
Minnesota Center
for Chemical
and Mental Health
Integrated Illness
Management and
Recovery Manual

Acknowledgements
Integrated Illness Management and
Recovery Manual
Page i
Integrated Illness Management and Recovery Manual
Acknowledgements
This manual was prepared for the Minnesota Center for Chemical and Mental Health (MNCAMH), locat-
ed within the School of Social Work, University of Minnesota, with funding provided by the Minnesota
Department of Human Services and Centers for Medicare and Medicaid Services. The Integrated Illness
Management and Recovery was built upon the SAMHSA Illness Management and Recovery Evidence-Based
Practices (EBP) KIT. The collaborative effort was a partnership between New Hampshire-Dartmouth
Psychiatric Research Center and the University of Minnesota. Primary authors are listed below.
Sarah Pratt, Ph.D.,
Assistant Professor in Psychiatry, Geisel School of Medicine at Dartmouth
Meghan Santos, LCSW,
Research Coordinator and Study Clinician, Geisel School of Medicine at Dartmouth
Kim Mueser, Ph.D.,
Executive Director, Center for Psychiatric Rehabilitation
Stephen Bartels, M.D., M.S.,
Geisel School of Medicine at Dartmouth, Department of Psychiatry
Piper Meyer-Kalos, Ph.D., LP,
MNCAMH Director, University of Minnesota
Disclaimer
The views, opinions, and content of this publication are those of the authors and contributors and do not
necessarily reflect the views, opinions, or policies of the Minnesota Department of Human Services.
Copyright ©
This material is copyright protected. If you have purchased or received this manual as part of the University
of Minnesota’s research project, you may make or distribute copies for the purpose of service delivery with-
in your agency only. You do not have permission to reproduce this for any other purpose without expressly
written permission granted by the authors or the University of Minnesota.
Electronic Access and Copies of Publication
This publication may be downloaded or ordered at http://www.mncamh.umn.org. Or, please contact the
center at [email protected], (612) 626-9042.
Recommended Citation
Pratt, S., Santos, M., Mueser, K., Bartels, S. and Meyer, P. Integrated Illness Management and Recovery
Manual. Minnesota Center for Chemical and Mental Health, St. Paul, MN.
Minnesota Center for Chemical and Mental Health
University of Minnesota
School of Social Work
170 Peters Hall,
St. Paul, MN 55108
(612) 626-9042

Table of Contents
Integrated Illness Management and
Recovery Manual
Page iii
Integrated Illness Management and Recovery Manual
Table of Contents
IntroductIon to the PractItIoner GuIdelInes ...........................................................................1
Modules
1. recovery strateGIes
Practitioner Guidelines for Handout #1: Recovery Strategies ........................................................7
Handout #1: Recovery Strategies .............................................................................................9
2. the BraIn Body connectIon
Practitioner Guidelines for Handout #2: The Stress-Vulnerability Model ...................................15
Handout #2: The Brain Body Connection ..............................................................................17
3. PractIcal Facts
Practitioner Guidelines for Handouts #3A-E: Practical Facts About Mental Illness .....................23
Handout #3A: Practical Facts About Schizophrenia ...............................................................25
Handout #3B: Practical Facts About Bipolar Disorder ............................................................31
Handout #3C: Practical Facts About Depression .................................................................... 37
Handout #3D: Practical Facts About Post-Traumatic Stress Disorder (PTSD) .........................41
Handout #3E: Practical Facts About Schizoaffective Disorder ................................................45
Practitioner Guidelines for Handouts #3F-P: Practical Facts About Health Issues ......................49
Handout #3F: Practical Facts on About Physical Health ........................................................51
Handout #3G: Practical Facts on About Diabetes ...................................................................53
Handout #3H: Practical Facts on About High Blood Pressure ................................................59
Handout #3I: Practical Facts on About High Cholesterol .......................................................63
Handout #3J: Practical Facts on About Osteoporosis .............................................................67
Handout #3K: Practical Facts on About Fibromyalgia ............................................................ 71
Handout #3L: Practical Facts About Gastro Esophageal Reflux Disease (GERD) ....................75
Handout #3M: Practical Facts About Osteoarthritis ...............................................................79
Handout #3N: Practical Facts About Chronic Obstructive Pulmonary Disease (COPD) .........83
Handout #3O: Practical Facts About Congestive Heart Failure ..............................................87
Handout #3P: Practical Facts About Coronary Artery Disease ................................................ 93
Handout #3Q: Practical Facts on About Obesity and Overweight .......................................... 97
Handout #3R: Practical Facts About Sexually Transmitted Infections (STI) ..........................101
Handout #3S: Practical Facts About Alcohol and Substance Use* ........................................ 105
4. healthy lIFestyles
Practitioner Guidelines for Handouts #4A-B: Healthy Lifestyles ...............................................113
Handout #4A: Practical Facts About Healthy Lifestyle .........................................................115
Handout #4B: Practical Facts About Tobacco Smoking ........................................................123
5. usInG MedIcatIon eFFectlvely
Practitioner Guidelines for Handout #5: Using Medication Effectively .....................................129
Handout #5: Using Medication Effectively ...........................................................................131

Table of Contents
Integrated Illness Management and
Recovery Manual
Page iv
6. socIal suPPort
Practitioner Guidelines for Handout #6: Social Support .......................................................... 155
Handout #6: Social Support ................................................................................................157
7. ManaGInG stress
Practitioner Guidelines for Handout #7: Managing Stress .......................................................163
Handout #7: Managing Stress .............................................................................................165
8. ManaGInG PhysIcal and Mental health
Practitioner Guidelines for Handout #8: Managing Persistent Physical and Mental Health .......173
Handout #8: Managing Persistent Physical and Mental Health Symptoms ...........................175
9. relaPse PreventIon
Practitioner Guidelines for Handout #9: Relapse Prevention ....................................................185
Handout #9: Relapse Prevention .......................................................................................... 187
10. selF advocacy
Practitioner Guidelines for Handout #10: Getting Your Needs Met in the Health Care System 193
Handout #10: Getting Your Needs Met in the Health Care System .......................................195
aPPendIx ......................................................................................................................................207
A. Guide to Thoughts and Feelings ..........................................................................................209
B. Common Styles of Thinking ................................................................................................211
C. The 5 Step of Cognitive Restructuring Worksheet ...............................................................213
D. Action Planning Worksheet .................................................................................................215
E. The 5 Steps of CR Note Card ...............................................................................................217
F. Readiness Ruler for Changes in Behavior .............................................................................219

Introduction
Integrated Illness Management and
Recovery Manual
Page 1
Introduction to the Practitioner Guidelines
for Integrated Illness Management
and Recovery
Integrated Illness Management and Recovery was developed in response to the high rates of medical
comorbidity in people who have a serious mental illness. The purpose of the program is to empower
consumers with knowledge and skills to better manage their health so that they can work on meaningful
life goals. The approach and curriculum was modeled after the Illness Management and Recovery Pro-
gram. At the start of the program, the concept of recovery is introduced and consumers start to explore
personally meaningful goals to work on during the program. This goal (or goals) is the foundation of the
program and where motivation may be harnessed to improve self-management of mental and physical
health.
In this introduction, some general suggestions for conducting I-IMR sessions are outlined as well as a
brief description of cognitive restructuring, some motivational interviewing basics, and some suggestions
for homework and delivery of handouts. Following the introduction, guidelines are provided for how to
cover each topic area in the I-IMR program.
The following is a list of the key elements of I-IMR:
1. Practitioners providing I-IMR should be trained in I-IMR and motivational interviewing. IMR
training is also highly recommended.
2. I-IMR may be delivered individually or in group. A hybrid of group and individual may be
ideal, with a focus on goal-setting/progress and individualized education for medical disor-
ders and mental illness in the individual sessions.
3. Practitioners should read the Practitioner Guidelines for I-IMR for each topic area prior to
conducting a session on the topic.
4. Practitioners should use the Goal Tracking Sheet, even if just referring to previously set goals
to check in on progress, as well as the Home Practice Sheets at each session.
5. It is recommended to follow the order of the topics unless there is a strong reason to move
a topic up. The first topics, Recovery and The Stress-Vulnerability Model, should always be
covered first because these topics are the framework for the model.
Structure of I-IMR Sessions
1. Informal socializing and identification of any major problems.
2. Review the previous session.
3. Discuss the homework from the previous session. Praise all efforts and problem-solve obstacles to
completing homework.
4. Set goals or follow-up on goals.
5. Set the agenda for the current session.
6. Teach new material (or review material from the previous session if necessary).
7. Summarize progress made in the current session.
8. Agree on homework to be completed before the next session.

Introduction
Integrated Illness Management and
Recovery Manual
Page 2
Using Cognitive Restructuring in I-IMR
Cognitive Restructuring is one of the core techniques from cognitive behavioral therapy and there may
be opportunities to use it in I-IMR sessions. Cognitive restructuring is based on the assumption that how
people react emotionally to different situations, especially in terms of negative feelings, is strongly influ-
enced by their thoughts and beliefs about themselves, other people, and the world in general. Teaching
people how to recognize the thoughts that underlie their negative feelings, and to examine those thoughts
critically, can often reduce the negative emotions associated with them. Cognitive Restructuring involves
questioning the automatic judgment that accompanies our thoughts. This is done by examining the evi-
dence to either support the judgment or determine the judgment faulty or false. This exercise can change
our perception of events which can impact our mood and behavior.
Cognitive Restructuring in 5 Simple Steps:
1. Ask the consumer to describe the situation.
2. Ask the consumer what he or she was feeling and thinking in the situation and as he/she de-
scribed the situation in session?
3. Ask the consumer to identify evidence that supports the thought.
4. Ask the consumer to brainstorm evidence that contradicts the thought.
5. Review, based on the evidence, whether or not the thought is
supported or not.
Before beginning cognitive restricting remember to explain the relationship between thoughts and feelings
to the consumer, and how inaccurate thoughts or beliefs can lead to strong negative feelings. Use generic
examples to first make these points, and then elicit from the consumer more personal examples. Then, ex-
plain that examining thoughts or beliefs resulting in negative feelings, and evaluating the evidence for and
against them, can change them and make them more accurate. Having more accurate thoughts and beliefs
decreases negative feelings. Explain to the consumer that the process of examining thoughts or beliefs,
evaluating evidence, and developing more accurate thoughts or beliefs is called cognitive restructuring.
In the attached Appendix you will find documents that can be used in session with a 5-step approach to
cognitive restructuring. These handouts can be helpful in recognizing and changing Common Styles of
Thinking. The 5 Step method will prompt consumers to develop an alternative more accurate thought
when the evidence does not support their upsetting thought, it also prompts them to develop an action
plan for dealing with situations in which a careful examination of the evidence indicates that the individu-
al’s concerns are realistic and need to be addressed. The following handouts are included in the appendix:
1. Guide to Thoughts and Feelings: Some consumers initially have difficulty differentiating between
thoughts and feelings. It is important to validate and normalize this issue with consumers, as this is
common, especially for people first learning this skill. This handout is specially designed to help peo-
ple recognize their thoughts and feelings and differentiate between the two.
2. Common Styles of Thinking: This handout helps consumers recognize common but inaccurate
thinking patterns. It’s most important that consumers understand what a “Common Style” is and why
it is something to look out for and address; it is less important that consumers are able to perfectly
define and differentiate between each of the categories. The Common Styles of Thinking described in
the handout can be reviewed and discussed with each consumer using the following probes:
- Why the style is inaccurate
- What might be a more accurate thought for the examples of the Common Style provided in the
handout
- Possible examples of when the client engaged in that Common Style of Thinking
- Possible alternative, more accurate thoughts for any personal examples of Common Styles of Thinking

Introduction
Integrated Illness Management and
Recovery Manual
Page 3
3. Cognitive Restructuring Worksheet: The Cognitive Restructuring Worksheet teaches a 5-step skill for
examining thoughts leading to upsetting feelings and either changing those thoughts (when they are
inaccurate) or developing an action plan to address the upsetting situation (when the thoughts are
accurate).
4. Action Planning Worksheet: The Action Planning Worksheet helps consumers develop an “action plan”
for dealing with situations in which a careful examination of consumer’s concerns reveals they are realis-
tic and need to be addressed. A step-by-step approach to developing an effective action plan is provided.
5. The 5 Steps of CR note card: This optional card can be photocopied and given to consumers once
they have a basic understanding of the CR skill and have used the 5 Steps of CR Worksheet with some
success. The purpose of the note card is to help consumers generalize the skills more easily within
their day-to-day activities. They can put copies of the note card where they can easily find them (e.g.,
place in their wallets or purses, post in their rooms, put in their backpacks) to serve as a reminder
of the steps of the skill. Consumers often appreciate having laminated copies, which are both more
attractive and sturdier.
Using Motivational Interviewing in I-IMR
Motivational interviewing is a type of conversation that focuses on exploring and resolving ambivalence
to strengthen a person’s motivation and commitment to change. The conversation should be collaborative
with the recognition that the power for change rests within the consumer. There are several helpful strat-
egies in motivational interviewing that include: developing discrepancy where practitioners explore the
difference between a current behavior and a core value as a motivator for change; use of reframing to help
consumers see past challenges and setbacks in a more positive light or as a source of strength; promoting
hope and supporting self-efficacy where practitioners have hope and positive expectations for consumers;
and exploring a consumer’s readiness and confidence to change through the readiness ruler included in the
appendix. The readiness ruler can help determine a consumer’s stage of change and explore both a con-
sumer’s desire to change and how willing the consumer is to make a change.
• OARS is a way to remember the basic approach to motivational interviewing:
• Open-ended questions help draw people out and explore feelings about making a change.
• Affirmations identify and highlight consumers’ strengths to help them feel like change is possible.
• Reflections are important to express empathy and can be used to guide the client toward change by
identifying the positives of making a change and the negatives of not making the change.
• Summaries are used to show interest and understanding to the consumer and to draw attention to
the important elements discussed. Summaries are also used to help acknowledge ambivalence.
Techniques for covering I-IMR curriculum
• Pause at the end of each topic (or more frequently depending on the person) to check for understanding
and to learn more about the person’s point of view. There are questions provided for this purpose at the
end of almost every topic in the handout. You can ask other questions such as:
• “What did you think of that section?” “What would you say is the main point of the section we just
read?”
• “Was there anything in this section you disagree with?”
• “Was this similar to your own experience?”
• “Do you have any comments about what we just read?”
• “What did you think of the examples? Which examples had the most meaning to you?”
• “Can you think of an example from your own experience about what we just read?”

Introduction
Integrated Illness Management and
Recovery Manual
Page 4
• Allow plenty of time for interaction. Make the communication a two-way street. You are both learning
something from each other about the topic. It is important not to ask questions too quickly, which the
person may experience as an “interrogation.”
• Pause to allow the person to complete the checklists and questionnaires and allow time for discussing
them. Some people need no help in completing them. Others may appreciate assistance, such as read-
ing words, spelling, or writing some of their answers.
• Break down the content into manageable “pieces.” It is important not to cover more than the individual
can absorb and to present information in small “chunks” at a comfortable pace.
• Show an appreciation for the person’s experience and knowledge. Thank the person for his or her
comments and clarifications. Recognizing the person’s expertise makes the relationship with the practi-
tioner collaborative, reinforcing, and motivating.
• Identify at least one way that information about that subject might be helpful to him or her. For ex-
ample, when reading about the topic “Coping with stress,” you might ask a general question, such as
“How could it be helpful to you to learn effective ways of coping with stress?” If the person has difficul-
ty answering, you might try one of the following probe questions, “Have there been times when you’ve
been under stress? What happened?” “Did you ever think that stress might be connected to having
more symptoms?”
Home Practice Strategies
• At the end of each session, help the person identify something he or she can do before the next session
to review or follow up on the information or skills that were just covered. Sometimes the homework
will involve furthering their knowledge or understanding, such as reviewing a section of the handout
or completing a questionnaire. Sometimes the homework will involve practicing or using a strategy
they developed.
• When homework involves practicing a strategy, it is very helpful for the person to make a specific plan
for how that will be accomplished. The more the practical the plan, the better. For example, if the per-
son identified that he or she would like to practice the strategy of exercising regularly, help make a plan
about what type of exercise, how many minutes, what days of the week, what time of day, and how to
overcome anticipated obstacles. This plan could be written down on a Step-by-step problem-solving
and goal achievement sheet (see the blank copy of this sheet in the “Recovery” handout).
• Help the person do some troubleshooting regarding what obstacles might interfere with completing the
homework. This gives the person some options and helps him or her avoid becoming distressed.
• When possible, encourage homework that involves family members and other supportive people. For
example, if the person is working on the goal of exercising more regularly, the homework might be to
invite a family member or another supportive person to go for a walk once a week.
• Follow up on each homework assignment by asking how it went. Praise the person for his or her
efforts and accomplishments on the homework. Explore the following questions: What was the person
able to do? What was the person not able to do? What might the person do differently in the future to
follow through with homework?
• If the person does not do the homework, you can help identify obstacles that he or she may have
encountered, and help problem-solve ways that these obstacles can be overcome. For example, if the
homework assignment was to attend a support group meeting and the person did not have transporta-
tion, you could help identify a bus or subway that the person could take to the meeting.

Introduction
Integrated Illness Management and
Recovery Manual
Page 5
• If the person did not complete the homework because the assignment was unrealistic, you can help
him or her to modify the assignment to be more achievable. For example, if the homework is to attend
a support group meeting, but the person is very apprehensive about being with people he doesn’t
know, a better assignment might be to start by calling up the contact person for the support group and
asking a few questions.
• Encourage homework that involves family members and supporters.

Module #1
Guidelines
Integrated Illness Management
and Recovery Manual
Page 7
Practitioner Guidelines for Handout #1:
Recovery Strategies
Goals
This topic area, which can usually be covered in 2 sessions, introduces the concept of the mind-body
connection and of “recovery,” encouraging people to develop personally meaningful goals to live the best
life possible. Therefore, it lays the foundation for the entire program. It is especially important for people
to understand that physical and mental illnesses are inextricably linked. Discuss the impact of health on
the ability to achieve other important goals. Help clients identify how working on wellness goals may
help them to reach other goals. It is also critical to establish individual definitions of recovery and ways
in which life could be better if illnesses were better managed because you may need to return to these to
harness motivation when it wanes during the course of the program.
Suggestions for Teaching
• Some people have been told or have come to believe that they cannot achieve meaningful life goals,
which is discouraging, and often results in people having very low expectations for themselves. The
notion that recovery is possible may not be consistent with some people’s self-concept of feeling like
“a failure.” Practitioners may need to help some people see that pursuing recovery is worth the effort.
Help people evaluate the advantages and disadvantages of keeping things the way they are, and the
advantages and disadvantages of changing.
• If people dwell on past setbacks and disappointments, gently re-direct them to think about the future.
Some people may need help in “re-framing” past challenges in order to see that the strategies they used to
cope with these difficulties reflect personal strength. Express empathy, but do not remain focused on the
past. For example, if someone frequently talks about not graduating from school after becoming ill, you
could say, “That must have been very difficult for you. You’ve had some setbacks, but that doesn’t mean
you cannot be successful now.” Encourage sharing about past accomplishments, which can be things like
household tasks, having knowledge about certain subjects, managing money well, or taking care of one’s
health.
• People may find it difficult to identify goals. Ask questions about different domains of life to identify
potential areas of dissatisfaction such as housing, finances, relationships, meaningful activities. It can
also be helpful to discuss what the person’s goals were before he or she became ill (such as, What did
you imagine yourself doing when you grew up? What types of things did you used to enjoy doing? Did
you want to go further in school? What were your dreams and hopes for your life?)
• People may identify very ambitious goals. It is important not to discourage people’s hopes. Instead,
help people break down goals into a series of smaller steps and encourage them to work towards those
steps, using a “shaping” approach. For example, if a person wants to lose 50 pounds in 6 weeks, en-
courage the person to focus on the first step that would be necessary to move towards that goal.

