Frequently Asked Questions Regarding Medicare and the Marketplace
August 1, 2014
1
This document is a compilation of the most frequently asked questions
(FAQs) regarding the intersection of Medicare and the Marketplace. These
FAQs have been cleared for use in response to public inquiries.
Please note that the frequently asked questions (FAQs) in this document
apply specifically to those individuals who:
have Medicare Part A only, Part B only, or neither, but who are
seeking coverage through a Marketplace plan,
had Marketplace coverage before becoming eligible for Medicare,
have retained a Marketplace plan after enrolling in Medicare.
These FAQs do not apply to those individuals who have both Medicare Parts
A & B and receive their health coverage exclusively through Medicare or a
Medicare health plan.
The majority of individuals with Medicare coverage have both Medicare Parts
A & B and do not have other private health insurance.
CMS added new FAQs to this document on April 21, 2016, in order to clarify
the benefit coordination between Medicare and certain types of employer-
based coverage. The new FAQs are D.7., D.8., and D.9.
Updated April 28, 2016
A. General Enrollment FAQs ......................................................................................................... 5
A.1. Can individuals who have Medicare enroll in individual market coverage, such as
coverage offered through the Individual Marketplace? .............................................................. 5
A.2. Can Medicare beneficiaries whose employer purchases insurance coverage through the
SHOP be enrolled in a SHOP Qualified Health Plan? ................................................................ 5
A.3. Does the prohibition against the sale or issuance of duplicate coverage to an individual
with Medicare apply to selling or issuing coverage to someone eligible for Medicare but not
yet signed up? ............................................................................................................................. 5
A.4. Do beneficiaries with Part B only meet the Affordable Care Act’s requirement to
maintain Minimum Essential Coverage? .................................................................................... 5
A.5. Does it make any difference to the Affordable Care Act’s requirement to maintain
Minimum Essential Coverage if an individual with Part B only is required to pay the Income
Related Monthly Adjustment Amount for Part B? ..................................................................... 5
A.6. The Individual Marketplace Qualified Health Plans (QHPs) may be cheaper than
Medicare for individuals who have to pay a premium for Part A. Can someone with Premium
Part A drop Medicare and enroll in the Individual Marketplace? .............................................. 5
A.7. Can a Medicare beneficiary purchase a stand-alone dental plan through the Individual
Marketplace? ............................................................................................................................... 6
Frequently Asked Questions Regarding Medicare and the Marketplace
August 1, 2014
2
A.8. If you have coverage in an Individual Marketplace Qualified Health Plan (QHP) and later
enroll in Medicare, can you keep your Marketplace coverage? ................................................. 6
A.9. Will individuals enrolled in an Individual Marketplace Qualified Health Plan (QHP) be
subject to the Part B or Premium Part A late enrollment penalty if they delay enrollment into
Medicare? .................................................................................................................................... 7
A.10. Can Medicare beneficiaries with coverage under SHOP plans delay enrollment in
Medicare Part B without penalty?............................................................................................... 7
A.11. Is prescription drug coverage in an Individual Marketplace or SHOP Qualified Health
Plan (QHP) considered creditable prescription drug coverage for purposes of Medicare Part
D? ................................................................................................................................................ 8
A.12. Is prescription drug coverage through the Marketplace considered creditable
prescription drug coverage for the purposes of determining whether an individual must pay the
late enrollment penalty upon enrollment in Medicare Part D? ................................................... 8
A.13. If a person is enrolled in Part A and has chosen not to enroll in Part B, can that person
purchase a QHP (or other individual market coverage) until their Part B is effective? ............. 8
A.14. If an individual is over age 65 and eligible for premium-free Part A, but is not collecting
Social Security benefits and has not enrolled in either Part A or Part B, can that person
purchase a QHP (or other individual market coverage)? ............................................................ 9
A.15. Is purchasing a QHP (or other individual market plan), instead of enrolling in Medicare
Part B, an option for individuals who fail to enroll in Part B in a timely manner and must pay a
Part B premium penalty, especially in those situations where the higher premium resulting
from the penalty may be more than the individual would pay for a QHP—with or without a tax
credit? .......................................................................................................................................... 9
A.16. A Qualified Health Plan (QHP) may be cheaper than Medicare for individuals who get
Part A for free but have to pay a late enrollment penalty or Income-Related Monthly
Adjustment Amount (IRMAA) for Part B. Can someone with free Part A drop Medicare and
enroll in a QHP?.......................................................................................................................... 9
B. ESRD ........................................................................................................................................ 10
B.1. Are Individuals with ESRD required to sign up for Medicare? ........................................ 10
B.2. Are individuals with ESRD who do not have Medicare coverage eligible to enroll in a
Marketplace Qualified Health Plan (QHP)? ............................................................................. 10
B.3. Are individuals with ESRD who do not have Medicare coverage eligible for the health
care Premium Tax Credit? ........................................................................................................ 10
B.4. Can beneficiaries who currently have Medicare coverage due to ESRD opt out of or
disenroll from Medicare? .......................................................................................................... 11
B.5. Is there a mechanism for individuals to cancel ESRD Medicare enrollment if applications
are initiated on their behalf without complete information about their options for QHPs? ..... 11
B.6. Please clarify whether individuals with ESRD who are currently enrolled in Medicare
based on ESRD can disenroll from both Part A and Part B. If yes, please specify the
requirements for doing so and the potential ramifications of this choice. ................................ 11
Frequently Asked Questions Regarding Medicare and the Marketplace
August 1, 2014
3
C. Consumer Messaging ............................................................................................................... 12
C.1. What is the message to Medicare beneficiaries who have questions about how the
