Lean Six Sigma for the
Healthcare Practice
A Pocket Guide
Also available from ASQ Quality Press:
The Certified Six Sigma Green Belt Handbook
Roderick A. Munro, Matthew J. Maio, Mohamed B. Nawaz, Govindarajan
Ramu, and Daniel J. Zrymiak
Six Sigma for the Office: A Pocket Guide
Roderick A. Munro
Six Sigma for the Shop Floor: A Pocket Guide
Roderick A. Munro
Automotive Internal Auditor Pocket Guide: Process Auditing to
ISO/TS 16949:2002
Roderick A. Munro
The Certified Six Sigma Black Belt Handbook, Second Edition
T. M. Kubiak and Donald W. Benbow
Applied Statistics for the Six Sigma Green Belt
Bhisham C. Gupta and H. Fred Walker
Statistical Quality Control for the Six Sigma Green Belt
Bhisham C. Gupta and H. Fred Walker
5S for Service Organizations and Offices: A Lean Look at Improvements
Debashis Sarkar
The Executive Guide to Understanding and Implementing Lean Six
Sigma: The Financial Impact
Robert M. Meisel, Steven J. Babb, Steven F. Marsh, and James
P. Schlichting
Transactional Six Sigma for Green Belts: Maximizing Service and
Manufacturing Processes
Samuel E. Windsor
Defining and Analyzing a Business Process: A Six Sigma Pocket Guide
Jeffrey N. Lowenthal
The Certified Manager of Quality/Organizational Excellence Handbook,
Third Edition
Russell T. Westcott, editor
To request a complimentary catalog of ASQ Quality Press publications,
call 800-248-1946, or visit our Web site at http://qualitypress.asq.org.
Lean Six Sigma for the
Healthcare Practice
A Pocket Guide
Roderick A. Munro, PhD
ASQ Quality Press
Milwaukee, Wisconsin

American Society for Quality, Quality Press, Milwaukee 53203
© 2009 by ASQ
All rights reserved. Published 2009
Printed in the United States of America
15 14 13 12 11 10 09 5 4 3 2 1
Library of Congress Cataloging-in-Publication Data
Munro, Roderick A.
Lean Six Sigma for the healthcare practice : a pocket guide / Roderick A. Munro.
p. cm.
Includes bibliographical references and index.
ISBN 978-0-87389-760-0 (soft cover, spiral bound : alk. paper)
1. Six sigma (Quality control standard) —Handbooks, manuals, etc.
2. Medical care—Quality control—United States—Statistical methods—
Handbooks, manuals, etc. I. Title.
[DNLM: 1. Health Services Administration—Handbooks. 2. Quality
Assurance, Health Care—Handbooks. 3. Efficiency, Organizational—
Handbooks. W 49 M968L 2009]
RA399.A3M66 2009
362.1068—dc22 2009000930
ISBN: 978-0-87389-760-0
No part of this book may be reproduced in any form or by any means, electronic,
mechanical, photocopying, recording, or otherwise, without the prior written
permission of the publisher.
Publisher: William A. Tony
Acquisitions Editor: Matt T. Meinholz
Project Editor: Paul O’Mara
Production Administrator: Randall Benson
ASQ Mission: The American Society for Quality advances individual,
organizational, and community excellence worldwide through learning, quality
improvement, and knowledge exchange.
Attention Bookstores, Wholesalers, Schools, and Corporations: ASQ Quality
Press books, videotapes, audiotapes, and software are available at quantity
discounts with bulk purchases for business, educational, or instructional use.
For information, please contact ASQ Quality Press at 800-248-1946, or write to
ASQ Quality Press, P.O. Box 3005, Milwaukee, WI 53201-3005.
To place orders or to request a free copy of the ASQ Quality Press Publications
Catalog, including ASQ membership information, call 800-248-1946. Visit our
Web site at www.asq.org or http://www.asq.org/quality-press.
Printed in the United States of America
Printed on acid-free paper
This book is dedicated to the Quality
Improvement Coaches (QICs) and Primary
Care Providers (PCPs) in Michigan
who have embarked on the Improving
Performance in Practice (IPIP) process.
The State of Michigan has combined the
reporting requirements of the Patient-
Centered Medical Home and the national
IPIP into one reporting process to
reduce redundancy and to focus more on
improvements in healthcare quality.
Most especially to the many overloaded,
stressed-out healthcare professionals who
may feel that they can not take on one more
task or new patient. The methodologies and
tools found in this book will help you.
(This page intentionally left blank)
vii
Contents
Acronym List ............................. xi
Preface.................................. xiii
Acknowledgments ........................ xv
Suggested Use of This Book................. xix
The DMAIC Matrix Guide................... 1
What Is Lean Six Sigma? ................... 5
Your Role in Lean Six Sigma ................ 11
What Is Variation? ........................ 17
Things You Might Be Involved With.......... 25
The DMAIC Model ........................ 29
Teams ................................... 41
The Lean Six Sigma Road Map for
the Practice ........................... 47
Summary ................................ 49
Tools.................................... 53
7S ................................... 53

Advanced Practice Quality Planning
(Healthcare APQP)................... 58
Auditing (Sampling, Sampling Plans) ...... 62
Benchmarking . . . . . . . . . . . . . . . . . . . . . . . . . 66
Brainstorming ......................... 71
Business Operating System (BOS) for
Healthcare Organizations ............. 76
Cause-and-Effect Diagram (Fishbone
Diagram, Ishikawa Diagram) .......... 79
Check Sheets .......................... 84
Continual Improvement (Kaizen,
Kaizen Events) ...................... 89
Cost–Benefit Analysis (Cost of Quality,
Quality Cost, Cost of Poor Quality,
Return on Investment) ............... 93
Cycle Time Analysis ..................... 98
Failure Mode and Effects Analysis......... 101
Flowchart (Flow Map, Process Map,
Current State/Could Be/Should
Be Map)............................ 113
Histogram ............................ 118
Kanban (Wait Time, Patient Pull-
Through)........................... 122
Lessons Learned ....................... 124
Management Involvement ............... 126
Measurement Systems Analysis (MSA) ..... 129
Mistake-Proofing (Error-Proofing,
Poka-Yoke) ......................... 133
Pareto Chart........................... 136
PDSA Cycle (Plan–Do–Study–Act) ......... 141
Practice Strategy (Future State) Project
Planning ........................... 145
Problem Solving ....................... 148
viii Table of Contents

Table of Contents ix
Process Behavior Charts (Statistical
Process Control) ..................... 152
Process Identification ................... 158
Process Improvement (PI) ................ 160
Run Chart ............................. 163
Scatter Diagram........................ 166
SIPOC Diagram......................... 170
Standard Operating Procedures (SOPs) .... 173
Standardization (SDCA—Standardize–
Do–Check–Adjust) ................... 175
Systems Thinking....................... 177
Team Meetings (Huddles) ............... 181
Teams (Employee Involvement,
Improvement, Self-Directed) .......... 185
Value Analysis ......................... 192
Value Stream Map (VSM) ................ 195
Variation Reduction .................... 199
Visual Controls, Aids .................... 202
Voice of the Customer (Patient
Feedback) .......................... 204
Walkaround/Walkthrough/Waste Walk .... 207
References............................... 211
Index ................................... 217
(This page intentionally left blank)
xi
Acronym List
7S—sort, set-in-order, shine, standardize,
sustain, safety, oversight
8D—eight disciplines to problem solving
APQP—healthcare advanced practice quality
planning
BOS—business operating system
C&E —cause-and-effect diagram
CI—continual improvement
COPQ—cost of poor quality
COQ—cost of quality
CPHQ—Certified Professional in Healthcare
Quality
CQIA—Certified Quality Improvement
Associate
DMAIC—define, measure, analyze, improve,
control
FMEA—failure mode and effects analysis

xii Acronym List
IPIP—improving performance in practice
IPO—input, process, output
ISO—International Organization for
Standardization
LCL—lower control limit (see “Process
Behavior Chart”)
M P CC—Michigan Primary Care Consortium
MSA—measurement systems analysis
PCMH—patient-centered medical home
PCP—Primary Care Provider
PDCA—plan–do–check–act
PDS A—plan–do–study–act
PI—process improvement
QIC—Quality Improvement Coach
ROI—return on investment
RPN—risk priority number (see “FMEA”)
SDCA—standardize–do–check–adjust
SIP OC—supplier, input, process, output,
customer
SOP—standard operating procedure
SPC—statistical process control
UCL—upper control limit (see “Process
Behavior Chart”)
VSM—value stream map
xiii
T
his book is a continuation of a series of
works started by the author, referred to as
QUIT—“Quality in Training.” It is hoped
that through this ongoing series people will be
helped in finding joy in the work that they do,
leading to healthier, happier lives.
A Zen Buddhist text on The Art of Living
states:
The Master in the art of living makes little
distinction between his work and his play,
his labor and his leisure, his mind and his
body, his education and his recreation,
his love and his religion. He hardly knows
which is which. He simply pursues his vision
of excellence in whatever he does, leaving
others to decide whether he is working or
playing. To him he is always doing both.
It will be left to the reader to decide at what point
the author is/was doing each in this text.
Preface

xiv Preface
We are discussing the concept of healthcare
quality sometimes called “quality of care and
services.” In this book, our focus is on how well
the organization performs the many activities
and functions involved in patient care. The term
“quality of care and services” is not limited to the
technical quality of care provided to patients;
“quality of care and services” is a broader, more
general category that includes not only the tech-
nical quality of care, but also includes how well
patient service needs are met.
If you would like to make comments to
the author about this book, please contact him at
authors@asq.org.
xv
A
s in any work, a lot of people were
involved in developing this book. I would
like to thank all the class participants,
suppliers, and peers that I have worked with in
the past 30 years. I continue to learn from all
your input.
I especially would like to thank Dr. Dean H.
Stamatis and Dr. Elizabeth J. Rice for their years
of friendship and their encouragement and sup-
port of this work.
Thanks also go to the staff at ASQ Quality
Press and the reviewers for their time, efforts,
and support in making this book a reality. Thanks
especially to Paul O’Mara and Matt Meinholz for
their ongoing support of this series.
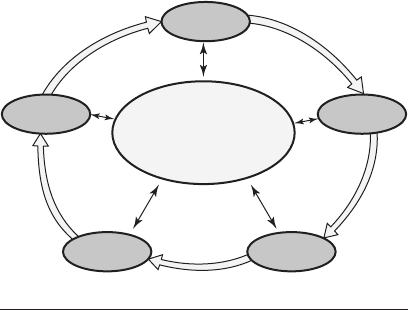
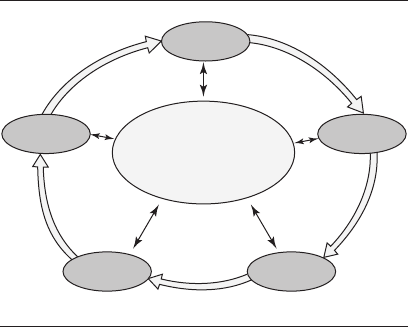
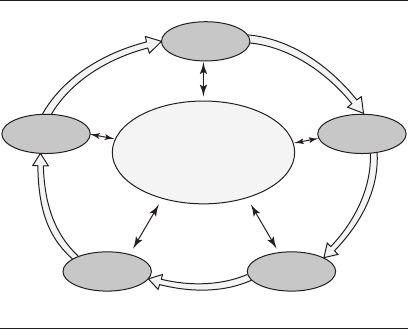
Special thanks goes to the Michigan IPIP team
of professionals. The Healthcare Improvement
Model on page xvi is a summary of some of the
early work that has been accomplished in assist-
ing Practices toward healthcare improvements.
Acknowledgments

xvi Acknowledgments
SA
DC
PA
DS/C
Health system
professionals
Community
Facilitate the project
using best processes
“Lean” the practice
Solve problems/
breakthrough improvement
Quality and lean
professionals
Informed,
activated
patients
Project
management
Needs
assessment
Team building
7 wastes
Kaizen
Value stream
Current state
Future state
DMAIC
Process mapping
5 whys Root cause analysis
Measurement systems
FMEA
Visual controls
7S
Waste walk
Value analysis
Error-proofing
Pull systems
Quick changeover
Standardized work
Set up controls
Kanban
Scoping
Cost of poor quality
Scheduling
Brainstorming
ROI
Training
Leadership
Productive
interactions
Improved outcomes
Patient-Centered
Medical Home
Prepared,
proactive
practice team

I would like to especially acknowledge the follow-
ing individuals:
Dr. Walt Talamonti, MD, Chair, Michigan
IPIP Steering Committee
Dr. Ernest Yoder, MD, Vice Chair,
Michigan IPIP Steering Committee
Dr. Joseph Fortuna, MD, Medical
Champion
Rose Steiner, RN, Director, Michigan IPIP
Dr. Kevin Piggott, MD, Chair, IPIP
Learning Collaborative
Quality Improvement Coach team volunteers:
Lou Ann Lathrop (General Motors), Chair
John Casey (Whitehall Group)
John Katona (Delphi)
Dave Lalain (AIAG)
Victor Lloyd (St. John Health)
Rebecca Snyder (Ford Motor Company)
Advisor to Michigan MPCC/AIAG IPIP process:
Barry Klein (GlaxoSmithKline
Pharmaceuticals)
Acknowledgments xvii
(This page intentionally left blank)
xix
T
his book is for those in the Practice or
staff activities of your organization whose
customers/payers may be encouraging or
requiring you to use Lean Six Sigma in your
workplace or to simply improve the way health-
care is being provided. The book is intended to
be a basic, easy-to-read, quick and handy ref-
erence to the process improvement topics that
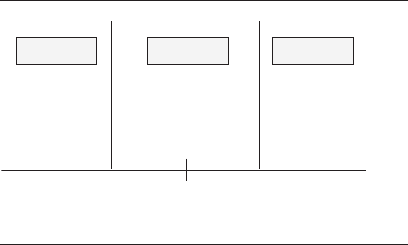
are so important in healthcare (page xx shows
a Venn diagram of tools found in this book). The
first seven sections of the book cover the basics
of Lean Six Sigma (“What Is Lean Six Sigma? ”
through “Lean Six Sigma Road Map for the Prac-
tice”) and how it can be applied and implemented
in the Practice. The tool matrix guide beginning
on page 2 has been arranged alphabetically for
ease of finding tools as needed. The remainder of
the pocket guide gives a brief description of the
various tools and methodologies used in Lean
Six Sigma. Each discussion has purposefully
Suggested Use of
This Book
xx Suggested Use of This Book
been kept short and simple to allow for a basic
understanding and includes some tips on how
or when to use the tool. If more detail is needed,
other references can be consulted to realize the
full impact of the tool.
Everyone in the organization, from the janitor
to the senior executive or Practice oversight com-
mittee, should know the basic information found
in this book. Some have felt in the past that this
type of information belonged only on the manu-
facturing floor. Today we have learned that there
is probably more opportunity within the Practice
than ever thought before (Berwick and Leape
Problem identification
Value stream map
Flowchart
Value analysis
Check sheet
Voice of the
customer
Histogram
Scatter diagram
Process
behavior chart
Measurement
systems analysis
Cycle time
Audit
Sampling
Pareto chart
Run chart
Stratification
Cause-and-effect chart
Brainstorming
Visual controls
Visual aids
7S
Problem analysis
Venn diagram of tools covered in this book.

Suggested Use of This Book xxi
1999). Especially since many healthcare practi-
tioners have received a large amount of scientific
training, the use of statistical tools to improve
processes in healthcare and quality of care and
services should be a natural combination.
Persons who can pass a designated test, either
internally created or one of many offered by var-
ious organizations, can be designated as Lean
Six Sigma Green Belts. Green Belts work with
teams to gather data and to analyze, improve,
and control the processes in the Practice. People
who become exceptionally expert in the use of
the Lean Six Sigma methods and processes and
who pass advanced testing are called Lean Six
Sigma Black Belts. Black Belts use experiments
and other advanced tools to help solve especially
difficult problems.
Your Practice may or may not have a Black
Belt (a full-time or part-time person dedicated to
doing Lean Six Sigma in your Practice). However,
everyone should become involved in continual
improvement efforts to help ensure your organiza-
tion’s survival and the improved care and health
of patients. Some process improvements can be
very simple to identify and implement while
others may take some time for the staff to fully
understand the dynamics of the issues involved.
These improvement efforts can be accomplished
by using this book and the tools within it to guide
your improvement projects.

xxii Suggested Use of This Book
In addition, you may deal with customer audit
personnel, government auditors, people desig-
nated as “rent a Black Belts,” or other coaches or
consultants to help with the advanced aspects of
Lean Six Sigma. By using all the resources that
are available, you can help your Practice stay
competitive in today’s global marketplace.
One of the biggest challenges in the Practice is
to allow time to understand the use of these tools
and to start collecting the data and information
that will be needed to make continual improve-
ment efforts a reality. Everything can be defined
as a process, and processes can be measured so
that they can be monitored for improvement. In
the past, you may not have thought about how to
measure work that is done in the Practice. Keep-
ing an open mind will be paramount to the suc-
cess of Lean Six Sigma in your Practice and to
making your work easier and more fulfilling.
Experience has shown that the journey can be
fun and rewarding for those who get honestly
involved in using the improvement tools and
methods. This effort is the “how to” of learning to
“work smarter, not harder!”
1
The DMAIC
Matrix Guide
T
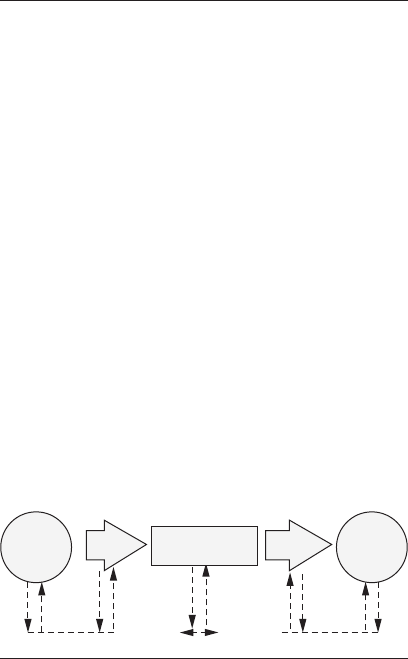
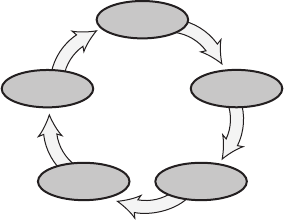
he DMAIC model (shown in Figure 1) is
referred to throughout this book. The acro-
nym stands for define, measure, analyze,
improve, and control. The reader will find the
Verify
Design
SDCA SDCA
PDSAPDSA
PDSA
MeasureControl
Improve Analyze
Define
Practice strategy
Employee involvement
Team meetings
Figure 1 The DMAIC model.
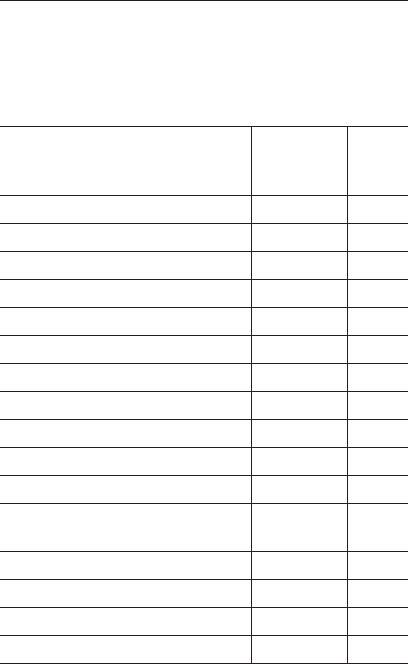
2 The DMAIC Matrix Guide
following matrix helpful as he or she matches
particular tools and approaches to particular
phases in the DMAIC process.
When used
in Lean
Name of tool/approach Six Sigma Page
7S DMAIC 53
Advanced practice quality planning D 58
Auditing DMAIC 62
Benchmarking MA 66
Brainstorming DAI 71
Business operating system (BOS) DMAIC 76
Cause-and-effect diagram DMA 79
Check sheets MA 84
Continual improvement AIC 89
Cost–benefit analysis DMAIC 93
Cycle time analysis DMIC 98
Failure mode and effects analysis DIC 101
(FMEA)
Flowchart DAI 113
Histogram M 118
Kanban IC 122
Lessons learned DIC 124
Continued

The DMAIC Matrix Guide 3
When used
in Lean
Name of tool/approach Six Sigma Page
Management involvement DMAIC 126
Measurement systems analysis MC 129
(MSA)
Mistake-proofing IC 133
Pareto chart M 136
PDSA cycle (plan–do–study–act) MAI 141
Practice strategy DMAIC 145
Problem solving I 148
Process behavior charts DC 152
Process identification D 158
Process improvement I 160
Run chart MC 163
Scatter diagram MAI 166
SIPOC diagram DM 170
Standard operating procedures IC 173
(SOPs)
Standardization DC 175
Systems thinking DI 177
Team meetings DMAIC 181
Teams D 185
Value analysis MAC 192
Continued
4 The DMAIC Matrix Guide
When used
in Lean
Name of tool/approach Six Sigma Page
Value stream map D 195
Variation reduction IC 199
Visual controls, aids IC 202
Voice of the customer DC 204
Walkaround/walkthrough/ DMAIC 207
waste walk

5
What Is Lean Six Sigma?
L6s
L
ean Six Sigma is a term describing the
overall concept of continual improvement
of everyday processes (Deming 1993). Con-
tinual improvement can be defined as the use of
problem-solving techniques and quick deploy-
ment to implement improvements, and then the
use of process behavior charts (Wheeler and
Poling 1998) to maintain the gains. Lean Six
Sigma is about strategic alignment, applied
learning, and culture or belief system transfor-
mation that uses four distinct but interrelated
characteristics: a strategy deployment approach,
a belief system, a statistical calculation, and a
suite of project improvement methods (Caldwell,
Brexler, and Gillem 2005). Lean Six Sigma is
being used in many organizations today in a
variety of applications (for example, schools, hos-
pitals, and private Practices). Basically, Lean Six
Sigma is about collecting data on a process and
using that data to analyze and interpret what

6 What Is Lean Six SIgma?
is happening in that process so that the process
can be improved to better satisfy the customer. A
basic process can be defined as an input, trans-
formation, and output (see Figure 2).
Lean Practice is simply the banishment of
waste. It is the elimination of waste by better
organizing and managing customer relations,
the supply chain, product development, and ser-
vice activities. Many service organizations, espe-
cially the larger ones, have been designed with
the idea of creating large service runs over short
periods of time (sometimes resulting in repetitive
checking of work done)—typically called mass
production. In Lean Practice, the organization
develops a process for processing/producing just
what is needed, as it is needed, by the patients/
customers that eliminates waste in time, energy,
effort, rechecking/verifying, inventories, mate-
rial handling, storage, and so on. This process is
also called the pull concept because the patient/
customer “pulls” what is needed from the suppli-
ers or Practice instead of the supplier making and
stockpiling large quantities until the customer
decides it wants some, as in mass production.
Transformation
(Process)
Input Output
Figure 2 The process model.

What Is Lean Six Sigma? 7
So, bringing these two concepts together we
get Lean Six Sigma for Healthcare. This is a pro-
cess that uses continual improvement techniques/
methodologies to eliminate waste in the Practice.
Waste is defined as anything that stifles health-
care staff personnel or patients, or results in
lost time, productivity, or simply sitting around
an office waiting for something to happen. But
is this really important in the way healthcare is
delivered today?
Dr. Donald Berwick has stated, “With the
rising complexity and reach of modern medi-
cine have come startling
levels of risk and harm
to patients” (Berwick and Leape 1999). Many
people who work in healthcare may not recog-
nize the things that they do as being part of a
process. Since they do not work repetitively as a
person in a factory running a machine, the Prac-
tice employee might be tempted to say, “I do not
have a process.” A process does not have to be a
repetitive task done exactly the same each and
every time. When we come into work each day,
we have general tasks that we do every day. The
specific items may change or be done in different
sequences; however, we do have procedures that
we follow to get our work done. This is what we
will be looking at and studying throughout this
guidebook.
Lean Six Sigma started at Motorola in the late
1980s as Six Sigma on the shop floor (process) and
8 What Is Lean Six SIgma?
then moved into the front office (transactional).
What we know today as Lean Six Sigma for
Healthcare has been honed with the addition
of lean methodologies at General Electric and a
growing number of other organizations. Following
a prescribed process, an entire organization starts
to look at everything that it does in the light of
reducing variation and waste—with the result
of increasing customer satisfaction. Customers
are defined as anyone from the next person who
uses the work we do (internal customer) to the
ultimate customer who uses the products or ser-
vices that our organization produces (external
customer). To assist in this process, sometimes
the supplier and customer are added to the basic
process flow (input, transformation, output),
creating the SIPOC (supplier, input, process,
output, customer) identification. This is espe-
cially useful in helping to define the boundaries
of what is to be studied (see Figure 3).
FeedbackFeedback
Transformation
(Process)
Input Output
Supplier Customer
Figure 3 The SIPOC model.

What Is Lean Six Sigma? 9
For some, the idea of improving a process
is a waste of time and should not be bothered
with (“we are already working the hardest that
we can”). Lean Six Sigma is not about working
harder, it is about working smarter! Juran (1964)
points out that the work we do is a result of the
fact that “changes creep up on us week by week,
a little bit at a time. Over a year or two, there
are 50 or 100 of these bits, which amounts to
quite a bit. The skills of the staff or managers
have not necessarily kept pace, and we wake up
to the existence of a wide gap.” This is one expla-
nation for why accidents and procedural errors
happen in healthcare today. If the root cause is
found for an accident or rejection of a product or
service, it usually can be traced back to either
many small changes that occurred in our orga-
nization or something having been omitted acci-
dentally between healthcare units.
Using Lean Six Sigma methodologies, we can
find those bits of change and decide which ones
should be fixed/modified and which ones need to
be improved. This process is not meant to be a
quick-fix (silver bullet) approach to the health-
care industry or individual patient care. The
methodical use of the tools over time will save
resources and effort (and lives) in doing our daily
jobs. This book provides an overview of the tools
and processes used in Lean Six Sigma. Detailed
explanations of the use of each tool or process can

10 What Is Lean Six SIgma?
be accessed readily in other references or on the
Internet. For many readers, this book will serve
as a quick reference to what you may already
have in your Practice that can be used by indi-
viduals and teams to improve overall processes.
11
Your Role in
Lean Six Sigma
I
n the Lean Six Sigma problem-solving pro-
cess, you may find a number of tools and
methods that you are already familiar with
and a few that are new to you. You may very well
ask, “How is this any different from what we
have done before?” The direct answer will need
to be given by your organization, and it depends
on the various programs that have already been
used. For many Practices, the Lean Six Sigma
effort is part of an ongoing evolution of how they
do their work to improve patient care. One of the
main things that you should notice is that every-
one will be more involved with problem-solving
efforts and with the everyday problems found in
patient care.
As we prepare for this exciting journey, first
look at Figure 4. What would you predict as the
golfer’s next score if you were looking only at
the top box of numbers? Maybe a golf score
within the range 100 to 105 would be a good
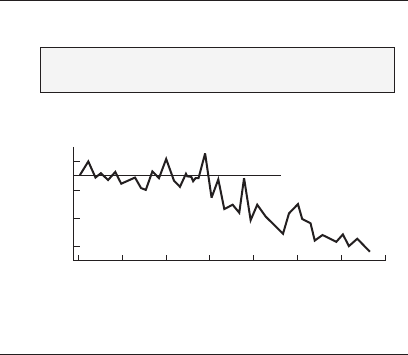
12 Your Role in Lean Six Sigma
guess. Could you say anything about the golfer
in general? Now take a look at the graph of the
same numbers (this is called a run chart), and a
lot of information becomes very clear. Your new
estimated score for game number 205 might be
within the range of 92 to 97. You could also say
that up through game 180 the golfer was rela-
tively consistent, scoring around 120. But then
something happened—maybe lessons were
taken, new clubs bought, or a new grip started
to be used—and things began to improve. The
Which provides more insight?
What is your prediction for game number 205?
Game number 180 185 190 195 200 205
Golf score 112 119 102 104 100 ?
or
Golf Scores
Game number
Score
125
115
105
95
170 190185180175 195 200 205
Figure 4 More insight.

