Winter 2020
Medicaid
Managed Care
Enrollment
and Program
Characteristics,
2018.
1

iii
CONTENTS
Medicaid Managed Care Enrollment and Program Characteristics, 2018 ............................................ 1
Errors and Corrections to the 2017 Report ........................................................................................... 2
Highlights ............................................................................................................................................. 10
Glossary .............................................................................................................................................. 11
Federal authorities (Waivers and State Plan Amendments) ............................................................... 11
Key Terms, Acronyms and Definitions ................................................................................................ 12
National Tables and Maps................................................................................................................... 16
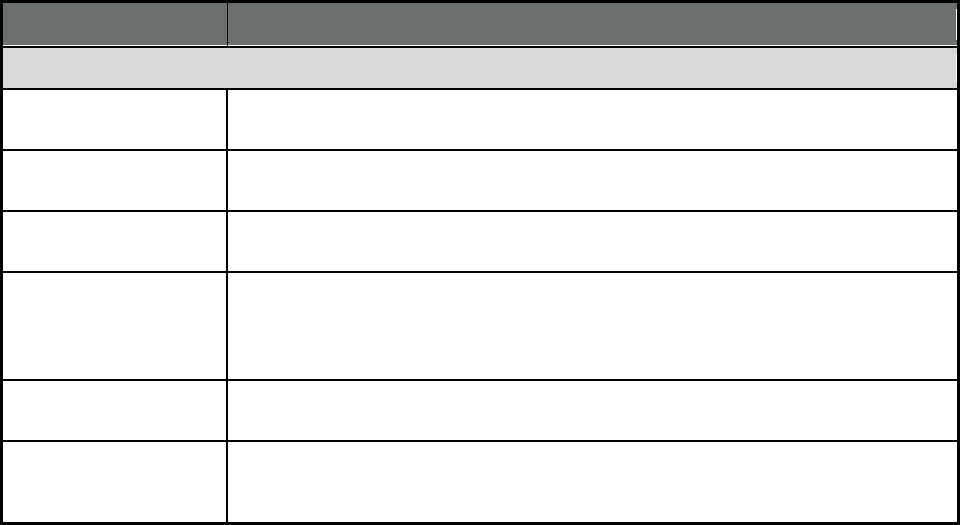
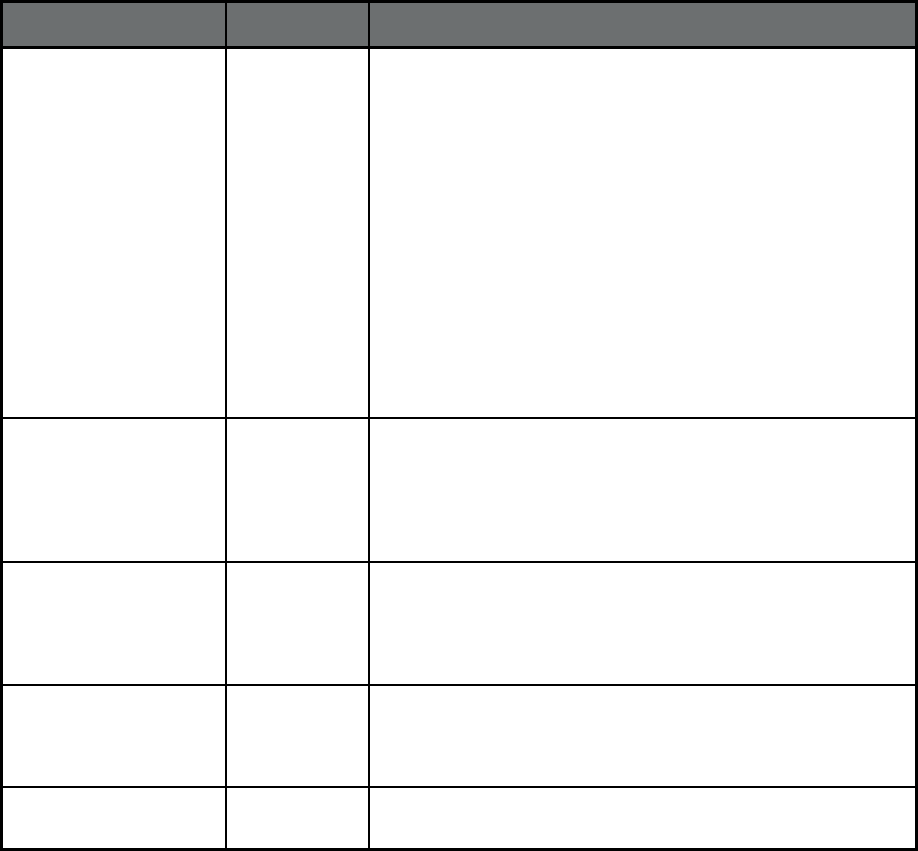
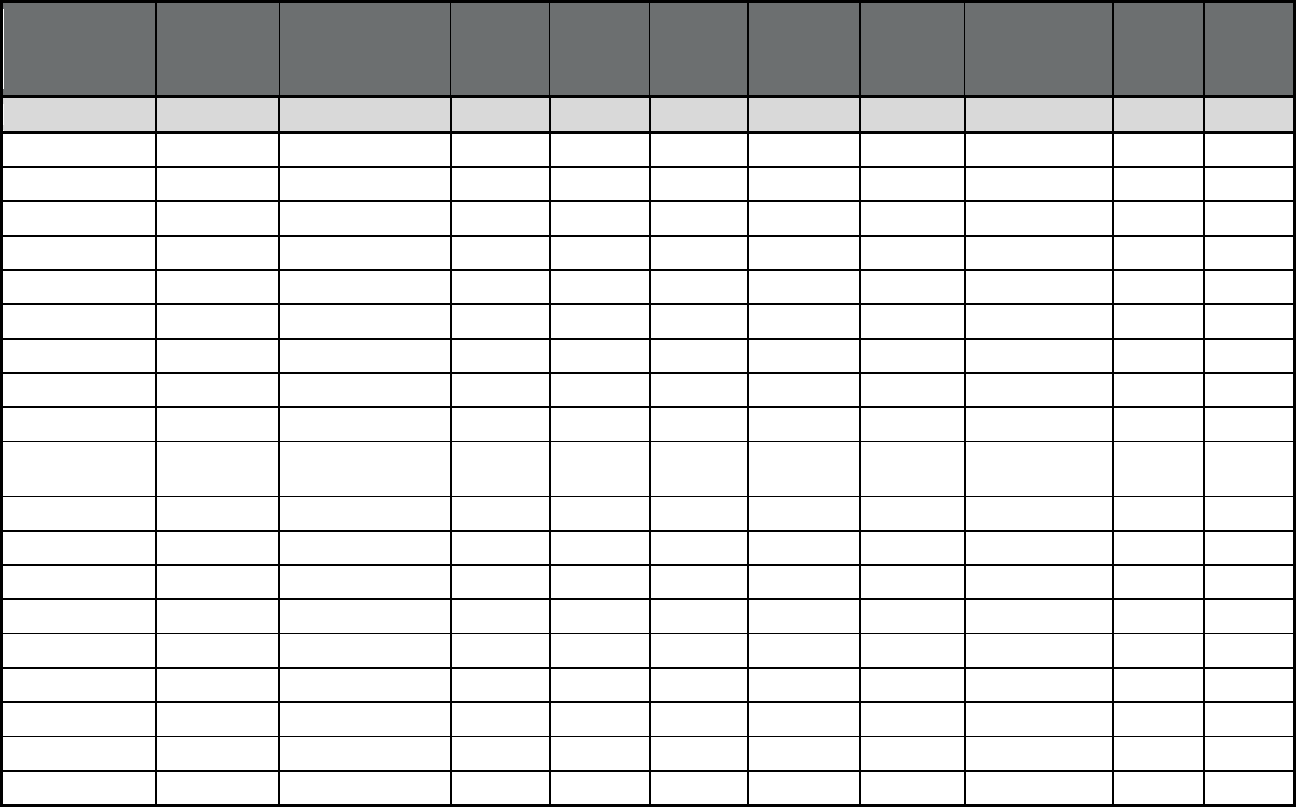
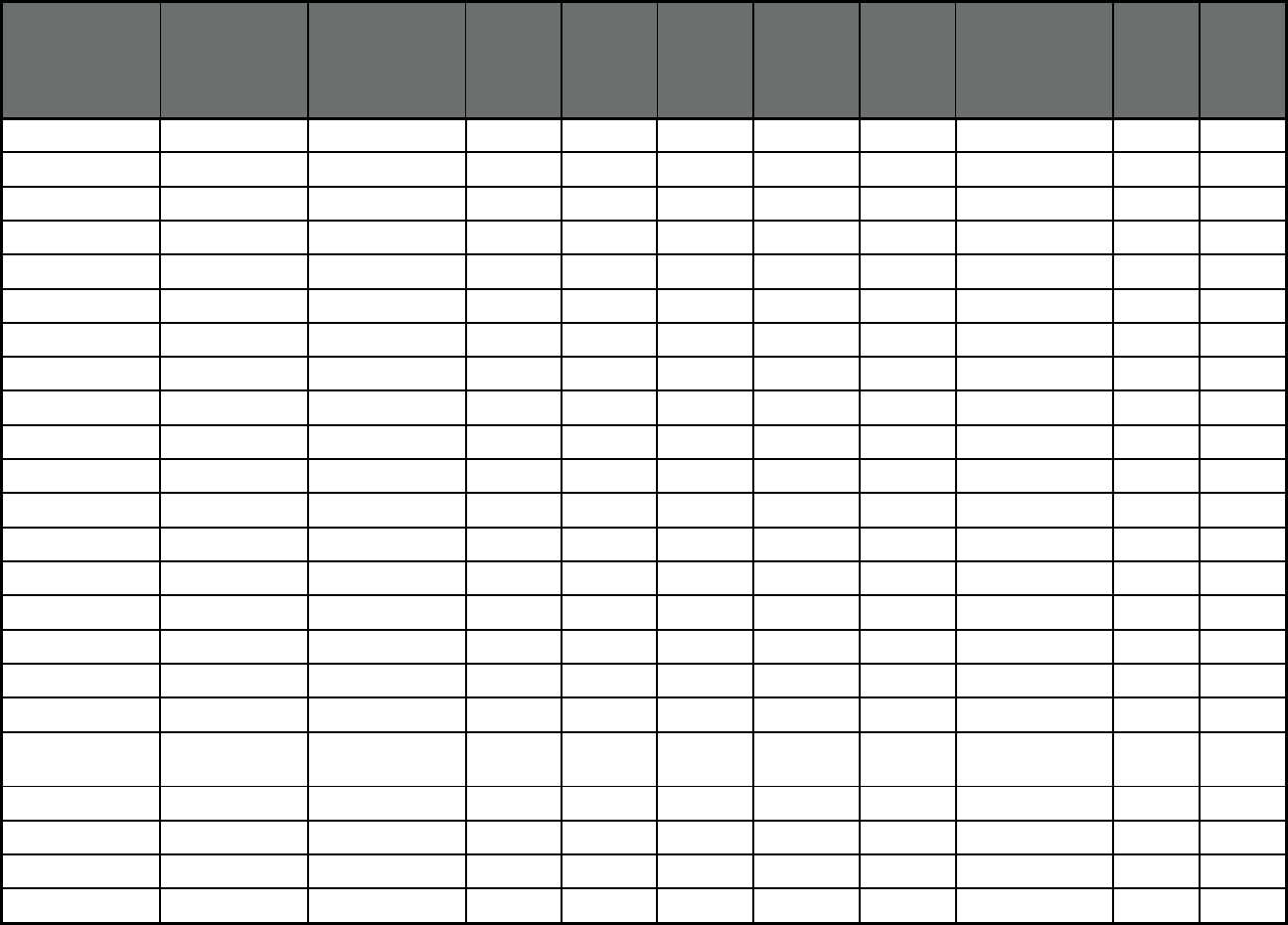
Table 1. State Medicaid Managed Care Enrollment Data Summary, as of July 1, 2018 .................. 16
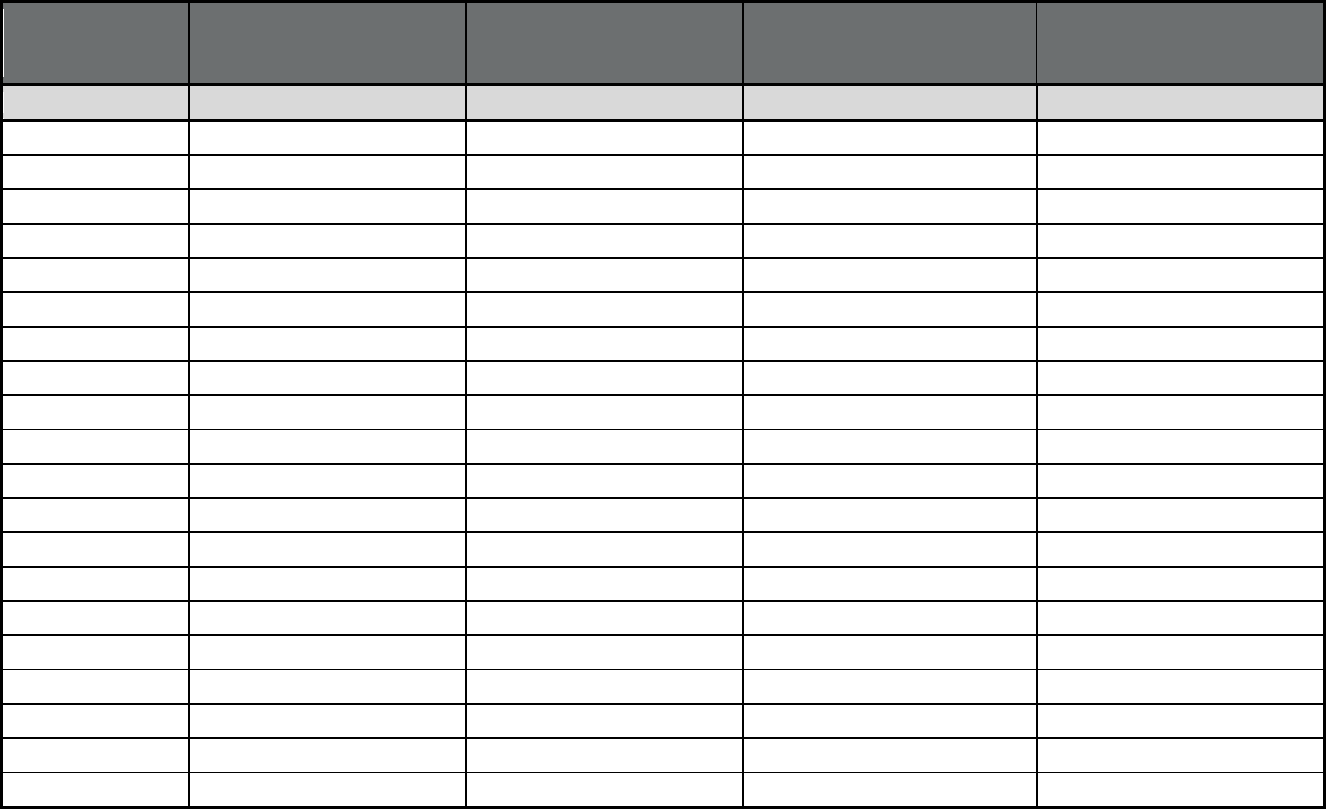
Table 2. State Managed Care Enrollment by Program Type, All Eligibles (Medicaid-only
and Medicare-Medicaid), as of July 1, 2018
1
................................................................................. 19
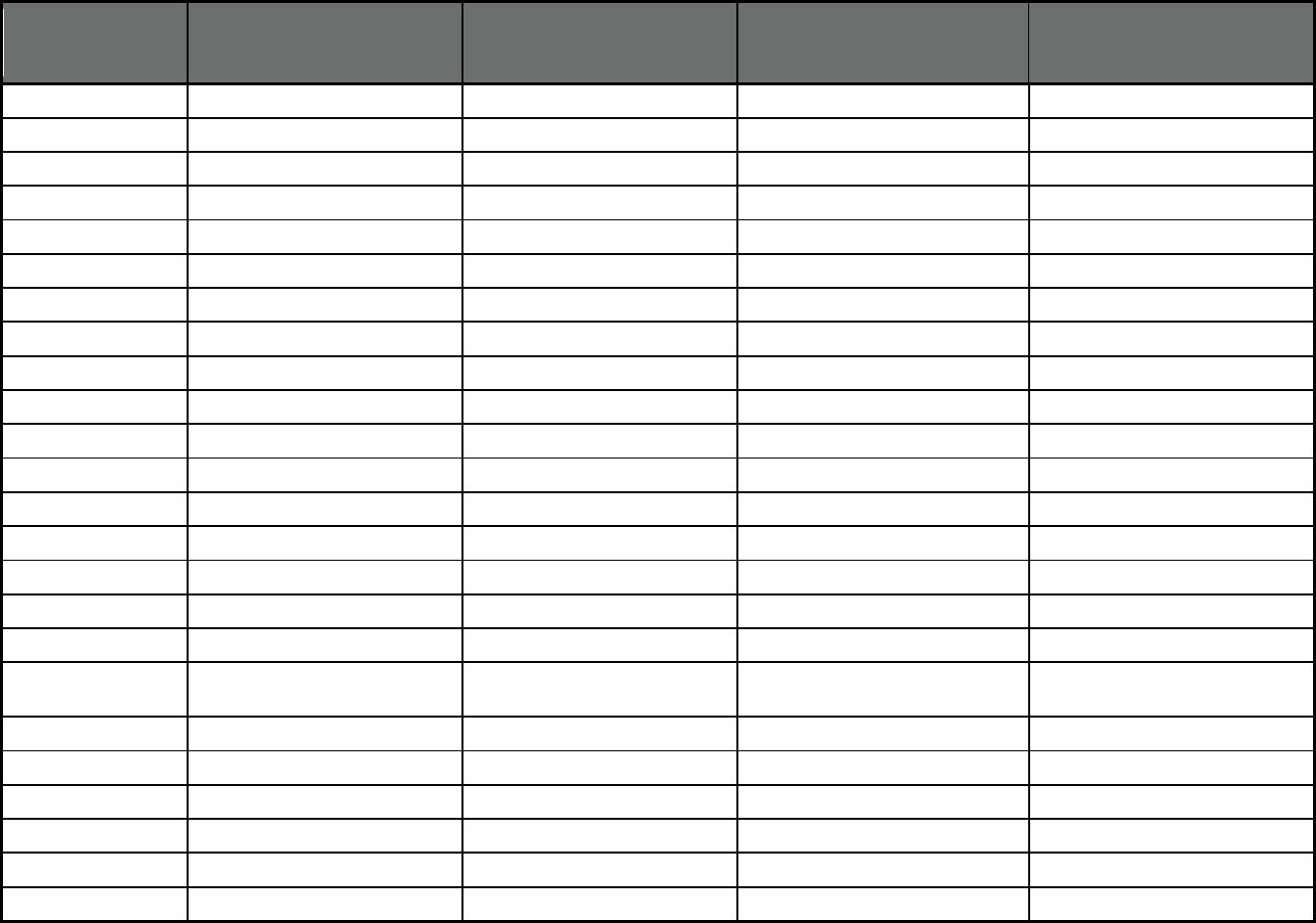
Table 3. Medicare-Medicaid Eligibles (Duals) Enrolled in Managed Care by Program
Type, as of July 1, 2018
1
................................................................................................................ 23
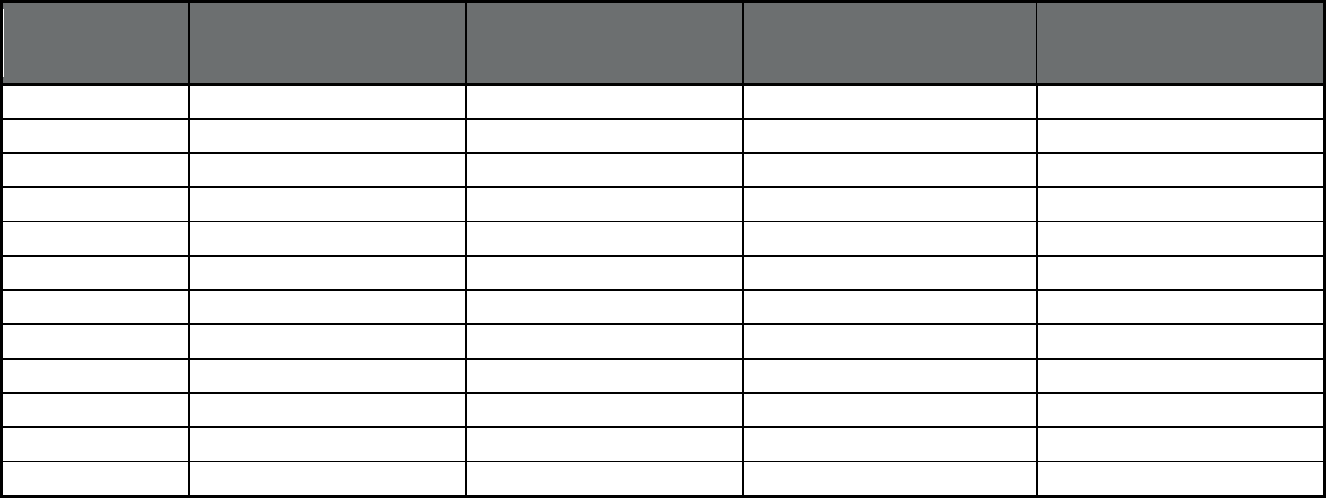
Table 4. Share of Medicaid Enrollees in Any Managed Care and in Comprehensive
Managed Care, as of July 1, 2018 ................................................................................................. 27
Map of State Comprehensive MCO Penetration as of July 1, 2018 ................................................. 30
Table 5. Enrollment by Program and Plan, as of 2018
1
.................................................................... 31
Table 6. Medicaid Managed Long Term Services and Supports (MLTSS) Program
Users or Enrollees, as of July 1, 2018
1.2
..................................................................................... 187
Map of State Counts of Users* of Managed Long-Term Services and Supports, as of
July 1, 2018 .................................................................................................................................. 191
Table 7 Number of Managed Care Programs Enrolling Certain Populations on a
Mandatory or Voluntary Basis, at any point in 2018 .................................................................... 192
Table 8. Number of Managed Care Program Types, by Quality Assurance
Requirements, Performance Incentives, and Provider Value-Based Purchasing
Status, at any point in 2018 ......................................................................................................... 193
State Tables ...................................................................................................................................... 194

1
Medicaid Managed Care Enrollment and Program Characteristics, 2018
Overview
This report is a production of the Division of Managed Care Programs (DMCP) in the
Center for Medicaid and CHIP Services at the Centers for Medicare & Medicaid Services, with
assistance from Mathematica Policy Research (contract # HHSM-500-2014-00034I/HHSM-500-
T0021).
The data and information presented in this report were collected directly from all states, the
District of Columbia, and US territories. Please see the Glossary for definitions of all terms and
acronyms used in this report.
• National tables provide summary data on Medicaid managed care: (1) enrollment at the state
and plan level, as of July 1, 2018, and (2) program features, including type of enrollment
(mandatory or voluntary) by population group enrolled, quality assurance requirements, and
use of performance incentives by managed care program type (see Glossary for definitions of
each type).
• State tables summarize the characteristics of each managed care program operating in each
state as of July 2018, including program type, geographic reach, federal operating authority,
start and end dates, beneficiary groups enrolled, services covered, quality assurance and
improvement provisions, and the names of participating plans or providers.
Data Limitations
Mathematica conducted quality assurance review and data validation on the enrollment data
and program features provided by state officials. While efforts were made to resolve apparent
errors, users of this report should be aware of some limitations. First, states may differ in how
they describe similar types of managed care programs; for example, some states listed the
benefits covered through primary care case management (PCCM) programs as all services that
are coordinated by primary care providers, while other states listed only case management. In
addition, states sometimes use different data systems to track the number of enrollees in each
type of managed care program or plan, and the number of unduplicated enrollees in any type of
managed care program, which may yield inconsistent results. In some cases, states reported
program or plan names that differ from those used in publicly available sources, including the
2017 edition of this report series. Questions regarding state-specific information in this report
should be directed to state/territorial Medicaid officials; contact information can be found on
state Medicaid agency websites in each state’s profile at this link:
http://medicaiddirectors.org/about/medicaid-directors/
If you have general questions concerning this report, please contact Alexis Gibson at
2
Acknowledgements
We wish to extend special thanks to the many state officials who contributed their time and
assistance for this data collection. We also appreciate the contributions of the Mathematica team
that participated in this effort: Kelsey Cowen, Cyrus Jadun, Jenna Libersky, Danielle
Chelminsky, Burke Hays, Sean Kirk, William Mulhern, Natasha Reese-McLaughlin, Megan
Reilly, Alena Tourtellotte, and Erin Weir Lakhmani.
Errors and Corrections to the 2017 Report
In the course of collecting data for the 2018 version of this report, Mathematica uncovered
several errors in the data contained in the 2017 Medicaid Managed Care Enrollment Report,
released in Winter 2019. That report was reissued and its errors are listed below.
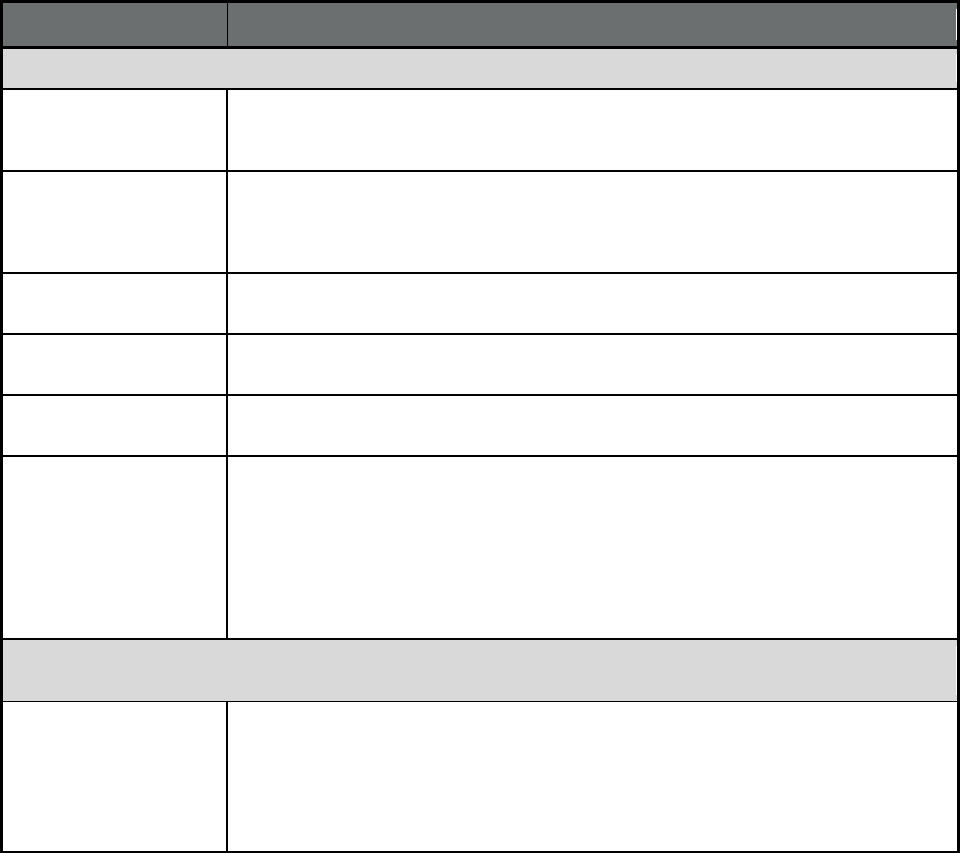
State/Domain Changes
Table 1: State Medicaid Managed Care Enrollment Data Summary, as of July 1, 2017
Georgia A footnote for Georgia has been added to the report that reads: “Georgia's Total Medicaid
Enrollment in Any Type of Managed Care does not include 1,556,221 NEMT enrollees; a
portion of these enrollees are simultaneously enrolled in other managed care programs.”
Indiana Total Medicaid enrollment in any type of managed care and total Medicaid enrollment in
comprehensive managed care were previously reported as 1,138,236. The corrected
figure for both enrollment in any type of managed care and enrollment in comprehensive
managed care is 1,138,368.
Nevada Medicaid enrollment in comprehensive MCOs under ACA Section VIII expansion was
previously reported as 190,510. The corrected figure is 183,853.
Oklahoma Total Medicaid enrollment in any type of managed care was previously reported as
653,362. The corrected figure is 652,952.
Texas Total Medicaid enrollment in comprehensive managed care was previously reported as
3,731,461. The corrected figure is 3,693,046.
All states As a result of these changes:
1. Total Medicaid enrollment in any type of managed care was previously reported as
65,796,616. The corrected figure is 65,796,338.
2. Medicaid enrollment in comprehensive managed care was previously reported as
55,601,033. The corrected figure is 55,562,750.
3. Medicaid enrollment in comprehensive MCOs under ACA Section VIII enrollment was
previously listed as 13,570,511. The corrected figure is 13,563,854.
Table 2. State Managed Care Enrollment by Program Type, All Eligibles (Medicaid-only and Medicare-
Medicaid), as of July 1, 2017
Georgia 1. Managed care enrollment in transportation programs was not previously reported. The
corrected figure is 1,556,221.
2. A footnote for Georgia has been added to the report that reads: “Georgia is unable to
provide separate counts of managed care and fee-for-service beneficiaries for their
NEMT program (which uses both payment models). As a result, enrollment counts
presented in this table include enrollees in both managed care and FFS.”
3
State/Domain Changes
Indiana Managed care enrollment in PACE programs was not previously reported. The corrected
figure is 132.
Louisiana Managed care enrollment in BHO (PIHP and/or PAHP) programs was previously reported
as 114,982. The corrected figure is 117,429.
Rhode Island Managed care enrollment in transportation programs was previously reported as 309,034.
The corrected figure is 278,402.
Texas Managed care enrollment in comprehensive MCO (with or without MLTSS) programs was
previously reported as 3,730,231. The corrected figure is 3,691,816.
All states As a result of these changes:
1. Total Medicaid enrollment in comprehensive MCOs (with or without MLTSS) was
previously reported as 55,558,073. The corrected figure is 55,519,658.
2. Managed care enrollment in BHO (PIHP and/or PAHP) programs was previously
reported as 10,727,803. The corrected figure is 10,730,250.
3. Managed care enrollment in transportation programs was previously reported as
12,847,769. The corrected figure is 14,373,358.
4. Managed care enrollment in PACE programs was previously reported as 42,960. The
corrected figure is 43,092.
Table 3: Medicare-Medicaid Eligibles (Duals) Enrolled in Managed Care by Program Type, as of July 1, 2017
Georgia 1. Medicare-Medicaid eligible (dual) enrollment in transportation programs was not
previously reported. The corrected figure is 0.
2. A footnote for Georgia has been added to the report that reads: “Georgia is unable to
provide separate counts of Medicaid-only and dually eligible beneficiaries for their
NEMT program. As a result, Medicare-Medicaid beneficiary enrollment is reported here
as zero.”
3. A footnote for Georgia has been added to the report that reads: “The total number of
dually eligible beneficiaries reported for Georgia only includes beneficiaries in the
QMB, SLMB, and QI programs.”
Idaho Total Medicare-Medicaid dually eligible beneficiaries was previously reported as 27,517.
The corrected figure is 46,342 to account for partial duals.
Indiana Medicare-Medicaid eligible (dual) enrollment in PACE programs was not previously
reported. The corrected figure is 127.
Nevada Total Medicare-Medicaid dually eligible beneficiaries was previously reported as 67,365.
The corrected figure is 76,221.
Ohio Total Medicare-Medicaid dually eligible beneficiaries was previously reported as 108,460.
The corrected figure is 251,004.
Rhode Island 1. Medicare-Medicaid eligible (dual) enrollment in transportation programs was
previously reported as 36,877. The corrected figure is 0.
Texas 2. Medicare-Medicaid eligible (dual) enrollment in comprehensive MCO (with or without
MLTSS) programs was previously reported as 38,427. The corrected figure is
296,462.
4
State/Domain Changes
All states As a result of these changes:
1. Total Medicare-Medicaid dually eligible enrollment was previously reported as
10,132,041. The corrected figure is 10,302,266.
2. Medicare-Medicaid eligible (dual) enrollment in comprehensive MCO (with or without
MLTSS) programs was previously reported as 2,577,209. The corrected figure is
2,835,244.
3. Medicare-Medicaid eligible (dual) enrollment in transportation programs was previously
reported as 1,167,035. The corrected figure is 1,130,158.
4. Medicare-Medicaid eligible (dual) enrollment in PACE programs was previously
reported as 34,809. The corrected figure is 34,936.
Table 4: Share of Medicaid Enrollees in Any Managed Care and in Comprehensive Managed Care, as of July 1,
2017
Georgia A footnote for Georgia has been added to the report that reads: “Georgia's Total Medicaid
Enrollment in Any Type of Managed Care does not include 1,556,221 NEMT enrollees; a
portion of these enrollees are simultaneously enrolled in other managed care programs.”
Indiana 1. Total Medicaid enrollment in any type of managed care and total Medicaid enrollment
in comprehensive managed care were previously reported as 1,138,236. The corrected
figure for both enrollment in any type of managed care and enrollment in
comprehensive managed care is 1,138,368.
2. The percent of all Medicaid enrollees in any type of managed care and comprehensive
managed care was previously reported as 77.1%. The corrected figure is 77.2%.
Oklahoma Total Medicaid enrollment in any type of managed care was previously reported as
653,362. The corrected figure is 652,952.
Texas 1. Total Medicaid enrollment in comprehensive managed care was previously reported
as 3,731,461. The corrected figure is 3,693,046.
2. The percent of all Medicaid enrollees in comprehensive managed care was previously
reported as 92.4%. The corrected figure is 91.5%.
All states As a result of these changes:
1. The number of individuals enrolled in any type of managed care was previously
reported as 65,796,616. The corrected figure is 65,796,338.
2. The number of individuals enrolled in comprehensive managed care was previously
reported as 55,601,033. The corrected figure is 55,562,750.
3. The percent of all Medicaid enrollees enrolled in comprehensive managed care was
previously reported as 69.3%. The corrected figure is 69.2%.
Table 5: Enrollment by Program and Plan, as of July 1, 2017
Alabama The Maternity Program has been updated to the Maternity Care Program for consistency
with future reporting years.
Georgia 1. The NEMT program and its associated plans were previously omitted from the 2017
reports. The program and its associated plans are now shown in the corrected reports
with a Medicaid-only enrollment of 1,556,221, a dual enrollment of 0, and a total
enrollment of 1,556,221.
2. A footnote for Georgia has been added to the report that reads: “Georgia is unable to
provide separate counts of Medicaid-only and dually eligible beneficiaries for their
NEMT program. As a result, Medicaid-only and total enrollment counts presented in
this table include both Medicaid-only and Medicare-Medicaid beneficiaries.”
5
State/Domain Changes
Indiana The PACE program and its associated plans were previously omitted from the 2017
reports. The program and its associated plans are now shown in the corrected reports with
a Medicaid-only enrollment of 5, a dual enrollment of 127, and a total enrollment of 132.
Kentucky The parent organization for the NEMT - Human Services Transportation Delivery plan was
previously reported as Humana CareSource. The corrected parent organization is NEMT –
Human Service Transportation Delivery.
Louisiana 1. The Dental program has been updated to the Dental Benefit Management program for
consistency with future reporting years.
2. The Coordinated System of Care program and its associated plans were previously
omitted from the 2017 reports. The program and its associated plans are now shown in
the corrected reports with a Medicaid-only enrollment of 2,447, a dual enrollment of 0,
and a total enrollment of 2,447.
New Jersey The FIDE SNP program and its associated plans were previously omitted from the 2017
reports. The program and its associated plans are now shown in the corrected reports with
a Medicaid-only enrollment of 0, a dual enrollment of 26,565, and a total enrollment of
26,565.
Rhode Island Medicaid-only, dually eligible, and total enrollment for the Transportation Broker program
were previously reported as 272,157; 36,877; and 309,034, respectively. The corrected
figures are 278,402; 0; and 278,402, respectively.
6
State/Domain Changes
Texas 1. Medicaid-only, dually eligible, and total enrollment for the STAR Health Superior Health
Plan was previously reported as 32,723; 12; and 32,735. The corrected figures are
32,735; 0; and 32,735, respectively.
2. Medicaid-only, dually eligible, and total enrollment for the STAR Kids Amerigroup plan
was previously reported as 27,735; 0; 27,735. The corrected figures are 27,592; 143;
and 27,735, respectively.
3. Medicaid-only, dually eligible, and total enrollment for the STAR Kids Superior Health
Plan was previously reported as 29,157; 0; and 29,157. The corrected figures are
28,967; 190; and 29,157, respectively.
4. Medicaid-only, dually eligible, and total enrollment for the STAR Kids Aetna plan was
previously reported as 5,124; 0; and 5,124. The corrected figures are 5,074; 50; and
5,124, respectively.
5. Medicaid-only, dually eligible, and total enrollment for the STAR Kids Community First
Health Plans plan was previously reported as 7,926; 0; and 7,926. The corrected
figures are 7,879; 47; 7,926, respectively.
6. Medicaid-only, dually eligible, and total enrollment for the STAR Kids United
Healthcare - Texas plan was previously reported as 30,364; 0; and 30,364. The
corrected figures are 30,208; 156; and 30,364, respectively.
7. Medicaid-only, dually eligible, and total enrollment for the STAR Kids Texas Children’s
Health Plan was previously reported as 25,577; 0; and 25,577. The corrected figures
are 25,476; 101; and 25,577, respectively.
8. Medicaid-only, dually eligible, and total enrollment for the STAR Kids Driscoll
Children’s Health Plan was previously reported as 10,611; 0; and 10,611. The
corrected figures are 10,565; 46; and 10,611, respectively.
9. Medicaid-only, dually eligible, and total enrollment for the STAR Kids Cook Children’s
Health Plan was previously reported as 8,993; 0; and 8,993. The corrected figures are
8,952; 41; and 8,993, respectively.
10. Medicaid-only, dually eligible, and total enrollment for the STAR Kids Blue Cross Blue
Shield plan was previously reported as 7,772; 0; and 7,772. The corrected figures are
7,735; 37; 7,772, respectively.
11. Medicaid-only, dually eligible, and total enrollment for the STAR Kids Children’s
Medical Center plan was previously reported as 9,688; 0; and 9,688. The corrected
figures are 9,658; 30; 9,688, respectively.
12. Medicaid-only, dually eligible, and total enrollment for the STAR+PLUS Amerigroup
plan was previously reported as 133,826; 13,053; and 146,879. The corrected figures
are 58,803; 75,023; and 133,826, respectively.
13. Medicaid-only, dually eligible, and total enrollment for the STAR+PLUS Cigna –
HealthSpring plan was previously reported as 50,149; 1,275; and 51,424. The
corrected figures are 19,706; 30,443; and 50,149, respectively.
14. Medicaid-only, dually eligible, and total enrollment for the STAR+PLUS Molina
Healthcare of Texas plan was previously reported as 87,652; 11,677; and 99,329. The
corrected figures are 35,012; 52,640; and 87,652, respectively.
15. Medicaid-only, dually eligible, and total enrollment for the STAR+PLUS Superior
Health Plan was previously reported as 139,417; 8,166; and 147,583. The corrected
figures are 65,115; 74,302; and 139,417, respectively.
16. Medicaid-only, dually eligible, and total enrollment for the STAR+PLUS United
Healthcare – Texas plan was previously reported as 115,686; 4,244; and 119,930. The
corrected figures are 52,473; 63,213; and 115,686, respectively.
7
State/Domain Changes
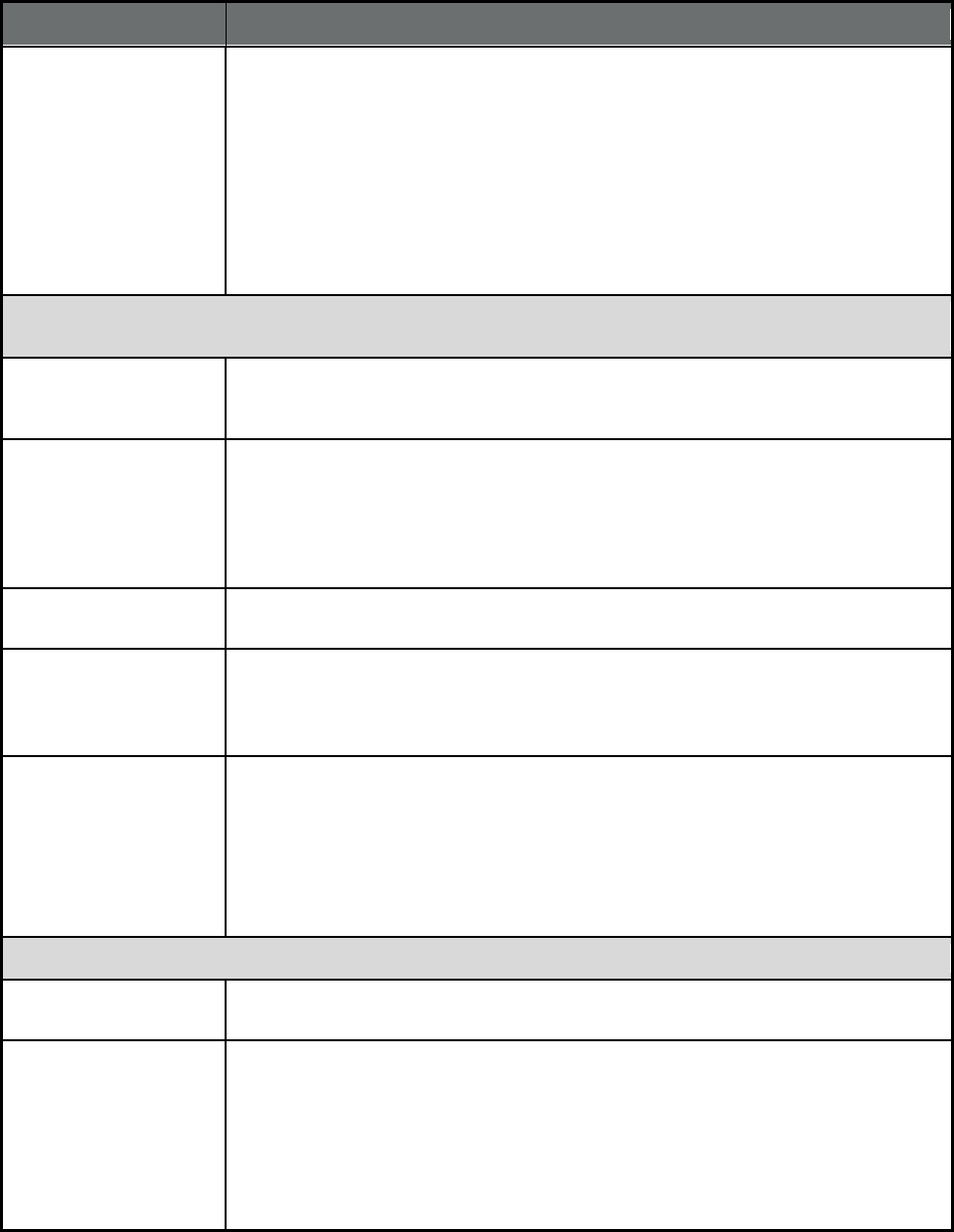
Table 6: Medicaid Managed Long Term Services and Supports (MLTSS) Program Users or Enrollees, as of July
1, 2017
Georgia A footnote for Georgia has been added to the report that reads: “Georgia's Total Medicaid
Enrollment in Any Type of Managed Care does not include 1,626,252 NEMT enrollees; a
portion of these enrollees are simultaneously enrolled in other managed care programs.”
Indiana Total Medicaid enrollment in any type of managed care was previously reported as
1,138,236. The corrected figure is 1,138,368.
Kansas A footnote for Kansas has been added to the report that reads: “Delaware, Idaho, Illinois,
Kansas, and Rhode Island report the number of enrollees in their MLTSS programs, some
of whom may not be using MLTSS. In previous years, they reported the number of users
of LTSS. The totals in this column do not include those six states because it is a count of
users, not enrollees.”
Ohio The number of enrollees using comprehensive managed care including LTSS was
previously reported as 45,135, which included users through Ohio’s FAI demonstration.
The corrected figure is 17,820 and does not include the state’s FAI demonstration.
Oklahoma Total Medicaid enrollment in any type of managed care was previously reported as
653,362. The corrected figure is 652,952.
All states As a result of these changes:
1. Total Medicaid enrollment in any type of managed care was previously reported as
65,796,616. The corrected figure is 65,796,338.
2. The number of enrollees using comprehensive managed care including LTSS was
previously reported as 871,052. The corrected figure is 814,450.
3. The percent of total managed care enrollees using comprehensive managed care
including LTSS was previously reported as 1.3%. The corrected figure is 1.2%
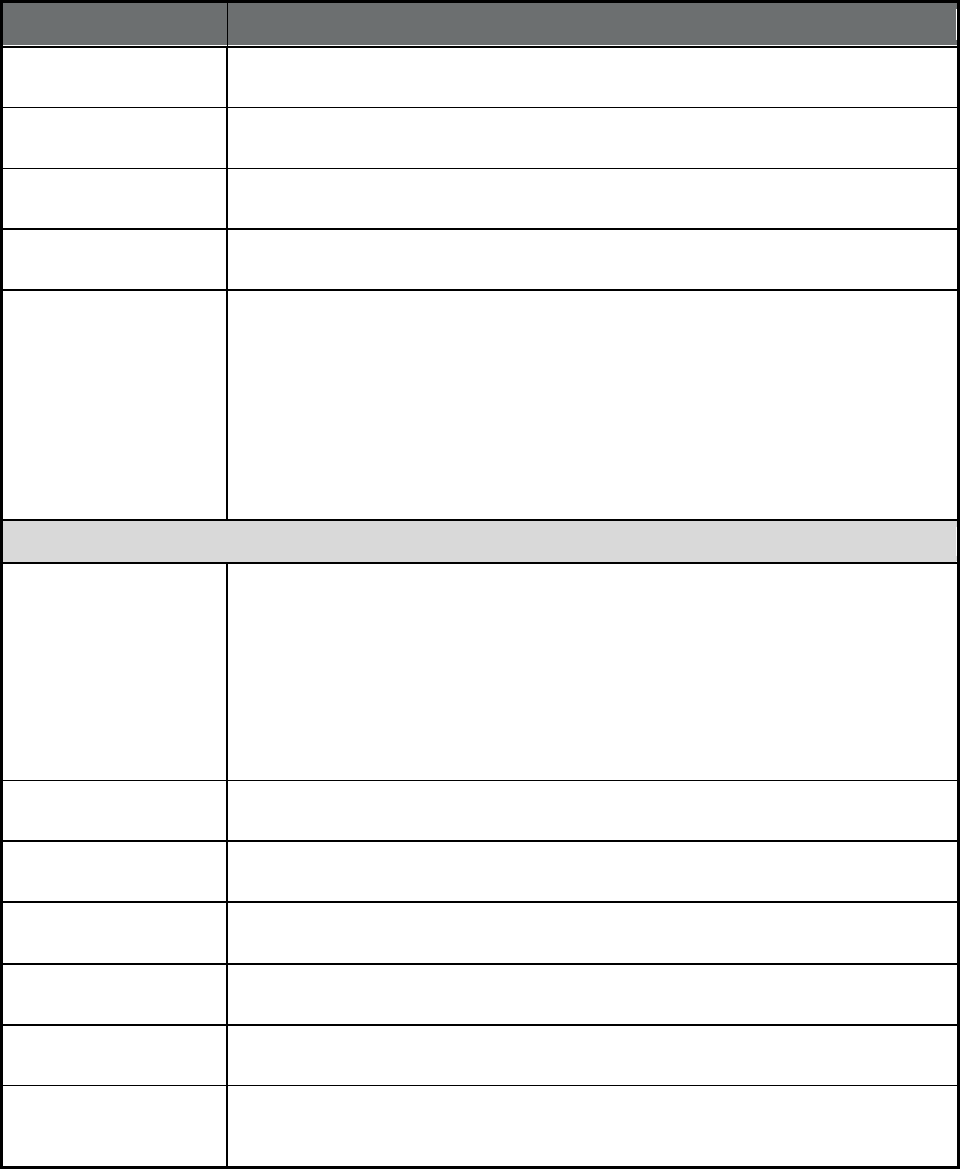
Table 7: Number of Managed Care Programs Enrolling Certain Populations on a Mandatory or Voluntary Basis,
at any point in 2017
The changes for Table 7 result from the errors and corrections described in Tables 1-6.
Comprehensive MCO with
or without MLTSS
1. The total number of comprehensive MCO programs with or without MLTSS has been
changed from 77 to 78.
2. The number of programs in which full duals are enrolled voluntarily has been changed
from 26 to 27.
3. The number of programs in which Native American/Alaskan Natives are exempt has
been changed from 12 to 13.
4. The number of programs in which foster care and adoption assistance children are
exempt has been changed from 26 to 27.
BHO (PIHP and/or PAHP) 1. The total number of BHO (PIHP and/or PAHP) programs has been changed from 14 to
15.
2. The number of programs in which children with special health care needs enrolled
voluntarily has been changed from 3 to 4.
8
State/Domain Changes
Transportation 1. The total number of transportation programs has been changed from 16 to 17.
2. The number of programs in which low-income adults are enrolled voluntarily has been
changed from 2 to 3.
3. The number of programs in which aged, blind, or disabled children or adults are
enrolled voluntarily has been changed from 2 to 3.
4. The number of programs in which non-disabled children (excluding children in foster
care or receiving adoption assistance) enrolled voluntarily has been changed from 2 to
3.
5. The number of programs in which individuals receiving limited benefits are enrolled
voluntarily has been changed from 2 to 3.
6. The number of programs in which full duals are enrolled voluntarily has been changed
from 2 to 3.
7. The number of programs in which children with special health care needs are enrolled
voluntarily has been changed from 2 to 3.
8. The number of programs in which foster care and adoption assistance children are
enrolled mandatorily has been changed from 12 to 13.
9. The number of programs in which Native American/Alaskan Natives are exempt has
been changed from 5 to 6.
PACE 1. The total number of PACE programs has been changed from 30 to 31.
2. The number of programs in which aged, blind, or disabled children or adults are
enrolled voluntarily has been changed from 23 to 24.
3. The number of programs in which full duals are enrolled voluntarily has been changed
from 29 to 30.
4. The number of programs in which partial duals are enrolled voluntarily has been
changed from 19 to 20.
5. The number of programs in which Native American/Alaskan Natives are enrolled
voluntarily has been changed from 21 to 22.
6. The number of programs in which foster care and adoption assistance children are
exempt has been changed from 20 to 21.
Table 8: Number of Managed Care Program Types, by Quality Assurance Requirements, Performance
Incentives, and Provider Value-Based Purchasing Status, at any point in 2017
The changes for Table 8 result from the errors and corrections described in Tables 1-6.
Comprehensive MCO with
or without MLTSS
1. The total number of comprehensive MCO programs with or without MLTSS has been
changed from 77 to 78.
2. The number of programs requiring HEDIS data has been changed from 70 to 71.
3. The number of programs requiring CAHPS data has been changed from 66 to 67.
4. The number of programs using an EQRO contractor has been changed from 72 to 73.
5. The number of programs using payment bonuses or differentials has been changed
from 32 to 33.
6. The number of programs using public reports comparing MCO performance on key
metrics has been changed from 42 to 43.
BHO (PIHP and/or PAHP) 1. The total number of BHO (PIHP and/or PAHP) programs has been changed from 14 to
15.
2. The number of programs requiring accreditation has been changed from 8 to 9.
Transportation The total number of transportation programs has been changed from 16 to 17.
PACE The total number of PACE programs has been changed from 30 to 31.
9
State/Domain Changes
State Tables
Alabama The Maternity Program has been updated to the Maternity Care Program for consistency
with future reporting years.
Georgia The NEMT program was previously omitted from the 2017 reports. The program is now
shown in the corrected report.
Indiana The PACE program was previously omitted from the 2017 reports. The program is now
shown in the corrected report.
Louisiana 1. The Dental program has been updated to the Dental Benefit Management program for
consistency with future reporting years.
2. The Coordinated System of Care program was previously omitted from the 2017
reports. The program is now shown in the corrected report.
New Jersey The FIDE SNP program was previously omitted from the 2017 reports. The program is
now shown in the corrected report.
New York HCBS waiver services were not previously reported as covered benefits under the
Medicaid Advantage Plus program. The benefits are included in the corrected 2017
reports.

10
Highlights
Data from the Medicaid Managed Care Data Collection System (MMCDCS) in 2018 and
previous years show the following trends:
• Medicaid enrollment in comprehensive MCOs increased by .7 percent – from 55.52
million in 2017 to 55.56 million in 2018, a smaller increase than in previous years. .
Comprehensive MCOs cover a broad range of Medicaid benefits, including acute,
primary and specialty care, and in some states, behavioral health and long-term services
and supports (LTSS) as well.
• The percentage of Medicaid beneficiaries enrolled in comprehensive managed care
plans as a result of the ACA Medicaid expansion increased for the third straight
year, although growth slowed in 2018. About 13.64 million low income adults eligible
for Medicaid under Section VIII of the ACA in 2018 were enrolled in comprehensive
MCOs, compared to 13.56 million in 2016 (a .54 percent increase). Enrollment in
comprehensive MCOs covered under Section VIII has more than tripled since 2014,
when just 4.8 million beneficiaries enrolled in such plans.
• Dual enrollment in comprehensive MCOs increased by 5.2 percent from 2017 to
2018. About 3 million dually eligible beneficiaries were enrolled in comprehensive
MCOs in 2018, an increase from about 2.8 million in 2017. Additionally, states expanded
the use of comprehensive MCOs for dually eligible beneficiaries. In 2018, about 29
percent of dually eligible beneficiaries were enrolled in comprehensive MCOs, compared
to about 28 percent in 2017.
• Use of Behavioral Health Organization (BHO) declined by 28.1 percent in 2018,
while use of Dental and MLTSS only programs continued to increase. 2018 marked
the fifth straight year of declined use in BHO programs. In 2018, about 9.7 percent of all
Medicaid beneficiaries were enrolled in BHO programs, down from 2013 enrollment of
17.0 percent. In contrast, enrollment in Dental and MLTSS only programs saw increased
enrollment similar to previous years. In 2018, about 10.4 percent of all Medicaid
beneficiaries were enrolled in Dental programs and .5 percent enrolled in MLTSS only
programs, up from 7.7 percent and .3 percent in 2014, respectively.
• Managed long-term services and supports (MLTSS) programs experienced growth.
Twenty-two states had managed LTSS (MLTSS) programs in operation as of July 1,
2018, consistent with the count in 2017
1
. As of July 1, 2018, there were over 1.3 million
(1,304,413) LTSS users, excluding a subset of 226,294 enrollees in Florida, Hawaii,
Idaho, Illinois, Kansas, and Pennsylvania, some of whom may not be LTSS users (these
states cannot report just LTSS users). 21 states reported LTSS users in both years, 14 of
which reported an increase in the number of LTSS users from 2017 to 2018.
1
The count of states in 2017 with MLTSS programs excludes South Carolina and Virginia whose only MLTSS
programs at that time were Medicare-Medicaid Financial Alignment demonstrations.
11
Glossary
Federal authorities (Waivers and State Plan Amendments)
1115(a) States can apply for a Section 1115 waiver to test experimental, pilot, or
demonstration projects that promote the objectives of the Medicaid and CHIP
programs.
1902(a)(70) NEMT States can use Section 1902(a)(70) statutory authority to amend their Medicaid state
plans to establish non‐emergency medical transportation (NEMT) brokerage
programs without regard to the statutory requirements for comparability, geographic
region served, and freedom of choice.
1905(t) States can use Section 1905(t) statutory authority to create voluntary primary care
case management (PCCM) managed care programs.
1915(a) States can use Section 1915(a) statutory authority to enter into a voluntary contract
with an entity to provide State plan services. Enrollment is voluntary.
1915(b) States can use Section 1915(b) waivers to mandate enrollment of special populations
into managed care delivery systems or otherwise limit beneficiaries’ choice of
providers.
1915(c) States can use Section 1915(c) waivers to provide long-term services and supports
(LTSS) in home and community settings rather than institutional settings. By using
1915(c) waivers concurrently with 1915(a), 1932(a), or 1915(b) authorities, states can
provide LTSS through managed care. Without a concurrent waiver allowing a state to
deliver these services through managed care, 1915(c) waiver services are paid fee-
for-service.
1915(i) States can use Section 1915(i) statutory authority to offer a variety of home and
community-based services through the state plan, regardless of whether enrollees
meet the institutional level of care. By using 1915(i) authority concurrently with
1915(a), 1932(a), or 1915(b) authorities, states can provide LTSS through managed
care.
1915(j) States can use Section 1915(j) statutory authority to offer self- directed personal
assistance services provided under the state plan and/or section 1915(c) waivers. By
using 1915(j) authority concurrently with 1915(a), 1932(a), or 1915(b) authorities,
states can provide LTSS through managed care.
1915(k) States can use Section 1915(k) statutory authority to provide home and community-
based attendant services and supports (the "Community First Choice Option") under
their state plan. By using 1915(k) authority concurrently with 1915(a), 1932(a), or
1915(b) authorities, states can provide LTSS through managed care.
1932(a) State can use Section 1932(a) statutory authority to mandate enrollment of Medicaid
beneficiaries in managed care entities without section 1915(b) or 1115 waiver
authority. However, certain groups are exempt from mandatory enrollment (for
example, Medicare-Medicaid dual enrollees, Native Americans and children with
special health care needs), and with exceptions for rural areas, the state must offer at
least two managed care options.
1937 Alternative Benefit
Plan
States can use Section 1937 statutory authority to provide alternative benefits tailored
to meet the needs of certain Medicaid population groups, target residents in certain
areas of the state, or provide services through specific delivery systems instead of
following the traditional Medicaid benefit plan. The Affordable Care Act of 2010
amended Section 1937 by requiring states to provide an alternative benefit package
to the newly eligible adult (Section VIII) Medicaid expansion population, which must
cover 10 essential health benefits described in ACA Section 1302(b).
1945 Health Homes States can use Section 1945 statutory authority to coordinate care for Medicaid
beneficiaries who have chronic conditions. Although Medicaid Health Homes are not
a managed care system, states can combine 1945 authority with a managed care
authority such as 1915(a), 1932(a), or 1915(b) to provide health home services
through managed care entities.
12
Key Terms, Acronyms and Definitions
Term Acronym Definition
Affordable Care Act ACA The Patient Protection and Affordable Care Act, is the federal law
that took full effect in 2014. Among other provisions, it authorized
states to expand Medicaid coverage to non-pregnant, childless,
low-income adults with household income up to 138 percent of the
federal poverty level, without a waiver or other special authority.
Behavioral Health
Organization
BHO A managed care entity specializing in behavioral health (mental
health and/or substance use disorder) services. Services are
covered on a prepaid basis.
Centers for Medicare &
Medicaid Services
CMS The federal agency that administers the Medicare and Medicaid
programs.
Comprehensive Managed
Care Organization
Compre-hensive
MCO
Comprehensive MCOs provide all acute, primary and specialty
medical services; some also cover behavioral health and long-term
services and supports. Entities that qualify as MCOs include Health
Maintenance Organizations (HMOs) and Health Insuring
Organizations (HIOs) in California.
Consumer Assessment of
Healthcare Providers and
Systems
CAHPS Surveys that ask consumers and patients about their experiences
with health care services and health plans. Some state Medicaid
agencies require health plans to submit data or results from
CAHPS surveys of managed care enrollees.
Dental Prepaid Ambulatory
Health Plan
A limited-benefit plan that only provides dental services.
Dual Eligibles (also
referred to as “Duals”, or
Medicare-Medicaid
Eligibles)
Individuals who are eligible for Medicare and either (1) eligible to
receive all state Medicaid benefits (“full duals”) or (2) the Medicaid
agency only pays for Medicare premiums and/or cost sharing
(“partial duals”).
Early and Periodic
Screening, Diagnostic and
Treatment
EPSDT States are required to cover the following services for all Medicaid-
eligible children under age 21: periodic screenings to identify
physical and mental conditions as well as vision, hearing, and
dental needs; and follow-up diagnostic and treatment services to
correct conditions identified during a screening.
External Quality Review
Organization
EQRO An organization that meets competence and independence
requirements and performs an external quality review of managed
care programs and plans.
Federally Qualified Health
Center
FQHC Federally Qualified Health Centers provide comprehensive health
services in underserved communities and must offer a sliding fee
scale. FQHCs receive grants under Section 330 of the Public
Health Service Act.
Fee-For-Service FFS A payment system in which the state reimburses providers directly
for each individual service rendered.
Healthcare Effectiveness
Data and Information Set
HEDIS A collection of performance measures and measurement
specifications which certain Medicaid managed care programs are
required to use and submit to the state. HEDIS measures and
definitions are produced by the National Committee for Quality
Assurance (NCQA).
13
Term Acronym Definition
Home and Community-
based Services
HCBS Long-term services and supports provided in homes or community
settings to Medicaid beneficiaries who are frail seniors, or with
mental illnesses, intellectual or developmental disabilities, and/or
physical disabilities in.
Intellectual /
Developmental Disabilities
IDD An individual with an intellectual or developmental disability has an
intellectual functioning level (IQ) below 70-75, limitations in
adaptive skills, and must have had the condition start before the
age of nineteen.
Intermediate Care
Facilities
ICF An optional Medicaid benefit to provide treatment in an institutional
care setting for individuals with intellectual disabilities.
Institution for Mental
Diseases
IMD Services furnished by a hospital, nursing facility, or other institution
of more than 16 beds that is primarily engaged in providing
diagnosis, treatment, or care of persons with mental diseases,
including medical attention, nursing care, and related services.
Whether an institution is an institution for mental diseases is
determined by its overall character as that of a facility established
and mai
ntained primarily for the care and treatment of individuals
with mental diseases, whether or not it is licensed as such. The
facility must be a hospital providing psychiatric or substance use
disorder inpatient care or a sub-acute facility providing psychi
atric
or substance use disorder crisis residential services, and length of
stay in the IMD must be for a short term stay of no more than 15
days during the period of the monthly capitation payment. The
provision of inpatient psychiatric or substance use disorder
treatment in an IMD must meet the requirements for in lieu of
services.
Long-term Services and
Supports
LTSS Long term services and supports assist individuals with activities of
daily living such as bathing, dressing and eating in institutional
settings, including nursing homes and ICFs-IDD, or in home and
community-based settings.
Managed Long Term
Services and Supports
MLTSS The delivery of LTSS, such as nursing home care and home and
community-based services, through capitated Medicaid managed
care programs. MLTSS programs can either provide LTSS in
addition to medical care through comprehensive MCOs, or they can
provide only LTSS benefits through PIHPs or PAHPs, referred to as
MLTSS-only programs.
Medicaid A health care program providing coverage for eligible low-income
adults, children, pregnant women, elderly adults and people with
disabilities. Medicaid is jointly administered and funded by states
and the federal government, according to federal rules.
Medicaid Managed Care Medicaid managed care provides for the delivery of Medicaid
health benefits and additional services through contracted
arrangements between state Medicaid agencies and managed care
entities, such as MCOs, that accept a set per member per month
(capitation) payment for these services, or with providers
responsible for coordinating a defined set of services.
Medicaid State Plan An agreement between a state and the federal government
describing how that state administers its Medicaid program,
including eligible individuals, services covered, reimbursement
methodologies, and administrative activities.
14
Term Acronym Definition
Medicaid State Plan
Amendment
SPA When a state is planning to make a change to its Medicaid program
policies or operational approach, states submit SPAs to CMS for
review and approval.
Medicaid Waivers Statutory authorities under which the Secretary of Health and
Human Services, upon the request of a state, may allow the state
to receive federal Medicaid matching funds for its expenditures
when the benefits or populations covered, or other program
features deviate from requirements or limitations of the federal
Medicaid statute.
Medicare A health care program for individuals ages 65 and older, and
individuals under age 65 with certain disabilities. Medicare is
administered and funded by the federal government.
Mental Health MH An individual’s psychological and emotional state. Mental disorders
affect how individuals relate to each other and make choices, and
may include changes in thinking, mood, and/or behavior.
Non-Emergency Medical
Transportation
NEMT A program that covers transportation to and from medically
necessary health care services.
Other Prepaid Health
Plans
PHP Prepaid ambulatory or inpatient health plans that cover a limited set
of benefits, such as behavioral health, long term care, dental, or
transportation benefits.
Prepaid Ambulatory Health
Plan
PAHP An entity that provides medical services to enrollees under contract
with the State agency and on the basis of prepaid capitation
payments or other payment arrangements that do not use State
plan payment rates. A PAHP does not provide or arrange for the
provision of any inpatient hospital or institutional services for its
enrollees.
Prepaid Inpatient Health
Plan
PIHP An entity that provides medical services to enrollees under contract
with the State agency and on the basis of prepaid capitation
payments or other payment arrangements that do not use State
plan payment rates. A PIHP provides, arranges for, or otherwise
has responsibility for, the provision of any inpatient hospital or
institutional services for its enrollees.
Presumptive Eligibility The option available to states to extend limited Medicaid coverage
at the point a provider determines that an individual’s income does
not exceed the eligibility threshold until a formal determination of
eligibility is made.
Primary Care Case
Management
PCCM A managed care arrangement in which primary care providers
contract with the state to provide a core set of case management
services to the enrollees assigned to them and to serve as the
enrollees’ home for medical care, in exchange for a small
administrative fee. All other services are reimbursed on a FFS
basis. Primary Care Providers (PCPs) can include primary care
physicians, clinics, group practices and nurse practitioners, among
others.
15
Term Acronym Definition
Primary Care Case
Management entity
PCCM entity In addition to providing primary care case management services for
the State, a PCCM entity is an organization that provides any of the
following functions: (1) Provision of intensive telephonic or face-to-
face case management, including operation of a nurse triage
advice line; (2) Development of enrollee care plans; (3) Execution
of contracts with and/or oversight resp
onsibilities for the activities of
FFS providers in the FFS program; (4) Provision of payments to
FFS providers on behalf of the State; (5) Provision of enrollee
outreach and education activities; (6) Operation of a customer
service call center; (7) Review of provider claims, utilization and
practice patterns to conduct provider profiling and/or practice
improvement; (8) Implementation of quality improvement activities
including administering enrollee satisfaction surveys or collecting
data necessary for per
formance measurement of providers; (9)
Coordination with behavioral health systems/providers; and/or (10)
Coordination with long-term services and supports systems/
providers.
Program for All-inclusive
Care for the Elderly
PACE A program that provides prepaid, capitated comprehensive medical
and social services in an adult day health center, as well as in-
home and referral services according to a participant’s needs. To
qualify, individuals must: (1) be 55 years of age or older, (2) meet a
nursing home level of care, and (3) live in a PACE organization
service area.
Section VIII Section VIII of the Affordable Care Act (ACA) authorized the
expansion of Medicaid coverage to non-pregnant, childless, low-
income adults with household income up to 138 percent of the
federal poverty level, who could previously be covered only under a
waiver or other special authority.
Substance Use Disorder SUD Individuals with an SUD recurrently use alcohol and/or drugs. As a
result, they experience significant clinical and functional impairment
that may include: health issues, disability and failure to meet
responsibilities.
Transportation Prepaid
Ambulatory Health Plan
NEMT PAHP A prepaid ambulatory health plan covering transportation services
only.
16
National Tables and Maps
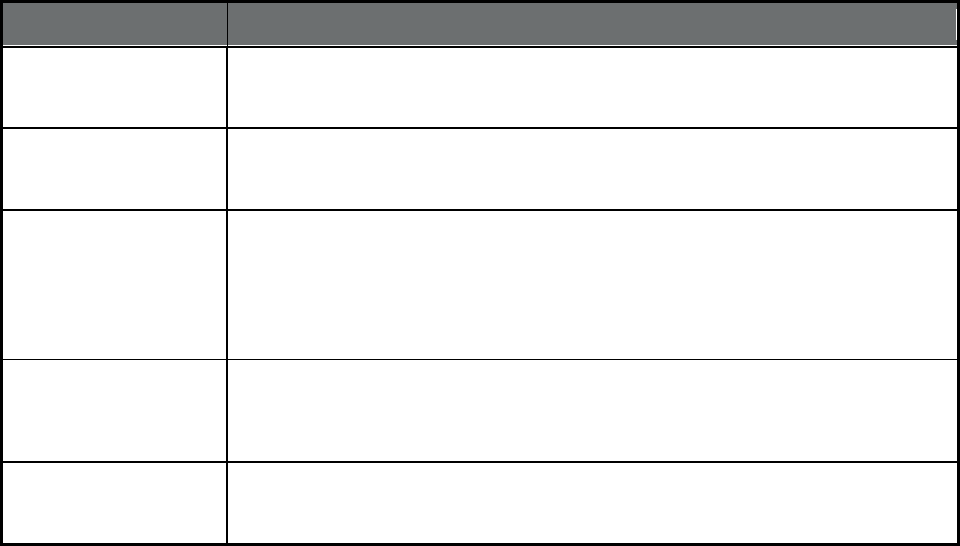
Table 1. State Medicaid Managed Care Enrollment Data Summary, as of July 1, 2018
State or Territory Total Medicaid Enrollees
1
Total Medicaid Enrollment in
Any Type of Managed Care
2
Medicaid Enrollment in
Comprehensive Managed Care
3
Medicaid Enrollment in
Comprehensive MCOs Under
ACA Section VIII Expansion
4
TOTALS 79,898,701 66,107,287 55,605,461 13,637,012
Alabama 1,019,417 638,221 174 0
Alaska
5
198,417 0 0 0
American Samoa n/a n/a n/a n/a
Arizona 1,849,465 1,560,593 1,560,593 383,615
Arkansas 979,619 871,262 258 0
California 13,140,347 10,670,306 10,661,382 3,144,393
Colorado
6
1,302,808 1,171,171 122,207 47,361
Connecticut
7
928,800 0 0 0
Delaware 236,760 208,802 199,887 57,851
District of Columbia 264,984 189,363 189,363 65,150
Florida 3,885,169 3,178,981 3,027,995 0
Georgia
8
2,074,310 1,485,250 1,445,804 0
Guam n/a n/a n/a n/a
Hawaii 355,873 351,685 351,685 23,714
Idaho 300,252 272,979 3,799 0
Illinois 3,110,093 2,176,902 2,145,760 476,583
Indiana 1,457,544 1,126,425 1,126,425 344,386
Iowa 626,011 580,507 564,926 166,755
Kansas 417,140 358,225 358,225 0
Kentucky 1,385,239 1,259,525 1,259,525 459,092
17
State or Territory Total Medicaid Enrollees
1
Total Medicaid Enrollment in
Any Type of Managed Care
2
Medicaid Enrollment in
Comprehensive Managed Care
3
Medicaid Enrollment in
Comprehensive MCOs Under
ACA Section VIII Expansion
4
Louisiana 1,640,075 1,504,540 1,385,242 473,308
Maine 270,243 234,327 0 0
Maryland 1,401,781 1,169,708 1,169,708 291,852
Massachusetts 1,865,755 1,211,485 750,573 180,657
Michigan 4,623,834 4,608,988 2,379,554 554,203
Minnesota 1,122,672 892,137 892,137 184,105
Mississippi 683,577 441,782 441,782 0
Missouri 971,143 954,603 712,335 0
Montana 291,890 215,475 0 0
Nebraska 250,056 249,024 249,022 0
Nevada 666,561 588,111 457,782 187,715
New Hampshire 200,850 133,829 133,829 9,046
New Jersey 1,668,451 1,569,344 1,569,344 523,347
New Mexico 842,138 666,050 666,050 224,743
New York 6,153,799 4,764,261 4,552,993 3,337,546
North Carolina 2,178,225 1,581,469 2,112 0
North Dakota 93,042 48,957 19,696 19,515
Northern Mariana
Islands
n/a n/a n/a n/a
Ohio 2,915,546 2,450,031 2,450,031 606,662
Oklahoma 880,954 649,023 466 0
Oregon 1,062,787 847,570 847,570 386,277
Pennsylvania 2,897,085 2,627,563 2,359,277 723,410
Puerto Rico
9
1,505,610 1,505,610 1,505,610 0
Rhode Island 313,095 302,407 248,278 73,323
18
State or Territory Total Medicaid Enrollees
1
Total Medicaid Enrollment in
Any Type of Managed Care
2
Medicaid Enrollment in
Comprehensive Managed Care
3
Medicaid Enrollment in
Comprehensive MCOs Under
ACA Section VIII Expansion
4
South Carolina 1,195,703 1,195,703 745,911 0
South Dakota 123,890 92,184 0 0
Tennessee 1,510,045 1,386,664 1,386,664 0
Texas 3,981,912 3,845,916 3,695,426 0
Utah 275,511 271,137 226,893 0
Vermont 174,682 123,310 123,310 48,637
Virgin Islands n/a n/a n/a n/a
Virginia 1,063,122 875,351 875,351 0
Washington 1,781,048 1,781,048 1,574,163 491,177
West Virginia 505,528 407,193 407,193 152,589
Wisconsin 1,197,453 811,920 759,015 0
Wyoming 58,390 370 136 0
1. Total Medicaid Enrollees represents an unduplicated count of all beneficiaries in FFS and any type of managed care, including Medicaid-only and Medicare-
Medicaid ("dual") enrollees receiving full Medicaid benefits or Medicaid cost sharing.
2. Total Medicaid Enrollment in Any Type of Managed Care represents an unduplicated count of beneficiaries enrolled in any Medicaid managed care program,
including comprehensive MCOs, limited benefit plans such as prepaid inpatient and ambulatory health plans, primary care case management (PCCM) programs,
and PCCM entities.
3. Medicaid Enrollment in Comprehensive Managed Care represents an unduplicated count of Medicaid beneficiaries enrolled in a managed care plan that
provides comprehensive benefits (acute, primary care, specialty, and any other), or PACE program. It excludes beneficiaries who are enrolled in a Financial
Alignment Demonstration Medicare-Medicaid Plan as their only form of managed care.
4. Medicaid Enrollment in Comprehensive MCOs under ACA Section VIII Expansion is a subset of the total reported in column C, and includes individuals who are
enrolled in comprehensive MCOs and are low-income adults, with or without dependent children, eligible for Medicaid under ACA Section VIII.
5. Alaska was not able to provide total Medicaid enrollment as of July 1, 2018. This figure is from the July - September 2018 enrollment data collected through the
Medicaid Budget and Expenditure System, updated December 2019, and accessed January 14, 2020. See https://data.medicaid.gov/Enrollment/2018-4Q-
Medicaid-MBES-Enrollment/qjmt-6zzy.
6. Colorado reported plan level enrollment as 0 for plans that had less than 30 beneficiaries. As a result, reported Medicaid Enrollment in Comprehensive
Managed Care may be lower than actual enrollment.
7. Connecticut was not able to provide total Medicaid enrollment as of July 1, 2018. This figure is from the July - September 2018 enrollment data collected
through the Medicaid Budget and Expenditure System, updated December 2019, and accessed January 14, 2020. See https://data.medicaid.gov/Enrollment/2018-
4Q-Medicaid-MBES-Enrollment/qjmt-6zzy.
19
8. Georgia's Total Medicaid Enrollment in Any Type of Managed Care does not include 1,626,252 NEMT enrollees; a portion of these enrollees are simultaneously
enrolled in other managed care programs.
9. Puerto Rico provides expanded Medicaid to 421,577 low-income, childless adults under an authority other than ACA Section VIII.
Note: "n/a" indicates that a state or territory was not able to report data.`
20
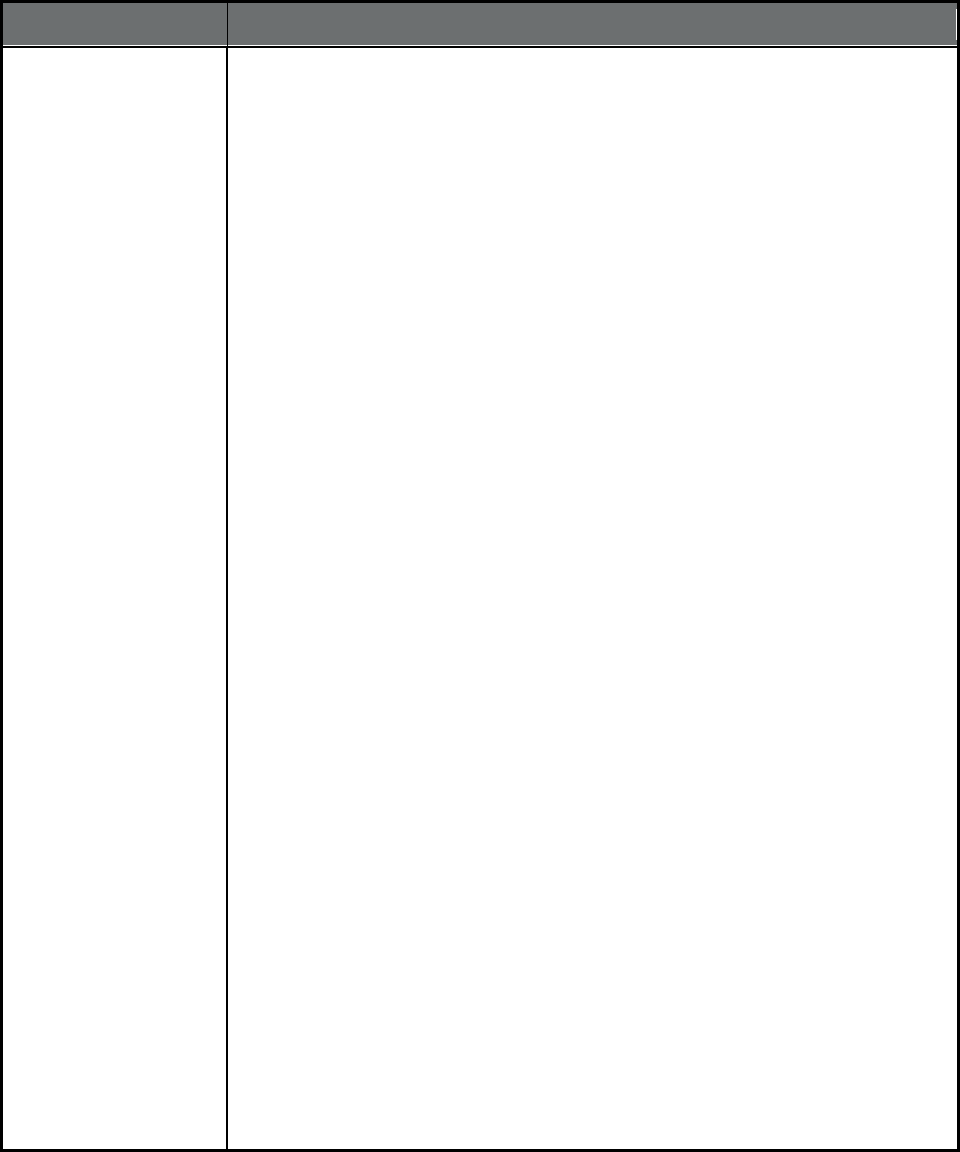
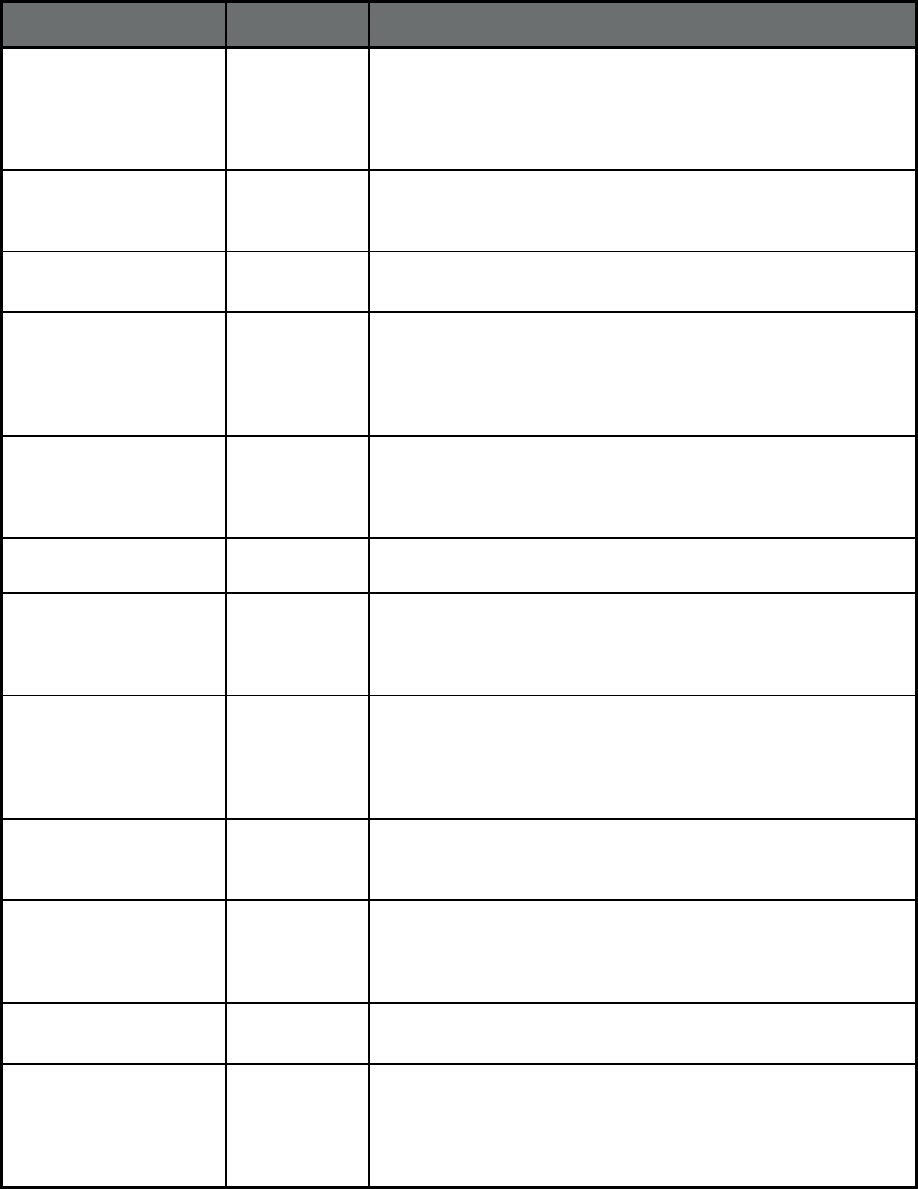
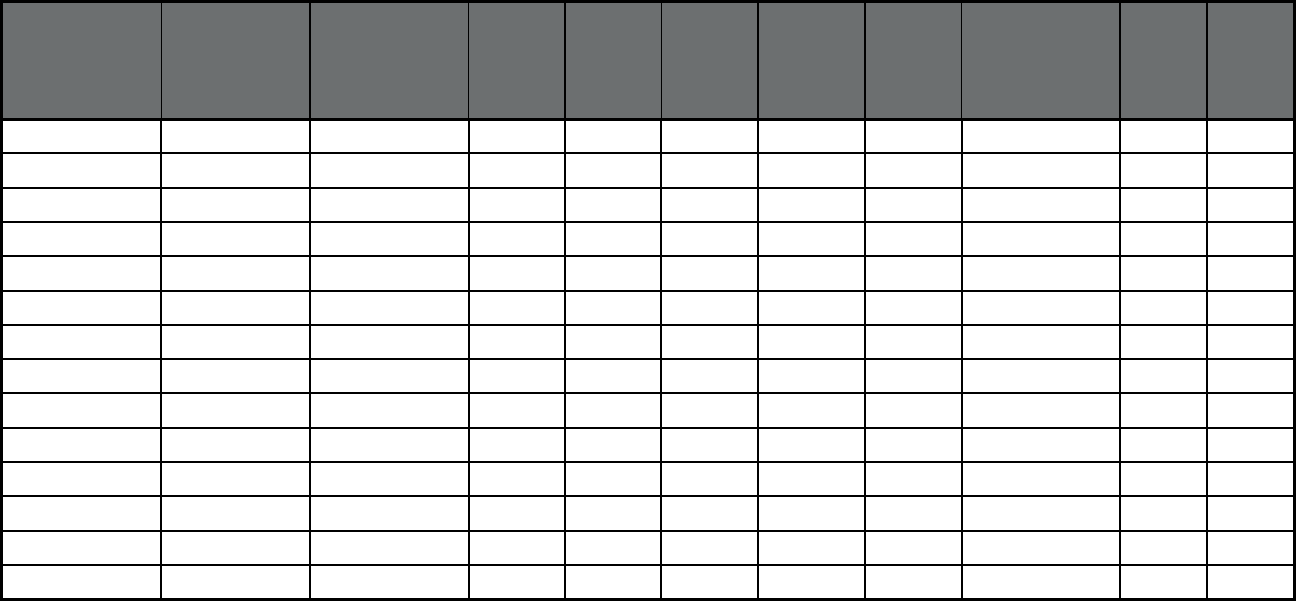
Table 2. State Managed Care Enrollment by Program Type, All Eligibles (Medicaid-only and Medicare-
Medicaid), as of July 1, 2018
1
State or
Territory
Total
Medicaid
Enrollees
2
Comprehensive
MCO (with or
without MLTSS)
3
PCCM
3
PCCM
entity
3
MLTSS
only
3
BHO (PIHP
and/or
PAHP)
3
Dental
3
Transportation
3
PACE Other
3
TOTALS 79,898,701 55,558,458 2,583,532 2,910,656 403,798 7,717,977 8,292,589 15,204,939 48,395 66,486
Alabama
4
1,019,417 -- 611,251 -- -- -- -- -- 174 22,844
Alaska
5
198,417 -- -- -- -- -- -- -- -- --
American Samoa n/a n/a n/a n/a n/a n/a n/a n/a n/a n/a
Arizona 1,849,465 1,560,593 -- -- -- -- -- -- -- --
Arkansas 979,619 -- 445,284 29,078 -- -- 576,970 579,996 258 --
California 13,140,347 10,653,598 -- -- -- 32 845,796 -- 7,784 670
Colorado
6
1,302,808 118,408 -- 1,048,881 -- 0 -- -- 3,799 --
Connecticut
7
928,800 -- -- -- -- -- -- -- -- --
Delaware 236,760 199,645 -- -- -- -- -- 208,802 242 --
District of
Columbia
264,984 189,363 -- -- -- -- -- 54,594 -- --
Florida 3,885,169 3,026,316 -- -- 101,524 -- -- -- 1,679 --
Georgia
8
2,074,310 1,445,804 -- -- -- -- -- 1,623,252 -- 39,446
Guam n/a n/a n/a n/a n/a n/a n/a n/a n/a n/a
Hawaii
9
355,873 351,685 -- -- -- -- -- -- -- --
Idaho 300,252 3,799 254,791 -- -- 269,240 272,979 272,979 -- --
Illinois 3,110,093 2,145,760 -- -- 31,143 -- -- -- -- --
Indiana 1,457,544 1,126,133 -- -- -- -- -- -- 292 --
Iowa 626,011 564,492 -- -- -- -- 302,681 15,581 434 --
Kansas 417,140 357,683 -- -- -- -- -- -- 542 --
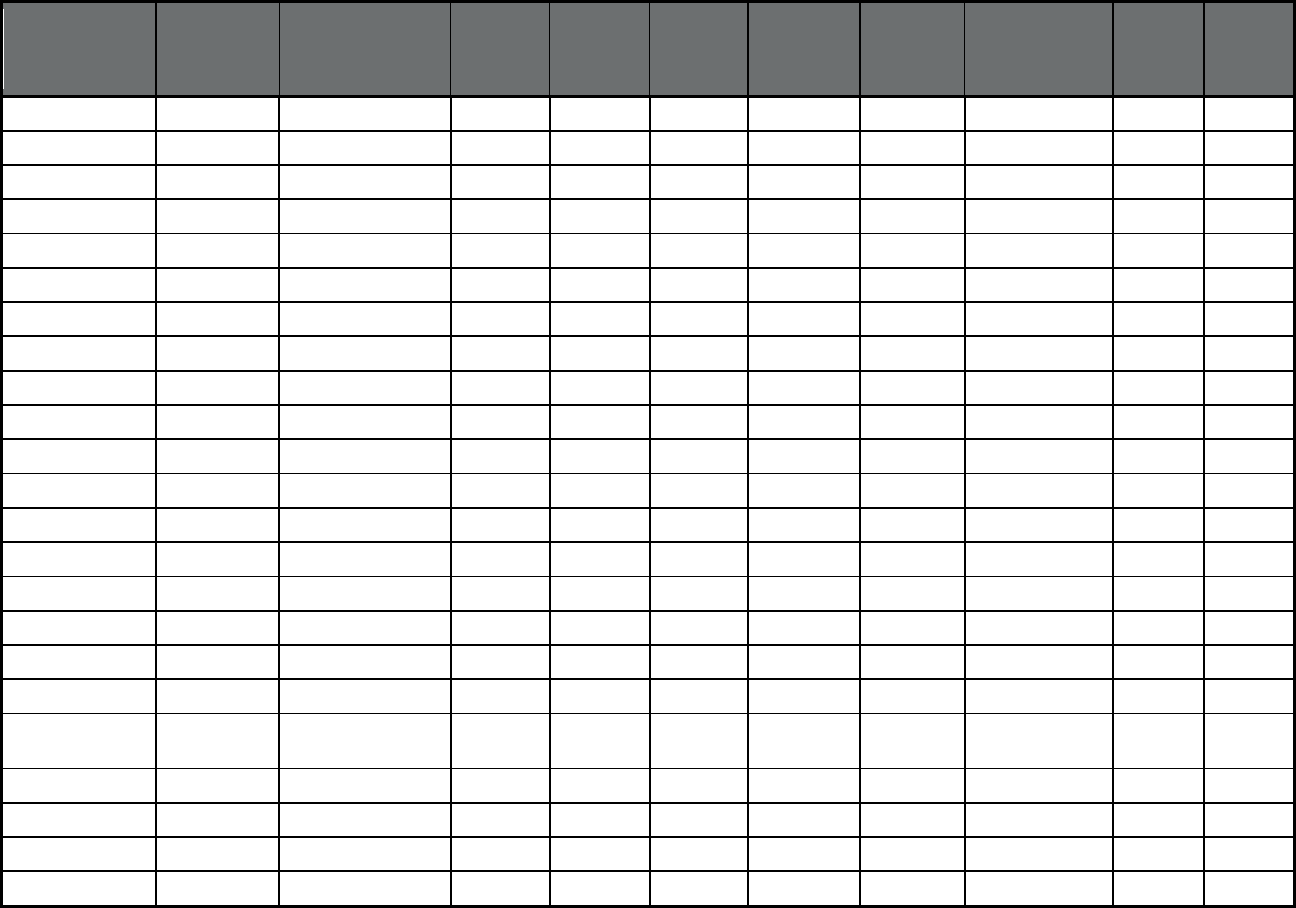
21
State or
Territory
Total
Medicaid
Enrollees
2
Comprehensive
MCO (with or
without MLTSS)
3
PCCM
3
PCCM
entity
3
MLTSS
only
3
BHO (PIHP
and/or
PAHP)
3
Dental
3
Transportation
3
PACE Other
3
Kentucky 1,385,239 1,259,525 -- -- -- -- -- 1,232,903 -- --
Louisiana 1,640,075 1,384,784 -- -- -- 118,107 1,503,192 -- 458 --
Maine 270,243 -- 141,777 -- -- -- -- 234,327 -- --
Maryland 1,401,781 1,169,603 -- -- -- -- -- -- 105 --
Massachusetts 1,865,755 746,051 119,512 339,350 -- 528,106 -- -- 4,522 --
Michigan
10
4,623,834 2,377,009 -- -- 11,295 2,276,353 969,152 -- 2,545 --
Minnesota 1,122,672 892,137 -- -- -- -- -- -- -- --
Mississippi 683,577 441,782 -- -- -- -- -- -- -- --
Missouri 971,143 712,335 -- -- -- -- -- 242,268 -- --
Montana 291,890 -- 215,475 -- -- -- -- -- -- --
Nebraska 250,056 248,832 -- -- -- -- 247,580 -- 190 --
Nevada
666,561 457,782 -- -- -- -- 457,782 588,111 -- --
New Hampshire 200,850 133,829 -- -- -- -- -- -- -- --
New Jersey 1,668,451 1,568,277 -- -- -- -- -- 1,561,266 1,067 --
New Mexico 842,138 665,250 -- -- -- -- -- -- 800 --
New York 6,153,799 4,547,299 -- -- 211,268 -- -- -- 5,694 --
North Carolina 2,178,225 -- -- 1,493,347 -- 1,578,977 -- -- 2,112 --
North Dakota 93,042 19,515 48,957 -- -- -- -- -- 181 0
Northern Mariana
Islands
n/a n/a n/a n/a n/a n/a n/a n/a n/a n/a
Ohio 2,915,546 2,449,577 -- -- -- -- -- -- 454 --
Oklahoma 880,954 -- 648,557 -- -- -- -- 648,557 466 --
Oregon
11
1,062,787 847,570 -- -- -- -- -- -- 1,392 --
Pennsylvania 2,897,085 2,352,627 -- -- -- 896,466 -- 622,053 6,650 151
22
State or
Territory
Total
Medicaid
Enrollees
2
Comprehensive
MCO (with or
without MLTSS)
3
PCCM
3
PCCM
entity
3
MLTSS
only
3
BHO (PIHP
and/or
PAHP)
3
Dental
3
Transportation
3
PACE Other
3
Puerto Rico 1,505,610 1,505,610 -- -- -- -- -- -- -- --
Rhode Island 313,095 247,983 -- -- -- -- 111,315 267,396 295 --
South Carolina 1,195,703 745,469 558 -- -- -- -- 1,195,703 442 --
South Dakota 123,890 -- 92,184 -- -- -- -- -- -- --
Tennessee
12
1,510,045 1,386,383 -- -- -- -- -- -- 281 --
Texas 3,981,912 3,694,211 -- -- -- -- 2,879,944 3,844,572 1,215 --
Utah 275,511 226,893 -- -- -- 268,452 125,198 231,531 -- --
Vermont 174,682 123,310 -- -- -- -- -- -- -- --
Virgin Islands n/a n/a n/a n/a n/a n/a n/a n/a n/a n/a
Virginia 1,063,122 872,408 -- -- -- -- -- -- 2,943 --
Washington 1,781,048 1,573,493 5,186 -- -- 1,781,048 -- 1,781,048 670 --
West Virginia
505,528 407,193 -- -- -- -- -- -- -- --
Wisconsin 1,197,453 758,442 -- -- 48,568 1,196 -- -- 573 3,141
Wyoming 58,390 -- -- -- -- -- -- -- 136 234
1. Because Medicaid beneficiaries may be enrolled concurrently in more than one type of managed care program (e.g., a Comprehensive MCO and a BHO), users
should not sum enrollment across all program types, since the total would count individuals more than once and, in some states, exceed the actual number of
Medicaid enrollees.
2. Total Medicaid Enrollees represents an unduplicated count of all beneficiaries in FFS and any type of managed care, including Medicaid-only and Medicare-
Medicaid ("dual") enrollees receiving full Medicaid benefits or Medicaid cost sharing.
3. Comprehensive MCOs cover acute, primary, and specialty medical care services; they may also cover behavioral health, long-term services and supports, and
other benefits in some states. Limited benefit managed care programs, including PCCM, PCCM entity, MLTSS only, BHO, Dental, Transportation, and Other cover
a narrower set of services.
4. Beneficiaries can simultaneously enroll in Alabama's two PCCM programs: Patient 1st and Health Homes. The de-duplicated Patient 1st enrollment is 380,285.
5. Alaska was not able to provide total Medicaid enrollment as of July 1, 2018. This figure is from the July - September 2018 enrollment data collected through the
Medicaid Budget and Expenditure System, updated December 2019, and accessed January 14, 2020. See https://data.medicaid.gov/Enrollment/2018-4Q-
Medicaid-MBES-Enrollment/qjmt-6zzy.
6. Colorado reported plan level enrollment as 0 for plans that had less than 30 beneficiaries. As a result, reported PACE program-level enrollment may be lower
than actual enrollment.
23
7. Connecticut was not able to provide total Medicaid enrollment as of July 1, 2018. This figure is from the July - September 2018 enrollment data collected
through the Medicaid Budget and Expenditure System, updated December 2019, and accessed January 14, 2020. See https://data.medicaid.gov/Enrollment/2018-
4Q-Medicaid-MBES-Enrollment/qjmt-6zzy.
8. Georgia is unable to provide separate counts of managed care and fee-for-service beneficiaries for their NEMT program (which uses both payment models). As
a result, enrollment counts presented in this table include enrollees in both managed care and FFS.
9. Hawaii's enrollment in comprehensive MCOs includes 4,470 beneficiaries who enrolled in an MCO plus Ohana Community Care Service for behavioral health
services.
10. Michigan has two programs that provide HCBS waiver services under capitation: MI Choice and the Specialty Prepaid Inpatient Health Plan (SPIHP). In this
table, MI Choice is reported as an MLTSS program and SPIHP is reported as a BHO. In Table 6, both programs are considered in the count of LTSS users.
11. Oregon’s enrollment in comprehensive MCOs includes beneficiaries in (1) Coordinated Care Organizations (CCOs); (2) Dental Care Organizations (DCOs), or
(3) a Mental Health Organization. CCO enrollees receive physical, dental and mental health services and may be enrolled in more than one plan type
simultaneously. Plan-level enrollment is found in Report 5.
12. Tennessee’s enrollment in comprehensive MCOs includes 1,241,360 beneficiaries who are also enrolled in an MCO plus Magellan Health Services for
pharmacy benefits and 802,783 beneficiaries who are also enrolled in an MCO plus DentaQuest USA Insurance Company for dental services.
Note: "n/a" indicates that a state or territory was not able to report data. "--" indicates states that do not operate programs of the given type. 0 signifies that a state
operated a program of this type in 2018, but it ended before July 1 or began after that date.
24
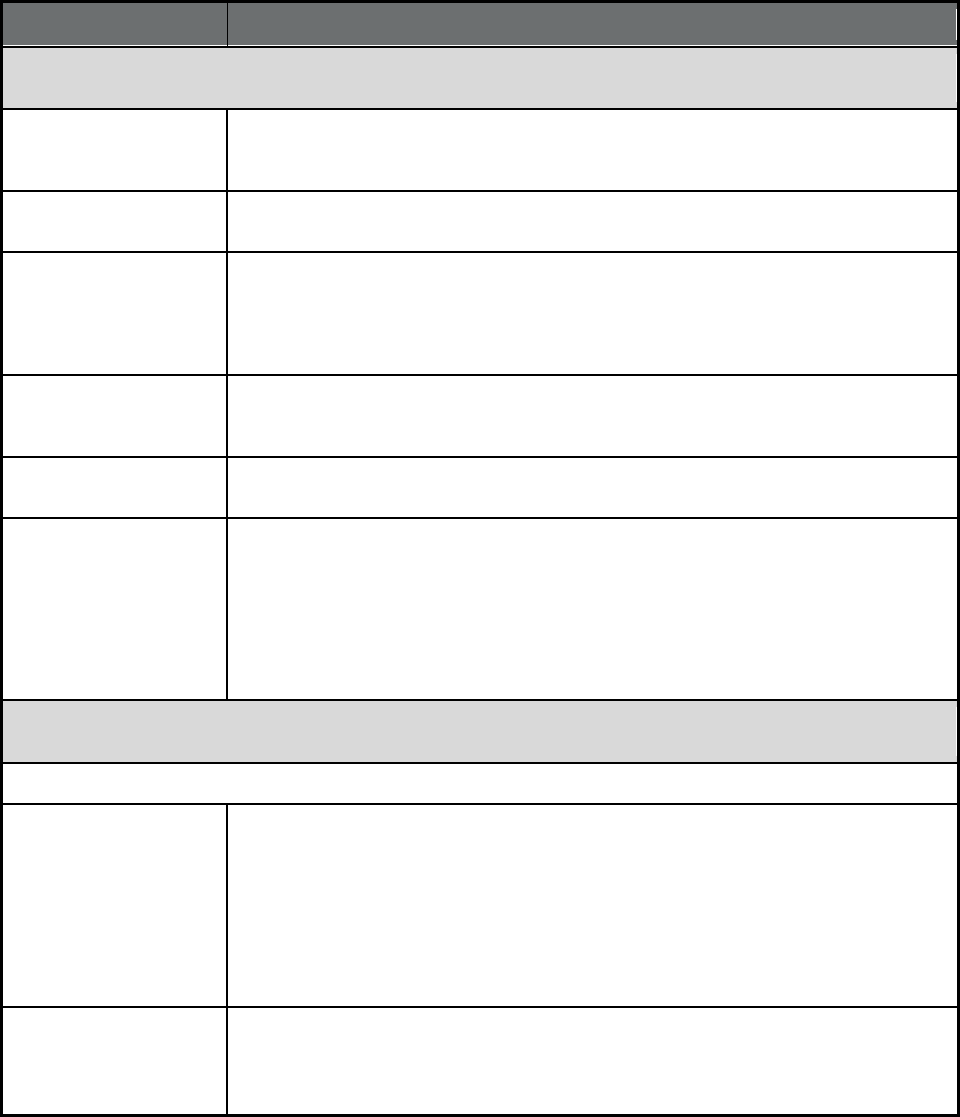
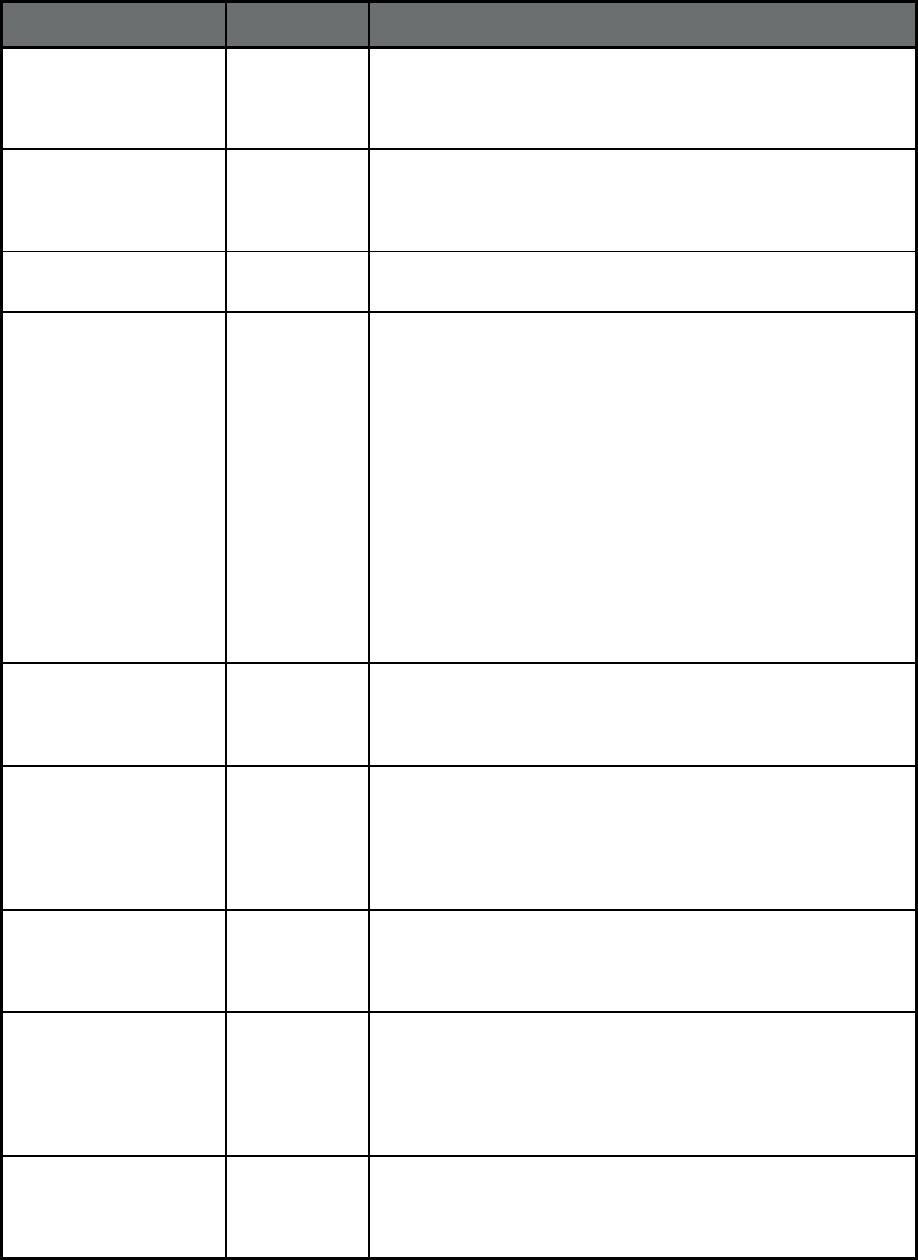
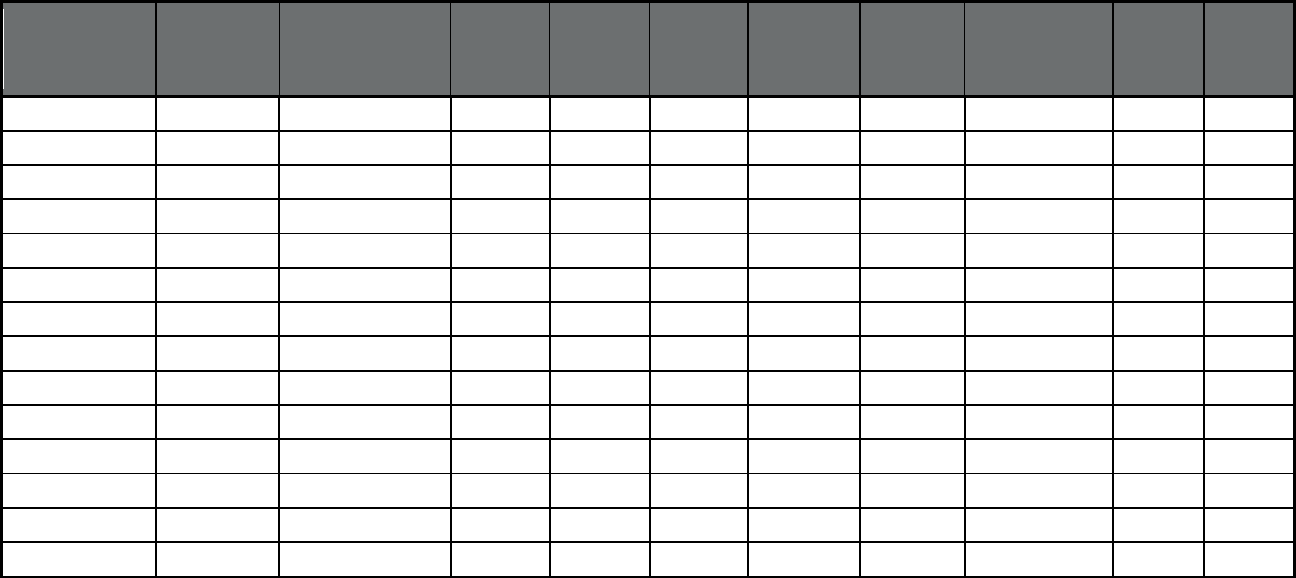
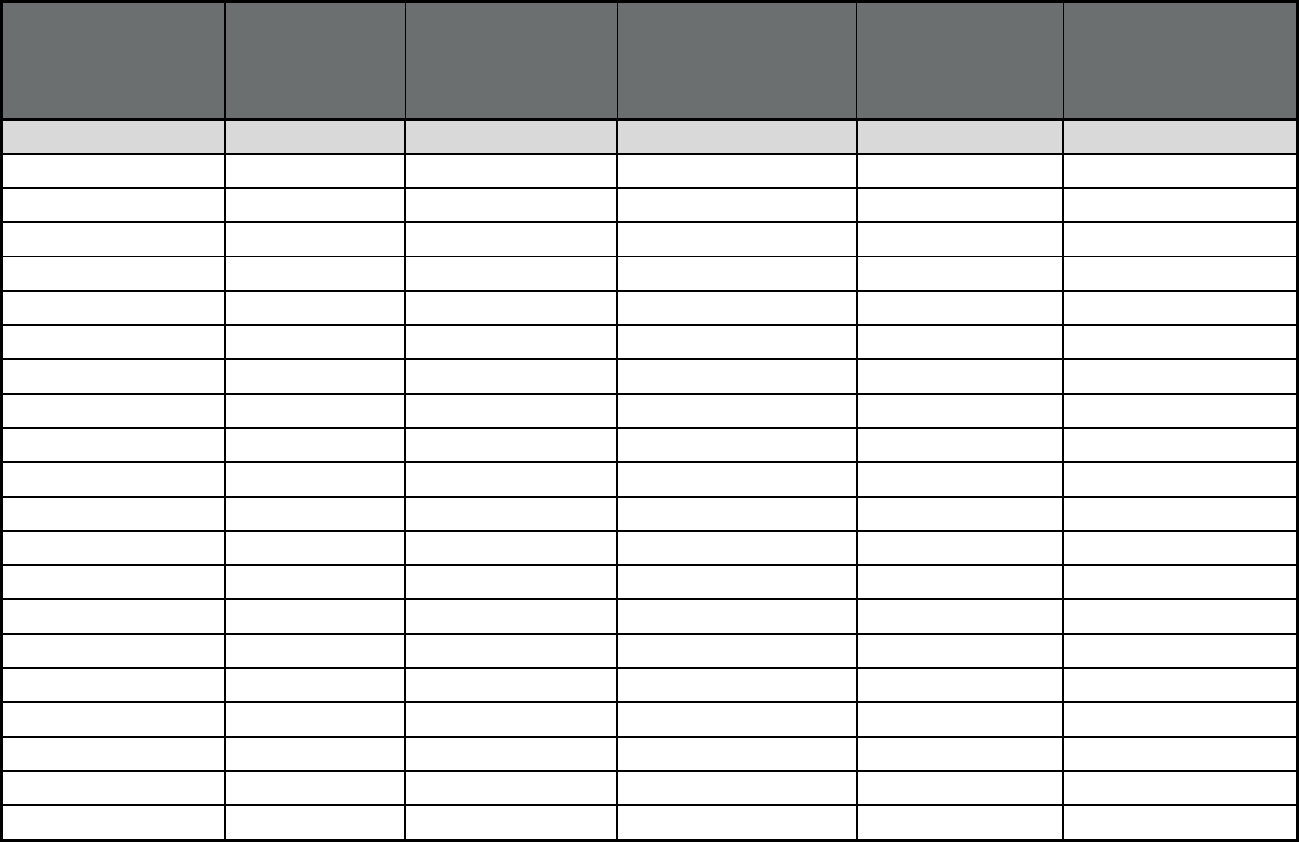
Table 3. Medicare-Medicaid Eligibles (Duals) Enrolled in Managed Care by Program Type, as of July 1, 2018
1
State or Territory
Total Medicare-
Medicaid dually
eligible
beneficiaries
2
Comprehensive
MCO (with or
without MLTSS)
3
PCCM
3
PCCM
entity
3
MLTSS
only
3
BHO (PIHP
and/or
PAHP)
3
Dental
3
Transportation
3
PACE Other
3
TOTALS 10,290,613 2,981,554 115,388 222,913 364,682 417,918 331,798 1,089,256 39,005 400
Alabama 213,678 -- 0 -- -- -- -- -- 149 0
Alaska n/a -- -- -- -- -- -- -- -- --
American Samoa n/a n/a n/a n/a n/a n/a n/a n/a n/a n/a
Arizona 220,474 149,900 -- -- -- -- -- -- -- --
Arkansas 134,914 -- 589 2,763 -- -- 53,473 67,099 248 --
California 1,343,891 962,791 -- -- -- 0 53,499 -- 6,068 339
Colorado
4
120,127 7,858 -- 68,703 -- 0 -- -- 3,646 --
Connecticut n/a -- -- -- -- -- -- -- -- --
Delaware 30,631 6,125 -- -- -- -- -- 6,125 232 --
District of
Columbia
21,621 125 -- -- -- -- -- 21,496 --
--
Florida 822,125 122,704 -- -- 93,529 -- -- -- 682 --
Georgia
5,6
218,337 427 -- -- -- -- -- 0 -- 0
Guam n/a n/a n/a n/a n/a n/a n/a n/a n/a n/a
Hawaii 34,596 34,596 -- -- -- -- -- -- -- --
Idaho 47,547 3,799 -- -- -- 23,425 27,240 27,240 -- --
Illinois 365,802 0 -- -- 31,143 -- -- -- -- --
Indiana 211,716 3,976 -- -- -- -- -- -- 283 --
Iowa 80,715 58,490 -- -- -- -- 58,547 1,275 409 --
Kansas 83,104 38,694 -- -- -- -- -- -- 0 --
25
State or Territory
Total Medicare-
Medicaid dually
eligible
beneficiaries
2
Comprehensive
MCO (with or
without MLTSS)
3
PCCM
3
PCCM
entity
3
MLTSS
only
3
BHO (PIHP
and/or
PAHP)
3
Dental
3
Transportation
3
PACE Other
3
Kentucky 152,336 55,918 -- -- -- -- -- 0 -- --
Louisiana 228,848 668 -- -- -- 103,234 104,724 443 --
Maine 92,256 -- 0 -- -- -- -- 51,453 -- --
Maryland 145,359 0 -- -- -- -- -- -- 93 --
Massachusetts 357,507 51,401 0 0 -- 0 -- -- 4,202 --
Michigan
7
327,697 39,166 -- -- 10,587 0 0 -- 2,429 --
Minnesota 142,348 81,117 -- -- -- -- -- -- -- --
Mississippi 161,017 0 -- -- -- -- -- -- -- --
Missouri 181,861 0 -- -- -- -- -- 143,578 -- --
Montana 28,634 -- 0 -- -- -- -- -- -- --
Nebraska 34,773 34,286 -- -- -- -- 34,246 -- 168 --
Nevada
74,484 0 -- -- -- -- 0 0 -- --
New Hampshire 31,816 16,321 -- -- -- -- -- -- -- --
New Jersey 221,266 179,446 -- -- -- -- -- 37,445 956 --
New Mexico 42,041 41,300 -- -- -- -- -- -- 741 --
New York 939,913 17,284 -- -- 189,890 -- -- -- 5,093 --
North Carolina 345,703 -- -- 151,447 -- 187,117 -- -- 680 --
North Dakota 16,909 0 0 -- -- -- -- -- 169 0
Northern Mariana
Islands
n/a n/a n/a n/a n/a n/a n/a n/a n/a n/a
Ohio 237,185 53,408 -- -- -- -- -- -- 359 --
Oklahoma 114,799 -- 114,799 -- -- -- -- 114,799 432 --
Oregon
8
76,067 52,057 -- -- -- -- -- 1,317 --
Pennsylvania 468,987 83,728 -- -- -- 73,364 -- 75,251 6,219 61
26
State or Territory
Total Medicare-
Medicaid dually
eligible
beneficiaries
2
Comprehensive
MCO (with or
without MLTSS)
3
PCCM
3
PCCM
entity
3
MLTSS
only
3
BHO (PIHP
and/or
PAHP)
3
Dental
3
Transportation
3
PACE Other
3
Puerto Rico 360,506 295,878 -- -- -- -- -- -- -- --
Rhode Island 35,733 0 -- -- -- -- 0 0 0 --
South Carolina 161,803 0 0 -- -- -- -- 161,803 391 --
South Dakota 12,188 -- 0 -- -- -- -- -- -- --
Tennessee
9
268,671 145,785 -- -- -- -- -- -- 267 --
Texas 649,495 293,046 -- -- -- -- 0 354,597 1,173 --
Utah 31,555 24,238 -- -- -- 30,775 69 27,095 -- --
Vermont
10
32,036 760 -- -- -- -- -- -- -- --
Virgin Islands n/a n/a n/a n/a n/a n/a n/a n/a n/a n/a
Virginia 108,805 108,805 -- -- -- -- -- -- 1,481 --
Washington
11
108,589 0 0 -- -- 0 -- 0 0 --
West Virginia 81,548 0 -- -- -- -- -- -- -- --
Wisconsin 57,536 17,457 -- -- 39,533 3 -- -- 543 0
Wyoming 11,064 -- -- -- -- -- -- -- 132 0
1. Because Medicare-Medicaid beneficiaries may be enrolled concurrently in more than one type of managed care program (e.g., a Comprehensive MCO and a
BHO), users should not sum enrollment across all program types, since the total would count individuals more than once and, in some states, exceed the actual
number of Medicaid enrollees.
2. Total Medicare-Medicaid dually eligible beneficiaries represents an unduplicated count of all beneficiaries in FFS and any type of managed care, including
enrollees receiving full Medicaid benefits or Medicaid cost sharing.
3. Comprehensive MCOs cover acute, primary, and specialty medical care services; they may also cover behavioral health, long-term services and supports, and
other benefits in some states. Limited benefit managed care programs, including PCCM, PCCM entity, MLTSS only, BHO, Dental, Transportation, and Other cover
a narrower set of services.
4. Colorado reported plan level enrollment as 0 for plans that had less than 30 beneficiaries. As a result, reported PACE program-level enrollment may be lower
than actual enrollment.
5. Georgia is unable to provide separate counts of Medicaid-only and dually eligible beneficiaries for their NEMT program. As a result, Medicare-Medicaid
beneficiary enrollment is reported here as zero.
6. The total number of dually eligible beneficiaries reported for Georgia only includes beneficiaries in the QMB, SLMB, and QI programs.
7. Michigan is not able to provide dual-eligible enrollment for the Specialty Prepaid Inpatient Health plan.
27
8. Oregon’s enrollment in comprehensive MCOs includes beneficiaries in (1) Coordinated Care Organizations (CCOs); (2) Dental Care Organizations (DCOs), or
(3) a Mental Health Organization. CCO enrollees receive physical, dental and mental health services and may be enrolled in more than one plan type
simultaneously. Plan-level enrollment is found in Report 5.
9. Tennessee’s enrollment in comprehensive MCOs includes 381 dually eligible beneficiaries who are also enrolled in an MCO plus Magellan Health Services for
pharmacy benefits and 381 dually eligible beneficiaries who are also enrolled in an MCO plus DentaQuest USA Insurance Company for dental services.
10. Vermont pays for Medicaid services for dually eligible enrollees on a FFS basis. Dually eligible enrollees reported in the Global Commitment to Health
Demonstration are Medicaid enrollees who have become newly eligible for Medicare and, as of July 1, have not yet transferred out of the program.
11. Washington is unable to provide separate counts of Medicaid-only and dual enrollment for their NEMT, ICMH comprehensive MCO, and PACE programs. As a
result, enrollment counts for Medicare-Medicaid beneficiaries are excluded from this report.
Note: "n/a" indicates that a state or territory was not able to report data. "--" indicates states that do not operate programs of the given type. 0 signifies that a state
operated a program of this type in 2018, but it ended before July 1 or began after that date.
28
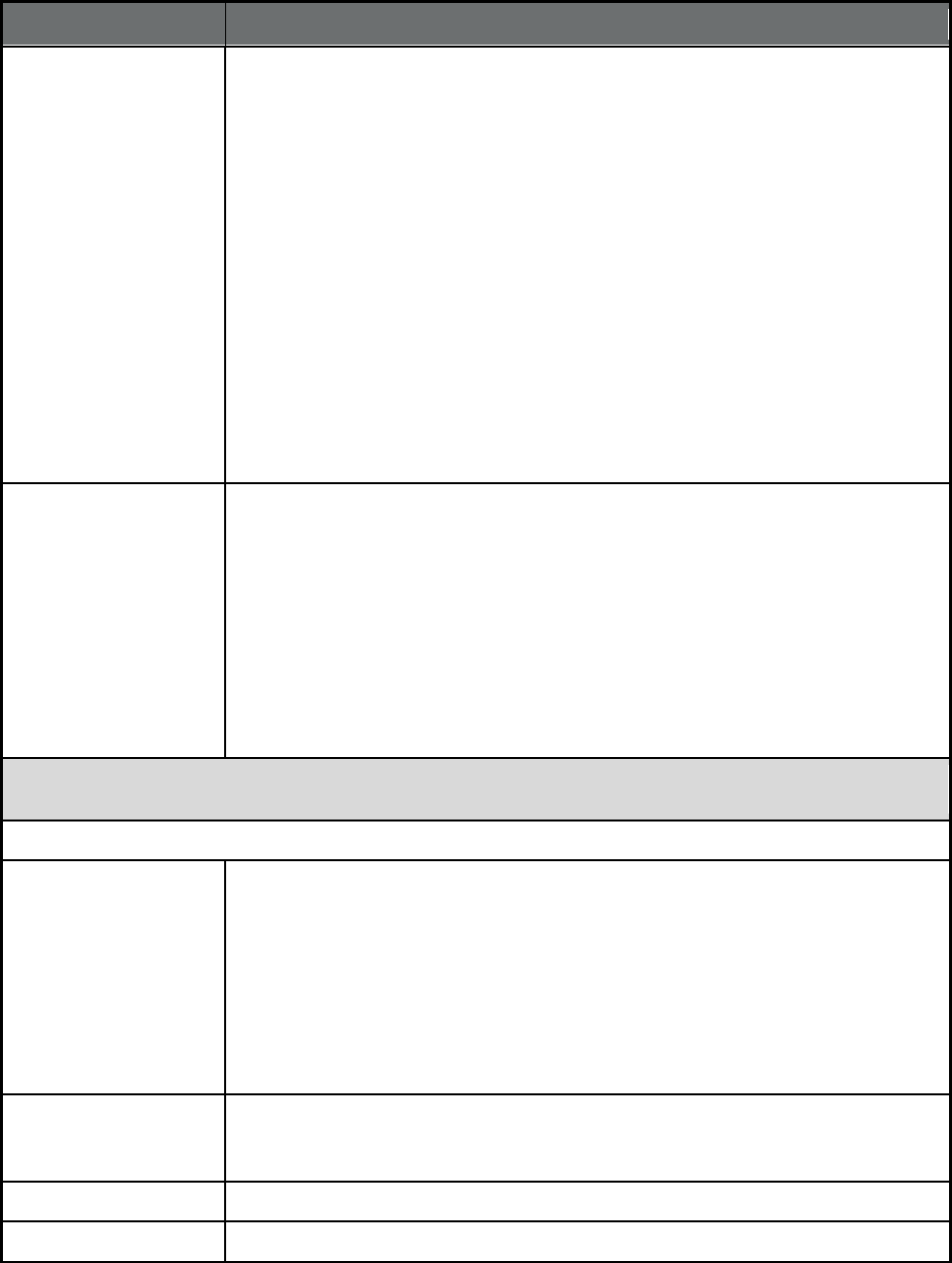
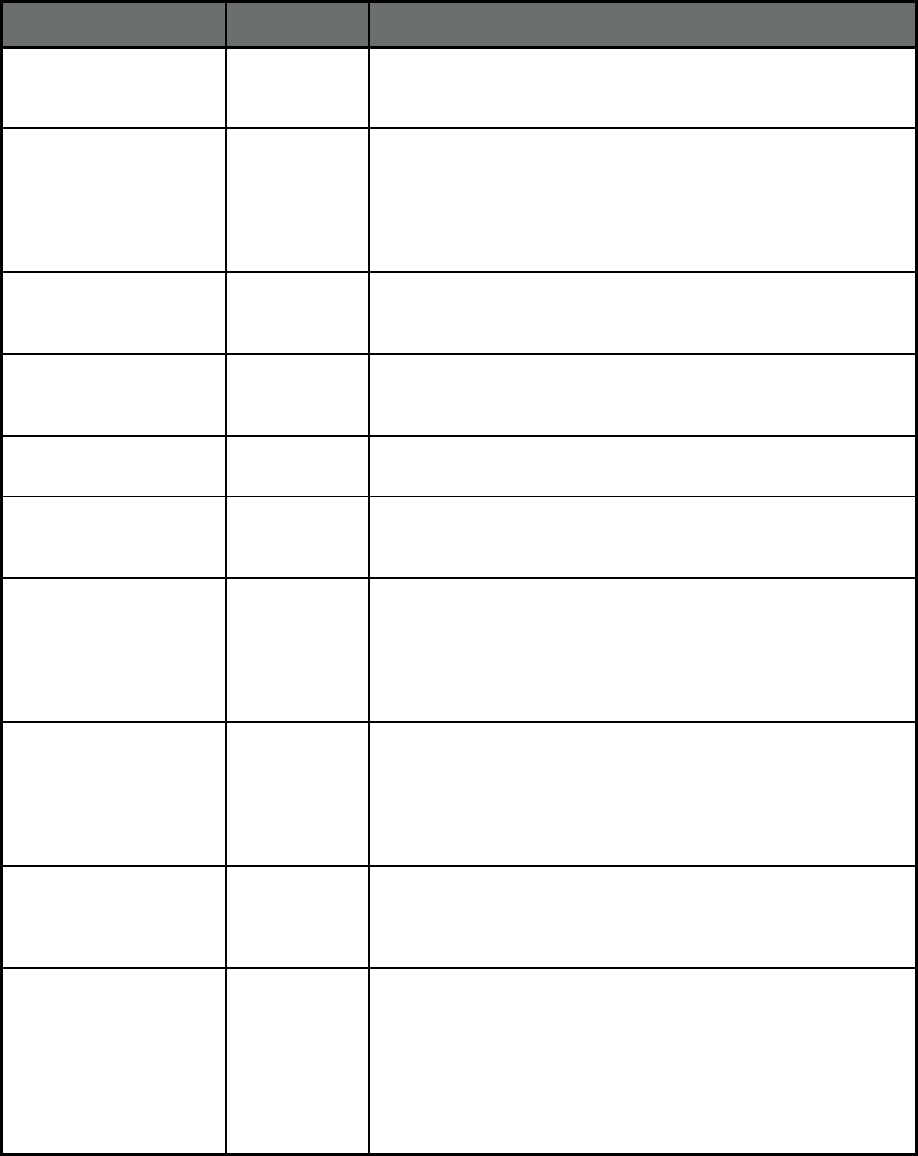
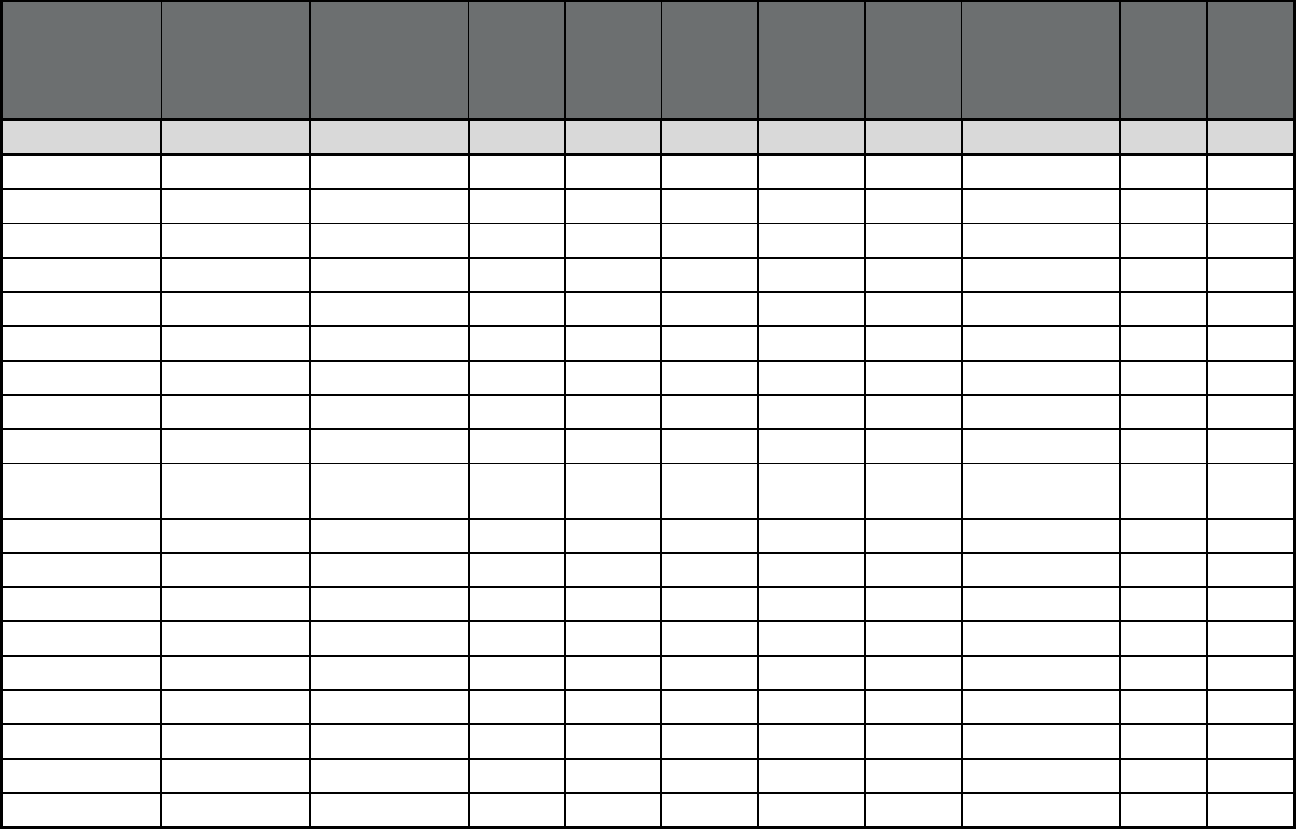
Table 4. Share of Medicaid Enrollees in Any Managed Care and in Comprehensive Managed Care, as of July
1, 2018
State or Territory
Total Medicaid
Enrollees
1
Total Medicaid
Enrollment in Any Type
of Managed Care
2
:
Number of Individuals
Total Medicaid Enrollment
in Any Type of Managed
Care
2
: Percent of all
Medicaid enrollees
Medicaid Enrollment in
Comprehensive
Managed Care
3
:
Number of Individuals
Medicaid Enrollment in
Comprehensive Managed
Care
3
: Percent of all
Medicaid enrollees
TOTALS 79,898,701 66,107,287 83% 55,605,461 70%
Alabama 1,019,417 638,221 62.6% 174 0.0%
Alaska
4
198,417 0 0.0% 0 0.0%
American Samoa n/a n/a n/a n/a n/a
Arizona 1,849,465 1,560,593 84.4% 1,560,593 84.4%
Arkansas 979,619 871,262 88.9% 258 0.0%
California 13,140,347 10,670,306 81.2% 10,661,382 81.1%
Colorado
5
1,302,808 1,171,171 89.9% 122,207 9.4%
Connecticut
6
928,800 0 0.0% 0 0.0%
Delaware 236,760 208,802 88.2% 199,887 84.4%
District of Columbia 264,984 189,363 71.5% 189,363 71.5%
Florida 3,885,169 3,178,981 81.8% 3,027,995 77.9%
Georgia
7
2,074,310 1,485,250 71.6% 1,445,804 69.7%
Guam n/a n/a n/a n/a n/a
Hawaii 355,873 351,685 98.8% 351,685 98.8%
Idaho 300,252 272,979 90.9% 3,799 1.3%
Illinois 3,110,093 2,176,902 70.0% 2,145,760 69.0%
Indiana 1,457,544 1,126,425 77.3% 1,126,425 77.3%
Iowa 626,011 580,507 92.7% 564,926 90.2%
Kansas 417,140 358,225 85.9% 358,225 85.9%
Kentucky 1,385,239 1,259,525 90.9% 1,259,525 90.9%
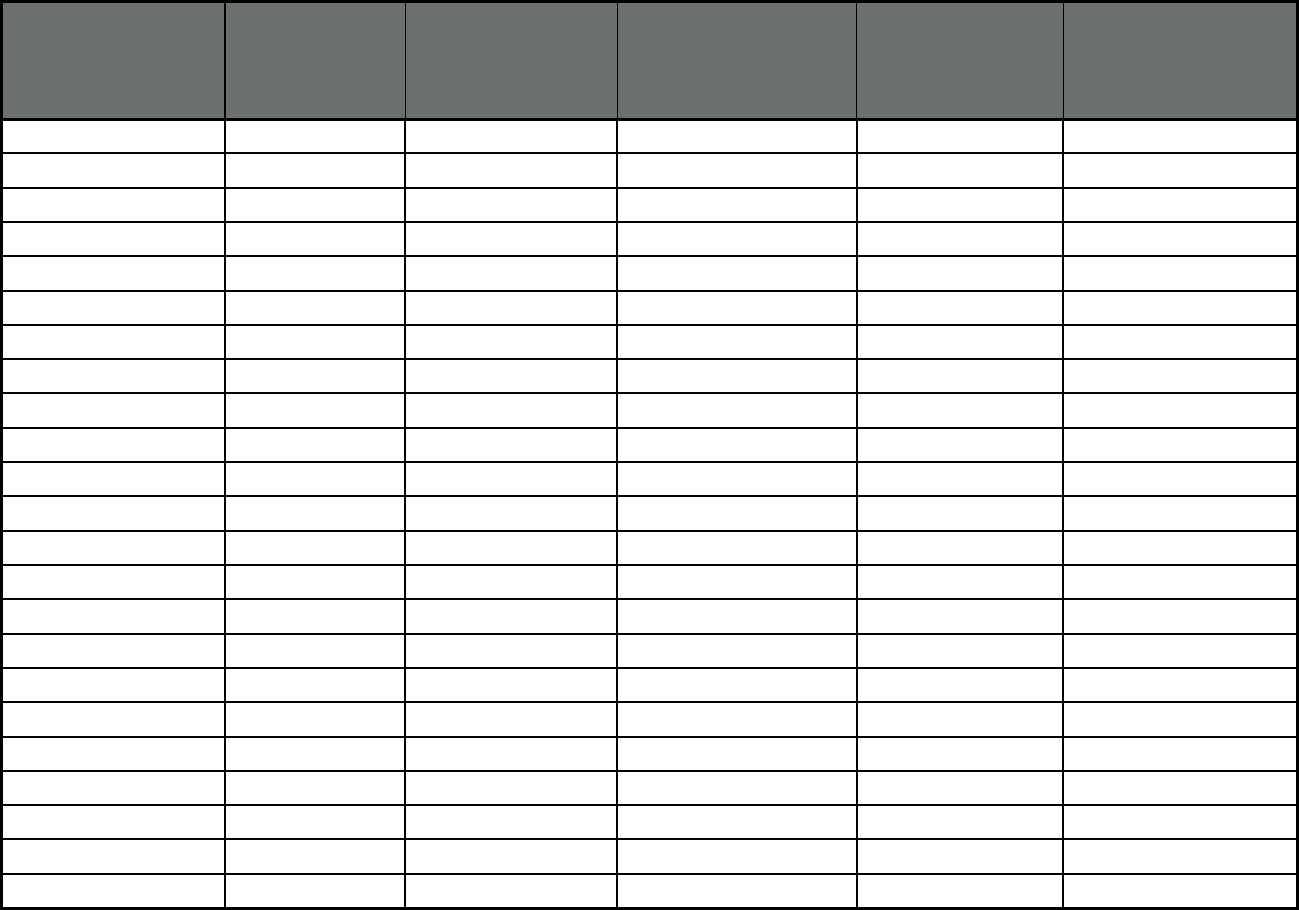
29
State or Territory
Total Medicaid
Enrollees
1
Total Medicaid
Enrollment in Any Type
of Managed Care
2
:
Number of Individuals
Total Medicaid Enrollment
in Any Type of Managed
Care
2
: Percent of all
Medicaid enrollees
Medicaid Enrollment in
Comprehensive
Managed Care
3
:
Number of Individuals
Medicaid Enrollment in
Comprehensive Managed
Care
3
: Percent of all
Medicaid enrollees
Louisiana 1,640,075 1,504,540 91.7% 1,385,242 84.5%
Maine 270,243 234,327 86.7% 0 0.0%
Maryland 1,401,781 1,169,708 83.4% 1,169,708 83.4%
Massachusetts 1,865,755 1,211,485 64.9% 750,573 40.2%
Michigan
7
4,623,834 4,608,988 99.7% 2,379,554 51.5%
Minnesota 1,122,672 892,137 79.5% 892,137 79.5%
Mississippi 683,577 441,782 64.6% 441,782 64.6%
Missouri 971,143 954,603 98.3% 712,335 73.4%
Montana 291,890 215,475 73.8% 0 0.0%
Nebraska 250,056 249,024 99.6% 249,022 99.6%
Nevada 666,561 588,111 88.2% 457,782 68.7%
New Hampshire 200,850 133,829 66.6% 133,829 66.6%
New Jersey 1,668,451 1,569,344 94.1% 1,569,344 94.1%
New Mexico 842,138 666,050 79.1% 666,050 79.1%
New York 6,153,799 4,764,261 77.4% 4,552,993 74.0%
North Carolina 2,178,225 1,581,469 72.6% 2,112 0.1%
North Dakota 93,042 48,957 52.6% 19,696 21.2%
Northern Mariana Islands n/a n/a n/a n/a n/a
Ohio 2,915,546 2,450,031 84.0% 2,450,031 84.0%
Oklahoma 880,954 649,023 73.7% 466 0.1%
Oregon 1,062,787 847,570 79.7% 847,570 79.7%
Pennsylvania
2,897,085 2,627,563 90.7% 2,359,277 81.4%
Puerto Rico 1,505,610 1,505,610 100.0% 1,505,610 100.0%

30
State or Territory
Total Medicaid
Enrollees
1
Total Medicaid
Enrollment in Any Type
of Managed Care
2
:
Number of Individuals
Total Medicaid Enrollment
in Any Type of Managed
Care
2
: Percent of all
Medicaid enrollees
Medicaid Enrollment in
Comprehensive
Managed Care
3
:
Number of Individuals
Medicaid Enrollment in
Comprehensive Managed
Care
3
: Percent of all
Medicaid enrollees
Rhode Island 313,095 302,407 96.6% 248,278 79.3%
South Carolina 1,195,703 1,195,703 100.0% 745,911 62.4%
South Dakota 123,890 92,184 74.4% 0 0.0%
Tennessee 1,510,045 1,386,664 91.8% 1,386,664 91.8%
Texas 3,981,912 3,845,916 96.6% 3,695,426 92.8%
Utah 275,511 271,137 98.4% 226,893 82.4%
Vermont 174,682 123,310 70.6% 123,310 70.6%
Virgin Islands n/a n/a n/a n/a n/a
Virginia 1,063,122 875,351 82.3% 875,351 82.3%
Washington 1,781,048 1,781,048 100.0% 1,574,163 88.4%
West Virginia 505,528 407,193 80.5% 407,193 80.5%
Wisconsin 1,197,453 811,920 67.8% 759,015 63.4%
Wyoming 58,390 370 0.6% 136 0.2%
1. Total Medicaid Enrollees represents an unduplicated count of all beneficiaries in FFS and any type of managed care, including Medicaid-only and Medicare-
Medicaid ("dual") enrollees receiving full Medicaid benefits or Medicaid cost sharing.
2. Total Medicaid enrollment in Any Type of Managed Care represents an unduplicated count of beneficiaries enrolled in any Medicaid managed care program,
including comprehensive MCOs, limited benefit MCOs, PCCMs, and PCCM entities.
3. Medicaid Enrollment in Comprehensive Managed Care represents an unduplicated count of Medicaid beneficiaries enrolled in a managed care plan that
provides comprehensive benefits (acute, primary care, specialty, and any other), as well as PACE programs. It excludes beneficiaries who are enrolled in a
Financial Alignment Initiative Medicare-Medicaid Plan as their only form of managed care.
4. Alaska was not able to provide total Medicaid enrollment as of July 1, 2018. This figure is from the July - September 2018 enrollment data collected through the
Medicaid Budget and Expenditure System, updated December 2019, and accessed January 14, 2020. See https://data.medicaid.gov/Enrollment/2018-4Q-
Medicaid-MBES-Enrollment/qjmt-6zzy.
5. Colorado reported plan level enrollment as 0 for plans that had less than 30 beneficiaries. As a result, reported Medicaid Enrollment in Comprehensive
Managed Care may be lower than actual enrollment.
6. Connecticut was not able to provide total Medicaid enrollment as of July 1, 2018. This figure is from the July - September 2018 enrollment data collected
through the Medicaid Budget and Expenditure System, updated December 2019, and accessed January 14, 2020. See https://data.medicaid.gov/Enrollment/2018-
4Q-Medicaid-MBES-Enrollment/qjmt-6zzy.
31
7. Georgia's Total Medicaid Enrollment in Any Type of Managed Care does not include 1,626,252 NEMT enrollees; a portion of these enrollees are simultaneously
enrolled in other managed care programs.
Note: "n/a" indicates that a state or territory was not able to report data.
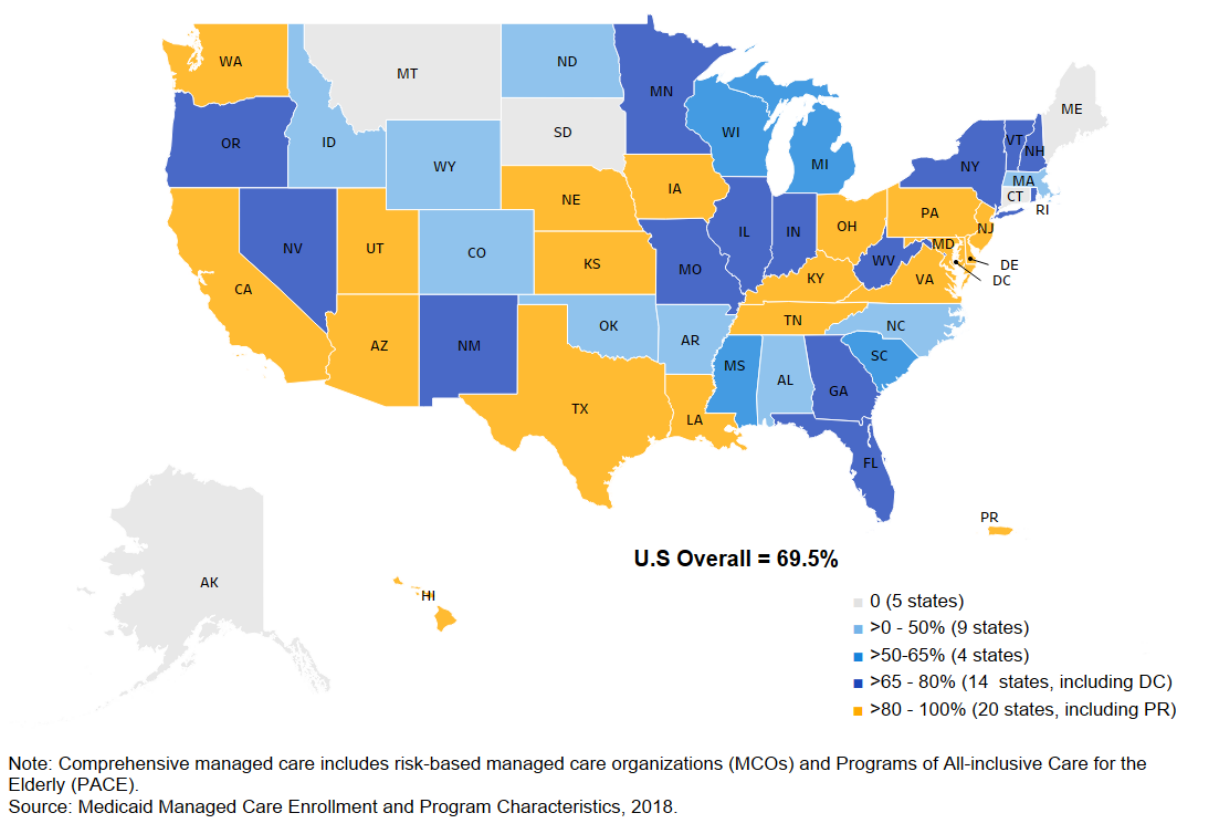
Note:
Comprehensive
managed
care
includes
risk-based
managed
care
organizations
(MCOs)
and
Programs
of
All-inclusive
Care
for
the
Elderly
(PACE).
Source:
Medicaid
Managed
Care
Enrollment
and
Program
Characteristics,
2018.
32
Map of State Comprehensive MCO Penetration as of July 1, 2018
33
Table 5. Enrollment by Program and Plan, as of 2018
1
State
Program Name
(Type) Plan Name
Parent
Organization
Geographic Region (state-
defined areas, counties, or
zip codes)
Medicaid-Only
Enrollment
Dual
Enrollment
Total
Enrollment
Alabama
2
Patient 1st (Primary
Care Case
Management (PCCM))
Patient 1st Alabama Medicaid
Agency
Statewide 611,251 0 611,251
Alabama
2
Health Homes
(Primary Care Case
Management (PCCM))
Health Homes Alabama Medicaid
Agency
Statewide 230,966 0 230,966
Alabama
2
Maternity Care
Program (Other
Prepaid Health Plan
(PHP) (limited
benefits))
Maternity Care Plan Alabama Medicaid
Agency
Barbour, Bibb, Blount,
Calhoun, Chambers,
Cherokee, Chilton, Choctaw,
Clay, Cleburne, Coffee,
Colbert, Coosa, Cullman,
Dale, Dallas, DeKalb,
Etowah, Fayette, Franklin,
Geneva, Greene, Hale,
Henry, Houston, Jackson,
Jefferson, Lamar,
Lauderdale, Lawrence, Lee,
Limestone, Macon,
Madison, Marengo, Marion,
Marshall, Mobile, Morgan,
Perry, Pickens, Randolph,
Russell, St. Clair, Shelby,
Sumter, Talladega,
Tallapoosa, Tuscaloosa,
Walker, Wilcox, and Winston
Counties
22,844 0 22,844
Alabama
2
PACE (Program of All-
inclusive Care for the
Elderly (PACE))
Mercy Life of Alabama PACE Mobile and Baldwin
Counties
25 149 174
Arizona Arizona Health Care
Cost Containment
System
(Comprehensive MCO
+ MLTSS)
United Healthcare Plan UnitedHealthcare Apache, Cochise, Coconino,
Graham, Greenlee, La Paz,
Maricopa, Mohave, Navajo,
Pima, Santa Cruz, Yavapai,
and Yuma Counties
469,579 46,866 516,445
34
State
Program Name
(Type) Plan Name
Parent
Organization
Geographic Region (state-
defined areas, counties, or
zip codes)
Medicaid-Only
Enrollment
Dual
Enrollment
Total
Enrollment
Arizona Arizona Health Care
Cost Containment
System
(Comprehensive MCO
+ MLTSS)
Care1st Health Plan WellCare Maricopa and Pima
Counties
130,829 7,821 138,650
Arizona Arizona Health Care
Cost Containment
System
(Comprehensive MCO
+ MLTSS)
DCS/CMDP Government
Agency/Non-Profit
Entity
Statewide 13,869 1 13,870
Arizona Arizona Health Care
Cost Containment
System
(Comprehensive MCO
+ MLTSS)
DES/Division of
Developmental
Disabilities (MLTSS)
Government
Agency/Non-Profit
Entity
Statewide 25,123 7,131 32,254
Arizona Arizona Health Care
Cost Containment
System
(Comprehensive MCO
+ MLTSS)
United Healthcare Plan
(MLTSS)
UnitedHealthcare Apache, Coconino, Gila,
Maricopa, Mohave, Navajo,
Pinal, and Yavapai Counties
1,171 7,538 8,709
Arizona Arizona Health Care
Cost Containment
System
(Comprehensive MCO
+ MLTSS)
Health Choice Arizona IASIS Healthcare
LLC/Steward
Apache, Coconino, Gila,
Maricopa, Mohave, Navajo,
Pima, and Pinal Counties
227,648 15,421 243,069
Arizona Arizona Health Care
Cost Containment
System
(Comprehensive MCO
+ MLTSS)
Health Net Access Centene
Corporation
Maricopa County 54,005 3,657 57,662
Arizona Arizona Health Care
Cost Containment
System
(Comprehensive MCO
+ MLTSS)
Mercy Care Plan Dignity Health and
Carondelet Health
Network
Maricopa and Pima
Counties
339,317 20,885 360,202
35
State
Program Name
(Type) Plan Name
Parent
Organization
Geographic Region (state-
defined areas, counties, or
zip codes)
Medicaid-Only
Enrollment
Dual
Enrollment
Total
Enrollment
Arizona Arizona Health Care
Cost Containment
System
(Comprehensive MCO
+ MLTSS)
Mercy Care Plan
(MLTSS)
Dignity Health and
Carondelet Health
Network
Gila, Maricopa, Pima, and
Pinal Counties
2,436 9,993 12,429
Arizona Arizona Health Care
Cost Containment
System
(Comprehensive MCO
+ MLTSS)
University Family Care Banner Health Cochise, Gila, Graham,
Greenlee, La Paz, Pima,
Pinal, Santa Cruz, Yavapai,
and Yuma Counties
119,538 10,815 130,353
Arizona Arizona Health Care
Cost Containment
System
(Comprehensive MCO
+ MLTSS)
Mercy Maricopa
Integrated Care
Mercy Care Maricopa County 13,905 7,776 21,681
Arizona Arizona Health Care
Cost Containment
System
(Comprehensive MCO
+ MLTSS)
Cenpatico Integrated
Care
Centene
Corporation
Cochise, Graham, Greenlee,
La Paz, Pima, Pinal, Santa
Cruz, and Yuma Counties
8,811 4,564 13,375
Arizona Arizona Health Care
Cost Containment
System
(Comprehensive MCO
+ MLTSS)
Health Choice
Integrated Care
Health Choice
Arizona/NARBHA
Apache, Coconino, Gila,
Mohave, Navajo, and
Yavapai Counties
3,571 2,151 5,722
Arizona Arizona Health Care
Cost Containment
System
(Comprehensive MCO
+ MLTSS)
Banner University
Family Care (MLTSS)
Banner Health Cochise, Gila, Graham,
Greenlee, La Paz, Maricopa,
Pima, Pinal, Santa Cruz,
and Yuma Counties
891 5,281 6,172
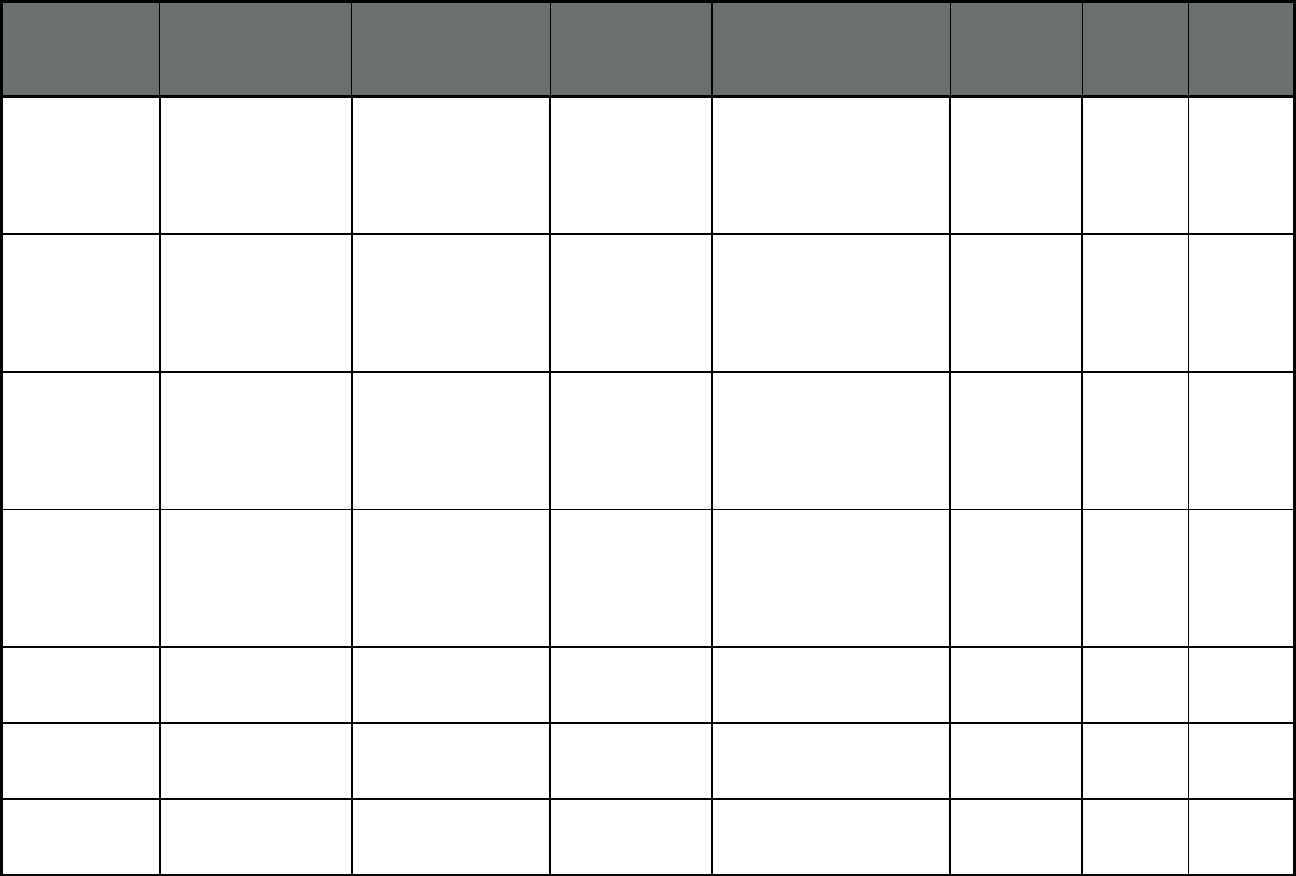
36
State
Program Name
(Type) Plan Name
Parent
Organization
Geographic Region (state-
defined areas, counties, or
zip codes)
Medicaid-Only
Enrollment
Dual
Enrollment
Total
Enrollment
Arkansas Provider-Led Arkansas
Shared Savings Entity
(PASSE) Program
(Primary Care Case
Management Entity
(PCCM Entity))
Summit Community
Care
Anthem Insurance
Companies, Inc.
Statewide 6,433 1,038 7,471
Arkansas Provider-Led Arkansas
Shared Savings Entity
(PASSE) Program
(Primary Care Case
Management Entity
(PCCM Entity))
Arkansas Total Care Centene
Corporation
Statewide 4,477 334 4,811
Arkansas Provider-Led Arkansas
Shared Savings Entity
(PASSE) Program
(Primary Care Case
Management Entity
(PCCM Entity))
Empower Healthcare
Solutions
Beacon Statewide 10,943 1,027 11,970
Arkansas Provider-Led Arkansas
Shared Savings Entity
(PASSE) Program
(Primary Care Case
Management Entity
(PCCM Entity))
Forevercare Gateway Health Statewide 4,462 364 4,826
Arkansas Connect Care
(Primary Care Case
Management (PCCM))
Multiple primary care
providers
Multiple Primary
Care Provider
(PCCM)
Statewide 444,695 589 445,284
Arkansas Arkansas Dental
Managed Care (Dental
only (PAHP))
Delta Dental of
Arkansas
Delta Dental Statewide 269,858 27,377 297,235
Arkansas Arkansas Dental
Managed Care (Dental
only (PAHP))
Managed Care of North
America (MCNA)
Dental
Managed Care of
North America
(MCNA), Inc.
Statewide 253,639 26,096 279,735
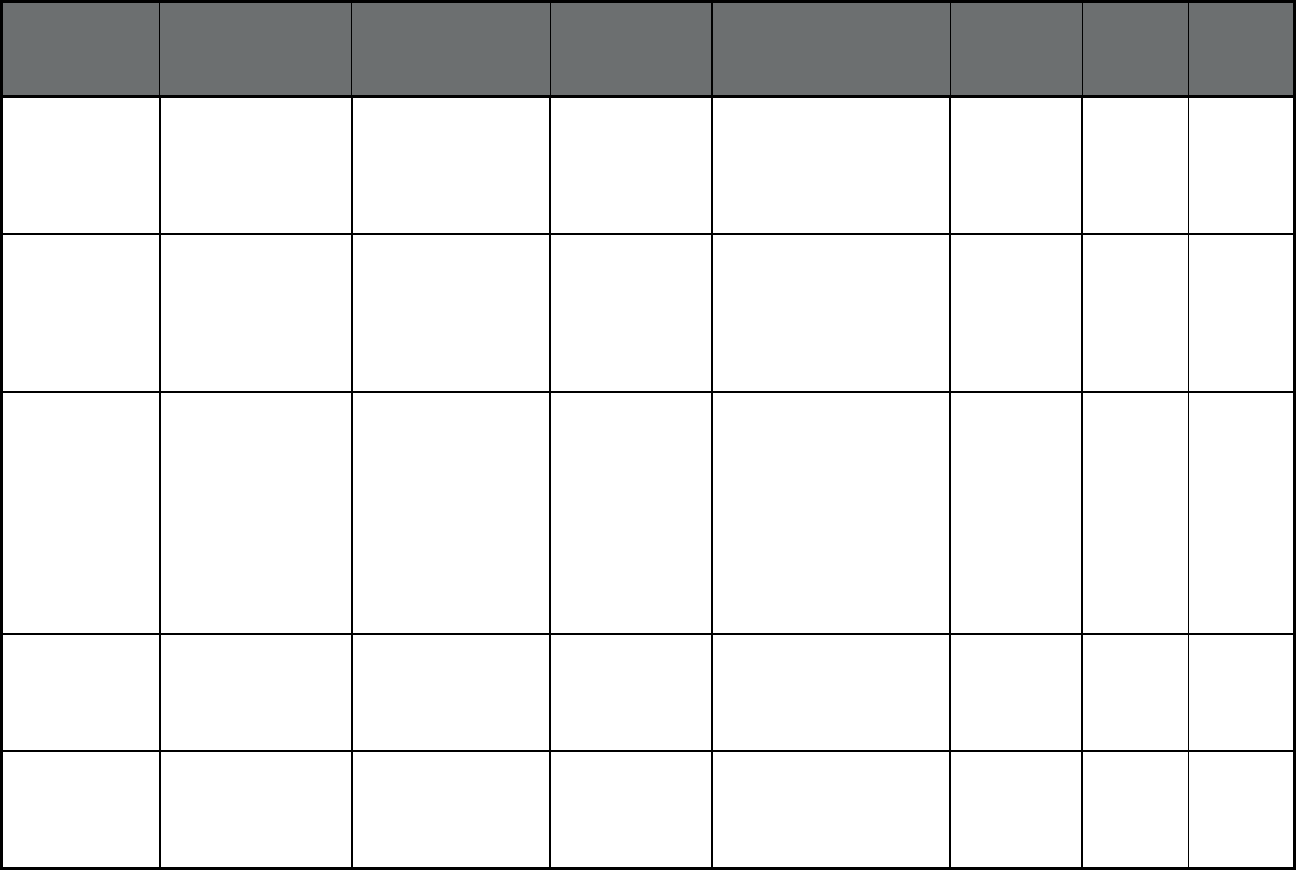
37
State
Program Name
(Type) Plan Name
Parent
Organization
Geographic Region (state-
defined areas, counties, or
zip codes)
Medicaid-Only
Enrollment
Dual
Enrollment
Total
Enrollment
Arkansas Arkansas Non-
Emergency Medical
Transport (NET) (Non-
Emergency Medical
Transportation)
Southeasttrans Southeasttrans Randolph, Clay, Lawrence,
Greene, Craighead,
Mississippi, Poinsett, Cross,
Crittenden, St. Francis,
Faulkner, Pulaski, and
Lonoke Counties
170,302 20,780 191,082
Arkansas Arkansas Non-
Emergency Medical
Transport (NET) (Non-
Emergency Medical
Transportation)
Central Arkansas
Development Council
Central Arkansas
Development
Council
Montgomery, Garland,
Saline, Hot Springs, Clark,
Pike, Sevier, Howard,
Hempstead, Little River,
Miller, Lafayette, Columbia,
Quachita, Dallas, Calhoun,
and Union Counties
89,447 12,239 101,686
Arkansas Arkansas Non-
Emergency Medical
Transport (NET) (Non-
Emergency Medical
Transportation)
Area Agency on Aging
of Western Arkansas
Area Agency on
Aging of Western
Arkansas
Benton, Washington,
Madison, Newton, Searcy,
Baxter, Boone, Carroll,
Fulton, Izard, Sharp, Stone,
Independence, Jackson,
Van Buren, Cleburne, White,
Woodruff, Crawford,
Franklin, Johnson, Pope,
Sebastian, Logan, Yell,
Scott, Polk, Perry, and
Conway Counties
202,853 25,959 228,812
Arkansas Arkansas Non-
Emergency Medical
Transport (NET) (Non-
Emergency Medical
Transportation)
Mid-Delta Mid-Delta Prairie, Monroe, Phillips,
and Lee Counties
9,132 1,966 11,098
Arkansas Arkansas Non-
Emergency Medical
Transport (NET) (Non-
Emergency Medical
Transportation)
Area Agency on Aging
of Southeast Arkansas
Area Agency on
Aging of Southeast
Arkansas
Grant, Jefferson, Arkansas,
Cleveland, Lincoln, Bradley,
Drew, Desha, Chicot, and
Ashley Counties
41,163 6,155 47,318
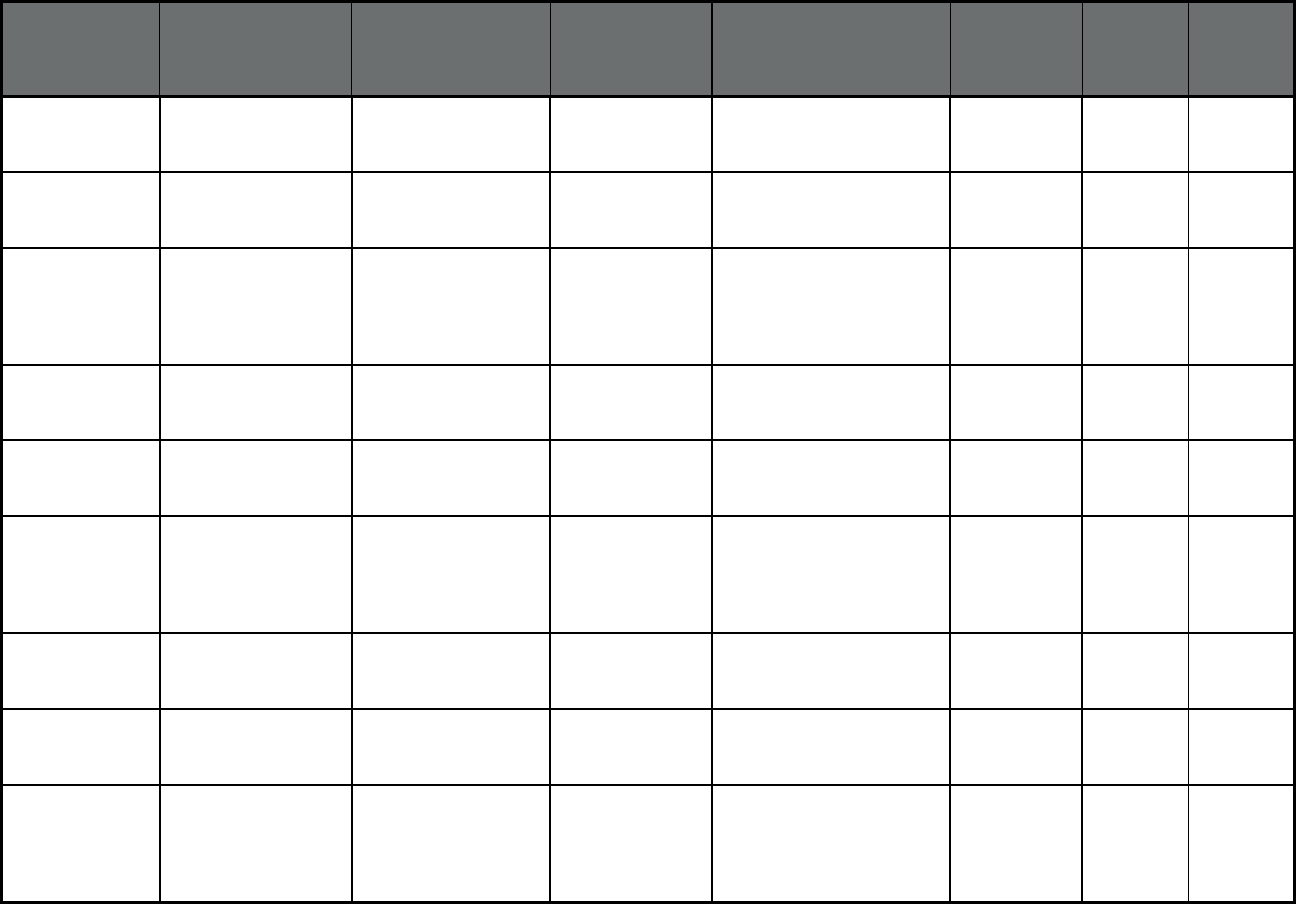
38
State
Program Name
(Type) Plan Name
Parent
Organization
Geographic Region (state-
defined areas, counties, or
zip codes)
Medicaid-Only
Enrollment
Dual
Enrollment
Total
Enrollment
Arkansas PACE (Program of All-
inclusive Care for the
Elderly (PACE))
Complete Health PACE Statewide 4 54 58
Arkansas PACE (Program of All-
inclusive Care for the
Elderly (PACE))
Total Life Healthcare PACE Statewide 6 194 200
California Health Plan of San
Mateo CCS Demo/San
Mateo
(Comprehensive
MCO)
Health Plan of San
Mateo CCS Demo
Health Plan of San
Mateo
San Mateo County 0 0 0
California Regional Model
(Comprehensive
MCO)
California Health &
Wellness Plan/Imperial
Centene
Corporation
Imperial County 59,377 2,439 61,816
California Regional Model
(Comprehensive
MCO)
California Health &
Wellness Plan/Region
1
Centene
Corporation
Butte, Colusa, Glenn,
Plumas, Sierra, Sutter, and
Tehama Counties
70,540 2,714 73,254
California Regional Model
(Comprehensive
MCO)
California Health &
Wellness Plan/Region
2
Centene
Corporation
Alpine, Amador, Calaveras,
El Dorado, Inyo, Mariposa,
Mono, Nevada, Placer,
Tuolumne, and Yuba
Counties
60,069 2,273 62,342
California Regional Model
(Comprehensive
MCO)
Molina Healthcare of
CA Partner
Plan/Imperial
Molina Healthcare Imperial County 14,159 807 14,966
California Regional Model
(Comprehensive
MCO)
Anthem Blue Cross
Partnership
Plan/Region 1
Anthem Insurance
Companies, Inc.
Butte, Colusa, Glenn,
Plumas, Sierra, Sutter, and
Tehama Counties
65,657 2,371 68,028
California Regional Model
(Comprehensive
MCO)
Anthem Blue Cross
Partnership
Plan/Region 2
Anthem Insurance
Companies, Inc.
Alpine, Amador, Calaveras,
El Dorado, Inyo, Mariposa,
Mono, Nevada, Placer,
Tuolumne, and Yuba
Counties
84,249 2,880 87,129
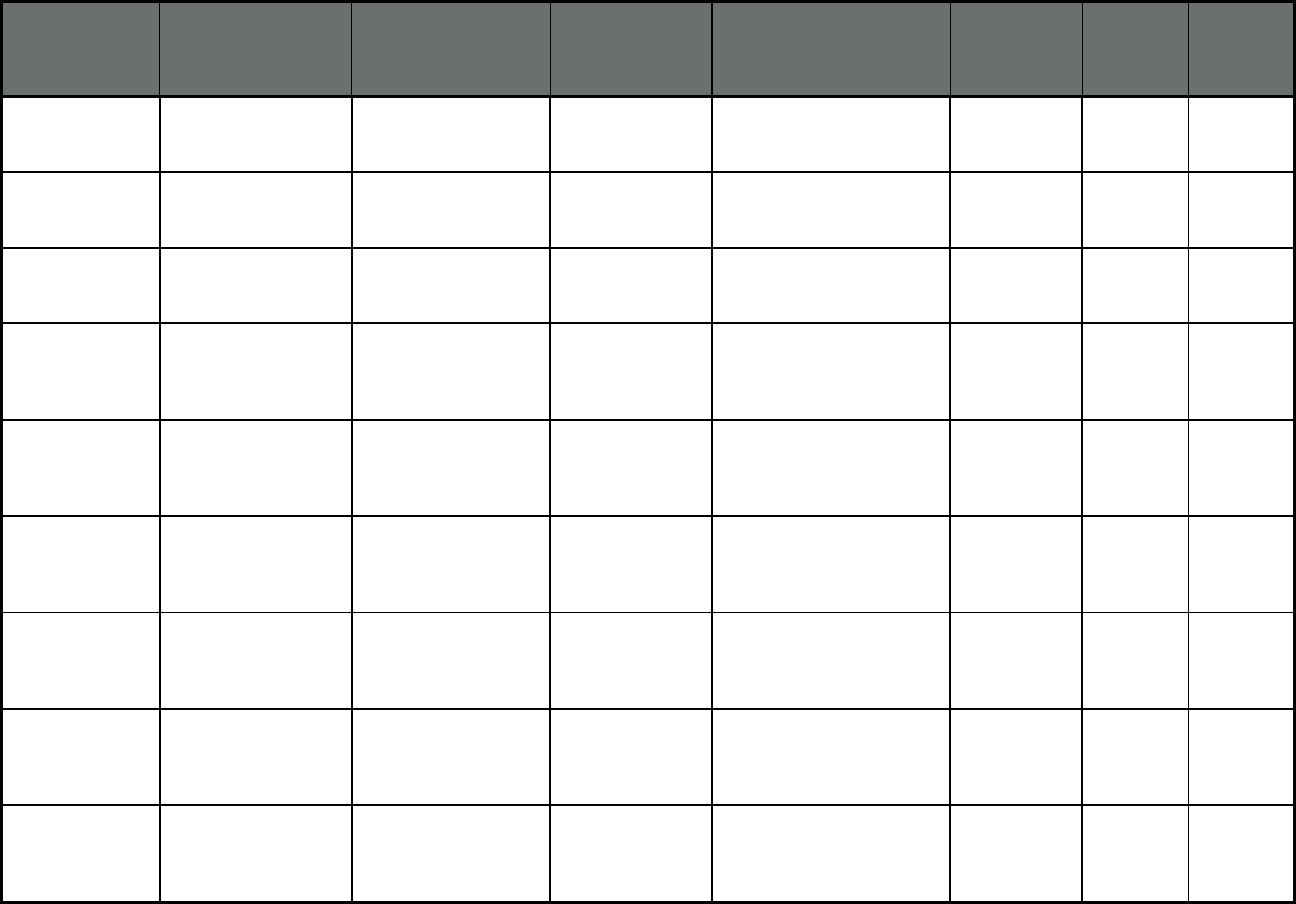
39
State
Program Name
(Type) Plan Name
Parent
Organization
Geographic Region (state-
defined areas, counties, or
zip codes)
Medicaid-Only
Enrollment
Dual
Enrollment
Total
Enrollment
California Regional Model
(Comprehensive
MCO)
KP Cal LLC/Amador Kaiser
Permanente
Amador County 94 0 94
California Regional Model
(Comprehensive
MCO)
KP Cal LLC/El Dorado Kaiser
Permanente
El Dorado County 1,950 48 1,998
California Regional Model
(Comprehensive
MCO)
KP Cal LLC/Placer Kaiser
Permanente
Placer County 7,153 211 7,364
California Geographic Managed
Care (GMC) Model
(Comprehensive MCO
+ MLTSS)
Care 1st Partner
Plan/San Diego
Blue Cross Blue
Shield
San Diego County 69,434 15,053 84,487
California Geographic Managed
Care (GMC) Model
(Comprehensive MCO
+ MLTSS)
Community Health
Group Partnership
Plan/San Diego
Community Health
Group
San Diego County 254,741 19,408 274,149
California Geographic Managed
Care (GMC) Model
(Comprehensive MCO
+ MLTSS)
Health Net/San Diego Centene
Corporation
San Diego County 58,742 14,473 73,215
California Geographic Managed
Care (GMC) Model
(Comprehensive MCO
+ MLTSS)
KP Cal LLC/San Diego Kaiser
Permanente
San Diego County 45,426 6,450 51,876
California Geographic Managed
Care (GMC) Model
(Comprehensive MCO
+ MLTSS)
Molina Healthcare of
CA Partner Plan/San
Diego
Molina Healthcare San Diego County 211,450 16,197 227,647
California Geographic Managed
Care (GMC) Model
(Comprehensive MCO
+ MLTSS)
Aetna Better Health of
CA/San Diego
Aetna San Diego County 4,606 53 4,659
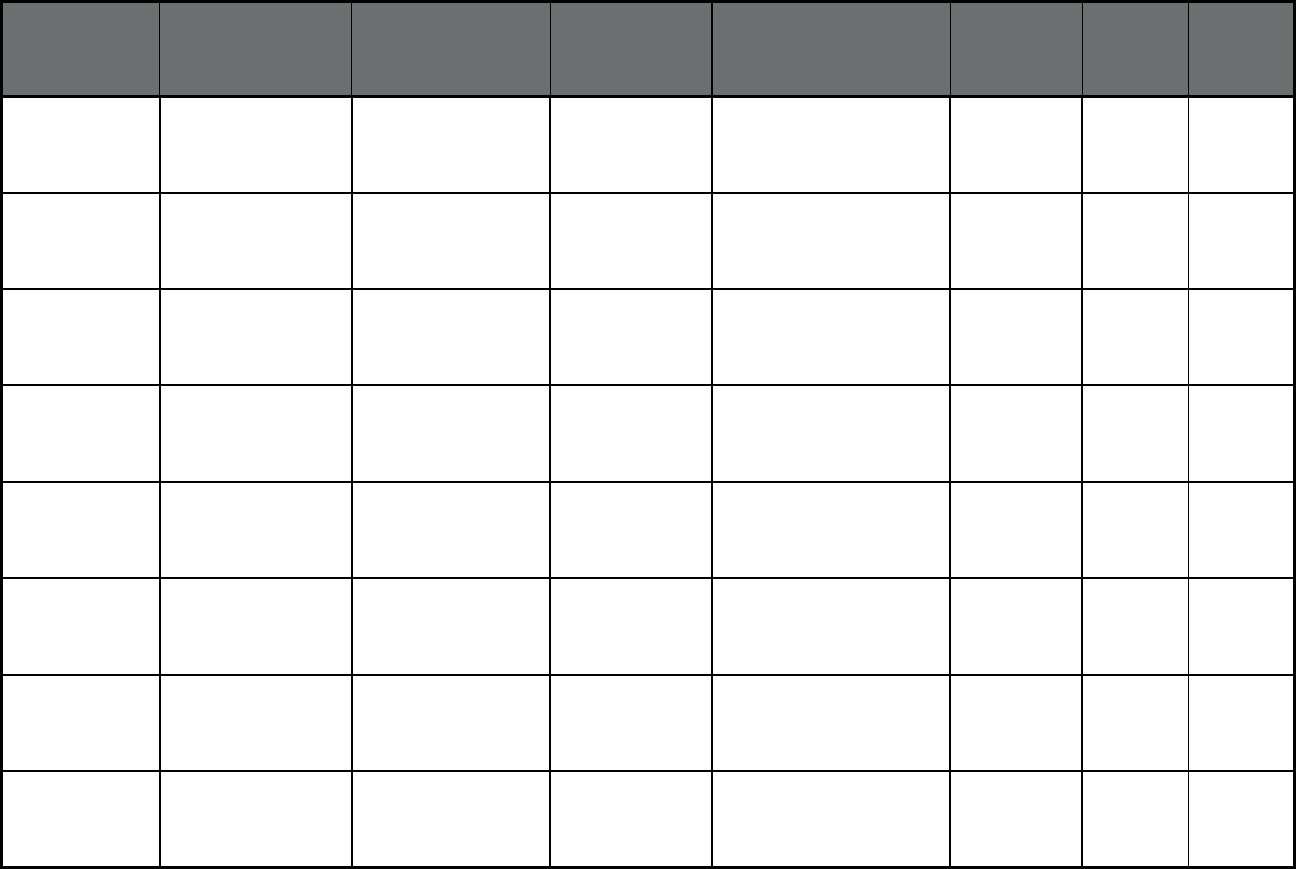
40
State
Program Name
(Type) Plan Name
Parent
Organization
Geographic Region (state-
defined areas, counties, or
zip codes)
Medicaid-Only
Enrollment
Dual
Enrollment
Total
Enrollment
California Geographic Managed
Care (GMC) Model
(Comprehensive MCO
+ MLTSS)
UnitedHealthcare
Community Plan/San
Diego
UnitedHealthcare San Diego County 5,988 138 6,126
California Geographic Managed
Care (GMC) Model
(Comprehensive MCO
+ MLTSS)
Anthem Blue Cross
Partnership
Plan/Sacramento
Anthem Insurance
Companies, Inc.
Sacramento County 170,285 7,533 177,818
California Geographic Managed
Care (GMC) Model
(Comprehensive MCO
+ MLTSS)
Health Net/Sacramento Centene
Corporation
Sacramento County 101,630 5,568 107,198
California Geographic Managed
Care (GMC) Model
(Comprehensive MCO
+ MLTSS)
KP Cal
LLC/Sacramento
Kaiser
Permanente
Sacramento County 79,367 6,557 85,924
California Geographic Managed
Care (GMC) Model
(Comprehensive MCO
+ MLTSS)
Molina Healthcare of
CA Partner
Plan/Sacramento
Molina Healthcare Sacramento County 52,675 3,832 56,507
California Geographic Managed
Care (GMC) Model
(Comprehensive MCO
+ MLTSS)
Aetna Better Health of
CA/Sacramento
Aetna Sacramento County 2,381 29 2,410
California Geographic Managed
Care (GMC) Model
(Comprehensive MCO
+ MLTSS)
UnitedHealthcare
Community
Plan/Sacramento
UnitedHealthcare Sacramento County 4,764 140 4,904
California Senior Care Action
Network (SCAN)
(Comprehensive MCO
+ MLTSS)
SCAN Health Plan/Los
Angeles
SCAN Health Plan Los Angeles County 0 7,423 7,423
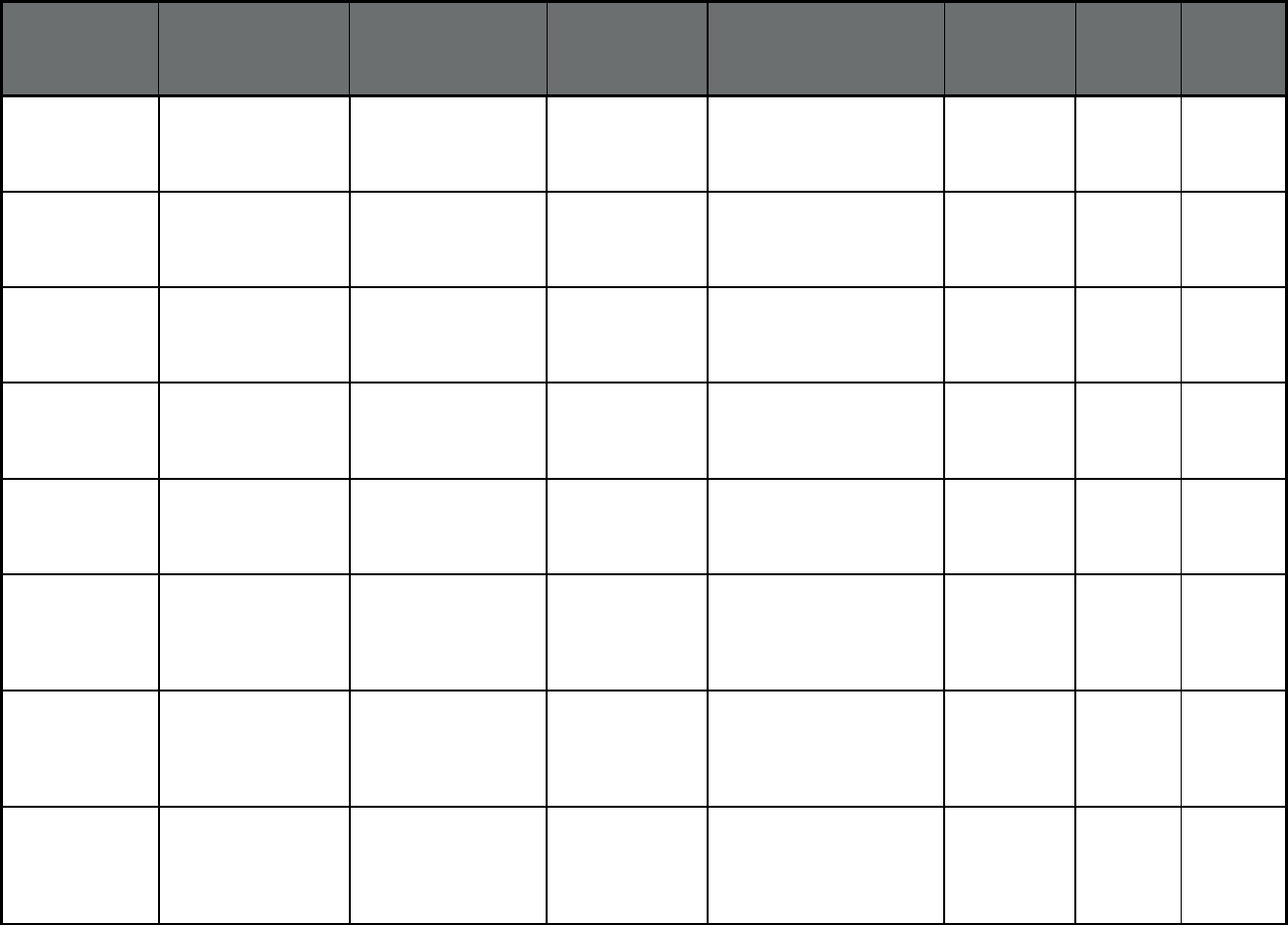
41
State
Program Name
(Type) Plan Name
Parent
Organization
Geographic Region (state-
defined areas, counties, or
zip codes)
Medicaid-Only
Enrollment
Dual
Enrollment
Total
Enrollment
California Senior Care Action
Network (SCAN)
(Comprehensive MCO
+ MLTSS)
SCAN Health
Plan/Riverside
SCAN Health Plan Riverside County 0 2,000 2,000
California Senior Care Action
Network (SCAN)
(Comprehensive MCO
+ MLTSS)
SCAN Health Plan/San
Bernardino
SCAN Health Plan San Bernardino County 0 1,327 1,327
California Senior Care Action
Network (SCAN)
(Comprehensive MCO
+ MLTSS)
SCAN Health Plan
(Nurs hm cert)/Los
Angeles
SCAN Health Plan Los Angeles County 0 1,596 1,596
California Senior Care Action
Network (SCAN)
(Comprehensive MCO
+ MLTSS)
SCAN Health Plan
(Nurs hm
cert)/Riverside
SCAN Health Plan Riverside County 0 531 531
California Senior Care Action
Network (SCAN)
(Comprehensive MCO
+ MLTSS)
SCAN Health Plan
(Nurs hm cert)/San
Bernardino
SCAN Health Plan San Bernardino County 0 328 328
California County Organized
Health Systems
(COHS) Model
(Comprehensive MCO
+ MLTSS)
CenCal Health/San
Luis Obispo
CenCal Health San Luis Obispo County 46,632 6,482 53,114
California County Organized
Health Systems
(COHS) Model
(Comprehensive MCO
+ MLTSS)
CenCal Health/Santa
Barbara
CenCal Health Santa Barbara County 113,107 12,078 125,185
California County Organized
Health Systems
(COHS) Model
(Comprehensive MCO
+ MLTSS)
Health Plan of San
Mateo
Health Plan of San
Mateo
San Mateo County 99,652 9,029 108,681
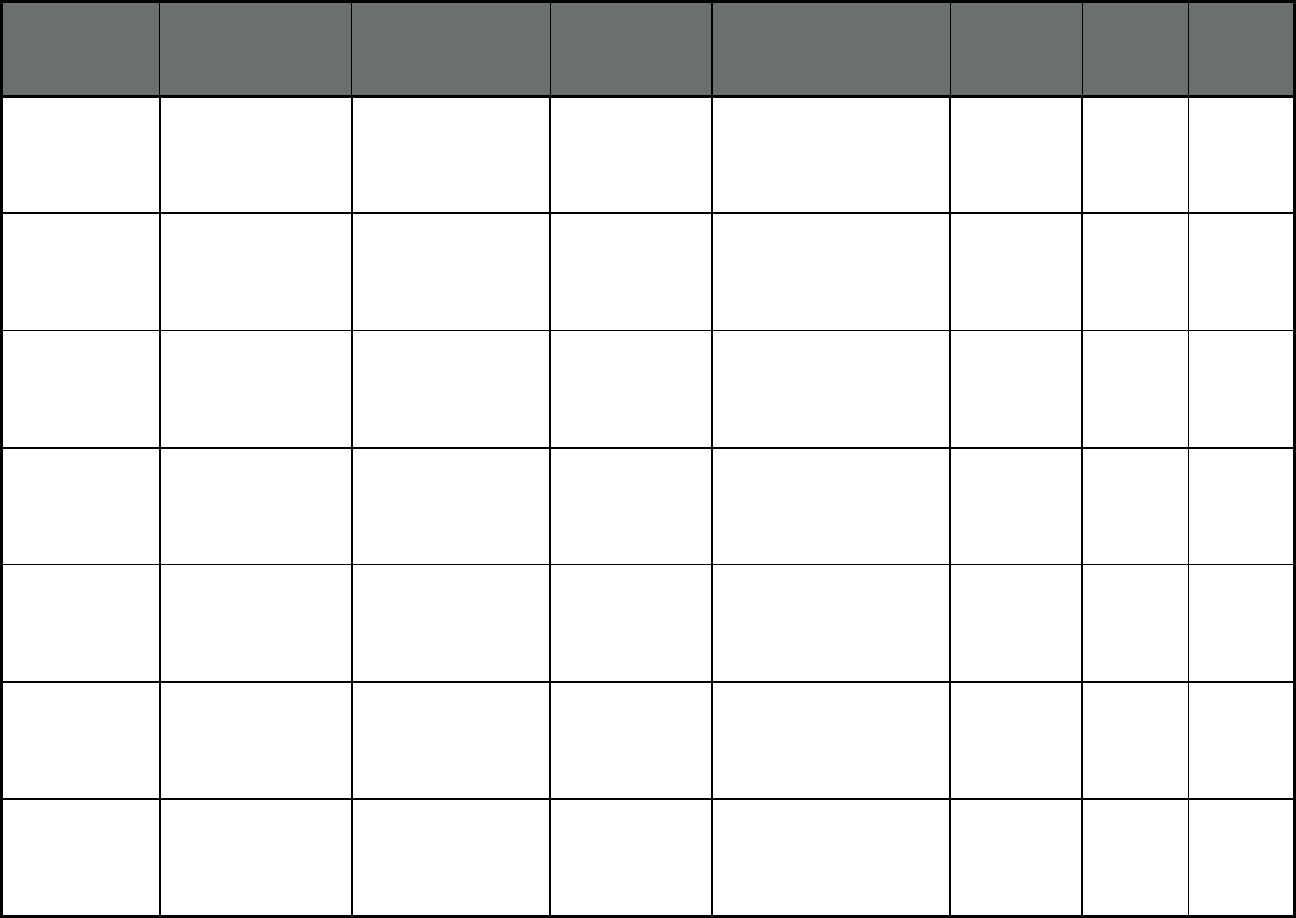
42
State
Program Name
(Type) Plan Name
Parent
Organization
Geographic Region (state-
defined areas, counties, or
zip codes)
Medicaid-Only
Enrollment
Dual
Enrollment
Total
Enrollment
California County Organized
Health Systems
(COHS) Model
(Comprehensive MCO
+ MLTSS)
Partnership HealthPlan
of CA/Northeast
Partnership
HealthPlan of
California
Lassen, Modoc, Shasta,
Siskiyou, and Trinity
Counties
78,321 13,696 92,017
California County Organized
Health Systems
(COHS) Model
(Comprehensive MCO
+ MLTSS)
Partnership HealthPlan
of CA/Northwest
Partnership
HealthPlan of
California
Del Norte and Humboldt
Counties
56,124 7,510 63,634
California County Organized
Health Systems
(COHS) Model
(Comprehensive MCO
+ MLTSS)
Partnership Health
Plan/Southeast
Partnership
HealthPlan of
California
Napa, Solano, and Yolo
Counties
166,390 23,437 189,827
California County Organized
Health Systems
(COHS) Model
(Comprehensive MCO
+ MLTSS)
Partnership Health
Plan/Southwest
Partnership
HealthPlan of
California
Lake, Marin, Mendocino,
and Sonoma Counties
187,299 28,104 215,403
California County Organized
Health Systems
(COHS) Model
(Comprehensive MCO
+ MLTSS)
Central California
Alliance for
Health/Merced
Central California
Alliance for Health
Merced County 113,142 10,795 123,937
California County Organized
Health Systems
(COHS) Model
(Comprehensive MCO
+ MLTSS)
Central California
Alliance for
Health/Monterey Santa
Cruz
Central California
Alliance for Health
Monterey and Santa Cruz
Counties
204,898 20,357 225,255
California County Organized
Health Systems
(COHS) Model
(Comprehensive MCO
+ MLTSS)
CalOptima/Orange CalOptima Orange County 678,532 80,327 758,859
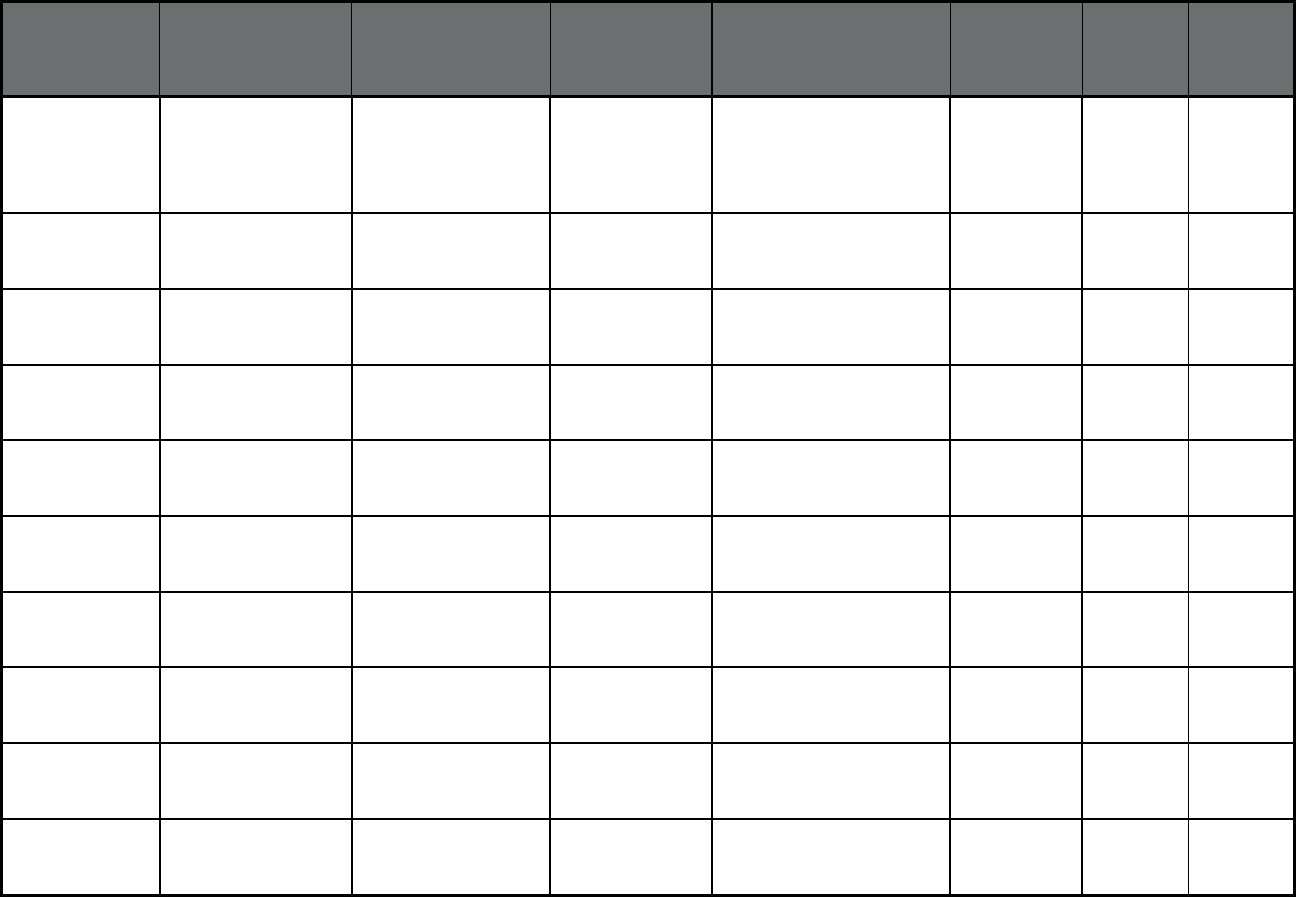
43
State
Program Name
(Type) Plan Name
Parent
Organization
Geographic Region (state-
defined areas, counties, or
zip codes)
Medicaid-Only
Enrollment
Dual
Enrollment
Total
Enrollment
California County Organized
Health Systems
(COHS) Model
(Comprehensive MCO
+ MLTSS)
Gold Coast Health
Plan/Ventura
Gold Coast Health
Plan
Ventura County 177,647 21,560 199,207
California Two-Plan Model
(Comprehensive MCO
+ MLTSS)
Health Net/Kern Centene
Corporation
Kern County 70,674 3,085 73,759
California Two-Plan Model
(Comprehensive MCO
+ MLTSS)
Health Net/Los Angeles Centene
Corporation
Los Angeles County 861,114 139,053 1,000,167
California Two-Plan Model
(Comprehensive MCO
+ MLTSS)
Health Net/San Joaquin Centene
Corporation
San Joaquin County 20,530 546 21,076
California Two-Plan Model
(Comprehensive MCO
+ MLTSS)
Health Net/Stanislaus Centene
Corporation
Stanislaus County 65,828 2,441 68,269
California Two-Plan Model
(Comprehensive MCO
+ MLTSS)
Health Net/Tulare Centene
Corporation
Tulare County 110,699 3,780 114,479
California Two-Plan Model
(Comprehensive MCO
+ MLTSS)
CalViva Health/Fresno CalViva Health Fresno County 286,356 10,881 297,237
California Two-Plan Model
(Comprehensive MCO
+ MLTSS)
CalViva Health/Kings CalViva Health Kings County 27,328 949 28,277
California Two-Plan Model
(Comprehensive MCO
+ MLTSS)
CalViva Health/Madera CalViva Health Madera County 35,920 1,090 37,010
California Two-Plan Model
(Comprehensive MCO
+ MLTSS)
Anthem Blue Cross
Partnership
Plan/Fresno
Anthem Insurance
Companies, Inc.
Fresno County 104,856 3,946 108,802
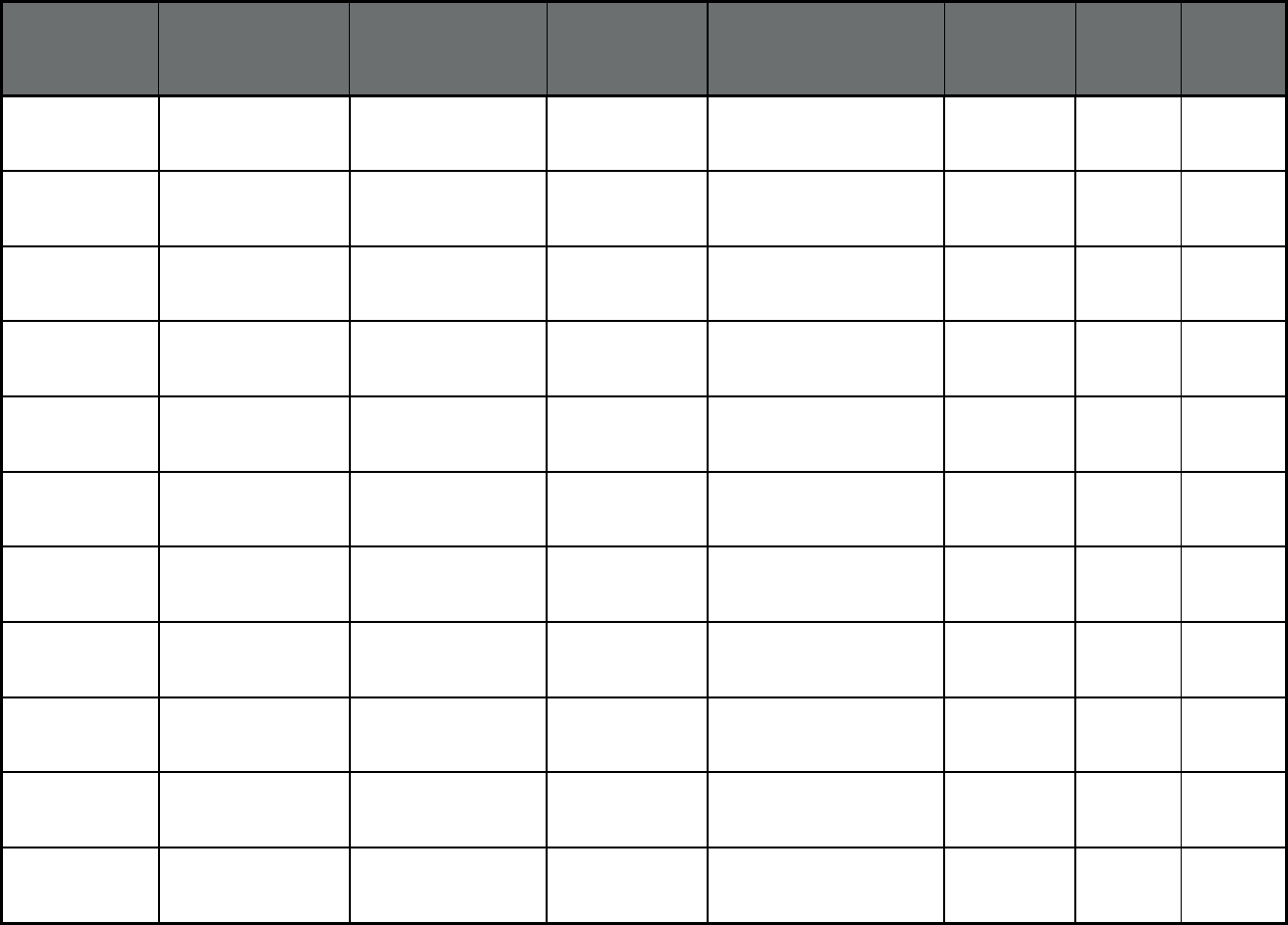
44
State
Program Name
(Type) Plan Name
Parent
Organization
Geographic Region (state-
defined areas, counties, or
zip codes)
Medicaid-Only
Enrollment
Dual
Enrollment
Total
Enrollment
California Two-Plan Model
(Comprehensive MCO
+ MLTSS)
Anthem Blue Cross
Partnership Plan/Kings
Anthem Insurance
Companies, Inc.
Kings County 19,155 589 19,744
California Two-Plan Model
(Comprehensive MCO
+ MLTSS)
Anthem Blue Cross
Partnership
Plan/Madera
Anthem Insurance
Companies, Inc.
Madera County 18,868 514 19,382
California Two-Plan Model
(Comprehensive MCO
+ MLTSS)
Anthem Blue Cross
Partnership
Plan/Alameda
Anthem Insurance
Companies, Inc.
Alameda County 58,024 2,661 60,685
California Two-Plan Model
(Comprehensive MCO
+ MLTSS)
Anthem Blue Cross
Partnership
Plan/Contra Costa
Anthem Insurance
Companies, Inc.
Contra Costa County 26,316 836 27,152
California Two-Plan Model
(Comprehensive MCO
+ MLTSS)
Anthem Blue Cross
Partnership Plan/San
Francisco
Anthem Insurance
Companies, Inc.
San Francisco County 16,513 2,427 18,940
California Two-Plan Model
(Comprehensive MCO
+ MLTSS)
Anthem Blue Cross
Partnership Plan/Santa
Clara
Anthem Insurance
Companies, Inc.
Santa Clara County 57,721 13,268 70,989
California Two-Plan Model
(Comprehensive MCO
+ MLTSS)
Anthem Blue Cross
Partnership Plan/Tulare
Anthem Insurance
Companies, Inc.
Tulare County 89,538 3,238 92,776
California Two-Plan Model
(Comprehensive MCO
+ MLTSS)
Kern Family Health
Care
Kern Health
Systems
Kern County 248,909 7,516 256,425
California Two-Plan Model
(Comprehensive MCO
+ MLTSS)
L.A. Care Health
Plan/Los Angeles
L.A. Care Los Angeles County 1,841,741 236,123 2,077,864
California Two-Plan Model
(Comprehensive MCO
+ MLTSS)
Contra Costa Health
Plan
Contra Costa
Health Plan
Contra Costa County 171,320 10,901 182,221
California Two-Plan Model
(Comprehensive MCO
+ MLTSS)
Alameda Alliance for
Health
Alameda Alliance
for Health
Alameda County 240,968 21,233 262,201
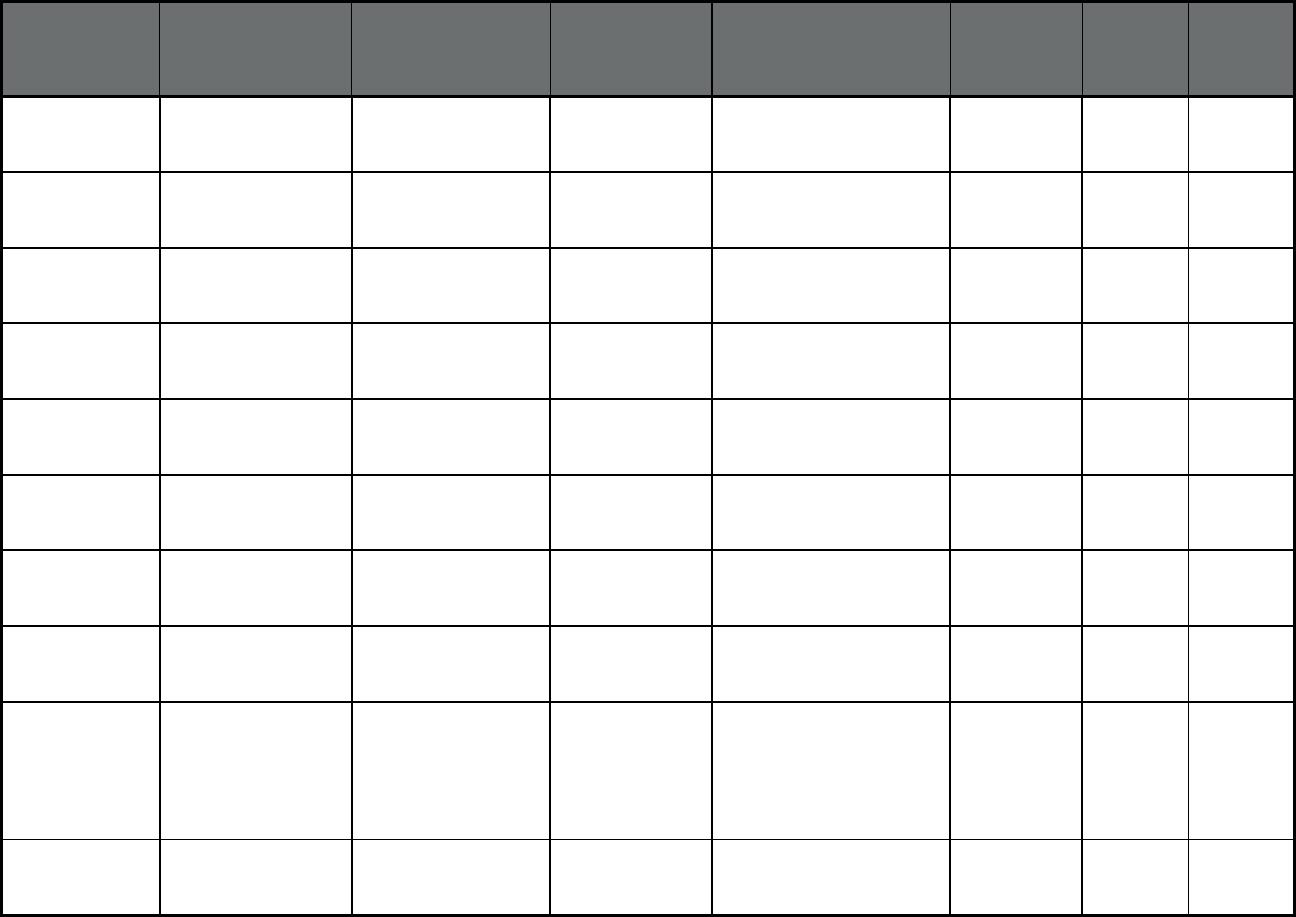
45
State
Program Name
(Type) Plan Name
Parent
Organization
Geographic Region (state-
defined areas, counties, or
zip codes)
Medicaid-Only
Enrollment
Dual
Enrollment
Total
Enrollment
California Two-Plan Model
(Comprehensive MCO
+ MLTSS)
Inland Empire Health
Plan/Riverside
Inland Empire
Health Plan
Riverside County 575,779 33,781 609,560
California Two-Plan Model
(Comprehensive MCO
+ MLTSS)
Inland Empire Health
Plan/San Bernardino
Inland Empire
Health Plan
San Bernardino County 586,801 34,322 621,123
California Two-Plan Model
(Comprehensive MCO
+ MLTSS)
Molina Healthcare of
CA Partner
Plan/Riverside
Molina Healthcare Riverside County 75,018 9,279 84,297
California Two-Plan Model
(Comprehensive MCO
+ MLTSS)
Molina Healthcare of
CA Partner Plan/San
Bernardino
Molina Healthcare San Bernardino County 64,751 7,588 72,339
California Two-Plan Model
(Comprehensive MCO
+ MLTSS)
San Francisco Health
Plan
San Francisco
Health Plan
San Francisco County 116,919 12,550 129,469
California Two-Plan Model
(Comprehensive MCO
+ MLTSS)
Health Plan of San
Joaquin/San Joaquin
Health Plan of San
Joaquin
San Joaquin County 208,433 9,576 218,009
California Two-Plan Model
(Comprehensive MCO
+ MLTSS)
Health Plan of San
Joaquin/Stanislaus
Health Plan of San
Joaquin
Stanislaus County 123,900 4,156 128,056
California Two-Plan Model
(Comprehensive MCO
+ MLTSS)
Santa Clara Family
Health Plan
Santa Clara
Family Health Plan
Santa Clara County 220,347 30,708 251,055
California Family Mosaic
Program/San
Francisco (Behavioral
Health Organization
(BHO) only (PIHP
and/or PAHP))
Family Mosaic
Project/San Francisco
San Francisco
Health Plan
San Francisco 32 0 32
California Dental Managed
Care/Los Angeles
(Dental only (PAHP))
Health Net Dental
Plan/Los Angeles
Health Net Los Angeles County 173,986 14,023 188,009
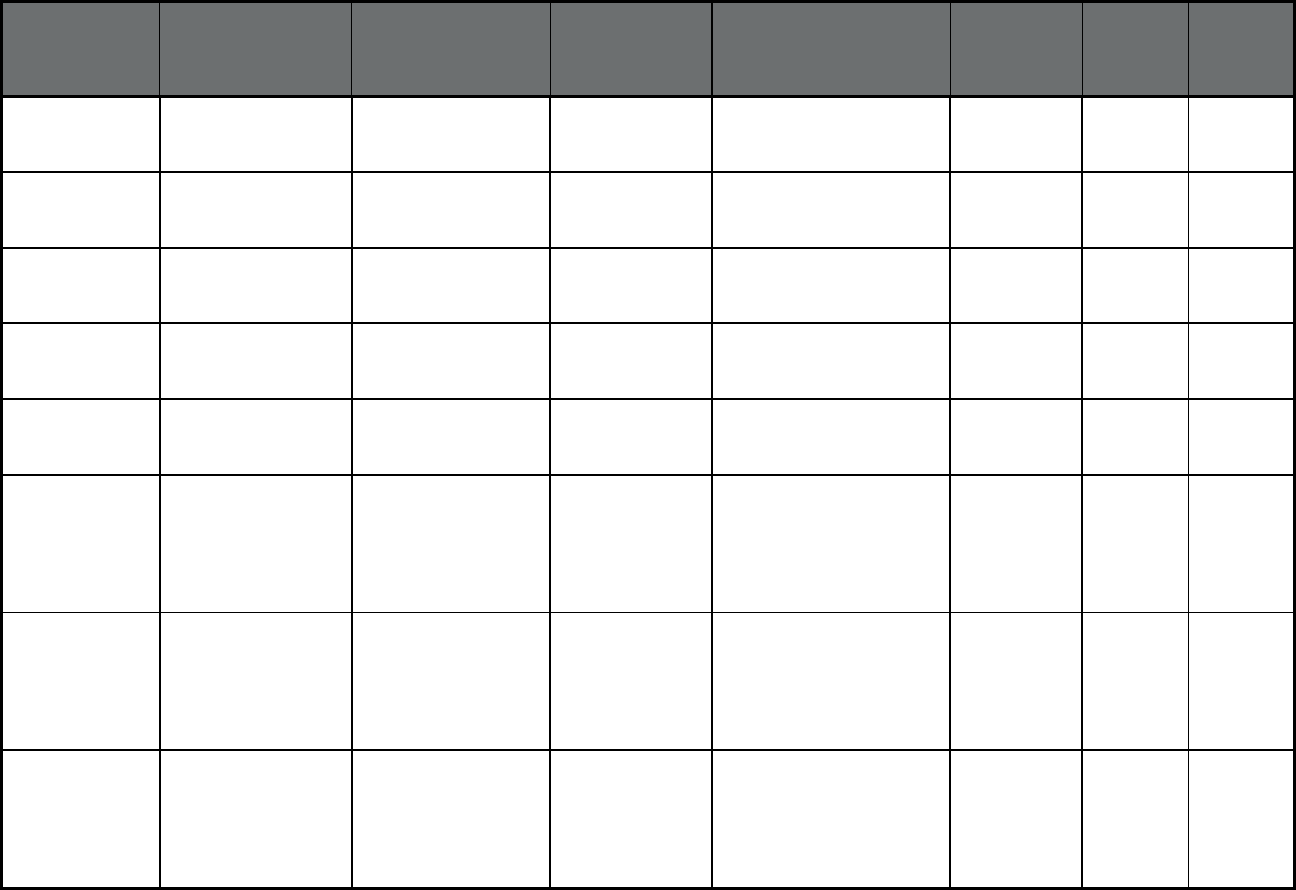
46
State
Program Name
(Type) Plan Name
Parent
Organization
Geographic Region (state-
defined areas, counties, or
zip codes)
Medicaid-Only
Enrollment
Dual
Enrollment
Total
Enrollment
California Dental Managed
Care/Los Angeles
(Dental only (PAHP))
Access Dental Plan/Los
Angeles
Access Dental,
Inc.
Los Angeles County 155,811 13,734 169,545
California Dental Managed
Care/Los Angeles
(Dental only (PAHP))
LIBERTY Dental
Plan/Los Angeles
LIBERTY Dental
Plan
Los Angeles County 58,936 5,269 64,205
California Dental Managed
Care/Sacramento
(Dental only (PAHP))
Health Net Dental
Plan/Sacramento
Health Net Sacramento County 121,027 6,671 127,698
California Dental Managed
Care/Sacramento
(Dental only (PAHP))
Access Dental
Plan/Sacramento
Access Dental,
Inc.
Sacramento County 127,500 6,115 133,615
California Dental Managed
Care/Sacramento
(Dental only (PAHP))
LIBERTY Dental
Plan/Sacramento
LIBERTY Dental
Plan
Sacramento County 155,037 7,687 162,724
California Positive
Healthcare/Los
Angeles (Other
Prepaid Health Plan
(PHP) (limited
benefits))
Positive Healthcare/Los
Angeles
AIDS Healthcare
Foundation
Los Angeles 331 339 670
California Program of All-
Inclusive Care for the
Elderly (PACE)
(Program of All-
inclusive Care for the
Elderly (PACE))
Redwood Coast
Pace/Humboldt
Humboldt Senior
Resource Center
Humboldt County 14 141 155
California Program of All-
Inclusive Care for the
Elderly (PACE)
(Program of All-
inclusive Care for the
Elderly (PACE))
San Diego PACE PACE San Diego County 86 236 322

47
State
Program Name
(Type) Plan Name
Parent
Organization
Geographic Region (state-
defined areas, counties, or
zip codes)
Medicaid-Only
Enrollment
Dual
Enrollment
Total
Enrollment
California Program of All-
Inclusive Care for the
Elderly (PACE)
(Program of All-
inclusive Care for the
Elderly (PACE))
St. Paul's PACE/San
Diego
Community
Eldercare of San
Diego
San Diego County 149 580 729
California Program of All-
Inclusive Care for the
Elderly (PACE)
(Program of All-
inclusive Care for the
Elderly (PACE))
Sutter SeniorCare
PACE/Sacramento
Sutter Health Sacramento County 31 263 294
California Program of All-
Inclusive Care for the
Elderly (PACE)
(Program of All-
inclusive Care for the
Elderly (PACE))
AltaMed Senior
Buenacare/Los
Angeles
AltaMed Health
Services
Corporation
Los Angeles County 673 1,858 2,531
California Program of All-
Inclusive Care for the
Elderly (PACE)
(Program of All-
inclusive Care for the
Elderly (PACE))
Brandman Centers for
Senior Care/Los
Angeles
Brandman Centers
for Senior Care
Los Angeles County 30 199 229
California Program of All-
Inclusive Care for the
Elderly (PACE)
(Program of All-
inclusive Care for the
Elderly (PACE))
CalOptima
PACE/Orange
CalOptima Orange County 110 164 274
California Program of All-
Inclusive Care for the
Elderly (PACE)
(Program of All-
inclusive Care for the
Elderly (PACE))
Center for Elders
Independence/Alameda
Center for Elders
Independence
Alameda County 68 558 626
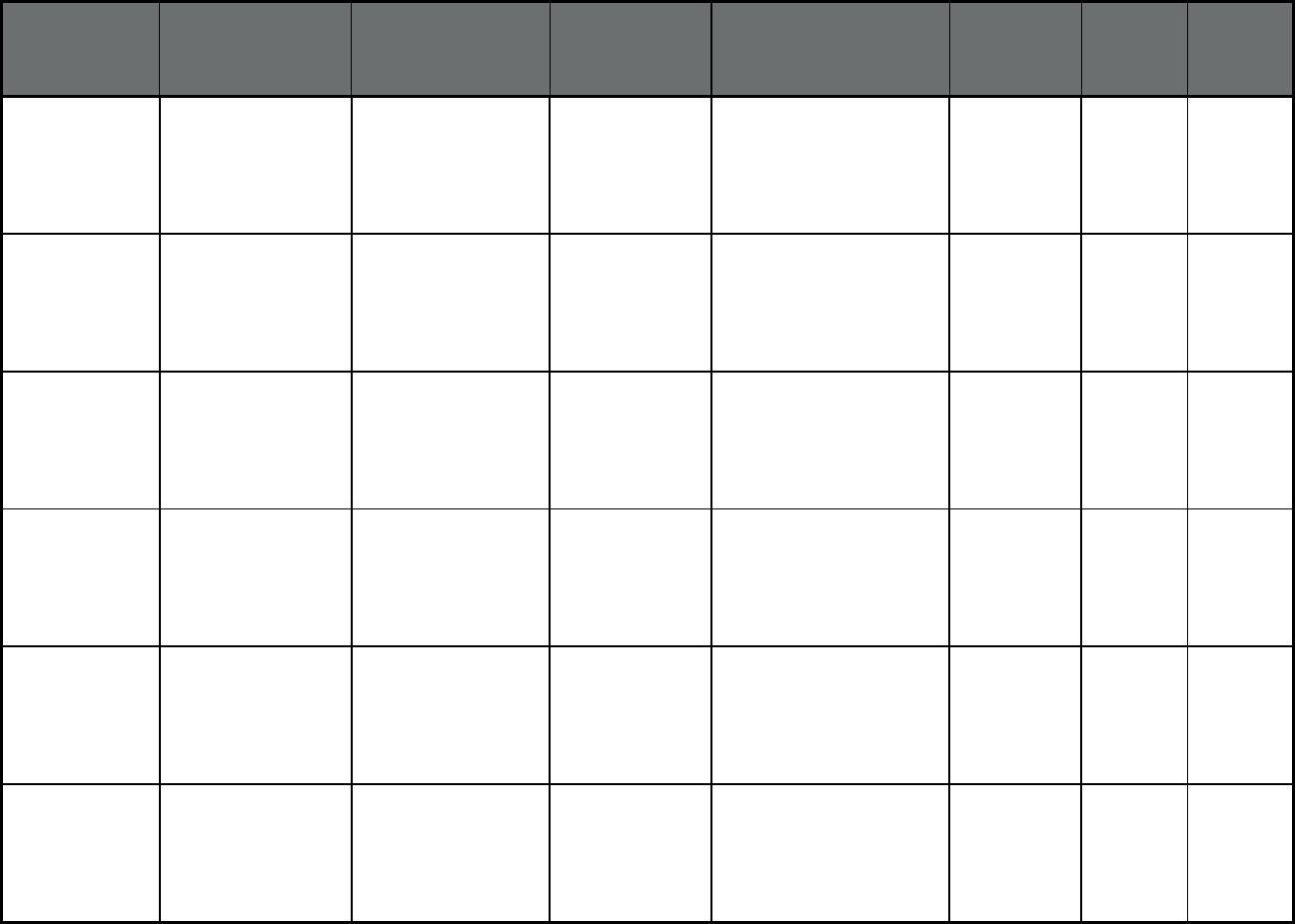
48
State
Program Name
(Type) Plan Name
Parent
Organization
Geographic Region (state-
defined areas, counties, or
zip codes)
Medicaid-Only
Enrollment
Dual
Enrollment
Total
Enrollment
California Program of All-
Inclusive Care for the
Elderly (PACE)
(Program of All-
inclusive Care for the
Elderly (PACE))
Center for Elders
Independence/Contra
Costa
Center for Elders
Independence
Contra Costa County 15 65 80
California Program of All-
Inclusive Care for the
Elderly (PACE)
(Program of All-
inclusive Care for the
Elderly (PACE))
Fresno PACE Central Valley
Medical Services
Corporation
Fresno County 213 307 520
California Program of All-
Inclusive Care for the
Elderly (PACE)
(Program of All-
inclusive Care for the
Elderly (PACE))
InnovAge
PACE/Riverside
InnovAge Riverside County 37 104 141
California Program of All-
Inclusive Care for the
Elderly (PACE)
(Program of All-
inclusive Care for the
Elderly (PACE))
InnovAge PACE/San
Bernardino County
InnovAge San Bernardino County 97 287 384
California Program of All-
Inclusive Care for the
Elderly (PACE)
(Program of All-
inclusive Care for the
Elderly (PACE))
On Lok
Lifeways/Alameda
On Lok Lifeways Alameda County 56 194 250
California Program of All-
Inclusive Care for the
Elderly (PACE)
(Program of All-
inclusive Care for the
Elderly (PACE))
On Lok Lifeways/Santa
Clara
On Lok Lifeways Santa Clara County 49 207 256
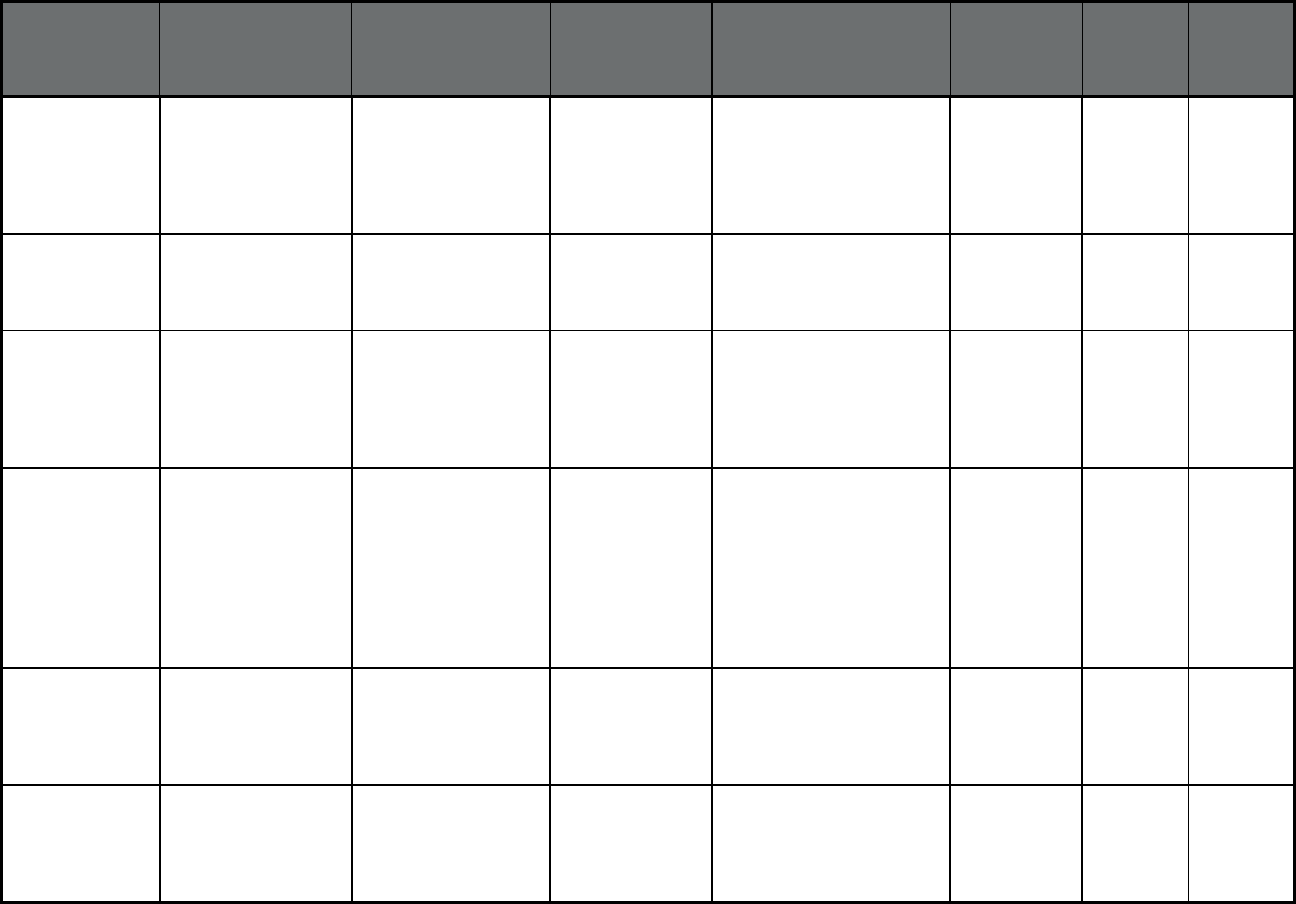
49
State
Program Name
(Type) Plan Name
Parent
Organization
Geographic Region (state-
defined areas, counties, or
zip codes)
Medicaid-Only
Enrollment
Dual
Enrollment
Total
Enrollment
California Program of All-
Inclusive Care for the
Elderly (PACE)
(Program of All-
inclusive Care for the
Elderly (PACE))
On Lok Lifeways/San
Francisco
On Lok Lifeways San Francisco County 88 905 993
Colorado
3,4
Denver Health
Medicaid Choice
(Comprehensive
MCO)
Denver Health
Medicaid Choice
Denver Health and
Hospital Authority
Denver, Arapahoe, Adams,
and Jefferson Counties
78,073 3,852 81,925
Colorado
3,4
Accountable Care
Collaborative: Rocky
Mountain Health Plans
Prime
(Comprehensive
MCO)
Accountable Care
Collaborative: Rocky
Mountain Health Plans
Prime
Rocky Mountain
Health
Garfield, Gunnison, Mesa,
Montrose, Pitkin, and Rio
Blanco Counties
32,477 4,006 36,483
Colorado
3,4
Accountable Care
Collaborative (ACC)
(Primary Care Case
Management Entity
(PCCM Entity))
RAE 1: Rocky
Mountain Health Plans
UnitedHealthcare Moffat, Routt, Jackson,
Grand, Summit, Eagle,
Garfield, Mesa, Delta, Pitkin,
Gunnison, Montrose, Ouray,
San Miguel, Hinsdale,
Dolores, San Juan,
Montezuma, La Plata,
Archuleta, and Larimer
Counties
137,867 8,669 146,536
Colorado
3,4
Accountable Care
Collaborative (ACC)
(Primary Care Case
Management Entity
(PCCM Entity))
RAE 2: Northeast
Health Partners
Northeast Health
Partners
Cheyenne, Kit Carson,
Lincoln, Logan, Morgan,
Phillips, Sedgwick,
Washington, Weld, and
Yuma Counties
81,472 6,132 87,604
Colorado
3,4
Accountable Care
Collaborative (ACC)
(Primary Care Case
Management Entity
(PCCM Entity))
RAE 3: Colorado
Access
Colorado Access Adams, Arapahoe, Douglas,
and Elbert Counties
238,753 13,526 252,279
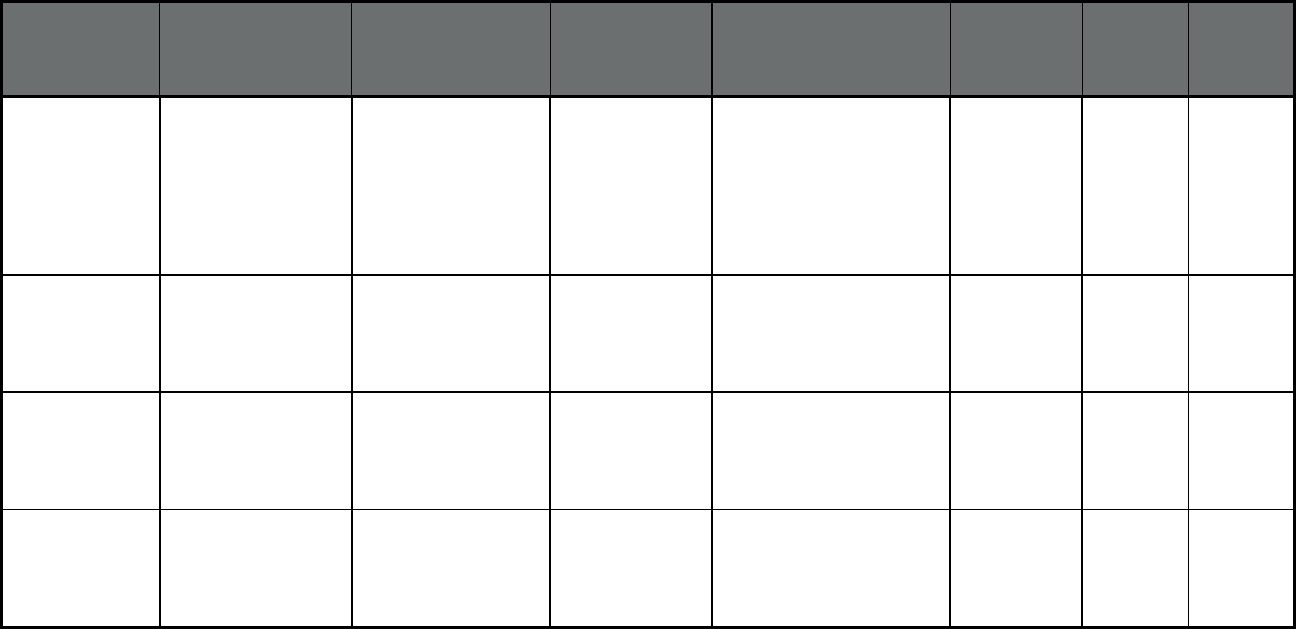
50
State
Program Name
(Type) Plan Name
Parent
Organization
Geographic Region (state-
defined areas, counties, or
zip codes)
Medicaid-Only
Enrollment
Dual
Enrollment
Total
Enrollment
Colorado
3,4
Accountable Care
Collaborative (ACC)
(Primary Care Case
Management Entity
(PCCM Entity))
RAE 4: Health
Colorado, Inc.
Health Colorado,
Inc.
Alamosa, Baca, Bent,
Chaffee, Conejos, Costilla,
Crowley, Custer, Fremont,
Huerfano, Kiowa, Lake, Las
Animas, Mineral, Otero,
Prowers, Pueblo, Rio
Grande, and Saguache
Counties
115,816 12,262 128,078
Colorado
3,4
Accountable Care
Collaborative (ACC)
(Primary Care Case
Management Entity
(PCCM Entity))
RAE 5: Colorado
Access
Colorado Access Denver County 115,179 8,614 123,793
Colorado
3,4
Accountable Care
Collaborative (ACC)
(Primary Care Case
Management Entity
(PCCM Entity))
RAE 6: Colorado
Community Health
Alliance
Colorado
Community Health
Alliance
Boulder, Clear Creek, Gilpin,
Broomfield, and Jefferson
Counties
132,836 10,673 143,509
Colorado
3,4
Accountable Care
Collaborative (ACC)
(Primary Care Case
Management Entity
(PCCM Entity))
RAE 7: Colorado
Community Health
Alliance
Colorado
Community Health
Alliance
El Paso, Park, and Teller
Counties
158,255 8,827 167,082
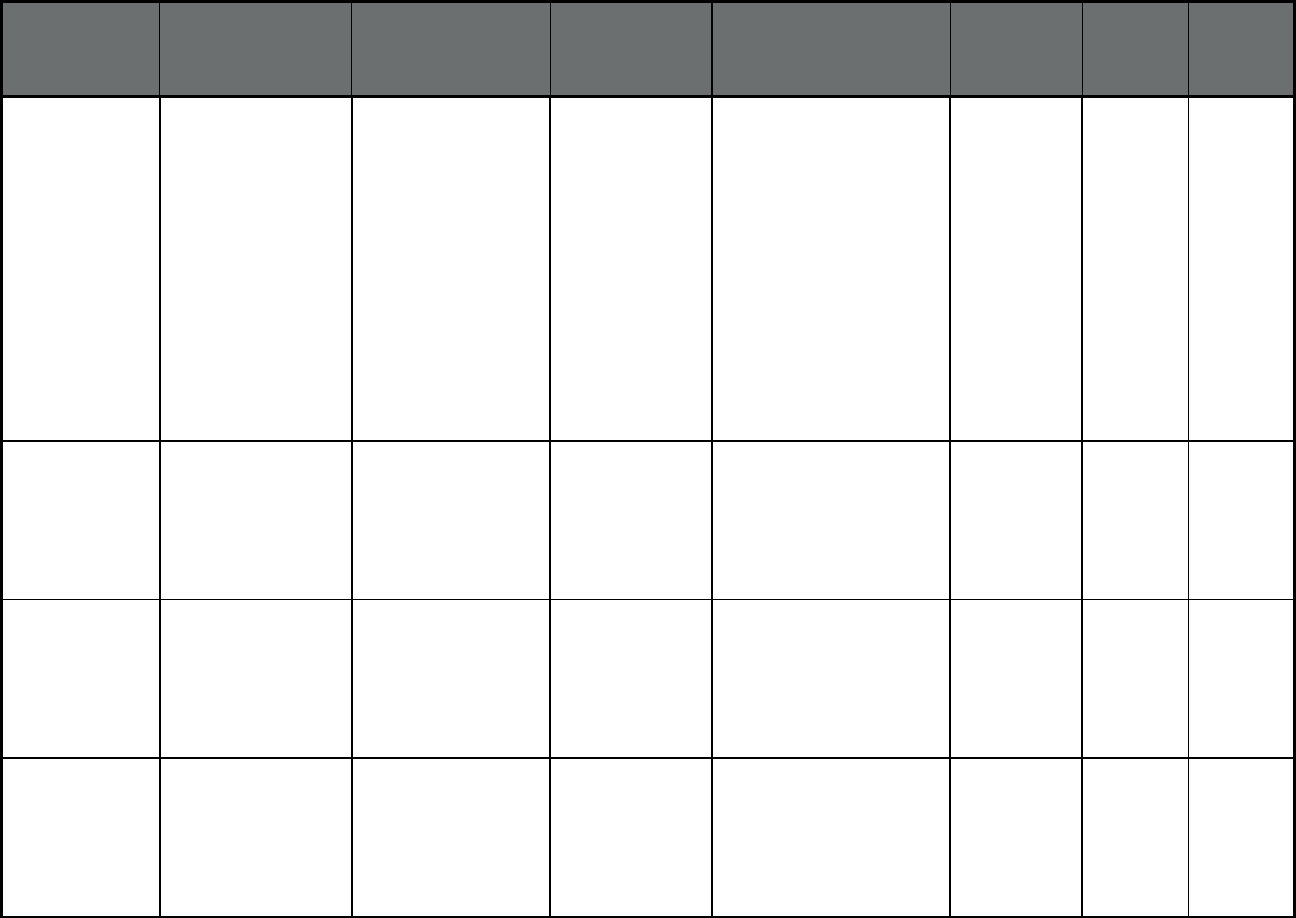
51
State
Program Name
(Type) Plan Name
Parent
Organization
Geographic Region (state-
defined areas, counties, or
zip codes)
Medicaid-Only
Enrollment
Dual
Enrollment
Total
Enrollment
Colorado
3,4
Colorado Medicaid
Community Behavioral
Health Services
Program (Behavioral
Health Organization
(BHO) only (PIHP
and/or PAHP))
Colorado Health
Partnerships
Colorado Health
Partnerships
Alamosta, Archuleta, Baca,
Bent, Chaffee, Conejos,
Costilla, Crowley, Custer,
Delta, Dolores, Eagle, El
Paso, Fremont, Garfield,
Grand, Gunnison, Hinsdale,
Huerfano, Jackson, Kiowa,
Lake, La Plata, Las Animas,
Mesa, Mineral, Moffat,
Montezuma, Montrose,
Ouray, Otero, Park, Pitkin,
Prowers, Pueblo, Rio
Blanco, Rio Grande, Routt,
Saguache, San Juan, San
Miguel, Summit and Teller
Counties
0 0 0
Colorado
3,4
Colorado Medicaid
Community Behavioral
Health Services
Program (Behavioral
Health Organization
(BHO) only (PIHP
and/or PAHP))
Behavioral Healthcare,
Inc.
Behavioral
Healthcare Inc.
Adams, Arapahoe, and
Douglas Counties
0 0 0
Colorado
3,4
Colorado Medicaid
Community Behavioral
Health Services
Program (Behavioral
Health Organization
(BHO) only (PIHP
and/or PAHP))
Foothills Behavioral
Health Partners
Foothills
Behavioral Health
Partners
Boulder, Broomfield, Clear
Creek, Gilpin, and Jefferson
Counties
0 0 0
Colorado
3,4
Colorado Medicaid
Community Behavioral
Health Services
Program (Behavioral
Health Organization
(BHO) only (PIHP
and/or PAHP))
Access Behavioral
Care - Denver
Access Behavioral
Care
Denver County 0 0 0
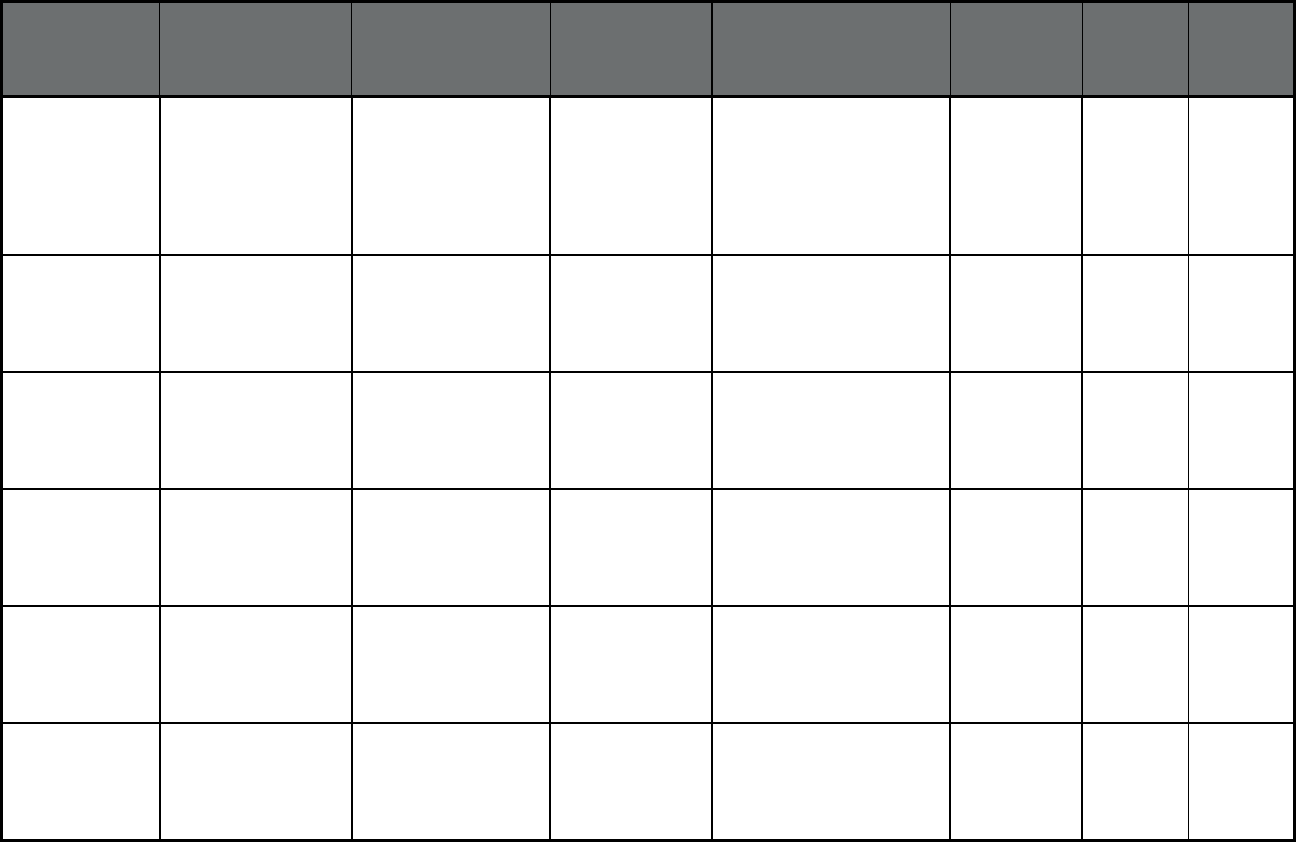
52
State
Program Name
(Type) Plan Name
Parent
Organization
Geographic Region (state-
defined areas, counties, or
zip codes)
Medicaid-Only
Enrollment
Dual
Enrollment
Total
Enrollment
Colorado
3,4
Colorado Medicaid
Community Behavioral
Health Services
Program (Behavioral
Health Organization
(BHO) only (PIHP
and/or PAHP))
Access Behavioral
Care - Northeast
Access Behavioral
Care
Cheyenne, Elbert, Kit
Carson, Larimer, Lincoln,
Logan, Morgan, Phillips,
Sedgwick, Washington,
Weld, and Yuma Counties
0 0 0
Colorado
3,4
Program of All-
Inclusive Care for the
Elderly (Program of
All-inclusive Care for
the Elderly (PACE))
Rocky Mountain Health
Care Services (PACE)
Health Care
Service
Corporation
El Paso County 41 531 572
Colorado
3,4
Program of All-
Inclusive Care for the
Elderly (Program of
All-inclusive Care for
the Elderly (PACE))
Total Longterm Care -
Pueblo DBA Innovage
Greater Colorado
PACE
Total Community
Options, Inc.
Pueblo County 0 451 451
Colorado
3,4
Program of All-
Inclusive Care for the
Elderly (Program of
All-inclusive Care for
the Elderly (PACE))
Total Longterm Care -
Innovage Aurora
(PACE)
Total Community
Options, Inc.
Aurora 112 1,916 2,028
Colorado
3,4
Program of All-
Inclusive Care for the
Elderly (Program of
All-inclusive Care for
the Elderly (PACE))
Volunteers of America
(VOANS) PACE DBA
Senior Community
Care
Volunteers of
America
Delta and Montrose
Counties
0 308 308
Colorado
3,4
Program of All-
Inclusive Care for the
Elderly (Program of
All-inclusive Care for
the Elderly (PACE))
Total Longterm Care -
Innovage Loveland
(PACE)
Total Community
Options, Inc.
Larimer and Weld Counties 0 216 216
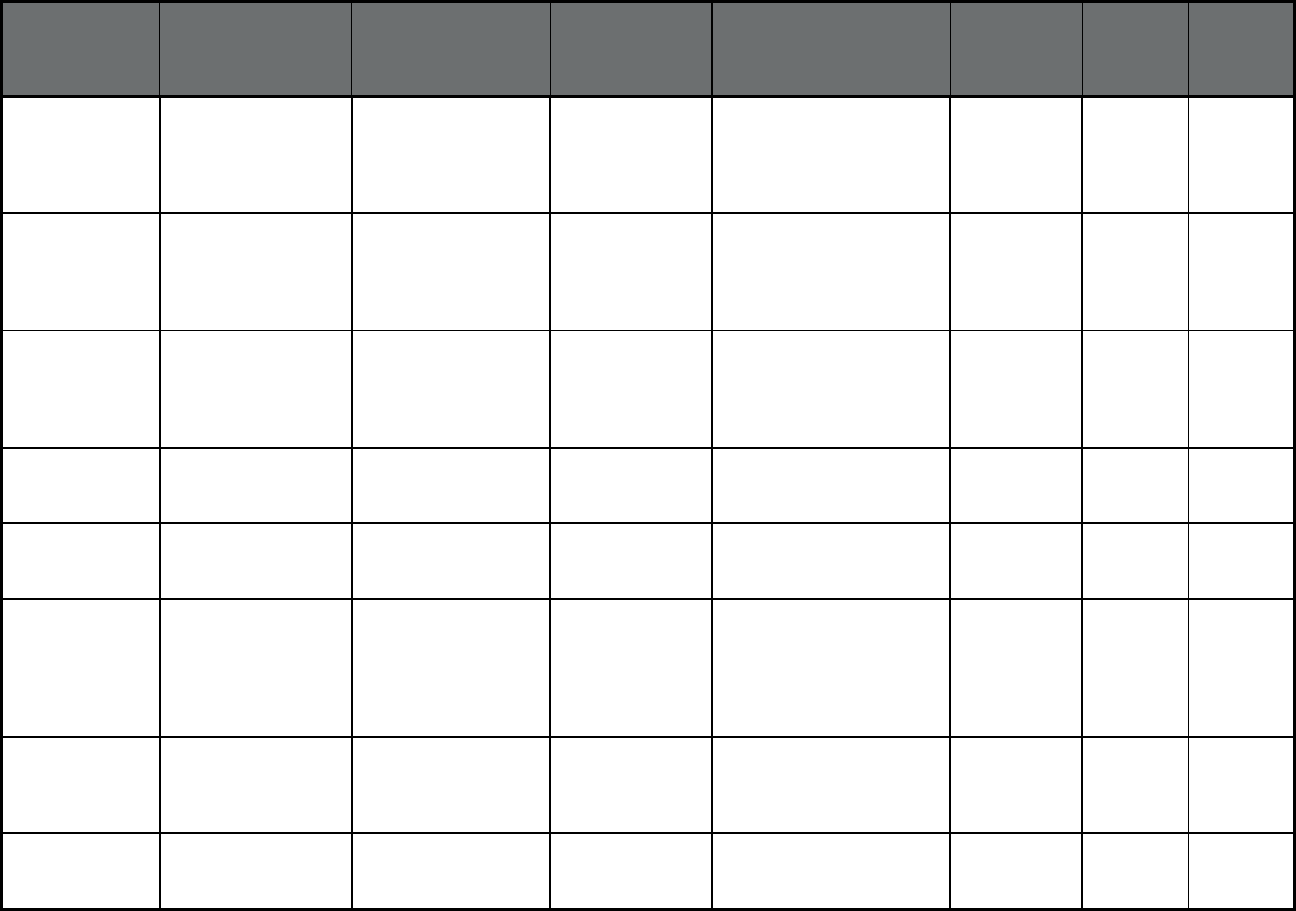
53
State
Program Name
(Type) Plan Name
Parent
Organization
Geographic Region (state-
defined areas, counties, or
zip codes)
Medicaid-Only
Enrollment
Dual
Enrollment
Total
Enrollment
Colorado
3,4
Program of All-
Inclusive Care for the
Elderly (Program of
All-inclusive Care for
the Elderly (PACE))
TRU Community Care Community Care
Health Plan (WI)
Boulder and Weld Counties 0 84 84
Colorado
3,4
Program of All-
Inclusive Care for the
Elderly (Program of
All-inclusive Care for
the Elderly (PACE))
Total Longterm Care -
Innovage Lakewood
(PACE)
Total Community
Options, Inc.
Lakewood 0 140 140
Colorado
3,4
Program of All-
Inclusive Care for the
Elderly (Program of
All-inclusive Care for
the Elderly (PACE))
Total Longterm Care -
Innovage Thornton
(PACE)
Total Community
Options, Inc.
Thornton 0 0 0
Delaware Diamond State Health
Plan (Comprehensive
MCO + MLTSS)
Highmark Health
Options of Delaware
Highmark Statewide 148,290 4,241 152,531
Delaware Diamond State Health
Plan (Comprehensive
MCO + MLTSS)
AmeriHealth Caritas of
Delaware
AmeriHealth Statewide 45,230 1,884 47,114
Delaware LogistiCare/Circulation
Non-Emergency
Medical Transportation
(Non-Emergency
Medical
Transportation)
LogistiCare/Circulation
Non-Emergency
Medical Transportation
LogistiCare Statewide 202,677 6,125 208,802
Delaware Saint Francis Life
(Program of All-
inclusive Care for the
Elderly (PACE))
Saint Francis Life Saint Francis
Healthcare
New Castle County 10 232 242
District of
Columbia
DC Healthy Families
(Comprehensive
MCO)
AmeriHealth Caritas
District of Columbia
AmeriHealth Statewide 110,092 7 110,099
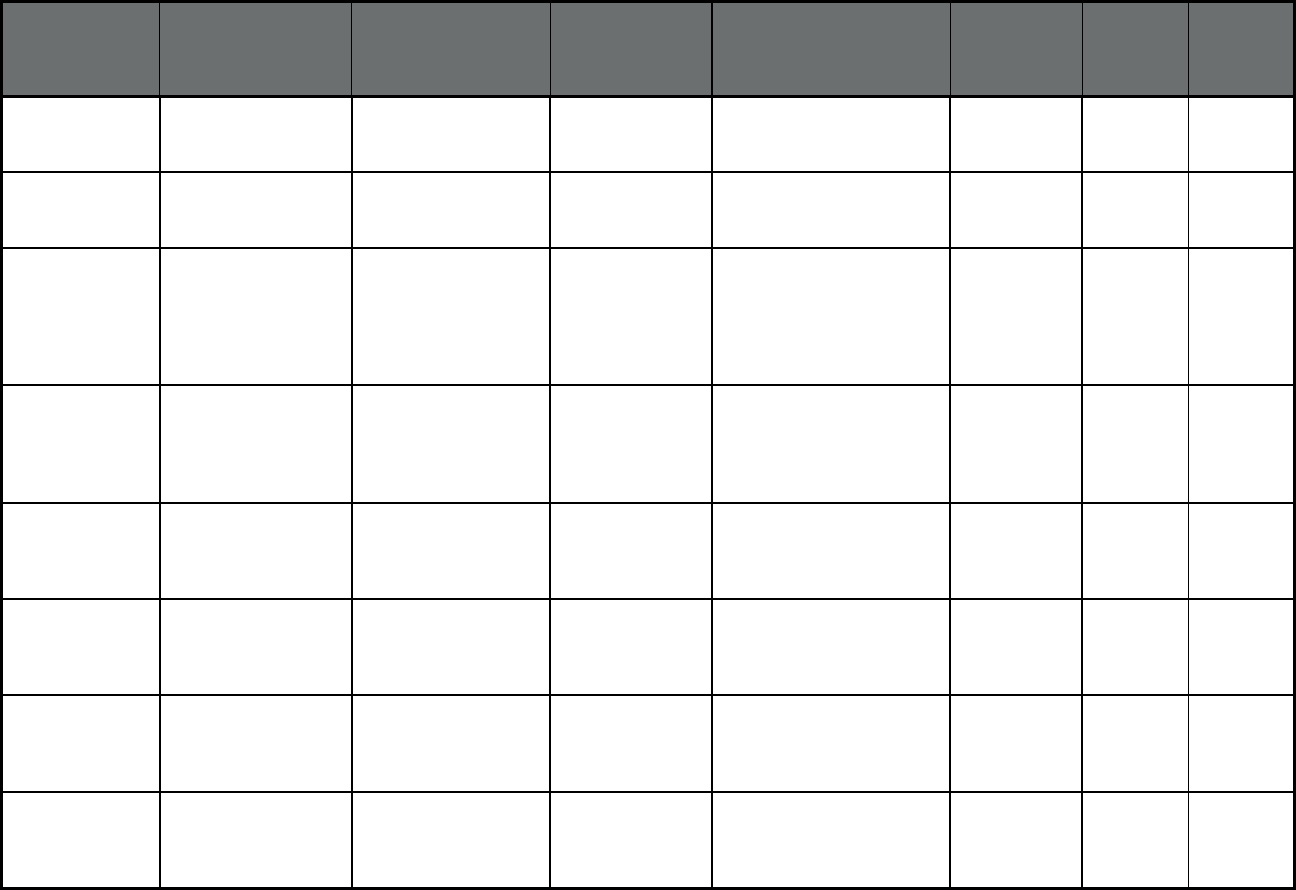
54
State
Program Name
(Type) Plan Name
Parent
Organization
Geographic Region (state-
defined areas, counties, or
zip codes)
Medicaid-Only
Enrollment
Dual
Enrollment
Total
Enrollment
District of
Columbia
DC Healthy Families
(Comprehensive
MCO)
Amerigroup District of
Columbia
Anthem Insurance
Companies, Inc.
Statewide 43,374 2 43,376
District of
Columbia
DC Healthy Families
(Comprehensive
MCO)
Trusted Health Plan Trusted Health
Plan, Inc.
Statewide 30,584 1 30,585
District of
Columbia
Child and Adolescent
Supplemental Security
Income Program
(CASSIP)
(Comprehensive
MCO)
Health Services for
Children with Special
Needs
The HSC
Foundation
Statewide 5,188 115 5,303
District of
Columbia
Non-Emergency
Medical Transportation
(NEMT) (Non-
Emergency Medical
Transportation)
Medical Transportation
Management, Inc.
Medical
Transportation
Management, Inc.
Statewide 33,098 21,496 54,594
Florida Managed Medical
Assistance Program
(Comprehensive
MCO)
Amerigroup Florida,
Inc.
Anthem Insurance
Companies, Inc.
Regions 5, 6, 7, and 11 297,550 7,794 305,344
Florida Managed Medical
Assistance Program
(Comprehensive
MCO)
Better Health, Inc. Anthem Insurance
Companies, Inc.
Regions 6 and 10 90,521 2,783 93,304
Florida Managed Medical
Assistance Program
(Comprehensive
MCO)
Aetna DBA Coventry
Healthcare of FL, Inc.
Aetna Region 11 48,206 1,966 50,172
Florida Managed Medical
Assistance Program
(Comprehensive
MCO)
Humana Medical Plan Humana Regions 1, 6, 9, 10, and 11 279,019 15,400 294,419
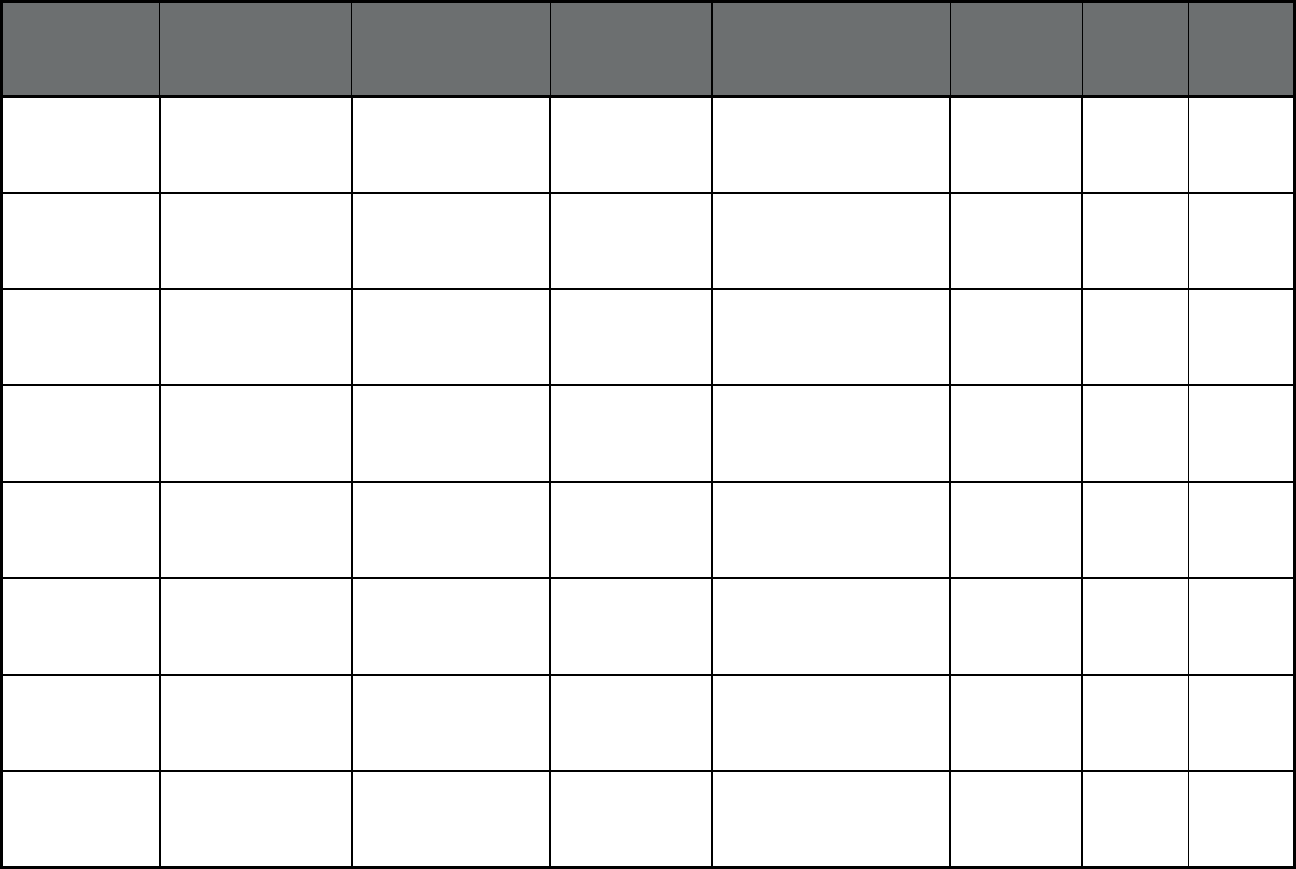
55
State
Program Name
(Type) Plan Name
Parent
Organization
Geographic Region (state-
defined areas, counties, or
zip codes)
Medicaid-Only
Enrollment
Dual
Enrollment
Total
Enrollment
Florida Managed Medical
Assistance Program
(Comprehensive
MCO)
Molina Healthcare of
Florida, Inc.
Molina Healthcare Regions 1, 4, 6, 7, 8, 9, and
11
279,019 15,400 294,419
Florida Managed Medical
Assistance Program
(Comprehensive
MCO)
Prestige Health Choice Prestige Health
Choice
Regions 2, 3, 5, 6, 7, 8, 9,
and 11
312,830 12,497 325,327
Florida Managed Medical
Assistance Program
(Comprehensive
MCO)
South Florida
Community Care
Network DBA
Community Care Plan
Community Care
Health Plan (WI)
Region 10 39,556 1,392 40,948
Florida Managed Medical
Assistance Program
(Comprehensive
MCO)
Simply Healthcare
Plans, Inc.
Anthem Insurance
Companies, Inc.
Region 11 64,436 6,823 71,259
Florida Managed Medical
Assistance Program
(Comprehensive
MCO)
Wellcare Health Plan of
Florida DBA Staywell
WellCare Regions 2, 3, 4, 5, 6, 7, 8,
and 11
615,568 18,213 633,781
Florida Managed Medical
Assistance Program
(Comprehensive
MCO)
Centene DBA Sunshine
State Health Plan, Inc.
Centene
Corporation
Regions 3, 4, 5, 6, 7, 8, 9,
10, and 11
462,503 14,259 476,762
Florida Managed Medical
Assistance Program
(Comprehensive
MCO)
United Healthcare of
Florida, Inc.
UnitedHealthcare Regions 3, 4, 7, and 11 247,869 12,803 260,672
Florida Managed Medical
Assistance Program
(Comprehensive
MCO)
AIDS Healthcare
Foundation DBA
Positive Healthcare,
Inc.
AIDS Healthcare
Foundation, Inc.
Regions 10 and 11 1,290 668 1,958
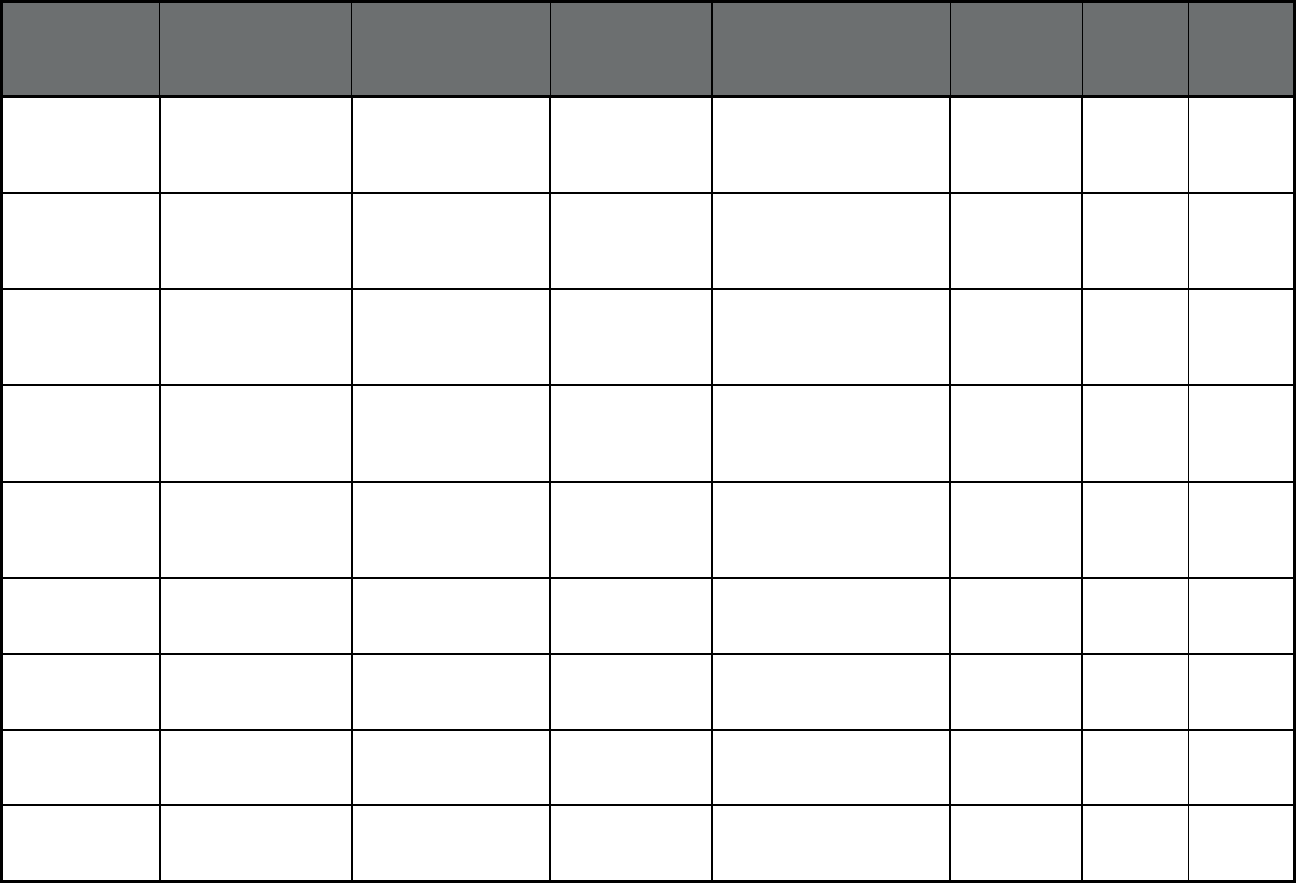
56
State
Program Name
(Type) Plan Name
Parent
Organization
Geographic Region (state-
defined areas, counties, or
zip codes)
Medicaid-Only
Enrollment
Dual
Enrollment
Total
Enrollment
Florida Managed Medical
Assistance Program
(Comprehensive
MCO)
Freedom Health, Inc. Freedom Health,
Inc.
Regions 3, 5, 6, 7, 8, 9, 10,
and 11
53 60 113
Florida Managed Medical
Assistance Program
(Comprehensive
MCO)
Magellan Complete
Care, LLC
Magellan Health Regions 2, 4, 5, 6, 7, 9, 10,
and 11
72,147 10,003 82,150
Florida Managed Medical
Assistance Program
(Comprehensive
MCO)
Simply Healthcare
Plans DBA Clear
Health Alliance
Anthem Insurance
Companies, Inc.
Regions 1, 2, 3, 5, 6, 7, 8, 9,
10, and 11
6,555 2,502 9,057
Florida Managed Medical
Assistance Program
(Comprehensive
MCO)
Sunshine State Health
Plan, Inc.
Centene
Corporation
Statewide 34,219 0 34,219
Florida Managed Medical
Assistance Program
(Comprehensive
MCO)
Children's Medical
Services
State of Florida,
Department of
Health
Statewide 52,271 141 52,412
Florida Long-term Care
Program (MLTSS only
(PIHP and/or PAHP))
Amerigroup Florida,
Inc.
Anthem Insurance
Companies, Inc.
Regions 10 and 11 512 4,857 5,369
Florida Long-term Care
Program (MLTSS only
(PIHP and/or PAHP))
Aetna DBA Coventry
Healthcare of FL, Inc.
Aetna Regions 6, 7, 9, and 11 430 4,748 5,178
Florida Long-term Care
Program (MLTSS only
(PIHP and/or PAHP))
Molina Healthcare of
FL, Inc.
Molina Healthcare Regions 5, 6, and 11 567 5,651 6,218
Florida Long-term Care
Program (MLTSS only
(PIHP and/or PAHP))
Centene DBA Sunshine
State Health Plan, Inc.
Centene
Corporation
Regions 1, 3,4, 5, 6, 7, 8, 9,
10, and 11
3,507 39,936 43,443
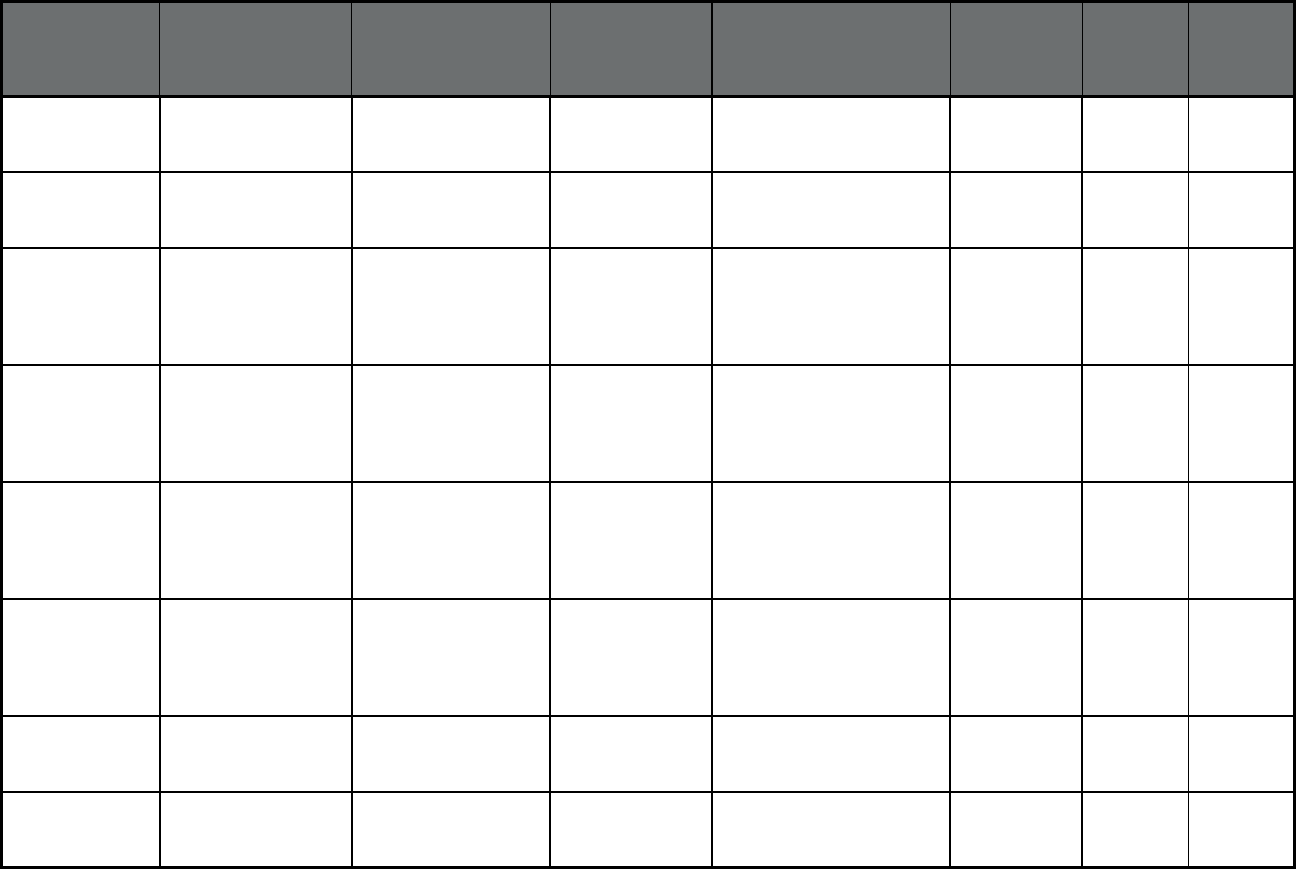
57
State
Program Name
(Type) Plan Name
Parent
Organization
Geographic Region (state-
defined areas, counties, or
zip codes)
Medicaid-Only
Enrollment
Dual
Enrollment
Total
Enrollment
Florida Long-term Care
Program (MLTSS only
(PIHP and/or PAHP))
United Healthcare of
FL, Inc.
UnitedHealthcare Regions 2, 3, 4, 5, 6, 7, 8, 9,
and 11
1,388 17,681 19,069
Florida Long-term Care
Program (MLTSS only
(PIHP and/or PAHP))
Humana Medical Plan,
Inc.
Humana Statewide 1,591 20,656 22,247
Florida Program of All-
Inclusive Care for the
Elderly (Program of
All-inclusive Care for
the Elderly (PACE))
Florida PACE Center Miami Jewish
Health
Miami-Dade County 90 651 741
Florida Program of All-
Inclusive Care for the
Elderly (Program of
All-inclusive Care for
the Elderly (PACE))
Hope Select Care Hope Healthcare Collier, Charlotte, and Lee
Counties
241 3 244
Florida Program of All-
Inclusive Care for the
Elderly (Program of
All-inclusive Care for
the Elderly (PACE))
Morselife Home Care,
Inc.
PACE Palm Beach County 386 13 399
Florida Program of All-
Inclusive Care for the
Elderly (Program of
All-inclusive Care for
the Elderly (PACE))
Suncoast Neighborly
Care, Inc.
Empath Health Pinellas County 280 15 295
Georgia Georgia Families
(Comprehensive
MCO)
Amerigroup Community
Care
Anthem Insurance
Companies, Inc.
Statewide 342,503 115 342,618
Georgia Georgia Families
(Comprehensive
MCO)
CareSource - Georgia CareSource Statewide 209,400 60 209,460
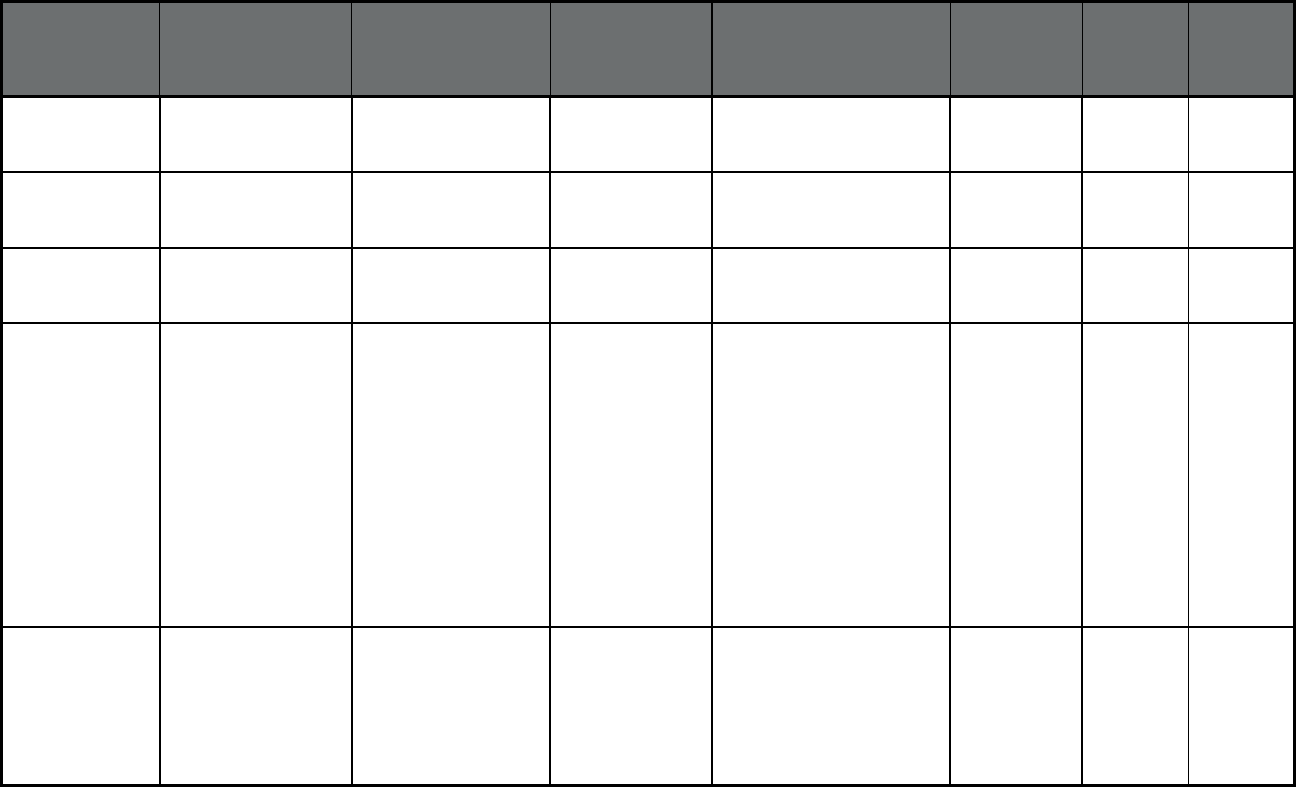
58
State
Program Name
(Type) Plan Name
Parent
Organization
Geographic Region (state-
defined areas, counties, or
zip codes)
Medicaid-Only
Enrollment
Dual
Enrollment
Total
Enrollment
Georgia Georgia Families
(Comprehensive
MCO)
Peach State Health
Plan
Centene
Corporation
Statewide 359,957 80 360,037
Georgia Georgia Families
(Comprehensive
MCO)
WellCare of Georgia WellCare Statewide 504,259 172 504,431
Georgia Georgia Families 360
(Comprehensive
MCO)
Amerigroup Anthem Insurance
Companies, Inc.
Statewide 29,258 0 29,258
Georgia
5
Non-Emergency
Medical Transportation
(NEMT) (Non-
Emergency Medical
Transportation)
Southeast Trans Southeastrans,
Inc. - Atlanta, GA
Atlanta, Georgia
30337
Banks, Barrow, Bartow,
Catoosa, Chattooga,
Cherokee, Cobb, Dade,
Dawson, Douglas, Fannin,
Floyd, Forsyth, Franklin,
Gilmer, Gordon,
Habersham, Hall, Haralson,
Jackson, Lumpkin, Morgan,
Murray, Paulding, Pickens,
Polk, Rabun, Stephens,
Towns, Union, Walker,
Walton, White, Whitfield,
Fulton, DeKalb, and
Gwinnett Counites
753,966 0 753,966
Georgia
5
Non-Emergency
Medical Transportation
(NEMT) (Non-
Emergency Medical
Transportation)
Logisticare LogistiCare Baldwin, Bibb, Bleckley,
Butts, Carroll, Clayton,
Coweta, Dodge, Fayette,
Heard, Henry, Jasper,
Jones, Lamar, Laurens,
Meriwether, Monroe,
Newton, Pike, Putnam,
869,286 0 869,286
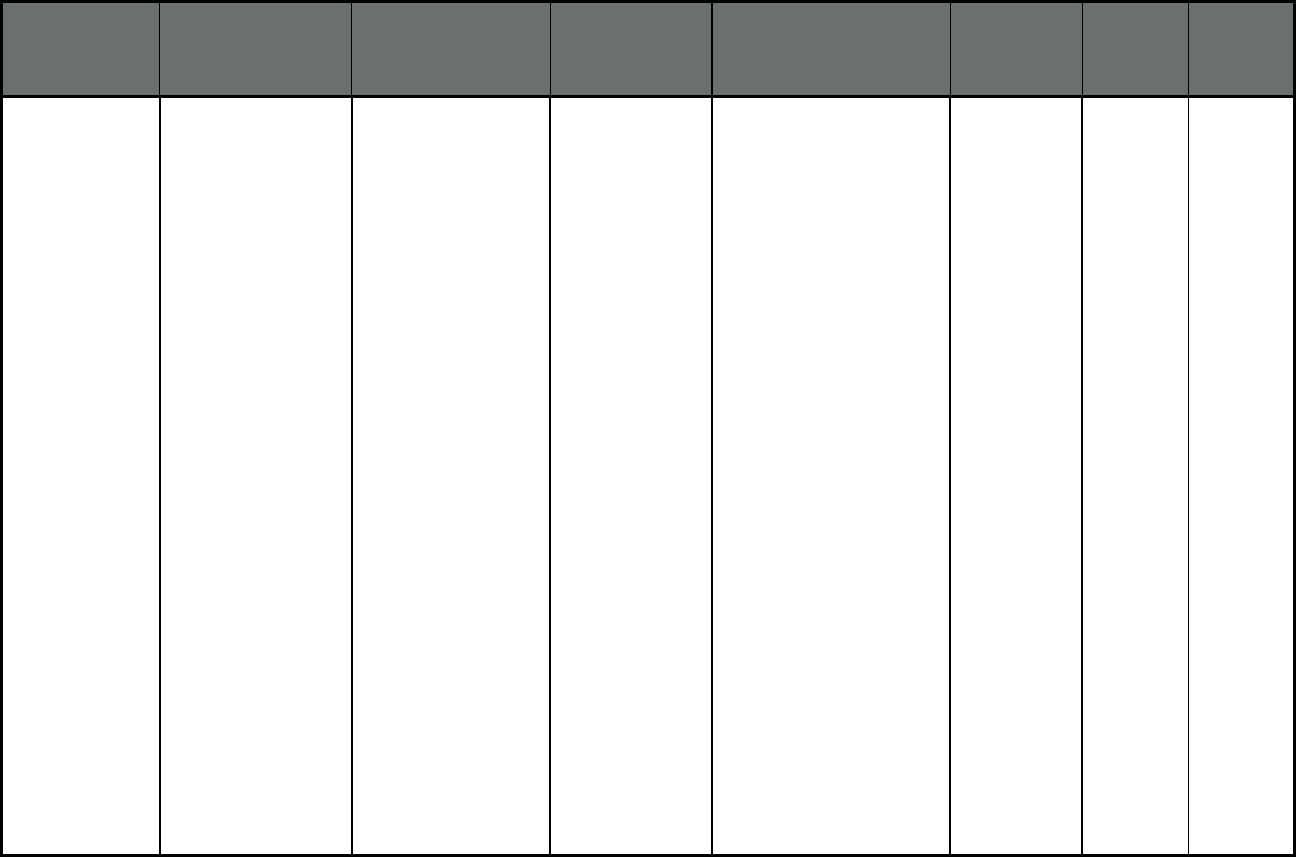
59
State
Program Name
(Type) Plan Name
Parent
Organization
Geographic Region (state-
defined areas, counties, or
zip codes)
Medicaid-Only
Enrollment
Dual
Enrollment
Total
Enrollment
Georgia
5
(cont
)
Non-Emergency
Medical Transportation
(NEMT) (Non-
Emergency Medical
Transportation)
Logisticare LogistiCare Rockdale, Spalding, Telfair,
Troup, Twiggs, Wilkinson,
Appling, Bacon, Brantley,
Bryan, Bulloch, Burke,
Camden, Candler, Charlton,
Chatham, Clarke, Columbia,
Effingham, Elbert, Emanuel,
Evans, Glascock, Glynn,
Greene, Hancock, Hart, Jeff
Davis, Jefferson, Jenkins,
Johnson, Liberty, Lincoln,
Long, Madison, McDuffie,
McIntosh, Montgomery,
Oconee, Oglethorpe
, Pierce,
Richmond, Screven,
Taliaferro, Tattnall, Toombs,
Treutlen, Ware, Warren,
Washington, Wayne,
Wheeler, Wilkes, Atkinson,
Baker, Ben Hill, Berrien,
Brooks, Calhoun,
Chattahoochee, Clay,
Clinch, Coffee, Colquitt,
Cook, Crawford, Crisp,
Decatur, Dooly, Dougherty,
Early, Echols, Grady, Harris,
Houston, Irwin, Lanier, Lee,
Lowndes, Macon, Marion,
Miller, Mitchell, Muscogee,
Peach, Pulaski, Quitman,
Randolph, Schley,
Seminole, Stewart, Sumter,
Talbot, Taylor, Terrell,
Thomas, Tift, Turner,
Upson, Webster, Wilcox,
and Worth Counties
869,286 0 869,286
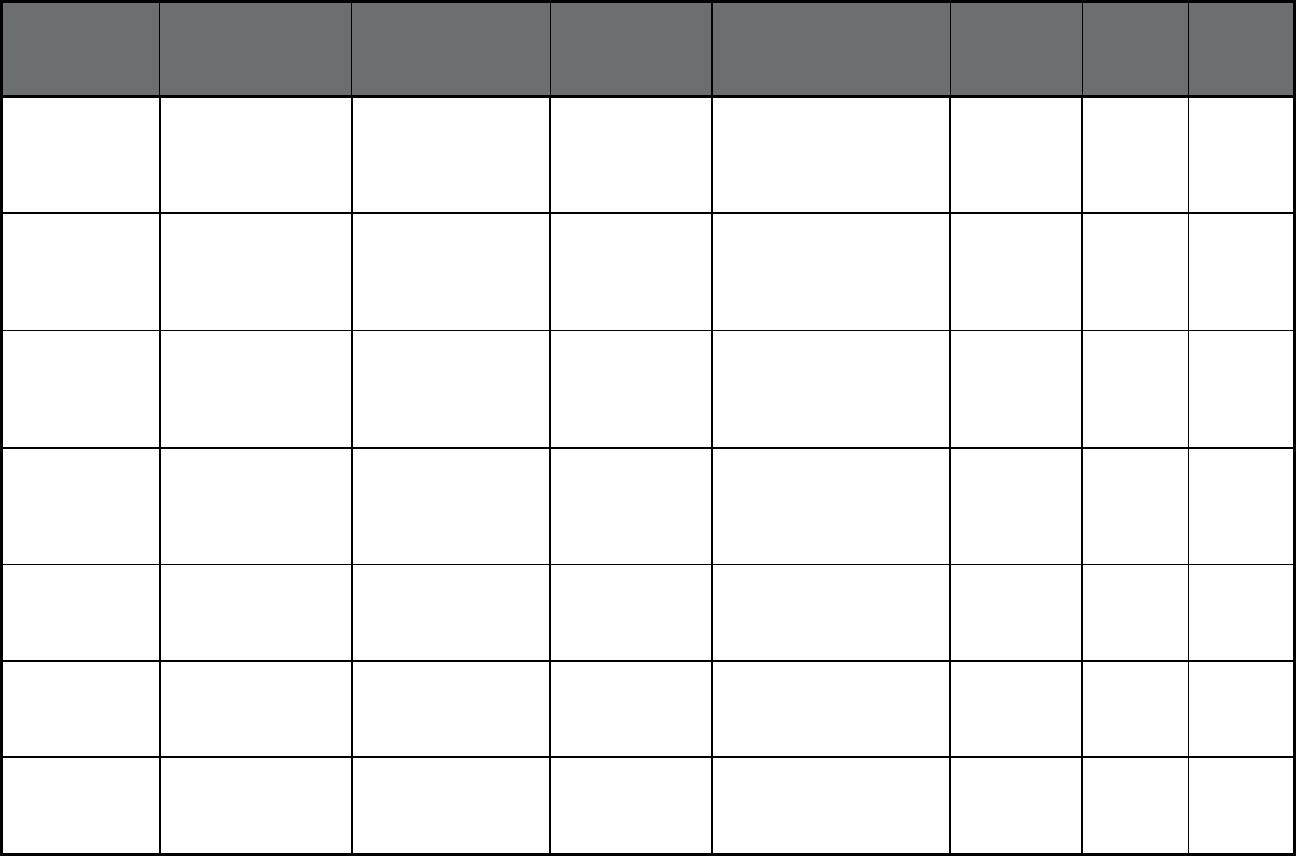
60
State
Program Name
(Type) Plan Name
Parent
Organization
Geographic Region (state-
defined areas, counties, or
zip codes)
Medicaid-Only
Enrollment
Dual
Enrollment
Total
Enrollment
Georgia Planning for Healthy
Babies (P4HB) (Other
Prepaid Health Plan
(PHP) (limited
benefits))
Amerigroup Anthem Insurance
Companies, Inc.
Statewide 10,556 0 10,556
Georgia Planning for Healthy
Babies (P4HB) (Other
Prepaid Health Plan
(PHP) (limited
benefits))
CareSource- Georgia CareSource Statewide 7,458 0 7,458
Georgia Planning for Healthy
Babies (P4HB) (Other
Prepaid Health Plan
(PHP) (limited
benefits))
Peach State Health
Plan
Centene
Corporation
Statewide 10,734 0 10,734
Georgia Planning for Healthy
Babies (P4HB) (Other
Prepaid Health Plan
(PHP) (limited
benefits))
WellCare of Georgia WellCare Statewide 10,698 0 10,698
Hawaii
6
Hawaii QUEST
Integration
(Comprehensive MCO
+ MLTSS)
AlohaCare QUEST AlohaCare Statewide 62,174 34 62,208
Hawaii
6
Hawaii QUEST
Integration
(Comprehensive MCO
+ MLTSS)
Hawaii Medical Service
Association (HMSA)
QUEST
HMSA Statewide 157,990 97 158,087
Hawaii
6
Hawaii QUEST
Integration
(Comprehensive MCO
+ MLTSS)
Kaiser Permanente
QUEST
Kaiser
Permanente
Oahu and Maui 29,268 20 29,288
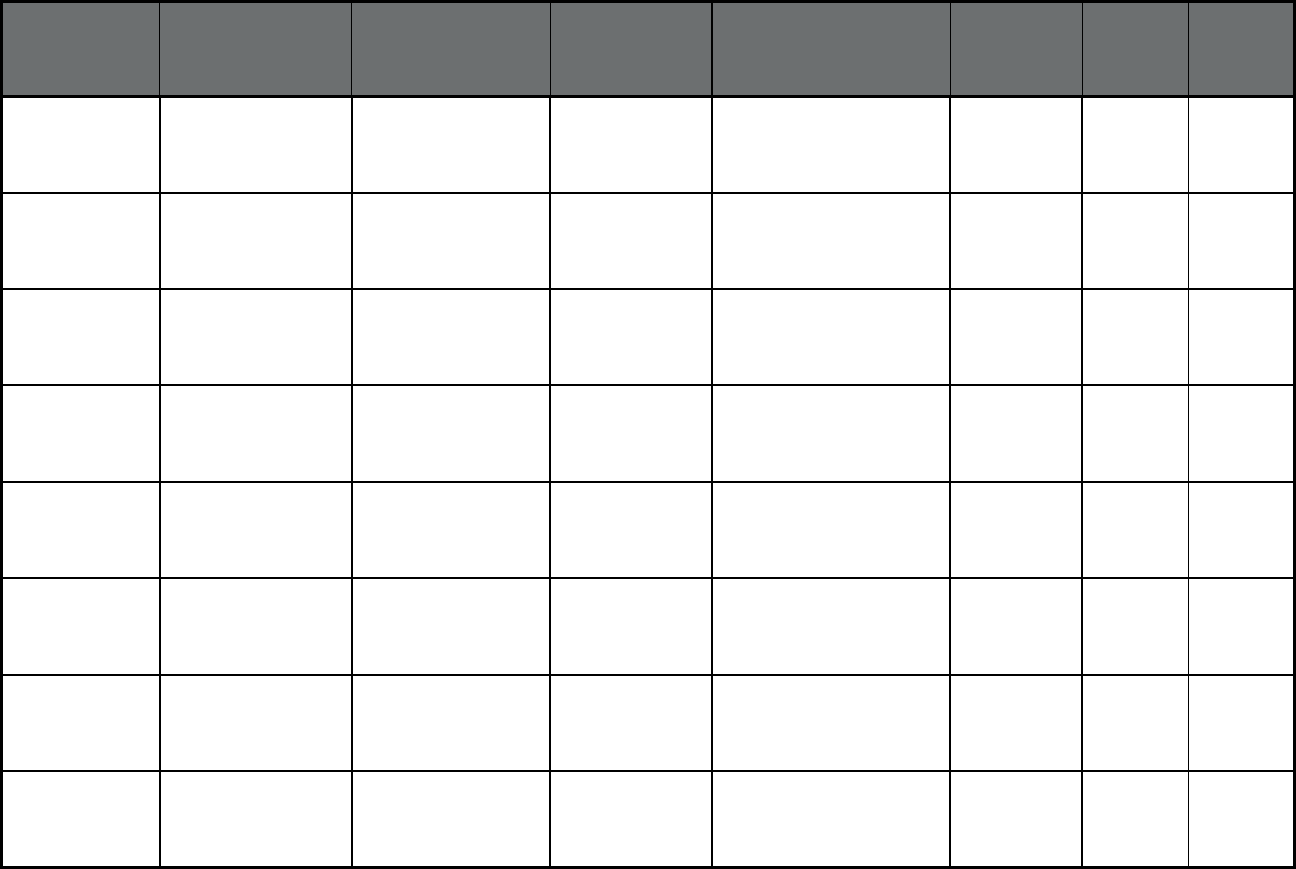
61
State
Program Name
(Type) Plan Name
Parent
Organization
Geographic Region (state-
defined areas, counties, or
zip codes)
Medicaid-Only
Enrollment
Dual
Enrollment
Total
Enrollment
Hawaii
6
Hawaii QUEST
Integration
(Comprehensive MCO
+ MLTSS)
Ohana Health Plan
QUEST
WellCare Statewide 22,235 40 22,275
Hawaii
6
Hawaii QUEST
Integration
(Comprehensive MCO
+ MLTSS)
UnitedHealthcare
Community Plan
QUEST
UnitedHealthcare Statewide 27,666 33 27,699
Hawaii
6
Hawaii QUEST
Integration
(Comprehensive MCO
+ MLTSS)
AlohaCare ABD AlohaCare Statewide 2,712 2,958 5,670
Hawaii
6
Hawaii QUEST
Integration
(Comprehensive MCO
+ MLTSS)
HMSA ABD HMSA Statewide 4,386 4,575 8,961
Hawaii
6
Hawaii QUEST
Integration
(Comprehensive MCO
+ MLTSS)
Kaiser ABD Kaiser
Permanente
Oahu and Maui 774 1,030 1,804
Hawaii
6
Hawaii QUEST
Integration
(Comprehensive MCO
+ MLTSS)
Ohana ABD WellCare Statewide 6,418 10,864 17,282
Hawaii
6
Hawaii QUEST
Integration
(Comprehensive MCO
+ MLTSS)
UnitedHealth ABD UnitedHealthcare Statewide 5,724 14,945 20,669
Hawaii
6
Hawaii QUEST
Integration
(Comprehensive MCO
+ MLTSS)
Ohana Community
Care Service (BHS)
WellCare Statewide 4,470 0 4,470
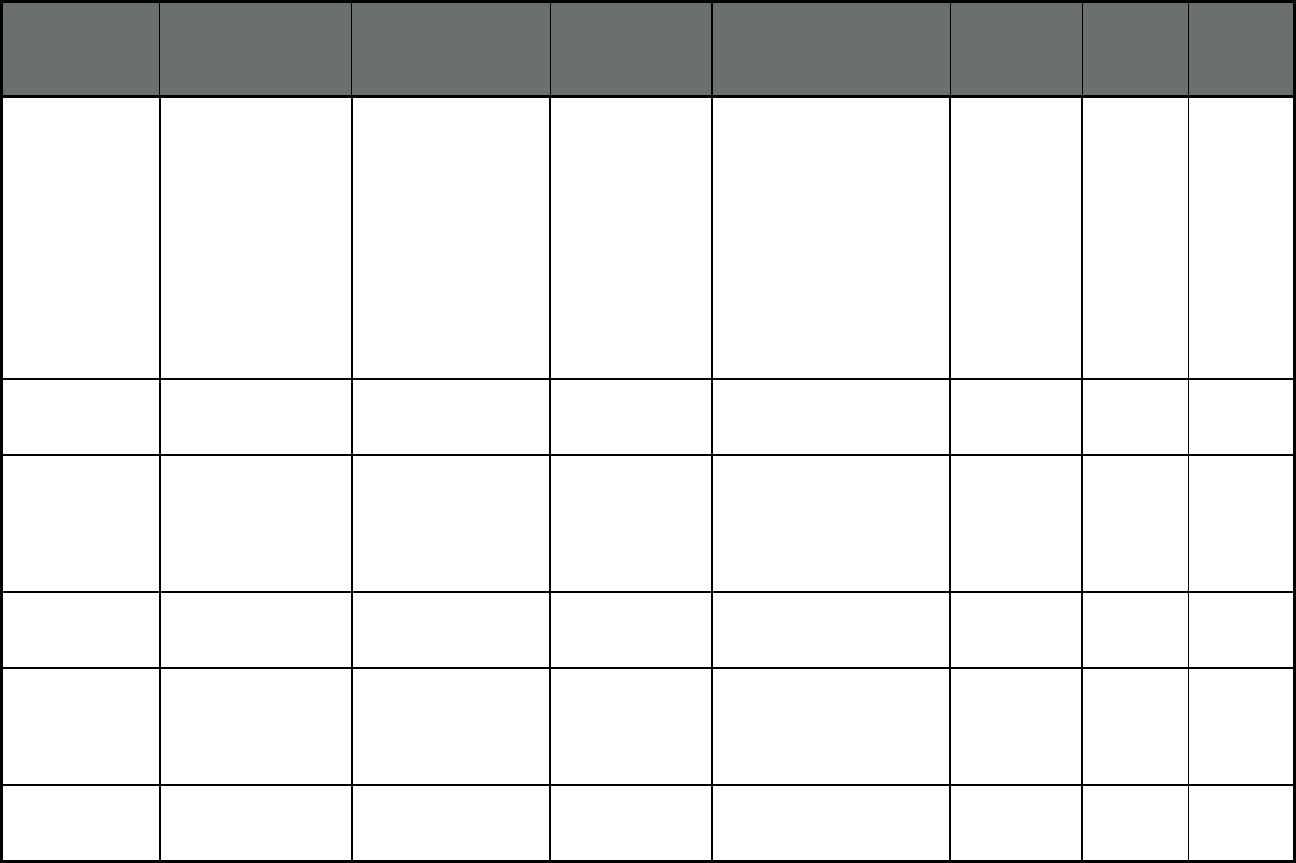
62
State
Program Name
(Type) Plan Name
Parent
Organization
Geographic Region (state-
defined areas, counties, or
zip codes)
Medicaid-Only
Enrollment
Dual
Enrollment
Total
Enrollment
Idaho Medicare/Medicaid
Coordinated Plan
(Comprehensive MCO
+ MLTSS)
Medicare/Medicaid
Coordinated Plan
Molina Healthcare Ada, Bannock, Bingham,
Bonner, Bonneville, Canyon,
Kootenai, Nez Perce, and
Twin Falls Counties. Blue
Cross of Idaho administers
the MMCP in additional
Idaho counties, including
Boise, Boundary, Cassia,
Clark, Elmore,
Fremont, Gem, Jefferson,
Madison, Minidoka,
Owyhee, Payette, and
Power Counties.
0 3,799 3,799
Idaho Healthy Connections
(Primary Care Case
Management (PCCM))
Healthy Connections Healthy
Connections
Statewide 235,469 19,322 254,791
Idaho Idaho Behavioral
Health Plan
(Behavioral Health
Organization (BHO)
only (PIHP and/or
PAHP))
Idaho Behavioral
Health Plan
UnitedHealthcare Statewide 245,815 23,425 269,240
Idaho Idaho Smiles (Dental
only (PAHP))
Idaho Smiles Managed Care of
North America
(MCNA), Inc.
Statewide 245,739 27,240 272,979
Idaho Non-Emergency
Medical Transportation
(Non-Emergency
Medical
Transportation)
Non-Emergency
Medical Transportation
Medical
Transportation
Management, Inc.
Statewide 245,739 27,240 272,979
Illinois HealthChoice Illinois
(Comprehensive MCO
+ MLTSS)
Blue Cross Blue Shield
of Illinois
Health Care
Service
Corporation
Statewide 414,925 0 414,925
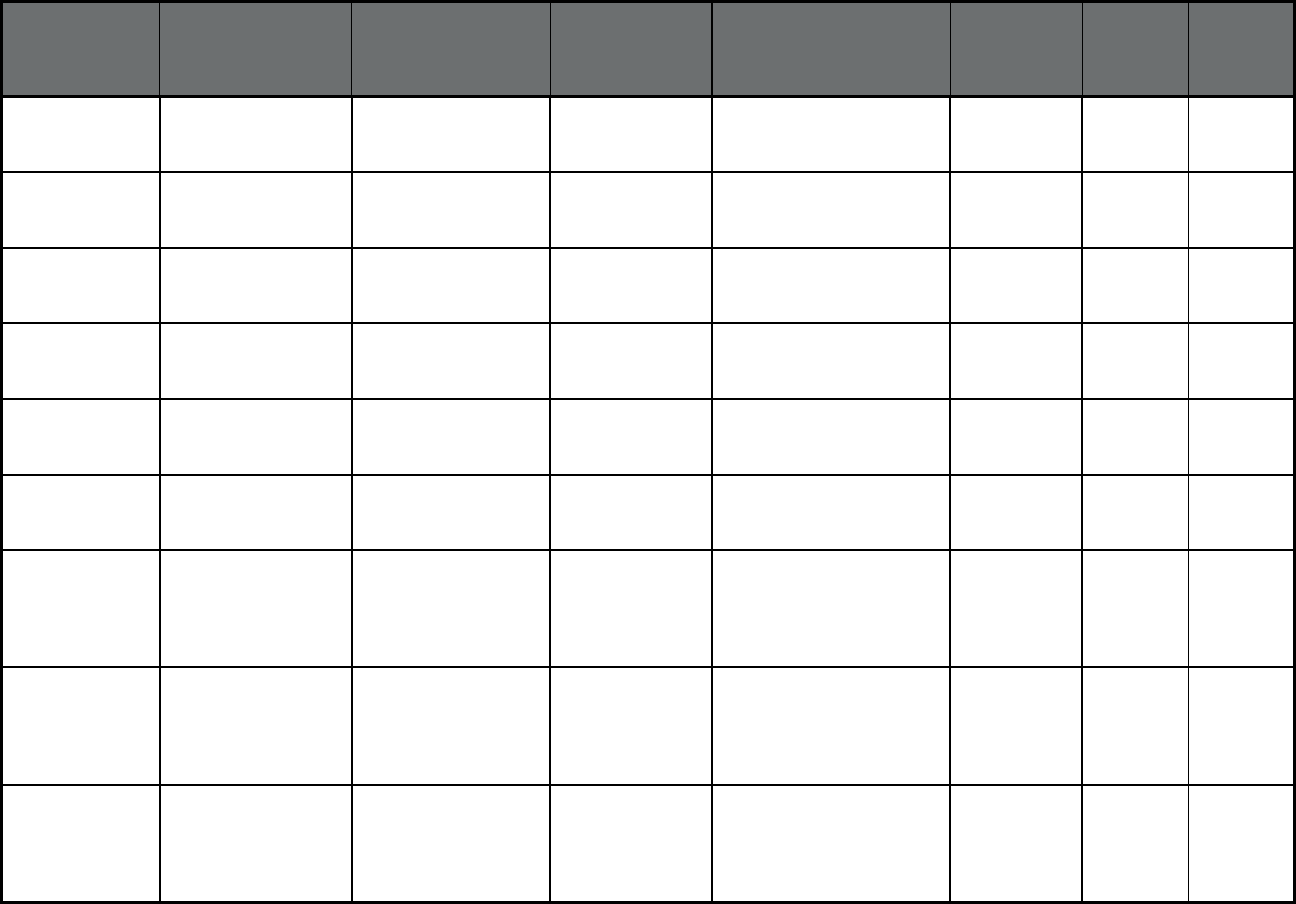
63
State
Program Name
(Type) Plan Name
Parent
Organization
Geographic Region (state-
defined areas, counties, or
zip codes)
Medicaid-Only
Enrollment
Dual
Enrollment
Total
Enrollment
Illinois HealthChoice Illinois
(Comprehensive MCO
+ MLTSS)
CountyCare Cook County
Health and
Hospitals System
Cook County 321,345 0 321,345
Illinois HealthChoice Illinois
(Comprehensive MCO
+ MLTSS)
IlliniCare Health Plan Centene
Corporation
Statewide 317,402 0 317,402
Illinois HealthChoice Illinois
(Comprehensive MCO
+ MLTSS)
Meridian Health Plan WellCare Statewide 572,164 0 572,164
Illinois HealthChoice Illinois
(Comprehensive MCO
+ MLTSS)
Molina Healthcare of
Illinois
Molina Healthcare Statewide 212,613 0 212,613
Illinois HealthChoice Illinois
(Comprehensive MCO
+ MLTSS)
NextLevel Health
Partners
NextLevel Health
Partners
Cook County 56,702 0 56,702
Illinois HealthChoice Illinois
(Comprehensive MCO
+ MLTSS)
Harmony Health Plan WellCare Statewide 250,609 0 250,609
Illinois HealthChoice Illinois -
Managed Long-Term
Services and Supports
(MLTSS only (PIHP
and/or PAHP))
Blue Cross Blue Shield
of Illinois
Health Care
Service
Corporation
Cook, DuPage, Kane,
Kankakee, Lake and Will
Counties
0 9,878 9,878
Illinois HealthChoice Illinois -
Managed Long-Term
Services and Supports
(MLTSS only (PIHP
and/or PAHP))
CountyCare Cook County
Health and
Hospitals System
Cook County 0 5,355 5,355
Illinois HealthChoice Illinois -
Managed Long-Term
Services and Supports
(MLTSS only (PIHP
and/or PAHP))
Harmony Health Plan WellCare Cook, DuPage, Kane,
Kankakee, Lake and Will
Counties
0 1,180 1,180
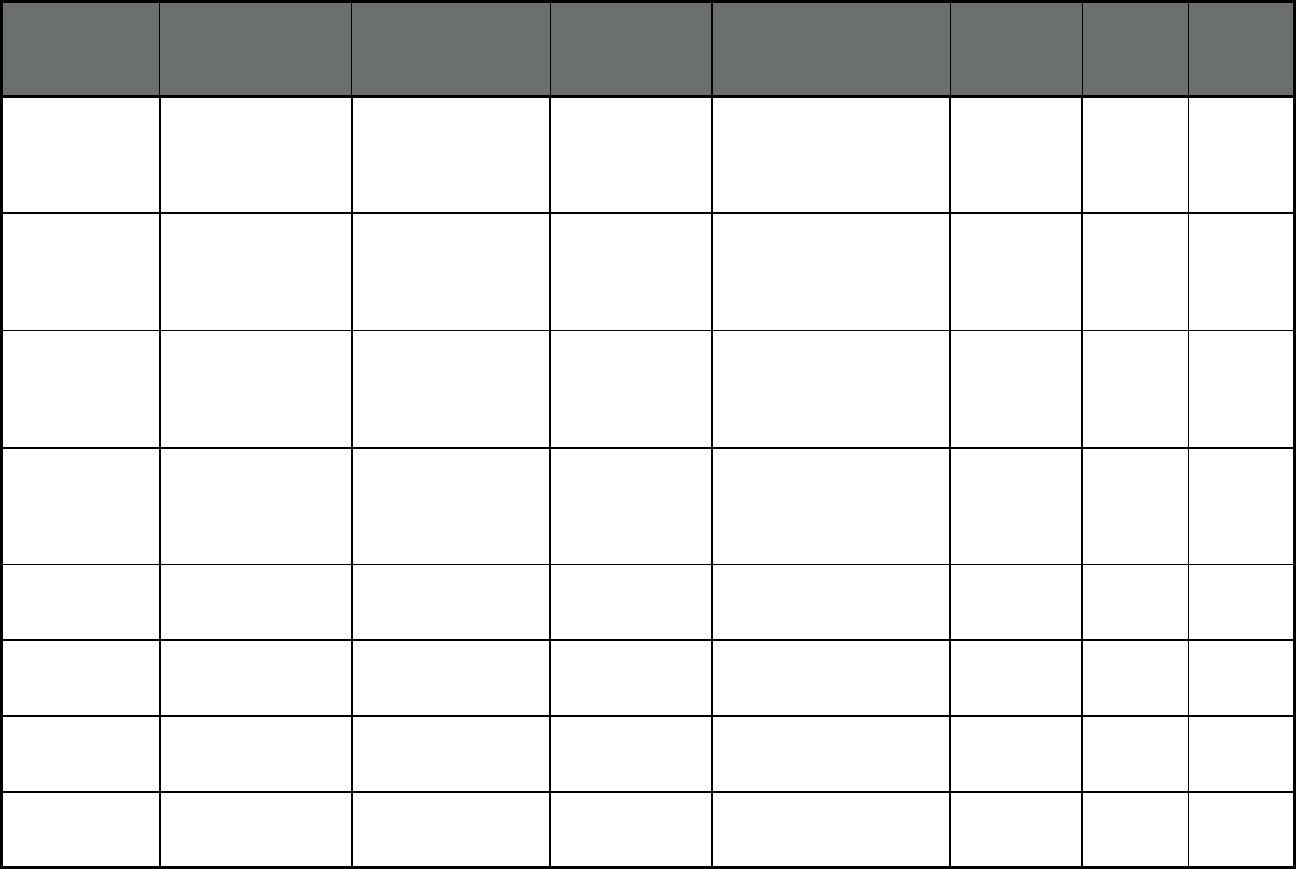
64
State
Program Name
(Type) Plan Name
Parent
Organization
Geographic Region (state-
defined areas, counties, or
zip codes)
Medicaid-Only
Enrollment
Dual
Enrollment
Total
Enrollment
Illinois HealthChoice Illinois -
Managed Long-Term
Services and Supports
(MLTSS only (PIHP
and/or PAHP))
IlliniCare Health Plan Centene
Corporation
Cook, DuPage, Kane,
Kankakee, Lake and Will
Counties
0 7,012 7,012
Illinois HealthChoice Illinois -
Managed Long-Term
Services and Supports
(MLTSS only (PIHP
and/or PAHP))
Meridian Health Plan WellCare Cook, DuPage, Kane,
Kankakee, Lake and Will
Counties
0 6,849 6,849
Illinois HealthChoice Illinois -
Managed Long-Term
Services and Supports
(MLTSS only (PIHP
and/or PAHP))
Molina Healthcare of
Illinois
Molina Healthcare Cook, DuPage, Kane,
Kankakee, Lake and Will
Counties
0 579 579
Illinois HealthChoice Illinois -
Managed Long-Term
Services and Supports
(MLTSS only (PIHP
and/or PAHP))
NextLevel Health
Partners
NextLevel Health
Partners
Cook County 0 290 290
Indiana Hoosier Care Connect
(Comprehensive
MCO)
Anthem Anthem Insurance
Companies, Inc.
Statewide 56,491 302 56,793
Indiana Hoosier Care Connect
(Comprehensive
MCO)
Managed Health
Services of Indiana
Cenete
Corporation
Statewide 34,059 138 34,197
Indiana Hoosier Healthwise
(Comprehensive
MCO)
Anthem Anthem Insurance
Companies, Inc.
Statewide 207,717 1 207,718
Indiana Hoosier Healthwise
(Comprehensive
MCO)
Caresource Indiana,
Inc
CareSource Statewide 61,413 1 61,414
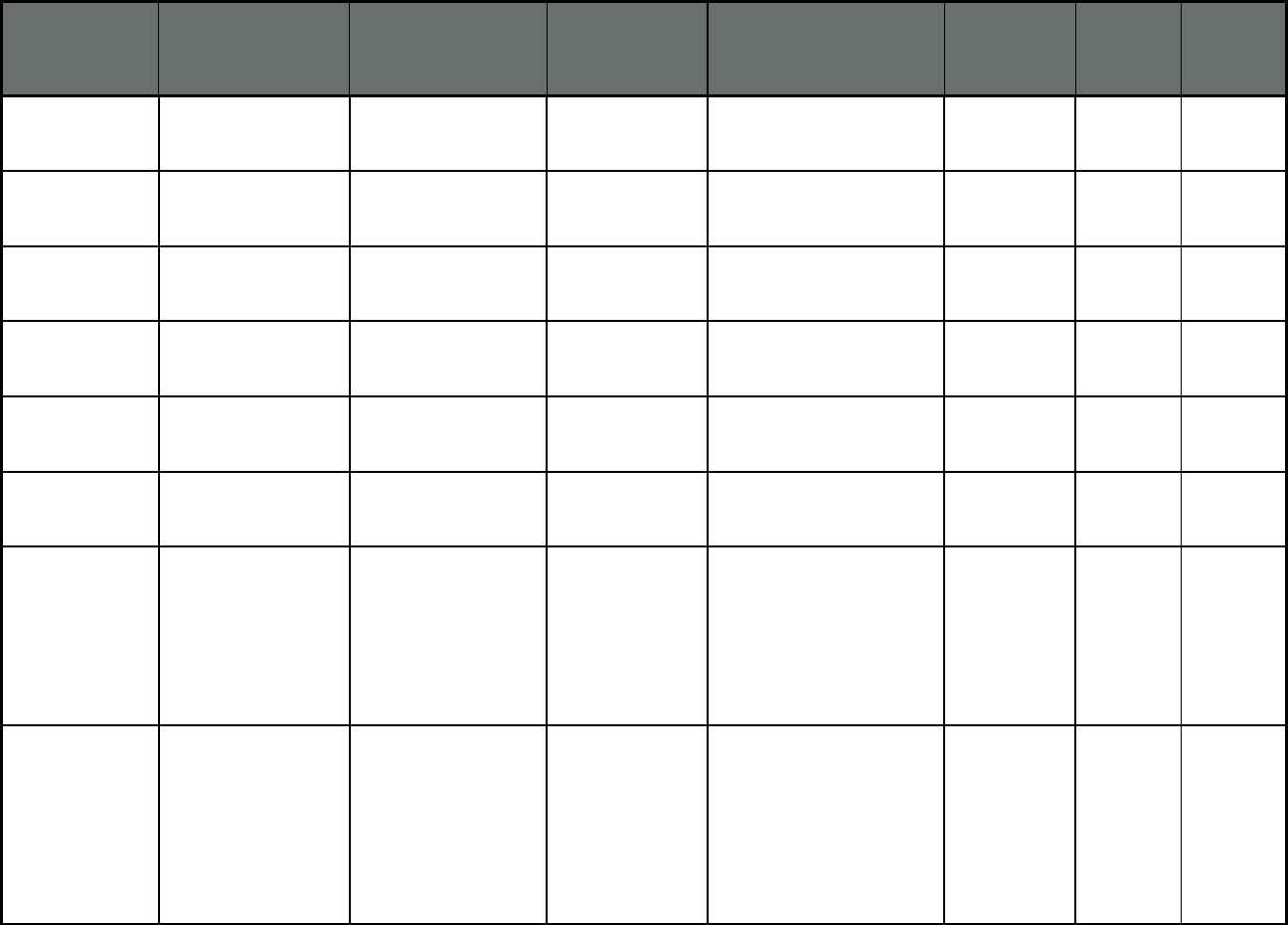
65
State
Program Name
(Type) Plan Name
Parent
Organization
Geographic Region (state-
defined areas, counties, or
zip codes)
Medicaid-Only
Enrollment
Dual
Enrollment
Total
Enrollment
Indiana Hoosier Healthwise
(Comprehensive
MCO)
Managed Health
Services of Indiana
Centene
Corporation
Statewide 150,441 2 150,443
Indiana Hoosier Healthwise
(Comprehensive
MCO)
MDWise McLaren Health
Plan
Statewide 213,253 0 213,253
Indiana Healthy Indiana Plan
(2.0) (Comprehensive
MCO)
Anthem Anthem Insurance
Companies, Inc.
Statewide 174,341 1,680 176,021
Indiana Healthy Indiana Plan
(2.0) (Comprehensive
MCO)
Caresource Indiana,
Inc
CareSource Statewide 44,850 216 45,066
Indiana Healthy Indiana Plan
(2.0) (Comprehensive
MCO)
Managed Health
Services of Indiana
Centene
Corporation
Statewide 70,153 644 70,797
Indiana Healthy Indiana Plan
(2.0) (Comprehensive
MCO)
MDWise McLaren Health
Plan
Statewide 109,439 992 110,431
Indiana PACE (Program of All-
inclusive Care for the
Elderly (PACE))
Franciscan Senior
Health and Wellness
PACE Lake and Johnson Counties,
and the following zip codes:
46107, 46201, 46202,
46203, 46204, 46217,
46218, 46219, 46221,
46222, 46225, 46227,
46229, 46237, 46239,
46241, 46259
3 173 176
Indiana PACE (Program of All-
inclusive Care for the
Elderly (PACE))
Saint Joseph PACE PACE 46506, 46514, 46516,
46517, 46526, 46530,
46536, 46544, 46545,
46552, 46554, 46556,
46561, 46574, 46601,
46613, 46614, 46615,
46616, 46617, 46619,
46628, 46635, 46637,
46563, 46573
6 110 116
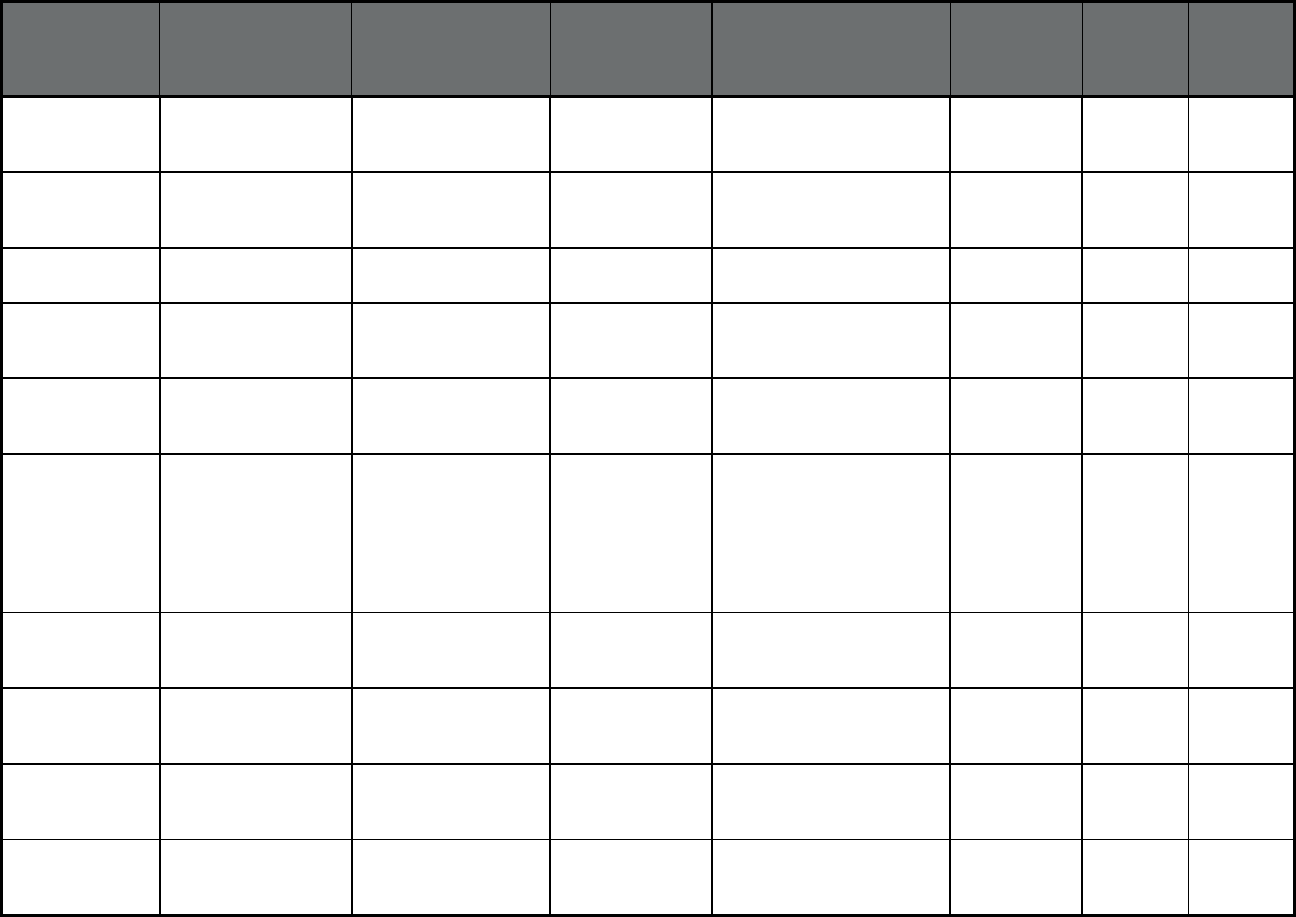
66
State
Program Name
(Type) Plan Name
Parent
Organization
Geographic Region (state-
defined areas, counties, or
zip codes)
Medicaid-Only
Enrollment
Dual
Enrollment
Total
Enrollment
Iowa IA Healthlink
(Comprehensive MCO
+ MLTSS)
UnitedHealthcare UnitedHealthcare Statewide 344,032 40,156 384,188
Iowa IA Healthlink
(Comprehensive MCO
+ MLTSS)
Amerigroup of Iowa,
Inc.
Amerigroup, Inc. Statewide 161,970 18,334 180,304
Iowa Dental Wellness Plan
(Dental only (PAHP))
Delta Dental of Iowa Delta Dental Statewide 169,173 38,695 207,868
Iowa Dental Wellness Plan
(Dental only (PAHP))
MCNA Dental Plans,
Inc.
Managed Care of
North America,
Inc.
Statewide 74,961 19,852 94,813
Iowa NEMT (Non-
Emergency Medical
Transportation)
Access2Care, LLC Mission Care
Services, LLC
Statewide 14,306 1,275 15,581
Iowa PACE (Program of All-
inclusive Care for the
Elderly (PACE))
PACE PACE Harrison, Mills,
Pottawattamie, Cherokee,
Monona, Plymouth,
Woodbury, Boone, Dallas,
Jasper, Marshall, Madison,
Marion, Polk, Story, and
Warren Counties
25 409 434
Kansas KanCare
(Comprehensive MCO
+ MLTSS)
Amerigroup Kansas,
Inc.
Anthem Insurance
Companies, Inc.
Statewide 102,427 12,182 114,609
Kansas KanCare
(Comprehensive MCO
+ MLTSS)
Sunflower State Health
Plan
Centene
Corporation
Statewide 104,857 13,655 118,512
Kansas KanCare
(Comprehensive MCO
+ MLTSS)
United HealthCare
Community Plan of
Kansas
UnitedHealthcare Statewide 111,705 12,857 124,562
Kansas PACE (Program of All-
inclusive Care for the
Elderly (PACE))
Via Christi PACE Sedgwick County 225 0 225
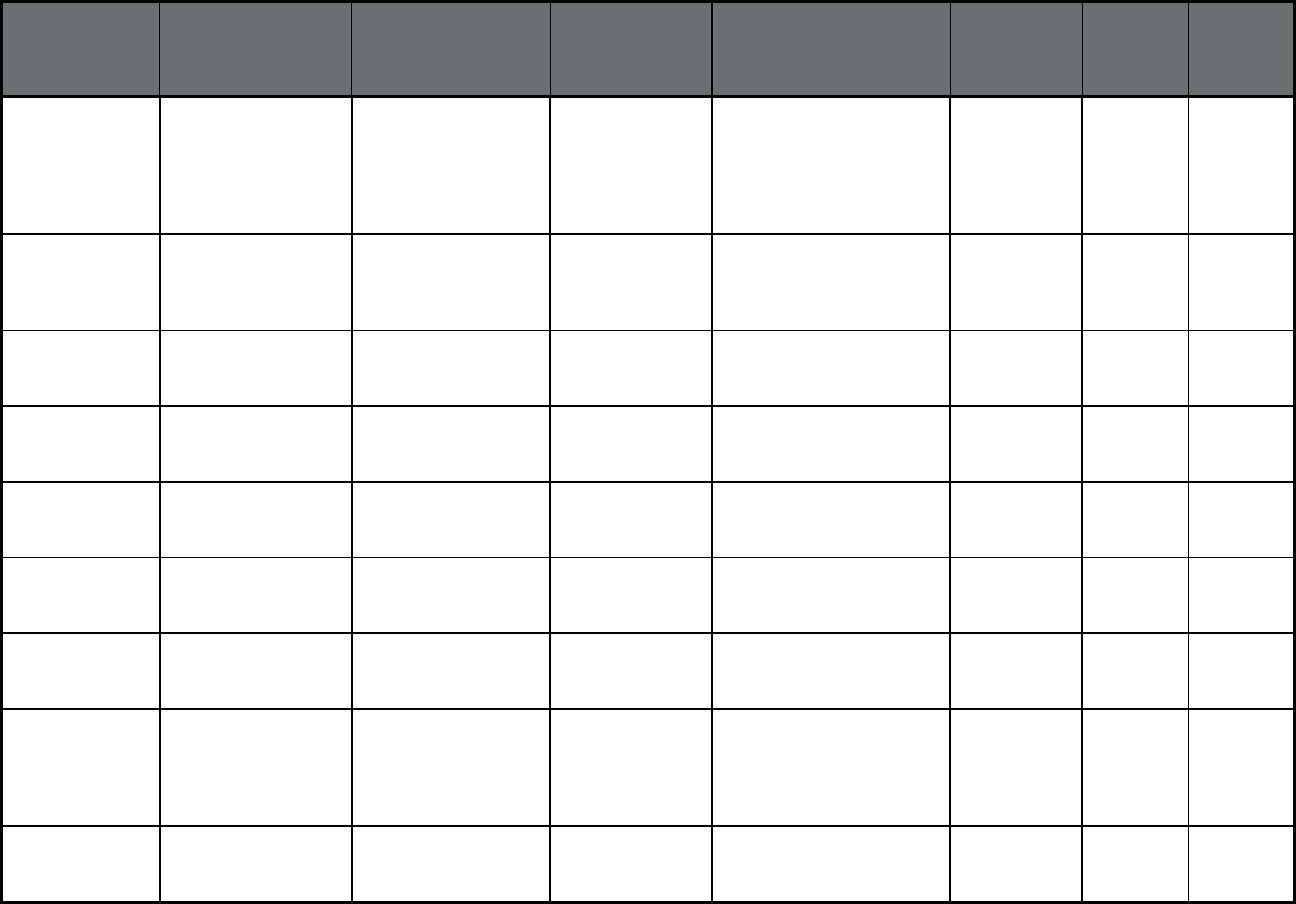
67
State
Program Name
(Type) Plan Name
Parent
Organization
Geographic Region (state-
defined areas, counties, or
zip codes)
Medicaid-Only
Enrollment
Dual
Enrollment
Total
Enrollment
Kansas PACE (Program of All-
inclusive Care for the
Elderly (PACE))
Midland Care PACE Douglas, Jackson,
Jefferson, Leavenworth,
Lyon, Marshall, Nemaha,
Osage, Shawnee,
Pottawatomie, Wabaunsee
and Wyandotte Counties
264 0 264
Kansas PACE (Program of All-
inclusive Care for the
Elderly (PACE))
Bluestem Pace, Inc. PACE McPherson, Ottawa,
Lincoln, Ellsworth, Saline,
Dickinson, Rice, Marion,
Reno and Harvey Counties
53 0 53
Kentucky Kentucky Managed
Care (Comprehensive
MCO)
Aetna Better Health of
Kentucky
Aetna Statewide 208,336 15,540 223,876
Kentucky Kentucky Managed
Care (Comprehensive
MCO)
Anthem Blue Cross
Blue Shield Medicaid
Anthem BCBS Statewide 126,166 3,591 129,757
Kentucky Kentucky Managed
Care (Comprehensive
MCO)
Humana-Caresource Humana Statewide 143,126 4,728 147,854
Kentucky Kentucky Managed
Care (Comprehensive
MCO)
Passport Health Plan Passport Health
Plan
Statewide 301,394 10,322 311,716
Kentucky Kentucky Managed
Care (Comprehensive
MCO)
WellCare of Kentucky WellCare Statewide 424,585 21,737 446,322
Kentucky Kentucky Non-
Emergency Medical
Transportation (Non-
Emergency Medical
Transportation)
NEMT - Human
Services Transportation
Delivery
NEMT - Human
Services
Transportation
Delivery
Statewide 1,232,903 0 1,232,903
Louisiana Healthy Louisiana
(Comprehensive
MCO)
Aetna Better Health Aetna Statewide 96,417 97 96,514
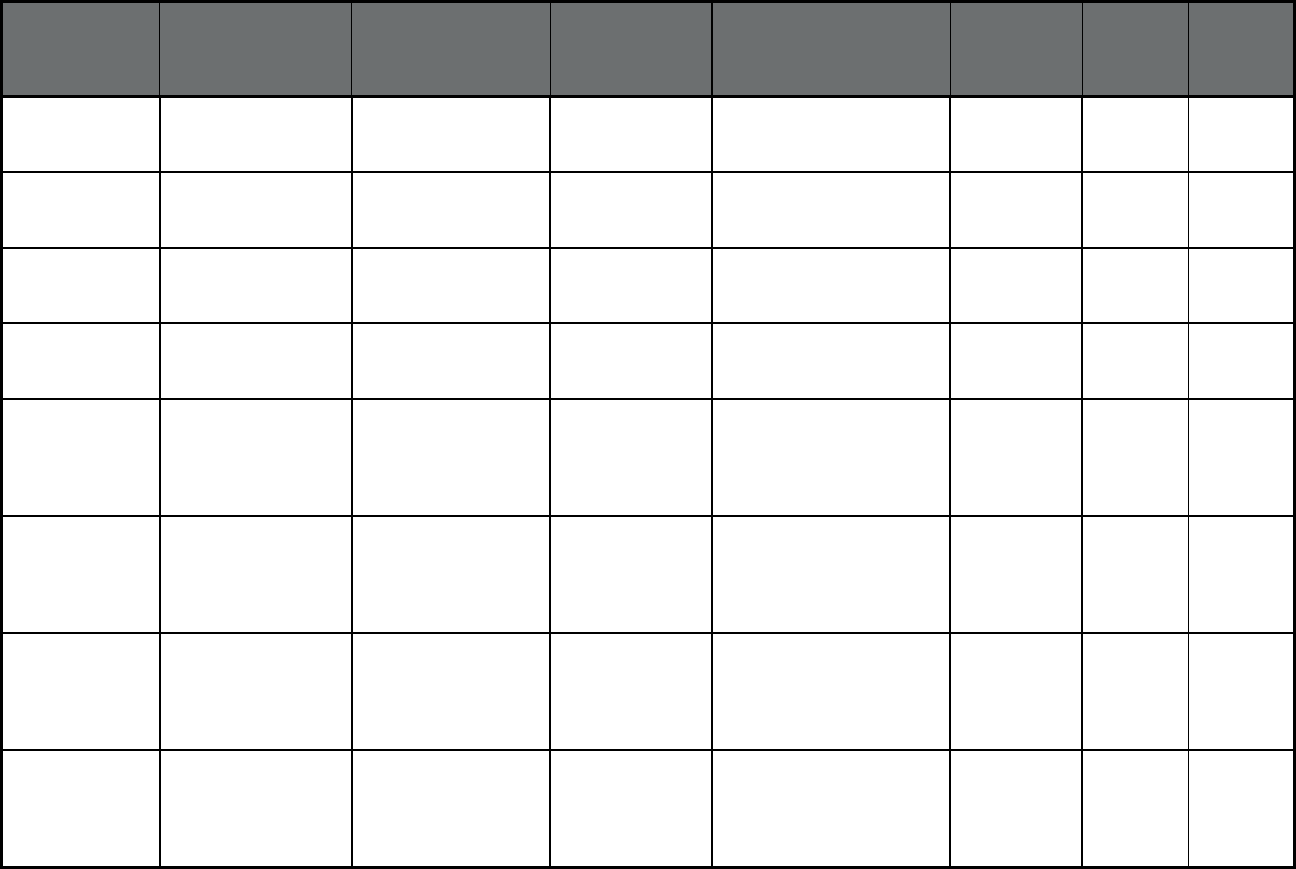
68
State
Program Name
(Type) Plan Name
Parent
Organization
Geographic Region (state-
defined areas, counties, or
zip codes)
Medicaid-Only
Enrollment
Dual
Enrollment
Total
Enrollment
Louisiana Healthy Louisiana
(Comprehensive
MCO)
AmeriHealth Caritas of
Louisiana
AmeriHealth Statewide 189,098 109 189,207
Louisiana Healthy Louisiana
(Comprehensive
MCO)
Healthy Blue Anthem Insurance
Companies, Inc.
Statewide 233,157 105 233,262
Louisiana Healthy Louisiana
(Comprehensive
MCO)
Louisiana Healthcare
Connections
Centene
Corporation
Statewide 450,896 191 451,087
Louisiana Healthy Louisiana
(Comprehensive
MCO)
UnitedHealthcare
Community Plan
UnitedHealthcare Statewide 414,548 166 414,714
Louisiana Healthy Louisiana
BHO (Behavioral
Health Organization
(BHO) only (PIHP
and/or PAHP))
Aetna Better Health Aetna Statewide 1,957 19,019 20,976
Louisiana Healthy Louisiana
BHO (Behavioral
Health Organization
(BHO) only (PIHP
and/or PAHP))
AmeriHealth Caritas of
Louisiana
AmeriHealth Statewide 2,025 18,576 20,601
Louisiana Healthy Louisiana
BHO (Behavioral
Health Organization
(BHO) only (PIHP
and/or PAHP))
Healthy Blue Anthem Insurance
Companies, Inc.
Statewide 2,325 19,355 21,680
Louisiana Healthy Louisiana
BHO (Behavioral
Health Organization
(BHO) only (PIHP
and/or PAHP))
Louisiana Healthcare
Connections
Centene
Corporation
Statewide 2,902 22,876 25,778
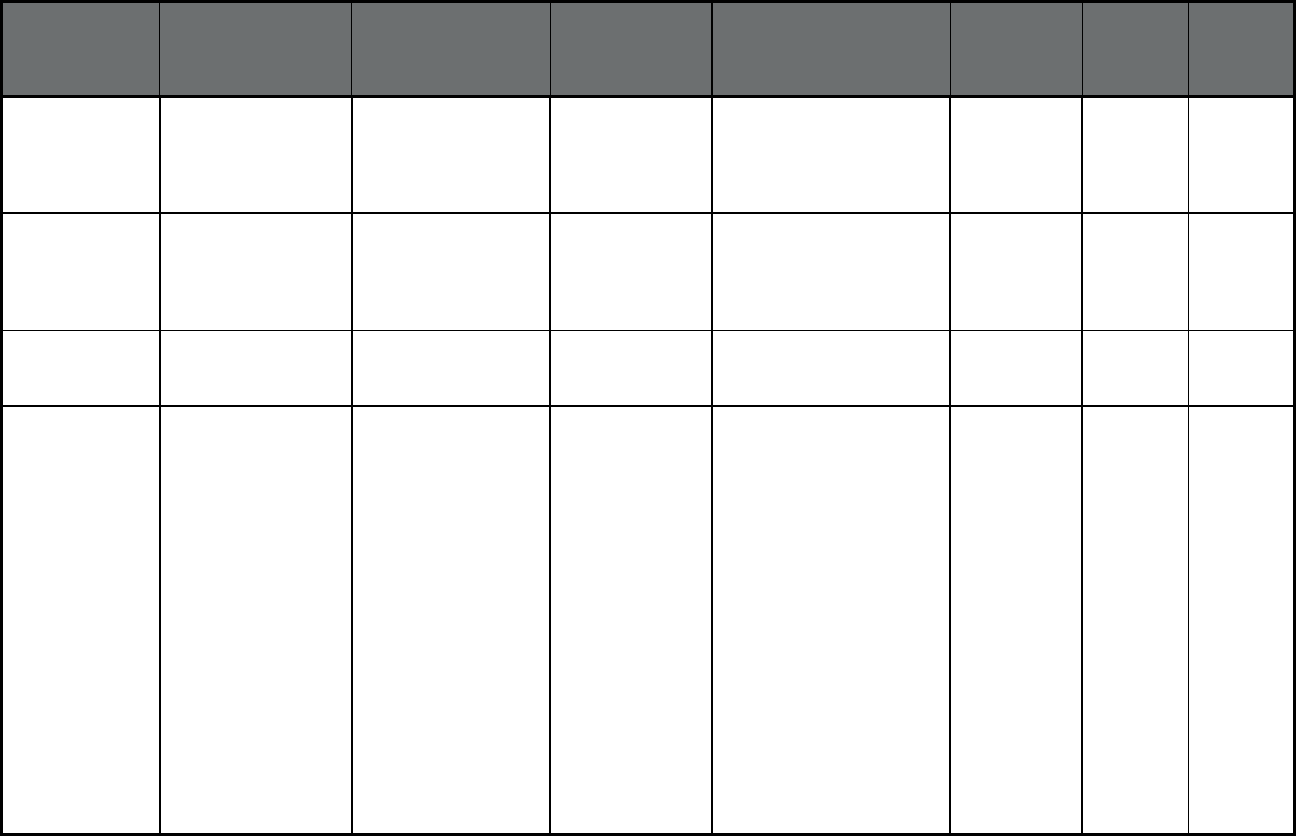
69
State
Program Name
(Type) Plan Name
Parent
Organization
Geographic Region (state-
defined areas, counties, or
zip codes)
Medicaid-Only
Enrollment
Dual
Enrollment
Total
Enrollment
Louisiana Healthy Louisiana
BHO (Behavioral
Health Organization
(BHO) only (PIHP
and/or PAHP))
UnitedHealthcare
Community Plan
UnitedHealthcare Statewide 3,132 23,408 26,540
Louisiana Coordinated System of
Care (Behavioral
Health Organization
(BHO) only (PIHP
and/or PAHP))
Magellan Magellan Health Statewide 2,532 0 2,532
Louisiana Dental Benefit
Management Program
(Dental only (PAHP))
MCNA of Louisiana Managed Care of
North America
(MCNA), Inc.
Statewide 1,398,468 104,724 1,503,192
Louisiana PACE (Program of All-
inclusive Care for the
Elderly (PACE))
Baton Rouge PACE 70704, 70710, 70714,
70719, 70720, 70722,
70729, 70736, 70739,
70748, 70767, 70770,
70775, 70777, 70791,
70801, 70802, 70803,
70804, 70805, 70806,
70807, 70808, 70809,
70810, 70811, 70812,
70813, 70814, 70815,
70816, 70817, 70818,
70819, 70820, 70821,
70822, 70823, 70825,
70826, 70827, 70831,
70833, 70835, 70836,
70837, 70873, 70874,
70879, 70883, 70884,
70891, 70892, 70893,
70894, 70895, 70896,
70898
0 196 196