Marketplace affects them? ........................................................................................................ 12
C.2. What do Medicare beneficiaries need to know about Medicare and the Individual
Marketplace? ............................................................................................................................. 12
C.3. I want to purchase health insurance through the Marketplace. What if I have Medicare? 12
C.4. Can I get a Marketplace plan if I already have Medicare? ................................................ 12
C.5. Can I choose Marketplace coverage instead of Medicare? ............................................... 12
C.6. If I’m getting Medicare Part A for free, can I drop Medicare to enroll in a Marketplace
plan? .......................................................................................................................................... 13
C.7. I have coverage through an Individual Marketplace Qualified Health Plan (QHP) and then
I enroll in Medicare. Once my coverage in Medicare starts, can the QHP disenroll me without
my consent? .............................................................................................................................. 13
C.8. Can an individual market health insurance issuer disenroll someone if it learns that
individual is a Medicare beneficiary prior to the individual's coverage effective date? ........... 13
C.9. What if I have only Medicare Part B? ............................................................................... 14
C.10. What if I have a Marketplace plan but will be eligible for Medicare soon? ................... 14
C.11. Medicare beneficiaries under age 65 don’t have federal guaranteed issue rights to
purchase Medicare Supplement (Medigap) insurance coverage. Can these beneficiaries enroll
in the Individual Marketplace to supplement their Medicare coverage? .................................. 15
D. Coordination of Benefits Policy ............................................................................................... 15
D.1. If someone is enrolled in both Medicare and an Individual Marketplace Qualified Health
Plan (QHP), will there be coordination of benefits? ................................................................. 15
D.2. Will Coordination of Benefits apply to someone who is enrolled in Medicare and a SHOP
Qualified Health Plan (QHP)? .................................................................................................. 15
D.3. What do employers participating in SHOP need to know about the Medicare Secondary
Payer rules? ............................................................................................................................... 15
D.4. What do SHOP Qualified Health Plans (QHPs) need to know about the Medicare
Secondary Payer rules? ............................................................................................................. 15
D.5. Will SHOP plans be required to inform beneficiaries of any benefit coordination? ........ 16
D.6. Will Marketplace coverage purchased prior to an individual enrolled in and/or entitled to
Medicare affect that individual’s eligibility for the Medicare Part D Low-Income Subsidy
(LIS) program?.......................................................................................................................... 16
D.7. An individual is enrolled in health insurance coverage based on active employment
through an employer that is defined (for purposes of the Affordable Care Act market reforms)
as small (including SHOP coverage) and is eligible for Medicare due to turning 65 but isn’t
enrolled in Medicare. Can the small group health plan change the payment level for or refuse
to pay for covered services for which Medicare would have paid had the person been enrolled
in Medicare?.............................................................................................................................. 16
Frequently Asked Questions Regarding Medicare and the Marketplace
August 1, 2014
4
D.8. An individual is enrolled in employer group “retiree only” coverage and is eligible for but
isn’t enrolled in Medicare. Can the group retiree health plan change the payment level for or
refuse to pay for covered services for which Medicare would have paid as the primary payer
had the person been enrolled in Medicare?............................................................................... 16
D.9. An individual who receives coverage through his employer’s self-insured group health
plan for active employees is eligible for Medicare due to turning age 65 but is not enrolled in
Medicare. The employer has fewer than twenty employees. Can the employer change the
payment level for or refuse to pay for otherwise covered services for which Medicare would
have paid as the primary payer had the individual been enrolled in Medicare? ...................... 17
E. Enrollment Operations ............................................................................................................. 18
E.1. Does the FFM application screen for Medicare enrollment? ............................................ 18
E.2. Will the Marketplace add a note to the Individual Marketplace paper application telling
people not to apply if they have Medicare? .............................................................................. 18

Frequently Asked Questions Regarding Medicare and the Marketplace
August 1, 2014
5
A. General Enrollment FAQs
A.1. Can individuals who have Medicare enroll in individual market coverage, such as
coverage offered through the Individual Marketplace?
No. Consistent with the longstanding prohibitions on the sale and issuance of duplicate
coverage to Medicare beneficiaries (section 1882(d) of the Social Security Act), it is
illegal to knowingly sell or issue an Individual Marketplace Qualified Health Plan (or an
individual market policy outside the Marketplace) to a Medicare beneficiary. This
prohibition does not apply in the SHOP market, or to employer coverage outside of the
SHOP market.
A.2. Can Medicare beneficiaries whose employer purchases insurance coverage through
the SHOP be enrolled in a SHOP Qualified Health Plan?
Yes, Medicare beneficiaries whose employers purchase SHOP coverage are treated the
same as any other person with employer Group Health Plan coverage. The statute
(Section 1882(d) of the Social Security Act) prohibits the sale or issuance of duplicate
coverage to an individual with Medicare, but employer-sponsored coverage is explicitly
exempted from this prohibition. SHOP coverage is sold to the employer. Note that for
Medicare beneficiaries who are active employees and are enrolled in SHOP coverage, the
Medicare Secondary Payer rules, which govern the coordination of benefits between
Medicare and the employer coverage, apply to employers with 20 or more employees.
A.3. Does the prohibition against the sale or issuance of duplicate coverage to an individual
with Medicare apply to selling or issuing coverage to someone eligible for Medicare but not
yet signed up?
No. The prohibition, set forth in Section 1882(d) of the Social Security Act, applies to
selling or issuing coverage to someone who has Medicare Part A or Part B. However, the
regulations at 26 CFR §1.36B-2(c)(i) state that an individual who is eligible to receive
benefits under government-sponsored minimum essential coverage (e.g. Medicare Part
A.4. Do beneficiaries with Part B only meet the Affordable Care Act’s requirement to
maintain Minimum Essential Coverage?
