Journal of Applied Research on Children: Informing Policy for Journal of Applied Research on Children: Informing Policy for
Children at Risk Children at Risk
Volume 2
Issue 2
Teen Pregnancy
Article 8
2011
Does Immediate Access to Birth Control Help Prevent Pregnancy? Does Immediate Access to Birth Control Help Prevent Pregnancy?
A Comparison of Onsite Provision Versus Off Campus Referral for A Comparison of Onsite Provision Versus Off Campus Referral for
Contraception at Two School-Based Clinics Contraception at Two School-Based Clinics
Peggy Smith
Baylor College of Medicine
Gabrielle Novello
Mariam R. Chacko
Follow this and additional works at: https://digitalcommons.library.tmc.edu/childrenatrisk
Recommended Citation Recommended Citation
Smith, Peggy; Novello, Gabrielle; and Chacko, Mariam R. (2011) "Does Immediate Access to Birth Control
Help Prevent Pregnancy? A Comparison of Onsite Provision Versus Off Campus Referral for
Contraception at Two School-Based Clinics,"
Journal of Applied Research on Children: Informing Policy for
Children at Risk
: Vol. 2: Iss. 2, Article 8.
DOI: https://doi.org/10.58464/2155-5834.1043
Available at: https://digitalcommons.library.tmc.edu/childrenatrisk/vol2/iss2/8
The Journal of Applied Research on Children is brought
to you for free and open access by CHILDREN AT RISK at
DigitalCommons@The Texas Medical Center. It has a "cc
by-nc-nd" Creative Commons license" (Attribution Non-
Commercial No Derivatives) For more information, please
contact [email protected].tmc.edu

Does Immediate Access to Birth Control Help Prevent Pregnancy? A Comparison Does Immediate Access to Birth Control Help Prevent Pregnancy? A Comparison
of Onsite Provision Versus Off Campus Referral for Contraception at Two School-of Onsite Provision Versus Off Campus Referral for Contraception at Two School-
Based Clinics Based Clinics
Acknowledgements Acknowledgements
Acknowledgments: This article was supported in part by a grant from St. Luke’s Episcopal Health
Charities, the Simmons Foundation and Maternal Child Health Bureau/Leadership Education in
Adolescent Health Grant - 2 T71 MC00011
This article is available in Journal of Applied Research on Children: Informing Policy for Children at Risk:
https://digitalcommons.library.tmc.edu/childrenatrisk/vol2/iss2/8

Introduction
Unplanned teen pregnancy and parenting continue to be issues
throughout the United States. In 2010, the national birth rate was 39.1 per
1,000 women aged 15-19.
1
The teen birth rate in Texas is particularly high
at 63.4 per 1,000, the third highest rate in the country. In Houston and
Harris County, Texas, teen birth rates of of 85 to 116 per thousand in
some zip codes are higher than the Texas rate in most areas, and in many
places in Houston and Harris County, teen birth rates are greater than 100
per 1,000 females.
2
High birth rates are indicative of even higher
pregnancy rates, as not all pregnancies are carried to term. In fact, Texas
has the fourth highest teen pregnancy rate in the nation at 101 per 1,000
teens ages 15-19, versus the national rate of 84 per 1,000.
3
This rate is
projected to increase by 13% by the year 2015, resulting in a projected
rate of 127 per 1,000.
4
Furthermore, the city of Houston has a high rate of
repeat pregnancies. In 2008, Houston had a repeat pregnancy rate of
23%, compared with other major cities in the U.S., which ranged from 12%
to 28%.
5
Minority groups, in particular blacks and Hispanics, are
disproportionately at-risk for teen pregnancy. Hispanics have the highest
teen birth rates in the country, followed by black teens. It is estimated that
52% of Hispanic girls and 50% of black girls under 20 years of age will
become pregnant, as opposed to 19% of non-Hispanic white girls.
6,7
For
teenage girls aged 15-19 in 2006, the birth rate among Hispanics was 83
per 1,000 and 64 per 1,000 among blacks, compared with 27 per 1,000
among non-Hispanic whites.
