
Washington Apple Health (Medicaid)
Paper Claim Billing
Resource
Every effort has been made to ensure this guide’s accuracy. If an actual or apparent conflict between this document
and an agency rule arises, the agency rules apply.

Paper Claim Billing Resource
Every effort has been made to ensure this guide’s accuracy. However, if a conflict exists between this resource and the agency’s rules, the agency’s
rules prevail. 2
About this resource
This resource provides general information that applies to most Apple Health providers. This guide is a
resource for the process of billing and submitting claims to the Washington Health Care Authority (HCA).
Effective October 1, 2016, HCA will accept only electronic claims for Apple Health (Medicaid) services,
except under limited circumstances.
Paper Claims Submission Practices Changing
All Apple Health (Medicaid) providers (excluding Tribal billing offices): Effective October 1, 2016, the
Health Care Authority (HCA) only accepts electronic claims for Apple Health (Medicaid) services, except
under very limited circumstances.
Providers may seek approval to submit paper claims if they are in a temporary or long-term situation outside
of their control that prevents submission of claims electronically. Examples of these unusual circumstances
may include but are not limited to:
• HCA notifies provider in writing that paper claims will be accepted due to ProviderOne System issues
preventing acceptance of electronic claims.
• The provider can demonstrate that the information needed for adjudication of an Apple Health
(Medicaid) claim cannot be submitted electronically using the claim formats required under the
ProviderOne Billing and Resource Guide.
• The provider is experiencing a disruption in their electricity or communication connection that is
outside of their control and is expected to last longer than two days. This exception applies only
while electricity or electronic communication is disrupted.
• Providers that have not submitted any electronic claims within the past state fiscal year (July 1, 2015
to June 30, 2016).
Providers who wish to ask for an exemption from submitting claims electronically may do so using the
Request a Waiver form. For more information see the ProviderOne Billing and Resource Guide webpage on
the agency’s website.
If you need further information regarding this notice, please contact: HCA Customer Service Center at 1-800-
562-3022.
Paper Claim Billing Resource
Every effort has been made to ensure this guide’s accuracy. However, if a conflict exists between this resource and the agency’s rules, the agency’s
rules prevail. 3
Table of Contents
About this resource .......................................................................................................................................... 1
Introduction ..................................................................................................................................................... 4
Who should use this resource? ........................................................................................................................ 4
Helpful information.......................................................................................................................................... 5
Section 1: Apple Health Overview ............................................................................................................ 8
What is Apple Health? ..................................................................................................................................... 8
Section 2: Submitting Paper Claims .......................................................................................................... 8
Guidelines/Instructions for Paper Claim Submission ...................................................................................... 8
Section 3: Claim Notes ............................................................................................................................. 9
Examples of claim notes and indicators .......................................................................................................... 9
Section 4: Claim Forms ........................................................................................................................... 10
Completing the CMS-1500 claim form ...........................................................................................................10
Completing the 2012 ADA Dental claim form ................................................................................................15
Completing the UB-04 claim form .................................................................................................................20

Paper Claim Billing Resource
Every effort has been made to ensure this guide’s accuracy. However, if a conflict exists between this resource and the agency’s rules, the agency’s
rules prevail. 4
Introduction
This resource provides general information to help understand the processes for submitting paper claims to
receive timely and accurate payments for covered services. This resource is to be used as a supplement to
the ProviderOne Billing and Resource Guide.
Disclaimer
A contract, known as the Core Provider Agreement (CPA), governs the relationship between HCA and
medical assistance providers. The CPA’s terms and conditions incorporate federal laws, rules and
regulations, state law, agency rules, regulations, program policies, provider alerts, and billing guides,
including this resource. Providers must submit a claim in accordance with agency rules, policies, provider
alerts, and billing guides in effect at the time they provided the service.
HCA does not assume responsibility for informing providers of national coding rules. ProviderOne will deny
claims billed in conflict with national coding rules. Consult the appropriate coding resources.
Who should use this resource?
The following providers will find this resource helpful:
• Providers temporarily approved to submit paper.
• Tribal billing offices. HCA complies with 25 U.S. Code § 1621e(h) and will not deny a claim for
benefits submitted by an Indian tribe or tribal organization based on the format in which the claim is
submitted.
Providers who do not meet one of the criteria above must submit claims electronically. The agency will not
process paper claims unless you have an approved waiver form for short-term temporary submission of
paper claims.
For more information about seeking an exception to electronic billing, review the Elimination of Paper
Claims – Frequently Asked Questions (FAQ).
This resource for paper claims assumes familiarity with standard medical billing practices and coding.
Paper Claim Billing Resource
Every effort has been made to ensure this guide’s accuracy. However, if a conflict exists between this resource and the agency’s rules, the agency’s
rules prevail. 5
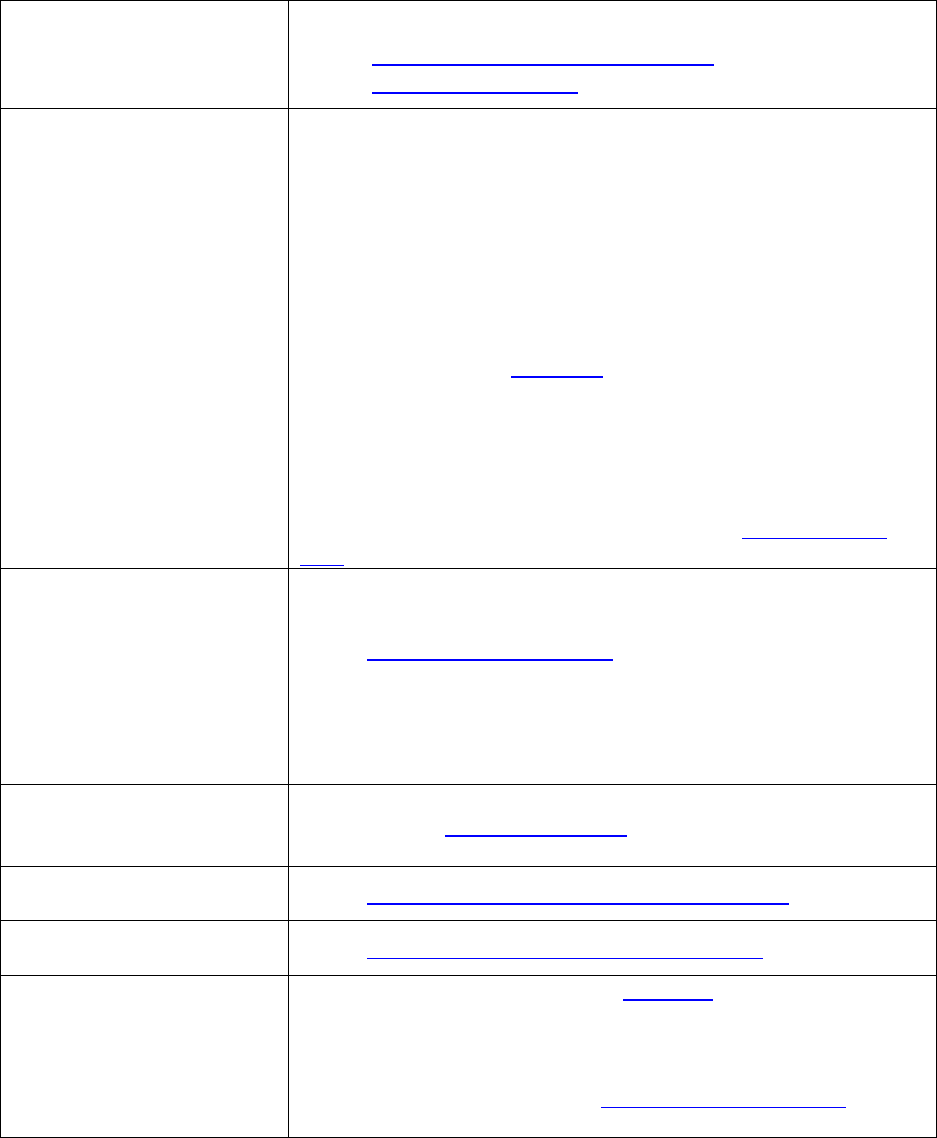
Helpful information
Where can I find billing guides
that explain program-specific
billing guidelines, coverage,
limitations, and fee schedules?
See the individual program-specific billing guides:
• Provider billing guides and fee schedules
• Hospital reimbursement
Who do I contact if I have
questions on payments,
denials, general questions
regarding claims processing, or
managed care plans?
The Medical Assistance Customer Service Center (MACSC) provider line is
available Monday through Friday 7 a.m. – 4:30 p.m. daily (claims line
open 8 a.m. to noon, closed noon to 1:30 p.m., and open 1:30 p.m. to
3:30 p.m.)
The interactive voice recognition (IVR) phone system is available 24 hours
a day, 7 days a week.
• Providers may contact MACSC at 1-800-562-3022; or
• Email MACSC at Contact Us
Note: Providers may use HCA's toll-free lines for questions regarding
its programs; however, HCA's response is based solely on the
information provided to the representative at the time of the call or
inquiry, and in no way exempts a provider from following the rules
and regulations that govern HCA's programs (see Chapter182-502
WAC).
Where can I get information
about becoming an Apple
Health provider, submitting a
change of address,
submitting a change of
ownership, or to ask
questions about the status of
an application?
See the Enroll as a Provider webpage.
1-800-562-3022 ext. 16137
Where can I find information
about HCA’s current rule
making activity?
See the agency’s Rulemaking webpage.
Where do I find all Washington
Administrative Codes?
See the Washington Administrative Code (WAC) webpage.
What is the Apple Health
web address?
See the Washington Apple Health (Medicaid) webpage.
Where can I ask questions
about private insurance or
third party liability?
For private insurance claims, submit a Contact us email. Choose Medical
Provider and use Private Commercial Insurance on the Select Topic
dropdown.
For casualty-related claims, see the Third Party Liability webpage, or call
1-800-562-3022.

