who has a master's degree in psychiatric
mental health nursing, and is registered as a Psychiatric Mental Health Nurse with the state board of
registered nurses.
Reconstructive Surgery is surgery performed to correct or repair abnormal structures of the body caused
by congenital defects, developmental abnormalities, trauma, infection, tumors, or disease to do either of the
following: (a) improve function; or (b) create a normal appearance, to the extent possible.
Residential Treatment Center is a Provider licensed and operated as required by law, which includes:
• Room, board and skilled nursing care (either an RN or LVN/LPN) available on-site at least eight hours
daily with 24 hour availability;
• A staff with one or more doctors available at all times;
• Residential treatment that takes place in a structured facility-based setting;
• The resources and programming to adequately diagnose, care and treat a Mental Health or substance
use disorder;
• Facilities that are designated for residential, sub-acute, or intermediate care and that may occur in care
systems that provide multiple levels of care; and
• Accreditation by The Joint Commission (TJC), the Commission on Accreditation of Rehabilitation
Facilities (CARF), the National Integrated Accreditation for Healthcare Organizations (NIAHO), or the
Council on Accreditation (COA).
The term Residential Treatment Center/Facility does not include a Provider, or that part of a Provider, used
mainly for:
• Nursing care
• Rest care
• Convalescent care
• Care of the aged
• Custodial Care
• Educational care
Retail Health Clinic is a facility that provides limited basic medical care services to Members -
basis. These clinics normally operate in major pharmacies or retail stores.
Skilled nursing facility is a facility licensed as a skilled nursing facility in the state in which it is located that
satisfies our accreditation requirements and is approved by us.
A Skilled Nursing Facility is not a place mainly for care of the aged, Custodial Care or domiciliary care, or a
place for rest, educational, or similar services.
Special Care Units are special areas of a Hospital which have highly skilled personnel and special
equipment for acute conditions that require constant treatment and observation.

101
Spouse as defined in Eligibility RequirementsUniversity of California
Group Insurance Regulations. A copy of this document is available in the HR Tools and Resources section
of UCnet (ucnet.universityofcalifornia.edu). Additional resources are also available in the Compensation and
Benefits section of UCnet to help you with your health and welfare plan decisions.
Stay is inpatient confinement which begins when you are admitted to a facility and ends when you are
discharged from that Facility.
Surprise Billing Claim is described in the
this booklet for details.
Urgent Care is the services received for a sudden, serious, or unexpected illness, injury or condition, other
than one which is life threatening, which requires immediate care for the relief of severe pain or diagnosis
and treatment of such condition.
Urgent Care Center is a Physician's office or a similar facility which meets established ambulatory care
criteria and provides medical care outside of a Hospital Emergency department, usually on an unscheduled,
walk-in basis. Urgent Care Centers are staffed by medical doctors, nurse practitioners and Physician
assistants primarily for the purpose of treating patients who have an injury or illness that requires immediate
care but is not serious enough to warrant a visit to an emergency room.
To find an Urgent Care Center, please call the Member Services number on the back of the identification
card. Please call the Urgent Care Center directly for hours of operation and to verify that the center can help
with the specific care that is needed.
We (us, our) refers to Anthem.
Year or Calendar Year is a 12 month period starting January 1 at 12:01 a.m. Pacific Standard Time.
You (your) refers to the Member and Dependents who are enrolled for Benefits under this Plan.
102
YOUR RIGHT TO APPEALS
The term includes both pre-service and post-service claims.
• A pre-service claim is a claim for benefits under the Plan for which you have not received the benefit or
for which you may need to obtain approval of Medical Necessity in advance.
• A post-service claim is any other claim for benefits under the Plan for which you have received the
service.
PRE-SERVICE CLAIMS
If your pre-service claim is denied or if your coverage is rescinded:
-service claim denial
The procedure Accolade will follow will satisfy following the minimum requirements for a full and fair review
under applicable federal regulations.
