BY ORDER OF THE
SECRETARY OF THE AIR FORCE
AIR FORCE MANUAL 44-144
20 JANUARY 2016
Medical Operations
NUTRITIONAL MEDICINE
COMPLIANCE WITH THIS PUBLICATION IS MANDATORY
ACCESSIBILITY:
Publications and forms are available for on the e-Publishing website at
www.e-Publishing.af.mil for downloading or ordering.
RELEASABILITY:
There are no releasability restrictions on this publication.
OPR: 559 MDG/CC
Supersedes: AFMAN44-144, 29 June 2011
Certified by: AF/SG3/5
(Maj Gen Roosevelt Allen)
Pages: 86
This Manual provides guidance for provision of nutrition education, medical nutrition therapy
(MNT), consultant services and management of manpower, subsistence, equipment, and
expendable supply resources in Nutritional Medicine (NM) operations in Air Force Medical
Treatment Facilities (MTF). This manual implements DODI 1338.10-M, Manual for the
Department of Defense Food Service Program, DODI 6025.24, Provision of Food and
Beverages to Certain Members and Dependents Not Receiving Inpatient Care in Medical
Treatment Facilities (MTFs), DODI 6130.50, DoD Nutrition Committee, and AFPD 44-1,
Medical Operations, and interfaces with AFPD 40-1, Health Promotion; AFI 40-101, Health
Promotion; AFI 40-104, Health Promotion Nutrition; AFI 41-120, Medical Resource
Management Operations. This Manual does not apply to the Air Force Reserve, except where
noted. This Manual does not apply to the Air National Guard. Send comments and suggested
improvements on AF Form 847, Recommendations for Change of Publication, through major
commands to the Air Force Surgeon General, HQ USAF/AFMSA, 7700 Arlington Blvd., Falls
Church, VA 22042-5158. Ensure that all records created as a result of processes prescribed in
this publication are maintained IAW Air Force Manual (AFMAN) 33-363, Management of
Records, and disposed of IAW Air Force Records Information Management System (AFRIMS)
Records Disposition Schedule (RDS). The authorities to waive wing/unit level requirements in
this publication are identified with a Tier (“T-0, T-1, T-2 or T-3”) number following the
compliance statement. See AFI 33-360, Publications and Forms Management, for a description
of the authorities associated with the Tier numbers. Submit requests for waivers through the
chain of command to the appropriate Tier waiver approval authority, or alternately, to the
Publication OPR for non-tiered compliance items. The use of the name or mark of any specific
manufacturer, commercial product, commodity, or service in this publication does not imply
endorsement by the Air Force.
2 AFMAN44-144 20 JANUARY 2016
SUMMARY OF CHANGES
This publication reflects significant changes in guidance and procedures in Nutritional Medicine
operations. Substantially revised, this document must be reviewed in its entirety. Major changes
include: added financial management billing error procedures, updated meal rates and meal day
values, the Joint Culinary Center for Excellence Quartermaster Basic Daily Food Allowance
(BDFA) calculation, Wounded Warrior meal reference guidance, and new DoDI 6025.24,,
Provision of Food and Beverages to Certain Members and Dependents Not Receiving Inpatient
Care in Medical Treatment Facilities, guidance. Additional changes include the removal of the
table of contents, updated mission statement, and removal of references to Health and Wellness
Centers. Chapter 2 was added detailing the roles and responsibilities of authority levels.
Nutrition in Prevention course attendance was removed and compliance with AFI 36-807,
Weekly and Daily Scheduling of Work and Holiday Observances was included. Nutrition
screening and outpatient therapeutic diet procedures were updated and Privacy Act requirements
were incorporated into inpatient meal service procedures. An attachment was added to the
chapter on subsistence account reporting and management as a compliance checklist for
purchasing, storing, inventorying, issuing, cost control, pricing, cashier operations, and ration
accounting. All chapters were updated per subject matter expert recommendations. The
document was also tiered in accordance with AFI 33-360.
Chapter 1—MISSION, VISION, AND ORGANIZATION 5
1.1. Mission and Vision. ............................................................................................... 5
1.2. Organization. .......................................................................................................... 5
Chapter 2—ROLES AND RESPONSIBILITIES 6
2.1. Air Force Surgeon General (AF/SG) shall: ............................................................ 6
2.2. Air Force Deputy Chief of Staff for Manpower and Personnel (AF/A1) shall: ..... 6
2.3. AF/SG Dietetics Consultant shall: ......................................................................... 6
2.4. Career Field Manager shall: ................................................................................... 6
2.5. Major Command (MAJCOM) Dietitian shall: ....................................................... 6
2.6. Medical Group Commander (MDG/CC) shall: ..................................................... 6
Chapter 3—PLANNING AND EVALUATION 8
3.1. NM Organizational Strategy. ................................................................................. 8
3.2. Performance Improvement (PI). ............................................................................ 8
3.3. Disaster and Contingency Planning. ...................................................................... 9
3.4. Menu Planning. ...................................................................................................... 9
Chapter 4—PERSONNEL ADMINISTRATION 11
4.1. Staffing, Utilization and Job Titles. ....................................................................... 11
Table 4.1. NM Officer Staffing and Duty Titles. .................................................................... 11
AFMAN44-144 20 JANUARY 2016 3
4.2. Duties. .................................................................................................................... 11
4.3. Job Descriptions. .................................................................................................... 12
4.4. Competency Assessment. ...................................................................................... 12
4.5. Work Schedules and Daily Assignments. .............................................................. 14
4.6. Education and Training. ......................................................................................... 14
4.7. Workload Reporting. ............................................................................................. 15
Chapter 5—NUTRITION CARE 18
5.1. Medical Nutrition Therapy (MNT). ....................................................................... 18
5.2. Patient Rights and Privacy. .................................................................................... 21
5.3. Nutrition Screening. ............................................................................................... 21
5.4. Documentation and Peer Review. .......................................................................... 22
5.5. Ordering Inpatient Meals and Nourishments. ........................................................ 23
5.6. Inpatient Meal Service ........................................................................................... 25
5.7. Dietary Kardex (AF Form 1741) or Electronic/MTF-Equivalent. ......................... 25
5.8. Meal Hours ............................................................................................................ 26
5.9. Bedside Tray Service. ............................................................................................ 26
5.10. Enteral Nutrition, Medical Foods, and Infant Formulas. ....................................... 27
5.11. Parenteral Nutrition (TPN, PPN). .......................................................................... 28
5.12. Therapeutic Diets for Outpatients. ......................................................................... 28
5.13. Patient and Family Education. ............................................................................... 28
5.14. Health Promotion Nutrition. .................................................................................. 29
Chapter 6—FOOD PRODUCTION AND SERVICE 30
6.1. Production Planning. .............................................................................................. 30
6.2. Purchasing Non-Food Supplies. ............................................................................. 31
6.3. Food Portion and Waste Control. ........................................................................... 31
6.4. Hazard Analysis and Critical Control Point (HACCP) .......................................... 32
6.5. Sanitation and Infection Control. ........................................................................... 33
6.6. Patient Tray Assembly. .......................................................................................... 33
Chapter 7—FINANCIAL MANAGEMENT 34
7.1. Budgets. ................................................................................................................. 34
7.2. Prime Vendor. ........................................................................................................ 34
7.3. Financial Accountability. ....................................................................................... 35
4 AFMAN44-144 20 JANUARY 2016
7.4. Subsistence Purchasing. ......................................................................................... 35
7.5. Unauthorized Uses of Subsistence Items. .............................................................. 37
7.6. Perpetual Inventory. ............................................................................................... 37
7.7. Physical Inventory. ................................................................................................ 37
7.8. Closing a NM Activity. .......................................................................................... 39
7.9. Issuing Subsistence. ............................................................................................... 39
7.10. Costing Subsistence Items. .................................................................................... 40
7.11. Excess Cost. ........................................................................................................... 40
7.12. Cashier Operations. ................................................................................................ 40
7.13. Eligibility and Identification of Diners. ................................................................. 43
7.14. ALACS Recipe Pricing Operations. ...................................................................... 45
7.15. Special Feeding Circumstances. ............................................................................ 46
7.16. NM Ration Accounting. ......................................................................................... 46
7.17. Subsistence Account Reporting and Management. ................................................ 48
Chapter 8—PROCEDURES FOR MEDICAL FACILITIES SUPPORTED BY BASE
FOOD SERVICE AND DIETETIC SHARING AGREEMENTS 51
8.1. Procedures for MTFs supported by Base Food Service. ........................................ 51
8.2. Dietetic Sharing Agreements. ................................................................................ 52
Chapter 9—CONSULTANT SERVICES 54
9.1. Purpose. .................................................................................................................. 54
9.2. The Consultant Dietitian. ....................................................................................... 54
9.3. Enlisted Consultant Roles. ..................................................................................... 57
9.4. NM Dietitian or Diet Therapy Personnel. .............................................................. 59
Attachment 1—GLOSSARY OF REFERENCES AND SUPPORTING INFORMATION 60
Attachment 2—4D0X1 DIET TECH DIET COUNSELING AUTHORIZATION GUIDE 71
Attachment 3—PERSONS AUTHORIZED TO EAT IN MILITARY TREATMENT
FACILITY DINING FACILITIES 75
Attachment 4—TABLE A4.1. NUTRITIONAL MEDICINE SUBSISTENCE REPORT
(EXCEL SPREADSHEET). 78
Attachment 5—SAMPLE MOA BETWEEN NM & BASE FOOD SERVICE 79
Attachment 6—NUTRITIONAL MEDICINE SERVICE OVERSIGHT CHECKLIST 82
AFMAN44-144 20 JANUARY 2016 5
Chapter 1
MISSION, VISION, AND ORGANIZATION
1.1. Mission and Vision. The mission of NM is to optimize health and performance through
nutrition. The NM vision is to be the global leaders in nutrition, fueling performance.
1.2. Organization. If a separate NM Element/Flight is feasible, then all NM personnel are
assigned to the NM unit under Functional Account Code (FAC) 5520 and matrixed to Health
Promotion as appropriate to complete health promotion nutrition interventions and provide MNT
when indicated. In clinics, the Medical Treatment Facility (MTF) Commander decides the best
location in the organization for NM personnel. Regardless of location, NM clinics with an
assigned Registered Dietitian/Registered Dietitian Nutritionist (RD/RDN) will simultaneously
provide health promotion nutrition education programs, as well as complete referrals for MNT
IAW AFI 44-102, Medical Care Management (T-2). Organizational structure for NM flights and
elements is more fully described in Chapter 3, Personnel Administration.
1.2.1. In Air Force Reserve Command (AFRC) units, NM personnel may be assigned to the
Medical Squadron or Aeromedical Staging Squadron (ASTS) where they may provide
nutrition education programs and support the Air Force Fitness Program. AFRC NM
personnel are also assigned to active duty NM units.
6 AFMAN44-144 20 JANUARY 2016
Chapter 2
ROLES AND RESPONSIBILITIES
2.1. Air Force Surgeon General (AF/SG) shall:
2.1.1. Ensure adequate programming, budget, training, and research to support nutritional
medicine.
2.1.2. Advocate for comprehensive and evidenced-based strategies to create a culture and
environment supportive of nutritional medicine.
2.1.3. Collaborate and coordinate nutrition policy with US Air Force Deputy Chief of Staff
for Manpower and Personnel (AF/A1).
2.2. Air Force Deputy Chief of Staff for Manpower and Personnel (AF/A1) shall:
2.2.1. Support AF/SG in developing Air Force nutrition policy.
2.2.2. Provide policy and guidance for integrating and vetting new/emerging institutional
education and training requirements or learning outcomes into accessions, Professional
Military Education (PME), Professional Continuing Education (PCE) and ancillary training.
2.3. AF/SG Dietetics Consultant shall:
2.3.1. Advise AF/SG on nutrition policy.
2.3.2. Coordinate with Air Force Medical Operations Agency (AFMOA) Health Promotion,
Air Force Medical Support Agency (AFMSA) Health Promotion, and Air Force Medical
Operations Agency/Biomedical Sciences Corps (AFMOA/SGB) on nutritional guidance and
programs.
2.4. Career Field Manager shall:
2.4.1. Advise AF/SG Dietetics Consultant on enlisted force matters.
2.4.2. Ensure career progression is being conducted across the career field.
2.5. Major Command (MAJCOM) Dietitian shall:
2.5.1. Coordinate with HP RDs on training, peer review, and mentorship on medical
nutrition therapy.
2.5.2. Advise the command and appropriate higher headquarters staff on nutrition issues, and
provide guidance and nutrition consultation to bases and MTFs.
2.5.3. Serve as clinical supervisor for HP RDs to include the credentialing process and diet
certification.
2.5.4. Direct the peer review process for nutritional medicine.
2.6. Medical Group Commander (MDG/CC) shall:
2.6.1. Advocate for comprehensive, evidence-based strategies to create a culture and
environment supportive of nutritional medicine (T-3).
AFMAN44-144 20 JANUARY 2016 7
2.6.2. Provide adequate programming, budget, training, and resourcing to achieve nutritional
medicine goals and objectives. (T-3).
2.6.3. In collaboration with the MAJCOM Dietitian, provide options to ensure all patients
have access to nutrition education. (T-3).
8 AFMAN44-144 20 JANUARY 2016
Chapter 3
PLANNING AND EVALUATION
3.1. NM Organizational Strategy. The purpose of long and short term strategy is to ensure
NM operations and associated activities are aligned with the Air Force Medical Service (AFMS)
strategy map. Individual NM organizational strategies should also be aligned with current,
overall strategic plans for the career field. Management strategies provide the NM flight an
opportunity to establish instruction and policies that focus and allocate NM resources. Strategies
should encompass both NM operations as well as efforts to make improvements. Strategic
planning sessions will include representation from airmen, civilians, contractors, NCOs, and
senior NM leaders. (T-3). The NM Organizational Strategy should be consistent with the MTF
Strategic Plan, and outline management objectives, improvement efforts, and resources. Each
NM flight should maintain a department strategic plan which includes a mission statement and
organizational chart, and goals/ objectives/action plans. (T-3)
3.1.1. Continuous communication with NM personnel and MTF senior leaders should take
place throughout the planning process and implementation of the NM action plans.
3.2. Performance Improvement (PI). Performance Improvement is a continuous activity that
involves measuring the function of important processes and services and when indicated,
identifies changes that enhance performance. These changes are incorporated into new and
existing processes, products, or services and are monitored to ensure improvements are
sustained. PI focuses on clinical, administrative and cost-of-care issues as well as patient
outcomes (results of care). The fundamental components of PI include staff education,
measuring performance through data collection, assessing current performance, utilizing the data
collected to improve organizational processes, services, and overall performance and re-
education. PI includes evaluating the following attributes: efficacy, appropriateness, availability,
timeliness, effectiveness, continuity, safety, efficiency, respect, and care. Performance measures
should focus on critical processes in nutrition care, food production and management of
personnel and financial resources. In addition, peer review is conducted and submitted in
accordance with local credentialing authority guidance to the appropriate MAJCOM Dietitian.
(T-3).
3.2.1. PI activities, based on facility scope of practice and capability, are focused on high-
risk, problem prone, high volume and high cost areas but are not limited to those areas.
3.2.1.1. Examples of high-risk patient process include: patient tray food temperatures,
NPO/clear liquid tracking, nutrient-drug interaction counseling documentation, inpatient
screening timeframes, and patient tray and menu accuracy.
3.2.1.2. Examples of problem prone processes include: nutrition clinic no-show rates,
kardex accuracy, absenteeism per time period, and number of work injuries per hours
worked.
3.2.1.3. Examples of high volume and high cost areas include: outcomes of MNT for
management of hyperlipidemia, diabetes, and weight control, cost per dining facility
meal, cost per patient meal, and cost per unit.
AFMAN44-144 20 JANUARY 2016 9
3.2.2. NM will have Performance Improvement Teams consisting of a team leader,
facilitator, recorder and team members as appropriate. Meeting minutes will be recorded and
maintained. (T-3).
3.3. Disaster and Contingency Planning. NM with in-patient feeding capabilities must have a
plan that establishes responsibilities and basic procedures for feeding patients and staff during
both wartime and peacetime contingency and disaster operations. (T-1). This plan is an annex in
the MTF's Medical Contingency Response Plan (MCRP).
3.4. Menu Planning. The Flight Commander/Element Chief is responsible for planning the
regular selective cycle and any special menus for the hospital to which they are assigned. (T-3).
The Chief, Clinical Dietetics is responsible for writing the therapeutic menus. All regular and
therapeutic menus will be approved by the NM Flight Commander/Element Chief. (T-3). At
hospitals with no dietitian assigned, regular and therapeutic menus will be written by the
NCOIC, NM and approved by the MAJCOM Dietitian. (T-3).
3.4.1. Cycle Menu Planning. Menu planning considerations should include subsistence
ordering and delivery schedules, subsistence storage capacity, available equipment,
subsistence budget, subsistence seasonal availability, personnel skills and abilities, seasonal
and religious holidays, patron preferences, average inpatient length of stay, disease
prevalence of patient population, patient age group considerations, cultural nutritional needs,
type of inpatient food service operation and facility menu style (room service, a la carte,
electronic menus, etc.).
3.4.1.1. All menus are designed to achieve or maintain optimal nutritional status. To the
greatest extent possible, regular/general menus will adhere to the Joint Subsistence Policy
Board, Department of Defense menu standards, which promote the United States
Department of Agriculture (USDA), and Department of Health and Human Service
(DHHS) Dietary Guidelines for Americans. (T-0). Therapeutic menus will follow
current recommendations for the MNT treatment of such acute and chronic disease states.
Consult the AND Nutrition Care Manual (NCM), Pediatric Nutrition Care Manual
(PNCM), Sports Nutrition Care Manual (SNCM), Dietary Guidelines for Americans, the
USDA Food and Nutrition Service’s Menu Magic for Children and/or other professional
sources for additional information on planning healthy menus.
3.4.1.2. Evaluate all menus for nutritional adequacy. (T-3). At a minimum, assess
compliance to Joint Subsistence Policy Board, Department of Defense Menu Standards
and compare nutrient content to the USDA MyPlate suggested servings for each food
group. Computrition and/or other commercial nutrient analysis programs may be used
for more detailed nutritional analysis as needed.
3.4.1.3. Develop the therapeutic cycle menu using items from the regular menu and in
the same sequence, as much as possible. (T-3). The content of the various therapeutic
diets are a function of and defined by the literature contained within the NCM.
3.4.1.4. Establish the type of inpatient food service operation as appropriate for the
facility. (T-3). Examples may include but are not limited to non-select menus, select
menus, buffet-style selection, hotel or room service, or any combination. Create a
hospital master menu in a format most appropriate to easily transfer to the style of menu
10 AFMAN44-144 20 JANUARY 2016
for the facility, i.e., AF Forms 1737 or 1739, Selective Menu, Hotel/Room Service menu,
Computrition, etc. (T-3). Reproduce menus as necessary.
3.4.1.5. Develop standard daily/weekly rotations for nutritional supplements and
food/snack items, as necessary, to ensure appropriate variety. (T-3).
3.4.1.6. At a minimum, update and modify menus annually. (T-3).
3.4.1.7. Develop a patient/customer feedback process to evaluate patient satisfaction
with menu items and NM service. (T-3). Results of patient satisfaction surveys and
customer feedback can be valuable when updating and modifying menus and food
production and service processes.
AFMAN44-144 20 JANUARY 2016 11
Chapter 4
PERSONNEL ADMINISTRATION
4.1. Staffing, Utilization and Job Titles. NM Flight Commander/Element Chief is the senior
dietitian (AFSC 43D3) assigned. In facilities where more than one dietitian is assigned, use
Table 4.1 to determine duty titles and functions.
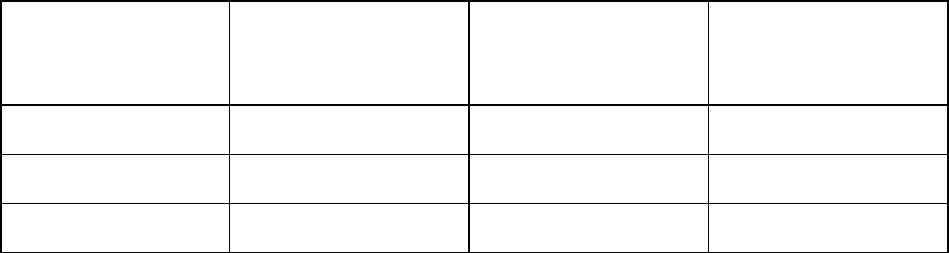
Table 4.1. NM Officer Staffing and Duty Titles.
Number of Dietitians
Assigned
NM Flight
Commander/Element
Chief
Clinical Dietetics
Element/Section
Chief
Clinical Dietitian
1
1
2
1
1
3 or more
1
1
1 or more
4.1.1. With the exception of organizations that support the AF SG Consultant
Dietitian/Biomedical Science Corps (BSC) Associate Chief for Dietetics or those supporting
the US Military Dietetic Internship Consortium and Graduate Program in Nutrition (GPN),
all RDs, other than the squadron or flight commander, will be assigned to patient care or
health promotion positions. Nutritional Medicine officer duty titles not listed above should
be approved by the AF SG Consultant Dietitian/BSC Associate Chief for Dietetics. In MTFs
where no dietitian is assigned, the MTF Commander designates an officer, not subject to
conflict of interest, as the NM Element Chief. (T-3).
4.1.2. The NM Manager/Superintendent/NCOIC is the most senior Diet Therapist (4D0X1).
Duty for enlisted personnel will conform to the standardized job and duty title guidance as
described in AFI 36-2618, The Enlisted Force Structure, and AFI 36-2201, Air Force
Training Program. (T-1). Exceptions must be approved by the Career Field Manager (CFM).
4.1.3. Considering the Unit Manpower Document (UMD), the Unit Personnel Management
Roster (UMPR), and the NM Product Line Analysis, a staffing plan must be developed and
available in each section to ensure an adequate number of personnel are assigned. (T-3).
4.2. Duties.
4.2.1. The NM Flight Commander/Element Chief is responsible for the planning,
organization, management, operation, performance improvement and coordination of NM
Flight/Element activities which include meal service to patients and authorized diners,
clinical nutrition and participation in health promotion programs. (T-3). The Flight
Commander/Element Chief also directs food procurement, production and service including
the planning, preparation and service of regular and therapeutic diets for MTF patients,
aeromedical evacuation patients, hospital personnel and dining facility patrons within
financial limitations; directs education activities including career development of dietitians
and proficiency development of NM personnel; oversees inpatient and outpatient clinical
dietetics activities including provision of MNT and community nutrition education. In NM
12 AFMAN44-144 20 JANUARY 2016
with one dietitian, the NM Element Chief has direct responsibility for food production and
service, along with providing clinical dietetics support by supervising and performing MNT
and nutrition education. (T-3).
4.2.2. Diet Therapy Superintendent/Chief Enlisted Manager (CEM) oversees the operation
of NM flight activities, plans and organizes nutrition care activities, directs food service
activities, inspects and evaluates nutrition care activities, performs technical nutrition care
functions, and plans and organizes nutrition care activities. (T-3). Consult the Career Field
Education and Training Plan (CFETP) 4D0X1 for more specific descriptions of duties for
diet therapy personnel assigned.
4.3. Job Descriptions. Job descriptions, including qualifications, responsibilities, and written
performance standards must be available for each duty position IAW AFI 44-119. (T-3).
4.4. Competency Assessment. The NM Flight Commander/Element Chief will ensure that
policies, procedural guidelines and national care standards are followed IAW AFI 44-119. (T-3).
4.4.1. Dietitian Credentialing and Privileging. RD competency is documented through the
credentialing and privileging process. Active duty, reserve, civilian, contract, and any
volunteer dietitians will be credentialed and awarded MTF clinical privileges IAW AFI 44-
119 before providing care to patients. (T-1). IAW AF Form 3930, Clinical Privileges-
Dietetics Providers, or the electronic equivalent form in Centralized Credentials Quality
Assurance System (CCQAS); an applicant’s ability to provide patient services within the
scope of clinical privileges requested will be based upon the following minimum criteria:
written verification of completion of a minimum of a baccalaureate degree from an
accredited college or university and completion of an AND-approved didactic program in
dietetics; written verification of successful completion of an AND-accredited supervised
practice program (Dietetic Internship OR Coordinated Program in Dietetics); written
verification of current registration by the AND OR written proof of eligibility to take the
AND registration examination. (T-0). Direct accession service members must obtain
registration prior to entry on active duty. Graduates of the US Military Dietetic Internship
Consortium/GPN must obtain registration within four months of graduation. (T-2). Once
dietitians achieve basic/core credentials and privileges, they should maintain currency and
competencies sufficient to support readiness/deployment missions.