Paper Claim Billing Resource
Every effort has been made to ensure this guide’s accuracy. However, if a conflict exists between this resource and the agency’s rules, the agency’s
rules prevail. 6
Where do I ask questions
about non-emergency
transportation services?
HCA provides access to non-emergency transportation services for
clients who need help with transportation to and from their
healthcare appointments.
For more information, see the Transportation Services (Non-Emergency)
webpage.
E-mail: HCA Transportation
Where do I ask questions
about Interpreter Services?
For spoken language access providers (LAP), register through
UniversalLanguage . Visit the spoken language access provider
webpage for more details.
For sign language interpretation, visit the sign language interpretation
webpage for more details.
E-mail: HCA Interpreter Services
Where do I obtain HCA’s
forms?
See the agency’s Forms and publications webpage.
Where can I find locations of
local Community Services
Offices (CSO)?
For more information, see the CSO webpage.
How do I find out where the
local Home and Community
Services (HCS) office is located?
For more information, see the HCS webpage.
How do I contact the local
Behavioral Health Organization
(BHO)?
For more information, see the BHO directory.
How do I find out what is
included in the nursing facility
per diem or general rate?
Contact Aging and Long Term Support Administration (ALTSA) or call at 1-
800-422-3263.
Where can I find information
about billing claims through
ProviderOne Direct Data Entry?
See the ProviderOne Billing and Resource Guide webpage.
Where can I find information
about billing HIPAA/EDI
Claims?
See the HIPAA webpage.
Paper Claim Billing Resource
Every effort has been made to ensure this guide’s accuracy. However, if a conflict exists between this resource and the agency’s rules, the agency’s
rules prevail. 7
How do I request
authorization?
Call 1-800-562-3022 using an extension listed below:
• Durable medical equipment and supplies, prosthetics and
orthotics, and oxygen: 15466
• Dental: 15468
• Pharmacy: 15483
• Medical – surgical: 52018
• All other medical services and enteral nutrition: 15471
See the program-specific billing guides for information on requesting
authorization.
• Provider billing guides and fee schedules
• Hospital reimbursement
For more assistance regarding authorization see the ProviderOne Billing
and Resource Guide.
Authorization forms can be sent by fax or mail:
Fax 1-866-668-1214
Attn: [enter one of the authorization areas above]
AUTHORIZATION SERVICES OFFICE
PO BOX 45535
OLYMPIA WA 98504-5535
If you are mailing/faxing supporting documentation without the original
authorization request form, a cover sheet is required. See the
ProviderOne Billing and Resource Guide for more information on cover
sheets.
Where can I access provider-
training materials?
See the Provider Resources webpage.

Paper Claim Billing Resource
Every effort has been made to ensure this guide’s accuracy. However, if a conflict exists between this resource and the agency’s rules, the agency’s
rules prevail. 8
Section 1: Apple Health overview
What is Apple Health?
Medical Assistance is the general name for Washington Apple Health programs administered by the Health
Care Authority (HCA).
Washington Apple Health includes Medicaid, mental health programs, chemical dependency and prevention
treatment programs, the Children’s Health Insurance Program (CHIP), family planning programs, and other
state-funded children’s healthcare programs. Medicaid is the federal entitlement program financed and
operated jointly by the states and the federal government.
For further information about eligibility, benefit packages and coverage limits please see the ProviderOne
Billing and Resource Guide.
Section 2: Submitting paper claims
Guidelines/instructions for paper claim submission
In order for the Optical Character Reader (OCR) feature of the scanner to read a paper claim, the blank claim form
must be a commercially produced form with either Sinclair Valentine J6983 or OCR Red Paper using these scan-
able red inks. These inks cannot be duplicated by a computer printer.
The following guidelines must be met to eliminate denials of a paper claim:
• Do not use red ink pens, highlighters, “post-it notes,” stickers, correction fluid, or tape anywhere on the
claim form or backup documentation. The scanner cannot read red ink and a yellow highlighter could turn
into a dark square covering the highlighted information during the scanning process.
• Use standard typewritten fonts that are 10 C.P.I. (characters per inch).
✓ Do not mix character fonts on the same claim form
✓ Do not use italics or script
• Use black printer ribbon, ink-jet, or laser printer cartridges.
✓ Make sure ink is not faded or too light
✓ Use of Dot Matrix printers may compromise the print quality
• Ensure all the claim information is entirely contained within the proper field on the claim form and on the
same horizontal plane. Misaligned data will delay processing and may even be missed.

Paper Claim Billing Resource
Every effort has been made to ensure this guide’s accuracy. However, if a conflict exists between this resource and the agency’s rules, the agency’s
rules prevail. 9
• For multiple page claims, please designate the page number on each page in the lower right hand
corner. Enter this information (e.g. 1 of 5, 2 of 5, 3 of 5, etc.) in the white space at the very bottom
of the claim form. This will help multiple page claims from being separated. The total dollar amount
needs to be listed on the last claim form for all combined pages.
• If the client has Medicare, complete the claim form as if billing for a non-Medicare client and attach
the Explanation of Medicare Benefits (EOMB).
• If the client has commercial private insurance, enter the private insurance payment on the claim
form and attach the private insurance Explanation of Benefits (EOB). Do not include any other
payment on the claim.
If you have an approved waiver to continue billing paper claims, the mailing address is noted on your approval
letter where these claims should be submitted to.
If you are a tribal biller, please visit the Tribal Affairs resources webpage for the appropriate address to submit
paper claims.
Note: The agency will not accept hand written or copied claim forms.
Section 3: Claim notes
Examples of claim notes and indicators
The following are examples of claim notes and indicators:
• SCI=B for baby on mom’s ID (can only be used the first 60 days of baby’s life)
o For multiple births use the following:
▪ SCI=BA for twin/triplet A
▪ SCI=BB for twin/triplet B
▪ SCI=BC for triplet C
• SCI=F for enteral nutrition – client not eligible for WIC
• SCI=I for Involuntary Treatment Act (ITA)
• SCI=V for voluntary (psych) treatment
Note: When using Special Claims Indicator (SCI) entries, everything following the “=” symbol will be read as part of
your indicator, so do not enter any additional data after that or ProviderOne will not recognize your entry. For
program-specific claim notes see the program-specific billing guides.