Notice of Adverse Pre-Service Claim Determination
If your pre--service claim determination (denial)
will include:
-service claim involved;
procedures and the time limits that apply to them if your appeal and the
pre-service claim denial is upheld;
the claim determination and about your right to request a copy of it free of charge, along with a discussion
of the claims denial decision; and
experimental treatment, or about your right to request this explanation free of charge, along with a
discussion of the pre-service claim denial decision; and
Appeals
You have the right to appeal an adverse benefit determination (pre-service claim denial). You, your Provider,
or your authorized representative must file your appeal within 180 calendar days after you are notified of the
pre-service claim denial. You will have the opportunity to submit written comments, documents, records, and
other information supporting your pre--service claim will take into
account all information you submit, regardless of whether it was submitted or considered in the initial benefit
determination.
Accolade offer two levels of pre-service claim appeal. The time frame allowed for Accolade to complete its
review is dependent upon the type of review requested either standard review or expedited/urgent review
To file an appeal for a pre-service claim, you, your Provider or your authorized representative must submit
the request in writing and provide at least the following information:
103
Benefits was sought; and
You or your authorized representative must submit the written pre-service claim to:
Accolade UM Appeals Department
7400 West Campus Road
Suite F-510
New Albany, OH 43054
You must include the pre-service claim Reference Number (included on the pre-service denial letter), and
Your Member Identification Number when submitting an appeal.
How Your Appeal will be Decided
When Accolade reviews your pre-service claim appeal, Accolade will not rely upon the initial benefit
determination or, for second-level pre-service claim appeals, to the earlier appeal determination. The review
will be conducted by an appropriate reviewer who did not make the initial determination and who does not
work for the person who made the initial determination. Any second-level pre-service claim reviews will be
conducted by an appropriate reviewer who did not make the initial determination or the first-level appeal
determination and who does not work for the person who made the initial determination or first-level appeal
determination.
If the pre-service claim denial was based in whole or in part on a medical judgment, including whether the
treatment is experimental, investigational, or not Medically Necessary, the reviewer will consult with a health
care professional who has the appropriate training and experience in the medical field involved in making
the judgment. This health care professional will not be one who was consulted in making an earlier
determination or who works for one who was consulted in making an earlier determination.
Notification of the Outcome of the Appeal
If you appeal a pre-service claim and it was an expedited/urgent review, Accolade will notify you of the
outcome of the pre-service claim appeal as soon as possible, but not later than 72 hours after receipt of your
request for appeal.
If you appeal a pre-service claim and it is a standard appeal, either first-level or second-level, Accolade will
notify you of the outcome of the both the first-level and second-level appeal within 15 days after receipt of
your request for appeal.
Pre-Service Claim Appeal Denial
-service claim appeal is denied, that denial will be considered an adverse benefit determination.
The notification from Accolade will include all of the information set forth in the above subsection entitled
-
Pre-Service Second Level Claim Appeals
-level appeal decision, a second level appeal is available. If you
would like to initiate a voluntary second level appeal, please write to the address listed above.
Voluntary second-level pre-service claim appeals must be submitted within 60 calendar days of the denial
of the first level appeal.
104
External Review
If the outcome of the mandatory first-level appeal is adverse to you and it was based on medical judgment,
or if it pertained to a recission of coverage, you may be eligible for an independent External Review pursuant
to federal law.
You must submit your request for External Review to Anthem within four (4) months of the notice of your
final internal adverse determination.
A request for an External Review must be in writing unless Anthem determines that it is not reasonable to
require a written statement. You do not have to re-send the information that you submitted for internal
appeal. However, you are encouraged to submit any additional information that you think is important for
review.
For pre-service claims involving urgent/concurrent care, you may proceed with an Expedited External
Review without filing an internal appeal or while simultaneously pursuing an expedited appeal through
telephone, facsimile, or other similar method. To proceed with an Expedited External Review, you or your
authorized representative must contact Accolade at the phone number listed on your ID card and provide at
least the following information:
All other requests for External Review should be submitted in writing unless Anthem determines that it is not
reasonable to require a written statement. Such requests should be submitted by you or your authorized
representative to:
Anthem Blue Cross Life and Health Insurance Company
ATTN: Appeals
P.O. Box 4310, Woodland Hills, CA 91365-4310
You must include Your Member Identification Number when submitting a request for External
Review.