Your Role in Lean Six Sigma 13
golfer still has not stabilized from whatever hap-
pened and may improve even more. The graph
should be continued to monitor the golfer’s prog-
ress. Thus, as the saying goes, this one picture (a
run chart) is worth a thousand words. Now think
about the large number of “scores”—patient tests
or numerical values—that we have in healthcare
for a patient. The human body is also a system,
and by using some simple graphs we can work
with patients to help improve an individual’s
system (process) of health. One quick note here:
if we record a patient’s vitals in an electronic
system (that is, registry, spreadsheet, database),
then the computer can give us these graphics
with a couple of simple clicks.
During the change process, and while using
this book, you will be able to use the Lean Six
Sigma model for improvement. It has been shown
that by following a model or road map we can
usually accomplish something much quicker
than we can without a guide. Some organizations
today use a model called MAIC (measure, ana-
lyze, improve, control) as a road map. They refer
to this process as being able to do “magic” with-
out the G (garbage) that we find in many activi-
ties. Many organizations have added a D (define)
stage at the beginning of the model to identify
the customer process, resulting in the DMAIC
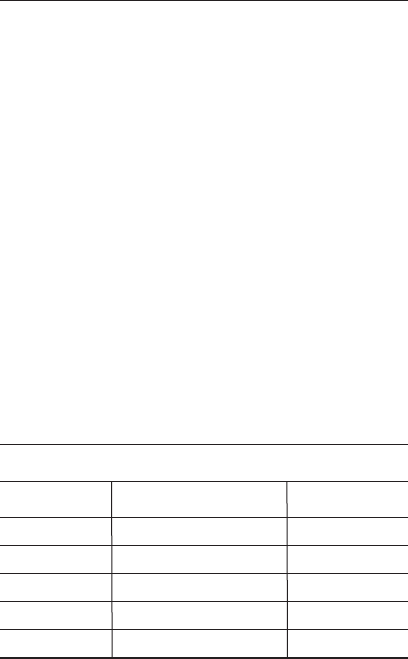
model (see Figure 5), which is commonly used in
the Lean Six Sigma approach.
14 Your Role in Lean Six Sigma
You may already use run charts, check-
lists, process sheets, standard operating proce-
dures, or any number of other such techniques in
your daily work. The use of the Lean Six Sigma
model for improvement should not replace any-
thing you’re currently doing. It should, however,
help you to review your daily work and look for
areas or methods to improve the process that
customers/patients want and need. Just because
we are doing the same things we have done
before, do our customers/patients still want the
same things from us? How many handwritten or
typed letters, memos, scripts, and so on, do you
Practice strategy
Employee involvement
Team meetings
Verify
Design
MeasureControl
Improve Analyze
Define
Figure 5 The DMAIC base model.

Your Role in Lean Six Sigma 15
see in a typical Practice today? Most work is now
done on computers and sent electronically.
We are beginning a journey of continual
improvement that can be used in our work and our
daily lives. Some of us have been on this journey
for some time while others may just be starting.
The process involves using what Deming (1993)
refers to as profound knowledge: appreciation
for a system, knowledge about variation, theory
of knowledge, and psychology. By following the
Lean Six Sigma methodology for improvement
you should see things around you work better, be
safer, and satisfy your customers more.
(This page intentionally left blank)
17
What Is Variation?
V
ariation is the basic principle that no two
things are exactly alike. There are usu-
ally many reasons for things not being
constant. Have you ever noticed while driving
that your vehicle does not stay exactly the same
distance between the white and yellow lines?
What causes this variation? Of course most of
us drive well, and the lines are on the road to
help us get to where we want to go without run-
ning into other vehicles or the ditch. But if we
could measure our vehicle’s distance between the
lines, we would find that minor drifts do occur
on a regular basis (common cause variation). If a
police officer pulls us over, however, some of the
reasons for drifting too far (special cause varia-
tion) might include these: wind velocity with a
high-profile vehicle, alcohol or drug involvement,
cell phone usage, inexperienced driver, poor
weather conditions, worn or damaged tires, or
other factors. The author was once pulled over by

18 What Is Variation?
the police because he was driving too close to the
white line. It seems that in that area, this could
only mean that the driver had been drinking
at the local casino! However, on dark, foggy
nights, the author prefers staying close to the
white line to give oncoming drivers more room on
two-lane country roads.
Similar things happen in healthcare. We have
procedures for how to do the work, but small
variations or personal preferences can and will
cause differences in the output of the process.
A common way to describe this is with the for-
mula Y = f(x), or Y equals the function of the x’s.
Graphically, this is most easily seen when using
the cause-and-effect (fishbone) diagram. The
effect (the head of the fish) is the “Y” of the for-
mula, and the causes (the bones of the fish) are
the x’s. Note that this process will actually help
improve creativity in your Practice as the inputs
will become less varied and the activities can
become more robust for the customer outputs, or
patient care.
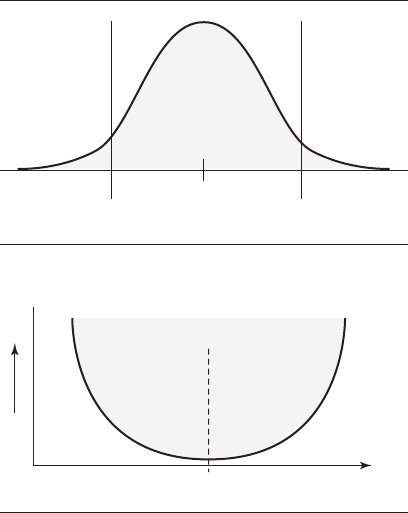
The traditional view of quality (sometimes
called the goalpost mentality—see Figure 6)
depicts the way many people regard varia-
tion when dealing with processes (for example,
blood pressure, HDL, LDL). It shows that some
processes (or items that are used) are clearly per-
formed within specifications or tolerances while
others are outside of specifications. There is no
What Is Variation? 19
relationship called out for Y = f(x), but the ques-
tion that should be asked is “What is the ‘real’
difference within the process or between a ser-
vice that is just inside the specification (a) and
another that is just outside the specification (b)?”
(See Figure 7.) Two competing services (say two
overnight delivery services) may be very simi-
lar and probably will function equally well when
used by your Practice. That is one of the reasons
companies who use this traditional model con-
tinue to provide services even if they are just out-
side the spec limits (that is, time of the actual
delivery)—because they think they can get a few
more sales to the customer and the deficiency
will not be noticed. This usually happens during
heavy office workload times when temporaries
are brought in and not trained very well.
No good Good No good
Loss No loss
Target
value
Lower
specification
limit
Upper
specification
limit
Loss
Y
Response
Figure 6 Traditional view of quality.
20 What Is Variation?
A different perspective on variation can be
seen in the Taguchi loss function model (see
Figure 8). This updated view of quality states
that all services (or processes), measured by the
x’s, should aim for a target value that is located
Target
value
Lower
specification
limit
Upper
specification
limit
ab
Figure 7 Part goodness.
Target
$
Loss
Y
Response
x
Poor Poor
Fair Fair
Good Good
Best
Figure 8 Taguchi loss function model.

What Is Variation? 21
at the middle of the specification limits (which
reflect customer expectations or healthcare spec-
ifications). In this case, services that are not
centered but similar to each other (for example
how well a report is written or the variation from
the expected wait time for a service) have nearly
the same “loss” to the customer (who may be a
manager or patient) and will not be accepted very
well if at the outer boundaries of the graph. As
the services offered move away from the target
value, the cost to the patient/customer (which
includes internal customers within the health-
care process), and thus society, increases as
issues or problems within the patient or with the
use of that service increase. The goal today is to
reduce variation (both common cause and special
cause—to be discussed later) so that the patient
feels better or the customer will see more service
delivery that is closer to the target value of what
they want versus what we can provide.
Recently, in ordering business cards from a
national office supply chain store, the author expe-
rienced a good example of poor service. The first
order was taken by a very knowledgeable sales-
person and was processed quickly and efficiently.
Then a couple of weeks later at the same store a
second order for a different card was placed. The
logistics manager for the store took the order
the second time and was totally unfamiliar
with the order process. Instead of a pleasant and

22 What Is Variation?
quick experience in ordering a simple item, the
experience was a long, drawn out, grueling effort
that left the author very frustrated and ready to
walk out of the store!
Another service example of the Taguchi loss
function is when people pay money to attend a
public seminar. The seminar is advertised to last
eight hours. If the seminar ends before the eight
hours, people may feel that they did not get their
money’s worth. If the seminar drags on beyond
the eight hours, people become upset because they
could miss their airplane, car pool, kids waiting
to be picked up, and so on. Thus, the seminar
leader must ensure that the attendees’ expecta-
tions are met within the boundaries advertised
and within the attendees’ wants and needs.
A patient may have been coming to a Practice
for a long period of time, and annual blood work
has shown that their HDL and LDL have been
within acceptable limits. Then, all of a sudden,
the numbers are not acceptable and a script is
written to help improve the numbers. However,
the cause of the just-out-of-specification num-
bers may be due to any number of variables rang-
ing from what the patient may have consumed,
contamination of the sample process, reading
of the blood work, or the instruments used to
make the measurements. However, if the annual
values of the HDL and LDL were available to the

What Is Variation? 23
doctor and patient in run chart format, then the
patient’s body process could be reviewed first to
see if there is something going on in the patient’s
life that actually requires medication, or to point
to a potential faulty reading and the need for
retesting.
Note: Be aware of the difference between
variation and variability. Variability comprises
three components: variation (discussed earlier),
instability (when a process has high amounts
of unknown [special cause] variation), and off-
target conditions (which happen when a process
is not centered between the engineering specifi-
cations) (Bajaria and Copp 1991).
(This page intentionally left blank)
25
Things You Might
Be Involved With
Y
our Practice may be using Six Sigma or
another quality methodology: lean office,
business operating system (BOS), contin-
uous improvement (CI), total quality manage-
ment (TQM), or a system known by some other
name. As a staff worker or supervisor of a pro-
cess, you will be asked by your Practice man-
agement to help implement improvement of the
activities or procedures that you work with. Your
challenge will be to look at the process with an
eye toward both simple improvements, which you
may already know need to be made (cleanliness,
too many signature requirements, information
just sitting around, recording data into a regis-
try, and so on), and how you can measure certain
factors to investigate better ways of performing
the process.
You will be asked to use the tools in this book,
and maybe others, to study your work area and
activities or procedures to look for improvement

26 Things You Might Be Involved With
ideas and ways to implement those ideas. You may
already be familiar with some of these tools; the
challenge will be in learning how to use them in
new ways to help your Practice to meet up coming
rule changes by payers, insurance programs, and
state or national programs or regulations.
Many of us find that by using a model or frame-
work we can do things more simply—“a picture
is worth a thousand words.” This is also true
when trying to improve processes. Dr. Kaoru
Ishikawa (the man who created the fishbone dia-
gram—see Figure 13, page 80) gave us a road
map to follow when first looking at a process that
needs to be improved. The words may not make
much sense right now, but as you work with pro-
cess improvement, you will come to understand
the importance of what is said here.
POINTERS IN
EXPRESSING QUALITY
1. Determine the assurance unit. (What is
to be measured?)
2. Determine the measuring method.
(How will we measure it?)
3. Determine the relative importance of
quality characteristics. (Is this key to
our process?)

Things You Might Be Involved With 27
4. Arrive at a consensus on defects and flaws.
(Does everyone agree on what is good
and bad?)
5. Expose latent deficiencies. (Look at the
process over time.)
6. Observe quality statistically. (Use process
behavior charting.)
7. Distinguish between “quality of design”
and “quality of conformance.” (Ishikawa
1976)
After we know what we can change (quality of
conformance) versus what we can not change
right now (quality of design—this is left to the
Design for Six Sigma [DFSS] process), we can
start working on our processes. Many Practice
personnel start out viewing this effort as only
more work, but many find that doing these stud-
ies actually saves them a lot of time and grief in
the future as things start to improve, work flows
better, and patients actually see results and
feel better. One question to ask yourself right
now is “How often does my process slow down or
stop because something is not working the way
it should?” Or “Is the output ever significantly
changed or even disregarded by someone down
the line (including my external customer/patient)
because something did not happen right at my
activity?” Note that this last question does not

28 Things You Might Be Involved With
ask if the business needs changed, which may
have caused the instance of variation. Working
on things that no one uses happens a lot for staff,
and dealing with this and the changing business
needs is also part of DFSS.
The next section discusses the DMAIC model,
where you will learn when to most appropri-
ately use the methods and tools presented in
this book to improve your or the patient’s pro-
cesses. As we proceed, please continue to keep an
open mind and be willing to experiment with the
tools. Be willing to look for ways to apply them in
your activities and procedures to learn as much
as you can about how a process operates. Also,
you may be expected to show patients, by use
of the graphical tools, how their health is being
affected, given the measurements that have been
taken over time. You will then be able to mod-
ify your work or instruct the patient as appropri-
ate and give your organization and your patients/
customers the best possible outcome.
29
The DMAIC Model
T
hroughout this book, you’ll find a number
of approaches and/or steps to assist you
in applying the tools or methods being
discussed. For the implementation of Lean Six
Sigma, a model has emerged that is well recog-
nized and which you’ll need to use in your Prac-
tice to show customers that Lean Six Sigma is
being used. The DMAIC model (see Figure 9)
stands for define, measure, analyze, improve, and
control, and is very similar to the PDSA (plan, do,
study, act) or PDCA (plan, do, check, act) models
that you may have heard of or are already using.
A key factor in each step of DMAIC is keep-
ing the focus of the Practice strategy in mind so
that all of the healthcare staff can work with the
methodology and focus the time and resources
to accomplish each of the phases and strive for
continual improvement. This is one of several
driving forces that make Lean Six Sigma differ-
ent from other quality improvement programs.
30 The DMAIC Model
Other driving forces include getting everyone in
the healthcare system involved (patients, pay-
ers, employers, and so on), getting the informa-
tion technology group to assist in supplying data
more quickly to everyone, and getting finan-
cial data in the form of cost-of-quality analysis.
Research (Stamatis 1996) is showing that many
organizations are finding more opportunity for
improvement to the bottom line in the office
than currently exists on many plant production
floors.
Practice strategy
Employee involvement
Team meetings
Verify
Design
SDCA SDCA
PDSAPDSA
PDSA
MeasureControl
Improve Analyze
Define
Figure 9 The DMAIC model.

The DMAIC Model 31
Staff personnel at all levels will be asked to
get involved with the Lean Six Sigma model and
look for continual improvement opportunities in
work areas. Basically, you will do the following:
Define Identify the issue causing
decreased customer satisfaction.
Measure Collect data from the process.
Analyze Study the process and data for
clues to what is going on.
Improve Act on the data to change the
process for the better.
Control Monitor the system to sustain
the gains.
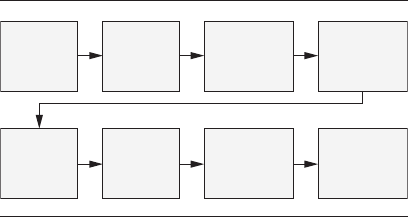
An example:
1. Select one important problem that you
have in the Practice.
2. Draw a flow diagram, or similar tool, of
the issue—how does it currently work?
3. Get concurrence from everyone who is
involved in that process that the flow
diagram is accurate. This in itself can
be a painful process of getting concurrence
and may actually solve some of the issues
as this process gets people aligned.

32 The DMAIC Model
4. Look over the flow diagram and ask
“Given what we know today, is this the
most effective way to do this?”
5. Make changes to the process as necessary
and update the process flow diagram
(note: this tool now becomes a simple job
aid, reminder, or training tool on how
that process works). Caution: be careful
about throwing technology at problems.
The process must work well first before
you computerize it. Otherwise, you
will only get the same problems as before—
only faster.
6. Now review the process and ask “What
could this process be?” or “How could this
process be more effective?”
7. Seek management approval and funding
for future changes.
8. Update the process flow diagram to match
the new flow. Train everyone in the new/
updated process flow using the flow
diagram/chart.
See Figure 10.
A number of tools and methods can be used in
the steps of the DMAIC model. This book gives
a quick overview of many of these items as they
relate to potential areas for improvement. More
The DMAIC Model 33
detailed information can be found in quality
control/assurance books, on the Internet, or in
quality improvement magazines or journals. The
DMAIC model uses the following tools:
Define
7S
Advanced practice quality planning
(healthcare APQP)
Auditing (sampling, sampling plans)
Brainstorming
Business operating system (BOS)
Cause-and-effect diagram (fishbone
diagram, Ishikawa diagram)
Look for
opportunities
for
improvement
Get staff
concurrence
Create
flowchart
Select
issue
Update
system
and train
staff
Future
improvements
Ask key
questions
Update
flowchart
Figure 10 Process improvement flowchart.

34 The DMAIC Model
Cost–benefit analysis (cost of quality,
quality cost, cost of poor quality, return
on investment)
Cycle time analysis
Failure mode and effects analysis (FMEA)
Flowcharts
Lessons learned—review
Practice strategy
Process behavior charts
Process identification—storyboards
SDCA (standardize, do, check, adjust)
SIPOC (supplier, input, process, output,
customer) diagram
Systems thinking
Team development
Team meetings (huddles)
Value stream mapping
Voice of the customer (patient feedback)
Walkaround/walkthrough/waste walk
Measure
7S

The DMAIC Model 35
Auditing (sampling, sampling plans)
Benchmarking—start by setting the
current baseline for the process
Business operating system (BOS)
Cause-and-effect diagram (fishbone
diagram, Ishikawa diagram)
Cost–benefit analysis—start collecting
information
Cycle time analysis
Data collection—check sheets, histograms,
Pareto charts, run charts, scatter
diagrams
Identifying a data collection plan
Identifying variability—instability,
variation, off-target, cause-and-effect
diagram, process capability
Measurement systems analysis (MSA)
PDSA (plan–do –study/check–act)
Practice strategy
SIPOC (supplier, input, process, output,
customer) diagram
Stratification
Team meetings (huddles)

36 The DMAIC Model
Value analysis
Walkaround/walkthrough/waste walk
Analyze
7S
Auditing (sampling, sampling plans)
Benchmarking—how others do things
Brainstorming
Business operating system (BOS)
Cause-and-effect diagram (fishbone
diagram, Ishikawa diagram)
Check sheets
Continual improvement
Cost–benefit analysis (cost of quality,
quality cost, cost of poor quality, return
on investment)
Flowcharts
Practice strategy
Scatter diagrams
Stratification
Team meetings (huddles)

The DMAIC Model 37
Value analysis
Walkaround/walkthrough/waste walk
Improve
7S
Auditing (sampling, sampling plans)
Brainstorming alternatives
Business operating system (BOS)
Continual improvement
Cost–benefit analysis (cost of quality,
quality cost, cost of poor quality, return
on investment)
Cycle time analysis
Flowcharts
Failure mode and effects analysis (FMEA)
Kanban (wait time, patient pull-through)
Lessons learned
Mistake-proofing
PDSA (plan–do–study/check–act)
Practice strategy
Problem solving

38 The DMAIC Model
Process improvement
Scatter diagrams
Standard operating procedures (SOPs)
Stratification
Systems thinking
Team meetings (huddles)
Variation reduction
Visual controls, aids
Walkaround/walkthrough/waste walk
Control
7S
Auditing (sampling, sampling plans)
Business operating system (BOS)
Continual improvement
Cost–benefit analysis (cost of quality,
quality cost, cost of poor quality, return
on investment)
Cycle time analysis
FMEA—update
Kanban

The DMAIC Model 39
Lessons learned—update
Measurement systems analysis (MSA)
Mistake-proofing
PDSA (plan–do–study/check–act)
Practice strategy
Process behavior charts
Run charts
Standard operating procedures
(SOPs)—update
Standardization (SDCA—standardize, do,
check, adjust)
Team meetings (huddles)
Value analysis
Variation reduction
Visual controls, aids
Voice of the customer (patient feedback)
Walkaround/walkthrough/waste walk
Most Practice staff members will find this pro-
cess very exciting as they will have the tools and
methods to demonstrate the improvements that
they are helping the organization to achieve.
There are times when a staff worker tries to tell

40 The DMAIC Model
a supervisor that something is wrong with a pro-
cess. Now we have the means to not only tell but
also show and demonstrate what needs to be
done. Following this process creates a road map
for continual improvement and, once started,
it is a never-ending journey. These tools and
methods have proven themselves useful every-
where: from shop floors to office settings, from
schools to hospitals, and even from churches to
the home. Also, if your Practice is currently plan-
ning on achieving ISO 9001 registration, Patient-
Centered Medical Home status, the Malcolm
Baldrige National Quality Award (or related
state-level award), or any number of other qual-
ity improvement–based awards or recognitions,
one of the baseline requirements is the ability to
demonstrate that continual improvement is actu-
ally being achieved.
41
Teams
T
he first thing we need to look at with respect
to teams is the difference between a team
and a group. A group (as in a natural work
group or department within the Practice) is a col-
lection of individuals who may be working toward
a common goal but who are not necessarily inter-
dependent. A team is a group of people who have
come together for a specific common purpose—
often to be accomplished within a specific time
frame—and has established a common definition
of what the members will be doing. Each person
understands and can discuss the common objec-
tive. Many philosophies and books are available
on teams, team building, and how to create effec-
tive teams. For example, the American Society
for Quality’s Team and Workplace Excellence
Forum has a lot of material.
An important problem many managers (those
who direct or run the Practice) face with respect
to teams is failing to ask individuals in the group

42 Teams
what they want from their experience on the
team! Lack of communication within the team
and between it and management thus causes a
vast number of failures. Finding a solution to
this should be the manager’s number one con-
cern any time groups of people come together.
Just saying the words one time is not enough for
effective communication to take place.
The second-most-important issue has to do
with the team itself. The members must be able
to answer three basic questions before they can
start and continue the process of teaming. These
questions are summed up in the acronym MCG.
M stands for “Who will be the members on the
team and why?” C stands for “Who will handle
what roles and responsibilities, and who is in
control?” G represents “What are the goals of the
team?” and ensuring that those goals are com-
municated to everyone who interacts with the
team. Each team needs to ask these three ques-
tions and ensure that its members share a com-
mon purpose.
MCG can be expanded by using another acro-
nym, SGRPI: systems, goals, roles, procedures,
and interpersonal relationships. The term systems
refers to thinking about how the team fits into
the structure of your Practice. Goals, as in MCG,
refers to what the team wants to accomplish
and communicating that to others. Roles, as in
the C of MCG, refers to the various roles involved
Teams 43
in a well-operating team and who will fill each.
Procedures refers to agreed-to and communi-
cated ground rules and logistical agreements
that the team has made with itself. Interpersonal
relationships refers to the relationships that any
team must work out in advance, as this becomes
a major issue if things are not resolved early.
People need to know how to relate to each other
and agree that they are all working for a common
purpose.
The following are some rationales for team
building from the National Training Laborato-
ries Institute (1984):
The Obvious
Goal clarity and
commitment
Surfacing control or
influence issues
Inclusion/cohesion
needs
Exploration of
working norms
Control/management
of destructive
competition
The Less Obvious
Identifying wants and
needs
Support needs
Creative
interdependence
(synergy)
Discovery of intrinsic
needs

44 Teams
Every team must go through a series of stages
toward group actualization. Five states com-
monly involved are: forming, storming, norming,
performing (producing), and ending. This process
usually takes a lot of time, and if at any point
something changes (for example, new managers,
new team members, economic conditions, a sig-
nificant emotional event experienced by one of
the existing members, and so on), the team as a
whole may need to go back to some prior stage
and repeat their efforts in order to become a top-
performing unit. Failure to follow these basic
stages is the most common reason why some
teams never achieve their full potential.
You should keep in mind several points at each
stage. Forming involves the people on the team
getting to know and trust each other. There can
be many frustrations here (for example, lack of
action, no clear assignment, poor communication,
and so on), and there is a lot for the team to work
through leading to the ultimate goal of accep-
tance and commitment of the group to becoming
a team. In storming, team members need to work
out their differences with each other. Because of
the forming activities, team members should feel
they are able to talk things out with each other
without hurting feelings or risking rejection just
because they see things differently. The pri-
mary outcome of this stage should be to clarify
the team’s major activities and develop members’

Teams 45
sense of belonging to the team. Norming occurs
when the team sets its boundaries and members
become more sensitive to each other and to the
goal or goals of the team. The team is now ready
to work on projects and enjoy a level of internal
support. In the performing stage the team can
work to full capacity to achieve its goals with
the pride that develops from performing well.
The last phase is ending. We all at various times
in our lives must deal with something coming to
an end. At the end of a team, or on losing a team
member, we want to be able to have satisfaction
with, and recognition of, a job well done.
Many managers want teams to immediately
jump into the performing stage of teamwork,
but this usually causes friction and a discon-
nect within the group, which has not been given
the opportunity to form into a team. Each team,
ideally during its formation phase, will identify
what its goal or purpose is for existing. There are
a number of team structures or types of teams:
• Cross-functional team. Members come
from various functional areas of the
organization and/or customers and
suppliers to achieve the goals of the team.
• Improvement team. Has a specific assigned
task of making one or more operational
improvements (cost, cycle time, quality) in
the Practice.

46 Teams
• Self-directed team. Operates with virtually
no management or supervisor involvement.
Its members have been given the time and
resources to accomplish the tasks assigned
to them.
• Quality circle. A team with the specific
assigned task of improving the quality of
an operation, service, or product. These
groups are commonly called improvement
teams today.
• Project team. A project-focused team that
has a specific goal to accomplish. It could
be a start-up of new activities, the launch
of a new product or service, a preventive
maintenance or cleaning program, or
other goal that may not involve a continual
improvement issue.
A team is far more than just a group of peo-
ple who happen to work in a given area. Well-
functioning teams take time to form and arrive
at their level of functionality, but once that has
taken place such teams have a lot of fun and take
pride in what they accomplish. Your overall goal
should be to develop well-functioning teams in
your Practice to achieve customer satisfaction
and continual improvement.
47
The Lean Six Sigma Road
Map for the Practice
A
s you prepare for the Lean Six Sigma
journey, you’ll do well to take a look at
the following suggested road map:
1. Develop a flowchart (or similar tool) of
a current significant process—“as is”—in
your Practice.
2. Recognize that variation exists in
everything you do—standardize the
process throughout the Practice.
3. Develop/refine measures of work for
customer satisfaction in the process.
4. Identify what the patient/customer wants
and needs—reduce variation around
this target.
5. Develop a “should be” or “preferred state”
process flow map.