Paper Claim Billing Resource
Every effort has been made to ensure this guide’s accuracy. However, if a conflict exists between this resource and the agency’s rules, the agency’s
rules prevail. 10
Section 4: Claim forms
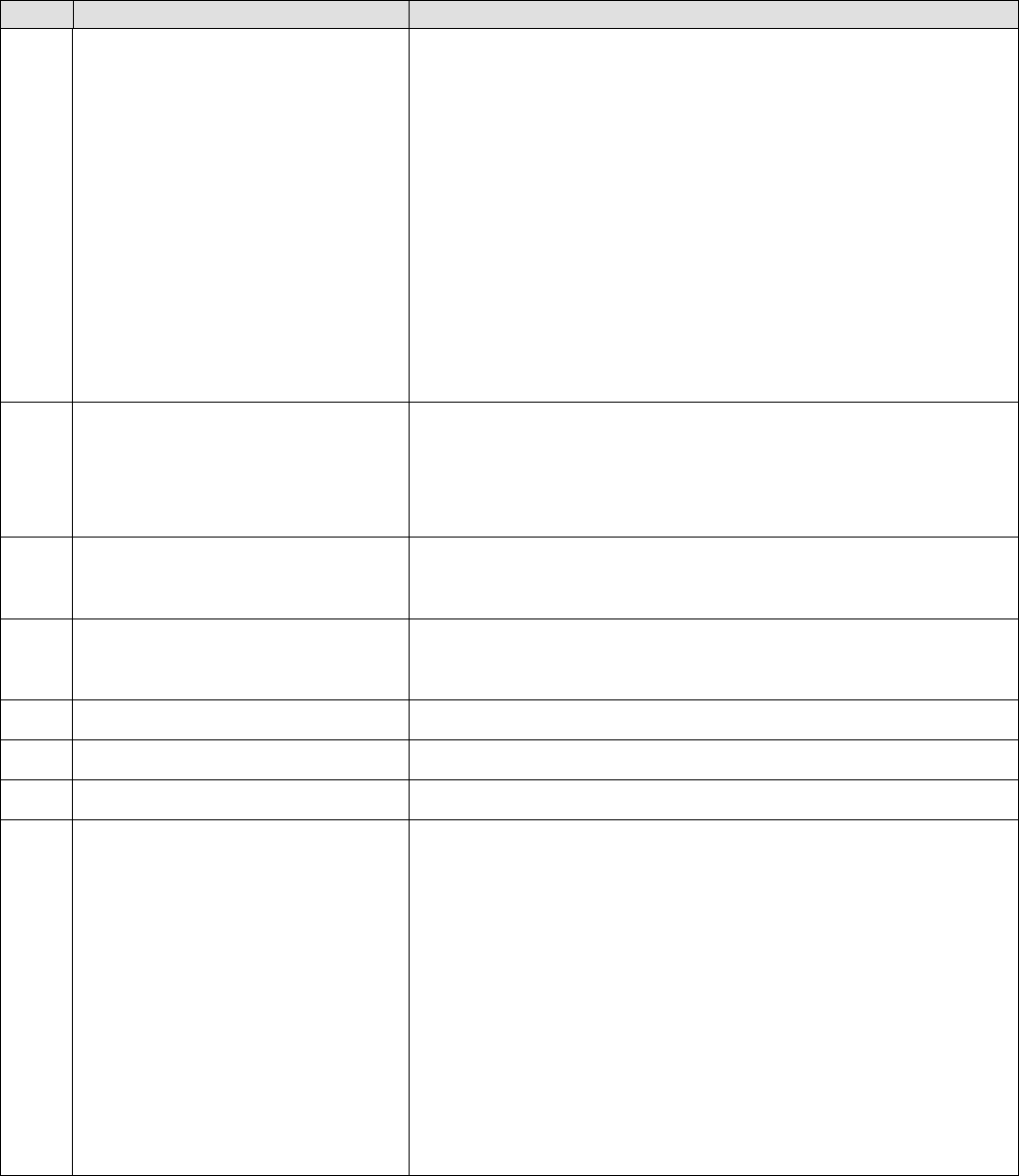
Completing the CMS-1500 claim form
The CMS-1500 claim form is a universal claim form and is the “approved” form that must be used when
billing for professional services. Approved forms will say “Approved OMB-0938-1197 FORM 1500 (02-12)” on
the bottom right hand corner. The numbered boxes on the claim form are referred to as fields. A number of
the fields on the form do not apply when billing the agency. Some field titles may not reflect their usage for
a particular claim type. This form is not available through Washington Health Care Authority but should be
available through your local office supplier.
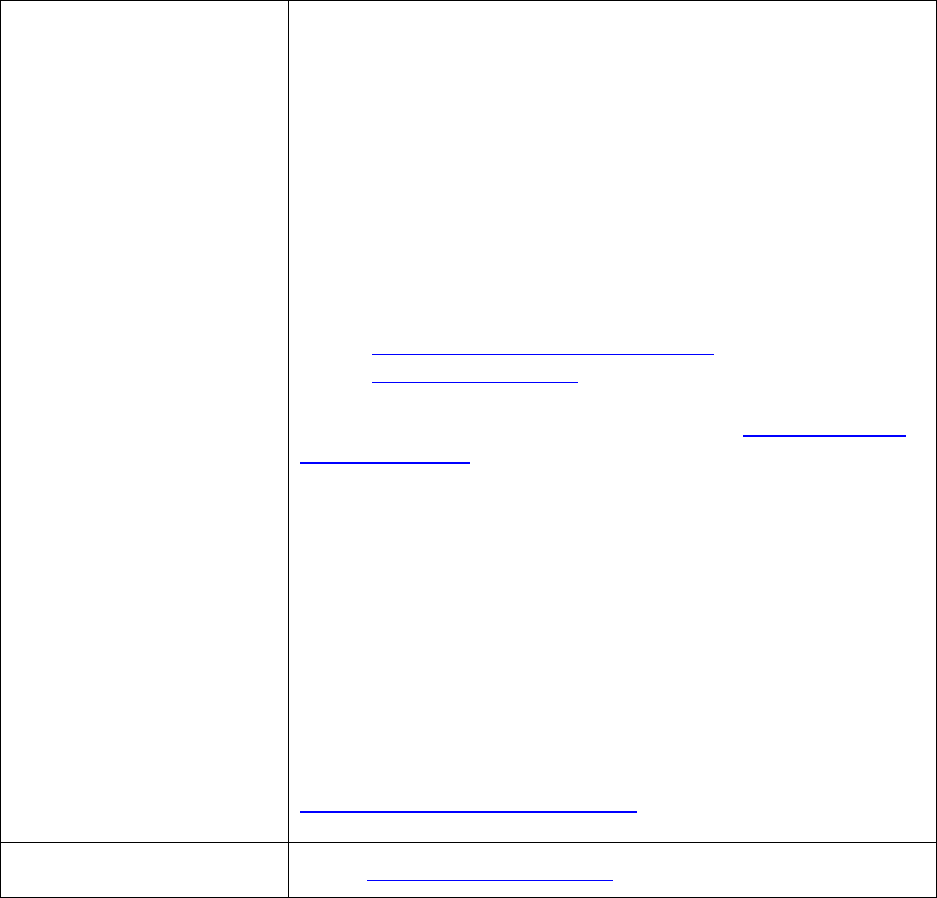
Field
Name
Action
1a
ProviderOne Client ID
Enter the ProviderOne Client ID (example 123456789WA).
2
Patient’s Name
Enter the last name, first name, and middle initial of the client
receiving services exactly as it appears on the client services card or
other proof of eligibility. If billing for a baby on mom’s ID, enter the
baby’s name here. If the baby is unnamed, use the mom’s last name
and “baby” as the first name.
Note: Be sure to insert commas separating sections of the name.
3
Patient’s Birthdate
Patient’s Sex
Enter the client’s birthdate in the following format: MMDDCCYY. Do
not include hyphens, dashes, etc. Enter the patient’s sex (gender). If
billing baby on mom’s ID, enter the baby’s birth date instead. If billing
baby on mom’s ID, enter the baby’s sex here.
4
Insured’s Name
When applicable. If the client has health insurance through
employment or another source (e.g., private insurance, Federal
Health Insurance Benefits, TRI-CARE, or TRI-CAREVA), enter the
name of the insured here. Enter the name of the insured except
when the insured and the client are the same – then the word
“Same” may be entered.
5
Patient’s Address
Enter the address of the client who received the services (the
person whose name is in Field 2).
6
Patient Relationship to Insured
Check the appropriate box.
7
Insured’s Address
Enter the address of the insured.
9
Other Insured’s Name
If there is other (primary) insurance (Field 11d), enter the last
name, first name and middle initial of the person who holds the
other insurance. If the client has other insurance and this field is not
completed, payment of the claim may be denied or delayed.
9a
Other Insured’s Policy or Group
Number
Enter the other insured’s policy or group number.
9b
Other Insured’s Date of Birth and
Gender
Check the appropriate box for the insured’s gender and enter the
birthdate in the following format: MMDDCCYY. Do not include
hyphens, dashes, etc.

Paper Claim Billing Resource
Every effort has been made to ensure this guide’s accuracy. However, if a conflict exists between this resource and the agency’s rules, the agency’s
rules prevail. 11
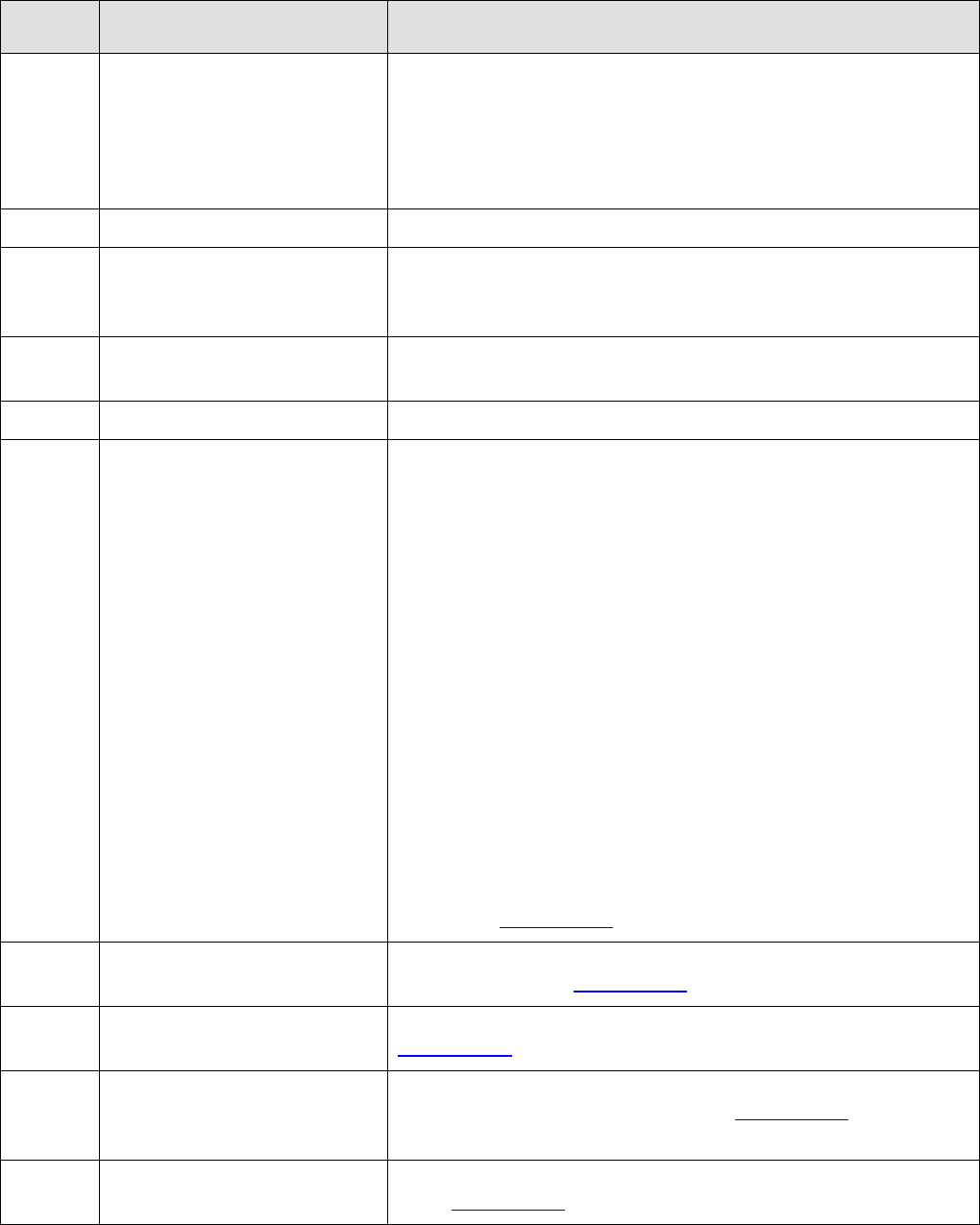
Field
Name
Action
9d
Insurance Plan Name or Program
Name
Enter the insurance plan name or program name (e.g., the insured's
health maintenance organization, private supplementary
insurance).
Please note: Apple Health, Medicaid, Welfare, Provider Services,
Healthy Options, First Steps, and Medicare, etc., are inappropriate
entries for this field.
10
Patient’s Condition Related To
Check yes or no to indicate whether employment, auto accident or
other accident involvement applies to one or more of the services
described in Field 24. Indicate the name of the coverage source in
field 10d (L&I, name of insurance company, etc.).
11
Insured's Policy Group or FECA
(Federal Employees Compensation
Act) Number
Primary insurance, when applicable. This information applies to the
insured person listed in Field 4. Enter the insured's policy and/or
group number and his/her social security number. The data in this
field will indicate the client has other insurance coverage and
Medicaid is the payer of last resort.
11a
Insured’s Date of Birth and Gender
Check the appropriate box when applicable for the insured’s gender
and enter the birthdate if different from field 3 in the following
format: MMDDCCYY. Do not include hyphens, dashes, etc.
11c
Insurance Plan Name or Program
Name
When applicable, show the insurance plan or program name to
identify the primary insurance involved. (Note: This may or may not
be associated with a group plan.)
11d
Is there another Health Benefit
Plan?
Required if the client has other insurance. Indicate yes or no. If yes,
you should have completed Fields 9a.-d. If the client has insurance,
and even if you know the insurance will not cover the service you
are billing, you must check yes. If 11d is left blank, the claim may be
processed and denied in error.
14
Date of Current Illness, Injury, or
Pregnancy
If applicable, enter the date in the following format: MMDDCCYY.
Do not include hyphens, dashes, etc.
15
If Patient Has Had Same or Similar
Illness
If applicable, enter the date in the following format: MMDDCCYY.
Do not include hyphens, dashes, etc.
16
Dates Patient Unable to Work in
Current Occupation
If applicable, enter the date in the following format: MMDDCCYY.
Do not include hyphens, dashes, etc.
17
Name of Referring Physician or
Other Source
When applicable, enter the referring physician or Primary Care Case
Manager (PCCM) name (Last Name, First Name).
17b
ID Number of Ordering/Referring
Physician
When applicable, enter the NPI number of the ordering/referring
physician. The provider reported here must be enrolled as a
Washington State Medicaid provider. When billing for services
provided to PCCM clients: enter the National Provider Identifier
(NPI) of the PCCM who referred the client for the service(s).
18
Hospitalization Dates Related to
Current Services
If applicable, enter the date in the following format: MMDDCCYY.
Do not include hyphens, dashes, etc.