8
In Houston, this disparity is particularly
pronounced. Texas Department of State Health Services reported that in
2003, 66% of all teen births were to Hispanic mothers and 23% were to
black mothers, while 11% were to white mothers.
9
The costs associated with teen childbearing are significant and
could potentially impact a school’s approach to teen pregnancy. Not only
does teen childbearing negatively affect mother and child, there are
significant consequences for the nation, states and districts. A 2008
analysis by The National Campaign to Prevent Teen and Unplanned
Pregnancy indicated teen childbearing cost U.S. taxpayers at least $10.9
billion each year, with the majority of costs incurred because of births to
teens 17 years and younger.
10
The public sector costs of teen childbearing
include lost tax revenues because of lower earnings from teen parents,
higher costs of public assistance to families with teen parents, and higher
costs of child welfare and health care for children born to teen mothers.
Furthermore, with approximately only 40% of teen mothers graduating
from high school, school districts with high teen pregnancy rates have a
1
Smith et al.: School-Based Birth Control Policy Comparison
Published by DigitalCommons@TMC, 2011
significantly increased risk of losing average daily attendance funding, as
well as enrollment funding.
11
A number of strategies have been employed with the goal of
reducing teenage pregnancy, with many taking place within schools.
Approximately 95% of all youth aged 5-17 was enrolled in school in 2008,
making the school system an ideal avenue through which to provide
pregnancy risk-reduction strategies.
12
The developmental period during
which students are in school is also conducive to introduction of
pregnancy prevention interventions, with the majority of students in school
at pre-sexual initiation or just post-sexual initiation phase. Educational
interventions, including abstinence-only, abstinence-plus and
comprehensive sex education curricula, have had some success in
helping to prevent teen pregnancy.
13
For students at high risk for teen
pregnancy, however, education curricula are not always enough. High-risk
youth tend to fall in lower socioeconomic groups and often do not have
regular access to primary and reproductive healthcare facilities.
Government funded and non-profit school-based health centers have
been established to provide these students with increased access to
reproductive health services in order to help them avoid unintended
pregnancy, sexually transmitted infections (STIs) and HIV. However, there
is often variation among these clinics in the services provided. For
example, many school-based clinics prohibit the dispensing of hormonal
birth control on-site.
Evidence shows that when hormonal birth control is not dispensed
on-site, teenage family planning clients take longer to come in to the clinic
for follow-up visits, are less likely to choose a birth control method during
their first or second visit and to select a consistent birth control method
over time.
14
-16
Ultimately, the delay or complete lack of access to
hormonal birth control on site at school-based clinics may have
deleterious effects on reproductive health outcomes among teens.
Zimmer-Gembeck, Doyle and Daniels
14
found that female teens who
visited school-based family planning clinics that initiated an on-site
dispensing policy were significantly more likely to select a contraceptive
method when compared to teens who visited the clinic before the on-site
dispensing policy was instituted. In addition, clients were more likely to
return for additional family planning visits after the on-site policy was
established. Sidebottom, Birnbaum and Stoddard
15
found that under a
voucher system for hormonal contraceptives in Minneapolis school-based
clinics, only 41% of students received all requested contraceptives. In
comparison, after a policy change to dispense hormonal contraceptives
on-site, 99% of students received all requested contraceptives. Ethier et
2
Journal of Applied Research on Children: Informing Policy for Children at Risk, Vol. 2 [2011], Iss. 2, Art. 8
https://digitalcommons.library.tmc.edu/childrenatrisk/vol2/iss2/8
DOI: 10.58464/2155-5834.1043
al.
16
found that female students who had access to a school-based health
center were more likely to have received pregnancy and disease-
prevention care, used hormonal contraception and emergency
contraception at last sexual encounter than female students who were
unable to access a school-based health center.
A limitation of existing studies is a lack of information on the overall
effects of these different dispensing policies on reproductive health
outcomes. Thus, the purpose of this paper is to compare the impact of
different policies for access to hormonal contraceptives among low-
income teens at two comparable school-based clinics. Specifically, the
objective of this exploratory comparison was to determine whether or not
receipt of hormonal contraception on site at a school-based clinic affected
subsequent pregnancy rates among student patients.
