______________________________________________________________________________________________________________
This document and others if attached contain information that is privileged, confidential and/or may contain protected health information (PHI). The Provider
named above is required to safeguard PHI by applicable law. The information in this document is for the sole use of Optum Rx. Proper consent to disclose
PHI between these parties has been obtained. If you received this document by mistake, please know that sharing, copying, distributing or using information
in this document is against the law. If you are not the intended recipient, please notify the sender immediately.
Office use only: General_CMS-Comm_2022Mar
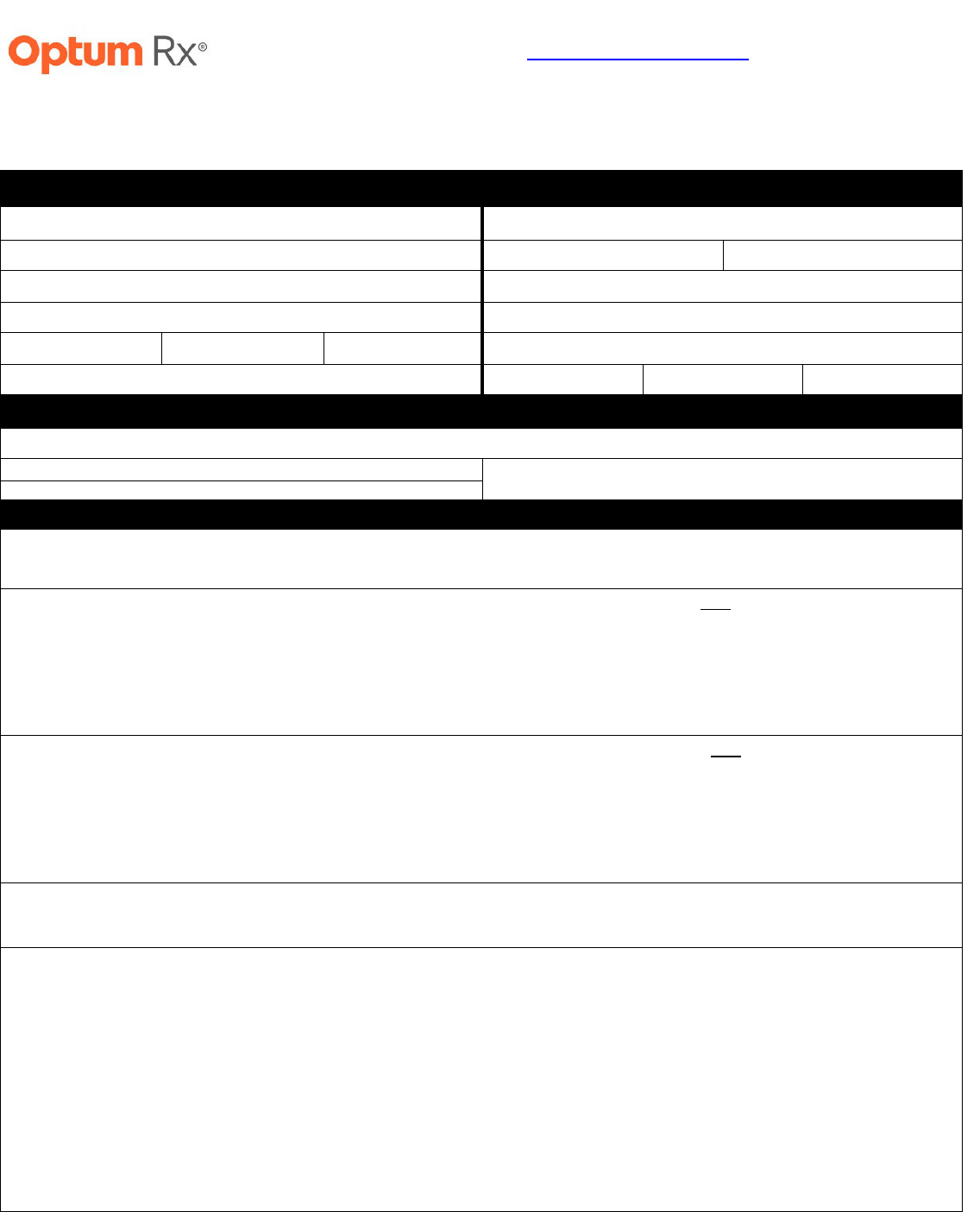
Prior Authorization Request Form (Page 1 of 2)
DO NOT COPY FOR FUTURE USE. FORMS ARE UPDATED FREQUENTLY AND MAY BE BARCODED
Member Information
(required)
Provider Information
(required)
Member Name:
Provider Name:
Insurance ID#:
NPI#:
Specialty:
Date of Birth:
Office Phone:
Street Address:
Office Fax:
City:
State:
Zip:
Office Street Address:
Phone:
City:
State:
Zip:
Medication Information
(required)
Medication Name/Dosage Form/Strength:
Check if requesting brand
Directions for Use:
Check if request is for continuation of therapy
Clinical Information (required)
What is the patient’s diagnosis for the medication being requested? ________________________________________________
ICD-10 Code(s): _____________________________________
What medication(s) has the patient tried and had an inadequate response to? (Please specify ALL medication(s)/strengths tried,
length of trial, and reason for discontinuation of each medication)
What medication(s) does the patient have a contraindication or intolerance to? (Please specify ALL medication(s) with the
associated contraindication to or specific issues resulting in intolerance to each medication)
Are there any supporting labs or test results? (Please specify)
Quantity limit requests:
What is the quantity requested per DAY? ______
What is the reason for exceeding the plan limitations?
Titration or loading-dose purposes
Patient is on a dose-alternating schedule (e.g., one tablet in the morning and two tablets at night, one to two tablets at bedtime)
Requested strength/dose is not commercially available
There is a medically necessary justification why the patient cannot use a higher commercially available strength to achieve
the same dosage and remain within the same dosing frequency. Please specify: _________________________________________
Patient requires a greater quantity for the treatment of a larger surface area [Topical applications only]
Other: ____________________________________________________________________________________________________