70
State
Program Name
(Type) Plan Name
Parent
Organization
Geographic Region (state-
defined areas, counties, or
zip codes)
Medicaid-Only
Enrollment
Dual
Enrollment
Total
Enrollment
Louisiana PACE (Program of All-
inclusive Care for the
Elderly (PACE))
Greater New Orleans PACE 70112, 70113, 70114,
70115, 70116, 70117,
70118, 70119, 70122,
70124, 70125, 70126,
70127, 70128, 70129,
70130, 70131, 70032,
70043, 70001, 70002,
70003, 70005, 70006,
70053, 70121
13 170 183
Louisiana PACE (Program of All-
inclusive Care for the
Elderly (PACE))
Lafayette PACE 70501, 70503, 70506,
70507, 70508, 70517,
70518, 70520, 70529,
70578, 70583, 70584,
70592
2 77 79
Maine MaineCare (Primary
Care Case
Management (PCCM))
Multiple Primary Care
Providers
MaineCare Statewide 141,777 0 141,777
Maine NET (Non-Emergency
Medical
Transportation)
Logisticare MaineCare NET Regions 1, 2, 6, 7, and 8 109,632 30,586 140,218
Maine NET (Non-Emergency
Medical
Transportation)
MidCoast Connector MaineCare NET Region 5 19,559 4,917 24,476
Maine NET (Non-Emergency
Medical
Transportation)
Penquis CAP MaineCare NET Regions 3 and 4 53,683 15,950 69,633
Maryland HealthChoice
(Comprehensive
MCO)
Amerigroup Community
Care
Anthem Insurance
Companies, Inc.
Statewide 276,054 0 276,054
Maryland HealthChoice
(Comprehensive
MCO)
Aetna Better Health of
Maryland
Aetna Statewide 7,203 0 7,203

71
State
Program Name
(Type) Plan Name
Parent
Organization
Geographic Region (state-
defined areas, counties, or
zip codes)
Medicaid-Only
Enrollment
Dual
Enrollment
Total
Enrollment
Maryland HealthChoice
(Comprehensive
MCO)
Jai Medical Systems Jai Medical
Systems
Baltimore City, Anne
Arundel and Baltimore
Counties
25,998 0 25,998
Maryland HealthChoice
(Comprehensive
MCO)
Kaiser Permanete Kaiser Permanete
of the Mid Atlantic
States
Anne Arundel, Baltimore,
Calver, Charles, Harford,
Howard, Montgomery, and
Prince George's Counties
63,724 0 63,724
Maryland HealthChoice
(Comprehensive
MCO)
Maryland Physician's
Care
Maryland Care Inc Statewide 213,677 0 213,677
Maryland HealthChoice
(Comprehensive
MCO)
MedStar MedStar Baltimore City, Anne
Arundel, Baltimore, Charles,
Harford, Montgomery,
Prince George's, and St.
Mary's Counties
90,488 0 90,488
Maryland HealthChoice
(Comprehensive
MCO)
Priority Partners Johns Hopkins
Health Care
Statewide 297,179 0 297,179
Maryland HealthChoice
(Comprehensive
MCO)
United HealthCare UnitedHealthcare Baltimore City, Anne
Arundel, Baltimore, Carroll,
Cecil, Charles, Harford,
Howard, Montgomery,
Prince George's, and St.
Mary's Counties
149,565 0 149,565
Maryland HealthChoice
(Comprehensive
MCO)
University of Maryland
Health Partners
University of
Maryland Medical
Systems
Statewide except for
Allegany, Garrett and
Washington Counties
45,715 0 45,715
Maryland Hopkins Elder Plus
(Program of All-
inclusive Care for the
Elderly (PACE))
Hopkins Elder Plus Johns Hopkins 21052, 21202, 21205,
21206, 21213, 21214,
21217, 21218, 21219,
21220, 21221, 21222,
21224, 21227, 21231,
21237
12 93 105
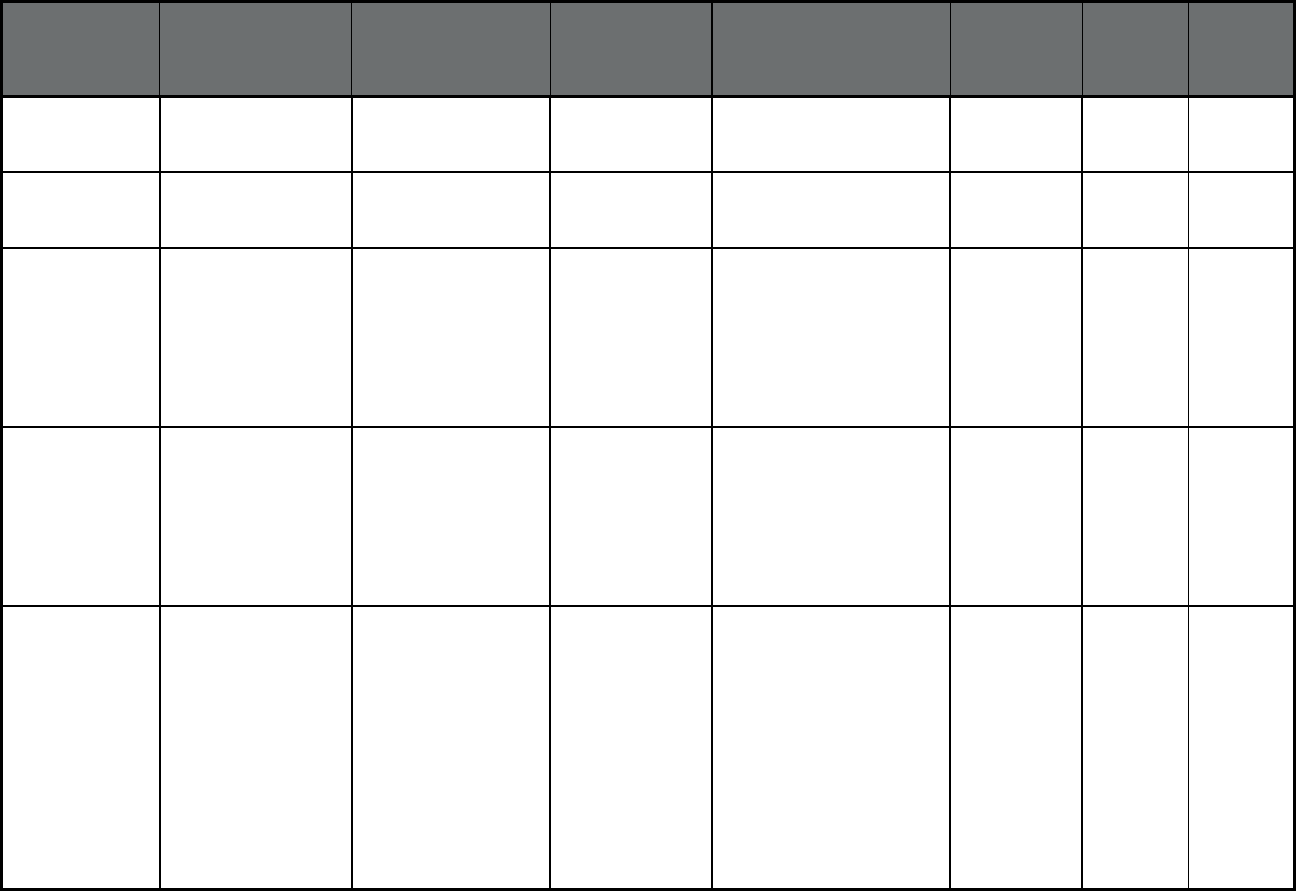
72
State
Program Name
(Type) Plan Name
Parent
Organization
Geographic Region (state-
defined areas, counties, or
zip codes)
Medicaid-Only
Enrollment
Dual
Enrollment
Total
Enrollment
Massachusetts MassHealth Managed
Care (Comprehensive
MCO)
Tufts Health Plan Tufts Health Plan Statewide (excluding
islands)
105,265 0 105,265
Massachusetts MassHealth Managed
Care (Comprehensive
MCO)
Boston Medical Center
Health Plan
Boston Medical
System
Statewide 72,409 0 72,409
Massachusetts Accountable Care
Partnership Plans
(Comprehensive
MCO)
Atrius Health in
partnership with Tufts
Health Public Plans
(THPP)
Tufts Health Plan Attleboro, Beverly, Boston,
Brockton, Falmouth,
Framingham. Gardner,
Fitchburg, Lawrence, Lowell,
Lynn, Malden, Plymouth,
Quincy, Revere, Salem,
Somerville, Waltham,
Wareham, Woburn
31,788 0 31,788
Massachusetts Accountable Care
Partnership Plans
(Comprehensive
MCO)
Beth Israel Deaconess
Care Organization
(BIDCO) in partnership
with Tufts Health Publi
c
Plans (THPP)
Tufts Health Plan Attleboro, Barnstable,
Beverly, Boston, Brockton,
Falmouth, Framingham,
Haverhill, Lowell, Lynn,
Malden, Orleans, Plymouth,
Quincy, Revere, Salem,
Somerville, Waltham,
Wareham, Woburn
33,629 0 33,629
Massachusetts Accountable Care
Partnership Plans
(Comprehensive
MCO)
Boston Children’s
Health ACO in
partnership with Tufts
Health Public Plans
(THPP)
Tufts Health Plan Attleboro, Barnstable,
Beverly, Boston, Brockton,
Fall River, Falmouth,
Framingham, Haverhill,
Holyoke, Lawrence, Lowell,
Lynn, Malden, New Bedford,
Northampton, Orleans,
Plymouth, Quincy, Revere,
Salem, Somerville,
Southbridge, Springfield,
Taunton, Waltham,
Wareham, Westfield,
Woburn, Worcester
83,442 0 83,442
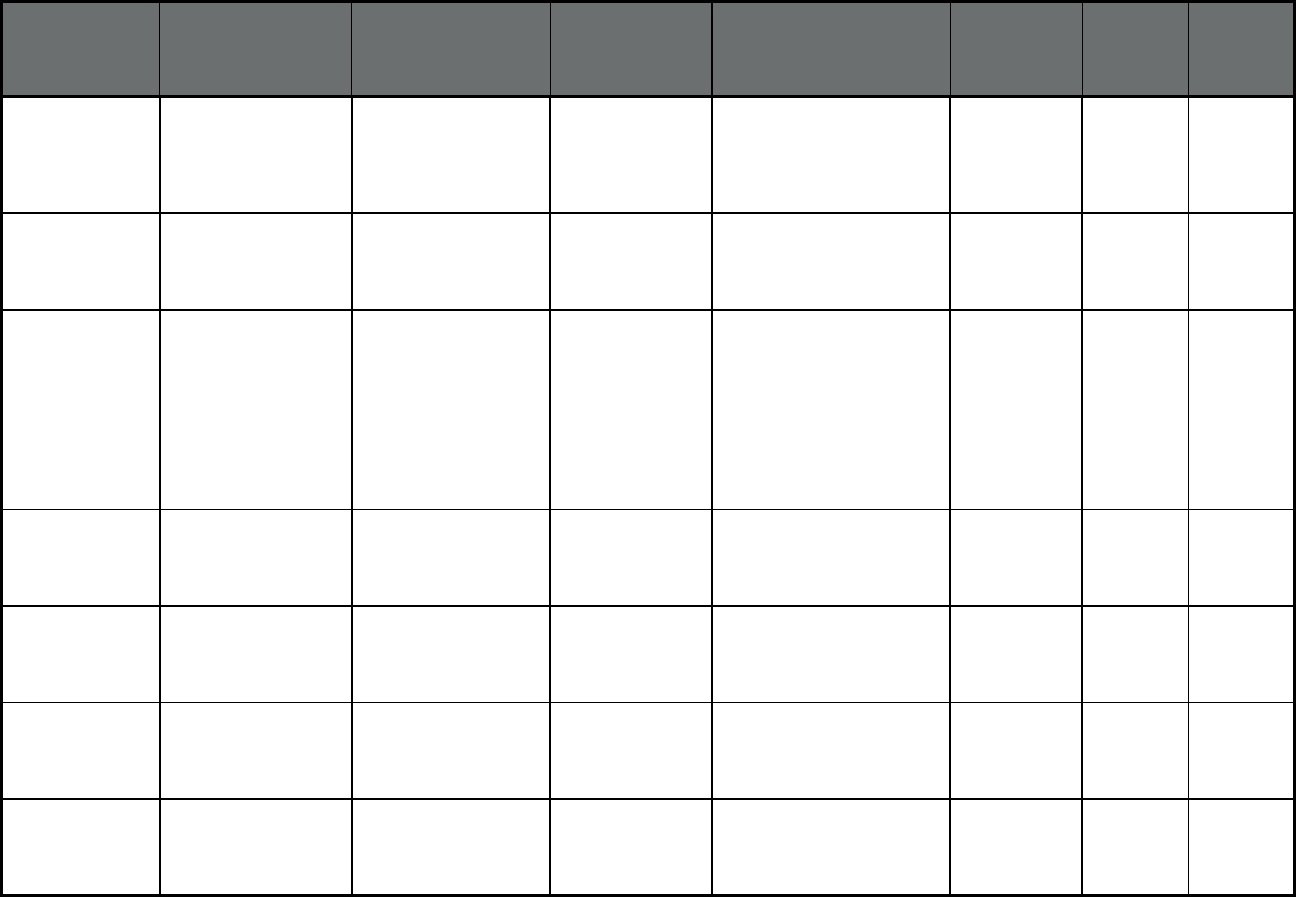
73
State
Program Name
(Type) Plan Name
Parent
Organization
Geographic Region (state-
defined areas, counties, or
zip codes)
Medicaid-Only
Enrollment
Dual
Enrollment
Total
Enrollment
Massachusetts Accountable Care
Partnership Plans
(Comprehensive
MCO)
Cambridge Health
Alliance (CHA) in
partnership with Tufts
Health Public Plans
(THPP)
Tufts Health Plan Boston, Lynn, Malden,
Revere, Somerville,
Waltham, Woburn
26,068 0 26,068
Massachusetts Accountable Care
Partnership Plans
(Comprehensive
MCO)
Merrimack Valley ACO
in partnership with
AllWays Health
Partners
Allways Health
Partners
Haverhill, Lawrence, Lowell 31,865 0 31,865
Massachusetts Accountable Care
Partnership Plans
(Comprehensive
MCO)
Boston Accountable
Care Organization in
partnership with BMC
HealthNet Plan
Boston Medical
Health Plan
Attleboro, Boston, Brockton,
Fall River, Falmouth,
Greenfield, Holyoke, Lynn,
Malden, New Bedford,
Northampton, Plymouth,
Quincy, Revere, Somerville,
Springfield, Taunton,
Waltham, Wareham,
Westfield, Woburn
107,081 0 107,081
Massachusetts Accountable Care
Partnership Plans
(Comprehensive
MCO)
Mercy Medical Center
in partnership with
BMC HealthNet Plan
Boston Medical
Health Plan
Holyoke, Northampton,
Springfield, Westfield
28,148 0 28,148
Massachusetts Accountable Care
Partnership Plans
(Comprehensive
MCO)
Signature Healthcare in
partnership with BMC
HealthNet Plan
Boston Medical
Health Plan
Brockton, Plymouth, Quincy,
Taunton
17,924 0 17,924
Massachusetts Accountable Care
Partnership Plans
(Comprehensive
MCO)
Southcoast Health in
partnership with BMC
HealthNet Plan
Boston Medical
Health Plan
Attleboro, Fall River,
Falmouth, New Bedford,
Plymouth, Taunton,
Wareham
16,044 0 16,044
Massachusetts Accountable Care
Partnership Plans
(Comprehensive
MCO)
Health Collaborative of
the Berkshires in
partnership with Fallon
Health
Fallon Health Plan Adams, Pittsfield 15,461 0 15,461
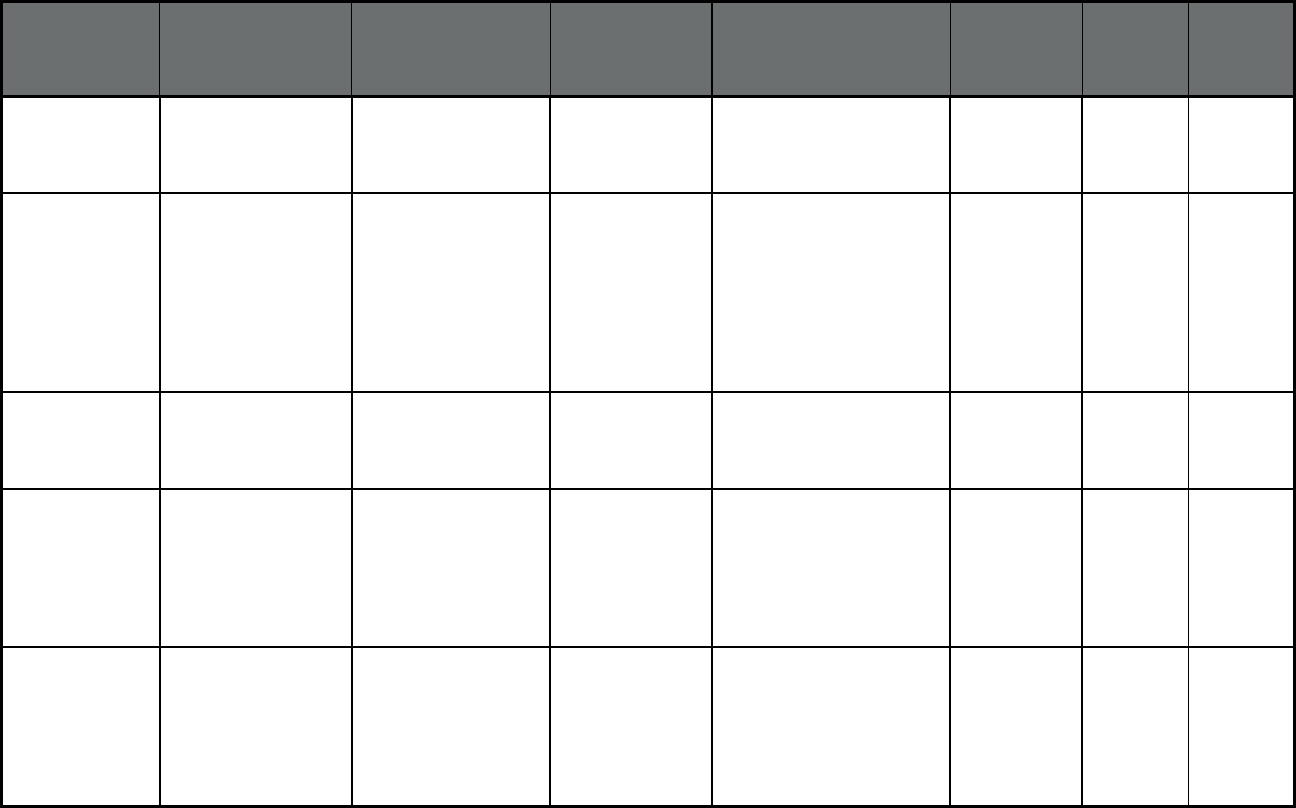
74
State
Program Name
(Type) Plan Name
Parent
Organization
Geographic Region (state-
defined areas, counties, or
zip codes)
Medicaid-Only
Enrollment
Dual
Enrollment
Total
Enrollment
Massachusetts Accountable Care
Partnership Plans
(Comprehensive
MCO)
Reliant Medical Group
in partnership with
Fallon Health
Fallon Health Plan Gardner-Fitchburg,
Framingham, Southbridge,
Worcester
30,168 0 30,168
Massachusetts Accountable Care
Partnership Plans
(Comprehensive
MCO)
Wellforce in partnership
with Fallon Health
Fallon Health Plan Attleboro, Barnstable,
Beverly, Boston, Brockton,
Falmouth, Framingham,
Haverhill, Lawrence, Lowell,
Lynn, Malden, Orleans,
Plymouth, Quincy, Revere,
Salem, Somerville,
Waltham, Wareham,
Woburn
52,821 0 52,821
Massachusetts Accountable Care
Partnership Plans
(Comprehensive
MCO)
Baystate Health Care
Alliance in partnership
with Health New
England
Health New
England
Holyoke, Northampton,
Springfield, Westfield
37,474 0 37,474
Massachusetts Primary Care
Accountable Care
Organizations
(Primary Care ACO)
(Primary Care Case
Management Entity
(PCCM Entity))
Community Care
Cooperative
Community Care
Health Plan (WI)
Statewide 112,875 0 112,875
Massachusetts Primary Care
Accountable Care
Organizations
(Primary Care ACO)
(Primary Care Case
Management Entity
(PCCM Entity))
Partners HealthCare
Choice
Partners
HealthCare Choice
Statewide 105,032 0 105,032
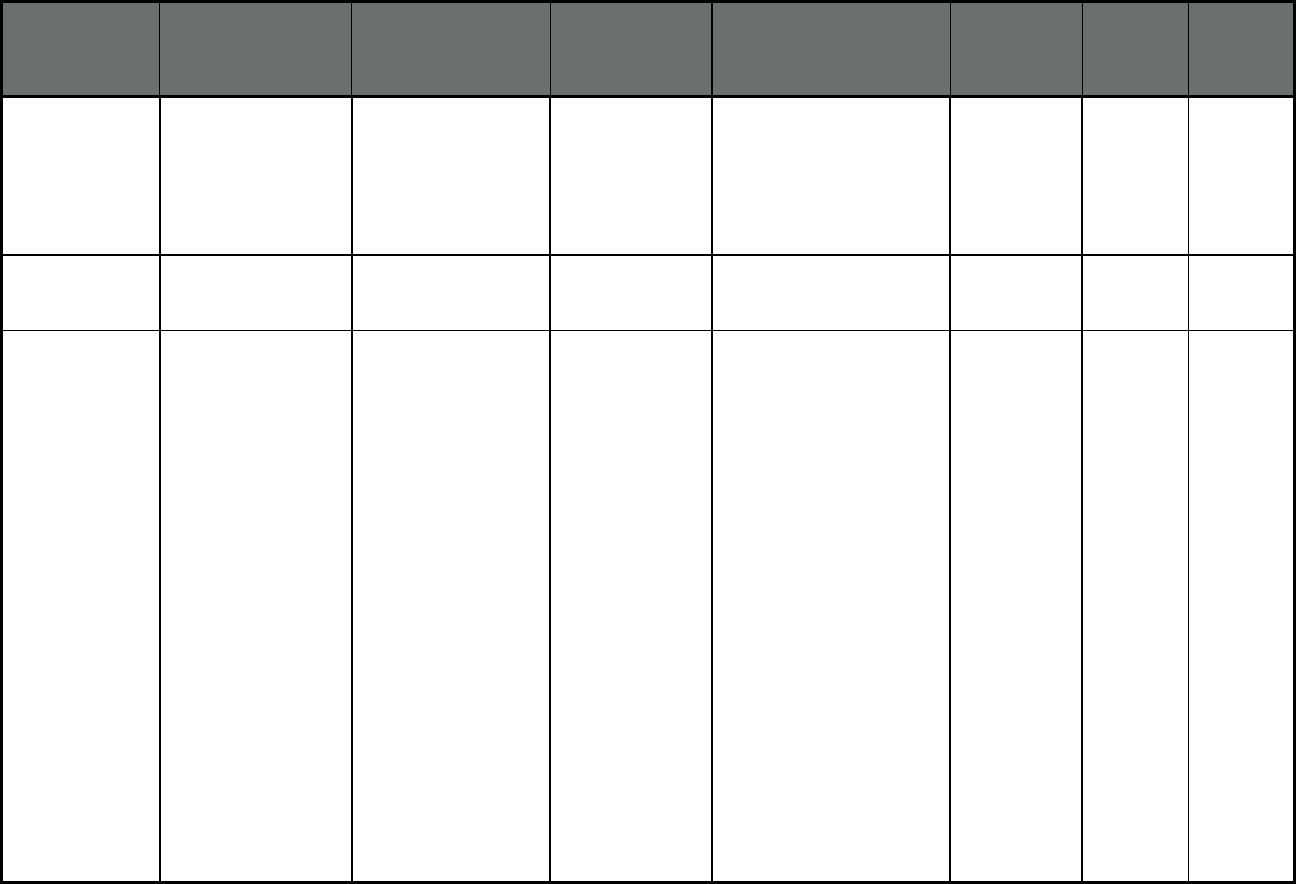
75
State
Program Name
(Type) Plan Name
Parent
Organization
Geographic Region (state-
defined areas, counties, or
zip codes)
Medicaid-Only
Enrollment
Dual
Enrollment
Total
Enrollment
Massachusetts Primary Care
Accountable Care
Organizations
(Primary Care ACO)
(Primary Care Case
Management Entity
(PCCM Entity))
Steward Health Choice Steward Health
Choice
Statewide 121,443 0 121,443
Massachusetts Senior Care Options
(Comprehensive MCO
+ MLTSS)
Boston Medical Center
Healthnet Plan
Boston Medical
Health Plan
Suffolk County 139 705 844
Massachusetts Senior Care Options
(Comprehensive MCO
+ MLTSS)
Commonwealth Care
Alliance
Commonwealth
Care Alliance
01330, 01337, 01338,
01339, 01340, 01341,
01342, 01344, 01354,
01301, 01302, 01039,
01346, 01347, 01054,
01349, 01350, 01351,
01360, 01367, 01369,
01370, 01072, 01373,
01375, 01376, 01379,
01380, 01093, 02322,
02157, 02457, 02184,
02185, 02146, 02445,
02446, 02147, 02447,
02021, 02467, 02025,
02026, 02027, 02030,
02032, 02035, 02343,
02052, 02053, 02054,
02186, 02187, 02192,
02194, 02492, 02494,
02056, 02171, 02062,
02762, 02169, 02170,
02171, 02269, 02368,
02067, 02070, 02071,
02072, 02081, 02181,
02481, 02482, 02090,
02188, 02189, 02190,
696 9,251 9,947
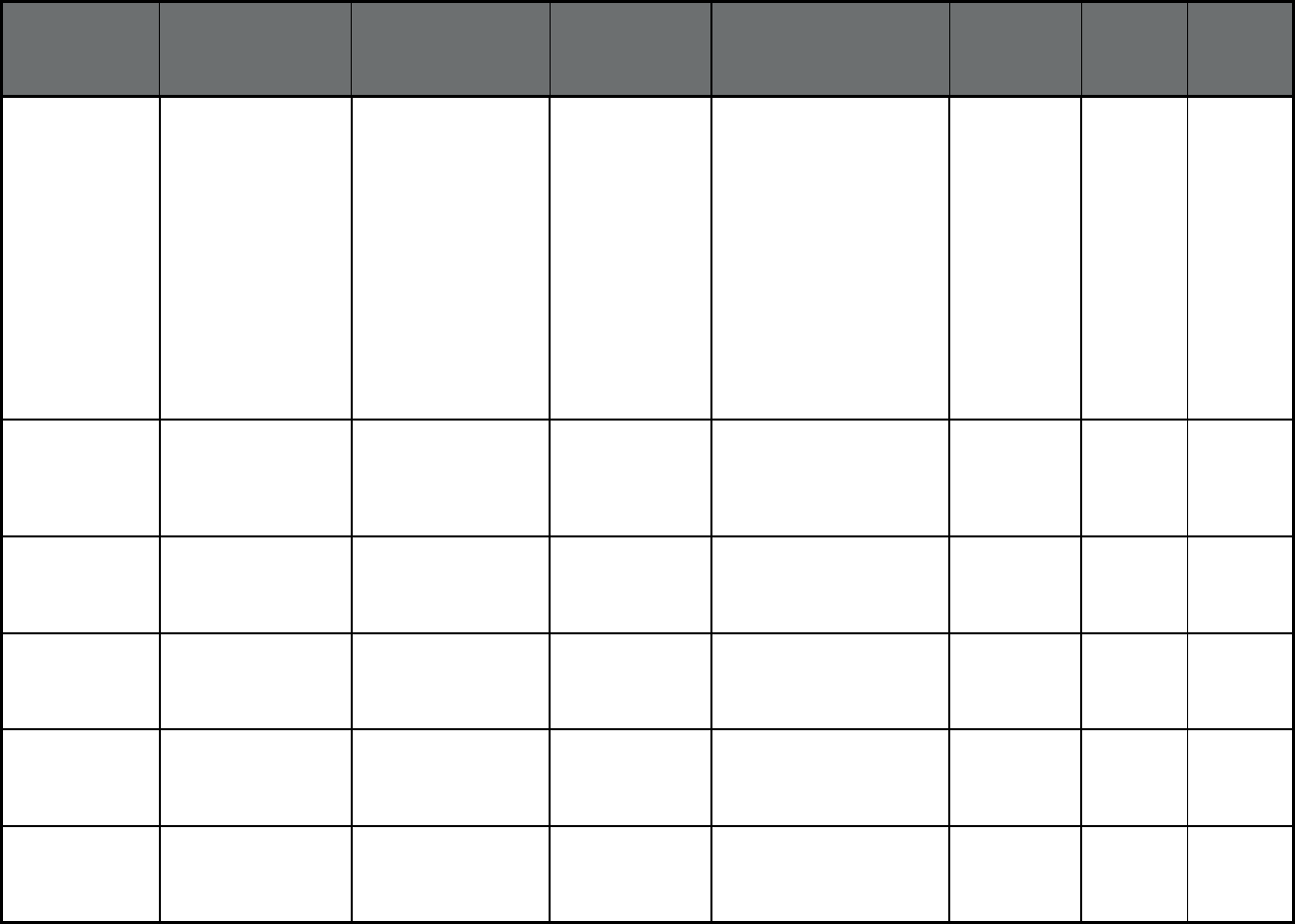
76
State
Program Name
(Type) Plan Name
Parent
Organization
Geographic Region (state-
defined areas, counties, or
zip codes)
Medicaid-Only
Enrollment
Dual
Enrollment
Total
Enrollment
Massachusetts
(cont)
Senior Care Options
(Comprehensive MCO
+ MLTSS)
Commonwealth Care
Alliance
02191, 02170, 02093,
02351, 02020, 02324,
02301, 02302, 02303,
02304, 02305, 02327,
02330, 02332, 02333,
02338, 02339, 02341,
02018, 02043, 02044,
02045, 02364, 02050,
02065, 02346, 02061,
02355, 02059, 02358,
02558, 02359, 02360,
02362, 02367, 02770,
02370, 02040, 02055,
02060, 02066, 02379,
02382
696 9,251 9,947
Massachusetts Senior Care Options
(Comprehensive MCO
+ MLTSS)
Navicare HMO Fallon Health Plan Barnstable, Brisol, Essex,
Franklin, Hampden,
Middlesex, Norfolk,
Plymouth, Suffolk, and
Worcester Counties
436 6,270 6,706
Massachusetts Senior Care Options
(Comprehensive MCO
+ MLTSS)
Senior Whole Health Magellan Health Bristol, Essex, Hampden,
Middlesex, Norfolk,
Plymouth, Suffolk, and
Worcester Counties
1,321 13,465 14,786
Massachusetts Senior Care Options
(Comprehensive MCO
+ MLTSS)
Tufts Health Plan Tufts Health Plan Barnstable, Bristol, Essex,
Hampden, Middlesex,
Norfolk, Plymouth, Suffolk,
and Worcester Counties
633 4,081 4,714
Massachusetts Senior Care Options
(Comprehensive MCO
+ MLTSS)
United Healthcare UnitedHealthcare Bristol, Essex, Hampden,
Middlesex, Norfolk,
Plymouth, Suffolk and
Worcester Counties
1,838 17,629 19,467
Massachusetts Primary Care Clinician
Program (PCC Plan)
(Primary Care Case
Management (PCCM))
Multiple Primary Care
Providers
Multiple Primary
Care Provider
(PCCM)
Statewide 119,512 0 119,512
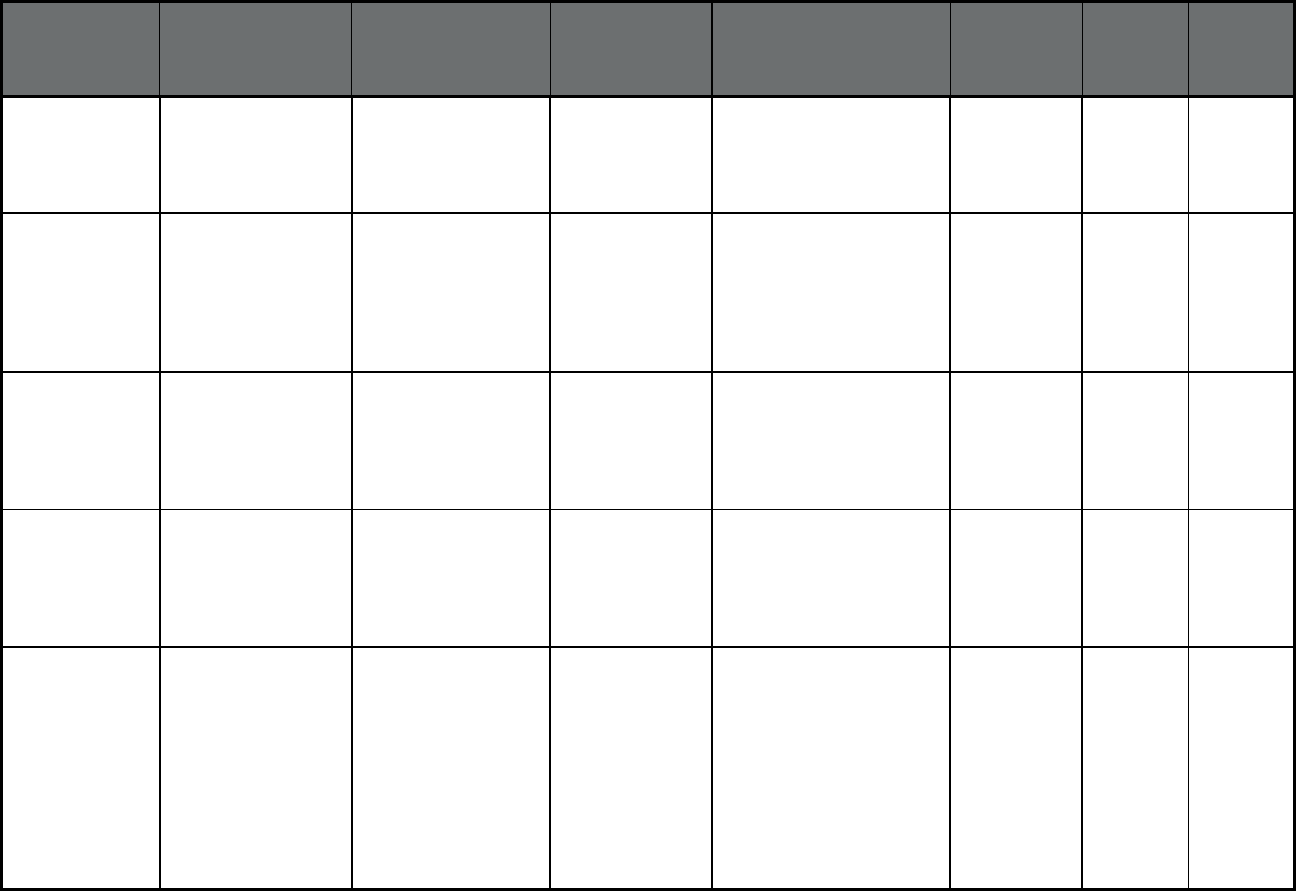
77
State
Program Name
(Type) Plan Name
Parent
Organization
Geographic Region (state-
defined areas, counties, or
zip codes)
Medicaid-Only
Enrollment
Dual
Enrollment
Total
Enrollment
Massachusetts MassHealth BH/SUD
PIHP (Behavioral
Health Organization
(BHO) only (PIHP
and/or PAHP))
Massachusetts
Behavioral Health
Partnership
Beacon Statewide 528,106 0 528,106
Massachusetts Money Follows the
Person- Behavioral
Health Supports
(MFP-BH) (Behavioral
Health Organization
(BHO) only (PIHP
and/or PAHP))
Money Follows the
Person- Behavioral
Health Supports (MFP-
BH)
Money Follows the
Person-
Behavioral Health
Supports (MFP-
BH)
Statewide 0 0 0
Massachusetts Program of All-
Inclusive Care for the
Elderly (PACE)
(Program of All-
inclusive Care for the
Elderly (PACE))
Elder Service Plan of
Cambridge Health
Alliance
Elder Service Plan Middlesex and Suffolk
Counties
32 396 428
Massachusetts Program of All-
Inclusive Care for the
Elderly (PACE)
(Program of All-
inclusive Care for the
Elderly (PACE))
Upham's Elder Service
Plan
Elder Service Plan 02108, 02445 30 246 276
Massachusetts Program of All-
Inclusive Care for the
Elderly (PACE)
(Program of All-
inclusive Care for the
Elderly (PACE))
Elder Service Plan of
Harbor Health
Elder Service Plan 02108, 02445, 02021,
02026, 02048, 02062,
02067, 02072, 02169,
02184, 02186, 02188,
02301, 02322, 02324,
02333, 02334, 02338,
02339, 02341, 02343,
02351, 02359, 02367,
02368, 02370, 02379,
02382, 02458, 02766,
02767, 02780
13 462 475
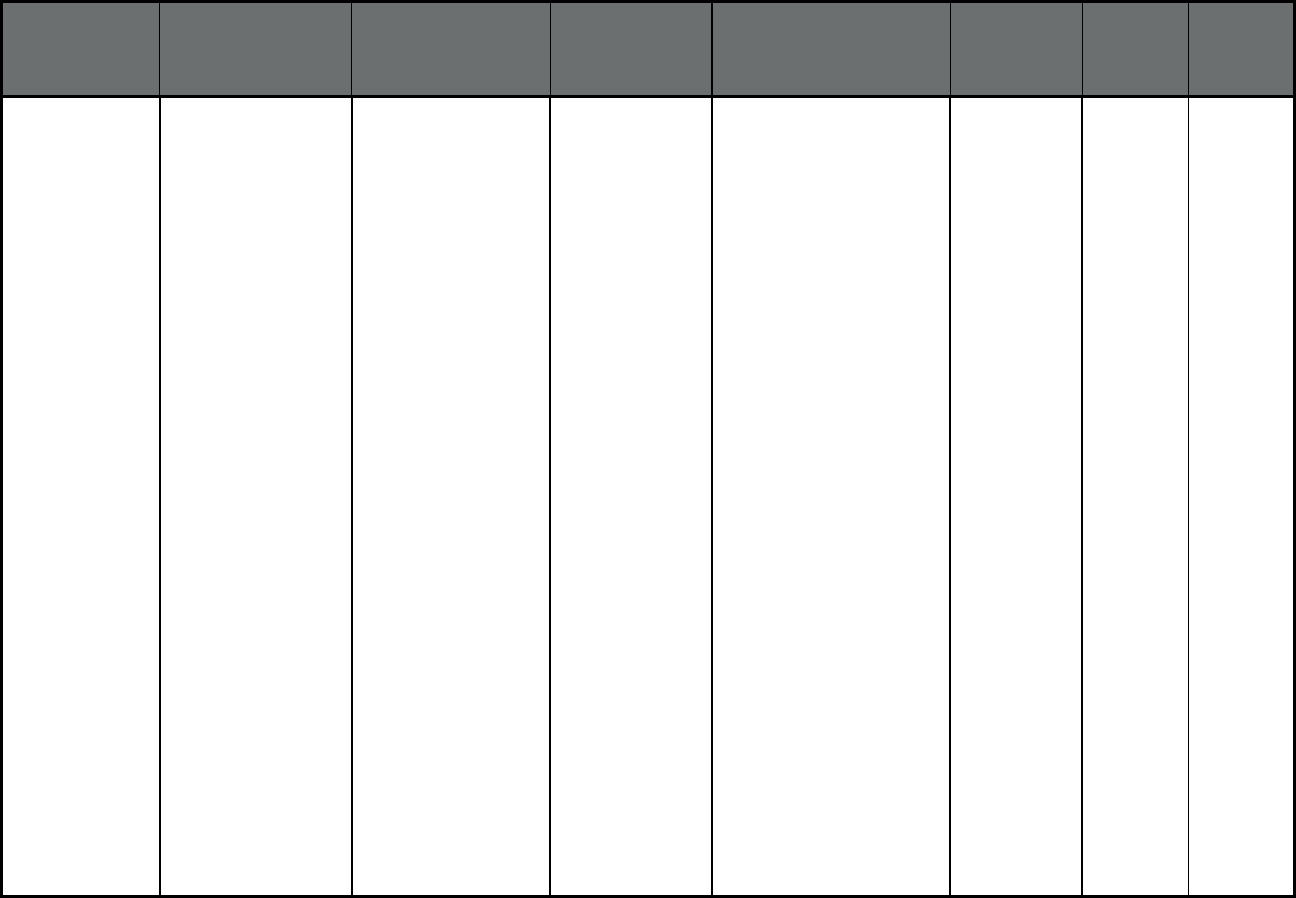
78
State
Program Name
(Type) Plan Name
Parent
Organization
Geographic Region (state-
defined areas, counties, or
zip codes)
Medicaid-Only
Enrollment
Dual
Enrollment
Total
Enrollment
Massachusetts Program of All-
Inclusive Care for the
Elderly (PACE)
(Program of All-
inclusive Care for the
Elderly (PACE))
Fallon Health Summit
Eldercare
Fallon Health Plan 01001, 01008, 01010,
01011, 01013, 01027,
01028, 01033, 01034,
01036, 01040, 01056,
01057, 01069, 01071,
01073, 01075, 01077,
01081, 01085, 01089,
01095, 01101, 01106,
01521, 01034, 01810,
01821, 01824, 01826,
01827, 01840, 01844,
01850, 01876, 01879,
01886, 01005, 01037,
01068, 01083, 01331,
01331, 01366, 01368,
01420, 01430, 01431,
01432, 01440, 01441,
01450, 01451, 01452,
01453, 01460, 01462,
01463, 01464, 01468,
01469, 01475, 01501,
01503, 01504, 01505,
01506, 01507, 01510,
01515, 01516, 01519,
01520, 01523, 01524,
01527, 01529, 01531,
01532, 01534, 01535,
01540, 01541, 01543,
01545, 01550, 01562,
01564, 01566, 01568,
01569, 01570, 01571,
01581, 01583, 01585,
01590, 01601, 01612,
01719, 01720, 01730,
01740, 01741, 01742,
01747, 01749, 01752,
01756, 01757, 01772,
01151, 01845
46 1,127 1,173
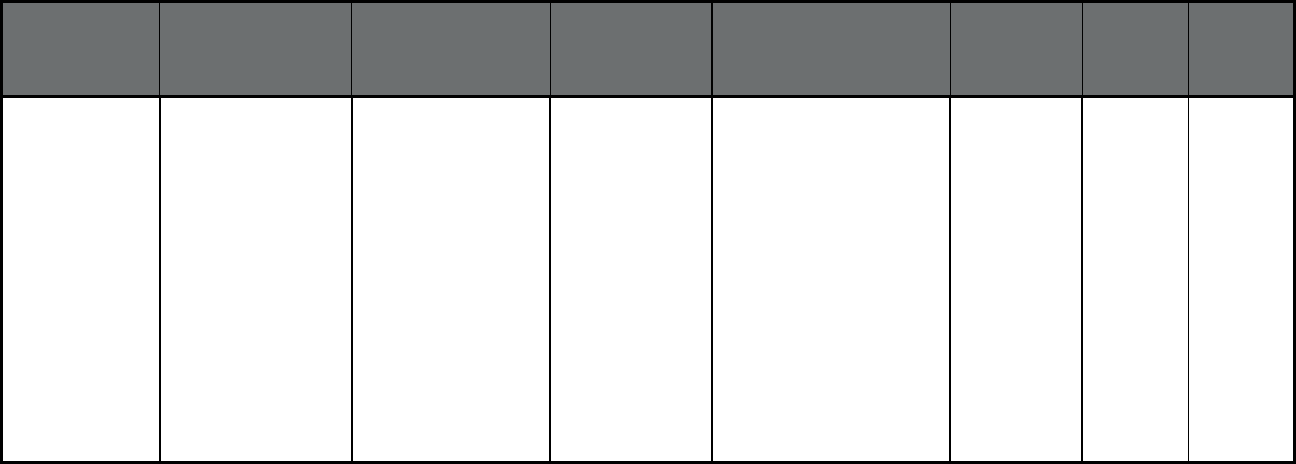
79
State
Program Name
(Type) Plan Name
Parent
Organization
Geographic Region (state-
defined areas, counties, or
zip codes)
Medicaid-Only
Enrollment
Dual
Enrollment
Total
Enrollment
Massachusetts Program of All-
Inclusive Care for the
Elderly (PACE)
(Program of All-
inclusive Care for the
Elderly (PACE))
Element Care Inc Element Care Inc 02176, 02180, 01810,
01821, 01824, 01826,
01827, 01840, 01844,
01850, 01876, 01879,
01886, 01845, 01801,
01803, 01830, 01833,
01834, 01860, 01864,
01867, 01880, 01887,
01890, 01901, 01906,
01907, 01908, 01913,
01915, 01921, 01923,
01929, 01930, 01936,
01938, 01940, 01944,
01945, 01949, 01950,
01951, 01952, 01960,
01966, 01969, 01970,
01983, 01984, 01985
67 927 994
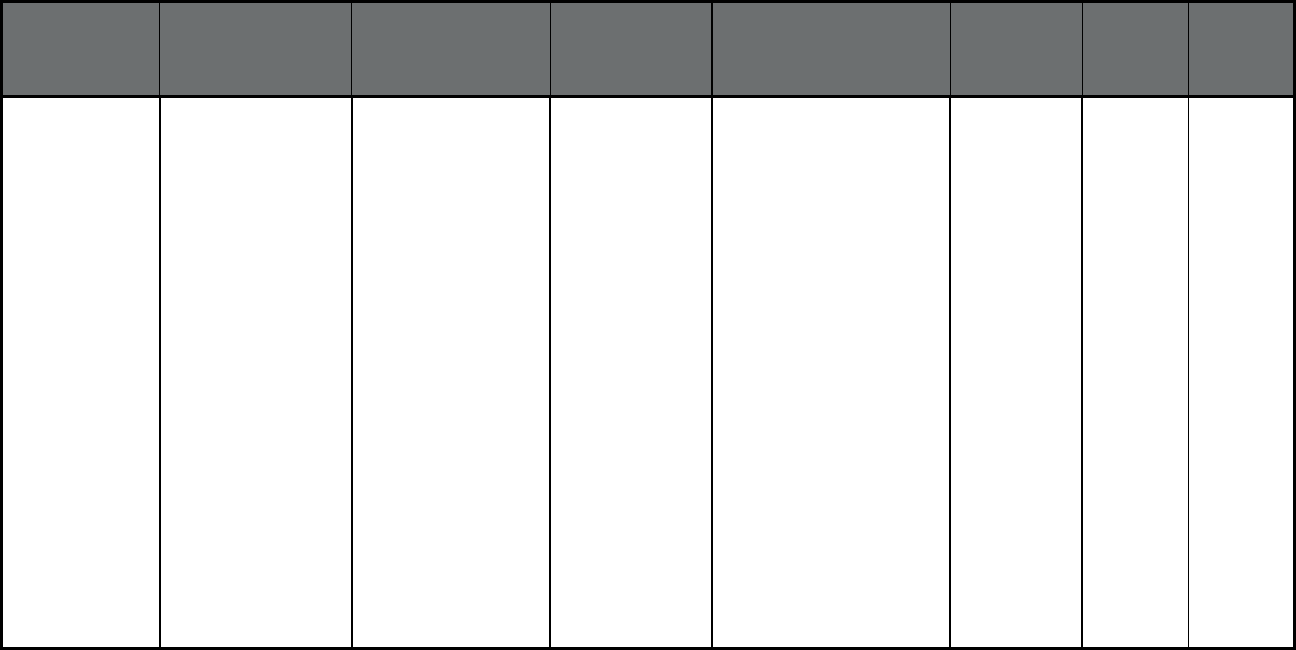
80
State
Program Name
(Type) Plan Name
Parent
Organization
Geographic Region (state-
defined areas, counties, or
zip codes)
Medicaid-Only
Enrollment
Dual
Enrollment
Total
Enrollment
Massachusetts Program of All-
Inclusive Care for the
Elderly (PACE)
(Program of All-
inclusive Care for the
Elderly (PACE))
Serenity Care PACE
Program
PACE 01002, 01027, 01350,
01001, 01002, 01007,
01008, 01010, 01011,
01012, 01013, 01026,
01027, 01028, 01032,
01033, 01034, 01035,
01036, 01038, 01040,
01050, 01056, 01057,
01060, 01069, 01070,
01071, 01073, 01075,
01077, 01081, 01082,
01085, 01089, 01095,
01096, 01098, 01101,
01106, 01151, 01243,
01521, 01009, 01030,
01039, 01053, 01054,
01059, 01062, 01066,
01072, 01079, 01080,
01084, 01088, 01093,
01097, 01301, 01330,
01337, 01338, 01339,
01340, 01341, 01342,
01344, 01346, 01351,
01354, 01355, 01360,
01364, 01367, 01370,
01375, 01378, 01379
66 325 391
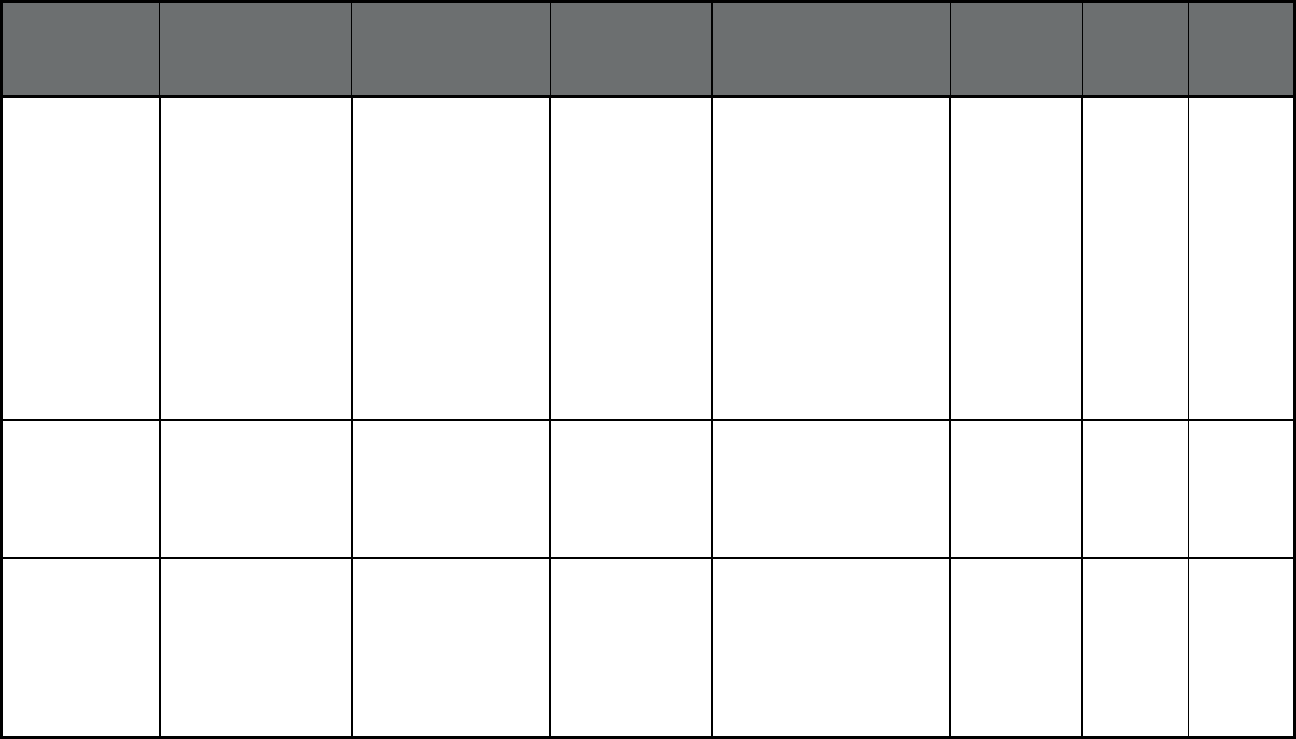
81
State
Program Name
(Type) Plan Name
Parent
Organization
Geographic Region (state-
defined areas, counties, or
zip codes)
Medicaid-Only
Enrollment
Dual
Enrollment
Total
Enrollment
Massachusetts Program of All-
Inclusive Care for the
Elderly (PACE)
(Program of All-
inclusive Care for the
Elderly (PACE))
Mercy Life Inc Mercy Life Inc 01008, 01010, 01011,
01013, 01027, 01028,
01033, 01034, 01036,
01040, 01056, 01057,
01069, 01071, 01073,
01075, 01077, 01081,
01085, 01089, 01095,
01101, 01106, 01521,
01151, 01002, 01027,
01350, 01002, 01007,
01012, 01026, 01032,
01035, 01038, 01050,
01060, 01070, 01082,
01096, 01098, 01243,
01034
11 223 234
Massachusetts Program of All-
Inclusive Care for the
Elderly (PACE)
(Program of All-
inclusive Care for the
Elderly (PACE))
Neighborhood PACE PACE Middlesex and Suffolk
Counties
55 496 551
Michigan Managed Care Plan
Division
(Comprehensive
MCO)
Aetna Better Health of
Michigan
Aetna Berrien, Branch, Calhoun,
Cass, Hillsdale, Jackson,
Kalamazoo, Lenawee,
Livingston, Macomb,
Monroe, Oakland, St.
Joseph, Van Buren,
Washtenaw, and Wayne
Counties
37,306 214 37,520
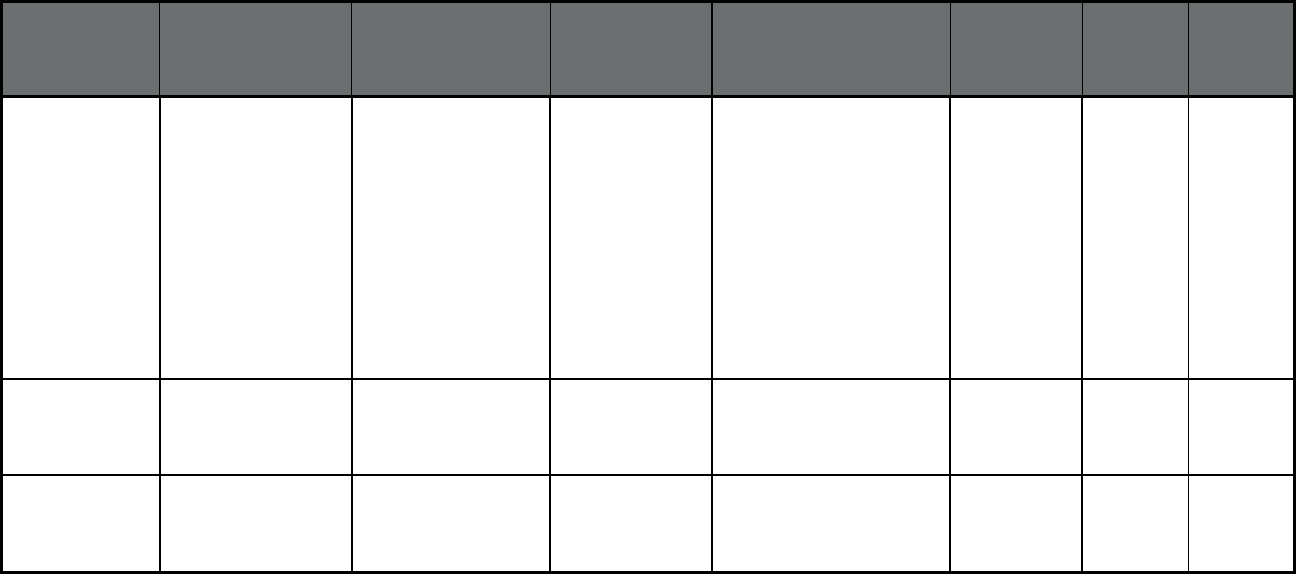
82
State
Program Name
(Type) Plan Name
Parent
Organization
Geographic Region (state-
defined areas, counties, or
zip codes)
Medicaid-Only
Enrollment
Dual
Enrollment
Total
Enrollment
Michigan Managed Care Plan
Division
(Comprehensive
MCO)
Blue Cross Complete of
Michigan
Blue Cross Blue
Shield
Allegan, Barry, Clinton,
Eaton, Genesee, Hillsdale,
Huron, Ingham, Ionia,
Jackson, Kent, Lake,
Lapeer, Lenawee,
Livingston, Macomb, Mason,
Mecosta, Monroe,
Montcalm, Muskegon,
Newaygo, Oakland,
Oceana, Osceola, St. Clair,
Sanilac, Shiawassee,
Tuscola, Washtenaw, and
Wayne Counties
209,603 3,535 213,138
Michigan Managed Care Plan
Division
(Comprehensive
MCO)
Harbor Health Plan Trusted Health
Plan
Macomb, Oakland, and
Wayne Counties
7,128 4 7,132
Michigan Managed Care Plan
Division
(Comprehensive
MCO)
HAP Midwest Health
Plan
Health Alliance
Plan
Genesee, Huron, Lapeer,
St. Clair, Sanilac,
Shiawassee, and Tuscola
Counties
3,031 33 3,064
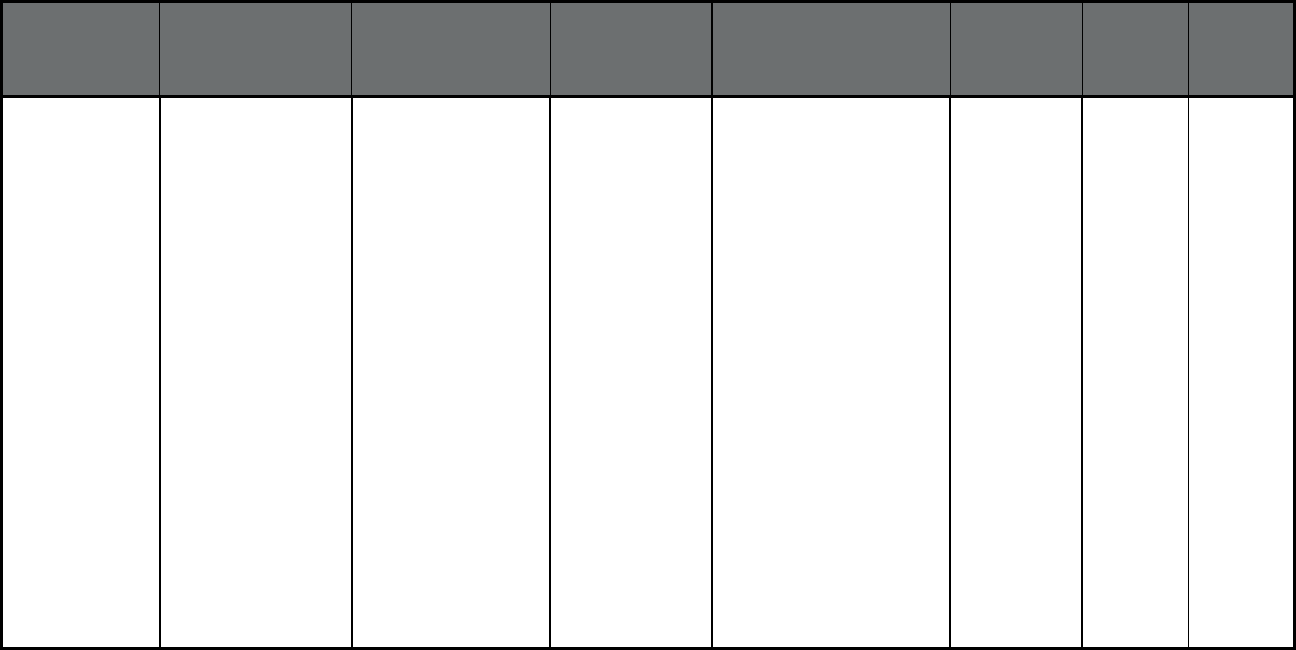
83
State
Program Name
(Type) Plan Name
Parent
Organization
Geographic Region (state-
defined areas, counties, or
zip codes)
Medicaid-Only
Enrollment
Dual
Enrollment
Total
Enrollment
Michigan Managed Care Plan
Division
(Comprehensive
MCO)
McLaren Health Plan McLaren Health
Plan
Alcona, Allegan, Alpena,
Antrim, Arenac, Barry, Bay,
Benzie, Berrien, Branch,
Calhoun, Cass, Charlevoix,
Cheboygan, Clare, Clinton,
Crawford, Eaton, Emmet,
Genesee, Gladwin, Grand
Traverse, Gratiot, Hillsdale,
Huron, Ingham, Ionia, Iosco,
Isabella, Jackson,
Kalamazoo, Kalkaska, Kent,
Lake, Lapeer, Leelanau,
Lenawee, Livingston,
Macomb, Manistee, Mason,
Mecosta, Midland,
Missaukee, Monroe,
Montcalm, Montmorency,
Muskegon, Newaygo,
Oakland, Oceana, Ogema,
Osceola, Oscoda, Otsego,
Ottawa, Presque Isle,
Roscommon, Saginaw, St.
Clair, St. Joseph, Sanilac,
Shiawassee, Tuscola, Van
Buren, Washtenaw, Wayne,
and Wexford Counties
201,833 6,022 207,855
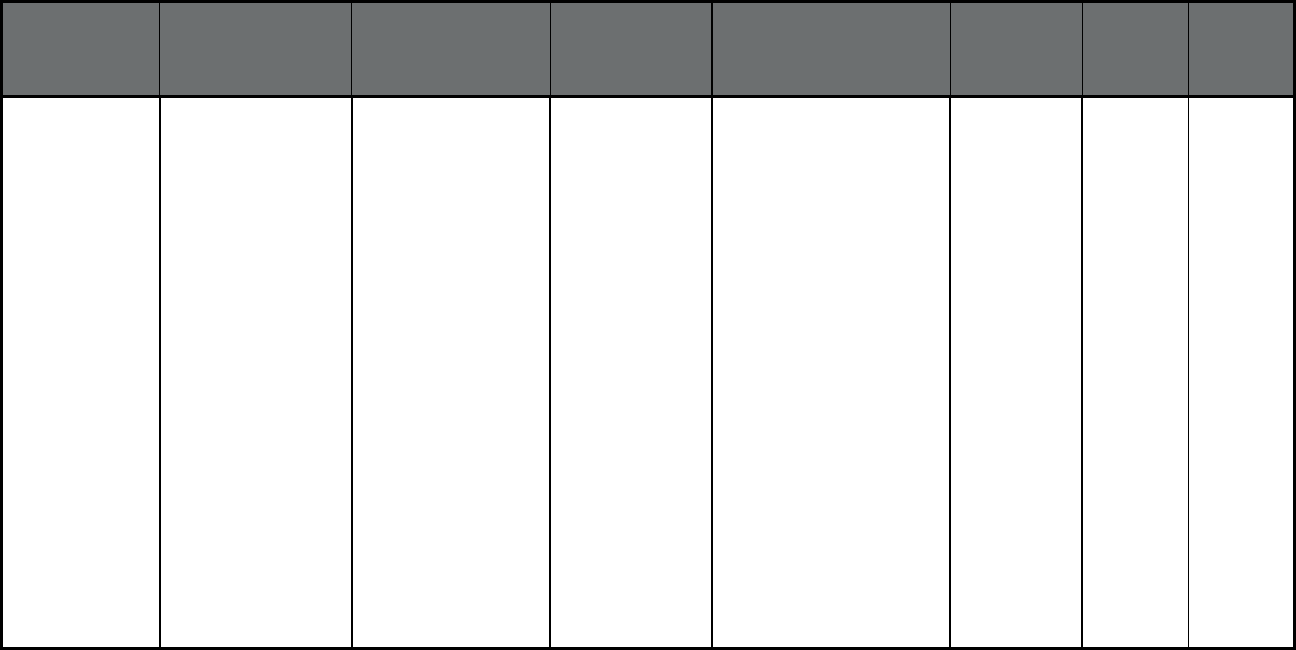
84
State
Program Name
(Type) Plan Name
Parent
Organization
Geographic Region (state-
defined areas, counties, or
zip codes)
Medicaid-Only
Enrollment
Dual
Enrollment
Total
Enrollment
Michigan Managed Care Plan
Division
(Comprehensive
MCO)
Meridian Health Plan of
Michigan
Meridian Alcona, Allegan, Alpena,
Antrim, Arenac, Barry, Bay,
Benzie, Berrien, Branch,
Calhoun, Cass, Charlevoix,
Cheboygan, Clare, Clinton,
Crawford, Eaton, Emmet,
Genesee, Gladwin, Grand
Traverse, Gratiot, Hillsdale,
Huron, Ingham, Ionia, Iosco,
Isabella, Jackson,
Kalamazoo, Kalkaska, Kent,
Lake, Lapeer, Leelanau,
Lenawee, Livingston
Macomb, Manistee, Mason,
Mecosta, Midland,
Missaukee, Monroe,
Montcalm, Montmorency,
Muskegon, Newaygo,
Oakland, Oceana, Ogemaw,
Osceola, Oscoda, Otsego,
Ottawa, Presque Isle,
Roscommon, Saginaw, St.
Clair, St. Joseph, Sanilac,
Shiawassee, Tuscola, Van
Buren, Washtenaw, Wayne,
and Wexford Counties
499,221 11,331 510,552
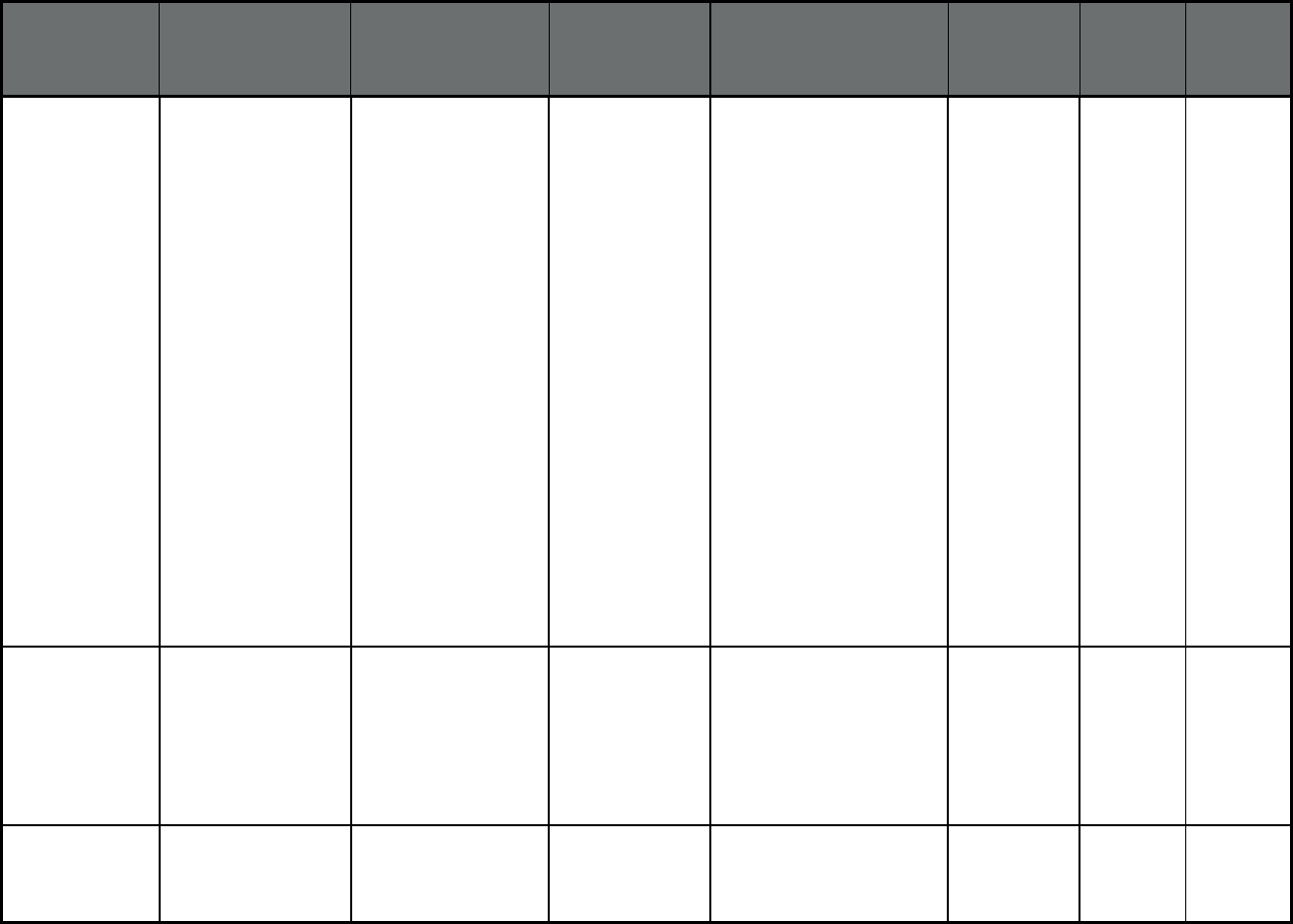
85
State
Program Name
(Type) Plan Name
Parent
Organization
Geographic Region (state-
defined areas, counties, or
zip codes)
Medicaid-Only
Enrollment
Dual
Enrollment
Total
Enrollment
Michigan
7
Managed Care Plan
Division
(Comprehensive
MCO)
Molina Healthcare of
Michigan
Molina Healthcare Alcona, Allegan, Alpena,
Antrim, Arenac, Barry, Bay,
Benzie, Berrien, Branch,
Calhoun, Cass, Charlevoix,
Cheboygan, Clare, Clinton,
Crawford, Eaton, Emmet,
Genesee, Gladwin, Grand
Traverse, Gratiot, Hillsdale,
Huron, Ingham, Ionia, Iosco,
Isabella, Jackson,
Kalamazoo, Kalkaska, Kent,
Lake, Lapeer, Leelanau,
Lenawee, Livingston,
Macomb, Manistee, Mason,
Mecosta, Midland,
Missaukee, Monroe,
Montcalm, Montmorency,
Muskegon, Newaygo,
Oakland, Oceana, Ogemaw,
Osceola, Oscoda, Otsego,
Ottawa, Presque Isle,
Roscommon, Saginaw, St.
Clair, St. Joseph, Sanilac,
Shiawassee, Tuscola, Van
Buren, Washtenaw, Wayne,
and Wexford Counties
351,204 9,960 361,164
Michigan Managed Care Plan
Division
(Comprehensive
MCO)
Priority Health Choice Priority Health
Choice, Inc.
Allegan, Barry, Berrien,
Branch, Calhoun, Cass,
Ionia, Kalamazoo, Kent,
Lake, Mason, Mecosta,
Montcalm, Muskegon,
Newaygo, Oceana, Osceola,
Ottawa, St. Joseph, and Van
Buren Counties
127,003 4,588 131,591
Michigan Managed Care Plan
Division
(Comprehensive
MCO)
Total Health Care Total Health Care Macomb, Oakland, and
Wayne Counties
52,441 231 52,672
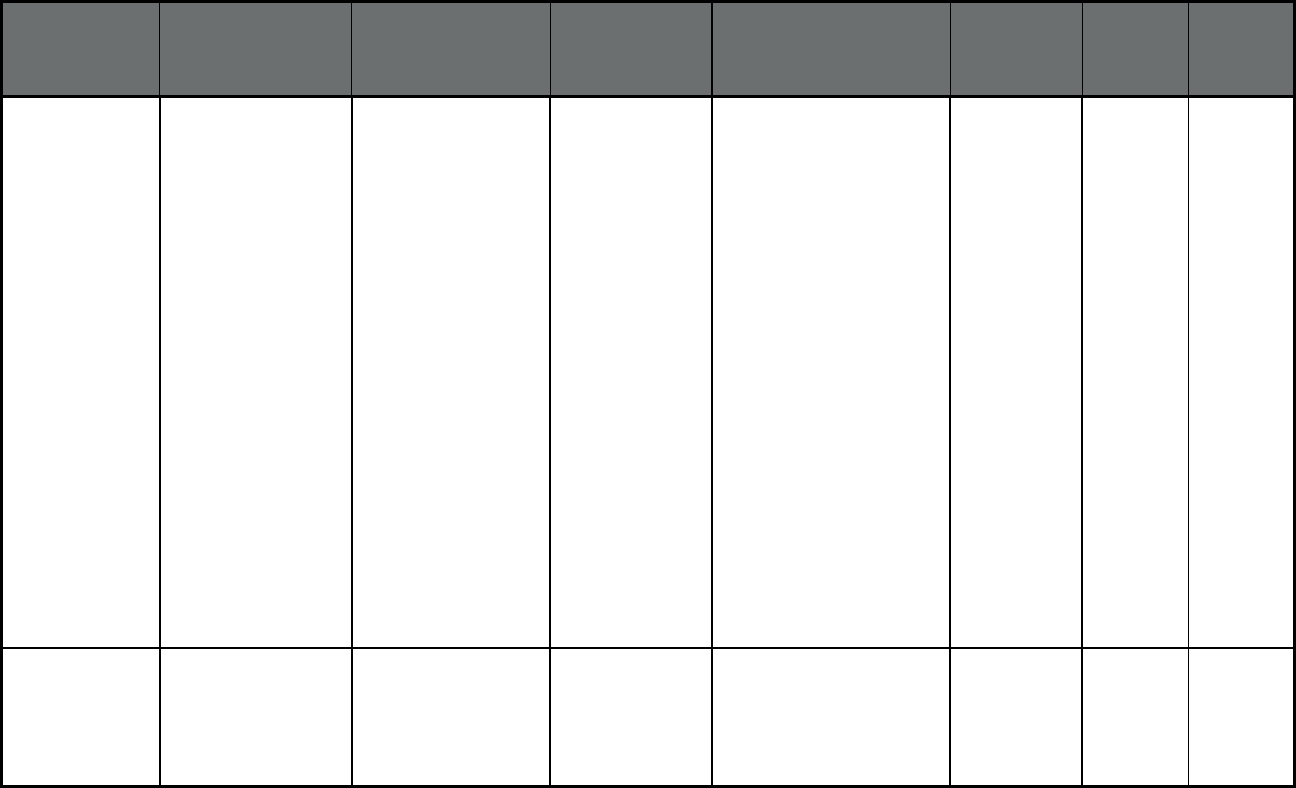
86
State
Program Name
(Type) Plan Name
Parent
Organization
Geographic Region (state-
defined areas, counties, or
zip codes)
Medicaid-Only
Enrollment
Dual
Enrollment
Total
Enrollment
Michigan Managed Care Plan
Division
(Comprehensive
MCO)
UnitedHealthcare
Community Plan
UnitedHealthcare Alcona, Allegan, Alpena,
Antrim, Arenac, Barry, Bay,
Benzie, Berrien, Branch,
Calhoun, Cass, Charlevoix,
Cheboygan, Clare,
Crawford, Emmet, Genesee,
Gladwin, Grand Traverse,
Gratiot, Hillsdale, Huron,
Ionia, Iosco, Isabella,
Jackson, Kalamazoo,
Kalkaska, Kent, Lake,
Lapeer, Leelanau, Lenewee,
Livingston, Macomb,
Manistee, Mason, Mecosta,
Midland, Missaukee,
Monroe, Montcalm,
Montmorency, Muskegon,
Newaygo, Oakland,
Oceana, Ogemaw, Osceola,
Oscoda, Otsego, Ottawa,
Presque Isle, Roscommon,
Saginaw, St. Clair, St.
Joseph, Sanilac,
Shiawassee, Tuscola, Van
Buren, Washtenaw, Wayne,
and Wexford Counties
251,312 3,240 254,552
Michigan Managed Care Plan
Division
(Comprehensive
MCO)
Upper Peninsula Health
Plan
Upper Peninsula
Health Plan
Alger, Baraga, Chippewa,
Delta, Dickinson, Gogebic,
Houghton, Iron, Keweenaw,
Luce, Mackinac, Marquette,
Menominee, Ontonagon,
and Schoolcraft Counties
43,558 8 43,566