48 The Lean Six Sigma Road Map for the Practice
6. Use a problem-solving methodology to
plan improvements.
7. Follow the PDSA model to deploy the
improvement.
8. Monitor the process using run charts or
process behavior charts.
9. Incorporate new technology where
appropriate.
10. Update standard operating procedures
or policies and lessons learned.
11. Celebrate successes.
12. Repeat the road map for continual
improvement—PDSA/SDCA.
49
Summary
W
e are starting a journey of continual
improvement in your Practice. The way
may be familiar to a lot of you as you
have been using the tools and methods for some
time. Others of you may be new to this path, and
through this book the author hopes to assist you
along the way. This book is designed to be a guide
rather than a detailed description of each tool
used. Follow the process, and use what seems
to be appropriate at each step. Every tool and
method will not be used each time a new study
starts. You may even find uses for these tools and
methods in different phases of the DMAIC model,
and that is encouraged. The goal of all this work
is to continually improve your procedures and
activities to satisfy your patients and customers
(both internally and externally) and increase the
effectiveness of your total Practice.

50 Summary
Here are some other points that healthcare
professionals should remember when using this
process:
1. If the method seems to be getting too
complicated, it probably is, and you should
step back to see if you can simplify what
you’re trying to study!
2. Asking patients to wait for long periods of
time is waste! Find a better way.
3. Most problems can be solved without using
designed experiments. If the process is
an old, established one and it used to work
okay, then keep asking why it isn’t now
until you find the problem!
4. Remember the KISS principle: keep it
simple (keep it simple staff, keep it simple
statistician, or keep it statistically simple)!
5. Sometimes all you need is an updated
histogram or flowchart to see the problem!
6. Never give up!
7. Have fun!
At times, your Practice might run into problems
that seemingly can not be solved, or you just don’t
have enough time and resources to handle every-
thing. It will be during those times that con-
sultants or other specialists may be called in to

Summary 51
assist with the issues at hand. Many times such
people will have advanced training in the tools
and methodologies discussed in this book. We
usually call these people “Lean Six Sigma Black
Belts,” and they may ask your team to start a
“Green Belt project.” Since that is what you are
doing with this book—Lean Six Sigma Green
Belt projects—you will be able to call yourself a
Lean Six Sigma Green Belt.
If you would like to earn a formal title in this
arena, check with a local quality practitioner or
contact the American Society for Quality (ASQ)
about the Certified Quality Improvement Asso-
ciate (CQIA) or other certification processes or
examinations for healthcare professionals. ASQ
can be reached at 800-248-1946 or http://www.
asq.org for more information.
(This page intentionally left blank)
53
Tools
Define
Measure
AnalyzeImprove
Control
7S
An old Japanese quality auditing technique,
after the initial greetings in the front office, is
to visit a rest room in the hourly working area
before conducting the rest of the audit. The
purpose of this detour, rather than to use the
facility, is to check for the cleanliness of the rest
room. The belief is that if management can not

54 7S
provide clean facilities for staff, then a number
of other processes may be at issue in the organi-
zation. Have you ever used a dirty restroom at a
gas station or a restaurant? What did you think
about how that organization handled other activ-
ities on the property?
How organized is your Practice and work
area? Is there dust, grease, food scraps, eye irri-
tants, trash, or other unclean issues in the work
space? An unclean office setting hides safety
hazards, health risks, and equipment problems,
shows a lack of pride in work, and signals a host
of other issues. If your office does look clean on
the surface, how about the way paperwork is
stored in your Practice? Does the doctor have all
of the correct files available at a single glance, or
is everything stored in patient files so that each
packet is different? How much time do patients
have to wait in the various waiting rooms in your
Practice? How about other personnel that work in
the Practice? Is everything available in a timely,
orderly manner, or is information typically miss-
ing or hard to find when needed to accomplish
the tasks at hand?
It has been researched and proven that
cleanliness/orderliness at home and work leads
to much more productive settings and more pride
in what we do. Some people feel that far too much
time is spent talking about uncleanliness and
7S 55
disorder; however, it has been shown to be one
of the more important factors contributing to
why things do not always work the way they are
supposed to. When things are not organized and
clean, the likelihood of something going wrong
increases exponentially.
The Japanese created a process referred to as
the 5S method, which work groups use to ensure
a clean, organized, and safe work environment
(see Table 1). Many work teams spend a specific
amount of time each day to ensure that their
work areas are cleaned. This has the added ben-
efit of allowing the staff who use the work area
to take a close look at their environment for signs
of future trouble.
The classic 5S includes sort, set in order, shine,
standardize, and sustain. For 7S, we are adding
safety, oversight.
Table 1 5S chart.
Japanese (S) Translation English (S)
Seiri Cleaning up Sort
Seiton Organizing Set
Seiso Cleaning Shine
Seiketsu Standardizing Standardize
Shitsuke Training & discipline Sustain

56 7S
The 5S method was created for a manufactur-
ing setting. In a medical Practice, we must also
be on high alert to ensure the safety of staff and
patients as well as the oversight of our processes.
Thus, we now have what can be called the 7S for
the healthcare Practice. These sets include:
• Sort. Review and sort work tools and
materials to ensure that all unnecessary
items are removed and to ensure
workplace organization. Look for
unnoticed dangers: unprotected moving
objects (such as file drawers), exposed
or damaged electrical wires, and other
issues that might get in the way of doing
the work safely.
• Set in order. Have a place for everything
and keep everything in its place when not
in use. People need to know where things
are supposed to be. Also, apply ergonomics
to help prevent movement injuries.
• Shine. Clean everything in the work area
inside and out regularly, inspecting each
item for signs of defects or wear or other
signs of future trouble.
• Standardize. Using the first three S’s,
establish a pattern of how things are to
be done. This is not meant to reduce
creativity, but to help ensure that things

7S 57
are done in a way that helps to reduce
variation in the process. Continually
maintain what has been accomplished
and ensure that standards are lived up to.
• Safety. The process of avoiding injuries to
patients from the care that is intended
to help them.
• Oversight. Medical oversight is the
process of reviewing care that is provided
to patients, to ensure their safety.
• Sustain. Reinforce all of the above to
ensure that this process becomes a part
of your daily work.
The task for you and your fellow staff is to clean
your work areas, address any unsafe issues that
currently exist, and prevent those that may occur
in the future. Put a red tag or other identification
on anything that should be addressed. If there is
a safety officer in your organization, ask him or
her to periodically check your work space to help
ensure a safe and clean working environment.
58 Advanced Practice Quality Planning (Healthcare APQP)
Define
Measure
AnalyzeImprove
Control
ADVANCED PRACTICE QUALITY
PLANNING (HEALTHCARE APQP)
Have you ever heard the old saying “a stitch in
time saves nine” or “an ounce of prevention is
worth a pound of cure”? How about “measure
twice, cut once”? What do these sayings mean?
Most people will answer by saying that if you
plan ahead of time, you can save time, money,
resources, and sometimes frustration. In my own
experience I have sometimes started a project
only to have the parameters change later and
have to redo work that was already done. The
idea that we can plan, as best as possible, ahead
of time to help prevent surprises and save valu-
able resources works in our jobs as well as in our
homes. Anything that is to be done can be thought
out first, or written plans can be completed to
lay out a blueprint of what we are going to do.

Advanced Practice Quality Planning (Healthcare APQP) 59
This concept is referred to as advanced practice
quality planning, or healthcare APQP.
APQP is a process whereby we first look at
the parameters of what we are going to do. Do we
have the right amount of resources or material
available? Do we have the right people to do the
job or provide the service? Do we have the right
tools or training to do the job well? Do we know
the correct way of using everything we have to
provide a safe environment for ourselves, our
patients, and other customers? All these ques-
tions, and many more, should be answered before
we start work! One of several tools you can use to
ensure that you have thought of all the elements
(causes) that will give you the desired output or
effect is the cause-and-effect diagram (see page
79). You can also think of APQP as the first step
of the PDSA cycle, where you are going to plan
before you do something.
In planning to meet future medical require-
ments, such as those espoused by the Committee
on Quality of Health Care in America in Crossing
the Quality Chasm (2001), we must ensure that
the six aims for improvement are addressed:
• Safe. Avoiding injuries to patients from
the care that is intended to help them.
• Effective. Providing services based on
scientific knowledge to all who could
benefit, and refraining from providing

60 Advanced Practice Quality Planning (Healthcare APQP)
services to those not likely to benefit
(avoiding underuse and overuse,
respectively).
• Patient-centered. Providing care that is
respectful of and responsive to individual
patient preferences, needs, and values,
and ensuring that patient values guide
all clinical decisions.
• Timely. Reducing waits and sometimes
harmful delays for both those who receive
and those who give care.
• Efficient. Avoiding waste, including waste
of equipment, suppliers, ideas, and energy.
• Equitable. Providing care that does not
vary in quality because of personal
characteristics such as gender, ethnicity,
geographic location, and socioeconomic
status.
Your organization may very well use some of
the traditional quality tools (check sheets, run
charts, Pareto diagrams, and so on) to ensure
that the elements of APQP are being done in
your organization prior to starting a new proj-
ect or job. Tools such as check sheets can take
on many forms and can be designed using the
cause-and-effect diagram as a guide to help
ensure completeness. You can and should use the
various tools reviewed in this guidebook to help
Advanced Practice Quality Planning (Healthcare APQP) 61
ensure that the work you are going to do is of
the best quality and reduces the greatest amount
of time and wasted effort possible. The typical
APQP model shown in Figure 11 incorporates a
lot of the tools and strategies found in this book.
Your role in this process is to ensure that the
work you will be doing is the best given the tools
and resources provided by management.
Act Plan
StudyDo
Take appropriate
action and
follow up
Determine
goals and
targets
Determine
methods of
reaching goals
Engage in
education and
training
Implement
work
Study the effects of
implementation
Figure 11 The APQP model.
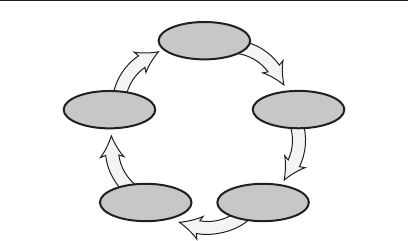
62 Auditing (Sampling, Sampling Plans)
Define
Measure
AnalyzeImprove
Control
AUDITING (SAMPLING,
SAMPLING PLANS)
Most people have heard of certified public accoun-
tants, or CPAs. A CPA maintains and checks
financial records to ensure accuracy of the num-
bers. We need to work with our management in
checking the working processes in our organiza-
tions to ensure that the processes are doing what
they are designed to do.
This checking process is sometimes called
quality auditing, and it is commonly done in orga-
nizations that are ISO 9001 registered or have
applied for a quality award (Baldrige or state-
level awards). Many customers require their sup-
pliers to check their products and services before
they are delivered. This is one reason your orga-
nization may have personnel designated to review
items in the Practice for accuracy. This is com-

Auditing (Sampling, Sampling Plans) 63
monly called inspection. Quality auditing is sim-
ilar to inspection in that we are looking at how
the process is doing instead of looking at specific
parts or services that have been provided. Some
organizations (as medical device manufactur-
ers and pharmaceutical companies) use supplier
quality engineers to visit their suppliers and/or
perform incoming inspection to check products
as parts are received from their suppliers.
The first thing you need to know if asked to
audit something is “What is the standard that
I will be auditing against?” If you are going to
conduct a process audit in another department,
you must ensure that there are standard operat-
ing procedures (SOPs) or some other form of pro-
cess sheets that are used to ensure that things
are being done in a standardized manner. If you
were to conduct a safety audit, then having the
written safety rules would be important. As you
are starting to see, there are a number of things
that can be audited. Some others are cleanliness,
quality of product, quality of service, knowledge
of the system, and emergency procedures. If your
Practice is ISO 9000 or ISO 14000 registered,
you already know a number of things that can
be audited. If you have not seen either of these
standards, you may wish to ask your supervisors
about getting a copy.
As organizations move to become registered
to national or international standards such as

64 Auditing (Sampling, Sampling Plans)
ISO 9001 or ISO 14001, they will train some of
their internal people to conduct quality system
audits. This is to ensure that the system that the
management has established is in fact working
the way it was intended to. As an employee in a
Practice you would be trained in auditing tech-
niques and assigned to auditing teams that will
periodically check the processes of other activi-
ties within your organization. This process of
quality auditing is very different from what the
Internal Revenue Service (IRS) does when they
call taxpayers in for a financial review. When
you are asked to be part of an audit team, you
need to be aware of some basic guidelines:
• Bepleasanttothepersonbeingaudited.
You are not a cop looking to catch him or
her doing something wrong.
• Befactualinwhatyouobserve.Hiding
things does not help the company improve,
and being too critical may harm personal
objectivity.
• Bethoroughinlookingattheprocess
as it relates to the standard. If you
miss something, customer satisfaction
may suffer or, worse yet, someone might
get hurt.
• Askquestionsforclarity.Youwanttobeas
positive as possible given the situation.

Auditing (Sampling, Sampling Plans) 65
• Recordyourobservationsfortherecordand
the next person who will audit the area.
• Followwhattheinternalleadauditor
directs you to do.
Being an internal auditor for your organization
can be both challenging and informative. We
usually get a better view of what our company is
doing if we have a chance to look at its activities.
For some of us, it breaks up our everyday routine
and gives us a chance to see how others might
be doing things and to benchmark (see the next
section) that against what we do.
Sampling is a methodology that reviews/
inspects a small segment of some larger pro-
cess/population to make a judgment/inference
about the entire process. This idea works in part
based on the central limit theorem, which basi-
cally states that over time, things tend to follow
patterns. An example of this would be to simply
flip a coin. Your basic assumption is that a coin is
fair and that for any group (say 10 to 50) of flips
that you should get roughly 50 percent heads and
50 percent tails. This is not always true, so we
could do samples of flipping a coin to verify how
“fair” the coin really is.
A sampling plan is a structured, planned
sequence of samples that are to be taken on a
given activity or process to verify the state of
goodness of the process.
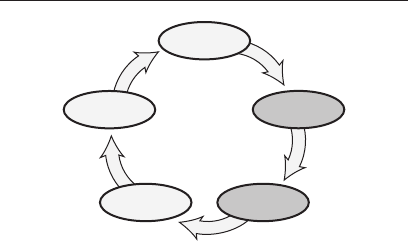
66 Benchmarking
Define
Measure
AnalyzeImprove
Control
BENCHMARKING
Benchmarking is the process of looking at a
system and applying some or all of its concepts
to another system. Granite Rock, a Malcolm
Baldrige National Quality Award–winning com-
pany located in California, has used benchmark-
ing in a dramatic way. Its processes had been the
same as those of nearly any gravel yard in
the United States. Any time a customer wanted
some road materials it sent a truck and driver
to the yard. The driver then placed the order at
the front office and waited for a Granite Rock
employee to get a front-end loader, go into the
yard to obtain the material, and fill the truck
with the appropriate amount. Then Granite
Rock decided to capitalize on the technology of
the ATM, the automated banking machine that

Benchmarking 67
allows a customer to walk up and, by inputting
some basic data, handle any number of banking
transactions. The new process that Granite Rock
developed allows the truck driver to pull into an
area with overhead filling stations (instead of
going to an office first) and punch in their cus-
tomer codes and the materials desired. The mate-
rial is automatically loaded into the truck. This
new process cuts wait time to minutes instead
of hours and allows customers to get materials
24 hours a day, seven days a week, year-round.
Some managers think benchmarking is only
about taking trips to competing organizations
and trying to copy something they do that is felt
to be better than what is currently being done in
their own organizations. During the late 1970s
and early 1980s many managers went to Japan
to learn what was being done there and to see
why Japanese quality was so much better than
that in the United States. Most of those trips
resulted in disappointment as you can’t always
see a physical difference in activities. Sometimes
it is the small, subtle things that Practice staff
have learned over time and shared with fellow
workers that make the big difference.
Here are the basic process steps of bench-
marking:
1. Flowchart the current process.
2. Identify the areas to be improved.

68 Benchmarking
3. Brainstorm ideas (blue sky—this term is
discussed under “Brainstorming”).
4. Investigate how others (internal and
external) do similar processes.
5. Develop plans for application of ideas.
6. Pilot test ideas.
7. Initiate the new process.
8. Evaluate the new process.
Before starting a benchmarking project, you are
advised to make sure you know exactly how your
current process works. That may sound funny,
but it has been shown that when people attempt
to flowchart a process (see “Flowchart” section),
there is often a lot of disagreement about the
exact steps and/or the order of those steps. Thus,
any time there is more than one person who per-
forms a task in or around your Practice, the
process should be flowcharted.
Once everyone agrees on how a process oper-
ates, you can start looking at the process for
bottle necks or other things that may not work or
flow as well as you might wish. This could be any-
thing about the current process from wanting to
reduce the amount of variation in one part of the
process to changing certain things about it that
may help employees’ ergonomics. In looking at
the process, it sometimes helps to get as creative

Benchmarking 69
as you can and ask, “What if ?” This is the “blue
sky” part of benchmarking. What might this
process look like in an ideal world? If money and
technology were no object, how might it work? If
we had the technology, what could happen?
Now it is time to do some research about how
others, internal or external to your organization,
may do similar things. By becoming internal
auditors (discussed in “Auditing”), we sometimes
get to see how others do similar things in our
own organizations. Also, as in the case of Granite
Rock (see “Auditing”), sometimes going outside
the industry helps give you ideas about a differ-
ent way of doing things. Say you need to move
something from one place to another; maybe
looking at mail service or delivery organizations
would help.
Once you have seen other ways of doing things,
it is time to figure out how you can do things
differently in your own operation. Establish a
plan for the changes, and acquire the needed
resources from management. The plan should
list the materials needed, when and where new
activities will be initiated, any training that may
be needed and when it will take place, and other
details that allow for the changeover to the new
idea. Then prepare and run a pilot test to ensure
that the plan will work. Generally it is unwise to
just jump right in with the new idea without test-
ing it first. Even the best-laid plans may have

70 Benchmarking
unforeseen bugs that can cause problems, so run
a small test first.
As you move forward into the new operation,
you should monitor it carefully to ensure that it
lives up to your hopes for the new process. Some-
times changeovers will be conducted in stages
instead of all at once. Either way, watch and eval-
uate the process to ensure that you are still meet-
ing the customer’s wants and needs—and doing
it faster, better, and/or cheaper than before.
A point to remember: Walt Disney was well
known for showing any carnival company exactly
how Disneyland was set up and operated. One day,
after being criticized for this, Walt said, “I hope
they copy me. That way as I create new things,
they will always be playing catch-up, while I
have the newest and greatest.” Benchmarking
is not just about copying something; it is about
looking at our processes for ways of doing things
better overall. The challenge is to distance your-
self from the way that it has always been done
to see if other methods or technologies now exist
that might help you in your work areas.
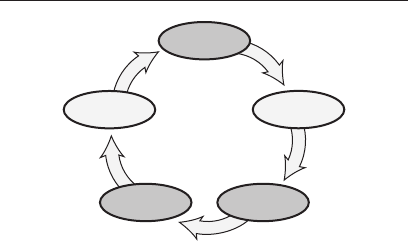
Brainstorming 71
Define
Measure
AnalyzeImprove
Control
BRAINSTORMING
Brainstorming is the process whereby an indi-
vidual, group, or team develops as many ideas
about a topic as possible using various creativity
techniques or methods. Two basic phases make
up brainstorming: the creative phase, which is
used to generate a large number of ideas, and
the evaluation phase, where the ideas generated
are evaluated for usefulness or practicality. Note
that the team should take a break time between
the two phases, as different parts of the brain are
used in each phase. At a minimum, a 10-minute
stretch break should be taken instead of going
directly into the evaluation mode after being
creative.
It is very important that during the creative
phase no criticism or other distractions are
allowed. Team members should keep their minds

72 Brainstorming
open to all possibilities, no matter how wild the
idea. One method here is to call for “blue sky”—
that is, if anything were possible, what might it
be? During this phase of brainstorming, the goal
is to generate as many ideas as possible. If ideas
are being put on a flip chart with a large group,
you should have two or more recorders available
to capture all the ideas as they develop. Other-
wise you can have each person say what he or she
is thinking and have him or her or another group
member record the idea on a sticky note and put
it on the wall. Facilitation can be used during the
creative phase, but freewheeling also works well.
Here are some basic guidelines for the creative
phase of brainstorming:
• Nocriticism,compliments,orquestions
allowed
• Wildideasarewelcome
• Don’twait
• Quantityisimportant(versusquality,at
this stage)
• Hitchhike—buildonpreviousideas
• Thinkbeyondthecurrentwayofdoing
things
• Thinkhowthingsmightbedone30years
from now
Brainstorming 73
During the evaluation phase it is best to have a
facilitator work with the group to look over the
ideas in a sequence. There are many ways to go
about evaluating the ideas you have generated.
One good starting point is to organize the list of
ideas into like groups or categories to help in the
evaluation process. The caution here is not to get
overly critical, as there may be something in one
of those “crazy” ideas that might actually work for
the given situation. This is often true because of
new technology or different ways of doing things
that are not common in your organization.
The brainstorming process can be fun and
hard work at the same time. The main purpose
is to “think outside the box” to get a new per-
spective on doing your own job. If you are unsure
what “outside the box” means, try this exer-
cise: In Figure 12, try connecting all the dots by
drawing four consecutive straight lines without
Figure 12 Nine dot exercise.

74 Brainstorming
lifting the pencil (or pen) off of the paper. One
possible answer appears on page 216.
The brainstorming technique can be very
helpful in looking at a process from all angles.
It is also helpful if the group working on the
project is cross-functional to the Practice, that
is, comprising people who work in different parts
of the healthcare community. And, optimally,
people from various areas and levels of respon-
sibility should be included in the brainstorming
group. But during this exercise there should be
no rank or level of employee recognized. Every-
one has an equal right to say what he or she
thinks, from the floor sweeper to the president.
However, a few comments to watch out for are
listed here as idea stoppers—they are warning
signals that the brainstorming process may not
be working as well as it could. If any of these idea
stoppers come up during the meeting, stop and
address them right away so the group or session
can move forward in a positive manner:
Brainstorming 75
Idea Stoppers
Don’t be ridiculous.
Let’s shelve it for
right now.
It won’t work here.
Our business is
different.
Let’s think about
it some more.
We did all right
without it.
It’s too radical
a change.
Management won’t
like it.
Where did you dig
up that idea?
It’s not practical.
It’s too expensive.
You can’t be serious.
You can’t do that.
The technology will
not allow that.
Where did you get . . .
We’ve never done it
before.
I have something
better.
It’s too risky.
Let’s be sensible.
We’ll never get it
approved.
They won’t like it.
It’s good, but . . .
Let’s check on it later.
Too much work.
Let’s get back to
reality.
That’s been tried
before.
That’s not my job.
You do not know
how we do things
around here.
That’s too high-tech
for us.
It will never work.
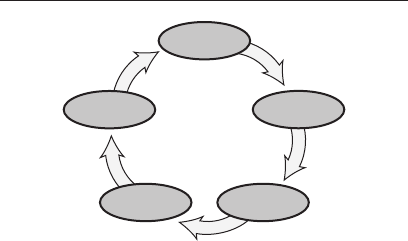
76 Business Operating System (BOS)
Define
Measure
AnalyzeImprove
Control
BUSINESS OPERATING SYSTEM
(BOS) FOR HEALTHCARE
ORGANIZATIONS
BOS (AIAG 2007) is a process that aims to aid in
the development or improvement of a fundamen-
tal management system for healthcare organi-
zations that provides for continual improvement,
emphasizing error or adverse- event prevention
and the reduction of variation and organizational
waste.
The BOS process focuses on the objectives of:
• Providingprocessimprovementsto
increase the value added to the
organization, customers, and stakeholders
• Improvingdeliveredhealthcare
quality and safety to complement
existing accreditation, or to aid in

Business Operating System (BOS) 77
achieving accreditation, certifications,
or registrations
• Improvingtheimageoftheorganization,
increasing customer confidence, and
having a tool to reward results
• Developing/incorporatingaprocessthat
is actionable
• Minimizingburdenonhealthcare
organizations
• AligningwiththeMalcomBaldrige
National Quality Award Program’s
Healthcare Criteria for Performance
Excellence to help the organization prepare
for state, national, or international
award programs.
The Healthcare Criteria are built on the follow-
ing set of interrelated core values and concepts:
• Visionaryleadership
• Patient-focusedexcellence
• Organizationalandpersonallearning
• Valuingstaffandpartners
• Agility
• Focusonthefuture
• Managingforinnovation

78 Business Operating System (BOS)
• Managementbyfact
• Socialresponsibilityandcommunity
health
• Focusonresultsandcreatingvalue
• Systemsperspective
Cause-and-Effect Diagram 79
Define
Measure
AnalyzeImprove
Control
CAUSE-AND-EFFECT DIAGRAM
(FISHBONE DIAGRAM,
ISHIKAWA DIAGRAM)
Originally developed in the 1940s by Kaoru
Ishikawa in Japan, the cause-and-effect diagram
is a graphical analysis tool that allows the user
to display the factors involved in a given situa-
tion. “Cause-and-effect diagrams are drawn to
clearly illustrate the various causes (x) affecting
product quality by sorting out and relating the
causes. Therefore, a good cause-and-effect dia-
gram is one that fits the purpose, and there is no
one definite form” (Ishikawa 1976). The causes
can be any item or occurrence that is related to
the effect (Y) being studied. Thus, the effect is a
function of the causes: Y = f(x). This tool is some-
times called an Ishikawa diagram (for its origi-
nator) or a fishbone diagram, or even a feather
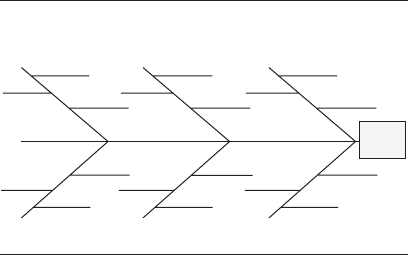
80 Cause-and-Effect Diagram
diagram, given the shape of the graphic (see
Figure 13).
Reminder: Ask the five W’s and H: what, why,
when, where, who, and how.
When creating this diagram, it is best to try
to keep an open mind and to work as a team to
view and discuss what the system or process is
doing. You want to capture everything you can
about the process, looking for all the actual activ-
ities in the process, not just what you think is
happening. Besides using the five W’s and H
in creating the cause-and-effect diagram, some
people use brainstorming, but many people start
by reviewing some of the eight M’s:
• Man(people—Practicestaff)
• Machine(equipment)
Causes
Effect
Man Machine Methods
Materials Mother Nature Measurement
Figure 13 A basic cause-and-effect diagram.