This is not an additional step that you must take in order to fulfill your appeal procedure obligations described
above. Your decision to seek External Review will not affect your rights to any other benefits under this
health care plan. There is no charge for you to initiate an independent External Review.
Requirement to file an Appeal before taking further legal action
No legal action of any kind related to a benefit decision may be filed by you in any other forum, unless it is
commenced within three years of the Plan's final decision on the claim or other request for benefits. If the
plan decides an appeal is untimely, the Plan's latest decision on the merits of the underlying claim or benefit
-level and second-level Appeals, and
External Review, but not including any voluntary level of appeal, before taking other legal action of any kind
against the plan.
105
POST-SERVICE CLAIMS
If your claim is denied or if your coverage is rescinded:
• you will be provided with a written notice of the denial or rescission; and
• you are entitled to a full and fair review of the denial or rescission.
Appeals Related to Medical Judgment
If the denial was based in whole or in part on a medical judgment, including whether the treatment is
experimental, investigational, or not Medically Necessary, you or your authorized representative must submit
the written appeal to:
Accolade UM Appeals Department
7400 West Campus Road
Suite F-510
New Albany, OH 43054
Notice of Adverse Benefit Determination
The procedure Anthem will follow will satisfy following the minimum requirements for a full and fair review
under applicable federal regulations.
If your claim is denied, notice of the adverse benefit determination (denial) will include:
• information sufficient to identify the claim involved;
• the specific reason(s) for the denial;
• a reference to the specific plan provision(s) on which determination is based;
• a description of any additional material or information needed to perfect your claim;
• an explanation of why the additional material or information is needed;
•
claim denial is upheld;
• information about any internal rule, guideline, protocol, or other similar criterion relied upon in making
the claim determination and about your right to request a copy of it free of charge, along with a discussion
of the claims denial decision; and
• the availability of, and contact information for, any applicable office of health insurance consumer
assistance or ombudsman who may assist you.
Appeals
You have the right to appeal an adverse benefit determination (claim denial or rescission of coverage). You
or your authorized representative must file your appeal within 180 calendar days after you are notified of the
denial or rescission. You will have the opportunity to submit written comments, documents, records, and
other information supporting your claim. Anthem's review of your claim will take into account all information
you submit, regardless of whether it was submitted or considered in the initial benefit determination.
• Anthem shall offer a single mandatory level of appeal and an additional voluntary second level of appeal
which may be a panel review, independent review, or other process consistent with the entity reviewing
the appeal. The time frame allowed for Anthem to complete its review is Dependent upon the type of
review involved (e.g. pre-service, concurrent, post-service, urgent, etc.).
106
All other requests for appeals
representative, except where the acceptance of oral appeals is otherwise required by the nature of the appeal
(e.g. Urgent Care). You or your authorized representative must submit a request for review to:
Anthem Blue Cross Life and Health Insurance Company
ATTN: Appeals
P.O. Box 4310, Woodland Hills, CA 91365-4310
You must include Your Member Identification Number when submitting an appeal.
Upon request, Anthem will provide, without charge, reasonable access to, and copies of, all documents,
information:
• was relied on in making the benefit determination; or
• was submitted, considered, or produced in the course of making the benefit determination; or
• demonstrates compliance with processes and safeguards to ensure that claim determinations are made
in accordance with the terms of the plan, applied consistently for similarly-situated claimants; or
•
Anthem will also provide you, free of charge, with any new or additional evidence considered, relied upon,
or generated in connection with your claim. In addition, before you receive an adverse benefit determination
on review based on a new or additional rationale, Anthem will provide you, free of charge, with the rationale.
For Out of State Appeals You have to file Provider appeals with the Host Plan. This means Providers must
file appeals with the same plan to which the claim was filed.
How Your Appeal will be Decided
When Anthem considers your appeal, Anthem will not rely upon the initial benefit determination or, for
voluntary second-level appeals, to the earlier appeal determination. The review will be conducted by an
appropriate reviewer who did not make the initial determination and who does not work for the person who
made the initial determination. A voluntary second-level review will be conducted by an appropriate reviewer
who did not make the initial determination or the first-level appeal determination and who does not work for
the person who made the initial determination or first-level appeal determination.