87
State
Program Name
(Type) Plan Name
Parent
Organization
Geographic Region (state-
defined areas, counties, or
zip codes)
Medicaid-Only
Enrollment
Dual
Enrollment
Total
Enrollment
Michigan Healthy Michigan Plan
(Comprehensive
MCO)
Aetna Better Health Aetna Berrien, Branch, Calhoun,
Cass, Hillsdale, Jackson,
Kalamazoo, Lenawee,
Livingston, Macomb,
Monroe, Oakland, St.
Joseph, Van Buren,
Washtenaw, and Wayne
Counties
9,975 0 9,975
Michigan Healthy Michigan Plan
(Comprehensive
MCO)
Blue Cross Complete of
Michigan
Blue Cross Blue
Shield
Allegan, Barry, Clinton,
Eaton, Genesee, Hillsdale,
Huron, Ingham, Ionia,
Jackson, Kent, Lake,
Lapeer, Lenawee,
Livingston, Macomb, Mason,
Mecosta, Monroe,
Montcalm, Muskegon,
Newaygo, Oakland,
Oceana, Osceola, St. Clair,
Sanilac, Shiawassee,
Tuscola, Washtenaw, and
Wayne Counties
85,852 0 85,852
Michigan Healthy Michigan Plan
(Comprehensive
MCO)
Harbor Health Plan Trusted Health
Plan
Macomb, Oakland, and
Wayne Counties
3,173 0 3,173
Michigan Healthy Michigan Plan
(Comprehensive
MCO)
HAP Midwest Health
Plan
Health Alliance
Plan
Genesee, Huron, Lapeer,
St. Clair, Sanilac,
Shiawassee, and Tuscola
Counties
1,501 0 1,501
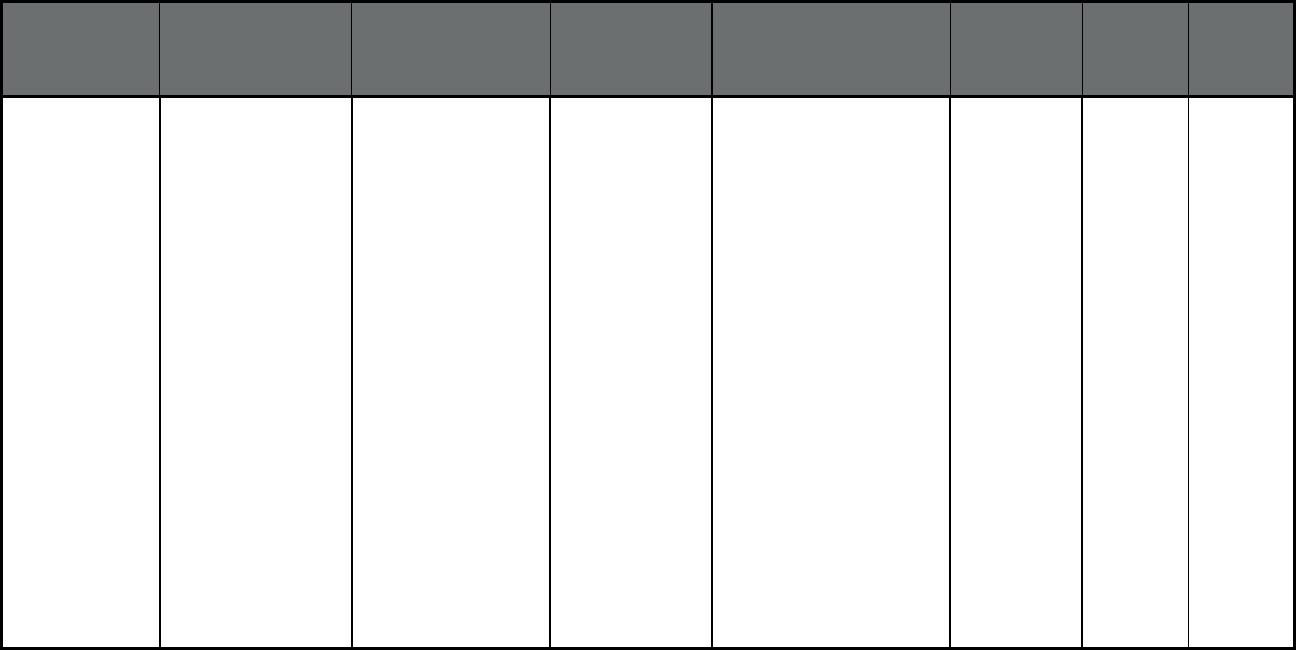
88
State
Program Name
(Type) Plan Name
Parent
Organization
Geographic Region (state-
defined areas, counties, or
zip codes)
Medicaid-Only
Enrollment
Dual
Enrollment
Total
Enrollment
Michigan Healthy Michigan Plan
(Comprehensive
MCO)
McLaren Health Plan McLaren Health
Plan
Alcona, Allegan, Alpena,
Antrim, Arenac, Barry, Bay,
Benzie, Berrien, Branch,
Calhoun, Cass, Charlevoix,
Cheboygan, Clare, Clinton,
Crawford, Eaton, Emmet,
Genesee, Gladwin, Grand
Traverse, Gratiot, Hillsdale,
Huron, Ingham, Ionia, Iosco,
Isabella, Jackson,
Kalamazoo, Kalkaska, Kent,
Lake, Lapeer, Leelanau,
Lenawee, Livingston,
Macomb, Manistee, Mason,
Mecosta, Midland,
Missaukee, Monroe,
Montcalm, Montmorency,
Muskegon, Newaygo,
Oakland, Oceana, Ogemaw,
Osceola, Oscoda, Otsego,
Ottawa, Presque Isle,
Roscommon, Saginaw, St.
Clair, St. Joseph, Sanilac,
Shiawassee, Tuscola, Van
Buren, Washtenaw, Wayne,
and Wexford Counties
68,214 0 68,214
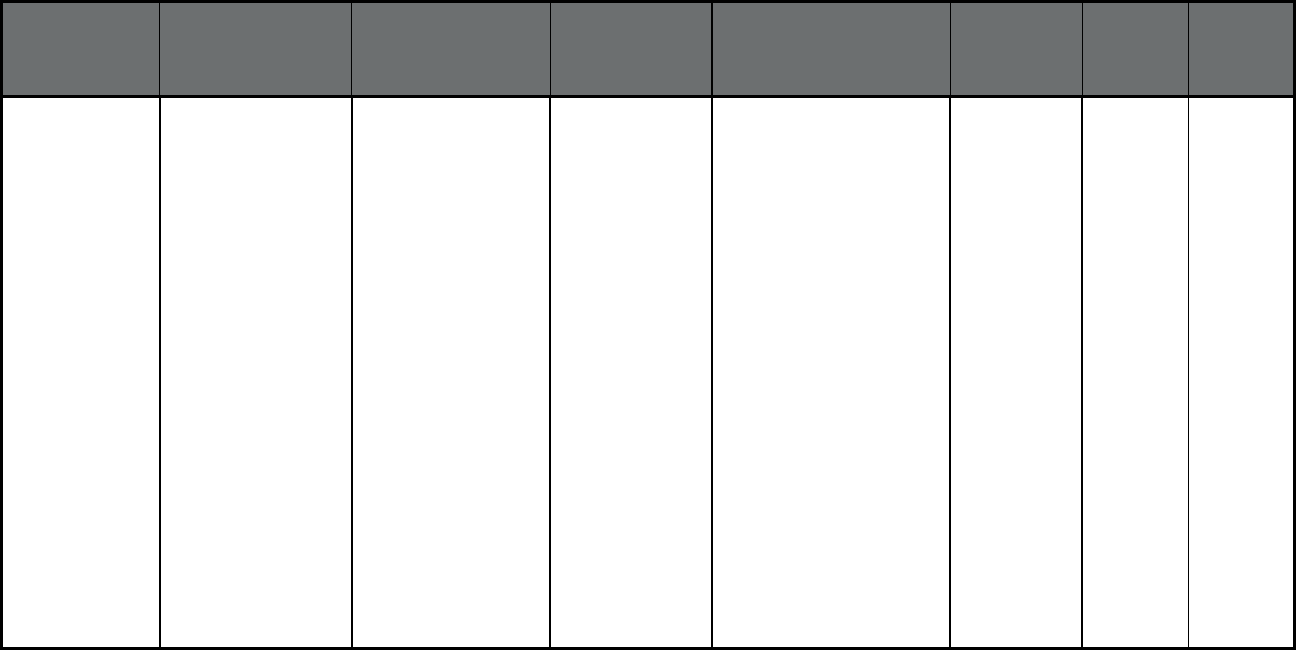
89
State
Program Name
(Type) Plan Name
Parent
Organization
Geographic Region (state-
defined areas, counties, or
zip codes)
Medicaid-Only
Enrollment
Dual
Enrollment
Total
Enrollment
Michigan Healthy Michigan Plan
(Comprehensive
MCO)
Meridian Health Plan of
Michigan
Meridian Alcona, Allegan, Alpena,
Antrim, Arenac, Barry, Bay,
Benzie, Berrien, Branch,
Calhoun, Cass, Charlevoix,
Cheboygan, Clare, Clinton,
Crawford, Eaton, Emmet,
Genesee, Gladwin, Grand
Traverse, Gratiot, Hillsdale,
Huron, Ingham, Ionia, Iosco,
Isabella, Jackson,
Kalamazoo, Kalkaska, Kent,
Lake, Lapeer, Leelanau,
Lenawee, Livingston,
Macomb, Manistee, Mason,
Mecosta, Midland,
Missaukee, Monroe,
Montcalm, Montmorency,
Muskegon, Newaygo,
Oakland, Oceana, Ogemaw,
Osceola, Oscoda, Otsego,
Ottawa, Presque Isle,
Roscommon, Saginaw, St.
Clair, St. Joseph, Sanilac,
Shiawassee, Tuscola, Van
Buren, Washtenaw, Wayne,
and Wexford Counties
152,706 0 152,706
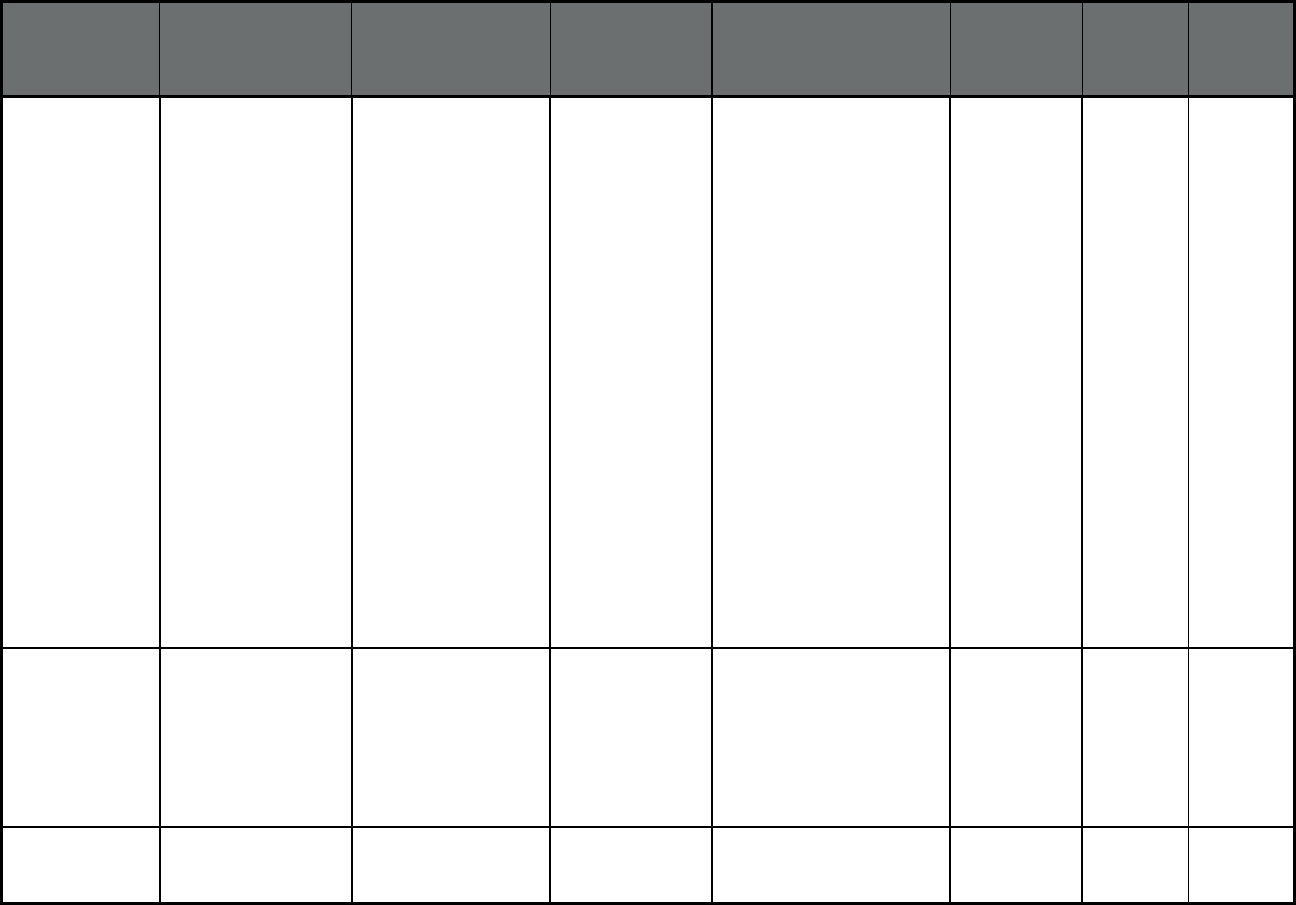
90
State
Program Name
(Type) Plan Name
Parent
Organization
Geographic Region (state-
defined areas, counties, or
zip codes)
Medicaid-Only
Enrollment
Dual
Enrollment
Total
Enrollment
Michigan Healthy Michigan Plan
(Comprehensive
MCO)
Molina Healthcare of
Michigan
Molina Healthcare Alcona, Allegan, Alpena,
Antrim, Arenac, Barry, Bay,
Benzie, Berrien, Branch,
Calhoun, Cass, Charlevoix,
Cheboygan, Clare, Clinton,
Crawford, Eaton, Emmet,
Genesee, Gladwin, Grand
Traverse, Gratiot, hillsdale,
Huron, Ingham, Ionia, Iosco,
Isabella, Jackson,
Kalamazoo, Kalkaska, Kent,
Lake, Lapeer, Leelanau,
Lenawee, Livingston,
Macomb, Manistee, Mason,
Mecosta, Midland,
Missaukee, Monroe,
Montcalm, Montmorency,
Muskegon, Newaygo,
Oakland, Oceana, Ogemaw,
Osceola, Oscoda, Otsego,
Ottawa, Presque Isle,
Roscommon, Saginaw, St.
Clair, St. Joseph, Sanilac,
Shiawassee, Tuscola, Van
Buren, Washtenaw, Wayne,
and Wexford Counties
93,375 0 93,375
Michigan Healthy Michigan Plan
(Comprehensive
MCO)
Priority Health Choice Priority Health
Choice, Inc.
Allegan, Barry, Berrien,
Branch, Calhoun, Cass,
Ionia, Kalamazoo, Kent,
Lake, Mason, Mecosta,
Montcalm, Muskegon,
Newaygo, Oceana, Osceola,
Ottawa, St. Joseph, and Van
Buren Counties
36,872 0 36,872
Michigan Healthy Michigan Plan
(Comprehensive
MCO)
Total Health Choice Total Health
Choice
Macomb, Oakland, and
Wayne Counties
16,804 0 16,804
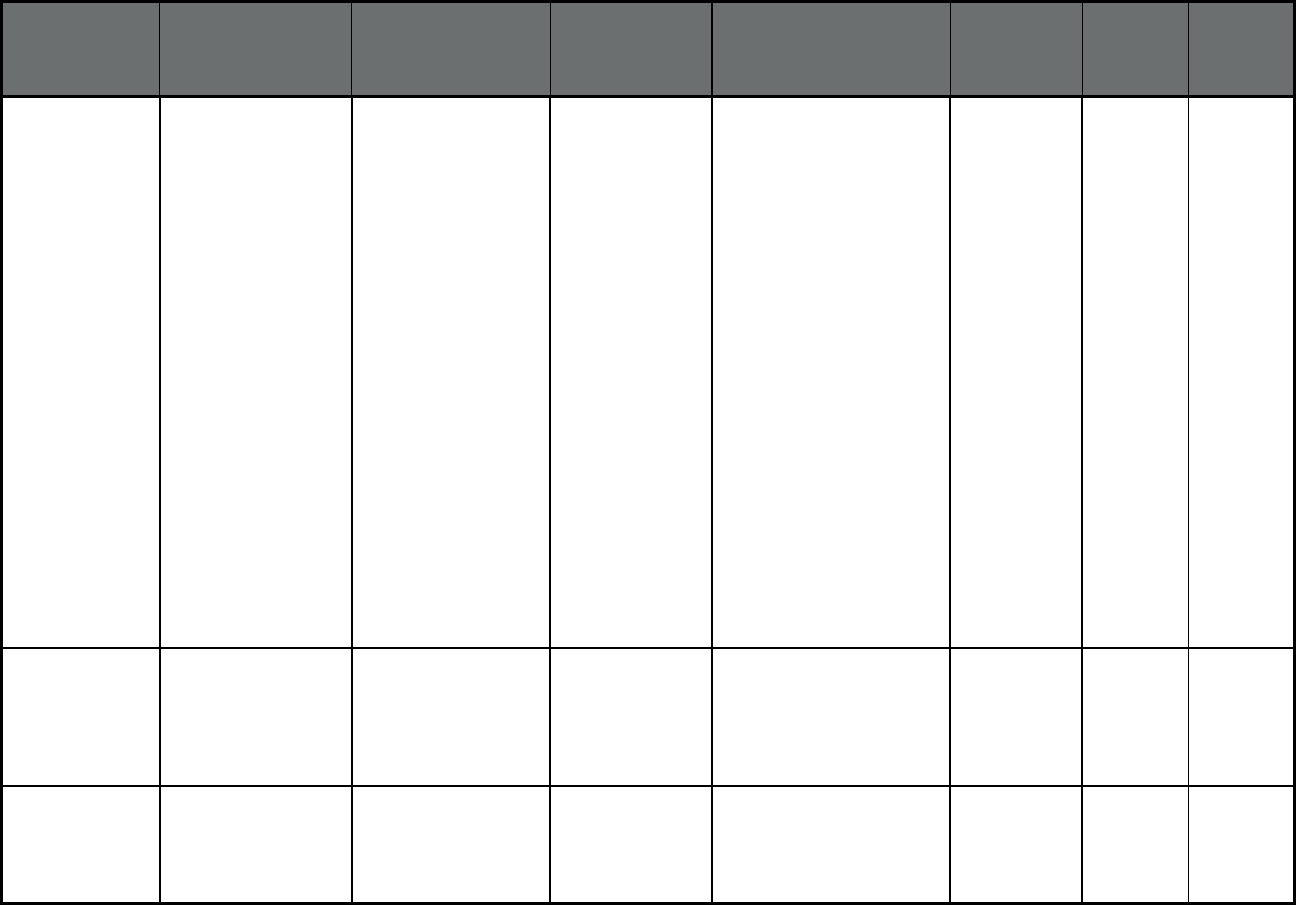
91
State
Program Name
(Type) Plan Name
Parent
Organization
Geographic Region (state-
defined areas, counties, or
zip codes)
Medicaid-Only
Enrollment
Dual
Enrollment
Total
Enrollment
Michigan Healthy Michigan Plan
(Comprehensive
MCO)
UnitedHealthcare
Community Plan
UnitedHealthcare Alcona, Allegan, Alpena,
Antrim, Arenac, Barry, Bay,
Benzie, Berrien, Branch,
Calhoun, Cass, Charlevoix,
Cheboygan, Clare,
Crawford, Emmet,
Genesee,
Gladwin, Grand Traverse,
Gratiot, Hillsdale, Huron,
Ionia, Iosco, Isabella,
Jackson, Kalamazoo,
Kalkaska, Kent, Lake
Lapeer, Leelanau, Lenawee,
Livingston, Macomb,
Manistee, Mason, Mecosta,
Midland, Missaukee,
Monroe, Montcalm,
Montmorency, Muskegon,
Newaygo, Oakland,
Oceana, Ogemaw, Osceola,
Oscoda, Otsego, Ottawa,
Presque Isle, Roscommon,
Saginaw, St. Clair, St.
Joseph, Sanilac,
Shiawassee, Tuscola, Van
Buren, Washtenaw, Wayne,
and Wexford Counties
70,061 0 70,061
Michigan Healthy Michigan Plan
(Comprehensive
MCO)
Upper Peninsula Health
Plan
Upper Peninsula
Health Plan
Alger, Baraga, Chippewa,
Delta, Dickinson, Gogebic,
Houghton, Iron, Keweenaw,
Luce, Mackinac, Marquette,
Menominee, Ontonagon,
and Schoolcraft Counties
15,670 0 15,670
Michigan MI Choice (MLTSS
only (PIHP and/or
PAHP))
Northern Healthcare
Management
Northern Lakes
Community Mental
Health
Antrim, Benzie, Charlevoix,
Emmet, Grand Traverse,
Kalkaska, Leelanau,
Manistee, Missaukee, and
Wexford Counties
29 304 333
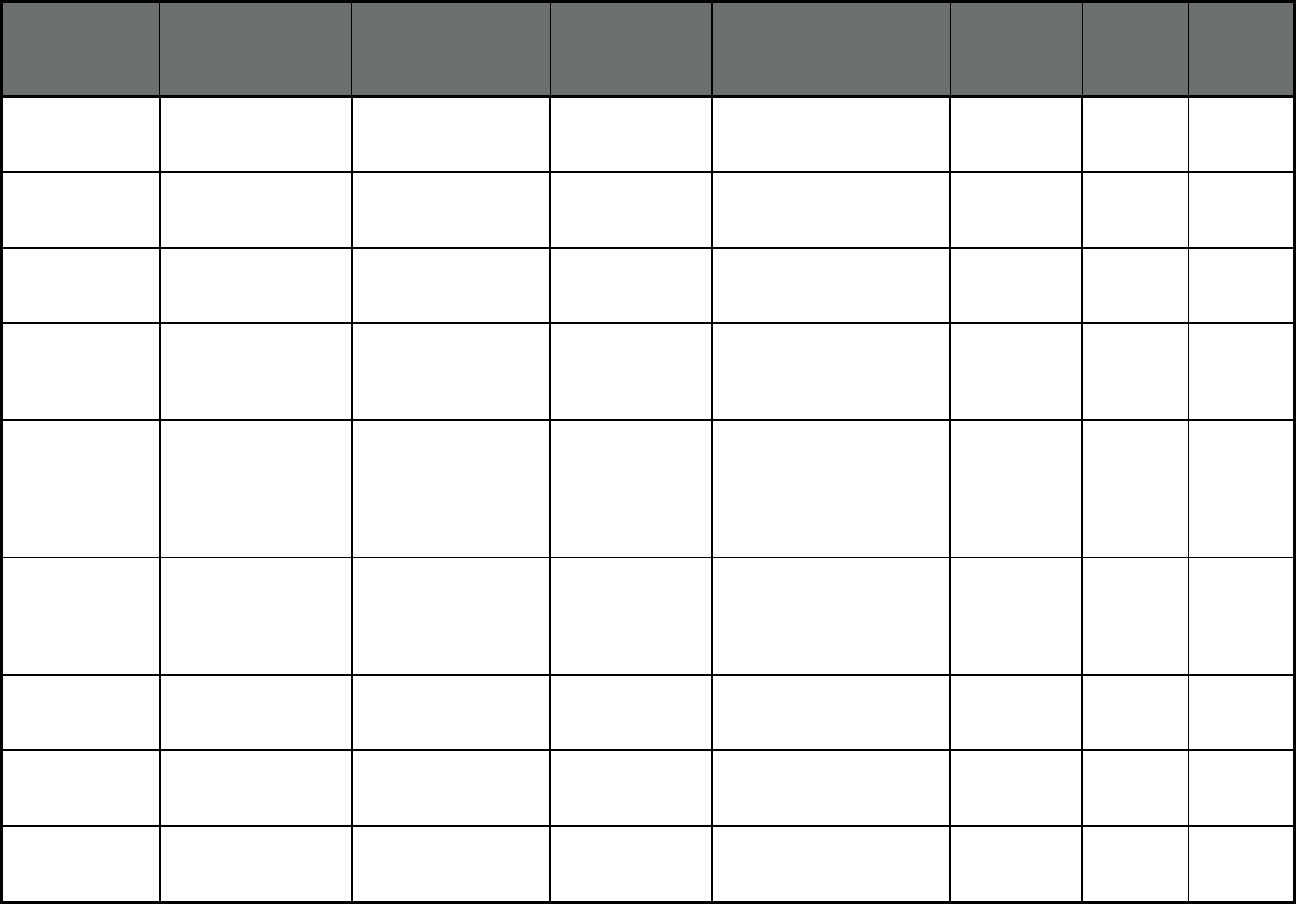
92
State
Program Name
(Type) Plan Name
Parent
Organization
Geographic Region (state-
defined areas, counties, or
zip codes)
Medicaid-Only
Enrollment
Dual
Enrollment
Total
Enrollment
Michigan MI Choice (MLTSS
only (PIHP and/or
PAHP))
Region 2 Area Agency
on Aging
Area Agencies on
Aging
Hillsdale, Jackson, and
Lenawee Counties
27 566 593
Michigan MI Choice (MLTSS
only (PIHP and/or
PAHP))
Region 3B Area
Agency on Aging
Area Agencies on
Aging
Barry, Berrien, Branch,
Calhoun, Cass, Kalamazoo,
and Van Buren Counties
34 448 482
Michigan MI Choice (MLTSS
only (PIHP and/or
PAHP))
Region 4 Area Agency
on Aging
Area Agencies on
Aging
Berrien, Cass, and Van
Buren Counties
24 433 457
Michigan MI Choice (MLTSS
only (PIHP and/or
PAHP))
Region 7 Area Agency
on Aging
Area Agencies on
Aging
Bay, Clare, Gladwin, Gratiot,
Huron, Isabella, Midland,
Saginaw, Sanilac, and
Tuscola Counties
56 802 858
Michigan MI Choice (MLTSS
only (PIHP and/or
PAHP))
Region 9 Area Agency
on Aging
Area Agencies on
Aging
Alcona, Alpena, Arenac,
Cheboygan, Crawford,
Iosco, Montmorency,
Ogemaw, Oscoda, Otsego,
Presque Isle, and
Roscommon Counties
25 379 404
Michigan MI Choice (MLTSS
only (PIHP and/or
PAHP))
Reliance Community
Care Partners
Community Care
Health Plan (WI)
Allegan, Ionia, Kent, Lake,
Mason, Mecosta,
Muskegon, Newaygo,
Oceana, Osceola, and
Ottawa Counties
43 573 616
Michigan MI Choice (MLTSS
only (PIHP and/or
PAHP))
Senior Resources of
West Michigan
Area Agencies on
Aging
Muskegon, Oceana, and
Ottawa Counties
32 646 678
Michigan MI Choice (MLTSS
only (PIHP and/or
PAHP))
Senior Services Inc. Senior Services
Inc.
Barry, Branch, Calhoun, and
Kalamazoo Counties
21 255 276
Michigan MI Choice (MLTSS
only (PIHP and/or
PAHP))
The Information Center The Information
Center
Wayne County 13 274 287
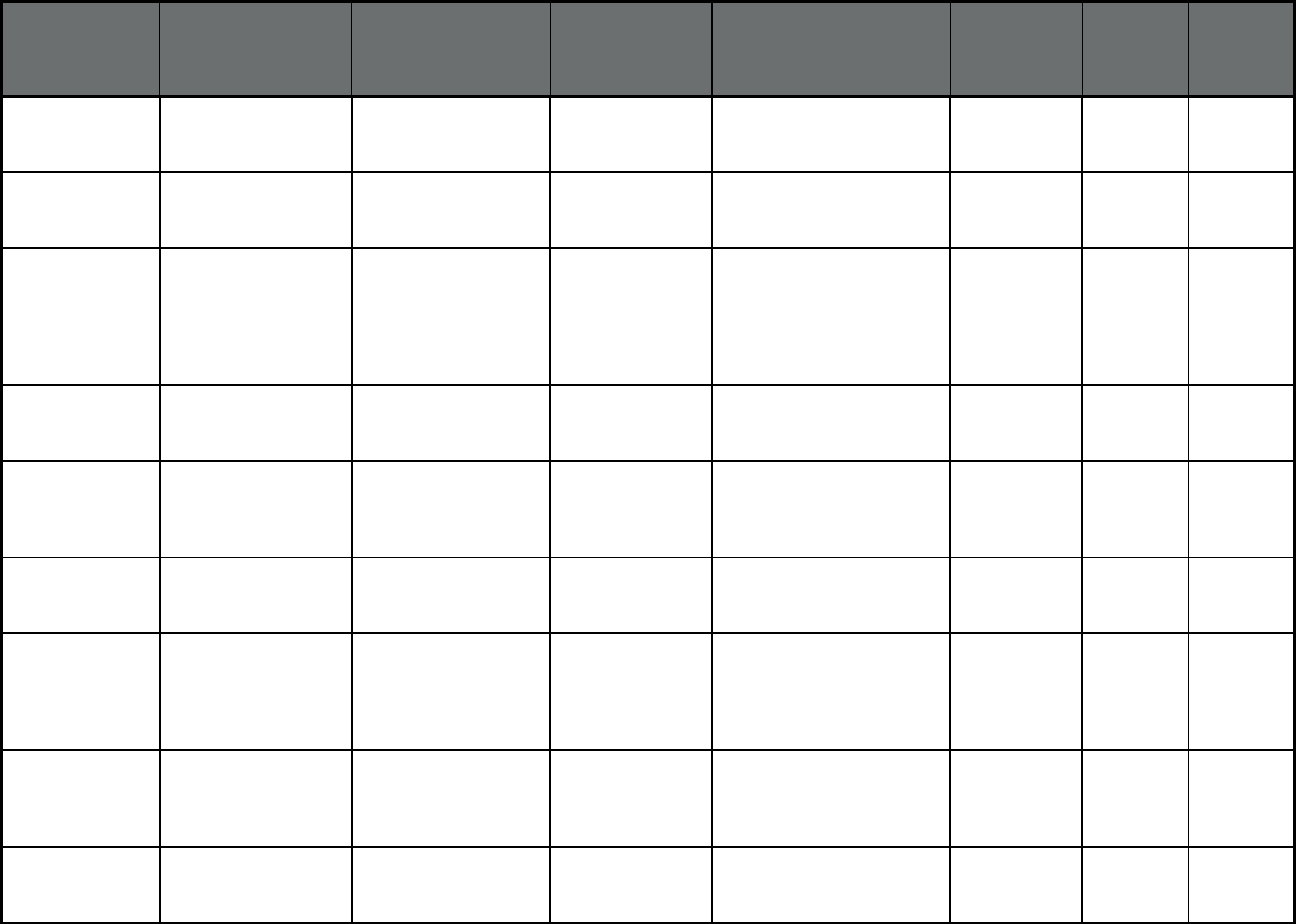
93
State
Program Name
(Type) Plan Name
Parent
Organization
Geographic Region (state-
defined areas, counties, or
zip codes)
Medicaid-Only
Enrollment
Dual
Enrollment
Total
Enrollment
Michigan MI Choice (MLTSS
only (PIHP and/or
PAHP))
The Senior Alliance Area Agencies on
Aging
Wayne County 20 506 526
Michigan MI Choice (MLTSS
only (PIHP and/or
PAHP))
Tri County Office on
Aging
Tri County Office
on Aging
Clinton, Eaton, and Ingham
Counties
81 649 730
Michigan MI Choice (MLTSS
only (PIHP and/or
PAHP))
UPCAP Area Agency
on Aging
Area Agencies on
Aging
Alger, Baraga, Chippewa,
Delta, Dickinson, Gogebic,
Houghton, Iron, Keweenaw,
Luce, Mackinac, Marquette,
Menominee, Ontonagon,
and Schoolcraft Counties
24 349 373
Michigan MI Choice (MLTSS
only (PIHP and/or
PAHP))
Valley Area Agency on
Aging
Area Agencies on
Aging
Genesee, Lapeer, and
Shiawassee Counties
26 309 335
Michigan MI Choice (MLTSS
only (PIHP and/or
PAHP))
A & D Home Health
Care, Inc.
A & D Home
Heatlh Care, Inc.
Bay, Clare, Gladwin, Huron,
Isabella, Midland, Saginaw,
Sanilac, and Tuscola
Counties
90 778 868
Michigan MI Choice (MLTSS
only (PIHP and/or
PAHP))
Area Agency on Aging
1-B
Area Agencies on
Aging
Livingston, Macomb,
Monroe, Oakland, and
Washtenaw Counties
42 768 810
Michigan MI Choice (MLTSS
only (PIHP and/or
PAHP))
Area Agency on Aging
of NW Michigan
Area Agencies on
Aging
Antrim, Benzie Charlevoix,
Emmet, Grand Traverse,
Kalkaska, Leelanau,
Manistee, Missaukee, and
Wexford Counties
21 316 337
Michigan MI Choice (MLTSS
only (PIHP and/or
PAHP))
Area Agency on Aging
of Western Michigan
Area Agencies on
Aging
Allegan, Ionia, Kent, Lake,
Mason, Mecosta, Montcalm,
Newaygo, and Osceola
Counties
35 799 834
Michigan MI Choice (MLTSS
only (PIHP and/or
PAHP))
Detroit Area Agency on
Aging
Area Agencies on
Aging
Wayne County 56 1,201 1,257
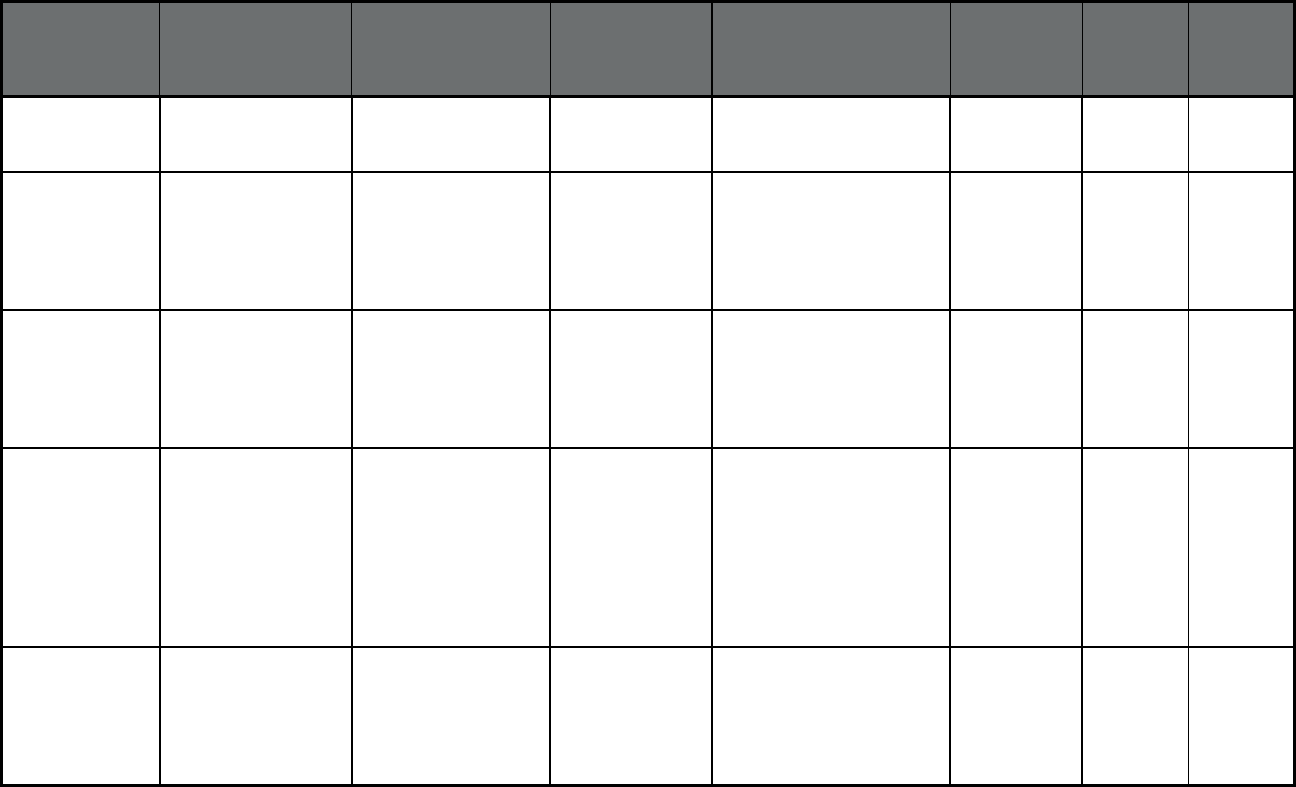
94
State
Program Name
(Type) Plan Name
Parent
Organization
Geographic Region (state-
defined areas, counties, or
zip codes)
Medicaid-Only
Enrollment
Dual
Enrollment
Total
Enrollment
Michigan MI Choice (MLTSS
only (PIHP and/or
PAHP))
MORC Home Care Inc. MORC Home Care
Inc.
Livingston, Macomb,
Monroe, Oakland, and
Washtenaw Counties
9 232 241
Michigan
7
Specialty Prepaid
Inpatient Health Plan
(Behavioral Health
Organization (BHO)
only (PIHP and/or
PAHP))
Lakeshore Regional
Entity
Lakeshore
Regional Entity
Allegan, Kent, Lake, Mason,
Muskegon, Oceana, and
Ottawa Counties
249,865 0 249,865
Michigan
7
Specialty Prepaid
Inpatient Health Plan
(Behavioral Health
Organization (BHO)
only (PIHP and/or
PAHP))
Macomb County CMH
Services
Macomb County
CMH Services
Macomb County 179,951 0 179,951
Michigan
7
Specialty Prepaid
Inpatient Health Plan
(Behavioral Health
Organization (BHO)
only (PIHP and/or
PAHP))
Mid-State Health
Network
Mid-State Health
Network
Arenac, Bay, Clare, Clinton,
Eaton, Gladwin, Gratiot,
Hillsdale, Huron, Ingham,
Ionia, Isabella, Jackson,
Mecosta, Midland,
Montcalm, Newaygo,
Oceola, Saginaw,
Shiawassee, and Tuscola
Counties
367,503 0 367,503
Michigan
7
Specialty Prepaid
Inpatient Health Plan
(Behavioral Health
Organization (BHO)
only (PIHP and/or
PAHP))
Northcare Network Northcare Network Alger, Baraga, Chippewa,
Delta, Dickinson, Houghton,
Iron, Keewanaw, Luce,
Mackinac, Marquette,
Menominee, Ontonagon,
and Schoolcraft Counties
63,431 0 63,431
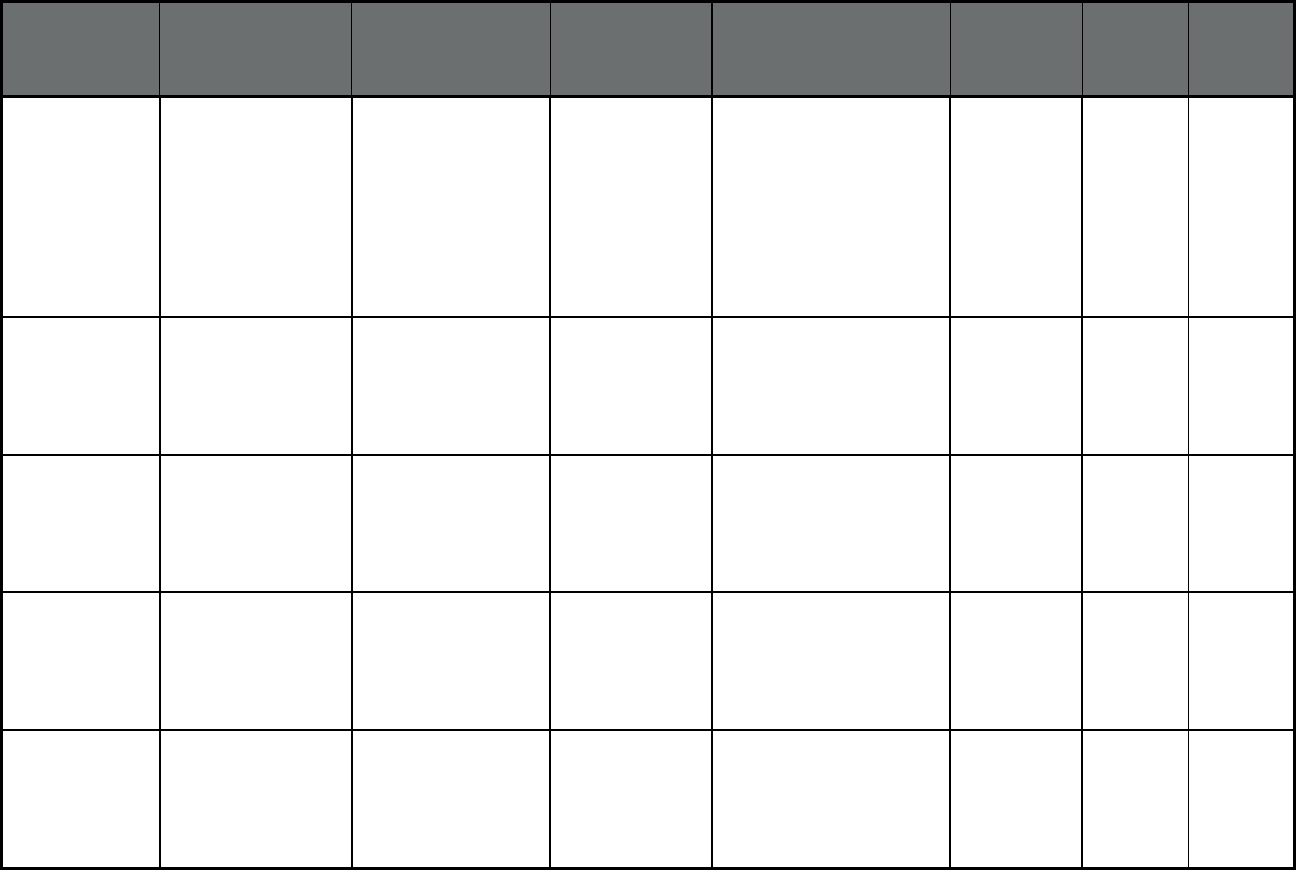
95
State
Program Name
(Type) Plan Name
Parent
Organization
Geographic Region (state-
defined areas, counties, or
zip codes)
Medicaid-Only
Enrollment
Dual
Enrollment
Total
Enrollment
Michigan
7
Specialty Prepaid
Inpatient Health Plan
(Behavioral Health
Organization (BHO)
only (PIHP and/or
PAHP))
Northern Michigan
Regional Entity
Northern Michigan
Regional Entity
Alcona, Alpena, Antrim,
Benzie, Charlevoix,
Cheboygan, Crawford,
Emmet, Grand Traverse,
Iosco, Kalkaska, Leelanau,
Manistee, Missaukee,
Montmorency, Ogemaw,
Oscoda, Otsego, Presque
Isle, Roscommon, and
Wexford Counties
115,735 0 115,735
Michigan
7
Specialty Prepaid
Inpatient Health Plan
(Behavioral Health
Organization (BHO)
only (PIHP and/or
PAHP))
Oakland County CMH
Authority
Oakland County
CMH Authority
Oakland County 170,905 0 170,905
Michigan
7
Specialty Prepaid
Inpatient Health Plan
(Behavioral Health
Organization (BHO)
only (PIHP and/or
PAHP))
Region 10 Region 10 Genesee, Lapeer, Sanilac,
and St. Clair Counties
187,376 0 187,376
Michigan
7
Specialty Prepaid
Inpatient Health Plan
(Behavioral Health
Organization (BHO)
only (PIHP and/or
PAHP))
Southwest Michigan
Behavioral Health
Southwest
Michigan
Behavioral Health
Berry, Berrien, Branch,
Calhoun, Cass, Kalamazoo,
St. Joseph, and Van Buren
Counties
193,479 0 193,479
Michigan
7
Specialty Prepaid
Inpatient Health Plan
(Behavioral Health
Organization (BHO)
only (PIHP and/or
PAHP))
CMH Partnership of
Southeast Michigan
CMH Partnership
of Southeast
Michigan
Lenawee, Livingston,
Monroe, and Washtenaw
Counties
115,556 0 115,556
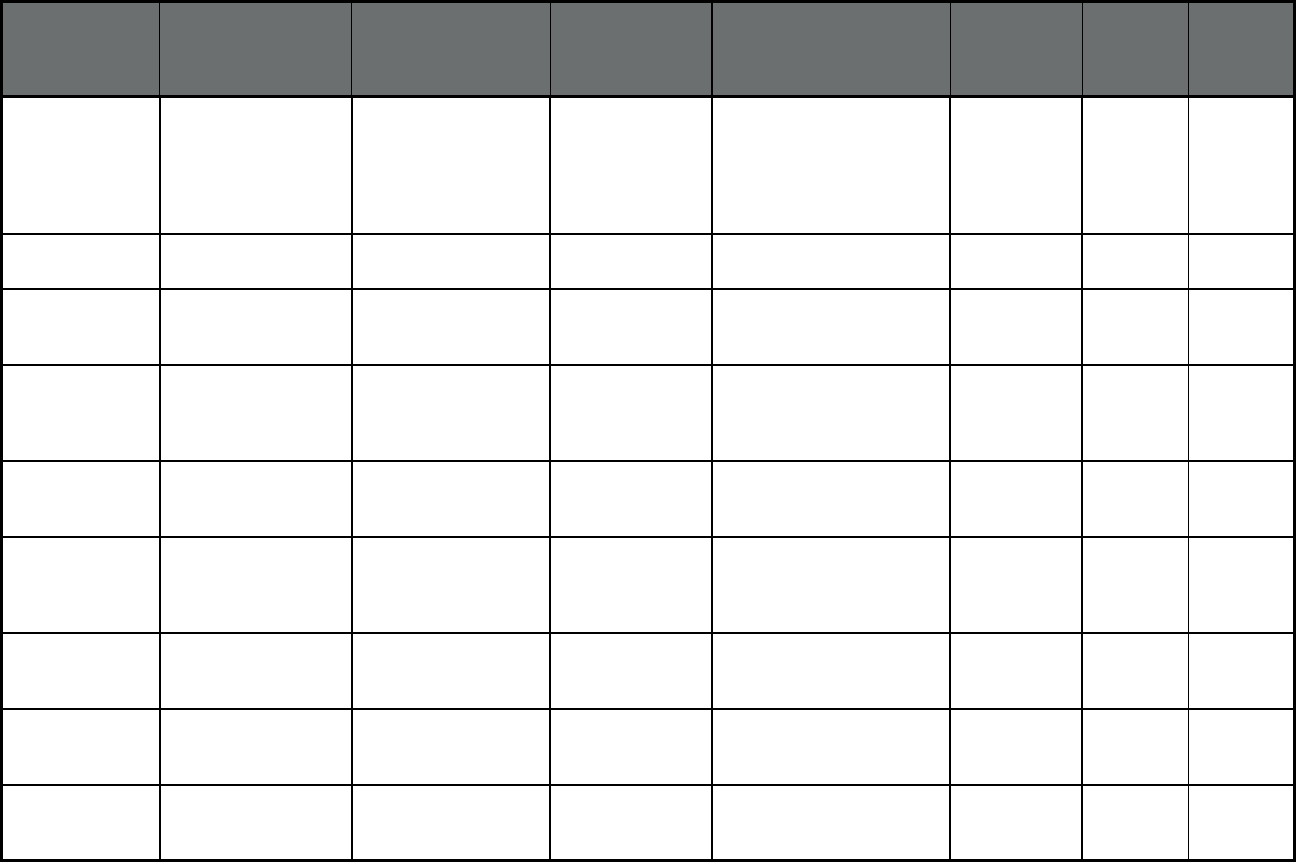
96
State
Program Name
(Type) Plan Name
Parent
Organization
Geographic Region (state-
defined areas, counties, or
zip codes)
Medicaid-Only
Enrollment
Dual
Enrollment
Total
Enrollment
Michigan
7
Specialty Prepaid
Inpatient Health Plan
(Behavioral Health
Organization (BHO)
only (PIHP and/or
PAHP))
Detroit Wayne Mental
Health Authority
Detroit Wayne
Mental Health
Authority
Wayne County 632,552 0 632,552
Michigan Healthy Kids Dental
(Dental only (PAHP))
Healthy Kids Dental Healthy Kids
Dental
Statewide 969,152 0 969,152
Michigan PACE (Program of All-
inclusive Care for the
Elderly (PACE))
Care Resources PACE Kent and Ottawa Counties 8 220 228
Michigan PACE (Program of All-
inclusive Care for the
Elderly (PACE))
Community PACE PACE Lake, Mason, Mecosta,
Montcalm, Newaygo,
Oceana, and Osceola
Counties
0 28 28
Michigan PACE (Program of All-
inclusive Care for the
Elderly (PACE))
Genesys PACE PACE Genesee County 8 77 85
Michigan PACE (Program of All-
inclusive Care for the
Elderly (PACE))
Great Lakes PACE PACE Arenac, Bay, Gratiot,
Midland, Saginaw,
Shiawassee, and Tuscola
Counties
12 109 121
Michigan PACE (Program of All-
inclusive Care for the
Elderly (PACE))
Huron Valley PACE PACE Livingston, Monroe,
Oakland, Wayne, and
Washtenaw Counties
1 174 175
Michigan PACE (Program of All-
inclusive Care for the
Elderly (PACE))
Life Circles PACE Muskegon County, parts of
Allegan and Ottawa
Counties
11 300 311
Michigan PACE (Program of All-
inclusive Care for the
Elderly (PACE))
PACE of Southeast MI PACE Macomb, Oakland, and
Wayne Counties
37 715 752
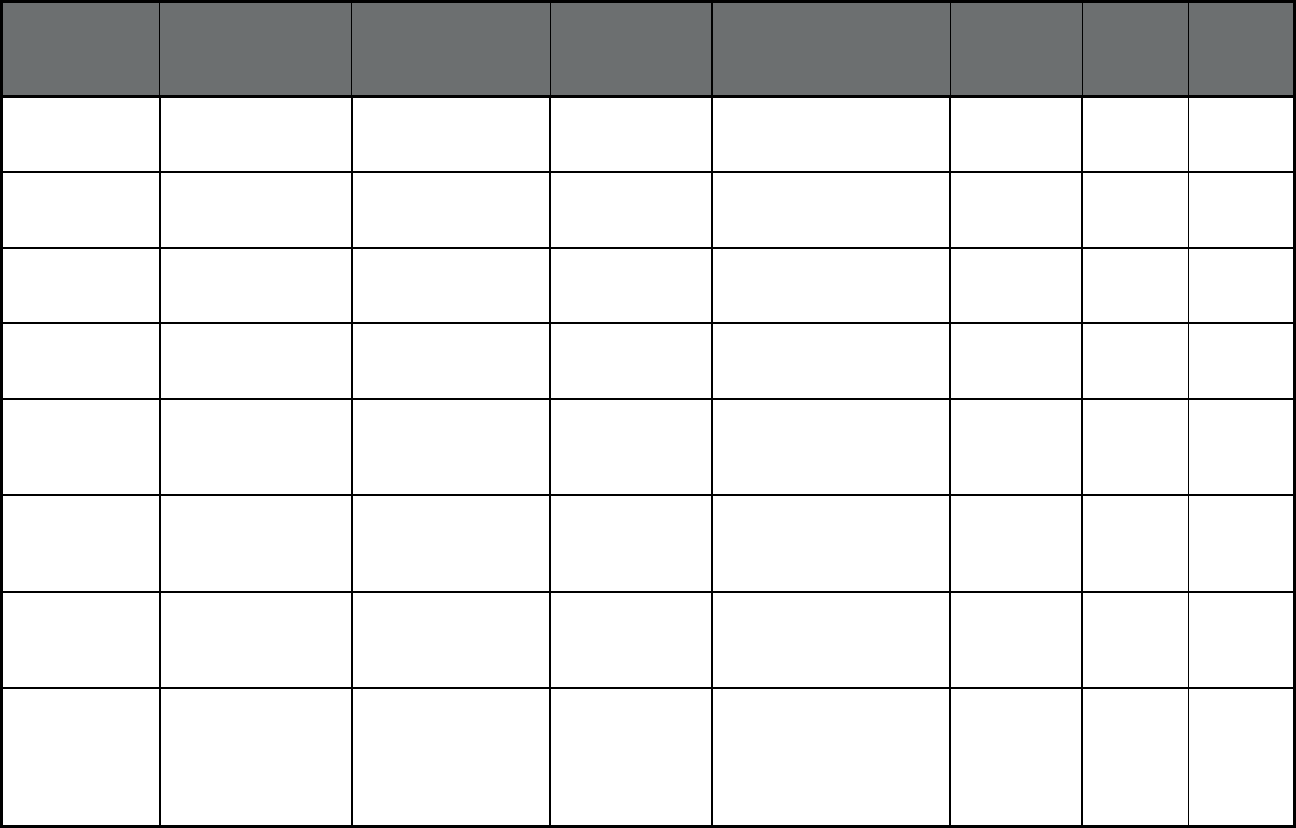
97
State
Program Name
(Type) Plan Name
Parent
Organization
Geographic Region (state-
defined areas, counties, or
zip codes)
Medicaid-Only
Enrollment
Dual
Enrollment
Total
Enrollment
Michigan PACE (Program of All-
inclusive Care for the
Elderly (PACE))
PACE of Southwest MI PACE Berrien, Cass, and Van
Buren Counties
4 167 171
Michigan PACE (Program of All-
inclusive Care for the
Elderly (PACE))
Senior Care Partners PACE Calhoun, Kalamazoo,
Allegan, Barry, and Van
Buren Counties
18 396 414
Michigan PACE (Program of All-
inclusive Care for the
Elderly (PACE))
Senior Community
Care
PACE Barry, Clinton, Eaton,
Ingham, Ionia, Livingston,
and Shiawassee Counties
11 139 150
Michigan PACE (Program of All-
inclusive Care for the
Elderly (PACE))
Thome PACE PACE Hillsdale, Jackson, and
Lenawee Counties
6 104 110
Minnesota Special Needs Basic
Care (SNBC)
(Comprehensive MCO
+ MLTSS)
Health Partners Health Partners,
Inc.
Statewide 2,387 2,795 5,182
Minnesota Special Needs Basic
Care (SNBC)
(Comprehensive MCO
+ MLTSS)
Hennepin Health Hennepin Health
Systems
Hennepin County 1,143 858 2,001
Minnesota Special Needs Basic
Care (SNBC)
(Comprehensive MCO
+ MLTSS)
Medica Medica Holding
Company
Statewide 5,956 6,833 12,789
Minnesota Special Needs Basic
Care (SNBC)
(Comprehensive MCO
+ MLTSS)
Prime West Prime West Health Beltrami, Bigstone,
Clearwater, Douglas, Grant,
Hubbard, McLeod, Meeker,
Pipestone, Pope, Renville,
Stevens, and Traverse
Counties
802 1,423 2,225
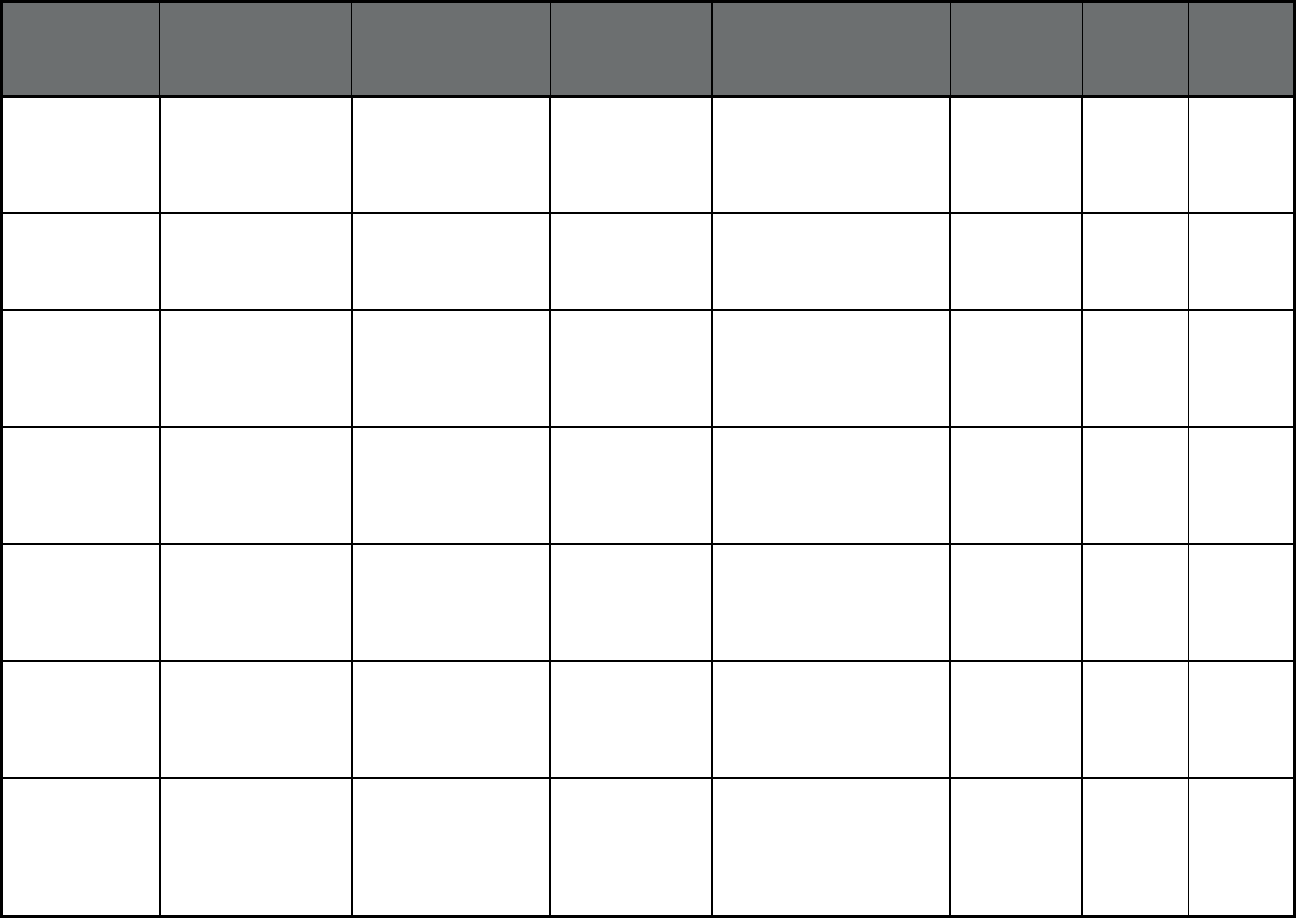
98
State
Program Name
(Type) Plan Name
Parent
Organization
Geographic Region (state-
defined areas, counties, or
zip codes)
Medicaid-Only
Enrollment
Dual
Enrollment
Total
Enrollment
Minnesota Special Needs Basic
Care (SNBC)
(Comprehensive MCO
+ MLTSS)
South Country South Country
Health Alliance
Brown, Dodge, Freeborn,
Kanabec, Morrison, Sibley,
Steele, Todd, Wabasha,
Wadena, and Waseca
Counties
987 1,957 2,944
Minnesota Special Needs Basic
Care (SNBC)
(Comprehensive MCO
+ MLTSS)
U Care U Care of
Minnesota
Statewide 13,781 14,795 28,576
Minnesota Prepaid Medical
Assistance Plan Plus
(PMAP+)
(Comprehensive MCO
+ MLTSS)
Blue Plus Blue Cross Blue
Shield
Statewide 325,097 0 325,097
Minnesota Prepaid Medical
Assistance Plan Plus
(PMAP+)
(Comprehensive MCO
+ MLTSS)
Health Partners Health Partners,
Inc.
Statewide 135,270 0 135,270
Minnesota Prepaid Medical
Assistance Plan Plus
(PMAP+)
(Comprehensive MCO
+ MLTSS)
Hennepin Health Hennepin Health
Systems
Hennepin County 23,811 0 23,811
Minnesota Prepaid Medical
Assistance Plan Plus
(PMAP+)
(Comprehensive MCO
+ MLTSS)
Itasca Medical Care Itasca Medical
Care
Itasca County 7,282 0 7,282
Minnesota Prepaid Medical
Assistance Plan Plus
(PMAP+)
(Comprehensive MCO
+ MLTSS)
Prime West Prime West Health Beltrami, Bigstone,
Clearwater, Douglas, Grant,
Hubbard, McLeod, Meeker,
Pipestone, Pope, Renville,
Stevens, and Traverse
Counties
34,842 0 34,842
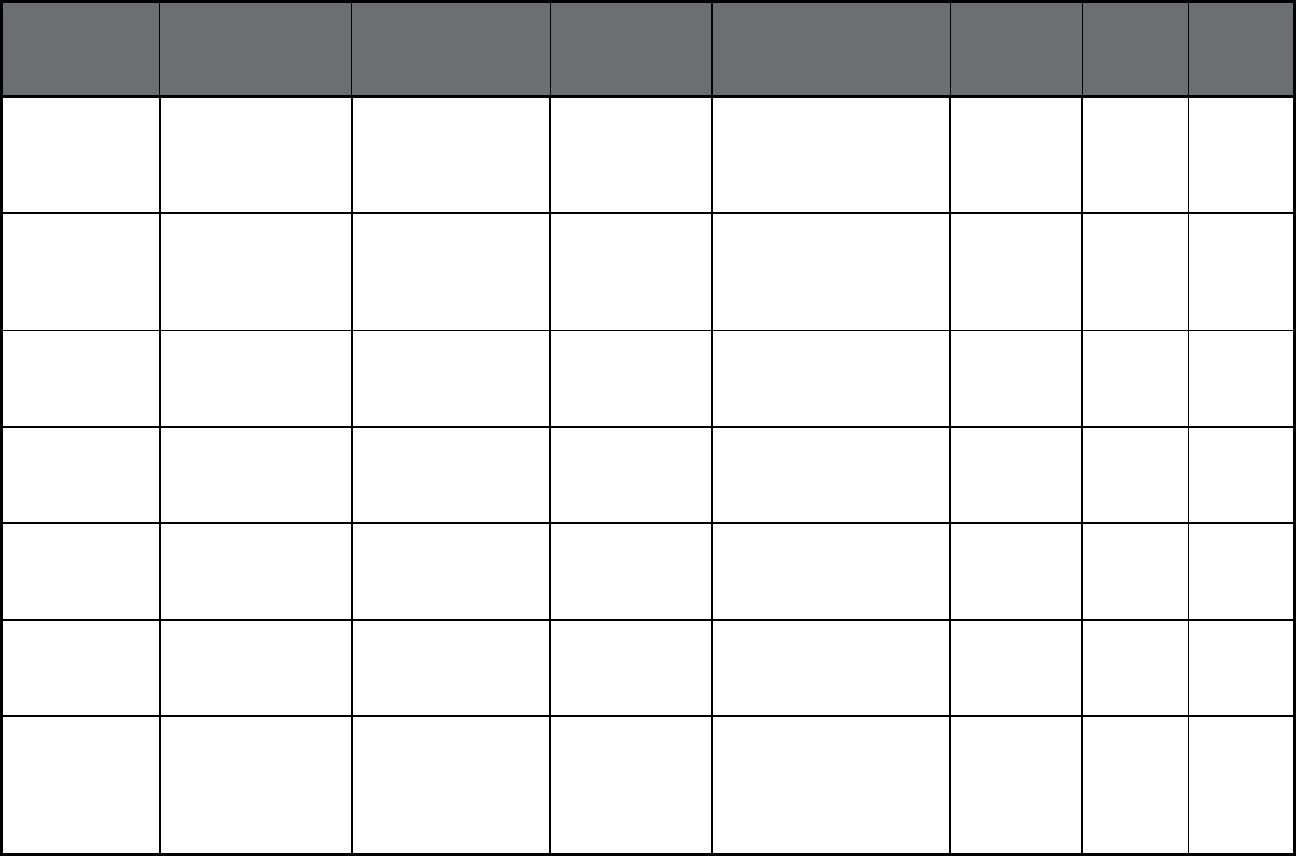
99
State
Program Name
(Type) Plan Name
Parent
Organization
Geographic Region (state-
defined areas, counties, or
zip codes)
Medicaid-Only
Enrollment
Dual
Enrollment
Total
Enrollment
Minnesota Prepaid Medical
Assistance Plan Plus
(PMAP+)
(Comprehensive MCO
+ MLTSS)
South Country South Country
Health Alliance
Brown, Dodge, Freeborn,
Kanabec, Morrison, Sibley,
Steele, Todd, Wabasha,
Wadena, and Waseca
Counties
32,964 0 32,964
Minnesota Prepaid Medical
Assistance Plan Plus
(PMAP+)
(Comprehensive MCO
+ MLTSS)
U Care U Care of
Minnesota
Statewide 224,055 0 224,055
Minnesota Minnesota Senior
Care Plus (MSC+)
(Comprehensive MCO
+ MLTSS)
Blue Plus Blue Cross Blue
Shield
Statewide 397 3,057 3,454
Minnesota Minnesota Senior
Care Plus (MSC+)
(Comprehensive MCO
+ MLTSS)
Health Partners Health Partners,
Inc.
Statewide 271 2,000 2,271
Minnesota Minnesota Senior
Care Plus (MSC+)
(Comprehensive MCO
+ MLTSS)
Itasca Medical Care Itasca Medical
Care
Itasca County 2 216 218
Minnesota Minnesota Senior
Care Plus (MSC+)
(Comprehensive MCO
+ MLTSS)
Medica Medica Holding
Company
Statewide 567 3,400 3,967
Minnesota Minnesota Senior
Care Plus (MSC+)
(Comprehensive MCO
+ MLTSS)
Prime West Prime West Health Beltrami, Bigstone,
Clearwater, Douglas, Grant,
Hubbard, McLeod, Meeker,
Pipestone, Pope, Renville,
Stevens, and Traverse
Counties
19 817 836
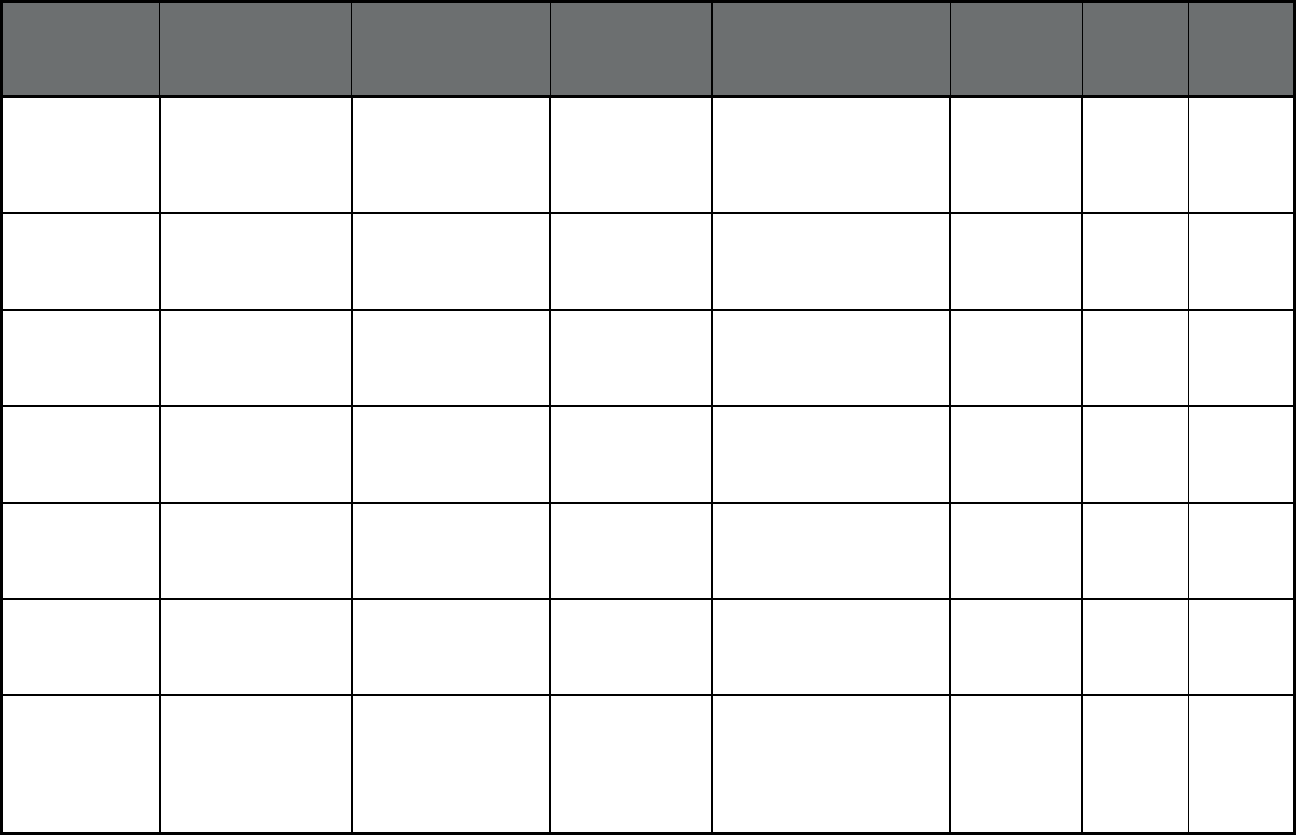
100
State
Program Name
(Type) Plan Name
Parent
Organization
Geographic Region (state-
defined areas, counties, or
zip codes)
Medicaid-Only
Enrollment
Dual
Enrollment
Total
Enrollment
Minnesota Minnesota Senior
Care Plus (MSC+)
(Comprehensive MCO
+ MLTSS)
South Country South Country
Health Alliance
Brown, Dodge, Freeborn,
Kanabec, Morrison, Sibley,
Steele, Todd, Wabasha,
Wadena, and Waseca
Counties
34 798 832
Minnesota Minnesota Senior
Care Plus (MSC+)
(Comprehensive MCO
+ MLTSS)
U Care U Care of
Minnesota
Statewide 1,353 3,360 4,713
Minnesota Minnesota Senior
Health Option (MSHO)
(Comprehensive MCO
+ MLTSS)
Blue Plus Blue Cross Blue
Shield
Statewide 0 8,607 8,607
Minnesota Minnesota Senior
Health Option (MSHO)
(Comprehensive MCO
+ MLTSS)
Health Partners Health Partners,
Inc.
Statewide 0 3,114 3,114
Minnesota Minnesota Senior
Health Option (MSHO)
(Comprehensive MCO
+ MLTSS)
Itasca Medical Care Itasca Medical
Care
Itasca County 0 453 453
Minnesota Minnesota Senior
Health Option (MSHO)
(Comprehensive MCO
+ MLTSS)
Medica Medica Holding
Company
Statewide 0 10,746 10,746
Minnesota Minnesota Senior
Health Option (MSHO)
(Comprehensive MCO
+ MLTSS)
Prime West Prime West Health Beltrami, Bigstone,
Clearwater, Douglas, Grant,
Hubbard, McLeod, Meeker,
Pipestone, Pope, Renville,
Stevens, and Traverse
Counties
0 1,920 1,920
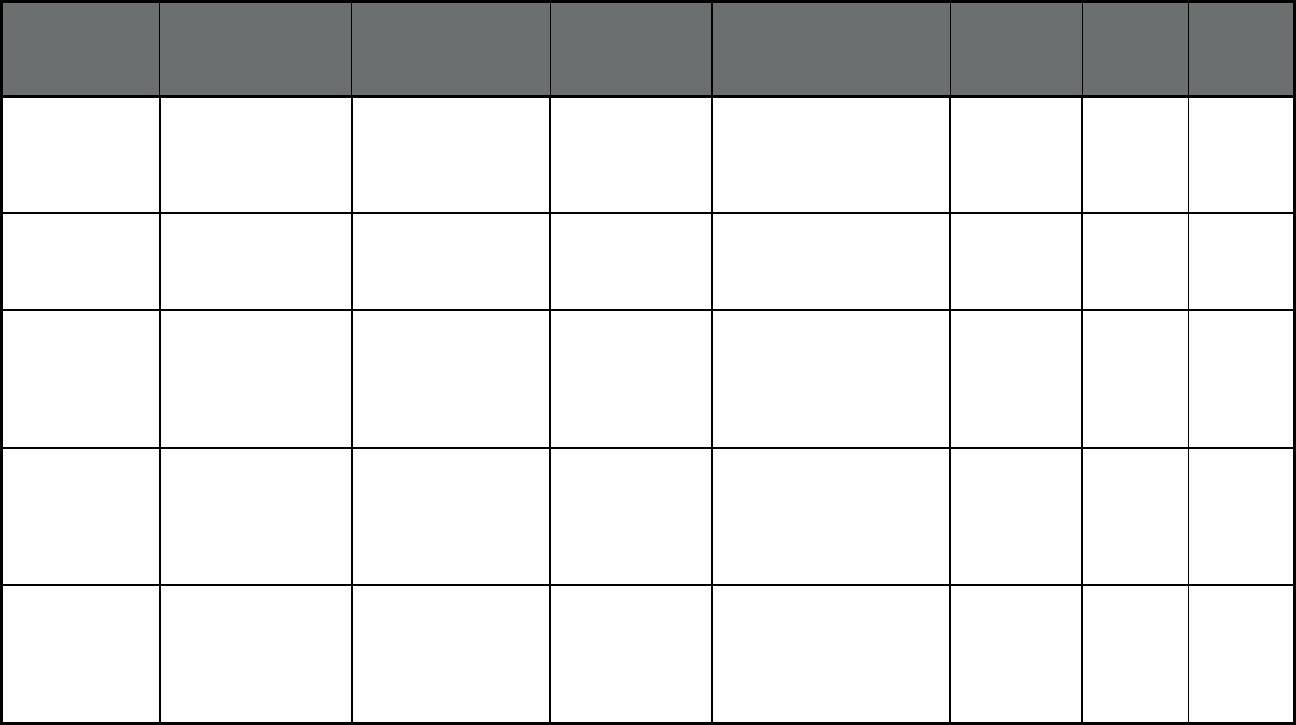
101
State
Program Name
(Type) Plan Name
Parent
Organization
Geographic Region (state-
defined areas, counties, or
zip codes)
Medicaid-Only
Enrollment
Dual
Enrollment
Total
Enrollment
Minnesota Minnesota Senior
Health Option (MSHO)
(Comprehensive MCO
+ MLTSS)
South Country South Country
Health Alliance
Brown, Dodge, Freeborn,
Kanabec, Morrison, Sibley,
Steele, Todd, Wabasha,
Wadena, and Waseca
Counties
0 1,828 1,828
Minnesota Minnesota Senior
Health Option (MSHO)
(Comprehensive MCO
+ MLTSS)
U Care U Care of
Minnesota
Statewide 0 12,140 12,140
Mississippi Mississippi
Coordinated Access
Network
(MississippiCAN)
(Comprehensive
MCO)
Magnolia Health Plan Centene
Corporation
Statewide 232,443 0 232,443
Mississippi Mississippi
Coordinated Access
Network
(MississippiCAN)
(Comprehensive
MCO)
UnitedHealthcare of
Mississippi Community
Plan
UnitedHealthcare Statewide 209,339 0 209,339
Missouri MO HealthNet
Managed Care/1915b
(Comprehensive
MCO)
Home State Health
Eastern
Centene
Corporation
Franklin, Jefferson, Lincoln,
Madison, Perry, Pike, St
Charles, St Francois, Ste
Genevieve, St Louis Co,
Warren, Washington, and St
Louis City
104,539 0 104,539
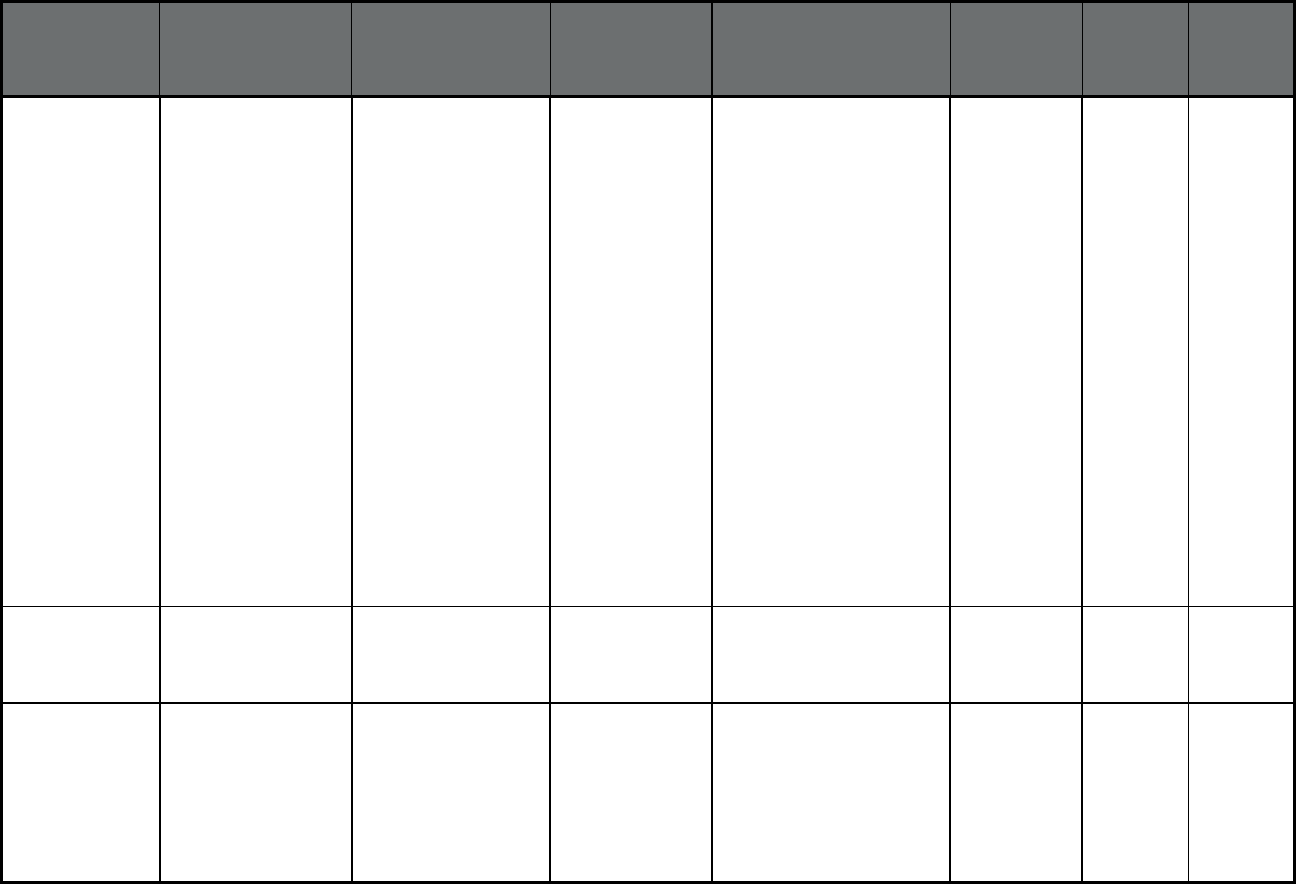
102
State
Program Name
(Type) Plan Name
Parent
Organization
Geographic Region (state-
defined areas, counties, or
zip codes)
Medicaid-Only
Enrollment
Dual
Enrollment
Total
Enrollment
Missouri MO HealthNet
Managed Care/1915b
(Comprehensive
MCO)
Home State Health
Central
Centene
Corporation
Adair, Andrew, Atchison,
Audrain, Benton, Bollinger,
Boone, Buchanan, Butler,
Caldwell, Callaway,
Camden, Cape Girardeau,
Carroll, Carter, Chariton,
Clark, Clinton, Cole, Cooper,
Crawford, Daviess, DeKalb,
Dent, Dunklin, Gasconade,
Gentry, Grundy, Harrison,
Holt, Howard, Iron, Knox,
Laclede, Lewis, Linn,
Livingston, Macon, Maries,
Marion, Mercer, Miller,
Mississippi, Moniteau,
Monroe, Montgomery,
Morgan, New Madrid,
Nodaway, Osage, Pettis,
Phelps, Pulaski, Putman,
Ralls, Randolph, Reynolds,
Ripley, Saline, Schuyler,
Scotland, Scott, Shelby,
Stoddard, Sullivan, Wayne
and Worth
63,646 0 63,646
Missouri MO HealthNet
Managed Care/1915b
(Comprehensive
MCO)
Home State Health
Western
Centene
Corporation
Bates, Cass, Cedar, Clay,
Henry, Jackson, Johnson,
Lafayette, Platte, Polk, Ray,
St Clair, and Vernon
50,541 0 50,541
Missouri MO HealthNet
Managed Care/1915b
(Comprehensive
MCO)
Home State Health
Southwest
Centene
Corporation
Barry, Barton, Christian,
Dade, Dallas, Douglas,
Greene, Hickory, Howell,
Jasper, Lawrence,
McDonald, Newton, Oregon,
Ozark, Shannon, Stone,
Taney, Texas, Webster and
Wright
46,983 0 46,983
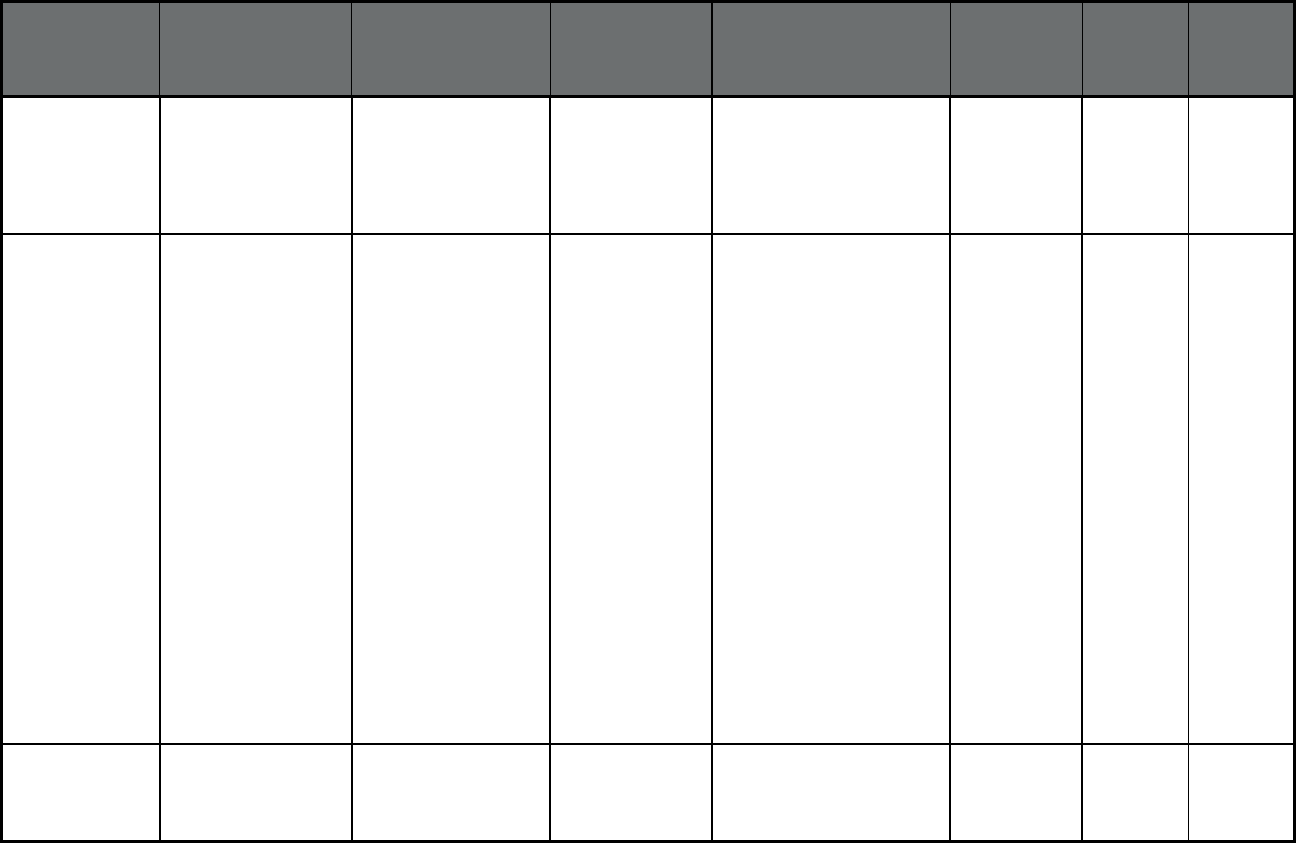
103
State
Program Name
(Type) Plan Name
Parent
Organization
Geographic Region (state-
defined areas, counties, or
zip codes)
Medicaid-Only
Enrollment
Dual
Enrollment
Total
Enrollment
Missouri MO HealthNet
Managed Care/1915b
(Comprehensive
MCO)
Missouri Care Eastern WellCare Franklin, Jefferson, Lincoln,
Madison, Perry, Pike, St
Charles, St Francois, Ste
Genevieve, St Louis Co,
Warren, Washington, and St
Louis City
75,195 0 75,195
Missouri MO HealthNet
Managed Care/1915b
(Comprehensive
MCO)
Missouri Care Central WellCare Adair, Andrew, Atchison,
Audrain, Benton, Bollinger,
Boone, Buchanan, Butler,
Caldwell, Callaway,
Camden, Cape Girardeau,
Carroll, Carter, Chariton,
Clark, Clinton, Cole, Co
oper,
Crawford, Daviess, DeKalb,
Dent, Dunklin, Gasconade,
Gentry, Grundy, Harrison,
Holt, Howard, Iron, Knox,
Laclede, Lewis, Linn,
Livingston, Macon, Maries,
Marion, Mercer, Miller,
Mississippi, Moniteau,
Monroe, Montgomery,
Morgan, New Madrid,
Nodaway, Osage, Pettis,
Phelps, Pulaski, Putman,
Ralls, Randolph, Reynolds,
Ripley, Saline, Schuyler,
Scotland, Scott, Shelby,
Stoddard, Sullivan, Wayne
and Worth
79,314 0 79,314
Missouri MO HealthNet
Managed Care/1915b
(Comprehensive
MCO)
Missouri Care Western WellCare Bates, Cass, Cedar, Clay,
Henry, Jackson, Johnson,
Lafayette, Platte, Polk, Ray,
St Clair, and Vernon
71,377 0 71,377
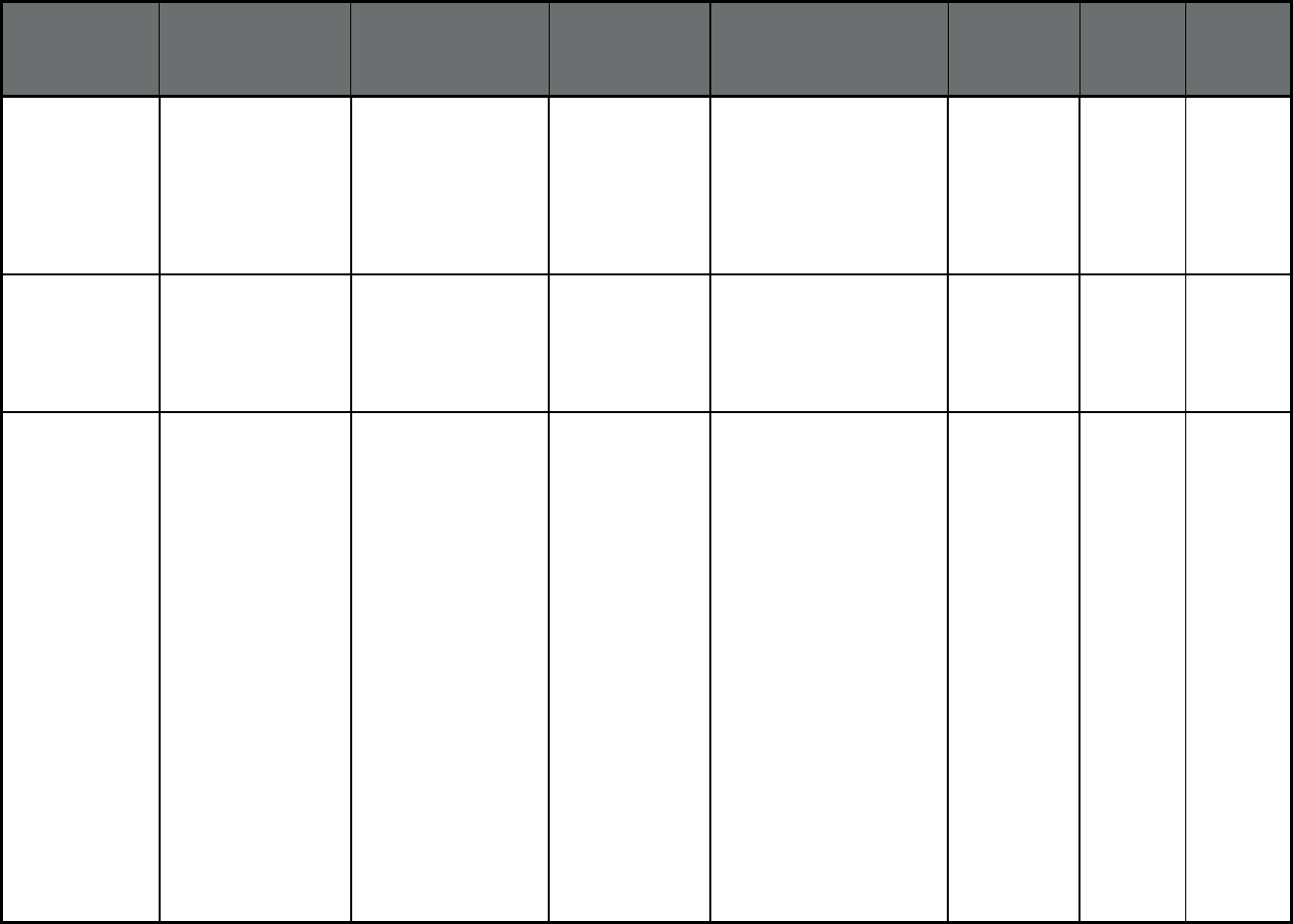
104
State
Program Name
(Type) Plan Name
Parent
Organization
Geographic Region (state-
defined areas, counties, or
zip codes)
Medicaid-Only
Enrollment
Dual
Enrollment
Total
Enrollment
Missouri MO HealthNet
Managed Care/1915b
(Comprehensive
MCO)
Missouri Care
Southwest
WellCare Barry, Barton, Christian,
Dade, Dallas, Douglas,
Greene, Hickory, Howell,
Jasper, Lawrence,
McDonald, Newton,
Oregon,
Ozark, Shannon, Stone,
Taney, Texas, Webster and
Wright
52,537 0 52,537
Missouri MO HealthNet
Managed Care/1915b
(Comprehensive
MCO)
United Healthcare
Eastern
UnitedHealthcare Franklin, Jefferson, Lincoln,
Madison, Perry, Pike, St
Charles, St Francois, Ste
Genevieve, St Louis Co,
Warren, Washington, and St
Louis City
51,016 0 51,016
Missouri MO HealthNet
Managed Care/1915b
(Comprehensive
MCO)
United Healthcare
Central
UnitedHealthcare Adair, Andrew, Atchison,
Audrain, Benton, Bollinger,
Boone, Buchanan, Butler,
Caldwell, Callaway,
Camden, Cape Girardeau,
Carroll, Carter, Chariton,
Clark, Clinton, Cole, Cooper,
Crawford, Daviess, DeKalb,
Dent, Dunklin, Gasconade,
Gentry, Grundy, Harrison,
Holt, Howard, Iron, Knox,
Laclede, Lewis, Linn,
Livingston, Macon, Maries,
Marion, Mercer, Miller,
Mississippi, Moniteau,
Monroe, Montgomery,
Morgan, New Madrid,
Nodaway, Osage, Pettis,
Phelps, Pulaski, Putman,
Ralls, Randolph, Reynolds,
Ripley, Saline, Schuyler,
Scotland, Scott, Shelby,
Stoddard, Sullivan, Wayne
and Worth
48,376 0 48,376
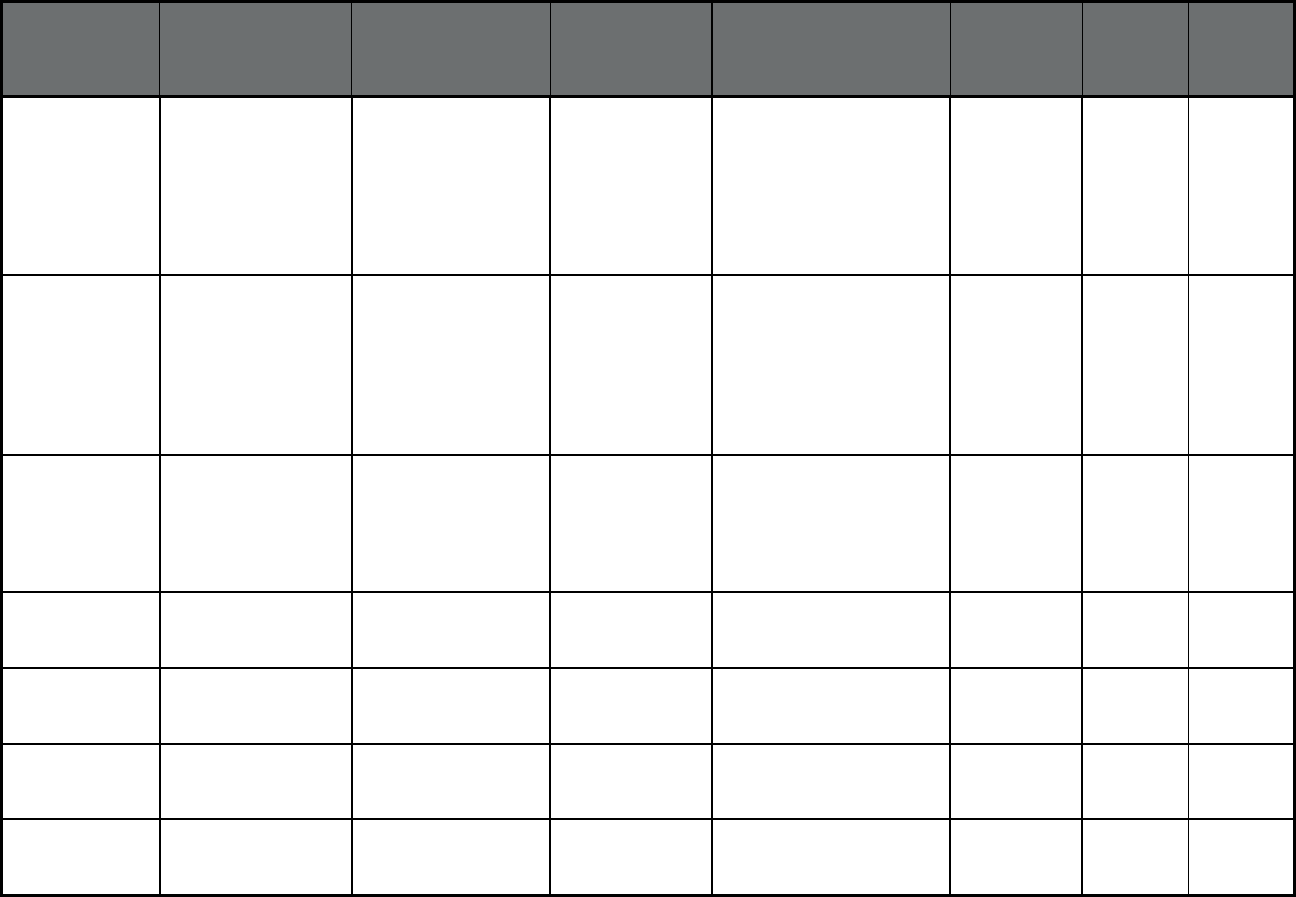
105
State
Program Name
(Type) Plan Name
Parent
Organization
Geographic Region (state-
defined areas, counties, or
zip codes)
Medicaid-Only
Enrollment
Dual
Enrollment
Total
Enrollment
Missouri MO HealthNet
Managed Care/1915b
(Comprehensive
MCO)
United Healthcare
Western
UnitedHealthcare Barry, Barton, Christian,
Dade, Dallas, Douglas,
Greene, Hickory, Howell,
Jasper, Lawrence,
McDonald, Newton, Oregon,
Ozark, Shannon, Stone,
Taney, Texas, Webster and
Wright
37,865 0 37,865
Missouri MO HealthNet
Managed Care/1915b
(Comprehensive
MCO)
United Healthcare
Southwest
UnitedHealthcare Barry, Barton, Christian,
Dade, Dallas, Douglas,
Greene, Hickory, Howell,
Jasper, Lawrence,
McDonald, Newton, Oregon,
Ozark, Shannon, Stone,
Taney, Texas, Webster and
Wright
30,946 0 30,946
Missouri Non-Emergency
Medical Transportation
Program (NEMT)
(Non-Emergency
Medical
Transportation)
Logisticare Solutions Providence
Service
Corporation
Statewide 98,690 143,578 242,268
Montana Passport to Health
(Primary Care Case
Management (PCCM))
Multiple Primary Care
Providers
Passport to Health Statewide 215,475 0 215,475
Nebraska Heritage Health
(Comprehensive
MCO)
UnitedHealthcare
Community Plan of
Nebraska
UnitedHealthcare Statewide 69,592 12,626 82,218
Nebraska Heritage Health
(Comprehensive
MCO)
WellCare of Nebraska WellCare Statewide 76,075 7,718 83,793
Nebraska Heritage Health
(Comprehensive
MCO)
Nebraska Total Care Nebraska Total
Care Inc.
Statewide 68,879 13,942 82,821
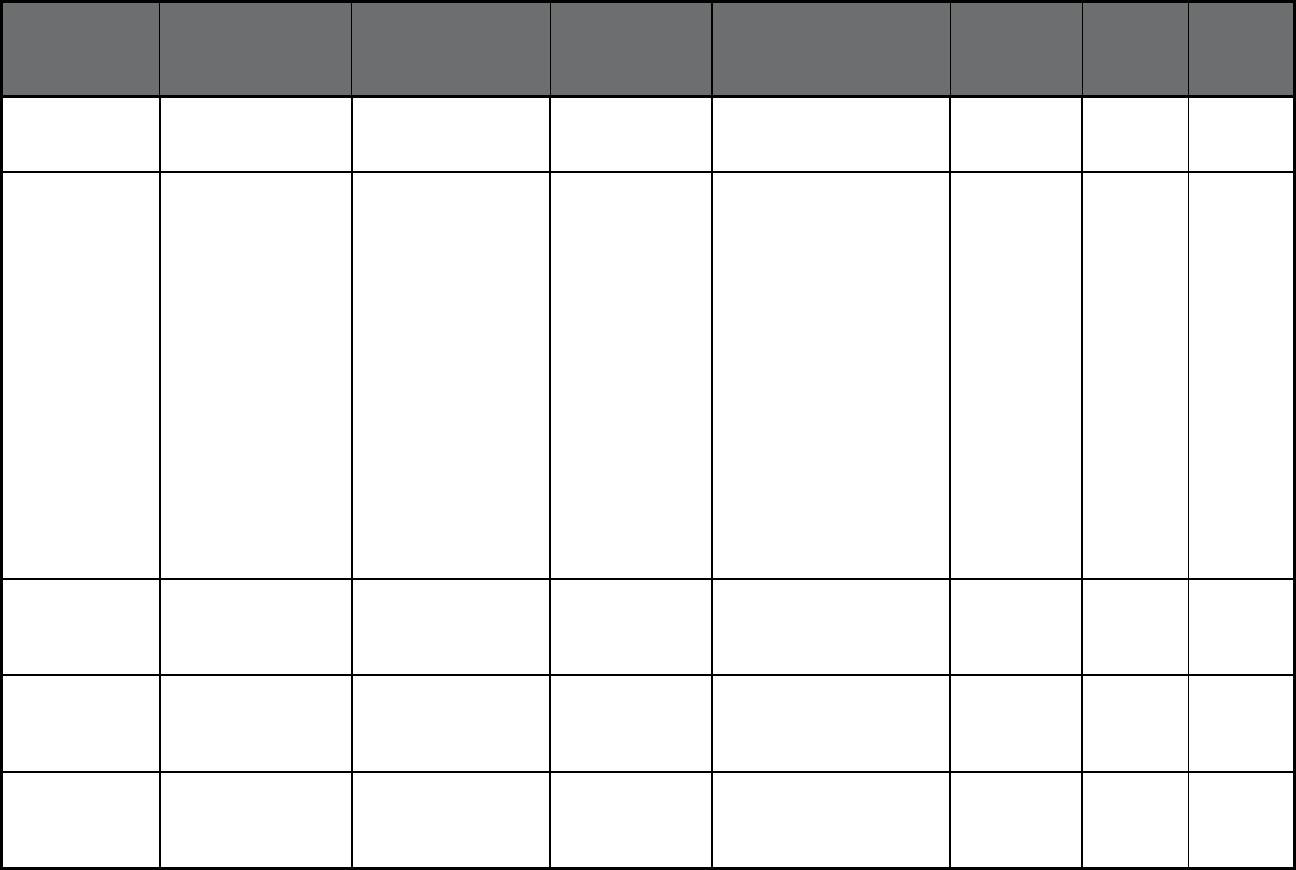
106
State
Program Name
(Type) Plan Name
Parent
Organization
Geographic Region (state-
defined areas, counties, or
zip codes)
Medicaid-Only
Enrollment
Dual
Enrollment
Total
Enrollment
Nebraska Dental Benefit
Manager (Dental only
(PAHP))
MCNA Nebraska Managed Care of
North America
(MCNA), Inc.
Statewide 213,334 34,246 247,580
Nebraska Program of All-
Inclusive Care for the
Elderly (PACE)
(Program of All-
inclusive Care for the
Elderly (PACE))
Immanuel Pathways Immanual
Pathways
68037, 68048, 68025,
68007, 68010, 68022,
68064, 68102, 68104,
68105, 68106, 68107,
68127, 68110, 68111,
68112, 68114, 68116,
68117, 68118, 68122,
68124, 68127, 68130,
68131, 68132, 68134,
68135, 68137, 68142,
68144, 68152, 68154,
68157, 68164, 68182,
68005, 68028, 68046,
68059, 68069, 68113,
68123, 68128, 68133,
68136, 68138, 68147,
68073, 68002, 68008,
68009, 68023, 68029,
68034, 68044, 68068
22 168 190
Nevada Mandatory Health
Maintenance Program
(Comprehensive
MCO)
Health Plan of Nevada
(HPN)
UnitedHealthcare Urban zip codes in Washoe
and Clark Counties
242,408 0 242,408
Nevada Mandatory Health
Maintenance Program
(Comprehensive
MCO)
Anthem Blue Cross
Blue Shield of Nevada
Anthem BCBS Urban zip codes in Washoe
and Clark Counties
165,519 0 165,519
Nevada Mandatory Health
Maintenance Program
(Comprehensive
MCO)
Silver Summit Health
Plan
Centene
Corporation
Urban zip codes in Washoe
and Clark Counties
49,855 0 49,855
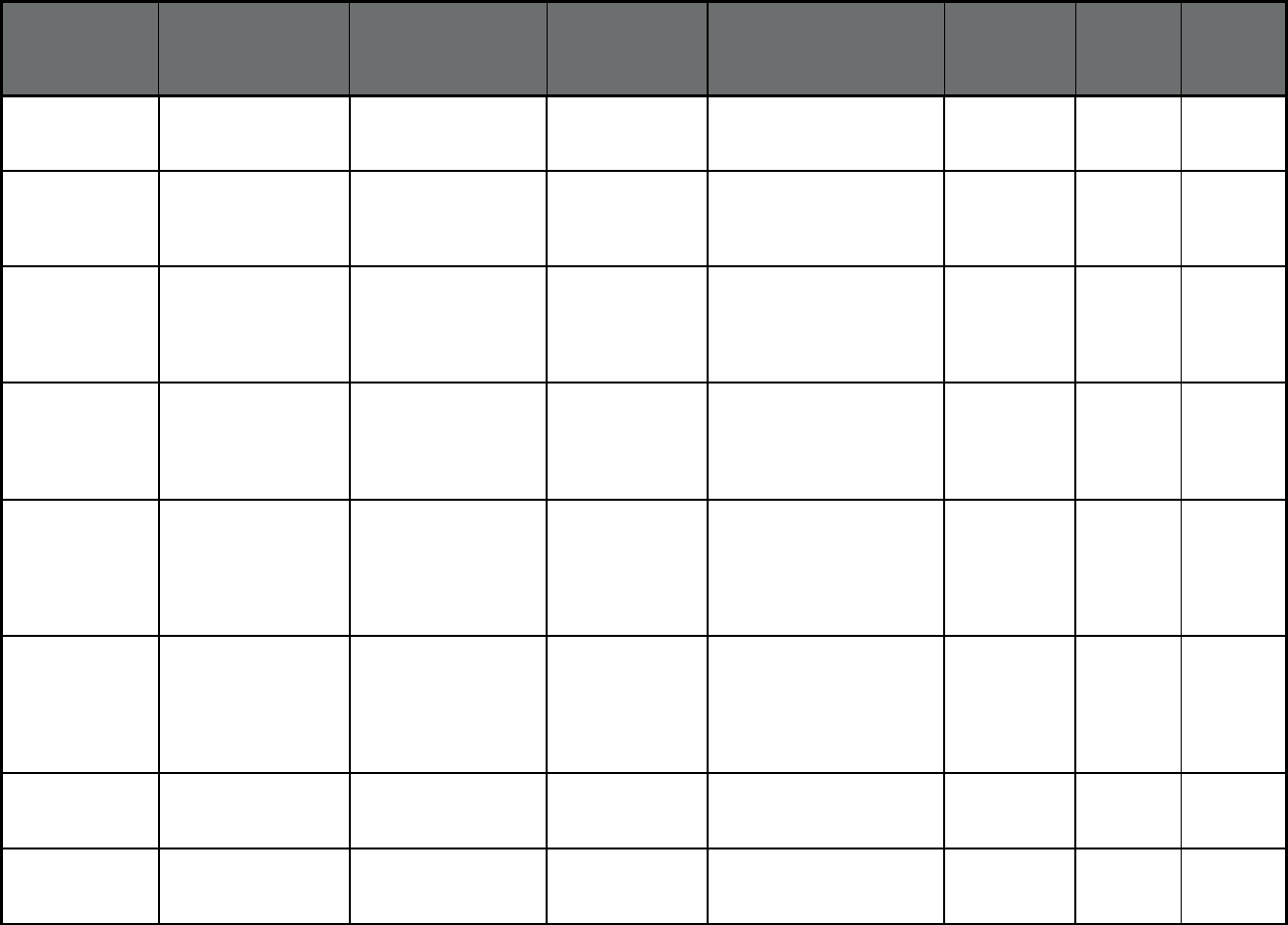
107
State
Program Name
(Type) Plan Name
Parent
Organization
Geographic Region (state-
defined areas, counties, or
zip codes)
Medicaid-Only
Enrollment
Dual
Enrollment
Total
Enrollment
Nevada Dental Benefits
Administrator (Dental
only (PAHP))
Liberty Dental Plan of
Nevada
Liberty Dental Plan
Corporation
Sufficiently populated Urban
Zip Codes in Washoe and
Clark counties
457,782 0 457,782
Nevada Non-Emergency
Transportation (Non-
Emergency Medical
Transportation)
Medical Transportation
Management (MTM
Nevada)
MTM Inc Statewide 588,111 0 588,111
New Hampshire New Hampshire
Medicaid Care
Management
(Comprehensive
MCO)
New Hampshire
Healthy Families
Centene
Corporation
Statewide 49,599 8,341 57,940
New Hampshire New Hampshire
Medicaid Care
Management
(Comprehensive
MCO)
Well Sense Health Plan Boston Medical
Health Plan
Statewide 60,024 7,980 68,004
New Hampshire New Hampshire
Health Protection
Program Medicaid
Care Management
ABP (Comprehensive
MCO)
New Hampshire
Healthy Families
Centene
Corporation
Statewide 3,158 0 3,158
New Hampshire New Hampshire
Health Protection
Program Medicaid
Care Management
ABP (Comprehensive
MCO)
Well Sense Health Plan Boston Medical
Health Plan
Statewide 4,727 0 4,727
New Jersey NJFamilyCare
(Comprehensive MCO
+ MLTSS)
Aetna Better Health NJ CVS Health Statewide 43,062 5,194 48,256
New Jersey NJFamilyCare
(Comprehensive MCO
+ MLTSS)
Amerigroup New
Jersey Inc
Anthem Insurance
Companies, Inc.
Statewide 148,670 16,743 165,413
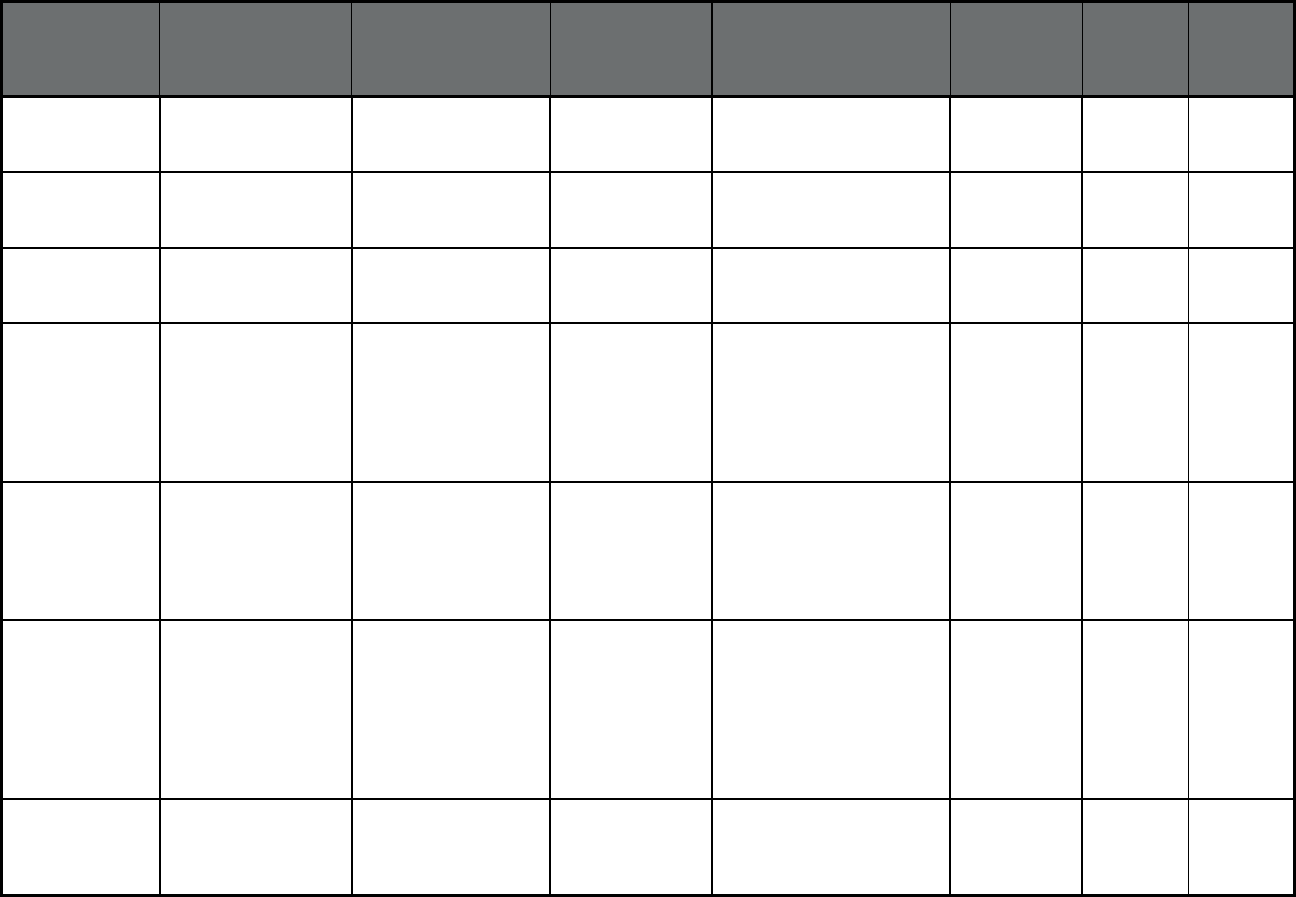
108
State
Program Name
(Type) Plan Name
Parent
Organization
Geographic Region (state-
defined areas, counties, or
zip codes)
Medicaid-Only
Enrollment
Dual
Enrollment
Total
Enrollment
New Jersey NJFamilyCare
(Comprehensive MCO
+ MLTSS)
Horizon NJ Health Blue Cross Blue
Shield
Statewide 748,954 72,804 821,758
New Jersey NJFamilyCare
(Comprehensive MCO
+ MLTSS)
UnitedHealthcare
Community Plan
UnitedHealthcare Statewide 396,903 34,653 431,556
New Jersey NJFamilyCare
(Comprehensive MCO
+ MLTSS)
WellCare of New
Jersey
WellCare All counties except
Hunterdon
51,242 12,195 63,437
New Jersey FIDE SNP
(Comprehensive MCO
+ MLTSS)
Amerivantage Dual
Coordination (HMO
SNP)
Amerigroup, Inc. Atlantic, Bergen, Burlington,
Camden, Cumberland,
Essex, Gloucester, Hudson,
Mercer, Middlesex,
Monmouth, Morris, Ocean,
Passaic, Somerset, and
Union Counties
0 9,221 9,221
New Jersey FIDE SNP
(Comprehensive MCO
+ MLTSS)
Horizon NJ TotalCare
(HMO SNP)
Horizon
Healthcare of New
Jersey, Inc.
Atlantic, Cumberland,
Essex, Gloucester, Hudson,
Hunterdon, Mercer,
Monmouth, Morris, Passaic,
Salem, Somerset, Sussex,
Union, and Warren Counties
0 6,781 6,781
New Jersey FIDE SNP
(Comprehensive MCO
+ MLTSS)
UnitedHealthcare Dual
Complete ONE (HMO
SNP)
UnitedHealthcare Atlantic, Bergen, Burlington,
Camden, Cumberland,
Essex, Gloucester, Hudson,
Hunterdon, Mercer,
Middlesex, Monmouth,
Morris, Ocean, Passaic,
Salem, Somerset, Sussex,
and Union Counties
0 19,158 19,158
New Jersey FIDE SNP
(Comprehensive MCO
+ MLTSS)
WellCare Liberty (HMO
SNP)
WellCare Bergen, Essex, Hudson,
Middlesex, Morris, Passaic,
Somerset, and Union
Counties
0 2,697 2,697
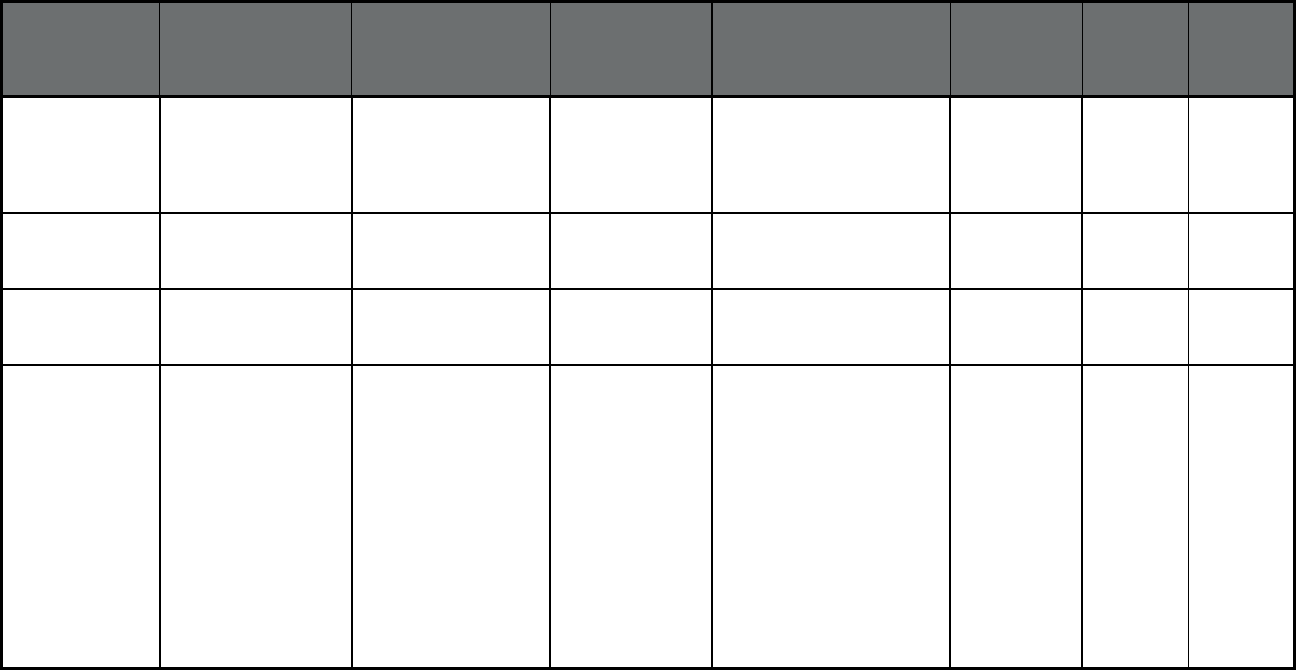
109
State
Program Name
(Type) Plan Name
Parent
Organization
Geographic Region (state-
defined areas, counties, or
zip codes)
Medicaid-Only
Enrollment
Dual
Enrollment
Total
Enrollment
New Jersey Non-Emergency
Medical Transportation
(Non-Emergency
Medical
Transportation)
Logisticare Providence
Service
Corporation
Statewide 1,523,821 37,445 1,561,266
New Jersey PACE (Program of All-
inclusive Care for the
Elderly (PACE))
Atlanticare LIFE PACE Atlantic and Cape May
Counties
9 35 44
New Jersey PACE (Program of All-
inclusive Care for the
Elderly (PACE))
Beacon of LIFE PACE Monmouth County 8 98 106
New Jersey PACE (Program of All-
inclusive Care for the
Elderly (PACE))
Inspira LIFE PACE Portions of Cumberland,
Gloucester and Salem
Counties, specifically,
residents of zip codes:
08028, 08062, 08071,
08094, 08098, 08302,
08311, 08312, 08314,
08316, 08318, 08321,
08322, 08323, 08324,
08327, 08328, 08329,
08332, 08343, 08344,
08345, 08348, 08349,
08352, 08353, 08360,
08361, 08362
23 245 268
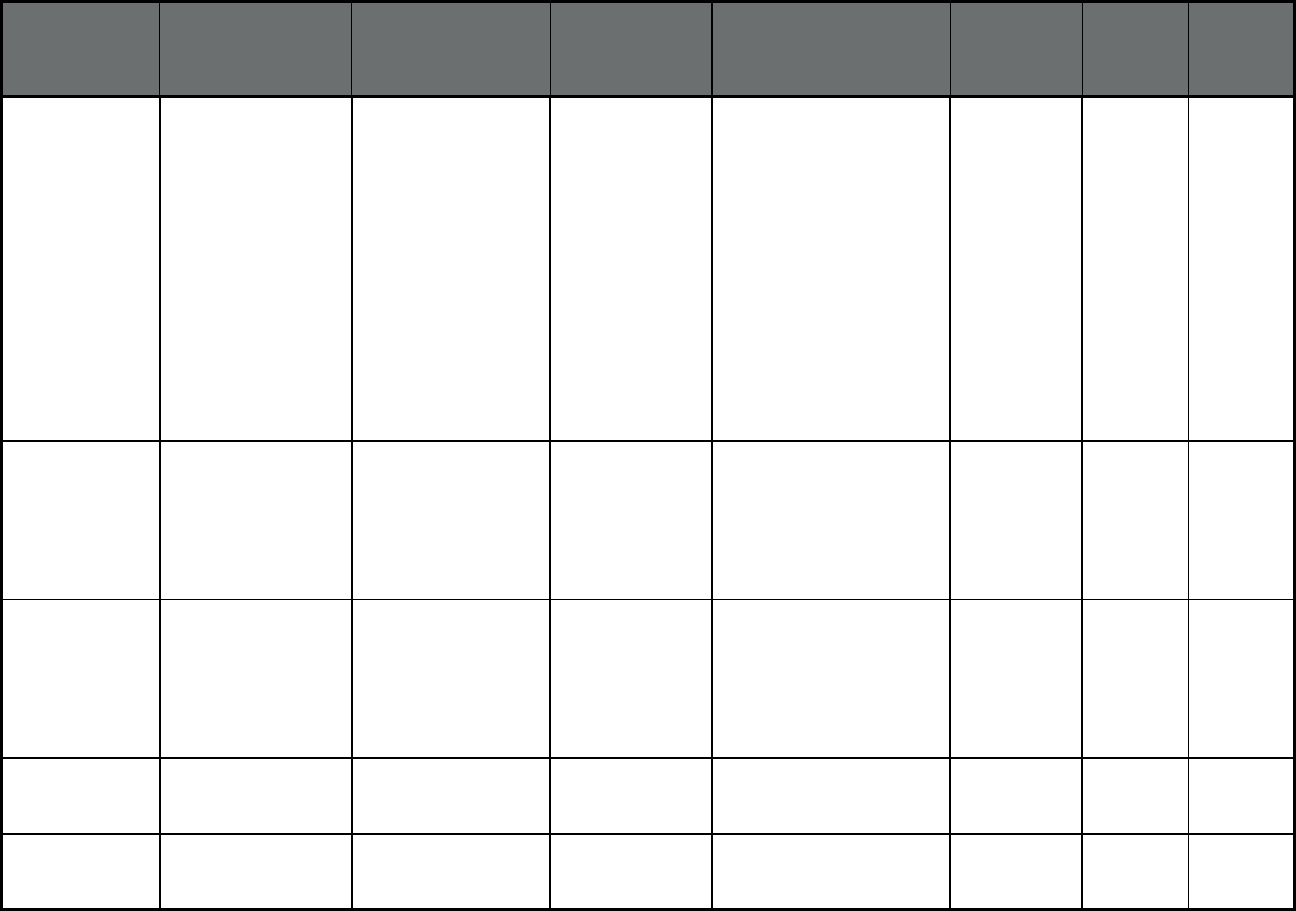
110
State
Program Name
(Type) Plan Name
Parent
Organization
Geographic Region (state-
defined areas, counties, or
zip codes)
Medicaid-Only
Enrollment
Dual
Enrollment
Total
Enrollment
New Jersey PACE (Program of All-
inclusive Care for the
Elderly (PACE))
LIFE at Lourdes PACE Most of Camden County,
some of Burlington County,
and zip codes: 08002,
08003, 08004, 08007,
08009, 08012, 08021,
08026, 08029, 08030,
08031, 08033, 08034,
08035, 08043, 08045,
08049, 08052, 08059,
08065, 08076, 08077,
08078, 08081, 08083,
08084, 08091, 08095,
08099, 08101, 08102,
08103, 08104, 08105,
08106, 08107, 08108,
08109, 08110
22 177 199
New Jersey PACE (Program of All-
inclusive Care for the
Elderly (PACE))
LIFE St. Francis PACE Mercer County and those
who reside in Burlington
County with one of the
following zip codes: 08015,
08016, 08022, 08060,
08068, 08505, 08515,
08518, 08554
36 281 317
New Jersey PACE (Program of All-
inclusive Care for the
Elderly (PACE))
Lutheran Senior Life PACE Most of Hudson County,
including residents of zip
codes: 07002, 07030,
07047, 07086, 07087,
07093, 07094, 07302,
07304, 07305, 07306,
07307, 07310, 07311
13 120 133
New Mexico Centennial Care
(Comprehensive MCO
+ MLTSS)
Blue Cross Blue Shield
of NM
Blue Cross Blue
Shield
Statewide 138,619 8,292 146,911
New Mexico Centennial Care
(Comprehensive MCO
+ MLTSS)
Molina Healthcare of
New Mexico Inc
Molina Healthcare Statewide 203,235 8,201 211,436
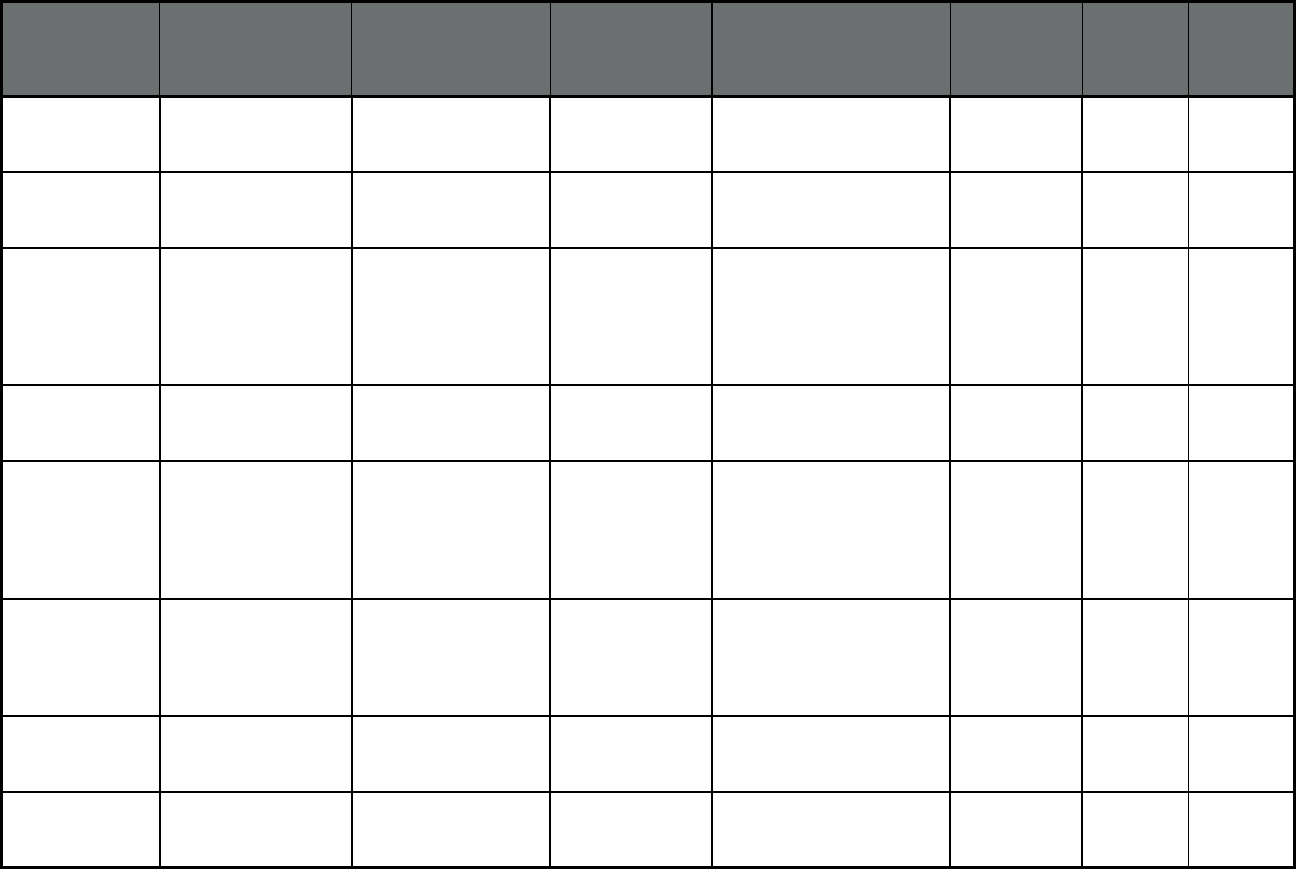
111
State
Program Name
(Type) Plan Name
Parent
Organization
Geographic Region (state-
defined areas, counties, or
zip codes)
Medicaid-Only
Enrollment
Dual
Enrollment
Total
Enrollment
New Mexico Centennial Care
(Comprehensive MCO
+ MLTSS)
Presbyterian Health
Plan
Presbyterian
Health Plan
Statewide 212,275 8,223 220,498
New Mexico Centennial Care
(Comprehensive MCO
+ MLTSS)
UnitedHealthcare
Community Plan
UnitedHealthcare Statewide 69,821 16,584 86,405
New Mexico Program of All-
Inclusive Care for the
Elderly (PACE)
(Program of All-
inclusive Care for the
Elderly (PACE))
Innovage New Mexico
PACE dba Total
Community Care
PACE Bernalillo County, Sandoval
County, Valencia County
59 741 800
New York Health and Recovery
Plans (Comprehensive
MCO)
Affinity Health Plan Affinity Health Plan Nassau, Orange, Rockland,
Suffolk and Westchester
Counties, New York City
4,355 0 4,355
New York Health and Recovery
Plans (Comprehensive
MCO)
Capital District
Physician's Health Plan
Capital District
Physician's Health
Plan
Albany, Broome, Columbia,
Fulton, Greene,
Montgomery, Rensselaer,
Saratoga, Schenectady,
Schoharie, Tioga, Warren
and Washington Counties
2,782 0 2,782
New York Health and Recovery
Plans (Comprehensive
MCO)
Excellus Health Plan Excellus Health
Plan
Broome, Erie, Herkimer,
Livingston, Monroe, Oneida,
Ontario, Orleans, Otsego,
Seneca, Wayne, and Yates
Counties
7,293 0 7,293
New York Health and Recovery
Plans (Comprehensive
MCO)
Fidelis Care Centene
Corporation
New York City and 57
counties
29,706 0 29,706
New York Health and Recovery
Plans (Comprehensive
MCO)
HealthFirst HealthFirst Nassau and Suffolk
Counties, New York City
23,526 0 23,526
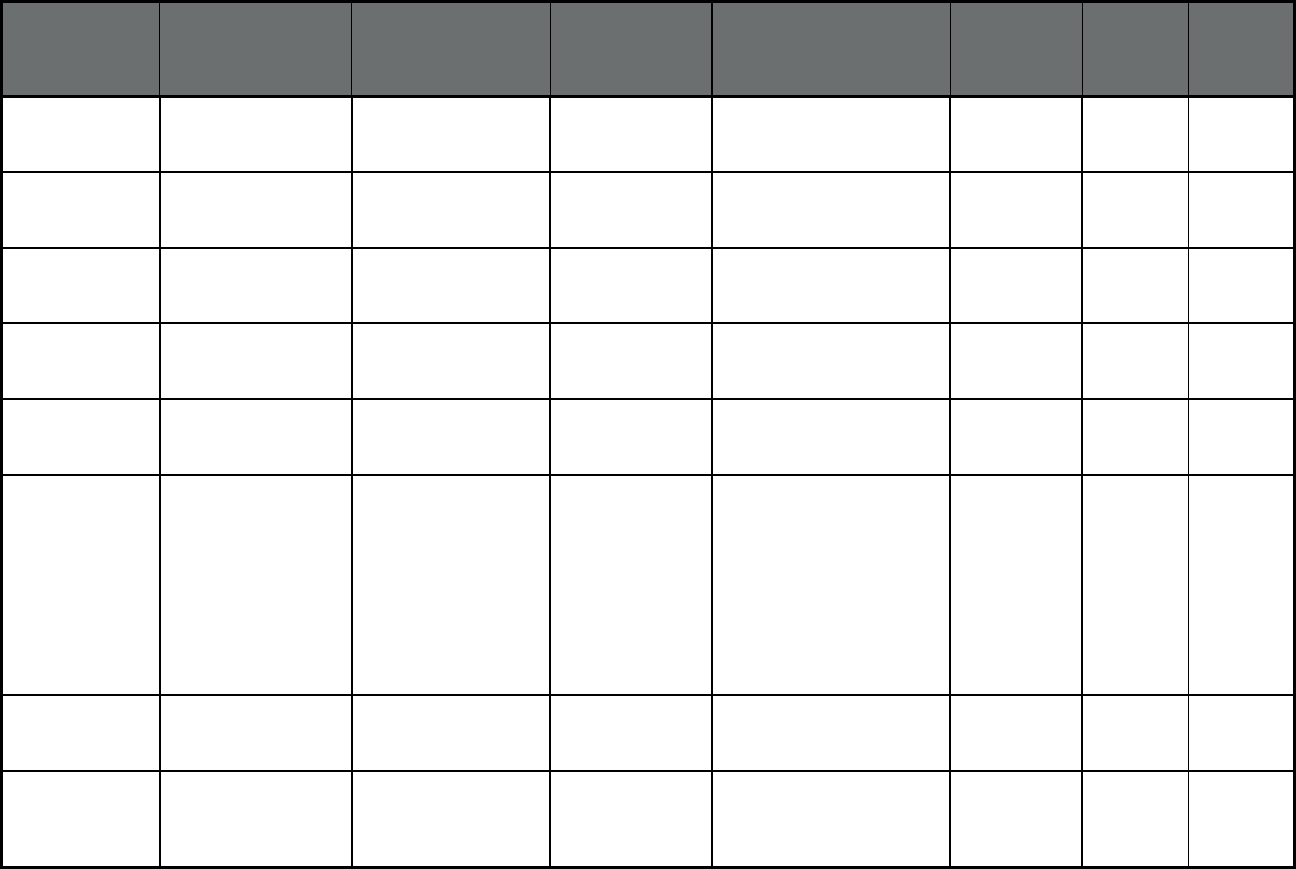
112
State
Program Name
(Type) Plan Name
Parent
Organization
Geographic Region (state-
defined areas, counties, or
zip codes)
Medicaid-Only
Enrollment
Dual
Enrollment
Total
Enrollment
New York Health and Recovery
Plans (Comprehensive
MCO)
HealthPlus Anthem Insurance
Companies, Inc.
Nassau and Putnam
Counties, New York City
5,935 0 5,935
New York Health and Recovery
Plans (Comprehensive
MCO)
HIP GNY HIP GNY Nassau, Suffolk, and
Westchester Counties, New
York City
4,635 0 4,635
New York Health and Recovery
Plans (Comprehensive
MCO)
Independent Health
Association
Independent
Health
Erie County 1,925 0 1,925
New York Health and Recovery
Plans (Comprehensive
MCO)
MetroPlus MetroPlus Health
Plan
New York City 10,901 0 10,901
New York Health and Recovery
Plans (Comprehensive
MCO)
Molina HealthCare of
New York
Molina Healthcare Cortland, Onondaga and
Tompkins Counties
1,484 0 1,484
New York Health and Recovery
Plans (Comprehensive
MCO)
MVP Health Plan MVP Health Plan Albany, Columbia,
Dutchess, Genesee,
Greene, Jefferson, Lewis,
Livingston, Monroe, Oneida,
Ontario, Orange, Putnam,
Rensselaer, Rockland,
Saratoga, Schenectady,
Sullivan, Ulster, Warren,
Washington, and
Westchester Counties
4,673 0 4,673
New York Health and Recovery
Plans (Comprehensive
MCO)
United HealthCare UnitedHealthcare New York City and 42
counties
6,813 0 6,813
New York Health and Recovery
Plans (Comprehensive
MCO)
YourCare Health Plan YourCare Health
Plan
Allegany, Cattaraugus,
Chautauqua, Erie, Monroe,
Ontario and Wyoming
Counties
1,785 0 1,785
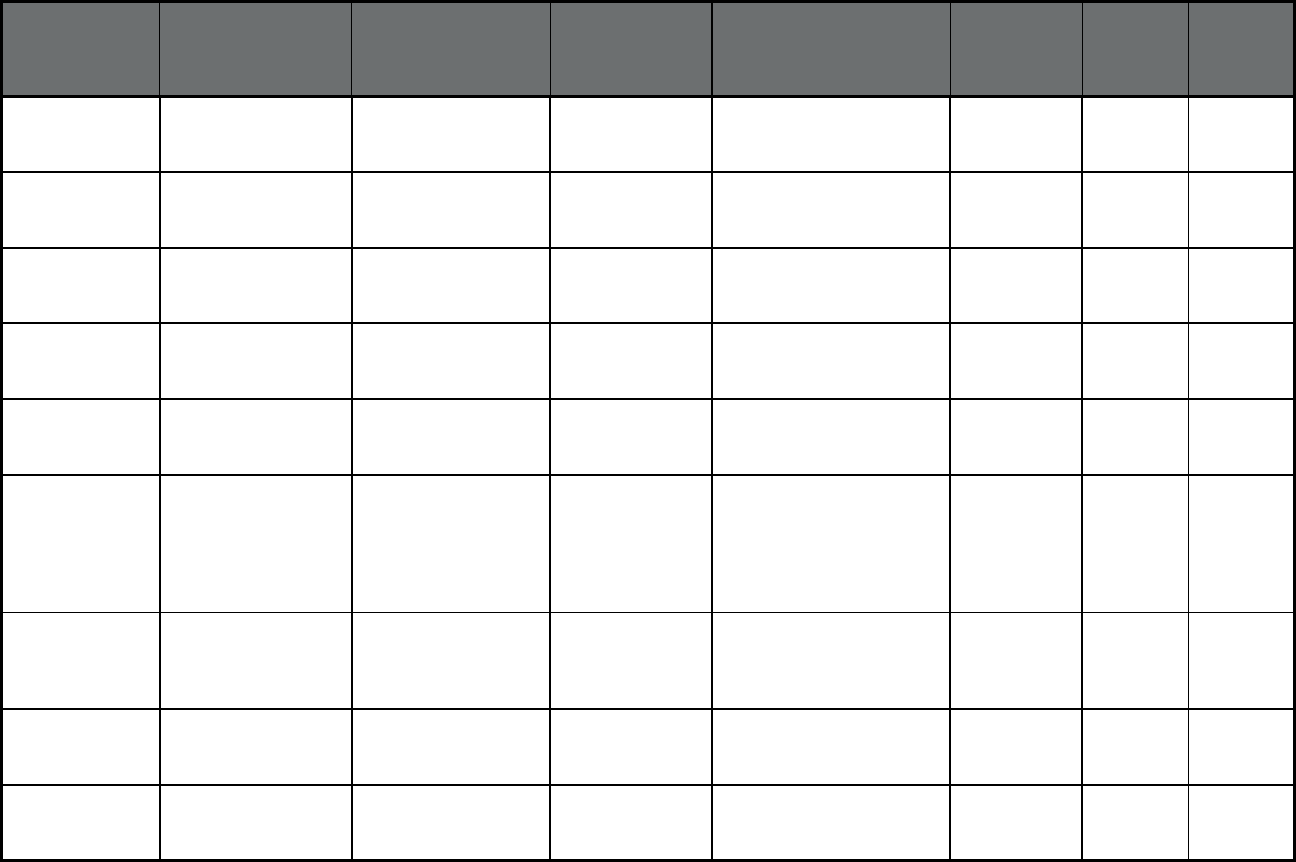
113
State
Program Name
(Type) Plan Name
Parent
Organization
Geographic Region (state-
defined areas, counties, or
zip codes)
Medicaid-Only
Enrollment
Dual
Enrollment
Total
Enrollment
New York Medicaid Advantage
(Comprehensive
MCO)
Affinity Affinity Health Plan New York City 0 0 0
New York Medicaid Advantage
(Comprehensive
MCO)
Fidelis Legacy Plan Fidelis Legacy
Plan
New York City and 35
counties
33 1,325 1,358
New York Medicaid Advantage
(Comprehensive
MCO)
Liberty Health
Advantage
Liberty Health
Advantage
New York City and Nassau
County
96 0 96
New York Medicaid Advantage
(Comprehensive
MCO)
United HealthCare UnitedHealthcare New York City and Nassau
County
21 2,920 2,941
New York Medicaid Advantage
(Comprehensive
MCO)
VNS Choice VNS Choice Nassau, Suffolk and
Westchester Counties, New
York City
15 298 313
New York Medicaid Advantage
(Comprehensive
MCO)
WellCare WellCare Albany, Broome, Erie,
Monroe, Niagara, Oneida,
Orange, Rensselaer,
Rockland, Saratoga,
Schenectady, Ulster, and
Wayne Counties
51 1,642 1,693
New York Medicaid Managed
Care (Comprehensive
MCO + MLTSS)
HealthNow HealthNow Allegany, Cattaraugus,
Chautauqua, Erie, Genesee,
Niagara, Orleans, and
Wyoming Counties
31,719 0 31,719
New York Medicaid Managed
Care (Comprehensive
MCO + MLTSS)
HealthPlus Anthem Insurance
Companies, Inc.
Nassau and Putnam
Counties, New York City
336,121 0 336,121
New York Medicaid Managed
Care (Comprehensive
MCO + MLTSS)
HIP Combined HIP Combined Nassau, Suffolk, and
Westchester Counties, New
York City
134,405 0 134,405
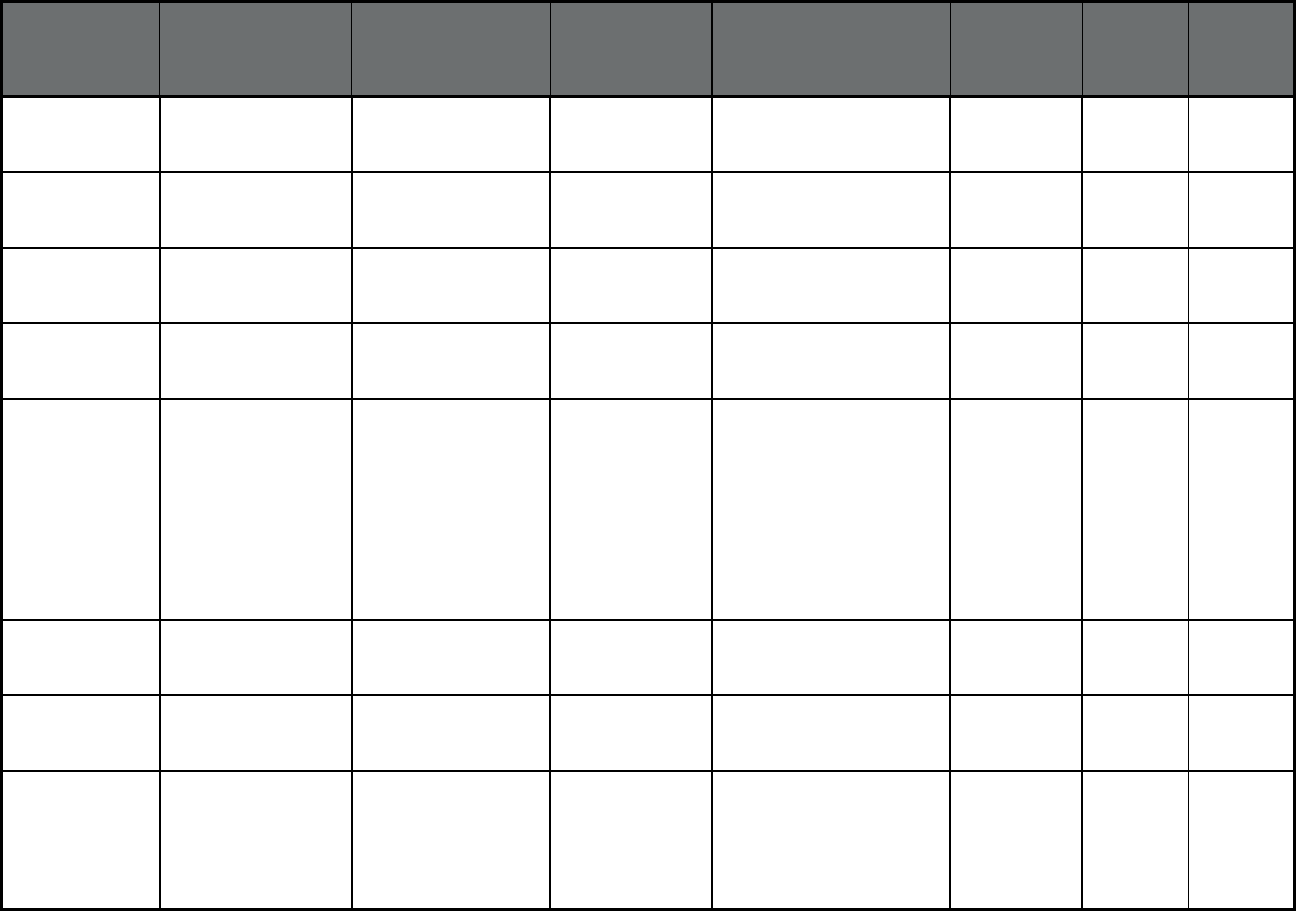
114
State
Program Name
(Type) Plan Name
Parent
Organization
Geographic Region (state-
defined areas, counties, or
zip codes)
Medicaid-Only
Enrollment
Dual
Enrollment
Total
Enrollment
New York Medicaid Managed
Care (Comprehensive
MCO + MLTSS)
Independent
Health/Hudson Valley &
WNY
Independent
Health
Erie County 57,271 0 57,271
New York Medicaid Managed
Care (Comprehensive
MCO + MLTSS)
MetroPlus Health Plan MetroPlus Health
Plan
New York City 374,574 0 374,574
New York Medicaid Managed
Care (Comprehensive
MCO + MLTSS)
MetroPlus Health Plan
Special Needs
MetroPlus Health
Plan
New York City 4,095 0 4,095
New York Medicaid Managed
Care (Comprehensive
MCO + MLTSS)
Molina Healthcare of
New York
Molina Healthcare Cortland, Onondaga, and
Tompkins Counties
28,592 0 28,592
New York Medicaid Managed
Care (Comprehensive
MCO + MLTSS)
MVP Health Plan MVP Health Plan Albany, Columbia,
Dutchess, Genesee,
Greene, Jefferson, Lewis,
Livingston, Monroe, Oneida,
Ontario, Orange, Putnam,
Rensselaer, Rockland,
Saratoga, Schenectady,
Sullivan, Ulster, Warren,
Washington, and
Westchester Counties
167,637 0 167,637
New York Medicaid Managed
Care (Comprehensive
MCO + MLTSS)
United HealthCare UnitedHealthcare New York City and 42
counties
481,881 0 481,881
New York Medicaid Managed
Care (Comprehensive
MCO + MLTSS)
VNS Choice Special
Needs
VNS Choice New York City 3,313 0 3,313
New York Medicaid Managed
Care (Comprehensive
MCO + MLTSS)
WellCare WellCare Albany, Dutchess, Erie,
Nassau, Niagara, Orange,
Rensselaer, Rockland,
Schenectady, Schuyler,
Steuben, and Ulster
Counties, New York City
104,961 0 104,961
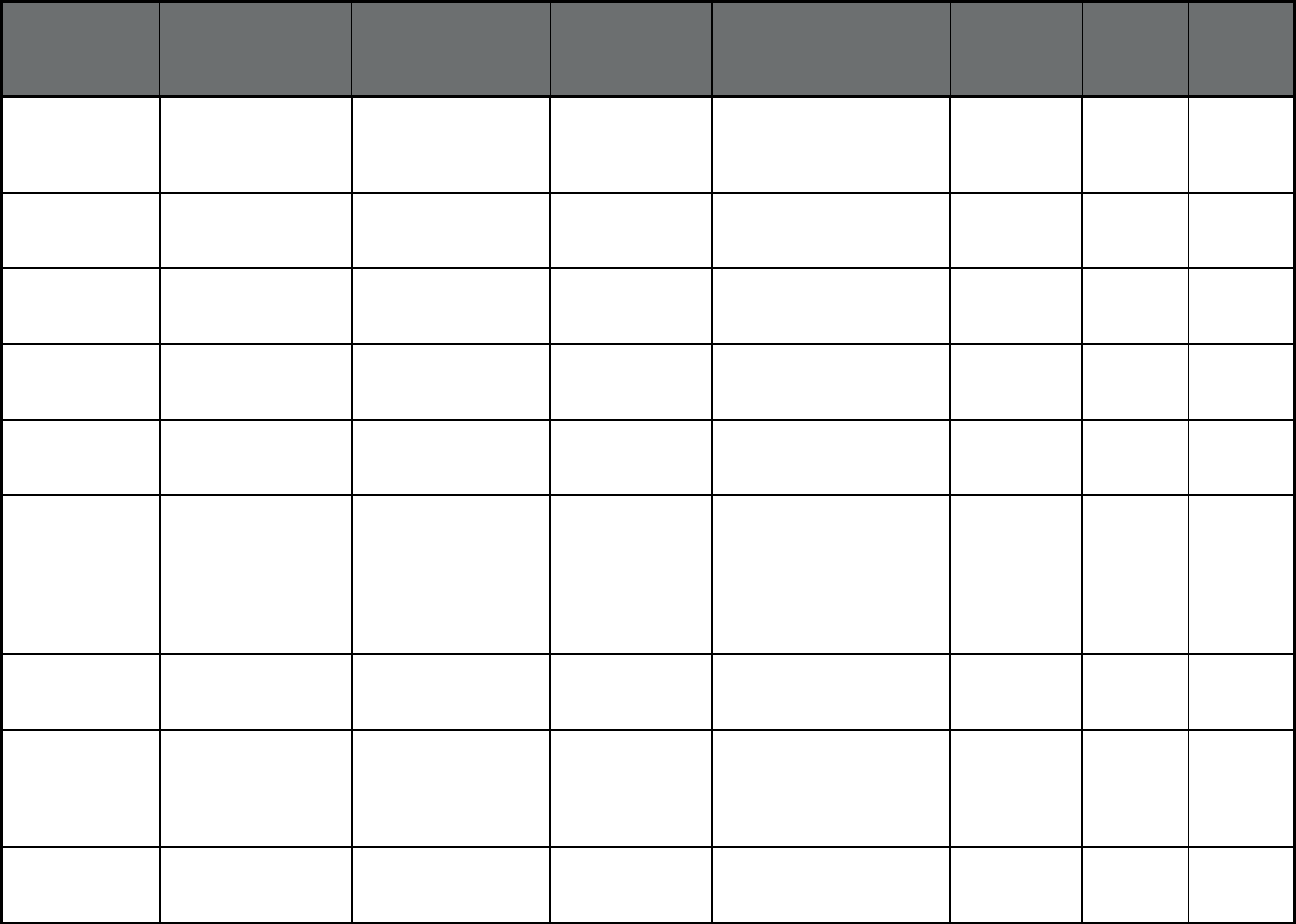
115
State
Program Name
(Type) Plan Name
Parent
Organization
Geographic Region (state-
defined areas, counties, or
zip codes)
Medicaid-Only
Enrollment
Dual
Enrollment
Total
Enrollment
New York Medicaid Managed
Care (Comprehensive
MCO + MLTSS)
YourCare Health Plan YourCare Health
Plan
Allegany, Cattaraugus,
Chautauqua, Erie, Monroe,
Ontario, and Wyoming
Counties
38,679 0 38,679
New York Medicaid Managed
Care (Comprehensive
MCO + MLTSS)
Fidelis Care Centene
Corporation
New York City and 57
Counties
1,244,926 0 1,244,926
New York Medicaid Managed
Care (Comprehensive
MCO + MLTSS)
HealthFirst HealthFirst Nassau and Suffolk
Counties, New York City
939,799 0 939,799
New York Medicaid Managed
Care (Comprehensive
MCO + MLTSS)
Affinity Health Plan Affinity Health Plan Nassau, Orange, Rockland,
Suffolk, and Westchester
Counties, New York City
213,679 0 213,679
New York Medicaid Managed
Care (Comprehensive
MCO + MLTSS)
Amida Care Special
Needs
Amida Care
Special Needs
New York City 6,488 0 6,488
New York Medicaid Managed
Care (Comprehensive
MCO + MLTSS)
Capital District
Physician's Health Plan
Capital District
Physician's Health
Plan
Albany, Broome, Clinton,
Columbia, Essex, Franklin,
Fulton, Greene,
Montgomery, Rensselaer,
Saratoga, Schenectady,
Schoharie, Tioga, Warren,
and Washington Counties
82,622 0 82,622
New York Medicaid Managed
Care (Comprehensive
MCO + MLTSS)
Crystal Run Health
Plan
Crystal Run Health
Plan
Orange and Sullivan
Counties
1,427 0 1,427
New York Medicaid Managed
Care (Comprehensive
MCO + MLTSS)
Excellus Health Plan Excellus Health
Plan
Broome, Erie, Herkimer,
Livingston, Monroe, Oneida,
Ontario, Orleans, Otsego,
Seneca, Wayne, and Yates
Counties
171,752 0 171,752
New York Medicaid Advantage
Plus (Comprehensive
MCO + MLTSS)
ElderPlan ElderPlan Nassau and Westchester
Counties, New York City
6 1,397 1,403
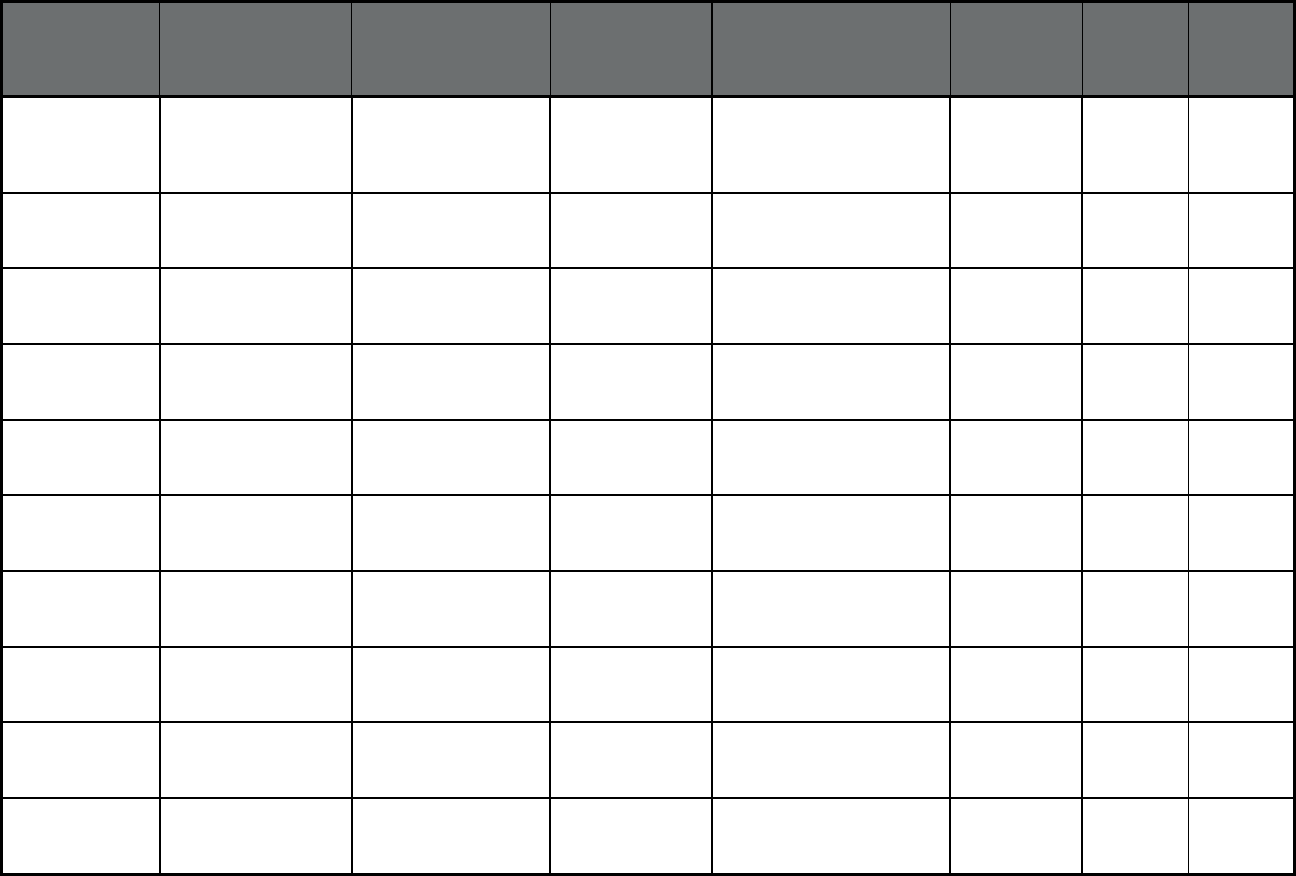
116
State
Program Name
(Type) Plan Name
Parent
Organization
Geographic Region (state-
defined areas, counties, or
zip codes)
Medicaid-Only
Enrollment
Dual
Enrollment
Total
Enrollment
New York Medicaid Advantage
Plus (Comprehensive
MCO + MLTSS)
Fidelis Legacy Plan Fidelis Legacy
Plan
Albany, Montgomery,
Rensselaer, and
Schenectady Counties, New
York City
2 94 96
New York Medicaid Advantage
Plus (Comprehensive
MCO + MLTSS)
GuildNet GuildNet New York City 2 453 455
New York Medicaid Advantage
Plus (Comprehensive
MCO + MLTSS)
HealthFirst HealthFirst Nassau County and New
York City
22 7,038 7,060
New York Medicaid Advantage
Plus (Comprehensive
MCO + MLTSS)
HealthPlus Advantage
Plus
HealthPlus
Advantage Plus
New York City 0 2 2
New York Medicaid Advantage
Plus (Comprehensive
MCO + MLTSS)
Senior Whole Health Senior Whole
Health
Nassau and Westchester
Counties, New York City
0 91 91
New York Medicaid Advantage
Plus (Comprehensive
MCO + MLTSS)
Village Care Village Care New York City 5 585 590
New York Medicaid Advantage
Plus (Comprehensive
MCO + MLTSS)
VNS Choice Plus VNS Choice Nassau, Suffolk, and
Westchester Counties, New
York City
8 1,439 1,447
New York Managed Long Term
Care (MLTSS only
(PIHP and/or PAHP))
Aetna Better Health Aetna Nassau and Suffolk
Counties, New York City
321 5,919 6,240
New York Managed Long Term
Care (MLTSS only
(PIHP and/or PAHP))
AgeWell New York AgeWell New York Nassau, Suffolk, and
Westchester Counties, New
York City
308 9,309 9,617
New York Managed Long Term
Care (MLTSS only
(PIHP and/or PAHP))
AlphaCare AlphaCare Westchester County and
New York City
3 0 3
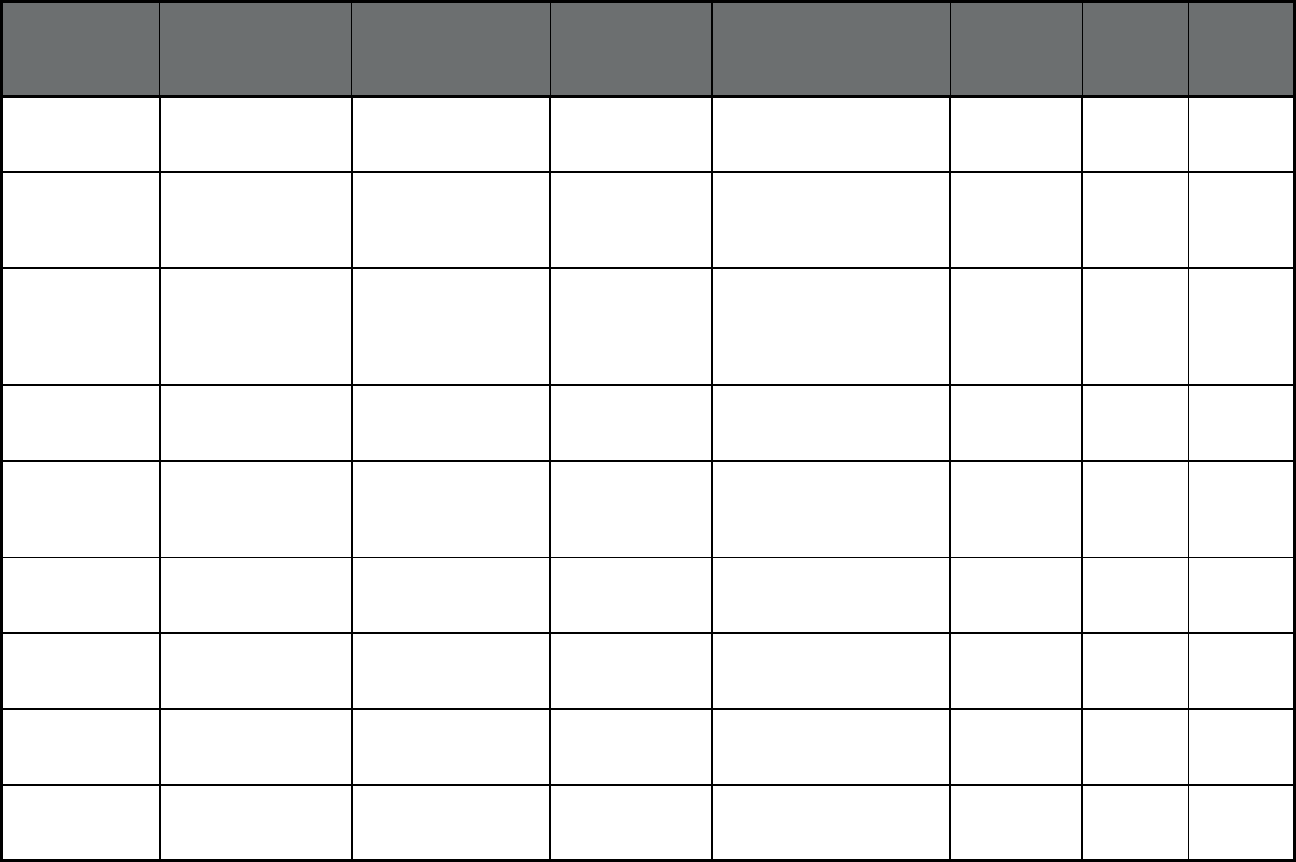
117
State
Program Name
(Type) Plan Name
Parent
Organization
Geographic Region (state-
defined areas, counties, or
zip codes)
Medicaid-Only
Enrollment
Dual
Enrollment
Total
Enrollment
New York Managed Long Term
Care (MLTSS only
(PIHP and/or PAHP))
ArchCare Community
Life
ArchCare Putnam and Westchester
Counties, New York City
441 3,422 3,863
New York Managed Long Term
Care (MLTSS only
(PIHP and/or PAHP))
Centers Plan for
Healthy Living
Centers Plan for
Healthy Living
Erie, Nassau, Niagara,
Rockland, Suffolk, and
Westchester Counties, New
York City
4,141 24,805 28,946
New York Managed Long Term
Care (MLTSS only
(PIHP and/or PAHP))
ElderPlan ElderPlan Dutchess, Nassau, Orange,
Putnam, Rockland, Suffolk,
Sullivan, Ulster, and
Westchester Counties, New
York City
807 12,095 12,902
New York Managed Long Term
Care (MLTSS only
(PIHP and/or PAHP))
ElderServe ElderServe Nassau, Suffolk, and
Westchester Counties, New
York City
1,025 11,319 12,344
New York Managed Long Term
Care (MLTSS only
(PIHP and/or PAHP))
ElderWood ElderWood Erie, Genesee, Monroe,
Niagara, Orleans, and
Wyoming Counties, New
York City
11 299 310
New York Managed Long Term
Care (MLTSS only
(PIHP and/or PAHP))
Extended MLTC Extended MLTC Nassau and Suffolk
Counties, New York City
507 4,217 4,724
New York Managed Long Term
Care (MLTSS only
(PIHP and/or PAHP))
Fallon Health Weinberg Fallon Health Plan Erie and Niagara Counties 69 657 726
New York Managed Long Term
Care (MLTSS only
(PIHP and/or PAHP))
Fidelis Care Fidelis Care New York City and 57
counties
1,366 20,000 21,366
New York Managed Long Term
Care (MLTSS only
(PIHP and/or PAHP))
GuildNet GuildNet Nassau, Suffolk, and
Westchester Counties, New
York City
557 6,892 7,449
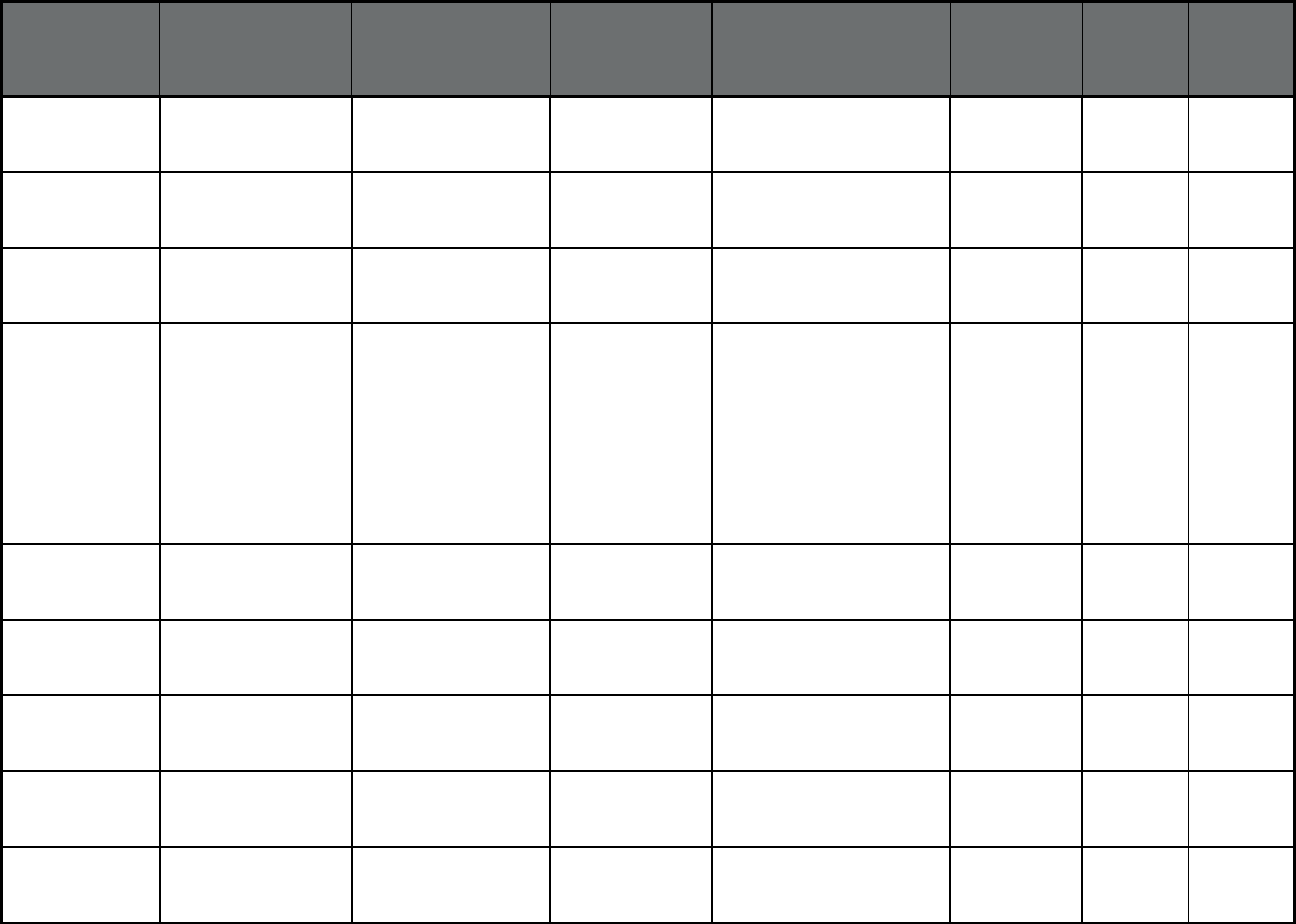
118
State
Program Name
(Type) Plan Name
Parent
Organization
Geographic Region (state-
defined areas, counties, or
zip codes)
Medicaid-Only
Enrollment
Dual
Enrollment
Total
Enrollment
New York Managed Long Term
Care (MLTSS only
(PIHP and/or PAHP))
Hamaspik Choice Hamaspik Choice Dutchess, Orange, Putnam,
Rockland, Sullivan, and
Ulster Counties
122 2,069 2,191
New York Managed Long Term
Care (MLTSS only
(PIHP and/or PAHP))
Health Advantage/Elant
Choice
Health
Advantage/Elant
Choice
Dutchess, Orange, and
Rockland Counties
80 907 987
New York Managed Long Term
Care (MLTSS only
(PIHP and/or PAHP))
HealthPlus HealthPlus New York City 429 4,621 5,050
New York Managed Long Term
Care (MLTSS only
(PIHP and/or PAHP))
iCircle Care iCircle Care Broome, Cayuga, Chemung,
Chenango, Cortland,
Genesee, Livingston,
Madison, Monroe,
Onondaga, Ontario,
Orleans, Oswego, Otsego,
Schuyler, Seneca, Steuben,
Tioga, Tompkins, Wayne,
Wyoming, and Yates
Counties
120 2,522 2,642
New York Managed Long Term
Care (MLTSS only
(PIHP and/or PAHP))
Independent Care
Systems
iCare New York City 982 5,292 6,274
New York Managed Long Term
Care (MLTSS only
(PIHP and/or PAHP))
Integra Integra Nassau, Suffolk, and
Westchester Counties, New
York City
1,868 9,879 11,747
New York Managed Long Term
Care (MLTSS only
(PIHP and/or PAHP))
Kalos Health Plan Kalos Health Plan Chautauqua, Erie, Genesee,
Monroe, Niagara, and
Orleans Counties
52 1,238 1,290
New York Managed Long Term
Care (MLTSS only
(PIHP and/or PAHP))
MetroPlus MetroPlus Health
Plan
New York City 561 1,291 1,852
New York Managed Long Term
Care (MLTSS only
(PIHP and/or PAHP))
Montefiore Montefiore Westchester County and
New York City
128 1,385 1,513
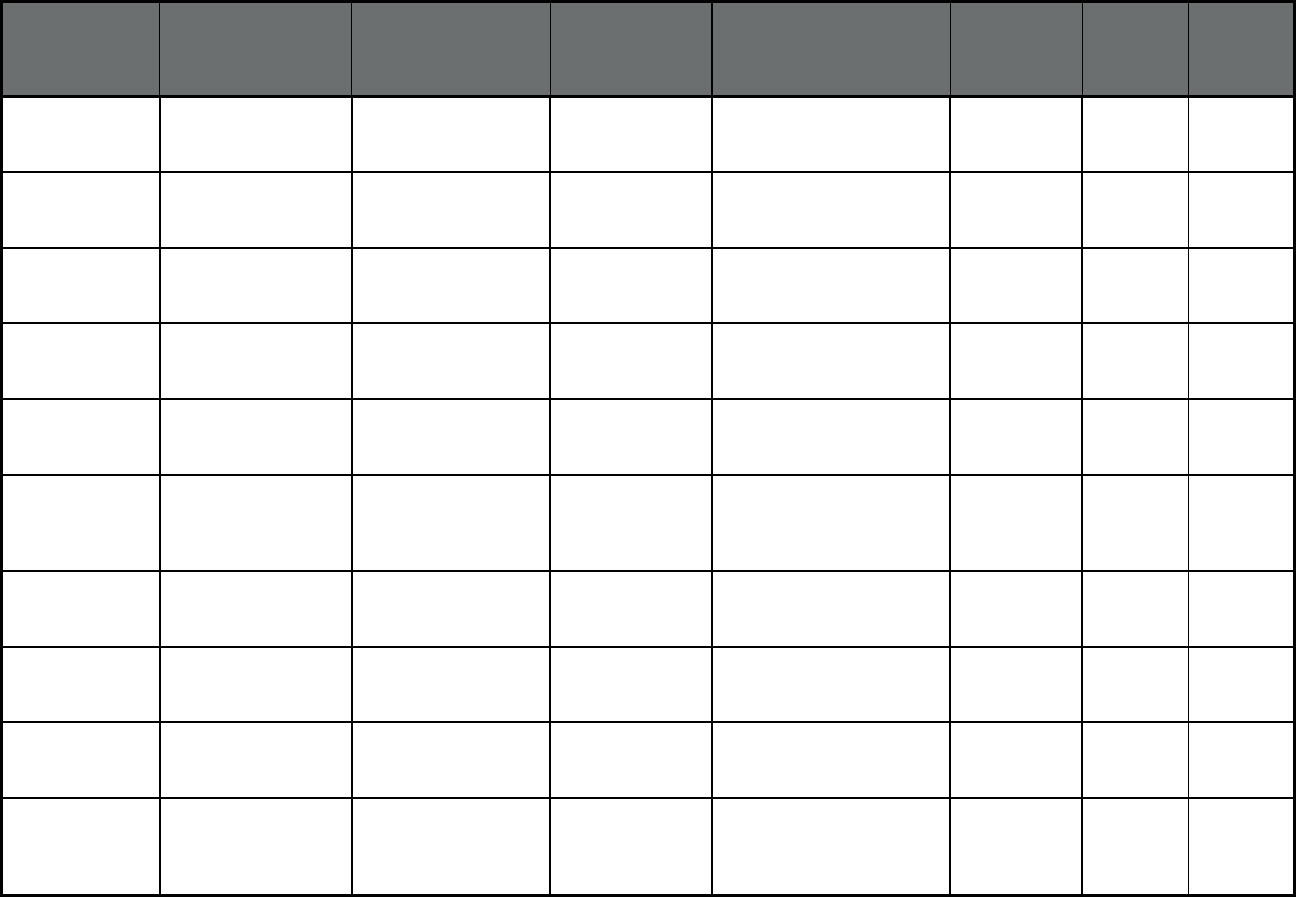
119
State
Program Name
(Type) Plan Name
Parent
Organization
Geographic Region (state-
defined areas, counties, or
zip codes)
Medicaid-Only
Enrollment
Dual
Enrollment
Total
Enrollment
New York Managed Long Term
Care (MLTSS only
(PIHP and/or PAHP))
North Shore - LIJ
Health Plan
North Shore - LIJ
Health Plan
Nassau and Suffolk
Counties, New York City
15 0 15
New York Managed Long Term
Care (MLTSS only
(PIHP and/or PAHP))
Prime Health Choice Prime Health
Choice
Albany, Dutchess, Orange,
Putnam, Rockland, Warren,
and Washington Counties
28 352 380
New York Managed Long Term
Care (MLTSS only
(PIHP and/or PAHP))
Senior Health Partners Senior Health
Partners
Nassau and Westchester
Counties, New York City
2,158 12,303 14,461
New York Managed Long Term
Care (MLTSS only
(PIHP and/or PAHP))
Senior Network Health Senior Network
Health
Herkimer and Oneida
Counties
23 526 549
New York Managed Long Term
Care (MLTSS only
(PIHP and/or PAHP))
Senior Whole Health Senior Whole
Health
Westchester County and
New York City
1,747 12,124 13,871
New York Managed Long Term
Care (MLTSS only
(PIHP and/or PAHP))
United HealthCare UnitedHealthcare Albany, Broome, Erie,
Monroe, Oneida, Onondaga,
Orange, and Rockland
Counties
167 4,066 4,233
New York Managed Long Term
Care (MLTSS only
(PIHP and/or PAHP))
Village Care Village Care New York City 2,004 8,679 10,683
New York Managed Long Term
Care (MLTSS only
(PIHP and/or PAHP))
VNA HomeCare
Options
VNA HomeCare
Options
48 counties 262 6,498 6,760
New York Managed Long Term
Care (MLTSS only
(PIHP and/or PAHP))
VNS Choice VNS Choice New York City and 28
counties
792 11,969 12,761
New York Managed Long Term
Care (MLTSS only
(PIHP and/or PAHP))
WellCare Advocate WellCare Albany, Erie, Nassau,
Orange, Rockland, Suffolk,
Ulster, and Westchester
Counties, New York City
284 5,235 5,519
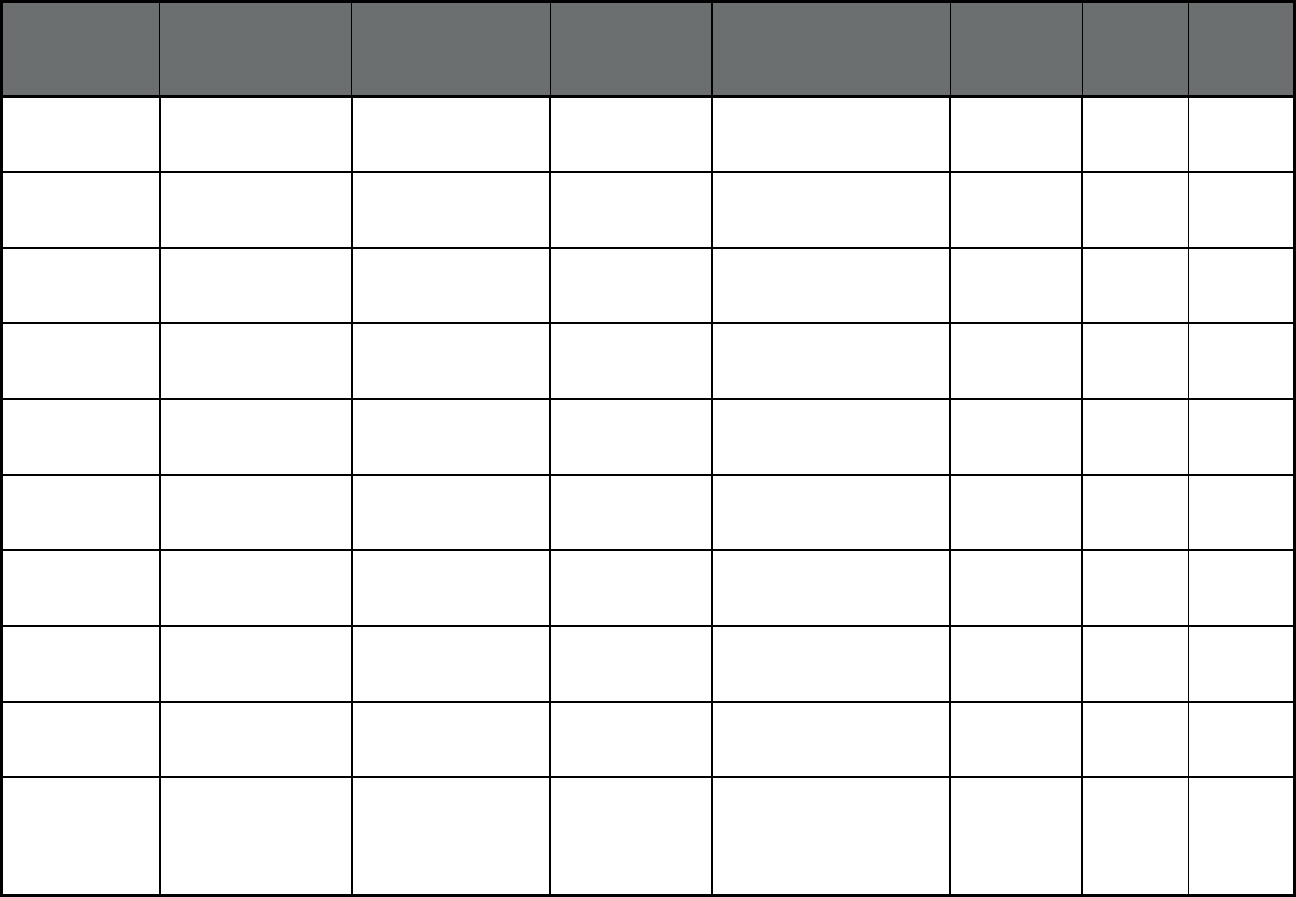
120
State
Program Name
(Type) Plan Name
Parent
Organization
Geographic Region (state-
defined areas, counties, or
zip codes)
Medicaid-Only
Enrollment
Dual
Enrollment
Total
Enrollment
New York PACE (Program of All-
inclusive Care for the
Elderly (PACE))
ArchCare Senior Life PACE Westchester County and
New York City
81 644 725
New York PACE (Program of All-
inclusive Care for the
Elderly (PACE))
Catholic Health - Life PACE Erie County 14 232 246
New York PACE (Program of All-
inclusive Care for the
Elderly (PACE))
CenterLight (CCM) PACE Nassau, Suffolk, and
Westchester Counties, New
York City
414 2,408 2,822
New York PACE (Program of All-
inclusive Care for the
Elderly (PACE))
Complete Senior Care PACE Niagara County 7 111 118
New York PACE (Program of All-
inclusive Care for the
Elderly (PACE))
Eddy Senior Care PACE Albany and Schenectady
Counties
17 199 216
New York PACE (Program of All-
inclusive Care for the
Elderly (PACE))
Fallon Health Weinberg PACE Erie County 4 116 120
New York PACE (Program of All-
inclusive Care for the
Elderly (PACE))
Independent Living for
Seniors
PACE Monroe, Ontario and Wayne
Counties
28 744 772
New York PACE (Program of All-
inclusive Care for the
Elderly (PACE))
PACE CNY PACE Onondaga County 22 541 563
New York PACE (Program of All-
inclusive Care for the
Elderly (PACE))
Total Senior Care PACE Allegany, Cattaraugus, and
Chautauqua Counties
14 98 112
North Carolina Community Care of
North Carolina
(Primary Care Case
Management Entity
(PCCM Entity))
North Carolina
Community Care
Carolina Access
Community Care
Health Plan (WI)
Statewide 1,341,900 151,447 1,493,347
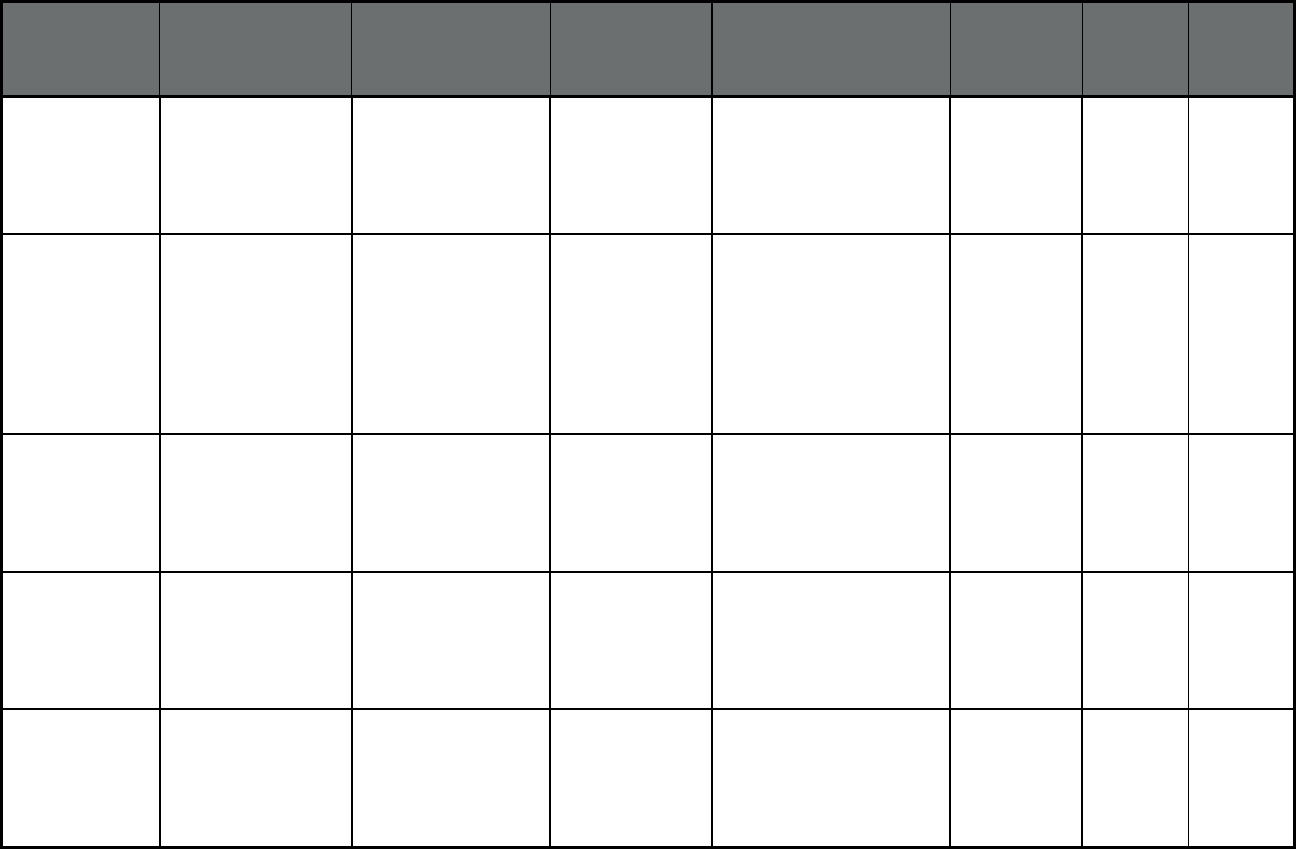
121
State
Program Name
(Type) Plan Name
Parent
Organization
Geographic Region (state-
defined areas, counties, or
zip codes)
Medicaid-Only
Enrollment
Dual
Enrollment
Total
Enrollment
North Carolina 1915(b)/(c) Medicaid
Waiver for MH/DD/SA
Services (Behavioral
Health Organization
(BHO) only (PIHP
and/or PAHP))
Alliance Behavioral
Healthcare
Alliance
Behavioral
Healthcare
Counties: Cumberland,
Durham, Johnston, Wake
212,280 22,741 235,021
North Carolina 1915(b)/(c) Medicaid
Waiver for MH/DD/SA
Services (Behavioral
Health Organization
(BHO) only (PIHP
and/or PAHP))
Cardinal Innovations
Healthcare Solutions
Cardinal
Innovations
Healthcare
Solutions
Counties: Alamance,
Cabarrus, Caswell,
Chatham, Davidson, Davie,
Forsyth, Franklin, Granville,
Halifax, Mecklenburg,
Orange, Rockingham,
Person, Rowan, Stanly,
Stokes, Union, Vance and
Warren
410,013 49,011 459,024
North Carolina 1915(b)/(c) Medicaid
Waiver for MH/DD/SA
Services (Behavioral
Health Organization
(BHO) only (PIHP
and/or PAHP))
Eastpointe Human
Services
Eastpointe Human
Services
Counties: Bladen,
Columbus, Duplin,
Edgecombe, Greene,
Lenoir, Nash, Robeson,
Sampson, Scotland, Wayne,
Wilson
149,171 23,487 172,658
North Carolina 1915(b)/(c) Medicaid
Waiver for MH/DD/SA
Services (Behavioral
Health Organization
(BHO) only (PIHP
and/or PAHP))
Partners Behavioral
Health Management
Partners
Behavioral Health
Management
Counties: Burke, Catawba,
Cleveland, Gaston, Iredell,
Lincoln, Surry, Yadkin
132,093 18,235 150,328
North Carolina 1915(b)/(c) Medicaid
Waiver for MH/DD/SA
Services (Behavioral
Health Organization
(BHO) only (PIHP
and/or PAHP))
Sandhills Center for
MH DD SA
Sandhills Center
for MH DD SA
Counties: Anson, Guilford,
Harnett, Hoke, Lee,
Montgomery, Moore,
Randolph, Richmond
168,686 20,816 189,502
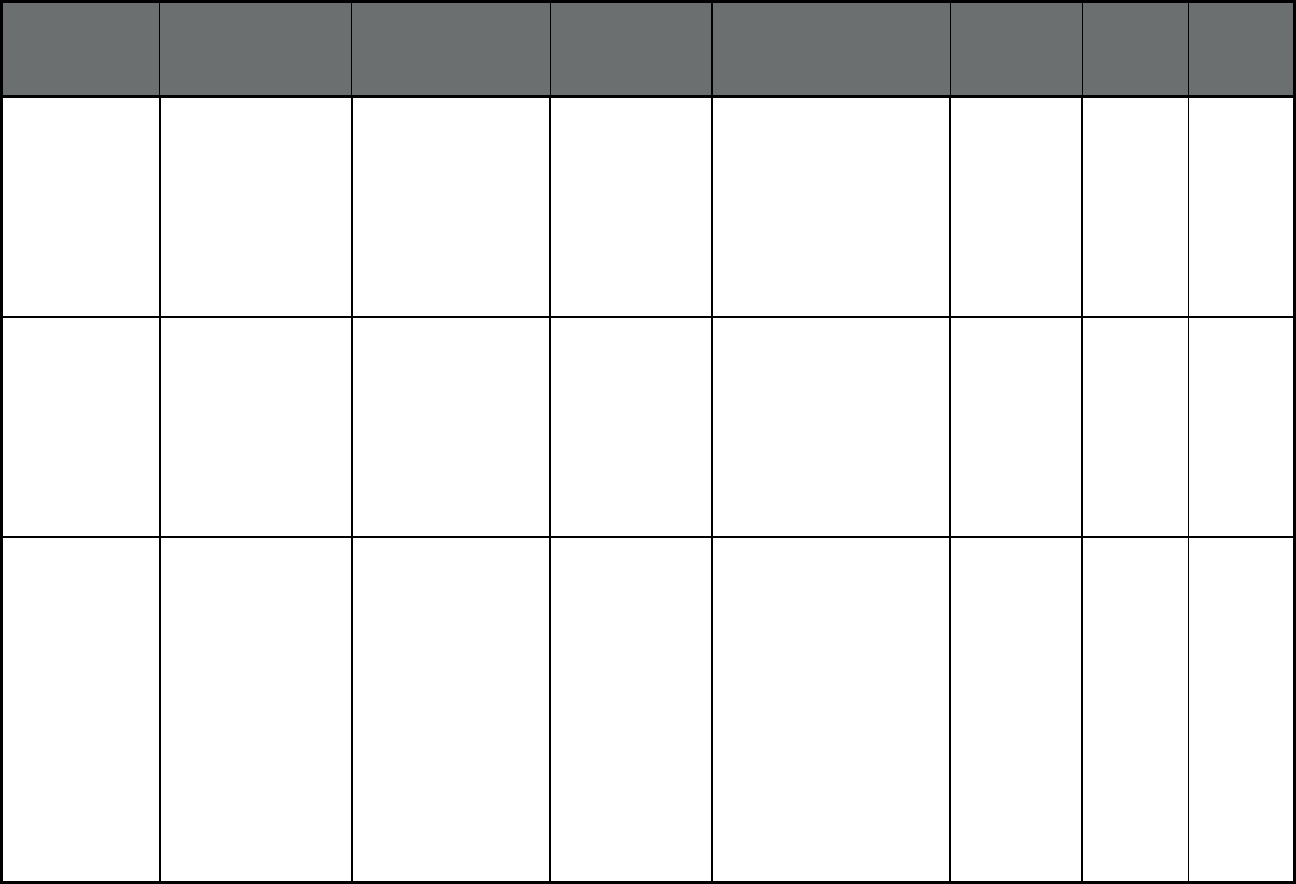
122
State
Program Name
(Type) Plan Name
Parent
Organization
Geographic Region (state-
defined areas, counties, or
zip codes)
Medicaid-Only
Enrollment
Dual
Enrollment
Total
Enrollment
North Carolina 1915(b)/(c) Medicaid
Waiver for MH/DD/SA
Services (Behavioral
Health Organization
(BHO) only (PIHP
and/or PAHP))
Trillium Health
Resources
Trillium Health Counties: Brunswick,
Carteret, New Hanover,
Onslow, Pender, Beaufort,
Bertie, Camden, Chowan,
Craven, Currituck, Dare,
Gates, Hertford, Hyde,
Jones, Martin, Northampton,
Pamlico, Pasquotank,
Perquimans, Pitt, Tyrrell,
Washington
181,765 28,257 210,022
North Carolina 1915(b)/(c) Medicaid
Waiver for MH/DD/SA
Services (Behavioral
Health Organization
(BHO) only (PIHP
and/or PAHP))
VAYA Health VAYA Health Counties: Alexander,
Alleghany, Ashe, Avery,
Buncombe, Caldwell,
Cherokee, Clay, Graham,
Haywood, Henderson,
Jackson, Macon, Madison,
McDowell, Mitchell, Polk,
Rutherford, Swain,
Transylvania, Watauga,
Wilkes, Yancey
137,852 24,570 162,422
North Carolina Program of All
Inclusive Care for the
Elderly (Program of
All-inclusive Care for
the Elderly (PACE))
Carolina Seniorcare Carolina
Seniorcare
Serving the following zip
codes in Davidson, Davie,
Iredell and Rowan Counties:
27012, 27107, 27127,
27239, 27262, 27265,
27284, 27292, 27295,
27299, 27360, 28127,
27013, 27054, 28023,
28071, 28081, 28083,
28088, 28125, 28137,
28138, 28144, 28146,
28147, 28159, 27006,
27028, 27013, 27020,
28115, 28117, 28166,
28625, 28634, 28636,
28660, 28677, 28689
145 61 206
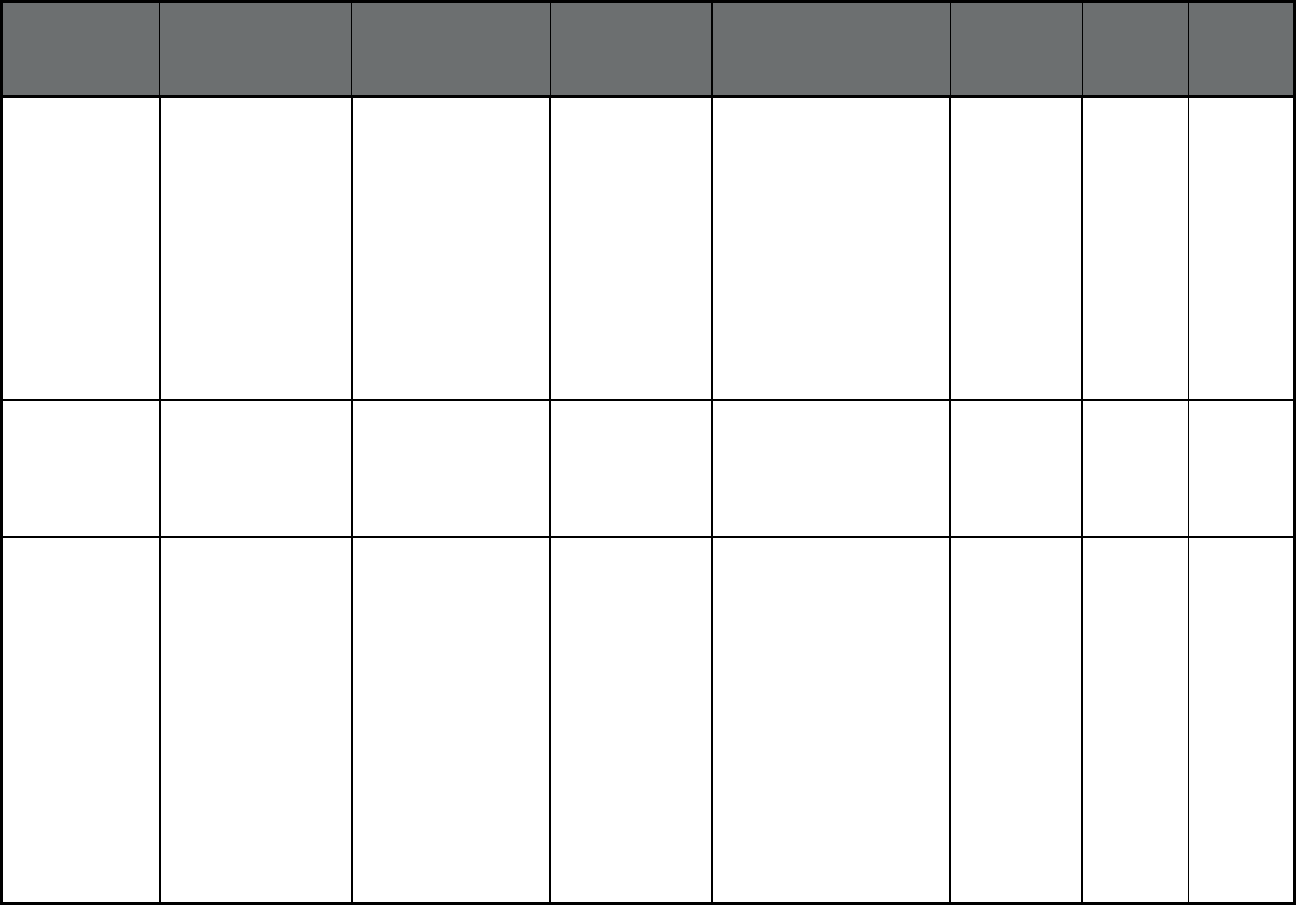
123
State
Program Name
(Type) Plan Name
Parent
Organization
Geographic Region (state-
defined areas, counties, or
zip codes)
Medicaid-Only
Enrollment
Dual
Enrollment
Total
Enrollment
North Carolina Program of All
Inclusive Care for the
Elderly (Program of
All-inclusive Care for
the Elderly (PACE))
Community
Carepartners, Inc.
Community Care
Health Plan (WI)
Serving the following zip
codes in Buncombe and
Henderson Counties: 28701,
28704, 28709, 28710,
28711, 28715, 28726,
28729, 28730, 28731,
28732, 28735, 28739,
28742, 28748, 28757,
28758, 28759, 28766,
28773, 28778, 28787,
28784, 28790, 28791,
28792, 28801, 28803,
28804, 28805, 28806,
28810
118 48 166
North Carolina Program of All
Inclusive Care for the
Elderly (Program of
All-inclusive Care for
the Elderly (PACE))
Elderhaus, Inc. Elderhaus, Inc. New Hanover County and
the following zip codes in
Brunswick County: 28422,
28451, 28461, 28479 and
the following zip code in
Pender County: 28443
89 34 123
North Carolina Program of All
Inclusive Care for the
Elderly (Program of
All-inclusive Care for
the Elderly (PACE))
Life St. Joseph of the
Pines, Inc.
Life St. Joseph of
the Pines, Inc.
Serving the following zip
codes in Cumberland,
Harnett Hoke, Moore and
Robeson Counties: 28301,
28302, 28303, 28304,
28305, 28306, 28307,
28308, 28309, 28310,
28311, 28312, 28314,
28318, 28342, 28344,
28348, 28356, 28371,
28382, 28390, 28391,
28395, 28315, 28326,
28373, 28376, 28357,
28371, 28377, 28384,
28315, 28357, 28376,
28377, 28386, 28314,
28334, 28339
176 98 274
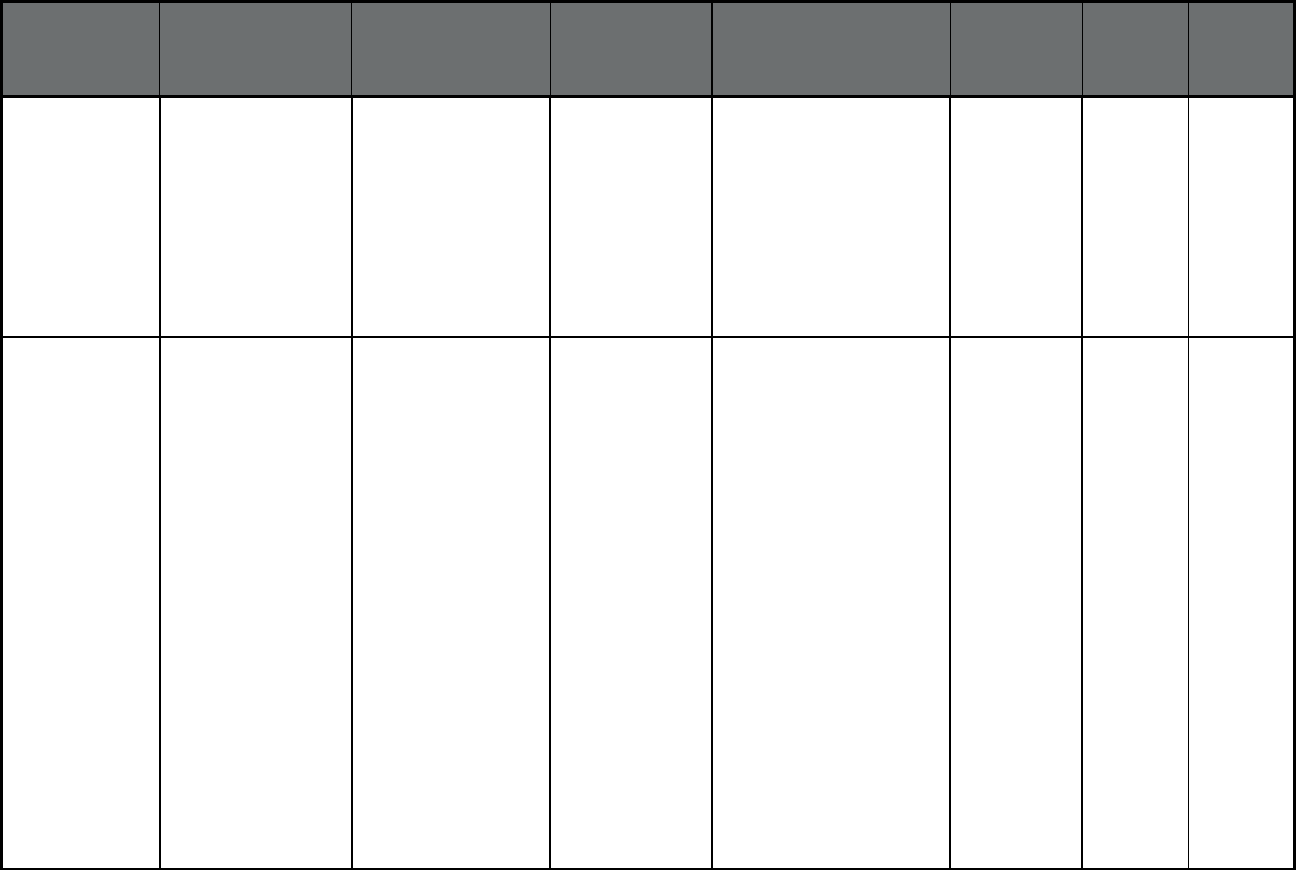
124
State
Program Name
(Type) Plan Name
Parent
Organization
Geographic Region (state-
defined areas, counties, or
zip codes)
Medicaid-Only
Enrollment
Dual
Enrollment
Total
Enrollment
North Carolina Program of All
Inclusive Care for the
Elderly (Program of
All-inclusive Care for
the Elderly (PACE))
PACE at Home, Inc. PACE Catawba County and
portions of zip codes in
Alexander, Burke, Caldwell
and Lincoln Counties:
28037, 28092, 28168,
28601, 28602, 28609,
28610, 28612, 28613,
28630, 28637, 28638,
28650, 28658, 28673,
28678, 28681, 28682,
28690
107 38 145
North Carolina Program of All
Inclusive Care for the
Elderly (Program of
All-inclusive Care for
the Elderly (PACE))
PACE of the Southern
Piedmont
PACE Serving the following zip
codes in Mecklenburg,
Cabarrus, Stanly and Union
Counties: 28025, 28027,
28031, 28036, 28071,
28075, 28078, 28079,
28081, 28083, 28097,
28103, 28104, 28105,
28107, 28109, 28110,
28112, 28124, 28129,
28134, 28137, 28138,
28215, 28163, 28173,
28174, 28202, 28203,
28204, 28205, 28206,
28207, 28208, 28209,
28210, 28211, 28212,
28213, 28214, 28216,
28217, 28223, 28226,
28227, 28244, 28226,
28227, 28244, 28246,
28254, 28262, 28269,
28270, 28273, 28274,
28277, 28278, 28280,
28281, 28282, 28284,
28285, 28287
121 41 162
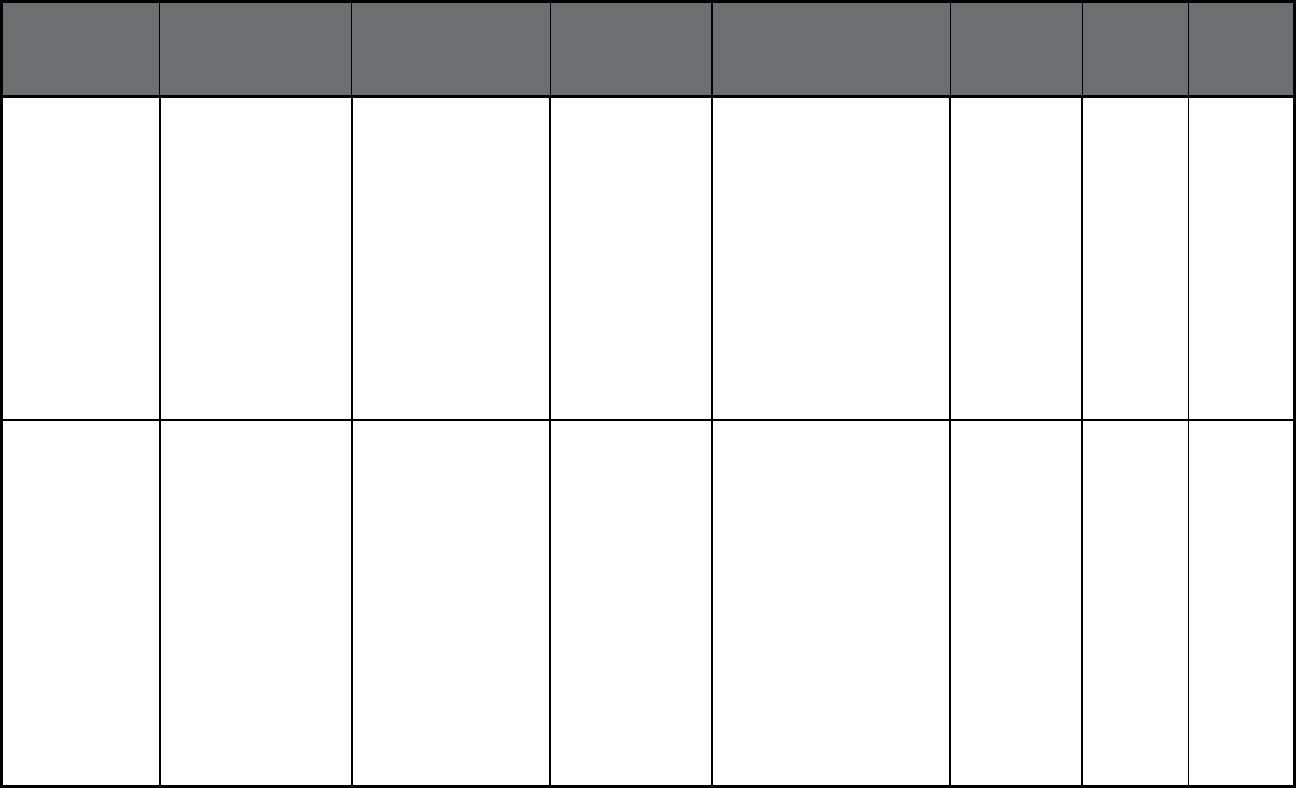
125
State
Program Name
(Type) Plan Name
Parent
Organization
Geographic Region (state-
defined areas, counties, or
zip codes)
Medicaid-Only
Enrollment
Dual
Enrollment
Total
Enrollment
North Carolina Program of All
Inclusive Care for the
Elderly (Program of
All-inclusive Care for
the Elderly (PACE))
PACE of the Triad PACE Serving the following zip
codes in Guilford and
Rockingham Counties:
27027, 27048, 27288,
27235, 27282, 27301,
27310, 27377, 27401,
27403, 27405, 27406,
27407, 27408, 27409,
27410, 27455, 27495,
27025, 27214, 27233,
27244, 27249, 27260,
27262, 27263, 27265,
27283, 27284, 27298,
27311, 27313, 27320,
27326, 27357, 27358
146 59 205
North Carolina Program of All
Inclusive Care for the
Elderly (Program of
All-inclusive Care for
the Elderly (PACE))
Piedmont Health
Services, Inc.
Piedmont Health
Services, Inc.
Serving the following zip
codes in Alamance,
Caswell, Orange, Chatham,
Lee Counties and the
portion of 27278 located in
Durham County: 27231,
27243, 27278, 27302,
27510, 27514, 27516,
27517, 27541, 27572,
27705, 27583, 27707,
27712, 27207, 27208,
27252, 27298, 27312,
27330, 27344, 27349,
27355, 27502, 27519,
27523, 27559, 27562,
27713, 27330, 27332,
27505, 28326
191 136 327
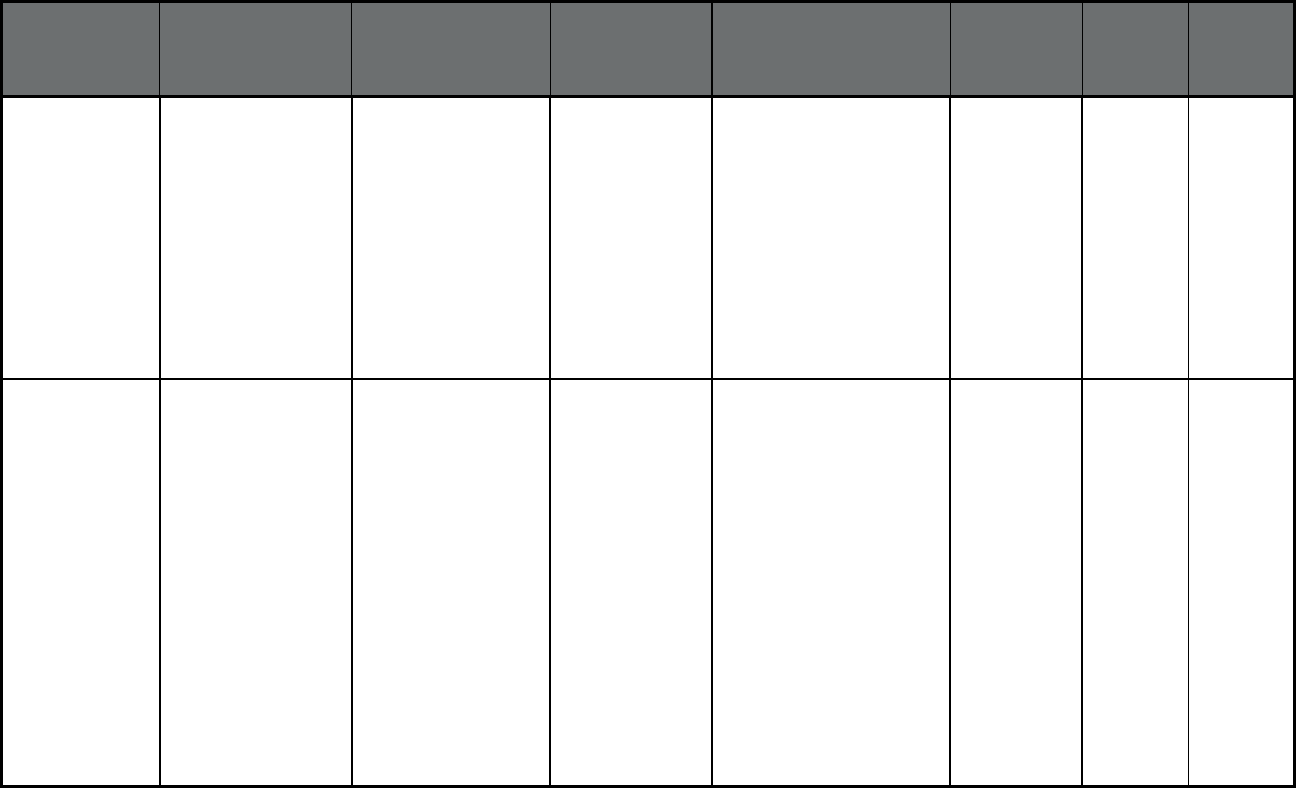
126
State
Program Name
(Type) Plan Name
Parent
Organization
Geographic Region (state-
defined areas, counties, or
zip codes)
Medicaid-Only
Enrollment
Dual
Enrollment
Total
Enrollment
North Carolina Program of All
Inclusive Care for the
Elderly (Program of
All-inclusive Care for
the Elderly (PACE))
Senior Total Life Care,
Inc.
Senior Total Life
Care, Inc.
Serving the following zip
codes in Cleveland, Gaston
and Lincoln Counties:
28006, 28012, 28016,
28021, 28032, 28033,
28034, 28052, 28053,
28054, 28055, 28056,
28077, 28080, 28086,
28092, 28098, 28101,
28120, 28164, 28021,
28073, 28086, 28150,
28152, 28006, 28021,
28033, 28080, 28164
147 64 211
North Carolina Program of All
Inclusive Care for the
Elderly (Program of
All-inclusive Care for
the Elderly (PACE))
Stay Well Senior Care Stay Well Senior
Care
Serving the following zip
codes in Montgomery,
Moore and Randolph
Counties: 27203, 27205,
27208, 27233, 27239,
27248, 27260, 27263,
27283, 27292, 27298,
27313, 27316, 27317,
27325, 27341, 27344,
27350, 27355, 27360,
27370, 27371, 28127,
27209, 27229, 27281,
27306, 27341, 27356,
27371, 28127, 27208,
27209, 27242, 27281,
27325, 27330, 27341,
27356, 27376, 28327,
28347, 28350, 28374,
28387, 28394
69 35 104
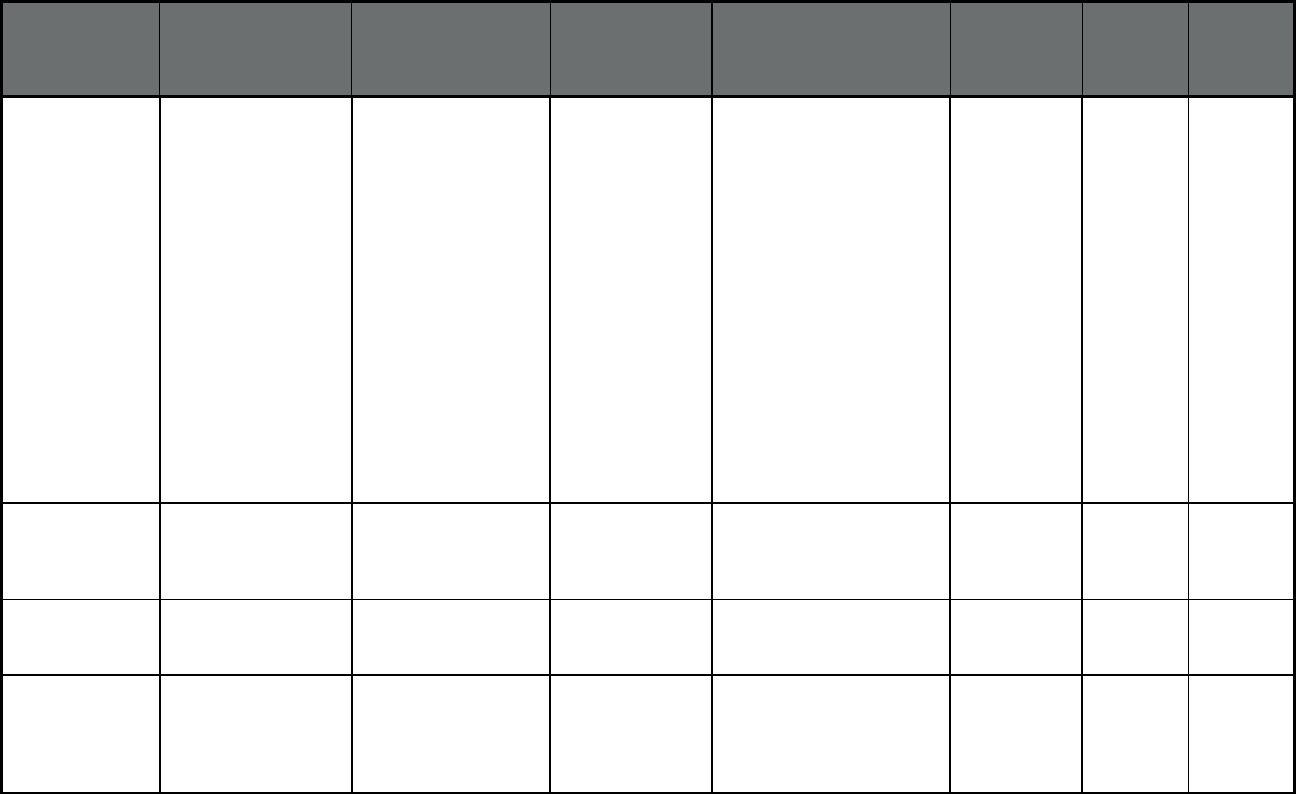
127
State
Program Name
(Type) Plan Name
Parent
Organization
Geographic Region (state-
defined areas, counties, or
zip codes)
Medicaid-Only
Enrollment
Dual
Enrollment
Total
Enrollment
North Carolina Program of All
Inclusive Care for the
Elderly (Program of
All-inclusive Care for
the Elderly (PACE))
VOANS Senior
Community Care
Community Care
Health Plan (WI)
Serving the following zip
codes in Durham, Wake
County: 27503, 27613,
27701, 27703, 27704,
27705, 27706, 27707,
27712, 27713, 27502,
27511, 27513, 27518,
27519, 27523, 27526,
27529, 27539, 27540,
27545, 27560, 27562,
27571, 27587, 27591,
27592, 27597, 27601,
27603, 27604, 27605,
27606, 27607, 27608,
27609, 27610, 27612,
27613, 27614, 27615,
27616, 27617 and Granville
County zip codes: 27509,
27522
123 66 189
North Dakota North Dakota Medicaid
Expansion
(Comprehensive
MCO)
ND Medicaid
Expansion MCO
Sanford Health
Plan
Statewide 19,515 0 19,515
North Dakota PCCM (Primary Care
Case Management
(PCCM))
Multiple Primary Care
Providers
Multiple Primary
Care Provider
(PCCM)
Statewide 48,957 0 48,957
North Dakota Health Management
Program (Other
Prepaid Health Plan
(PHP) (limited
benefits))
Health Management US Care
Management
Statewide 0 0 0
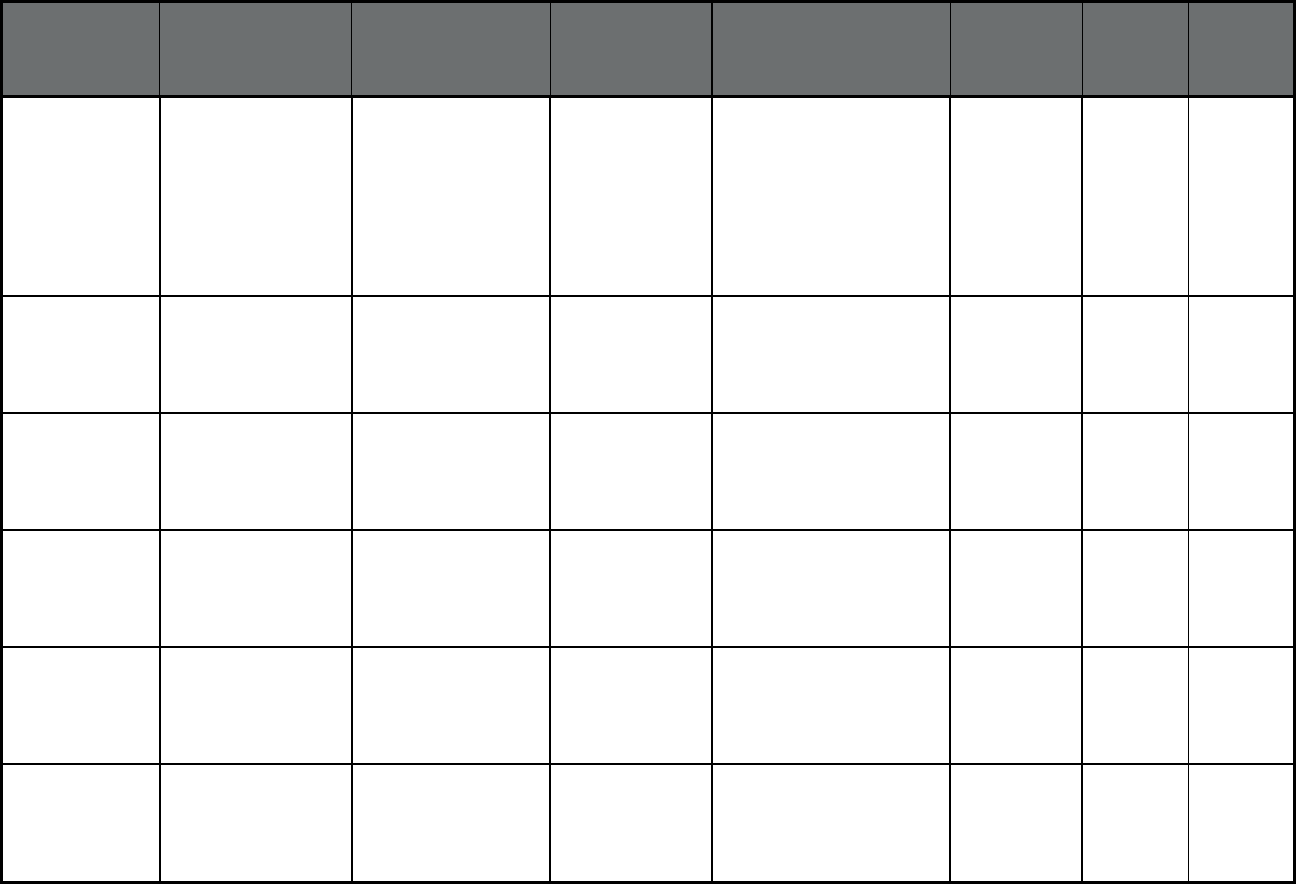
128
State
Program Name
(Type) Plan Name
Parent
Organization
Geographic Region (state-
defined areas, counties, or
zip codes)
Medicaid-Only
Enrollment
Dual
Enrollment
Total
Enrollment
North Dakota PACE (Program of All-
inclusive Care for the
Elderly (PACE))
PACE PACE Zip codes: 58501, 58502,
58503 (Bismarck), 58504
(Lincoln), 58554 (Mandan),
58558 (Menoken), 58601,
58602 (Dickinson), 58652
(Richardton), 58655 (South
Heart), 58656 (Taylor),
58701, 58702, 58703,
58722, 58785 (Minot)
12 169 181
Ohio Ohio Medicaid
Managed Care
Program
(Comprehensive
MCO)
Buckeye Health Plan Centene
Corporation
Statewide 307,779 0 307,779
Ohio Ohio Medicaid
Managed Care
Program
(Comprehensive
MCO)
CareSource CareSource Statewide 1,254,635 0 1,254,635
Ohio Ohio Medicaid
Managed Care
Program
(Comprehensive
MCO)
Molina Healthcare of
Ohio, Inc.
Molina Healthcare Statewide 292,128 0 292,128
Ohio Ohio Medicaid
Managed Care
Program
(Comprehensive
MCO)
Paramount Advantage Promedica Statewide 244,867 0 244,867
Ohio Ohio Medicaid
Managed Care
Program
(Comprehensive
MCO)
UnitedHealthcare
Community Plan of
Ohio, Inc.
UnitedHealthcare Statewide 296,760 0 296,760
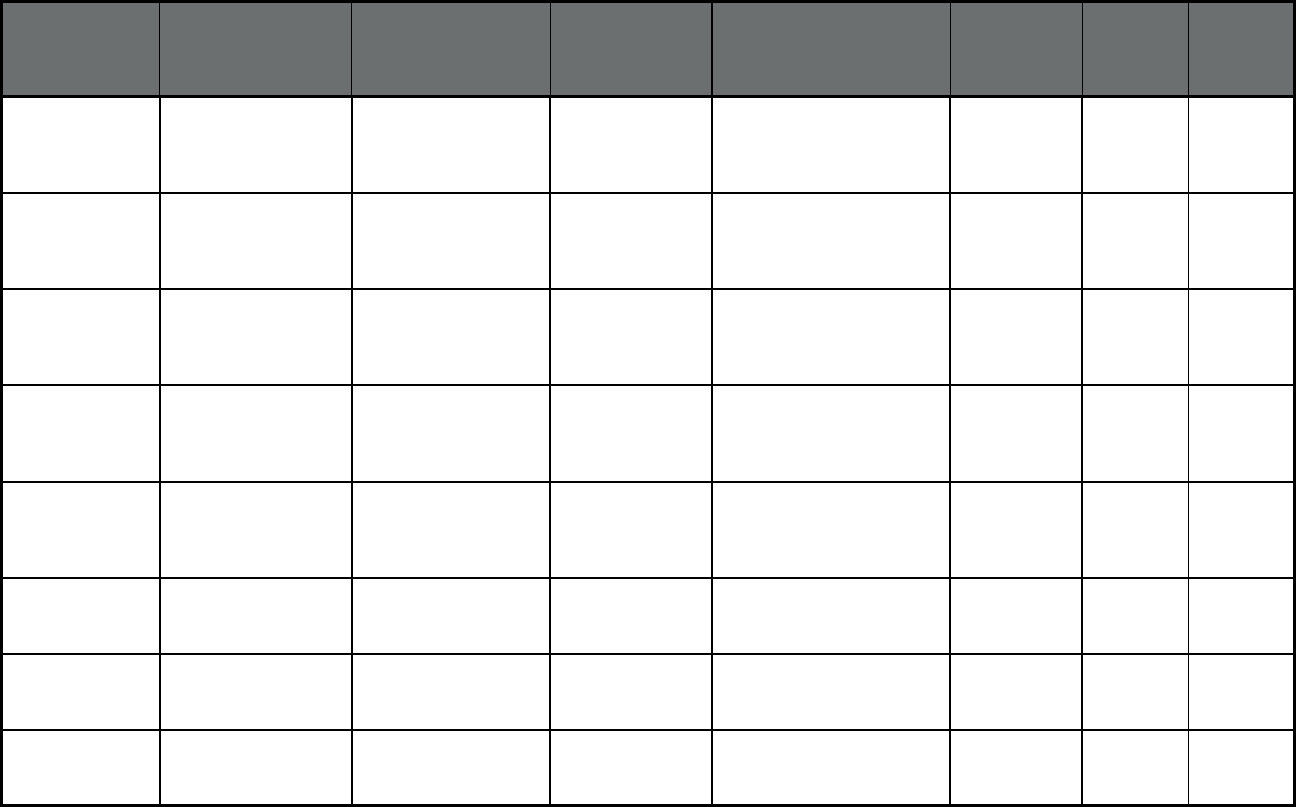
129
State
Program Name
(Type) Plan Name
Parent
Organization
Geographic Region (state-
defined areas, counties, or
zip codes)
Medicaid-Only
Enrollment
Dual
Enrollment
Total
Enrollment
Ohio MyCare Ohio Opt-Out
Program
(Comprehensive MCO
+ MLTSS)
Aetna Better Health of
Ohio
Aetna Central, Northwest,
Southwest
0 11,117 11,117
Ohio MyCare Ohio Opt-Out
Program
(Comprehensive MCO
+ MLTSS)
Buckeye Health Plan Centene
Corporation
Northeast, Northwest, West
Central
0 9,647 9,647
Ohio MyCare Ohio Opt-Out
Program
(Comprehensive MCO
+ MLTSS)
CareSource CareSource East Central, Northeast,
Northeast Central
0 11,233 11,233
Ohio MyCare Ohio Opt-Out
Program
(Comprehensive MCO
+ MLTSS)
Molina Healthcare of
Ohio, Inc.
Molina Healthcare Central, Southwest, West
Central
0 9,531 9,531
Ohio MyCare Ohio Opt-Out
Program
(Comprehensive MCO
+ MLTSS)
UnitedHealthcare
Community Plan of
Ohio, Inc.
UnitedHealthcare East Central, Northeast,
Northeast Central
0 11,880 11,880
Ohio Ohio PACE (Program
of All-inclusive Care
for the Elderly (PACE))
McGregor PACE PACE Cuyahoga County 95 359 454
Oklahoma SoonerCare Choice
(Primary Care Case
Management (PCCM))
SoonerCare Choice Oklahoma Health
Care Authority
Statewide 533,758 114,799 648,557
Oklahoma SoonerRide (Non-
Emergency Medical
Transportation)
SoonerRide Oklahoma Health
Care Authority
Statewide 533,758 114,799 648,557
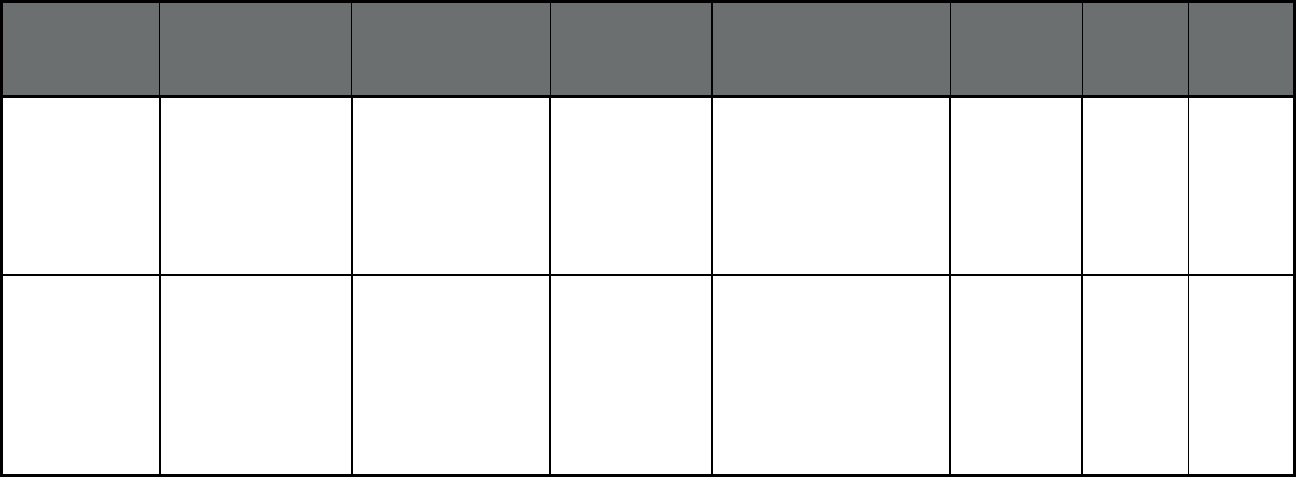
130
State
Program Name
(Type) Plan Name
Parent
Organization
Geographic Region (state-
defined areas, counties, or
zip codes)
Medicaid-Only
Enrollment
Dual
Enrollment
Total
Enrollment
Oklahoma PACE (Program of All-
inclusive Care for the
Elderly (PACE))
Cherokee Elder Care
(CEC)
PACE 74464, 74441, 74423,
74960, 74427, 74465,
74403, 74457, 74451,
74352, 74434, 74401,
74471, 74364, 74347,
74402, 74444, 74368,
74964, 74446, 74452,
74359, 74965, 74439
14 134 148
Oklahoma PACE (Program of All-
inclusive Care for the
Elderly (PACE))
Life PACE PACE 74103, 74104, 74105,
74106, 74107, 74110,
74112, 74114, 74115,
74119, 74120, 74126,
74127, 74128, 74129,
74130, 74132, 74133,
74136, 74137, 74145,
74146, 74134, 74135,
74117, 74116, 74108
14 117 131
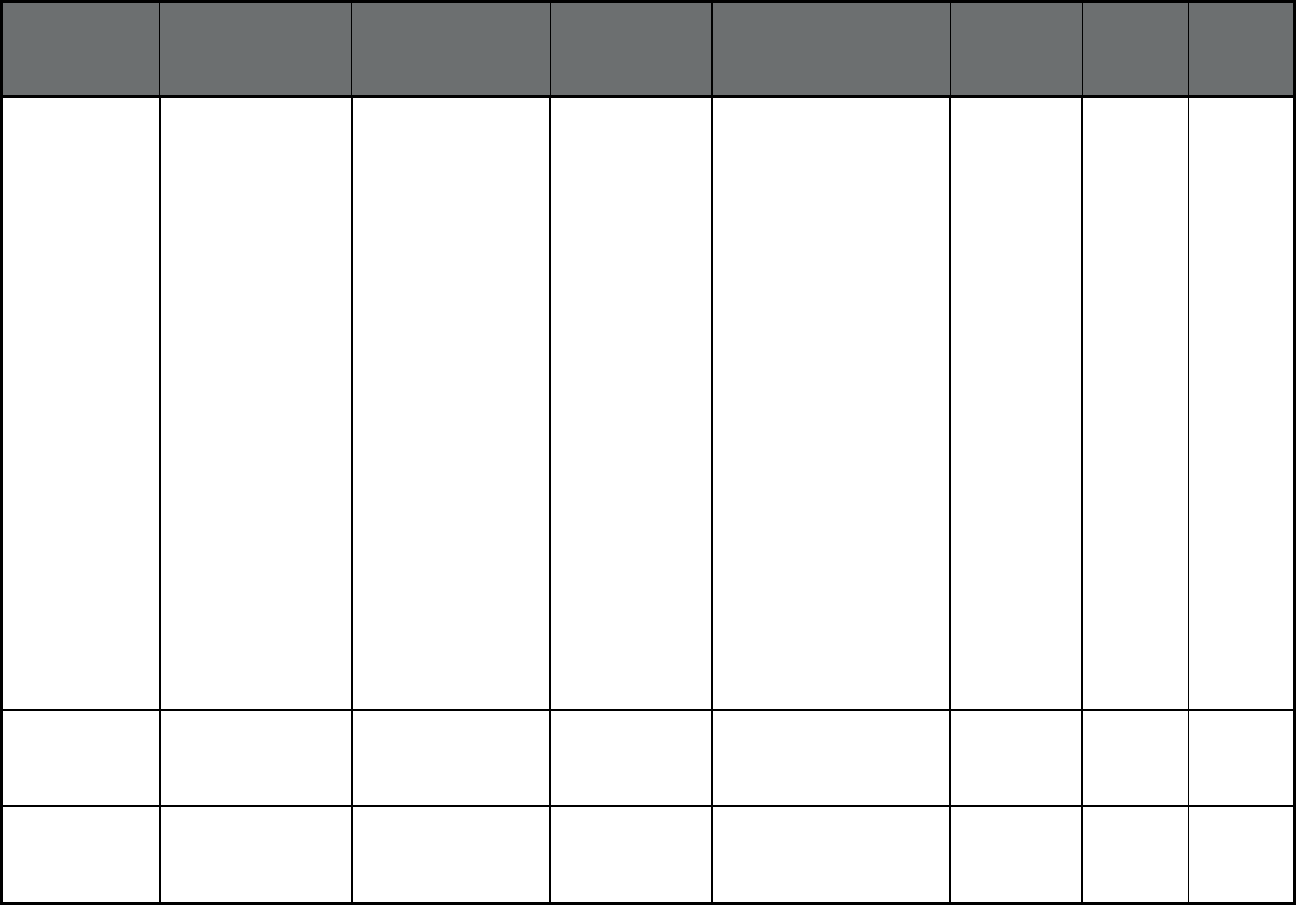
131
State
Program Name
(Type) Plan Name
Parent
Organization
Geographic Region (state-
defined areas, counties, or
zip codes)
Medicaid-Only
Enrollment
Dual
Enrollment
Total
Enrollment
Oklahoma PACE (Program of All-
inclusive Care for the
Elderly (PACE))
Valir PACE PACE 73008, 73106, 73143,
73003, 73147, 73025,
73134, 73084, 73119,
73140, 73124, 73157,
73170, 73163, 73066,
73150, 73110, 73139,
73105, 73142, 73185,
73109, 73194, 73113,
73169, 73103, 73154,
73121, 73156, 73165,
73127, 73013, 73131,
73198, 73118, 73178,
73141, 73184, 73160,
73146, 73120, 73149,
73083, 73137, 73122,
73155, 73132, 73108,
73162, 73112, 73167,
73102, 73152, 73012,
73179, 73135, 73126,
73190, 73129, 73196,
73117, 73173, 73123,
73153, 73144, 73116,
73148, 73034, 73136,
73120, 73115, 73107,
73159, 73111, 73164,
73101, 73151, 73130,
73145, 73125, 73189,
73128, 73195, 73114,
73172, 73104
6 181 187
Oregon
8
Oregon Health Plan
(OHP)
(Comprehensive
MCO)
Access Dental Plan,
LLC
Access Dental,
Inc.
Clackamas, Multnomah, and
Washington Counties
1,490 72 1,562
Oregon
8
Oregon Health Plan
(OHP)
(Comprehensive
MCO)
Advantage Dental
Services
Advantage Dental
Services
Statewide except Tillamook
County
14,280 4,160 18,440
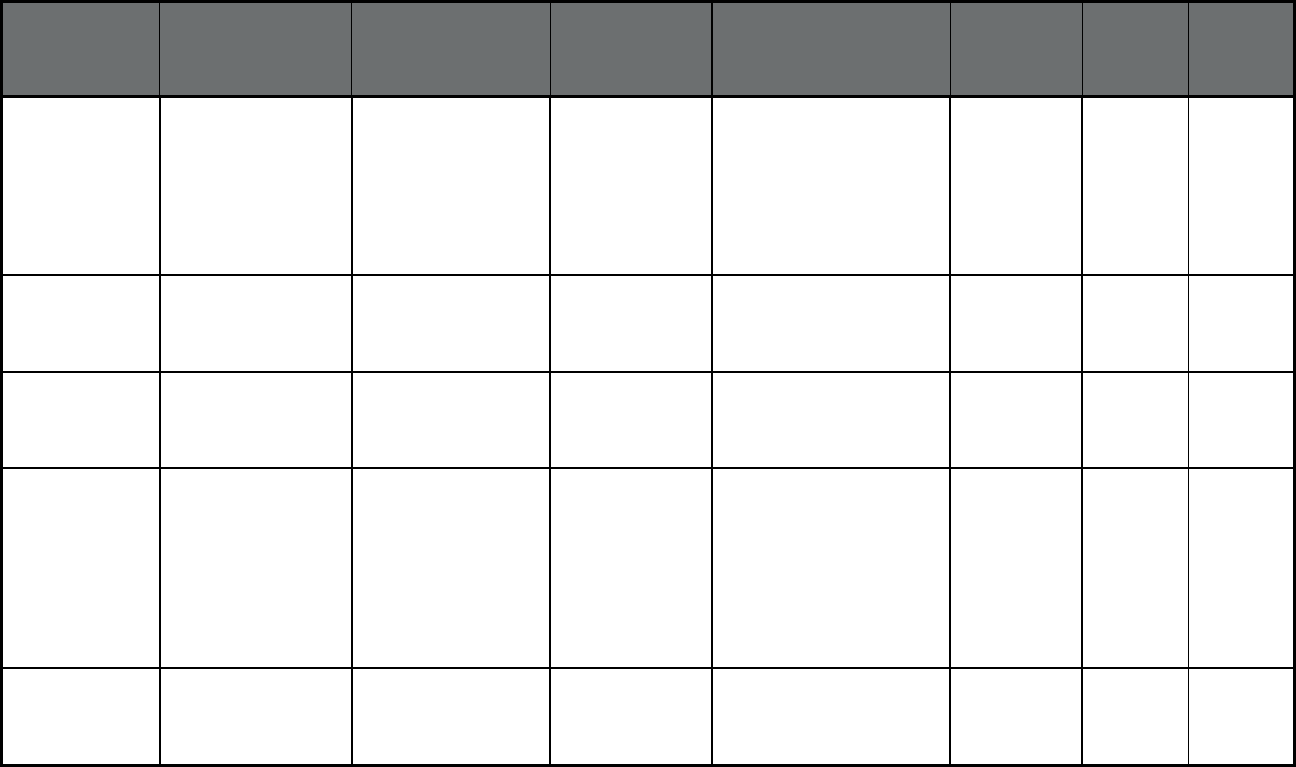
132
State
Program Name
(Type) Plan Name
Parent
Organization
Geographic Region (state-
defined areas, counties, or
zip codes)
Medicaid-Only
Enrollment
Dual
Enrollment
Total
Enrollment
Oregon
8
Oregon Health Plan
(OHP)
(Comprehensive
MCO)
Capitol Dental Care,
Inc.
HealthShare of
Oregon
Benton, Clackamas,
Clatsop, Columbia, Hood
River, Jackson, Josephine,
Klamath, Lane, Lincoln,
Linn, Marion, Multnomah,
Polk, Umatilla, Wasco,
Washington, and Yamhill
Counties
10,319 974 11,293
Oregon
8
Oregon Health Plan
(OHP)
(Comprehensive
MCO)
CareOregon Dental CareOregon Clackamas, Multnomah, and
Washington Counties
1,522 95 1,617
Oregon
8
Oregon Health Plan
(OHP)
(Comprehensive
MCO)
Family Dental Care HealthShare of
Oregon
Clackamas, Multnomah, and
Washington Counties
1,542 70 1,612
Oregon
8
Oregon Health Plan
(OHP)
(Comprehensive
MCO)
Greater Oregon
Behavioral Health, Inc.
Greater Oregon
Behavioral Health,
Inc.
Baker (97869 excluded),
Clatsop, Columbia, Douglas,
Gilliam, Grant, Harney,
Hood River, Lake, Malheur
(97710 excluded), Morrow,
Sherman, Umatilla, Union,
Wallowa, Wasco, and
Wheeler (97848 excluded)
Counties
507 3,076 3,583
Oregon
8
Oregon Health Plan
(OHP)
(Comprehensive
MCO)
Managed Dental Care
of Oregon
HealthShare of
Oregon
Clackamas, Multnomah, and
Washington Counties
1,534 66 1,600
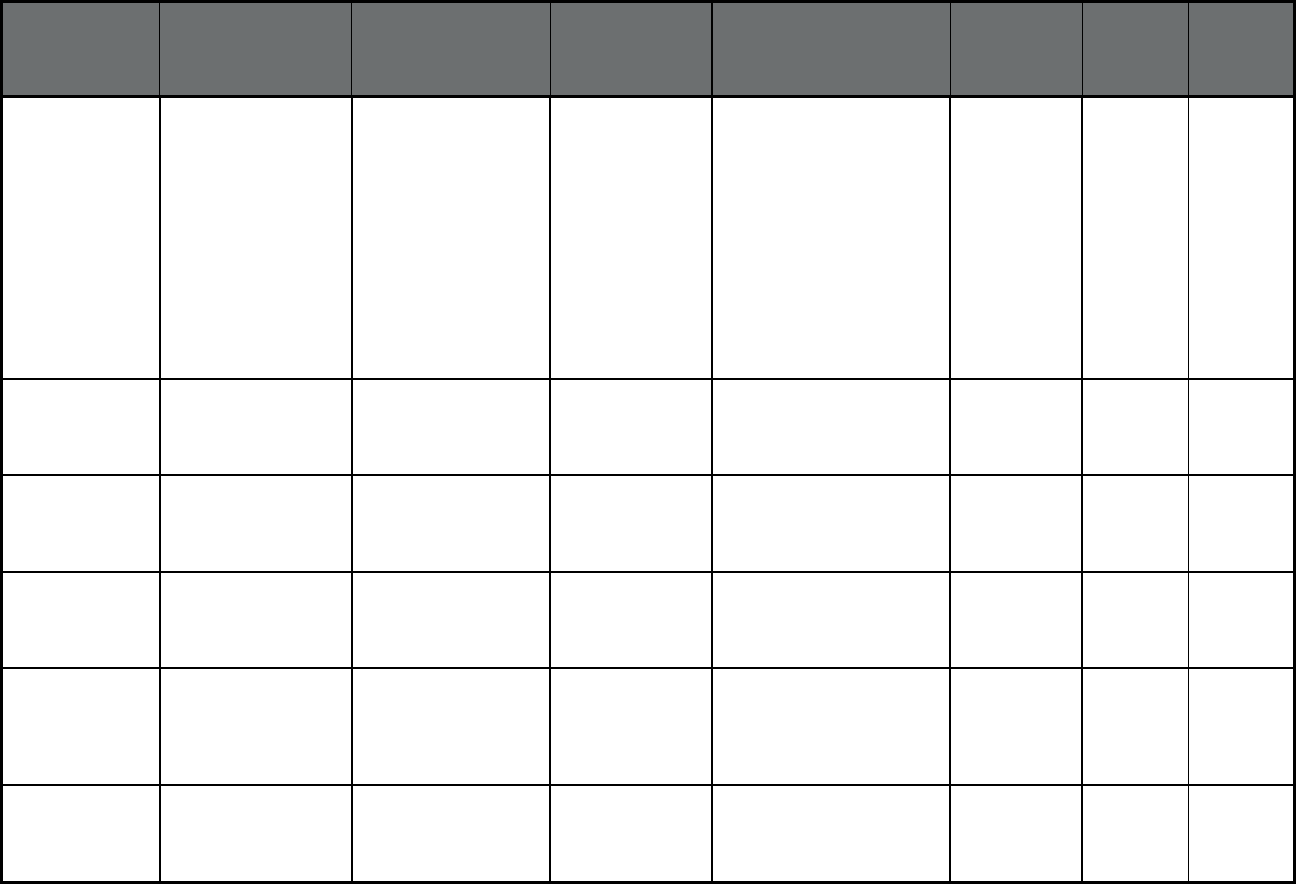
133
State
Program Name
(Type) Plan Name
Parent
Organization
Geographic Region (state-
defined areas, counties, or
zip codes)
Medicaid-Only
Enrollment
Dual
Enrollment
Total
Enrollment
Oregon
8
Oregon Health Plan
(OHP)
(Comprehensive
MCO)
ODS Community
Health Inc.
MODA Health Baker, Benton, Clackamas,
Clatsop, Columbia, Crook,
Deschutes (97733, 97735
excluded), Hood River,
Jackson, Jefferson,
Josephine, Lane, Linn
(97759 excluded), Malheur,
Marion, Multnomah, Polk
(97370 excluded),
Tillamook, Wallowa (97828,
97846 only), Wasco,
Washington, and Yamhill
Counties
6,452 1,224 7,676
Oregon
8
Oregon Health Plan
(OHP)
(Comprehensive
MCO)
AllCare Health Plan AllCare Health
Plan
Curry, Douglas (97410,
97442 only), Jackson, and
Josephine Counties
46,073 2,199 48,272
Oregon
8
Oregon Health Plan
(OHP)
(Comprehensive
MCO)
Cascade Health
Alliance
Cascade Health
Alliance
Klamath (97731, 97733,
97737, 97739, 97425
excluded) County
16,230 683 16,913
Oregon
8
Oregon Health Plan
(OHP)
(Comprehensive
MCO)
Columbia Pacific Columbia Pacific Clatsop, Columbia, and
Tillamook Counties
22,762 749 23,511
Oregon
8
Oregon Health Plan
(OHP)
(Comprehensive
MCO)
Eastern Oregon CCO Eastern Oregon
CCO
Baker, Gilliam, Grant,
Harney, Lake, Malheur,
Morrow, Sherman, Umatilla,
Union, Wallowa, and
Wheeler Counties
46,209 1,557 47,766
Oregon
8
Oregon Health Plan
(OHP)
(Comprehensive
MCO)
HealthShare of Oregon HealthShare of
Oregon
Clackamas, Multnomah, and
Washington Counties
290,073 18,525 308,598
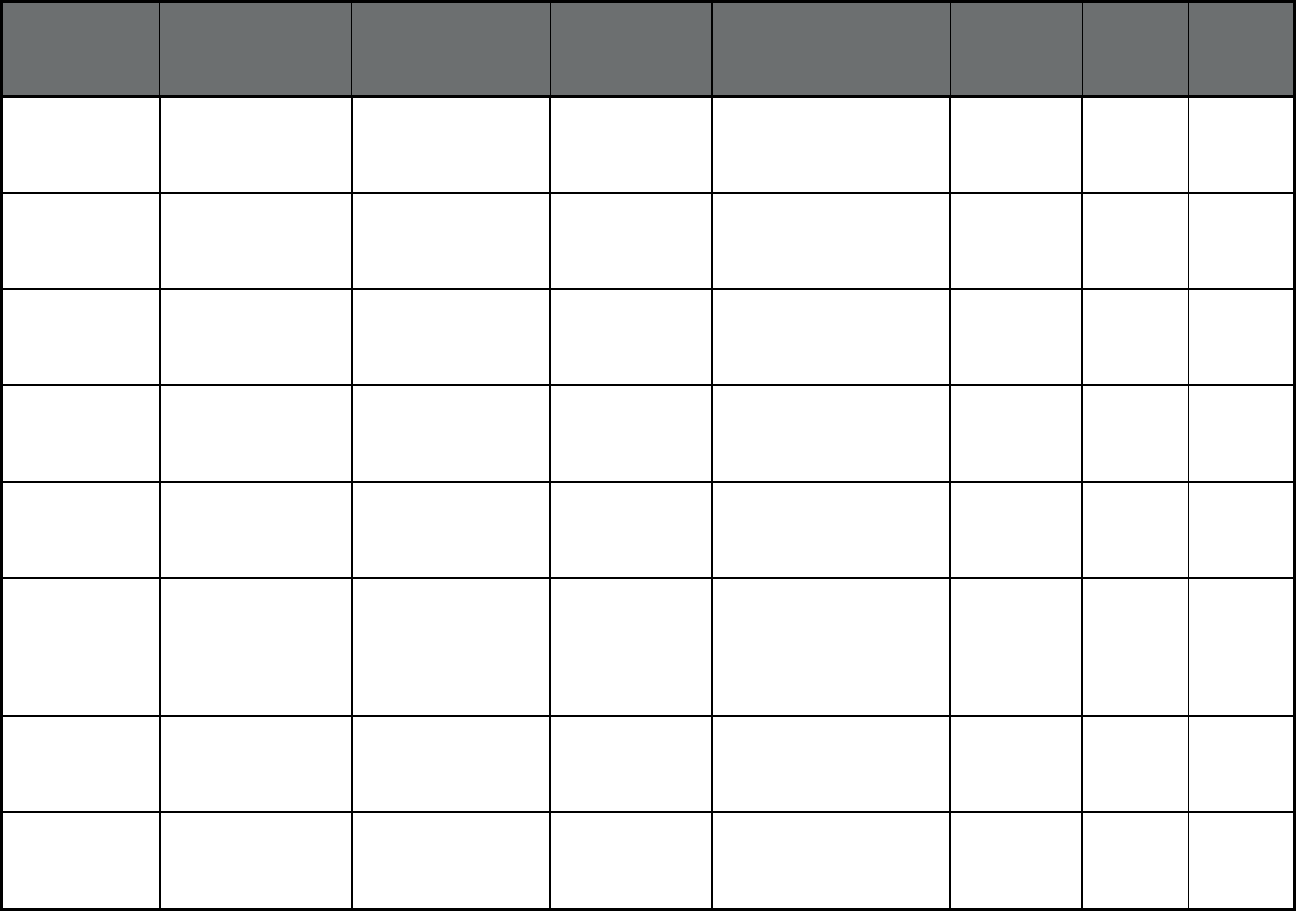
134
State
Program Name
(Type) Plan Name
Parent
Organization
Geographic Region (state-
defined areas, counties, or
zip codes)
Medicaid-Only
Enrollment
Dual
Enrollment
Total
Enrollment
Oregon
8
Oregon Health Plan
(OHP)
(Comprehensive
MCO)
InterCommunity Health
Network
InterCommunity
Health Network
Benton, Lincoln, and Linn
Counties
50,152 2,432 52,584
Oregon
8
Oregon Health Plan
(OHP)
(Comprehensive
MCO)
Jackson Care Connect Jackson Care
Connect
Jackson County 28,814 1,109 29,923
Oregon
8
Oregon Health Plan
(OHP)
(Comprehensive
MCO)
PacificSource
Community Solutions -
Central Oregon
PacificSource
Community
Solutions
Crook, Deschutes,
Jefferson, and Klamath
(97731, 97733, 97737,
97739 only)
45,636 2,249 47,885
Oregon
8
Oregon Health Plan
(OHP)
(Comprehensive
MCO)
PacificSource
Community Solutions -
Columbia Gorge
PacificSource
Community
Solutions
Hood River and Wasco
Counties
11,569 322 11,891
Oregon
8
Oregon Health Plan
(OHP)
(Comprehensive
MCO)
PrimaryHealth of
Josephine County
PrimaryHealth of
Josephine County
Douglas (97410, 97442
only), Jackson and
Josephine Counties
9,148 521 9,669
Oregon
8
Oregon Health Plan
(OHP)
(Comprehensive
MCO)
Trillium Community
Health Plan
Trillium Health Benton (97448, 97456 only),
Coos (97449 only), Douglas
(97424, 97493, 97436,
97441, 97467, 97473 only),
Lane, and Linn (97446 only)
Counties
81,804 4,227 86,031
Oregon
8
Oregon Health Plan
(OHP)
(Comprehensive
MCO)
Umpqua Health
Alliance
Umpqua Health
Alliance
Douglas (97441, 97467,
97473 excluded) County
24,879 1,345 26,224
Oregon
8
Oregon Health Plan
(OHP)
(Comprehensive
MCO)
Advanced Health Advanced Health Coos, Curry, and Douglas
(97459 only) Counties
17,866 1,173 19,039
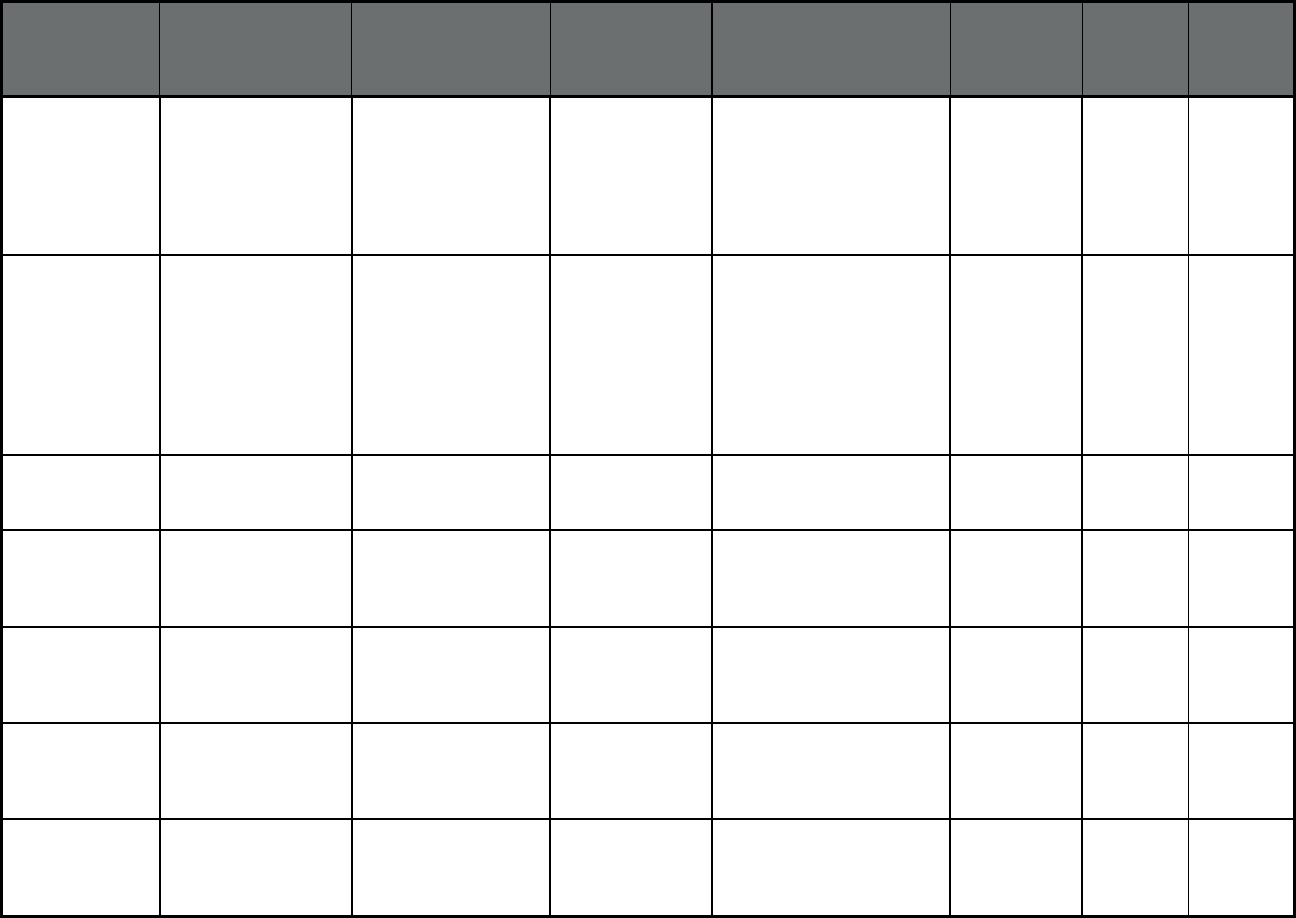
135
State
Program Name
(Type) Plan Name
Parent
Organization
Geographic Region (state-
defined areas, counties, or
zip codes)
Medicaid-Only
Enrollment
Dual
Enrollment
Total
Enrollment
Oregon
8
Oregon Health Plan
(OHP)
(Comprehensive
MCO)
Willamette Valley
Community Health
Willamette Valley
Community Health
Benton (97361 only),
Clackamas (97002, 97032,
97071, 97362, 97375 only),
Linn (97346, 97350, 97352,
97358, 97360, 97383 only),
Marion, Polk, and Yamhill
(97304 only)
94,312 4,560 98,872
Oregon
8
Oregon Health Plan
(OHP)
(Comprehensive
MCO)
Yamhill Community
Care
Community Care
Health Plan (WI)
Clackamas (97002, 97071,
97140 only), Marion (97137
only), Polk (97101, 97304,
97347, 97371, 97378,
97396 only), Tillamook
(97347 only), Washington
(97119, 97123, 97132,
97140 only), and Yamhill
Counties
22,668 669 23,337
Oregon PACE (Program of All-
inclusive Care for the
Elderly (PACE))
Providence Elder Place PACE Multnomah, Washington,
Clatsop, Clackamas and
Tillamook Counties
75 1,317 1,392
Pennsylvania HealthChoices -
Physical Health
(Comprehensive
MCO)
Aetna Better Health Aetna Southeast zone, Southwest
zone, Lehigh/Capital zone,
Northwest zone, Northeast
zone
199,482 631 200,113
Pennsylvania HealthChoices -
Physical Health
(Comprehensive
MCO)
Gateway Health Gateway Health Southwest zone,
Lehigh/Capital zone,
Northwest zone
289,736 996 290,732
Pennsylvania HealthChoices -
Physical Health
(Comprehensive
MCO)
Health Partners Plan Health Partners
Plan
Southeast zone 244,990 752 245,742
Pennsylvania HealthChoices -
Physical Health
(Comprehensive
MCO)
United Healthcare
Community Plan, Inc.
UnitedHealthcare Southeast zone, Southwest
zone, Lehigh/Capital zone
222,275 747 223,022
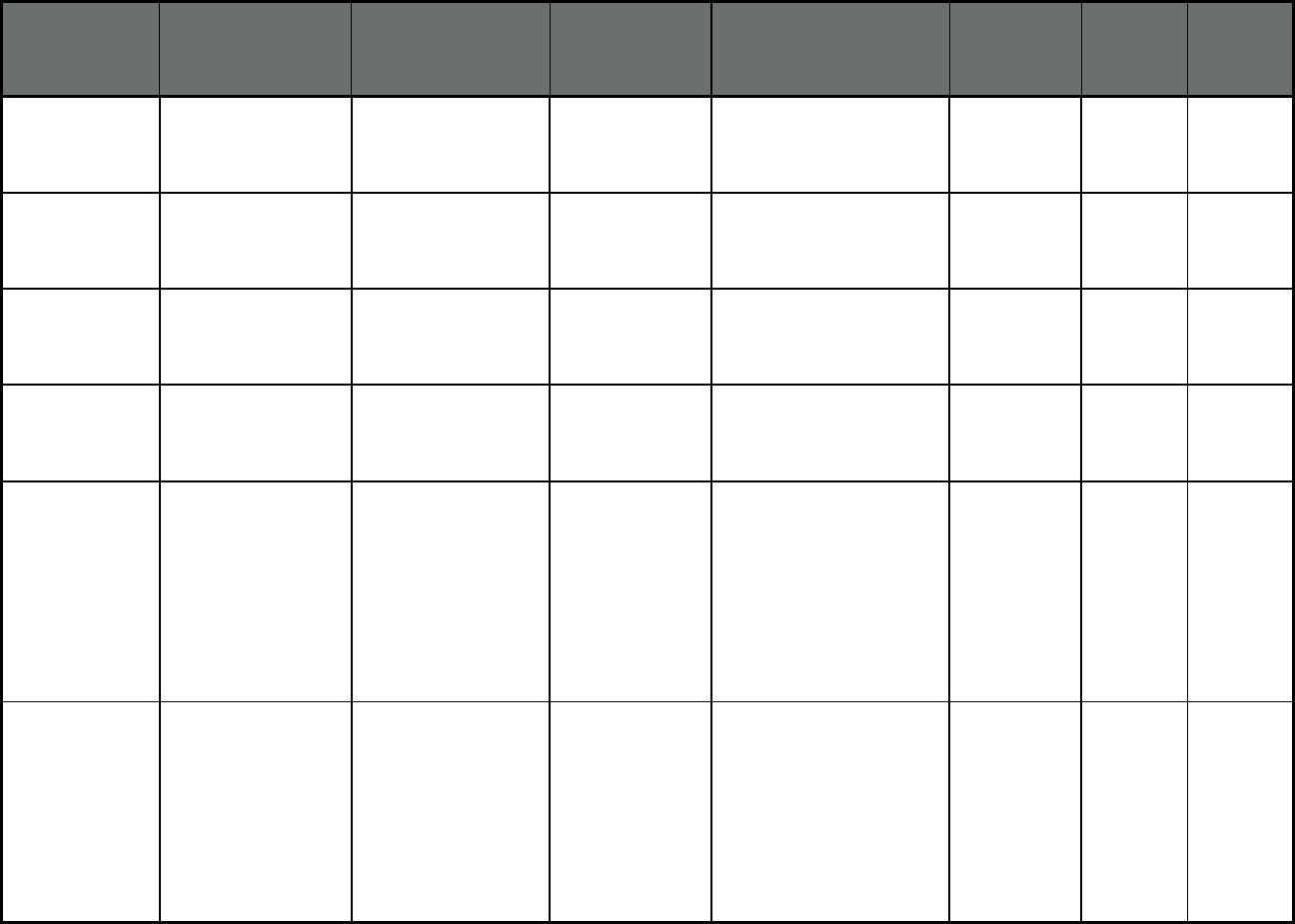
136
State
Program Name
(Type) Plan Name
Parent
Organization
Geographic Region (state-
defined areas, counties, or
zip codes)
Medicaid-Only
Enrollment
Dual
Enrollment
Total
Enrollment
Pennsylvania HealthChoices -
Physical Health
(Comprehensive
MCO)
UPMC for You UPMC Health Plan Southwest zone,
Lehigh/Capital zone,
Northwest zone
413,437 1,817 415,254
Pennsylvania HealthChoices -
Physical Health
(Comprehensive
MCO)
Geisinger Health Plan Geisinger Health
Plan
Northeast 183,218 556 183,774
Pennsylvania HealthChoices -
Physical Health
(Comprehensive
MCO)
AmeriHealth
Caritas/AmeriHealth
Caritas Northeast
Vista Lehigh/Capital, Northwest,
Northeast
281,763 848 282,611
Pennsylvania HealthChoices -
Physical Health
(Comprehensive
MCO)
Keystone First Vista Southeast 430,155 1,306 431,461
Pennsylvania Community
HealthChoices
(Comprehensive MCO
+ MLTSS)
UPMC Community
HealthChoices
UPMC Southwest PA: Allegheny
County, Armstrong County,
Beaver County, Bedford
County, Blair County, Butler
County, Cambria County,
Fayette County, Greene
County, Indiana County,
Lawrence County, Somerset
County, Washington County
and Westmoreland County
2,401 40,643 43,044
Pennsylvania Community
HealthChoices
(Comprehensive MCO
+ MLTSS)
Pennsylvania Health &
Wellness
Centene
Corporation
Southwest PA: Allegheny
County, Armstrong County,
Beaver County, Bedford
County, Blair County, Butler
County, Cambria County,
Fayette County, Greene
County, Indiana County,
Lawrence County, Somerset
County, Washington County
and Westmoreland County
812 20,908 21,720
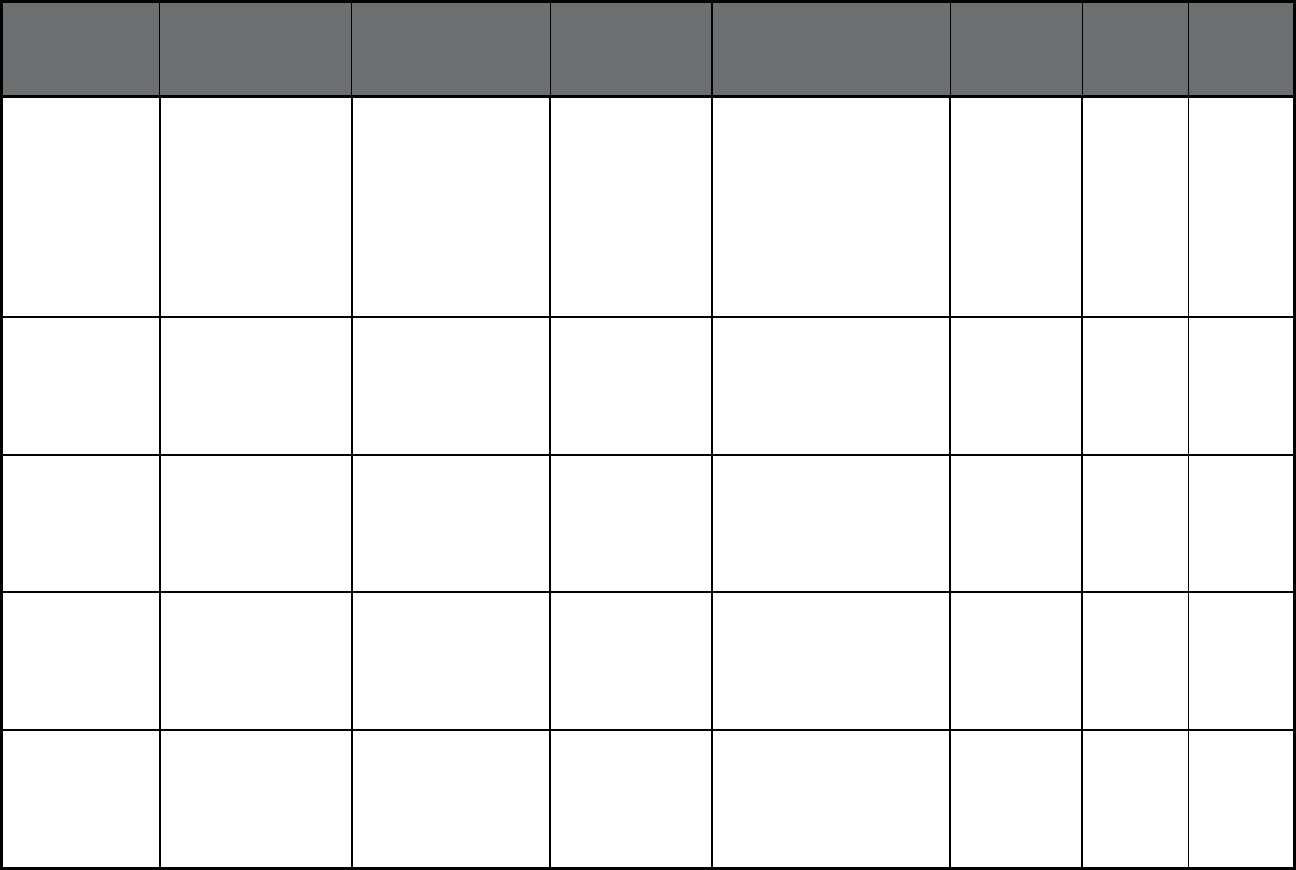
137
State
Program Name
(Type) Plan Name
Parent
Organization
Geographic Region (state-
defined areas, counties, or
zip codes)
Medicaid-Only
Enrollment
Dual
Enrollment
Total
Enrollment
Pennsylvania Community
HealthChoices
(Comprehensive MCO
+ MLTSS)
Amerihealth Caritas /
Keystone First
Vista Southwest PA: Allegheny
County, Armstrong County,
Beaver County, Bedford
County, Blair County, Butler
County, Cambria County,
Fayette County, Greene
County, Indiana County,
Lawrence County, Somerset
County, Washington County
and Westmoreland County
630 14,524 15,154
Pennsylvania Behavioral Health
HealthChoices
(Behavioral Health
Organization (BHO)
only (PIHP and/or
PAHP))
Allegheny County
HealthChoices
Community Care
Health Plan (WI)
Allegheny County 59,156 7,508 66,664
Pennsylvania Behavioral Health
HealthChoices
(Behavioral Health
Organization (BHO)
only (PIHP and/or
PAHP))
Beaver County
HealthChoices
Beacon Beaver County 9,848 1,338 11,186
Pennsylvania Behavioral Health
HealthChoices
(Behavioral Health
Organization (BHO)
only (PIHP and/or
PAHP))
Behavioral Health
Services of Bedford
and Somerset
PerformCare Bedford and Somerset
Counties
7,722 1,289 9,011
Pennsylvania Behavioral Health
HealthChoices
(Behavioral Health
Organization (BHO)
only (PIHP and/or
PAHP))
Berks County
HealthChoices
Community Care
Health Plan (WI)
Berks County 27,868 2,255 30,123
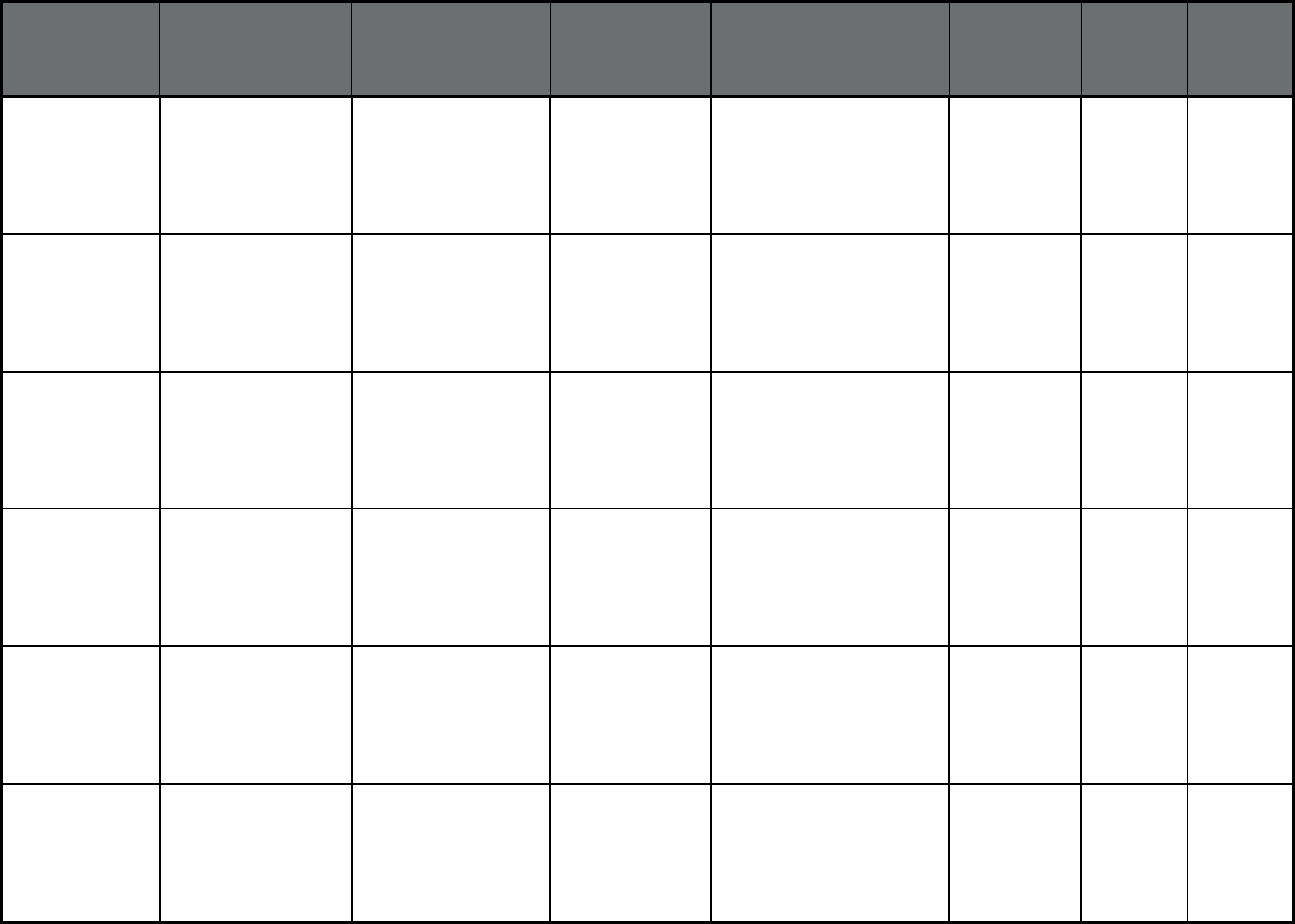
138
State
Program Name
(Type) Plan Name
Parent
Organization
Geographic Region (state-
defined areas, counties, or
zip codes)
Medicaid-Only
Enrollment
Dual
Enrollment
Total
Enrollment
Pennsylvania Behavioral Health
HealthChoices
(Behavioral Health
Organization (BHO)
only (PIHP and/or
PAHP))
Blair County
HealthChoices
Community Care
Health Plan (WI)
Blair County 8,717 1,266 9,983
Pennsylvania Behavioral Health
HealthChoices
(Behavioral Health
Organization (BHO)
only (PIHP and/or
PAHP))
Bucks County
HealthChoices
Magellan Health Bucks County 21,897 1,909 23,806
Pennsylvania Behavioral Health
HealthChoices
(Behavioral Health
Organization (BHO)
only (PIHP and/or
PAHP))
Cambria County
HealthChoices
Beacon Cambria County 9,517 1,262 10,779
Pennsylvania Behavioral Health
HealthChoices
(Behavioral Health
Organization (BHO)
only (PIHP and/or
PAHP))
Carbon-Monroe-Pike
Joinder Board
Community Care
Health Plan (WI)
Carbon, Monroe and Pike
Counties
21,392 1,540 22,932
Pennsylvania Behavioral Health
HealthChoices
(Behavioral Health
Organization (BHO)
only (PIHP and/or
PAHP))
Chester County
HealthChoices
Community Care
Health Plan (WI)
Chester County 15,562 1,229 16,791
Pennsylvania Behavioral Health
HealthChoices
(Behavioral Health
Organization (BHO)
only (PIHP and/or
PAHP))
Cumberland County
HealthChoices
PerformCare Cumberland County 11,803 928 12,731
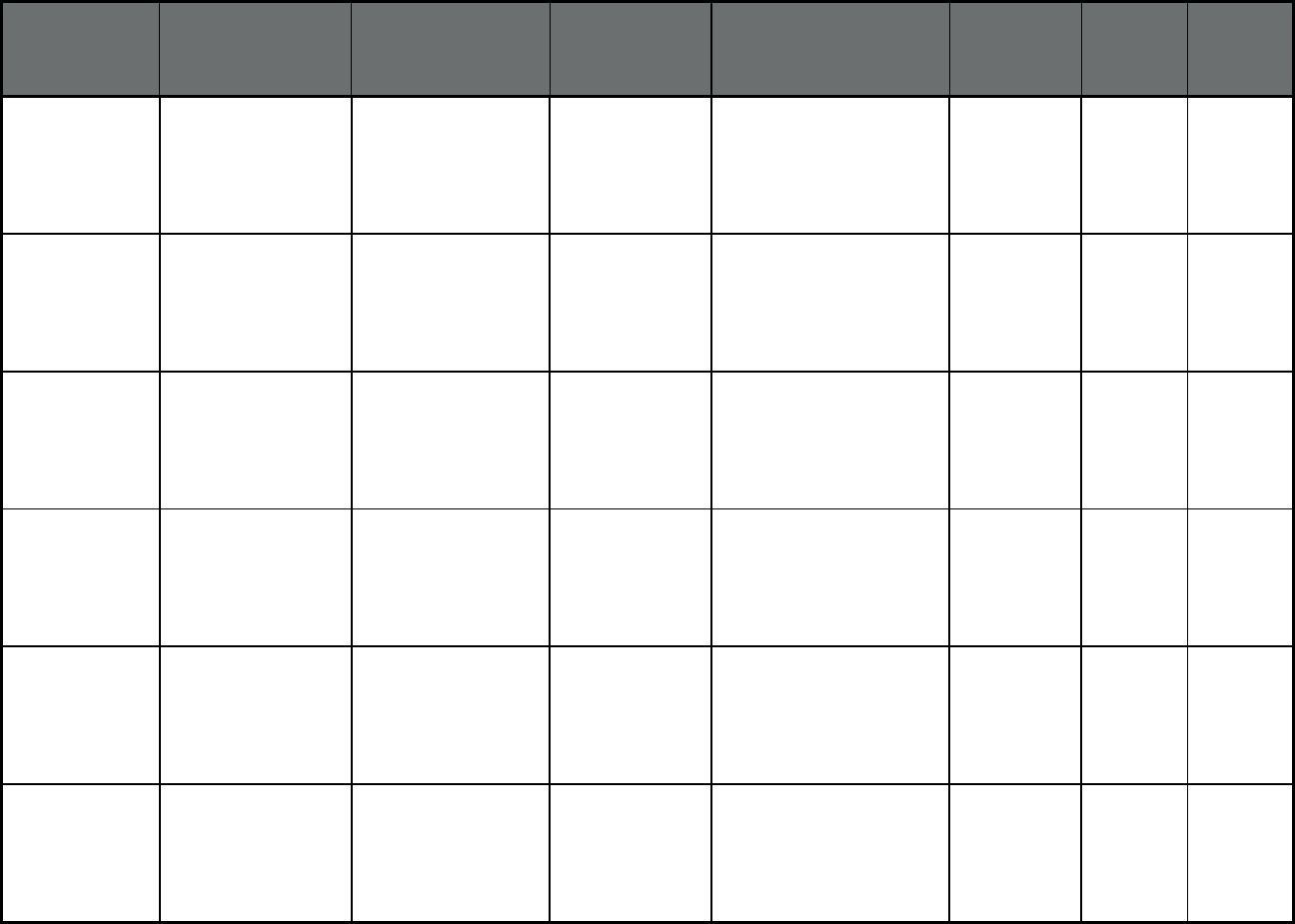
139
State
Program Name
(Type) Plan Name
Parent
Organization
Geographic Region (state-
defined areas, counties, or
zip codes)
Medicaid-Only
Enrollment
Dual
Enrollment
Total
Enrollment
Pennsylvania Behavioral Health
HealthChoices
(Behavioral Health
Organization (BHO)
only (PIHP and/or
PAHP))
Dauphin County
HealthChoices
PerformCare Dauphin County 22,532 1,856 24,388
Pennsylvania Behavioral Health
HealthChoices
(Behavioral Health
Organization (BHO)
only (PIHP and/or
PAHP))
Delaware County
HealthChoices
Magellan Health Delaware County 37,229 2,548 39,777
Pennsylvania Behavioral Health
HealthChoices
(Behavioral Health
Organization (BHO)
only (PIHP and/or
PAHP))
Erie County
HealthChoices
Community Care
Health Plan (WI)
Erie County 21,200 1,612 22,812
Pennsylvania Behavioral Health
HealthChoices
(Behavioral Health
Organization (BHO)
only (PIHP and/or
PAHP))
Fayette County
HealthChoices
Beacon Fayette County 11,701 1,531 13,232
Pennsylvania Behavioral Health
HealthChoices
(Behavioral Health
Organization (BHO)
only (PIHP and/or
PAHP))
Greene County
(Commonwealth)
Beacon Greene County 2,907 397 3,304
Pennsylvania Behavioral Health
HealthChoices
(Behavioral Health
Organization (BHO)
only (PIHP and/or
PAHP))
Lancaster County
HealthChoices
PerformCare Lancaster County 29,600 2,015 31,615
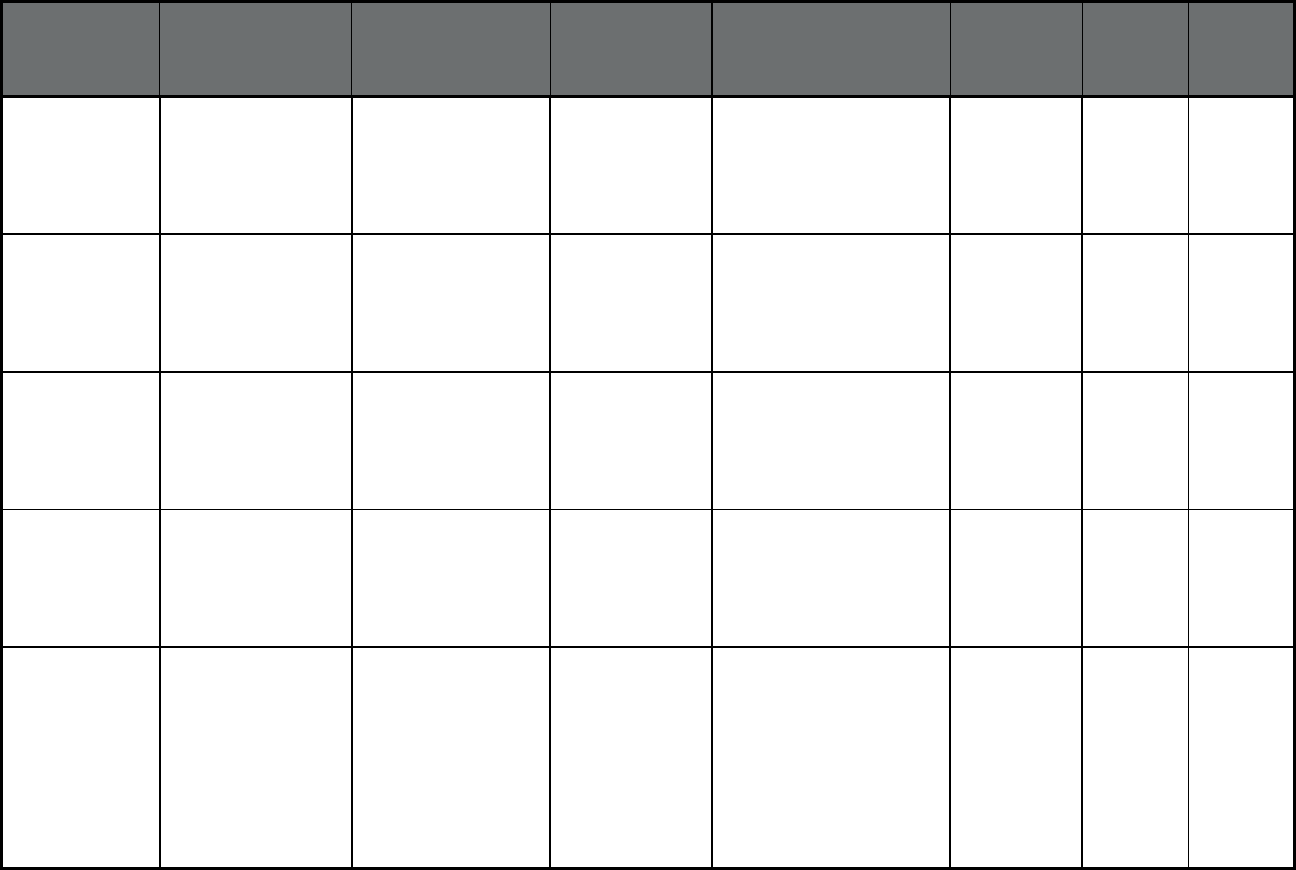
140
State
Program Name
(Type) Plan Name
Parent
Organization
Geographic Region (state-
defined areas, counties, or
zip codes)
Medicaid-Only
Enrollment
Dual
Enrollment
Total
Enrollment
Pennsylvania Behavioral Health
HealthChoices
(Behavioral Health
Organization (BHO)
only (PIHP and/or
PAHP))
Lebanon County
HealthChoices
PerformCare Lebanon County 9,425 647 10,072
Pennsylvania Behavioral Health
HealthChoices
(Behavioral Health
Organization (BHO)
only (PIHP and/or
PAHP))
Lehigh County
HealthChoices
Magellan Health Lehigh County 27,976 2,151 30,127
Pennsylvania Behavioral Health
HealthChoices
(Behavioral Health
Organization (BHO)
only (PIHP and/or
PAHP))
Lycoming-Clinton
Joinder Board
Community Care
Health Plan (WI)
Clinton and Lycoming
Counties
10,603 944 11,547
Pennsylvania Behavioral Health
HealthChoices
(Behavioral Health
Organization (BHO)
only (PIHP and/or
PAHP))
Montgomery County
HealthChoices
Magellan Health Montgomery County 30,823 2,495 33,318
Pennsylvania Behavioral Health
HealthChoices
(Behavioral Health
Organization (BHO)
only (PIHP and/or
PAHP))
North Central State
Option
Community Care
Health Plan (WI)
Bradford, Cameron, Centre,
Clarion, Clearfield,
Columbia, Elk, Forest,
Huntingdon, Jefferson,
Juniata, McKean, Mifflin,
Montour, Northumberland,
Potter, Schuylkill, Snyder,
Sullivan, Tioga, Union,
Warren and Wayne
Counties
70,567 7,153 77,720
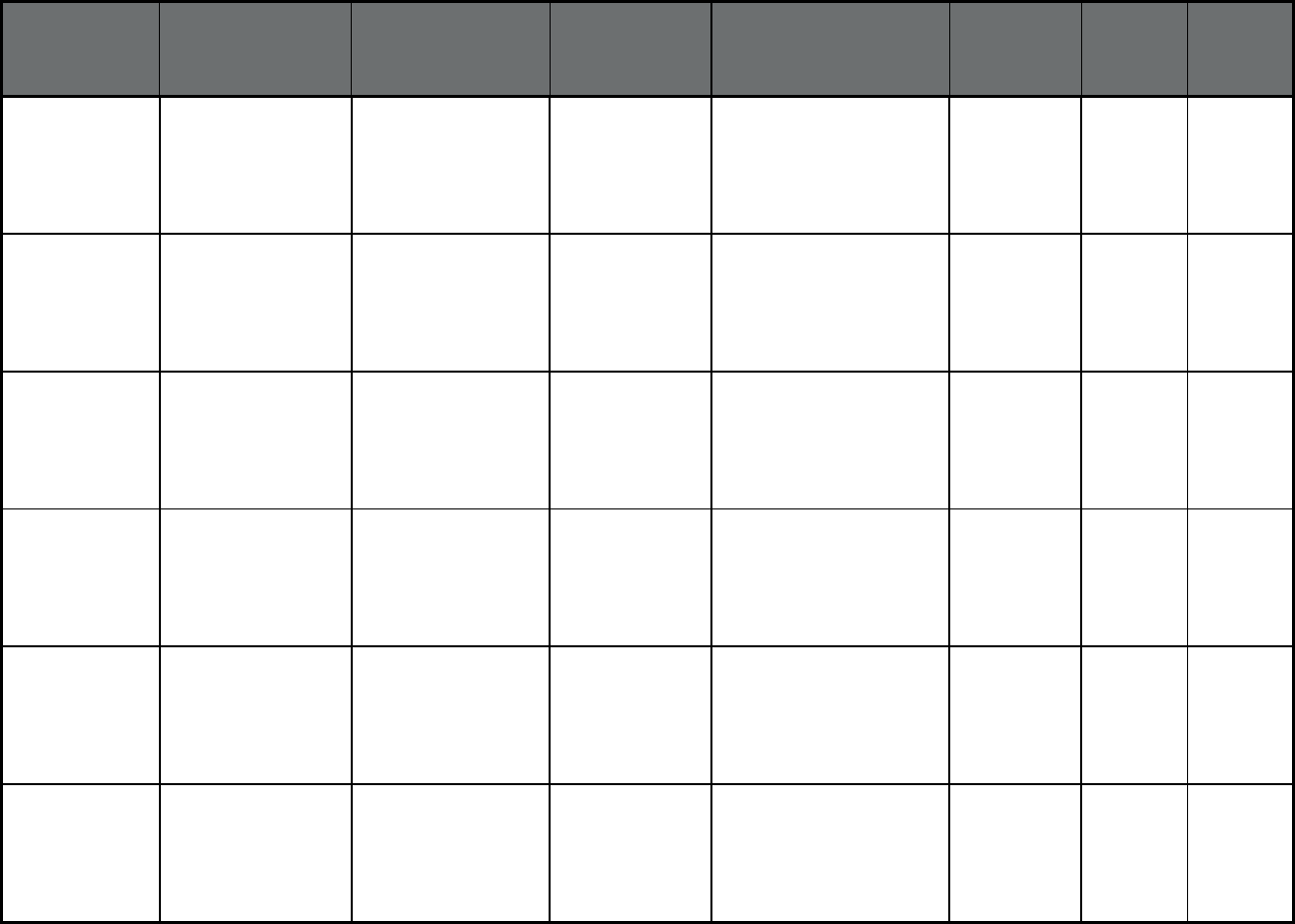
141
State
Program Name
(Type) Plan Name
Parent
Organization
Geographic Region (state-
defined areas, counties, or
zip codes)
Medicaid-Only
Enrollment
Dual
Enrollment
Total
Enrollment
Pennsylvania Behavioral Health
HealthChoices
(Behavioral Health
Organization (BHO)
only (PIHP and/or
PAHP))
Northampton County
HealthChoices
Magellan Health Northampton County 17,993 1,520 19,513
Pennsylvania Behavioral Health
HealthChoices
(Behavioral Health
Organization (BHO)
only (PIHP and/or
PAHP))
Northeast Behavioral
Health Care
Consortium
Community Care
Health Plan (WI)
Lackawanna, Luzerne,
Susquehanna and Wyoming
Counties
46,956 3,777 50,733
Pennsylvania Behavioral Health
HealthChoices
(Behavioral Health
Organization (BHO)
only (PIHP and/or
PAHP))
Northwest Behavioral
Health Partnership
Beacon Crawford, Mercer and
Venango Counties
17,873 1,829 19,702
Pennsylvania Behavioral Health
HealthChoices
(Behavioral Health
Organization (BHO)
only (PIHP and/or
PAHP))
Perry County
HealthChoices
PerformCare Perry County 2,484 224 2,708
Pennsylvania Behavioral Health
HealthChoices
(Behavioral Health
Organization (BHO)
only (PIHP and/or
PAHP))
Philadelphia County
HealthChoices
Community
Behavioral Health
Philadelphia County 173,309 11,945 185,254
Pennsylvania Behavioral Health
HealthChoices
(Behavioral Health
Organization (BHO)
only (PIHP and/or
PAHP))
Southwest Behavioral
Health Management
Beacon Armstrong, Butler, Indianna,
Lawrence, Washington and
Westmoreland Counties
52,461 7,154 59,615
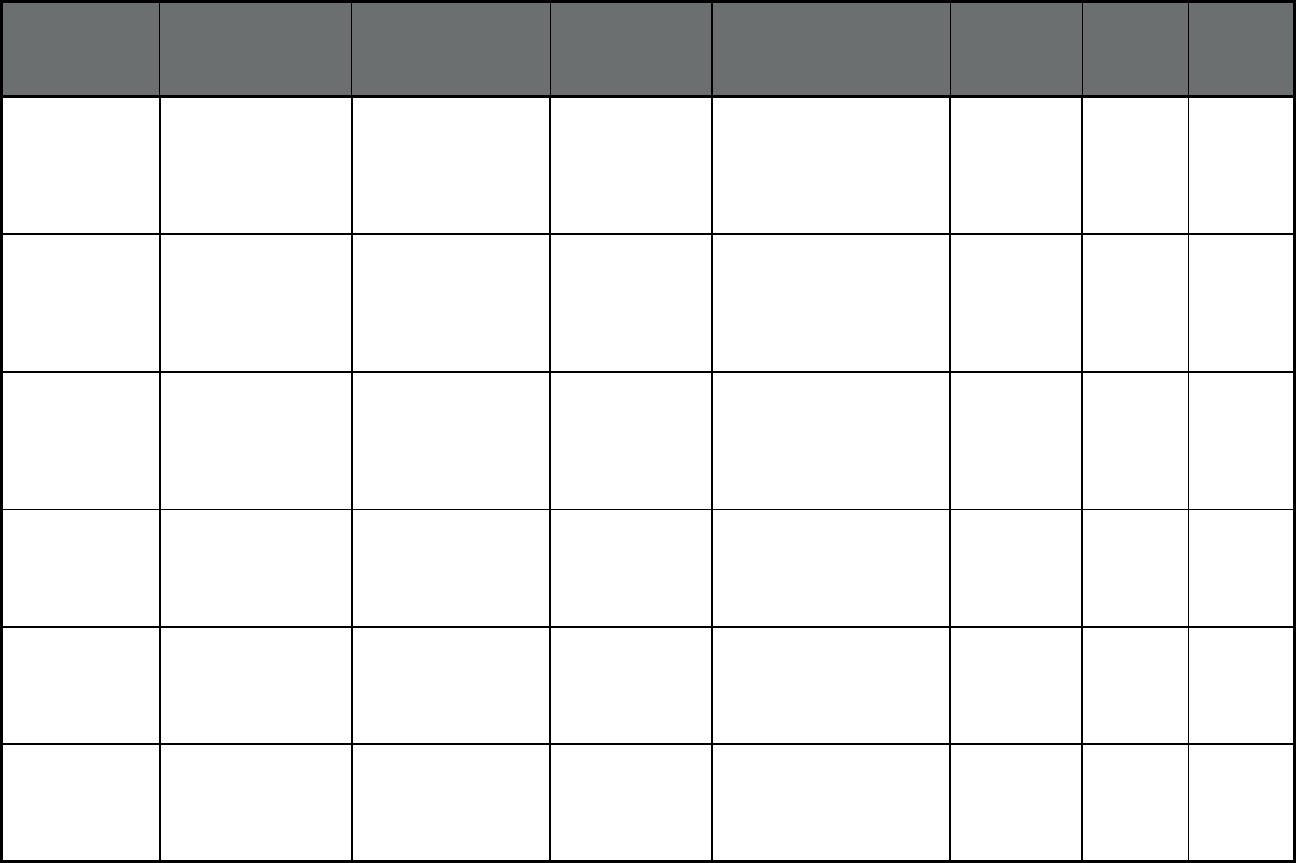
142
State
Program Name
(Type) Plan Name
Parent
Organization
Geographic Region (state-
defined areas, counties, or
zip codes)
Medicaid-Only
Enrollment
Dual
Enrollment
Total
Enrollment
Pennsylvania Behavioral Health
HealthChoices
(Behavioral Health
Organization (BHO)
only (PIHP and/or
PAHP))
Tuscarora Managed
Care Alliance
PerformCare Franklin and Fulton
Counties
10,210 752 10,962
Pennsylvania Behavioral Health
HealthChoices
(Behavioral Health
Organization (BHO)
only (PIHP and/or
PAHP))
York/Adams County
HealthChoices
Community Care
Health Plan (WI)
York and Adams Counties 33,771 2,290 36,061
Pennsylvania MATP (Medical
Assistance
Transportation
Program) (Non-
Emergency Medical
Transportation)
LogistiCare LogistiCare Philadelphia 546,802 75,251 622,053
Pennsylvania Adult Community
Autism Program
(Other Prepaid Health
Plan (PHP) (limited
benefits))
Adult Community
Autism Program
Keystone Autism
Services
Dauphin, Cumberland,
Lancaster and Chester
Counties
90 61 151
Pennsylvania PA Living
Independence for the
Elderly (Program of
All-inclusive Care for
the Elderly (PACE))
Senior LIFE
Greensburg H-2937
Senior LIFE Westmoreland County 6 195 201
Pennsylvania PA Living
Independence for the
Elderly (Program of
All-inclusive Care for
the Elderly (PACE))
Senior LIFE Johnstown
H-3925
Senior LIFE Cambria County, Somerset
County (partial)
24 197 221
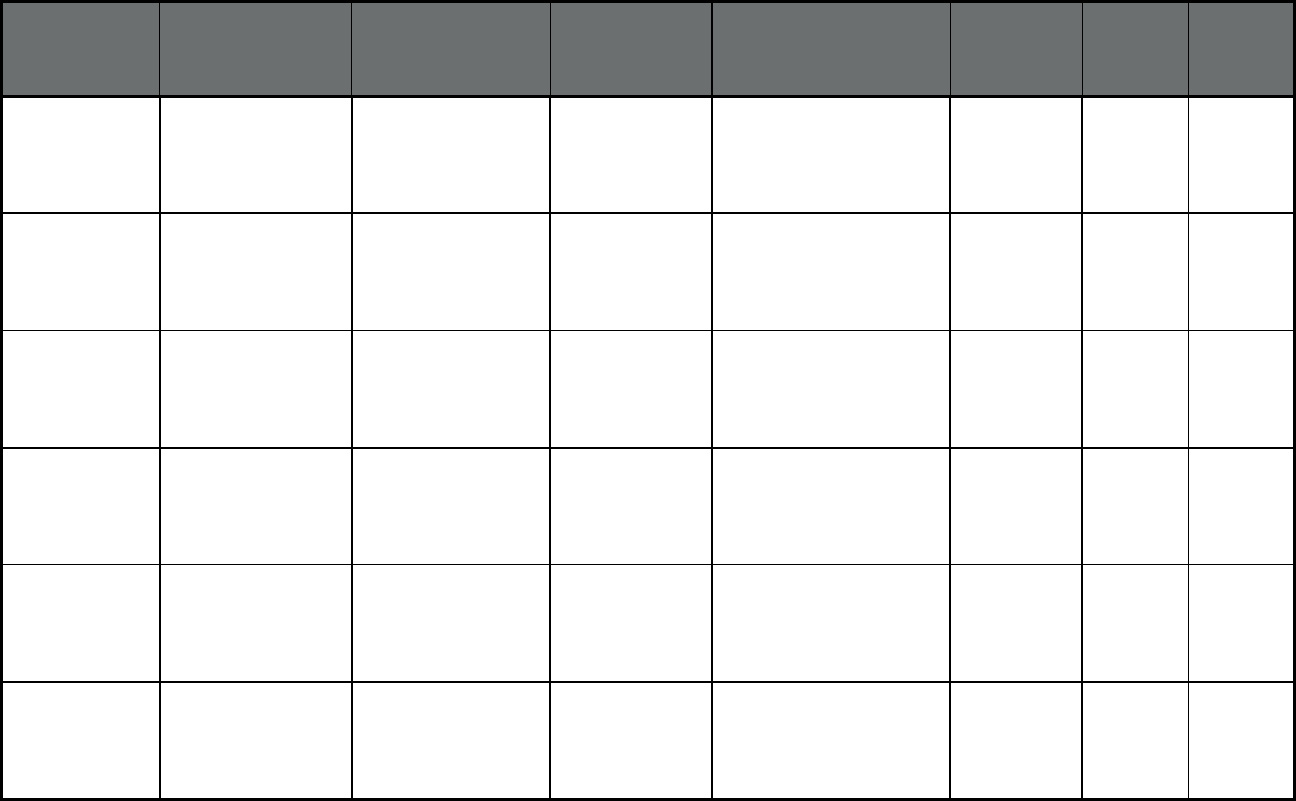
143
State
Program Name
(Type) Plan Name
Parent
Organization
Geographic Region (state-
defined areas, counties, or
zip codes)
Medicaid-Only
Enrollment
Dual
Enrollment
Total
Enrollment
Pennsylvania PA Living
Independence for the
Elderly (Program of
All-inclusive Care for
the Elderly (PACE))
Senior LIFE Altonna H-
5902
Senior LIFE Blair, Cambria and Indiana
Counties
17 284 301
Pennsylvania PA Living
Independence for the
Elderly (Program of
All-inclusive Care for
the Elderly (PACE))
Senior LIFE York H-
0819
Senior LIFE York County and Dauphin
County
13 209 222
Pennsylvania PA Living
Independence for the
Elderly (Program of
All-inclusive Care for
the Elderly (PACE))
Senior LIFE Lehigh H-
5978
Senior LIFE Lehigh County, Berks
County and Northampton
County
19 315 334
Pennsylvania PA Living
Independence for the
Elderly (Program of
All-inclusive Care for
the Elderly (PACE))
Senior LIFE
Washington H-2992
Senior LIFE Washington County, Fayette
County and Greene County
76 531 607
Pennsylvania PA Living
Independence for the
Elderly (Program of
All-inclusive Care for
the Elderly (PACE))
SpiriTrust LIFE H-2537 SpiriTrust LIFE H-
2537
Franklin County,
Cumberland County and
Perry County
2 95 97
Pennsylvania PA Living
Independence for the
Elderly (Program of
All-inclusive Care for
the Elderly (PACE))
LIFE NWPA H-4999 LIFE NWPA H-
4999
Erie County, Mercer County,
Crawford County and
Warren County
9 207 216
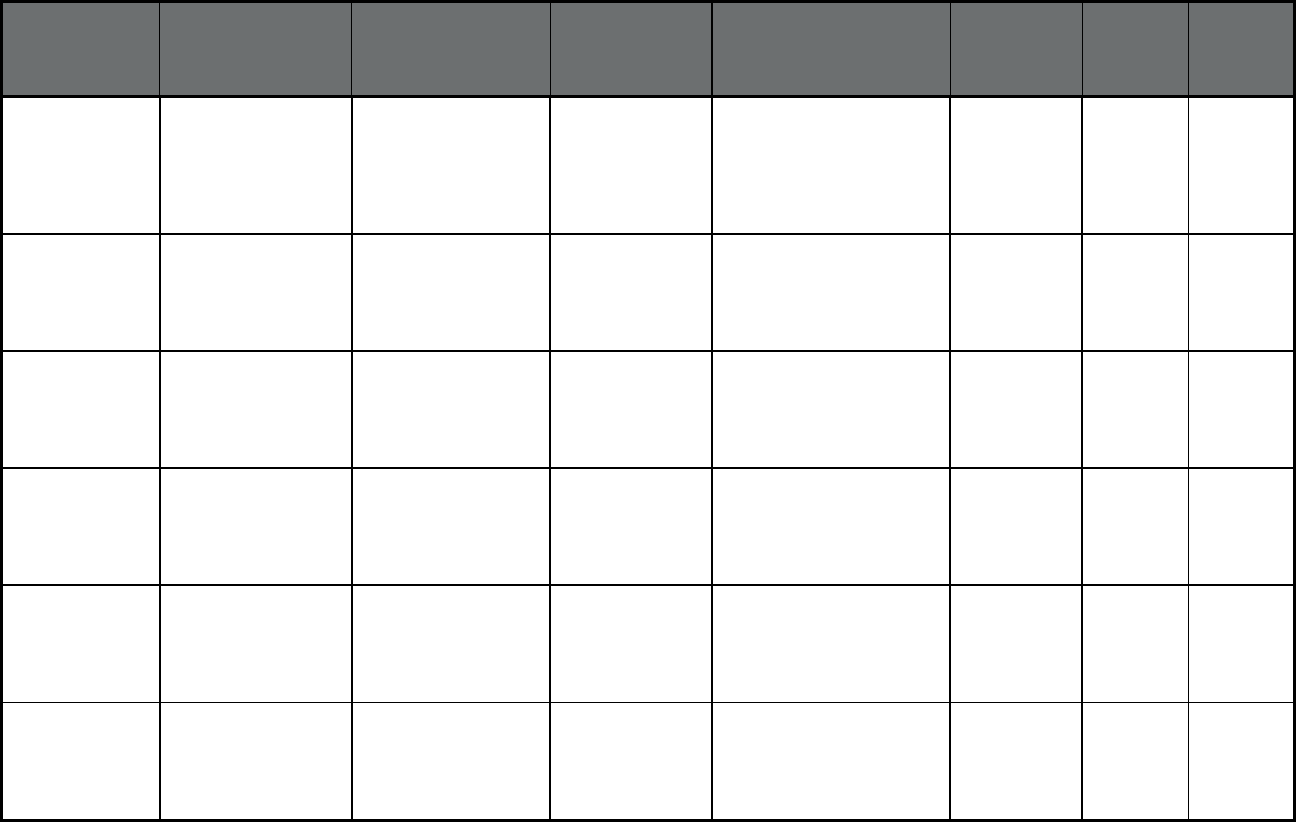
144
State
Program Name
(Type) Plan Name
Parent
Organization
Geographic Region (state-
defined areas, counties, or
zip codes)
Medicaid-Only
Enrollment
Dual
Enrollment
Total
Enrollment
Pennsylvania PA Living
Independence for the
Elderly (Program of
All-inclusive Care for
the Elderly (PACE))
LIFE Geisinger H-2064 Geisinger Health
Plan
Luzerne County,
Lackawanna County,
Columbia County, Montour
County, Northumberland
County and Schuylkill
County
4 197 201
Pennsylvania PA Living
Independence for the
Elderly (Program of
All-inclusive Care for
the Elderly (PACE))
Mercy LIFE H-3919 Mercy LIFE H-
3919
Philadelphia County and
Delaware County
59 690 749
Pennsylvania PA Living
Independence for the
Elderly (Program of
All-inclusive Care for
the Elderly (PACE))
Mercy LIFE West
Philadelphia H-3908
Mercy LIFE West
Philadelphia H-
3908
Philadelphia County 36 476 512
Pennsylvania PA Living
Independence for the
Elderly (Program of
All-inclusive Care for
the Elderly (PACE))
LIFE St. Mary H-6551 LIFE St. Mary H-
6551
Bucks County 11 219 230
Pennsylvania PA Living
Independence for the
Elderly (Program of
All-inclusive Care for
the Elderly (PACE))
Innovage LIFE H-9830 Innovage LIFE H-
9830
Philadelphia County 41 605 646
Pennsylvania PA Living
Independence for the
Elderly (Program of
All-inclusive Care for
the Elderly (PACE))
Albright LIFE H-9068 Albright LIFE H-
9068
Lancaster County, Lebanon
County, Lycoming County,
Clinton County, Union
County and Chester County
5 180 185
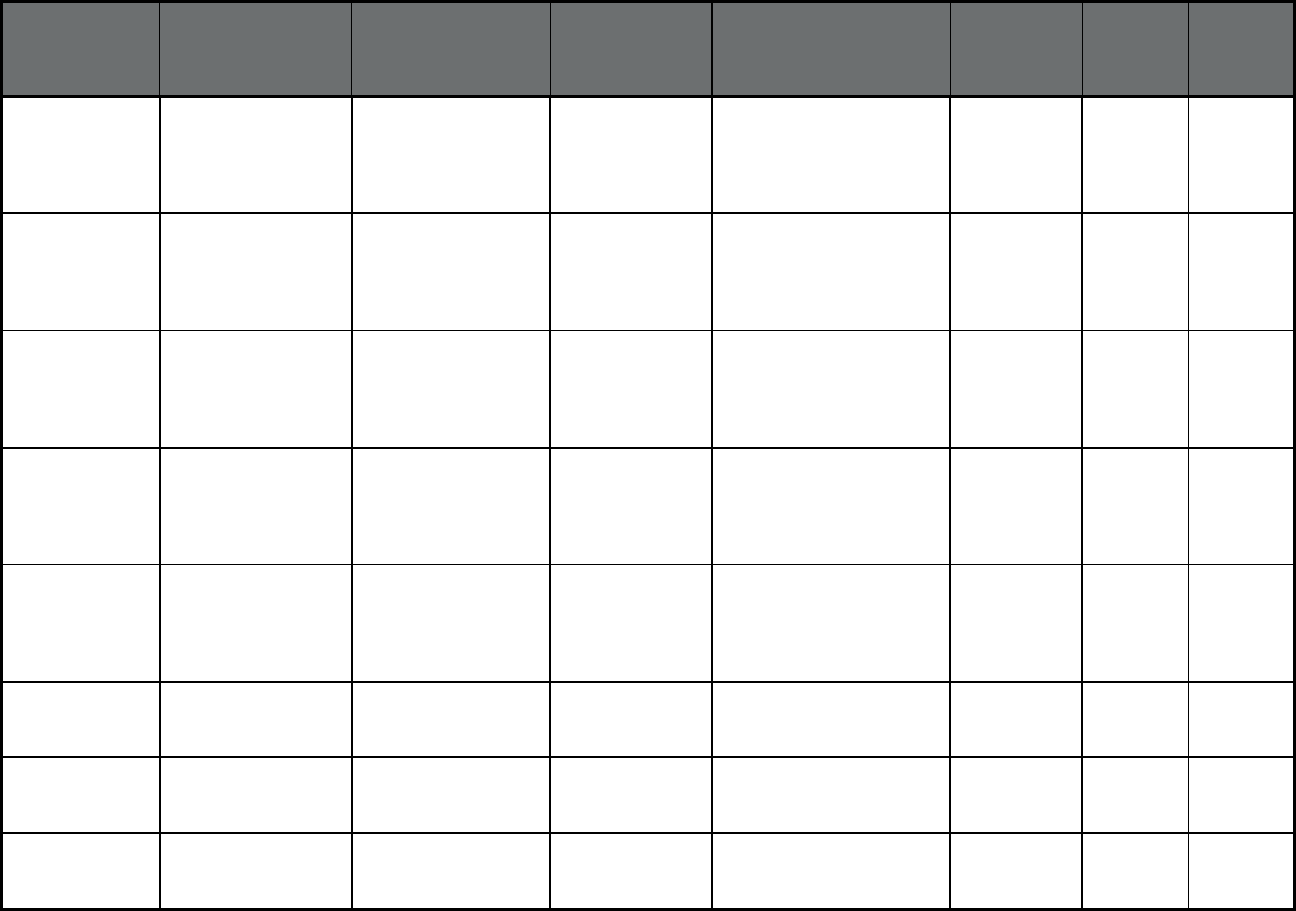
145
State
Program Name
(Type) Plan Name
Parent
Organization
Geographic Region (state-
defined areas, counties, or
zip codes)
Medicaid-Only
Enrollment
Dual
Enrollment
Total
Enrollment
Pennsylvania PA Living
Independence for the
Elderly (Program of
All-inclusive Care for
the Elderly (PACE))
Community LIFE H-
3917
Community LIFE
H-3917
Allegheny County,
Westmoreland County and
Washington County
25 563 588
Pennsylvania PA Living
Independence for the
Elderly (Program of
All-inclusive Care for
the Elderly (PACE))
LIFE Pittsburgh H-3918 LIFE Pittsburgh H-
3918
Allegheny County 40 552 592
Pennsylvania PA Living
Independence for the
Elderly (Program of
All-inclusive Care for
the Elderly (PACE))
VieCare Butler H-3060 VieCare Butler H-
3060
Butler County 12 189 201
Pennsylvania PA Living
Independence for the
Elderly (Program of
All-inclusive Care for
the Elderly (PACE))
VieCare Beaver H-
7660
VieCare Beaver H-
7660
Beaver County and
Lawrence County
29 451 480
Pennsylvania PA Living
Independence for the
Elderly (Program of
All-inclusive Care for
the Elderly (PACE))
VieCare Armstrong H-
6118
VieCare
Armstrong H-6118
Armstrong County 3 64 67
Puerto Rico Government Health
Plan (Comprehensive
MCO)
First Medical Plan Inc. First Medical Plan
Inc.
North, San Juan, Special 270,421 16,614 287,035
Puerto Rico Government Health
Plan (Comprehensive
MCO)
Triple S Salud, Inc. Blue Cross Blue
Shield
Metro North, West 382,031 20,090 402,121
Puerto Rico Government Health
Plan (Comprehensive
MCO)
Molina Health Care PR,
Inc.
Molina Healthcare East, Southwest 302,829 17,840 320,669
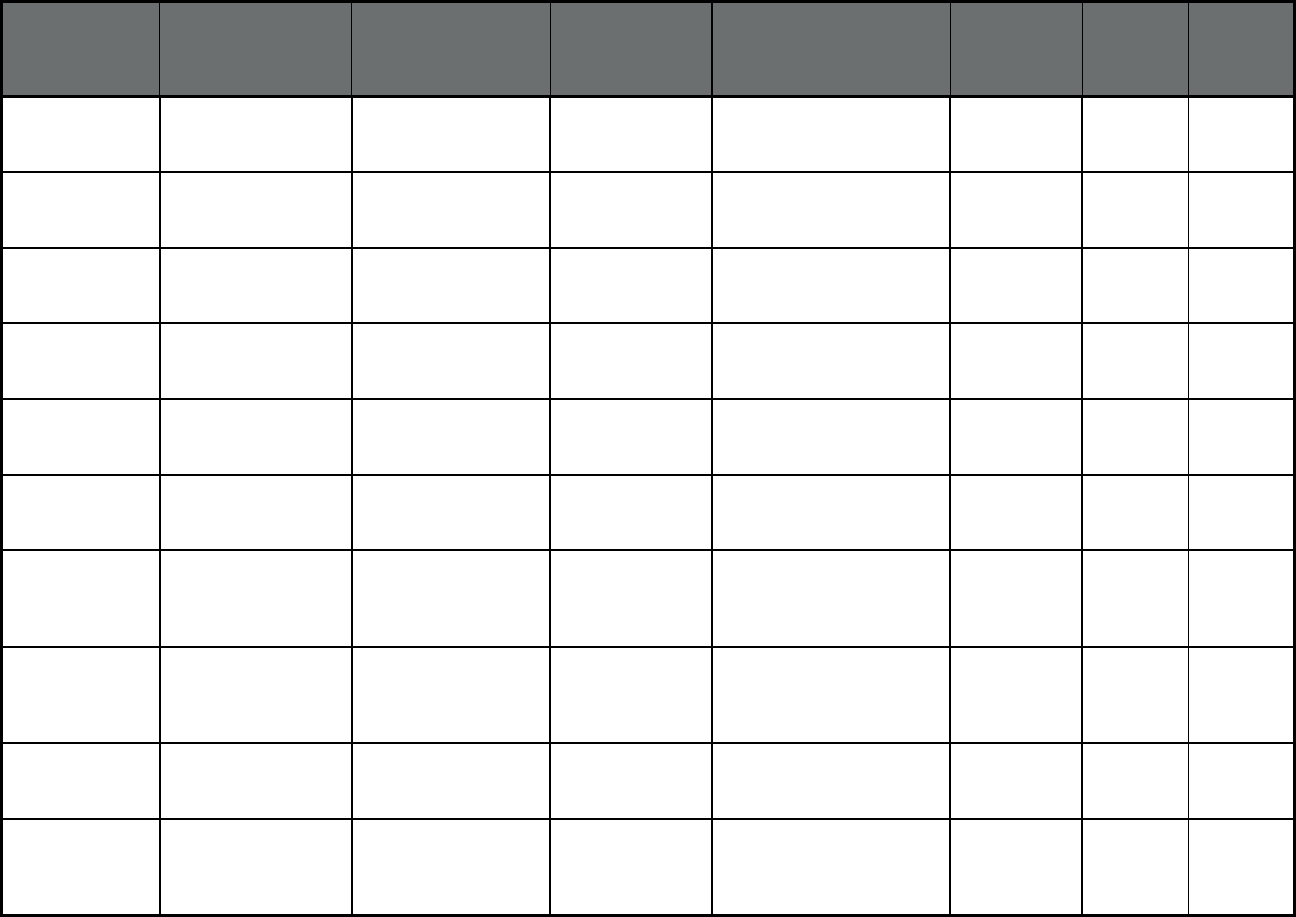
146
State
Program Name
(Type) Plan Name
Parent
Organization
Geographic Region (state-
defined areas, counties, or
zip codes)
Medicaid-Only
Enrollment
Dual
Enrollment
Total
Enrollment
Puerto Rico Government Health
Plan (Comprehensive
MCO)
MMM MultiHealth, Inc. Medicare and
Much More
(MMM), Inc.
Northeast, Southeast 254,451 14,969 269,420
Puerto Rico Medicare Platino
(Comprehensive
MCO)
Triple S Advantage Blue Cross Blue
Shield
Statewide 0 40,996 40,996
Puerto Rico Medicare Platino
(Comprehensive
MCO)
Humana Health Plan of
PR Inc.
Humana Statewide 0 22,276 22,276
Puerto Rico Medicare Platino
(Comprehensive
MCO)
MCS Advantage Inc. MCS Advantage
Inc.
Statewide 0 88,379 88,379
Puerto Rico Medicare Platino
(Comprehensive
MCO)
MMM Health Care Inc. Medicare and
Much More
(MMM), Inc.
Statewide 0 64,161 64,161
Puerto Rico Medicare Platino
(Comprehensive
MCO)
Constellation Health
LLC
Constellation
Health LLC
Statewide 0 10,553 10,553
Rhode Island RIte Care, RHP and
Medicaid Expansion
(Comprehensive
MCO)
Neighborhood Health
Plan of RI
Neighborhood
Health Plan of RI
Statewide 155,216 0 155,216
Rhode Island RIte Care, RHP and
Medicaid Expansion
(Comprehensive
MCO)
UnitedHealthCare of
Rhode Island
Community Plan
UnitedHealthcare Statewide 92,767 0 92,767
Rhode Island Rite Smiles Dental
Program (Dental only
(PAHP))
UnitedHealthCare
Dental of Rhode Island
UnitedHealthcare Statewide 111,315 0 111,315
Rhode Island Transportation Broker
(Non-Emergency
Medical
Transportation)
Logisticare, Inc. LogistiCare Statewide 267,396 0 267,396
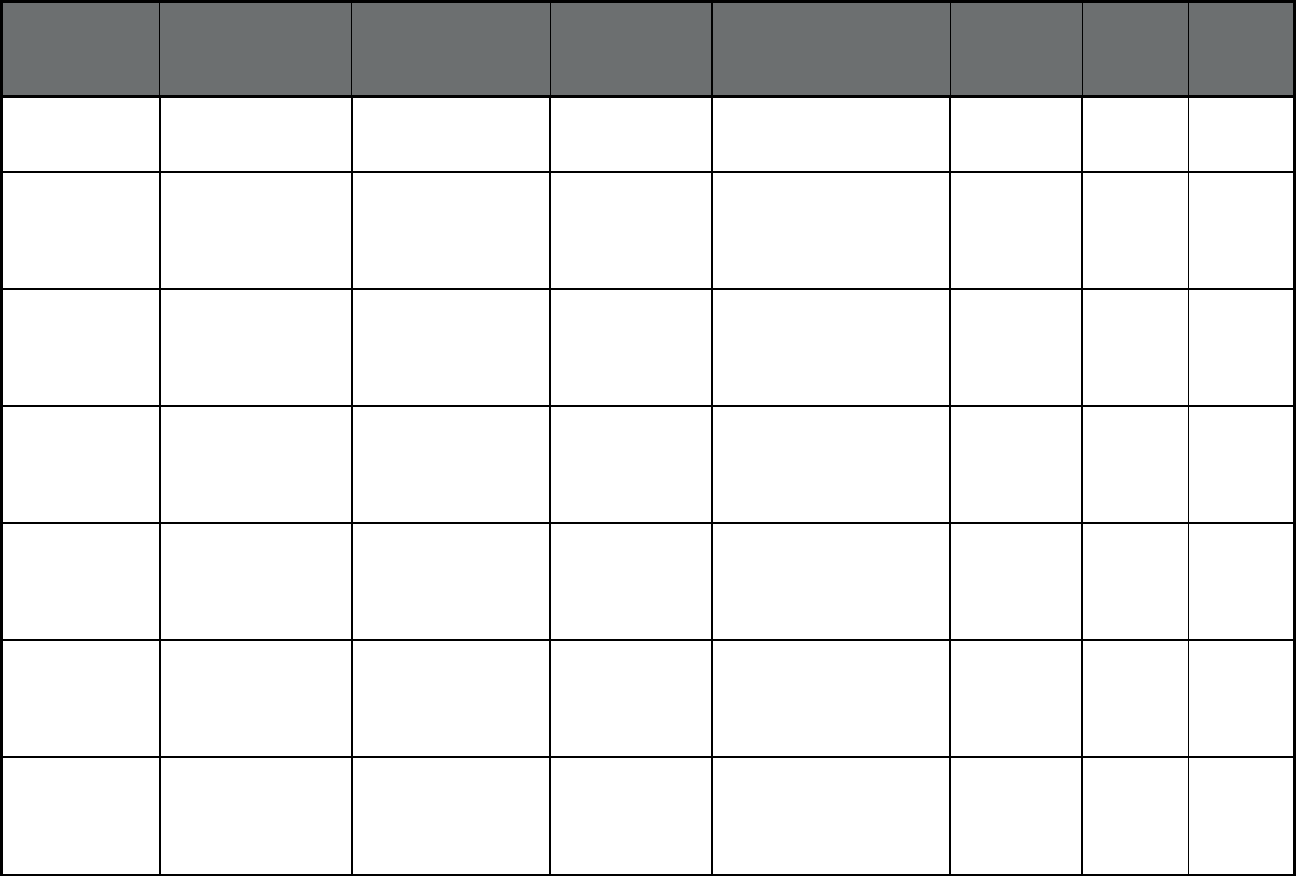
147
State
Program Name
(Type) Plan Name
Parent
Organization
Geographic Region (state-
defined areas, counties, or
zip codes)
Medicaid-Only
Enrollment
Dual
Enrollment
Total
Enrollment
Rhode Island PACE (Program of All-
inclusive Care for the
Elderly (PACE))
PACE Organization of
RI
PACE Statewide 295 0 295
South Carolina South Carolina
Managed Care
Organizations
(Comprehensive
MCO)
Select Health of South
Carolina
AmeriHealth Statewide 354,400 0 354,400
South Carolina South Carolina
Managed Care
Organizations
(Comprehensive
MCO)
Absolute Total Care Centene
Corporation
Statewide 108,032 0 108,032
South Carolina South Carolina
Managed Care
Organizations
(Comprehensive
MCO)
BlueChoice Healthplan
Medicaid
Blue Cross Blue
Shield
Statewide 96,346 0 96,346
South Carolina South Carolina
Managed Care
Organizations
(Comprehensive
MCO)
Molina Healthcare of
South Carolina
Molina Healthcare Statewide 111,302 0 111,302
South Carolina South Carolina
Managed Care
Organizations
(Comprehensive
MCO)
WellCare of South
Carolina
WellCare Statewide 75,389 0 75,389
South Carolina South Carolina
Medical Homes
Network (Primary Care
Case Management
(PCCM))
South Carolina
Solutions
Community Health
Solutions America
Statewide 558 0 558
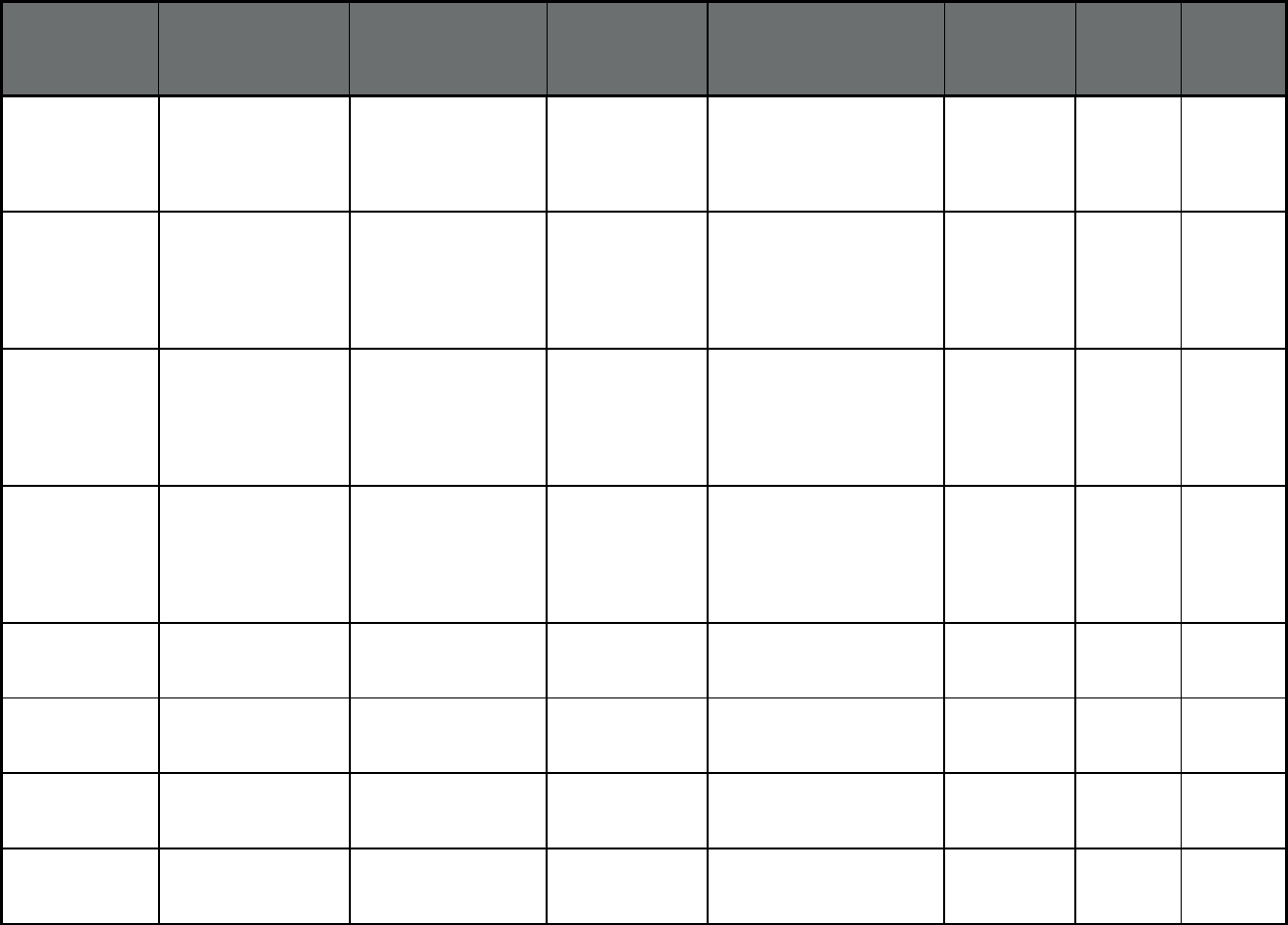
148
State
Program Name
(Type) Plan Name
Parent
Organization
Geographic Region (state-
defined areas, counties, or
zip codes)
Medicaid-Only
Enrollment
Dual
Enrollment
Total
Enrollment
South Carolina South Carolina Non-
Emergency Medical
Transportation (Non-
Emergency Medical
Transportation)
Logisticare LogistiCare Statewide 1,033,900 161,803 1,195,703
South Carolina South Carolina
Program for All
Inclusive Care for the
Elderly (Program of
All-inclusive Care for
the Elderly (PACE))
Palmetto Senior Care PRISMA Health Richland and Lexington
County
32 247 279
South Carolina South Carolina
Program for All
Inclusive Care for the
Elderly (Program of
All-inclusive Care for
the Elderly (PACE))
The Methodist Oaks The Methodist
Oaks
Orangeburg County 14 93 107
South Carolina South Carolina
Program for All
Inclusive Care for the
Elderly (Program of
All-inclusive Care for
the Elderly (PACE))
Greenville Health
System Senior Care
PRISMA Health Greenville Anderson
Pickens Counties
5 51 56
South Dakota PRIME (Primary Care
Case Management
(PCCM))
Multiple Primary Care
Providers
Multiple Primary
Care Provider
(PCCM)
Statewide 92,184 0 92,184
Tennessee
9
TennCare II
(Comprehensive MCO
+ MLTSS)
Amerigroup Amerigroup, Inc. Statewide 337,584 38,699 376,283
Tennessee
9
TennCare II
(Comprehensive MCO
+ MLTSS)
DentaQuest USA
Insurance Company
DentaQuest USA
Insurance
Company
Statewide 802,783 381 803,164
Tennessee
9
TennCare II
(Comprehensive MCO
+ MLTSS)
Magellan Health
Services
Magellan Health Statewide 1,241,360 381 1,241,741
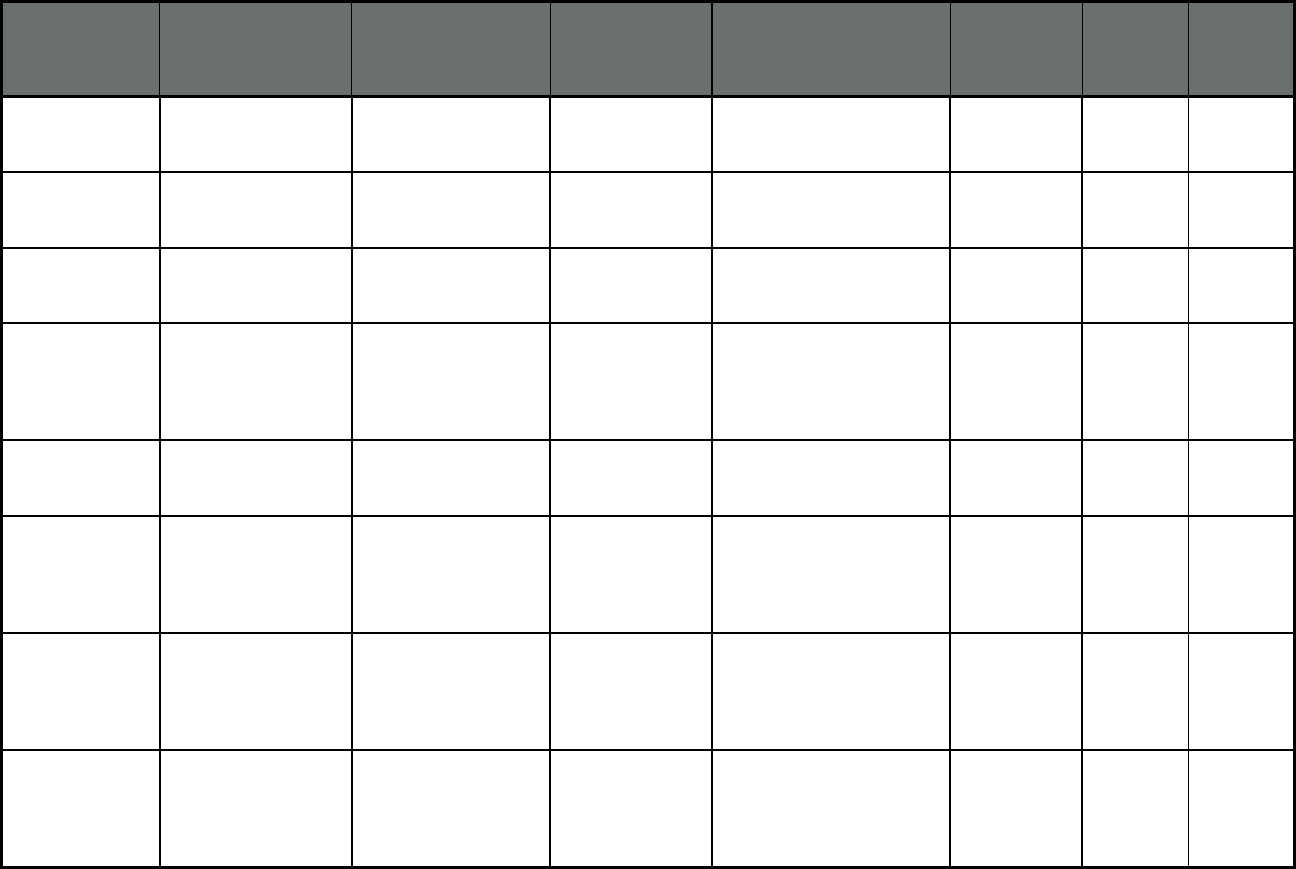
149
State
Program Name
(Type) Plan Name
Parent
Organization
Geographic Region (state-
defined areas, counties, or
zip codes)
Medicaid-Only
Enrollment
Dual
Enrollment
Total
Enrollment
Tennessee
9
TennCare II
(Comprehensive MCO
+ MLTSS)
UnitedHealthcare
Community Plan
UnitedHealthcare Statewide 381,108 52,094 433,202
Tennessee
9
TennCare II
(Comprehensive MCO
+ MLTSS)
Volunteer State Health
Plan (BlueCare)
Blue Cross Blue
Shield
Statewide 459,478 51,512 510,990
Tennessee
9
TennCare II
(Comprehensive MCO
+ MLTSS)
Volunteer State Health
Plan (TennCare Select)
Blue Cross Blue
Shield
Statewide 63,190 2,718 65,908
Tennessee
9
Program of All-
Inclusive Care for the
Elderly (Program of
All-inclusive Care for
the Elderly (PACE))
Alexian Brothers
Community Services
Alexian Brothers
Community
Services
Hamilton County 14 267 281
Texas STAR Health
(Comprehensive
MCO)
Superior HealthPlan Centene
Corporation
Statewide 34,117 0 34,117
Texas STAR
(Comprehensive
MCO)
Amerigroup Texas, Inc. Amerigroup, Inc. Bexar SDA, Dallas SDA,
Harris SDA, Jefferson SDA,
Lubbock SDA, MRSA
Central, MRSA Northeast,
MRSA West, Tarrant SDA
539,812 0 539,812
Texas STAR
(Comprehensive
MCO)
Superior Health Plan,
Inc.
Centene
Corporation
Bexar SDA, El Paso SDA,
Hidalgo SDA, Lubbock SDA,
MRSA Central, MRSA
Northeast, MRSA West,
Nueces SDA, Travis SDA
737,410 0 737,410
Texas STAR
(Comprehensive
MCO)
El Paso Health Plans,
Inc., dba El Paso
Health
El Paso County
Hospital District -
DBA University
Medical Center of
El Paso
Bexar SDA, El Paso SDA 66,563 0 66,563
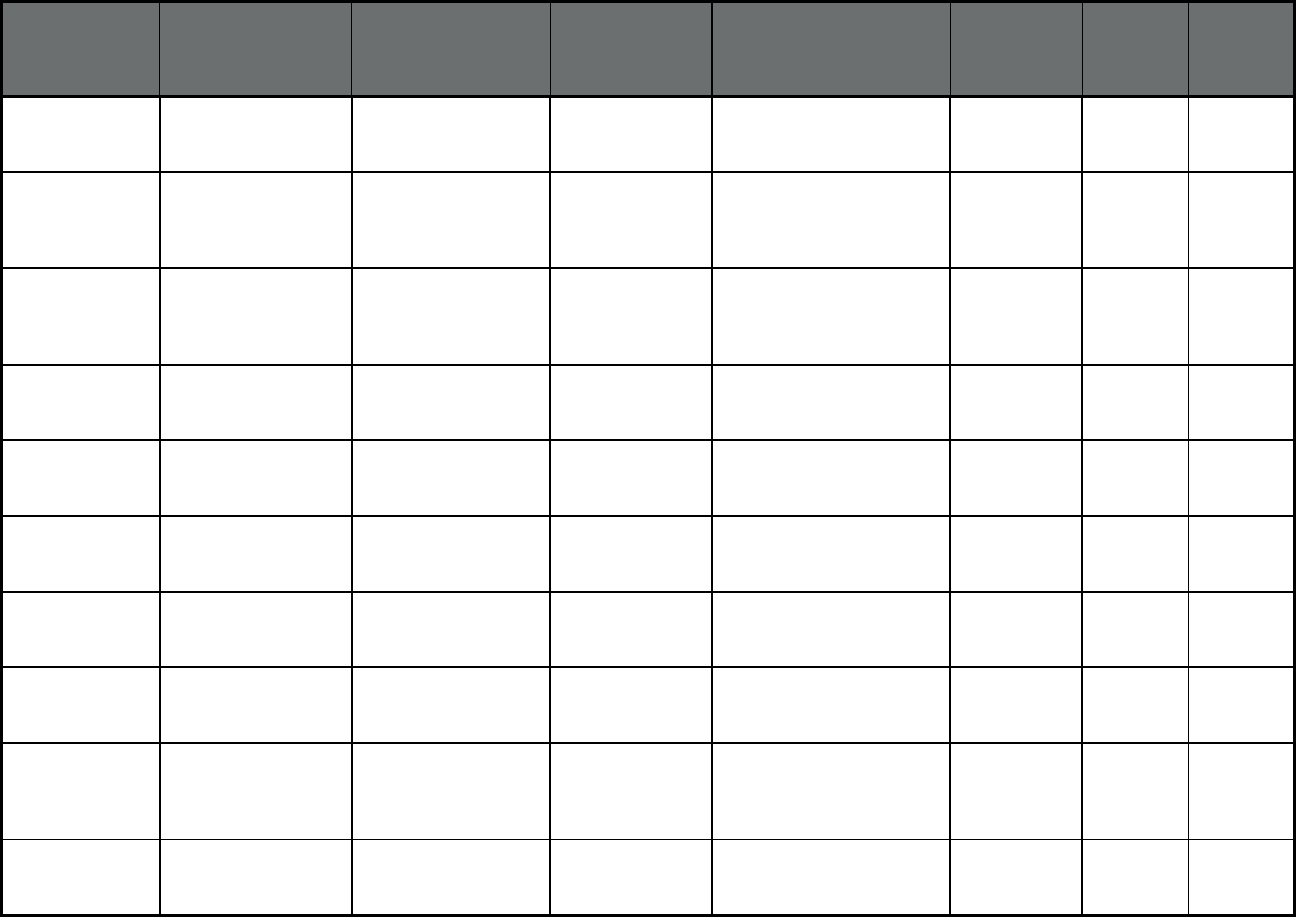
150
State
Program Name
(Type) Plan Name
Parent
Organization
Geographic Region (state-
defined areas, counties, or
zip codes)
Medicaid-Only
Enrollment
Dual
Enrollment
Total
Enrollment
Texas STAR
(Comprehensive
MCO)
Aetna Better Health of
Texas, Inc.
Aetna Bexar SDA, Tarrant SDA 74,678 0 74,678
Texas STAR
(Comprehensive
MCO)
Community First Health
Plans, Inc.
Bexar County
Hospital District,
dba University
Health System
Bexar SDA 108,453 0 108,453
Texas STAR
(Comprehensive
MCO)
UnitedHealthcare
Insurance Company,
dba United Healthcare
Community Plan
UnitedHealthcare Harris SDA, Hidalgo SDA,
Jefferson SDA
139,036 0 139,036
Texas STAR
(Comprehensive
MCO)
Texas Children's
Health Plan, Inc.
Texas Children's Harris SDA, Jefferson SDA 348,467 0 348,467
Texas STAR
(Comprehensive
MCO)
Molina Healthcare of
Texas, Inc.
Molina Healthcare Dallas SDA, El Paso SDA,
Harris SDA, Hidalgo SDA,
Jefferson SDA
95,739 0 95,739
Texas STAR
(Comprehensive
MCO)
Driscoll Children's
Health Plan
Driscoll Hidalgo SDA, Nueces SDA 157,744 0 157,744
Texas STAR
(Comprehensive
MCO)
Parkland Community
Health Plan, Inc.
Dallas County
Hospital District
Dallas SDA 165,083 0 165,083
Texas STAR
(Comprehensive
MCO)
Cook Children's Health
Plan
Cook Children's
Health Care
System
Tarrant SDA 107,151 0 107,151
Texas STAR
(Comprehensive
MCO)
Community First Health
Plans, Inc.
Bexar County
Hospital District,
dba University
Health System
Harris SDA, Jefferson SDA 245,466 0 245,466
Texas STAR
(Comprehensive
MCO)
Seton Health Plan, Inc.,
dba Dell Childrens
Health Plan
Seton Insurance
Services
Corporation
Travis SDA 23,122 0 23,122
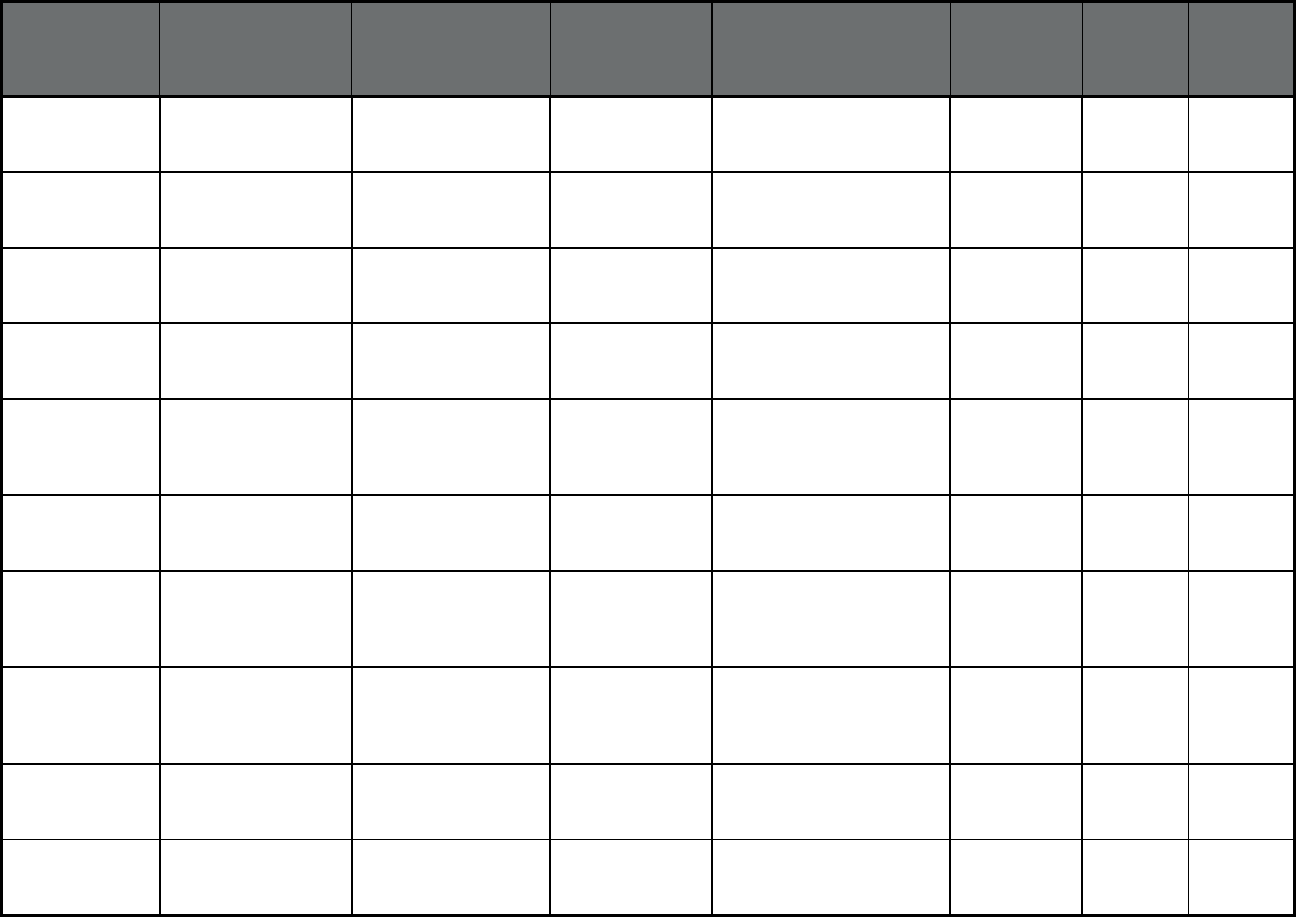
151
State
Program Name
(Type) Plan Name
Parent
Organization
Geographic Region (state-
defined areas, counties, or
zip codes)
Medicaid-Only
Enrollment
Dual
Enrollment
Total
Enrollment
Texas STAR
(Comprehensive
MCO)
Health Care Service
Corp. (dba Blue Cross
Blue Shield)
Health Care
Service
Corporation
Travis SDA 31,971 0 31,971
Texas STAR
(Comprehensive
MCO)
SHA. LLC, dba
FirstCare Health Plans
Scott and White
Health Plan
Lubbock SDA, MRSA West 84,226 0 84,226
Texas STAR
(Comprehensive
MCO)
Scott & White Health
Plan
Baylor Scott &
White Holdings
MRSA Central 45,067 0 45,067
Texas STAR Kids
(Comprehensive MCO
+ MLTSS)
Amerigroup Insurance
Company
Amerigroup, Inc. Dallas SDA, El Paso SDA,
Harris SDA, MRSA West,
Lubbock SDA
26,925 147 27,072
Texas STAR Kids
(Comprehensive MCO
+ MLTSS)
Superior HealthPlan,
Inc.
Centene
Corporation
Bexar SDA, El Paso SDA,
Hidalgo SDA, Lubbock SDA,
MRSA West SDA, Travis
SDA, Nueces SDA
28,479 189 28,668
Texas STAR Kids
(Comprehensive MCO
+ MLTSS)
Aetna Better Health of
Texas Inc.
Aetna Tarrant SDA 4,807 36 4,843
Texas STAR Kids
(Comprehensive MCO
+ MLTSS)
Community First Health
Plans, Inc.
Bexar County
Hospital District,
dba University
Health System
Bexar SDA 7,858 41 7,899
Texas STAR Kids
(Comprehensive MCO
+ MLTSS)
UnitedHealthcare
Insurance Company,
dba United Healthcare
Community Plan
UnitedHealthcare Harris SDA, Hidalgo SDA,
Jefferson SDA, MRSA
Central SDA, MRSA
Northeast SDA
30,436 159 30,595
Texas STAR Kids
(Comprehensive MCO
+ MLTSS)
Texas Children’s
Health Plan, Inc.
Texas Children's Harris SDA, Jefferson SDA,
MRSA Northeast SDA
26,084 100 26,184
Texas STAR Kids
(Comprehensive MCO
+ MLTSS)
Driscoll Children’s
Health Plan
Driscoll Hidalgo SDA, Nueces SDA 10,396 45 10,441
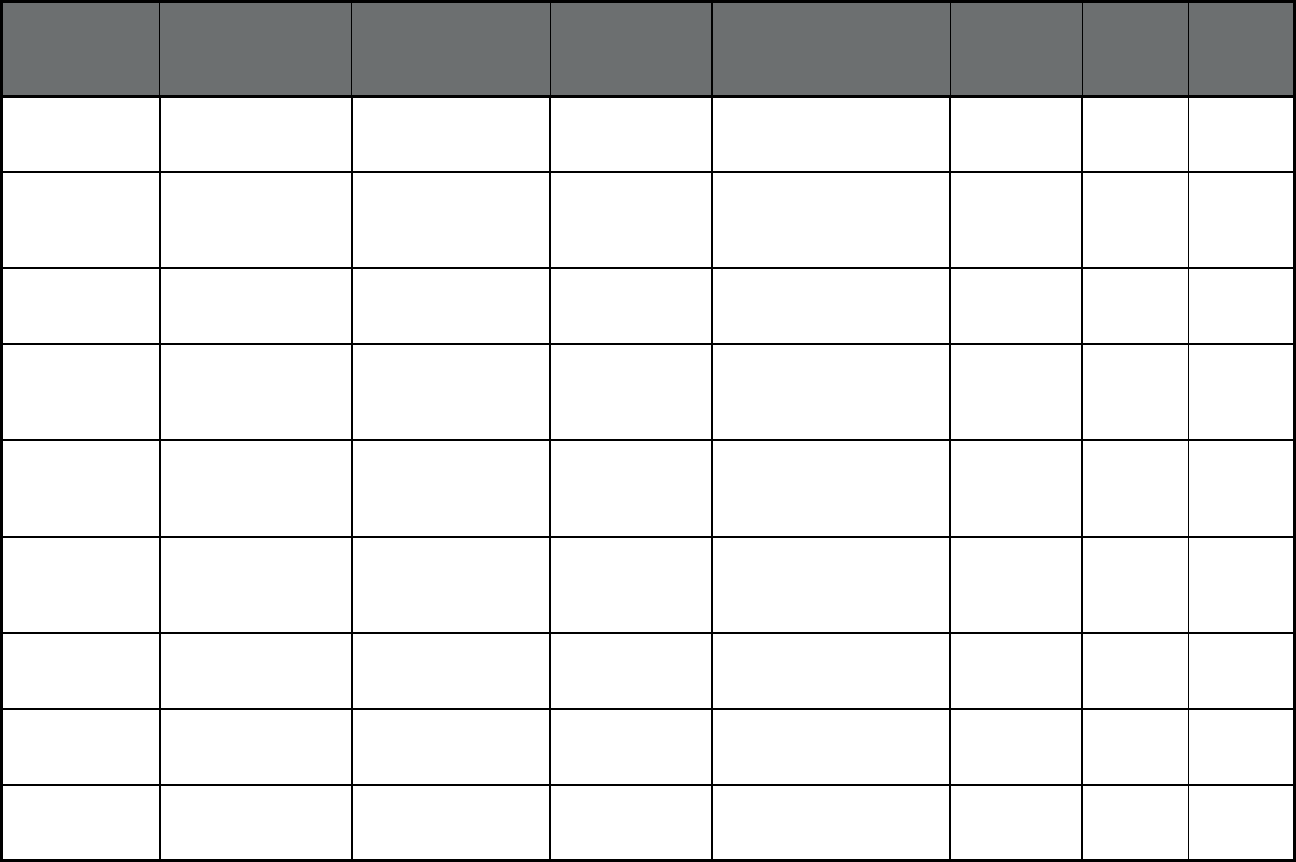
152
State
Program Name
(Type) Plan Name
Parent
Organization
Geographic Region (state-
defined areas, counties, or
zip codes)
Medicaid-Only
Enrollment
Dual
Enrollment
Total
Enrollment
Texas STAR Kids
(Comprehensive MCO
+ MLTSS)
Cook Children's Health
Plan
Cook Children's
Health Care
System
Tarrant SDA 9,447 46 9,493
Texas STAR Kids
(Comprehensive MCO
+ MLTSS)
Health Care Service
Corporation DBA Blue
Cross and Blue Shield
of Texas (BCBSTX)
Health Care
Service
Corporation
MRSA Central SDA, Travis
SDA
7,870 48 7,918
Texas STAR Kids
(Comprehensive MCO
+ MLTSS)
Children’s Medical
Center Health Plan
Children's Health
System of Texas
Dallas SDA 9,202 34 9,236
Texas STAR+PLUS
(Comprehensive MCO
+ MLTSS)
Amerigroup Texas, Inc. Anthem Insurance
Companies, Inc.
Bexar SDA, El Paso SDA,
Harris SDA, Jefferson SDA,
Lubbock SDA, MRSA West,
Tarrant SDA, Travis SDA
58,450 72,405 130,855
Texas STAR+PLUS
(Comprehensive MCO
+ MLTSS)
Superior HealthPlan,
Inc
Centene
Corporation
Bexar SDA, Dallas SDA,
Hidalgo SDA, Lubbock SDA,
Nueces SDA, MRSA
Central, MRSA West
65,788 73,702 139,490
Texas STAR+PLUS
(Comprehensive MCO
+ MLTSS)
UnitedHealthcare
Insurance Company,
dba United Healthcare
Community Plan
UnitedHealthcare Harris SDA, Jefferson SDA,
Nueces SDA, Travis SDA,
MRSA Central, MRSA
Northeast
55,929 64,561 120,490
Texas STAR+PLUS
(Comprehensive MCO
+ MLTSS)
Molina Healthcare of
Texas, Inc.
Molina Healthcare Bexar SDA, Dallas SDA, El
Paso SDA, Harris SDA,
Hidalgo SDA, Jefferson SDA
35,570 51,751 87,321
Texas STAR+PLUS
(Comprehensive MCO
+ MLTSS)
HealthSpring Life &
Health Insurance Co.,
Inc.
Cigna Hidalgo SDA, MRSA
Northeast, Tarrant SDA
19,819 29,782 49,601
Texas Children's Medicaid
Dental Services
(Dental only (PAHP))
MCNA Insurance
Company
Managed Care of
North America
(MCNA), Inc.
Statewide 1,229,546 0 1,229,546
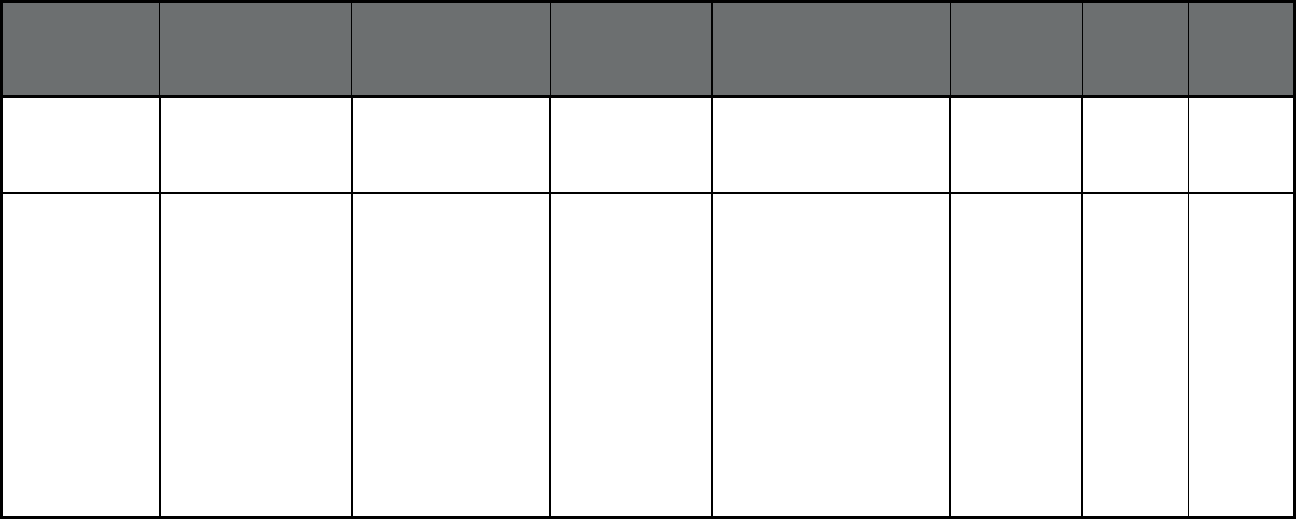
153
State
Program Name
(Type) Plan Name
Parent
Organization
Geographic Region (state-
defined areas, counties, or
zip codes)
Medicaid-Only
Enrollment
Dual
Enrollment
Total
Enrollment
Texas Children's Medicaid
Dental Services
(Dental only (PAHP))
DentaQuest USA
Insurance Company,
Inc.
DentaQuest, LLC
(owned by
DentaQuest
Group, Inc.)
Statewide 1,650,398 0 1,650,398
Texas Medical Transportation
Program (Non-
Emergency Medical
Transportation)
American Medical
Response
American Medical
Response
Brown, Callahan, Coke,
Coleman, Comanche,
Concho, Crockett, Dimmit,
Eastland, Edwards, Fisher,
Haskell, Irion, Jones, Kent,
Kimble, Kinney, Knox,
Maverick, Mcculloch,
Menard, Mitchell, Nolan,
Reagan, Real, Runnels,
Schleicher, Scurry,
Shackelford, Stephens,
Sterling, Stonewall, Sutton,
Taylor, Throckmorton, Tom
Green, Uvalde, Val Verde,
Zavala
93,639 14,863 108,502
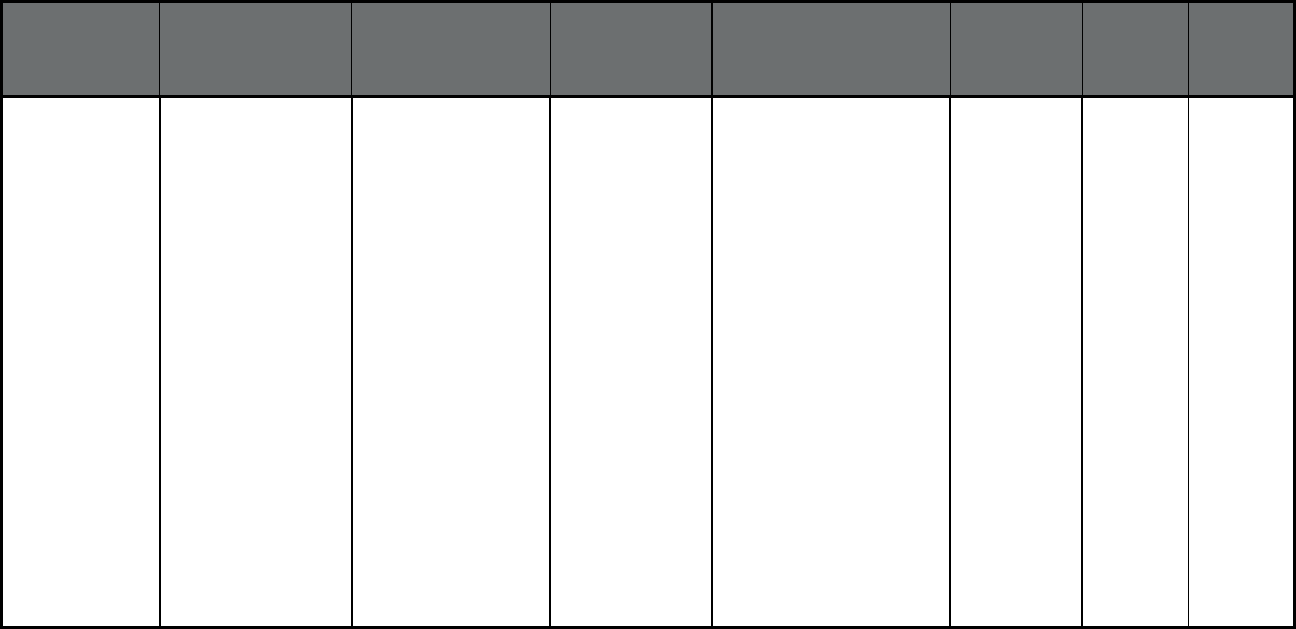
154
State
Program Name
(Type) Plan Name
Parent
Organization
Geographic Region (state-
defined areas, counties, or
zip codes)
Medicaid-Only
Enrollment
Dual
Enrollment
Total
Enrollment
Texas Medical Transportation
Program (Non-
Emergency Medical
Transportation)
LogistiCare LogistiCare Aransas, Armstrong,
Atascosa, Bailey, Bandera,
Bastrop, Bee, Bell, Bexar,
Blanco, Bosque, Brazos,
Brisco, Brooks, Burleson,
Burnet, Caldwell, Cameron,
Carson, Castro, Childress,
Collingsworth, Cochran,
Comal, Coryell, Crosby,
Dallas, Dallam, Deaf Smith,
Denton, Dickens, Donley,
Duval, Ellis, Erath, Falls,
Fayette, Floyd, Freestone,
Frio, Garza, Gray, Gillespie,
Grimes, Guadalupe, Hall,
Hale, Hamilton, Hansford,
Hartley, Hays, Hemphill,
Hidalgo, Hill, Hockley, Hood,
Hunt, Hutchinson, Jim Hogg,
Jim Wells, Johnson, Karnes,
Kaufman, Kendall, Kenedy,
Kerr, King, Kleberg, Lamb,
Lampasas, Lee, Leon,
Lipscomb, Limestone, Live
Oak, Llano, Lubbock,
2,022,031 202,581 2,224,612
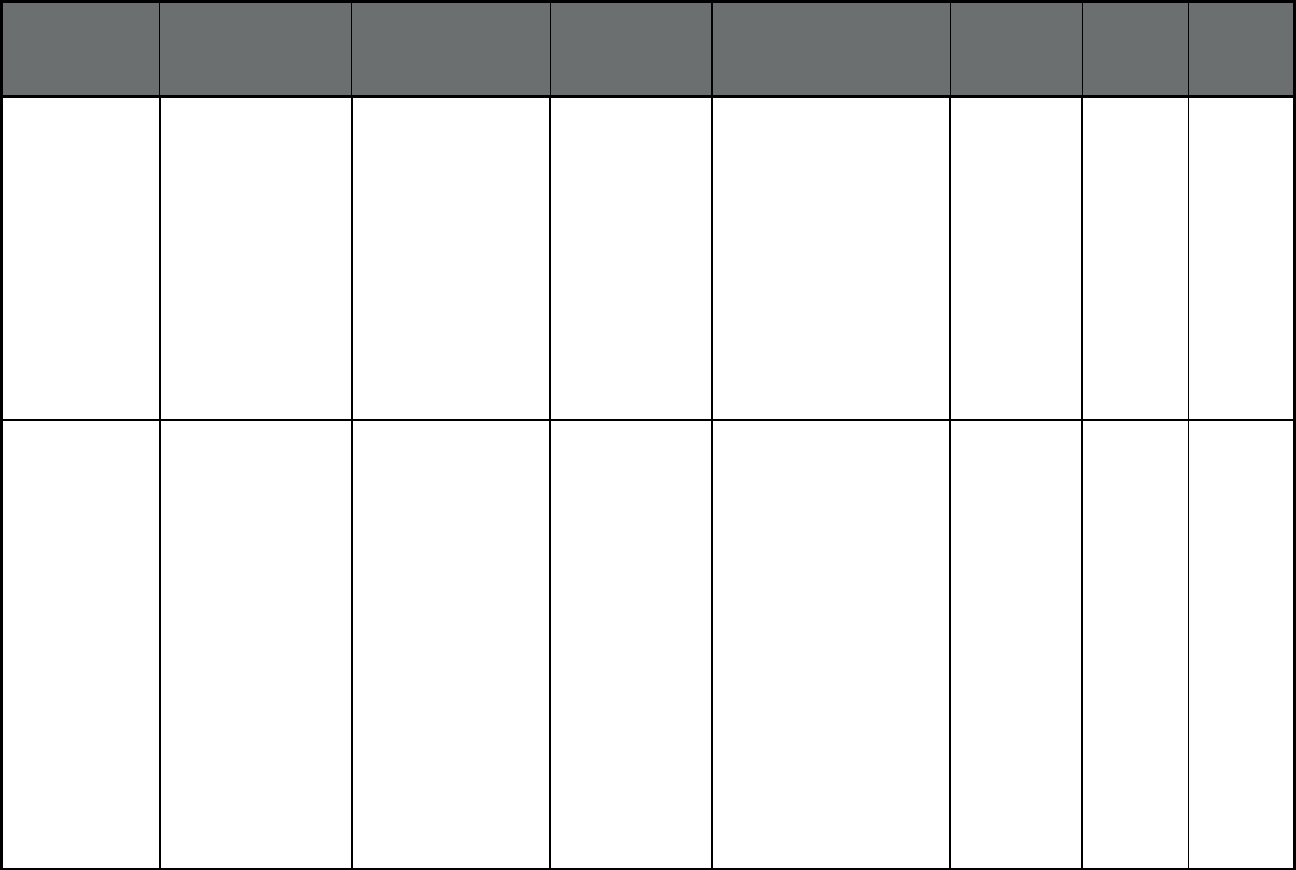
155
State
Program Name
(Type) Plan Name
Parent
Organization
Geographic Region (state-
defined areas, counties, or
zip codes)
Medicaid-Only
Enrollment
Dual
Enrollment
Total
Enrollment
Texas (cont.) Medical Transportation
Program (Non-
Emergency Medical
Transportation)
LogistiCare LogistiCare Lynn, Madison, Mason,
Mclennan, McMullen,
Medina, Milam, Mills, Moore,
Motley, Navarro, Nueces,
Ochiltree, Oldham, Palo
Pinto, Parker, Parmer,
Potter, Randall, Refugio,
Roberts, Robertson,
Rockwall, San Patricio, San
Saba, Sherman, Somervell,
Starr, Swisher, Tarrant,
Terry, Travis, Washington,
Webb, Wheeler, Willacy,
Williamson, Wilson,
Yoakum, Zapata
2,022,031 202,581 2,224,612
Texas Medical Transportation
Program (Non-
Emergency Medical
Transportation)
Medical Transportation
Management
Medical
Transportation
Management, Inc.
Anderson, Angelina, Austin,
Bowie, Brazoria, Calhoun,
Camp, Cass, Chambers,
Cherokee, Colorado, De
Witt, Delta, Fort Bend,
Franklin, Galveston, Goliad,
Gonzales, Gregg, Hardin,
Harris, Harrison, Henderson,
Hopkins, Houston, Jackson,
Jasper, Jefferson, Lamar,
Lavaca, Liberty, Marion,
Matagorda, Montgomery,
Morris, Nacogdoches,
Newton, Orange, Panola,
Polk, Rains, Red River,
Rusk, Sabine, San
Augustine, San Jacinto,
Shelby, Smith, Titus, Trinity,
Tyler, Upshur, Van Zandt,
Victoria, Walker, Waller,
Wharton, Wood
1,174,476 110,262 1,284,738
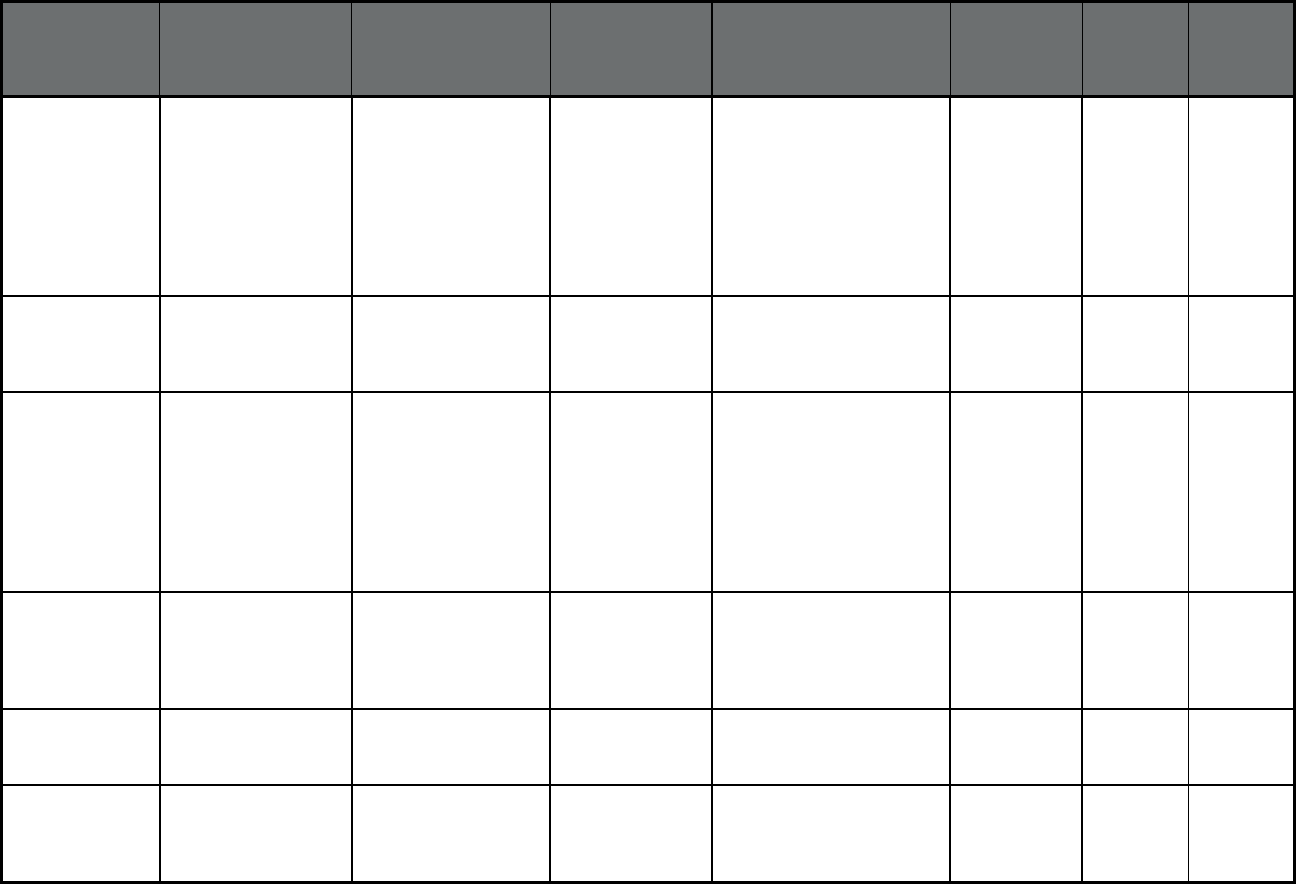
156
State
Program Name
(Type) Plan Name
Parent
Organization
Geographic Region (state-
defined areas, counties, or
zip codes)
Medicaid-Only
Enrollment
Dual
Enrollment
Total
Enrollment
Texas Medical Transportation
Program (Non-
Emergency Medical
Transportation)
Project Armistad Project Armistad Andrews, Borden, Brewster,
Crane, Culberson, Dawson,
Ector, El Paso, Gaines,
Glasscock, Howard,
Hudspeth, Jeff Davis,
Loving, Martin, Midland,
Pecos, Presidio, Reeves,
Terrell, Upton, Ward,
Winkler
199,829 26,891 226,720
Texas PACE (Program of All-
inclusive Care for the
Elderly (PACE))
Bienvivir Senior Health
Services (El Paso)
PACE 79901, 79902, 79903,
79904, 79905, 79907,
79915, 79924, 79925,
79930, 79935, 79936
28 892 920
Texas PACE (Program of All-
inclusive Care for the
Elderly (PACE))
Silver Star Health
Network (Lubbock)
PACE 79401, 79402, 79403,
79404, 79405, 79406,
79407, 79408, 79409,
79410, 79411, 79412,
79413, 79414, 79415,
79416, 79423, 79424,
79430, 79452, 79453,
79454, 79464, 79490,
79491, 79493, 79499
12 156 168
Texas PACE (Program of All-
inclusive Care for the
Elderly (PACE))
Werner (Amarillo) PACE 9015, 79101, 79102, 79103,
79104, 79106, 79107,
79108, 79109, 79110,
79111, 79118, 79119,
79121, 79124
2 125 127
Utah UNI HOME
(Comprehensive
MCO)
HOME University of Utah
Health Plans
Statewide 720 475 1,195
Utah Choice of Health Care
Delivery
(Comprehensive
MCO)
Healthy U University of Utah
Health Plans
Statewide 42,297 6,446 48,743
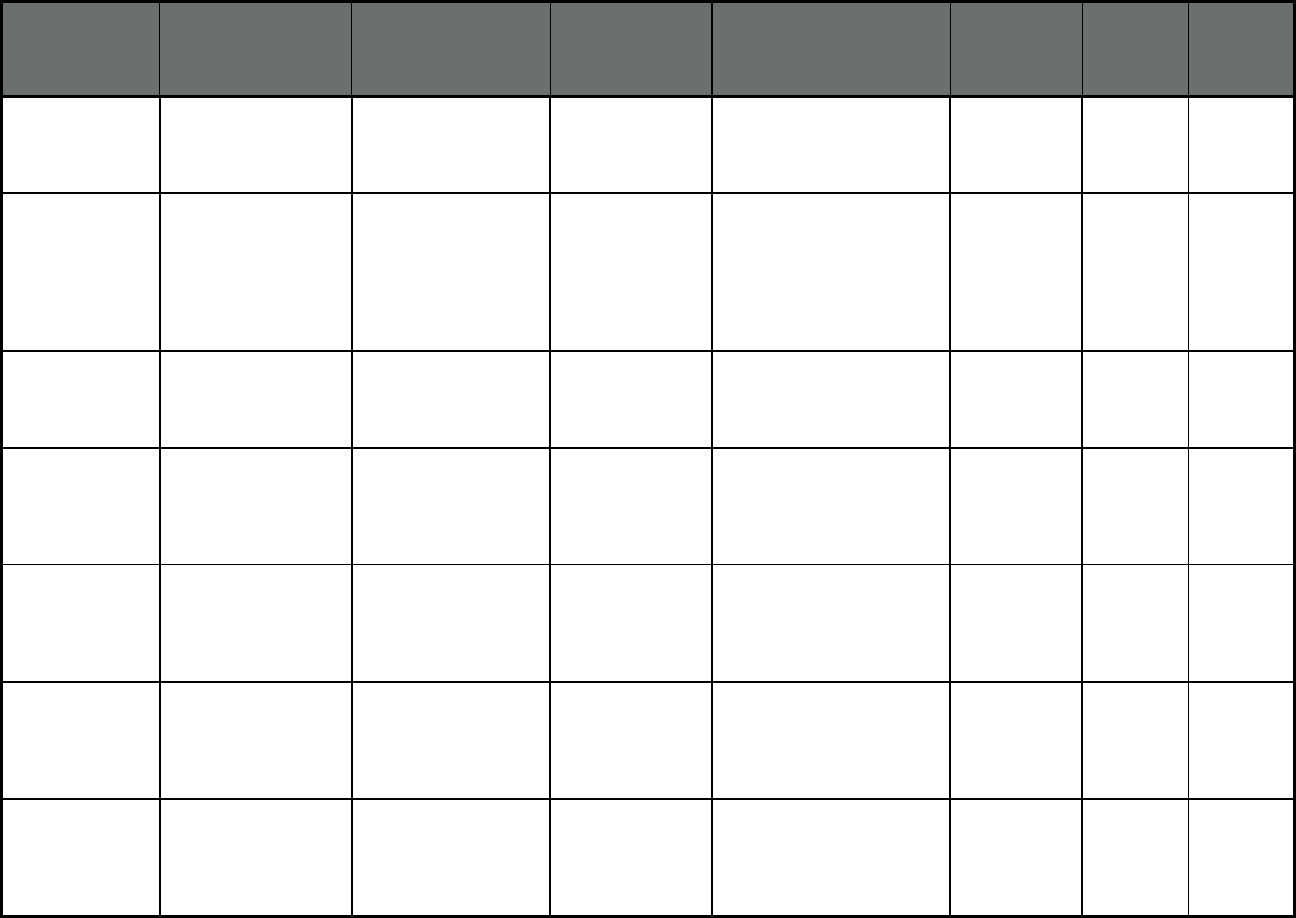
157
State
Program Name
(Type) Plan Name
Parent
Organization
Geographic Region (state-
defined areas, counties, or
zip codes)
Medicaid-Only
Enrollment
Dual
Enrollment
Total
Enrollment
Utah Choice of Health Care
Delivery
(Comprehensive
MCO)
Molina Molina Healthcare Statewide 58,234 6,479 64,713
Utah Choice of Health Care
Delivery
(Comprehensive
MCO)
Health Choice Steward Health
Care System
Beaver, Box Elder, Cache,
Davis, Iron, Juab, Miller,
Morgan, Rich, Salt Lake,
Sanpete, Sevier, Summit,
Tooele, Utah, Wasatch,
Washington and Weber
Counties
16,895 1,563 18,458
Utah Choice of Health Care
Delivery
(Comprehensive
MCO)
SelectHealth Select Health, Inc. Statewide 84,509 9,275 93,784
Utah Prepaid Mental Health
(Behavioral Health
Organization (BHO)
only (PIHP and/or
PAHP))
Bear River Mental
Health
Bear River Mental
Health
Box Elder, Cache, and Rich
Counties
15,133 1,507 16,640
Utah Prepaid Mental Health
(Behavioral Health
Organization (BHO)
only (PIHP and/or
PAHP))
Central Utah Mental
Health
Central Utah
Mental Health
Juab, Millard, Piute,
Sanpete, Sevier and Wayne
Counties
8,177 1,059 9,236
Utah Prepaid Mental Health
(Behavioral Health
Organization (BHO)
only (PIHP and/or
PAHP))
Davis Behavioral
Health
Davis Behavioral
Health
Davis County 19,907 2,366 22,273
Utah Prepaid Mental Health
(Behavioral Health
Organization (BHO)
only (PIHP and/or
PAHP))
Four Corners
Community Behavioral
Health
Four Corners
Community
Behavioral Health
Grand, Emery and Carbon
Counties
4,362 822 5,184
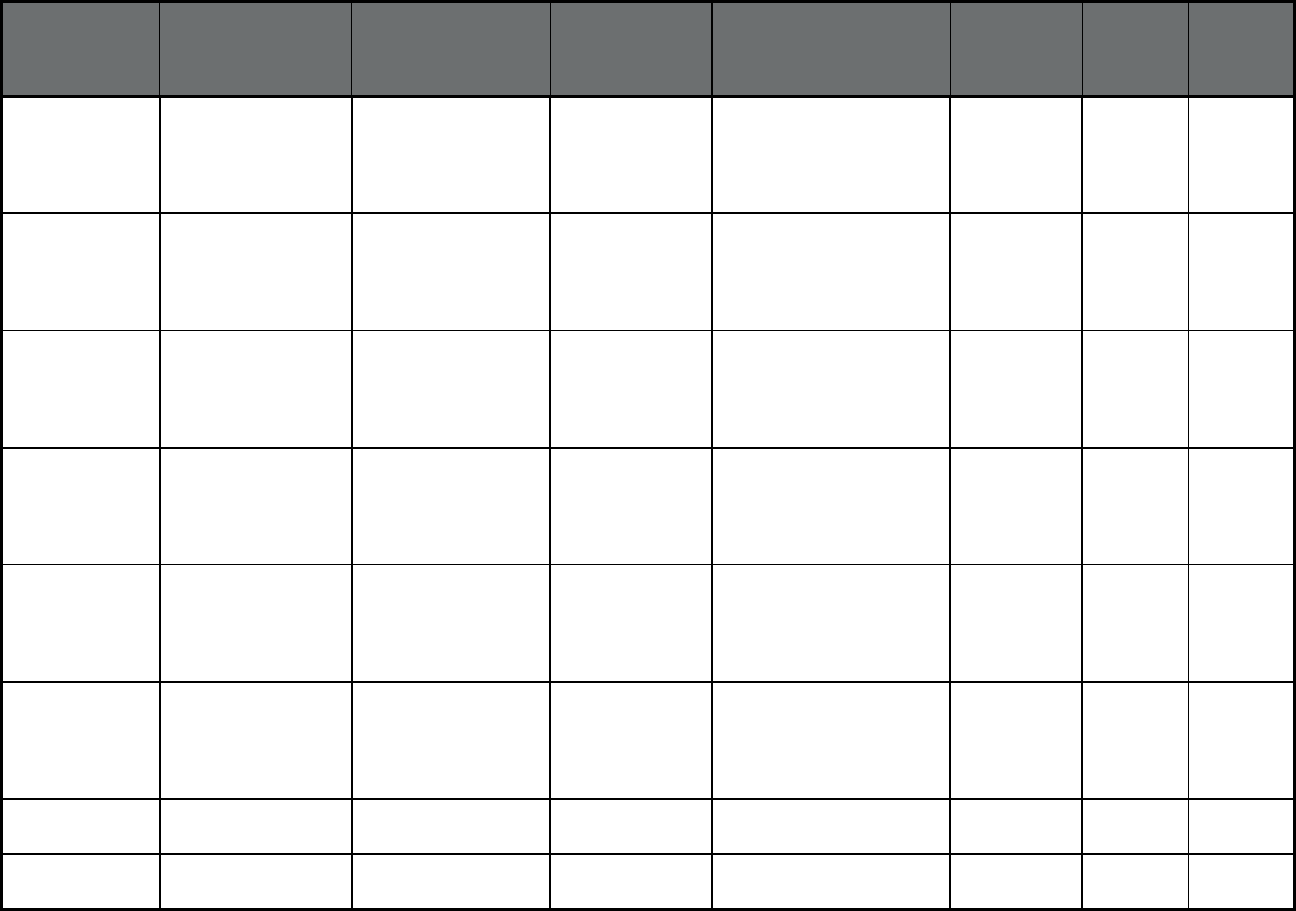
158
State
Program Name
(Type) Plan Name
Parent
Organization
Geographic Region (state-
defined areas, counties, or
zip codes)
Medicaid-Only
Enrollment
Dual
Enrollment
Total
Enrollment
Utah Prepaid Mental Health
(Behavioral Health
Organization (BHO)
only (PIHP and/or
PAHP))
Northeastern
Counseling
Northeastern
Counseling
Duchesne, Uintah, Daggett,
and San Juan Counties
9,189 1,163 10,352
Utah Prepaid Mental Health
(Behavioral Health
Organization (BHO)
only (PIHP and/or
PAHP))
Optum Health Optum Health Salt Lake County 86,925 13,130 100,055
Utah Prepaid Mental Health
(Behavioral Health
Organization (BHO)
only (PIHP and/or
PAHP))
Southwest Behavioral
Health
Southwest
Behavioral Health
Beaver, Garfield, Kane, Iron
and Washington Counties
22,546 2,659 25,205
Utah Prepaid Mental Health
(Behavioral Health
Organization (BHO)
only (PIHP and/or
PAHP))
Valley Behavioral
Health
Valley Behavioral
Health
Summit and Tooele
Counties
6,931 773 7,704
Utah Prepaid Mental Health
(Behavioral Health
Organization (BHO)
only (PIHP and/or
PAHP))
Wasatch Mental Health Wasatch Mental
Health
Utah County 41,758 3,871 45,629
Utah Prepaid Mental Health
(Behavioral Health
Organization (BHO)
only (PIHP and/or
PAHP))
Weber Mental Health Weber Mental
Health
Weber and Morgan
Counties
22,749 3,425 26,174
Utah Dental (Dental only
(PAHP))
Premier Access Avesis
Incorporated
Salt Lake, Weber, Davis and
Utah Counties
64,738 37 64,775
Utah Dental (Dental only
(PAHP))
Delta Dental Delta Dental Davis, Salt Lake, Weber and
Utah Counties
60,391 32 60,423
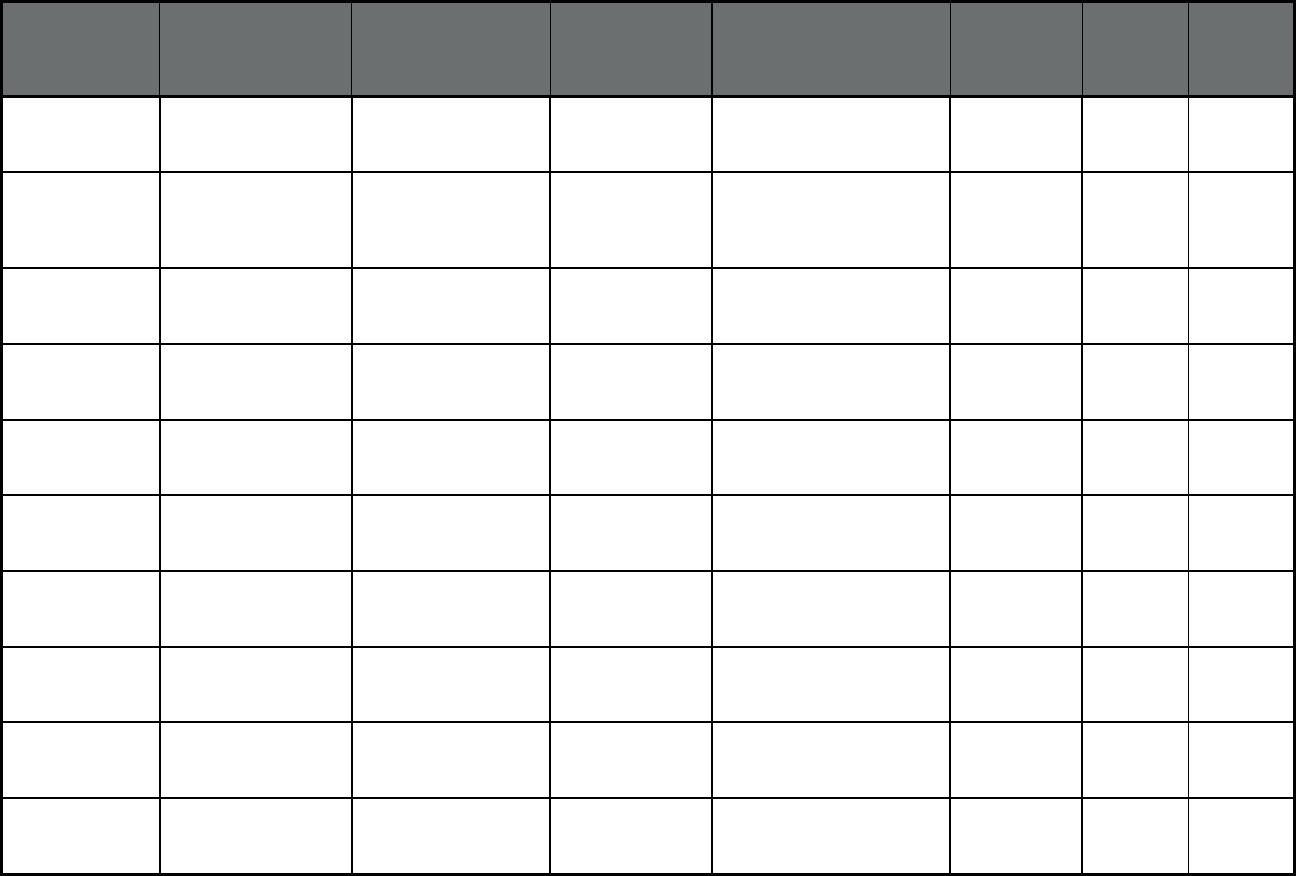
159
State
Program Name
(Type) Plan Name
Parent
Organization
Geographic Region (state-
defined areas, counties, or
zip codes)
Medicaid-Only
Enrollment
Dual
Enrollment
Total
Enrollment
Utah Transportation (Non-
Emergency Medical
Transportation)
Logisticare Solutions Providence
Service
Corporation
Statewide 204,436 27,095 231,531
Vermont
10
Global Commitment to
Health Demonstration
(Comprehensive MCO
+ MLTSS)
Department of Vermont
Health Access
Vermont Agency
of Human Services
Statewide 122,550 760 123,310
Virginia Medallion 3.0
(Comprehensive
MCO)
Virginia Premier Health
Plan
Virginia Premier
Health Plan
Statewide 158,008 0 158,008
Virginia Medallion 3.0
(Comprehensive
MCO)
Anthem Anthem Insurance
Companies, Inc.
Statewide 251,115 0 251,115
Virginia Medallion 3.0
(Comprehensive
MCO)
Intotal Health Inova Health
System
Statewide 52,799 0 52,799
Virginia Medallion 3.0
(Comprehensive
MCO)
Kaiser Kaiser Statewide 12,887 0 12,887
Virginia Medallion 3.0
(Comprehensive
MCO)
Optima Health Care PACE Statewide 149,500 0 149,500
Virginia Medallion 3.0
(Comprehensive
MCO)
Coventry Health Plan Coventry Health
Plan
Statewide 35,658 0 35,658
Virginia CCC Plus
(Comprehensive MCO
+ MLTSS)
Aetna Better Health for
Virginia
Aetna Statewide 14,431 16,160 30,591
Virginia CCC Plus
(Comprehensive MCO
+ MLTSS)
Anthem HealthKeepers Anthem Insurance
Companies, Inc.
Statewide 27,059 33,254 60,313
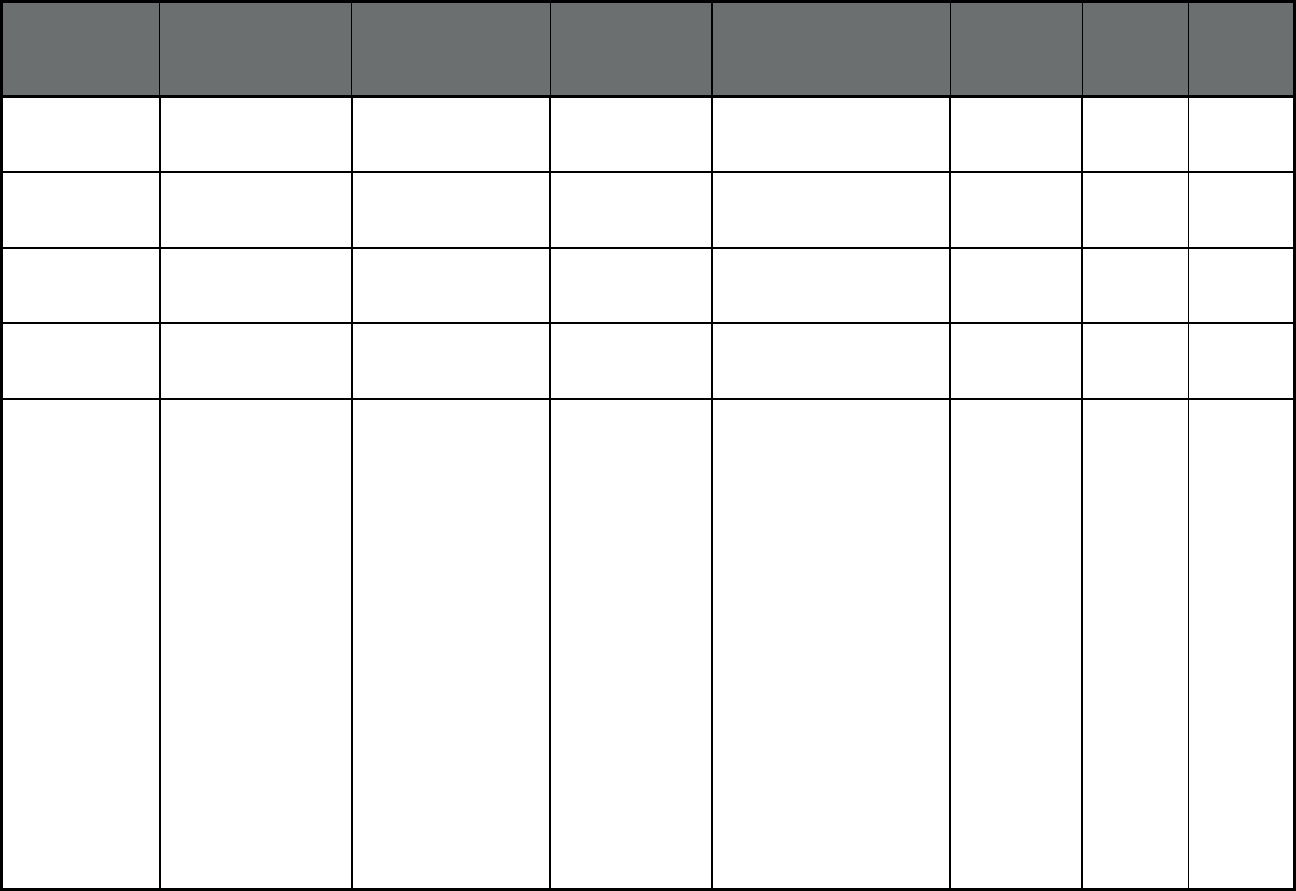
160
State
Program Name
(Type) Plan Name
Parent
Organization
Geographic Region (state-
defined areas, counties, or
zip codes)
Medicaid-Only
Enrollment
Dual
Enrollment
Total
Enrollment
Virginia CCC Plus
(Comprehensive MCO
+ MLTSS)
Magellan Complete
Care of Virginia
Magellan Health Statewide 10,213 11,746 21,959
Virginia CCC Plus
(Comprehensive MCO
+ MLTSS)
Optima Health Optima Health Statewide 19,949 14,395 34,344
Virginia CCC Plus
(Comprehensive MCO
+ MLTSS)
United Health Care UnitedHealthcare Statewide 10,607 12,899 23,506
Virginia CCC Plus
(Comprehensive MCO
+ MLTSS)
Virginia Premier Virginia Premier Statewide 21,377 20,351 41,728
Virginia DMAS PACE
(Program of All-
inclusive Care for the
Elderly (PACE))
Innovage Innovage 23112 23113 23114
23120 23124 23129
23139 23140 23141
23146 23173 23181
23221 23224 23225
23226 23227 23228
23231 23232 23234
23235 23236 23237
23238 23240 23241
23249 23260 23261
23269 23273 23274
23276 23278 23279
23282 23284 23285
23286 23289 23290
23291 23293 23295
22546 23005 23009
23011 23015 23030
23039 23047 23058
23059 23060 23069
23075 23086 23089
23102 23103 23106
23111 23116 23150
23162 23192 23218
0 134 134
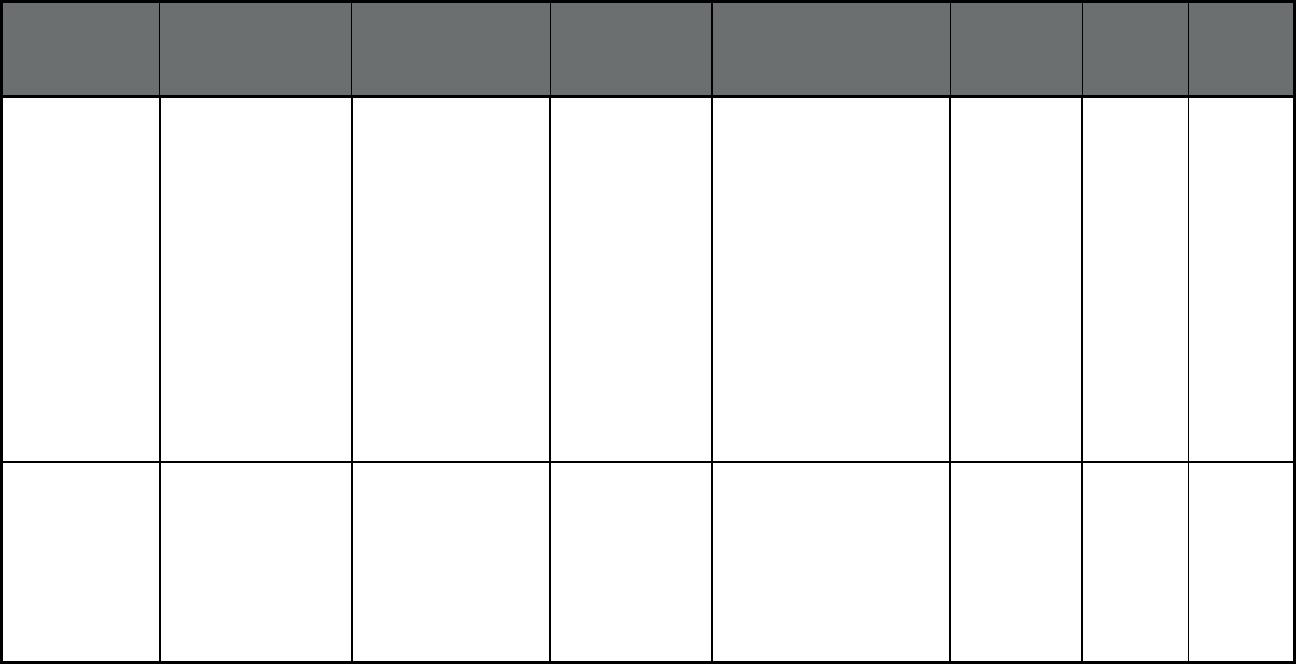
161
State
Program Name
(Type) Plan Name
Parent
Organization
Geographic Region (state-
defined areas, counties, or
zip codes)
Medicaid-Only
Enrollment
Dual
Enrollment
Total
Enrollment
Virginia (cont) DMAS PACE
(Program of All-
inclusive Care for the
Elderly (PACE))
Innovage Innovage 23219 23220 23222
23223 23229 23230
23233 23242 23250
23255 23288 23801
23803 23804 23805
23806 23830 23831
23832 23833 23834
23836 23838 23840
23841 23842 23850
23860 23875 23882
23885 23601 23605
23607 23651 23661
23662 23663 23664
23665 23666 23669 23602
23603 23604 23606
23608 23692 23693
23696
0 134 134
Virginia DMAS PACE
(Program of All-
inclusive Care for the
Elderly (PACE))
Mountain Empire/All
Care PACE
PACE 24215 24216 24218
24219 24221 24230
24243 24244 24245
24246 24248 24250
24251 24258 24263
24265 24271 24273
24277 24279 24281
24282 24283 24290
24293
4 189 193
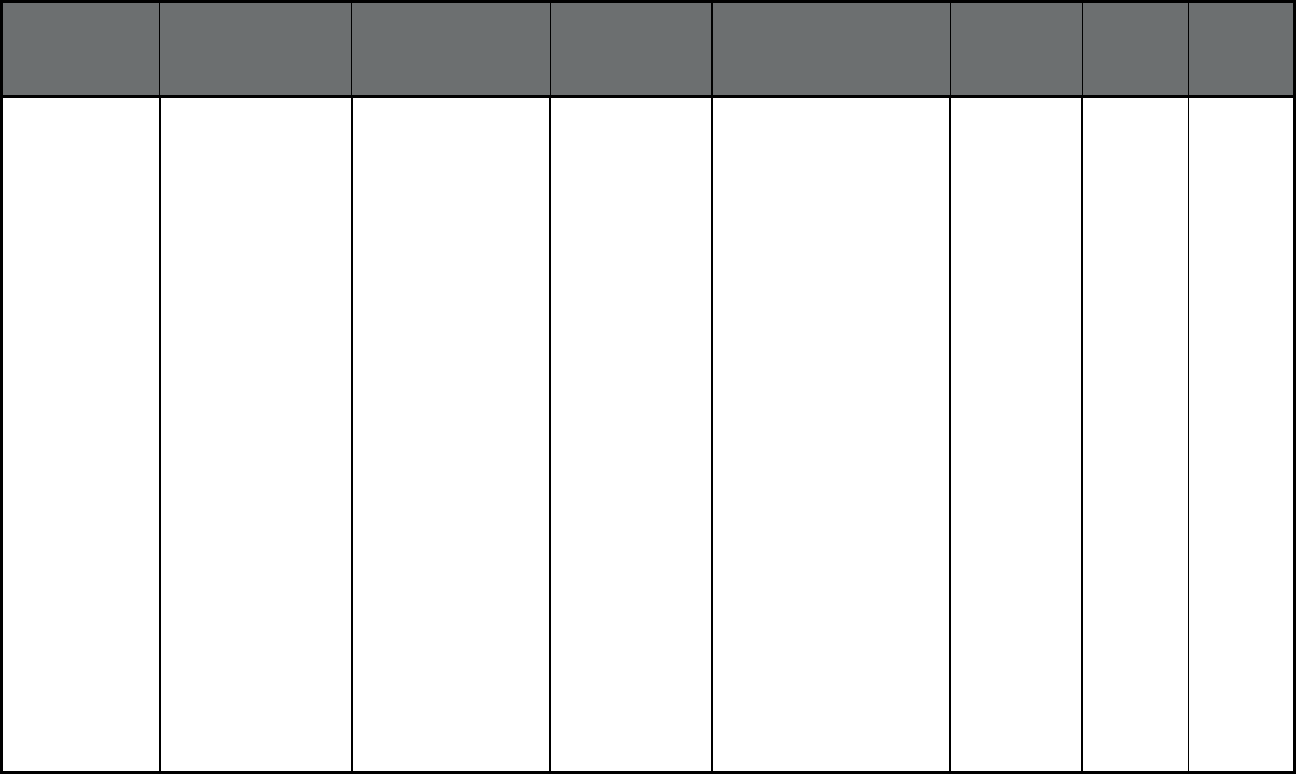
162
State
Program Name
(Type) Plan Name
Parent
Organization
Geographic Region (state-
defined areas, counties, or
zip codes)
Medicaid-Only
Enrollment
Dual
Enrollment
Total
Enrollment
Virginia DMAS PACE
(Program of All-
inclusive Care for the
Elderly (PACE))
INOVA PACE Inova Health
System
22034 22035 22036
22037 22038 22039
22040 22041 22042
22043 22044 22046
22047 22060 22066
22067 22079 22081
22082 22092 22093
22095 22096 22101
22102 22103 22106
22107 22108 22109
22116 22118 22119
22120 22121 22122
22124 22125 22134
22135 22150 22151
22152 22153 22156
22158 22159 22160
22161 22172 22180
22181 22182 22183
22184 22185 22191
22192 22193 22194
22195 22199 22201
22202 22203 22204
22205 22206 22207
22209 22210 22211
22212 22213 22214
22215 22216 22217
22218 22219 22222
22223 22225 22226
22227 22229 22230
22234 22240 22241
22242 22243 22244
22245 22246 22301
1,405 60 1,465
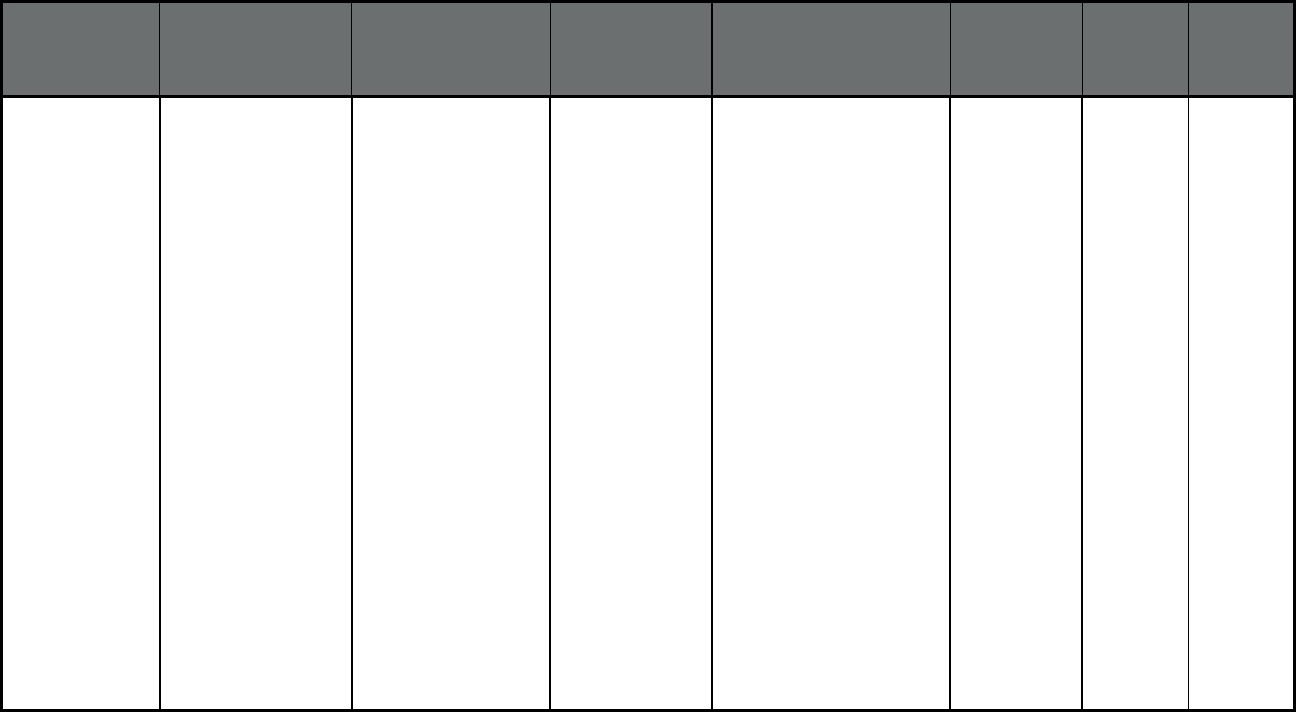
163
State
Program Name
(Type) Plan Name
Parent
Organization
Geographic Region (state-
defined areas, counties, or
zip codes)
Medicaid-Only
Enrollment
Dual
Enrollment
Total
Enrollment
Virginia DMAS PACE
(Program of All-
inclusive Care for the
Elderly (PACE))
Riverside PACE Riverside Health
System
23112 23113 23114
23120 23124 23129
23139 23140 23141
23146 23173 23181
23221 23224 23225
23226 23227 23228
23231 23232 23234
23235 23236 23237
23238 23240 23241
23249 23260 23261
23269 23273 23274
23276 23278 23279
23282 23284 23285
23286 23289 23290
23291 23293 23295
22546 23005 23009
23011 23015 23030
23039 23047 23058
23059 23060 23069
23075 23086 23089
23102 23103 23106
23111 23116 23150
23162 23192 23218
23219 23220 23222
23223 23229 23230
23233 23242 23250
23255 23288 23801
23803 23804 23805
23806 23830 23831
5 401 406
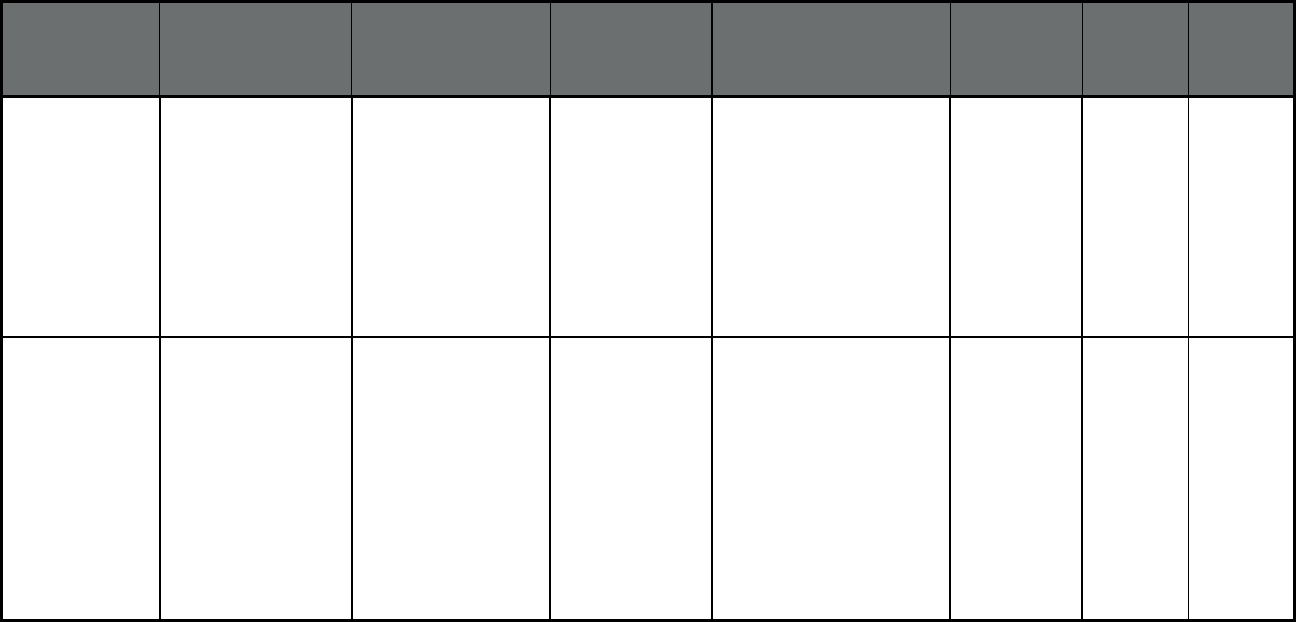
164
State
Program Name
(Type) Plan Name
Parent
Organization
Geographic Region (state-
defined areas, counties, or
zip codes)
Medicaid-Only
Enrollment
Dual
Enrollment
Total
Enrollment
Virginia (cont) DMAS PACE
(Program of All-
inclusive Care for the
Elderly (PACE))
Riverside PACE Riverside Health
System
23832 23833 23834
23836 23838 23840
23841 23842 23850
23860 23875 23882
23885 23601 23605
23607 23651 23661
23662 23663 23664
23665 23666 23669
23602 23603 23604
23606 23608 23692
23693 23696
5 401 406
Virginia DMAS PACE
(Program of All-
inclusive Care for the
Elderly (PACE))
Innovage PACE Innovage 24011 24012 24013
24014 24015 24016
24017 24018 24019
24020 24059 24060
24064 24065 24066
24067 24070 24073
24077 24079 24083
24087 24090 24092
24095 24101 24121
24122 24138 24149
24151 24153 24162
24174 24175 24176
24179 24184
19 263 282
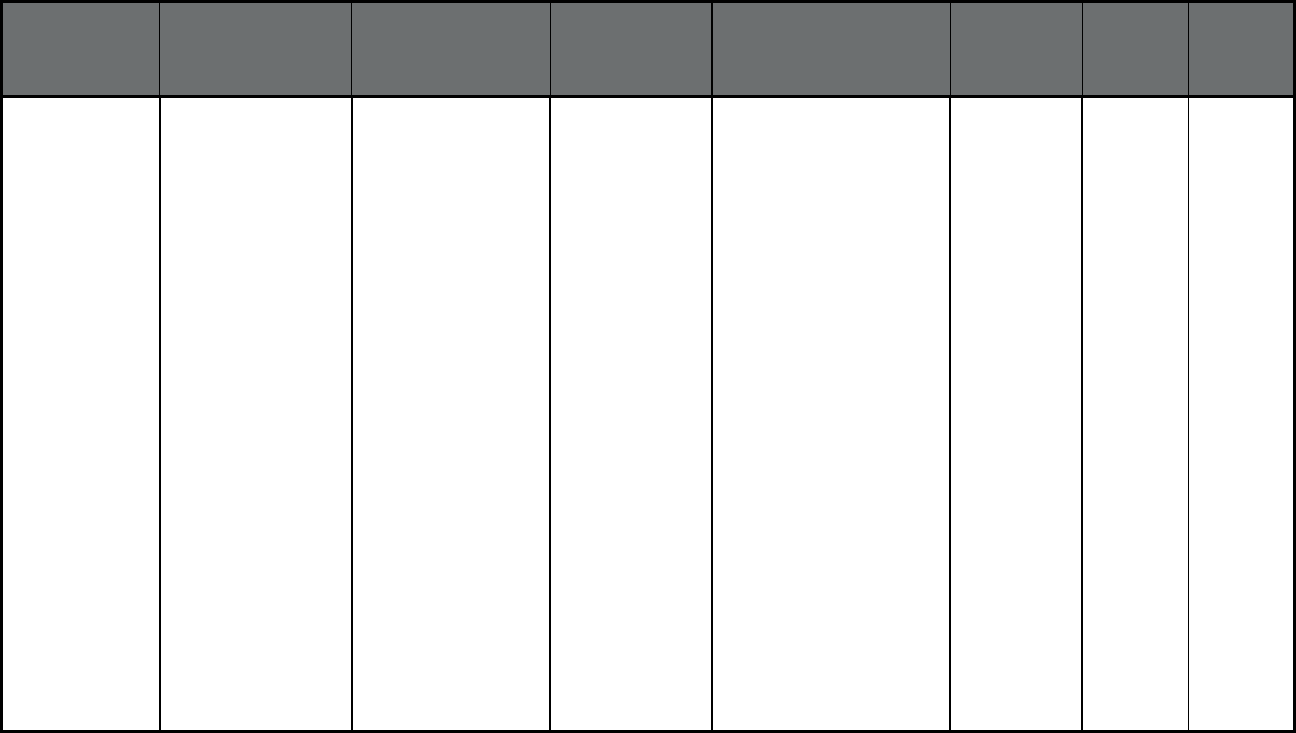
165
State
Program Name
(Type) Plan Name
Parent
Organization
Geographic Region (state-
defined areas, counties, or
zip codes)
Medicaid-Only
Enrollment
Dual
Enrollment
Total
Enrollment
Virginia DMAS PACE
(Program of All-
inclusive Care for the
Elderly (PACE))
Centra PACE Centra 23002 23004 23027
23040 23083 23123
23824 23894 23901
23909 23921 23922
23923 23930 23934
23936 23937 23939
23941 23942 23943
23947 23952 23954
23955 23958 23959
23960 23963 23966
23974 23976 24599
24501 24502 24503
24504 24521 24522
24523 24536 24538
24550 24551 24553
24554 24556 24570
24572 24574 24588
24593 24054 24055
24069 24078 24082
24089 24102 24104
24112 24137 24139
24146 24148 24161
24165 24168 24517
24527 24528 24530
24531 24540 24541
24549 24557 24563
24565 24566 24569
24571 24586 24594
24133 24176 24543
24576
5 208 213
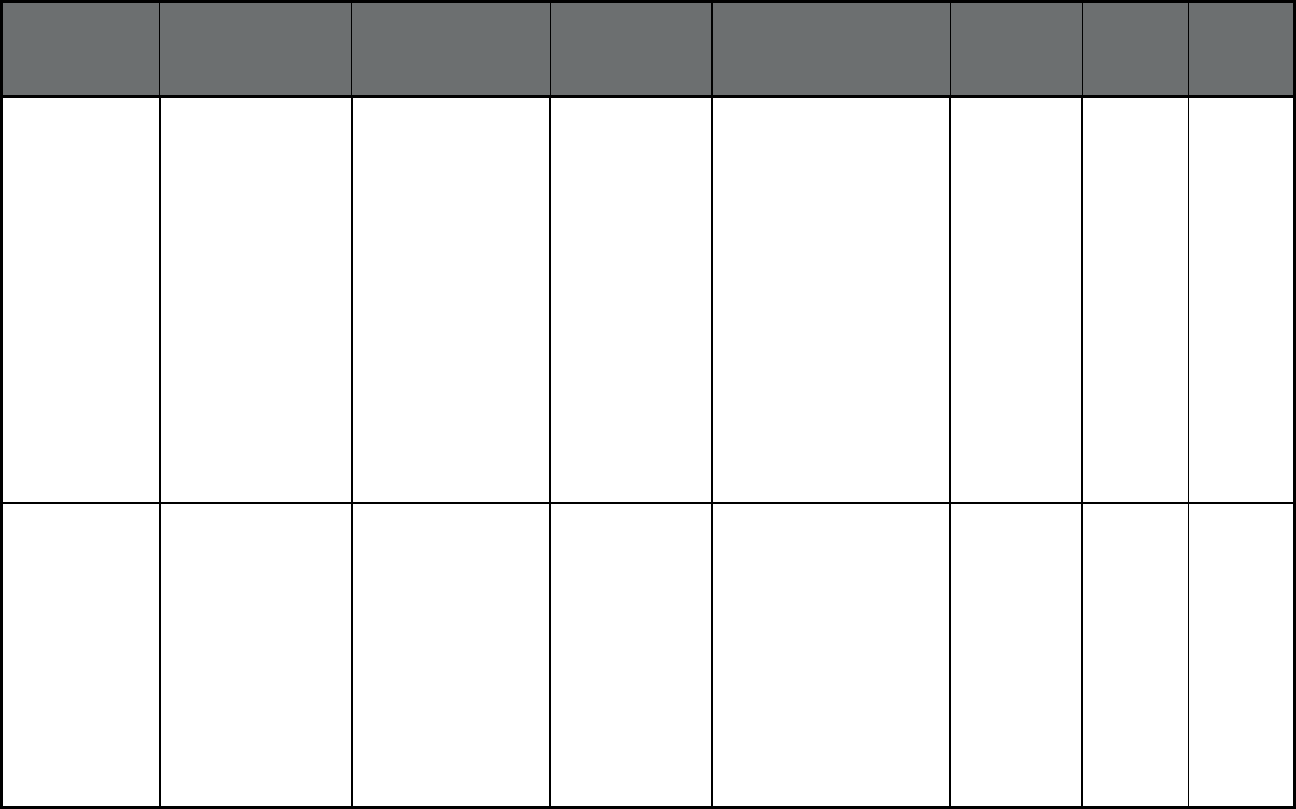
166
State
Program Name
(Type) Plan Name
Parent
Organization
Geographic Region (state-
defined areas, counties, or
zip codes)
Medicaid-Only
Enrollment
Dual
Enrollment
Total
Enrollment
Virginia DMAS PACE
(Program of All-
inclusive Care for the
Elderly (PACE))
Sentara PACE Sentara
Healthcare
23320 23321 23322
23323 23324 23325
23432 23433 23434
23435 23436 23437
23438 23701 23702
23703 23704 23707
23709 23314 23315
23430 23487 23846
23851 23883 23898
23451 23452 23453
23454 23455 23456
23457 23459 23460
23461 23462 23463
23464 23502 23503
23504 23505 23507
23508 23509 23510
23511 23513 23517
23518 23521 23523
23529
24 226 250
Washington
11
Apple Health/Healthy
Options Health Home
Program
(Comprehensive
MCO)
Multiple Sites Multiple Sites Adams, Asotin, Benton,
Chelan, Clallam, Clark,
Columbia, Cowlitz, Douglas,
Ferry, Franklin, Garfield,
Grant, Grays Harbor, Island,
Jefferson, King, Kitsap,
Kittitas, Klickitat, Lewis,
Lincoln, Mason, Okanogan,
Pacific, Pend Oreille, Pierce,
San Juan, Snohomish,
Skagit, Skamania, Spokane,
Stevens, Thurston,
Wahkiakum, Walla Walla,
Whatcom, Whitman, Yakima
22,412 0 22,412
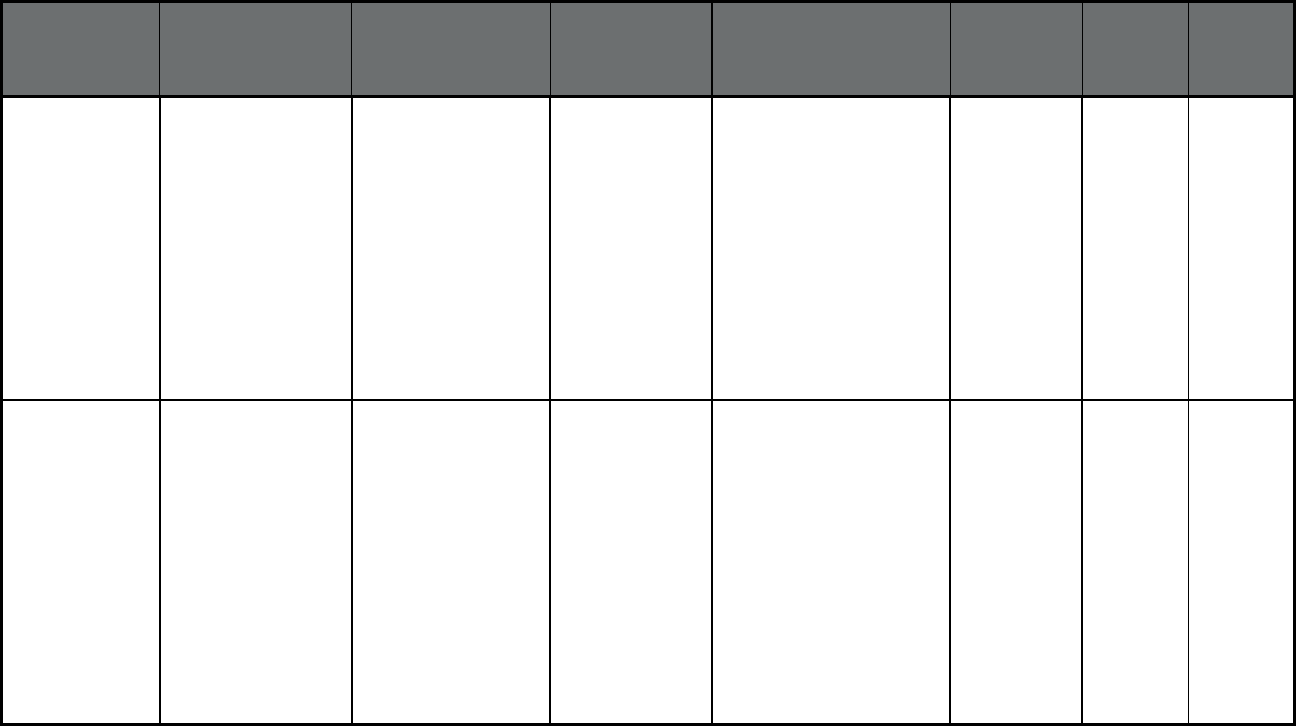
167
State
Program Name
(Type) Plan Name
Parent
Organization
Geographic Region (state-
defined areas, counties, or
zip codes)
Medicaid-Only
Enrollment
Dual
Enrollment
Total
Enrollment
Washington Apple Health
(Comprehensive
MCO)
Amerigroup Amerigroup, Inc. Adams, Asotin, Benton,
Chelan, Columbia, Cowlitz,
Douglas, Ferry, Franklin,
Garfield, Grant, Grays
Harbor, Island, Jefferson,
King, Kitsap, Kittitas,
Klickitat, Lewis, Lincoln,
Mason, Okanogan, Pacific,
Pend Oreille, Pierce, San
Juan, Skagit, Snohomish,
Spokane, Stevens,
Thurston, Wahkiakum,
Walla Walla, Whatcom,
Whitman, Yakima
126,669 0 126,669
Washington Apple Health
(Comprehensive
MCO)
Community Health Plan
of Washington
Community Health
Plan of
Washington
Adams, Asotin, Benton,
Chelan, Clark, Columbia,
Cowlitz, Douglas, Ferry,
Franklin, Grant, Grays
Harbor, Island, Jefferson,
King, Kitsap, Kittitas,
Klickitat, Lewis, Lincoln,
Mason, Okanogan, Pacific,
Pend Oreille, Pierce, San
Juan, Skagit, Skamania,
Snohomish, Spokane,
Stevens, Thurston,
Wahkiakum, Walla Walla,
Whatcom, Whitman,
Yakima.
226,519 0 226,519
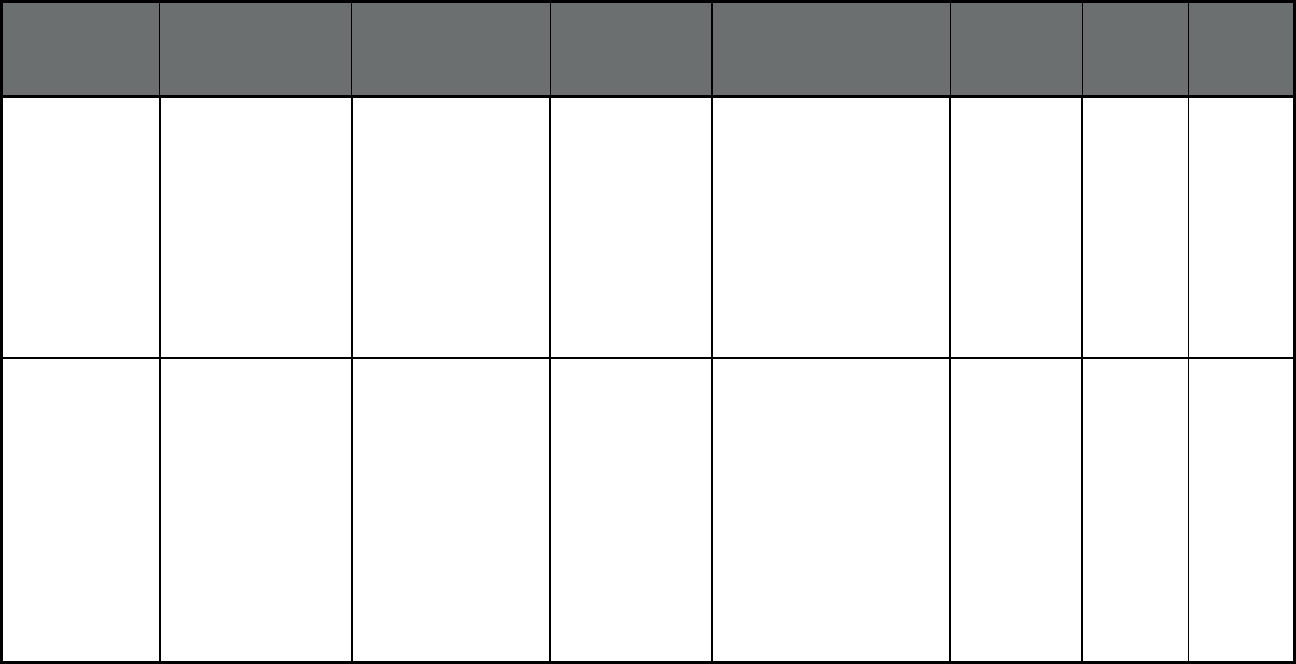
168
State
Program Name
(Type) Plan Name
Parent
Organization
Geographic Region (state-
defined areas, counties, or
zip codes)
Medicaid-Only
Enrollment
Dual
Enrollment
Total
Enrollment
Washington Apple Health
(Comprehensive
MCO)
Coordinated Care of
Washington
Coordinated Care
of Washington
Adams, Asotin, Benton,
Chelan, Columbia,
Douglas, Franklin, Grant,
Island, Jefferson, King,
Kitsap, Kittitas, Lewis,
Lincoln, Mason, Okanogan,
Pacific, Pierce, San Juan,
Skagit, Snohomish,
Spokane, Stevens,
Thurston, Wahkiakum,
Walla Walla, Whatcom,
Whitman, Yakima.
173,341 0 173,341
Washington Apple Health
(Comprehensive
MCO)
Molina Health Care of
Washington
Molina Healthcare Adams, Asotin, Benton,
Chelan, Clallam, Clark,
Columbia, Cowlitz, Douglas,
Ferry, Franklin, Garfield,
Grant, Grays Harbor
, Island,
King, Kitsap, Kittitas,
Klickitat, Lewis, Lincoln,
Mason, Okanogan, Pacific,
Pend Oreille, Pierce, San
Juan, Skagit, Skamania,
Snohomish, Spokane,
Stevens, Thurston,
Wahkiakum, Walla Walla,
Whatcom, Whitman, Yakima
569,871 0 569,871
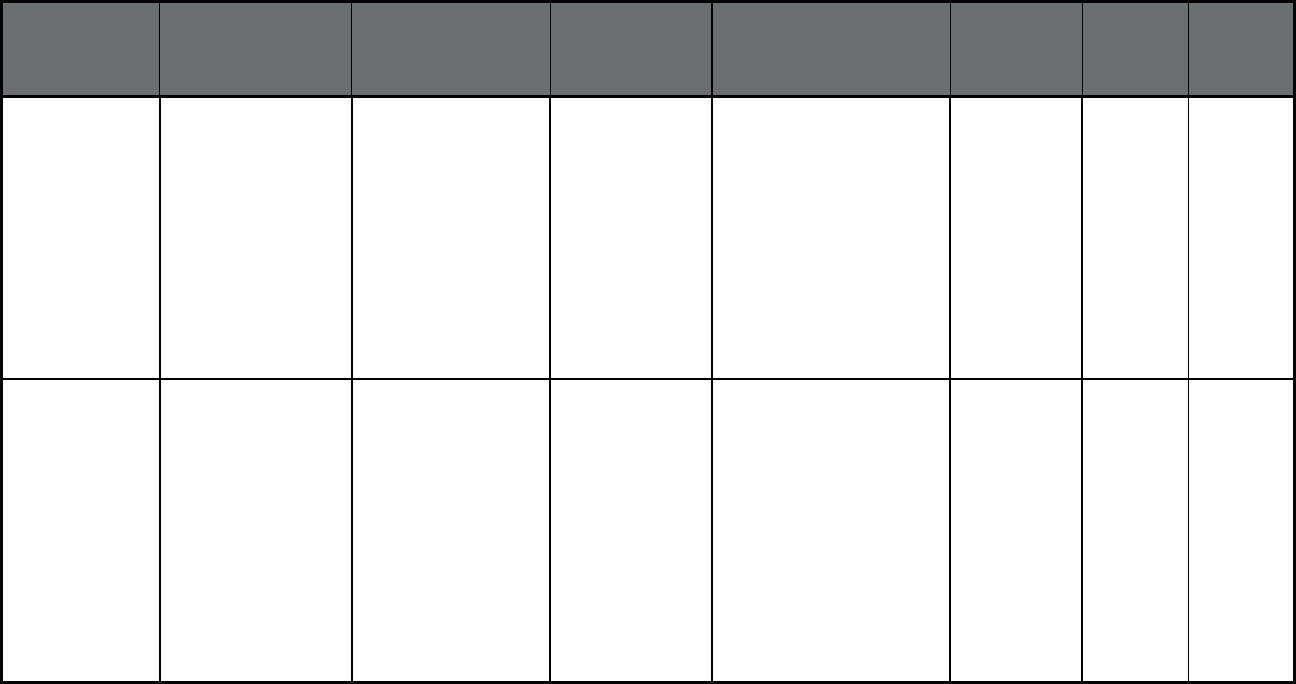
169
State
Program Name
(Type) Plan Name
Parent
Organization
Geographic Region (state-
defined areas, counties, or
zip codes)
Medicaid-Only
Enrollment
Dual
Enrollment
Total
Enrollment
Washington Apple Health
(Comprehensive
MCO)
United Health Care UnitedHealthcare Adams, Asotin, Benton,
Chelan, Clallam, Columbia,
Cowlitz, Douglas, Ferry,
Franklin, Garfield, Grant,
Grays Harbor, Island,
Jefferson, King, Kitsap,
Kittitas, Lewis, Lincoln,
Mason, Okanogan, Pacific,
Pierce, Skagit, Snohomish,
Spokane, Stevens,
Thurston, Wahkiakum,
Walla Walla, Whatcom,
Whitman, Yakima
201,693 0 201,693
Washington Healthy Options -
Blind Disabled
(Comprehensive
MCO)
Amerigroup Amerigroup, Inc. Adams, Asotin, Benton,
Chelan, Columbia, Cowlitz,
Douglas, Ferry, Franklin,
Garfield, Grant, Grays
Harbor, Island, Jefferson,
King, Kitsap, Kittitas,
Klickitat, Lewis, Lincoln,
Mason, Okanogan, Pacific,
Pend Oreille, Pierce, San
Juan, Skagit, Snohomish,
Spokane, Stevens,
Thurston, Wahkiakum,
Walla Walla, Whatcom,
Whitman, Yakima
10,146 0 10,146
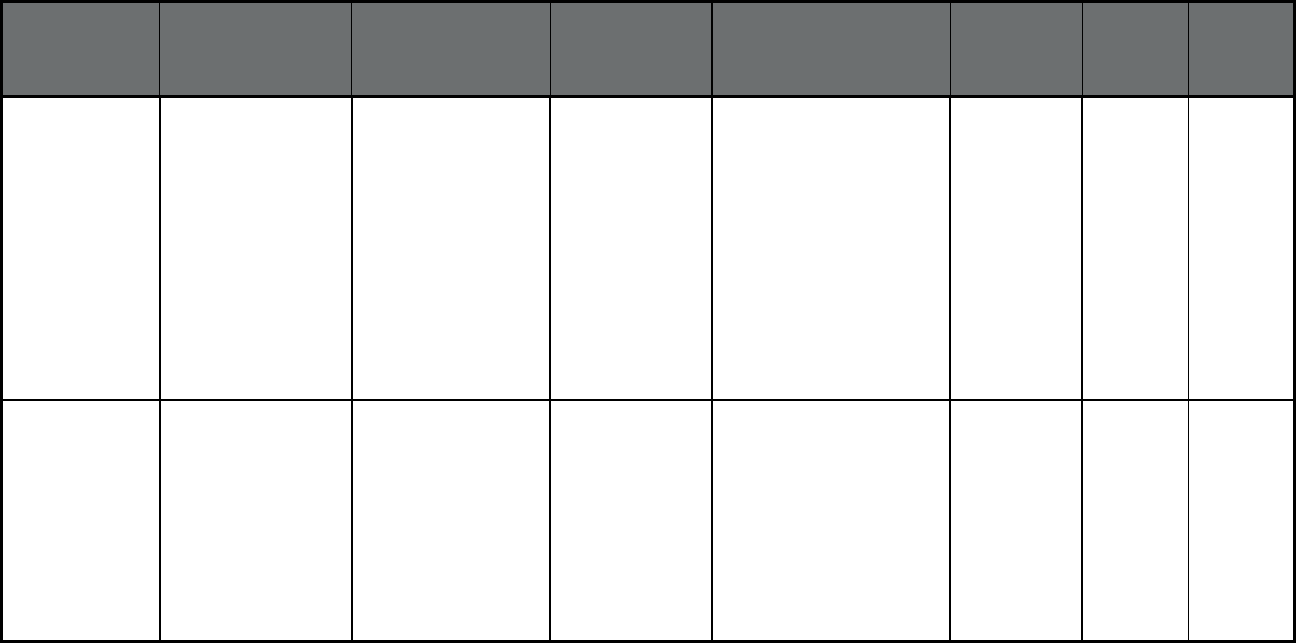
170
State
Program Name
(Type) Plan Name
Parent
Organization
Geographic Region (state-
defined areas, counties, or
zip codes)
Medicaid-Only
Enrollment
Dual
Enrollment
Total
Enrollment
Washington Healthy Options -
Blind Disabled
(Comprehensive
MCO)
Community Health Plan
of WA
Community Health
Plan of WA
Adams, Asotin, Benton,
Chelan, Clark, Columbia,
Cowlitz, Douglas, Ferry,
Franklin, Grant, Grays
Harbor, Island, Jefferson,
King, Kitsap, Kittitas,
Klickitat, Lewis, Lincoln,
Mason, Okanogan, Pacific,
Pend Oreille, Pierce, San
Juan, Skagit, Skamania,
Snohomish, Spokane,
Stevens, Thurston,
Wahkiakum, Walla Walla,
Whatcom, Whitman, Yakima
16,372 0 16,372
Washington Healthy Options -
Blind Disabled
(Comprehensive
MCO)
Coordinated Care of
Washington
Coordinated Care
of Washington
Adams, Asotin, Benton,
Chelan, Columbia, Douglas,
Franklin, Grant, Island,
Jefferson, King, Kitsap,
Kittitas, Lewis, Lincoln,
Mason, Okanogan, Pacific,
Pierce, San Juan, Skagit,
Snohomish, Spokane,
Stevens, Thurston,
Wahkiakum, Walla Walla,
Whatcom, Whitman, Yakima
11,465 0 11,465
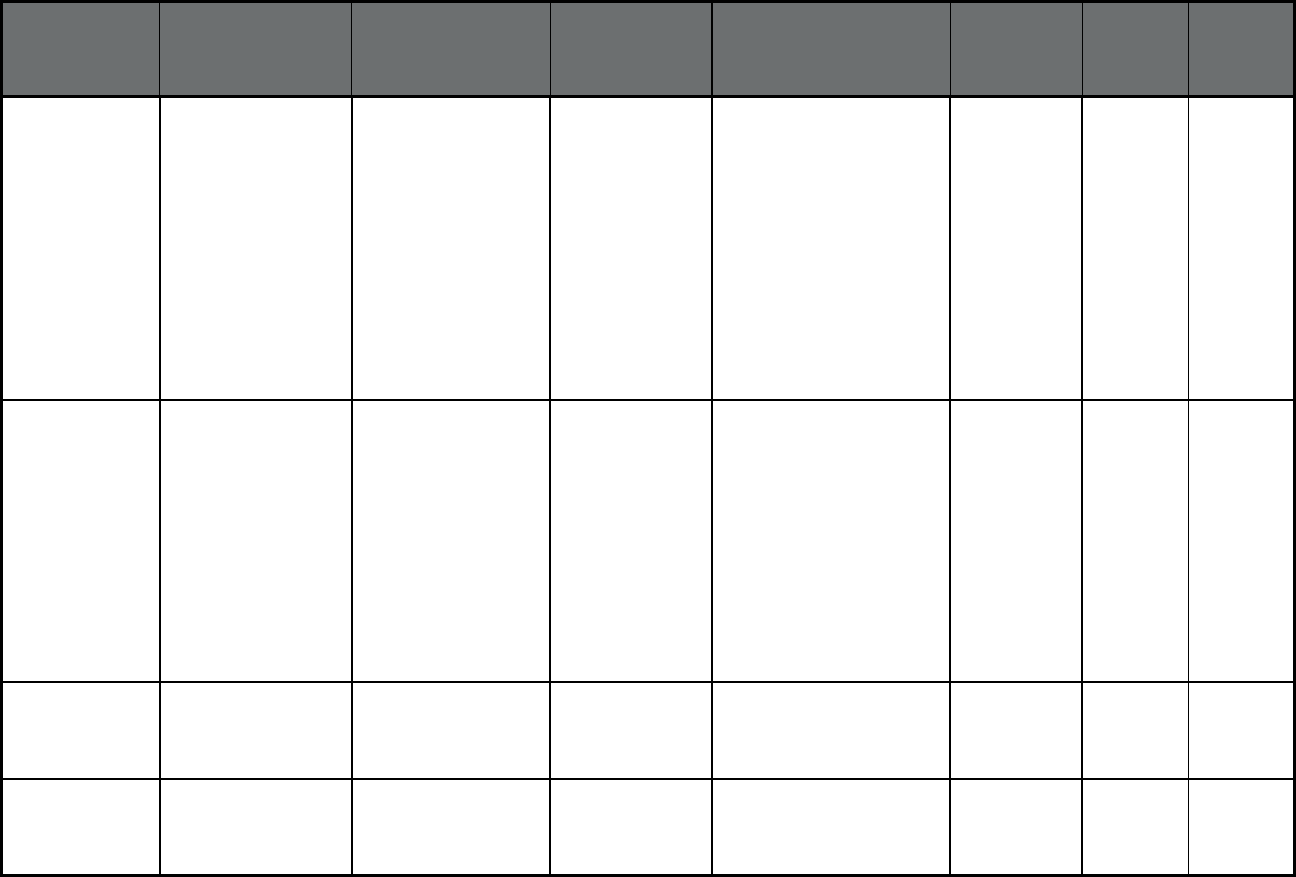
171
State
Program Name
(Type) Plan Name
Parent
Organization
Geographic Region (state-
defined areas, counties, or
zip codes)
Medicaid-Only
Enrollment
Dual
Enrollment
Total
Enrollment
Washington Healthy Options -
Blind Disabled
(Comprehensive
MCO)
Molina Health Care Molina Healthcare Adams, Asotin, Benton,
Chelan, Clallam, Clark,
Columbia, Cowlitz, Douglas,
Ferry, Franklin, Garfield,
Grant, Grays Harbor, Island,
King, Kitsap, Kittitas,
Klickitat, Lewis, Lincoln,
Mason, Okanogan, Pacific,
Pend Oreille, Pierce, San
Juan, Skagit, Skamania,
Snohomish, Spokane,
Stevens, Thurston,
Wahkiakum, Walla Walla,
Whatcom, Whitman, Yakima
32,295 0 32,295
Washington Healthy Options -
Blind Disabled
(Comprehensive
MCO)
United Health Care UnitedHealthcare Adams, Asotin, Benton,
Chelan, Clallam, Columbia,
Cowlitz, Douglas, Ferry,
Franklin, Garfield, Grant,
Grays Harbor, Island,
Jefferson, King, Kitsap,
Kittitas, Lewis, Lincoln,
Mason, Okanogan, Pacific,
Pierce, Skagit, Snohomish,
Spokane, Stevens,
Thurston, Wahkiakum,
Walla Walla, Whatcom,
Whitman, Yakima
13,890 0 13,890
Washington Fully Integrated
Managed Care (FIMC)
(Comprehensive
MCO)
Amerigroup Amerigroup, Inc. Grant, Chelan, Douglas 3,831 0 3,831
Washington Fully Integrated
Managed Care (FIMC)
(Comprehensive
MCO)
Coordinated Care of
Washington
Coordinated Care
of Washington
Grant, Chelan, Douglas 14,165 0 14,165
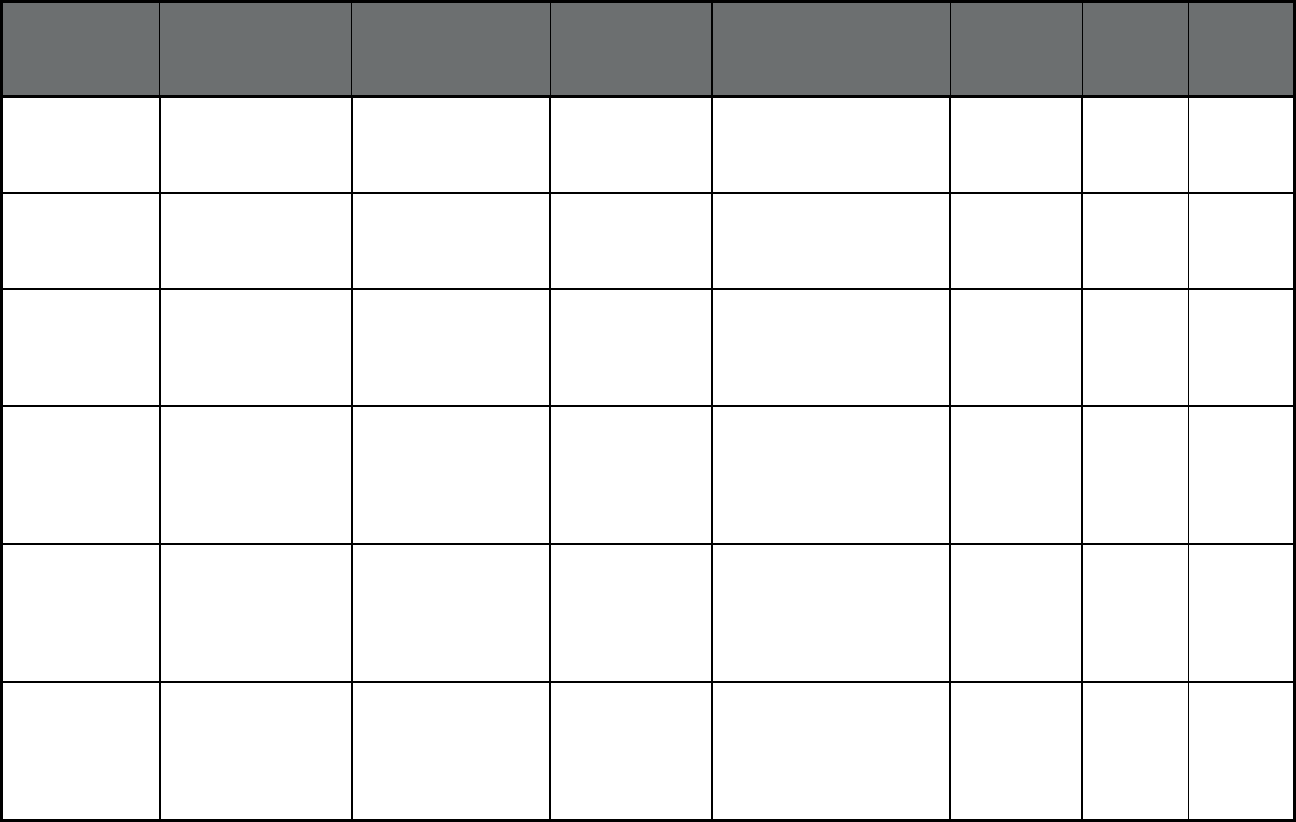
172
State
Program Name
(Type) Plan Name
Parent
Organization
Geographic Region (state-
defined areas, counties, or
zip codes)
Medicaid-Only
Enrollment
Dual
Enrollment
Total
Enrollment
Washington Fully Integrated
Managed Care (FIMC)
(Comprehensive
MCO)
Community Health Plan
of Washington
Community Health
Plan of
Washington
Chelan, Clark, Douglas,
Grant, Skamania
16,576 0 16,576
Washington Fully Integrated
Managed Care (FIMC)
(Comprehensive
MCO)
Molina Health Care Molina Healthcare Chelan, Clark, Douglas,
Grant, Skamania
134,248 0 134,248
Washington PCCM (Primary Care
Case Management
(PCCM))
Multiple Primary Care
Providers
Multiple Primary
Care Provider
(PCCM)
Clallam, Grays Harbor, King,
Snohomish, Whatcom,
Okanogan, Ferry, Stevens,
Lincoln, Spokane, Benton
and Yakima
5,186 0 5,186
Washington
12
Behavioral Health
Services Only (BHSO)
(Behavioral Health
Organization (BHO)
only (PIHP and/or
PAHP))
Amerigroup Amerigroup, Inc. Grant, Chelan, Douglas 1,398 0 1,398
Washington
12
Behavioral Health
Services Only (BHSO)
(Behavioral Health
Organization (BHO)
only (PIHP and/or
PAHP))
Coordinated Care of
Washington
Coordinated Care
of Washington
Grant, Chelan, Douglas 2,381 0 2,381
Washington
12
Behavioral Health
Services Only (BHSO)
(Behavioral Health
Organization (BHO)
only (PIHP and/or
PAHP))
Molina Health Care Molina Healthcare Chelan, Clark, Douglas,
Grant, Skamania
7,081 0 7,081
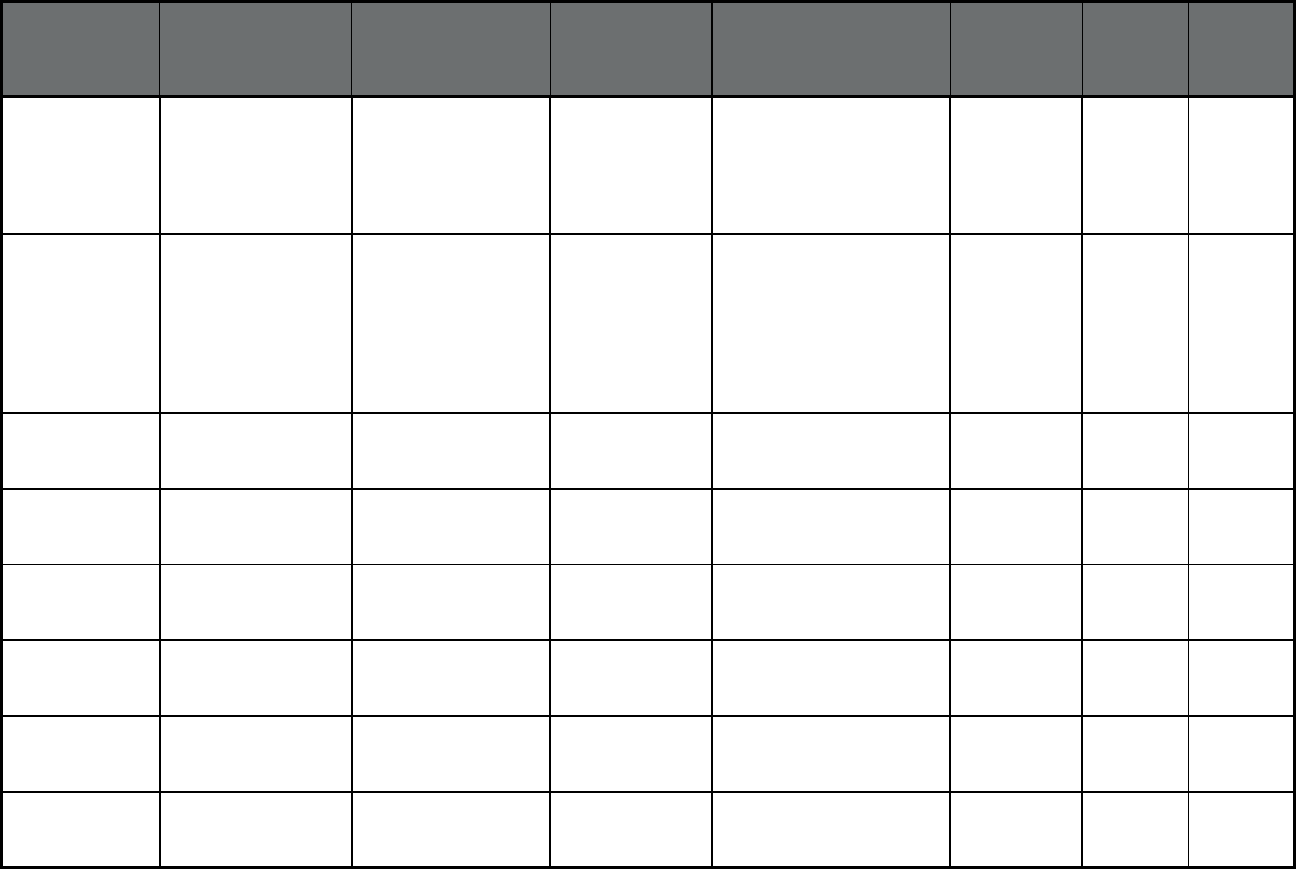
173
State
Program Name
(Type) Plan Name
Parent
Organization
Geographic Region (state-
defined areas, counties, or
zip codes)
Medicaid-Only
Enrollment
Dual
Enrollment
Total
Enrollment
Washington
12
Behavioral Health
Services Only (BHSO)
(Behavioral Health
Organization (BHO)
only (PIHP and/or
PAHP))
Community Health
Care Plan of WA
Community Health
Care Plan of
Washington
Chelan, Clark, Douglas,
Grant, Skamania
4,813 0 4,813
Washington
12
Washington State
Integrated Community
Mental Health
Program (ICMH)
(Behavioral Health
Organization (BHO)
only (PIHP and/or
PAHP))
BHO Behavorial Health
Organizations of
WA
Statewide 1,765,375 0 1,765,375
Washington
12
NEMT (Non-
Emergency Medical
Transportation)
Multiple Transportation
Brokers
Multiple
Transportation
Brokers
Statewide 1,781,048 0 1,781,048
Washington
12
PACE (Program of All-
inclusive Care for the
Elderly (PACE))
Providence Elder Place PACE Statewide 670 0 670
West Virginia Mountain Health Trust
(Comprehensive
MCO)
Aetna Better Health of
WV
Aetna Statewide 122,563 0 122,563
West Virginia Mountain Health Trust
(Comprehensive
MCO)
The Health Plan The Health Plan Statewide 80,725 0 80,725
West Virginia Mountain Health Trust
(Comprehensive
MCO)
Unicare Anthem Insurance
Companies, Inc.
Statewide 139,509 0 139,509
West Virginia Mountain Health Trust
(Comprehensive
MCO)
West Virginia Family
Health
West Virginia
Family
Health/Highmark
Statewide 64,396 0 64,396
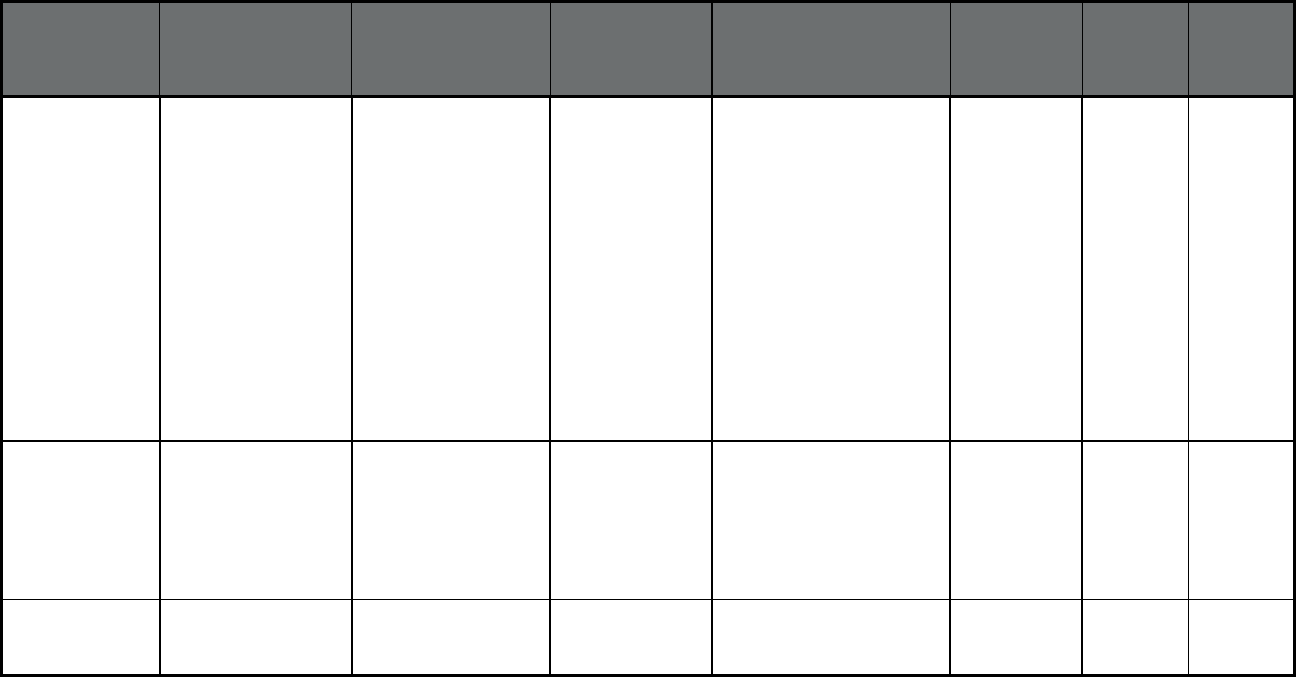
174
State
Program Name
(Type) Plan Name
Parent
Organization
Geographic Region (state-
defined areas, counties, or
zip codes)
Medicaid-Only
Enrollment
Dual
Enrollment
Total
Enrollment
Wisconsin BadgerCare Plus
(Comprehensive
MCO)
Anthem Blue Cross
Blue Shield
Anthem BCBS Counties: Brown, Calumet,
Dane, Dodge, Door,
Florence, Fond du Lac,
Forest, Green Lake,
Jefferson, Kenosha,
Kewaunee, Langlade,
Manitowoc, Marinette,
Marquette, Menominee,
Milwaukee, Oconto,
Outagamie, Ozaukee, Polk,
Portage, Racine, Rock,
Shawano, Sheboygan,
Taylor, Walworth,
Washington, Waukesha,
Waupaca, Waushara,
Winnebago, Wood
83,735 91 83,826
Wisconsin BadgerCare Plus
(Comprehensive
MCO)
Children’s Community
Health Plan
Children’s
Community Health
Plan
Counties: Brown, Calumet,
Kenosha, Milwaukee,
Outagamie, Ozaukee,
Racine, Sheboygan,
Walworth, Washington,
Waukesha, Waupaca,
Winnebago
124,131 59 124,190
Wisconsin BadgerCare Plus
(Comprehensive
MCO)
Dean Health Plan Dean Health Plan Counties: Columbia, Dane,
Dodge, Grant, Iowa,
Jefferson, Rock, Sauk
37,613 43 37,656
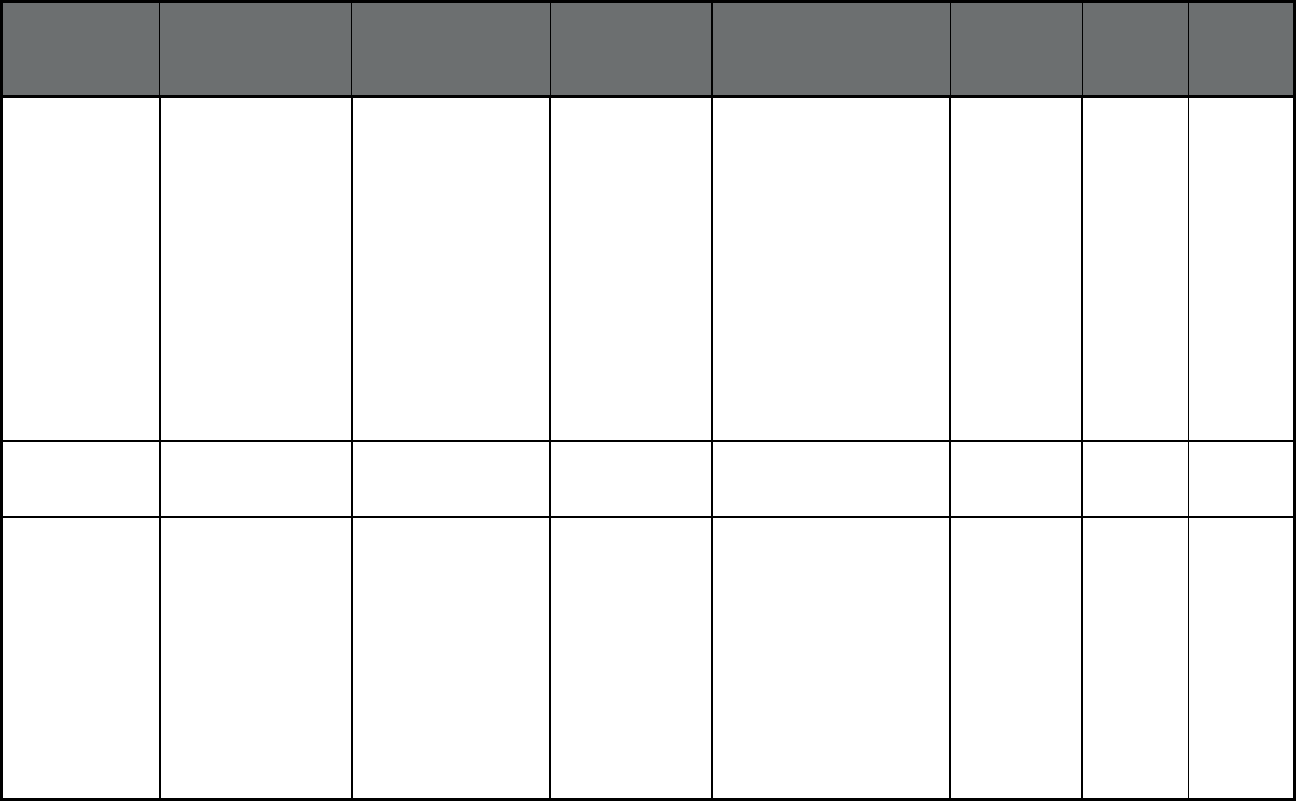
175
State
Program Name
(Type) Plan Name
Parent
Organization
Geographic Region (state-
defined areas, counties, or
zip codes)
Medicaid-Only
Enrollment
Dual
Enrollment
Total
Enrollment
Wisconsin BadgerCare Plus
(Comprehensive
MCO)
Group Health
Cooperative Of Eau
Claire
Group Health
Cooperative
Counties: Adams, Ashland,
Barron, Bayfield, Buffalo,
Burnett, Chippewa, Clark,
Columbia, Crawford,
Douglas, Dunn, Eau Claire,
Forest, Grant, Green, Iowa,
Iron, Jackson, Juneau, La
Crosse, Lafayette,
Langlade, Lincoln,
Marathon, Monroe, Oneida,
Pepin, Pierce, Polk,
Portage, Price, Rusk, St.
Croix, Sawyer, Shawano,
Taylor, Trempealeau,
Vernon, Vilas, Washburn,
Wood
48,194 91 48,285
Wisconsin BadgerCare Plus
(Comprehensive
MCO)
Group Health
Cooperative Of South
Central WI
Group Health
Cooperative
County: Dane 5,435 14 5,449
Wisconsin BadgerCare Plus
(Comprehensive
MCO)
Independent Care
(iCare)
iCare Counties: Adams, Brown,
Door, Fond du Lac, Grant,
Green, Jackson, Juneau,
Kenosha, Kewaunee, La
Crosse, Manitowoc,
Marinette, Milwaukee,
Monroe, Oconto,
Outagamie, Ozaukee,
Racine, Sheboygan,
Trempealeau, Vernon,
Walworth, Washington,
Waukesha, Waupaca,
Winnebago
15,921 18 15,939
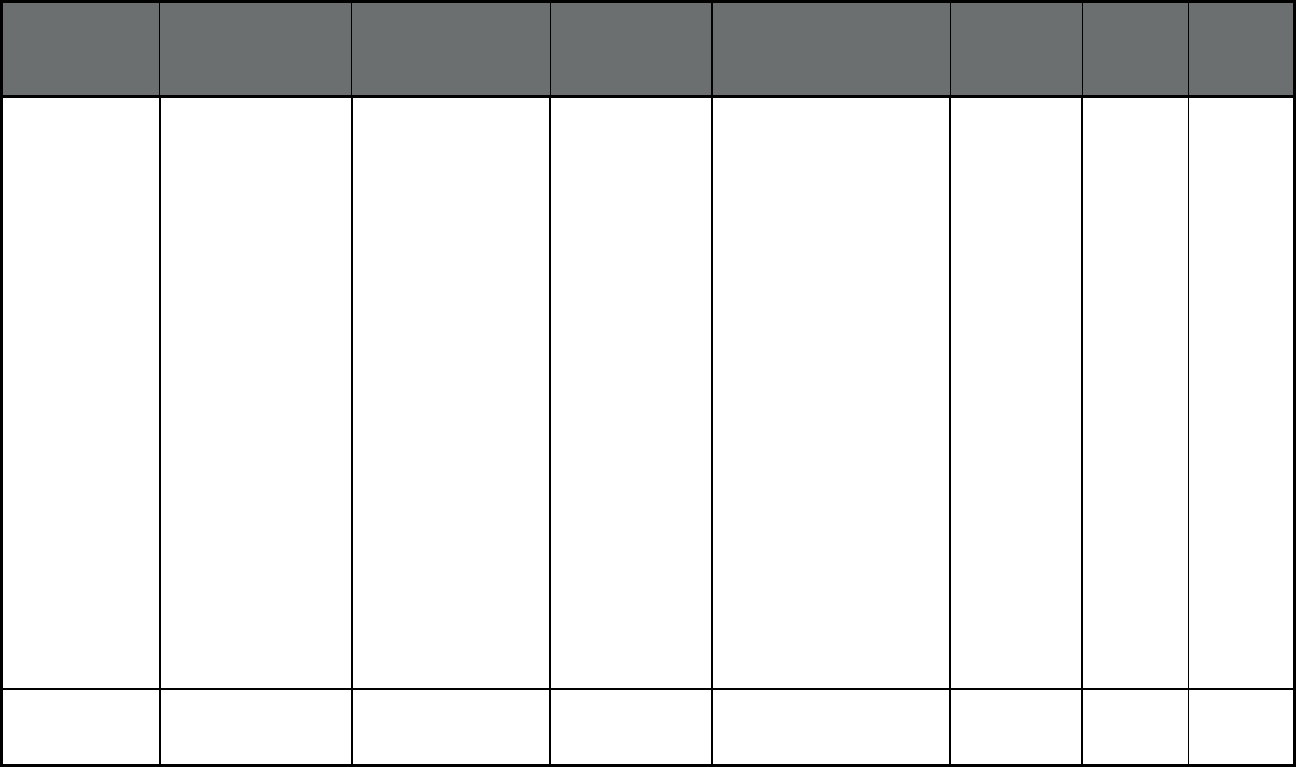
176
State
Program Name
(Type) Plan Name
Parent
Organization
Geographic Region (state-
defined areas, counties, or
zip codes)
Medicaid-Only
Enrollment
Dual
Enrollment
Total
Enrollment
Wisconsin BadgerCare Plus
(Comprehensive
MCO)
MHS of Wisconsin MHS of Wisconsin Counties: Ashland, Adams,
Barron, Bayfield, Brown,
Buffalo, Calumet, Chippewa,
Clark, Crawford, Dane,
Dodge, Door, Douglas,
Dunn, Eau Claire, Fond du
Lac, Forest, Grant, Green,
Green Lake, Iowa, Iron,
Jackson, Jefferson, Juneau,
Kenosha, Kewaunee, La
Crosse, Lafayette,
Langlade, Lincoln,
Manitowoc, Marathon,
Marinette, Marquette,
Menominee, Milwaukee,
Monroe, Oconto, Oneida,
Outagamie, Ozaukee,
Pepin, Pierce, Polk,
Portage, Price, Racine,
Richland, Rock, Rusk,
Sawyer, Shawano,
Sheboygan, St. Croix, Sauk,
Taylor, Trempealeau,
Vernon, Vilas, Walworth,
Washburn, Washington,
Waukesha, Waupaca,
Waushara, Winnebago,
Wood
32,431 37 32,468
Wisconsin BadgerCare Plus
(Comprehensive
MCO)
MercyCare Insurance
Company
Mercy Care Counties: Dane, Green,
Jefferson, Rock, Walworth
12,310 28 12,338
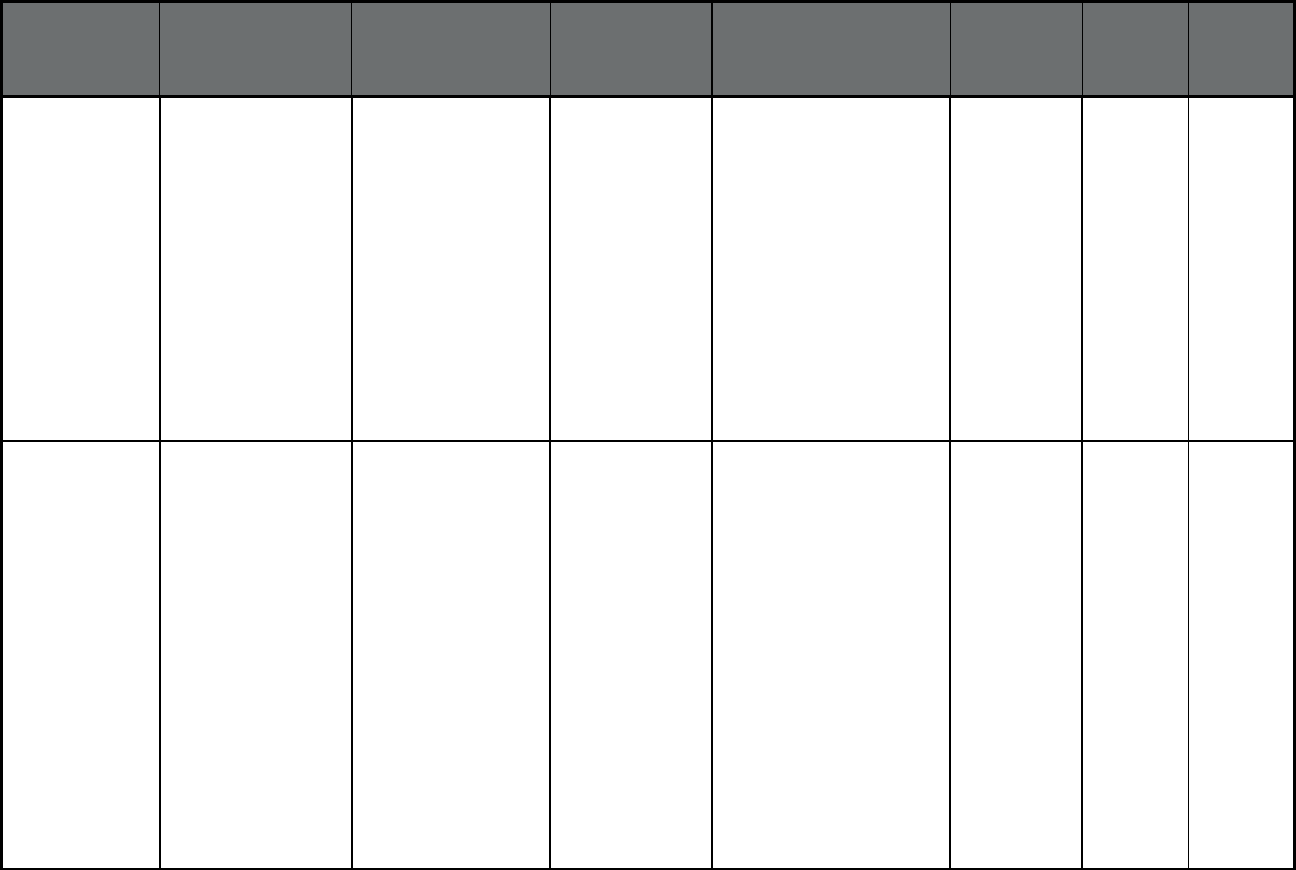
177
State
Program Name
(Type) Plan Name
Parent
Organization
Geographic Region (state-
defined areas, counties, or
zip codes)
Medicaid-Only
Enrollment
Dual
Enrollment
Total
Enrollment
Wisconsin BadgerCare Plus
(Comprehensive
MCO)
Molina Health Plan Molina Healthcare Counties: Brown, Calumet,
Clark, Dodge, Door,
Florence, Fond du Lac,
Forest, Green Lake,
Jefferson, Kenosha,
Kewaunee, Langlade,
Lincoln, Manitowoc,
Marathon, Marinette,
Marquette, Milwaukee,
Oconto, Oneida, Outagamie,
Ozaukee, Portage, Racine,
Shawano, Sheboygan,
Taylor, Vilas, Walworth,
Washington, Waukesha,
Waupaca, Waushara,
Winnebago, Wood
56,542 23 56,565
Wisconsin BadgerCare Plus
(Comprehensive
MCO)
Network Health Plan Network Health
Plan
Counties: Ashland, Bayfield,
Brown, Calumet, Chippewa,
Clark, Crawford, Dodge,
Door, Douglas, Eau Claire,
Fond du Lac, Forest, Green
Lake, Iron, Jefferson,
Kenosha, Kewaunee,
Langlade, Lincoln,
Manitowoc, Marathon,
Marinette, Marquette,
Menominee, Milwaukee,
Oconto, Oneida, Outagamie,
Ozaukee, Polk, Portage,
Price, Racine, Rock, Rusk,
Sawyer, Shawano,
Sheboygan, Taylor, Vilas,
Walworth, Washburn,
Waukesha, Waupaca,
Waushara, Winnebago,
Wood
33,530 31 33,561
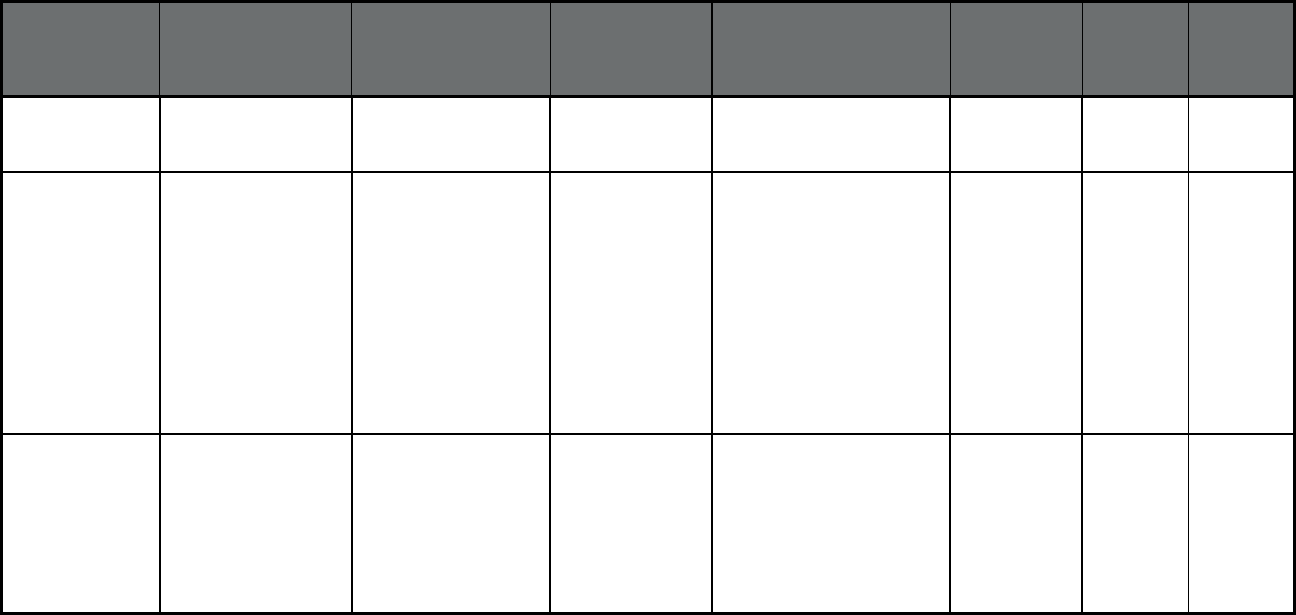
178
State
Program Name
(Type) Plan Name
Parent
Organization
Geographic Region (state-
defined areas, counties, or
zip codes)
Medicaid-Only
Enrollment
Dual
Enrollment
Total
Enrollment
Wisconsin BadgerCare Plus
(Comprehensive
MCO)
Physicians Plus Health
Plan
Physicians Plus
Health Plan
County: Dane 9,314 17 9,331
Wisconsin BadgerCare Plus
(Comprehensive
MCO)
Security Health Plan Security Health
Plan
Counties: Adams, Ashland,
Barron, Bayfield, Burnett,
Chippewa, Clark, Douglas,
Dunn, Eau Claire, Forest,
Iron, Jackson, Juneau,
Langlade, Lincoln,
Marathon, Monroe, Oneida,
Pepin, Portage, Price, Rusk,
Sawyer, Shawano, Taylor,
Trempealeau, Vilas,
Washburn, Waupaca,
Waushara, Wood
55,634 94 55,728
Wisconsin BadgerCare Plus
(Comprehensive
MCO)
Trilogy Health
Insurance
Trilogy Health
Insurance
Counties: Brown, Dodge,
Green Lake, Kenosha,
Marinette, Milwaukee,
Oconto, Outagamie,
Ozaukee, Racine, Shawano,
Sheboygan, Washington,
Waukesha, Waupaca,
Waushara, Winnebago
10,787 6 10,793
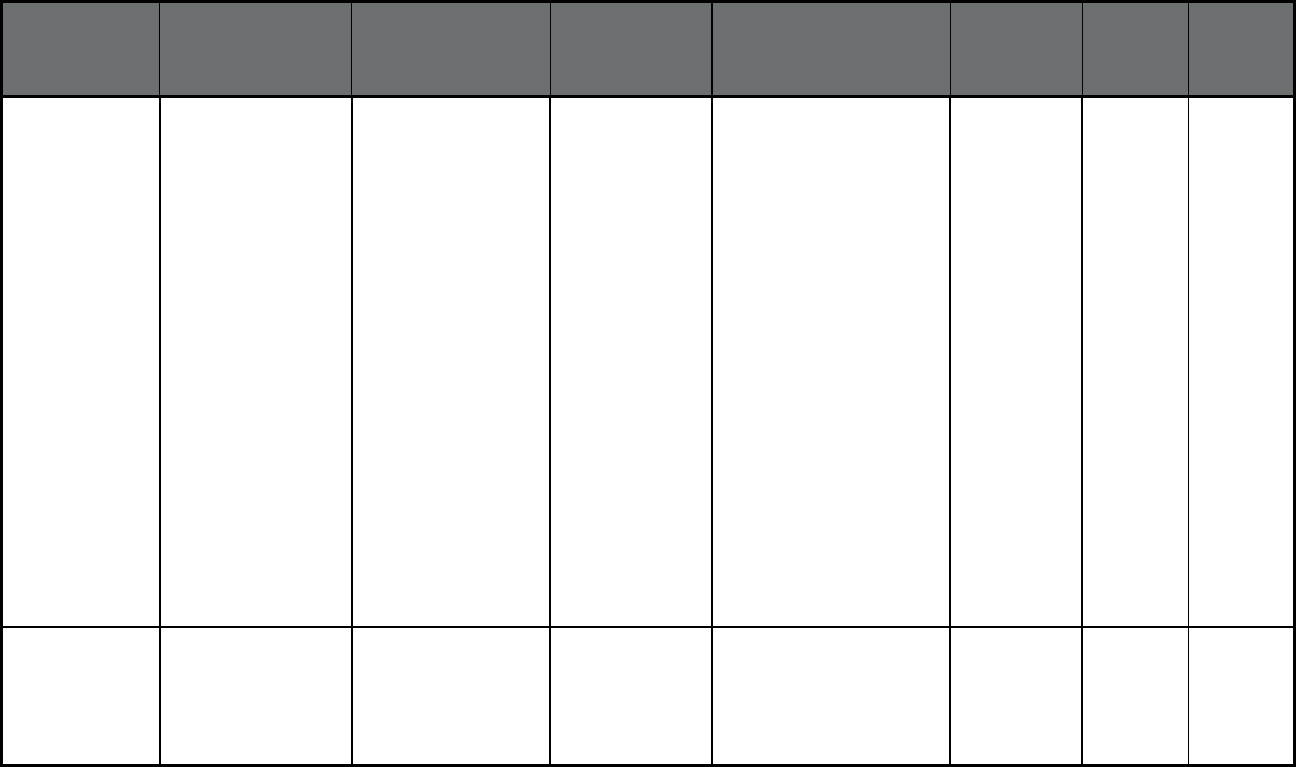
179
State
Program Name
(Type) Plan Name
Parent
Organization
Geographic Region (state-
defined areas, counties, or
zip codes)
Medicaid-Only
Enrollment
Dual
Enrollment
Total
Enrollment
Wisconsin BadgerCare Plus
(Comprehensive
MCO)
UnitedHealthcare
Community Plan
UnitedHealthcare Counties: Adams, Ashland,
Barron, Bayfield, Brown,
Burnett, Calumet,
Chippewa, Columbia,
Crawford, Dane, Dodge,
Door, Douglas, Eau Claire,
Florence, Fond du Lac,
Forest, Green, Green Lake,
Jefferson, Kenosha,
Kewaunee, La Crosse,
Langlade, Lincoln,
Manitowoc, Marathon,
Marinette, Marquette,
Menominee, Milwaukee,
Monroe, Oconto, Oneida,
Outagamie, Ozaukee,
Pierce, Polk, Portage, Price,
Racine, Rock, St. Croix,
Sauk, Sawyer, Shawano,
Sheboygan, Taylor,
Trempealeau, Vernon, Vilas,
Walworth, Washburn,
Washington, Waukesha,
Waupaca, Waushara,
Winnebago, Wood
144,764 191 144,955
Wisconsin BadgerCare Plus
(Comprehensive
MCO)
Quartz Quartz Counties: Buffalo, Columbia,
Crawford, Dane, Dodge,
Fond du Lac, Grant, Green,
Jackson, Jefferson, Juneau,
La Crosse, Monroe, Rock,
Sauk, Trempealeau, Vernon
29,797 42 29,839
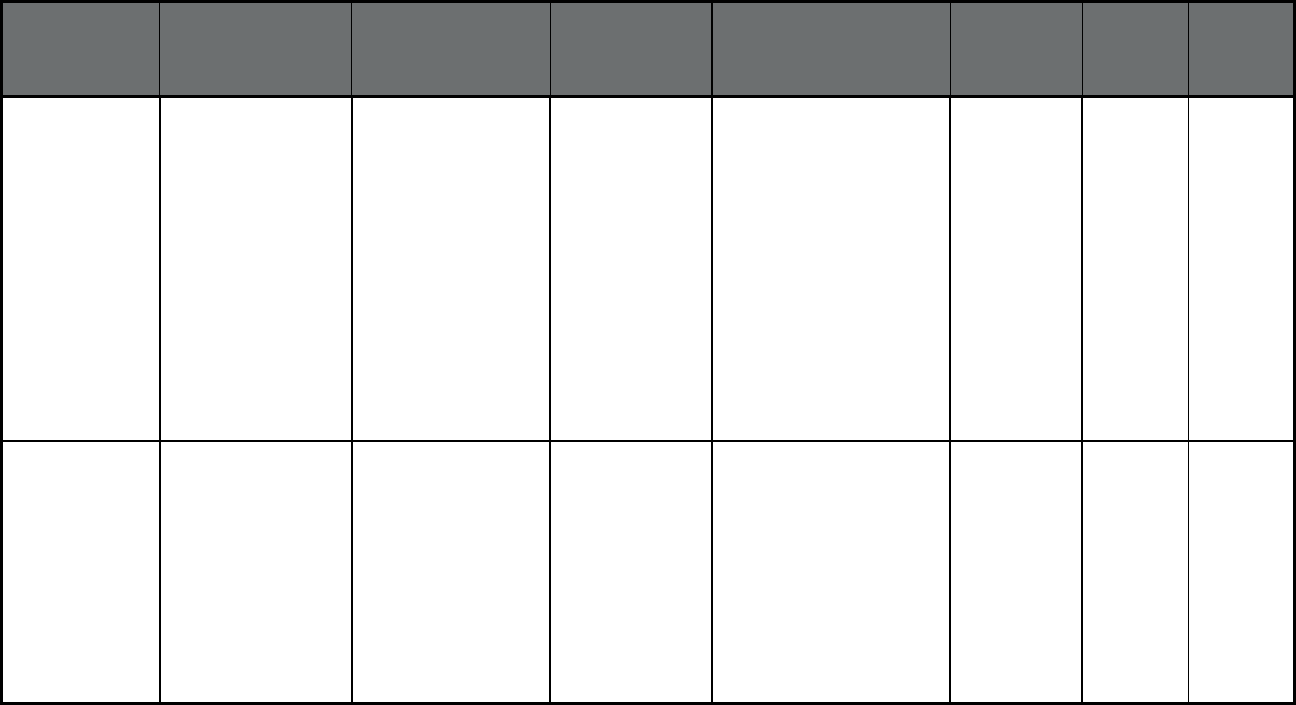
180
State
Program Name
(Type) Plan Name
Parent
Organization
Geographic Region (state-
defined areas, counties, or
zip codes)
Medicaid-Only
Enrollment
Dual
Enrollment
Total
Enrollment
Wisconsin SSI Managed Care
(Comprehensive
MCO)
Anthem Blue Cross
Blue Shield
Anthem BCBS Counties: Brown, Calumet,
Dane, Dodge, Door,
Florence, Fond du Lac,
Forest, Green Lake,
Jefferson, Kenosha,
Kewaunee, Langlade,
Manitowoc, Marinette,
Marquette, Menominee,
Milwaukee, Oconto,
Outagamie, Ozaukee, Polk,
Portage, Racine, Rock,
Shawano, Sheboygan,
Taylor, Walworth,
Washington, Waukesha,
Waupaca, Waushara,
Winnebago, Wood
4,977 654 5,631
Wisconsin SSI Managed Care
(Comprehensive
MCO)
Care Wisconsin Community Care
Health Plan (WI)
Counties: Adams, Calumet,
Clark, Columbia, Crawford,
Dane, Dodge, Fond du Lac,
Grant, Green, Green Lake,
Iowa, Jackson, Jefferson,
Juneau, La Crosse,
Lafayette, Marquette,
Monroe, Outagamie,
Ozaukee, Richland, Rock,
Trempealeau, Vernon,
Waukesha, Waupaca,
Waushara, Winnebago
2,426 369 2,795
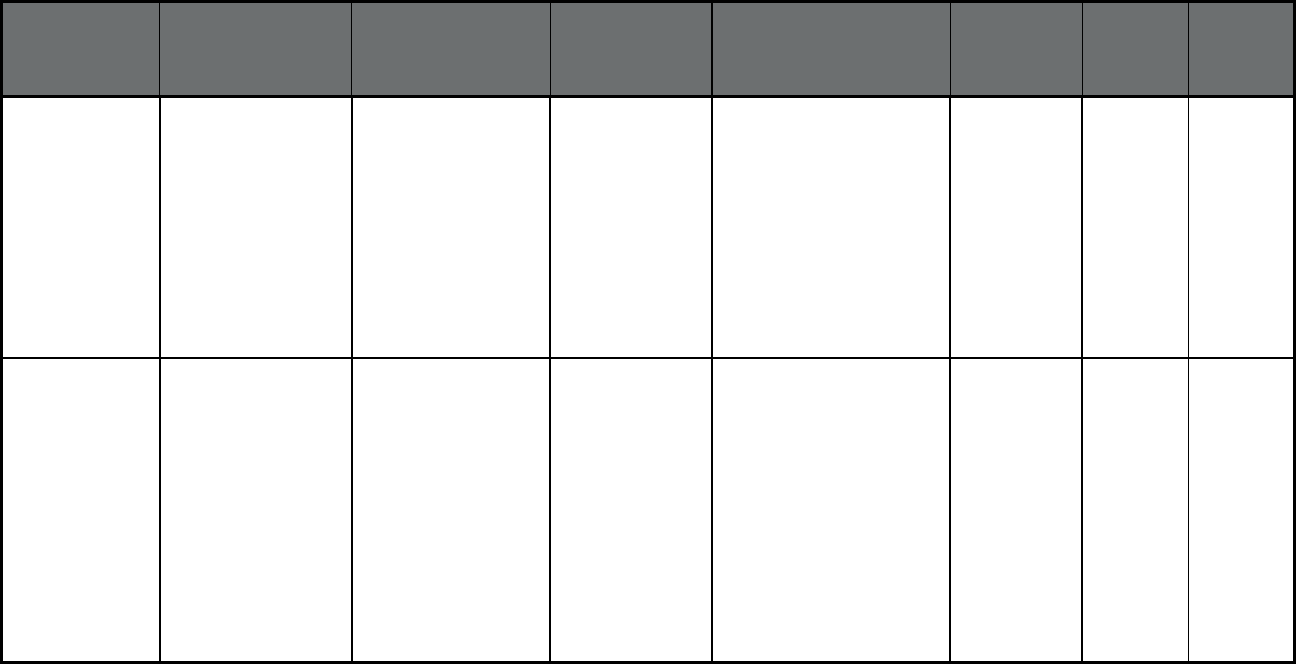
181
State
Program Name
(Type) Plan Name
Parent
Organization
Geographic Region (state-
defined areas, counties, or
zip codes)
Medicaid-Only
Enrollment
Dual
Enrollment
Total
Enrollment
Wisconsin SSI Managed Care
(Comprehensive
MCO)
Group Health
Cooperative Of Eau
Claire
Group Health
Cooperative
Counties: Ashland, Buffalo,
Chippewa, Columbia,
Crawford, Douglas, Eau
Claire, Forest, Grant, Green,
Iowa, Iron, Jackson, Juneau,
La Crosse, Lafayette,
Langlade, Lincoln,
Marathon, Oneida, Pepin,
Polk, Portage, Price,
Richland, Shawano,
Trempealeau, Vernon, Vilas
,
Washburn, Wood
2,674 640 3,314
Wisconsin SSI Managed Care
(Comprehensive
MCO)
Independent Care
(iCare)
iCare Counties: Adams, Brown,
Dane, Dodge, Door, Fond
Du Lac, Grant, Green,
Jackson, Jefferson, Juneau,
Kenosha, Kewaunee, La
Crosse, Manitowoc,
Marinette, Milwaukee,
Monroe, Oconto,
Outagamie, Ozaukee,
Racine, Rock, Sheboygan,
Trempealeau, Vernon,
Walworth, Washington,
Waukesha, Waupaca,
Winnebago
6,387 3,906 10,293
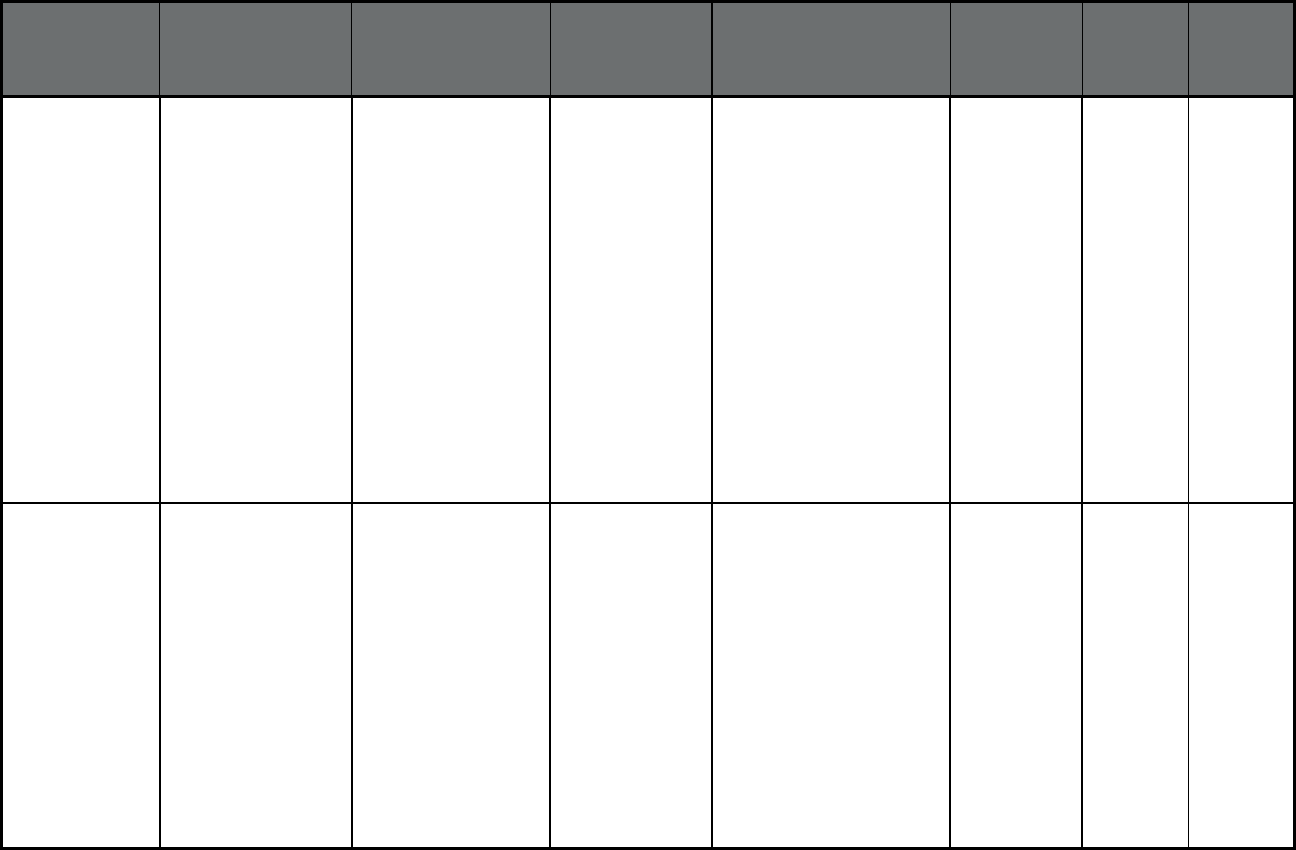
182
State
Program Name
(Type) Plan Name
Parent
Organization
Geographic Region (state-
defined areas, counties, or
zip codes)
Medicaid-Only
Enrollment
Dual
Enrollment
Total
Enrollment
Wisconsin SSI Managed Care
(Comprehensive
MCO)
MHS of Wisconsin MHS of Wisconsin Counties: Ashland, Bayfield,
Brown, Calumet, Chippewa,
Clark, Dodge, Door,
Douglas, Eau Claire, Fond
du Lac, Forest, Green Lake,
Iron, Jefferson, Kenosha,
Kewaunee, Langlade,
Lincoln, Manitowoc,
Marathon, Marinette,
Marquette, Menominee,
Milwaukee, Oconto, Oneida,
Outagamie, Ozaukee, Polk,
Portage, Price, Racine,
Rock, Rusk, Sawyer,
Shawano, Sheboygan,
Taylor, Vilas, Walworth,
Washburn, Waukesha,
Waupaca, Waushara,
Winnebago, Wood
4,834 1,346 6,180
Wisconsin SSI Managed Care
(Comprehensive
MCO)
Molina Health Plan Molina Healthcare Counties: Brown, Calumet,
Clark, Dodge, Door,
Florence, Fond du Lac,
Forest, Green Lake,
Jefferson, Kenosha,
Kewaunee, Langlade,
Lincoln, Manitowoc,
Marathon, Marinette,
Marquette, Milwaukee,
Oconto, Oneida, Outagamie,
Ozaukee, Portage, Racine,
Shawano, Sheboygan,
Taylor, Vilas, Walworth,
Washington, Waukesha,
Waupaca, Waushara,
Winnebago, Wood
2,593 595 3,188
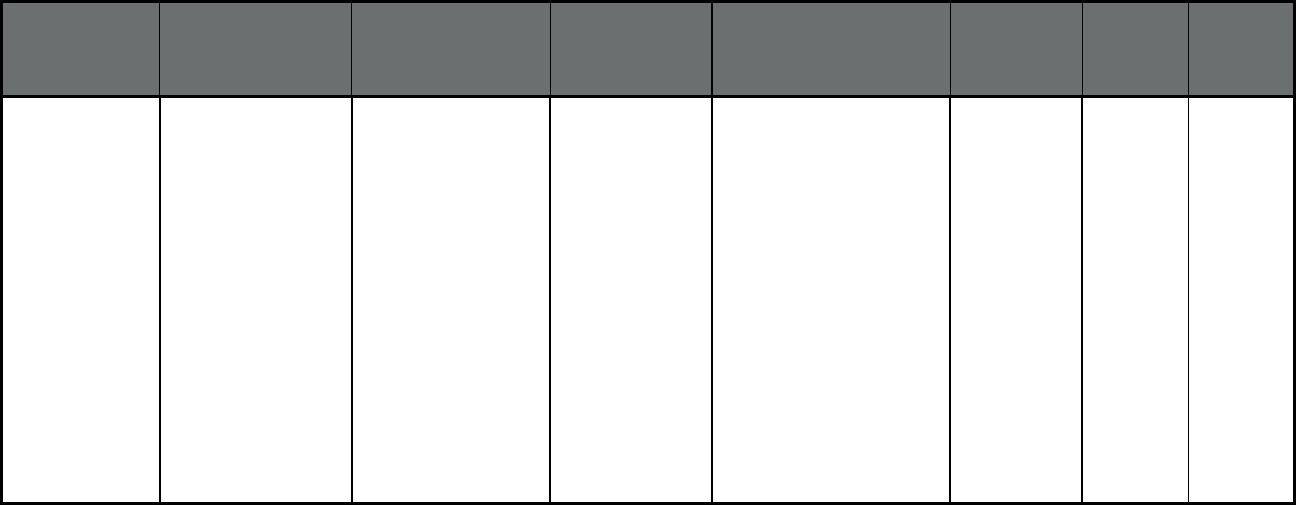
183
State
Program Name
(Type) Plan Name
Parent
Organization
Geographic Region (state-
defined areas, counties, or
zip codes)
Medicaid-Only
Enrollment
Dual
Enrollment
Total
Enrollment
Wisconsin SSI Managed Care
(Comprehensive
MCO)
Network Health Plan Network Health
Plan
Counties: Ashland, Bayfield,
Brown, Calumet, Chippewa,
Clark, Dodge, Door,
Douglas, Eau Claire, Fond
du Lac, Forest, Green Lake,
Iron, Jefferson, Kenosha,
Kewaunee, Langlade,
Lincoln, Manitowoc,
Marathon, Marinette,
Marquette, Menominee,
Milwaukee, Oconto, Oneida,
Outagamie, Ozaukee, Polk,
Portage, Price, Racine,
Rock, Rusk, Sawyer,
Shawano, Sheboygan,
Taylor, Vilas, Walworth,
Washburn, Waukesha,
Waupaca, Waushara,
Winnebago, Wood
3,052 785 3,837
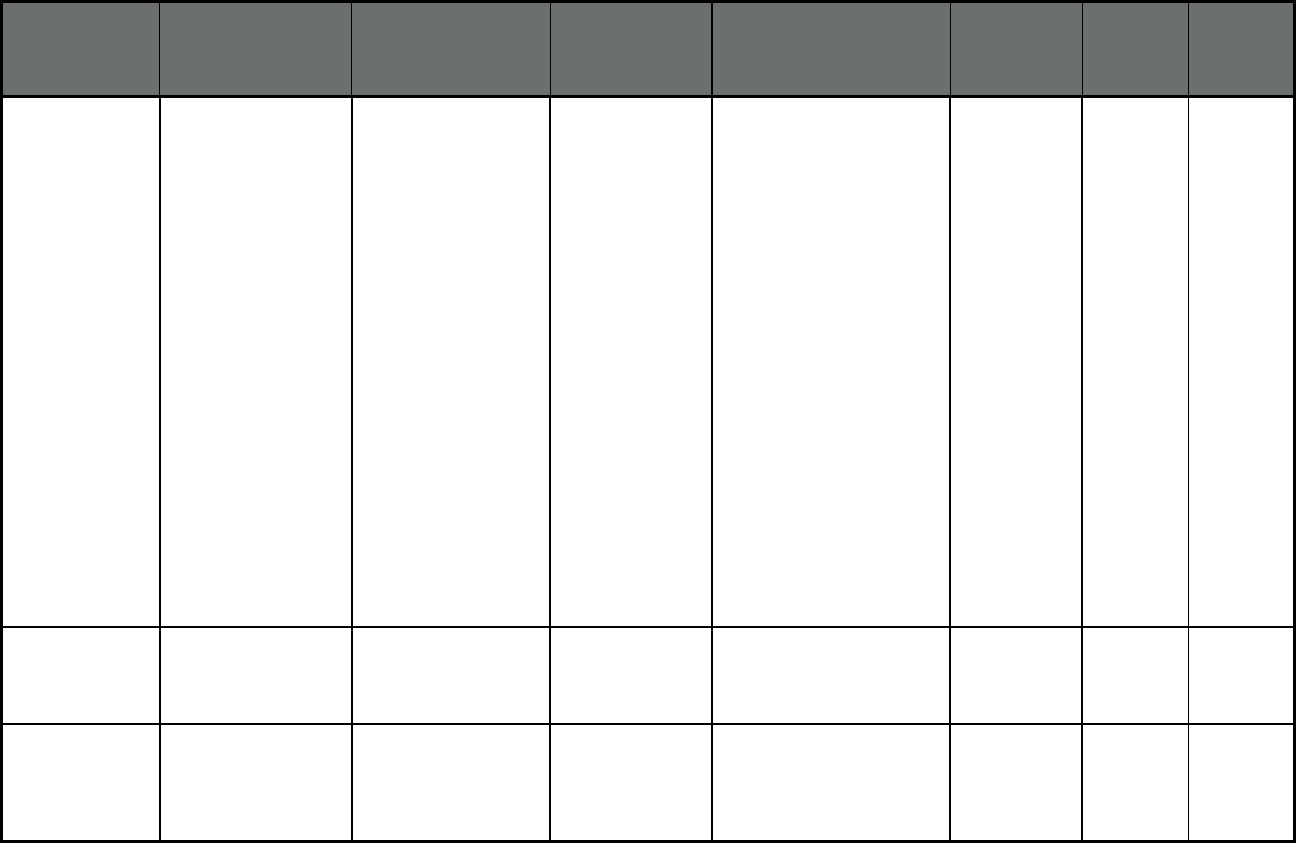
184
State
Program Name
(Type) Plan Name
Parent
Organization
Geographic Region (state-
defined areas, counties, or
zip codes)
Medicaid-Only
Enrollment
Dual
Enrollment
Total
Enrollment
Wisconsin SSI Managed Care
(Comprehensive
MCO)
UnitedHealthcare
Community Plan
UnitedHealthcare Counties: Adams, Ashland,
Barron, Bayfield, Brown,
Burnett, Calumet,
Chippewa, Columbia,
Crawford, Dane, Dodge,
Door, Douglas, Eau Claire,
Florence, Fond du Lac,
Forest, Green, Green Lake,
Jefferson, Kenosha,
Kewaunee, La Crosse,
Langlade, Lincoln,
Manitowoc, Marathon,
Marinette, Marquette,
Menominee, Milwaukee,
Monroe, Oconto, Oneida,
Outagamie, Ozaukee,
Pierce, Polk, Portage, Price,
Racine, Rock, St. Croix,
Sauk, Sawyer, Shawano,
Sheboygan, Taylor,
Trempealeau, Vernon,
Vilas,
Walworth, Washburn,
Washington, Waukesha,
Waupaca, Waushara,
Winnebago, Wood
13,187 5,727 18,914
Wisconsin Family Care
Partnership Program
(Comprehensive MCO
+ MLTSS)
Care Wisconsin Community Care
Health Plan (WI)
Counties: Columbia, Dane,
Dodge, Jefferson, Ozaukee,
Sauk, Waukesha
273 1,534 1,807
Wisconsin Family Care
Partnership Program
(Comprehensive MCO
+ MLTSS)
Community Care, Inc. Community Care
Health Plan (WI)
Counties: Calumet,
Kenosha, Milwaukee,
Outagamie, Ozaukee,
Racine, Washington,
Waukesha, Waupaca
145 483 628