Methods
Program Description
The school-based adolescent clinics are under the aegis of an academic
medical institution and operate in collaboration with a metropolitan
independent school district. The primary health care model used at two
school clinics is comprehensive, focuses on both teenage girls and boys
and incorporates elements of prevention, intervention and education
through meaningful collaboration with school and other community
partners. The clinics’ primary goal is to provide access to preventive
health care services to uninsured students through delivery of on-site
medical, gynecological, nutritional, and mental health services. Written
parental consent is obtained at initial entry into the clinic and preferably at
the beginning of the academic year. As part of this goal, the clinics attempt
to reduce pregnancy rates through standardized screening for sexual
activity and risk of pregnancy at every clinic visit. Brief contraceptive
counseling for teens who engage in sexual activity is also provided. The
clinic in one school (School A) has been in existence since 2005. The
contraceptive dispensing policy at School A’s clinic is on site, where those
seeking birth control can receive free and confidential contraceptive
services (including hormonal contraception using the same-day or Quick
Start method, emergency contraception and condoms) at the clinic
(supported by Title X funding). The other school clinic (School B) has been
in existence since 2007 and uses a referral policy, by which students
cannot receive hormonal contraception, emergency contraception or
condoms on the school campus and must travel to another affiliated teen
clinic to receive free hormonal contraception. However, Well Woman
examinations are conducted, and STI testing and treatment is provided.
3
Smith et al.: School-Based Birth Control Policy Comparison
Published by DigitalCommons@TMC, 2011
The contraceptive service policy was determined by the principal of each
school based on political and personal factors.
Participants
The schools are located in comparable inner city urban
neighborhoods. The majority of students was of Hispanic ethnicity and had
no private health insurance coverage. The number of students enrolled in
School A in 2008-2009 was 1928 and in 2009-2010 1891; School B in
2008-2009 was 2606 and in 2009-2010 was 2763. The number of
unduplicated visits made by students to the School A clinic in 2008-2009
was 988 and in 2009-2010 was 980. Visits to the School B clinic in 2008-
2009 were 988 and in 2009-2010, 1253. Over 80% of students who
attend both school clinics participate in the federal free and reduced lunch
program, an indicator of low-income status.
Data Collection
Using a retrospective chart review and an electronic database
review (AHLERS Integrated System), patients seen in both clinics from
9/2008-12/2009 for primary care and reproductive health symptoms were
reviewed. Charts of all female patients seen during this time period were
reviewed by a research assistant. Charts of sexually active females were
identified and the following data was extracted: demographic data, history
of prior pregnancy, record of providing birth control counseling, the
outcome of the counseling; documentation of interest in seeking hormonal
contraception; evidence of a return visit and dispensing of hormonal
contraception in school clinic A; and a referral appointment to an affiliated
teen clinic off campus and evidence of appointment kept and hormonal
contraception dispensed in school clinic B. Whenever possible, the nurse
practitioner at clinic B and who worked at more than one clinic site
referred students to herself at the referral clinic site. Outcome measures
included positive pregnancy test results at any point during or after birth
control use. The authors made the assumption that since these students
had sought services at the school clinic, they would likely utilize their
school clinic or the referral clinic to seek pregnancy testing. The clinics
were known for their ability to provide confidential pregnancy testing and
facilitate prenatal care for pregnant girls. Patients were tracked via the
electronic database system through 3/31/2010.The data collected was
second checked by the authors. Human Subjects approval was obtained
from the institution to review medical records and electronic data (Protocol
#H26846).
4
Journal of Applied Research on Children: Informing Policy for Children at Risk, Vol. 2 [2011], Iss. 2, Art. 8
https://digitalcommons.library.tmc.edu/childrenatrisk/vol2/iss2/8
DOI: 10.58464/2155-5834.1043

Data Analysis
Data were entered in IBM SPSS Statistics 19.0. Data analysis
included calculation of mean age, frequency of students with a prior
history of pregnancy, appointments kept, hormonal contraception started ,
mean duration of follow up period, positive pregnancy tests. The duration
of the observation period for a participant in each setting was determined
as the time between the first visit, when contraceptive counseling was
conducted, through 3/31/2010. An independent t-test was used to
compare the mean duration of the observation period between School
clinics A and B. Fisher’s Exact Test was used to compare the
appointment-keeping rate and the type of hormonal contraceptive method
dispensed between school clinics A and B, In addition Fisher’s Exact Test
was used to compare the overall pregnancy rates and the association
between a prior history of pregnancy and pregnancy rates.