Cause-and-Effect Diagram 81
• Methods(operatingprocedures)
• Materials
• Measurement
• MotherNature(environment)
• Management(person[s]whorunsor
directs the Practice)
• Money
This tool is relatively simple to use, yet it is very
powerful. Once completed, it graphically portrays
the factors of the process to management and
other teams. Imagine you want to have donuts
at your next team meeting. What are some of the
factors that would be involved? You first need to
decide where the donuts will come from, what
type you want, who will make or buy them, and
other issues. A simple cause-and-effect diagram
for this appears in Figure 14.
As the team works on the process, more detail
can be added to the diagram. Let’s say that in
our donut example the team wants to look at
the measurement stem of the diagram to see
how the amount of cream in the donut could
vary. Some factors you might add are consis-
tency of the cream, types of cream used, size of
insertion equipment, cooking temperature effect
on cream, and so on (see Figure 15). This allows
the team to get as detailed as needed to ensure
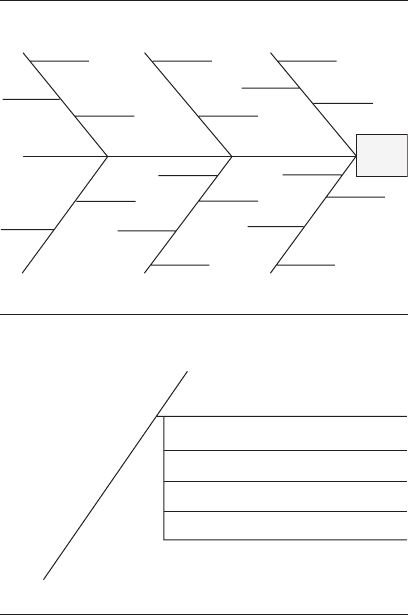
82 Cause-and-Effect Diagram
Cooking
location
Room temp.
Amount
jelly filled
Good
donuts
Man Machine Methods
Materials Mother Nature Measurement
Training Deep fryer model Convenience store
bought
Care
Individual mastery
Equipment
placement
Donut shop
Homemade
Type of
oil
Fresh dough
Room humidity
Age of donuts
Amount
cream filled
Light
intensity
Measurement
plan
Figure 14 Cause-and-effect diagram for donuts.
Measurement
Amount of cream filled
Consistency of cream
Types of cream used
Size of insertion equipment
Cooking temperature effect on cream
Figure 15 Cause-and-effect stem: measurement
breakdown.

Cause-and-Effect Diagram 83
that it understands the process and can show the
causes and effects of the given situation. Once
completed, the cause-and-effect diagram can
be shown to other groups (for example, accoun-
tants, maintenance, administrators, other Prac-
tice staff, management, customers, suppliers)
as a visual aid or training aid so that everyone
involved in the activity understands what the
process is doing.
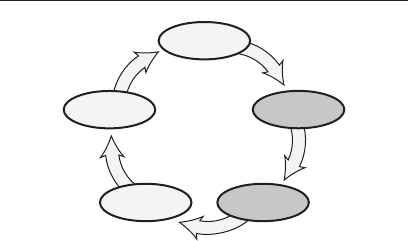
84 Check Sheets
Define
Measure
AnalyzeImprove
Control
CHECK SHEETS
A check sheet (sometimes called a checklist) is
any set of words, tally lists, or graphics designed
to assist us in conducting a planned review or
observation of our process or system. An air-
craft pilot, before taking off or landing a plane,
is required to use a check sheet to ensure proper
operation of the airplane (see Figure 16). For
us in the healthcare Practice, check sheets can
either be a list of things to do or a data collection
method that allows us to tally the issues/items
being monitored on a list or on a pictorial image.
As can be seen in Figures 17 and 18, these
check sheets are designed to collect data for
analytical purposes from our work areas. Prac-
tice staff need to have simple tools that allow
for quick and easy collection of data. During the
Check Sheets 85
Preflight Inspection: Cessna 152
1) CABIN
1. Control Wheel Lock—Remove
2. Ignition Switch—OFF
3. Master Switch—ON
4. Fuel Quantity Indicators—CHECK
QUANTITY
5. Fuel Shutoff Valve—ON
2) EMPENNAGE
1. Rudder Gust Lock—REMOVE
2. Tail Tie-Down—DISCONNECT
3. Control Surfaces—CHECK freedom
of movement and security
3) RIGHT WING Trailing Edge
1. Aileron—CHECK freedom of movement
and security
4) RIGHT WING
1. Wing Tie-Down—DISCONNECT
2. Main Wheel Tire—CHECK for proper
inflation
3. Before first flight of the day and after
each refueling, use sampler cup and
drain small quantity of fuel from fuel tank
sump quick-drain valve to check for
water, sediment, and proper fuel grade.
4. Fuel Quantity—CHECK VISUALLY for
desired level
5. Fuel Filler Cup—SECURE
5) NOSE
1. Engine Oil Level—CHECK, do not
operate with less than four quarts. Fill to
six quarts for extended flight.
Figure 16 Cessna 152 checklist.
86 Check Sheets
Game day: 6/1/09
Opponent: Falcons Game Stats Tally
Final score: 4 to 2 W
Fielder
Strike Walk 1st 2nd 3rd Home RBI out Other
Pitcher l l ll
Catcher ll l
1st base l l l
2nd base l l l l
Short l l l l l
3rd base ll l l
Left field ll l
Center
field l l l
Right
field l ll
Other 1 ll l l
Other 2 l ll
Other 3 ll
Other 4 ll
Other 5 ll
Totals 11 5 3 4 2 1 3 16
Figure 17 Traditional check sheet.
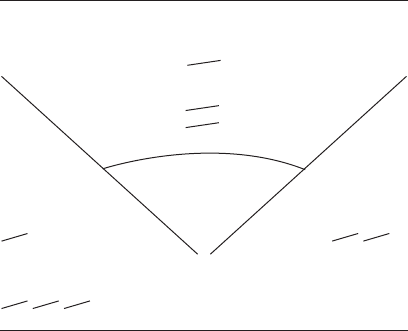
Check Sheets 87
collection of data on a check sheet, it is common
to see developing patterns or trends that may
affect the outcome of a process. This is especially
true in healthcare settings where we do not see
repetitive activities on a daily basis. You want
to make this data collection as easy as possible;
otherwise the information you obtain may not be
as reliable as you need or the time it takes you to
collect the data may be prohibitive. Here are the
basic steps in making a check sheet:
1. Identify and agree on the causes or
conditions that are to be collected.
Game day: 6/1/09
Opponent: Falcons
Final score: 4 to 2 W
Game Stats Tally
Walks
l l l l
Out by fielder
l l l l l l l l l l l l l
Strikeouts
l l l l l l l l l
Home runs
l l l l
x = On-base hits
s = Stranded
o = Field location of "out"
ooo o
oooo
xxxx
ssss ss
oo
xx
s
o
xxx
sss
oooo
Figure 18 Pictorial check sheet.

88 Check Sheets
2. Decide who will collect the data, over what
time period or periods, and how the data
will be collected.
3. Create a check sheet that will work in the
area where it is to be used.
4. Collect the data as designed to ensure
consistency and accuracy of the
information.
Check sheets can be the basis for other analyt-
ical tools and are often incorporated into attri-
bute process behavior charts (discussed under
“Process Behavior Charts”). It is sometimes sur-
prising how just creating and using a check sheet
can help you focus on continual improvement and
how changes may occur just because of the use
of the check sheet. As you strive to improve your
organization using the tools of Lean Six Sigma,
check sheets become a powerful tool.
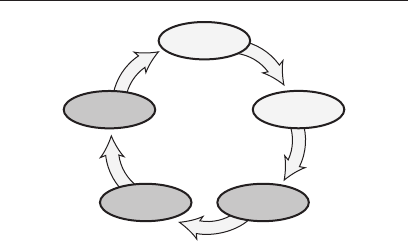
Continual Improvement (Kaizen, Kaizen Events) 89
Define
Measure
AnalyzeImprove
Control
CONTINUAL IMPROVEMENT
(KAIZEN, KAIZEN EVENTS)
Continual improvement (CI) is the process of keep-
ing an open mind and looking for ways to make
the things that you do better, do them less expen-
sively, or do them faster. As the Industrial Revo-
lution progressed into the early 1900s, Frederick
Taylor developed a method of work specializa-
tion that many organizations still use today. It
was during this time that workers first stopped
checking their own work, and specialized inspec-
tors were employed in inspection teams. This
process developed for several decades, and pro-
fessional organizations were born that focused
on doing inspection better.
During the late 1920s Walter Shewhart devel-
oped the first control chart, and statistical pro-
cess control (SPC) was born (some now call this

90 Continual Improvement (Kaizen, Kaizen Events)
process behavior charting). Many organizations
continued to rely on inspectors, but the use of
charting, which could bring the staff back into
the process of looking at the quality of their work,
became a requirement in the United States dur-
ing World War II. It was in 1951 that Armand
Feigenbaum first published his book Total Qual-
ity Control, and the TQM (total quality manage-
ment) age commenced.
During the 1960s and 1970s the use of qual-
ity circles and employee involvement became the
next evolutionary phase in continual improve-
ment. This was followed by a major resurgence
of SPC during the 1980s. During the 1990s the
International Organization for Standardiza-
tion’s quality management system (QMS) ISO
9000, and the Malcolm Baldrige National Qual-
ity Award were the major advances in continual
improvement. With the turn of the century, Six
Sigma started receiving a lot of attention.
Other terms used of late include value
analysis/value engineering, lean manufacturing/
lean office, kaizen, poka-yoke, and others. Lean
Six Sigma is the latest wave in the ongoing con-
tinual improvement movement and is bringing
together many fields of study and putting them
in the hands of the people doing the work.
Some people refer to these various methods
as continuous improvement because they feel

Continual Improvement (Kaizen, Kaizen Events) 91
we should always make breakthrough strides
in everything we do. Unfortunately, nature and
human beings do not work that way. Even in evo-
lution, things have to step back or level off every
now and then. As we learn new things, some-
times humans have to relearn old knowledge.
Thus Dr. Deming changed the term continuous
to continual.
Concurrent with this change, Dr. Deming also
developed a system he called profound knowledge.
This concept involves the following: appreciation
for a system, knowledge about variation, theory
of knowledge, and psychology. By using each of
these aspects of profound knowledge, continual
improvement can and will become a reality in
our organizations. Our goal is always to main-
tain and improve the quality of the products or
services we provide to customers, both internal
and external.
One common way of implementing continual
improvement is to use the PDSA cycle (see) and
SDCA cycle (see “Standardization”) together (see
Figure 19): the Practice staffer will see a com-
plete process for identifying processes, improving
those processes, and applying lessons learned.
The two cycles working together with the other
tools in this book will help the Practice worker to
continually improve the work that is done with
an eye to satisfying the customer.
92 Continual Improvement (Kaizen, Kaizen Events)
Kaizen is a Japanese terms that literally
means continuous improvement.
A kaizen event is a preplanned activity or
sequence of actions to be taken over a short period
of time to make/allow for a desired outcome to
occur. An example of a kaizen event could be the
planned rearrangement of the Practice furni-
ture based on studies conducted to improve the
workflow to better satisfy patients or the work-
flow of the Practice. Another example might be
a special one- or two-day effort to load patient
chart data into a registry to allow for better
utilization of information and for preplanning of
patient visits.
C
D
A
S
S
D
A
P
Figure 19 PDSA and SDCA working together.
Cost–Benefit Analysis 93
Define
Measure
AnalyzeImprove
Control
COST–BENEFIT ANALYSIS
(COST OF QUALITY, QUALITY
COST, COST OF POOR QUALITY,
RETURN ON INVESTMENT)
Cost–benefit analysis is a financial tool that
reports how quality levels are being sustained in
the Practice and its patient base. Many costs
in the Practice can be classified into one of four cat-
egories: prevention costs, appraisal costs, internal
failure costs, or external failure costs. However,
not all expenses of the company are used for the
cost–benefit analysis, only those that relate in
some way to products or services that we deliver
to our customers (see Table 2). The real power of
this tool is not so much in our using the exact or
“right” measures for each expense, but in looking
at trends over time to see how the organization
94 Cost–Benefit Analysis
Table 2 Costs of quality.
Prevention costs Appraisal costs Internal failure costs External failure costs
Marketing/customer/ Purchasing appraisal Product/service design Complaint investigations/
user costs failure costs (internal) customer or user service
Product/service/ Operations (manufacturing Purchasing failure Returned goods
design development or service) appraisal costs costs
Purchasing External appraisal Operations (product Retrofit costs
prevention costs costs or service) failure costs
Operations Review of test and Other internal Warranty claims
(manufacturing or inspection data failure costs
service) prevention
costs
Quality Miscellaneous quality Liability costs
administration evaluations
Other prevention costs Penalties
Customer/user goodwill
Lost sales
Other external failure costs
Source: ASQ Quality Costs Committee, Jack Campanella, editor. 1999. Principles of Quality Costs: Principles,
Implementation, and Use. 3rd ed. Reprinted with permission of ASQ Quality Press, Milwaukee, Wisconsin.
Cost–Benefit Analysis 95
is doing. We want to look at what the total
cost is to provide our customers with products
and services.
Traditionally, when cost of quality is first cal-
culated for an organization, a picture such as that
in Figure 20 will emerge. This is partly because
many accountants and managers have not been
taught about this tool in their formal education,
nor does any government or professional organi-
zation require the reporting of financial data in
this format.
Organizations that have learned to use the
cost–benefit analysis of quality costs typically
are very surprised at the amount of waste that
they’re producing. By focusing on prevention and
Dollars $
Prevention Appraisal Internal
failure
External
failure
Figure 20 Traditional quality costs.

96 Cost–Benefit Analysis
appraisal activities, the failure costs will slowly
start to come down. This will not happen over-
night, and it may take years in some stubborn
cases to show improvement as the old proce-
dures work their way out of your organization’s
system.
No one should be blamed for the poor results
of the first measurement. It is important to look
at those numbers as a benchmark against which
to measure improvement. The results of the first
measurement should be made available to every-
one in the Practice so that people can start to
generate ideas about what can be done and how
to go about doing it. There’s an old adage: “What
gets measured, gets done!” Thus, if everyone
knows that management is watching the num-
bers of the cost–benefit analysis, things should
start to improve.
The ultimate goal is to change the overall pic-
ture to look like the one in Figure 21. As an orga-
nization continually improves its operations, it
will see an overall reduction in the total cost to
provide its products and services.
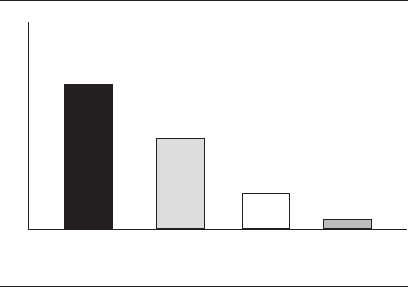
Cost–Benefit Analysis 97
Dollars $
Prevention Appraisal Internal
failure
External
failure
Figure 21 Quality costs—moving to continual
improvement.
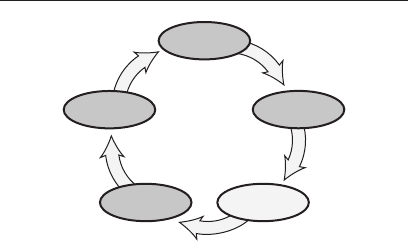
98 Cycle Time Analysis
Define
Measure
AnalyzeImprove
Control
CYCLE TIME ANALYSIS
Once you identify the boundaries of your process
(see “SIPOC Diagram” and “Process Identifica-
tion”), you can now set a starting benchmark for
what is being done. Knowing what is happen-
ing currently will give you a base from which to
evaluate the effect of future improvements. It is
surprising to note that many healthcare organi-
zations do not know what their cycle times are
nor what the yield of the process is. Yield can be
defined as the total number of units handled cor-
rectly (with no rework or rechecking) through the
process step(s).
In using the cycle time or yield tool, one com-
mon approach is to look at the value added for
each step in the process. Do items, people, or
information sit around in holding patterns

Cycle Time Analysis 99
waiting for something to be done? Are multiple
reviews or signatures required where no value is
added(doestheitemreallyneedtheVP’ssigna-
ture, which in reality is only a rubber stamp)?
How long is it currently taking to accomplish
all the process steps versus how long it should
take the information or item to go through the
system? A common suggestion is to imagine
yourself as the object or item going through your
system and see what is really going on. From this
perspective, you can then look for possible areas
of improvement.
The four basic principles of cycle time reduc-
tion are: eliminate, combine, simplify, and change.
Can certain steps be eliminated? These could
be sorting, storage, or movement of the item or
information. Can some of the steps be combined?
This could be having the same person do mul-
tiple activities at the same time or having the
customer speak to only one person instead of
several. Can the steps or information be simpli-
fied in some way? Is a complicated form really
necessary or is it just the way things are done?
Finally, should things or the process be changed?
The “current state,” “could be,” and “should be”
flowchart maps are useful at this point to look at
ways to make changes (see “Flowchart”).
Your manager or supervisor may have you
collect information about the cycle times in

100 Cycle Time Analysis
your process to calculate something call rolled
throughput yield. This is a measure used to track
the overall process as to the quality output of your
system. It is a good metric to use to evaluate your
success in how the process is being improved.
A cycle time analysis was conducted at a
Practice where a quality improvement coach
(QIC) noted that a lot of billing errors were being
returned from the payer. In following the trail
back through the various personnel in the
Practice, the root cause was discovered to be the
poor handwriting of the doctor and the first per-
son to have to input the information into the com-
puter system for billing purposes. Since it was
so hard to track down the doctor each time the
person had a question (which was happening
many time each day), the person had to guess
at what they thought the doctor intended. The
data clerk was able to guess correctly only some
of the time. Thus the Practice was forced to hire
two people (one data entry clerk and one person
to chase down the errors for correcting billing
issues) to handle the workload. Finding a better
way for the doctor to communicate his/her intent
to the computer system would allow for one full-
time person to be better utilized to add value to
the Practice instead of chasing down errors.
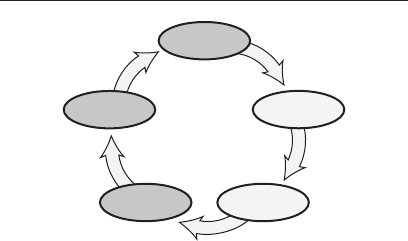
Failure Mode and Effects Analysis (FMEA) 101
Define
Measure
AnalyzeImprove
Control
FAILURE MODE AND
EFFECTS ANALYSIS (FMEA)
The failure mode and effects analysis (FMEA)
was first extensively used in the aerospace indus-
try in the 1960s to look at all the possible effects
of failure of a given piece of equipment. (The con-
cept of FMEA was first developed in 1949.) These
documents typically have been created by engi-
neers or the quality officer and often do not get
down to the shop floor or to the work areas where
they are needed. Sometimes three versions of
the FMEA are created during the design, devel-
opment, and implementation of a new service.
The system FMEA looks at the concept of creat-
ing a new service, what the effects on the service
might be, and what Practice staff may need to go
through to be able to provide the service. Design
engineers use the design FMEA to determine

102 Failure Mode and Effects Analysis (FMEA)
how the service should be offered. The process
FMEA (the one staff should have available to
them) looks at how the service actually is pro-
vided and the various effects that can arise.
The process FMEA is useful because it ana-
lyzes the operation to determine what could go
wrong if things are not controlled, maintained,
and set up properly, and what to do about each
issue. If done well, the FMEA should predict
what could happen if something goes wrong in
the process and assign a priority number for each
issue raised. One of the more famous FMEAs
was done on O-rings used in the space shuttle
program. Engineers predicted that if a certain
series of environmental circumstances occurred,
the shuttle would blow up on takeoff. Sadly, we
all know what eventually happened.
If you have never seen an FMEA for your oper-
ation (see Figure 22), you should ask your super-
visor or local expert if one exists. Otherwise, you
might ask whether someone could work with
you to create a process FMEA for your work
area. The process of developing this document
will assist you in a number of ways: it will help
ensure that the processes in your work area are
running as smoothly as they can given the cur-
rent environment, and it will help you look for
initial areas of improvement in your Practice.
The FMEA is a matrix of process issues that
could happen in the system. A numerical scale
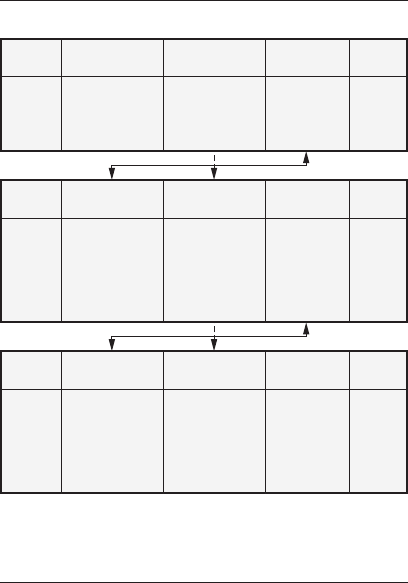
Failure Mode and Effects Analysis (FMEA) 103
System FMEA
Failure
mode Effect Cause
The problem The The
ramifications cause(s)
of the of the
problem problem
Design FMEA
Failure
mode Effect Cause
The causes The effect New root
of the from the causes for
problem system FMEA the design
from the with perhaps failure
system FMEA a better modes
definition
Process FMEA
Note: It is not unusual to have an iteration of the causes in a
process FMEA. The flow of the iteration is demonstrated. The
iteration stops when the RPN is sufficiently low—less than 50 in
a 1 to 10 guideline scale.
Failure
mode Effect Cause
The causes The same Specific
of the effect as the root causes
problem design for the
from the FMEA process
design FMEA failure
modes
Figure 22 Relationships of a process FMEA in an
iteration mode of failure identification.
Source: Stamatis, D. H. 2003. Failure Mode and Effect Analysis:
FMEA from Theory to Execution, 2nd ed. Reprinted with
permission of ASQ Quality Press, Milwaukee, Wisconsin.