Module #1
Guidelines
Integrated Illness Management
and Recovery Manual
Page 8
Review Questions
What helps you feel confident or optimistic about the future?
What advice would you give to someone with a mental illness who is discouraged about recovery?
What advice would you give to someone with a physical illness who is discouraged about recovery?
What aspects of your health would you like to improve?
How does health impact your life and your activities?
Suggestions for Home Practice
1. Ask people to formulate their own definition of recovery and write it down before the next meeting.
2. Ask people to discuss the concept of recovery with a family member or other
supportive person.
3. Ask people to brainstorm ideas about personally meaningful life goals and steps to achieve them.
Module #1
Handout
Integrated Illness Management
and Recovery Manual
Page 9
Integrated Illness Management and Recovery
Handout #1: Recovery Strategies
Living Life to the Fullest!
People are entitled to live the best lives they can imagine. Being healthy and
achieving “recovery” can make it easier to get the most out of life.
Let’s Discuss!
The word recovery can mean many things. What does “recovery” mean
to you?
Do you feel like you are getting the most out of your life?
What makes life worth living for you?
What gives you meaning in life?
The Brain-Body Connection
There is a powerful connection between the brain and the body. Mental health affects
physical health and vice versa. For example, stress and depression can cause physical
pain, make people more vulnerable to catching colds, lead to ulcers, cause migraines,
and increase blood pressure. Being physically ill (for example having chronic pain, cancer,
diabetes, or COPD) can cause mentalhealth symptoms like depression, irritability, or
confusion. When someone has a mental and a physical illness, it is important to manage
BOTH of them because a relapse in one can cause a relapse in the other. Recovery from
illness, which you can achieve if you learn how to manage your symptoms and work on goals,
can help you move closer to the life you want to lead.
Let’s Discuss!
How do your mental and physical illnesses affect each other?
How do you feel physically when you are stressed or in a bad mood?
What happens to your mood when you are not feeling good physically?
Module #1
Handout
Integrated Illness Management
and Recovery Manual
Page 10
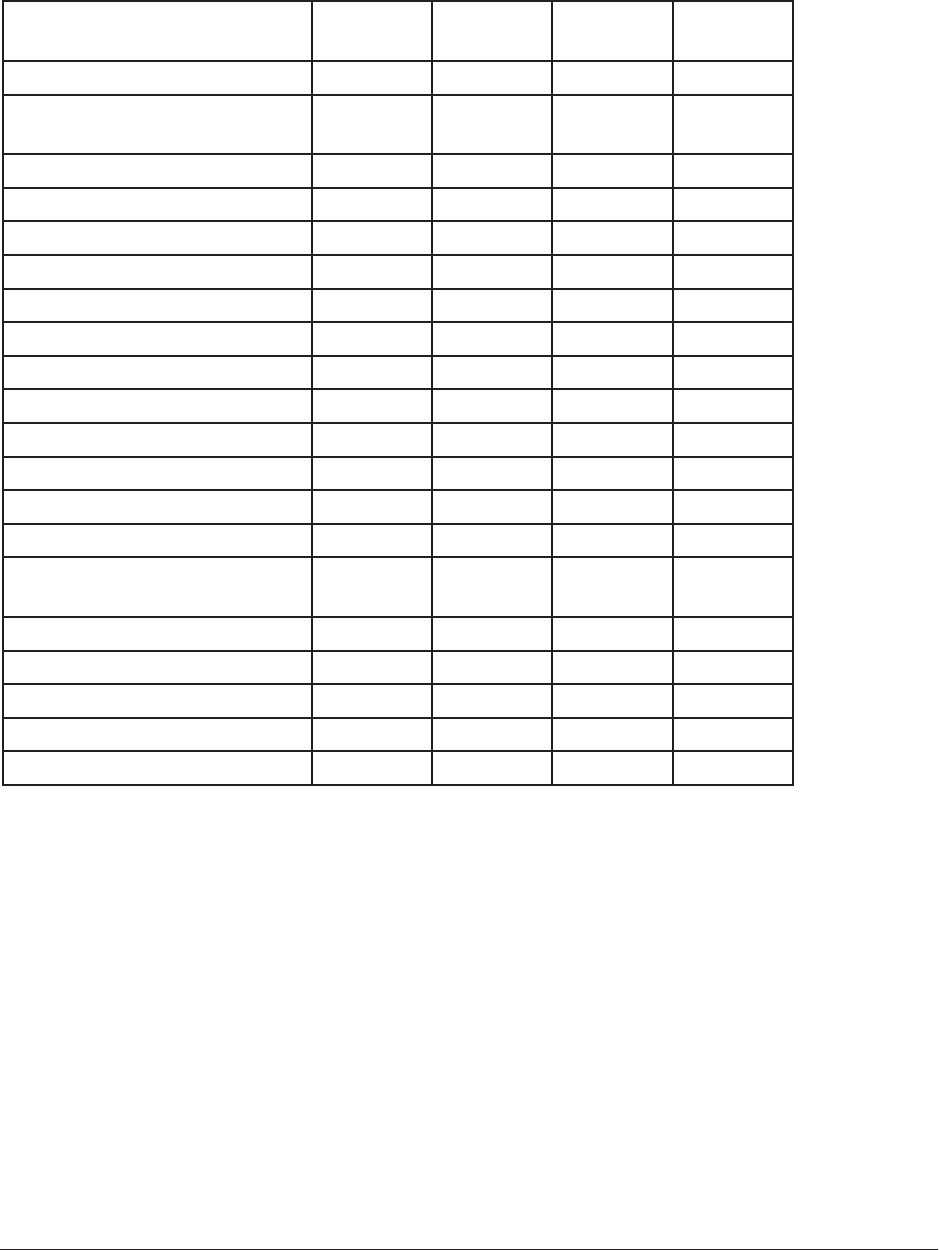
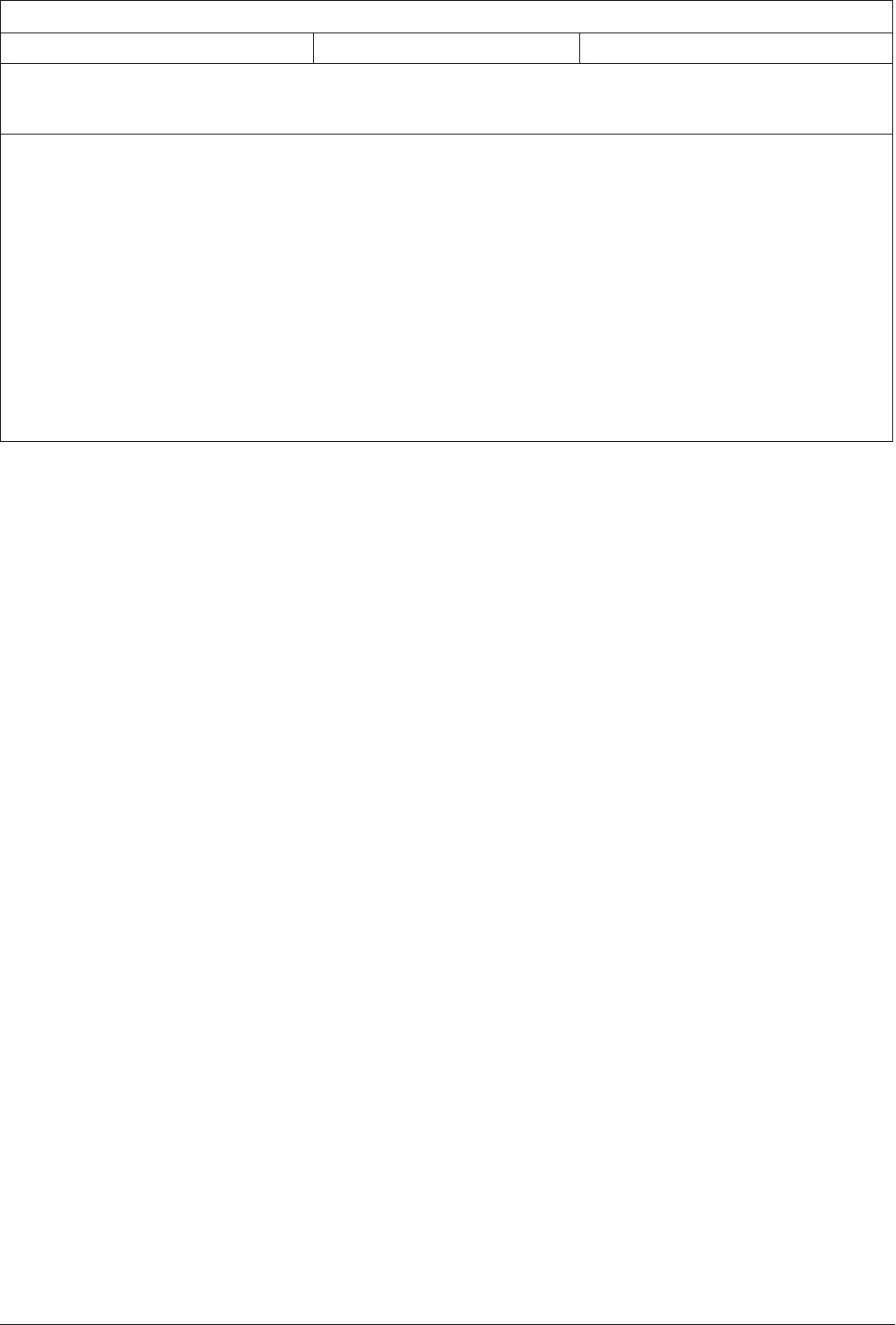
Rate Your Satisfaction With Areas of Your Life
When thinking about how to get the most out of life, it is helpful to rate your satisfaction
with various areas such as those listed below. Put a check in the column that describes
how satised you are with the following areas of your life.
Area of my life
not
satised
moderately
satised
very
satised
I want to
change
Friendships
Meaningful work
(paid or unpaid)
Enjoyable activities
Family relationships
Living situation
Spirituality
Finances
Belonging to a community
Intimate relationships
Expressing creativity
Education
Eating Habits
Exercise
Sleep Habits
Stress Level /
Coping Strategies
Mental health / Symptoms
Substance Use
Physical Health
Health Care
Other areas:
If you checked “not satised” for any of the areas above, think about whether you might
want to make a change or set a goal that is related to that area. If you do, put a check in
the last column next to that area where it says “I want to change.”
Dream Big!
After you have identied an aspect of your life that you want to change, think about how
your life could be different, or better, if you make the change. Don’t be afraid to dream
big!
Go For It!
People who are most successful at getting what they want from life usually have set clear
long-term goals for themselves and have worked on a step-by-step plan to get there.
Module #1
Handout
Integrated Illness Management
and Recovery Manual
Page 11
Let’s Discuss!
What is an example of a goal that you have set in the past?
Have you ever used a step-by-step plan for achieving a goal?
Have you had success in achieving a goal in your life?
Now that you have identied an area of your life that you might want to change in order to
get more out of life, think about how your life will be better if you make that change. For
example, what things will you be able to do that you do not do now? Use the Goal Tracking
Sheet on page 4 to write down the goal that you would like to accomplish in the area that
you have identied. Write it under “Long-term Goal.”
Keys to Success
• Break your long-term goal into short-term goals. Then, break
those short-term goals into steps that you can achieve in 1-2
weeks.
• Start with the rst step and try to stay focused only on that
step.
• Get support with the steps; other people’s ideas and participation can make a big
difference.
• Working on more than one long-term goal at one time might be difcult.
• Don’t be discouraged if it takes longer than you think to accomplish a long-term goal;
this is very common.
• Set-backs and even failures are normal and can give you a chance to learn what NOT to
do when you try again!
Keeping Track
One of the most important keys to success in reaching a goal is keeping
track of progress on your step-by-step plan and WRITING DOWN the
plan. Use the Goal Tracking Sheet on the next page to keep track of how
you are doing after you start working on a goal.
Module #1
Handout
Integrated Illness Management
and Recovery Manual
Page 12
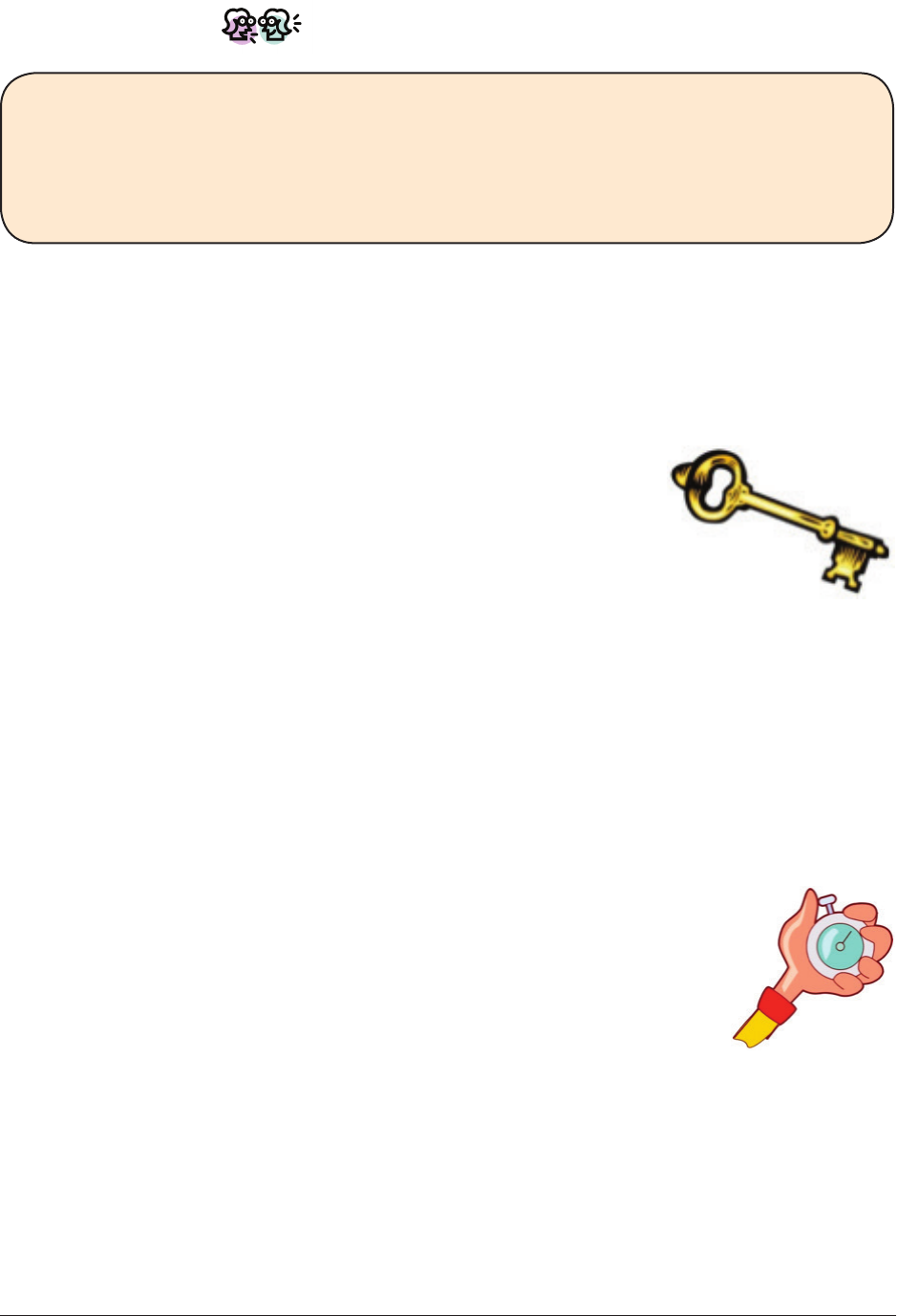
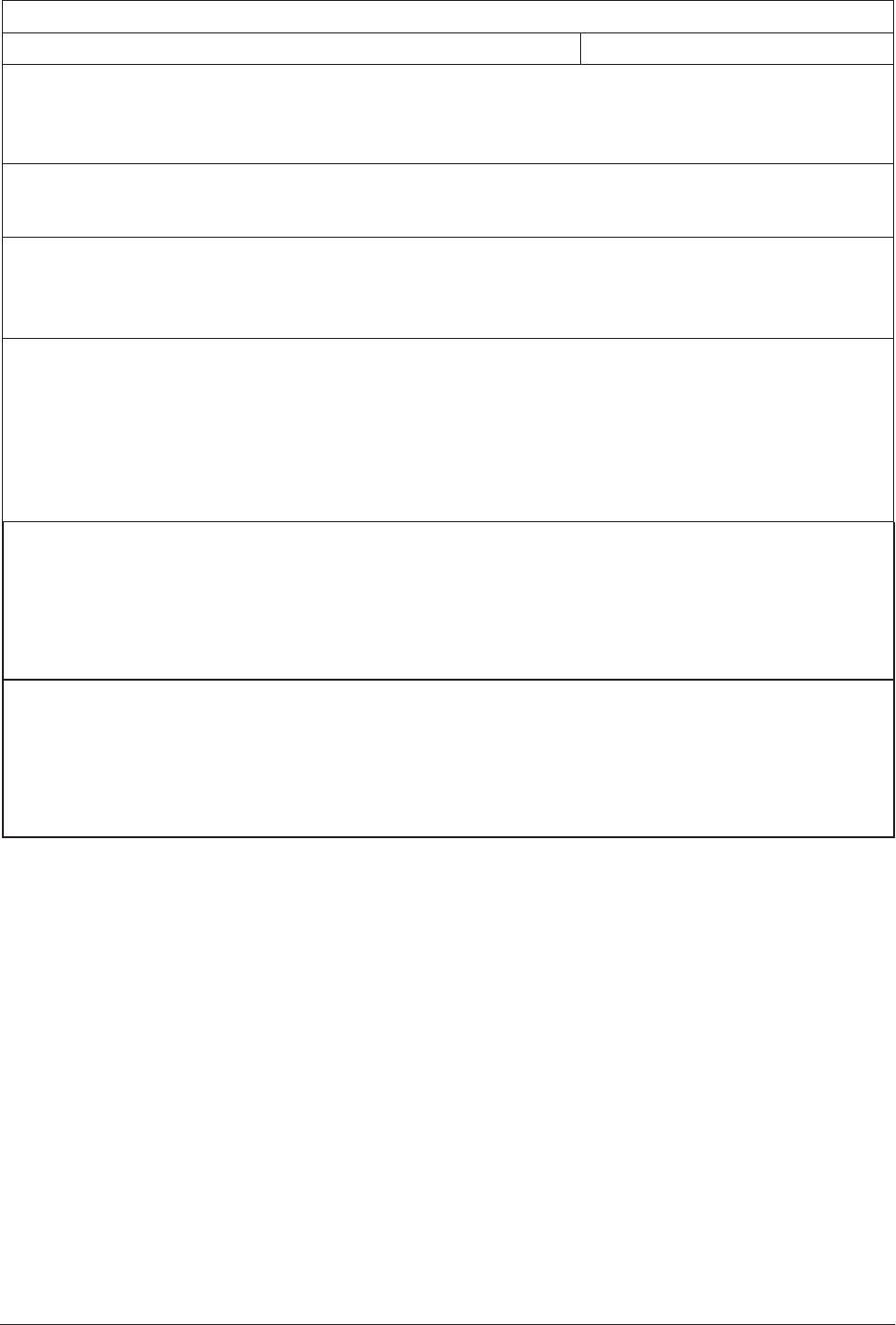
IMR Goal Tracking Sheet
A completed copy should be kept by the IMR participant
and by the practitioner.
Name:
Review
at least
monthly
Date:
Long-term (Meaningful) Goal (LTG):
Date Achieved:
Note: Start a new Goal Tracking Sheet
if the Long-term Goal is modied or a
new goal is set.
Date Modied:
Short-term Goals (STGs) Related to the Long-term Goal
Place a √ after steps achieved
Goal 1: Goal 2:
Steps:
1.
2.
3.
4.
Date Started:
Date Reviewed:
Achieved: o Fully
o Partially
o Not at all
o Continue working on STG
o Set new STG
Start Date:
Next Steps:
1.
2.
3.
4.
Date Reviewed:
Achieved: o Fully
o Partially
o Not at all
o Continue working on STG
o Set new STG
Steps:
1.
2.
3.
4.
Date Started:
Date Reviewed:
Achieved: o Fully
o Partially
o Not at all
o Continue working on STG
o Set new STG
Start Date:
Next Steps:
1.
2.
3.
4.
Date Reviewed:
Achieved: o Fully
o Partially
o Not at all
o Continue working on STG
o Set new STG
Module #1
Handout
Integrated Illness Management
and Recovery Manual
Page 13
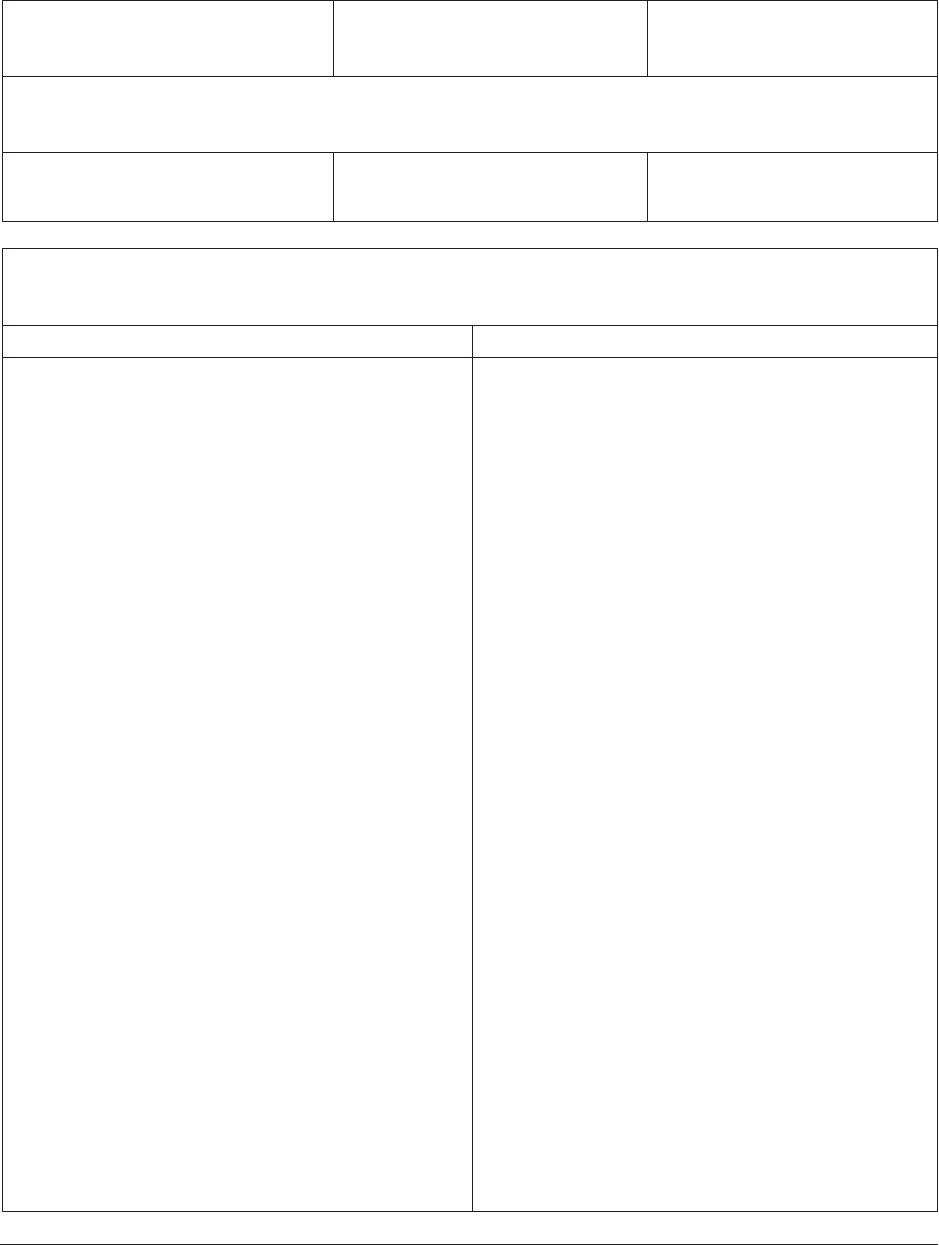
Revisiting the Long-term Goal
Name:
Complete every 3 months
Date:
Restate Long-term Goal:
Is this goal still meaningful? o No. o Yes.
If “Yes”, what Short Term Goals need to continue to be worked on?
If “No”, what is the new Long-Term goal?
Complete a new IMR Goal-tracking for this goal.
Module #1
Handout
Integrated Illness Management
and Recovery Manual
Page 14
End of Treatment Goal Progress Review
Name: Date:
Reason for end of treatment (e.g., completed curriculum, moving to a new location, got a
job and cannot sessions any more):
What was the client’s goal?
Did the client achieve his/her goal?
o Fully
o Partially
o Not at all
Brief description of progress made (for behavioral changes, indicate how long changes
have been maintained):
Next steps (if needed):
Plans to maintain behavior change (if needed):

Module #2
Guidelines
Integrated Illness Management
and Recovery Manual
Page 15
Practitioner Guidelines for Handout #2:
The Stress-Vulnerability Model
Goals
This topic builds on the prior topic represents another opportunity to emphasize the relationship between
mental and physical illness. Discuss the impact of poor physical health on psychiatric symptoms. Under-
standing the interaction of psychiatric and medical problems may increase motivation to better manage
illness. For example, a poorly managed medical illness such as diabetic hypoglycemia may cause irrita-
bility that can mimic hypomania or even irritability seen in depression. People may be unaware that both
problems are happening concurrently, believing that their psychiatric problem is responsible for their feel-
ings/behaviors and neglecting to care for their diabetes. Likewise, poorly managed psychiatric illness can
negatively impact medical problems. It is helpful to relate the information in the handout to the person’s
own situation. For example, learning more about the stress-vulnerability model might help someone
recognize that stress contributed to an increase in symptoms or a re-hospitalization in the past.
Suggestions for Teaching
• People may say that they do not have a mental illness and believe that they do not need treatment.
Even when people do not believe they have an illness, they may recognize the negative effects of stress
in their lives. They are often receptive to talking about treatment options as a way of reducing stress or
coping with life problems.
• Many people who do not think they have a mental illness are nonetheless comfortable talking about
medical or other problems they are experiencing, and are interested in hearing ideas about how they
might solve those problems.
Review Questions
According to the stress-vulnerability model, what are the main factors that contribute to symptoms?
How can people reduce their biological vulnerability?
What are some protective factors that can keep you from getting sick?
Suggestions for Home Practice
1. Identify protective factors that could help you avoid illness.
2. Identify risk factors that have contributed to your physical and mental illness.
Module #2
Handout
Integrated Illness Management
and Recovery Manual
Page 17
Integrated Illness Management and Recovery
Handout #2: The Brain Body Connection
Stress-Vulnerability and Mind-Body
The “stress-vulnerability model” is a way of explaining how the mind-body
connection works. It is also a way of understanding how mental and physical
illnesses can develop. Learning about this can help you limit the bad effects of
illness so you can get what you want out of life.
What Causes Illnesses?
According to the “stress-vulnerability model,” some people have a tendency to
develop a problem or illness. For example, someone might be more likely to have
high blood pressure because both of their parents have it, even if they live a healthy lifestyle.
In the same way, someone might be more likely to have depression if it runs in the family. Or,
something about a person’s body or the chemicals in their brain could cause illness. For exam-
ple, people with Type 1 diabetes do not make insulin in their bodies, and people with schizo-
phrenia or depression may not have the right balance of chemicals in their brains.
Let’s Discuss!
Can you think of any illnesses that you might have a tendency to develop because of
family history or because of something about your physical body?
Biological factors like genes don’t completely explain why some people develop an illness.
Stress also plays an important part because it can trigger symptoms or make them worse.
For example, if someone with a family history of depression experiences something stressful
like losing a loved one or being the victim of a sexual or physical assault, that person may be
more likely to develop depression. Or, someone with a tendency to have high blood pressure
may have more health problems if they are under a lot of stress.
Let’s Discuss!
What are some examples of stressful things that have happened to you or that you have
to deal with much of the time?
How do these stressful things affect your physical and mental health?