Medicare Part B alone does not constitute Minimum Essential Coverage.
A.5. Does it make any difference to the Affordable Care Act’s requirement to maintain
Minimum Essential Coverage if an individual with Part B only is required to pay the
Income Related Monthly Adjustment Amount for Part B?
No, the same principles apply.
A.6. The Individual Marketplace Qualified Health Plans (QHPs) may be cheaper than
Medicare for individuals who have to pay a premium for Part A. Can someone with
Premium Part A drop Medicare and enroll in the Individual Marketplace?
Yes. Individuals who are not eligible to get Medicare Part A for free may drop both their
Premium Part A and their Part B coverage (or choose not to enroll when first eligible).
An individual who does not have Medicare (either Part A or Part B) can enroll in a QHP.
Frequently Asked Questions Regarding Medicare and the Marketplace
August 1, 2014
6
Note that individuals who get free Part A cannot drop it without dropping their retiree
benefits (social security or railroad retirement) and paying back all retirement benefits
received and costs incurred by the Medicare program as well.
Before making this choice, there are 2 important points for individuals to consider:
Individuals who do not enroll in Medicare when first eligible (during their initial
enrollment period) may have to pay late enrollment penalties if they later apply
for both Premium Part A and Part B. The Part B penalty applies for as long as the
individual has Part B coverage.
In addition, individuals who enroll in Medicare after their initial enrollment
period ends can enroll in Medicare only during the Medicare general enrollment
period (from January 1 to March 31) and coverage does not begin until July of
that year.
A.7. Can a Medicare beneficiary purchase a stand-alone dental plan through the Individual
Marketplace?
Even though Medicare does not provide dental coverage, and therefore a stand-alone
dental plan would not duplicate Medicare benefits, the Federally-facilitated Marketplaces
(FFMs) require that individuals buy a comprehensive medical Qualified Health Plan
(QHP) before they can purchase a separate dental plan. Because it is illegal to sell or
issue a comprehensive medical QHP to a Medicare beneficiary, Medicare beneficiaries
cannot currently buy a stand-alone dental plan through the FFMs. Nothing in federal law
prohibits issuers from generally selling or issuing stand-alone dental plans through State
Based Marketplaces that can support this functionality, or outside the Marketplaces, to
Medicare beneficiaries.
A.8. If you have coverage in an Individual Marketplace Qualified Health Plan (QHP) and
later enroll in Medicare, can you keep your Marketplace coverage?
Yes. The prohibition on selling or issuing duplicative coverage set forth in Section
1882(d) of the Social Security Act applies to the sale or issuance of a (QHP) or other
individual market coverage to a Medicare beneficiary. It does not require an individual
who was not a Medicare beneficiary when the QHP was purchased to drop coverage
when he or she becomes a Medicare beneficiary.
Once Medicare Part A coverage begins, however, any premium tax credits and reduced
cost-sharing the individual receives through the Marketplace will be discontinued.
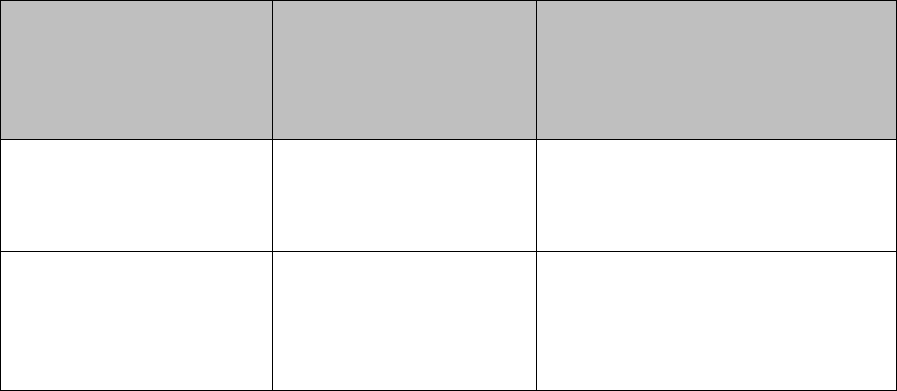
See the chart below for details.
Frequently Asked Questions Regarding Medicare and the Marketplace
August 1, 2014
7
Chart A: Maintaining Enrollment in an Individual Marketplace Qualified Health Plan
(QHP) Once Medicare Coverage Begins
If you are:
Can you keep your
Individual
Marketplace QHP
after enrolling in
Medicare?
Are you eligible to continue
receiving tax credits and
reduced cost-sharing?
Currently enrolled in a
QHP and become entitled
to free Part A
Yes
No. Any tax credits the individual
is receiving in the QHP will be
discontinued once Part A coverage
begins.
Currently enrolled in a
QHP and become eligible
to buy Premium Part A
and Part B
Yes
Yes, if you only enroll in Part B,
because Part B does not constitute
Minimum Essential Coverage.
No, if you enroll in Premium Part
A.
A.9. Will individuals enrolled in an Individual Marketplace Qualified Health Plan (QHP)
be subject to the Part B or Premium Part A late enrollment penalty if they delay
enrollment into Medicare?
Yes. Individuals who do not enroll in Medicare during their Initial Enrollment Period
(either for Part B or Premium Part A) will only be able to enroll in Medicare during the
Medicare General Enrollment Period and may be subject to the late enrollment penalties.
The Part B penalty applies for as long as the individual has Part B.
A.10. Can Medicare beneficiaries with coverage under SHOP plans delay enrollment in
Medicare Part B without penalty?
