
125
VOLUME 45 : NUMBER 4 : AUGUST 2022
ARTIC LE
This article is peer-reviewed© 2022 NPS MedicineWise
Helen K Reddel
Research leader and
Director, Australian Centre
for Airways Disease
Monitoring
1
Honorary visiting physician
2
Gloria J Foxley
Clinical trials coordinator
1,2
Sharon R Davis
Postdoctoral research
fellow, Australian Centre for
Airways Disease Monitoring
1
1
Woolcock Institute of
Medical Research and The
University of Sydney
2
Royal Prince Alfred
Hospital
Sydney
Keywords
asthma, drug dose
calculation, inhaled
corticosteroids, metered
dose inhalers
Aust Prescr 2022;45:125–9
https://doi.org/10.18773/
austprescr.2022.033
How to step down asthma preventer
treatment in patients with well-controlled
asthma – more is not always better
SUMMARY
Most of the benefit of asthma preventer inhalers is seen with low doses. However, many Australian
patients are prescribed doses of inhaled corticosteroids that are higher than necessary to control
their asthma.
Prescribing unnecessarily high preventer doses increases the patient’s risk of adverse effects.
Theymay also increase the patient’s out-of-pocket costs.
Asthma guidelines recommend considering a step-down in preventer treatment after asthma has
been well controlled for two to three months in adults and for six months in children. The step-
down process should be individualised for each patient.
Preventive therapy should not be stopped completely.
LABA.
4
There are several possible explanations for this
deviation from the recommendations. Some patients
with frequent symptoms at diagnosis may have
been prescribed a high-dose preventer, without the
dose being reviewed after the symptoms improved.
Many patients have their preventer dose increased
during a flare-up, but few return for review after
they have recovered, so they remain indefinitely on
unnecessarily high doses.
5
In some cases, clinicians,
given the substantial pressures on their time, feel that
switching asthma treatment may not be a worthwhile
use of their time, especially if there is a risk that
asthma control will be worse after the switch.
6
Why consider stepping down
asthmatreatment?
Most of the benefits of ICSs are achieved with low
doses which are associated with very little risk of
adverse effects. Long-term treatment with high doses
is associated with a small increase in the background
risk of conditions such as cataract and osteoporosis.
7
Some patients are concerned about any type of
corticosteroid treatment,
8
with some concerns
mistakenly driven by information about anabolic
steroids. Patients may not be aware that the risks
described in Consumer Medicines Information are
seen only with high ICS doses taken for a long period
of time, or with oral corticosteroids. When starting
treatment, prescribers should emphasise to the patient
that one of the goals of asthma management is to first
achieve good control and then find the lowest dose for
them that will keep the asthma well controlled.
Introduction
Asthma management is not a case of ‘one size fits all’.
A key goal is to customise treatment for the needs
of each patient. This involves finding the lowest dose
that will keep asthma symptoms well controlled and
reduce the risk of severe attacks (also called severe
flare-ups or exacerbations), while minimising the risk
of adverse effects.
Inhaled corticosteroids
Australian asthma guidelines recommend that most
adult and adolescent patients should be prescribed
a low-dose inhaled corticosteroid (ICS) or an
as-needed combination of low-dose ICS and low-dose
formoterol.
1
Only some patients need daily treatment
with a combination of low-dose ICS with a long-acting
beta
2
agonist (LABA). Few patients require medium or
high doses of the ICS–LABA combination, or add-on
treatment (for ICS doses for adults and adolescents,
see Table 1).
2
For children 6–11 years, regular ICS is
recommended for those who have symptoms more
than once weekly, or frequent or moderately severe
exacerbations. Few children require high doses (for
ICS doses for children, see Table 2).
3
Guidelines
recommend the consideration of stepping down
the dose of therapy when asthma has been stable
and well controlled for 2–3 months in adults, and six
months in children.
1
Despite these guidelines, a recent study found
that 71% of Australian adults and adolescents with
asthma who were prescribed preventer inhalers had
been dispensed a high-dose combination of ICS–
126
ARTIC LE
VOLUME 45 : NUMBER 4 : AUGUST 2022
Full text free online at nps.org.au/australian-prescriber
An additional reason for considering stepping down
the dose is that it may substantially reduce out-of-
pocket costs for patients. This may improve their
adherence to therapy.
9,10
Which patients should be
consideredfor a step-down?