Module #2
Handout
Integrated Illness Management
and Recovery Manual
Page 18
Addressing Both Mind and Body to Succeed in Life
The mind and the body are so connected that sometimes it can be hard to
determine the cause of a symptom that you might be having. But, it is
important to identify the cause (something related to the mind or something
related to the body) so that you will know what steps to take to make it
better. Treatment for illness needs to address all of the following:
• Identifying the cause of the symptom
• Reducing biological vulnerability
• Reducing stress
• Coping with stress more effectively
Identifying the Source
Sometimes a physical problem can be similar to a mental health symptom and vice versa.
Here are some examples:
1. Thyroid problems can create symptoms that are like depression such as fatigue,
nervousness, low mood, and slow thinking.
2. Not getting enough oxygen (from COPD or congestive heart failure) or infections of
various kinds (for example, bladder infection) can cause confusion, irritability, inability
to stay focused on a topic, getting stuck on a topic, being easily distracted, or being
withdrawn, which resemble some symptoms of schizophrenia.
3. Low blood sugar can cause irritability or anger that can resemble hypomania or
depression.
4. Chronic depression can cause headaches or pains in the body that could be mistaken
for migraines, injuries, arthritis, bromyalgia or other muscle or bone problems.
5. Chest pain can be caused by anxiety or by heart conditions such as heart attack,
or by gastrointestinal esophageal reux disease.
6. Anxiety can cause problems with breathing that might be mistaken for an asthma
attack.
7. Depression can cause fatigue or slowed speech or movements that could be confused
with a variety of medical illnesses that produce these kinds of symptoms.
8. Depression can cause problems with memory, thinking, and decision making that could
be mistaken for early signs of dementia.
9. Anxiety or depression can cause diarrhea that could be confused with a medical
problem.
10. Congestive heart failure can cause symptoms of anxiety and irritability
or restlessness that could resemble hypomania.
Module #2
Handout
Integrated Illness Management
and Recovery Manual
Page 19
Reducing Biological Vulnerability
Medications are one of the most powerful tools for treating problems with the body or
brain that are causing illness. The educational handout “Using Medication Effectively”
provides more specic information about medications and how to get the best results from
them. Your need to decide whether your medications are working for you. Medications are
not perfect: they don’t always get rid of illness and they have side effects. Medications
also help some people more than others.
Another way to reduce biological vulnerability is to avoid alcohol and drug use. Alcohol and
drug use affect chemicals in the brain, which can lead to worse symptoms and relapses. Al-
cohol and drug use can also lead to legal, nancial, and health problems, resulting in stress
that can trigger symptoms. In addition, using alcohol and drugs can interfere with the
benecial effects of medication.
Reducing and Coping With Stress
There is no such thing as a stress-free life, so you can’t avoid all stress. In fact, to pur-
sue important goals in life, it is essential to be willing to take on new challenges, which can
be stressful. But it is helpful to be aware of times when you’re under too much stress and
to learn strategies for coping with it effectively. The following strategies might help you
reduce stress:
• Identify things that caused stress for you in the past and prepare for them.
• Set reasonable expectations for yourself—not too much or too little.
• Find activities that are meaningful to you.
• Maintain good health habits by eating well, getting enough sleep, and exercising
regularly.
• Find supportive people and tell them what you are feeling and thinking.
• Avoid situations where people argue with you or criticize you.
• Give yourself credit for your talents and strengths
• Use relaxation techniques, such as deep breathing, meditation, picturing a pleasant
scene, progressive muscle relaxation.
• Use “positive self-talk,” such as “This is a challenge, but I can handle it.”
• Use religion or another form of spiritual inspiration.
• Engage in a hobby such as cooking, gardening, reading, or listening to music.
Let’s Discuss!
What do you do to reduce stress?
Have you considered any of the strategies above?
Module #2
Handout
Integrated Illness Management
and Recovery Manual
Page 20
The next page lists categories of “Protective Factors,” things that can help you stay happy
and healthy, and “Risk Factors,” things that can make it more likely that you will become
sick. Using these categories, make a list of your Protective Factors and Risk Factors:
Protective Factors Risk Factors
Module #2
Handout
Integrated Illness Management
and Recovery Manual
Page 21
Protective Factors
Social and Leisure Activities
Medication
Healthcare
Healthy Lifestyle Habits
(Eating Healthy, Exercise, Sleep)
Risk Factors
Alcohol or Drug Use
Smoking
Family History
Excess Stress
Module #2
Handout
Integrated Illness Management
and Recovery Manual
Page 22
Integrated Illness Management and Recovery
Home Practice Sheet
My home practice for this week is:
To complete this home practice, I will use the following plan:
When:
Where:
With Whom:
What do I need to do the practice?
Today’s Date: _ _ / _ _ /_ _ _ _
Participant: ____________________ IIMR Specialist:_________________________
Integrated Illness Management and Recovery
Home Practice Sheet
My home practice for this week is:
To complete this home practice, I will use the following plan:
When:
Where:
With Whom:
What do I need to do the practice?
Today’s Date: _ _ / _ _ /_ _ _ _
Participant: ____________________ IIMR Specialist:_________________________

Module #3A-E
Guidelines
Integrated Illness Management
and Recovery Manual
Page 23
Practitioner Guidelines for Handouts #3A-E:
Practical Facts About Mental Illness
Goals
People are empowered by knowledge. The more they understand the basic facts about their disorder, the
better equipped they are to take an active role in their treatment, self-management of their psychiatric or
medical condition, and recovery. Cover only the handouts describing the conditions that people have.
Make sure to emphasize the relationship between mental illnesses and medical problems.
Suggestions for Teaching
• Before this topic, people may not have understood that some of their experiences were caused by
symptoms. For example, people may have thought that their lack of energy and motivation was caused
by personal weakness or “laziness” or that the voices they heard were some kind of “punishment.”
Helping people choose and practice alternative self-statement such as, “The voices I’m hearing are a
symptom of my illness.”
• After completing the topic “What are the symptoms of mental illness?” the practitioner could ask the
person if it might be helpful to be able to describe his or her symptoms to someone in their support
system, such as another practitioner or a family member. In the session, the person could practice what
he or she might say to the family member or treatment team member.
• People may be reluctant to acknowledge that they have a specific mental illness, that they have par-
ticular symptoms, or that they have any mental illness. Recognizing that one has a mental illness or a
specific type of mental illness can be helpful, but is not a prerequisite for participating in IIMR. Respect
the person’s opinion and seek common ground to facilitate working together. Point out that psychiatric
diagnoses are just a way of describing a group of symptoms that occur together. Ase different words
or phrases that are acceptable to the person, such as “having problems with stress,” “having a nervous
condition,” or “having problems with anxiety.”
• Some people already know a great deal about their mental illness. It is still desirable to go over the
handout to check people’s understanding and ensure that they are able to use the information
effectively.
Review Questions
What are some of the symptoms of ______________?
Does everyone who has ___________ have the same experience with symptoms?
What causes ___________________?
What information would be helpful to someone who just received a diagnosis of
_____________________?

Module #3A-E
Guidelines
Integrated Illness Management
and Recovery Manual
Page 24
Suggestions for Home Practice
1. Help people select a specific individual to talk to about the symptoms he or she has experienced. Go
over a list of symptoms from the educational handout to help the person plan what they will cover.
2. Help people plan how he or she can practice positive self-statements based on new information to
combat self-blame.
3. If people want more information about their mental illness, encourage them to seek out information
from community resources, the library, or the internet.

Module #3A
Handout
Integrated Illness Management
and Recovery Manual
Page 25
Integrated Illness Management and Recovery
Handout #3A: Practical Facts About
Schizophrenia
What do you know about schizophrenia?
• A mental illness that usually starts in adolescence or adulthood.
• About one in every one hundred people (1%) develops schizophrenia.
• Causes upsetting symptoms (hearing voices, lack of motivation)
• Can lead to problems with working, interpersonal relationships, and having fun.
• Can cause problems with concentration, organization, and planning.
• It is not “curable,” but you can experience recovery and lead a meaningful life.
• Diagnosed based on a clinical interview by a mental health professional.
• Doctors may do a physical exam and/or certain lab tests or blood tests to see if there
could be other causes for the symptoms, such as a medical problem.
What are the most common signs/symptoms of schizophrenia?
Some symptoms of schizophrenia are the same as those that happen in other mental
disorders. Making a diagnosis of schizophrenia is based on which different symptoms are
happening, how long they have been present, and how bad they are. No one has exactly the
same symptoms or is bothered the same amount by them.
1) Hallucinations: Hearing, seeing, feeling or smelling something that is not actually there.
Hearing voices is the most common kind of hallucination. When people hear voices, they
seem very real, like they can actually hear them.
2) Delusions. Firmly believing something, even when there is evidence that it is not
true. These beliefs can be about anything and can seem very real to the person with
schizophrenia, but they seem impossible and untrue to others. Common delusions
include:
Paranoia. Mistakenly believing that others want to hurt them.
Ideas of Reference. Mistakenly thinking that others are talking about them or taking
special notice of them.
Somatic Delusions. Mistakenly thinking something is wrong with their body.
Grandiosity. Mistakenly thinking they have special talents or powers.
3) Thought Disorder. Confused thinking that can make it hard to stay focused on a topic
of conversation, use the correct words, form complete sentences, or talk in an
organized way that other people can understand.
4) Negative Symptoms. Problems with motivation, energy, having fun, and expressing
emotions (especially facial expression and voice tone).
Module #3A
Handout
Integrated Illness Management
and Recovery Manual
Page 26
5) Cognitive Problems. Trouble with concentration, memory, planning, organizing, and
judgment.
6) Disorganized Behavior. Behaving strangely or doing things that seem to have no
purpose.
What other problems are often associated with schizophrenia?
1) Medical Problems. People with schizophrenia have more medical problems than people
without mental illness. These include diabetes, high blood pressure, high cholesterol,
and cancer. Many of these problems are caused by unhealthy lifestyle practices (eating
foods high in fat and calories, lack of exercise, poor sleep habits, lack of treatment for
medical problems).
2) Problems with Social or Role Functioning. When people have trouble making or
keeping friends, maintaining close relationships, taking care of themselves (hygiene)
or their children, household chores, getting or keeping a job, leaving the house, getting
exercise, eating healthy, taking care of medical problems.
3) Substance Abuse. People with schizophrenia are more likely to have problems with
abusing alcohol and/or drugs than people without a mental illness.
4) Smoking. More than twice as many people with schizophrenia smoke (70-85%)
compared with people without a mental illness (20-25%).
Let’s Discuss!
Which of these symptoms or other problems have you had?
How does schizophrenia affect physical health and vice versa?
• Having a mental illness can make it hard to take care of physical health problems, espe-
cially during a relapse.
• Negative symptoms can make it hard for people to feel motivated to take care of them-
selves, like showering, exercising (even though exercise can make people feel more ener-
getic), or eating regular and healthy meals, which can make people feel bad physically.
• Negative symptoms can also make it hard for people to motivate themselves to do the
things that are important to do to take care of medical problems like going to medical
appointments, taking medications as prescribed, taking glucose readings, or taking blood
pressure readings.
• Paranoia can also make it hard for people to get out of the house and get to medical
appointments or pick up important medications from the pharmacy
• Some people with schizophrenia have mistaken beliefs (delusions) about their physical
health like thinking they are very ill when they are not.
• Thethinkingproblems(difcultywithmemory,planning,scheduling,etc.)thatcanhap-
pen with schizophrenia can make it harder to do the things people need to do to manage
medical problems, like follow a treatment plan, take medications as prescribed, schedule
and go to medical appointments, monitor blood pressure or blood sugar.
Module #3A
Handout
Integrated Illness Management
and Recovery Manual
Page 27
What steps can you can take to manage symptoms of
schizophrenia?
• Learning how to cope with stress
• Having social support
• Making a relapse prevention plan
• Using medication effectively
• Taking care of your physical health
• Leading a healthy lifestyle (getting enough sleep, exercise, and eating healthy)
• Many types of therapies that involve talking to a trained counselor help with symptoms
of schizophrenia (Cognitive Behavioral Therapy, Skills Training, Cognitive Remediation).
What causes schizophrenia?
• Itisnoone’sfault.Youdidnotcauseitandneitherdidyourfamilymembersoranyone
else.
• Scientistsdon’tcompletelyunderstandit,buttheythinkitiscausedbyproblemswith
thewaysomepeople’sbrainswork(“biological
vulnerability”).
• Chemicals called “neurotransmitters” send messages in the brain.
When they are out of balance, they can cause the brain to send
messages that contain wrong information. These problems in the
brain probably exist
atbirtheventhoughthesignsofschizophreniausuallydon’tappear
until people are teenagers or adults.
• In addition to this biological vulnerability, stress probably plays a
role in people
developing schizophrenia and how well people cope with it. The theory of how
vulnerability and stress interact with each other is called the “stress-vulnerability
model” and is covered in more detail in the handout “The Stress-Vulnerability Model.”
Famous people who have been diagnosed with schizophrenia:
John Nash (born in 1928) is an American mathematician who made discoveries that were
importanttotheeldofEconomics.HewontheNobelPrizeforEconomicsin1994.His
story is told in
A Beautiful Mind
, a book that was made into a movie.
William Chester Minor (1834 - 1920) was an American Army surgeon who also made major
contributionstotheOxfordEnglishDictionary.
Vaslav Nijinski (1890 - 1950) was a Russian dancer who is legendary because of his
physical strength, light movements and expressive body language. He is especially
remembered for a dance piece called “Afternoon of a Faun.”

Module #3A
Handout
Integrated Illness Management
and Recovery Manual
Page 28
What is “Stigma”?
• Negative opinions and attitudes that some people have about mental illness.
• Research shows that as the general public gets to know more about mental illnesses
and as they get to know people who have experienced them, their negative beliefs
decrease.
• Two major laws protect against discrimination against people with physical or psychiatric
disabilities. The Americans with Disabilities Act (ADA) makes it against the law to
discriminate in the areas of employment, transportation, communication or recreation.
The Fair Housing Act (FHA) prohibits housing discrimination.

Module #3A
Handout
Integrated Illness Management
and Recovery Manual
Page 29
Integrated Illness Management and Recovery
Home Practice Sheet
My home practice for this week is:
To complete this home practice, I will use the following plan:
When:
Where:
With Whom:
What do I need to do the practice?
Today’sDate:__/__/____
Participant:____________________IIMRSpecialist:_________________________
Integrated Illness Management and Recovery
Home Practice Sheet
My home practice for this week is:
To complete this home practice, I will use the following plan:
When:
Where:
With Whom:
What do I need to do the practice?
Today’sDate:__/__/____
Participant:____________________IIMRSpecialist:_________________________

Module #3B
Handout
Integrated Illness Management
and Recovery Manual
Page 31
Integrated Illness Management and Recovery
Handout #3B: Practical Facts About
Bipolar Disorder
What do you know about bipolar disorder?
• A mental illness that affects about one person in every one hundred
people (1%).
• Used to be called “manic depression.”
• Causes upsetting symptoms such as severe mood swings, from the highest of highs
(mania) to the lowest of the lows (depression).
• People usually develop it as teenagers or young adults, age 16 to age 30. People can also
havetheirrstsymptomswhentheyareintheir40’sor50’s.
• It is not “curable,” but there are effective treatments for it.
• People can learn to manage it and can lead meaningful and productive lives.
• Diagnosed based on a clinical interview by a mental health professional.
• Doctors may do a physical exam and/or certain lab tests or blood tests to see if there
could be other causes for the symptoms, such as a medical problem.
• Some people have a mild form of it and only have symptoms a few times in their lives.
Other people have a more severe form of it.
• It tends to be “episodic,” with symptoms getting worse then better over time. When
symptoms reappear or get worse, this is called a “symptom exacerbation” or an “acute
episode” or a “relapse.” (More information on relapse is provided in the handout, “Relapse
Prevention.”) Some relapses can be managed at home, but other relapses may require
hospitalization.
What are the symptoms of bipolar disorder?
Some symptoms of bipolar disorder are the same as those that happen in other mental
disorders. Making a diagnosis of bipolar disorder is based on which symptoms are
happening, how long they have been present, and how bad they are. No one has exactly
the same symptoms or is bothered the same amount by them.
1. Extremely high mood (“mania”). When people experience any or all of the following:
Extreme happiness or excitement. Feeling extremely happy, on top of the world,
like everything was falling into place.
Irritability. Feeling very irritated, even over little things.
Unrealistic self-condence. Feeling like you can do virtually anything, even things
thatyoudon’treallyhavetheskillstodo.
No need for sleep. Feelinglikeyoudon’tneedtosleepasmuchasusualorthatyou
can even go for days without sleep.

Module #3B
Handout
Integrated Illness Management
and Recovery Manual
Page 32
Talking a lot. Talking a lot more than usual, so much that it is hard for people to
interrupt you.
Racing thoughts. Having thoughts that go so fast in your head that it is hard to
keep up with them.
Being easily distracted. Being distracted by every sound (for example, the ticking
of the clock, the air conditioner humming, a car driving by, someone walking by in the
hall, a bird singing outside the window).
Extreme energy and activity. Spending an excessive amount of time awake and
working on tasks, hobbies, or activities.
Bad judgment and/or risk taking. Behaving in ways that are dangerous or risky like
going on spending sprees, going home with strangers, hitchhiking,
2. Extremely low mood (“depression”). “Depression”isdenedasincluding:
Sad mood. Feeling very down, like there is nothing positive in life. Crying a lot.
Eating too little or too much. Having very little appetite or eating too much.
Sleeping too little or too much. Sleeping much more than usual or having insomnia
most nights.
Feeling tired and low energy. Feeling physically tired or exhausted most days.
Feeling helpless, hopeless, worthless. Feeling like you are powerless to make your
life better and/or that you are not an important person.
Feeling guilty for things that aren’t your fault. Feeling that you are responsible
for things that you did not cause or do.
Suicidal thoughts or actions. Feeling like you are tired of life, would be better off
dead, or having thoughts of wanting to hurt or kill yourself.
Trouble concentrating and making decisions. Having a hard time staying focused or
making even very simple decisions like what to wear or eat.
3. “Psychotic symptoms.” Some people with bipolar disorder have one or more of these:
Hallucinations. When people hear, see, feel or smell things that are not actually
there. Hearing voices is the most common kind of hallucination. When people hear
voices, they seem very real, and like they can actually hear them.
Delusions. Whenpeoplermlybelievesomething,evenwhenthereisevidencethat
it is not true. These beliefs can be about anything and seem very real to the person,
but seem impossible and untrue to others. Common delusions include:
Paranoia. Mistakenly believing that others want to hurt you.
Ideas of Reference. Mistakenly thinking that others are talking about or taking
special notice of you.
Somatic Delusions. Mistakenly thinking something is wrong with your body.
Grandiosity. Mistakenly thinking you have special talents or powers.
Thought Disorder. When people have confused thinking. This can make it hard to
stay focused on a topic of conversation, use the correct words, form complete
sentences, or talk in an organized way that other people can understand.
Cognitive Problems. When people have trouble with concentration, memory, planning,
organizing, and judgment.
Module #3B
Handout
Integrated Illness Management
and Recovery Manual
Page 33
Let’s Discuss!
Which of these symptoms or other problems have you had?
How does bipolar disorder affect physical health and vice versa?
• Having a mental illness can make it hard to take care of physical health problems,
especially during a relapse.
• Depression can make people feel too tired to take care of themselves, like showering,
exercising (even though exercise can make people feel less depressed), or eating regular
and healthy meals, which can make people feel bad physically.
• Depression can make it hard for people to motivate themselves to do the things that
are important to do to take care of medical problems like going to medical appointments,
taking medications as prescribed, taking glucose readings, or taking blood pressure
readings.
• Peoplewhodon’tgetenoughsleepbecauseofmaniaaremorelikelytogetsick.
• Depression can cause physical pain like aching muscles.
• Being physically sick or in pain can make people feel depressed, hopeless, or helpless.
Let’s Discuss!
Have you noticed other ways that your bipolar disorder has affected your physical
health or vice versa?
What are steps can you take to manage symptoms of bipolar
disorder?
• Learning how to cope with stress
• Having social support
• Making a relapse prevention plan
• Using medication effectively
• Taking care of your physical health
• Leading a healthy lifestyle (getting enough sleep, exercise, and eating healthy)
• Many types of therapies that involve talking to a trained counselor help with bipolar
disorder (Cognitive Behavioral Therapy, Problem Solving Therapy, Interpersonal
Therapy)

Module #3B
Handout
Integrated Illness Management
and Recovery Manual
Page 34
What causes bipolar disorder?
• Itisnoone’sfault.Youdidnotcauseitandneitherdidyourfamilymembersoranyone
else.
• Scientistsdon’tcompletelyunderstandit,buttheythinkitiscausedbyproblemswith
thewaysomepeople’sbrainswork(“biologicalvulnerability”).
• “Neurotransmitters” are chemicals that send messages in the brain. When they are out
of balance, they can cause the brain to send messages that contain wrong information.
These problems probably exist at birth even though signs of bipolar disorder usually
don’tappearuntilpeopleareteenagersoradults.
• In addition to this biological vulnerability, stress probably plays a role in people
developing bipolar disorder and how well people cope with it. The theory of how
vulnerability and stress interact with each other is called the “stress-vulnerability
model” and is covered in more detail in the handout “The Stress-Vulnerability Model.”
Examples of famous people who have been diagnosed with bipolar
disorder
Patti Duke is an American actress who had her own television series and has starred in
movies, including “The Miracle Worker.”
Robert Boorstin was a special assistant to President Clinton.
Vincent Van Gogh was one of the most famous painters who ever lived.
Kay Redeld Jamison is a psychologist, researcher and writer. In 2001 she won a
MacArthur Fellowship, sometimes referred to as “the genius award.”
What is “Stigma”?
• Negative opinions and attitudes that some people have about mental illness.
• Research shows that as the general public gets to know more about mental illnesses
and as they get to know people who have experienced them, their negative beliefs
decrease.
• Two major laws protect against discrimination against people with physical or psychiatric
disabilities. The Americans with Disabilities Act (ADA) makes it against the law to
discriminate in the areas of employment, transportation, communication or recreation.
The Fair Housing Act (FHA) prohibits housing discrimination.
Module #3B
Handout
Integrated Illness Management
and Recovery Manual
Page 35
Integrated Illness Management and Recovery
Home Practice Sheet
My home practice for this week is:
To complete this home practice, I will use the following plan:
When:
Where:
With Whom:
What do I need to do the practice?
Today’sDate:__/__/____
Participant:____________________IIMRSpecialist:_________________________
Integrated Illness Management and Recovery
Home Practice Sheet
My home practice for this week is:
To complete this home practice, I will use the following plan:
When:
Where:
With Whom:
What do I need to do the practice?
Today’sDate:__/__/____
Participant:____________________IIMRSpecialist:_________________________

Module #3C
Handout
Integrated Illness Management
and Recovery Manual
Page 37
Integrated Illness Management and Recovery
Handout #3C: Practical Facts About
Depression
What do you know about depression?
• One of the most common psychiatric problems.
• 15-20 people out of every 100 have a period of serious depression at some time in their
lives.
• Causes extremely low moods (feeling very sad or “blue”)
• May also cause problems with appetite, sleeping and energy level.
• For some people, it can seriously interfere with self-care, work and social life.
• It is very treatable and people can learn to manage it so they can lead meaningful lives.
• Diagnosed based on a clinical interview by a mental health professional.
• Doctors may do a physical exam and/or certain lab tests or blood tests to see if there
could be other causes for the symptoms, such as a medical problem.
• Some people have a mild form of it and only have symptoms a few times in their lives.
Other people have “Major Depression,” which is more severe.
• It tends to be “episodic,” with symptoms getting worse then better over time. When
symptoms reappear or get worse, this is called a “symptom exacerbation” or an “acute
episode” or a “relapse.” (More information on relapse is provided in the handout, “Reduc-
ing Relapses.”) Some relapses can be managed at home, but other relapses may require
hospitalization.
What are the symptoms of depression?
Some symptoms of depression are the same as those that happen in other mental disorders.
Making a diagnosis of depression is based on which different symptoms are happening, how
long they have been present, and how bad they are. This handout focuses on the diagnosis
of “major depression,” which requires having a group of symptoms for at least two weeks.
No one has exactly the exact symptoms or is bothered the same amount by them.
1. Sad mood. Feeling very down, like there is nothing positive in life.
Crying a lot.
2. Eating too little or too much. Having very little appetite or eating
too much.
3. Sleeping too little or too much. Sleeping much more than usual or
having insomnia most nights.
4. Feeling tired and low energy. Feeling physically tired or exhausted most days.
5. Feeling helpless, hopeless, worthless. Feeling like you are powerless to make your
life better and/or that you are not an important person.
Module #3C
Handout
Integrated Illness Management
and Recovery Manual
Page 38
6. Feeling guilty for things that aren’t your fault. Feeling that you are responsible for
things that you did not cause or do.
7. Suicidal thoughts or actions. Feeling like you are tired of life, would be better off
dead, or having thoughts of wanting to hurt or kill yourself.
8. Trouble concentrating and making decisions. Having a hard time staying focused or
making even very simple decisions like what to wear or eat.
Let’s Discuss!
Which of these symptoms or other problems have you had?
How does depression affect physical health and vice versa?
• Having a mental illness can make it hard to take care of physical
health problems, especially during a relapse.
• Depression can make people feel too tired to take care of them-
selves, like showering, exercising (even though exercise can make
people feel less depressed), or eating regular and healthy meals,
which can make people feel bad physically.
• Depression can make it hard for people to motivate themselves to do the things that
are important to do to take care of medical problems like going to medical appointments,
taking medications as prescribed, taking glucose readings, or taking blood pressure
readings.
• Depression can cause physical pain like aching muscles.
• Peoplewithinsomniawhodon’tgetenoughsleeparemorelikelytogetsick.
• Being physically sick or in pain can make people feel more depressed, hopeless and
helpless.
What are steps can you take to manage symptoms of depression?
• Learning how to cope with stress
• Having social support
• Making a relapse prevention plan
• Using medication effectively
• Taking care of your physical health
• Leading a healthy lifestyle (getting enough sleep, exercise, and eating healthy)
• Many types of therapies that involve talking to a trained counselor help with depression
(Cognitive Behavioral Therapy, Problem-Solving Therapy, Interpersonal Therapy)