Note: If the patient exceeds the maximum FDA approved dosing of 4 grams of acetaminophen per day because he/she needs extra medication due to
reasons such as going on a vacation, replacement for a stolen medication, provider changed to another medication that has acetaminophen, or provider
changed the dosing of the medication that resulted in acetaminophen exceeding 4 grams per day, please have the patient’s pharmacy contact the
Optum Rx Pharmacy Helpdesk at (800) 788-7871 at the time they are filling the prescription for a one-time override.
Optum Rx has partnered with CoverMyMeds to receive prior authorization requests,
saving you time and often delivering real-time determinations.
Visit go.covermymeds.com/OptumRx to begin using this free service.
Please note: All information below is required to process this request.
Mon-Fri: 5am to 10pm Pacific / Sat: 6am to 3pm Pacific

______________________________________________________________________________________________________________
This document and others if attached contain information that is privileged, confidential and/or may contain protected health information (PHI). The Provider
named above is required to safeguard PHI by applicable law. The information in this document is for the sole use of Optum Rx. Proper consent to disclose
PHI between these parties has been obtained. If you received this document by mistake, please know that sharing, copying, distributing or using information
in this document is against the law. If you are not the intended recipient, please notify the sender immediately.
Office use only: General_CMS-Comm_2022Mar
Prior Authorization Request Form (Page 2 of 2)
DO NOT COPY FOR FUTURE USE. FORMS ARE UPDATED FREQUENTLY AND MAY BE BARCODED
Are there any other comments, diagnoses, symptoms, medications tried or failed, and/or any other information the physician feels is important to
this review?
________________________________________________________________________________________________________________
________________________________________________________________________________________________________________
Please note: This coverage determination request is not for a buy and bill drug. Optum Rx is not authorized to review requests for medications
Supplied by the physician's office. For additional information, please contact the patient's medical benefit.
This request may be denied unless all required information is received.
If the patient is not able to meet the above standard prior authorization requirements, please call 1-800-711-4555.
For urgent or expedited requests please call 1-800-711-4555.
This form may be used for non-urgent requests and faxed to 1-844-403-1028.