Evidence shows that preventer treatment can be
stepped down safely. Systematic reviews of studies in
properly selected patients found no overall increase
in the risk of exacerbations.
11
However, the dose of ICS
that will keep asthma well controlled varies between
patients, so consider each step-down as a treatment
trial and monitor the patient closely afterwards. There
is much less evidence about stepping down treatment
in children.
11
Consider stepping down therapy when asthma
has been well controlled by a stable dose of ICS
or ICS–LABA for at least 2–3 months in adults
and adolescents and after six months in children,
particularly if the ICS dose is medium or high by
age group (see Tables 1 and 2).
2,3
All patients should
have a written asthma action plan before starting a
step-down.
To assess symptom control, use a tool such as the
Asthma Control Test. This evaluates symptoms,
reliever use and perceived control over four weeks.
12
Also ask patients if they have had any flare-ups in
the last 12 months, as these increase the risk of future
exacerbations. A flare-up more than three months ago
that was triggered by an isolated upper respiratory
infection would not necessarily be a contraindication
to stepping down the dose, provided symptoms had
been well controlled since then.
Poor adherence is not necessarily a barrier to stepping
down, provided the patient has well-controlled
asthma and no exacerbations. A greater reduction in
the prescribed dose may be considered if the patient
has been using their preventer infrequently. However,
if a patient notices more symptoms after missing
only one or two doses of their current preventer, they
are likely to need their current dose, so it should not
bereduced.
During pregnancy, consider stepping down only if
the woman has well-controlled asthma and is taking