4.4.1.1. Specialized board certifications are encouraged, but are not mandatory, for all
dietitians. RDs may be eligible for the following recognized board certifications:
Certified Nutrition Support Clinician (CNSC), Certified Diabetes Educator (CDE),
Certified Health Education Specialist (CHES), Registered Clinical Exercise Physiologist
(RCEP), Registered Exercise Specialist (RES), and the following AND certifications:
Certified Specialist in Gerontological Nutrition (CSG), Certified Specialist in Sports
Dietetics (CSSD), Certified Specialist in Pediatric Nutrition (CSP), Certified Specialist in
Renal Nutrition (CSR), and Certified Specialist in Oncology Nutrition (CSO) the Fellow
of American Nutrition and Dietetics (FAND). Many board certifications are eligible for
Non-Physician Health Care Provider Board Certified Pay. Some specialized positions
within the AFMS may require board certification, and board certified CNSC and CDE
dietitians may receive additional clinical privileges. In addition, advanced privileges may
be granted by the institution-specific privileging body.
AFMAN44-144 20 JANUARY 2016 13
4.4.1.1.1. Additional clinical privileges for CNSC dietitians may include: ordering
enteral feedings, including type of formula, rate, strength, type/size of feeding tube,
gastrointestinal location of feeding tube and evaluation of tolerance; total and
peripheral parenteral nutrition (TPN & PPN), including macronutrients, rate, volume,
additives and cycling schedule; transitional feedings; blood glucose checks for cyclic
TPN; and 24 hour urine collections for nitrogen balance studies.
4.4.1.1.2. Additional clinical privileges for CDE dietitians include: practicing as a
case manager; regulating insulin; and, educating patients on the use of a glucometer.
4.4.1.1.3. When privileged to perform as a CNSC or CDE, the individual will meet
the following criteria: provide written verification of initial certification from the
granting agency, show evidence of meeting continuing education requirements in the
respective specialty and provide evidence of completion of recertification
requirements as mandated by the granting agency. (T-0).
4.4.1.1.4. Dietitians may have more advanced privileges; such as, performing
indirect calorimetry, ordering dual energy X-Ray Absorptiometry (DXA), or
performing advanced nutrition focused physical exam. The dietitian will provide
written verification of training or education supporting the privilege being requested.
(T-3).
4.4.1.2. Recommendation for reappointment of privileges will be based upon the
following criteria: maintaining registration status as a RD, active practice of dietetics,
evidence of demonstrated proficiency based upon quarterly peer reviews that show no
negative trends nor validated occurrences that would warrant privilege limitations,
current Basic Life Support (BLS) training and evidence of completion of required
Continuing Education Units (CEU). (T-0).
4.4.2. Diet Therapy Personnel Competency. Diet therapy personnel competency is assessed
initially for everyone within the first 60 days of assignment to determine proficiency level.
(T-3). This may be demonstrated through attendance at formal military diet therapy courses,
nationally accredited certifications, enlisted specialty training and assessment/authorization
of diet therapy skills by a RD.
4.4.2.1. The NM Manager/Superintendent, and NCOIC must obtain and maintain the
skill level commensurate with their grade and attend Professional Military Education
appropriate for their grade. (T-3). Diet Therapy Craftsmen (active duty or reserve)
should attend our Nutrition Management Accounting Course as soon as possible once
assigned to a MTF. (T-3).
4.4.2.2. Diet Authorizations. Credentialed RDs use AF Form 628, Diet
Instruction/Assessment Authorization, to evaluate and authorize diet therapists for:
nutrition screenings, nutrition assessments, nutrition progress notes, and individual,
group, or family education. (T-2). See Attachment 2, Diet Counseling Authorization
Guide, for a list of approved diet authorizations. Exceptions to Attachment 2 must be
approved by the MAJCOM Dietitian. Diet authorizations may be valid for up to two
years. When significant changes in diet instruction materials or nutrition practice occur
within the two-year period, a RD must accomplish reauthorization. (T-2). The leader of
the MNT Work Group will inform the AF SG Consultant Dietitian/BSC Associate Chief
14 AFMAN44-144 20 JANUARY 2016
for Dietetics when significant changes occur that warrant reauthorization of diet
technicians. (T-1). In turn, the AF SG Consultant Dietitian/BSC Associate Chief for
Dietetics will inform the MAJCOM Dietitians. (T-3).
4.4.2.3. Dietary Manager’s Association (DMA), Certified Dietary Manager (CDM), and
Certified Food Protection Professional (CFPP) certifications, and Diet Technician
Register (DTR) for diet therapy personnel are highly encouraged. Diet therapists who
earn the above mentioned certifications will also be taken into consideration for advanced
enlisted leadership positions through the annual Diet Therapy Enlisted Development
evaluation board.
4.5. Work Schedules and Daily Assignments.
4.5.1. NM work schedules will comply with AFI 36-807, Weekly and Daily Scheduling of
Work and Holiday Observances.
4.6. Education and Training.
4.6.1. Orientation. Employee Orientation will be performed and documented for each new
military, civilian, and contract employee within the first 30 days of employment IAW AFI,
44-119, Medical Quality Operations. (T-0).
4.6.2. Age-specific training. Age-specific training focuses on the ages of patients/clients
served and includes the ability to obtain and interpret information in terms of patient needs,
knowledge, growth and development as well as range of treatment options. This training
must be provided before staff may work with specialized age groups, and must be repeated
annually. (T-3).
4.6.3. In-Service Training.
4.6.3.1. Base recurring in-service training on required annual training, type and nature of
services provided, individual NM needs, information from performance improvement
activities, infection control activities, safety program, performance appraisals and peer
review.
4.6.3.2. Establish and document an annual in-service training schedule. (T-3).
4.6.3.2.1. Record date training was conducted, learning objectives, detailed topic
outline, names of attendees at initial and make up sessions and the instructor. (T-3).
4.6.3.2.2. Establish a method of training for personnel not in attendance at the initial
session to ensure all personnel receive training. (T-3).
4.6.3.3. A dietitian or NCO will ensure the effectiveness of preparation, presentations,
and documentation of each session. (T-3).
4.6.3.3.1. Evaluate in-service training using written post-quizzes, skill demonstration,
group discussion or other evaluation methods. (T-3).
4.6.3.4. At a minimum, the following training must be provided on an annual basis,
unless otherwise noted.
4.6.3.4.1. Fire Safety. Develop a Job Safety Training Outline that identifies and
addresses section specific safety hazards IAW AFI 91-301, Air Force Occupational
AFMAN44-144 20 JANUARY 2016 15
Safety, Fire Protection and Health Program. Documented on AF Form 55, Employee
Safety and Health Record. (T-3).
4.6.3.4.2. Federal Hazard Communication Training and Workplace Specific Hazard
Communication Training (HAZMAT). Handling of hazardous materials is also
briefed on employees’ initial and annual Occupational Safety and Health
Administration (OSHA) training. The job specific training will be given individually
and in small groups by authorized trainers. (T-0). Documented on AF Form 55.
4.6.3.4.3. Disaster Preparedness/MCRP. The NM Team Chief, IAW AFI 41-106,
Unit Level Management of Medical Readiness Programs, is responsible to develop
the MCRP team annual training plan that ensures each team member receives annual
and make-up training to maintain proficiency standards and ensure training is
documented in Medical Readiness Decision Support System (MRDSS) ULTRA. (T-
3).
4.6.3.4.4. Readiness Skills Verification (RSV). The AFSC functional training
managers at the unit level, IAW AFI 41-106, are responsible for developing the
annual RSV training plan for their AFSC, complete annual gap-analysis, ensure RSV
and make-up training are conducted using standardized career field materials and
documented in MRDSS ULTRA. (T-3).
4.6.3.4.5. Anti-Robbery/Resource Protection. (T-3).
4.6.3.4.6. Food Handlers Training IAW AFI 48-116, Food Safety Program and the
AFMAN 48-147_IP, Tri-Service Food Code. (T-3).
4.6.3.4.7. Infection Control/Bloodborne Pathogens. (T-3).
4.6.3.4.8. BLS/Obstructed airway conducted biennially. (T-3).
4.6.4. Coordination of Support to Formal Training Programs. Support for coordinated
undergraduate, professional practice, advanced degree dietitian programs, or independent
study programs for dietary managers must be coordinated through the AF SG Consultant
Dietitian/BSC Associate Chief for Dietetics. Additional staffing will not be authorized to
support these programs.
4.7. Workload Reporting.
4.7.1. Medical Expense Personnel Reporting System (MEPRS). MEPRS is an accounting
system used by the AF Medical Service that provides NM managers with manpower, cost
distribution, expense and workload reporting data. NM expense, personnel utilization and
workload data are collected for this system through manual and automated processes. Since
MEPRS data are used to determine manpower requirements, expense allocation and
productivity, NM input needs to be current, accurate and complete.
4.7.1.1. Personnel Time/Utilization. The timely and accurate control of personnel data is
essential for the total success of the MEPRS as personnel costs are the largest expense in
the MTF budget. Time (hours) worked is reported through manual entry into the Defense
Medical Human Resources System-internet (DMHRSi). Each individual is responsible
for accurately reporting hours worked to the correct Functional Cost Codes (FCC). (T-3).
A work center monitor should be appointed whose job it is to review DMHRSi for
16 AFMAN44-144 20 JANUARY 2016
accuracy, consistency, and appropriate FCCs, before they are submitted to the DMHRSi
Program Manager.
4.7.1.2. Contract Services/Sharing Agreements. For contracts in any area within dietetics
services, the cost should be allocated in the appropriate MEPRS account codes based on
the type of work accomplished. This allocation may be based on contractor estimates or
any method that NM management deems appropriate to reflect the percent of cost
allocated in each code based on the cost of labor and supplies used.
4.7.2. Functional Cost Codes (FCCs) and Usage. FCCs are used for all DoD Nutritional
Medicine organizations. FCCs are used to record NM expenditures, personnel time, and
workload. Specific written guidance governs MEPRS procedures and FCC usage: DoD
6010-13-M, Medical Expense and Performance Reporting System for Fixed Military Medical
and Dental Treatment Facilities Manual, and AFI 41-102, AF Medical Expense and
Performance Reporting System (MEPRS) for Fixed Military Medical and Dental Treatment
Facilities. The FCCs that are used most frequently in NM are as follows:
4.7.2.1. (EIA) Patient Food Operations. Provides meal service to inpatients, outpatients,
and transient patients. It includes activities such as routine inpatient rounds, therapeutic
menu development, patient tray assembly, and any activities related to patient feeding.
Supply expenditures include the following examples: enteral nutrition formulas, diet kits,
paper products for patient tray use only, insulated mugs and bowls used for the patient
tray line, selective menus, tray mats, office supplies used solely for inpatient feeding.
4.7.2.2. (EIB) Combined Food Operations. Includes subsistence, food preparation, and
services that are used for inpatient or non-patient feeding in the dining facility. This may
include menu and recipe development for regular menu items, sanitation of combined
areas, and subsistence accounting. Supply expenditures include the following examples:
cleaning supplies, plastic wrap, cooks’ knives, flatware, china, glassware, general office
supplies, and paper products used for both patient tray assembly and the dining facility.
4.7.2.3. (EIC) Inpatient Clinical Dietetics. Includes basic and comprehensive nutritional
care for patients. Activities include coordination of changes in diet requirements;
developing nutrition care plans; nutritional assessment and counseling, and clinical
nutrition management activities. Supply expenditures include pocket computers for
inpatient dietitians.
4.7.2.4. (FDC) Non-patient Food Operations. Includes nutrition management expenses
unrelated to patient care, but in support of staff and visitors. To include cashiers, serving
line, and dining facility functions. Supply expenses include dining facility trays, supplies
for cafeteria serving line, cash register tape, and napkins for dining facility use.
4.7.2.5. (BAL) Outpatient Nutrition Clinic. Includes comprehensive nutritional care to
outpatients including appointment scheduling, assessing and planning nutrition care,
individual and group instruction, and publication management of instruction materials
and handouts. Supply expenses include nutrient analysis programs used for weight
management, nutrition clinic office supplies, instructional materials used for outpatient
counseling.
4.7.2.6. (FCGH) Health Promotion. Includes awareness, education, and interventions
that support the Health Promotion target areas of Tobacco-Free Living, Nutritional
AFMAN44-144 20 JANUARY 2016 17
Fitness, Physical Activity, Healthy Weight and other Health Promotion initiatives as
indicated. EBBH should be used for administrative oversight of Health Promotion
programs. Non-MNT nutrition education should be counted as FCGH versus BALA.
4.7.3. Inpatient weighted nutrition procedures are provided to RMO monthly for inclusion in
MEPRS. This is critical manpower data and should be reviewed monthly by NM leadership
to ensure accuracy. (T-3).
18 AFMAN44-144 20 JANUARY 2016
Chapter 5
NUTRITION CARE
5.1. Medical Nutrition Therapy (MNT).
5.1.1. MNT is the development and provision of specific nutrition procedures in the
treatment of a disease or condition, or as a means to prevent or delay disease or
complications and optimize health and performance. MNT includes performing a
comprehensive nutrition assessment to determine a nutrition diagnosis, planning and
implementing a nutrition intervention using evidence-based nutrition practice guidelines, and
monitoring and evaluating an individual’s progress over subsequent visits. The level, content
and frequency of nutrition services that are appropriate for optimal care and nutrition
outcomes are individualized by the nutrition professional providing the MNT.
5.1.1.1. MNT is provided using the Nutrition Care Process (NCP) developed and
advocated for by AND. Documentation of care within the NCP utilizes established
terminology, with the goal of effectively communicating well defined components of
MNT. The NCP is a systematic approach to providing high quality nutrition care and
consists of four distinct and interrelated steps: nutrition assessment, diagnosis,
intervention, and monitoring/evaluation.
5.1.1.2. Evidence-Based Dietetics Practice and Standards. MNT is provided based on an
integration of the best available and up-to-date scientific evidence, professional expertise
and client values to improve outcomes. The AND’s NCM and PNCM are the preferred
source for evidence-based dietetics practice and patient education. However, other
professional sources may include but are not limited to: the AND’s Evidence Analysis
Library, Veteran’s Health Administration (VA)/DoD Clinical Practice Guidelines,
National Kidney Foundation, American Society for Parenteral and Enteral Nutrition
(ASPEN), American Heart Association, American Diabetes Association, the National
Institutes of Health (NIH), TRICARE Online, Medline Plus, Military One Source, and
the U.S. National Library of Medicine.
5.1.1.3. The NCM, PNCM, and SNCM are comprehensive online resources that cover all
aspects of nutrition management, and each MTF is encouraged to purchase each manual
that is appropriate to service their specific patient population, in the volume of
subscriptions adequate for their facility. Prior to purchasing, coordinate with AND and
the local Information Technology (IT)/Systems department to ensure the MTF’s range of
computer URLs can access the manual(s) at any one time up to the limit of subscriptions
purchased. Ideally, access to the NCM should be through the local intranet (vs. with a
username and password), but local IT guidance should be sought. Ensure the link to the
care manuals are centrally located, i.e., Medical Group (MDG) Intranet, for all MTF
personnel and providers to access, and market the availability and use of these resources.
5.1.2. Reproducible patient education materials from sources other than those listed above
may be utilized at the discretion of the credentialed RD.
5.1.3. Providing MNT.
AFMAN44-144 20 JANUARY 2016 19
5.1.3.1. Credentialed RDs and/or authorized diet therapy personnel (under the
supervision of a credentialed RD) provide MNT. (T-0). MNT is an essential component
of comprehensive healthcare. Appropriate screening processes should be developed to
identify those beneficiaries who would benefit from MNT in either the inpatient or
outpatient setting.
5.1.3.2. The screening and referral process should be coordinated to involve appropriate
medical, nursing and ancillary personnel, and to identify those patients who would most
benefit from the provision of MNT. .
5.1.3.3. Patients who will benefit from MNT include (but are not limited to) those with
diabetes, pediatric failure to thrive, dyslipidemia, hypertension, malnutrition, high-risk
pregnancy, renal disease, inflammatory bowel disease, celiac disease, liver disease,
obesity or pre or post bariatric surgery, metabolic syndrome, or are receiving enteral
and/or parenteral nutrition.
5.1.4. RDs and other providers such as physicians, dentists, certified nurse-midwives
(CNM), physician assistants (PA), nurse practitioners, and pharmacists may provide nutrition
education IAW their MTF clinical privileges and AFI 44-119, however this information
should be consistent with evidence based care guidelines and appropriate to the patient
condition or disease state.
5.1.4.1. Diet therapy craftsmen provide MNT as authorized by AF Form 628 and can be
authorized to provide MNT IAW Attachment 2, Diet Counseling Authorization Guide.
(T-3). Using this guide, the authorizing/credentialed RD determines what diets a diet
therapy craftsman may be certified on based on their assessment of the diet therapy
craftsman’s knowledge, ability, and skills. In addition, the authorizing/credentialed RD
defines the diet therapy craftsman’s scope of practice and required level of supervision
for each diet authorization.
5.1.4.2. MNT for inpatients may be provided without consult based on the patient’s
assessed nutrition risk per the MTF’s inpatient nutrition screening procedures. Medical
staff can also consult for inpatient NM services using SF 513, Medical Record –
Consultation Sheet, or electronic/MTF equivalent.
5.1.4.3. Inpatient diet orders, to include enteral nutrition support, nourishments, and
nutritional supplements, are ordered via the inpatient electronic medical record system.
(T-3).
5.1.4.4. Diet orders will be for regular or therapeutic diets offered at the facility. The
available therapeutic diets will be based upon the needs of the population served.
Components and defining characteristics of therapeutic diets will be consistent with
guidance from the Nutrition Care Manual. (T-0). Nonstandard diets requested by the
ordering provider to meet unique patient needs will be coordinated with the RD providing
care to that patient and/or the NM Flight Commander/Element Chief. See paragraph 5.3.
(T-3).
5.1.4.5. For Nutritional Medicine Clinics (NMCs) with an assigned RD, MNT for
outpatients is provided based on provider referral using SF 513 or electronic/MTF
equivalent. (T-3). Clients may also self-refer IAW MTF/Outpatient Nutrition Clinic
guidance. Generally, self-referrals to the outpatient nutrition clinic are limited to
20 AFMAN44-144 20 JANUARY 2016
participation in group classes. Local considerations, including characteristics of the
beneficiary population, resource constraints and MTF leadership priorities, will drive
decisions regarding provision of outpatient MNT. The MTF Commander will consider
options to ensure that all patients receive high quality nutrition services when the MTF
does not have an outpatient RD or diet therapist assigned, or when the need for MNT
within the beneficiary population exceeds resources available. (T-3). Possible options
include hiring a full-time or part-time civilian RD, contracting for nutrition services, tele-
wellness referral (if available/appropriate), or referral to an off-base provider if the MNT
benefit is covered by TRICARE. The MAJCOM Dietitian is also a resource for
coordinating MNT.
5.1.5. MNT Outcomes and Outcomes Management
5.1.5.1. MNT outcomes are measurable benefits and include: improvements in patients’
clinical, functional/behavioral, quality of life/satisfaction, or financial status as a direct
result of MNT. Tracking and documenting MNT outcomes is important because in
managed care, medical services are reimbursable insurance benefits only if they produce
positive outcomes in a cost-effective manner.
5.1.5.2. For NMCs with an assigned RD, each MTF will identify, prioritize and track
MNT outcomes significant for their patient population and relevant to the AF and/or the
MTF’s interdisciplinary teams, case managers, and disease and condition management
programs. (T-3). Committees such as the Integrated Delivery System (IDS), Population
Health Working Group, and Environment of Care, may be resourceful avenues for
tracking and marketing MNT outcomes.
5.1.5.3. The USAF Dietetics Benchmarking Tool can be used to track key metrics within
USAF dietetics. Within the domain of MNT and clinical dietetics, relevant metrics for
inpatients include: number of inpatient meals, number of inpatients, weighted diet
census, inpatient weighted nutrition procedures, and staffing metrics. For outpatient
MNT, RVU generation, Defense Enrollment Eligibility Reporting System (DEERS)
population numbers, presence of civilian and contracted RDs providing outpatient MNT,
and relevant MEPRS data should be tracked. This information is reported up from each
NM to the MAJCOM Dietitian and to the AF SG Consultant Dietitian. (T-3). Metrics
being tracked by the Population Health Working Group, such as patients with abnormal
HgbA
1
C values or elevated lipid levels, may be appropriate targets for MNT outcomes
collection. For RDs or Diet Therapy Craftsman who must divide their time between
population health and MNT, this information may assist in prioritizing patient
populations to serve and time spent. The NM Flight Commander/Element Chief should
be aware of unique factors within the population (e.g., related to the mission of the
installation), top 5 or top 10 ICD-9 diagnosis codes pertinent to nutrition, stated concerns
or objectives of the MTF leadership or installation leadership that are pertinent to
dietetics, and should use this information when establishing local outcomes for tracking.
The NM Flight Commander/Element Chief should also consult with MTF coding experts,
Resource Management Office (RMO) personnel, and other MTF personnel, to understand
expectations regarding RVU generation, tracking and facility standards which will
pertain to the NM Flight/Element. NM Flight Commander/Element Chief should look to
optimize coding and documentation in accordance with local and USAF guidance. When
selecting appropriate local outcomes for tracking MNT effectiveness, the NM Flight
AFMAN44-144 20 JANUARY 2016 21
Commander/Element Chief should consider use of the Nutrition Care Process (NCP).
The NCP is appropriate for use at the individual patient level, or for populations and
groups. Appropriate population assessment, establishing specific nutrition problems
which require nutrition intervention, and selection of meaningful monitoring and
evaluation criteria are part of effective outcomes management.
5.2. Patient Rights and Privacy.
5.2.1. All patients have the right to be informed about and participate in their nutrition care.
Reasonable efforts should be made to ensure patients’ food preferences are noted, menus
individualized, learning needs accommodated and special needs are met when applicable.
NM personnel will comply with all Privacy Act guidance and instructions such as AFI 33-
332, Air Force Privacy Act Program, and the Health Insurance Portability and
Accountability Act (HIPAA). (T-0).
5.3. Nutrition Screening.
5.3.1. MTF/NM will develop a nutrition screening process to determine the nutritional risk
for both inpatients and outpatients. (T-0). The screening and referral process should include
appropriate medical, nursing and ancillary personnel both in development and
implementation to best capture those patients who would most benefit from the provision of
MNT.
5.3.2. MTF policies and operating instructions will detail both inpatient and outpatient
populations to be screened, screening criteria and local processes and documentation
techniques. (T-3). A RD will educate the MTF staff on nutrition screening policies and
procedures as applicable. (T-3). Regardless of the screening process developed, the NM
Flight Commander/Element Chief should ensure that existing policies (inpatient and
outpatient) are updated appropriately, compliance with the policy is enforced, training is
conducted regularly, and modifications to the process are reflected in policy revisions.
5.3.2.1. Nutrition screening is not considered part of the Nutrition Care Process, but is an
essential precursor to the NCP. A selected nutrition screening process should reflect the
unique needs of the population served as well as the resources and considerations of the
facility. The AND’s Evidence Analysis Library (EAL) can serve as a resource to locate
validated, reliable screening and assessment tools. Other resources for use in developing
a nutrition screening process include, but are not limited to, the AND’s Pocket Guide to
Nutrition Assessment, ASPEN Core Curriculum or practice guidelines, and the CNM
Nutrition Screening Practices in Health Care Organizations.
5.3.3. Inpatient screening.
5.3.3.1. It is advisable that the existing admission assessment documentation (e.g., initial
nursing assessment and/or the history and physical) be reviewed and incorporated into a
nutrition screening process. This documentation may be a standard Essentris form and
modifications should be coordinated with Information Technology (IT) staff.
5.3.3.2. Inpatient nutrition screening is completed within 24 hours of admission to the
MTF. (T-0). This screening can be conducted by medical personnel outside of NM
according to locally developed processes. NM Flight Commander/Element Chief should
22 AFMAN44-144 20 JANUARY 2016
regularly monitor the performance of the local screening process to ensure compliance
and efficacy.
5.3.3.3. Pre-admission screening procedures are developed depending upon NM
resources and facility needs.
5.3.3.4. Dietitians will initiate the provision of MNT for inpatients identified as being at
nutrition risk, based upon local procedures and timelines. (T-3).
5.3.4. Outpatient screening
5.3.4.1. Diagnoses of interest should include: diabetes, pediatric failure to thrive,
dyslipidemia, hypertension, malnutrition, high-risk pregnancy, renal disease,
inflammatory bowel disease, celiac disease, liver disease, obesity or pre or post bariatric
surgery, metabolic syndrome, or those requiring enteral and/or parenteral nutrition. Other
diagnoses could be added based upon local population needs as determined by providers.