Notification of the Outcome of the Appeal
If you appeal a post-service claim, the reviewer will notify you of the outcome of the appeal within 60 days
after receipt of your request for appeal.
Appeal Denial
• If your appeal is denied, that denial will be considered an adverse benefit determination. The notification
from the reviewer
Adverse Benefit Determination.
107
Voluntary Second Level Appeals
If you are dissatisfied with the plan's mandatory first level appeal decision, a voluntary second level appeal
may be available. If you would like to initiate a second level appeal, please write to the address listed above.
Voluntary appeals must be submitted within 60 calendar days of the denial of the first level appeal. You are
not required to complete a voluntary second level appeal prior to submitting a request for an independent
External Review.
External Review
If the outcome of the mandatory first level appeal is adverse to you and it was based on medical judgment,
or if it pertained to a rescission of coverage, you may be eligible for an independent External Review pursuant
to federal law.
You must submit your request for External Review to Anthem within four (4) months of the notice of your
final internal adverse determination.
A request for an External Review must be in writing unless Anthem determines that it is not reasonable to
require a written statement. You do not have to re-send the information that you submitted for internal
appeal. However, you are encouraged to submit any additional information that you think is important for
review.
All other requests for External Review should be submitted in writing unless Anthem determines that it is not
reasonable to require a written statement. Such requests should be submitted by you or your authorized
representative to:
Anthem Blue Cross Life and Health Insurance Company
ATTN: Appeals
P.O. Box 4310, Woodland Hills, CA 91365-4310
You must include Your Member Identification Number when submitting an appeal.
This is not an additional step that you must take in order to fulfill your appeal procedure obligations described
above. Your decision to seek External Review will not affect your rights to any other benefits under this
health care plan. There is no charge for you to initiate an independent External Review.
Requirement to file an Appeal before taking further legal action
No legal action of any kind related to a benefit decision may be filed by you in any other forum, unless it is
commenced within three years of the plan's final decision on the claim or other request for benefits. If the
plan decides an appeal is untimely, the plan's latest decision on the merits of the underlying claim or benefit
request is the final decision date. You must exhaust the plan's internal Appeals Procedure but not including
any voluntary level of appeal, before taking other legal action of any kind against the plan.
The policies, procedures and timeframes in this section may be modified upon further clarification
from Department of Health and Human Services and Department of Labor.

108
FOR YOUR INFORMATION
ANTHEM BLUE CROSS WEB SITE
web site to access Benefit information, claims payment status, Benefit maximum status, In-Network
Providers or to order an identification card. Simply log on to www.anthem.com/caLog In
the "Register now" link on your first visit to establish a User ID and Password to access the personalized and
secure MemberAccess Web site. Once registered, simply click the "Log In" button and enter your User ID
and Password to access the MemberAccess Web site.
Identity Protection Services
Anthem has made identity protection services available to Members. To learn more about these services,
please visit www.anthem.com/ resources.
LANGUAGE ASSISTANCE PROGRAM
Requesting a written or oral translation is easy. Just contact Member Services by calling the phone number
on your identification card to update your language preference to receive future translated documents or to
request interpretation assistance.
STATEMENT OF RIGHTS UNDER THE NEWBORNS AND MOTHERS HEALTH PROTECTION ACT
Under federal law, group health plans and health insurance issuers offering group health insurance coverage
generally may not restrict benefits for any Hospital length of Stay in connection with childbirth for the mother
or newborn child to less than 48 hours following a vaginal delivery or less than 96 hours following a delivery
by cesarean section. However the plan or issuer may pay for a shorter Stay if the attending Physician (e.g.,
your Physician, nurse midwife, or physician assistant), after consultation with the mother, discharges the
mother or newborn earlier.
Also, under federal law, plans and issuers may not set the level of benefits or out-of-pocket costs so that any
later portion of the 48 hour (or 96 hour) Stay is treated in a manner less favorable to the mother or newborn
than any earlier portion of the Stay.