a high-dose preventer. Otherwise, postpone stepping
down until after delivery.
13
Stepping down in patients with
severeasthma
For patients with severe asthma, careful step-down
ofinhaled therapy can be considered if symptom
control and exacerbations respond to add-on
biologic therapy such as benralizumab, dupilumab,
mepolizumab or omalizumab. The highest priority
is to gradually reduce and stop oral corticosteroids.
Reducing the ICS dose can be considered after
3–6months, but not to below a medium dose.
14
In
severe asthma, any dose reduction should be in
consultation with a specialist.
A step-by-step guide to
steppingdown
Depending on the patient’s current therapy, there are
several step-down options (see Table 3). The step-
down process is individualised for each patient.
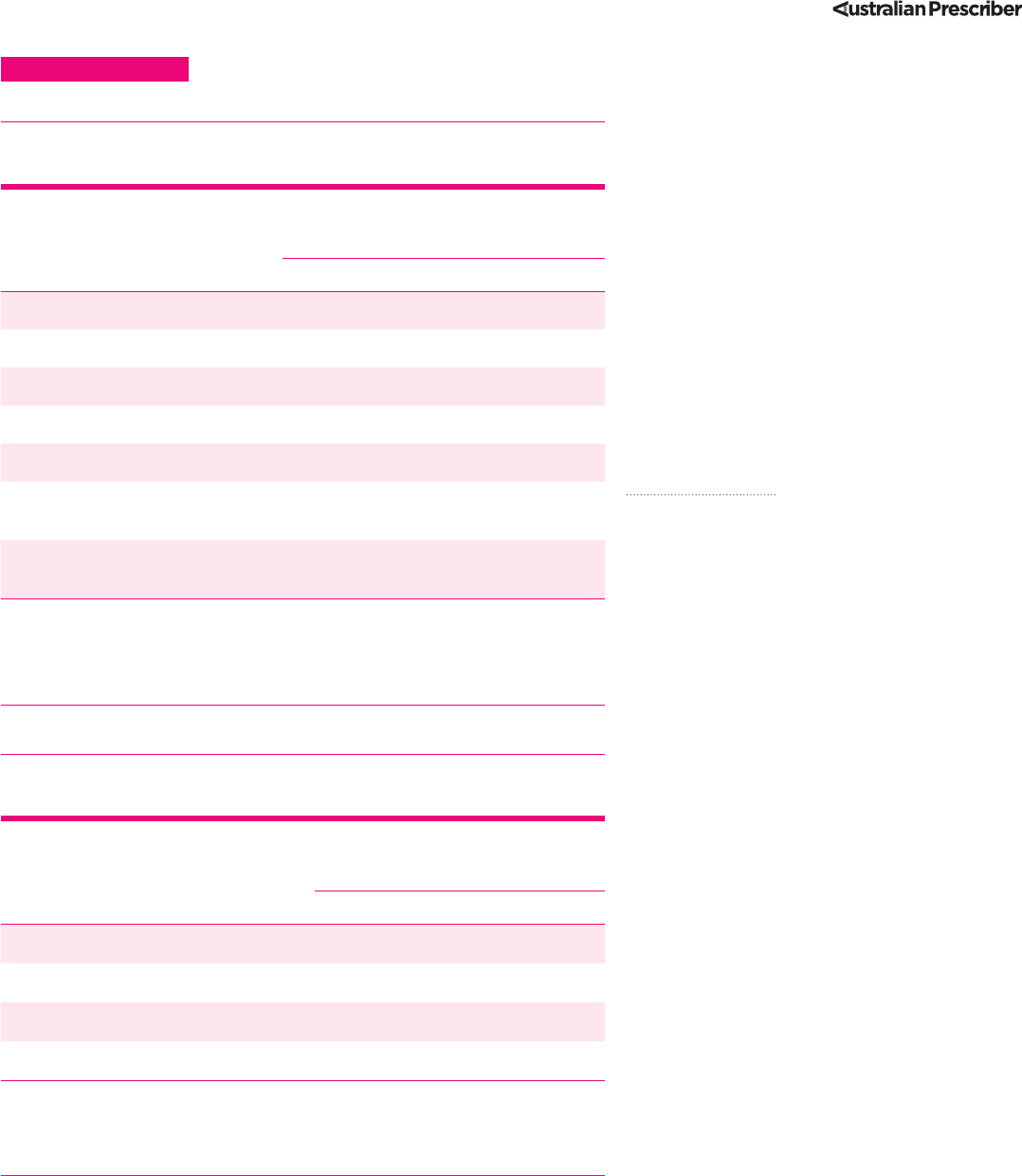
Table 1 Inhaled corticosteroid dose levels for adults
andadolescents
2
Inhaled corticosteroid Total daily metered dose (micrograms)
foradults and adolescents 12 years and
over with asthma
Low Medium High
Beclometasone dipropionate 100–200 250–400 >400
Budesonide 200–400 500–800 >800
Ciclesonide 80–160 240–320 >320
Fluticasone furoate – 100 200
Fluticasone propionate 100–200 250–500 >500
Mometasone furoate* in combination
with indacaterol
62.5 127.5 260
Mometasone furoate*† in combination
with indacaterol and glycopyrronium
– 68 136
This is not a table of equivalence, but instead it shows the doses of inhaled
corticosteroid that are classified as low, medium or high for each drug.
* Delivered doses not metered doses
† Approved only for adults 18 years and over
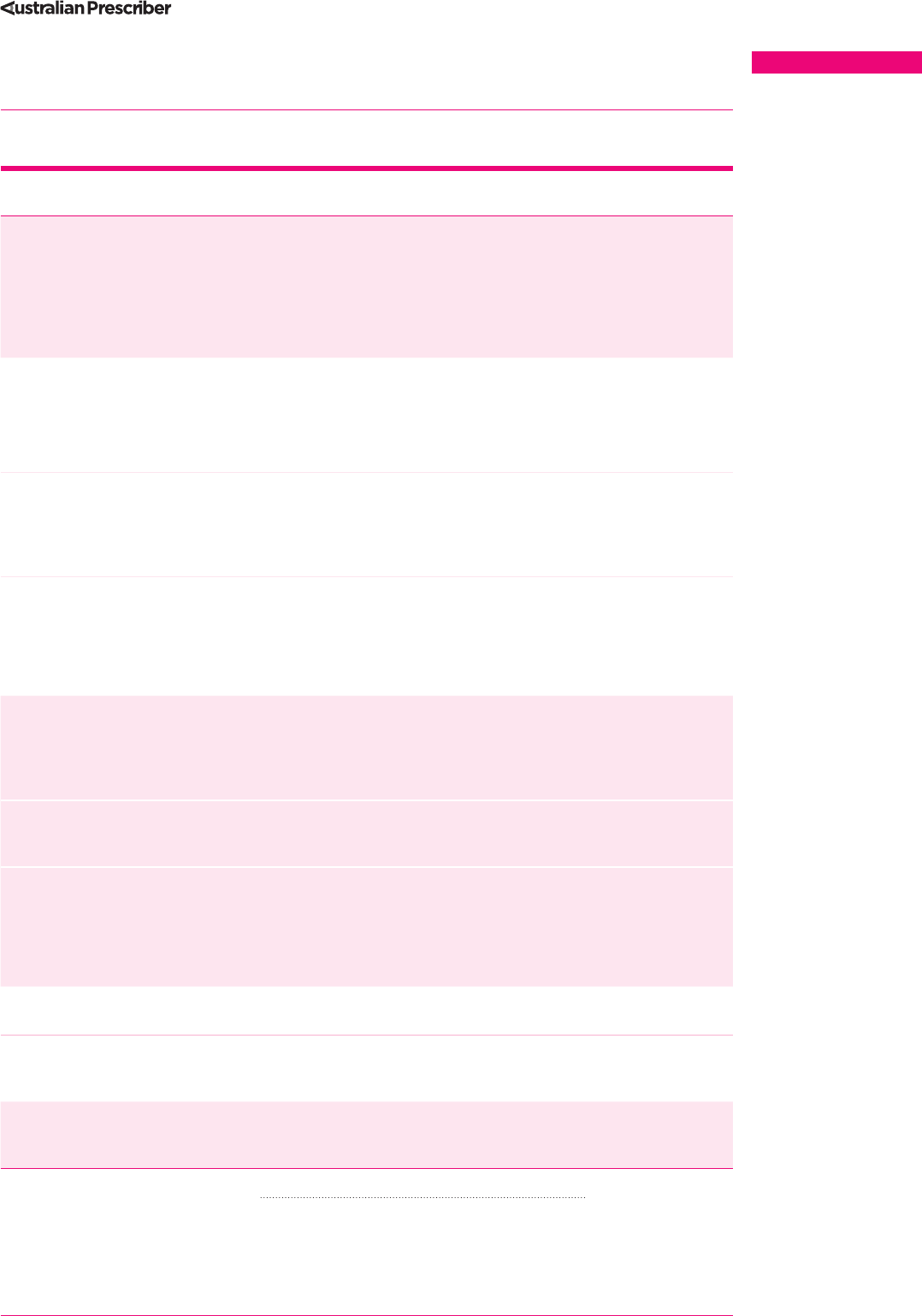
Table 2 Inhaled corticosteroid dose levels for children
6–11years
3
Inhaled corticosteroid Total daily metered dose
(micrograms) for children 6–11 years
with asthma