185
State
Program Name
(Type) Plan Name
Parent
Organization
Geographic Region (state-
defined areas, counties, or
zip codes)
Medicaid-Only
Enrollment
Dual
Enrollment
Total
Enrollment
Wisconsin Family Care
Partnership Program
(Comprehensive MCO
+ MLTSS)
Independent Care
(iCare)
iCare Counties: Dane, Kenosha,
Milwaukee, Racine
299 633 932
Wisconsin Family Care (MLTSS
only (PIHP and/or
PAHP))
Care Wisconsin Community Care
Health Plan (WI)
Counties: Brown, Buffalo,
Chippewa, Clark, Columbia,
Crawford, Dodge, Door,
Dunn, Eau Claire, Grant,
Green, Green Lake, Iowa,
Jackson, Jefferson, Juneau,
Kewaunee, La Crosse,
Lafayette, Marinette,
Marquette, Menominee,
Monroe, Oconto, Ozaukee,
Pepin, Pierce, Richland, St.
Croix, Sauk, Shawano,
Sheboygan, Taylor,
Trempealeau, Vernon,
Walworth, Washington,
Waukesha, Waushara
1,587 6,894 8,481
Wisconsin Family Care (MLTSS
only (PIHP and/or
PAHP))
Community Care, Inc. Community Care
Health Plan (WI)
Counties: Calumet, Fond du
Lac, Kenosha, Milwaukee,
Manitowoc, Outagamie,
Ozaukee, Racine,
Sheboygan, Walworth,
Washington, Waukesha,
Waupaca, Winnebago
2,429 8,459 10,888
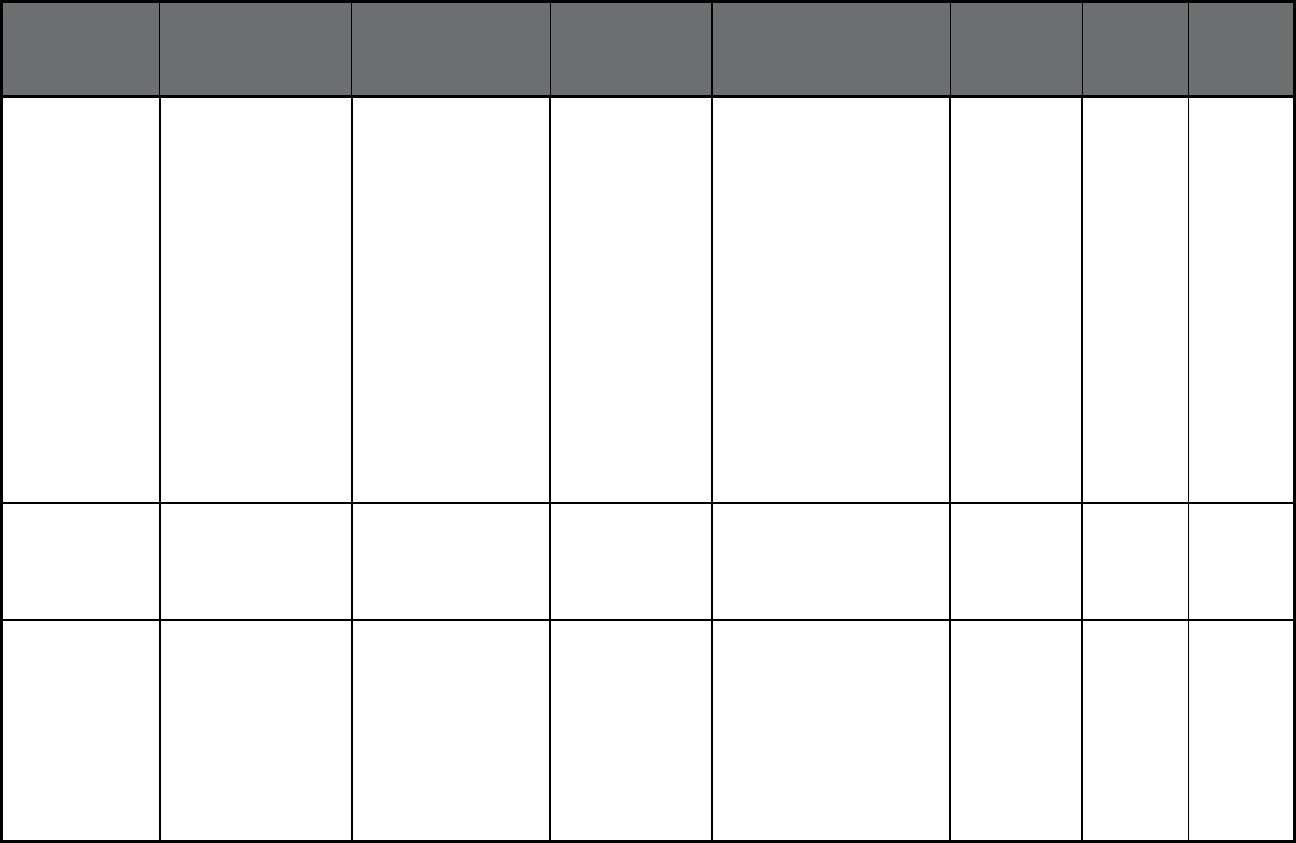
186
State
Program Name
(Type) Plan Name
Parent
Organization
Geographic Region (state-
defined areas, counties, or
zip codes)
Medicaid-Only
Enrollment
Dual
Enrollment
Total
Enrollment
Wisconsin Family Care (MLTSS
only (PIHP and/or
PAHP))
CommunityLink
(became Inclusa in
September 2017)
CommunityLink
(became Inclusa in
September 2017)
Counties: Ashland, Barron,
Bayfield, Buffalo, Burnett,
Chippewa, Clark, Columbia,
Crawford, Dodge, Douglas,
Dunn, Eau Claire, Florence,
Forest, Grant, Green, Green
Lake, Iowa, Iron, Jackson,
Jefferson, Juneau, La
Crosse, Lafayette,
Langlade, Lincoln,
Marathon, Marquette,
Monroe, Oneida, Pepin,
Pierce, Polk, Portage, Price,
Richland, Rock, Rusk, Sauk,
Sawyer, St. Croix,
Trempealeau, Vernon, Vilas,
Washington, Waukesha,
Washburn, Waushara,
Wood
2,442 12,527 14,969
Wisconsin Family Care (MLTSS
only (PIHP and/or
PAHP))
My Choice Family Care My Choice Family
Care
Counties: Kenosha,
Milwaukee, Ozaukee,
Racine, Rock, Sheboygan,
Walworth, Washington,
Waukesha
1,575 7,074 8,649
Wisconsin Family Care (MLTSS
only (PIHP and/or
PAHP))
Lakeland Care District Lakeland Care
District
Counties: Brown, Calumet,
Door, Florence, Fond du
Lac, Forest, Kewaunee,
Langlade, Lincoln,
Manitowoc, Marathon,
Marinette, Menominee,
Oconto, Oneida, Outagamie,
Portage, Shawano, Vilas,
Waupaca, Winnebago,
Wood
1,002 4,579 5,581
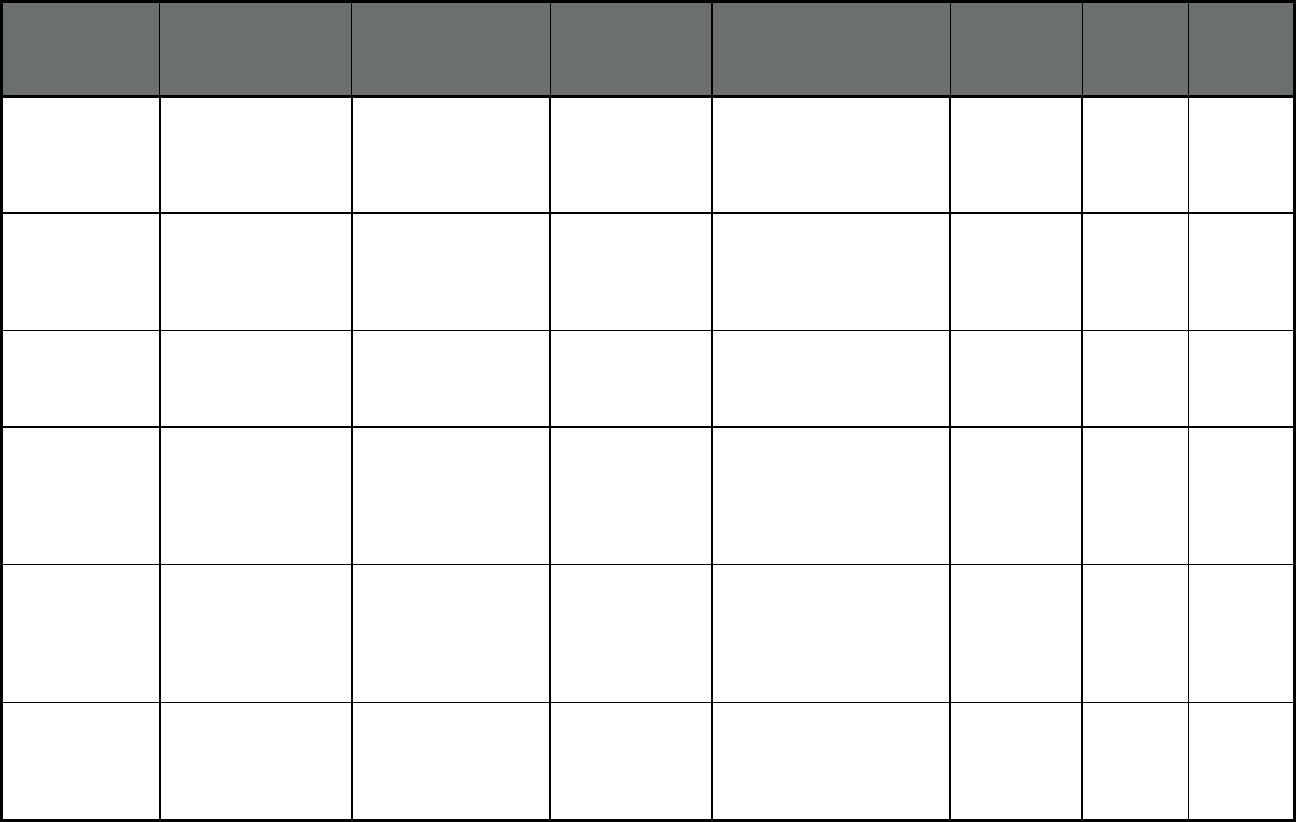
187
State
Program Name
(Type) Plan Name
Parent
Organization
Geographic Region (state-
defined areas, counties, or
zip codes)
Medicaid-Only
Enrollment
Dual
Enrollment
Total
Enrollment
Wisconsin Children Come First
(CCF) (Behavioral
Health Organization
(BHO) only (PIHP
and/or PAHP))
Children Come First Children Come
First
County: Dane 122 0 122
Wisconsin WrapAround
Milwaukee (Behavioral
Health Organization
(BHO) only (PIHP
and/or PAHP))
WrapAround
Milwaukee
WrapAround
Milwaukee
County: Milwaukee 1,071 3 1,074
Wisconsin Care4Kids (Other
Prepaid Health Plan
(PHP) (limited
benefits))
Children's Community
Health Plan
Children's
Community Health
Plan
Counties: Milwaukee,
Kenosha, Racine,
Washington, Ozaukee,
Waukesha
3,141 0 3,141
Wisconsin Program of All-
inclusive Care for the
Elderly (PACE)
(Program of All-
inclusive Care for the
Elderly (PACE))
Community Care, Inc. Community Care
Health Plan (WI)
Counties: Milwaukee and
Waukesha
30 543 573
Wyoming Care Management
Entity for Emotionally
Disturbed Children
(Other Prepaid Health
Plan (PHP) (limited
benefits))
CME Statewide Magellan Health Statewide 234 0 234
Wyoming Wyoming PACE at
Cheyenne Medical
Center (Program of
All-inclusive Care for
the Elderly (PACE))
Cheyenne Regional
Medical Center PACE
Cheyenne
Regional Medical
Center
Laramie County 4 132 136
1. The information in this table was provided by state officials. In some cases, program or plan names in this table differ from those used in publicly available
sources. Questions regarding state-specific information in this table should be directed to State/territorial Medicaid officials.
2. Beneficiaries can simultaneously enroll in Alabama's Patient 1st and Health Homes plans. The de-duplicated Patient 1st plan enrollment is 380,285.
188
3. Colorado reported plan level enrollment as 0 for plans that had less than 30 beneficiaries. As a result, reported plan-level enrollment in PACE may be lower than
actual enrollment.
4. Colorado's comprehensive MCOs, Rocky Mountain Health Plans PRIME and Denver Health Medicaid Choice, are contracted under Regional Accountable
Entity (RAE) 1 and RAE 5 of the state's PCCM Entity program, Accountable Care Collaborative.
5. Georgia is unable to provide separate counts of Medicaid-only and dually eligible beneficiaries for their NEMT program. As a result, Medicaid-only and total
enrollment counts presented in this table include both Medicaid-only and Medicare-Medicaid beneficiaries.
6. Beneficiaries can concurrently enroll in Ohana Community Care Service and another medical or dental plan under the Quest program. The de-duplicated
comprehensive MCO enrollment is 351,685.
7. Michigan is not able to provide dual-eligible enrollment for the Specialty Prepaid Inpatient Health plan.
8. Oregon Health Plan includes (1) Coordinated Care Organizations (CCOs); (2) Dental Care Organizations (DCOs), like Access Dental Plan, LLC; Advantage
Dental Services; Capitol Dental Care, Inc.; CareOregon Dental; Family Dental Care; Managed Dental Care or Oregon; and ODS Community Health, Inc., or (3) the
Mental Health Organization called Greater Oregon Behavioral Health, Inc. CCO enrollees receive physical, dental and mental health services and may be enrolled
in more than one plan type simultaneously.
9. Beneficiaries can simultaneously enroll in (1) Magellan Health services, (2) DentaQuest USA Insurance Company, and (3) another comprehensive MCO. The
de-duplicated comprehensive MCO enrollment is 1,386,664.
10. The Department of Vermont Health Access, a state agency, acts as Vermont's single MCO entity. Vermont pays for Medicaid services for dually eligible
enrollees on a FFS basis. Dually eligible enrollees reported in the Global Commitment to Health Demonstration are Medicaid enrollees who have become newly
eligible for Medicare and, as of July 1, have not yet transferred out of the program.
11. The 22,412 enrollees reported in the Health Home program excludes 72,261 beneficiaries who are enrolled in both comprehensive MCO programs and the
Health Home program.
12. Washington is unable to provide separate counts of Medicaid-only and dual enrollment for their NEMT, BHSO, and PACE programs. As a result, Medicaid-only
and total enrollment counts presented in this table include both Medicaid-only and Medicare-Medicaid beneficiaries.
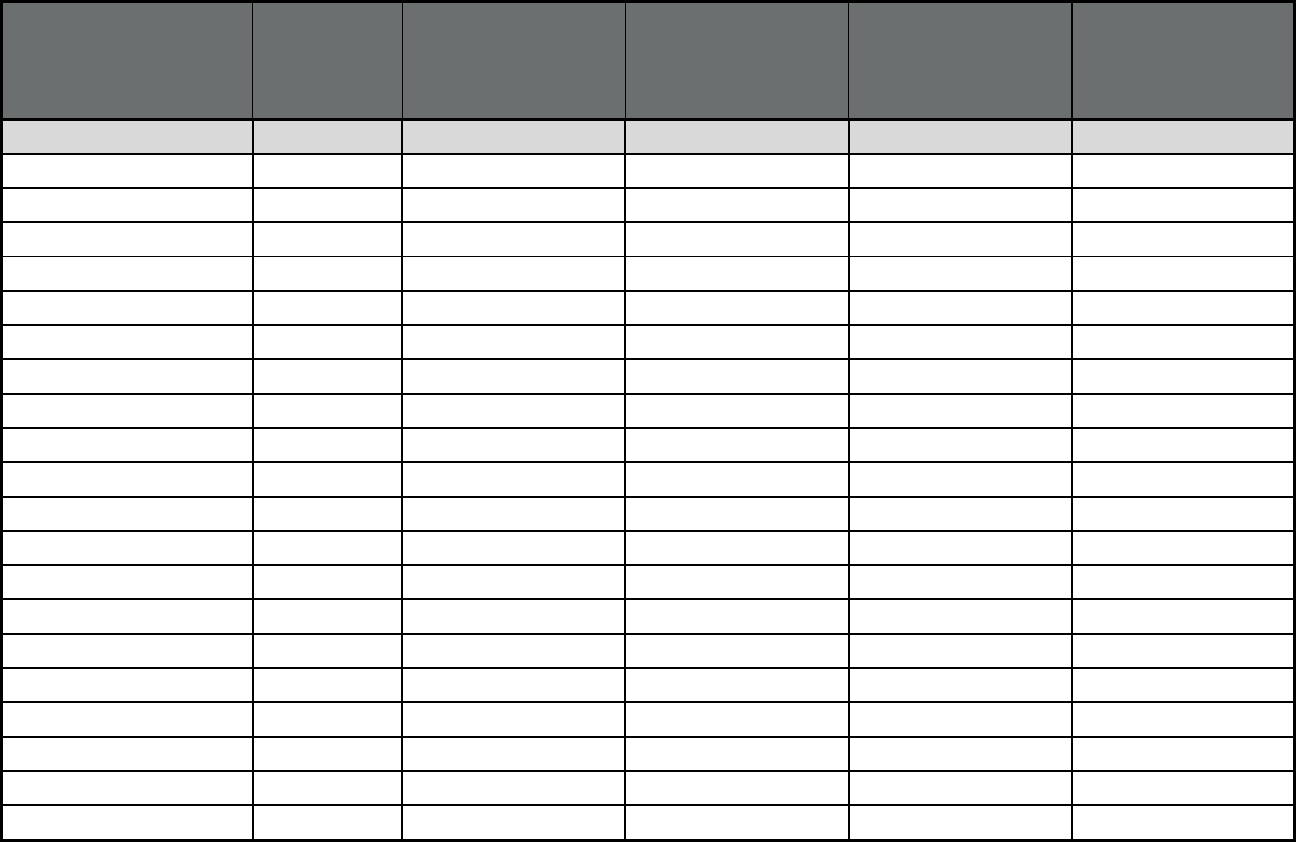
189
Table 6. Medicaid Managed Long Term Services and Supports (MLTSS) Program Users or Enrollees, as of
July 1, 2018
1.2
State or Territory
Total Medicaid
Enrollment in
Any Type of
Managed Care
Comprehensive
Managed Care Including
LTSS
2
: Number of
Enrollees Using LTSS
3,4
Comprehensive
Managed Care Including
LTSS
2
: Percent of Total
Managed LTSS (MLTSS)
Only: Number of
Enrollees Using LTSS
3,4
Managed LTSS (MLTSS)
Only: Percent of Total
TOTALS 66,107,287 1,025,522 1.6% 278,891 0.4%
Alabama 638,221 0 0.0% 0 0.0%
Alaska 0 0 0.0% 0 0.0%
American Samoa n/a n/a n/a n/a n/a
Arizona 1,560,593 60,015 3.8% 0 0.0%
Arkansas 871,262 0 0.0% 0 0.0%
California 10,670,306 346,031 3.2% 0 0.0%
Colorado 1,171,171 0 0.0% 0 0.0%
Connecticut 0 0 0.0% 0 0.0%
Delaware 208,802 13,542 6.5% 0 0.0%
District of Columbia 189,363 0 0.0% 0 0.0%
Florida
4
3,178,981 0 0.0% 101,524 3.2%
Georgia
5
1,485,250 0 0.0% 0 0.0%
Guam n/a n/a n/a n/a n/a
Hawaii
4
351,685 9,466 2.7% 0 0.0%
Idaho
4
272,979 3,799 1.4% 0 0.0%
Illinois
4
2,176,902 28,756 1.3% 31,143 1.4%
Indiana 1,126,425 0 0.0% 0 0.0%
Iowa 580,507 41,421 7.1% 0 0.0%
Kansas
4
358,225 29,083 8.1% 0 0.0%
Kentucky 1,259,525 0 0.0% 0 0.0%
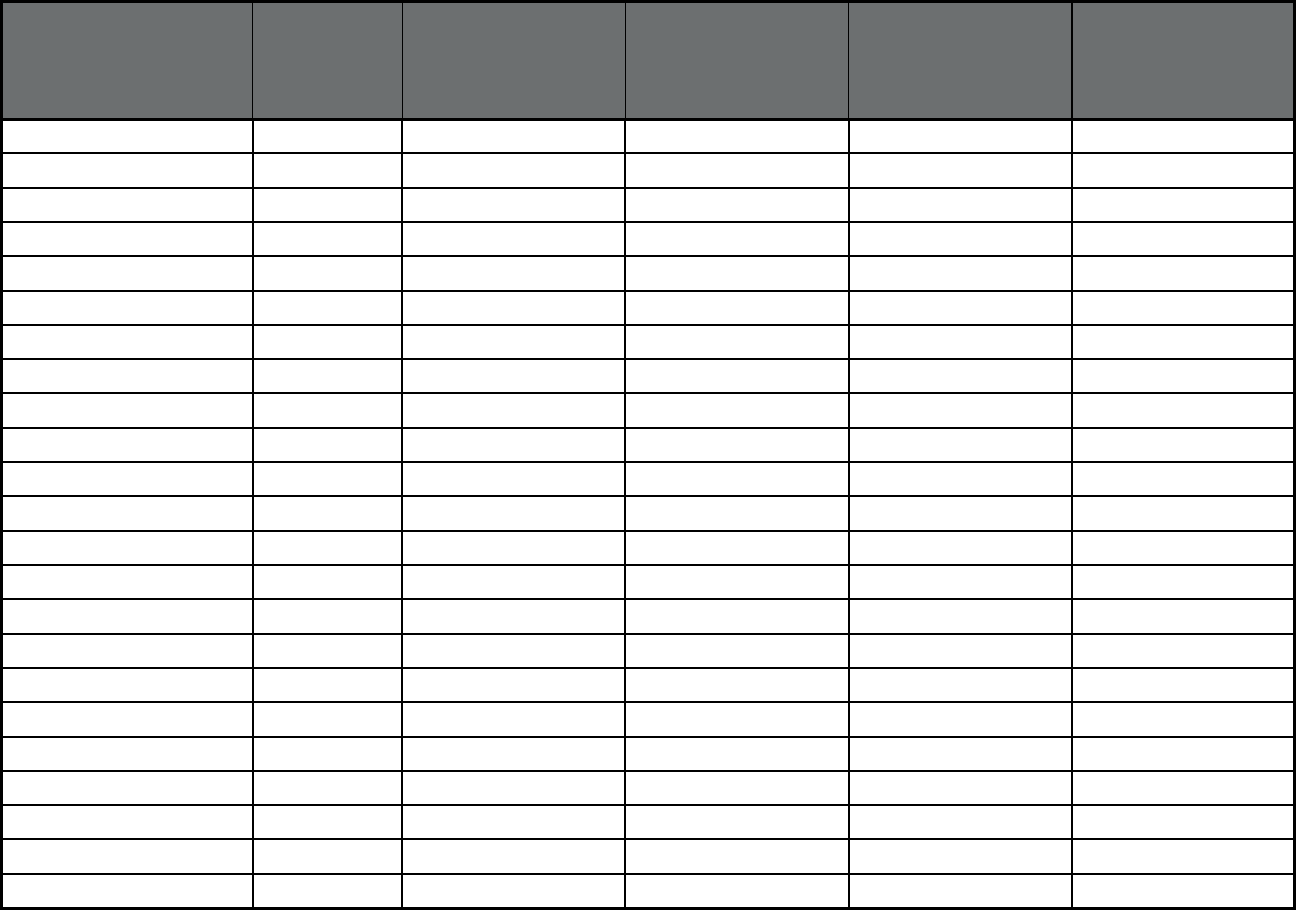
190
State or Territory
Total Medicaid
Enrollment in
Any Type of
Managed Care
Comprehensive
Managed Care Including
LTSS
2
: Number of
Enrollees Using LTSS
3,4
Comprehensive
Managed Care Including
LTSS
2
: Percent of Total
Managed LTSS (MLTSS)
Only: Number of
Enrollees Using LTSS
3,4
Managed LTSS (MLTSS)
Only: Percent of Total
Louisiana 1,504,540 0 0.0% 0 0.0%
Maine 234,327 0 0.0% 0 0.0%
Maryland 1,169,708 0 0.0% 0 0.0%
Massachusetts 1,211,485 61,367 5.1% 0 0.0%
Michigan
6
4,608,988 0 0.0% 19,055 0.4%
Minnesota
7
892,137 33,382 3.7% 0 0.0%
Mississippi 441,782 0 0.0% 0 0.0%
Missouri 954,603 0 0.0% 0 0.0%
Montana 215,475 0 0.0% 0 0.0%
Nebraska 249,024 0 0.0% 0 0.0%
Nevada 588,111 0 0.0% 0 0.0%
New Hampshire 133,829 0 0.0% 0 0.0%
New Jersey
8
1,569,344 44,715 2.8% 0 0.0%
New Mexico 666,050 28,957 4.3% 0 0.0%
New York
9
4,764,261 11,144 0.2% 211,268 4.4%
North Carolina 1,581,469 0 0.0% 0 0.0%
North Dakota 48,957 0 0.0% 0 0.0%
Northern Mariana Islands n/a n/a n/a n/a n/a
Ohio
10
2,450,031 20,050 0.8% 0 0.0%
Oklahoma 649,023 0 0.0% 0 0.0%
Oregon 847,570 0 0.0% 0 0.0%
Pennsylvania
4
2,627,563 22,523 0.9% 0 0.0%
Puerto Rico 1,505,610 0 0.0% 0 0.0%
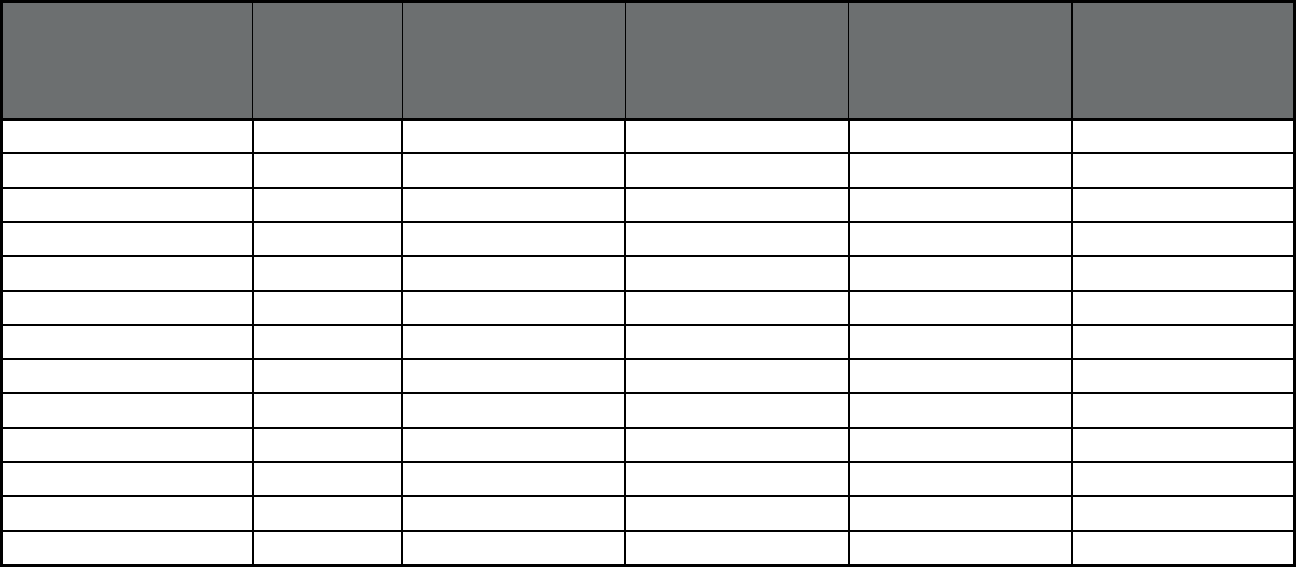
191
State or Territory
Total Medicaid
Enrollment in
Any Type of
Managed Care
Comprehensive
Managed Care Including
LTSS
2
: Number of
Enrollees Using LTSS
3,4
Comprehensive
Managed Care Including
LTSS
2
: Percent of Total
Managed LTSS (MLTSS)
Only: Number of
Enrollees Using LTSS
3,4
Managed LTSS (MLTSS)
Only: Percent of Total
Rhode Island 302,407 0 0.0% 0 0.0%
South Carolina 1,195,703 0 0.0% 0 0.0%
South Dakota 92,184 0 0.0% 0 0.0%
Tennessee 1,386,664 24,289 1.8% 0 0.0%
Texas 3,845,916 124,552 3.2% 0 0.0%
Utah 271,137 0 0.0% 0 0.0%
Vermont 123,310 202 0.2% 0 0.0%
Virgin Islands n/a n/a n/a n/a n/a
Virginia 875,351 212,460 24.3% 0 0.0%
Washington 1,781,048 0 0.0% 0 0.0%
West Virginia 407,193 0 0.0% 0 0.0%
Wisconsin 811,920 3,395 0.4% 48,568 6.0%
Wyoming 370 0 0.0% 0 0.0%
1. Enrollment and user counts include both Medicaid-only and Medicare-Medicaid (“dual”) enrollees. For both types of enrollees, Medicaid covers LTSS. For dual
enrollees, Medicaid may also cover Medicare cost-sharing for acute, primary care, and specialty services covered by Medicare, and other non-LTSS services that
are not covered by Medicare.
2. Comprehensive Managed Care Including LTSS does not include PACE programs.
3. Some comprehensive managed care programs enroll beneficiaries who may be at risk of needing LTSS but do not receive any LTSS. The counts of LTSS users
only include individuals that receive LTSS. States differ in their ability to report individuals who use MLTSS versus those who are enrolled (and may or may not be
using LTSS). This table reports MLTSS users unless otherwise noted.
4. Florida, Hawaii, Idaho, Illinois, Kansas, and Pennsylvania report the number of enrollees in their MLTSS programs, some of whom may not be using MLTSS.
The totals in this column do not include those six states because it is a count of users, not enrollees.
5. Georgia's Total Medicaid Enrollment in Any Type of Managed Care does not include 1,626,252 NEMT enrollees; a portion of these enrollees are simultaneously
enrolled in other managed care programs.
6. 7,760 of Michigan's MLTSS users are receiving capitated HCBS under the state's Specialty Prepaid Inpatient Health Plan, a BHO. The remainder are receiving
MLTSS under MI Choice, an MLTSS Only program.
7. Minnesota's MLTSS user count includes 3,867 dually eligible Medicare-Medicaid beneficiaries who received skilled nursing visits in the home, some of which
may be paid for by Medicare rather than Medicaid.
192
8. LTSS users in New Jersey are enrolled in either the FamilyCare program or the FIDE SNP program. Total LTSS users include enrollees from both of these
program who use LTSS services.
9. New York provides LTSS services through a comprehensive MCO+MLTSS program and a separate MLTSS-only program.
10. Since 2014, Ohio has operated an MLTSS program for dually eligible beneficiaries who chose not to participate in (i.e., opt out of) the MyCare Financial
Alignment Demonstration. Ohio began reporting the MyCare Opt-Out as an MLTSS program in 2016.
Note: "n/a" indicates that a state or territory was not able to report data.
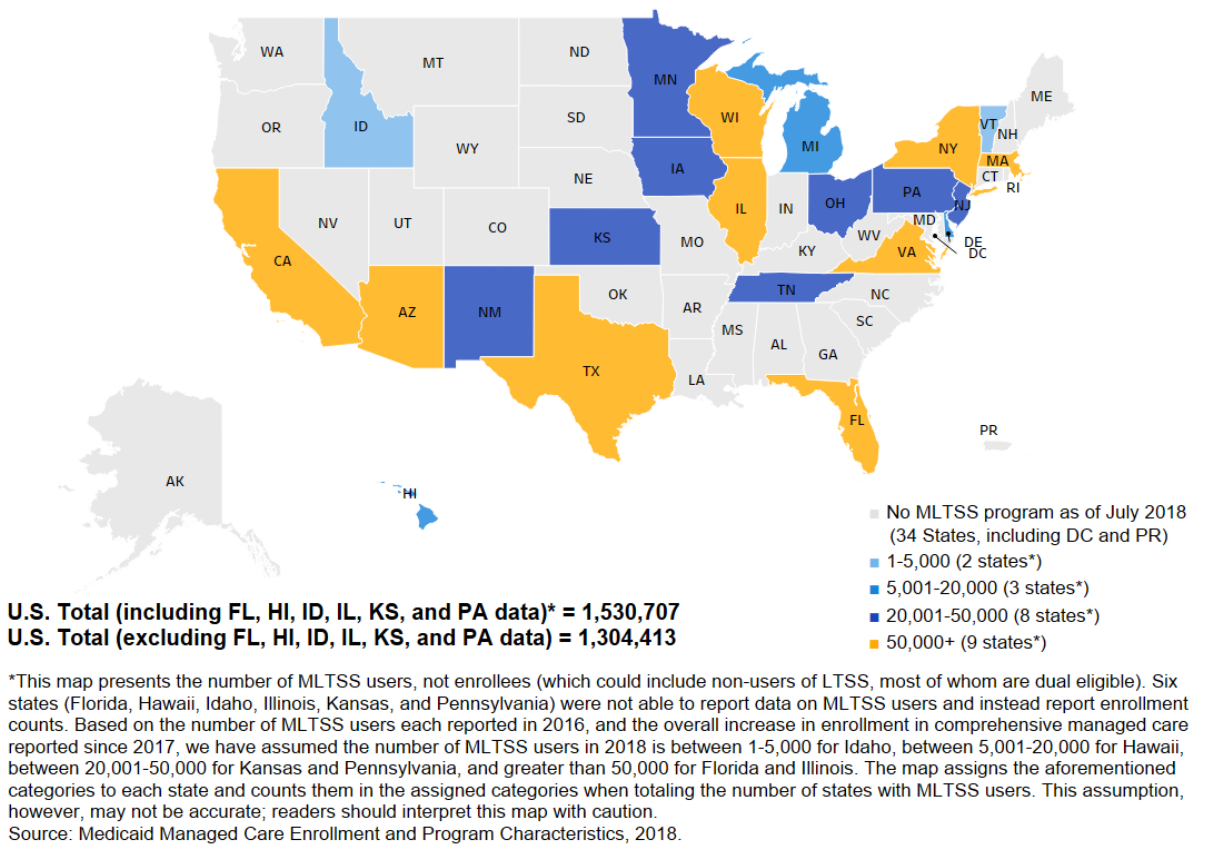
U.S.
Total
(including
FL,
HI,
ID,
IL,
KS,
and
PA
data)*
=
1,530,707
U.S.
Total
(excluding
FL,
HI,
ID,
IL,
KS,
and
PA
data)
=
1,304,413
*This
map
presents
the
number
of
MLTSS
users,
not
enrollees
(which
could
include
non-users
of
LTSS,
most
of
whom
are
dual
eligible).
Six
states
(Florida,
Hawaii,
Idaho,
Illinois,
Kansas,
and
Pennsylvania)
were
not
able
to
report
data
on
MLTSS
users
and
instead
report
enrollment
counts.
Based
on
the
number
of
MLTSS
users
each
reported
in
2016,
and
the
overall
increase
in
enrollment
in
comprehensive
managed
care
reported
since
2017,
we
have
assumed
the
number
of
MLTSS
users
in
2018
is
between
1-5,000
for
Idaho,
between
5,001-20,000
for
Hawaii,
between
20,001-50,000
for
Kansas
and
Pennsylvania,
and
greater
than
50,000
for
Florida
and
Illinois.
The
map
assigns
the
aforementioned
categories
to
each
state
and
counts
them
in
the
assigned
categories
when
totaling
the
number
of
states
with
MLTSS
users.
This
assumption,
however,
may
not
be
accurate;
readers
should
interpret
this
map
with
caution.
Source:
Medicaid
Managed
Care
Enrollment
and
Program
Characteristics,
2018.
193
Map of State Counts of Users* of Managed Long-Term Services and Supports, as of July 1, 2018
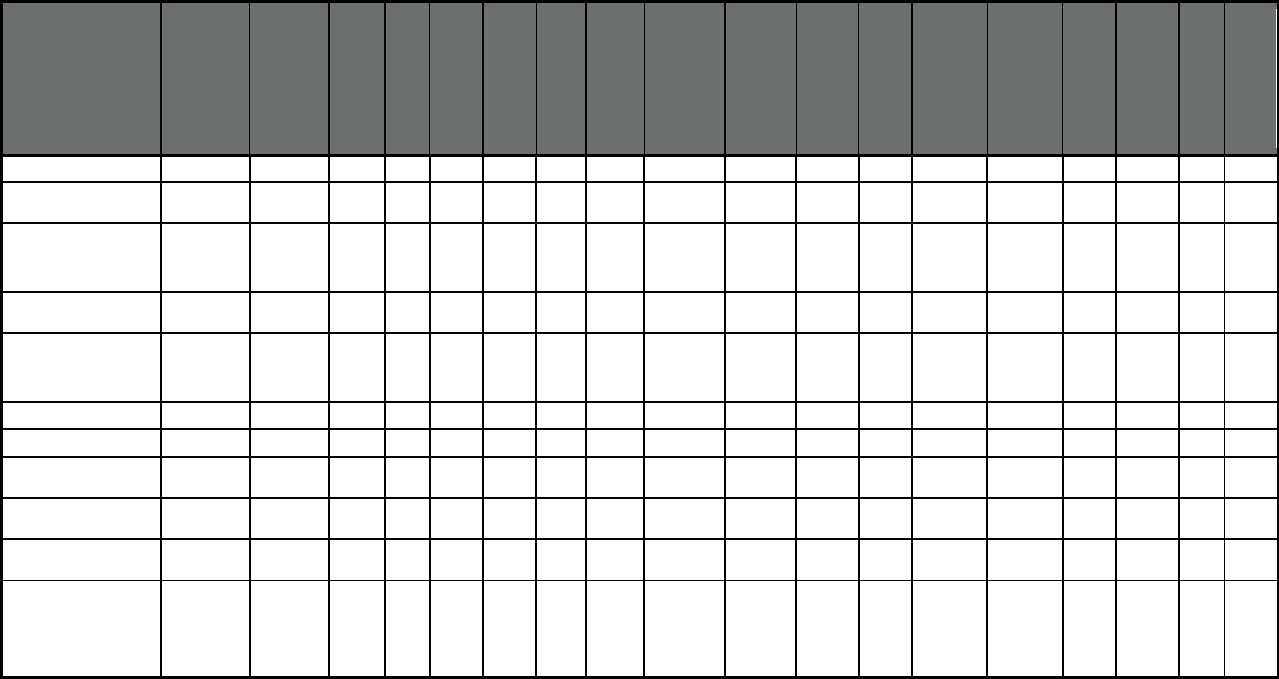
194
Table 7. Number of Managed Care Programs Enrolling Certain Populations on a Mandatory or Voluntary
Basis, at any point in 2018
Features
(N = total number of
programs)
Enrollment
(M=Mandatory,
V=Voluntary)1
Comprehen-
sive MCO
with or
without
MLTSS
(76):
M
Comprehen-
sive MCO
with or
without
MLTSS
(76):
V
PCCM
(13):
M
PCCM
(13):
V
PCCM
Entity
(4):
M
PCCM
Entity
(4):
V
MLTSS
(5):
M
MLTSS
(5):
V
BHO (PIHP
and/or
PAHP)
(15):
M
BHO (PIHP
and/or
PAHP)
(15):
V
Dental
(12):
M
Dental
(12):
V
Transporta-
tion
(18):
M
Transporta-
tion
(18):
V
Other
PHP
(7):
M
Other
PHP
(7):
V
PACE
(31):
M
PACE
(31):
V
Low-income Adults 40 4 6 1 4 0 1 0 9 0 7 2 11 3 0 2 0 0
Aged, Blind or Disabled
Children or Adults
45 13 10 2 3 1 2 1 11 0 8 2 15 3 1 1 0 24
Non-Disabled Children
(excluding children in foster
care or receiving adoption
assistance)
43 3 10 1 4 0 1 0 9 0 8 2 13 3 1 2 0 0
Individuals receiving Limited
Benefits
12 2 4 1 1 0 0 0 3 0 2 2 7 3 1 2 0 0
Low-income adults not
otherwise eligible and
covered prior to 2014 under
a waiver or other authority
39 5 4 1 2 0 0 0 8 0 5 2 9 1 0 1 0 0
Full Duals 26 25 0 1 2 1 3 2 9 2 5 2 13 3 0 1 0 30
Partial Duals 6 5 0 1 0 0 0 1 4 2 3 0 6 2 0 1 0 20
Children with Special Health
Care Needs
32 14 4 3 3 1 1 0 8 4 6 3 14 3 1 2 0 0
Native American/Alaskan
Natives
23 42 4 7 2 1 2 2 5 7 5 7 7 5 0 5 0 23
Foster Care and Adoption
Assistance Children
32 19 2 6 2 2 1 0 8 4 6 2 14 0 0 4 0 1
Exempt populations
(NA/AN=Native
American/Alaskan Native,
FC/AA=Foster Care and
Adoption Assistance
Children)
2
NA/AN
11
FC/AA
22
NA/AN
2
FC/AA
4
NA/AN
1
FC/AA
0
NA/AN
1
FC/AA
4
NA/AN
3
FC/AA
2
NA/AN
0
FC/AA
4
NA/AN
6
FC/AA
1
NA/AN
2
FC/AA
2
NA/AN
8
FC/AA
21
1. In some cases, the sum of mandatory and voluntary enrollment populations for any given program type is greater than the total number of programs of that type. That is because a state may treat individuals within a specific group, such as
aged, blind, or disabled adults, differently. For example, a state can mandate enrollment of aged adults, while allowing blind and disabled adults to enroll voluntarily.
2. Certain federal statutory authorities do not allow enrollment of American Indians/Alaska Natives or Foster Care Children. Where states use these authorities to operate Medicaid managed care, American Indians/Alaska Natives or Foster Care
Children are considered "exempt.
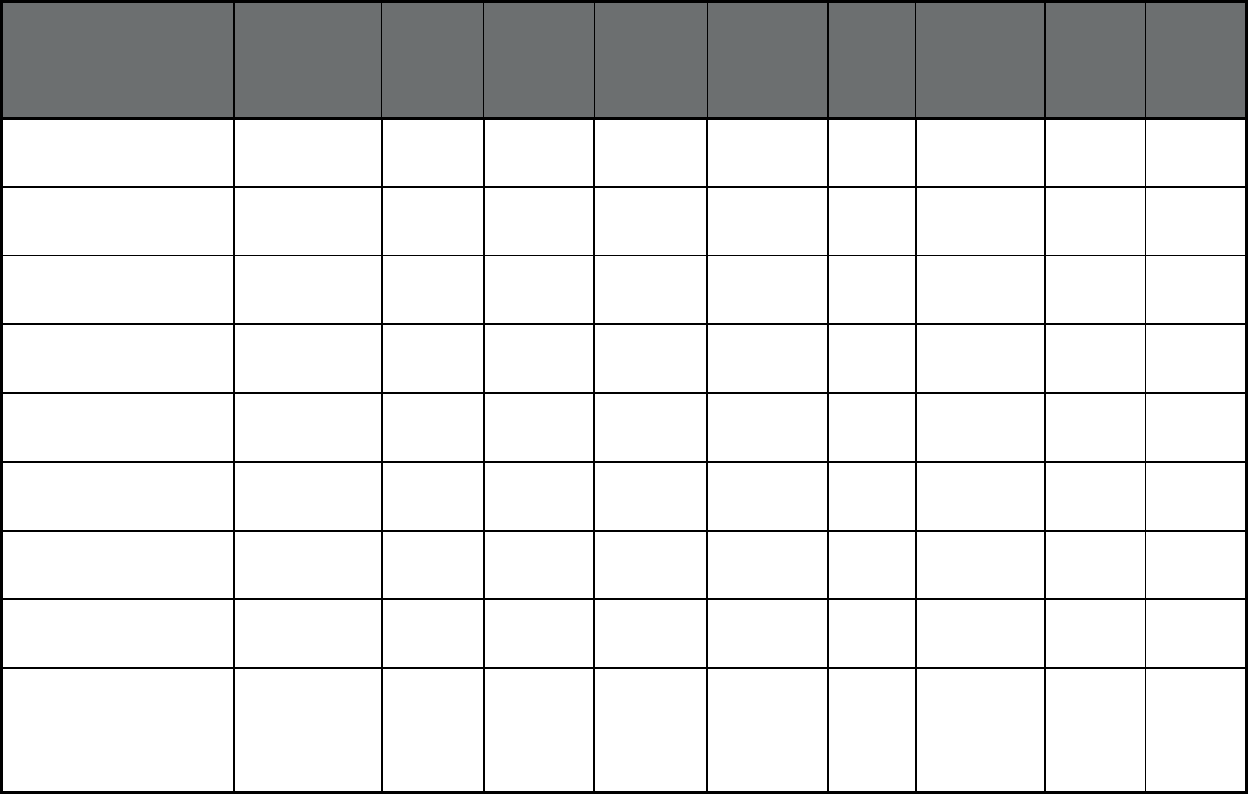
195
Table 8. Number of Managed Care Program Types, by Quality Assurance Requirements, Performance
Incentives, and Provider Value-Based Purchasing Status, at any point in 2018
Features
(total number of programs)
Comprehensive
MCO with or
without MLTSS
(76)
PCCM
(13)
PCCM Entity
(4)
MLTSS
(5)
BHO (PIHP
and/or PAHP)
(15)
Dental
(12)
Transportation
(18)
Other PHP
(7)
PACE
(31)
Quality Assurance and Data
Collection: HEDIS data
required
68 3 2 1 8 8 0 3 2
Quality Assurance and Data
Collection: CAHPS data
required
66 3 2 1 4 9 0 3 1
Quality Assurance and Data
Collection: Accreditation
required
39 0 0 2 8 3 0 1 1
Quality Assurance and Data
Collection: EQRO contractor
used
71 3 2 4 9 6 1 3 2
Performance incentives:
Payment bonuses/differentials
to reward MCOs
30 2 1 3 4 1 2 1 1
Performance incentives:
Preferential auto-enrollment to
reward MCOs
20 0 0 1 0 0 0 0 0
Performance incentives: Public
reports comparing MCO
performance on key metrics
42 2 2 1 4 4 1 0 0
Performance incentives:
Withholds tied to performance
metrics
35 1 1 2 3 4 0 1 0
Performance incentives:
MCOs/PHPs required or
encouraged to pay providers
for value/quality outcomes
using shared-risk or shared-
savings methods
45 0 2 1 3 4 0 0 0
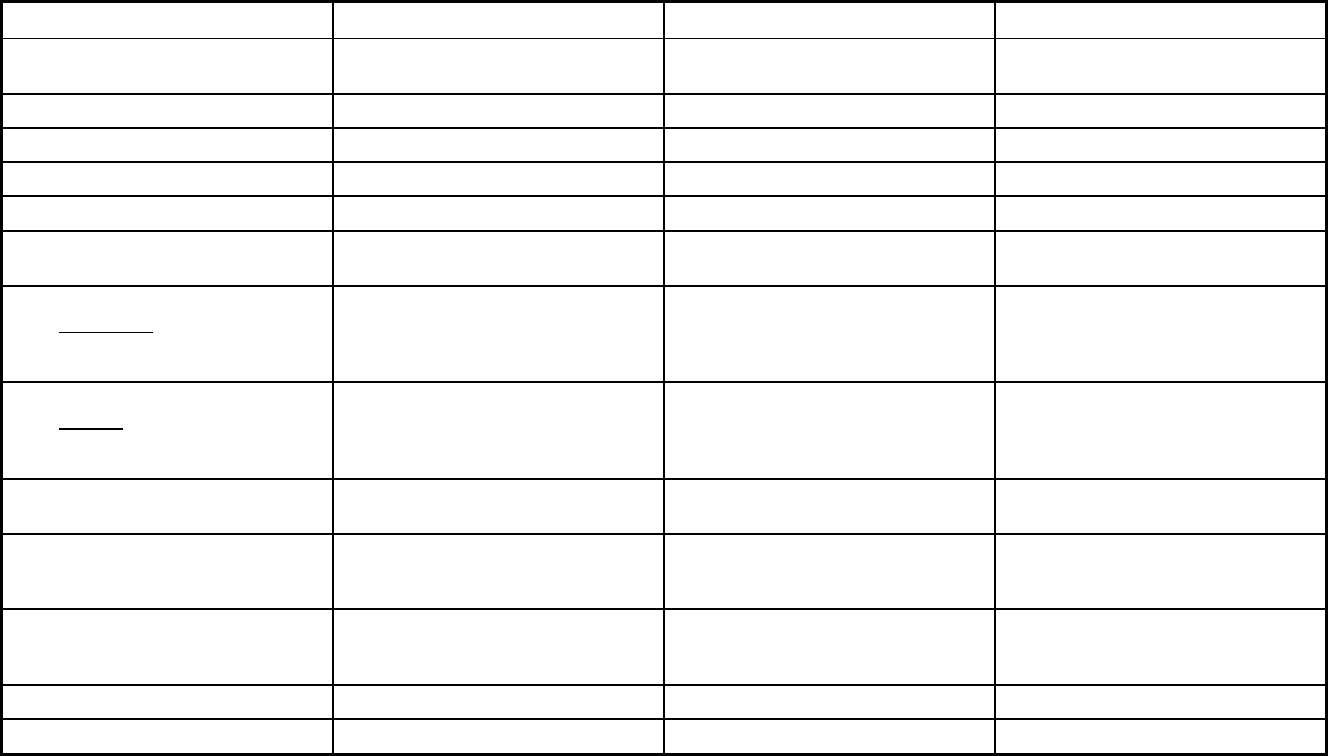
194
State Tables
Alabama Managed Care Program Features, as of 2018
Features Maternity Care Program PACE Patient 1st
Program type Other Prepaid Health Plan (PHP)
(limited benefits)
Program of All-inclusive Care for the
Elderly (PACE)
Primary Care Case Management
(PCCM)
Statewide or region-specific? Statewide Mobile and Baldwin County Statewide
Federal operating authority 1915(b) PACE 1932(a)
Program start date 09/01/1988 01/01/2012 10/01/2004
Waiver expiration date (if applicable) 08/30/2019
If the program ended in 2018, indicate
the end date
Populations enrolled: Low-income
adults not covered under ACA Section
VIII (excludes pregnant women and
people with disabilities)
Populations enrolled: Low-income
adults covered under ACA Section VIII
(excludes pregnant women and people
with disabilities)
Populations enrolled: Aged, Blind or
Disabled Children or Adults
Mandatory Voluntary Mandatory
Populations enrolled: Non-Disabled
Children (excludes children in foster
care or receiving adoption assistance)
Mandatory Mandatory
Populations enrolled: Individuals
receiving Limited Benefits (excludes
partial duals)
Mandatory Mandatory
Populations enrolled: Full Duals Voluntary
Populations enrolled: Partial Duals Voluntary

195
Features Maternity Care Program PACE Patient 1st
Populations enrolled: Children with
Special Health Care Needs
Mandatory Voluntary
Populations enrolled: Native
American/Alaskan Natives
Voluntary Voluntary Voluntary
Populations enrolled: Foster Care and
Adoption Assistance Children
Exempt Exempt
Populations enrolled: Enrollment choice
period
Pre-assigned N/A N/A
Populations enrolled: Enrollment broker
name (if applicable)
Populations enrolled: Notes on
enrollment choice period
Open enrollment begins the first of
every month, and disenrollment is
effective the last day of the chosen
month.
Benefits covered: Inpatient hospital
physical health
X
Benefits covered: Inpatient hospital
behavioral health (MH and/or SUD)
X
Benefits covered: Outpatient hospital
physical health
X
Benefits covered: Outpatient hospital
behavioral health (MH and/or SUD)
X
Benefits covered: Partial hospitalization X
Benefits covered: Physician X X X
Benefits covered: Nurse practitioner X
Benefits covered: Rural health clinics
and FQHCs
X
Benefits covered: Clinic services X X
Benefits covered: Lab and x-ray X X
Benefits covered: Prescription drugs X
Benefits covered: Prosthetic devices
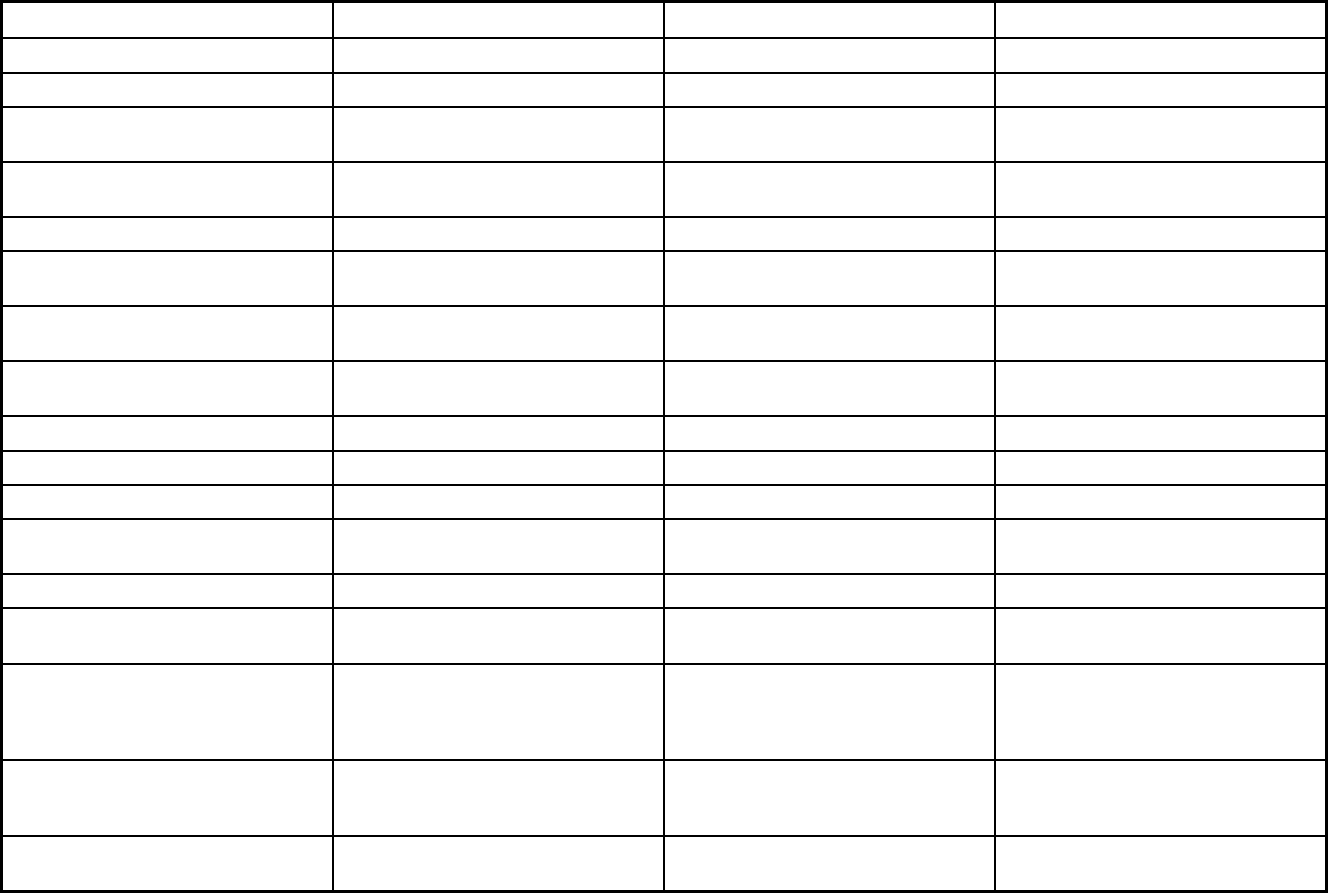
196
Features Maternity Care Program PACE Patient 1st
Benefits covered: EPSDT
Benefits covered: Case management X X X
Benefits covered: SSA Section 1945-
authorized health home
Benefits covered: Health home care
(services in home)
X
Benefits covered: Family planning X
Benefits covered: Dental services
(medical/surgical)
X
Benefits covered: Dental (preventative
or corrective)
X
Benefits covered: Personal care (state
plan option)
X
Benefits covered: HCBS waiver services
Benefits covered: Private duty nursing X
Benefits covered: ICF-IDD
Benefits covered: Nursing facility
services
X
Benefits covered: Hospice care X
Benefits covered: Non-Emergency
Medical Transportation
X
Benefits covered: Institution for Mental
Disease inpatient treatment for people
ages 21-64 defined by 42 CFR
§438.6(e) as an 'in lieu of' benefit
Benefits covered: Other (e.g., nurse
midwife services, freestanding birth
centers, podiatry, etc.)
Freestanding birth centers Other medically necessary services as
determined by the interdiscplinary team
Quality assurance and improvement:
HEDIS data required?
No No No
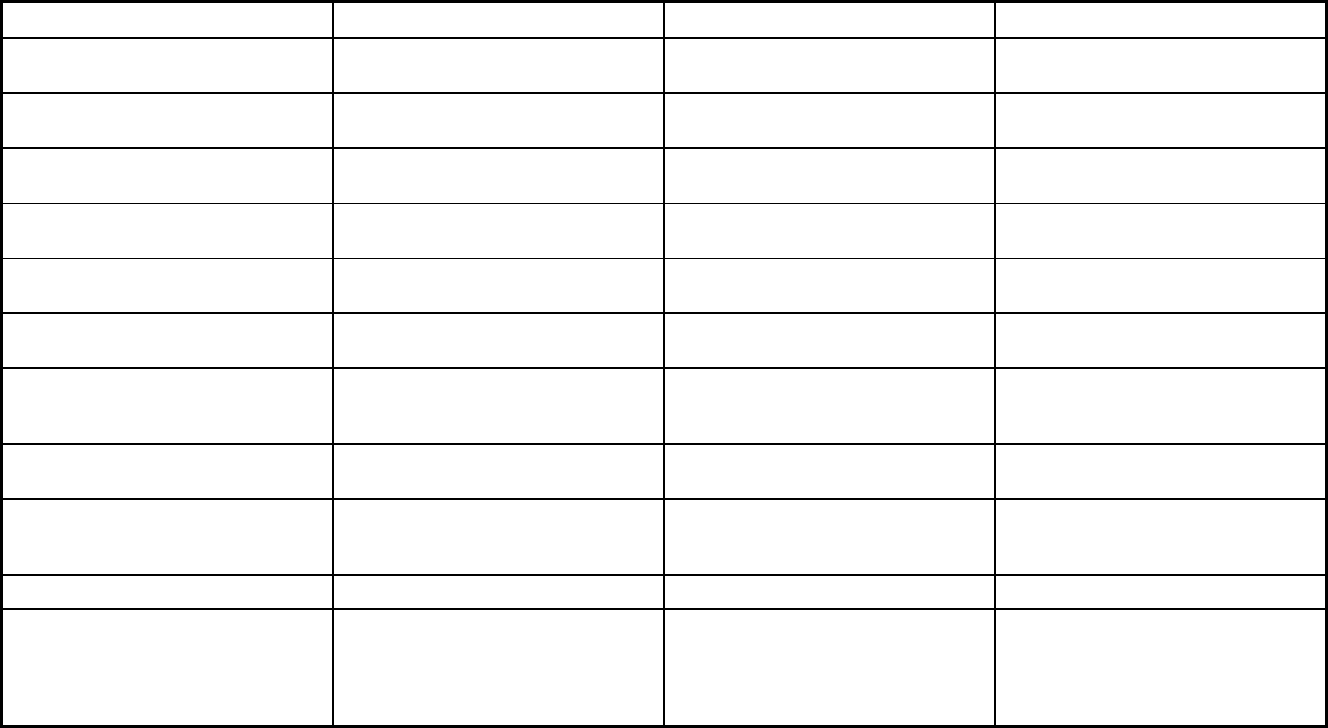
197
Features Maternity Care Program PACE Patient 1st
Quality assurance and improvement:
CAHPS data required?
Yes No No
Quality assurance and improvement:
Accreditation required?
No No No
Quality assurance and improvement:
Accrediting organization
Quality assurance and improvement:
EQRO contractor name (if applicable)
Performance incentives: Payment
bonuses/differentials to reward plans
Performance incentives: Preferential
auto-enrollment to reward plans
Performance incentives: Public reports
comparing plan performance on key
metrics
Performance incentives: Withholds tied
to performance metrics
Performance incentives: MCOs/PHPs
required or encouraged to pay providers
for value/quality outcomes
Participating plans: Plans in Program Maternity Care Plan Mercy Life of Alabama Patient 1st
Notes: Program notes This is only a maternity care program. It
is a PAHP only program. Maternity
services are provided FFS, not under
1915(b) authority in the above excluded
counties.
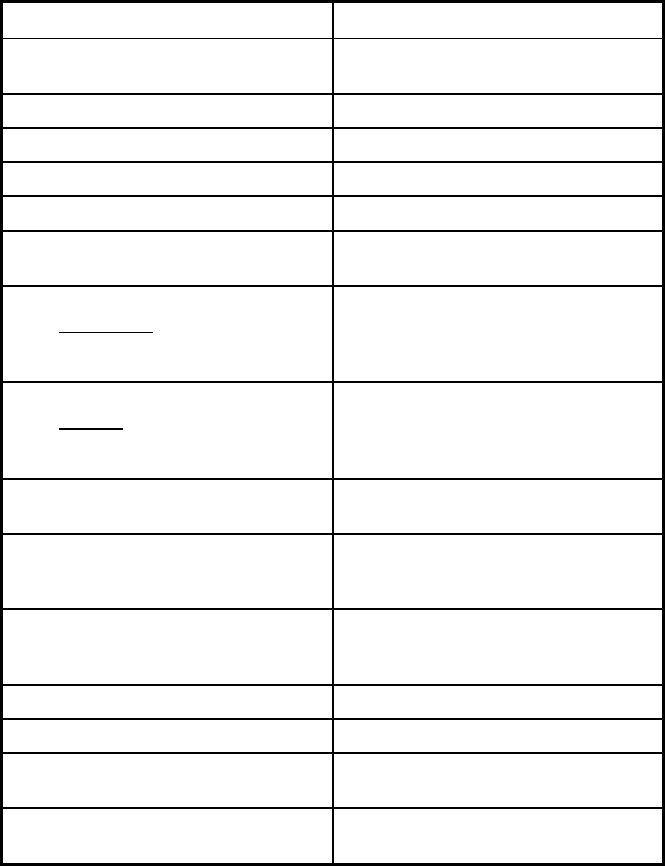
198
Alabama Managed Care Program Features, as of 2018 (2 of 2)
Features Health Homes
Program type Primary Care Case Management
(PCCM)
Statewide or region-specific? Statewide
Federal operating authority 1945 Health Homes
Program start date 04/01/2015
Waiver expiration date (if applicable)
If the program ended in 2018, indicate
the end date
Populations enrolled: Low-income
adults not covered under ACA Section
VIII (excludes pregnant women and
people with disabilities)
Populations enrolled: Low-income
adults covered under ACA Section VIII
(excludes pregnant women and people
with disabilities)
Populations enrolled: Aged, Blind or
Disabled Children or Adults
Mandatory
Populations enrolled: Non-Disabled
Children (excludes children in foster
care or receiving adoption assistance)
Mandatory
Populations enrolled: Individuals
receiving Limited Benefits (excludes
partial duals)
Mandatory
Populations enrolled: Full Duals
Populations enrolled: Partial Duals
Populations enrolled: Children with
Special Health Care Needs
Mandatory
Populations enrolled: Native
American/Alaskan Natives
Voluntary
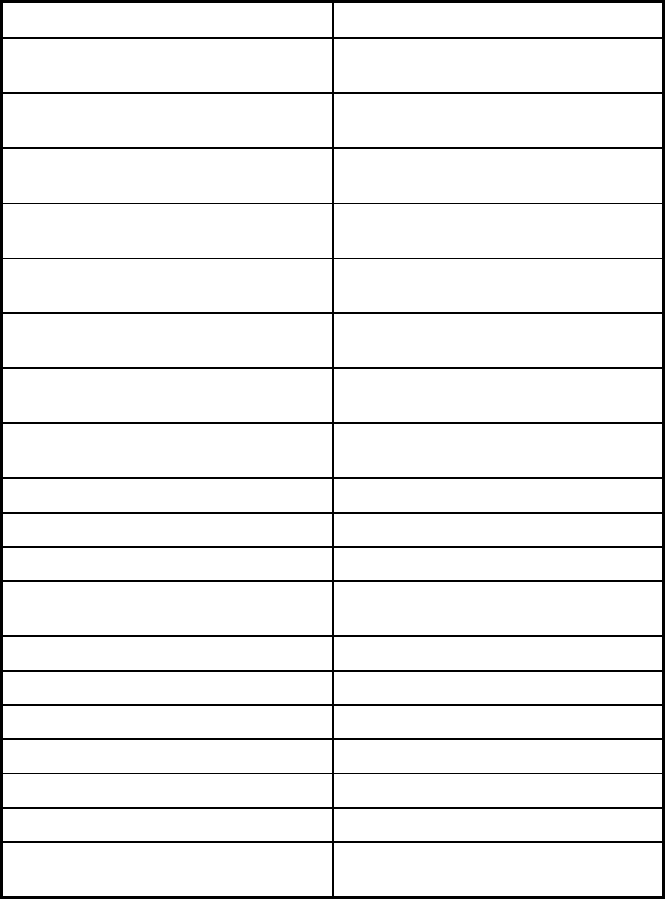
199
Features Health Homes
Populations enrolled: Foster Care and
Adoption Assistance Children
Exempt
Populations enrolled: Enrollment choice
period
N/A
Populations enrolled: Enrollment broker
name (if applicable)
Populations enrolled: Notes on
enrollment choice period
Benefits covered: Inpatient hospital
physical health
Benefits covered: Inpatient hospital
behavioral health (MH and/or SUD)
Benefits covered: Outpatient hospital
physical health
Benefits covered: Outpatient hospital
behavioral health (MH and/or SUD)
Benefits covered: Partial hospitalization
Benefits covered: Physician
Benefits covered: Nurse practitioner
Benefits covered: Rural health clinics
and FQHCs
Benefits covered: Clinic services
Benefits covered: Lab and x-ray
Benefits covered: Prescription drugs
Benefits covered: Prosthetic devices
Benefits covered: EPSDT
Benefits covered: Case management X
Benefits covered: SSA Section 1945-
authorized health home
X
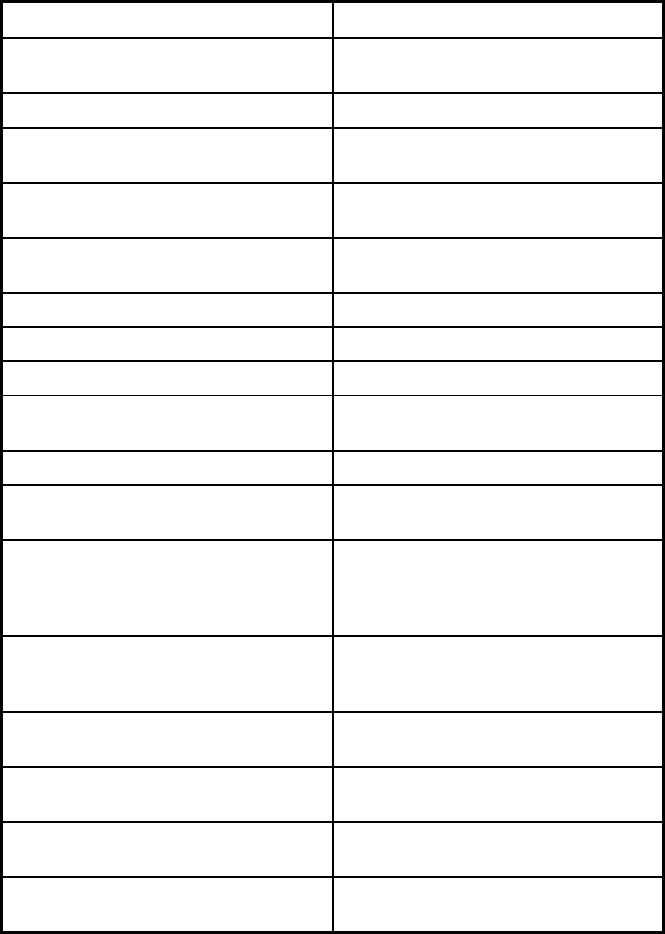
200
Features Health Homes
Benefits covered: Health home care
(services in home)
Benefits covered: Family planning
Benefits covered: Dental services
(medical/surgical)
Benefits covered: Dental (preventative
or corrective)
Benefits covered: Personal care (state
plan option)
Benefits covered: HCBS waiver services
Benefits covered: Private duty nursing
Benefits covered: ICF-IDD
Benefits covered: Nursing facility
services
Benefits covered: Hospice care
Benefits covered: Non-Emergency
Medical Transportation
Benefits covered: Institution for Mental
Disease inpatient treatment for people
ages 21-64 defined by 42 CFR
§438.6(e) as an 'in lieu of' benefit
Benefits covered: Other (e.g., nurse
midwife services, freestanding birth
centers, podiatry, etc.)
Quality assurance and improvement:
HEDIS data required?
Yes
Quality assurance and improvement:
CAHPS data required?
Yes
Quality assurance and improvement:
Accreditation required?
No
Quality assurance and improvement:
Accrediting organization
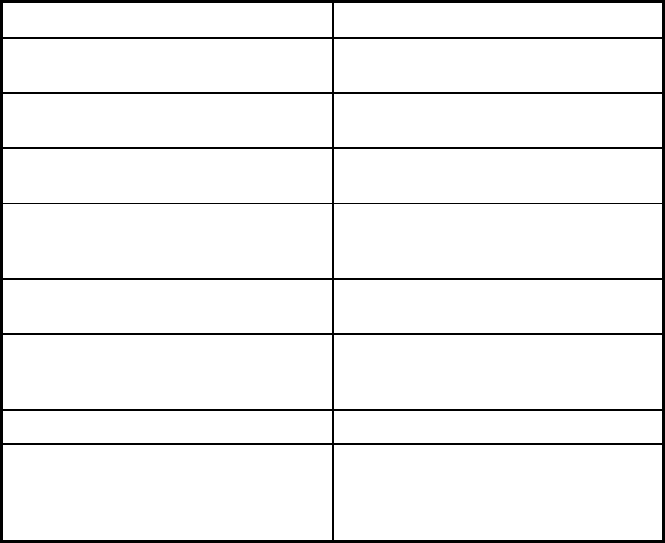
201
Features Health Homes
Quality assurance and improvement:
EQRO contractor name (if applicable)
Performance incentives: Payment
bonuses/differentials to reward plans
Performance incentives: Preferential
auto-enrollment to reward plans
Performance incentives: Public reports
comparing plan performance on key
metrics
Performance incentives: Withholds tied
to performance metrics
Performance incentives: MCOs/PHPs
required or encouraged to pay providers
for value/quality outcomes
Participating plans: Plans in Program Health Homes
Notes: Program notes To be eligible for the Health Home, a
recipient must be enrolled in Patient 1st
and their assigned PMP must also be
participating in the Health Home.
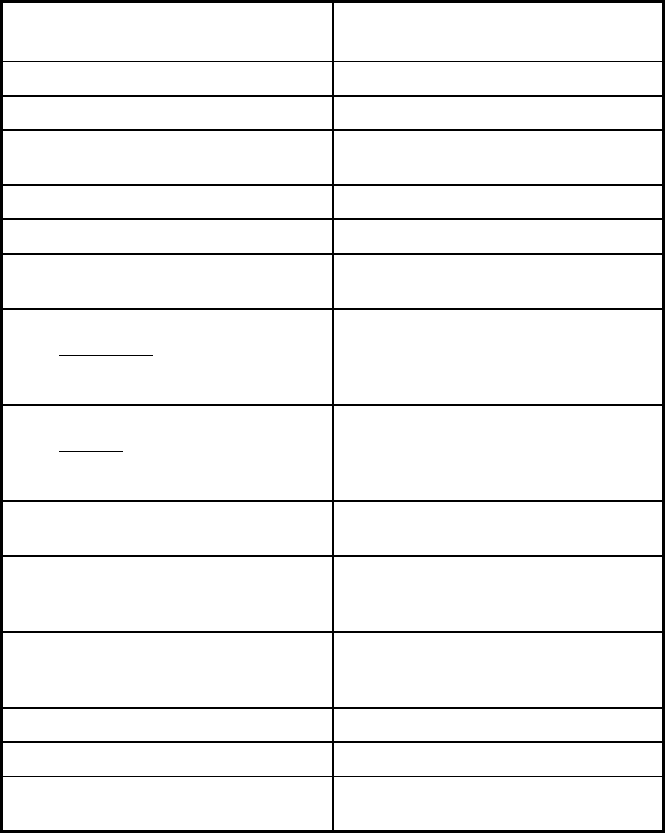
202
Arizona Managed Care Program Features, as of 2018
Features
Arizona Health Care Cost
Containment System
Program type Comprehensive MCO + MLTSS
efStatewide or region-specific? Statewide
Federal operating authority 1115(a) (Medicaid demonstration
waivers)
Program start date 07/13/1982
Waiver expiration date (if applicable) 09/30/2021
If the program ended in 2018, indicate
the end date
Populations enrolled: Low-income
adults not covered under ACA Section
VIII (excludes pregnant women and
people with disabilities)
Mandatory
Populations enrolled: Low-income
adults covered under ACA Section VIII
(excludes pregnant women and people
with disabilities)
Mandatory
Populations enrolled: Aged, Blind or
Disabled Children or Adults
Mandatory
Populations enrolled: Non-Disabled
Children (excludes children in foster
care or receiving adoption assistance)
Mandatory
Populations enrolled: Individuals
receiving Limited Benefits (excludes
partial duals)
Populations enrolled: Full Duals Mandatory
Populations enrolled: Partial Duals
Populations enrolled: Children with
Special Health Care Needs
Mandatory
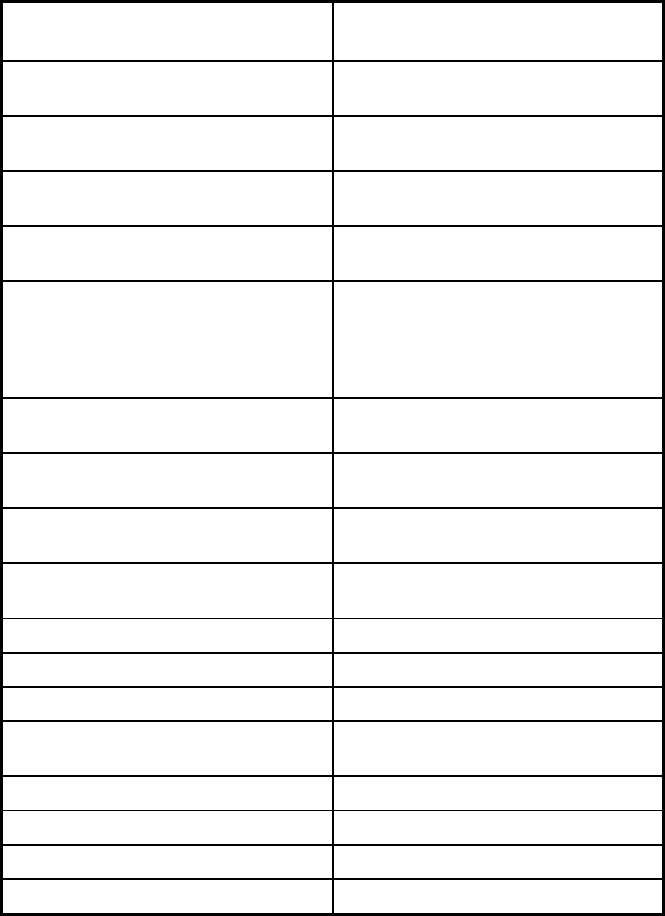
203
Features
Arizona Health Care Cost
Containment System
Populations enrolled: Native
American/Alaskan Natives
Voluntary
Populations enrolled: Foster Care and
Adoption Assistance Children
Mandatory
Populations enrolled: Enrollment choice
period
Other
Populations enrolled: Enrollment broker
name (if applicable)
Populations enrolled: Notes on
enrollment choice period
The enrollment choice period for
members who are auto-assigned is 90
days. After the initial enrollment choice
period, members receive an annual
enrollment choice period of 60 days.
Benefits covered: Inpatient hospital
physical health
X
Benefits covered: Inpatient hospital
behavioral health (MH and/or SUD)
X
Benefits covered: Outpatient hospital
physical health
X
Benefits covered: Outpatient hospital
behavioral health (MH and/or SUD)
X
Benefits covered: Partial hospitalization
Benefits covered: Physician X
Benefits covered: Nurse practitioner X
Benefits covered: Rural health clinics
and FQHCs
X
Benefits covered: Clinic services X
Benefits covered: Lab and x-ray X
Benefits covered: Prescription drugs X
Benefits covered: Prosthetic devices X
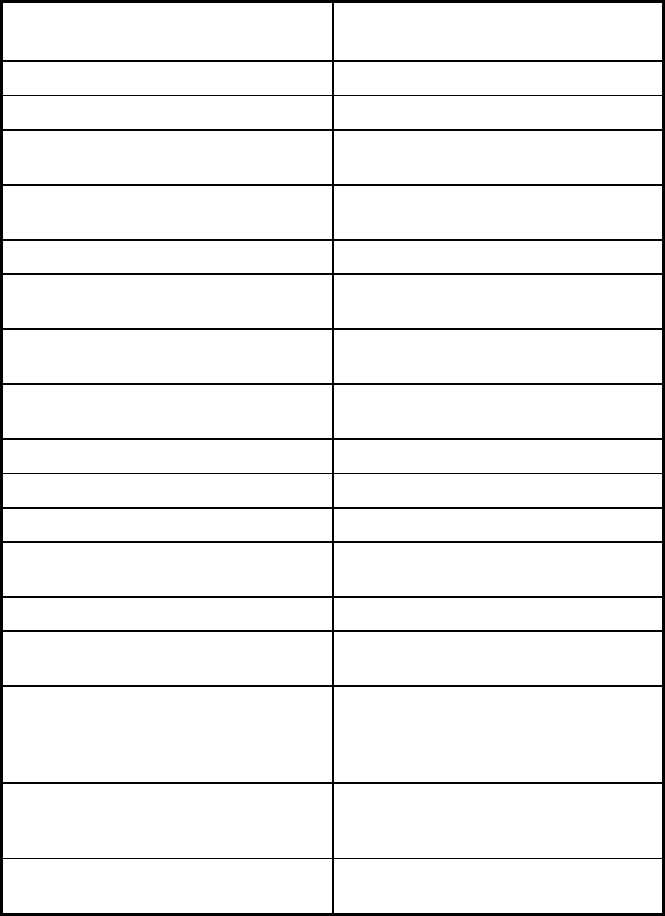
204
Features
Arizona Health Care Cost
Containment System
Benefits covered: EPSDT X
Benefits covered: Case management X
Benefits covered: SSA Section 1945-
authorized health home
Benefits covered: Health home care
(services in home)
X
Benefits covered: Family planning X
Benefits covered: Dental services
(medical/surgical)
X
Benefits covered: Dental (preventative
or corrective)
X
Benefits covered: Personal care (state
plan option)
X
Benefits covered: HCBS waiver services X
Benefits covered: Private duty nursing X
Benefits covered: ICF-IDD X
Benefits covered: Nursing facility
services
X
Benefits covered: Hospice care X
Benefits covered: Non-Emergency
Medical Transportation
X
Benefits covered: Institution for Mental
Disease inpatient treatment for people
ages 21-64 defined by 42 CFR
§438.6(e) as an 'in lieu of' benefit
X
Benefits covered: Other (e.g., nurse
midwife services, freestanding birth
centers, podiatry, etc.)
Freestanding birth centers & podiatry
Quality assurance and improvement:
HEDIS data required?
Yes
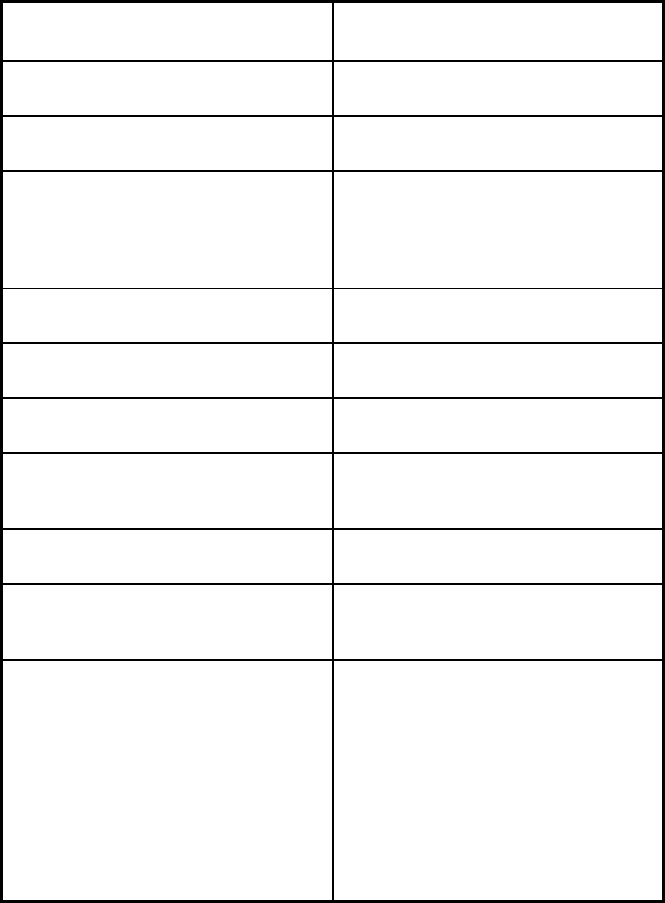
205
Features
Arizona Health Care Cost
Containment System
Quality assurance and improvement:
CAHPS data required?
Yes
Quality assurance and improvement:
Accreditation required?
No
Quality assurance and improvement:
Accrediting organization
Please note that HEDIS and CAHPS
are run by the EQRO not the MCO.
CAHPS is completed by our EQRO, but
AHCCCS does not request that every
population be evaluated every year.
Quality assurance and improvement:
EQRO contractor name (if applicable)
Health Services Advisory Group
Performance incentives: Payment
bonuses/differentials to reward plans
X
Performance incentives: Preferential
auto-enrollment to reward plans
X
Performance incentives: Public reports
comparing plan performance on key
metrics
X
Performance incentives: Withholds tied
to performance metrics
X
Performance incentives: MCOs/PHPs
required or encouraged to pay providers
for value/quality outcomes
X
Participating plans: Plans in Program United Healthcare Plan; Care1st Health
Plan; DCS/CMDP; DES/Division of
Developmental Disabilities (MLTSS);
United Healthcare Plan (MLTSS);
Health Choice Arizona; Health Net
Access; Mercy Care Plan; Mercy Care
Plan (MLTSS); University Family Care;
Mercy Maricopa Integrated Care;
Cenpatico Integrated Care; Health
Choice Integrated Care; Banner
University Family Care (MLTSS)
206
Features
Arizona Health Care Cost
Containment System
Notes: Program notes Enrollment (voluntary with auto-
enrollment) – members have choice,
and if they do not choose then there are
rules for where they are auto-enrolled
depending on the program. If an
individual does not choose their plan
prior to eligibility being determined, they
are auto-enrolled in a health plan and
given 30 days to choose a different
plan. Most members in these groups are
mandatorily enrolled, but American
Indian/Alaska Native members of these
populations are voluntarily enrolled.
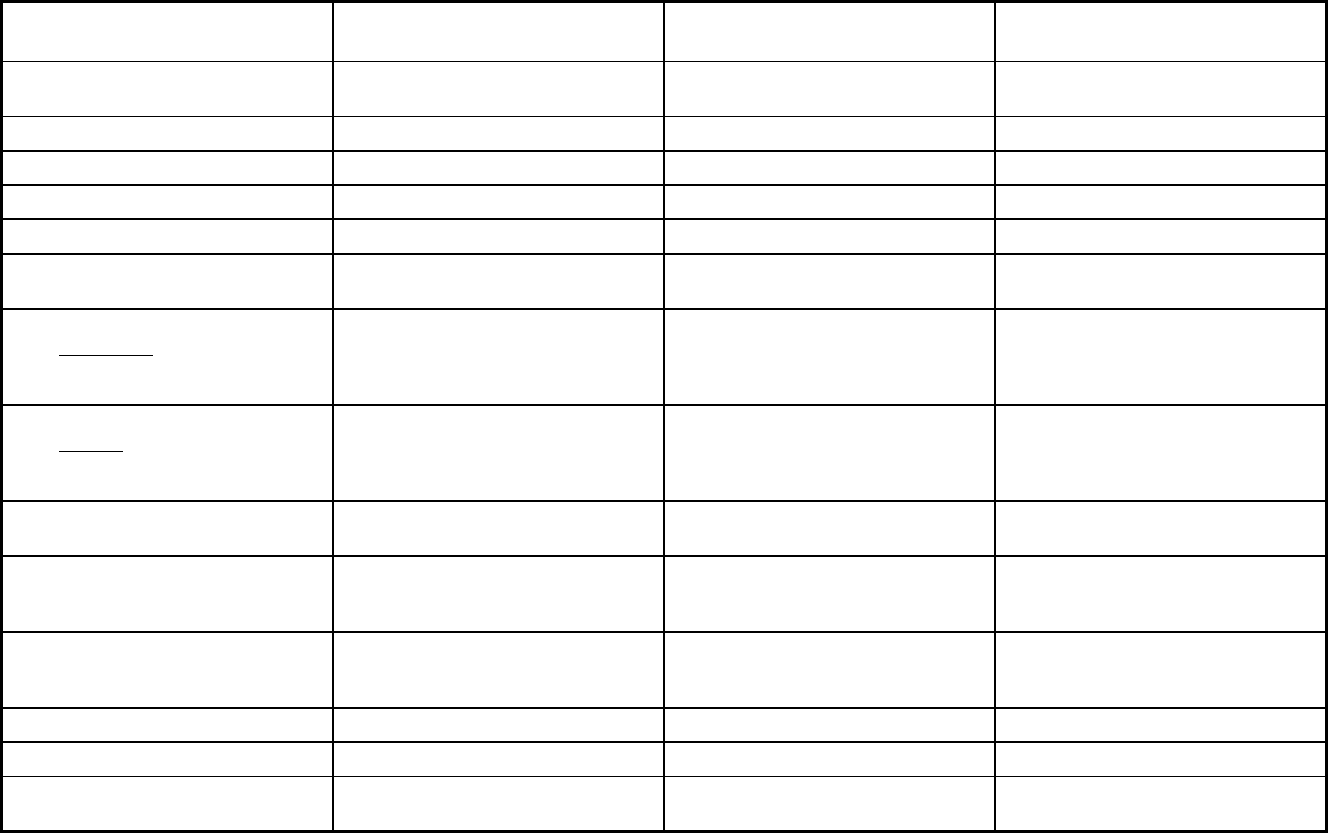
207
Arkansas Managed Care Program Features, as of 2018 (1 of 2)
Features Connect Care PACE
Provider-Led Arkansas Shared
Savings Entity (PASSE) Program
Program type Primary Care Case Management
(PCCM)
Program of All-inclusive Care for the
Elderly (PACE)
Primary Care Case Management Entity
(PCCM Entity)
Statewide or region-specific? Statewide Statewide Statewide
Federal operating authority 1932(a) PACE 1915(b)
Program start date 01/01/2014 04/01/2016 02/01/2018
Waiver expiration date (if applicable) 03/01/2019
If the program ended in 2018, indicate
the end date
Populations enrolled: Low-income
adults not covered under ACA Section
VIII (excludes pregnant women and
people with disabilities)
Mandatory Mandatory
Populations enrolled: Low-income
adults covered under ACA Section VIII
(excludes pregnant women and people
with disabilities)
Mandatory
Populations enrolled: Aged, Blind or
Disabled Children or Adults
Mandatory Voluntary Mandatory
Populations enrolled: Non-Disabled
Children (excludes children in foster
care or receiving adoption assistance)
Mandatory
Populations enrolled: Individuals
receiving Limited Benefits (excludes
partial duals)
Populations enrolled: Full Duals Voluntary Mandatory
Populations enrolled: Partial Duals
Populations enrolled: Children with
Special Health Care Needs
Mandatory
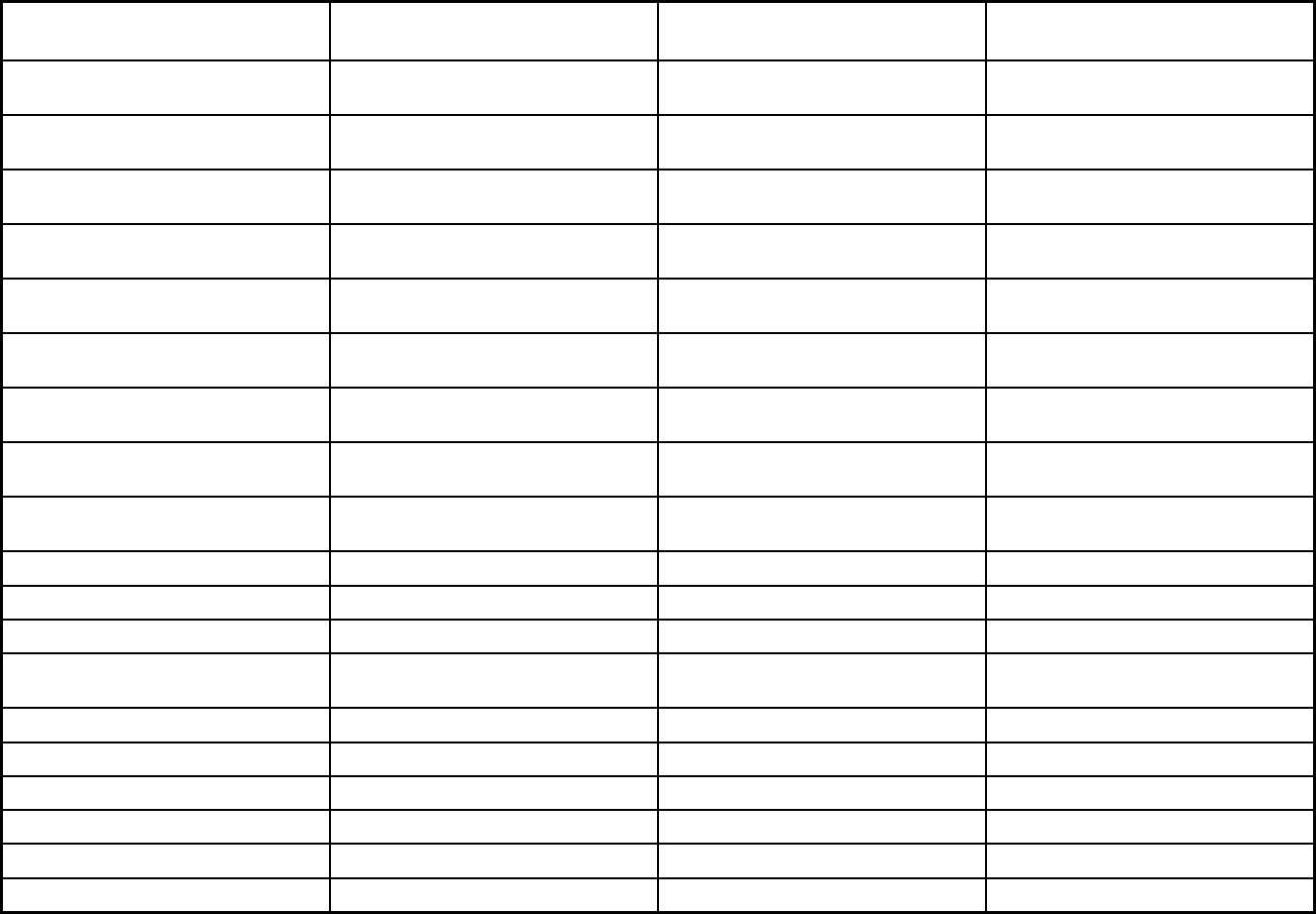
208
Features Connect Care PACE
Provider-Led Arkansas Shared
Savings Entity (PASSE) Program
Populations enrolled: Native
American/Alaskan Natives
Exempt Exempt Exempt
Populations enrolled: Foster Care and
Adoption Assistance Children
Mandatory Mandatory
Populations enrolled: Enrollment choice
period
N/A N/A Pre-assigned
Populations enrolled: Enrollment broker
name (if applicable)
Populations enrolled: Notes on
enrollment choice period
Benefits covered: Inpatient hospital
physical health
Benefits covered: Inpatient hospital
behavioral health (MH and/or SUD)
Benefits covered: Outpatient hospital
physical health
Benefits covered: Outpatient hospital
behavioral health (MH and/or SUD)
Benefits covered: Partial hospitalization X
Benefits covered: Physician X
Benefits covered: Nurse practitioner
Benefits covered: Rural health clinics
and FQHCs
Benefits covered: Clinic services X
Benefits covered: Lab and x-ray X
Benefits covered: Prescription drugs
Benefits covered: Prosthetic devices
Benefits covered: EPSDT
Benefits covered: Case management X X X
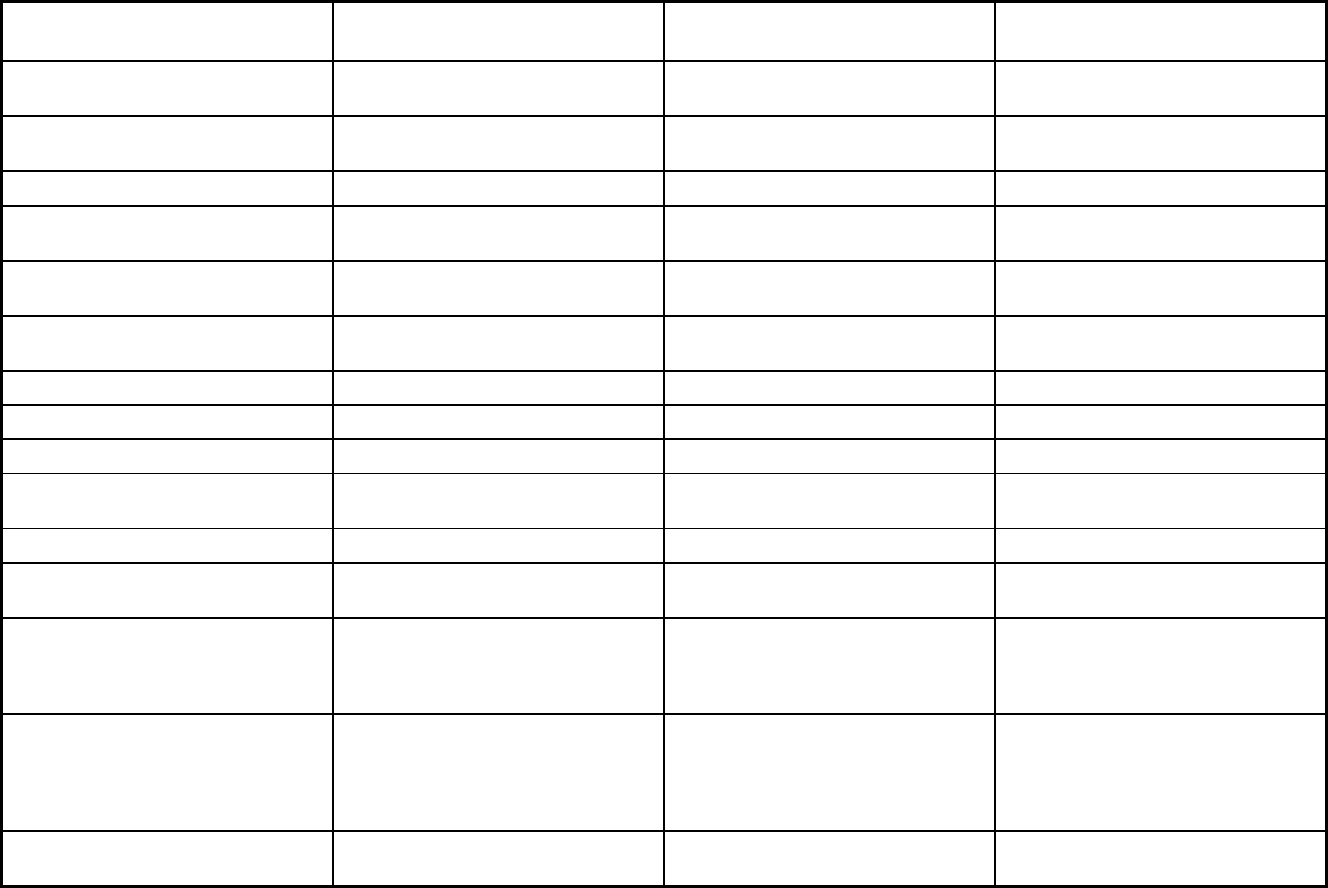
209
Features Connect Care PACE
Provider-Led Arkansas Shared
Savings Entity (PASSE) Program
Benefits covered: SSA Section 1945-
authorized health home
Benefits covered: Health home care
(services in home)
Benefits covered: Family planning
Benefits covered: Dental services
(medical/surgical)
X
Benefits covered: Dental (preventative
or corrective)
Benefits covered: Personal care (state
plan option)
X
Benefits covered: HCBS waiver services
Benefits covered: Private duty nursing
Benefits covered: ICF-IDD
Benefits covered: Nursing facility
services
Benefits covered: Hospice care
Benefits covered: Non-Emergency
Medical Transportation
Benefits covered: Institution for Mental
Disease inpatient treatment for people
ages 21-64 defined by 42 CFR
§438.6(e) as an 'in lieu of' benefit
Benefits covered: Other (e.g., nurse
midwife services, freestanding birth
centers, podiatry, etc.)
Capitated comprehensive medical and
social services in adult day health
centers and in-home and referral
services according to the participants
needs.
Quality assurance and improvement:
HEDIS data required?
No No No
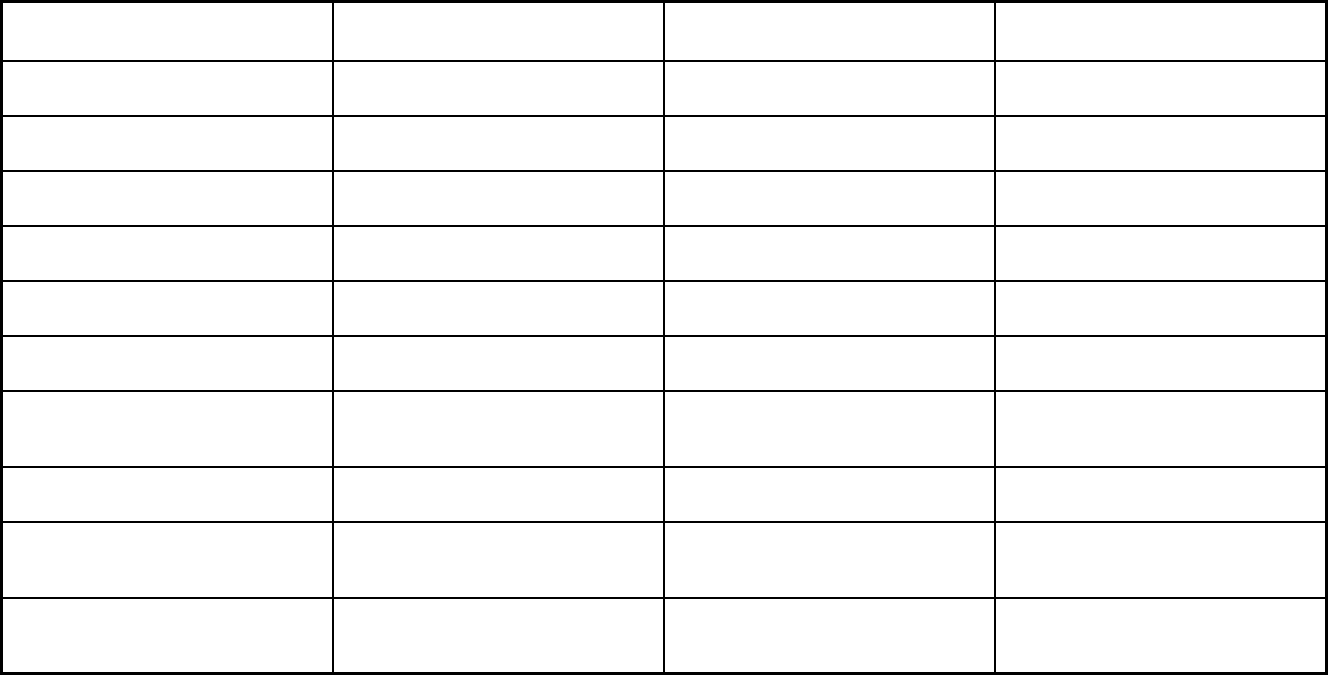
210
Features Connect Care PACE
Provider-Led Arkansas Shared
Savings Entity (PASSE) Program
Quality assurance and improvement:
CAHPS data required?
Yes No No
Quality assurance and improvement:
Accreditation required?
No Yes No
Quality assurance and improvement:
Accrediting organization
Health Management Plan (CMS)
Quality assurance and improvement:
EQRO contractor name (if applicable)
Performance incentives: Payment
bonuses/differentials to reward plans
Performance incentives: Preferential
auto-enrollment to reward plans
Performance incentives: Public reports
comparing plan performance on key
metrics
Performance incentives: Withholds tied
to performance metrics
Performance incentives: MCOs/PHPs
required or encouraged to pay providers
for value/quality outcomes
Participating plans: Plans in Program Multiple primary care providers Complete Health; Total Life Healthcare Summit Community Care; Arkansas
Total Care; Empower Healthcare
Solutions; Forevercare
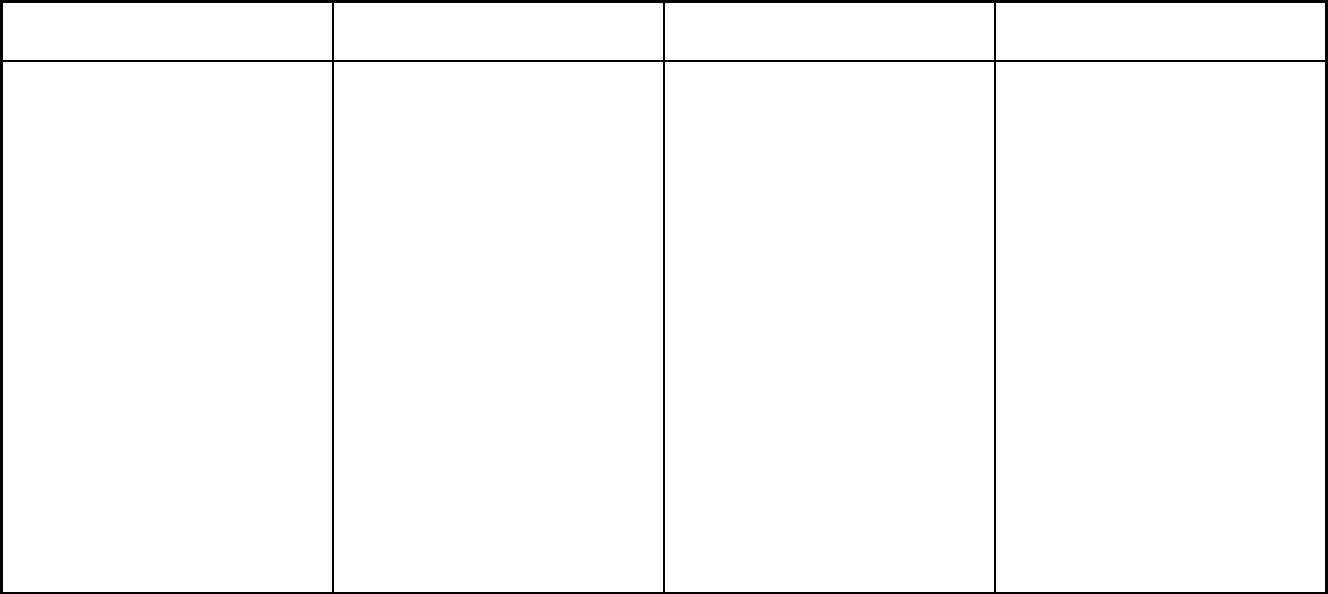
211
Features Connect Care PACE
Provider-Led Arkansas Shared
Savings Entity (PASSE) Program
Notes: Program notes The PASSE is designed to address the
needs of Medicaid beneficiaries who
have complex behavioral health and
intellectual and developmental
disabilities service needs. Providers of
specialty and medical services will enter
into pa
rtnerships with each other and an
experienced organization that performs
administrative functions similar to
insurance companies. Providers retain
majority ownership of each PASSE.
The
governing body of each PASSE must
include several types of providers
including a Developmental Disabilities
Services provider, a Behavioral Health
Services provider, a hospital, a
physician, and a pharmacist. There are
2 phases of implementation. Phase I,
which began on February 1, 2018, is
when each PASSE is responsible for
providing care coordination to every
individual that has been assigned to
them. Phase II, which began March 1,
2019, is when the PASSE entered into a
full-risk contract as an MCO.
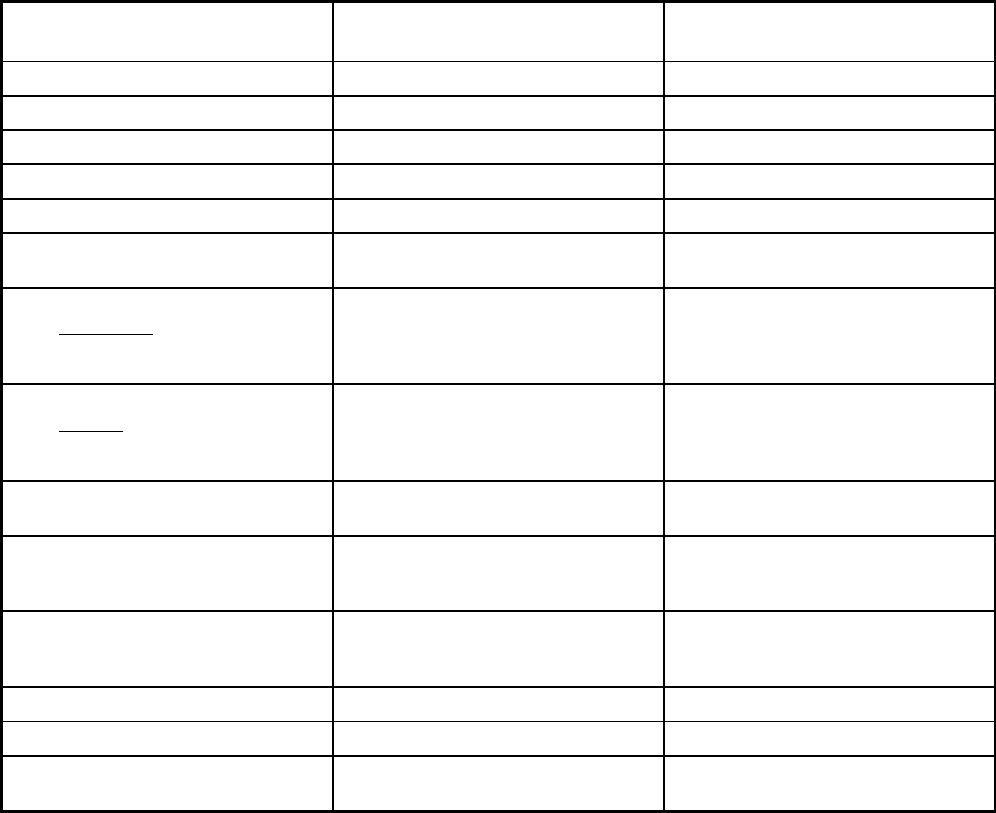
212
Arkansas Managed Care Program Features, as of 2018 (2 of 2)
Features Arkansas Dental Managed Care
Arkansas Non-Emergency Medical
Transport (NET)
Program type Dental only (PAHP) Non-Emergency Medical Transportation
Statewide or region-specific? Statewide Statewide
Federal operating authority 1915(b) 1915(b),1902(a)(70) NEMT
Program start date 01/01/2018 03/01/1998
Waiver expiration date (if applicable) 12/31/2022 09/30/2019
If the program ended in 2018, indicate
the end date
Populations enrolled: Low-income
adults not covered under ACA Section
VIII (excludes pregnant women and
people with disabilities)
Mandatory Mandatory
Populations enrolled: Low-income
adults covered under ACA Section VIII
(excludes pregnant women and people
with disabilities)
Mandatory
Populations enrolled: Aged, Blind or
Disabled Children or Adults
Mandatory Mandatory
Populations enrolled: Non-Disabled
Children (excludes children in foster
care or receiving adoption assistance)
Mandatory Mandatory
Populations enrolled: Individuals
receiving Limited Benefits (excludes
partial duals)
Populations enrolled: Full Duals Mandatory Mandatory
Populations enrolled: Partial Duals
Populations enrolled: Children with
Special Health Care Needs
Mandatory Mandatory
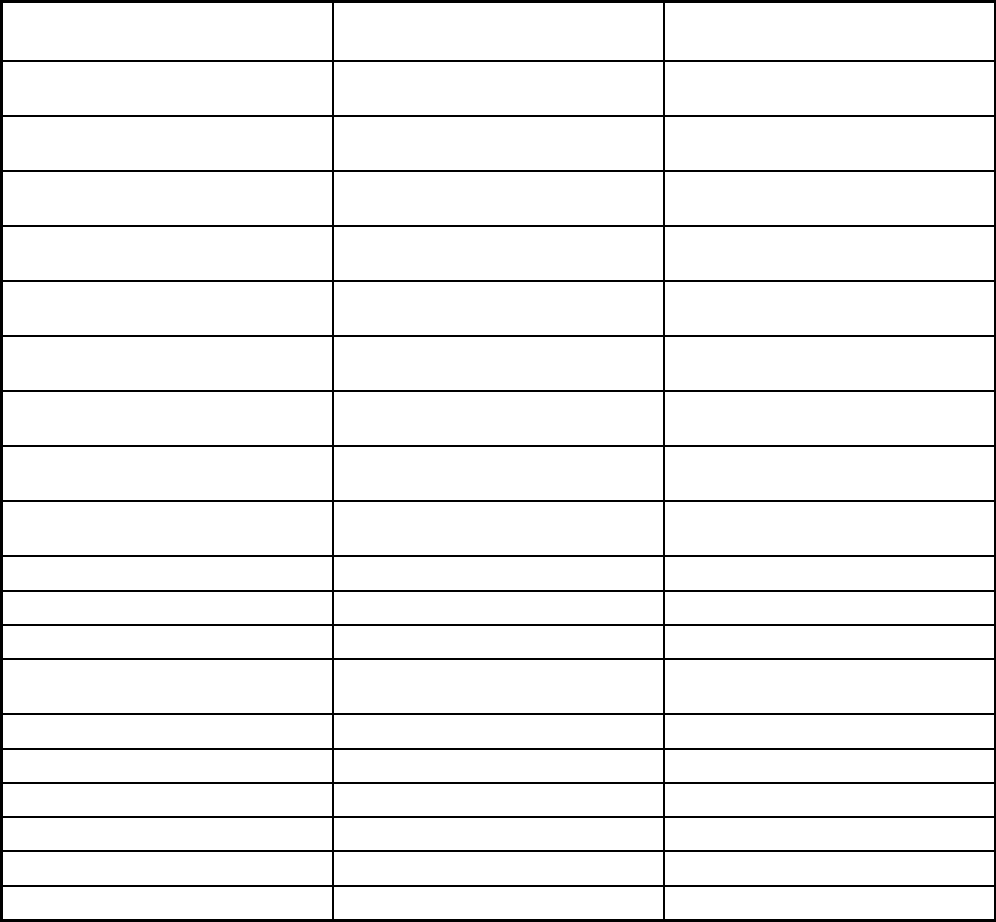
213
Features Arkansas Dental Managed Care
Arkansas Non-Emergency Medical
Transport (NET)
Populations enrolled: Native
American/Alaskan Natives
Voluntary Exempt
Populations enrolled: Foster Care and
Adoption Assistance Children
Mandatory Mandatory
Populations enrolled: Enrollment choice
period
Pre-assigned
Populations enrolled: Enrollment broker
name (if applicable)
Populations enrolled: Notes on
enrollment choice period
Benefits covered: Inpatient hospital
physical health
Benefits covered: Inpatient hospital
behavioral health (MH and/or SUD)
Benefits covered: Outpatient hospital
physical health
Benefits covered: Outpatient hospital
behavioral health (MH and/or SUD)
Benefits covered: Partial hospitalization
Benefits covered: Physician
Benefits covered: Nurse practitioner
Benefits covered: Rural health clinics
and FQHCs
Benefits covered: Clinic services
Benefits covered: Lab and x-ray
Benefits covered: Prescription drugs
Benefits covered: Prosthetic devices
Benefits covered: EPSDT
Benefits covered: Case management
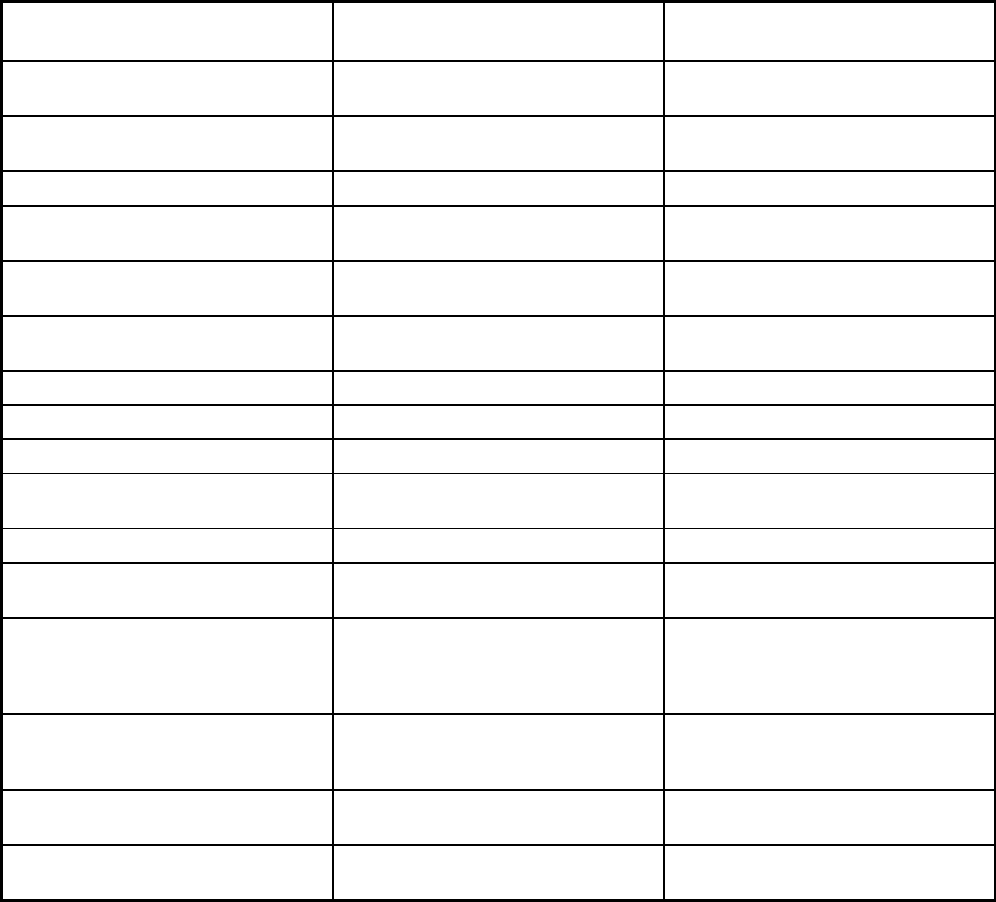
214
Features Arkansas Dental Managed Care
Arkansas Non-Emergency Medical
Transport (NET)
Benefits covered: SSA Section 1945-
authorized health home
Benefits covered: Health home care
(services in home)
Benefits covered: Family planning
Benefits covered: Dental services
(medical/surgical)
X
Benefits covered: Dental (preventative
or corrective)
X
Benefits covered: Personal care (state
plan option)
Benefits covered: HCBS waiver services
Benefits covered: Private duty nursing
Benefits covered: ICF-IDD
Benefits covered: Nursing facility
services
Benefits covered: Hospice care
Benefits covered: Non-Emergency
Medical Transportation
X
Benefits covered: Institution for Mental
Disease inpatient treatment for people
ages 21-64 defined by 42 CFR
§438.6(e) as an 'in lieu of' benefit
Benefits covered: Other (e.g., nurse
midwife services, freestanding birth
centers, podiatry, etc.)
Quality assurance and improvement:
HEDIS data required?
Yes No
Quality assurance and improvement:
CAHPS data required?
Yes No
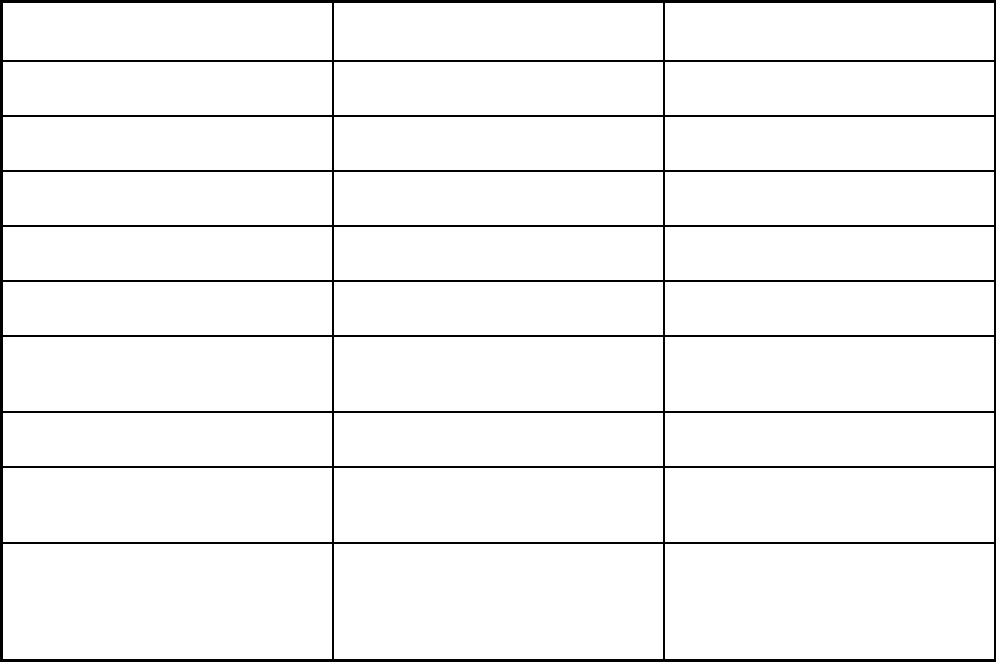
215
Features Arkansas Dental Managed Care
Arkansas Non-Emergency Medical
Transport (NET)
Quality assurance and improvement:
Accreditation required?
Yes No
Quality assurance and improvement:
Accrediting organization
URAC
Quality assurance and improvement:
EQRO contractor name (if applicable)
Performance incentives: Payment
bonuses/differentials to reward plans
Performance incentives: Preferential
auto-enrollment to reward plans
Performance incentives: Public reports
comparing plan performance on key
metrics
Performance incentives: Withholds tied
to performance metrics
Performance incentives: MCOs/PHPs
required or encouraged to pay providers
for value/quality outcomes
X
Participating plans: Plans in Program Delta Dental of Arkansas; Managed
Care of North America (MCNA) Dental
Southeasttrans; Central Arkansas
Development Council; Area Agency on
Aging of Western Arkansas; Mid-Delta;
Area Agency on Aging of Southeast
Arkansas
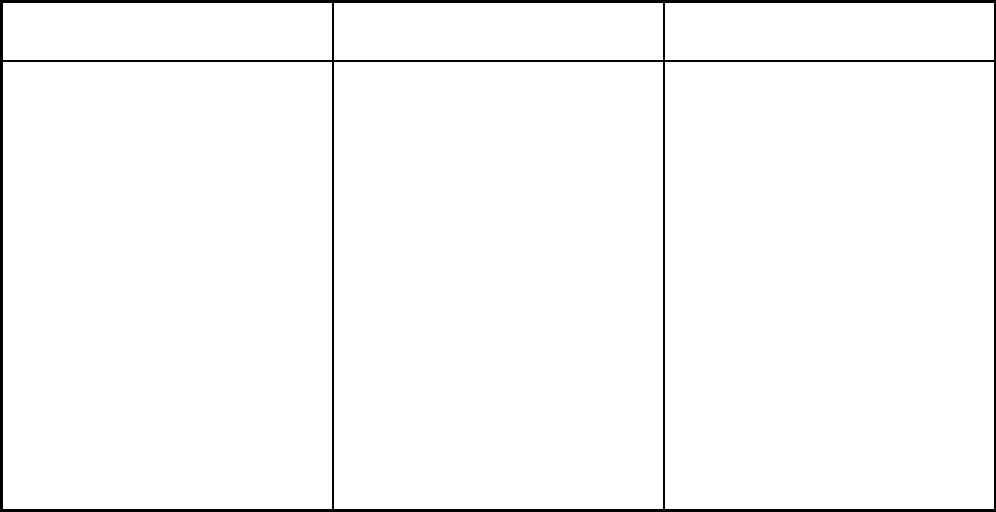
216
Features Arkansas Dental Managed Care
Arkansas Non-Emergency Medical
Transport (NET)
Notes: Program notes In early December 2017, all Arkansas
Medicaid beneficiaries who are eligible
for dental benefits were randomly and
evenly assigned to one of the two dental
managed care plans. Members were
able to access plan providers starting
January 1, 2018 for covered dental
services. If members wish to switch
plans, they have 90 days to do so. The
vendors will serve all members who
receive dental services through
Medicaid except for those residing in
Human Development Centers,
individuals enrolled in the Program for
All Inclusive Care for the Elderly
(PACE), members who reside in a
nursing home setting, and individuals
who are eligible for Medicaid only after
incurring medical expenses that cause
them to “spend down” to Medicaid
eligibility levels.
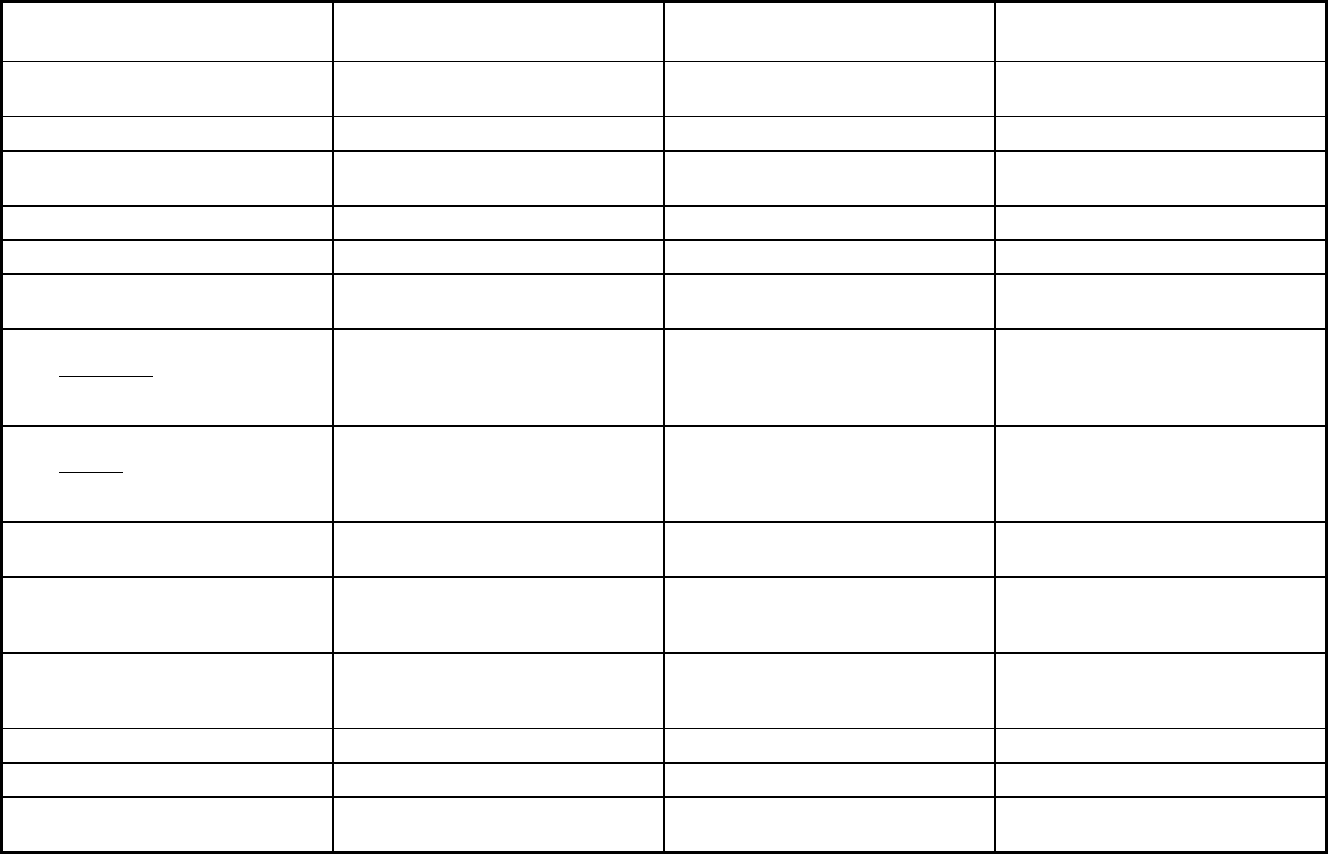
217
California Managed Care Program Features, as of 2018 (1 of 4)
Features Positive Healthcare/Los Angeles
Family Mosaic Program/San
Francisco
Health Plan of San Mateo CCS
Demo/San Mateo
Program type Other Prepaid Health Plan (PHP)
(limited benefits)
Behavioral Health Organization (BHO)
only (PIHP and/or PAHP)
Comprehensive MCO
Statewide or region-specific? Los Angeles San Francisco San Mateo
Federal operating authority 1937 Alt Benefit Plan 1915(a) 1115(a) (Medicaid demonstration
waivers)
Program start date 04/01/2002 12/01/1992 06/01/2012
Waiver expiration date (if applicable) 04/01/2018
If the program ended in 2018, indicate
the end date
04/01/2018
Populations enrolled: Low-income
adults not covered under ACA Section
VIII (excludes pregnant women and
people with disabilities)
Voluntary
Populations enrolled: Low-income
adults covered under ACA Section VIII
(excludes pregnant women and people
with disabilities)
Voluntary
Populations enrolled: Aged, Blind or
Disabled Children or Adults
Populations enrolled: Non-Disabled
Children (excludes children in foster
care or receiving adoption assistance)
Voluntary
Populations enrolled: Individuals
receiving Limited Benefits (excludes
partial duals)
Populations enrolled: Full Duals
Populations enrolled: Partial Duals
Populations enrolled: Children with
Special Health Care Needs
Voluntary Mandatory
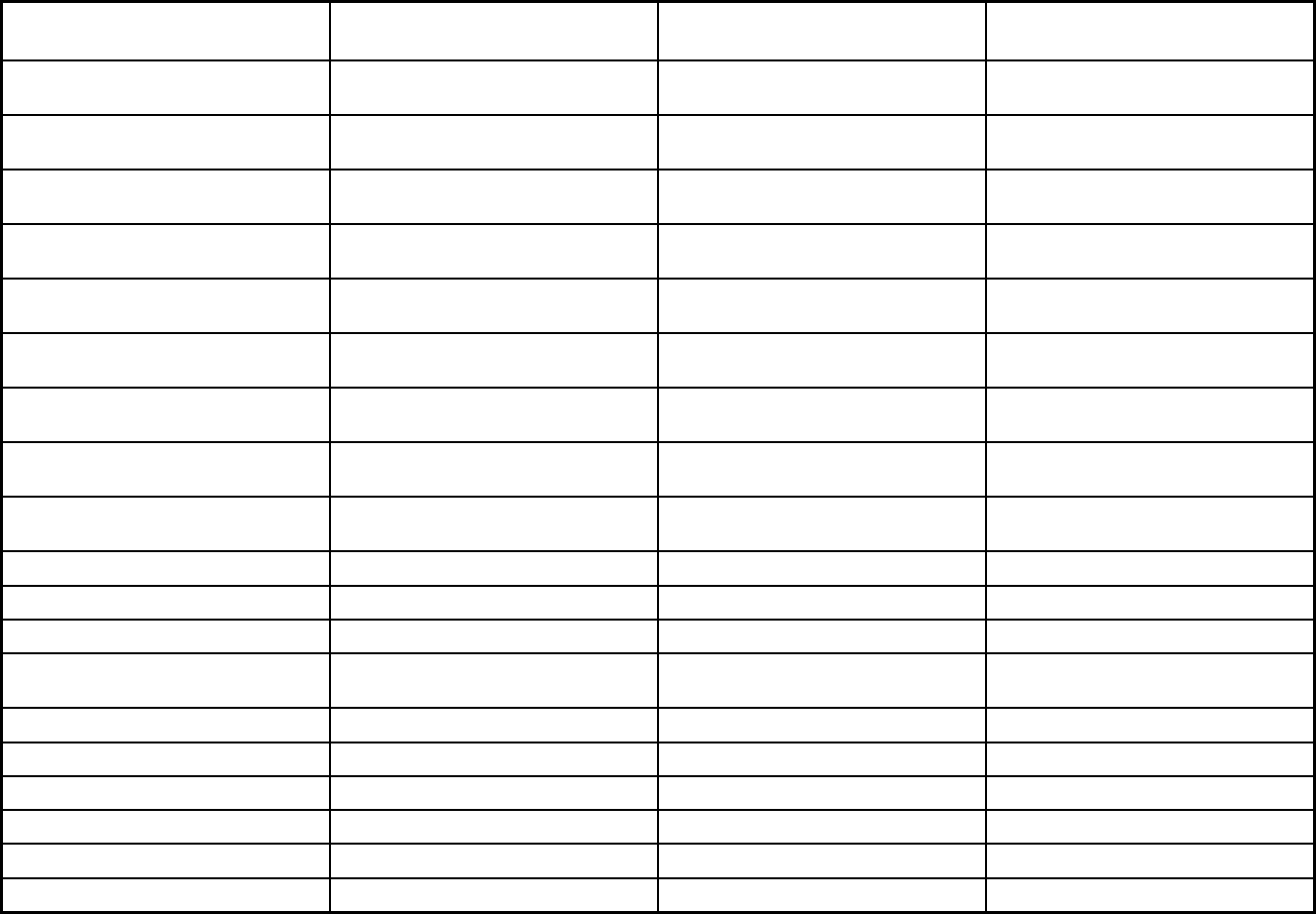
218
Features Positive Healthcare/Los Angeles
Family Mosaic Program/San
Francisco
Health Plan of San Mateo CCS
Demo/San Mateo
Populations enrolled: Native
American/Alaskan Natives
Voluntary Voluntary Exempt
Populations enrolled: Foster Care and
Adoption Assistance Children
Voluntary Voluntary Voluntary
Populations enrolled: Enrollment choice
period
Pre-assigned
Populations enrolled: Enrollment broker
name (if applicable)
Populations enrolled: Notes on
enrollment choice period
Benefits covered: Inpatient hospital
physical health
X
Benefits covered: Inpatient hospital
behavioral health (MH and/or SUD)
Benefits covered: Outpatient hospital
physical health
X X
Benefits covered: Outpatient hospital
behavioral health (MH and/or SUD)
X
Benefits covered: Partial hospitalization
Benefits covered: Physician X X
Benefits covered: Nurse practitioner X X X
Benefits covered: Rural health clinics
and FQHCs
X X
Benefits covered: Clinic services X X X
Benefits covered: Lab and x-ray X X X
Benefits covered: Prescription drugs X X X
Benefits covered: Prosthetic devices X X X
Benefits covered: EPSDT X X X
Benefits covered: Case management X X X
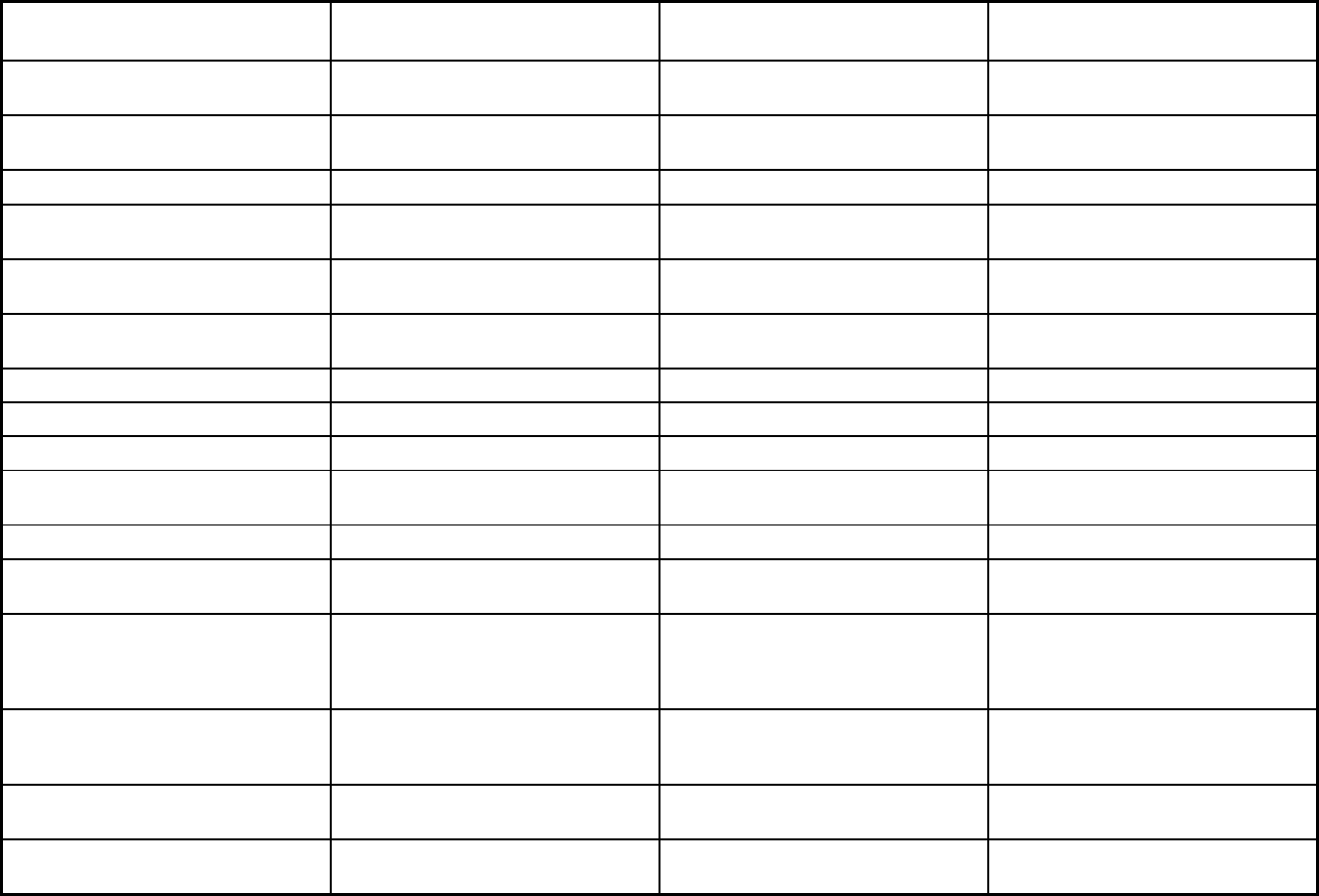
219
Features Positive Healthcare/Los Angeles
Family Mosaic Program/San
Francisco
Health Plan of San Mateo CCS
Demo/San Mateo
Benefits covered: SSA Section 1945-
authorized health home
Benefits covered: Health home care
(services in home)
Benefits covered: Family planning X X
Benefits covered: Dental services
(medical/surgical)
Benefits covered: Dental (preventative
or corrective)
Benefits covered: Personal care (state
plan option)
Benefits covered: HCBS waiver services
Benefits covered: Private duty nursing
Benefits covered: ICF-IDD
Benefits covered: Nursing facility
services
Benefits covered: Hospice care X X
Benefits covered: Non-Emergency
Medical Transportation
X X X
Benefits covered: Institution for Mental
Disease inpatient treatment for people
ages 21-64 defined by 42 CFR
§438.6(e) as an 'in lieu of' benefit
Benefits covered: Other (e.g., nurse
midwife services, freestanding birth
centers, podiatry, etc.)
Quality assurance and improvement:
HEDIS data required?
Yes Yes Yes
Quality assurance and improvement:
CAHPS data required?
Yes No No
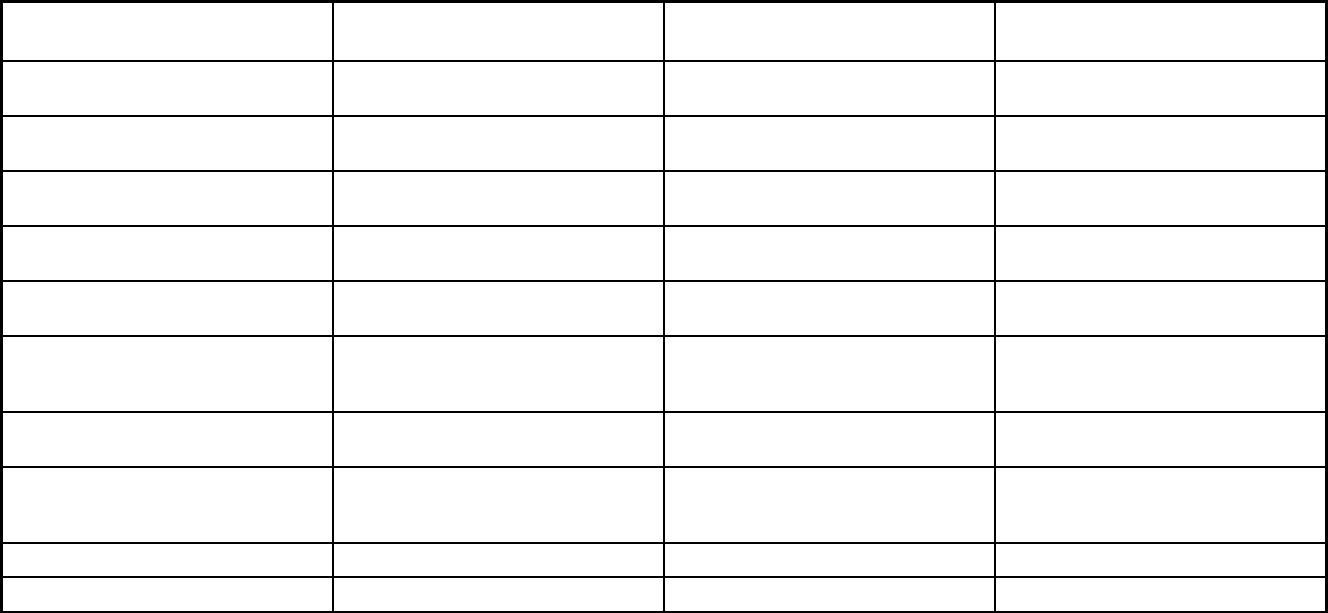
220
Features Positive Healthcare/Los Angeles
Family Mosaic Program/San
Francisco
Health Plan of San Mateo CCS
Demo/San Mateo
Quality assurance and improvement:
Accreditation required?
No No No
Quality assurance and improvement:
Accrediting organization
Quality assurance and improvement:
EQRO contractor name (if applicable)
Performance incentives: Payment
bonuses/differentials to reward plans
Performance incentives: Preferential
auto-enrollment to reward plans
Performance incentives: Public reports
comparing plan performance on key
metrics
Performance incentives: Withholds tied
to performance metrics
Performance incentives: MCOs/PHPs
required or encouraged to pay providers
for value/quality outcomes
Participating plans: Plans in Program Positive Healthcare/Los Angeles Family Mosaic Project/San Francisco Health Plan of San Mateo CCS Demo
Notes: Program notes
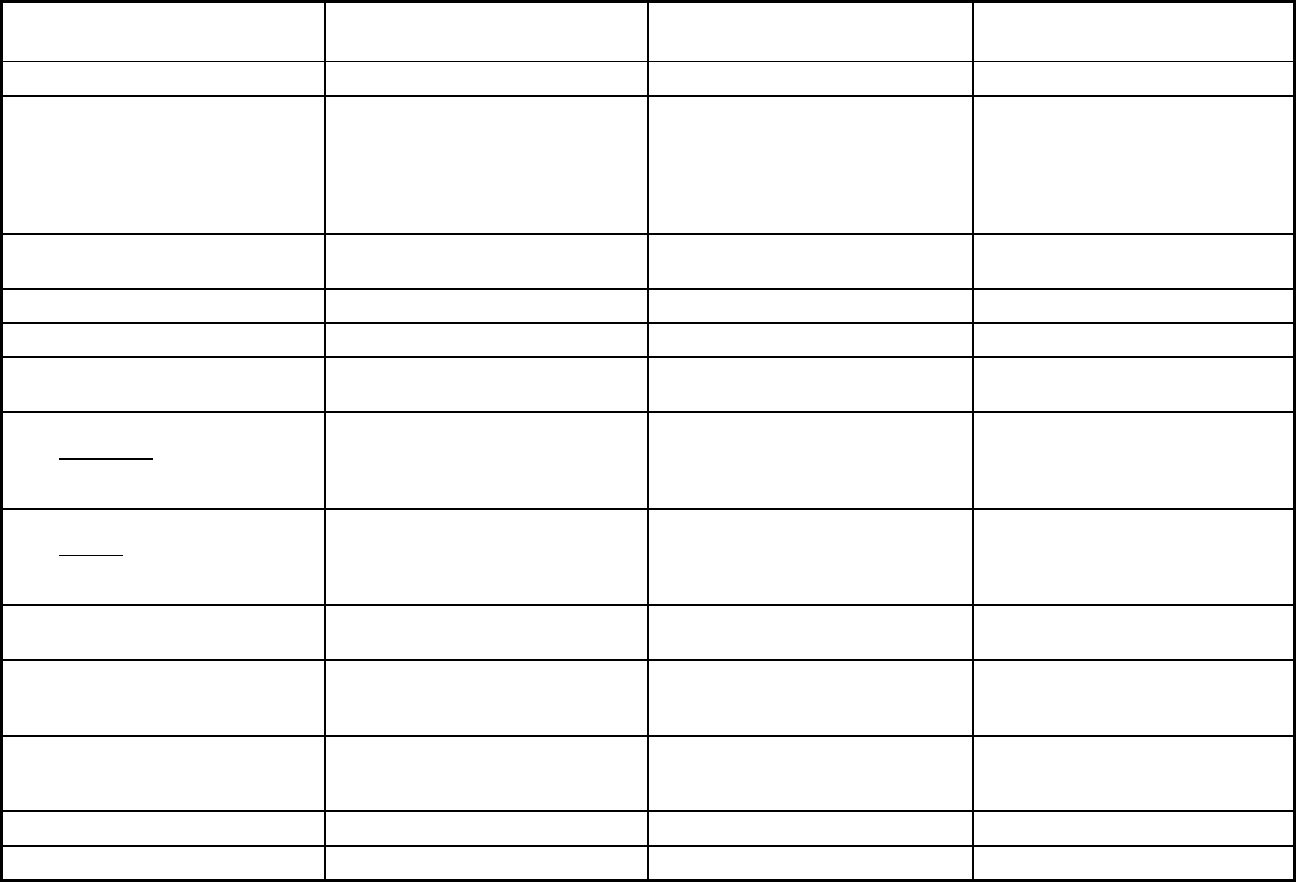
221
California Managed Care Program Features, as of 2018 (2 of 4)
Features
County Organized Health Systems
(COHS) Model Two-Plan Model Regional Model
Program type Comprehensive MCO + MLTSS Comprehensive MCO + MLTSS Comprehensive MCO
Statewide or region-specific? Del Norte, Humboldt, Lake, Lassen,
Marin, Medocino, Merced, Modoc,
Monterey, Napa, Orange, San Luis
Obispo, San Mateo, Santa Barbara,
Santa Cruz, Shasta, Siskiyou, Solano,
Sonoma, Trinity, Ventura, Yolo
Alameda, Contra Costa, Fresno, Kern,
Kings, Los Angeles, Madera, Riverside,
San Bernardino, San Francisco, San
Joaquin, Santa Clara, Stanislaus,
Tulare
Alpine, Amador, Butte, Calaveras,
Colusa, El Dorado, Glenn, Imperial,
Inyo, Mariposa, Mono, Nevada, Placer,
Plumas, San Benito, Sierra, Sutter,
Tehama, Tuolumne, Yuba
Federal operating authority 1115(a) (Medicaid demonstration
waivers)
1115(a) (Medicaid demonstration
waivers),1915(b)/1915(c)
1115(a) (Medicaid demonstration
waivers)
Program start date 10/01/1995 01/01/1996 10/02/2013
Waiver expiration date (if applicable) 12/31/2020 12/31/2020 12/31/2020
If the program ended in 2018, indicate
the end date
Populations enrolled: Low-income
adults not covered under ACA Section
VIII (excludes pregnant women and
people with disabilities)
Mandatory Mandatory
Populations enrolled: Low-income
adults covered under ACA Section VIII
(excludes pregnant women and people
with disabilities)
Mandatory Mandatory Mandatory
Populations enrolled: Aged, Blind or
Disabled Children or Adults
Mandatory Mandatory Mandatory
Populations enrolled: Non-Disabled
Children (excludes children in foster
care or receiving adoption assistance)
Mandatory Mandatory Mandatory
Populations enrolled: Individuals
receiving Limited Benefits (excludes
partial duals)
Mandatory
Populations enrolled: Full Duals Varies Varies Voluntary
Populations enrolled: Partial Duals Mandatory
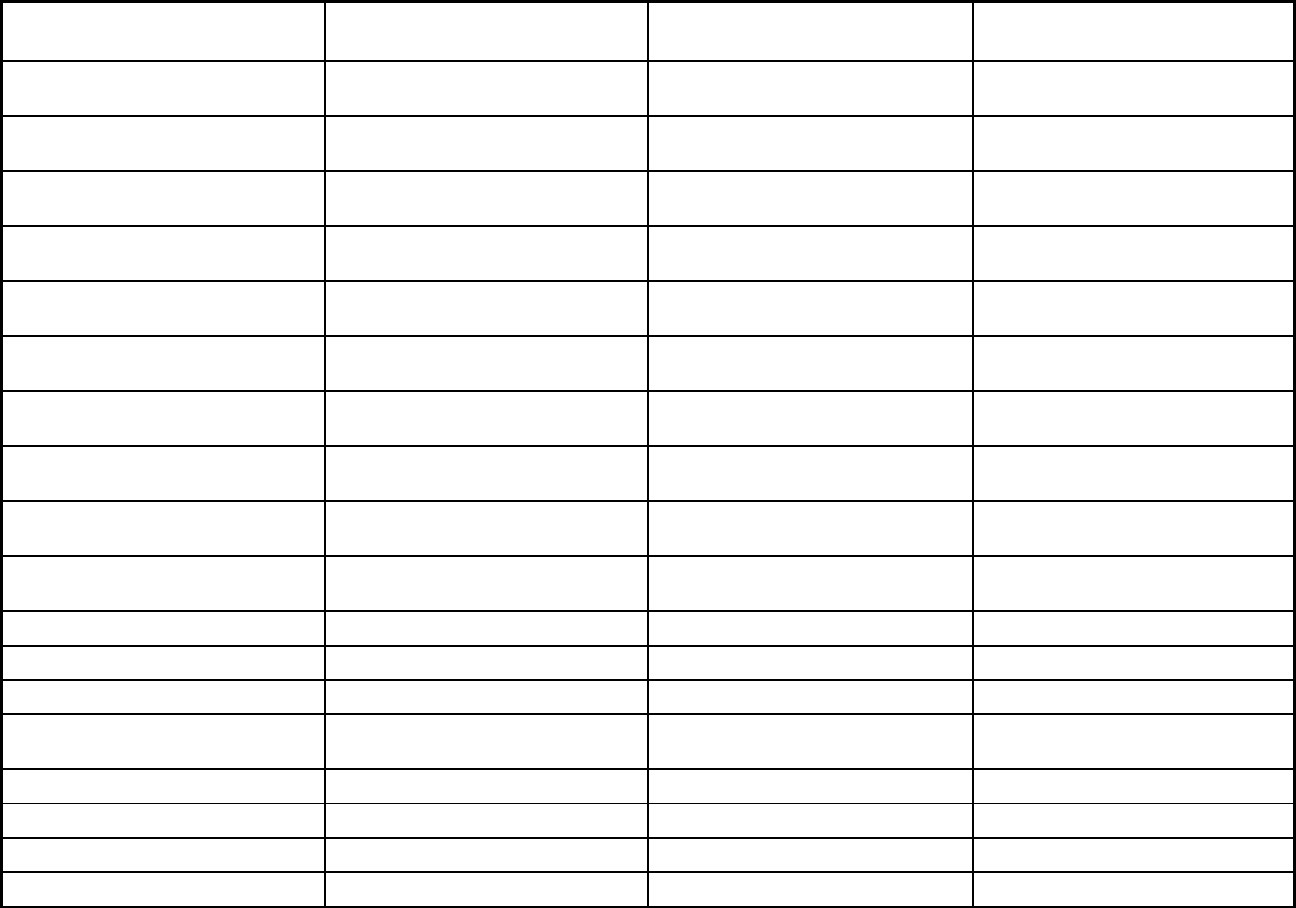
222
Features
County Organized Health Systems
(COHS) Model Two-Plan Model Regional Model
Populations enrolled: Children with
Special Health Care Needs
Mandatory Voluntary Voluntary
Populations enrolled: Native
American/Alaskan Natives
Mandatory Voluntary Voluntary
Populations enrolled: Foster Care and
Adoption Assistance Children
Voluntary Voluntary Voluntary
Populations enrolled: Enrollment
choice period
Pre-assigned Other Other
Populations enrolled: Enrollment
broker name (if applicable)
Populations enrolled: Notes on
enrollment choice period
Approximately 45 days Approximately 45 days
Benefits covered: Inpatient hospital
physical health
X X X
Benefits covered: Inpatient hospital
behavioral health (MH and/or SUD)
X
Benefits covered: Outpatient hospital
physical health
X X X
Benefits covered: Outpatient hospital
behavioral health (MH and/or SUD)
X
Benefits covered: Partial hospitalization
Benefits covered: Physician X X X
Benefits covered: Nurse practitioner X X X
Benefits covered: Rural health clinics
and FQHCs
X X X
Benefits covered: Clinic services X X
Benefits covered: Lab and x-ray X X X
Benefits covered: Prescription drugs X X X
Benefits covered: Prosthetic devices X X X
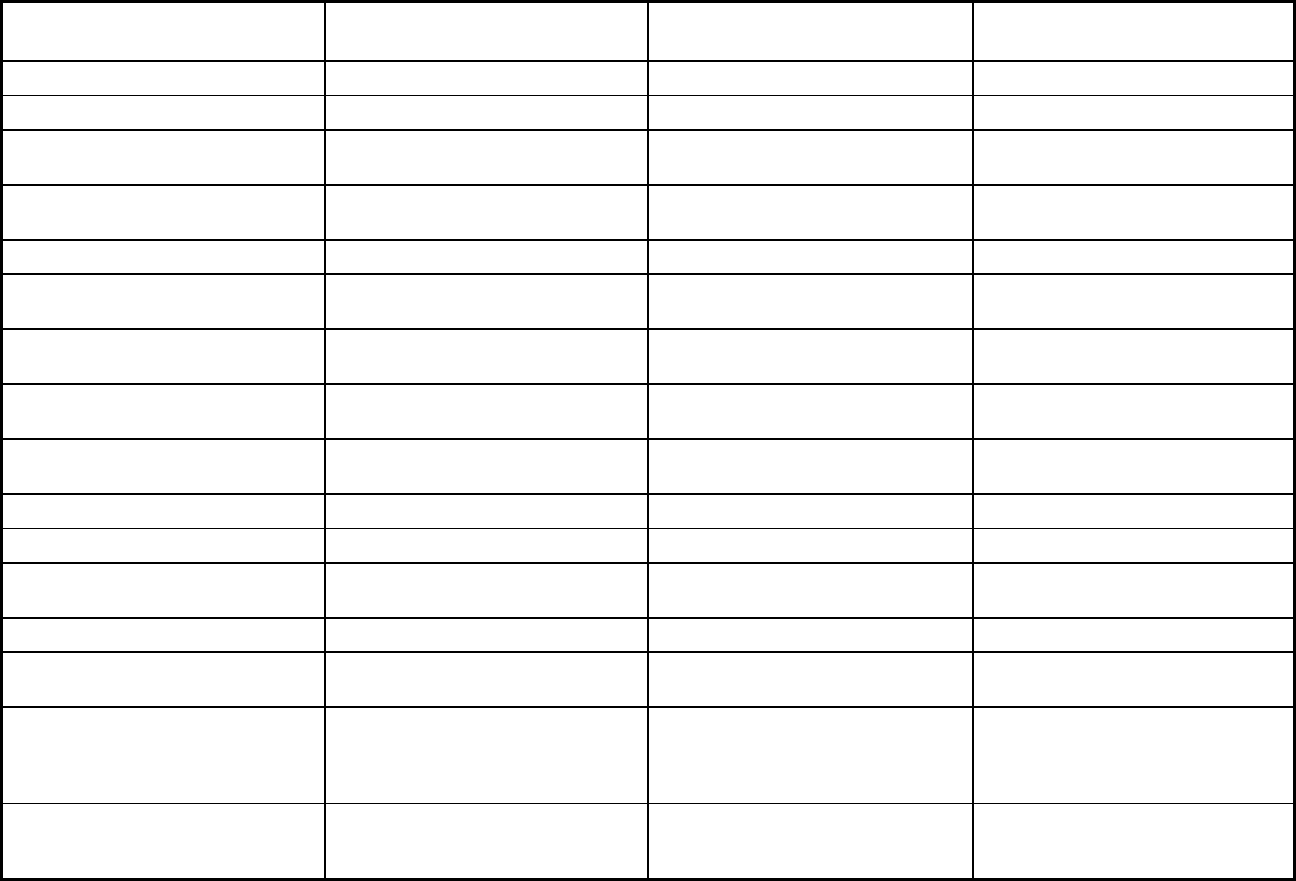
223
Features
County Organized Health Systems
(COHS) Model Two-Plan Model Regional Model
Benefits covered: EPSDT X X X
Benefits covered: Case management X X X
Benefits covered: SSA Section 1945-
authorized health home
Benefits covered: Health home care
(services in home)
Benefits covered: Family planning X X X
Benefits covered: Dental services
(medical/surgical)
Benefits covered: Dental (preventative
or corrective)
X
Benefits covered: Personal care (state
plan option)
X
Benefits covered: HCBS waiver
services
X
Benefits covered: Private duty nursing X
Benefits covered: ICF-IDD X X
Benefits covered: Nursing facility
services
X X
Benefits covered: Hospice care X X X
Benefits covered: Non-Emergency
Medical Transportation
X X X
Benefits covered: Institution for Mental
Disease inpatient treatment for people
ages 21-64 defined by 42 CFR
§438.6(e) as an 'in lieu of' benefit
Benefits covered: Other (e.g., nurse
midwife services, freestanding birth
centers, podiatry, etc.)
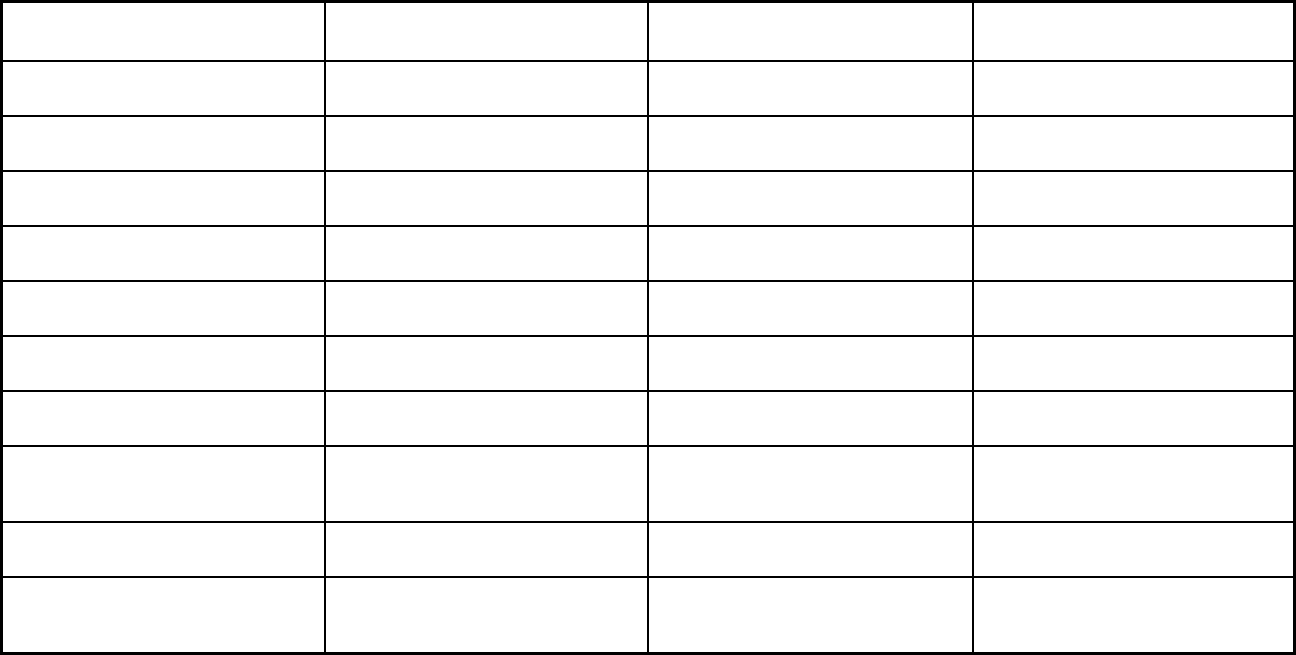
224
Features
County Organized Health Systems
(COHS) Model Two-Plan Model Regional Model
Quality assurance and improvement:
HEDIS data required?
Yes Yes Yes
Quality assurance and improvement:
CAHPS data required?
Yes Yes Yes
Quality assurance and improvement:
Accreditation required?
No No No
Quality assurance and improvement:
Accrediting organization
Quality assurance and improvement:
EQRO contractor name (if applicable)
Health Services Advisory Group Health Services Advisory Group Health Services Advisory Group
Performance incentives: Payment
bonuses/differentials to reward plans
Performance incentives: Preferential
auto-enrollment to reward plans
X X
Performance incentives: Public reports
comparing plan performance on key
metrics
X X X
Performance incentives: Withholds tied
to performance metrics
Performance incentives: MCOs/PHPs
required or encouraged to pay
providers for value/quality outcomes
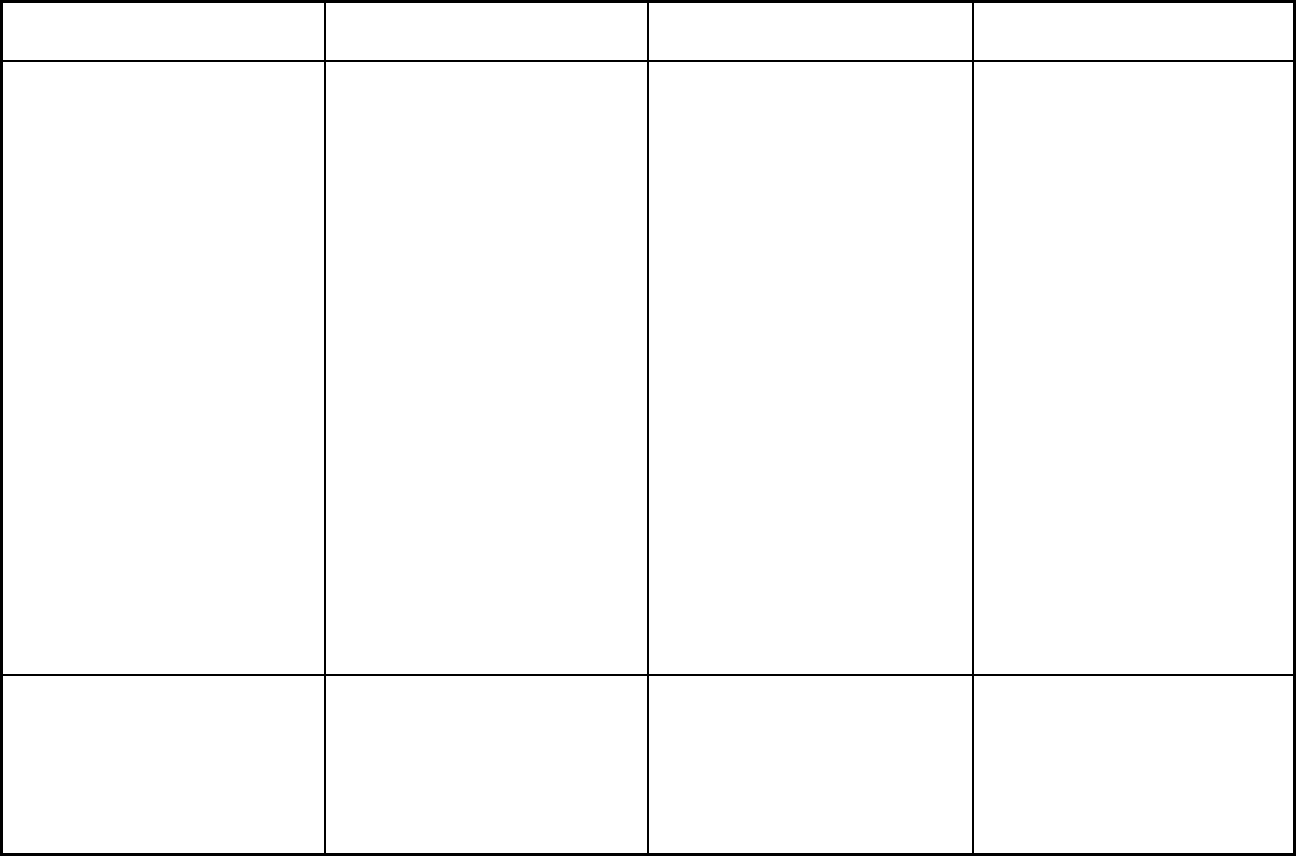
225
Features
County Organized Health Systems
(COHS) Model Two-Plan Model Regional Model
Participating plans: Plans in Program CenCal Health/San Luis Obispo;
CenCal Health/Santa Barbara; Health
Plan of San Mateo; Partnership
HealthPlan of CA/Northeast;
Partnership HealthPlan of
CA/Northwest; Partnership Health
Plan/Southeast; Partnership Health
Plan/Southwest; Central California
Alliance for Health/Merced; Central
California Alliance for Health/Monterey
Santa Cru
z; CalOptima/Orange; Gold
Coast Health Plan/Ventura
Health Net/Kern; Health Net/Los
Angeles; Health Net/San Joaquin;
Health Net/Stanislaus; Health
Net/Tulare; CalViva Health/Fresno;
CalViva Health/Kings; CalViva
Health/Madera; Anthem Blue Cross
Partnership
Plan/Fresno; Anthem Blue
Cross Partnership Plan/Kings; Anthem
Blue Cross Partnership Plan/Madera;
Anthem Blue Cross Partnership
Plan/Alameda; Anthem Blue Cross
Partnership Plan/Contra Costa; Anthem
Blue Cross Partnership Plan/San
Francisco; Anthem Blue Cross
Partnership Plan/Santa Clara; Anthem
Blue Cross Partnership Plan/Tulare;
Kern Family Health Care; L.A. Care
Health Plan/Los Angeles; Contra Costa
Health Plan; Alameda Alliance for
Health; Inland Empire Health
Plan/Riverside; Inland Empire Health
Plan/S
an Bernardino; Molina
Healthcare of CA Partner
Plan/Riverside; Molina Healthcare of
CA Partner Plan/San Bernardino; San
Francisco Health Plan; Health Plan of
San Joaquin/San Joaquin; Health Plan
of San Joaquin/Stanislaus; Santa Clara
Family Health Plan
California Health & Wellness
Plan/Imperial; California Health &
Wellness Plan/Region 1; California
Health & Wellness Plan/Region 2;
Molina Healthcare of CA Partner
Plan/Imperial; Anthem Blue Cross
Partnership Plan/Region 1; Anthem
Blue Cross Partner
ship Plan/Region 2;
KP Cal LLC/Amador; KP Cal LLC/El
Dorado; KP Cal LLC/Placer
Notes: Program notes Full duals are mandatory for managed
care enrollment in CCI Counties
(Orange and San Mateo) and voluntary
for all other Counties.
Full duals are mandatory for managed
care enrollment in CCI Counties (Los
Angeles, Riverside, San Bernardino,
and Santa Clara) and voluntary for all
other counties (Alameda, Contra Costa,
Fresno, Kern, Kings, Madera, San
Francisco, San Joaquin, Stanislaus and
Tulare).
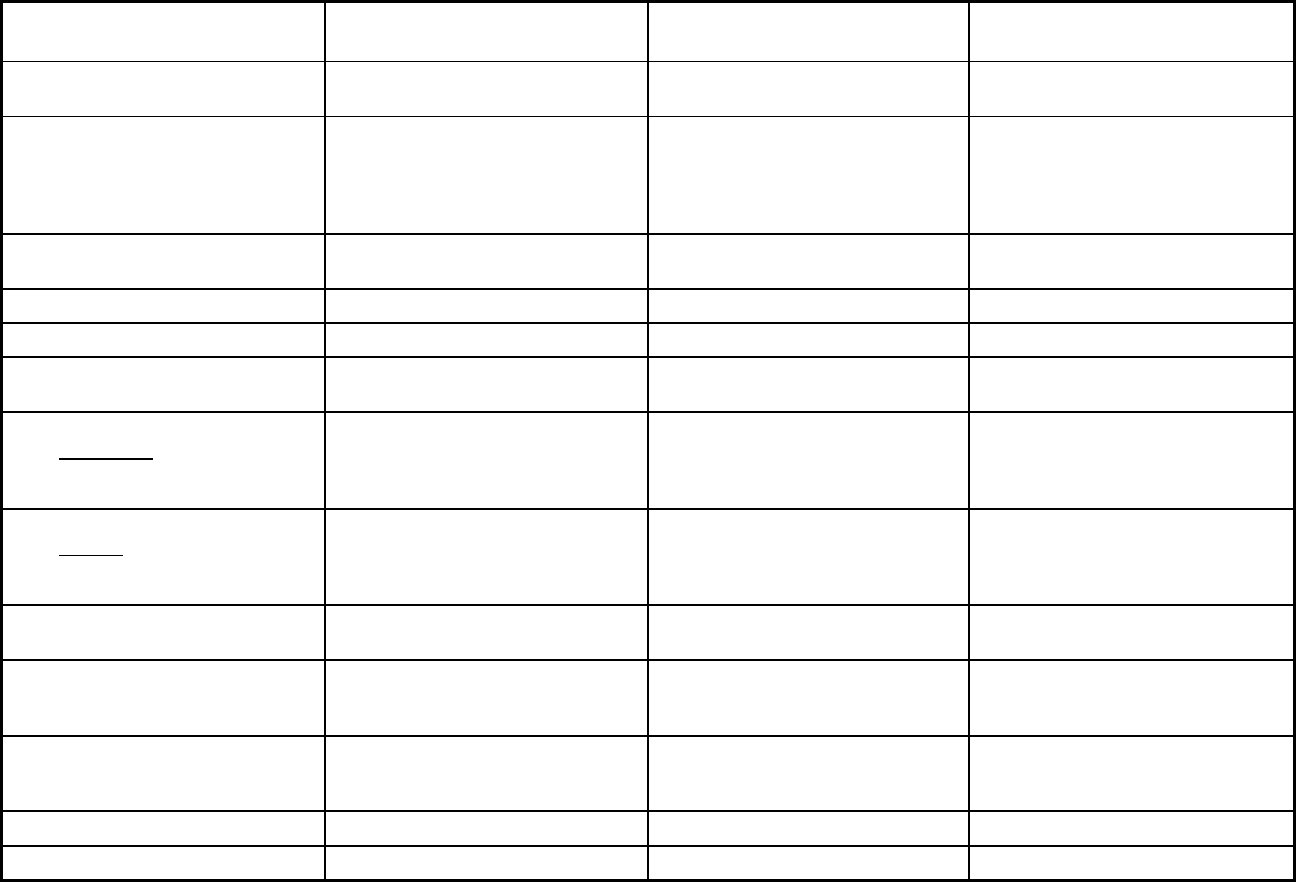
226
California Managed Care Program Features, as of 2018 (3 of 4)
Features
Geographic Managed Care (GMC)
Model Senior Care Action Network (SCAN)
Program of All-Inclusive Care for the
Elderly (PACE)
Program type Comprehensive MCO + MLTSS Comprehensive MCO + MLTSS Program of All-inclusive Care for the
Elderly (PACE)
Statewide or region-specific? Sacramento, San Diego Los Angeles, Riverside, San
Bernardino
Alameda, Contra Costa, Fresno,
Humboldt, Los Angeles, Orange,
Riverside, Sacramento, San
Bernardino, San Diego, San Francisco,
Santa Clara
Federal operating authority 1115(a) (Medicaid demonstration
waivers)
1115(a) (Medicaid demonstration
waivers)
PACE
Program start date 06/01/1991 01/01/1996 06/01/1991
Waiver expiration date (if applicable) 12/31/2020 12/31/2020
If the program ended in 2018, indicate
the end date
Populations enrolled: Low-income
adults not covered under ACA Section
VIII (excludes pregnant women and
people with disabilities)
Mandatory
Populations enrolled: Low-income
adults covered under ACA Section VIII
(excludes pregnant women and people
with disabilities)
Mandatory
Populations enrolled: Aged, Blind or
Disabled Children or Adults
Mandatory Voluntary Voluntary
Populations enrolled: Non-Disabled
Children (excludes children in foster
care or receiving adoption assistance)
Mandatory
Populations enrolled: Individuals
receiving Limited Benefits (excludes
partial duals)
Populations enrolled: Full Duals Varies Voluntary Voluntary
Populations enrolled: Partial Duals Voluntary
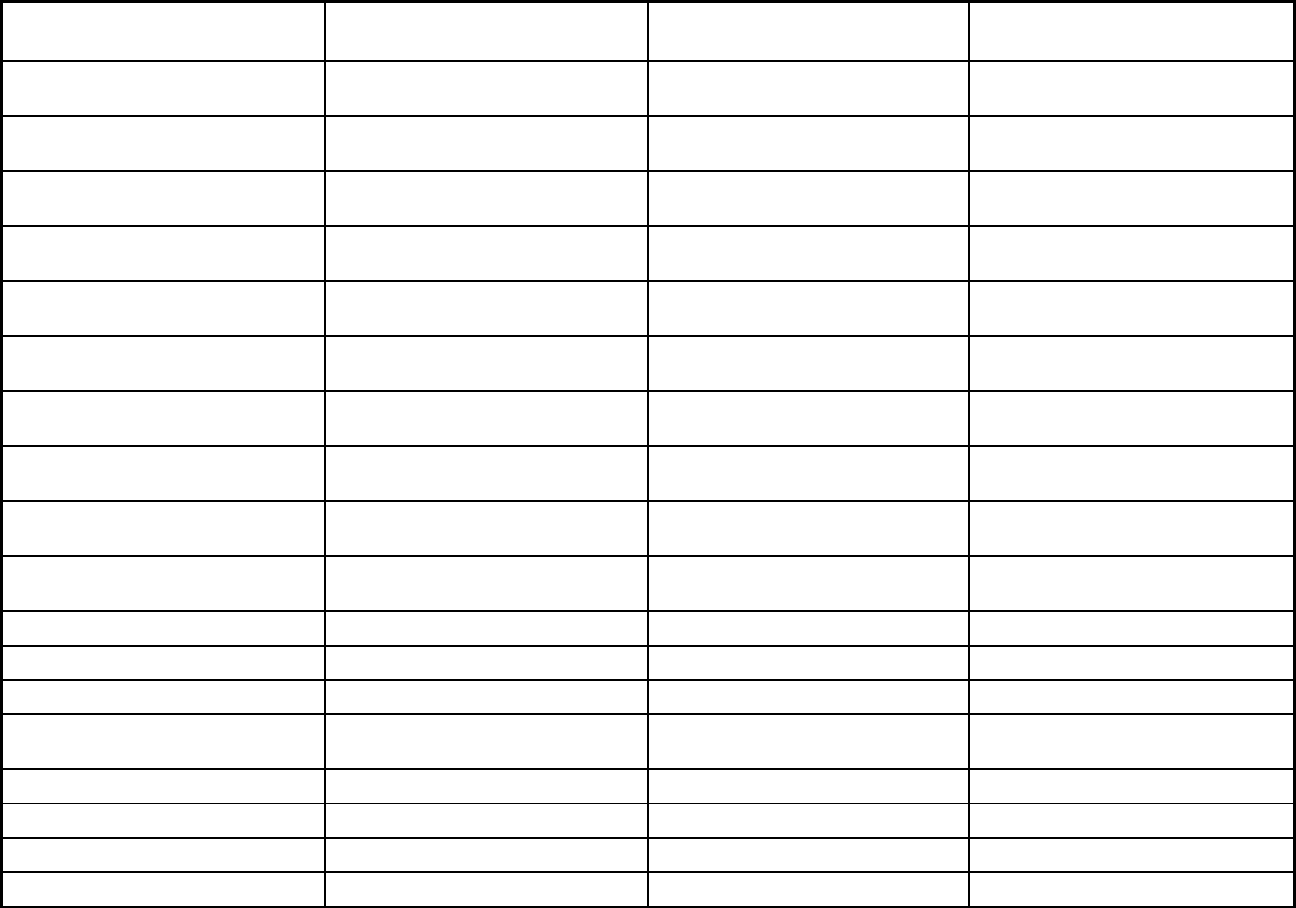
227
Features
Geographic Managed Care (GMC)
Model Senior Care Action Network (SCAN)
Program of All-Inclusive Care for the
Elderly (PACE)
Populations enrolled: Children with
Special Health Care Needs
Voluntary
Populations enrolled: Native
American/Alaskan Natives
Voluntary Voluntary Voluntary
Populations enrolled: Foster Care and
Adoption Assistance Children
Voluntary Exempt Exempt
Populations enrolled: Enrollment
choice period
Other N/A
Populations enrolled: Enrollment
broker name (if applicable)
Health Care Options (Maximus)
Populations enrolled: Notes on
enrollment choice period
Approximately 45 days
Benefits covered: Inpatient hospital
physical health
X X X
Benefits covered: Inpatient hospital
behavioral health (MH and/or SUD)
X
Benefits covered: Outpatient hospital
physical health
X X X
Benefits covered: Outpatient hospital
behavioral health (MH and/or SUD)
X X X
Benefits covered: Partial hospitalization X X
Benefits covered: Physician X X X
Benefits covered: Nurse practitioner X X X
Benefits covered: Rural health clinics
and FQHCs
X X
Benefits covered: Clinic services X X X
Benefits covered: Lab and x-ray X X X
Benefits covered: Prescription drugs X X X
Benefits covered: Prosthetic devices X X X
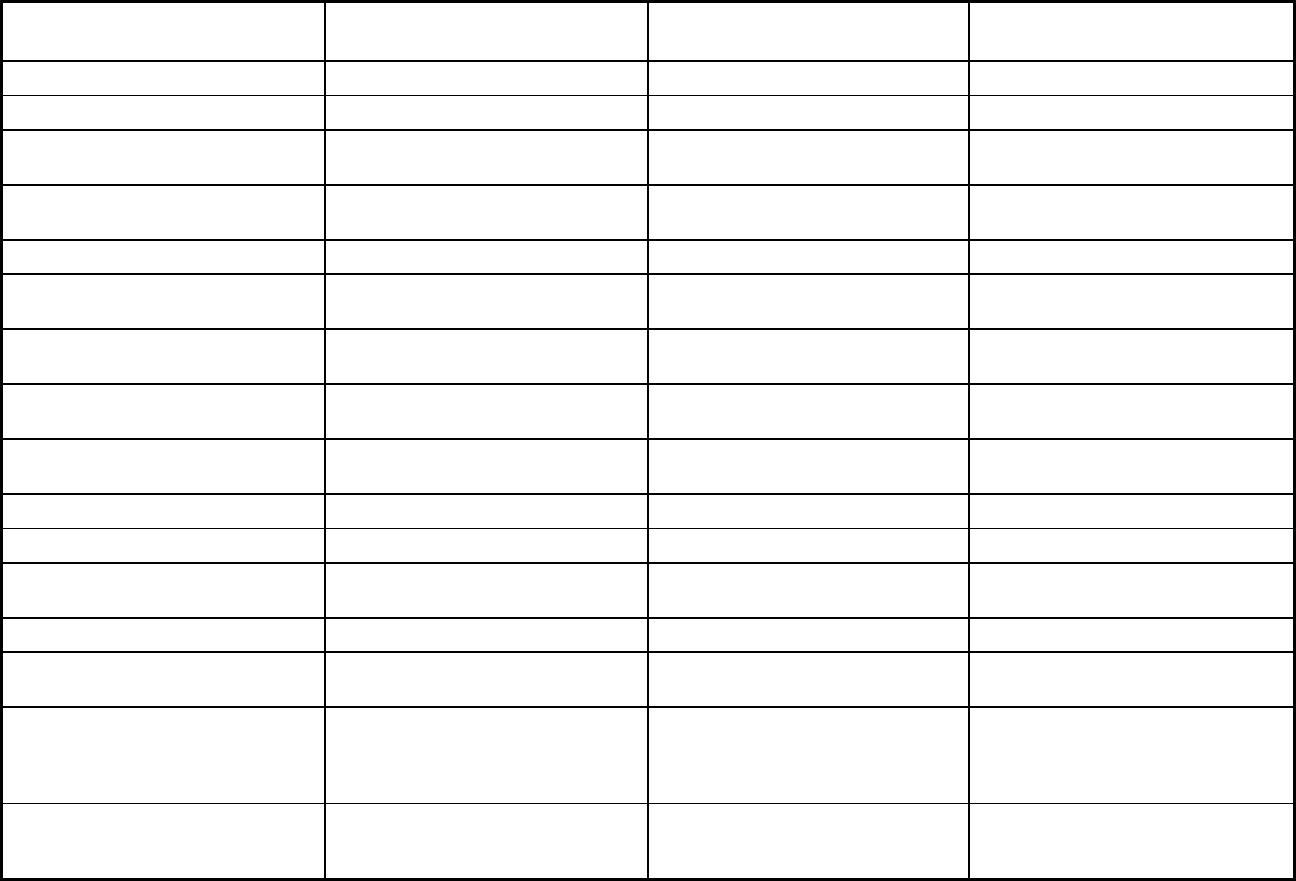
228
Features
Geographic Managed Care (GMC)
Model Senior Care Action Network (SCAN)
Program of All-Inclusive Care for the
Elderly (PACE)
Benefits covered: EPSDT X X
Benefits covered: Case management X X X
Benefits covered: SSA Section 1945-
authorized health home
Benefits covered: Health home care
(services in home)
X X
Benefits covered: Family planning X X
Benefits covered: Dental services
(medical/surgical)
X X
Benefits covered: Dental (preventative
or corrective)
X X
Benefits covered: Personal care (state
plan option)
X X X
Benefits covered: HCBS waiver
services
X
Benefits covered: Private duty nursing X
Benefits covered: ICF-IDD X
Benefits covered: Nursing facility
services
X X X
Benefits covered: Hospice care X X X
Benefits covered: Non-Emergency
Medical Transportation
X X X
Benefits covered: Institution for Mental
Disease inpatient treatment for people
ages 21-64 defined by 42 CFR
§438.6(e) as an 'in lieu of' benefit
Benefits covered: Other (e.g., nurse
midwife services, freestanding birth
centers, podiatry, etc.)
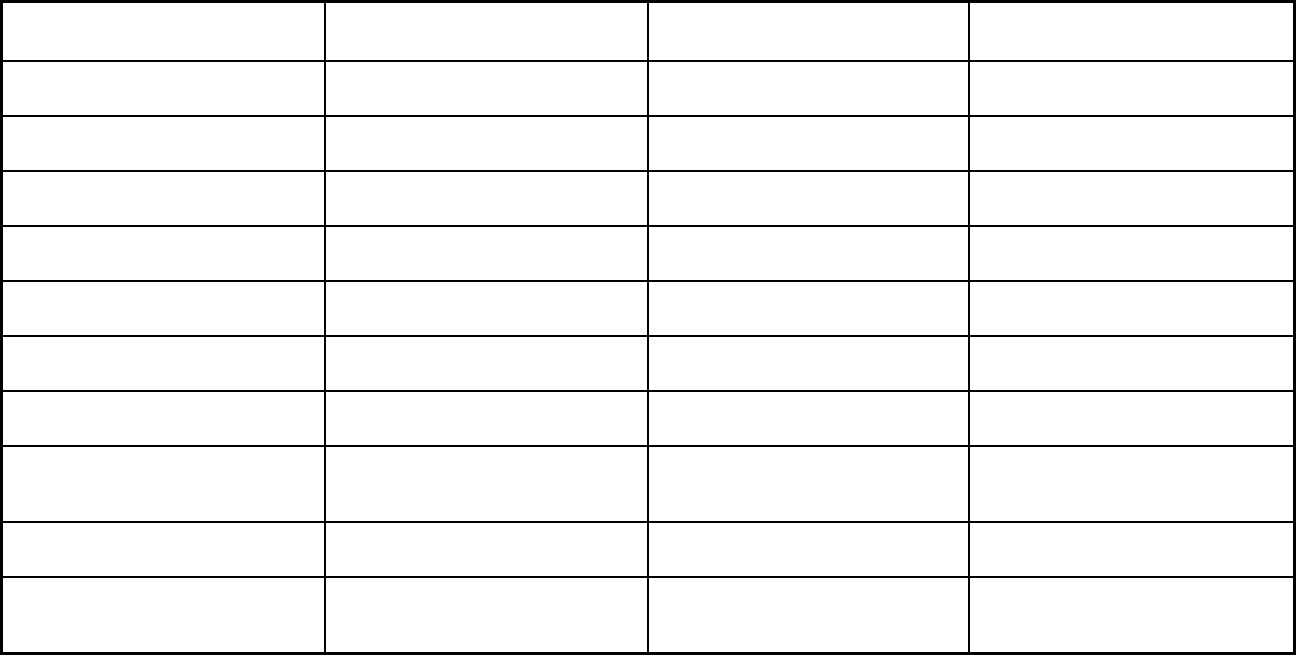
229
Features
Geographic Managed Care (GMC)
Model Senior Care Action Network (SCAN)
Program of All-Inclusive Care for the
Elderly (PACE)
Quality assurance and improvement:
HEDIS data required?
Yes No No
Quality assurance and improvement:
CAHPS data required?
Yes No No
Quality assurance and improvement:
Accreditation required?
No No No
Quality assurance and improvement:
Accrediting organization
Quality assurance and improvement:
EQRO contractor name (if applicable)
Health Services Advisory Group
Performance incentives: Payment
bonuses/differentials to reward plans
Performance incentives: Preferential
auto-enrollment to reward plans
X
Performance incentives: Public reports
comparing plan performance on key
metrics
X
Performance incentives: Withholds tied
to performance metrics
Performance incentives: MCOs/PHPs
required or encouraged to pay
providers for value/quality outcomes
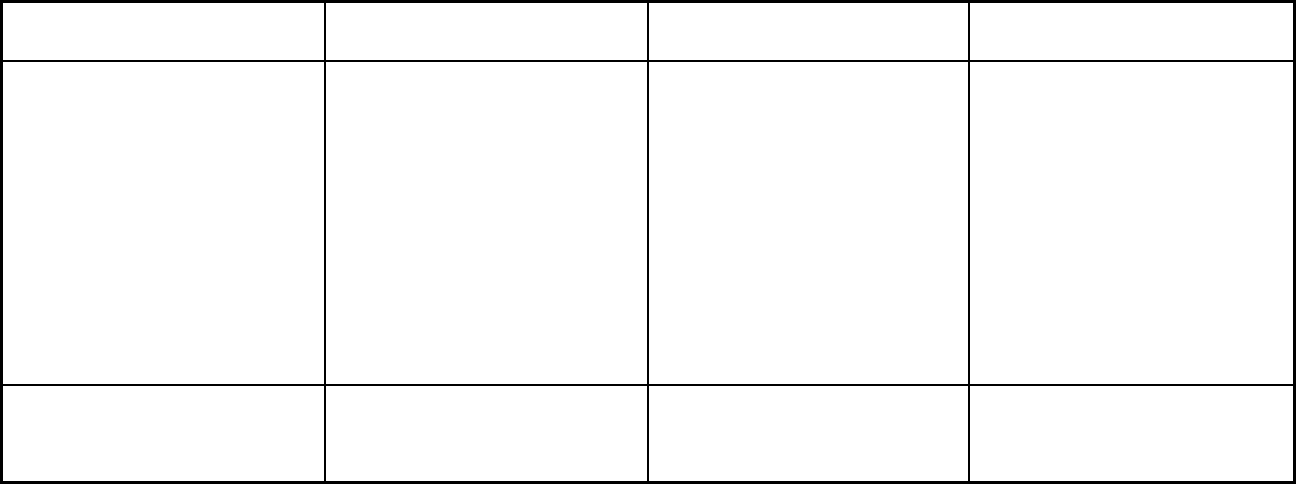
230
Features
Geographic Managed Care (GMC)
Model Senior Care Action Network (SCAN)
Program of All-Inclusive Care for the
Elderly (PACE)
Participating plans: Plans in Program Care 1st Partner Plan/San Diego;
Community Health Group Partnership
Plan/San Diego; Health Net/San
Diego; KP Cal LLC/San Diego; Molina
Healthcare of CA Partner Plan/San
Diego; Aetna Better Health of CA/San
Diego; UnitedHealthcare Community
Plan/San Diego; Anthem Blue Cross
Partnership Plan/Sacramento; Health
Net/Sacramento; KP Cal
LLC/Sacramento; Molina Healthcare of
CA Partner Plan/Sacramento; Aetna
Better Health of CA/Sacramento;
UnitedHealthcare Community
Plan/Sacramento
SCAN Health Plan/Los Angeles; SCAN
Health Plan/Riverside; SCAN Health
Plan/San Bernardino; SCAN Health
Plan (Nurs hm cert)/Los Angeles;
SCAN Health Plan (Nurs hm
cert)/Riverside; SCAN Health Plan
(Nurs hm cert)/San Bernardino
Redwood Coast Pace/Humboldt; San
Diego PACE; St. Paul's PACE/San
Diego; Sutter SeniorCare
PACE/Sacramento; AltaMed Senior
Buenacare/Los Angeles; Brandman
Centers for Senior Care/Los Angeles;
CalOptima PACE/Orange; Center for
Elders Independence/Alameda; Center
for Elders Independence/Contra Costa;
Fres
no PACE; InnovAge
PACE/Riverside; InnovAge PACE/San
Bernardino County; On Lok
Lifeways/Alameda; On Lok
Lifeways/Santa Clara; On Lok
Lifeways/San Francisco
Notes: Program notes Full duals are mandatory for managed
care enrollment in CCI Counties (San
Diego) and voluntary for all other
counties (Sacramento).
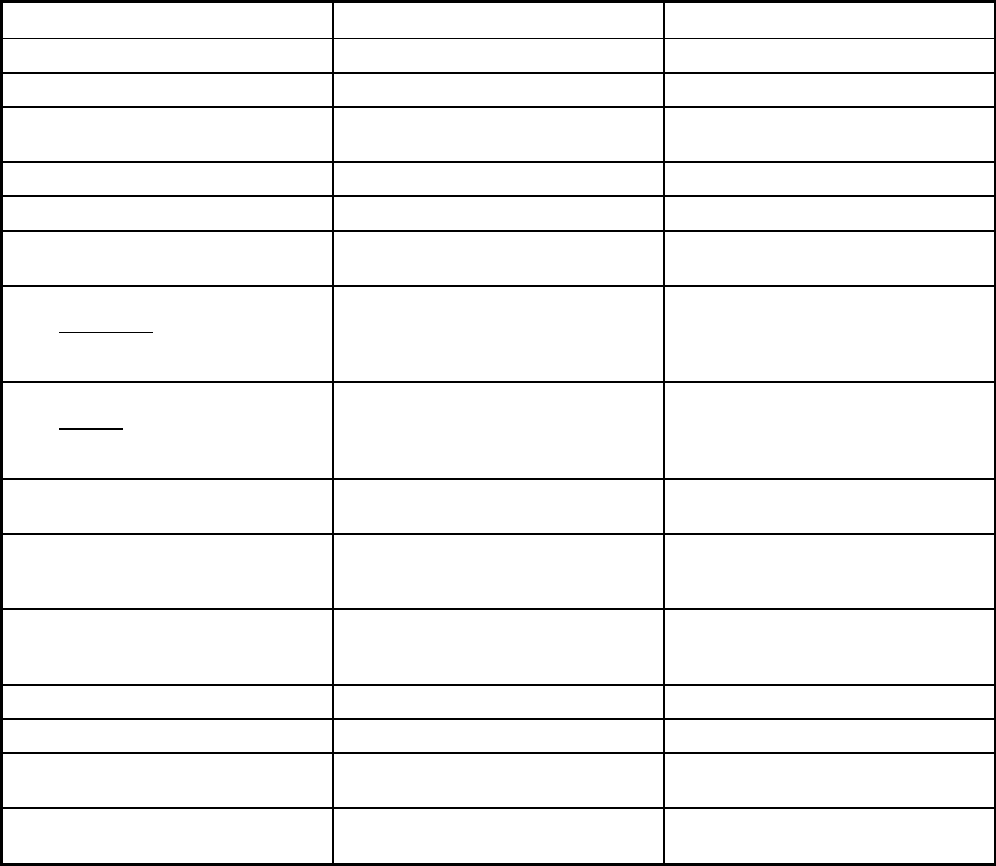
231
California Managed Care Program Features, as of 2018 (4 of 4)
Features Dental Managed Care/Los Angeles Dental Managed Care/Sacramento
Program type Dental only (PAHP) Dental only (PAHP)
Statewide or region-specific? Los Angeles Sacramento
Federal operating authority 1915(a)/1915(i) 1115(a) (Medicaid demonstration
waivers)
Program start date 04/01/1998 12/01/1998
Waiver expiration date (if applicable) 12/31/2020 12/31/2020
If the program ended in 2018, indicate
the end date
Populations enrolled: Low-income
adults not covered under ACA Section
VIII (excludes pregnant women and
people with disabilities)
Voluntary Voluntary
Populations enrolled: Low-income
adults covered under ACA Section VIII
(excludes pregnant women and people
with disabilities)
Voluntary Voluntary
Populations enrolled: Aged, Blind or
Disabled Children or Adults
Voluntary Voluntary
Populations enrolled: Non-Disabled
Children (excludes children in foster
care or receiving adoption assistance)
Voluntary Voluntary
Populations enrolled: Individuals
receiving Limited Benefits (excludes
partial duals)
Voluntary Voluntary
Populations enrolled: Full Duals Voluntary Voluntary
Populations enrolled: Partial Duals
Populations enrolled: Children with
Special Health Care Needs
Voluntary Voluntary
Populations enrolled: Native
American/Alaskan Natives
Voluntary Voluntary
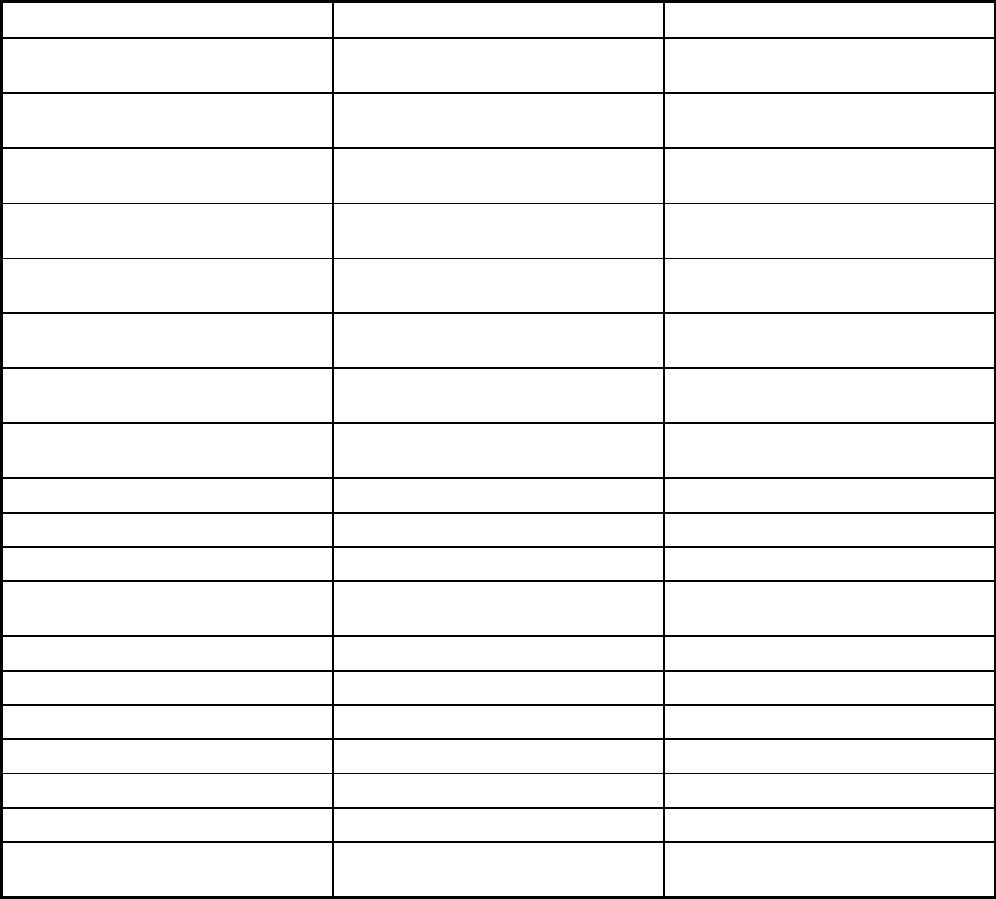
232
Features Dental Managed Care/Los Angeles Dental Managed Care/Sacramento
Populations enrolled: Foster Care and
Adoption Assistance Children
Voluntary Voluntary
Populations enrolled: Enrollment choice
period
60 days 60 days
Populations enrolled: Enrollment broker
name (if applicable)
Health Care Operations (Maximus) Health Care Operations (Maximus)
Populations enrolled: Notes on
enrollment choice period
Benefits covered: Inpatient hospital
physical health
Benefits covered: Inpatient hospital
behavioral health (MH and/or SUD)
Benefits covered: Outpatient hospital
physical health
Benefits covered: Outpatient hospital
behavioral health (MH and/or SUD)
Benefits covered: Partial hospitalization
Benefits covered: Physician
Benefits covered: Nurse practitioner
Benefits covered: Rural health clinics
and FQHCs
X X
Benefits covered: Clinic services
Benefits covered: Lab and x-ray
Benefits covered: Prescription drugs
Benefits covered: Prosthetic devices
Benefits covered: EPSDT X X
Benefits covered: Case management X X
Benefits covered: SSA Section 1945-
authorized health home
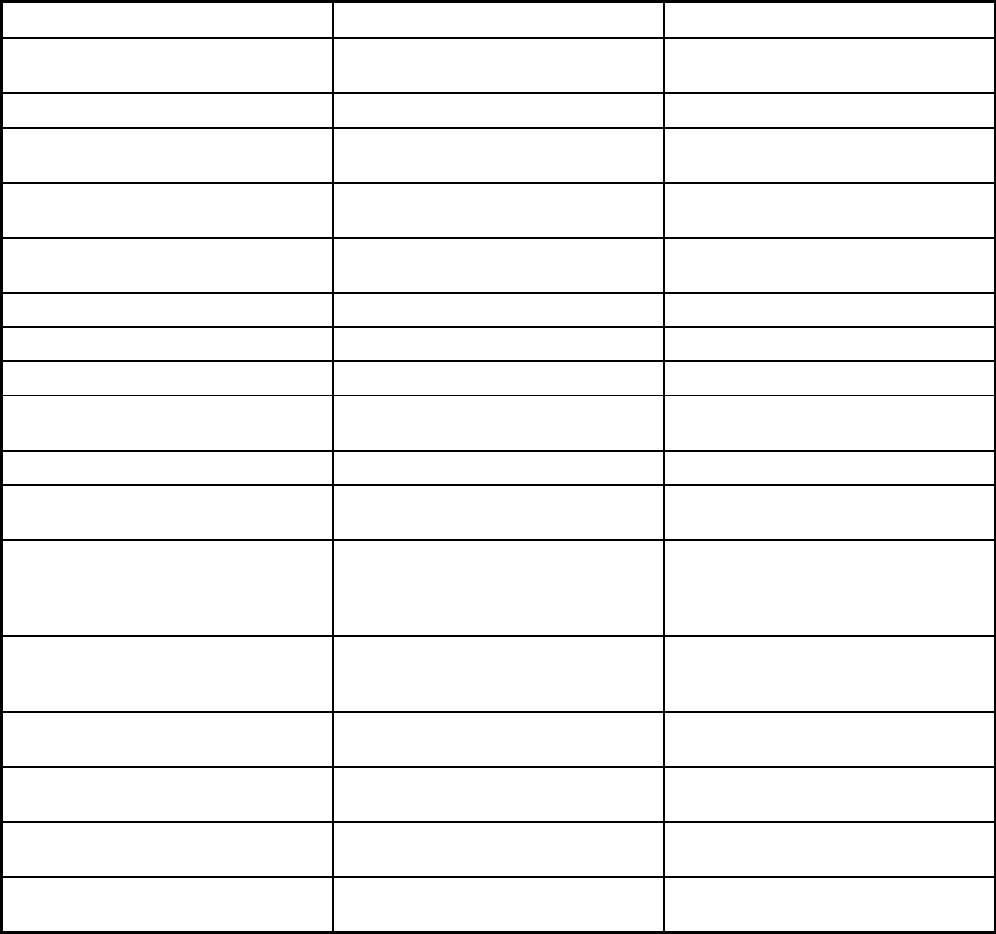
233
Features Dental Managed Care/Los Angeles Dental Managed Care/Sacramento
Benefits covered: Health home care
(services in home)
Benefits covered: Family planning
Benefits covered: Dental services
(medical/surgical)
X X
Benefits covered: Dental (preventative
or corrective)
X X
Benefits covered: Personal care (state
plan option)
Benefits covered: HCBS waiver services
Benefits covered: Private duty nursing
Benefits covered: ICF-IDD
Benefits covered: Nursing facility
services
Benefits covered: Hospice care
Benefits covered: Non-Emergency
Medical Transportation
X X
Benefits covered: Institution for Mental
Disease inpatient treatment for people
ages 21-64 defined by 42 CFR
§438.6(e) as an 'in lieu of' benefit
Benefits covered: Other (e.g., nurse
midwife services, freestanding birth
centers, podiatry, etc.)
Quality assurance and improvement:
HEDIS data required?
Yes Yes
Quality assurance and improvement:
CAHPS data required?
Yes Yes
Quality assurance and improvement:
Accreditation required?
No No
Quality assurance and improvement:
Accrediting organization
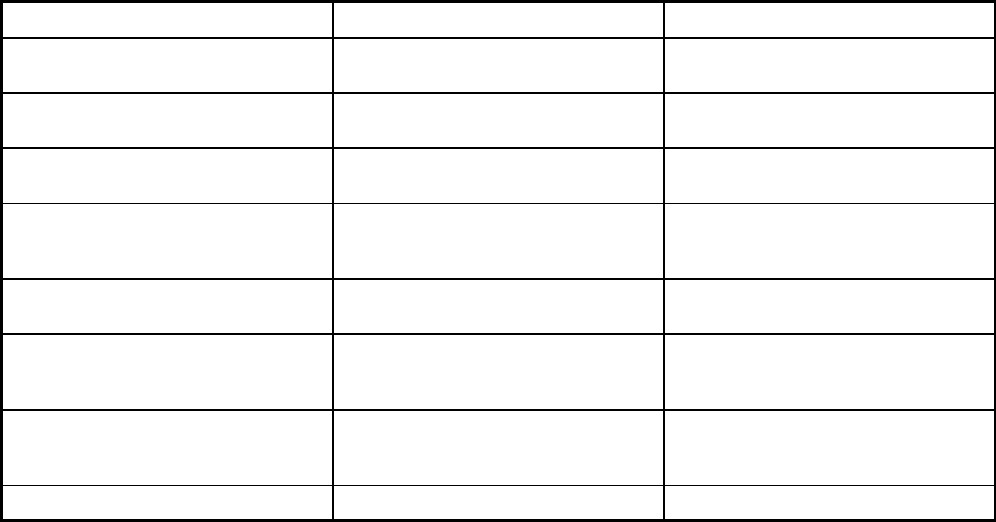
234
Features Dental Managed Care/Los Angeles Dental Managed Care/Sacramento
Quality assurance and improvement:
EQRO contractor name (if applicable)
Performance incentives: Payment
bonuses/differentials to reward plans
Performance incentives: Preferential
auto-enrollment to reward plans
Performance incentives: Public reports
comparing plan performance on key
metrics
X X
Performance incentives: Withholds tied
to performance metrics
Performance incentives: MCOs/PHPs
required or encouraged to pay providers
for value/quality outcomes
Participating plans: Plans in Program Health Net Dental Plan/Los Angeles;
Access Dental Plan/Los Angeles;
LIBERTY Dental Plan/Los Angeles
Health Net Dental Plan/Sacramento;
Access Dental Plan/Sacramento;
LIBERTY Dental Plan/Sacramento
Notes: Program notes
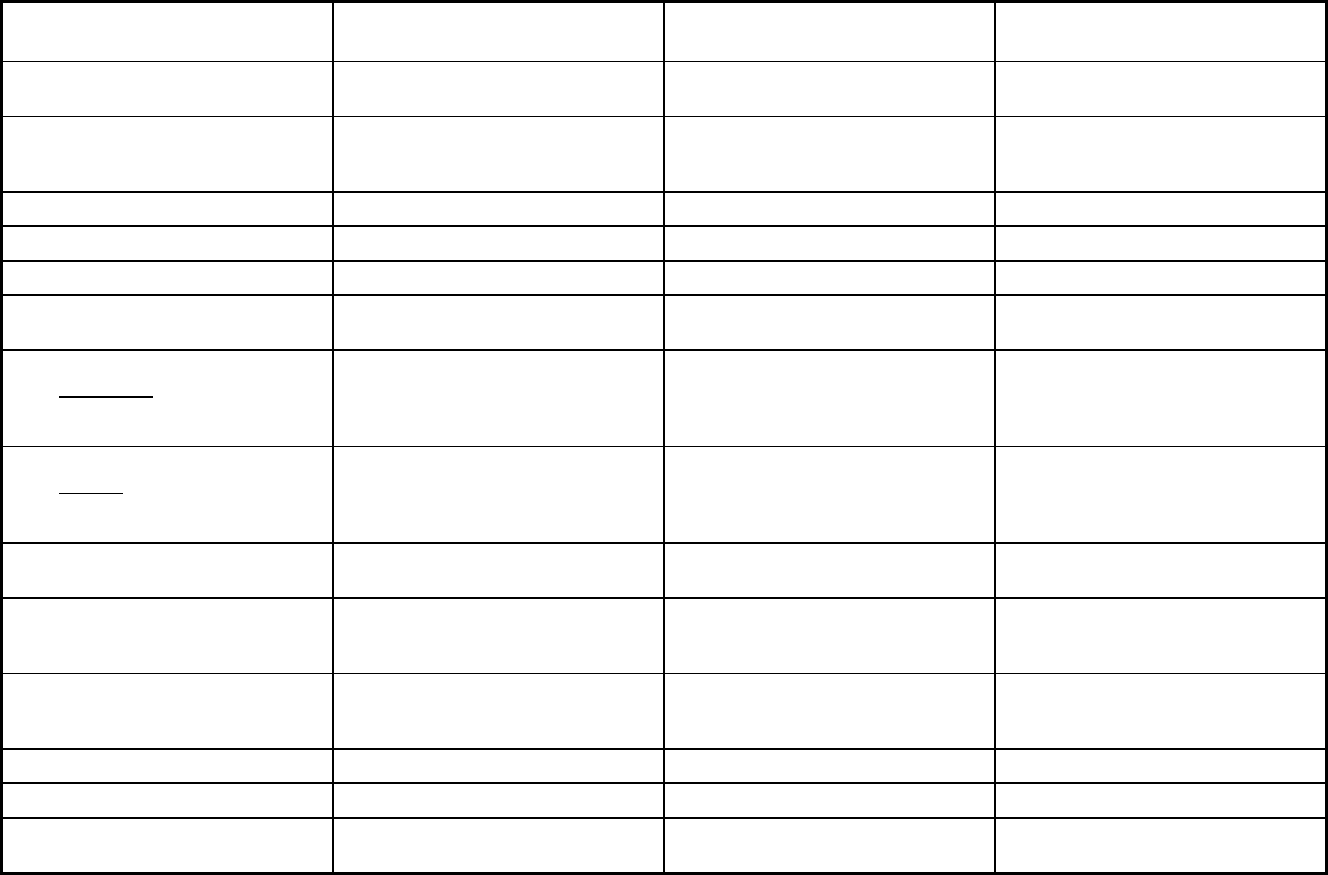
235
Colorado Managed Care Program Features, as of 2018 (1 of 2)
Features
Program of All-Inclusive Care for the
Elderly
Accountable Care Collaborative
(ACC)
Colorado Medicaid Community
Behavioral Health Services Program
Program type Program of All-inclusive Care for the
Elderly (PACE)
Primary Care Case Management Entity
(PCCM Entity)
Behavioral Health Organization (BHO)
only (PIHP and/or PAHP)
Statewide or region-specific? Adams, Arapahoe, Broomfield, Denver,
Jefferson, Boulder, Weld (Southwest),
Pueblo, El Paso, Delta, Montrose
Statewide Statewide
Federal operating authority PACE 1915(b) 1915(b)
Program start date 10/01/1991 07/01/2018 07/01/1995
Waiver expiration date (if applicable) 06/30/2023 06/30/2019
If the program ended in 2018, indicate
the end date
06/30/2018
Populations enrolled: Low-income
adults not covered under ACA Section
VIII (excludes pregnant women and
people with disabilities)
Mandatory Mandatory
Populations enrolled: Low-income
adults covered under ACA Section VIII
(excludes pregnant women and people
with disabilities)
Mandatory Mandatory
Populations enrolled: Aged, Blind or
Disabled Children or Adults
Voluntary Mandatory Mandatory
Populations enrolled: Non-Disabled
Children (excludes children in foster
care or receiving adoption assistance)
Mandatory Mandatory
Populations enrolled: Individuals
receiving Limited Benefits (excludes
partial duals)
Mandatory
Populations enrolled: Full Duals Voluntary Mandatory Mandatory
Populations enrolled: Partial Duals Voluntary
Populations enrolled: Children with
Special Health Care Needs
Mandatory Mandatory
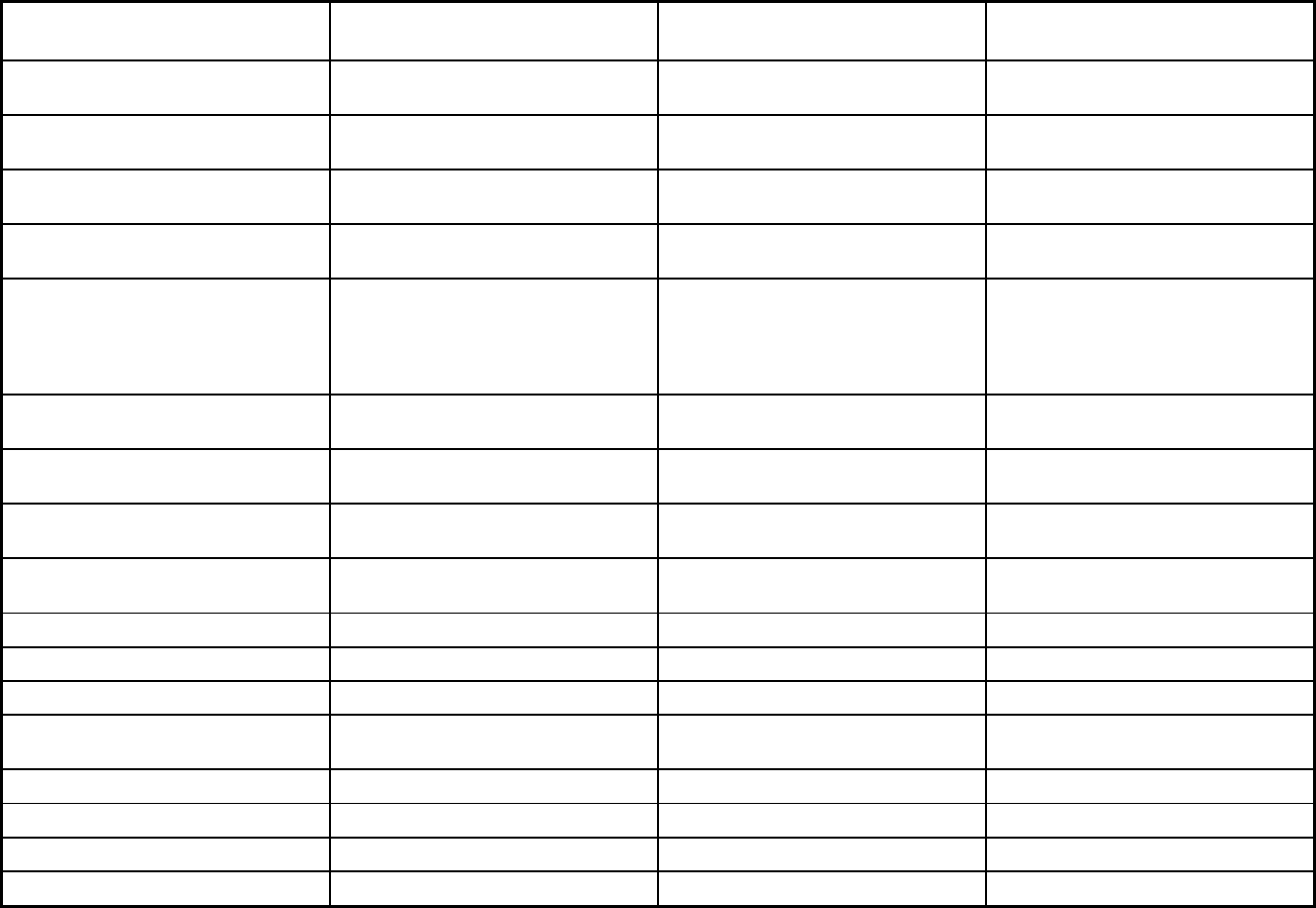
236
Features
Program of All-Inclusive Care for the
Elderly
Accountable Care Collaborative
(ACC)
Colorado Medicaid Community
Behavioral Health Services Program
Populations enrolled: Native
American/Alaskan Natives
Voluntary Mandatory Mandatory
Populations enrolled: Foster Care and
Adoption Assistance Children
Exempt Mandatory Mandatory
Populations enrolled: Enrollment choice
period
N/A Other Pre-assigned
Populations enrolled: Enrollment broker
name (if applicable)
Maximus Health Services, Inc. Maximus Health Services, Inc.
Populations enrolled: Notes on
enrollment choice period
There is no enrollment period; existing
Medicaid members that meet the level
of care may apply for PACE at any time.
Members are enrolled on the first of the
month.
Beneficiaries are passively enrolled and
can choose their primary care provider
at any time.
Benefits covered: Inpatient hospital
physical health
X X
Benefits covered: Inpatient hospital
behavioral health (MH and/or SUD)
X X X
Benefits covered: Outpatient hospital
physical health
X X
Benefits covered: Outpatient hospital
behavioral health (MH and/or SUD)
X X X
Benefits covered: Partial hospitalization X X X
Benefits covered: Physician X X
Benefits covered: Nurse practitioner X X
Benefits covered: Rural health clinics
and FQHCs
X X
Benefits covered: Clinic services X X X
Benefits covered: Lab and x-ray X X X
Benefits covered: Prescription drugs X X
Benefits covered: Prosthetic devices X X
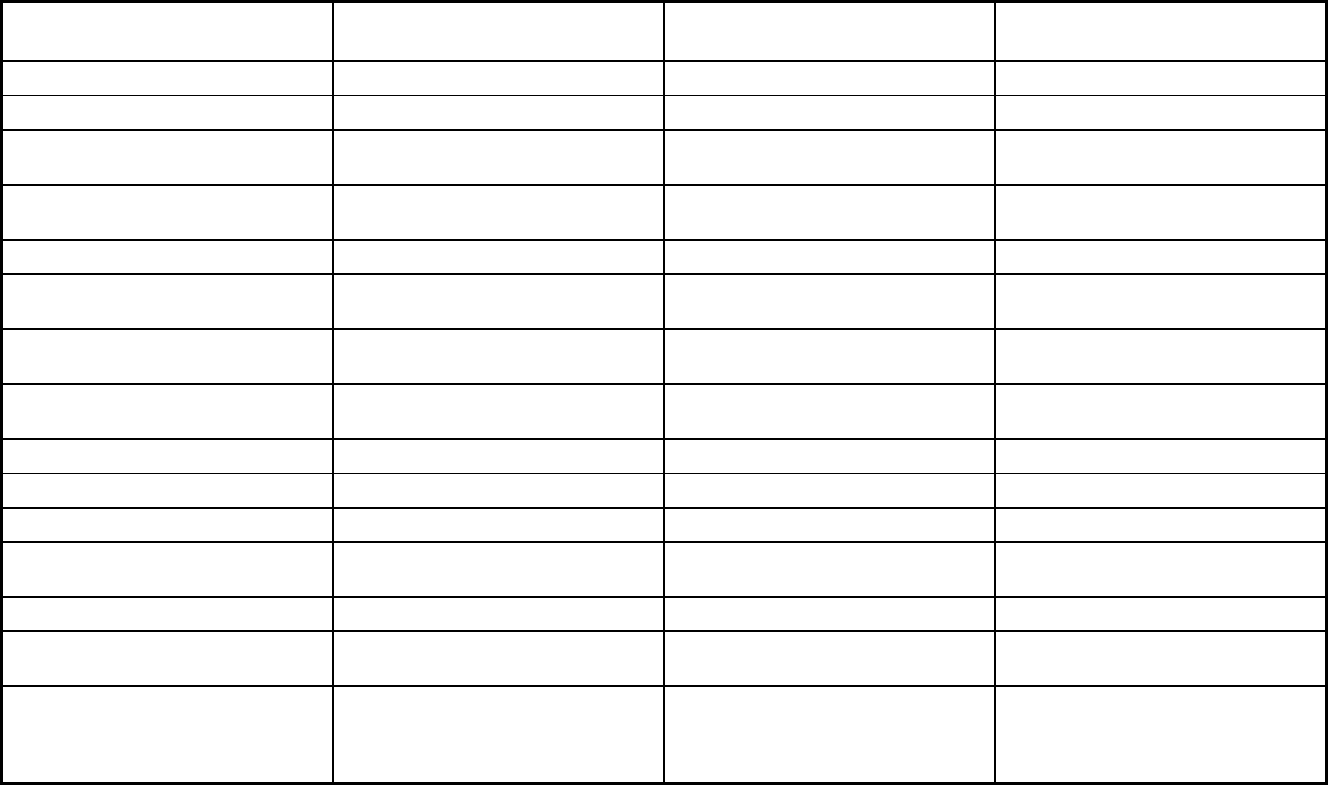
237
Features
Program of All-Inclusive Care for the
Elderly
Accountable Care Collaborative
(ACC)
Colorado Medicaid Community
Behavioral Health Services Program
Benefits covered: EPSDT X X
Benefits covered: Case management X X X
Benefits covered: SSA Section 1945-
authorized health home
Benefits covered: Health home care
(services in home)
X X
Benefits covered: Family planning X
Benefits covered: Dental services
(medical/surgical)
X X
Benefits covered: Dental (preventative
or corrective)
X X
Benefits covered: Personal care (state
plan option)
X X
Benefits covered: HCBS waiver services X
Benefits covered: Private duty nursing X X
Benefits covered: ICF-IDD X
Benefits covered: Nursing facility
services
X X
Benefits covered: Hospice care X X
Benefits covered: Non-Emergency
Medical Transportation
X X
Benefits covered: Institution for Mental
Disease inpatient treatment for people
ages 21-64 defined by 42 CFR
§438.6(e) as an 'in lieu of' benefit
X X
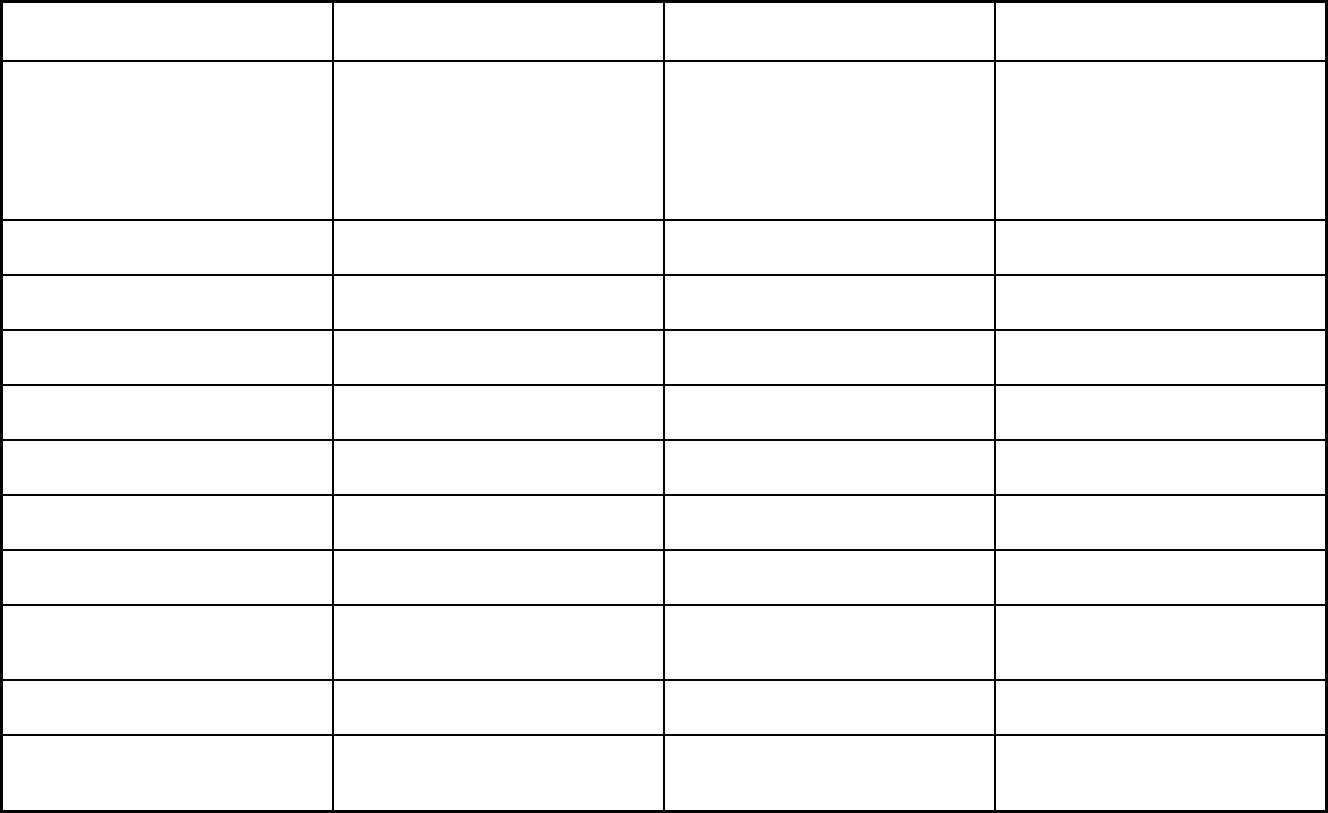
238
Features
Program of All-Inclusive Care for the
Elderly
Accountable Care Collaborative
(ACC)
Colorado Medicaid Community
Behavioral Health Services Program
Benefits covered: Other (e.g., nurse
midwife services, freestanding birth
centers, podiatry, etc.)
PACE is an all-inclusive program. Some
of the other available services include
optometry, podiatry, rehabilitative
services, adult day health center
services, and transportation.
All members enrolled in ACC are
eligible for all 1932(a) state plan
benefits. They also get benefits covered
under the 1915(b) waiver. All plans are
responsible for providing behavioral
health benefits under the 1915(b)
waiver.
Quality assurance and improvement:
HEDIS data required?
No Yes No
Quality assurance and improvement:
CAHPS data required?
No Yes No
Quality assurance and improvement:
Accreditation required?
No No No
Quality assurance and improvement:
Accrediting organization
Quality assurance and improvement:
EQRO contractor name (if applicable)
Health Services Advisory Group, Inc.
Performance incentives: Payment
bonuses/differentials to reward plans
X X
Performance incentives: Preferential
auto-enrollment to reward plans
Performance incentives: Public reports
comparing plan performance on key
metrics
X
Performance incentives: Withholds tied
to performance metrics
X
Performance incentives: MCOs/PHPs
required or encouraged to pay providers
for value/quality outcomes
X
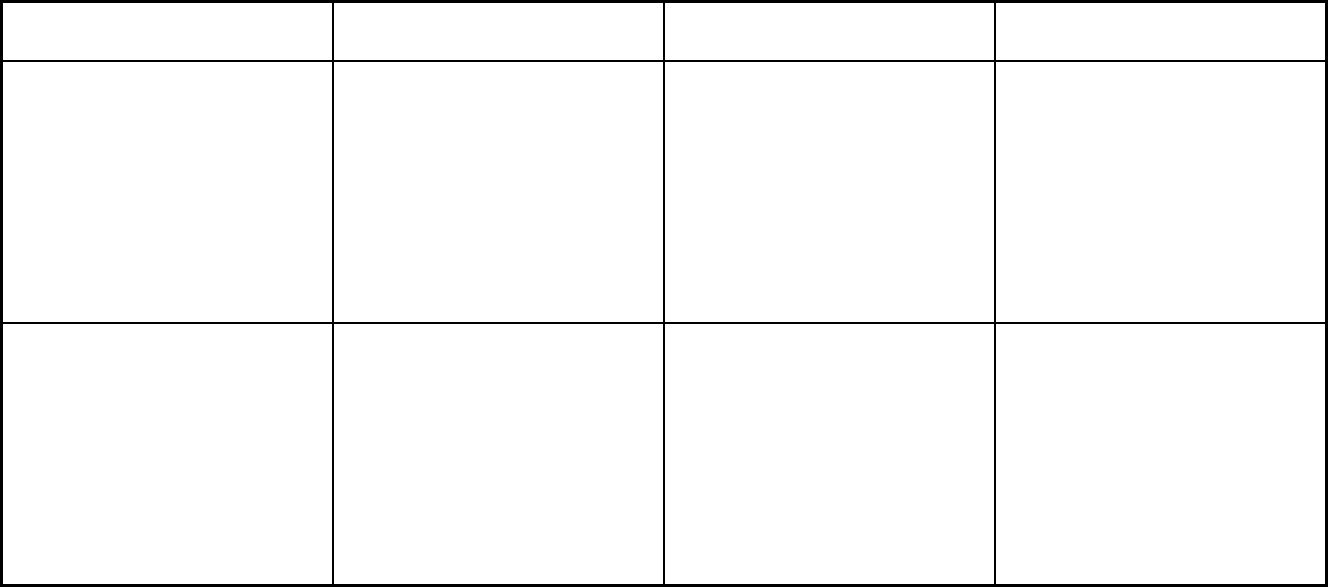
239
Features
Program of All-Inclusive Care for the
Elderly
Accountable Care Collaborative
(ACC)
Colorado Medicaid Community
Behavioral Health Services Program
Participating plans: Plans in Program Rocky Mountain Health Care Services
(PACE); Total Longterm Care - Pueblo
DBA Innovage Greater Colorado PACE;
Total Longterm Care - Innovage Aurora
(PACE); Volunteers of America
(VOANS) PACE DBA Senior
Community Care; Total Longterm Care -
Innovage Loveland (PACE); TRU
Community Care; Total Longterm Care -
Innovage Lakewood (PACE); Total
Longterm Care - Innovage Thornton
(PACE)
RAE 1: Rocky Mountain Health Plans;
RAE 2: Northeast Health Partners; RAE
3: Colorado Access; RAE 4: Health
Colorado, Inc.; RAE 5: Colorado
Access; RAE 6: Colorado Community
Health Alliance; RAE 7: Colorado
Community Health Alliance
Colorado Health Partnerships;
Behavioral Healthcare, Inc.; Foothills
Behavioral Health Partners; Access
Behavioral Care - Denver; Access
Behavioral Care - Northeast
Notes: Program notes The Accountable Care Collaborative
(ACC) program has seven regional
plans called Regional Accountable
Entities (RAEs). The RAEs operate as
both PCCM Entity and PIHP program
types. The state pays the RAEs a full-
risk capitation payment for behavioral
health services under the PIHP
authority. The RAEs also get an
administrative (not risk-based) per
member per month payment for
functions performed as a PCCM Entity.
The Colorado Medicaid Community
Behavioral Health Services Program
contracts with BHOs to arrange for or
provide medically necessary mental
health services to clients in five service
areas. In each area, the program is
managed by a different behavioral
health organization BHO. Medicaid
members are assigned to a BHO based
on where they live.
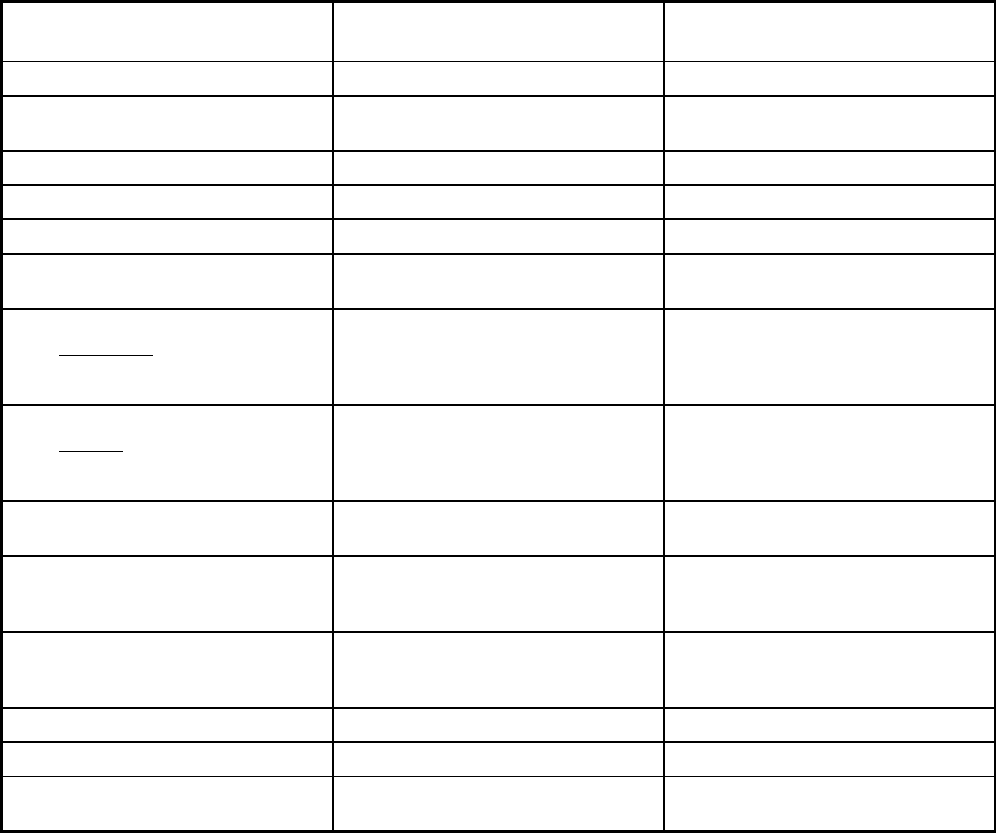
240
Colorado Managed Care Program Features, as of 2018 (2 of 2)
Features Denver Health Medicaid Choice
Accountable Care Collaborative:
Rocky Mountain Health Plans Prime
Program type Comprehensive MCO Comprehensive MCO
Statewide or region-specific? Denver, Arapahoe, Adams, Jefferson
Counties
Garfield, Gunnison, Mesa, Montrose,
Pitkin, Rio Blanco Counties
Federal operating authority 1915(a) 1932(a)
Program start date 01/01/1997 09/01/2014
Waiver expiration date (if applicable)
If the program ended in 2018, indicate
the end date
Populations enrolled: Low-income
adults not covered under ACA Section
VIII (excludes pregnant women and
people with disabilities)
Voluntary Mandatory
Populations enrolled: Low-income
adults covered under ACA Section VIII
(excludes pregnant women and people
with disabilities)
Voluntary Mandatory
Populations enrolled: Aged, Blind or
Disabled Children or Adults
Voluntary Mandatory
Populations enrolled: Non-Disabled
Children (excludes children in foster
care or receiving adoption assistance)
Voluntary
Populations enrolled: Individuals
receiving Limited Benefits (excludes
partial duals)
Populations enrolled: Full Duals Voluntary Mandatory
Populations enrolled: Partial Duals
Populations enrolled: Children with
Special Health Care Needs
Voluntary
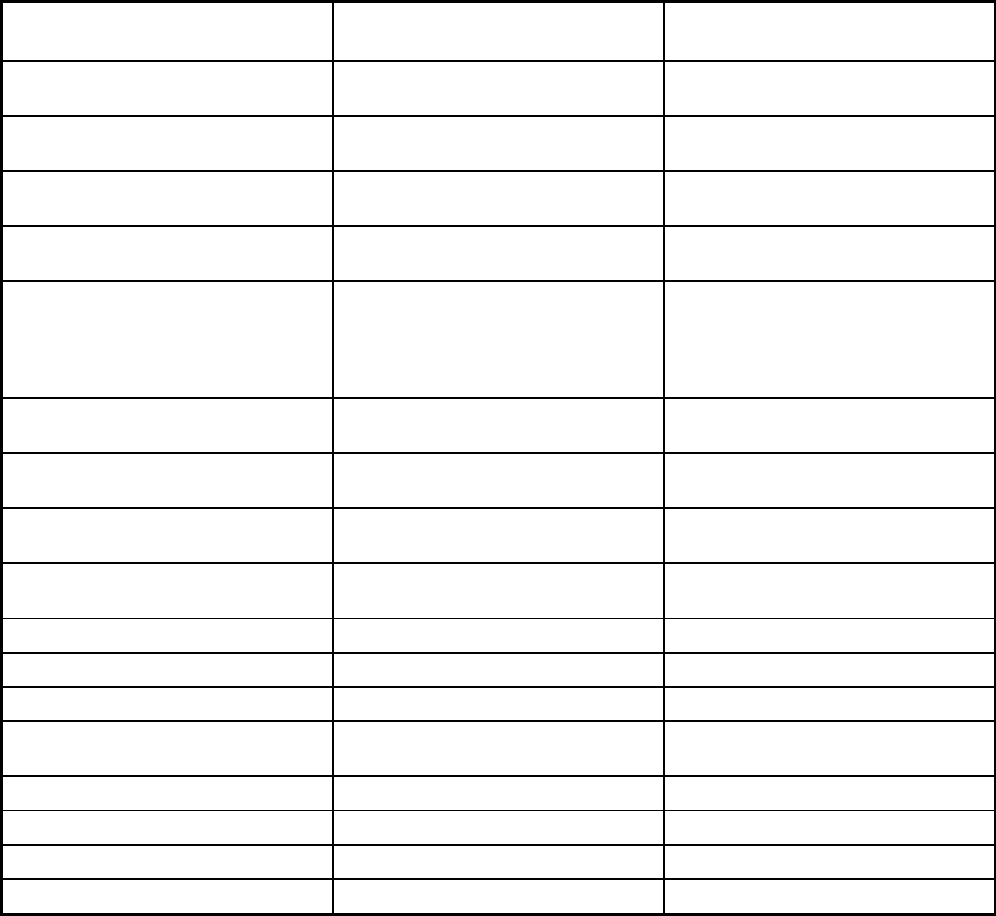
241
Features Denver Health Medicaid Choice
Accountable Care Collaborative:
Rocky Mountain Health Plans Prime
Populations enrolled: Native
American/Alaskan Natives
Voluntary Voluntary
Populations enrolled: Foster Care and
Adoption Assistance Children
Voluntary Voluntary
Populations enrolled: Enrollment choice
period
Other Other
Populations enrolled: Enrollment broker
name (if applicable)
Maximus Health Services, Inc. Maximus Health Services, Inc.
Populations enrolled: Notes on
enrollment choice period
Clients are passively enrolled with 90
days to opt-out after enrollment. Each
year, clients are given notice 60 days
prior to the first day of their birth month
that they can disenroll.
Clients are passively enrolled with 90
days to opt-out after enrollment. Each
year, clients are given notice 60 days
prior to the first day of their birth month
that they can disenroll.
Benefits covered: Inpatient hospital
physical health
X X
Benefits covered: Inpatient hospital
behavioral health (MH and/or SUD)
Benefits covered: Outpatient hospital
physical health
X X
Benefits covered: Outpatient hospital
behavioral health (MH and/or SUD)
Benefits covered: Partial hospitalization
Benefits covered: Physician X X
Benefits covered: Nurse practitioner X X
Benefits covered: Rural health clinics
and FQHCs
X X
Benefits covered: Clinic services X X
Benefits covered: Lab and x-ray X X
Benefits covered: Prescription drugs X X
Benefits covered: Prosthetic devices
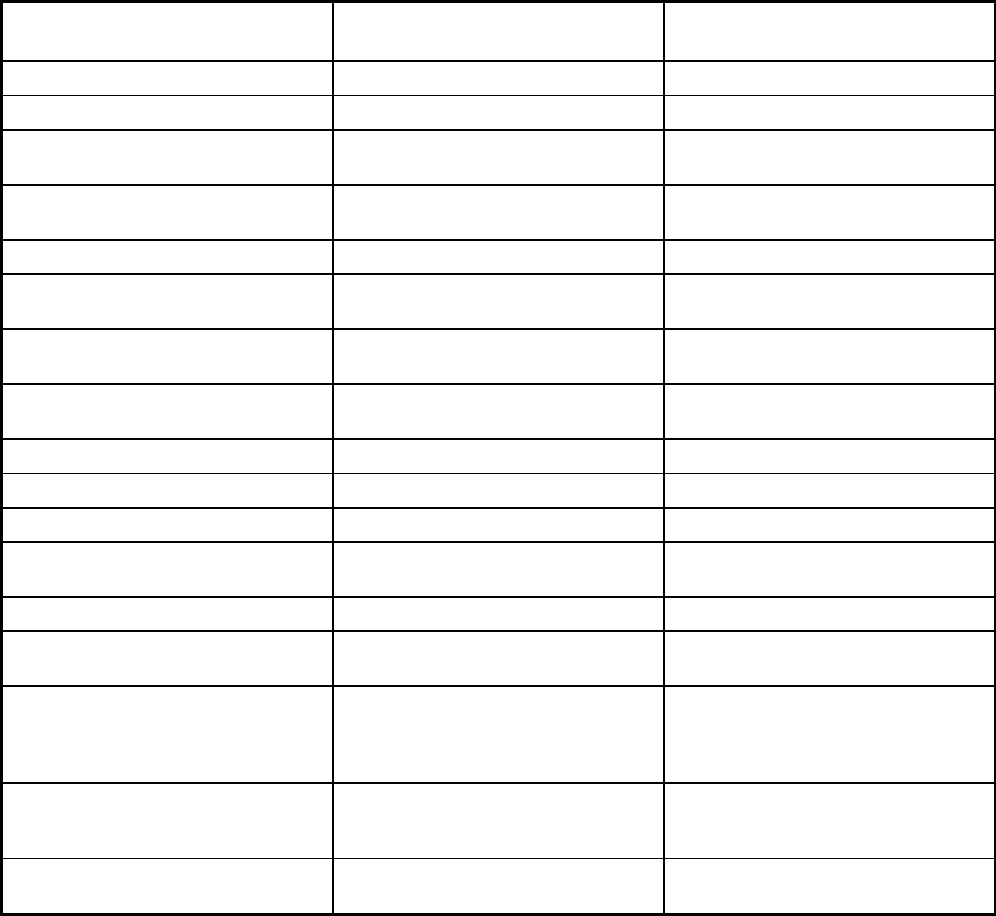
242
Features Denver Health Medicaid Choice
Accountable Care Collaborative:
Rocky Mountain Health Plans Prime
Benefits covered: EPSDT X X
Benefits covered: Case management
Benefits covered: SSA Section 1945-
authorized health home
Benefits covered: Health home care
(services in home)
X X
Benefits covered: Family planning X X
Benefits covered: Dental services
(medical/surgical)
Benefits covered: Dental (preventative
or corrective)
Benefits covered: Personal care (state
plan option)
X X
Benefits covered: HCBS waiver services
Benefits covered: Private duty nursing
Benefits covered: ICF-IDD
Benefits covered: Nursing facility
services
Benefits covered: Hospice care
Benefits covered: Non-Emergency
Medical Transportation
Benefits covered: Institution for Mental
Disease inpatient treatment for people
ages 21-64 defined by 42 CFR
§438.6(e) as an 'in lieu of' benefit
Benefits covered: Other (e.g., nurse
midwife services, freestanding birth
centers, podiatry, etc.)
Durable medical equipment Durable medical equipment
Quality assurance and improvement:
HEDIS data required?
Yes Yes
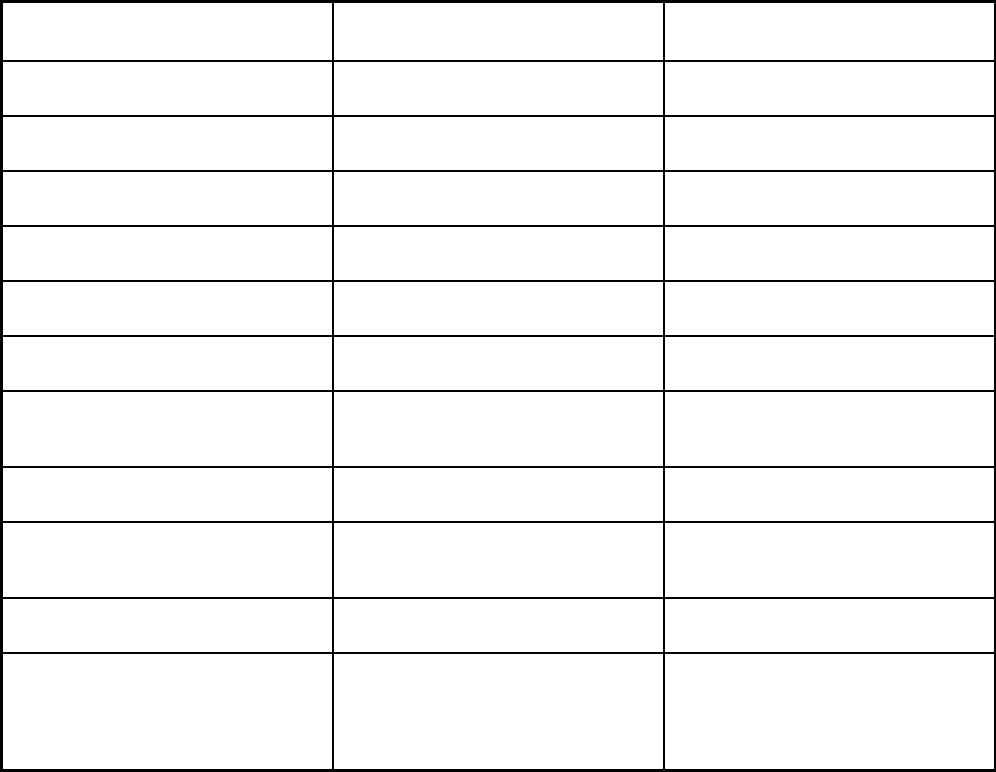
243
Features Denver Health Medicaid Choice
Accountable Care Collaborative:
Rocky Mountain Health Plans Prime
Quality assurance and improvement:
CAHPS data required?
Yes Yes
Quality assurance and improvement:
Accreditation required?
No No
Quality assurance and improvement:
Accrediting organization
Quality assurance and improvement:
EQRO contractor name (if applicable)
Health Services Advisory Group, Inc. Health Services Advisory Group, Inc.
Performance incentives: Payment
bonuses/differentials to reward plans
X
Performance incentives: Preferential
auto-enrollment to reward plans
Performance incentives: Public reports
comparing plan performance on key
metrics
X
Performance incentives: Withholds tied
to performance metrics
Performance incentives: MCOs/PHPs
required or encouraged to pay providers
for value/quality outcomes
X
Participating plans: Plans in Program Denver Health Medicaid Choice Accountable Care Collaborative: Rocky
Mountain Health Plans Prime
Notes: Program notes Denver Health Medicaid Choice is
contracted and operates under RAE 5
(Colorado Access) of the Accountable
Care Collaborative program.
Rocky Mountain Health Plans Prime is
contracted and operates under RAE 1
(Rocky Mountain Health Plans) of the
Accountable Care Collaborative
program.
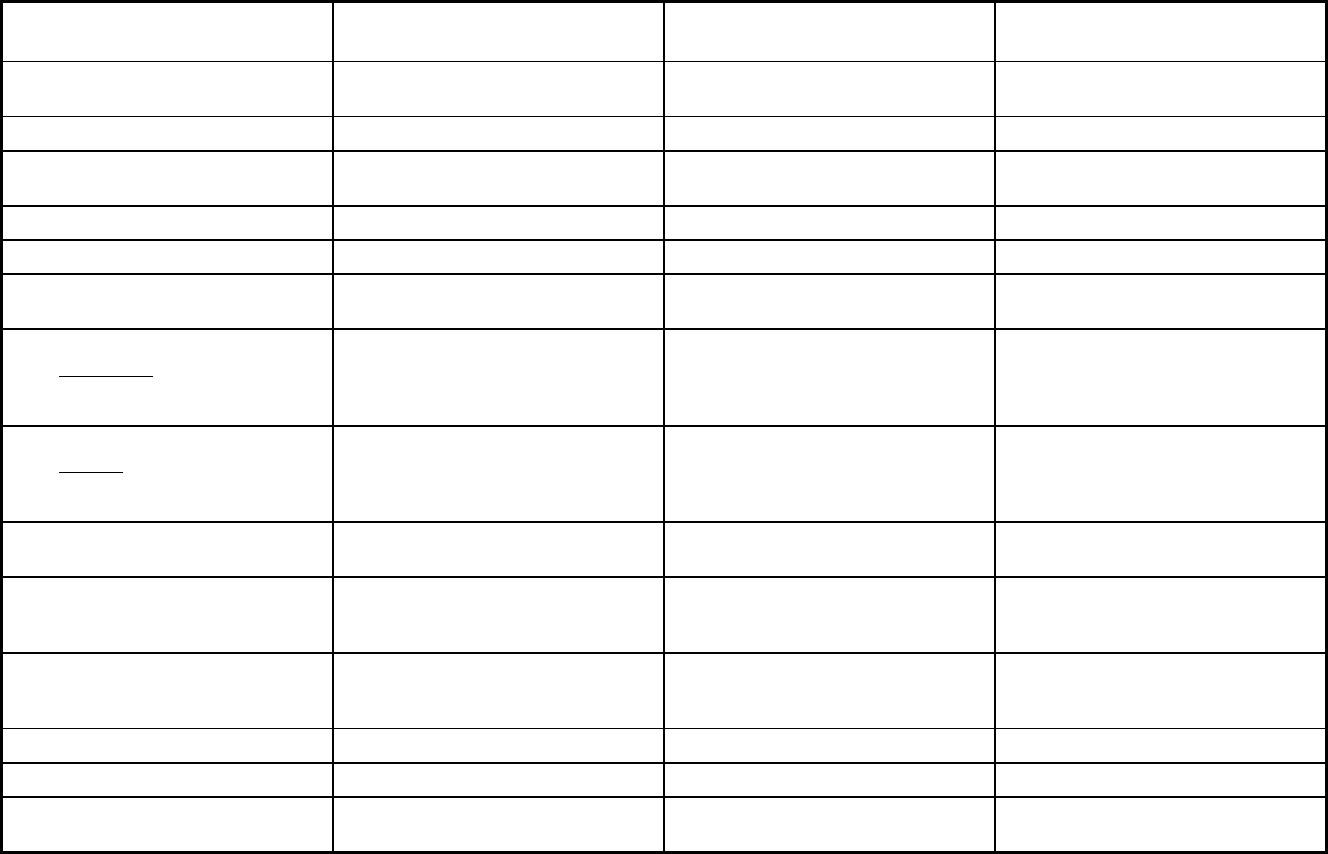
244
Delaware Managed Care Program Features, as of 2018
Features
LogistiCare/Circulation Non-
Emergency Medical Transportation Diamond State Health Plan Saint Francis Life
Program type Non-Emergency Medical Transportation Comprehensive MCO + MLTSS Program of All-inclusive Care for the
Elderly (PACE)
Statewide or region-specific? Statewide Statewide New Castle County
Federal operating authority 1902(a)(70) NEMT 1115(a) (Medicaid demonstration
waivers)
PACE
Program start date 07/01/2002 01/01/1996 02/01/2013
Waiver expiration date (if applicable) 07/31/2019
If the program ended in 2018, indicate
the end date
Populations enrolled: Low-income
adults not covered under ACA Section
VIII (excludes pregnant women and
people with disabilities)
Mandatory Mandatory
Populations enrolled: Low-income
adults covered under ACA Section VIII
(excludes pregnant women and people
with disabilities)
Mandatory Mandatory
Populations enrolled: Aged, Blind or
Disabled Children or Adults
Mandatory Mandatory Voluntary
Populations enrolled: Non-Disabled
Children (excludes children in foster
care or receiving adoption assistance)
Mandatory Mandatory
Populations enrolled: Individuals
receiving Limited Benefits (excludes
partial duals)
Mandatory
Populations enrolled: Full Duals Mandatory Mandatory Voluntary
Populations enrolled: Partial Duals
Populations enrolled: Children with
Special Health Care Needs
Mandatory Mandatory
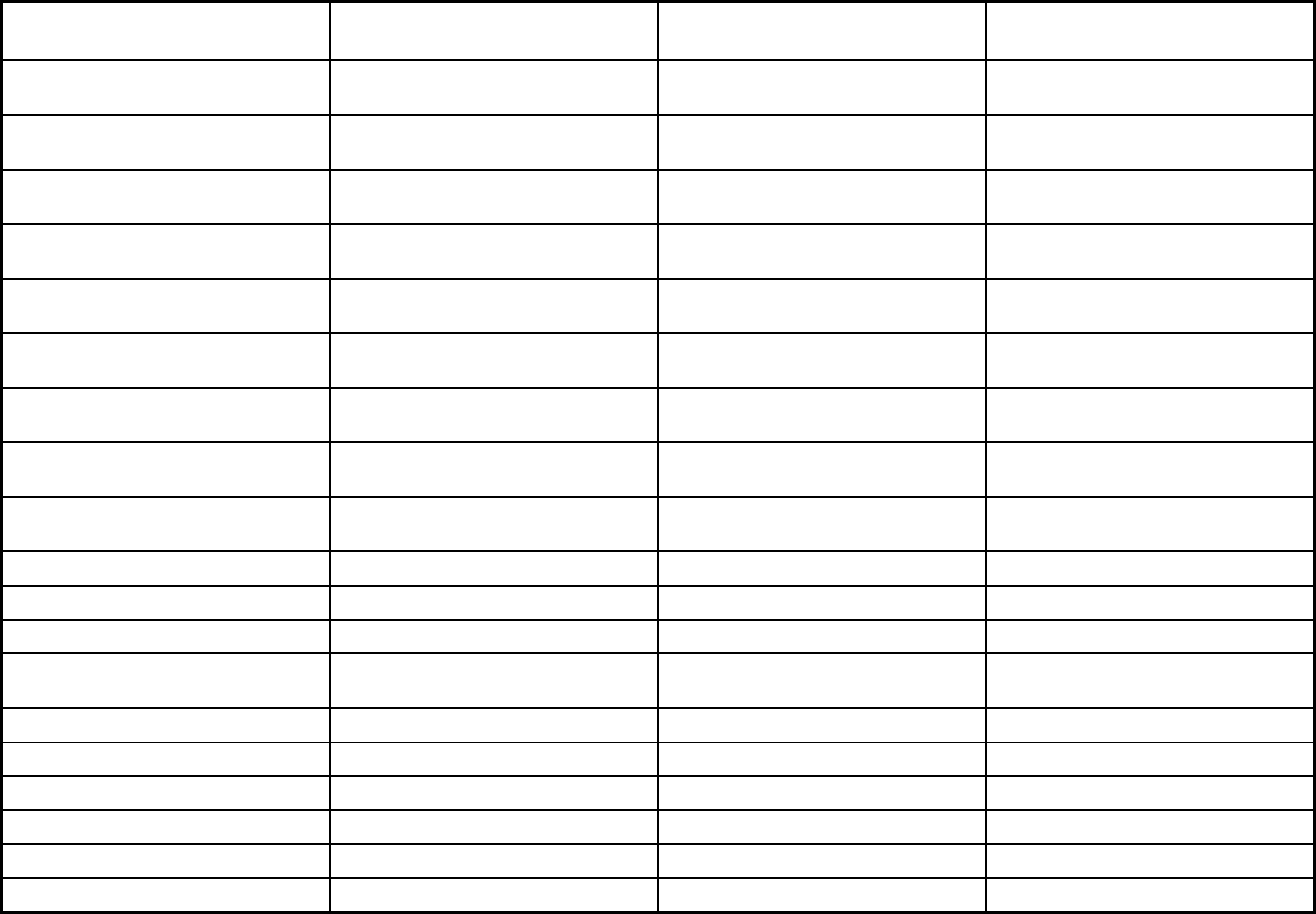
245
Features
LogistiCare/Circulation Non-
Emergency Medical Transportation Diamond State Health Plan Saint Francis Life
Populations enrolled: Native
American/Alaskan Natives
Exempt Mandatory Voluntary
Populations enrolled: Foster Care and
Adoption Assistance Children
Mandatory Mandatory Exempt
Populations enrolled: Enrollment choice
period
Pre-assigned N/A
Populations enrolled: Enrollment broker
name (if applicable)
DXC Technology DXC Technology
Populations enrolled: Notes on
enrollment choice period
Benefits covered: Inpatient hospital
physical health
X X
Benefits covered: Inpatient hospital
behavioral health (MH and/or SUD)
X X
Benefits covered: Outpatient hospital
physical health
X X
Benefits covered: Outpatient hospital
behavioral health (MH and/or SUD)
X X
Benefits covered: Partial hospitalization X X
Benefits covered: Physician X X
Benefits covered: Nurse practitioner X X
Benefits covered: Rural health clinics
and FQHCs
X X
Benefits covered: Clinic services X X
Benefits covered: Lab and x-ray X X
Benefits covered: Prescription drugs X X
Benefits covered: Prosthetic devices X X
Benefits covered: EPSDT X
Benefits covered: Case management X X
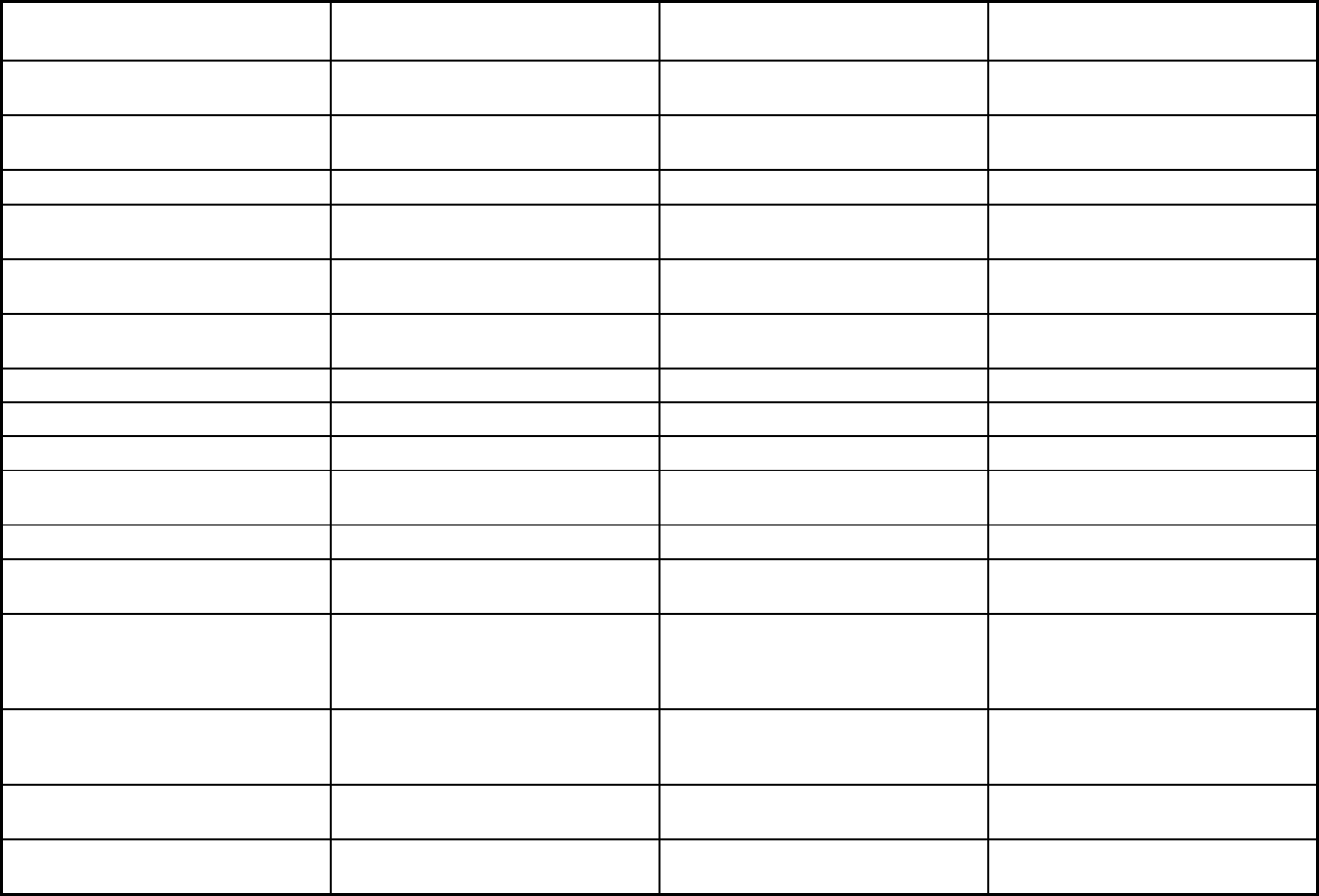
246
Features
LogistiCare/Circulation Non-
Emergency Medical Transportation Diamond State Health Plan Saint Francis Life
Benefits covered: SSA Section 1945-
authorized health home
Benefits covered: Health home care
(services in home)
X X
Benefits covered: Family planning X X
Benefits covered: Dental services
(medical/surgical)
X
Benefits covered: Dental (preventative
or corrective)
X
Benefits covered: Personal care (state
plan option)
X X
Benefits covered: HCBS waiver services X X
Benefits covered: Private duty nursing X X
Benefits covered: ICF-IDD X
Benefits covered: Nursing facility
services
X X
Benefits covered: Hospice care X X
Benefits covered: Non-Emergency
Medical Transportation
X X
Benefits covered: Institution for Mental
Disease inpatient treatment for people
ages 21-64 defined by 42 CFR
§438.6(e) as an 'in lieu of' benefit
X X
Benefits covered: Other (e.g., nurse
midwife services, freestanding birth
centers, podiatry, etc.)
Freestanding birth centers, home-
delivered meals, emergency response
system, home modifications
Quality assurance and improvement:
HEDIS data required?
No Yes Yes
Quality assurance and improvement:
CAHPS data required?
No Yes Yes
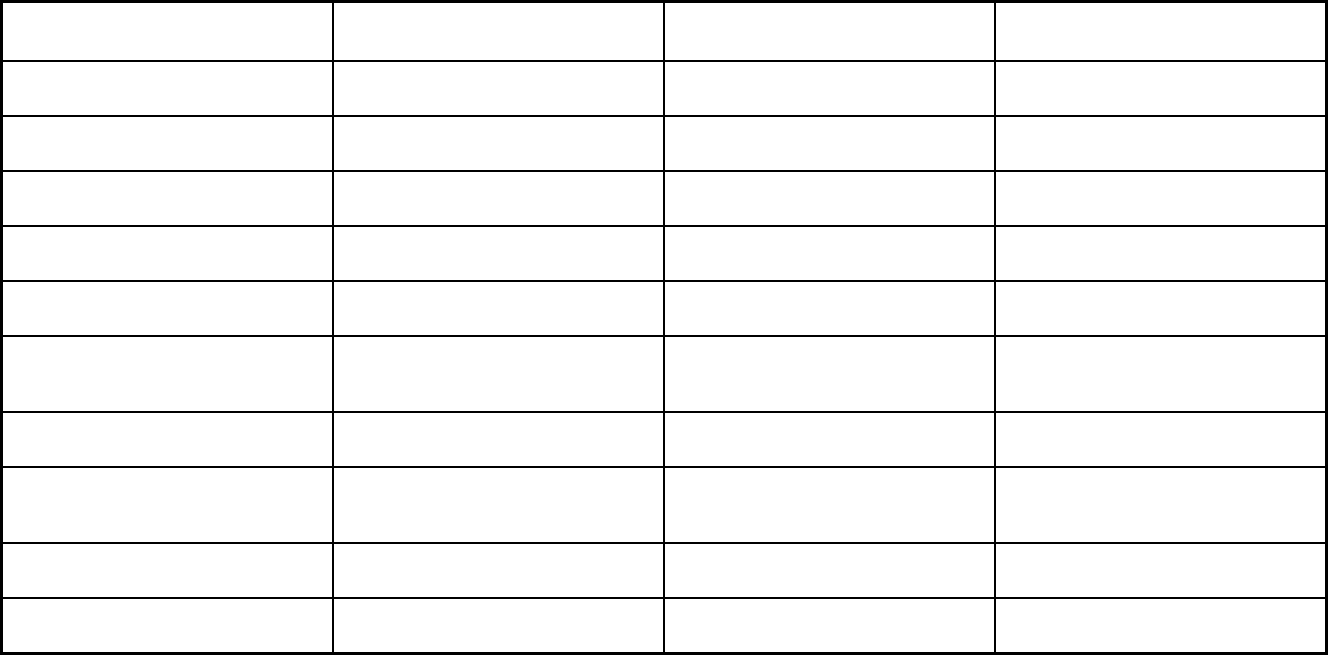
247
Features
LogistiCare/Circulation Non-
Emergency Medical Transportation Diamond State Health Plan Saint Francis Life
Quality assurance and improvement:
Accreditation required?
No Yes No, but accreditation considered in plan
selection criteria
Quality assurance and improvement:
Accrediting organization
NCQA
Quality assurance and improvement:
EQRO contractor name (if applicable)
Mercer Government Human Services
Consulting
Performance incentives: Payment
bonuses/differentials to reward plans
X
Performance incentives: Preferential
auto-enrollment to reward plans
Performance incentives: Public reports
comparing plan performance on key
metrics
X
Performance incentives: Withholds tied
to performance metrics
Performance incentives: MCOs/PHPs
required or encouraged to pay providers
for value/quality outcomes
X
Participating plans: Plans in Program LogistiCare/Circulation Non-Emergency
Medical Transportation
Highmark Health Options of Delaware;
AmeriHealth Caritas of Delaware
Saint Francis Life
Notes: Program notes AmeriHealth Caritas contract began on
1/1/2018.
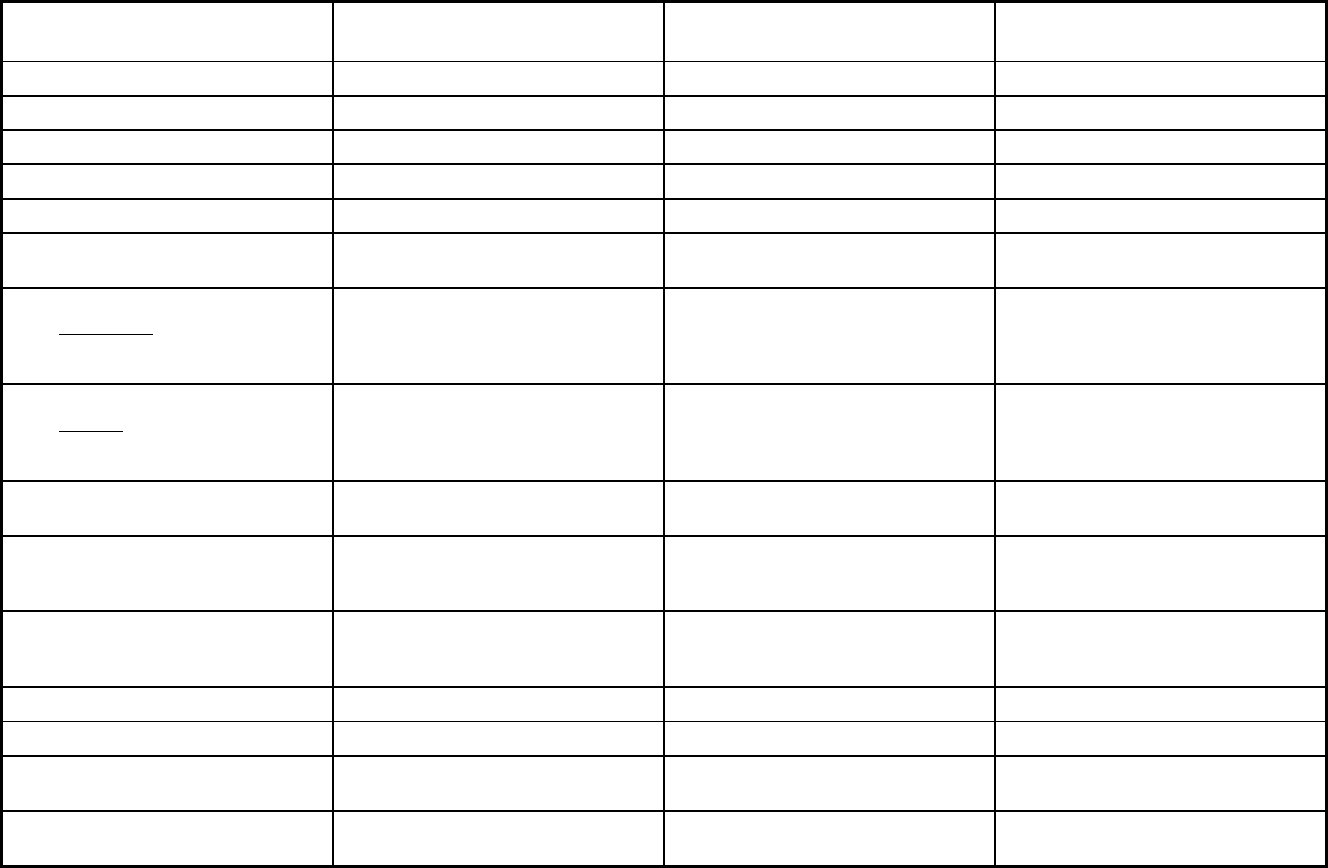
248
District of Columbia Managed Care Program Features, as of 2018
Features DC Healthy Families
Child and Adolescent Supplemental
Security Income Program (CASSIP)
Non-Emergency Medical
Transportation (NEMT)
Program type Comprehensive MCO Comprehensive MCO Non-Emergency Medical Transportation
Statewide or region-specific? Statewide Statewide Statewide
Federal operating authority 1932(a),1945 Health Homes 1915(a) 1902(a)(70) NEMT
Program start date 04/01/1994 01/01/1996 10/01/2007
Waiver expiration date (if applicable)
If the program ended in 2018, indicate
the end date
Populations enrolled: Low-income
adults not covered under ACA Section
VIII (excludes pregnant women and
people with disabilities)
Mandatory
Populations enrolled: Low-income
adults covered under ACA Section VIII
(excludes pregnant women and people
with disabilities)
Mandatory
Populations enrolled: Aged, Blind or
Disabled Children or Adults
Voluntary Voluntary Mandatory
Populations enrolled: Non-Disabled
Children (excludes children in foster
care or receiving adoption assistance)
Mandatory
Populations enrolled: Individuals
receiving Limited Benefits (excludes
partial duals)
Mandatory
Populations enrolled: Full Duals Voluntary Voluntary Mandatory
Populations enrolled: Partial Duals
Populations enrolled: Children with
Special Health Care Needs
Voluntary Mandatory
Populations enrolled: Native
American/Alaskan Natives
Mandatory Voluntary Exempt
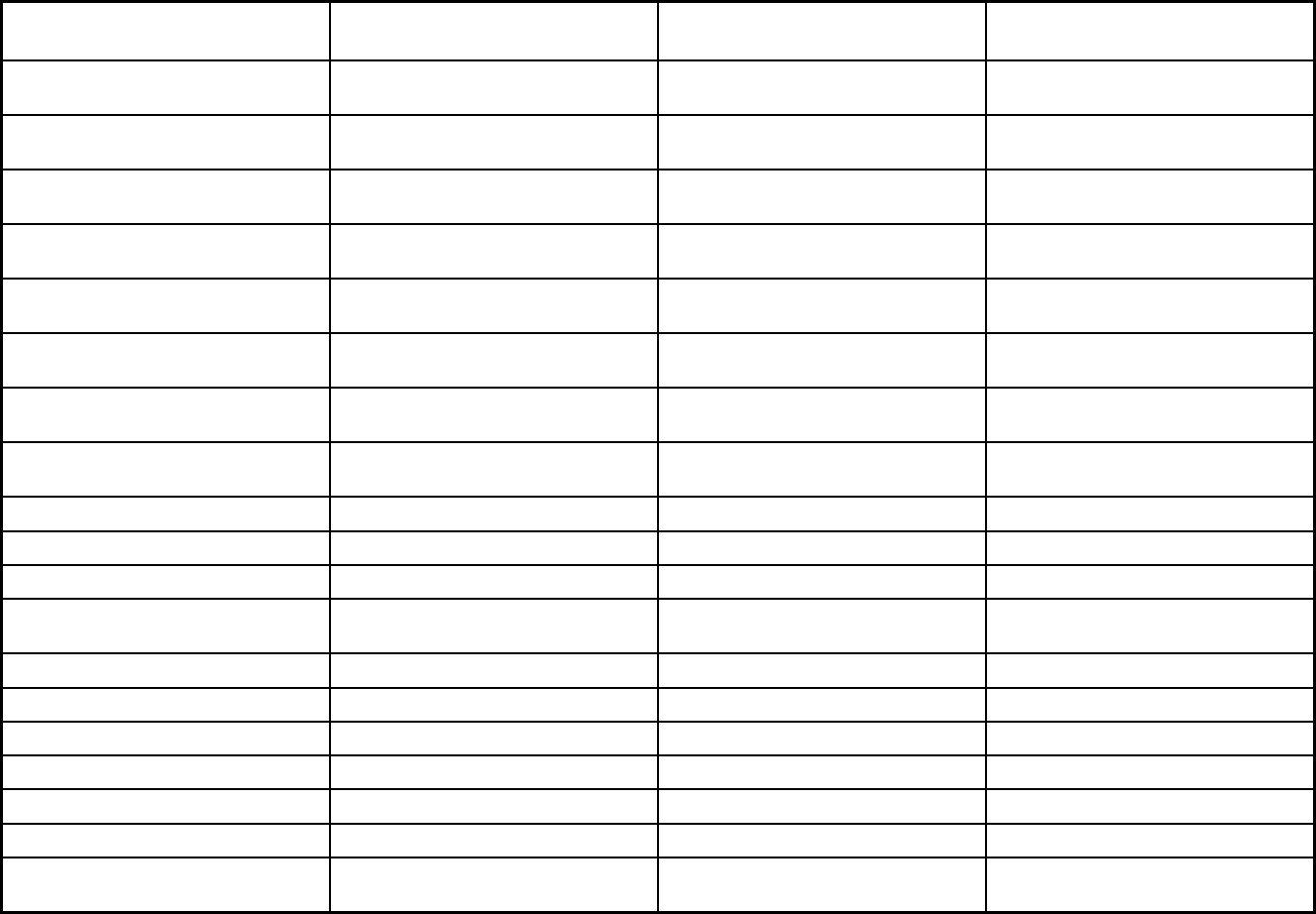
249
Features DC Healthy Families
Child and Adolescent Supplemental
Security Income Program (CASSIP)
Non-Emergency Medical
Transportation (NEMT)
Populations enrolled: Foster Care and
Adoption Assistance Children
Exempt Voluntary Mandatory
Populations enrolled: Enrollment choice
period
30 days Other
Populations enrolled: Enrollment broker
name (if applicable)
Maximus
Populations enrolled: Notes on
enrollment choice period
Enrollment is voluntary. All other
beneficiaries stay in fee-for-service.
Benefits covered: Inpatient hospital
physical health
X X
Benefits covered: Inpatient hospital
behavioral health (MH and/or SUD)
X X
Benefits covered: Outpatient hospital
physical health
X X
Benefits covered: Outpatient hospital
behavioral health (MH and/or SUD)
X X
Benefits covered: Partial hospitalization X X
Benefits covered: Physician X X
Benefits covered: Nurse practitioner X X
Benefits covered: Rural health clinics
and FQHCs
X X
Benefits covered: Clinic services X X
Benefits covered: Lab and x-ray X X
Benefits covered: Prescription drugs X X
Benefits covered: Prosthetic devices X X
Benefits covered: EPSDT X X
Benefits covered: Case management X X
Benefits covered: SSA Section 1945-
authorized health home
X
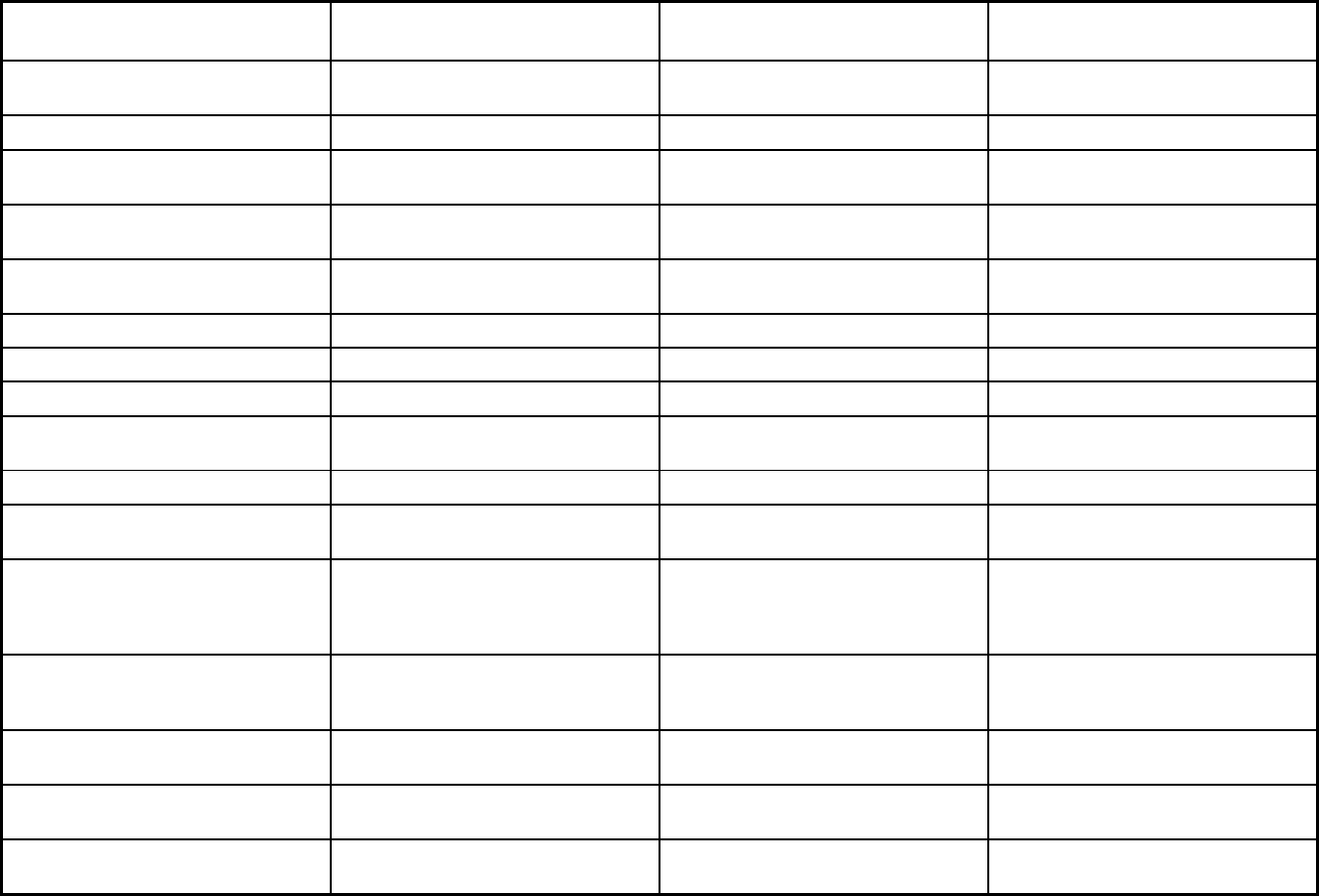
250
Features DC Healthy Families
Child and Adolescent Supplemental
Security Income Program (CASSIP)
Non-Emergency Medical
Transportation (NEMT)
Benefits covered: Health home care
(services in home)
X X
Benefits covered: Family planning X X
Benefits covered: Dental services
(medical/surgical)
X X
Benefits covered: Dental (preventative
or corrective)
X X
Benefits covered: Personal care (state
plan option)
X X
Benefits covered: HCBS waiver services X
Benefits covered: Private duty nursing X
Benefits covered: ICF-IDD X
Benefits covered: Nursing facility
services
X
Benefits covered: Hospice care X X
Benefits covered: Non-Emergency
Medical Transportation
X X X
Benefits covered: Institution for Mental
Disease inpatient treatment for people
ages 21-64 defined by 42 CFR
§438.6(e) as an 'in lieu of' benefit
X X
Benefits covered: Other (e.g., nurse
midwife services, freestanding birth
centers, podiatry, etc.)
Freestanding birth centers Freestanding birth centers
Quality assurance and improvement:
HEDIS data required?
Yes Yes No
Quality assurance and improvement:
CAHPS data required?
Yes Yes No
Quality assurance and improvement:
Accreditation required?
Yes No No
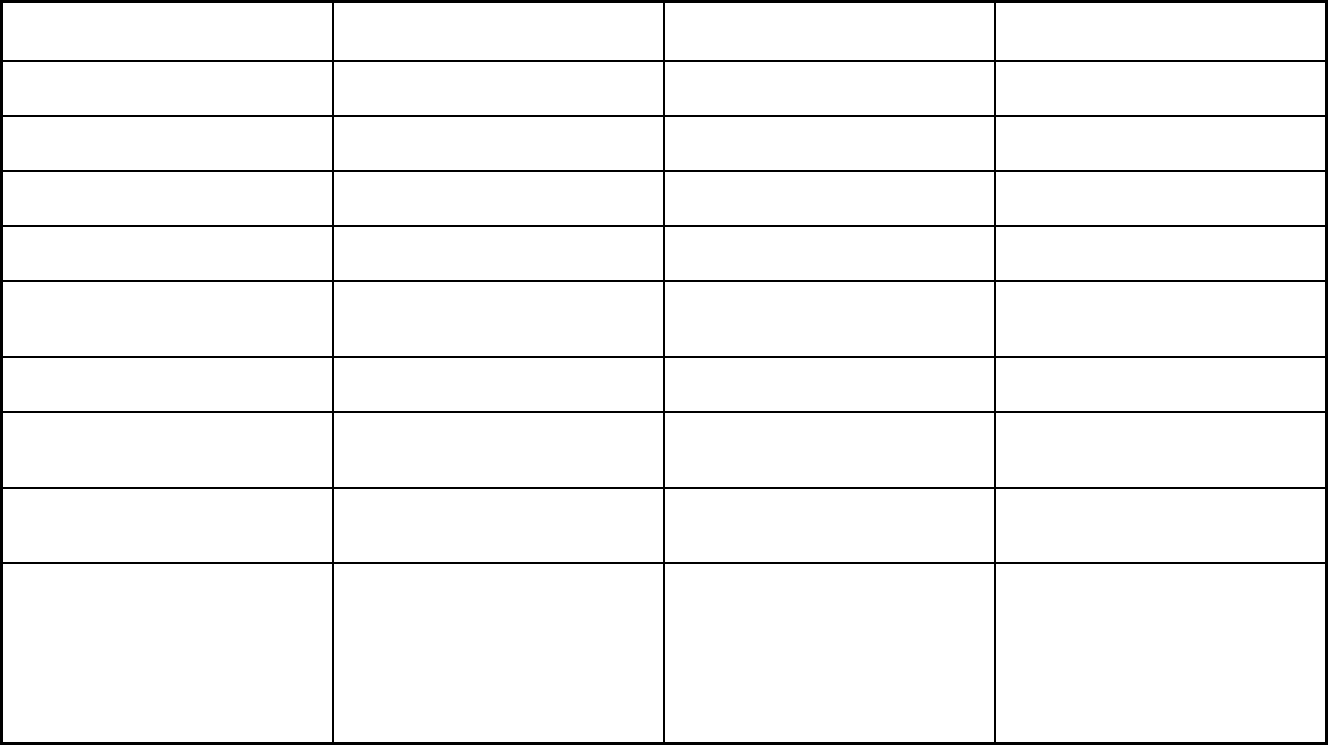
251
Features DC Healthy Families
Child and Adolescent Supplemental
Security Income Program (CASSIP)
Non-Emergency Medical
Transportation (NEMT)
Quality assurance and improvement:
Accrediting organization
NCQA
Quality assurance and improvement:
EQRO contractor name (if applicable)
Qlarant
Performance incentives: Payment
bonuses/differentials to reward plans
X
Performance incentives: Preferential
auto-enrollment to reward plans
Performance incentives: Public reports
comparing plan performance on key
metrics
X
Performance incentives: Withholds tied
to performance metrics
X
Performance incentives: MCOs/PHPs
required or encouraged to pay providers
for value/quality outcomes
X
Participating plans: Plans in Program AmeriHealth Caritas District of
Columbia; Amerigroup District of
Columbia; Trusted Health Plan
Health Services for Children with
Special Needs
Medical Transportation Management,
Inc.
Notes: Program notes Full duals are eligible for enrollment if
there is a Medicaid-enrolled dependent
child in the household. Nursing facilities
are covered by MCO for the first 30
consecutive days. DC Healthy Families
was previously reported as the Medicaid
Managed Care Program.
Aged, blind, or disabled children and
adults are eligible up to the age of 26.
CASSIP was previously reported as
Health Services for Children with
Special Needs.
The DC Department of Health Care
Finance pays for non-emergency
medical transportation only for its fee-
for-service members. Non-emergency
medical transportation for managed
care members is paid by the District's
Medicaid managed care organizations
for low-income adults and children.
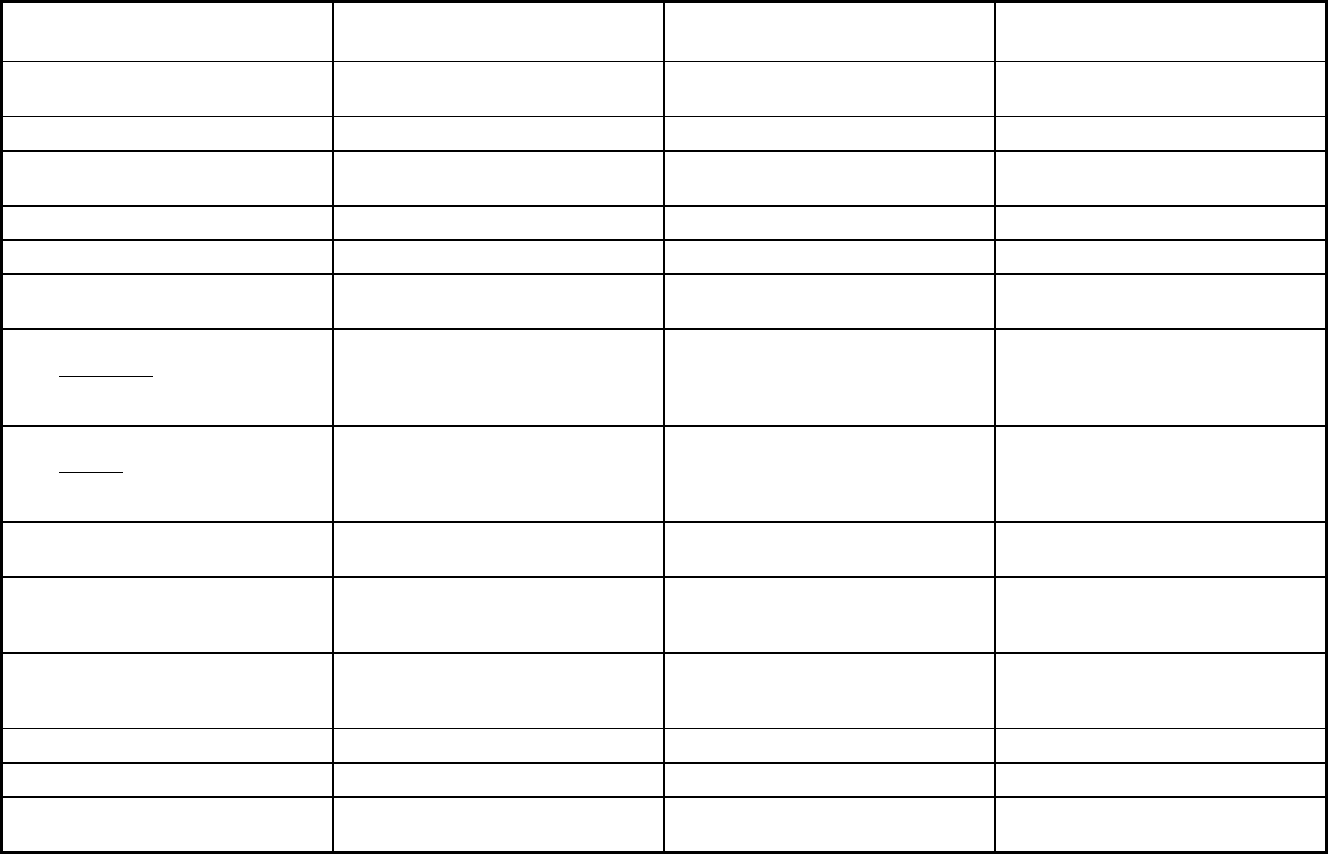
252
Florida Managed Care Program Features, as of 2018
Features
Managed Medical Assistance
Program Long-term Care Program
Program of All-Inclusive Care for the
Elderly
Program type Comprehensive MCO MLTSS only (PIHP and/or PAHP) Program of All-inclusive Care for the
Elderly (PACE)
Statewide or region-specific? Statewide Statewide Statewide
Federal operating authority 1115(a) (Medicaid demonstration
waivers)
1915(b)/1915(c) PACE
Program start date 08/01/2014 03/01/2014 01/01/2003
Waiver expiration date (if applicable) 06/30/2022 12/27/2021
If the program ended in 2018, indicate
the end date
Populations enrolled: Low-income
adults not covered under ACA Section
VIII (excludes pregnant women and
people with disabilities)
Mandatory Mandatory
Populations enrolled: Low-income
adults covered under ACA Section VIII
(excludes pregnant women and people
with disabilities)
Populations enrolled: Aged, Blind or
Disabled Children or Adults
Mandatory Mandatory Voluntary
Populations enrolled: Non-Disabled
Children (excludes children in foster
care or receiving adoption assistance)
Mandatory Mandatory
Populations enrolled: Individuals
receiving Limited Benefits (excludes
partial duals)
Populations enrolled: Full Duals Mandatory Mandatory Voluntary
Populations enrolled: Partial Duals
Populations enrolled: Children with
Special Health Care Needs
Mandatory Mandatory
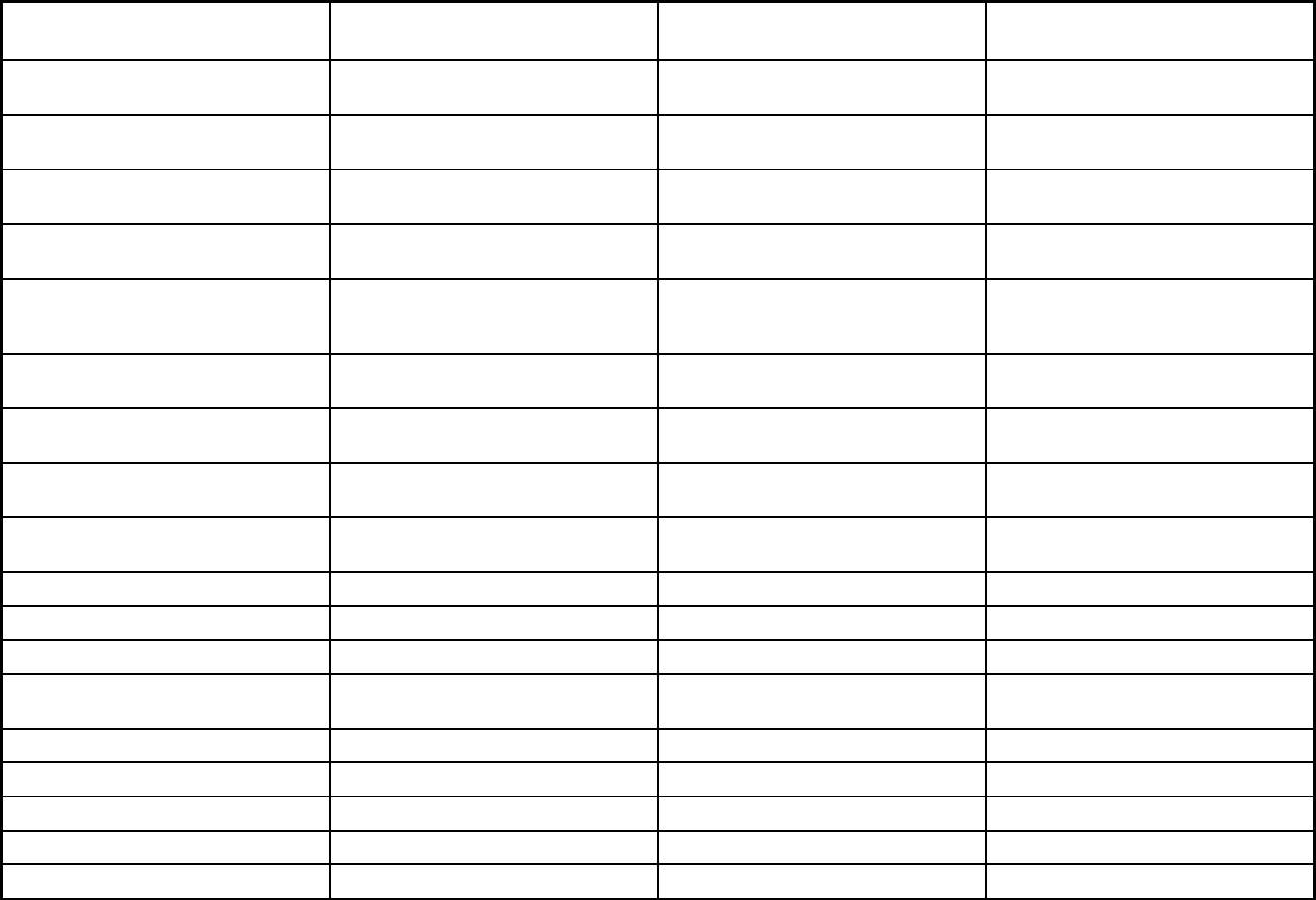
253
Features
Managed Medical Assistance
Program Long-term Care Program
Program of All-Inclusive Care for the
Elderly
Populations enrolled: Native
American/Alaskan Natives
Mandatory Mandatory Voluntary
Populations enrolled: Foster Care and
Adoption Assistance Children
Mandatory Mandatory Exempt
Populations enrolled: Enrollment choice
period
Other 60 days N/A
Populations enrolled: Enrollment broker
name (if applicable)
Automated Health Systems Automated Health Systems Automated Health Systems
Populations enrolled: Notes on
enrollment choice period
Beneficiaries are enrolled immediately
after determined eligible. Beneficiaries
are then given 120 days to pick a plan.
Continuous while slots are available
Benefits covered: Inpatient hospital
physical health
X X
Benefits covered: Inpatient hospital
behavioral health (MH and/or SUD)
X X
Benefits covered: Outpatient hospital
physical health
X X
Benefits covered: Outpatient hospital
behavioral health (MH and/or SUD)
X X
Benefits covered: Partial hospitalization X X
Benefits covered: Physician X X
Benefits covered: Nurse practitioner X X
Benefits covered: Rural health clinics
and FQHCs
X X
Benefits covered: Clinic services X X
Benefits covered: Lab and x-ray X X
Benefits covered: Prescription drugs X X
Benefits covered: Prosthetic devices X X
Benefits covered: EPSDT X
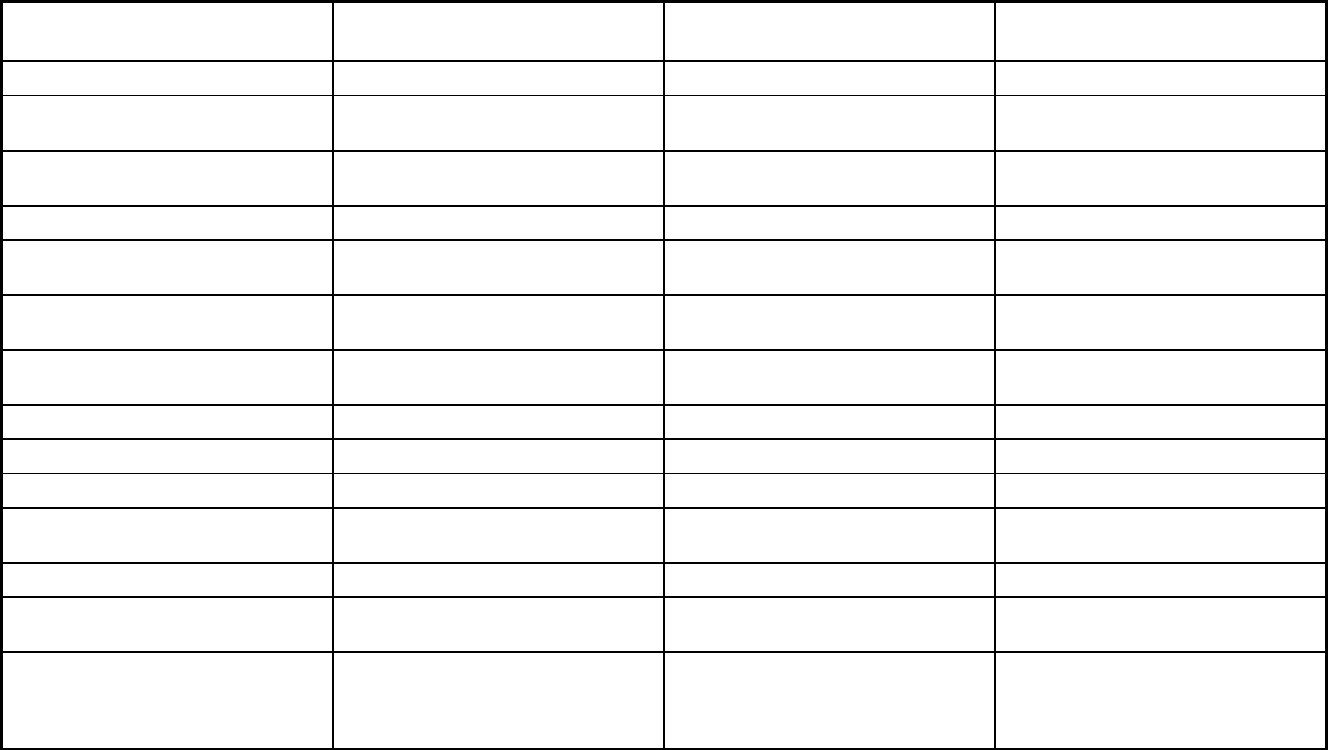
254
Features
Managed Medical Assistance
Program Long-term Care Program
Program of All-Inclusive Care for the
Elderly
Benefits covered: Case management X X
Benefits covered: SSA Section 1945-
authorized health home
Benefits covered: Health home care
(services in home)
X X X
Benefits covered: Family planning X X
Benefits covered: Dental services
(medical/surgical)
X X
Benefits covered: Dental (preventative
or corrective)
X X
Benefits covered: Personal care (state
plan option)
X X
Benefits covered: HCBS waiver services X X
Benefits covered: Private duty nursing X X
Benefits covered: ICF-IDD
Benefits covered: Nursing facility
services
X X
Benefits covered: Hospice care X X X
Benefits covered: Non-Emergency
Medical Transportation
X X X
Benefits covered: Institution for Mental
Disease inpatient treatment for people
ages 21-64 defined by 42 CFR
§438.6(e) as an 'in lieu of' benefit
X
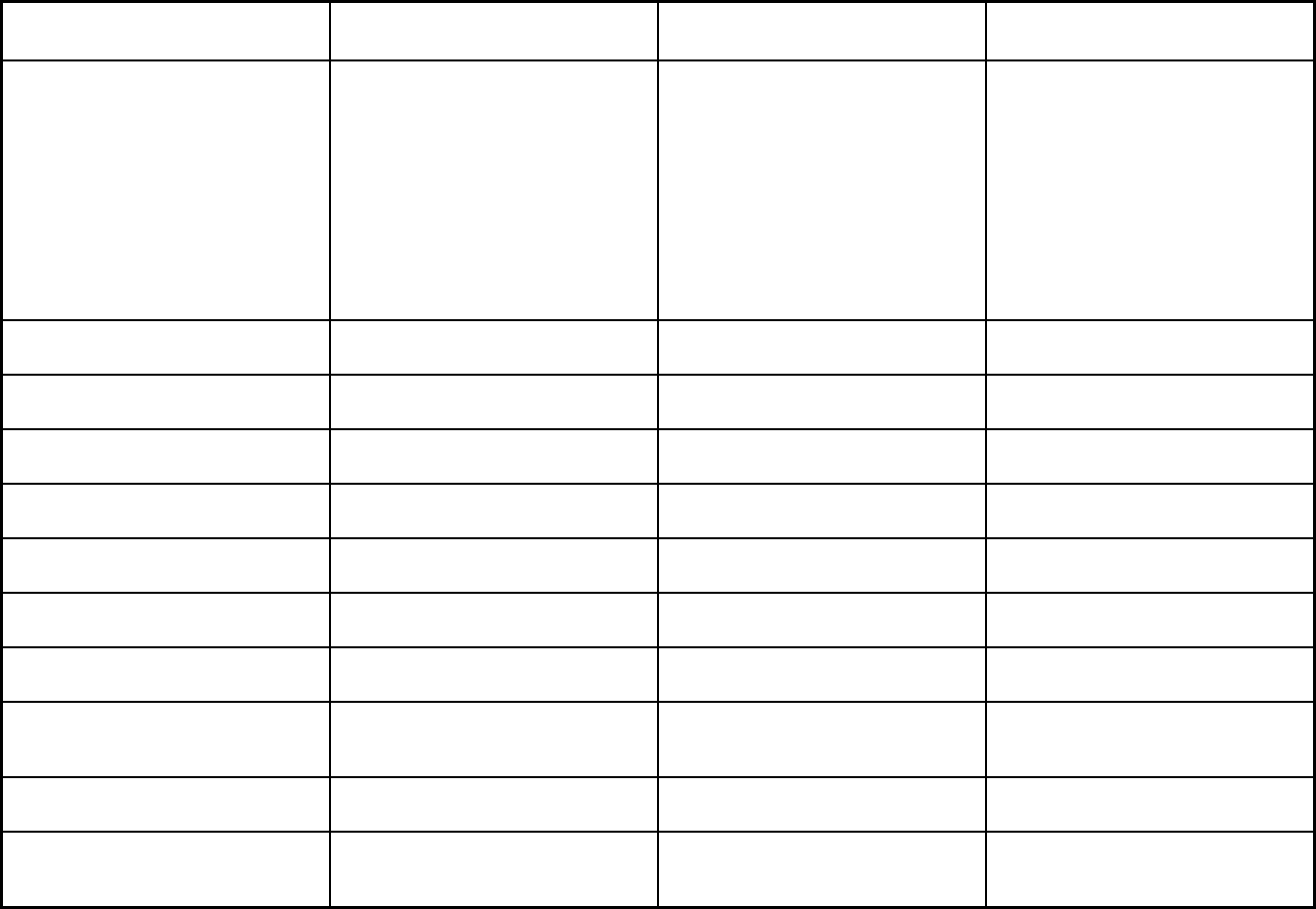
255
Features
Managed Medical Assistance
Program Long-term Care Program
Program of All-Inclusive Care for the
Elderly
Benefits covered: Other (e.g., nurse
midwife services, freestanding birth
centers, podiatry, etc.)
Midwife, birth center, podiatry, and
targeted case management. In addition,
the agency also negotiated expanded
benefits above the Medicaid state plan
service package. These expanded
benefits vary by plan and can include,
but are not necessarily limited to,
expanded adult dental services,
expanded outpatient hospital visits,
physician home visits, nutritional
counseling, and home and community-
based services.
Home health prosthetic devices,
intermittent and skilled nursing services.
In addition, the agency also negotiated
expanded benefits above the Medicaid
state plan service package and 1915(c).
These expanded benefits vary by plan
and include, but are not limited to,
cellular phone service, mobile personal
emergency response system, over-the-
counter medications and supplies, and
support to transition out of nursing
facilities.
All other FL Medicaid covered services
and other services as determined by the
multidisciplinary team
Quality assurance and improvement:
HEDIS data required?
Yes Yes No
Quality assurance and improvement:
CAHPS data required?
Yes No No
Quality assurance and improvement:
Accreditation required?
Yes Yes No
Quality assurance and improvement:
Accrediting organization
NCQA, AAAHC, Nationally recognized
accrediting organizations
NCQA, AAAHC, Nationally recognized
accrediting organizations
Quality assurance and improvement:
EQRO contractor name (if applicable)
Health Services Advisory Group Health Services Advisory Group
Performance incentives: Payment
bonuses/differentials to reward plans
X
Performance incentives: Preferential
auto-enrollment to reward plans
Performance incentives: Public reports
comparing plan performance on key
metrics
X
Performance incentives: Withholds tied
to performance metrics
Performance incentives: MCOs/PHPs
required or encouraged to pay providers
for value/quality outcomes
X
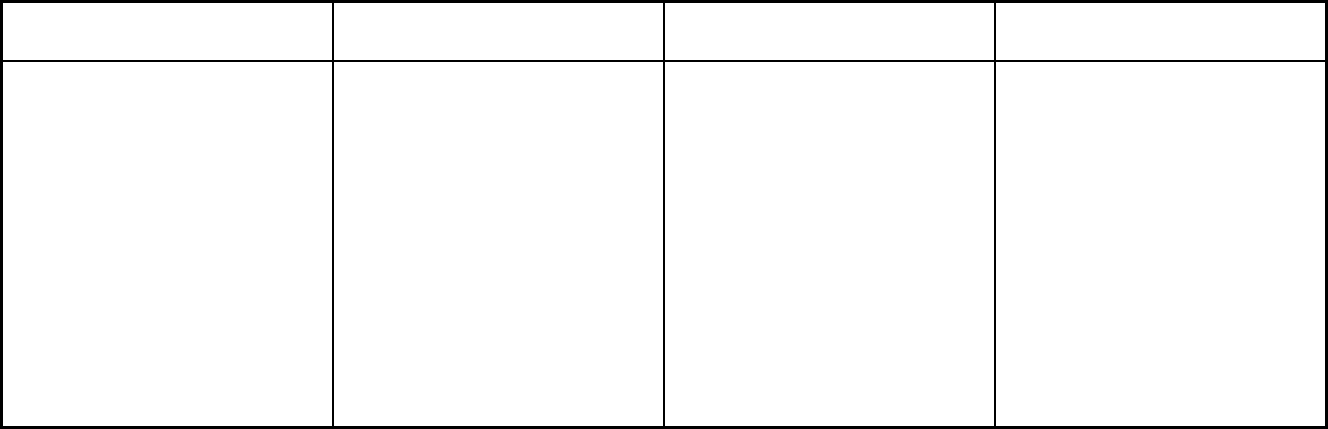
256
Features
Managed Medical Assistance
Program Long-term Care Program
Program of All-Inclusive Care for the
Elderly
Participating plans: Plans in Program Amerigroup Florida, Inc.; Better Health,
Inc.; Aetna DBA Coventry Healthcare of
FL, Inc.; Humana Medical Plan; Molina
Healthcare of Florida, Inc.; Prestige
Health Choice; South Florida
Community Care Network DBA
Community Care Plan; Simply
Healthcare Plans, Inc.; Wellcare Health
Plan of Florida DBA Staywell; Centene
DBA Sunshine State Health Plan, Inc.;
United Healthcare of Florida, Inc.; AIDS
Healthcare Foundation DBA Positive
Healthcare, Inc.; Freedom Health, Inc.;
Magellan Complete Care, LLC; Simply
Healthcare Plans DBA Clear Health
Alliance; Sunshine State Health Plan,
Inc.; Children's Medical Services
Amerigroup Florida, Inc.; Aetna DBA
Coventry Healthcare of FL, Inc.; Molina
Healthcare of FL, Inc.; Centene DBA
Sunshine State Health Plan, Inc.; United
Healthcare of FL, Inc.; Humana Medical
Plan, Inc.
Florida PACE Center; Hope Select
Care; Morselife Home Care, Inc.;
Suncoast Neighborly Care, Inc.
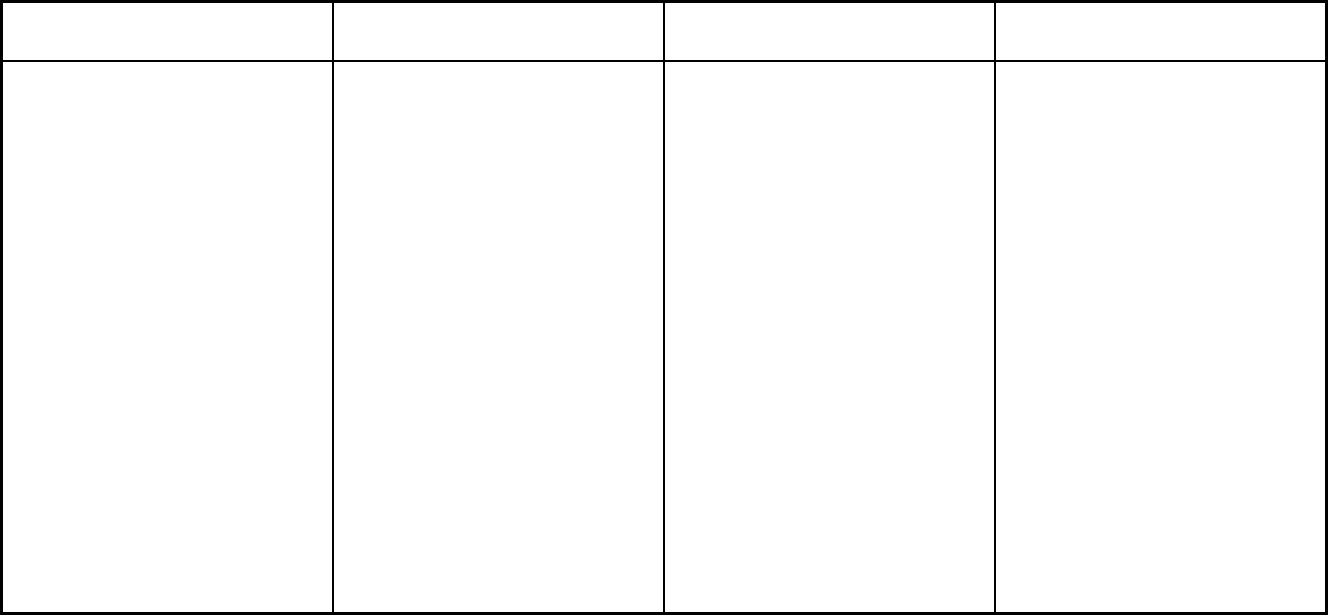
257
Features
Managed Medical Assistance
Program Long-term Care Program
Program of All-Inclusive Care for the
Elderly
Notes: Program notes The following populations are enrolled
automatically in the Managed Medical
Assistance (MMA) program. Pregnant
women who meet all other criteria for
Medicaid eligibility are automatically
enrolled, however presumptively eligible
pregna
nt women are excluded. Full dual
recipients receiving fee-for-service
Medicare or beneficiareis who are
enrolled in a Medicare Advantage plan
are automatically enrolled, however
duals who are not fully liable but who
are enrolled in a fully liable Medicare
Advantage plan or in a Medicare
Advantage Special Needs plan are
excluded. The MMA program includes
MMA specialty plans for recipients in the
child welfare system, recipients under
the age of 21 with chronic conditions,
recipients with HIV or AIDS, recipients
with a serious mental illness, and adults
with chronic conditions who have both
Medicare and full Medicaid (also called
“full duals”). The MMA specialty plans
cover the same health care services as
the standard MMA plans.
A recipient must be 18 years of age or
older and meet Nursing Facility level of
care in order to enroll in the Long-term
Care program. Recipients aged 18 to
64 must be eligible for Medicaid by
reason of a disability as determined by
the Social Security Administration in
order to enroll in the Long-term Care
program. In addition to the 60 day
enrollment period, once a recipient is
enrolled with a plan they have 120 days
to change plans if they wish to do so.
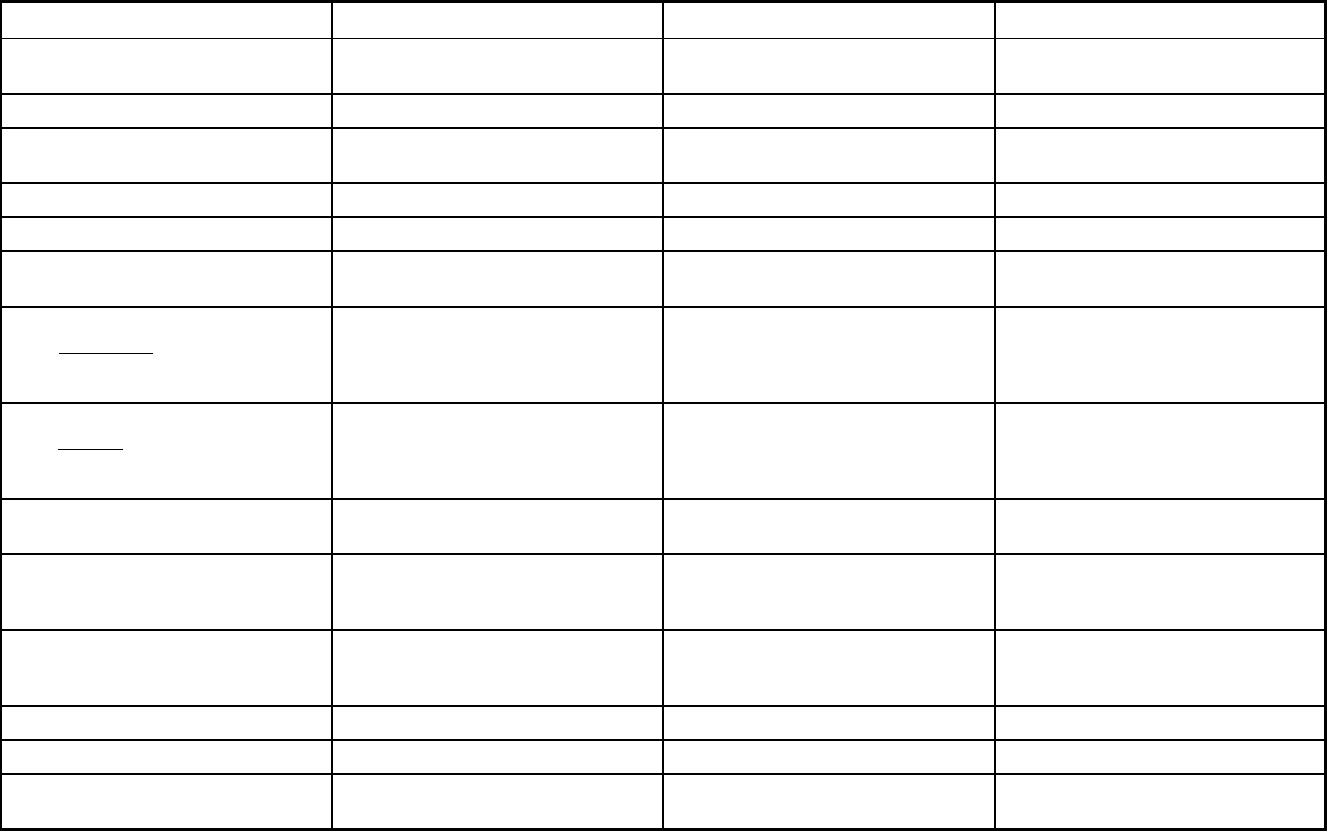
258
Georgia Managed Care Program Features, as of 2018 (1 of 2)
Features Georgia Families Georgia Families 360 Planning for Healthy Babies (P4HB)
Program type Comprehensive MCO Comprehensive MCO Other Prepaid Health Plan (PHP)
(limited benefits)
Statewide or region-specific? Statewide Statewide Statewide
Federal operating authority 1932(a)/1915(i) 1932(a),1932(a)/1915(i) 1115(a) (Medicaid demonstration
waivers)
Program start date 06/01/2006 03/03/2014 01/01/2011
Waiver expiration date (if applicable) 12/31/2020
If the program ended in 2018, indicate
the end date
Populations enrolled: Low-income
adults not covered under ACA Section
VIII (excludes pregnant women and
people with disabilities)
Mandatory
Populations enrolled: Low-income
adults covered under ACA Section VIII
(excludes pregnant women and people
with disabilities)
Populations enrolled: Aged, Blind or
Disabled Children or Adults
Populations enrolled: Non-Disabled
Children (excludes children in foster
care or receiving adoption assistance)
Mandatory
Populations enrolled: Individuals
receiving Limited Benefits (excludes
partial duals)
Voluntary Voluntary
Populations enrolled: Full Duals
Populations enrolled: Partial Duals
Populations enrolled: Children with
Special Health Care Needs
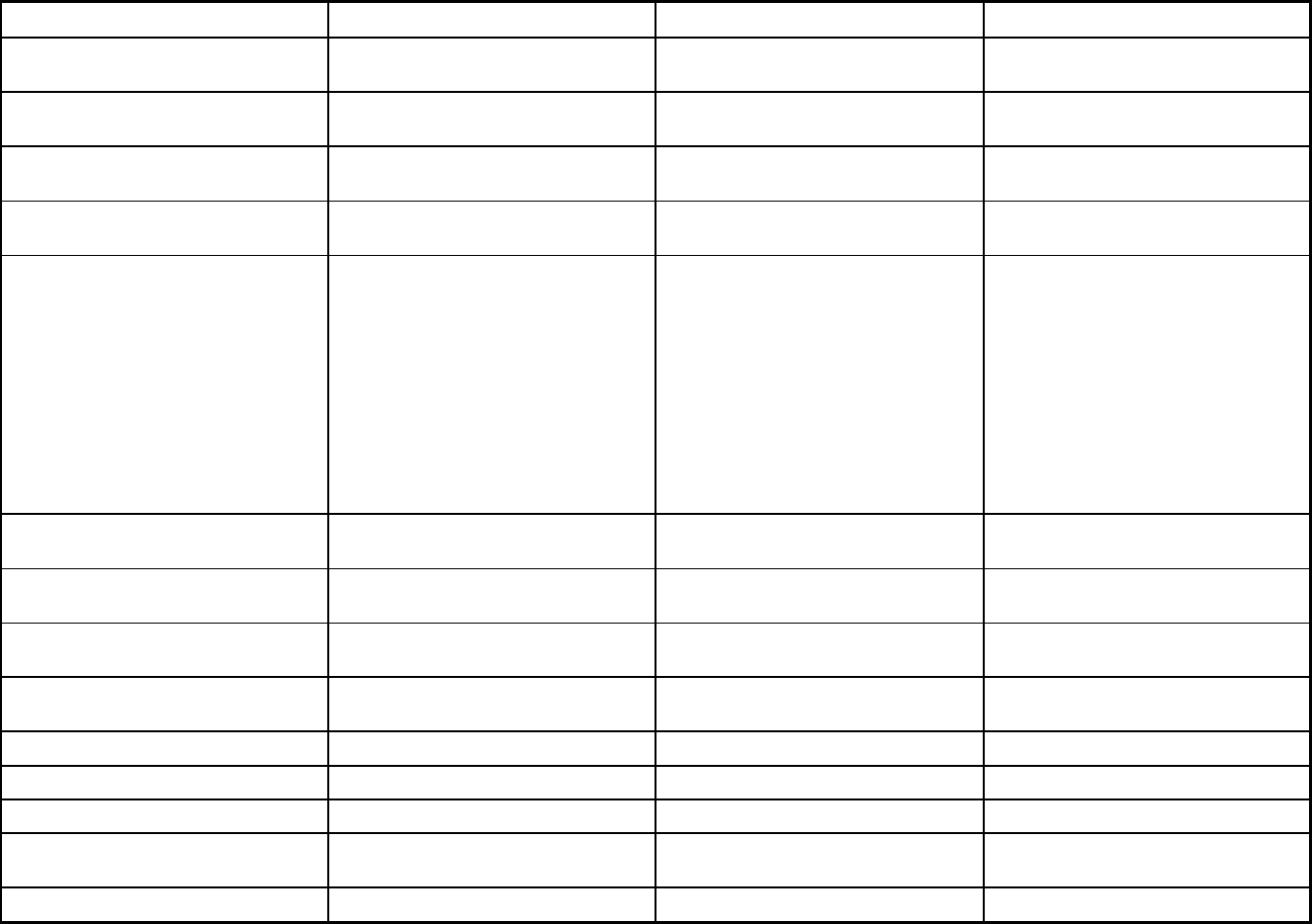
259
Features Georgia Families Georgia Families 360 Planning for Healthy Babies (P4HB)
Populations enrolled: Native
American/Alaskan Natives
Exempt Exempt Exempt
Populations enrolled: Foster Care and
Adoption Assistance Children
Exempt Mandatory Exempt
Populations enrolled: Enrollment choice
period
30 days 30 days Other
Populations enrolled: Enrollment broker
name (if applicable)
maximus Maximus
Populations enrolled: Notes on
enrollment choice period
Women who are enrolled in the P4HB
program are granted a 30 days period to
select a care management organization
(CMO) of their choice. Furthermore,
once a woman selects a CMO, she
transitions to her selected CMO the day
following her CMO selection. If the
woman does not select a CMO within
the 30 day choice period, she is
autoassigned to a CMO, in order to
receive P4HB services, based on the
state's auto-assignment algorithm.
Benefits covered: Inpatient hospital
physical health
X X
Benefits covered: Inpatient hospital
behavioral health (MH and/or SUD)
X X
Benefits covered: Outpatient hospital
physical health
X X
Benefits covered: Outpatient hospital
behavioral health (MH and/or SUD)
X X
Benefits covered: Partial hospitalization
Benefits covered: Physician X X
Benefits covered: Nurse practitioner X X
Benefits covered: Rural health clinics
and FQHCs
X X
Benefits covered: Clinic services X X
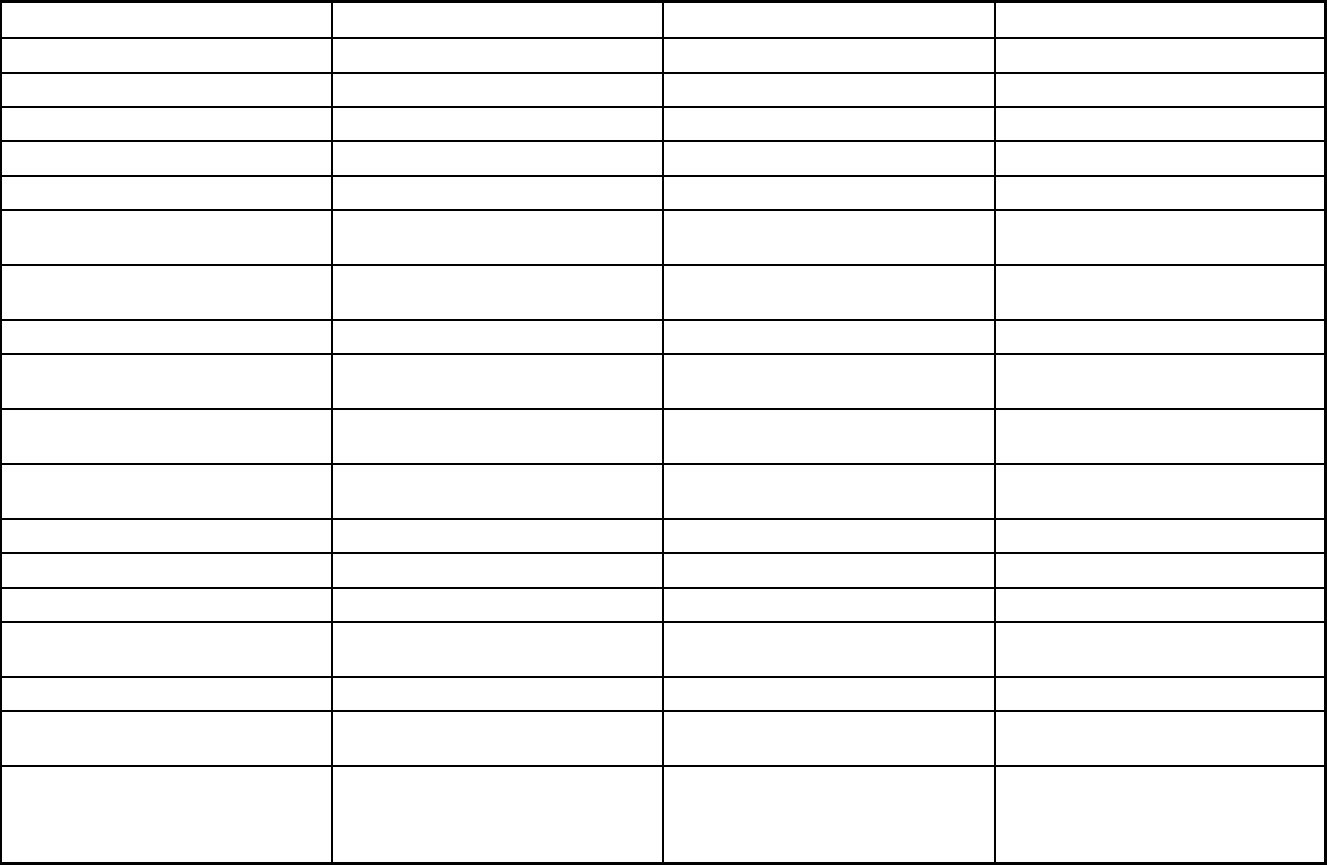
260
Features Georgia Families Georgia Families 360 Planning for Healthy Babies (P4HB)
Benefits covered: Lab and x-ray X X
Benefits covered: Prescription drugs X X
Benefits covered: Prosthetic devices X X
Benefits covered: EPSDT X X
Benefits covered: Case management X X
Benefits covered: SSA Section 1945-
authorized health home
Benefits covered: Health home care
(services in home)
Benefits covered: Family planning X X X
Benefits covered: Dental services
(medical/surgical)
X X
Benefits covered: Dental (preventative
or corrective)
X X
Benefits covered: Personal care (state
plan option)
Benefits covered: HCBS waiver services
Benefits covered: Private duty nursing
Benefits covered: ICF-IDD
Benefits covered: Nursing facility
services
X
Benefits covered: Hospice care
Benefits covered: Non-Emergency
Medical Transportation
Benefits covered: Institution for Mental
Disease inpatient treatment for people
ages 21-64 defined by 42 CFR
§438.6(e) as an 'in lieu of' benefit