Yes. A Medicare beneficiary who is enrolled in employer purchased SHOP coverage is
treated the same as any other person with employer group health plan coverage.
Individuals can delay enrollment if they are covered under a group health plan based on
their or their spouse’s current employment. These individuals have a special enrollment
period to sign up for Part B without penalty:
Any time they are still covered by the group health plan.
During the 8-month period that begins the month after the employment ends or
the coverage ends, whichever happens first.
If the individual does not sign up during this special enrollment period, enrollment will
only be possible during the General Enrollment Period which occurs annually from
January through March with coverage beginning July 1. The individual may also have to
pay a late enrollment penalty for as long as he or she has Part B.
Frequently Asked Questions Regarding Medicare and the Marketplace
August 1, 2014
8
A.11. Is prescription drug coverage in an Individual Marketplace or SHOP Qualified
Health Plan (QHP) considered creditable prescription drug coverage for purposes of
Medicare Part D?
While prescription drug coverage is an essential health benefit, there is no requirement
under the Affordable Care Act or its implementing regulations that prescription drug
coverage in an Individual Marketplace or SHOP QHP be at least as good as Medicare
Part D coverage, which is the general test for whether coverage is creditable. However,
all private insurers offering prescription drug coverage, including Individual Marketplace
and SHOP QHPs, are required to determine annually if their prescription drug coverage is
creditable and notify CMS and their Medicare-eligible enrollees in writing of the
determination.
All private insurers offering prescription drug coverage are required to notify their
Medicare-eligible enrollees of the plan’s creditable coverage status in writing annually
prior to the start of the Medicare open enrollment period that begins on October 15, and
in the following situations:
Prior to an individual’s Initial Enrollment Period for Part D;
Prior to the effective date of enrollment in the insurer’s prescription drug
coverage;
Upon any change that affects whether the coverage is creditable; and
Upon request by the individual.
A.12. Is prescription drug coverage through the Marketplace considered creditable
prescription drug coverage for the purposes of determining whether an individual must
pay the late enrollment penalty upon enrollment in Medicare Part D?
While prescription drug coverage is an essential health benefit, prescription drug
coverage in a Marketplace or SHOP plan isn’t required to be expected to pay, on average,
at least as much as Medicare’s standard prescription drug coverage (creditable). All
private plans offering prescription drug coverage, including Marketplace and SHOP
plans, must determine if their prescription drug coverage is creditable each year and let
you know in writing.
A.13. If a person is enrolled in Part A and has chosen not to enroll in Part B, can that
person purchase a QHP (or other individual market coverage) until their Part B is
effective?
For beneficiaries who would purchase their plan on the individual market, no. Consistent
with the longstanding prohibitions on the sale and issuance of duplicate coverage to
Medicare beneficiaries (section 1882(d) of the Social Security Act), it is illegal for an
insurer to sell or issue to a Medicare beneficiary a QHP (or other individual market
coverage) that the insurer knows would duplicate Medicare benefits. This is true even if
the beneficiary has only Part A or only Part B.
This prohibition does not apply in the small group market, including plans sold through
the Small Business Health Options Program (SHOP). Medicare beneficiaries whose
Frequently Asked Questions Regarding Medicare and the Marketplace
August 1, 2014
9
employers purchase SHOP coverage are treated the same as any other person with
employer-sponsored Group Health Plan (GHP) coverage. The statute
(Section 1882(d) of the Social Security Act) prohibits the sale or issuance of coverage
that the insurer knows duplicates Medicare benefits to an individual with Medicare, but
employer-sponsored (GHP) coverage is explicitly exempted from this prohibition. SHOP
coverage is sold to the employer. Note that for Medicare beneficiaries who are active
employees and are enrolled in SHOP coverage, the Medicare Secondary Payer rules
govern the coordination of benefits between Medicare and the employer coverage as
appropriate.
A.14. If an individual is over age 65 and eligible for premium-free Part A, but is not
collecting Social Security benefits and has not enrolled in either Part A or Part B, can that
person purchase a QHP (or other individual market coverage)?
Yes. If the individual is not collecting Social Security benefits, and is not covered by
Medicare (that is, he or she does not have either Part A or Part B), then the anti-
duplication statute in section 1882(d) of the Social Security Act would not prohibit the
issuer of a QHP (or other individual market coverage) from issuing or selling coverage to
the individual. Please note, not enrolling in Part B when an individual is first eligible
may result in paying late enrollment penalties. The Part B late enrollment penalty applies
for as long as the individual has Part B.
A.15. Is purchasing a QHP (or other individual market plan), instead of enrolling in
Medicare Part B, an option for individuals who fail to enroll in Part B in a timely manner
and must pay a Part B premium penalty, especially in those situations where the higher
premium resulting from the penalty may be more than the individual would pay for a
QHP—with or without a tax credit?
Generally, no. If an individual already has Medicare coverage (including Part A and/or
Part B coverage), consistent with the longstanding prohibitions on the sale and issuance
of duplicate coverage to Medicare beneficiaries (section 1882(d) of the Social Security
Act), it is illegal for an insurer to knowingly sell or issue to a Medicare beneficiary an
individual market plan that the insurer knows would duplicate Medicare benefits,
regardless of the cost of the Part B premium amount. An individual who does not have
Medicare (neither Part A nor Part B) and who is otherwise eligible can enroll in a QHP.
An individual who does not enroll in Medicare during his or her Medicare Initial
Enrollment Period (either for Part B or Premium Part A) will only be able to enroll in
Medicare during the Medicare General Enrollment Period. In addition, if the individual
chooses to enroll later, he or she may be subject to late enrollment penalties. The Part B
late enrollment penalty applies for as long as the individual has Part B.
