The evolution of the
medical workforce

THE FUTURE OF THE MEDICAL WORKFORCE 32 ANZ—MELBOURNE INSTITUTE HEALTH SECTOR REPORT
Contents
Background and key findings 4
Growth in the medical workforce 6
Is self-suciency realistic? 8
Not enough GPs, too many
non-GP specialists? 9
Doctor’s earnings 10
Bulk billing and fees rising 11
Telehealth use falling 12
Conclusions 17
References 18

4 ANZ—MELBOURNE INSTITUTE HEALTH SECTOR REPORT THE EVOLUTION OF THE MEDICAL WORKFORCE 5
BACKGROUND
During the past 18 months, many doctors have
experienced significant changes to their workload
and practice patterns. Most successfully pivoted their
working practices and business models to adjust to the
pandemic, and many have bounced back but recognise
that much has changed. Though Australia has been less
aected by COVID-19 than other countries, many issues
have been raised about flexibility and adaptation of
health care providers to ensure the appropriate supply
of medical care in ‘business as usual’ times, as well as
during future pandemics and natural disasters.
This report examines some key trends for the medical
workforce after around 20 years of expansion in supply
(Geen, 2014). In an era of increased medical workforce
supply, it is essential to ensure that additional doctors
are used to meet population needs for healthcare,
rather than reinforcing a paradox of overtreatment
and overdiagnosis for some of the population existing
alongside undertreatment for those most in need. This
includes trying to get the ‘right’ balance of the medical
workforce between urban and rural areas, between
specialties, and between generalism and specialised
care. Flexibility and adaptation are central to this, and
are key ongoing themes of the new National Medical
Workforce Strategy (Department of Health, 2019).
The Strategy has recognised the problems with the
current way the medical workforce is trained, organised
and funded, and how these diculties significantly
reduce the ability of the medical workforce to meet
population needs for healthcare.
KEY FINDINGS
• The number of doctors continues to grow, with the
number of non-GP specialists growing faster than
the number of GPs.
• Higher numbers of doctors in training and non-
GP specialists are beginning to spill over into rural
areas. More doctors are working outside of major
metropolitan areas. Growth in the number of doctors
outside major metropolitan areas outstrips the growth
inside these areas for all doctors except for GPs. This is
despite decades of policy targeted to persuade more
GPs to go rural.
• Spillovers into rural and regional areas could be
caused by increased supply and competition pushing
doctors out of major cities. There has also been
increased investment in regional training of GPs and
non-GP specialists and other policies that help pull
doctors away from major cities. In addition, spillovers
could be caused by existing non-GP specialists
spending more time in public hospitals reducing job
opportunities for newly qualified non-GP specialists in
major cities.
• A stated national policy objective is self-suciency
of the medical workforce, but the number of
international medical graduates (GPs and non-GP
specialists) continued to grow faster than the number
of domestically trained GPs and non-GP specialists
until the end of 2019. COVID-19, however, has sharply
reduced total immigration into Australia, though
medical practitioners remain on the new Priority
Migration Skilled Occupation List introduced in
late 2020.
• Specialty choice remains an issue, as applications for
GP training places fall and the number of specialists
continues to grow faster than GPs. Non-GP specialists
earned almost twice as much as GPs, with their
earnings growing twice as fast such that the gap
between GP and non-GP specialist earnings has
widened over time, probably aided by the Medicare
Fee Freeze. The earnings gap is likely to widen
further as there are no specific national policies to
address this.
• Annual fee revenue per doctor has been falling over
time. The most likely reason is that the number of GPs
and non-GP specialists (supply) has been growing
leading to more competition, whilst the number of
patients per doctor (demand) has been falling even
as the population increases. The Medicare fee freeze
and fall in growth of private hospital care could have
contributed to this.
• Whilst fee revenue has been falling, doctors’ self-
reported annual earnings (after practice costs and
before tax) have been increasing. This suggests that
doctors are managing to maintain their take home
pay by either reducing practice costs per doctor or
increasing income in other ways.
• Doctors have also been slowly changing their billing
patterns over time, with higher rates of bulk billing,
especially for non-GP specialists, as well as higher
fees charged for non-bulk billed services. This is likely
to reflect lower fees and more bulk billing for less
auent patients balanced out by higher fees for more
auent patients.
• Telehealth consultations continue to be used and
funding has been extended to the end of 2021,
but their use overall has been slowly falling. Video
consultations are still used much less than
telephone, though are more likely to be used by
non-GP specialists.
• For GPs, the proportion of attendances using
telehealth for GP Mental Health Plans and Chronic
Disease Management Plans are slightly lower than
for usual GP visits, suggesting no additional need
for telehealth for these specific patient populations.
Level A (short) telehealth consultations remain high
and are much more likely to be phone calls. Medicare
telehealth funding is expected to be continued in the
longer term where there is a need from patients, and
higher rebates for video consultations could help to
increase their use by GPs. However, there remains little
evidence on the appropriateness of telehealth.
Medical practitioners have continued to adapt to
significant increases in medical workforce supply as
well as COVID-19. Increased supply leads to more
competition, and the eects of this are beginning to be
seen as doctors spill over into rural and regional areas
and increasing pressure on fee revenue. But after 20
years, issues such as specialty choice have not been
addressed, rural practice needs continued support,
and the benefits of telehealth need to be better utilised.

6 ANZ—MELBOURNE INSTITUTE HEALTH SECTOR REPORT
ignores the costs of a general expansion in the doctor
supply and ignores the strong preferences of most
doctors to remain in major cities and auent areas that
we have found in our research (McIsaac et al., 2015;
Scott et al., 2013).
It has been dicult to implement the required
complementary policies to change career pathways,
medical training, and models of care that encourage
doctors to work in underserved areas. Though much has
been done including financial incentives, rural pathways
for GPs, as well as regional training hubs for non-GP
specialists, many of the issues have not been solved
and there remains uncertainty about their eectiveness.
There are currently no national policies to encourage
doctors to practice in disadvantaged areas within
major cities.
There is some evidence of an increase in the proportion
of doctors working outside of major cities. In 2019,
79,543 doctors were working in major cities in Australia,
compared to 23,470 outside of major cities. Since 2013,
the number of doctors working outside of major cities
has grown by 4.8 per cent - faster than the growth in the
number of doctors in major cities of 3.9 per cent over
the same period. This has contributed to a slight increase
in the percentage of all doctors working outside major
cities from 22 per cent in 2013 to 22.8 per cent in 2019.
Figure 2 shows the average annual growth in the number
of doctors working outside of major cities compared to
the growth of those in major cities. For all doctors except
GPs, growth in the number of doctors is faster outside of
major cities. For hospital non-specialists and specialists
in training, this provides evidence that training has been
successfully shifted outside of main metropolitan
tertiary hospitals which have a fixed capacity and
may have been unable to absorb the sharp increase in
medical graduates. National policies have also included
training doctors in private hospitals. The growth in the
numbers of non-GP specialists outside of capital cities
is more surprising and could reflect an oversupply of
doctors in major cities beginning to spill over into large
regional towns.
However, despite the eorts by policy makers to
persuade more GPs to go rural, the per centage of GPs
outside of major cities areas has fallen slightly from 29.2
per cent in 2013 to 28.7 per cent in 2019. This is because
the growth in the number of GPs in major cities (3.9 per
cent between 2013 and 2019) has been slightly higher
than the growth in the number of GPs outside of major
cities (3.4 per cent per year between 2013 and 2019).
This is not necessarily evidence of policy failure as it
could be that without these policies, the situation might
be much worse.