Low High
Beclometasone dipropionate 100–200 >200 (maximum 400)
Budesonide 200–400 >400 (maximum 800)
Ciclesonide 80–160 >160 (maximum 320)
Fluticasone propionate 100–200 >200 (maximum 500)
This is not a table of equivalence, but instead it shows the doses of inhaled
corticosteroids that are classified as low or high for each drug. The only dose of
fluticasone furoate indicated for children (50 micrograms/day) is not available
inAustralia.
How to step down asthma preventer treatment in patients with well-controlled asthma – more is not always better
127
ARTIC LE
VOLUME 45 : NUMBER 4 : AUGUST 2022
Full text free online at nps.org.au/australian-prescriber
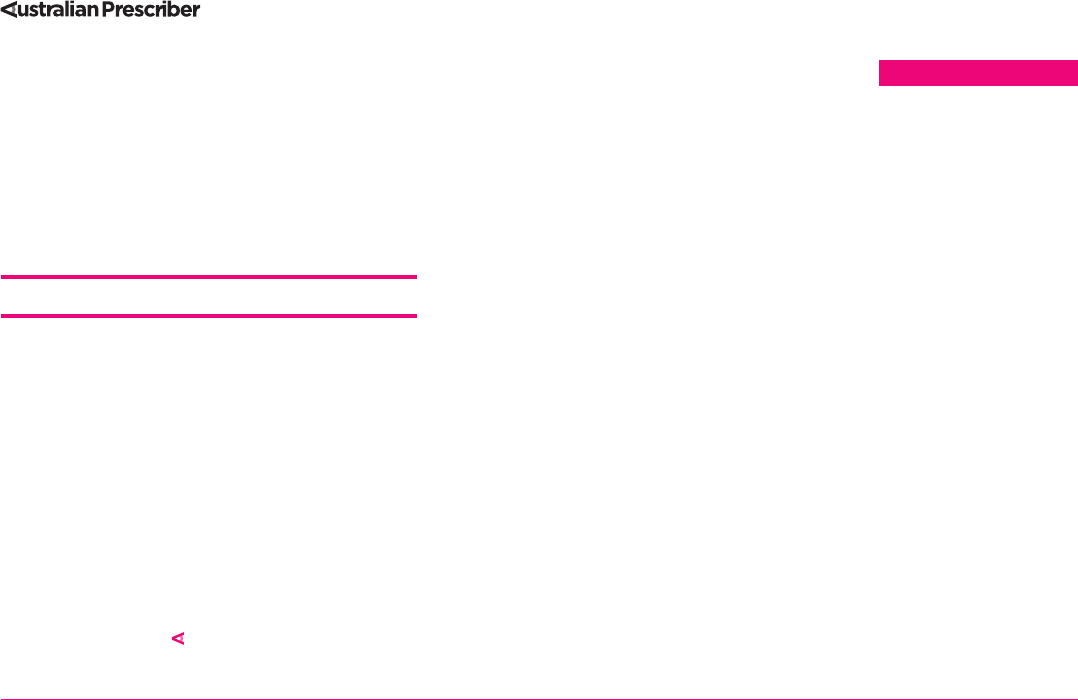
Table 3 Step-down options for preventer therapy in adults and adolescents who
have had well-controlled asthma for at least 2–3 months
1
Treatment
level
Current preventer treatment Suggested step-down options
5 High-dose combination ICS–LABA plus
add-on therapy such as biologic therapy or
oral corticosteroids for severe asthma
Discuss with the specialist who prescribed the add-on
treatment. Once asthma is well controlled, the highest
priority for stepping down is to gradually reduce and
then cease oral corticosteroids (if prescribed); check for
adrenal suppression. Advise patients not to stop their
combination ICS–LABA treatment. Do not reduce ICS–
LABA below a medium dose.
4 Medium- or high-dose ICS–LABA–LAMA
maintenance, plus as-needed SABA
Consider ceasing the LAMA, and continuing the same
dose of ICS–LABA.
OR
If the ICS dose is high, consider reducing to a medium
dose (but not to low dose) while continuing LAMA.
4 Medium-dose MART, i.e. 2 inhalations
twice daily of budesonide/formoterol
200/6micrograms or beclometasone/
formoterol 100/6 micrograms, plus 1
inhalation taken as needed for symptom relief