5.3.4.2. Coordination with the local contracted entity performing appointment scheduling
is recommended. Additionally, the provider staff should be educated on appropriate
wording and information to include in consults to NM. This will minimize inappropriate
self-referrals or unclear provider referrals.
5.3.4.3. NM/MTF will develop operating guidance for an outpatient nutrition clinic to
include patient referral, scheduling, class preparation, patient/family check-in procedures,
lesson plans, education evaluation tools, communication with other health care
professionals, and documentation. (T-3). Upon outpatient check in, two patient
identifiers need to be requested to validate the patient’s identify. (T-0).
5.3.5. Additional considerations for specific inpatient populations such as obstetrics or
pediatrics are considered as appropriate.
5.4. Documentation and Peer Review.
5.4.1. MNT is documented in the inpatient EHR (Essentris) and outpatient electronic health
record (AHLTA) or other MTF equivalent using the Assessment, Diagnosis, Intervention,
Monitoring, Evaluation (A.D.I.M.E.) format, as applicable. (T-3).
5.4.1.1. Additional hard-copy document forms include SF 513, SF 509, Medical Record
Progress Note, and SF 600, Chronological Record of Medical Care.
5.4.1.2. All medical record entries must include date and time, signature block, and
nutrition care provider signature, or as applicable with the local EHR. (T-3).
5.4.1.2.1. When documenting MNT via hard-copy forms the signature block format
will be (T-3):
Name, Grade, USAF, BSC
AFSC 43D3, Registered Dietitian
or
Name, Grade, USAF
AFSC 4D0X1, Diet Therapy Journeyman/Craftsman
5.4.2. Assessment data is found on the following forms or electronic/MTF equivalent: AF
Form 2572, Nutritional Assessment of Dietary Intake; AF Form 2508, Calorie Count; DD
AFMAN44-144 20 JANUARY 2016 23
Form 792, Twenty-four Hour Patient Intake and Output Worksheet; and AF Form 3067,
Intravenous Record.
5.4.3. Peer review is conducted quarterly. See paragraphs 9.2.4.4 and 9.2.4.4.1-3 for peer
review details. (T-3).
5.4.4. RDs conduct and attend inpatient dietary patient rounds, medical patient rounds,
nutrition support committee rounds, and discharge planning whenever possible. (T-3).
Pertinent patient data/notes are recorded in the MTF electronic health record. (T-3).
5.4.5. Participation in such interdisciplinary, patient-centered activities enhances
communication between care providers and allows the RD to obtain additional patient
information for assessments and re-assessments, menu selection assistance, information
regarding food preferences or intolerances, food allergies, educational needs, etc. In
addition, nutrition needs after discharge can be coordinated as needed.
5.5. Ordering Inpatient Meals and Nourishments.
5.5.1. Nursing Service uses AF Form 1094, Diet Order, AF Form 2567, Diet Order Change,
Composite Health Care System (CHCS), Essentris or electronic/MTF equivalent to order or
communicate the following to NM: therapeutic and non-therapeutic diets, Nothing Per Oral
(NPO), or out on pass; tube feedings; Total Parenteral Nutrition (TPN); food allergies; age of
pediatric patients; special tray preparations; and new patient admissions, discharges, or
transfers.
5.5.1.1. Local NM/MTF establishes guidance when diet orders and diet order changes
are required by NM to properly and effectively serve patient meals and nourishments.
Ideally, Nursing Service submits diet orders daily NLT 0500 hours, and diet order
changes NLT 1000 and 1500 hours.
5.5.1.2. All diet orders will comply with the AND as well as both print and online
versions of the NCM, PNCM, and SNCM. (T-0).
5.5.1.3. Therapeutic in-flight meals (TIM) for patients in the aeromedical evacuation
system are ordered using AF Form 2464, CTIM Telephone Diet Order, or electronic/MTF
equivalent. (T-3).
5.5.2. Nourishment Service.
5.5.2.1. Individual Nourishments.
5.5.2.1.1. The RD or other authorized health care provider will order additional
individual patient nourishments on AF Form 2568, Nourishment Request, on AF
Form 1094 or electronic/MTF-equivalent as appropriate. (T-3).
5.5.2.1.2. NM personnel ensure the individual nourishment is in compliance with the
current diet order. (T-3). NM will call the RD, Nursing Service, and/or patient’s
provider to clarify all ambiguous nourishment requests. (T-3).
5.5.2.1.3. All individual nourishments, diet specific or additionally ordered, will be
maintained on AF Form 1741 or electronic/MTF-equivalent. (T-3).
24 AFMAN44-144 20 JANUARY 2016
5.5.2.1.4. NM prepares nourishments and nourishment labels to include: patient’s
name, inpatient unit, room number, hour to serve, food item(s), preparation date and
time, and expiration date. (T-3).
5.5.2.1.5. NM delivers nourishments to Nursing Service or patients based on local
guidance. (T-3).
5.5.2.2. Bulk Nourishments.
5.5.2.2.1. NM will develop guidance for Nursing Service to order bulk nourishments
for supplemental patient feeding. (T-3). For example, frozen meals are commonly
obtained by nutritional medicine and distributed to the inpatient units on a nightly
basis in case a patient is admitted after the evening meal tray collection, ensuring
these patients receive a hot meal as needed. In addition, meals for residents working
overnight are commonly prepared and delivered IAW facility-specific guidance.
5.5.2.2.1.1. Outpatient clinics will procure their own supply of patient
nourishments using their own Government Purchase Card (GPC) and funding
source. (T-3). NM does not furnish outpatients or outpatient clinics with
nourishments. (T-3).
5.5.2.2.1.2. Nursing Service will order bulk nourishments on AF Form 2568 or
electronic/MTF-equivalent. NM will approve, prepare, and deliver bulk
nourishment requests IAW local guidance. (T-3). Nursing will sign for receipt of
nourishment delivery. (T-3).
5.5.2.2.1.3. All bulk nourishment items are labeled with the following: Inpatient
unit, food item, date and time prepared, and expiration date. (T-3).
5.5.2.3. All nourishments, individual or bulk, are for patient feeding only. Nourishments
are not to be consumed by hospital staff or visitors. (T-3).
5.5.2.4. Nourishments are modified based on food tolerances, food allergies, preferences
and diet order as appropriate and whenever possible. (T-3).
5.5.2.5. Inpatient Nourishment Refrigerators.
5.5.2.5.1. Nursing Service will monitor temperatures for inpatient refrigerators and
freezers used for patient nourishments. (T-3).
5.5.2.5.2. Temperatures are monitored three times a day with thermometers located
in the interior of the refrigerator and freezer compartments. (T-3). The outside
temperature gauge on the equipment is not always reliable and will not be used to
monitor interior temperatures. (T-3).
5.5.2.5.3. Record temperatures on a temperature chart according to local guidance.
(T-3).
5.5.2.5.4. Acceptable temperature range for refrigerators is 34 to 40˚ Fahrenheit. The
acceptable temperature range for freezers is -10 to 10˚ Fahrenheit. Acceptable
temperature ranges should adhere to AFMAN 48-147_IP, Tri-Service Food Code.
5.5.2.5.5. Local guidance must indicate specific procedures to be followed should
temperatures fall below standards. (T-3).
AFMAN44-144 20 JANUARY 2016 25
5.6. Inpatient Meal Service
5.6.1. NM will develop local procedures for providing inpatient meal service. (T-3). Several
variations of service are available and may include selective menus, nonselective menus,
room service or hotel style, or a combination of them all.
5.6.1.1. Procedures will outline how often patients on non-selective therapeutic diets are
visited on inpatient dietary rounds as applicable. (T-3).
5.6.2. Menu tickets, hard copy or electronic (Computrition), are used to assemble and
identify food trays for inpatients. (T-3). In accordance with Joint Commission standards,
menu tickets are to contain two patient identifiers. (T-0). As such, menu tickets are treated
as personal information and are protected under the Health Insurance Portability and
Accountability Act (HIPAA) and must be either filed or disposed of in an appropriate and
consistent manner (i.e. shredded upon discharge). (T-3). In addition, menu tickets must
contain the appropriate privacy act information, such as: “FOR OFFICIAL USE ONLY.
This page contains information protected under the Privacy Act of 1974, as amended. Do not
disclose without authorization”. (T-0).
5.6.2.1. The NM flight of each MTF generates their own menu tickets based on type of
menus offered, type food service operation employed, and existing specific therapeutic
diets. (T-3). This allows for personalization of menu items relative the diet-types offered
and enables menus to be updated as needed based on food item availability from their
prime vendor.
5.6.3. Menu patterns are modified based on food tolerances, food allergies, preferences and
diet order as appropriate and whenever possible. (T-3).
5.6.4. Salt Substitute. Do not give salt substitute to patients unless ordered by the healthcare
provider. Use mixtures of appropriate herbs and spices (non-sodium and non-potassium
based) instead. (T-3).
5.6.5. Disposable Tray Service. Isolation trays need not be routinely used for patients with
contagious diseases or infections per AFI 44-108, Infection Control Program. (T-3). Use
disposable tray service for radiation ablation therapy patients according to local procedures.
(T-3).
5.6.6. Psychiatric Patients. Nursing Service orders “paper products for precautionary
measures” for patients who could hurt themselves or others. Identify these patients by
stamping menu slips with “paper products.” (T-3). Other patient populations (e.g., radiation
ablation) may also require similar considerations; policies should reflect patient needs.
5.6.7. Mothers of breastfed pediatric inpatients are authorized inpatient meal service.
Follow all procedures outlined above for inpatients. (T-3).
5.6.7.1. Provisions may be made to provide postpartum mothers and their guest a one-
time “Proud Parent” meal. One guest of the post-partum mother may purchase a meal at
the proportional BDFA rate and must pay for the meal prior to the meal service.
5.7. Dietary Kardex (AF Form 1741) or Electronic/MTF-Equivalent.
5.7.1. NM will establish local procedures for use of AF Form 1741 or electronic/MTF-
equivalent. (T-3).
26 AFMAN44-144 20 JANUARY 2016
5.7.2. Create and complete a patient Kardex to communicate current and future nutritional
care to other dietitians and diet therapy personnel. (T-3).
5.7.2.1. Patient information to record, maintain, and update on the Kardex include
patient’s name, age, gender, diet order, nutritional risk level, food preferences, food
allergies, scheduled nourishments, nutrient/drug interactions, etc. As appropriate, these
considerations will be incorporated into provision of patient meals (see 5.5). (T-3).
5.7.3. Initial/sign each entry made to the patient Kardex when more than one person
performs dietary rounds or charting procedures. (T-3).
5.7.4. A patient Kardex is maintained until the patient is discharged. (T-3). Create
procedures to maintain a Kardex file for patients who are frequently re-admitted to ensure
continuity of care. (T-3).
5.7.5. Use the reverse side of AF Form 1741 to compute nonstandard therapeutic diets. (T-
3).
5.7.5.1. Modify the therapeutic menu pattern to reflect dietary restrictions and patient
preferences for use when writing the therapeutic menu patterns, as applicable. (T-3).
5.8. Meal Hours
5.8.1. The MTF Commander approves meal hours for inpatients and the NM dining facility.
(T-3).
5.8.2. For inpatients, the number of hours between the evening meal time and breakfast the
following morning must not exceed 15 hours. (T-3).
5.8.3. Adjust meal hours slightly to provide adequate preflight support of patients being
moved in the aeromedical evacuation system. (T-3). Feed post-flight aeromedical evacuation
patients at normal meal hours or as needed, depending on when the patients last ate a meal.
(T-3). If frozen meals are available, they may be given to such patients or medical center
residents that missed regular meal times due to duty or travel.
5.9. Bedside Tray Service.
5.9.1. NM prepares and delivers patient meal trays per diet order and patient preferences and
delivers to Nursing Service or patient’s bedside based on local guidance. (T-3).
5.9.2. Nursing Service prepares patients for eating, checks trays against diet orders before
serving according to local policy, and helps patients with feeding as needed. (T-3). Preparing
patients for the meal includes raising the bed, clearing bedside tables, etc. Note: This
instruction does not relieve the NM Officer or diet therapy supervisor of the responsibility for
checking patient tray service.
5.9.3. Nursing Service removes soiled trays from bedsides and returns trays to the food cart,
and checks trays for possible contamination prior to returning them to NM. (T-3).
5.9.3.1. Dishware and trays visibly contaminated with vomit, blood, drainage, secretions,
etc., will be wiped clean with hospital-approved cleaning solution before returning them
to the food service cart. (T-3). All contaminated medical supplies will be removed from
meal trays and disposed of on the inpatient unit. (T-3).
AFMAN44-144 20 JANUARY 2016 27
5.9.4. Nursing Service will check the food cart to ensure no contaminated paper service trays
are returned to the kitchen. (T-3). If a contaminated tray and/or its components are returned
to NM staging area, NM personnel will contact the responsible inpatient unit, and nursing
service personnel will be asked to retrieve and properly dispose of the contaminated material
on the tray. (T-3).
5.9.5. For patients receiving radiation ablation therapy, dispose of all disposable dishware on
the inpatient unit. (T-3). Do not return to NM any items taken into the patient’s room. (T-3).
5.9.6. For patients on precautions to prevent injury to self or others, all disposable dishware
is returned to NM on the food cart and disposed of in the usual manner. (T-3).
5.10. Enteral Nutrition, Medical Foods, and Infant Formulas.
5.10.1. Enteral formulas and other medical foods, and infant formulas are supply items
purchased by NM via the Government Purchase Card (GPC) for inpatient use. (T-3).
5.10.2. Providers will order appropriate enteral nutrition on AF Form 3066 or
electronic/MTF-equivalent, indicating product name, strength, and rate. (T-3). If feeding rate
is less than 24 hours, indicate the times of feedings and total number of milliliters per day.
5.10.2.1. Clinical dietitians will advise providers regarding the nutrient composition and
administration rates of enteral formulas available and will provide MNT to patients
receiving enteral nutrition following available evidence-based practice guidelines and
clinical judgment. (T-3).
5.10.3. Nursing Service personnel will order enteral nutrition on AF Form 1094, AF Form
2567, or electronic/MTF-equivalent, and include patient’s name, Uniform Cost Accounting
(UCA) code, unit, room number, enteral formula name, strength, and rate required. (T-3).
5.10.4. Nursing service will administer all enteral nutrition IAW the physician’s orders. (T-
3).
5.10.5. Enteral formula feeding bags and administration sets are procured by the inpatient
unit/ASF from Medical Materiel, as applicable. (T-3).
5.10.6. Feeding sets should be changed out according to local policy and manufacturer
guidelines.
5.10.7. NM will maintain an adequate supply of enteral formula products and deliver enteral
formulas to the inpatient unit. (T-3). Enteral formulas are routinely provided for a 24-hour
period. Enteral formula should be administered in such a way as to minimize waste (e.g. do
not hang 24 hours’ worth of formula when the maximum hang time for that system is 8
hours).
5.10.7.1. In MTFs without an assigned inpatient dietitian, enteral formulas and medical
foods may be purchased, prepared and dispensed by the Pharmacy or Nursing Service.
5.10.7.2. Infant formulas are supply items and are not procured, stored, or supplied by
NM. (T-3).
5.10.8. Enteral formulas and medical foods are not routinely issued to outpatients in CONUS
medical facilities. Arrangements for home enteral nutrition may be available through
28 AFMAN44-144 20 JANUARY 2016
discharge planning; however, the MTF Commander has the authority to approve Pharmacy to
dispense these items on a patient-by-patient basis. (T-3).
5.10.8.1. Medical foods for outpatients with inborn errors of metabolism may be
requested and dispensed by the Pharmacy on the written prescription of a provider IAW
AFI 44-102, Medical Care Management.
5.10.9. The MTF’s enteral formulary must be approved by a multi-disciplinary committee,
such as the Pharmacy and Therapeutics (P&T) Committee. (T-3). It is recommended that
there be a RD on the P&T Committee.
5.11. Parenteral Nutrition (TPN, PPN).
5.11.1. Providers will order TPN or PPN on AF Form 3066 or electronic/MTF-equivalent.
(T-3).
5.11.1.1. Clinical dietitians will advise providers regarding the nutrient composition and
administration rates of parenteral nutrition and will provide MNT to patients receiving
parenteral nutrition following available evidence based practice guidelines and clinical
judgment. (T-3).
5.11.2. Nursing Service personnel will order parenteral nutrition on AF Form 1094, AF
Form 2567, or electronic/MTF-equivalent. (T-3).
5.11.3. Inpatient pharmacy is responsible for preparing and delivering parenteral formulas to
the inpatient unit. (T-3). NM does not prepare, provide, or administer parenteral nutrition
solutions. (T-3).
5.11.4. Arrangements for home TPN are available through discharge planning.
5.12. Therapeutic Diets for Outpatients.
5.12.1. Outpatients are generally not provided meals at the expense of the NMF. There are
situations that vary between installations wherein meals or snacks are provided to diabetic
patients who have been in the Emergency Department (ED) for over 4 hours and admission
to the hospital is anticipated.
5.12.2. Various outpatient locations (i.e. ED, Hematology/Oncology) may request snack
items for patients for whom they anticipate an extended stay in the MTF while in nursing
care that require nutrition, and may be requested on SF 513 or electronic/MTF equivalent.
5.13. Patient and Family Education.
5.13.1. Patient and family education is provided throughout the continuum of care to meet
ongoing nutritional and behavioral needs. (T-3). It should include interactive, collaborative,
and interdisciplinary processes that promote healthy behavior and encourage patient/family
involvement in the nutritional plan of care.
5.13.2. The need for patient and family education for inpatients is assessed during
implementation of the NCP. (T-3). The need for outpatient education is assessed at clinic
encounters. (T-3).
5.13.3. Nutrition intervention takes into consideration cultural and religious practices,
emotional barriers, desire and motivation to learn, physical and cognitive limitations,
language barriers, and financial implication of care choices.
AFMAN44-144 20 JANUARY 2016 29
5.13.4. Patient and family education is interactive and addresses potential nutrient-drug
interactions, nutrition interventions, modified diets, patient and family responsibilities, and
follow-up information on accessing future care or community resources. (T-3).
5.13.5. Patient education is documented as part of the care provided, in the inpatient or
outpatient EHR as appropriate. (T-3). Additional hard-copy document forms include SF
513, SF 509, and SF 600. Nutrition education and MNT for patients/families commonly
offered should be IAW AFI 44-102 and/or based on the needs of the MTF/base patient
population and NM staffing and resources.
5.14. Health Promotion Nutrition.
5.14.1. Nutrition plays an important role in the AF Health Promotion Program (HPP).
Health status is dependent upon the collective behaviors, attitudes, knowledge, and beliefs of
family and community. To meet nutrition and fitness goals and outcomes, all interventions
should use multiple modalities of the Intervention Pyramid (see AFI 40-101, Guidance
Document). Delivery of programs and services are provided in locations where target
populations live, work, and play with emphasis on high population reach programs and
strategies.
5.14.2. The scope of practice for Health Promotion is to assess base population and
environmental nutrition needs, plan, collaborate, implement and evaluate community
nutrition strategies, interventions and programs and use multiple, evidence-based strategies
and interventions with the largest reach to impact population eating behaviors and outcomes.
Health Promotion Nutrition is addressed in AFI 40-104.
30 AFMAN44-144 20 JANUARY 2016
Chapter 6
FOOD PRODUCTION AND SERVICE
6.1. Production Planning.
6.1.1. (Automated) Production Planning. NM personnel will utilize Computrition to
automate their production planning processes IAW the current instructions outlined in the
Computrition Training & Reference Guide and Food Operations Management (FOM) User’s
Reference Guide. (T-3).
6.1.1.1. Menu Maintenance.
6.1.1.1.1. All meal changes and assignment of meals to cycle days is performed
under the Menu Maintenance function in Computrition. (T-3).
6.1.1.1.2. All recipes and food items are verified as being on the menu either by
crosschecking the screen or by using the View at Glance Report. (T-3).
6.1.1.1.3. Once the recipes and food items are verified, run the Menu Item Cost
Report. (T-3). This report must be run at least monthly, however, running the report
weekly to update the food costs in the system is recommended. (T-3).
6.1.1.1.4. Next, run the Recipe Price Report to obtain the updated costs. (T-3). Note:
The Menu Cost Report must be run prior to running the Recipe Price Report. (T-3).
6.1.1.2. Forecasting.
6.1.1.2.1. Forecasting is available when the menu is corrected and verified.
6.1.1.2.2. Forecast for menu items that require controlled quantity production. (T-3).
Daily consumables such as PC condiments, fountain soda, fresh fruit and other
similar items do not need to be forecasted within Computrition, but can be monitored
each month in Computrition to better help with ordering. To monitor daily
consumables, create a Cost Center in the Cost Center Table (system
setup>tables>items>cost centers) and use the Requisition Out to show how much was
used during the week. The review of the previous month’s daily consumables
utilization should assist with ordering/forecasting.
6.1.1.2.3. The Menu Maintenance function of Computrition is where the site
manager identifies what courses are to be forecasted (soup, entree, vegetable, etc.).
6.1.1.2.4. In Computrition, go to Menus Post Meal Count function and enter the
number of meals served into the actual count fields. (T-3). Click calculated prepared
button to automatically populate amounts in the prepared field. (T-3). There are three
options for forecasting to choose from: 1. Do not apply batching, Forecast equals
Prepared (selected by default). This option sets all prepared amounts to forecasts
amounts. 2. Batch (each menu meal separately). Select this option if batching should
be included for prepared amounts. 3. Overwrite existing prepared figures. Select this
option to overwrite any numbers that have been entered in the prepared fields. Once
an option is chosen, click in the Served field of each recipe and type the amounts
served. When amounts are placed in this field, figures are automatically entered into
AFMAN44-144 20 JANUARY 2016 31
the Leftover and Next Time fields. The Percent Count field is active if the Served
amount is less than the prepared amount. Click the Review Counts button to show
counts and have the ability to copy them forward to the next time the menu is served.
A number must be in the Served and Next Time fields of each recipe in order for
counts to be copy forward.
6.1.1.3. Calculate Yield Adjust. The post meal count function of Computrition to
forecast must be used at least five days prior to the day that the user would like to yield
adjust. (T-3). This is necessary for the pulling of food items three days prior to use (early
withdrawal; frozen meats, etc.) and prepping of items two days prior to actual meal
service (pre-preparation; gelatins, etc.).
6.1.1.4. Run Production Reports. Once the Post Meal Counts have been completed and
copied forward, run the Production Worksheet Report. (T-3). This report provides a list
of recipes and amounts required for producing the selected menus and meals for the
selected dates. Also, print the Menu Scaled Recipes Report this will print recipes for the
date and meal selected scaled to the amount required in the menus. (T-3).
6.1.2. (Manual) Production Planning. The Production Worksheet Report (Computrition) is
normally used to perform production planning. If Computrition or computer systems are
down, temporarily perform manual production planning (forecast food production needs for
the meals in the cycle menu, establish a food use monitoring system, and communicate
instructions to food production personnel in the planning, preparing, cooking and serving of
meals) according to local procedures. (T-3). Facilities with inpatient feeding only should
establish an alternate method of creating an audit trail for food use, AF Form 543, Food Issue
Record, menus and tally sheets. If the NM cash register does not have the capability of
inputting patient meal counts, menu items served to patients and the total number of servings
provided to patients must be documented according to local procedures. (T-3). The tally
sheet for patient meals and late trays, to include therapeutic menus, should also be tracked
and recorded according to local procedures.
6.2. Purchasing Non-Food Supplies.
6.2.1. Items for Patient Tray Service. Establish local operating procedures to request and
purchase nonfood supplies needed for patient tray service, dining facility operations, food
production, and sanitation. (T-3). These procedures must reflect types of items needed,
amounts used, replacement factors, stock levels, and delivery times. (T-3). Prepackaged
flatware sets and dining packets containing straw, napkin and condiments (sugar, salt, pepper
and sugar substitute) are allowed and are ordered by NM as supply items. (T-3).
6.2.2. Enteral Formulas and other Medical Foods, and Infant Formulas. See Chapter 5,
Section 5.10 for information on purchasing these items.
6.3. Food Portion and Waste Control.
6.3.1. Standardized recipes, serving utensils, and dishes are used to control portions, quality,
and cost of food served. (T-3). Foods should be cooked progressively, in small amounts as
needed to help ensure a fresher, more acceptable product. This practice also results in less
waste by cooking only what is needed as it is needed. NM production managers should
periodically observe plate waste in the dish room from dining facility service and patient
32 AFMAN44-144 20 JANUARY 2016
trays to evaluate patient’s consumption related to food quality, taste, portion control, quantity
prepared and acceptability.
6.4. Hazard Analysis and Critical Control Point (HACCP) HACCP is the prevention-based
food service safety system that must be used in NM. HACCP systems are designed to prevent
the occurrence of potential food safety problems. HACCP involves seven principles.