104 Failure Mode and Effects Analysis (FMEA)
has been developed to look at the severity of an
issue, the likelihood of occurrence, and the pos-
sibility of detecting an issue during the current
operation before it gets downstream. One typical
set of scores is shown in Figures 23 through 25.
(Granted that these are manufacturing exam-
ples; adaptation will have to be made to your
Practice setting.)
The three scores in the tables are then mul-
tiplied across the matrix to get a single number
called the risk priority number (RPN), which is
used by management to decide what issues, if
any, need to be addressed further. This document
should give the Practice worker a clear picture
of the operation and how the service should be
provided.
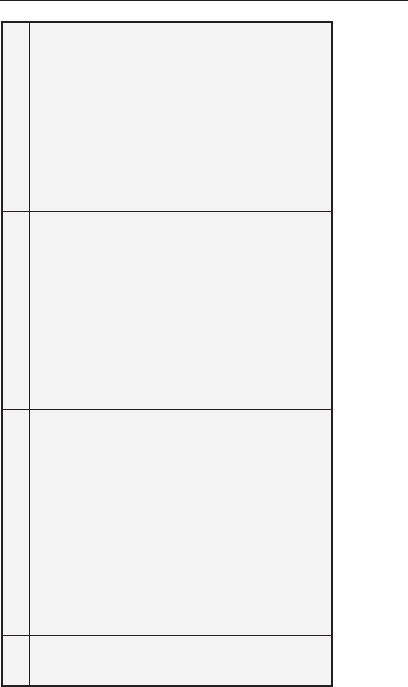
Failure Mode and Effects Analysis (FMEA) 105
Rank Resolution
1 Minor: Unreasonable to expect Unreasonable to expect that If the numerical value falls
that the minor nature of this failure the minor nature of the failure between two numbers,
would cause any real effect on would cause any noticeable always select the higher
the product and/or service. effect on the product and/or number.
Customer will probably not even the service. Customer most If the team has a
notice the failure. likely will not be able to disagreement in the ranking
detect the failure. value, the following
may help:
2–3 Low: Low severity ranking due Low severity ranking due to 1. If the disagreement
to nature of failure causing only slight annoyance of the is an adjacent category,
a slight customer annoyance. failure. Customer probably average out the
Customer probably will notice a will notice a very minor difference. For example,
slight deterioration of the product deterioration of the product if one member says 2
and/or service, a slight and/or service. and someone else says
inconvenience in the next 6, the ranking in this
process, or minor rework action. case should be 4 (2
and 6 are adjacent
categories. Therefore
2 + 6 = 8, 8/2 = 4).
Figure 23 Severity process and/or service guideline.*
*All of the above guidelines and rankings may be changed to reflect specific situations.
Source: Stamatis, D. H. 2003. Failure Mode and Effect Analysis: FMEA from Theory to Execution, 2nd ed.
Reprinted with permission of ASQ Quality Press, Milwaukee, Wisconsin.
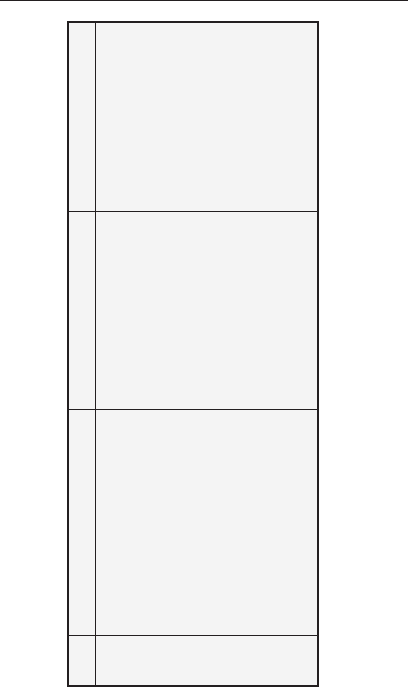
106 Failure Mode and Effects Analysis (FMEA)
Rank Resolution
4–6 Moderate: Moderate ranking Moderate failure causes 2. If the disagreement
because failure causes some customer dissatisfaction. jumps one category,
dissatisfaction. Customer is made Customer is made then consensus must
uncomfortable or is annoyed by uncomfortable and/or be reached. Even with
the failure. May cause the use of annoyed by the failure. Some one person holding out,
unscheduled repairs and/or degradation of performance total consensus must
damage to equipment. is noticeable. be reached. No average,
no majority. Everyone
in the team must have
ownership of the
ranking. They may not
agree 100 percent, but
they can live with it.
Figure 23 Continued.
Failure Mode and Effects Analysis (FMEA) 107
Rank Resolution
7–8 High: High degree of customer High degree of customer If the numerical value falls
dissatisfaction due to the nature of dissatisfaction due to the between two numbers,
the failure, such as an inoperable nature of the failure. No always select the higher
product or inoperative safety or government number.
convenience. Does not involve regulations issues. If the team has a
safety issues or government disagreement in the ranking
regulations. May cause value, the following
disruptions to subsequent may help:
processes and/or services.
1. If the disagreement
is an adjacent category,
average out the
difference. For example,
if one member says 2
and someone else says
6, the ranking in this
case should be 4 (2
and 6 are adjacent
categories. Therefore
2 + 6 = 8, 8/2 = 4).
Figure 23 Continued.
108 Failure Mode and Effects Analysis (FMEA)
Rank Resolution
9–10 Very high: Very high severity is Very high severity ranking 2. If the disagreement
when the failure affects safety or when safety issues are jumps one category,
involves noncompliance with involved or compliance to then consensus must
government regulations. government regulations is be reached. Even with
ignored. one person holding out,
total consensus must
In this scale 9–10 is reserved be reached. No average,
only for safety and government no majority. Everyone
compliance requirements. All in the team must have
other rankings may be used as ownership of the
they seem applicable. ranking. They may not
agree 100 percent, but
they can live with it.
Figure 23 Continued.
Failure Mode and Effects Analysis (FMEA) 109
Resolution
If the numerical value falls
between two numbers,
always select the higher
number.
If the team has a
disagreement in the ranking
value, the following
may help:
1. If the disagreement
is an adjacent category,
average out the
difference. For example,
if one member says 2
and someone else says
6, the ranking in this
case should be 4 (2
and 6 are adjacent
categories. Therefore
2 + 6 = 8, 8/2 = 4).
Rank
1 Failure is unlikely. C
pk
greater than or equal to
1.67 (<1 in 10
6
or ≈ ±5s)
2 Very low: Process in statistical
control. Isolated failures exist.
C
pk
is greater than or equal
to 1.33 (1 in 20,000 or ≈ ±4s)
3 Low: Process in statistical
control. Isolated failures
occur sometimes. C
pk
is
greater than or equal to
1.00 (1 in 4000 or ≈ ±3.5s)
4–6 Moderate: Process in
statistical control with
occasional failures but not in
major proportions. C
pk
is less
than or equal to 1.00 (1 in
1000 or 1 in 80 or ≈ ±3s)
Rank
1 Remote probability of
occurence. Capability shows
at least X-bar ±3s within
specifications (1/10,000).
2–5 Low probability of
occurrence. Process in
statistical control. Capability
shows at least X-bar ±3s
within specifications
(1/5000–1/500).
6–7 Moderate probability of
occurrence. Process in
statistical control with
occasional failures, but not
in major proportions.
Capability shows more
than X-bar ± 2.5s within
specifications (1/20–1/200).
Figure 24 Occurrence process and/or service guideline.*
*All of the above guidelines and rankings may be changed to reflect specific situations.
Source: Stamatis, D. H. 2003. Failure Mode and Effect Analysis: FMEA from Theory to Execution, 2nd ed.
Reprinted with permission of ASQ Quality Press, Milwaukee, Wisconsin.
110 Failure Mode and Effects Analysis (FMEA)
Resolution
2. If the disagreement
jumps one category,
then consensus must
be reached. Even with
one person holding out,
total consensus must
be reached. No average,
no majority. Everyone
in the team must have
ownership of the
ranking. They may not
agree 100 percent, but
they can live with it.
Rank
7–8 High: Process not in
statistical control. Have
failures often (1/40–1/20).
9–10 Very high: Failures are
inevitable.
Rank
8–9 High probability of
occurrence. Process in
statistical control with
failures often occurring.
Capability shows X-bar
±1.5s (1/100–1/20)
10 Very high probability of
occurrence. Failure is
almost certain. (1/10+)
Note: To use a criteria scale such as this, one must have a substantial amount of data to support
statistical control and C
pk
values. This is a very powerful scale if one has the data; if not, do not try to
generate the data to support the scale. Use a theoretical scale that is more qualitative but through the
synergy of the team becomes just as powerful.
Figure 24 Continued.
Failure Mode and Effects Analysis (FMEA) 111
Resolution
If the numerical value falls
between two numbers,
always select the higher
number.
If the team has a
disagreement in the ranking
value, the following
may help:
1. If the disagreement
is an adjacent category,
average out the
difference. For example,
if one member says 2
and someone else says
6, the ranking in this
case should be 4 (2
and 6 are adjacent
categories. Therefore
2 + 6 = 8, 8/2 = 4).
Rank
Remote likelihood that the product
or service will be delivered
(1/10,000). The defect is
functionally obvious and readily
detected. Detection reliability at
least 99.99 percent.
Low likelihood that the product
would be delivered with the defect.
The defect is obvious
(1/5000–1/500). Detection
reliability at least 99.80 percent.
Moderate likelihood that the
product will be delivered with the
defect. The defect is easily
identified (1/200–1/50). Detection
reliability at least 98.00 percent.
Rank
1 Very high: Controls almost
certainly will detect the
existence of a defect.
2–5 High: Controls have a good
chance of detecting the
existence of a failure.
6–8 Moderate: Controls may
detect the existence of
a defect.
Figure 25 Detection process and/or service guideline.*
*All of the above guidelines and rankings may be changed to reflect specific situations.
Source: Stamatis, D. H. 2003. Failure Mode and Effect Analysis: FMEA from Theory to Execution, 2nd ed.
Reprinted with permission of ASQ Quality Press, Milwaukee, Wisconsin.
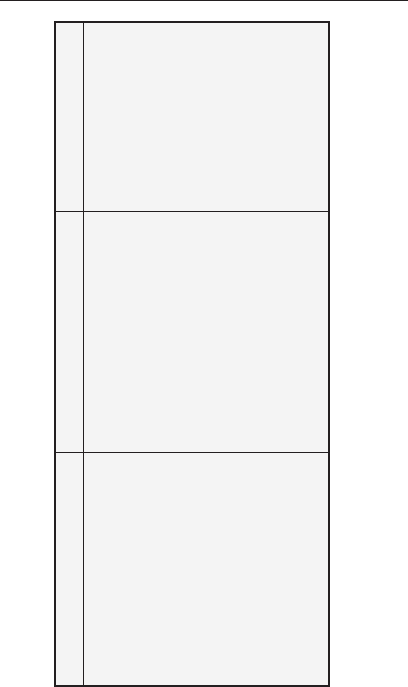
112 Failure Mode and Effects Analysis (FMEA)
Resolution
2. If the disagreement
jumps one category,
then consensus must
be reached. Even with
one person holding out,
total consensus must
be reached. No average,
no majority. Everyone
in the team must have
ownership of the
ranking. They may not
agree 100 percent, but
they can live with it.
Rank
High likelihood that the product
would be delivered with the defect.
The defect is subtle (1/20).
Detection reliability greater than
90 percent.
Very high likelihood that the
product and/or service will be
delivered with the defect. Item is
usually not checked or not
checkable. Quite often the defect
is latent and would not appear
during the process or service
(1/10+). Detection reliability
90 percent or less.
Rank
9 Low: Controls more than
likely will not detect the
existence of a defect.
10 Very low: Controls very
likely will not detect the
existence of a defect.
Figure 25 Continued.
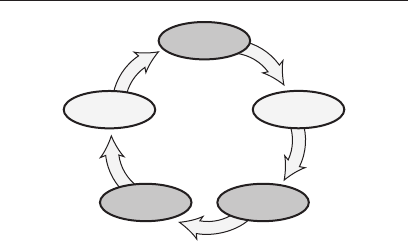
Flowchart 113
Define
Measure
AnalyzeImprove
Control
FLOWCHART (FLOW MAP,
PROCESS MAP, CURRENT STATE/
COULD BE/SHOULD BE MAP)
When you create a flowchart, you are creating
a picture of the steps in a process or system as
it actually operates or is supposed to operate.
Given the old adage that a picture is worth a
thousand words, this tool allows you to commu-
nicate, using standard symbols (see Figure 26),
how your process works (see Figure 27). The flow-
chart is very useful when looking at a process
that you want to improve (note that it is included
in the control plan—if done in your Practice). By
actually creating three flowcharts—1) what you
think it is (before you check reality), 2) what it
actually is, and 3) what you would like it to be
(see Figure 28)—you can analyze what changes
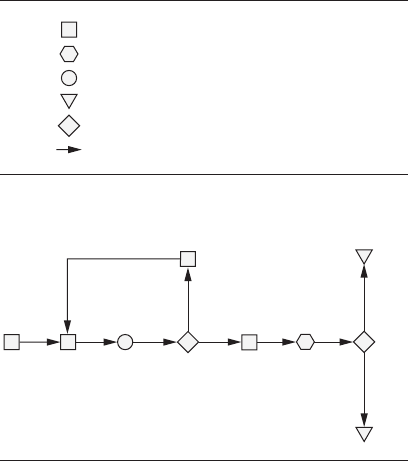
114 Flowchart
need to be made and study whether the changes
are doable given your training and resources.
Each organization should decide for itself
what symbols to use, as there are many versions
available today. After you decide what symbols
to use, you can follow some basic steps to create
the flowchart:
Bad
Bad
Good
Good
Scrap
Warehouse
Figure 27 Basic flowchart structure.
Process step or operation
Delay
Quality check, inspection, or measurement
Storage
Decision
Movement of material
Figure 26 Typical flowchart symbols.
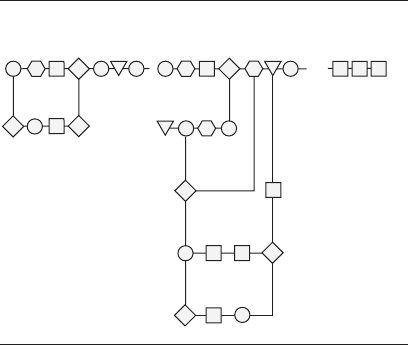
Flowchart 115
1. Create the boundaries of the process that
you intend to flowchart. This might involve
identifying the inputs and outputs of the
process or identifying who the suppliers
and customers are for the process.
2. Determine the various steps in the process.
Do not worry about sequence here, but
do collect all the steps. The foundation
material from a failure mode and effects
analysis (FMEA) or control plan can
be used if available to help start this
process. If a group is brainstorming ideas,
What you think it is… What it actually is…
What you would
like it to be…
Figure 28 Three versions of a process.

116 Flowchart
you could list each idea on a flip chart or
a wall using sticky notes.
3. Build the sequence of the process, putting
everything into the appropriate order.
4. Draw the flowchart using the symbols
appropriate for your organization.
5.Verifythattheflowchartiscompleteand
appropriate for the given operation. This
can be very important if more than one
group is working on similar processes.
Overlaps or deletions may otherwise occur
between processes.
Flowcharts are a good analytical tool for moni-
toring a process over time and also in conducting
training for new Practice staff or supervisors. By
referencing the flowcharts on a regular basis, you
can use them as visual standards to help ensure
that things are still running as they are supposed
to. Note that if a change is made to the process,
it is important to update the flowchart to reflect
the change. Regular audits may be done in your
area for any number of issues (safety, quality,
environmental, and so on), so having the flow-
charts readily available helps everyone involved.
Tip: Some organizations like to start with the
“what you think it is” flowchart to get a sense of
what is happening in the Practice. Other groups

Flowchart 117
like to start with “what you would like it to be”
so that they can set the vision for the future.
The challenge for many organizations is to final-
ize the “what it actually is” flowchart, as there
are often many viewpoints within the Practice as
to how and why things work the way they do.
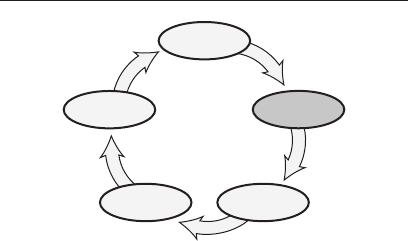
118 Histogram
Define
Measure
AnalyzeImprove
Control
HISTOGRAM
A histogram is a frequency distribution that
graphically displays the measurements taken
from a process and shows how those data are dis-
tributed and centered over a measurement scale
(usually horizontally—see Figure 29). Histo-
grams give us a picture of what a process is pro-
ducing over a specified period of time and how
much variation exists. This picture can then
be compared with our expectations of the pro-
cess, or older histograms, to see if it is operating
within specifications and to the desired plan for
that particular process. Sometimes you will see a
normal bell-shaped curve included with the his-
togram to show the theoretical placement of the
numbers as compared with the actual measure-
ments taken from the process (see Figure 30).
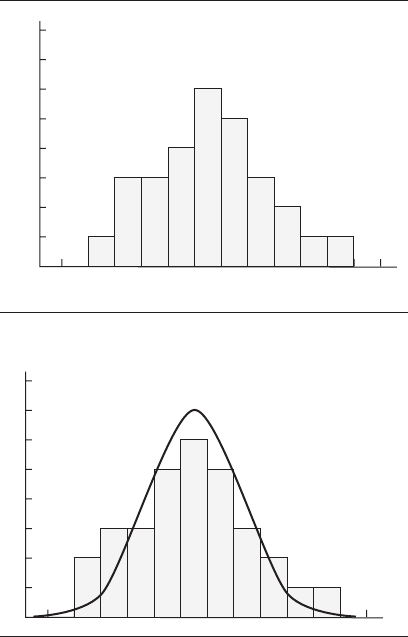
Histogram 119
Value—measurement
Count #
Figure 29 Basic histogram.
Figure 30 Histogram with bell-shaped curve.

120 Histogram
A histogram is usually quick and easy to con-
struct and is typically one of the first tools you
will use in looking at the output of a process. It
can be created by hand or with the aid of a com-
puter. Given that some test equipment can now
be tied directly to computers, a wealth of infor-
mation becomes available very quickly using the
histogram as the base. Using the histogram,
calculations can be made on the process’s mean
(average), median (middle number), and stan-
dard deviation (measure of how the numbers
are distributed in the data, sometimes compared
with the normal curve expectations).
If the Practice staffer needs to make a histo-
gram by hand, here are the basic steps:
• Setupachecksheettocollectthe
data—this could be the histogram
graph itself.
• Collectthemeasurementsastheyoccur
and record them on the check sheet.
• Orderthedataonthehistogramgraph,
if not already done through the check
sheet.
• Postthehistogramwhereotherscansee
the process.
• Interpretthedata.

Histogram 121
Since the histogram is made up of individual
numbers, it is possible to show the specification
limits for the parts on the histogram. This is
done to look for shifts in the process or the over-
all capability of the process.

122 Kanban (Wait Time, Patient Pull-Through)
Define
Measure
AnalyzeImprove
Control
KANBAN (WAIT TIME,
PATIENT PULL-THROUGH)
A system is best controlled when material, people,
and information flow into and out of the process
in a smooth and rational manner (without peri-
ods of waiting). If process inputs (patients, staff
members, supplies, and so on) arrive before they
are needed, unnecessary confusion, inventory,
wasted time, and costs generally occur. If process
outputs are not synchronized with downstream
processes, delays, disappointed customers/
patients, and associated costs may occur.
A properly administered kanban system will
improve system control by assuring timely move-
ment of products, people, and information. This
method is used in a process to signal an upstream
supplier (internal or external) that more material
or product is needed downstream. Originally, it

Kanban (Wait Time, Patient Pull-Through) 123
was just a manual card system, but has evolved
into more sophisticated signaling methods for
some organizations (by use of patient charts, col-
ored lighting systems, and so on). It is referred to
as a pull system because it serves to pull mate-
rial or product from a supplier rather than rely-
ing on a scheduling system to push the material
or product forward at predetermined intervals.
It is said that the kanban method was inspired
by Toyota’s Taiichi Ohno visiting a United States
supermarket.
In the past, many Practices were designed
with large patient waiting rooms and areas
where needed supplies were stored. If you see the
patient waiting area filled with people on a daily
basis (versus once in a while), then this is an indi-
cation of a systemic problem. The physical layout
of the office area may need to be discussed in the
Lean Six Sigma team meeting to brainstorm pos-
sible rearrangements to the way we approach the
scheduling of patients and how we move patients
and staff around the office, to allow doctors and
other staff to better utilize everyone’s time. Ask-
ing anyone (patients, doctors, staff members, and
so on) to wait is a form of waste and needs to be
minimized.
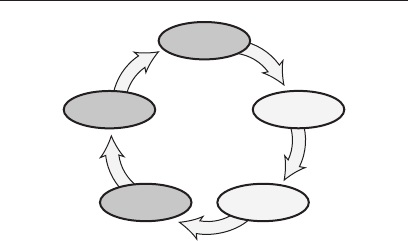
124 Lessons Learned
Define
Measure
AnalyzeImprove
Control
LESSONS LEARNED
We have all learned to do things through our
experiences, the people we have met, and the
articles or books we have read. We now apply this
learning to the work that we do every day. Some
things are repetitive, while others take thought
to accomplish. Either way, there is a standard
process that we use to accomplish our work. If we
were to take a vacation day or be out sick, could
the work be done reasonably well without us?
We are not talking about replacing ourselves
here; however, there should be a way for someone
else to be able to figure out how to do our work if
we are not there. Some companies rely on stan-
dard operating procedures (SOPs) to tell new or
replacement staff what to do. But those rarely
tell the whole truth about a job. Lessons learned
is a system that allows for the collection, storage,

Lessons Learned 125
retrieval, and distribution of knowledge—the
important learnings—to other people to use when
needed. This could be used for many purposes: to
do someone’s job in his or her absence, to conduct
internal benchmarks, or to look for better ways of
doing another job in the organization.
Learning just to gather knowledge is part
of what a learning organization is all about. In
lessons learned, companies formally establish a
system for collecting important learnings about
particular customers, activities, or processes
for use at a later time. The author’s dentist,
after each checkup, records what he has talked
about with the patient on cards that stay with
the patient’s dental records. This allows him
to review what has been or is happening in the
patient’s life prior to the next dental visit. This
process could be captured for use by any service
organization. A process should exist for collect-
ing and using these “Aha!” insights, for example,
the Ritz Carlton is well known for greeting
returning guests with personalized service
learned from prior visits. “What are we going
to do differently in this Practice regarding this
process, and for our customers, based on what we
have learned?” Thus, we learn to not repeat our
past mistakes.
In the ideal setting, the culmination of lessons
learned should lead your Practice to becoming
the best healthcare organization that it can be.
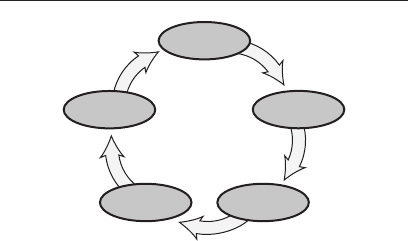
126 Management Involvement
Define
Measure
AnalyzeImprove
Control
MANAGEMENT INVOLVEMENT
In the study of economics, one finds the theories
of bubble up (worker taking the lead to do things)
and trickle down (management taking the lead
to do things). In either case, as we have seen in
the Practice, we need to have management’s buy-
in and support to ensure that things last over
time. Management involvement, then, is the way
that supervisors and managers support employ-
ees through time and resource allowances to not
only do the job well, but to study how to do an
even better job for the customer. Merely asking
staff to work harder or work better will not be
enough over time to make a real difference for
the customer.
To demonstrate management involvement,
managers and leaders need to operate with
integrity and be guided by moral principle. To be

Management Involvement 127
involved, they must be courageous, be willing to
ask the tough questions (even if they do not like
the answers), be willing to defend the decisions
of teams and employees who work for them, and
be willing to instruct upper managers to do what
is right. Employees must know that the environ-
ment is safe, that the system is being well taken
care of, and the business is being managed fairly.
Also, the managers and leaders must be willing
to uphold processes and principles that say, in
effect, that this organization will be successful
and people will be proud to work here.
Dr. J. M. Juran (1989) points out in his Juran
on Leadership for Quality that managers should:
• Establishqualitygoals
• Provideresources
• Reviewprogress
• Giverecognition
• Revisetherewardsystem
• Serveonprojectteams
• Faceuptoemployeeapprehensions
This is an area where you will “know it when you
see it.” If supervisors continually try to push staff
to only work harder to make their numbers, then
you know that quality and customer concerns are
minimal. On the other hand, if supervisors care

128 Management Involvement
that the services and products that are presented
to customers are the best they can be, and they
show concern for satisfying or delighting the cus-
tomer, then managers are showing commitment
to quality and how work is being done.
For Lean Six Sigma to work well in your orga-
nization, management must be committed during
all phases of the process to ensure that adequate
time and resources are allocated to achieve
continual improvement. Practice staff will notice
that managers are not cutting corners to save
costs, that safety remains a prime concern, and
that they, the Practice staff, are being treated
fairly. Also, Practice staff will see workload dis-
tribution and expectations being managed in an
equitable fashion and that employment agree-
ments are managed equitably.
Peter Senge’s comment on the subject is worth
repeating here: “Top management buy-in is a poor
substitute for genuine commitment and learning
capabilities at all levels in an organization. In
fact, if management authority is used unwisely,
it can make such commitment and capability less
likely to develop” (Senge 1990).
Measurement Systems Analysis (MSA) 129
Define
Measure
AnalyzeImprove
Control
MEASUREMENT SYSTEMS
ANALYSIS (MSA)
In healthcare environments, we do not often
think about analyzing the equipment or pro-
cesses we use to study or verify work that has
been done according to a standard or specifi-
cation. Whenever we measure anything with a
gage or a scale, we typically assume that it will
give us a true reading or measurement. Have
you ever put an envelope on a postage scale and
then put the same envelope back on again to see
if you get the same postage reading? Usually you
will, but more often than you might think,
you can actually get a different reading. This is
especially true if you are just between two differ-
ent rate codes. Or have you stepped on a bath-
room scale only to try it again a little later to see
if you get the same reading? Depending on the

130 Measurement Systems Analysis (MSA)
scale (some newer electronic scales have blockers
in them to prevent variation) you may very well
see different readings. What is happening?
Any form of measurement has variation in it.
Even if a gage or scale is being used, results can
be different. If you have multiple people review-
ing data entry information, the odds are that
incorrect information will get through! That is
why many accounting processes have so many
rework and rechecking loops in them. Why does
this happen? It is a well proven fact that inspec-
tion is only about 80 percent effective. Also, even
if you have a standard to work to (say, a written
procedure that is to be followed for some out-
come), there is always a chance for something
to not be evaluated the same way by different
people. Ask almost any police officer who has had
to take eyewitness testimony of a traffic accident
from a number of people. The officer will prob-
ably tell you that there were as many versions of
the story as people interviewed!
Each of us relies on measurement processes
(visual inspection, verification loops, actual
testing equipment, and so on) to measure our
processes and the outcomes of our work. The
question measurement systems analysis (MSA)
addresses is “How effective are those measure-
ment processes?” It is surprising how quickly
a measurement process can get out of calibra-
tion or otherwise give poor readings. Even after

Measurement Systems Analysis (MSA) 131
installing the measurement system properly and
using it the way that it was designed, things can
still go wrong with how the measurement pro-
cess performs. Sometimes we will see two identi-
cal processes that will give different outcomes for
the same thing being studied. In other cases, two
or more Practice staff will use the same or simi-
lar processes but get different results.
Measurement systems analysis is a method
of checking how well people are using a measure-
ment process and judging whether the mea-
surement system is effective and efficient, in
order to provide your customers with the services
they want. The process of testing is sometimes
called gage repeatability and reproducibility
(GR&R), and through the use of software we
can look at the gage’s accuracy, repeatability,
reproducibility, and stability. If the MSA shows
problems, then you must take action to ensure
that the service you provide will meet customer
requirements.
One common MSA method involves a group
of people (two or more) using the same or simi-
lar measurement processes and testing a blind
set of numbered samples (around 10 or so). The
test items (reports, financial information, timed
events, and so on) are given to the people ran-
domly with only the tester knowing which item
is which. Each person tests each item a total of
three times in a random order so that the person

132 Measurement Systems Analysis (MSA)
will not know what outcome the item may have
had on a prior test. After all items have been
measured the appropriate number of times, the
data can be put into any of a number of computer
software programs for analysis.
Other methods of MSA are used for processes
that can only be checked once for each item. The
main point here is that checking processes can
vary, and our methods of verifying or validating
what is done must be understood so that deci-
sions can be made on the overall effectiveness of
how things are being evaluated. With this infor-
mation, we can start studying the variation of
the processes with confidence that we know the
variation of the measurement system.
Mistake-Proofing (Error-Proofing, Poka-Yoke) 133
Define
Measure
AnalyzeImprove
Control
MISTAKE-PROOFING (ERROR-
PROOFING, POKA-YOKE)
Mistake-proofing (also called error-proofing or
poka-yoke) is the process of either ensuring that
there is only one way (or limited ways) to do any
given task in a process or ensuring that any mis-
take is very obvious as soon as it happens. Such
efforts help reduce variation in the process and
help prevent nonconformity issues from arising
in the process downstream or when a customer
uses the product or service. Have you ever noticed
that when you try to plug an electrical appliance
into an electrical outlet, the plug can go in only
one way (this is true for either two- or three-
pronged plugs)? This is an example of mistake-
proofing that allows the electronics industry to
ensure proper usage of appliances in the office
or home.

134 Mistake-Proofing (Error-Proofing, Poka-Yoke)
Jobs in your organization can be looked at in
the same way. Is it possible for a process to be
completed in more than one way? Can the process
be done in a different order than what the pro-
cess design states (or worse yet, does each person
develop their own method for doing the work)? If
any of these issues or any number of others exist,
you should help ensure that things are done more
consistently to help reduce variation in the pro-
cess. Note: We are not talking about reducing or
stopping independent thought or creativity here!
Some things can be done differently with little to
no impact on the outcome of the process. What
we want to look at is how to give customers more
consistency in what they see.
You may need to get quality assurance or man-
agement involved with some changes to your pro-
cesses; however, some changes you can do with
the help of your natural work groups. If there is
a series of similar processes that comes through
your area, look over the paperwork that accom-
panies these processes. Is everything arranged
logically for your work space? Is the paperwork
aligned to show similar steps in the same order
or sequence? Do some reports sit in in-boxes for
long periods of time with no value added? If you
could change anything about your work area,
what would it be? Tell your supervisor or team
your ideas.