Low-dose MART, i.e. 1 inhalation twice daily of
budesonide/formoterol 200/6 micrograms or
beclometasone/formoterol 100/6 micrograms, plus 1
inhalation taken as needed for symptom relief.
4 Medium- or high-dose ICS–LABA
maintenance, plus as-needed SABA
Continue ICS–LABA, reducing the ICS dose by 25–50% by:
• prescribing a lower dose ICS-LABA formulation
OR
• for ICS–LABA combinations prescribed more than once
daily, by reducing the number of inhalations per day.
3 Low-dose MART, 1 inhalation twice daily of
budesonide/formoterol 200/6micrograms
or beclomethasone/formoterol
100/6micrograms, plus 1 inhalation taken
as needed for symptom relief
As-needed only low-dose budesonide/formoterol
200/6micrograms.
[Note: as-needed only treatment has not been studied
with beclometasone/formoterol]
3 Low-dose fluticasone furoate vilanterol
(a once-daily ICS–LABA) plus as-needed
SABA
Consider stepping down to once-daily fluticasone
furoate (ICS alone) plus as-needed SABA.
3 Low-dose combination ICS–LABA
maintenance (twice-daily formulations),
plus as-needed SABA
Reduce ICS–LABA dose by 25–50% by:
• reducing from twice-daily to once-daily
OR
• for patients prescribed 2 pus per dose, reducing to
1pu per dose.
2 Maintenance low-dose ICS plus as-needed
SABA
Continue daily low-dose ICS (with a lower dose if
available), plus as-needed SABA.
2 As-needed low-dose budesonide/
formoterol 200/6 micrograms taken as
needed for symptom relief
Reduce to as-needed low-dose budesonide/formoterol
100/6 micrograms per dose.
1 As-needed SABA alone (not a preventer) SABA-only treatment is not recommended, except for
the very few patients who have symptoms less than
twice a month and no risk factors for exacerbations.
Treatment levels in the table correspond to Australian asthma guidelines for adults andadolescents.