6.4.1. Analyze hazards. Potential food-related hazards and measures to control potential
hazards are identified. (T-0). The hazard could be biological, such as a microbe; chemical,
such as a toxin; or physical, such as ground glass or metal fragments.
6.4.2. Identify critical control points. (T-0). These are points in a food's production, from its
raw state through processing and shipping to consumption by the consumer, at which the
potential hazard can be controlled or eliminated. Examples are cooking, cooling, and
packaging.
6.4.3. Establish preventive measures with critical limits for each control point. (T-0). For
example, for a cooked food this might include setting the minimum cooking temperature and
time required to ensure the elimination of any harmful microbes.
6.4.4. Establish procedures to monitor the critical control points. (T-0). Such procedures
might include determining how and by whom cooking time and temperature should be
monitored.
6.4.5. Establish corrective actions to take when monitoring shows that a critical limit has not
been met. (T-0). For example, reprocessing or disposing of food if the minimum cooking
temperature is not met.
6.4.6. Establish procedures to verify that the system is working properly--for example,
testing time-and-temperature recording devices to verify that a cooking unit is working
properly. (T-0).
6.4.7. Establish effective record keeping documenting the HACCP system. (T-0). This
would include records of hazards and their control methods, the monitoring of safety
requirements and action taken to correct potential problems.
6.4.8. Food Temperatures. NM personnel complete AF Form 2582, Food Temperature
Chart, or local equivalent, before and during each meal to ensure foods are served at
appropriate temperatures IAW the AFMAN 48-147_IP, Tri-Service Food Code. (T-0).
Foods at other than optimal temperatures must be reheated or chilled as appropriate. (T-0).
6.4.9. Storing Subsistence Items. Subsistence storage rooms and refrigerators/freezers
MUST remain locked at all times when not in use. (T-0). Entry for all but authorized
personnel must be prohibited. (T-0). NM refrigerators should have the following: an
accurate thermometer inside the unit which can be viewed from outside the
refrigerator/freezer, a temperature chart to record readings taken at specific times IAW local
guidance unless centrally monitored by Facilities Management, a warning sign such as
“Determine No One is Inside Before Locking,” a safety lock release that lets the door open
from inside when externally locked, an electric light preferably mounted overhead with a
glass-dome bulb protector and a grid-type metal cover, and a sign indicating the type of
food(s) stored within and the required temperature range IAW the AFMAN 48-147_IP, Tri-
Service Food Code.
AFMAN44-144 20 JANUARY 2016 33
6.5. Sanitation and Infection Control. Sanitation and Infection Control. Refer to AFI 48-116,
Food Safety Program, AFMAN 48-147_IP, Tri-Service Food Code, AFI 48-117, Public Facility
Sanitation, and AFI 44-108, Infection Prevention and Control Program, for NM sanitation and
infection control policies. Limit access to food preparation and service areas by unauthorized
personnel. NM personnel performing dishwashing duties must always wear gloves as a
protective device against possible infections or contamination. (T-3).
6.6. Patient Tray Assembly. Patient trays are assembled using a centralized food service,
which places all food service workers under the supervision of the NM officer or diet therapy
supervisor. (T-3). Using the right patient tray service system aids in the appropriate use of
employees assigned. The size of the medical treatment facility determines the type of patient
tray assembly system used.
6.6.1. Heated Base With Enclosed Pellet System. Larger MTFs use the heated base with
enclosed pellet system. (T-3). This system can also be used to augment the hot and cold cart
system used in smaller facilities, if the tray carts cannot maintain a high enough temperature
for hot foods.
6.6.2. Hot and Cold Tray Cart System. The hot and cold tray cart systems are typically used
at smaller facilities due to reduced labor requirements. One person can prepare all trays and
additional personnel are needed only to deliver trays to patient inpatient units. If an MTF's
number of operational beds would normally dictate using a hot/cold food cart system, but the
contingency plan calls for an expansion capacity making the heated base with pellet system
desirable, retain and use the heated base with enclosed pellets system and conveyor belt.
6.6.3. Insulated Stacking Trays System. The Insulated Stacking Tray System is generally
used at small facilities that are supported by base food service.
6.6.4. Point of Service Trolley/Cart System. This system is intended for cook-serve meals to
be plated on the patient care units by food service workers. Food service workers will obtain
meal orders from patients at the bedside and then plate the food from a trolley/cart outside
the room. The trolley/cart typically has heated wells and refrigeration compartments to keep
foods at proper temperature. This system is designed to cater to patient food preferences at
mealtimes.
34 AFMAN44-144 20 JANUARY 2016
Chapter 7
FINANCIAL MANAGEMENT
7.1. Budgets. The purpose of an operations and maintenance budget is to plan for the
expenditure of funds in a manner that meets mission objectives within financial limitations. The
budget planning process requires time and effort to ensure sufficient funds are available for NM
operations. The MTF budget cycle usually begins a few months before the start of the fiscal
year. NM operating budgets are developed to include projections for supplies, equipment
purchases and maintenance costs, and required travel. To develop an operating budget the
following steps are followed:
7.1.1. Collect data, to include the previous year’s budget, actual expenses for the last year,
projections for new programs or services, inflation rate, and workload trends. (T-3).
7.1.2. Compare data: Analyze last year’s budget versus expenditures, and reasons for
variation. (T-3).
7.1.3. Compile data: Obtain current cost data for equipment and supplies, projected supply
usage, anticipating needs in all NM areas, including educational materials. (T-3). Obtain
input from key NM personnel. (T-3).
7.1.4. Draft the budget: Determine annual and quarterly costs. (T-3).
7.2. Prime Vendor. Prime Vendor is a concept of support whereby a single commercial
distributor serves as the major provider of products to various federal customers within a
geographical region or zone. The vendor supplies commercially available subsistence items
under a contractual agreement established by the Defense Supply Center Philadelphia (DSCP) or
Department of Veterans Affairs (DVA).
7.2.1. NM personnel must have a thorough knowledge of their Prime Vendor contract,
especially renewal timeframes. (T-3). Prime Vendor contracts are developed by DSCP in a
number of steps called the acquisition process. NM communication throughout this process
for generating new or renewing existing contracts is essential ensure specific NM subsistence
purchasing needs are met. Further information on establishing Prime Vendor contracts can
be found in the DSCP Prime Vendor Manual available on the DSCP website.
7.2.2. NM must communicate to DSCP specific subsistence needs such as low-fat dairy
products, special bread items, ice cream novelties and any dietetic items (low sodium, low-
fat, sugar-free). (T-3). NM must detail what is unique to its operation and the support
needed. (T-3). Any special requests or unusually large orders must be communicated to the
vendor. (T-3). Problems with vendors should be reported to DSCP for resolution, after
reasonable attempts to arrive at settlement have occurred with the vendor. Communication in
writing with DSCP on vendor’s performance, both positive and negative, is essential in
determining continuing contracts or future awards. Vendors must communicate with NM
and DSCP representatives during all phases of the contract award process. (T-3). It is the
prime vendor’s responsibility to communicate his terms not only to DSCP but also to NM.
(T-3). The Contractor Representative must be accessible to NM and the vendor’s customer
service must be available and easily reached by phone. (T-0). Vendor communication and
the level of service should be the same with government customers as it is with all others.
AFMAN44-144 20 JANUARY 2016 35
DSCP is responsible for explaining the contract and identifying the customer’s requirements.
DSCP is responsible for communications with all parties during the acquisition process.
DSCP must act as the customers’ advocate in communicating with the vendors and must
require vendors to adhere to the conditions and terms of the contract.
7.3. Financial Accountability. The duties of personnel purchasing subsistence will be
separated from the duties of personnel completing ration accounting so that no one individual is
responsible for both originating data (source records) and inputting/processing data. (T-3).
Therefore, individuals who issue food will not be authorized to close verify or issue/return
documents to the official inventory. (T-3). Storeroom personnel will not be responsible for
completing the NM Accounting Spreadsheet. (T-3).
7.4. Subsistence Purchasing. NM will purchase subsistence through DSCP or DVA prime
vendor contracts and local direct delivery contracts. (T-0). Small facilities with limited NM
operations may use Government Purchase Card (GPC) accounts to purchase subsistence items
needed for patient feeding. The cost of food purchased is charged to the medical sub-account of
04(X), Essential Station Messing (ESM), Military Personnel Appropriation. (Example: 5703500
320 48 562 525725). The correct ESM accounting classification number is updated annually and
is effective 1 October. A letter from the Air Force Services Activity (AFSVA), coordinated
through the AF SG Consultant Dietitian/BSC Associate Chief for Dietetics, and distributed to
MAJCOMs and MTFs indicates the updated ESM account classification number.
7.4.1. Subsistence orders are submitted according to locally established procedure. (T-3).
7.4.2. Subsistence acceptance authority is assigned to NM. (T-3). NM must designate
individuals authorized to accept or reject subsistence or supplies delivered under prime
vendor programs or other DSCP contracts. (T-3).
7.4.2.1. Designated personnel should verify the hard copy purchase order with the
vendor invoice from the driver. Ensure that products received match those ordered at
time of receipt so that the vendor’s delivery ticket may be annotated with any
discrepancies. (T-3). When discrepancies are detected upon receipt, the vendor’s invoice
will be annotated to indicate actual quantities received by striking through the listed
quantity and entering the received quantity and reasons for the differences (i.e., damaged,
short quantity, missing, substitution, high temperature, etc.). (T-3). These changes must
also be made in STORES before the STORES receipt is sent for payment. (T-3). If the
vendor substitutes more expensive food items, NM personnel should follow procedures
outlined in the prime vendor contract for resolution. The individual making the change
should initial all corrections to the distributor’s invoice. The carrier’s representative
should sign the invoice when such corrections are made. Any invoice changes must be
verified with prime vendor. When discrepancies are detected after receipt confirmation,
NM personnel should phone the distributor’s customer representative to request a one for
one replacement for the discrepant quantity.
7.4.2.1.1. Invoices must reflect only items/quantities accepted and signed for by the
NM receiving official. (T-3).
7.4.2.1.2. Invoices must be receipted through STORES DLA. (T-3).

36 AFMAN44-144 20 JANUARY 2016
7.4.2.1.3. STORES receipt prices must be used to upload data into Computrition
(Vendor receipts are used to verify items and quantity of items received, but vendor
prices are not used). (T-3).
7.4.2.1.4. Check each function in the billing chain: NM storeroom personnel, DSCP
or VA Account Manager and Contract Specialist, and Prime Vendor Billing
Department, to make sure all codes and billing/accounting information are correct.
(T-3).
7.4.2.1.4.1. Billing errors may result from many causes: invalid Department of
Defense Activity Address Code (DODAAC), incorrect Military Standard
Requisitioning and Issue Procedure (MILSTRIP) profile, TAC 3 billing address,
and/or ESM accounting classification.
7.4.2.1.4.2. The DODAAC is the unique code that identifies the NM activity. All
NM activities must have a DODAAC beginning with "FT" and followed by a
four-digit number. Codes with other two-letter prefixes, such as "FB” or "FM”
are incorrect. Questions or concerns about this code should be referred to the
MAJCOM Dietitian.
7.4.2.1.4.3. MILSTRIP PROFILES are the “ship to” address for delivering food.
The NM MILSTRIP profile must be current in the DSCP system for proper
billing and payment.
7.4.2.1.5. Each month the SF 1080, Voucher for Transfers Between Appropriations
and/or Funds, will be verified. (T-0). The SF 1080 is obtained from DFAS-
JDCBB/CO-EBS (Address: Defense Finance and Accounting Service; Attn: DFAS-
JDCBB/CO-EBS; P.O. Box 182204; Columbus, OH 43218-2204). Any billing
errors are corrected through the DSCP account manager. Procedures to verify the SF
1080 may vary from base to base. Each base must coordinate with their DSCP
account manager to determine the correct method. The typical method is as follows:
The SF 1080 will be verified with Computrition reports and vendor receipts. (T-1).
At the end of each month, the NM accountant or NCOIC will compare the amount
disbursed by DFAS to the amount of subsistence purchased as shown on the invoices.
(T-0). This is accomplished by comparing the total subsistence purchases recorded in
Computrition with total disbursements for the month. Each invoice paid will be
verified and marked if accurate payment was made. (T-0). A Memorandum for
Record will be attached to the report indicating invoices from previous months paid
during the current month and an annotation made by invoices to be paid in the next
month. Any discrepancies in amounts reimbursed by DFAS or invoices not paid
within two months will be submitted in a letter format to the regional DFAS office for
correction. (T-0). NOTE: Throughout the month the accountant may want to record
each invoice number and dollar value to facilitate reconciliation at the end of the
month. Invoices must reflect only items/quantities accepted and signed for by the
NM receiving official.
7.4.3. The subsistence GPC card in NM activities will be used for the purchase of
subsistence items only. (T-3). This card is not authorized for any other purchases. Items
other than subsistence to support the preparation or serving of foods may not be purchased
with this card. The government purchase card can typically only be used to purchase items
AFMAN44-144 20 JANUARY 2016 37
from DeCA. The NM government purchase card is for urgent clinically driven nutritional
requirements. Urgent purchases include foods for patient feeding when these foods are not
available through the prime vendor or DECA. If they are available through the prime
vendor, then the prime vendor must be used. The GPC cannot be used to purchase
subsistence from any other local sources unless approved by Corporate Food Service with
coordination with the Deputy Assistant Secretary Financial Operations.
7.4.3.1. Contact the base contracting office and request the GPC Procurement Program
Cardholder and Approving Official Account Set-Up Information application forms. Each
cardholder and each approving official must complete an application form. For address,
use the duty section address. Submit a letter of request for GPC card listing all
individuals responsible for subsistence procurement. Identify the primary approving
official as well as all designated alternates. All cardholders will receive monthly
statements of their account activity. The approving officials can view a monthly
summary statement on line. The approving official will not be a cardholder. (T-3).
7.4.3.2. Each cardholder must maintain a GPC account documentation binder IAW AFI
64-117, Air Force Government-Wide Purchase Card Program. (T-3).
7.5. Unauthorized Uses of Subsistence Items. MTF staff and visitors are not authorized to
consume unused trays, leftover food, or nourishments on inpatient care units. (T-3). Food items
purchased for use by NM activities will not be issued or given to the Pharmacy or nursing
service for making medications or coloring tube feedings. (T-3). Food items for blood sugar
testing, gastric emptying studies, etc. are purchased through their respective departments.
Pharmacy, nursing service and any other departments may purchase necessary subsistence items,
such as sugar, baking soda, cornstarch, or food coloring from DeCA or other vendors via their
own GPC accounts. Nonfood items such as charcoal and lighter fluid for NM theme meals
should be purchased with NM supply funds. (T-3). Subsistence funds and food items purchased
with subsistence funds are not used for guest meals, snacks, coffee breaks, cooking
demonstrations, parties of any type, blood donor or health promotion programs. Food items for
health promotion activities are purchased via separate health promotion GPC accounts. (T-3). If
food items for blood donor or health promotion programs are purchased by other departments
and are stored in NM, they will not be posted, included in the NM subsistence inventory, or
physically located with other subsistence. (T-3). These items will be controlled, specially
marked, and used only in support of the programs for which they were purchased. (T-3).
7.6. Perpetual Inventory. The Storeroom Manager is responsible for keeping the perpetual
inventory system of subsistence stock records and source documents for subsistence purchases
and issues. (T-3). Entries include vendor receipts and purchase invoices, GPC statements and
receipts, or AF Forms 543, Food Issue Record.
7.6.1. (Automated) . Access the Computrition online user manual for appropriate
procedures by pressing F1 while logged into Computrition. (T-3).
7.6.2. (Manual) . AF Form 542, Subsistence Stock Record, is used to maintain a perpetual
inventory of all food items in the storeroom. (T-3).
7.7. Physical Inventory.
7.7.1. A physical inventory is performed each month on one of the last three normal duty
days and is representative as of the date of the inventory (with the exception of FY close-out
38 AFMAN44-144 20 JANUARY 2016
when the inventory is performed on the last duty day of the month). (T-3). Pre-pulled
subsistence to be used for the weekend through the last calendar day must be issued on the
actual day used. Any inventory adjustment is to be posted to AF Form 546, Food Cost
Record, or NM Accounting Spreadsheet as of the date of inventory. (T-3). Post the
remaining days of the month and close out the AF Form 546 or NM Accounting Spreadsheet
on the last day of the month. The FY close-out in September should be conducted on the last
day of the fiscal year when possible; otherwise, it is taken on the last duty day and the above
procedures followed for closing out the account.
7.7.2. The MTF Commander or designee appoints a disinterested person (officer or
noncommissioned officer in grades E-7 or above) to perform a physical inventory of all food
items. (T-3). The inventory officer must be trained on their responsibilities and inventory
procedures. (T-3). This training should include directions on using the wall-to-wall
inventory method (shelf-by-shelf, top to bottom) to count and record the total quantity of
each item on hand. A NM representative will assist the inventory officer. The storeroom is
closed and no food issues are made until the inventory is completed. (T-3). Any food issues
made after the inventory are dated for the following day. (T-3). A physical count is taken of
each unissued food item on the inventory listing obtained from Computrition. (T-3). The
inventory officer delivers the completed and signed inventory listing to the Commander’s
Support Staff and NM Officer/NCOIC. (T-3).
7.7.3. Inventory Certification. After the inventory is done, the inventory officer and NM
inventory representative sign the following statement on the last page of the inventory listing:
"I certify this physical count of inventory is correct." (T-3).
7.7.4. If the physical count and the inventory records do not agree, attempt to recount the
item(s) and reconcile the differences using purchase invoices, issue logs, GPC receipts,
and/or Computrition reports. (T-3). When differences cannot be reconciled, an Inventory
Adjustment Report is prepared. (T-3).
7.7.4.1. Inventory Adjustment Report. When approved, this report is a valid accounting
document used to adjust discrepancies found during a regularly scheduled inventory.
NM will keep a copy of the approved report. (T-3).
7.7.4.1.1. The MSA officer and NM Accountant prepares the Inventory Adjustment
Report from the costed inventory listing to show actual overages and shortages by
item and the net total monetary adjustment. It must also show the total value of all
subsistence issued since the last inventory and the value of one half of one percent
(0.005) of that total. NM Storeroom personnel are not authorized to prepare this
report. (T-3).
7.7.4.1.2. NM submits the report to the squadron commander, who is authorized to
approve net dollar discrepancies of not more than one-half of one percent (0.005) of
the total dollar value of food used since the last inventory. (T-3). Food items that are
not approved for adjustment by the squadron commander as well as losses or
damages due to other than normal NM operations (fire or theft) may require Report of
Survey action by the commander.
7.7.5. Inventory Control. At the end of each quarter and the fiscal year, the dollar value of
the closing inventory, as reported on AF Form 541, Nutritional Medicine Service Subsistence
AFMAN44-144 20 JANUARY 2016 39
Cost Report, or NM Accounting Spreadsheet, will be between 15 and 30 percent of the
cumulative average monthly cost of food used for the fiscal year to date. (T-3). MTFs using
Prime Vendor for subsistence will reduce inventory levels to 2-3 days’ supply, or not more
than 15 to 30 percent of the cumulative average monthly cost of food used for the fiscal year
to date. (T-3). Optimal inventory levels must be determined locally to ensure that adequate
food is on hand/available in case of disaster or emergency situations when deliveries are
likely to be disrupted. (T-3). Additionally, it is important to review cumulative (versus
exclusively quarterly) dollar value of the closing inventory to meet monetary standards at FY
close out.
7.7.5.1. Additionally OCONUS locations may have special circumstance that preclude
strict adherence to a closing inventory value of 15-30 percent, secondary to varying costs
and transportation time, depending on availability and location of the prime vendor
utilized.
7.8. Closing a NM Activity. No less than four months prior to closing, start dropping the
inventory level to below the 25 percent level. (T-3). Adapt menus to use food in stock instead of
purchasing more food. (T-3). Gradually drop the inventory level so that two months prior to
closure, the inventory level is approximately 15 percent. At closure, transfer the last bit of
inventory to other base dining facilities. (T-3).
7.9. Issuing Subsistence.
7.9.1. (Automated) Items are issued in Computrition. (T-3). Access the Computrition
online user manual for appropriate procedures by pressing F1 while logged into
Computrition.
7.9.2. (Manual) AF Form 543 is used to issue food supplies manually. Once able to access
Computrition, transcribe all information. AF Form 543 is a source document used by the
MSA officer and NM storeroom personnel to maintain the official perpetual inventory of
food items. Storeroom personnel complete AF Form 543 for each day of the week and issue
direct delivery items on the day they are received. Perishable fresh fruits and vegetables may
be issued the day of purchase and receipt. High volume, low-cost items may be issued as
needed each day, or for a longer use period. Food items being issued should be listed by
food groups or some other internal order on the form to expedite issuing, posting, pricing,
and receiving.
7.9.2.1. The person receiving the food items from the storeroom counts and verifies food
received and signs the form in the “received” block. (T-3). If more food items are issued
than needed, return to inventory under “returned” column of form.
7.9.2.2. No later than the day following issue of food, post issues to AF Form 542
writing the balance of the item issued in column 1 as the item is posted, and the signed
forms are reviewed and checked by NM management. MSA office gets the original and a
copy; NM keeps a copy. (T-3).
7.9.2.3. The MSA office cost-extends the two copies of AF Form 543 marking column 2
of the form as each item is posted. One copy of the cost-extended form is returned to
NM for review and filing.
40 AFMAN44-144 20 JANUARY 2016
7.9.2.4. The MSA office retains on file the original cost-extended form and returns the
duplicate to NM for filing. NM retains the file for three years for audit purposes. (T-3).
7.10. Costing Subsistence Items. All MTFs use the Last-In First-Out (LIFO) costing method
for recording purchases and costing items. (T-3). With this method, the value of the inventory is
based on the last purchase price of each line item and as food items are purchased, the new unit
price, if applicable, is used to re-value the entire balance of that line item in the inventory. This
practice is designed into the automated system. (Note: First-In First-Out is still the preferred
method for rotating food items.)
7.11. Excess Cost. Excess Costs are feeding costs that exceed the monetary allowance
authorized for individual food components or needs. Examples of situations where
reimbursements are authorized include: use of operational rations (the cost of the operational
ration that exceeds actual earnings), substituted food items, unsatisfactory subsistence (spoilage
upon delivery), beverages for medical readiness exercises, and lost meals due to disaster or
exercise situations. These credits are not added to earnings, but rather subtracted from issues.
(T-3). The resulting dollar amount, Food Served, is used to calculate monetary status. (T-3).
Monetary credit is taken and annotated on the NM Accounting Spreadsheet in the excess cost
column; this is calculated into the earnings minus issues. The dollar value of issues will not
reflect any cost of subsistence items that were credited. (T-3).
7.11.1. The NM officer or diet therapy supervisor prepares a statement to support the other
income (credit), including the date and hour of the disaster, combat mission or field, alert or
medical readiness exercise. Certification of this statement is required by the MTF
Commander. (T-3).
7.12. Cashier Operations. Separation of financial duties and responsibilities in authorizing,
processing, recording and receiving cash transactions is essential to prevent loss of funds. NM
must develop a local instruction to detail how cashiering and accounting duties are separated so
as to establish adequate internal controls to prevent theft and abuse. (T-3).
7.12.1. Change Fund. DoD Financial Management Regulation 7000.14-R, Vol 5, Disbursing
Policy and Procedures, Chapter 3, Keeping and Safeguarding Public Funds, authorizes and
states how the NM Officer requests a change fund.
7.12.2. Cash Control. For A la Carte (ALACS) operations, a cash control supervisor must be
designated in writing. An adequate funds storage safe must be available to hold the change
fund, cash sales, and controlled forms. (T-3).
7.12.2.1. AF Form 2570, Nutritional Medicine Service Cash and Forms Receipt, is used
to issue the cash drawer, and AF IMT 79, Headcount Record, to the cashier as required.
The same AF Form 2570 is used by the cashier to return the cash drawer, cash collected,
and AF IMT 79 to the cash control officer after the meal. (T-3). Discrepancies are also
noted on AF IMT 79. (T-3).
7.12.3. Control of signature and cash collection forms and cash. The cash control supervisor
indicates funds and controlled forms (AF IMT 79) for turn in to MSA using AF Form 1305,
Receipt for Transfer of Cash and Vouchers, for cash collected and AF Form 1254, Register
of Cash Collection Sheets, for controlled forms used to document the transfer of
responsibility from NM to MSA. (T-3). If the forms used vary by installation, comply with
local policies.
AFMAN44-144 20 JANUARY 2016 41
7.12.3.1. The AF IMT 79 is a controlled form used to obtain the signatures of all persons
who eat in NM dining facilities at government expense (i.e., ESM), except inpatients.