Mistake-Proofing (Error-Proofing, Poka-Yoke) 135
The originator of this method was a Japanese
engineer named Shigeo Shingo, and there is now
a yearly prize (Shingo Prize) in the United States
to promote the use of mistake-proofing and other
world-class operational excellence strategies.
136 Pareto Chart
Define
Measure
AnalyzeImprove
Control
PARETO CHART
Dr. J. M. Juran applied the concept of the Pareto
principle (based on the work of a 19th-century
economist and priest named Vilfredo Pareto)
to industry during the 1950s. Basically, the
Pareto principle, or 80/20 rule, states that 80
percent of effect(s) are the result of 20 percent
of causes. The result of this work is a graphi-
cal tool—called a Pareto chart—that shows fre-
quency of occurrences (or ranks the effects of
problems). See Figure 31.
The Pareto chart organizes data to show
which items or issues have the greatest fre-
quency in the process, system, or service. The
chart stratifies the data to show the ranking of
the groups, starting with the largest and work-
ing across to the smallest group (see Figure 32
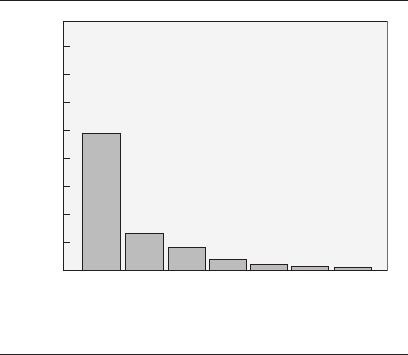
Pareto Chart 137
for a pictorial version of the Pareto chart). The
idea is that by organizing the data in this format,
we can develop a plan to work on problems that
will give us the biggest return on our process
improvement efforts.
A Pareto chart is easy to develop by hand; how-
ever, there are computer software programs that
can do this as well. Here are the basic steps:
• Collectthedata—thePracticestaffercan
again start with the check sheet to collect
information.
80
70
60
50
40
30
20
10
0
Count
Defect
Count 49 13 75433
Element 7
Element 6
Element 3
Element 1
Element 8
Element 2
Others
Figure 31 Pareto chart.
138 Pareto Chart
• Organizeandgroupthedatafromhighest
frequency to lowest frequency.
• DrawtheParetochart.
• Analyzethedata.
• Workontheissues.
Once the Pareto chart has been created, the
Practice staffer and team can start develop-
ing plans and actions (use a problem-solving
method) for improving the process, starting with
the most frequently occurring issue or problem.
As that problem is improved (you may not be able
to totally eliminate the problem, but you still
A
B
C
D
E
F
G
H
Patient: ___________
Address: ___________
___________
___________
Phone: ___________
Email: ___________
BackFront
Figure 32 Pictorial Pareto chart—patient
chart audit.
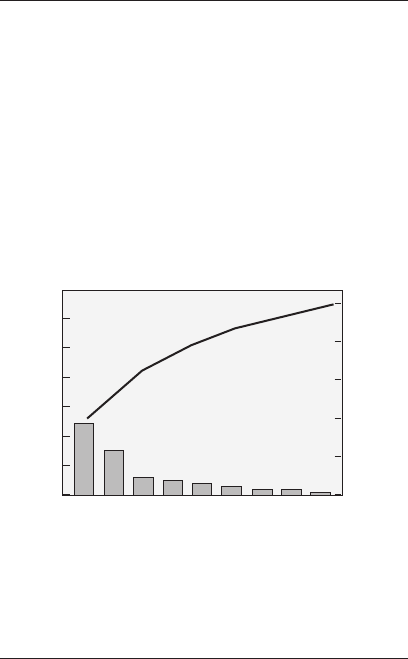
Pareto Chart 139
try), the team can go to the next most frequently
occurring problem and work on that, and so on.
When creating multiple Pareto charts over
time for the same process, it is helpful to main-
tain the same scale (see Figures 33 and 34). If
a computer is used, the Practice staffer may
have to manually set the scale. This will allow
for easier comparisons to demonstrate continual
improvement.
60
50
40
30
20
10
0
100
80
60
40
20
0
Count
Percent
Defect
Before Improvement
Addition error
Wrong city
Customer not verified
Spelling error
Wrong $ value
Customer info wrong
Wrong state
Wrong salesperson
Other
Count 24 15 6 5 4 3 2 2 1
Figure 33 “Before” Pareto chart.
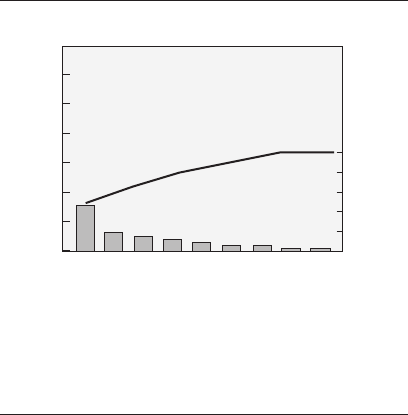
140 Pareto Chart
0
Count
Percent
Defect
Wrong city
Customer not verified
Spelling error
Wrong $ value
Customer info wrong
Wrong state
Wrong salesperson
Additional error
Other
Count 15 6 5 4 3 2 2 1 1
100
80
60
40
20
After Improvement
60
50
40
30
20
10
0
Figure 34 “After” Pareto chart.
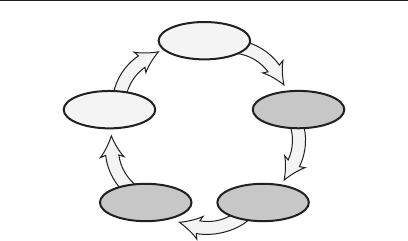
PDSA Cycle (Plan–Do–Study–Act) 141
Define
Measure
AnalyzeImprove
Control
PDSA CYCLE
(PLAN–DO–STUDY–ACT)
PDSA is a strategy intended to be a guiding light
for the way we work and do our jobs. Building on
the work of Walter Shewhart in the 1930s, Dr. W.
Edwards Deming changed the PDCA improve-
ment model (plan–do–check–act) to PDSA (plan–
do–study–act). The latter model is the foundation
for various methods such as advanced quality
planning, problem solving, Lean Six Sigma, and
process improvement (see Figure 35).
The PDSA cycle is used as a road map to work
through a process to identify possible aspects
that can be improved. First, a plan is estab-
lished regarding what is to be worked on. In the
do phase, we do the work of the process. Then
we can study the process and outputs of the pro-
cess to identify possible improvements. Finally,
142 PDSA Cycle (Plan–Do–Study–Act)
we take some actions on what we have seen and
observed. This cycle should be repeated until
the process is as good as it can be given the cur-
rent process parameters and materials. The
challenge is that as new methods, materials, and
technology become available, we keep open minds
to allow for changing the way we do our work.
Another view of the PDSA cycle is represented
by the data–knowledge–action cycle (see Figure
A
C
T
P
L
A
N
S
T
U
D
Y
D
O
Figure 35 PDSA cycle.
PDSA Cycle (Plan–Do–Study–Act) 143
36). This may allow the Practice staffer or man-
ager to understand PDSA by starting with the
basic building blocks of the process. You need
to have knowledge about the process, have data
from the process, and be willing and able to take
action to make necessary changes. Without all
three components, nothing will change. Just as
a three-legged stool will give solid support, once
all three parts are present, you can work with
the process to understand what it is doing. Then
you can work to improve it.
A fascinating point that the author has noted
while observing people such as Deming, Juran,
and Feigenbaum is that each of them applied the
Knowledge
Action
Data
Figure 36 Continuous improvement model.
Source: Cutcher-Gershenfeld, J., and K. Ford. 2005. Valuable
Disconnects in Organizational Learning Systems. New York:
Oxford University Press. Used with permission.

144 PDSA Cycle (Plan–Do–Study–Act)
PDSA technique to his own life and work. Each
of them continually challenged their beliefs and
training to look for new and better ways of doing
any work or assignment. The point is to continu-
ally improve everything that we do, both on the
job and in our life.
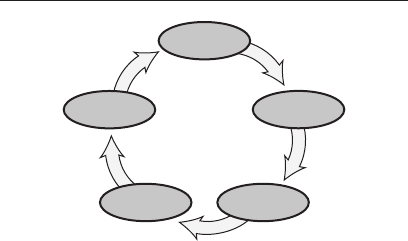
Practice Strategy (Future State) Project Planning 145
Define
Measure
AnalyzeImprove
Control
PRACTICE STRATEGY (FUTURE
STATE) PROJECT PLANNING
Building a practice strategy involves a lot of proj-
ect planning to ensure that the desired goals
and outcomes of the Practice will be achieved.
The old adage that “failing to plan is planning
to fail” applies to medical Practices as much as
anywhere else. If we give little to no forethought
to how we run our Practice to deliver quality and
safe healthcare for our patients, then the out-
comes can not be predicted. In the books Curing
Health Care (Berwick, Godfrey, and Roessner
1990) and Crossing the Quality Chasm (Commit-
tee on Quality Healthcare in America 2001), a
bleak picture is presented on how well, or poorly,
we in the United States as a society design and
deliver our healthcare to patients. The challenge
here is for Six Sigma team members to utilize

146 Practice Strategy (Future State) Project Planning
the tools outlined in this pocket guide to set a
strategic plan in place to help ensure that your
Practice is delivering the very best quality and
safest healthcare available to your patients.
Project planning is the disciplined monitor-
ing of how and when a practice strategy will
be accomplished. If you want to go on a long
trip, do you just jump in the car and go? Some
people do because they like the spontaneity of
adventure. Most of us, however, would rather
plan the trip, some in more detail than others.
We do so to know what needs to be taken, how
long we will be gone, and any number of other
details. Those of you with young children know
that this is very important.
Too often, Practice staff use the tools and pro-
cesses listed in this book as independent events
to satisfy some issue of the moment. Using project
planning, you should look at the entire system and
strive for synergy as you use communication
and the tools and processes to contribute to con-
tinual improvement. Project planning becomes
the tracking system to ensure that all the
elements, tools, processes, communications, and
so forth, are brought together as a whole system
for doing the work that you do in your Practice.
Effective project planning requires skills in
the following areas (Kerzner 1995):
• Informationprocessing

Practice Strategy (Future State) Project Planning 147
• Communication
• Resourcenegotiations
• Securingcommitments
• Incrementalandmodularplanning
• Assuringmeasurablemilestones
• Facilitatingtopmanagementinvolvement
At times Practice staff may become part of proj-
ect plans that are developed in your Practice or
aligned healthcare units. Working with such
plans should help ensure the successful demon-
stration of continual improvement and the satis-
faction of customer’s wants and needs.
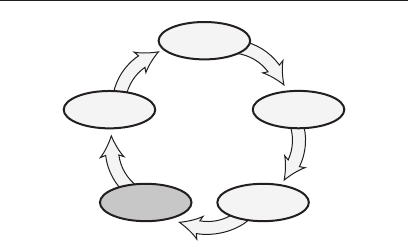
148 Problem Solving
Define
Measure
AnalyzeImprove
Control
PROBLEM SOLVING
Some of the more successful attempts to solve
problems have been accomplished through the
use of a model or strategy that outlines the steps
that should be followed in investigating and con-
taining issues, and fixing the problems so that
they will not return. Unfortunately, many of us
have seen situations in which a problem has been
fixed, only for the same issue to crop up again in
a week, month, or year. The question is “How do
we permanently solve problems?”
One common approach to problem solving
is called the eight discipline (8D) approach
( Stamatis 1996). The steps commonly followed in
this process are:
1. Use a team approach. Organize a small
group of people (note that we did not say

Problem Solving 149
that you have a team at this point—this
is just a starting group) with knowledge
of the process/product, authority to make
changes in the Practice, and skill in the
technical disciplines required to solve
the problem and implement corrective
actions. The group must have a designated
Champion.
2. Describe the problem. Specify the internal/
external customer problem by identifying
the quantifiable terms—the who, what,
when, where, why, how, and how many
(five W’s and two H’s) for the problem.
Use SIPOC, brainstorming, flowcharts,
and any other methods that the group
feels is appropriate.
3. Start and check interim (containment)
actions. Define and implement
containment actions to isolate the
effect or issue from the problem “right
now.”Verifytheeffectivenessofthis
containment action to ensure that the
internal or external customer does not
see further problems.
4. Define and check root causes. Identify
all potential causes of the problem
(a cause-and-effect chart is useful here).
Isolate and verify the root causes by

150 Problem Solving
testing each potential cause (sampling is
used here) against the problem description
and test data (individual test or a DOE
if needed). Identify alternative corrective
actions to eliminate root causes, using a
process behavior chart to ensure that
the process remains stable.
5. Check corrective action. Through a
sampling plan, quantitatively confirm
that the selected corrective actions will
resolve the problem for the customer and
will not cause undesirable issues (FMEA
and control plans).
6. Start permanent corrective action.
Once a corrective action is verified to
be working, update all procedures
and processes to incorporate the new
process. This should include training
where appropriate.
7. Stop future problems. Modify the
management systems, operating systems,
preventive maintenance, processes,
and procedures and documentation to
prevent recurrence of this and all similar
problems. Note: If similar processes are
found in the Practice, look closely at them
also to ensure that they do not develop the
same issue.

Problem Solving 151
8. Congratulate your team. Improvements
happen only because many people work
together. Everyone deserves credit.
Your external customers may have a prescribed
problem- solving methodology other than 8D that
they want your organization to use. Other meth-
ods that can be used in problem solving are the
PDSA cycle and, although not recommended, the
scientific method that you probably learned in
high school.
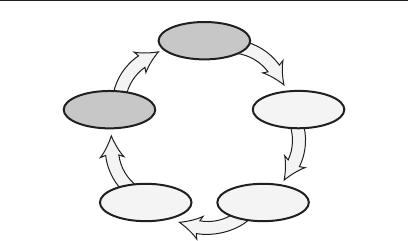
152 Process Behavior Charts (Statistical Process Control)
Define
Measure
AnalyzeImprove
Control
PROCESS BEHAVIOR CHARTS
(STATISTICAL PROCESS CONTROL)
The foundation for process behavior charts was
laid by Walter Shewhart (called the father of
modern-day quality control) in the late 1920s.
The charts were originally called control charts
as they were thought to help control the pro-
cess. Today, more than 30 different charts can be
used; however, we typically use only six or seven
on a regular basis; Practice staff will find the
IMR, p, and u the most useful. These charts fol-
low the premise of creating a picture of the pro-
cess variation while the work is being done (see
“Run Chart”). This allows the Practice staffer
to ensure that the process is stable and continu-
ing to operate within the process boundaries (not
necessarily specification limits) that have been
established for that process. If something does

Process Behavior Charts (Statistical Process Control) 153
start to deteriorate or change in the process,
the process behavior chart will give the Practice
staffer an early warning that something needs
to be adjusted or changed to bring the process
back into control. Note: the healthcare worker
should remember that in pursuing continual
improvement, you want the process to change for
the better; thus, instead of a stable process you
should see the variation on the process behav-
ior chart follow the standard out-of-control rules
(found in many texts)!
This book will not go into the details of creat-
ing and maintaining process behavior charts as
you can find many references on the subject (see
“control charts” in most texts). We will discuss in
general the basic charts and some of the ways to
use them. Table 3 lists these basic charts.
The “Data type” column in Table 3 indicates
twodifferenttypesofdata.Variabledataareinfor-
mation in number format that comes from scales
(for example, length measures, weighing devices,
temperature controls, distance measures, or time
measures). Attribute data are information on the
goodness of something (for example, pass/fail cri-
teria, acceptance standards, accuracy of proce-
dure, or accuracy of counts).
Variable data are usually considered more
valuable in understanding process behavior than
attribute data as more information is available
and trends and patterns are more easily and
154 Process Behavior Charts (Statistical Process Control)
Table 3 Process behavior chart types.
Chart name Data type Measure* Description
X-bar and R Variable Averages of Subtract the smallest sample value
variable data from the largest to identify the range
X-bar and s Variable Averages of Use a computer to identify the
variable data standard deviation
Individual moving Variable Individual variable Used when averages are not
range (IMR) data available
p Attribute Fraction of Percentage of all units checked
nonconforming units
np Attribute Number of total Number of units found to have issues
nonconforming units
c Attribute Number of Number of issues found
nonconforming
u Attribute Number of Average number of issues found per
nonconforming per unit the number of units checked
*
Some references refer to nonconforming as “defect” or “defective.” Your industry may have a product liability
issue with the terms “defect” or “defective,” so “nonconforming” is used in this text.
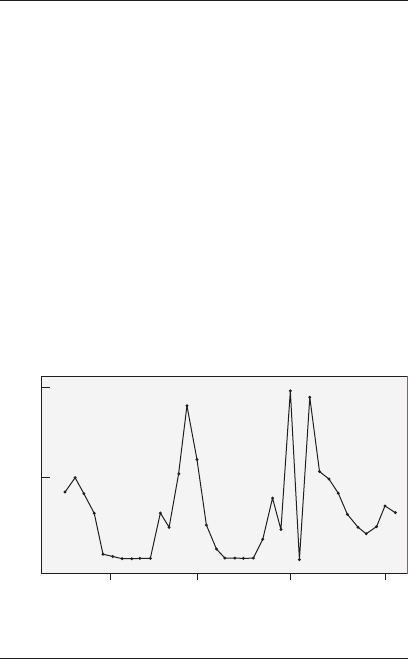
Process Behavior Charts (Statistical Process Control) 155
more quickly seen in the variables. The home gas
usage run chart (see Figure 37) is an example of
plotting using variable data.
In either type of process behavior chart (vari-
able or attribute), the healthcare worker or super-
visor needs to ensure that the measurements
from the process are recorded, calculated, and
plotted appropriately. In variable data charts the
healthcare worker should ensure that the process
average is calculated and then refer to an appro-
priate table to calculate the upper (UCL) or lower
(LCL) control limits (see Figure 38), which can
be found in most SPC books (Stamatis 1997).
100
50
0
Units
May
98
Mar
99
Jan
00
Nov
00
Month
Figure 37 Home gas usage.
156 Process Behavior Charts (Statistical Process Control)
When working with attribute charts, calculat-
ing the control limits with a handheld calculator
can be relatively simple. See Figures 39 and 40
for the steps to follow on the calculator for the p
and u charts (most commonly used in the Practice
setting) without having to learn the technical
formulas found in many reference books.
T he mo st i mp or t a nt t h i n g a bout p r o c es s b eh av-
ior charts is that you actually use them to under-
stand what your process is doing. Just ma king the
charts and posting them on the wall is often sar-
castically called statistical process display (SPD)
and does little to help the healthcare worker
monitor or improve the process. Learning to use
and read the charts can go a long way toward
helping your Practice maintain and/or improve
the quality of services that you provide. The term
“being in statistical control” refers to the plot
points on the chart following a random pattern
between the upper and lower control limits.
First add up all the x’s and divide by the total num-
ber; this equals x
–
. Record this number. The UCL
and LCL can be calculated using a standardized
table that can be found in many control chart refer-
ences or in SPC software.
Figure 38 Calculating process average, UCL, and
LCL for variable data.
Process Behavior Charts (Statistical Process Control) 157
First add up all the u’s and divide by the total num-
ber; this equals u
–
.
On your calculator, follow these steps:
1. Enter u
–
into the display.
2. Divide by the total number of u’s.
3. √
_____
4. Times 3 equals some value; record this
value.
5. Add the value to u
–
for UCL.
6. Subtract the value from u
–
for LCL.
Figure 40 u chart control limit calculations.
First add up all the p’s and divide by the total num-
ber; this equals p
–
. Record this number.
On your calculator, follow these steps:
1. 1 minus p
–
.
2. Times p
–
.
3. Divide by the total number of p’s.
4. √
_____
5. Times 3 equals some value; record this
value.
6. Add the value to p
–
for UCL.
7. Subtract the value from p
–
for LCL.
Figure 39 p chart control limit calculations.
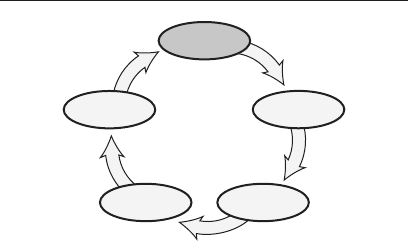
158 Process Identification
Define
Measure
AnalyzeImprove
Control
PROCESS IDENTIFICATION
Anything we do can be defined in terms of a pro-
cess or system. Many of the tools discussed in
this book can be used to help identify causes and
effects, frequency and distribution of measures,
most frequently occurring data, process flow as
it is occurring, and other aspects of the process.
If you plan to study a process, it is very impor-
tant that you first identify the boundaries that
you will work within. Many books talk about the
basic “input, process, output” model for process
identification (shown earlier in Figure 2, page
6). Today, some people use the SIPOC model (see
Figure 3, page 8)—supplier, input, process, out-
put, customer—which gives defined boundaries
to the old model.
In any sporting event, besides knowing the
rules of the game, you must know the boundaries

Process Identification 159
of the game field. This does not prevent us from
thinking outside the box (boundaries), but it does
give us guidelines for what we are dealing with
as we go about our daily tasks and endeavors.
Taking the time to actually list or draw compo-
nents of the process will help us find issues more
quickly than might otherwise be possible.
One common method of identifying the pro-
cess is called the storyboard method. This tool is
similar to flowcharting but involves drawing pic-
tures of the various tasks instead of just using
words. This technique is used by movie produc-
ers to sequence scenes of a film prior to shooting
to ensure that everyone on the set (actors, sound
technicians, cinematographer, support person-
nel, and so on) knows what is supposed to happen
ahead of time. The same scenario can be used in
the Practice to lay out a pictorial sequence of the
process as it should happen. This technique can
be especially useful if you have customers from
different cultures visiting your Practice who may
not speak your language as their native tongue.
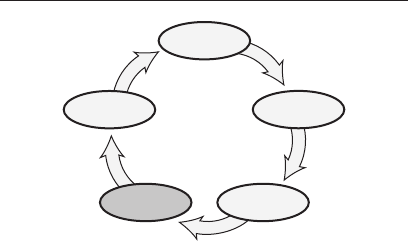
160 Process Improvement (PI)
Define
Measure
AnalyzeImprove
Control
PROCESS IMPROVEMENT (PI)
Process improvement is the method of making
a system work better to satisfy customer wants
and needs. It is vital if continual improvement is
to become a reality. In process improvement you
should look at reducing overall variability, not
just the variation. Variability is made up of three
components: instability, variation, and off-target
conditions.
In dealing with variability, most practitio-
ners traditionally have addressed only the varia-
tionquestion.Variationisimportant,andweuse
the tools listed in this book to help reduce it as
much as possible. But the other two components
are also important. Without knowledge of these
two—instability and off-target conditions—

Process Improvement (PI) 161
we could miss some very important factors and
even cause major problems in the Practice.
Instability is the lack of a stable operating pro-
cess; common cause and special cause variation
are unchecked and not responded to. Without a
stable process, capability values are not worth
calculating and customers can, and do, see any
number of issues come and go without rhyme or
reason. The best method for monitoring a pro-
cess is to use process behavior charts, but far too
often the charts either are not kept up-to-date or
are not used at all. Practice staff play a big role
in monitoring the processes to ensure that the
jobs they perform are stable and in control.
Whether a process is off target is often deter-
mined by the managers who design the operation
or services. The Practice staffer can only mon-
itor whether the process is centered within the
specifications and/or control limits. Even though
today we talk about the Taguchi loss func-
tion and how processes should be centered with
regard to what the customer wants and needs,
many jobs we work in today were designed years
ago when managers put the target wherever it
made the most economic sense for the company
at that time, instead of for the customer. In other
cases, we have done something the same way for
so long that it is now assumed that there is a rule

162 Process Improvement (PI)
or even a governmental law that it must be done
that way. So the Practice staffer should moni-
tor the process and be ready to give up-to-date
information to managers when processes are to
be redesigned, so that the new thinking becomes
a reality in your Practice.
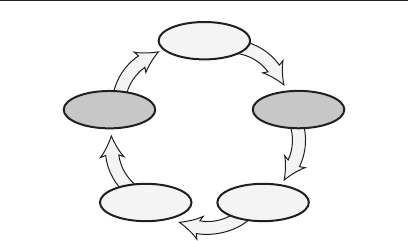
Run Chart 163
Define
Measure
AnalyzeImprove
Control
RUN CHART
A run chart is a graph that shows measurements
from an operation or process in relationship to
time.Virtually no calculations are required for
this chart, and it is very useful in monitoring
process variation for patterns, trends, and shifts.
The run chart, sometimes called a trend chart or
line graph, is the basis for a number of the pro-
cess behavior charts and can be used almost
anywhere (try tracking the utility usage of your
home, and then look for ways to cut energy usage
to save cost—see Figure 41).
The run chart is created by setting up a time-
line and a measurement scale. Then, as mea-
surements are taken from the process during
production runs, the data can be plotted on the
grid to form a graph of the process. The health-
care worker can then monitor the process as it is

164 Run Chart
running to see the process variation and deter-
mine whether the process is changing with
sudden shifts (spikes) or moving up or down over
time (trends). The home gas usage run chart
was made with actual numbers for a northern
state. Notice the general trend of summer versus
winter usage. The winter of 1998 used less energy
than either the winters of 1999 or 2000 because
an elderly father came to live in the home during
the last two years. You can also see a spike in
February 2000, which was caused by an esti-
mated bill being generated instead of an actual
gas reading taken during January. During the
summer months, the furnace is not used very
100
50
0
Units
May
98
Mar
99
Jan
00
Nov
00
Month
Figure 41 Home gas usage.

Run Chart 165
much, but the gas dryer is being used more and
more to handle additional laundry needs.
Other uses of the run chart show the health-
care worker if there are cycles (as in the gas
usage example above) or how events around the
work area may be affecting the operation or pro-
cess. Sometimes we work with an operation for so
long that we don’t notice little things happening
around us that may have an impact on how the
process works. By monitoring a run chart, we can
get a picture of what is going on in the system.
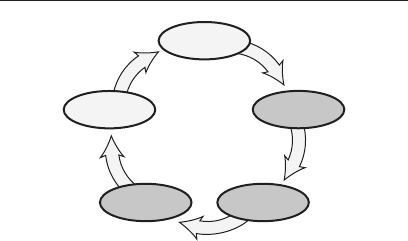
166 Scatter Diagram
Define
Measure
AnalyzeImprove
Control
SCATTER DIAGRAM
The scatter diagram is a graphic display used to
identify a relationship or association between two
variables, cause and effect, and so on. To create
the diagram, you plot the intersection of the two
data points, maintaining one variable on the
x-axis and the other variable on the y-axis. Once
all of the data is on the graph, the observer can
eyeball a line of best fit (which can also be calcu-
lated on a computer for accuracy). The plot pat-
tern (line of best fit) identifies whether there is a
positive, negative, or no correlation in the data.
There is also the possibility for a nonlinear rela-
tionship between the variables (see Figure 42).
One caution in the use of this tool is to ensure
that the two variables being compared actu-
ally are related to each other. By accident, you
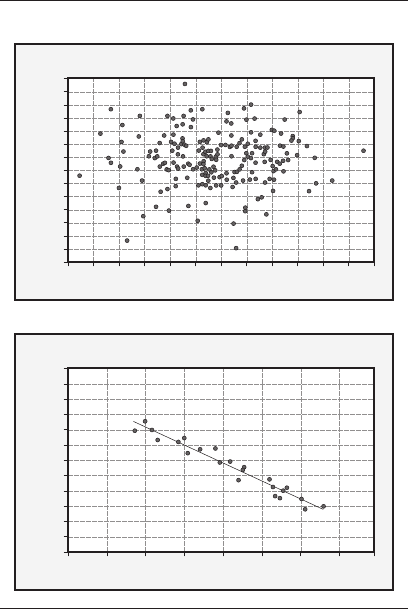
Scatter Diagram 167
–1.0
–1.5
–2.0
–2.5
–3.0
–3.5
–4.0
100 200 300
X
Scatter plot
400 500
Y
No correlation:
Strong negative correlation:
3
2
1
0
–1
–2
–3
–4
–3 –2 –1 0
X
Scatter plot
21 3
Y
Figure 42 Scatter diagrams.
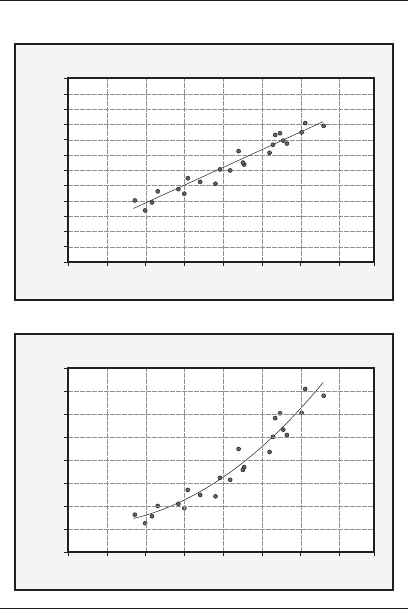
168 Scatter Diagram
Strong positive correlation:
Quadratic relationship:
4.0
3.5
3.0
2.5
2.0
1.5
1.0
100 200 300
X
Scatter plot
400 500
Y
40
30
20
10
0
100 200 300
X
Scatter plot
400 500
Y
Figure 42 Continued.