Though the number of GPs is growing, it is their
distribution that matters most to improving access to
populations most in need. Some policies have been
introduced only recently, such as rural generalist training
pathways and will not yet show an eect, but other
policies such as financial incentives have been in place
for a long time. Evidence shows that financial incentives
may not be eective (Scott et al., 2013), or if they are it is
only for GP Registrars who are the most mobile (Yong et
al., 2018) whilst financial support for locum relief may be
particularly eective (Li et al., 2014).
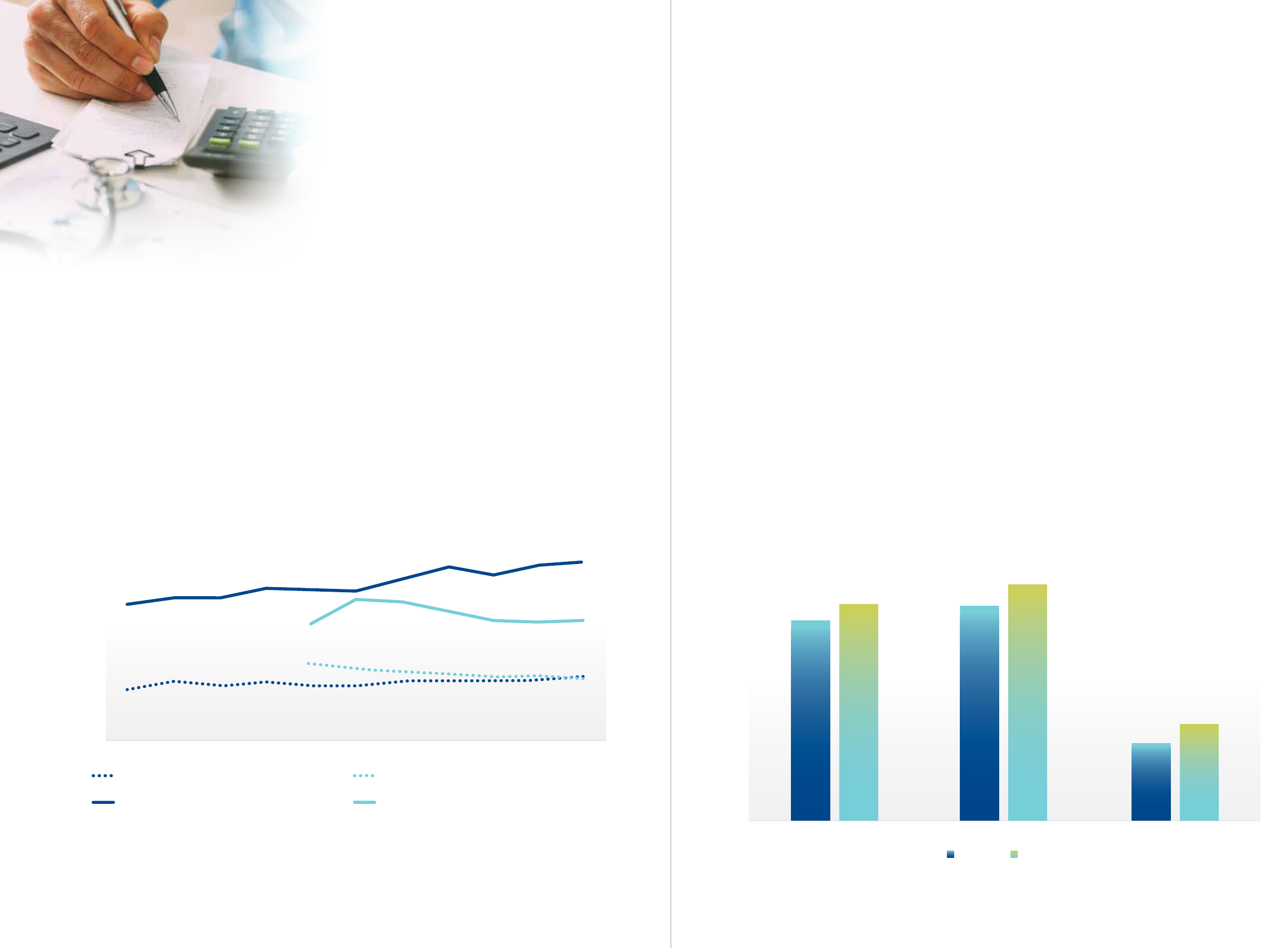
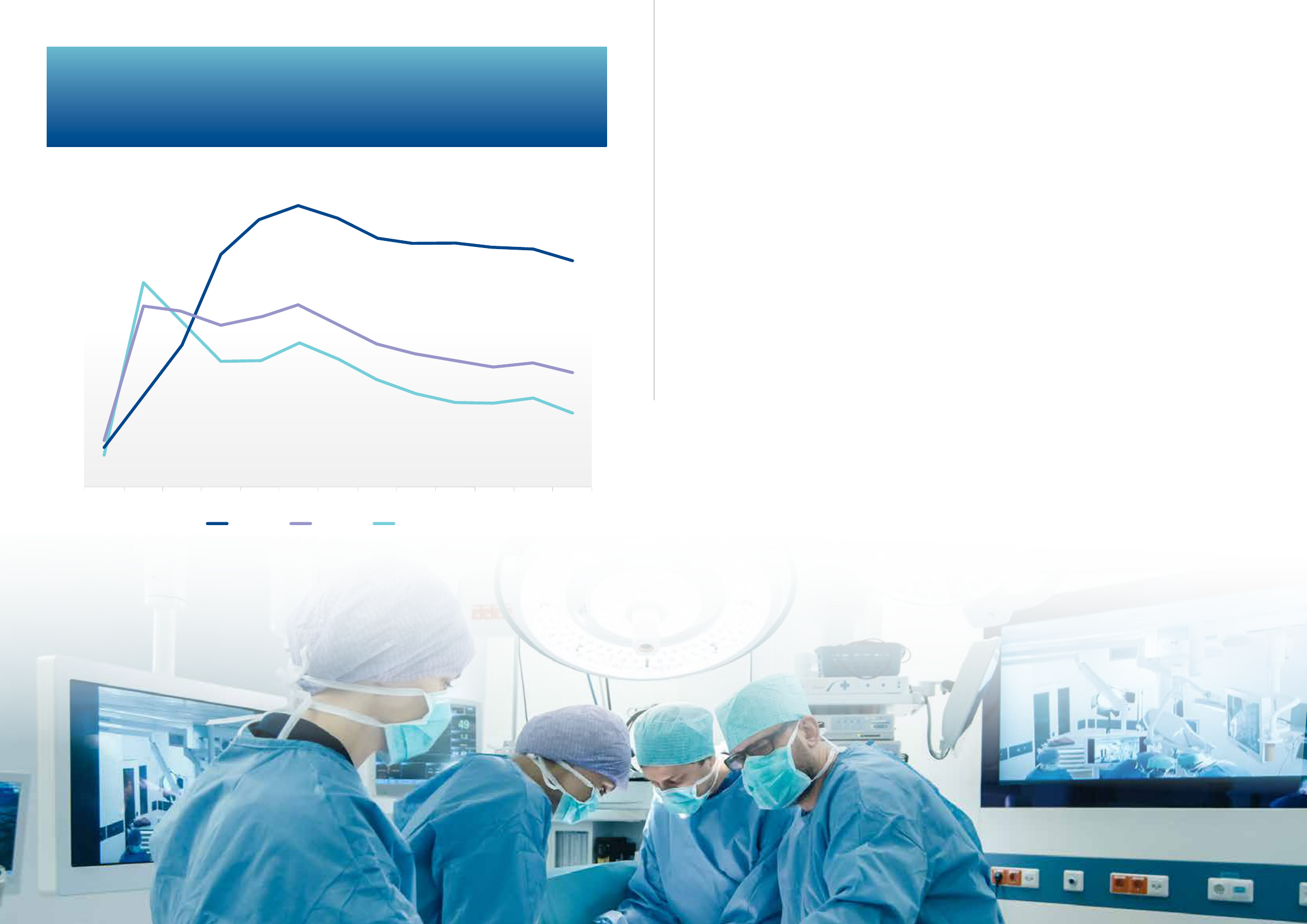
GROWTH IN THE MEDICAL WORKFORCE
For the first time, the number of doctors in clinical
practice exceeded 100,000 in 2019 (Figure 1), a growth
of 3.9 per cent over the 5 years 2014 to 2019 whilst
population growth was 1.6 per cent per year. The number
of hospital non-specialists, including interns and doctors
in training who have yet to enter specialty training,
exhibited the fastest growth of 5.5 per cent per year
over the same period.