261
Features Georgia Families Georgia Families 360 Planning for Healthy Babies (P4HB)
Benefits covered: Other (e.g., nurse
midwife services, freestanding birth
centers, podiatry, etc.)
Podiatry, nurse midwife
Quality assurance and improvement:
HEDIS data required?
Yes Yes Yes
Quality assurance and improvement:
CAHPS data required?
Yes Yes Yes
Quality assurance and improvement:
Accreditation required?
Yes Yes No
Quality assurance and improvement:
Accrediting organization
NCQA, URAC NCQA, JCAHO, URAC
Quality assurance and improvement:
EQRO contractor name (if applicable)
Health Services Advisory Group Health Services Advisory Group
Performance incentives: Payment
bonuses/differentials to reward plans
X
Performance incentives: Preferential
auto-enrollment to reward plans
X
Performance incentives: Public reports
comparing plan performance on key
metrics
Performance incentives: Withholds tied
to performance metrics
Performance incentives: MCOs/PHPs
required or encouraged to pay providers
for value/quality outcomes
Participating plans: Plans in Program Amerigroup Community Care;
CareSource - Georgia; Peach State
Health Plan; WellCare of Georgia
Amerigroup Amerigroup; CareSource- Georgia;
Peach State Health Plan; WellCare of
Georgia
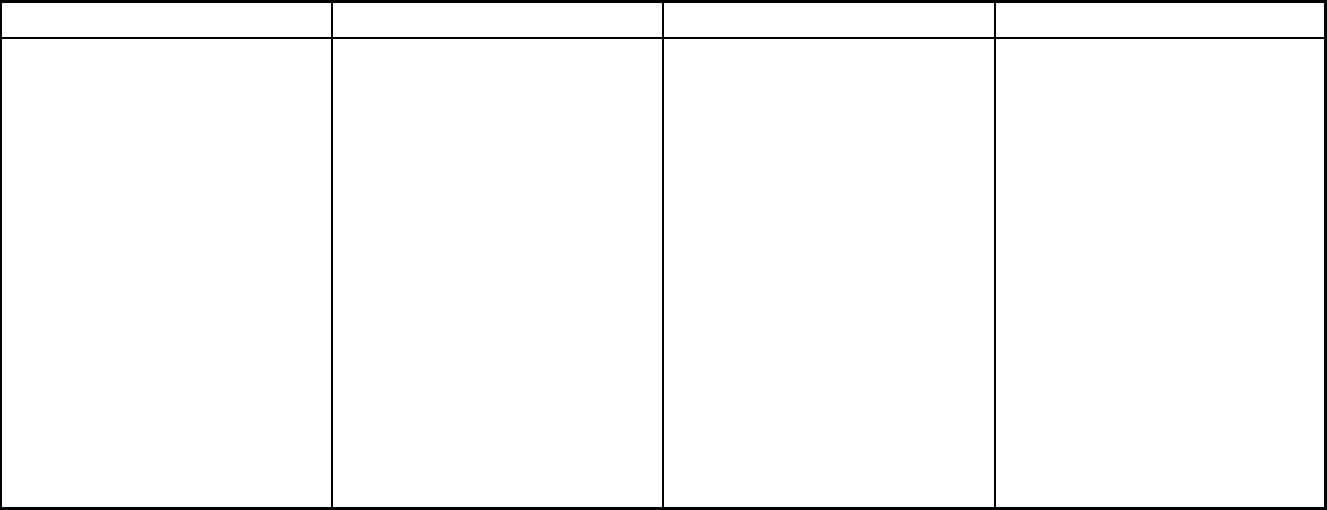
262
Features Georgia Families Georgia Families 360 Planning for Healthy Babies (P4HB)
Notes: Program notes Georgia Families is a program that
delivers health care services to
members of Medicaid and PeachCare
for Kids. (PeachCare for Kids is an S-
CHIP program. The enrollment data
provided in this report do not include
enrollment data for PeachCare for Kids.)
The program is a partnership between
the Department of Community Health
(DCH) and private care management
organizations (CMOs). Georgia Families
provides members a choice of health
plans, allowing them to select a health
care plan that fits their needs. Dually
eligible beneficiaries are not eligible to
enroll in Georgia Families. However, if
an individual becomes dually eligible
while already enrolled in a Georgia
Families plan, a short delay in
disenrollment results in the inclusion of
a small number of dually eligible
enrollees in Georgia Families plans.
Georgia Families 360 enrolls children,
youth, and young adults in foster care;
children and youth receiving adoption
assistance; and select youth involved in
the juvenile justice system.
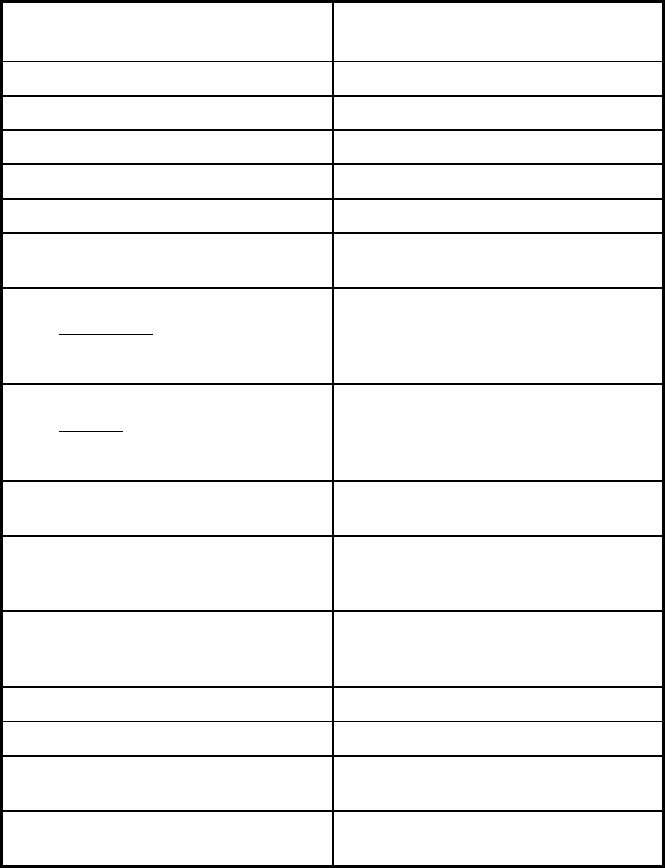
263
Georgia Managed Care Program Features, as of 2018 (2 of 2)
Features
Non-Emergency Medical
Transportation (NEMT)
Program type Non-Emergency Medical Transportation
Statewide or region-specific? Statewide
Federal operating authority 1902(a)(70) NEMT
Program start date 10/07/1997
Waiver expiration date (if applicable)
If the program ended in 2018, indicate
the end date
Populations enrolled: Low-income
adults not covered under ACA Section
VIII (excludes pregnant women and
people with disabilities)
Voluntary
Populations enrolled: Low-income
adults covered under ACA Section VIII
(excludes pregnant women and people
with disabilities)
Populations enrolled: Aged, Blind or
Disabled Children or Adults
Voluntary
Populations enrolled: Non-Disabled
Children (excludes children in foster
care or receiving adoption assistance)
Voluntary
Populations enrolled: Individuals
receiving Limited Benefits (excludes
partial duals)
Voluntary
Populations enrolled: Full Duals Voluntary
Populations enrolled: Partial Duals
Populations enrolled: Children with
Special Health Care Needs
Voluntary
Populations enrolled: Native
American/Alaskan Natives
Exempt
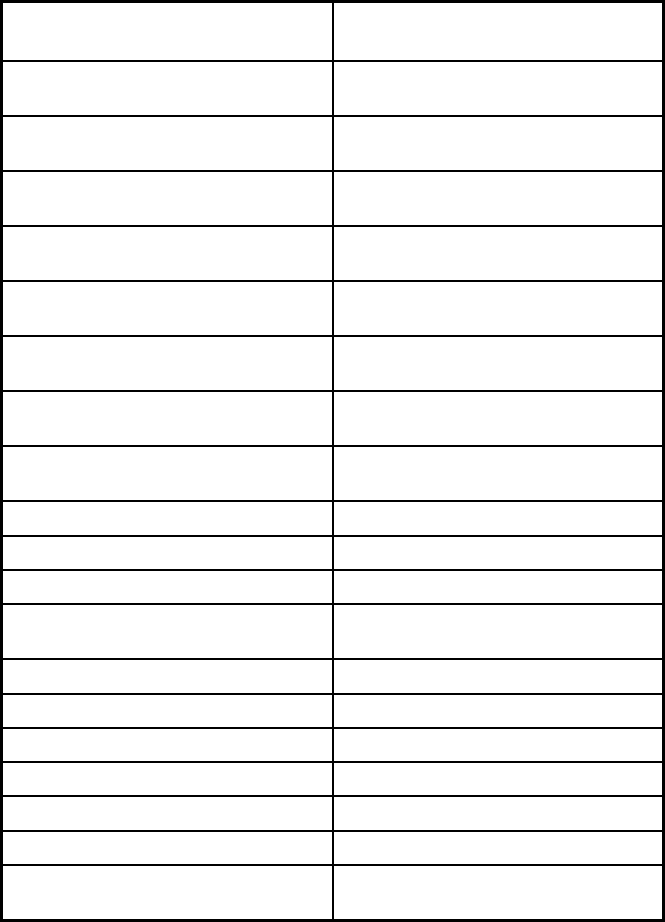
264
Features
Non-Emergency Medical
Transportation (NEMT)
Populations enrolled: Foster Care and
Adoption Assistance Children
Mandatory
Populations enrolled: Enrollment choice
period
Populations enrolled: Enrollment broker
name (if applicable)
Populations enrolled: Notes on
enrollment choice period
Benefits covered: Inpatient hospital
physical health
Benefits covered: Inpatient hospital
behavioral health (MH and/or SUD)
Benefits covered: Outpatient hospital
physical health
Benefits covered: Outpatient hospital
behavioral health (MH and/or SUD)
Benefits covered: Partial hospitalization
Benefits covered: Physician
Benefits covered: Nurse practitioner
Benefits covered: Rural health clinics
and FQHCs
Benefits covered: Clinic services
Benefits covered: Lab and x-ray
Benefits covered: Prescription drugs
Benefits covered: Prosthetic devices
Benefits covered: EPSDT
Benefits covered: Case management
Benefits covered: SSA Section 1945-
authorized health home
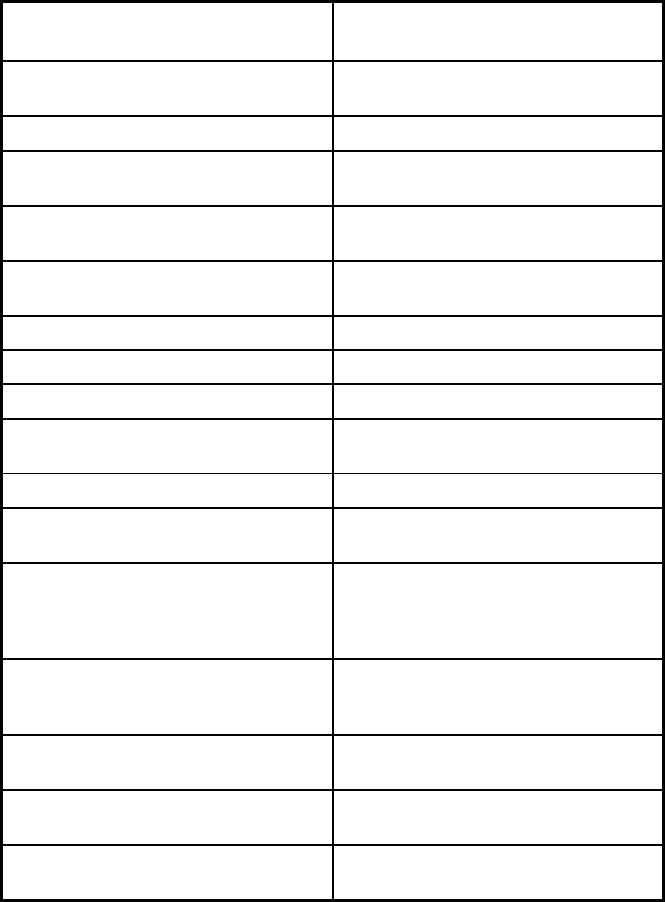
265
Features
Non-Emergency Medical
Transportation (NEMT)
Benefits covered: Health home care
(services in home)
Benefits covered: Family planning
Benefits covered: Dental services
(medical/surgical)
Benefits covered: Dental (preventative
or corrective)
Benefits covered: Personal care (state
plan option)
Benefits covered: HCBS waiver services
Benefits covered: Private duty nursing
Benefits covered: ICF-IDD
Benefits covered: Nursing facility
services
Benefits covered: Hospice care
Benefits covered: Non-Emergency
Medical Transportation
X
Benefits covered: Institution for Mental
Disease inpatient treatment for people
ages 21-64 defined by 42 CFR
§438.6(e) as an 'in lieu of' benefit
Benefits covered: Other (e.g., nurse
midwife services, freestanding birth
centers, podiatry, etc.)
Quality assurance and improvement:
HEDIS data required?
No
Quality assurance and improvement:
CAHPS data required?
No
Quality assurance and improvement:
Accreditation required?
No
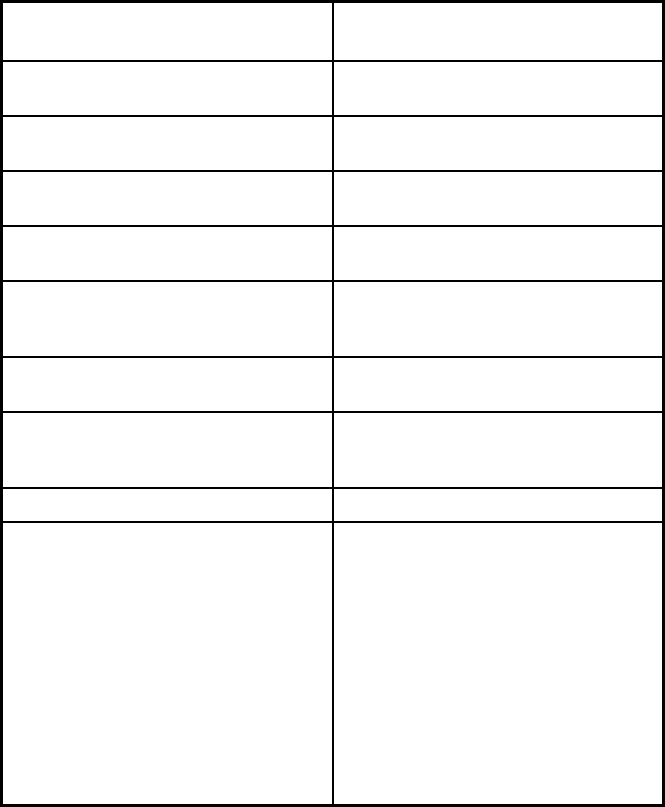
266
Features
Non-Emergency Medical
Transportation (NEMT)
Quality assurance and improvement:
Accrediting organization
Quality assurance and improvement:
EQRO contractor name (if applicable)
Performance incentives: Payment
bonuses/differentials to reward plans
Performance incentives: Preferential
auto-enrollment to reward plans
Performance incentives: Public reports
comparing plan performance on key
metrics
Performance incentives: Withholds tied
to performance metrics
Performance incentives: MCOs/PHPs
required or encouraged to pay providers
for value/quality outcomes
Participating plans: Plans in Program Southeast Trans; Logisticare
Notes: Program notes To provide the necessary non-
emergency medical transportation, DCH
utilizes a brokerage system and it is
these two Brokers, LogistiCare and
Southeastrans, who coordinate and
provide NEMT services for the state's
five regions (North, Atlanta, Central,
East and Southwest). NEMT brokers
are paid a monthly capitated rate based
on the number of eligible Medicaid
members residing in their contracted
region(s). Transportation services are
provided at no cost.
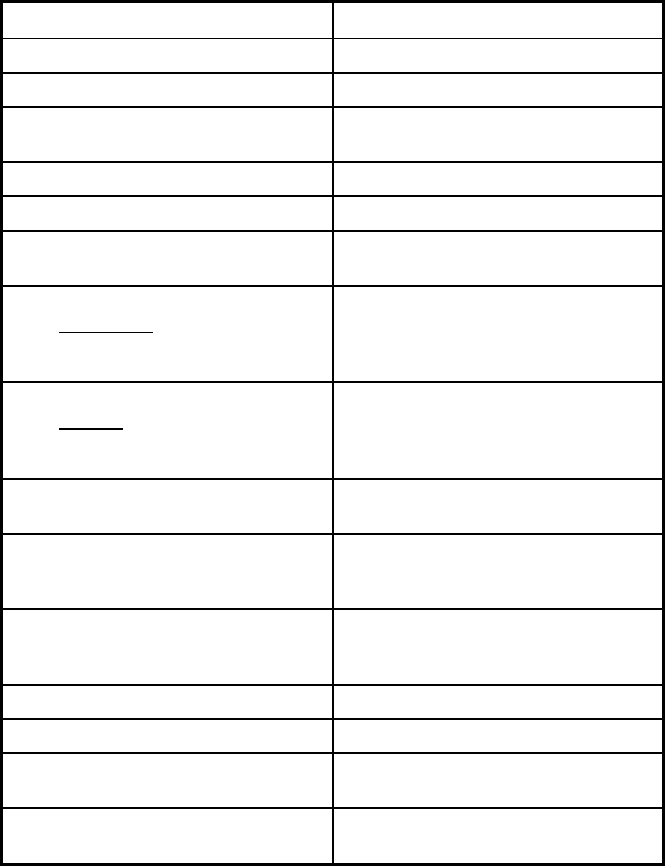
267
Hawaii Managed Care Program Features, as of 2018
Features Hawaii QUEST Integration
Program type Comprehensive MCO + MLTSS
Statewide or region-specific? Statewide
Federal operating authority 1115(a) (Medicaid demonstration
waivers)
Program start date 09/01/1994
Waiver expiration date (if applicable) 07/31/2024
If the program ended in 2018, indicate
the end date
Populations enrolled: Low-income
adults not covered under ACA Section
VIII (excludes pregnant women and
people with disabilities)
Mandatory
Populations enrolled: Low-income
adults covered under ACA Section VIII
(excludes pregnant women and people
with disabilities)
Mandatory
Populations enrolled: Aged, Blind or
Disabled Children or Adults
Mandatory
Populations enrolled: Non-Disabled
Children (excludes children in foster
care or receiving adoption assistance)
Mandatory
Populations enrolled: Individuals
receiving Limited Benefits (excludes
partial duals)
Mandatory
Populations enrolled: Full Duals Mandatory
Populations enrolled: Partial Duals Mandatory
Populations enrolled: Children with
Special Health Care Needs
Mandatory
Populations enrolled: Native
American/Alaskan Natives
Mandatory
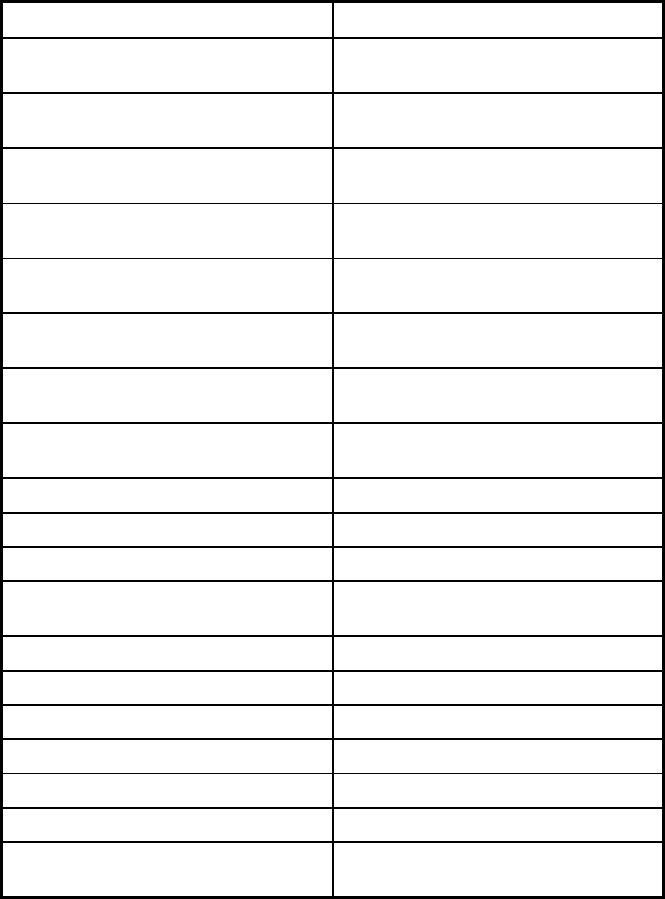
268
Features Hawaii QUEST Integration
Populations enrolled: Foster Care and
Adoption Assistance Children
Mandatory
Populations enrolled: Enrollment choice
period
30 days
Populations enrolled: Enrollment broker
name (if applicable)
Populations enrolled: Notes on
enrollment choice period
Benefits covered: Inpatient hospital
physical health
X
Benefits covered: Inpatient hospital
behavioral health (MH and/or SUD)
X
Benefits covered: Outpatient hospital
physical health
X
Benefits covered: Outpatient hospital
behavioral health (MH and/or SUD)
X
Benefits covered: Partial hospitalization X
Benefits covered: Physician X
Benefits covered: Nurse practitioner X
Benefits covered: Rural health clinics
and FQHCs
X
Benefits covered: Clinic services X
Benefits covered: Lab and x-ray X
Benefits covered: Prescription drugs X
Benefits covered: Prosthetic devices X
Benefits covered: EPSDT X
Benefits covered: Case management X
Benefits covered: SSA Section 1945-
authorized health home
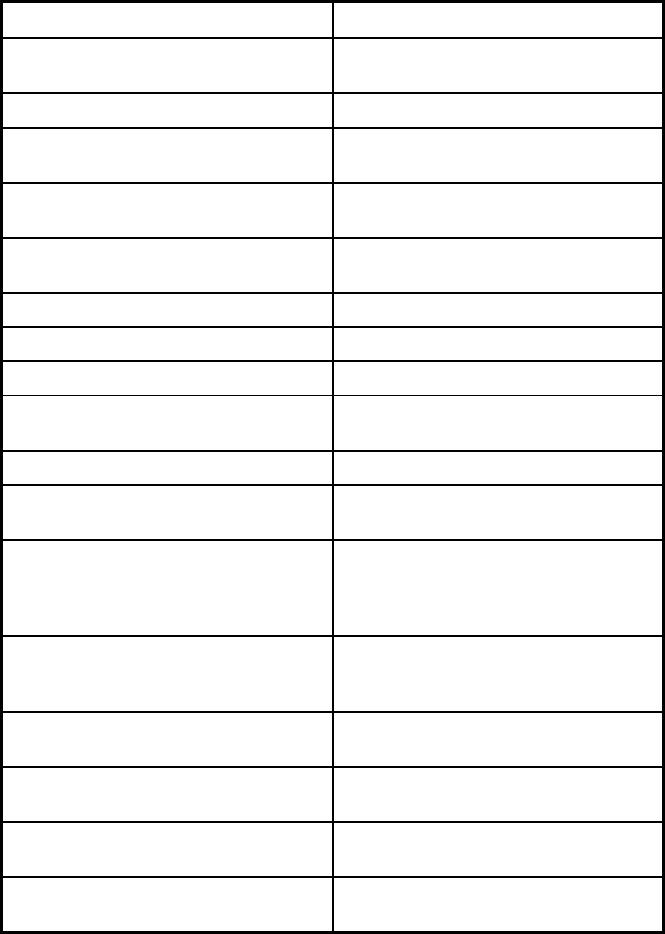
269
Features Hawaii QUEST Integration
Benefits covered: Health home care
(services in home)
X
Benefits covered: Family planning X
Benefits covered: Dental services
(medical/surgical)
X
Benefits covered: Dental (preventative
or corrective)
X
Benefits covered: Personal care (state
plan option)
X
Benefits covered: HCBS waiver services X
Benefits covered: Private duty nursing X
Benefits covered: ICF-IDD X
Benefits covered: Nursing facility
services
X
Benefits covered: Hospice care X
Benefits covered: Non-Emergency
Medical Transportation
X
Benefits covered: Institution for Mental
Disease inpatient treatment for people
ages 21-64 defined by 42 CFR
§438.6(e) as an 'in lieu of' benefit
Benefits covered: Other (e.g., nurse
midwife services, freestanding birth
centers, podiatry, etc.)
Quality assurance and improvement:
HEDIS data required?
Yes
Quality assurance and improvement:
CAHPS data required?
Yes
Quality assurance and improvement:
Accreditation required?
Yes
Quality assurance and improvement:
Accrediting organization
NCQA
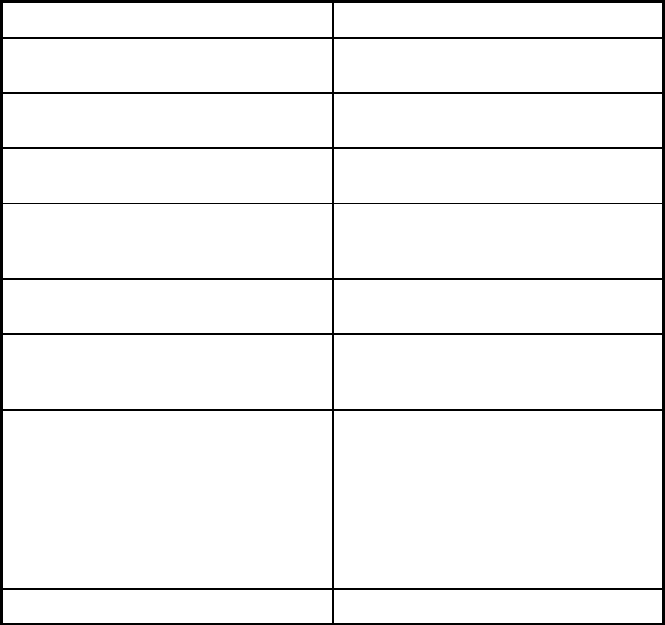
270
Features Hawaii QUEST Integration
Quality assurance and improvement:
EQRO contractor name (if applicable)
Health Services Advisory Group
Performance incentives: Payment
bonuses/differentials to reward plans
Performance incentives: Preferential
auto-enrollment to reward plans
X
Performance incentives: Public reports
comparing plan performance on key
metrics
Performance incentives: Withholds tied
to performance metrics
X
Performance incentives: MCOs/PHPs
required or encouraged to pay providers
for value/quality outcomes
X
Participating plans: Plans in Program AlohaCare QUEST; Hawaii Medical
Service Association (HMSA) QUEST;
Kaiser Permanente QUEST; Ohana
Health Plan QUEST; UnitedHealthcare
Community Plan QUEST; AlohaCare
ABD; HMSA ABD; Kaiser ABD; Ohana
ABD; UnitedHealth ABD; Ohana
Community Care Service (BHS)
Notes: Program notes
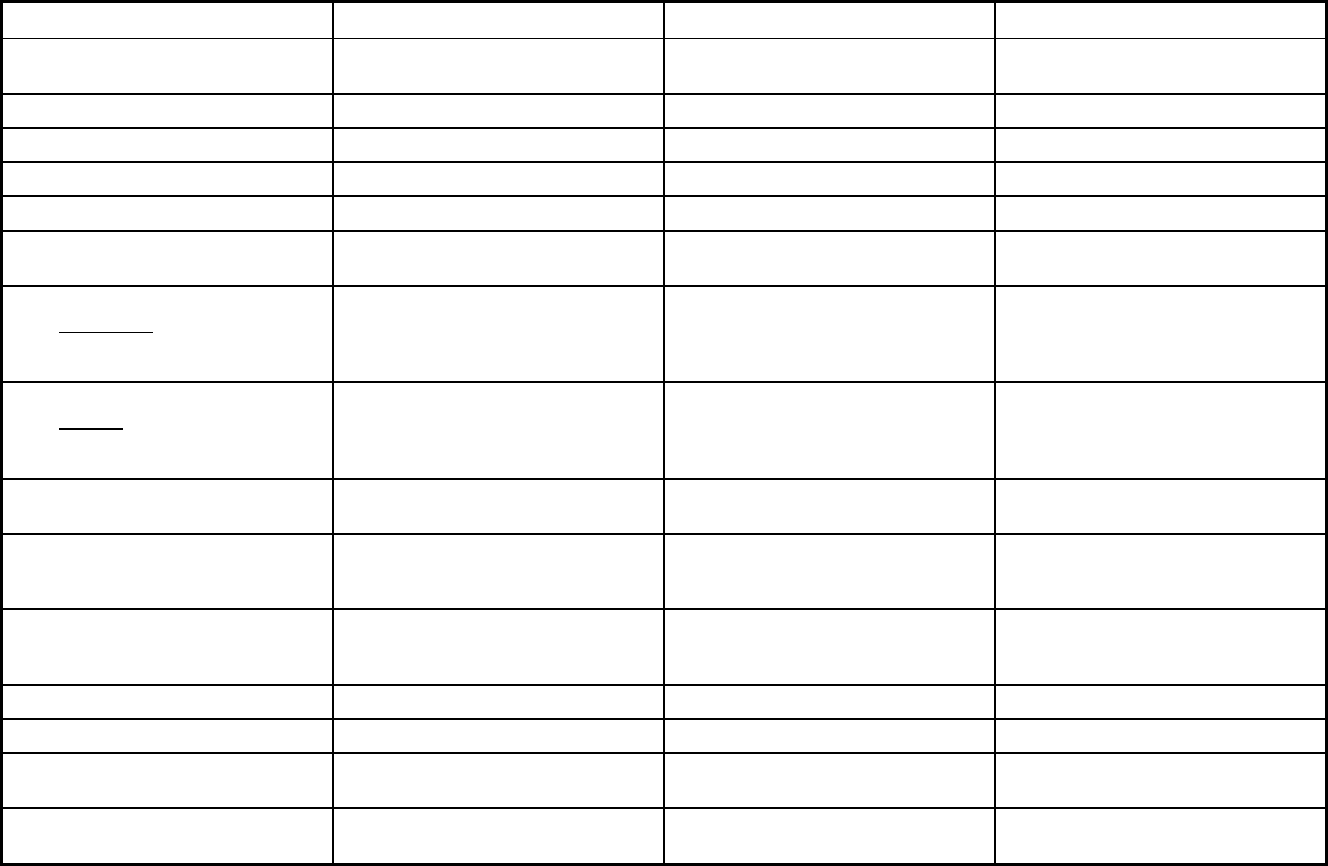
271
Idaho Managed Care Program Features, as of 2018 (1 of 2)
Features Idaho Behavioral Health Plan Healthy Connections Medicare/Medicaid Coordinated Plan
Program type Behavioral Health Organization (BHO)
only (PIHP and/or PAHP)
Primary Care Case Management
(PCCM)
Comprehensive MCO + MLTSS
Statewide or region-specific? Statewide Statewide Counties
Federal operating authority 1915(b),1915(b)/1915(i) 1932(a) 1915(a)/1915(c)
Program start date 09/01/2013 10/01/2006 07/01/2014
Waiver expiration date (if applicable) 03/21/2022 12/31/2019
If the program ended in 2018, indicate
the end date
Populations enrolled: Low-income
adults not covered under ACA Section
VIII (excludes pregnant women and
people with disabilities)
Mandatory Mandatory
Populations enrolled: Low-income
adults covered under ACA Section VIII
(excludes pregnant women and people
with disabilities)
Populations enrolled: Aged, Blind or
Disabled Children or Adults
Mandatory Mandatory
Populations enrolled: Non-Disabled
Children (excludes children in foster
care or receiving adoption assistance)
Mandatory Mandatory
Populations enrolled: Individuals
receiving Limited Benefits (excludes
partial duals)
Populations enrolled: Full Duals Voluntary Voluntary Voluntary
Populations enrolled: Partial Duals Voluntary Voluntary
Populations enrolled: Children with
Special Health Care Needs
Populations enrolled: Native
American/Alaskan Natives
Mandatory Voluntary Voluntary
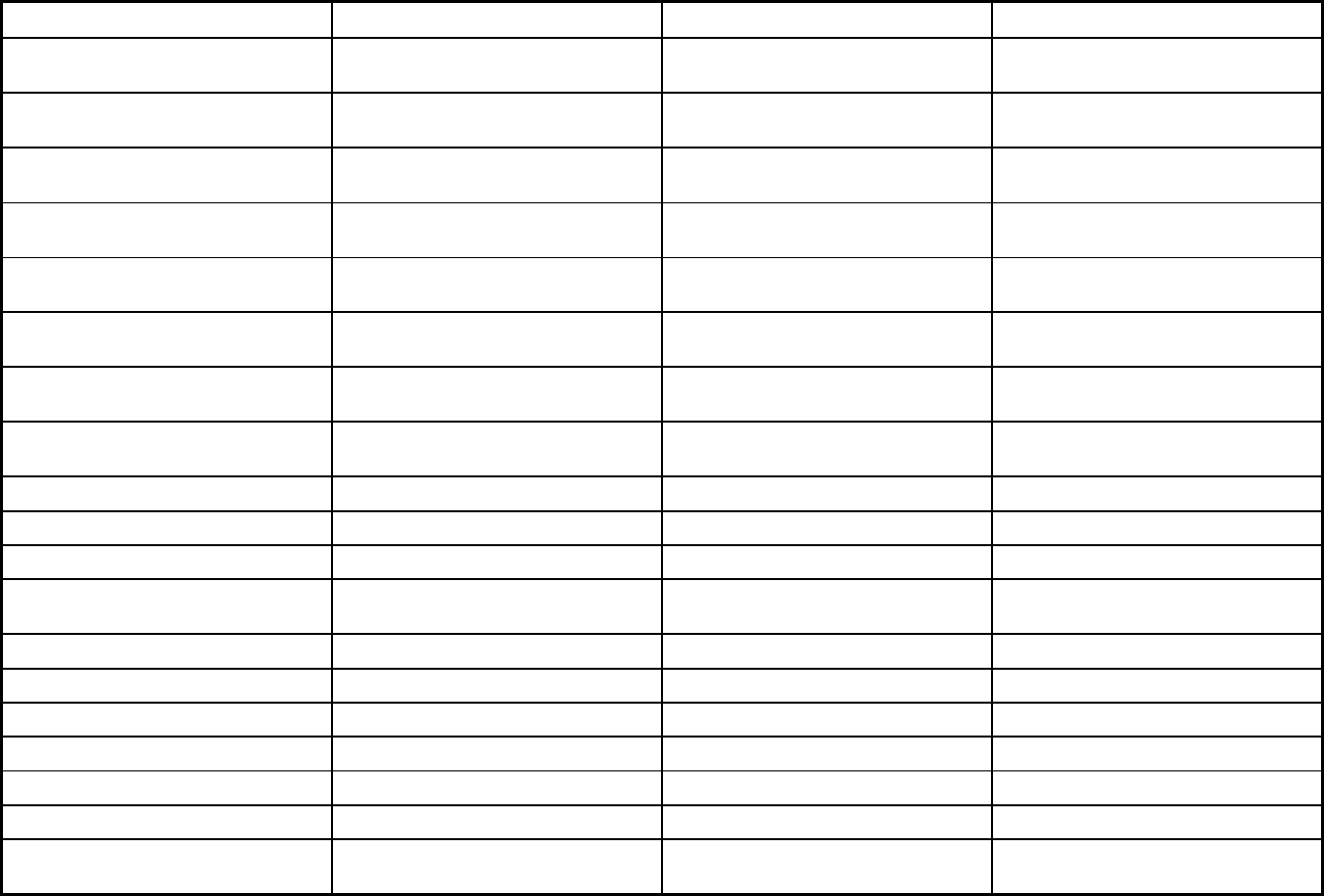
272
Features Idaho Behavioral Health Plan Healthy Connections Medicare/Medicaid Coordinated Plan
Populations enrolled: Foster Care and
Adoption Assistance Children
Mandatory Voluntary Exempt
Populations enrolled: Enrollment choice
period
N/A
Populations enrolled: Enrollment broker
name (if applicable)
Populations enrolled: Notes on
enrollment choice period
Benefits covered: Inpatient hospital
physical health
X
Benefits covered: Inpatient hospital
behavioral health (MH and/or SUD)
X
Benefits covered: Outpatient hospital
physical health
X
Benefits covered: Outpatient hospital
behavioral health (MH and/or SUD)
X X
Benefits covered: Partial hospitalization X
Benefits covered: Physician X X
Benefits covered: Nurse practitioner X X
Benefits covered: Rural health clinics
and FQHCs
X X
Benefits covered: Clinic services X
Benefits covered: Lab and x-ray X
Benefits covered: Prescription drugs X
Benefits covered: Prosthetic devices X
Benefits covered: EPSDT X
Benefits covered: Case management X X X
Benefits covered: SSA Section 1945-
authorized health home
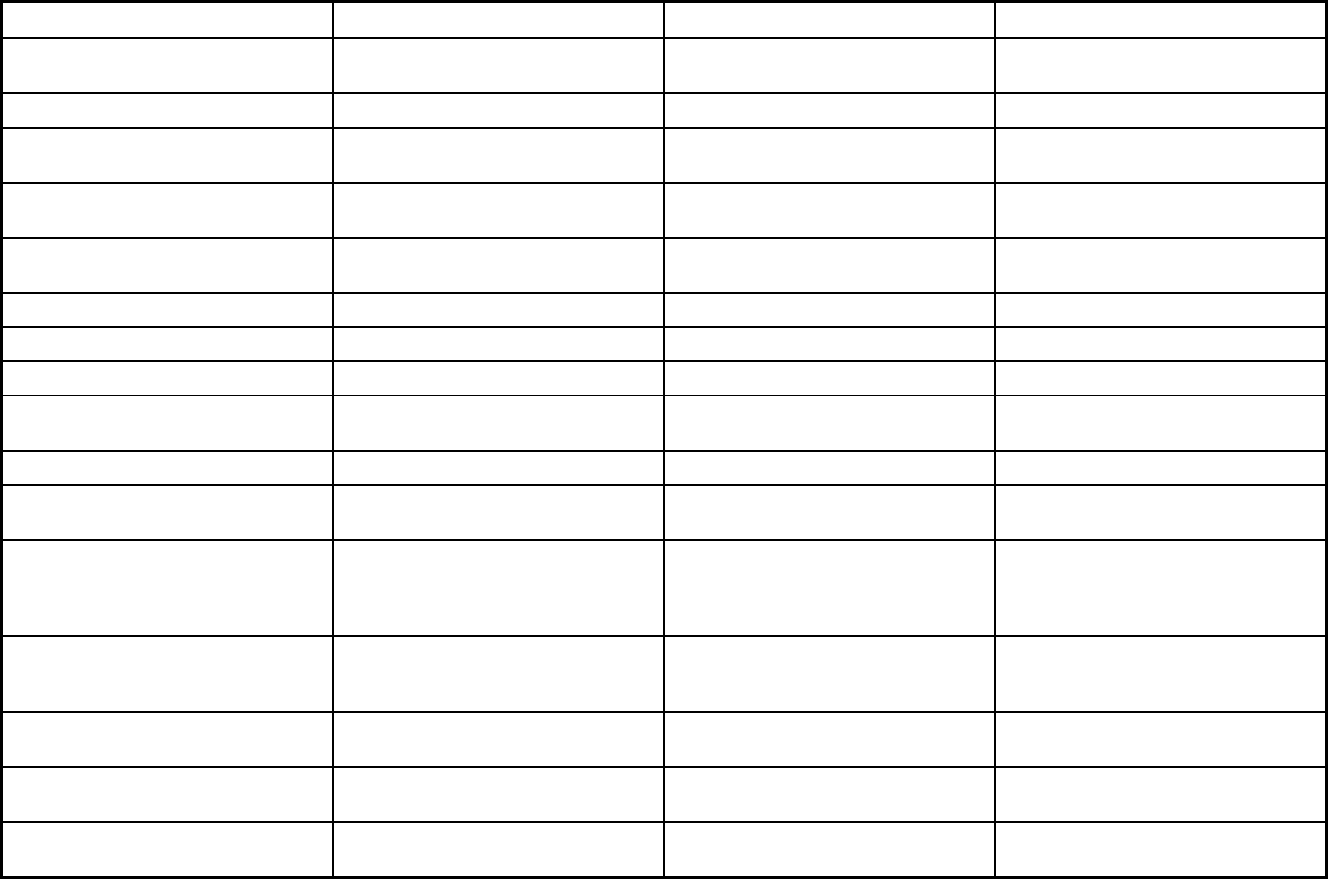
273
Features Idaho Behavioral Health Plan Healthy Connections Medicare/Medicaid Coordinated Plan
Benefits covered: Health home care
(services in home)
X
Benefits covered: Family planning X
Benefits covered: Dental services
(medical/surgical)
Benefits covered: Dental (preventative
or corrective)
Benefits covered: Personal care (state
plan option)
X
Benefits covered: HCBS waiver services X
Benefits covered: Private duty nursing
Benefits covered: ICF-IDD X
Benefits covered: Nursing facility
services
X
Benefits covered: Hospice care X
Benefits covered: Non-Emergency
Medical Transportation
Benefits covered: Institution for Mental
Disease inpatient treatment for people
ages 21-64 defined by 42 CFR
§438.6(e) as an 'in lieu of' benefit
Benefits covered: Other (e.g., nurse
midwife services, freestanding birth
centers, podiatry, etc.)
Peer support; family support Medicaid-Primary services not covered
by Medicare
Quality assurance and improvement:
HEDIS data required?
Yes No No
Quality assurance and improvement:
CAHPS data required?
Yes No No
Quality assurance and improvement:
Accreditation required?
Yes No Yes
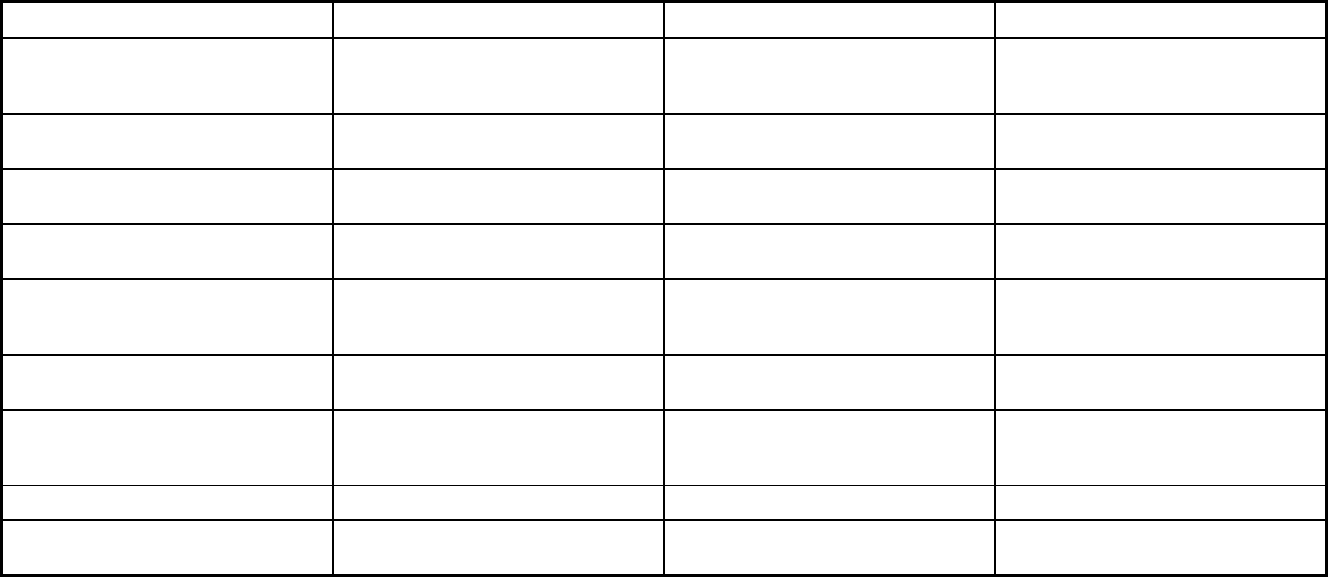
274
Features Idaho Behavioral Health Plan Healthy Connections Medicare/Medicaid Coordinated Plan
Quality assurance and improvement:
Accrediting organization
NCQA For those participating at tiers 3 or 4 of
our PCMH model, national accreditation
is required.
NCQA
Quality assurance and improvement:
EQRO contractor name (if applicable)
Telligen
Performance incentives: Payment
bonuses/differentials to reward plans
X
Performance incentives: Preferential
auto-enrollment to reward plans
Performance incentives: Public reports
comparing plan performance on key
metrics
X X
Performance incentives: Withholds tied
to performance metrics
X X
Performance incentives: MCOs/PHPs
required or encouraged to pay providers
for value/quality outcomes
X X
Participating plans: Plans in Program Idaho Behavioral Health Plan Healthy Connections Medicare/Medicaid Coordinated Plan
Notes: Program notes HCBS Services are not covered under
this program.
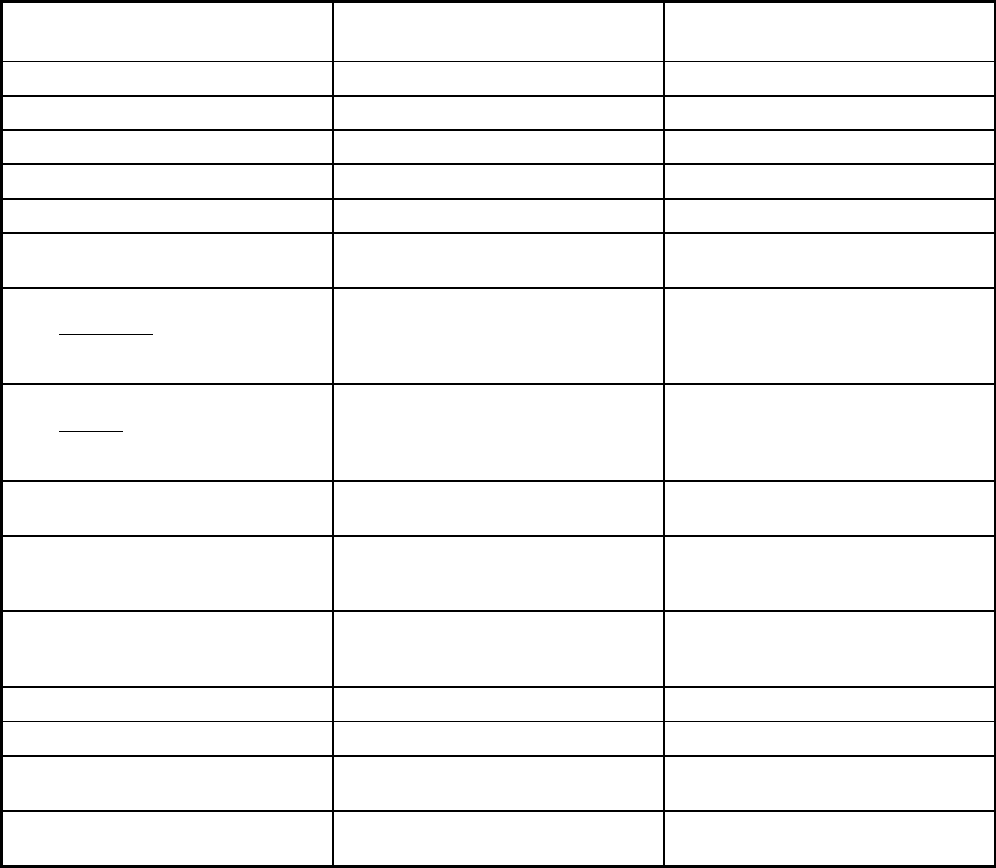
275
Idaho Managed Care Program Features, as of 2018 (2 of 2)
Features Idaho Smiles
Non-Emergency Medical
Transportation
Program type Dental only (PAHP) Non-Emergency Medical Transportation
Statewide or region-specific? Statewide Statewide
Federal operating authority 1915(b) 1902(a)(70) NEMT
Program start date 08/01/2010 09/01/2010
Waiver expiration date (if applicable) 06/30/2022
If the program ended in 2018, indicate
the end date
Populations enrolled: Low-income
adults not covered under ACA Section
VIII (excludes pregnant women and
people with disabilities)
Mandatory Mandatory
Populations enrolled: Low-income
adults covered under ACA Section VIII
(excludes pregnant women and people
with disabilities)
Populations enrolled: Aged, Blind or
Disabled Children or Adults
Mandatory Mandatory
Populations enrolled: Non-Disabled
Children (excludes children in foster
care or receiving adoption assistance)
Mandatory Mandatory
Populations enrolled: Individuals
receiving Limited Benefits (excludes
partial duals)
Mandatory
Populations enrolled: Full Duals
Populations enrolled: Partial Duals
Populations enrolled: Children with
Special Health Care Needs
Mandatory Mandatory
Populations enrolled: Native
American/Alaskan Natives
Mandatory Mandatory
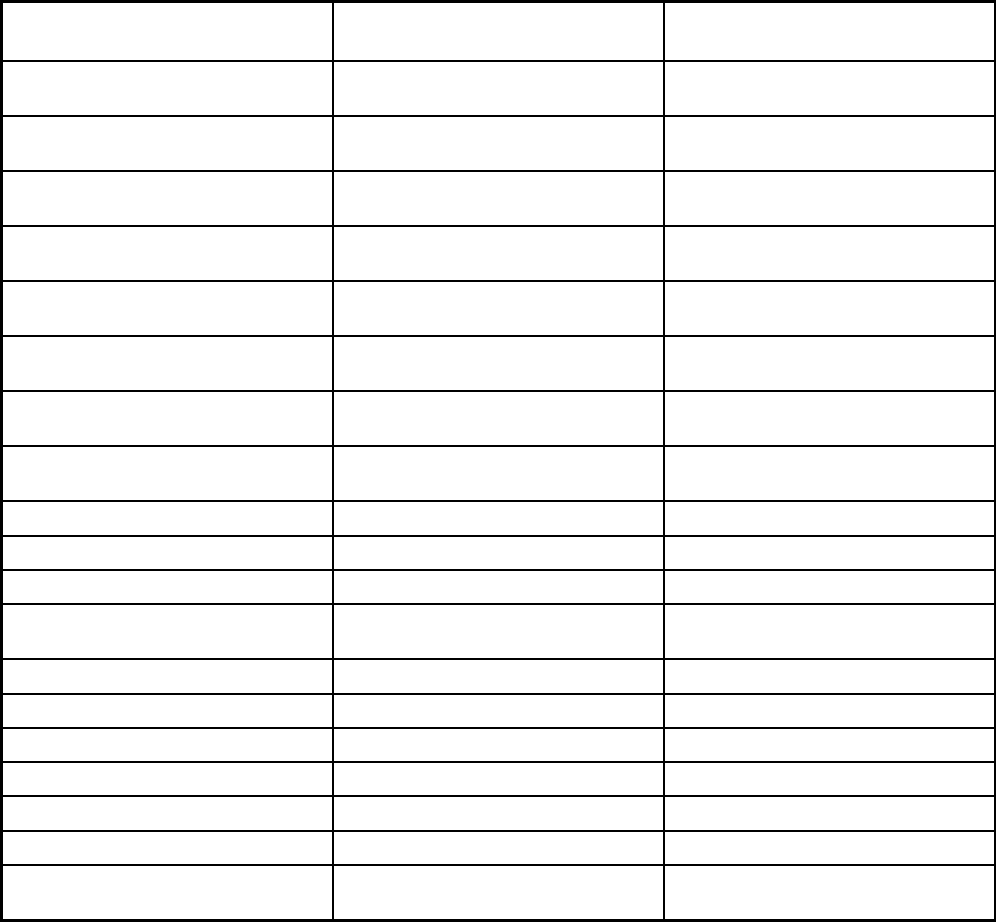
276
Features Idaho Smiles
Non-Emergency Medical
Transportation
Populations enrolled: Foster Care and
Adoption Assistance Children
Mandatory Mandatory
Populations enrolled: Enrollment choice
period
Populations enrolled: Enrollment broker
name (if applicable)
Populations enrolled: Notes on
enrollment choice period
Benefits covered: Inpatient hospital
physical health
Benefits covered: Inpatient hospital
behavioral health (MH and/or SUD)
Benefits covered: Outpatient hospital
physical health
Benefits covered: Outpatient hospital
behavioral health (MH and/or SUD)
Benefits covered: Partial hospitalization
Benefits covered: Physician
Benefits covered: Nurse practitioner
Benefits covered: Rural health clinics
and FQHCs
Benefits covered: Clinic services
Benefits covered: Lab and x-ray
Benefits covered: Prescription drugs
Benefits covered: Prosthetic devices
Benefits covered: EPSDT
Benefits covered: Case management
Benefits covered: SSA Section 1945-
authorized health home
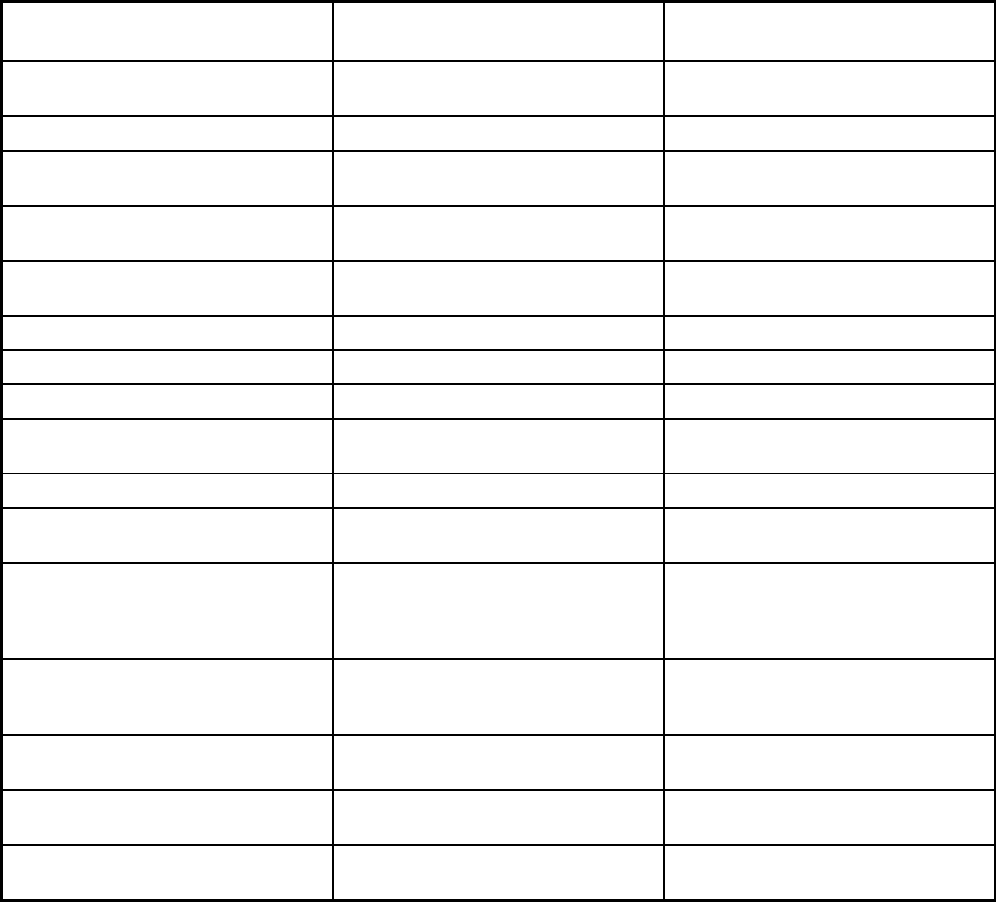
277
Features Idaho Smiles
Non-Emergency Medical
Transportation
Benefits covered: Health home care
(services in home)
Benefits covered: Family planning
Benefits covered: Dental services
(medical/surgical)
X
Benefits covered: Dental (preventative
or corrective)
X
Benefits covered: Personal care (state
plan option)
Benefits covered: HCBS waiver services
Benefits covered: Private duty nursing
Benefits covered: ICF-IDD
Benefits covered: Nursing facility
services
Benefits covered: Hospice care
Benefits covered: Non-Emergency
Medical Transportation
X
Benefits covered: Institution for Mental
Disease inpatient treatment for people
ages 21-64 defined by 42 CFR
§438.6(e) as an 'in lieu of' benefit
Benefits covered: Other (e.g., nurse
midwife services, freestanding birth
centers, podiatry, etc.)
Quality assurance and improvement:
HEDIS data required?
No No
Quality assurance and improvement:
CAHPS data required?
Yes No
Quality assurance and improvement:
Accreditation required?
No No
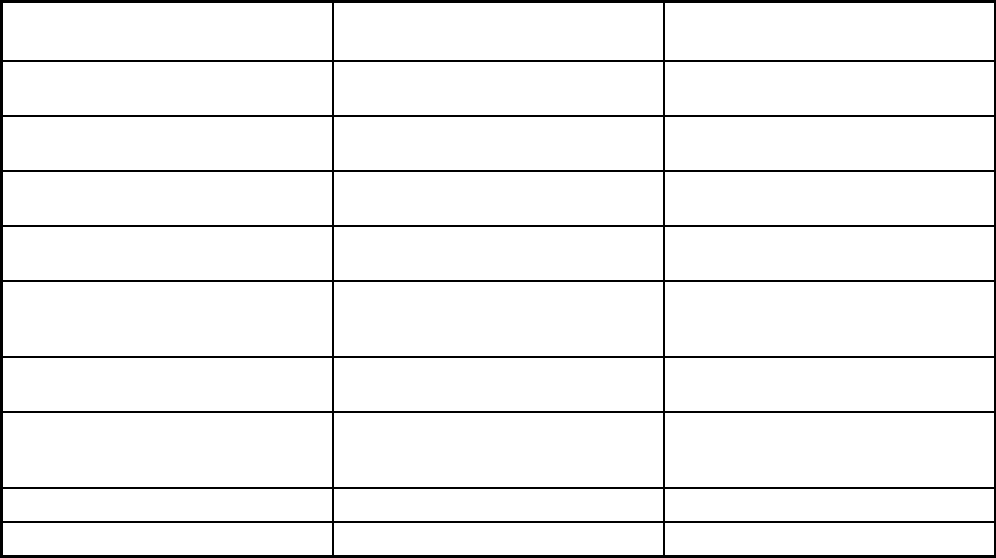
278
Features Idaho Smiles
Non-Emergency Medical
Transportation
Quality assurance and improvement:
Accrediting organization
NCQA, AAAHC URAC
Quality assurance and improvement:
EQRO contractor name (if applicable)
Performance incentives: Payment
bonuses/differentials to reward plans
Performance incentives: Preferential
auto-enrollment to reward plans
Performance incentives: Public reports
comparing plan performance on key
metrics
Performance incentives: Withholds tied
to performance metrics
X
Performance incentives: MCOs/PHPs
required or encouraged to pay providers
for value/quality outcomes
Participating plans: Plans in Program Idaho Smiles Non-Emergency Medical Transportation
Notes: Program notes
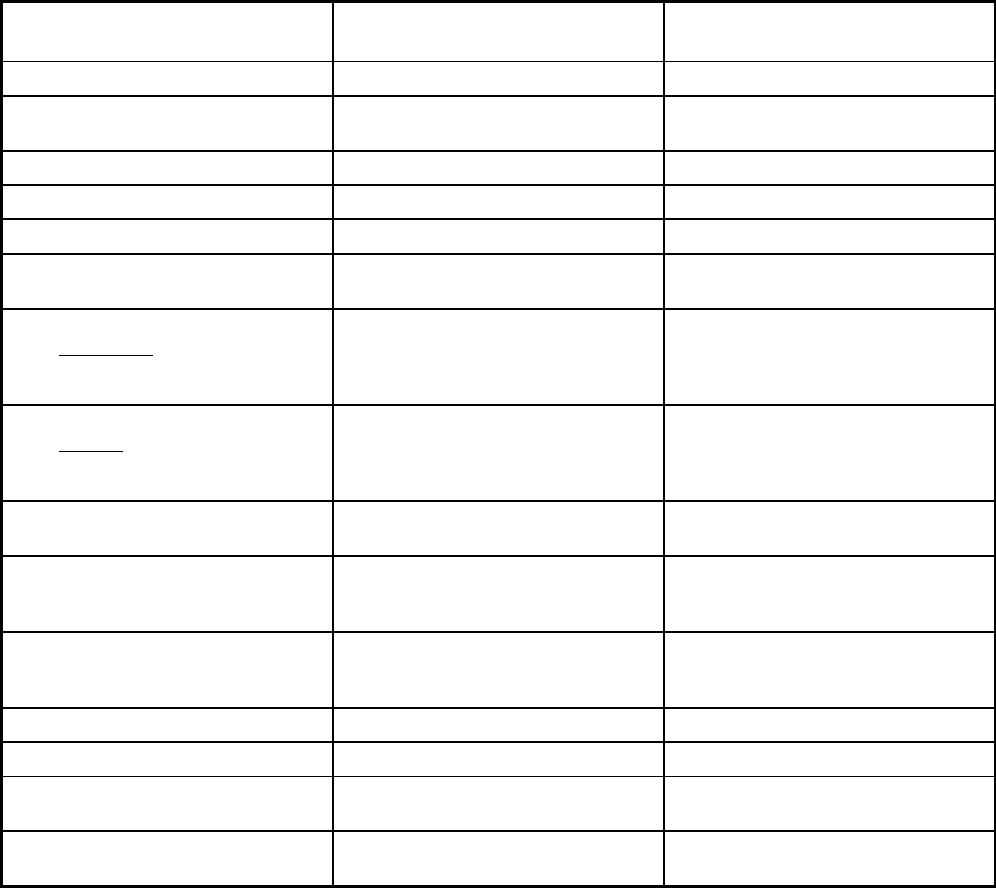
279
Illinois Managed Care Program Features, as of 2018
Features HealthChoice Illinois
HealthChoice Illinois - Managed
Long-Term Services and Supports
Program type Comprehensive MCO + MLTSS MLTSS only (PIHP and/or PAHP)
Statewide or region-specific? Statewide Cook, DuPage, Kane, Kankakee, Lake
and Will counties
Federal operating authority 1932(a)/1915(c) 1915(b)
Program start date 01/01/2018 01/01/2018
Waiver expiration date (if applicable) 07/11/2021 12/31/2019
If the program ended in 2018, indicate
the end date
Populations enrolled: Low-income
adults not covered under ACA Section
VIII (excludes pregnant women and
people with disabilities)
Populations enrolled: Low-income
adults covered under ACA Section VIII
(excludes pregnant women and people
with disabilities)
Mandatory
Populations enrolled: Aged, Blind or
Disabled Children or Adults
Mandatory
Populations enrolled: Non-Disabled
Children (excludes children in foster
care or receiving adoption assistance)
Mandatory
Populations enrolled: Individuals
receiving Limited Benefits (excludes
partial duals)
Populations enrolled: Full Duals Mandatory
Populations enrolled: Partial Duals
Populations enrolled: Children with
Special Health Care Needs
Mandatory
Populations enrolled: Native
American/Alaskan Natives
Voluntary Voluntary
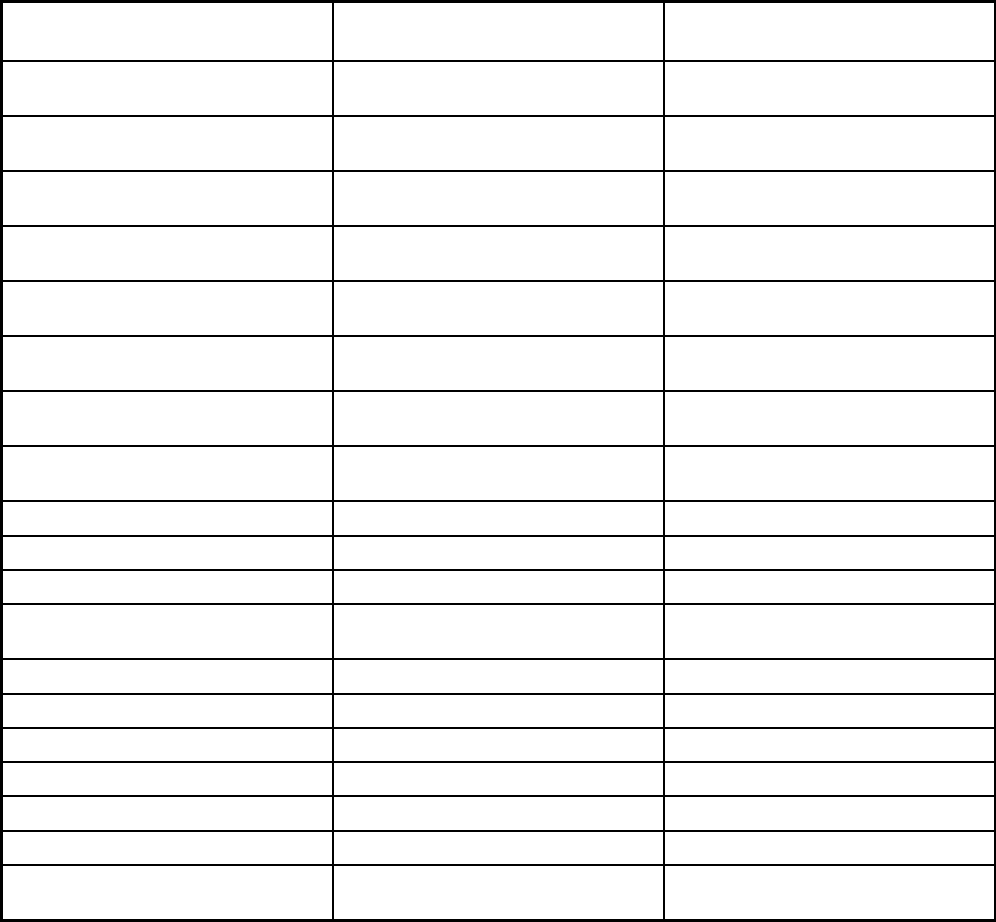
280
Features HealthChoice Illinois
HealthChoice Illinois - Managed
Long-Term Services and Supports
Populations enrolled: Foster Care and
Adoption Assistance Children
Exempt Exempt
Populations enrolled: Enrollment choice
period
60 days 60 days
Populations enrolled: Enrollment broker
name (if applicable)
MAXIMUS MAXIMUS
Populations enrolled: Notes on
enrollment choice period
Benefits covered: Inpatient hospital
physical health
X
Benefits covered: Inpatient hospital
behavioral health (MH and/or SUD)
X
Benefits covered: Outpatient hospital
physical health
X
Benefits covered: Outpatient hospital
behavioral health (MH and/or SUD)
X
Benefits covered: Partial hospitalization X
Benefits covered: Physician X
Benefits covered: Nurse practitioner X
Benefits covered: Rural health clinics
and FQHCs
X
Benefits covered: Clinic services X
Benefits covered: Lab and x-ray X
Benefits covered: Prescription drugs X
Benefits covered: Prosthetic devices X
Benefits covered: EPSDT X
Benefits covered: Case management X
Benefits covered: SSA Section 1945-
authorized health home
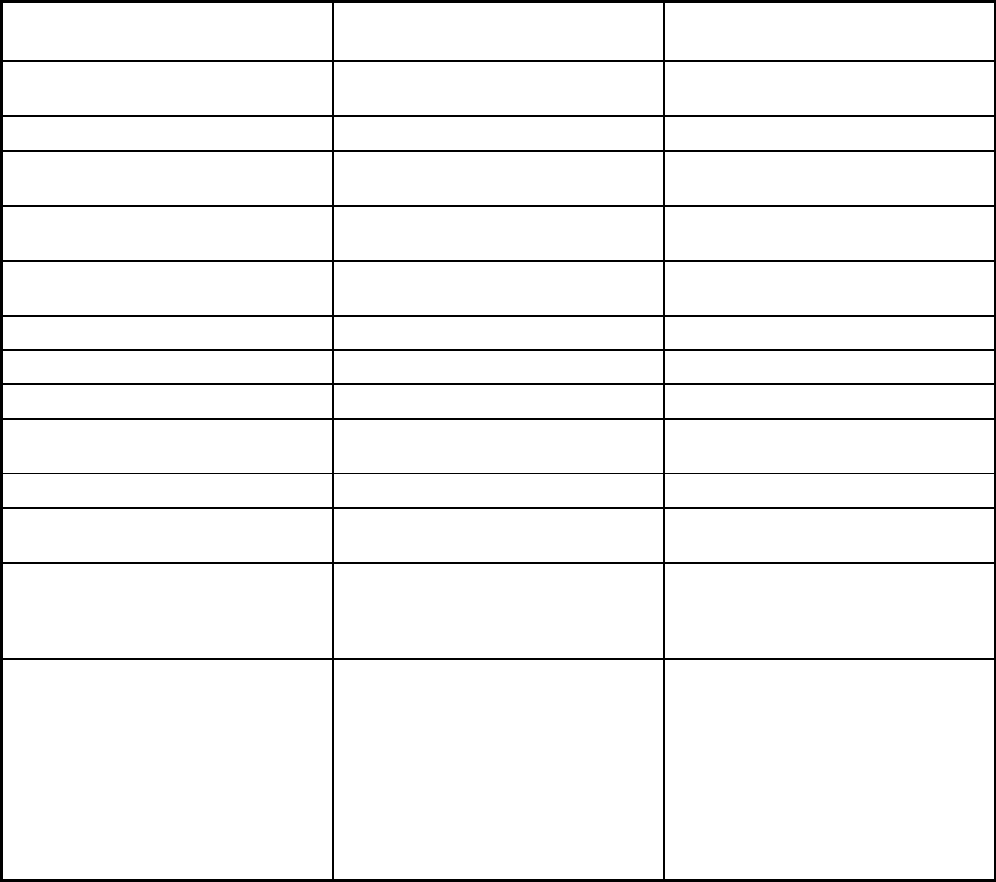
281
Features HealthChoice Illinois
HealthChoice Illinois - Managed
Long-Term Services and Supports
Benefits covered: Health home care
(services in home)
X
Benefits covered: Family planning X
Benefits covered: Dental services
(medical/surgical)
X
Benefits covered: Dental (preventative
or corrective)
X
Benefits covered: Personal care (state
plan option)
Benefits covered: HCBS waiver services X X
Benefits covered: Private duty nursing X
Benefits covered: ICF-IDD
Benefits covered: Nursing facility
services
X X
Benefits covered: Hospice care X
Benefits covered: Non-Emergency
Medical Transportation
X X
Benefits covered: Institution for Mental
Disease inpatient treatment for people
ages 21-64 defined by 42 CFR
§438.6(e) as an 'in lieu of' benefit
X
Benefits covered: Other (e.g., nurse
midwife services, freestanding birth
centers, podiatry, etc.)
Ambulatory surgical treatment center,
assisted living, assistive/augmentative
communication devices, audiology,
behavioral, blood and blood
components, chiropractic, durable
medical equipment, environmental
accessibility, immunization,
physical/occupational and speech
therapy, podiatry, renal, specialized
medical equipment and supplies, vision
Non-Medicare behavioral health
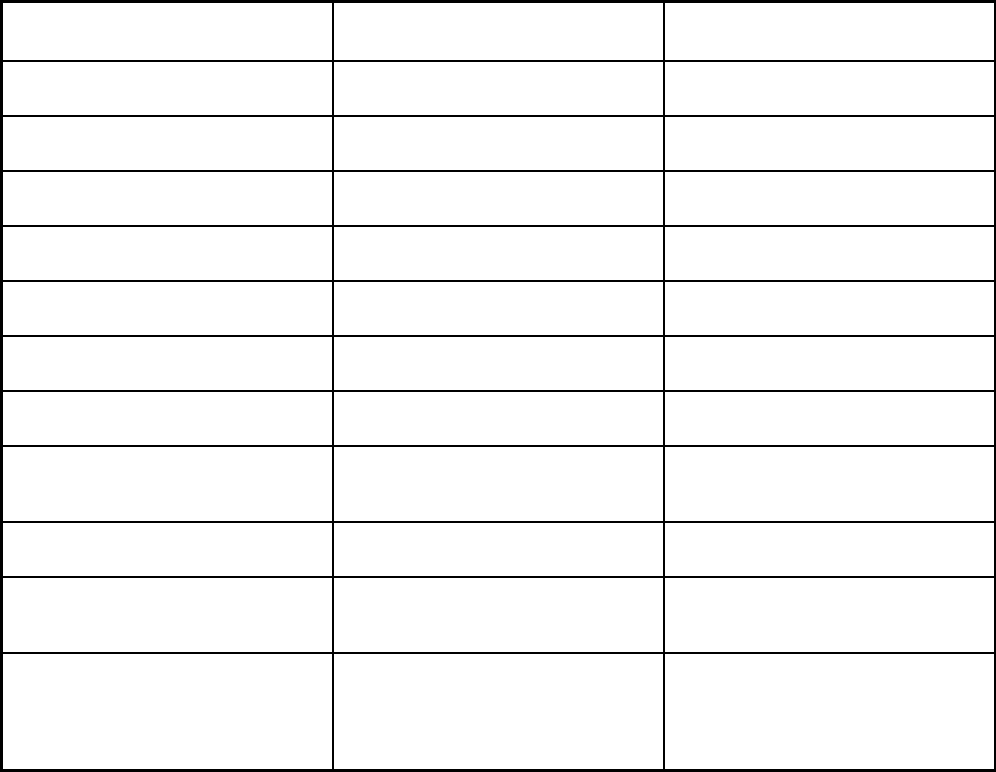
282
Features HealthChoice Illinois
HealthChoice Illinois - Managed
Long-Term Services and Supports
Quality assurance and improvement:
HEDIS data required?
Yes No
Quality assurance and improvement:
CAHPS data required?
Yes Yes
Quality assurance and improvement:
Accreditation required?
Yes Yes
Quality assurance and improvement:
Accrediting organization
NCQA NCQA
Quality assurance and improvement:
EQRO contractor name (if applicable)
Health Services Advisory Group Health Services Advisory Group
Performance incentives: Payment
bonuses/differentials to reward plans
X
Performance incentives: Preferential
auto-enrollment to reward plans
Performance incentives: Public reports
comparing plan performance on key
metrics
X
Performance incentives: Withholds tied
to performance metrics
X X
Performance incentives: MCOs/PHPs
required or encouraged to pay providers
for value/quality outcomes
X X
Participating plans: Plans in Program Blue Cross Blue Shield of Illinois;
CountyCare; IlliniCare Health Plan;
Meridian Health Plan; Molina Healthcare
of Illinois; NextLevel Health Partners;
Harmony Health Plan
Blue Cross Blue Shield of Illinois;
CountyCare; Harmony Health Plan;
IlliniCare Health Plan; Meridian Health
Plan; Molina Healthcare of Illinois;
NextLevel Health Partners
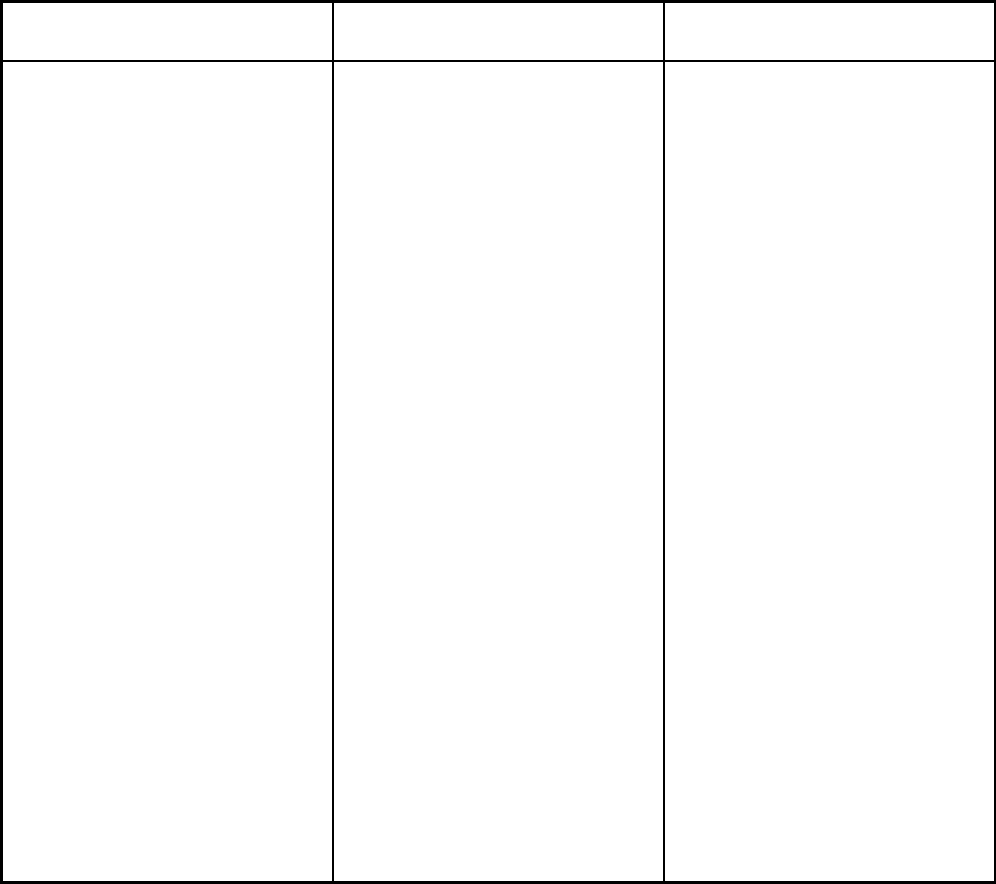
283
Features HealthChoice Illinois
HealthChoice Illinois - Managed
Long-Term Services and Supports
Notes: Program notes HealthChoice Illinois is a statewide
program, effective 1/1/2018, comprised
of the populations previously included in
the Integrated Care Program, the Family
Health Plan/Affordable Care Act
Program, and the Managed Long Term
Services and Supports Program. Low-
income pregnant women are enrolled
mandatorily in this program. Pursuant to
305 ILCS 5/5-30 (a) and (h), if a
managed care organization (MCO) is
serving at least 5,000 SPDs (Seniors or
Persons with Disabilities) or 15,000
individuals in other populations covered
by Illinois Medicaid and has received
full-risk capitation for at least one (1)
year, the MCO is considered eligible for
accreditation and shall achieve
accreditation by the NCQA within two
(2) years after the date the MCO
became eligible for accreditation.
HealthChoice Illinois enrolls several
populations through 1915(c) waiver
authority, via five different 1915(c)
waivers, each of which has a different
start and expiration date. The current
Persons with Disabilities 1915(c) waiver
began on 7/12/2016 and will expire on
7/11/2021; the current Elderly 1915(c)
waiver began on 11/1/2016 and will
expire on 10/31/2021; the current
Traumatic Brain Injury 1915(c) waiver
began on 7/1/2017 and will expire on
6/30/2022; the current Supportive Living
Facility 1915(c) waiver began on
10/23/2017 and will expire on
10/22/2022; and the current HIV/AIDS
1915© waiver began on 10/1/2018 and
will expire on 9/30/2023.
Dually eligible adults enrolled in the
state’s Financial Alignment Initiative
Demonstration (MMAI) are not allowed
to enroll in this program. Pursuant to
305 ILCS 5/5-30 (a) and (h), if a
managed care organization (MCO) is
serving at least 5,000 SPDs (Seniors or
Persons with Disabilities) or 15,000
individuals in other populations covered
by Illinois Medicaid and has received
full-risk capitation for at least one (1)
year, the MCO is considered eligible for
accreditation and shall achieve
accreditation by the NCQA within two
(2) years after the date the MCO
became eligible for accreditation.
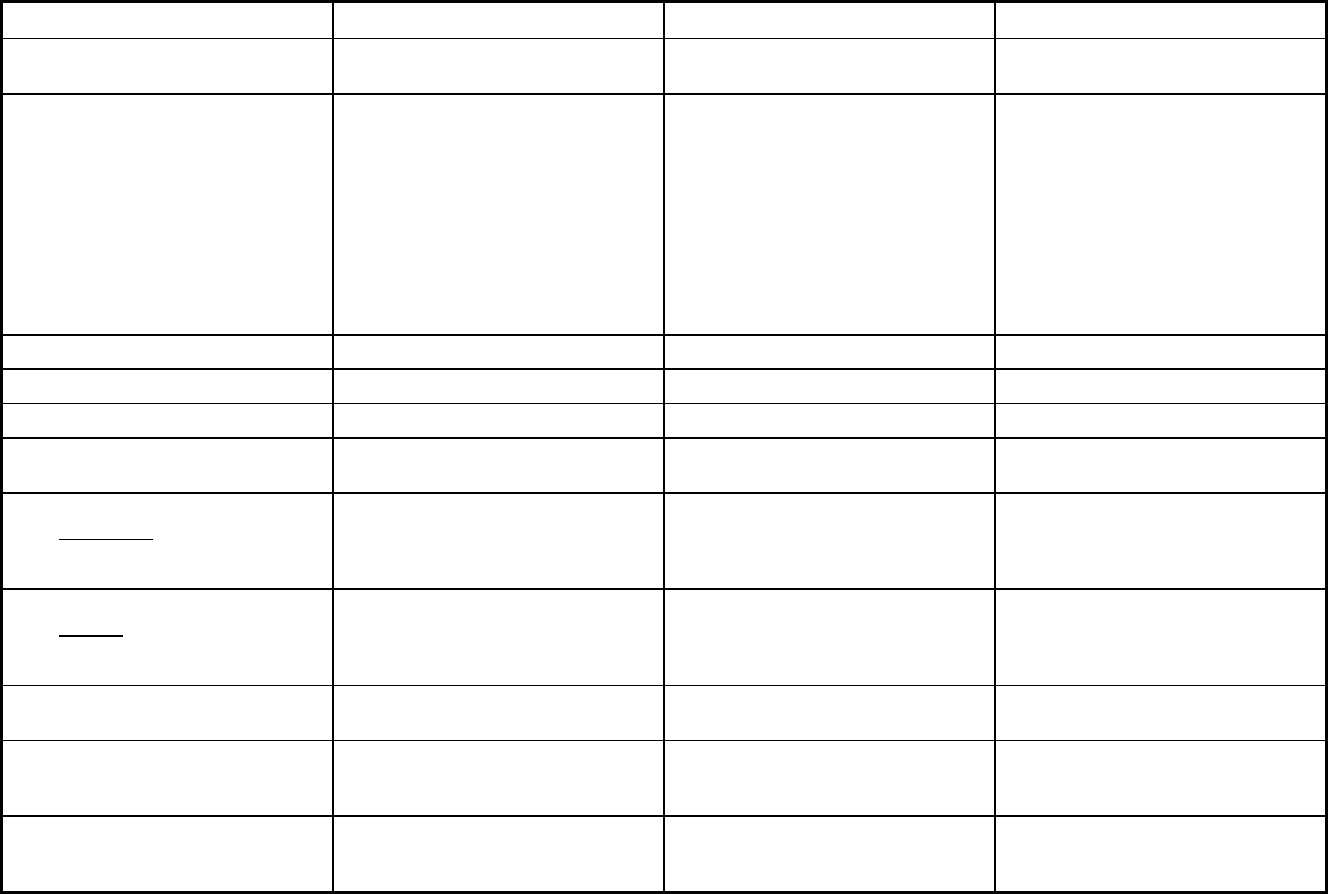
284
Indiana Managed Care Program Features, as of 2018 (1 of 2)
Features PACE Hoosier Care Connect Hoosier Healthwise
Program type Program of All-inclusive Care for the
Elderly (PACE)
Comprehensive MCO Comprehensive MCO
Statewide or region-specific? Lake and Johnson Counties, and the
following zip codes: 46107, 46201,
46202, 46203, 46204, 46217, 46218,
46219, 46221, 46222, 46225, 46227,
46229, 46237, 46239, 46241, 46259,
46506, 46514, 46516, 46517,
46526,46530, 46536, 46544, 46545,
46552, 46554, 46556, 46561, 46574,
46601, 46613, 46614, 46615, 46616,
46617, 46619, 46628, 46635, 46637,
46563, 46573
Statewide Statewide
Federal operating authority PACE 1915(b) 1932(a)
Program start date 10/01/2012 04/01/2015 01/01/2000
Waiver expiration date (if applicable) 06/30/2019
If the program ended in 2018, indicate
the end date
Populations enrolled: Low-income
adults not covered under ACA Section
VIII (excludes pregnant women and
people with disabilities)
Populations enrolled: Low-income
adults covered under ACA Section VIII
(excludes pregnant women and people
with disabilities)
Populations enrolled: Aged, Blind or
Disabled Children or Adults
Voluntary Mandatory
Populations enrolled: Non-Disabled
Children (excludes children in foster
care or receiving adoption assistance)
Mandatory
Populations enrolled: Individuals
receiving Limited Benefits (excludes
partial duals)
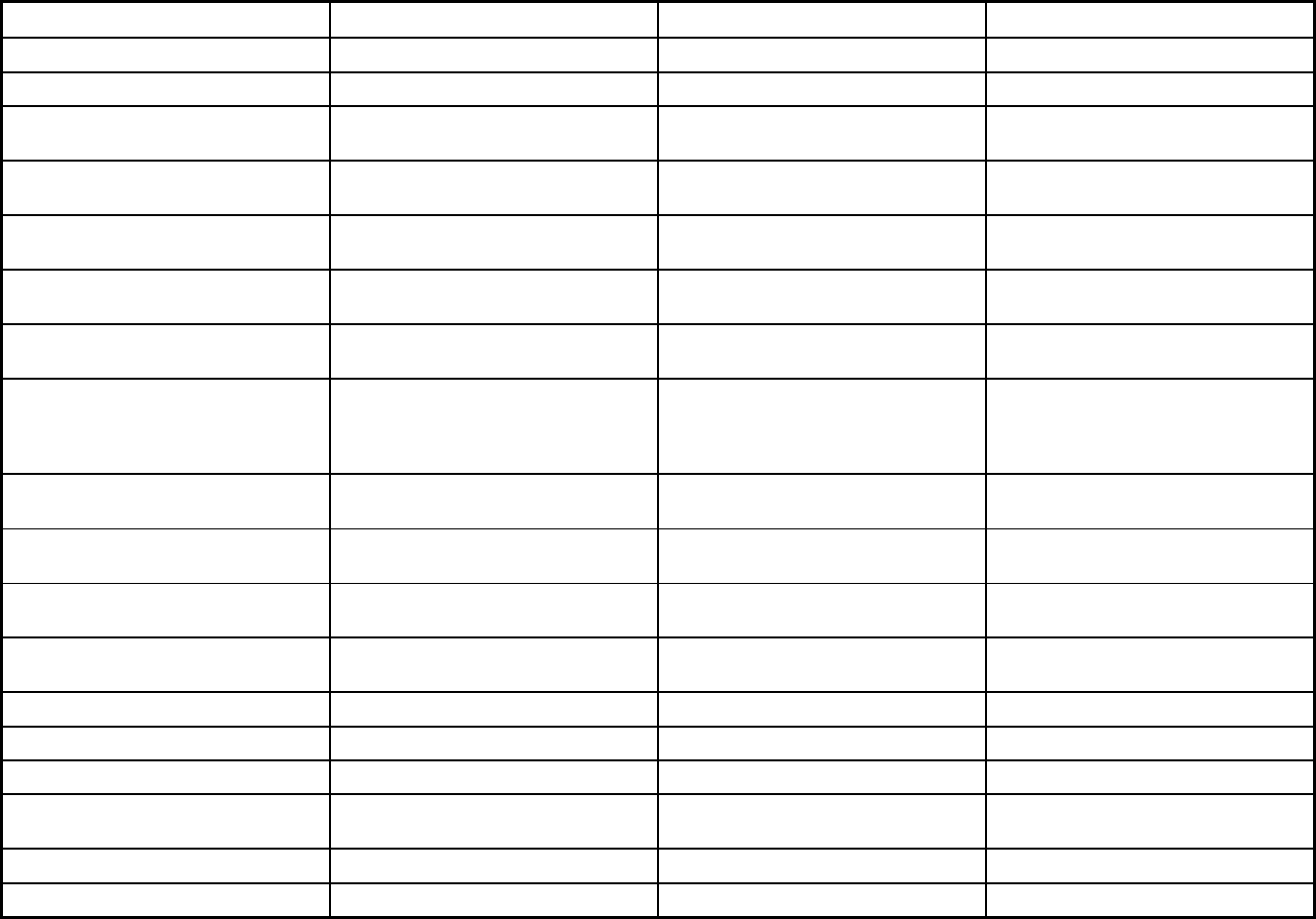
285
Features PACE Hoosier Care Connect Hoosier Healthwise
Populations enrolled: Full Duals Voluntary
Populations enrolled: Partial Duals Voluntary
Populations enrolled: Children with
Special Health Care Needs
Populations enrolled: Native
American/Alaskan Natives
Voluntary Voluntary Voluntary
Populations enrolled: Foster Care and
Adoption Assistance Children
Exempt Voluntary Exempt
Populations enrolled: Enrollment choice
period
N/A Other Other
Populations enrolled: Enrollment broker
name (if applicable)
Maximus Maximus
Populations enrolled: Notes on
enrollment choice period
If members do select a health plan upon
application, they are auto-assigned.
They have a 90-day window to change
their health plan.
If members do select a health plan upon
application, they are auto-assigned.
They have a 90-day window to change
their health plan.
Benefits covered: Inpatient hospital
physical health
X X X
Benefits covered: Inpatient hospital
behavioral health (MH and/or SUD)
X X X
Benefits covered: Outpatient hospital
physical health
X X X
Benefits covered: Outpatient hospital
behavioral health (MH and/or SUD)
X X X
Benefits covered: Partial hospitalization X X X
Benefits covered: Physician X X X
Benefits covered: Nurse practitioner X X X
Benefits covered: Rural health clinics
and FQHCs
X X X
Benefits covered: Clinic services X X X
Benefits covered: Lab and x-ray X X X
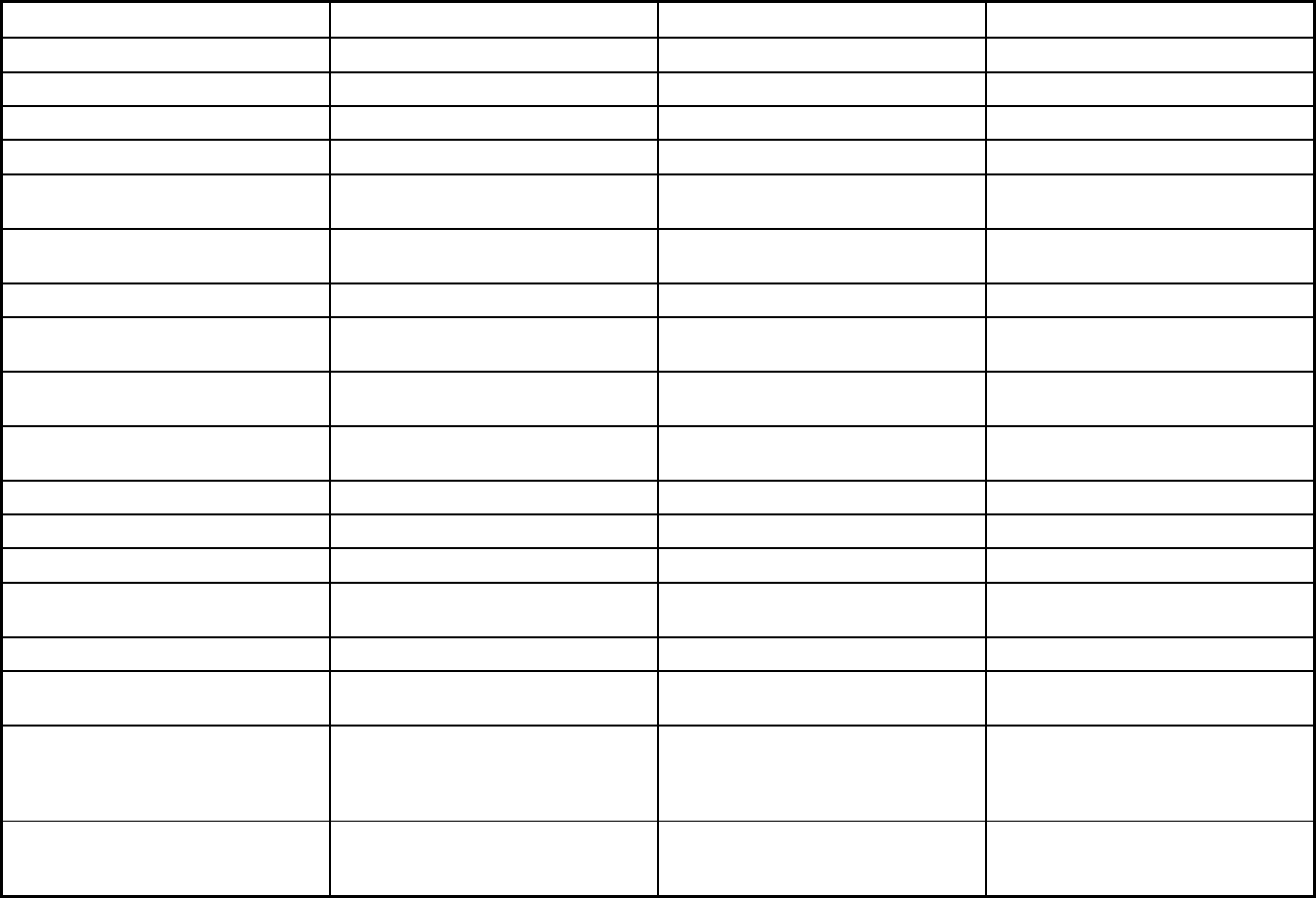
286
Features PACE Hoosier Care Connect Hoosier Healthwise
Benefits covered: Prescription drugs X X X
Benefits covered: Prosthetic devices X X X
Benefits covered: EPSDT X X
Benefits covered: Case management X X X
Benefits covered: SSA Section 1945-
authorized health home
Benefits covered: Health home care
(services in home)
X X X
Benefits covered: Family planning X X X
Benefits covered: Dental services
(medical/surgical)
X X X
Benefits covered: Dental (preventative
or corrective)
X X X
Benefits covered: Personal care (state
plan option)
X
Benefits covered: HCBS waiver services
Benefits covered: Private duty nursing X
Benefits covered: ICF-IDD
Benefits covered: Nursing facility
services
X X
Benefits covered: Hospice care X X
Benefits covered: Non-Emergency
Medical Transportation
X X X
Benefits covered: Institution for Mental
Disease inpatient treatment for people
ages 21-64 defined by 42 CFR
§438.6(e) as an 'in lieu of' benefit
X X
Benefits covered: Other (e.g., nurse
midwife services, freestanding birth
centers, podiatry, etc.)
Podiatry Podiatry
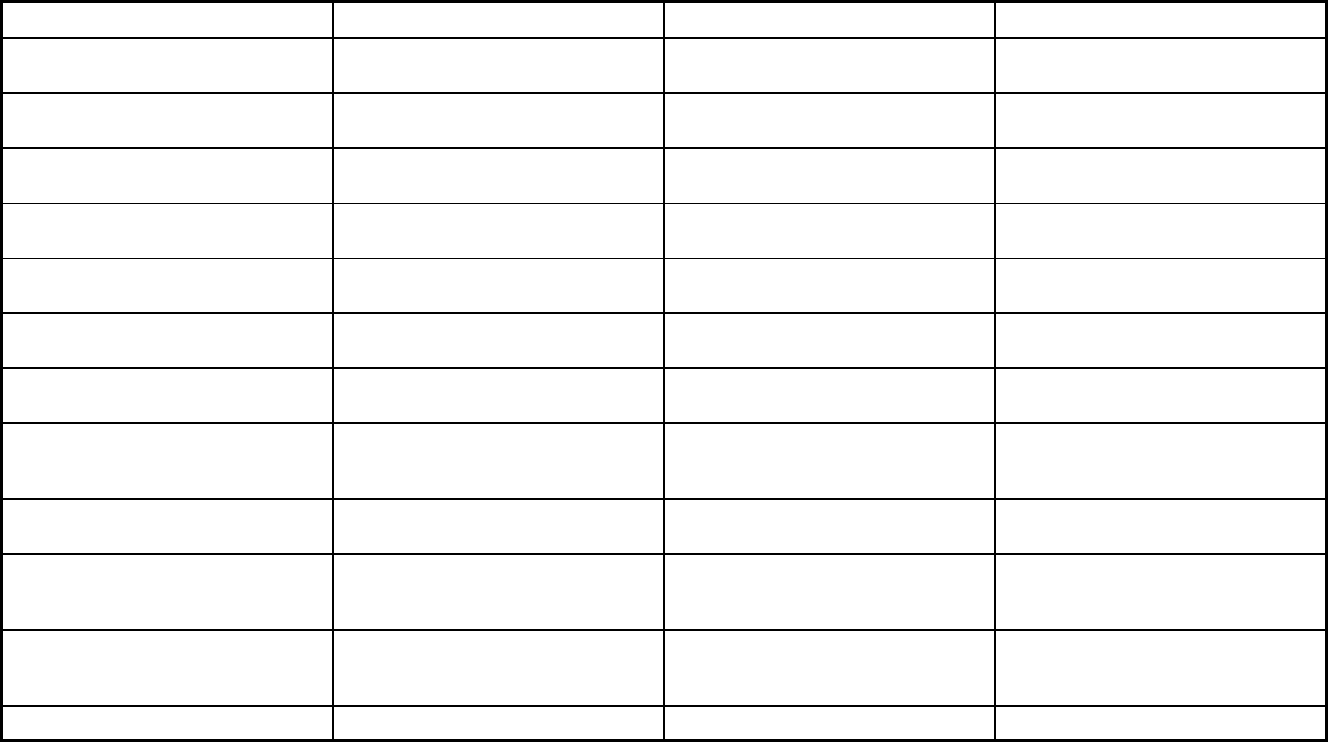
287
Features PACE Hoosier Care Connect Hoosier Healthwise
Quality assurance and improvement:
HEDIS data required?
No Yes Yes
Quality assurance and improvement:
CAHPS data required?
No Yes Yes
Quality assurance and improvement:
Accreditation required?
No Yes Yes
Quality assurance and improvement:
Accrediting organization
NCQA NCQA
Quality assurance and improvement:
EQRO contractor name (if applicable)
Burns and Associates Burns and Associates
Performance incentives: Payment
bonuses/differentials to reward plans
X X
Performance incentives: Preferential
auto-enrollment to reward plans
Performance incentives: Public reports
comparing plan performance on key
metrics
Performance incentives: Withholds tied
to performance metrics
X X
Performance incentives: MCOs/PHPs
required or encouraged to pay providers
for value/quality outcomes
X X
Participating plans: Plans in Program Franciscan Senior Health and Wellness;
Saint Joseph PACE
Anthem; Managed Health Services of
Indiana
Anthem; Caresource Indiana, Inc;
Managed Health Services of Indiana;
MDWise
Notes: Program notes
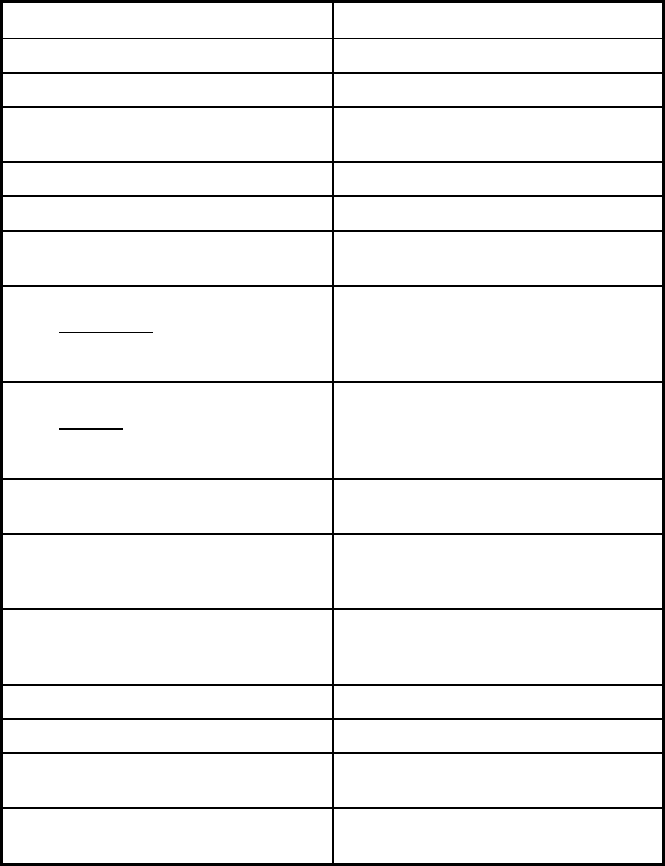
288
Indiana Managed Care Program Features, as of 2018 (2 of 2)
Features Healthy Indiana Plan (2.0)
Program type Comprehensive MCO
Statewide or region-specific? Statewide
Federal operating authority 1115(a) (Medicaid demonstration
waivers)
Program start date 02/01/2015
Waiver expiration date (if applicable) 12/31/2020
If the program ended in 2018, indicate
the end date
Populations enrolled: Low-income
adults not covered under ACA Section
VIII (excludes pregnant women and
people with disabilities)
Mandatory
Populations enrolled: Low-income
adults covered under ACA Section VIII
(excludes pregnant women and people
with disabilities)
Mandatory
Populations enrolled: Aged, Blind or
Disabled Children or Adults
Populations enrolled: Non-Disabled
Children (excludes children in foster
care or receiving adoption assistance)
Populations enrolled: Individuals
receiving Limited Benefits (excludes
partial duals)
Populations enrolled: Full Duals
Populations enrolled: Partial Duals
Populations enrolled: Children with
Special Health Care Needs
Populations enrolled: Native
American/Alaskan Natives
Voluntary
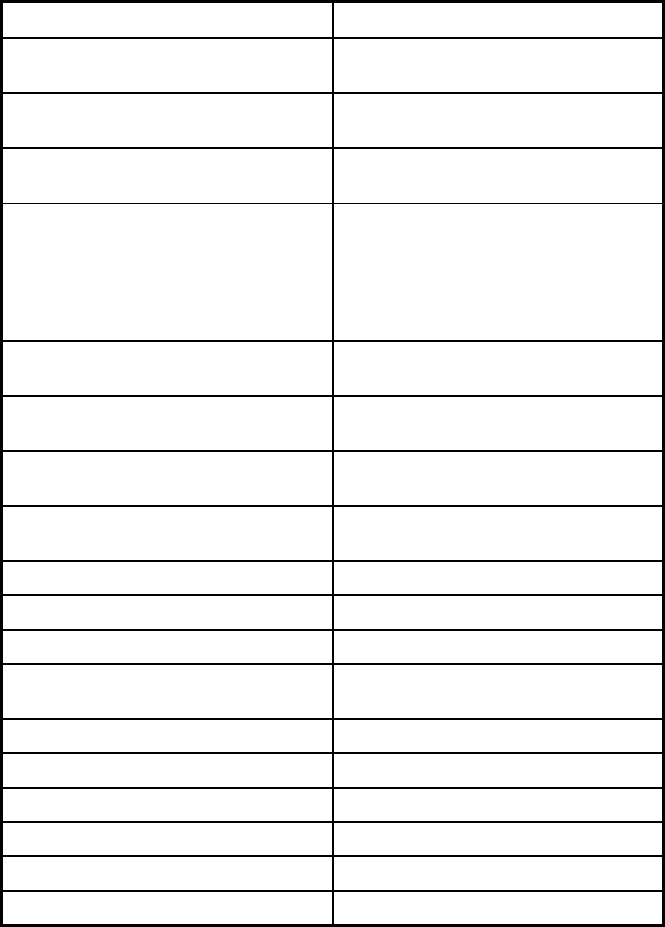
289
Features Healthy Indiana Plan (2.0)
Populations enrolled: Foster Care and
Adoption Assistance Children
Exempt
Populations enrolled: Enrollment choice
period
Other
Populations enrolled: Enrollment broker
name (if applicable)
Maximus
Populations enrolled: Notes on
enrollment choice period
If members do select a health plan upon
application, they are auto-assigned.
They have a 60-day window to change
their health plan. Members cannot
change plans after having made a
POWER account contribution.
Benefits covered: Inpatient hospital
physical health
X
Benefits covered: Inpatient hospital
behavioral health (MH and/or SUD)
X
Benefits covered: Outpatient hospital
physical health
X
Benefits covered: Outpatient hospital
behavioral health (MH and/or SUD)
X
Benefits covered: Partial hospitalization X
Benefits covered: Physician X
Benefits covered: Nurse practitioner X
Benefits covered: Rural health clinics
and FQHCs
X
Benefits covered: Clinic services X
Benefits covered: Lab and x-ray X
Benefits covered: Prescription drugs X
Benefits covered: Prosthetic devices X
Benefits covered: EPSDT X
Benefits covered: Case management X
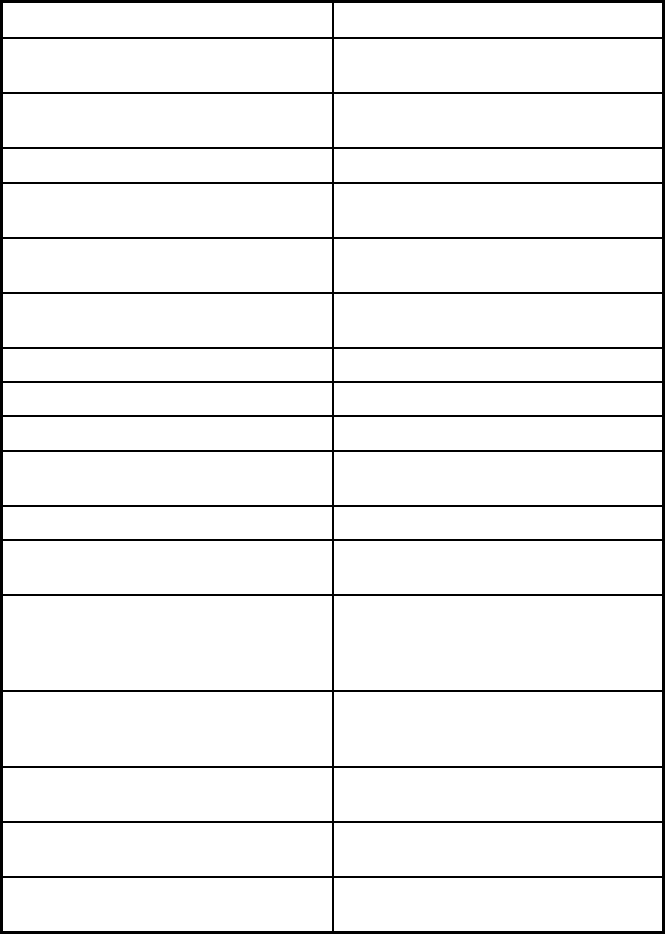
290
Features Healthy Indiana Plan (2.0)
Benefits covered: SSA Section 1945-
authorized health home
Benefits covered: Health home care
(services in home)
X
Benefits covered: Family planning X
Benefits covered: Dental services
(medical/surgical)
X
Benefits covered: Dental (preventative
or corrective)
X
Benefits covered: Personal care (state
plan option)
X
Benefits covered: HCBS waiver services
Benefits covered: Private duty nursing X
Benefits covered: ICF-IDD
Benefits covered: Nursing facility
services
X
Benefits covered: Hospice care X
Benefits covered: Non-Emergency
Medical Transportation
X
Benefits covered: Institution for Mental
Disease inpatient treatment for people
ages 21-64 defined by 42 CFR
§438.6(e) as an 'in lieu of' benefit
X
Benefits covered: Other (e.g., nurse
midwife services, freestanding birth
centers, podiatry, etc.)
Podiatry
Quality assurance and improvement:
HEDIS data required?
Yes
Quality assurance and improvement:
CAHPS data required?
Yes
Quality assurance and improvement:
Accreditation required?
Yes
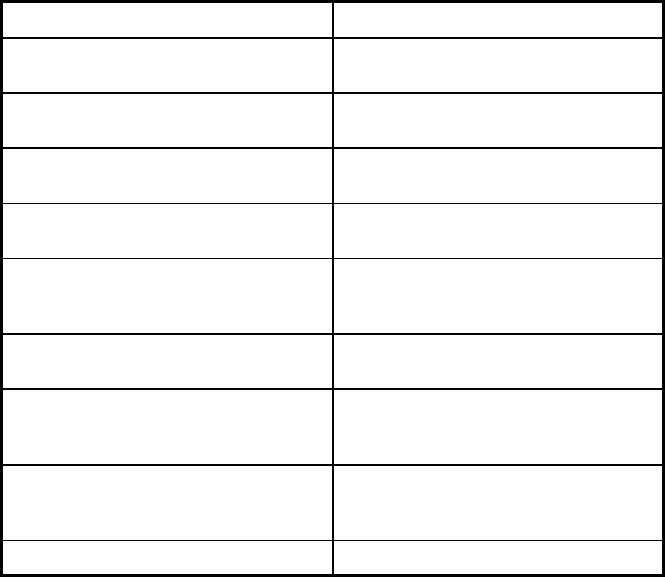
291
Features Healthy Indiana Plan (2.0)
Quality assurance and improvement:
Accrediting organization
NCQA
Quality assurance and improvement:
EQRO contractor name (if applicable)
Burns and Associates
Performance incentives: Payment
bonuses/differentials to reward plans
X
Performance incentives: Preferential
auto-enrollment to reward plans
Performance incentives: Public reports
comparing plan performance on key
metrics
Performance incentives: Withholds tied
to performance metrics
X
Performance incentives: MCOs/PHPs
required or encouraged to pay providers
for value/quality outcomes
X
Participating plans: Plans in Program Anthem; Caresource Indiana, Inc;
Managed Health Services of Indiana;
MDWise
Notes: Program notes
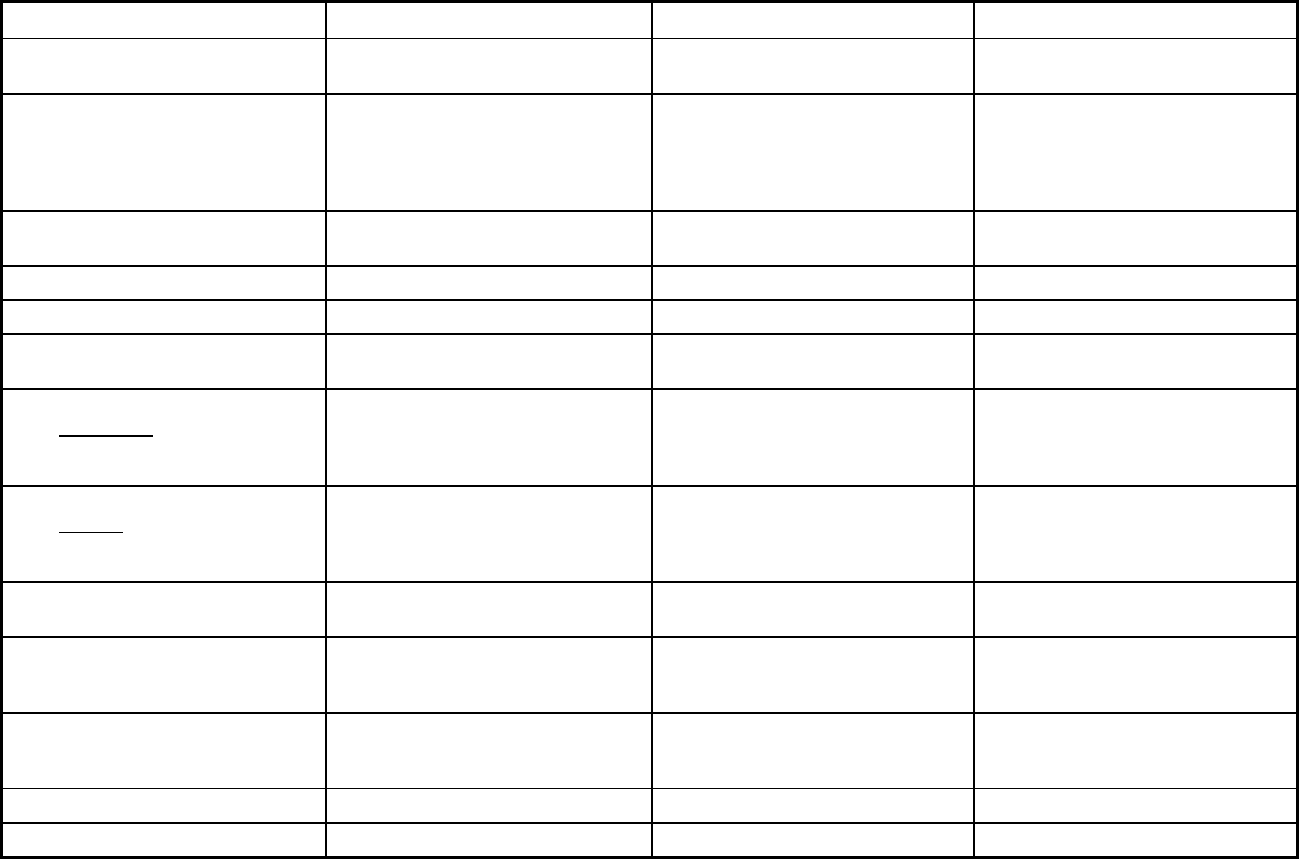
292
Iowa Managed Care Program Features, as of 2018 (1 of 2)
Features IA Healthlink Dental Wellness Plan PACE
Program type Comprehensive MCO + MLTSS Dental only (PAHP) Program of All-inclusive Care for the
Elderly (PACE)
Statewide or region-specific? Statewide Statewide Harrison, Mills, Pottawattamie,
Cherokee, Monona, Plymouth,
Woodbury, Boone, Dallas, Jasper,
Marshall, Madison, Marion, Polk, Story,
and Warren Counties
Federal operating authority 1915(b)/1915(c),1937 Alt Benefit
Plan,1945 Health Homes
1115(a) (Medicaid demonstration
waivers)
PACE
Program start date 04/01/2016 05/01/2014 09/01/2009
Waiver expiration date (if applicable) 03/31/2021 01/01/2020
If the program ended in 2018, indicate
the end date
Populations enrolled: Low-income
adults not covered under ACA Section
VIII (excludes pregnant women and
people with disabilities)
Mandatory Mandatory
Populations enrolled: Low-income
adults covered under ACA Section VIII
(excludes pregnant women and people
with disabilities)
Mandatory Mandatory
Populations enrolled: Aged, Blind or
Disabled Children or Adults
Mandatory Voluntary
Populations enrolled: Non-Disabled
Children (excludes children in foster
care or receiving adoption assistance)
Mandatory
Populations enrolled: Individuals
receiving Limited Benefits (excludes
partial duals)
Populations enrolled: Full Duals Mandatory Mandatory Voluntary
Populations enrolled: Partial Duals Mandatory
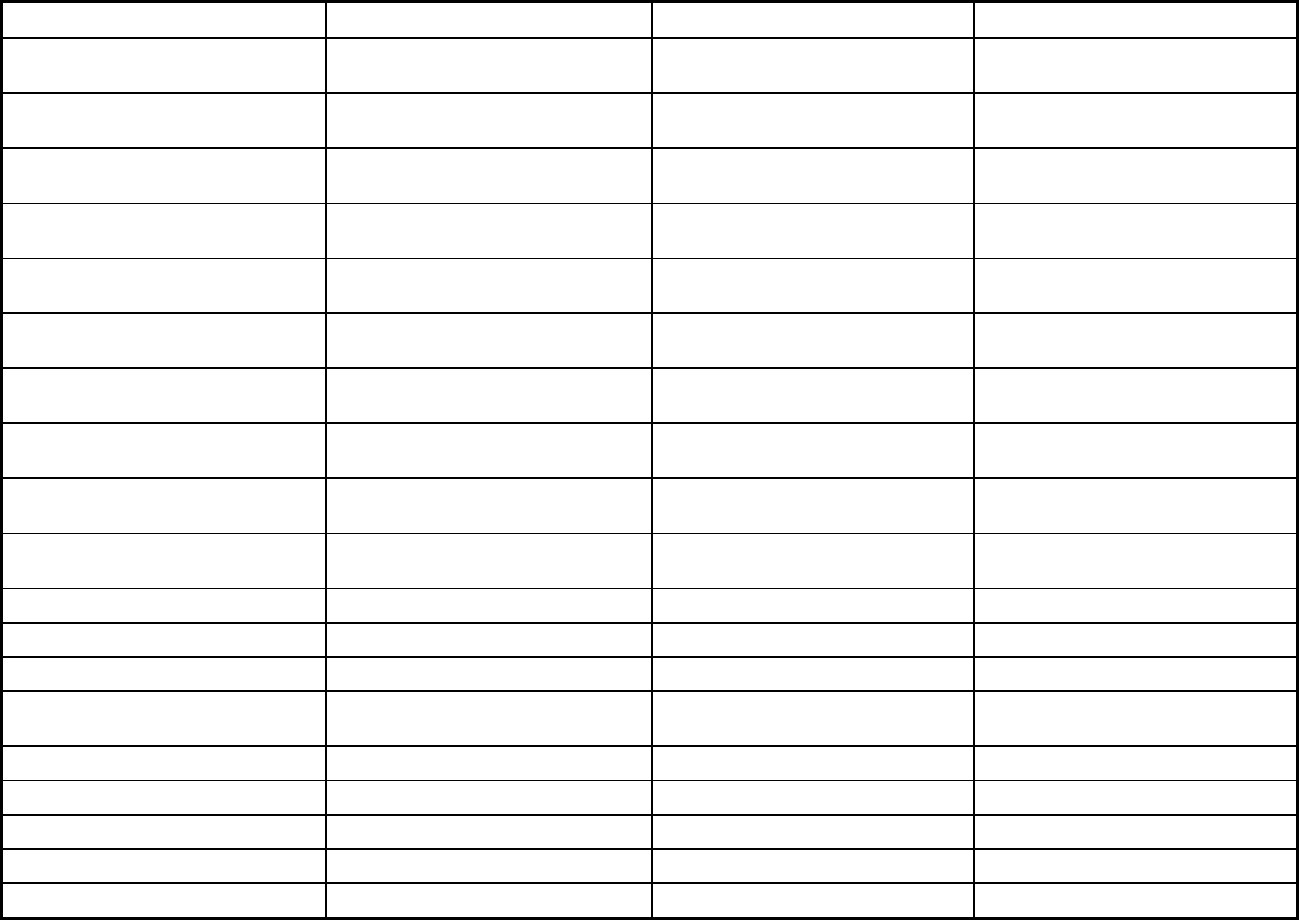
293
Features IA Healthlink Dental Wellness Plan PACE
Populations enrolled: Children with
Special Health Care Needs
Mandatory
Populations enrolled: Native
American/Alaskan Natives
Voluntary Voluntary Exempt
Populations enrolled: Foster Care and
Adoption Assistance Children
Mandatory Exempt Exempt
Populations enrolled: Enrollment choice
period
Pre-assigned Pre-assigned N/A
Populations enrolled: Enrollment broker
name (if applicable)
Maximus (Iowa Medicaid Member
Services contractor)
Maximus (Iowa Medicaid Member
Services contractor)
Populations enrolled: Notes on
enrollment choice period
Benefits covered: Inpatient hospital
physical health
X X
Benefits covered: Inpatient hospital
behavioral health (MH and/or SUD)
X X
Benefits covered: Outpatient hospital
physical health
X X
Benefits covered: Outpatient hospital
behavioral health (MH and/or SUD)
X X
Benefits covered: Partial hospitalization X X
Benefits covered: Physician X X
Benefits covered: Nurse practitioner X X
Benefits covered: Rural health clinics
and FQHCs
X X
Benefits covered: Clinic services X X
Benefits covered: Lab and x-ray X X
Benefits covered: Prescription drugs X X
Benefits covered: Prosthetic devices X X
Benefits covered: EPSDT X
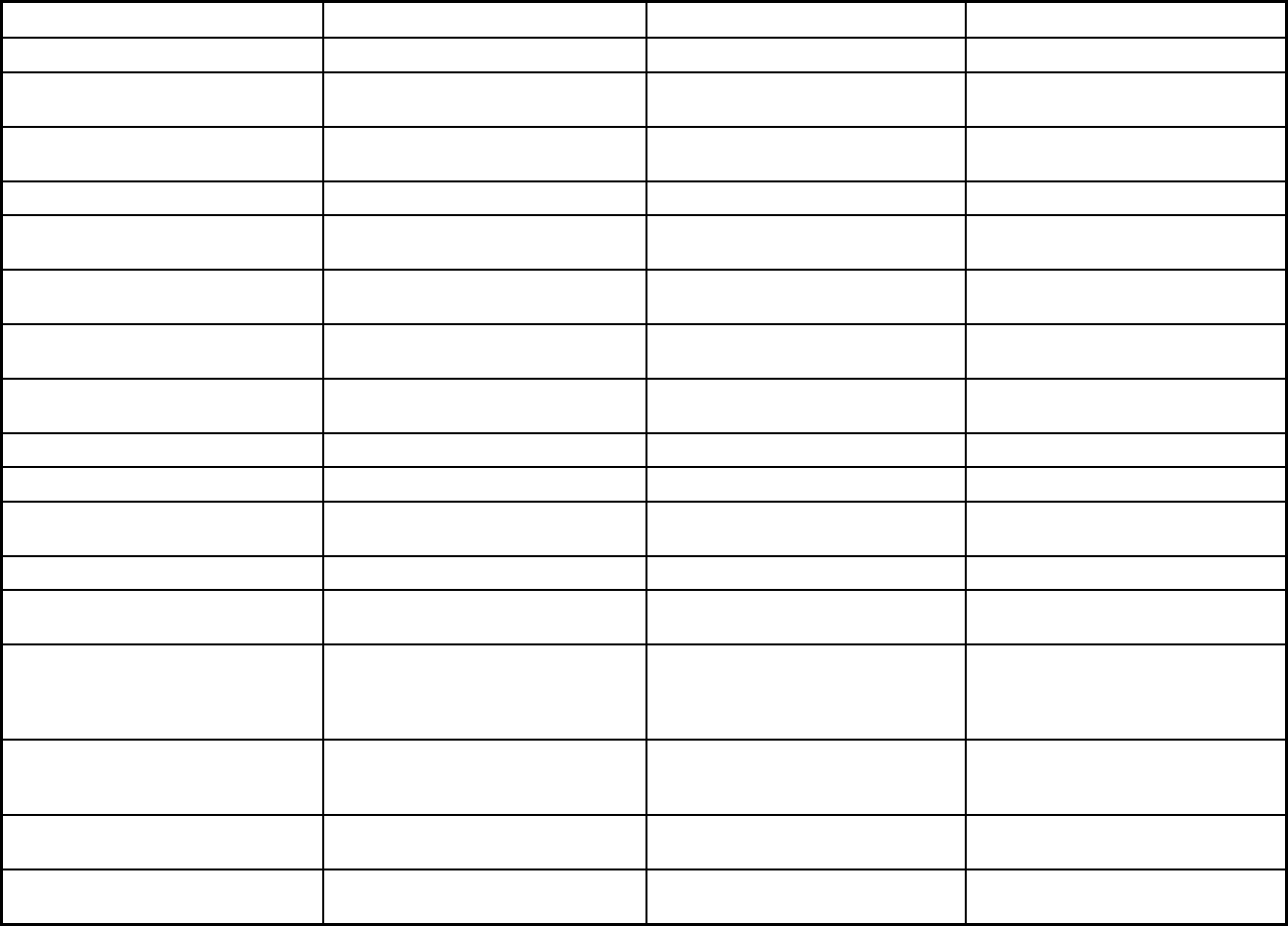
294
Features IA Healthlink Dental Wellness Plan PACE
Benefits covered: Case management X X
Benefits covered: SSA Section 1945-
authorized health home
X
Benefits covered: Health home care
(services in home)
X X
Benefits covered: Family planning X
Benefits covered: Dental services
(medical/surgical)
X
Benefits covered: Dental (preventative
or corrective)
X X
Benefits covered: Personal care (state
plan option)
Benefits covered: HCBS waiver
services
X
Benefits covered: Private duty nursing X X
Benefits covered: ICF-IDD X
Benefits covered: Nursing facility
services
X X
Benefits covered: Hospice care X X
Benefits covered: Non-Emergency
Medical Transportation
X X
Benefits covered: Institution for Mental
Disease inpatient treatment for people
ages 21-64 defined by 42 CFR
§438.6(e) as an 'in lieu of' benefit
Benefits covered: Other (e.g., nurse
midwife services, freestanding birth
centers, podiatry, etc.)
Quality assurance and improvement:
HEDIS data required?
Yes No No
Quality assurance and improvement:
CAHPS data required?
Yes No No

