1
According to research, signs and symptoms of as many as 120 medical conditions can be first detected by an examination of the mouth, throat and neck –
and earlier detection means earlier treatment. (Source: Oral Diagnosis, Oral Medicine and Treatment Planning, 1994, S. Bricker, R. Langlais, C. Miller.)
2
Family out-of-pocket maximum applies if there are two or more children per family only; there is no out-of-pocket maximum for children receiving out-of-network
services.
3
Child orthodontic coverage begins at age eight. This means that the child must have been banded after age eight in order to receive coverage.
ABCBS_CO_Ped_Basic
Anthem Dental Pediatric Plan
Individuals and Small Groups
Good health starts with a healthy mouth.
1
Good dental health and routine visits to your dentist can pay off in a bigger
way than just having a healthy smile. Conditions in the mouth can, and
often do, affect the rest of the body. Dental exams can help recognize as
many as 120 medical conditions, making them extremely important to your
overall health.
This benefit summary outlines the basics of your Anthem Dental Pediatric
Plan, providing you with a quick reference of deductibles, coinsurance,
limitations and exclusions when you receive covered services from a
participating dental provider. Please refer to the plan certificate for a more
complete explanation of the specific services covered by the plan.
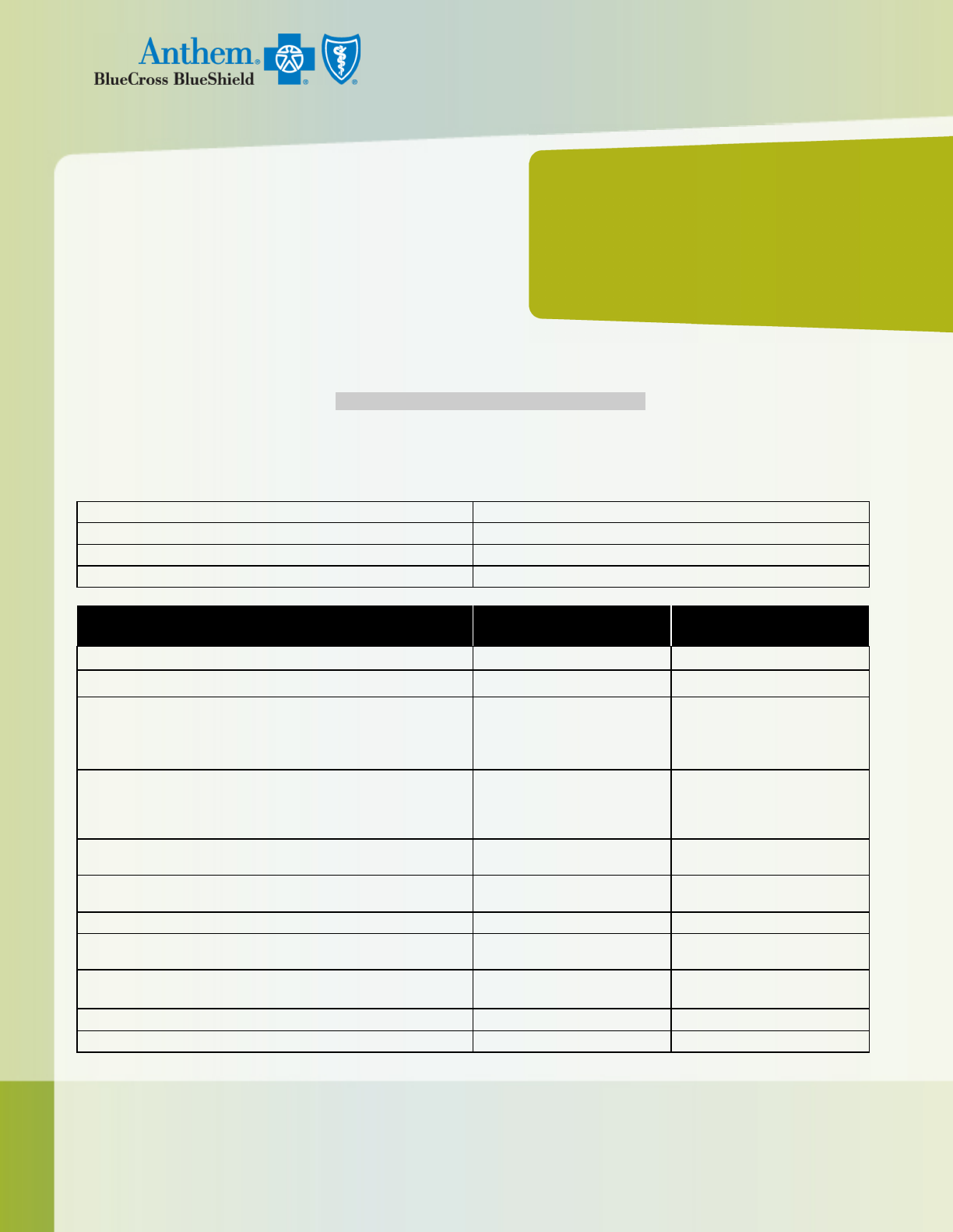
PEDIATRIC DENTAL BENEFITS AT A GLANCE:
The following benefits are available to pediatric members through age 18. After you have met your annual deductible, Anthem will pay for
Dental services at the listed coinsurance amounts up to the Maximum Allowed Charge (MAC) as determined by Anthem for each covered
service. However, there may be different levels of coinsurance, depending on whether you choose to receive services from a Participating
(In-Network) or a Nonparticipating (Out-of-Network) dentist.