The number of non-GP specialists continues to grow
faster (4.5 per cent per year) than the number of GPs
(3.5 per cent per year). In 2014 there were 3,143 more
specialists than GPs, and this grew to 5,283 in 2019.
This is despite the growing burden of chronic disease
and a recognised need for more generalist doctors
(with a wide range of skills across dierent disease
areas) inside, but especially outside, of major cities.
At this aggregate level, there is no evidence of increasing
generalism in the Australian medical workforce – indeed
the contrary seems to be the case.
More doctors outside of cities
The proposed solution to medical workforce
maldistribution was thought to be ‘flooding the market’
to achieve self-suciency, with a more than doubling
of medical graduates from the early 2000s, fuelling the
growth of doctor numbers in Figure 1 (Australian Health
Ministers Council, 2004). The expectation was that
excess doctors in overserved areas would eventually spill
over into underserved rural and regional areas and lower
socioeconomic status areas in major cities. Such a policy
2005
10,000
15,000
20,000
25,000
30,000
Number of doctors
Years
Non-GP specialists
Figure 1
Figure 2
GPs Doctors-in-training
35,000
40,000
45,000
2006 2007 2008 2009 2010 2011 2012 2013 2014 2015 2016 2017 2018 2019 2020 2021
2.92%
6.50%
4.27%
6.07%
4.44%
5.26%
3.88%
3.37%
Non-GP specialists
Major cities Outside major cities
Specialist-in-training Hospital non-specialists GPs
Figure 1. Number of doctors 2005 to 2019 (linear projections to 2021).
2005
10,000
15,000
20,000
25,000
30,000
Number of doctors
Years
Non-GP specialists
Figure 1
Figure 2
GPs Doctors-in-training
35,000
40,000
45,000
2006 2007 2008 2009 2010 2011 2012 2013 2014 2015 2016 2017 2018 2019 2020 2021
2.92%
6.50%
4.27%
6.07%
4.44%
5.26%
3.88%
3.37%
Non-GP specialists
Major cities Outside major cities
Specialist-in-training Hospital non-specialists GPs
Figure 2. Average annual percentage increase in the number of doctors working
outside and inside major cities (between 2013 to 2019).
Source: Health Workforce Planning Tool, Department of Health.
Source: Health Workforce Planning Tool, Department of Health. Major cities defined as Modified Monash Model 1.

Figure 5
Figure 6
74.3%
80.1%
79.8%
87.7%
Non-GP specialistsGPsAll Medicare
35.6%
28.7%
0.105
0.131
0.079
If income increased by $50,000
If procedural work increased from ‘none’ to ‘some’
If opportunities for academic work increased from
‘poor’ to ‘average’
2009-10 2019-20
domestic supply, many employers - including public
hospitals as well as medical practices – wish to maintain
flexibility in hiring IMGs to fill gaps. The fall in the
number and percentage of junior doctors who are IMGs
should eventually flow through to the qualified medical
workforce in the future provided the number of new
IMGs does not increase.
COVID-19 might have at least temporarily reduced
the pre-COVID-19 increase in IMGs, whilst overall
immigration to Australia fell by around 90 per cent
in 2020. However, doctors have been added to the
Priority Migration Skilled Occupation List since late
2020 , suggesting a continuing reliance on IMGs to fill
gaps in supply. It remains to be seen whether Australia’s
reputation as a COVID free country continues to increase
immigration to Australia in the future once international
travel restrictions are gradually lifted.
IS SELF-SUFFICIENCY REALISTIC?
A key aspect of medical workforce distribution policy
over the past 15-20 years has been self-suciency
(O’Sullivan et al., 2019). This includes not only increasing
domestic supply but at the same time reducing the
immigration of doctors from other countries to ensure
training positions and jobs are available for the increased
domestic supply.
In 2018 changes to the temporary skilled visa
program made it more dicult for visa holders to stay
permanently in Australia. In 2019, additional policies as
part of the ‘Stronger Rural Health Strategy’ included
proposals to reduce immigration intakes for GPs and
resident medical ocers (primarily working in hospitals
in major cities). This was intended to help create
opportunities for locally trained doctors in training to
practice in rural and regional areas. However, a new
Priority Migration Skilled Occupation List introduced
in 2020 during COVID-19 seems to have reversed this
policy as it includes GPs, Resident Medical Ocers,
Psychiatrists, and Other Medical Practitioners.
The reliance on international medical graduates (IMGs)
in rural and regional areas is likely to continue as long as
domestically trained doctors have strong preferences
to work in major cities. Still, COVID-19 might have
unexpectedly accelerated the policy of self-suciency
because of restrictions on international travel reducing
immigration and leaving ‘space’ for domestically trained
doctors. However, this could also potentially make it
more dicult to recruit doctors to rural and regional
areas if city doctors do not want to move.
International medical graduates (IMGs) comprised 35.1
per cent of the total Australian medical workforce in
clinical practice in 2019, a fall from 37.5 per cent in 2013
because of faster growth in domestic supply rather than
falls in immigration (4.9 per cent per year compared to
2.8 per cent per year for IMGs). Figure 3 shows that the
overall number of GPs and non-GP specialists who are
IMGs has continued to increase steadily over time, by 4.5
per cent and 6 per cent respectively, whilst the number
of IMGs who are doctors in training has fallen. Combined
with increased domestic supply of doctors in training,
this has contributed to a fall in the proportion of hospital
non-specialists who are IMGs (this group includes
medical ocers) from 39.3 per cent in 2013 to 26.3 per
cent in 2019, with a similar fall in this percentage for
specialists in training (39.3 per cent to 28.1 per cent).
For both GPs and non-GP specialists, continuing
immigration means that the growth in numbers of
IMGs has been higher than the growth in the number of
Australian-trained doctors. The proportion of specialists
who are IMGs continued to increase from 30.8 per cent in
2013 to 32.9 per cent in 2019. This is because the growth
in the number of IMG non-GP specialists (6 per cent per
year) continues to outstrip the growth in the numbers of
Australian trained non-GP specialists (3.9 per cent). The
percentage of GPs who are IMGs has grown slightly from
43.1 per cent in 2013 to 44.8 per cent in 2019.
Despite some policy changes designed to reduce
immigration, IMGs continue to represent a very flexible
and cost-eective solution for employers in rural and
regional areas who often drive temporary immigration
through sponsorship of visas. Even with an increase in
NOT ENOUGH GPS, TOO MANY NON-GP
SPECIALISTS?
Figure 1 shows that a higher proportion of junior doctors
are continuing to choose non-GP specialty training, as
the number of specialists grows faster than the number
of GPs. Over the past 20 years there have been no
explicit policies designed to alter specialty choices.
More GP training places do not alter doctors’ preferences
or the relative attractiveness of general practice.
There is recent evidence that the number of GP training
places are not being filled, with falls in the numbers of
applicants for GP training (RACGP, 2020).
Our previous research has shown that relative earnings
can play a key role in specialty choice (Sivey et al.,
2012). Doctors’ annual earnings (annual income from
all medical work after practice costs but before tax) are
increasing in real terms, by an average of 1.1 per cent per
year for GPs and by 2.2 per cent for non-GP specialists.