Paper Claim Billing Resource
Every effort has been made to ensure this guide’s accuracy. However, if a conflict exists between this resource and the agency’s rules, the agency’s
rules prevail. 12
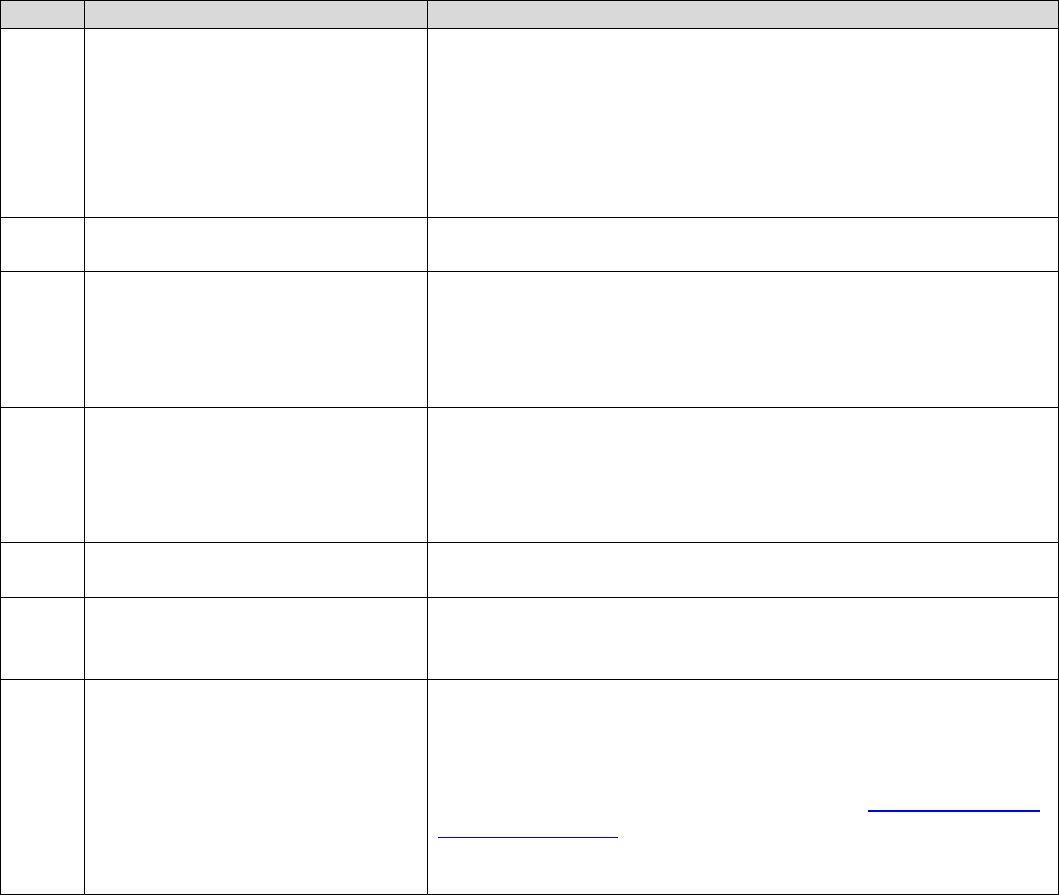
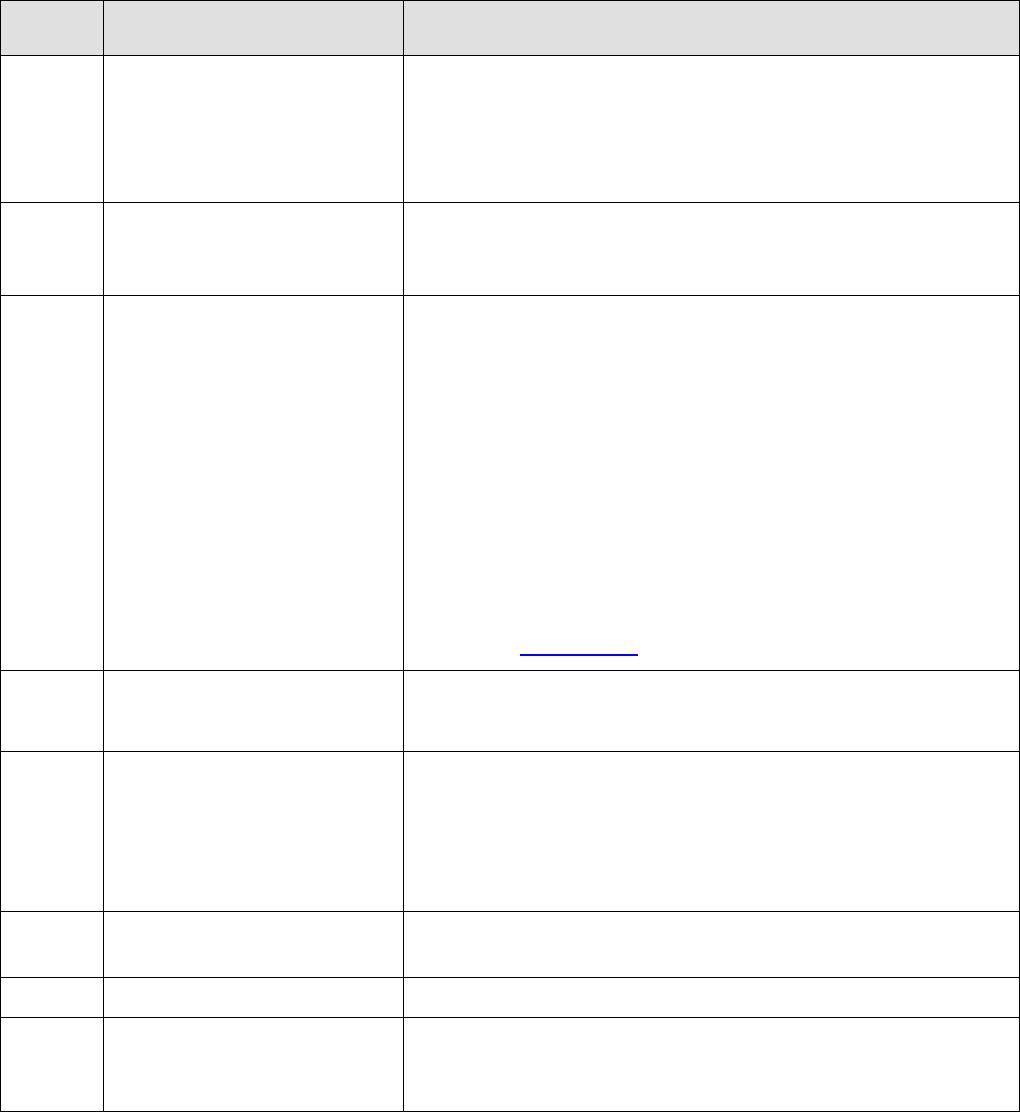
Field
Name
Action
19
Reserved for Local Use
This field is used for notes that require an Apple Health claims
specialist to review a claim before payment is made. To make any
of the following comments, enter “SCI=” and the corresponding
letter on the list below:
• B – BABY ON MOMS CLIENT ID
BA for twin/triplet A
BB for twin/triplet B
BC for triplet C
• F – ENTERAL NUTRITION – CLIENT NOT ELIGIBLE FOR WIC
• H – CHILDREN WITH SPECIAL HEALTHCARE NEEDS
• I – INVOLUNTARY TREATMENT ACT (ITA)(Legal Status)
• K – NOT RELATED TO TERMINAL ILLNESS (Hospice Client)
• V – VOLUNTARY TREATMENT (Legal Status)
This is also the location to enter NDCs, if applicable. Indicate what
line the NDC is for by putting “LN#” before the NDC.
If the client is on a spenddown, enter “Spenddown” here and the $
amount.
When billing multiple PA or EPA numbers, enter the authorization
number as follows:
19. Line 1: 870000XXX/ Line 2: 870000XXX
Note: Baby on Mom’s Client ID can only be used during the first 60
days of baby’s life.
20
Outside Lab?
If applicable, check the appropriate box and enter charges.
21
Diagnosis or Nature of Illness or
Injury
Enter the appropriate diagnosis code(s) in areas A-L, with A being
primary.
22
Medicaid Resubmission
When applicable. If this billing is being submitted beyond the 365
day timely filing deadline, enter the TCN that verifies that the claim
was originally submitted within the time limit. (The TCN number is
the claim number listed on the Remittance and Status Report.)
Also enter TCN numbers in this field for adjusting or voiding claims.
They must be in the following format:
• 7-101629600000340000 (replace/adjustment)
• 8-101629600000340000 (void/cancel)
23
Prior Authorization Number
When applicable. If the service or hardware being billed requires
authorization, enter the assigned number. For billing multiple
authorization numbers, see Field 19.
24a
Date(s) of Service
Enter the "from" and "to" dates of service.
Paper Claim Billing Resource
Every effort has been made to ensure this guide’s accuracy. However, if a conflict exists between this resource and the agency’s rules, the agency’s
rules prevail. 13
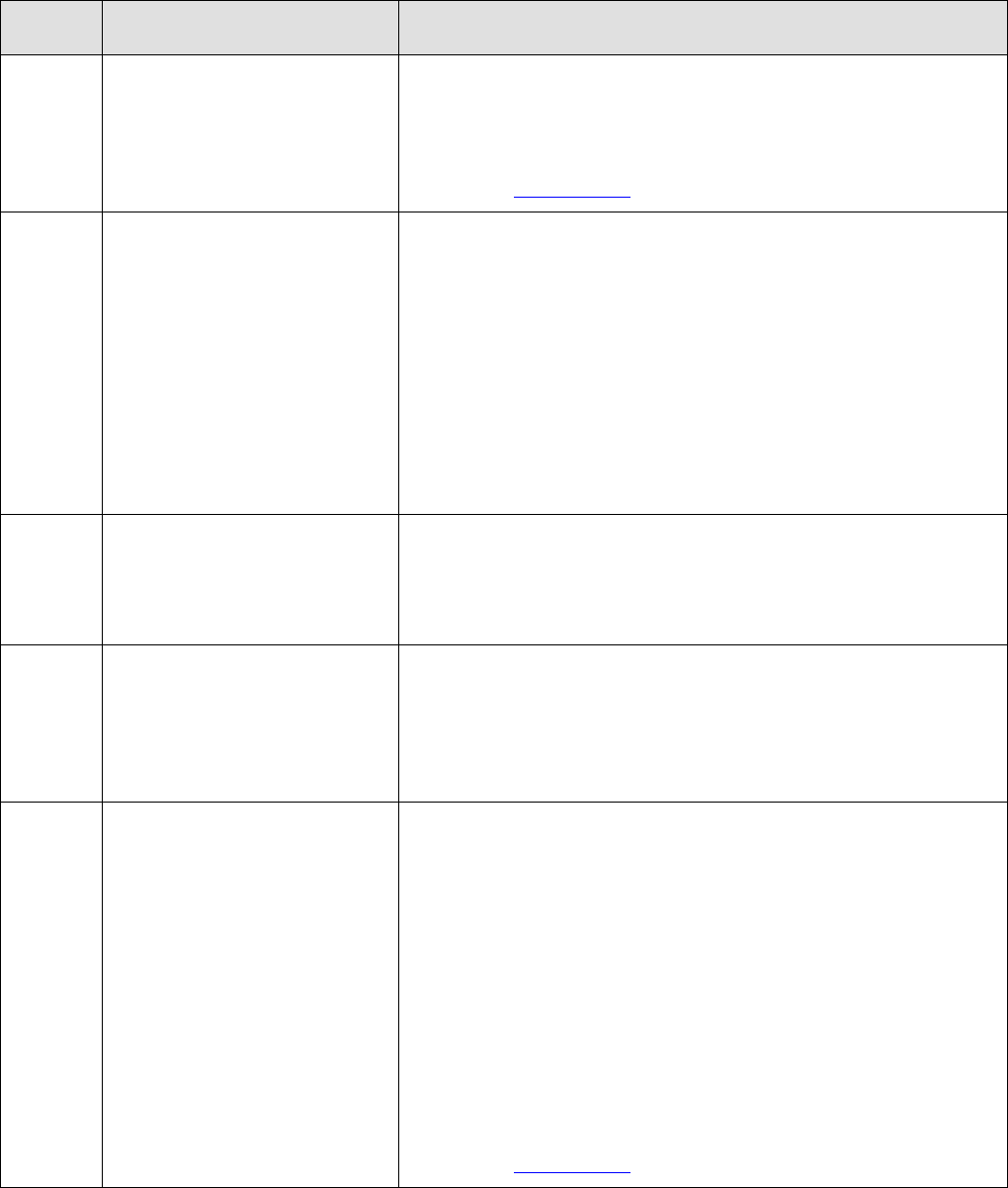
Field
Name
Action
24b
Place of Service
Enter the appropriate two digit code. For example:
11- Office
31- Skilled Nursing Facility
32- Nursing Facility
The agency requires that a valid two-digit place of service be
indicated that accurately reflects the place of service. Claims with
inaccurate place of service designations will be denied.
24d
Procedures, Services or Supplies
CPT/HCPCS
Enter the appropriate procedure code for the service(s) being
billed. When appropriate enter a modifier(s).
24e
Diagnosis Pointer
Enter the diagnosis pointer by entering A-L to correspond to field
21. The first diagnosis should be the principal diagnosis. Follow
additional digit requirements per ICD-10. Do not enter the actual
diagnosis code in this field. Please do not enter a comma or any
other punctuation in this field.
24f
Charges
Enter your usual and customary charge for the service performed. If
billing for more than one unit, enter the total charge of the units
being billed. Do not include dollar signs or decimals in this field. Do
not add sales tax. Sales tax is automatically calculated by the system
and included with the remittance amount.
24g
Days or Units
Enter the total number of days or units for each line. These figures
must be whole units.
24i
ID Qualifier
Enter the taxonomy qualifier ZZ if required by Medicare or any
other primary carrier. ProviderOne ignores this field but some
carriers require it in order for field 24j to be forwarded to HCA.
24j
Rendering Provider ID#
If applicable, reference (outside)
laboratory
Enter the taxonomy code in the top half of the field for the
rendering provider, if applicable. Enter the NPI for the rendering
provider in the bottom half of the field. This information is only
needed if it is different than fields 33a and 33b. For more
information on taxonomy codes, please see the ProviderOne Billing
and Resource Guide. The rendering provider must be enrolled as a
Washington State Medicaid provider prior to start of treatment.
Enter the NPI number of the reference (outside) laboratory here.