Module #3C
Handout
Integrated Illness Management
and Recovery Manual
Page 39
What causes depression?
• Itisnoone’sfault.Youdidnotcauseitandneitherdidyourfamilymembersoranyone
else.
• Scientistsdon’tcompletelyunderstandit,buttheythinkitiscausedbyproblemswith
thewaysomepeople’sbrainswork(“biologicalvulnerability”).
• Chemicals called “neurotransmitters” send messages in the brain. When they are out
of balance, they can cause the brain to send messages that contain wrong information.
These problems in the brain probably exist at birth even though the signs of depression
usuallydon’tappearuntilpeopleareteenagersoradults.
• In addition to this biological vulnerability, stress probably plays a role in people develop-
ing depression and how well people cope with it. For example, losing a loved one, losing a
job, or being the victim of abuse or violence can increase the chances of a person devel-
oping depression. The theory of how vulnerability and stress interact with each other is
called the “stress-vulnerability model” and is covered in more detail in the handout “The
Stress-Vulnerability Model.”
• Many people develop depression after they suffer major medical problems like cancer or
chronic pain, among others.
Examples of famous people who have been diagnosed with major
depression
WinstonChurchillwasthePrimeMinisterofEnglandduringWorldWarII.
Mike Wallace is an American television journalist, well known for conducting interviews on
the show “60 Minutes.”
What is “Stigma”?
• Negative opinions and attitudes that some people have about mental illness.
• Research shows that as the general public gets to know more about mental illnesses and
as they get to know people who have experienced them, their negative beliefs decrease.
• Two major laws protect against discrimination against people with physical or psychiatric
disabilities. The Americans with Disabilities Act (ADA) makes it against the law to dis-
criminate in the areas of employment, transportation, communication or recreation. The
Fair Housing Act (FHA) prohibits housing discrimination.
Module #3C
Handout
Integrated Illness Management
and Recovery Manual
Page 40
Integrated Illness Management and Recovery
Home Practice Sheet
My home practice for this week is:
To complete this home practice, I will use the following plan:
When:
Where:
With Whom:
What do I need to do the practice?
Today’sDate:__/__/____
Participant:____________________IIMRSpecialist:_________________________
Integrated Illness Management and Recovery
Home Practice Sheet
My home practice for this week is:
To complete this home practice, I will use the following plan:
When:
Where:
With Whom:
What do I need to do the practice?
Today’sDate:__/__/____
Participant:____________________IIMRSpecialist:_________________________

Module #3D
Handout
Integrated Illness Management
and Recovery Manual
Page 41
Integrated Illness Management and Recovery
Handout #3D: Practical Facts About
Post-traumatic Stress Disorder (PTSD)
What do you know about Post-traumatic Stress Disorder (PTSD)?
• Serious problems and symptoms that last for a long time and are related to experienc-
ing a traumatic event such as physical or sexual abuse, combat, serious accident, natural
disaster(earthquake,tsunami,re,etc.).
• More than just feeling bad about an upsetting event.
• About 12 in every 100 people (7-12%) in the general population gets PTSD
• Can lead to problems with working, interpersonal relationships, and having fun.
• People can recover and lead a meaningful life.
• Diagnosed based on a clinical interview by a mental health professional.
• Doctors may do a physical exam and/or certain lab tests or blood tests to see if there
could be other causes for the symptoms, such as a medical problem.
What are the most common signs/symptoms of PTSD?
Some symptoms of PTSD are the same as those that happen in other mental disorders.
Making a diagnosis of PTSD is based on which different symptoms are happening, how long
they have been present, and how bad they are. No one has exactly the same symptoms or
is bothered the same amount by them.
1. Re-experiencingtheeventthroughunwantedmemories,dreams,orashbacks.
2. Avoidance of people, places or things that remind you of the traumatic event,
OR feeling numb or detached from other people.
3. Increased Arousal. This includes symptoms like increased heart rate and muscular
tension,restlessness,difcultysleeping,irritability,poorconcentration,feelingon
guard or hypervigilant, or having an exaggerated startle response.
What other problems are often associated with PTSD?
1. Medical Problems. People with PTSD often have more medical problems than people
without mental illness. These include diabetes, high blood pressure, high cholesterol,
and cancer. Many of these problems are caused by unhealthy lifestyle practices
(eating foods high in fat and calories, lack of exercise, poor sleep habits, lack of
treatment for medical problems).
2. Problems with Social or Role Functioning. Some people have trouble making or
keeping friends, maintaining close relationships, taking care of themselves (hygiene) or
their children, household chores, getting or keeping a job, leaving the house, getting
exercise, eating healthy, taking care of medical problems.

Module #3D
Handout
Integrated Illness Management
and Recovery Manual
Page 42
3. Depression. Some people with PTSD develop symptoms of depression such as sadness,
problems with sleeping and/or eating, trouble concentrating, losing interest in fun
things.
4. Substance Abuse. People with PTSD are more likely to have problems with abusing
alcohol and/or drugs than people without a mental illness.
Which of these symptoms or other problems have you had?
How does PTSD affect physical health and vice versa?
• Having a mental illness can make it hard to take care of physical health problems, espe-
cially during a relapse.
• Avoidance symptoms can make it hard for people to feel motivated to take care of
themselves, like showering, exercising (even though exercise can make people feel more
energetic), or eating regular and healthy meals, which can make people feel bad physical-
ly.
• Avoidance or depressive symptoms can also make it hard for people to motivate them-
selves to do the things that are important to do to take care of medical problems like
going to medical appointments, taking medications as prescribed, taking glucose read-
ings, or taking blood pressure readings.
• Depression can cause physical pain such as achy muscles.
• Thethinkingproblems(difcultywithmemory,planning,scheduling,etc.)thatcanhap-
pen with depression can make it harder to do the things people need to do to manage
medical problems, like follow a treatment plan, take medications as prescribed, schedule
and go to medical appointments, monitor blood pressure or blood sugar.
What are steps can you take to manage symptoms of PTSD?
• Learning how to cope with stress
• Having social support
• Making a relapse prevention plan
• Using medication effectively
• Taking care of your physical health
• Leading a healthy lifestyle (getting enough sleep, exercise, and eating healthy)
• Many types of therapies that involve talking to a trained counselor help with PTSD
symptoms(ExposureTherapy,CognitiveRestructuring)
What causes PTSD?
• Scientistsdon’tcompletelyunderstandit,buttheythinkitiscausedbyacombination
oftheproblemswiththewaysomepeople’sbrainswork(“biologicalvulnerability”)and
stress. The theory of how vulnerability and stress interact with each other is called
the “stress-vulnerability model” and is covered in more detail in the handout “The
Stress-Vulnerability Model.”

Module #3D
Handout
Integrated Illness Management
and Recovery Manual
Page 43
• People who have a serious mental illness (schizophrenia, depression, bipolar disorder) are
more likely to have had a major trauma (over 90%) and are more likely to develop PTSD
at some point in their lives (40%).
• People who have been the victims of abuse during childhood are more likely to suffer
abuse during adulthood, which can make them more vulnerable to developing PTSD.
What is “Stigma”?
• Negative opinions and attitudes that some people have about mental illness.
• Research shows that as the general public gets to know more about mental illnesses and
as they get to know people who have experienced them, their negative beliefs decrease.
• Two major laws protect against discrimination against people with physical or psychiatric
disabilities. The Americans with Disabilities Act (ADA) makes it against the law to
discriminate in the areas of employment, transportation, communication or recreation.
The Fair Housing Act (FHA) prohibits housing discrimination.

Module #3E
Handout
Integrated Illness Management
and Recovery Manual
Page 45
Integrated Illness Management and Recovery
Handout #3E: Practical Facts About
Schizoaffective Disorder
What do you know about schizoaffective disorder?
• A mental illness that usually starts in adolescence or adulthood.
• Can lead to problems with working, interpersonal relationships, and having fun.
• Can cause problems with concentration, organization, and planning.
• It is not “curable,” but you can experience recovery and lead a meaningful life.
• Diagnosed based on a clinical interview by a mental health professional.
• Doctors may do a physical exam and/or certain lab tests or blood tests to see if there
could be other causes for the symptoms, such as a medical problem.
What are the most common signs/symptoms of schizoaffective
disorder?
People who have schizoaffective disorder have symptoms of schizophrenia PLUS symptoms
of either bipolar disorder or major depression. Making a diagnosis of schizoaffective
disorder is based on which different symptoms are happening, how long they have been
present, and how bad they are. No one has exactly the same symptoms or is bothered
the same amount by them
For information about symptoms of schizoaffective disorder, refer to the handouts on
schizophrenia, major depression, and/or bipolar disorder.
What other problems are often associated with schizoaffective
disorder?
1. Medical Problems. People with schizoaffective disorder have more medical problems
than people without mental illness. These include diabetes, high blood pressure, high
cholesterol, and cancer. Many of these problems are caused by unhealthy lifestyle
practices (eating foods high in fat and calories, lack of exercise, poor sleep habits,
lack of treatment for medical problems).
2. Problems with Social or Role Functioning. Some people have trouble making or
keeping friends, maintaining close relationships, taking care of themselves (hygiene) or
their children, household chores, getting or keeping a job, leaving the house, getting
exercise, eating healthy, taking care of medical problems.
3. Substance Abuse. Some people are more likely to have problems with abusing alcohol
and/or drugs than people without a mental illness.
4. Smoking. More than twice as many people with schizoaffective disorder smoke
(70-85%) compared with people without a mental illness (20-25%).

Module #3E
Handout
Integrated Illness Management
and Recovery Manual
Page 46
Which of these symptoms or other problems have you had?
How does schizoaffective disorder affect physical health and vice
versa?
• Having a mental illness can make it hard to take care of physical health problems,
especially during a relapse.
• Negative symptoms can make it hard for people to feel motivated to take care of
themselves, like showering, exercising (even though exercise can make people feel
more energetic), or eating regular and healthy meals, which can make people feel bad
physically.
• Negative symptoms can also make it hard for people to motivate themselves to do the
things that are important to do to take care of medical problems like going to medical
appointments, taking medications as prescribed, taking glucose readings, or taking blood
pressure readings.
• Paranoia can also make it hard for people to get out of the house and get to medical
appointments or pick up important medications from the pharmacy
• Some people with schizoaffective disorder have mistaken beliefs (delusions) about their
physical health like thinking they are very ill when they are not.
• Thethinkingproblems(difcultywithmemory,planning,scheduling,etc.)thatcanhappen
with schizoaffective disorder can make it harder to do the things people need to do to
manage medical problems, like follow a treatment plan, take medications as prescribed,
schedule and go to medical appointments, monitor blood pressure or blood sugar.
What are steps can you take to manage symptoms of
schizoaffective disorder?
• Learning how to cope with stress
• Having social support
• Making a relapse prevention plan
• Using medication effectively
• Taking care of your physical health
• Leading a healthy lifestyle (getting enough sleep, exercise, and eating healthy)
• Many types of therapies that involve talking to a trained counselor help with
schizoaffective disorder (Cognitive Behavioral Therapy, Skills Training, Cognitive
Remediation)
What causes schizoaffective disorder?
• Itisnoone’sfault.Youdidnotcauseitandneitherdidyourfamilymembersoranyone
else.
• Scientistsdon’tcompletelyunderstandit,buttheythinkitiscausedbyproblemswith
thewaysomepeople’sbrainswork(“biologicalvulnerability”).

Module #3E
Handout
Integrated Illness Management
and Recovery Manual
Page 47
• Chemicals called “neurotransmitters” send messages in the brain. When they are out
of balance, they can cause the brain to send messages that contain wrong information.
These problems in the brain probably exist at birth even though the signs of s
chizoaffectivedisorderusuallydon’tappearuntilpeopleareteenagersoradults.
• In addition to this biological vulnerability, stress probably plays a role in people
developing schizoaffective disorder and how well people cope with it. The theory of
how vulnerability and stress interact with each other is called the “stress-vulnerability
model” and is covered in more detail in the handout “The Stress-Vulnerability Model.”
What is “Stigma”?
• Negative opinions and attitudes that some people have about mental illness.
• Research shows that as the general public gets to know more about mental illnesses and
as they get to know people who have experienced them, their negative beliefs decrease.
• Two major laws protect against discrimination against people with physical or psychiatric
disabilities. The Americans with Disabilities Act (ADA) makes it against the law to
discriminate in the areas of employment, transportation, communication or recreation.
The Fair Housing Act (FHA) prohibits housing discrimination.

Module #3F-S
Guidelines
Integrated Illness Management
and Recovery Manual
Page 49
Practitioner Guidelines for Handouts #3F-S:
Practical Facts About Health Issues
Goals
The amount of time this topic area takes to cover depends on how many health concerns a person wants
to learn about or is currently managing. Each handout covers a medical/health issue and you may be
able to cover 1-3 medical issues in a session. The handouts provide the opportunity to learn about health
issues and answer some of the common questions. This is also an important place to make connections
between a person’s personally meaningful goal and better management of health. In this topic, clients
should be encouraged to make routine visits to the doctor and discussion should focus on the necessity of
routine visits to screen for medical conditions and to prevent complications of illnesses.
Suggestions for Teaching
• Some people may not manage existing medical problems because they lack symptoms (e.g., hyperten-
sion often has few or no symptoms). Discuss the long-term consequences and complications that may
arise if medical problems are not managed properly. More importantly, link better disease management
to making progress towards the person’s meaningful goal will help build motivation.
• If a person does not see a doctor regularly or does not, discuss the advantages and disadvantages of
regular doctor visits to screen for and treat medical problems. If feasible and if the client is interested,
it may helpful to attend a medical appointment with the client to assess skills around sharing health
information and give feedback following the appointment.
• Many people will need preventive health care such as a pneumonia vaccine, mammogram, PSA test,
flu shot, etc. Discuss the advantages and disadvantages of getting these tests/procedures and a plan for
obtaining these tests/vaccines.
Review Questions
What are some of the symptoms of ______________?
What causes ___________________?
What can you do to better manage _______________?
Which of the following is a risk factor for many illnesses that you cannot change?
• Smoking
• Age
• Lack of exercise
• Stress
Suggestions for Home Practice
1. Develop a list of questions to bring to the client’s next medical appointment. Prioritize the list form
most to least important.
2. Use the health issue management worksheet at the end of each handout to identify areas the client
wants to work on to improve management of the medical problem.

Module #3F-S
Guidelines
Integrated Illness Management
and Recovery Manual
Page 50
Additional Resources
Diabetes, High Blood Pressure,
High Cholesterol, Heart Disease, Obesity
American Diabetes Association
1 888 DIABETES
www.diabetes.org
National Diabetes Education Program
One Diabetes Way
Bethesda, MD 20814-9692
(301) 496-3583
http://ndep.nih.gov
National Heart, Blood and Lung Institute
NHBLI Health Information Center
P.O. Box 30105
Bethesda, MD 20824-0105
(301) 592-8573
www.nhlbi.nih.gov
American Heart Association
www.americanheart.org
Hypertension Education Foundation, Inc.
Box 651
Scarsdale, NY 10583
www.hypertensionfoundation.org
Osteoarthritis, Fibromyalgia,
and Osteoporosis
National Osteoporosis Foundation
1232 22nd Street N.W.
Washington, D.C. 20037-1292
(202) 223-2226
www.nof.org
National Institutes of Health
Osteoporosis and Related Bone Diseases
2 AMS Circle
Bethesda, MD
20892-3676
800-624-BONE
www.osteo.org
Arthritis Foundation
www.arthritis.org
National Institute of Arthritis and
Musculoskeletal and Skin Diseases
National Institutes of Health
1 AMS Circle
Bethesda, MD 20892-3675
(301) 495-4484
www.niams.nih.gov
Chronic Obstructive Pulmonary Disease (COPD)
American Lung Association
www.lungusa.org
National Emphysema Foundation
15 Belden Avenue
Norwalk, CT 06850
(203) 849-9000
www.emphysemafoundation.org
National Lung Health Education Program
American Association for Respiratory Care
9425 MacArthur Boulevard
Irving, TX 75063
(972) 910-8555
www.nlhep.org
National Heart, Lung, and Blood Institute
P.O. Box 30105
Bethesda, MD 20824-0105
(301) 592-8573
www.nhlbi.nih.gov
Sexually Transmitted Infections (STIs)
Centers for Disease Control and Prevention
http://www.cdc.gov/std/
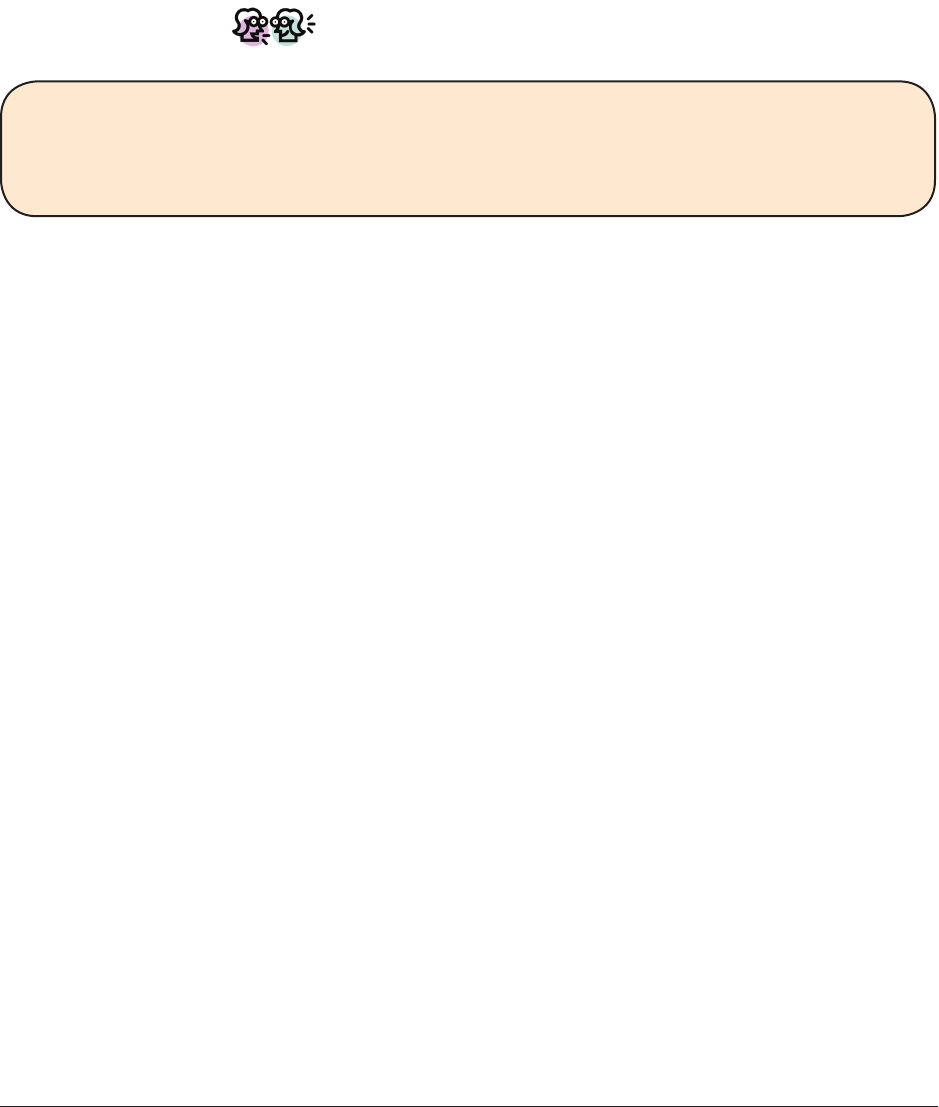
Module #3F
Handout
Integrated Illness Management
and Recovery Manual
Page 51
Integrated Illness Management and Recovery
Handouts #3F: Practical Facts About
Physical Health
In the following handouts, you will learn information on a variety of medical conditions and
health issues.
Let’s Discuss!
Why do you think it is important to learn about your medical condition?
How do you think learning about your health issues might help you to better manage
them?
Look at the list of medical conditions below and check off the ones that you have. Then
look through the list again and think about what issues are the most challenging to manage
or preventing you from taking steps towards your goal. Circle those medical conditions.
We will try to review all the topics of interest to you starting with the circled conditions.
• Diabetes
• High Blood Pressure
• High Cholesterol
• Osteoporosis
• Fibromyalgia
• GERD(AcidReux)
• Osteoarthritis
• ChronicObstructivePulmonaryDisease(COPD)
• Congestive Heart Failure
• Coronary Artery Disease
• Overweight and Obesity
• SexuallyTransmittedInfections
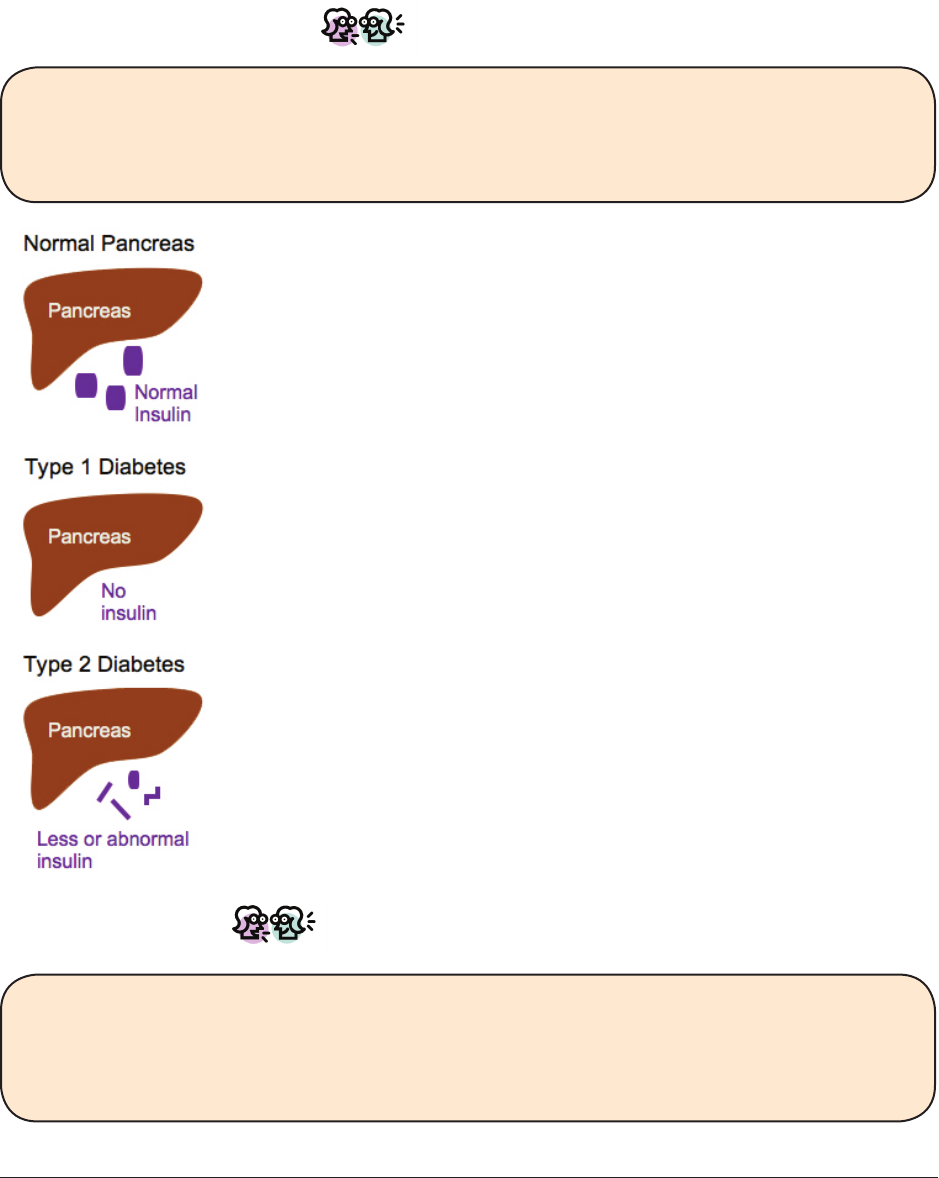
Module #3G
Handout
Integrated Illness Management
and Recovery Manual
Page 53
Integrated Illness Management and Recovery
Handout #3G: Practical Facts About
Diabetes
First, Let’s Discuss!
What is diabetes? What do you know about this medical condition? What has it been
like for you to live with diabetes? What effect has living and managing diabetes had
on reaching your meaningful goals?
The pancreas normally makes a hormone called insulin. Insulin helps
break down food so you will have enough energy. Sometimes the
pancreas stops producing insulin normally and causes high blood
sugar, which is also called “glucose.” This is called diabetes. There
are two types of diabetes: type 1 and type 2.
In type 1 diabetes, the pancreas makes no insulin. This is often
diagnosed in children or young adults. People with type 1 diabetes
have to inject insulin into their bodies and to make careful food
choices.
Intype2diabetes,thereislessinsulin,oritdoesn’tworkaswellso
sugar in the blood is not broken down and changed to energy you can
use. It is mainly diagnosed in adulthood. Most people with diabetes
havetype2diabetes.Beingoverweightandnotexercisingcanlead
totype2diabetes.Type2diabetescanbemanagedwithexercise,
diet, and taking prescription medication, but if it is not managed
well, people have to inject themselves with insulin.
If your doctor thinks that you may have diabetes, you will probably
have a fasting blood glucose test. Fasting means not eating or
drinking for some period of time. A normal fasting blood glucose is
below 100. A fasting blood glucose greater than 126 mg/dL on two
occasions is usually an indicator of diabetes. Blood sugar between
101 and 125 is called pre-diabetes, which may be reversed with diet
andexercise.
Let’s Discuss!
Whatsymptomsofdiabeteshaveyouexperienced?Haveyouhadanylong-term
consequences of diabetes? What are you doing now to manage your blood sugar?
What would you like to start doing to better manage your blood sugar?
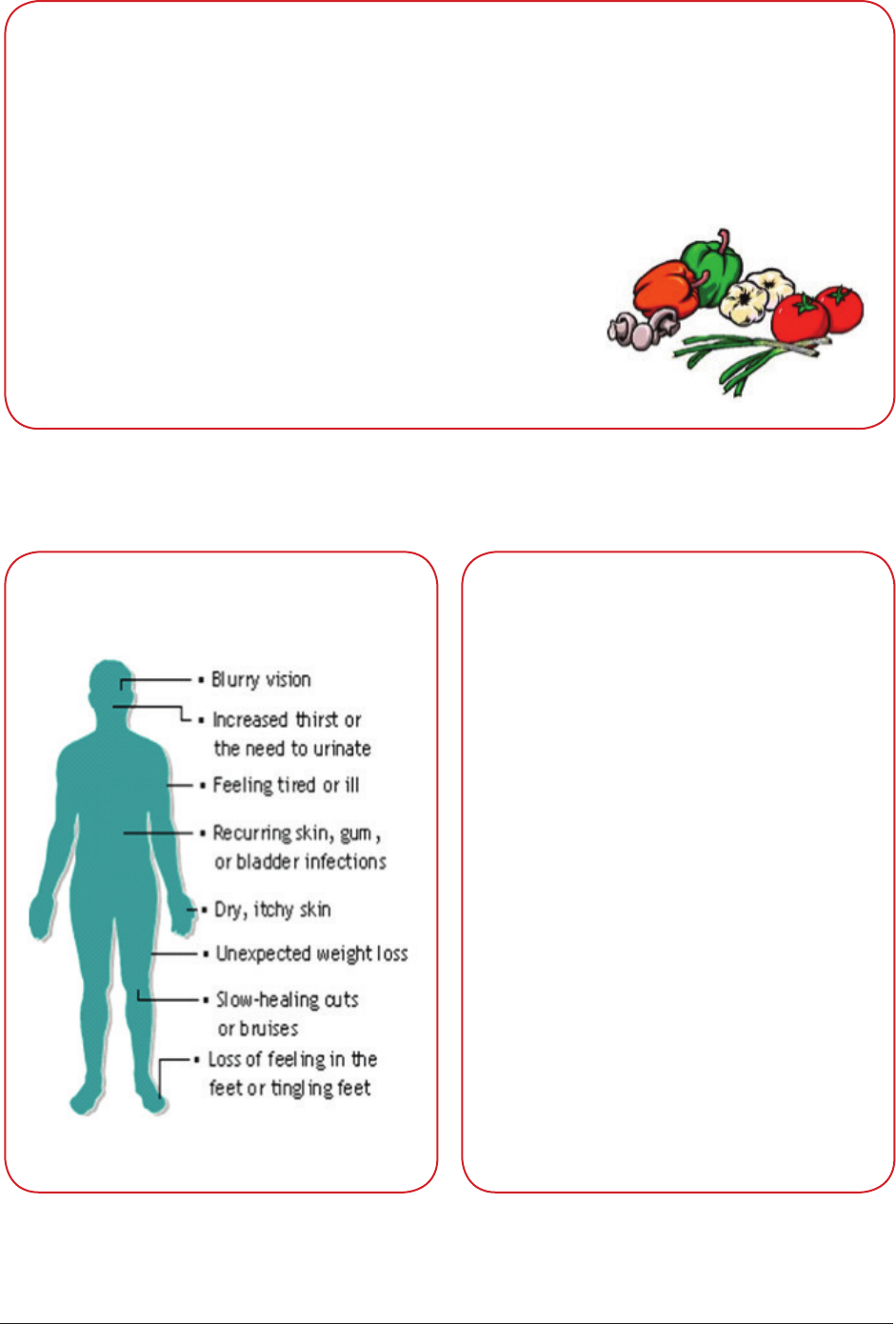
Module #3G
Handout
Integrated Illness Management
and Recovery Manual
Page 54
Staying Healthy With Diabetes
• Eat a balanced diet. A diabetes educator or nutritionist may help you develop a
meal plan that is right for you.
• Stayactive.Checkwithyourdoctorbeforestartinganewexerciseplan.
• Take medications as prescribed.
• Avoid alcohol and tobacco.
• Monitor your blood pressure and blood sugar levels.
• Have cholesterol checked regularly.
• See your doctor and specialists as needed. These may
includedentists,podiatrists(footdoctor),andeye
doctors.
Below are the symptoms of diabetes and long-term consequences
of high blood sugar.
Symptoms of Diabetes
Consequences of Diabetes
• Heart disease
• Stroke
• Neuropathy (nerve damage that
causes numbness, tingling or
weaknessinthelegsorarms)
• More infections
• Damage to the kidneys
• Damage to the eyes
People who have diabetes and
high blood pressure are more
likely to have complications like
heart disease.
The best way to avoid complica-
tions is to have good blood sugar
control.
Module #3G
Handout
Integrated Illness Management
and Recovery Manual
Page 55
Managing Diabetes
Peoplewithdiabetesneedtoeathealthyandgetregularexercise.Theyalsohaveto
watchforsignsthattheirbloodsugaristoolow(aconditioncalledhypoglycemia),ortoo
high(aconditioncalledhyperglycemia).Bothoftheseconditionscanbedangerous,even
life-threatening. In type 2 diabetes that is not treated with insulin, it is more common to
experiencehighbloodsugar(glucose),howeveritisalsoimportanttoknowthesymptoms
of low blood sugar and to take diabetes medications as prescribed to avoid low blood sugar.
Hemoglobin A1c: Know Your Number
This is your Average Blood Sugar over the past 2-3 months and can be measured by a
blood test. A Hemoglobin A1c of 7 or less is ideal.
RED: “Stop and Think” 10.0%
YELLOW: “Caution” Be Careful 8.0%
GREEN: “Good Going” Great Control 7.0%
HbA1c Over years of high HbA1c,
these problems can occur:
Avg Blood
Sugar
16.0 420
15.0 Amputation 390
14.0 Kidney Failure 360
13.0 Blindness 330
12.0 Heart Attack 300
11.0 Stroke 270
10.0 Increased Risk of Alzheimer’s Disease 240
9.0 Decreased Healing 210
8.0 180
7.0 150
6.0 120
5.0 90