Coverage Year
Calendar Year
Insured Age Limit
End of month in which insured turns age 19
Annual Deductible (per child; applies to all services)
$50
Waiting Periods
None
DENTAL SERVICES
(examples of what is/is not covered by the plan):
IN-NETWORK
Anthem pays:
OUT-OF-NETWORK
Anthem pays:
Annual Benefit Maximum
No maximum
No maximum
Annual Out-of-Pocket Maximum $350 / $700 per family
2
Not applicable
Diagnostic & Preventive Services, for example:
• Periodic oral exam
• Teeth cleaning
• Bitewing X-rays
100%
70%
Basic Services, for example:
• Composite (tooth-colored) fillings on anterior (front) teeth
• Amalgam (silver-colored) fillings on posterior (back) teeth
• Posterior (back) composite fillings covered at amalgam allowance
60%
50%
Endodontic Services, for example:
•
Root canal
50% 50%
Periodontal Services, for example:
• Scaling and root planing
Not covered
Not covered
Oral Surgery Services
50%
50%
Major Services, for example:
•
Crowns
50%
50%
Prosthodontic Services, for example:
• Dentures and bridges
Not covered Not covered
Dentally Necessary Orthodontic Services
3
50%
50%
Dentally Necessary Orthodontic Lifetime Maximum
No maximum
No maximum
Anthem Blue Cross and Blue Shield is the trade name of Rocky Mountain Hospital and Medical Service, Inc. HMO products underwritten by HMO Colorado, Inc. Independent
licensees of the Blue Cross and Blue Shield Association. ANTHEM is a registered trademark of Anthem Insurance Companies, Inc. The Blue Cross and Blue Shield names and
symbols are registered marks of the Blue Cross and Blue Shield Association. 10/2014
Choice of dentists
While your dental plan lets you choose any dentist, you may end up paying more for a service if you visit an out-of-network dentist. Why?
Because in-network dentists have agreed to payment rates for various services and cannot charge you more. On the other hand, out-of-network
dentists don’t have a contract with us and are able to bill you for the difference between the total amount we allow to be paid for a service –
called the “maximum allowed amount” – and the amount they usually charge for a service. When they bill you for this difference, it is called
“balance billing.”
How Anthem dental decides on maximum allowed amounts
Anthem develops an out-of-network dental fee schedule/rate to determine the maximum allowed cost (MAC) for services provided by
an out-of-network dentist. This schedule may be changed or updated based on such things as reimbursement amounts accepted by
dentists contracted with our dental plans, or other industry cost and usage data.
Here’s an example of higher costs for out-of-network dental services
This is an example only. Your experience may be different, depending on your insurance plan, the services you receive and the
dentist who provides the services.
Ted gets a stainless steel crown from an out-of-network dentist, who charges $1,200 for the service and bills Anthem for that amount.
Anthem’s maximum allowed charge for this dental service is $800. That means there will be a $400 difference, which the dentist can
“balance bill” Ted.
Since Ted will also need to pay $400 coinsurance, the total he’ll pay the out-of-network dentist is $800. Here’s the math:
• Dentist’s charge: $1,200
• Anthem’s maximum allowed amount: $800
• Anthem pays 50%: $400
• Ted pays 50% (coinsurance): $400
• Balance Ted owes the provider: $1,200 - $800 = $400
• Ted’s total cost: $400 coinsurance + $400 provider balance = $800
In the example, if Ted had gone to an in-network dentist, his cost would be only $400 for the coinsurance because he would not have
been “balance billed” the $400 difference.