In addition, a plan or issuer may not, under federal law, require that a Physician or Other Health Care Provider
obtain authorization for prescribing a length of Stay of up to 48 hours (or 96 hours). However, to use certain
Providers or facilities, or to reduce your out-of-pocket costs, you may be required to obtain pre-certification.
For information on pre-certification, please call the Member Services number on the back of the identification
card.
STATEMENT OF RIGHTS UNDER THE WOMEN’S HEALTH AND CANCER RIGHTS ACT OF 1998
This Plan benefits for
mastectomy-related services including all stages of reconstruction and surgery to achieve symmetry
between the breasts, prostheses, and complications resulting from a mastectomy (including lymphedema).
If you have any questions about this coverage, please call the Member Services number on the back of the
identification card.
Language Assistance Services for Self-Funded PPO Plans
English: Language assistance services, free of charge, are available to you. Call the Member Services
number on the back of the identification card. TTY Users Call 711.
Arabic: . 1-866-406-1182 711 .
Armenian: Լեզվի օգնության ծառայությունները մատչելի են ձեզ համար անվճար:
Զանգահարեք 1-866-406-1182 TTY Users զանգահարեք 711:
Farsi: . 1-866-406-1182 TTY 711 .
Hindi: :
1-866-406-1182
711
Hmong: Cov kev pabcuam hauv kev txhais lus muaj rau koj dawb xwb. Hu rau 1-866-406-1182 TTY Cov
Neeg Siv Hu Xov tooj 711.
Japanese: 言語支援サービスは無料でご利用いただけます。電話1-866-406-1182 TTYユーザーは
711に電話をかける。
Khmer: 1-866-406-
1182 TTY 711
Korean: 언어 지원 서비스는 무료로 이용하실 수 있습니다. 전화 1-866-406-1182 TTY
사용자는 711에 전화하십시오.
Punjabi: . 1-866-406-1182 TTY 711.
Russian: Языковые услуги предоставляются вам бесплатно. Вызов 1-866-406-1182 Пользователи TTY
Вызов 711.
Spanish: Los servicios de asistencia lingüística están disponibles gratuitamente. Llame al 1-866-406-1182
Usuarios de TTY Llame al 711.
Tagalog: Ang mga serbisyo ng tulong sa wika ay libre sa iyo. Tumawag sa 1-866-406-1182 Mga gumagamit
ng TTY Tumawag sa 711.
Thai: มีบริการช่วยเหลือด้านภาษาโดยไม่เสียค่าใช้จ่าย โทร 1-866-406-1182 ผู้ใช้ TTY โทร. 711
Chinese: 免费提供语言援助服务。致电1-866-406-1182 TTY用户致电711。
Vietnamese: Các dịch vụ hỗ trợ ngôn ngữ có sẵn cho bạn miễn phí. Gọi số 1-866-406-1182 Người sử dụng
TTY Gọi số 711.

Notice Informing Individuals About Nondiscrimination and
Accessibility Requirements
-Funded Plans comply with applicable Federal civil rights laws
and do not discriminate on the basis of race, color, national origin, age, disability, or sex. The UC Self-
Funded Plans do not exclude people or treat them differently because of race, color, national origin, age,
disability, or sex.
-Funded Plans:
• Provide free aids and services to people with disabilities to communicate effectively with us, such
as:
o Qualified sign language interpreters
o Written information in other formats (large print, audio, accessible electronic formats, other
formats)
• Provide free language services to people whose primary language is not English, such as:
o Qualified interpreters
o Information written in other languages
If you need these services, contact the Member Services number on the back of the identification card
(TTY 711).
-Funded Plans have failed to provide these services or discriminated in another
way on the basis of race,
Lead Discrimination Affirmative Action Title IX Officer, 1111 Franklin St., 5
th
Floor, Oakland, CA 94607,
Phone Number: (510) 987-0477, Fax Number: (510) 217-9114, Email: John.Sim[email protected]. You can file
Discrimination, Affirmative Action Title IX Officer is available to help you.