A.16. A Qualified Health Plan (QHP) may be cheaper than Medicare for individuals who
get Part A for free but have to pay a late enrollment penalty or Income-Related Monthly

Frequently Asked Questions Regarding Medicare and the Marketplace
August 1, 2014
10
Adjustment Amount (IRMAA) for Part B. Can someone with free Part A drop Medicare
and enroll in a QHP?
Generally, no. Individuals generally can choose to stop Medicare coverage only if
they’re paying a premium for Part A or have only Part B. Individuals with free Part A
can’t drop Medicare without also dropping their retiree benefits (Social Security or
Railroad retirement) and paying back all retirement or disability benefits they received
and all costs spent for their care by the Medicare program.
Before making this choice, there are two important points for individuals to consider:
An individual who does not enroll in Medicare during his or her Medicare Initial
Enrollment Period (either for Part B or Premium Part A) will only be able to enroll in
Medicare during the Medicare General Enrollment Period. The General Enrollment
Period occurs from January 1 to March 31 with coverage beginning on July 1 of that
year. In addition, if the individual chooses to enroll later, he or she may be subject to late
enrollment penalties. The Part B late enrollment penalty applies for as long as the
individual has Part B.
B. ESRD
B.1. Are Individuals with ESRD required to sign up for Medicare?
No. Individuals with ESRD are not required to sign up for Medicare; it is voluntary. In
order to get Medicare coverage, the individual must meet the necessary eligibility
requirement and apply. If you don’t apply, you do not get Medicare coverage.
B.2. Are individuals with ESRD who do not have Medicare coverage eligible to enroll in a
Marketplace Qualified Health Plan (QHP)?
Individuals with ESRD who do not have either Medicare Part A or Part B are eligible to
enroll in individual market coverage because the Medicare anti-duplication statute does
not apply; therefore, individual market guaranteed issue rights apply under the ACA. In
order to enroll in a QHP through the Marketplace, the individual must meet the eligibility
requirements for enrollment (i.e., criteria related to citizenship, lawful presence,
incarceration, and residency).
B.3. Are individuals with ESRD who do not have Medicare coverage eligible for the health
care Premium Tax Credit?
An individual may be eligible for the health care Premium Tax Credit if he or she is not
eligible for minimum essential coverage, as outlined in the IRS Notice 2013-41 at the
following web link: http://www.irs.gov/pub/irs-drop/n-13-41.pdf
However, individuals will lose their eligibility for the health care Premium Tax Credit
when coverage in Medicare Part A begins.
Frequently Asked Questions Regarding Medicare and the Marketplace
August 1, 2014
11
B.4. Can beneficiaries who currently have Medicare coverage due to ESRD opt out of or
disenroll from Medicare?
Generally, no. Following the application for Medicare, the law provides that Medicare
coverage ends one year after the termination of regular dialysis or 36 months after a
successful kidney transplant. However, a beneficiary may withdraw their original
Medicare application. The individual is required to repay all costs covered by Medicare,
pay any outstanding balances, and refund any benefits received from the SSA or RRB.
Once all repayments have been made, the withdrawal can be processed as though the
individual was never enrolled in Medicare at all (i.e., retroactively).
B.5. Is there a mechanism for individuals to cancel ESRD Medicare enrollment if
applications are initiated on their behalf without complete information about their options
for QHPs?
A dialysis facility or attending physician may not complete an application for Medicare
entitlement on behalf of the beneficiary. While these providers may submit the medical
evidence form for an individual applying for Medicare based on ESRD, the individual
must also contact the Social Security Administration (SSA) to complete the Medicare
application.
If an individual wants to enroll in a QHP after the medical evidence form is submitted by
the provider, the individual can choose to not complete his or her application for
Medicare. If the individual has Medicare currently based on ESRD, he or she may
withdraw their original Medicare application. The individual is required to repay all
costs covered by Medicare, pay any outstanding balances, and refund any benefits
received from the SSA or RRB. Once all repayments have been made, the withdrawal
can be processed as though the individual was never enrolled in Medicare at all (i.e.,
retroactively).
B.6. Please clarify whether individuals with ESRD who are currently enrolled in Medicare
based on ESRD can disenroll from both Part A and Part B. If yes, please specify the
requirements for doing so and the potential ramifications of this choice.
Generally, individuals with ESRD who are currently enrolled in Medicare based on
ESRD cannot disenroll prospectively. Following the application for Medicare, the law
provides that Medicare coverage ends one year after the termination of regular dialysis or
36 months after a successful kidney transplant. However, a beneficiary may withdraw
their original Medicare application. The individual is required to repay all costs covered
by Medicare, pay any outstanding balances, and refund any benefits received from the
SSA or RRB. Once all repayments have been made, the withdrawal can be processed as
though the individual was never enrolled in Medicare at all (i.e., retroactively).

Frequently Asked Questions Regarding Medicare and the Marketplace
August 1, 2014
12
C. Consumer Messaging
C.1. What is the message to Medicare beneficiaries who have questions about how the
Marketplace affects them?
Medicare isn’t part of the Health Insurance Marketplace. If you have Medicare, you are
covered, and do not need to do anything about the Marketplace.
The Marketplace won’t affect your Medicare choices and benefits. No matter how you
get Medicare, whether through Original Medicare or a Medicare Advantage Plan, you
won’t have to make any changes.
C.2. What do Medicare beneficiaries need to know about Medicare and the Individual
Marketplace?
Individuals with Medicare need to know that if they have Medicare, an Individual
Marketplace plan is not appropriate for them. If individuals want coverage designed to
supplement Medicare, they can visit Medicare.gov to learn more about Medigap policies.