This is similar to wage growth in the rest of the economy.
But what is the evidence that if GP earnings were
higher, more doctors would choose to become a GP?
Our previous review of evidence of medical career
choices suggest a range of factors play a role, with
advice from supervisors and senior doctors playing
a major role (Scott et al., 2014). MABEL research
found that expected future earnings was an important
factor, along with opportunities for procedural work,
hours worked, control over hours worked, on-call,
opportunities for academic work and continuity of care
(Sivey et al., 2012). Future earnings were more important
for the 33 per cent of junior doctors reporting any
educational debt.
Our research simulated that if GP earnings were to
increase by $50 000 per year (around $280,000 in
2020 prices), the percentage of junior doctors choosing
general practice would increase by 10.5 percentage
points (Figure 4). More procedural work and academic
work had similar sized eects (13.1 and 7.9 percentage
point increases) as a $50,000 increase in earnings,
suggesting that other factors matter at least as much
as earnings (Sivey et al., 2012).
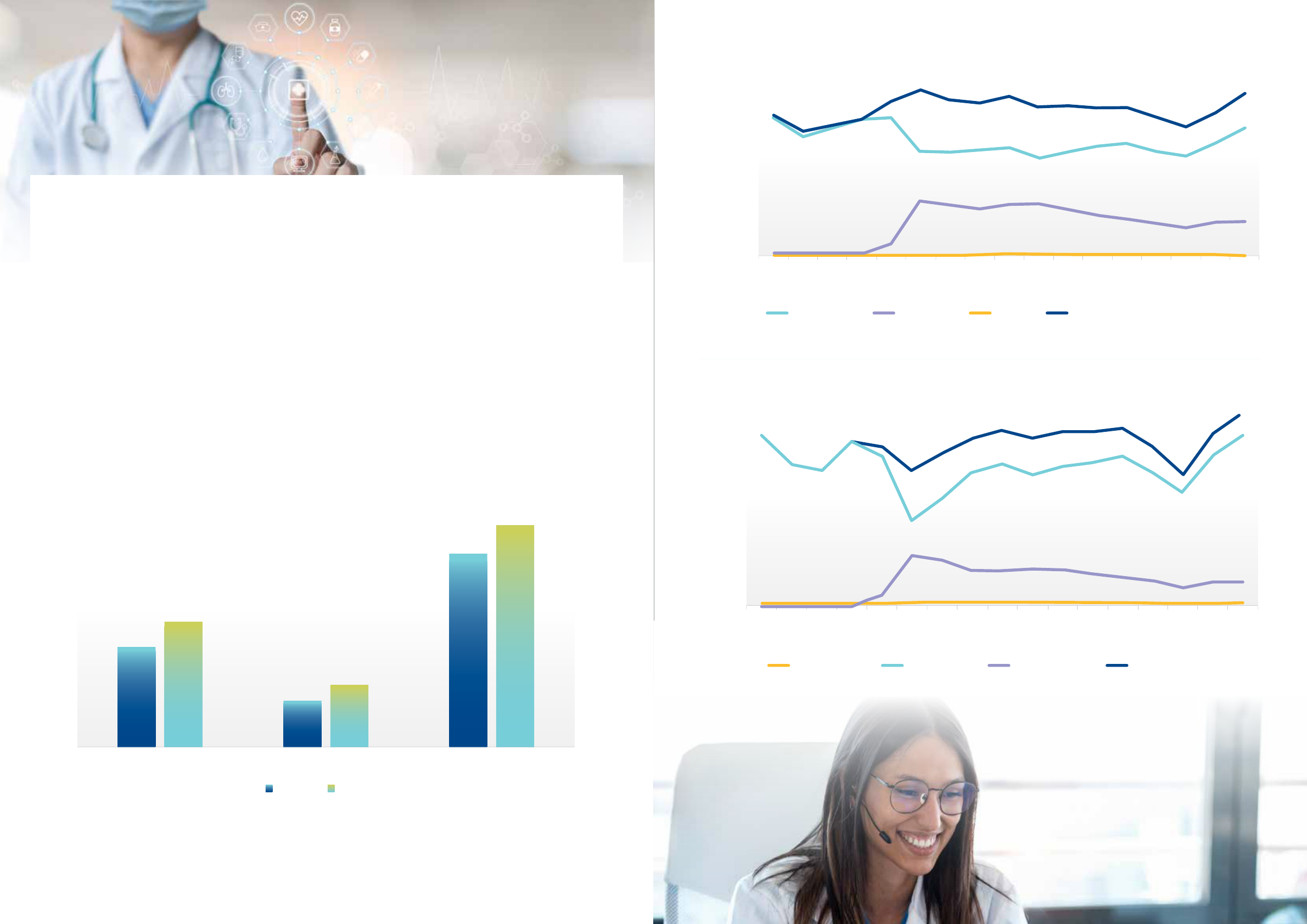
Figure 5 shows that the remuneration of non-GP
specialists remains high relative to GPs. In 2018, non-
GP specialists earned almost double as much as GPs.
Importantly, this gap has widened over time.
These trends are similar if we adjust for dierences in
hours worked. In 2008 mean GPs earnings were $189,574
per year, increasing by 10.7 per cent to $209,938 in 2018.
Non-GP specialists mean annual earnings were $338,554
in 2008, with this increasing by 21.5 per cent to $411,575
in 2018 – double the rate of earnings growth for GPs.
Where earnings matter, this is making it more dicult to
persuade more junior doctors to become GPs.
Policies such as the Medicare fee freeze, where the
indexing of Medicare rebates in line with inflation
was frozen between 2014 and 2018, are likely to have
widened the gap in earnings, compounding these
issues. Though the fee freeze was applied to all doctors,
this was more likely to have adversely aected the
remuneration and morale of GPs, since they bulk-bill
more and face more competition (Gravelle et al., 2016)
compared to non-GP specialists, potentially further
widening the gap in remuneration and reducing the
attractiveness of general practice as a speciality.
More generally, policies that attempt to reduce Medicare
spending on GPs will likely mean fewer junior doctors
will end up choosing general practice training.
Figure 3
Figure 4
$450,000
$400,000
$350,000
$300,000
$250,000
$200,000
$150,000
$100,000
2008 2009 2010 2011 2012 2013 2014 2015 2016 2017 2018
GP self-reported annual income
(before tax, after practice costs)
GP annual total fee revenue: Medicare
Non-GP specialist self-reported annual income
(before tax, after practice costs)
Non-GP specialist annual total fee revenue: Medicare
16,000
14,000
12,000
10,000
8,000
6,000
4,000
2,000
2013 2014 2015 2016 2017 2018 2019
0
General practitioner (GP)
Hospital non-specialist
Specialist
Specialist-in-training
Figure 3. Number of doctors who are international
medical graduates, by doctor type (2013 to 2019).
THE EVOLUTION OF THE MEDICAL WORKFORCE 98 ANZ—MELBOURNE INSTITUTE HEALTH SECTOR REPORT
Source: Health Workforce Planning Tool, Department of Health.
Figure 4. The increase in the probability of junior doctors
choosing GP training under specific scenarios.
Source: Sivey et al (2012).
DOCTORS’ EARNINGS
Fee revenue per doctor falling
Figure 5 also includes data on fee revenue per doctor.
Using data from Medicare, this is the total fee revenue
from private practice each year divided by the number
of doctors. This includes revenue received from Medicare
benefits plus patients’ out of pocket costs (and for non-
GP specialists, from private health insurers who may
cover patient’s in-hospital out of pocket costs using gap
cover). Note that for GPs, fee revenue does not include
revenue paid to the practice from the Practice Incentive
Program (around 10 per cent of revenue), and so this line
is an underestimate of the level of fee revenue per GP.