Module #3G
Handout
Integrated Illness Management
and Recovery Manual
Page 56
Name __________________________________________ Date _ _ / _ _ / _ _ _ _
To achieve good control of your _________, it is important to take practical step towards
better management. Take one step now, and after you have achieved it, move on to another.
Diet Exercise LoseWeight Takemedications Monitor
properly blood sugar
Quitsmoking Annualeyeexam Checkfeet DentalExam Personal
Goal
Getaushot Practicehealthy AnnualExams ReduceStress Avoid
sleep habits Alcohol
Selected Step:
Action Plan:
CondenceRuler:12345678910
Not Somewhat Extremely
condent condent condent
Module #3G
Handout
Integrated Illness Management
and Recovery Manual
Page 57
Integrated Illness Management and Recovery
Home Practice Sheet
My home practice for this week is:
To complete this home practice, I will use the following plan:
When:
Where:
With Whom:
What do I need to do the practice?
Today’sDate:__/__/____
Participant: ____________________ IIMR Specialist:_________________________
Integrated Illness Management and Recovery
Home Practice Sheet
My home practice for this week is:
To complete this home practice, I will use the following plan:
When:
Where:
With Whom:
What do I need to do the practice?
Today’sDate:__/__/____
Participant: ____________________ IIMR Specialist:_________________________
Module #3H
Handout
Integrated Illness Management
and Recovery Manual
Page 59
Integrated Illness Management and Recovery
Handout #3H: Practical Facts About
High Blood Pressure
Theheartpumpsbloodthroughthebody’sarteries–likeapumppushing
water through pipes. When the heart pumps, the arteries open, allowing
blood to pass through. If the arteries are too narrow, the heart has to
pump harder to push the blood through. This increases the pressure on
the arteries. We call the amount of pressure on the arteries the “blood
pressure”.Wemeasure2differentbloodpressures–asystolicpressure
anddiastolicpressure.Thesystolicpressure(topnumber)isameasureofthepressure
onthearterieswhentheheartisbeating.Thediastolicpressure(bottomnumber)is
ameasureofthepressureonthearterieswhentheheartisatrest(betweenbeats).
A “normal” blood pressure is usually less than 120/80.
Let’s Discuss!
What is high blood pressure? What do you know about it?
What has it been like for you to live with high blood pressure?
What effect has living and managing high blood pressure had on reaching your
meaningful goals?
Manypeopledon’trealizetheyhavehighbloodpressurebecausethereareusuallyno
symptoms.Somepeoplemaynoticeheadachesordizziness.Theorgansofthebody,
theheartforexample,canhandlehighbloodpressureforalongtime.But,eventually
the pressure causes damage to organs and can lead to stroke, heart attack, heart failure,
eye disease and kidney failure.
Causes of High Blood Pressure
Thespeciccauseisunknownin95%of
people with high blood pressure, but is
more likely to occur in people with the
following risk factors:
• Age–beingover
35 years old
• Race–African
Americans are
at higher risk
• Family history
• Sedentary
lifestyle
• High salt diet
• Being
overweight
• High cholesterol
• Drinking alcohol
• Smoking
Symptoms of
High Blood Pressure
High blood pressure is a “silent killer”
because there are often no symptoms
until it is very advanced.
High blood pressure damages the heart,
arteries, and blood vessels to the brain.
Untreated hypertension can cause a
“stroke”, which means blood is unable
to reach the brain. Symptoms of stroke
include:
Module #3H
Handout
Integrated Illness Management
and Recovery Manual
Page 60
If you have high blood pressure, educate support people
on the signs of a stroke!
If a support person notices any symptoms of stroke,
they should call 9-1-1 immediately.
Seetheboxbelow.Adiagnosisofhighbloodpressureisgivenwhenbloodpressureis
above 120/80 on a few different days. The acceptable range for people with diabetes may
be different and should be discussed with a doctor.
Blood Pressure Category Systolic(mmHg) Diastolic(mmHg)
Normal Less than 120 And Less than 80
Pre-Hypertension 120 – 139 Or 80 – 89
Stage 1 Hypertension 140 – 159 Or 90 – 99
Stage 2 Hypertension 160 or higher Or 100 or higher
Managing High Blood Pressure
There are many lifestyle changes people can make to help manage blood pressure. Your
doctor may also consider prescribing medications to control high blood pressure. Things
you can do:
• Take medications as prescribed.
• Keep health care appointments.
• Quit smoking.
• Avoid alcohol and caffeine.
• Maintain a healthy weight.
• Eat a low-fat, lower sodium, plant based diet.
• Stayphysicallyactive.Aerobicexerciseisthebestexerciseforloweringblood
pressure.
Module #3H
Handout
Integrated Illness Management
and Recovery Manual
Page 61
Name __________________________________________ Date _ _ / _ _ / _ _ _ _
To achieve good control of your _________, it is important to take practical step towards
better management. Take one step now, and after you have achieved it, move on to another.
Diet Exercise LoseWeight Takemedications Monitor
properly blood sugar
Quitsmoking Annualeyeexam Checkfeet DentalExam Personal
Goal
Getaushot Practicehealthy AnnualExams ReduceStress Avoid
sleep habits Alcohol
Selected Step:
Action Plan:
CondenceRuler:12345678910
Not Somewhat Extremely
condent condent condent
Module #3H
Handout
Integrated Illness Management
and Recovery Manual
Page 62
Integrated Illness Management and Recovery
Home Practice Sheet
My home practice for this week is:
To complete this home practice, I will use the following plan:
When:
Where:
With Whom:
What do I need to do the practice?
Today’sDate:__/__/____
Participant: ____________________ IIMR Specialist:_________________________
Integrated Illness Management and Recovery
Home Practice Sheet
My home practice for this week is:
To complete this home practice, I will use the following plan:
When:
Where:
With Whom:
What do I need to do the practice?
Today’sDate:__/__/____
Participant: ____________________ IIMR Specialist:_________________________
Module #3I
Handout
Integrated Illness Management
and Recovery Manual
Page 63
Integrated Illness Management and Recovery
Handout #3I: Practical Facts About
High Cholesterol
Cholesterolisasoft,waxysubstance.Itisusedtoformthe
wallsofthebody’scellsandtomakeseveralimportanthor-
mones.Itisalsofoundinthefat(orlipid)thatisintheblood.
Some cholesterol comes from the food we eat and some is
made by our bodies. Although cholesterol is needed to live, hav-
ingtoomuchofitisunhealthy.Extracholesterolstickstothe
lining of the blood vessels and builds up over time. As a result, the blood vessels become
narrower.Thispreventstheowofblood,aconditioncalledatherosclerosis.Peoplewith
atherosclerosis have a higher risk of heart attack, stroke and circulatory problems.
Let’s Discuss!
What is high cholesterol? What do you know about it?
What has it been like for you to live with high blood pressure?
What effect has living and managing high blood pressure had on reaching your
meaningful goals?
High cholesterol does not produce symptoms and is diagnosed by a routine blood test.
If you have high blood pressure or diabetes, your doctor may recommend a lower target
cholesterol.Althoughthevaluesreportedintheboxbelowaregoodguidelinestofollow,
it is best to talk with your doctor about target levels that are best for you.
Cholesteroliscarriedinthebloodby“lipoproteins”.Thereis“good”(HDL)and“bad”
(LDL)cholesterol.Abloodtestforcholesterolmeasures:
•Yourtotalcholesterollevel–shouldbelessthan200
•Yourhighdensitylipoprotein,orHDLlevel–betterifabove40
• Your low density lipoprotein, or LDL level - recommended below 130 (or lower for
somemedicalconditions)
Cholesterol
Module #3I
Handout
Integrated Illness Management
and Recovery Manual
Page 64
Have you had any symptoms from related medical problems or long-term consequences
of high cholesterol? What are you doing now to manage your cholesterol now? What
would you like to start doing to better manage your cholesterol?
The Facts on Fats
There are several kinds of fats in the foods you eat. You should try avoid the ones that
raise LDL levels, including:
Saturated Fat: Foundinanimalfats,milk,cheese,andtropical(palmandcoconut)oils.
Trans Fat: Found in fast foods, margarine, peanut butter, crackers, cookies, and other
packaged food.
Fats that do not increase LDL cholesterol:
Monounsaturated & Polyunsaturated Fat: Found in vegetable oils such as olive oil, corn oil,
and canola oil.
Manage Your Cholesterol
Risk Factors for High Cholesterol
Risk Factors You Can Change
Smoking - Cigarette smoking increases LDL.
Diets high in saturated fat -
Saturated fat is the main dietary cause
of high blood cholesterol and high LDL.
Sedentary lifestyle - Physical inactivity
can contribute to a decrease in HDL.
High blood pressure - High blood
pressure in combination with high
cholesterol can accelerate the buildup
of fatty deposits.
Being overweight-Excessweightcan
lower your HDL level.
Diabetes - Individuals with diabetes are
more likely to develop high cholesterol.
Risk Factors You Can’t Change
Age - Men over age 45 and women over
age 55 are at increased risk of high
cholesterol.
Family history - A family history of
heart disease or high cholesterol
increases risk, even for people who
do not eat foods high in fats.
• Quit smoking.
• Exercise!Regular
exercisemayincrease
HDL and cause weight
loss, which lowers LDL.
• Eat a heart healthy diet. Watch your
intake of fat, sweets, eggs, and sodium.
• Eat lots of vegetables, fruits, and
whole grains and stick with leaner
meatssuchaschickenandsh.
• Maintain a healthy weight.
• Take medications as prescribed.
• Reduce sugar intake.

Module #3I
Handout
Integrated Illness Management
and Recovery Manual
Page 65
Name __________________________________________ Date _ _ / _ _ / _ _ _ _
To achieve good control of your _________, it is important to take practical step towards
better management. Take one step now, and after you have achieved it, move on to another.
Diet Exercise LoseWeight Takemedications Monitor
properly blood sugar
Quitsmoking Annualeyeexam Checkfeet DentalExam Personal
Goal
Getaushot Practicehealthy AnnualExams ReduceStress Avoid
sleep habits Alcohol
Selected Step:
Action Plan:
CondenceRuler:12345678910
Not Somewhat Extremely
condent condent condent
Module #3I
Handout
Integrated Illness Management
and Recovery Manual
Page 66
Integrated Illness Management and Recovery
Home Practice Sheet
My home practice for this week is:
To complete this home practice, I will use the following plan:
When:
Where:
With Whom:
What do I need to do the practice?
Today’sDate:__/__/____
Participant: ____________________ IIMR Specialist:_________________________
Integrated Illness Management and Recovery
Home Practice Sheet
My home practice for this week is:
To complete this home practice, I will use the following plan:
When:
Where:
With Whom:
What do I need to do the practice?
Today’sDate:__/__/____
Participant: ____________________ IIMR Specialist:_________________________
Module #3J
Handout
Integrated Illness Management
and Recovery Manual
Page 67
Integrated Illness Management and Recovery
Handout #3J: Practical Facts About
Osteoporosis
“Osteoporosis” means “porous bone.” It is caused by a loss of calcium in the body, making
bones too fragile to handle ordinary stresses. Osteoporosis increases the likelihood of
broken bones particularly in the spine, hip and wrists and can cause compression fractures
in the spine, which may occur without any warning. A compression fracture results when
one of the backbones collapses on itself and can cause severe pain.
Let’s Discuss!
What is osteoporosis? What do you know about it?
What has it been like for you to live with osteoporosis? What effect has living and
managing osteoporosis had on reaching your meaningful goals?
Approximately 10 million Americans have osteoporosis.
Bone strength depends on the amount of calcium, phosphorous and other minerals in the
bone. A decrease in the amount of these minerals may result in a decrease in the strength
of the bone. Bone, which is continuously breaking down and rebuilding, does not rebuild at
the same rate as people get older, resulting in a lower bone density, or bone mass.
Usinginformationfromyourmedicalhistoryandaphysicalexamincludingheight,weight,
and lab tests, your doctor may determine that you are at risk for osteoporosis and order
teststomakeadiagnosis.Aspecializedx-raycalledabonemineraldensitytest(orbone
scan)isoftenperformedtodiagnoseosteoporosis.Themostcommonofthesetestsisa
DEXAscanwhichislikeanX-raythatexaminesthehipandspinetodeterminethebone
densityoftheseareas.Twoscoresareobtainedforthehipandthespine.Therstscore,
called a “T-score,” compares your bone density to a healthy, 30 year-old adult and assesses
risk of bone fracture. The second score, the “Z-score,” compares the bone density to what
isexpectedforapersonofyourageandbodysize.
Your doctor may suggest a bone density test if you have risk factors such as:
• Prolonged use of steroid or thyroid medications.
• Diagnosis of type 1 diabetes, liver disease or kidney disease.
• Family history of osteoporosis.
• Youexperiencedearlymenopause.
• If you are postmenopausal, over 50, and have at least one other risk factor.
• If you are postmenopausal and over 65.
• Tobaccouseorexcessivealcoholuse.

Module #3J
Handout
Integrated Illness Management
and Recovery Manual
Page 68
Osteoporosis often doesn’t produce symptoms. Sometimes people experience pain or
may notice a change in height as a result of compression fractures in the back.
Let’s Discuss!
Have you had any symptoms from osteoporosis? What are you doing now to manage
your osteoporosis? What would you like to start doing to better manage your
osteoporosis?
Managing Osteoporosis
Doctors will often prescribe medication to prevent the progression of osteoporosis.
Inaddition,shemayrecommendweightbearingexercise,suchaswalkingorlifting
weights, and increasing intake of calcium and vitamin D either through pills or diet.
There are steps you can take to prevent osteoporosis from developing or from worsening.
It is important to try to prevent falling. Things you can do to prevent falling and
osteoporosis-related fractures are:
• Keepoorsfreeofclutterandelectricalcords.
• Use a rubber mat in the bathtub.
• Wear shoes with good traction even when at home.
• When out in the community, carry a backpack or shoulder bag. This leaves hands free
for balance and to break a fall.
• If recommended by the doctor, use a cane or walker and wear hip padding.
Some other things that can help to prevent osteoporosis and its complications:
• Quit smoking if you smoke.
• Limit alcohol intake.
• Workonbalance(practicestandingononelegoronyourtoes).
• Doweightbearingexercisessuchaswalkingorliftinglightweights.
Stretching can also improve balance.
• EatadietrichincalciumandvitaminD(milkanddairyproducts,fortiedcerealsand
leafygreenvegetables).AskyourdoctorifyoushouldtakevitaminD.
• Take prescription medications for osteoporosis, if prescribed.

Module #3J
Handout
Integrated Illness Management
and Recovery Manual
Page 69
Name __________________________________________ Date _ _ / _ _ / _ _ _ _
To achieve good control of your _________, it is important to take practical step towards
better management. Take one step now, and after you have achieved it, move on to another.
Diet Exercise LoseWeight Takemedications Monitor
properly blood sugar
Quitsmoking Annualeyeexam Checkfeet DentalExam Personal
Goal
Getaushot Practicehealthy AnnualExams ReduceStress Avoid
sleep habits Alcohol
Selected Step:
Action Plan:
CondenceRuler:12345678910
Not Somewhat Extremely
condent condent condent

Module #3J
Handout
Integrated Illness Management
and Recovery Manual
Page 70
Integrated Illness Management and Recovery
Home Practice Sheet
My home practice for this week is:
To complete this home practice, I will use the following plan:
When:
Where:
With Whom:
What do I need to do the practice?
Today’sDate:__/__/____
Participant: ____________________ IIMR Specialist:_________________________
Integrated Illness Management and Recovery
Home Practice Sheet
My home practice for this week is:
To complete this home practice, I will use the following plan:
When:
Where:
With Whom:
What do I need to do the practice?
Today’sDate:__/__/____
Participant: ____________________ IIMR Specialist:_________________________
Module #3K
Handout
Integrated Illness Management
and Recovery Manual
Page 71
Integrated Illness Management and Recovery
Handout #3K: Practical Facts About
Fibromyalgia
Let’s Discuss!
Whatisbromyalgia?Whatdoyouknowaboutit?
Whathasitbeenlikeforyoutolivewithbromyalgia?
What,ifany,effecthaslivingandmanagingbromyalgiahadonreachingyour
meaningful goals?
Fibromyalgiaisachronicconditioncharacterizedbyfatigue,musclepainandtenderness.
Often the pain is focused in areas known as “tender points” in the neck, shoulders, legs,
hips,arms,andback.Peoplewithbromyalgiaoftenalsohaveotherproblemssuchas
sleepdisturbances,depression,anxiety,andgastrointestinaldistress.
Theexactcauseofbromyalgiaisunknown,howeverseveralfactorsmayberelatedtothe
development of the condition including:
• Injury - Previous injury to a part of the body may trigger the development
ofbromyalgia.
• Infection -Someresearchindicatesthatbromyalgiacouldbetriggeredby
a bacterial or viral infection.
• Neurotransmitters - Changes in the levels of neurotransmitters, particularly
seratonin,maybeinvolvedinthedevelopmentofbromyalgia.
• Sleep Disturbance–Someresearchersthinkthatthismaybeacauserather
thanasymptomofbromyalgia.
Thereisnolabtestorx-raythatcanbeperformedtodiagnosebromyalgia.Often,the
symptomsofbromyalgiaoverlapwithotherproblemsandbromyalgiaisdiagnosedonly
after other conditions have been ruled out. To make things more complicated, not all peo-
pleexperiencethesamesymptoms.But,mostpeoplehave:
• Widespread pain for 3 or more months.
• Pain in at least 11 of 18 “tender points.”
• No other possible cause for the condition.
Module #3K
Handout
Integrated Illness Management
and Recovery Manual
Page 72
Let’s Discuss!
Describethesymptomsyouhaveexperiencedwithbromyalgia.
Whatareyoudoingnowtomanageyourbromyalgia?
Whatwouldyouliketostartdoingtobettermanageyourbromyalgia?
How can you manage bromyalgia?
Your doctor may prescribe a variety of types medications to help manage symptoms of
bromyalgiaincluding:
• Analgesics–Aspirin,ibuprofen,orTylenolaresometimesprescribedtorelievepain.
• Antidepressants - These can help to regulate levels of neurotransmitters.
• Muscle relaxants-MedicationssuchasFlexerilmaybeprescribedtoreducemuscle
spasms.
• Anti-seizure -MedicationsusedtopreventseizuressuchasNeurontin,mayalsobe
helpful for managing pain.
There are also things you can do to help manage bromyalgia including:
• Exercise.Workslowlytowardssmallexercisegoalstoavoidexacerbatingpainand
fatigue. Watch out for signs that you may be overdoing it.
• Take medications as prescribed.
• Eat a healthy, nutrient-rich diet.
• Get an adequate amount of sleep.
• Practicerelaxationandstressmanagement.