You can also file a civil rights complaint with the U.S. Department of Health and Human Services, Office for
Civil Rights, electronically through the Office for Civil Rights Complaint Portal, available at
https://ocrportal.hhs.gov/ocr/portal/lobby.jsf, or by mail or phone at:
U.S. Department of Health and Human Services
200 Independence Avenue, SW
Room 509F, HHH Building
Washington, D.C. 20201
1-800-368-1019, 800-537-7697 (TDD)
Complaint forms are available at http://www.hhs.gov/ocr/office/file/index.html.
Consolidated Appropriations Act of 2021 Notice
Consolidated Appropriations Act of 2021 (CAA)
The Consolidated Appropriations Act of 2021 (CAA) is a federal law that includes the No Surprises Act as
well as the Provider transparency requirements that are described below.
Surprise Billing Claims
Surprise Billing Claims are claims that are subject to the No Surprises Act requirements:
• Emergency Services provided by Out-of-Network Providers;
• Covered Services provided by an Out-of-Network Provider at an In-Network Facility; and
• Out-of-Network Air Ambulance Services.
No Surprises Act Requirements
Emergency Services
As required by the CAA, Emergency Services are covered under your Plan:
• Without the need for Precertification;
• Whether the Provider is In-Network or Out-of-Network;
If the Emergency Services you receive are provided by an Out-of-Network Provider, Covered Services will
be processed at the In-Network benefit level.
Note that if you receive Emergency Services from an Out-of-Network Provider, your Out-of-Pocket costs
will be limited to amounts that would apply if the Covered Services had been furnished by an In-Network
Provider. However, Out-of-Network cost-shares (i.e., Copayments, Deductibles and/or Coinsurance) will
apply to your claim if the treating Out-of-Network Provider determines you are stable, meaning you have
been provided necessary Emergency Care such that your condition will not materially worsen and the Out-
of-Network Provider determines: (i) that you are able to travel to an In-Network Facility by non-emergency
transport; (ii) the Out-of-Network Provider complies with the notice and consent requirement; and (iii) you
are in condition to receive the information and provide informed consent. If you continue to receive
services from the Out-of-Network Provider after you are stabilized, you will be responsible for the Out-of-
Network cost-shares, and the Out-of-Network Provider will also be able to charge you any difference
between the Maximum Allowed Amount and the Out-of- This notice and
consent exception does not apply if the Covered Services furnished by an Out-of-Network Provider result
from unforeseen and urgent medical needs arising at the time of service.
Out-of-Network Services Provided at an In-Network Facility
When you receive Covered Services from an Out-of-Network Provider at an In-Network Facility, your Out-
of-Pocket costs will be limited to amounts that would apply if the Covered Service had been furnished by
an In-Network Provider. However, if the Out-of-Network Provider gives you proper notice of its charges,
and you give written consent to such charges, claims will be paid at the Out-of-Network benefit level. This
means you will be responsible for Out-of-Network cost-shares for those services and the Out-of-Network
Provider can also charge you any difference between the Maximum Allowed Amount and the Out-of-
This Notice and Consent process described below does not apply to
Ancillary Services furnished by an Out-of-Network Provider at an In-Network Facility. Your Out-of-Pocket
costs for claims for Covered Ancillary Services furnished by an Out-of-Network Provider at an In-Network
Facility will be limited to amounts that would apply if the Covered Service had been furnished by an In-
Network Provider. Ancillary Services are one of the following services: (A) Emergency Services; (B)
anesthesiology; (C) laboratory and pathology; (D) radiology; (E) neonatology; (F) diagnostic services; (G)
assistant surgeons; (H) Hospitalists; (I) Intensivists; and (J) any services set out by the U.S. Department of
Health & Human Services. In addition, The Claims Administrator will not apply this notice and consent
process to you if the Claims Administrator does not have an In-Network Provider in your area who can
perform the services you require.
Out-of-Network Providers satisfy the notice and consent requirement as follows:
1. By obtaining your written consent not later than 72 hours prior to the delivery of services; or
2. If the notice and consent is given on the date of the service, if you make an appointment within 72
hours of the services being delivered.