They can also visit Medicare.gov to learn more about other Medicare options, like
Medicare Advantage Plans.
C.3. I want to purchase health insurance through the Marketplace. What if I have
Medicare?
Medicare isn’t part of the Health Insurance Marketplace, so you don’t need to do
anything. If you have Medicare, you’re considered covered. The Marketplace won’t
affect your Medicare choices or benefits. No matter how you get Medicare, whether
through Original Medicare or a Medicare Advantage Plan (like an HMO or PPO), you
won’t have to make any changes. Note: The Marketplace doesn’t offer Medicare
supplement (Medigap) insurance or Part D drug plans.
C.4. Can I get a Marketplace plan if I already have Medicare?
No. It’s against the law for someone who knows that you have Medicare to sell or issue
you a Marketplace policy. This is true even if you have only Medicare Part A or only Part
B. If you want coverage designed to supplement Medicare, you can find out more about
Medigap policies. You can also learn about other Medicare options, like Medicare
Advantage Plans. For prescription drug coverage, you can buy a Medicare Part D drug
plan.
C.5. Can I choose Marketplace coverage instead of Medicare?
Generally, no. It’s against the law for someone who knows you have Medicare to sell you
a Marketplace plan. But there are a few situations where you can choose a Marketplace
private health plan instead of Medicare:
If you’re paying a premium for Part A. In this case you can drop your Part A and
Part B coverage and get a Marketplace plan instead.
If you’re eligible for Medicare but haven’t enrolled in it. This could be because:
o You’d have to pay a premium
Frequently Asked Questions Regarding Medicare and the Marketplace
August 1, 2014
13
o You have a medical condition that qualifies you for Medicare, like end-
stage renal disease (ESRD), but haven’t applied for Medicare coverage
o You’re not collecting Social Security retirement or disability benefits
before you’re eligible for Medicare
Before choosing a Marketplace plan over Medicare, there are 2 important points to
consider:
If you enroll in Medicare after your initial enrollment period ends, you may have
to pay a late enrollment penalty for as long as you have Medicare.
Generally you can enroll in Medicare only during the Medicare general
enrollment period (from January 1 to March 31 each year). Your coverage won’t
start until July. This may cause a gap in your coverage.
C.6. If I’m getting Medicare Part A for free, can I drop Medicare to enroll in a
Marketplace plan?
Generally, no. You can choose to have your Medicare stop only if you’re paying a premium
for Part A or have only Part B. If you get Part A for free, you can’t drop Medicare without
also dropping your retiree or disability benefits (Social Security or railroad retirement) and
paying back all retirement or disability benefits you’ve received and all costs spent for your
care by the Medicare program. Before making this choice, there are 2 important points to
consider:
If you enroll in Medicare after your initial enrollment period ends, you may have to
pay a late enrollment penalty for as long as you have Medicare.
Generally you can enroll in Medicare only during the Medicare general enrollment
period (from January 1 to March 31 each year). Your coverage won’t start until July.
This may cause a gap in your coverage.
C.7. I have coverage through an Individual Marketplace Qualified Health Plan (QHP) and
then I enroll in Medicare. Once my coverage in Medicare starts, can the QHP disenroll me
without my consent?
No, issuers may not terminate enrollees whom they subsequently find to be eligible for or
enrolled in Medicare, unless the enrollee requests the termination.
C.8. Can an individual market health insurance issuer disenroll someone if it learns that
individual is a Medicare beneficiary prior to the individual's coverage effective date?
Consistent with the longstanding prohibitions on the sale and issuance of duplicate
coverage to Medicare beneficiaries (section 1882(d) of the Social Security Act), it is
illegal to knowingly sell or issue an Individual Marketplace Qualified Health Plan (or an
individual market policy outside the Marketplace) to a Medicare beneficiary. The issuer
should cancel an enrollment prior to the policy being issued if the issuer learns that the
enrollment is for someone who has Medicare coverage. That is, the start date for the
individual’s Part A and/or Part B was before the effective date of the individual market
coverage. However, if the applicant’s Medicare coverage has not started yet, then the
issuer issue the coverage on a guaranteed available basis.
Frequently Asked Questions Regarding Medicare and the Marketplace
August 1, 2014
14
Issuers may not, however, terminate the individual market coverage of enrollees who
they find to be eligible for or enrolled in Medicare after the coverage has been issued,
even if the individual was eligible for or enrolled in Medicare before enrollment into the
individual market coverage, unless the enrollee requests the termination or another legal
basis for termination applies.
C.9. What if I have only Medicare Part B?
If you have only Medicare Part B, you are not considered to have minimum essential
coverage. This means you may have to pay the penalty that people who don't have
coverage may have to pay. If you have Medicare Part A only, you are considered
covered. If you have both Medicare Part A and Part B, you are also considered covered.
C.10. What if I have a Marketplace plan but will be eligible for Medicare soon?
If you have a Marketplace plan, you can keep it until your Medicare coverage starts.
Then you can cancel it without penalty. If you like, you can keep your Marketplace plan
too. But if you’ve been getting tax credits or lower out-of-pocket costs on a plan you
bought through the Marketplace, these savings will end once your Medicare Part A
coverage starts. You’d have to pay full price for the Marketplace plan.
Let’s assume you have a Marketplace plan and are turning 65 sometime this year. Once
you’re eligible for Medicare, you’ll have an initial enrollment period to sign up for
Medicare. For most people, the initial enrollment period starts 3 months before their 65th
birthday and ends 3 months after their 65th birthday. In most cases it’s to your advantage
to sign up for Medicare when you’re first eligible because:
Once your Medicare Part A coverage starts, you won’t be able to keep any
premium tax credits or lower out of pocket costs for a Marketplace plan based on
your income. You’ll have to pay full price for the Marketplace plan.