Module #3K
Handout
Integrated Illness Management
and Recovery Manual
Page 73
Name __________________________________________ Date _ _ / _ _ / _ _ _ _
To achieve good control of your _________, it is important to take practical step towards
better management. Take one step now, and after you have achieved it, move on to another.
Diet Exercise LoseWeight Takemedications Monitor
properly blood sugar
Quitsmoking Annualeyeexam Checkfeet DentalExam Personal
Goal
Getaushot Practicehealthy AnnualExams ReduceStress Avoid
sleep habits Alcohol
Selected Step:
Action Plan:
CondenceRuler:12345678910
Not Somewhat Extremely
condent condent condent
Module #3K
Handout
Integrated Illness Management
and Recovery Manual
Page 74
Integrated Illness Management and Recovery
Home Practice Sheet
My home practice for this week is:
To complete this home practice, I will use the following plan:
When:
Where:
With Whom:
What do I need to do the practice?
Today’sDate:__/__/____
Participant: ____________________ IIMR Specialist:_________________________
Integrated Illness Management and Recovery
Home Practice Sheet
My home practice for this week is:
To complete this home practice, I will use the following plan:
When:
Where:
With Whom:
What do I need to do the practice?
Today’sDate:__/__/____
Participant: ____________________ IIMR Specialist:_________________________
Module #3L
Handout
Integrated Illness Management
and Recovery Manual
Page 75
Integrated Illness Management and Recovery
Handout #3L: Practical Facts About
Gastro Esophageal Reux Disease
(GERD)
Let’s Discuss!
What is GERD? What do you know about it?
What has it been like for you to live with GERD?
What, if any, effect has living and managing GERD had on reaching your meaningful
goal?
GastroEsophagealReuxDiseaseorGERDisanirritationorinammationofthe
esophagus when stomach acid, liquid found in the stomach to assist in the digestion of
food, backs up into the esophagus. If not treated, the acid can damage the esophagus
over time. Complications of GERD include:
• Barrett’s esophagus - A rare complication of GERD involving changes in the color and
compositionoftheliningoftheesophagus.Barrett’sesophagusisariskfactorfor
esophageal cancer.
• Esophageal stricture - Caused by the narrowing of the esophagus; can make swallowing
difcult.
• Esophageal ulcer–Apainfulopensoreontheesophagusthatcanmakeswallowingmore
difcult.
10-20% of adults have symptoms of acid reux once a week.
GERD is caused when the esophageal sphincter, which is the opening that allows food from
the esophagus to enter the stomach and prevents food from the stomach from entering
backintotheesophagus,weakensandallowsstomachacidtoowbackupintotheesopha-
gus. The presence of acid in the esophagus can irritate the lining and eventually wear away
and narrow the esophagus, causing pain and discomfort. There are certain risk factors
that may increase the chance of developing GERD such as diabetes, obesity, hiatal hernia,
asthma, pregnancy, or peptic ulcer.
A diagnosis is usually made by reporting the classic symptoms of heartburn
andregurgitation(feelingthatfoodcomesupagaininthethroat)tothedoc-
tor. However, other testing procedures such as a barium X-ray or endoscopy
maybeperformediftreatmentdoesn’tworkorifsymptomsaresevere.A
bariumX-rayinvolvesswallowingaspecialtypeofliquidthatshowsuponanx-ray.Endos-
copyinvolvesswallowingathin,exible,lightedtubethattakespicturesoftheesophagus.
Module #3L
Handout
Integrated Illness Management
and Recovery Manual
Page 76
Let’s Discuss!
GERDisassociatedwithheartburn,nausea,belching,difcultyswallowing,andasour
taste in the mouth. Some people report coughing and a sore throat as well.
DescribethesymptomsyouhaveexperiencedwithGERD.Whatareyoudoingnowto
manage your GERD? What would you like to start doing to better manage your GERD?
How can you manage GERD?
Over-the-counter medications may control mild GERD symptoms however, if they are not
effective, the doctor may prescribe other medications. If medications do not provide
relief and symptoms are severe, surgery may be considered. Usually before doing surgery,
thedoctorwilldomoretestingtoconrmadiagnosisofGERD.
There are things you can do to help manage GERD including:
Maintain a healthy weight.
Avoid eating large meals.
Avoid lying down soon after eating.
Use a pillow to elevate the head when sleeping.
Avoid smoking.

Module #3L
Handout
Integrated Illness Management
and Recovery Manual
Page 77
Name __________________________________________ Date _ _ / _ _ / _ _ _ _
To achieve good control of your _________, it is important to take practical step towards
better management. Take one step now, and after you have achieved it, move on to another.
Diet Exercise LoseWeight Takemedications Monitor
properly blood sugar
Quitsmoking Annualeyeexam Checkfeet DentalExam Personal
Goal
Getaushot Practicehealthy AnnualExams ReduceStress Avoid
sleep habits Alcohol
Selected Step:
Action Plan:
CondenceRuler:12345678910
Not Somewhat Extremely
condent condent condent
Module #3L
Handout
Integrated Illness Management
and Recovery Manual
Page 78
Integrated Illness Management and Recovery
Home Practice Sheet
My home practice for this week is:
To complete this home practice, I will use the following plan:
When:
Where:
With Whom:
What do I need to do the practice?
Today’sDate:__/__/____
Participant: ____________________ IIMR Specialist:_________________________
Integrated Illness Management and Recovery
Home Practice Sheet
My home practice for this week is:
To complete this home practice, I will use the following plan:
When:
Where:
With Whom:
What do I need to do the practice?
Today’sDate:__/__/____
Participant: ____________________ IIMR Specialist:_________________________
Module #3M
Handout
Integrated Illness Management
and Recovery Manual
Page 79
Integrated Illness Management and Recovery
Handout #3M: Practical Facts About
Osteoarthritis
Let’s Discuss!
WhatisOsteoarthritis(arthritis)?Whatdoyouknowaboutit?
What has it been like for you to live with arthritis?
What effect has living and managing arthritis had on reaching your meaningful goals?
Osteoarthritis, which is sometimes referred to as degenerative joint disease, is the most
common form of arthritis. Osteoarthritis involves a gradual breakdown of cartilage in the
jointsthatmostoftenaffectsthehips,knees,ngers,hands,andback.Cartilageisthe
exiblematerialfoundbetweenbonesthatenablearms,legs,andngerstobend.Arthri-
tis often gets worse over time.
Adoctormaytakeamedicalhistory,doaphysicalexam,andorder
teststondoutifsomeonehasosteoarthritis.Thereareblood
teststhatcanprovideinformationaswellasx-rays,bonescans,or
anMRI(MagneticResonanceImaging).Yourdoctormayalsosug-
gest a test called arthrocentesis or another test called arthrogra-
phy.Arthrocentesisinvolvesdraininguidfromthejointtolook
forsignsofdegeneration.Arthrographyinvolvestakinganx-ray
after dye has been injected into the joint.
The cause of osteoarthritis is not always clear however, risk factors may include:
• Age - Risk for the condition increases with age.
• Gender - More women than men have osteoarthritis.
• A history of injury - Injury to the joints increases risk for osteoarthritis.
• Obesity-Excessweightcanputextrastressonthejoints.
• Other joint diseases - Diseases such as Rheumatoid Arthritis increase risk.
Let’s Discuss!
Osteoarthritis is associated with pain and stiffness in the joints, swelling, and lumps
orbumpsinngersorthumbs.Describethesymptomsofosteoarthritisyouhave.
What are you doing now to manage your osteoarthritis? What would you like to start
doing to better manage your osteoarthritis?

Module #3M
Handout
Integrated Illness Management
and Recovery Manual
Page 80
Osteoarthritis affects approximately 21 million Americans.
How can you manage osteoarthritis?
There are treatments for osteoarthritis that can help people maintain their daily activi-
ties. Treatments may reduce pain and increase joint movement.
There are also things you can do to better manage your arthritis including:
• Exerciseregularly.(Discusswithyourdoctorbeforebeginninganexerciseprogram).
• Yourdoctormayrecommendphysicaltherapy.Completephysicaltherapyexercisesas
instructed.
• Control your weight.
• Take medications as prescribed.
• Userelaxationanddeep-breathingtechniques.
• Apply heat or cold to painful areas.

Module #3M
Handout
Integrated Illness Management
and Recovery Manual
Page 81
Name __________________________________________ Date _ _ / _ _ / _ _ _ _
To achieve good control of your _________, it is important to take practical step towards
better management. Take one step now, and after you have achieved it, move on to another.
Diet Exercise LoseWeight Takemedications Monitor
properly blood sugar
Quitsmoking Annualeyeexam Checkfeet DentalExam Personal
Goal
Getaushot Practicehealthy AnnualExams ReduceStress Avoid
sleep habits Alcohol
Selected Step:
Action Plan:
CondenceRuler:12345678910
Not Somewhat Extremely
condent condent condent
Module #3M
Handout
Integrated Illness Management
and Recovery Manual
Page 82
Integrated Illness Management and Recovery
Home Practice Sheet
My home practice for this week is:
To complete this home practice, I will use the following plan:
When:
Where:
With Whom:
What do I need to do the practice?
Today’sDate:__/__/____
Participant: ____________________ IIMR Specialist:_________________________
Integrated Illness Management and Recovery
Home Practice Sheet
My home practice for this week is:
To complete this home practice, I will use the following plan:
When:
Where:
With Whom:
What do I need to do the practice?
Today’sDate:__/__/____
Participant: ____________________ IIMR Specialist:_________________________
Module #3N
Handout
Integrated Illness Management
and Recovery Manual
Page 83
Integrated Illness Management and Recovery
Handout #3N: Practical Facts About
Chronic Obstructive Pulmonary Disease
(COPD)
Let’s Discuss!
What is do you know about COPD? What has it been like for you to live with COPD?
What effect has living and managing COPD had on reaching your meaningful goals?
What are you doing now to manage your COPD?
Chronic Obstructive Pulmonary Disease, or COPD, refers to two lung
diseases: emphysema and chronic bronchitis. These lung diseases block
airowinandoutofthelungs.Thismakesbreathingmoredifcult.
Overtime,theowofaircanbecomemoreblocked,makingiteven
moredifculttobreathe.COPDisthefourthleadingcauseofdeathin
the US.
A Pulmonary Function Test is the best way to diagnose COPD. Your doctor may recommend
this if you had risk factors or symptoms of COPD. A Pulmonary Function Test usually
involves breathing into a mouthpiece. It compares how much air your lungs can hold and
howfastaircarmoveinandoutofyourlungs.Italsolooksathowwellcarbondioxide
(whichiswhatyouexhale)andoxygen(whichiswhatyouinhale)istransferredbetween
the air and blood.
Causes of COPD
***Smoking–majorriskfactor
Family History
History of respiratory infections as a
child
Secondhandsmokeexposure
Exposuretopollution
Alpha-1-antitrypsindeciency–
aninheritedproteindeciency
80%-90%ofCOPDdeathsarecaused
by smoking
Symptoms of COPD
Wheezing
Loss of appetite and weight loss
Decreaseinabilitytoexercise
Cough, with or without phlegm
Chronic fatigue
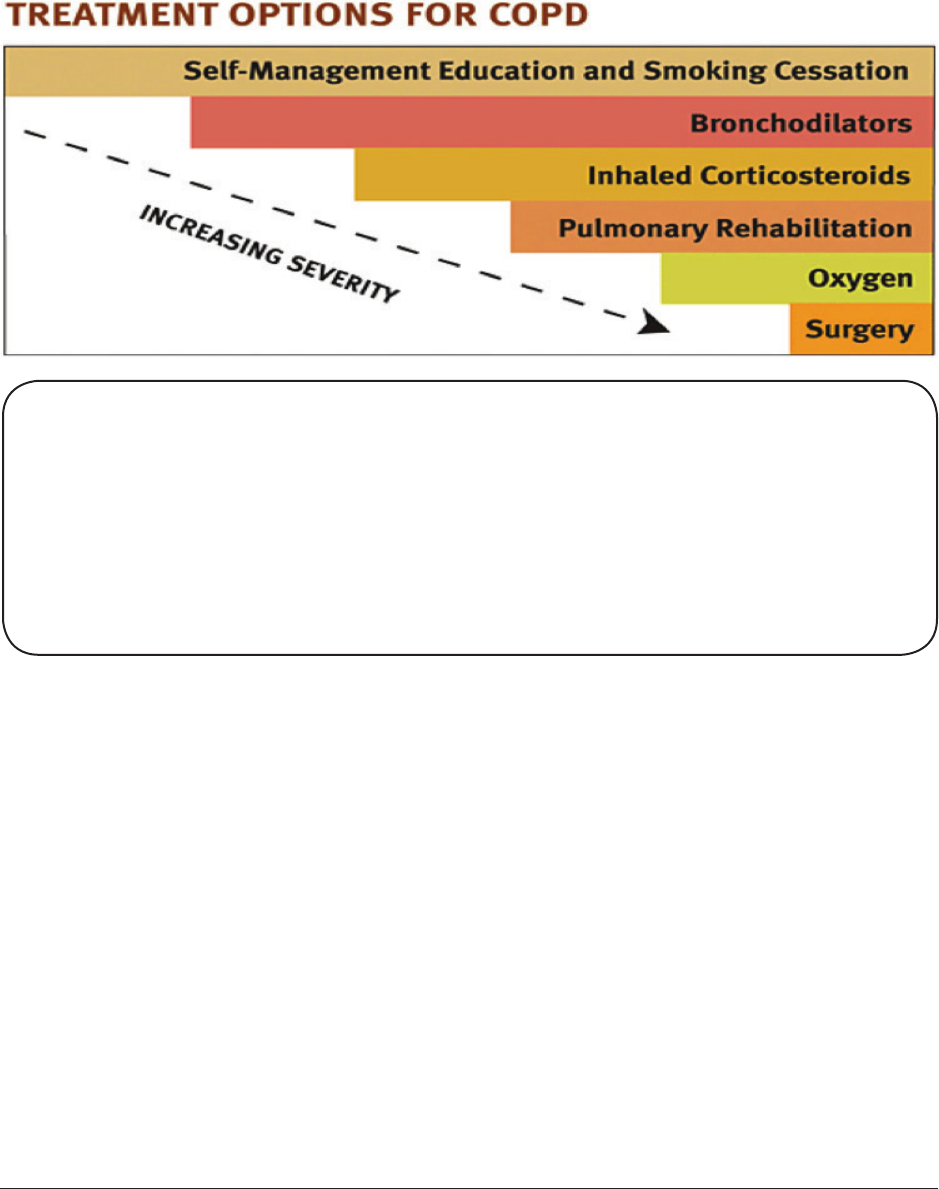
Module #3N
Handout
Integrated Illness Management
and Recovery Manual
Page 84
How can you manage COPD?
There is no cure for COPD, however there are treatments. These treatments may
decrease symptoms, make breathing easier and reduce complications that may result
fromCOPDsuchaspneumonia.Yourdoctormayrecommendaushoteveryyearanda
pneumonia vaccine to prevent certain causes of pneumonia. Consultation with a lung
specialist, or pulmonologist, may also be recommended.
Steps to manage COPD
• Ifyousmoke,QUIT!
• Take medications as prescribed.
• Getushotsandapneumoniavaccine
• Performdailyexercise,suchaswalking.Talktoyourdoctoraboutstarting
a program with initial modest goals.

Module #3N
Handout
Integrated Illness Management
and Recovery Manual
Page 85
Name __________________________________________ Date _ _ / _ _ / _ _ _ _
To achieve good control of your _________, it is important to take practical step towards
better management. Take one step now, and after you have achieved it, move on to another.
Diet Exercise LoseWeight Takemedications Monitor
properly blood sugar
Quitsmoking Annualeyeexam Checkfeet DentalExam Personal
Goal
Getaushot Practicehealthy AnnualExams ReduceStress Avoid
sleep habits Alcohol
Selected Step:
Action Plan:
CondenceRuler:12345678910
Not Somewhat Extremely
condent condent condent
Module #3N
Handout
Integrated Illness Management
and Recovery Manual
Page 86
Integrated Illness Management and Recovery
Home Practice Sheet
My home practice for this week is:
To complete this home practice, I will use the following plan:
When:
Where:
With Whom:
What do I need to do the practice?
Today’sDate:__/__/____
Participant: ____________________ IIMR Specialist:_________________________
Integrated Illness Management and Recovery
Home Practice Sheet
My home practice for this week is:
To complete this home practice, I will use the following plan:
When:
Where:
With Whom:
What do I need to do the practice?
Today’sDate:__/__/____
Participant: ____________________ IIMR Specialist:_________________________
Module #3O
Handout
Integrated Illness Management
and Recovery Manual
Page 87
Integrated Illness Management and Recovery
Handout #3O: Practical Facts About
Congestive Heart Failure
Let’s Discuss!
What is CHF? What do you know about it?
What has it been like for you to live with CHF?
What effect has living and managing CHF had on reaching your meaningful goals?
Congestiveheartfailure(CHF)occurswhentheheartisnolongerable
topumpbloodtothebody’scells.OnetypeofCHFinvolvestheheart’s
inability to pump enough blood through the body. The second type of
CHF occurs when the heart cannot pump enough blood to the lungs where
itpicksupoxygenforthebody’scells.CHFismostoftencausedby
coronary artery disease or another chronic medical condition that causes
gradual damage to the heart, like high blood pressure or diabetes.
In order to diagnose CHF, the doctor will take a health history, consider your risk factors,
anddoaphysicalexam.Yourdoctormaydofurthertestsincluding:
Electrocardiogram (EKG) - measures electrical impulses given off by the heart and can
determine if someone is having a heart attack or has had a heart attack in the past.
Exercise Stress Test–involvesbeingmonitoredwhiledoingsomekindofexerciseor
activity.Thiscandetermineiftheheartisgettingsufcientbloodandoxygensupply.
Echocardiogram - uses sound waves to form an image of your heart, this can determine if
partofyourheartisdamagedbyablockage,andifandwherethebloodishavingdifculty
owing.
Blood Test–canshowahormonecalledBrainNatriureticPeptide(BNP).Highlevelsof
this hormone is an indication of CHF.
Chest X-ray–candetermineifthereisanyuidaroundtheheartorinthelungs.
There are many factors that may contribute to the development of CHF. Some of the
factors that cannot be changed are:
• Age - Older people are more likely to develop CHF.
• Gender - Men are at greater risk than women.
• Medical problems - CHF can be the result of long-term effects of medical problems such
as coronary artery disease, high blood pressure, high cholesterol, diabetes and other
problems.
Module #3O
Handout
Integrated Illness Management
and Recovery Manual
Page 88
Some of the factors that may be changed or improved include:
• Smoking - Increases risk of heart disease.
• High blood pressure - Increases the workload of the heart.
• High cholesterol - Increases risk for heart disease.
• Diabetes - Poor blood sugar control may increase risk for CHF
• Alcoholuse–Serious,long-termalcoholusecancontributetoCHF.
• Sedentarylifestyle-LackofexerciseisariskfactorforCHF.Regularexercisecan
help protect the heart from disease.
• Being overweight - Increases risk for developing high blood pressure, high cholesterol
and diabetes. It also increases the workload of the heart.
Let’s Discuss!
Symptoms of CHF may go unnoticed when the condition is in its early stages.
As the condition progresses, shortness of breath and fatigue are the most common
symptoms. Nausea, irregular heartbeat and cough can also be present as well as
swelling in the abdomen, legs, ankles and feet.
DescribethesymptomsyouhaveexperiencedwithCHF.Whatareyoudoingnowto
manage your CHF? What would you like to start doing to better manage your CHF?
How can you manage CHF?
If you have medical condition that affects your heart, the doctor will begin to treat or
continue to treat that medical condition. The doctor will likely consider the cause of CHF
and the stage when determining other treatment options. Medications, many of which are
used in the treatment of high blood pressure, are a likely option. Surgery may be needed
in cases of severe CHF or CHF that has not responded to other treatment. Sometimes
cardiologists,doctorsthatspecializeintreatingdiseaseoftheheart,maydecideto
implantadebrillatortoavoidlife-threateningarrhythmias.
There are many things YOU can do to manage CHF. Steps you can take include:
• Eat a low-fat diet.
• Eat a low-sodium diet.
• Ifyourdoctorrecommendsit,watchyouruidintake.
• Weigh yourself every day and report sudden increases to your doctor right away.
• Avoid alcohol.
• Increaseintakeoffruits,vegetables,whole-grains,andsh.
• Maintain a healthy weight.
• Quit smoking.
• Take medications prescribed by your doctor.

Module #3O
Handout
Integrated Illness Management
and Recovery Manual
Page 89
• Avoidanti-inammatorymedicationssuchasaspirinoribuprofen,whichmaycauseyou
to retain salt and make CHF worse.
• Talkwithyourdoctoraboutthepossibilityofincorporatingexerciseintoyourroutine.
Exercisemaybepartofacardiacrehabilitationprogram.

Module #3O
Handout
Integrated Illness Management
and Recovery Manual
Page 90
Name __________________________________________ Date _ _ / _ _ / _ _ _ _
To achieve good control of your _________, it is important to take practical step towards
better management. Take one step now, and after you have achieved it, move on to another.
Diet Exercise LoseWeight Takemedications Monitor
properly blood sugar
Quitsmoking Annualeyeexam Checkfeet DentalExam Personal
Goal
Getaushot Practicehealthy AnnualExams ReduceStress Avoid
sleep habits Alcohol
Selected Step:
Action Plan:
CondenceRuler:12345678910
Not Somewhat Extremely
condent condent condent
Module #3O
Handout
Integrated Illness Management
and Recovery Manual
Page 91
Integrated Illness Management and Recovery
Home Practice Sheet
My home practice for this week is:
To complete this home practice, I will use the following plan:
When:
Where:
With Whom:
What do I need to do the practice?
Today’sDate:__/__/____
Participant: ____________________ IIMR Specialist:_________________________
Integrated Illness Management and Recovery
Home Practice Sheet
My home practice for this week is:
To complete this home practice, I will use the following plan:
When:
Where:
With Whom:
What do I need to do the practice?
Today’sDate:__/__/____
Participant: ____________________ IIMR Specialist:_________________________
Module #3P
Handout
Integrated Illness Management
and Recovery Manual
Page 93
Integrated Illness Management and Recovery
Handout #3P: Practical Facts About
Coronary Artery Disease
Let’s Discuss!
What is Coronary Artery Disease? What do you know about it?
What has it been like for you to live with Coronary Artery Disease?
What effect has living and managing Coronary Artery Disease had on reaching your
meaningful goals?
Coronaryarterydisease(CAD)isthemostcommontypeofheartdisease
in the United States. It is also the leading cause of death for both men
and women. Coronary artery disease is caused by atherosclerosis, a grad-
ual buildup of plaque in the blood vessels connected to your heart. This
plaque narrows the blood vessels, reducing the amount of blood that is
abletogettotheheartandreducingoxygentotheheart.
There are many factors, often working in combination, which may contribute to the
development of coronary artery disease. Some of the factors that are not changeable
include:
• Age- Older people are more likely to develop CAD.
• Gender- Men are at greater risk than women.
• Heredity- Family history is an important factoring developing CAD.
Some of the factors that may be changed or improved include:
• Smoking-IncreasesriskofdevelopingCADbyupto4times!
• High blood pressure - Increases the workload of the heart.
• High cholesterol - Increases risk for CAD.
• Diabetes - Poor blood sugar control may increases risk of CAD.
• Sedentarylifestyle-LackofexerciseisariskfactorforCAD.
• Regularexercisecanhelpprotecttheheartfromdisease.
• Being overweight - Increases risk for developing high blood pressure, high cholesterol
and diabetes. It also increases the workload of the heart.
In order to diagnose coronary artery disease, the doctor will take a health history,
consideryourriskfactors,anddoaphysicalexam.Ifyourdoctordeterminesthatyou
have risk factors for coronary artery disease, further tests may be ordered including:

Module #3P
Handout
Integrated Illness Management
and Recovery Manual
Page 94
Electrocardiogram (EKG) - measures electrical impulses given off by the heart and can
determine if someone had a heart attack in the past or is presently having a heart attack.
Exercise Stress Test-involvesbeingmonitoredwhiledoingsomekindofexerciseorac-
tivity.Thiscandetermineiftheheartisgettingsufcientbloodandoxygensupply.
Echocardiogram - uses sound waves to form an image of your heart, this can determine if
partofyourheartisdamagedbyablockage,andifandwherethebloodishavingdifculty
owing.
Other tests that may be ordered include a coronary angiography, a test that shows the
narrowing of arteries, and a nuclear scan, which can determine the amount of blood able to
owtotheheart.
Let’s Discuss!
Symptoms of CAD are chest pain, also called angina, and shortness of breath.
However,sometimespeoplewillnotexperienceanysymptomsthoughtheyare
still at risk for cardiac events such as a heart attack.
DescribethesymptomsyouhaveexperiencedwithCAD.
What are you doing now to manage your CAD?
What would you like to start doing to better manage your CAD?
How can I manage coronary artery disease?
The doctor will likely suggest a combination of treatments including lifestyle changes,
medications, and, depending on the severity of blockage, possibly surgical procedures.
There are many things you can do to treat and even prevent coronary artery disease.
Steps you can take include:
• Eat a low-fat diet.
• Eat a low-sodium diet.
• Increaseintakeoffruits,vegetables,whole-grains,andsh.
• Maintain a healthy weight.
• Quit smoking.
• Take medications prescribed by your doctor.
• Talkwithyourdoctoraboutthepossibilityofincorporatingexerciseintoyourroutine.