1
ICS inhaled corticosteroid
LABA long-acting beta
2
agonist
LAMA long-acting muscarinic antagonist, as separate inhaler or in triple ICS–LABA–LAMA combination
MART maintenance and reliever therapy with budesonide/formoterol or beclometasone/formoterol. In this regimen, the
patient takes ICS/formoterol combination as both their maintenance treatment and as their reliever (instead of a SABA)
SABA short-acting beta
2
agonist

128
ARTIC LE
VOLUME 45 : NUMBER 4 : AUGUST 2022
Full text free online at nps.org.au/australian-prescriber
How to step down asthma preventer treatment in patients with well-controlled asthma – more is not always better
Use shared decision making
Explain the rationale and the process for stepping
down the dose, and understand the patient’s or
parent’s willingness or concerns. Discuss how the
dose required for the prevention of flare-ups will be
individualised for them.
Timing
Choose an appropriate time to reduce the dose. For
example, do not step down if the patient is developing
a cold, or about to travel, or just before a holiday
period. For patients who are allergic to rye grass
and live in an area where thunderstorm asthma may
occur, it would not be advisable to step down their
treatment during the pollen season. Step down before
the previous inhaler is completely empty, so the
patient can resume their previous dose promptly if
asthma worsens.
Assess the patient’s risk factors
Risk factors include a history of previous
exacerbations and allergen exposure in sensitised
patients.
Record the patient’s baseline asthma status
Use the Asthma Control Test or document how many
days each week the patient has asthma symptoms,
or needs to use their inhaler to relieve symptoms.
Document lung function if available.
Make small dose adjustments gradually
The ICS dose can be reduced by 25–50%, by
prescribing a lower dose formulation or reducing
thefrequency of use. Consider reducing in two
steps of 25% rather than a single 50% reduction. For
example, if the patient is taking two puffs twice a
day, suggest they drop one of the evening puffs. If
they remain stable after one month, drop the other
evening dose so they would then be taking two puffs
once a day.
Self-monitoring
Ask the patient to monitor symptoms and reliever
use,and record the date of the step-down in their
diary or calendar. Advise them that if, over a few
weeks, they experience an overall increase in
symptoms or reliever use, or start waking at night
due to asthma, they should resume their previous
dose. For patients who are anxious, or about whom
one is concerned, consider asking for two weeks of
peak expiratory flow monitoring as a baseline, then
mark the step-down date and continue recording
for another 3–4 weeks. The Woolcock peak flow
chart makes it easy to detect exacerbations and
gradual changes.
15
Monitoring peak expiratory
flow isparticularly useful given reduced access to
spirometry during the COVID-19 pandemic. The
National Asthma Council has information to assist
with self-monitoring.
Action plan
Make sure the patient’s written asthma action plan is
up to date, so that they know what to do and who to
contact if they have a flare-up.
Review
Book a follow-up visit for two or three months
afterstepping down (or earlier if there is concern)
and prompt the patient to contact their GP sooner
iftheir asthma worsens. At the follow-up visit, assess
symptom control, adherence, reliever use and lung
function (if test available). If the patient’s asthma is still
stable, consider stepping down by another 25–50%.
Do not completely stop inhaled
corticosteroids
In adults or adolescents, completely stopping
preventive therapy increases the risk of severe
exacerbations.
New step-down options in
mildasthma
For adults and adolescents with well-controlled
asthma on a low-dose ICS or low-dose ICS–LABA,
with an as-needed short-acting beta
2
agonist (SABA)
reliever, one option is to continue daily treatment
indefinitely.
16
However, patients with few symptoms
are often poorly adherent to therapy, increasing their
risk of severe exacerbations.
A new step-down option available in Australia since
2020 is to switch to an as-needed combination of
low-dose budesonide with formoterol. The patient
uses the low-dose budesonide/formoterol inhaler
whenever needed for symptom relief, instead of
a SABA. This option is supported by three large
studies including step-down in mild asthma, that
showed symptom control and lung function were
similar, and the risk of severe exacerbations was the
same or lower, compared with continuing regular
daily ICS with as-needed SABA.
17-20
Importantly, the
risk of severe exacerbations was reduced by more
than 60% compared with switching to SABA-only
treatment.
17
Patients took an average of three to four
doses of budesonide/formoterol 200/6 micrograms
per week, so in clinical practice, one inhaler would
last an average of six months. Although the initial
out-of-pocket cost to the patient would be higher, the
average daily cost to the patient over the life of the
inhaler would be much lower than with daily ICS or
daily ICS–LABA, plus an as-needed SABA.