Paper Claim Billing Resource
Every effort has been made to ensure this guide’s accuracy. However, if a conflict exists between this resource and the agency’s rules, the agency’s
rules prevail. 14
Field
Name
Action
25
Federal Tax ID Number
Enter in the Federal Tax ID or Social Security number and indicate
via the check boxes which number is being used.
26
Patient's Account Number
Not required (optional field for your internal purposes). Enter alpha
and/or numeric characters only. For example, a medical record
number or patient account number. This number will be printed on
your Remittance and Status Report (RA) under the heading Patient
Account Number.
27
Accept Assignment?
Check the appropriate box.
28
Total Charge
Enter the sum of all charges indicated in Field 24F. Do not use dollar
signs or decimals in this field.
29
Amount Paid
If there is a private insurance payment, show the amount here and
attach a copy of the private insurance EOB. If payment is received
from a source other than insurance, specify the source in Field 10d.
Do not use dollar signs or decimals in this field or enter prior
Medicare, Medicare Advantage, or Medicaid payments here.
30
Rsvd for NUCC Use
Enter total charges minus any amount(s) in Field 29. Do not use
dollar signs or decimals in this field.
32
Service Facility Location
Information
Enter the location address if different from Field 33
• Enter the location NPI
• Enter the location Taxonomy. For more information on
taxonomy codes, please see the ProviderOne Billing and
Resource Guide.
This field is required for Sleep Centers, Birthing Facilities, and
Centers of Excellence when the location of service is different from
the billing NPI’s location.
33
Physician's, Supplier's Billing Name,
Address, Zip Code And Phone #
Enter the provider’s Name and Address on all claim forms.
• Enter the Billing Provider NPI
• Enter the Billing Provider Taxonomy. For more information
on taxonomy codes, please see the ProviderOne Billing and
Resource Guide.
Paper Claim Billing Resource
Every effort has been made to ensure this guide’s accuracy. However, if a conflict exists between this resource and the agency’s rules, the agency’s
rules prevail. 15
Completing the 2012 ADA Dental claim form
The 2012 ADA dental claim form is the only form approved by Washington Health Care Authority for dental
billing. Approved forms will say "(c) 2012 American Dental Association" in the lower right-hand corner. The
numbered boxes on the claim form are referred to as fields. A number of the fields on the form do not apply
when billing the agency. This form is not available through Washington Health Care Authority but should be
available through your local office supplier.
Field
Name
Action
2
Predetermination/Preauthorization
Number
Place the required prior authorization number or EPA number in this
field.
3
Company/Plan Name, Address, City,
State, Zip Code
Enter the claims address for the Health Care Authority.
4
Other Dental or Medical Coverage
Check the appropriate box.
5
Name of Policyholder/Subscriber
(Last, First, Middle Initial, Suffix)
If different from the patient, enter the name of the subscriber.
6
Date of Birth
Enter the subscriber’s date of birth. Hyphens, dashes, etc. are not
needed.
8
Policyholder/Subscriber Identifier
(SSN or ID#)
Enter the subscriber’s SSN or other identifier assigned by the payer.
9
Plan/Group Number
If the client has third party coverage, enter the dental plan number of
the subscriber.
10
Relationship to Primary
Policyholder/Subscriber
Check the applicable box.
11
Other Insurance Company/Dental
Benefit Plan Name, Address, City,
State, Zip Code
Enter any other applicable third party insurance.
12
Policyholder/Subscriber Name (Last,
First, Middle Initial, Suffix), Address,
City, State, Zip Code
Enter the last name, first name, and middle initial of the client
receiving services exactly as it appears on the client services card
or other proof of eligibility.
Note: Be sure to insert commas separating sections of the name.
13
Date of Birth (MMDDCCYY)
Enter the client’s date of birth. Hyphens, dashes, etc. are not
needed.
14
Gender
Check the applicable box.
15
Policyholder/Subscriber Identifier
(SSN or ID#)
Enter the patient’s ProviderOne Client ID (for example
123456789WA)
16
Plan/Group Number
Enter the subscriber’s group Plan or Policy Number.
18
Relationship to
Policyholder/Subscriber
Check the appropriate box.