If you enroll in Medicare after your initial enrollment period ends, you may have
to pay a late enrollment penalty for as long as you have Medicare. In addition,
you can enroll in Medicare Part B (and Part A if you have to pay a premium for it)
only during the Medicare general enrollment period (from January 1 to March 31
each year). Coverage doesn’t start until July of that year. This may create a gap in
your coverage.
If you want coverage to supplement Medicare, you can get Medicare supplement
(Medigap) insurance. For prescription drug coverage, you can buy a Medicare Part D
drug plan. You can learn about other Medicare options, like Medicare Advantage Plans.
Once your Medicare coverage starts, you can cancel your Marketplace health plan
without penalty. You can do this by contacting the Marketplace call center or cancelling
your coverage online. If you have Medicare coverage, you’re considered covered under
the health care law. You won’t have to pay the fee that some people without insurance
must pay. Be sure not to cancel your Marketplace plan before your Medicare coverage
begins. Otherwise you may have a gap in coverage.

Frequently Asked Questions Regarding Medicare and the Marketplace
August 1, 2014
15
C.11. Medicare beneficiaries under age 65 don’t have federal guaranteed issue rights to
purchase Medicare Supplement (Medigap) insurance coverage. Can these beneficiaries
enroll in the Individual Marketplace to supplement their Medicare coverage?
No, consistent with the longstanding prohibitions on the sale and issuance of duplicate
coverage to Medicare beneficiaries (section 1882(d) of the Social Security Act), it is
illegal to knowingly sell or issue a Qualified Health Plan (QHP) to a Medicare
beneficiary. If individuals are seeking supplemental coverage for their Medicare, and do
not have retiree coverage, they should consult Medicare.gov about enrolling in a
Medicare Advantage plan, or check with their State department of insurance to see if
their state requires the sale of Medigap policies to people under age 65.
D. Coordination of Benefits Policy
D.1. If someone is enrolled in both Medicare and an Individual Marketplace Qualified
Health Plan (QHP), will there be coordination of benefits?
If someone is enrolled in both Medicare and an Individual Marketplace QHP, Medicare is
the primary payer. Medicare does not provide coordination of benefits.
D.2. Will Coordination of Benefits apply to someone who is enrolled in Medicare and a
SHOP Qualified Health Plan (QHP)?
Medicare beneficiaries whose employer purchases SHOP coverage are treated the same
as any other person with employer coverage. If the employer has 20 or more employees,
the employer-provided health coverage generally will be primary for a Medicare
beneficiary who is covered through active employment.
D.3. What do employers participating in SHOP need to know about the Medicare
Secondary Payer rules?
An employer participating in SHOP will be impacted by the Medicare Secondary Payer
(MSP) rules if the employer has 20 or more employees, and any of its employees are
Medicare beneficiaries. When offering health coverage to its employees, the employer
cannot “take Medicare into account” when determining if an individual is eligible for
enrollment in the employer-sponsored plan. This means that the employer can’t exclude
the individual’s opportunity to participate in the employer-sponsored Group Health Plan
coverage on the basis that the employee is a Medicare beneficiary.
D.4. What do SHOP Qualified Health Plans (QHPs) need to know about the Medicare
Secondary Payer rules?
If the employer has 20 or more employees, the SHOP QHP insurer will be required to
participate in the Medicare program’s “Section 111 Group Health Plan Reporting”
program, which is mandated by applicable Medicare Secondary Payer (MSP) regulations.
Insurers under these circumstances will be required to register with CMS’ Medicare
Secondary Payer Coordination of Benefits Contractor and report its coverage of the
working people with Medicare to CMS under the MSP reporting requirements.

Frequently Asked Questions Regarding Medicare and the Marketplace
August 1, 2014
16
D.5. Will SHOP plans be required to inform beneficiaries of any benefit coordination?
Yes. SHOP insurers are required to notify their enrollees of the coordination of benefits
between Medicare and the employer coverage.
D.6. Will Marketplace coverage purchased prior to an individual enrolled in and/or
entitled to Medicare affect that individual’s eligibility for the Medicare Part D Low-Income
Subsidy (LIS) program?
Having Marketplace coverage is not a factor in determining whether or a beneficiary is
eligible for the Low-Income Subsidy (LIS) program.
D.7. An individual is enrolled in health insurance coverage based on active employment
through an employer that is defined (for purposes of the Affordable Care Act market
reforms) as small (including SHOP coverage) and is eligible for Medicare due to turning 65
but isn’t enrolled in Medicare. Can the small group health plan change the payment level
for or refuse to pay for covered services for which Medicare would have paid had the
person been enrolled in Medicare?
No. In the absence of other primary coverage (such as Medicare), a SHOP QHP (or other
non-grandfathered, small group market coverage) is expected to pay for covered services
as the primary payer. Per the essential health benefits and actuarial value requirements
under the Affordable Care Act, a small group market insurance plan may not limit
coverage based on the theoretical possibility of an individual’s enrollment in other
coverage. Additionally, modifying a benefit design based on Medicare eligibility could
be considered discriminatory in violation of the federal non-discrimination prohibitions.
1
As such, a SHOP QHP or other non-grandfathered small group health plan must pay for
services for an enrollee who is eligible for but not enrolled in other primary coverage as if
the enrollee were not eligible for such coverage.