295
Features IA Healthlink Dental Wellness Plan PACE
Quality assurance and improvement:
Accreditation required?
Yes No No
Quality assurance and improvement:
Accrediting organization
NCQA
Quality assurance and improvement:
EQRO contractor name (if applicable)
Health Services Advisory Group Health Services Advisory Group
Performance incentives: Payment
bonuses/differentials to reward plans
Performance incentives: Preferential
auto-enrollment to reward plans
Performance incentives: Public reports
comparing plan performance on key
metrics
X
Performance incentives: Withholds tied
to performance metrics
X X
Performance incentives: MCOs/PHPs
required or encouraged to pay
providers for value/quality outcomes
X
Participating plans: Plans in Program UnitedHealthcare; Amerigroup of Iowa,
Inc.
Delta Dental of Iowa; MCNA Dental
Plans, Inc.
PACE
Notes: Program notes
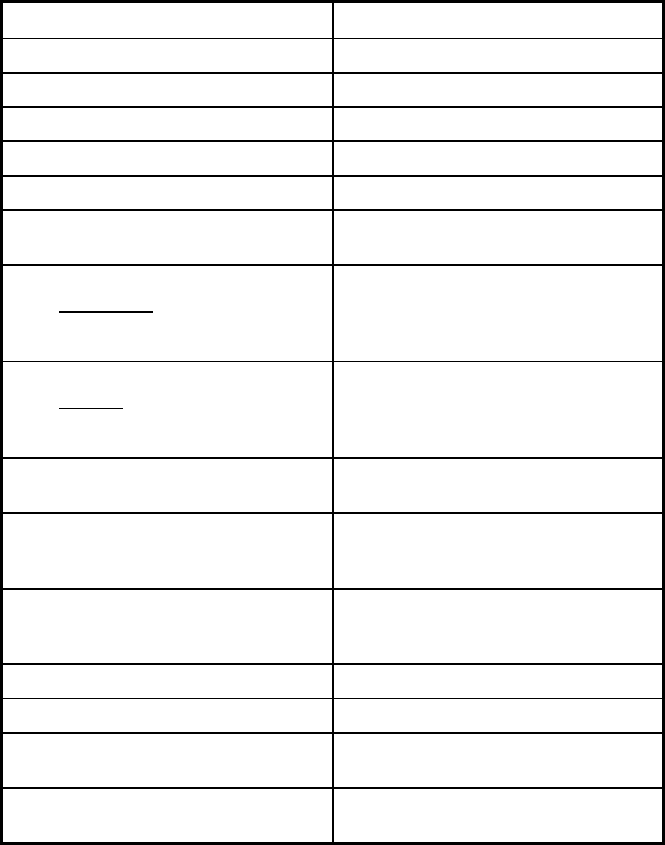
296
Iowa Managed Care Program Features, as of 2018 (2 of 2)
Features NEMT
Program type Non-Emergency Medical Transportation
Statewide or region-specific? Statewide
Federal operating authority 1902(a)(70) NEMT
Program start date 01/01/2009
Waiver expiration date (if applicable)
If the program ended in 2018, indicate
the end date
Populations enrolled: Low-income
adults not covered under ACA Section
VIII (excludes pregnant women and
people with disabilities)
Mandatory
Populations enrolled: Low-income
adults covered under ACA Section VIII
(excludes pregnant women and people
with disabilities)
Mandatory
Populations enrolled: Aged, Blind or
Disabled Children or Adults
Mandatory
Populations enrolled: Non-Disabled
Children (excludes children in foster
care or receiving adoption assistance)
Mandatory
Populations enrolled: Individuals
receiving Limited Benefits (excludes
partial duals)
Populations enrolled: Full Duals Mandatory
Populations enrolled: Partial Duals
Populations enrolled: Children with
Special Health Care Needs
Mandatory
Populations enrolled: Native
American/Alaskan Natives
Voluntary
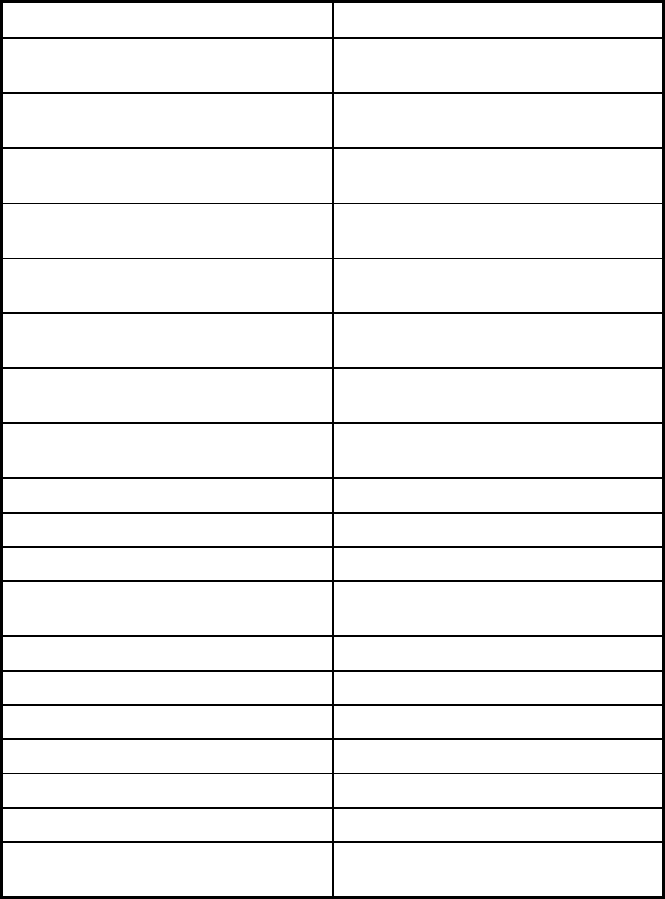
297
Features NEMT
Populations enrolled: Foster Care and
Adoption Assistance Children
Mandatory
Populations enrolled: Enrollment choice
period
Populations enrolled: Enrollment broker
name (if applicable)
Populations enrolled: Notes on
enrollment choice period
Benefits covered: Inpatient hospital
physical health
Benefits covered: Inpatient hospital
behavioral health (MH and/or SUD)
Benefits covered: Outpatient hospital
physical health
Benefits covered: Outpatient hospital
behavioral health (MH and/or SUD)
Benefits covered: Partial hospitalization
Benefits covered: Physician
Benefits covered: Nurse practitioner
Benefits covered: Rural health clinics
and FQHCs
Benefits covered: Clinic services
Benefits covered: Lab and x-ray
Benefits covered: Prescription drugs
Benefits covered: Prosthetic devices
Benefits covered: EPSDT
Benefits covered: Case management
Benefits covered: SSA Section 1945-
authorized health home
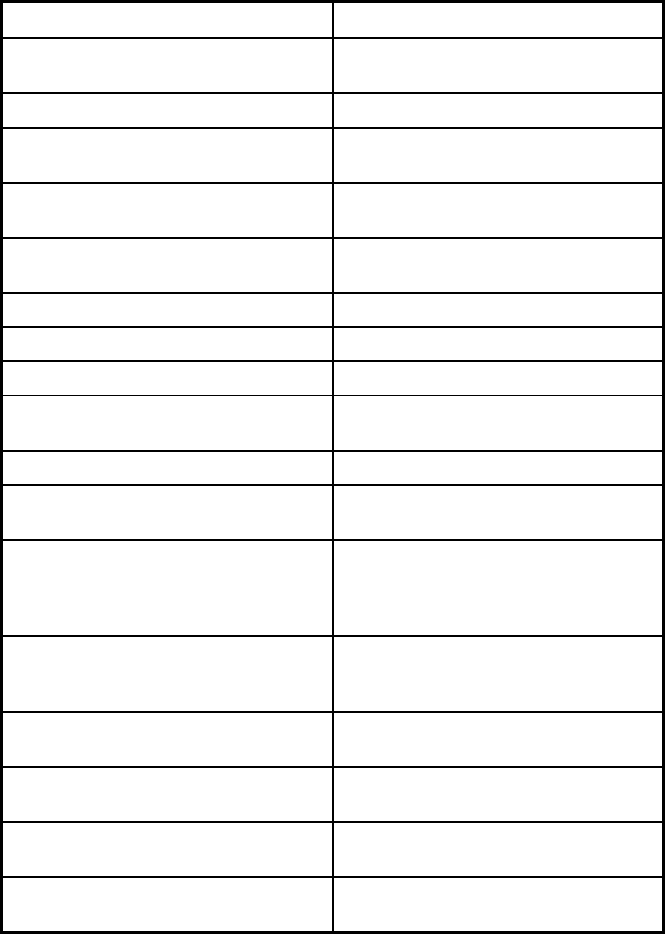
298
Features NEMT
Benefits covered: Health home care
(services in home)
Benefits covered: Family planning
Benefits covered: Dental services
(medical/surgical)
Benefits covered: Dental (preventative
or corrective)
Benefits covered: Personal care (state
plan option)
Benefits covered: HCBS waiver services
Benefits covered: Private duty nursing
Benefits covered: ICF-IDD
Benefits covered: Nursing facility
services
Benefits covered: Hospice care
Benefits covered: Non-Emergency
Medical Transportation
X
Benefits covered: Institution for Mental
Disease inpatient treatment for people
ages 21-64 defined by 42 CFR
§438.6(e) as an 'in lieu of' benefit
Benefits covered: Other (e.g., nurse
midwife services, freestanding birth
centers, podiatry, etc.)
Quality assurance and improvement:
HEDIS data required?
No
Quality assurance and improvement:
CAHPS data required?
No
Quality assurance and improvement:
Accreditation required?
No
Quality assurance and improvement:
Accrediting organization
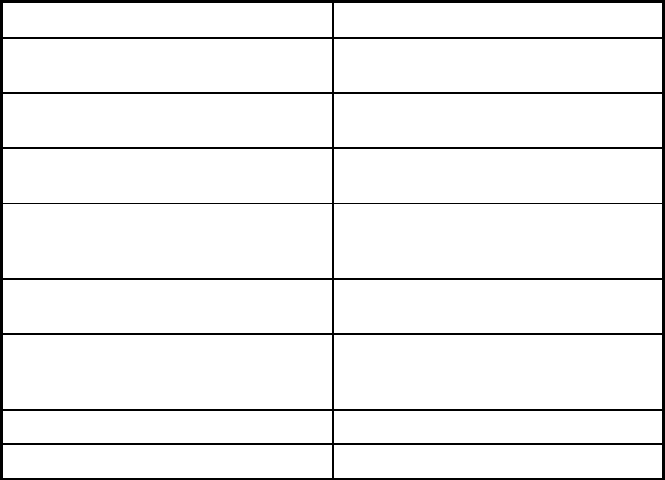
299
Features NEMT
Quality assurance and improvement:
EQRO contractor name (if applicable)
Performance incentives: Payment
bonuses/differentials to reward plans
Performance incentives: Preferential
auto-enrollment to reward plans
Performance incentives: Public reports
comparing plan performance on key
metrics
Performance incentives: Withholds tied
to performance metrics
Performance incentives: MCOs/PHPs
required or encouraged to pay providers
for value/quality outcomes
Participating plans: Plans in Program Access2Care, LLC
Notes: Program notes
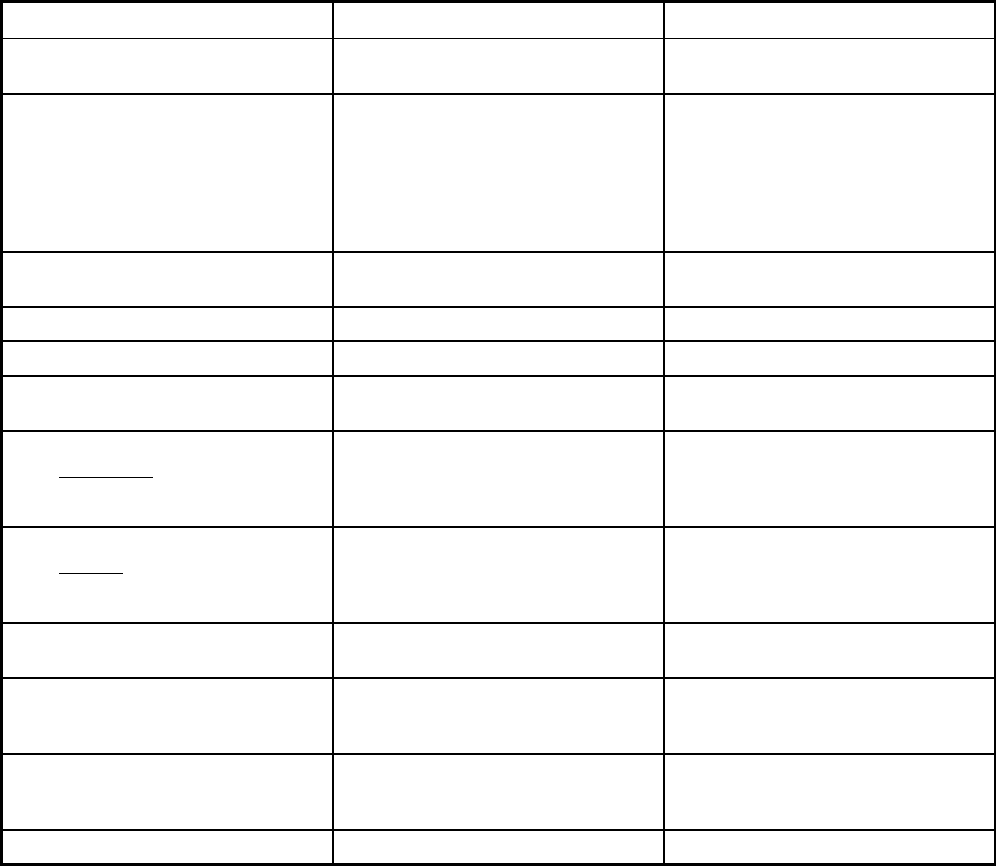
300
Kansas Managed Care Program Features, as of 2018
Features KanCare PACE
Program type Comprehensive MCO + MLTSS Program of All-inclusive Care for the
Elderly (PACE)
Statewide or region-specific? Statewide Dickinson, Douglas, Ellsworth, Harvey,
Jackson, Jefferson, Leavenworth,
Lincoln, Lyon, Marion, Marshall,
McPherson, Nemaha, Osage, Ottawa,
Reno, Rice, Saline, Sedgwick,
Shawnee, Pottawatomie, Wabaunsee
and Wyandotte counties
Federal operating authority 1115(a) (Medicaid demonstration
waivers)
PACE
Program start date 01/01/2013 08/01/2002
Waiver expiration date (if applicable) 12/31/2018
If the program ended in 2018, indicate
the end date
Populations enrolled: Low-income
adults not covered under ACA Section
VIII (excludes pregnant women and
people with disabilities)
Populations enrolled: Low-income
adults covered under ACA Section VIII
(excludes pregnant women and people
with disabilities)
Mandatory
Populations enrolled: Aged, Blind or
Disabled Children or Adults
Mandatory Voluntary
Populations enrolled: Non-Disabled
Children (excludes children in foster
care or receiving adoption assistance)
Mandatory
Populations enrolled: Individuals
receiving Limited Benefits (excludes
partial duals)
Populations enrolled: Full Duals Mandatory Voluntary
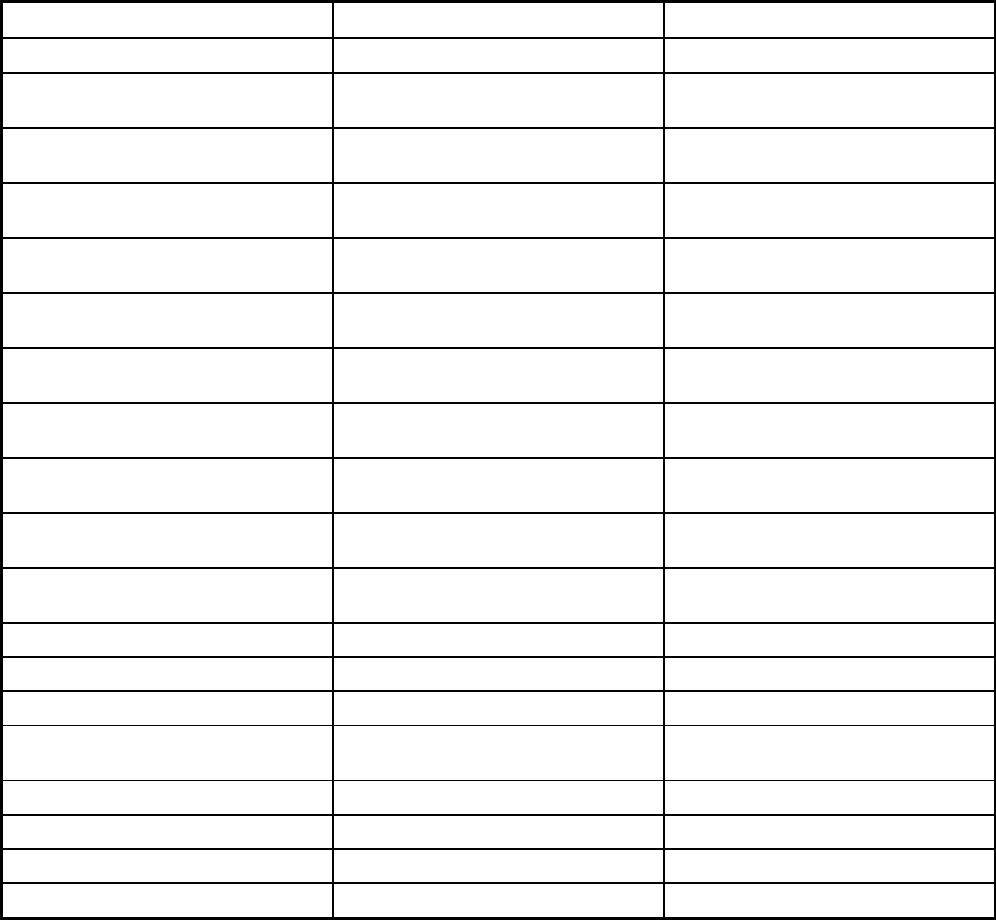
301
Features KanCare PACE
Populations enrolled: Partial Duals Voluntary
Populations enrolled: Children with
Special Health Care Needs
Mandatory
Populations enrolled: Native
American/Alaskan Natives
Voluntary Voluntary
Populations enrolled: Foster Care and
Adoption Assistance Children
Mandatory Exempt
Populations enrolled: Enrollment choice
period
60 days N/A
Populations enrolled: Enrollment broker
name (if applicable)
DXC Technology DXC Technologies
Populations enrolled: Notes on
enrollment choice period
Benefits covered: Inpatient hospital
physical health
X X
Benefits covered: Inpatient hospital
behavioral health (MH and/or SUD)
X X
Benefits covered: Outpatient hospital
physical health
X X
Benefits covered: Outpatient hospital
behavioral health (MH and/or SUD)
X X
Benefits covered: Partial hospitalization X
Benefits covered: Physician X X
Benefits covered: Nurse practitioner X X
Benefits covered: Rural health clinics
and FQHCs
X
Benefits covered: Clinic services X X
Benefits covered: Lab and x-ray X X
Benefits covered: Prescription drugs X X
Benefits covered: Prosthetic devices X X
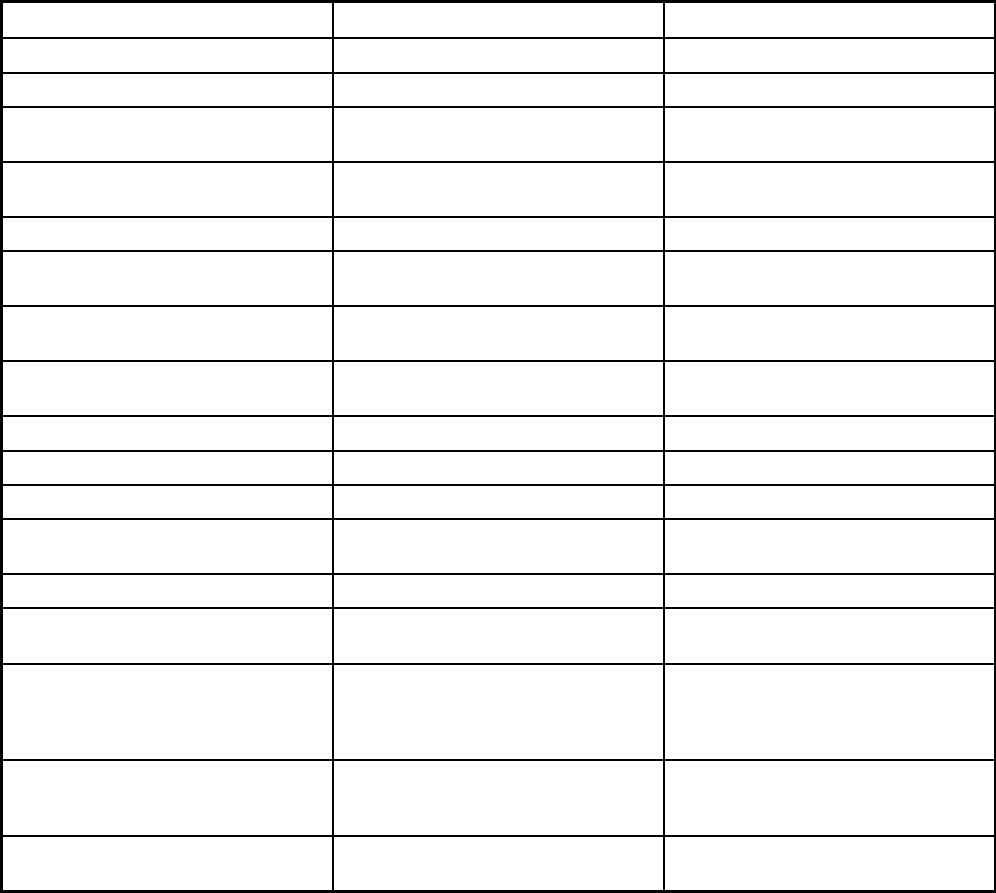
302
Features KanCare PACE
Benefits covered: EPSDT X
Benefits covered: Case management X
Benefits covered: SSA Section 1945-
authorized health home
Benefits covered: Health home care
(services in home)
X X
Benefits covered: Family planning X
Benefits covered: Dental services
(medical/surgical)
X X
Benefits covered: Dental (preventative
or corrective)
X X
Benefits covered: Personal care (state
plan option)
X
Benefits covered: HCBS waiver services X
Benefits covered: Private duty nursing
Benefits covered: ICF-IDD X
Benefits covered: Nursing facility
services
X X
Benefits covered: Hospice care X X
Benefits covered: Non-Emergency
Medical Transportation
X X
Benefits covered: Institution for Mental
Disease inpatient treatment for people
ages 21-64 defined by 42 CFR
§438.6(e) as an 'in lieu of' benefit
Benefits covered: Other (e.g., nurse
midwife services, freestanding birth
centers, podiatry, etc.)
Adult day care, recreational therapy,
meals, social services, social work
counseling, etc.
Quality assurance and improvement:
HEDIS data required?
Yes No
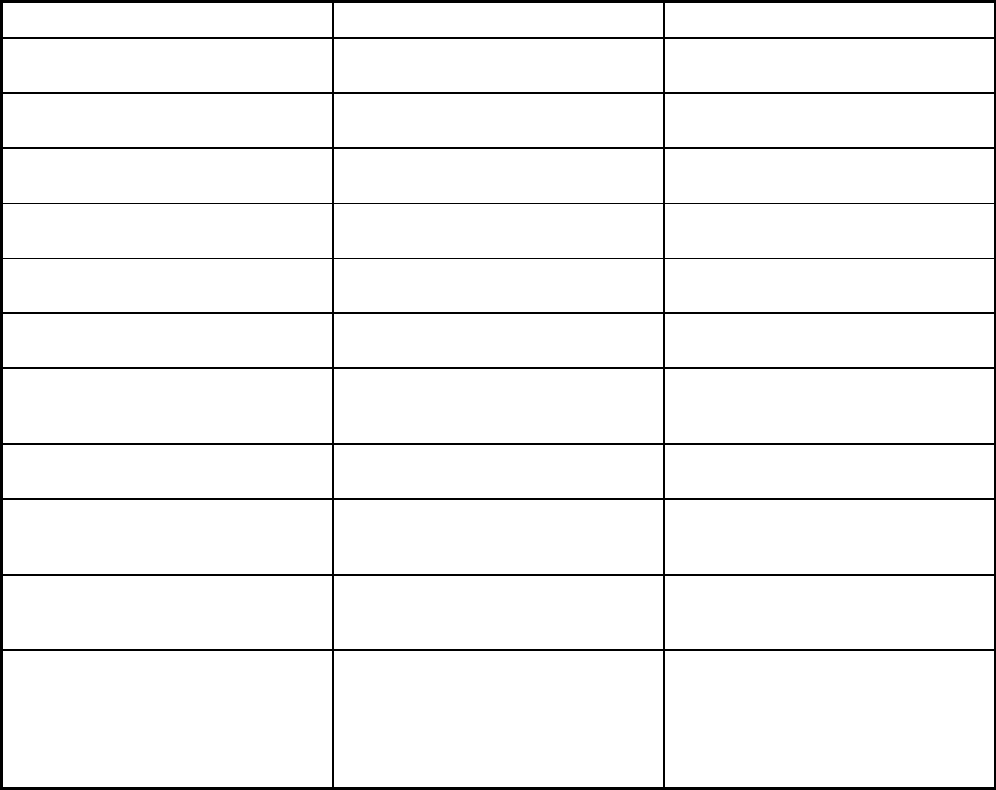
303
Features KanCare PACE
Quality assurance and improvement:
CAHPS data required?
Yes No
Quality assurance and improvement:
Accreditation required?
Yes No
Quality assurance and improvement:
Accrediting organization
NCQA
Quality assurance and improvement:
EQRO contractor name (if applicable)
Kansas Foundation for Medical Care
Performance incentives: Payment
bonuses/differentials to reward plans
Performance incentives: Preferential
auto-enrollment to reward plans
Performance incentives: Public reports
comparing plan performance on key
metrics
X
Performance incentives: Withholds tied
to performance metrics
X
Performance incentives: MCOs/PHPs
required or encouraged to pay providers
for value/quality outcomes
X
Participating plans: Plans in Program Amerigroup Kansas, Inc.; Sunflower
State Health Plan; United HealthCare
Community Plan of Kansas
Via Christi; Midland Care; Bluestem
Pace, Inc.
Notes: Program notes Kansas operates Kancare under the
1115(a) demonstration waiver
concurrently with seven 1915(c)
waivers. Personal Care Benefits are
covered through one or more of the
1915(c) waivers.
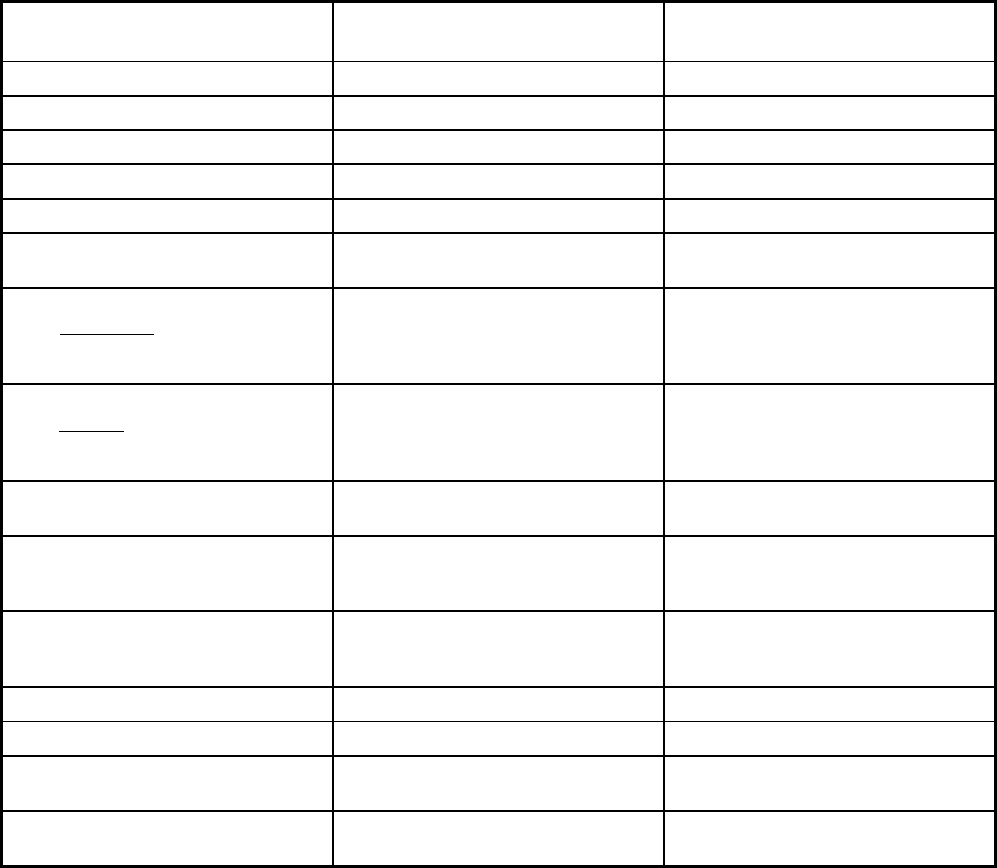
304
Kentucky Managed Care Program Features, as of 2018
Features Kentucky Managed Care
Kentucky Non-Emergency Medical
Transportation
Program type Comprehensive MCO Non-Emergency Medical Transportation
Statewide or region-specific? Statewide Statewide
Federal operating authority 1915(b) 1915(b)
Program start date 11/01/2011 12/01/1998
Waiver expiration date (if applicable) 09/30/2019 09/30/2019
If the program ended in 2018, indicate
the end date
Populations enrolled: Low-income
adults not covered under ACA Section
VIII (excludes pregnant women and
people with disabilities)
Mandatory Mandatory
Populations enrolled: Low-income
adults covered under ACA Section VIII
(excludes pregnant women and people
with disabilities)
Mandatory Mandatory
Populations enrolled: Aged, Blind or
Disabled Children or Adults
Mandatory Mandatory
Populations enrolled: Non-Disabled
Children (excludes children in foster
care or receiving adoption assistance)
Mandatory Mandatory
Populations enrolled: Individuals
receiving Limited Benefits (excludes
partial duals)
Mandatory Mandatory
Populations enrolled: Full Duals Mandatory
Populations enrolled: Partial Duals
Populations enrolled: Children with
Special Health Care Needs
Mandatory Mandatory
Populations enrolled: Native
American/Alaskan Natives
Voluntary Voluntary
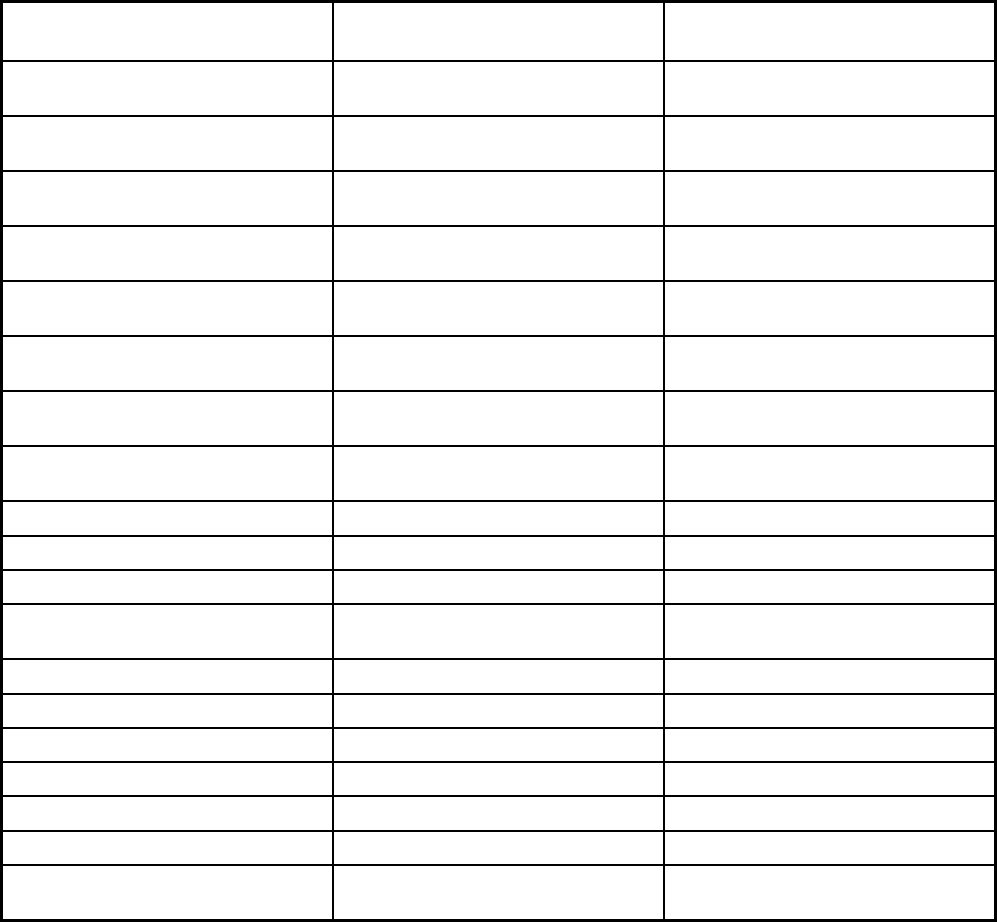
305
Features Kentucky Managed Care
Kentucky Non-Emergency Medical
Transportation
Populations enrolled: Foster Care and
Adoption Assistance Children
Mandatory Mandatory
Populations enrolled: Enrollment choice
period
Populations enrolled: Enrollment broker
name (if applicable)
Populations enrolled: Notes on
enrollment choice period
Benefits covered: Inpatient hospital
physical health
X
Benefits covered: Inpatient hospital
behavioral health (MH and/or SUD)
X
Benefits covered: Outpatient hospital
physical health
X
Benefits covered: Outpatient hospital
behavioral health (MH and/or SUD)
X
Benefits covered: Partial hospitalization X
Benefits covered: Physician X
Benefits covered: Nurse practitioner X
Benefits covered: Rural health clinics
and FQHCs
X
Benefits covered: Clinic services X
Benefits covered: Lab and x-ray X
Benefits covered: Prescription drugs X
Benefits covered: Prosthetic devices X
Benefits covered: EPSDT X
Benefits covered: Case management
Benefits covered: SSA Section 1945-
authorized health home
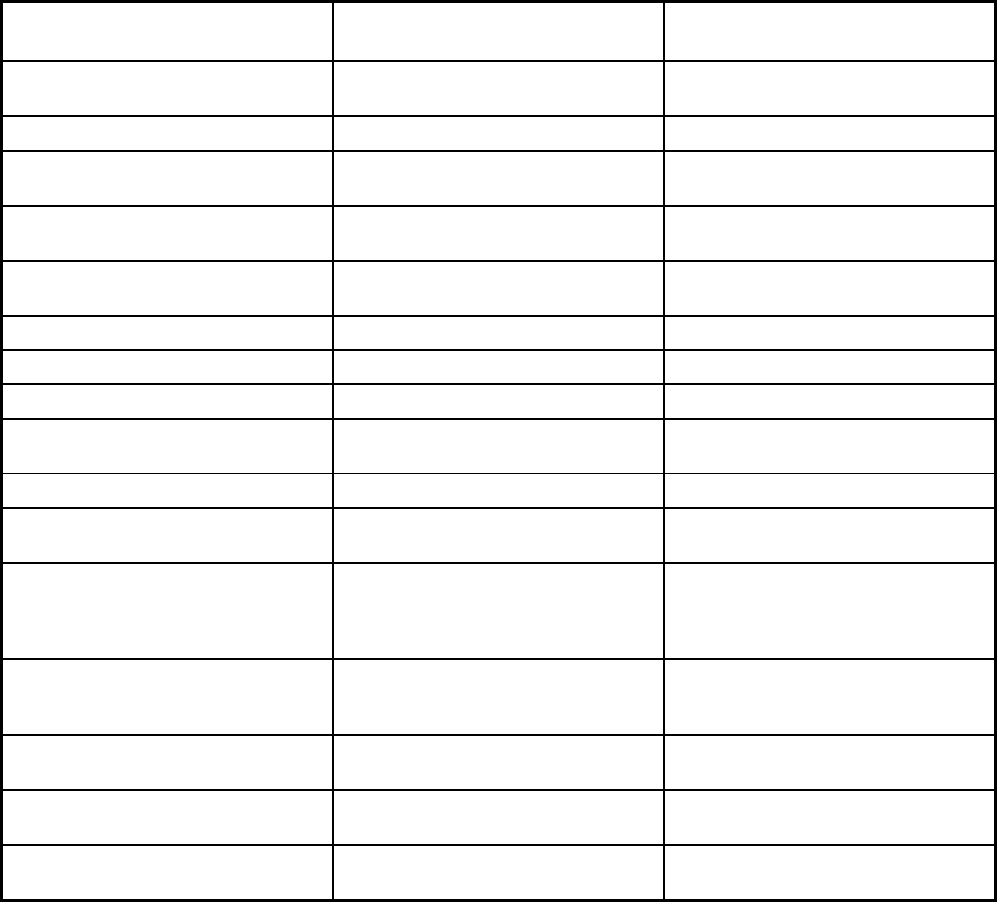
306
Features Kentucky Managed Care
Kentucky Non-Emergency Medical
Transportation
Benefits covered: Health home care
(services in home)
X
Benefits covered: Family planning X
Benefits covered: Dental services
(medical/surgical)
X
Benefits covered: Dental (preventative
or corrective)
X
Benefits covered: Personal care (state
plan option)
Benefits covered: HCBS waiver services
Benefits covered: Private duty nursing X
Benefits covered: ICF-IDD
Benefits covered: Nursing facility
services
Benefits covered: Hospice care X
Benefits covered: Non-Emergency
Medical Transportation
X
Benefits covered: Institution for Mental
Disease inpatient treatment for people
ages 21-64 defined by 42 CFR
§438.6(e) as an 'in lieu of' benefit
Benefits covered: Other (e.g., nurse
midwife services, freestanding birth
centers, podiatry, etc.)
Quality assurance and improvement:
HEDIS data required?
Yes No
Quality assurance and improvement:
CAHPS data required?
Yes No
Quality assurance and improvement:
Accreditation required?
Yes No
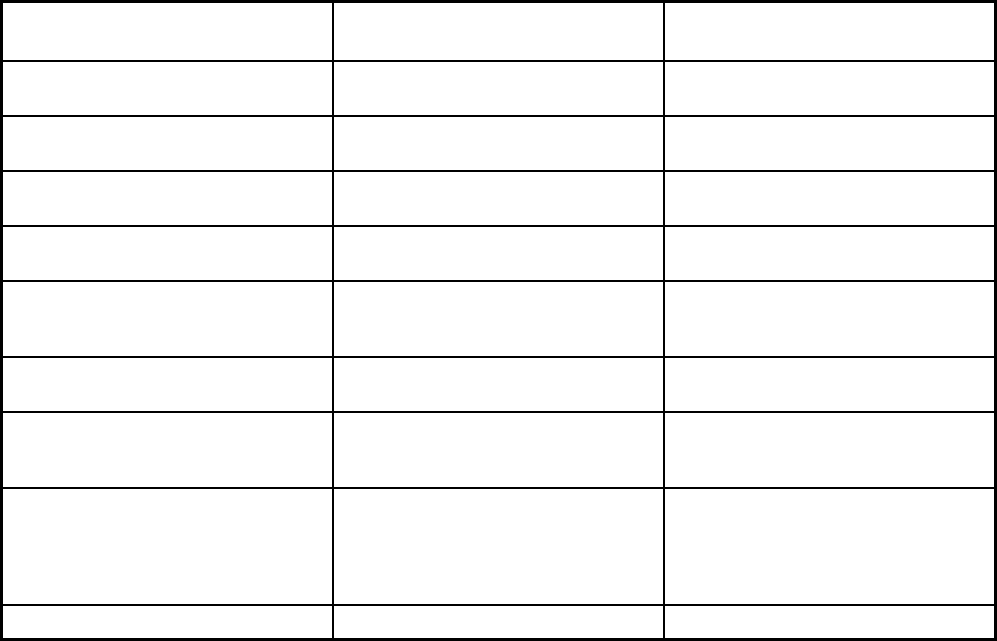
307
Features Kentucky Managed Care
Kentucky Non-Emergency Medical
Transportation
Quality assurance and improvement:
Accrediting organization
NCQA
Quality assurance and improvement:
EQRO contractor name (if applicable)
Island Peer Review Organization
Performance incentives: Payment
bonuses/differentials to reward plans
X
Performance incentives: Preferential
auto-enrollment to reward plans
Performance incentives: Public reports
comparing plan performance on key
metrics
X
Performance incentives: Withholds tied
to performance metrics
Performance incentives: MCOs/PHPs
required or encouraged to pay providers
for value/quality outcomes
X
Participating plans: Plans in Program Aetna Better Health of Kentucky;
Anthem Blue Cross Blue Shield
Medicaid; Humana-Caresource;
Passport Health Plan; WellCare of
Kentucky
NEMT - Human Services Transportation
Delivery
Notes: Program notes
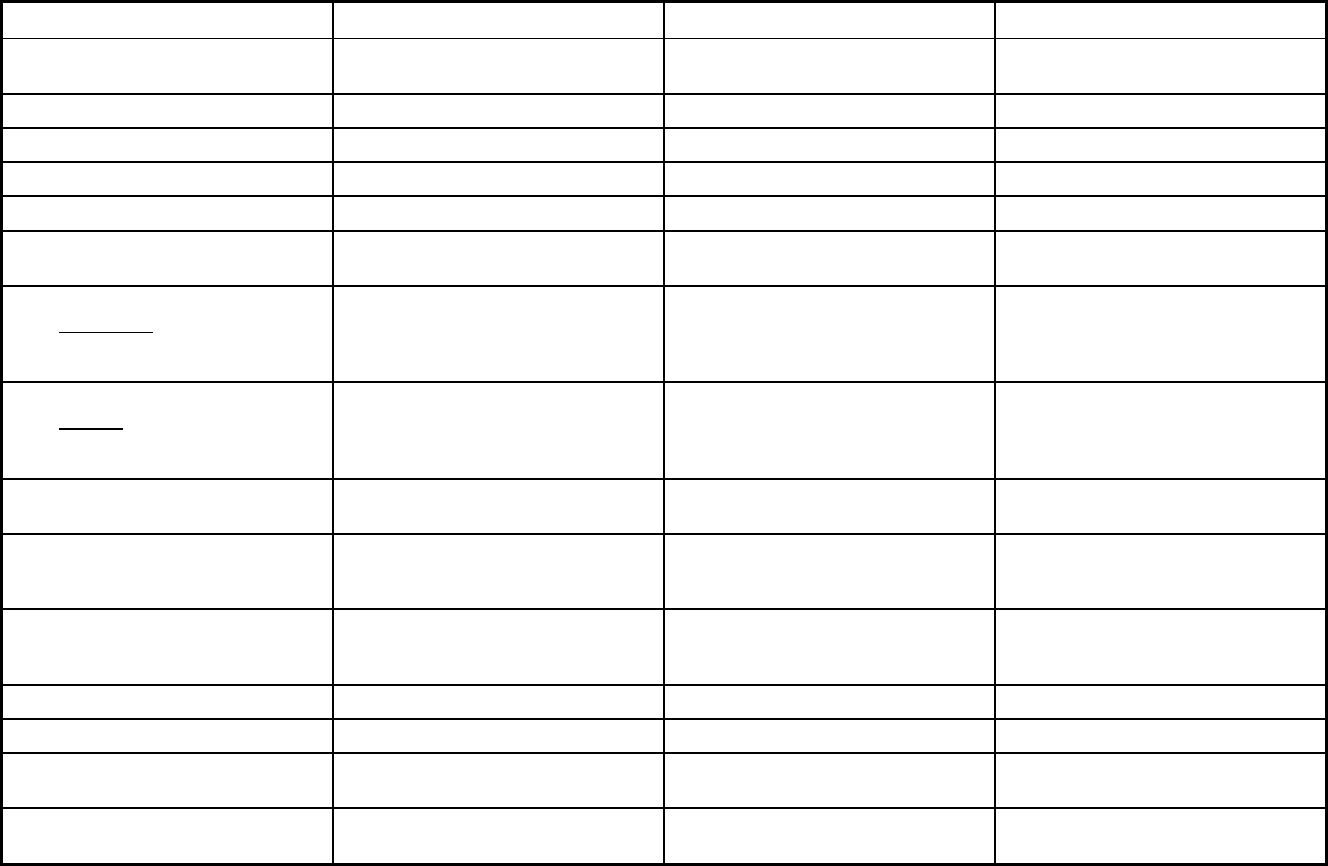
308
Louisiana Managed Care Program Features, as of 2018 (1 of 2)
Features Healthy Louisiana Healthy Louisiana BHO Coordinated System of Care
Program type Comprehensive MCO Behavioral Health Organization (BHO)
only (PIHP and/or PAHP)
Behavioral Health Organization (BHO)
only (PIHP and/or PAHP)
Statewide or region-specific? Statewide Statewide Statewide
Federal operating authority 1932(a) 1915(b) 1915(b)/1915(c)
Program start date 02/01/2012 12/01/2015 03/01/2012
Waiver expiration date (if applicable) 10/31/2022 06/30/2022
If the program ended in 2018, indicate
the end date
Populations enrolled: Low-income
adults not covered under ACA Section
VIII (excludes pregnant women and
people with disabilities)
Mandatory
Populations enrolled: Low-income
adults covered under ACA Section VIII
(excludes pregnant women and people
with disabilities)
Mandatory
Populations enrolled: Aged, Blind or
Disabled Children or Adults
Varies Mandatory
Populations enrolled: Non-Disabled
Children (excludes children in foster
care or receiving adoption assistance)
Mandatory
Populations enrolled: Individuals
receiving Limited Benefits (excludes
partial duals)
Populations enrolled: Full Duals Mandatory
Populations enrolled: Partial Duals
Populations enrolled: Children with
Special Health Care Needs
Mandatory Voluntary
Populations enrolled: Native
American/Alaskan Natives
Voluntary Exempt Exempt
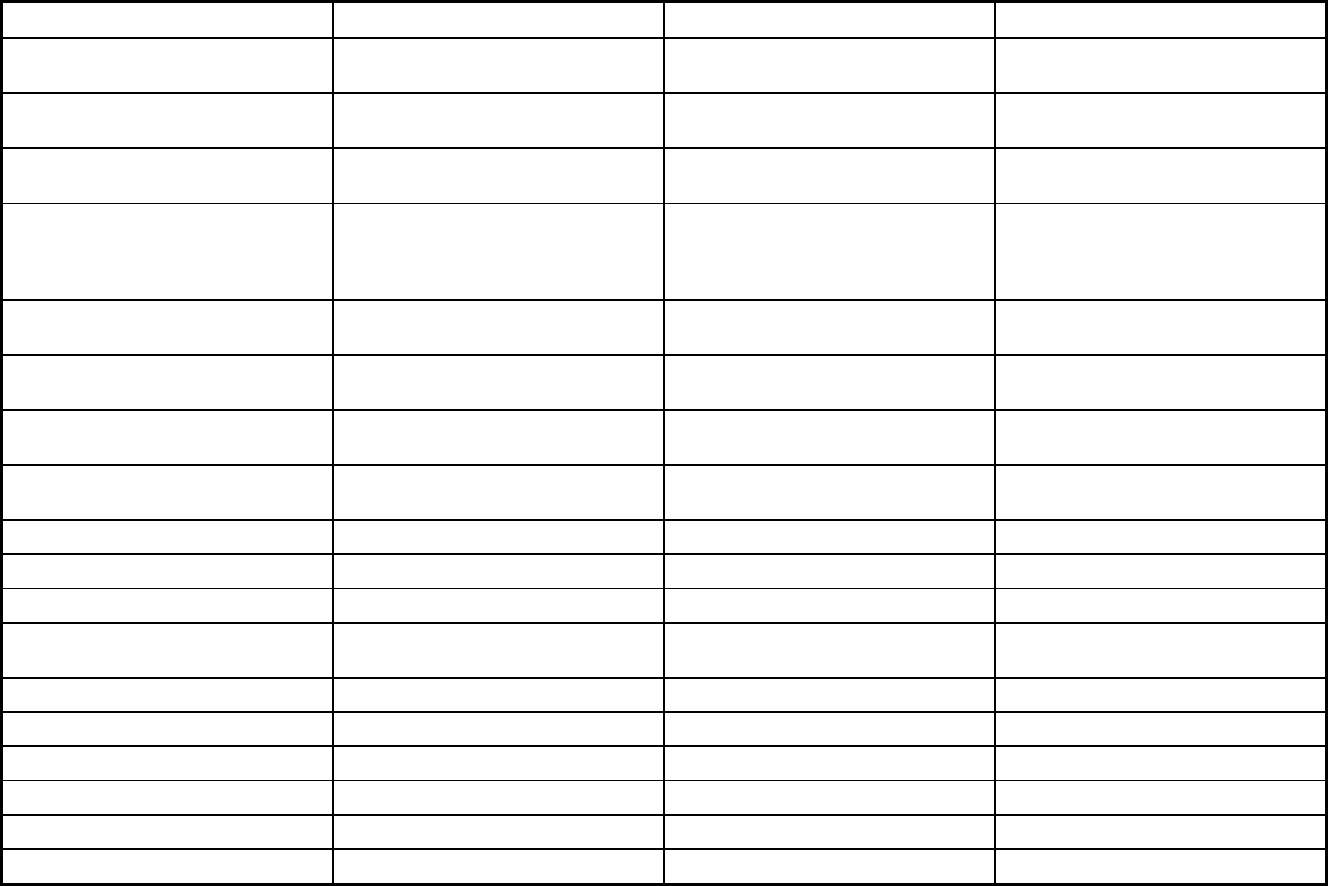
309
Features Healthy Louisiana Healthy Louisiana BHO Coordinated System of Care
Populations enrolled: Foster Care and
Adoption Assistance Children
Mandatory Mandatory
Populations enrolled: Enrollment choice
period
Other Pre-assigned
Populations enrolled: Enrollment broker
name (if applicable)
Maximus Health Services Maximus Health Services
Populations enrolled: Notes on
enrollment choice period
The enrollee has the opportunity to
choose an MCO at the time of
application. If they do not choose an
MCO, the enrollee is pre-assigned.
Benefits covered: Inpatient hospital
physical health
X
Benefits covered: Inpatient hospital
behavioral health (MH and/or SUD)
X X X
Benefits covered: Outpatient hospital
physical health
X
Benefits covered: Outpatient hospital
behavioral health (MH and/or SUD)
X X X
Benefits covered: Partial hospitalization
Benefits covered: Physician X X X
Benefits covered: Nurse practitioner X X X
Benefits covered: Rural health clinics
and FQHCs
X X X
Benefits covered: Clinic services X X X
Benefits covered: Lab and x-ray X
Benefits covered: Prescription drugs X
Benefits covered: Prosthetic devices X
Benefits covered: EPSDT X X X
Benefits covered: Case management X X X
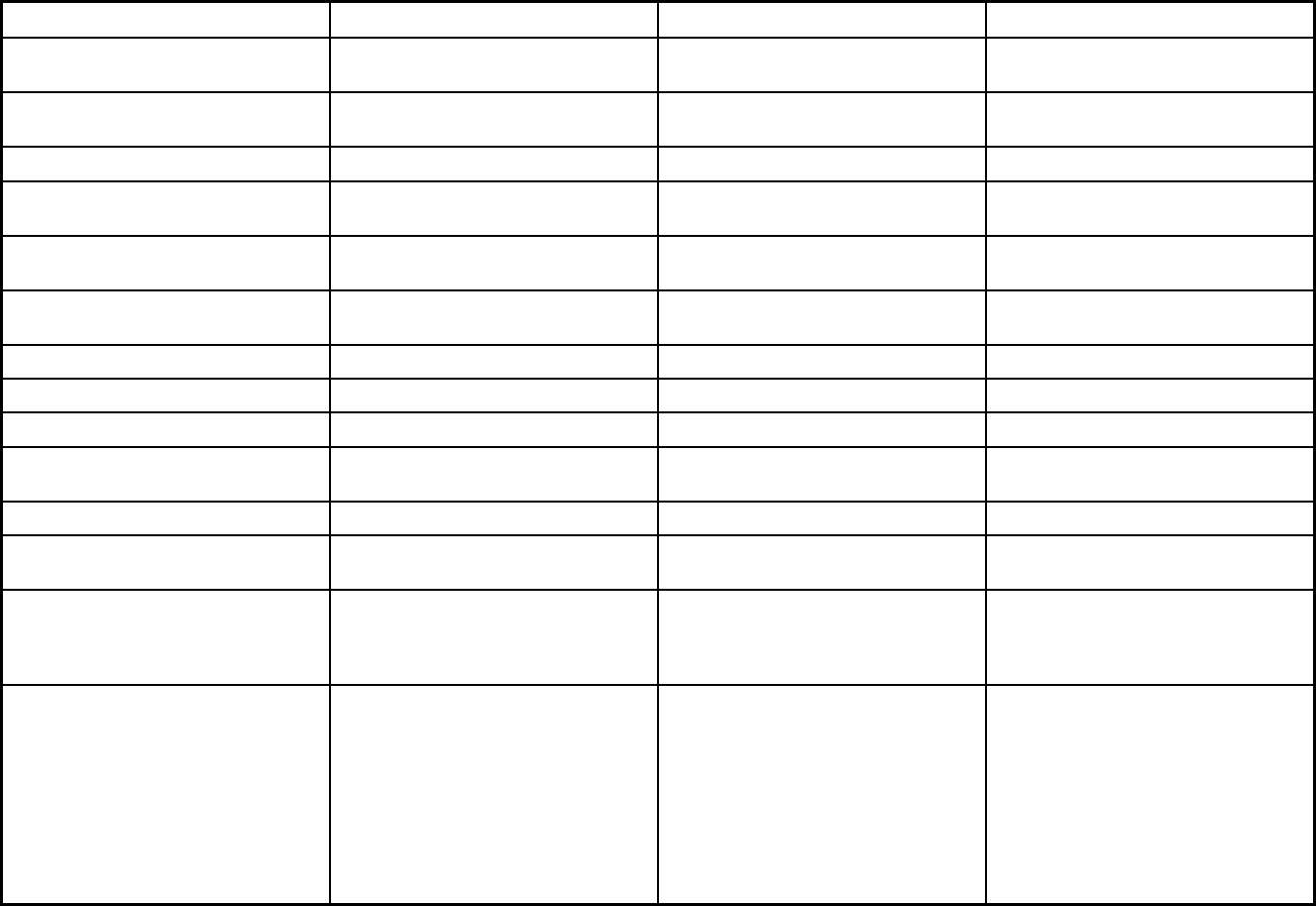
310
Features Healthy Louisiana Healthy Louisiana BHO Coordinated System of Care
Benefits covered: SSA Section 1945-
authorized health home
Benefits covered: Health home care
(services in home)
X
Benefits covered: Family planning X
Benefits covered: Dental services
(medical/surgical)
X
Benefits covered: Dental (preventative
or corrective)
Benefits covered: Personal care (state
plan option)
X
Benefits covered: HCBS waiver services X X
Benefits covered: Private duty nursing
Benefits covered: ICF-IDD
Benefits covered: Nursing facility
services
Benefits covered: Hospice care X
Benefits covered: Non-Emergency
Medical Transportation
X X
Benefits covered: Institution for Mental
Disease inpatient treatment for people
ages 21-64 defined by 42 CFR
§438.6(e) as an 'in lieu of' benefit
X X
Benefits covered: Other (e.g., nurse
midwife services, freestanding birth
centers, podiatry, etc.)
Similar to Private Duty Nursing,
Louisiana offers Extended Home
Nursing to recipients under 21 only.
Certified Nurse Midwives are covered
and practice within the scope of their
license. Podiatry services are covered,
but limited to a list of payable
procedures. Personal care (state plan
option) services are available to
enrollees aged 0 - 20.
Youth Support and Training (YST);
Parent Support and Training (PST);
short-term respite; Independent
Living/Skills Building (ILSB) services;
mental health rehabilitation services
including: psychosocial rehabilitation,
crisis intervention, crisis stabilization.
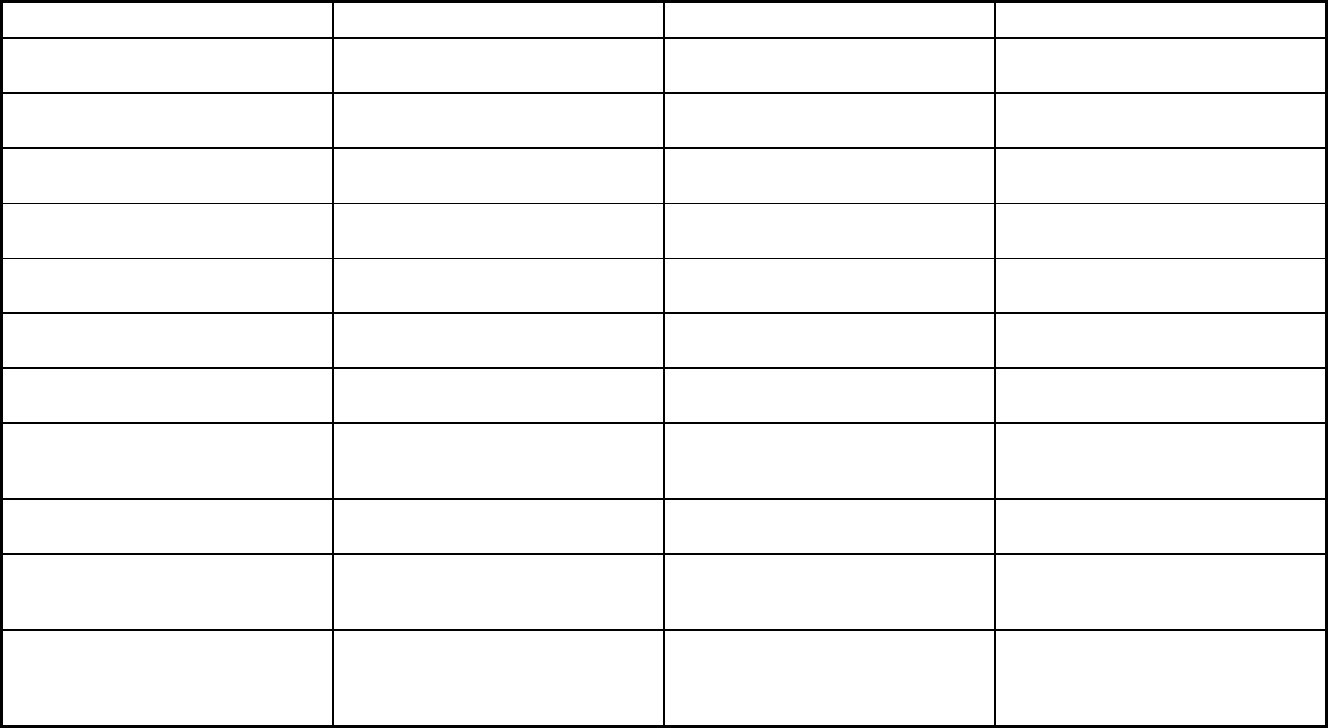
311
Features Healthy Louisiana Healthy Louisiana BHO Coordinated System of Care
Quality assurance and improvement:
HEDIS data required?
Yes Yes No
Quality assurance and improvement:
CAHPS data required?
Yes Yes No
Quality assurance and improvement:
Accreditation required?
Yes Yes Yes
Quality assurance and improvement:
Accrediting organization
NCQA, URAC NCQA NCQA
Quality assurance and improvement:
EQRO contractor name (if applicable)
IPRO IPRO
Performance incentives: Payment
bonuses/differentials to reward plans
Performance incentives: Preferential
auto-enrollment to reward plans
Performance incentives: Public reports
comparing plan performance on key
metrics
X X
Performance incentives: Withholds tied
to performance metrics
X X
Performance incentives: MCOs/PHPs
required or encouraged to pay providers
for value/quality outcomes
X X
Participating plans: Plans in Program Aetna Better Health; AmeriHealth
Caritas of Louisiana; Healthy Blue;
Louisiana Healthcare Connections;
UnitedHealthcare Community Plan
Aetna Better Health; AmeriHealth
Caritas of Louisiana; Healthy Blue;
Louisiana Healthcare Connections;
UnitedHealthcare Community Plan
Magellan
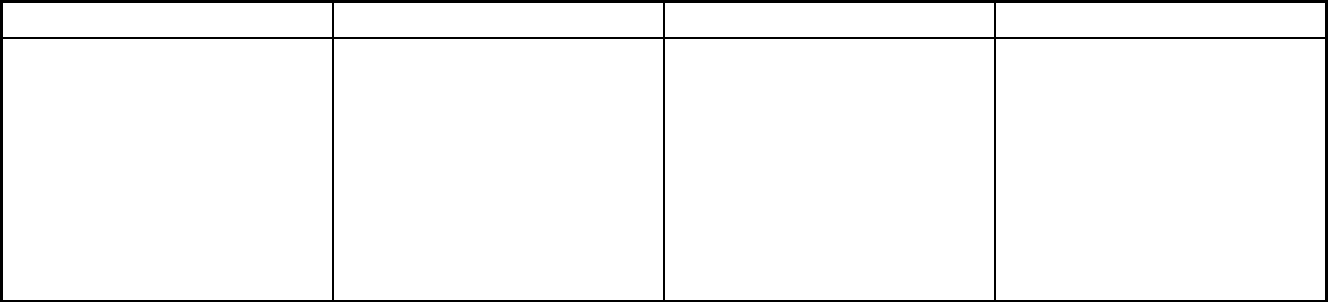
312
Features Healthy Louisiana Healthy Louisiana BHO Coordinated System of Care
Notes: Program notes Some of the disabled children
population can voluntarily opt out of
enrolling.
This is a limited benefit MCO program,
which is reported as a BHO since only
behavioral health services and NEMT
are covered. These enrollees are
individuals who receive fee-for-service
Medicaid for most of their health
services, including physical health
services and prescription benefits. The
limited benefit MCO program covers
behavioral health services for residents
in long term care facilities as well as
those outside of long term care facilities.
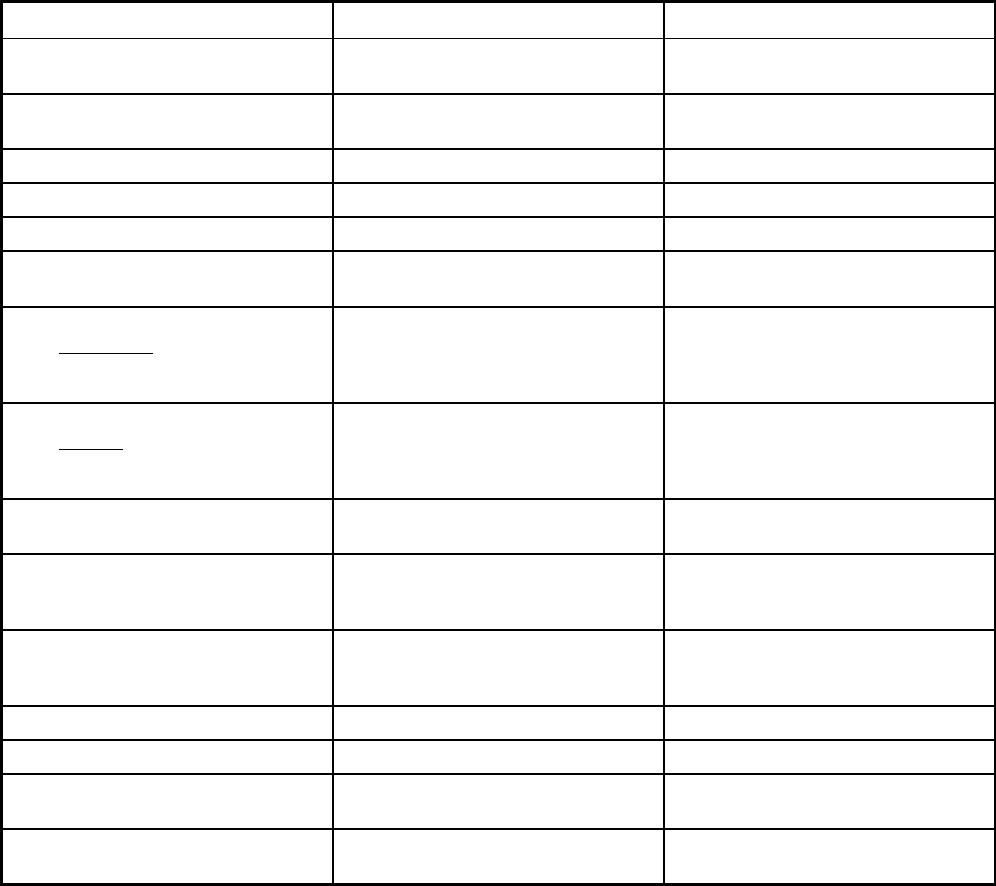
313
Louisiana Managed Care Program Features, as of 2018 (2 of 2)
Features Dental Benefit Management Program PACE
Program type Dental only (PAHP) Program of All-inclusive Care for the
Elderly (PACE)
Statewide or region-specific? Statewide Baton Rouge, Greater New Orleans,
Lafayette
Federal operating authority 1915(b) PACE
Program start date 07/01/2014 09/01/2007
Waiver expiration date (if applicable) 06/30/2021
If the program ended in 2018, indicate
the end date
Populations enrolled: Low-income
adults not covered under ACA Section
VIII (excludes pregnant women and
people with disabilities)
Mandatory
Populations enrolled: Low-income
adults covered under ACA Section VIII
(excludes pregnant women and people
with disabilities)
Mandatory
Populations enrolled: Aged, Blind or
Disabled Children or Adults
Mandatory
Populations enrolled: Non-Disabled
Children (excludes children in foster
care or receiving adoption assistance)
Mandatory
Populations enrolled: Individuals
receiving Limited Benefits (excludes
partial duals)
Mandatory
Populations enrolled: Full Duals Mandatory Voluntary
Populations enrolled: Partial Duals Voluntary
Populations enrolled: Children with
Special Health Care Needs
Mandatory
Populations enrolled: Native
American/Alaskan Natives
Mandatory Voluntary
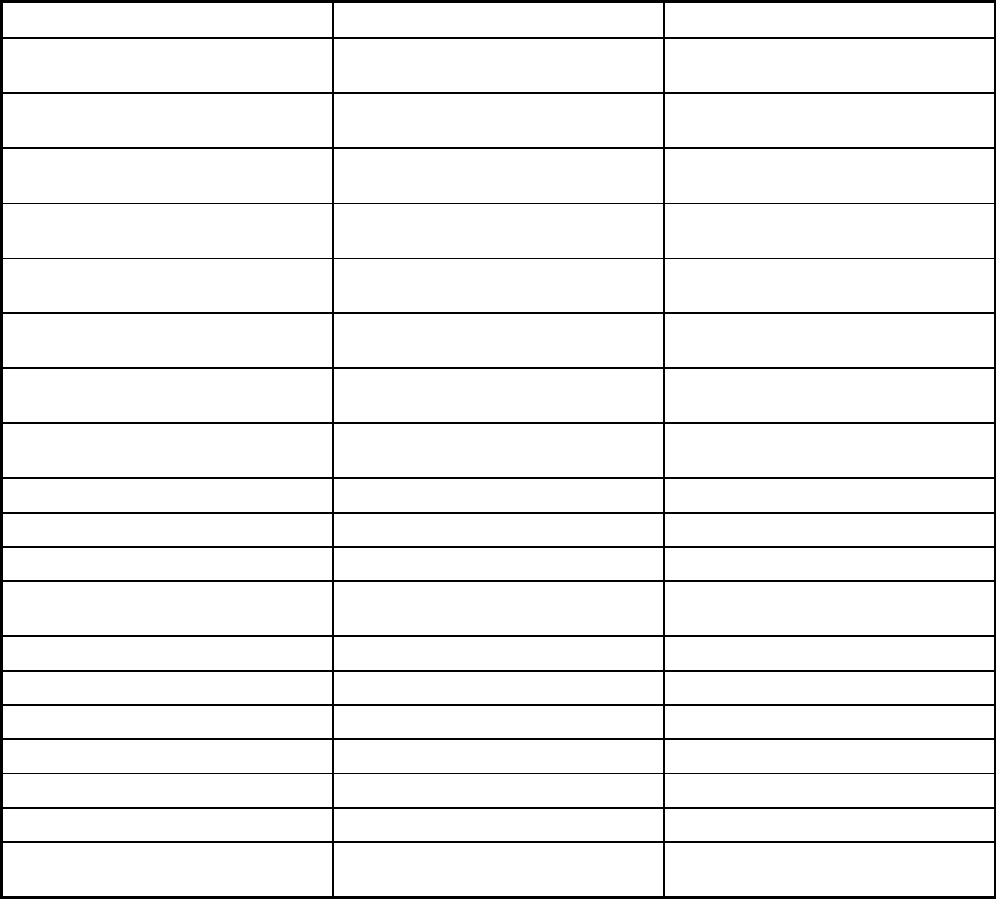
314
Features Dental Benefit Management Program PACE
Populations enrolled: Foster Care and
Adoption Assistance Children
Mandatory
Populations enrolled: Enrollment choice
period
N/A
Populations enrolled: Enrollment broker
name (if applicable)
Populations enrolled: Notes on
enrollment choice period
Benefits covered: Inpatient hospital
physical health
X
Benefits covered: Inpatient hospital
behavioral health (MH and/or SUD)
X
Benefits covered: Outpatient hospital
physical health
X
Benefits covered: Outpatient hospital
behavioral health (MH and/or SUD)
X
Benefits covered: Partial hospitalization
Benefits covered: Physician X
Benefits covered: Nurse practitioner X
Benefits covered: Rural health clinics
and FQHCs
X X
Benefits covered: Clinic services X X
Benefits covered: Lab and x-ray X X
Benefits covered: Prescription drugs X
Benefits covered: Prosthetic devices X
Benefits covered: EPSDT X
Benefits covered: Case management X
Benefits covered: SSA Section 1945-
authorized health home
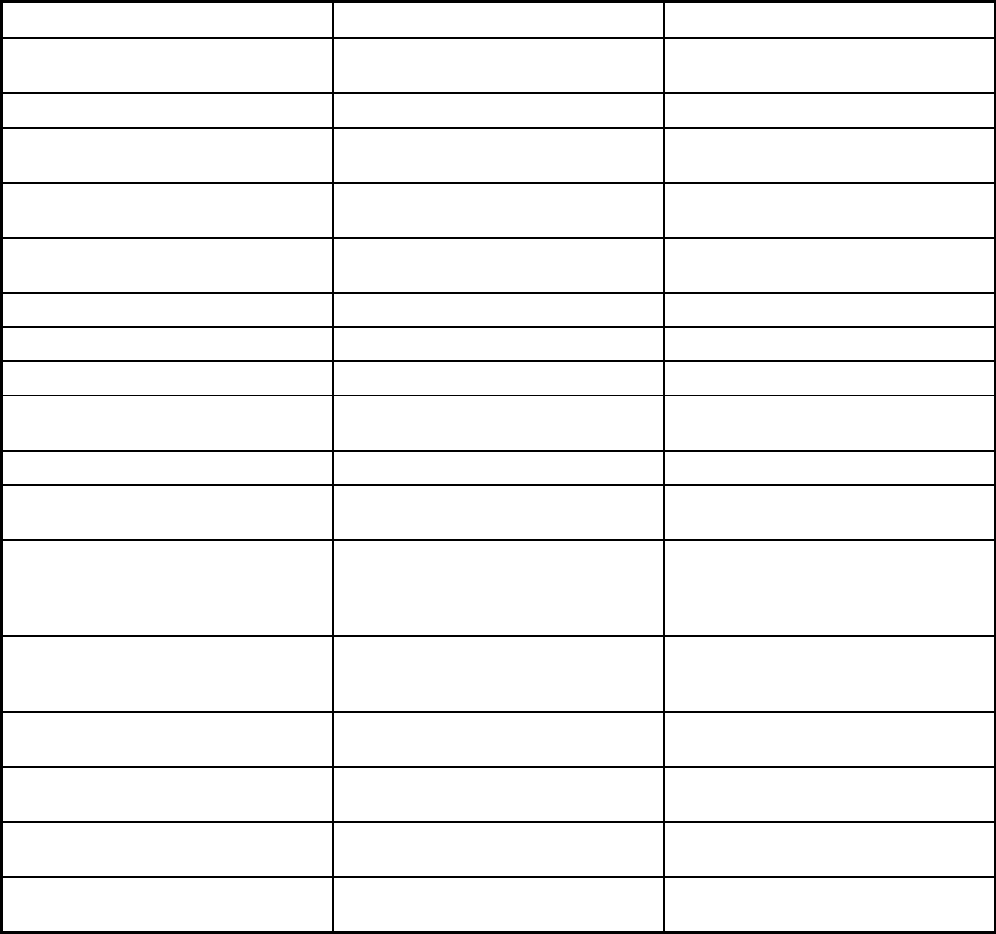
315
Features Dental Benefit Management Program PACE
Benefits covered: Health home care
(services in home)
X
Benefits covered: Family planning
Benefits covered: Dental services
(medical/surgical)
X X
Benefits covered: Dental (preventative
or corrective)
X X
Benefits covered: Personal care (state
plan option)
X
Benefits covered: HCBS waiver services X
Benefits covered: Private duty nursing X
Benefits covered: ICF-IDD
Benefits covered: Nursing facility
services
X
Benefits covered: Hospice care X
Benefits covered: Non-Emergency
Medical Transportation
X
Benefits covered: Institution for Mental
Disease inpatient treatment for people
ages 21-64 defined by 42 CFR
§438.6(e) as an 'in lieu of' benefit
Benefits covered: Other (e.g., nurse
midwife services, freestanding birth
centers, podiatry, etc.)
All specialized services authorized by
IDT, including podiatry.
Quality assurance and improvement:
HEDIS data required?
Yes No
Quality assurance and improvement:
CAHPS data required?
Yes No
Quality assurance and improvement:
Accreditation required?
No No
Quality assurance and improvement:
Accrediting organization
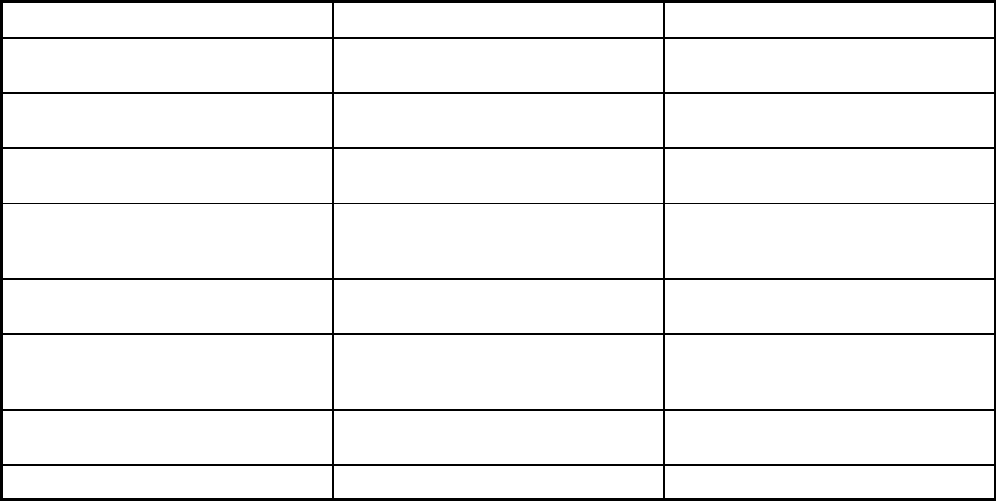
316
Features Dental Benefit Management Program PACE
Quality assurance and improvement:
EQRO contractor name (if applicable)
Myers & Stauffer LC
Performance incentives: Payment
bonuses/differentials to reward plans
Performance incentives: Preferential
auto-enrollment to reward plans
Performance incentives: Public reports
comparing plan performance on key
metrics
Performance incentives: Withholds tied
to performance metrics
Performance incentives: MCOs/PHPs
required or encouraged to pay providers
for value/quality outcomes
Participating plans: Plans in Program MCNA of Louisiana Baton Rouge; Greater New Orleans;
Lafayette
Notes: Program notes
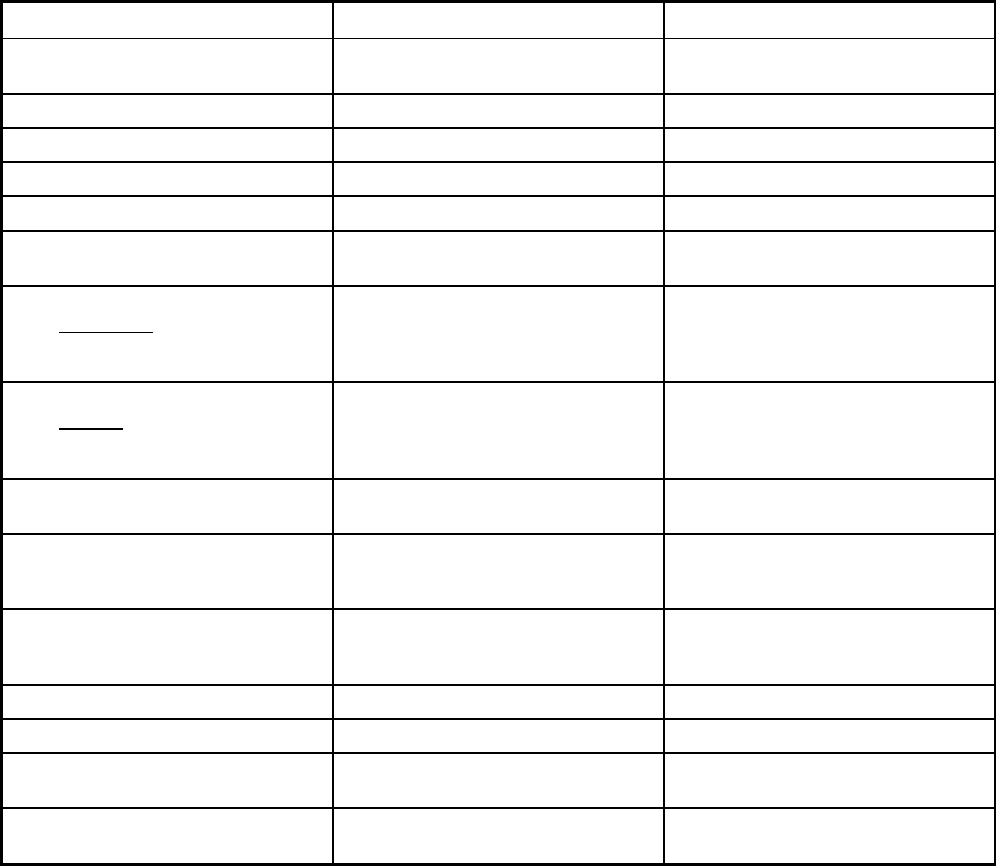
317
Maine Managed Care Program Features, as of 2018
Features MaineCare NET
Program type Primary Care Case Management
(PCCM)
Non-Emergency Medical Transportation
Statewide or region-specific? Statewide Statewide
Federal operating authority 1932(a) 1915(b)
Program start date 05/01/1999 08/01/2011
Waiver expiration date (if applicable) 03/31/2022
If the program ended in 2018, indicate
the end date
Populations enrolled: Low-income
adults not covered under ACA Section
VIII (excludes pregnant women and
people with disabilities)
Populations enrolled: Low-income
adults covered under ACA Section VIII
(excludes pregnant women and people
with disabilities)
Populations enrolled: Aged, Blind or
Disabled Children or Adults
Mandatory Mandatory
Populations enrolled: Non-Disabled
Children (excludes children in foster
care or receiving adoption assistance)
Mandatory Mandatory
Populations enrolled: Individuals
receiving Limited Benefits (excludes
partial duals)
Populations enrolled: Full Duals Mandatory
Populations enrolled: Partial Duals
Populations enrolled: Children with
Special Health Care Needs
Mandatory
Populations enrolled: Native
American/Alaskan Natives
Voluntary Mandatory
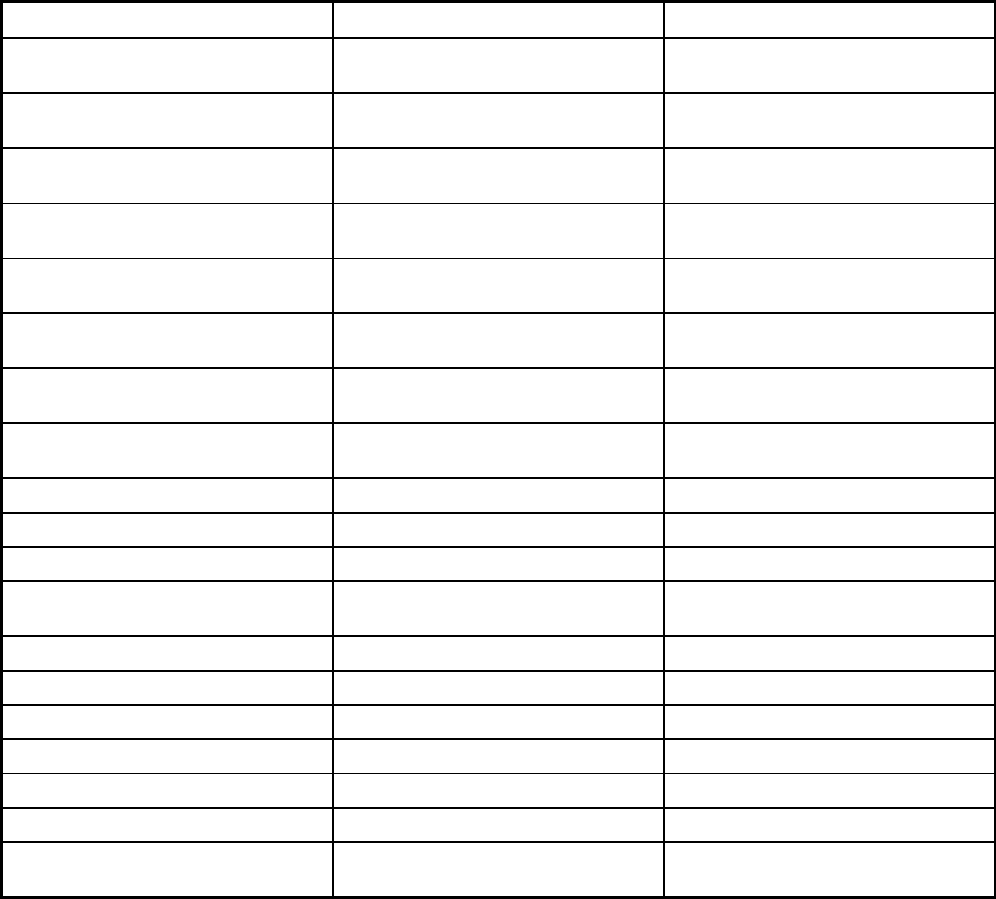
318
Features MaineCare NET
Populations enrolled: Foster Care and
Adoption Assistance Children
Voluntary Mandatory
Populations enrolled: Enrollment choice
period
N/A Pre-assigned
Populations enrolled: Enrollment broker
name (if applicable)
Populations enrolled: Notes on
enrollment choice period
28 days
Benefits covered: Inpatient hospital
physical health
Benefits covered: Inpatient hospital
behavioral health (MH and/or SUD)
Benefits covered: Outpatient hospital
physical health
Benefits covered: Outpatient hospital
behavioral health (MH and/or SUD)
Benefits covered: Partial hospitalization
Benefits covered: Physician X
Benefits covered: Nurse practitioner
Benefits covered: Rural health clinics
and FQHCs
X
Benefits covered: Clinic services
Benefits covered: Lab and x-ray
Benefits covered: Prescription drugs
Benefits covered: Prosthetic devices
Benefits covered: EPSDT
Benefits covered: Case management X
Benefits covered: SSA Section 1945-
authorized health home
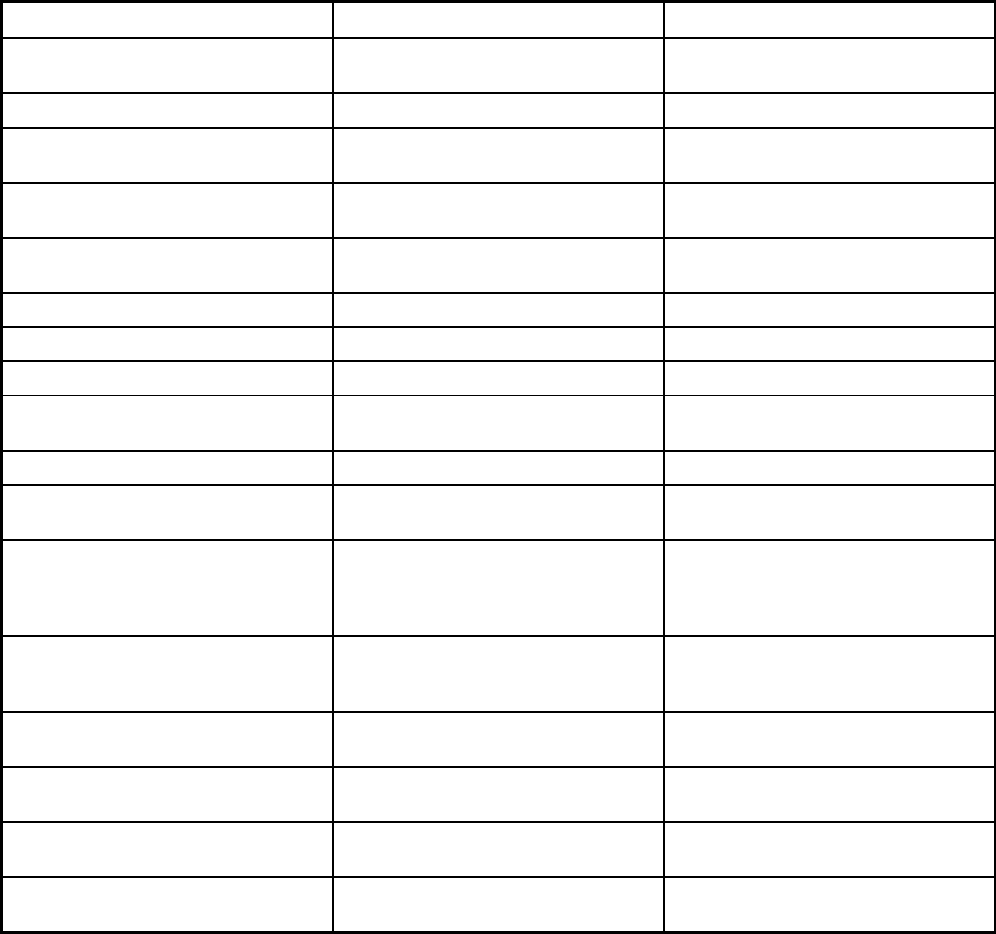
319
Features MaineCare NET
Benefits covered: Health home care
(services in home)
Benefits covered: Family planning
Benefits covered: Dental services
(medical/surgical)
Benefits covered: Dental (preventative
or corrective)
Benefits covered: Personal care (state
plan option)
Benefits covered: HCBS waiver services
Benefits covered: Private duty nursing
Benefits covered: ICF-IDD
Benefits covered: Nursing facility
services
Benefits covered: Hospice care
Benefits covered: Non-Emergency
Medical Transportation
X
Benefits covered: Institution for Mental
Disease inpatient treatment for people
ages 21-64 defined by 42 CFR
§438.6(e) as an 'in lieu of' benefit
Benefits covered: Other (e.g., nurse
midwife services, freestanding birth
centers, podiatry, etc.)
Quality assurance and improvement:
HEDIS data required?
Yes No
Quality assurance and improvement:
CAHPS data required?
Yes No
Quality assurance and improvement:
Accreditation required?
No No
Quality assurance and improvement:
Accrediting organization
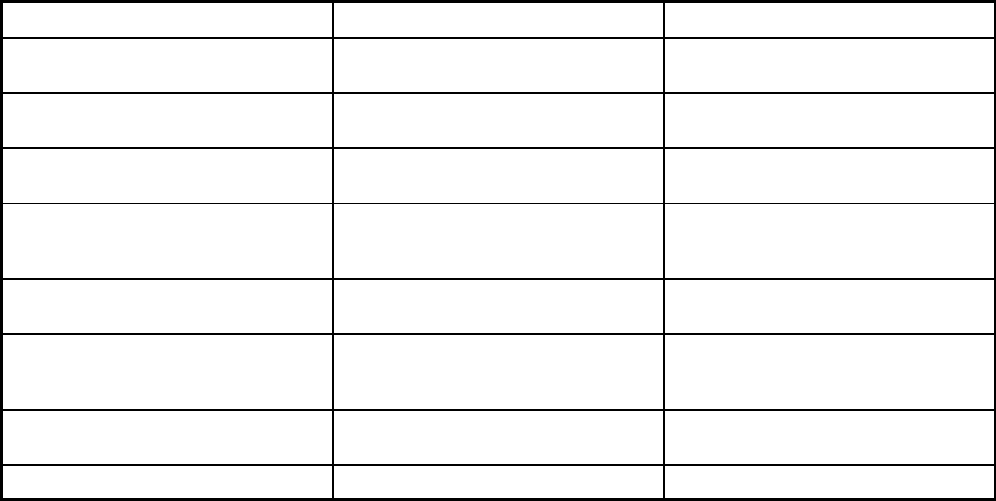
320
Features MaineCare NET
Quality assurance and improvement:
EQRO contractor name (if applicable)
Performance incentives: Payment
bonuses/differentials to reward plans
X
Performance incentives: Preferential
auto-enrollment to reward plans
Performance incentives: Public reports
comparing plan performance on key
metrics
X
Performance incentives: Withholds tied
to performance metrics
Performance incentives: MCOs/PHPs
required or encouraged to pay providers
for value/quality outcomes
Participating plans: Plans in Program Multiple Primary Care Providers Logisticare; MidCoast Connector;
Penquis CAP
Notes: Program notes
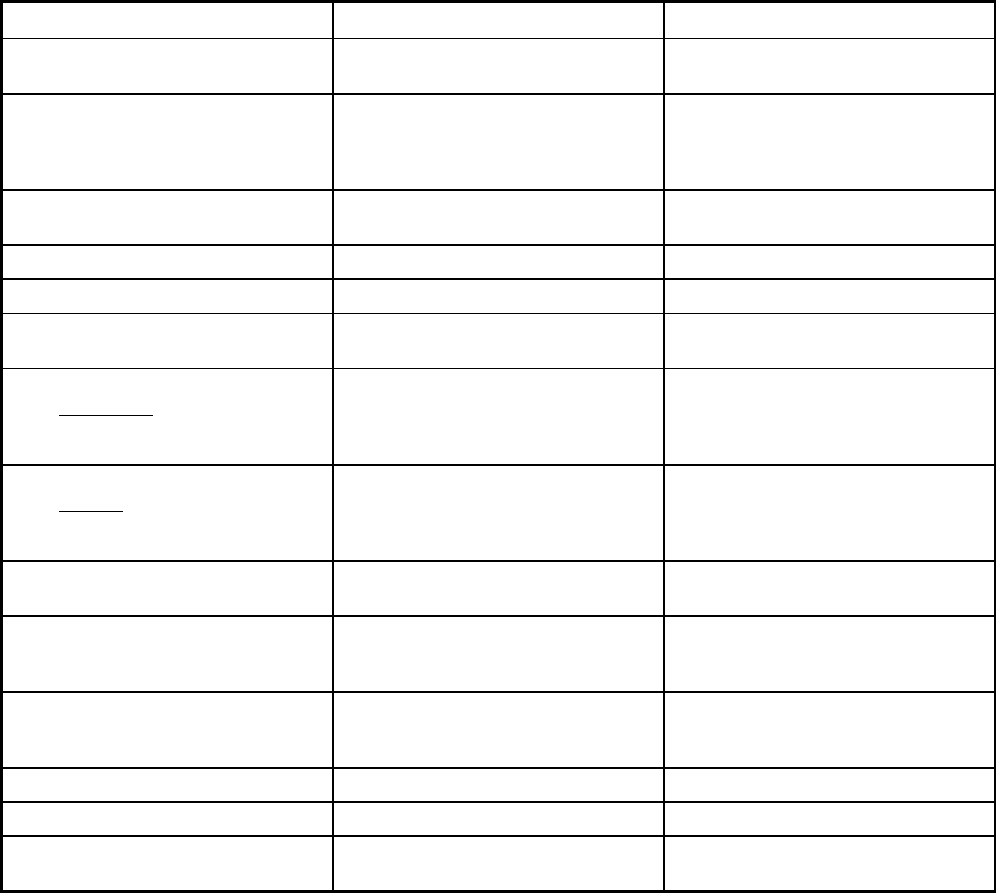
321
Maryland Managed Care Program Features, as of 2018
Features HealthChoice Hopkins Elder Plus
Program type Comprehensive MCO Program of All-inclusive Care for the
Elderly (PACE)
Statewide or region-specific? Statewide 21052, 21202, 21205, 21206, 21213,
21214, 21217, 21218, 21219, 21220,
21221, 21222, 21224, 21227, 21231,
21237
Federal operating authority 1115(a) (Medicaid demonstration
waivers)
PACE
Program start date 06/02/1997 11/01/2002
Waiver expiration date (if applicable) 12/31/2021
If the program ended in 2018, indicate
the end date
Populations enrolled: Low-income
adults not covered under ACA Section
VIII (excludes pregnant women and
people with disabilities)
Mandatory
Populations enrolled: Low-income
adults covered under ACA Section VIII
(excludes pregnant women and people
with disabilities)
Mandatory
Populations enrolled: Aged, Blind or
Disabled Children or Adults
Mandatory
Populations enrolled: Non-Disabled
Children (excludes children in foster
care or receiving adoption assistance)
Mandatory
Populations enrolled: Individuals
receiving Limited Benefits (excludes
partial duals)
Populations enrolled: Full Duals Voluntary
Populations enrolled: Partial Duals Voluntary
Populations enrolled: Children with
Special Health Care Needs
Mandatory
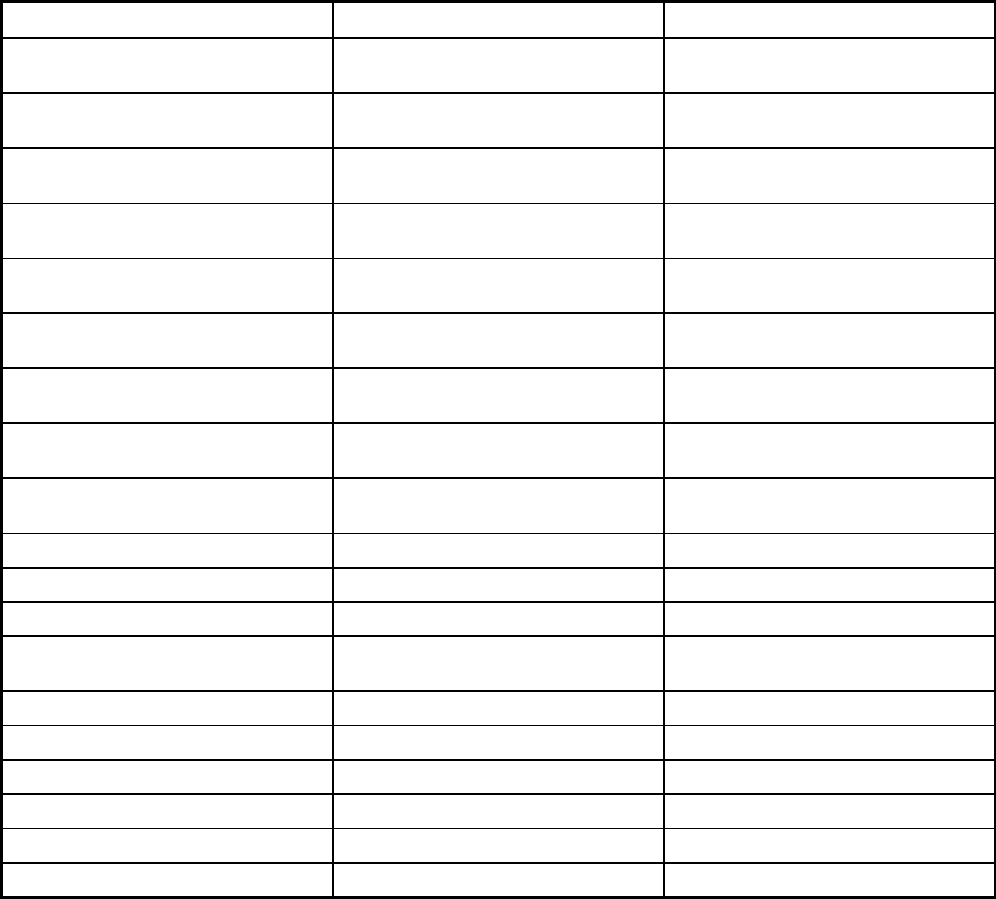
322
Features HealthChoice Hopkins Elder Plus
Populations enrolled: Native
American/Alaskan Natives
Mandatory Voluntary
Populations enrolled: Foster Care and
Adoption Assistance Children
Mandatory Exempt
Populations enrolled: Enrollment choice
period
Other N/A
Populations enrolled: Enrollment broker
name (if applicable)
Maryland Health Connection
Populations enrolled: Notes on
enrollment choice period
If participants don't choose at the time
of application they are auto-assigned.
Benefits covered: Inpatient hospital
physical health
X
Benefits covered: Inpatient hospital
behavioral health (MH and/or SUD)
Benefits covered: Outpatient hospital
physical health
X
Benefits covered: Outpatient hospital
behavioral health (MH and/or SUD)
Benefits covered: Partial hospitalization
Benefits covered: Physician X
Benefits covered: Nurse practitioner X
Benefits covered: Rural health clinics
and FQHCs
X
Benefits covered: Clinic services X
Benefits covered: Lab and x-ray X
Benefits covered: Prescription drugs X
Benefits covered: Prosthetic devices X
Benefits covered: EPSDT X
Benefits covered: Case management X
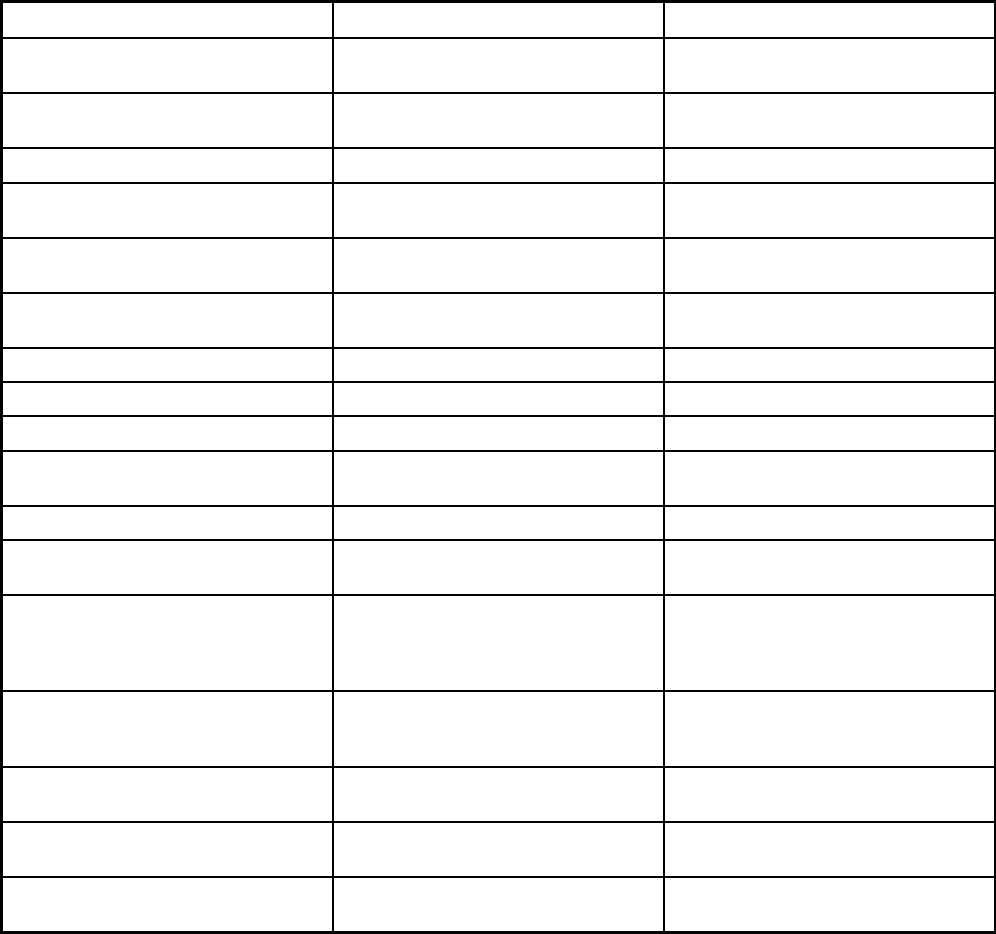
323
Features HealthChoice Hopkins Elder Plus
Benefits covered: SSA Section 1945-
authorized health home
Benefits covered: Health home care
(services in home)
X
Benefits covered: Family planning X
Benefits covered: Dental services
(medical/surgical)
Benefits covered: Dental (preventative
or corrective)
Benefits covered: Personal care (state
plan option)
Benefits covered: HCBS waiver services
Benefits covered: Private duty nursing X
Benefits covered: ICF-IDD
Benefits covered: Nursing facility
services
Benefits covered: Hospice care X
Benefits covered: Non-Emergency
Medical Transportation
Benefits covered: Institution for Mental
Disease inpatient treatment for people
ages 21-64 defined by 42 CFR
§438.6(e) as an 'in lieu of' benefit
Benefits covered: Other (e.g., nurse
midwife services, freestanding birth
centers, podiatry, etc.)
Nurse midwife, freestanding birthing
centers, podiatry (routine foot care
under 21 and diabetics)
All benefits listed under 42 CFR 460.90
- 460.106
Quality assurance and improvement:
HEDIS data required?
Yes No
Quality assurance and improvement:
CAHPS data required?
Yes No
Quality assurance and improvement:
Accreditation required?
Yes No
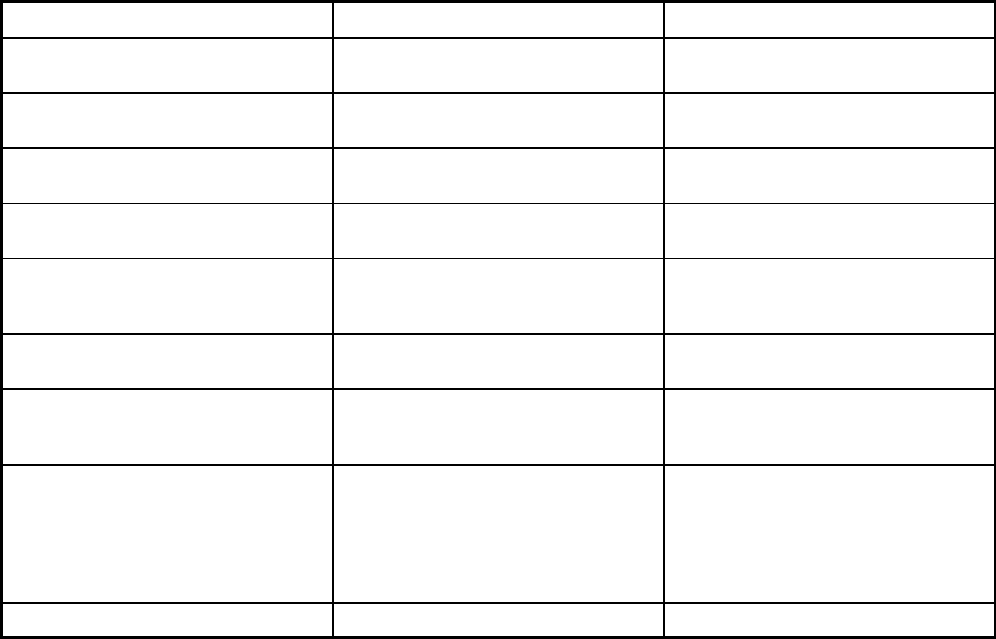
324
Features HealthChoice Hopkins Elder Plus
Quality assurance and improvement:
Accrediting organization
NCQA
Quality assurance and improvement:
EQRO contractor name (if applicable)
Qlarant
Performance incentives: Payment
bonuses/differentials to reward plans
X
Performance incentives: Preferential
auto-enrollment to reward plans
Performance incentives: Public reports
comparing plan performance on key
metrics
X
Performance incentives: Withholds tied
to performance metrics
X
Performance incentives: MCOs/PHPs
required or encouraged to pay providers
for value/quality outcomes
Participating plans: Plans in Program Amerigroup Community Care; Aetna
Better Health of Maryland; Jai Medical
Systems; Kaiser Permanete; Maryland
Physician's Care; MedStar; Priority
Partners; United HealthCare; University
of Maryland Health Partners
Hopkins Elder Plus
Notes: Program notes
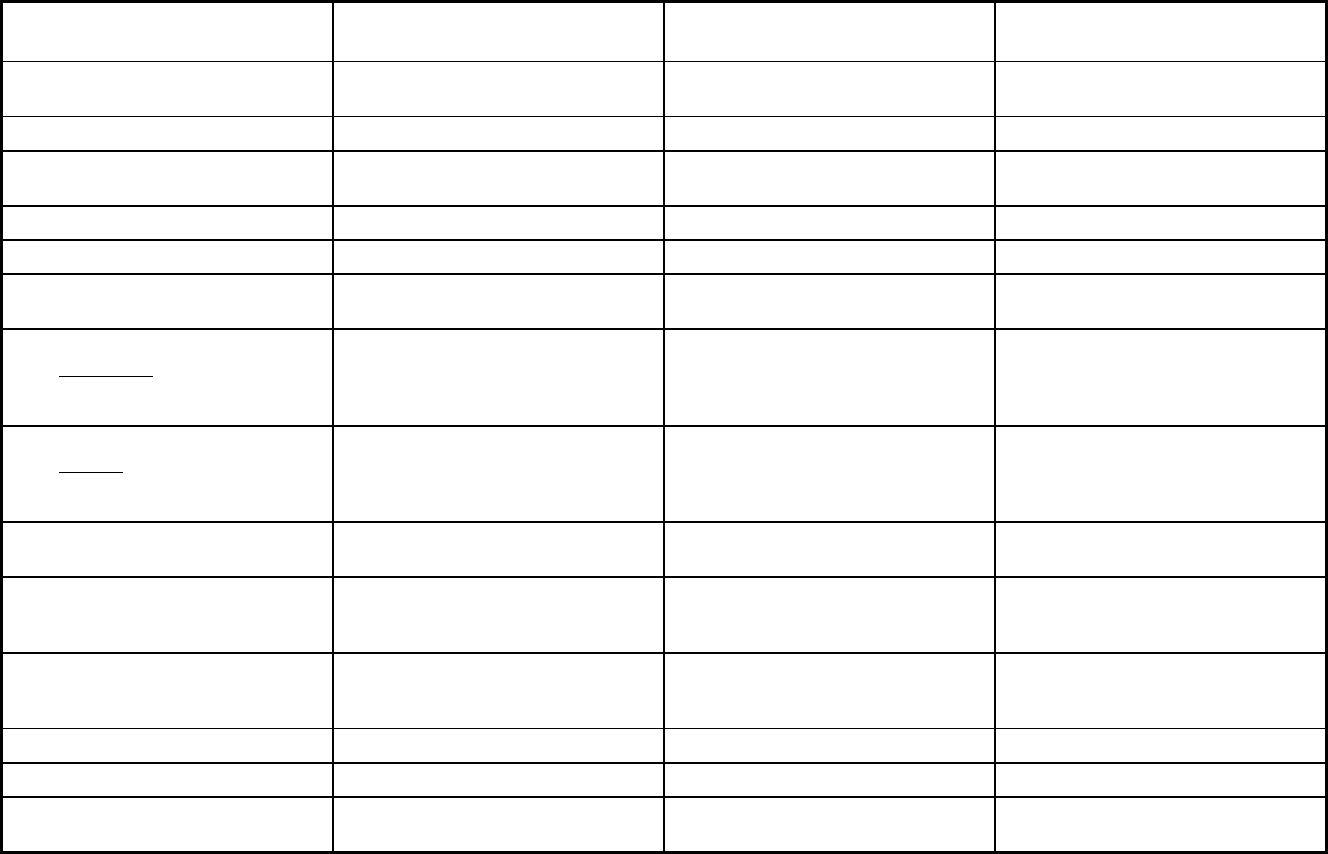
325
Massachusetts Managed Care Program Features, as of 2018 (1 of 3)
Features MassHealth Managed Care
Primary Care Clinician Program (PCC
Plan)
Primary Care Accountable Care
Organizations (Primary Care ACO)
Program type Comprehensive MCO Primary Care Case Management
(PCCM)
Primary Care Case Management Entity
(PCCM Entity)
Statewide or region-specific? Statewide Statewide Statewide
Federal operating authority 1115(a) (Medicaid demonstration
waivers)
1115(a) (Medicaid demonstration
waivers)
1115(a) (Medicaid demonstration
waivers)
Program start date 07/07/1998 01/01/1995 03/01/2018
Waiver expiration date (if applicable) 06/30/2019 06/30/2022 06/30/2022
If the program ended in 2018, indicate
the end date
Populations enrolled: Low-income
adults not covered under ACA Section
VIII (excludes pregnant women and
people with disabilities)
Mandatory Mandatory Mandatory
Populations enrolled: Low-income
adults covered under ACA Section VIII
(excludes pregnant women and people
with disabilities)
Mandatory Mandatory Mandatory
Populations enrolled: Aged, Blind or
Disabled Children or Adults
Mandatory Mandatory Mandatory
Populations enrolled: Non-Disabled
Children (excludes children in foster
care or receiving adoption assistance)
Mandatory Mandatory Mandatory
Populations enrolled: Individuals
receiving Limited Benefits (excludes
partial duals)
Populations enrolled: Full Duals
Populations enrolled: Partial Duals
Populations enrolled: Children with
Special Health Care Needs
Mandatory Mandatory Mandatory
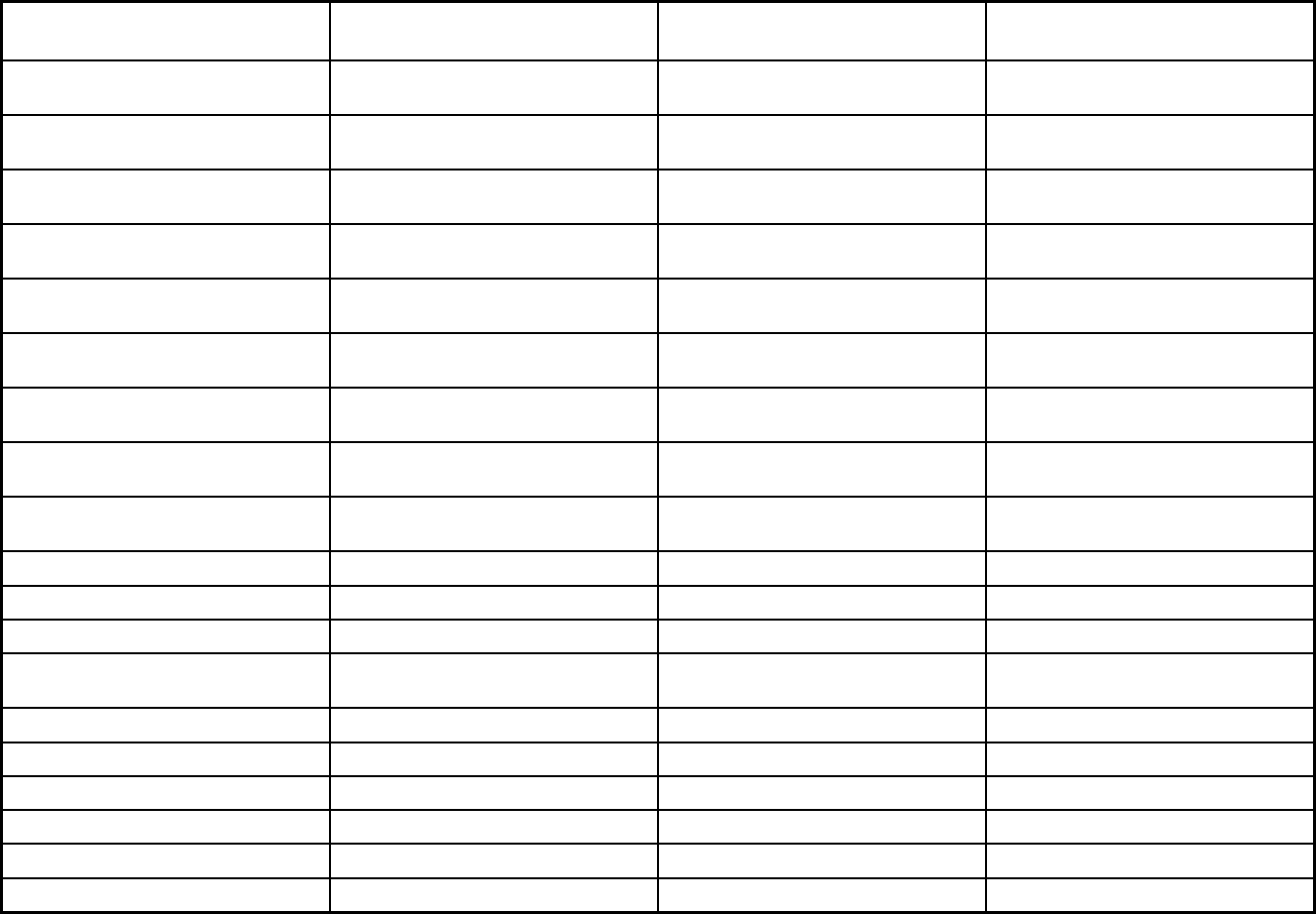
326
Features MassHealth Managed Care
Primary Care Clinician Program (PCC
Plan)
Primary Care Accountable Care
Organizations (Primary Care ACO)
Populations enrolled: Native
American/Alaskan Natives
Mandatory Mandatory Mandatory
Populations enrolled: Foster Care and
Adoption Assistance Children
Voluntary Voluntary Voluntary
Populations enrolled: Enrollment choice
period
Other N/A Other
Populations enrolled: Enrollment broker
name (if applicable)
Maximus Maximus Maximus
Populations enrolled: Notes on
enrollment choice period
14 days with a 90 day plan selection
period.
14 days
Benefits covered: Inpatient hospital
physical health
X
Benefits covered: Inpatient hospital
behavioral health (MH and/or SUD)
X
Benefits covered: Outpatient hospital
physical health
X
Benefits covered: Outpatient hospital
behavioral health (MH and/or SUD)
X
Benefits covered: Partial hospitalization X
Benefits covered: Physician X
Benefits covered: Nurse practitioner X
Benefits covered: Rural health clinics
and FQHCs
X
Benefits covered: Clinic services X
Benefits covered: Lab and x-ray X
Benefits covered: Prescription drugs X
Benefits covered: Prosthetic devices X
Benefits covered: EPSDT X
Benefits covered: Case management X X
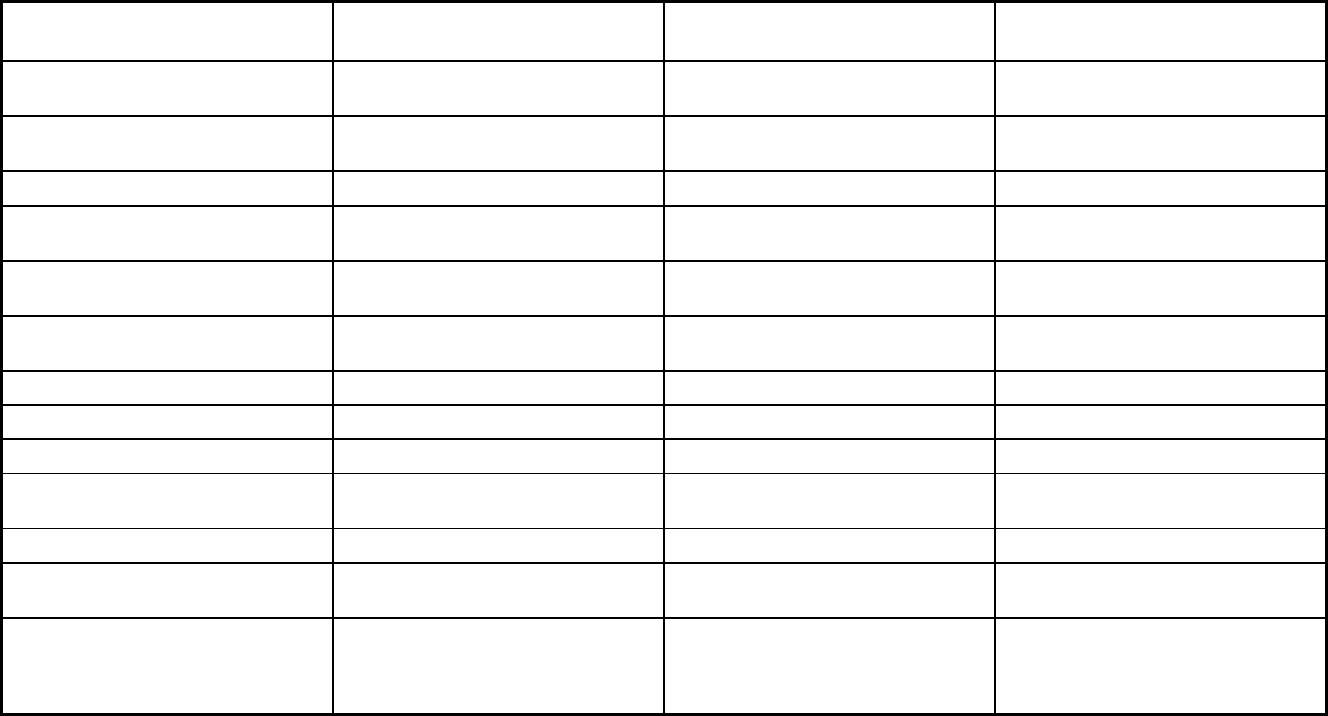
327
Features MassHealth Managed Care
Primary Care Clinician Program (PCC
Plan)
Primary Care Accountable Care
Organizations (Primary Care ACO)
Benefits covered: SSA Section 1945-
authorized health home
Benefits covered: Health home care
(services in home)
X
Benefits covered: Family planning X
Benefits covered: Dental services
(medical/surgical)
X
Benefits covered: Dental (preventative
or corrective)
Benefits covered: Personal care (state
plan option)
X
Benefits covered: HCBS waiver services
Benefits covered: Private duty nursing
Benefits covered: ICF-IDD
Benefits covered: Nursing facility
services
X
Benefits covered: Hospice care X
Benefits covered: Non-Emergency
Medical Transportation
X
Benefits covered: Institution for Mental
Disease inpatient treatment for people
ages 21-64 defined by 42 CFR
§438.6(e) as an 'in lieu of' benefit
X
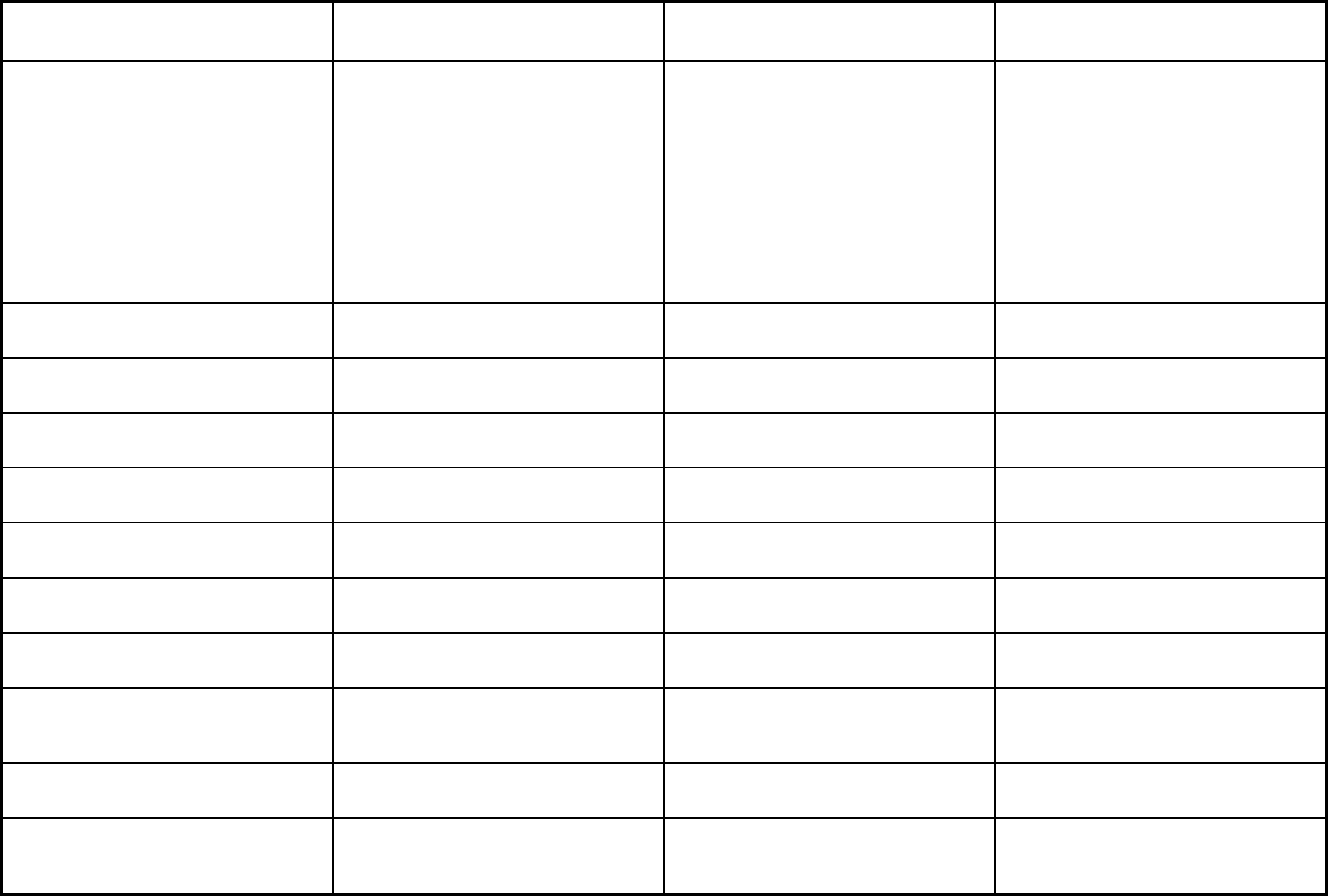
328
Features MassHealth Managed Care
Primary Care Clinician Program (PCC
Plan)
Primary Care Accountable Care
Organizations (Primary Care ACO)
Benefits covered: Other (e.g., nurse
midwife services, freestanding birth
centers, podiatry, etc.)
Acupuncture, audiology, breast pump,
chiropractic, diabetes self-management
training, dialysis, DME, early
intervention, emergency services,
fluoride varnish, hearing aids, infertility
diagnosis, dentures, medical nutrition
therapy, orthotics, podiatry, radiology
and diagnostic tests, tobacco cessation,
vision care, speech therapy,
occupational therapy, physical therapy,
SNF, chronic or rehab, others
Quality assurance and improvement:
HEDIS data required?
Yes No No
Quality assurance and improvement:
CAHPS data required?
Yes No No
Quality assurance and improvement:
Accreditation required?
Yes No No
Quality assurance and improvement:
Accrediting organization
NCQA Voluntary participation in EQR
performance measure validation
Quality assurance and improvement:
EQRO contractor name (if applicable)
Innovative Resource Group, LLC D/B/A
KEPRO
Innovative Resource Group, LLC D/B/A
KEPRO
Innovative Resource Group, LLC D/B/A
KEPRO
Performance incentives: Payment
bonuses/differentials to reward plans
Performance incentives: Preferential
auto-enrollment to reward plans
Performance incentives: Public reports
comparing plan performance on key
metrics
X X
Performance incentives: Withholds tied
to performance metrics
Performance incentives: MCOs/PHPs
required or encouraged to pay providers
for value/quality outcomes
X X
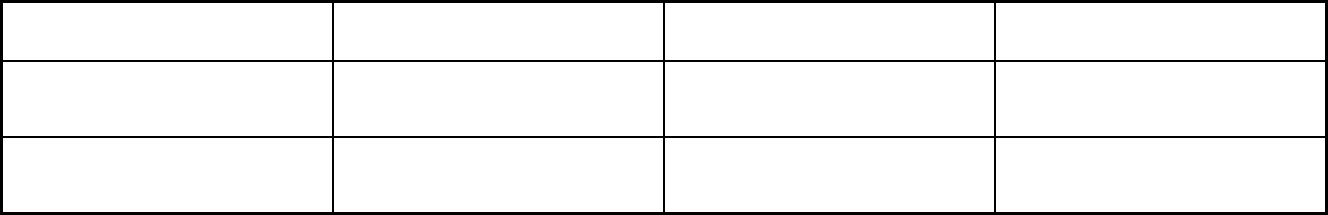
329
Features MassHealth Managed Care
Primary Care Clinician Program (PCC
Plan)
Primary Care Accountable Care
Organizations (Primary Care ACO)
Participating plans: Plans in Program Tufts Health Plan; Boston Medical
Center Health Plan
Multiple Primary Care Providers Community Care Cooperative; Partners
HealthCare Choice; Steward Health
Choice
Notes: Program notes Services provided in this program are
covered by total cost of care rather than
capitation.
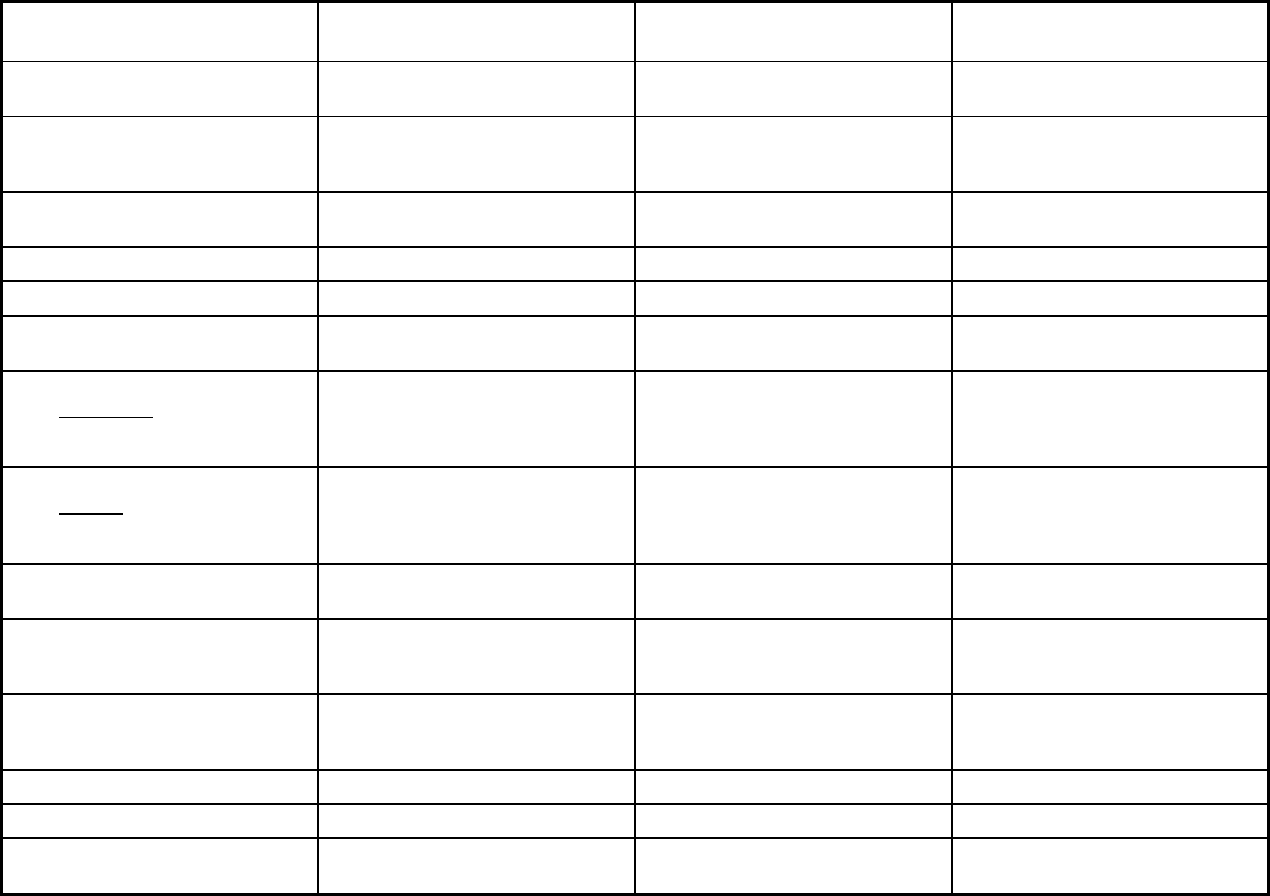
330
Massachusetts Managed Care Program Features, as of 2018 (2 of 3)
Features
Program of All-Inclusive Care for
the Elderly (PACE)
Accountable Care Partnership
Plans MassHealth BH/SUD PIHP
Program type Program of All-inclusive Care for the
Elderly (PACE)
Comprehensive MCO Behavioral Health Organization (BHO)
only (PIHP and/or PAHP)
Statewide or region-specific? Bristol, Essex, Franklin, Hampden,
Hampshire, Middlesex, Norfolk,
Plymouth, Suffolk, Worcestor
Statewide Statewide
Federal operating authority PACE 1115(a) (Medicaid demonstration
waivers)
1115(a) (Medicaid demonstration
waivers)
Program start date 07/10/1990 03/01/2018 07/01/1997
Waiver expiration date (if applicable) 06/30/2022 06/30/2022
If the program ended in 2018, indicate
the end date
Populations enrolled: Low-income
adults not covered under ACA Section
VIII (excludes pregnant women and
people with disabilities)
Mandatory Mandatory
Populations enrolled: Low-income
adults covered under ACA Section VIII
(excludes pregnant women and
people with disabilities)
Mandatory Mandatory
Populations enrolled: Aged, Blind or
Disabled Children or Adults
Voluntary Mandatory Mandatory
Populations enrolled: Non-Disabled
Children (excludes children in foster
care or receiving adoption assistance)
Mandatory Mandatory
Populations enrolled: Individuals
receiving Limited Benefits (excludes
partial duals)
Populations enrolled: Full Duals Voluntary Mandatory
Populations enrolled: Partial Duals Voluntary
Populations enrolled: Children with
Special Health Care Needs
Mandatory Mandatory
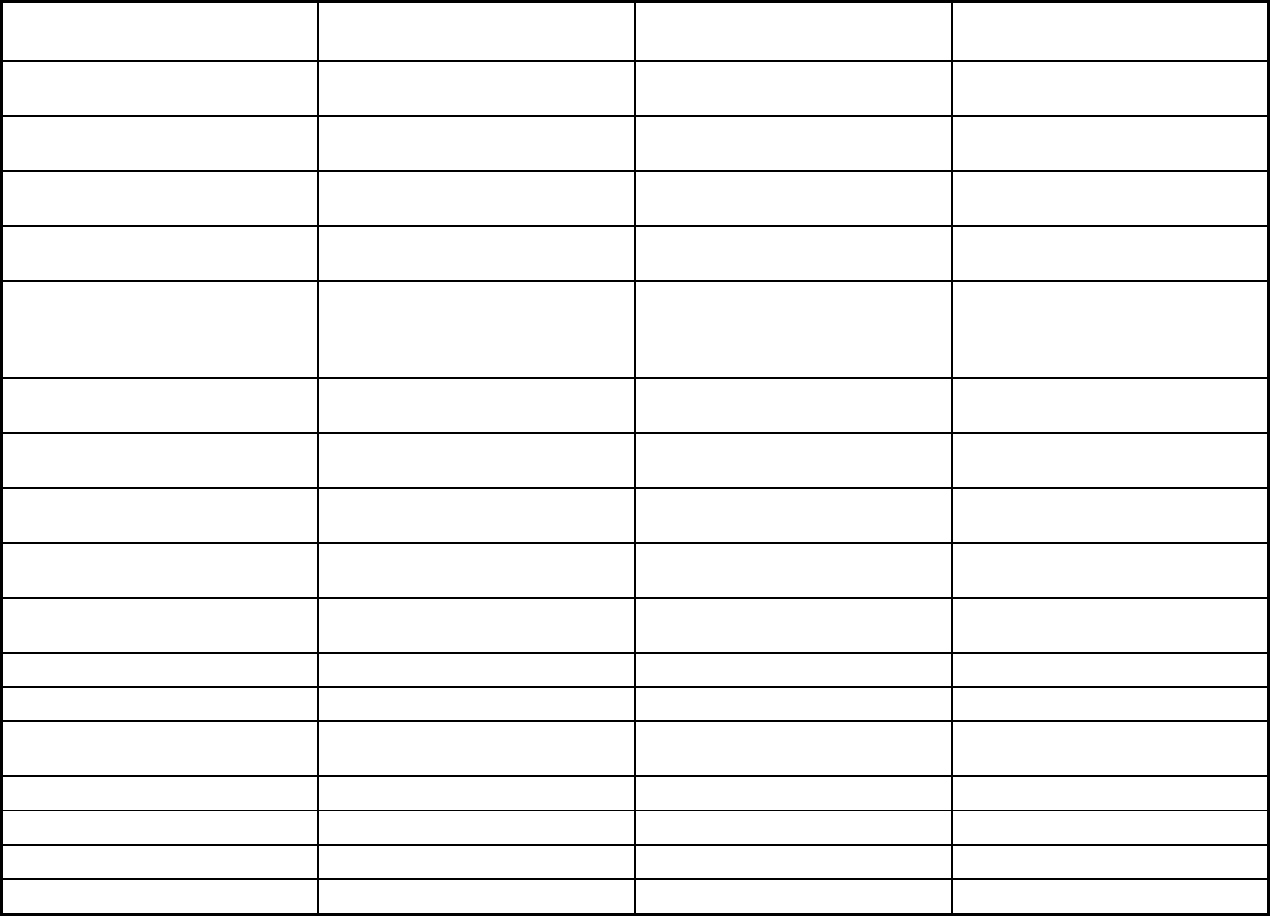
331
Features
Program of All-Inclusive Care for
the Elderly (PACE)
Accountable Care Partnership
Plans MassHealth BH/SUD PIHP
Populations enrolled: Native
American/Alaskan Natives
Voluntary Mandatory Mandatory
Populations enrolled: Foster Care and
Adoption Assistance Children
Voluntary Voluntary
Populations enrolled: Enrollment
choice period
N/A Other Other
Populations enrolled: Enrollment
broker name (if applicable)
Maximus Maximus
Populations enrolled: Notes on
enrollment choice period
Enrollment open all year, effective the
first day of the next month following
the date on which the member elects
to enroll.
14 days with 90 day plan selection
period.
Daily
Benefits covered: Inpatient hospital
physical health
X X
Benefits covered: Inpatient hospital
behavioral health (MH and/or SUD)
X X X
Benefits covered: Outpatient hospital
physical health
X X
Benefits covered: Outpatient hospital
behavioral health (MH and/or SUD)
X X X
Benefits covered: Partial
hospitalization
X X X
Benefits covered: Physician X X X
Benefits covered: Nurse practitioner X X X
Benefits covered: Rural health clinics
and FQHCs
X X
Benefits covered: Clinic services X X X
Benefits covered: Lab and x-ray X X
Benefits covered: Prescription drugs X X X
Benefits covered: Prosthetic devices X X
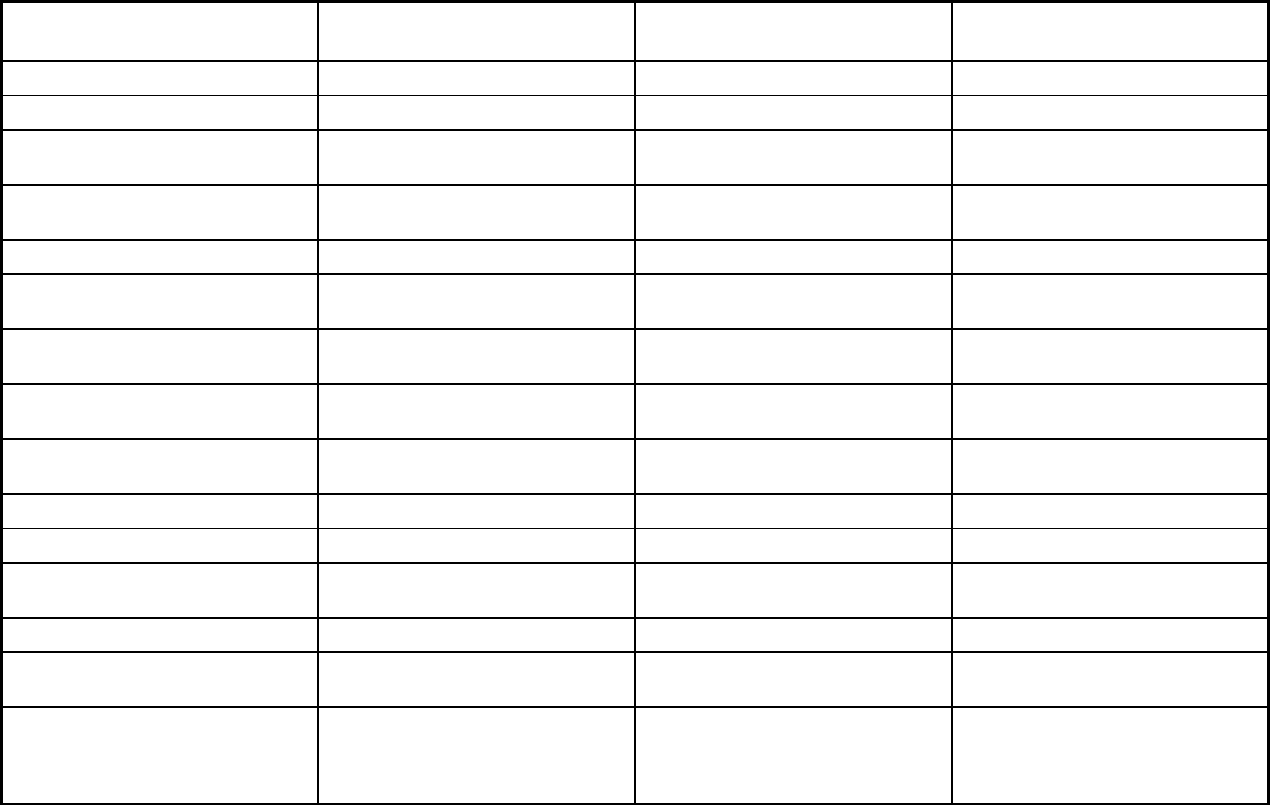
332
Features
Program of All-Inclusive Care for
the Elderly (PACE)
Accountable Care Partnership
Plans MassHealth BH/SUD PIHP
Benefits covered: EPSDT X
Benefits covered: Case management X X X
Benefits covered: SSA Section 1945-
authorized health home
Benefits covered: Health home care
(services in home)
X X
Benefits covered: Family planning X X
Benefits covered: Dental services
(medical/surgical)
X X
Benefits covered: Dental (preventative
or corrective)
X
Benefits covered: Personal care (state
plan option)
X
Benefits covered: HCBS waiver
services
X
Benefits covered: Private duty nursing X
Benefits covered: ICF-IDD
Benefits covered: Nursing facility
services
X X
Benefits covered: Hospice care X X
Benefits covered: Non-Emergency
Medical Transportation
X X
Benefits covered: Institution for Mental
Disease inpatient treatment for people
ages 21-64 defined by 42 CFR
§438.6(e) as an 'in lieu of' benefit
X X
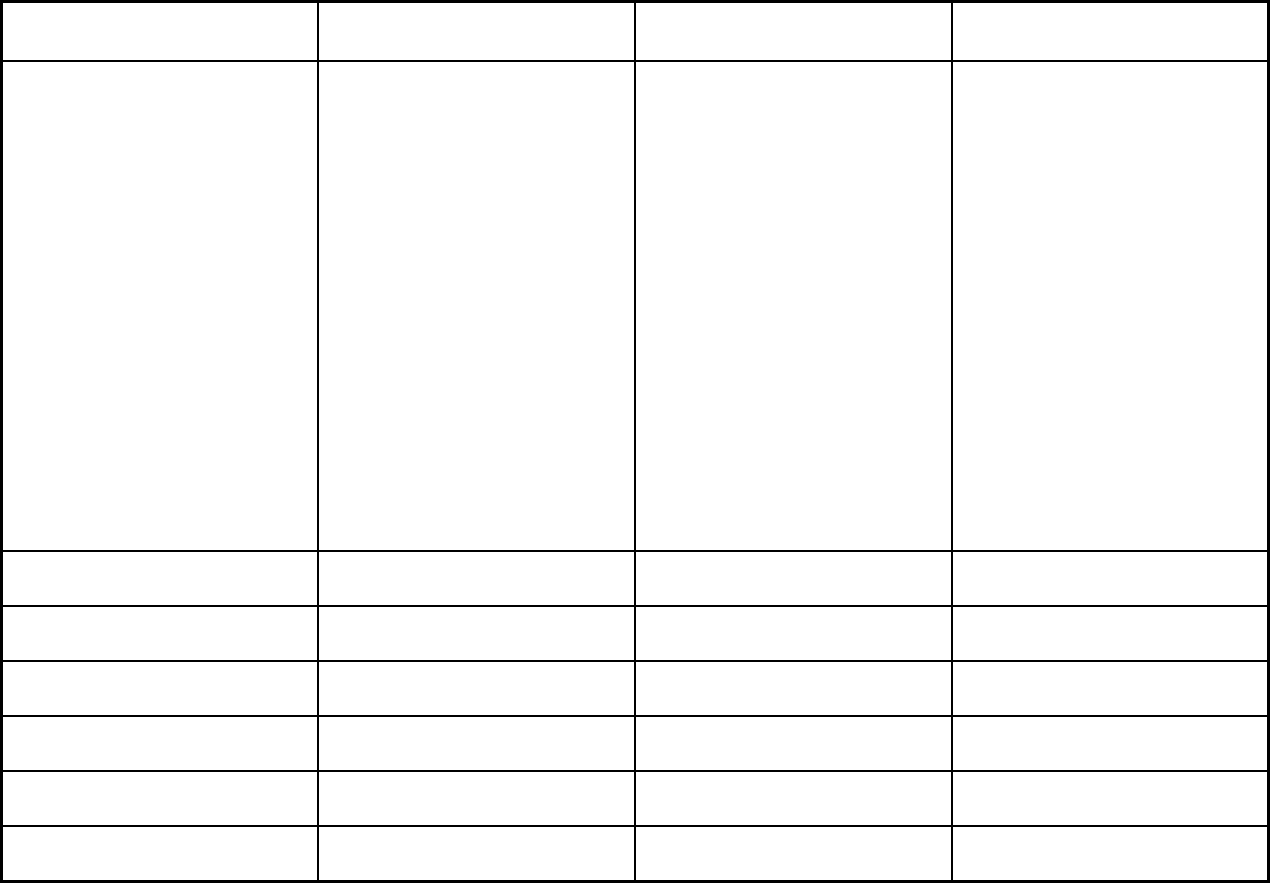
333
Features
Program of All-Inclusive Care for
the Elderly (PACE)
Accountable Care Partnership
Plans MassHealth BH/SUD PIHP
Benefits covered: Other (e.g., nurse
midwife services, freestanding birth
centers, podiatry, etc.)
The PACE program covers all
medically necessary services for the
enrolled population, including but not
limited to all covered Medicare and
Medicaid services.
Acupuncture, audiology, breast pump,
chiropractic, diabetes self-
management training, dialysis, DME,
early intervention, emergency
services, fluoride varnish, hearing
aids, infertility diagnosis, dentures,
medical nutrition therapy, orthotics,
podiatry, radiology and diagnostic
tests, tobacco cessation, vision care,
speech therapy, occupational therapy,
physical therapy, SNF up to 100 days
per contract year, chronic or rehab,
and Home Health (nursing and
therapies). LTSS are covered through
FFS. (Note: this list is not fully
inclusive).
Children’s Behavioral Health Initiative
(CBHI) services, Emergency Services
Program, and Diversionary Services:
Community Crisis Stabilization,
Community-Based Acute Treatment
for Children and Adolescents (CBAT),
Acute Treatment Services (ATS) for
Substance Use Disorders (Level III-
7),
Clinical Support Services (CSS) for
Substance Use Disorders (Level III.5),
and Transitional Care Unit (TCU),
Community Support Program (CSP),
Partial Hospitalization, Psychiatric Day
Treatment, Structure Outpatient
Addiction Program (SOAP), Program
of Assertive Community Treatment,
and Intensive Outpatient Treatment,
Transitional Support Services (TSSW)
for Substance Use Disorders,
Residential Rehabilitation Services for
Substance Use Disorder and
Enhanced Residential Rehabilitation
Services for Dually Diagnosed.
Quality assurance and improvement:
HEDIS data required?
No Yes Yes
Quality assurance and improvement:
CAHPS data required?
No Yes No
Quality assurance and improvement:
Accreditation required?
No Yes Yes
Quality assurance and improvement:
Accrediting organization
NCQA NCQA
Quality assurance and improvement:
EQRO contractor name (if applicable)
Innovative Resource Group, LLC
D/B/A KEPRO
Innovative Resource Group, DBA
KEPRO
Performance incentives: Payment
bonuses/differentials to reward plans
X
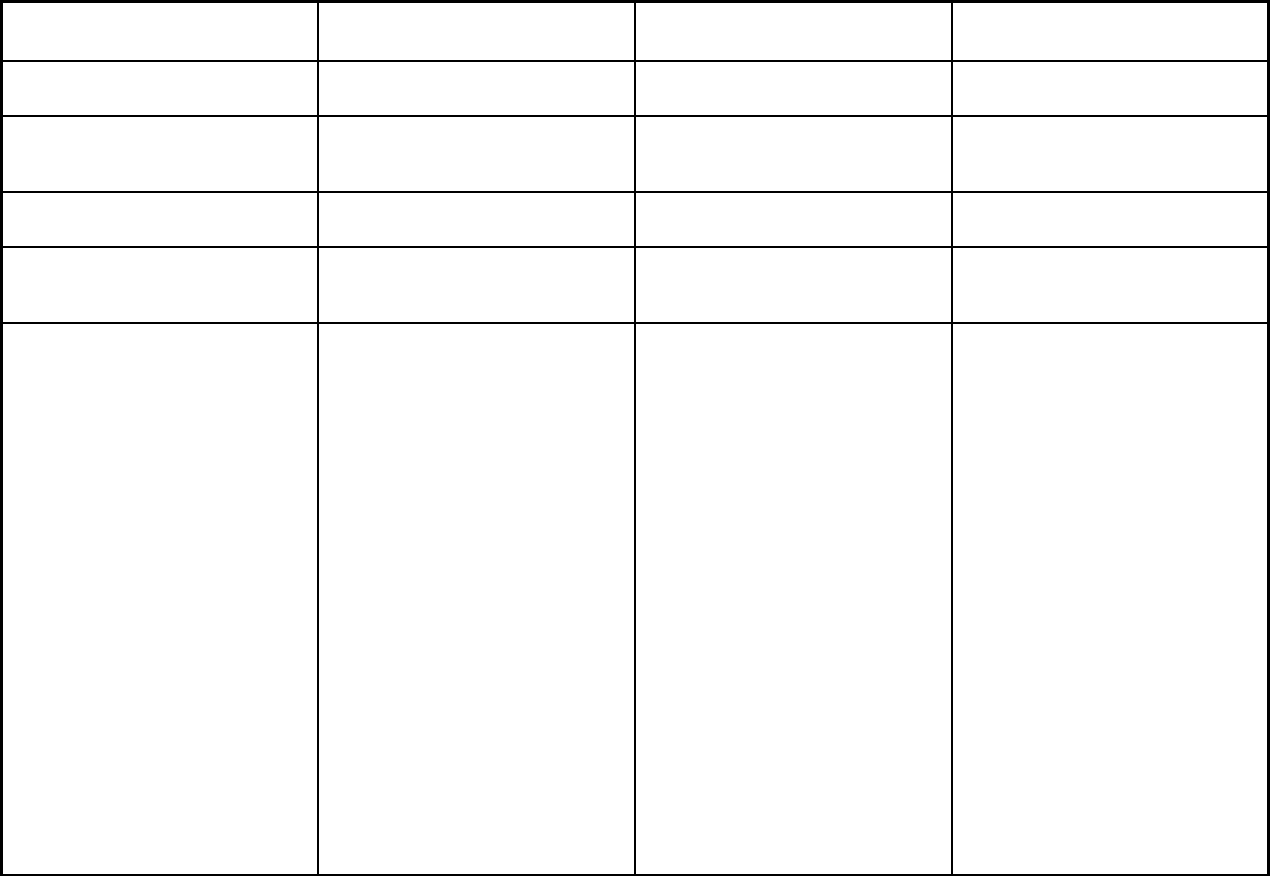
334
Features
Program of All-Inclusive Care for
the Elderly (PACE)
Accountable Care Partnership
Plans MassHealth BH/SUD PIHP
Performance incentives: Preferential
auto-enrollment to reward plans
Performance incentives: Public reports
comparing plan performance on key
metrics
X X
Performance incentives: Withholds
tied to performance metrics
Performance incentives: MCOs/PHPs
required or encouraged to pay
providers for value/quality outcomes
X
Participating plans: Plans in Program Elder Service Plan of Cambridge
Health Alliance; Upham's Elder
Service Plan; Elder Service Plan of
Harbor Health; Fallon Health Summit
Eldercare; Element Care Inc; Serenity
Care PACE Program; Mercy Life Inc;
Neighborhood PACE
Atrius Health in partnership with Tufts
Health Public Plans (THPP); Beth
Israel Deaconess Care Organization
(BIDCO) in partnership with Tufts
Health Public Plans (THPP); Boston
Children’s Health ACO in partnership
with Tufts Health Public Plans (THPP);
Cambridge Health Alliance (CHA) in
partnership with Tufts Health Public
Plans (THPP); Merrimack Valley ACO
in partnership with AllWays Health
Partners; Boston Accountable Care
Organization in partnership with BMC
HealthNet Plan; Mercy Medical Center
in partnership with BMC HealthNet
Plan; Signature Healthcare in
partnership with BMC HealthNet Plan;
Southcoast Health in partnership with
BMC HealthNet Plan; Health
Collaborative of the Berkshires in
partnership with Fallon Health; Reliant
Medical Group in partnership with
Fallon Health; Wellforce in partnership
with Fallon Health; Baystate Health
Care Alliance in partnership with
Health New England
Massachusetts Behavioral Health
Partnership
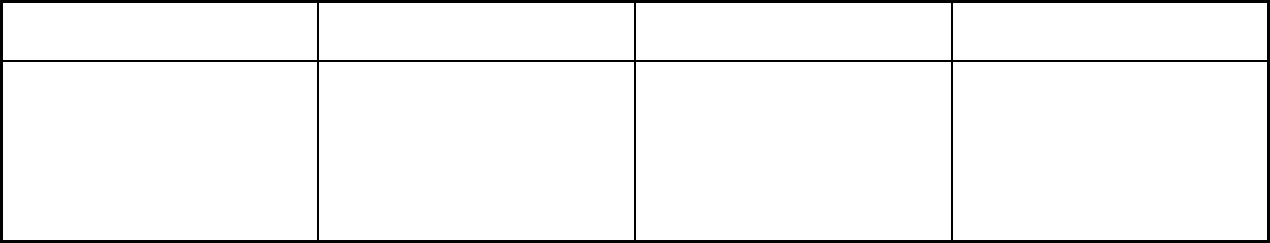
335
Features
Program of All-Inclusive Care for
the Elderly (PACE)
Accountable Care Partnership
Plans MassHealth BH/SUD PIHP
Notes: Program notes Enrollment numbers do not include
private pay enrollees, if any.
Full duals are only enrolled
mandatorily if less than 21 years of
age. The 1915(b) waiver provides
managed behavioral health benefits
for participants enrolled in the MFP-
CL
and MFP-RS 1915(c) waivers. All
other 1915(c) waiver HCBS are
provided on a fee-for-service basis.
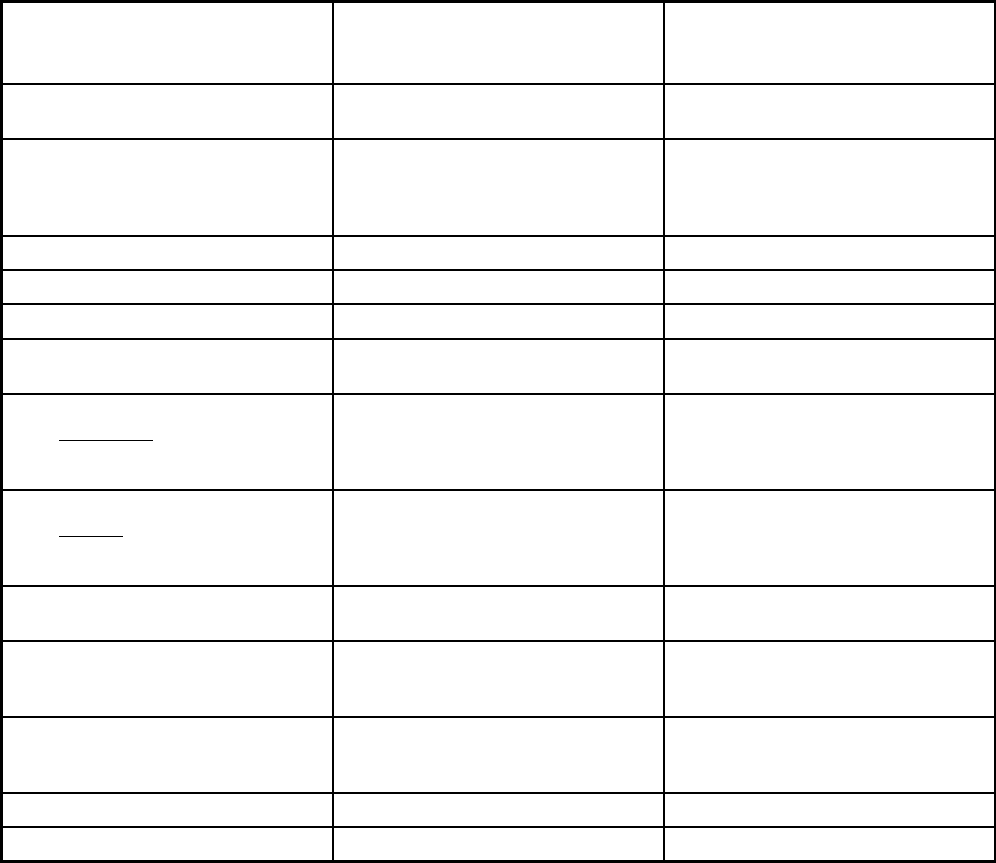
336
Massachusetts Managed Care Program Features, as of 2018 (3 of 3)
Features
Money Follows the Person-
Behavioral Health Supports (MFP-
BH) Senior Care Options
Program type Behavioral Health Organization (BHO)
only (PIHP and/or PAHP)
Comprehensive MCO + MLTSS
Statewide or region-specific? Statewide Counties of Barnstable, Bristol, Essex,
Franklin, Hampden, Hampshire,
Middlesex, Norfolk, Plymouth, Suffolk,
Worcester and Berkshire
Federal operating authority 1915(b)/1915(c) 1915(a)/1915(c)
Program start date 04/01/2013 07/01/2004
Waiver expiration date (if applicable) 03/31/2018 12/31/2018
If the program ended in 2018, indicate
the end date
03/31/2018
Populations enrolled: Low-income
adults not covered under ACA Section
VIII (excludes pregnant women and
people with disabilities)
Mandatory
Populations enrolled: Low-income
adults covered under ACA Section VIII
(excludes pregnant women and people
with disabilities)
Mandatory
Populations enrolled: Aged, Blind or
Disabled Children or Adults
Mandatory Voluntary
Populations enrolled: Non-Disabled
Children (excludes children in foster
care or receiving adoption assistance)
Populations enrolled: Individuals
receiving Limited Benefits (excludes
partial duals)
Populations enrolled: Full Duals Mandatory Voluntary
Populations enrolled: Partial Duals Mandatory Voluntary
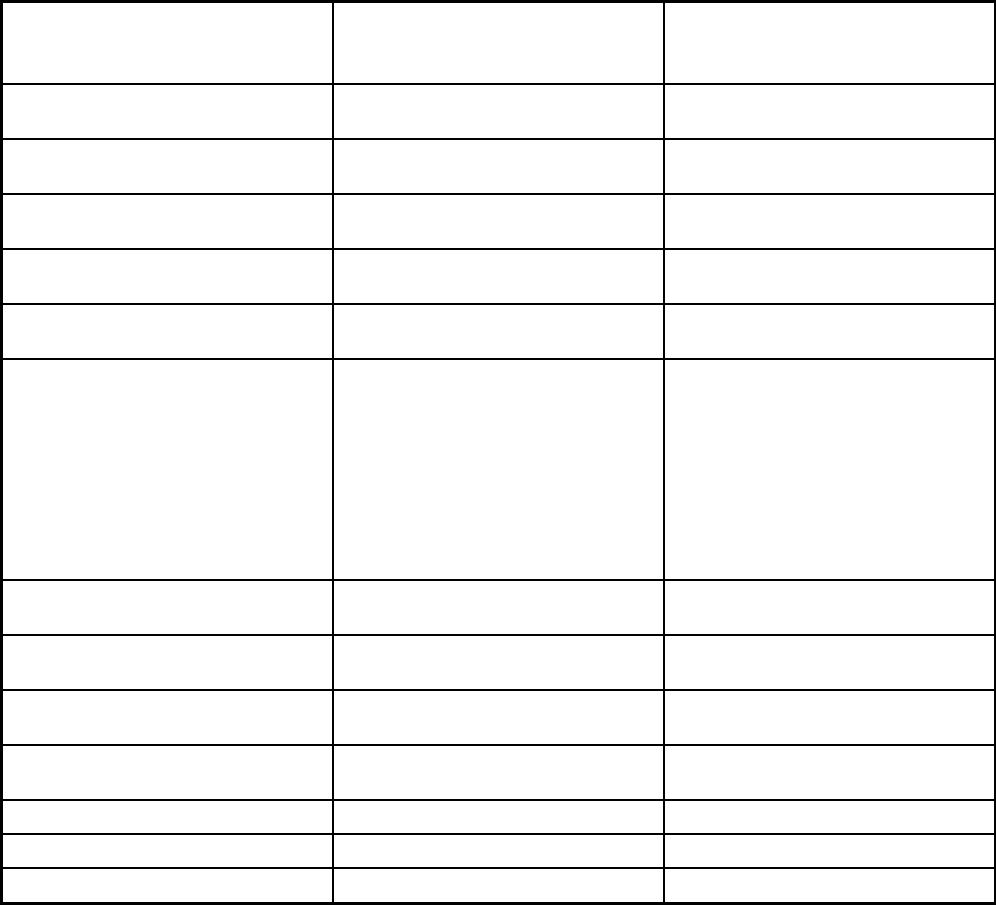
337
Features
Money Follows the Person-
Behavioral Health Supports (MFP-
BH) Senior Care Options
Populations enrolled: Children with
Special Health Care Needs
Populations enrolled: Native
American/Alaskan Natives
Mandatory Voluntary
Populations enrolled: Foster Care and
Adoption Assistance Children
Exempt
Populations enrolled: Enrollment choice
period
Other
Populations enrolled: Enrollment broker
name (if applicable)
Populations enrolled: Notes on
enrollment choice period
Medicaid members are eligible to enroll
all year, with enrollment effective the
first day of the month following the
month in which the member decided to
enroll. Dual eligible members are
eligible to enroll in accordance with the
Medicare Advantage enrollment period,
with enrollment effective the first day of
the month following the month in which
the member decided to enroll.
Benefits covered: Inpatient hospital
physical health
X
Benefits covered: Inpatient hospital
behavioral health (MH and/or SUD)
X X
Benefits covered: Outpatient hospital
physical health
X
Benefits covered: Outpatient hospital
behavioral health (MH and/or SUD)
X X
Benefits covered: Partial hospitalization X X
Benefits covered: Physician X
Benefits covered: Nurse practitioner X
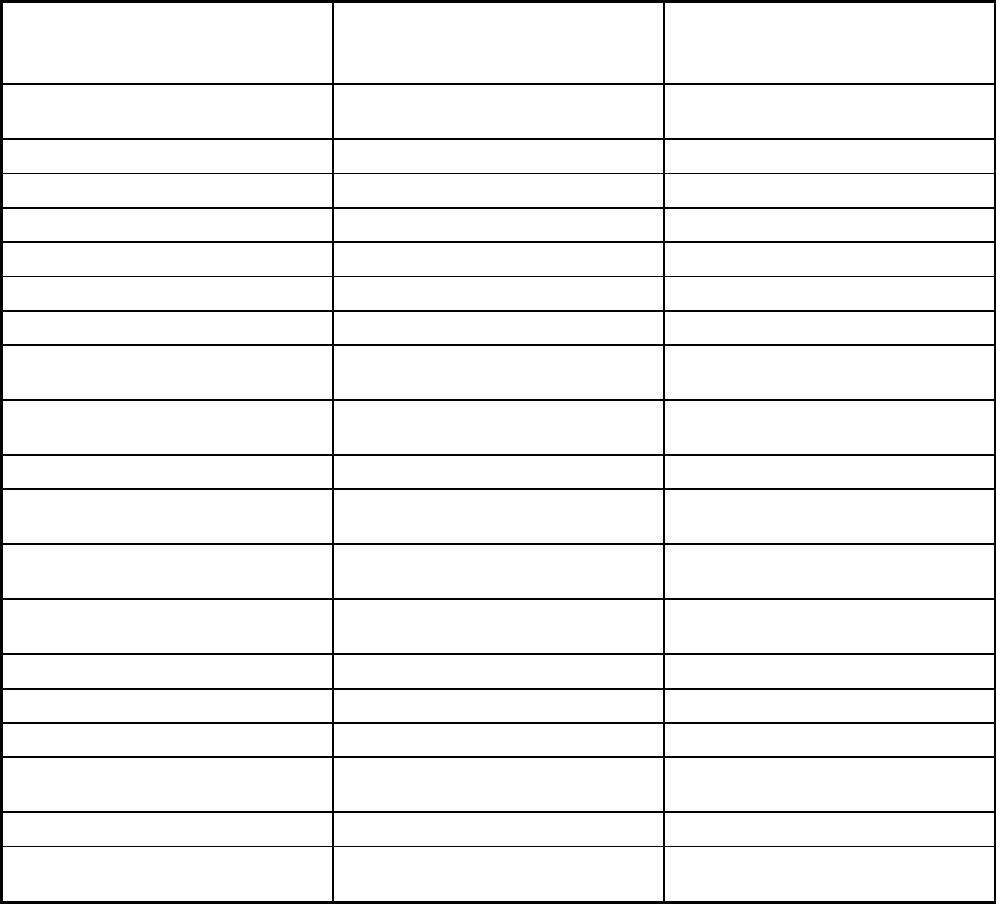
338
Features
Money Follows the Person-
Behavioral Health Supports (MFP-
BH) Senior Care Options
Benefits covered: Rural health clinics
and FQHCs
X
Benefits covered: Clinic services X X
Benefits covered: Lab and x-ray X
Benefits covered: Prescription drugs X
Benefits covered: Prosthetic devices X
Benefits covered: EPSDT
Benefits covered: Case management X X
Benefits covered: SSA Section 1945-
authorized health home
Benefits covered: Health home care
(services in home)
X
Benefits covered: Family planning X
Benefits covered: Dental services
(medical/surgical)
X
Benefits covered: Dental (preventative
or corrective)
X
Benefits covered: Personal care (state
plan option)
X
Benefits covered: HCBS waiver services X
Benefits covered: Private duty nursing X
Benefits covered: ICF-IDD
Benefits covered: Nursing facility
services
X
Benefits covered: Hospice care X
Benefits covered: Non-Emergency
Medical Transportation
X
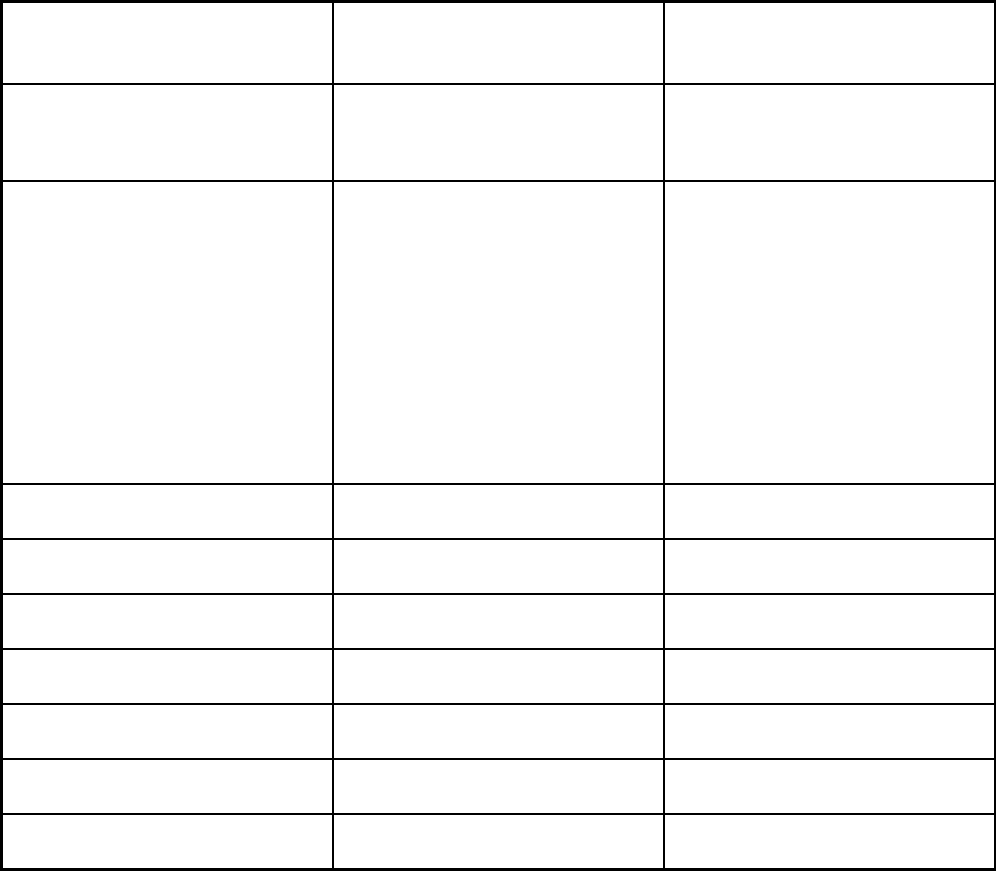
339
Features
Money Follows the Person-
Behavioral Health Supports (MFP-
BH) Senior Care Options
Benefits covered: Institution for Mental
Disease inpatient treatment for people
ages 21-64 defined by 42 CFR
§438.6(e) as an 'in lieu of' benefit
Benefits covered: Other (e.g., nurse
midwife services, freestanding birth
centers, podiatry, etc.)
Emergency Services Program and
Diversionary Services, Community
Crisis Stabilization, Acute Treatment
Services (ATS) for Substance Use
Disorders (Level III-7), Clinical Support
Services (CSS) for Substance Use
Disorders (Level III-5) and Transitional
Care Unit (TCU), Community Support
Program (CSP), Partial Hospitalization,
Partial Psychiatric Day Treatment,
Structure Outpatient Addiction Program
(SOAP), Program of Assertive
Community Treatment and Intensive
Outpatient Treatment
All MassHealth covered LTSS and all
services described in the
Commonwealth 1915(c) Frail Elder
Waiver
Quality assurance and improvement:
HEDIS data required?
No Yes
Quality assurance and improvement:
CAHPS data required?
No Yes
Quality assurance and improvement:
Accreditation required?
No No
Quality assurance and improvement:
Accrediting organization
Quality assurance and improvement:
EQRO contractor name (if applicable)
KEPRO
Performance incentives: Payment
bonuses/differentials to reward plans
Performance incentives: Preferential
auto-enrollment to reward plans
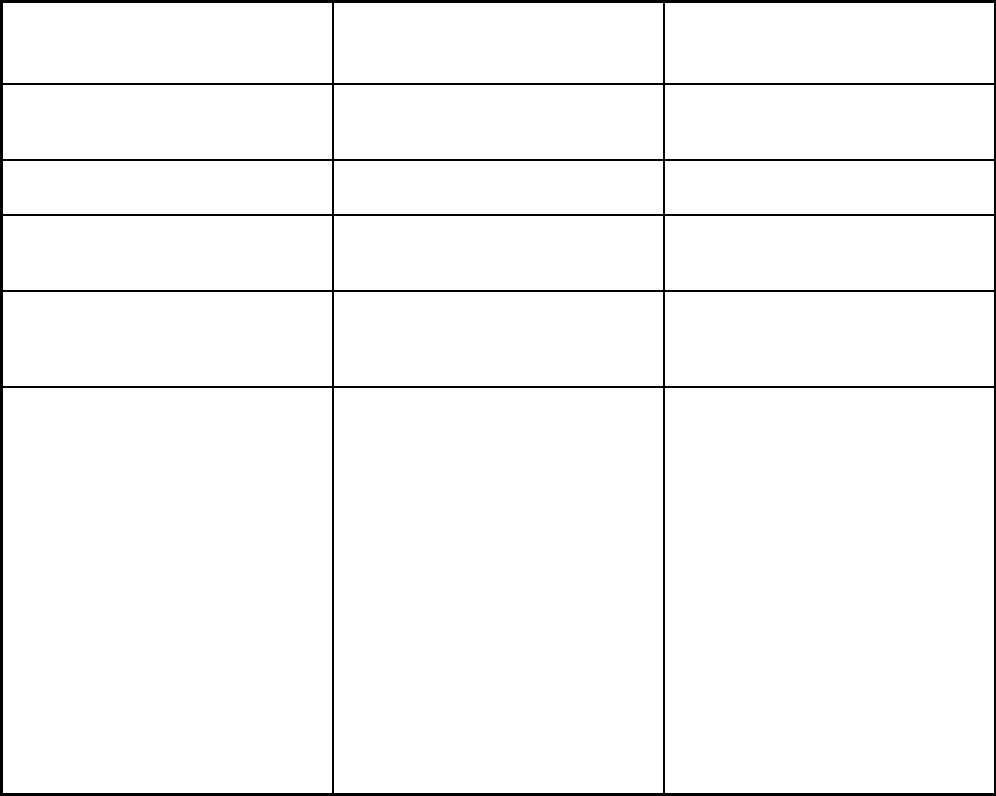
340
Features
Money Follows the Person-
Behavioral Health Supports (MFP-
BH) Senior Care Options
Performance incentives: Public reports
comparing plan performance on key
metrics
X
Performance incentives: Withholds tied
to performance metrics
Performance incentives: MCOs/PHPs
required or encouraged to pay providers
for value/quality outcomes
Participating plans: Plans in Program Money Follows the Person- Behavioral
Health Supports (MFP-BH)
Boston Medical Center Healthnet Plan;
Commonwealth Care Alliance; Navicare
HMO; Senior Whole Health; Tufts
Health Plan; United Healthcare
Notes: Program notes MassHealth members enrolled in the
two 1915(c) MFP Waivers who are not
otherwise eligible for the 1115
demonstration were mandatorily
enrolled in this 1915(b) Waiver. The
1915(c) waivers included both the MFP
Community Living (MFP-CL, waiver
control number MA.1027) and the MFP
Residential Supports (MFP-RS, waiver
control number MA.1028) Waivers. The
MFP-BH Waiver (MFP-BH, waiver
control number MA.0002) ran
concurrently with these 1915(c) waivers.
MFP waiver participants must be age
18-64 with disabilities or age 65 or over
and must be on MassHealth Standard.
The SCO Program is a voluntary
program offered to MassHealth
members age 65 and older residing in
the service area of a Senior Care
Oganization. The SCO program is
available in 12 of the 14 counties in
Massachusetts. The SCO program
covers all medically necessary Medicaid
and Medicare covered services through
its provider network. Each enrollee
selects a PCP upon enrollment,
receives care coordination, and
participates in and signs off on the
development of his/her care plan. Each
Senior Care Organization is also
designated by CMS as a Medicare
Advantage Special Needs Plan for
individuals dually eligible for Medicare
and Medicaid.
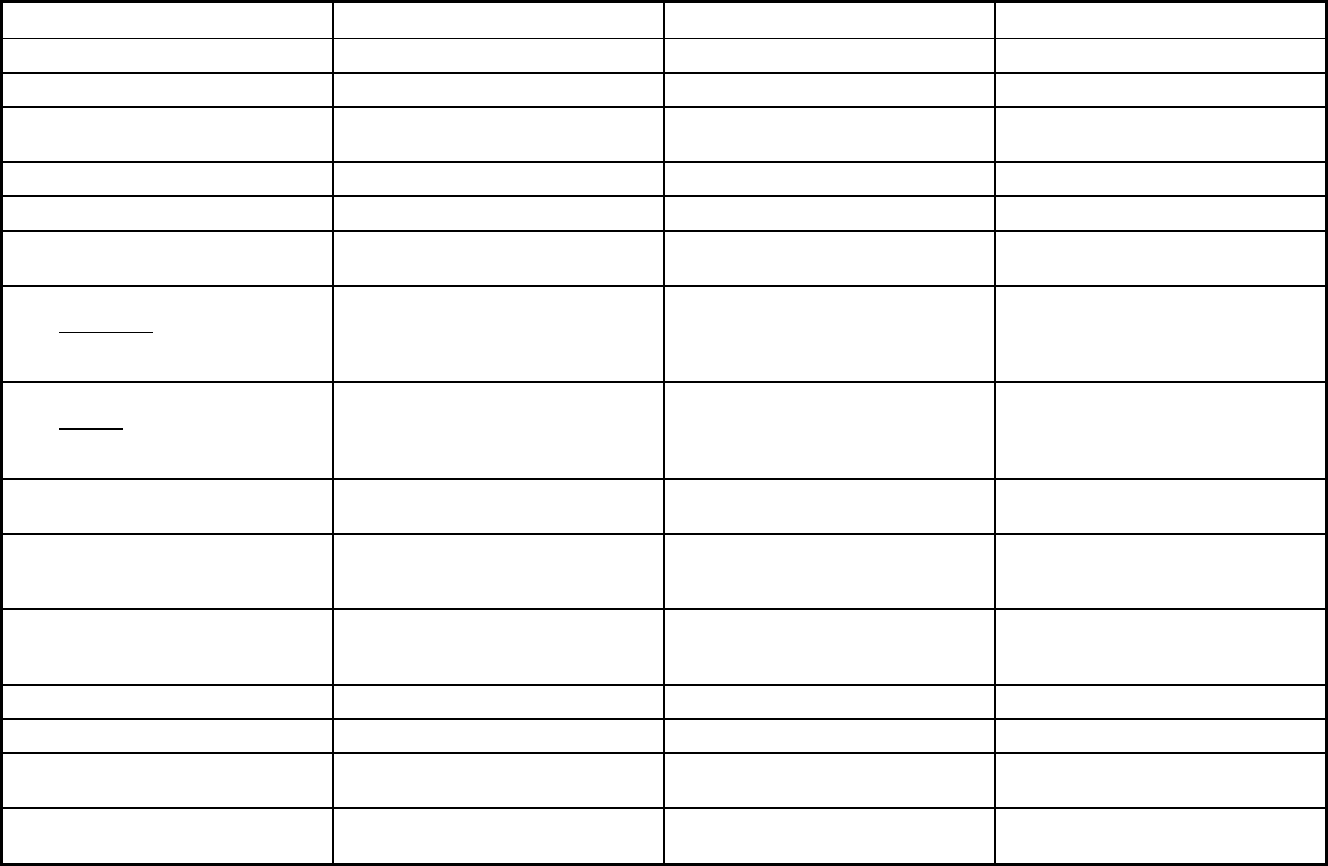
341
Michigan Managed Care Program Features, as of 2018 (1 of 2)
Features MI Choice Managed Care Plan Division Healthy Michigan Plan
Program type MLTSS only (PIHP and/or PAHP) Comprehensive MCO Comprehensive MCO
Statewide or region-specific? Statewide Statewide Statewide
Federal operating authority 1915(b)/1915(c) 1915(b) 1115(a) (Medicaid demonstration
waivers)
Program start date 10/01/2003 07/01/1997 04/01/2014
Waiver expiration date (if applicable) 09/30/2019 12/31/2019 12/31/2023
If the program ended in 2018, indicate
the end date
Populations enrolled: Low-income
adults not covered under ACA Section
VIII (excludes pregnant women and
people with disabilities)
Mandatory
Populations enrolled: Low-income
adults covered under ACA Section VIII
(excludes pregnant women and people
with disabilities)
Voluntary
Populations enrolled: Aged, Blind or
Disabled Children or Adults
Voluntary Mandatory
Populations enrolled: Non-Disabled
Children (excludes children in foster
care or receiving adoption assistance)
Mandatory
Populations enrolled: Individuals
receiving Limited Benefits (excludes
partial duals)
Mandatory
Populations enrolled: Full Duals Voluntary Voluntary
Populations enrolled: Partial Duals Voluntary Voluntary
Populations enrolled: Children with
Special Health Care Needs
Voluntary
Populations enrolled: Native
American/Alaskan Natives
Voluntary Voluntary Voluntary
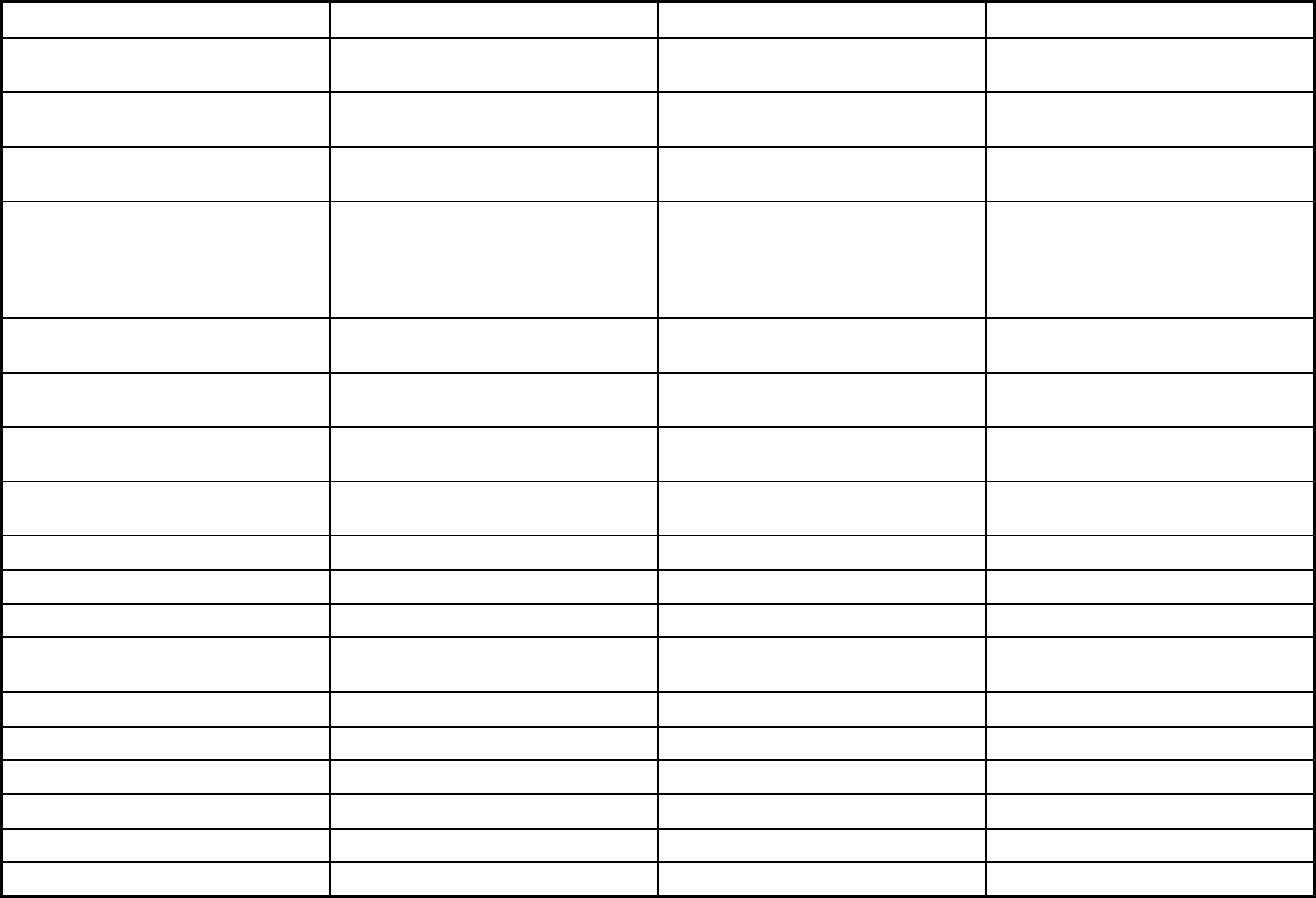
342
Features MI Choice Managed Care Plan Division Healthy Michigan Plan
Populations enrolled: Foster Care and
Adoption Assistance Children
Exempt Mandatory Exempt
Populations enrolled: Enrollment choice
period
Other Other Other
Populations enrolled: Enrollment broker
name (if applicable)
Michigan Enrolls Michigan Enrolls
Populations enrolled: Notes on
enrollment choice period
Enrollments and disenrollments are
allowed at any time. Enrollments are
always voluntary for qualified
individuals. Must meet NFLOC to
qualify.
New enrollees have up to 90 days to
switch Medicaid Health Plans, otherwise
there is a rolling open enrollment based
on the last digit of the individual's case
number.
New enrollees have up to 90 days to
switch Medicaid Health Plans, otherwise
there is a rolling open enrollment based
on the last digit of the individual's case
number.
Benefits covered: Inpatient hospital
physical health
X X
Benefits covered: Inpatient hospital
behavioral health (MH and/or SUD)
Benefits covered: Outpatient hospital
physical health
X X
Benefits covered: Outpatient hospital
behavioral health (MH and/or SUD)
X X X
Benefits covered: Partial hospitalization
Benefits covered: Physician X X
Benefits covered: Nurse practitioner X X
Benefits covered: Rural health clinics
and FQHCs
X X
Benefits covered: Clinic services X X
Benefits covered: Lab and x-ray X X
Benefits covered: Prescription drugs X X
Benefits covered: Prosthetic devices X X
Benefits covered: EPSDT X X
Benefits covered: Case management X X X
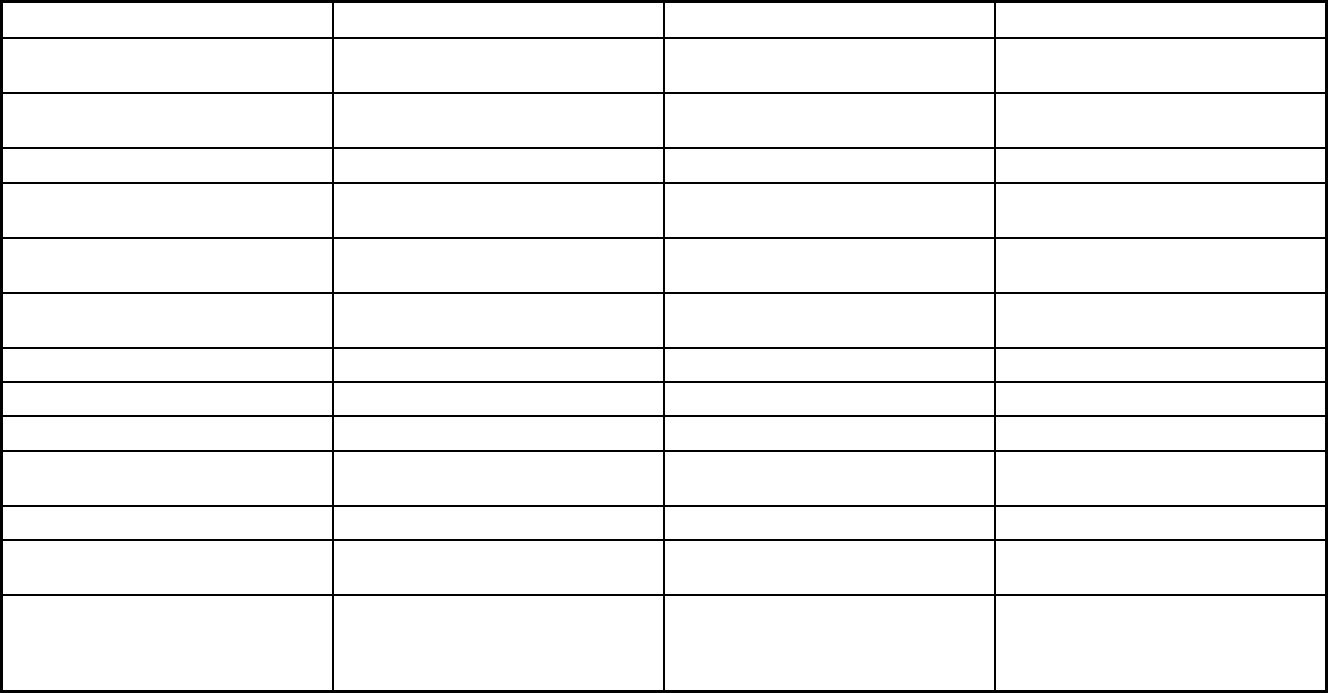
343
Features MI Choice Managed Care Plan Division Healthy Michigan Plan
Benefits covered: SSA Section 1945-
authorized health home
Benefits covered: Health home care
(services in home)
X
Benefits covered: Family planning X X
Benefits covered: Dental services
(medical/surgical)
X X
Benefits covered: Dental (preventative
or corrective)
X
Benefits covered: Personal care (state
plan option)
Benefits covered: HCBS waiver services X
Benefits covered: Private duty nursing X
Benefits covered: ICF-IDD
Benefits covered: Nursing facility
services
X
Benefits covered: Hospice care X
Benefits covered: Non-Emergency
Medical Transportation
X X
Benefits covered: Institution for Mental
Disease inpatient treatment for people
ages 21-64 defined by 42 CFR
§438.6(e) as an 'in lieu of' benefit
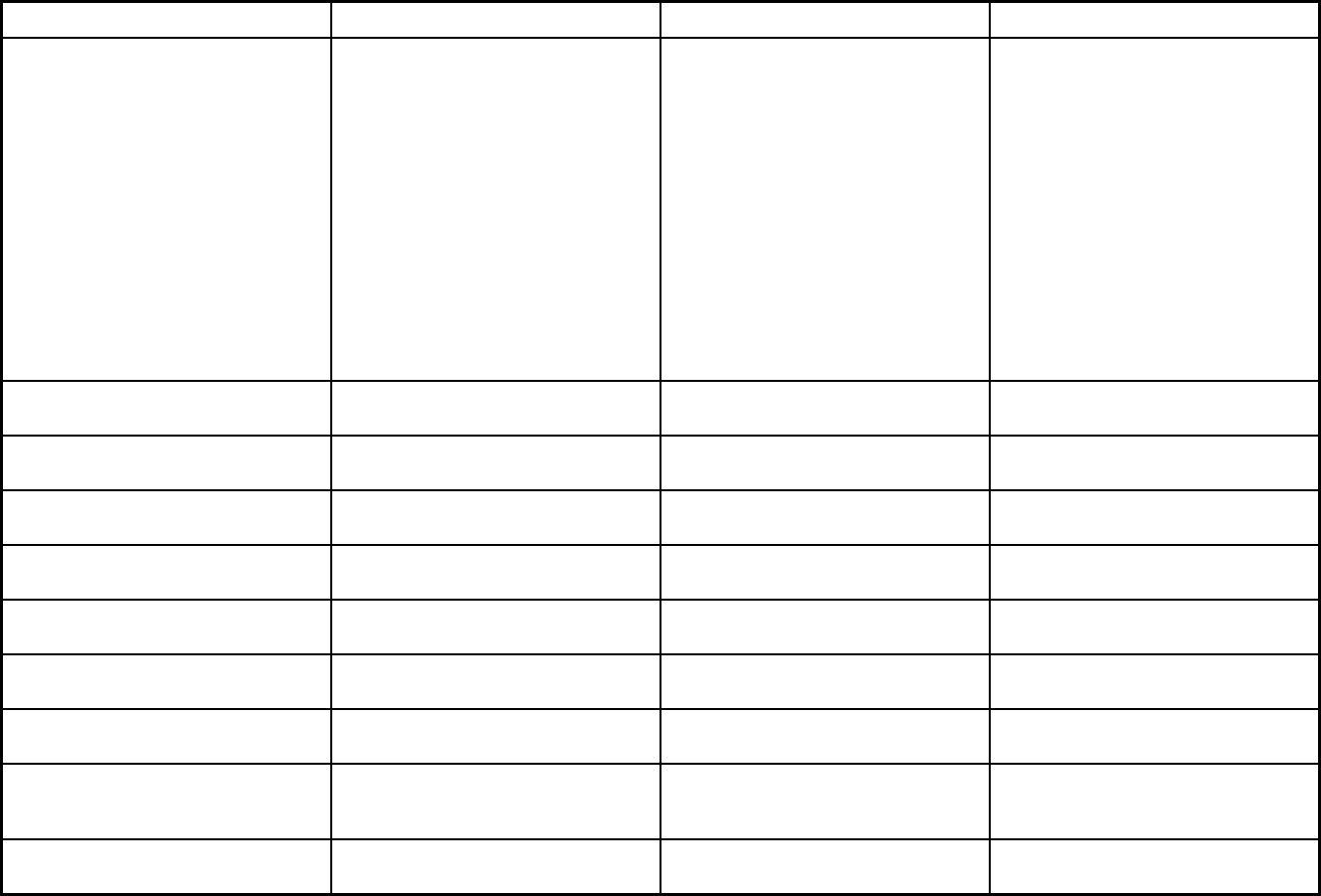
344
Features MI Choice Managed Care Plan Division Healthy Michigan Plan
Benefits covered: Other (e.g., nurse
midwife services, freestanding birth
centers, podiatry, etc.)
Adult Day Health, chore, community
living support, community transition,
counseling, home modifications, fiscal
intermediary, goods and services, home
delivered meals, non-medical
transportation, nursing services, PERS,
private duty nursing, respite, specialized
medical equipment and supplies,
supports coordination and trainers
Ambulance and other emergency
medical transportation, certified midwife
services, chiropractic services, DME
and supplies, emergency services, end
stage renal disease services, health
education, hearing and speech services,
hearing aids (under 21 years old),
medically necessary weight reduction
services, parenting and birthing classes,
podiatry services, prosthetics and
orthotics, tobacco cessation treatment,
speech, language, physical and
occupational therapies, transplant
services, transportation for medically
necessary covered services, treatment
for STDs, vision services
Ambulance and other emergency
medical transportation, certified midwife
services, chiropractic services, DME
and supplies, emergency services, end
stage renal disease services, health
educa
tion, hearing and speech services,
hearing aids (under 21 years old),
medically necessary weight reduction
services, parenting and birthing classes,
podiatry services, prosthetics and
orthotics, tobacco cessation treatment,
speech, language, physical and
occupational therapies, transplant
services, transportation for medically
necessary covered services, treatment
for STDs, vision services
Quality assurance and improvement:
HEDIS data required?
No Yes Yes
Quality assurance and improvement:
CAHPS data required?
No Yes Yes
Quality assurance and improvement:
Accreditation required?
No Yes Yes
Quality assurance and improvement:
Accrediting organization
NCQA, URAC NCQA, URAC
Quality assurance and improvement:
EQRO contractor name (if applicable)
Health Services Advisory Group Health Services Advisory Group
Performance incentives: Payment
bonuses/differentials to reward plans
X X
Performance incentives: Preferential
auto-enrollment to reward plans
X X
Performance incentives: Public reports
comparing plan performance on key
metrics
X X
Performance incentives: Withholds tied
to performance metrics
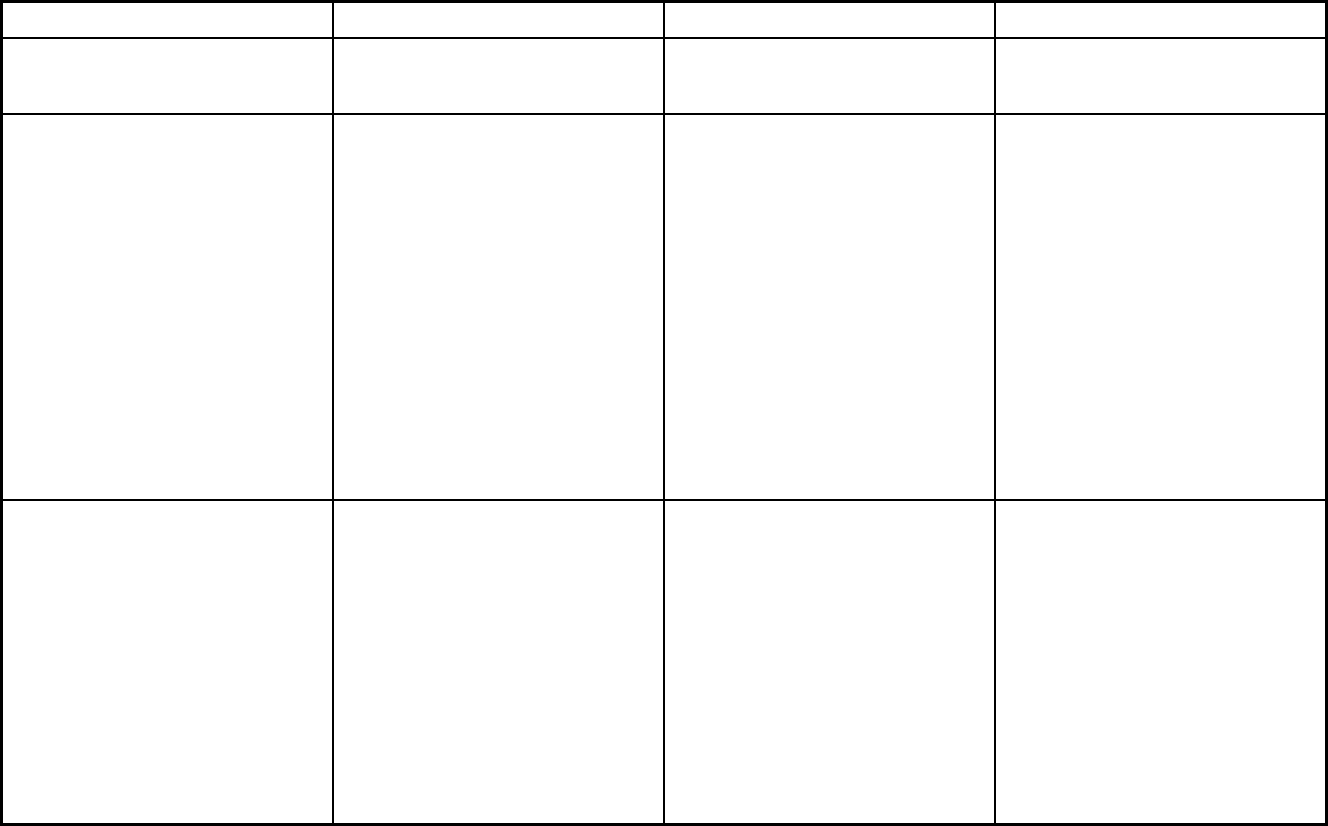
345
Features MI Choice Managed Care Plan Division Healthy Michigan Plan
Performance incentives: MCOs/PHPs
required or encouraged to pay providers
for value/quality outcomes
X X
Participating plans: Plans in Program Northern Healthcare Management;
Region 2 Area Agency on Aging;
Region 3B Area Agency on Aging;
Region 4 Area Agency on Aging;
Region 7 Area Agency on Aging;
Region 9 Area Agency on Aging;
Reliance Community Care Partners;
Senior Resources of West Michigan;
Senior Services Inc.; The Information
Center; The Senior Alliance; Tri County
Office on Aging; UPCAP Area Agency
on Aging; Valley Area Agency on Aging;
A & D Home Health Care, Inc.; Area
Agency on Aging 1-B; Area Agency on
Aging of NW Michigan; Area Agency on
Aging of Western Michigan; Detroit Area
Agency on Aging; MORC Home Care
Inc.
Aetna Better Health of Michigan; Blue
Cross Complete of Michigan; Harbor
Health Plan; HAP Midwest Health Plan;
McLaren Health Plan; Meridian Health
Plan of Michigan; Molina Healthcare of
Michigan; Priority Health Choice; Total
Health Care; UnitedHealthcare
Community Plan; Upper Peninsula
Health Plan
Aetna Better Health; Blue Cross
Complete of Michigan; Harbor Health
Plan; HAP Midwest Health Plan;
McLaren Health Plan; Meridian Health
Plan of Michigan; Molina Healthcare of
Michigan; Priority Health Choice; Total
Health Choice; UnitedHealthcare
Community Plan; Upper Peninsula
Health Plan
Notes: Program notes Cover HCBS only. Must be elderly or
disabled adult (at least age 18), meet
Nursing Facility Level of Care (NFLOC),
and require supports coordination and
at least one additional waiver service to
qualify. Accreditation is not required, but
some plans do this voluntarily.
In order to provide greater access and
to support coordination of care for
behavioral health services, the Michigan
Department of Health and Human
Services (MDHHS) has removed the 20-
visit maximum limitation for outpatient
behavioral health services
(psychotherapy services). The
restriction is lifted for both Fee-for-
Service and Medicaid Health Plan
beneficiaries effective for dates of
service on or after October 1, 2017.
Due to a policy change, Medicare
Eligibles are excluded from Healthy
Michigan Plan. In order to provide
greater access and to support
coordination of care for behavioral
health services, the Michigan
Department of Health and Human
Services (MDHHS) has removed the 20-
visit maximum limitation for outpatient
behavioral services (psychotherapy
services). The restriction is lifted for
both Fee-for-Service and Medicaid
Health Plan beneficiaries effective for
dates of service on or after October 1,
2017.
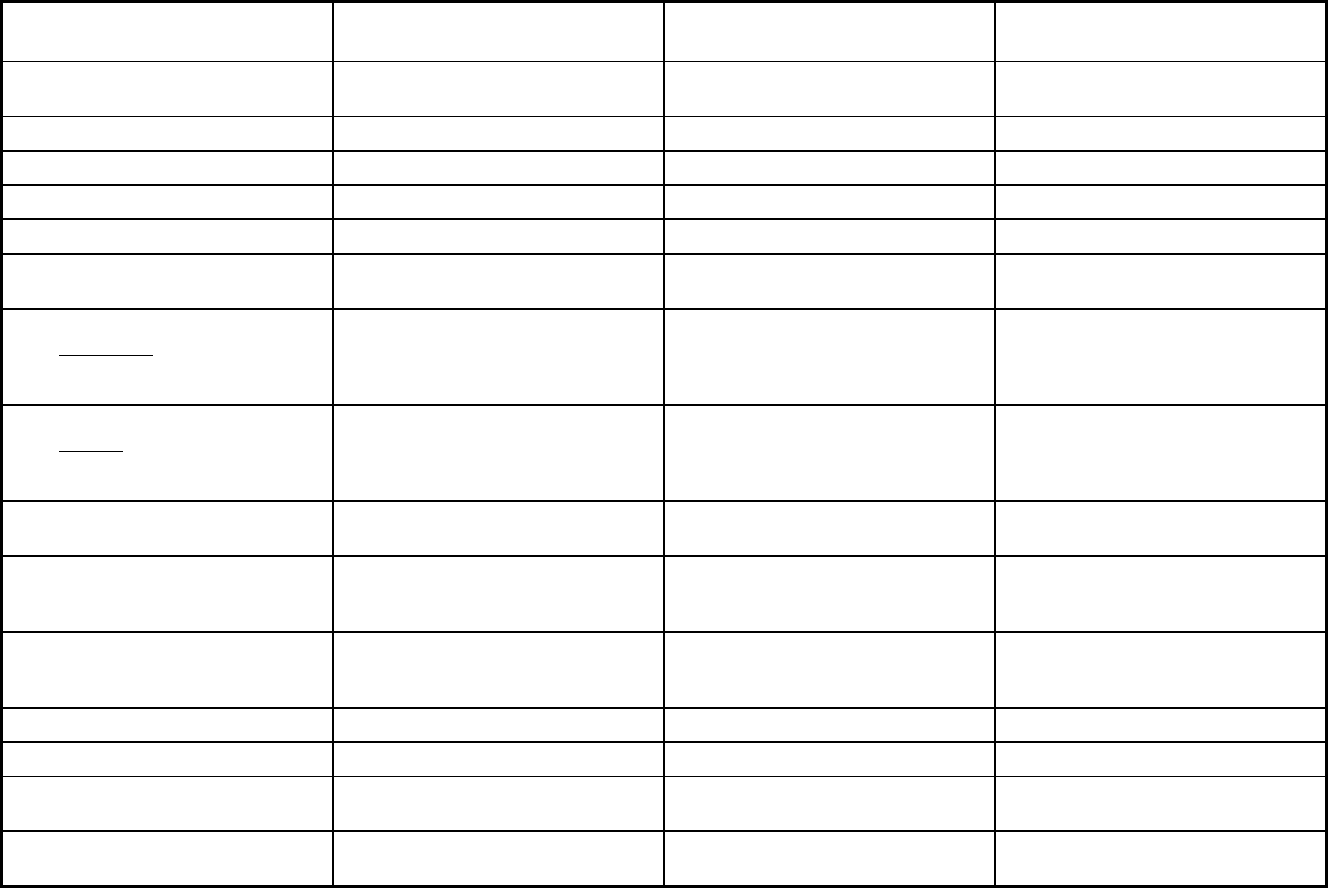
346
Michigan Managed Care Program Features, as of 2018 (2 of 2)
Features Healthy Kids Dental
Specialty Prepaid Inpatient Health
Plan PACE
Program type Dental only (PAHP) Behavioral Health Organization (BHO)
only (PIHP and/or PAHP)
Program of All-inclusive Care for the
Elderly (PACE)
Statewide or region-specific? Statewide Statewide Statewide
Federal operating authority 1915(b) 1915(b)/1915(c) PACE
Program start date 04/01/2009 10/01/1998 11/01/2003
Waiver expiration date (if applicable) 09/30/2020 09/30/2019
If the program ended in 2018, indicate
the end date
Populations enrolled: Low-income
adults not covered under ACA Section
VIII (excludes pregnant women and
people with disabilities)
Mandatory
Populations enrolled: Low-income
adults covered under ACA Section VIII
(excludes pregnant women and people
with disabilities)
Mandatory
Populations enrolled: Aged, Blind or
Disabled Children or Adults
Mandatory Mandatory Voluntary
Populations enrolled: Non-Disabled
Children (excludes children in foster
care or receiving adoption assistance)
Mandatory Mandatory
Populations enrolled: Individuals
receiving Limited Benefits (excludes
partial duals)
Mandatory
Populations enrolled: Full Duals Voluntary Voluntary
Populations enrolled: Partial Duals Voluntary Voluntary
Populations enrolled: Children with
Special Health Care Needs
Populations enrolled: Native
American/Alaskan Natives
Voluntary Voluntary Exempt
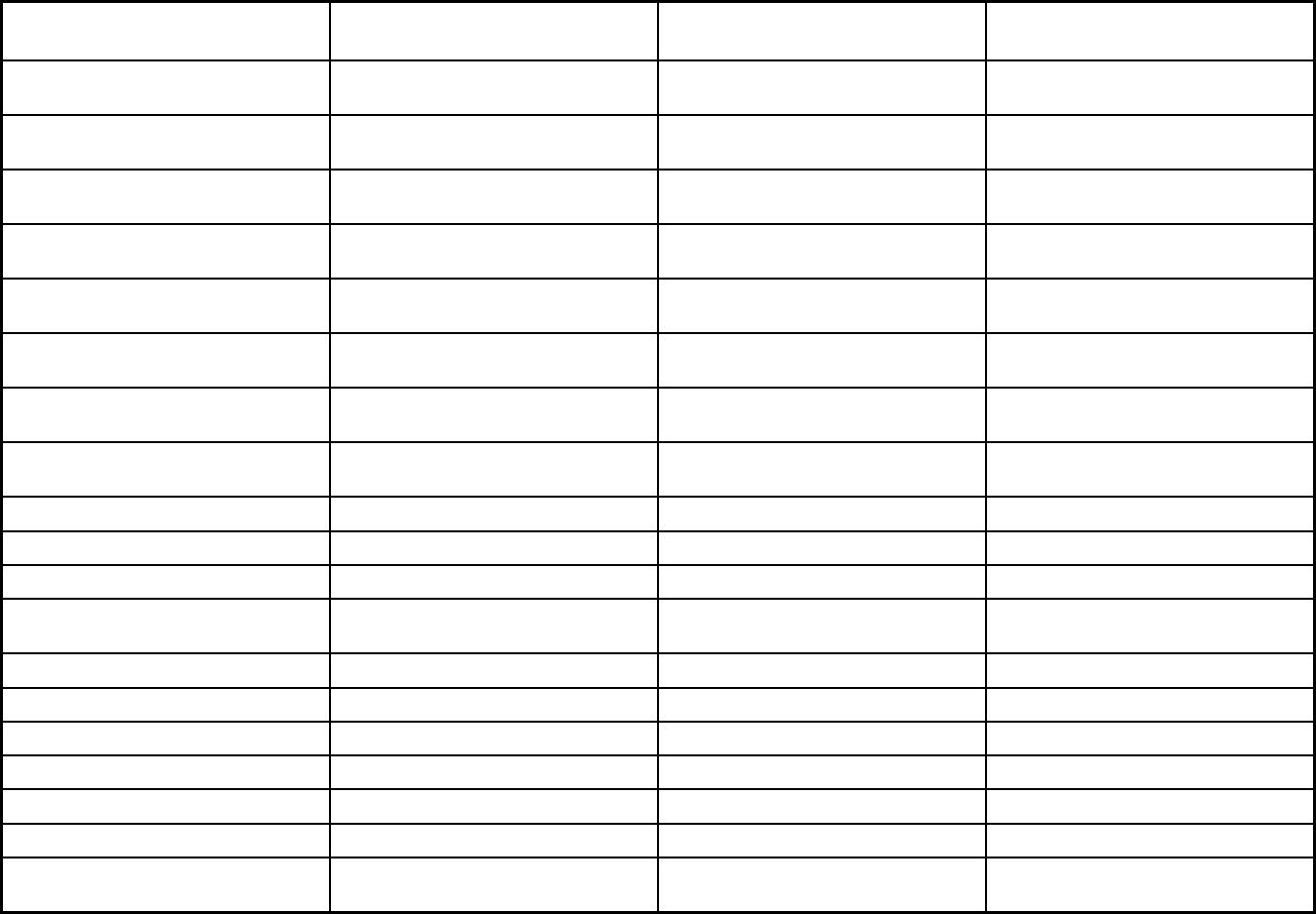
347
Features Healthy Kids Dental
Specialty Prepaid Inpatient Health
Plan PACE
Populations enrolled: Foster Care and
Adoption Assistance Children
Mandatory Mandatory Exempt
Populations enrolled: Enrollment choice
period
Other Other N/A
Populations enrolled: Enrollment broker
name (if applicable)
Populations enrolled: Notes on
enrollment choice period
Does not apply because the State only
contracts with one managed care entity.
No lock-in period.
Benefits covered: Inpatient hospital
physical health
X
Benefits covered: Inpatient hospital
behavioral health (MH and/or SUD)
X X
Benefits covered: Outpatient hospital
physical health
X
Benefits covered: Outpatient hospital
behavioral health (MH and/or SUD)
X X
Benefits covered: Partial hospitalization
Benefits covered: Physician X
Benefits covered: Nurse practitioner
Benefits covered: Rural health clinics
and FQHCs
Benefits covered: Clinic services
Benefits covered: Lab and x-ray X
Benefits covered: Prescription drugs X
Benefits covered: Prosthetic devices X
Benefits covered: EPSDT
Benefits covered: Case management X
Benefits covered: SSA Section 1945-
authorized health home
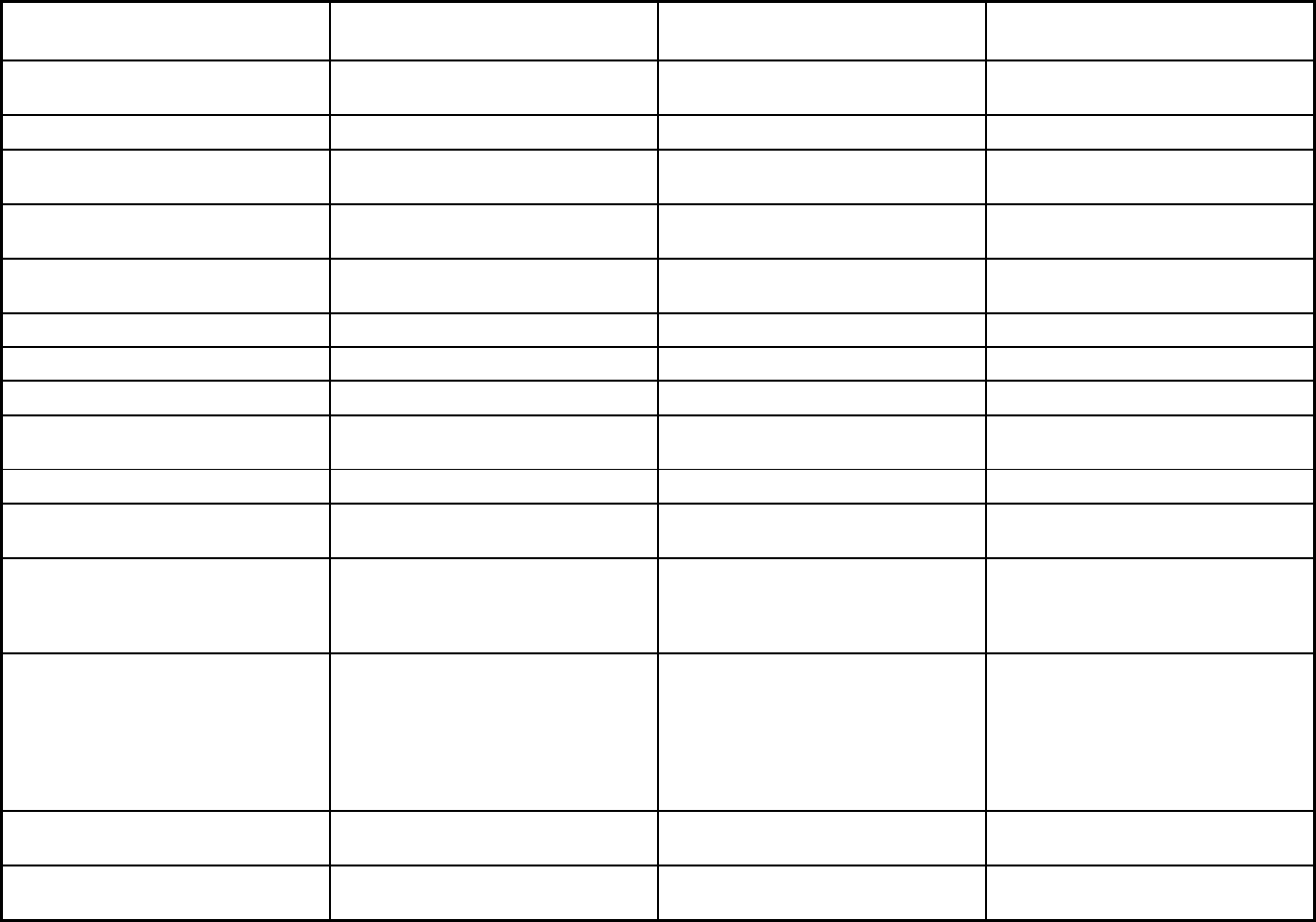
348
Features Healthy Kids Dental
Specialty Prepaid Inpatient Health
Plan PACE
Benefits covered: Health home care
(services in home)
X
Benefits covered: Family planning
Benefits covered: Dental services
(medical/surgical)
X
Benefits covered: Dental (preventative
or corrective)
X X
Benefits covered: Personal care (state
plan option)
X
Benefits covered: HCBS waiver services X X
Benefits covered: Private duty nursing
Benefits covered: ICF-IDD
Benefits covered: Nursing facility
services
X
Benefits covered: Hospice care
Benefits covered: Non-Emergency
Medical Transportation
X
Benefits covered: Institution for Mental
Disease inpatient treatment for people
ages 21-64 defined by 42 CFR
§438.6(e) as an 'in lieu of' benefit
Benefits covered: Other (e.g., nurse
midwife services, freestanding birth
centers, podiatry, etc.)
Assertive community treatment,
assessments, assistive technology,
behavior management review, child
therapy, clubhouse, community living
supports, crisis interventions, crisis
residential, enhanced pharmacy,
environmental modifications
Transportation
Quality assurance and improvement:
HEDIS data required?
No No No
Quality assurance and improvement:
CAHPS data required?
No No No
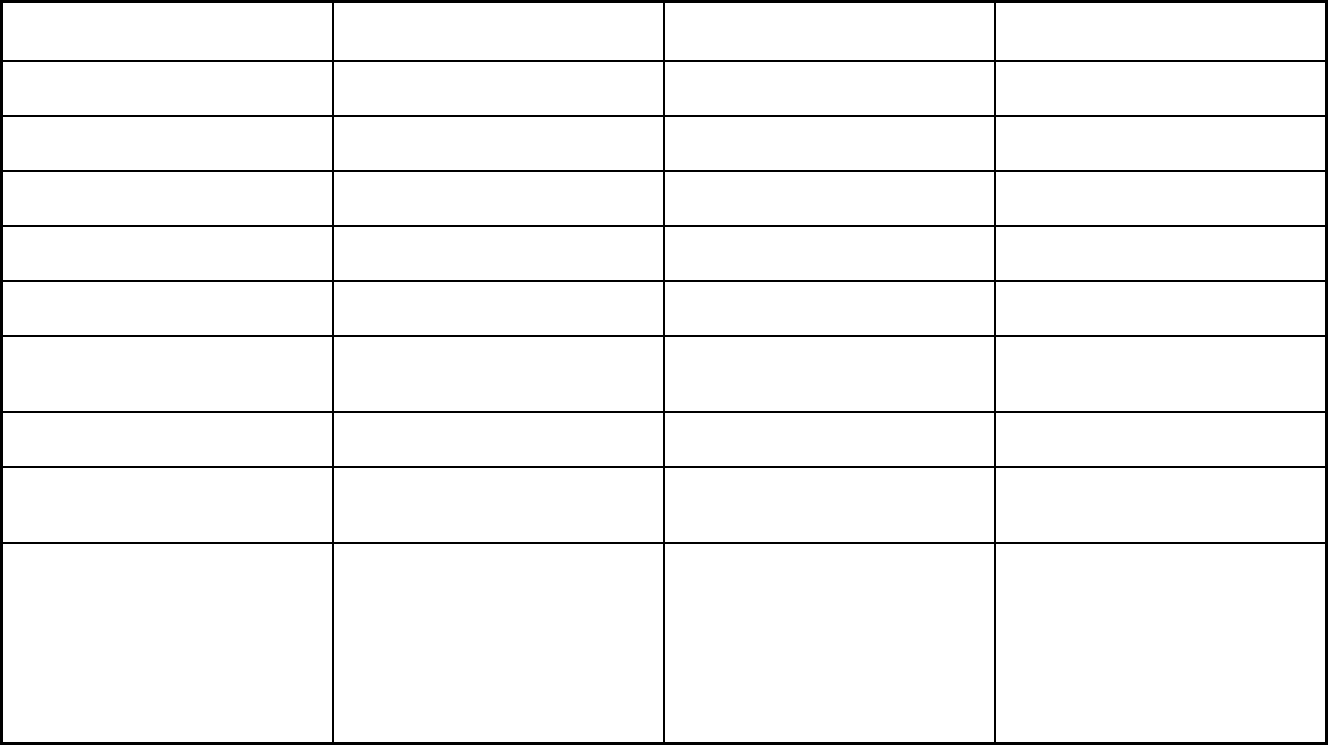
349
Features Healthy Kids Dental
Specialty Prepaid Inpatient Health
Plan PACE
Quality assurance and improvement:
Accreditation required?
No No No
Quality assurance and improvement:
Accrediting organization
Quality assurance and improvement:
EQRO contractor name (if applicable)
Performance incentives: Payment
bonuses/differentials to reward plans
Performance incentives: Preferential
auto-enrollment to reward plans
Performance incentives: Public reports
comparing plan performance on key
metrics
Performance incentives: Withholds tied
to performance metrics
Performance incentives: MCOs/PHPs
required or encouraged to pay providers
for value/quality outcomes
Participating plans: Plans in Program Healthy Kids Dental Lakeshore Regional Entity; Macomb
County CMH Services; Mid-State Health
Network; Northcare Network; Northern
Michigan Regional Entity; Oakland
County CMH Authority; Region 10;
Southwest Michigan Behavioral Health;
CMH Partnership of Southeast
Michigan; Detroit Wayne Mental Health
Authority
Care Resources; Community PACE;
Genesys PACE; Great Lakes PACE;
Huron Valley PACE; Life Circles; PACE
of Southeast MI; PACE of Southwest
MI; Senior Care Partners; Senior
Community Care; Thome PACE
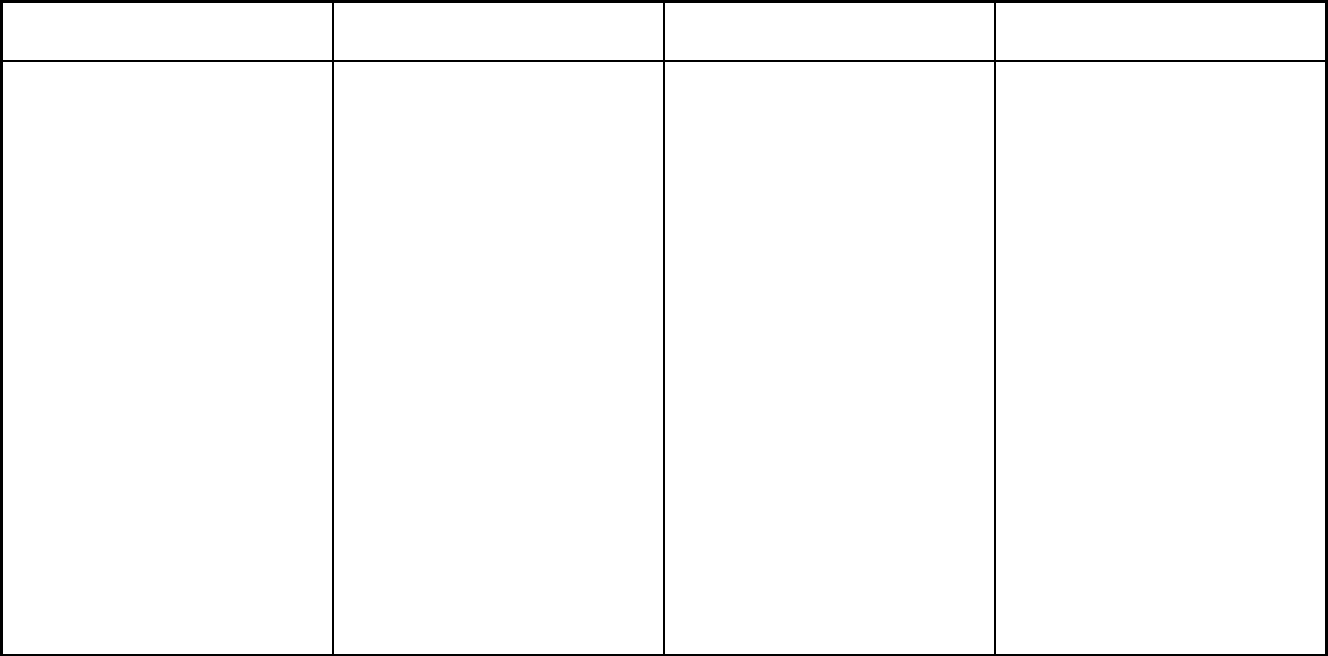
350
Features Healthy Kids Dental
Specialty Prepaid Inpatient Health
Plan PACE
Notes: Program notes MDHHS contracts for the administration
of the Medicaid dental benefit called
Healthy Kids Dental in all 83 counties.
The contractor administers the Medicaid
dental benefit to all Medicaid
beneficiaries under age 21 in the
participating counties. The dental
services provided through the contractor
mimic the dental services provided
through the Fee-For-Service Medicaid
program. Medicaid beneficiaries have
access to dentists through the
contractor's participating dental
networks. Beneficiaries must see a
dentist who participates with the Healthy
Kids Dental contract.
7,760 beneficiaries received HCBS
services as of 07/01/18.
Enrollment is voluntary and is not
restricted to individuals who are
Medicare beneficiaries and/or Medicaid
recipients. The PACE organization
receives a prospective monthly payment
for each Medicare participant based on
a rate similar to the rate paid to
Medicare Advantage, and a prospective
monthly payment for each Medicaid
participant that is negotiated between
the PACE organization and the State
administering agency. The Medicaid
capitation must be less than the amount
that would have been paid under the
State plan if the individuals were not
enrolled in PACE. PACE organizations
may charge a premium to individuals
who do not have Medicaid eligibility.
The PACE benefit package for all
participants, regardless of the source of
payment, must include all Medicaid-
covered services, as specified in the
State's approved Medicaid individual's
overall health status. While enrolled in
a PACE program, the participant must
receive all Medicare and Medicaid
benefits solely through the PACE
organization.

351
Minnesota Managed Care Program Features, as of 2018 (1 of 2)
Features Special Needs Basic Care (SNBC)
Prepaid Medical Assistance Plan
Plus (PMAP+) Minnesota Senior Care Plus (MSC+)
Program type Comprehensive MCO + MLTSS Comprehensive MCO + MLTSS Comprehensive MCO + MLTSS
Statewide or region-specific? Statewide Statewide Statewide
Federal operating authority 1915(a),1945 Health Homes 1915(b),1932(a),1945 Health Homes 1915(b)/1915(c),1945 Health Homes
Program start date 01/01/2008 07/01/1985 06/01/2005
Waiver expiration date (if applicable) 06/30/2021 06/30/2021
If the program ended in 2018, indicate
the end date
Populations enrolled: Low-income
adults not covered under ACA Section
VIII (excludes pregnant women and
people with disabilities)
Mandatory
Populations enrolled: Low-income
adults covered under ACA Section VIII
(excludes pregnant women and people
with disabilities)
Mandatory
Populations enrolled: Aged, Blind or
Disabled Children or Adults
Voluntary Mandatory
Populations enrolled: Non-Disabled
Children (excludes children in foster
care or receiving adoption assistance)
Mandatory
Populations enrolled: Individuals
receiving Limited Benefits (excludes
partial duals)
Populations enrolled: Full Duals Voluntary Mandatory
Populations enrolled: Partial Duals
Populations enrolled: Children with
Special Health Care Needs
Voluntary
Populations enrolled: Native
American/Alaskan Natives
Voluntary Mandatory Mandatory
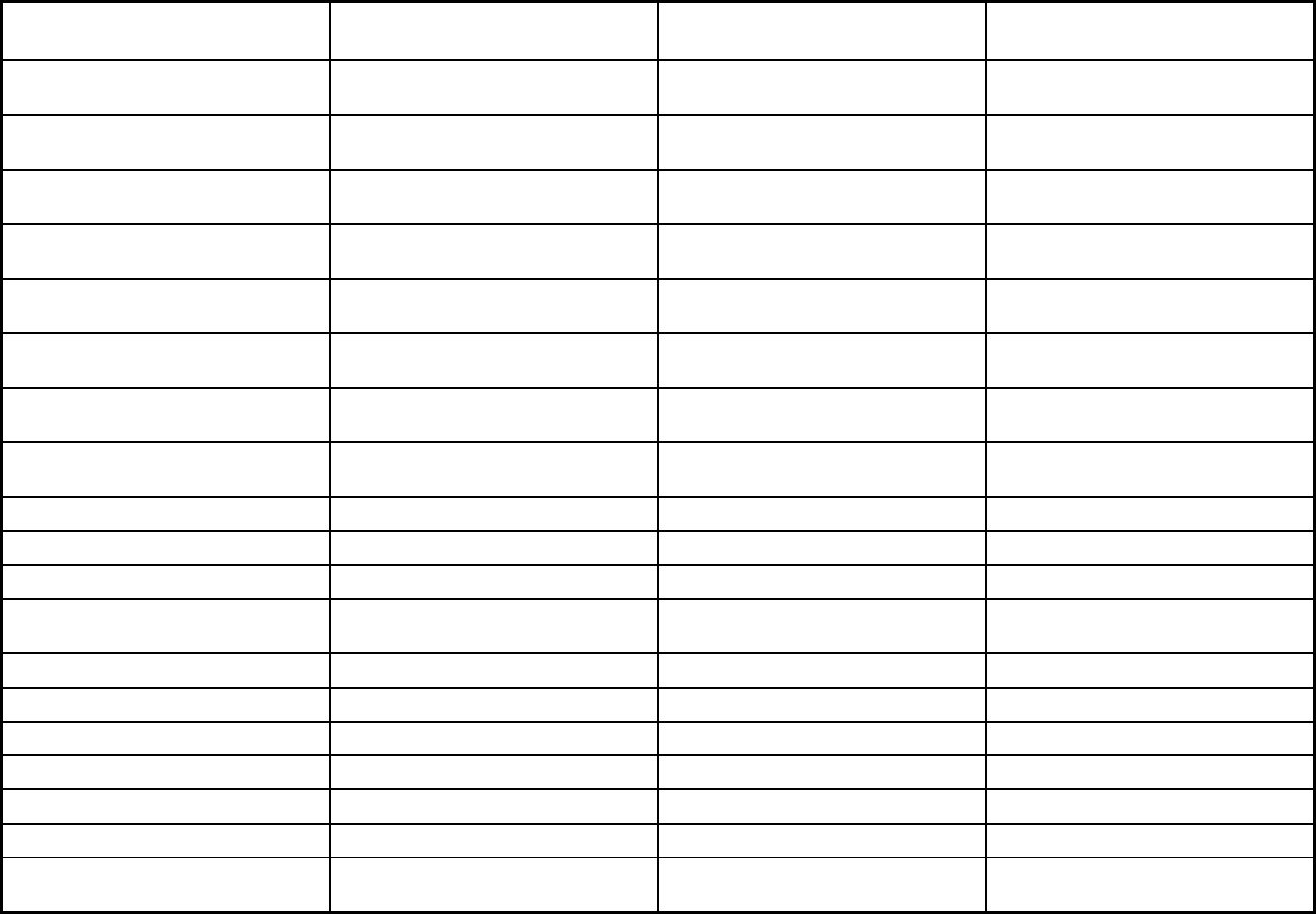
352
Features Special Needs Basic Care (SNBC)
Prepaid Medical Assistance Plan
Plus (PMAP+) Minnesota Senior Care Plus (MSC+)
Populations enrolled: Foster Care and
Adoption Assistance Children
Voluntary Mandatory Exempt
Populations enrolled: Enrollment choice
period
30 days 30 days 30 days
Populations enrolled: Enrollment broker
name (if applicable)
Populations enrolled: Notes on
enrollment choice period
Benefits covered: Inpatient hospital
physical health
X X X
Benefits covered: Inpatient hospital
behavioral health (MH and/or SUD)
X X X
Benefits covered: Outpatient hospital
physical health
X X X
Benefits covered: Outpatient hospital
behavioral health (MH and/or SUD)
X X X
Benefits covered: Partial hospitalization X X X
Benefits covered: Physician X X X
Benefits covered: Nurse practitioner X X X
Benefits covered: Rural health clinics
and FQHCs
Benefits covered: Clinic services X X X
Benefits covered: Lab and x-ray X X X
Benefits covered: Prescription drugs X X X
Benefits covered: Prosthetic devices X X X
Benefits covered: EPSDT X X
Benefits covered: Case management X X X
Benefits covered: SSA Section 1945-
authorized health home
X X X
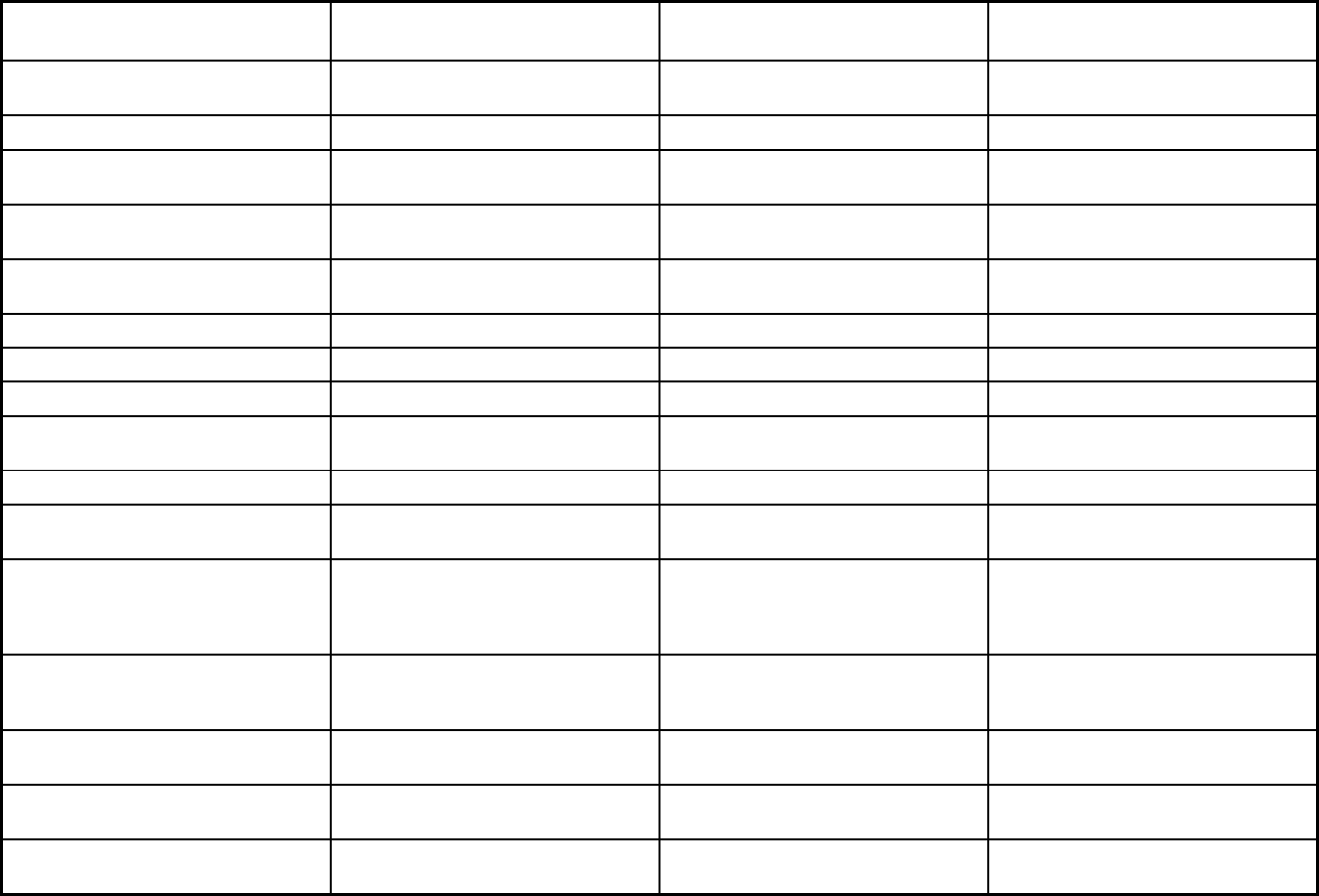
353
Features Special Needs Basic Care (SNBC)
Prepaid Medical Assistance Plan
Plus (PMAP+) Minnesota Senior Care Plus (MSC+)
Benefits covered: Health home care
(services in home)
X X X
Benefits covered: Family planning X X X
Benefits covered: Dental services
(medical/surgical)
X X X
Benefits covered: Dental (preventative
or corrective)
X X X
Benefits covered: Personal care (state
plan option)
X X
Benefits covered: HCBS waiver services X
Benefits covered: Private duty nursing X X
Benefits covered: ICF-IDD
Benefits covered: Nursing facility
services
X X X
Benefits covered: Hospice care X X X
Benefits covered: Non-Emergency
Medical Transportation
X X X
Benefits covered: Institution for Mental
Disease inpatient treatment for people
ages 21-64 defined by 42 CFR
§438.6(e) as an 'in lieu of' benefit
X X
Benefits covered: Other (e.g., nurse
midwife services, freestanding birth
centers, podiatry, etc.)
Quality assurance and improvement:
HEDIS data required?
Yes Yes Yes
Quality assurance and improvement:
CAHPS data required?
Yes Yes Yes
Quality assurance and improvement:
Accreditation required?
No No No
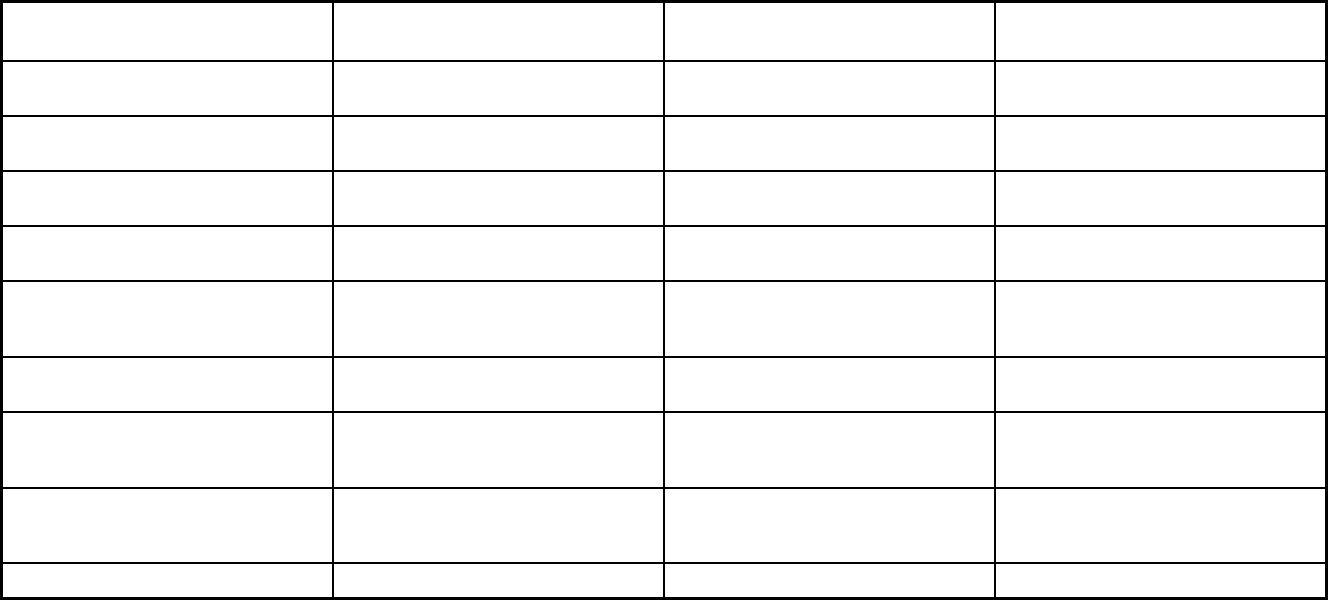
354
Features Special Needs Basic Care (SNBC)
Prepaid Medical Assistance Plan
Plus (PMAP+) Minnesota Senior Care Plus (MSC+)
Quality assurance and improvement:
Accrediting organization
Quality assurance and improvement:
EQRO contractor name (if applicable)
Michigan Peer Review Organization Michigan Peer Review Organization Michigan Peer Review Organization
Performance incentives: Payment
bonuses/differentials to reward plans
Performance incentives: Preferential
auto-enrollment to reward plans
X X X
Performance incentives: Public reports
comparing plan performance on key
metrics
Performance incentives: Withholds tied
to performance metrics
X X
Performance incentives: MCOs/PHPs
required or encouraged to pay providers
for value/quality outcomes
X X X
Participating plans: Plans in Program Health Partners; Hennepin Health;
Medica; Prime West; South Country; U
Care
Blue Plus; Health Partners; Hennepin
Health; Itasca Medical Care; Prime
West; South Country; U Care
Blue Plus; Health Partners; Itasca
Medical Care; Medica; Prime West;
South Country; U Care
Notes: Program notes
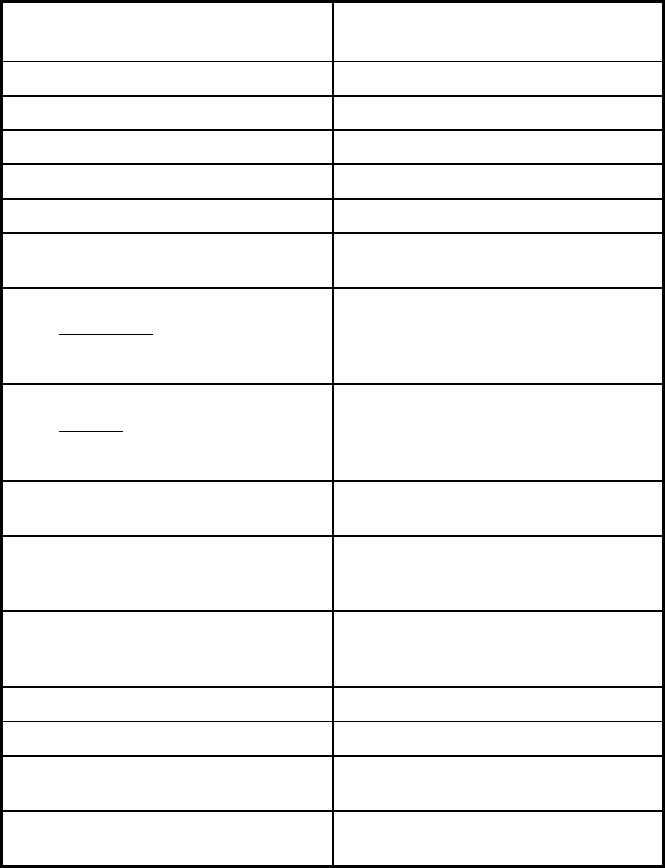
355
Minnesota Managed Care Program Features, as of 2018 (2 of 2)
Features
Minnesota Senior Health Option
(MSHO)
Program type Comprehensive MCO + MLTSS
Statewide or region-specific? Statewide
Federal operating authority 1915(a)/1915(c),1945 Health Homes
Program start date 03/01/1997
Waiver expiration date (if applicable) 12/31/2020
If the program ended in 2018, indicate
the end date
Populations enrolled: Low-income
adults not covered under ACA Section
VIII (excludes pregnant women and
people with disabilities)
Populations enrolled: Low-income
adults covered under ACA Section VIII
(excludes pregnant women and people
with disabilities)
Populations enrolled: Aged, Blind or
Disabled Children or Adults
Voluntary
Populations enrolled: Non-Disabled
Children (excludes children in foster
care or receiving adoption assistance)
Populations enrolled: Individuals
receiving Limited Benefits (excludes
partial duals)
Populations enrolled: Full Duals Voluntary
Populations enrolled: Partial Duals
Populations enrolled: Children with
Special Health Care Needs
Populations enrolled: Native
American/Alaskan Natives
Voluntary
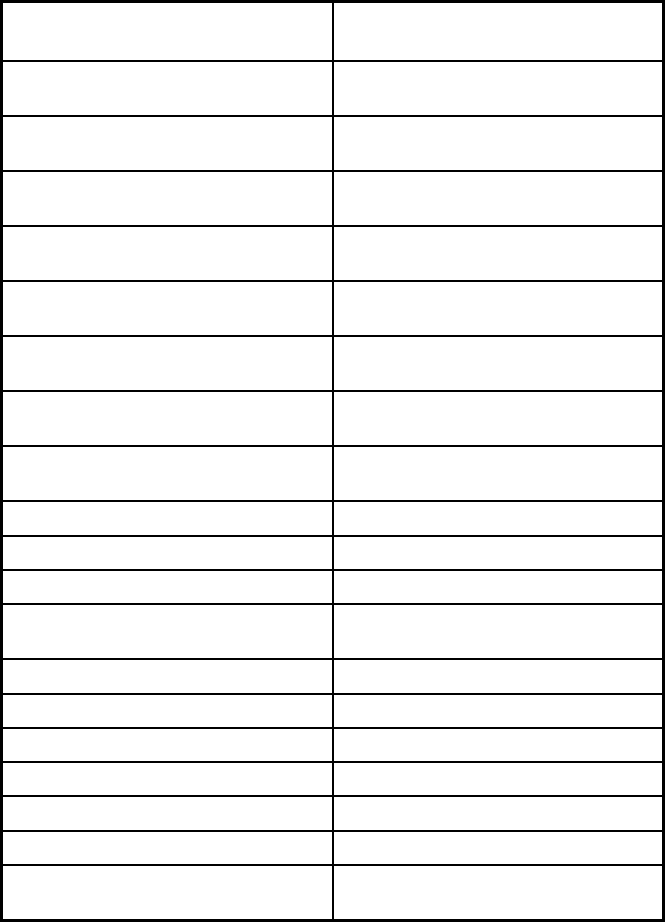
356
Features
Minnesota Senior Health Option
(MSHO)
Populations enrolled: Foster Care and
Adoption Assistance Children
Exempt
Populations enrolled: Enrollment choice
period
30 days
Populations enrolled: Enrollment broker
name (if applicable)
Populations enrolled: Notes on
enrollment choice period
Benefits covered: Inpatient hospital
physical health
X
Benefits covered: Inpatient hospital
behavioral health (MH and/or SUD)
X
Benefits covered: Outpatient hospital
physical health
X
Benefits covered: Outpatient hospital
behavioral health (MH and/or SUD)
X
Benefits covered: Partial hospitalization X
Benefits covered: Physician X
Benefits covered: Nurse practitioner X
Benefits covered: Rural health clinics
and FQHCs
Benefits covered: Clinic services X
Benefits covered: Lab and x-ray X
Benefits covered: Prescription drugs X
Benefits covered: Prosthetic devices X
Benefits covered: EPSDT
Benefits covered: Case management X
Benefits covered: SSA Section 1945-
authorized health home
X
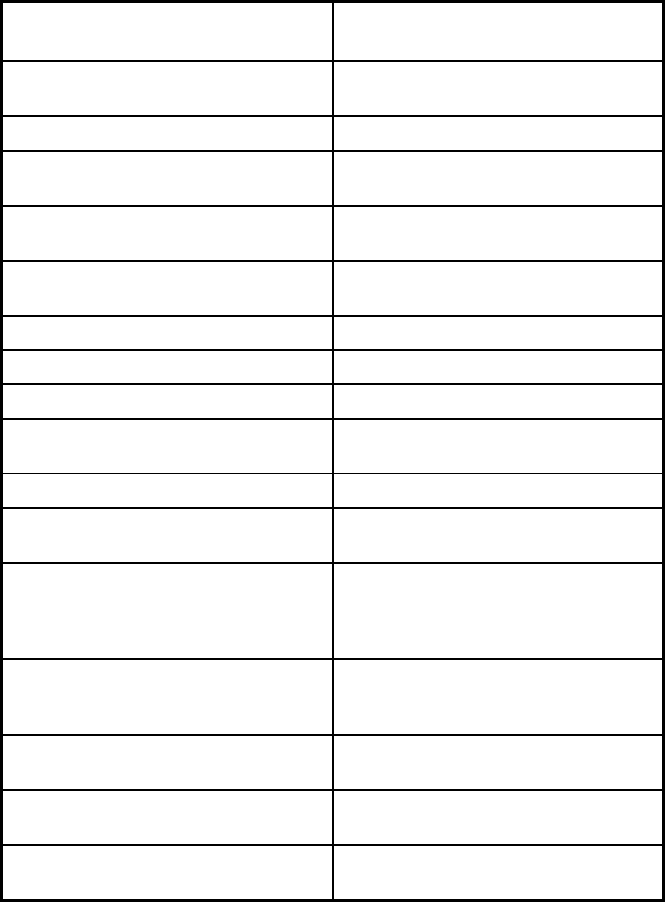
357
Features
Minnesota Senior Health Option
(MSHO)
Benefits covered: Health home care
(services in home)
X
Benefits covered: Family planning X
Benefits covered: Dental services
(medical/surgical)
X
Benefits covered: Dental (preventative
or corrective)
X
Benefits covered: Personal care (state
plan option)
X
Benefits covered: HCBS waiver services X
Benefits covered: Private duty nursing X
Benefits covered: ICF-IDD
Benefits covered: Nursing facility
services
X
Benefits covered: Hospice care X
Benefits covered: Non-Emergency
Medical Transportation
X
Benefits covered: Institution for Mental
Disease inpatient treatment for people
ages 21-64 defined by 42 CFR
§438.6(e) as an 'in lieu of' benefit
Benefits covered: Other (e.g., nurse
midwife services, freestanding birth
centers, podiatry, etc.)
Quality assurance and improvement:
HEDIS data required?
Yes
Quality assurance and improvement:
CAHPS data required?
Yes
Quality assurance and improvement:
Accreditation required?
No
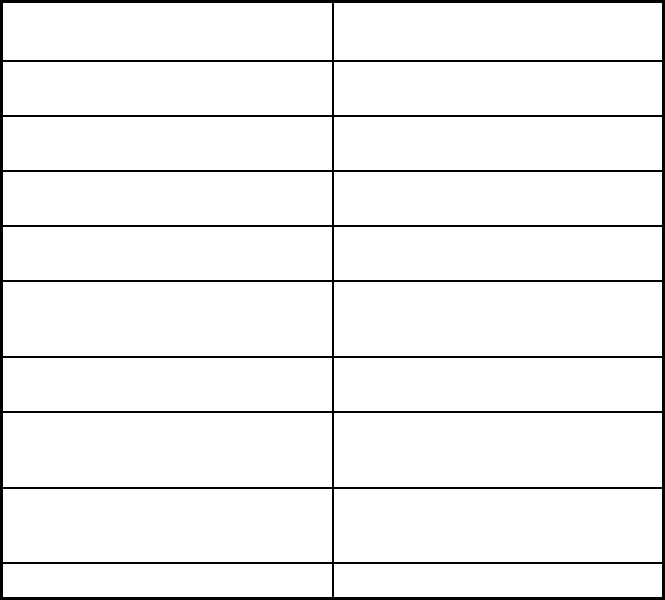
358
Features
Minnesota Senior Health Option
(MSHO)
Quality assurance and improvement:
Accrediting organization
Quality assurance and improvement:
EQRO contractor name (if applicable)
Michigan Peer Review Organization
Performance incentives: Payment
bonuses/differentials to reward plans
Performance incentives: Preferential
auto-enrollment to reward plans
X
Performance incentives: Public reports
comparing plan performance on key
metrics
Performance incentives: Withholds tied
to performance metrics
X
Performance incentives: MCOs/PHPs
required or encouraged to pay providers
for value/quality outcomes
X
Participating plans: Plans in Program Blue Plus; Health Partners; Itasca
Medical Care; Medica; Prime West;
South Country; U Care
Notes: Program notes
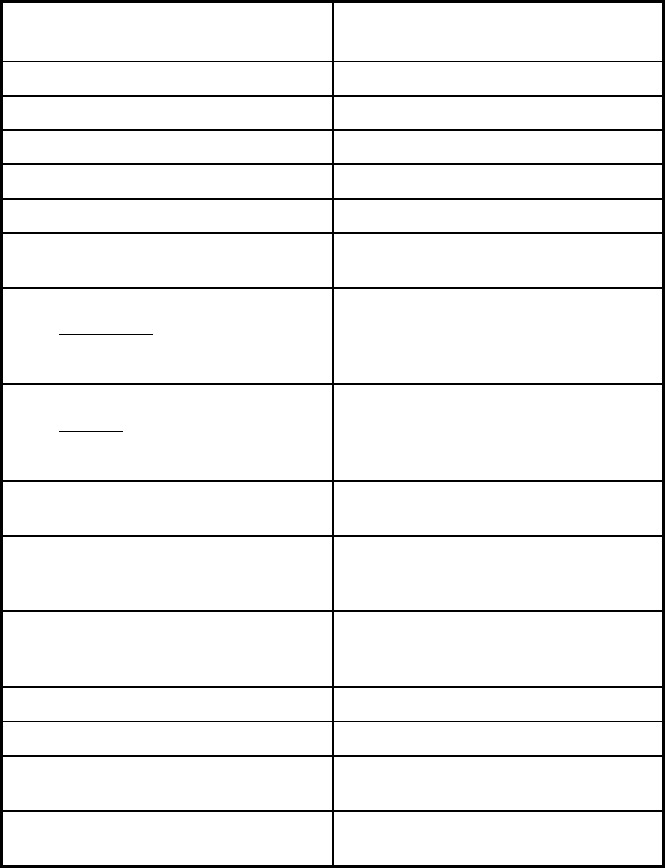
359
Mississippi Managed Care Program Features, as of 2018
Features
Mississippi Coordinated Access
Network (MississippiCAN)
Program type Comprehensive MCO
Statewide or region-specific? Statewide
Federal operating authority 1932(a)
Program start date 01/01/2011
Waiver expiration date (if applicable)
If the program ended in 2018, indicate
the end date
Populations enrolled: Low-income
adults not covered under ACA Section
VIII (excludes pregnant women and
people with disabilities)
Mandatory
Populations enrolled: Low-income
adults covered under ACA Section VIII
(excludes pregnant women and people
with disabilities)
Populations enrolled: Aged, Blind or
Disabled Children or Adults
Mandatory
Populations enrolled: Non-Disabled
Children (excludes children in foster
care or receiving adoption assistance)
Mandatory
Populations enrolled: Individuals
receiving Limited Benefits (excludes
partial duals)
Populations enrolled: Full Duals
Populations enrolled: Partial Duals
Populations enrolled: Children with
Special Health Care Needs
Voluntary
Populations enrolled: Native
American/Alaskan Natives
Voluntary
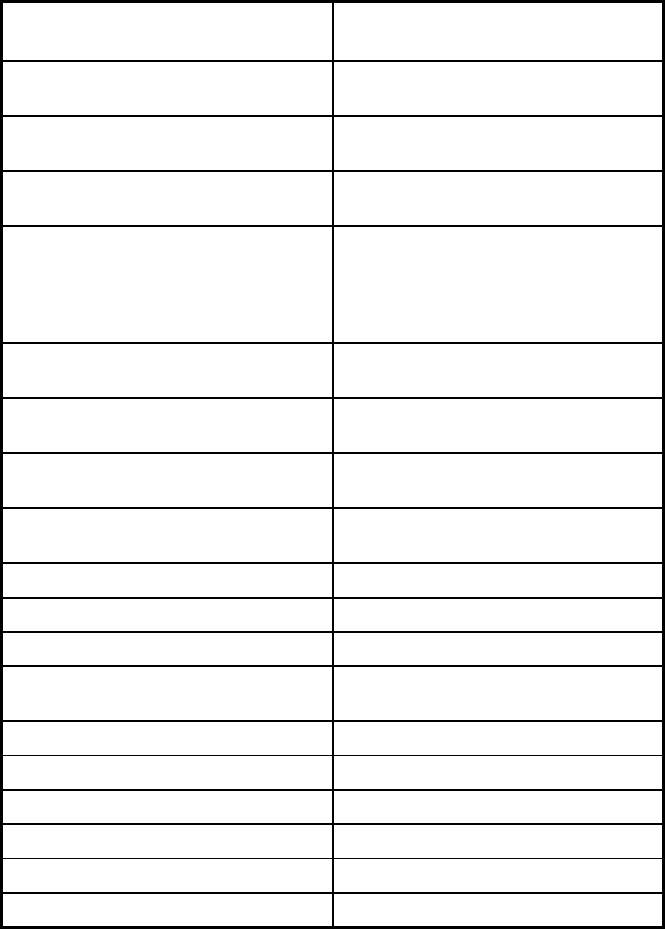
360
Features
Mississippi Coordinated Access
Network (MississippiCAN)
Populations enrolled: Foster Care and
Adoption Assistance Children
Voluntary
Populations enrolled: Enrollment choice
period
Other
Populations enrolled: Enrollment broker
name (if applicable)
Conduent
Populations enrolled: Notes on
enrollment choice period
Members are allowed 30 days to
choose an MCO or be autoassigned.
After MCO assignment, members are
allowed to change MCO during initial 90
days.
Benefits covered: Inpatient hospital
physical health
X
Benefits covered: Inpatient hospital
behavioral health (MH and/or SUD)
X
Benefits covered: Outpatient hospital
physical health
X
Benefits covered: Outpatient hospital
behavioral health (MH and/or SUD)
X
Benefits covered: Partial hospitalization
Benefits covered: Physician X
Benefits covered: Nurse practitioner X
Benefits covered: Rural health clinics
and FQHCs
X
Benefits covered: Clinic services X
Benefits covered: Lab and x-ray X
Benefits covered: Prescription drugs X
Benefits covered: Prosthetic devices X
Benefits covered: EPSDT X
Benefits covered: Case management X
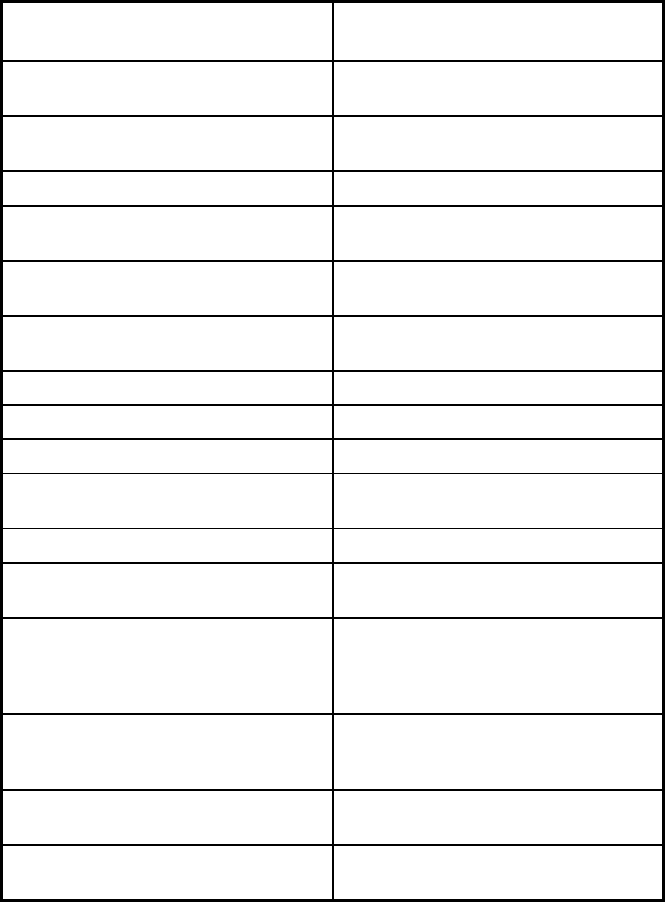
361
Features
Mississippi Coordinated Access
Network (MississippiCAN)
Benefits covered: SSA Section 1945-
authorized health home
Benefits covered: Health home care
(services in home)
X
Benefits covered: Family planning X
Benefits covered: Dental services
(medical/surgical)
X
Benefits covered: Dental (preventative
or corrective)
X
Benefits covered: Personal care (state
plan option)
X
Benefits covered: HCBS waiver services
Benefits covered: Private duty nursing X
Benefits covered: ICF-IDD
Benefits covered: Nursing facility
services
Benefits covered: Hospice care X
Benefits covered: Non-Emergency
Medical Transportation
X
Benefits covered: Institution for Mental
Disease inpatient treatment for people
ages 21-64 defined by 42 CFR
§438.6(e) as an 'in lieu of' benefit
Benefits covered: Other (e.g., nurse
midwife services, freestanding birth
centers, podiatry, etc.)
Quality assurance and improvement:
HEDIS data required?
Yes
Quality assurance and improvement:
CAHPS data required?
Yes
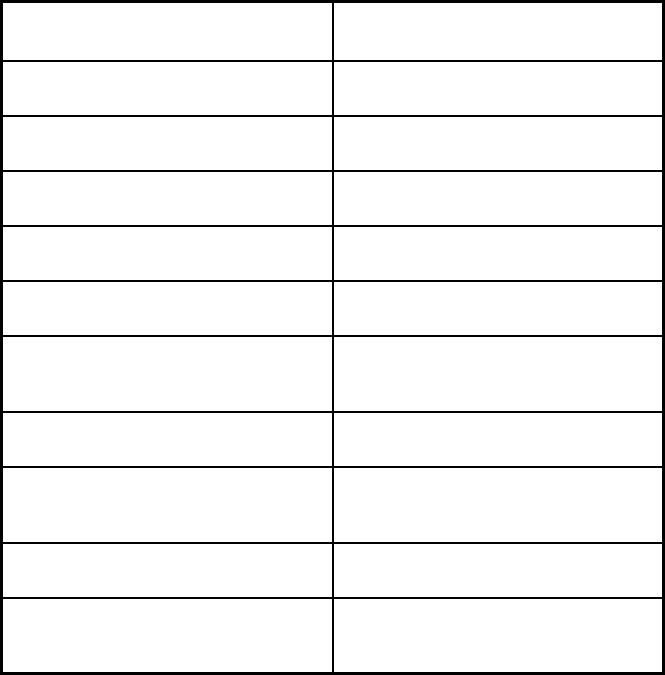
362
Features
Mississippi Coordinated Access
Network (MississippiCAN)
Quality assurance and improvement:
Accreditation required?
No, but accreditation considered in plan
selection criteria
Quality assurance and improvement:
Accrediting organization
NCQA, JCAHO, URAC
Quality assurance and improvement:
EQRO contractor name (if applicable)
The Carolinas Center for Medical
Excellence
Performance incentives: Payment
bonuses/differentials to reward plans
Performance incentives: Preferential
auto-enrollment to reward plans
Performance incentives: Public reports
comparing plan performance on key
metrics
Performance incentives: Withholds tied
to performance metrics
X
Performance incentives: MCOs/PHPs
required or encouraged to pay providers
for value/quality outcomes
X
Participating plans: Plans in Program Magnolia Health Plan; UnitedHealthcare
of Mississippi Community Plan
Notes: Program notes A third MCO was added to the
MississippiCAN program on October 1,
2018: Molina Healthcare of Mississippi.
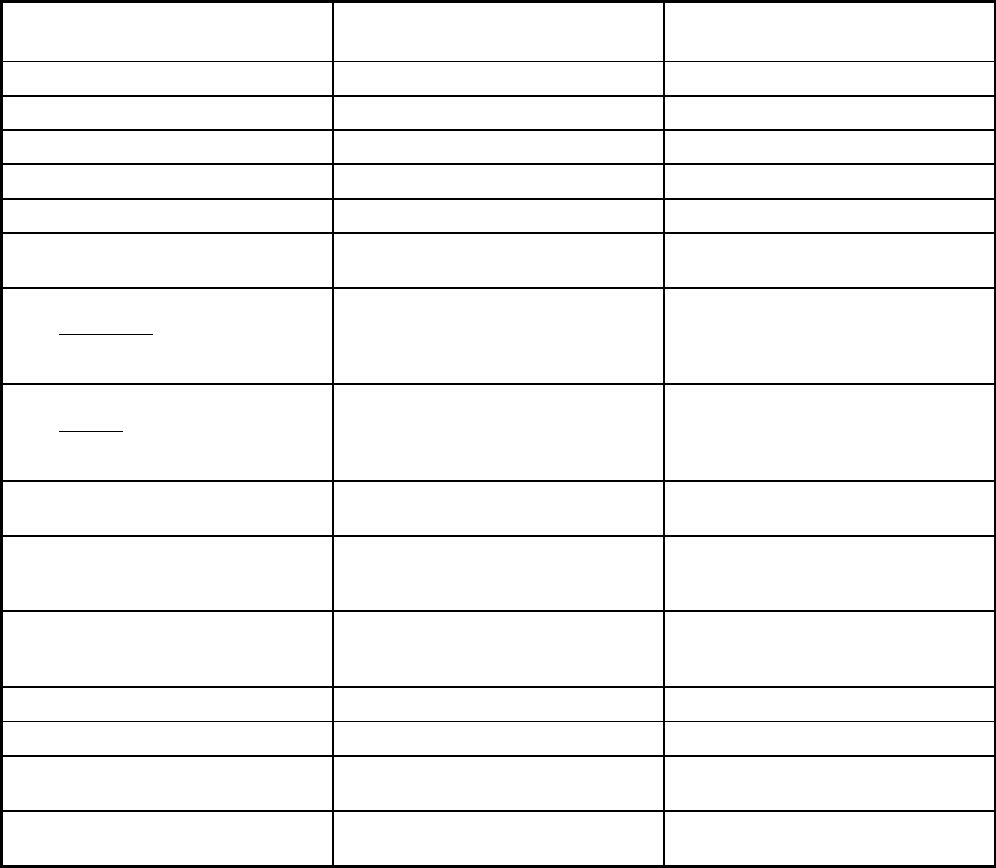
363
Missouri Managed Care Program Features, as of 2018
Features MO HealthNet Managed Care/1915b
Non-Emergency Medical
Transportation Program (NEMT)
Program type Comprehensive MCO Non-Emergency Medical Transportation
Statewide or region-specific? Statewide Statewide
Federal operating authority 1915(b) 1902(a)(70) NEMT
Program start date 09/01/1995 10/01/2006
Waiver expiration date (if applicable) 06/30/2020
If the program ended in 2018, indicate
the end date
Populations enrolled: Low-income
adults not covered under ACA Section
VIII (excludes pregnant women and
people with disabilities)
Mandatory Mandatory
Populations enrolled: Low-income
adults covered under ACA Section VIII
(excludes pregnant women and people
with disabilities)
Populations enrolled: Aged, Blind or
Disabled Children or Adults
Mandatory Mandatory
Populations enrolled: Non-Disabled
Children (excludes children in foster
care or receiving adoption assistance)
Mandatory Mandatory
Populations enrolled: Individuals
receiving Limited Benefits (excludes
partial duals)
Populations enrolled: Full Duals Mandatory
Populations enrolled: Partial Duals Mandatory
Populations enrolled: Children with
Special Health Care Needs
Mandatory Mandatory
Populations enrolled: Native
American/Alaskan Natives
Mandatory Mandatory
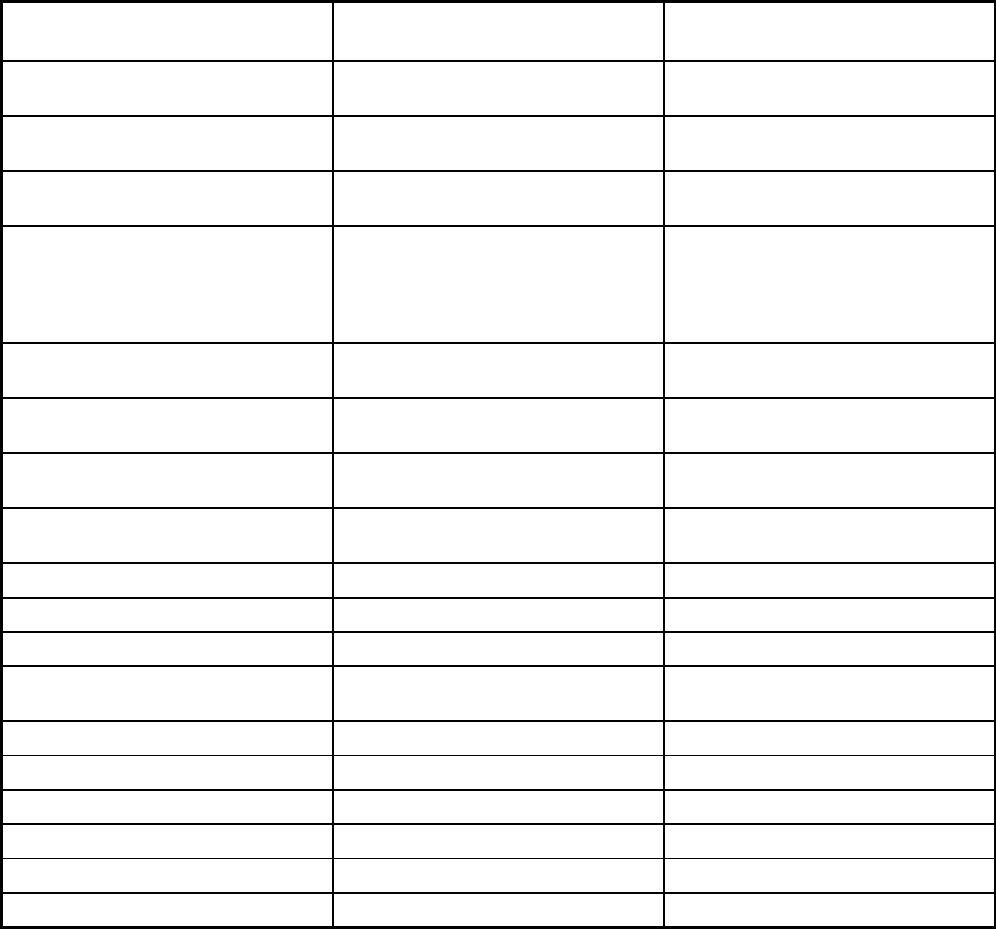
364
Features MO HealthNet Managed Care/1915b
Non-Emergency Medical
Transportation Program (NEMT)
Populations enrolled: Foster Care and
Adoption Assistance Children
Mandatory Mandatory
Populations enrolled: Enrollment choice
period
Other
Populations enrolled: Enrollment broker
name (if applicable)
WIPRO Infocrossing Medicaid State Plan
Populations enrolled: Notes on
enrollment choice period
Pregnant Women have 7 days while the
rest of the population has 15 days.
Children in the care and custody of the
State of Missouri are enrolled the same
day.
Benefits covered: Inpatient hospital
physical health
X
Benefits covered: Inpatient hospital
behavioral health (MH and/or SUD)
X
Benefits covered: Outpatient hospital
physical health
X
Benefits covered: Outpatient hospital
behavioral health (MH and/or SUD)
X
Benefits covered: Partial hospitalization X
Benefits covered: Physician X
Benefits covered: Nurse practitioner X
Benefits covered: Rural health clinics
and FQHCs
X
Benefits covered: Clinic services X
Benefits covered: Lab and x-ray X
Benefits covered: Prescription drugs X
Benefits covered: Prosthetic devices X
Benefits covered: EPSDT X
Benefits covered: Case management X
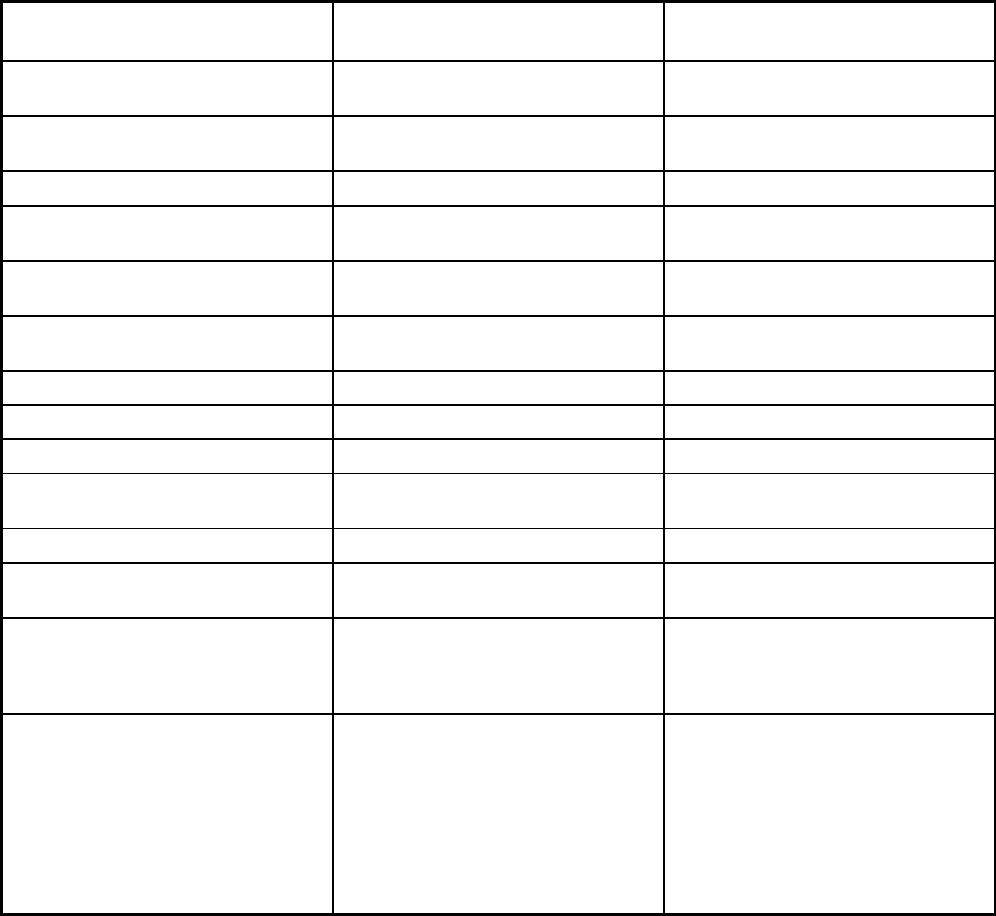
365
Features MO HealthNet Managed Care/1915b
Non-Emergency Medical
Transportation Program (NEMT)
Benefits covered: SSA Section 1945-
authorized health home
Benefits covered: Health home care
(services in home)
X
Benefits covered: Family planning X
Benefits covered: Dental services
(medical/surgical)
Benefits covered: Dental (preventative
or corrective)
X
Benefits covered: Personal care (state
plan option)
X
Benefits covered: HCBS waiver services
Benefits covered: Private duty nursing
Benefits covered: ICF-IDD
Benefits covered: Nursing facility
services
Benefits covered: Hospice care X
Benefits covered: Non-Emergency
Medical Transportation
X X
Benefits covered: Institution for Mental
Disease inpatient treatment for people
ages 21-64 defined by 42 CFR
§438.6(e) as an 'in lieu of' benefit
X
Benefits covered: Other (e.g., nurse
midwife services, freestanding birth
centers, podiatry, etc.)
Ambulatory surgical care, asthma
education and in-home environmental
assessments, comprehensive day
rehabilitation, durable medical
equipment, emergency, hearing,
immunization, inpatient substance use
disorders, outpatient substance use
disorders, obesity, prenatal case
management, podiatry, vision
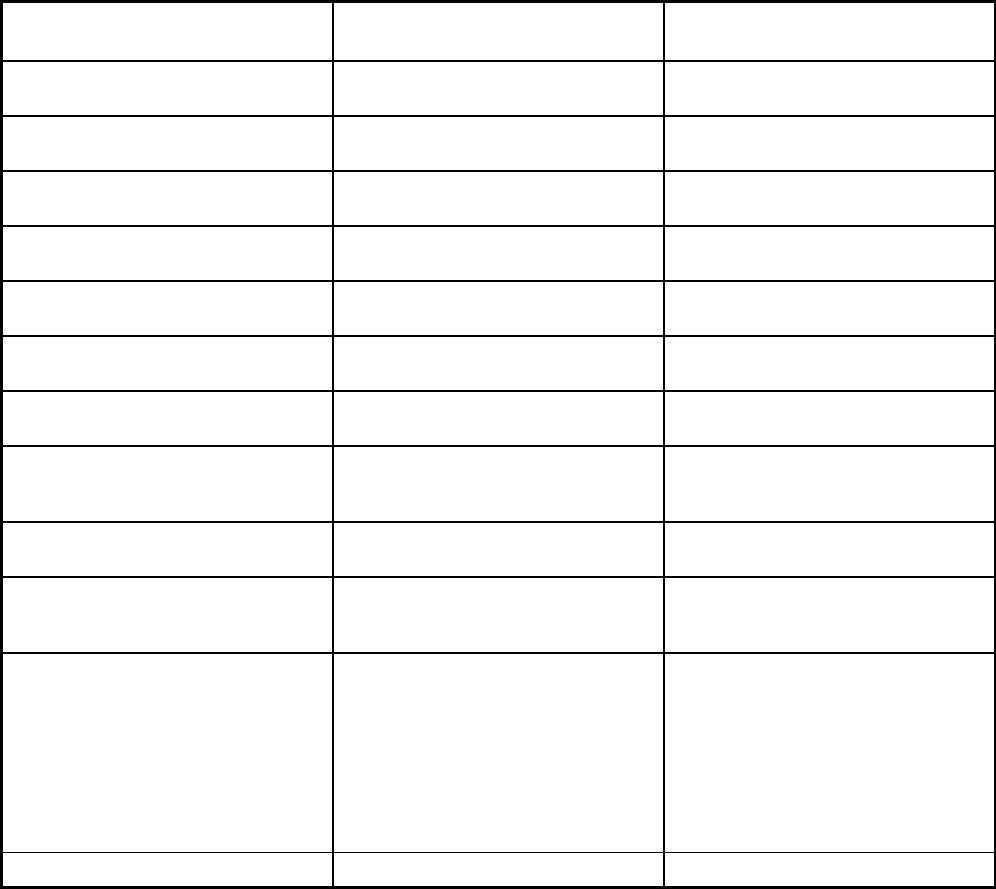
366
Features MO HealthNet Managed Care/1915b
Non-Emergency Medical
Transportation Program (NEMT)
Quality assurance and improvement:
HEDIS data required?
Yes No
Quality assurance and improvement:
CAHPS data required?
Yes No
Quality assurance and improvement:
Accreditation required?
Yes No
Quality assurance and improvement:
Accrediting organization
NCQA
Quality assurance and improvement:
EQRO contractor name (if applicable)
Primaris Holdings, Inc.
Performance incentives: Payment
bonuses/differentials to reward plans
X
Performance incentives: Preferential
auto-enrollment to reward plans
X
Performance incentives: Public reports
comparing plan performance on key
metrics
X
Performance incentives: Withholds tied
to performance metrics
X
Performance incentives: MCOs/PHPs
required or encouraged to pay providers
for value/quality outcomes
Participating plans: Plans in Program Home State Health Eastern; Home
State Health Central; Home State
Health Western; Home State Health
Southwest; Missouri Care Eastern;
Missouri Care Central; Missouri Care
Western; Missouri Care Southwest;
United Healthcare Eastern; United
Healthcare Central; United Healthcare
Western; United Healthcare Southwest
Logisticare Solutions
Notes: Program notes
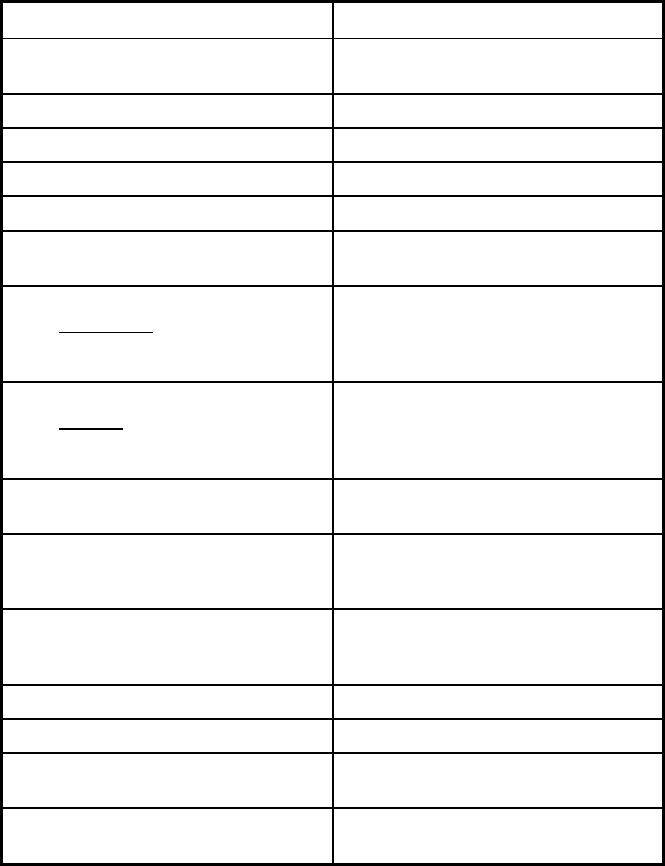
368
Montana Managed Care Program Features, as of 2018
Features Passport to Health
Program type Primary Care Case Management
(PCCM)
Statewide or region-specific? Statewide
Federal operating authority 1915(b)
Program start date 01/01/1994
Waiver expiration date (if applicable) 03/31/2019
If the program ended in 2018, indicate
the end date
Populations enrolled: Low-income
adults not covered under ACA Section
VIII (excludes pregnant women and
people with disabilities)
Populations enrolled: Low-income
adults covered under ACA Section VIII
(excludes pregnant women and people
with disabilities)
Mandatory
Populations enrolled: Aged, Blind or
Disabled Children or Adults
Mandatory
Populations enrolled: Non-Disabled
Children (excludes children in foster
care or receiving adoption assistance)
Mandatory
Populations enrolled: Individuals
receiving Limited Benefits (excludes
partial duals)
Populations enrolled: Full Duals
Populations enrolled: Partial Duals
Populations enrolled: Children with
Special Health Care Needs
Mandatory
Populations enrolled: Native
American/Alaskan Natives
Mandatory
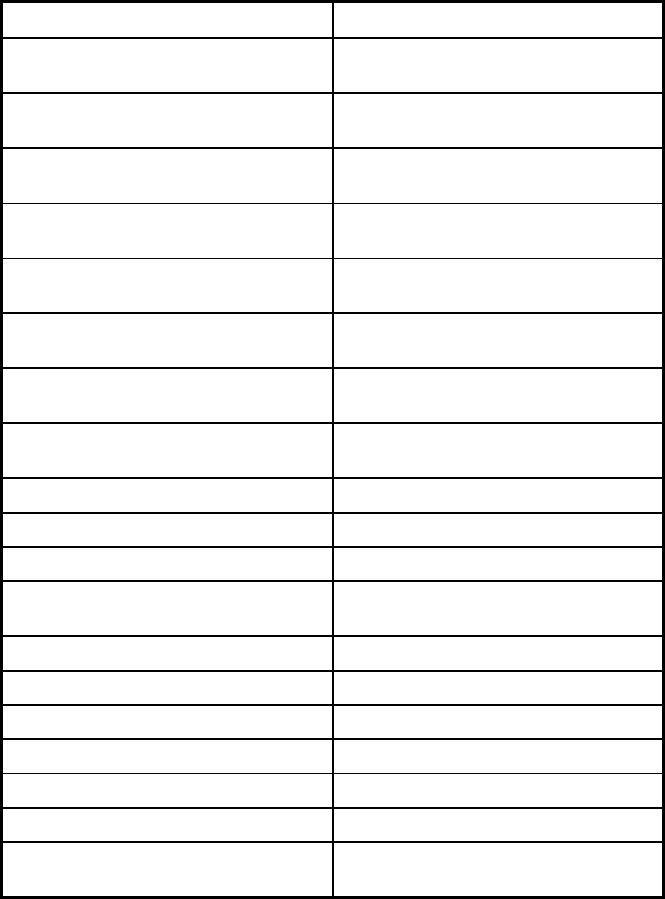
369
Features Passport to Health
Populations enrolled: Foster Care and
Adoption Assistance Children
Mandatory
Populations enrolled: Enrollment choice
period
N/A
Populations enrolled: Enrollment broker
name (if applicable)
Conduent
Populations enrolled: Notes on
enrollment choice period
Benefits covered: Inpatient hospital
physical health
Benefits covered: Inpatient hospital
behavioral health (MH and/or SUD)
Benefits covered: Outpatient hospital
physical health
Benefits covered: Outpatient hospital
behavioral health (MH and/or SUD)
Benefits covered: Partial hospitalization
Benefits covered: Physician X
Benefits covered: Nurse practitioner
Benefits covered: Rural health clinics
and FQHCs
Benefits covered: Clinic services
Benefits covered: Lab and x-ray
Benefits covered: Prescription drugs
Benefits covered: Prosthetic devices
Benefits covered: EPSDT
Benefits covered: Case management X
Benefits covered: SSA Section 1945-
authorized health home
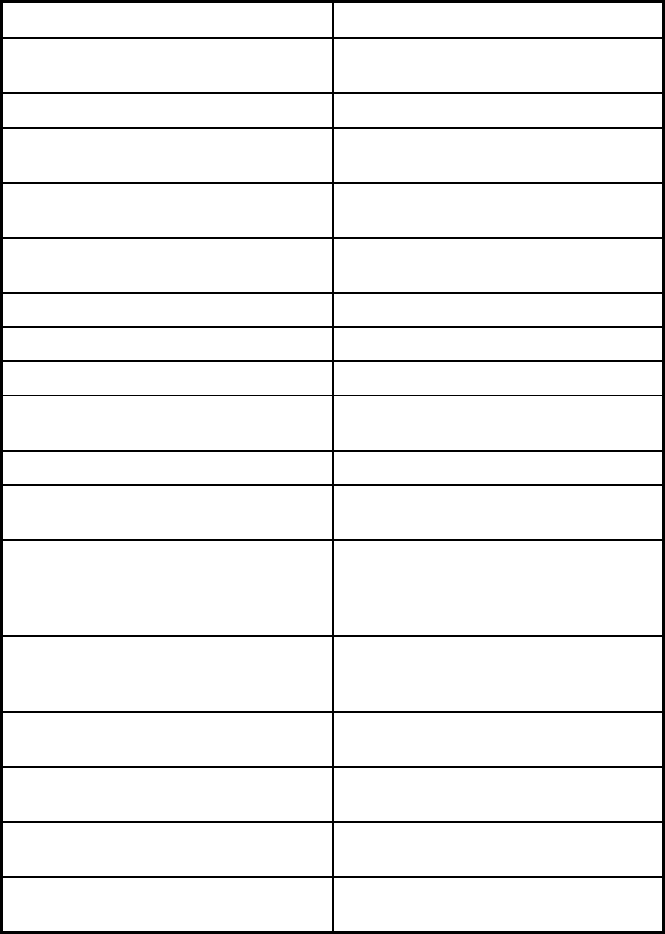
370
Features Passport to Health
Benefits covered: Health home care
(services in home)
Benefits covered: Family planning
Benefits covered: Dental services
(medical/surgical)
Benefits covered: Dental (preventative
or corrective)
Benefits covered: Personal care (state
plan option)
Benefits covered: HCBS waiver services
Benefits covered: Private duty nursing
Benefits covered: ICF-IDD
Benefits covered: Nursing facility
services
Benefits covered: Hospice care
Benefits covered: Non-Emergency
Medical Transportation
Benefits covered: Institution for Mental
Disease inpatient treatment for people
ages 21-64 defined by 42 CFR
§438.6(e) as an 'in lieu of' benefit
Benefits covered: Other (e.g., nurse
midwife services, freestanding birth
centers, podiatry, etc.)
Quality assurance and improvement:
HEDIS data required?
No
Quality assurance and improvement:
CAHPS data required?
No
Quality assurance and improvement:
Accreditation required?
No
Quality assurance and improvement:
Accrediting organization
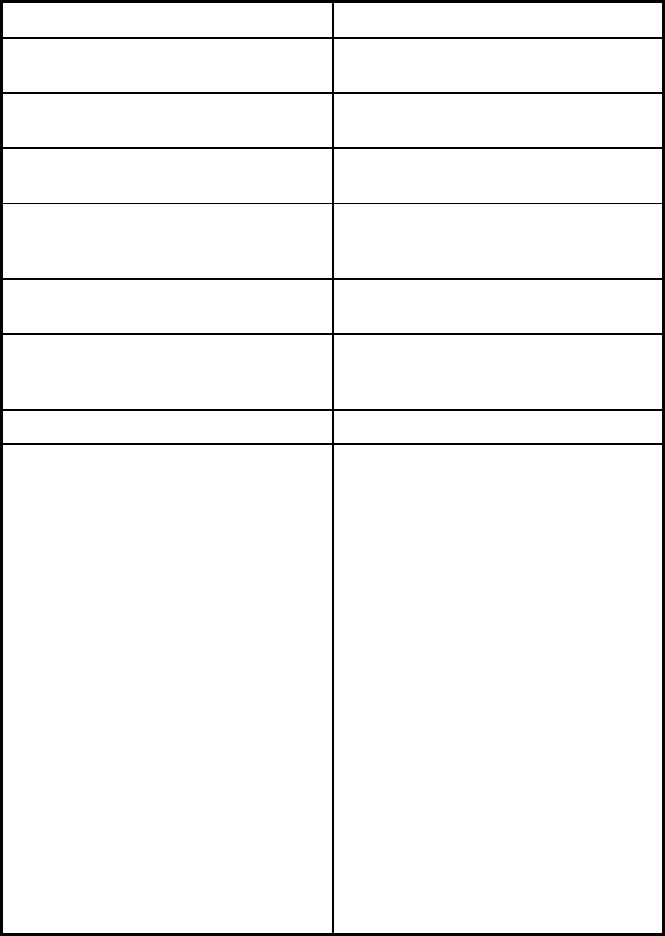
371
Features Passport to Health
Quality assurance and improvement:
EQRO contractor name (if applicable)
Performance incentives: Payment
bonuses/differentials to reward plans
Performance incentives: Preferential
auto-enrollment to reward plans
Performance incentives: Public reports
comparing plan performance on key
metrics
Performance incentives: Withholds tied
to performance metrics
Performance incentives: MCOs/PHPs
required or encouraged to pay providers
for value/quality outcomes
Participating plans: Plans in Program Multiple Primary Care Providers
Notes: Program notes Montana has four programs that operate
under the authority of the 1915(b)
waiver. The Passport to Health
program is the Primary Care Case
Management (PCCM) program. Benefits
covered include those that are covered
by both the monthly PMPM and FFS
benefits that could be delivered by a
primary provider participating in the
Passport to Health Program. The Team
Care program is a sub-program of
Passport which began in 2004. The
Health Improvement program, the
EPCCM program, began in 2009 as an
enhancement to Passport. The Tribal
HIP program was created in April 2007
as a partnership between the Tribal,
State and Federal government to
address factors that contribute to health
disparities in American Indians eligible
for Medicaid residing on a reservation.
The Nurse First program is the nurse
advice line that began in 2004.
372
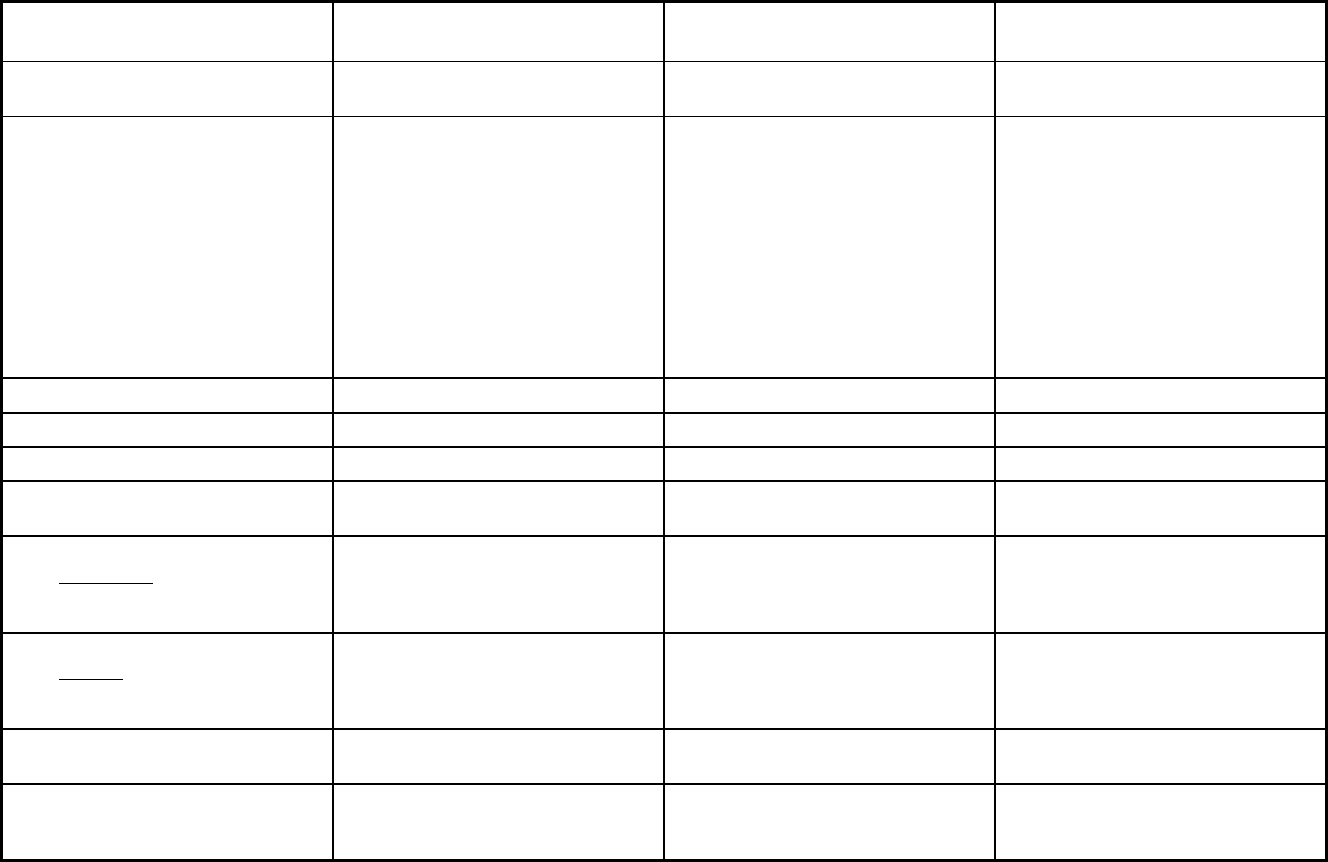
373
Nebraska Managed Care Program Features, as of 2018
Features Dental Benefit Manager Heritage Health
Program of All-Inclusive Care for the
Elderly (PACE)
Program type Dental only (PAHP) Comprehensive MCO Program of All-inclusive Care for the
Elderly (PACE)
Statewide or region-specific? Statewide Statewide 68037, 68048, 68025, 68007, 68010,
68022, 68064, 68102, 68104, 68105,
68106, 68107, 68127, 68110, 68111,
68112, 68114, 68116, 68117, 68118,
68122, 68124, 68127, 68130, 68131,
68132, 68134, 68135, 68137, 68142,
68144, 68152, 68154, 68157, 68164,
68182, 68005, 68028, 68046, 68059,
68069, 68113, 68123, 68128, 68133,
68136, 68138, 68147, 68073, 68002,
68008, 68009, 68023, 68029, 68034,
68044, 68068
Federal operating authority 1915(b) 1915(b) PACE
Program start date 10/01/2017 01/01/2017 05/01/2013
Waiver expiration date (if applicable) 06/30/2019 06/30/2019
If the program ended in 2018, indicate
the end date
Populations enrolled: Low-income
adults not covered under ACA Section
VIII (excludes pregnant women and
people with disabilities)
Mandatory Mandatory
Populations enrolled: Low-income
adults covered under ACA Section VIII
(excludes pregnant women and people
with disabilities)
Mandatory Mandatory
Populations enrolled: Aged, Blind or
Disabled Children or Adults
Mandatory Mandatory Voluntary
Populations enrolled: Non-Disabled
Children (excludes children in foster
care or receiving adoption assistance)
Mandatory Mandatory
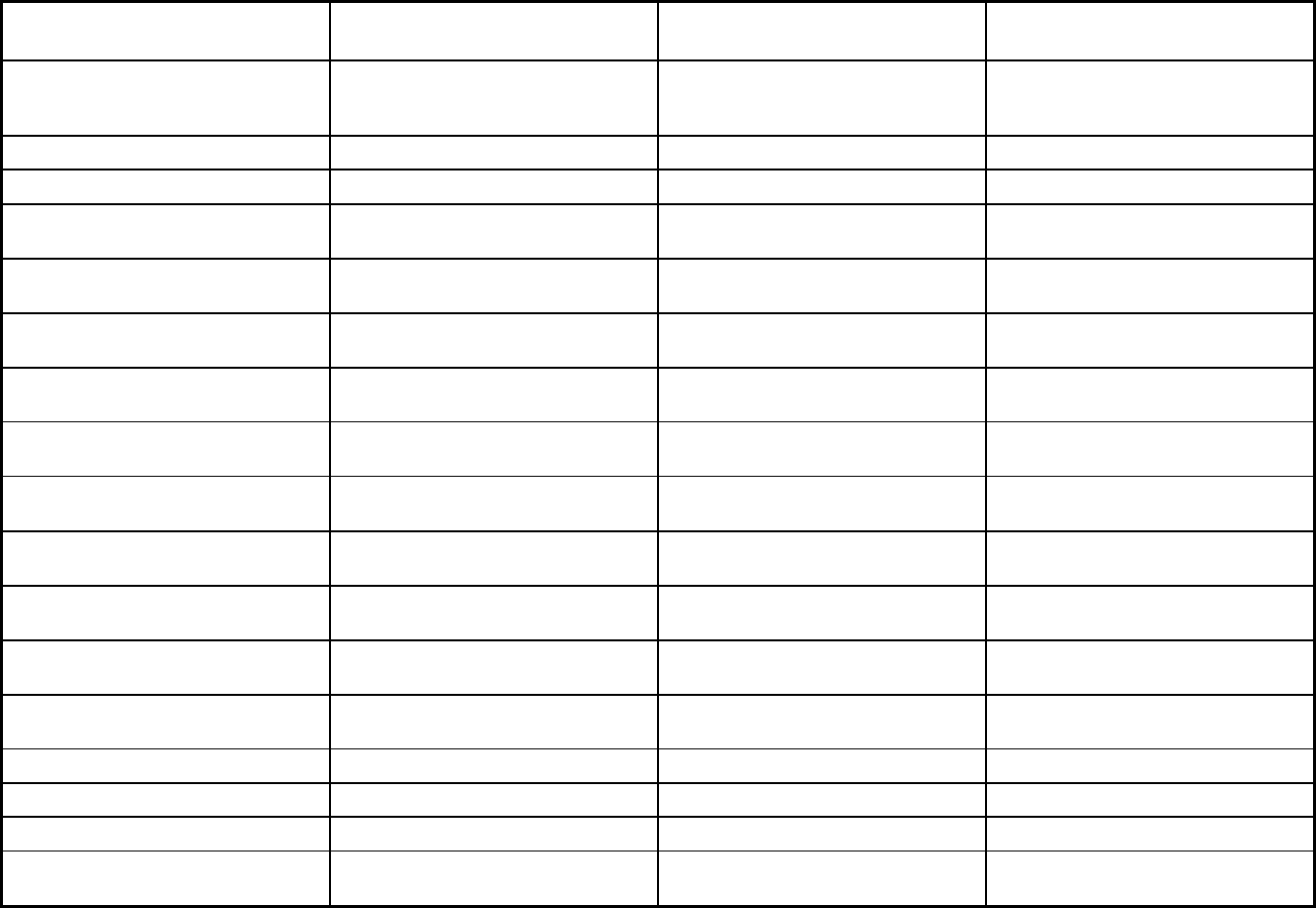
374
Features Dental Benefit Manager Heritage Health
Program of All-Inclusive Care for the
Elderly (PACE)
Populations enrolled: Individuals
receiving Limited Benefits (excludes
partial duals)
Mandatory Mandatory
Populations enrolled: Full Duals Mandatory Mandatory
Populations enrolled: Partial Duals Mandatory Mandatory
Populations enrolled: Children with
Special Health Care Needs
Mandatory Mandatory
Populations enrolled: Native
American/Alaskan Natives
Mandatory Mandatory Voluntary
Populations enrolled: Foster Care and
Adoption Assistance Children
Mandatory Mandatory Voluntary
Populations enrolled: Enrollment choice
period
Pre-assigned Pre-assigned N/A
Populations enrolled: Enrollment broker
name (if applicable)
Automated Health Systems (AHS)
Populations enrolled: Notes on
enrollment choice period
Benefits covered: Inpatient hospital
physical health
X X
Benefits covered: Inpatient hospital
behavioral health (MH and/or SUD)
X X
Benefits covered: Outpatient hospital
physical health
X X
Benefits covered: Outpatient hospital
behavioral health (MH and/or SUD)
X X
Benefits covered: Partial hospitalization X X
Benefits covered: Physician X X
Benefits covered: Nurse practitioner X X
Benefits covered: Rural health clinics
and FQHCs
X X
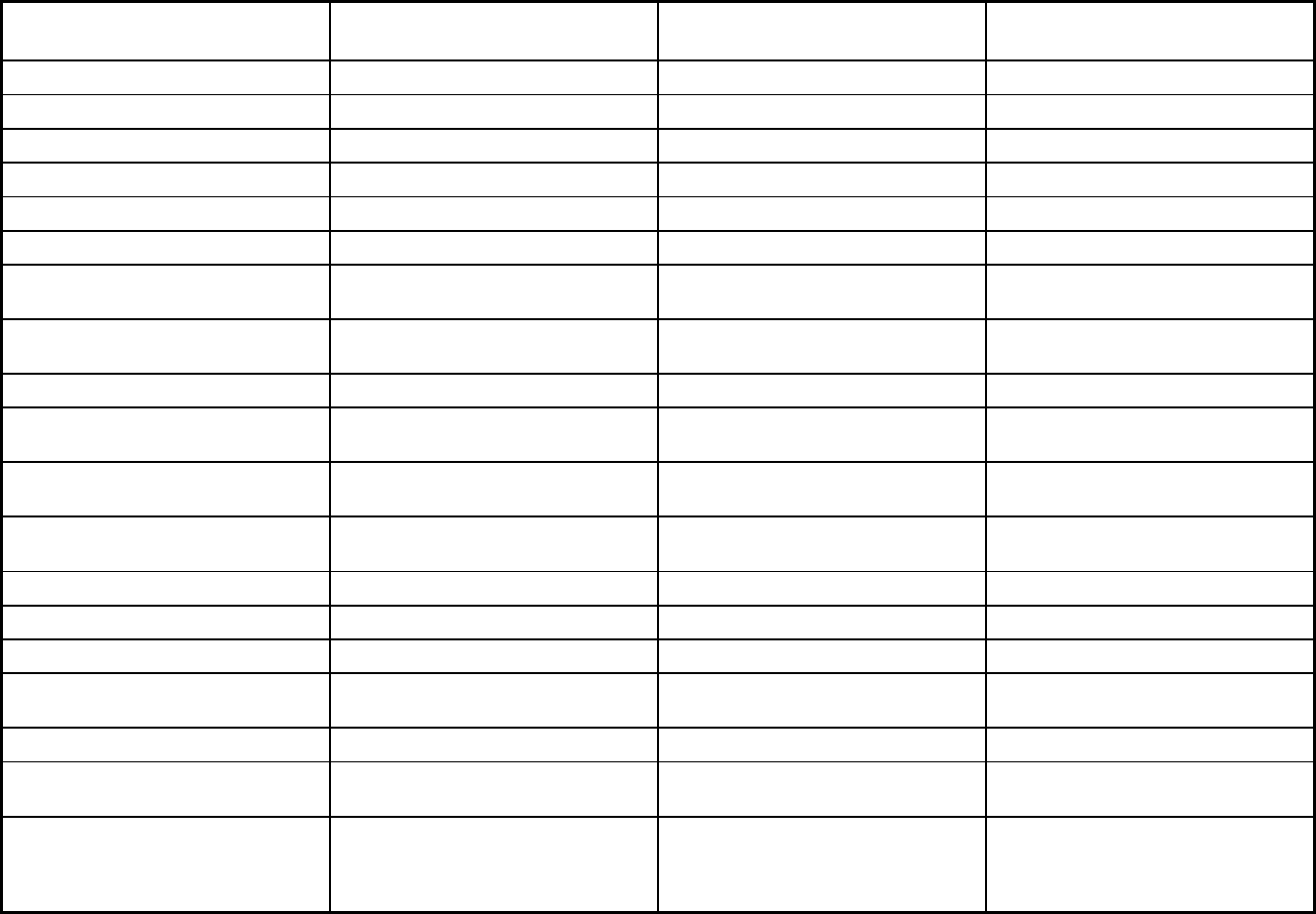
375
Features Dental Benefit Manager Heritage Health
Program of All-Inclusive Care for the
Elderly (PACE)
Benefits covered: Clinic services X X
Benefits covered: Lab and x-ray X X
Benefits covered: Prescription drugs X X
Benefits covered: Prosthetic devices X X
Benefits covered: EPSDT X X
Benefits covered: Case management X X
Benefits covered: SSA Section 1945-
authorized health home
Benefits covered: Health home care
(services in home)
X X
Benefits covered: Family planning X X
Benefits covered: Dental services
(medical/surgical)
X X
Benefits covered: Dental (preventative
or corrective)
X X
Benefits covered: Personal care (state
plan option)
X
Benefits covered: HCBS waiver services X
Benefits covered: Private duty nursing X X
Benefits covered: ICF-IDD X
Benefits covered: Nursing facility
services
X
Benefits covered: Hospice care X X
Benefits covered: Non-Emergency
Medical Transportation
X
Benefits covered: Institution for Mental
Disease inpatient treatment for people
ages 21-64 defined by 42 CFR
§438.6(e) as an 'in lieu of' benefit
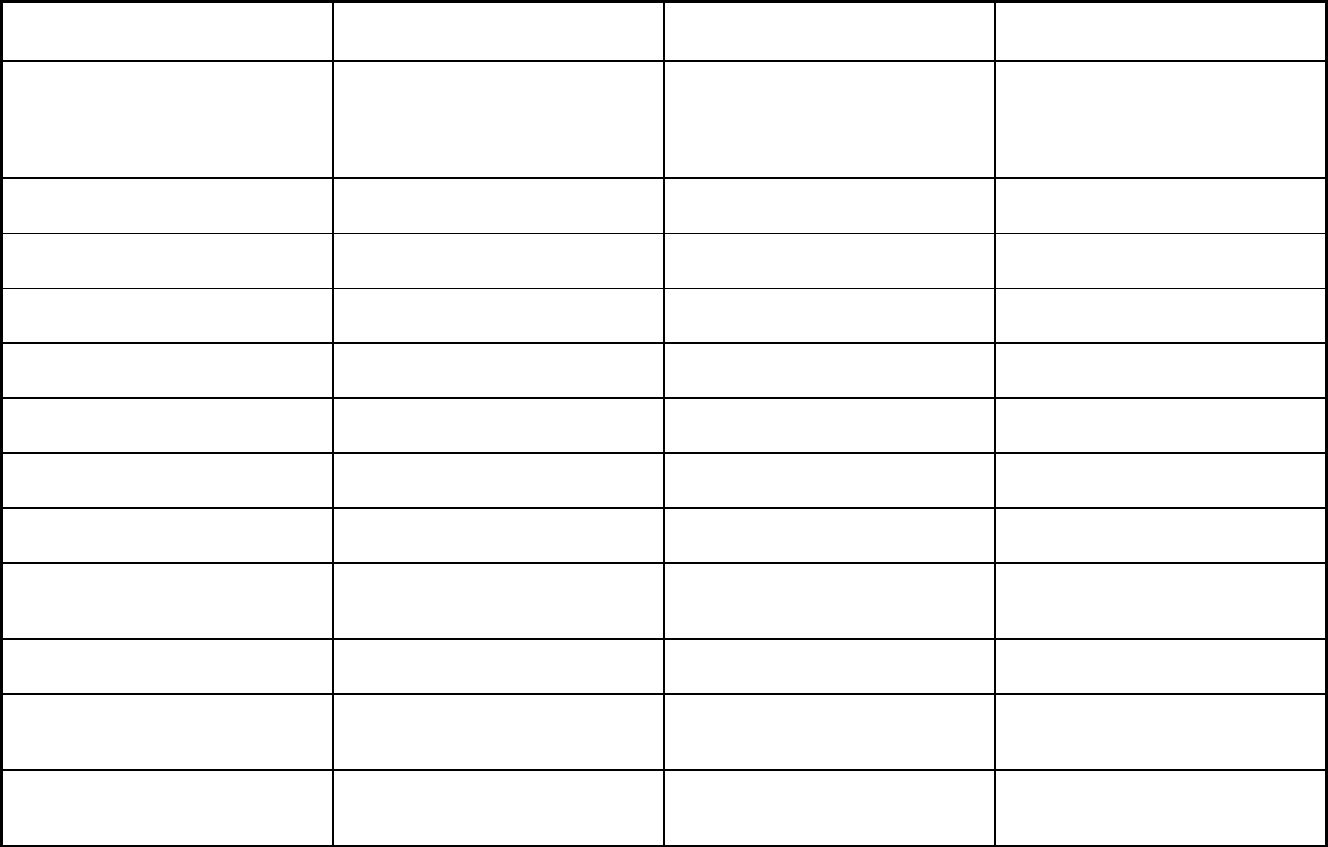
376
Features Dental Benefit Manager Heritage Health
Program of All-Inclusive Care for the
Elderly (PACE)
Benefits covered: Other (e.g., nurse
midwife services, freestanding birth
centers, podiatry, etc.)
Podiatry, hearing, immunization, speech
therapy, physical therapy, vision,
chiropractic, durable medical
equipment, occupational therapy,
freestanding birth center
Quality assurance and improvement:
HEDIS data required?
No Yes No
Quality assurance and improvement:
CAHPS data required?
No Yes No
Quality assurance and improvement:
Accreditation required?
Yes Yes No
Quality assurance and improvement:
Accrediting organization
URAC NCQA
Quality assurance and improvement:
EQRO contractor name (if applicable)
Island Peer Review Organization Island Peer Review Organization
Performance incentives: Payment
bonuses/differentials to reward plans
Performance incentives: Preferential
auto-enrollment to reward plans
Performance incentives: Public reports
comparing plan performance on key
metrics
Performance incentives: Withholds tied
to performance metrics
X X
Performance incentives: MCOs/PHPs
required or encouraged to pay providers
for value/quality outcomes
X
Participating plans: Plans in Program MCNA Nebraska UnitedHealthcare Community Plan of
Nebraska; WellCare of Nebraska;
Nebraska Total Care
Immanuel Pathways
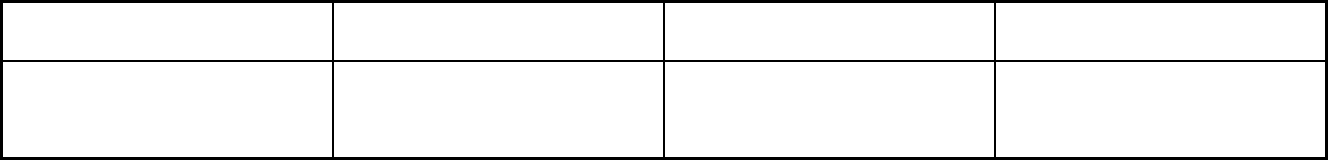
377
Features Dental Benefit Manager Heritage Health
Program of All-Inclusive Care for the
Elderly (PACE)
Notes: Program notes Voluntary program in select zip codes
throughout Cass, Dodge, Douglas,
Sarpy, Saunders, and Washington
Counties.
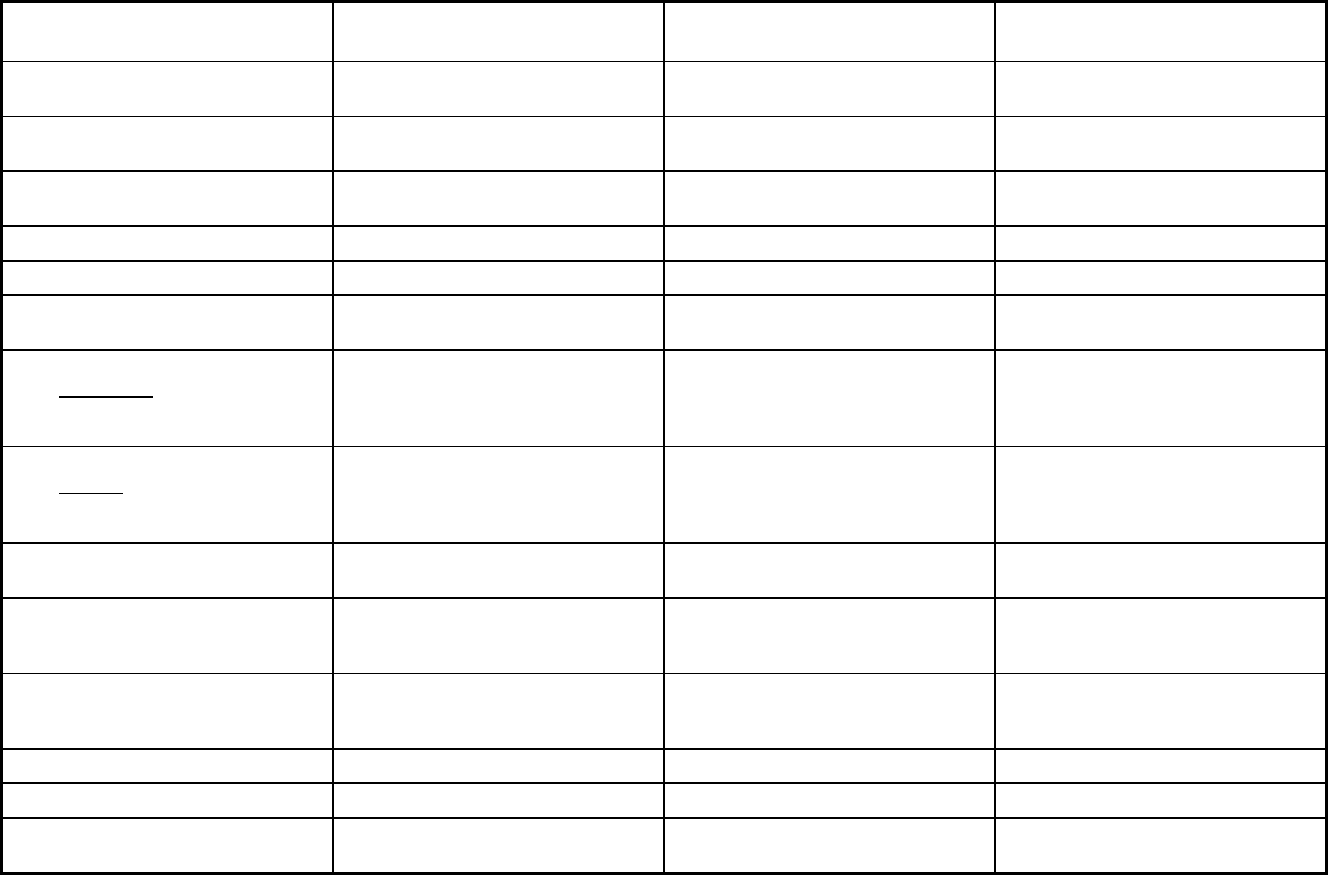
378
Nevada Managed Care Program Features, as of 2018 (1 of 2)
Features Non-Emergency Transportation
Health Care Guidance Program
(HCGP) Dental Benefits Administrator
Program type Non-Emergency Medical Transportation Primary Care Case Management
(PCCM)
Dental only (PAHP)
Statewide or region-specific? Statewide Statewide Sufficiently populated Urban Zip Codes
in Washoe and Clark counties.
Federal operating authority 1902(a)(70) NEMT 1115(a) (Medicaid demonstration
waivers)
1932(a),1937 Alt Benefit Plan
Program start date 10/01/2003 07/01/2014 01/01/2018
Waiver expiration date (if applicable)
If the program ended in 2018, indicate
the end date
06/30/2018
Populations enrolled: Low-income
adults not covered under ACA Section
VIII (excludes pregnant women and
people with disabilities)
Mandatory Mandatory Mandatory
Populations enrolled: Low-income
adults covered under ACA Section VIII
(excludes pregnant women and people
with disabilities)
Mandatory Mandatory Mandatory
Populations enrolled: Aged, Blind or
Disabled Children or Adults
Mandatory Mandatory
Populations enrolled: Non-Disabled
Children (excludes children in foster
care or receiving adoption assistance)
Mandatory Mandatory Mandatory
Populations enrolled: Individuals
receiving Limited Benefits (excludes
partial duals)
Mandatory
Populations enrolled: Full Duals Mandatory
Populations enrolled: Partial Duals
Populations enrolled: Children with
Special Health Care Needs
Mandatory Mandatory Voluntary
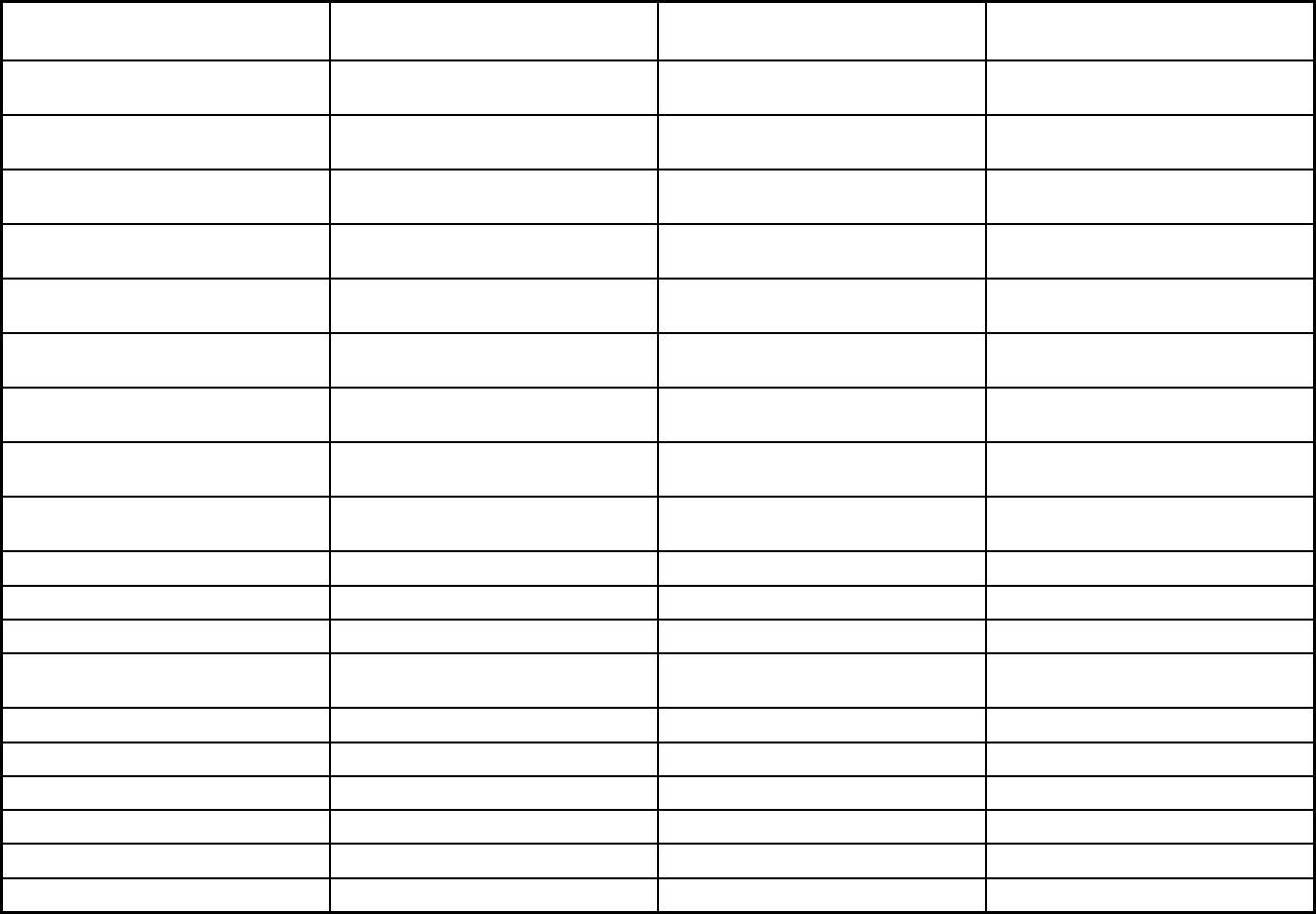
379
Features Non-Emergency Transportation
Health Care Guidance Program
(HCGP) Dental Benefits Administrator
Populations enrolled: Native
American/Alaskan Natives
Mandatory Exempt Voluntary
Populations enrolled: Foster Care and
Adoption Assistance Children
Mandatory Exempt Exempt
Populations enrolled: Enrollment choice
period
N/A 30 days
Populations enrolled: Enrollment broker
name (if applicable)
DXC
Populations enrolled: Notes on
enrollment choice period
Benefits covered: Inpatient hospital
physical health
Benefits covered: Inpatient hospital
behavioral health (MH and/or SUD)
Benefits covered: Outpatient hospital
physical health
Benefits covered: Outpatient hospital
behavioral health (MH and/or SUD)
Benefits covered: Partial hospitalization
Benefits covered: Physician
Benefits covered: Nurse practitioner
Benefits covered: Rural health clinics
and FQHCs
Benefits covered: Clinic services
Benefits covered: Lab and x-ray
Benefits covered: Prescription drugs
Benefits covered: Prosthetic devices
Benefits covered: EPSDT
Benefits covered: Case management X
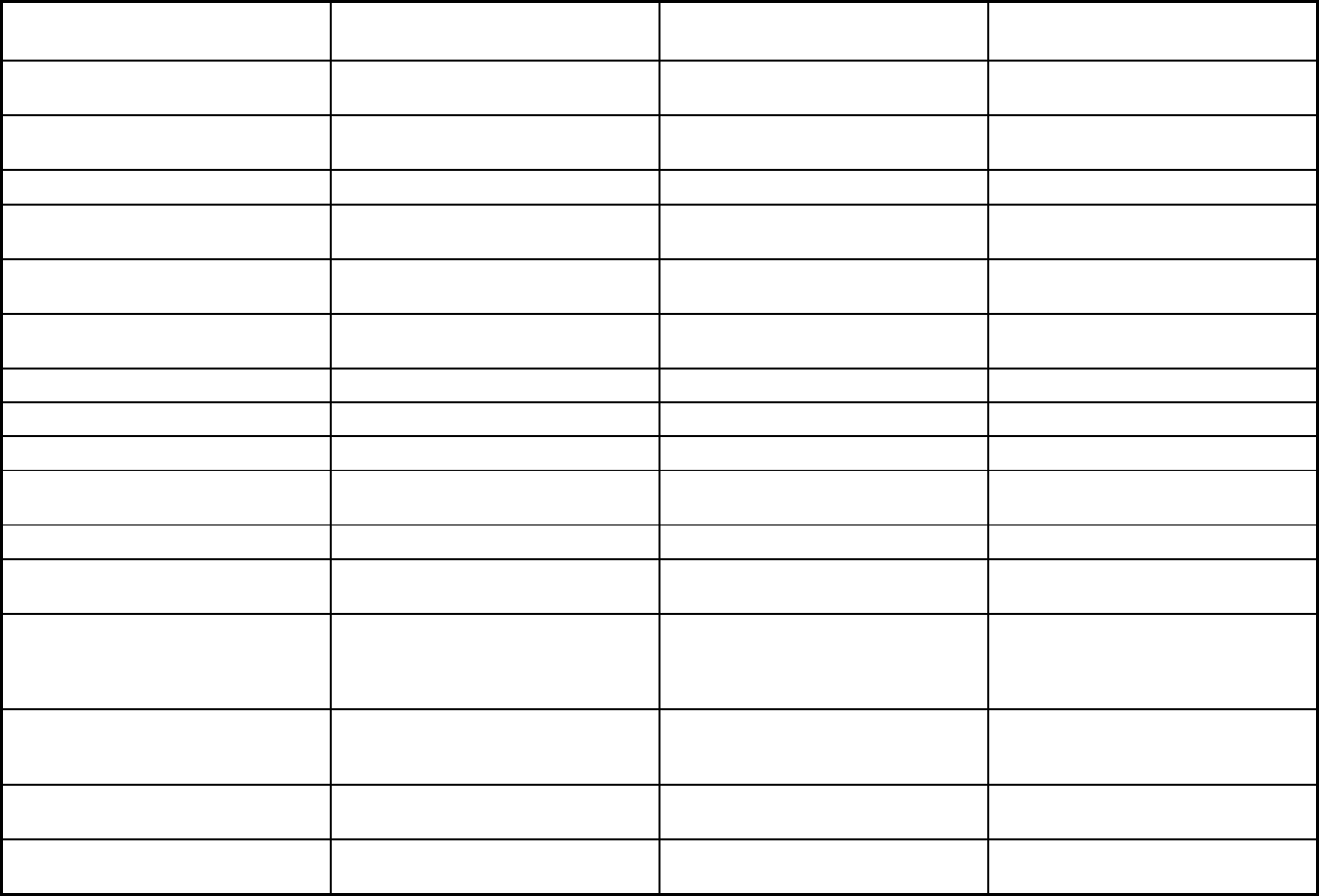
380
Features Non-Emergency Transportation
Health Care Guidance Program
(HCGP) Dental Benefits Administrator
Benefits covered: SSA Section 1945-
authorized health home
Benefits covered: Health home care
(services in home)
Benefits covered: Family planning
Benefits covered: Dental services
(medical/surgical)
X
Benefits covered: Dental (preventative
or corrective)
X
Benefits covered: Personal care (state
plan option)
Benefits covered: HCBS waiver services
Benefits covered: Private duty nursing
Benefits covered: ICF-IDD
Benefits covered: Nursing facility
services
Benefits covered: Hospice care
Benefits covered: Non-Emergency
Medical Transportation
X
Benefits covered: Institution for Mental
Disease inpatient treatment for people
ages 21-64 defined by 42 CFR
§438.6(e) as an 'in lieu of' benefit
Benefits covered: Other (e.g., nurse
midwife services, freestanding birth
centers, podiatry, etc.)
Quality assurance and improvement:
HEDIS data required?
No Yes Yes
Quality assurance and improvement:
CAHPS data required?
No No Yes
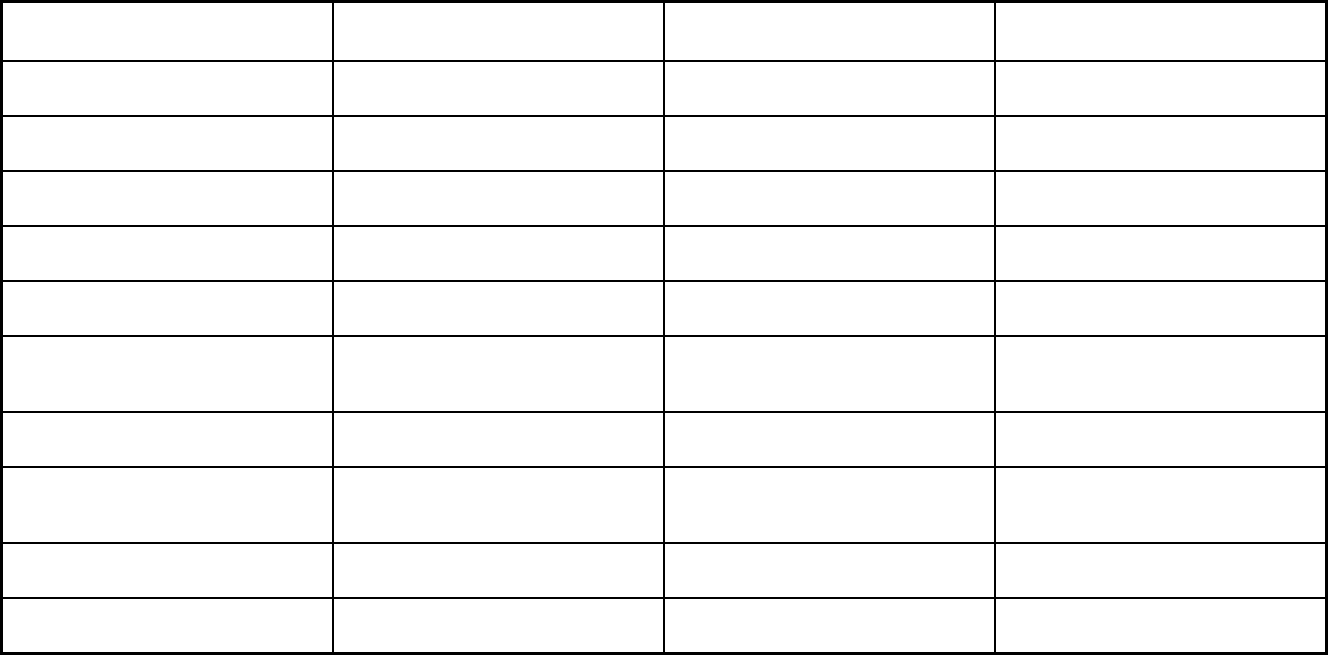
381
Features Non-Emergency Transportation
Health Care Guidance Program
(HCGP) Dental Benefits Administrator
Quality assurance and improvement:
Accreditation required?
No, but accreditation considered in plan
selection criteria
No, but accreditation considered in plan
selection criteria
No, but accreditation considered in plan
selection criteria
Quality assurance and improvement:
Accrediting organization
Any vetted accreditation that relates to
plan’s transportation mission
NCQA NCQA
Quality assurance and improvement:
EQRO contractor name (if applicable)
Health Services Advisory Group Health Services Advisory Group Health Services Advisory Group
Performance incentives: Payment
bonuses/differentials to reward plans
X
Performance incentives: Preferential
auto-enrollment to reward plans
Performance incentives: Public reports
comparing plan performance on key
metrics
X X
Performance incentives: Withholds tied
to performance metrics
X X
Performance incentives: MCOs/PHPs
required or encouraged to pay providers
for value/quality outcomes
X
Participating plans: Plans in Program Medical Transportation Management
(MTM Nevada)
Liberty Dental Plan of Nevada
Notes: Program notes Contract ended 06/30/2018; no
enrollees 07/01/2018.
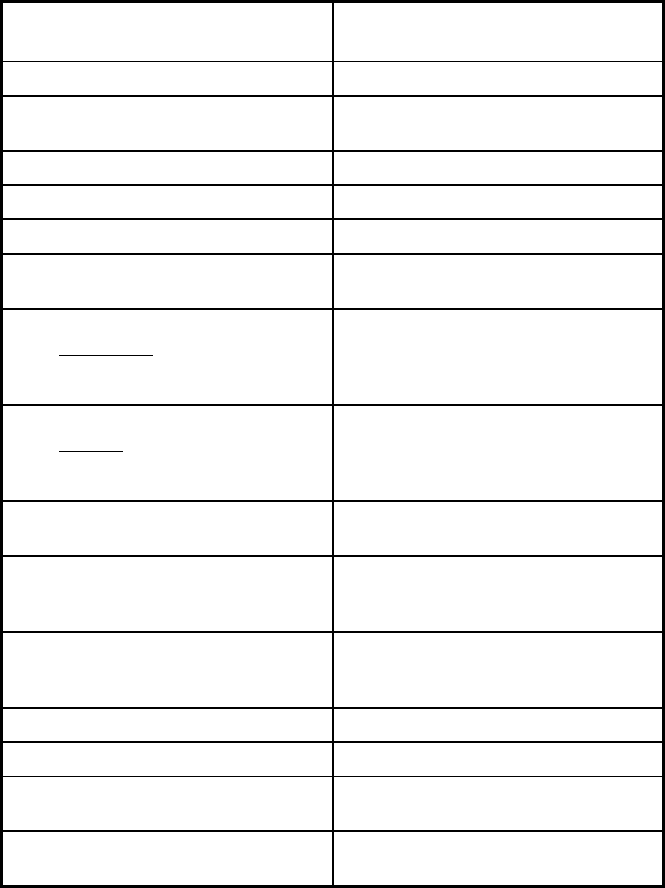
382
Nevada Managed Care Program Features, as of 2018 (2 of 2)
Features
Mandatory Health Maintenance
Program
Program type Comprehensive MCO
Statewide or region-specific? Sufficiently populated Urban Zip Codes
in Washoe and Clark counties.
Federal operating authority 1932(a)
Program start date 10/31/1988
Waiver expiration date (if applicable)
If the program ended in 2018, indicate
the end date
06/30/2018
Populations enrolled: Low-income
adults not covered under ACA Section
VIII (excludes pregnant women and
people with disabilities)
Mandatory
Populations enrolled: Low-income
adults covered under ACA Section VIII
(excludes pregnant women and people
with disabilities)
Mandatory
Populations enrolled: Aged, Blind or
Disabled Children or Adults
Populations enrolled: Non-Disabled
Children (excludes children in foster
care or receiving adoption assistance)
Mandatory
Populations enrolled: Individuals
receiving Limited Benefits (excludes
partial duals)
Populations enrolled: Full Duals
Populations enrolled: Partial Duals
Populations enrolled: Children with
Special Health Care Needs
Voluntary
Populations enrolled: Native
American/Alaskan Natives
Voluntary
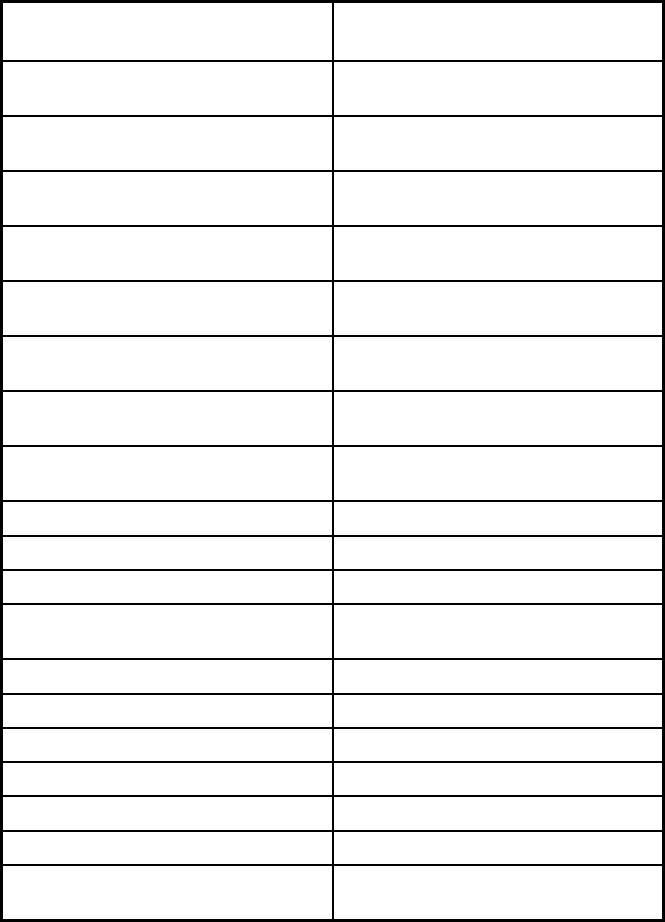
383
Features
Mandatory Health Maintenance
Program
Populations enrolled: Foster Care and
Adoption Assistance Children
Exempt
Populations enrolled: Enrollment choice
period
30 days
Populations enrolled: Enrollment broker
name (if applicable)
DXC
Populations enrolled: Notes on
enrollment choice period
Benefits covered: Inpatient hospital
physical health
X
Benefits covered: Inpatient hospital
behavioral health (MH and/or SUD)
X
Benefits covered: Outpatient hospital
physical health
X
Benefits covered: Outpatient hospital
behavioral health (MH and/or SUD)
X
Benefits covered: Partial hospitalization X
Benefits covered: Physician X
Benefits covered: Nurse practitioner X
Benefits covered: Rural health clinics
and FQHCs
X
Benefits covered: Clinic services X
Benefits covered: Lab and x-ray X
Benefits covered: Prescription drugs X
Benefits covered: Prosthetic devices X
Benefits covered: EPSDT X
Benefits covered: Case management X
Benefits covered: SSA Section 1945-
authorized health home
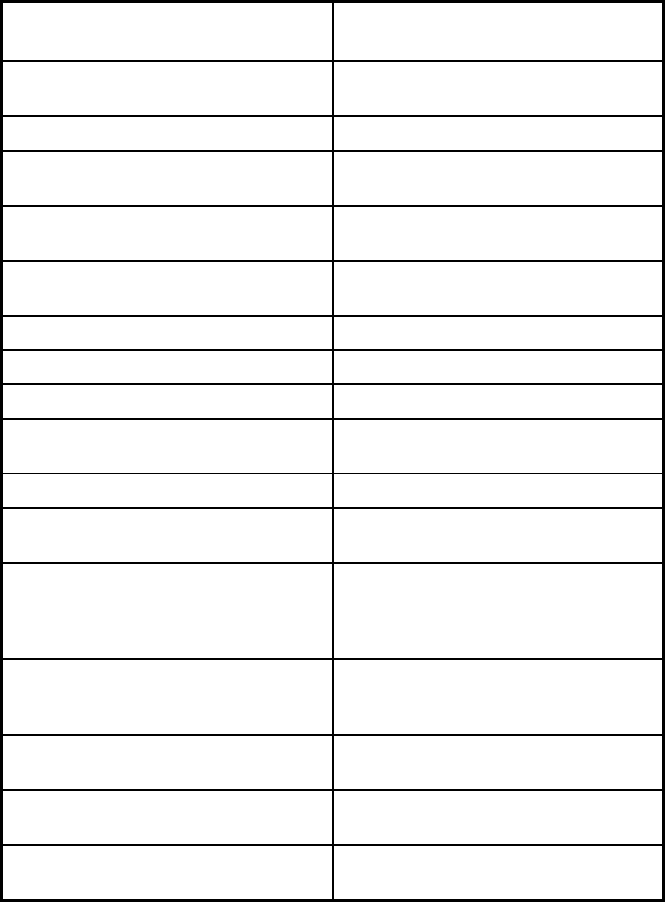
384
Features
Mandatory Health Maintenance
Program
Benefits covered: Health home care
(services in home)
X
Benefits covered: Family planning X
Benefits covered: Dental services
(medical/surgical)
Benefits covered: Dental (preventative
or corrective)
Benefits covered: Personal care (state
plan option)
X
Benefits covered: HCBS waiver services
Benefits covered: Private duty nursing X
Benefits covered: ICF-IDD X
Benefits covered: Nursing facility
services
Benefits covered: Hospice care X
Benefits covered: Non-Emergency
Medical Transportation
Benefits covered: Institution for Mental
Disease inpatient treatment for people
ages 21-64 defined by 42 CFR
§438.6(e) as an 'in lieu of' benefit
X
Benefits covered: Other (e.g., nurse
midwife services, freestanding birth
centers, podiatry, etc.)
Quality assurance and improvement:
HEDIS data required?
Yes
Quality assurance and improvement:
CAHPS data required?
Yes
Quality assurance and improvement:
Accreditation required?
No, but accreditation considered in plan
selection criteria
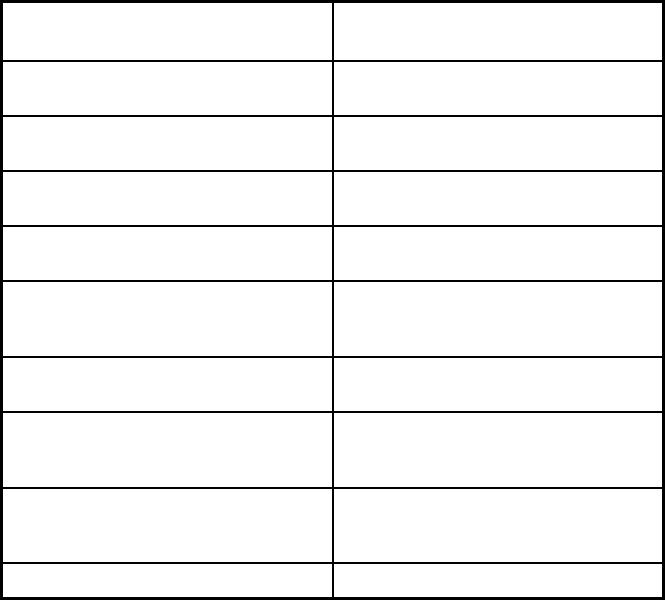
385
Features
Mandatory Health Maintenance
Program
Quality assurance and improvement:
Accrediting organization
NCQA
Quality assurance and improvement:
EQRO contractor name (if applicable)
Health Services Advisory Group
Performance incentives: Payment
bonuses/differentials to reward plans
Performance incentives: Preferential
auto-enrollment to reward plans
X
Performance incentives: Public reports
comparing plan performance on key
metrics
X
Performance incentives: Withholds tied
to performance metrics
X
Performance incentives: MCOs/PHPs
required or encouraged to pay providers
for value/quality outcomes
X
Participating plans: Plans in Program Health Plan of Nevada (HPN); Anthem
Blue Cross Blue Shield of Nevada;
Silver Summit Health Plan
Notes: Program notes
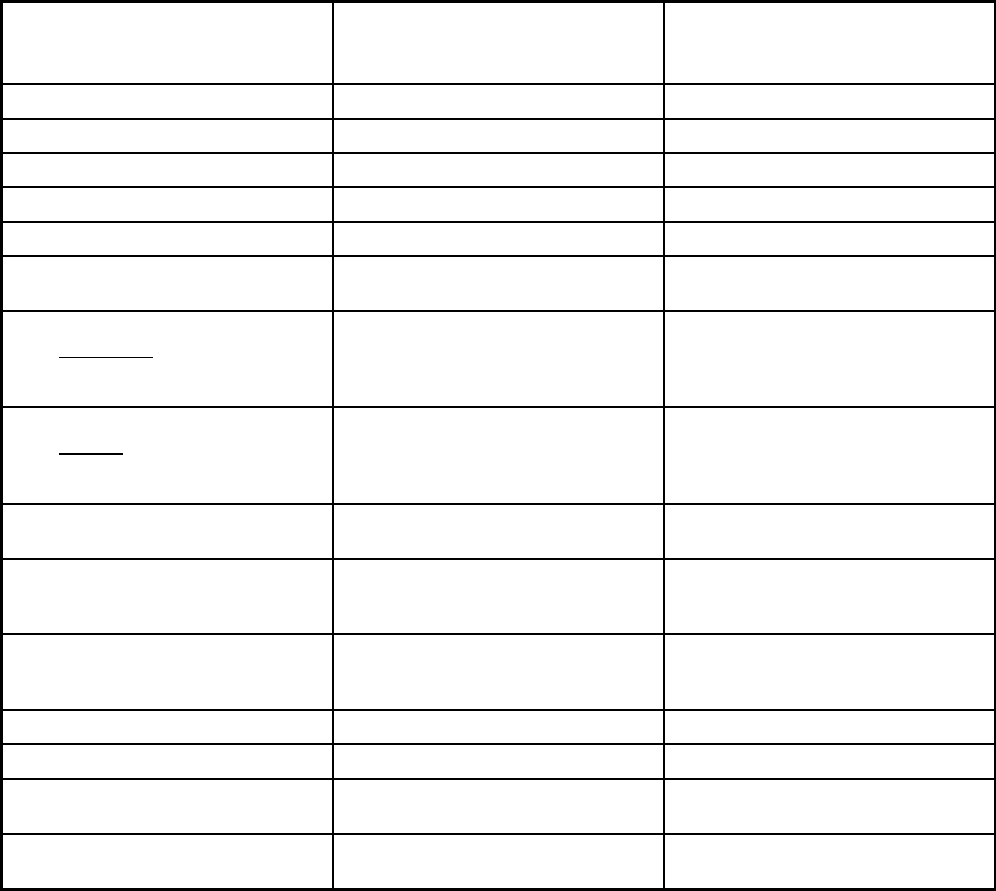
386
New Hampshire Managed Care Program Features, as of 2018
Features
New Hampshire Medicaid Care
Management
New Hampshire Health Protection
Program Medicaid Care Management
ABP
Program type Comprehensive MCO Comprehensive MCO
Statewide or region-specific? Statewide Statewide
Federal operating authority 1915(b),1932(a) 1932(a),1937 Alt Benefit Plan
Program start date 12/01/2013 08/01/2014
Waiver expiration date (if applicable) 03/31/2020
If the program ended in 2018, indicate
the end date
12/31/2018
Populations enrolled: Low-income
adults not covered under ACA Section
VIII (excludes pregnant women and
people with disabilities)
Mandatory
Populations enrolled: Low-income
adults covered under ACA Section VIII
(excludes pregnant women and people
with disabilities)
Mandatory Mandatory
Populations enrolled: Aged, Blind or
Disabled Children or Adults
Mandatory
Populations enrolled: Non-Disabled
Children (excludes children in foster
care or receiving adoption assistance)
Populations enrolled: Individuals
receiving Limited Benefits (excludes
partial duals)
Populations enrolled: Full Duals Mandatory
Populations enrolled: Partial Duals
Populations enrolled: Children with
Special Health Care Needs
Mandatory
Populations enrolled: Native
American/Alaskan Natives
Mandatory Mandatory
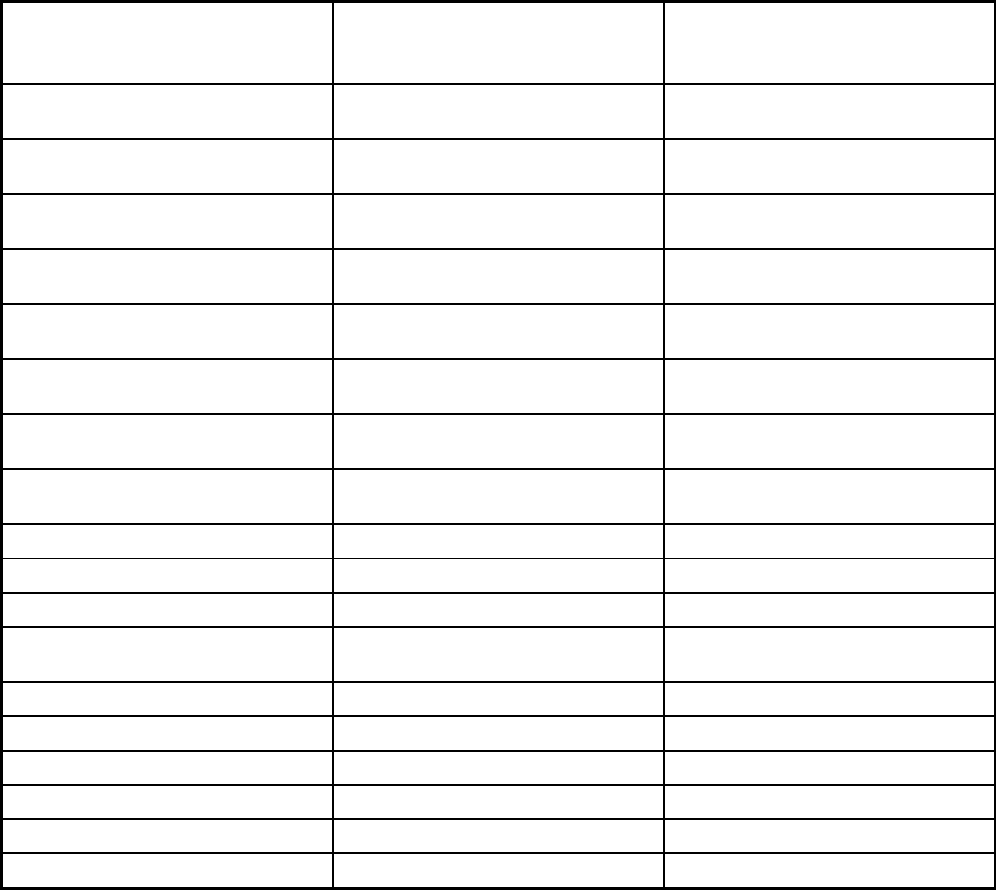
387
Features
New Hampshire Medicaid Care
Management
New Hampshire Health Protection
Program Medicaid Care Management
ABP
Populations enrolled: Foster Care and
Adoption Assistance Children
Mandatory Mandatory
Populations enrolled: Enrollment choice
period
60 days 60 days
Populations enrolled: Enrollment broker
name (if applicable)
Maximus
Populations enrolled: Notes on
enrollment choice period
Benefits covered: Inpatient hospital
physical health
X X
Benefits covered: Inpatient hospital
behavioral health (MH and/or SUD)
X X
Benefits covered: Outpatient hospital
physical health
X X
Benefits covered: Outpatient hospital
behavioral health (MH and/or SUD)
X X
Benefits covered: Partial hospitalization X X
Benefits covered: Physician X X
Benefits covered: Nurse practitioner X X
Benefits covered: Rural health clinics
and FQHCs
X X
Benefits covered: Clinic services X X
Benefits covered: Lab and x-ray X X
Benefits covered: Prescription drugs X X
Benefits covered: Prosthetic devices X X
Benefits covered: EPSDT X X
Benefits covered: Case management X X
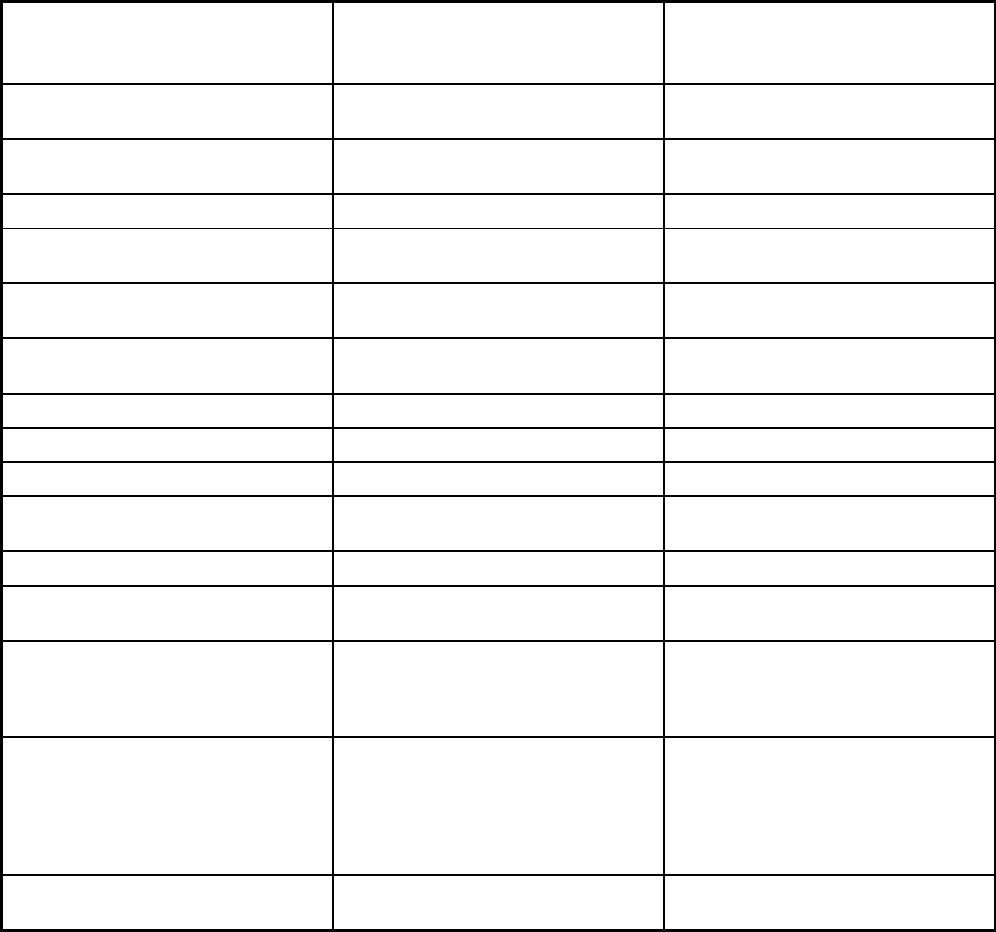
388
Features
New Hampshire Medicaid Care
Management
New Hampshire Health Protection
Program Medicaid Care Management
ABP
Benefits covered: SSA Section 1945-
authorized health home
Benefits covered: Health home care
(services in home)
X X
Benefits covered: Family planning X X
Benefits covered: Dental services
(medical/surgical)
Benefits covered: Dental (preventative
or corrective)
Benefits covered: Personal care (state
plan option)
X
Benefits covered: HCBS waiver services
Benefits covered: Private duty nursing X
Benefits covered: ICF-IDD
Benefits covered: Nursing facility
services
Benefits covered: Hospice care X X
Benefits covered: Non-Emergency
Medical Transportation
X
Benefits covered: Institution for Mental
Disease inpatient treatment for people
ages 21-64 defined by 42 CFR
§438.6(e) as an 'in lieu of' benefit
X X
Benefits covered: Other (e.g., nurse
midwife services, freestanding birth
centers, podiatry, etc.)
Nurse midwife, non-nurse midwife,
freestanding birth centers, podiatry,
PT/OT/ST, ambulance, adult medical
day care, DME, eyeglasses, full
substance use disorder treatment
Nurse midwife, non-nurse midwife,
freestanding birth centers, podiatry,
PT/OT/ST, ambulance, adult medical
day care, DME, eyeglasses,
chiropractic, full substance use disorder
treatment
Quality assurance and improvement:
HEDIS data required?
Yes Yes
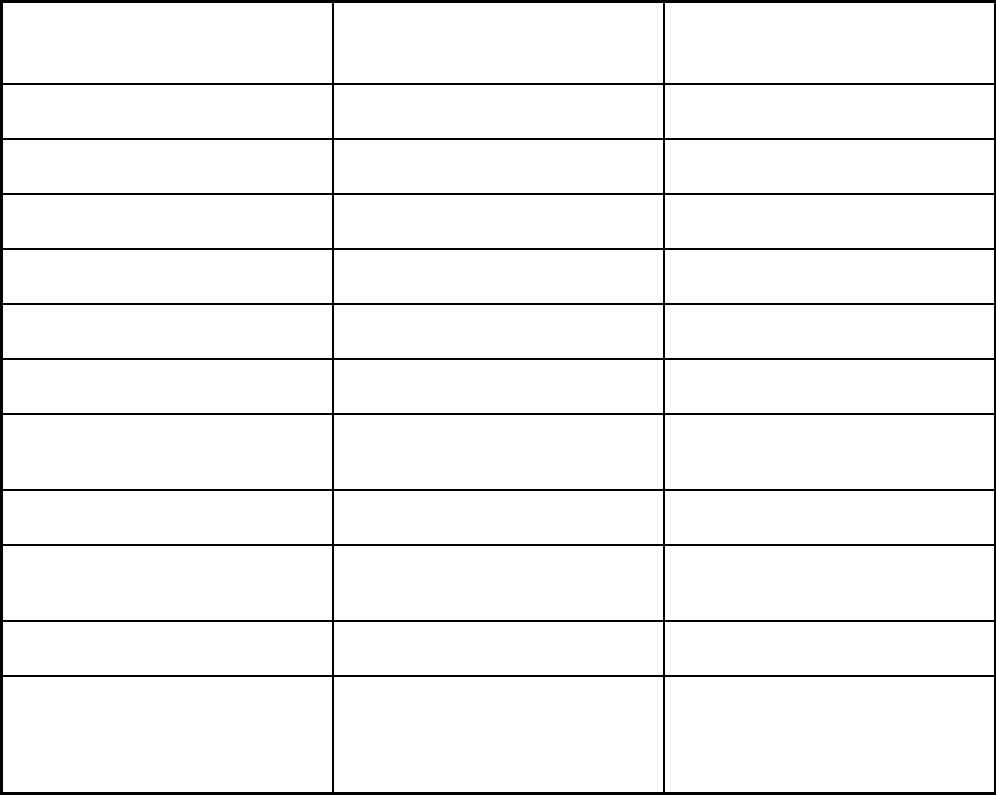
389
Features
New Hampshire Medicaid Care
Management
New Hampshire Health Protection
Program Medicaid Care Management
ABP
Quality assurance and improvement:
CAHPS data required?
Yes Yes
Quality assurance and improvement:
Accreditation required?
Yes Yes
Quality assurance and improvement:
Accrediting organization
NCQA NCQA
Quality assurance and improvement:
EQRO contractor name (if applicable)
Health Services Advisory Group Health Services Advisory Group
Performance incentives: Payment
bonuses/differentials to reward plans
Performance incentives: Preferential
auto-enrollment to reward plans
Performance incentives: Public reports
comparing plan performance on key
metrics
Performance incentives: Withholds tied
to performance metrics
Performance incentives: MCOs/PHPs
required or encouraged to pay providers
for value/quality outcomes
Participating plans: Plans in Program New Hampshire Healthy Families; Well
Sense Health Plan
New Hampshire Healthy Families; Well
Sense Health Plan
Notes: Program notes Individuals in the New Hampshire
Medicaid Care Management program
can be enrolled under either a 1915(b)
waiver or a 1932(a) federal operating
authority.
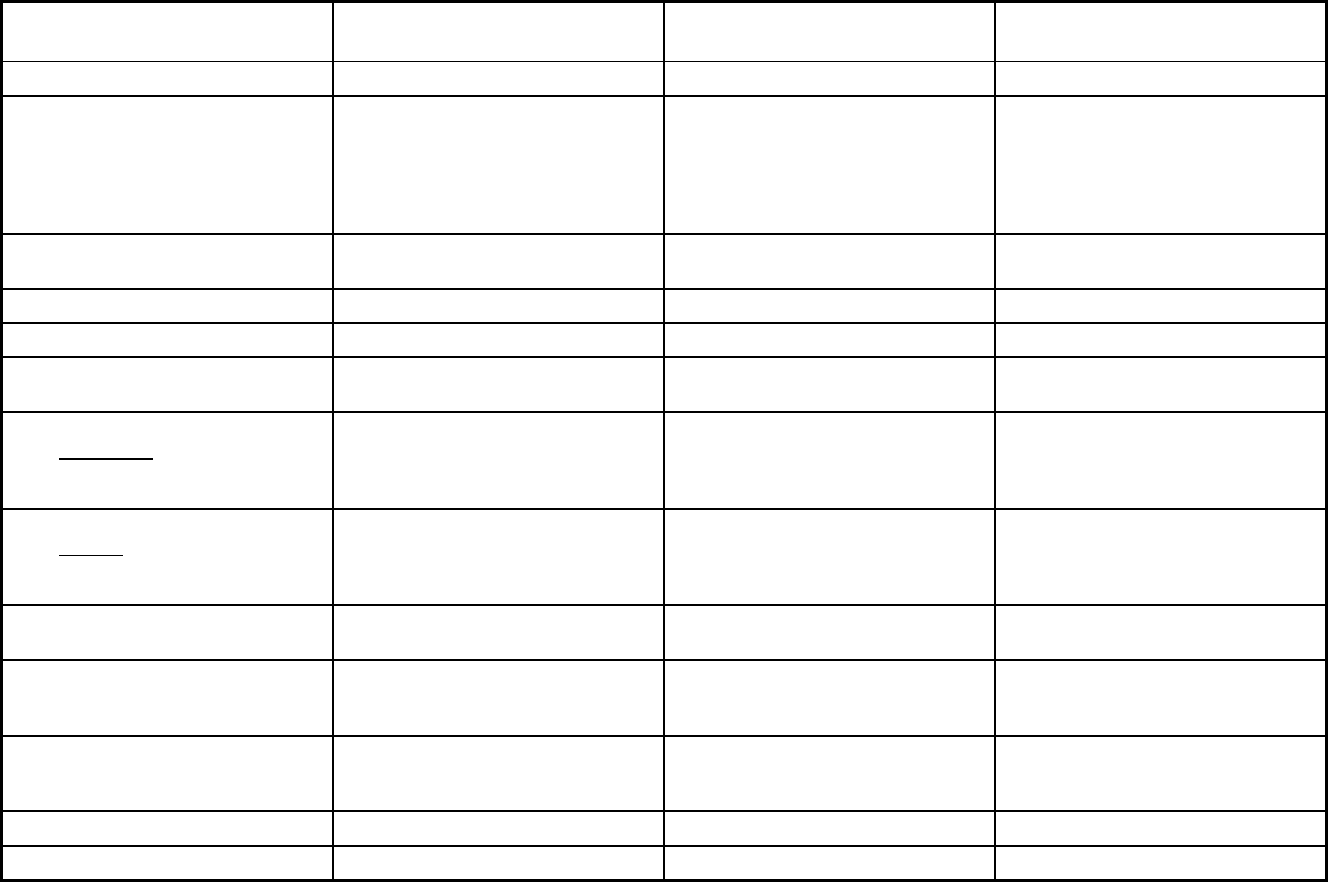
390
New Jersey Managed Care Program Features, as of 2018 (1 of 2)
Features NJFamilyCare FIDE SNP
Non-Emergency Medical
Transportation
Program type Comprehensive MCO + MLTSS Comprehensive MCO + MLTSS Non-Emergency Medical Transportation
Statewide or region-specific? Statewide Atlantic, Bergen, Burlington, Camden,
Cumberland, Essex, Gloucester,
Hudson, Hunterdon, Mercer, Middlesex,
Monmouth, Morris, Ocean, Passaic,
Salem, Somerset, Sussex, Union, and
Warren counties.
Statewide
Federal operating authority 1115(a) (Medicaid demonstration
waivers),1937 Alt Benefit Plan
1115(a) (Medicaid demonstration
waivers)
1902(a)(70) NEMT
Program start date 09/01/1995 01/01/2012 07/01/2009
Waiver expiration date (if applicable) 06/30/2022 06/30/2022
If the program ended in 2018, indicate
the end date
Populations enrolled: Low-income
adults not covered under ACA Section
VIII (excludes pregnant women and
people with disabilities)
Mandatory
Populations enrolled: Low-income
adults covered under ACA Section VIII
(excludes pregnant women and people
with disabilities)
Mandatory Mandatory
Populations enrolled: Aged, Blind or
Disabled Children or Adults
Mandatory Mandatory
Populations enrolled: Non-Disabled
Children (excludes children in foster
care or receiving adoption assistance)
Mandatory Mandatory
Populations enrolled: Individuals
receiving Limited Benefits (excludes
partial duals)
Populations enrolled: Full Duals Mandatory Voluntary Mandatory
Populations enrolled: Partial Duals Mandatory
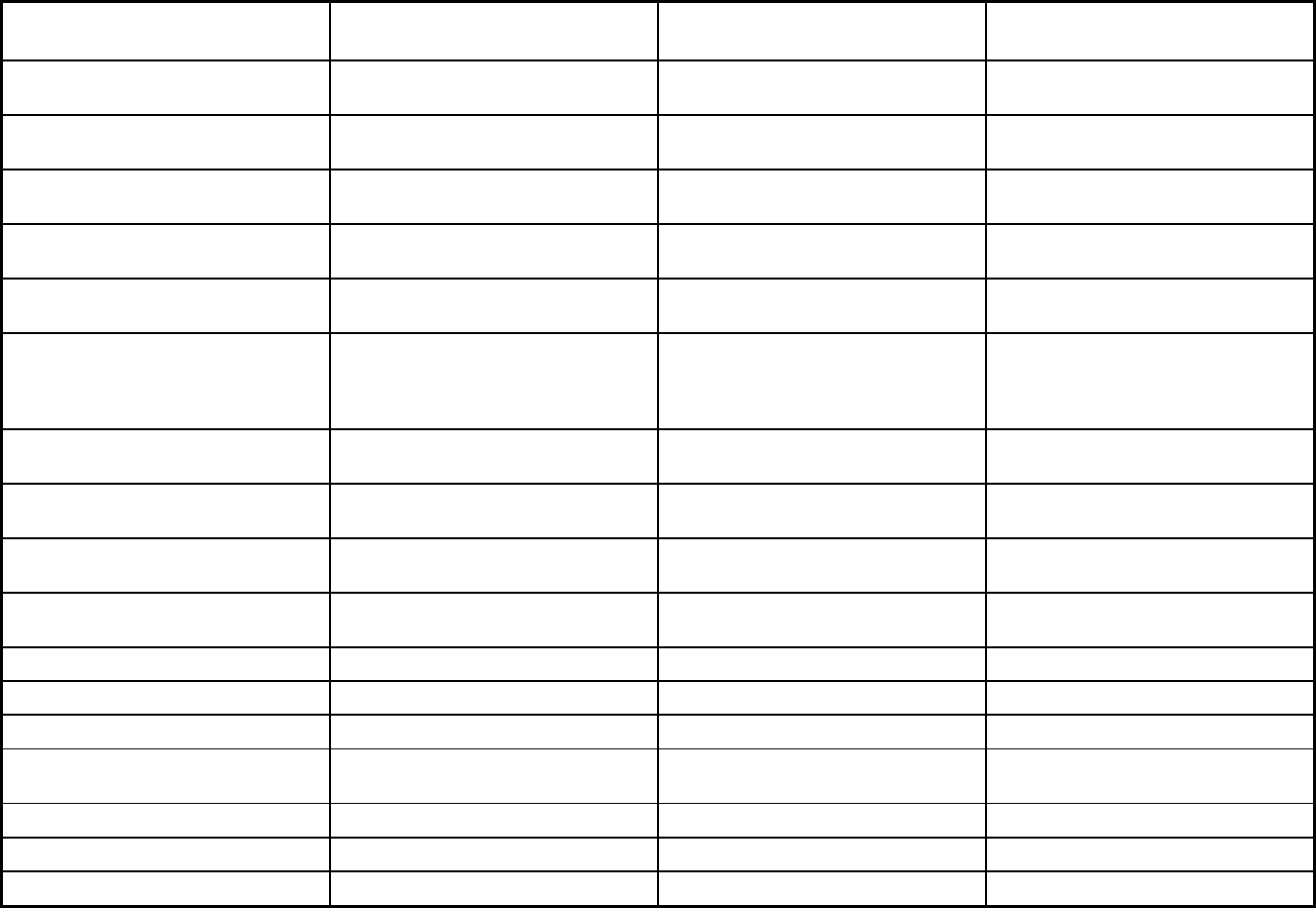
391
Features NJFamilyCare FIDE SNP
Non-Emergency Medical
Transportation
Populations enrolled: Children with
Special Health Care Needs
Mandatory Mandatory
Populations enrolled: Native
American/Alaskan Natives
Voluntary Exempt Voluntary
Populations enrolled: Foster Care and
Adoption Assistance Children
Mandatory Exempt Mandatory
Populations enrolled: Enrollment choice
period
10 days Other
Populations enrolled: Enrollment broker
name (if applicable)
Conduent
Populations enrolled: Notes on
enrollment choice period
Enrollee may enroll or disenroll without
cause once per quarter for the first three
quarters of the year. Annual enrollment
period rules apply thereafter.
Benefits covered: Inpatient hospital
physical health
X X
Benefits covered: Inpatient hospital
behavioral health (MH and/or SUD)
X X
Benefits covered: Outpatient hospital
physical health
X X
Benefits covered: Outpatient hospital
behavioral health (MH and/or SUD)
X X
Benefits covered: Partial hospitalization X X
Benefits covered: Physician X X
Benefits covered: Nurse practitioner X X
Benefits covered: Rural health clinics
and FQHCs
X X
Benefits covered: Clinic services X X
Benefits covered: Lab and x-ray X X
Benefits covered: Prescription drugs X X
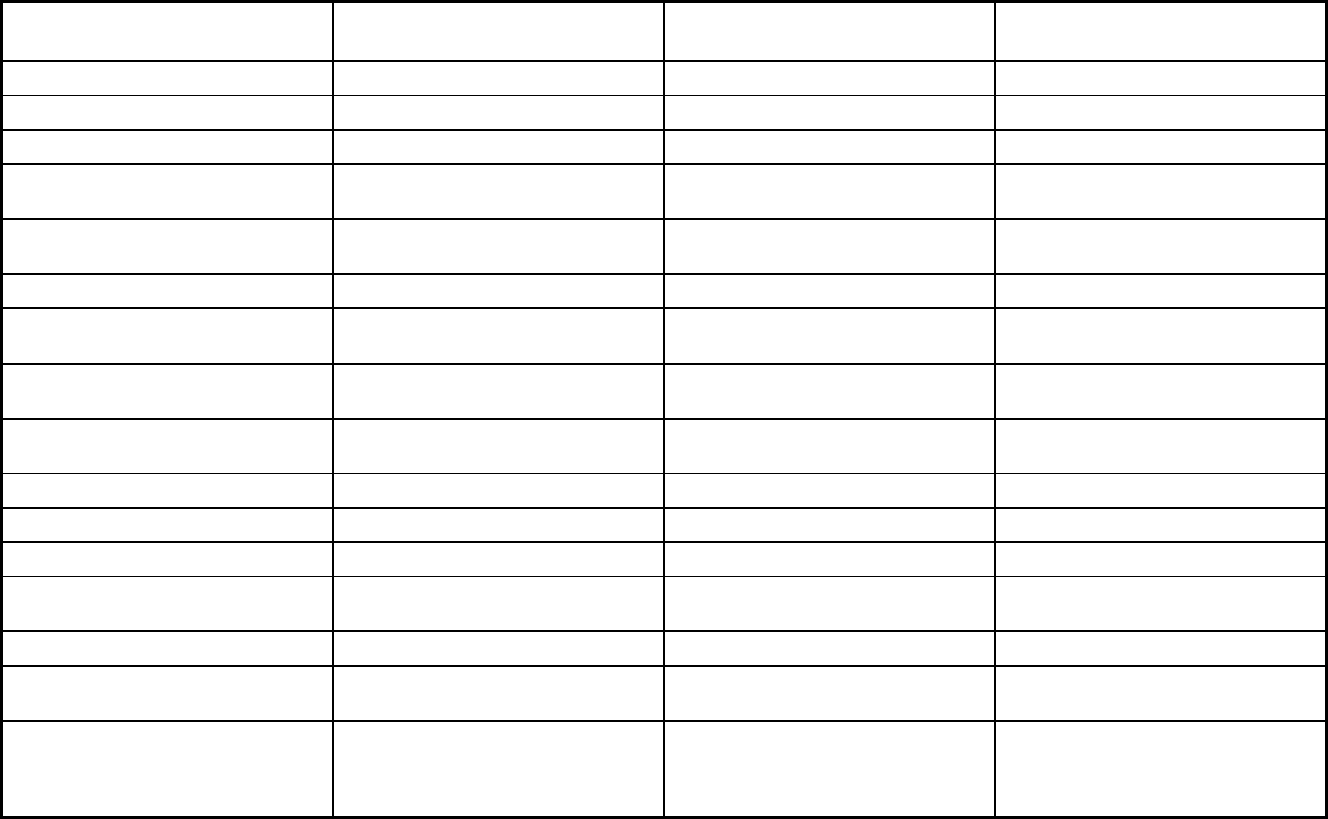
392
Features NJFamilyCare FIDE SNP
Non-Emergency Medical
Transportation
Benefits covered: Prosthetic devices X X
Benefits covered: EPSDT X X
Benefits covered: Case management X X
Benefits covered: SSA Section 1945-
authorized health home
Benefits covered: Health home care
(services in home)
X X
Benefits covered: Family planning X X
Benefits covered: Dental services
(medical/surgical)
X X
Benefits covered: Dental (preventative
or corrective)
X X
Benefits covered: Personal care (state
plan option)
X X
Benefits covered: HCBS waiver services X X
Benefits covered: Private duty nursing X X
Benefits covered: ICF-IDD X X
Benefits covered: Nursing facility
services
X X
Benefits covered: Hospice care X X
Benefits covered: Non-Emergency
Medical Transportation
X X X
Benefits covered: Institution for Mental
Disease inpatient treatment for people
ages 21-64 defined by 42 CFR
§438.6(e) as an 'in lieu of' benefit
X X
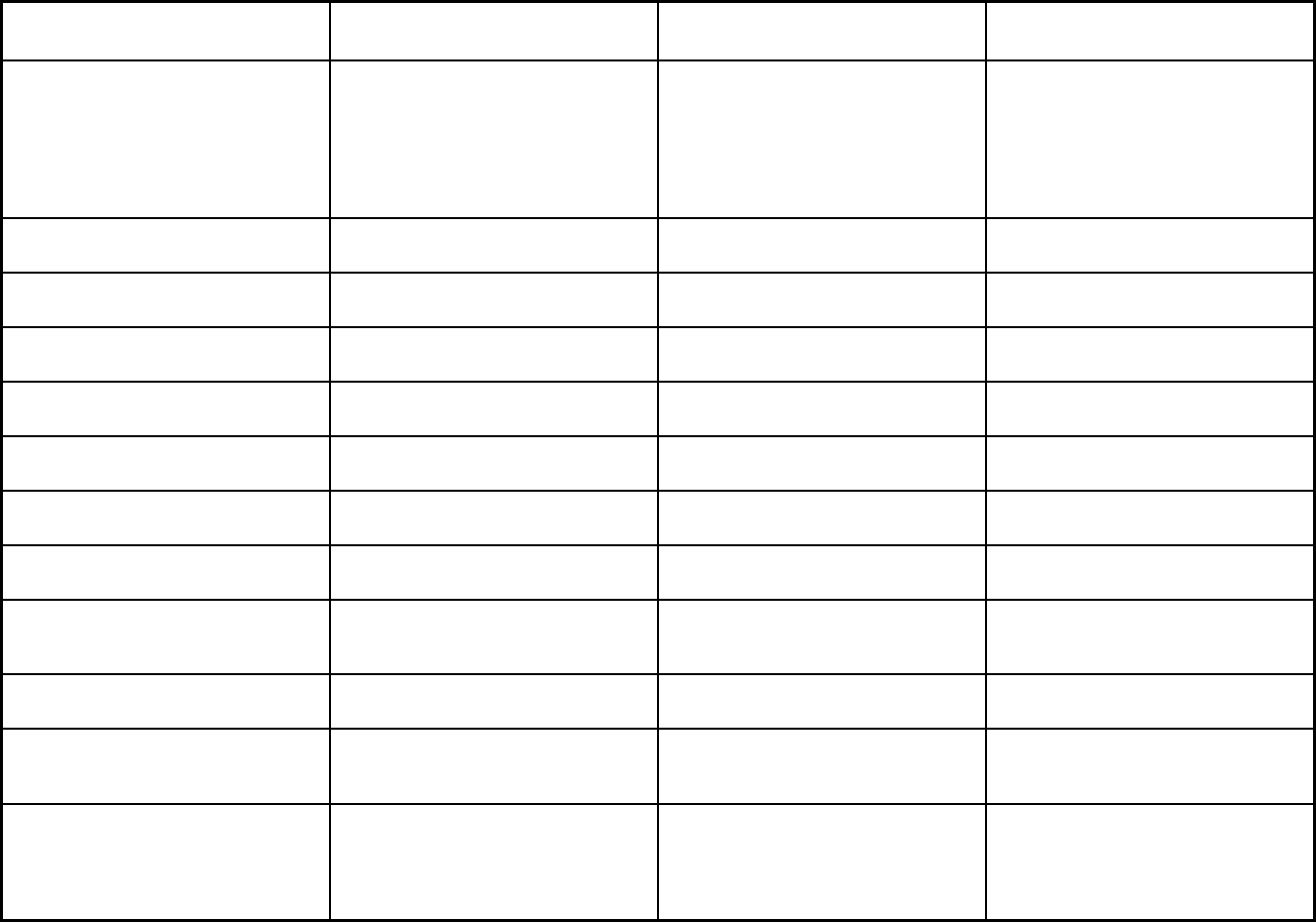
393
Features NJFamilyCare FIDE SNP
Non-Emergency Medical
Transportation
Benefits covered: Other (e.g., nurse
midwife services, freestanding birth
centers, podiatry, etc.)
Assistive tech, audiology, chiropractic,
DME, hearing aid, immunization, MDC,
medical supplies, optical appliances,
optometrist, organ transplants, orthotics,
rehab/sp hosp, outpatient rehab, non-
routine podiatrist, post-acute care,
preventive health, spec hosp, vision
Assistive tech, audiology, chiropractic,
DME, hearing aid, immunization, MDC,
medical supplies, optical appliances,
optometrist, organ transplants, orthotics,
rehab/sp hosp, outpatient rehab, non-
routine podiatrist, post-acute care,
preventive health, spec hosp, vision
Quality assurance and improvement:
HEDIS data required?
Yes Yes No
Quality assurance and improvement:
CAHPS data required?
Yes Yes No
Quality assurance and improvement:
Accreditation required?
Yes No No
Quality assurance and improvement:
Accrediting organization
NCQA
Quality assurance and improvement:
EQRO contractor name (if applicable)
Island Peer Review Organization Island Peer Review Organization
Performance incentives: Payment
bonuses/differentials to reward plans
X X
Performance incentives: Preferential
auto-enrollment to reward plans
Performance incentives: Public reports
comparing plan performance on key
metrics
X X
Performance incentives: Withholds tied
to performance metrics
Performance incentives: MCOs/PHPs
required or encouraged to pay providers
for value/quality outcomes
Participating plans: Plans in Program Aetna Better Health NJ; Amerigroup
New Jersey Inc; Horizon NJ Health;
UnitedHealthcare Community Plan;
WellCare of New Jersey
Amerivantage Dual Coordination (HMO
SNP); Horizon NJ TotalCare (HMO
SNP); UnitedHealthcare Dual Complete
ONE
 (HMO SNP); WellCare
Liberty (HMO SNP)
Logisticare
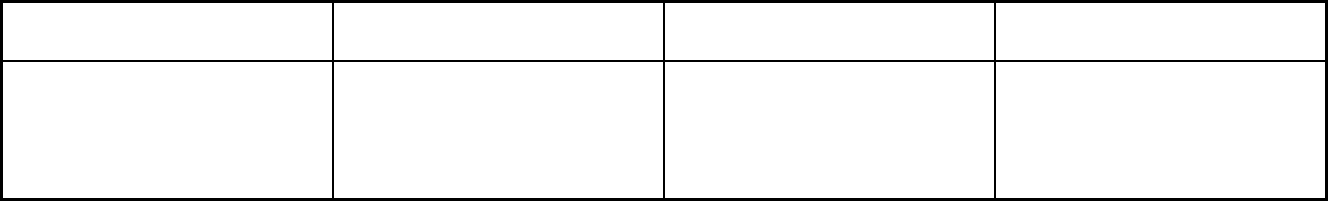
394
Features NJFamilyCare FIDE SNP
Non-Emergency Medical
Transportation
Notes: Program notes HCBS services are part of the MLTSS
program which is available to qualified
beneficiaries under NJFamilyCare. All
NJFamilyCare MCOs are statewide
except WellCare, which is not available
in Hunterdon County.
Members may only enroll through
Medicare or with the FIDE SNP plan
directly.
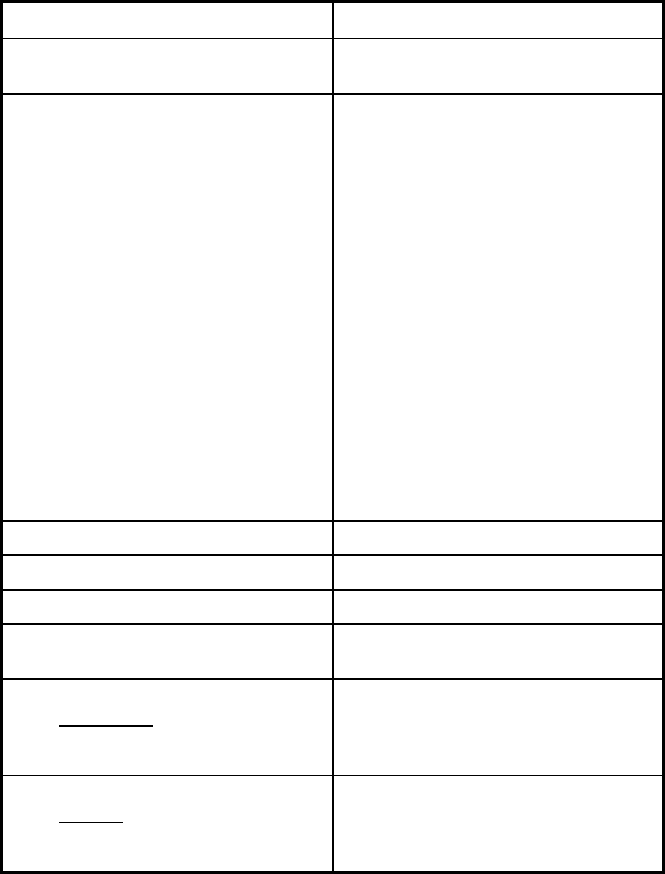
395
New Jersey Managed Care Program Features, as of 2018 (2 of 2)
Features PACE
Program type Program of All-inclusive Care for the
Elderly (PACE)
Statewide or region-specific? Atlantic, Cape May, Monmouth, and
Mercer Counties. Zip codes: 08028,
08062, 08071, 08094, 08098, 08302,
08311, 08312, 08314, 08316, 08318,
08321, 08322, 08323, 08324, 08327,
08328, 08329, 08332, 08343, 08344,
08345, 08348, 08349, 08352, 08353,
08360, 08361, 08362, 08002, 08003,
08004, 08007, 08009, 08012, 08021,
08026, 08029, 08030, 08031, 08033,
08034, 08035, 08043, 08045, 08049,
08052, 08059, 08065, 08076, 08077,
08078, 08081, 08083, 08084, 08091,
08095, 08099, 08101, 08102, 08103,
08104, 08105, 08106, 08107, 08108,
08109, 08110, 08015, 08016, 08022,
08060, 08068, 08505, 08515, 08518,
08554, 07002, 07030, 07047, 07086,
07087, 07093, 07094, 07302, 07304,
07305, 07306, 07307, 07310, 07311
Federal operating authority PACE
Program start date 04/09/2009
Waiver expiration date (if applicable)
If the program ended in 2018, indicate
the end date
Populations enrolled: Low-income
adults not covered under ACA Section
VIII (excludes pregnant women and
people with disabilities)
Populations enrolled: Low-income
adults covered under ACA Section VIII
(excludes pregnant women and people
with disabilities)
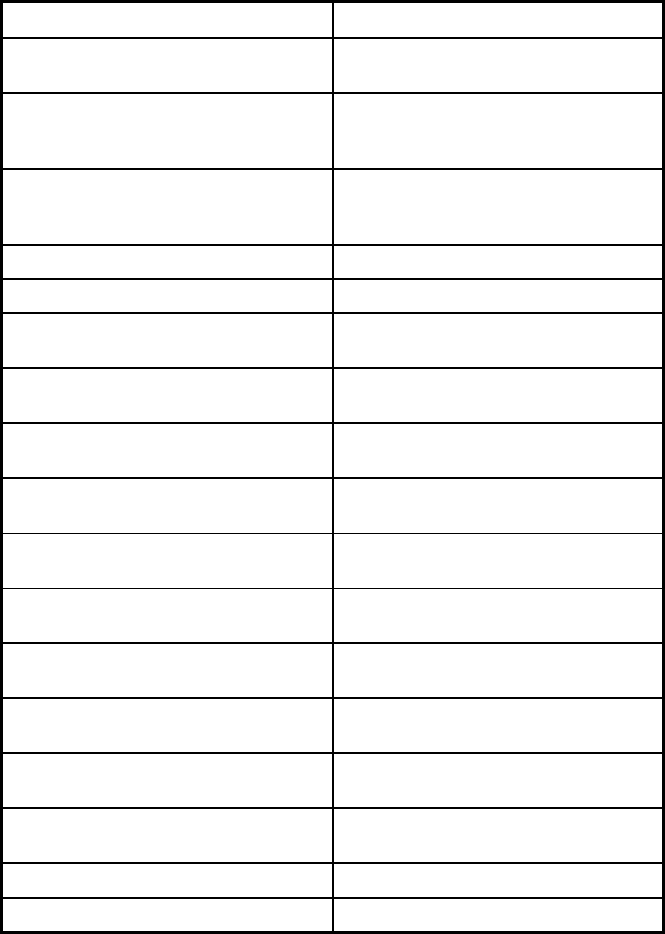
396
Features PACE
Populations enrolled: Aged, Blind or
Disabled Children or Adults
Voluntary
Populations enrolled: Non-Disabled
Children (excludes children in foster
care or receiving adoption assistance)
Populations enrolled: Individuals
receiving Limited Benefits (excludes
partial duals)
Populations enrolled: Full Duals Voluntary
Populations enrolled: Partial Duals Voluntary
Populations enrolled: Children with
Special Health Care Needs
Populations enrolled: Native
American/Alaskan Natives
Voluntary
Populations enrolled: Foster Care and
Adoption Assistance Children
Exempt
Populations enrolled: Enrollment choice
period
N/A
Populations enrolled: Enrollment broker
name (if applicable)
Populations enrolled: Notes on
enrollment choice period
Benefits covered: Inpatient hospital
physical health
X
Benefits covered: Inpatient hospital
behavioral health (MH and/or SUD)
X
Benefits covered: Outpatient hospital
physical health
X
Benefits covered: Outpatient hospital
behavioral health (MH and/or SUD)
X
Benefits covered: Partial hospitalization X
Benefits covered: Physician X
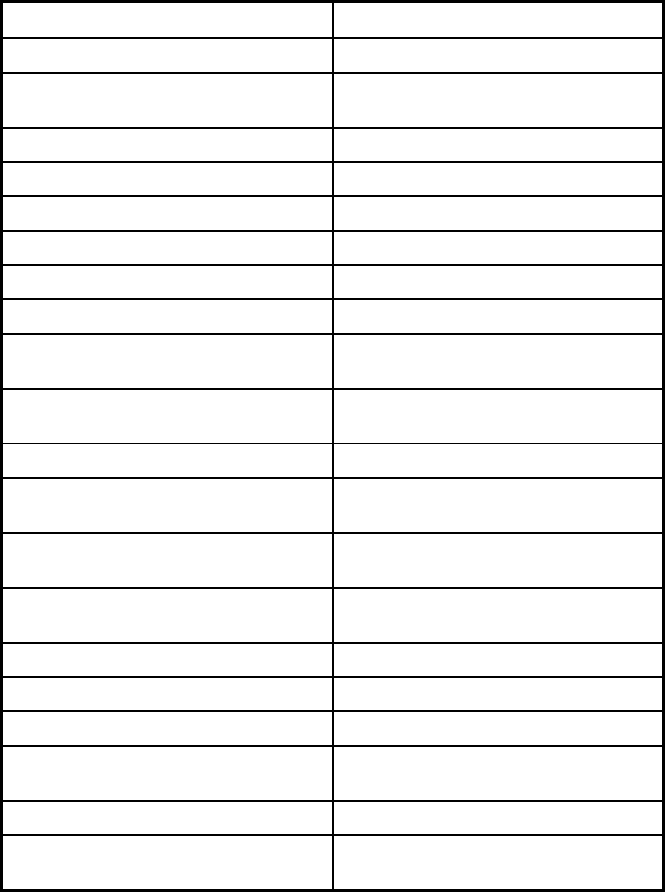
397
Features PACE
Benefits covered: Nurse practitioner X
Benefits covered: Rural health clinics
and FQHCs
Benefits covered: Clinic services X
Benefits covered: Lab and x-ray X
Benefits covered: Prescription drugs X
Benefits covered: Prosthetic devices X
Benefits covered: EPSDT
Benefits covered: Case management X
Benefits covered: SSA Section 1945-
authorized health home
Benefits covered: Health home care
(services in home)
X
Benefits covered: Family planning X
Benefits covered: Dental services
(medical/surgical)
X
Benefits covered: Dental (preventative
or corrective)
X
Benefits covered: Personal care (state
plan option)
X
Benefits covered: HCBS waiver services X
Benefits covered: Private duty nursing
Benefits covered: ICF-IDD
Benefits covered: Nursing facility
services
X
Benefits covered: Hospice care X
Benefits covered: Non-Emergency
Medical Transportation
X
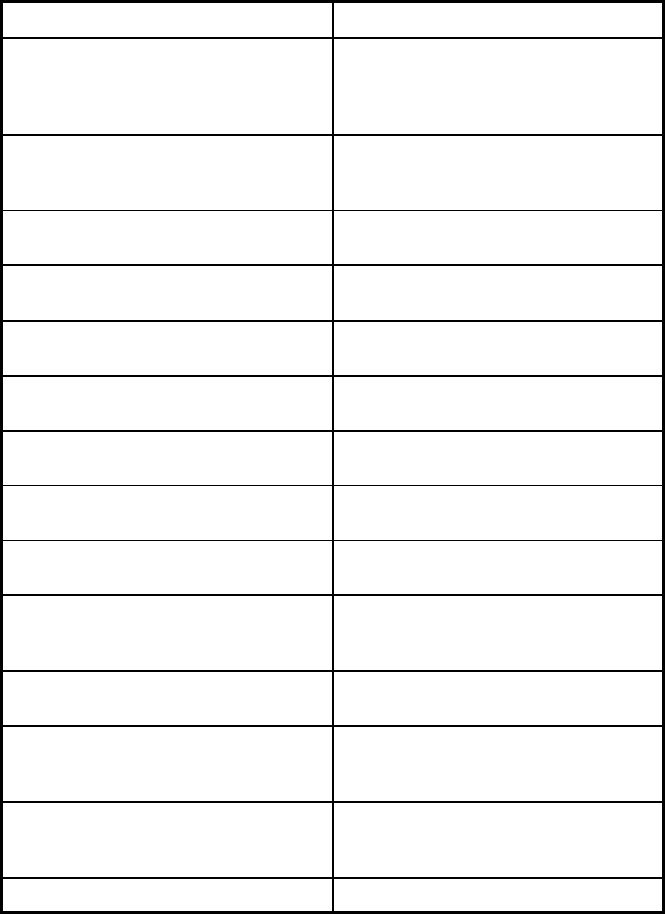
398
Features PACE
Benefits covered: Institution for Mental
Disease inpatient treatment for people
ages 21-64 defined by 42 CFR
§438.6(e) as an 'in lieu of' benefit
Benefits covered: Other (e.g., nurse
midwife services, freestanding birth
centers, podiatry, etc.)
Quality assurance and improvement:
HEDIS data required?
No
Quality assurance and improvement:
CAHPS data required?
No
Quality assurance and improvement:
Accreditation required?
No
Quality assurance and improvement:
Accrediting organization
Quality assurance and improvement:
EQRO contractor name (if applicable)
Performance incentives: Payment
bonuses/differentials to reward plans
Performance incentives: Preferential
auto-enrollment to reward plans
Performance incentives: Public reports
comparing plan performance on key
metrics
Performance incentives: Withholds tied
to performance metrics
Performance incentives: MCOs/PHPs
required or encouraged to pay providers
for value/quality outcomes
Participating plans: Plans in Program Atlanticare LIFE; Beacon of LIFE;
Inspira LIFE; LIFE at Lourdes; LIFE St.
Francis; Lutheran Senior Life
Notes: Program notes
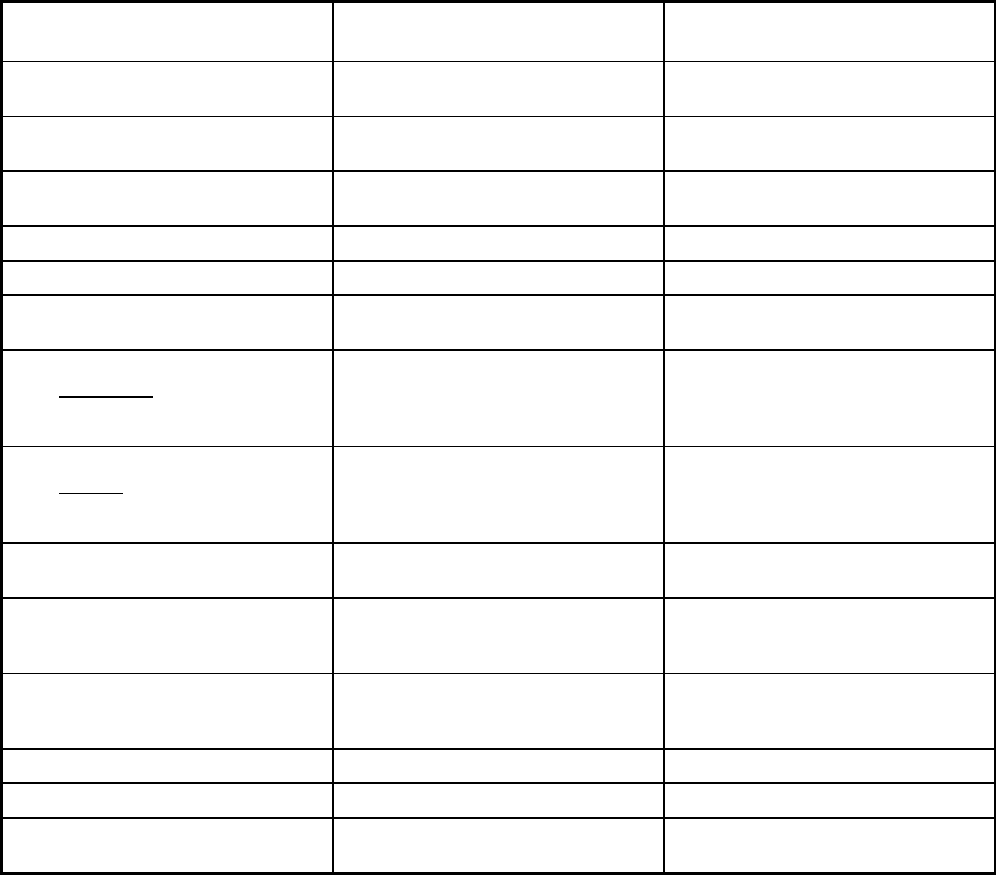
400
New Mexico Managed Care Program Features, as of 2018
Features Centennial Care
Program of All-Inclusive Care for the
Elderly (PACE)
Program type Comprehensive MCO + MLTSS Program of All-inclusive Care for the
Elderly (PACE)
Statewide or region-specific? Statewide Bernalillo County, Sandoval County,
Valencia County
Federal operating authority 1115(a) (Medicaid demonstration
waivers)
PACE
Program start date 01/01/2014 07/01/2004
Waiver expiration date (if applicable) 12/31/2018
If the program ended in 2018, indicate
the end date
12/31/2018
Populations enrolled: Low-income
adults not covered under ACA Section
VIII (excludes pregnant women and
people with disabilities)
Mandatory
Populations enrolled: Low-income
adults covered under ACA Section VIII
(excludes pregnant women and people
with disabilities)
Mandatory
Populations enrolled: Aged, Blind or
Disabled Children or Adults
Mandatory
Populations enrolled: Non-Disabled
Children (excludes children in foster
care or receiving adoption assistance)
Mandatory
Populations enrolled: Individuals
receiving Limited Benefits (excludes
partial duals)
Mandatory
Populations enrolled: Full Duals Mandatory Voluntary
Populations enrolled: Partial Duals
Populations enrolled: Children with
Special Health Care Needs
Mandatory
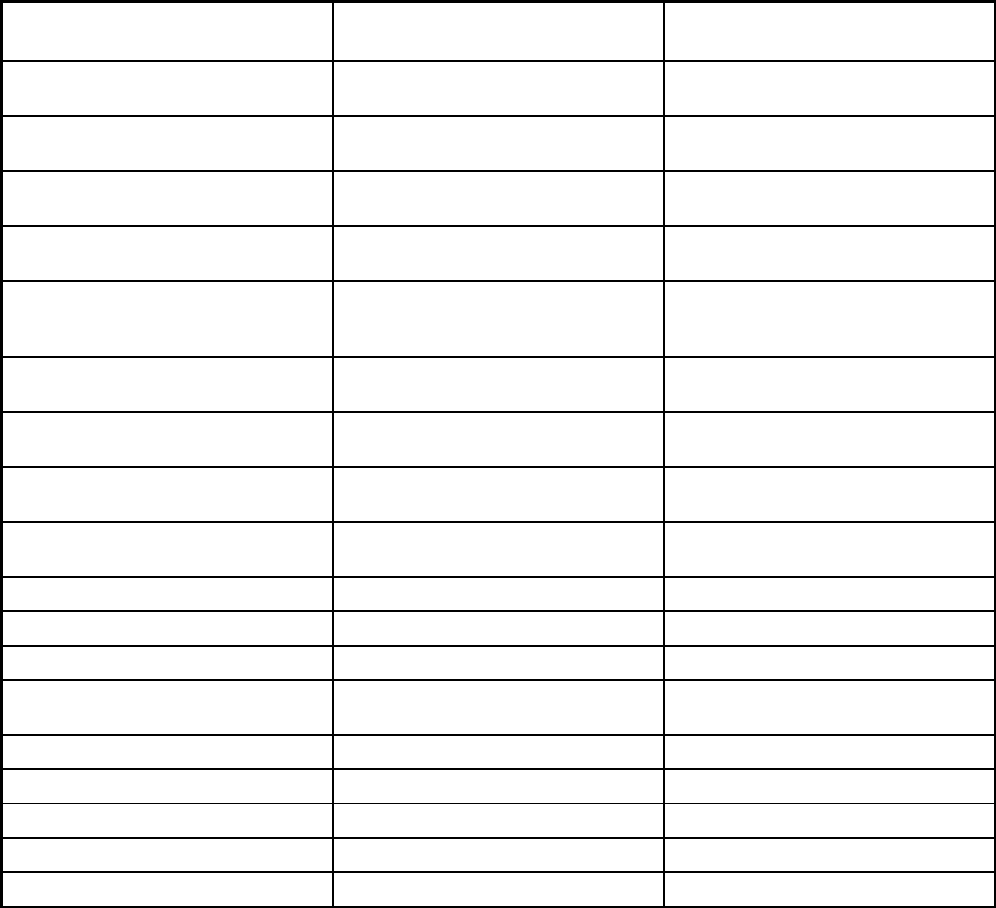
401
Features Centennial Care
Program of All-Inclusive Care for the
Elderly (PACE)
Populations enrolled: Native
American/Alaskan Natives
Voluntary Exempt
Populations enrolled: Foster Care and
Adoption Assistance Children
Mandatory
Populations enrolled: Enrollment choice
period
Other N/A
Populations enrolled: Enrollment broker
name (if applicable)
Populations enrolled: Notes on
enrollment choice period
Members have 90 days to switch MCO's
when initially enrolled and during
recertification.
Disenrollment permitted every 30 days.
Benefits covered: Inpatient hospital
physical health
X X
Benefits covered: Inpatient hospital
behavioral health (MH and/or SUD)
X X
Benefits covered: Outpatient hospital
physical health
X X
Benefits covered: Outpatient hospital
behavioral health (MH and/or SUD)
X X
Benefits covered: Partial hospitalization X X
Benefits covered: Physician X X
Benefits covered: Nurse practitioner X X
Benefits covered: Rural health clinics
and FQHCs
X X
Benefits covered: Clinic services X X
Benefits covered: Lab and x-ray X X
Benefits covered: Prescription drugs X X
Benefits covered: Prosthetic devices X X
Benefits covered: EPSDT X
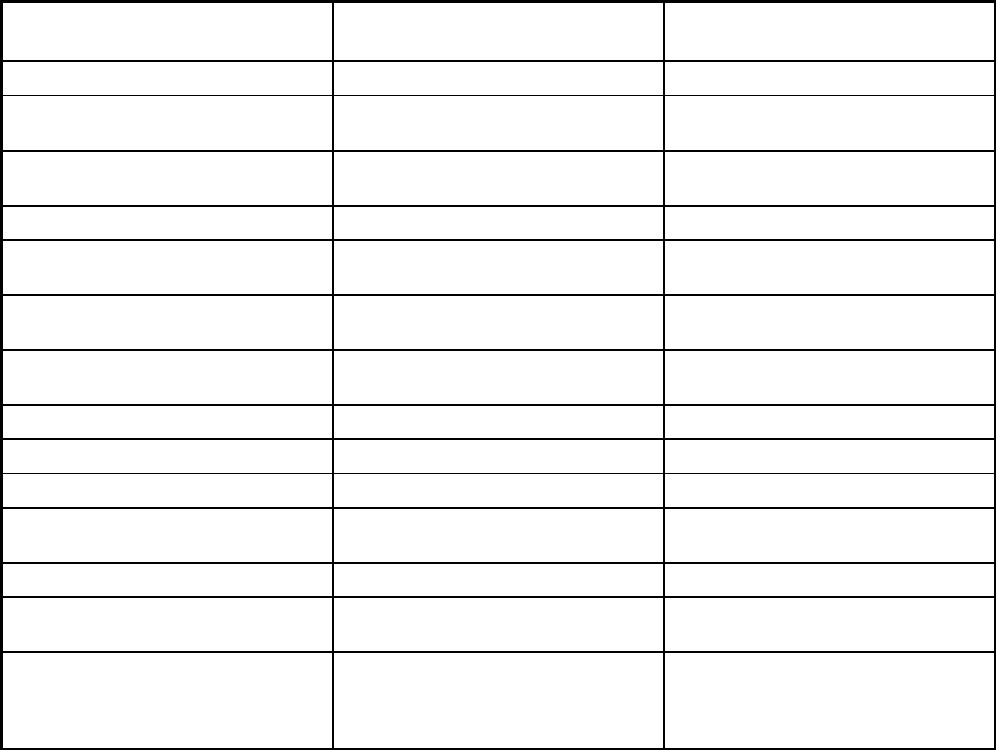
402
Features Centennial Care
Program of All-Inclusive Care for the
Elderly (PACE)
Benefits covered: Case management X X
Benefits covered: SSA Section 1945-
authorized health home
Benefits covered: Health home care
(services in home)
X X
Benefits covered: Family planning X
Benefits covered: Dental services
(medical/surgical)
X X
Benefits covered: Dental (preventative
or corrective)
X X
Benefits covered: Personal care (state
plan option)
X X
Benefits covered: HCBS waiver services X
Benefits covered: Private duty nursing X X
Benefits covered: ICF-IDD
Benefits covered: Nursing facility
services
X X
Benefits covered: Hospice care X
Benefits covered: Non-Emergency
Medical Transportation
X X
Benefits covered: Institution for Mental
Disease inpatient treatment for people
ages 21-64 defined by 42 CFR
§438.6(e) as an 'in lieu of' benefit
X
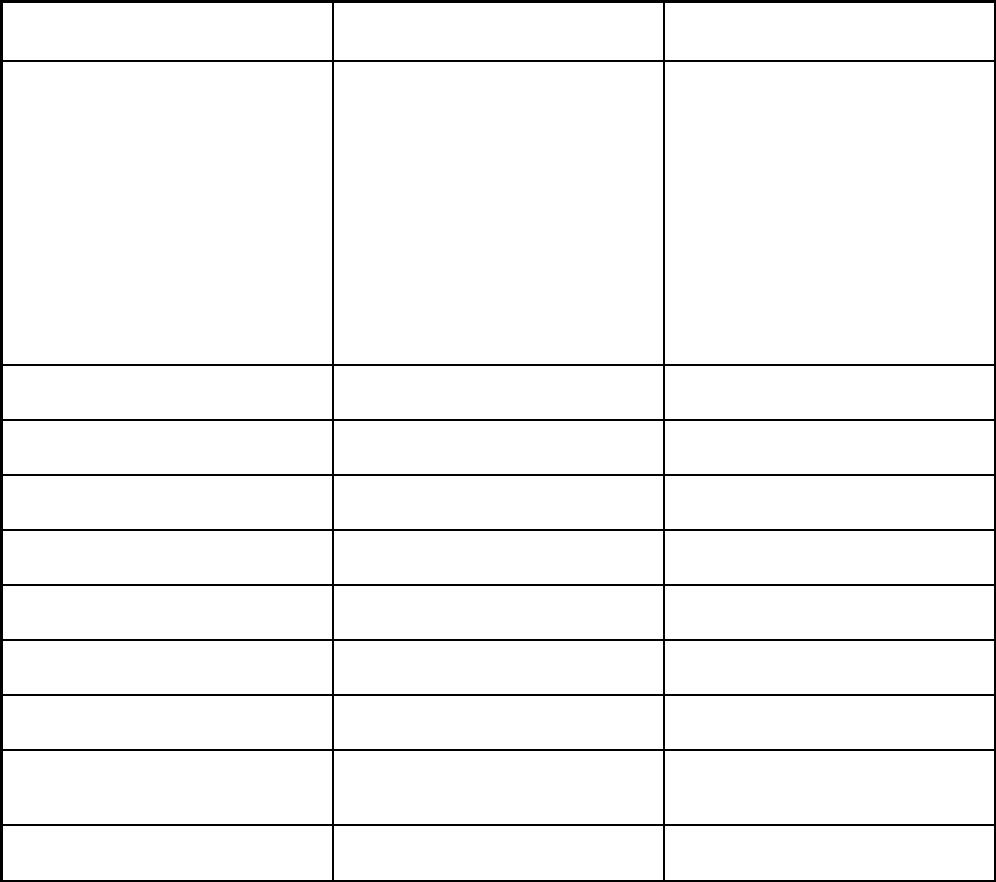
403
Features Centennial Care
Program of All-Inclusive Care for the
Elderly (PACE)
Benefits covered: Other (e.g., nurse
midwife services, freestanding birth
centers, podiatry, etc.)
Ambulatory, surgical, anesthesia,
diagnostic imaging, imaging and
therapeutic radiology services, dialysis,
durable medical equipment and medical
supplies, hearing and audiology,
immunization, medical service
providers, midwife, nutritional,
occupational therapy, physical therapy,
podiatry, pregnancy termination (state
funded), prosthetics and orthotics,
rehabilitation, reproductive health,
school based, speech therapy,
telehealth, transplant, transportation,
vision, pediatricians
Quality assurance and improvement:
HEDIS data required?
Yes Yes
Quality assurance and improvement:
CAHPS data required?
Yes No
Quality assurance and improvement:
Accreditation required?
Yes No
Quality assurance and improvement:
Accrediting organization
NCQA
Quality assurance and improvement:
EQRO contractor name (if applicable)
IPRO
Performance incentives: Payment
bonuses/differentials to reward plans
Performance incentives: Preferential
auto-enrollment to reward plans
X
Performance incentives: Public reports
comparing plan performance on key
metrics
X
Performance incentives: Withholds tied
to performance metrics
X
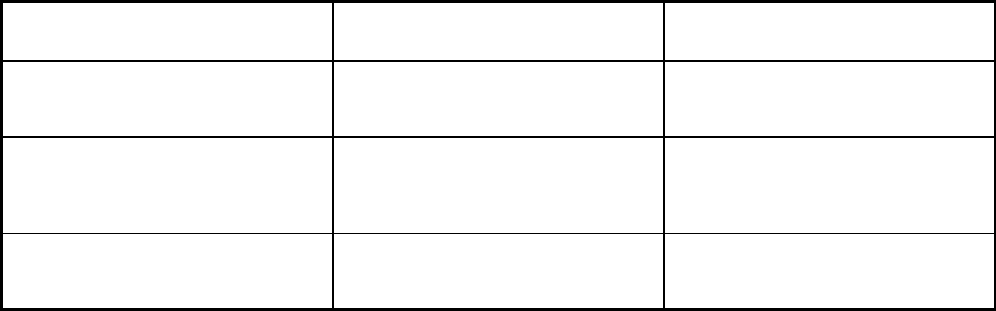
404
Features Centennial Care
Program of All-Inclusive Care for the
Elderly (PACE)
Performance incentives: MCOs/PHPs
required or encouraged to pay providers
for value/quality outcomes
X
Participating plans: Plans in Program Blue Cross Blue Shield of NM; Molina
Healthcare of New Mexico Inc;
Presbyterian Health Plan;
UnitedHealthcare Community Plan
Innovage New Mexico PACE dba Total
Community Care
Notes: Program notes Native American/Alaskan Native
Enrollment would be manditorily
enrolled if receiving LTSS.
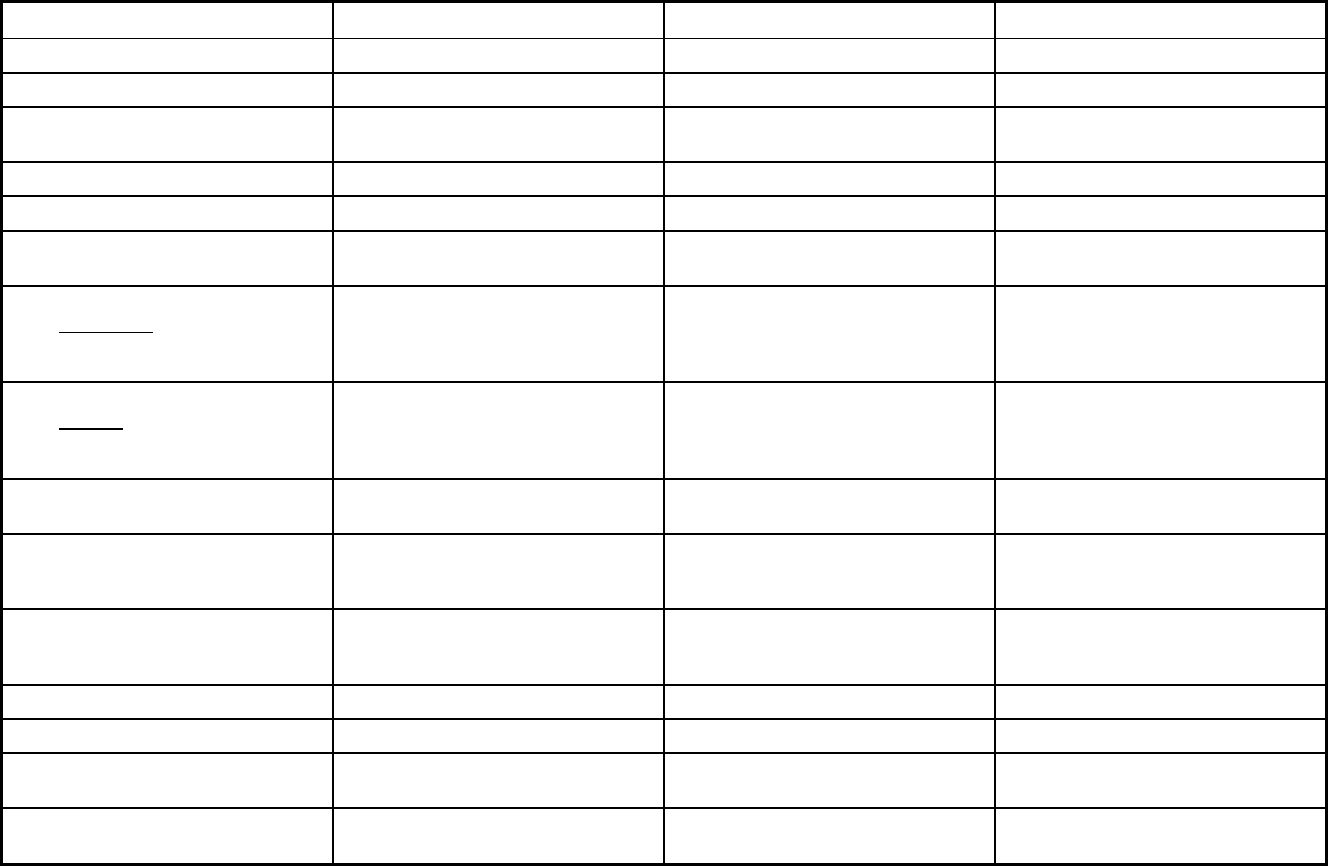
405
New York Managed Care Program Features, as of 2018 (1 of 2)
Features Health and Recovery Plans Managed Long Term Care Medicaid Advantage Plus
Program type Comprehensive MCO MLTSS only (PIHP and/or PAHP) Comprehensive MCO + MLTSS
Statewide or region-specific? Statewide Statewide Statewide
Federal operating authority 1115(a) (Medicaid demonstration
waivers)
1115(a) (Medicaid demonstration
waivers)
1115(a) (Medicaid demonstration
waivers)
Program start date 10/01/2015 01/01/1998 01/01/2007
Waiver expiration date (if applicable) 03/31/2021 03/31/2021 03/31/2021
If the program ended in 2018, indicate
the end date
Populations enrolled: Low-income
adults not covered under ACA Section
VIII (excludes pregnant women and
people with disabilities)
Voluntary
Populations enrolled: Low-income
adults covered under ACA Section VIII
(excludes pregnant women and people
with disabilities)
Voluntary
Populations enrolled: Aged, Blind or
Disabled Children or Adults
Populations enrolled: Non-Disabled
Children (excludes children in foster
care or receiving adoption assistance)
Populations enrolled: Individuals
receiving Limited Benefits (excludes
partial duals)
Populations enrolled: Full Duals Mandatory Voluntary
Populations enrolled: Partial Duals
Populations enrolled: Children with
Special Health Care Needs
Populations enrolled: Native
American/Alaskan Natives
Exempt Exempt Exempt
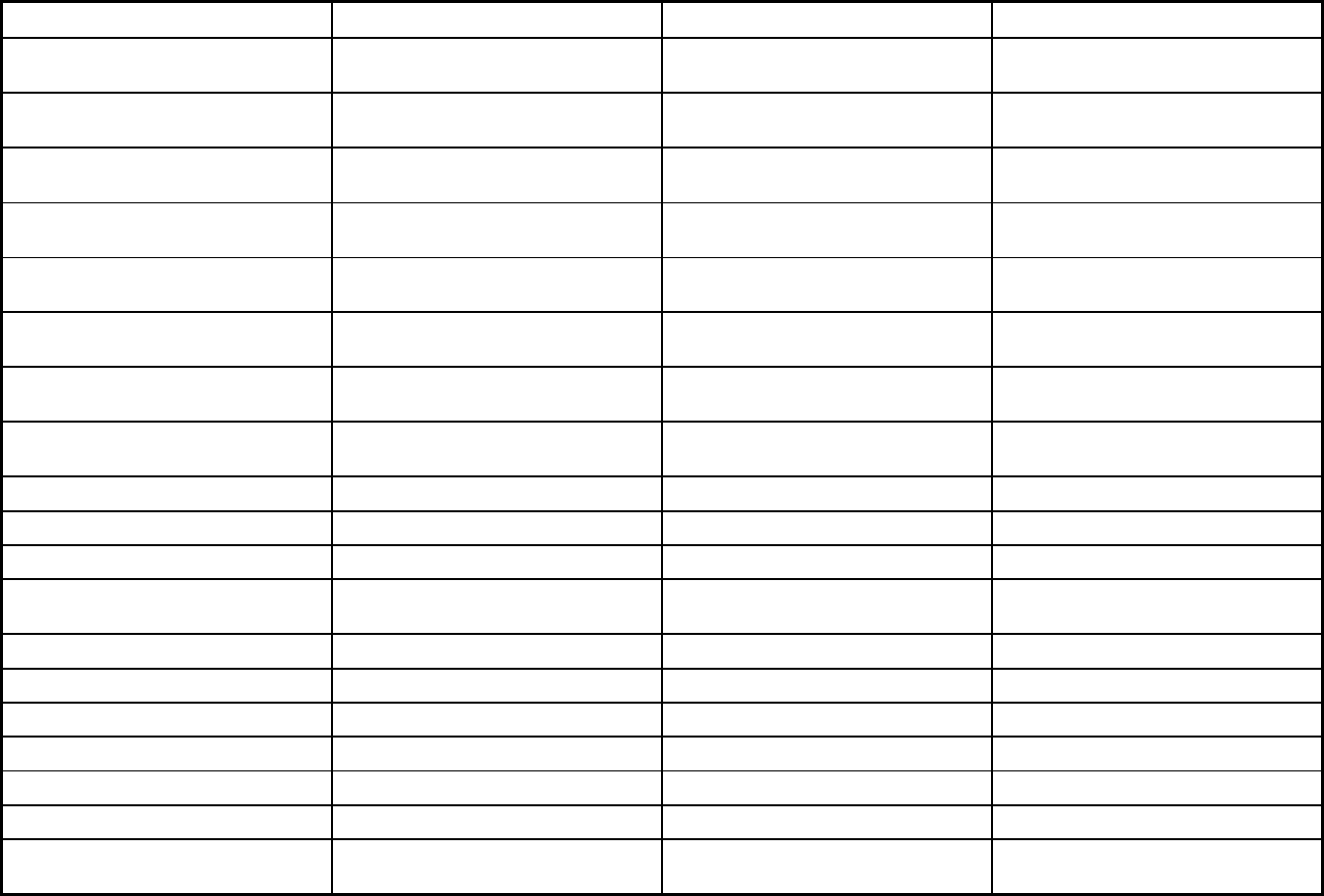
406
Features Health and Recovery Plans Managed Long Term Care Medicaid Advantage Plus
Populations enrolled: Foster Care and
Adoption Assistance Children
Exempt Exempt Exempt
Populations enrolled: Enrollment choice
period
30 days 60 days 60 days
Populations enrolled: Enrollment broker
name (if applicable)
NY Medicaid Choice/Maximus NY Medicaid Choice/Maximus NY Medicaid Choice/Maximus
Populations enrolled: Notes on
enrollment choice period
Benefits covered: Inpatient hospital
physical health
X X
Benefits covered: Inpatient hospital
behavioral health (MH and/or SUD)
X X
Benefits covered: Outpatient hospital
physical health
X X
Benefits covered: Outpatient hospital
behavioral health (MH and/or SUD)
X X
Benefits covered: Partial hospitalization X
Benefits covered: Physician X X X
Benefits covered: Nurse practitioner X X X
Benefits covered: Rural health clinics
and FQHCs
X
Benefits covered: Clinic services X X X
Benefits covered: Lab and x-ray X X
Benefits covered: Prescription drugs X X
Benefits covered: Prosthetic devices X X
Benefits covered: EPSDT
Benefits covered: Case management X X X
Benefits covered: SSA Section 1945-
authorized health home
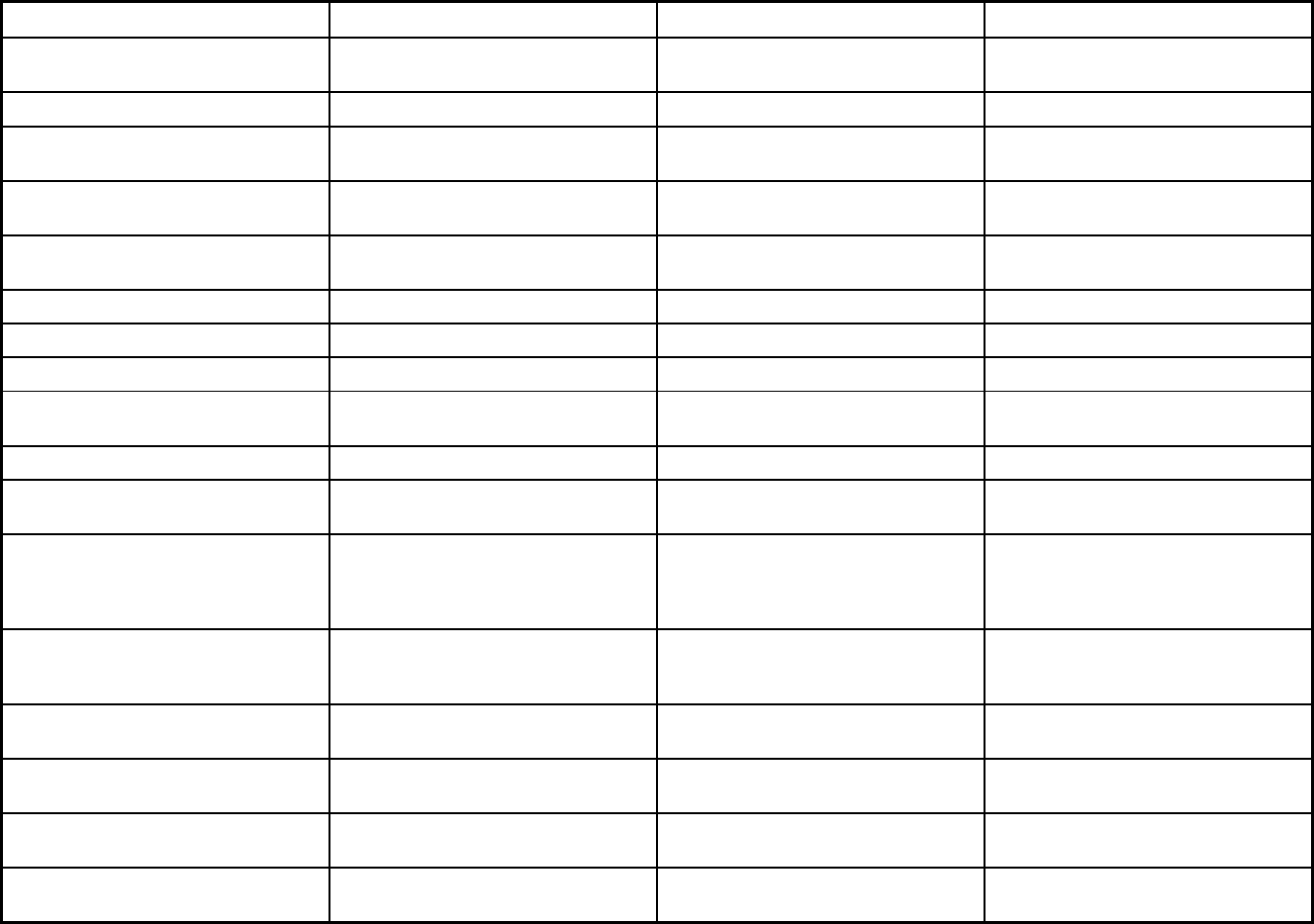
407
Features Health and Recovery Plans Managed Long Term Care Medicaid Advantage Plus
Benefits covered: Health home care
(services in home)
X X X
Benefits covered: Family planning X
Benefits covered: Dental services
(medical/surgical)
X X X
Benefits covered: Dental (preventative
or corrective)
X X X
Benefits covered: Personal care (state
plan option)
X X X
Benefits covered: HCBS waiver services X X X
Benefits covered: Private duty nursing X X X
Benefits covered: ICF-IDD
Benefits covered: Nursing facility
services
X X
Benefits covered: Hospice care X X
Benefits covered: Non-Emergency
Medical Transportation
X X
Benefits covered: Institution for Mental
Disease inpatient treatment for people
ages 21-64 defined by 42 CFR
§438.6(e) as an 'in lieu of' benefit
Benefits covered: Other (e.g., nurse
midwife services, freestanding birth
centers, podiatry, etc.)
Midwife Services, audiology, vision,
occupational therapy
Podiatry
Quality assurance and improvement:
HEDIS data required?
Yes No No
Quality assurance and improvement:
CAHPS data required?
Yes No No
Quality assurance and improvement:
Accreditation required?
No No No
Quality assurance and improvement:
Accrediting organization
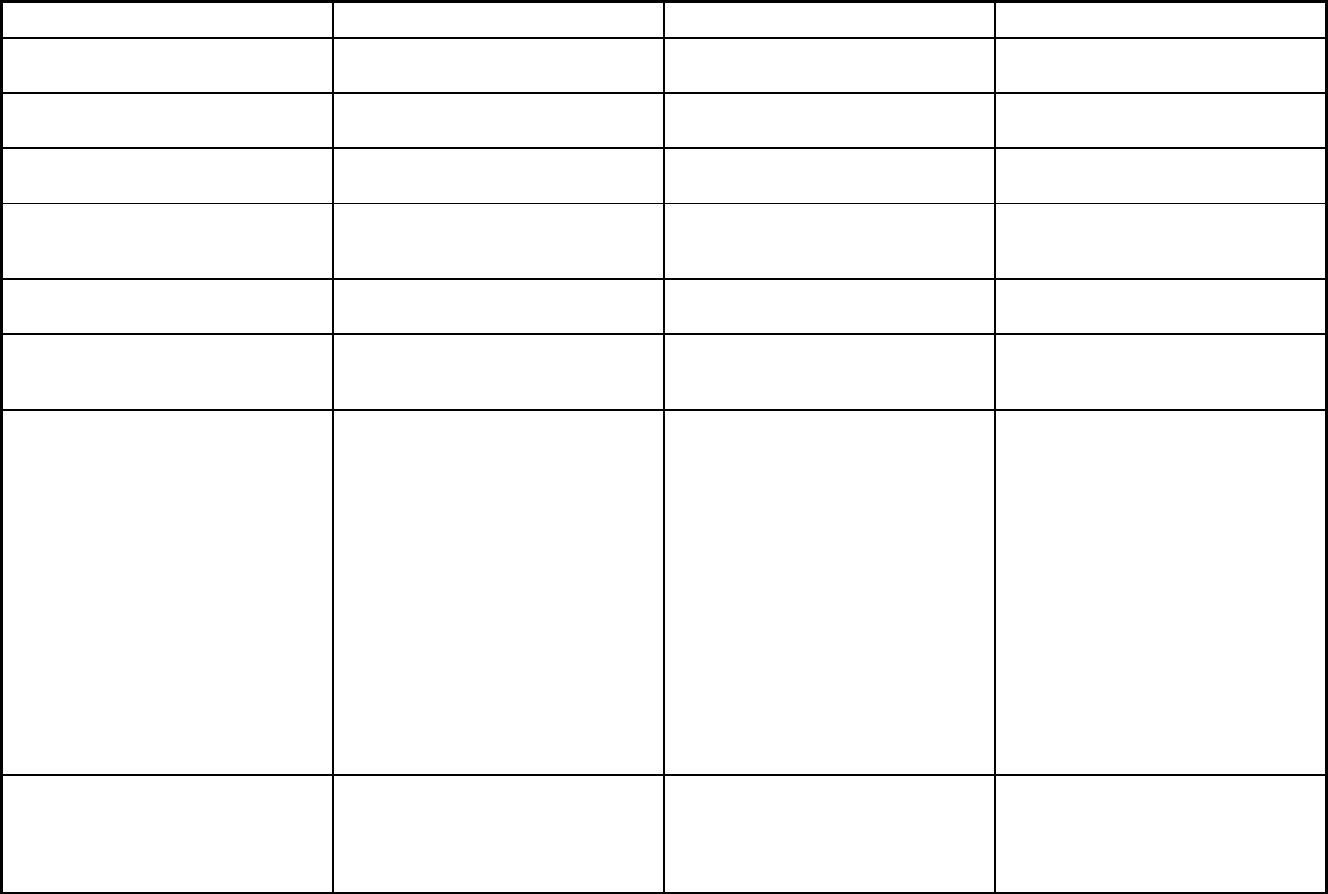
408
Features Health and Recovery Plans Managed Long Term Care Medicaid Advantage Plus
Quality assurance and improvement:
EQRO contractor name (if applicable)
Island Peer Review Organization Island Peer Review Organization Island Peer Review Organization
Performance incentives: Payment
bonuses/differentials to reward plans
X X
Performance incentives: Preferential
auto-enrollment to reward plans
X X
Performance incentives: Public reports
comparing plan performance on key
metrics
X X
Performance incentives: Withholds tied
to performance metrics
Performance incentives: MCOs/PHPs
required or encouraged to pay providers
for value/quality outcomes
X
Participating plans: Plans in Program Affinity Health Plan; Capital District
Physician's Health Plan; Excellus Health
Plan; Fidelis Care; HealthFirst;
HealthPlus; HIP GNY; Independent
Health Association; MetroPlus; Molina
HealthCare of New York; MVP Health
Plan; United HealthCare; YourCare
Health Plan
Aetna Better Health; AgeWell New York;
AlphaCare; ArchCare Community Life;
Centers Plan for Healthy Living;
ElderPlan; ElderServe; ElderWood;
Extended MLTC; Fallon Health
Weinberg; Fidelis Care; GuildNet;
Hamaspik Choice; Health
Advantage/Elant Choice; HealthPlus;
iCircle Care; Independent Care
Systems; Integra; Kalos Health Plan;
MetroPlus; Montefiore; North Shore -
LIJ Health Plan; Prime Health Choice;
Senior Health Partners; Senior Network
Health; Senior Whole Health; United
HealthCare; Village Care; VNA
HomeCare Options; VNS Choice;
WellCare Advocate
ElderPlan; Fidelis Legacy Plan;
GuildNet; HealthFirst; HealthPlus
Advantage Plus; Senior Whole Health;
Village Care; VNS Choice Plus
Notes: Program notes The covered benefit of partial
hospitalization only applies to enrollees
21 years of age and older. CMS has
approved HCBS within the HARP
program under 1115(a) authority.
MLTC enrollees may elect hospice care,
but a hospice enrollee cannot enroll in
MLTC. Some, but not all, HCBS waiver
services are covered by MLTC plans.
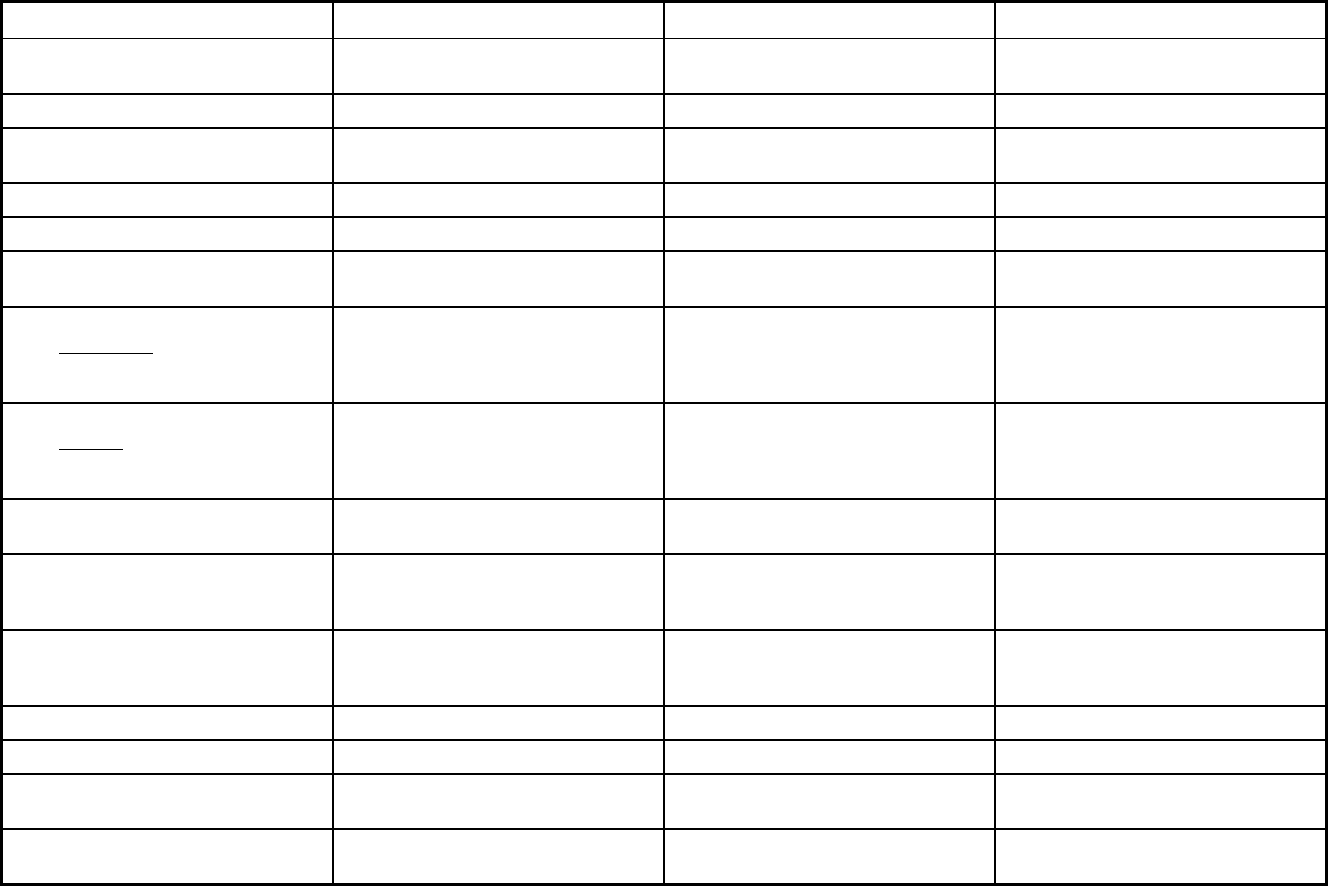
410
New York Managed Care Program Features, as of 2018 (2 of 2)
Features PACE Medicaid Advantage Medicaid Managed Care
Program type Program of All-inclusive Care for the
Elderly (PACE)
Comprehensive MCO Comprehensive MCO + MLTSS
Statewide or region-specific? Statewide Statewide Statewide
Federal operating authority PACE 1115(a) (Medicaid demonstration
waivers)
1115(a) (Medicaid demonstration
waivers)
Program start date 01/01/2001 10/01/2006 10/01/1997
Waiver expiration date (if applicable) 03/31/2021 03/31/2021
If the program ended in 2018, indicate
the end date
Populations enrolled: Low-income
adults not covered under ACA Section
VIII (excludes pregnant women and
people with disabilities)
Mandatory
Populations enrolled: Low-income
adults covered under ACA Section VIII
(excludes pregnant women and people
with disabilities)
Mandatory
Populations enrolled: Aged, Blind or
Disabled Children or Adults
Mandatory
Populations enrolled: Non-Disabled
Children (excludes children in foster
care or receiving adoption assistance)
Mandatory
Populations enrolled: Individuals
receiving Limited Benefits (excludes
partial duals)
Populations enrolled: Full Duals Voluntary Voluntary
Populations enrolled: Partial Duals Voluntary
Populations enrolled: Children with
Special Health Care Needs
Populations enrolled: Native
American/Alaskan Natives
Exempt Exempt Exempt
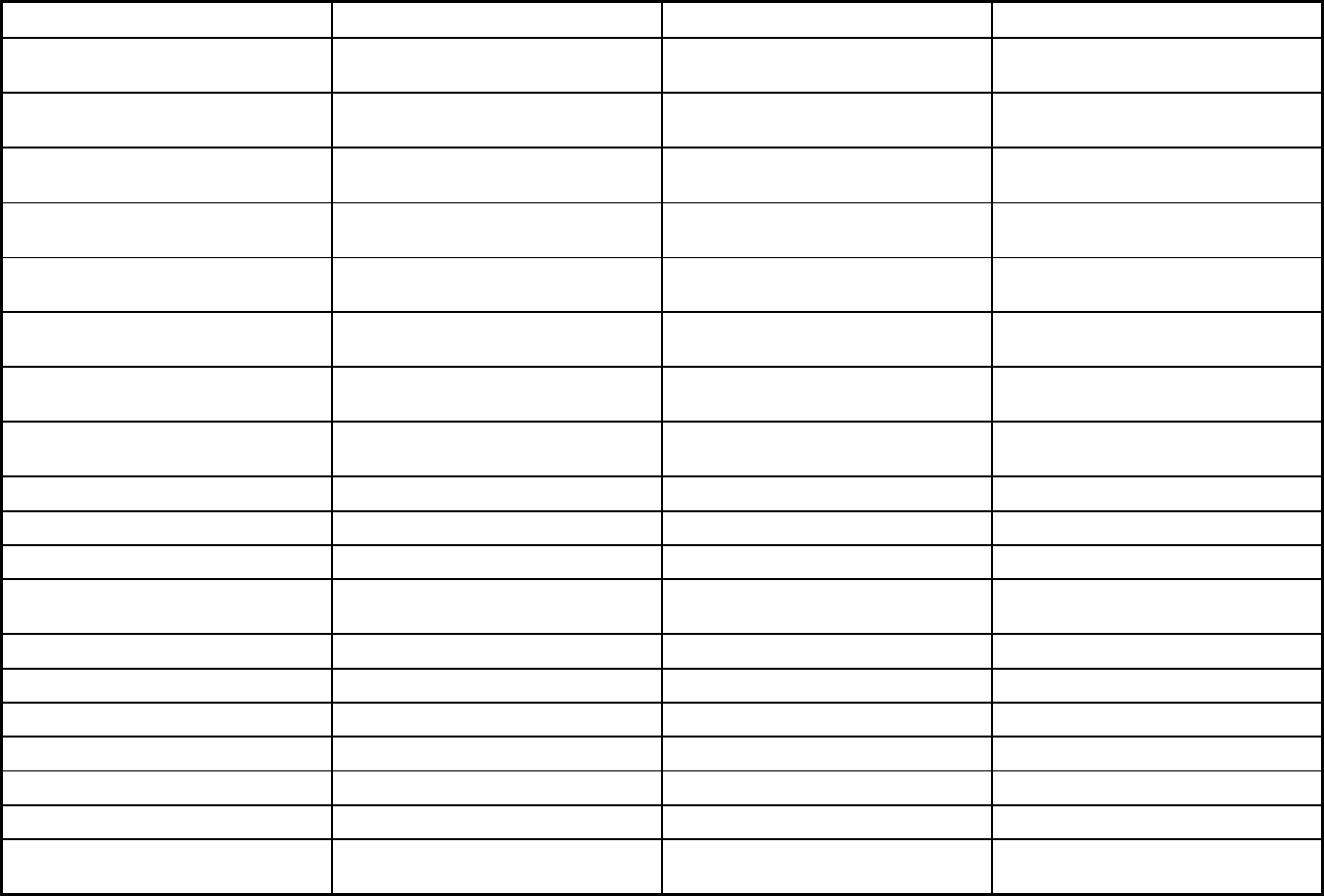
411
Features PACE Medicaid Advantage Medicaid Managed Care
Populations enrolled: Foster Care and
Adoption Assistance Children
Exempt Exempt Mandatory
Populations enrolled: Enrollment choice
period
N/A 60 days 30 days
Populations enrolled: Enrollment broker
name (if applicable)
NY Medicaid Choice/Maximus NY Medicaid Choice/Maximus NY Medicaid Choice/Maximus
Populations enrolled: Notes on
enrollment choice period
Benefits covered: Inpatient hospital
physical health
X X X
Benefits covered: Inpatient hospital
behavioral health (MH and/or SUD)
X X X
Benefits covered: Outpatient hospital
physical health
X X X
Benefits covered: Outpatient hospital
behavioral health (MH and/or SUD)
X X X
Benefits covered: Partial hospitalization X X
Benefits covered: Physician X X X
Benefits covered: Nurse practitioner X X X
Benefits covered: Rural health clinics
and FQHCs
X
Benefits covered: Clinic services X X X
Benefits covered: Lab and x-ray X X X
Benefits covered: Prescription drugs X X X
Benefits covered: Prosthetic devices X X X
Benefits covered: EPSDT X
Benefits covered: Case management X X X
Benefits covered: SSA Section 1945-
authorized health home
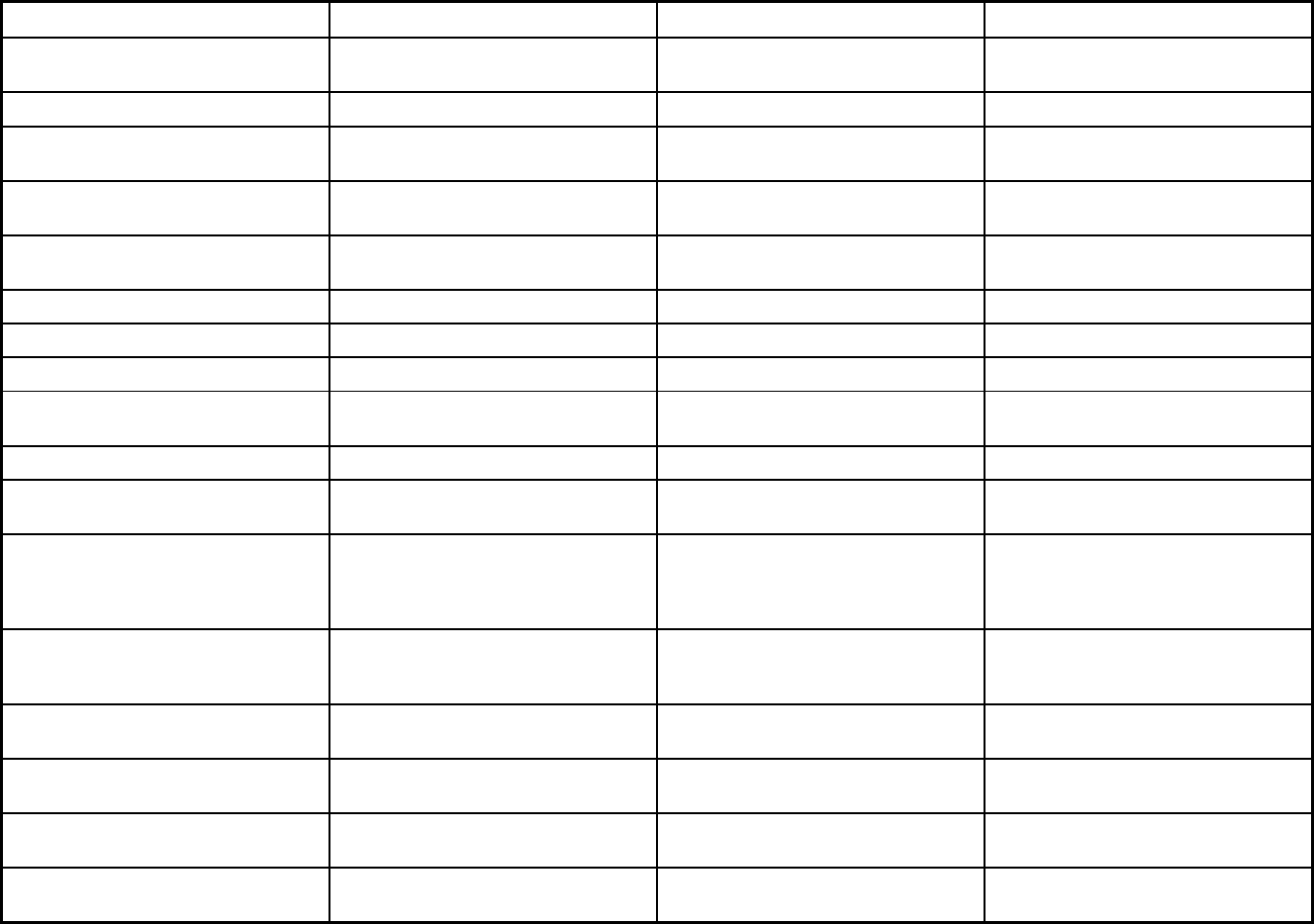
412
Features PACE Medicaid Advantage Medicaid Managed Care
Benefits covered: Health home care
(services in home)
X X X
Benefits covered: Family planning X
Benefits covered: Dental services
(medical/surgical)
X X X
Benefits covered: Dental (preventative
or corrective)
X X X
Benefits covered: Personal care (state
plan option)
X X X
Benefits covered: HCBS waiver services X
Benefits covered: Private duty nursing X X X
Benefits covered: ICF-IDD
Benefits covered: Nursing facility
services
X X
Benefits covered: Hospice care X
Benefits covered: Non-Emergency
Medical Transportation
X X
Benefits covered: Institution for Mental
Disease inpatient treatment for people
ages 21-64 defined by 42 CFR
§438.6(e) as an 'in lieu of' benefit
Benefits covered: Other (e.g., nurse
midwife services, freestanding birth
centers, podiatry, etc.)
Podiatry, physical therapy, occupational
therapy
Podiatry, outpatient rehabilitation,
hearing services, vision care services
Nurse midwife services, vision care, foot
care services
Quality assurance and improvement:
HEDIS data required?
No No Yes
Quality assurance and improvement:
CAHPS data required?
No No Yes
Quality assurance and improvement:
Accreditation required?
No No No
Quality assurance and improvement:
Accrediting organization
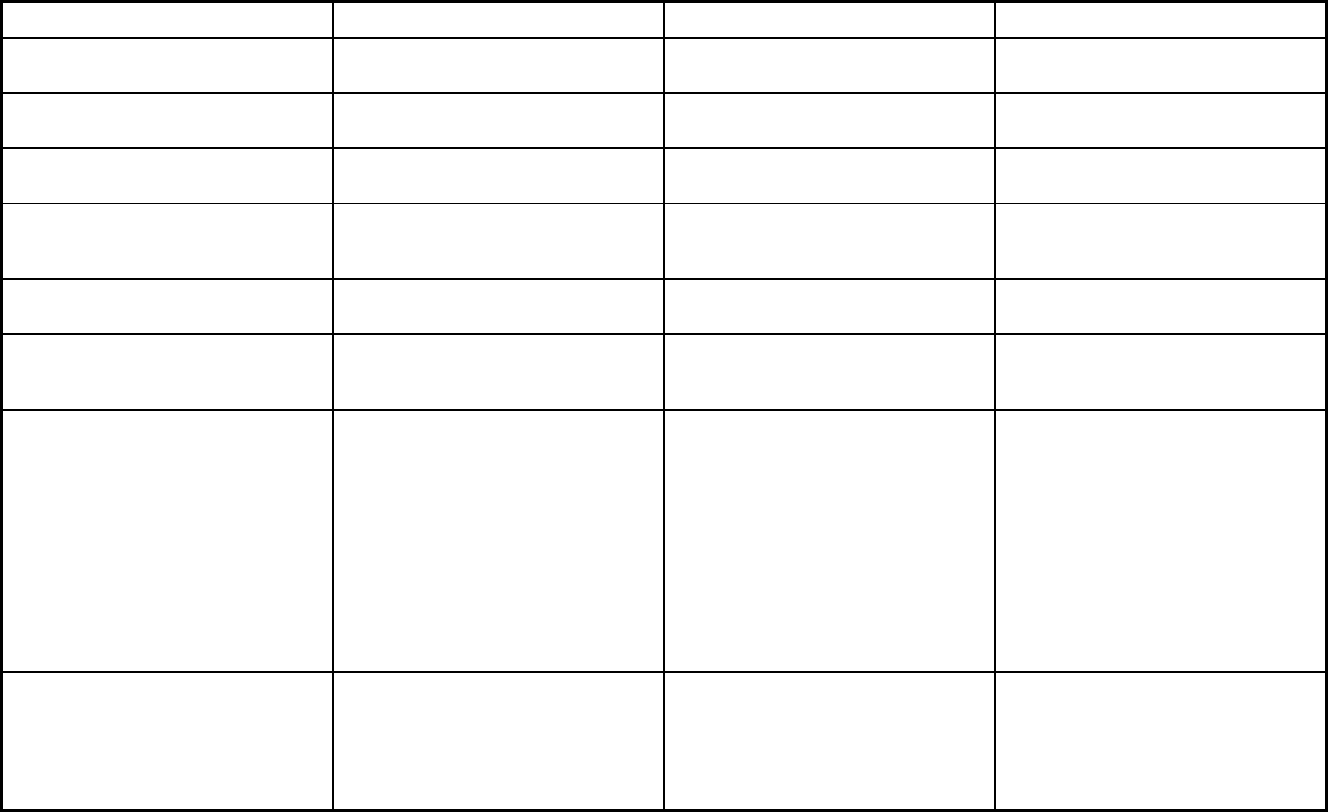
413
Features PACE Medicaid Advantage Medicaid Managed Care
Quality assurance and improvement:
EQRO contractor name (if applicable)
Island Peer Review Organization Island Peer Review Organization Island Peer Review Organization
Performance incentives: Payment
bonuses/differentials to reward plans
X
Performance incentives: Preferential
auto-enrollment to reward plans
X
Performance incentives: Public reports
comparing plan performance on key
metrics
X
Performance incentives: Withholds tied
to performance metrics
Performance incentives: MCOs/PHPs
required or encouraged to pay providers
for value/quality outcomes
X
Participating plans: Plans in Program ArchCare Senior Life; Catholic Health -
Life; CenterLight (CCM); Complete
Senior Care; Eddy Senior Care; Fallon
Health Weinberg; Independent Living for
Seniors; PACE CNY; Total Senior Care
Affinity; Fidelis Legacy Plan; Liberty
Health Advantage; United HealthCare;
VNS Choice; WellCare
HealthNow; HealthPlus; HIP Combined;
Independent Health/Hudson Valley;
WNY; MetroPlus Health Plan; MetroPlus
Health Plan Special Needs; Molina
Healthcare of New York; MVP Health
Plan; United HealthCare; VNS Choice
Special Needs; WellCare; YourCare
Health Plan; Fidelis Care; HealthFirst;
Affinity Health Plan; Amida Care Special
Needs; Capital District Physician's
Health Plan; Crystal Run Health Plan;
Excellus Health Plan
Notes: Program notes Covered Benefits include non-hospice
palliative care. OB/GYN is mandated
with a minimum age of 55 years. Quality
Assurance measures would include
PACE home health agency, a federally
mandated internal program.
The covered benefit of partial
hospitalization only applies to enrollees
21 years of age and older. Fidelis Care
covers emergency and non-emergency
transportation in Rockland County only.
`
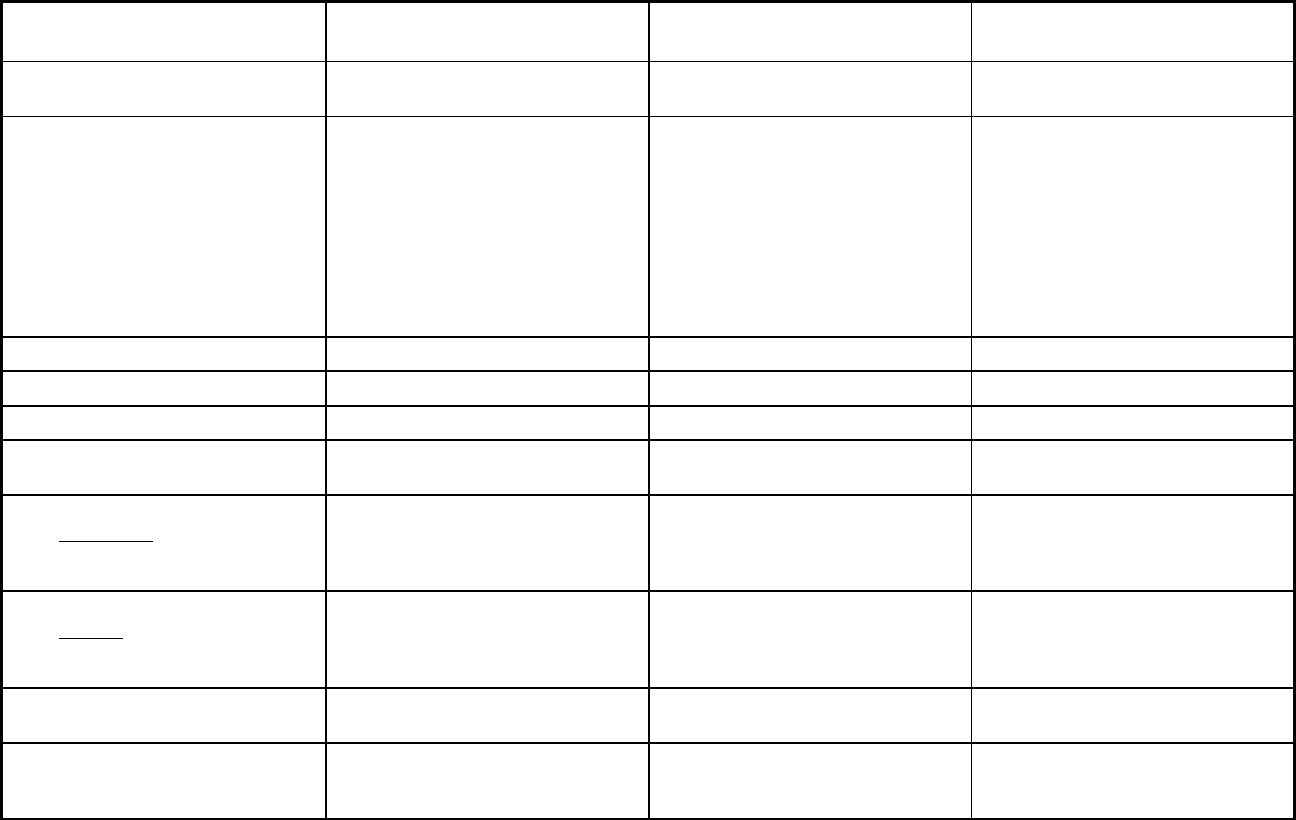
414
North Carolina Managed Care Program Features, as of 2018
Features Community Care of North Carolina
Program of All Inclusive Care for the
Elderly
1915(b)/(c) Medicaid Waiver for
MH/DD/SA Services
Program type Primary Care Case Management Entity
(PCCM Entity)
Program of All-inclusive Care for the
Elderly (PACE)
Behavioral Health Organization (BHO)
only (PIHP and/or PAHP)
Statewide or region-specific? Statewide Alamance, Alexander, Brunswick,
Burke, Cabarrus, Caldwell, Caswell,
Catawba, Chatham, Cleveland,
Cumberland, Davidson, Davie,
Durham, Gaston, Granville, Guilford,
Harnett, Hoke, Iredell, Lee, Lincoln,
Mecklenburg, Moore, New Hanover,
Orange, Robeson, Rockingham,
Rowan, Stanley, Union, and Wake
counties
Statewide
Federal operating authority 1932(a) PACE 1915(b)/1915(c)
Program start date 04/01/1991 02/01/2008 01/01/2012
Waiver expiration date (if applicable) 06/30/2018
If the program ended in 2018, indicate
the end date
Populations enrolled: Low-income
adults not covered under ACA Section
VIII (excludes pregnant women and
people with disabilities)
Mandatory Mandatory
Populations enrolled: Low-income
adults covered under ACA Section VIII
(excludes pregnant women and people
with disabilities)
Populations enrolled: Aged, Blind or
Disabled Children or Adults
Voluntary Voluntary Mandatory
Populations enrolled: Non-Disabled
Children (excludes children in foster
care or receiving adoption assistance)
Mandatory Mandatory
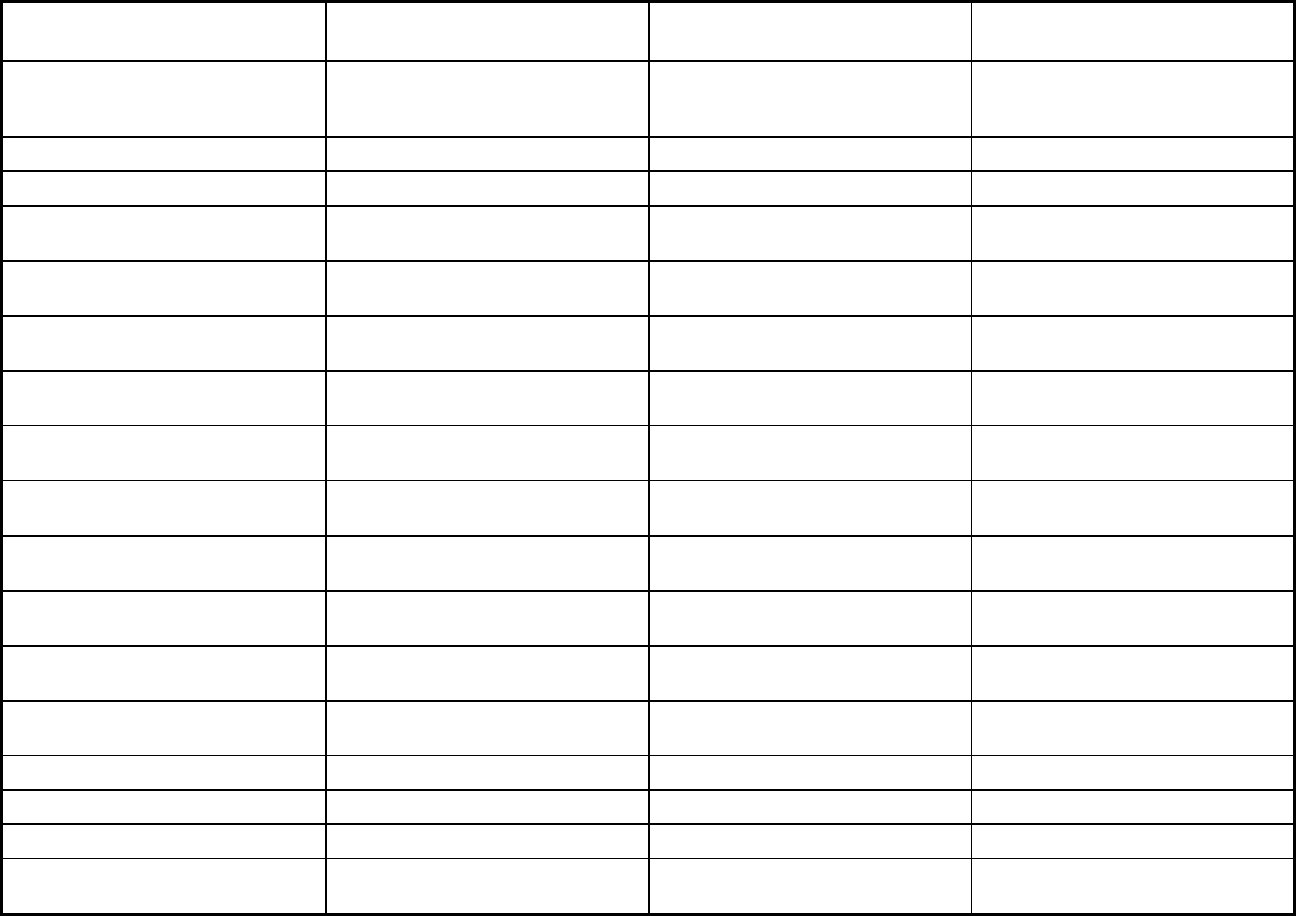
415
Features Community Care of North Carolina
Program of All Inclusive Care for the
Elderly
1915(b)/(c) Medicaid Waiver for
MH/DD/SA Services
Populations enrolled: Individuals
receiving Limited Benefits (excludes
partial duals)
Populations enrolled: Full Duals Voluntary Voluntary Mandatory
Populations enrolled: Partial Duals Voluntary
Populations enrolled: Children with
Special Health Care Needs
Voluntary Mandatory
Populations enrolled: Native
American/Alaskan Natives
Voluntary Voluntary Voluntary
Populations enrolled: Foster Care and
Adoption Assistance Children
Voluntary Exempt Mandatory
Populations enrolled: Enrollment
choice period
Other N/A Pre-assigned
Populations enrolled: Enrollment broker
name (if applicable)
Populations enrolled: Notes on
enrollment choice period
Beneficiaries have 90 days to enroll
into the PCCM program.
Benefits covered: Inpatient hospital
physical health
X
Benefits covered: Inpatient hospital
behavioral health (MH and/or SUD)
X X
Benefits covered: Outpatient hospital
physical health
X
Benefits covered: Outpatient hospital
behavioral health (MH and/or SUD)
X X
Benefits covered: Partial hospitalization X
Benefits covered: Physician X
Benefits covered: Nurse practitioner X
Benefits covered: Rural health clinics
and FQHCs
X
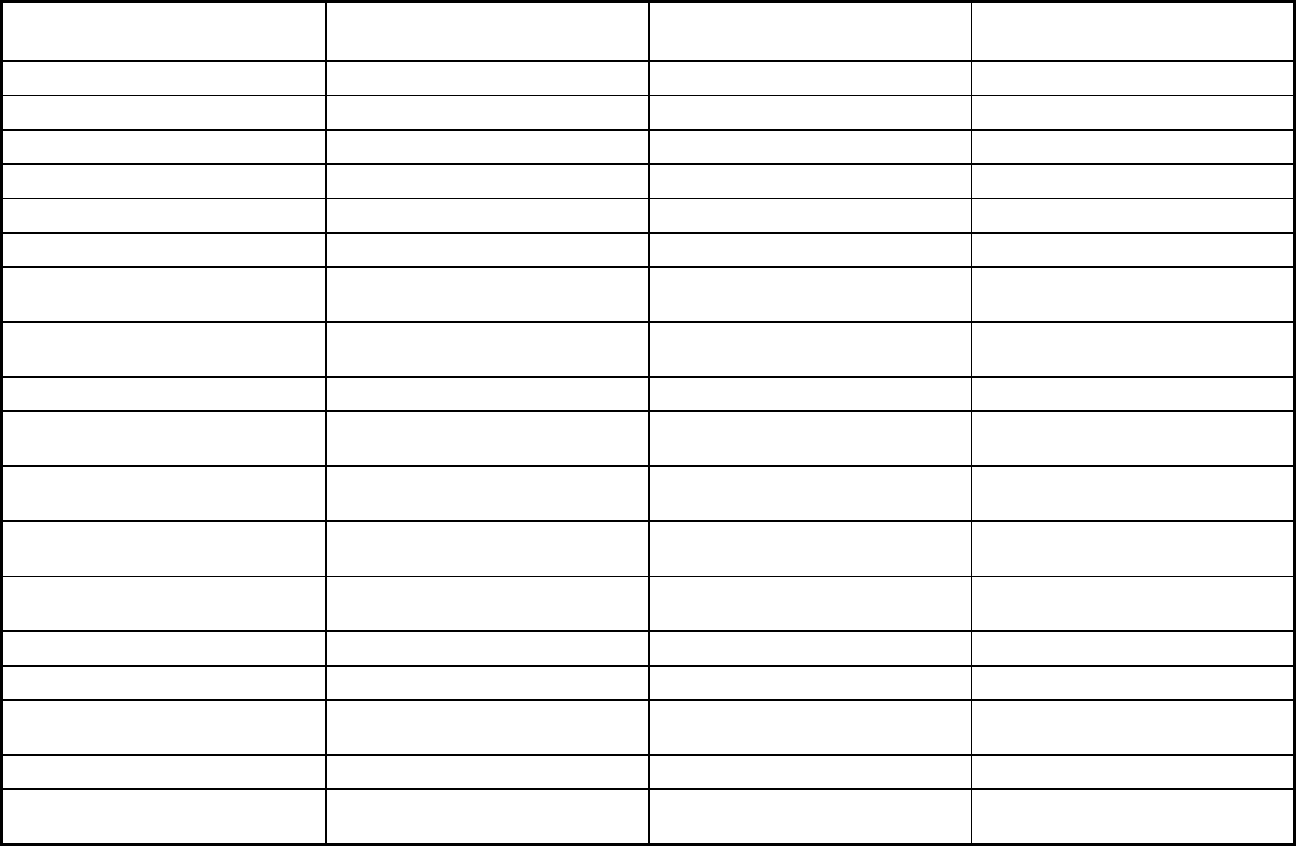
416
Features Community Care of North Carolina
Program of All Inclusive Care for the
Elderly
1915(b)/(c) Medicaid Waiver for
MH/DD/SA Services
Benefits covered: Clinic services X
Benefits covered: Lab and x-ray X
Benefits covered: Prescription drugs X
Benefits covered: Prosthetic devices X
Benefits covered: EPSDT X
Benefits covered: Case management X X
Benefits covered: SSA Section 1945-
authorized health home
Benefits covered: Health home care
(services in home)
X
Benefits covered: Family planning
Benefits covered: Dental services
(medical/surgical)
X
Benefits covered: Dental (preventative
or corrective)
X
Benefits covered: Personal care (state
plan option)
X
Benefits covered: HCBS waiver
services
X X
Benefits covered: Private duty nursing X
Benefits covered: ICF-IDD X
Benefits covered: Nursing facility
services
X
Benefits covered: Hospice care X
Benefits covered: Non-Emergency
Medical Transportation
X
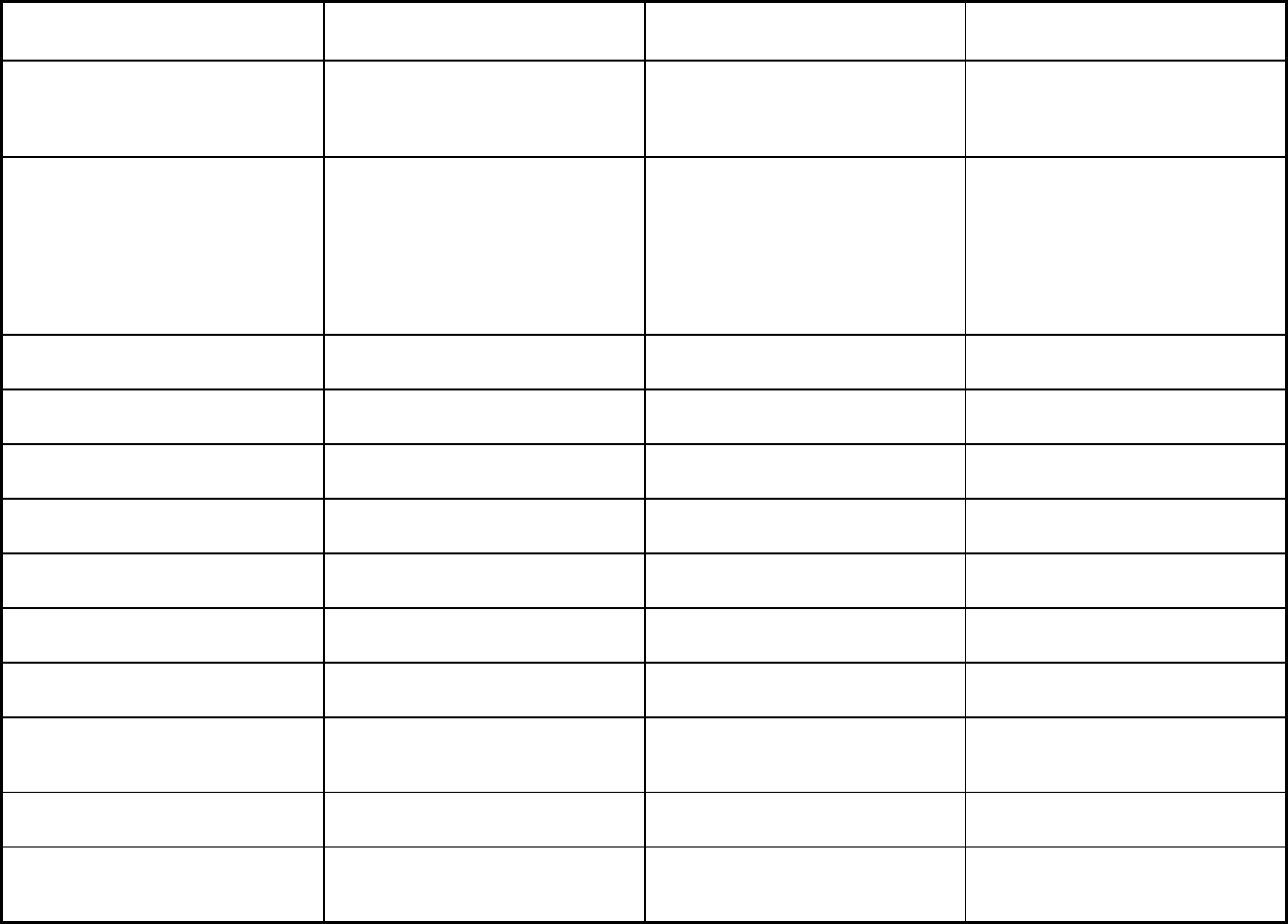
417
Features Community Care of North Carolina
Program of All Inclusive Care for the
Elderly
1915(b)/(c) Medicaid Waiver for
MH/DD/SA Services
Benefits covered: Institution for Mental
Disease inpatient treatment for people
ages 21-64 defined by 42 CFR
§438.6(e) as an 'in lieu of' benefit
X
Benefits covered: Other (e.g., nurse
midwife services, freestanding birth
centers, podiatry, etc.)
Restorative therapies; nutrition
counseling; recreational therapies;
meals
Outpatient behavioral health services
including services provided by
psychiatrists for recipients with a
diagnosis in the 290-319 range;
psychiatric residential treatment
facilities; therapeutic foster care;
residential child care; hospital
emergency dept
Quality assurance and improvement:
HEDIS data required?
Yes No Yes
Quality assurance and improvement:
CAHPS data required?
Yes No Yes
Quality assurance and improvement:
Accreditation required?
No No Yes
Quality assurance and improvement:
Accrediting organization
NCQA, URAC
Quality assurance and improvement:
EQRO contractor name (if applicable)
Carolina Center for Medical Excellence
Performance incentives: Payment
bonuses/differentials to reward plans
Performance incentives: Preferential
auto-enrollment to reward plans
Performance incentives: Public reports
comparing plan performance on key
metrics
X
Performance incentives: Withholds tied
to performance metrics
Performance incentives: MCOs/PHPs
required or encouraged to pay
providers for value/quality outcomes
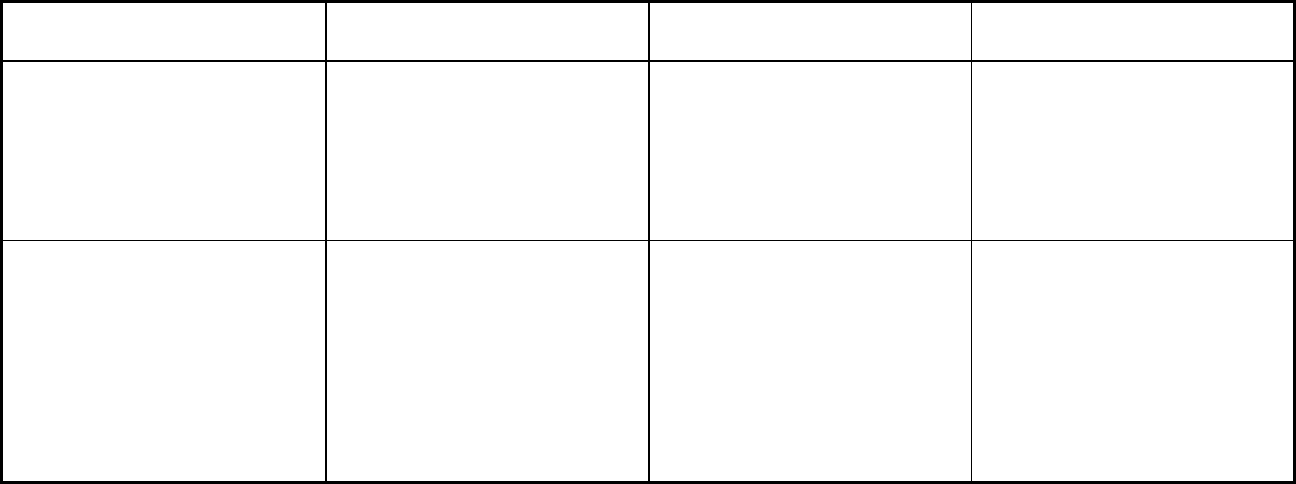
418
Features Community Care of North Carolina
Program of All Inclusive Care for the
Elderly
1915(b)/(c) Medicaid Waiver for
MH/DD/SA Services
Participating plans: Plans in Program North Carolina Community Care
Carolina Access
Carolina Seniorcare; Community
Carepartners, Inc.; Elderhaus, Inc.; Life
St. Joseph of the Pines, Inc.; PACE at
Home, Inc.; PACE of the Southern
Piedmont; PACE of the Triad;
Piedmont Health Services, Inc.; Senior
Total Life Care, Inc.; Stay Well Senior
Care; VOANS Senior Community Care
Alliance Behavioral Healthcare;
Cardinal Innovations Healthcare
Solutions; Eastpointe Human Services;
Partners Behavioral Health
Management; Sandhills Center for MH
DD SA; Trillium Health Resources;
VAYA Health
Notes: Program notes Plan consists of independently
contracted medical home/primary care
providers who receive a PMPM
management fee for coordinationing
care at the medical home provider
office.
IMD: PACE serves individuals 55 and
over in pre-approved service areas/zip
codes. With regards to inpatient psych
placements, a PACE organization can
be contracted with a particular hospital
or psychiatric clinic in their approved
service area and network. Most
psychiatric inpatient placements placed
participants in local contracted
hospitals that had psychiatric unit/wing
within the facility.
Waiver expiration date (if applicable) -
6/30/2018 (currently under Technical
Extension). All Medicaid recipients are
covered by a Behavioral Healthcare
(BHO). Enrollment in one of seven
plans is based on the enrollee's county
of residence.
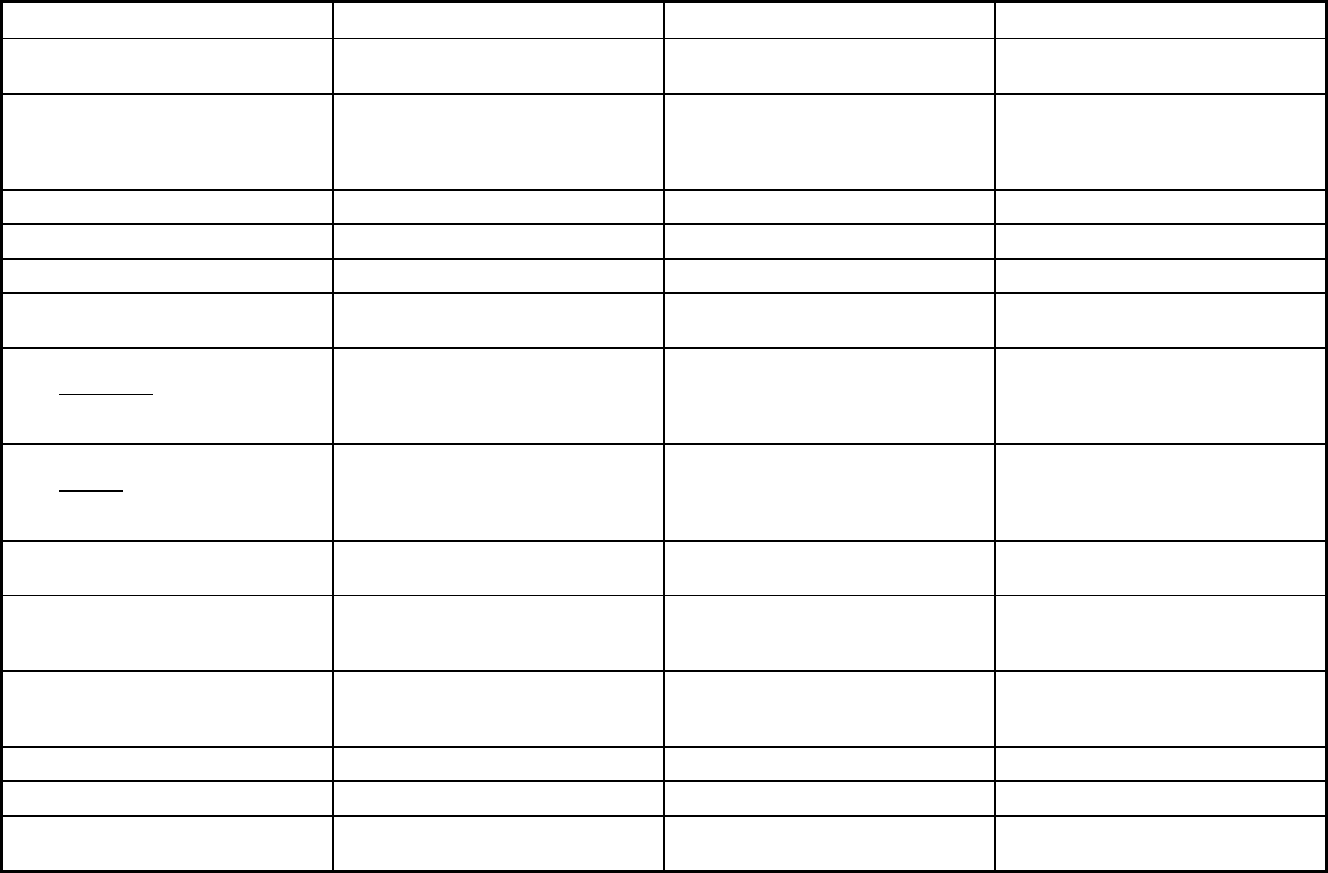
419
North Dakota Managed Care Program Features, as of 2018 (1 of 2)
Features Health Management Program PACE PCCM
Program type Other Prepaid Health Plan (PHP)
(limited benefits)
Program of All-inclusive Care for the
Elderly (PACE)
Primary Care Case Management
(PCCM)
Statewide or region-specific? Statewide Ward: 58701, 58702, 58703, 58722,
58785. Burleigh: 58501, 58502, 58503,
58504. Morton: 58554. Stark: 58601,
58602, 58630, 58652, 58655, 58656.
Statewide
Federal operating authority 1932(a) PACE 1932(a)/1915(i)
Program start date 08/01/2007 08/01/2008 01/10/1994
Waiver expiration date (if applicable)
If the program ended in 2018, indicate
the end date
06/30/2018
Populations enrolled: Low-income
adults not covered under ACA Section
VIII (excludes pregnant women and
people with disabilities)
Voluntary Mandatory
Populations enrolled: Low-income
adults covered under ACA Section VIII
(excludes pregnant women and people
with disabilities)
Populations enrolled: Aged, Blind or
Disabled Children or Adults
Voluntary Voluntary
Populations enrolled: Non-Disabled
Children (excludes children in foster
care or receiving adoption assistance)
Voluntary Mandatory
Populations enrolled: Individuals
receiving Limited Benefits (excludes
partial duals)
Voluntary Mandatory
Populations enrolled: Full Duals Voluntary
Populations enrolled: Partial Duals Voluntary
Populations enrolled: Children with
Special Health Care Needs
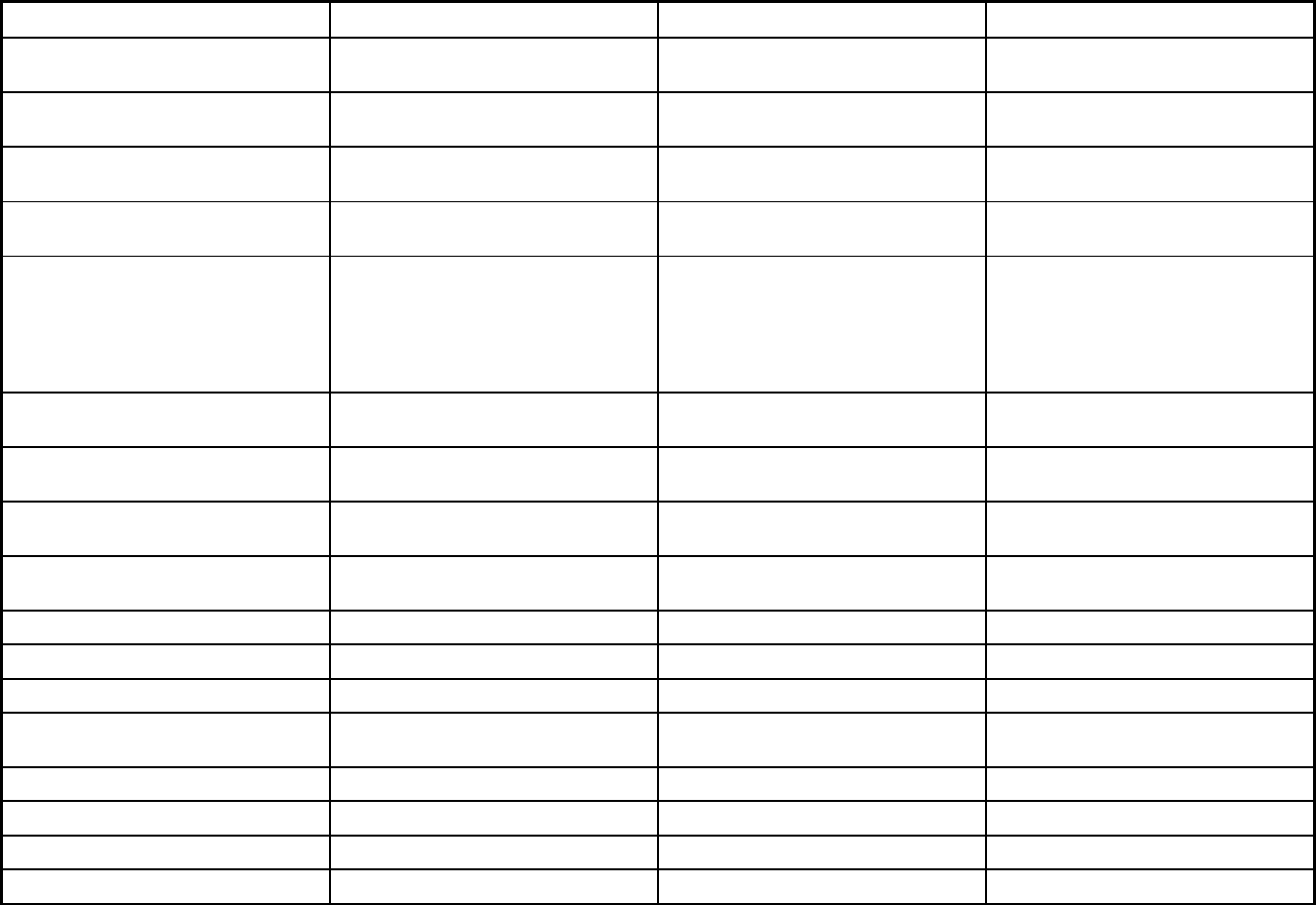
420
Features Health Management Program PACE PCCM
Populations enrolled: Native
American/Alaskan Natives
Voluntary Voluntary Mandatory
Populations enrolled: Foster Care and
Adoption Assistance Children
Voluntary Exempt
Populations enrolled: Enrollment choice
period
N/A N/A
Populations enrolled: Enrollment broker
name (if applicable)
Populations enrolled: Notes on
enrollment choice period
Enrollment begins on the first day of the
month following the determination that
they are eligible.
Once enrolled the recipient has 14 days
to choose a PCP or one will be
assigned. They can change PCP
without good cause for the first 90 days
and every 12 months during the 60 day
annual open enrollment period.
Benefits covered: Inpatient hospital
physical health
X
Benefits covered: Inpatient hospital
behavioral health (MH and/or SUD)
X
Benefits covered: Outpatient hospital
physical health
X X
Benefits covered: Outpatient hospital
behavioral health (MH and/or SUD)
X
Benefits covered: Partial hospitalization
Benefits covered: Physician X X
Benefits covered: Nurse practitioner X X
Benefits covered: Rural health clinics
and FQHCs
X X
Benefits covered: Clinic services X X
Benefits covered: Lab and x-ray X
Benefits covered: Prescription drugs X
Benefits covered: Prosthetic devices X
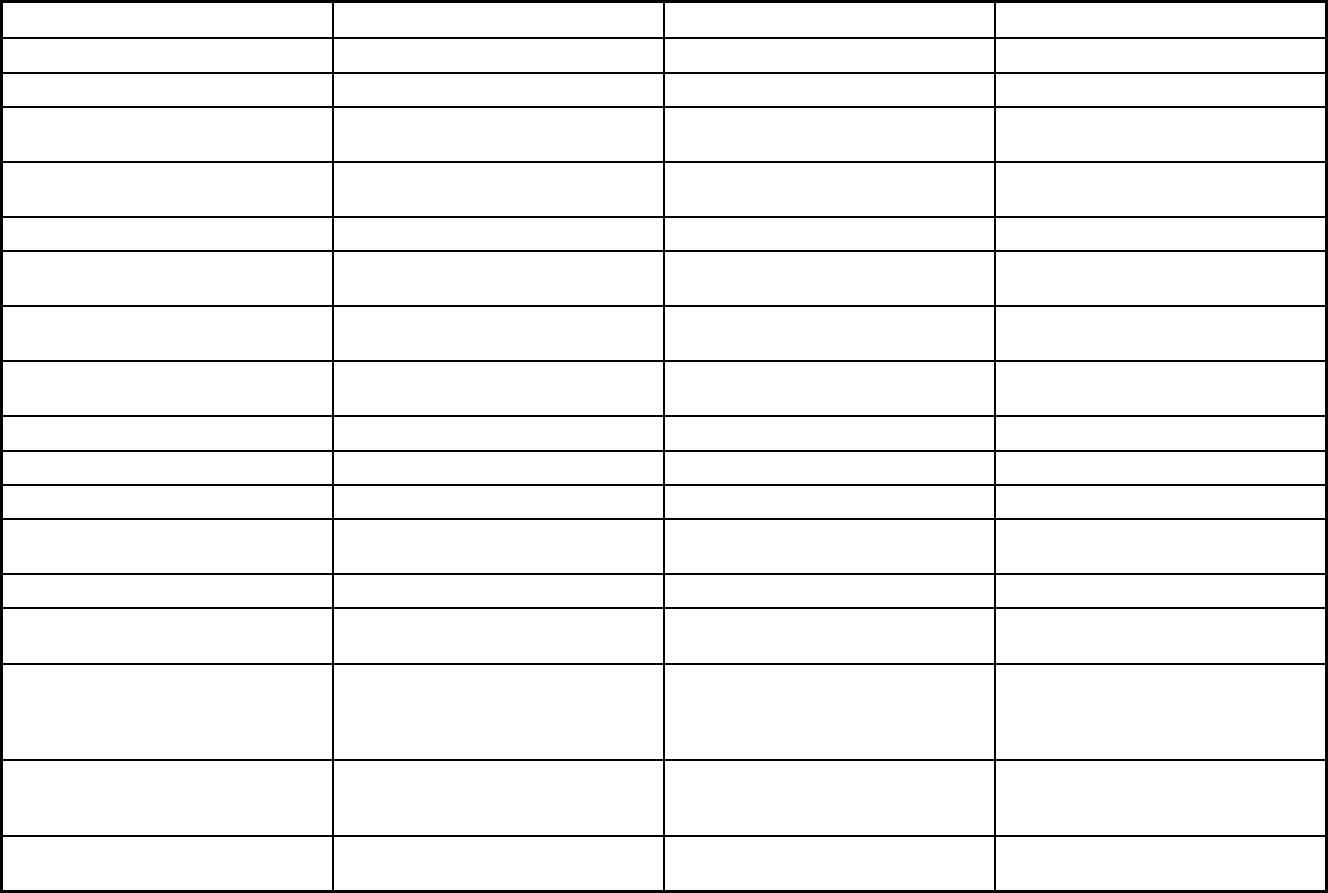
421
Features Health Management Program PACE PCCM
Benefits covered: EPSDT
Benefits covered: Case management X X X
Benefits covered: SSA Section 1945-
authorized health home
Benefits covered: Health home care
(services in home)
X
Benefits covered: Family planning
Benefits covered: Dental services
(medical/surgical)
X
Benefits covered: Dental (preventative
or corrective)
X
Benefits covered: Personal care (state
plan option)
X
Benefits covered: HCBS waiver services
Benefits covered: Private duty nursing
Benefits covered: ICF-IDD
Benefits covered: Nursing facility
services
Benefits covered: Hospice care
Benefits covered: Non-Emergency
Medical Transportation
Benefits covered: Institution for Mental
Disease inpatient treatment for people
ages 21-64 defined by 42 CFR
§438.6(e) as an 'in lieu of' benefit
Benefits covered: Other (e.g., nurse
midwife services, freestanding birth
centers, podiatry, etc.)
Quality assurance and improvement:
HEDIS data required?
No No No
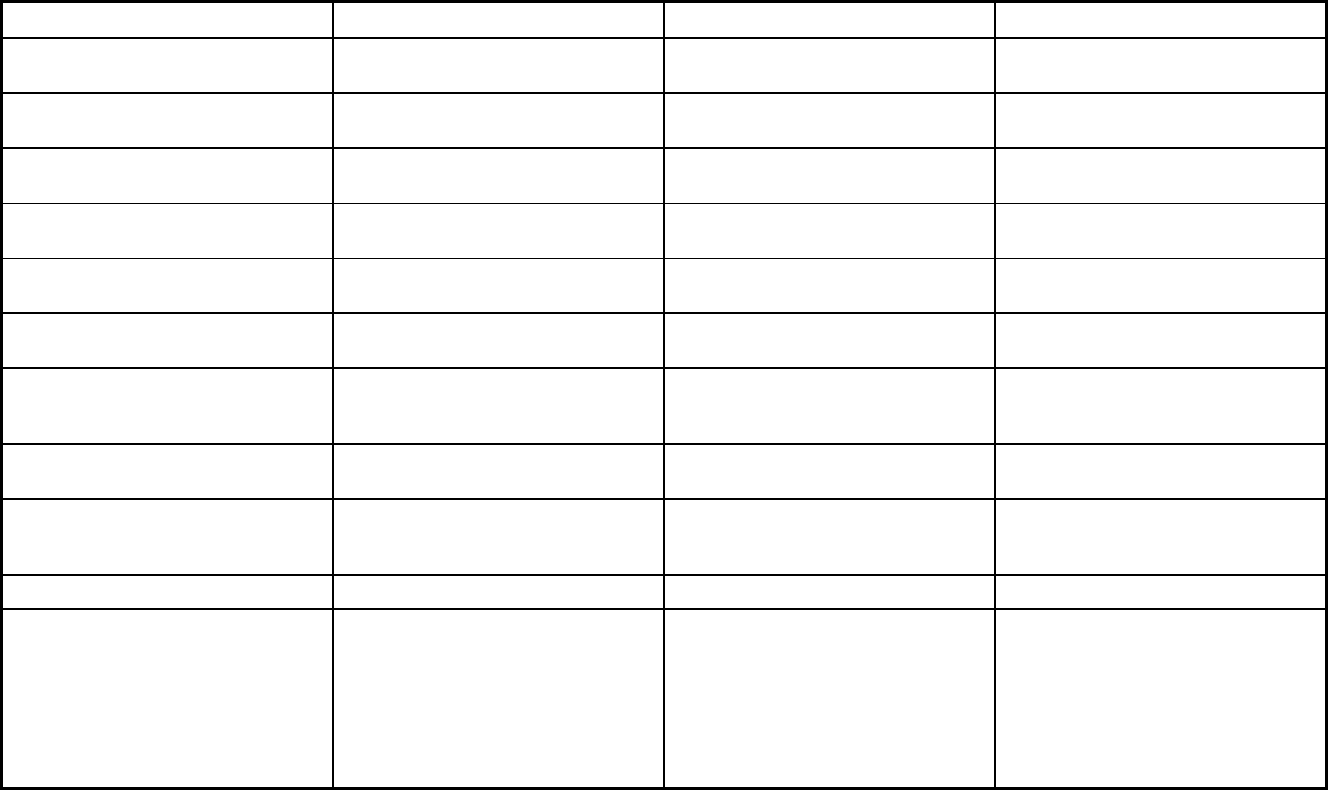
422
Features Health Management Program PACE PCCM
Quality assurance and improvement:
CAHPS data required?
No No No
Quality assurance and improvement:
Accreditation required?
No No No
Quality assurance and improvement:
Accrediting organization
North Dakota
Quality assurance and improvement:
EQRO contractor name (if applicable)
Performance incentives: Payment
bonuses/differentials to reward plans
Performance incentives: Preferential
auto-enrollment to reward plans
Performance incentives: Public reports
comparing plan performance on key
metrics
Performance incentives: Withholds tied
to performance metrics
Performance incentives: MCOs/PHPs
required or encouraged to pay providers
for value/quality outcomes
Participating plans: Plans in Program Health Management PACE Multiple Primary Care Providers
Notes: Program notes Effective July 1, 2018 the Health
Management Program was no longer an
authorized service with it being removed
from North Dakota's Medicaid State
Plan with authority granted by the
Center for Medicare and Medicaid
Services as of August 9, 2019. Thus, no
enrollment as of July 1, 2018.
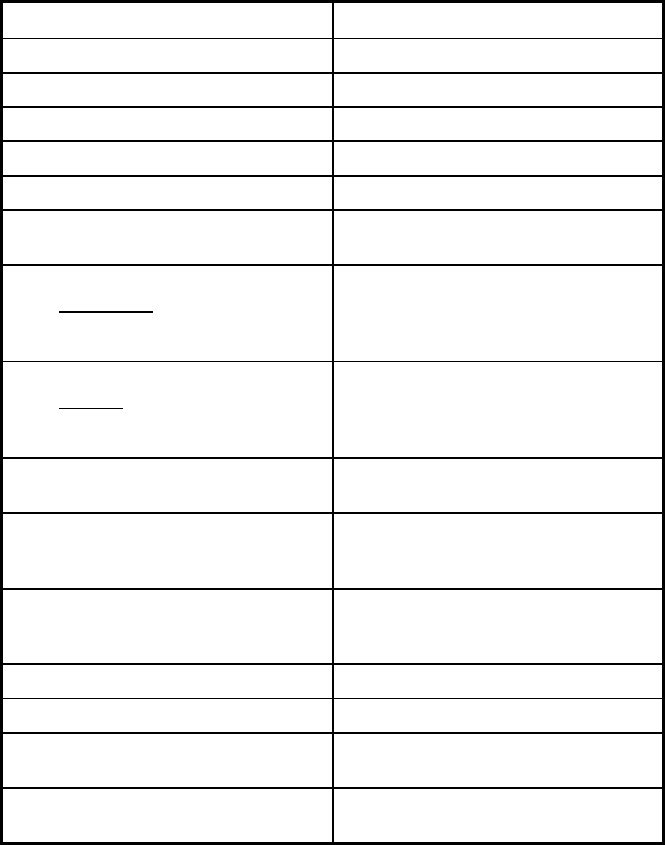
423
North Dakota Managed Care Program Features, as of 2018 (2 of 2)
Features North Dakota Medicaid Expansion
Program type Comprehensive MCO
Statewide or region-specific? Statewide
Federal operating authority 1915(b),1937 Alt Benefit Plan
Program start date 01/01/2014
Waiver expiration date (if applicable) 12/31/2019
If the program ended in 2018, indicate
the end date
Populations enrolled: Low-income
adults not covered under ACA Section
VIII (excludes pregnant women and
people with disabilities)
Populations enrolled: Low-income
adults covered under ACA Section VIII
(excludes pregnant women and people
with disabilities)
Mandatory
Populations enrolled: Aged, Blind or
Disabled Children or Adults
Populations enrolled: Non-Disabled
Children (excludes children in foster
care or receiving adoption assistance)
Populations enrolled: Individuals
receiving Limited Benefits (excludes
partial duals)
Populations enrolled: Full Duals
Populations enrolled: Partial Duals
Populations enrolled: Children with
Special Health Care Needs
Populations enrolled: Native
American/Alaskan Natives
Mandatory
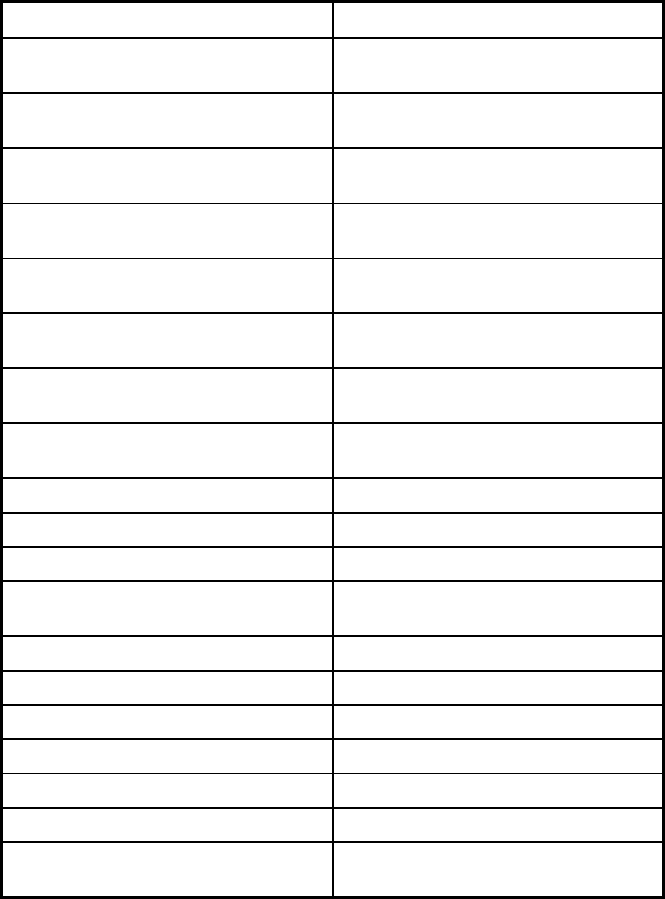
424
Features North Dakota Medicaid Expansion
Populations enrolled: Foster Care and
Adoption Assistance Children
Mandatory
Populations enrolled: Enrollment choice
period
Pre-assigned
Populations enrolled: Enrollment broker
name (if applicable)
Populations enrolled: Notes on
enrollment choice period
Benefits covered: Inpatient hospital
physical health
X
Benefits covered: Inpatient hospital
behavioral health (MH and/or SUD)
X
Benefits covered: Outpatient hospital
physical health
X
Benefits covered: Outpatient hospital
behavioral health (MH and/or SUD)
X
Benefits covered: Partial hospitalization
Benefits covered: Physician X
Benefits covered: Nurse practitioner X
Benefits covered: Rural health clinics
and FQHCs
X
Benefits covered: Clinic services X
Benefits covered: Lab and x-ray
Benefits covered: Prescription drugs X
Benefits covered: Prosthetic devices X
Benefits covered: EPSDT X
Benefits covered: Case management X
Benefits covered: SSA Section 1945-
authorized health home
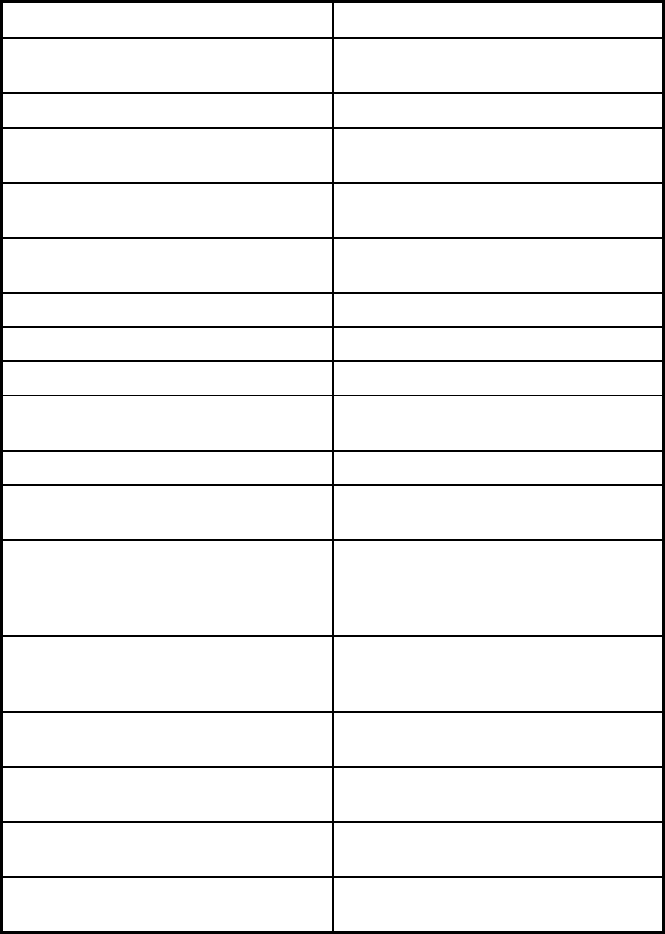
425
Features North Dakota Medicaid Expansion
Benefits covered: Health home care
(services in home)
X
Benefits covered: Family planning X
Benefits covered: Dental services
(medical/surgical)
X
Benefits covered: Dental (preventative
or corrective)
X
Benefits covered: Personal care (state
plan option)
Benefits covered: HCBS waiver services
Benefits covered: Private duty nursing
Benefits covered: ICF-IDD
Benefits covered: Nursing facility
services
Benefits covered: Hospice care X
Benefits covered: Non-Emergency
Medical Transportation
X
Benefits covered: Institution for Mental
Disease inpatient treatment for people
ages 21-64 defined by 42 CFR
§438.6(e) as an 'in lieu of' benefit
Benefits covered: Other (e.g., nurse
midwife services, freestanding birth
centers, podiatry, etc.)
Up to 30 days SNF within a 12 month
period
Quality assurance and improvement:
HEDIS data required?
Yes
Quality assurance and improvement:
CAHPS data required?
Yes
Quality assurance and improvement:
Accreditation required?
No
Quality assurance and improvement:
Accrediting organization