Emergency dental treatment for the international traveler
As an Anthem dental member, you and your eligible, covered dependents automatically have access to the International Emergency Dental
Program.* With this program, you may receive emergency dental care from our listing of credentialed dentists while traveling or working nearly
anywhere in the world.
* The International Emergency Dental Program is managed by DeCare Dental, an independent company offering dental-management services to Anthem.
Finding a dentist is easy.
To select a dentist by name or location: • Go to anthem.com/mydentalvision • Call Anthem dental Customer Service
TO CONTACT US:
Call Write
Call the toll-free number on the back of your member ID card to speak with a U.S.-
based customer service representative during normal business hours. Calling after
hours? We may still be able to assist you with our interactive voice-response system.
Refer to the back of your member
ID card for the address.
Anthem Blue Cross and Blue Shield is the trade name of Rocky Mountain Hospital and Medical Service, Inc. HMO products underwritten by HMO Colorado, Inc. Independent
licensees of the Blue Cross and Blue Shield Association. ANTHEM is a registered trademark of Anthem Insurance Companies, Inc. The Blue Cross and Blue Shield names and
symbols are registered marks of the Blue Cross and Blue Shield Association. 10/2014
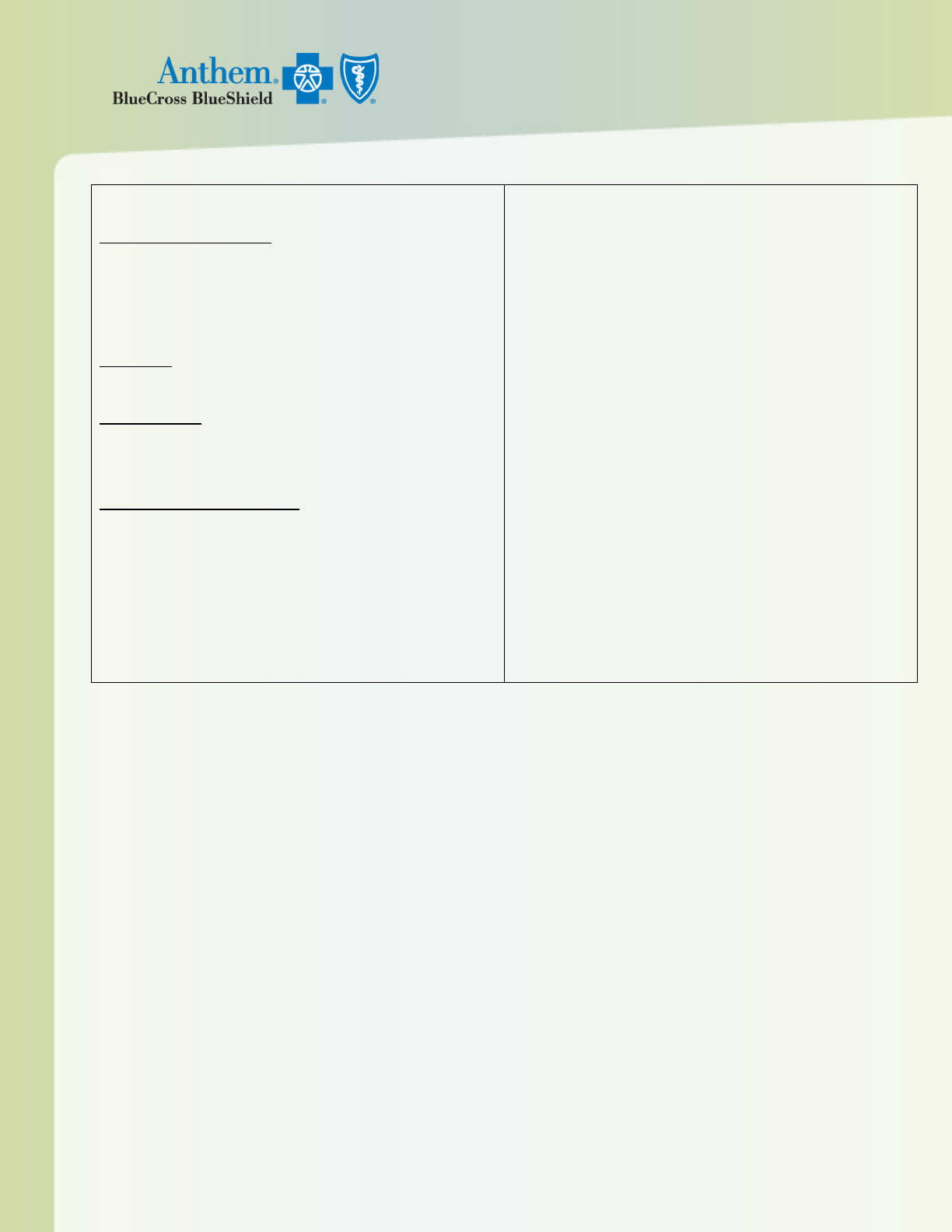
Limitations & Exclusions
Limitations – Below is a partial listing of dental plan limitations. Please see your
certificate of coverage for a full list.