EXAMPLE: Ms. Lee is still working and has SHOP coverage through her employer. She
turns 65 and becomes eligible to get Medicare, but she has not enrolled in Medicare. She
sees a health care provider for a service that the SHOP plan covers and that Medicare
would have covered as well. The provider charges $150 for the service. Medicare does
not pay anything since Ms. Lee has not enrolled in Medicare. The health plan’s contract
indicates that Ms. Lee has a $30 copay for this service. The health plan is responsible for
$120 and Ms. Lee is responsible for her $30 copay.
D.8. An individual is enrolled in employer group “retiree only” coverage and is eligible for
but isn’t enrolled in Medicare. Can the group retiree health plan change the payment level
for or refuse to pay for covered services for which Medicare would have paid as the
primary payer had the person been enrolled in Medicare?
Yes, if the retiree coverage has a contractual stipulation that allows the plan to pay at a
different rate (or not at all), as long as Medicare would have been primary. Retiree
coverage is exempt from the market reforms implemented under the Affordable Care Act,
1
Non-discrimination provisions that may apply to non-grandfathered small group health insurance coverage include
those in the guaranteed availability regulation (45 CFR 147.104(e)); the essential health benefits regulations (45
CFR 156.125); and the QHP certification standards (45 CFR 156.200(e)), as applicable.

Frequently Asked Questions Regarding Medicare and the Marketplace
August 1, 2014
17
including the essential health benefits and actuarial value requirements and the non-
discrimination provision at 45 CFR §147.104(e). Therefore, the ACA market reforms do
not prohibit retiree-only plans
2
from paying at a different rate or not at all if a member
becomes eligible for other insurance coverage that would have paid as primary, even if
the member chooses not to enroll in the other coverage. MSP rules do not apply to
retirees who do not have current employment status.
EXAMPLE: Ms. Casserly has retiree-only coverage through her former employer. She
turns 65 and becomes eligible to get Medicare, but she has not enrolled in Medicare. She
sees her health care provider for a service that her retiree insurance covers and that
Medicare would have covered as well. The health care provider charges $150 for the
service. Medicare doesn’t pay anything since Ms. Casserly has not enrolled in Medicare.
The retiree health plan’s contract indicates that Ms. Casserly has a $20 copay for this
service. However, it also indicates that if Ms. Casserly becomes eligible for other
coverage (whether she enrolls in it or not), the plan will pay at a lesser rate. In this case,
the retiree health plan’s contract says it will only pay 50% of the fee leaving Ms. Casserly
with a $75 cost-sharing obligation.
D.9. An individual who receives coverage through his employer’s self-insured group health
plan for active employees is eligible for Medicare due to turning age 65 but is not enrolled
in Medicare. The employer has fewer than twenty employees. Can the employer change the
payment level for or refuse to pay for otherwise covered services for which Medicare would
have paid as the primary payer had the individual been enrolled in Medicare?
Yes, if the employer’s group health plan contractual terms allow the employer to pay at a
different rate (or not at all) and Medicare would have been primary (i.e., when the
employer has fewer than twenty employees). A self-insured group health plan offered by
an employer is not subject to the essential health benefits and actuarial value
requirements or various non-discrimination provisions of the Affordable Care Act and its
implementing regulations. As such, those ACA requirements do not prohibit an employer
health plan from paying at a different rate or not at all if a member becomes eligible for
other coverage that would have paid as primary to the employer, even if the member
chooses not to take that other coverage.
EXAMPLE: Mr. Ludwig has coverage through his employer. His employer has fewer
than twenty employees. He turns 65 and becomes eligible to get Medicare, but he hasn’t
enrolled in Medicare. He sees his health care provider for a service the employer’s
contract covers and that Medicare would have covered as well. The health care provider
charges $150 for the service. Medicare doesn’t pay anything since Mr. Ludwig doesn’t
have Medicare. The self-insured employer’s contract indicates that Mr. Ludwig has a $30
copay for this service. However, it also indicates that in the event Mr. Ludwig becomes
eligible for other coverage (whether he enrolls in it or not), the employer will pay at a
2
See FAQ dated October 12, 2010 which addresses the exemption from the Affordable Care Act for group health
plans with less than 2 current employees, which can be found here: https://www.cms.gov/CCIIO/Resources/Fact-
Sheets-and-FAQs/aca_implementation_faqs3.html.

Frequently Asked Questions Regarding Medicare and the Marketplace
August 1, 2014
18
lesser rate. In this case, the terms of the employer’s plan says it will only pay 20% of the
fee leaving Mr. Ludwig with a $120 cost-sharing obligation.
E. Enrollment Operations
E.1. Does the FFM application screen for Medicare enrollment?
The FFM application verifies enrollment in Medicare for individuals who have requested
financial assistance. However, the FFM systems are not currently set up to prevent
Medicare beneficiaries from enrolling in a Qualified Health Plan.
E.2. Will the Marketplace add a note to the Individual Marketplace paper application
telling people not to apply if they have Medicare?
Specific Medicare messaging isn’t included in the online or paper applications; however,
in the 2014 Medicare & You Handbook, the Medicare call center, Medicare.gov, and
HealthCare.gov, we have reassured beneficiaries that they are covered, their Medicare
benefits aren’t changing, and the Marketplace doesn’t require them to do anything
differently. In our public messaging, individuals are informed that Medicare isn’t part of
the Health Insurance Marketplace. If you have Medicare, you are covered, and do not
need to explore coverage through the Marketplace. The Marketplace won’t affect your
Medicare choices, and your benefits won’t be changing. No matter how you get
Medicare, whether through Original Medicare or a Medicare Advantage Plan, you’ll still
have the same benefits and security you have now. You won’t have to make any changes.