Results
School A clinic: As seen in Table 1 (see Appendix), of 79 students who
requested hormonal contraception the mean age was 17.5 years (range
15 to 22 years); 68% >
18 years, 77% were Hispanic, and 21% (16/79)
reported prior pregnancy. As seen in Table 2, all 79 students (100%)
returned for onsite hormonal contraception (65% pill and 35% long acting
progestin injection by appointment within one week. The mean duration of
the observation period for participants in this setting was 13 months
(range 4-19 months).
School B clinic: As seen in Table 1, of the 40 students who
requested and were referred for hormonal contraception, the mean age
was 17.5 years (range 14 to 20 years); 52% were >
18 years, 88% were
Hispanic, and 7.5% reported prior pregnancy. As seen in Table 2, only
50% (20/40) kept their appointment for hormonal contraception. The time
taken to follow up for these appointments ranged from the same day to
126 days (mean 7.25 days); 75% (15/20) were seen within 7 days and
85% (17/20) were seen within 14 days. The remaining three students took
39 to 126 days to keep their appointment. Pills were dispensed to 85%
(17/20) and 15% (3/20) received long acting progestin injection. The mean
duration of the observation period for participants in this setting was 11.9
months (range 4-19 months).
A significantly higher frequency of students kept their appointments
for hormonal contraception at School A clinic as compared to School B
clinic (p <0.05). The difference between the mean duration of the
observation period and type of birth control used (pills versus long acting
progestin injection) between School clinics A and B was not statistically
5
Smith et al.: School-Based Birth Control Policy Comparison
Published by DigitalCommons@TMC, 2011
significant. Combining the data of both schools, the overall pregnancy rate
for students in both clinics was 10.9% (13/119). There was no statistically
significant difference between the mean age of students who did and did
not have a documented positive pregnancy test (18. 0 vs. 17.5 years). As
seen in Table 2, the pregnancy rate was significantly higher at the school
that referred its students for contraception compared to the school with
onsite services (p< 0.05). The pregnancy rate was also significantly higher
for students without a prior history of pregnancy in the school with a
referral policy for contraception (21.6%) versus the school with onsite
contraceptive services (4.7%) (p< 0.05).
Discussion
This study was a preliminary attempt to evaluate outcomes of differing
policies regarding the provision of hormonal birth control at school-based
health clinics. The main findings were: (1) the follow up appointment rate
for hormonal contraception among students who sought birth control at a
school clinic was significantly higher at the school clinic with onsite
contraceptive services compared to the school clinic with a referral policy
for contraception. In addition, at the school clinic with a referral policy of
those who kept their appointments, the majority (85%) were able to keep
their appointment within 14 days; (2) the school clinic with a referral policy
for contraception had a significantly higher pregnancy rate than the school
clinic with on-site contraceptive services and; (3) the pregnancy rate was
also significantly higher for students without a prior history of pregnancy in
the school with a referral policy for contraception compared to the school
with onsite contraceptive services.
The first finding in this study helps to strengthen other published
studies that found the provision of on-site access to birth control was more
likely to promote birth control use.
14-16
It also appears that at least half the
students are able to follow through with appointments when a successful
referral mechanism is in place. However, it is concerning that almost half
of the students were unable to follow through, despite indicating their
interest in seeking hormonal contraception. In this context, it is likely that
these students had difficulty accessing the offsite services that were
offered for multiple reasons. We can speculate that the challenges
included difficulty with arranging appointments to initiate and obtain refills
for hormonal contraception, lack of transportation and inability to seek
confidential services on one’s own after school.