Paper Claim Billing Resource
Every effort has been made to ensure this guide’s accuracy. However, if a conflict exists between this resource and the agency’s rules, the agency’s
rules prevail. 16
Field
Name
Action
20
Name (Last, First, Middle Initial,
Suffix) Address, City, State, Zip Code
Enter the last name, first name, and middle initial of the client
receiving services exactly as it appears on the client services card
or other proof of eligibility.
Note: This field is not required if “self” is checked in box 18.
21
Date of Birth (MMDDCCYY)
Enter the client’s date of birth. Hyphens, dashes, etc. are not
needed.
Note: This field is not required if “self” is checked in box 18.
22
Gender
Check the appropriate box.
Note: This field is not required if “self” is checked in box 18.
23
Patient ID/Account #
Not required (optional field for your internal purposes). Enter an
alpha or numeric character only. For example, a medical record
number or patient account number. This number will be printed
on the Remittance Advice (RA) under the heading Patient
Account Number.
24
Procedure Date (MMDDCCYY)
Enter the eight-digit date of service, indicating
month, day, and year (e.g., April 1, 2007 =
04012007). Hyphens, dashes, etc. are not needed.
25
Area of Oral Cavity
If the procedure code requires an arch or a quadrant designation,
enter one of the following:
01 Maxillary area
02 Mandibular area
10 Upper right quadrant
20 Upper left quadrant
30 Lower left quadrant
40 Lower right quadrant
27
Tooth Number(s) or Letter(s)
Enter the appropriate tooth number, letter(s):
1. 1 through 32 for permanent teeth
2. A through T for primary teeth
3. 51 through 82 or AS through TS for supernumerary teeth
4. Only one tooth number may be billed per line
Do not fill in preceding zeros for tooth numbers (e.g. tooth 1).
Paper Claim Billing Resource
Every effort has been made to ensure this guide’s accuracy. However, if a conflict exists between this resource and the agency’s rules, the agency’s
rules prevail. 17
Field
Name
Action
28
Tooth Surface
Enter the appropriate letter from the list below to indicate the
tooth surface. Up to five surfaces may be listed in this column
(separate with a comma):
B = Buccal
D = Distal
F = Facial
I = Incisal
L = Lingual
M = Mesial
O = Occlusal
Note: Make entries in this field only if the procedure requires a
tooth surface.
29
Procedure Code
Enter the appropriate current CDT procedure code that represents
the procedure or service performed. The use of any other procedure
code(s) will result in denial of payment.
Note: The agency only covers procedure codes listed on our Fee
Schedule that has a dollar amount indicated.
30
Description
Give a brief written description of the services rendered. When billing
for general anesthesia or IV sedation, enter the actual beginning and
ending time.
31
Fee
Enter your usual and customary fee (not the agency's maximum
allowable rate) for each service rendered. If the Fee Schedule
indicates to bill Acquisition Cost (AC), please bill your acquisition cost.
31a
Other Fee(s)
This field is not used by the agency.
32
Total Fee
Enter the total charges. Do not include decimal points or dollar signs.
33
Missing Teeth Information
Place an “X” on the appropriate missing teeth.
35
Remarks
Enter appropriate comments in this field
• To indicate a payment by a private insurance, enter “insurance
payment” and the amount. Attach the private insurance EOB
to the claim.
• If processing a void, enter the TCN in this field preceded by an
8 (e.g. 8-123456789012345678).
• If processing an adjustment or replacement, enter the TCN in
this field preceded by a 7 (e.g. 7-123456789012345678).
• If the claim is an adjustment and indicating an insurance
payment, use the following format – 7-123456789012345678
- $123.45.
• Indicate the client’s Spenddown amount - enter “Spenddown”
and then the $ amount.

Paper Claim Billing Resource
Every effort has been made to ensure this guide’s accuracy. However, if a conflict exists between this resource and the agency’s rules, the agency’s
rules prevail. 18
Field
Name
Action
38
Place of Treatment
The agency defines the following places of service for paper
claims when a place of treatment box is checked but no two-digit
place of service is indicated:
Box checked
Place of Service (POS)
Office
Dental office (POS 11)
Hospital
Outpatient hospital (POS 22)
ECF
Skilled nursing facility (POS 31)
Other
The agency will not allow “other” without a
two-digit place of service indicated.
If the services rendered are not in one of the places of service
indicated above, then the two-digit POS must be indicated in
field 38.
The agency considers the following places of service for dental
claims (not all services are covered in all places of service):
Place of Service
Two digit Indicator code
Office
11 - Dentist office
Hospital
21 - Inpatient hospital
22 - Outpatient hospital
23 - Hospital emergency room
31 - Skilled nursing facility
54 - Intermediate care facility
Other
03 - School based services
12 - Client’s residence
24 - Professional Services in an
Ambulatory Service Center
50 - Federally Qualified Health Center
71 - State or public health clinic
The agency requires that the use of a valid two-digit place of service
be indicated that accurately reflects the place of service. Inaccurate
place of service designations result in claim denials.
39
Enclosures
Indicate “Y” if you are attaching backup documents and “N” if not
attaching backup documents. (Do not send X-rays when billing for
services).
40
Is Treatment for Orthodontics?
Check the appropriate box.
41
Date Appliance Placed (MMDDCCYY)
This field must be completed for orthodontic treatment.
42
Months of Treatment Remaining
If applicable, enter the months of treatment remaining.
43
Replacement of Prosthesis?
Check appropriate box. If “yes,” enter the reason for replacement in
field 35 (Remarks).

Paper Claim Billing Resource
Every effort has been made to ensure this guide’s accuracy. However, if a conflict exists between this resource and the agency’s rules, the agency’s
rules prevail. 19
Field
Name
Action
44
Date Prior Placement (MMDDCCYY)
Enter the appropriate date if “yes” is checked for field 43.
45
Treatment Resulting from
Check the appropriate box.
46
Date of Accident (MMDDCCYY)
If applicable, enter the date of accident.
47
Auto Accident State
Enter the two letter abbreviation for the state the accident occurred
in, if applicable.
48
Name, Address, City, State, Zip Code
Enter the practice or business name and address as recorded with
the agency. If a solo practice, enter the dentist name and business
address as recorded with the agency.
49
NPI
Enter the National Provider Identifier (NPI). Providers are identified
by this code and not by provider name. Omitting this number will
result in claim denial
The provider must be enrolled as a Medicaid contracted provider
prior to start of treatment.
50
License Number
Enter the billing dentist’s license number.
51
SSN or TIN
Enter the billing dentist’s SSN or TIN.
52a
Additional Provider ID
Enter the taxonomy for the billing provider. For more information on
taxonomy codes, please see the ProviderOne Billing and Resource
Guide.
53
Treating Dentist and Treatment
Location Information
Enter the treating dentist’s signature and date.
54
NPI
Enter the treating provider NPI if it is different from the billing
provider NPI. The treating provider must be enrolled as a Medicaid
contracted provider prior to start of treatment.
55
License Number
Enter the treating dentist’s license number.
56
Address, City, State, Zip Code
Enter the treating dentist’s address, city, state and zip code.
56a
Provider Specialty Code
Enter in the treating provider taxonomy if an NPI was entered in box
54.
58
Additional Provider ID
This field is not used by the agency.