Doctors may also receive other revenue not captured
here such as rent paid by pathology companies. For non-
GP specialists working across both public hospitals and
private practice, income received from public hospitals
is included in the self-reported earnings data, whilst fee
revenue includes only revenue from private practice.
Fee revenue per doctor has been falling over time after
adjusting for CPI. This downward trend remains, but is
slightly flatter, after we adjust for a fall in hours worked
over time. This squeeze in revenue could be due to a
combination of several factors. First, this could partly be
a function of the Medicare fee freeze that started in July
2014, especially for GPs, but the fall starts before that.
Second, there is evidence of a reduction in the growth
in the volume of private hospital care after 2016, when
the fall in private health insurance membership started
and debate about egregious fees and high out of pocket
costs began (Bai et al., 2020). But the fall in annual
revenue begins in 2013, before these issues started.
Third, and most likely, is that the fall of fee revenue
over time could be because of the increasing number
of doctors over time (Figure 1) leading to increased
competition. The overall number of patients and services
per patient grew between 2009-2010 and 2019-2020
(both by 1.8 per cent per year), but this growth was
much slower than the growth in the number of GPs (3.5
per cent) and non-GP specialists (4.5 per cent).
This seems to be the case: the total number of patients
using Medicare per doctor (GP plus non-GP specialist)
peaked in 2011 at 384 and fell by 1.9 per cent per year
to 327 by 2019. Similarly, the number of Medicare
services per doctor fell by 0.8 per cent, from 7,002 in
2009 to 6,320 in 2019. Supply has been increasing faster
than demand suggesting there were fewer patients to
go around.
Figure 5
Figure 6
74.3%
80.1%
79.8%
87.7%
Non-GP specialistsGPsAll Medicare
35.6%
28.7%
0.105
0.131
0.079
If income increased by $50,000
If procedural work increased from ‘none’ to ‘some’
If opportunities for academic work increased from
‘poor’ to ‘average’
2009-10 2019-20
Figure 6. Percentage of services bulk billed, 2009-2010 to 2019-2020.
Why are earnings (after practice costs) rising,
but fee revenue per doctor falling?
In the context of falling fee revenue per doctor, the
only way that doctors can maintain their self-reported
earnings (after practice costs but before tax) in Figure
5 is if practice owners are reducing costs to maintain
their take home pay, or if they are earning more medical
income from other sources.
Unfortunately, no data are routinely collected on
practice costs. Some cost reductions could have been
achieved through practices becoming larger over time
(Scott, 2017) such that the sharing of fixed costs across
more GPs could lead to lower practice costs per doctor
(economies of scale).
For non-GP specialists in Figure 5, self-reported earnings
are for work in both public hospitals and the private
sector, whilst fee revenue is only for private work
from the MBS. Figure 4 shows that the gap between
fee revenue and self-reported earnings is widening
over time, suggesting an increasing share of earnings
from their work in the public sector over time, and/
or reductions in practice costs. This is consistent with
evidence showing that non-GP specialists have been
spending a higher proportion of their time in public
hospitals since 2015 (Bai et al., 2020).
If non-GP specialists have been spending more time
in public hospitals, this also has implications for the
availability of public hospital positions for newly qualified
specialists, which might also explain the increasing share
of non-GP specialists working outside of major cities in
Figure 2. There is also anecdotal evidence that non-GP
specialists are forming into larger groups with corporate
ownership, again possibly leading to lower costs per
doctor enabling them to maintain earnings after practice
costs whilst fee revenue declines.
THE EVOLUTION OF THE MEDICAL WORKFORCE 1110 ANZ—MELBOURNE INSTITUTE HEALTH SECTOR REPORT
Source: Own calculations from ‘MBS statistics financial year 2019-2020 Geo.xls’ downloaded from: https://www1.health.gov.au/internet/main/publishing.nsf/
Content/32CC6EB4BCC0BB1CCA257BF0001FEB92/$File/MBS%20Statistics%20Financial%20Year%202019-20%20Geo.xlsx. GP bulk-billing rate includes
out-of-hospital unreferred attendances. Non-GP specialist bulk billing rate includes specialist attendances, obstetrics, anaesthetics, and operations
(excludes pathology, diagnostic imaging, radiotherapy and therapeutic nuclear medicine).
Figure 3
Figure 4
$450,000
$400,000
$350,000
$300,000
$250,000
$200,000
$150,000
$100,000
2008 2009 2010 2011 2012 2013 2014 2015 2016 2017 2018
GP self-reported annual income
(before tax, after practice costs)
GP annual total fee revenue: Medicare
Non-GP specialist self-reported annual income
(before tax, after practice costs)
Non-GP specialist annual total fee revenue: Medicare
16,000
14,000
12,000
10,000
8,000
6,000
4,000
2,000
2013 2014 2015 2016 2017 2018 2019
0
General practitioner (GP)
Hospital non-specialist
Specialist
Specialist-in-training
Figure 5. Annual earnings and fee revenue of GPs and Non-GP specialists, 2008 to 2018 (weighted and adjusted for CPI).
Source: Self-reported annual income is from the Medicine in Australia: Balancing Employment of Life (MABEL) survey on annual income before tax but after practice
costs – essentially gross take home pay. This uses data from between 1,813 and 3,270 GPs per year, and from between 2,206 to 4,261 non-GP specialists per year, and
is adjusted for CPI, and also weighted to be representative of the doctor population. Fee revenue reported is from Medicare data linked to MABEL survey respondents
who consented to data linkage. For GPs, this does not include practice-level payments from the Practice Incentive Program (which would add about 10 per cent to
these figures) or other sources of income. Fee revenue data are from between 661 and 988 GPs per year, and between 713 and 943 non-GP specialists per year, and is
adjusted for CPI, and also weighted to be representative of the doctor population. The findings are very similar if we use the same doctors for the MABEL self-reported
earnings as for the fee revenue.
BULK BILLING AND FEES RISING
Against a backdrop of lower fee revenue, decisions
such as changing the fees charged, including choosing
whether to bulk bill and choosing whether to use gap
cover arrangements with private health insurers, are
important business decisions for influencing revenue
but are also decisions that impact on patients’ access
to healthcare. The balance between maintaining the
number of patients seen and what they are charged can
be dicult, more so for GPs who face more competition.
Figure 6 shows that bulk-billed services, where there
is no out of pocket cost to the patient, as a percentage
of all Medicare services have increased from 74.3 per
cent in 2009-2010 to 80.1 per cent in 2019-2020. Bulk
billing rates for non-GP specialists (including specialist
attendances, obstetrics, anaesthetics, operations) remain
much lower than for GPs (35.6 per cent compared to
87.7 per cent), though have increased at a faster rate
compared to those for GPs, by 23.9 per cent over the
period compared to 7.7 per cent for GPs.
The increase in bulk billing rates reduces revenue per
service, but this can be balanced by an increase in fees
for non-bulk billed services, as shown in Figure 7. More
auent patients are still likely to attend if fees rise,
whilst increasing bulk billing may lead to an increase
in utilisation for patients who are less well-o. There is
evidence that some doctors care about their patients’
financial circumstances (Ge et al., 2019), and that doctors
in less auent areas of Australia charge lower fees
(Gravelle et al., 2016; Johar, 2012; Johar et al., 2017).
TELEHEALTH USE FALLING
During COVID-19 there were high hopes that telehealth
might become part of routine care. The rapid
introduction of telehealth brought the future slightly
closer as many healthcare providers and patients had a
taste for how this could work. Telehealth can potentially
solve not only issues arising during pandemics, but also
how to improve access to healthcare for vulnerable and
underserved populations. The use of telehealth would
also make the system more responsive and flexible to
patients’ needs.