The difference in pregnancy rates between the two schools was
significant and highlights the potential for easy access to affordable
reproductive services and a wide range of contraceptive services in a
6
Journal of Applied Research on Children: Informing Policy for Children at Risk, Vol. 2 [2011], Iss. 2, Art. 8
https://digitalcommons.library.tmc.edu/childrenatrisk/vol2/iss2/8
DOI: 10.58464/2155-5834.1043
school clinic to positively affect health outcomes among high-risk
populations. Reduced compliance with oral contraceptive pills (as
compared to injectable long acting progestin) may have negatively
affected the pregnancy rates at both school clinics. This is supported by
data that demonstrate higher compliance rates and lower pregnancies
rates with injectable long acting progestin involving same day or Quick
Start method as compared to oral contraceptive pill use.
17
In addition, the
availability of condoms and emergency contraception or method switching
may have lowered the pregnancy rate at the school with onsite hormonal
contraceptive services. Finally, pregnant girls may have dropped out of
both schools and use of other medications interfering with oral
contraceptive pills may have affected rates in both locations.
Unfortunately, these data are not retrievable.
A prior history of pregnancy appeared to encourage seeking of
hormonal contraception and thus affected the outcome measure at both
school clinics. This finding suggests that these teen and young adult
mothers were motivated to prevent further pregnancies and wanted to
graduate from high school.
18
In contrast, the pregnancy rate was
significantly higher for students without a prior history of pregnancy in the
school with a referral policy for contraception compared to the school with
onsite contraceptive services. Improving access to hormonal
contraception for sexually active high school females without a prior
history of pregnancy who are motivated to prevent unintended pregnancy
is important. Our research supports the need for a greater focus by
communities on prevention of unintended pregnancy among high school
students with no prior history of pregnancy. Evidence exists that school
enrollment functions as a protective factor in the reduction of risk
behaviors. This is especially true for high school settings in which sexual
risk-taking related to unintended pregnancy has significant consequences
for the completion of secondary education and the matriculation to
colleges and universities.
19
However, college aspirations may not be
protective against initiation of sexual activity in neighborhoods with a high
concentration of poverty.
20
It would be logical that school-based clinics
collaborate with high schools that predominantly enroll students from low
income neighborhoods to address this adolescent health issue.
The provision of comprehensive adolescent-focused health care,
components of on-site medical services should include medical services,
case management and social support, and accessibility and convenience
to enhance the possibility that adolescents will obtain and use prescriptive
and long acting methods of hormonal contraception (LARC) to prevent
unintended pregnancy. The convenience of on-site service is especially
7
Smith et al.: School-Based Birth Control Policy Comparison
Published by DigitalCommons@TMC, 2011
important for time-sensitive emergency contraception. This preventive
method, by being available to students, maximizes pregnancy prevention
services for teens who otherwise would not have access to a private
physician or are under 18 years of age and could not receive the method
without a prescription.
In fact, individual school policy as well as school district policy
appears to be a major factor determining the prohibition of on-site
contraceptive dispensing among school-based health centers across the
country, as 30% and 74% of prohibitions were determined by these
factors, respectively.
21,22
One may wonder if those in the educational field
and parents are either unwilling or unable to see the consequences of
unintended pregnancy on the educational attainment of their students.
The low number of students seeking hormonal contraceptive
services over a 12-month period is striking, especially at the school clinic
with onsite contraceptive services. Several factors may be at play here.
Per school district policy. all adolescents who received services at both
school clinics must have a signed parental consent. Because students
know this, it may be a barrier to seeking confidential contraceptive
services (even prior to an initial clinic visit) by all students, including those
who have parental permission and those unwilling or unable to obtain
parental permission. In addition, the school clinic with a referral policy for
contraception had been in existence for two years at the time of this study
and may not have been familiar to many students and parents. Some
students could have also had private providers or gone to other health
facilities such as a federally qualified health center.
Limitations
The major limitations of this study are the retrospective chart review
method for data collection, the small sample size in the school with a
referral policy for contraception and the limited number of variables
extracted for data analysis. The small sample size also precluded
multivariable analysis to control for confounding variables. In addition,
important variables such as condom use and emergency contraception
were not tracked during the study period. Finally, cultural values
surrounding pregnancy at younger ages among certain minority immigrant
populations are shown to affect pregnancy rates and were not controlled
for in the statistical analysis.