The AF IMT 79 is also used to collect and record all funds of cash paying customers.
The designated NM representative, who must be a government employee, keeps a
separate file of completed AF IMT 79 forms in numerical order by serial number. This
file must be physically checked at least once each month to see that all forms are
accounted for by number. (T-3). No two AF IMT 79 forms bear the same number in the
same fiscal year. All numbered and unused forms must be kept in a locked safe. (T-3).
The MSA clerk furnishes the NM representative as many numbered AF IMT 79 forms as
may be required. The AF IMT 79 forms issued to NM are tracked on AF Form 1254 by
MSA. (T-3). Completed AF IMT 79 forms are turned in by the NM cash control
supervisor by listing the serial numbers on the same AF Form 1305 used to turn in AF
IMT 79 forms and cash to MSA.
7.12.4. Cash and Forms turn in to MSA. All cash collected and AF IMT 79 forms used must
be turned in to the MSA office daily, excluding weekends. (T-3). However, if the storage
limit on the safe/funds storage container is inadequate to support the amount of cash
collected over a 2 or 3 day weekend, make arrangements with the MSA office to turn in
excess cash to the MSA office during the weekend period, or request an increase, through
Finance, in the amount of funds the safe/funds storage container can store.
7.12.4.1. Cash deposit paperwork (AF Form 544, Nutritional Medicine Daily Facility
Summary Report, AF Form 1305, and AF Form 2570) must be done on a daily basis,
even if the money must be held over the weekend. (T-3).
7.12.5. ALACS Cash Register Operations. Cash registers are used with the capacity to
identify ESM diners by their last four social security numbers; record meal charges; produce
daily cumulative reports of total charges to each social security number; calculate discount
and standard meal prices; receive cash; record diner head count by category, including
transient patients, inpatients eating in the dining facility, and second servings from ESM
customers; produce both patient and dining facility food consumption reports; and record
totals for Food Service Operating Expenses collected. Care must be taken that the cash
registers are correctly programmed to both calculate and charge cash patrons the standard,
with surcharge rate as well as the discount rate, and correctly total the surcharges from each
meal period. See section 6.13. ALACS Recipe Pricing Operations, for additional information
on standard and discount rates.
7.12.5.1. The DoD subsistence surcharge (operating expense) is proportionately divided
between the AF Military Personnel Appropriation (MPA) and the Defense Health
Program (DHP) O&M appropriation based on the percentage of the MTF dining hall’s
military and civilian manpower authorizations (per the Unit Manning Document). MTF
military personnel are funded by the AF MPA and civilians are funded by the DHP O&M
appropriation. MTF MSA officers will proportionately divide the surcharge accordingly
with the start of each FY. (T-3). For example, if the FY surcharge collected is $100 and
the MTF dining hall manpower authorizations are three military and seven civilian
personnel, then the proportionate amount to deposit to MPA is $30 and the amount to
deposit to the DHP O&M is $70 (e.g., out of 10 employees, 30 percent are military and
70 percent are civilian, therefore $100 would be divided respectively).

42 AFMAN44-144 20 JANUARY 2016
7.12.5.2. Cash register maintenance contracts are established and adequate supplies of
tapes and ribbons are procured locally through Medical Logistics. (T-3).
7.12.5.3. Cashiers must offer all customers a receipt for their purchases. (T-3).
7.12.6. Subsistence Credit Allowance Management System (SCAMS) Cashier Operations.
In SCAMS operations, all diners in a government dining facility, except ambulatory and
transient patients, sign for meals. The cashier verifies the diner's identification. In overseas
areas, authorized medical facility local national employees will pay for meals according to
the Status of Forces Agreement (SOFA) for that country. (T-0). Local disaster plans may
address use of personal checks and/or lost meals due to disaster situations.
7.12.6.1. Meal rates at appropriated fund facilities using SCAMS. Meal rates at SCAMS
facilities are established by the Office of Under Secretary of Defense (Comptroller).
Meal rates are posted annually effective 1 January and can be downloaded from Tab G of
the Department of Defense FY Reimbursable Rates table,
http://comptroller.defense.gov/rates/. This table also describes who is eligible for the
standard or discount rate.
7.12.6.2. All non-ESM persons entering the dining facility must pay the posted price of
the meal being served, regardless of the type of meal items or quantity selected. (T-3).
Some small volume feeding overseas facilities do not have cash registers and use the AF
IMT 79, Headcount Record, to record patron meals. Separate AF IMT 79 forms are used
for cash and ESM diners. (T-3).
7.12.6.3. The cashier ensures the AF IMT 79 forms are completed daily for each meal
period. (T-3). A separate AF IMT 79 is used for non-U.S. citizen civilian employees
overseas who are allowed to eat in the dining facility. (T-3). Use a separate AF IMT 79
for breakfast, lunch, and dinner. (T-3). These forms will not be "carried over" from one
meal to another. Therefore, in facilities where an authorized change fund is allotted for
both dollars and the local currency, three AF IMT 79 forms are issued per meal (one for
meal card holders, one for dollars, and one for local currency). (T-3).
7.12.6.4. Air Force Reserve members must present verification of eligibility for ESM
meals (reserve active duty orders or AF Form 40a, Record of Individual Inactive Duty
Training) while on active duty training or inactive duty for training, sign AF IMT 79 as
required, and write their names and last four social security numbers legibly on the forms.
(T-3). NM will make a copy of the member’s orders and turn in copies to MSA with the
AF IMT 79s for the day. (T-3). AD and Reserve members who receive the subsistence
portion of per diem are not authorized to subsist at government expense and must pay for
their meals. (T-3). When a guard or reserve unit member does not receive the subsistence
portion of per diem, they do not pay for their meals, but instead sign a separate AF Form
79 (separated by unit). (T-3). Note: Billing may be required by MSA.
7.12.6.5. After the meal, the NM supervisor verifies entries on the AF IMT 79, signs the
form, and then transfers the number of meals for each different category onto the
appropriate entries in the NM Accounting Spreadsheet (automated) and AF Form 544.
(T-3).
7.12.6.6. When the amount of cash collected varies from the number of signatures and
total amount due, the supervisor investigates and states the explanation for overages or
AFMAN44-144 20 JANUARY 2016 43
shortages on AF IMT 79. (T-3). Include the name(s) of the cashier(s) during the meal.
(T-3). If no reason for the cash variance is apparent, state that there is no apparent reason
for the cash variance. (T-3). NMs should establish local policies and procedures to track
cashier overages and shortages so corrective action or training can be initiated.
7.12.6.7. The completed AF IMT 79 forms and collected cash are delivered to the MSA
officer at least once each normal duty day. The MSA officer will, upon receipt of
completed AF IMT 79 forms, and the cash from the NM cash control supervisor, verify
the cash receipts against the total amount of cash received. (T-3).
7.12.6.8. Small volume feeding facilities will use Computrition to track inventory, as
well as all purchases and requisitions. (T-3). The NM Accounting Spreadsheet
(automated) is used to record daily earnings, issues, and purchases, as well as all relevant
patient feeding activities (APV/SDS) and patient bed days.
7.12.6.8.1. In the event the computer systems were down for an extended period of
time, the SCAMS facility would utilize standardized AF Form processes (i.e., AF
Form 542, AF Form 543, AF Form 544, and AF Form 541) to track earnings and
issues until appropriate entries could be made in the NM Accounting Spreadsheet or
Computrition, once automated operations resumed. (T-3).
7.13. Eligibility and Identification of Diners. DOD 1338.1 0-M, Manual for the Department
of Defense Food Service Program, AFI 41-115, Authorized Health Care and Health Care
Benefits in the Military Health Services System, and AFH 41-114, Military Health Services
System Matrix, state who is eligible for medical care in AF medical facilities, prescribe the extent
of care allowed, provide guidance for care, and delineate who pays standard and discount meal
rates (see Attachment 3). Meal rates are published annually by the Office of Under Secretary of
Defense (Comptroller) and are typically released by HQ USAF/SG3 to resource management
officers in December, with an effective date of 1 January. All meal rate prices must be posted at
the dining facility entrance or serving areas. All MTF staff members must pay for all food
consumed.
7.13.1. Transient patient. Transient patients in the aeromedical evacuation system or Non-
Medical Attendants (NMAs) do not pay or sign for meals. They are identified by the patient
identification wristband or IAW local procedures. A patient ceases to be a transient patient
when admitted to a MTF. The number of transient patients at each meal is recorded as a
Remain Over Night (RON) patient on the NM Accounting Spreadsheet (automated) and AF
Form 544, Nutritional Medicine Daily Facility Summary Report (manual). (T-3). Breakfast
meals are calculated to receive .20 meal credit; lunch and dinner, .40 meal credit. (T-3).
7.13.2. Nonmedical attendant (NMA). The nonmedical attendant of a hospitalized patient
pays the appropriate charges for all meals consumed.
7.13.3. Essential Station Messing (ESM). ESM diners are enlisted members authorized to eat
at government expense. Medical enlisted personnel and airmen assigned to the MTF present
their DoD Common Access Card (CAC) Identification Card. (T-3). Enlisted personnel in
TDY status must show valid orders and their DoD CAC Identification Card. (T-3). Follow
installation-specific guidance for identifying eligible personnel as appropriate.
7.13.3.1. The OIC/NCOIC of NM validates ESM diners using last name and last four of
Social Security Numbers for identification and spot check signature/cashier records to

44 AFMAN44-144 20 JANUARY 2016
ensure that only authorized personnel are subsisting at government expense. (T-3). A
current listing of ESM diners from the base Force Support Squadron should be received
and reviewed at least monthly.
7.13.4. Inpatients and ambulatory procedures visit (APV)/same day surgery (SDS).
Inpatients and APV/SDS patients are identified by nursing staff using AF Form 1094 or
through the Essentris-Computrition interface. (T-3).
7.13.5. Outpatients. Outpatients in the MTF for treatment may purchase meals from vending
machines or directly from NM as guests.
7.13.6. Wounded Warrior (WW) Meals. In accordance with the National Defense
Authorization Act for Fiscal Year 2009, section 602, MTFs provide meals at no cost (and no
surcharge) to certain injured members of the Armed Forces while receiving healthcare
services for an injury, illness, or disease incurred in support of OPERATION IRAQI
FREEDOM, OPERATION ENDURING FREEDOM, or any other operation or area
designated by the Secretary of Defense. (T-0). Healthcare services include medical
recuperation or therapy or other continuous care as an inpatient or outpatient.
7.13.6.1. Wounded Warriors (WW) will present DoD Form 714, Meal Card, indicating
that member is a WW entitled to a meal free of charge. (T-0). In addition, WW’s must
present CAC Military Identification Card. (T-3).
7.13.6.1.1. For bases that do not have a local WW Liaison Office or Coordinator to
issue WW meal card (DoD Form 714, Meal Card), NM will establish a local
guidance to properly identify eligible WWs to help prevent fraud, waste and abuse of
this privilege. (T-3).
7.13.6.2. The NM cashier will process the WW’s meal at no cost and input meal
purchase into the cash register system IAW local procedures. (T-3).
7.13.6.3. WW will sign a separate AF IMT 79 entitled, “Wounded Warrior”. (T-3). AF
IMT 79 will include at a minimum WW name, rank, unit of assignment, and contact
information. (T-3).
7.13.6.4. The number of WW meals served will be entered daily as a wounded warrior
into the AF Accounting Spreadsheet. (T-3).
7.13.6.5. A tally of total WW meals will be tracked on the AF Accounting Spreadsheet
and NM will provide monthly cost and service summaries per local guidance obtained
from AFSVA. (T-3).
7.13.6.6. NM will advertise the WW meal program by posting the Assistant Secretary of
Defense for Health Affairs Memorandum dated 4 February 2009 on bulletin board(s) in
the NM department visible to patrons. (T-0). The memorandum can be located at
http://www.tricare.mil/ocfo/_docs/20090204%20Permanent%20Waiver%20of%20
Meal%20Surcharge.PDF.
7.13.7. Non-admitted meals (NAMs). This is a category of meal accounting for designated
outpatients in the MTF. The Diet Therapist will annotate on AF Form 2573, Weighted Diet
Census. (T-3). Follow local infection control policy when providing food to non-admitted
patients. (T-3).

AFMAN44-144 20 JANUARY 2016 45
7.13.7.1. Outpatients in the MTF for treatment (not APV or SDS) for greater than 4
hours (i.e. chemotherapy clinic, dialysis clinic, emergency room) who by virtue of their
care cannot leave the area to obtain food or beverage may be provided
nourishment/meals. Meals/nourishments provided are accounted for under “non-
admitted meals” on the accounting spreadsheet. NAM eligible outpatients do not visit the
dining facility to obtain a “free” meal. The NDAA 2012 provision of food guidance can
be found at: http://www.gpo.gov/fdsys/pkg/BILLS-112hr1540enr/pdf/BILLS-
112hr1540enr.pdf. The guidance can be located on page 175, section 704, 0178b
(Provision of food to certain members and dependents not receiving inpatient care in
military medical treatment facilities).
7.13.7.2. Parents (non-patients) who are required by the physician to stay on the pediatric
inpatient unit to be with their child (the patient) may be served meals on the unit. Meals
are accounted for under “non-admitted meals” on the accounting spreadsheet. (T-3).
7.13.7.3. Breastfeeding mothers (non-patients) of infants admitted to the hospital may
receive a tray in place of the infant. Meal cost is tracked on the accounting spreadsheet in
the “non-admitted meals” column.
7.13.7.4. When requesting food and beverages from the MTF’s Food Service
Department it is important that: (1) communication is accomplished in a timely manner to
take care of the patient’s nutritional needs, (2) dietary restrictions are addressed at the
time the order is placed, and (3) food and beverages are provided in a timely manner in
accordance with the MTF’s routine food service procedures.
7.14. ALACS Recipe Pricing Operations. In ALACS each recipe item is priced and sold on
an individual item basis. Computerized menu pricing reports such as the Computrition Recipe
Price Report must be available. (T-3). Each recipe cost that is not available from these programs
must be manually calculated, per DoD guidance: When using an “a la carte” menu, the price of
every item on the menu shall be established at 133 percent (surcharge) of the food cost (i.e., the
cost of unprepared food multiplied by a factor of 1.33). The following category of diners will be
charged a discount price. (T-3). This discount price is the menu cost minus the 33% surcharge.
The discount rate shall not be charged to:
(a) spouses and other dependents of enlisted personnel in pay grades E-1 through E-4.
(b) members of organized nonprofit youth groups sponsored at either the national or local level
and permitted to eat in the general dining facility by the Commanding Officer of the installation.
Such groups include: Civil Air Patrol, Junior ROTC and Scouting units.
(c) officers, enlisted members, and federal civilian employees who are not receiving the meal
portion of per diem and who are either: (1) Performing duty on a U.S. Government vessel, (2) On
field duty, (3) In a group travel status, or (4) Included in essential unit messing (EUM) as defined
in the JFTR, Volume 1.
(d) officers, enlisted members, and federal employees who are not receiving the meal portion of
per diem, and who are on a U.S. Government aircraft on official duty either as a passenger or as
a crew member engaged in flight operations.
(e) officers, enlisted members, and federal employees on Joint Task Force operations other than
training at temporary U.S. installations, or using temporary dining facilities.
In addition, when calculating the base menu item cost, an additional 20% condiment fee may be
added to the basic cost per portion of all items served in appropriated fund food activities. This
46 AFMAN44-144 20 JANUARY 2016
addition is intended to cover condiments, and items that are not recipe ingredients (nonstick
spray, fryer oil), and food preparation losses from spillage, burning, discarded, etc. Ideally this
variable percent should be adjusted per menu item. As an example, if French Fries cost $0.50
per serving from the prime vendor, a 33% surcharge is added. In addition, since this is a non-
ready-to-eat food (needs to be fried), a 20% condiment charge is added, making the cost to the
patron $0.80. Conversely, a pre-portioned ready-to-eat food item such as an 8 oz carton of milk
should have a surcharge of 33% (per DoD ALL menu items are assessed surcharge) and
condiment additive of 0% since it is ready to eat.
7.14.1. ALACS facilities are encouraged to round menu item prices at the registers to the
nearest $0.05.
7.15. Special Feeding Circumstances. Responsibilities for control measures, when feeding
under disaster and combat conditions or during field, alert, and medical readiness exercises, are
the same as those under normal circumstances. Personnel who receive monetary allowance for
subsistence must pay for their meals, including paying for operational meals such as MREs. In
normal NM management procedures apply during disasters, in combat areas, and during field,
alert or medical readiness exercises as often as possible. Special cashier procedures may have to
be instituted during disaster or emergency conditions. The installation commander provides the
MTF Commander with a statement (verbal, followed in writing) that emergency or disaster
conditions prevail and that it is essential to furnish food to persons other than those normally
allowed. (T-3). Those persons able to pay for meals sign AF IMT 79 if required, and pay
according to Attachment 3 of this Manual. (T-3). Those persons unable to pay for meals sign a
separate AF IMT 79. (T-3). The diet therapy supervisor or other specified person writes the
name of the group of persons being fed on the AF IMT 79 above the title. (T-3). If it is not
feasible to obtain signatures, as in the case where food support is provided to another civilian
hospital, the NM officer certifies the number of meals furnished on a separate AF IMT 79 and
includes the statement: “I certify that (number of meals) were provided to (the name hospital) in
(location) due to (situation, such as hurricane) for (the meal period, meal date).” (T-3). The
number of meals is included on AF Form 544 and NM Accounting Spreadsheet. (T-3). Credit is
taken for all meals. (T-3). The MSA officer and NM accountant maintains documentation to
prove entries on AF IMT 79 and 544 and NM Accounting Spreadsheet. (T-3). If feasible, the
MSA officer bills the appropriate agency for the costs of meals provided.
7.16. NM Ration Accounting. For accurate NM financial reports, NM accounting parameters
must be accurate and up to date, whether calculated on the AF Accounting Spreadsheet or
manually. (T-3).
7.16.1. A ration is the quantity of nutritionally adequate food required to subsist or feed one
person for one day.
7.16.2. The Food Cost Index is a DoD prescribed list of food components and quantities that
represent the allowance for fifty-five standard ration food items, which is used to compute
the Basic Daily Food Allowance (BDFA). (T-3).
7.16.3. The BDFA is a prescribed quantity of food, as defined by components and monetary
value, required to provide a nutritionally adequate diet for one person for one day.
7.16.3.1. (Automated) . The MTF BDFA is calculated monthly on the NM Accounting
Spreadsheet using the most current Food Cost Index. (T-3). The BDFA can also be

AFMAN44-144 20 JANUARY 2016 47
calculated using the Joint Culinary Center For Excellence Quartermaster Website at
http://www.quartermaster.army.mil/jccoe/operations_directorate/quad/BDFA/bdfa
_main.html. The template built into the NM Accounting Spreadsheet must follow the
Food Cost Index obtained from the Defense Logistics Agency. (T-3). For correct
computation of this allowance, using prime vendor contracts or DeCA, the exact
subsistence items referred to by the National Stock Number (NSN) need to be verified.
(T-0). When verifying items and calculating the BDFA, food substitutions may only be
used if the exact food item listed by the stock number is unavailable through prime
vendor. (T-3). Even if the item is not used, if it is available, it must be priced for BDFA
calculation. Do not substitute higher cost items not intended for use to artificially raise
the BDFA, and do not substitute higher cost items because of personal preference. (T-3).
7.16.4. Patient Basic Daily Food Allowance (Patient BDFA) is the MTF BDFA with an
added 15 percent supplemental allowance (Patient Supplemental Percentage) to help defray
the cost of bulk nourishments. The Patient BDFA is only used to calculate patient meal day
earnings. Only one Patient BDFA applies for the full calendar month.
7.16.4.1. (Automated) Use NM Accounting Spreadsheet to compute Patient BDFA for
patient meal days served each day. (T-3).
7.16.5. Small Volume Feeding Allowance/Percentage. NM activities using SCAMS and
serving less than 100 average daily meal days for both patient and dining facility patron
rations are authorized an additional supplemental allowance of 15 percent of the MTF BDFA
in order to adjust for the increased costs of feeding a smaller number of people. (T-3). This
eligibility is determined at the end of each month using the previous months average daily
meal days, and is applied to ESM and SCAMS dining facility patrons only. It is not
authorized for ALACS cash sales. (T-3). If allowed, the 15 percent supplemental allowance
is used to figure the next month’s MTF BDFA. As an example, if calculating the small
volume allowance for August, you would take the total meal days for July, divide by 31
(days in month), if the total is less than 100, then the allowance is authorized.
7.16.6. Therapeutic In-flight Meal (TIM) Allowance. A special monetary allowance equal to
80 percent of the MTF BDFA is authorized for each TIM furnished by the NM activity for
aeromedical evacuation patients to be consumed in flight. Additional guidance may be found
in AFI 41-301, Worldwide Aeromedical Evacuation System, and AFI 41-307, Aeromedical
Evacuation Patient Considerations and Standards of Care.
7.16.7. Holiday and Special Meal Percentages/Allowances. An additional meal allowance is
permitted for certain federal holidays, typically Christmas and Thanksgiving, the Air Force
birthday, and Airmen appreciation meals. The extra earnings allowed for holidays and
special meals are designed to recoup additional costs incurred, to include serving items in the
dining facility to ESM patrons at all facilities and cash patrons at SCAMS facilities, as well
as for holiday meal enhancements for inpatients (e.g., nut cups, ice cream, cake, candy, etc.).
For these meals, an additional 25% meal allowance is permitted. For Airman appreciation
meals, an additional 15% is allowed. Christmas and Thanksgiving holiday meals must be
served at the lunch meal. If holiday or special meals are served on dates other than the
holiday, the Accounting Spreadsheet manager should be informed. There must be a special
menu planned and served to qualify for the additional allowance. A la Carte facilities do not
48 AFMAN44-144 20 JANUARY 2016
receive an additional 25% on cash customers as any additional cost associated should be
calculated into the cost of the food.
7.16.7.1. (Automated) NM Accounting Spreadsheet automatically calculates the
additional 25 percent holiday lunch percentage for Thanksgiving and Christmas. To
calculate extra earnings for other holidays and special meals in SCAMS facilities, the
number of ESM lunch meals served is added to the number of cash patron lunch meals
served and this is then multiplied by 25 percent (or 15 percent for airman appreciation
meals) to equal the additional number of meal days. This additional number of meal days
multiplied by the current MTF BDFA will equal the amount of additional earnings for the
holiday lunch meal. For ALACS facilities the same procedure is followed, only the
additional meal day earnings for other federal holidays is determined only by the number
of ESM customers, and patients served.
7.16.8. Occupied Bed Day refers to the number of inpatients subsisting in the MTF and
equals beds occupied minus bassinets from the Admission and Disposition Recapitulation
Report.
7.16.9. A Meal Day is a value in which the number of meals is weighted by a predetermined
percentage (IAW DOD 1338.10-M) to balance the cost and attendance variances between the
meals. The number of meal days for a given day is figured by multiplying the number of
breakfast, lunch, and dinner meals served by the factored percentages of 20, 40, and 40
percent, respectively, and totaling the results. TIMs are valued at 80 percent, APV/SDS
meals at 40 percent, holiday meals at 65 percent, and, if served, midnight meal at 20 percent.
If APV patrons utilize the dining facility for breakfast, they are valued at 20 percent of the
BDFA. Beginning in Fiscal Year 2016, the number of meal days for a given day is figured
by multiplying the number of breakfast, lunch, and dinner meals served by the factored
percentages of 25, 40, and 35 percent, respectively, and totaling the results.
7.16.10. Patient Meal Days are obtained by multiplying the occupied bed days times the
appropriate meal factors.
7.16.11. ESM Meal Days are obtained by multiplying the number of ESM patrons multiplied
by the appropriate meal factors.
7.16.12. Cash Patron Meal Days are obtained by multiplying the number of cash customers
times the appropriate meal factors.
7.17. Subsistence Account Reporting and Management.
7.17.1. AF Forms 544, Rations Earning Record, the NM Accounting Spreadsheet and
Computrition are used to assist NM managers and the MSA Officer in overseeing the
subsistence account, inventory value, earnings and collections. AF Form 544 or electronic
equivalent, and the NM Accounting Spreadsheet will be made available to the MSA Officer
to facilitate daily, monthly, quarterly, and end of fiscal year oversight of subsistence
accounting. (T-3). NM operations are encouraged to place electronic versions of the 544,
and the NM Accounting Spreadsheet on a shared drive, with limited access to key personnel
within NM and MSA.
7.17.1.1. (Automated) . AF Form 544 and the NM Accounting Spreadsheet have all of
the information needed to monitor key financial indicators in NM.