New telehealth items were funded from March 2020 to
help protect patients and providers from COVID-19, as
well as help circumvent the fall in demand for healthcare
that led to substantial falls in income for many providers
in 2020 (Scott, 2020). Since then, the use of telehealth
has fallen overall as the pandemic in Australia has
subsided. Figures 8 and 9 show the use of telehealth
MBS items between March 2020 and March 2021.
The use of telehealth reached its peak in April 2020
when 36 per cent of all Medicare consultation items
for GPs and non-GP specialists were conducted using
telehealth. Figure 8 for GPs and Figure 9 for other
specialists show a gradual fall in the use of telehealth
since then. By March 2021, the proportion of GP
attendances using telehealth had fallen at 21.6
per cent, and to 13.4 per cent for other specialists.
These are still very large proportions at a time when
Australia is essentially free of COVID-19, but the trend
is still downward, and it is unclear when it will stabilise
and find its ‘natural’ rate. Partly this will be determined
by expectations and the exact details of policy changes
beyond 2021.
Non-GP SpecialistsGPsAll Medicare
$79.27
$63.95
$39.33
$29.35
$141.41
$123.41
Figure 7
Figure 8
0
3,500,000
7,000,000
10,500,000
14,000,000
Face-to-face Telephone Video Total unreferred attendances
Nov 19
Dec 19
Jan 20
Feb 20
Mar 20
Apr 20
May 20
Jun 20
Jul 20
Aug 20
Sep 20
Oct 20
Nov 20
Dec 20
Jan 21
Feb 21
Mar 21
2009-10 2019-20
Non-GP SpecialistsGPsAll Medicare
$79.27
$63.95
$39.33
$29.35
$141.41
$123.41
Figure 7
Figure 8
0
3,500,000
7,000,000
10,500,000
14,000,000
Face-to-face Telephone
Video Total unreferred attendances
Nov 19
Dec 19
Jan 20
Feb 20
Mar 20
Apr 20
May 20
Jun 20
Jul 20
Aug 20
Sep 20
Oct 20
Nov 20
Dec 20
Jan 21
Feb 21
Mar 21
2009-10 2019-20
Figure 10
7%
6%
4%
1%
5%
2%
3%
0%
3,000,000
2,250,000
1,150,000
750,000
0
Face-to-face
New telehealthOld telehealth Total attendances
Jun 19 Jun 20Apr 20Feb 20Dec 19Oct 19Aug 19 Aug 20 Oct 20 Dec 20 Feb 21
Old telehealth (Non-GP specialists) Non-GP specialists GPs
Nov 19
Dec 19
Jan 20
Feb 20
Mar 20
Apr 20
May 20
Jun 20
Jul 20
Aug 20
Sep 20
Oct 20
Nov 20
Dec 20
Jan 21
Feb 21
Mar 21
Figure 7. Fee charged per non-bulk-billed service, adjusted for CPI, 2009-2010 to 2019-2020.
Figure 8. Number of MBS items claimed for GP attendances, November 2019 to March 2021.
Figure 9. Number of MBS items claimed for Specialist attendances, November 2019 to March 2021.
12 ANZ—MELBOURNE INSTITUTE HEALTH SECTOR REPORT
Source: Own calculations from ‘MBS statistics financial year 2019-2020 Geo.xls’ downloaded from: https://www1.health.gov.au/internet/main/publishing.nsf/
Content/32CC6EB4BCC0BB1CCA257BF0001FEB92/$File/MBS%20Statistics%20Financial%20Year%202019-20%20Geo.xlsx. GP data include out-of-hospital
unreferred attendances. Non-GP specialist data include specialist attendances, obstetrics, anaesthetics, and operations (excludes pathology, diagnostic imaging,
radiotherapy and therapeutic nuclear medicine). Fee charged per non-bulk billed service = (Fee charged – Benefit paid) / (All services – Bulk billed services).
Source: MBS Statistics Item Reports http://medicarestatistics.humanservices.gov.au/statistics/mbs_item.jsp using telehealth item numbers:
http://www.mbsonline.gov.au/internet/mbsonline/publishing.nsf/Content/news-2020-03-29-latest-news-March.
Source: MBS Statistics Item Reports http://medicarestatistics.humanservices.gov.au/statistics/mbs_item.jsp using telehealth item numbers:
http://www.mbsonline.gov.au/internet/mbsonline/publishing.nsf/Content/news-2020-03-29-latest-news-March.
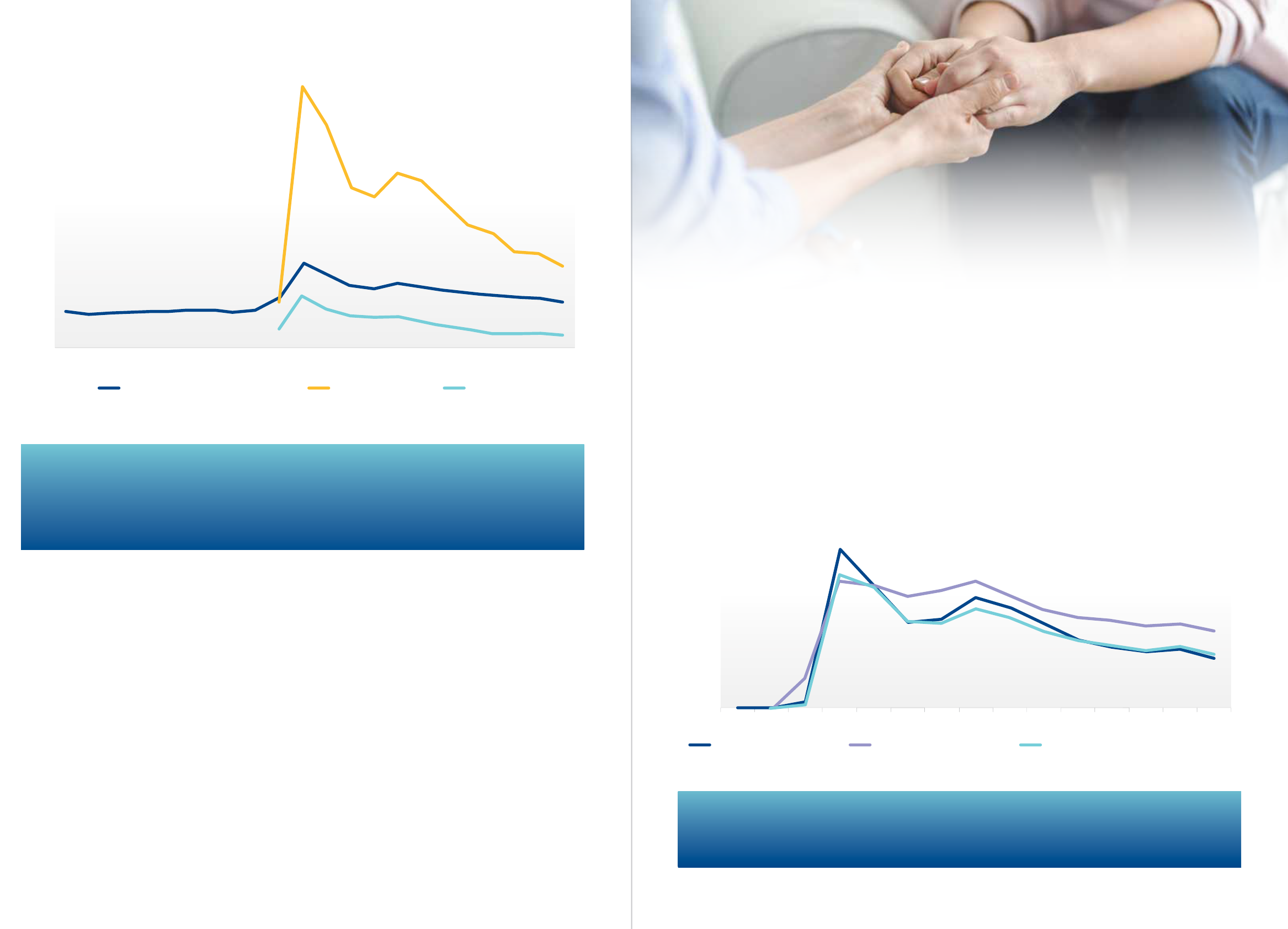
Video consultations remain low
Though there was much promise about the increased
use of telehealth heralding advances in technology,
the vast majority of telehealth consultations used phone
calls rather than video, especially for GPs. Department
of Health guidance states that video is the preferred
method of conducting a telehealth consultation, yet the
use of video has remained stubbornly low and is falling
(Figure 8 and 9).