Paper Claim Billing Resource
Every effort has been made to ensure this guide’s accuracy. However, if a conflict exists between this resource and the agency’s rules, the agency’s
rules prevail. 20
Completing the UB-04 claim form
The following instructions explain how to complete the UB-04 claim form and the “approved” form must be
used when billing. The form will say “Approved OMB No. 0938-0997” on the bottom left hand corner. The
instructions should be used to supplement the information in the National Uniform Billing Committee
(NUBC) official UB-04 Data Specifications Manual. For fields that are situational and for code usage details
not covered below please refer to the NUBC Manual. This form is not available through the Washington
Health Care Authority but should be available through your local office supplier.
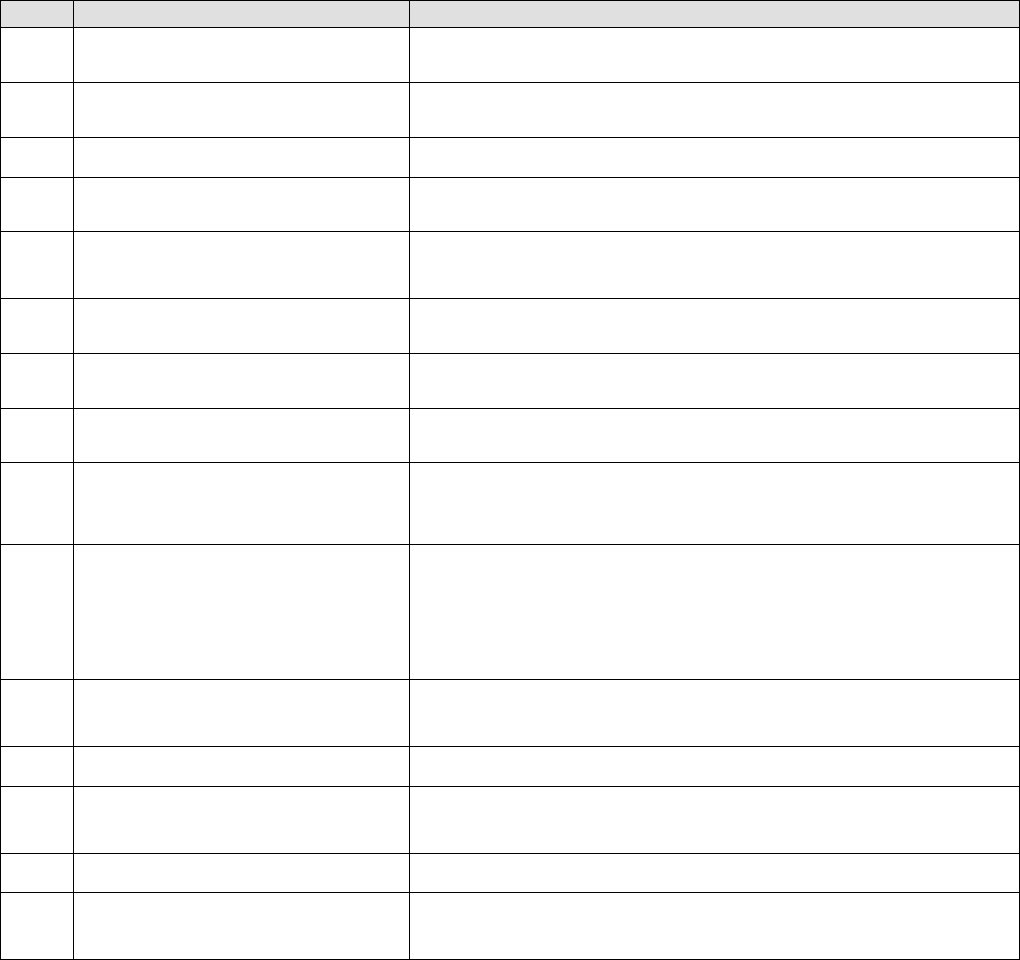
Form
Locator
Name
Action
1
Billing Provider Name
Line 1: Provider Name
Line 2: Street Address or Post Office Box
Line 3: City, State, and Zip Code plus 4
Line 4:Telephone (& Fax)
2
Pay-to Name and Address
Report only if different from form Locator 1.
3a
Patient Control Number
Enter patient’s unique (alpha and/or numeric) number assigned
by the provider. This number will be printed on the Remittance
and Status Report (RA) under the heading Patient Account
Number.
3b
Medical/Health Record Number
Optional item. Enter alpha and/or numeric characters only. This
entry is not returned on the RA.
4
Type of Bill
ProviderOne uses the Type of Bill for adjudication and pricing. The
ProviderOne recommended TOBs are:
Type of service
Type of bill code
Hospice
81X, 82X
Home Health
32X, 34X
Kidney Center
72X
Inpatient Hospital
11X
Outpatient Hospital
13X
Nursing Home
21X
Swing Bed
18X
FQHC Crossover
77X
RHC Crossover
71X
5
Federal Tax Number
Enter the Federal tax identification number.
6
Statement Covers Period
Enter from and to dates of service (MMDDCCYY). Overlapping
fiscal/calendar years do not require split billing.
8a
Patient Name/Identifier
Enter the patient’s ProviderOne Client ID (for example,
123456789WA).
Paper Claim Billing Resource
Every effort has been made to ensure this guide’s accuracy. However, if a conflict exists between this resource and the agency’s rules, the agency’s
rules prevail. 21
Form
Locator
Name
Action
8b
Patient Name/Identifier
Enter the last name, first name, and middle initial of the client
receiving services exactly as it appears on the client services card
or other proof of eligibility. If billing for a baby on mom’s ID enter
the baby’s name here. If the baby is un-named use the mom’s last
name and “baby” as the first name.
Note: Be sure to insert commas separating sections of the name.
9
Patient Address
Enter the address of the client who received the services.
10
Birthdate
Enter in the patient’s date of birth in the following format:
MMDDCCYY. (Example: 05102003 for May 10, 2003.) If billing baby on
mom’s ID enter the baby’s birth date instead.
11
Sex
Indicate if the patient is male (M) or female (F). If billing baby on
mom’s ID enter the baby’s sex here.
12
Admission Date
Indicate the start date of admission.
13
Admission Hour
Enter the code for the hour of admission converted to 24 hour
time as shown below:
CODE
TIME AM
CODE
TIME PM
00
12:00-12:59
12
12:00-12:59
(Midnight)
(Noon)
01
01:00-01:59
13
01:00-01:59
02
02:00-02:59
14
02:00-02:59
03
03:00-03:59
15
03:00-03:59
04
04:00-04:59
16
04:00-04:59
05
05:00-05:59
17
05:00-05:59
06
06:00-06:59
18
06:00-06:59
07
07:00-07:59
19
07:00-07:59
08
08:00-08:59
20
08:00-08:59
09
09:00-09:59
21
09:00-09:59
10
10:00-10:59
22
10:00-10;59
11
11:00-11:59
23
11:00-11:59
Refer to the NUBC manual for more information.
14
Priority(Type) of Visit
Required when patient is being admitted to the hospital for inpatient
services. Refer to the NUBC manual for more information.
15
Admission Source
Indicate the source of referral for admission or visit. Refer to the
NUBC manual for more information.
16
Discharge Hour
Enter the hour of discharge. Refer to the 24-hour time as shown in the
coding table for Form Locator 13 and the NUBC manual for more
information.
17
Status
Enter the code indicating patient status as of the discharge date. Refer
to the NUBC manual for more information.

Paper Claim Billing Resource
Every effort has been made to ensure this guide’s accuracy. However, if a conflict exists between this resource and the agency’s rules, the agency’s
rules prevail. 22
Form
Locator
Name
Action
18-28
Condition Codes
Refer to the NUBC manual for Codes other than below:
Washington State assigned Condition Codes
Trauma - Qualified Trauma cases are identified by the following
codes:
TP
Indicates a pediatric client (through age 14 only) with an
Injury Severity Score (ISS) in the range of 9-12
TT
Indicates a transferred client with an ISS that is less than
13 for adults or less than 9 for pediatric clients
TV
Indicates an ISS in the range of 13 to 15
TW
Indicates an ISS in the range of 16 to 24
TX
Indicates an ISS in the range of 25 to 34
TY
Indicates an ISS in the range of 35 to 44
TZ
Indicates an ISS of 45 or greater
29
Accident State
If applicable, enter the state in which the accident occurred.
(Example: OR, CA, etc.)
31-34
Occurrence Code and Dates
Refer to the NUBC manual for more information. Not required on a
Hospice, Kidney Center, Home Health or SNF claims.
35-36
Occurrence Span Codes and
Dates
Refer to the NUBC manual for more information.
38
Responsible Party name and
address
Enter the information for the claim addressee.

Paper Claim Billing Resource
Every effort has been made to ensure this guide’s accuracy. However, if a conflict exists between this resource and the agency’s rules, the agency’s
rules prevail. 23
Form
Locator
Name
Action
39-41
Value codes and Amounts
Refer to the NUBC manual for codes other than below:
Value Code 66: For EMER patient liability on Inpatient Hospital
claims, then enter the Patient Participation Amount.
Value Code 66: For Spenddown on Institutional Hospital claims
then enter the Patient Participation Amount.
Value Code 24: Enter this code in the code field with the Patient
Class immediately following in the amount field. See the Nursing
Facilities Billing Guide for valid Patient Class codes. (e.g.,
20.00=class code 20).
Value Code 31: Enter this code in the code field with the Patient
Participation amount for the entire month immediately following
in the amount field for Nursing Home claims.
Value Code 31: For Hospice claims indicating the Skilled Nursing
Facility room and board charge, enter this code in the code field only
once per claim and if there is more than one patient participation
amount, sum the amounts and enter only one value amount.
Value Code 54: Enter this code in the code field with the newborn
birth weight in grams in the amount field (no decimals). Right justify
the weight in grams to the left of the dollars/cents delimiter. If your
billing software requires the decimal in the Value Code field, enter the
weight in grams followed by “.00” (e.g. 2499.00).
42
Revenue Code
Revenue Codes must be valid for the Type of Bill or facility. For
example, revenue code usage for Hospice may differ from a
hospital.
a. For Hospice, Home Health, Kidney Center and Nursing Home
billing, see the individual Billing Guides.
b. For Inpatient and Outpatient Hospital services, see the Apple
Health Revenue Code Grid.
c. On the final page of your claim, form locator 42, line 23 will
require revenue code 0001 with your claim total in form locator
47, line 23.