Module #3P
Handout
Integrated Illness Management
and Recovery Manual
Page 95
Name __________________________________________ Date _ _ / _ _ / _ _ _ _
To achieve good control of your _________, it is important to take practical step towards
better management. Take one step now, and after you have achieved it, move on to another.
Diet Exercise LoseWeight Takemedications Monitor
properly blood sugar
Quitsmoking Annualeyeexam Checkfeet DentalExam Personal
Goal
Getaushot Practicehealthy AnnualExams ReduceStress Avoid
sleep habits Alcohol
Selected Step:
Action Plan:
CondenceRuler:12345678910
Not Somewhat Extremely
condent condent condent
Module #3P
Handout
Integrated Illness Management
and Recovery Manual
Page 96
Integrated Illness Management and Recovery
Home Practice Sheet
My home practice for this week is:
To complete this home practice, I will use the following plan:
When:
Where:
With Whom:
What do I need to do the practice?
Today’sDate:__/__/____
Participant: ____________________ IIMR Specialist:_________________________
Integrated Illness Management and Recovery
Home Practice Sheet
My home practice for this week is:
To complete this home practice, I will use the following plan:
When:
Where:
With Whom:
What do I need to do the practice?
Today’sDate:__/__/____
Participant: ____________________ IIMR Specialist:_________________________
Module #3Q
Handout
Integrated Illness Management
and Recovery Manual
Page 97
Integrated Illness Management and Recovery
Handout #3Q: Practical Facts About
Obesity and Overweight
Let’s Discuss!
What is obesity? What do you know about it?
Describe any symptoms you have had as a result of being overweight or obese.
Have you had medical problems because of your weight?
What are you doing now to manage your weight?
What would you like to start doing to better manage your weight?
Whateffect has being overweight or obese had on reaching your meaningful goals?
Obesity is when a person both weighs too much for their height and has too much body
fat. It occurs gradually over many years from consuming more calories than needed, and as
weight increases so does the risk of developing other medical problems. Usually it refers
tohavingmorethan30%bodyfat.
Obesity may not cause any symptoms, however some people may
notice shortness of breath, back or joint pain, or fatigue. Even if
apersondoesnotexperienceanyphysicalsymptoms,obesityhas
long-term health consequences and puts people at risk for
developing many other medical problems including: high blood
pressure,highcholesterol,acidreux(GERD),diabetes,heart
disease, stroke, and sleep disorders. Arthritis and other joint
problemsareoftenworsenedbecauseofexcessweight.
SometimesobesityisdeterminedbyameasurementcalledtheBodyMassIndexorBMI.
This is not necessarily an accurate measure of body fat because BMI only takes into
consideration,aperson’sheightandweight.Itdoesnotaccountformusclemass.Ahealthy
BMI is considered to be 19-25. A BMI of 25-30 is overweight and above 30 is considered
obese. A doctor may use other ways to measure obesity such as the waist to hip ratio.
Thewaisttohipratioisperformedbymeasuringaperson’shipcircumferenceandwaist
circumference. Generally, a waist to hip ratio of .7 is considered healthy for women and
.9 is considered healthy for men. This is based on evidence that having more body fat in
the belly or abdomen raises risk of many diseases. There are other tests that are more
accurate measures of body fat. The most commonly used is the skinfold caliper test.

Module #3Q
Handout
Integrated Illness Management
and Recovery Manual
Page 98
How can you manage your weight?
• Make changes to your diet - Making small, gradual but permanent changes to your diet
may reduce the amount of calories you consume each day. Remember that you need to
use more calories than you consume in order to lose weight.
• Increase activity level - Increasing activity not only burns calories, but some types of
exercise,likeweighttraining,buildleanmusclemasswhichwillincreasethebody’sme-
tabolism. The term metabolism means the rate at which a person burns calories.
• Determine your calorie needs-Therearemanymethodsusedtodetermineaperson’s
dailycalorieneeds.Ifyouareaimingtoloseweight,askyourdoctoratyournextvisit
how many calories you should be aiming for to lose 4-8 pounds per month (healthy weight
loss).
• Plan to lose weight slowly - A healthy rate to lose weight is ½-2 pounds per week. Losing
weightfasterthanthismaymakeitdifculttokeeptheweightoffinthelongrun.
• Don’t skip breakfast - Breakfast is called the most important meal of the day for a
reason!Studieshaveshownthatpeoplewhoeatbreakfastaremorelikelytobeat
a healthy weight than people who do not eat breakfast. Eating breakfast helps prevent
over-eating and may boost your metabolism.

Module #3Q
Handout
Integrated Illness Management
and Recovery Manual
Page 99
Name __________________________________________ Date _ _ / _ _ / _ _ _ _
To achieve good control of your _________, it is important to take practical step towards
better management. Take one step now, and after you have achieved it, move on to another.
Diet Exercise LoseWeight Takemedications Monitor
properly blood sugar
Quitsmoking Annualeyeexam Checkfeet DentalExam Personal
Goal
Getaushot Practicehealthy AnnualExams ReduceStress Avoid
sleep habits Alcohol
Selected Step:
Action Plan:
CondenceRuler:12345678910
Not Somewhat Extremely
condent condent condent
Module #3Q
Handout
Integrated Illness Management
and Recovery Manual
Page 100
Integrated Illness Management and Recovery
Home Practice Sheet
My home practice for this week is:
To complete this home practice, I will use the following plan:
When:
Where:
With Whom:
What do I need to do the practice?
Today’sDate:__/__/____
Participant: ____________________ IIMR Specialist:_________________________
Integrated Illness Management and Recovery
Home Practice Sheet
My home practice for this week is:
To complete this home practice, I will use the following plan:
When:
Where:
With Whom:
What do I need to do the practice?
Today’sDate:__/__/____
Participant: ____________________ IIMR Specialist:_________________________
Module #3R
Handout
Integrated Illness Management
and Recovery Manual
Page 101
Integrated Illness Management and Recovery
Handout #3R: Practical Facts About
Sexually Transmitted Infections (STI)
Let’s Discuss!
Whatdoyouknowaboutsexuallytransmittedinfections(STIs)?
How do people get STIs?
How might a STI interfere with reaching your meaningful goals?
Asexuallytransmittedinfection(STI)isaninfectioncausedbya
bacteriaoravirusthatisspreadthroughsexualcontact.Sexually
transmitted infections are very common.
Sexuallytransmittedinfectionsarediagnosedbyahealthcare
professional.Adetailedhistorymaybetakenandaphysicalexammight
beperformed.Manytestsforsexuallytransmittedinfectionsrequire
either a urine test or blood test.
There are a variety of STIs including:
Chlamydia - caused by bacteria. It is the most common STI (3 million men and women are
diagnosedeachyear).Itoftencausesnosymptoms,butcanleadtoseriouscomplications.
Symptoms can include: abnormal discharge from penis or vagina, pain during urination, low
grade fever, and vaginal bleeding. Chlamydia is treated with antibiotics.
Gonorrhea - caused by bacteria. It is sometimes referred to as “the clap.” Symptoms may
include: abdominal pain, fever, pus or discharge from penis or vagina, painful urination, and
menstrual irregularities. Gonorrhea is treated with antibiotics.
HPV or human papillomavirus - a virus that is spread by skin-to-skin contact. It is
extremelycommonandtherearemorethan100types.Someofthevirusesdonotcause
symptoms and are not harmful. Others may result in genital warts or may increase risk
of some genital and throat cancers. There is no treatment for “high risk” HPV, which may
increase risk of cancer, however treatments for changes in cervical cells found on a pap
smear can be treated. This is why routine pap smears are very important. “Low-risk” HPV
that causes warts can be treated.
Syphillis - caused by bacteria. Symptoms depend on the stage of the infection and it
oftentakesweeksafterexposuretoexperiencesymptoms.Symptomscanincludethe
following: sores, rashes, fatigue, sore throat, fever, swollen lymph nodes, and headaches.
Other symptoms can be present with symptoms or the infection can progress to a stage
where there are no symptoms at all. It can be treated with antibiotics, but the earlier
the infection is diagnosed, the simpler the treatment.

Module #3R
Handout
Integrated Illness Management
and Recovery Manual
Page 102
Herpes - caused by a virus. Symptoms of herpes can be mild and go unnoticed. Often, peo-
ple will notice one or more blisters in the genitals, anus, or mouth. The blisters break and
leave sores that can take 2-4 weeks to heal. Blisters often reoccur. There is no cure for
herpes, but treatments are available to reduce the amount and severity of outbreaks.
HIV/AIDS-HIVisthehumanimmunodeciencyvirus.Itisthevirusthatcanleadtoac-
quiredimmunedeciencysyndrome,orAIDS.Thevirusweakensaperson’sabilitytoght
offinfectionsandcancers.Itistransmittedthroughexchangeofbodilyuidsorblood.
Sexualtransmissionmostcommonlyoccursduringunprotectedvaginaloranalsex.
How can you prevent sexually transmitted infections?
• Useacondomeachandeverytimeyouhavesex,includingoralsex.Consistentand
correctcondomusereducesthelikelihoodofcatchingmostsexuallytransmitted
infections.
• Abstainfromsexualactivity.
• Havesexonlywithonlyonepartner.BothpartnersshouldbetestedforSTDsbefore
havingsex.

Module #3R
Handout
Integrated Illness Management
and Recovery Manual
Page 103
Name __________________________________________ Date _ _ / _ _ / _ _ _ _
To achieve good control of your _________, it is important to take practical step towards
better management. Take one step now, and after you have achieved it, move on to another.
Diet Exercise LoseWeight Takemedications Monitor
properly blood sugar
Quitsmoking Annualeyeexam Checkfeet DentalExam Personal
Goal
Getaushot Practicehealthy AnnualExams ReduceStress Avoid
sleep habits Alcohol
Selected Step:
Action Plan:
CondenceRuler:12345678910
Not Somewhat Extremely
condent condent condent
Module #3R
Handout
Integrated Illness Management
and Recovery Manual
Page 104
Integrated Illness Management and Recovery
Home Practice Sheet
My home practice for this week is:
To complete this home practice, I will use the following plan:
When:
Where:
With Whom:
What do I need to do the practice?
Today’sDate:__/__/____
Participant: ____________________ IIMR Specialist:_________________________
Integrated Illness Management and Recovery
Home Practice Sheet
My home practice for this week is:
To complete this home practice, I will use the following plan:
When:
Where:
With Whom:
What do I need to do the practice?
Today’sDate:__/__/____
Participant: ____________________ IIMR Specialist:_________________________
Module #3S
Handout
Integrated Illness Management
and Recovery Manual
Page 105
* If this is an area of interest and need, there are additional materials available in the Illness
Management and Recovery curriculum.
Let’s Discuss!
Whydopeopleusealcoholandothersubstances?Whathasbeenyourexperience?
What are some of the effects, positive and negative, of alcohol and other substances?
Usingalcohol,suchasdrinkingabeer,aglassofwine,oramixeddrink,iscommoninmodern
society. Using certain types of street drugs, such as marijuana, cocaine, amphetamines
(“speed”),andhallucinogens(suchasLSDand“ecstasy”),islesscommon.Althoughusing
these types of substances can make people feel good, they can also cause problems and make
itmoredifcultforpeopletomanagetheirpsychiatricillness.Lookatthechecklistbelow
and check off some of the reasons you use alcohol or other substances.
• Tosocialize
• To improve mood
• To cope with symptoms
• Distract from problems
• Part of daily routine
Substances can also have negative effects and can interfere with having a good quality of
life. Understanding both the positive and negative effects of using substances can help in
deciding whether to stop using them. Some of the common problems related to drug and
alcohol use are listed below.
• Increased symptoms/relapses
• Social problems
• Interference with work or school
• Daily living problems
• Legal problems
• Health problems
• Safety problems
• Psychological dependence
• Physical dependence
Commonly used substances and their effects
Itishelpfultounderstandwhatpeoplecommonlyexperiencewhentheyusealcoholand
drugs. The following table lists both the positive and negative effects of alcohol and drugs.
Integrated Illness Management and Recovery
Handout #3S: Alcohol and Substance Use
*
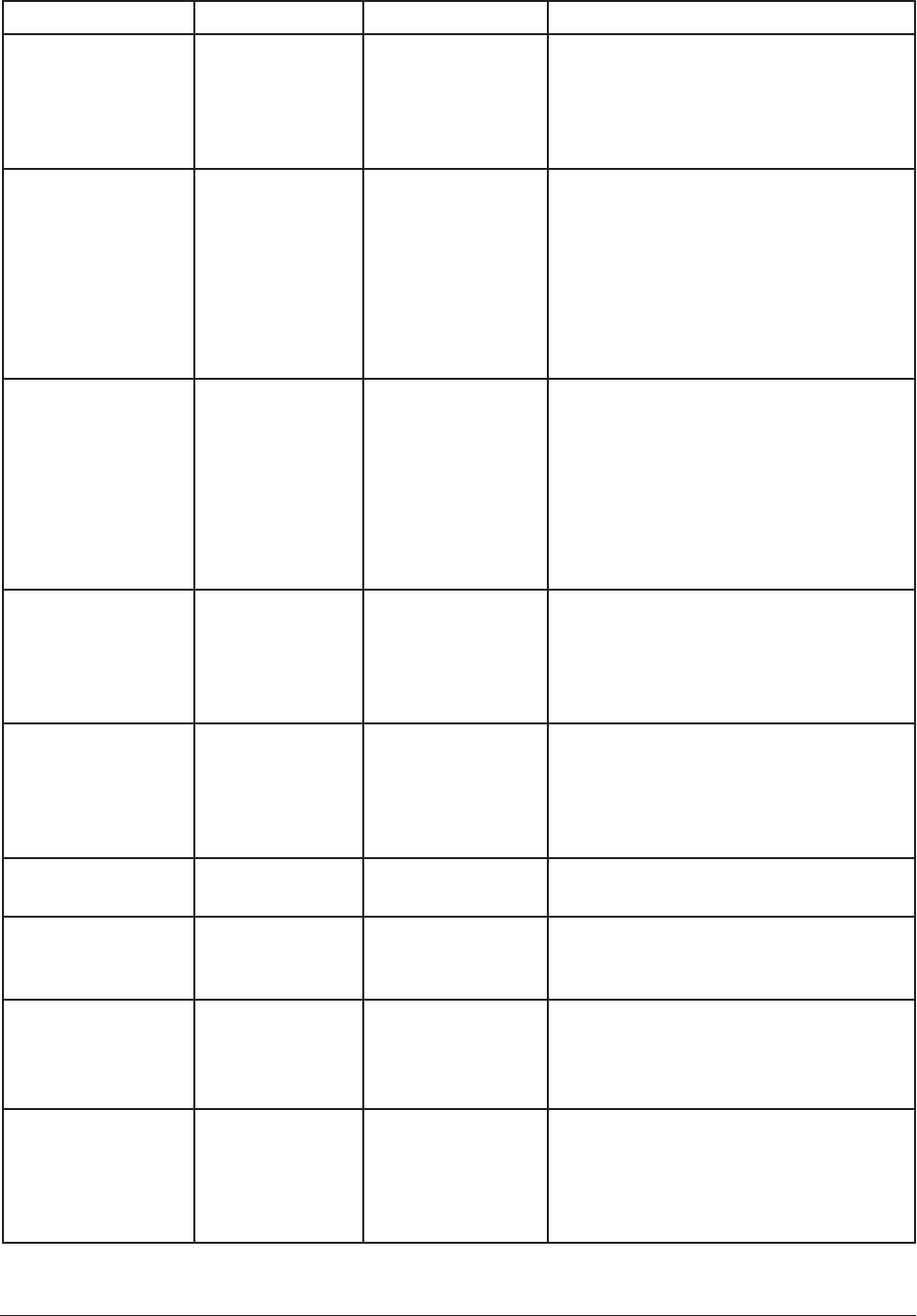
Module #3S
Handout
Integrated Illness Management
and Recovery Manual
Page 106
Commonly used substances and their effects
Substance Type Examples Positive Effects Negative Effects
Alcohol Beer, wine, gin,
whiskey, vodka,
tequila
•Relaxation
• Lighter mood
• Slower reaction time, drowsiness
• Socially embarrassing behavior
• May increase the risk of heart
disease, cancer, and liver
problems
Cannabis Marijuana,
hash, THC
•Relaxation
• “High” feeling
• Slower reaction time and poor
coordination
• Apathy and fatigue
• Paranoia
•Anxietyorpanicfeelings
• Long term risk to health of lungs,
may cause COPD or chronic
bronchitis
Stimulants Cocaine
(powder/or
crack),
amphetamines
(crystal meth.,
Dexedrine)
• Alert feeling
• Euphoria, good
feelings
•Anxiety
• Paranoia and psychosis
• Sleeplessness
• Some may have long term effect
on gastrointestinal system.
• Long-term use of methamphet-
amine may cause many health
and dental problems.
Hallucinogens LSD, ecstasy,
peyote,
mescaline
• Heightened
sensory
awareness
• Feeling of
well-being
• Bad “trips”
• Psychotic symptoms
Opiates Heroin, opium
morphine,
Vicodin,
Demerol,
Oxycontin
• Feeling of
well-being
•Relaxation
• Reduced pain
sensitivity
• Drowsiness
• Highly addictive
• Risk of overdose
Inhalants Glue, aerosols,
paint
• “High” feeling • Severe disorientation
•Toxic/braindamage
Caffeine Coffee, some
teas, some
sodas
• Alert feeling • Feeling jittery
• Can interfere with sleep
Nicotine Smoking,
chewing
tobacco
• Feeling alert
• Feels good
• Causes many health problems
including: lung disease, heart
disease, and increase chance of
developing a variety of cancers.
Benzodiazepines
(Anti-anxiety
medication)
Valium,
Xanax,
Klonopin,
Ativan
• Reduced
anxiety
•Relaxation
•Reboundanxietywhenmedication
wears off
• Loss of inhibition and
coordination
• Dulled senses
Module #3S
Handout
Integrated Illness Management
and Recovery Manual
Page 107
Substance use and the stress-vulnerability model
The stress-vulnerability model of mental illness, which was covered earlier in I-IMR,
explainshowusingsubstancescanmakethesymptomsofmentalillnessworse.Hereisa
brief review of the model below:
Thesymptomsofmentalillnessarecausedbybiologicalfactors(orvulnerabilities).These
biological factors can be made worse from:
• alcohol and drugs
• stress
These biological factors can be made better with:
• medications
• effective coping
• social support
• meaningful activities
Alcohol and drug use can make symptoms worse and cause relapses. Using these substances
can also interfere with medications, making them less effective at reducing symptoms and
preventing relapses. Because even small amounts of alcohol or drug use can cause these
problems, people with psychiatric illness can be described as putting themselves at a real
risk of setting off symptoms when they use substances.
Weighing the Pros and Cons of using substances
Decidingtostopusingalcoholanddrugscanbeadifcultdecisiontomake.Onewayto
helpyoumakethatdecisionistocomeupwithalistofallthe“pros”(advantages)ofusing
substances,andallthe“cons”(disadvantages)ofusingsubstances.Tobetterunderstand
your own reasons for using substances, complete the worksheet below.
“PROS” of using substances
List all the advantages of continuing
to use drugs and alcohol. (Consider
advantagessuchas:socializing,feelinggood,
escaping, coping with symptoms, something
to look forward to, habit, and any others
thatmightbeimportant.)
“CONS” of using substances
List all the disadvantages you can think
of for using substances. (Consider
disadvantages such as: worse symptoms
orrelapseofmentalillness,conictwith
family or friends, trouble with work or
school,parentingdifculties,problemswith
health,legalsystem,housing,ormoney.)
Module #3S
Handout
Integrated Illness Management
and Recovery Manual
Page 108
Considering all the “Pros” and “Cons”, do you want to cut down or
stop?
______ NO. I do not want to cut down or stop
______MAYBE.IthinkImightwanttocutdownorstopbutI’mnotsure.
______ YES. I would like to cut down or stop.
Deciding whether to cut down or stop using substances
Understanding the “pros” and “cons” of using substances can help you decide whether you
want to continue using. It is also helpful to consider the “pros” and “cons” of not using sub-
stances. What are the advantages of developing a sober lifestyle? What would you have to
give up in order to have such a lifestyle? Complete the worksheet below to
consider the “pros” and “cons” of becoming sober.
PROS of becoming sober
List the advantages of developing a sober
lifestyle. Consider how sobriety may help
you achieve personal recovery goals.
CONS of becoming sober
List what you think you might have to
give up if you stopped using substances.
Consider the “costs” of sobriety, such as
losing friends, nothing fun to do, troubling
symptoms, no escape, and feeling bad.
Considering all the “pros” and “cons” of sobriety and the “pros” and “cons” of using
substances(Worksheet1),wouldyouliketocutdownorstop?
_____ NO. I do not want to cut down or stop.
_____MAYBE.IthinkImightwanttocutdownorstopbutI’mnotsure.
_____ YES. I would like to stop.
Developing a sober lifestyle
When people decide to develop a sober lifestyle, it takes planning and practice. Sometimes
there can be setbacks along the way, such as urges to use substances or relapses in
substance use. Developing your own personal plan for a sober lifestyle is an important
part of managing your mental illness and achieving your personal recovery goals. There
are three important steps to achieving sobriety:
• Remember your reasons for not using substances.
• Develop a plan to prevent going back to using substances in “high risk” situations.
• Identify new ways of getting your needs met.
Module #3S
Handout
Integrated Illness Management
and Recovery Manual
Page 109
Whom do you know who has made positive changes by developing a
sober lifestyle?
Abstinence or Cutting Down?
Decidingtotakecontroloverone’slifebyaddressingproblemsrelatedtodrugoralcohol
use is an important decision that involves changing your lifestyle. Part of making such a
decisioninvolvesdecidingwhethertostopusingsubstancesaltogether(abstinence)orto
cut down but not stop using entirely.
Peoplewithsubstanceuseproblemsoftennditdifculttocutdownonusingsubstances,
because using even a small amount makes them want to have more. In addition, because
of the biological nature of psychiatric disorders, people with a mental illness can be very
sensitive to the effects of even small amounts of alcohol and drugs. This means that those
small amounts of substances can have drastic effects. For this reason, many people with
drug and alcohol problems are more successful developing a sober lifestyle rather than
cutting down how much they use.
Some people want to work on their substance use problems, but are not ready to stop using
completely. For these people, reducing the amount of alcohol or drugs that they use can
beagoodrststeptowardssobriety.
Making a Personal Sobriety Plan
Inordertoachieveyoursobrietygoals,itishelpfultodevelopaspecicplan.
The worksheet below can be used to help you develop your personal sobriety plan.
Personal Sobriety Plan
CONGRATULATIONS! You’ve taken the rst and most important step toward ridding
your life of problems related to alcohol and drugs. You can change or modify your
plan based on how well it is working for you. Share your plan with people who are
close to you so they can support you in achieving your sobriety.
Step 1. List one to three reasons how your life will be better by stopping using
substances. Consider how sobriety may help you achieve your personal recovery goals.
Step 2. Identify one to three “high risk” situations that can lead to unwanted use of
substances. Consider situations in which you have used substances in the past, such as
people offering you substances, being pressured to use, feeling bad, having nothing to do,
and cravings.
Module #3S
Handout
Integrated Illness Management
and Recovery Manual
Page 110
Step 3. Make a plan for how to deal with those “high risk” substance use situations.
For each “high risk” situation, identify one or two ways of dealing with it.
Situation 1:
Plan for dealing with it:
Situation 2:
Plan for dealing with it:
Situation 3:
Plan for dealing with it:
Module #3S
Handout
Integrated Illness Management
and Recovery Manual
Page 111
Step 4. Find new ways of getting your needs met. Consider the ways substances have met
yourneedsinthepast,suchashangingoutwithfriends,feelingrelaxedor“high,”dealing
with symptoms, or having something to do. What needs did they meet? For each need you
identify, think of at least one new strategy for getting that need met.
Need 1:
Strategy for meeting this need:
Need 2:
Strategy for meeting this need:
Need 3:
Strategy for meeting this need:
Recovery from Substance Use Problems
Taking control over your life and tackling your substance use problems can be hard work,
and there may be setbacks along the way. However, your strength and determination will
pay off as you become sober and reclaim your life. You have every right to be hopeful
that recovery is possible, and that you can take charge of your own life and grow past the
effectsthatsubstanceshavehadonit!
Module #3S
Handout
Integrated Illness Management
and Recovery Manual
Page 112
Integrated Illness Management and Recovery
Home Practice Sheet
My home practice for this week is:
To complete this home practice, I will use the following plan:
When:
Where:
With Whom:
What do I need to do the practice?
Today’sDate:__/__/____
Participant: ____________________ IIMR Specialist:_________________________
Integrated Illness Management and Recovery
Home Practice Sheet
My home practice for this week is:
To complete this home practice, I will use the following plan:
When:
Where:
With Whom:
What do I need to do the practice?
Today’sDate:__/__/____
Participant: ____________________ IIMR Specialist:_________________________