6,7
However, the schools were comparable in
terms of ethnicity.
8
Journal of Applied Research on Children: Informing Policy for Children at Risk, Vol. 2 [2011], Iss. 2, Art. 8
https://digitalcommons.library.tmc.edu/childrenatrisk/vol2/iss2/8
DOI: 10.58464/2155-5834.1043
Recommendations
Health professionals and community leaders may need to accept the
additional responsibility of informing the public school community of the
value of providing reproductive health care services on campus to at-risk
adolescents at the high school level. While historically schools have been
seen as the source of added value services to students who receive
education under their purview, broad endorsement of providing medical
care as well is not universal. One strategy to advance this concept is to
redefine health care from the point of view of access. Therefore, a
potential strategy for advocating for comprehensive school-based clinics
can be embedded in the concept of the medical home. The medical home
model implemented in a teen clinic or family planning clinic setting can be
an efficient way to deliver both well and sick child care for communities
with large numbers of uninsured youth.
23
Creating a medical home within
a school venue can be an efficient way not only to initiate and complete
series of vaccinations, for instance, but also to involve parents through the
consenting process required for the care of minors. Using the medical
home model can also provide a forum for the detection and treatment of
sexually transmitted infections, the prevention and screening of HIV, and
the prevention of unintended pregnancy through contraceptive dispensing
and counseling in this at-risk group. Therefore, the authors recommend
the collaboration between schools and teen-focused clinics to create a
medical home for high-risk teens. Recently enacted national legislation
has yet to be interpreted as to whether or not such recommendations can
be practically actualized on a broad scale.
Conclusions
This was a preliminary attempt to evaluate outcomes of differing policies
regarding the provision of hormonal birth control at school-based health
clinics to students seeking hormonal contraception. Results indicate that
the school clinic with a referral policy for contraception had a significantly
higher pregnancy rate than the school clinic with on-site contraceptive
services. Further study with a larger sample size is necessary. This study
has implications for reproductive health policy, especially as directed
toward high-risk teenage populations.
9
Smith et al.: School-Based Birth Control Policy Comparison
Published by DigitalCommons@TMC, 2011
References
1. Child Trends. Facts at a glance: A fact sheet reporting national,
state, and city trends in teen childbearing. Publication 2011-10.
2011.
2. Texas Department of State Health Services, Bureau of Vital
Statistics, 2008. Harris County Teen Birth Rates (Instant Atlas):
Accessed August 16, 2011. http://www.sph.uth.tmc.edu/tprc/tprc-
default-inner.aspx?id=10662
3. Guttmacher Institute. US Teenage Pregnancies, Births and
Abortions: National and State Trends and Trends by Race and
Ethnicity. http://www.guttmacher.org/pubs/USTPtrends.pdf.
Accessed July 12, 2011.
4. Sayegh MA, Castrucci BC, Lewis K, Hobbs-Lopez A. Teen
pregnancy in Texas: 2005 to 2015. Matern Child Health J.
2010;14:94-101.
5. Child Trends. Percentage of all teen births that are repeat births,
and number of births to mothers under 20, in large cities*, 2008.
National Center for Health Statistics, 2008. Natality Special
Research File. 2011.
6. National Campaign to Prevent Teen Pregnancy. Teen Pregnancy
and Childbearing among Latino Teens.
http://www.thenationalcampaign.org/resources/pdf/FastFacts_TPC
hildbearing_Latinos.pdf. Accessed July 12, 2011.
7. National Campaign to Prevent Teen Pregnancy. Teen Pregnancy
and Childbearing among Black Teens.
http://www.thenationalcampaign.org/resources/pdf/FastFacts_TPC
hildbearing_Blacks.pdf. Accessed July 12, 2011.
8. Martin JA, Hamilton BE, Sutton PD, et al. Births: final data for
2006. National Vital Statistics Reports, 57(7). Hyattsville, MD:
National Center for Health Statistics; 2009.
9. City of Houston. The state of health in Houston/Harris County.
http://www.houstontx.gov/health/HoustonHealth/StateOfHealth2007
.pdf. Published 2007. Accessed September 9, 2010.