426
Features North Dakota Medicaid Expansion
Quality assurance and improvement:
EQRO contractor name (if applicable)
Qlarant Quality Solutions
Performance incentives: Payment
bonuses/differentials to reward plans
Performance incentives: Preferential
auto-enrollment to reward plans
Performance incentives: Public reports
comparing plan performance on key
metrics
Performance incentives: Withholds tied
to performance metrics
Performance incentives: MCOs/PHPs
required or encouraged to pay providers
for value/quality outcomes
Participating plans: Plans in Program ND Medicaid Expansion MCO
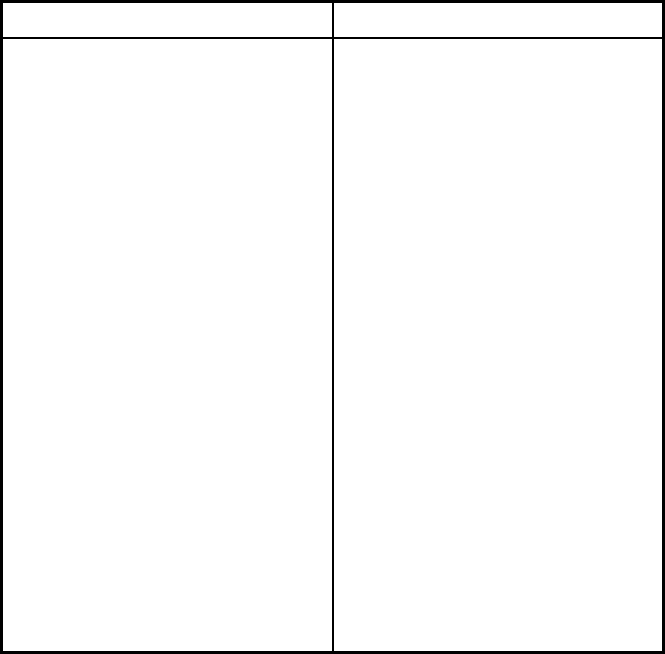
427
Features North Dakota Medicaid Expansion
Notes: Program notes In order for the State to provide
Medicaid Expansion MCO through
private carriers including mandatory
enrollment, an initial 1915(b) waiver
allowing managed care enrollment of
the new adult group for Medicaid
expansion was submitted to CMS with
authority granted. The 1915(b) waiver
renewal was submitted to CMS for
2016-2017 and 2018-2019 with
authority granted. In addition, CMS
granted initial authority through an 1115
waiver to ensure compliance related to
having one health plan choice for those
Medicaid Expansion recipeints in urban
areas of the state. CMS extended this
1115 waiver authority until such time
that the Final Medicaid Managed Care
CFR were published (May 6, 2016) -
with the changes noted at 42 CFR §
438.52(b)(1) and (b)(3) the 1115 waiver
was no longer needed thus it was
allowed to expire. Per the Medicare
Advantage Health Service Delivery
(HSD) Reference file for the applicable
calendar year, ND no longer has any
counties designated as being urban
thus the state may limit rural area
residents to a single MCO.
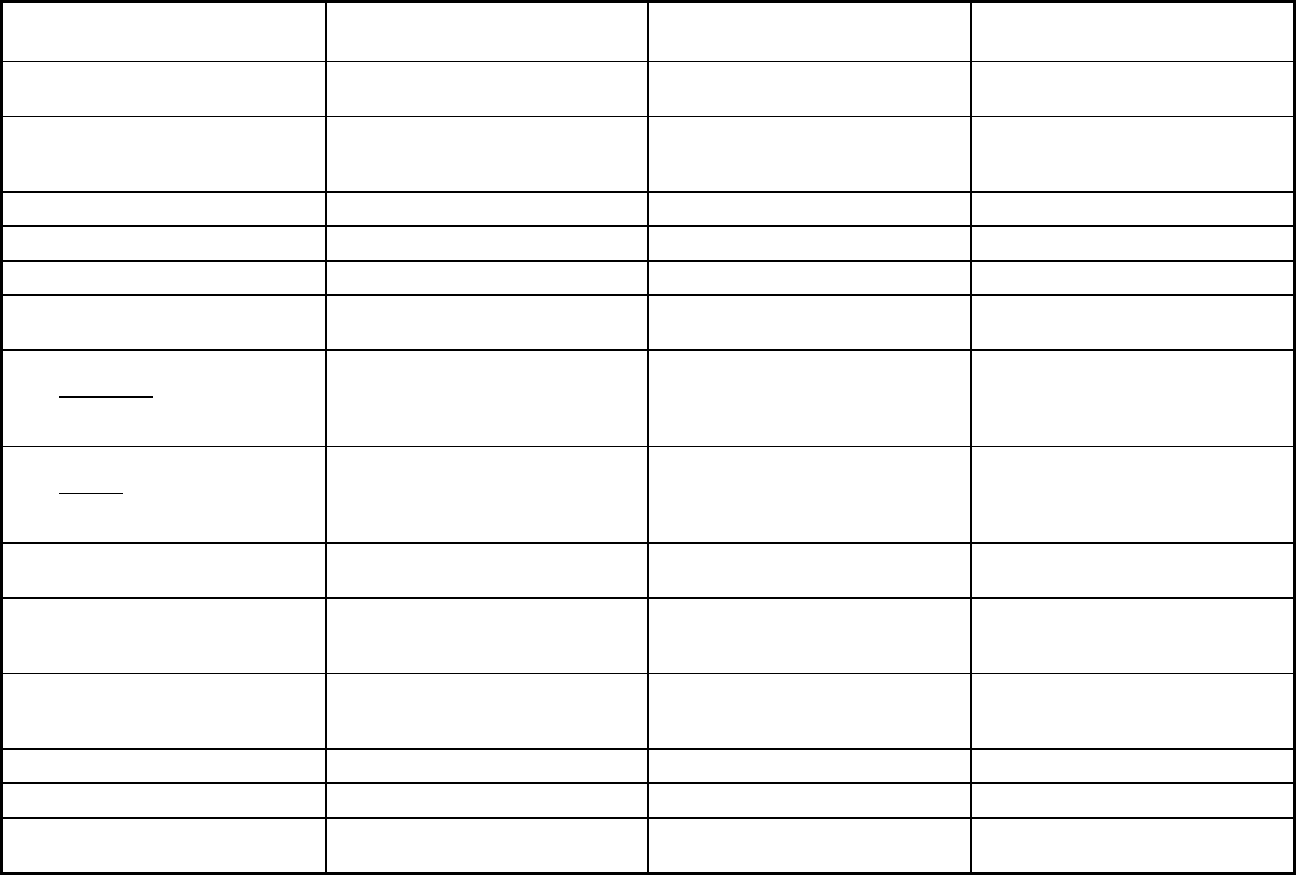
428
Ohio Managed Care Program Features, as of 2018
Features Ohio PACE
Ohio Medicaid Managed Care
Program MyCare Ohio Opt-Out Program
Program type Program of All-inclusive Care for the
Elderly (PACE)
Comprehensive MCO Comprehensive MCO + MLTSS
Statewide or region-specific? Cuyahoga County Statewide Central, Northwest, Northeast,
Northeast Central, Southwest, West
Central, East Central
Federal operating authority PACE 1915(b),1932(a) 1915(b)/1915(c)
Program start date 11/01/2002 07/01/2006 05/01/2014
Waiver expiration date (if applicable) 03/31/2020 12/31/2023
If the program ended in 2018, indicate
the end date
Populations enrolled: Low-income
adults not covered under ACA Section
VIII (excludes pregnant women and
people with disabilities)
Mandatory
Populations enrolled: Low-income
adults covered under ACA Section VIII
(excludes pregnant women and people
with disabilities)
Mandatory
Populations enrolled: Aged, Blind or
Disabled Children or Adults
Voluntary Mandatory
Populations enrolled: Non-Disabled
Children (excludes children in foster
care or receiving adoption assistance)
Mandatory
Populations enrolled: Individuals
receiving Limited Benefits (excludes
partial duals)
Populations enrolled: Full Duals Voluntary Mandatory
Populations enrolled: Partial Duals Voluntary
Populations enrolled: Children with
Special Health Care Needs
Mandatory
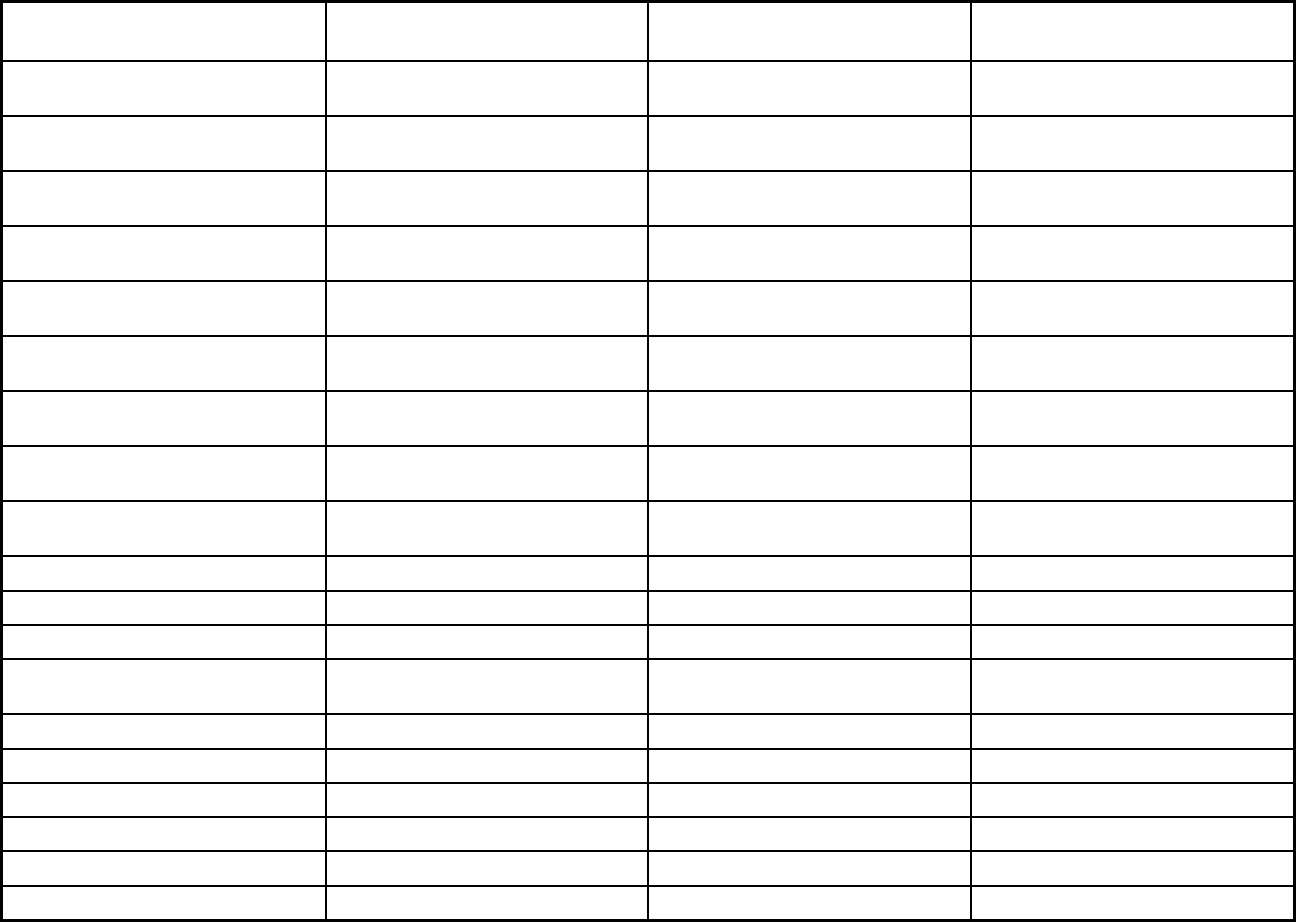
429
Features Ohio PACE
Ohio Medicaid Managed Care
Program MyCare Ohio Opt-Out Program
Populations enrolled: Native
American/Alaskan Natives
Exempt Voluntary Exempt
Populations enrolled: Foster Care and
Adoption Assistance Children
Mandatory Mandatory
Populations enrolled: Enrollment
choice period
N/A Other Other
Populations enrolled: Enrollment broker
name (if applicable)
Automated Health Systems, Inc. Automated Health Systems, Inc.
Populations enrolled: Notes on
enrollment choice period
Ohio PACE operates under an open-
enrollment model.
Medicaid enrollees are pre-assigned to
a plan with 90 days to change plans.
Enrollees are pre-assigned to a plan
and have 90 days to change plans.
Benefits covered: Inpatient hospital
physical health
X X X
Benefits covered: Inpatient hospital
behavioral health (MH and/or SUD)
X X X
Benefits covered: Outpatient hospital
physical health
X X
Benefits covered: Outpatient hospital
behavioral health (MH and/or SUD)
X X X
Benefits covered: Partial hospitalization X X
Benefits covered: Physician X X X
Benefits covered: Nurse practitioner X X X
Benefits covered: Rural health clinics
and FQHCs
X X
Benefits covered: Clinic services X X
Benefits covered: Lab and x-ray X X X
Benefits covered: Prescription drugs X X
Benefits covered: Prosthetic devices X X
Benefits covered: EPSDT X X
Benefits covered: Case management X X
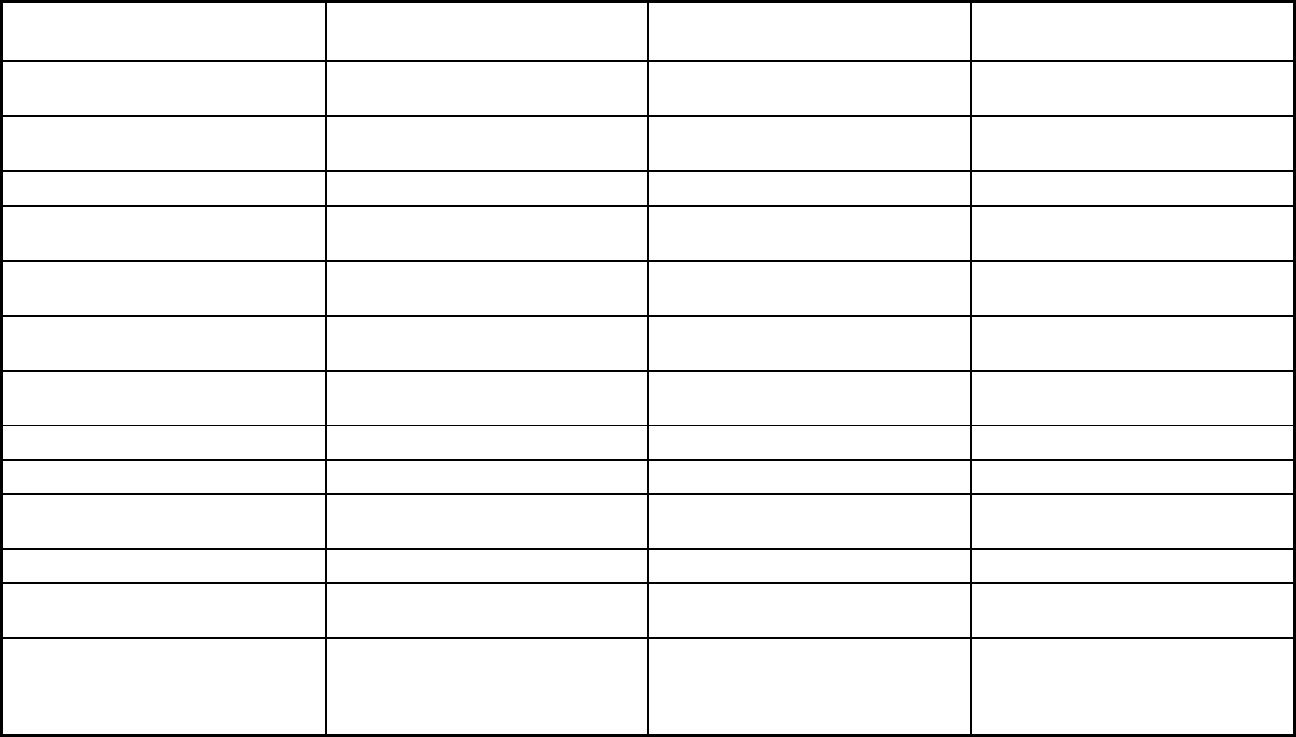
430
Features Ohio PACE
Ohio Medicaid Managed Care
Program MyCare Ohio Opt-Out Program
Benefits covered: SSA Section 1945-
authorized health home
Benefits covered: Health home care
(services in home)
X X X
Benefits covered: Family planning X X
Benefits covered: Dental services
(medical/surgical)
X X X
Benefits covered: Dental (preventative
or corrective)
X X X
Benefits covered: Personal care (state
plan option)
X X
Benefits covered: HCBS waiver
services
X X
Benefits covered: Private duty nursing X X X
Benefits covered: ICF-IDD
Benefits covered: Nursing facility
services
X X X
Benefits covered: Hospice care X X X
Benefits covered: Non-Emergency
Medical Transportation
X X X
Benefits covered: Institution for Mental
Disease inpatient treatment for people
ages 21-64 defined by 42 CFR
§438.6(e) as an 'in lieu of' benefit
X X
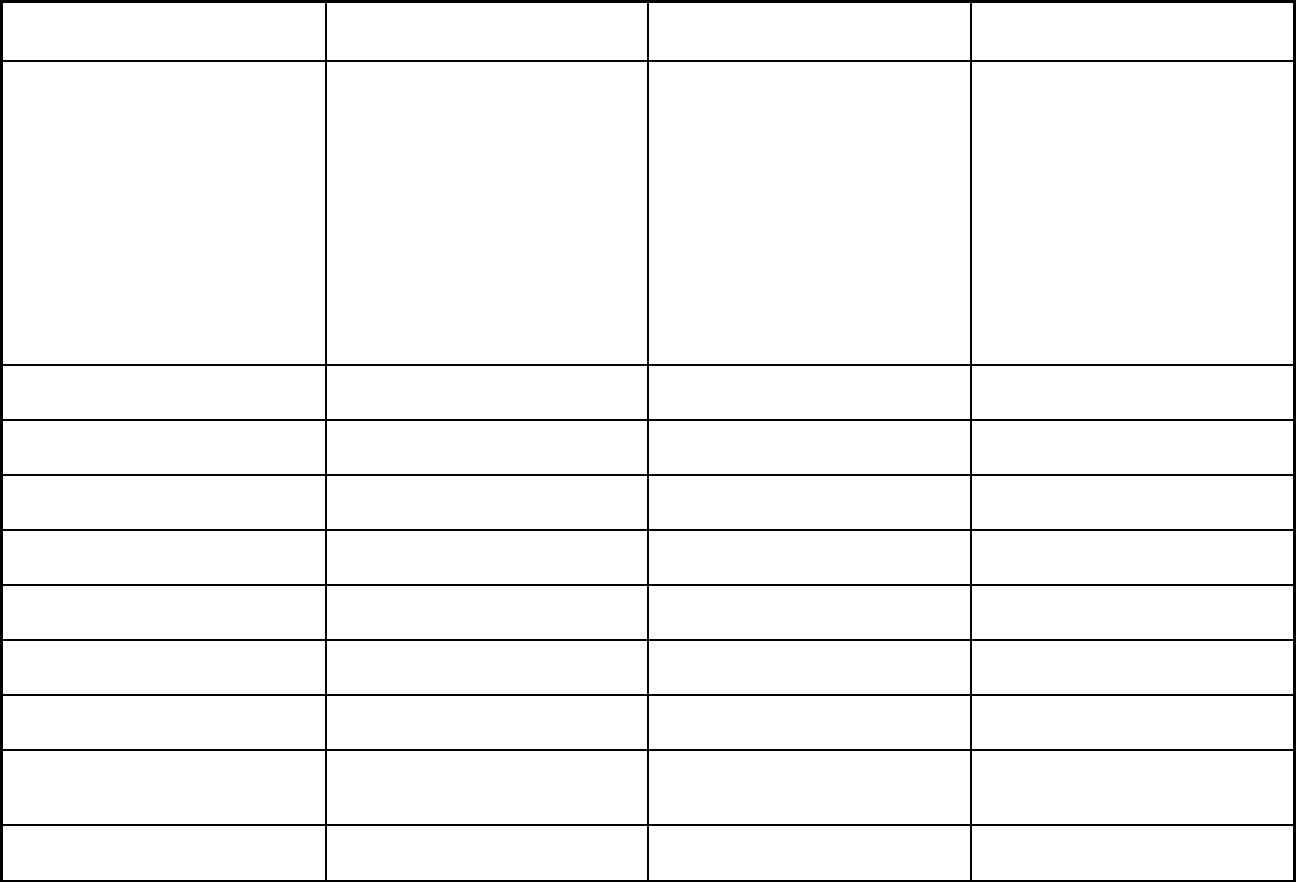
431
Features Ohio PACE
Ohio Medicaid Managed Care
Program MyCare Ohio Opt-Out Program
Benefits covered: Other (e.g., nurse
midwife services, freestanding birth
centers, podiatry, etc.)
Immunizations, nurse midwife services,
freestanding birth centers, certified
family nurse practitioner, certified
pediatric nurse practitioner, physical
therapy, speech therapy, occupational
therapy, developmental therapy,
chiropractic, podiatry, vision, DME and
medical supplies, ambulance,
ambulette, care management,
telemedicine, respite services for
eligible children receiving SSI, se
rvices
for members with a primary diagnosis
of Autism Spectrum Disorder,
screening and counseling for obesity
Immunizations, nurse midwife services,
freestanding birth centers, care
management, DME and medical
supplies, vision, physical therapy,
speech t
herapy, occupational therapy,
developmental therapy, certified family
nurse practitioner, certified pediatric
nurse practitioner, ambulance,
ambulette, podiatry, telemedicine,
services for members with a primary
diagnosis of autism spectrum disorder,
screeni
ng and counseling for obesity
Quality assurance and improvement:
HEDIS data required?
No Yes Yes
Quality assurance and improvement:
CAHPS data required?
No Yes Yes
Quality assurance and improvement:
Accreditation required?
No Yes Yes
Quality assurance and improvement:
Accrediting organization
NCQA NCQA
Quality assurance and improvement:
EQRO contractor name (if applicable)
Health Services Advisory Group Health Services Advisory Group
Performance incentives: Payment
bonuses/differentials to reward plans
Performance incentives: Preferential
auto-enrollment to reward plans
X
Performance incentives: Public reports
comparing plan performance on key
metrics
X X
Performance incentives: Withholds tied
to performance metrics
X X
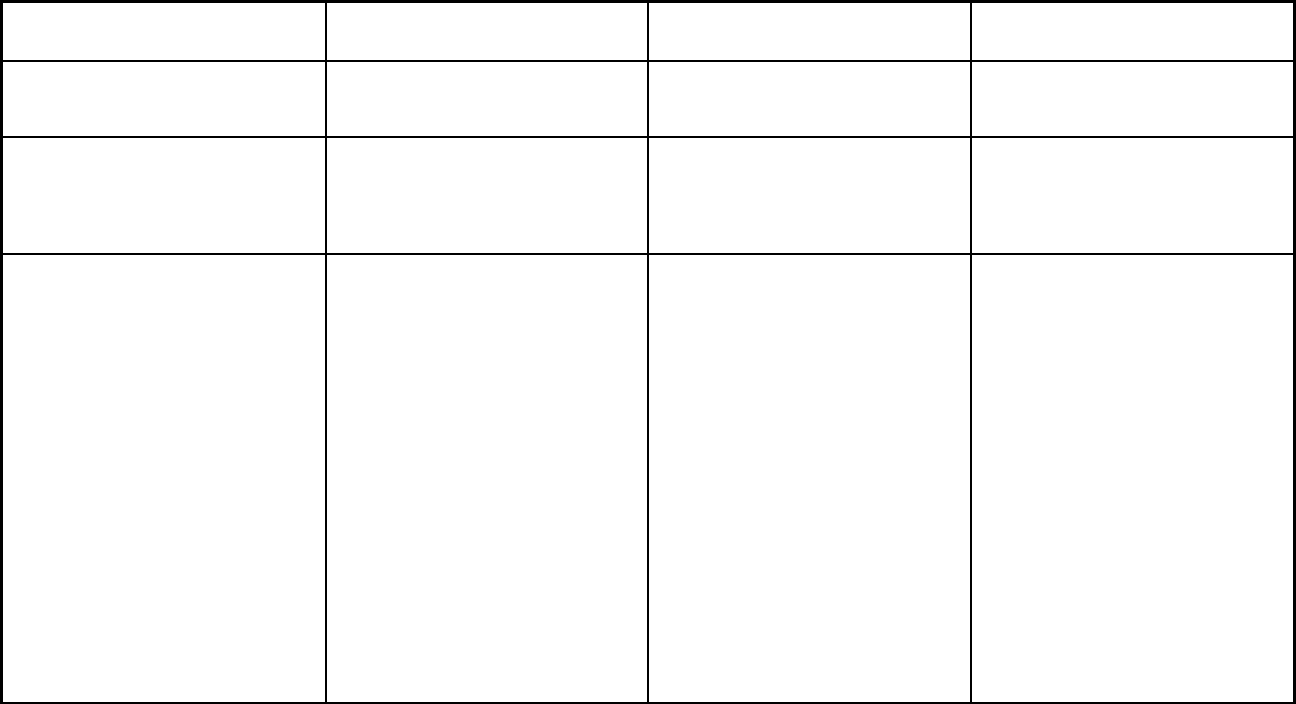
432
Features Ohio PACE
Ohio Medicaid Managed Care
Program MyCare Ohio Opt-Out Program
Performance incentives: MCOs/PHPs
required or encouraged to pay
providers for value/quality outcomes
X X
Participating plans: Plans in Program McGregor PACE Buckeye Health Plan; CareSource;
Molina Healthcare of Ohio, Inc.;
Paramount Advantage;
UnitedHealthcare Community Plan of
Ohio, Inc.
Aetna Better Health of Ohio; Buckeye
Health Plan; CareSource; Molina
Healthcare of Ohio, Inc.;
UnitedHealthcare Community Plan of
Ohio, Inc.
Notes: Program notes Regarding the coverage of HCBS
services - Ohio has chosen to offer the
same covered benefits in the PACE
program that are available to
individuals enrolled on a 1915(c)
waiver to better ensure the assessed
needs of individuals with an
intermediate level of care are met, and
better pr
omote the health and welfare
of PACE participants.
Ohio Medicaid managed care plans are
responsible for payment of medically
necessary nursing facility services for
ABD and MAGI enrollees until
discharge or until the member is
disenrolled, in accordance w
ith the
processes set forth in rule 5160-26-
02.1 of the Ohio Administrative Code.
For enrollees in the newly eligible
category (ACA Section VIII expansion
group, up to 138% federal poverty
level), nursing facility stays are covered
for the length of time medically
necessary. Individuals enrolled in
1915 (c) receiving HCBS services
through the Ohio Department of
Developmental Disabilities may enroll
in this Medicaid managed care
program voluntarily, with HCBS carved
out to fee-for-
service (not provided
through managed care).
Ohio Medicaid's waiver for this
program was renewed in the second
half of 2018, and the waiver authority
expiration date was changed from
3/31/2019 to 12/31/2023. The
individuals that must enroll in this
program are full duals who are age 18
and older. This includes children in
foster care and children receiving
adoption assistance who are full duals
and age 18 and older.
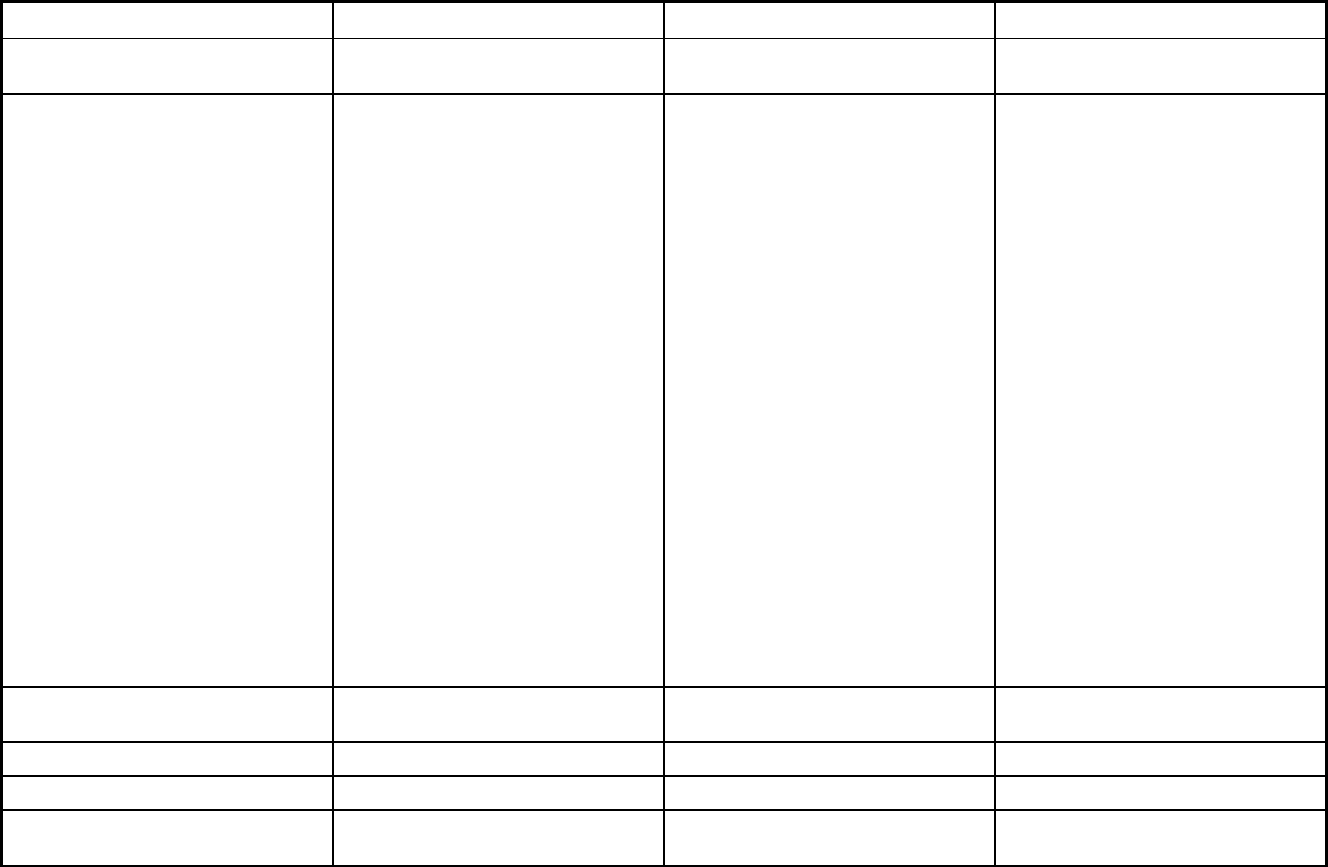
433
Oklahoma Managed Care Program Features, as of 2018
Features SoonerRide SoonerCare Choice PACE
Program type Non-Emergency Medical Transportation Primary Care Case Management
(PCCM)
Program of All-inclusive Care for the
Elderly (PACE)
Statewide or region-specific? Statewide Statewide 74464, 74441, 74423, 74960, 74427,
74465, 74403, 74457, 74451, 74352,
74434, 74401, 74471, 74364, 74347,
74402, 74444, 74368, 74964, 74446,
74452, 74359, 74965, 74439 74103,
74104, 74105, 74106, 74107, 74110,
74112, 74114, 74115, 74119, 74120,
74126, 74127, 74128, 74129, 74130,
74132, 74133, 74136, 74137, 74145,
74146, 74134, 74135, 74117, 74116,
74108 73008, 73106, 73143, 73003,
73147, 73025, 73134, 73084, 73119,
73140, 73124, 73157, 73170, 73163,
73066, 73150, 73110, 73139, 73105,
73142, 73185, 73109, 73194, 73113,
73169, 73103, 73154, 73121, 73156,
73165, 73127, 73013, 73131, 73198,
73118, 73178, 73141, 73184, 73160,
73146, 73120, 73149, 73083, 73137,
73122, 73155, 73132, 73108, 73162,
73112, 73167, 73102, 73152, 73012,
73179, 73135, 73126, 73190, 73129,
73196, 73117, 73173, 73123, 73153,
73144, 73116, 73148, 73034, 73136,
73120, 73115, 73107, 73159, 73111,
73164, 73101, 73151, 73130, 73145,
73125, 73189, 73128, 73195, 73114,
73172, 73104
Federal operating authority 1902(a)(70) NEMT 1115(a) (Medicaid demonstration
waivers)
PACE
Program start date 06/01/2006 01/01/1996 08/01/2008
Waiver expiration date (if applicable) 12/31/2023
If the program ended in 2018, indicate
the end date
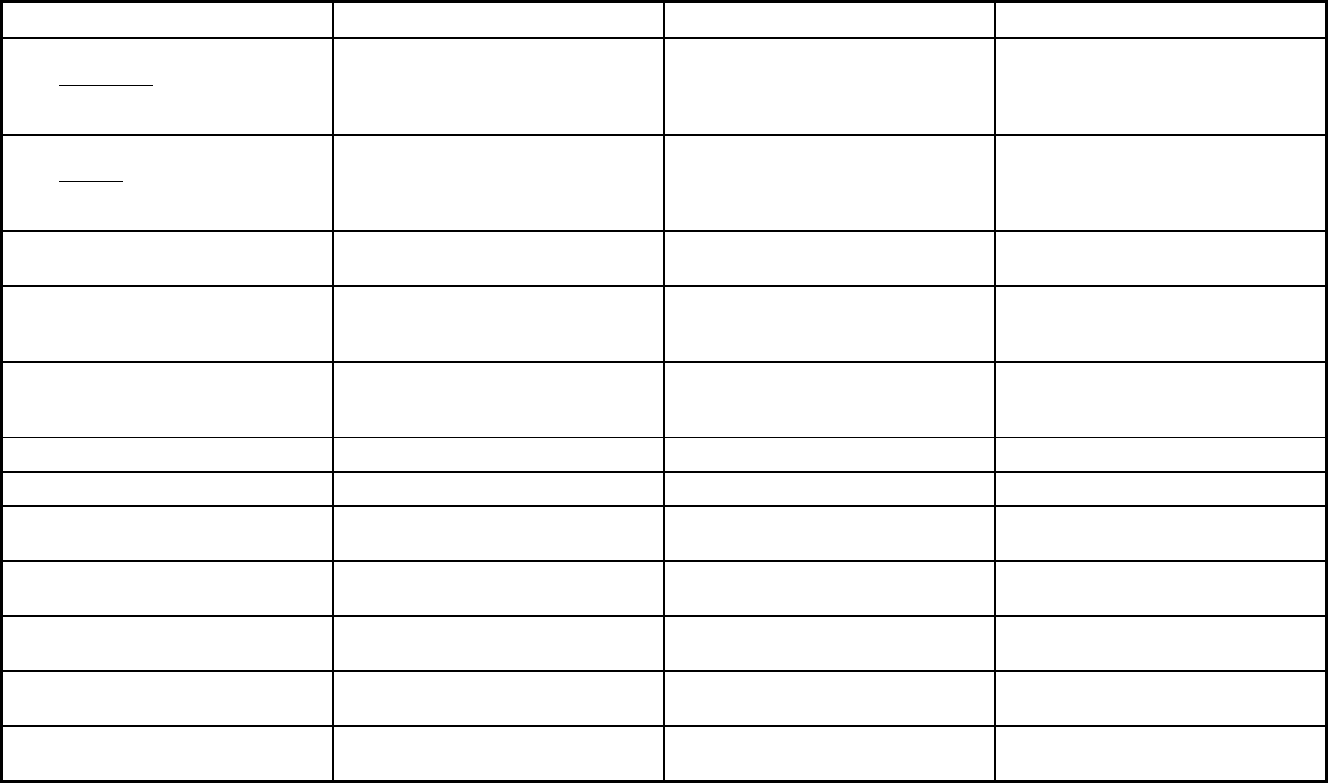
434
Features SoonerRide SoonerCare Choice PACE
Populations enrolled: Low-income
adults not covered under ACA Section
VIII (excludes pregnant women and
people with disabilities)
Mandatory Mandatory
Populations enrolled: Low-income
adults covered under ACA Section VIII
(excludes pregnant women and people
with disabilities)
Populations enrolled: Aged, Blind or
Disabled Children or Adults
Mandatory Mandatory Voluntary
Populations enrolled: Non-Disabled
Children (excludes children in foster
care or receiving adoption assistance)
Mandatory
Populations enrolled: Individuals
receiving Limited Benefits (excludes
partial duals)
Voluntary
Populations enrolled: Full Duals Mandatory Voluntary
Populations enrolled: Partial Duals Voluntary
Populations enrolled: Children with
Special Health Care Needs
Populations enrolled: Native
American/Alaskan Natives
Mandatory Voluntary Voluntary
Populations enrolled: Foster Care and
Adoption Assistance Children
Exempt Voluntary Exempt
Populations enrolled: Enrollment choice
period
Pre-assigned N/A N/A
Populations enrolled: Enrollment broker
name (if applicable)
Logisticare Maximus
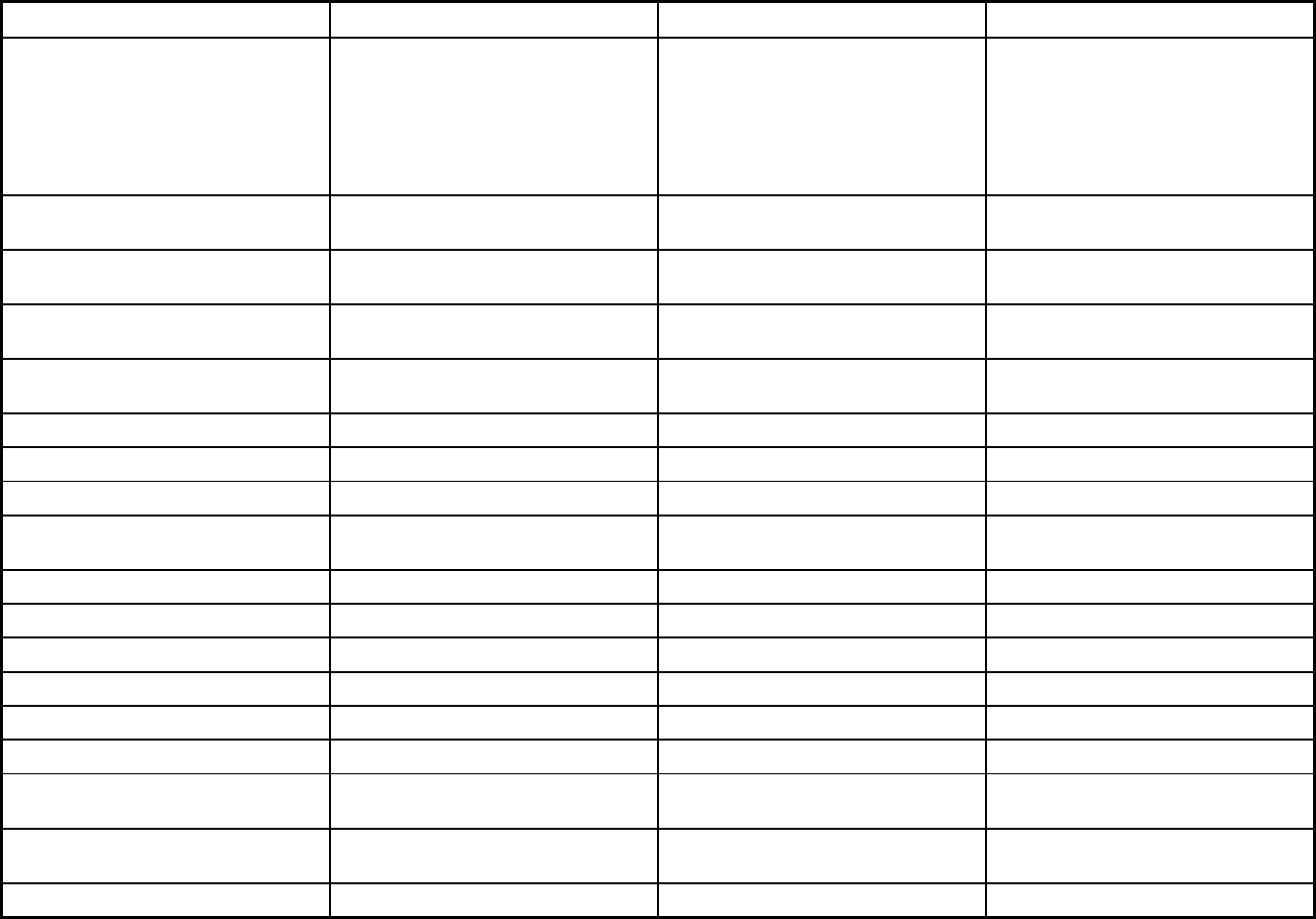
435
Features SoonerRide SoonerCare Choice PACE
Populations enrolled: Notes on
enrollment choice period
Members are enrolled within 72 hours of
application.
Enrollment process takes approximately
4-6 weeks. Members are enrolled on the
14th of every month to be effective the
first day of the following month.
Members go through the PACE
Organizations for the entire enrollment
process.
Benefits covered: Inpatient hospital
physical health
X X
Benefits covered: Inpatient hospital
behavioral health (MH and/or SUD)
X X
Benefits covered: Outpatient hospital
physical health
X X
Benefits covered: Outpatient hospital
behavioral health (MH and/or SUD)
X X
Benefits covered: Partial hospitalization X X
Benefits covered: Physician X X
Benefits covered: Nurse practitioner X X
Benefits covered: Rural health clinics
and FQHCs
X
Benefits covered: Clinic services X X
Benefits covered: Lab and x-ray X X
Benefits covered: Prescription drugs X X
Benefits covered: Prosthetic devices X X
Benefits covered: EPSDT X
Benefits covered: Case management X X
Benefits covered: SSA Section 1945-
authorized health home
Benefits covered: Health home care
(services in home)
X X
Benefits covered: Family planning X
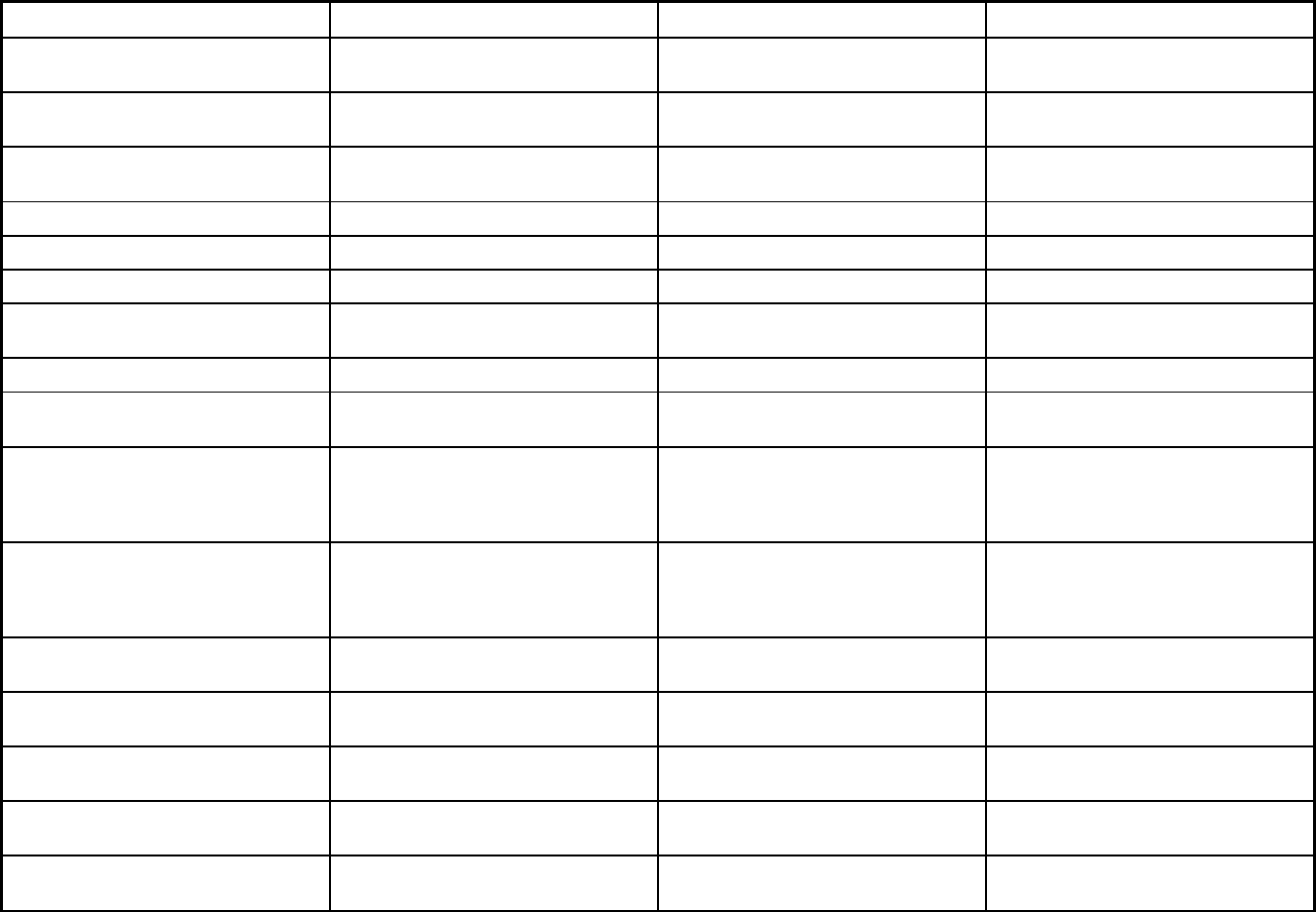
436
Features SoonerRide SoonerCare Choice PACE
Benefits covered: Dental services
(medical/surgical)
X X
Benefits covered: Dental (preventative
or corrective)
X X
Benefits covered: Personal care (state
plan option)
X X
Benefits covered: HCBS waiver services
Benefits covered: Private duty nursing X X
Benefits covered: ICF-IDD
Benefits covered: Nursing facility
services
X
Benefits covered: Hospice care X X
Benefits covered: Non-Emergency
Medical Transportation
X X
Benefits covered: Institution for Mental
Disease inpatient treatment for people
ages 21-64 defined by 42 CFR
§438.6(e) as an 'in lieu of' benefit
Benefits covered: Other (e.g., nurse
midwife services, freestanding birth
centers, podiatry, etc.)
Podiatry, speech therapy, disease
management, hearing, institutional,
occupational therapy, physical therapy,
skilled nursing facility, vision
Podiatry, speech therapy, disease
management, hearing, institutional,
occupational therapy, physical therapy,
skilled nursing facility, vision
Quality assurance and improvement:
HEDIS data required?
No No No
Quality assurance and improvement:
CAHPS data required?
No No No
Quality assurance and improvement:
Accreditation required?
No No No
Quality assurance and improvement:
Accrediting organization
State Specific PCMH
Quality assurance and improvement:
EQRO contractor name (if applicable)
Telligen
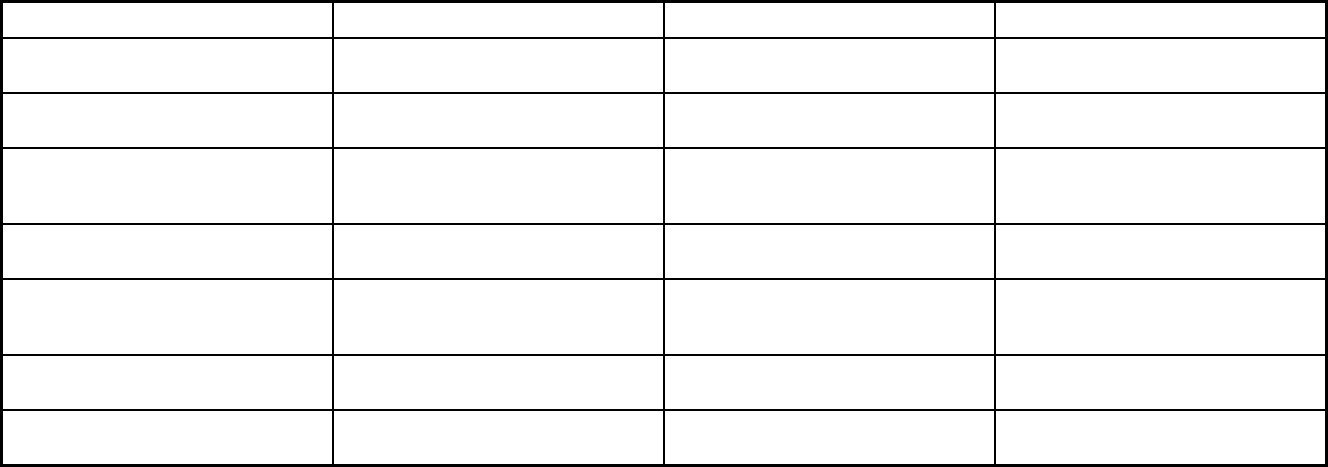
437
Features SoonerRide SoonerCare Choice PACE
Performance incentives: Payment
bonuses/differentials to reward plans
Performance incentives: Preferential
auto-enrollment to reward plans
Performance incentives: Public reports
comparing plan performance on key
metrics
Performance incentives: Withholds tied
to performance metrics
Performance incentives: MCOs/PHPs
required or encouraged to pay providers
for value/quality outcomes
Participating plans: Plans in Program SoonerRide SoonerCare Choice Cherokee Elder Care (CEC); Life PACE;
Valir PACE
Notes: Program notes PACE members are not eligible for
SoonerRide.
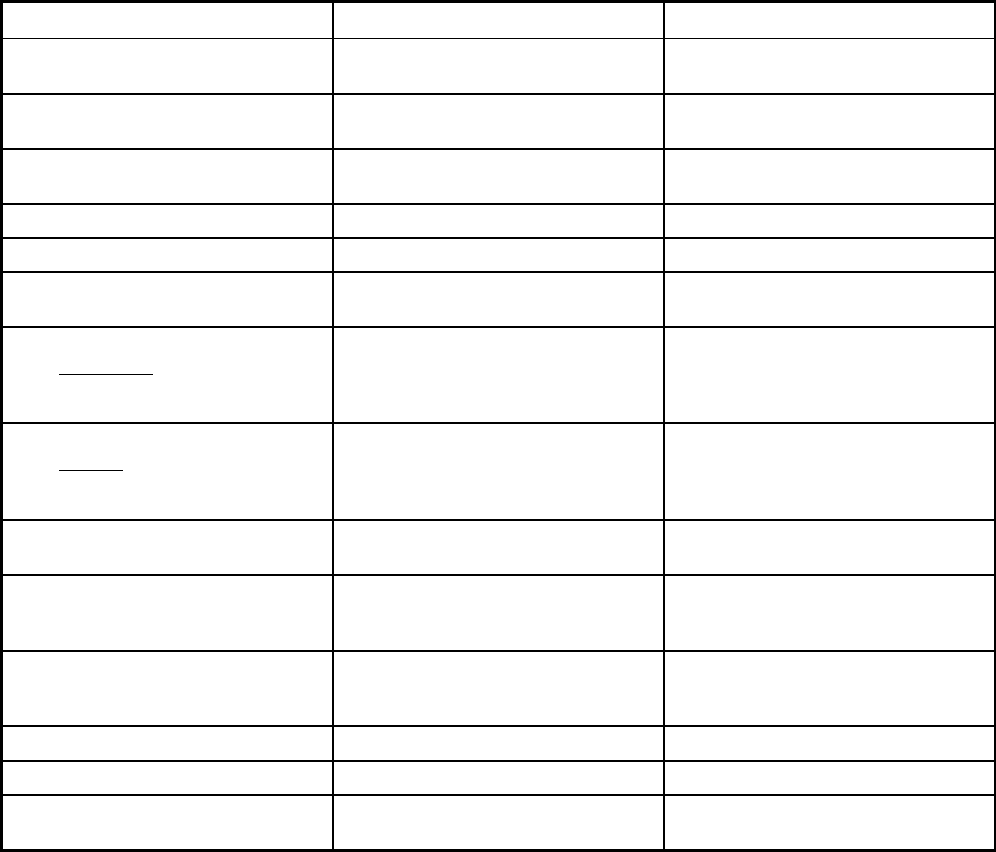
438
Oregon Managed Care Program Features, as of 2018
Features Oregon Health Plan (OHP) PACE
Program type Comprehensive MCO Program of All-inclusive Care for the
Elderly (PACE)
Statewide or region-specific? Statewide Multnomah, Washington, Clatsop,
Clackamas and Tillamook Counties
Federal operating authority 1115(a) (Medicaid demonstration
waivers)
PACE
Program start date 02/01/1994 01/01/1986
Waiver expiration date (if applicable) 06/30/2022
If the program ended in 2018, indicate
the end date
Populations enrolled: Low-income
adults not covered under ACA Section
VIII (excludes pregnant women and
people with disabilities)
Mandatory
Populations enrolled: Low-income
adults covered under ACA Section VIII
(excludes pregnant women and people
with disabilities)
Mandatory
Populations enrolled: Aged, Blind or
Disabled Children or Adults
Voluntary
Populations enrolled: Non-Disabled
Children (excludes children in foster
care or receiving adoption assistance)
Voluntary
Populations enrolled: Individuals
receiving Limited Benefits (excludes
partial duals)
Mandatory
Populations enrolled: Full Duals Voluntary Voluntary
Populations enrolled: Partial Duals Voluntary Voluntary
Populations enrolled: Children with
Special Health Care Needs
Mandatory
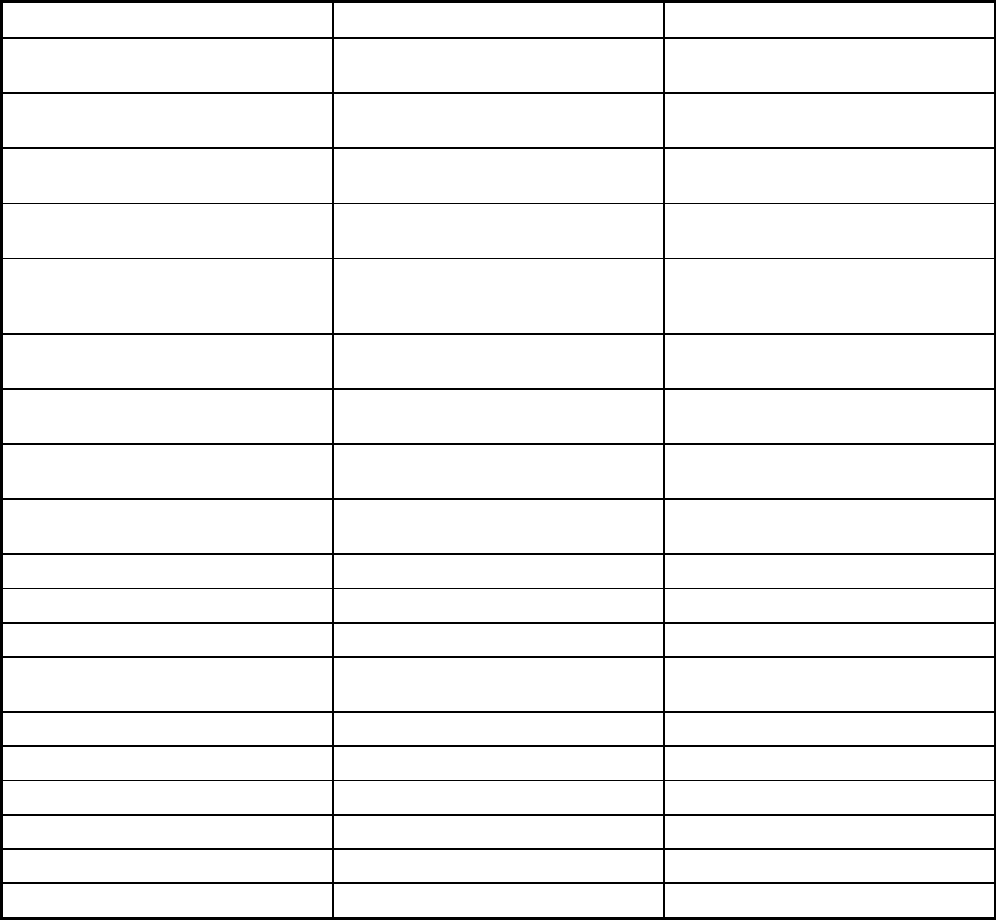
439
Features Oregon Health Plan (OHP) PACE
Populations enrolled: Native
American/Alaskan Natives
Voluntary Voluntary
Populations enrolled: Foster Care and
Adoption Assistance Children
Voluntary
Populations enrolled: Enrollment choice
period
Pre-assigned N/A
Populations enrolled: Enrollment broker
name (if applicable)
Populations enrolled: Notes on
enrollment choice period
Flexible enrollment eligibility - rolling
enrollment to be effective on the 1st of
the following month.
Benefits covered: Inpatient hospital
physical health
X X
Benefits covered: Inpatient hospital
behavioral health (MH and/or SUD)
X X
Benefits covered: Outpatient hospital
physical health
X X
Benefits covered: Outpatient hospital
behavioral health (MH and/or SUD)
X X
Benefits covered: Partial hospitalization X
Benefits covered: Physician X X
Benefits covered: Nurse practitioner X
Benefits covered: Rural health clinics
and FQHCs
Benefits covered: Clinic services X
Benefits covered: Lab and x-ray X X
Benefits covered: Prescription drugs X X
Benefits covered: Prosthetic devices X X
Benefits covered: EPSDT X
Benefits covered: Case management X X
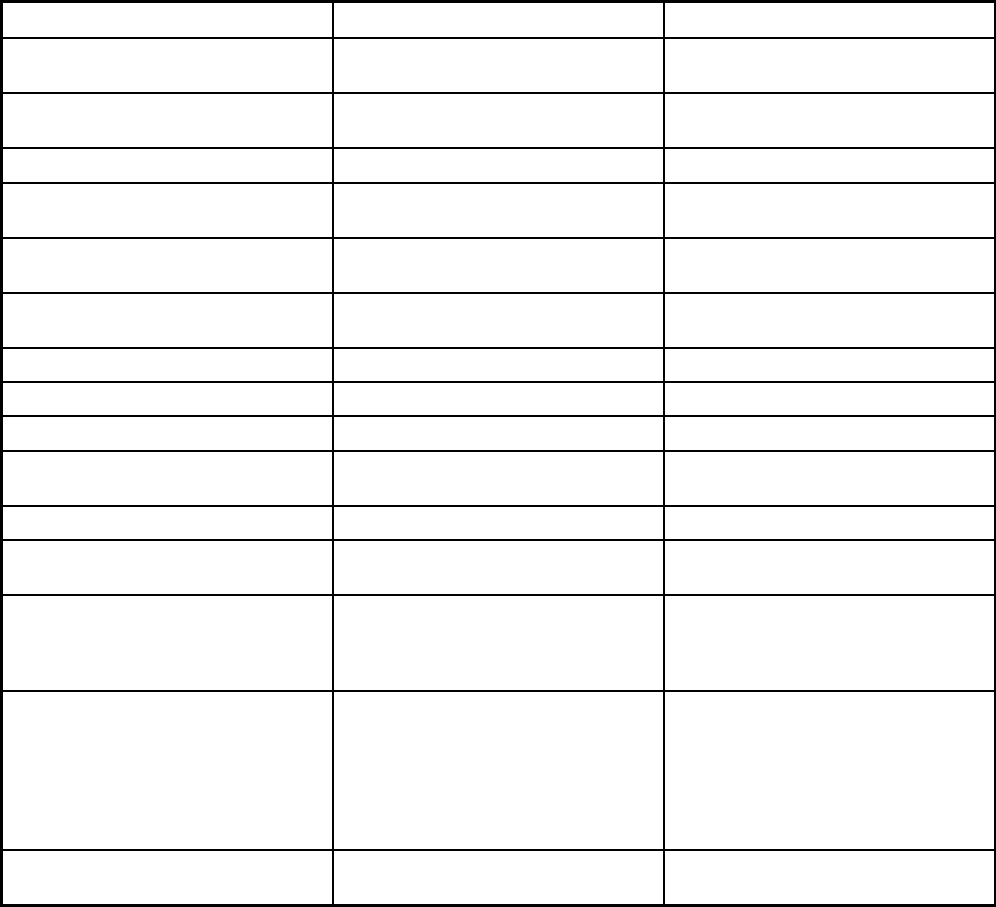
440
Features Oregon Health Plan (OHP) PACE
Benefits covered: SSA Section 1945-
authorized health home
Benefits covered: Health home care
(services in home)
X X
Benefits covered: Family planning X
Benefits covered: Dental services
(medical/surgical)
X X
Benefits covered: Dental (preventative
or corrective)
X X
Benefits covered: Personal care (state
plan option)
X
Benefits covered: HCBS waiver services X
Benefits covered: Private duty nursing
Benefits covered: ICF-IDD
Benefits covered: Nursing facility
services
X X
Benefits covered: Hospice care X X
Benefits covered: Non-Emergency
Medical Transportation
X X
Benefits covered: Institution for Mental
Disease inpatient treatment for people
ages 21-64 defined by 42 CFR
§438.6(e) as an 'in lieu of' benefit
Benefits covered: Other (e.g., nurse
midwife services, freestanding birth
centers, podiatry, etc.)
Hearing, immunization, vision Medications (OTC and RX), mental
health care, DME,
speech/physical/occupational/
recreational theraputic services,
audiology/optical/podiatry specialty
medical care, occupational and physical
therapy and social services
Quality assurance and improvement:
HEDIS data required?
No No
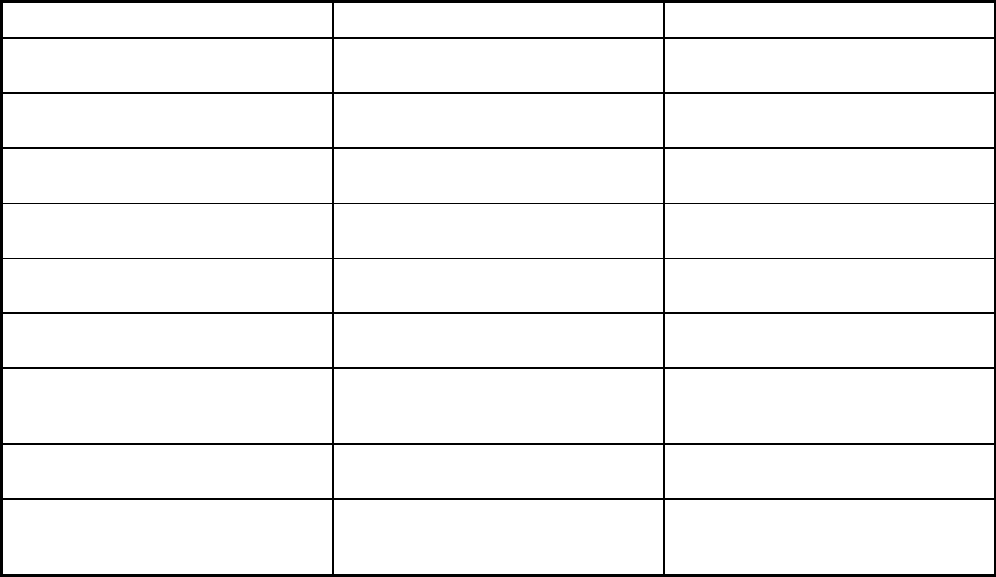
441
Features Oregon Health Plan (OHP) PACE
Quality assurance and improvement:
CAHPS data required?
Yes No
Quality assurance and improvement:
Accreditation required?
No No
Quality assurance and improvement:
Accrediting organization
NCQA, URAC NCQA
Quality assurance and improvement:
EQRO contractor name (if applicable)
Health Insight
Performance incentives: Payment
bonuses/differentials to reward plans
X X
Performance incentives: Preferential
auto-enrollment to reward plans
Performance incentives: Public reports
comparing plan performance on key
metrics
X
Performance incentives: Withholds tied
to performance metrics
X
Performance incentives: MCOs/PHPs
required or encouraged to pay providers
for value/quality outcomes
442
Features Oregon Health Plan (OHP) PACE
Participating plans: Plans in Program Access Dental Plan, LLC; Advantage
Dental Services; Capitol Dental Care,
Inc.; CareOregon Dental; Family Dental
Care; Greater Oregon Behavioral
Health, Inc.; Managed Dental Care of
Oregon; ODS Community Health Inc.;
AllCare Health Plan; Cascade Health
Alliance; Columbia Pacific; Eastern
Oregon CCO; HealthShare of Oregon;
InterCommunity Health Network;
Jackson Care Connect; PacificSource
Community Solutions - Central Oregon;
PacificSource Community Solutions -
Columbia Gorge; PrimaryHealth of
Josephine County; Trillium Community
Health Plan; Umpqua Health Alliance;
Advanced Health; Willamette Valley
Community Health; Yamhill Community
Care
Providence Elder Place
Notes: Program notes In the Oregon Health Plan/Medicaid
program, a person can be enrolled
simultaneously in two or three plans.
For example, a client can be enrolled in
the PACE program for physical health, a
dental plan (DCO) for dental care and a
mental health plan (CCO) for mental
health care. FamilyCare (CCO) had
closed to enrollment prior to June 2018.
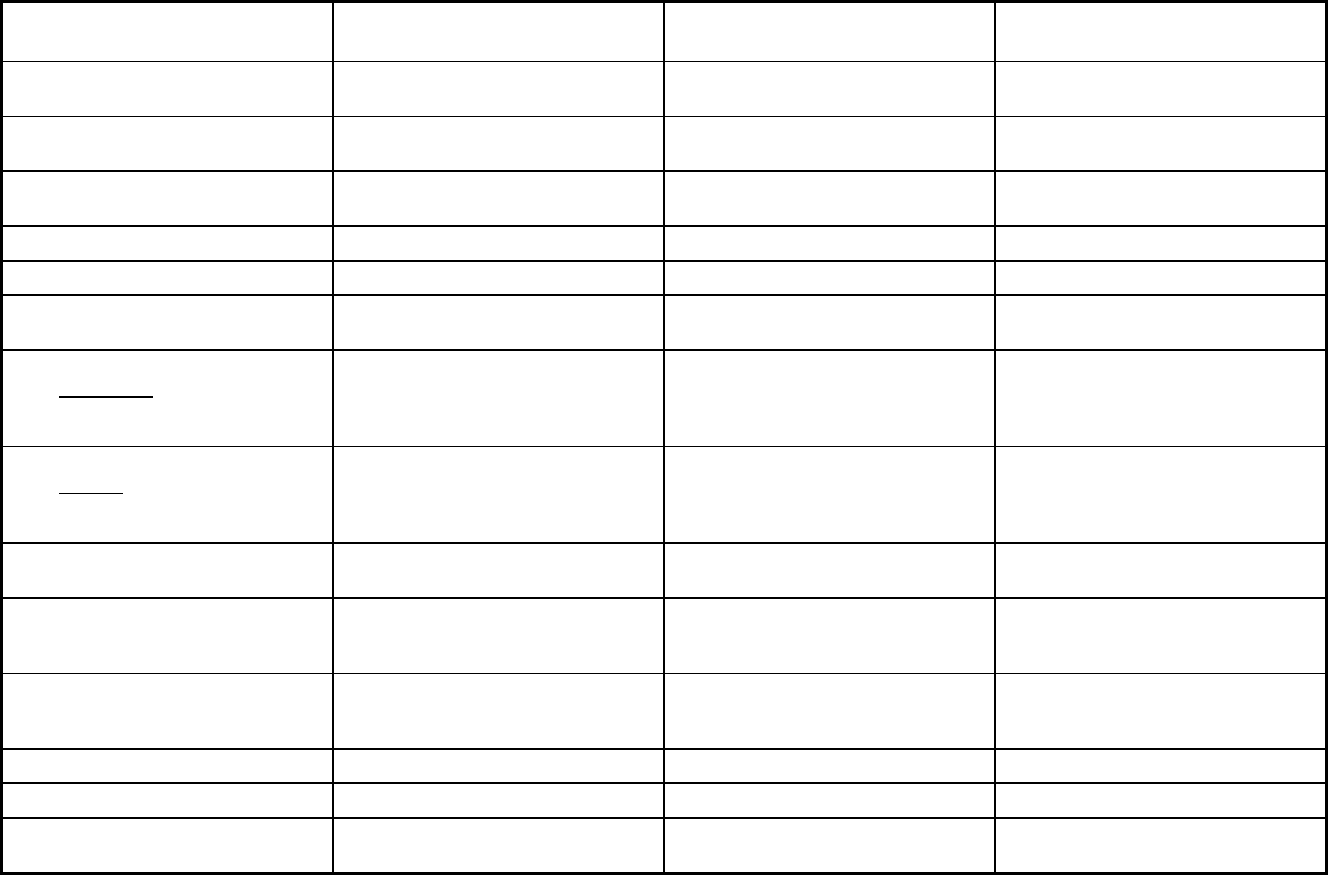
443
Pennsylvania Managed Care Program Features, as of 2018 (1 of 2)
Features Adult Community Autism Program
MATP (Medical Assistance
Transportation Program) Behavioral Health HealthChoices
Program type Other Prepaid Health Plan (PHP)
(limited benefits)
Non-Emergency Medical Transportation Behavioral Health Organization (BHO)
only (PIHP and/or PAHP)
Statewide or region-specific? Dauphin, Cumberland, Lancaster and
Chester counties
Philadelphia Statewide
Federal operating authority 1915(a) 1902(a)(70) NEMT 1115(a) (Medicaid demonstration
waivers),1915(b)
Program start date 08/01/2009 11/01/2005 01/01/1999
Waiver expiration date (if applicable) 12/31/2021 12/31/2021
If the program ended in 2018, indicate
the end date
Populations enrolled: Low-income
adults not covered under ACA Section
VIII (excludes pregnant women and
people with disabilities)
Voluntary Mandatory
Populations enrolled: Low-income
adults covered under ACA Section VIII
(excludes pregnant women and people
with disabilities)
Voluntary Mandatory
Populations enrolled: Aged, Blind or
Disabled Children or Adults
Voluntary Mandatory
Populations enrolled: Non-Disabled
Children (excludes children in foster
care or receiving adoption assistance)
Voluntary Mandatory
Populations enrolled: Individuals
receiving Limited Benefits (excludes
partial duals)
Voluntary Mandatory
Populations enrolled: Full Duals Voluntary Voluntary Mandatory
Populations enrolled: Partial Duals Voluntary Voluntary Mandatory
Populations enrolled: Children with
Special Health Care Needs
Voluntary Mandatory
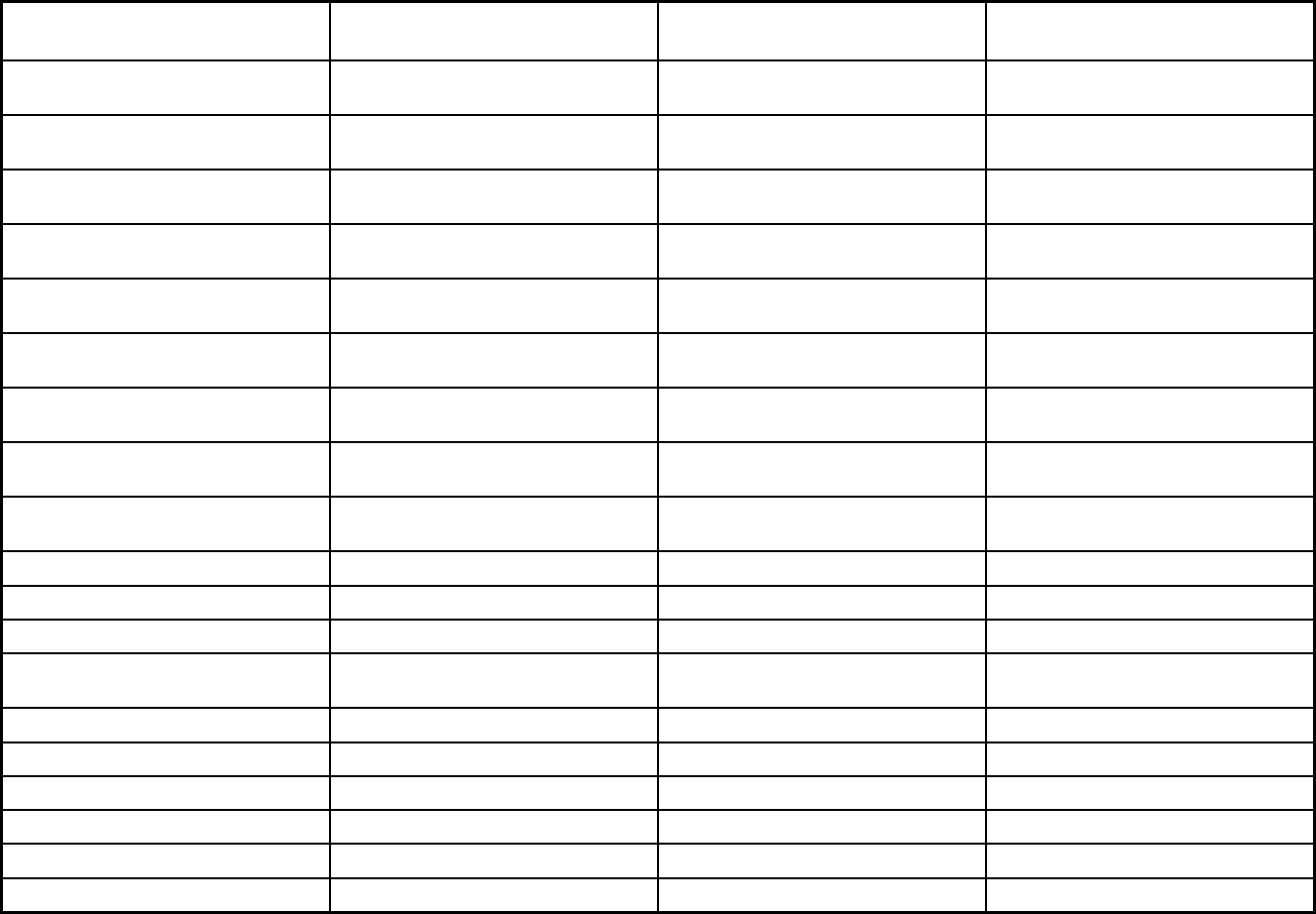
444
Features Adult Community Autism Program
MATP (Medical Assistance
Transportation Program) Behavioral Health HealthChoices
Populations enrolled: Native
American/Alaskan Natives
Exempt Exempt Exempt
Populations enrolled: Foster Care and
Adoption Assistance Children
Exempt Mandatory
Populations enrolled: Enrollment choice
period
Pre-assigned
Populations enrolled: Enrollment broker
name (if applicable)
LogistiCare
Populations enrolled: Notes on
enrollment choice period
Benefits covered: Inpatient hospital
physical health
Benefits covered: Inpatient hospital
behavioral health (MH and/or SUD)
X
Benefits covered: Outpatient hospital
physical health
Benefits covered: Outpatient hospital
behavioral health (MH and/or SUD)
X
Benefits covered: Partial hospitalization X
Benefits covered: Physician X X
Benefits covered: Nurse practitioner
Benefits covered: Rural health clinics
and FQHCs
X
Benefits covered: Clinic services X
Benefits covered: Lab and x-ray
Benefits covered: Prescription drugs
Benefits covered: Prosthetic devices
Benefits covered: EPSDT X
Benefits covered: Case management X
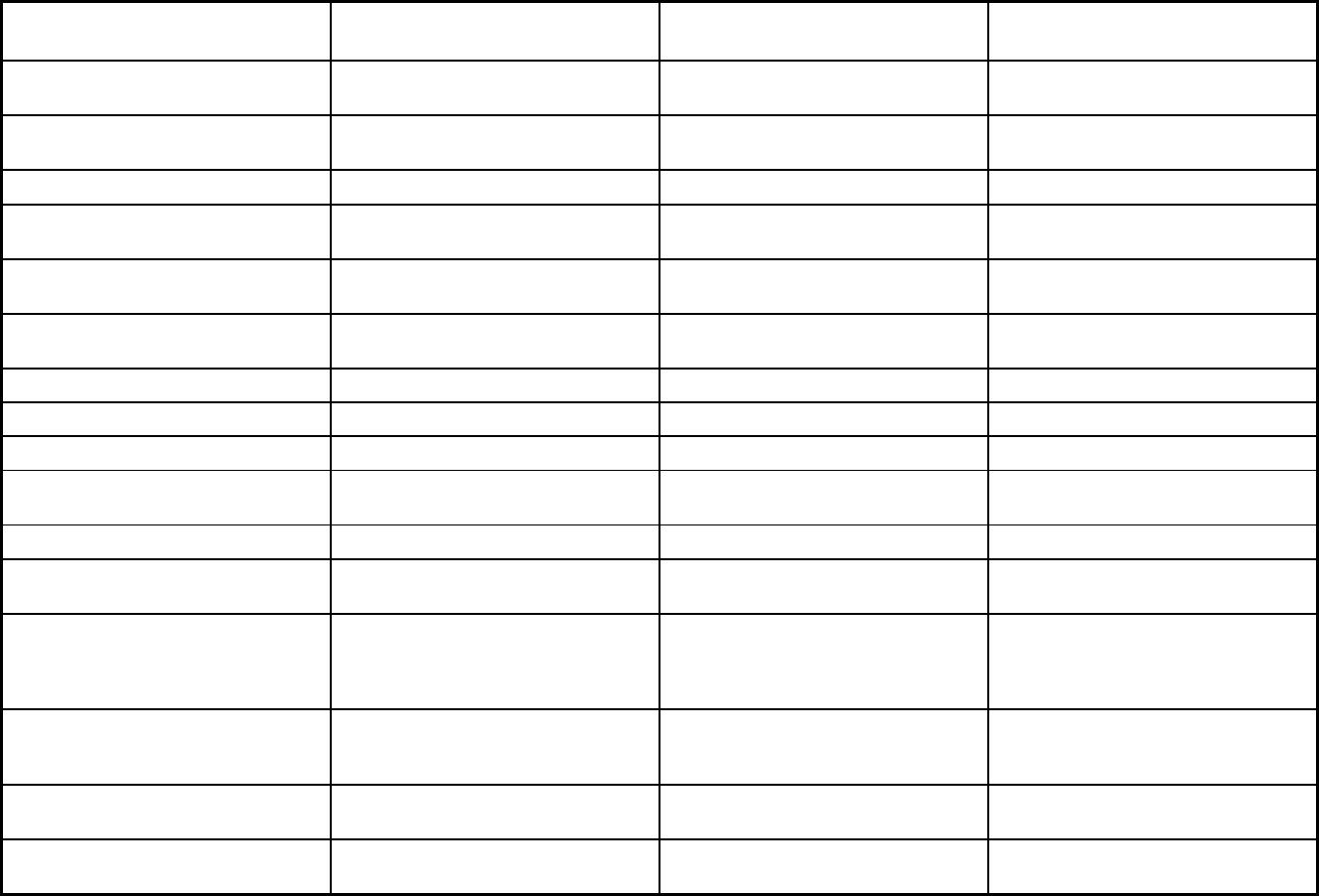
445
Features Adult Community Autism Program
MATP (Medical Assistance
Transportation Program) Behavioral Health HealthChoices
Benefits covered: SSA Section 1945-
authorized health home
Benefits covered: Health home care
(services in home)
Benefits covered: Family planning
Benefits covered: Dental services
(medical/surgical)
X
Benefits covered: Dental (preventative
or corrective)
X
Benefits covered: Personal care (state
plan option)
Benefits covered: HCBS waiver services X
Benefits covered: Private duty nursing
Benefits covered: ICF-IDD
Benefits covered: Nursing facility
services
Benefits covered: Hospice care
Benefits covered: Non-Emergency
Medical Transportation
X
Benefits covered: Institution for Mental
Disease inpatient treatment for people
ages 21-64 defined by 42 CFR
§438.6(e) as an 'in lieu of' benefit
X
Benefits covered: Other (e.g., nurse
midwife services, freestanding birth
centers, podiatry, etc.)
Podiatry, speech therapy, occupational
therapy, language therapy, counseling,
respite, supported employment
Psychiatric rehabilitation, peer specialist
services
Quality assurance and improvement:
HEDIS data required?
No No Yes
Quality assurance and improvement:
CAHPS data required?
No No No
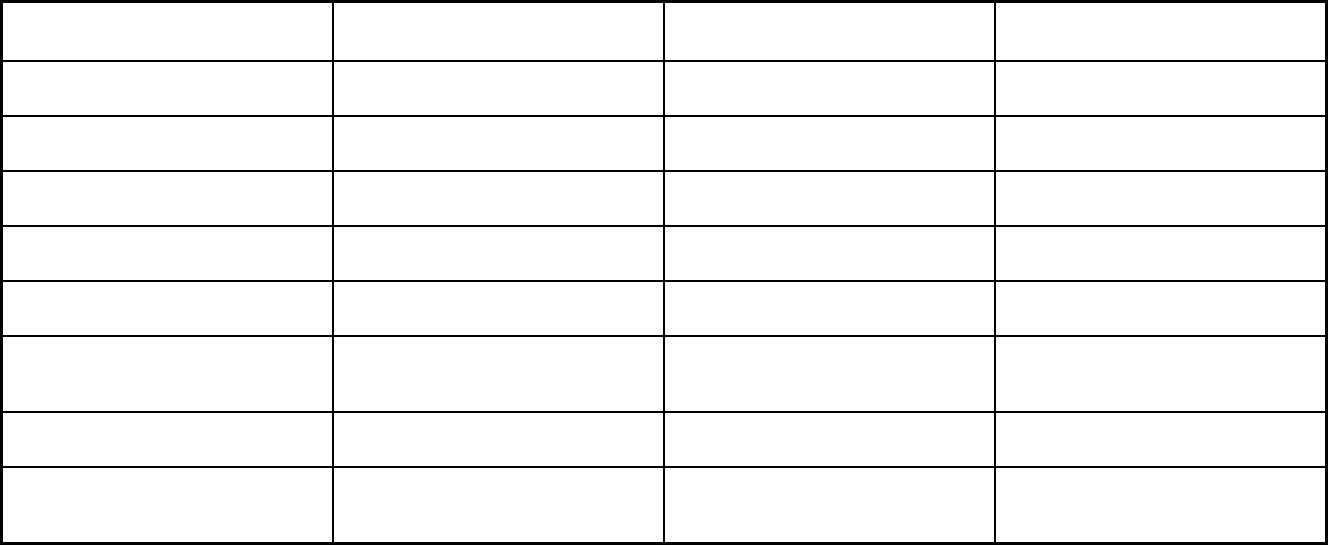
446
Features Adult Community Autism Program
MATP (Medical Assistance
Transportation Program) Behavioral Health HealthChoices
Quality assurance and improvement:
Accreditation required?
No No Yes
Quality assurance and improvement:
Accrediting organization
NCQA, JCAHO, URAC, for Inpatient,
Outpatient
Quality assurance and improvement:
EQRO contractor name (if applicable)
Island Peer Review Organization Island Peer Review Organization
Performance incentives: Payment
bonuses/differentials to reward plans
X
Performance incentives: Preferential
auto-enrollment to reward plans
Performance incentives: Public reports
comparing plan performance on key
metrics
Performance incentives: Withholds tied
to performance metrics
X
Performance incentives: MCOs/PHPs
required or encouraged to pay providers
for value/quality outcomes
X
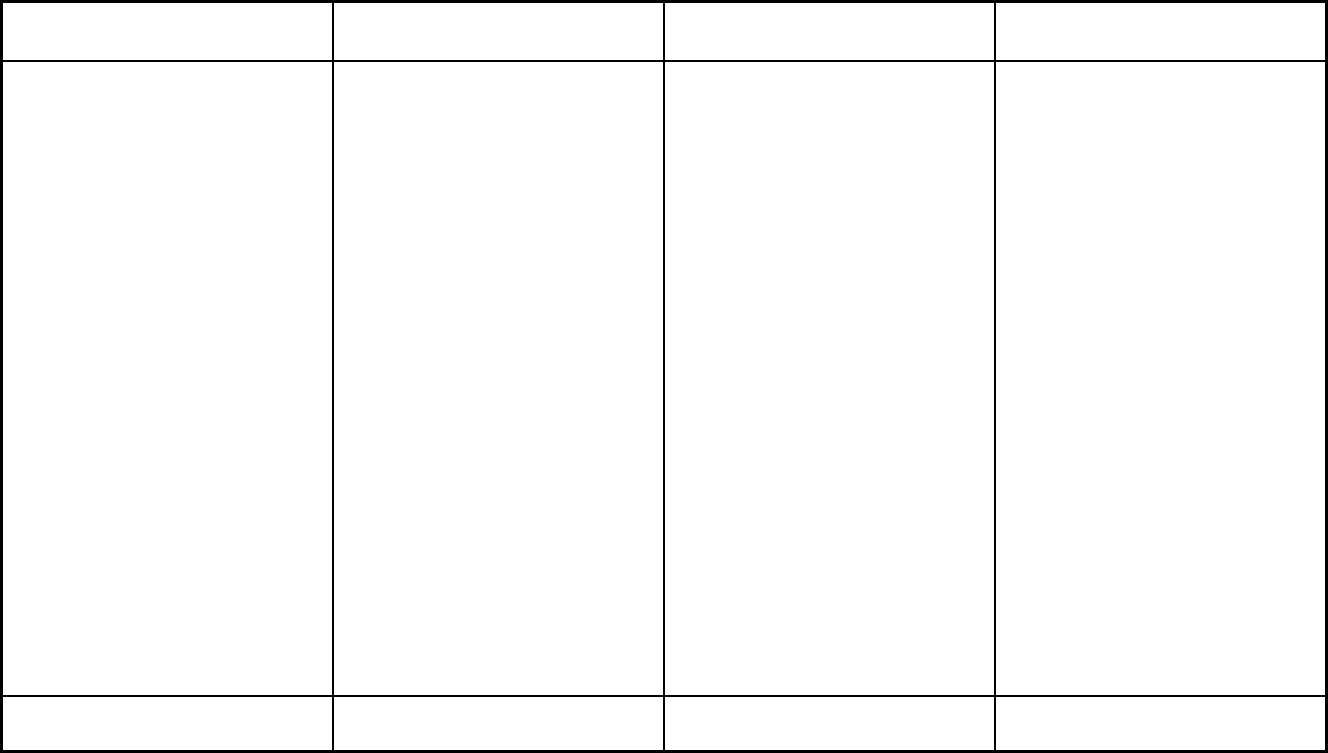
447
Features Adult Community Autism Program
MATP (Medical Assistance
Transportation Program) Behavioral Health HealthChoices
Participating plans: Plans in Program Adult Community Autism Program LogistiCare Allegheny County HealthChoices;
Beaver County HealthChoices;
Behavioral Health Services of Bedford
and Somerset; Berks County
HealthChoices; Blair County
HealthChoices; Bucks County
HealthChoices; Cambria County
HealthChoices; Carbon-Monroe-Pike
Joinder Board; Chester County
HealthChoices; Cumberland County
HealthChoices; Dauphin County
HealthChoices; Delaware County
HealthChoices; Erie County
HealthChoices; Fayette County
HealthChoices; Greene County
(Commonwealth); Lancaster County
HealthChoices; Lebanon County
HealthChoices; Lehigh County
HealthChoices; Lycoming-Clinton
Joinder Board; Montgomery County
HealthChoices; North Central State
Option; Northampton County
HealthChoices; Northeast Behavioral
Health Care Consortium; Northwest
Behavioral Health Partnership; Perry
County HealthChoices; Philadelphia
County HealthChoices; Southwest
Behavioral Health Management;
Tuscarora Managed Care Alliance;
York/Adams County HealthChoices
Notes: Program notes ACAP is a PAHP with MLTSS. 1115(a) authority is for Residential Drug
and Alcohol services.
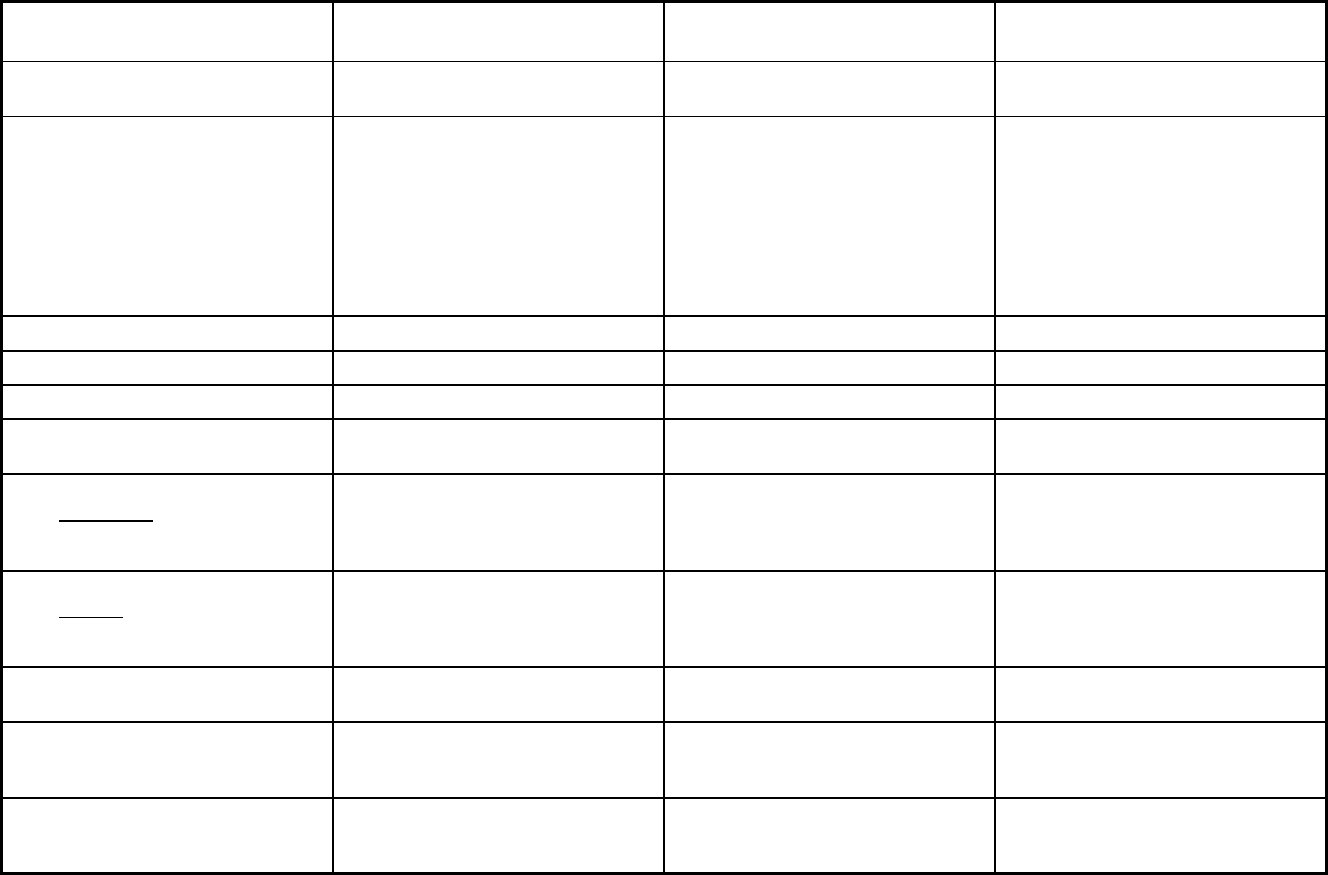
448
Pennsylvania Managed Care Program Features, as of 2018 (2 of 2)
Features
PA Living Independence for the
Elderly Community HealthChoices HealthChoices - Physical Health
Program type Program of All-inclusive Care for the
Elderly (PACE)
Comprehensive MCO + MLTSS Comprehensive MCO
Statewide or region-specific? Statewide Community HealthChoices will be
phased in over a three year period
beginning in Southwest Pennsylvania
on January 1, 2018. The following
counties were included in Phase 1:
Allegheny, Armstrong, Beaver, Bedford,
Blair, Butler, Cambria, Fayette, Greene,
Indiana, Lawrence, Somerset,
Washington and Westmoreland.
Statewide
Federal operating authority PACE 1915(b)/1915(c) 1915(b)
Program start date 07/24/1998 01/01/2018 02/01/1997
Waiver expiration date (if applicable) 07/01/2020 12/31/2021
If the program ended in 2018, indicate
the end date
Populations enrolled: Low-income
adults not covered under ACA Section
VIII (excludes pregnant women and
people with disabilities)
Mandatory
Populations enrolled: Low-income
adults covered under ACA Section VIII
(excludes pregnant women and people
with disabilities)
Mandatory
Populations enrolled: Aged, Blind or
Disabled Children or Adults
Mandatory Mandatory
Populations enrolled: Non-Disabled
Children (excludes children in foster
care or receiving adoption assistance)
Mandatory
Populations enrolled: Individuals
receiving Limited Benefits (excludes
partial duals)
Mandatory
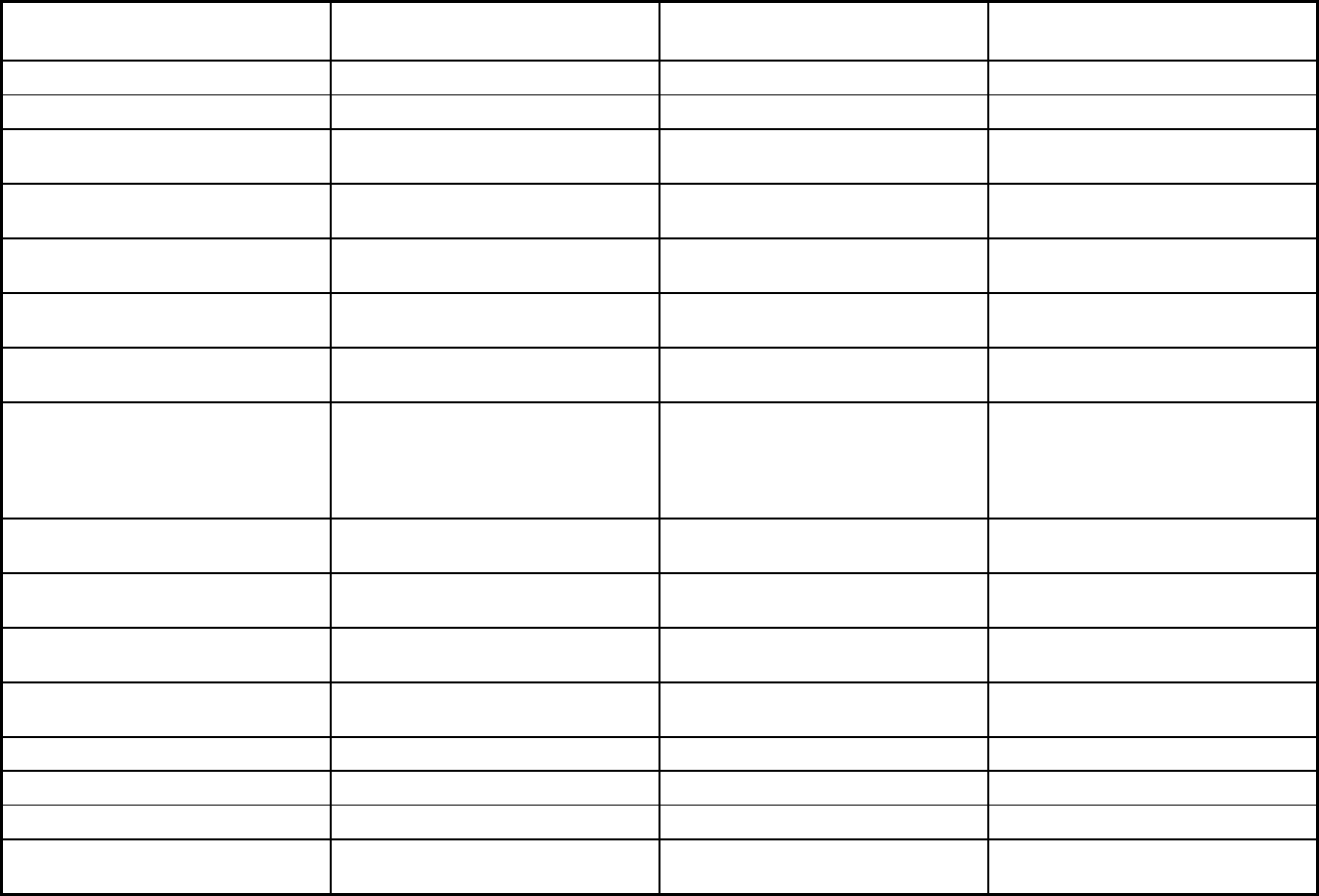
449
Features
PA Living Independence for the
Elderly Community HealthChoices HealthChoices - Physical Health
Populations enrolled: Full Duals Voluntary Mandatory Mandatory
Populations enrolled: Partial Duals Voluntary Mandatory
Populations enrolled: Children with
Special Health Care Needs
Mandatory
Populations enrolled: Native
American/Alaskan Natives
Voluntary Mandatory Mandatory
Populations enrolled: Foster Care and
Adoption Assistance Children
Exempt Exempt Mandatory
Populations enrolled: Enrollment choice
period
N/A Other Other
Populations enrolled: Enrollment broker
name (if applicable)
Maximus Maximus
Populations enrolled: Notes on
enrollment choice period
Open enrollment all year. Participants go through choice
counseling at initial enrollment and can
change their plan at any time. Dating
rules affect when the member will be
enrolled.
Consumers have the right to change
MCOs at any time.
Benefits covered: Inpatient hospital
physical health
X X X
Benefits covered: Inpatient hospital
behavioral health (MH and/or SUD)
X
Benefits covered: Outpatient hospital
physical health
X X X
Benefits covered: Outpatient hospital
behavioral health (MH and/or SUD)
X
Benefits covered: Partial hospitalization X
Benefits covered: Physician X X X
Benefits covered: Nurse practitioner X X X
Benefits covered: Rural health clinics
and FQHCs
X X
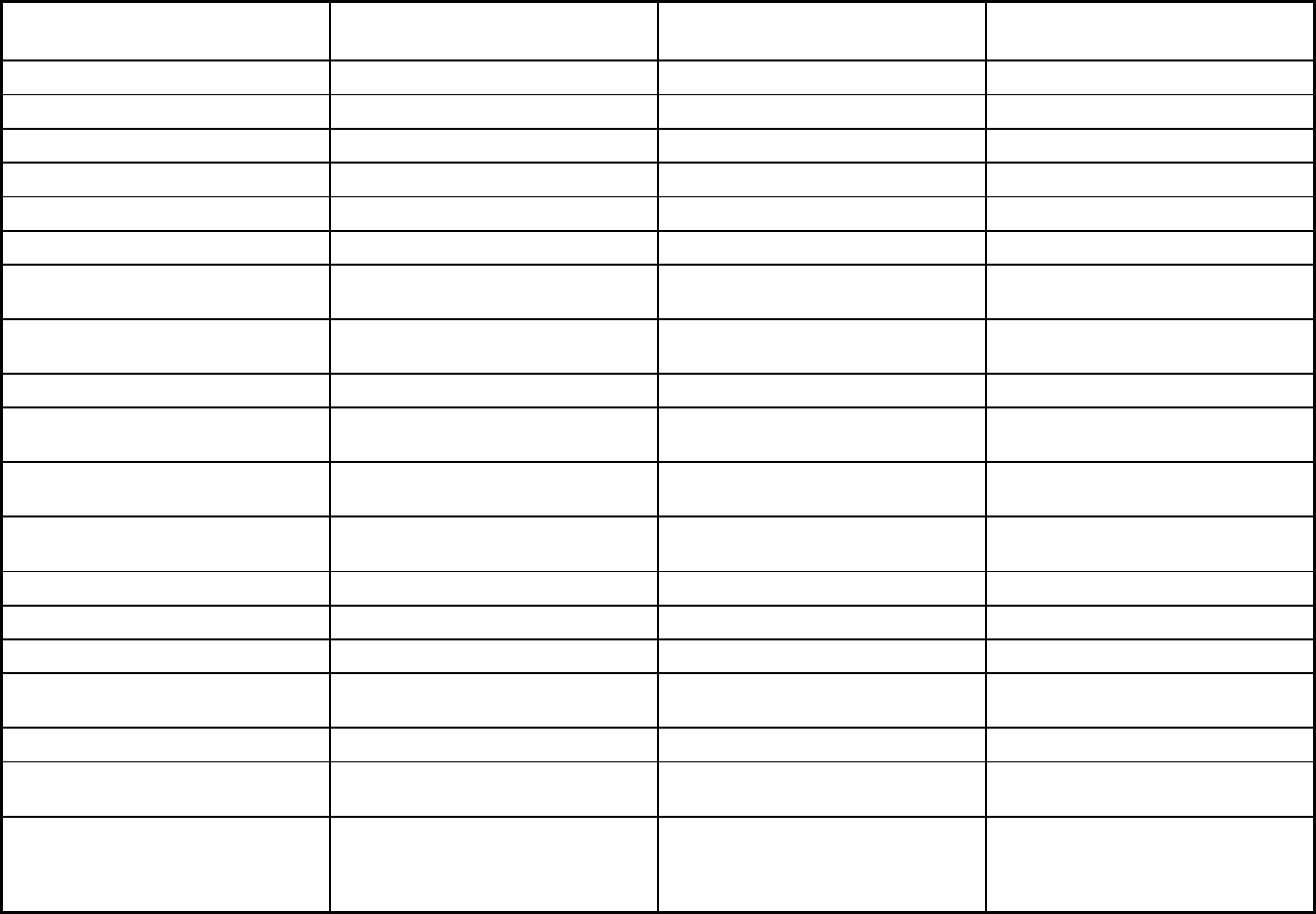
450
Features
PA Living Independence for the
Elderly Community HealthChoices HealthChoices - Physical Health
Benefits covered: Clinic services X X X
Benefits covered: Lab and x-ray X X X
Benefits covered: Prescription drugs X X X
Benefits covered: Prosthetic devices X X X
Benefits covered: EPSDT X
Benefits covered: Case management X X X
Benefits covered: SSA Section 1945-
authorized health home
Benefits covered: Health home care
(services in home)
X X X
Benefits covered: Family planning X X
Benefits covered: Dental services
(medical/surgical)
X X X
Benefits covered: Dental (preventative
or corrective)
X X X
Benefits covered: Personal care (state
plan option)
X X
Benefits covered: HCBS waiver services X X
Benefits covered: Private duty nursing X X
Benefits covered: ICF-IDD X
Benefits covered: Nursing facility
services
X X X
Benefits covered: Hospice care X X X
Benefits covered: Non-Emergency
Medical Transportation
X X X
Benefits covered: Institution for Mental
Disease inpatient treatment for people
ages 21-64 defined by 42 CFR
§438.6(e) as an 'in lieu of' benefit
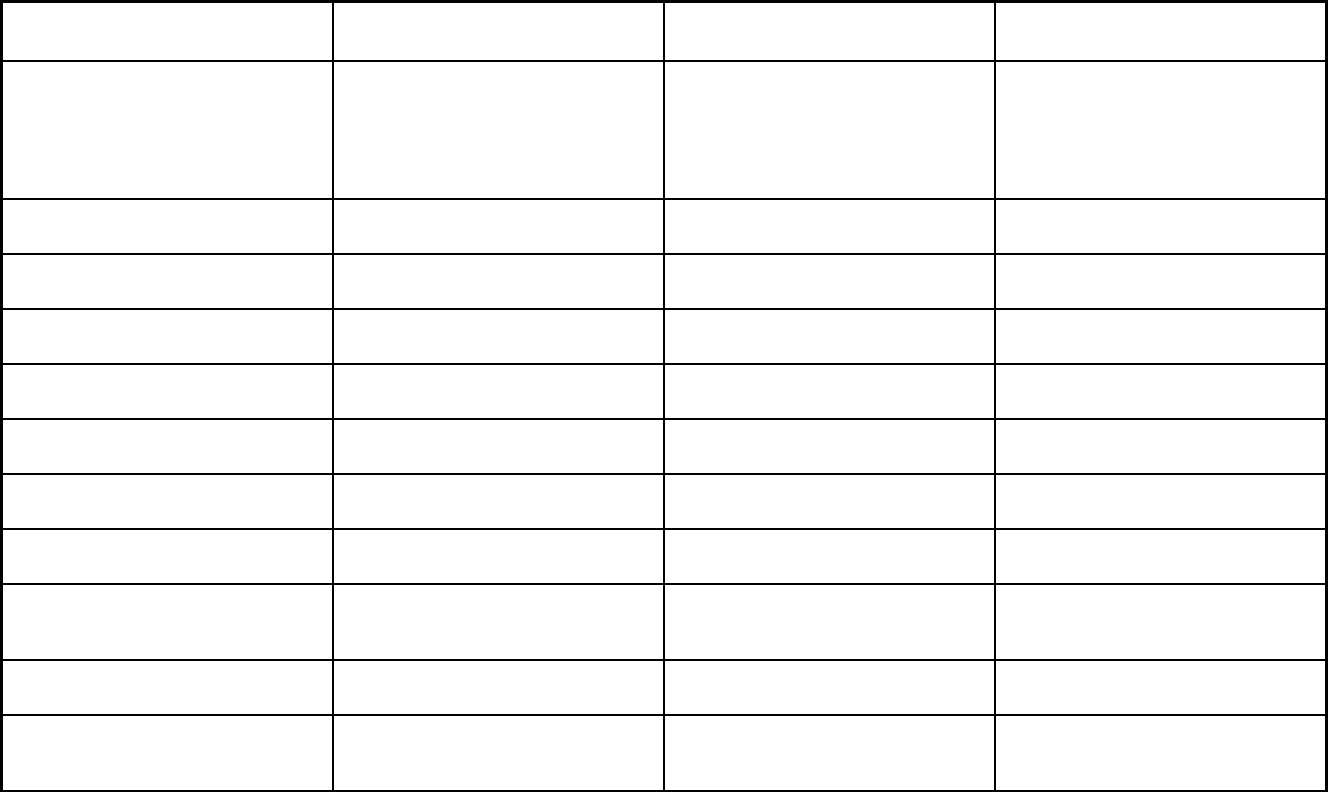
451
Features
PA Living Independence for the
Elderly Community HealthChoices HealthChoices - Physical Health
Benefits covered: Other (e.g., nurse
midwife services, freestanding birth
centers, podiatry, etc.)
PACE programs cover specialists of all
disiplines as needed. PACE does not
operate under a waiver.
Chiropractic services, mobile mental
health treatment, maternity services,
podiatrist services
Nurse midwife services, freestanding
birth centers, podiatry, chiropractic
services, optometrists, renal dialysis
centers, ambulatory surgical centers,
medical supplies & equipment, home
health (visiting nurses)
Quality assurance and improvement:
HEDIS data required?
No Yes Yes
Quality assurance and improvement:
CAHPS data required?
No Yes Yes
Quality assurance and improvement:
Accreditation required?
No Yes Yes
Quality assurance and improvement:
Accrediting organization
PACE Quality Assurance and
Performance Improvement (QAPI)
NCQA NCQA, Nationally Recognized
Organization
Quality assurance and improvement:
EQRO contractor name (if applicable)
IPRO Island Peer Review Organization
Performance incentives: Payment
bonuses/differentials to reward plans
X
Performance incentives: Preferential
auto-enrollment to reward plans
Performance incentives: Public reports
comparing plan performance on key
metrics
X
Performance incentives: Withholds tied
to performance metrics
X
Performance incentives: MCOs/PHPs
required or encouraged to pay providers
for value/quality outcomes
X
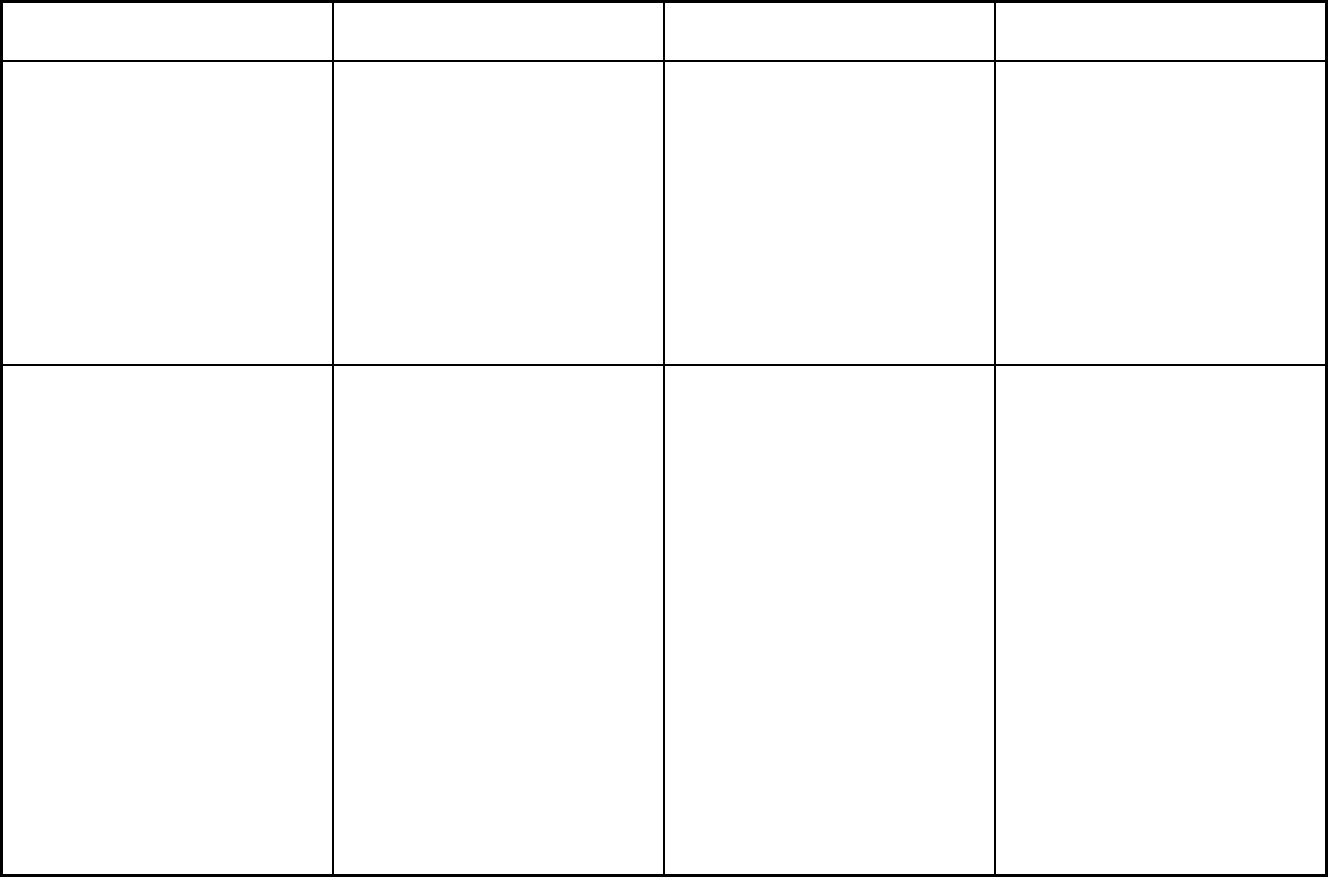
452
Features
PA Living Independence for the
Elderly Community HealthChoices HealthChoices - Physical Health
Participating plans: Plans in Program Senior LIFE Greensburg H-2937; Senior
LIFE Johnstown H-3925; Senior LIFE
Altonna H-5902; Senior LIFE York H-
0819; Senior LIFE Lehigh H-5978;
Senior LIFE Washington H-2992;
SpiriTrust LIFE H-2537; LIFE NWPA H-
4999; LIFE Geisinger H-2064; Mercy
LIFE H-3919; Mercy LIFE West
Philadelphia H-3908; LIFE St. Mary H-
6551; Innovage LIFE H-9830; Albright
LIFE H-9068; Community LIFE H-3917;
LIFE Pittsburgh H-3918; VieCare Butler
H-3060; VieCare Beaver H-7660;
VieCare Armstrong H-6118
UPMC Community HealthChoices;
Pennsylvania Health & Wellness;
Amerihealth Caritas / Keystone First
Aetna Better Health; Gateway Health;
Health Partners Plan; United Healthcare
Community Plan, Inc.; UPMC for You;
Geisinger Health Plan; AmeriHealth
Caritas/AmeriHealth Caritas Northeast;
Keystone First
Notes: Program notes 1. Under "Benefits Covered", Private
Duty Nursing is only covered for
children under 21 years old. In addition,
in counties that have not implemented
the Community HealthChoices program,
the first 30 days of nursing facility
services are covered by the
HealthChoices plan. Beneficiaries with
stays beyond the initial 30 days are
disenrolled from HealthChoices and
their stay is covered by FFS. For
counties that have implemented
Community HealthChoices, nursing
facility services for days 31+ are
covered by the Physical HealthChoices
plan up to the day the Member is
enrolled into Community HealthChoices.
2. Under "Enrollment", only those under
21 years of age, Full Dual and Partial
Dual are enrolled mandatorily in
HealthChoices. PA HealthChoices
Physical and Behavioral Health operate
under a single statewide 1915(b) waiver
but are administered separately.
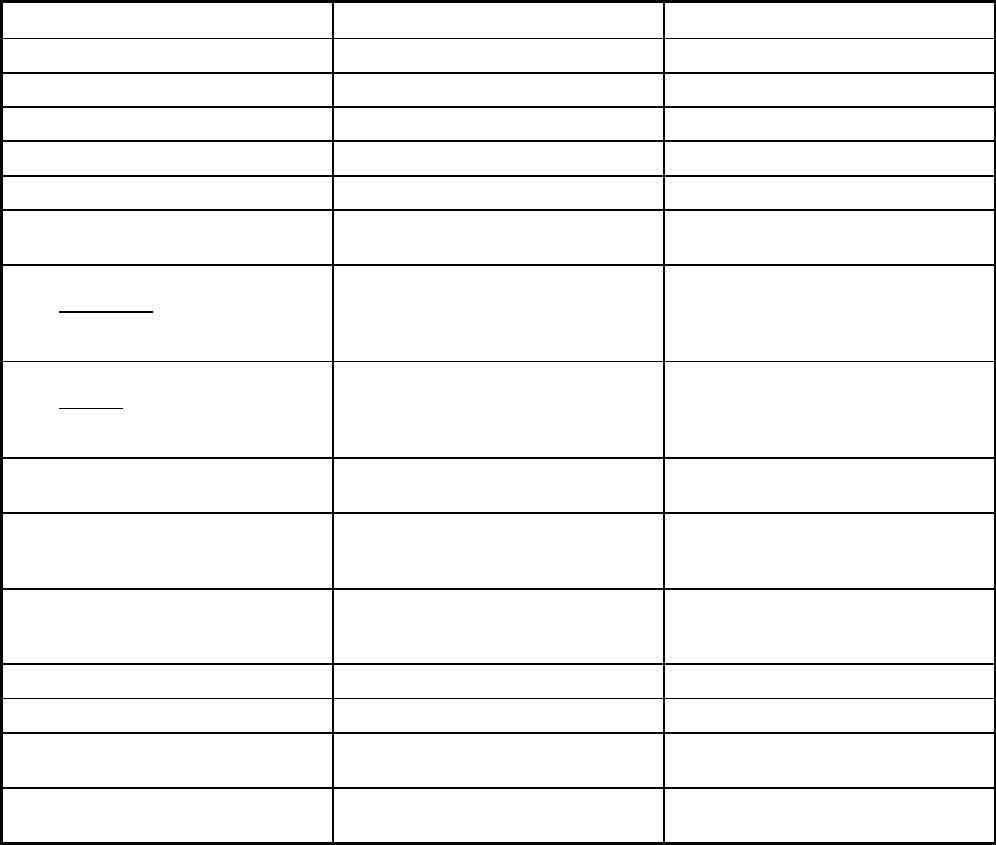
453
Puerto Rico Managed Care Program Features, as of 2018
Features Government Health Plan Medicare Platino
Program type Comprehensive MCO Comprehensive MCO
Statewide or region-specific? Statewide Statewide
Federal operating authority 1932(a),1937 Alt Benefit Plan 1915(b)
Program start date 02/01/1994 01/01/2006
Waiver expiration date (if applicable)
If the program ended in 2018, indicate
the end date
Populations enrolled: Low-income
adults not covered under ACA Section
VIII (excludes pregnant women and
people with disabilities)
Mandatory
Populations enrolled: Low-income
adults covered under ACA Section VIII
(excludes pregnant women and people
with disabilities)
Mandatory
Populations enrolled: Aged, Blind or
Disabled Children or Adults
Mandatory
Populations enrolled: Non-Disabled
Children (excludes children in foster
care or receiving adoption assistance)
Mandatory
Populations enrolled: Individuals
receiving Limited Benefits (excludes
partial duals)
Populations enrolled: Full Duals Mandatory Voluntary
Populations enrolled: Partial Duals
Populations enrolled: Children with
Special Health Care Needs
Mandatory
Populations enrolled: Native
American/Alaskan Natives
Mandatory Voluntary

454
Features Government Health Plan Medicare Platino
Populations enrolled: Foster Care and
Adoption Assistance Children
Mandatory Exempt
Populations enrolled: Enrollment choice
period
Pre-assigned Other
Populations enrolled: Enrollment broker
name (if applicable)
Populations enrolled: Notes on
enrollment choice period
No specific time
Benefits covered: Inpatient hospital
physical health
X X
Benefits covered: Inpatient hospital
behavioral health (MH and/or SUD)
X X
Benefits covered: Outpatient hospital
physical health
X X
Benefits covered: Outpatient hospital
behavioral health (MH and/or SUD)
X X
Benefits covered: Partial hospitalization X X
Benefits covered: Physician X X
Benefits covered: Nurse practitioner
Benefits covered: Rural health clinics
and FQHCs
X X
Benefits covered: Clinic services X X
Benefits covered: Lab and x-ray X X
Benefits covered: Prescription drugs X X
Benefits covered: Prosthetic devices X X
Benefits covered: EPSDT X
Benefits covered: Case management X X
Benefits covered: SSA Section 1945-
authorized health home
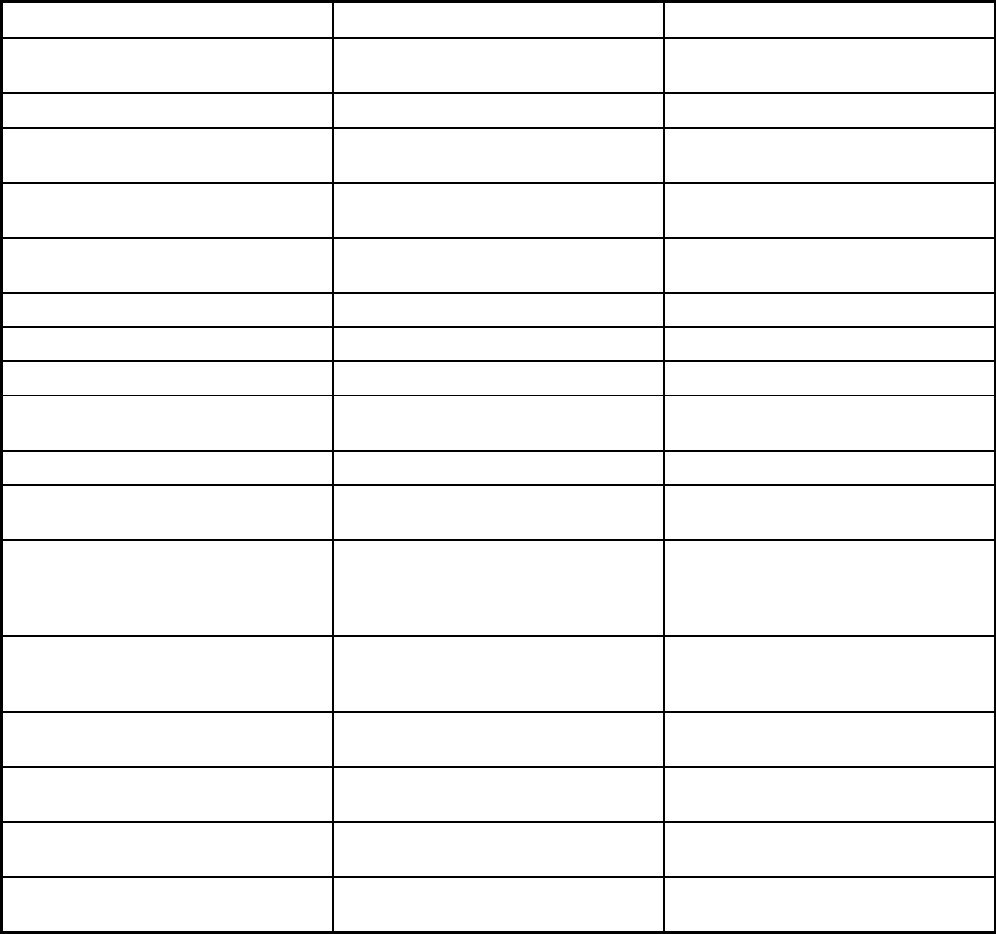
455
Features Government Health Plan Medicare Platino
Benefits covered: Health home care
(services in home)
Benefits covered: Family planning X X
Benefits covered: Dental services
(medical/surgical)
X X
Benefits covered: Dental (preventative
or corrective)
X X
Benefits covered: Personal care (state
plan option)
Benefits covered: HCBS waiver services
Benefits covered: Private duty nursing
Benefits covered: ICF-IDD
Benefits covered: Nursing facility
services
Benefits covered: Hospice care
Benefits covered: Non-Emergency
Medical Transportation
Benefits covered: Institution for Mental
Disease inpatient treatment for people
ages 21-64 defined by 42 CFR
§438.6(e) as an 'in lieu of' benefit
Benefits covered: Other (e.g., nurse
midwife services, freestanding birth
centers, podiatry, etc.)
Quality assurance and improvement:
HEDIS data required?
Yes Yes
Quality assurance and improvement:
CAHPS data required?
Yes Yes
Quality assurance and improvement:
Accreditation required?
No No
Quality assurance and improvement:
Accrediting organization
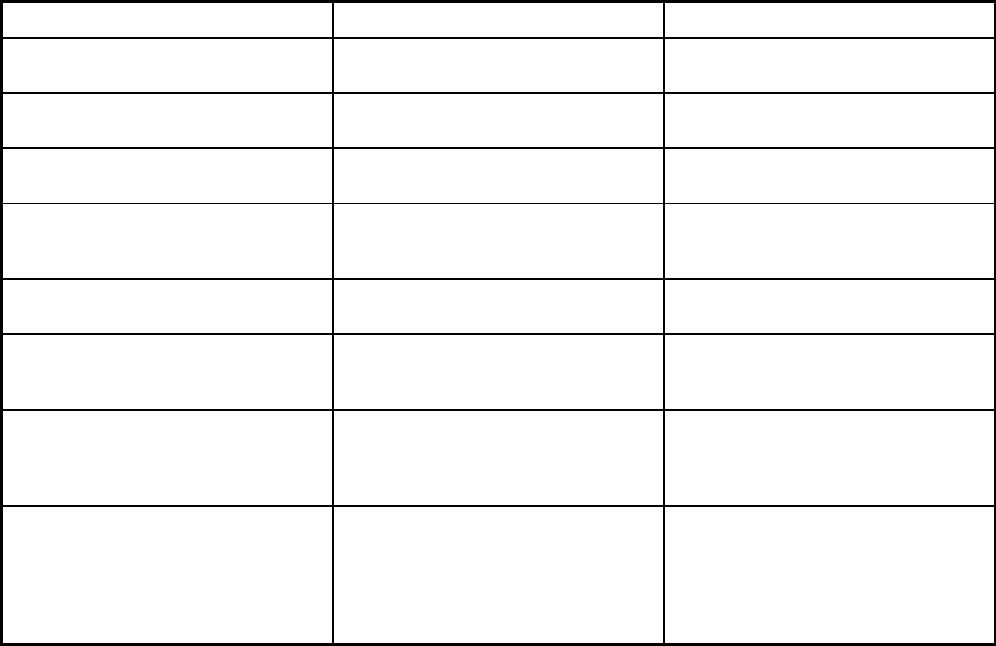
456
Features Government Health Plan Medicare Platino
Quality assurance and improvement:
EQRO contractor name (if applicable)
Island Peer Review Organization Island Peer Review Organization
Performance incentives: Payment
bonuses/differentials to reward plans
Performance incentives: Preferential
auto-enrollment to reward plans
Performance incentives: Public reports
comparing plan performance on key
metrics
Performance incentives: Withholds tied
to performance metrics
X
Performance incentives: MCOs/PHPs
required or encouraged to pay providers
for value/quality outcomes
X X
Participating plans: Plans in Program First Medical Plan Inc.; Triple S Salud,
Inc.; Molina Health Care PR, Inc.; MMM
MultiHealth, Inc.
Triple S Advantage; Humana Health
Plan of PR Inc.; MCS Advantage Inc.;
MMM Health Care Inc.; Constellation
Health LLC
Notes: Program notes Medicare Platino is a Medicare
Advantage product that provides
Medicaid wrap around benefits to
enrollees. The benefits above include
those covered by Medicaid and
Medicare.
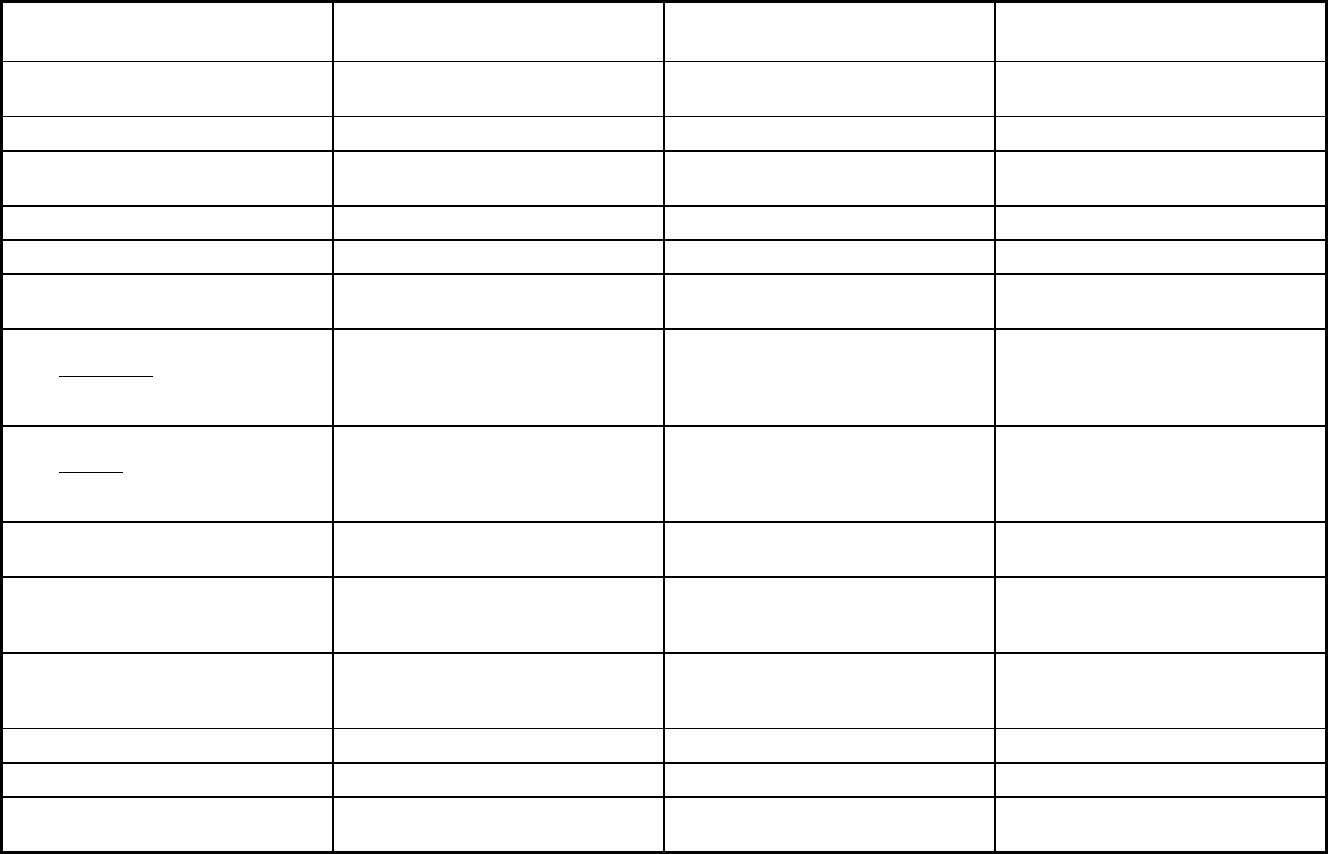
457
Rhode Island Managed Care Program Features, as of 2018 (1 of 2)
Features PACE
RIte Care, RHP and Medicaid
Expansion Transportation Broker
Program type Program of All-inclusive Care for the
Elderly (PACE)
Comprehensive MCO Non-Emergency Medical Transportation
Statewide or region-specific? Statewide Statewide Statewide
Federal operating authority PACE 1115(a) (Medicaid demonstration
waivers)
1902(a)(70) NEMT
Program start date 11/01/2005 08/01/1994 05/01/2014
Waiver expiration date (if applicable) 12/31/2023
If the program ended in 2018, indicate
the end date
Populations enrolled: Low-income
adults not covered under ACA Section
VIII (excludes pregnant women and
people with disabilities)
Mandatory Mandatory
Populations enrolled: Low-income
adults covered under ACA Section VIII
(excludes pregnant women and people
with disabilities)
Mandatory Mandatory
Populations enrolled: Aged, Blind or
Disabled Children or Adults
Voluntary Mandatory Mandatory
Populations enrolled: Non-Disabled
Children (excludes children in foster
care or receiving adoption assistance)
Mandatory Mandatory
Populations enrolled: Individuals
receiving Limited Benefits (excludes
partial duals)
Mandatory Mandatory
Populations enrolled: Full Duals Voluntary Mandatory
Populations enrolled: Partial Duals Mandatory
Populations enrolled: Children with
Special Health Care Needs
Mandatory Mandatory
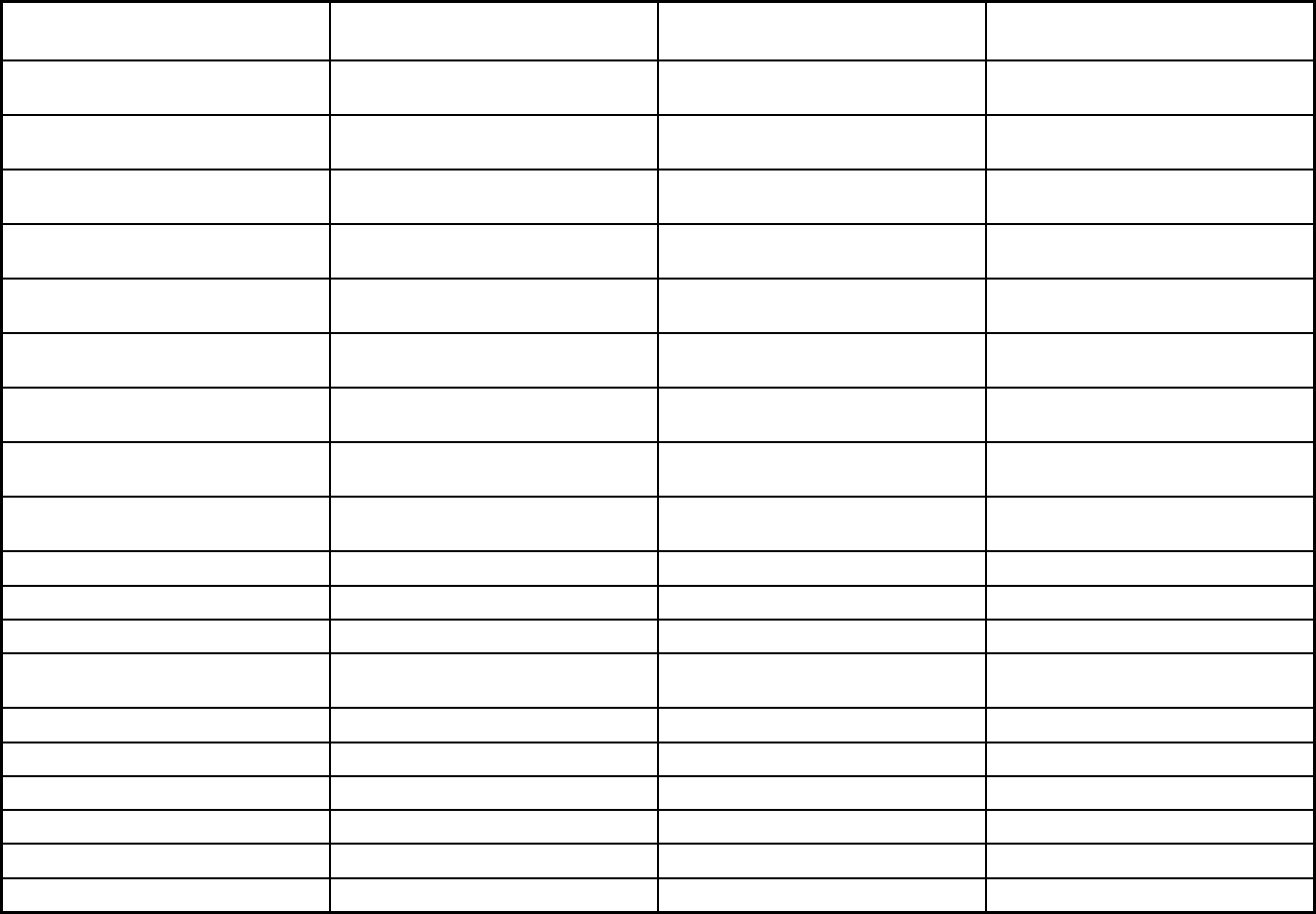
458
Features PACE
RIte Care, RHP and Medicaid
Expansion Transportation Broker
Populations enrolled: Native
American/Alaskan Natives
Voluntary Mandatory Exempt
Populations enrolled: Foster Care and
Adoption Assistance Children
Mandatory
Populations enrolled: Enrollment choice
period
N/A Other Pre-assigned
Populations enrolled: Enrollment broker
name (if applicable)
Populations enrolled: Notes on
enrollment choice period
90 Days 90 Days
Benefits covered: Inpatient hospital
physical health
X X
Benefits covered: Inpatient hospital
behavioral health (MH and/or SUD)
X X
Benefits covered: Outpatient hospital
physical health
X X
Benefits covered: Outpatient hospital
behavioral health (MH and/or SUD)
X
Benefits covered: Partial hospitalization X X
Benefits covered: Physician X X
Benefits covered: Nurse practitioner X X
Benefits covered: Rural health clinics
and FQHCs
X
Benefits covered: Clinic services X X
Benefits covered: Lab and x-ray X X
Benefits covered: Prescription drugs X X
Benefits covered: Prosthetic devices X X
Benefits covered: EPSDT X X
Benefits covered: Case management X X
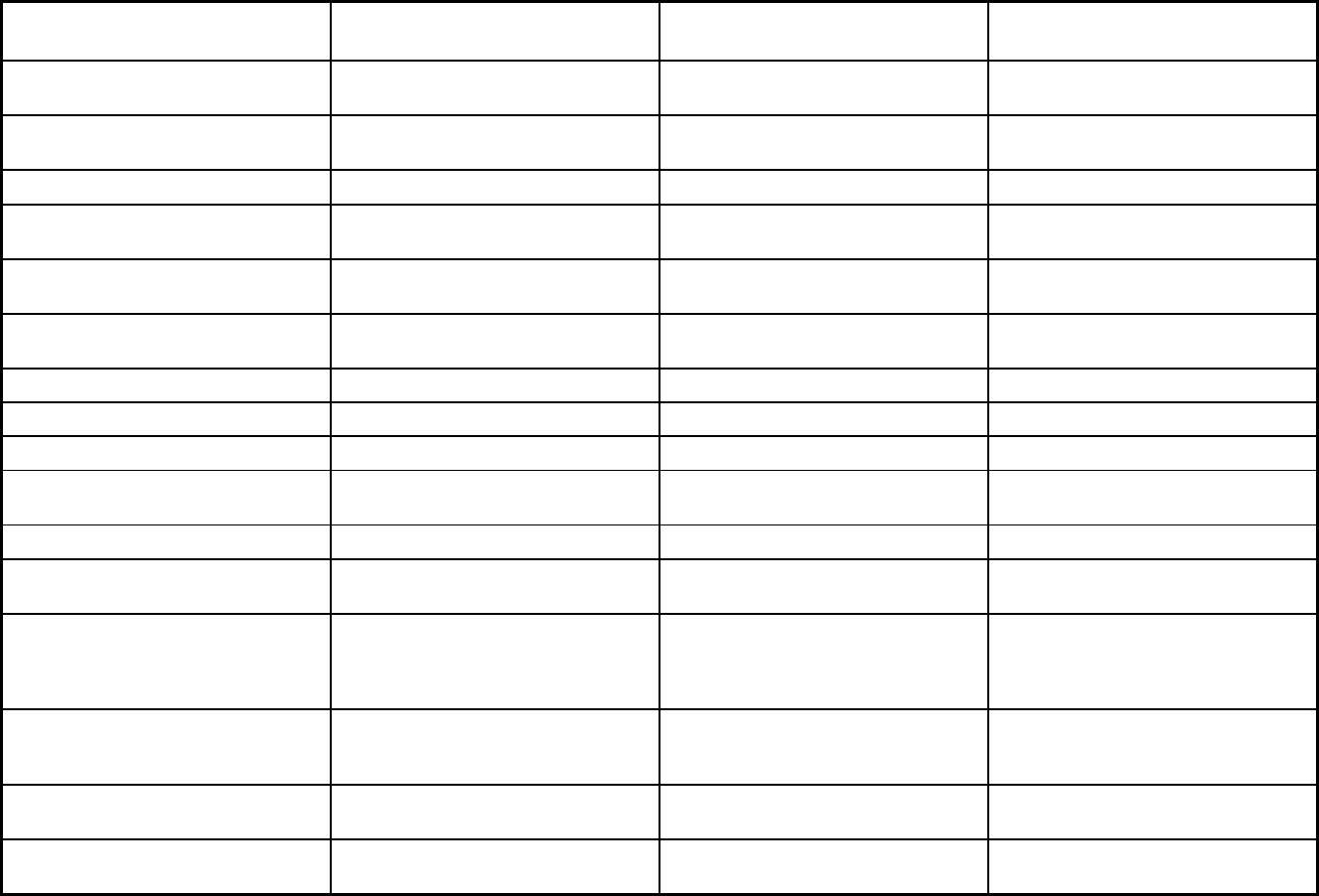
459
Features PACE
RIte Care, RHP and Medicaid
Expansion Transportation Broker
Benefits covered: SSA Section 1945-
authorized health home
Benefits covered: Health home care
(services in home)
X X
Benefits covered: Family planning X
Benefits covered: Dental services
(medical/surgical)
X X
Benefits covered: Dental (preventative
or corrective)
X
Benefits covered: Personal care (state
plan option)
X X
Benefits covered: HCBS waiver services X
Benefits covered: Private duty nursing X X
Benefits covered: ICF-IDD
Benefits covered: Nursing facility
services
X X
Benefits covered: Hospice care X
Benefits covered: Non-Emergency
Medical Transportation
X X
Benefits covered: Institution for Mental
Disease inpatient treatment for people
ages 21-64 defined by 42 CFR
§438.6(e) as an 'in lieu of' benefit
X
Benefits covered: Other (e.g., nurse
midwife services, freestanding birth
centers, podiatry, etc.)
Quality assurance and improvement:
HEDIS data required?
No No No
Quality assurance and improvement:
CAHPS data required?
No Yes No