AFMAN44-144 20 JANUARY 2016 49
7.17.1.1.1. The Computrition Inventory Movement Summary Report provides
detailed information pertaining to food purchases. The report can be sorted by food
categories or dollar value. The verified total from this report should be compared to
the cost of food purchased for the day from invoices received.
7.17.1.1.2. The Computrition Inventory Cost Report lists inventory items by
category, NSN, vendor issue unit, issue cost, quantity on hand, and value of current
inventory. This value is entered on the NM Accounting Spreadsheet.
7.17.1.1.3. AF Form 544 is used to record the number of meals served in MTFs. The
information on AF Form 544 is used as a guide for determining the number of meals
to prepare, deciding on quantities of food to purchase, store and issue, helping to
control food costs, and providing cumulative daily, monthly, quarterly, and yearly
cost data. The form covers categories of inpatients and categories of diners in the
dining facility, and TIMs. A separate form is used daily and then taken to the MSA
office. Note: At minimum a copy of the AF Form 544 or electronic equivalent
showing the categories of diners, ration earnings by meal, and daily food cost data
will be submitted to MSA daily, or by the first duty day following a weekend. (T-3).
The form will be signed by the NCOIC, Nutritional Medicine, or equivalent, and the
MSA officer. Both MSA and NM file a copy. (T-3).
7.17.1.2. (Manual) . The following three manual cost data records and financial reports
may be used in NM and the MSA office to determine financial status. Follow specific
instructions on forms for completion. Manual accounting will only be accomplished
when computer access and the NM Accounting Spreadsheet are unavailable. (T-3). This
would not include short term system failures, as the NM Accounting Spreadsheet can be
updated when systems come back online.
7.17.1.2.1. AF Form 544 is completed by following the instructions on the back of
the form.
7.17.1.2.2. When documenting manually, AF Form 541 is used to provide quarterly
and cumulative fiscal year summary data on food purchased in NM. It shows the
financial status operating under the SCAMS management system. The AF Form 541
is only used in facilities performing manual accounting. If required, the AF Form 541
is completed quarterly by the MSA Officer using data provided by NM on AF Forms
544, and 546.
7.17.1.2.3. AF Form 546 provides an overview of daily financial transactions and
current monthly cumulative totals. AF Form 546 will be provided to the MSA
Officer each month, on a date mutually agreed upon. (T-3).
7.17.1.3. Inpatient Diet Census. Workload figures for the number of trays served to
patients on the nursing units and the number and types of therapeutic diets served will be
documented on AF Form 2573, Diet Census, or electronic substitute, once daily, using
breakfast, lunch, or dinner data (typically lunch is used). (T-3). Additional instructions
are printed on the reverse side of the form. NM gives the workload figures and weighted
diet census from AF Form 2573 to the MSA Office per local guidance. The AF Form
2573 provides critical manpower data and should be reviewed monthly by NM leadership
to ensure accuracy.
50 AFMAN44-144 20 JANUARY 2016
7.17.1.4. Air Force Medical Operations Agency (AFMOA) Reporting. On a monthly
basis, MTFs with food service operations will submit a spreadsheet including the
information/data in Attachment 4 to their MTF MSA Office and Functional Manager. (T-
3). The MAJCOM Functional Manager (MFM) will submit a consolidated report (Excel
spreadsheet), for their MAJCOM, by MTF, to the AFMOA Uniform Business Office
IAW AFI 41-120, Medical Resource Management Operations. (T-3). The consolidated
MAJCOM report will be submitted to AFMOA by the MFM by no later than close of
business on the 5th calendar day following the last day of the month. (T-3). Example, the
April report will be submitted by no later than 5 May. (T-3).
7.17.2. Subsistence Account Management. Primary indicators which evaluate the financial
status of the NM operation are: earnings less cost of food served, earnings minus purchases,
inventory level, and periodic inventory adjustment.
7.17.2.1. Financial Parameters. The financial status of the NM subsistence account is
measured using food issues adjusted for spoilage and supplemental/other income, which
is referred to as cost of food served. The status of earnings minus cost of food served
must not exceed plus or minus 5 percent of the average monthly ration earnings at the end
of each of the first three quarters of the fiscal year, as annotated on the AF Accounting
Spreadsheet. At the end of the fiscal year, earnings minus cost of food served must not
be more than $100.00 or plus or minus 2 percent of the average monthly credit earnings,
whichever is greater. (T-3). When calculating the 5 percent for the quarter or the 2
percent for the end of fiscal year, always use fiscal year to-date figures. As an example,
at the end of March take the total earnings fiscal year to-date and divide by 6 to get the
monthly average, then multiply that number by 5% or 0.05 to get the plus or minus range.
Your fiscal year to-date earnings, minus cost of food served, must fall within that range.
7.17.2.2. Fiscal Year Close-out. If, at the end of the fiscal year, the earnings minus cost
of food served on the NM Accounting Spreadsheet exceeds (plus or minus) 2 percent of
the average monthly earnings (total earnings, fiscal year to date, divided by 12), the MTF
Commander may consider initiating a Report of Survey action.
7.17.2.3. Transferring a Subsistence Account when Food Served Exceeds Credit
Earnings. A report of survey is initiated when a NM officer or NCOIC (when no dietitian
is assigned), accepts a subsistence account where the authorized parameters for the
current quarter have not been met. The officer who writes the report of survey
determines if there is an excessive loss, the cause of the loss, and any financial liability.
If financial liability is found, the commander can take disciplinary action. If the
investigation shows an excessive loss, the MTF commander may request MAJCOM/SG
authority to over purchase at the end of the subsequent fiscal quarters and at the end of
the fiscal year, that portion of the loss that exceeds 2 percent of the monthly monetary
credit earnings. The request must show that the MTF cannot absorb the loss over a
period of 3 months or by the end of the fiscal year unless it reduces food services or menu
quality to the point where it would harm the morale and welfare of the subsisting patients
and enlisted personnel.
7.17.2.4. Nutritional Medicine Service Oversight Checklist can be found at Attachment
6.
AFMAN44-144 20 JANUARY 2016 51
Chapter 8
PROCEDURES FOR MEDICAL FACILITIES SUPPORTED BY BASE FOOD
SERVICE AND DIETETIC SHARING AGREEMENTS
8.1. Procedures for MTFs supported by Base Food Service.
8.1.1. MTF Commander or designated NM representative responsibilities:
8.1.1.1. In cooperation with the Base Food Service activity, develops and maintains a
written list of personnel who may certify meal requests. (T-3).
8.1.1.2. Ensures that a letter of agreement outlining the responsibilities of both Base
Food Service and NM personnel are on file with both activities. Reviews the agreement
annually or whenever changes are indicated. (T-3).
8.1.1.3. Arranges for Nursing Service personnel to complete an original and one copy of
the AF Form 1094 for each meal. (T-3).
8.1.1.4. Arranges for an enclosed vehicle to transport NM personnel and supplies to Base
Food Service and back three times daily, at a minimum. The closed vehicle will be used
for transporting patient meal trays and nourishments from Base Food Service to the MTF
and back. (T-3).
8.1.1.5. Ensures that an appropriate healthcare provider prescribes any diets and
supplemental feedings. Per local guidance, NM in coordination with Medical Logistics
personnel, purchase enteral feedings. (T-3).
8.1.1.6. Ensures food items and meals are used only for patient feeding. (T-3).
8.1.1.7. Coordinates in advance the number and types of meals required and arranges
pickup times with the Base Food Service Supervisor. Prepares a separate (by meal
period) request for meals on AF IMT 79. Prepares, or assists NM personnel with meal
preparation. (T-3).
8.1.1.8. Notifies Base Food Service Supervisor in advance, or as soon as possible, when
menu items cannot be used for therapeutic diets and specifies substitutes. (T-3).
Substitute items must not cause the total cost of meals for patients to exceed the total
meal rate allowance. (T-3).
8.1.1.9. Assigns an individual to pick up meals, serve meals to patients in the MTF, and
return soiled dishes and equipment to Base Food Service. (T-3).
8.1.1.10. Establishes a medical sub-account and purchases special patient feeding items,
such as crackers, juice, baby food, and dietetic foods. (T-3). See paragraphs 6.3.3 and 6.5
on medical subsistence funds and procedures for purchasing food using a GPC account.
8.1.1.11. Accounts for meals served. Prepare duplicate copies of AF Form 3516, Food
Service Inventory Transfer Receipt. (T-3). For Meals Ready to Eat (MREs) transfer, use
AF Form 28, War Reserve Materiel (WRM) Ration Report, obtained from the Base Food
Service for each meal period according to instructions on the form. NOTE: Do not cost
out each menu item or the total cost of the meal. For each meal, attach the original AF
IMT 79 to a copy of AF Form 1094. (T-3). Base Food Service retains these forms for
52 AFMAN44-144 20 JANUARY 2016
audit purposes. AF Form 3516 will reflect the food items for meals and between-meal
feedings. (T-3). The Admission & Disposition list should not be used to request meals,
but should be used as a check to make sure that meals and nourishments requested are
appropriate given the number of patients admitted.
8.1.1.12. Uses AF Form 1741 to record food likes and dislikes and any food allergies for
every patient requiring meals. Include therapeutic meal patterns or substitute as required
for menu writing purposes and meal ticket preparation. (T-3).
8.1.1.13. Provides appropriate patient tray service. (T-3). The use of disposable
tableware should be minimized. If disposable dishes must be used, an insulated, stacking
patient tray delivery system is recommended to best maintain the temperature of hot and
cold foods.
8.1.1.14. Ensures that an inpatient selective menu, based on the Base Food Service
menu, is prepared in advance for patients. (T-3).
8.1.1.15. Ensures that sufficient equipment is available to prepare and/or hold foods at
the proper temperatures for food quality and safety. (T-3).
8.1.2. Base Food Service Officer or designated representative responsibilities:
8.1.2.1. Provides the NCOIC, NM, with the menu for the base dining facility at least
three days in advance and notifies the NCOIC of any menu changes at least 24 hours in
advance. Works with the NCOIC, NM, to offer at least two entree choices not served at
the previous meal. Works with NM diet therapist to determine an appropriate substitute
for therapeutic diets when regular menu items are not suitable.
8.1.2.2. Calculates and receives the appropriate earnings for reimbursement for meals
provided. Each meal provided is counted as an ESM customer. Ensures the cost of food
issued for patient feeding does not exceed the BDFA plus 15 percent. Retains the
original AF IMT 79 with attached copy of AF Form 1094.
8.1.2.3. Coordinates the number and types of meals. (T-3). Reviews certified meal
requests. (T-3). Prepares and issues regular meals. (T-3). Provides portion control
condiments for patient feeding on a "by-meal" basis. (T-3).
8.1.2.4. Provides NM personnel with a designated parking space and a work area to
assemble trays and prepare therapeutic diet food; NM section/work area should be
segregated as much as possible from Services dining and serving areas. (T-3).
8.1.2.4.1. Provides NM personnel with adequate, secure storage space for subsistence
and supplies to prevent pilferage and misappropriated use by unauthorized personnel
if available. (T-3).
8.1.2.5. Provides warewashing support area to NM activities without warewashing
facilities. (T-3).
8.2. Dietetic Sharing Agreements.
8.2.1. The MTF Commander or designee coordinates dietetic sharing agreements with the
MAJCOM Dietitian. (T-3).
AFMAN44-144 20 JANUARY 2016 53
8.2.2. The MAJCOM Dietitian reviews all sharing agreements to ensure they include all
appropriate Process Improvement programs and internal controls demonstrating services are
provided in accordance with the sharing agreement. (T-3). See Attachment 5, SAMPLE
MOA.
8.2.3. Sharing agreements must specify responsibilities and procedures. (T-3). Examples of
services available include:
8.2.4. Inpatient clinical dietetics services.
8.2.4.1. Basic, intermediate, complex, and extensive nutritional care.
8.2.4.2. Nutrition screening, assessment, and reassessment.
8.2.4.3. Use of MNT evidence-based guides for practice, protocols, and clinical care
guidelines.
8.2.5. Inpatient and outpatient consultation.
8.2.5.1. Use of SF 513 for inpatient consultation requests, or electronic/MTF-equivalent.
8.2.5.2. Use of approved form for outpatient individual and group diet consultations and
follow-up requests.
8.2.6. Patient meal service.
8.2.6.1. Meal services to include: trays, menus, ordering diets, meal service, delivering
and returning trays, and providing nourishments to patients.
8.2.7. Outcome measures and Process Improvement.
8.2.7.1. Data collection, analysis, and implementation procedures to continuously
improve quality of care and measure and monitor performance and outcomes.
8.2.7.2. Standards for patient satisfaction, tray accuracy, and quality of nutrition care.
8.2.8. Internal controls to ensure patients receive care at a standard comparable to those
received by patients at a larger AF MTF and in accordance with this AFMAN.
54 AFMAN44-144 20 JANUARY 2016
Chapter 9
CONSULTANT SERVICES
9.1. Purpose. The purpose of the AF Dietetic Consultant Program is to support the AFMS
mission through efficient NM operations that provide quality services. Consultant services are
available at various levels of operations. The Consultant Dietitian advises the AFMS, AF/SG,
AFMOA, and MAJCOM SGs, and provides consultant services to bases where NM personnel
(diet technicians) are assigned without a credentialed RD and where no NM capabilities or
personnel are assigned. The AF Career Field Manager (CFM) is the senior enlisted consultant to
the Associate Chief for Dietetics, AF SG Chief, Enlisted Medical Force (CMEF), MAJCOM
CMEF, and Diet Therapy MAJCOM Functional Managers (MFM), ensuring the development of
all enlisted personnel.
9.2. The Consultant Dietitian.
9.2.1. AF SG Consultant Dietitian/BSC Associate Chief for Dietetics. Consultant to AF SG
on all matters related to nutrition and dietetics. The Individual Mobilization Augmentee
(IMA) to the AF SG Consultant Dietitian serves as the Air Reserve Component (ARC)
advisor for Reserve dietitian career field issues.
9.2.2. MAJCOM Dietitians collaborate with DoD, AF/A1, AF SG Consultant Dietitian/BSC
Associate Chief for Dietetics, AFMOA Dietitian, HP Support Office stakeholders, subject
matter experts, and other agencies (e.g., Defense Commissary Agency, Army and Air Force
Exchange Service, national organizations, such as AND, and DoD/AF-level working groups,
such as the DoD Nutrition Committee, Community Action Information Board) as applicable
to research, develop, implement, market and evaluate evidence-based strategies and
interventions and initiatives to meet health promotion nutrition objectives.
9.2.3. MAJCOM Dietitians. MAJCOM Dietitians (senior active duty officers or civilians)
are appointed upon recommendation by the AF SG Consultant Dietitian. The MAJCOM
Dietitians, duties also include:
9.2.3.1. Serves as clinical supervisor to dietitians for credentialing purposes. The
MAJCOM Dietitian may approve a local credentialed provider to serve as clinical
supervisor.
9.2.3.2. Coordinates with AFMOA for training of HP dietitians and implementation of
HP nutrition strategies and interventions/initiatives as outlined in AFI 40-104.
9.2.3.3. Ensures credentialed RDs within the MAJCOM are trained to perform diet
technician diet authorizations/certifications as needed.
9.2.3.4. Ensures quarterly peer reviews of 15 patient notes or 100%, whichever is less,
are completed for all credentialed RDs and diet therapists assigned to the MAJCOM.
9.2.3.4.1. Submits Memorandum for Record (MFR) and hard copy peer review
reports (as applicable) quarterly to the member subject to peer review and to the
member’s Credentials Office as necessary.
9.2.3.4.2. Develops procedure to include MAJCOM-specific peer review schedule
and process for obtaining patient notes to review. (T-2). Requests those being peer
AFMAN44-144 20 JANUARY 2016 55
reviewed to provide a list of patients seen within the quarter (listing full patient’s
name and last four of SSN) is recommended which will allow the dietitian to select
which patient notes to review. Peer reviews on dietitians may be performed, if
required, by a local credentialed provider after coordination with the MAJCOM
Dietitian. A MFR or e-mail stating what peer reviews were accomplished and the
overall outcome will be provided to the MAJCOM Dietitian.
9.2.3.4.3. The electronic peer review system may be used as available and applicable.
9.2.3.5. Maintains quality communications with NM and facility personnel.
Communications should be frequent and well documented, as it is necessary to show
oversight and training by a RD to inspecting agencies. The consultant dietitian and each
NM section within their respective command must keep records of all communication
including e-mails, teleconferences, and video conferences.
9.2.3.6. Provides oversight of all NM activities/services at bases/facilities without a
credentialed dietitian assigned (only diet technician(s) assigned).
9.2.3.6.1. In coordination with AFMOA, reviews capability to provide rapid
telemedicine services to provide RD consultation if needed.
9.2.3.6.2. Ensures that NM services provided and compliance to regulations are
reviewed at least annually via Virtual Consultant Assistance (VCA) or more
frequently as requested by the facility.
9.2.3.6.3. Virtual Consultant Assistance (VCA). If it is not feasible to perform an in-
person Staff Assistance Visit (SAV), a VCA may be performed by webinar and/or
teleconference. Virtual consultation will be performed annually to continuously
evaluate NM services and compliance to regulations.
9.2.3.6.4. A specified member of the NM section undergoing the VCA is responsible
for ensuring all items identified below, that will be evaluated by the dietitian
providing the VCA, are sent electronically to the dietitian at least one month prior to
the VCA. (Evaluation of NM services by the MAJCOM Dietitian, or dietitian
designated by the MAJCOM Dietitian to perform the VCA, will include (but not
limited to) the following:
9.2.3.6.4.1. Any Medical Group Instruction involving NM service.
9.2.3.6.4.2. Internal Operating Instructions and Position Descriptions.
9.2.3.6.4.3. Training documentation (in-service plans and documentation, such as
lesson plans, competency assessment, attendee signatures, annual training
schedule), AF Training Record (AFTR) with emphasis on AF Form 628, Diet
Instruction/Assessment Authorization, and Competency/RSV Training
documentation.
9.2.3.6.4.4. Section organizational chart.
9.2.3.6.4.5. Last the JC/AAAHC/SAC/SAV reports.
9.2.3.6.4.6. Strategic planning documentation to include nutrition services
mission/vision/goals/objectives.
56 AFMAN44-144 20 JANUARY 2016
9.2.3.6.4.7. Process Improvement Program and nutrition program outcomes data.
9.2.3.6.4.8. Nutrition lesson plans and presentations used for group classes,
inpatient and outpatient forms, nutrition care overprints/screenings, etc.
9.2.3.6.4.9. Patient education materials and reference books.
9.2.3.6.4.10. Data quality/productivity reports.
9.2.3.6.4.11. Typical CHCS appointment schedule for RD and diet technicians.
9.2.3.6.4.12. Consultant dietitian communication log.
9.2.3.6.4.13. Compliance with TRICARE access to care standards.
9.2.3.6.4.14. Management tool monthly reports (as applicable) and management
plan.
9.2.3.6.4.15. Letter of agreement with base food services, patient menu, and
dining facility menu (if applicable).
9.2.3.6.4.16. Customer satisfaction surveys (inpatient/outpatient/dining facility).
9.2.3.6.4.17. Public Health Flight monthly sanitation inspection reports (one year
if applicable).
9.2.3.6.4.18. Equipment replacement plan.
9.2.3.6.4.19. Self-inspection documentation.
9.2.3.6.4.20. Food temperature charts (one year if applicable) and
refrigerator/freezer temperature charts (one year if applicable).
9.2.3.7. The VCA will be performed by an assigned credentialed dietitian at least
annually or as required. When a VCA includes the Health Promotion Program, the
assigned dietitian will coordinate the evaluation and final report with the Health
Promotion at AFMSA or AFMOA. (Each respective MAJCOM Consultant Dietitian is
responsible for creating a VCA/peer review schedule outlining which dietitian within
their command is responsible to conduct the VCA on which installations and when the
respective VCAs are due. After the VCA concludes, a copy of the final report must be
sent to the NM NCOIC, Squadron/Group Commander, the AF SG Consultant Dietitian,
and the nutrition staff at AFMSA and AFMOA. The final report is due within 1 month
after the VCA is conducted.
9.2.3.7.1. In-Person Staff Assistance Visits (SAV). Evaluation may be done through
face-to-face visits if virtual consultation is not sufficient to meet the facility needs at
the request of the WG Commander.
9.2.3.7.2. The same documents will be reviewed in the SAV as in the VCA and the
assigned credentialed dietitian performing the SAV must send a MFR to the facility
undergoing the SAV one month in advance. (T-3). An inbrief and outbrief with the
key leadership (to include the unit commander) of the facility undergoing the SAV is
encouraged. At the conclusion of the SAV, the final report is due within one month
and is sent to the same members identified in 8.2.3.10. Diet certifications may also
be performed during the in-person SAV or via telephone during a VCA.
AFMAN44-144 20 JANUARY 2016 57
9.2.3.8. Provides guidance, monitoring, and evaluation of nutrition services at MTFs
without any NM personnel assigned (no NM operation), and, when nutrition education in
HP programs is involved, collaborates with Health Promotion staff at AFMSA or
AFMOA.
9.3. Enlisted Consultant Roles.
9.3.1. Diet Therapy Career Field Manager Responsibilities are as follows: The Diet Therapy
AF CFM is appointed by the AF Surgeon General to ensure development, implementation,
and maintenance of the CFETP for the Diet Therapy career field. The CFM will
communicate directly with the Associate Chief for Dietetics, MFMs, ARC, and AETC
Training Pipeline Manager (TPM) to disseminate AF and career field policies and program
requirements. (
9.3.1.1. Use the Utilization and Training Workshop (U&TW)/Specialty Training
Requirements Team (STRT) meeting as forums and quality control tools to determine
and manage career field education and training (E&T) requirements.
9.3.1.2. Chair the portion of the STRT/U&TW for utilization, authorization, and general
career field mission issues, and partner with the AETC TPM throughout the
STRT/U&TW.
9.3.1.3. Ensure the direct involvement and participation of Subject Matter Experts
(SMEs) from the field.
9.3.1.4. Develop the CFETP as the core document for E&T requirements.
9.3.1.5. Establish the framework for managing career field E&T by specifying career
field progress.
9.3.1.6. Develop criteria to accelerate individual training when it is in the best interest of
the AF.
9.3.1.7. Oversee the Career Development Course (CDC) program for the Diet Therapy
career field. The AF CFM also reviews CDCs for accuracy and initiates actions to
develop new or revised CDCs to meet new requirements.
9.3.1.8. Ensure, when feasible, the direct involvement and participation of HQ Air
University A4L Extension Course Program personnel in U&TW proceedings impacting
development, revision, or deletion of CDCs or Specialized Courses used for career field
upgrade training.
9.3.1.9. Work closely with SG Chief, Enlisted Medical Force, MAJCOM CMEFs,
MFMs and Command Chief Master Sergeants (CCM) on training, development, manning
and personnel issues impacting NM personnel.
9.3.1.10. Support NM personnel with base initiatives and concerns while working with
MFM/MAJCOM RDs.
9.3.1.11. Advise HQ AFMPC/DPMRAD2 and the “Chiefs’ Group” on personnel
assignments.
58 AFMAN44-144 20 JANUARY 2016
9.3.2. Diet Therapy MAJCOM Functional Manager’s Responsibilities.
9.3.2.1. The primary duties and responsibilities of a MFM are outlined in AFI 36-2101,
Classifying Military Personnel (Officer and Enlisted), and AFI 36-2201. These duties
include, but are not limited to:
9.3.2.2. Assist in development and maintaining currency of CFETP. Establish review
procedures. Coordinate on new and proposed classification changes and publicizing
approved changes.
9.3.2.3. Serve as MAJCOM representative at AFSC 4D0X1 U&TW.
9.3.2.4. Assist technical training managers and course personnel with planning,
developing, implementing, and maintaining all 4D0X1 AFSC-specific training courses.
9.3.2.5. Assist the AF CFM, Air Force Occupational Measurement Squadron (AFOMS),
and CMEF in identifying subject matter experts for Specialty Knowledge Test rewrite
projects.
9.3.2.6. Assist AFOMS in developing and administering Job Surveys and interpreting
Occupational Survey Report data.
9.3.2.7. Coordinate and implement career field classification and structure changes.
9.3.2.8. Disseminate AF and career field policies and program requirements.
9.3.2.9. Maintain regular and consistent contact with MAJCOM MTF personnel to
include, but not limited to:
(1) Compilation and dissemination of information concerning process improvements.
(2) Compilation and dissemination of information concerning recent inspections.
(3) Address AFSC concerns/issues within the command and forward them to the CMEF who will
forward to the AF CFM.