Figure 10 shows the proportion of attendances using
video conferencing for GPs and specialists.
Before COVID-19, non-GP specialists could already claim
MBS items for video consultations for patients in rural
and regional areas, and GPs as well could access some
items for aged care. Interestingly, Figure 10 also shows
that the proportion of specialist attendances using
these ‘old’ telehealth items seems to have increased,
compared to before COVID-19, suggesting better access
to care for patients in rural and regional areas. However,
our previous research during COVID-19 showed that the
use of new telehealth items by GPs in May 2020 was no
higher for patients in rural and regional areas compared
to those in major cities (Scott et al., 2021).
In terms of the low use of video consultations, especially
by GPs, our previous research showed that a lack of
infrastructure may be an important the reason for
this (Scott et al., 2021). A continuing lack of certainty
about the permanence of Medicare funding could have
discouraged GP practices to invest in this infrastructure
during 2020. Furthermore, our research showed that
GPs with a higher share of elderly patients were less
likely to use video consultations, presumably because
of diculties for some elderly patients, who are perhaps
those most in need, in using this technology and so
preferring the phone. The MBS rebates for video and
phone consultations are also the same, and so there
is scope to change financial incentives to encourage a
higher proportion of video consultations.
Figure 10
7%
6%
4%
1%
5%
2%
3%
0%
3,000,000
2,250,000
1,150,000
750,000
0
Face-to-face New telehealthOld telehealth Total attendances
Jun 19 Jun 20Apr 20Feb 20Dec 19Oct 19Aug 19 Aug 20 Oct 20 Dec 20 Feb 21
Old telehealth (Non-GP specialists)
Non-GP specialists GPs
Nov 19
Dec 19
Jan 20
Feb 20
Mar 20
Apr 20
May 20
Jun 20
Jul 20
Aug 20
Sep 20
Oct 20
Nov 20
Dec 20
Jan 21
Feb 21
Mar 21
Figure 11
Figure 12
50%
30%
35%
40%
45%
25%
20%
5%
10%
15%
0%
15%
30%
45%
60%
0%
Jan 20 Feb 20 Mar 20 Apr 20 May 20Jun 20 Jul 20 Aug 20 Sep 20 Oct 20 Nov 20 Dec 20 Jan 21 Feb 21 Mar 21
Mental Health telehealth GP attendances telehealth Chronic Disease Management telehealth
Mar 20 Apr 20 May 20 Jun 20 Jul 20 Aug 20 Sep 20 Oct 20 Nov 20 Dec 20 Jan 21 Feb 21 Mar 21
Level A Level B Level C+D
Figure 10. Percentage of attendances using video conferencing, June 2019 to March 2021.
Figure 11. Percentage of GP Mental Health and Chronic Disease Management Plans using telehealth,
March 2020 to March 2021.
The use of video has been much lower for GPs as a proportion of total attendances compared to
other specialists. In April 2020, 1.3 per cent of all GP attendances used video, and this had fell to
0.32 per cent by March 2021. For non-GP specialists in private practice, use has been much higher
than GPs, with 6.8 per cent of attendances using video in April 2020, falling to 2.1 per cent by
March 2021.
Data for the use of telehealth for specific populations shows that in March 2021, telehealth was
used in 14 per cent of GP Mental Health plans and 14.9 of GP Chronic Disease Management Plans.
This compares to the use of telehealth in 21.6 per cent of all GP attendances.
Use of video for specific populations
For specific population groups that could be more in
need, the use of telehealth was lower than usual GP
consultations. This is shown in Figure 11 that highlights a
declining trend in the proportion on mental health and
chronic disease items using telehealth, no dierent from
the fall in use for GP attendances overall.
Though there is a focus on higher quality video
conferencing, there also seems to be a role for short
telephone consultations, used to provide follow-up
to patients for test results or repeat prescriptions and
referrals, and for shorter acute presentations that
do not require a physical examination or non-verbal
communication. This is work that some GPs may have
undertaken before COVID-19 to an extent but did not
receive a fee, with other GPs requesting that the patient
visited the practice to receive a fee.
The further development of policy around the use
of telehealth beyond the end of 2021 needs to be
supported by more clear evidence of benefit for
population sub-groups. For GPs, encouraging the higher
use of video and the value of short consultations over
the phone seem to be clear and of benefit to patients.
There are no national data on the use of telehealth
by non-GP specialists for public hospital outpatient
appointments. The need for telehealth to remain
available for any further disease outbreaks is important,
even though there has been a steady fall in utilisation
over time.
THE EVOLUTION OF THE MEDICAL WORKFORCE 1514 ANZ—MELBOURNE INSTITUTE HEALTH SECTOR REPORT
Source: MBS Statistics Item Reports: http://medicarestatistics.humanservices.gov.au/statistics/mbs_item.jsp using telehealth item numbers:
http://www.mbsonline.gov.au/internet/mbsonline/publishing.nsf/Content/news-2020-03-29-latest-news-March.
Source: MBS Statistics Item Reports: http://medicarestatistics.humanservices.gov.au/statistics/mbs_item.jsp using telehealth item numbers:
http://www.mbsonline.gov.au/internet/mbsonline/publishing.nsf/Content/news-2020-03-29-latest-news-March.
CONCLUSIONS
The rapid expansion of the medical workforce has
led to a number of policy issues about how best to
direct the medical workforce to areas of highest need.
Twenty years after this expansion began, including the
introduction and then abolition of Health Workforce
Australia, a National Medical Workforce Strategy has
been developed to try and tackle some of these issues
(Department of Health, 2019).
The strategy has five priorities with exact details and
plans for implementation to be published: i) collaborate
on planning and design, ii) rebalance supply and
distribution, iii) reform the training pathway, iv)
building the generalist capability of the medical
workforce, and v) a flexible and responsive medical
workforce. These are lofty aims but do set out a clear
vision for where to head. If the last 20 years is anything
to go by, addressing these priorities will take time.
Australia’s fractured health care system has significantly
delayed eective national policy action to help ensure
the best use of the medical workforce.
Issues of specialty choice, rural and regional
maldistribution, and self-suciency remain very
important, with market forces continuing to dominate
doctors’ decisions about their specialty and location of
practice. Doctor’s decisions are underpinned by a largely
unaltered fee-for-service payment model that rewards
procedural work and sub-specialisation more than
generalism and holistic care.
Our analysis suggests that, 20 years later, the increase
in supply of medical practitioners is finally beginning
to spill over to rural and regional areas, though this is
not the case for GPs. This could be explained by the
increased supply and competition that is eventually
pushing doctors out of major cities, caused by the
increased investment in regional training of GPs and
non-GP specialists and other policies pulling doctors
away from major cities, or caused by existing non-
GP specialists spending more time in public hospitals
reducing opportunities for newly qualified non-GP
specialists in major cities.
Regionally-based training should continue to be an
essential part of all medical training. Self-suciency
still seems a long way o as the number of international
medical graduates continues to grow. The disruption to
immigration due to COVID-19 may make it more dicult
for rural and regional areas to fill vacant positions, but on
the other hand could also create more vacancies in major
cities that will prevent domestically trained doctors from
going rural.