Out-of-Network Air Ambulance Services
When you receive Covered Services from an Out-of-Network Air Ambulance Provider, your Out-of-Pocket
costs will be limited to amounts that would apply if the Covered Service had been furnished by an In-
Network Air Ambulance Provider.
How Cost-Shares Are Calculated
Your cost shares for Surprise Billing Claims will be calculated based on the Recognized Amount. Any Out-
of-Pocket cost shares you pay to an Out-of-Network Provider for either Emergency Services or for Covered
Services provided by an Out-of-Network Provider at an In-Network Facility or for Covered Services
provided by an Out-of-Network Air Ambulance Service Provider will be applied to your In-Network Out-of-
Pocket Limit.
Appeals
If you receive Emergency Services from an Out-of-Network Provider or Covered Services from an Out-of-
Network Provider at an In-Network Facility or Out-of-Network Air Ambulance Services and believe those
services are covered by the No Surprises Act, you have the right to appeal that claim. If your appeal of a
Surprise Billing Claim is denied, then you have a right to appeal the adverse decision to an Independent
Review Organization as set out in the section of this Benefit Book.
Provider Directories
The Claims Administrator is required to confirm the list of In-Network Providers in its Provider Directory
every 90 days. If you can show that you received inaccurate information from The Claims Administrator
that a Provider was In-Network on a particular claim, then you will only be liable for In-Network cost shares
(i.e., Copayments, Deductibles, and/or Coinsurance) for that claim. Your In-Network cost shares will be
calculated based upon the Maximum Allowed Amount.
Transparency Requirements
The Claims Administrator provides the following information on its website:
• Protections with respect to Surprise Billing Claims by Providers, including information on how to
contact state and federal agencies if you believe a Provider has violated the No Surprises Act.
You may also obtain the following information on The Claims Administratoror by calling Member
Services at the phone number on the back of your ID Card:
• Cost sharing information for 500 defined services, as required by the Centers for Medicare & Medicaid
Services (CMS); and
• A listing / directory of all In-Network Providers.
In addition, the Claims Administrator will provide access through its website to the following information:
• In-Network negotiated rates; and
• Historical Out-of-Network rates.
Claims Administered by:
ANTHEM BLUE CROSS
on behalf of
ANTHEM BLUE CROSS LIFE AND HEALTH INSURANCE COMPANY
By authority of the Regents, University of California Human Resources, located in Oakland, administers all
benefit plans in accordance with applicable plan documents and regulations, custodial agreements,
University of California Group Insurance Regulations for Faculty and Staff, group insurance contracts, and
state and federal laws. No person is authorized to provide benefits information not contained in these
source documents, and information not contained in these source documents cannot be relied upon as
having been authorized by the Regents. Source documents are available for inspection upon request (800-
888-8267). What is written here does not constitute a guarantee of plan coverage or benefits—particular
rules and eligibility requirements must be met before benefits can be received. The University of California
intends to continue the benefits described here indefinitely; however, the benefits of all employees,
retirees, and plan beneficiaries are subject to change or termination at the time of contract renewal or at
any other time by the University or other governing authorities. The University also reserves the right to
determine new premiums, employer contributions and monthly costs at any time. Health and welfare
benefits are not accrued or vested benefit entitlements. UC’s contribution toward the monthly cost of the
coverage is determined by UC and may change or stop altogether, and may be affected by the state of
California’s annual budget appropriation. If you belong to an exclusively represented bargaining unit, some
of your benefits may differ from the ones described here. For more information, employees should contact
their Human Resources Office and retirees should call the Retirement Administration Service Center (800-
888-8267).
In conformance with applicable law and University policy, the University is an affirmative action/equal
opportunity employer. Please send inquiries regarding the University’s affirmative action and equal
opportunity policies for staff to Systemwide AA/EEO Policy Coordinator, University of California, Office of
the President, 1111 Franklin Street, 5th Floor, Oakland, CA 94607, and for faculty to the Office of Academic
Personnel and Programs, University of California Office of the President, 1111 Franklin Street, Oakland, CA
94607.