9.3.2.10. Assignments: MFMs are only advisors and do not control assignments and
should not be considered as individuals who can manipulate the assignment system. The
medical enlisted assignment system is the responsibility of HQ AFMPC/DPMRAD2 and
the “Chiefs’ Group.” However, it is imperative that MFMs be knowledgeable of
authorizations and assignments within the MAJCOM to better serve as consultants to
MAJCOM assignment managers regarding assignment actions. As such, they may:
(1) Identify candidates for PCS/PCA/TDY assignments.
(2) Advertise position vacancies for urgent (short notice separations/discharges, etc.) and routine fill
requirements.
(3) Recommend/initiate resolution of staffing imbalances between MTFs (command leveling).
(4) Assist assignment staffers by fielding inquiries pertaining to career progression and classification.
(5) Be knowledgeable of authorizations and assignments within the MAJCOM and identify special
needs.
9.3.2.11. Notify CMEF and AF CFM of areas of concern within assigned MAJCOM
such as early discharge/dismissal, chronic shortages, inspections resulting in marginal or
unsatisfactory scores, two-time CDC failures, etc.
AFMAN44-144 20 JANUARY 2016 59
9.3.2.12. Participate in monthly teleconferences, relaying manning, training and any
personnel issues which need to be communicated to a higher level or just shared for
informational purposes.
9.3.2.13. Participate in annual strategic planning initiatives and provide input to shape
the future direction of the career field. (
9.3.2.14. Work closely with the MAJCOM Dietitian to ensure all enlisted member’s
concerns are addressed.
9.3.2.15. Fulfill any other duties as required by the CMEF and AF CFM.
9.4. NM Dietitian or Diet Therapy Personnel.
9.4.1. The dietitian or diet therapy personnel serve as a nutrition advisor to local media, HP,
base and community organizations. (T-3). Only a dietitian shall serve as nutrition advisor to
the MTF Commander. NM advisor responsibilities include:
9.4.1.1. Medical Staff. Serves as a nutrition resource for the medical and support staff
and the MTF Commander regarding diet prescriptions, nutritional supplements, medical
foods, nutrition assessment, MNT, current nutrition concepts and research. (T-2).
9.4.1.2. Health Promotion Program. Coordinate with Headquarters staff on guidance
related to HP nutrition program activities as nutrition advisor for other components of the
HP program involving nutrition education and disease prevention. (T-2). Provide
nutrition advice to Force Support Squadron to create an environment conducive to
healthy eating. Also serves as a community nutrition resource for base agencies such as
the Child and Youth Programs. (T-2). These responsibilities are performed by the health
promotion nutrition specialist if the capability exists. (T-2).
9.4.1.3. Professional Assistance. Provides interim professional assistance to the NM
operations by telephone or electronically. (T-2). NM staff in MTFs without dietitians
must record interim communications with the consultant in a log book or maintain copies
of electronic communications, noting subjects discussed and information communicated
by the consultant. (T-2).
MARK A. EDIGER
Lieutenant General, USAF, MC, CFS
Surgeon General
60 AFMAN44-144 20 JANUARY 2016
Attachment 1
GLOSSARY OF REFERENCES AND SUPPORTING INFORMATION
References
DOD 1338.10-M, Manual for the Department of Defense Food Service Program, March 1990
DOD 6010.13-M, Medical Expense and Performance Reporting System for Fixed Military
Medical and Dental Treatment Facilities Manual, 7 April 2008
DOD Financial Management Regulation 7000.14-R, Vol 5, Disbursing Policy and Procedures,
Chapter 3, Keeping and Safeguarding Public Funds, January 2010
DODI 6025.24, Provision of Food and Beverages to Certain Members and Dependents Not
Receiving Inpatient Care in Medical Treatment Facilities, 07 March 2014
DODI 6130.50, DoD Nutrition Committee, 18 February 18 2011
AFPD 40-1, Health Promotion, 17 December 2009
AFPD 44-1, Medical Operations, 1 September 1999
AFI 33-332, Air Force Privacy and Civil Liberties Program, 12 January 2015
AFI 36-807, Weekly and Daily Scheduling of Work and Holiday Observances, 21 June 1999
AFI 36-1001, Managing the Civilian Performance Program, 1 July 1999
AFI 36-2101, Classifying Military Personnel (Officer and Enlisted), 25 June 2013
AFI 36-2201, Air Force Training Program, 15 September 2010
AFI 36-2406, Officer and Enlisted Evaluation Systems, 2 January 2013
AFI 36-2618, The Enlisted Force Structure, 27 February 2009
AFI 36-2905, Fitness Program, 21 October 2013
AFI 38-101, Air Force Organization, 16 March 2011
AFI 40-101, Health Promotion, 17 October 2014
AFI 40-104, Health Promotion Nutrition, 17 October 2014
AFI 41-102, Air Force Medical Expense and Performance Reporting System (MEPRS) For
Fixed Military Medical and Dental Treatment Facilities, 9 May 2014
AFI 41-106, Medical Readiness Program Management, 22 April 2014
AFI 41-301, Worldwide Aeromedical Evacuation System, 1 August 1996
AFI 41-307, Aeromedical Evacuation Patient Considerations and Standards of Care, 20 August
2003
AFI 44-102, Medical Care Management, 17 March 2015
AFI 44-108, Infection Prevention and Control Program, 11 December 2014
AFI 44-119, Medical Quality Operations, 16 August 2011
AFI 44-141, Nutrition Standards and Education, 15 June 2001
AFMAN44-144 20 JANUARY 2016 61
AFI 48-116, Food Safety Program, 19 August 2014
AFI 48-117, Public Facility Sanitation, 26 June 2014
AFI 64-117, Air Force Government-Wide Purchase Card (GPC) Program, 20 September 2011
AFI 90-201, The Air Force Inspection System, 21 April 2015
AFJMAN 34-406V2, Index of Recipes, Armed Forces Recipe Service, 1 September 1992
AFMAN 41-120, Medical Resource Management Operations, 6 November 2014
AFMAN 48-147_IP, Tri-Service Food Code, 30 April 2014
AF NM Accounting Spreadsheet (https://kx.afms.mil/nutritionalmedicine)
AFMS Flight Path (https://kx.afms.mil/bsc)
AND Evidence Analysis Library (www.andeal.org)
AND Nutrition Care Manual (www.nutritioncaremanual.org)
AND Nutrition Care Process (www.eatright.org/HealthProfessionals/content.aspx?id=7077)
AND Patient Education Materials (www.eatright.org)
AND Pediatric Nutrition Care Manual (www.nutritioncaremanual.org)
AND Sports Nutrition Care Manual (www.nutritioncaremanual.org)
AND Pocket Guide to Nutrition Assessment (www.eatright.org)
ASPEN Nutrition Support Core Curriculum (www.nutritioncare.org)
Career Field Education and Training Plan (CFETP) 4D0X1, Diet Therapy
(https://kx.afms.mil/nutritionalmedicine)
CNM Nutrition Screening Practices in Health Care Organizations (www.cnmdpg.org)
Computrition On-Line User Manual (https://kx.afms.mil/nutritionalmedicine)
DSCP Prime Vendor Guide Book (www.dscp.dla.mil/subs/pv/pvguide.pdf)
Health Services Inspection Standards (https://kx.afms.mil/afia)
International Dietetics & Nutrition Terminology Reference Manual (www.eatright.org)
Joint Commission for the Accreditation of Healthcare Organizations Standards
(www.jointcommission.org)
Memorandum from the Assistant Secretary of Defense for Health Affairs, Diplomate Pay for
Psychologists and Board Certification Pay for Non-Physician Health Care Providers, 9 March 09
(https://kx.afms.mil/bsc)
Memorandum from the Assistant Secretary of Defense for Health Affairs, National Defense
Authorization Act for Fiscal Year 2009 Permanent Prohibition Against Requiring Certain Injured
Members to Pay for Meals Provided by Military Treatment Facilities
(https://kx.afms.mil/nutritionalmedicine)
NM KX Website (https://kx.afms.mil/nutritionalmedicine)
USDA My Plate (http://myplate.gov)

62 AFMAN44-144 20 JANUARY 2016
USDA Dietary Guidelines for Americans (www.health.gov/dietaryguidelines)
Prescribed Forms
AF Form 541, Nutritional Medicine Service Subsistence Cost Report
AF Form 542, Subsistence Stock Record
AF Form 543, Food Issue Record
AF Form 544, Nutritional Medicine Daily Facility Summary Report
AF Form 546, Food Cost Record
AF Form 628, Diet Instruction/Assessment Authorization
AF Form 1094, Diet Order
AF Form 1737, Selective Menu (White) (3-way perforation)
AF Form 1738, Therapeutic Menu (Yellow) (3-way perforation)
AF Form 1739, Selective Menu (White) (6-way perforation)
AF Form 1740, Therapeutic Menu (Yellow) (6-way perforation)
AF Form 1741, Diet Record
AF Form 2464, CTIM Telephone Diet Order
AF Form 2478, Sodium Restricted (Pink) (3-way perforation)
AF Form 2479, Diabetic (Green) (3-way perforation)
AF Form 2480, Diabetic (Green) (6-way perforation)
AF Form 2481, Liquid (Yellow) (3-way perforation)
AF Form 2482, Liquid (Yellow) (6-way perforation)
AF Form 2485, Sodium Restricted (Pink) (6-way perforation)
AF Form 2487, Step 1 Moderate; Step 2 Strict Cholesterol and Fat Diet (Blue) (3-way
perforation)
AF Form 2488, Step 1 Moderate; Step 2 Strict Cholesterol and Fat Diet (Blue) (6-way
perforation)
AF Form 2497, Fat Restricted (Blue) (3-way perforation)
AF Form 2498, Fat Restricted (Blue) (6-way perforation)
AF Form 2499, Calorie Restricted (Green) (3-way perforation)
AF Form 2500, Calorie Restricted (Green) (6-way perforation)
AF Form 2503, Nutritional Medicine Service Patient Evaluation
AF Form 2504, Nutritional Medicine Service Patron Evaluation
AF Form 2508, Patient Calorie Count Sheet
AF Form 2567, Diet Order Change
AFMAN44-144 20 JANUARY 2016 63
AF Form 2568, Nourishment Request (Bulk)
AF Form 2570, Nutritional Medicine Service Cash and Forms Receipt
AF Form 2582, Food Temperature Chart
AF Form 2572, Nutritional Assessment of Dietary Intake
AF Form 2573, Diet Census
AF Form 2577, Medical Food Service – Daily Work Assignment
AF Form 2579, Nourishment
AF Form 3574, Pureed/Blenderized Liquid (Yellow) (3-way perforation)
AF Form 3575, Pureed/Blenderized Liquid (Yellow) (6-way perforation)
AF IMT 79, Headcount Record
Adopted Forms
DD Form 714, Meal Card
DD Form 792, Twenty-Four Hour Patient Intake and Output Worksheet
AF Form 28, War Reserve Materiel (WRM) Ration Report
AF Form 40a, Record of Individual Inactive Duty Training
AF Form 55, Employee Safety and Health Record
AF Form 847, Recommendation for Change of Publication
AF Form 1254, Register of Cash Collection Sheets
AF Form 1305, Receipt for Transfer of Cash and Vouchers
AF Form 2581, Daily Absenteeism Record
AF Form 3066, Doctor’s Order
AF Form 3067, Intravenous Record
AF Form 3516, Food Service Inventory Transfer Receipt
AF Form 3930, Clinical Privileges – Dietetics Providers
OPM Form 71, Application for Leave
SF 509, Medical Record Progress Note
SF 513, Medical Record – Consultation Sheet
SF 600, Chronological Record of Medical Care
Abbreviations and Acronyms
AAAHC—Accreditation Association for Ambulatory Health Care
AND—Academy of Nutrition and Dietetics
ADIME—Assessment, Diagnosis, Intervention, Monitoring, Evaluation
64 AFMAN44-144 20 JANUARY 2016
AETC—Air Education and Training Command
AF—Air Force
AFI—Air Force Instruction
AFMOA—Air Force Medical Operations Agency
AFOMS—Air Force Occupational Measurement Squadron
AFOSH—Air Force Occupational Safety and Health
AFPD—Air Force Policy Directive
AFMS—Air Force Medical Service
AFRIMS—Air Force Records Information Management Systems
AFSC—Air Force Specialty Code
AFSVA—Air Force Services Activity
AFTR—Air Force Training Records
AIDS—Acquired Immune Deficiency Syndrome
ALACS—A la Carte System
AMA—American Medical Association
APV—Ambulatory Procedure Visit
ARC—Air Reserve Component
ASF—Aeromedical Staging Facility
ASPEN—Association of Enteral and Parenteral Nutrition
ASTS—Aeromedical Staging Squadron
BDFA—Basic Daily Food Allowance
BLS—Basic Life Support
BSC—Biomedical Sciences Corps
CAC—Common Access Card
CBRN—Chemical, Biological, Radiological, and Nuclear
CCM—Command Chief Master Sergeant
CDC—Career Development Course
CDE—Certified Diabetes Educator
CDM—Certified Dietary Manager
CFETP—Career Field Education and Training Plan
CFM—Career Field Manager
CEU—Continuing Education Unit
AFMAN44-144 20 JANUARY 2016 65
CFM—Career Field Manager
CHCS—Composite Health Care System
CHES—Certified Health Education Specialist
CMEF—Chief, Enlisted Medical Force
CNM—Certified Nurse Midwife
CNSC—Certified Nutrition Support Clinician
CONUS—Continental United States
COPD—Chronic Obstructive Pulmonary Disease
CPG—Clinical Practice Group
CSG—Certified Specialist in Gerontological Nutrition
CSO—Certified Specialist in Oncology Nutrition
CSP—Certified Specialist in Pediatric Nutrition
CSR—–Certified Specialist in Renal Nutrition
CSSD—Certified Specialist in Sports Dietetics
DCO—Defense Connect Online
DeCA—Defense Commissary Agency
DFAC—Dining Facility
DFAS—CO—Defense Finance & Accounting Service – Columbus
DHP—Defense health Program
DMA—Dietary Managers Association
DMRSHi—Defense Medical Human Resources System-internet
DoD—Department of Defense
DODAAC—Department of Defense Activity Address Code
DSCP—Defense Supply Center Philadelphia
DVA—Department of Veterans Affairs
ECR—Electronic Cash Registers
ED—Emergency Department
EHR—Electronic Health Record
EMEDS—Expeditionary Medical Support
ESM—Essential Station Messing
FAC—Functional Account Code
FAND—Fellow of the Academy of Nutrition and Dietetics
66 AFMAN44-144 20 JANUARY 2016
FCC—Functional Cost Codes
FDA—Food and Drug Administration
FOM—Food Operations Management
FOUO—For Official Use Only
GPC—Government Purchase Card
GPN—Graduate Program in Nutrition
HACCP—Hazard Analysis Critical Control Points
HAZMAT—Hazardous Material
HCP—Health Care Provider
HIPAA—Health Insurance Portability and Accountability Act
HIV—Human Immunodeficiency Virus
HPP—Health Promotion Program
IDNT—International Dietetics and Nutrition Terminology
IDS—Integrated Delivery System
IT—Information Technology
JC—Joint Commission
KX—Knowledge Exchange
LIFO—Last In First Out
MAJCOM—Major Command
MAOI—Monoamine Oxidase Inhibitors
MCRP—Medical Contingency Response Plan
MedFACTS—Medical Facility Assessment and Compliance Tracking System
MEPRS—Medical Expense Performance Reporting System
MFM—MAJCOM Functional Manager
MFR—Memorandum for Record
MILSTRIP—Military Standard Requisitioning and Issue Procedure
MNT—Medical Nutrition Therapy
MOA—Memorandum of Agreement
MPA—Military Personnel Appropriation
MRDSS—Medical Readiness Decision Support System
MRE—Meals Ready to Eat
MTF—Medical Treatment Facility
AFMAN44-144 20 JANUARY 2016 67
NCM—Nutrition Care Manual
NCP—Nutrition Care Process
NCOIC—Noncommissioned Officer in Charge
NDC—Nutritional Diagnostic Category
NIH—National Institutes of Health
NM—Nutritional Medicine
NMC—Nutritional Medicine Clinic
NMIS—-Nutrition Management Information System
NMA—Non-Medical Attendant
NPBCP—Non-Physician Health Care Provider Board Certified Pay
NPI—National Provider Identifier
NPO—Nothing Per Oral
NSN—National Stock Number
OPM—Office of Personnel Management
OIC—Officer in Charge
OMG—Objective Medical Group
OPAC—On-Line Payment & Collection
OSHA—Occupational Safety and Health Administration
PA—Privacy Act
PA—Physician Assistant
PAS—Privacy Act Statement
PDO—Publications Distribution Office
PES—Problem Etiology Signs/Symptoms
PI—Performance Improvement
PNCM—Pediatric Nutrition Care Manual
PPN—Peripheral Parenteral Nutrition
PTS—Patient Tray Service
QTP—Qualification Training Package
RCEP—Registered Clinical Exercise Physiologist
RD—Registered Dietitian
RDS—Records Disposition Schedule
REE—Resting Energy Expenditure
68 AFMAN44-144 20 JANUARY 2016
RES—Registered Exercise Specialist
RMO—Resource Management Office
RON—Remain over night
RSV—Readiness Skills Verification
RTH—Ready to Hang
SAC—–Self-Assessment Checklist
SAV—Staff Assistance Visit
SCAMS—Subsistence Credit Allowance Management System
SDS—Same Day Surgery
SF—Standard Form
SIMS—Services Information Management System
SME—Subject Matter Expert
SNCM—Sports Nutrition Care Manual
SOFA—Status of Forces Agreement
STORES—Subsistence Total Receipt Electronic System
STRT—Specialty Training Requirements Team
TF—Tube Feeding
TIM—Therapeutic Inflight Meal
TPM—Training Pipeline Manager
TPN—Total Parenteral Nutrition
UCA—Uniform Cost Accounting
UGR—Unitized Group Ration
UMD—Unit Manning Document
UMPR—Unit Personnel Management Roster
URL—Uniform Resource Locator
USAF—US Air Force
USDA—United States Department of Agriculture
U&TW—Utilization and Training Workshop
VA—Veterans Administration
VCA—Virtual Consultant Visit
WW—Wounded Warrior
AFMAN44-144 20 JANUARY 2016 69
Terms
A La Carte System (ALACS)—A system in which the dining facility cash patrons are charged
for each menu item selected. Each food item is priced and sold by the individual portion.
Essential Station Messing (ESM) patrons “pay” by meal card number or social security number
instead of cash, as under conventional food service policies.
Academy of Nutrition and Dietetics (AND)—The parent professional organization that
establishes standards of practice for the training and performance of RDs.
Ambulatory Procedure Visit (APV)—Formerly known as same day surgery, refers to the
immediate (day of procedure), pre-procedure and immediate post-procedure care in an
ambulatory setting. Care is in the facility for less than 24 hours.
Burlodge—The Burlodge company supplies specialized patient meal assembly and delivery
systems particularly suited to conventional hot-line/cook-serve and cook-chill applications.
Computrition—Computrition’s Hospitality Suite Commercial-off-the-shelf (COTS) software
solution replaces the legacy Government off-the-shelf (GOTS) system originally deployed in
1994 and is comprised of two key products: Foodservice Operations Management (FOM) and
Nutrition Care Management (NCM). The FOM provides automated daily functions such as
menu planning, purchasing, inventory, production, recipe management, and forecasting that the
former NMIS GOTS application once handled, as well as new features such as food and labor
costing, nutrient labeling, and HACCP compliance procedures. The NCM includes the ability to
track patient demographics, acuity levels, diet orders, weight history, as well as any likes,
dislikes, or allergies, menu and tray ticket production, comprehensive nutrient analysis, recipe
and menu management, the generation of automated HACCP guidelines. The software
application is designed to interface with the Electronic Health Record (Essentris) and the
Subsistence Total Order and Receipt Electronic System (STORES).
Food Cost Index— A representative list of specified quantities of food items (components)
prescribed by DOD and used to compute the monetary value of the operational basic daily food
allowance (Operational BDFA).
Food Service Operating Expenses—A charge established to comply with the congressional
requirement to recover a part of personnel and operational-maintenance costs. Food service
operating expense is generally charged to officers, civilians, and enlisted personnel not receiving
ESM who eat in appropriated fund facilities (formerly known as surcharge).
Government Purchase Card (GPC)—The Government Purchase Card is the official
government-wide purchase credit card.
Hazard Analysis Critical Control Point (HACCP)—A systematic approach to the
identification, evaluation, and control of food safety hazards.
Joint Commission (JC)—The accreditation body for medical treatment facilities.
Meal—A portion of food taken at one time.
Meal Day—A value in which the number of meals is weighted by a predetermined percentage to
balance the cost and attendance variances between the meals. The number of meal days for a
given day is figured by multiplying the number of breakfast, lunch, and dinner meals served by
70 AFMAN44-144 20 JANUARY 2016
the factored percentages of 20, 40, and 40 percent, respectively, and totaling the results (formerly
called ration).
Meal Periods—Breakfast: The meal served during the morning hours and considered the first
meal of the day. Lunch: The meal served at midday and considered the second meal of the day.
Dinner: The meal served during the evening hours and considered the third meal of the day.
Night Meal: The meal served between the dinner and breakfast meals. Dinner or breakfast type
meals may be served. The meal credit and reimbursement rates are based on the menu actually
served. The night meal is for persons on night duty.
Medical Foods—Enteral feedings and dietary supplements which enhance or replace regular
foods for patients with special feeding requirements.
"Nil per os" or "Nothing By Mouth"(NPO)—The patient will receive no food or beverages
from Nutritional Medicine Flight when this diet order is written.
Nutrition Management Information System (NMIS)—NMIS is a joint service multifunctional
management information system designed to replace the TRIFOOD system. NMIS provides the
following functions: data maintenance, production planning, menu cycle planning, NM
accounting, forecasting, inventory management, management reporting, a la carte/conventional
meal service pricing, diet office functions and nutrition outcomes management functionality.
Nutritional Diagnostic Category (NDC)—A fundamental class of nutritional problems, used to
categorize a patient’s nutritional condition.
Prime Vendor—Customized contracts developed with commercial distributors that are designed
to furnish a full range of subsistence goods and delivery services with emphasis on quality,
availability and minimum delivery lead time.
Ration—Refers to a portion or type of food.
Subsistence—Food products as packaged, bought, sold, and issued.
Therapeutic In—flight Meals (TIMs)—Therapeutic diet foods provided by the medical
treatment facility to patients receiving a prescribed therapeutic diet who are embarking on
aeromedical evacuation flights. There is no longer CTIMS, Cooked Therapeutic In-Flight Meals
Unitized Group Ration—A pre-packaged, heat and serve ration designed to feed a complete
meal for 50 persons. This combination ration replaces the B and T rations and makes maximum
use of commercial items.
Virtual Consultant Assistance (VCA)—A virtual means to conduct what was formally known
as a SAV to ensure NM operations are inspection ready specifically in locations without a RD.
Weighted Diet Census—Total of diet census after applying weighted percentages to certain
therapeutic patients based on difficulty of procedures.
Weighted Meal Days—The total of the percentage of a whole meal day multiplied by a
particular meal count(s).
AFMAN44-144 20 JANUARY 2016 71
Attachment 2
4D0X1 DIET TECH DIET COUNSELING AUTHORIZATION GUIDE
Table A2.1. 4D0X1 Diet Tech Diet Counseling Authorization Guide.
GENERAL
CATEGORY
DIET TECH AUTHORIZATION
ALLOWED
DIET TECH AUTHORIZATION
NOT ALLOWED; MUST BE
PERFORMED BY REGISTERED
DIETITIAN ONLY
Adverse Reactions to
Food
Food
Allergies/Hypersensitivities in
Adults
Lactose Intolerance
Food Allergies/Hypersensitivities in
Pediatric Patients Under 18 Years
of Age
Multiple Food Allergies
Cancer
Cancer Prevention
Cancer
Cardiovascular
Disease
Cardiovascular Disease (Diet
for dyslipidemia)
Hypertension (DASH Diet)
Metabolic Syndrome
Congestive Heart Failure-
COPD
COPD
Cystic Fibrosis
Cystic Fibrosis
Diabetes/Endocrine
Adult Type 1 and 2 with no
complications (renal,
hypoglycemia, etc.)
Gestational Diabetes not on
insulin
Reactive Hypoglycemia
Adult Type 1 and 2 WITH
complications (renal,
hypoglycemia, etc.)
Gestational Diabetes on Insulin
Diabetes (Under 18 years of Age)
Disaccharidase Deficiencies
Diet-Drug Nutrient
Interactions
Coumadin
MAOIs
All Others
Eating
Disorders/Feeding
Problems
High Calorie/Protein for weight
maintenance (malnutrition not
present)
All Eating Disorders (Bulimia,
Anorexia Nervosa, Compulsive
Overeating, etc.)