Scatter Diagram 169
could show that there is a relationship between
two variables when there may be a third factor
in play. An example of this would be to say that
drowning is caused by increased ice cream sales.
On the graph, it might be noted that as drown-
ings go up, so do ice cream sales. However, as
everyone could guess, both of these events occur
more frequently during summer months versus
winter. So drowning and ice cream sales are actu-
ally factors of warmer weather, versus having a
causal relationship to each other.
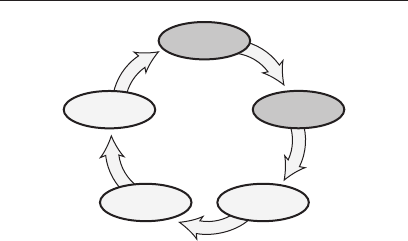
170 SIPOC Diagram
Define
Measure
AnalyzeImprove
Control
SIPOC DIAGRAM
The SIPOC (supplier–input–process–output–
customer) diagram can be a flowchart, quasi–
value stream map, turtle diagram, and so on,
that shows the variables involved in a given pro-
cess (see Figure 43). Traditionally, we would
have mapped the IPO (inputs, process, out-
puts) of a process, which could be the entire
Practice or one aspect of the Practice. Today,
we typically include the items, people/patients,
or processes that are needed at the beginning
of the process flow and then list the items,
people, or processes that are a result of what is
being done/studied in the core event. One of the
primary uses of the SIPOC diagram is to ensure
that everyone in the system has a clear, visual
reference for what is to be done in the process (a
road map of how things are supposed to work).
SIPOC Diagram 171
Suppliers
Providers of the required inputs/
resources to ensure that the process
executes as planned.
Inputs
Resources required by the process to
obtain the intended output.
Process
Top-level description of activity.
Outputs
Deliverables from the process.
Note: deliverables can be hardware,
software, systems, services, data,
information, and so on.
Customers
Any organization that receives an
output or deliverable from the process.
Note: can also capture systems/
databases that receive outputs,
information, data, and so on.
Input
boundaries
Process being
reviewed
Output
boundaries
Figure 43 Basic SIPOC diagram.

172 SIPOC Diagram
This is a method of aligning everyone to a com-
mon goal (what is to be accomplished).
To develop a SIPOC diagram, start by defin-
ing the process and its boundaries. Next, iden-
tify the outputs of the process, including data,
services, products, information, records, and so
on. For each identified output, identify all of the
associated inputs. Then move on to the internal
and external customers—those that receive the
identified outputs. Finally, move back to the sup-
plier column to identify the internal and external
suppliers for each identified input. Although it
may seem odd to bounce back and forth from side
to side on the chart, this is done to help stimulate
thinking. For example, new outputs are often
identified when discussing inputs or customers.
External suppliers to a process are those out-
side the enterprise that provide process inputs,
including materials, purchased parts, contracted
services, electrical power, and so on. Internal sup-
pliers to a process are departments or processes
inside the enterprise that provide process inputs.
Similarly, a process’s external customers are
those outside the enterprise who receive process
outputs while internal customers are those inside
the enterprise who receive process outputs. Sup-
pliers of either type are responsible for meeting
the requirements of their customers. Customers
of either type are responsible for communicating
their requirements to their suppliers.
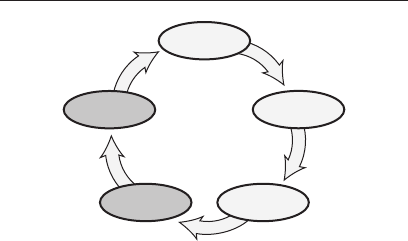
Standard Operating Procedures (SOPs) 173
Define
Measure
AnalyzeImprove
Control
STANDARD OPERATING
PROCEDURES (SOPs)
Standard operating procedures (SOPs) are known
by many names: work instructions, level three
ISO 9001 documentation, operating guides, job
aids, standard job procedures, and more. Your
Practice may already have a policy and proce-
dures manual (sometimes called a quality man-
ual) that can include at least some of the SOPs
for your Practice. In your Practice, what do you
call the step-by-step description of how to carry
out a task? These descriptions should give the
details of how you do your various jobs. They
should address such things as: What is the job?
Where does the SOP apply? When does the SOP
apply? Who is responsible? And so on.
Practice staff are responsible for following
SOPs as written. If any deviations are made,

174 Standard Operating Procedures (SOPs)
the healthcare worker needs to document what
was done and why (either in the patient charts
or other designated area for such information).
This will be a big help if at a later date a problem
arises and an investigation is done in the health-
care worker’s area. Documented evidence will
go a long way toward preventing finger-pointing
or faultfinding and the healthcare worker being
blamed for something out of his or her control.
The SOP should be a living document, chang-
ing as Practice staff change the work that they
do. If something changes in the system, the
healthcare worker should ensure that the SOP
is updated. Once something changes in the pro-
cess, and a new, desirable level is achieved, the
healthcare worker should help update all docu-
ments relating to that process appropriately and
destroy the old documents.
Standardization (SDCA) 175
Define
Measure
AnalyzeImprove
Control
STANDARDIZATION
(SDCA—STANDARDIZE–DO–
CHECK–ADJUST)
Standardization is the process of locking in the
gains that you have made during the improve-
ment process. It is commonly referred to as the
SDCA cycle (standardize–do–check–adjust). This
tool is generally used once a process has been
improved, to update the control plans, FMEA,
process sheets, and other process documentation
to lock in the improvements and standardize the
changes throughout the organization (see Figure
44). Thus, everyone who is involved with the pro-
cess in question will provide the service in the
same basic way.
The SDCA cycle involves updating (standard-
izing) any documentation related to the process
that has been improved, then doing the work
176 Standardization (SDCA)
to ensure that it runs smoothly. The process is
then checked or inspected to ensure accuracy
and, finally, adjusted to ensure that the pro-
cess output satisfies the customer’s wants and
needs. This cycle should be used any time that
improvements have been achieved and the Prac-
tice wants to ensure that the lessons learned will
become part of everyday work.
A
D
J
U
S
T
S
T
A
N
D
A
R
D
I
Z
E
C
H
E
C
K
D
O
Figure 44 Standardization cycle.
Systems Thinking 177
Define
Measure
AnalyzeImprove
Control
SYSTEMS THINKING
Systems thinking is recognition/identification
and consideration of all the various individual
elements that interrelate with a common pur-
pose toward the whole function of a unit (Rice
1997). Many of us are so busy doing our daily jobs
that we have little time to think about what we
are actually doing. In systems thinking, you use
all the tools and methods around you to look at
what is being done in a given operation. You must
examine the operation as it is for aspects of the
process, equipment, methods, procedures, envi-
ronment, or other factors, that could be changed
to give faster, better, and cheaper service to cus-
tomers (internal and external). Often, however,
we notice that someone (maybe even yourself)
has made a change in one part of an operation
only to cause new problems somewhere else.

178 Systems Thinking
Using systems thinking, you can understand
the process and know that if one factor is changed
or influenced in some particular way, then some-
thing different might happen downstream in the
process. For example, if a computer glitch occurs
in one Practice, will that prevent other tasks in
other healthcare units from being completed?
If one healthcare worker changes something in
the way data is collected, but does not let others
know, what might happen to the integrity of the
information downstream? If programming is
changed on a database with little or no updated
training provided, how long will it take to get
accurate and reliable information? All of this is
part of systems thinking.
You should constantly be looking at the vari-
ability in the system for opportunities for con-
tinual improvement. As the author has noted
in other sections of this guide, variability is
made up of three factors: instability, variation,
and off- target conditions. Instability of a pro-
cess says that you can not be sure what it will
do at any given time. Process behavior charts
are useful tools to graphically show how the pro-
cess is operating and whether the process is in
a state of statistical control. However, instabil-
ity goes beyond just statistical control. A process
can become unstable for any number of reasons.
Some of these include lack of poor housekeeping
disciplines, poor materials from suppliers, vague

Systems Thinking 179
or unknown customer requirements, inadequate
procedure definition, or equipment shortages.
Learning about your process and how it fits into
the overall activities in your Practice is the foun-
dation of systems thinking.
Variation is discussed in the “What Is Vari-
ation” section of this book, so let’s look at off-
target conditions. Given today’s views on quality
processes, process designers should always set
target values of characteristic measurements.
With tools such as quality function deployment
(not discussed in this book), specialists should be
able to center the target values according to what
the customer wants and needs. But this has not
always been the case.
A service call recently experienced by the
author may be a good example of a lack of systems
thinking. In making an appointment, I was told
to expect a wait of a couple of hours. I arrived at
the organization a little early with a book to read.
A person took the order and sent the information
to the back for the service to be performed. After
three hours of not hearing anything (the first
person had noted that I was waiting on the prem-
ises), I went to check on how things were going.
I was told that things were not right and that I
must have done something, but that the service
should be completed shortly. After another hour,
I again went to check on the service to find that
things had been completed, but I had not been

180 Systems Thinking
called yet. It seems that there was some need to
transfer paperwork between a number of people
before I could be called. A couple of days later,
a quality representative called me to see how I
liked the service. After recounting the above
story, the rep repeatedly apologized and said
that she would look into what might have caused
the long delay, which should not have occurred.
It turned out that part of the delay was due to
someone taking a lunch break and my paperwork
being buried on their desk. After they returned
from lunch, the person started from the top of
the pile and they worked their way down to my
file at the bottom.
Team Meetings (Huddles) 181
Define
Measure
AnalyzeImprove
Control
TEAM MEETINGS (HUDDLES)
Useful and productive team meetings are struc-
tured events with a purpose. Just meeting for
the sake of meeting wastes time and energy that
could be used more productively in other areas.
Many of us do not think much about meetings
since we attend so many of them that it seems
almost second nature. We rarely ask if the meet-
ing is necessary and a valuable use of the attend-
ees’ time. Any time two or more people come
together to conduct business, we should remem-
ber that time, energy, and resources are being
spent. For an in-depth study of the topic, see How
to Make Meetings Work by Michael Doyle and
David Straus (1976).
The first question should always be, “Why
are we having this meeting?” There are actually
many good reasons to hold meetings, and there

182 Team Meetings (Huddles)
are different meeting types. Five of the most
basic are problem solving, information sharing
(both gathering and/or giving), planning and
coordination, decision making, and reaction or
feedback. Any meeting can be a combination
of these types. Each type of meeting may require
different roles, more or fewer people, and a vari-
ety of meeting methods. It is important to be
clear about the type of meeting you want and
to plan accordingly. Be sure everyone who will
be attending knows the type of meeting it will be
and why it’s being held so that they can arrive
with a common set of expectations.
You should always set an agenda because:
• Itisanessentialstepindetermining
whether a meeting is needed and, if it is,
to building a successful one
• Ithelpsdefinewhatneedstobe
accomplished (outcomes)
• Itspellsouthowtheoutcomescanbe
accomplished (process)
• Anagendaestablishesatimeframe
• Ithelpsidentifywhoneedstobepresent
Here are some rules to ensure that you have a
good meeting:
1. Treat others as equals, not as inferiors.

Team Meetings (Huddles) 183
2. Be sincere, not manipulative and sneaky.
3. Genuinely care about others; don’t be
indifferent.
4. Keep an open mind rather than being
certain and dogmatic.
5. Be descriptive and specific, not evaluative
and vague.
6. Concentrate on solving problems, not
blaming others.
7. Assume that others have good intentions
rather than assuming that they are
devious.
8. Explain the what and the why; don’t
assume that your intentions or purpose
are automatically understood.
9. Listen for the other person’s point of view;
we don’t always share the same reality.
10. Encourage everyone to give their input;
don’t dominate.
11. Accept and appreciate the differences in
others; don’t let stereotypes run your life.
12. Watch and respond to the way people
interact at every meeting; how people work
together affects the outcome and the
meeting’s effectiveness.

184 Team Meetings (Huddles)
Here are the typical roles of meeting
participants:
• Leader
• Facilitator
• Timekeeper
• Recorder
• Teammember
• Historian—lessonslearned
Planned and handled properly, meetings do not
have to be a waste of time and energy. Ensuring
that there is a good reason to hold the meeting
and establishing a good agenda are the best ways
to use everyone’s time well.
Teams 185
Define
Measure
AnalyzeImprove
Control
TEAMS (EMPLOYEE
INVOLVEMENT, IMPROVEMENT,
SELF-DIRECTED)
Employee Involvement Teams
Some companies call their employees their most
valuable assets. When this is true, managers
spend time and resources to coach and train
the employees to be better at whatever they do.
This is especially true when it comes to allowing
employees to become more involved with the work
that is done in healthcare. Employee involvement
is about encouraging and allowing all employees
to do better work by using their minds as well as
their hands to do the job. This notion is feared
by many managers who were trained in classical
management theory—they may think they will
lose control over the work environment. By using

186 Teams
the whole person instead of having the employee
check his or her brain at the door when they enter
work, managers actually can have more produc-
tive processes and better activities. Going from
“do what I say” to “what will it take to satisfy our
customers?” will go a long way toward developing
an environment where continual improvement is
a way of life.
Thus, a basic definition of employee involve-
ment is the process of including employees at
a variety of levels and across functional areas
for the purpose of having meaningful input/
involvement in the business (Rice 1998). This is
different from prior business models (for exam-
ple, Theory X, Taylorism) where managers sat in
their offices and dictated their wisdom to employ-
ees and directed them to “just go do it” or “do it
exactly as I told you.” Empowerment is about
personal responsibility and having personal and
organizational goals aligned.
Evidence that employee involvement is alive
in your Practice includes but is not limited to
the following: no surprise decisions are made,
as input is sought from many people; instead
of managers ordering employees what to do,
an atmosphere of cooperation is evident in the
Practice; if something does go wrong, groups of
people work on fixing the issue versus the man-
ager or supervisor assigning blame; employees
are not afraid to approach managers or even the

Teams 187
owner of the organization. Every Practice needs
to define employee involvement given its culture,
its organizational goals, and its customer base.
Just as real teams take a long time to become
efficient operating units, so too it takes time to
build employee involvement into the culture of
the Practice. But the personal and productivity
rewards for doing so can be outstanding.
Improvement Teams
An improvement team consists of a group of
appropriate individuals who have been chosen to
work on a specific process to find ways of improv-
ing the operation (cost, cycle time, quality of
product or service). These teams are meant to be
active for a certain time frame, working on spe-
cific processes, and then report to management
their findings and recommendations.
This is the team that works to make the big
changes (what Juran calls managerial break-
throughs) in processes for continual improve-
ments. These changes usually will be on the
order of a factor of 10 or more change in the pro-
cess as measured in process capability or in cus-
tomer delight (versus satisfaction). It is important
for members of this team to keep an open mind
and think out of the box, and not be afraid to call
in experts as needed to make the big improve-
ments. Use of the “could be” process map is

188 Teams
useful here to help with brainstorming ideas of
what is possible.
The improvement team’s members usually
will be highly trained in the use of the tools and
methodologies surveyed in this book (as well as
in other techniques) and probably will be some
of the teachers of these tools to other Practice
personnel. Practice staff and improvement team
members do not need to be certified to be able
to use these tools, and because of their work-
ing every day with the process, they can some-
times solve problems better than those who are
certified. When more expertise is needed, some
of the highest mastery certifications that exist
for using these tools are the Lean Six Sigma
Master Black Belt and the ASQ Certified Six
Sigma Black Belt.
Self-Directed Teams
A self-directed team is a group of people who
have been authorized by management to work on
a process or to improve a process using all the
resources available to them and to manage their
own time and energy, as a self-operating unit,
for the good of the organization. Self-directed
teams tend to share leadership equally among
the group members; thus, rather than one person
being the leader, they are all responsible for the
output of the team.

Teams 189
These teams tend to be more important in a
company that has evolved into a lean manufac-
turing or lean Practice organization. Whereas
the old system of mass review does not require
people to be prepared to change anything
quickly, in a lean organization changeover of pro-
duction must be quick and often, and sometimes
occurs many times each shift. Mass customiza-
tion has become a new buzzword for manufactur-
ing, given customer demand for large quantities
of service transactions made to individual cus-
tomers’ requirements.
In lean Practice organizations, natural work
cells or groups are usually formed around a cer-
tain service area. These groups are ideal candi-
dates to become self-directed teams as they work
closely together and can work as a single unit to
satisfy customers instead of as individual staff.
The team then is able to provide its own reward
and recognition to each of its members. The team
members have shared goals and take respon-
sibility for communication with the rest of the
organization.
Team Basics
Remember the famous quote, “There is no ‘I’
in ‘team’”? The essence of this idea is to imply
that a team is a collective effort of individuals.
To harness the best of each individual, the

190 Teams
team members need to understand each other’s
strengths, roles, responsibilities, and the scope
of the task. There are a number of books that go
into detail about how to form a team, organize
meetings, manage projects, and accomplish the
desired goals. In the context of Six Sigma, we
will cover areas important to a Green Belt. Pro-
tocols such as setting the team agenda, record-
ing the minutes of the meeting (with proposed
actions), sticking to the set meeting time, and
enforcing meeting attendance need to be fol-
lowed for an effective team meeting. An initial
meeting to kick off the team with introductions
and high-level discussion on the goals, objectives,
milestones, and so on, will provide an opportu-
nity for the team to get to know each other and
understand the expectations. A team agenda can
be flexible but you need to have one.
Some teams have their team goals, objectives,
and scope/boundaries visibly displayed at every
meeting to keep the members on track. Man-
agement presence during kickoff and at regu-
lar intervals during the project helps enforce the
importance of the team objective.
Team Formation
A team usually comprises five to nine members
(seven is considered an ideal size) with comple-
mentary skills to achieve the goals and objectives

Teams 191
of the team. Team composition should be driven
by the size and scope of the project; it is possible
to have a team of one or two for a smaller project
and a large team with sub-teams for a big project.
The team includes subject matter experts and
stakeholders. Subject matter experts sometimes
remain outside the team as resources or extended
team members. Stakeholders are always part of
the team. The team will not be able to implement
their ideas and solutions without having stake-
holders represented on the team. Teams smaller
than five reduce the opportunity for interaction
problems and are easier to manage, whereas
teams greater than nine produce a lot of inter-
action that can be counterproductive to a team’s
progress. Teams with greater diversity tend to
produce better interaction between team mem-
bers. Some teams also bring in individuals who
are neither subject matter experts nor stakehold-
ers but are outsiders to the team. The outsider
helps the team ask questions that might never be
explored by the team members closer to the pro-
cess. This needs to be moderated as the outsider
might ask too many questions and frustrate the
core members. Typically, Six Sigma teams are
cross-functional so as to address the issues from
every angle.
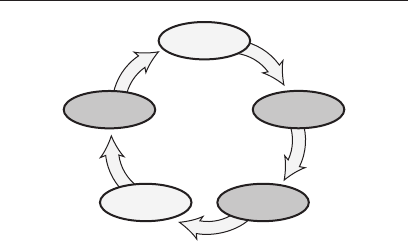
192 Value Analysis
Define
Measure
AnalyzeImprove
Control
VALUE ANALYSIS
A value analysis is a review of a process to iden-
tify what parts or steps of a process actually add
value for interested parties that need access to
that portion of the healthcare system. The issue
here is that our current tasks and assignments
take a certain amount of time. What if we could
eliminate some of the steps that are deemed
unnecessary so that more time could be spent
doing the things that really mean something to
the patients, clients, stakeholders, and so on, of
the Practice? One of many possible ideas here
would be to eliminate the need to constantly go
to a fax machine (which could be at the other end
of a long hallway) to receive information that
could just as easily be sent directly to the com-
puter that the person is working on.

Value Analysis 193
To do a value analysis, it helps to imagine your-
self as the thing going through a process (such
as information, blood test results, or some other
patient evaluation). What happens from the very
first thought of getting the process accomplished?
If a doctor orders a blood work request, what are
the steps that are actually needed to allow the
doctor to discuss the results with the patient?
To start this analysis, create a list of all of the
actions/steps that need to be accomplished and
the amount of time each takes from the view-
point of the thing going through the process (for
example, blood test—doctor’s request, script,
patient goes to have blood drawn, waiting time,
actual blood draw event, samples labeled prop-
erly, travel to laboratory, tests conducted, results
recorded, records sent to doctor, wait for next
patient visit, doctor remembers to discuss results
with patient, any follow-up actions needed).
Once the process has been mapped and times
recorded, review each entry to see which ones
meet all three criteria below to say that the step
actually adds some value:
• Doesacustomer(patient,stakeholder,
other important person) recognize the step
as being important?
• Doesthestepaddvaluetothethinggoing
through the process? (For example,
signatures do not add value.)

194 Value Analysis
• Wasthestepdonerightthefirsttime?
Only when an item meets all three criteria (you
can say yes to each) is that step considered a
value-add to the process. All of the other items
are non-value-added steps and need to be con-
sidered for elimination or at least diminished
impact as they relate to the process.
Please note that we are “leaning” the pro-
cess with the value analysis instead of trying to
make the Practice staff work harder or longer
hours to complete the tasks as we have them cur-
rently established. There are many process steps
in every Practice, which have developed for any
number of reasons, that do not add value to the
process. Eliminating as many of the non-value-
added steps as possible will free up a lot of time
of the Practice staff and allow them to do the
most important work. It has been estimated that
many offices can eliminate 50 percent to 80 per-
cent of their current time requirements in doing
nearly any task by conducting a value analy-
sis. This is typically one of the first places (low-
hanging fruit) for the Six Sigma team to look
when analyzing a Practice for possible improve-
ment efforts.
Value Stream Map (VSM) 195
Define
Measure
AnalyzeImprove
Control
VALUE STREAM MAP (VSM)
A value stream is the series of activities that an
organization performs, such as scheduling, orga-
nizing, ordering, counseling, record keeping, and
accounting, to provide the healthcare services. A
value stream often starts with a first contact with
a patient or supplier’s supplier and ends with the
payment for services or customer’s customer (as
the SIPOC diagram will show). Wastes are both
explicit and hidden along this value stream.
The three main components of a value stream
are:
1. Flow of information/materials, from
receipt of supplier material to delivery of
finished goods and services to customers.
Examples:

196 Value Stream Map
• Schedulingpatientsforofficevisitsand
then ensuring that they are checked in
when they arrive
• Rawmaterial/suppliesshippedweekly
from a supplier to the organization
by truck
• Movementofmaterialfromrawmaterial
storage to areas where it is needed in
the Practice
• Shippingoffinishedgoodstoan
overseas customer via customs
2. The transformation of raw materials/
information into completed services, or
inputs into outputs. Examples:
• Gettingthepatientroutedaroundthe
Practice to ensure that a full evaluation
is completed
• Sendingpatientstoaspecialistifneeded
for further testing/consultations
3. The flow of information required to
support the flow of information/material
and transformation of goods and services.
Examples:
• Patientchartsupdatedproperlyand
stored in an appropriate location (not
being left on desks)

Value Stream Map 197
• Billingdoneappropriatelyandall
payments timely received
This concept is visually illustrated via a lean
tool called the value stream map. This map uses
simple graphics and icons to illustrate the move-
ment of material, information, inventory, work-
in-progress, operators, and so on. Value stream
mapping is a very powerful tool. The analy-
sis subsequent to value stream mapping, called
value stream analysis, can help uncover hidden
wastes within the organization. An organization
that effectively uses lean thinking and applies
lean tools to reduce waste throughout the value
stream and offer value to their customers is a
lean enterprise organization.
Figure 45 shows a quasi value stream map
(VSM) without the time allocations inserted in
each box. The time is an important factor in com-
pletingafullVSM,andeachprocess,onceflow-
charted, needs to be studied to understand the
actual time averages and variation found at each
step in the process. This will allow you to under-
stand the bottlenecks better and to see the pro-
cess as a whole functioning system.
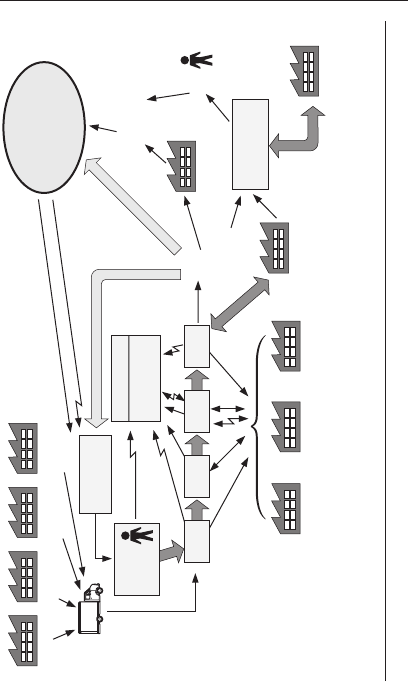
198 Value Stream Map
Hospital
Insurance
organizations
Billing
Fee collection
$
Patient
repeats cycle
as needed
Pharmas
Pharmacy
Home self care
Family member care
Medical
devices
Office
supplies
Medical
supplies
Wellness
Quality healthcare
of patient
Patient
visits
practice
Patient
PCMH
Education
and learning
Practice
scheduling
Tests Nurse Doc Tests
• Optometry
• Dentistry
• Podiatry
Specialist
Specialist
• Cardiology
• Neurology
• Pathology
• Radiology
• Laboratory services
• Pharmaceutical
Specialist
Figure 45 Total quality assurance management value stream map.
Variation Reduction 199
Define
Measure
AnalyzeImprove
Control
VARIATION REDUCTION
Variation is a fact of life. If the measurement
instrument (gage) or process that you are using
does not show that the process is varying, then it
is not sensitive enough and needs to be replaced.
If you get one complaint about something, you
can be assured that there are probably 10 more
complaints that your system did not pick up. The
author is aware of one organization who thinks
that it provides pretty good service to customers.
But one long-time customer (nearly 20 years) has
recently become very upset about the overall ser-
vice being received, and on one particular order
was triple-charged for a wrong product sent that
took an excessive amount of time to arrive. It
wasn’t until the author made a call to the presi-
dent of the organization that the vice president
of customer service got involved in trying to
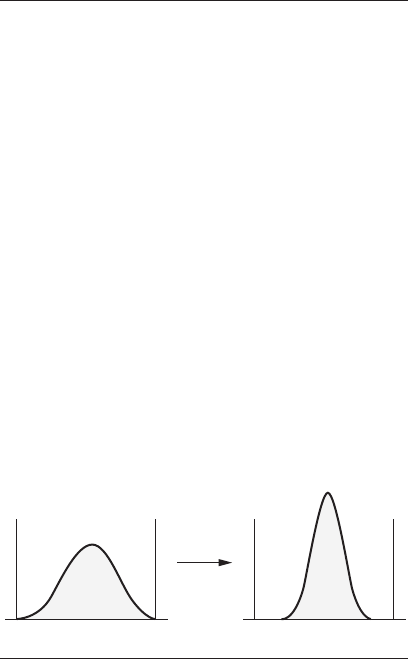
200 Variation Reduction
straighten things out. The organization still does
not have a good method to accurately collect cus-
tomer concerns, and the customer in question is
still very unhappy.
Since all processes vary, the question becomes
how to improve the process by reducing the
amount of variation that is currently present
(see Figure 46). This book lists various tools and
methods to help identify variation. In variation
reduction, you use those same tools to identify
and monitor your progress toward improving
what you do. Does the run chart show a reduction
in variation? What can be seen in the cause-and-
effect diagram, the histogram, the Pareto chart,
or other tools? These and many other questions
should be answered to understand the process as
well as possible.
Just buying a new electronic instrument may
actually cause more variation in the system due to
UCL LCL UCL LCL
Improvement
Figure 46 Variation reduction curves.