460
Features PACE
RIte Care, RHP and Medicaid
Expansion Transportation Broker
Quality assurance and improvement:
Accreditation required?
No Yes No
Quality assurance and improvement:
Accrediting organization
NCQA
Quality assurance and improvement:
EQRO contractor name (if applicable)
iPro
Performance incentives: Payment
bonuses/differentials to reward plans
X
Performance incentives: Preferential
auto-enrollment to reward plans
X
Performance incentives: Public reports
comparing plan performance on key
metrics
X
Performance incentives: Withholds tied
to performance metrics
X
Performance incentives: MCOs/PHPs
required or encouraged to pay providers
for value/quality outcomes
X
Participating plans: Plans in Program PACE Organization of RI Neighborhood Health Plan of RI;
UnitedHealthCare of Rhode Island
Community Plan
Logisticare, Inc.
Notes: Program notes
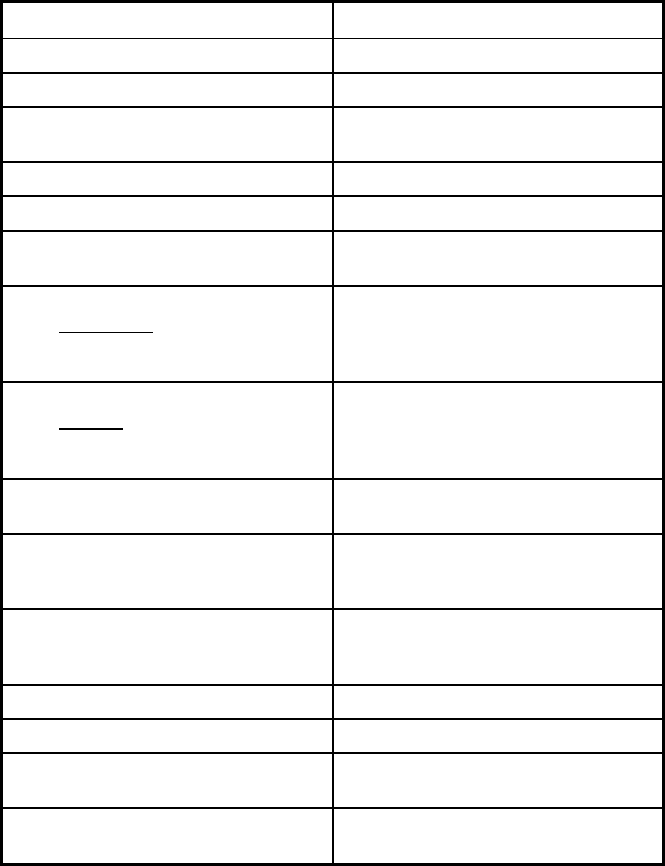
461
Rhode Island Managed Care Program Features, as of 2018 (1 of 2)
Features Rite Smiles Dental Program
Program type Dental only (PAHP)
Statewide or region-specific? Statewide
Federal operating authority 1115(a) (Medicaid demonstration
waivers)
Program start date 05/01/2006
Waiver expiration date (if applicable) 12/31/2023
If the program ended in 2018, indicate
the end date
Populations enrolled: Low-income
adults not covered under ACA Section
VIII (excludes pregnant women and
people with disabilities)
Mandatory
Populations enrolled: Low-income
adults covered under ACA Section VIII
(excludes pregnant women and people
with disabilities)
Mandatory
Populations enrolled: Aged, Blind or
Disabled Children or Adults
Mandatory
Populations enrolled: Non-Disabled
Children (excludes children in foster
care or receiving adoption assistance)
Populations enrolled: Individuals
receiving Limited Benefits (excludes
partial duals)
Populations enrolled: Full Duals
Populations enrolled: Partial Duals
Populations enrolled: Children with
Special Health Care Needs
Mandatory
Populations enrolled: Native
American/Alaskan Natives
Mandatory
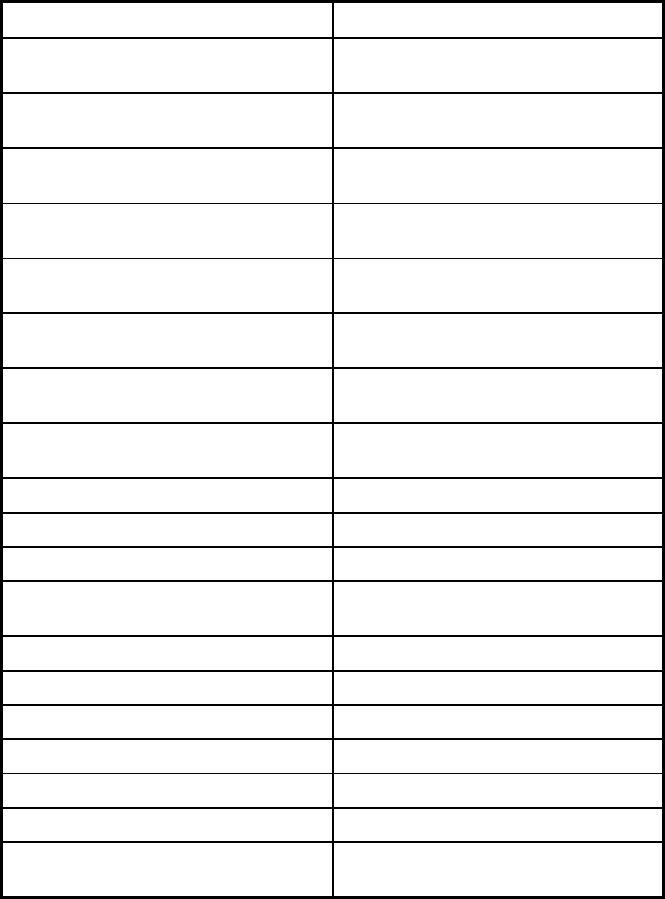
462
Features Rite Smiles Dental Program
Populations enrolled: Foster Care and
Adoption Assistance Children
Mandatory
Populations enrolled: Enrollment choice
period
Pre-assigned
Populations enrolled: Enrollment broker
name (if applicable)
Populations enrolled: Notes on
enrollment choice period
Benefits covered: Inpatient hospital
physical health
Benefits covered: Inpatient hospital
behavioral health (MH and/or SUD)
Benefits covered: Outpatient hospital
physical health
Benefits covered: Outpatient hospital
behavioral health (MH and/or SUD)
Benefits covered: Partial hospitalization
Benefits covered: Physician
Benefits covered: Nurse practitioner
Benefits covered: Rural health clinics
and FQHCs
Benefits covered: Clinic services
Benefits covered: Lab and x-ray
Benefits covered: Prescription drugs
Benefits covered: Prosthetic devices
Benefits covered: EPSDT
Benefits covered: Case management
Benefits covered: SSA Section 1945-
authorized health home
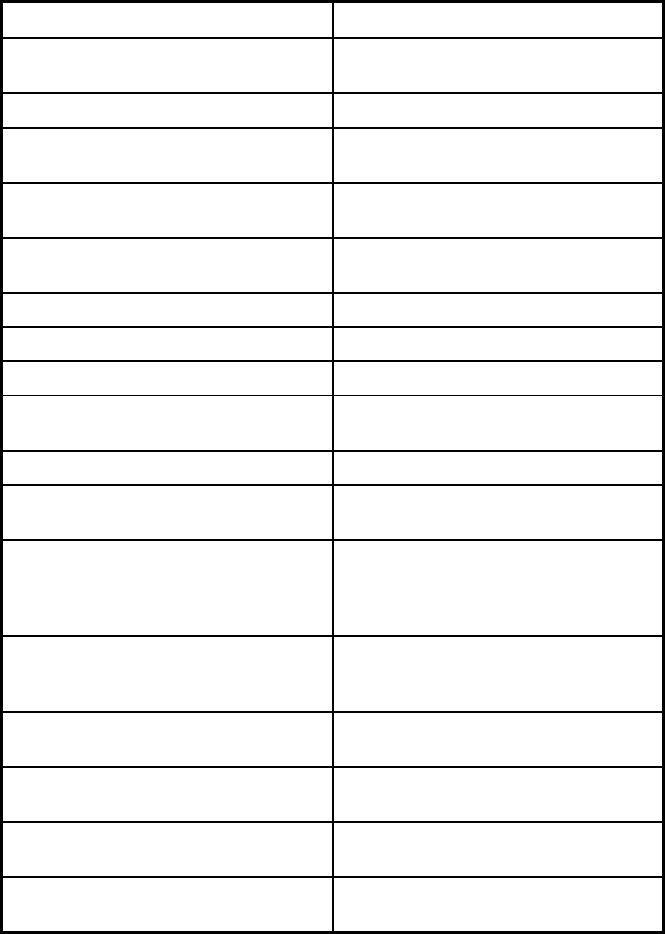
463
Features Rite Smiles Dental Program
Benefits covered: Health home care
(services in home)
Benefits covered: Family planning
Benefits covered: Dental services
(medical/surgical)
Benefits covered: Dental (preventative
or corrective)
X
Benefits covered: Personal care (state
plan option)
Benefits covered: HCBS waiver services
Benefits covered: Private duty nursing
Benefits covered: ICF-IDD
Benefits covered: Nursing facility
services
Benefits covered: Hospice care
Benefits covered: Non-Emergency
Medical Transportation
Benefits covered: Institution for Mental
Disease inpatient treatment for people
ages 21-64 defined by 42 CFR
§438.6(e) as an 'in lieu of' benefit
Benefits covered: Other (e.g., nurse
midwife services, freestanding birth
centers, podiatry, etc.)
Quality assurance and improvement:
HEDIS data required?
Yes
Quality assurance and improvement:
CAHPS data required?
Yes
Quality assurance and improvement:
Accreditation required?
Yes
Quality assurance and improvement:
Accrediting organization
NCQA
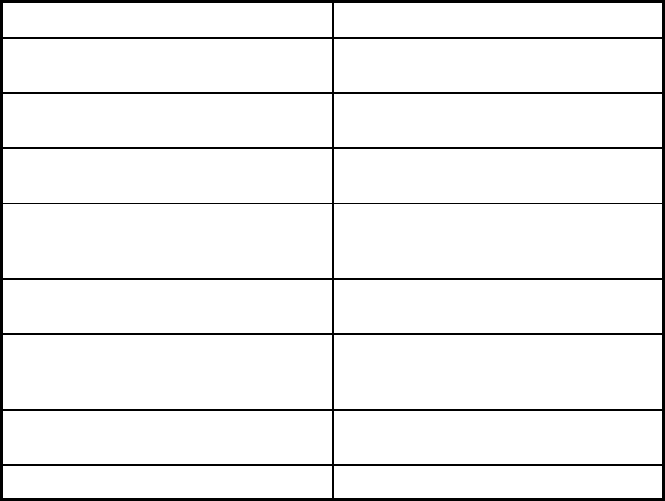
464
Features Rite Smiles Dental Program
Quality assurance and improvement:
EQRO contractor name (if applicable)
Performance incentives: Payment
bonuses/differentials to reward plans
Performance incentives: Preferential
auto-enrollment to reward plans
Performance incentives: Public reports
comparing plan performance on key
metrics
X
Performance incentives: Withholds tied
to performance metrics
Performance incentives: MCOs/PHPs
required or encouraged to pay providers
for value/quality outcomes
X
Participating plans: Plans in Program UnitedHealthCare Dental of Rhode
Island
Notes: Program notes
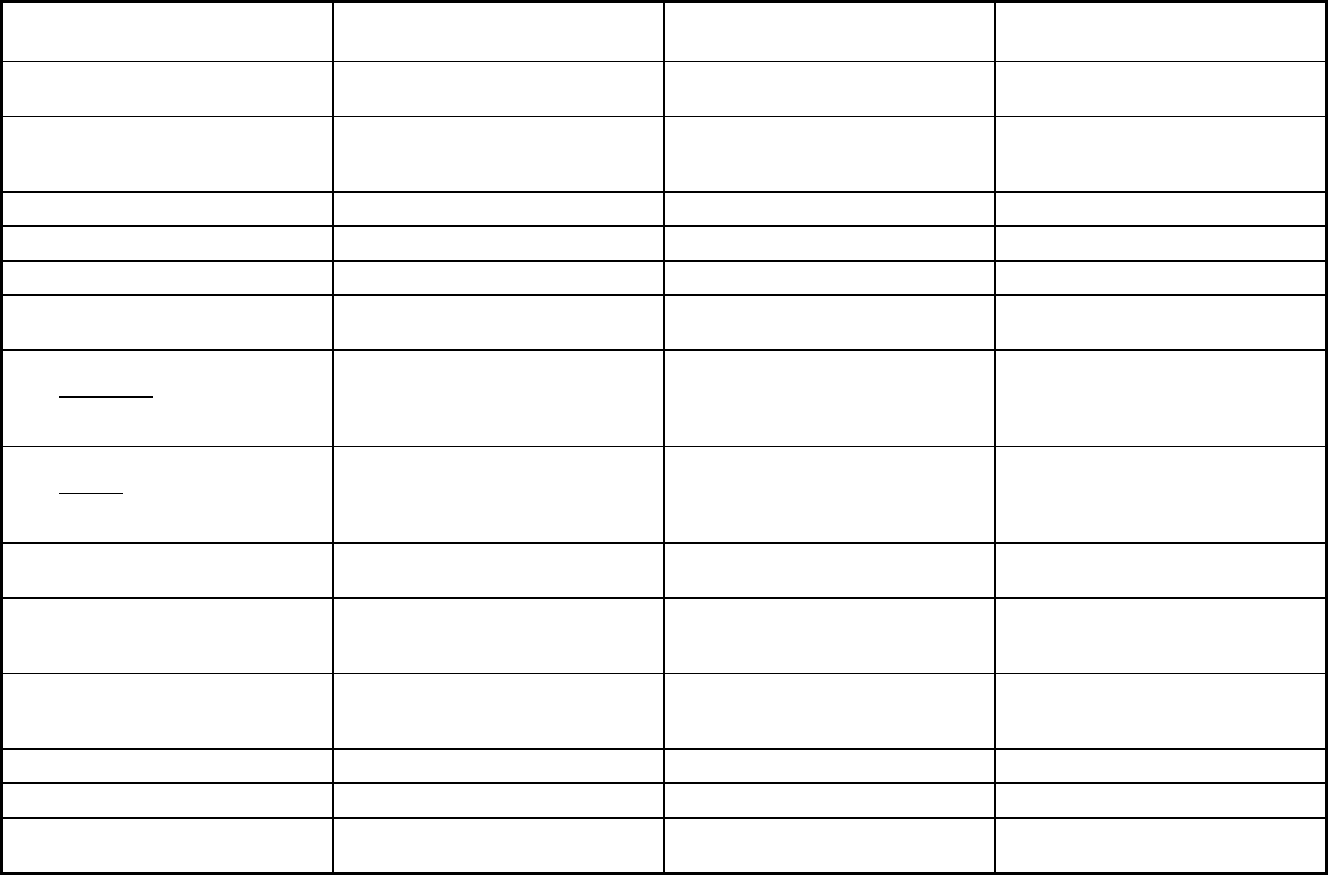
465
South Carolina Managed Care Program Features, as of 2018 (1 of 2)
Features
South Carolina Managed Care
Organizations
South Carolina Medical Homes
Network
South Carolina Program for All
Inclusive Care for the Elderly
Program type Comprehensive MCO Primary Care Case Management
(PCCM)
Program of All-inclusive Care for the
Elderly (PACE)
Statewide or region-specific? Statewide Statewide Lexington County, Richland County,
Orangeburg County, Greenville County,
Anderson County, Pickens County
Federal operating authority 1932(a) 1932(a) PACE
Program start date 09/01/1996 08/01/2007 01/01/1990
Waiver expiration date (if applicable)
If the program ended in 2018, indicate
the end date
Populations enrolled: Low-income
adults not covered under ACA Section
VIII (excludes pregnant women and
people with disabilities)
Mandatory Voluntary
Populations enrolled: Low-income
adults covered under ACA Section VIII
(excludes pregnant women and people
with disabilities)
Populations enrolled: Aged, Blind or
Disabled Children or Adults
Mandatory Voluntary Voluntary
Populations enrolled: Non-Disabled
Children (excludes children in foster
care or receiving adoption assistance)
Mandatory Voluntary
Populations enrolled: Individuals
receiving Limited Benefits (excludes
partial duals)
Populations enrolled: Full Duals Voluntary
Populations enrolled: Partial Duals
Populations enrolled: Children with
Special Health Care Needs
Voluntary Voluntary
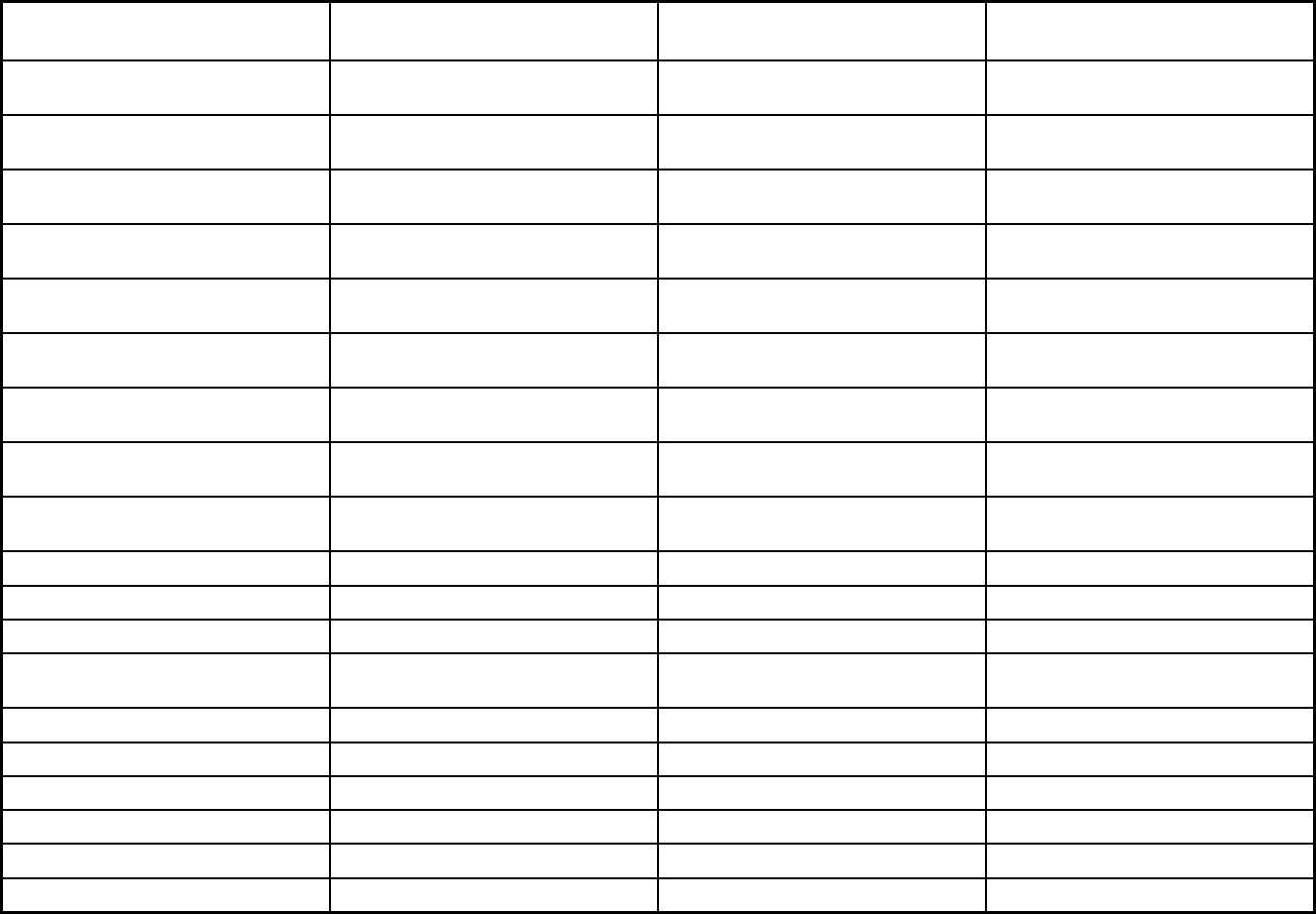
466
Features
South Carolina Managed Care
Organizations
South Carolina Medical Homes
Network
South Carolina Program for All
Inclusive Care for the Elderly
Populations enrolled: Native
American/Alaskan Natives
Voluntary Voluntary Voluntary
Populations enrolled: Foster Care and
Adoption Assistance Children
Voluntary Voluntary Exempt
Populations enrolled: Enrollment choice
period
Other N/A N/A
Populations enrolled: Enrollment broker
name (if applicable)
Maximus Maximus
Populations enrolled: Notes on
enrollment choice period
90 days 90 days
Benefits covered: Inpatient hospital
physical health
X X
Benefits covered: Inpatient hospital
behavioral health (MH and/or SUD)
X X
Benefits covered: Outpatient hospital
physical health
X X
Benefits covered: Outpatient hospital
behavioral health (MH and/or SUD)
X X
Benefits covered: Partial hospitalization X X
Benefits covered: Physician X X
Benefits covered: Nurse practitioner X X
Benefits covered: Rural health clinics
and FQHCs
X X
Benefits covered: Clinic services X X
Benefits covered: Lab and x-ray X X
Benefits covered: Prescription drugs X X
Benefits covered: Prosthetic devices X X
Benefits covered: EPSDT X X
Benefits covered: Case management X X
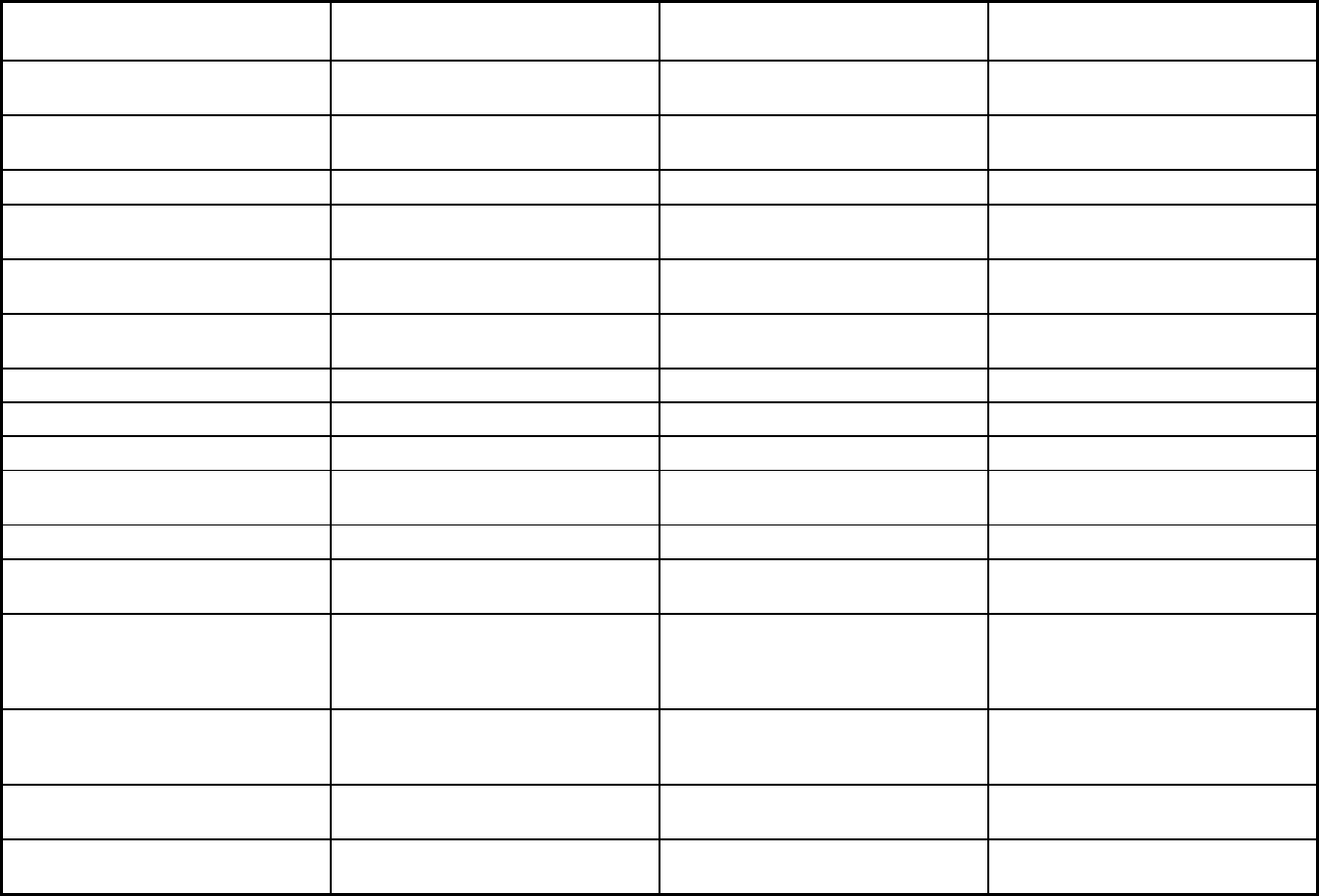
467
Features
South Carolina Managed Care
Organizations
South Carolina Medical Homes
Network
South Carolina Program for All
Inclusive Care for the Elderly
Benefits covered: SSA Section 1945-
authorized health home
Benefits covered: Health home care
(services in home)
X X
Benefits covered: Family planning X
Benefits covered: Dental services
(medical/surgical)
Benefits covered: Dental (preventative
or corrective)
X
Benefits covered: Personal care (state
plan option)
Benefits covered: HCBS waiver services X
Benefits covered: Private duty nursing
Benefits covered: ICF-IDD
Benefits covered: Nursing facility
services
X
Benefits covered: Hospice care
Benefits covered: Non-Emergency
Medical Transportation
Benefits covered: Institution for Mental
Disease inpatient treatment for people
ages 21-64 defined by 42 CFR
§438.6(e) as an 'in lieu of' benefit
X
Benefits covered: Other (e.g., nurse
midwife services, freestanding birth
centers, podiatry, etc.)
Nurse midwife, birth centers,
chiropractic services, therapy services
(speech, hearing, language, etc.), vision
Quality assurance and improvement:
HEDIS data required?
Yes No No
Quality assurance and improvement:
CAHPS data required?
Yes No No
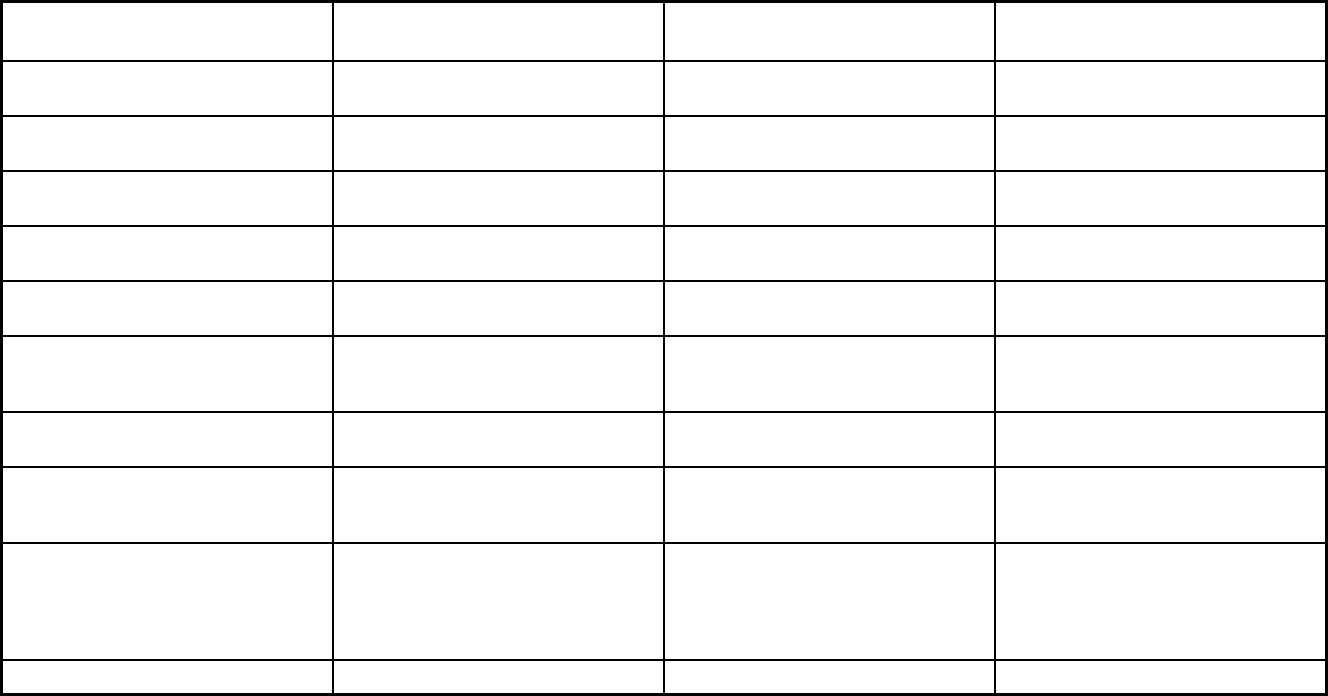
468
Features
South Carolina Managed Care
Organizations
South Carolina Medical Homes
Network
South Carolina Program for All
Inclusive Care for the Elderly
Quality assurance and improvement:
Accreditation required?
Yes No No
Quality assurance and improvement:
Accrediting organization
NCQA
Quality assurance and improvement:
EQRO contractor name (if applicable)
The Carolina Center for Medical
Excellence
Performance incentives: Payment
bonuses/differentials to reward plans
X
Performance incentives: Preferential
auto-enrollment to reward plans
X
Performance incentives: Public reports
comparing plan performance on key
metrics
X
Performance incentives: Withholds tied
to performance metrics
X
Performance incentives: MCOs/PHPs
required or encouraged to pay providers
for value/quality outcomes
X
Participating plans: Plans in Program Select Health of South Carolina;
Absolute Total Care; BlueChoice
Healthplan Medicaid; Molina Healthcare
of South Carolina; WellCare of South
Carolina
South Carolina Solutions Palmetto Senior Care; The Methodist
Oaks; Greenville Health System Senior
Care
Notes: Program notes
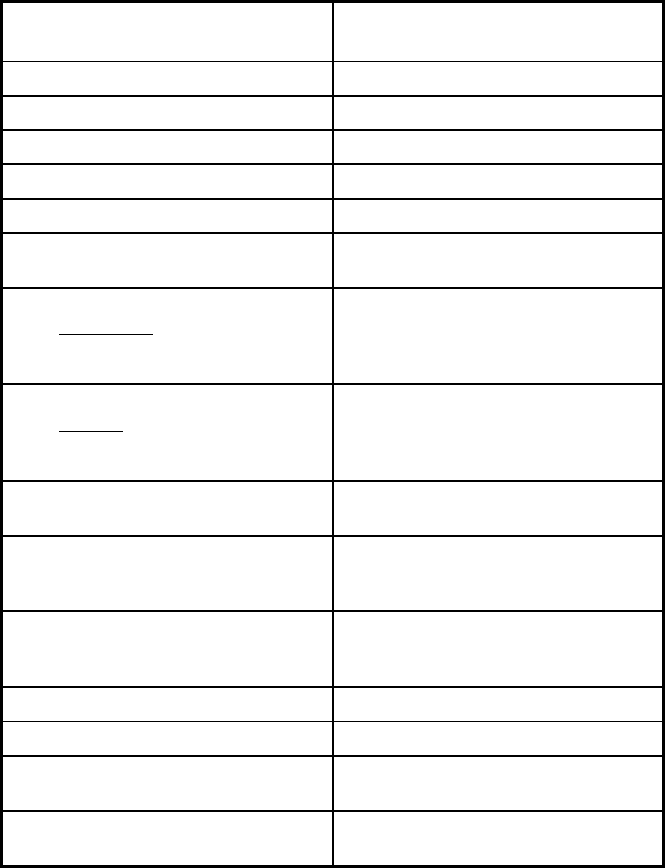
469
South Carolina Managed Care Program Features, as of 2018 (2 of 2)
Features
South Carolina Non-Emergency
Medical Transportation
Program type Non-Emergency Medical Transportation
Statewide or region-specific? Statewide
Federal operating authority
Program start date 05/01/2007
Waiver expiration date (if applicable)
If the program ended in 2018, indicate
the end date
Populations enrolled: Low-income
adults not covered under ACA Section
VIII (excludes pregnant women and
people with disabilities)
Mandatory
Populations enrolled: Low-income
adults covered under ACA Section VIII
(excludes pregnant women and people
with disabilities)
Mandatory
Populations enrolled: Aged, Blind or
Disabled Children or Adults
Mandatory
Populations enrolled: Non-Disabled
Children (excludes children in foster
care or receiving adoption assistance)
Mandatory
Populations enrolled: Individuals
receiving Limited Benefits (excludes
partial duals)
Mandatory
Populations enrolled: Full Duals Mandatory
Populations enrolled: Partial Duals Mandatory
Populations enrolled: Children with
Special Health Care Needs
Mandatory
Populations enrolled: Native
American/Alaskan Natives
Mandatory
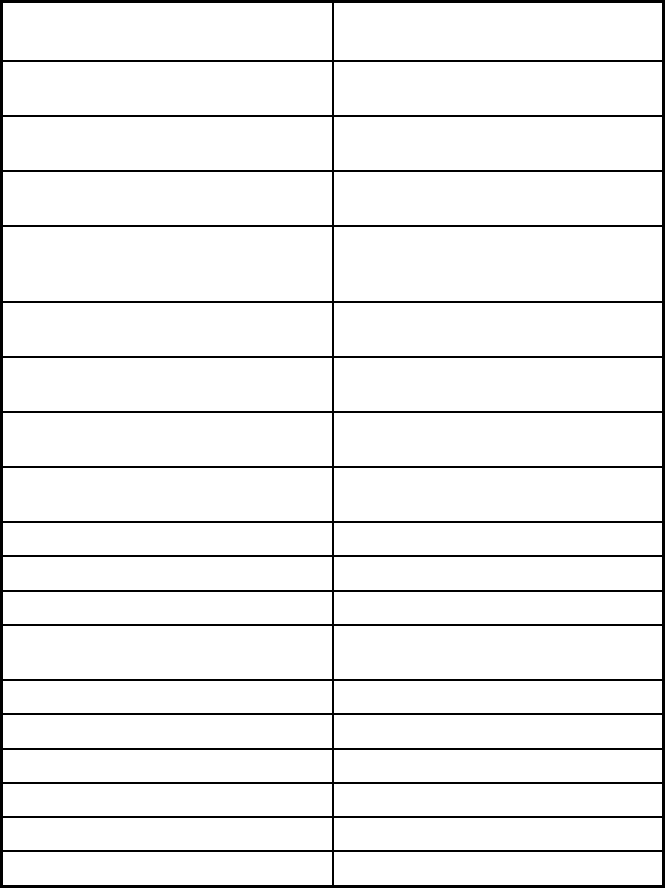
470
Features
South Carolina Non-Emergency
Medical Transportation
Populations enrolled: Foster Care and
Adoption Assistance Children
Mandatory
Populations enrolled: Enrollment choice
period
Other
Populations enrolled: Enrollment broker
name (if applicable)
Populations enrolled: Notes on
enrollment choice period
Recipient chooses to use transportation
services based on identifying the need
to access service providers.
Benefits covered: Inpatient hospital
physical health
Benefits covered: Inpatient hospital
behavioral health (MH and/or SUD)
Benefits covered: Outpatient hospital
physical health
Benefits covered: Outpatient hospital
behavioral health (MH and/or SUD)
Benefits covered: Partial hospitalization
Benefits covered: Physician
Benefits covered: Nurse practitioner
Benefits covered: Rural health clinics
and FQHCs
Benefits covered: Clinic services
Benefits covered: Lab and x-ray
Benefits covered: Prescription drugs
Benefits covered: Prosthetic devices
Benefits covered: EPSDT
Benefits covered: Case management
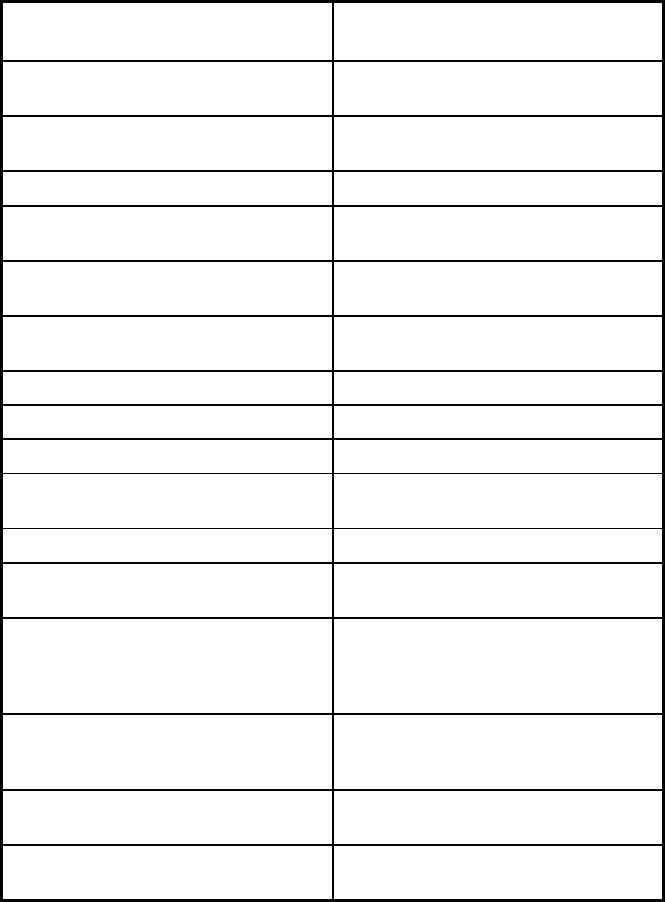
471
Features
South Carolina Non-Emergency
Medical Transportation
Benefits covered: SSA Section 1945-
authorized health home
Benefits covered: Health home care
(services in home)
Benefits covered: Family planning
Benefits covered: Dental services
(medical/surgical)
Benefits covered: Dental (preventative
or corrective)
Benefits covered: Personal care (state
plan option)
Benefits covered: HCBS waiver services
Benefits covered: Private duty nursing
Benefits covered: ICF-IDD
Benefits covered: Nursing facility
services
Benefits covered: Hospice care
Benefits covered: Non-Emergency
Medical Transportation
X
Benefits covered: Institution for Mental
Disease inpatient treatment for people
ages 21-64 defined by 42 CFR
§438.6(e) as an 'in lieu of' benefit
Benefits covered: Other (e.g., nurse
midwife services, freestanding birth
centers, podiatry, etc.)
Quality assurance and improvement:
HEDIS data required?
No
Quality assurance and improvement:
CAHPS data required?
No
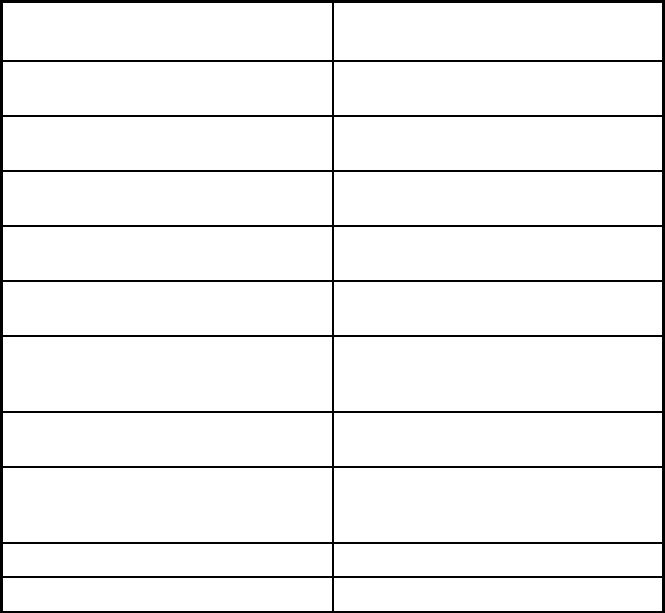
472
Features
South Carolina Non-Emergency
Medical Transportation
Quality assurance and improvement:
Accreditation required?
No
Quality assurance and improvement:
Accrediting organization
Quality assurance and improvement:
EQRO contractor name (if applicable)
Performance incentives: Payment
bonuses/differentials to reward plans
X
Performance incentives: Preferential
auto-enrollment to reward plans
Performance incentives: Public reports
comparing plan performance on key
metrics
X
Performance incentives: Withholds tied
to performance metrics
Performance incentives: MCOs/PHPs
required or encouraged to pay providers
for value/quality outcomes
Participating plans: Plans in Program Logisticare
Notes: Program notes
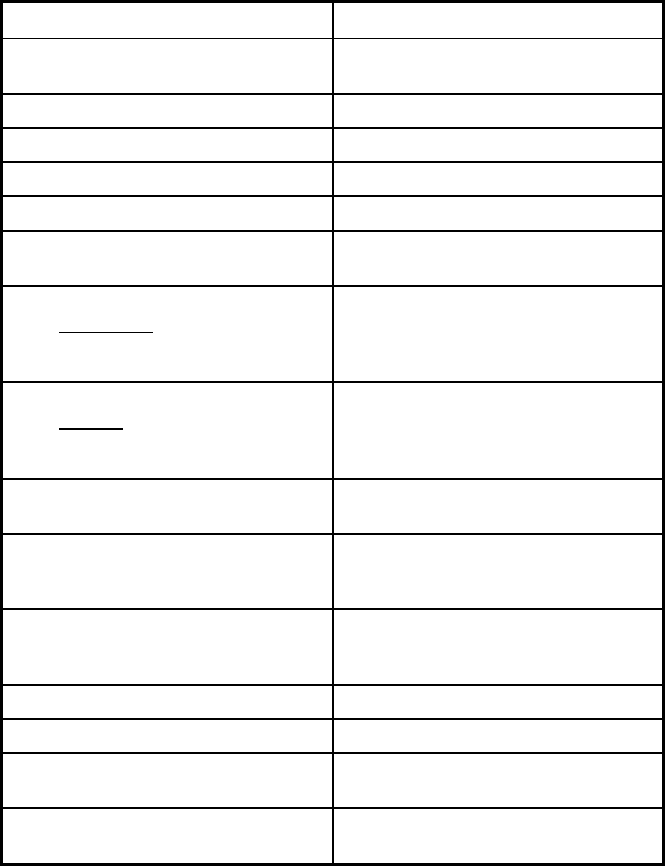
473
South Dakota Managed Care Program Features, as of 2018
Features PRIME
Program type Primary Care Case Management
(PCCM)
Statewide or region-specific? Statewide
Federal operating authority 1932(a)
Program start date 10/02/2002
Waiver expiration date (if applicable)
If the program ended in 2018, indicate
the end date
Populations enrolled: Low-income
adults not covered under ACA Section
VIII (excludes pregnant women and
people with disabilities)
Populations enrolled: Low-income
adults covered under ACA Section VIII
(excludes pregnant women and people
with disabilities)
Populations enrolled: Aged, Blind or
Disabled Children or Adults
Mandatory
Populations enrolled: Non-Disabled
Children (excludes children in foster
care or receiving adoption assistance)
Mandatory
Populations enrolled: Individuals
receiving Limited Benefits (excludes
partial duals)
Mandatory
Populations enrolled: Full Duals
Populations enrolled: Partial Duals
Populations enrolled: Children with
Special Health Care Needs
Populations enrolled: Native
American/Alaskan Natives
Mandatory
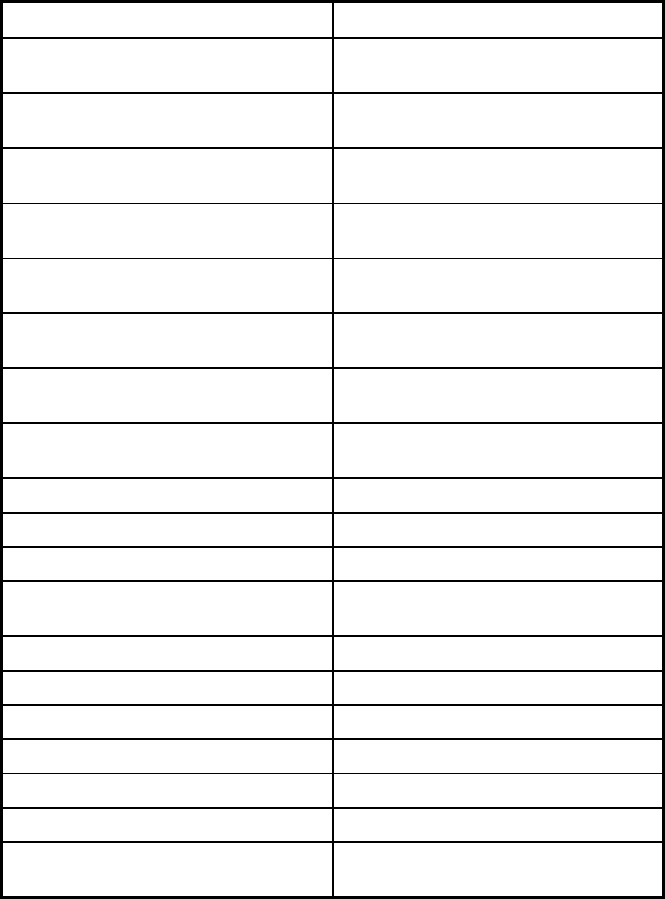
474
Features PRIME
Populations enrolled: Foster Care and
Adoption Assistance Children
Exempt
Populations enrolled: Enrollment choice
period
N/A
Populations enrolled: Enrollment broker
name (if applicable)
Populations enrolled: Notes on
enrollment choice period
Benefits covered: Inpatient hospital
physical health
Benefits covered: Inpatient hospital
behavioral health (MH and/or SUD)
Benefits covered: Outpatient hospital
physical health
Benefits covered: Outpatient hospital
behavioral health (MH and/or SUD)
Benefits covered: Partial hospitalization
Benefits covered: Physician
Benefits covered: Nurse practitioner
Benefits covered: Rural health clinics
and FQHCs
Benefits covered: Clinic services
Benefits covered: Lab and x-ray
Benefits covered: Prescription drugs
Benefits covered: Prosthetic devices
Benefits covered: EPSDT
Benefits covered: Case management X
Benefits covered: SSA Section 1945-
authorized health home
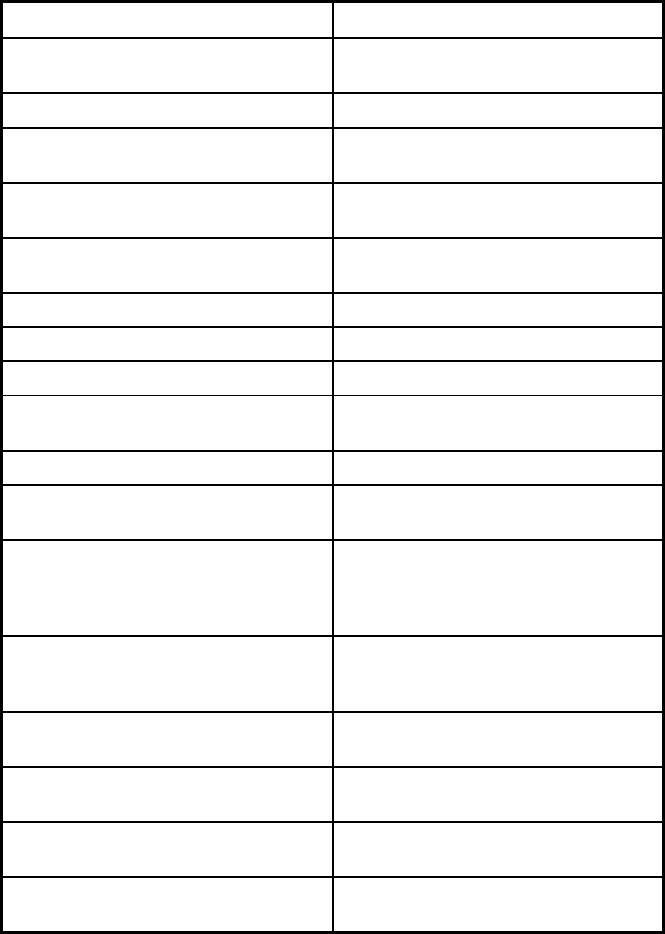
475
Features PRIME
Benefits covered: Health home care
(services in home)
Benefits covered: Family planning
Benefits covered: Dental services
(medical/surgical)
Benefits covered: Dental (preventative
or corrective)
Benefits covered: Personal care (state
plan option)
Benefits covered: HCBS waiver services
Benefits covered: Private duty nursing
Benefits covered: ICF-IDD
Benefits covered: Nursing facility
services
Benefits covered: Hospice care
Benefits covered: Non-Emergency
Medical Transportation
Benefits covered: Institution for Mental
Disease inpatient treatment for people
ages 21-64 defined by 42 CFR
§438.6(e) as an 'in lieu of' benefit
Benefits covered: Other (e.g., nurse
midwife services, freestanding birth
centers, podiatry, etc.)
Quality assurance and improvement:
HEDIS data required?
No
Quality assurance and improvement:
CAHPS data required?
No
Quality assurance and improvement:
Accreditation required?
No
Quality assurance and improvement:
Accrediting organization
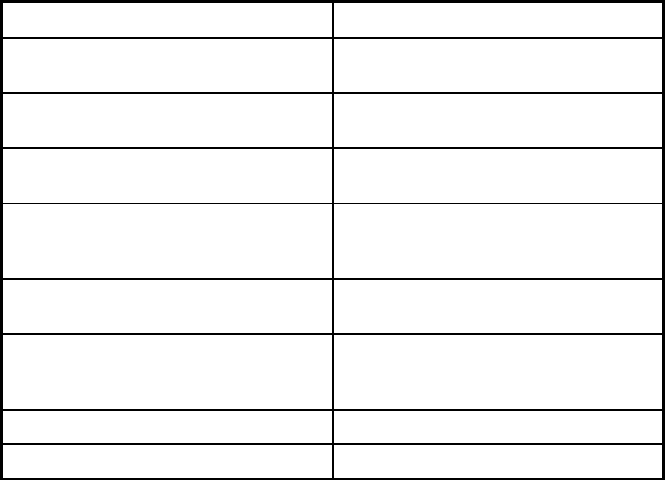
476
Features PRIME
Quality assurance and improvement:
EQRO contractor name (if applicable)
Performance incentives: Payment
bonuses/differentials to reward plans
Performance incentives: Preferential
auto-enrollment to reward plans
Performance incentives: Public reports
comparing plan performance on key
metrics
Performance incentives: Withholds tied
to performance metrics
Performance incentives: MCOs/PHPs
required or encouraged to pay providers
for value/quality outcomes
Participating plans: Plans in Program Multiple Primary Care Providers
Notes: Program notes
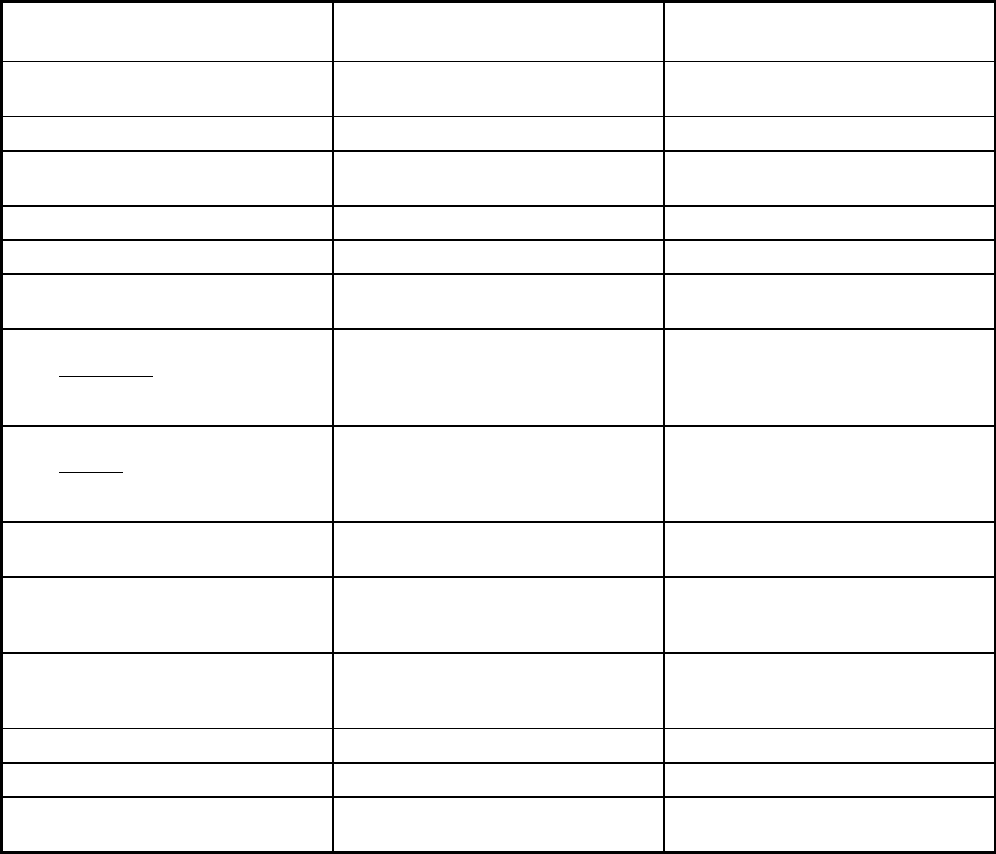
477
Tennessee Managed Care Program Features, as of 2018
Features TennCare II
Program of All-Inclusive Care for the
Elderly
Program type Comprehensive MCO + MLTSS Program of All-inclusive Care for the
Elderly (PACE)
Statewide or region-specific? Statewide Hamilton County
Federal operating authority 1115(a) (Medicaid demonstration
waivers),1945 Health Homes
PACE
Program start date 07/01/2002 04/07/1999
Waiver expiration date (if applicable) 06/30/2021
If the program ended in 2018, indicate
the end date
Populations enrolled: Low-income
adults not covered under ACA Section
VIII (excludes pregnant women and
people with disabilities)
Mandatory
Populations enrolled: Low-income
adults covered under ACA Section VIII
(excludes pregnant women and people
with disabilities)
Populations enrolled: Aged, Blind or
Disabled Children or Adults
Mandatory Voluntary
Populations enrolled: Non-Disabled
Children (excludes children in foster
care or receiving adoption assistance)
Mandatory
Populations enrolled: Individuals
receiving Limited Benefits (excludes
partial duals)
Populations enrolled: Full Duals Mandatory Voluntary
Populations enrolled: Partial Duals
Populations enrolled: Children with
Special Health Care Needs
Mandatory
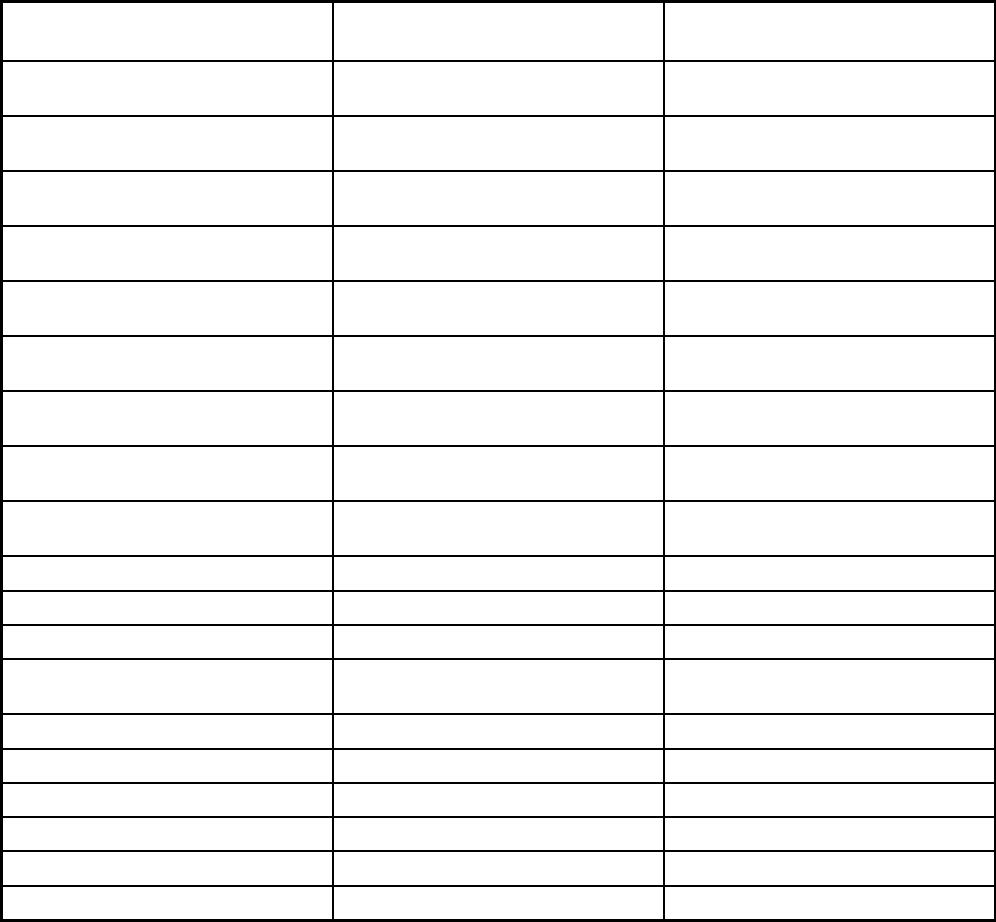
478
Features TennCare II
Program of All-Inclusive Care for the
Elderly
Populations enrolled: Native
American/Alaskan Natives
Exempt Exempt
Populations enrolled: Foster Care and
Adoption Assistance Children
Voluntary
Populations enrolled: Enrollment choice
period
Pre-assigned N/A
Populations enrolled: Enrollment broker
name (if applicable)
Populations enrolled: Notes on
enrollment choice period
Benefits covered: Inpatient hospital
physical health
X X
Benefits covered: Inpatient hospital
behavioral health (MH and/or SUD)
X X
Benefits covered: Outpatient hospital
physical health
X X
Benefits covered: Outpatient hospital
behavioral health (MH and/or SUD)
X X
Benefits covered: Partial hospitalization X X
Benefits covered: Physician X X
Benefits covered: Nurse practitioner X X
Benefits covered: Rural health clinics
and FQHCs
X
Benefits covered: Clinic services X X
Benefits covered: Lab and x-ray X X
Benefits covered: Prescription drugs X X
Benefits covered: Prosthetic devices X X
Benefits covered: EPSDT X
Benefits covered: Case management X X
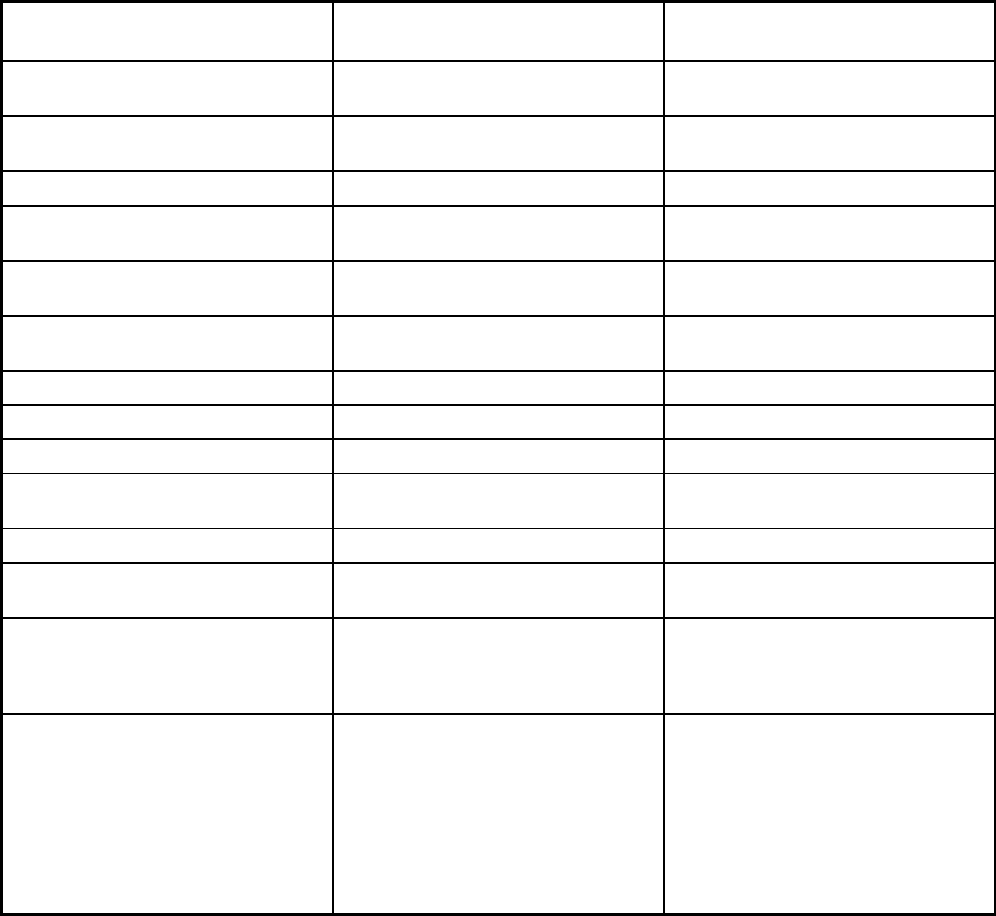
479
Features TennCare II
Program of All-Inclusive Care for the
Elderly
Benefits covered: SSA Section 1945-
authorized health home
X
Benefits covered: Health home care
(services in home)
X X
Benefits covered: Family planning X
Benefits covered: Dental services
(medical/surgical)
X X
Benefits covered: Dental (preventative
or corrective)
X
Benefits covered: Personal care (state
plan option)
X X
Benefits covered: HCBS waiver services X X
Benefits covered: Private duty nursing X X
Benefits covered: ICF-IDD
Benefits covered: Nursing facility
services
X X
Benefits covered: Hospice care X X
Benefits covered: Non-Emergency
Medical Transportation
X X
Benefits covered: Institution for Mental
Disease inpatient treatment for people
ages 21-64 defined by 42 CFR
§438.6(e) as an 'in lieu of' benefit
X
Benefits covered: Other (e.g., nurse
midwife services, freestanding birth
centers, podiatry, etc.)
Freestanding birth centers, podiatry
services, and other services as
indicated in Tennessee's approved
Medicaid State Plan.
Podiatry, nutrition counseling,
recreational therapy and social
activities, spiritual care, transportation
and escort to and from the PACE
center, audiology and hearing aids,
optometry and eyeglasses, and medical
equipment and supplies are additional
services covered by Tennessee's PACE
program.
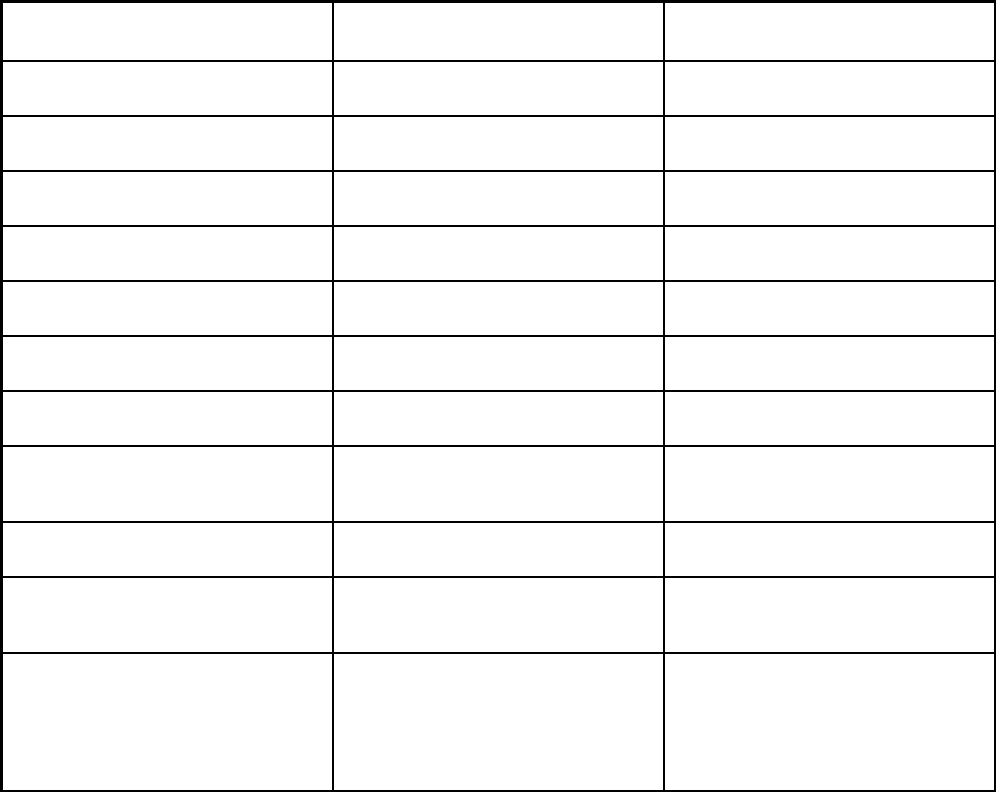
480
Features TennCare II
Program of All-Inclusive Care for the
Elderly
Quality assurance and improvement:
HEDIS data required?
Yes No
Quality assurance and improvement:
CAHPS data required?
Yes No
Quality assurance and improvement:
Accreditation required?
Yes No
Quality assurance and improvement:
Accrediting organization
NCQA
Quality assurance and improvement:
EQRO contractor name (if applicable)
Qsource
Performance incentives: Payment
bonuses/differentials to reward plans
X
Performance incentives: Preferential
auto-enrollment to reward plans
Performance incentives: Public reports
comparing plan performance on key
metrics
X
Performance incentives: Withholds tied
to performance metrics
X
Performance incentives: MCOs/PHPs
required or encouraged to pay providers
for value/quality outcomes
X
Participating plans: Plans in Program Amerigroup; DentaQuest USA
Insurance Company; Magellan Health
Services; UnitedHealthcare Community
Plan; Volunteer State Health Plan
(BlueCare); Volunteer State Health Plan
(TennCare Select)
Alexian Brothers Community Services
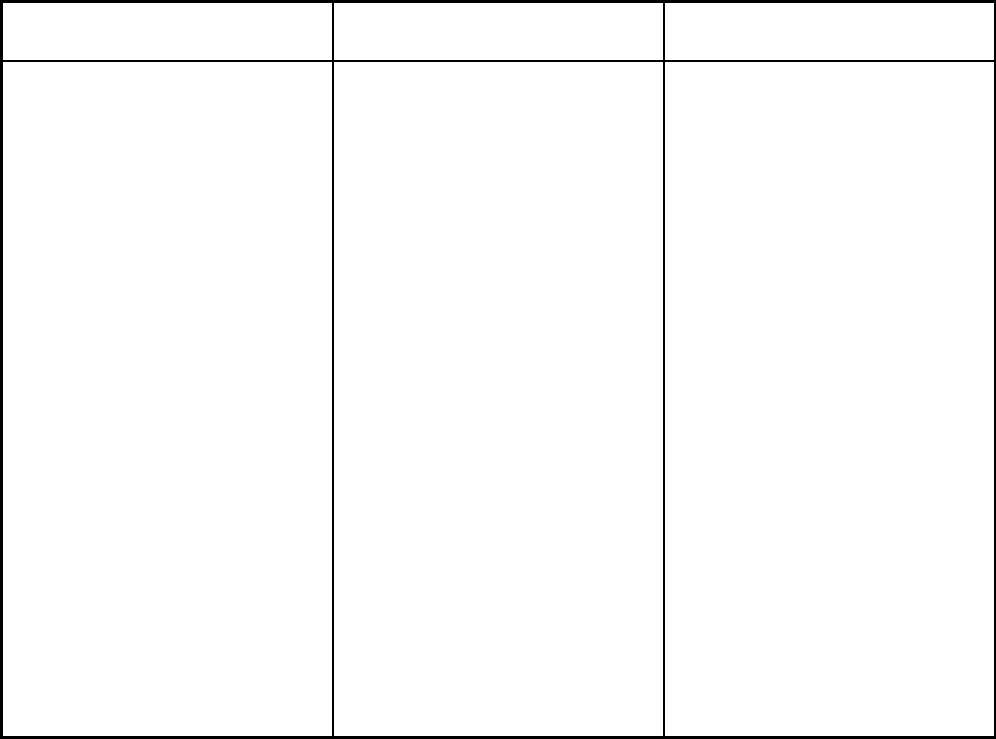
481
Features TennCare II
Program of All-Inclusive Care for the
Elderly
Notes: Program notes Dental services (preventive, diagnostic,
and treatment) are available to
TennCare enrollees under age 21, and
included within the EPSDT benefit. ICF-
IDD benefits are reimbursed outside the
TennCare II Demonstration, although
recipients of the benefit are still enrolled
in managed care for other benefits.
Individuals eligible for coverage solely
by virtue of the TennCare II
Demonstration are not entitled to certain
State Plan services but still receive a
wide range of physical health services,
behavioral health services, and long-
term services and supports. Partial
duals do not qualify for TennCare and,
therefore, are not enrolled in a
TennCare MCO. Most TennCare
members are enrolled in more than one
of the six plans identified. Each member
is enrolled in one Managed Care Entity
(MCE) for physical health services,
behavioral health services, and long-
term services and supports. Adults
(excluding PACE members) are also
enrolled in a second MCE for pharmacy
benefits. Children are enrolled in one
MCE for physical health services,
behavioral health services, and long-
term services and supports; a second
MCE for pharmacy benefits; and a third
MCE for dental benefits.
A segment of Tennessee's PACE
population qualifies for coverage solely
by virtue of the TennCare II
Demonstration (Tennessee's 1115
Medicaid demonstration waiver) and not
via Tennessee's Medicaid State Plan.
TennCare II has a demonstration-only
population referred to as the "PACE
Carryover Group", which consists of
individuals who were enrolled in a
PACE program as of June 30, 2012, but
who upon redetermination no longer
qualify for enrollment due solely to the
state's modification of its nursing facility
level of care criteria. Individuals enroll in
the PACE program voluntarily, but, once
enrolled, are required to participate in
managed care. Individuals who enroll in
TennCare but opt not to participate in
PACE are mandatorily enrolled in an
MCO. PACE applicants and recipients
must meet the nursing facility level of
care criteria (i.e., be disabled) to qualify
for the program.
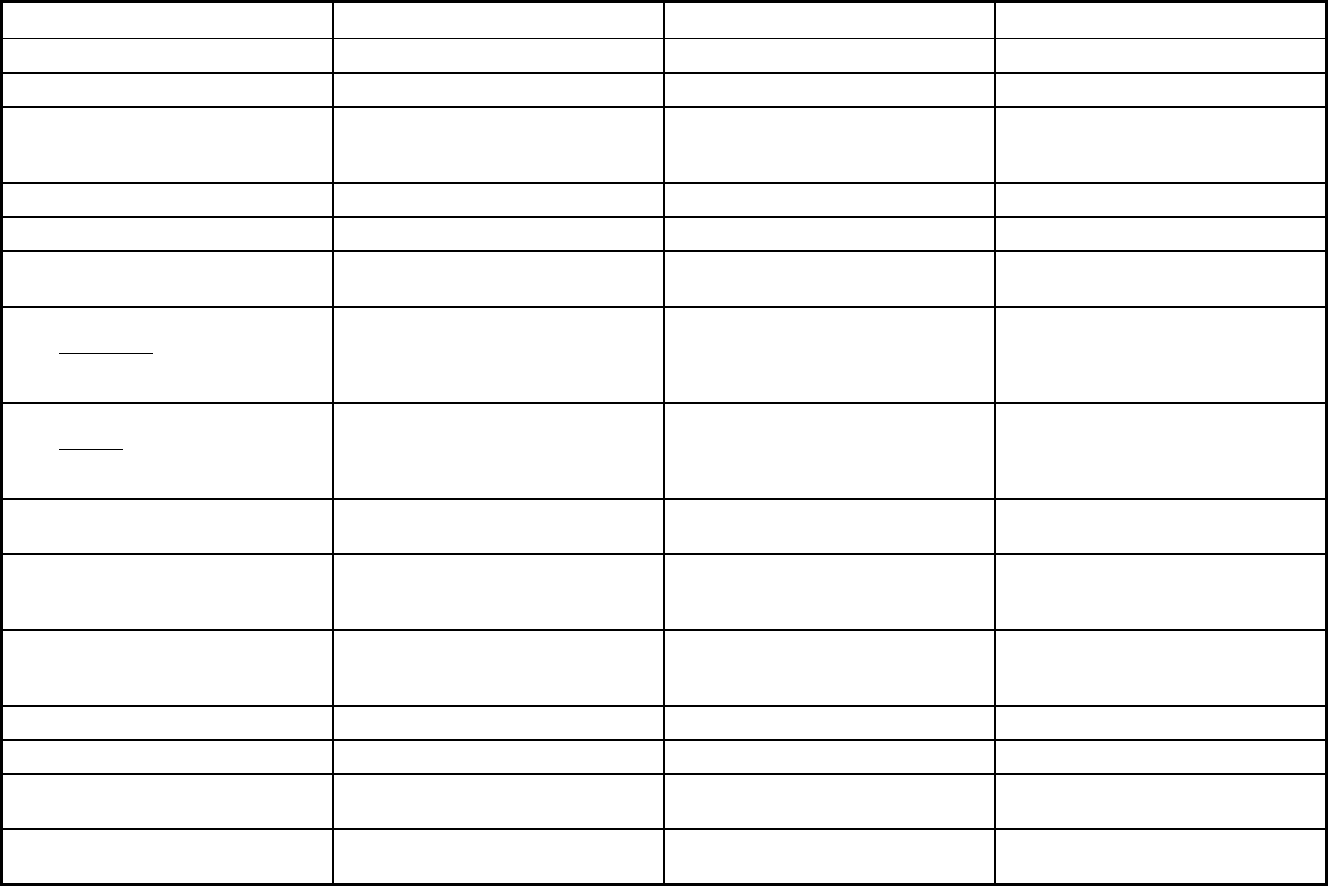
482
Texas Managed Care Program Features, as of 2018 (1 of 3)
Features STAR Health STAR STAR Kids
Program type Comprehensive MCO Comprehensive MCO Comprehensive MCO + MLTSS
Statewide or region-specific? Statewide Statewide Statewide
Federal operating authority 1915(a) 1115(a) (Medicaid demonstration
waivers)
1115(a) (Medicaid demonstration
waivers),1915(b)/1915(c),1945 Health
Homes
Program start date 04/01/2008 12/11/2011 11/01/2016
Waiver expiration date (if applicable) 09/30/2022 09/30/2022
If the program ended in 2018, indicate
the end date
Populations enrolled: Low-income
adults not covered under ACA Section
VIII (excludes pregnant women and
people with disabilities)
Mandatory
Populations enrolled: Low-income
adults covered under ACA Section VIII
(excludes pregnant women and people
with disabilities)
Populations enrolled: Aged, Blind or
Disabled Children or Adults
Mandatory Mandatory
Populations enrolled: Non-Disabled
Children (excludes children in foster
care or receiving adoption assistance)
Mandatory
Populations enrolled: Individuals
receiving Limited Benefits (excludes
partial duals)
Populations enrolled: Full Duals Voluntary Mandatory
Populations enrolled: Partial Duals
Populations enrolled: Children with
Special Health Care Needs
Mandatory
Populations enrolled: Native
American/Alaskan Natives
Voluntary Voluntary Voluntary
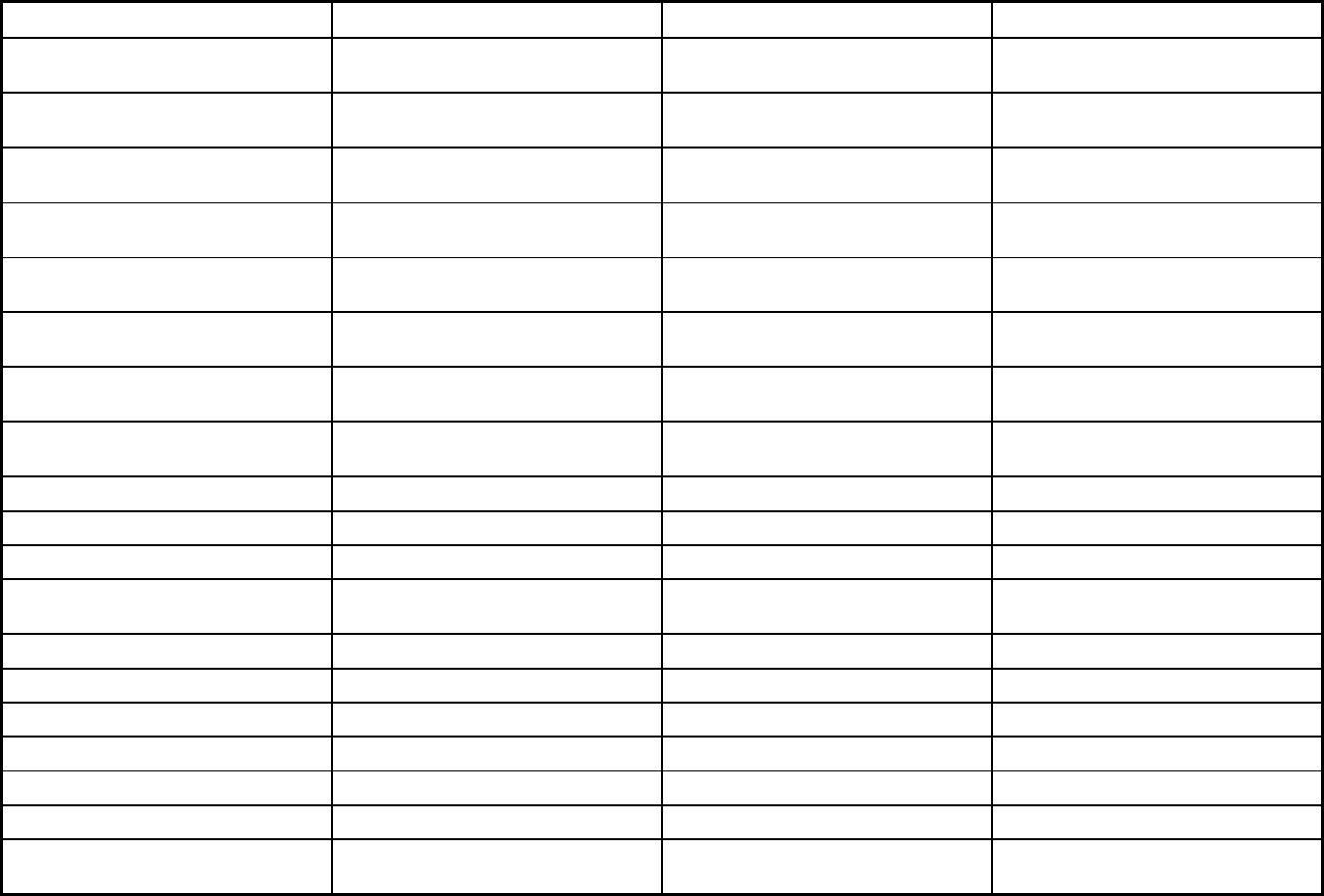
483
Features STAR Health STAR STAR Kids
Populations enrolled: Foster Care and
Adoption Assistance Children
Mandatory Mandatory Mandatory
Populations enrolled: Enrollment choice
period
Other 15 days 15 days
Populations enrolled: Enrollment broker
name (if applicable)
MAXIMUS MAXIMUS MAXIMUS
Populations enrolled: Notes on
enrollment choice period
Members are auto-enrolled by the
enrollment broker
Benefits covered: Inpatient hospital
physical health
X X X
Benefits covered: Inpatient hospital
behavioral health (MH and/or SUD)
X X X
Benefits covered: Outpatient hospital
physical health
X X X
Benefits covered: Outpatient hospital
behavioral health (MH and/or SUD)
X X X
Benefits covered: Partial hospitalization X X X
Benefits covered: Physician X X X
Benefits covered: Nurse practitioner X X X
Benefits covered: Rural health clinics
and FQHCs
X X X
Benefits covered: Clinic services X X X
Benefits covered: Lab and x-ray X X X
Benefits covered: Prescription drugs X X X
Benefits covered: Prosthetic devices X X X
Benefits covered: EPSDT X X X
Benefits covered: Case management X X X
Benefits covered: SSA Section 1945-
authorized health home
X
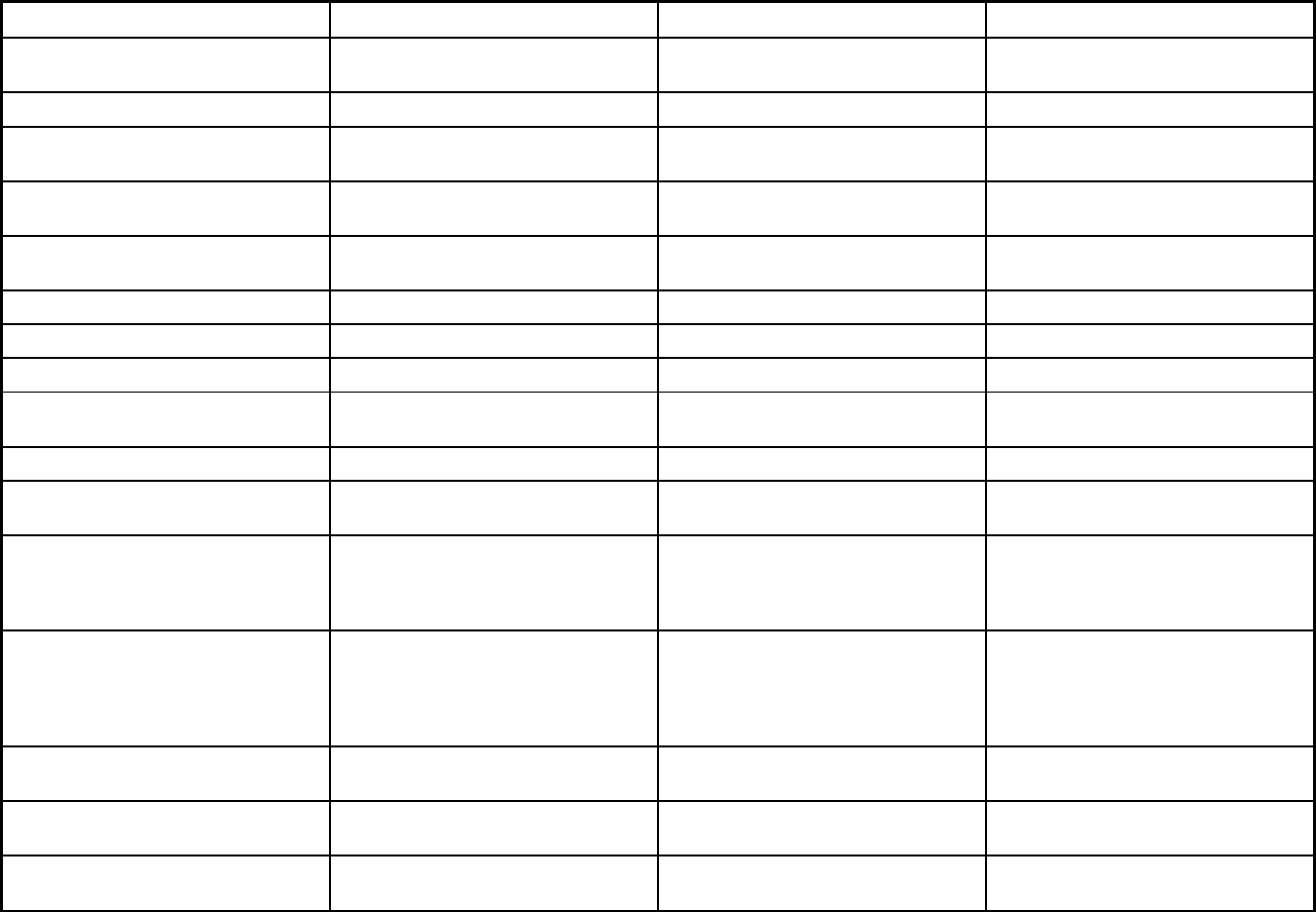
484
Features STAR Health STAR STAR Kids
Benefits covered: Health home care
(services in home)
X
Benefits covered: Family planning X X X
Benefits covered: Dental services
(medical/surgical)
X X
Benefits covered: Dental (preventative
or corrective)
X X
Benefits covered: Personal care (state
plan option)
X X
Benefits covered: HCBS waiver services X
Benefits covered: Private duty nursing X X X
Benefits covered: ICF-IDD X
Benefits covered: Nursing facility
services
X
Benefits covered: Hospice care X X
Benefits covered: Non-Emergency
Medical Transportation
X X
Benefits covered: Institution for Mental
Disease inpatient treatment for people
ages 21-64 defined by 42 CFR
§438.6(e) as an 'in lieu of' benefit
Benefits covered: Other (e.g., nurse
midwife services, freestanding birth
centers, podiatry, etc.)
Diagnostic services, podiatrist services,
medical supplies, non-prescription
drugs, eye glasses, preventive services,
nurse midwife services, and pediatric or
family nurse practitioner services
Diagnostic services, podiatrist services,
medical supplies, non-prescription
drugs, eye glasses, preventive services,
nurse midwife services, and pediatric or
family nurse practitioner services
Diagnostic services, podiatrist services,
medical supplies, non-prescription
drugs, eye glasses, preventive services,
nurse midwife services, and pediatric or
family nurse practitioner services
Quality assurance and improvement:
HEDIS data required?
Yes Yes Yes
Quality assurance and improvement:
CAHPS data required?
Yes Yes Yes
Quality assurance and improvement:
Accreditation required?
No, but accreditation considered in plan
selection criteria
No, but accreditation considered in plan
selection criteria
No, but accreditation considered in plan
selection criteria
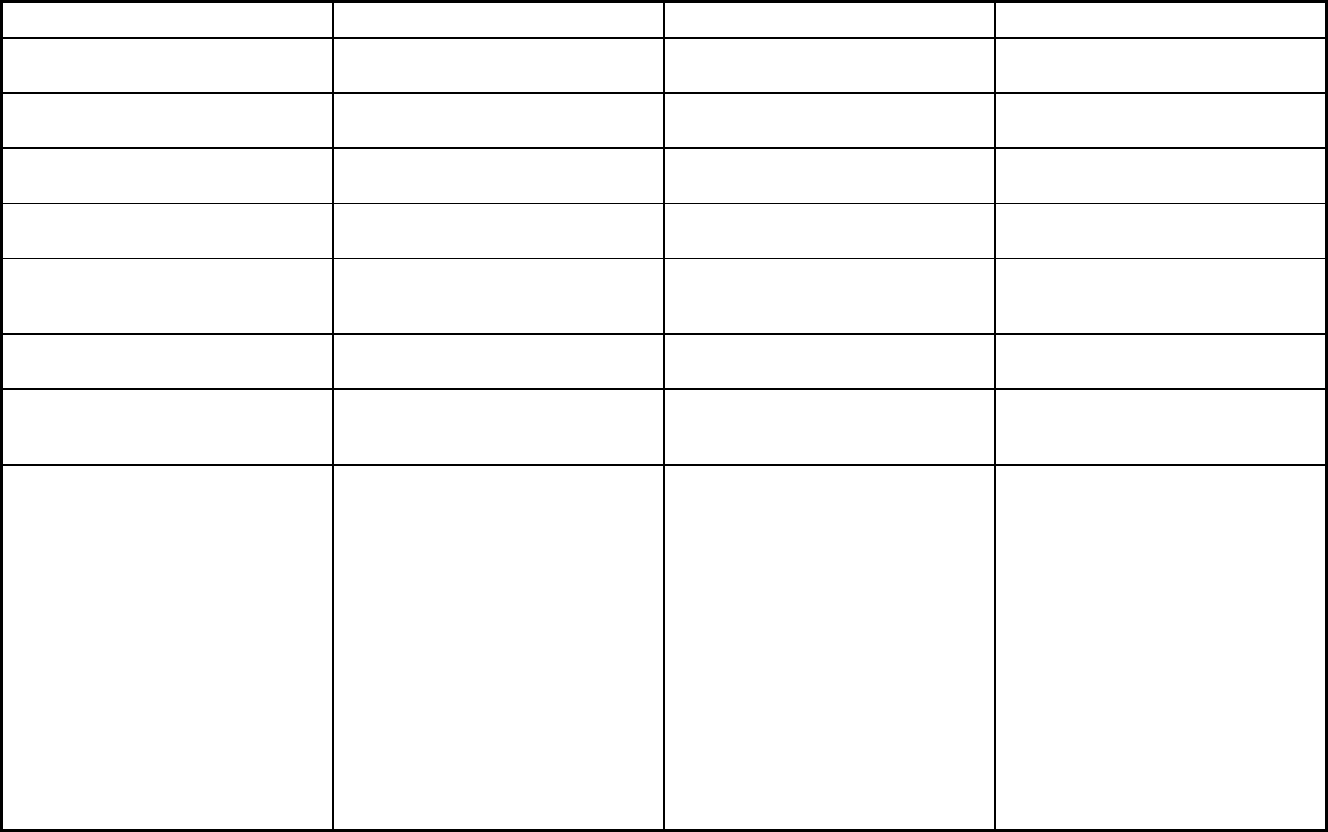
485
Features STAR Health STAR STAR Kids
Quality assurance and improvement:
Accrediting organization
NCQA, URAC NCQA, URAC NCQA, URAC
Quality assurance and improvement:
EQRO contractor name (if applicable)
Institute for Child Health Policy Institute for Child Health Policy Institute for Child Health Policy
Performance incentives: Payment
bonuses/differentials to reward plans
X
Performance incentives: Preferential
auto-enrollment to reward plans
Performance incentives: Public reports
comparing plan performance on key
metrics
X X
Performance incentives: Withholds tied
to performance metrics
Performance incentives: MCOs/PHPs
required or encouraged to pay providers
for value/quality outcomes
X X X
Participating plans: Plans in Program Superior HealthPlan Amerigroup Texas, Inc.; Superior Health
Plan, Inc.; El Paso Health Plans, Inc.,
dba El Paso Health; Aetna Better Health
of Texas, Inc.; Community First Health
Plans, Inc.; UnitedHealthcare Insurance
Company, dba United Healthcare
Community Plan; Texas Children's
Health Plan, Inc.; Molina Healthcare of
Texas, Inc.; Driscoll Children's Health
Plan; Parkland Community Health Plan,
Inc.; Cook Children's Health Plan;
Community First Health Plans, Inc.;
Seton Health Plan, Inc., dba Dell
Childrens Health Plan; Health Care
Service Corp. (dba Blue Cross Blue
Shield); SHA. LLC, dba FirstCare Health
Plans; Scott & White Health Plan
Amerigroup Insurance Company;
Superior HealthPlan, Inc.; Aetna Better
Health of Texas Inc.; Community First
Health Plans, Inc.; UnitedHealthcare
Insurance Company, dba United
Healthcare Community Plan; Texas
Children’s Health Plan, Inc.; Driscoll
Children’s Health Plan; Cook Children's
Health Plan; Health Care Service
Corporation DBA Blue Cross and Blue
Shield of Texas (BCBSTX); Children’s
Medical Center Health Plan
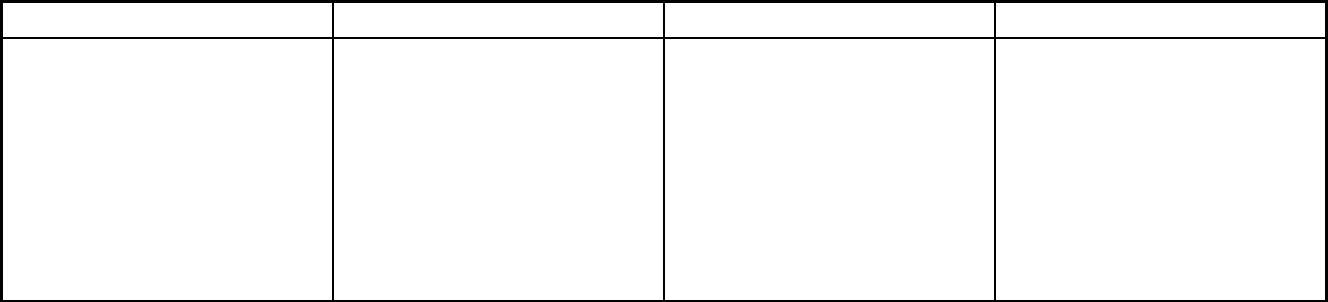
486
Features STAR Health STAR STAR Kids
Notes: Program notes Enrollment in the STAR Health Program
is voluntary for the following population
categories: 1) Children and young
adults in DFPS conservatorship; 2)
Emancipated minors or members age
18-22 who voluntarily agree to continue
in foster placement; 3) Young adults
age 18-
21 who have exited care and are
participating in the Medicaid for
Transitional Foster Care Youth
(MTFCY) or Former Foster Care
Children (FFCC) program.
STAR population also includes pregnant
women. Dental benefits covered by the
STAR program are administered by
Dental Maintenance Organizations.
1115 and 1915 (c) waivers are applied
to this program.
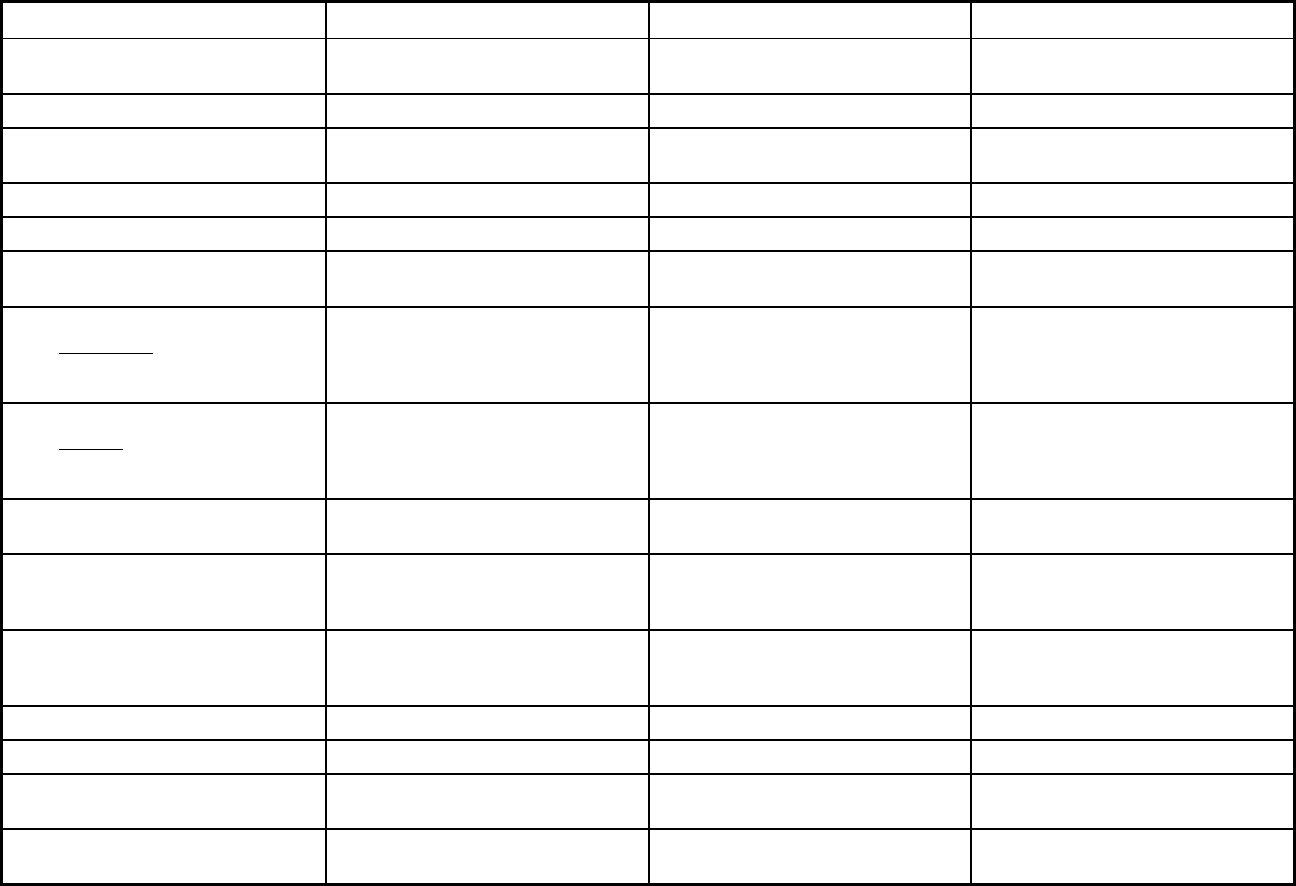
487
Texas Managed Care Program Features, as of 2018 (2 of 3)
Features STAR+PLUS Children's Medicaid Dental Services PACE
Program type Comprehensive MCO + MLTSS Dental only (PAHP) Program of All-inclusive Care for the
Elderly (PACE)
Statewide or region-specific? Statewide Statewide Statewide
Federal operating authority 1115(a) (Medicaid demonstration
waivers)
1115(a) (Medicaid demonstration
waivers)
PACE
Program start date 12/11/2011 12/11/2011 06/01/2001
Waiver expiration date (if applicable) 09/30/2022 09/30/2022
If the program ended in 2018, indicate
the end date
Populations enrolled: Low-income
adults not covered under ACA Section
VIII (excludes pregnant women and
people with disabilities)
Populations enrolled: Low-income
adults covered under ACA Section VIII
(excludes pregnant women and people
with disabilities)
Populations enrolled: Aged, Blind or
Disabled Children or Adults
Mandatory Mandatory Voluntary
Populations enrolled: Non-Disabled
Children (excludes children in foster
care or receiving adoption assistance)
Mandatory
Populations enrolled: Individuals
receiving Limited Benefits (excludes
partial duals)
Populations enrolled: Full Duals Mandatory Voluntary
Populations enrolled: Partial Duals Voluntary
Populations enrolled: Children with
Special Health Care Needs
Populations enrolled: Native
American/Alaskan Natives
Voluntary Voluntary Voluntary
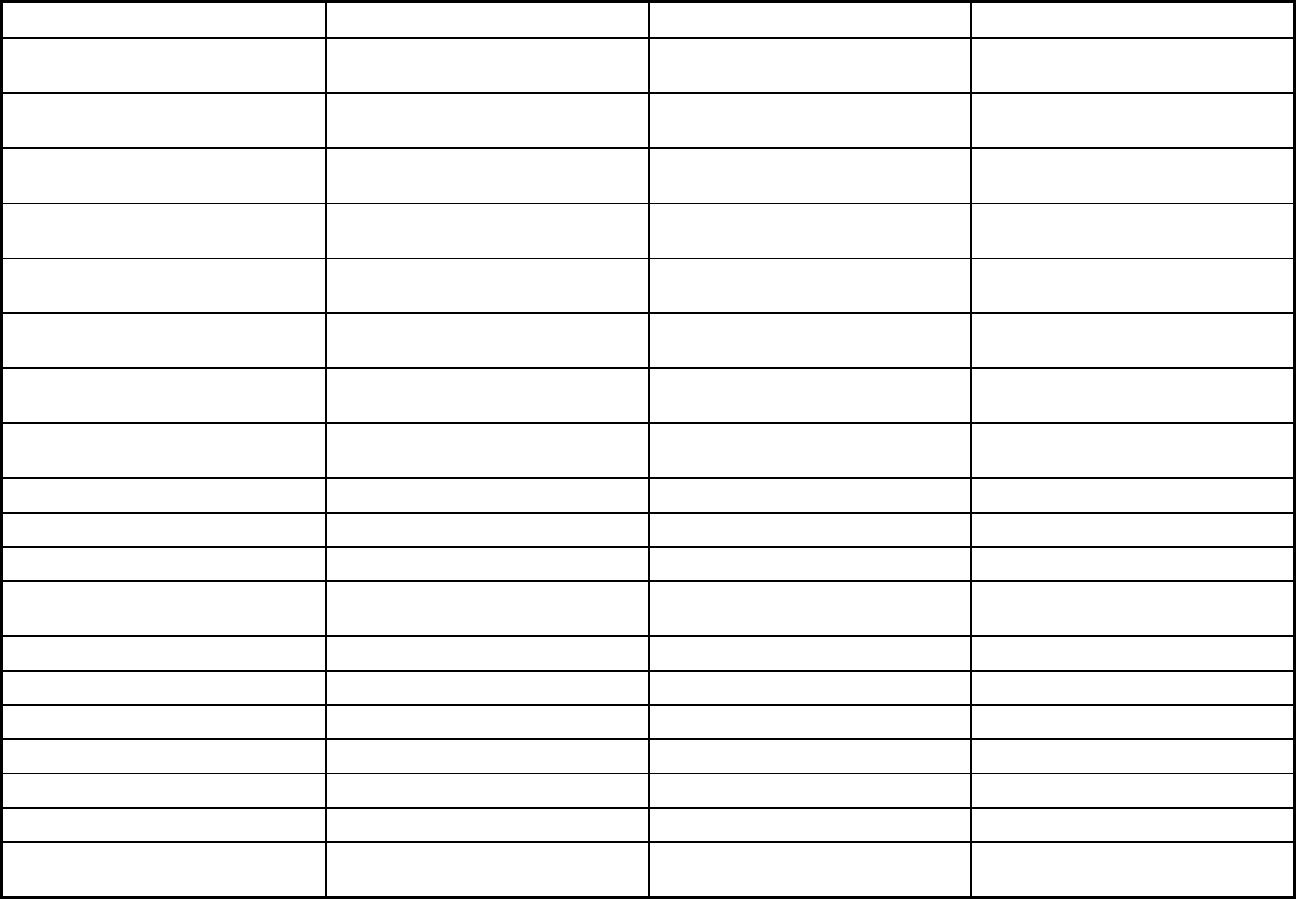
488
Features STAR+PLUS Children's Medicaid Dental Services PACE
Populations enrolled: Foster Care and
Adoption Assistance Children
Exempt Exempt
Populations enrolled: Enrollment
choice period
15 days 15 days N/A
Populations enrolled: Enrollment broker
name (if applicable)
MAXIMUS MAXIMUS
Populations enrolled: Notes on
enrollment choice period
Benefits covered: Inpatient hospital
physical health
X X
Benefits covered: Inpatient hospital
behavioral health (MH and/or SUD)
X X
Benefits covered: Outpatient hospital
physical health
X X
Benefits covered: Outpatient hospital
behavioral health (MH and/or SUD)
X X
Benefits covered: Partial hospitalization X
Benefits covered: Physician X X
Benefits covered: Nurse practitioner X X
Benefits covered: Rural health clinics
and FQHCs
X X
Benefits covered: Clinic services X X
Benefits covered: Lab and x-ray X X
Benefits covered: Prescription drugs X X
Benefits covered: Prosthetic devices X X
Benefits covered: EPSDT X
Benefits covered: Case management X X
Benefits covered: SSA Section 1945-
authorized health home
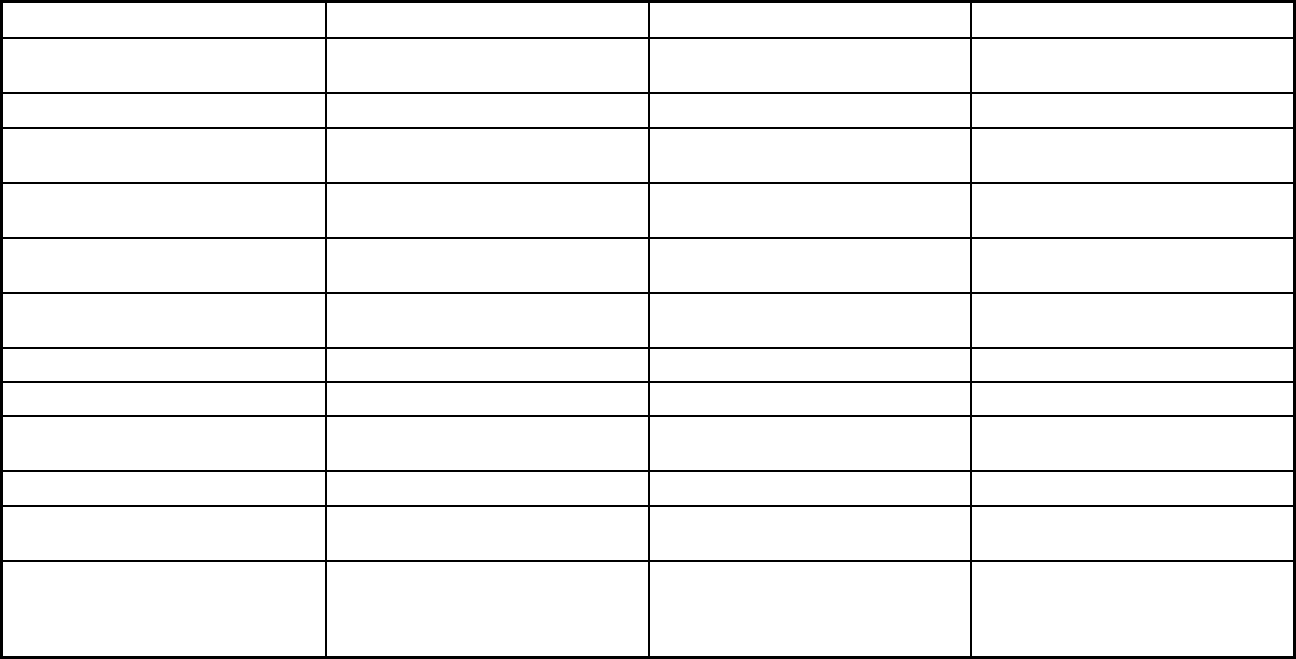
489
Features STAR+PLUS Children's Medicaid Dental Services PACE
Benefits covered: Health home care
(services in home)
X
Benefits covered: Family planning X
Benefits covered: Dental services
(medical/surgical)
X X
Benefits covered: Dental (preventative
or corrective)
X X
Benefits covered: Personal care (state
plan option)
X X
Benefits covered: HCBS waiver
services
X X
Benefits covered: Private duty nursing X
Benefits covered: ICF-IDD
Benefits covered: Nursing facility
services
X X
Benefits covered: Hospice care X X
Benefits covered: Non-Emergency
Medical Transportation
X X
Benefits covered: Institution for Mental
Disease inpatient treatment for people
ages 21-64 defined by 42 CFR
§438.6(e) as an 'in lieu of' benefit
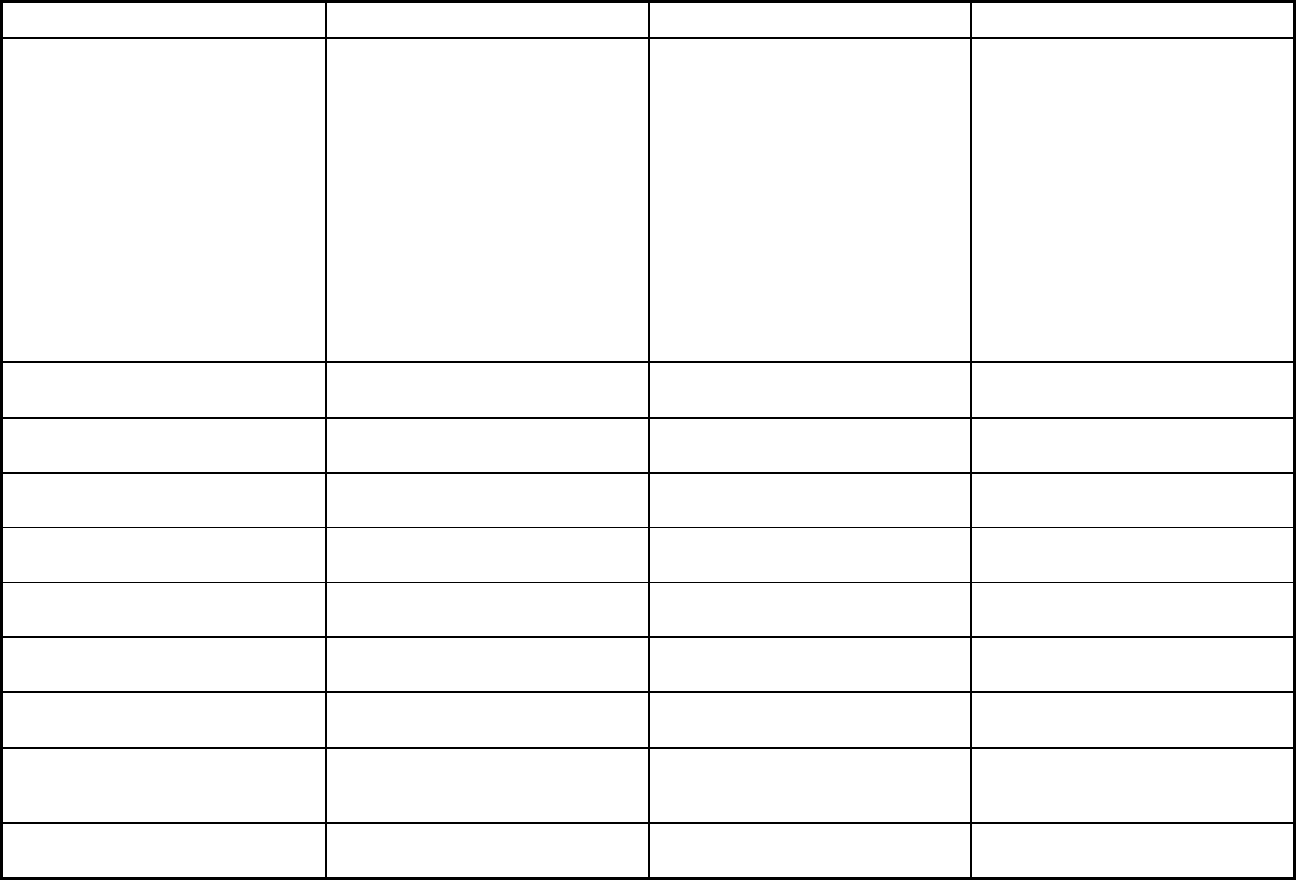
490
Features STAR+PLUS Children's Medicaid Dental Services PACE
Benefits covered: Other (e.g., nurse
midwife services, freestanding birth
centers, podiatry, etc.)
Diagnostic services, podiatrist services,
medical supplies, non-prescription
drugs, eye glasses, preventive
services, nurse midwife services, and
pediatric or family nurse practitioner
services
Adult day care/adult foster care,
nursing, restorative therapies: physical,
occupational, and recreational
therapies, meals and nutrition
counseling, social work/social services,
medical supplies/adaptive aids and
minor home modifications,
transportation to and from medical
appointments, medical specialists,
such as audiology, dentistry,
optometry, podiatry, speech therapy,
respite care, Medical care provided by
a PACE physician familiar with the
history, needs, and preferences of
each participant
Quality assurance and improvement:
HEDIS data required?
Yes Yes No
Quality assurance and improvement:
CAHPS data required?
Yes Yes No
Quality assurance and improvement:
Accreditation required?
No, but accreditation considered in
plan selection criteria
No, but accreditation considered in
plan selection criteria
No
Quality assurance and improvement:
Accrediting organization
NCQA, URAC NCQA, URAC
Quality assurance and improvement:
EQRO contractor name (if applicable)
Institute for Child Health Policy Institute for Child Health Policy
Performance incentives: Payment
bonuses/differentials to reward plans
X X
Performance incentives: Preferential
auto-enrollment to reward plans
Performance incentives: Public reports
comparing plan performance on key
metrics
X
Performance incentives: Withholds tied
to performance metrics
X
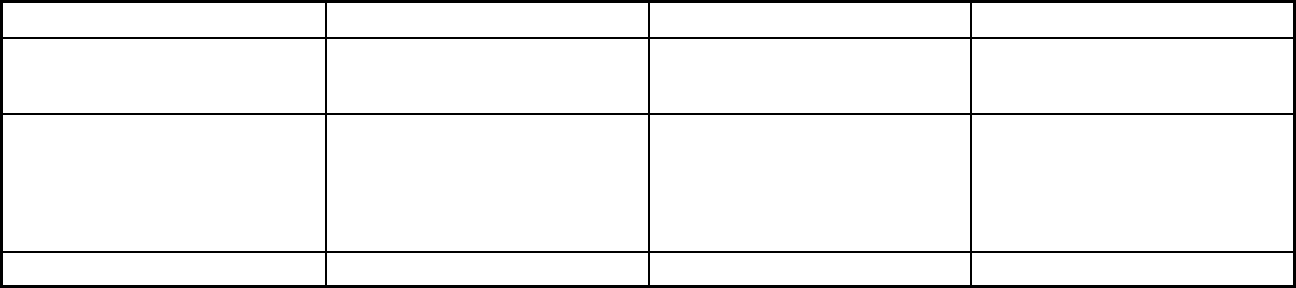
491
Features STAR+PLUS Children's Medicaid Dental Services PACE
Performance incentives: MCOs/PHPs
required or encouraged to pay
providers for value/quality outcomes
X X
Participating plans: Plans in Program Amerigroup Texas, Inc.; Superior
HealthPlan, Inc; UnitedHealthcare
Insurance Company, dba United
Healthcare Community Plan; Molina
Healthcare of Texas, Inc.; HealthSpring
Life & Health Insurance Co., Inc.
MCNA Insurance Company;
DentaQuest USA Insurance Company,
Inc.
Bienvivir Senior Health Services (El
Paso); Silver Star Health Network
(Lubbock); Werner (Amarillo)
Notes: Program notes
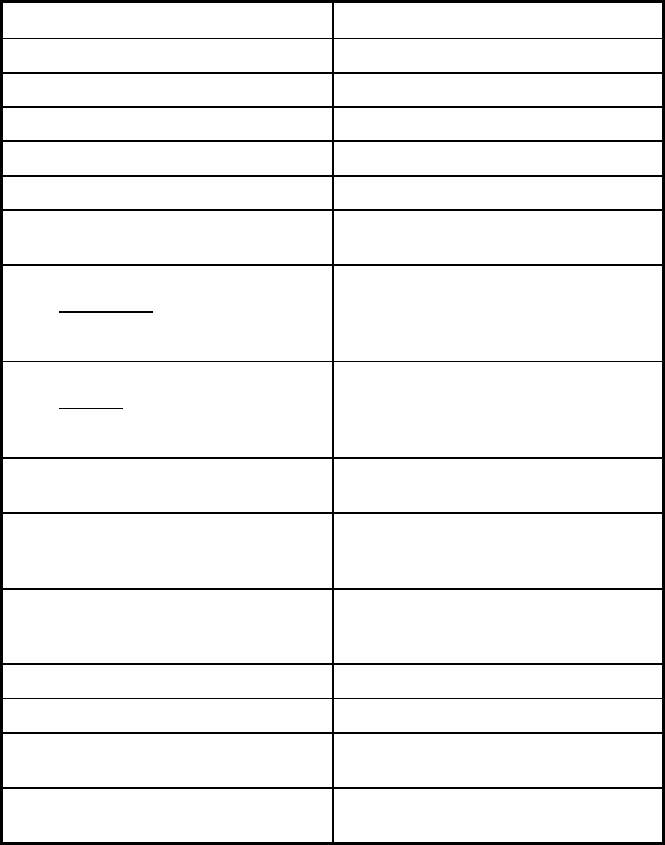
492
Texas Managed Care Program Features, as of 2018 (3 of 3)
Features Medical Transportation Program
Program type Non-Emergency Medical Transportation
Statewide or region-specific? Statewide
Federal operating authority 1915(b)
Program start date 09/01/2014
Waiver expiration date (if applicable) 03/31/2022
If the program ended in 2018, indicate
the end date
Populations enrolled: Low-income
adults not covered under ACA Section
VIII (excludes pregnant women and
people with disabilities)
Voluntary
Populations enrolled: Low-income
adults covered under ACA Section VIII
(excludes pregnant women and people
with disabilities)
Populations enrolled: Aged, Blind or
Disabled Children or Adults
Voluntary
Populations enrolled: Non-Disabled
Children (excludes children in foster
care or receiving adoption assistance)
Voluntary
Populations enrolled: Individuals
receiving Limited Benefits (excludes
partial duals)
Voluntary
Populations enrolled: Full Duals Voluntary
Populations enrolled: Partial Duals Voluntary
Populations enrolled: Children with
Special Health Care Needs
Voluntary
Populations enrolled: Native
American/Alaskan Natives
Voluntary
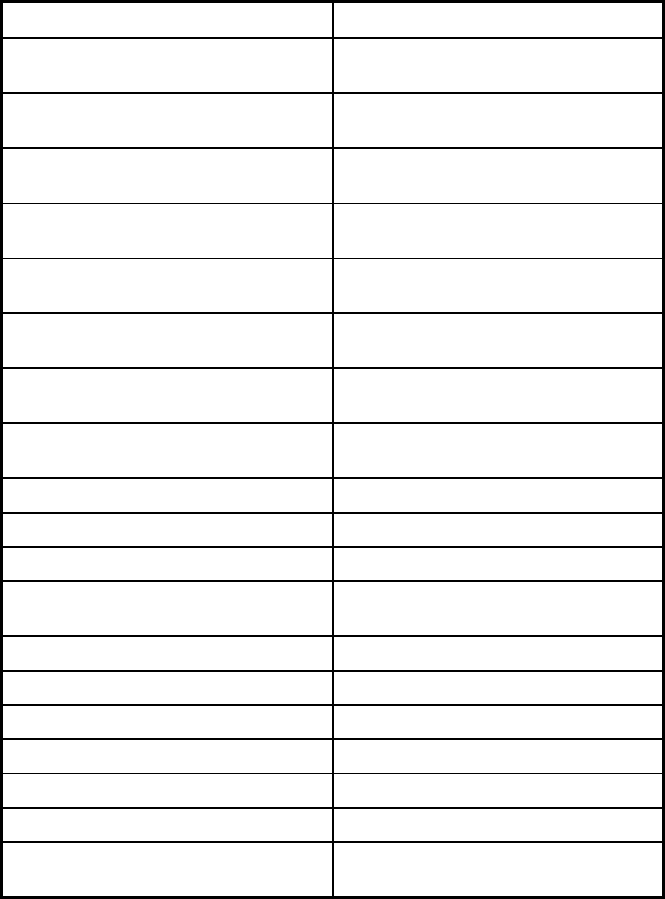
493
Features Medical Transportation Program
Populations enrolled: Foster Care and
Adoption Assistance Children
Populations enrolled: Enrollment choice
period
Pre-assigned
Populations enrolled: Enrollment broker
name (if applicable)
Populations enrolled: Notes on
enrollment choice period
Benefits covered: Inpatient hospital
physical health
Benefits covered: Inpatient hospital
behavioral health (MH and/or SUD)
Benefits covered: Outpatient hospital
physical health
Benefits covered: Outpatient hospital
behavioral health (MH and/or SUD)
Benefits covered: Partial hospitalization
Benefits covered: Physician
Benefits covered: Nurse practitioner
Benefits covered: Rural health clinics
and FQHCs
Benefits covered: Clinic services
Benefits covered: Lab and x-ray
Benefits covered: Prescription drugs
Benefits covered: Prosthetic devices
Benefits covered: EPSDT
Benefits covered: Case management
Benefits covered: SSA Section 1945-
authorized health home
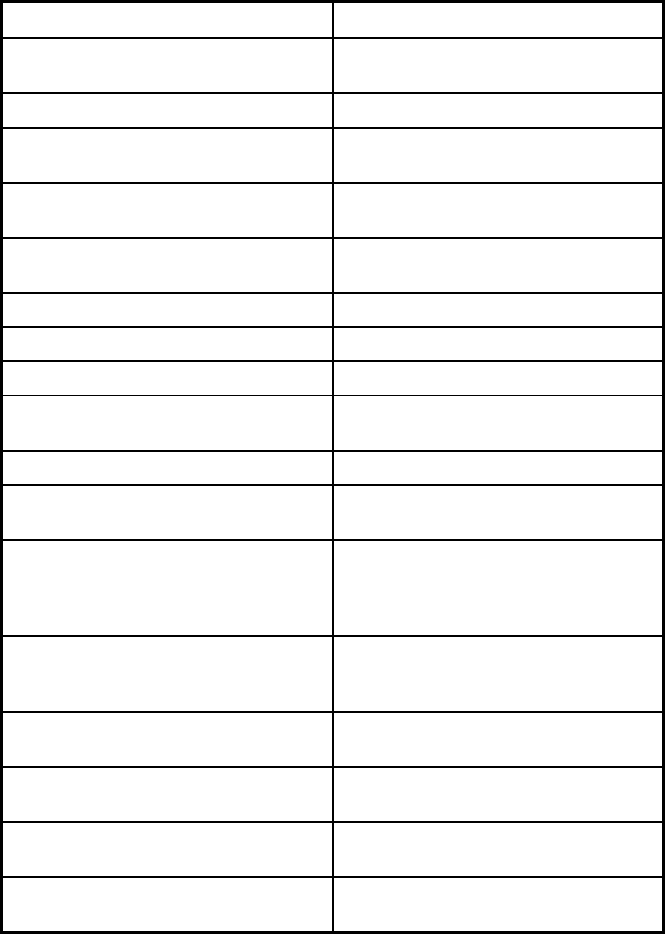
494
Features Medical Transportation Program
Benefits covered: Health home care
(services in home)
Benefits covered: Family planning
Benefits covered: Dental services
(medical/surgical)
Benefits covered: Dental (preventative
or corrective)
Benefits covered: Personal care (state
plan option)
Benefits covered: HCBS waiver services
Benefits covered: Private duty nursing
Benefits covered: ICF-IDD
Benefits covered: Nursing facility
services
Benefits covered: Hospice care
Benefits covered: Non-Emergency
Medical Transportation
X
Benefits covered: Institution for Mental
Disease inpatient treatment for people
ages 21-64 defined by 42 CFR
§438.6(e) as an 'in lieu of' benefit
Benefits covered: Other (e.g., nurse
midwife services, freestanding birth
centers, podiatry, etc.)
Quality assurance and improvement:
HEDIS data required?
No
Quality assurance and improvement:
CAHPS data required?
No
Quality assurance and improvement:
Accreditation required?
No
Quality assurance and improvement:
Accrediting organization
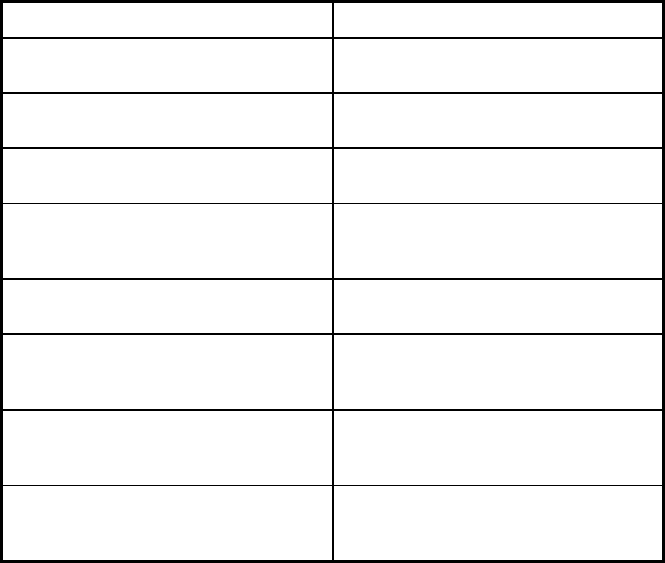
495
Features Medical Transportation Program
Quality assurance and improvement:
EQRO contractor name (if applicable)
Performance incentives: Payment
bonuses/differentials to reward plans
Performance incentives: Preferential
auto-enrollment to reward plans
Performance incentives: Public reports
comparing plan performance on key
metrics
Performance incentives: Withholds tied
to performance metrics
Performance incentives: MCOs/PHPs
required or encouraged to pay providers
for value/quality outcomes
Participating plans: Plans in Program American Medical Response;
LogistiCare; Medical Transportation
Management; Project Armistad
Notes: Program notes Based on the client's county of
residence, the client is assigned to the
single broker in the region.
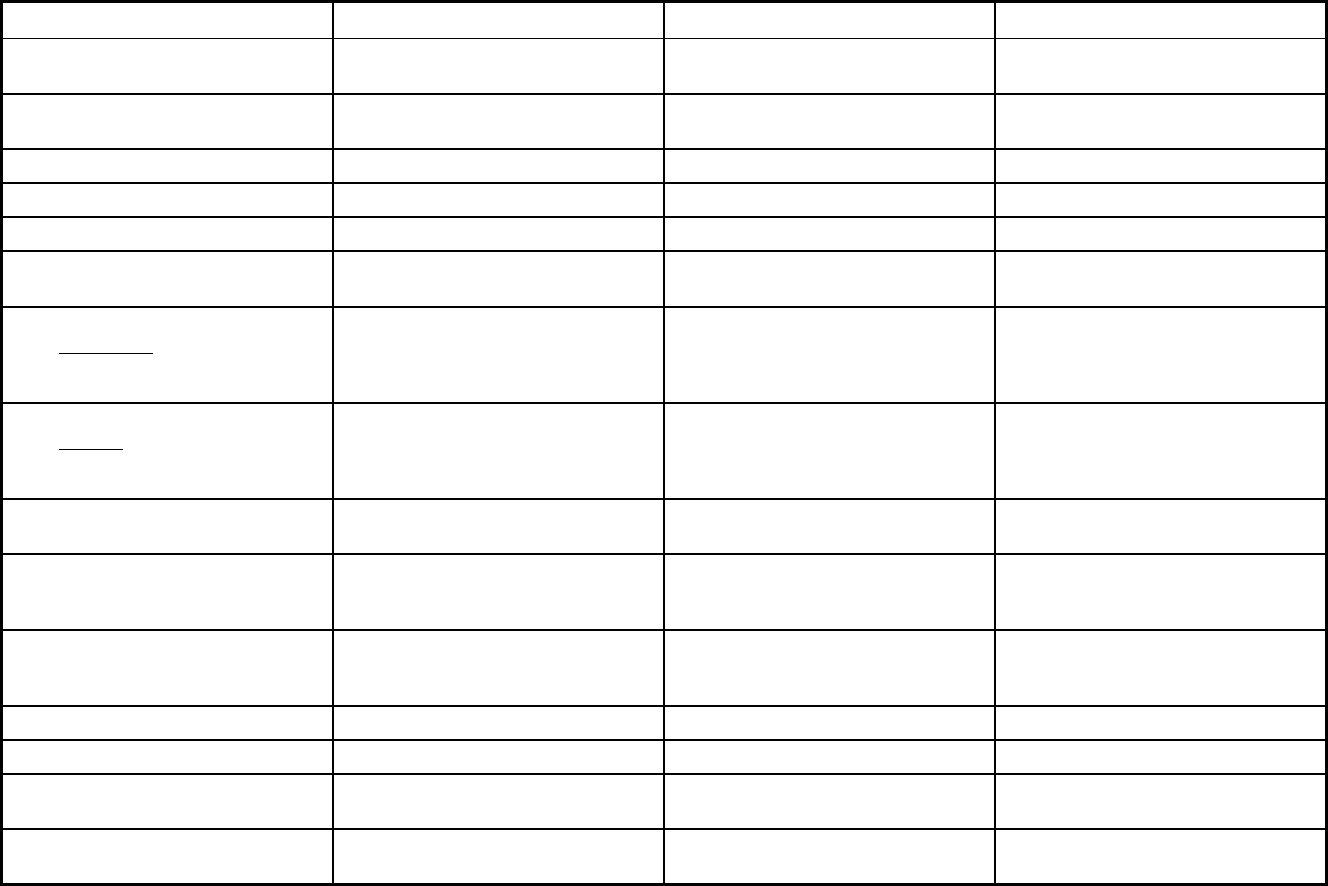
496
Utah Managed Care Program Features, as of 2018 (1 of 2)
Features Prepaid Mental Health Dental UNI HOME
Program type Behavioral Health Organization (BHO)
only (PIHP and/or PAHP)
Dental only (PAHP) Comprehensive MCO
Statewide or region-specific? Based on state counties and some
multi-county partnerships
Statewide Statewide
Federal operating authority 1915(b) 1915(b) 1915(a)
Program start date 07/01/1991 09/01/2013 07/01/2011
Waiver expiration date (if applicable) 06/30/2022 12/31/2023 06/30/2021
If the program ended in 2018, indicate
the end date
Populations enrolled: Low-income
adults not covered under ACA Section
VIII (excludes pregnant women and
people with disabilities)
Mandatory
Populations enrolled: Low-income
adults covered under ACA Section VIII
(excludes pregnant women and people
with disabilities)
Mandatory
Populations enrolled: Aged, Blind or
Disabled Children or Adults
Mandatory Mandatory Voluntary
Populations enrolled: Non-Disabled
Children (excludes children in foster
care or receiving adoption assistance)
Mandatory Mandatory
Populations enrolled: Individuals
receiving Limited Benefits (excludes
partial duals)
Mandatory
Populations enrolled: Full Duals Mandatory Mandatory Voluntary
Populations enrolled: Partial Duals Mandatory Mandatory Voluntary
Populations enrolled: Children with
Special Health Care Needs
Mandatory Mandatory Voluntary
Populations enrolled: Native
American/Alaskan Natives
Mandatory Mandatory Voluntary
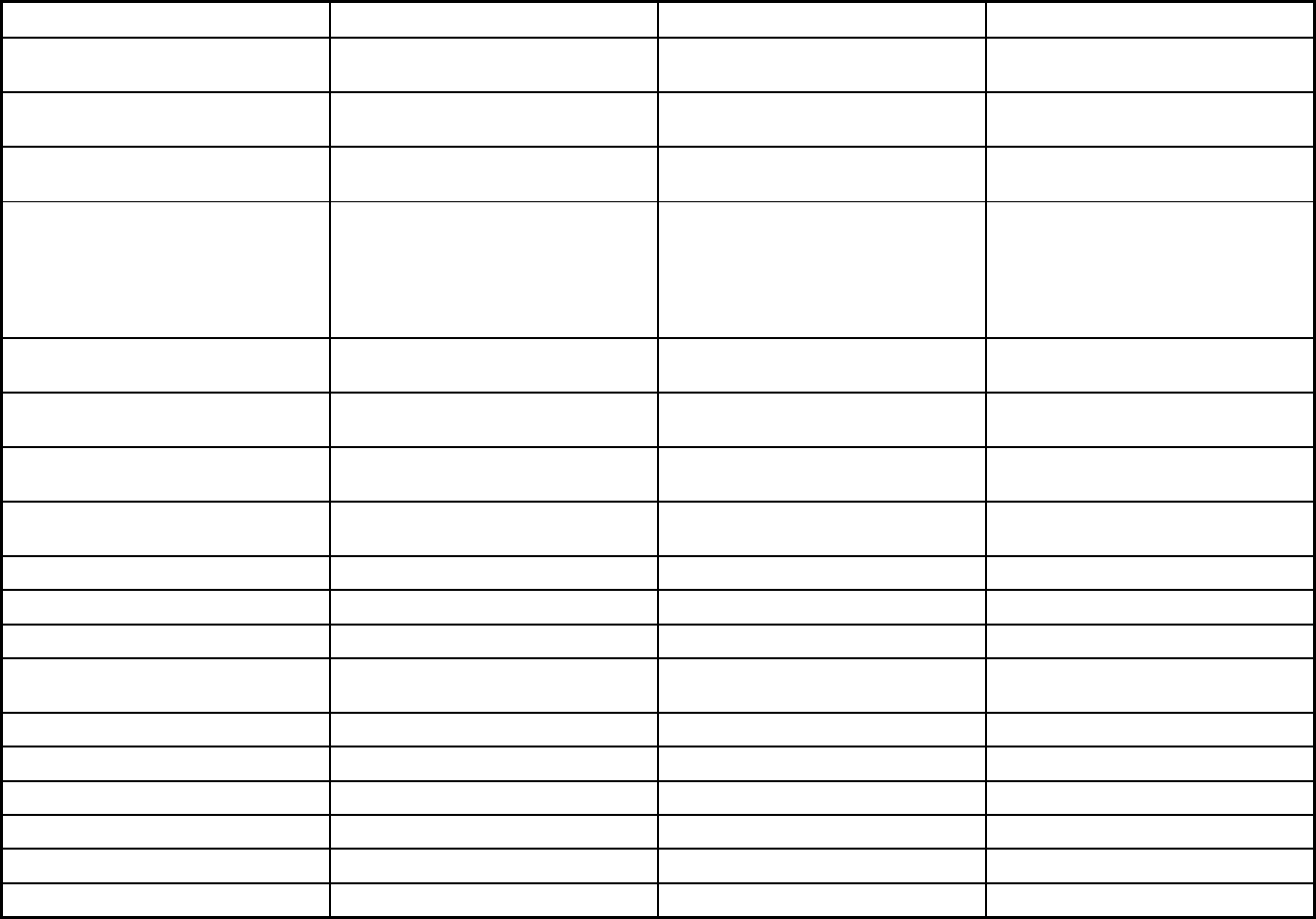
497
Features Prepaid Mental Health Dental UNI HOME
Populations enrolled: Foster Care and
Adoption Assistance Children
Mandatory Exempt Voluntary
Populations enrolled: Enrollment choice
period
Pre-assigned Other Other
Populations enrolled: Enrollment broker
name (if applicable)
Populations enrolled: Notes on
enrollment choice period
15-45 days. Enrollment choice date will
vary depending on when the enrollment
file transaction takes place. In addition,
the enrollee will be able to change to
another plan within the first 90 days of
enrollment in the plan.
No enrollment period. There is a waiting
list for the program. Enrollees apply. If
there is room, they are enrolled.
Benefits covered: Inpatient hospital
physical health
X
Benefits covered: Inpatient hospital
behavioral health (MH and/or SUD)
X X
Benefits covered: Outpatient hospital
physical health
X
Benefits covered: Outpatient hospital
behavioral health (MH and/or SUD)
X X
Benefits covered: Partial hospitalization X
Benefits covered: Physician X
Benefits covered: Nurse practitioner X
Benefits covered: Rural health clinics
and FQHCs
X
Benefits covered: Clinic services X
Benefits covered: Lab and x-ray X
Benefits covered: Prescription drugs X
Benefits covered: Prosthetic devices X
Benefits covered: EPSDT X
Benefits covered: Case management X
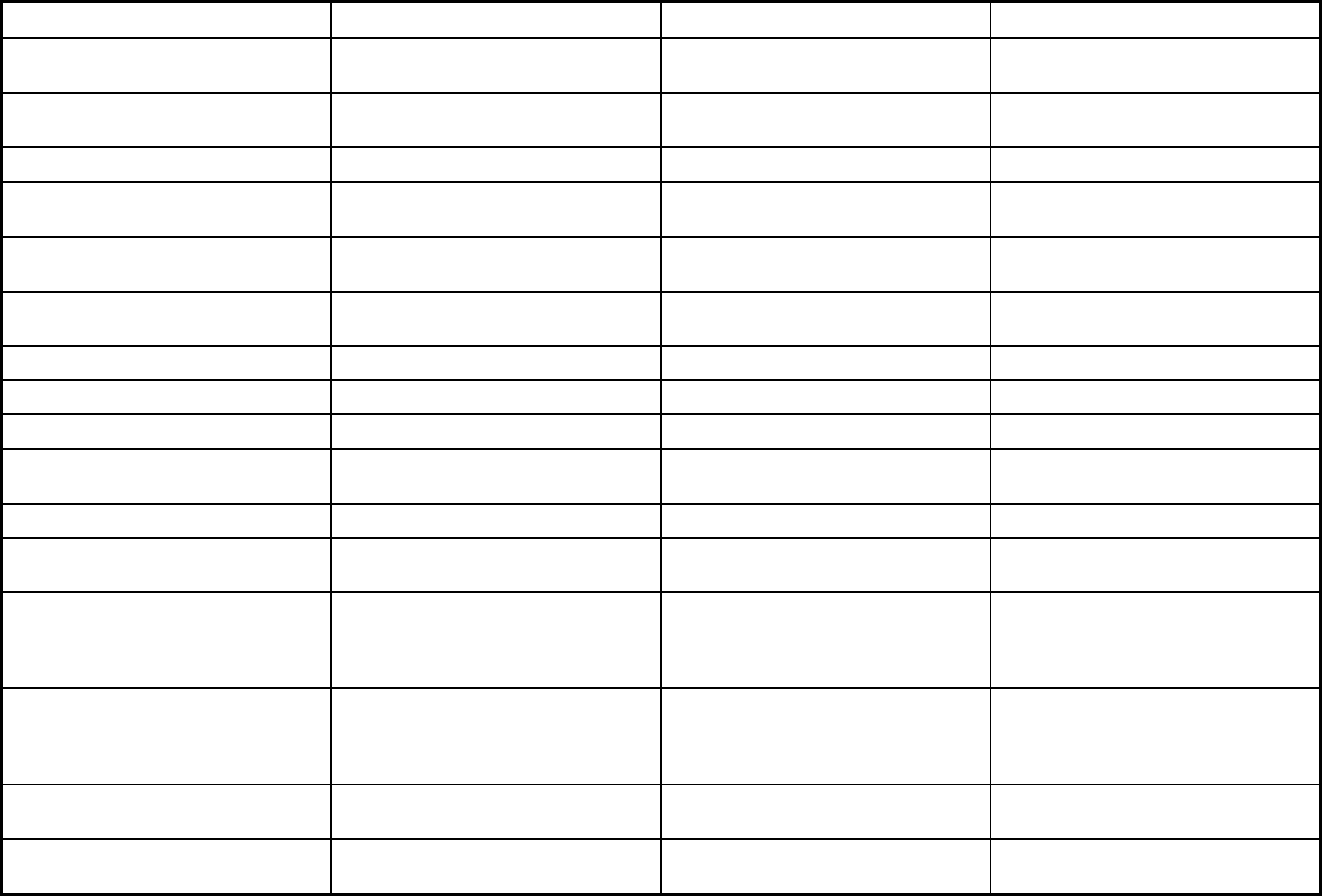
498
Features Prepaid Mental Health Dental UNI HOME
Benefits covered: SSA Section 1945-
authorized health home
Benefits covered: Health home care
(services in home)
X
Benefits covered: Family planning X
Benefits covered: Dental services
(medical/surgical)
Benefits covered: Dental (preventative
or corrective)
X
Benefits covered: Personal care (state
plan option)
Benefits covered: HCBS waiver services
Benefits covered: Private duty nursing X
Benefits covered: ICF-IDD
Benefits covered: Nursing facility
services
Benefits covered: Hospice care X
Benefits covered: Non-Emergency
Medical Transportation
Benefits covered: Institution for Mental
Disease inpatient treatment for people
ages 21-64 defined by 42 CFR
§438.6(e) as an 'in lieu of' benefit
Benefits covered: Other (e.g., nurse
midwife services, freestanding birth
centers, podiatry, etc.)
Vision, podiatry, dialysis, DME, inpatient
medical detox, nurse midwife services,
freestanding birth centers, ambulatory
surgical centers
Quality assurance and improvement:
HEDIS data required?
Yes Yes Yes
Quality assurance and improvement:
CAHPS data required?
Yes Yes Yes
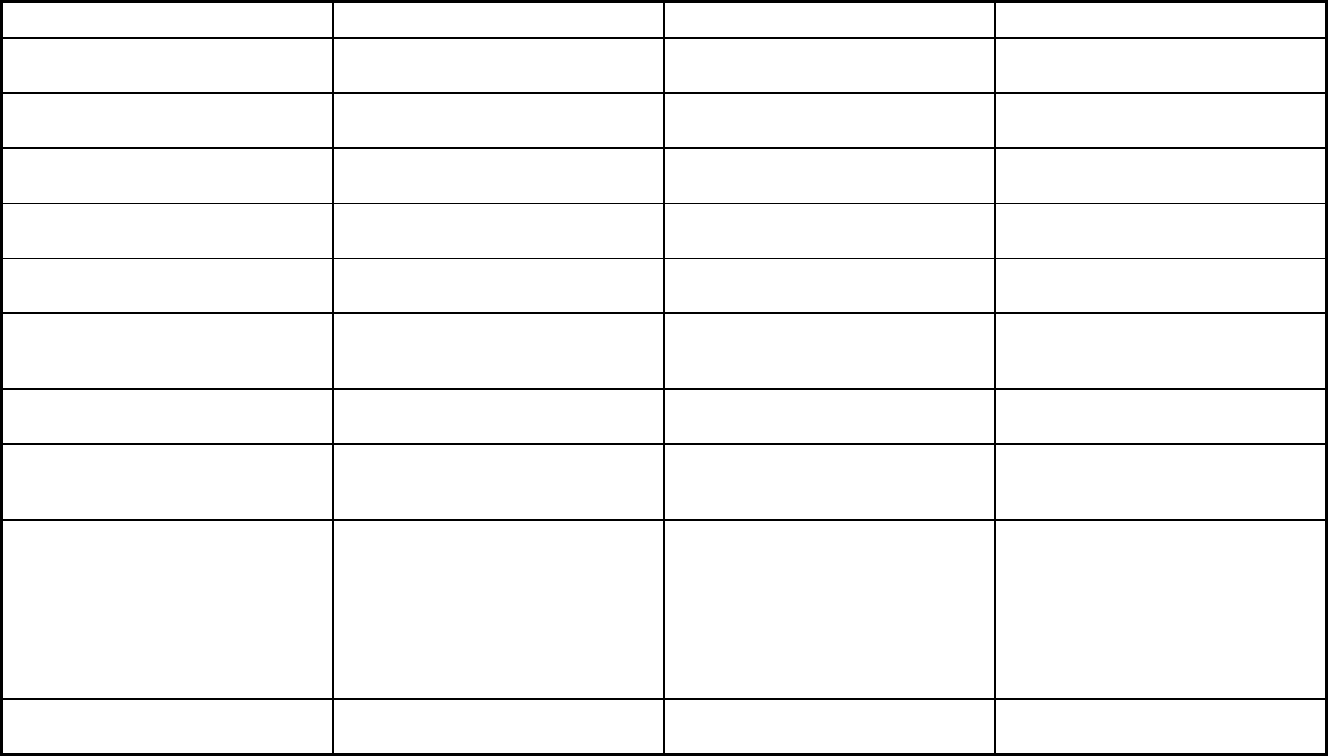
499
Features Prepaid Mental Health Dental UNI HOME
Quality assurance and improvement:
Accreditation required?
No No No
Quality assurance and improvement:
Accrediting organization
Quality assurance and improvement:
EQRO contractor name (if applicable)
Health Services Advisory Group Health Services Advisory Group
Performance incentives: Payment
bonuses/differentials to reward plans
Performance incentives: Preferential
auto-enrollment to reward plans
Performance incentives: Public reports
comparing plan performance on key
metrics
Performance incentives: Withholds tied
to performance metrics
Performance incentives: MCOs/PHPs
required or encouraged to pay providers
for value/quality outcomes
Participating plans: Plans in Program Bear River Mental Health; Central Utah
Mental Health; Davis Behavioral Health;
Four Corners Community Behavioral
Health; Northeastern Counseling;
Optum Health; Southwest Behavioral
Health; Valley Behavioral Health;
Wasatch Mental Health; Weber Mental
Health
Premier Access; Delta Dental HOME
Notes: Program notes Pregnant women are also covered
through this program.
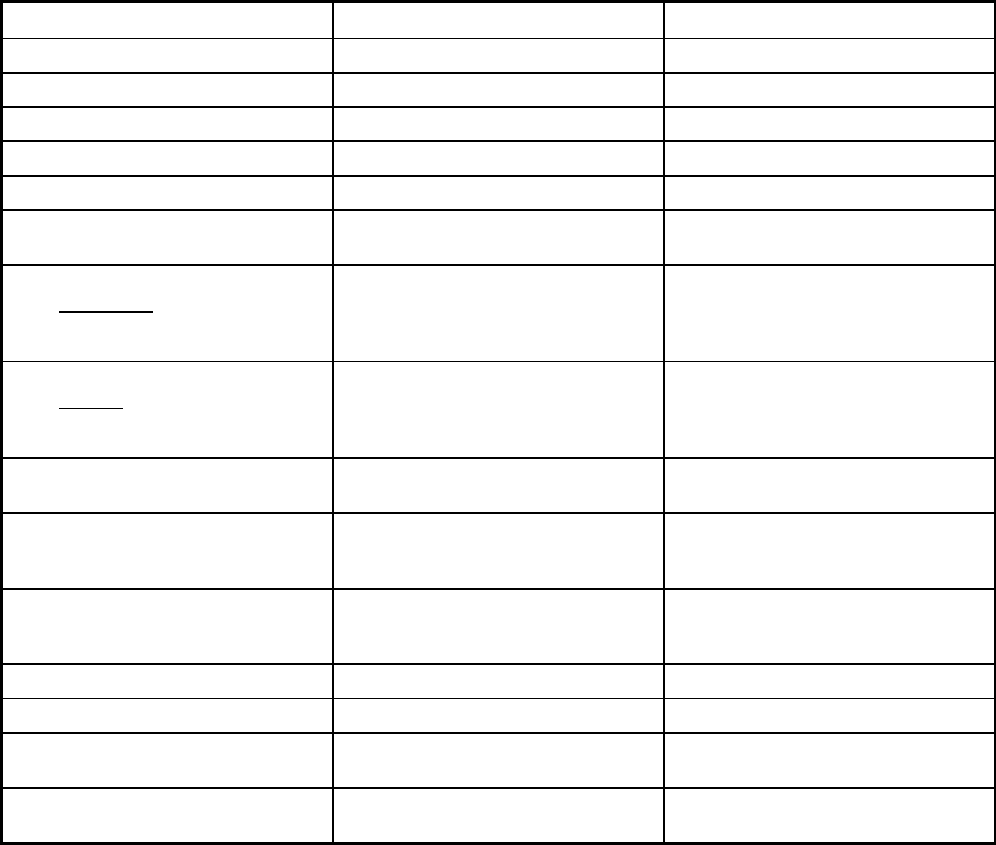
500
Utah Managed Care Program Features, as of 2018 (2 of 2)
Features Choice of Health Care Delivery Transportation
Program type Comprehensive MCO Non-Emergency Medical Transportation
Statewide or region-specific? Statewide Statewide
Federal operating authority 1915(b) 1902(a)(70) NEMT
Program start date 03/23/1983 07/12/2001
Waiver expiration date (if applicable) 06/30/2022
If the program ended in 2018, indicate
the end date
Populations enrolled: Low-income
adults not covered under ACA Section
VIII (excludes pregnant women and
people with disabilities)
Varies
Populations enrolled: Low-income
adults covered under ACA Section VIII
(excludes pregnant women and people
with disabilities)
Varies
Populations enrolled: Aged, Blind or
Disabled Children or Adults
Varies Mandatory
Populations enrolled: Non-Disabled
Children (excludes children in foster
care or receiving adoption assistance)
Varies Mandatory
Populations enrolled: Individuals
receiving Limited Benefits (excludes
partial duals)
Varies
Populations enrolled: Full Duals Varies Mandatory
Populations enrolled: Partial Duals Varies Mandatory
Populations enrolled: Children with
Special Health Care Needs
Varies Mandatory
Populations enrolled: Native
American/Alaskan Natives
Mandatory Voluntary

501
Features Choice of Health Care Delivery Transportation
Populations enrolled: Foster Care and
Adoption Assistance Children
Mandatory Mandatory
Populations enrolled: Enrollment choice
period
Other Pre-assigned
Populations enrolled: Enrollment broker
name (if applicable)
Populations enrolled: Notes on
enrollment choice period
15-45 days. Enrollment choice date will
vary depending on when the enrollment
file transaction takes place. In addition,
the enrollee will be able to change to
another plan within the first 90 days of
enrollment in the plan.
Benefits covered: Inpatient hospital
physical health
X
Benefits covered: Inpatient hospital
behavioral health (MH and/or SUD)
Benefits covered: Outpatient hospital
physical health
X
Benefits covered: Outpatient hospital
behavioral health (MH and/or SUD)
Benefits covered: Partial hospitalization X
Benefits covered: Physician X
Benefits covered: Nurse practitioner X
Benefits covered: Rural health clinics
and FQHCs
X
Benefits covered: Clinic services X
Benefits covered: Lab and x-ray X
Benefits covered: Prescription drugs X
Benefits covered: Prosthetic devices X
Benefits covered: EPSDT X
Benefits covered: Case management X
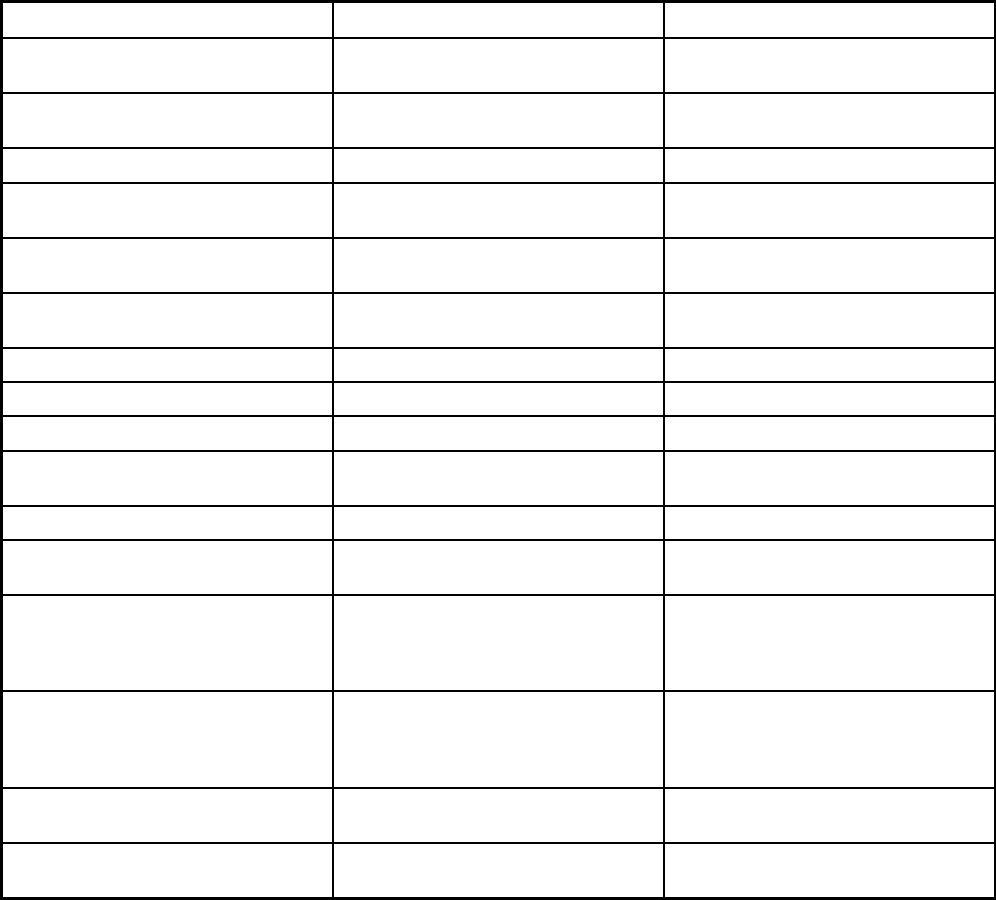
502
Features Choice of Health Care Delivery Transportation
Benefits covered: SSA Section 1945-
authorized health home
Benefits covered: Health home care
(services in home)
X
Benefits covered: Family planning X
Benefits covered: Dental services
(medical/surgical)
Benefits covered: Dental (preventative
or corrective)
Benefits covered: Personal care (state
plan option)
Benefits covered: HCBS waiver services
Benefits covered: Private duty nursing X
Benefits covered: ICF-IDD
Benefits covered: Nursing facility
services
Benefits covered: Hospice care X
Benefits covered: Non-Emergency
Medical Transportation
X
Benefits covered: Institution for Mental
Disease inpatient treatment for people
ages 21-64 defined by 42 CFR
§438.6(e) as an 'in lieu of' benefit
Benefits covered: Other (e.g., nurse
midwife services, freestanding birth
centers, podiatry, etc.)
Vision, podiatry, dialysis, DME, inpatient
medical detox, nurse midwife services,
freestanding birth centers, ambulatory
surgical centers
Quality assurance and improvement:
HEDIS data required?
Yes No
Quality assurance and improvement:
CAHPS data required?
Yes No
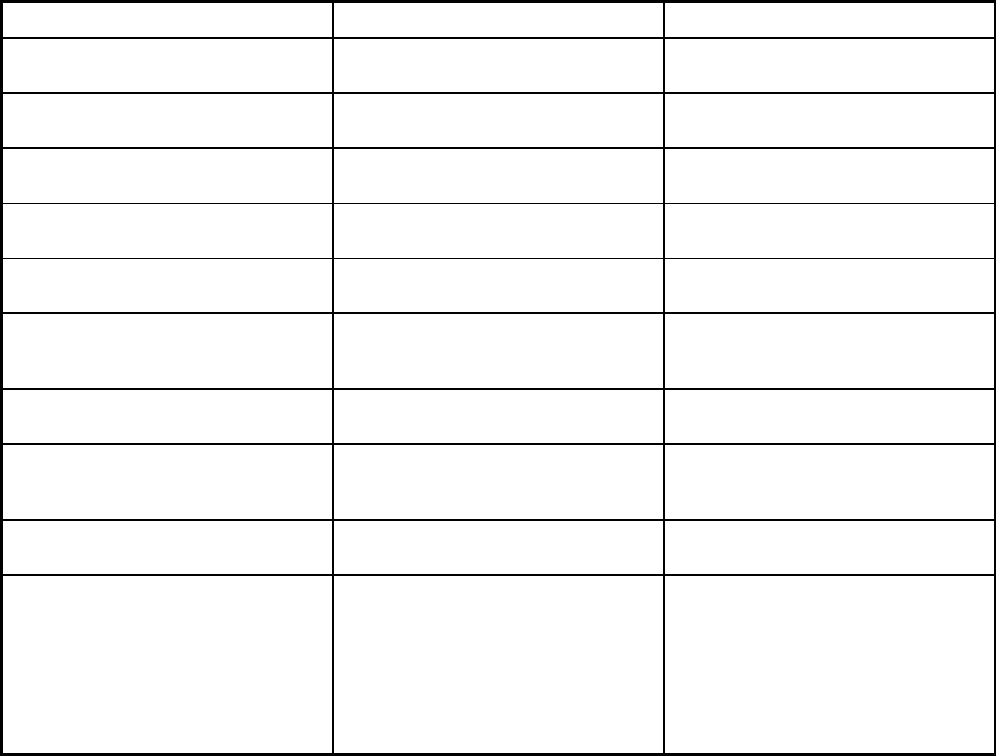
503
Features Choice of Health Care Delivery Transportation
Quality assurance and improvement:
Accreditation required?
No No
Quality assurance and improvement:
Accrediting organization
Quality assurance and improvement:
EQRO contractor name (if applicable)
Health Services Advisory Group
Performance incentives: Payment
bonuses/differentials to reward plans
Performance incentives: Preferential
auto-enrollment to reward plans
Performance incentives: Public reports
comparing plan performance on key
metrics
Performance incentives: Withholds tied
to performance metrics
Performance incentives: MCOs/PHPs
required or encouraged to pay providers
for value/quality outcomes
Participating plans: Plans in Program Healthy U; Molina; Health Choice;
SelectHealth
Logisticare Solutions
Notes: Program notes Enrollment is mandatory in the following
13 counties: Box Elder, Cache, Davis,
Iron, Morgan, Rich, Salt Lake, Summit,
Tooele, Utah, Wasatch, Washington,
and Weber. Enrollment is voluntary in all
other counties.
Specific Native American populations
are exempted from enrollment with the
contracted transportation provider by
race, and zip code and/or county code.
However, they are provided
transportation through other means.
Pregnant women are also covered
through this program.
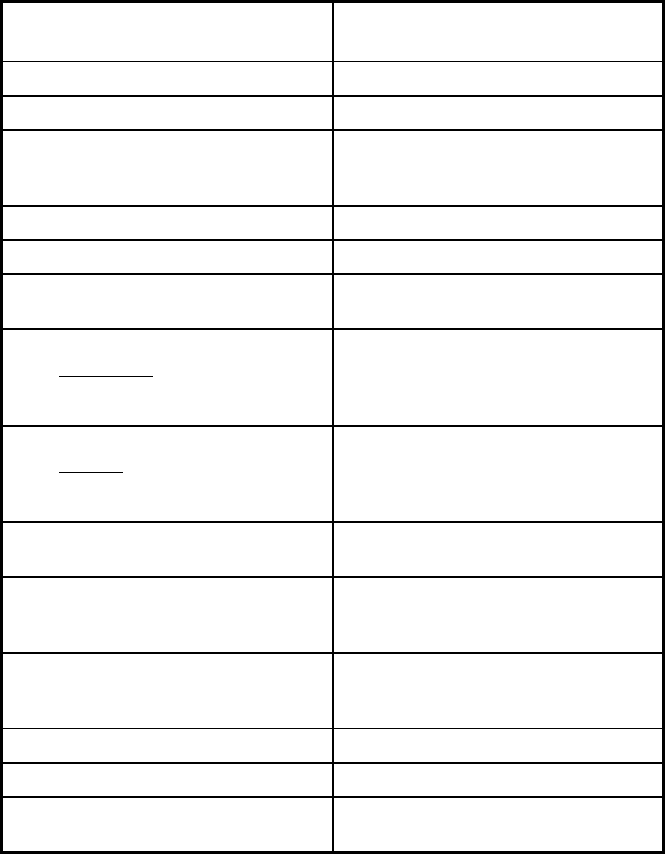
504
Vermont Managed Care Program Features, as of 2018
Features
Global Commitment to Health
Demonstration
Program type Comprehensive MCO + MLTSS
Statewide or region-specific? Statewide
Federal operating authority 1115(a) (Medicaid demonstration
waivers),1937 Alt Benefit Plan,1945
Health Homes
Program start date 10/01/2005
Waiver expiration date (if applicable) 12/31/2021
If the program ended in 2018, indicate
the end date
Populations enrolled: Low-income
adults not covered under ACA Section
VIII (excludes pregnant women and
people with disabilities)
Mandatory
Populations enrolled: Low-income
adults covered under ACA Section VIII
(excludes pregnant women and people
with disabilities)
Mandatory
Populations enrolled: Aged, Blind or
Disabled Children or Adults
Mandatory
Populations enrolled: Non-Disabled
Children (excludes children in foster
care or receiving adoption assistance)
Mandatory
Populations enrolled: Individuals
receiving Limited Benefits (excludes
partial duals)
Mandatory
Populations enrolled: Full Duals Mandatory
Populations enrolled: Partial Duals Mandatory
Populations enrolled: Children with
Special Health Care Needs
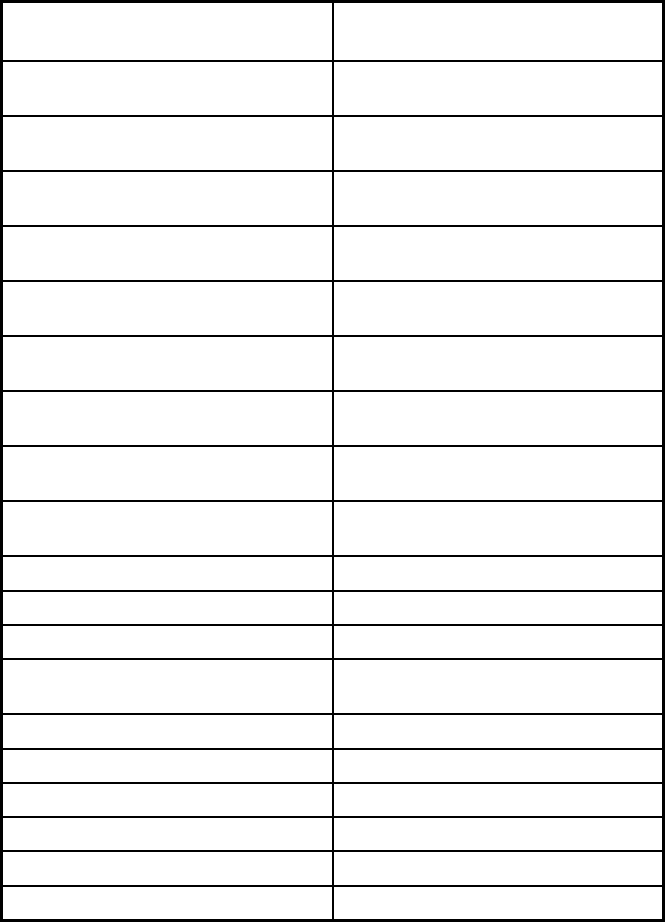
505
Features
Global Commitment to Health
Demonstration
Populations enrolled: Native
American/Alaskan Natives
Mandatory
Populations enrolled: Foster Care and
Adoption Assistance Children
Mandatory
Populations enrolled: Enrollment choice
period
Pre-assigned
Populations enrolled: Enrollment broker
name (if applicable)
Populations enrolled: Notes on
enrollment choice period
Benefits covered: Inpatient hospital
physical health
X
Benefits covered: Inpatient hospital
behavioral health (MH and/or SUD)
X
Benefits covered: Outpatient hospital
physical health
X
Benefits covered: Outpatient hospital
behavioral health (MH and/or SUD)
X
Benefits covered: Partial hospitalization X
Benefits covered: Physician X
Benefits covered: Nurse practitioner X
Benefits covered: Rural health clinics
and FQHCs
X
Benefits covered: Clinic services X
Benefits covered: Lab and x-ray X
Benefits covered: Prescription drugs X
Benefits covered: Prosthetic devices X
Benefits covered: EPSDT X
Benefits covered: Case management X
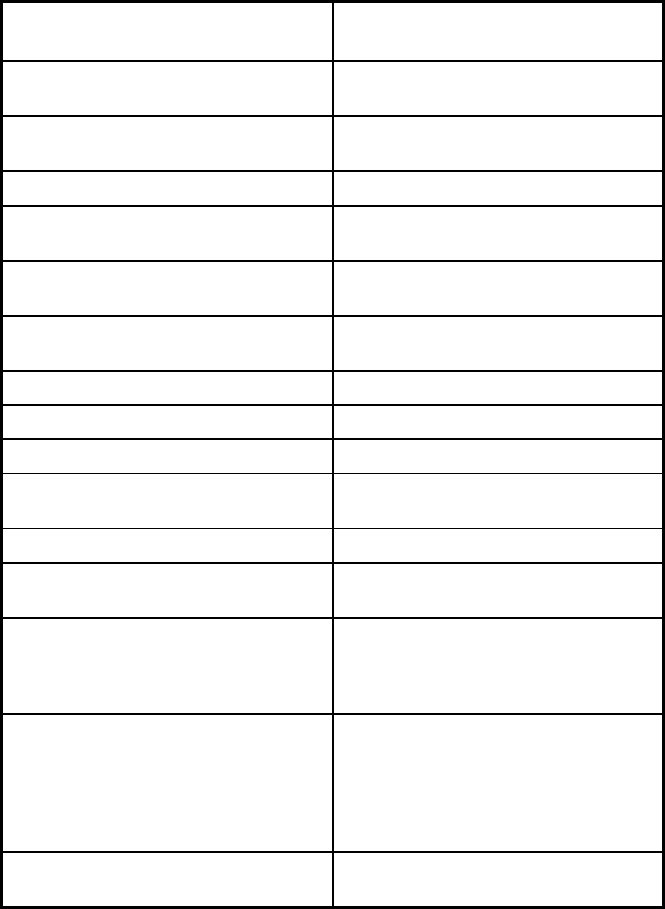
506
Features
Global Commitment to Health
Demonstration
Benefits covered: SSA Section 1945-
authorized health home
X
Benefits covered: Health home care
(services in home)
X
Benefits covered: Family planning X
Benefits covered: Dental services
(medical/surgical)
X
Benefits covered: Dental (preventative
or corrective)
X
Benefits covered: Personal care (state
plan option)
X
Benefits covered: HCBS waiver services X
Benefits covered: Private duty nursing X
Benefits covered: ICF-IDD X
Benefits covered: Nursing facility
services
X
Benefits covered: Hospice care X
Benefits covered: Non-Emergency
Medical Transportation
X
Benefits covered: Institution for Mental
Disease inpatient treatment for people
ages 21-64 defined by 42 CFR
§438.6(e) as an 'in lieu of' benefit
X
Benefits covered: Other (e.g., nurse
midwife services, freestanding birth
centers, podiatry, etc.)
Nurse midwives, chiropractic,
PT/OT/SP, tobacco cessation
counseling, optometrist services, high
tech nursing services, optician services,
naturopathic physician services, and
behavioral health services
Quality assurance and improvement:
HEDIS data required?
Yes
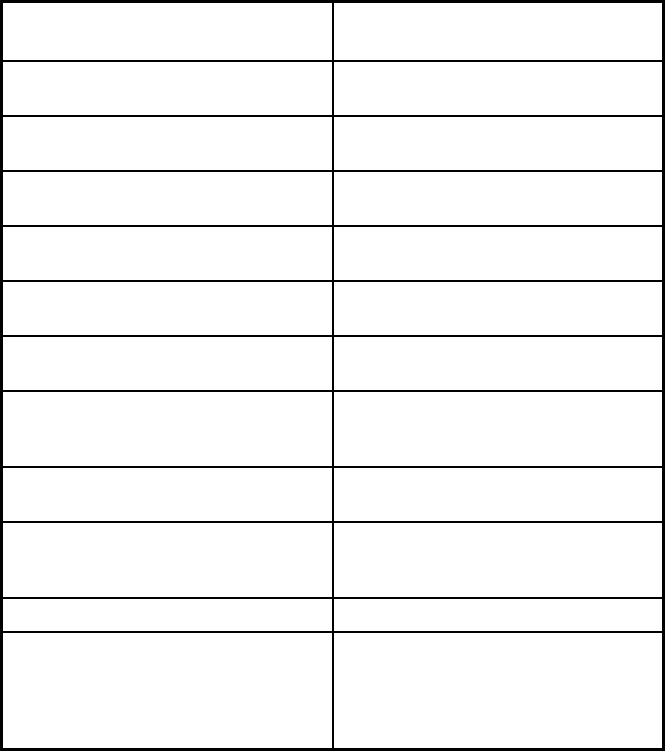
507
Features
Global Commitment to Health
Demonstration
Quality assurance and improvement:
CAHPS data required?
No
Quality assurance and improvement:
Accreditation required?
No
Quality assurance and improvement:
Accrediting organization
Quality assurance and improvement:
EQRO contractor name (if applicable)
Health Services Advisory Group
Performance incentives: Payment
bonuses/differentials to reward plans
Performance incentives: Preferential
auto-enrollment to reward plans
Performance incentives: Public reports
comparing plan performance on key
metrics
Performance incentives: Withholds tied
to performance metrics
X
Performance incentives: MCOs/PHPs
required or encouraged to pay providers
for value/quality outcomes
Participating plans: Plans in Program Department of Vermont Health Access
Notes: Program notes Health homes provide coordinated,
systemic, whole-person care to VT
Medicaid beneficiaries who receive
medication assisted therapy (MAT) for
opiod dependency.
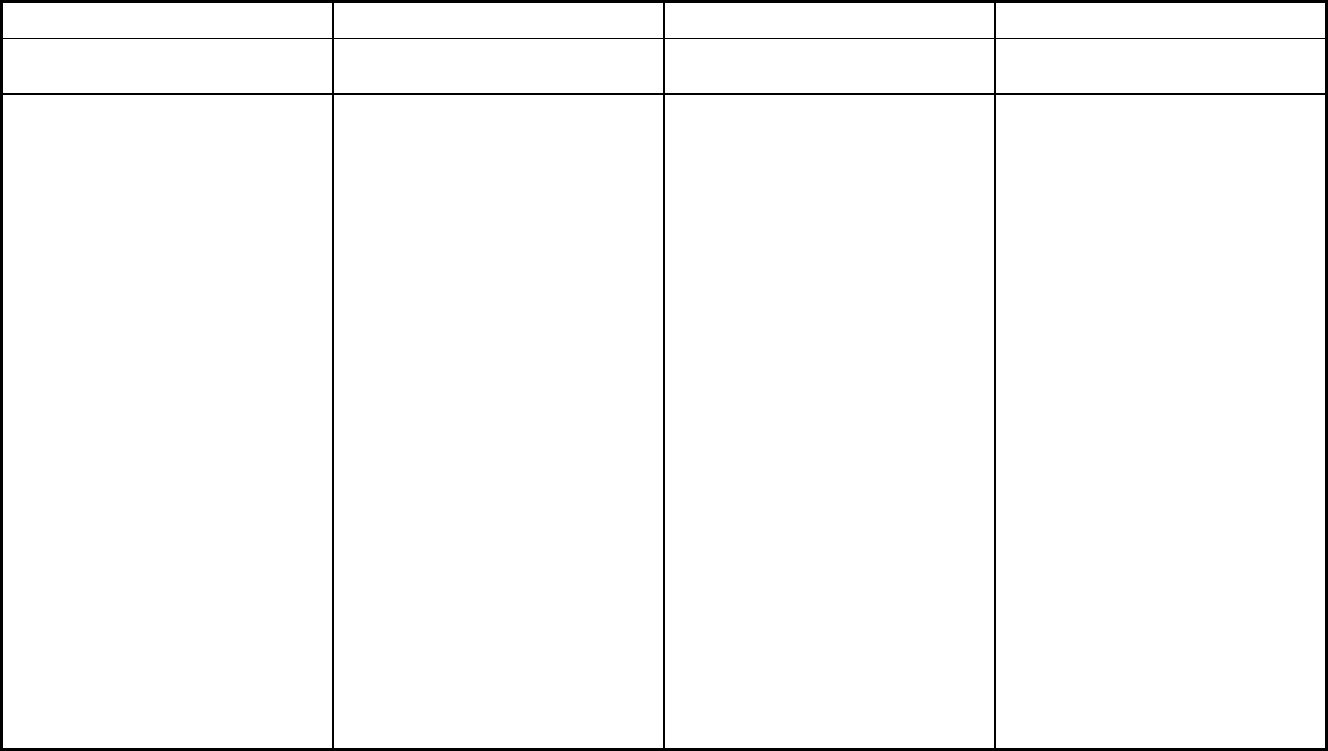
508
Virginia Managed Care Program Features, as of 2018
Features
CCC Plus
Medallion 3.0
DMAS PACE
Program type
Comprehensive MCO + MLTSS
Comprehensive MCO
Program of All-inclusive Care for the
Elderly (PACE)
Statewide or region-specific?
Statewide
Statewide
22901 22902 22903 22904 22911
22920 22922 22923 22931 22932
22935 22936 22937 22938 22940
22942 22943 22946 22947 22949
22958 22959 22963 22964 22967
22968 22969 22971 22973 22974
22976 23022 23024 23055 23065
23084 23093 23117 24464 24562
24590 23002 23004 23027 23040
23083 23123 23824 23894 23901
23909 23921 23922 22901 22902
22903 22904 22911 22920 22922
22923 22931 22932 22935 22936
22937 22938 22940 22942 22943
22946 22947 22949 22958 22959
22963 22964 22967 22968 22969
22971 22973 22974 22976 23022
23024 23055 23065 23084 23093
23117 24464 24562 24590 23002
23004 23027 23040 23083 23123
23824 23894 23901 23909 23921
23922 23923 23930 23934 23936
23937 23939 23941 23942 23943
23947 23952 23954 23955 23958
23959 23960 23963 23966 23974
23976 24599 24501 24502 24503
24504 24521 24522 24523 24536
24538 24550 24551 24553 24554
24556 24570 24572 24574 24588
24593 24054 24055 24069 24078
24082 24089 24102 24104 24112
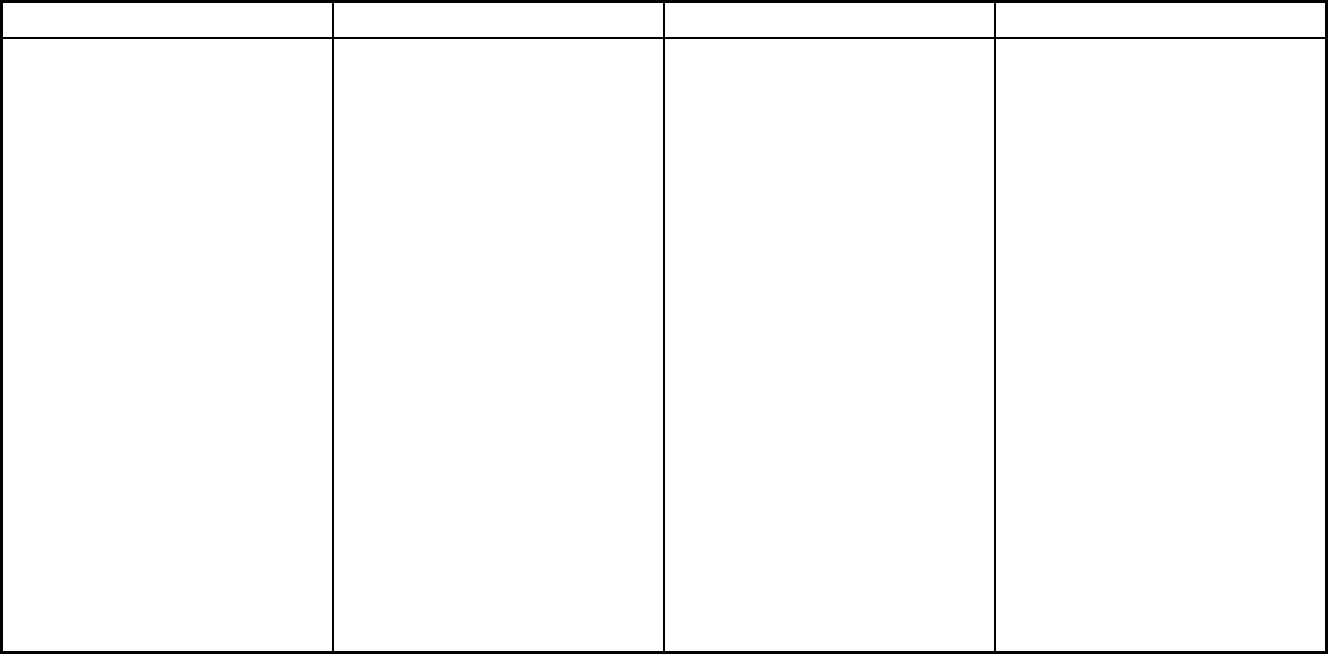
509
Features CCC Plus Medallion 3.0 DMAS PACE
Statewide or region-specific? (cont.) Statewide Statewide 24137 24139 24146 24148 24161
24165 24168 24517 24527 24528
24530 24531 24540 24541 24549
24557 24563 24565 24566 24569
24571 24586 24594 24133 24176
24543 24576 24011 24012 24013
24014 24015 24016 24017 24018
24019 24020 24059 24060 24064
24065 24066 24067 24070 24073
24077 24079 24083 24087 24090
24092 24095 24101 24121 24122
24138 24149 24151 24153 24162
24174 24175 24176 24179 24184
23112 23113 23114 23120 23124
23129 23139 23140 23141 23146
23173 23181 23221 23224 23225
23226 23227 23228 23231 23232
23234 23235 23236 23237 23238
23240 23241 23249 23260 23261
23269 23273 23274 23276 23278
23279 23282 23284 23285 23286
23289 23290 23291 23293 23295
22546 23005 23009 23011 23015
23030 23039 23047 23058 23059
23060 23069 23075 23086 23089
23102 23103 23106 23111 23116
23150 23162 23192 23218 23219
23220 23222 23223 23229
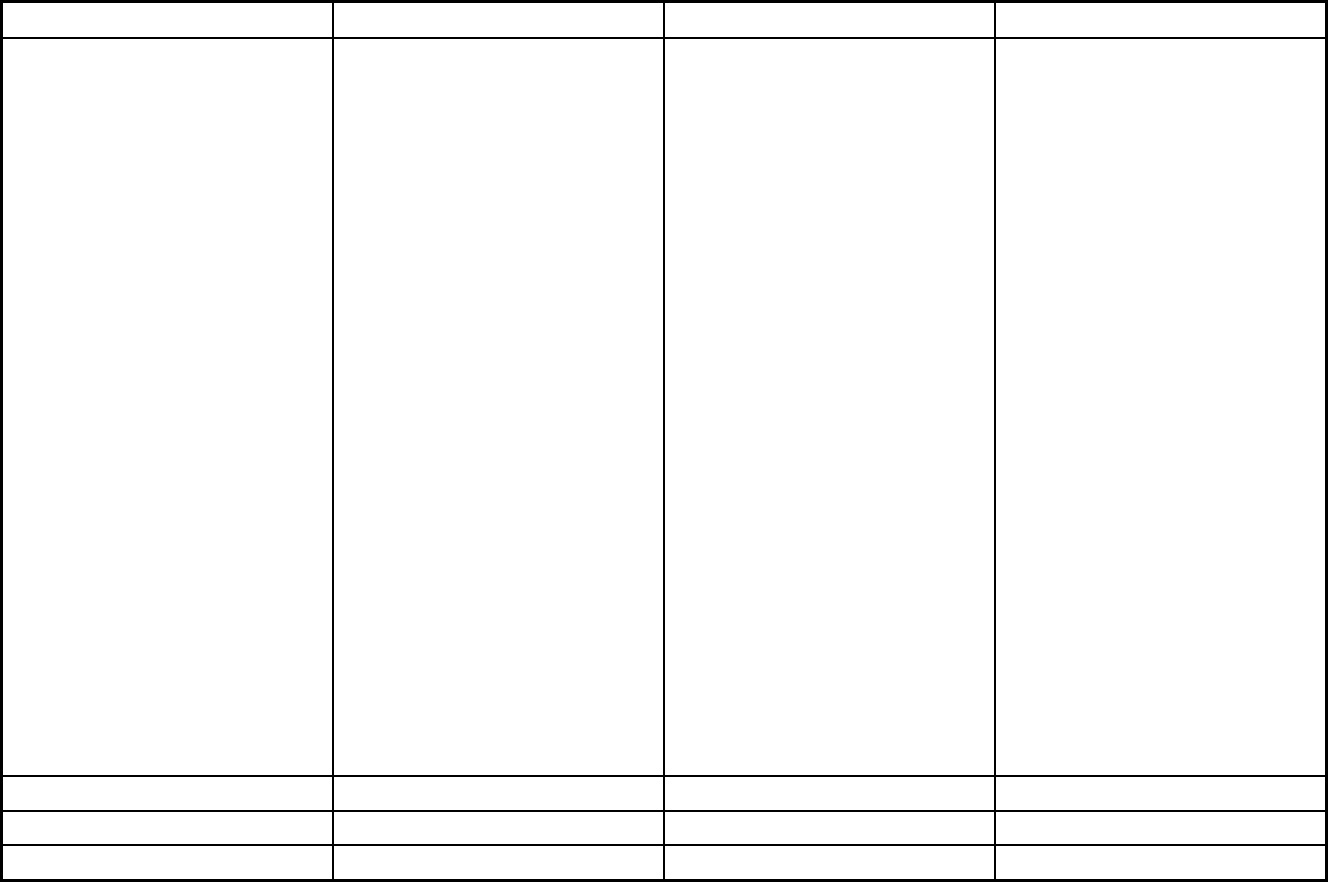
510
Features CCC Plus Medallion 3.0 DMAS PACE
Statewide or region-specific? (cont.) Statewide Statewide 23230 23233 23242 23250 23255
23288 23801 23803 23804 23805
23806 23830 23831 23832 23833
23834 23836 23838 23840 23841
23842 23850 23860 23875 23882
23885 23601 23605 23607 23651
23661 23662 23663 23664 23665
23666 23669 23602 23603 23604
23606 23608 23692 23693 23696
23320 23321 23322 23323 23324
23325 23432 23433 23434 23435
23436 23437 23438 23701 23702
23703 23704 23707 23709 23314
23315 23430 23487 23846 23851
23883 23898 23451 23452 23453
23454 23455 23456 23457 23459
23460 23461 23462 23463 23464
23502 23503 23504 23505 23507
23508 23509 23510 23511 23513
23517 23518 23521 23523 23529
24215 24216 24218 24219 24221
24230 24243 24244 24245 24246
24248 24250 24251 24258 24263
24265 24271 24273 24277 24279
24281 24282 24283 24290 24293
24217 24220 24224 24225 24226
24228 24237 24239 24256 24260
24266 24269 24272 24280 24377
24601 24602 24603 24604 24605
24606 24607 24608 24609 24612
24613 24614 24619 24620 24622
24624 24627 24628 24630 24631
24634 24635 24637 24639 24640
24641 24646 24647 24649 24651
24656 24657 24658
Federal operating authority 1915(b)/1915(c) 1915(b) PACE
Program start date 08/01/2017 07/01/2017 11/01/2007
Waiver expiration date (if applicable) 07/01/2022 06/30/2019
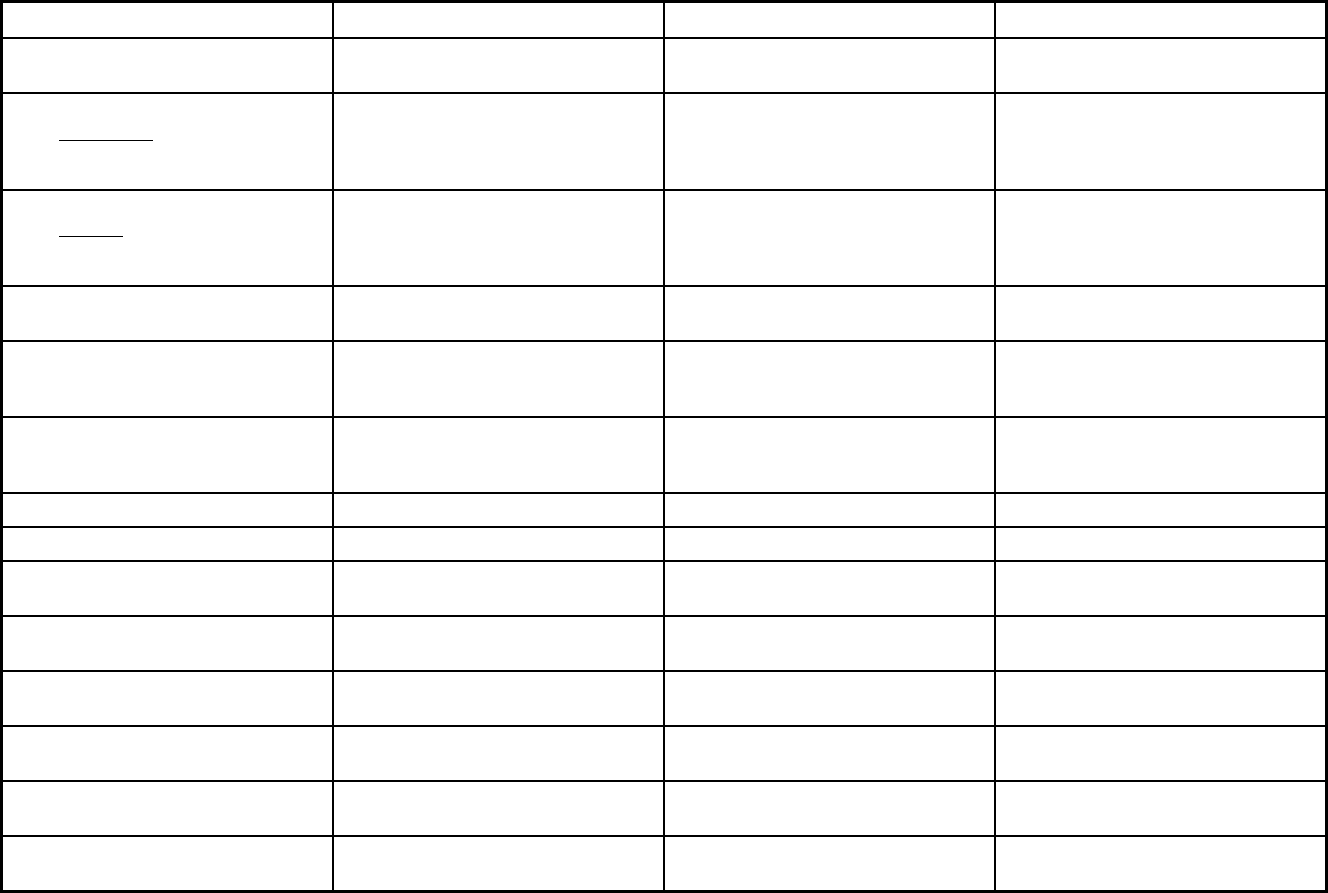
511
Features CCC Plus Medallion 3.0 DMAS PACE
If the program ended in 2018, indicate
the end date
Populations enrolled: Low-income
adults not covered under ACA Section
VIII (excludes pregnant women and
people with disabilities)
Mandatory Mandatory
Populations enrolled: Low-income
adults covered under ACA Section VIII
(excludes pregnant women and people
with disabilities)
Mandatory
Populations enrolled: Aged, Blind or
Disabled Children or Adults
Mandatory
Populations enrolled: Non-Disabled
Children (excludes children in foster
care or receiving adoption assistance)
Mandatory Mandatory
Populations enrolled: Individuals
receiving Limited Benefits (excludes
partial duals)
Populations enrolled: Full Duals Mandatory Voluntary
Populations enrolled: Partial Duals Voluntary
Populations enrolled: Children with
Special Health Care Needs
Mandatory Mandatory
Populations enrolled: Native
American/Alaskan Natives
Mandatory Exempt Voluntary
Populations enrolled: Foster Care and
Adoption Assistance Children
Mandatory Mandatory
Populations enrolled: Enrollment choice
period
Pre-assigned Pre-assigned N/A
Populations enrolled: Enrollment broker
name (if applicable)
Maximus Maximus
Populations enrolled: Notes on
enrollment choice period
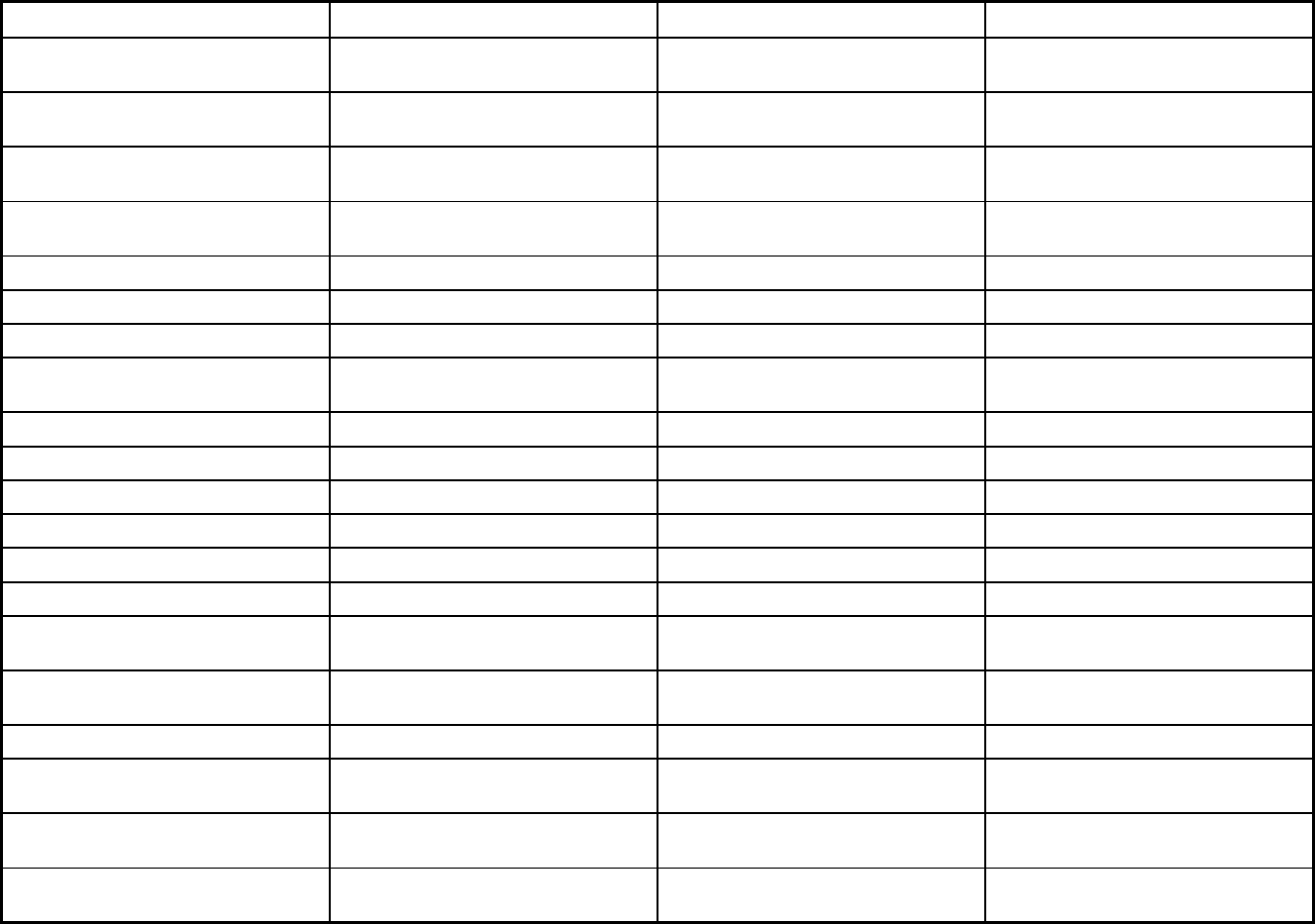
512
Features CCC Plus Medallion 3.0 DMAS PACE
Benefits covered: Inpatient hospital
physical health
X X X
Benefits covered: Inpatient hospital
behavioral health (MH and/or SUD)
X X X
Benefits covered: Outpatient hospital
physical health
X X
Benefits covered: Outpatient hospital
behavioral health (MH and/or SUD)
X X
Benefits covered: Partial hospitalization X X
Benefits covered: Physician X X X
Benefits covered: Nurse practitioner X X X
Benefits covered: Rural health clinics
and FQHCs
X X
Benefits covered: Clinic services X X X
Benefits covered: Lab and x-ray X X X
Benefits covered: Prescription drugs X X X
Benefits covered: Prosthetic devices X X
Benefits covered: EPSDT X X
Benefits covered: Case management X X X
Benefits covered: SSA Section 1945-
authorized health home
Benefits covered: Health home care
(services in home)
X X X
Benefits covered: Family planning X X
Benefits covered: Dental services
(medical/surgical)
X X X
Benefits covered: Dental (preventative
or corrective)
Benefits covered: Personal care (state
plan option)
X X X
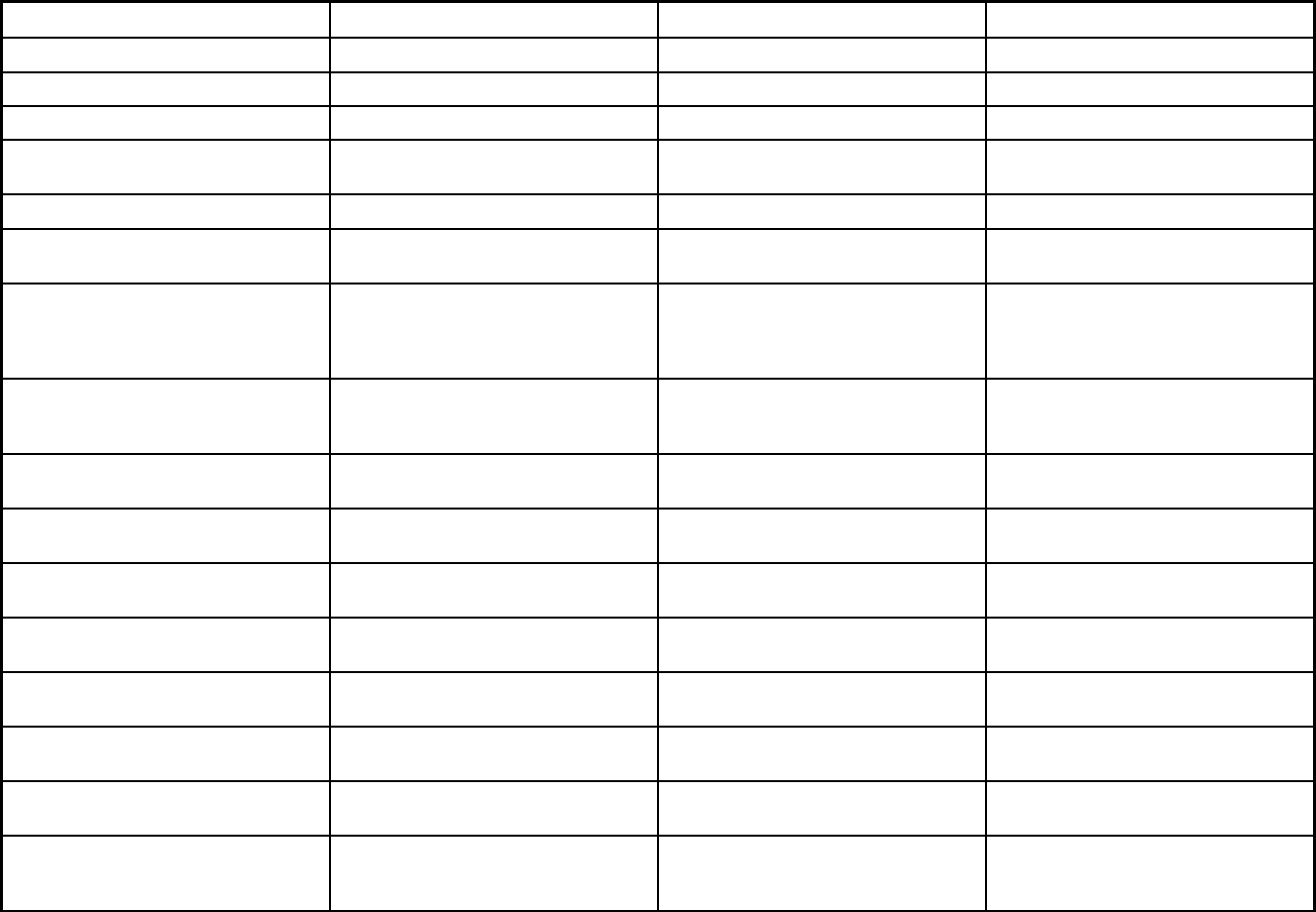
513
Features CCC Plus Medallion 3.0 DMAS PACE
Benefits covered: HCBS waiver services X
Benefits covered: Private duty nursing X
Benefits covered: ICF-IDD
Benefits covered: Nursing facility
services
X X
Benefits covered: Hospice care X X
Benefits covered: Non-Emergency
Medical Transportation
X X
Benefits covered: Institution for Mental
Disease inpatient treatment for people
ages 21-64 defined by 42 CFR
§438.6(e) as an 'in lieu of' benefit
Benefits covered: Other (e.g., nurse
midwife services, freestanding birth
centers, podiatry, etc.)
Quality assurance and improvement:
HEDIS data required?
Yes Yes No
Quality assurance and improvement:
CAHPS data required?
Yes Yes No
Quality assurance and improvement:
Accreditation required?
Yes Yes No
Quality assurance and improvement:
Accrediting organization
NCQA NCQA JCAHO
Quality assurance and improvement:
EQRO contractor name (if applicable)
HSAG HSAG
Performance incentives: Payment
bonuses/differentials to reward plans
X X
Performance incentives: Preferential
auto-enrollment to reward plans
Performance incentives: Public reports
comparing plan performance on key
metrics
X
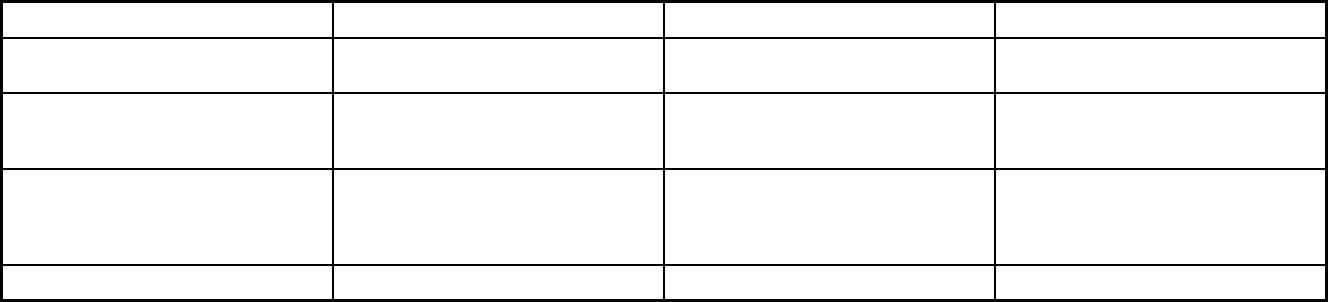
514
Features CCC Plus Medallion 3.0 DMAS PACE
Performance incentives: Withholds tied
to performance metrics
X X
Performance incentives: MCOs/PHPs
required or encouraged to pay providers
for value/quality outcomes
X X
Participating plans: Plans in Program Aetna Better Health for Virginia; Anthem
HealthKeepers; Magellan Complete
Care of Virginia; Optima Health; United
Health Care; Virginia Premier
Virginia Premier Health Plan; Anthem;
Intotal Health; Kaiser; Optima Health
Care; Coventry Health Plan
Innovage; Mountain Empire/All Care
PACE; INOVA PACE; Riverside PACE;
Innovage PACE; Centra PACE; Sentara
PACE
Notes: Program notes
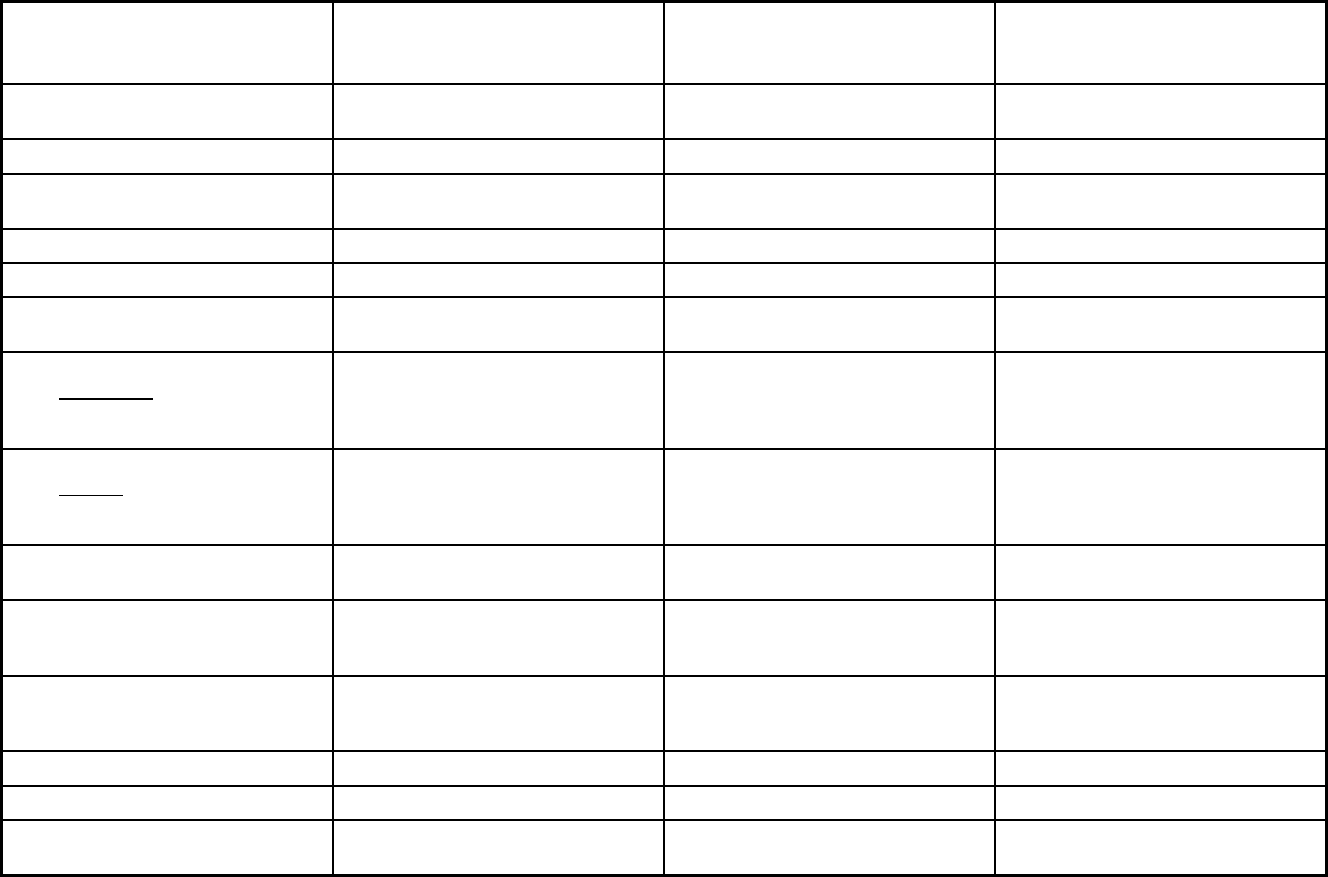
515
Washington Managed Care Program Features, as of 2018 (1 of 3)
Features
Washington State Integrated
Community Mental Health Program
(ICMH) NEMT Apple Health
Program type Behavioral Health Organization (BHO)
only (PIHP and/or PAHP)
Non-Emergency Medical Transportation Comprehensive MCO
Statewide or region-specific? Statewide Statewide Statewide
Federal operating authority 1115(a) (Medicaid demonstration
waivers)
1902(a)(70) NEMT 1932(a)
Program start date 10/01/2014 10/01/2008 07/01/1994
Waiver expiration date (if applicable) 12/31/2022
If the program ended in 2018, indicate
the end date
Populations enrolled: Low-income
adults not covered under ACA Section
VIII (excludes pregnant women and
people with disabilities)
Mandatory
Populations enrolled: Low-income
adults covered under ACA Section VIII
(excludes pregnant women and people
with disabilities)
Mandatory Mandatory Mandatory
Populations enrolled: Aged, Blind or
Disabled Children or Adults
Mandatory Mandatory Mandatory
Populations enrolled: Non-Disabled
Children (excludes children in foster
care or receiving adoption assistance)
Mandatory Mandatory Mandatory
Populations enrolled: Individuals
receiving Limited Benefits (excludes
partial duals)
Mandatory
Populations enrolled: Full Duals Mandatory Mandatory
Populations enrolled: Partial Duals Mandatory Mandatory
Populations enrolled: Children with
Special Health Care Needs
Mandatory Mandatory Mandatory
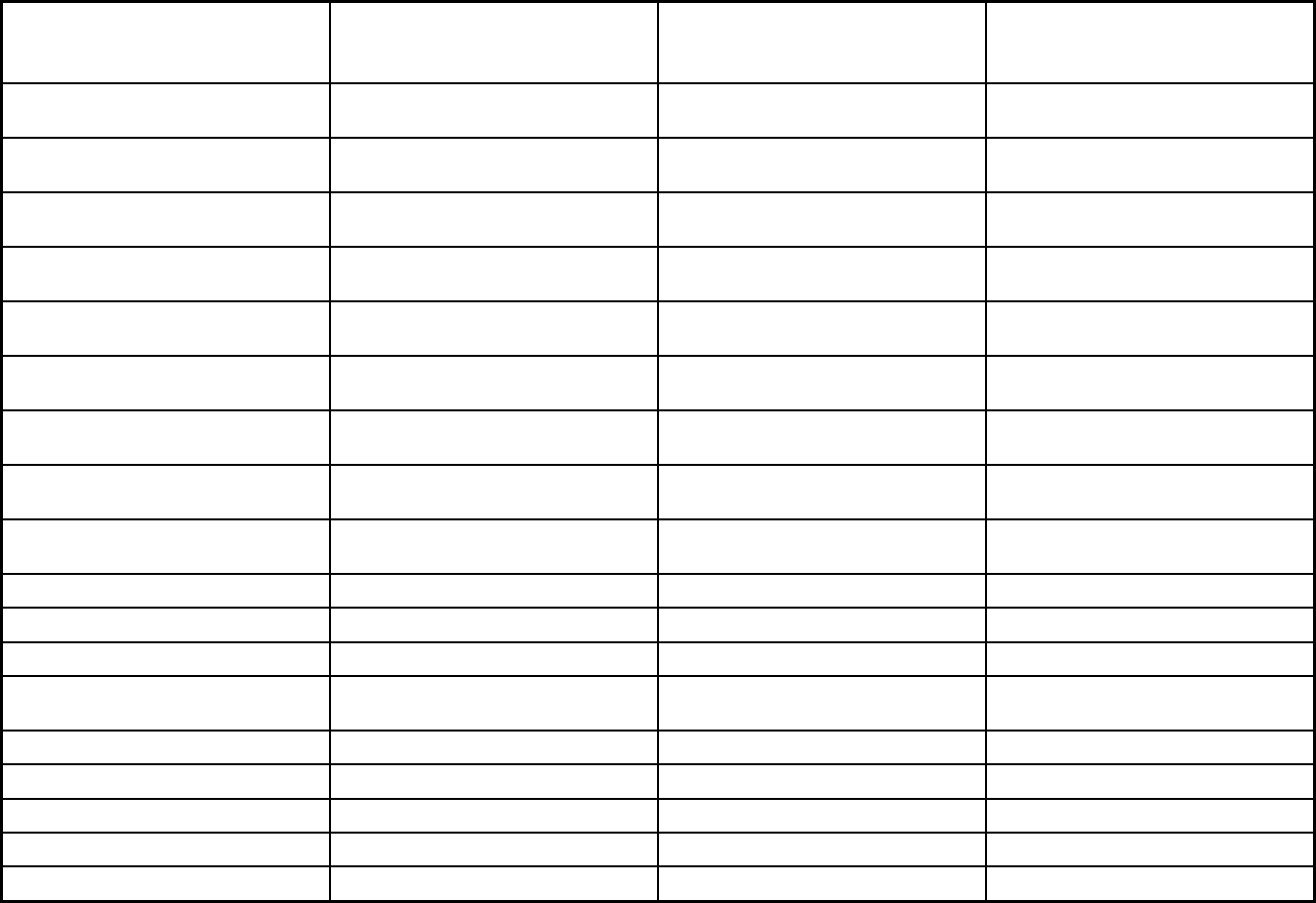
516
Features
Washington State Integrated
Community Mental Health Program
(ICMH) NEMT Apple Health
Populations enrolled: Native
American/Alaskan Natives
Voluntary Mandatory Voluntary
Populations enrolled: Foster Care and
Adoption Assistance Children
Mandatory Mandatory Voluntary
Populations enrolled: Enrollment choice
period
Pre-assigned Other
Populations enrolled: Enrollment broker
name (if applicable)
Regional Support Networks
Populations enrolled: Notes on
enrollment choice period
Enrollment open continuously
Benefits covered: Inpatient hospital
physical health
X
Benefits covered: Inpatient hospital
behavioral health (MH and/or SUD)
Benefits covered: Outpatient hospital
physical health
X
Benefits covered: Outpatient hospital
behavioral health (MH and/or SUD)
X X
Benefits covered: Partial hospitalization X X
Benefits covered: Physician X
Benefits covered: Nurse practitioner X
Benefits covered: Rural health clinics
and FQHCs
X X
Benefits covered: Clinic services X X
Benefits covered: Lab and x-ray X
Benefits covered: Prescription drugs X
Benefits covered: Prosthetic devices X
Benefits covered: EPSDT X X
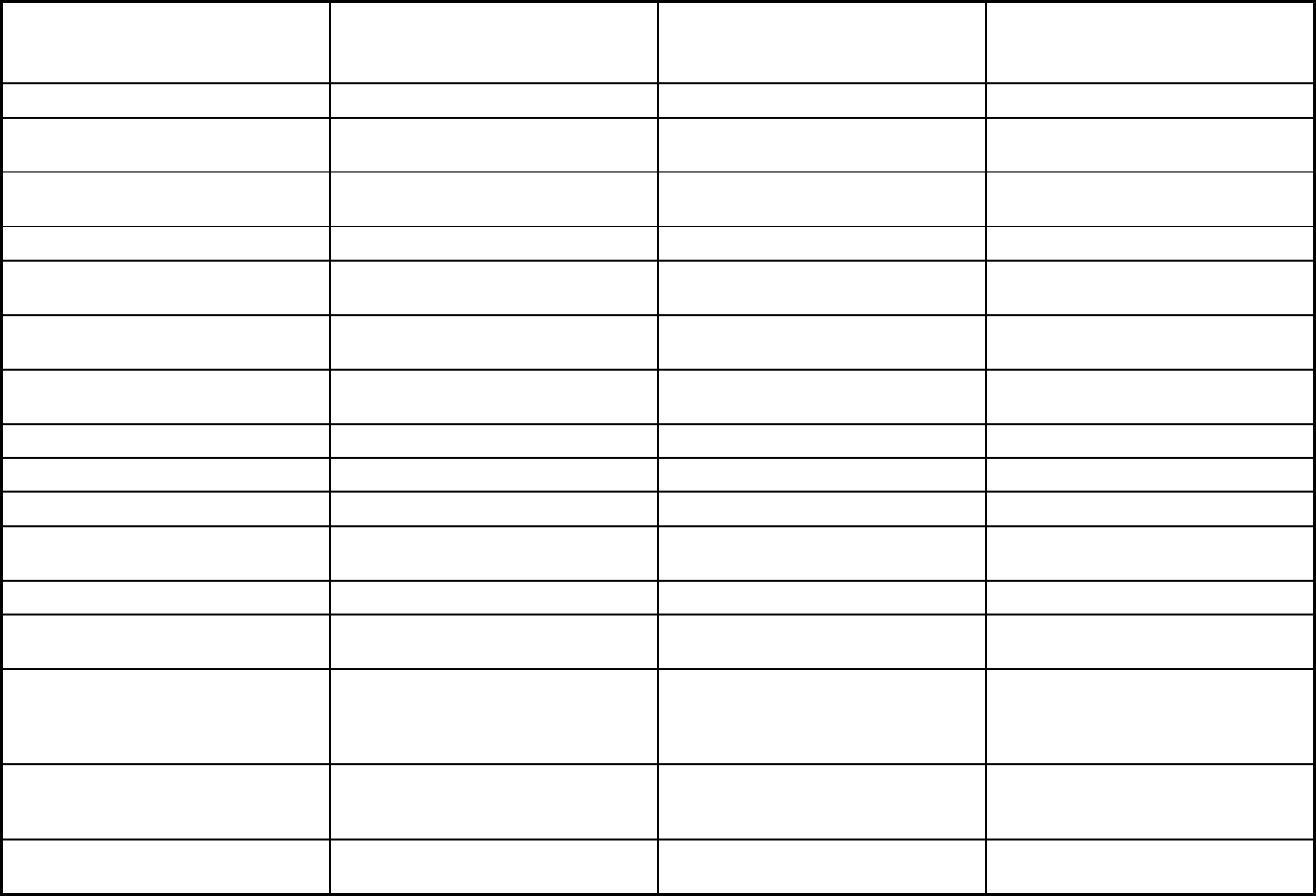
517
Features
Washington State Integrated
Community Mental Health Program
(ICMH) NEMT Apple Health
Benefits covered: Case management X X
Benefits covered: SSA Section 1945-
authorized health home
Benefits covered: Health home care
(services in home)
X
Benefits covered: Family planning X
Benefits covered: Dental services
(medical/surgical)
X
Benefits covered: Dental (preventative
or corrective)
Benefits covered: Personal care (state
plan option)
Benefits covered: HCBS waiver services
Benefits covered: Private duty nursing X
Benefits covered: ICF-IDD
Benefits covered: Nursing facility
services
X
Benefits covered: Hospice care X
Benefits covered: Non-Emergency
Medical Transportation
X X
Benefits covered: Institution for Mental
Disease inpatient treatment for people
ages 21-64 defined by 42 CFR
§438.6(e) as an 'in lieu of' benefit
Benefits covered: Other (e.g., nurse
midwife services, freestanding birth
centers, podiatry, etc.)
Quality assurance and improvement:
HEDIS data required?
No No Yes
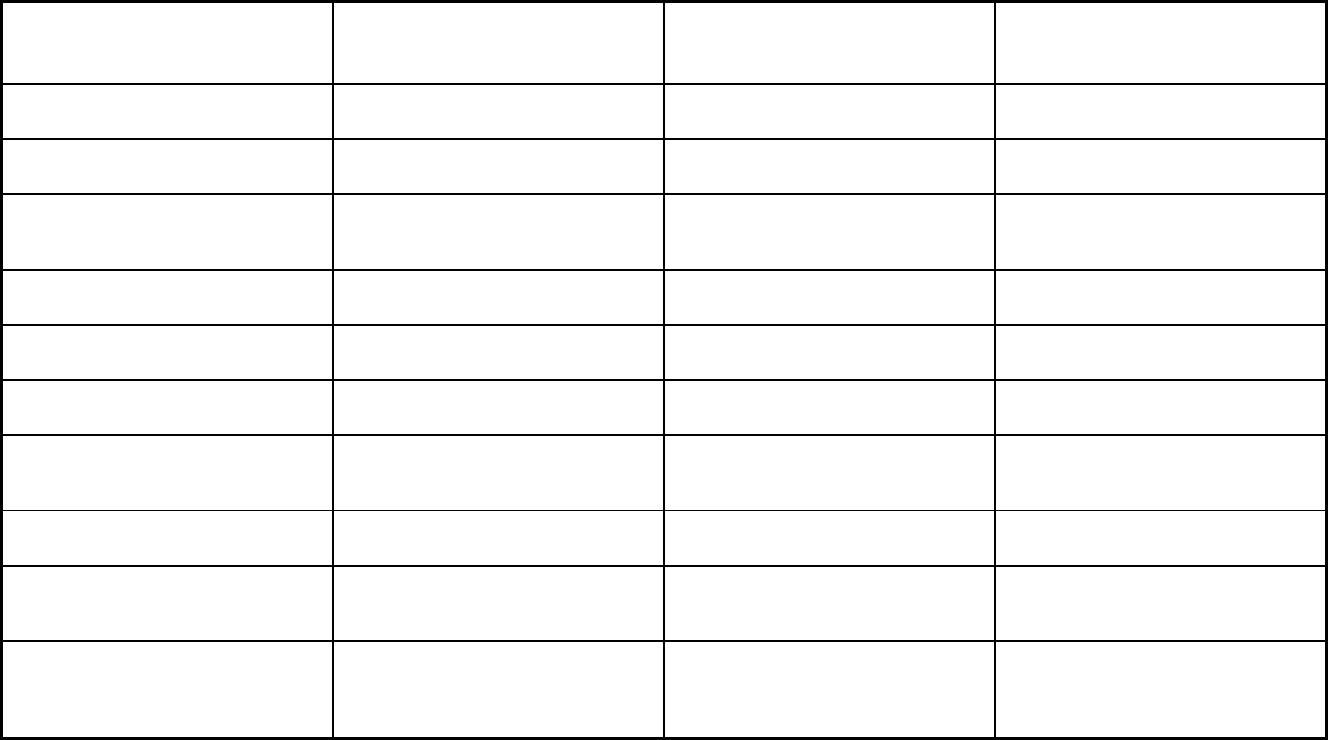
518
Features
Washington State Integrated
Community Mental Health Program
(ICMH) NEMT Apple Health
Quality assurance and improvement:
CAHPS data required?
No No Yes
Quality assurance and improvement:
Accreditation required?
Yes No Yes
Quality assurance and improvement:
Accrediting organization
Regional support network's contract with
accredited community mental health
agencies.
NCQA
Quality assurance and improvement:
EQRO contractor name (if applicable)
Qualis Health Qualis
Performance incentives: Payment
bonuses/differentials to reward plans
X
Performance incentives: Preferential
auto-enrollment to reward plans
Performance incentives: Public reports
comparing plan performance on key
metrics
Performance incentives: Withholds tied
to performance metrics
Performance incentives: MCOs/PHPs
required or encouraged to pay providers
for value/quality outcomes
Participating plans: Plans in Program BHO Multiple Transportation Brokers Amerigroup; Community Health Plan of
Washington; Coordinated Care of
Washington; Molina Health Care of
Washington; United Health Care
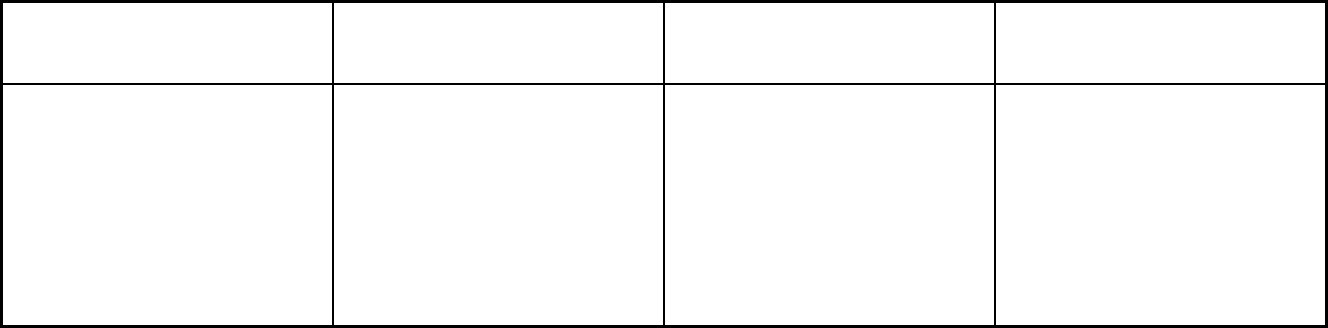
519
Features
Washington State Integrated
Community Mental Health Program
(ICMH) NEMT Apple Health
Notes: Program notes Effective 07/01/2017: The AI/AN
population was removed from
mandatory enrollment in behavioral
health managed care. That meant the
majority of AI/AN individuals were
transferred to the FFS system for
behavioral health. That FFS system is
not part of the waiver. The 1115 waiver
(an amendment to the larger 1115) that
allows us to use federal funds in SUD
IMDs was effective 7/1/2018.
Brokers are based on county. NEMT is
provided for anyone covered on
Medicaid that meet the enrollment
criteria.
Please note managed care plans only
cover rehabilitation care in nursing
home facilities. Custodial care is is
covered under FFS.
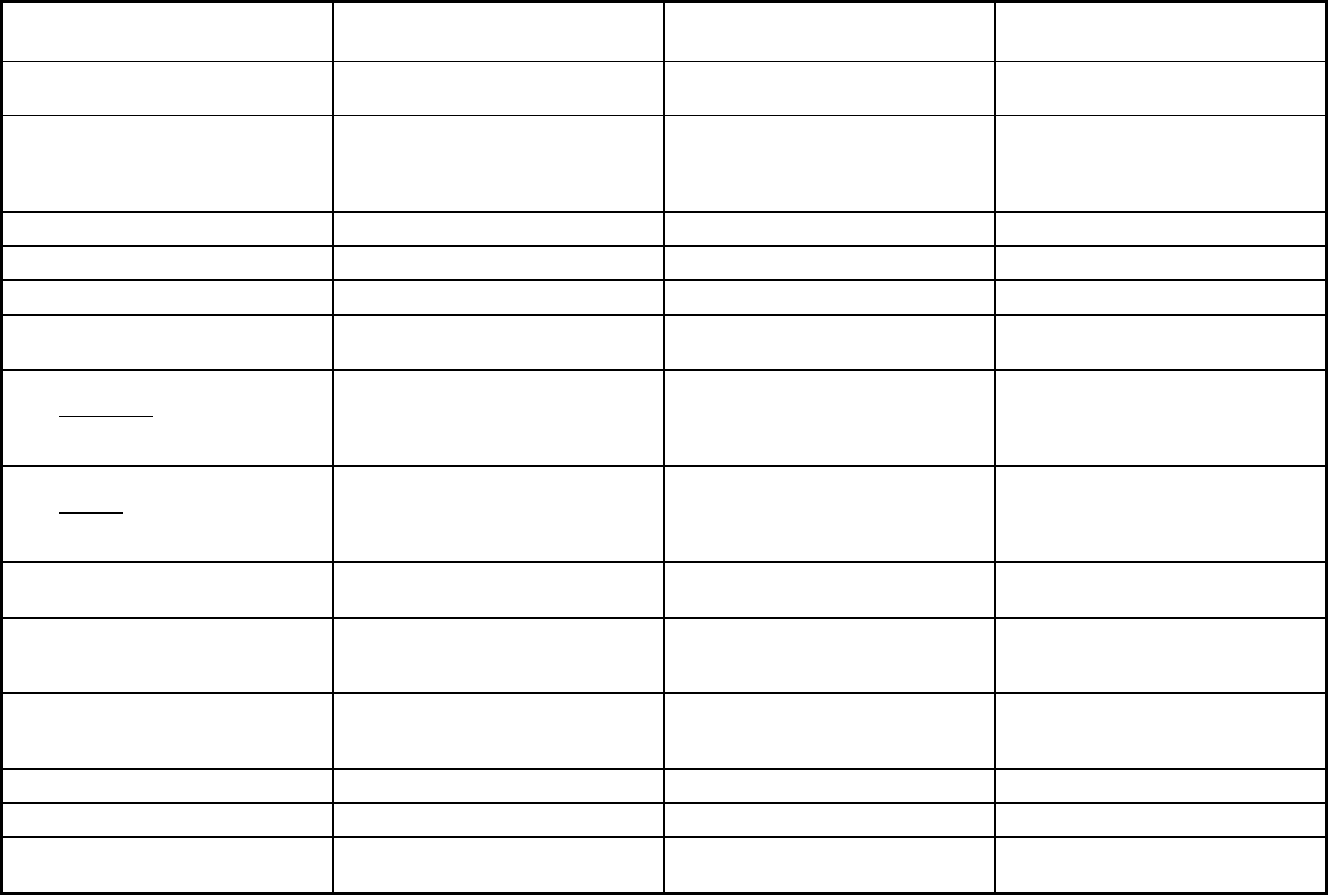
520
Washington Managed Care Program Features, as of 2018 (2 of 3)
Features Healthy Options - Blind Disabled
Behavioral Health Services Only
(BHSO) PCCM
Program type Comprehensive MCO Behavioral Health Organization (BHO)
only (PIHP and/or PAHP)
Primary Care Case Management
(PCCM)
Statewide or region-specific? Statewide Chelan, Clark, Douglas, Grant, and
Skamania Counties
Clallam, Grays Harbor, King,
Snohomish, Whatcom, Okanogan,
Ferry, Stevens, Lincoln, Spokane,
Benton and Yakima Counties
Federal operating authority 1932(a) 1915(b) 1932(a)
Program start date 07/01/2012 04/01/2016 07/01/1995
Waiver expiration date (if applicable) 06/30/2022
If the program ended in 2018, indicate
the end date
Populations enrolled: Low-income
adults not covered under ACA Section
VIII (excludes pregnant women and
people with disabilities)
Populations enrolled: Low-income
adults covered under ACA Section VIII
(excludes pregnant women and people
with disabilities)
Mandatory Voluntary
Populations enrolled: Aged, Blind or
Disabled Children or Adults
Mandatory Mandatory Voluntary
Populations enrolled: Non-Disabled
Children (excludes children in foster
care or receiving adoption assistance)
Mandatory
Populations enrolled: Individuals
receiving Limited Benefits (excludes
partial duals)
Populations enrolled: Full Duals Mandatory
Populations enrolled: Partial Duals
Populations enrolled: Children with
Special Health Care Needs
Mandatory Mandatory Voluntary
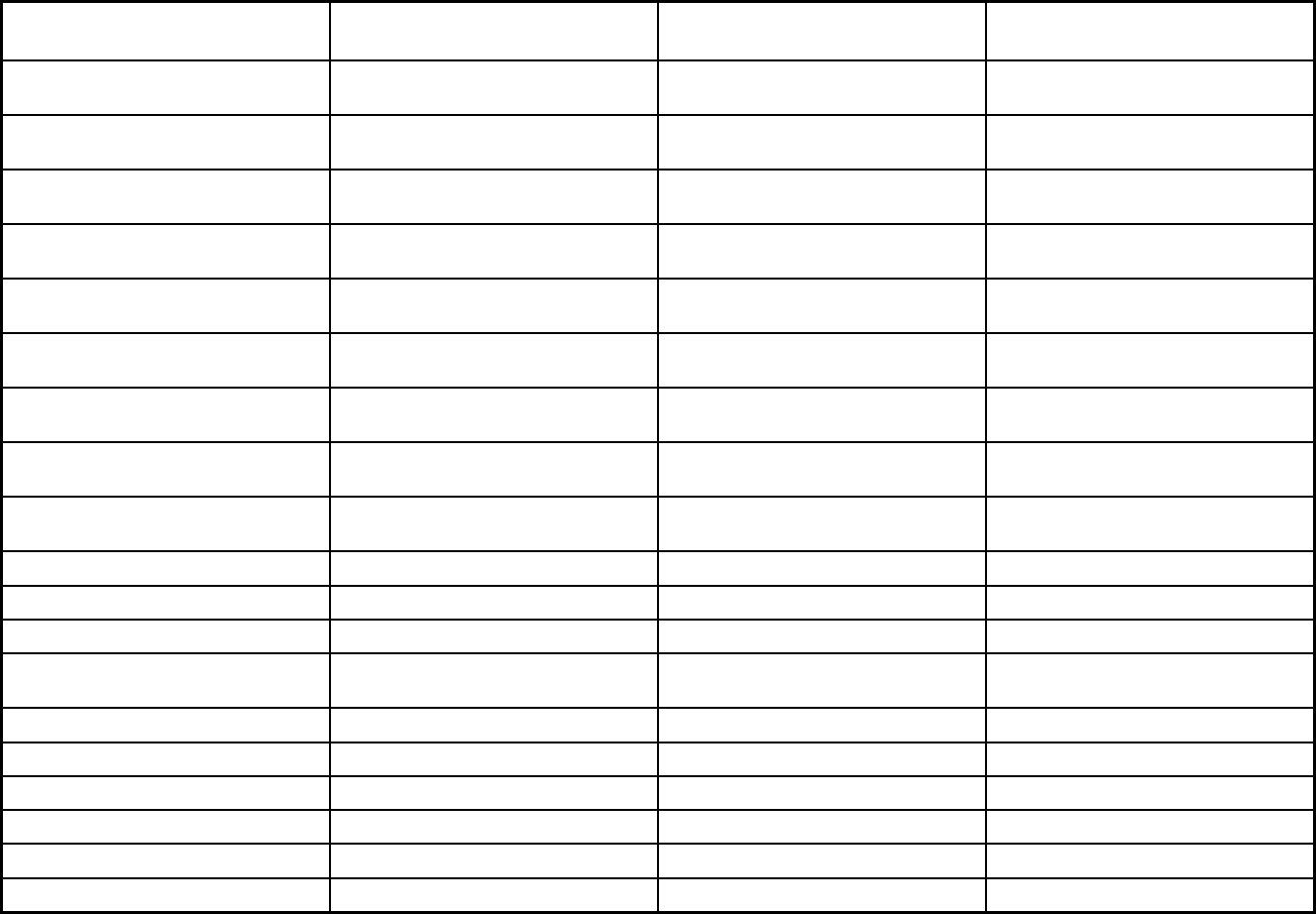
521
Features Healthy Options - Blind Disabled
Behavioral Health Services Only
(BHSO) PCCM
Populations enrolled: Native
American/Alaskan Natives
Voluntary Voluntary Voluntary
Populations enrolled: Foster Care and
Adoption Assistance Children
Voluntary Exempt Voluntary
Populations enrolled: Enrollment choice
period
Other Other N/A
Populations enrolled: Enrollment broker
name (if applicable)
Populations enrolled: Notes on
enrollment choice period
Enrollment open continuously Enrollment open continuously Enrollment open continuously
Benefits covered: Inpatient hospital
physical health
X X
Benefits covered: Inpatient hospital
behavioral health (MH and/or SUD)
X
Benefits covered: Outpatient hospital
physical health
X X
Benefits covered: Outpatient hospital
behavioral health (MH and/or SUD)
X X X
Benefits covered: Partial hospitalization X X
Benefits covered: Physician X X
Benefits covered: Nurse practitioner X X
Benefits covered: Rural health clinics
and FQHCs
X X
Benefits covered: Clinic services X X
Benefits covered: Lab and x-ray X X
Benefits covered: Prescription drugs X X
Benefits covered: Prosthetic devices X X
Benefits covered: EPSDT X X
Benefits covered: Case management X X X
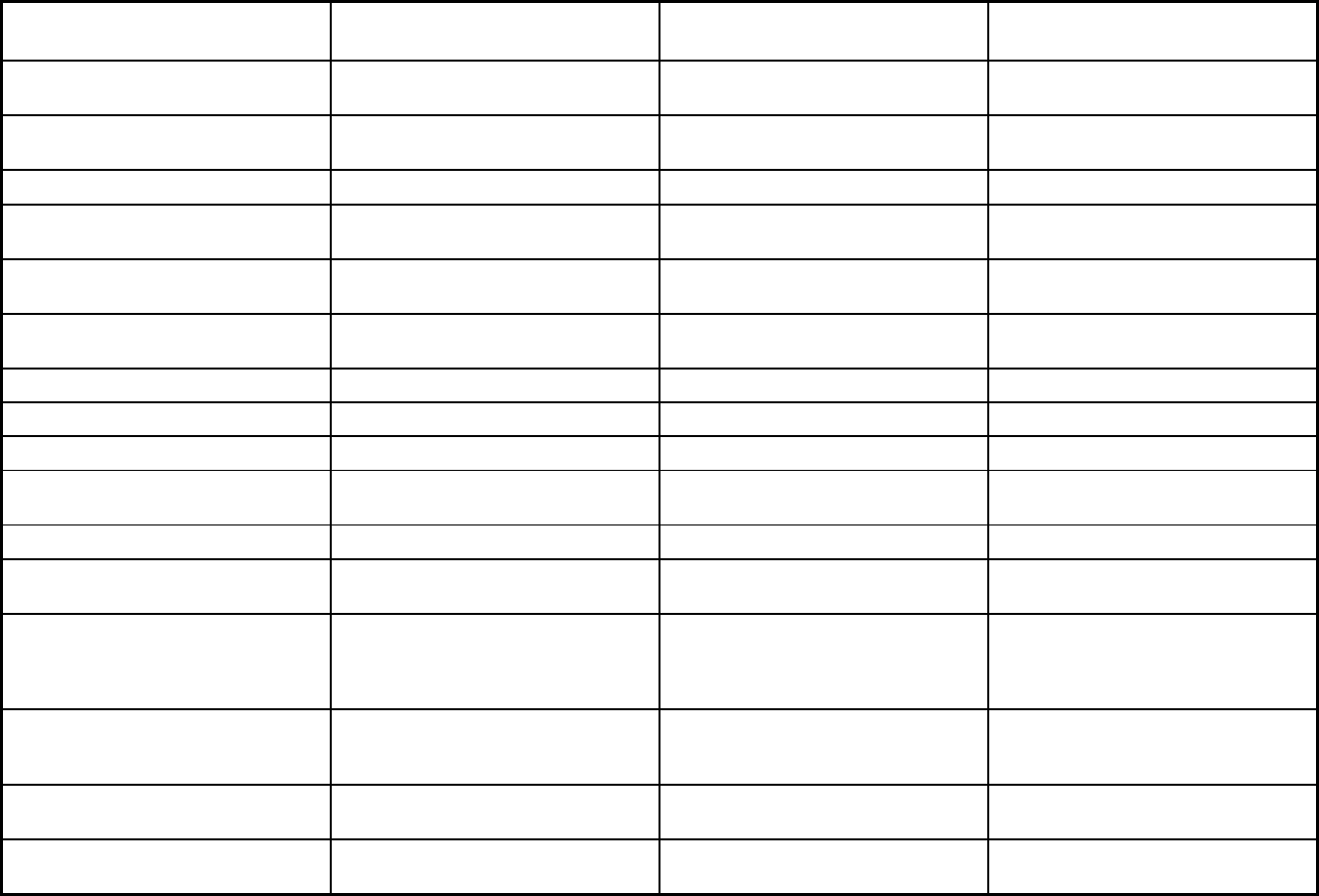
522
Features Healthy Options - Blind Disabled
Behavioral Health Services Only
(BHSO) PCCM
Benefits covered: SSA Section 1945-
authorized health home
Benefits covered: Health home care
(services in home)
X X
Benefits covered: Family planning X X
Benefits covered: Dental services
(medical/surgical)
X
Benefits covered: Dental (preventative
or corrective)
Benefits covered: Personal care (state
plan option)
Benefits covered: HCBS waiver services
Benefits covered: Private duty nursing X X
Benefits covered: ICF-IDD
Benefits covered: Nursing facility
services
X X
Benefits covered: Hospice care X X
Benefits covered: Non-Emergency
Medical Transportation
Benefits covered: Institution for Mental
Disease inpatient treatment for people
ages 21-64 defined by 42 CFR
§438.6(e) as an 'in lieu of' benefit
Benefits covered: Other (e.g., nurse
midwife services, freestanding birth
centers, podiatry, etc.)
Quality assurance and improvement:
HEDIS data required?
Yes Yes No
Quality assurance and improvement:
CAHPS data required?
Yes No No
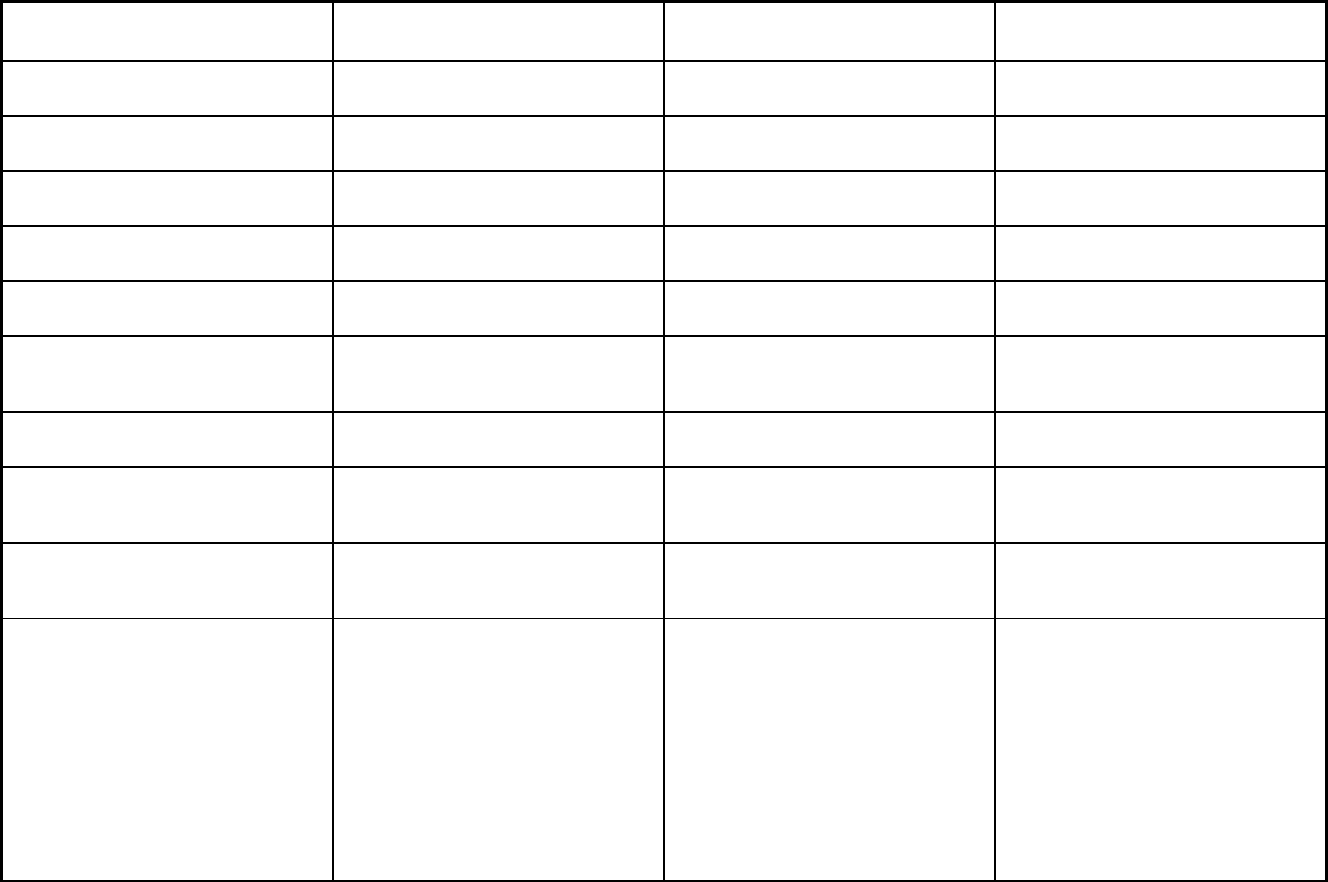
523
Features Healthy Options - Blind Disabled
Behavioral Health Services Only
(BHSO) PCCM
Quality assurance and improvement:
Accreditation required?
Yes Yes No
Quality assurance and improvement:
Accrediting organization
NCQA NCQA
Quality assurance and improvement:
EQRO contractor name (if applicable)
Qualis Qualis
Performance incentives: Payment
bonuses/differentials to reward plans
Performance incentives: Preferential
auto-enrollment to reward plans
Performance incentives: Public reports
comparing plan performance on key
metrics
Performance incentives: Withholds tied
to performance metrics
Performance incentives: MCOs/PHPs
required or encouraged to pay providers
for value/quality outcomes
Participating plans: Plans in Program Amerigroup; Community Health Plan of
WA; Coordinated Care of Washington;
Molina Health Care; United Health Care
Amerigroup; Coordinated Care of
Washington; Molina Health Care;
Community Health Care Plan of WA
Multiple Primary Care Providers
Notes: Program notes Please note managed care plans only
cover rehabilitation care in nursing
home facilities. Custodial care is is
covered under FFS.
IHS administers this program for
Yakima, Spokane, and Confederated
Tribes of the Colville Reservation. There
are two FQHCs: Seattle Indian Health
Board and Native Project. The tribal
clinics are as follows: Lower Elwha
Klallam, Lummi Nation, Nooksack Tribe,
Tulalip Nation, Confederated Tribes of
the Colville Reservation (non-IHS
managed facility), Puyallup Tribe,
Quileute Tribe, Quinault Indian Nation
and Port Gamble S'Klallam Tribe.
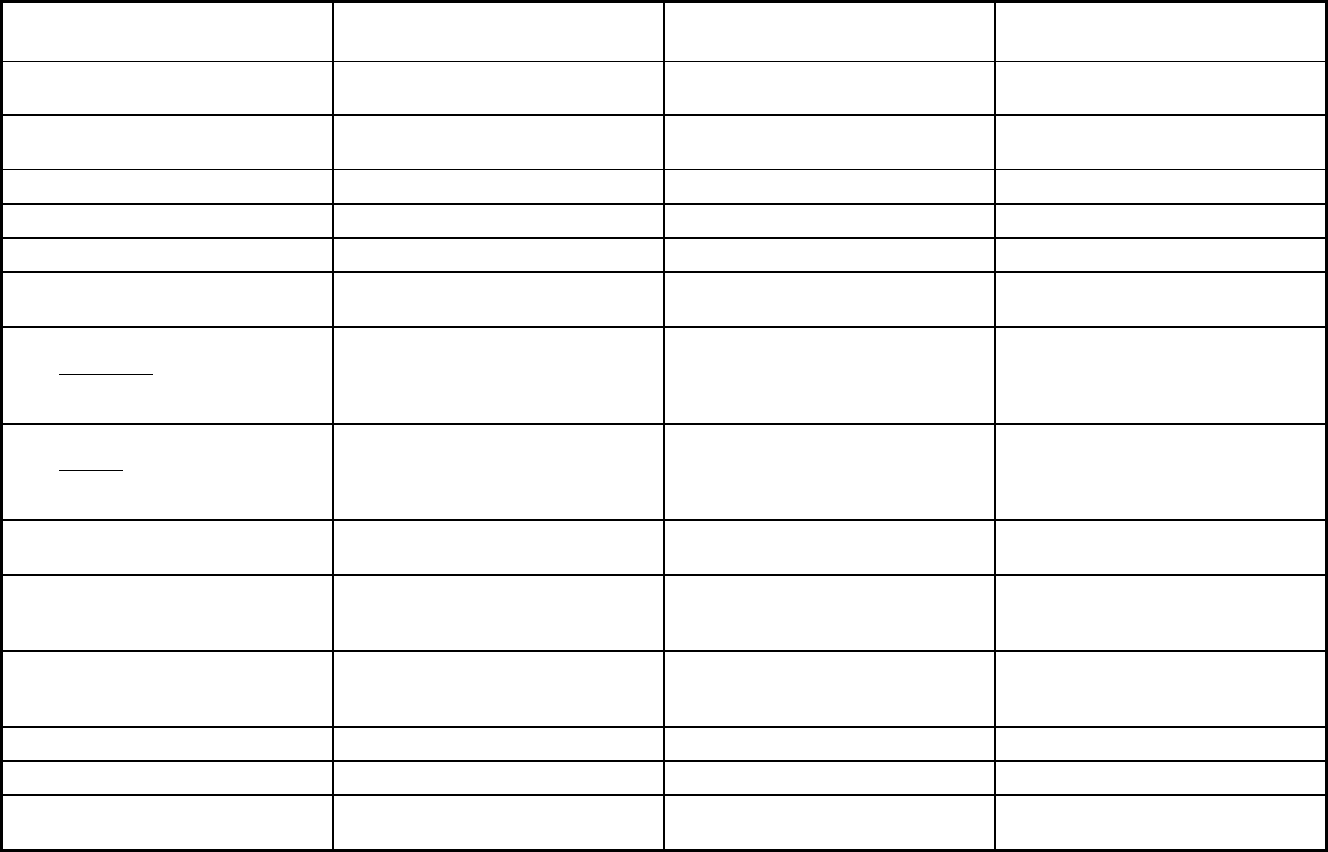
524
Washington Managed Care Program Features, as of 2018 (3 of 3)
Features
Fully Integrated Managed Care
(FIMC) PACE
Apple Health/Healthy Options Health
Home Program
Program type Comprehensive MCO Program of All-inclusive Care for the
Elderly (PACE)
Comprehensive MCO
Statewide or region-specific? Chelan, Clark, Douglas, Grant, and
Skamania Counties
Statewide Statewide
Federal operating authority 1932(a),1945 Health Homes PACE 1945 Health Homes
Program start date 04/01/2016 01/01/1997 07/01/2013
Waiver expiration date (if applicable)
If the program ended in 2018, indicate
the end date
Populations enrolled: Low-income
adults not covered under ACA Section
VIII (excludes pregnant women and
people with disabilities)
Voluntary
Populations enrolled: Low-income
adults covered under ACA Section VIII
(excludes pregnant women and people
with disabilities)
Mandatory Voluntary
Populations enrolled: Aged, Blind or
Disabled Children or Adults
Mandatory Voluntary Voluntary
Populations enrolled: Non-Disabled
Children (excludes children in foster
care or receiving adoption assistance)
Mandatory
Populations enrolled: Individuals
receiving Limited Benefits (excludes
partial duals)
Populations enrolled: Full Duals Voluntary Voluntary
Populations enrolled: Partial Duals
Populations enrolled: Children with
Special Health Care Needs
Mandatory Voluntary
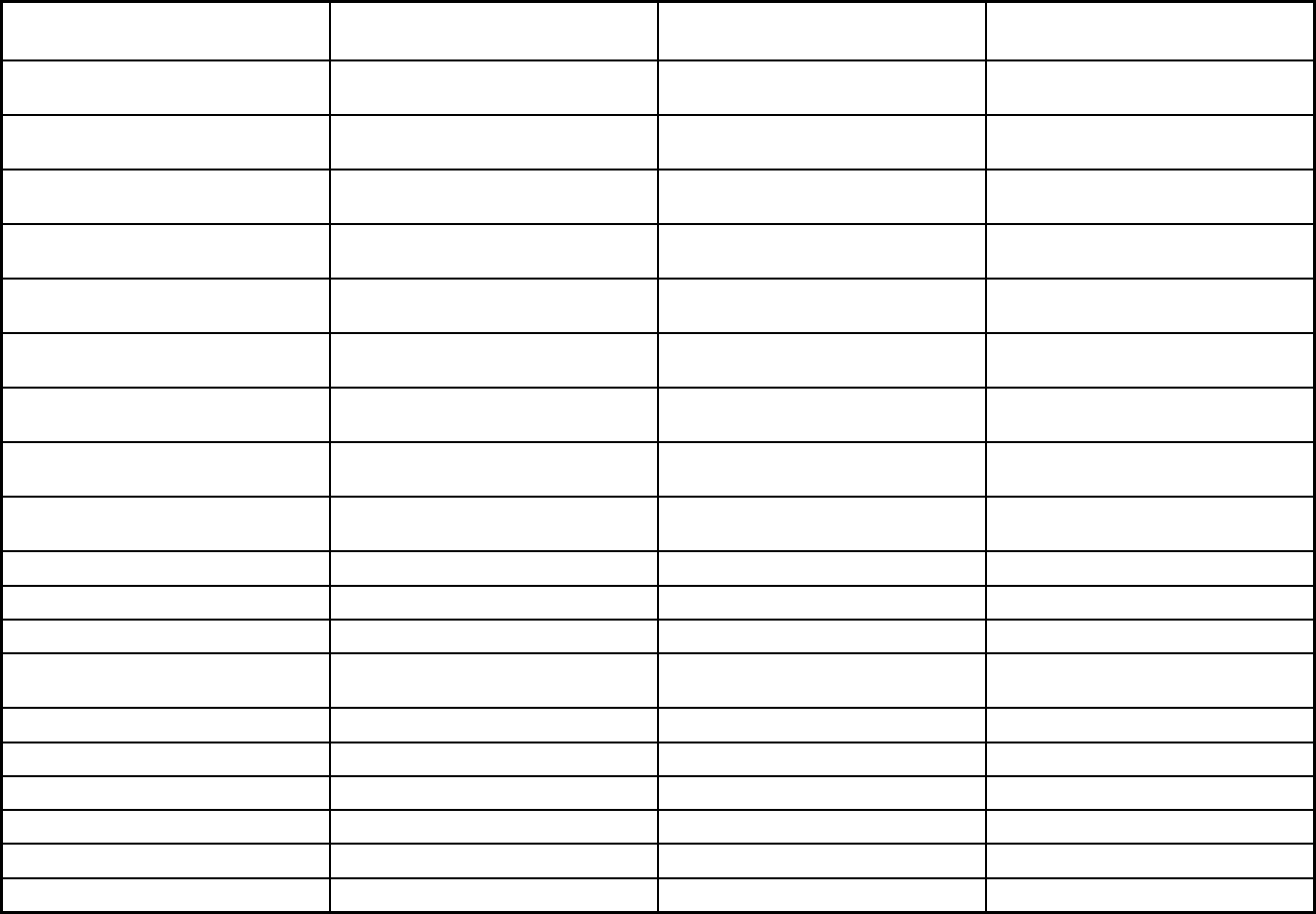
525
Features
Fully Integrated Managed Care
(FIMC) PACE
Apple Health/Healthy Options Health
Home Program
Populations enrolled: Native
American/Alaskan Natives
Voluntary Voluntary Voluntary
Populations enrolled: Foster Care and
Adoption Assistance Children
Exempt Exempt Exempt
Populations enrolled: Enrollment choice
period
Other N/A Pre-assigned
Populations enrolled: Enrollment broker
name (if applicable)
Populations enrolled: Notes on
enrollment choice period
Enrollment open continuously
Benefits covered: Inpatient hospital
physical health
X X
Benefits covered: Inpatient hospital
behavioral health (MH and/or SUD)
X
Benefits covered: Outpatient hospital
physical health
X X
Benefits covered: Outpatient hospital
behavioral health (MH and/or SUD)
X X
Benefits covered: Partial hospitalization X X
Benefits covered: Physician X
Benefits covered: Nurse practitioner X X
Benefits covered: Rural health clinics
and FQHCs
X X
Benefits covered: Clinic services X X
Benefits covered: Lab and x-ray X X
Benefits covered: Prescription drugs X X
Benefits covered: Prosthetic devices X
Benefits covered: EPSDT X
Benefits covered: Case management X X
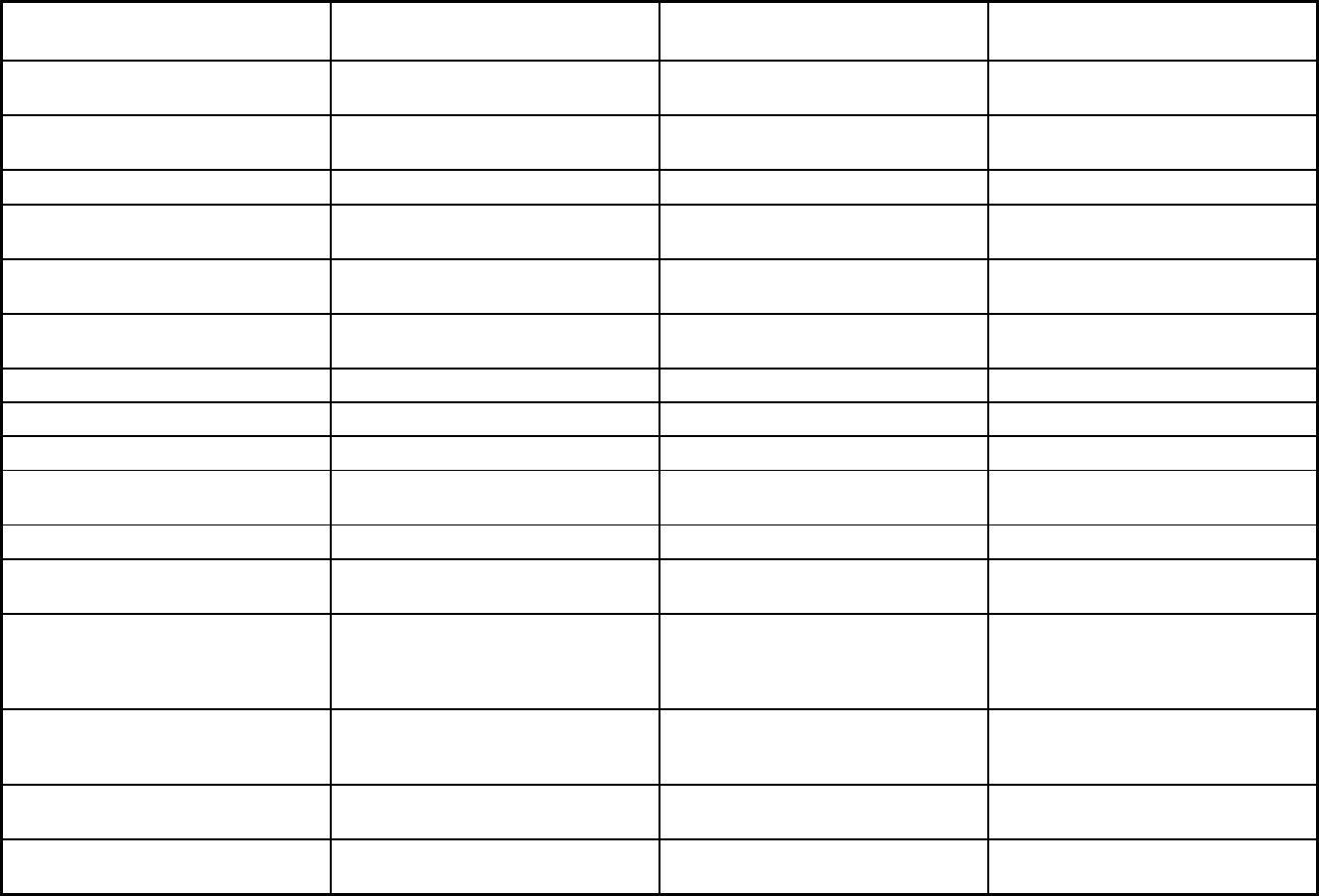
526
Features
Fully Integrated Managed Care
(FIMC) PACE
Apple Health/Healthy Options Health
Home Program
Benefits covered: SSA Section 1945-
authorized health home
X X
Benefits covered: Health home care
(services in home)
X X
Benefits covered: Family planning X
Benefits covered: Dental services
(medical/surgical)
X X
Benefits covered: Dental (preventative
or corrective)
X
Benefits covered: Personal care (state
plan option)
X X
Benefits covered: HCBS waiver services X
Benefits covered: Private duty nursing X
Benefits covered: ICF-IDD
Benefits covered: Nursing facility
services
X X
Benefits covered: Hospice care X
Benefits covered: Non-Emergency
Medical Transportation
X
Benefits covered: Institution for Mental
Disease inpatient treatment for people
ages 21-64 defined by 42 CFR
§438.6(e) as an 'in lieu of' benefit
X
Benefits covered: Other (e.g., nurse
midwife services, freestanding birth
centers, podiatry, etc.)
Comfort Care and Podiatry
Quality assurance and improvement:
HEDIS data required?
Yes No No
Quality assurance and improvement:
CAHPS data required?
Yes No No
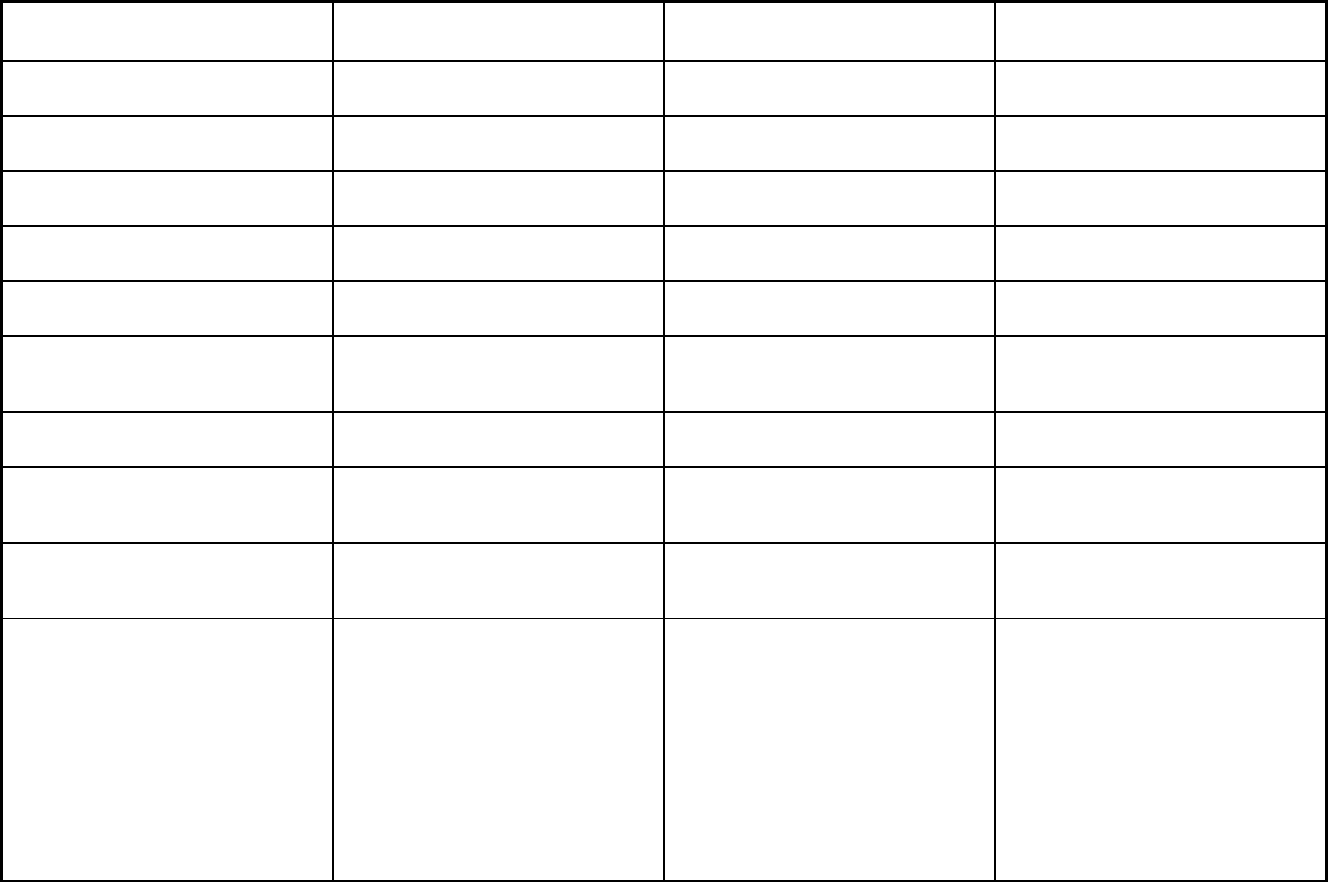
527
Features
Fully Integrated Managed Care
(FIMC) PACE
Apple Health/Healthy Options Health
Home Program
Quality assurance and improvement:
Accreditation required?
Yes No No
Quality assurance and improvement:
Accrediting organization
NCQA
Quality assurance and improvement:
EQRO contractor name (if applicable)
Qualis
Performance incentives: Payment
bonuses/differentials to reward plans
Performance incentives: Preferential
auto-enrollment to reward plans
Performance incentives: Public reports
comparing plan performance on key
metrics
Performance incentives: Withholds tied
to performance metrics
Performance incentives: MCOs/PHPs
required or encouraged to pay providers
for value/quality outcomes
Participating plans: Plans in Program Amerigroup; Coordinated Care of
Washington; Community Health Plan of
Washington; Molina Health Care
Providence Elder Place Multiple Sites
Notes: Program notes Please note managed care plans only
cover rehabilitation care in nursing
home facilities. Custodial care is is
covered under FFS.
Washington delivers the optional Health
Home Medicaid/Medical Benefit both in
the fee-for-service system and through
MCOs. For individuals in Apple Health
comprehensive MCOs, the MCOs are at
risk for health home services plus a
broad array of benefits including
inpatient, outpatient, physician services,
pharmacy, etc. For individuals in
PCCMs, the MCOs administer health
homes services separate from the
PCCM program.
528
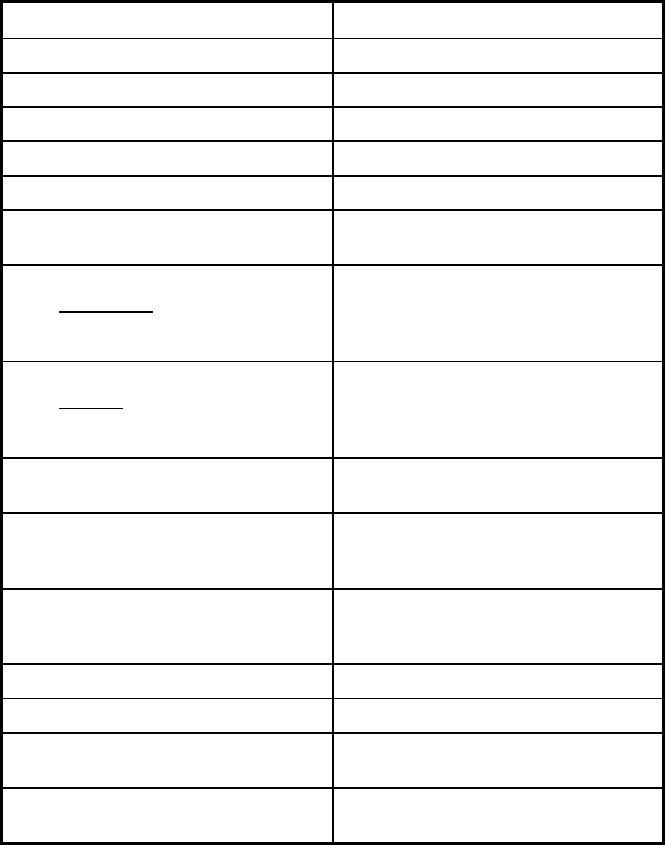
529
West Virginia Managed Care Program Features, as of 2018
Features Mountain Health Trust
Program type Comprehensive MCO
Statewide or region-specific? Statewide
Federal operating authority 1915(b)
Program start date 09/01/1996
Waiver expiration date (if applicable) 06/30/2019
If the program ended in 2018, indicate
the end date
Populations enrolled: Low-income
adults not covered under ACA Section
VIII (excludes pregnant women and
people with disabilities)
Mandatory
Populations enrolled: Low-income
adults covered under ACA Section VIII
(excludes pregnant women and people
with disabilities)
Mandatory
Populations enrolled: Aged, Blind or
Disabled Children or Adults
Mandatory
Populations enrolled: Non-Disabled
Children (excludes children in foster
care or receiving adoption assistance)
Mandatory
Populations enrolled: Individuals
receiving Limited Benefits (excludes
partial duals)
Populations enrolled: Full Duals
Populations enrolled: Partial Duals
Populations enrolled: Children with
Special Health Care Needs
Mandatory
Populations enrolled: Native
American/Alaskan Natives
Mandatory
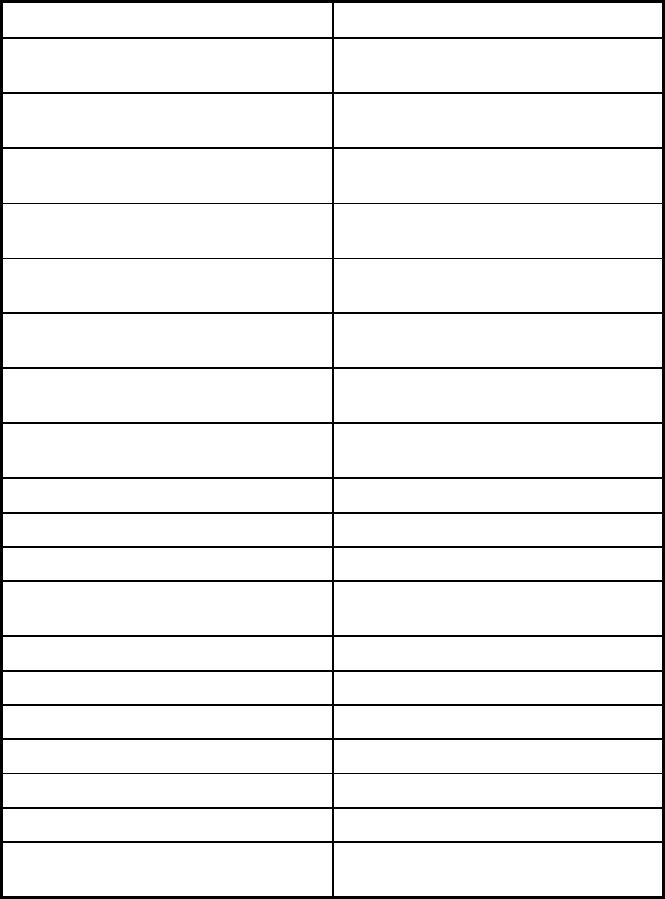
530
Features Mountain Health Trust
Populations enrolled: Foster Care and
Adoption Assistance Children
Exempt
Populations enrolled: Enrollment choice
period
Other
Populations enrolled: Enrollment broker
name (if applicable)
MAXIMUS
Populations enrolled: Notes on
enrollment choice period
45-60 days depending on packet
receival date
Benefits covered: Inpatient hospital
physical health
X
Benefits covered: Inpatient hospital
behavioral health (MH and/or SUD)
X
Benefits covered: Outpatient hospital
physical health
X
Benefits covered: Outpatient hospital
behavioral health (MH and/or SUD)
X
Benefits covered: Partial hospitalization X
Benefits covered: Physician X
Benefits covered: Nurse practitioner X
Benefits covered: Rural health clinics
and FQHCs
X
Benefits covered: Clinic services X
Benefits covered: Lab and x-ray X
Benefits covered: Prescription drugs X
Benefits covered: Prosthetic devices X
Benefits covered: EPSDT X
Benefits covered: Case management
Benefits covered: SSA Section 1945-
authorized health home
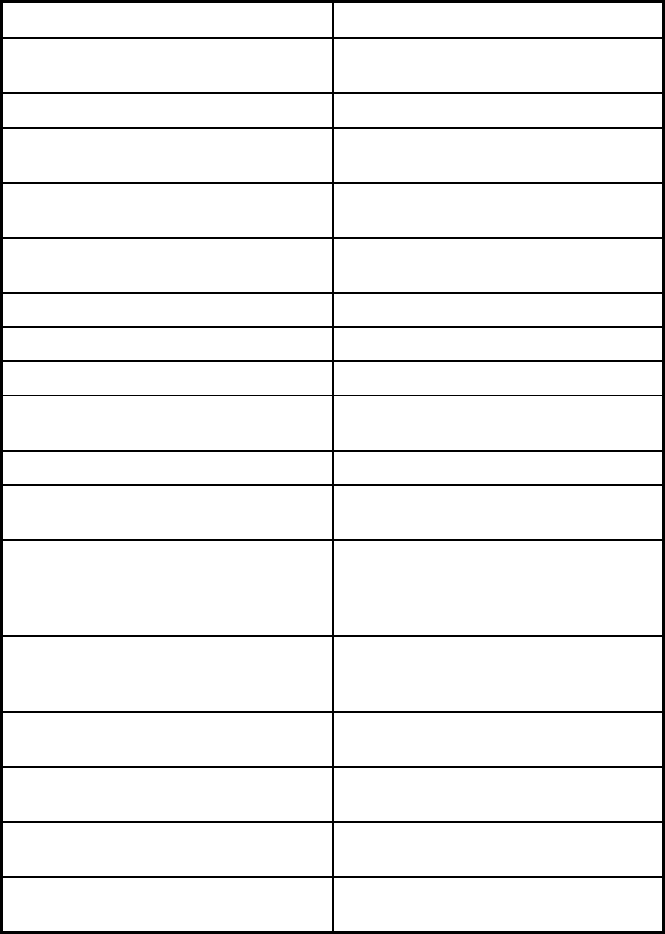
531
Features Mountain Health Trust
Benefits covered: Health home care
(services in home)
X
Benefits covered: Family planning X
Benefits covered: Dental services
(medical/surgical)
X
Benefits covered: Dental (preventative
or corrective)
X
Benefits covered: Personal care (state
plan option)
Benefits covered: HCBS waiver services
Benefits covered: Private duty nursing X
Benefits covered: ICF-IDD
Benefits covered: Nursing facility
services
Benefits covered: Hospice care X
Benefits covered: Non-Emergency
Medical Transportation
Benefits covered: Institution for Mental
Disease inpatient treatment for people
ages 21-64 defined by 42 CFR
§438.6(e) as an 'in lieu of' benefit
Benefits covered: Other (e.g., nurse
midwife services, freestanding birth
centers, podiatry, etc.)
Quality assurance and improvement:
HEDIS data required?
Yes
Quality assurance and improvement:
CAHPS data required?
Yes
Quality assurance and improvement:
Accreditation required?
Yes
Quality assurance and improvement:
Accrediting organization
NCQA
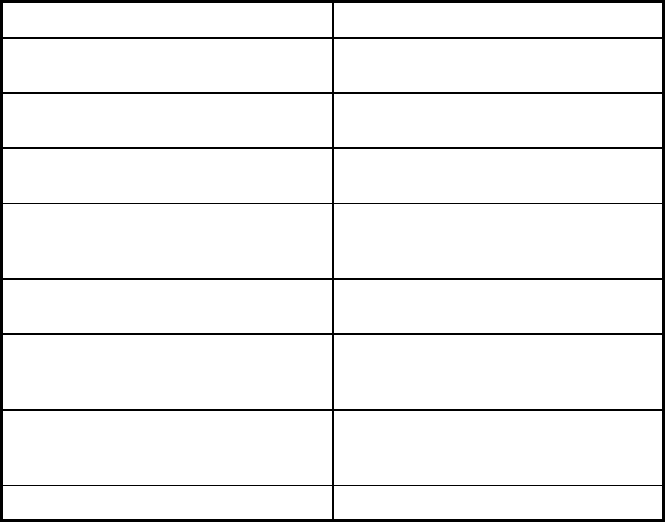
532
Features Mountain Health Trust
Quality assurance and improvement:
EQRO contractor name (if applicable)
Qlarant (formerly Delmarva)
Performance incentives: Payment
bonuses/differentials to reward plans
Performance incentives: Preferential
auto-enrollment to reward plans
Performance incentives: Public reports
comparing plan performance on key
metrics
X
Performance incentives: Withholds tied
to performance metrics
Performance incentives: MCOs/PHPs
required or encouraged to pay providers
for value/quality outcomes
X
Participating plans: Plans in Program Aetna Better Health of WV; The Health
Plan; Unicare; West Virginia Family
Health
Notes: Program notes
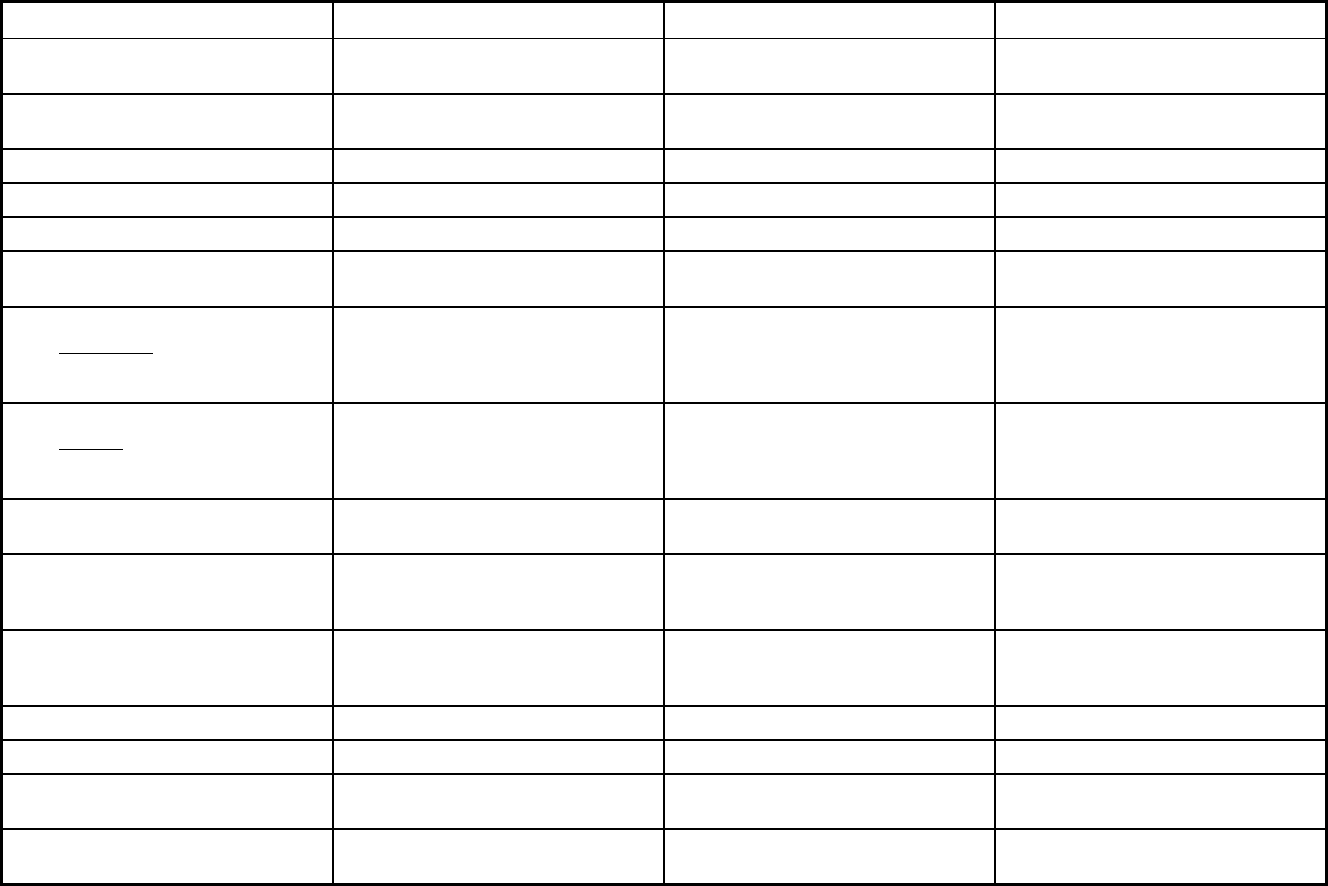
533
Wisconsin Managed Care Program Features, as of 2018 (1 of 3)
Features BadgerCare Plus Care4Kids Children Come First (CCF)
Program type Comprehensive MCO Other Prepaid Health Plan (PHP)
(limited benefits)
Behavioral Health Organization (BHO)
only (PIHP and/or PAHP)
Statewide or region-specific? Statewide Kenosha, Milwaukee, Ozaukee, Racine,
Washington, and Washington Counties
County: Dane
Federal operating authority 1932(a) 1937 Alt Benefit Plan 1915(a)
Program start date 02/01/2008 01/01/2014 04/01/1993
Waiver expiration date (if applicable)
If the program ended in 2018, indicate
the end date
Populations enrolled: Low-income
adults not covered under ACA Section
VIII (excludes pregnant women and
people with disabilities)
Mandatory
Populations enrolled: Low-income
adults covered under ACA Section VIII
(excludes pregnant women and people
with disabilities)
Mandatory
Populations enrolled: Aged, Blind or
Disabled Children or Adults
Populations enrolled: Non-Disabled
Children (excludes children in foster
care or receiving adoption assistance)
Mandatory
Populations enrolled: Individuals
receiving Limited Benefits (excludes
partial duals)
Populations enrolled: Full Duals Voluntary
Populations enrolled: Partial Duals
Populations enrolled: Children with
Special Health Care Needs
Voluntary Voluntary Voluntary
Populations enrolled: Native
American/Alaskan Natives
Voluntary Voluntary Voluntary
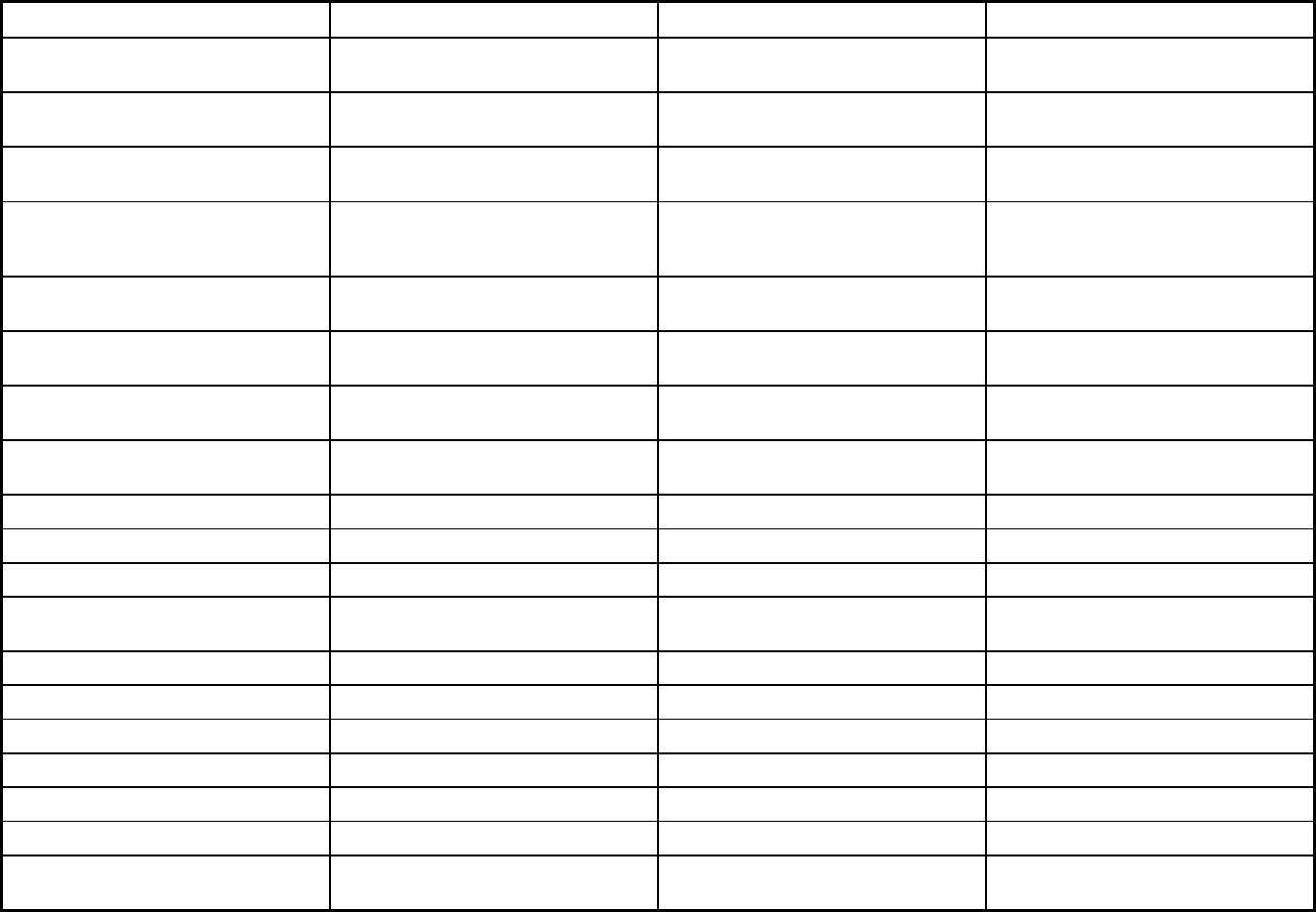
534
Features BadgerCare Plus Care4Kids Children Come First (CCF)
Populations enrolled: Foster Care and
Adoption Assistance Children
Exempt Voluntary Voluntary
Populations enrolled: Enrollment choice
period
Other Other Other
Populations enrolled: Enrollment broker
name (if applicable)
MAXIMUS MAXIMUS
Populations enrolled: Notes on
enrollment choice period
90 days open enrollment period Open enrollment period as long as child
remains in out of home care and resides
in eligible placement setting/county.
Enrollment may occur at any time
Benefits covered: Inpatient hospital
physical health
X X
Benefits covered: Inpatient hospital
behavioral health (MH and/or SUD)
X X X
Benefits covered: Outpatient hospital
physical health
X X
Benefits covered: Outpatient hospital
behavioral health (MH and/or SUD)
X X X
Benefits covered: Partial hospitalization X X
Benefits covered: Physician X X
Benefits covered: Nurse practitioner X X
Benefits covered: Rural health clinics
and FQHCs
X X
Benefits covered: Clinic services X X
Benefits covered: Lab and x-ray X X
Benefits covered: Prescription drugs
Benefits covered: Prosthetic devices X
Benefits covered: EPSDT X X
Benefits covered: Case management X X X
Benefits covered: SSA Section 1945-
authorized health home
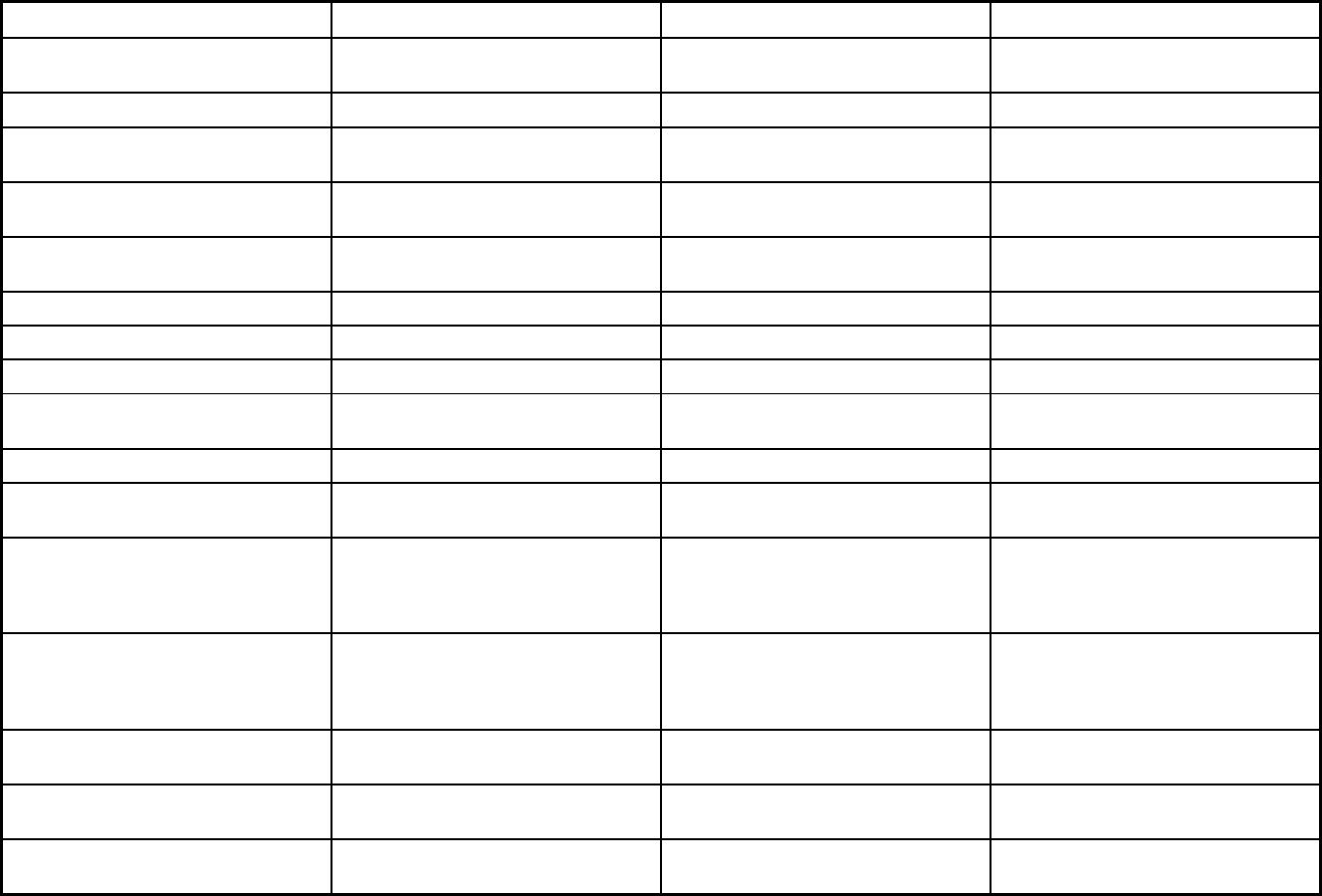
535
Features BadgerCare Plus Care4Kids Children Come First (CCF)
Benefits covered: Health home care
(services in home)
X X
Benefits covered: Family planning X X
Benefits covered: Dental services
(medical/surgical)
X X
Benefits covered: Dental (preventative
or corrective)
X X
Benefits covered: Personal care (state
plan option)
X X
Benefits covered: HCBS waiver services
Benefits covered: Private duty nursing X X
Benefits covered: ICF-IDD
Benefits covered: Nursing facility
services
X X
Benefits covered: Hospice care X X
Benefits covered: Non-Emergency
Medical Transportation
Benefits covered: Institution for Mental
Disease inpatient treatment for people
ages 21-64 defined by 42 CFR
§438.6(e) as an 'in lieu of' benefit
X
Benefits covered: Other (e.g., nurse
midwife services, freestanding birth
centers, podiatry, etc.)
Prosthetic devices, nurse midwife
services, podiatry, chiropractic (varies
by plan), and dental (varies by
geographic region)
Prosthetic devices, nurse midwife
services, and podiatry
Quality assurance and improvement:
HEDIS data required?
Yes Yes No
Quality assurance and improvement:
CAHPS data required?
No No No
Quality assurance and improvement:
Accreditation required?
No No No
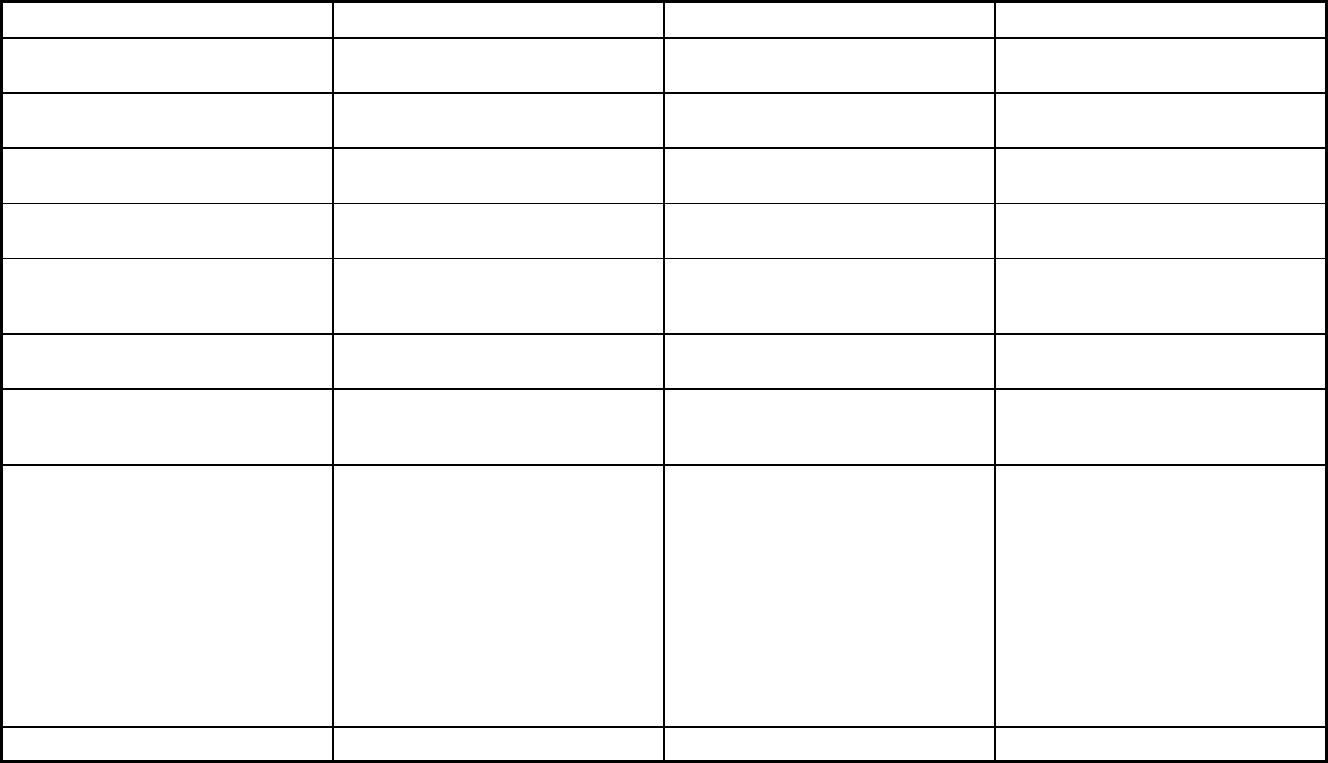
536
Features BadgerCare Plus Care4Kids Children Come First (CCF)
Quality assurance and improvement:
Accrediting organization
Quality assurance and improvement:
EQRO contractor name (if applicable)
MetaStar, Inc. MetaStar, Inc. MetaStar, Inc.
Performance incentives: Payment
bonuses/differentials to reward plans
X
Performance incentives: Preferential
auto-enrollment to reward plans
Performance incentives: Public reports
comparing plan performance on key
metrics
X
Performance incentives: Withholds tied
to performance metrics
X
Performance incentives: MCOs/PHPs
required or encouraged to pay providers
for value/quality outcomes
X
Participating plans: Plans in Program Anthem Blue Cross Blue Shield;
Children’s Community Health Plan;
Dean Health Plan; Group Health
Cooperative Of Eau Claire; Group
Health Cooperative Of South Central
WI; Independent Care (iCare); MHS of
Wisconsin; MercyCare Insurance
Company; Molina Health Plan; Network
Health Plan; Physicians Plus Health
Plan; Security Health Plan; Trilogy
Health Insurance; UnitedHealthcare
Community Plan; Quartz
Children's Community Health Plan Children Come First
Notes: Program notes
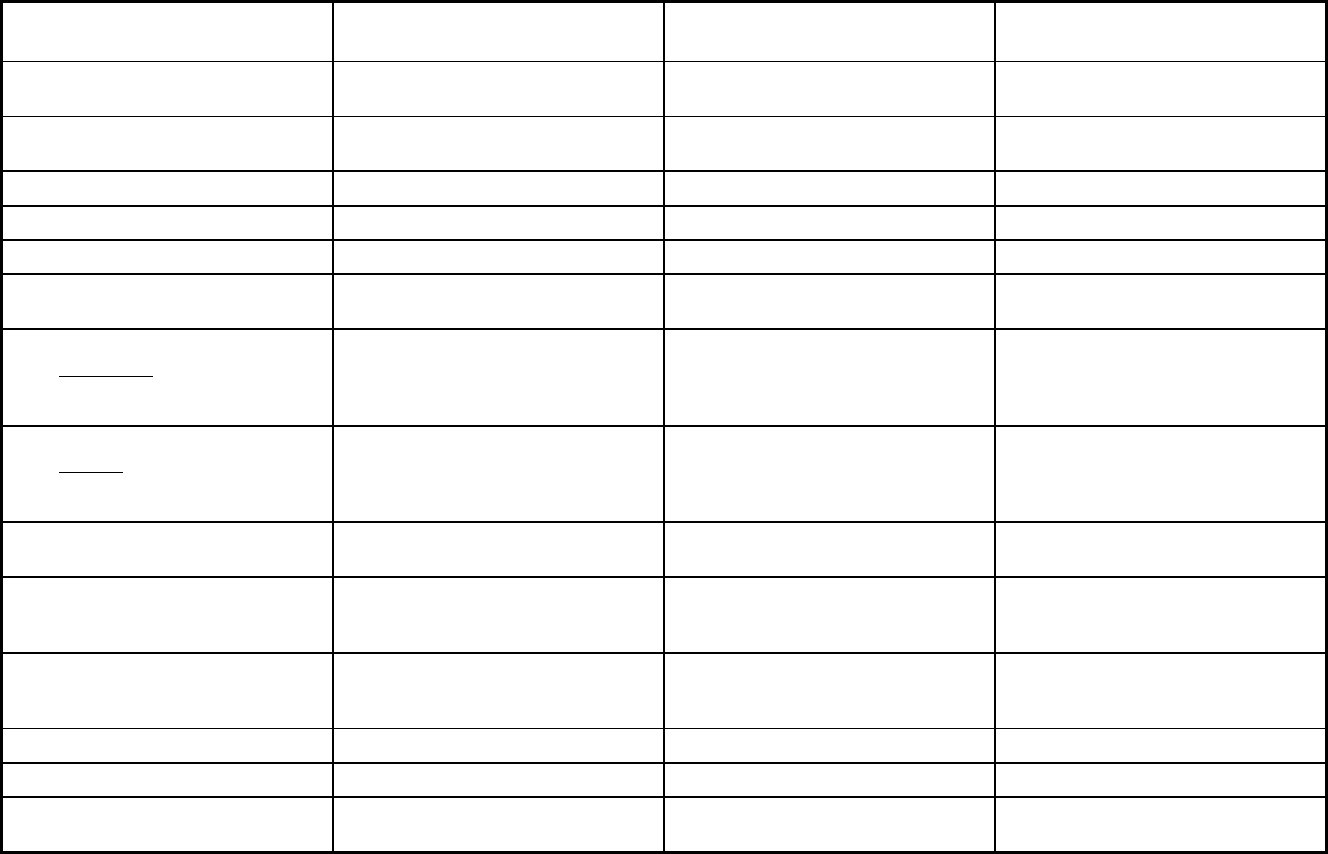
537
Wisconsin Managed Care Program Features, as of 2018 (2 of 3)
Features SSI Managed Care WrapAround Milwaukee
Program of All-inclusive Care for the
Elderly (PACE)
Program type Comprehensive MCO Behavioral Health Organization (BHO)
only (PIHP and/or PAHP)
Program of All-inclusive Care for the
Elderly (PACE)
Statewide or region-specific? Statewide County: Milwaukee Milwaukee Racine and Waukesha
Counties
Federal operating authority 1932(a) 1915(a) PACE
Program start date 04/01/2005 03/01/1997 11/01/1990
Waiver expiration date (if applicable)
If the program ended in 2018, indicate
the end date
Populations enrolled: Low-income
adults not covered under ACA Section
VIII (excludes pregnant women and
people with disabilities)
Populations enrolled: Low-income
adults covered under ACA Section VIII
(excludes pregnant women and people
with disabilities)
Populations enrolled: Aged, Blind or
Disabled Children or Adults
Mandatory Voluntary
Populations enrolled: Non-Disabled
Children (excludes children in foster
care or receiving adoption assistance)
Populations enrolled: Individuals
receiving Limited Benefits (excludes
partial duals)
Populations enrolled: Full Duals Voluntary Voluntary
Populations enrolled: Partial Duals
Populations enrolled: Children with
Special Health Care Needs
Voluntary
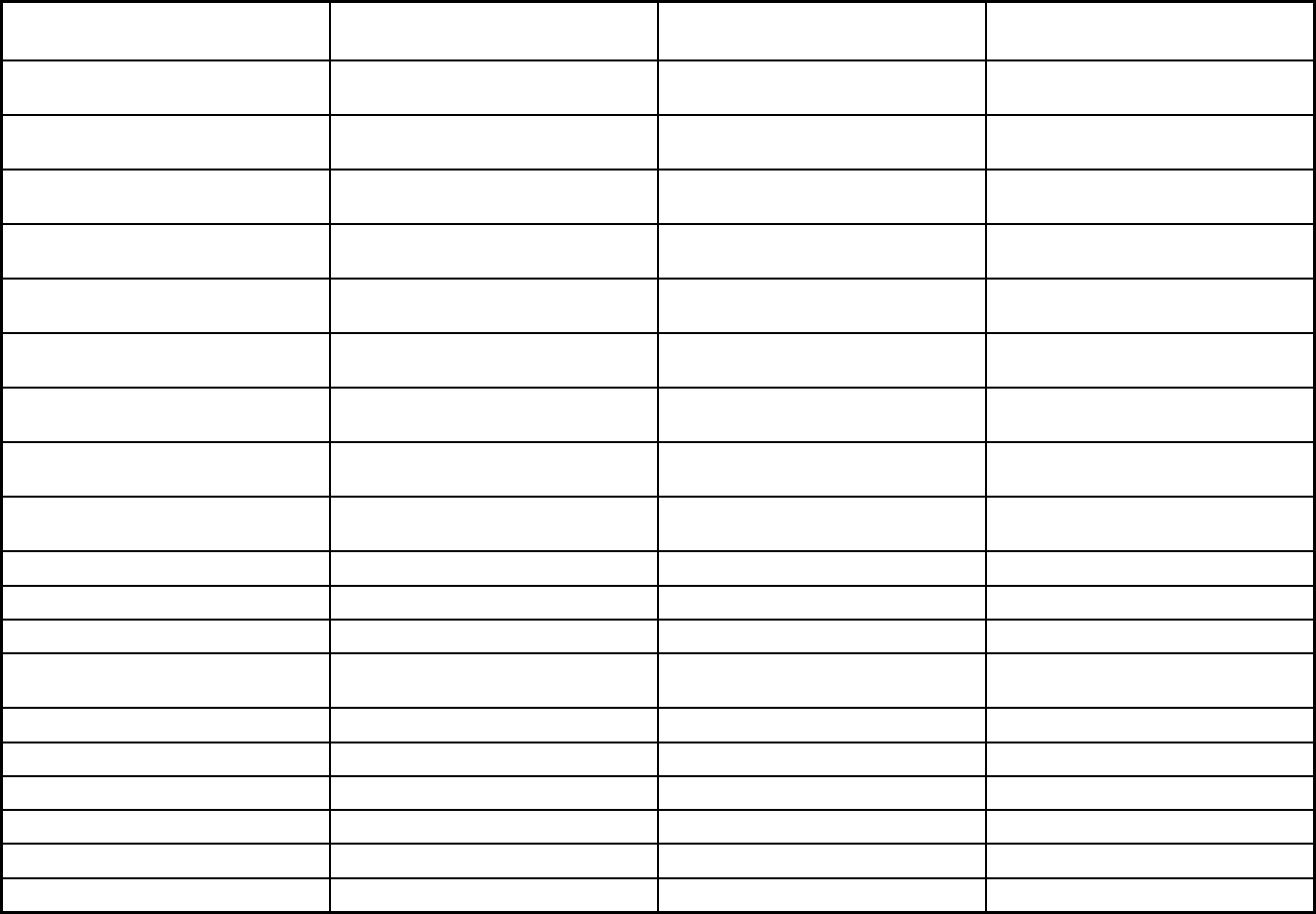
538
Features SSI Managed Care WrapAround Milwaukee
Program of All-inclusive Care for the
Elderly (PACE)
Populations enrolled: Native
American/Alaskan Natives
Voluntary Voluntary Exempt
Populations enrolled: Foster Care and
Adoption Assistance Children
Voluntary Exempt
Populations enrolled: Enrollment choice
period
Other Other N/A
Populations enrolled: Enrollment broker
name (if applicable)
Automated Health Systems
Incorporated (AHSI)
Populations enrolled: Notes on
enrollment choice period
90 days open enrollment period Voluntary enrollment can occur at any
time
Open enrollment
Benefits covered: Inpatient hospital
physical health
X X
Benefits covered: Inpatient hospital
behavioral health (MH and/or SUD)
X X X
Benefits covered: Outpatient hospital
physical health
X X
Benefits covered: Outpatient hospital
behavioral health (MH and/or SUD)
X X X
Benefits covered: Partial hospitalization X X
Benefits covered: Physician X X
Benefits covered: Nurse practitioner X X
Benefits covered: Rural health clinics
and FQHCs
X X
Benefits covered: Clinic services X X
Benefits covered: Lab and x-ray X X
Benefits covered: Prescription drugs X
Benefits covered: Prosthetic devices X
Benefits covered: EPSDT X
Benefits covered: Case management X X X
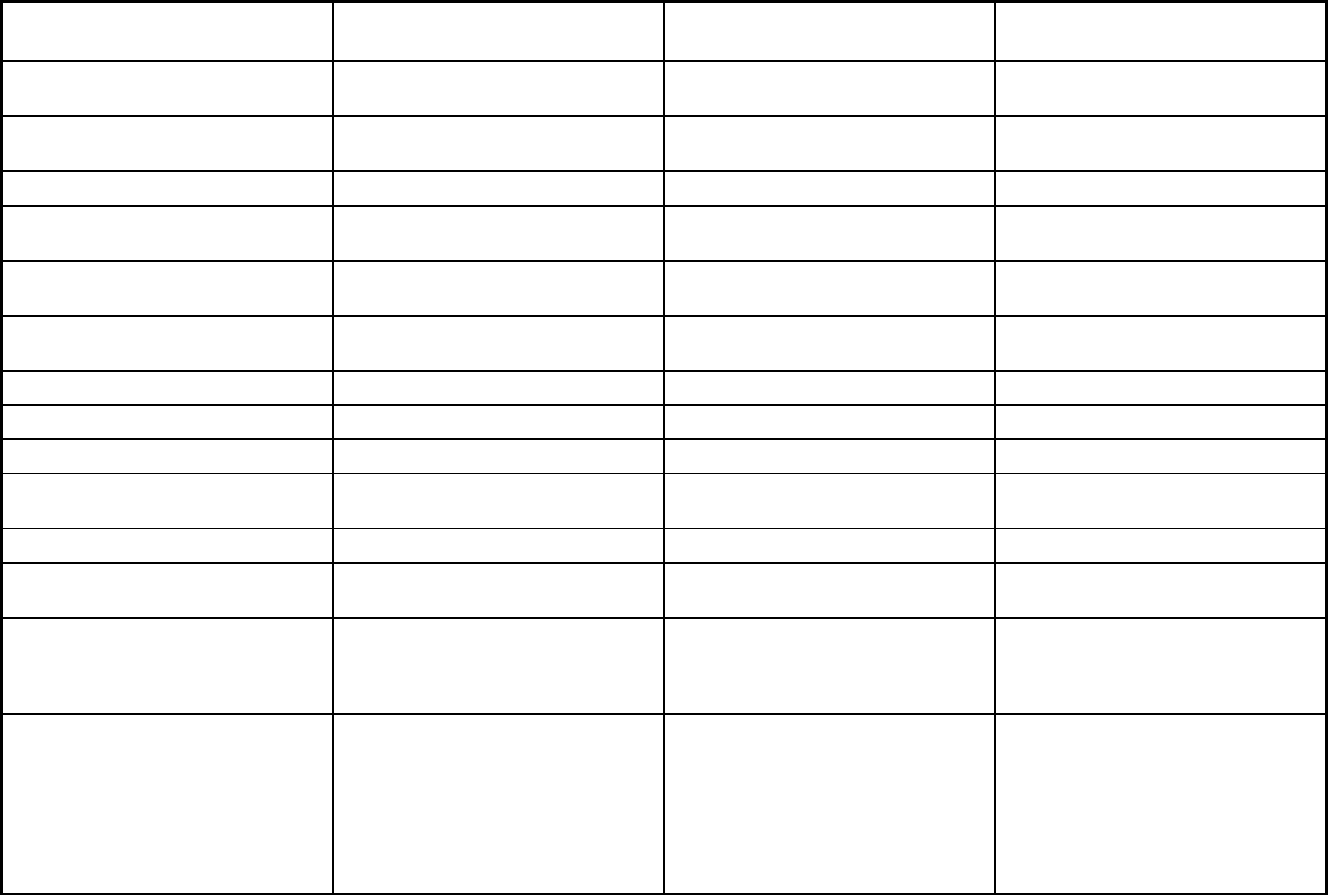
539
Features SSI Managed Care WrapAround Milwaukee
Program of All-inclusive Care for the
Elderly (PACE)
Benefits covered: SSA Section 1945-
authorized health home
Benefits covered: Health home care
(services in home)
X X
Benefits covered: Family planning X X
Benefits covered: Dental services
(medical/surgical)
X X
Benefits covered: Dental (preventative
or corrective)
X X
Benefits covered: Personal care (state
plan option)
X X
Benefits covered: HCBS waiver services X
Benefits covered: Private duty nursing X X
Benefits covered: ICF-IDD X
Benefits covered: Nursing facility
services
X X
Benefits covered: Hospice care X X
Benefits covered: Non-Emergency
Medical Transportation
X
Benefits covered: Institution for Mental
Disease inpatient treatment for people
ages 21-64 defined by 42 CFR
§438.6(e) as an 'in lieu of' benefit
X
Benefits covered: Other (e.g., nurse
midwife services, freestanding birth
centers, podiatry, etc.)
Nurse midwife services, podiatry and
chiropractic, and dental varies by
geographic region
Ambulatory surgical center, audiology,
chiropractic, community mental health
services, durable medical equipment
and medical supplies, occupational
therapy, physical therapy, podiatry,
respiratory care for ventilator dependent
persons, speech & language pathology,
and vision care
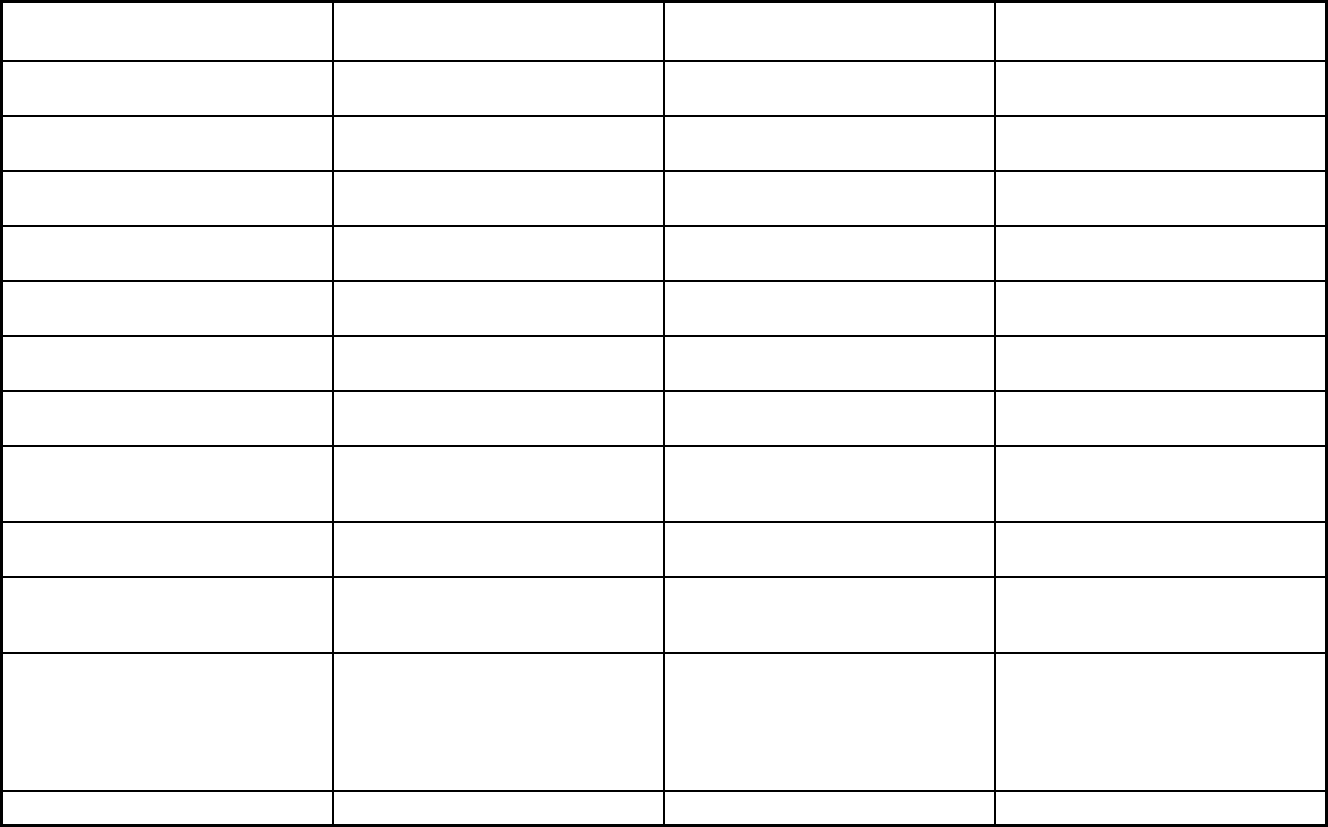
540
Features SSI Managed Care WrapAround Milwaukee
Program of All-inclusive Care for the
Elderly (PACE)
Quality assurance and improvement:
HEDIS data required?
Yes No No
Quality assurance and improvement:
CAHPS data required?
No No No
Quality assurance and improvement:
Accreditation required?
No, but accreditation considered in plan
selection criteria
No No
Quality assurance and improvement:
Accrediting organization
Majority of HMOs are accredited by
NCQA
Quality assurance and improvement:
EQRO contractor name (if applicable)
MetaStar, Inc. MetaStar, Inc. MetaStar Inc
Performance incentives: Payment
bonuses/differentials to reward plans
X
Performance incentives: Preferential
auto-enrollment to reward plans
Performance incentives: Public reports
comparing plan performance on key
metrics
X
Performance incentives: Withholds tied
to performance metrics
X
Performance incentives: MCOs/PHPs
required or encouraged to pay providers
for value/quality outcomes
Participating plans: Plans in Program Anthem Blue Cross Blue Shield; Care
Wisconsin; Group Health Cooperative
Of Eau Claire; Independent Care
(iCare); MHS of Wisconsin; Molina
Health Plan; Network Health Plan;
UnitedHealthcare Community Plan
WrapAround Milwaukee Community Care, Inc.
Notes: Program notes
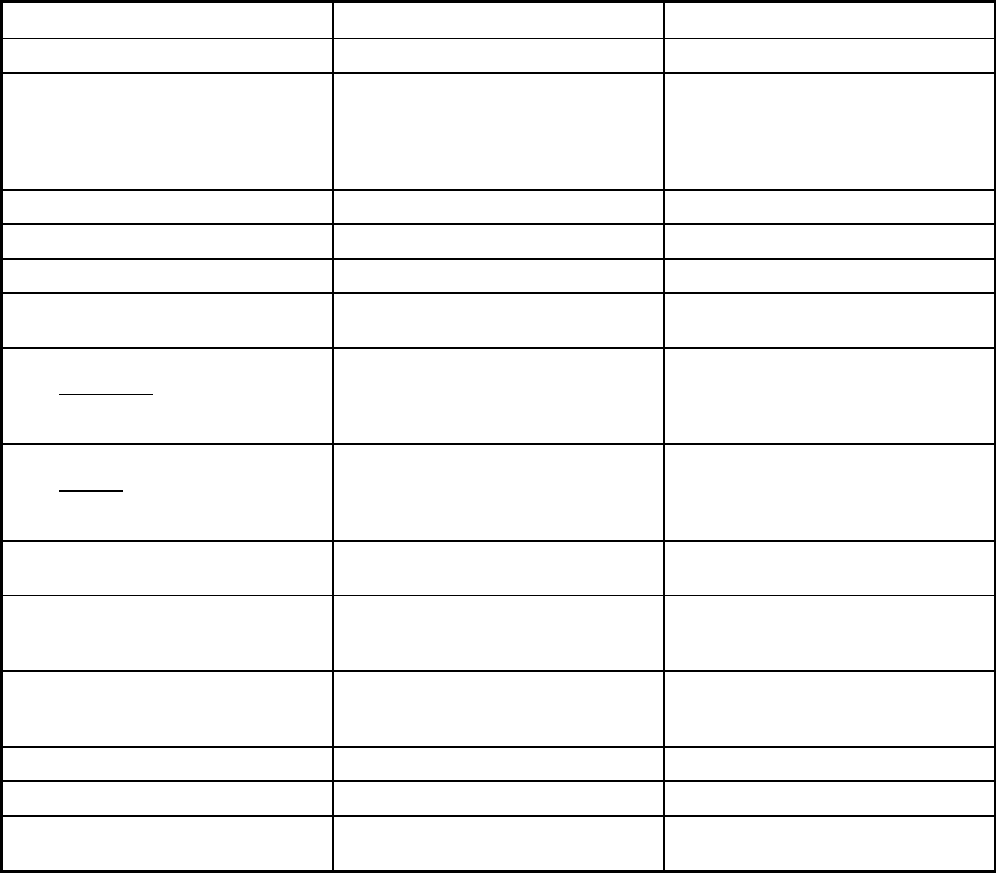
541
Wisconsin Managed Care Program Features, as of 2018 (3 of 3)
Features Family Care Partnership Program Family Care
Program type Comprehensive MCO + MLTSS MLTSS only (PIHP and/or PAHP)
Statewide or region-specific? Calumet, Columbia, Dane, Dodge,
Jefferson, Kenosha, Milwaukee.
Outagamie, Ozaukee, Racine, Sauk,
Washington, Waukesha, and Waupaca
Counties
Statewide
Federal operating authority 1932(a)/1915(c) 1915(b)/1915(c)
Program start date 02/01/1995 02/01/2000
Waiver expiration date (if applicable) 12/31/2019 12/31/2019
If the program ended in 2018, indicate
the end date
Populations enrolled: Low-income
adults not covered under ACA Section
VIII (excludes pregnant women and
people with disabilities)
Populations enrolled: Low-income
adults covered under ACA Section VIII
(excludes pregnant women and people
with disabilities)
Populations enrolled: Aged, Blind or
Disabled Children or Adults
Voluntary Mandatory
Populations enrolled: Non-Disabled
Children (excludes children in foster
care or receiving adoption assistance)
Populations enrolled: Individuals
receiving Limited Benefits (excludes
partial duals)
Populations enrolled: Full Duals Voluntary Voluntary
Populations enrolled: Partial Duals
Populations enrolled: Children with
Special Health Care Needs
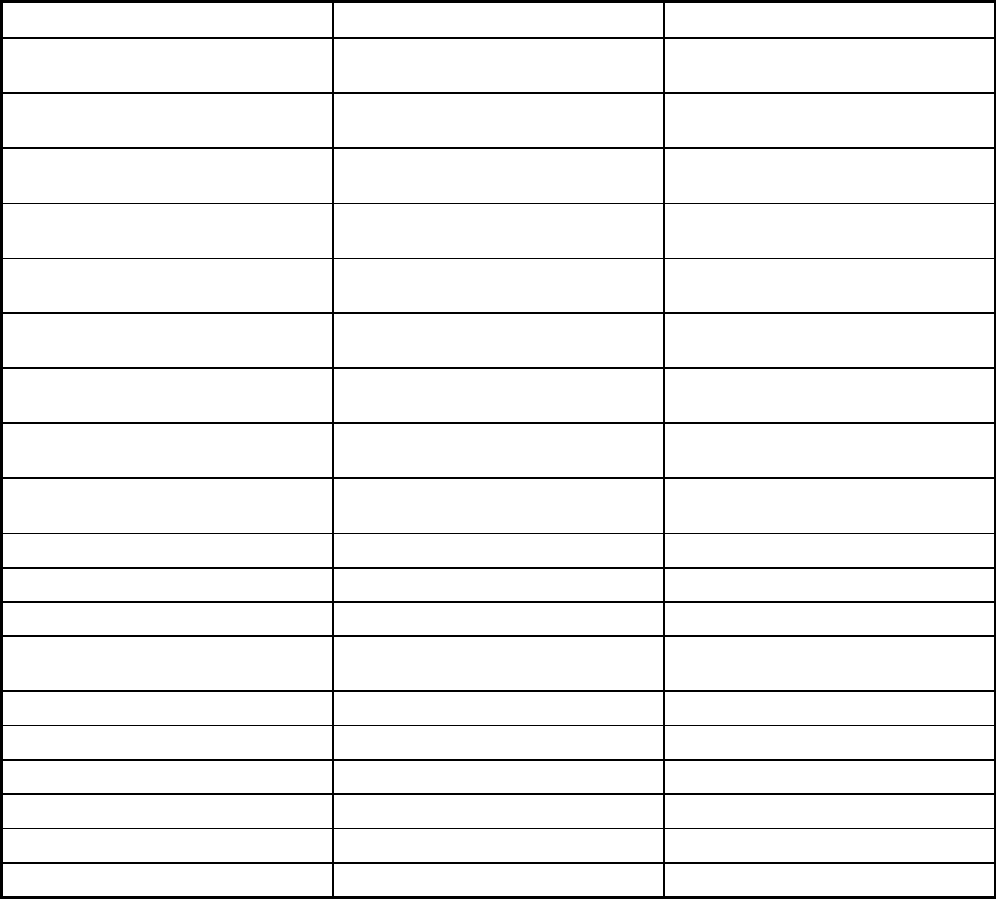
542
Features Family Care Partnership Program Family Care
Populations enrolled: Native
American/Alaskan Natives
Voluntary Mandatory
Populations enrolled: Foster Care and
Adoption Assistance Children
Exempt Exempt
Populations enrolled: Enrollment choice
period
Other Other
Populations enrolled: Enrollment broker
name (if applicable)
Populations enrolled: Notes on
enrollment choice period
Open enrollment Open enrollment
Benefits covered: Inpatient hospital
physical health
X
Benefits covered: Inpatient hospital
behavioral health (MH and/or SUD)
X
Benefits covered: Outpatient hospital
physical health
X
Benefits covered: Outpatient hospital
behavioral health (MH and/or SUD)
X X
Benefits covered: Partial hospitalization X X
Benefits covered: Physician X
Benefits covered: Nurse practitioner X X
Benefits covered: Rural health clinics
and FQHCs
X
Benefits covered: Clinic services X
Benefits covered: Lab and x-ray X
Benefits covered: Prescription drugs X
Benefits covered: Prosthetic devices X
Benefits covered: EPSDT X
Benefits covered: Case management X X
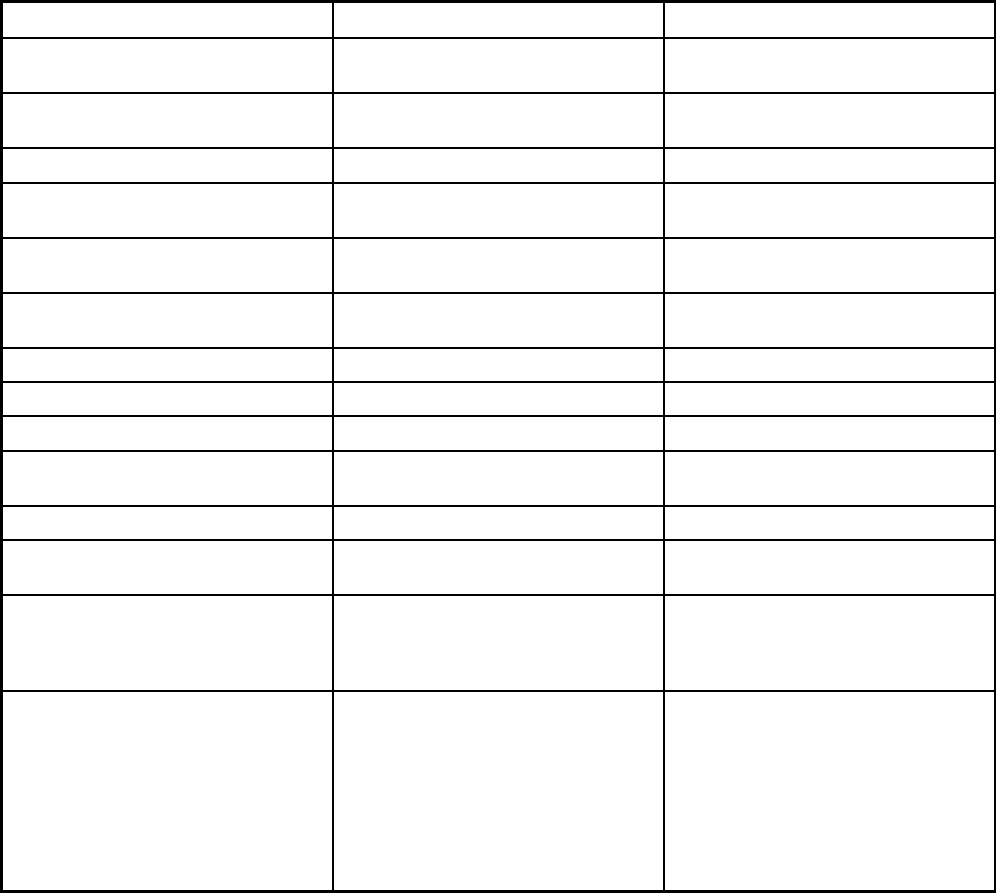
543
Features Family Care Partnership Program Family Care
Benefits covered: SSA Section 1945-
authorized health home
Benefits covered: Health home care
(services in home)
X X
Benefits covered: Family planning X
Benefits covered: Dental services
(medical/surgical)
X
Benefits covered: Dental (preventative
or corrective)
X
Benefits covered: Personal care (state
plan option)
X X
Benefits covered: HCBS waiver services X X
Benefits covered: Private duty nursing X X
Benefits covered: ICF-IDD X X
Benefits covered: Nursing facility
services
X X
Benefits covered: Hospice care X
Benefits covered: Non-Emergency
Medical Transportation
X X
Benefits covered: Institution for Mental
Disease inpatient treatment for people
ages 21-64 defined by 42 CFR
§438.6(e) as an 'in lieu of' benefit
Benefits covered: Other (e.g., nurse
midwife services, freestanding birth
centers, podiatry, etc.)
Ambulatory surgical center, audiology,
chiropractic, community mental health
services, durable medical equipment
and medical supplies, nurse-midwife,
occupational therapy, physical therapy,
podiatry, prenatal care coordination,
respiratory care for ventilator dependent
persons, school-
based services, speech
and language pathology, vision care
Community mental health services,
durable medical equipment and medical
supplies, occupational therapy, physical
therapy, respiratory care for ventilator
dependent persons, and speech and
language pathology
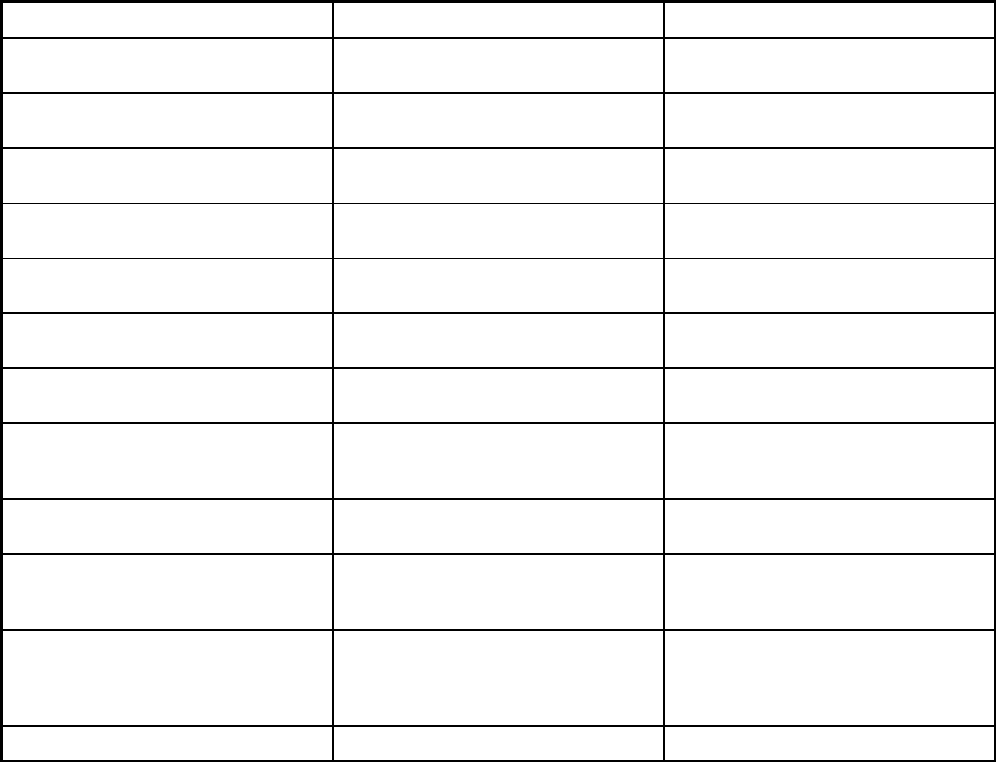
544
Features Family Care Partnership Program Family Care
Quality assurance and improvement:
HEDIS data required?
No No
Quality assurance and improvement:
CAHPS data required?
No No
Quality assurance and improvement:
Accreditation required?
No No
Quality assurance and improvement:
Accrediting organization
Quality assurance and improvement:
EQRO contractor name (if applicable)
MetaStar Inc MetaStar, Inc
Performance incentives: Payment
bonuses/differentials to reward plans
X X
Performance incentives: Preferential
auto-enrollment to reward plans
Performance incentives: Public reports
comparing plan performance on key
metrics
Performance incentives: Withholds tied
to performance metrics
X X
Performance incentives: MCOs/PHPs
required or encouraged to pay providers
for value/quality outcomes
Participating plans: Plans in Program Care Wisconsin; Community Care, Inc.;
Independent Care (iCare)
Care Wisconsin; Community Care, Inc.;
CommunityLink (became Inclusa in
September 2017); My Choice Family
Care; Lakeland Care District
Notes: Program notes
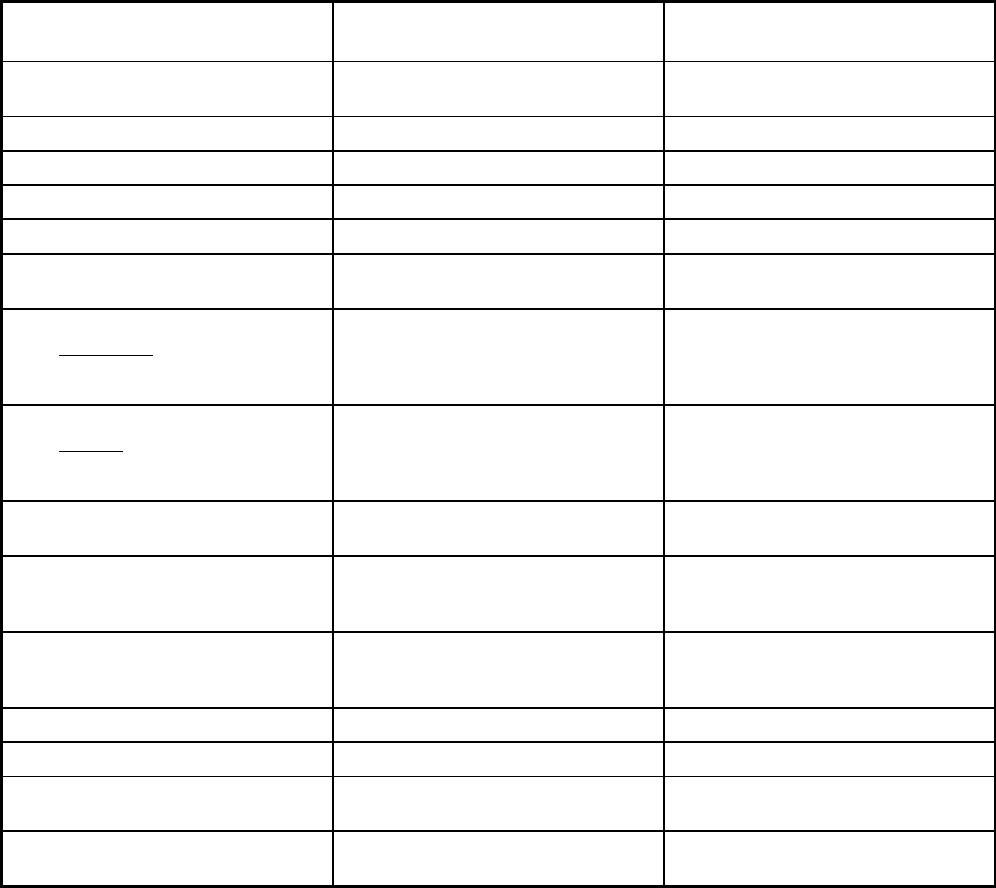
545
Wyoming Managed Care Program Features, as of 2018
Features
Wyoming PACE at Cheyenne Medical
Center
Care Management Entity for
Emotionally Disturbed Children
Program type Program of All-inclusive Care for the
Elderly (PACE)
Other Prepaid Health Plan (PHP)
(limited benefits)
Statewide or region-specific? Laramie County Statewide
Federal operating authority PACE 1915(b)/1915(c)
Program start date 02/01/2013 09/01/2015
Waiver expiration date (if applicable) 06/30/2020
If the program ended in 2018, indicate
the end date
Populations enrolled: Low-income
adults not covered under ACA Section
VIII (excludes pregnant women and
people with disabilities)
Populations enrolled: Low-income
adults covered under ACA Section VIII
(excludes pregnant women and people
with disabilities)
Populations enrolled: Aged, Blind or
Disabled Children or Adults
Voluntary
Populations enrolled: Non-Disabled
Children (excludes children in foster
care or receiving adoption assistance)
Populations enrolled: Individuals
receiving Limited Benefits (excludes
partial duals)
Populations enrolled: Full Duals Voluntary
Populations enrolled: Partial Duals Voluntary
Populations enrolled: Children with
Special Health Care Needs
Voluntary
Populations enrolled: Native
American/Alaskan Natives
Voluntary Voluntary
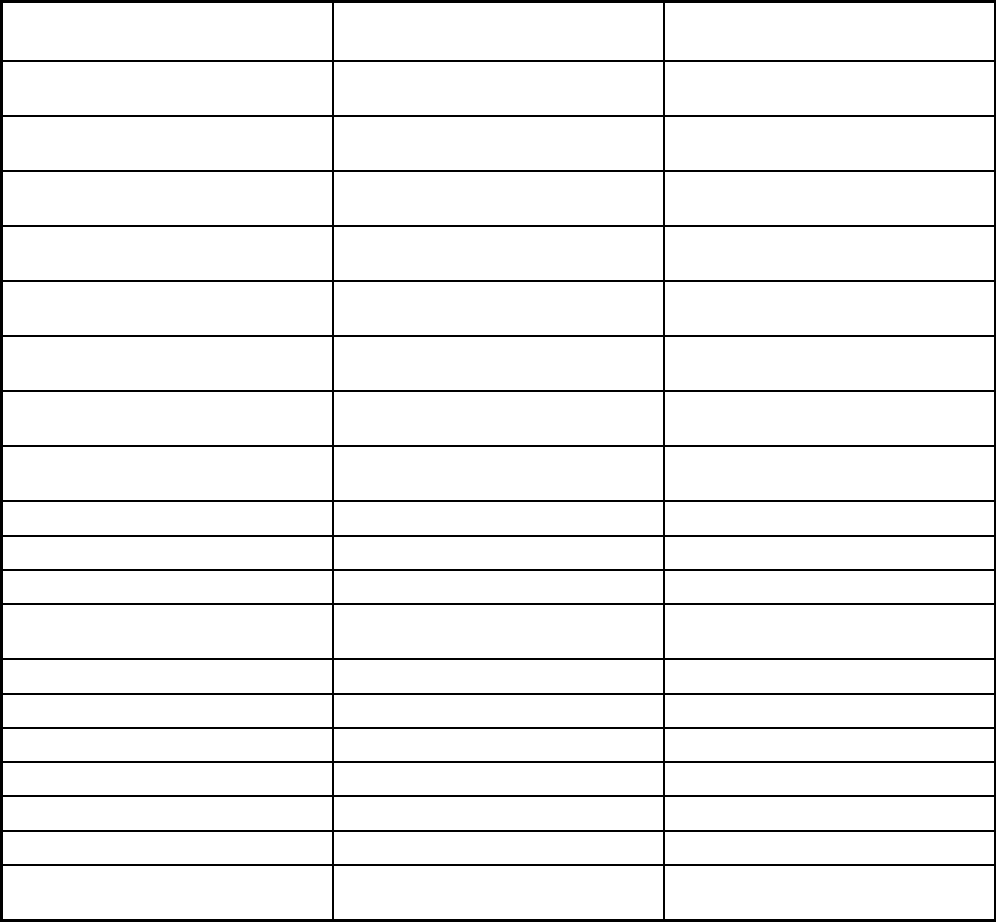
546
Features
Wyoming PACE at Cheyenne Medical
Center
Care Management Entity for
Emotionally Disturbed Children
Populations enrolled: Foster Care and
Adoption Assistance Children
Exempt Voluntary
Populations enrolled: Enrollment choice
period
N/A
Populations enrolled: Enrollment broker
name (if applicable)
Populations enrolled: Notes on
enrollment choice period
Benefits covered: Inpatient hospital
physical health
X
Benefits covered: Inpatient hospital
behavioral health (MH and/or SUD)
X
Benefits covered: Outpatient hospital
physical health
X
Benefits covered: Outpatient hospital
behavioral health (MH and/or SUD)
X
Benefits covered: Partial hospitalization X
Benefits covered: Physician X
Benefits covered: Nurse practitioner X
Benefits covered: Rural health clinics
and FQHCs
Benefits covered: Clinic services X
Benefits covered: Lab and x-ray X
Benefits covered: Prescription drugs X
Benefits covered: Prosthetic devices X
Benefits covered: EPSDT
Benefits covered: Case management X X
Benefits covered: SSA Section 1945-
authorized health home
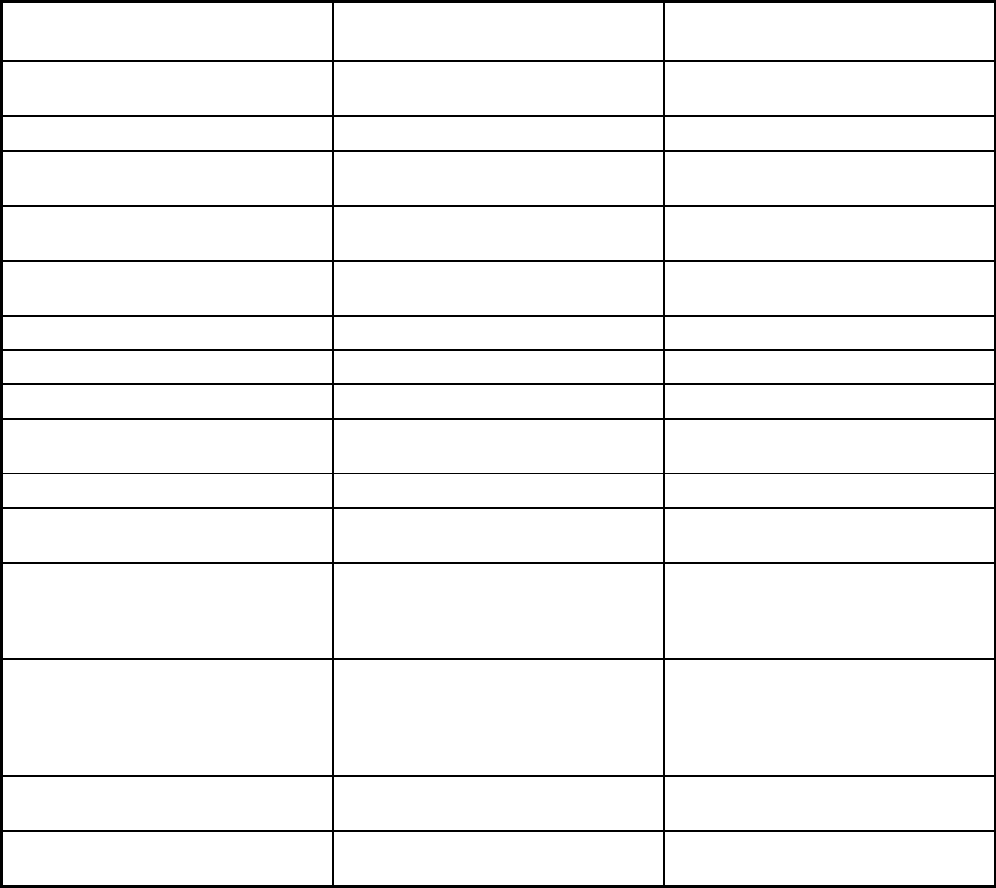
547
Features
Wyoming PACE at Cheyenne Medical
Center
Care Management Entity for
Emotionally Disturbed Children
Benefits covered: Health home care
(services in home)
X
Benefits covered: Family planning X
Benefits covered: Dental services
(medical/surgical)
X
Benefits covered: Dental (preventative
or corrective)
X
Benefits covered: Personal care (state
plan option)
Benefits covered: HCBS waiver services X X
Benefits covered: Private duty nursing
Benefits covered: ICF-IDD
Benefits covered: Nursing facility
services
X
Benefits covered: Hospice care X
Benefits covered: Non-Emergency
Medical Transportation
X
Benefits covered: Institution for Mental
Disease inpatient treatment for people
ages 21-64 defined by 42 CFR
§438.6(e) as an 'in lieu of' benefit
Benefits covered: Other (e.g., nurse
midwife services, freestanding birth
centers, podiatry, etc.)
Any other service determined by the
interdisciplinary team (IDT) as
necessary to meet the participant’s
needs and which improve or maintain
the participant’s overall health status.
Targeted case management State Plan
Authority including family care
coordinators, youth peer support
partners, and family support partners.
All individuals receive respite.
Quality assurance and improvement:
HEDIS data required?
No No
Quality assurance and improvement:
CAHPS data required?
No No
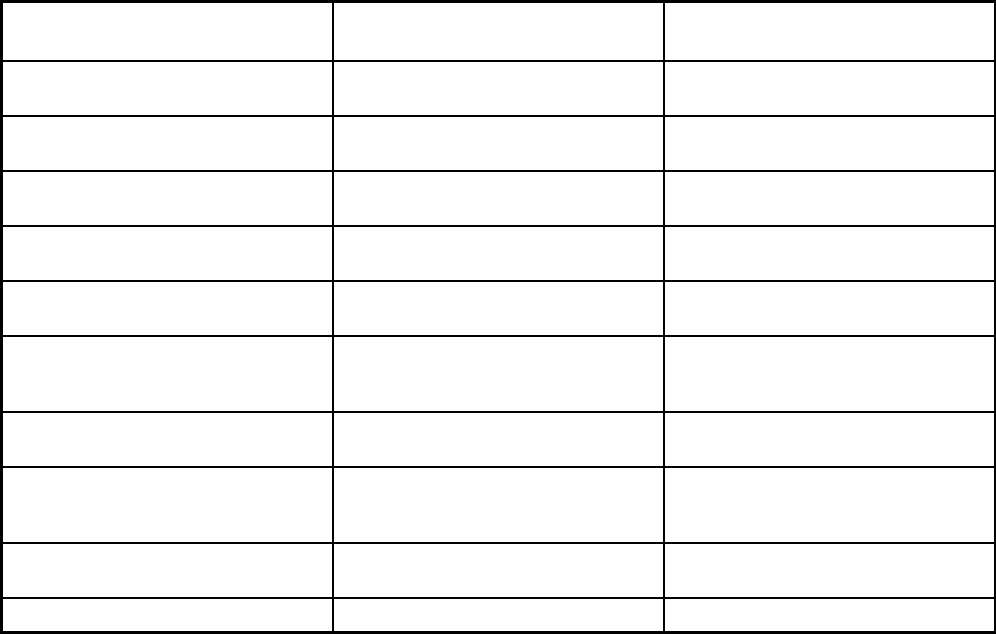
548
Features
Wyoming PACE at Cheyenne Medical
Center
Care Management Entity for
Emotionally Disturbed Children
Quality assurance and improvement:
Accreditation required?
No Yes
Quality assurance and improvement:
Accrediting organization
NCQA, JCAHO, URAC, Council on
Accreditation COA
Quality assurance and improvement:
EQRO contractor name (if applicable)
Navigant
Performance incentives: Payment
bonuses/differentials to reward plans
X
Performance incentives: Preferential
auto-enrollment to reward plans
Performance incentives: Public reports
comparing plan performance on key
metrics
Performance incentives: Withholds tied
to performance metrics
X
Performance incentives: MCOs/PHPs
required or encouraged to pay providers
for value/quality outcomes
Participating plans: Plans in Program Cheyenne Regional Medical Center
PACE
CME Statewide
Notes: Program notes