Failure To Thrive (Pediatric and
72 AFMAN44-144 20 JANUARY 2016
GENERAL
CATEGORY
DIET TECH AUTHORIZATION
ALLOWED
DIET TECH AUTHORIZATION
NOT ALLOWED; MUST BE
PERFORMED BY REGISTERED
DIETITIAN ONLY
Adult)
Diet for Dysphagia
Fitness Nutrition
Fitness Improvement Program
Gastrointestinal
Disease
Peptic Ulcer Disease
Gastroesophagheal Reflux
Disease
Celiac Disease
Irritable Bowel Syndrome
Colitis
Crohn’s Disease
Malabsorption, intestinal
Postop Surg Syndromes/By-Pass
Gluten-Restricted
Gliadin-Free Diet
Postgastrectomy
HIV/AIDS
HIV/AIDS
Lifecycle Nutrition
Breast Feeding/Lactation
Vegetarian Diets
Healthy Prenatal Nutrition
(including calorie controlled)
Vegan
Vegetarian Diets During Pregnancy
Hyperemesis Gravidarium
Liver Disease
Hepatitis
Liver Disease
Nephrotic Syndrome
Malnutrition
Marasmus, Nutritional
Kwashiorkor
Protein – Calorie Malnutrition
AFMAN44-144 20 JANUARY 2016 73
GENERAL
CATEGORY
DIET TECH AUTHORIZATION
ALLOWED
DIET TECH AUTHORIZATION
NOT ALLOWED; MUST BE
PERFORMED BY REGISTERED
DIETITIAN ONLY
Miscellaneous
Therapeutic Diets
Fat-Restricted
Fiber-Restricted
High-Fiber
High-Calorie, High-Protein
Purine-Restricted Diet
Tyramine-Restricted Diet
All Others
Modified Consistency
Blenderized
Mechanically Altered Diet
Modified Mineral
Calcium
Potassium
Iron
Sodium Restricted
Overall Dietary Inadequacies
Warranting Use of Multi-
vitamin
All Others
Ascites (Sodium Restriction Under
2 gm)
Nutrition Screening
Nutrition Screening
Nutrition Assessment of Patients at
High Nutritional Risk. Nutrition
assessment of other patients per
local guidance and diet technician
authorization.
Nutrition Support
Tube Feeding
Total Parenteral Nutrition
Renal Disease
Urolithiasis
Chronic Renal Failure
Acute Renal Failure
Dialysis
Substance Abuse
Healthy Nutrition for substance
74 AFMAN44-144 20 JANUARY 2016
GENERAL
CATEGORY
DIET TECH AUTHORIZATION
ALLOWED
DIET TECH AUTHORIZATION
NOT ALLOWED; MUST BE
PERFORMED BY REGISTERED
DIETITIAN ONLY
abuse, chemical dependency
Supplements
General information and
awareness about supplements
Specific/prescriptive guidance on
supplements
Transplant Diets
All
Weight Management
Calorie Controlled Diet for
Weight Management
Pediatric Healthy Weight
Management Principles (no
assigned calorie level) with
parent/guardian present; <5 yrs
old requires contact with
MAJCOM Dietitian.
Very Low Calorie Diets <1200
Calories for Female, <1500 for
Males)
Pediatric Weight Management
(Assigned Calorie Level) (<18 yrs
old)
AFMAN44-144 20 JANUARY 2016 75
Attachment 3
PERSONS AUTHORIZED TO EAT IN MILITARY TREATMENT FACILITY DINING
FACILITIES
A3.1. Authority. DOD 1338.10-M.
A3.2. Category Definition. Charges for persons authorized to eat in a USAF MTF dining
facility vary, depending on the status of each person. The five major categories of personnel are:
officers, enlisted personnel, military dependents, federal civilian employees, and others.
A3.3. General Entitlements. See Table.
A3.4. Special Considerations:
A3.4.1. Outpatients and visitors may eat in MTF dining facility when authorized to do so by
the MTF commander, but must pay either the discount or full meal rate, depending on their
status.
A3.4.2. Inpatients traveling in the aeromedical evacuation system are not charged for their
meals.
A3.4.3. Outpatients traveling in the aeromedical evacuation system pay the full rate for their
meals in the dining facility.
A3.4.4. Nonmedical attendants traveling in the aeromedical evacuation system pay the full
meal rate, regardless of category. (Exception: Dependents of E-4 and below pay the discount
rate).
A3.4.5. Military members of foreign governments pay the same rates as their US
counterparts.
A3.4.6. National Guard and Air National Guard, the ROTC (all services), and the Army, Air
Force, Navy, Marine, and Coast Guard Reserves, on active duty or inactive duty for training,
pay the same rates as their active duty counterparts. They can pay for meals with cash or by
cross service billing.
A3.4.7. Wounded Warriors (WW). With proper identification, WWs receiving inpatient or
outpatient care at the MTF are not charged for meals.
A3.4.8. Outpatients undergoing medical procedures involving extended (4 hours or as per
recommended dietary requirements) periods, a who are unable to purchase food or beverages
by virtue of receiving such care, must pay either the discount or full meal rate, depending on
their status .
A3.4.9. A family member who provides care to an infant receiving inpatient medical care,
who is unable to purchase food or beverages by virtue of providing such care to the infant,
must pay either the discount or full meal rate, depending on their status.
A3.4.10. The discount rate includes the cost of food only.
A3.4.11. The full rate includes the cost of food and a proportional charge for food service
operating expenses.
76 AFMAN44-144 20 JANUARY 2016
A3.4.12. Charges for meals are based on annual DOD rates. HQ USAF/SGMC provides the
rates to medical resource management officers by message in October.
A3.4.13. Food Service Operating Expenses waiver authority is at DOD level. Request for
waivers should be submitted to SAF/FMF, 1130 Air Force Pentagon, Washington, DC
20330-1130.
Table A3.1. Persons Authorized To Eat In MTF Dining Facilities.
These Customers
Pay This Amount
Discount Rate
Full Rate
Enlisted members drawing Basic Allowance for Subsistence (BAS).
X
Officers on duty in the MTF
X
Federal civilian employees on duty in the MTF.
X
Federal civilian employees on official duty as a result of an act of providence
or civil disturbance when no other comparable food service facilities are
available.
X
International Military Education Training (IMET) and Foreign Military Sales
(FMS) students not receiving the meal portion of per diem and the meal
operating charges are recovered through tuition charges.
X
IMET and FMS students when the operating charge is not included in tuition.
X
Officer candidate, cadet, midshipman, or ROTC/NROTC/AFROTC students in
training.
X
Members and chaperones of organized nonprofit youth groups extended the
privilege of visiting a base or who are operating on base and the installation
commander permits them to eat.
X
Students in DoD Dependents Schools overseas and alternative student meal
facilities are not available.
X
Family members of E-1 through E-4.
X
Active duty and nonactive duty aeromedical evacuation patients not receiving
per diem.
X
Active or nonactive duty non-medical attendant (NMA) to an aeromedical
evacuation patient, not receiving per diem.
X
Active duty aeromedical evacuation patients or NMAs on orders and receiving
per diem.
X
Anyone receiving the subsistence portion of per diem.
X
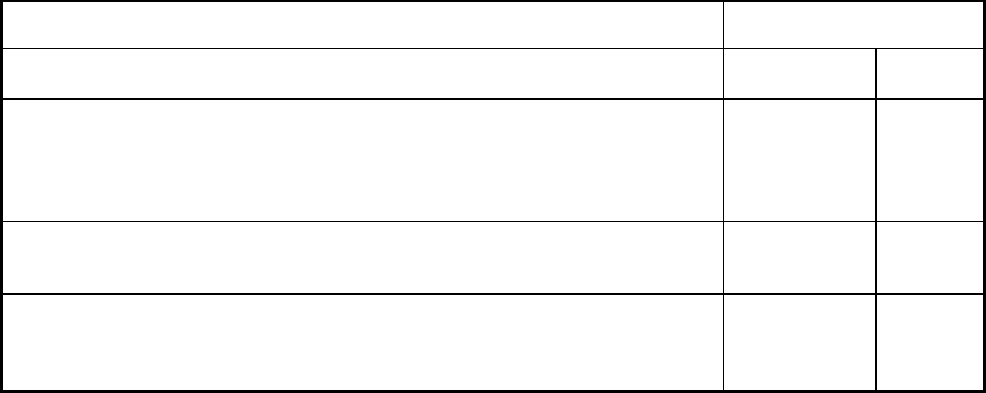
AFMAN44-144 20 JANUARY 2016 77
These Customers
Pay This Amount
Discount Rate
Full Rate
Full-time paid professional field and headquarters Red Cross staff workers,
full-time paid secretarial and clerical Red Cross workers on duty in Red Cross
offices, Red Cross volunteers, uniformed and non-uniformed, in CONUS and
overseas.
X
United Service Organization (USO) personnel authorized by the installation
commander.
X
Anyone who the installation commander allows when considered to be in the
best interest of the Air Force and no other adequate food service facilities are
available.
X
78 AFMAN44-144 20 JANUARY 2016
Attachment 4
TABLE A4.1 NUTRITIONAL MEDICINE SUBSISTENCE REPORT (EXCEL
SPREADSHEET).
MAJCOM
MTF
OBDFA
MBDFA
PBDFA
TOTAL
PURCHASES
COST OF
ISSUES
TOTAL
EARNINGS
TOTAL MEALS
TOTAL MEAL
DAYS
PATIENT MEAL
DAYS
OTHER MEAL
DAYS
OPERATIONAL
MEAL DAYS
TOTAL:
Instructions for completion:
MAJCOMs will submit a consolidated report, by MTF, on a monthly basis to AFMOA Uniform
Business Office. (T-1).
Definitions:
4a. OBDFA: Operational Basic Daily Food Allowance, provided by the base food services
officer,
without any modifications. Use to calculate operational rations.
4b. MBDFA: MTF Basic Daily Food Allowance. The OBDFA modified to include the cost
of 100% ground beef. Used to calculate SIK and CTIM meal earnings.
4c. PBDFA: Patient Basic Daily Food Allowance. MBDFA plus an additional 15% for patient
feedings. Used to calculate patient meal earnings.
4d. Total Meals: Total Meals served each month per AF Accounting Spreadsheet.
4e. Total Meal Days: Replaces the term "ration". Equivalent of 3 meals served in 24 hours. One
bed
day = one meal day.
4f. Patient Meal Day: Equals one bed day or the Ambulatory Procedure Visit (APV)
Equivalent, normally 40% per meal.
4g. Other Meal Day: All other meals served by the MTF dining facility.
4h. Operational Meal Day: Meals issued for exercises.

AFMAN44-144 20 JANUARY 2016 79
Attachment 5
SAMPLE MOA BETWEEN NM & BASE FOOD SERVICE
DEPARTMENT OF THE AIR FORCE
DATE
MEMORANDUM FOR (FORCE SUPPORT SQUADRON CC)
FROM: (REQUESTING CC)
SUBJECT: Patient Feeding Memorandum of Agreement (MOA)
1. The Patient Feeding MOA applies to the XXth Medical Support Squadron (MDSS),
Nutritional Medicine Flight (NMF), and the XXth Force Support Squadron (FSS), (name of
dining facility). The NCOIC of each activity will be the designated representatives. This MOA
addresses responsibilities and local procedures for routine hospital patient feeding under normal
conditions and patient feeding requirements during exercises, war, and disaster contingencies.
The MOA should be reviewed or renewed annually, upon transfer of NCOICs, and change in
agreement of responsibility or procedures.
2. Responsibilities and procedures for food support under normal conditions:
a. The (name of dining facility) will:
(1) Provide menus and notice of menu changes by calling the NMF at XXX-XXXX, or by
faxing the menus and changes to XXX-XXXX as soon as available. Ideally menu changes
should be provided to NMF at least 24 hours in advance.
(2) Provide hot meals along with the condiments to include: desserts, assorted fruits,
beverages etc.
(3) Assist NMF staff in packing food items in insulated food containers to be transported
to the medical facility.
(4) Contact NMF supervisor when procedures need revision or problems arise needing
resolution by either party.
80 AFMAN44-144 20 JANUARY 2016
(5) The (name of dining facility) will not prepare or cook any therapeutic diet menu
items, but will allow NMF staff the space and equipment to prepare therapeutic items in the
dining facility kitchen.
b. NMF will:
(1) Provide the (name of dining facility) a list of NMF personnel authorized to pick up
meals. The NMF NCOIC is responsible for preparing and updating the authorization letter(s)
which are signed by (NMF Chief) (Atch 2).
(2) Inform the dining facility supervisor or food production manager of the number of
meals needed no less than 1 hour prior to that specific meal hour. The number of meals
requested will correspond with those listed on the AF Form 79, Head Count Record (Atch 1).
AF Form 79 is used for accountability of meals and signed by the NMF technician.
(3) Assemble all meal trays for patients using available food from the dining facility’s
daily menu.
(4) Sanitize food preparation/tray assembly areas after each use and maintain designated
NMF storage areas in a neat and sanitary manner.
(5) Sanitize all insulated containers after each meal period. When insulated containers are
not used for more than a 24-hour time period they will be sanitized prior to use.
(6) Ensure all meals and food supplies obtained from the dining facility are secured in a
controlled area and used for patient feeding only.
(7) Whenever necessary, using MDG funds, purchase all supplements and special feeding
terms such as Ensure, Boost, Resource, and other items for patient snacks or specialty diet meals
from the base commissary for patients.
(8) Ensure dining facility is informed of all changes, additions or deletions to the patient
count within an appropriate amount of time so as to avoid an over-production of food or the
unnecessary waste of manpower assets.
3. Responsibilities and procedures for patient feeding during exercises.
a. NMF will: continue to pick up food from the base dining facility to feed patients.
b. The (Name of dining facility) will continue patient meal preparation as usual whenever
meals are requested.
4. The undersigned agrees to the terms of this MOA.
5. This letter supersedes all previous MOAs established between the two parties.
AFMAN44-144 20 JANUARY 2016 81
SIGNATURE BLOCK
Commander, XX Medical Support Squadron
2 Attachments:
1. AF Form 79, Head Count Record (controlled form)
2. List of Personnel Authorized to pick up meals
lst Ind, XX FSS/CC, Patient Feeding Memorandum of Agreement (MOA), (enter date)
MEMORANDUM FOR XX MDSS/CC
Approved/Disapproved
SIGNATURE BLOCK
Commander, XX Force Support Squadron
Annual Review Dates:
___________________________________
___________________________________
___________________________________
___________________________________
82 AFMAN44-144 20 JANUARY 2016
Attachment 6
NUTRITIONAL MEDICINE SERVICE OVERSIGHT CHECKLIST
(Reference: AFMAN 44-144, Nutritional Medicine)
Purchasing Subsistence:
Do the appropriate Nutritional Medicine (NM) personnel have a thorough
knowledge/understanding of their Prime Vendor contract to include renewal timeframes?
Are the duties of personnel purchasing subsistence separated from the duties of personnel
completing ration accounting so that no one individual is responsible for both originating
data and inputting/processing data?
Has NM designated individuals authorized to accept or reject subsistence or supplies
delivered under prime vendor programs or other DSCP (Defense Supply Center Philadelphia)
contracts?
Do designated personnel verify the hard copy purchase order with the vendor invoice from
the driver and ensure that products received match those ordered at the time of receipt so that
the vendor’s delivery ticket may be annotated with any discrepancies?
Do invoices reflect only items and quantities accepted and signed for by the NM receiving
official?
If /when discrepancies are detected upon receipt, is the vendor’s invoice annotated to indicate
actual quantities received by striking through the listed quantity and entering the received
quantity and reason for the differences?
Each month, is SF 1080 verified?
If available, is the NM subsistence GPC card appropriately (only for subsistence items to
support the preparation or serving of foods)?
Storing Subsistence:
Are subsistence storage rooms, refrigerators, and freezers secure (locked) when not in use;
(exception: produce, and direct deliver/milk refrigerator)?
Is entry for unauthorized personnel controlled, prohibited?
Inventory Controls:
AFMAN44-144 20 JANUARY 2016 83
Is the storeroom manager maintaining the perpetual inventory system of subsistence stock
records, source documents for subsistence purchase and issues (entries include vendor
receipts and purchase invoices, GPC statements and receipts, or AF Forms 543, Food Issue
Record)?
Is a physical inventory performed each month (except September) on one of the last three
normal duty days and representative as of the date of the inventory (with the exception of FY
close-out)? The FY close-out in September should be conducted on the last day of the FY
when possible (if not possible, then on the last duty day).
Does the MTF Commander appoint a disinterested, trained person (officer or SNCO) to
perform a physical inventory of all food items? The inventory official delivers the completed
and signed inventory listing to the MSA Officer and NM Officer/NCOIC.
If there are discrepancies/differences between the physical count and inventory records (that
cannot be resolved), is an Inventory Adjustment Report prepared?
At the end of each quarter and the FY, is the dollar value of the closing inventory between
(not more than) 15% and 30% of the cumulative average monthly cost of food used for the
FY to date? MTFs using Prime Vendor should reduce inventory levels to 2-3 days’ supply.
Optimal inventory levels should be determined locally to ensure that adequate food is on
hand/available in case of disaster or emergency situations when deliveries may be disrupted.
Issuing and Costing Subsistence:
Do storeroom personnel issue subsistence using Computrition (automated) or AF Form 543
(manual)? Direct delivery items may be issued on the day they are received. Perishable
fresh fruits and vegetables may be issued the day of purchase and receipt. High volume, low-
cost items may be issued as needed each day, or for a longer use period.
Does the person receiving the food items from the storeroom count and verify food received
and sign the form in the received block? If more food items are issued than needed, are they
returned to inventory under the returned column?
Does the MTF use the Last-In First-Out (LIFO) costing method for recording purchases and
costing items?
Cashier Operations:
Is there separation of financial duties and responsibilities in authorizing, processing,
recording, and receiving cash transactions? Cashiering and accounting duties must be
separated to ensure adequate internal controls to prevent loss of funds.
Does NM have: appropriate and authorized change fund (IAW DoD Financial Management
Regulation 7000.14-R, Vol 5); for a la carte operations, a cash control supervisor designated
84 AFMAN44-144 20 JANUARY 2016
in writing; and, an adequate funds storage safe to hold the change fund, cash sales, and
guarded forms (such as AF IMT 79)?
Is AF Form 2570 used to issue the cash drawer and AF IMT 79 to the cashier? Is the same
AF Form 2570 used by the cashier to return the cash drawer, cash collected, and AF IMT 79
to the cash control officer after the meal? Are any discrepancies noted on the AF IMT 79?
Does the cash control supervisor indicate funds and guarded forms (AF IMT 79) for turn in
to MSA Office using AF Form 1305 for cash collected and AF Form 1254 for guarded forms
used to document the transfer of responsibility from NM to the MSA Office?
Does the cash control supervisor indicate funds and guarded forms (AF IMT 79) for turn in
to MSA Office using AF Form 1305 for case collected and AF Form 1254 for guarded forms
used to document the transfer of responsibility from NM to MSA?
Is all cash collected and AF IMT 79 forms used turned in to the MSA office daily, excluding
weekends? If the storage limit on the safe/funds storage container is inadequate to support
the amount of cash collected over a 2 or 3 day weekend, NM should make arrangements with
the MSA Office to turn in cash during the weekend or request an increase in the amount of
funds that can be stored. In any case, cash deposit paperwork must be done on a daily basis,
even if the funds must be held over the weekend.
Are cash registers correctly programmed to calculate both the charge cash patrons the DoD-
directed surcharge and correctly total the surcharges from each meal period?
Is the MTF MSA Office correctly dividing the surcharge between the AF Military Personnel
Appropriation and the Defense Health Program O&M appropriation? MSA Office is
supposed to proportionately divide the surcharge accordingly with the start of each FY.
If the NM DFAC does not have cash registers (SCAMS operations), do all diners, except
ambulatory and transient patients, sign for meals using the appropriate number of AF IMT
79s for each meal? Does the cashier verify the diner’s identification?
Are completed AF IMT 79 forms and collected cash delivered to the MSA Office at least
once each normal duty day and the MSA Office verifies the cash receipts against the total
amount of cash received as annotated on AF IMT 79s?
Eligibility and Identification of Diners:
Is diner eligibility and identification correctly verified?
Are diners appropriately processed based on their status?
Recipe Pricing:
AFMAN44-144 20 JANUARY 2016 85
1. For a la carte operations, is each recipe item priced and sold on an individual item basis?
Computrition menu pricing reports such as the Computrition Recipe Price Report should
be used/available; if not, each recipe cost must be manually calculated. Menu item
pricing must include DoD surcharges.
NM Ration Accounting:
Are NM accounting parameters accurate and up to date, whether calculated/using the AF
Accounting Spreadsheet (Excel) or manually?
Is the MTF Basic Daily Food Allowance (BDFA) accurately calculated, on a monthly basis,
using the most current monthly Food Cost Index (FCI)?
Is the Patient BDFA correctly calculated (BDFA plus 15% supplemental allowance)? Is the
Patient BFDA only used to calculate patient meal day earnings?
If applicable, were NM activities using SCAMS and serving less than 100 average daily meal
days for both patient and DFAC patron rations applying the authorized additional
supplemental allowance of 15% of the MTF BDFA (this is called the small volume feeding
allowance/percentage)? This eligibility is determined at the end of each month and is applied
to ESM and SCAMS DFAC patrons only. It is not authorized for a la carte cash sales. If
allowed, the 15% supplemental allowance is used to figure the next month’s MTF BDFA.
If applicable, was the Therapeutic In-flight Meals (TIMs) allowance appropriately
applied/used? A special monetary allowance equal to 80% of the MTF BDFA is authorized
for each TIM furnished by NM for aeromedical evacuation patients to consume in-flight.
Were holiday and special meal percentages/allowances of an additional 25% (for federal
holidays, the AF birthday, and Easter) and 15% (for airman appreciation meals) appropriately
applied to ESM DFAC patrons at all facilities and cash patrons at SCAMS facilities (a la
carte facilities do not receive an additional 25% for cash customers of patients during these
meals)? To claim the additional percentage, holiday meals must be served on the actual day
designated as the holiday. Christmas and Thanksgiving holiday meals must be served at the
lunch meal. There must be a special menu planned and served to qualify for the allowance.
Are occupied bed days accurately calculated? Occupied bed day refers to the number of
inpatients subsisting in the MTF and equals beds occupied minus bassinets from the
Admission and Disposition Recapitulation Report.
Are meal days accurately calculated? A meal day is a value in which the number of meals is
weighted by a predetermined percentage. The number of meal days for a given day is
figured by multiplying the number of breakfast, lunch and dinner meals served by the
factored percentages of 20, 40 and 40 percent, respectively, and totaling the results. If/as
applicable, TIMs are valued at 80%, Ambulatory Procedures Visit (APV)/Same Day Surgery
(SDS) meals at 40%, holiday meals at 65%, and midnight meal at 20%.
86 AFMAN44-144 20 JANUARY 2016
Are patient meal days appropriately obtained by multiplying the occupied bed days by the
appropriate meal factors?
Are ESM meal days appropriately obtained by multiplying the number of ESM patrons by
the appropriate meal factors?
Are cash patron meal days appropriately obtained by multiplying the number of cash patrons
by the appropriate meal factors?
Subsistence Account Reporting and Management:
For automated operations, are the AF Accounting Spreadsheet and Computrition used to
assist NM managers in overseeing their subsistence account, inventory value, earnings and
collections?
For manual operations, are the following three manual cost data records and financial reports
used in NM and the MSA Office to determine financial status: AF Form 544, AF Form 541,
and AF Form 546?
Is AF Form 2573, Diet Census, documented once daily (following procedures printed on the
reverse side of the form) used for workload figures for the number of trays served to patients
on the nursing units and the number and types of therapeutic diets served to patients on the
nursing units?
On a monthly basis, is the NM Flight submitting their financial data on the appropriate
spreadsheet (reference AFMAN 44-144, Attachment 4 and AFMOA spreadsheet) to the
AFMOA Uniform Business Office, via their Functional Manager? Is NM also providing a
copy of this info/spreadsheet to their MTF MSA Office every month?
Subsistence account management. Primary indicators to evaluate the financial status of the
NM operation are: earnings less food served, earnings minus purchases, inventory level, and
periodic inventory adjustment.
Financial Parameters. Does the status of earnings minus issues not exceed (plus or minus)
5% of the average monthly ration earnings at the end of each of the first three quarters of the
FY as annotated on the AF Accounting Spreadsheet? At the end of the FY, do earnings
minus issues not exceed $100.00 or (plus or minus) 2% of the average monthly credit
earnings, whichever is greater?
FY Close-out. If at the end of the FY, the earnings minus issues on the AF Accounting
Spreadsheet or line 57 of AF Form 544 exceeds (plus or minus) 2% of the average monthly
earnings, did the MTF Commander investigate?