The widening gap between non-GP specialists’ and
GPs’ earnings, exacerbated by the Medicare Fee Freeze,
is important context in an area where there has been
no national policy to correct the imbalance in the
numbers of GPs and non-GP specialists in Australia.
It is clear that over 20 years, the increased supply has
disproportionately been funnelled away from
primary care.
There is evidence that fee revenue per doctor is also now
falling, likely due to increased supply as the growth in the
number of doctors is higher than the growth in demand
from patients. Whilst doctors’ earnings (after practice
costs) are still increasing, falls in fee revenue per doctor
suggest that practice costs per doctor are falling and/or
income is increasing in other ways.
How doctors in private practice manage their billing
and workload is a key issue. Doctors are continuing to
increase their bulk-billing rates, especially for non-GP
specialists, to help maintain volume, whilst fees for non-
bulk billed services increase. Whilst discretion on setting
fees has provided some flexibility, there is only so much
that can be done if there are fewer patients to go around.
The impact of COVID-19 on some of these long term
trends is still unclear but has highlighted how flexible the
medical workforce (and the health care system) needs
to be to meet patients’ needs in an uncertain world.
Though patterns of disease have remained largely the
same, the introduction of telehealth has changed how
the population interacts with doctors and going back
to what it was before COVID-19 does not seem to be an
option. Flexibility and adaptation is the key to ensuring
that the population’s changing health needs are met.
16 ANZ—MELBOURNE INSTITUTE HEALTH SECTOR REPORT
Figure 11
Figure 12
50%
30%
35%
40%
45%
25%
20%
5%
10%
15%
0%
15%
30%
45%
60%
0%
Jan 20 Feb 20 Mar 20 Apr 20 May 20Jun 20 Jul 20 Aug 20 Sep 20 Oct 20 Nov 20 Dec 20 Jan 21 Feb 21 Mar 21
Mental Health telehealth GP attendances telehealth Chronic Disease Management telehealth
Mar 20 Apr 20 May 20 Jun 20 Jul 20 Aug 20 Sep 20 Oct 20 Nov 20 Dec 20 Jan 21 Feb 21 Mar 21
Level A
Level B Level C+D
Figure 12. Percentage of GP telehealth consultations which are Level A, B, C and D, March 2020 to March 2021.
Figure 12 shows that Level A (short) consultations make up almost 50 per cent of all telehealth
consultations and remain quite high in March 2021, and that the share of Level B, C and D
telehealth consultations are much lower. In March 2021 there were 225,542 Level A face to face
GP consultations, a similar level compared to before COVID-19, and 435,314 Level A GP telehealth
consultations (4,270 using video). This suggests that the telehealth consultations are additional to
what was previously undertaken.
Source: MBS Statistics Item Reports http://medicarestatistics.humanservices.gov.au/statistics/mbs_item.jsp using telehealth item numbers:
http://www.mbsonline.gov.au/internet/mbsonline/publishing.nsf/Content/news-2020-03-29-latest-news-March.

THE FUTURE OF THE MEDICAL WORKFORCE 1918 ANZ—MELBOURNE INSTITUTE HEALTH SECTOR REPORT
ACKNOWLEDGEMENT
This report was funded by Australia and New Zealand
Banking Group Limited. Funding for MABEL comes
from the National Health and Medical Research
Council (2007 to 2016: 454799 and 1019605); the
Australian Department of Health and Ageing (2008);
Health Workforce Australia (2013); and in 2017 The
University of Melbourne, Medibank Better Health
Foundation, the NSW Ministry of Health, and the
Victorian Department of Health and Human Services.
This report was prepared by Professor Anthony Scott
with assistance from Mr Terence Bai of the Melbourne
Institute: Applied Economic & Social Research at The
University of Melbourne.
1. Australian Health Ministers’ Council. 2004. National
Health Workforce Strategic Framework. Australian
Health Ministers Council, Sydney.
2. Bai, T., Mendez, S., Scott, A., Yong, J., 2020. The falling
growth in the use of private hospitals in Australia.
Working Paper 18/20, The University of Melbourne,
Melbourne.
3. Department of Health, 2019. Scoping Framework
for the National Medical Workforce Strategy, 2019,
Australian Government, Canberra.
4. Ge, G., Godager, G., Wang, J., 2019. Ge, Ge & Godager,
Geir & Wang, Jian, 2019. “Do physicians care about
patients’ utility? Evidence from an experimental
study of treatment choices under demand-side cost
sharing,” , University of Oslo, Health Economics
Research Programme., Universirty of Oslo, Oslo.
5. Gravelle, H., Scott, A., Sivey, P., Yong, J., 2016.
Competition, prices and quality in the market for
physician consultations. The Journal of Industrial
Economics, 64(1), 135-169.
6. Johar, M., 2012. Do doctors charge high income
patients more? Economics Letters, 117, 596-599.
7. Johar, M., Mu, C., Van Gool, K., Wong, C.Y., 2017.
Bleeding Hearts, Profiteers, or Both: Specialist
Physician Fees in an Unregulated Market. Health
Economics, 26(4), 528-535.
8. Li, J.H., Scott, A., McGrail, M., Humphreys, J., Witt, J.,
2014. Retaining rural doctors: Doctors’ preferences
for rural medical workforce incentives. Social Science
& Medicine, 121, 56-64.
9. McIsaac, M., Scott, A., Kalb, G., 2015. The supply of
general practitioners across local areas: accounting
for spatial heterogeneity. BMC Health Services
Research, 15(1).
10. O’Sullivan, B., Russell, D.J., McGrail, M.R., Scott, A.,
2019. Reviewing reliance on overseas-trained doctors
in rural Australia and planning for self-suciency:
applying 10 years’ MABEL evidence. Human
Resources for Health, 17(1), 8.
REFERENCES
18 ANZ—MELBOURNE INSTITUTE HEALTH SECTOR REPORT
11. Scott, A., 2017. General Practice Trends. ANZ-Melbourne
Institue Health Sector Report, Melbourne Institute: Applied
Economic and Social Research, The University of Melbourne,
Melbourne.
12. Scott, A., 2020. The impact of COVID-19 on GPs and non-GP
specialists. ANZ-Melbourne Institute Health Sector Report,
Melbourne Institute: Aplied Economic and Social Research,
The University of Melbourne, Melbourne.
13. Scott, A., Bai, T., Zhang, Y., 2021. Association between
telehealth use and general practitioner characteristics during
COVID-19: findings from a nationally representative survey of
Australian doctors. BMJ Open, 11(3), e046857.
14. Scott, A., Joyce, C., Cheng, T., Wang, W., 2014. Medical Career
Path Decision Making: A Rapid Review. Evidence Check
Review, Sax Institute, Sydney.
15. Scott, A., Witt, J., Humphreys, J., Joyce, C., Kalb, G., Jeon,
S.H., McGrail, M., 2013. Getting doctors into the bush: General
Practitioners’ preferences for rural location. Social Science &
Medicine, 96, 33-44.
16. Sivey, P., Scott, A., Witt, J., Joyce, C., Humphreys, J., 2012.
Junior doctors’ preferences for specialty choice. Journal of
Health Economics, 31(6), 813-823.
17. Yong, J., Scott, A., Gravelle, H., Sivey, P., McGrail, M., 2018. Do
rural incentives payments aect entries and exits of general
practitioners? Social Science & Medicine, 214, 197-205.
18. Geen, L. 2014. A brief history of medical education and
training in Australia. Medical Journal of Australia, 201 (1):
S19-S22

20 ANZ—MELBOURNE INSTITUTE HEALTH SECTOR REPORT
© 2021
Melbourne Institute: Applied Economic & Social Research