Diagnostic and Preventive Services
Oral evaluations (exams) Limited to 2 per 12-month period
Teeth cleaning (prophylaxis) Limited to one per 12-month period
Bitewing X-rays Limited to one series of films per 12-month period
Complete series X-rays (panoramic or full-mouth) Limited to one series in any 60-
month period
Sealants Limited to permanent molars
Space maintainers Covered only for premature loss of primary posterior (back) teeth
Basic Services
Fillings Covered once per tooth surface per 24-month period
Extractions Basic removal of teeth
Major/Other Services
Stainless steel crowns Covered once per tooth in a 24-month period
Root canal therapy Coverage is for permanent teeth only.
Surgical extractions Removal of impacted teeth covered only with evidence of
pathology
Dentally Necessary Orthodontic Services
Limited to one course of treatment per member per lifetime for dentally necessary
orthodontic services only; to be considered dentally necessary orthodontic care, at least
one of the following criteria must be present:
a. There is spacing between adjacent teeth that interferes with the biting function;
b. There is an overbite to the extent that the lower anterior teeth impinge on the roof of
the mouth when child bites;
c. Positioning of the jaws or teeth impair chewing or biting function;
d. On an objective professionally recognized dental orthodontic severity index, the
condition scores at a level consistent with the need for orthodontic care; or
e. Based on a comparable assessment of items a through d, there is an overall
orthodontic problem that interferes with the biting function.
Exclusions – Below is a partial listing of noncovered services. Please see your
certificate of coverage for a full list.
Services provided before or after the term of this coverage Services received
before your effective date or after coverage ends, unless otherwise specified in the
dental plan certificate
Cosmetic orthodontic services Orthodontic braces, appliances and all related
services that are not considered dentally necessary
Cosmetic dentistry Services provided by dentists solely for the purpose of improving
the appearance of the tooth when tooth structure and function are satisfactory and no
pathologic conditions (cavities) exist
Drugs and medications Intravenous conscious sedation, IV sedation and general
anesthesia when performed with nonsurgical dental care; analgesia, analgesic agents,
anxiolysis nitrous oxide, therapeutic drug injections, medicines or drugs for nonsurgical
or surgical dental care
Prosthodontic services Such as dentures and bridges
Periodontal services Such as scaling and root planing
This is not a contract; it is a partial listing of benefits and services. All covered services are subject to the conditions, limitations, exclusions, terms and provisions of your certificate of
coverage. In the event of a discrepancy between the information in this summary and the certificate of coverage, the certificate will prevail.
The in-network dental providers mentioned in this communication are independently contracted providers who exercise independent professional judgment.
They are not agents or employees of Anthem Blue Cross Blue Shield.
IMPORTANT NOTE: There are currently no Participating Dentists available in Baca, Chaffee, Cheyenne, Crowley, Dolores, Eagle, Elbert, Gilpin, Grand, Hinsdale,
Jackson, Kiowa, Lake, Mineral, Moffat, Ouray, Phillips, Pitkin, Rio Blanco, Saguache, San Juan, San Miguel, Sedgwick, Washington, and Yuma Counties.
Anthem does not discriminate based on race, color, ethnicity, national origin, religion, age, gender, gender identity, mental or physical
disabilities, sexual orientation, genetic information, including pregnancy and expected length of life, present or predicted disability, degree of
medical dependency, quality of life, or other health condition or health status in the administration of the plan (including enrollment, marketing
practices, benefit designs, and benefit determinations).