Variation Reduction 201
measurement error (see “Measurement Systems
Analysis”). Throwing money at the system (say, a
gift certificate for a future purchase) rarely helps
improve the process. Studies will need to be done
to understand all aspects of the process varia-
tion (for example, equipment, Practice supplies,
people, communications, or paperwork), and you’ll
need to work to reduce the causes in the system.
The key is to identify and provide what the cus-
tomer wants and needs from your process to the
best of your abilities, given any limitations of
the process.
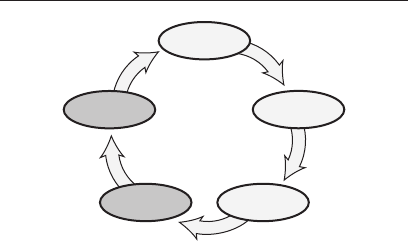
202 Visual Controls, Aids
Define
Measure
AnalyzeImprove
Control
VISUAL CONTROLS, AIDS
When you drive a motor vehicle, what visual con-
trols help you get to where you are going? This
could be a great thought starter in asking Prac-
tice staff what would help them accomplish their
tasks better. In an automobile, we have vari-
ous monitoring devices inside the vehicle. Then
there are numerous street signs, traffic lights,
construction barriers or other warning devices,
law enforcement personnel, and signals (hope-
fully) from other drivers on their intentions. In
our Practice, we can include any number of tech-
niques (some very simple) and ways to help our
fellow staff to know what is coming through the
Practice or what is going to happen next.
Remember the old adage “a picture is worth
1000 words?” The author has a copy of one of the
first Toyota manuals used in the United States

Visual Controls, Aids 203
for what is called the Toyota Production System.
It contains mostly pictures! Why might this
be? If you were to go to Japan, or any other coun-
try where you could not speak the language, how
would you communicate with others? Now think
about your patients. Do they speak the medical
language that you do? The odds are, they do not,
and some of our patients may even feel threat-
ened by all of the medical terminology that they
hear in the Practice even though it is in English.
Many of our Practices already have models
and pictures in the examination rooms to help
clinicians explain to patients how the body
works. Can this be expanded? Using computers
any number of things can be done to show how
the body is or should be functioning. There are
even high-end holographic devices today that can
show the actual organs of the body in real time.
How about simpler techniques—pictures or mod-
els that a patient can touch and feel to get the
information to them as needed?
The challenge then is to set up a system that
allows anyone to quickly see where information,
people, supplies/materials, and so on, belong and
where they are going next. Use pictures, direc-
tional indicators (how do you feel when you walk
into a new hospital for the first time), and any
other indicators to assist everyone in knowing
how things work or how to get from point A to
point B.
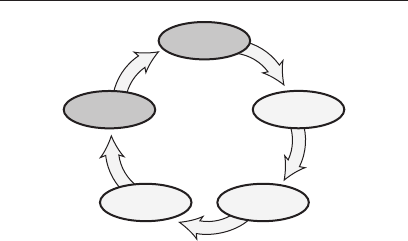
204 Voice of the Customer (Patient Feedback)
Define
Measure
AnalyzeImprove
Control
VOICE OF THE CUSTOMER
(PATIENT FEEDBACK)
Customer feedback is a method or process of find-
ing out what the customer actually thinks of your
products or services. It is said that for every cus-
tomer who actively complains to you, there are
at least 10 others who for one reason or another
will speak badly to others of your products and
services. Finding out what the customer thinks,
wants, and needs is a time-consuming effort, and
many customers are getting tired of filling out
surveys. Sometimes when customers (internal or
external) do tell us something, we can not do any-
thing about it, we do not want to hear what they
are saying, or they expect something other than
what we offer.
There traditionally have been many tech-
niques for talking with customers, and with the

Voice of the Customer (Patient Feedback) 205
advent of e-mail and the Internet, even more
exist today. The problem with many surveys is
that we really do not know what proportion of
our customers or which of our customers actually
bothered to send them back. Also, paper surveys
tend to have a very low return rate overall; thus,
they really do not give us a very good picture. The
point is that we must keep trying to talk with
customers as often as possible to ensure that we
know what their wants and needs are.
The most effective method still seems to be
actually getting out into the world with your
customers to experience what they experience
and to interact with them as they use your prod-
ucts and services. Have you ever thought about
what you do? What is it like for the next person in
the organization to use your work? For Practice
staff, finding this out should be a lot easier than
it is for shop floor personnel, as staff can simply
communicate with the next person in the health-
care chain. Practice staff might want to talk
with that person directly, observe how he or she
uses the information supplied to him or her, and
study the data that are collected in the process
to look for better ways to do work to make things
easier for the internal customer.
A good starting point for collecting customer
feedback is to set up a display for all employees
and visitors to see. On that display, have sam-
ples of the ultimate products/services that are

206 Voice of the Customer (Patient Feedback)
produced in your Practice. It has often been noted
that employees work all day yet do not know
how their work is used. Once the display is up,
employees can point out their work to others and
take pride in what they do. Some of this infor-
mation may not relate to the services provided
by your Practice, so it should be passed along to
an immediate customer who buys the services.
Doing this well will allow your Practice to pro-
vide additional services to your immediate cus-
tomers that they did not ask or pay for, giving
you an advantage over your competition.
Walkaround/Walkthrough/Waste Walk 207
Define
Measure
AnalyzeImprove
Control
WALKAROUND/WALKTHROUGH/
WASTE WALK
If you attended grade school in the United States,
somewhere in the early grades you probably had
a teacher play the telephone game with the class.
The telephone game involves the teacher put-
ting the class in a semicircle and whispering a
short phrase to the first student. Then each stu-
dent in turn whispers what they heard (or think
that they heard) into the ear of the next student
in line. By the time the last student received the
message and repeated what they heard, it usually
sounded nothing like what the teacher started
with. Note: the author has done the same with
degreed engineers and they still can not keep the
phrase consistent.
So, given this scenario, think about your own
work area. Are things being done the same way

208 Walkaround/Walkthrough/Waste Walk
as they were a year ago, two, five, or even 10?
Small things are changing all of the time. Unless
some form of standard (visual, written, and so on)
is employed, the odds are that things will change
over time. The purpose of the walkaround is to
identify these areas of change or to highlight
areas or things that should be or could be changed
to improve the operation of the Practice.
Avedis Donabedian (2003) defined quality
assurance as “all actions taken to establish, pro-
tect, promote, and improve the quality of health
care.” With this in mind, walk around your
Practice and start asking the question, “What
if?” We are often limited by our perceptions of
money, time, physical surroundings, and so on.
What if we could change something? How would
that impact the staff’s ability to provide a better
experience for the patient?
One primary challenge with this technique is
to be able to view your work area with an open
mind and stay out of the mind-set that we do
things this way because of some preconceived
notion that it must be that way. Continually ask
yourself, “If we could do this better for the custo-
mer (internal or external), how might the cus-
tomer appreciate the better service?” If a doctor
could open any patient folder in the Practice and
find everything in the same order, with sum-
mary run charts at the front giving an overview

Walkaround/Walkthrough/Waste Walk 209
of the patient’s health, how might that affect the
doctor’s work and the patient’s experience?
During the walkaround of the Practice, one
thing to keep in mind is elimination of what the
Japanese call muda, or waste.
Eight Categories of Muda
1. Overproduction above demand
2. Waiting for processing, use, work
3. Material and/or information movement
4. Overprocessing
5. Excess inventory
6. Unnecessary motion
7. Inaccurate work (defectives)
8. Underutilized people
Causes of Waiting Waste
• Unbalancedworkload
• Waitingforinformation
• Queuingdelays
• Latedeliveries
• Upstreamqualityproblems

210 Walkaround/Walkthrough/Waste Walk
• Unleveledscheduling
Causes of Processing Waste
• SOPchangeswithoutcommunication
• Just-in-caselogic
• Truecustomerrequirementsundefined
• Overprocessingtoaccommodatedowntime
• Lackofcommunication
• Redundantapprovals
• Extracopies/excessiveinformation
211
References
ASQ Quality Cost Committee, J. Campanella,
editor. 1999. Principles of Quality Costs:
Principles, Implementation, and Use. 3rd ed.
Milwaukee: ASQ Quality Press.
Automotive Industry Action Group. 2007. HF-2
Business Operating Systems (BOS) for
Health Care Organizations: Requirements for
Process Improvements to Achieve Excellence.
Southfield, MI: AIAG.
Bajaria, H. J., and R. P. Copp. 1991. Statistical
Problem Solving; A Team Process for
Identifying and Resolving Problems. Garden
City, MI: Multiface.
Berwick, D. M., and L. L. Leape. 1999.
“ Reducing Errors in Medicine: It’s Time
to Take This More Seriously.” BMJ, 1999,
319 (July 17): 136–37.

212 References
Berwick, D. M., A. B. Godfrey, and J. Roessner.
1990. Curing Health Care: New Strategies
for Quality Improvement. San Francisco:
Jossey-Bass.
Burke, W. W. 1987. Organization Development:
A Normative View. Reading, MA: Addison-
Wesley. (Part of a series of books on OD.)
Caldwell, C., J. Brexler, and T. Gillem. 2005.
Lean-Six Sigma for Healthcare. Milwaukee:
ASQ Quality Press.
Chowdhury, S. 2001. The Power of Lean Six
Sigma. Chicago: Dearborn.
Committee on Quality Health Care in America,
Institute of Medicine. 2001. Crossing the
Quality Chasm: A New Health System for
the 21st Century. Washington, DC: National
Academy Press.
Cutcher-Gershenfeld, J., and K. Ford. 2005.
Valuable Disconnects in Organizational
Learning Systems: Integrating Bold Visions
and Harsh Realities. New York: Oxford
University Press.
Deming, W. E. 1993. The New Economics:
For Industry, Government, Education.
Cambridge, MA: MIT, Center for Advanced
Engineering Study.
———. 1999. Lean Manufacturing Workshop.
Dearborn, MI: Ford Motor Company.

References 213
Donabedian, A. 2003. An Introduction to Quality
Assurance in Health Care. New York: Oxford
University Press.
Doyle, M., and D. Straus. 1976. How to Make
Meetings Work: The New Interaction Method.
New York: Jove.
If Japan Can, Why Can’t We . . . 1980. VHS.
Washington, DC: CC-M Productions.
(To purchase a videocassette, go to
http:www.managementwisdom.com/ifjapan
canwhyc.html.)
Ishikawa, K. 1976. Guide to Quality Control.
Tokyo: Asian Productivity Organization.
Juran, J. M. 1964. Managerial Breakthrough:
A New Concept of the Manager’s Job. New
York: McGraw-Hill.
———. 1989. Juran on Leadership for Quality:
An Executive Handbook. New York: The Free
Press.
Kerzner, H. 1995. Project Management: A
Systems Approach to Planning, Scheduling,
and Controlling. 5th ed. New York: Van
Nostrand Reinhold.
Munro, R.A. 2000. “Linking Lean Six Sigma
with QS-9000.” Quality Progress (May).
———. 2002. Six Sigma for the Office: A Pocket
Guide. Milwaukee: ASQ Quality Press.

214 References
National Demonstration Project on Quality
Improvement in Healthcare. 1990. Curing
Health Care: New Strategies for Quality
Improvement. San Francisco: Jossey-Bass.
National Training Laboratories Institute. 1984.
Team-Building Readings. Arlington, VA:
NTLI.
Quality or Else. 1980. VHS. Washington,
DC: CC-M Productions. (To purchase a
videocassette, go to http:www.management
wisdom.com/qualityorelse.html.)
Rice, E. J. 1984. A Quick Reference Guide for
Team Building: Which Path Is Your Team
Taking. Dearborn, MI: Ford Motor Company.
(Note: The June 1999 issue of Quality
Progress was dedicated to teams. Also the
American Quality and Participation [AQP],
an affiliate of ASQ, has much available on
teams and team building).
———. 1997. “Automotive Excellence: Know the
History of Training to Promote Learning.”
ASQ Automotive Division 3, no. 4 (Fall):
12–15.
———. 1998. “Are You Listening?” Quality
P r o g r e s s 31, no. 5 (May): 25.
Senge, P. M. 1990. The Fifth Discipline: The Art
and Practice of the Learning Organization.
New York: Jove.

References 215
Stamatis, D. H. 1996. Total Quality Service:
Principles, Practices, and Implementation.
Delray Beach, FL: St. Lucie Press.
———. 1997. TQM Engineering Handbook. New
York: Marcel Dekker.
———. 2003. Failure Mode and Effect Analysis:
FMEA from Theory to Execution. 2nd ed.
Milwaukee: ASQ Quality Press.
Time: The Next Dimension of Quality. 1993.
VHS. CRM Films. http://www.crmlearning.
com/time-the-next-dimension-of-quality.
Wheeler, D. J., and S. R. Poling. 1998. Building
Continual Improvement: A Guide for
Business. Knoxville, TN: SPC Press.
Womack, J. P., and D. T. Jones. 1996. Lean
Thinking. New York: Simon & Schuster.
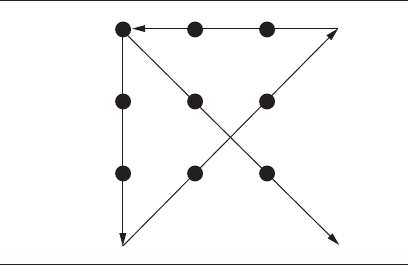
216 Answer from puzzle on page 73.
Start
Figure 46 Nine dots exercise solved.
217
Index
A
advanced practice quality planning (healthcare APQP),
58–61
analyze, phase of DMAIC, tools used in, 36–37
Art of Living, The, xiii
attribute data, 153–56
auditing, 62–65
B
benchmarking, 66–70
Black Belt, Lean Six Sigma, xxi, 51
brainstorming, 71–75
breakthrough improvement, 187
business operating system (BOS), for healthcare
organizations, 76–78
C
cause-and-effect diagram, 18, 79–83
check sheets, 84–88
checklist, 84–88
common cause variation, 17
continual improvement, 89–91
versus continuous improvement, 90–91
continual improvement process, tips, 50

218 Index
continuous improvement, versus continual improvement,
90–91
control, phase of DMAIC, tools used in, 38–39
cost of quality, 93
cost of poor quality, 93
costs, categories of, 93–96
could be map, 113–17, 187–88
cross-functional team, 45
current state map, 113–17
customer, definition, 8
customer feedback, 204–6
cycle time analysis, 98–100
cycle time reduction, principles, 99
D
data collection, with check sheets, 84–87
data–knowledge–action cycle, 143
define, phase of DMAIC, tools used in, 33–34
Deming, W. E., 91, 141, 144
design FMEA, 101–2
Design for Six Sigma (DFSS), 27–28
Disney, Walt, 70
DMAIC (define–measure–analyze–improve–control)
matrix guide, 2–4
model, 1, 13, 29–40
driving forces of, 29–30
problem-solving steps, 31–32
E
eight discipline (8D) problem solving process, 148–51
eight M’s, in cause-and-effect diagram, 80–81
80/20 rule, 136
employee involvement teams, 185–87
F
failure mode and effects analysis (FMEA), 101–4
in flowcharting, 115
Feigenbaum, Armand, 90, 144

Index 219
fishbone diagram, 18, 79–83
5S method, 53, 55–56
five W’s and H, in cause-and-effect diagram, 80
five W’s and two H’s, 149
flow map, 113–17
flowchart, 113–17
in benchmarking, 68
G
gage repeatability and reproducibility (GR&R), 131
goalpost mentality, 18–19
Granite Rock, 66–67
Green Belt, Lean Six Sigma, xxi, 51
group, versus team, 41
H
histogram, 118–21
I
idea stoppers, in brainstorming, 74–75
improve, phase of DMAIC, tools used in, 37–38
improvement teams, 45, 187–88
inspection, 62–63
instability, in variability, 23, 160–61, 178–79
internal audit, guidelines, 63–65
International Organization for Standardization (ISO), 90
Ishikawa, Kaoru, 26, 79
Ishikawa diagram, 18, 79–83
ISO 9001 registration, 40
J
job aids, 32, 173
Juran, J. M., 127, 136, 143
K
kaizen, 89–91

220 Index
kaizen events, 89–91
kanban, 122–23
L
lean organization, 197
structure, 189
Lean Six Sigma
Black Belt, xxi, 51
definition, 5–6
Green Belt, xxi, 51
in Practice, xxi–xxii, 6–10
road map for Practice, 47–48
your role in, 11–15
Lean Six Sigma for Healthcare, 7
lessons learned, 124–25
line graph, 163–65
loss function, 20, 22, 161
lower control limit, 155-157
M
MAIC (measure–analyze–improve–control) improvement
model, 13
Malcolm Baldrige National Quality Award (MBNQA),
40, 90
Healthcare Criteria for Performance Excellence, 77–78
MCG (members–control–goals), and teams, 42
measure, phase of DMAIC, tools used in, 34–36
measurement systems analysis (MSA), 129–32
meetings, team, 181–84
mistake-proofing, 133–35
muda, 209–10
O
off-target conditions, in variability, 23, 160–62, 179
Ohno, Taiichi, 123
output, of process (Y = f/x), 18, 79

Index 221
P
p chart, control limit calculations, 157
Pareto, Vilfredo, 136
Pareto chart, 136–39
patient feedback, 204–6
Patient-Centered Medical Home, 40
PDCA (plan–do–check–act) cycle, 141
PDSA (plan–do–study–act) cycle, 59
in continual improvement, 91
poka-yoke, 90, 133
practice strategy (future state) project planning, 145–47
problem solving, 148–51
steps in DMAIC, 31–32
process
in healthcare, 7
output of, (Y = f/x), 18, 79
process behavior charting, 89–90
process FMEA, 102
process improvement, 160–62
process map, 113–17
process model, 6
profound knowledge, Deming’s, 15, 91
project planning, 146–47
project team, 46
pull concept, in lean Practice, 6
Q
quality
expressing, 26–27
traditional view of, 18–19
quality auditing, 62–63
quality circle, 46
quality improvement, in the Practice, 25–26
six aims of, 59–60
quality of care and services, healthcare, xiv
quality of conformance, 27
quality of design, 27
quality system audit, guidelines, 63–65

222 Index
R
risk priority number (RPN), 104
Ritz Carlton, 125
road map for Practice, Lean Six Sigma, 47–48
rolled throughput yield, 99–100
run chart, 12–13, 163–65
S
scatter diagram, 166–69
SDCA (standardize–do–check–adjust) cycle, 175–76
in continual improvement, 91
self-directed teams, 46, 188–89
Senge, Peter, 128
7S method, 53–57
SGRPI (systems–goals–roles–procedures–interpersonal
relationships), 42–43
Shewhart, Walter, 89, 141, 152
Shingo prize, 135
Shingo, Shigeo, 135
should be map, 133–17
SIPOC diagram, 170–72
SIPOC (supplier–input–process–output–customer) model,
8, 158
special cause variation, 17
specifications, and quality, 19, 20–21
standard operating procedures (SOPs), 173–74
standardization, 175–76
standards, in auditing, 63–64
statistical process control (SPC), 89–90
statistical process display (SPD), 156
storyboard method, of process identification, 159
systems FMEA, 101
systems thinking, 177–80
T
Taguchi loss function, 20–21, 22
Taylor, Frederick, 89

Index 223
team building, rationales, 43
team meetings, 181–84
teams, 41–46, 185–91
formation, 190–91
versus a group, 41
stages of, 44–45
types of, 45–46
thinking outside the box, in brainstorming, 73–74
tools, Lean Six Sigma, 53–210
advanced practice quality planning, 58–61
auditing, 62–65
benchmarking, 66–70
brainstorming, 71–75
business operating system (BOS) for healthcare
organizations, 76–78
cause-and-effect diagram, 79–83
check sheets, 84–88
continual improvement, 89–91
cost of poor quality, 93–96
cost of quality, 93–96
cost–benefit analysis, 93–96
current state/could be/should be map, 113–17
cycle time analysis, 98–100
employee involvement teams, 185–87
error-proofing, 133–35
failure mode and effects analysis (FMEA), 101–4
fishbone diagram, 79–83
flow map, 113–17
flowchart, 113–17
healthcare APQP, 58–61
histogram, 118–21
huddles, 181–84
improvement teams, 187–88
Ishikawa diagram, 79–83
kaizen, 89–91
kaizen events, 89–91
kanban, 122–23
lessons learned, 124–25
line graph, 163–65
management involvement, 126–28

224 Index
measurement systems analysis (MSA), 129–32
mistake-proofing, 133–35
Pareto chart, 136–39
patient feedback, 204–6
patient pull-through, 122–23
PDSA (plan–do–study–act) cycle, 141–44
poka-yoke, 133–35
practice strategy (future state) project planning, 145–47
problem solving, 148–51
process behavior charts, 152–56
process identification, 158–59
process improvements, 160–62
process map, 113–17
quality cost, 93–96
return on investment, 93–96
run chart, 163–65
sampling, 62–65
sampling plans, 62–65
scatter diagram, 166–69
SDCA (standardize–do–check–adjust) cycle, 175–76
self-directed teams, 188–89
7S method, 53–57
SIPOC diagram, 170–72
standard operating procedures (SOPs), 173–74
standardization, 175–76
statistical process control (SPC), 152–56
systems thinking, 177–80
team meetings, 181–84
teams, 185–91
trend chart, 163–65
used in analyze phase of DMAIC, 36–37
used in control phase of DMAIC, 38–39
used in define phase of DMAIC, 33–34
used in improve phase of DMAIC, 37–38
used in measure phase of DMAIC, 34–36
value analysis, 192–94
value stream map, 195–97
variation reduction, 199–201
visual aids, 202–3
visual controls, 202–3

Index 225
voice of the customer, 204–6
wait time, 122–23
walkaround/walkthrough/waste walk, 207–10
trend chart, 163–65
U
u chart, control limit calculations, 157
upper control limit, 155–57
V
value analysis, 192–94, 197
value stream map, 195–97
variability, 160–61, 178
versus variation, 23
variable data, 153–56
variation, 160
description and definition, 17–23
versus variability, 23
variation reduction, 199–201
visual aids, 202–3
visual controls, 202–3
voice of the customer, 204–6
W
wait time, 122–23
walkaround, 207–10
walkthrough, 207–10
waste, 209–10
in Lean Practice, 6
waste walk, 207–10
Y
yield, definition, 98
(This page intentionally left blank)

ASQ is…
More than 90,000 •
individuals and 700
companies in more than
100 countries
The world’s largest •
organization dedicated to
promoting quality
A community of •
professionals striving to
bring quality to their work
and their lives
The administrator of •
the Malcolm Baldrige
National Quality Award
A supporter of quality •
in all sectors including
manufacturing, service,
healthcare, government,
and education
YOU•
Belong to the Quality Community!
Established in 1946, ASQ
is a global community of
quality experts in all fields and
industries. ASQ is dedicated to
the promotion and advancement
of quality tools, principles, and
practices in the workplace
and in the community.
The Society also serves as an
advocate for quality. Its members
have informed and advised
the U.S. Congress, government
agencies, state legislatures,
and other groups and
individuals worldwide on
quality-related topics.
Vision
By making quality a global
priority, an organizational
imperative, and a personal
ethic, ASQ becomes the
community of choice for
everyone who seeks quality
technology, concepts, or tools
to improve themselves and
their world.
Visit www.asq.org for more information.

Visit www.asq.org/membership for more information on ASQ membership.
*2008, The William E. Smith Institute for Association Research
Research shows that people who
join associations experience
increased job satisfaction,
earn more, and are generally
happier*. ASQ membership
can help you achieve this while
providing the tools you need to
be successful in your industry
and to distinguish yourself
from your competition. So why
wouldn’t you want to be a part
of ASQ?
Networking
Have the opportunity to meet,
communicate, and collaborate
with your peers within the
quality community through
conferences and local ASQ
section meetings, ASQ forums
or divisions, ASQ Communities
of Quality discussion boards,
and more.
Professional
Development
Access a wide variety of
professional development tools
such as books, training, and
certifications at a discounted
price. Also, ASQ certifications
and the ASQ Career Center
help enhance your quality
knowledge and take your career
to the next level.
Solutions
Find answers to all your
quality problems, big and
small, with ASQ’s Knowledge
Center, mentoring program,
various e-newsletters, Quality
Progress magazine, and
industry-specific products.
Access to Information
Learn classic and current quality
principles and theories in ASQ’s
Quality Information Center
(QIC), ASQ Weekly e-newsletter,
and product offerings.
Advocacy Programs
ASQ helps create a better
community, government, and
world through initiatives that
include social responsibility,
Washington advocacy, and
Community Good Works.
ASQ Membership

Visit www.asq.org/certifi cation to fi nd out more or to apply today!
ASQ certifi cation is formal
recognition by ASQ that an
individual has demonstrated
a profi ciency within, and
comprehension of, a specifi ed
body of knowledge at a
point in time. ASQ offers 15
certifi cations to choose from.
Nearly 150,000 certifi cations
have been issued. ASQ has
members in 100 countries,
in all industries, and in all
cultures. ASQ certifi cation is
internationally accepted
and recognized.
Benefi ts to the Individual
New skills gained and •
profi ciency upgraded
Investment in your career•
Mark of technical excellence•
Assurance that you •
are current with
emerging technologies
Discriminator in •
the marketplace
Certifi ed professionals •
earn more than their
uncertifi ed counterparts
Certifi cation is endorsed by •
more than 125 companies
Benefi ts to the
Organization
Investment in the •
company’s future
Certifi ed individuals can •
perfect and share new
techniques in the workplace
Certifi ed staff are •
knowledgeable and able
to assure product and
service quality
Quality is a global concept. It
spans borders, cultures, and
languages. No matter what
country your customers live in
or what language they speak,
they demand quality products
and services. You and your
organization also benefi t from
quality tools and practices.
Acquire the knowledge to
position yourself and your
organization ahead of
your competition.
ASQ Certifi cation

Visit www.asq.org/training for more information.
ASQ Training
Classroom-based
Training
ASQ offers training in a
traditional classroom setting
on a variety of topics. Our
instructors are quality experts
and lead courses that range
from one day to four weeks,
in several different cities.
Classroom-based training is
designed to improve quality
and your organization’s bottom
line. Benefit from quality
experts; from comprehensive,
cutting-edge information; and
from peers eager to share
their experiences.
Web-based Training
Virtual Courses
ASQ’s virtual courses provide
the same expert instructors,
course materials, interaction
with other students, and ability
to earn CEUs and RUs as our
classroom-based training,
without the hassle and expenses
of travel. Learn in the comfort of
your own home or workplace.
All you need is a computer with
Internet access and a telephone.
Self-paced Online
Programs
These online programs allow
you to work at your own pace
while obtaining the quality
knowledge you need. Access
them whenever it is convenient
for you, accommodating
your schedule.
Some Training Topics Include
Auditing•BasicQuality
Engineering•Education
Healthcare•Government
FoodSafety•ISO
Leadership•Lean
Quality Management
Reliability•SixSigma
Social Responsibility