10. National Campaign to Prevent Teen Pregnancy. Counting it up: The
Public Cost of Teen Childbearing. Available at:
http://www.thenationalcampaign.org/costs/default.aspx. Published
2011. Accessed July 12, 2011.
11. Hoffman, S.D. (2006). By the numbers: the public costs of teen
childbearing. National Campaign to Prevent Teen Pregnancy:
Washington, DC.
10
Journal of Applied Research on Children: Informing Policy for Children at Risk, Vol. 2 [2011], Iss. 2, Art. 8
https://digitalcommons.library.tmc.edu/childrenatrisk/vol2/iss2/8
DOI: 10.58464/2155-5834.1043
http://www.thenationalcampaign.org/costs/pdf/report/1-
BTN_Front_Matter.pdf. Accessed September 9, 2010.
12. US Department of Commerce, Census Bureau, Current Population
Survey (CPS), October Supplement, 1970–2008.
http://nces.ed.gov/programs/coe/2010/section1/table-ope-1.asp.
Accessed September 9, 2010.
13. Kirby D. The impact of schools and school programs upon
adolescent sexual behavior. J Sex Res. 2002;39(1):27-33.
14. Zimmer-Gembeck, MJ, Doyle L, Daniels JA. Contraceptive
dispensing and selection in school-based health centers. J Adolesc
Health. 2001;29:177-185.
15. Sidebottom A, Birnbaum AS, Nafstad SS. Decreasing barriers for
teens: evaluation of a new teenage pregnancy prevention strategy
in school-based clinics. Am J Public Health. 2003;93:1890-1892.
16. Ethier KA, Dittus, PJ, DeRosa CJ et al. School-based health center
access, reproductive health care, and contraceptive use among
sexually experienced high school students. J Adolesc Health.
2011;48:562-565.
17. Rickert VI, Tiezzi L, Lipshutz J, et al. Depo Now: Preventing
unintended pregnancies among adolescents and young adults. J
Adolesc Health. 2007;40:22-28.
18. Kern SEU, Pullmann MD, Walker SC, et al. Adolescent use of
school-based health centers and high school dropout. Arch Pediatr
Adolesc Med. 2011;165: 617-623.
19. Hoffert, SL, Reid L, Mott FL, The Effects of Early Childbearing on
Schooling over time.Fam Plann Perspect. 2001; 33:259-67.
20. Cubbin C, Brindis CD, Jain S, Santelli J, Braverman P.
Neighborhood poverty, aspirations and expectations, and initiation
of sex. J Adolesc Health; 2010;47;399-406.
21. The Guttmacher Report on Public Policy. School - Based Health
Centers and the Birth Control Debate- Special Analysis. October
2000. http://www.guttmacher.org/pubs/pdf. Accessed July 12,
2011.
22. Santelli JS, Nystrom RJ, Brindis C, et al. Reproductive health in
school-based health centers: findings from the 1998-99 census of
school-based health centers. J Adolesc Health. 2003;32:443-451.
23. Schaffer SJ, Fontanesi J, Rickert D, et al. How effectively can
health care settings beyond the traditional medical home provide
vaccines to adolescents? Pediatrics, 2008;121(Supp 1):S35-S45.