Smaller studies in adults and children have found
that it is possible to step down from daily ICS to
129
ARTIC LE
VOLUME 45 : NUMBER 4 : AUGUST 2022
Full text free online at nps.org.au/australian-prescriber
taking low-dose ICS only when the patient takes their
SABA for symptom relief. This is more effective than
SABA alone at preventing exacerbations.
21,22
This
approach is not currently recommended in Australian
asthmaguidelines.
Conclusion
A key goal of asthma management is to customise
the treatment to the patient’s needs, by first
achievinggood asthma control and then finding
the minimum effective dose that, together with an
asthmaaction plan, will minimise the patient’s risk
of severe exacerbations. This approach optimises
the benefit for patients, reduces the risk of adverse
effects, and reduces costs for the patient and
the healthcare system. With shared decision-
making anda careful plan, many patients are
keen to engage in the process of optimising their
asthmamanagement.
Conflicts of interest:
In the last three years, Helen Reddel’s institute has
received independent research funding from AstraZeneca,
GlaxoSmithKline and Novartis.She or her institute has
received honoraria for participation in advisory boards
for AstraZeneca, Chiesi, GlaxoSmithKline, Novartis and
Sanofi-Genzyme; honoraria from AstraZeneca, Boehringer
Ingelheim, Chiesi, GlaxoSmithKline, Sanofi-Genzyme and
Teva for independent medical educational presentations;
consulting fees from AstraZeneca and Novartis. Helen
Reddel is Chair of the Global Initiative for Asthma(GINA)
Science Committee, and a member ofthe Australian
Asthma Handbook Guidelines Committee.
In the last three years, Gloria Foxley’s institute
has received independent research funding from
AstraZeneca, GlaxoSmithKline and Novartis.
In the last three years, Sharon R Davis’s institute
has received independent research funding from
AstraZeneca, GlaxoSmithKline and Novartis.
1. National Asthma Council Australia. Figure – Selecting and adjusting
medication for adults and adolescents. In: Australian asthma handbook.
Version 2.2. Melbourne: National Asthma Council Australia; 2022.
https://www.asthmahandbook.org.au/management/adults [cited 2022 Jul 1]
2. National Asthma Council Australia. Table - Definitions of ICS dose levels in
adults. In: Australian asthma handbook. Version 2.2. Melbourne: National
Asthma Council Australia; 2022. https://www.asthmahandbook.org.au/
management/adults/initial-treatment/preventers/ics-based-preventers
[cited
2022 Jul 1
]
3. National Asthma Council Australia. Table - Definitions of ICS dose levels in
children. In: Australian asthma handbook. Version 2.2. Melbourne: National
Asthma Council Australia; 2022. https://www.asthmahandbook.org.au/
management/children/6-years-and-over/reliever-and-preventer [cited 2022
Jul 1]
4. Hew M, McDonald VM, Bardin PG, Chung LP, Farah CS, Barnard A, et al.
Cumulative dispensing of high oral corticosteroid doses for treating asthma in
Australia. Med J Aust 2020;213:316-20. https://doi.org/10.5694/mja2.50758
5. Yawn BP, Wollan PC, Bertram SL, Lowe D, Butterfield JH, Bonde D, et al.
Asthma treatment in a population-based cohort: putting step-up and step-
down treatment changes in context. Mayo Clin Proc 2007;82:414-21.
https://doi.org/10.4065/82.4.414
6. Tudball J, Reddel HK, Laba TL, Jan S, Flynn A, Goldman M, et al. General
practitioners’ views on the influence of cost on the prescribing of asthma
preventer medicines: a qualitative study. Aust Health Rev 2019;43:246-53.
https://doi.org/10.1071/AH17030
7. Leone FT, Fish JE, Szefler SJ, West SL; Expert Panel on Corticosteroid Use.
Systematic review of the evidence regarding potential complications of
inhaled corticosteroid use in asthma: collaboration of American College of
Chest Physicians, American Academy of Allergy, Asthma, and Immunology,
and American College of Allergy, Asthma, and Immunology. Chest
2003;124:2329-40. https://doi.org/10.1378/chest.124.6.2329
8. Horne R, Chapman SC, Parham R, Freemantle N, Forbes A, Cooper V.
Understanding patients’ adherence-related beliefs about medicines
prescribed for long-term conditions: a meta-analytic review of the Necessity-
Concerns Framework. PLoS One 2013;8:e80633. https://doi.org/10.1371/
journal.pone.0080633
9. Davis SR, Tudball J, Flynn A, Lembke K, Zwar N, Reddel HK. “You’ve got
to breathe, you know” - asthma patients and carers’ perceptions around
purchase and use of asthma preventer medicines. Aust N Z J Public Health
2019;43:207-13. https://doi.org/10.1111/1753-6405.12865
10. Laba TL, Jan S, Zwar NA, Roughead E, Marks GB, Flynn AW, et al. Cost-related
underuse of medicines for asthma-opportunities for improving adherence.