Paper Claim Billing Resource
Every effort has been made to ensure this guide’s accuracy. However, if a conflict exists between this resource and the agency’s rules, the agency’s
rules prevail. 24
Form
Locator
Name
Action
43
Description
Enter a written description of the related revenue categories included
on the bill.
The agency is collecting NDC information on Centers for Medicare
and Medicaid Services designated, physician administered drugs
in the outpatient hospital setting and for Kidney Centers (revenue
Codes 0634-0637 drugs with procedures).
See the Physician-Related Services /Health Care Professional Services
Billing Guide for the description of the NDC reporting format criteria.
When reporting a drug, enter identifier N4, the eleven-digit NDC
code, Unit Qualifier, and number of units from the package of the
dispensed drug for the specified detail line. Do not enter a space,
hyphen, or other separator between N4, the NDC code, Unit
Qualifier, and number of units.
Refer to the NUBC manual for more information.
44
HCPCS/CPT/RATE Codes
When applicable, enter the HCPCS/CPT/RATE codes.
Outpatient HCPCS – see the Apple Health Revenue Code Grid for
Revenue code/HCPCS combination requirements.
Inpatient rates – required when a room and board revenue code
is reported.
Modifiers are entered in this field, when applicable, and attached
to the qualifying code line.
45
Service Date
Required on outpatient hospital, kidney center, hospice, nursing
home, and home health claims. On each line, enter the date of
service.
46
Service Units
Enter the units of service for each revenue code. Please do not use
decimal points (e.g. 1 unit = 1).
47
Total Charges
Enter the total charge for each revenue code or procedure code
entry.
Line 23: This entry must be the sum of the individual charges.
48
Non-Covered Charges
Enter the amount required by contract with the agency.
Enter charges for non-covered services performed during the stay or
charges paid by another payer (Medicare) when all services must be
reported on the inpatient claims.
Paper Claim Billing Resource
Every effort has been made to ensure this guide’s accuracy. However, if a conflict exists between this resource and the agency’s rules, the agency’s
rules prevail. 25
Form
Locator
Name
Action
50 a-c
Payer Name
Enter Washington Medicaid for the Medicaid payer identification.
Enter the name of the third party payer if applicable:
50a–Primary payer
50b–Secondary payer
50c–Tertiary payer
51
Health Plan ID
For Apple Health Medicaid, leave blank. Enter the health plan
identification number (if known) in 51 a, b, c depending on whether
the insurance is primary, secondary, or tertiary.
52 a-c
Release of Information
Certification Indicator
Required
Indicate whether the patient or patient’s legal representative has
signed a statement permitting the provider to release data to
other organizations. The Release of Information is limited to the
information carried on the claim.
I = Informed Consent to Release Medical Information.
(Required when the provider has not collected a signature and
state or federal laws do not supersede the HIPAA Privacy Rule by
requiring a signature be collected.)
Y = Yes, provider has a Signed Statement Permitting Release of
Medical Billing Data Related to a Claim.
Refer to the NUBC manual for more information.
53 a-c
Assignment of Benefits
Certification Indicator
Required
Not used by the agency.
54 a-c
Prior Payments
Enter the amount that has been received (if any) toward payment
of the claim from another payer prior to billing the agency.
54a–Primary payment
54b–Secondary payment
54c–Tertiary payment
55
Estimate Amount Due
The amount estimated by the provider to be due from the indicated
payer (estimated responsibility less prior payments).
56
NPI
Enter the NPI for the billing provider.
57 a-c
Other Billing Provider ID
A unique identification number assigned to the provider submitting
the bill by the health plan. Not Required. The agency does not assign
or require a unique identification number other than the NPI.

Paper Claim Billing Resource
Every effort has been made to ensure this guide’s accuracy. However, if a conflict exists between this resource and the agency’s rules, the agency’s
rules prevail. 26
Form
Locator
Name
Action
58 a-c
Insured’s Name
Enter the insured’s last name, first name, and middle initial
exactly as it appears on the client services card or other proof of
eligibility.
Note: Be sure to insert commas separating sections of the name.
If the recipient is covered by insurance other than Medicaid, enter
the name of the individual in whose name the insurance is
carried.
Carry through the payer line scheme reported in Form Locator 50
A-C.
Refer to the NUBC manual for more information.
59 a-c
Patient’s Relationship to Insured
Enter 18 when the subscriber is the same person as the patient. If
the subscriber is not the same person as the patient, do not use
this field.
60 a-c
Insured’s Unique ID
Enter all of the insured’s unique identification numbers assigned by
any payer organizations.
Carry through the payer line scheme reported in Form Locator 50 A-C.
Enter the ProviderOne Client ID exactly as it appears on the
ProviderOne Services card or other proof of eligibility (example:
123456789WA).
Refer to the NUBC manual for more information.
61 a-c
Group Name
Refer to the NUBC manual for more information.
62 a-c
Insurance Group Number
Refer to the NUBC manual for more information.
63 a-c
Treatment Authorization Codes
Enter the Prior Authorization (PA) number issued by the agency or
Expedited Authorization Number (EPA) located in the appropriate
program-specific billing guides for the billed service if required.
Carry through the payer line scheme reported in Form Locator 50 A-C.
If the claim meets the qualifications for Medical Inpatient
Detoxification (MID) use the following EPA numbers. Please see the
Inpatient Hospital Services Billing Guide for additional information.
• Acute alcohol detoxification use 870000433
• Acute drug detoxification use 870000435
Claims for MID services without one of the above EPA numbers will be
denied.

Paper Claim Billing Resource
Every effort has been made to ensure this guide’s accuracy. However, if a conflict exists between this resource and the agency’s rules, the agency’s
rules prevail. 27
Form
Locator
Name
Action
64 a-c
Document Control Number
When applicable. If the submission date for the claim is over the
365-day time limit, enter the TCN that verifies that the claim was
originally submitted within the time limit. (The TCN number is the
claim number listed on the Remittance Advice.)
Also enter TCN numbers in this field for adjusting or voiding
claims. They must be in the following format:
• 7-101629600000340000 (replace/adjustment)
• 8-101629600000340000 (void/cancel)
65 a-c
Employer Name
If applicable, enter the employer name of the insured.
Carry through the payer line scheme reported in Form Locator 50 a-c.
66
Diagnosis and Procedure Code
Qualifier
Required. Enter the qualifier that identifies the version of the
International Classification of Diseases (ICD) reported:
9 – Ninth Revision
0 – Tenth Revision
67
Principal Diagnosis Code
Principal Diagnosis Code (the condition established after
study to be chiefly responsible for causing the use of facility
services). Required:
• Present on Admission (POA) Indicator - see NUBC manual for
usage guidelines.
• Please see the Inpatient Hospital Services Billing Guide for
additional information.
67a-q
Other Diagnosis Codes
Enter the most specific ICD diagnosis codes that correspond to
additional conditions that co-exist at the time of service or affect
the length of stay.
• For preterm infants, include the appropriate birth weight code
(765.11 to 765.19).
• POA Indicator for applicable secondary diagnosis.
• Refer to the NUBC manual for more information.
69
Admitting Diagnosis Code
Enter the presenting symptom (diagnosis) and the reason for the
patient’s visit.
Refer to the NUBC manual for more information.
70a-c
Patient’s Reason for Visit
Refer to the NUBC manual for more information.
72a-c
External Cause of Injury
Refer to the NUBC manual for more information.
74
Other Procedure Codes and
Date
Inpatient: Enter the code identifying the principal ICD surgical or
obstetrical procedure and the date on which either was
performed. Enter the date in MMDDYY format.
Refer to the NUBC manual for more information.
Paper Claim Billing Resource
Every effort has been made to ensure this guide’s accuracy. However, if a conflict exists between this resource and the agency’s rules, the agency’s
rules prevail. 28
Form
Locator
Name
Action
74a-e
Other Procedure Codes and
Date
Inpatient: Enter the codes identifying all other significant
procedures performed during the billing period covered by the
claim and the dates on which the procedures were performed. Do
not use decimal points.
Refer to the NUBC manual for more information.
76
Attending Provider Name and
Identifiers
Enter the NPI number for the attending physician (the physician
primarily responsible for the care of the patient) or the resident
physician. The NPI number of the Advanced Registered Nurse
Practitioners (ARNPs) may also be reported in this form locator if
they were primarily responsible for services in the hospital
setting.
Report in this form locator the NPI number of the physician
ordering lab tests or X-ray services.
Note: All providers reported here must be enrolled as a
Washington State Medicaid Provider.
77
Operating Physician Name and
Identifiers
Required. Enter the NPI number for the operating physician when
a surgical procedure code is listed on the claim.
Note: All providers reported here must be enrolled as a
Washington State Medicaid Provider.
78-79
Other Provider (Individual)
Name and Identifiers
Enter the NPI number of other treating providers or the referring
provider. Enter the NPI number for a Primary Care Case Management
(PCCM), or Skilled Nursing Facility (SNF).
Note: All providers reported here must be enrolled as a
Washington State Medicaid Provider.
80
Remarks
Enter any notes that would help in processing a claim for payment.
Possible comments include:
• SCI=B – Baby on Moms ID
o SCI=BA for twin/triplet A
o SCI=BB for twin/triplet B
o SCI=BC for triplet C
• SCI=I – Involuntary Treatment Act (ITA)
• SCI=V – Voluntary Treatment
Note: Baby on Mom’s Client ID can only be used during the first
60 days of baby’s life.
Refer to the NUBC manual for more information.

Paper Claim Billing Resource
Every effort has been made to ensure this guide’s accuracy. However, if a conflict exists between this resource and the agency’s rules, the agency’s
rules prevail. 29
Form
Locator
Name
Action
81 a-d
Code-Code
The billing provider’s NPI entered in Form Locator 56 is mapped to
a taxonomy code(s) that is needed to identify the provider in the
ProviderOne claims processing system. The provider must enter
qualifier code B3 and the reported taxonomy code in this Form
Locator that corresponds to the service billed on the claim. For
more information on taxonomy codes, please see the ProviderOne
Billing and Resource Guide.
For any other code qualifiers, please refer to the NUBC manual for
more information.