11
Smith et al.: School-Based Birth Control Policy Comparison
Published by DigitalCommons@TMC, 2011
Appendix
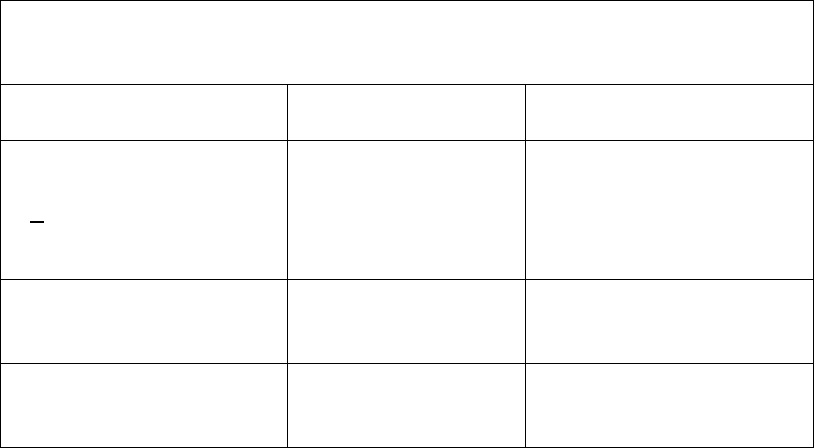
Table 1. Characteristics of Students Seeking Hormonal
Contraception
September 2008 – December 2009 at two school clinics
Characteristics
School
A
clinic
(N=79)
School
B
clinic
(N=40)
Age:
(years)
Mean(range)
> 18 years (%)
17.5 (15-22)
53 (68)
17.5 (14- 20)
21 (52)
Race/Ethnicity:
Hispanic (%)
60 (77)
35 (88)
Prior Pregnancy (%) 16 (21.9)
[95% C.I. 12% -
30%]
3 (7.5)
[95% C.I. 1% -20%]
12
Journal of Applied Research on Children: Informing Policy for Children at Risk, Vol. 2 [2011], Iss. 2, Art. 8
https://digitalcommons.library.tmc.edu/childrenatrisk/vol2/iss2/8
DOI: 10.58464/2155-5834.1043
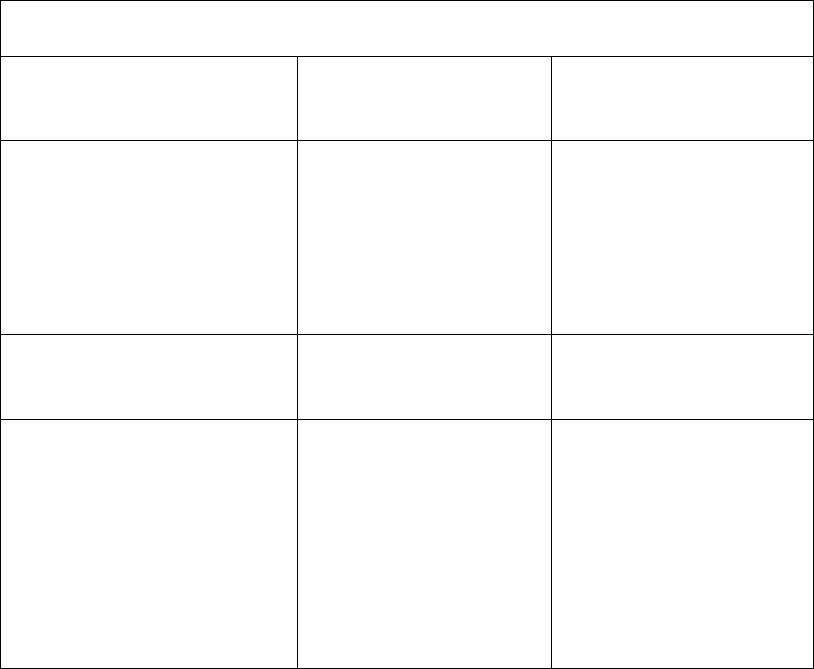
Table 2.
Comparison between two school clinics for
Appointments
Rates, Method Type and Pregnancy Rates
School
A
clinic
(N=79)
(%)
School
B
clinic
(N=40)
(%)
Contraception
Appointment
Observation period
Mean/(range)
months
79 (100)
13.3(4-19)
20 (50)*
11.9(4-19)
Method
received
Oral Contraceptive Pill
Long acting
progestin
51 (65)
28 (35)
17 (85)
3 (15)
Pregnancy rate
No prior history of
Pregnancy
Received
contraception
5 (6 )
[95% C.I. 2% -14%]
4 (4.7)
[95% C.I. 0.9% -13%]
5 (6) [95% C.I. 2% -
14%]
8 (20)*
[95% C.I. 9% -35%]
8 (21.6 )*
[95% C.I. 9% -38%]
3 (15) [95% C.I. 3% -
37%]
*p<0.05
13
Smith et al.: School-Based Birth Control Policy Comparison
Published by DigitalCommons@TMC, 2011