JAllergy Clin Immunol Pract 2019;7:2298-2306.e12. https://doi.org/10.1016/
j.jaip.2019.03.024
11. Gionfriddo MR, Hagan JB, Rank MA. Why and how to step down chronic
asthma drugs. BMJ 2017;359:j4438. https://doi.org/10.1136/bmj.j4438
12. Ko FW, Hui DS, Leung TF, Chu HY, Wong GW, Tung AH, et al. Evaluation of the
asthma control test: a reliable determinant of disease stability and a predictor
of future exacerbations. Respirology 2012;17:370-8. https://doi.org/10.1111/
j.1440-1843.2011.02105.x
13. National Asthma Council Australia. Managing asthma actively during
pregnancy. In: Australian asthma handbook. Version 2.2. Melbourne: National
Asthma Council Australia; 2022. https://www.asthmahandbook.org.au/
populations/pregnant-women/pregnancy/asthma-care [cited 2022 Jul 1]
14. Global Initiative for Asthma. Difficult-to-treat and severe asthma in adults
and adolescents. In: Global strategy for asthma management and prevention.
Fontana, WI, USA: GINA; 2022. https://ginasthma.org/reports [cited 2022
Jul1]
15. Jansen J, McCaffery KJ, Hayen A, Ma D, Reddel HK. Impact of graphic format
on perception of change in biological data: implications for health monitoring
in conditions such as asthma. Prim Care Respir J 2012;21:94-100.
https://doi.org/10.4104/pcrj.2012.00004
16. Reddel HK. Updated Australian guidelines for mild asthma: what’s
changed and why? Aust Prescr 2020;43:220-4. https://doi.org/10.18773/
austprescr.2020.076
17. Bateman ED, O’Byrne PM, FitzGerald JM, Barnes PJ, Zheng J, Lamarca R,
etal. Positioning as-needed budesonide-formoterol for mild asthma: effect of
prestudy treatment in pooled analysis of SYGMA 1 and 2. Ann Am Thorac Soc
2021;18:2007-17. https://doi.org/10.1513/AnnalsATS.202011-1386OC
18. Bateman ED, Reddel HK, O’Byrne PM, Barnes PJ, Zhong N, Keen C, etal.
As-needed budesonide-formoterol versus maintenance budesonide in
mild asthma. N Engl J Med 2018;378:1877-87. https://doi.org/10.1056/
NEJMoa1715275
19. Hardy J, Baggott C, Fingleton J, Reddel HK, Hancox RJ, Harwood M, et al.;
PRACTICAL study team. Budesonide-formoterol reliever therapy versus
maintenance budesonide plus terbutaline reliever therapy in adults with
mild to moderate asthma (PRACTICAL): a 52-week, open-label, multicentre,
superiority, randomised controlled trial. Lancet 2019;394:919-28.
https://doi.org/10.1016/S0140-6736(19)31948-8
20. O’Byrne PM, FitzGerald JM, Bateman ED, Barnes PJ, Zhong N, Keen C,
etal. Inhaled combined budesonide-formoterol as needed in mild asthma.
NEnglJMed 2018;378:1865-76. https://doi.org/10.1056/NEJMoa1715274
21. Martinez FD, Chinchilli VM, Morgan WJ, Boehmer SJ, Lemanske RF Jr,
MaugerDT, et al. Use of beclomethasone dipropionate as rescue treatment for
children with mild persistent asthma (TREXA): a randomised, double-blind,
placebo-controlled trial. Lancet 2011;377:650-7. https://doi.org/10.1016/
S0140-6736(10)62145-9
22. Papi A, Canonica GW, Maestrelli P, Paggiaro P, Olivieri D, Pozzi E, et al.; BEST
Study Group. Rescue use of beclomethasone and albuterol in a single inhaler
for mild asthma. N Engl J Med 2007;356:2040-52. https://doi.org/10.1056/
NEJMoa063861
REFERENCES