Module #4
Guidelines
Integrated Illness Management
and Recovery Manual
Page 113
Practitioner Guidelines for Handouts #4A-B:
Healthy Lifestyles
Goals
The Healthy Lifestyles handouts should take between 2-4 sessions to complete depending on whether
or not the Tobacco Smoking handout needs to be covered. The goal of this topic area is to provide some
very basic information on different elements of a healthy lifestyle: diet, exercise and physical activity, and
sleep habits. At the end of the Practitioner Guidelines for this section, there are suggestions of resources
you may want to access depending on the participant’s interest and knowledge about healthy lifestyle
change. Many consumers may identify healthy lifestyle goals and so this topic may be one that is revisit-
ed throughout the program. The purpose of the information in the handout is to increase motivation to
engage in health behavior changes by linking changes to improving self-management of medical problems
and psychiatric problems.
Suggestions for Teaching
• All smokers should also cover the Tobacco Smoking handout regardless of readiness to quit. If not
interested in quitting, emphasis should be on the decisional balance exercise and preparing to quit
strategies may be revisited if the client becomes motivated to try to quit smoking.
• Extensive resources exist both in the community and online for enhancing nutritional
and fitness education. Ask the client if there are aspects of fitness and or nutrition that he or she would
like to learn more about and support the client in accessing these resources.
• This topic has many potential opportunities for in vivo practices. In a group setting or working indi-
vidually, light stretching exercises could be practiced together. Grocery store visits and home visits to
assess knowledge and skill around preparing healthy foods could be invaluable.
• If sleep or eating habits are extremely dysfunctional and impacting the client’s life in a significant way,
exploring the possibility of a referral to a sleep clinic or to a therapist/treatment center that focuses on
eating disorders may be necessary.
Review Questions
What are some strategies you learned for eating a healthier diet?
What is the difference between physical activity and exercise?
What is it important to have a bedtime/sleep routine?
Suggestions for Home Practice
1. Ask the client if he or she would be willing to track eating habits by using a food log (simply writing
what is eaten on a calendar perhaps) to increase awareness about current eating habits and identify
areas for change.
2. Ask the client to think about exercise or physical activities enjoyed in the past or things that he or
she might like to try and brainstorm a list.
3. Identify one healthy sleep habit that the client is not doing and develop a plan for implementing it in
the upcoming week.
4. Monitor smoking/tobacco use by using the pack wraps in the handouts.

Module #4
Guidelines
Integrated Illness Management
and Recovery Manual
Page 114
Additional Resources
Nutrition and Diet
7 Ways to Jumpstart Healthy Life Changes
http://www.health.harvard.edu/healthbeat/7-ways-to-jumpstart-healthy-change-in-your-life
Website with links to various nutrition resources online
http://www.nutrition.gov/
Overeaters Anonymous
http://www.oa.org/
Exercise and Physical Activity
The President’s (Activity) Challenge
https://www.presidentschallenge.org/participate/index.shtml
Interesting tips for overcoming barriers to being more active
http://www.healthyalberta.com/activeliving.htm
Physical activity guidelines
http://www.health.gov/paguidelines/
Healthy Sleep Habits
Harvard Medical School-Division of Sleep Medicine
http://healthysleep.med.harvard.edu/need-sleep/what-can-you-do/good-sleep-habits
Healthy Sleep Awareness Project
http://www.sleepeducation.org/
American Sleep Apnea Association
http://www.sleepapnea.org/
National Sleep Foundation
http://sleepfoundation.org/
Smoking Cessation
SmokeFree.Gov
http://smokefree.gov/
American Lung Association
http://www.lung.org/stop-smoking/
Module #4A
Handout
Integrated Illness Management
and Recovery Manual
Page 115
Integrated Illness Management and Recovery
Handout #4A: Practical Facts About
Healthy Lifestyle
Let’s Discuss!
What is a healthy lifestyle?
What makes someone a “healthy person”?
How might being physically healthy help you to reach your goals?
How are mental health and physical health connected?
Are there healthy changes you have been thinking about making in your life?
A healthy lifestyle can support your physical and emotional well-being
to help you feel and do your best. A healthy lifestyle includes
behaviors such as eating healthy, getting enough sleep, being
physically active, and becoming a non-smoker. A healthy lifestyle is an
important part of managing medical problems and can also help with
your mood. For example, exercise can make you feel more energetic
and happier so you can do the things you want to do. Being physically
healthy can also make it easier to reach your life goals.
Module #4A
Handout
Integrated Illness Management
and Recovery Manual
Page 116
Healthy Eating
Let’s Discuss!
Why is eating healthier important part of a healthy lifestyle?
Would/Is eating healthier a step towards your personal goal? Why?
What changes would you like to make to your diet? Why are those changes important?
Making changes to your eating habits takes effort, but the results are very rewarding for
your emotional and physical well-being. Think of specic changes you would like to make
and develop a plan to accomplish the changes.
Place a checkmark next to each of the steps you would like to make to your eating habits
in the next 6 months. You may decide to work on one step at a time or more than one step
at a time, but it is best to avoid trying to make more than 2-3 changes at once. You may be
doing some of these behaviors already. If so, don’t check them off.
o Eat more fruits and vegetables
o Eat less sugary foods i.e. cookies, pies, cakes, high sugar cereals, etc.
o Eat smaller portion sizes
o Drink more water (versus juices, sodas, or caffeinated beverages)
o Eat fewer snacks foods or eat healthier snacks
o Reduce night eating
o Learn how to read nutrition labels
o Eat fewer high sodium food such as packaged/prepared foods and snacks
Let’s Discuss!
How much do you need to eat each day?
Have you ever tracked how much you were eating each day? How was that for you?
Why do you think it might be important?
Having a sense of how much you are eating each day can be an important part of main-
taining a healthy weight. Determining how much you need to eat each day will depend on
whether you want to lose weight or stay at your current weight. You will also need to con-
sider how much activity you get each day. How much you eat differs if you are very physi-
cally active versus spend most of the day sitting.
Module #4A
Handout
Integrated Illness Management
and Recovery Manual
Page 117
First, Let’s Discuss!
What are some ways you could eat less each day?
Can you think of what you ate yesterday?
Are there any substitutions you can think of that would make your eating healthier?
Here are some examples:
Drink water instead of soda!
Chicken instead of hamburger
Fruit instead of cookies.
Healthy breakfast ideas:
• Plain oatmeal is a wonderful breakfast food. It is low in fat
and high in ber. Whole-grain cereals are also healthy and
have vitamins and minerals. Look for low-fat, low sugar, and
high ber cereals and always use low fat or skim milk to
keep fat intake down. Try adding fruit to your oatmeal or
cereal such as peaches or berries.
• Mix 1/2-cup low-fat cottage cheese with ½ cup of fruit.
• Make an egg white omelet or use Egg Beaters (see package for serving
size) and top with 1-tablespoon salsa or try an omelet with a small
handful of chopped mushrooms or other vegetables.

Module #4A
Handout
Integrated Illness Management
and Recovery Manual
Page 118
Healthy lunch and dinner ideas:
• Choose chicken, sh, or beans instead of red
meat and cheese.
• Cook with oils that contain a lot of
polyunsaturated and monounsaturated fats,
like olive and canola oil instead of cooking with
butter.
• Eat vegetables and fruits at every meal. In fact,
most of your plate should be lled with vegetables
(or fruit).
Healthy snacks options:
• Microwave popcorn (snack size “light” bag)
• Veggie sticks (raw carrots, celery, cucumbers, red peppers, etc.)
• Fruit
• Unsalted (low-salt) pretzels (2 handfuls)
• Vanilla wafers or gingersnaps (no more than 6)
• Graham crackers (2 cracker sheets)
• Single slice of toast with tablespoon or less of
peanut butter
• Reduced-sodium Saltines or other crackers and low-fat cheese
(six crackers and six thin, small slices of cheese)
• A small handful of nuts (2 tablespoons)
Healthy restaurant eating:
• Before going to a restaurant, ask for a copy of the menu and identify the lower fat
items the restaurant has to offer before ordering. Many restaurants now offer menus
with nutritional content or special symbols that identify the healthy options.
• Most restaurants serve at least twice as much food as you need to eat. So, at the start
of the meal, ask the wait staff to pack up ½ of your meal. This way, you have another
meal to eat the next day!
Module #4A
Handout
Integrated Illness Management
and Recovery Manual
Page 119
Get Moving! Becoming More Physically Active
Let’s Discuss!
Why is being more physically active an important part of physical and emotional
health? What is the difference between exercise and physical activity?
How could getting more exercise and physical activity help you to reach your life
goals?
What kind of exercise or activity do you do now or have you enjoyed in the past?
What changes would you like to make to your activity level?
Exercise is planned physical activity lasting more than 10 minutes that is done for the sole
purpose of working on your tness that causes you to breathe heavy and/or make your
heart beat faster and/or sweat. There are many activities that are physically challenging,
like raking leaves or grocery shopping in a large store, but they are not exercise. In order
to stay healthy, you should try to do both: increase physical activity AND get regular
exercise.
Types of exercise
Stretching helps to keep joints healthy and exible and can also
improve balance and circulation. Improving exibility is important to
help us avoid injuries and make it easier to perform daily activities.
5-10 minutes is all you need to improve your felxibility. Stretching
can also be helpful for people with medical conditions such as arthritis
and other joint problems. Examples of stretching exercises: range of
motion exercise, yoga, tai chi, etc.
Aerobic exercise increases your heart rate, increases breathing and causes
you to perspire. It is the most effective form of exercise for weight loss
and is important for the management of many medical problems including:
high blood pressure, diabetes, high cholesterol, etc. Examples of aerobic
exercise: brisk walking, active yard work, jogging, dancing, bicycling, etc.
Strengthening or resistance exercises are important for building muscle
and keeping bones strong. If done 2 or 3 times per week, strength
exercises can help you to lose weight. Examples of resistance exercises:
weight lifting, swimming, bicycling, etc.
You don’t have to go to a gym to exercise. You can do exercises at home or in your
neighborhood. Can you think of ways to get more exercise?
Module #4A
Handout
Integrated Illness Management
and Recovery Manual
Page 120
Healthy Sleep Habits
Let’s Discuss!
What is a “good night’s sleep?”
Why is it important to physical and emotional health to get a good night’s sleep?
Would you like to improve your sleep habits?
How might improving sleep habits help you reach your life goals?
There are many factors that can make it difcult to fall asleep or stay asleep. However,
it is important to get enough sleep each night because poor sleep may affect our emotion-
al health as well as our physical health. For example, you might not have enough energy to
participate in exercise or other physical activity if you do not get enough sleep. You might
get depressed or irritable or have trouble concentrating or remembering things if you are
not sleeping well.
Place a checkmark next to each of the steps you would like to take to sleep better in the
next 6 months. You may decide to work on one step at a time or more than one step at a
time, but it is best to avoid trying to make more than 2-3 changes at once. You may be
doing some of these behaviors already. If so, don’t check them off.
o Go to bed and get up at the same times every day.
o Avoid caffeine after 6 PM and smoking within an hour of going to bed.
o Exercise so you feel tired at night, but try not to exercise right before bedtime. Finish
up all exercise 2-3 hours prior to bed.
o Don’t nap during the day.
o Avoid alcohol. It often causes early awakening.
o Do something relaxing before going to bed, such as reading, listening to music, having
herbal tea or warm milk, or watching something funny on TV (but not something
dramatic or stimulating).
o Make sure your room is dark and quiet; use an eye mask or earplugs.
o If you have trouble sleeping for more than 30 minutes, get out of bed and do something
relaxing for 15 minutes or more before returning to bed.
o Avoid screen time (TV, computer, electronic devices) too close to bedtime.
o Get outside. Exposure to natural light during the day may improve sleep.
o Experiment with “white noise” like a fan. White noise can help mask other noises in the
environment that might disturb sleep such as a car alarm or a dog barking.
o Make sure your room is dark. Light sends a message to the brain to wake up, even alarm
clock lights or other light from electronics in the room.
o Discuss with your doctor, whether or not you should get a referral to a sleep specialist.
Sleep disorders like sleep apnea (when people stop breathing while sleeping) are medical
issues for which treatment does exist.
o Research shows that the perfect temperature for sleeping is on the cooler side, about
65 degrees. Consider your room temperature when developing a plan for better sleep.

Module #4A
Handout
Integrated Illness Management
and Recovery Manual
Page 121
Integrated Illness Management and Recovery
Home Practice Sheet
My home practice for this week is:
To complete this home practice, I will use the following plan:
When:
Where:
With Whom:
What do I need to do the practice?
Today’s Date: _ _ / _ _ /_ _ _ _
Participant: ____________________ IIMR Specialist:_________________________
Integrated Illness Management and Recovery
Home Practice Sheet
My home practice for this week is:
To complete this home practice, I will use the following plan:
When:
Where:
With Whom:
What do I need to do the practice?
Today’s Date: _ _ / _ _ /_ _ _ _
Participant: ____________________ IIMR Specialist:_________________________
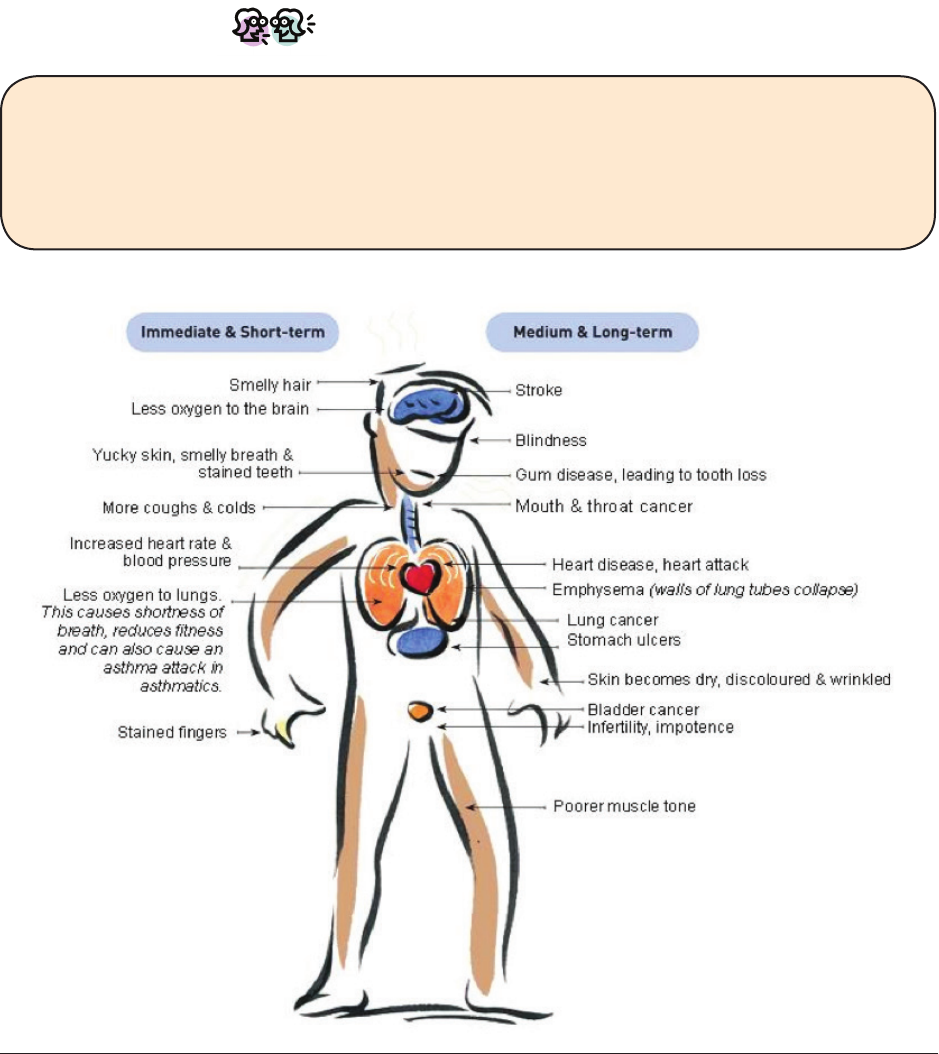
Module #4B
Handout
Integrated Illness Management
and Recovery Manual
Page 123
Integrated Illness Management and Recovery
Handout #4B: Practical Facts About
Tobacco Smoking
Smoking increases the risk of developing many health problems. Quitting smoking is
probably one of the best ways to better manage medical problems such as diabetes,
heart disease, arthritis, COPD, high blood pressure, and high cholesterol. You can also
reduce your risk of developing illnesses by quitting smoking.
Let’s Discuss!
How long have you been a smoker? What do you like about smoking? What do you
dislike about smoking? Have you ever tried to quit smoking? Tell me about your quit
attempt(s). Have you had any symptoms or health problems related to smoking?
How might smoking interfere with reaching your goals?
This diagram shows the bad effects of smoking on the body.
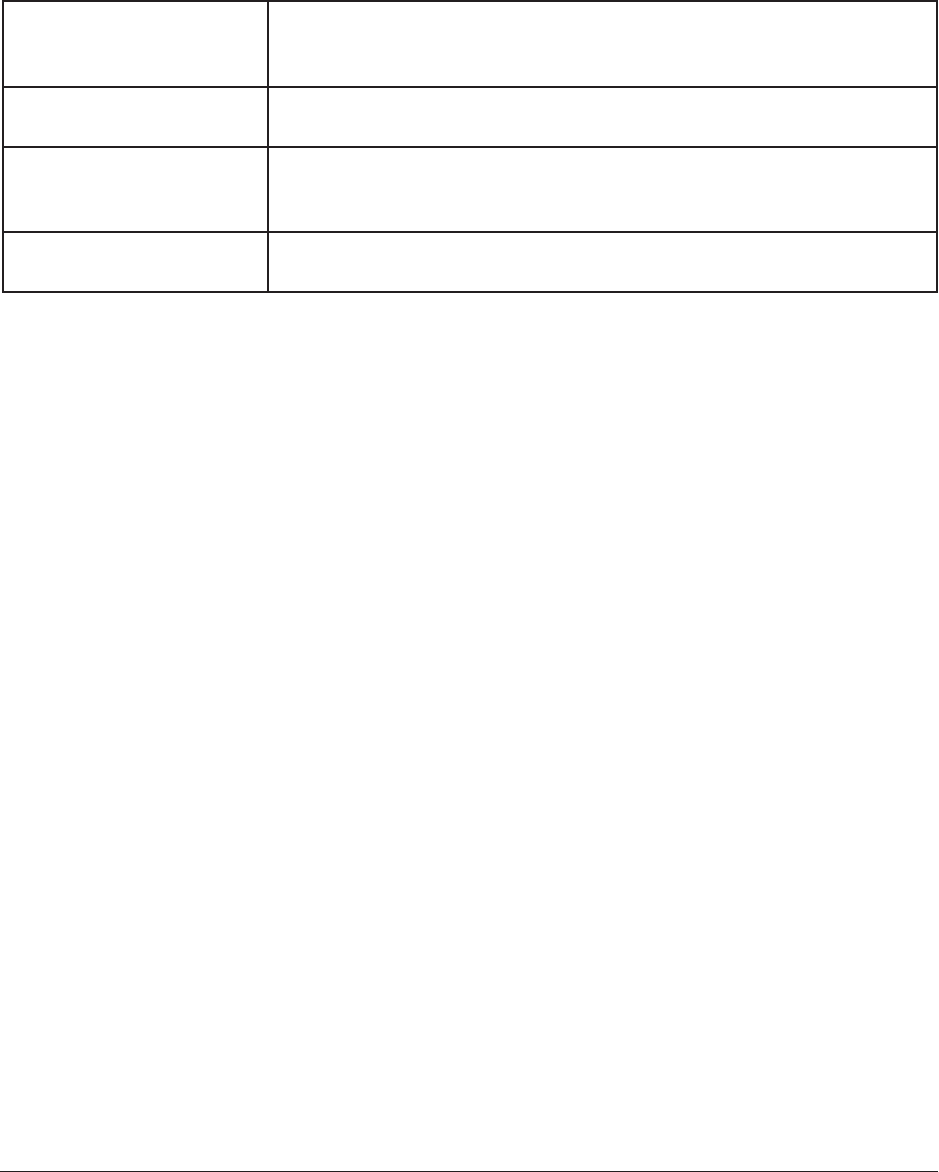
Module #4B
Handout
Integrated Illness Management
and Recovery Manual
Page 124
Deciding to quit smoking
Deciding to quit or to keep smoking is a very personal choice. Most people have to try to
quit many times before they are successful. There are several treatments available to
help people quit smoking. Research shows that people are more successful when they use
treatment versus trying to quit “cold turkey.” If you do quit, tell your doctor because the
level of some of your medications might increase as a result of quitting, so your dose might
have to be decreased.
Nicotine replacement
therapy (NRT)
• Contains nicotine and helps people with withdrawal symptoms
• Available as a gum, lozenge, patch, inhaler, or nasal spray
• Very few side effects, which depend on the form of NRT
Bupropion
(Zyban or Wellbutrin)
• Helps reduce physical withdrawal symptoms
• Can be used with nicotine replacement therapy
Varenicline (Chantix) • Twice daily medication that decreases cravings for nicotine
• Does not have nicotine
• Side effects may include nausea and vivid dreams
Counseling • Group or individual counseling offered locally
• Call 1-800-QUIT-NOW for free telephone counseling
Tips for preparing to quit smoking
• Monitor your smoking - Track what happens before you light up using the worksheet
below. Complete a worksheet every day for 1-2weeks. This will help you prepare for
situations that will be challenging when you try to quit.
• Think about why you smoke - Using the worksheet below, think about what makes you
want to continue to smoke and what makes you want to quit.
• Pick a treatment - Research shows that people have more success quitting if they use
treatment. Talk to your doctor about your options and use the treatment as prescribed.
• Drink water - Drinking lots of water can help ush out nicotine and other chemicals
from smoking and will also give you something else to do if you have an urge to smoke.
• Deep breathe - Quitting smoking may temporarily increase feelings of anxiety, but
these feelings are probably just your boy’s reaction to not having nicotine, which is
called “withdrawal.” Deep breathing can help with physical symptoms of withdrawal from
nicotine.
• Find other activities you enjoy - You get some enjoyment from smoking and you will
need to replace that with other activities, so think of hobbies and activities enjoy that
you can do.
• Spring clean - Cleaning your house thoroughly will help you get ready to quit because it
will make your environment smell fresh and clean. Get rid of ashtrays and lighters.
• Find a support - Let your friends and family members know that you are planning to quit.
People may offer encouragement. If people know ahead of time, they may not smoke
when you are around. Consider making plans with a friend on your quit date either to talk
to or do a fun activity.
• Set a quit date - Decide on a day you would like to quit. Plan out your day hour-by-hour
so that you have plenty to do on your quit day and so that you will be distracted and less
likely to think about smoking. Plan to see or talk to your supports and to do an activity
you enjoy.

Module #4B
Handout
Integrated Illness Management
and Recovery Manual
Page 125
Track Your Smoking: Pack Wraps
Write the date here ____________________
Morning Cigarette
1. What time is it? ___________________
2. What I am doing? (Circle activity or write in an activity)
Waking up Eating or drinking Socializing Driving Write in other____________
3. What is your mood? (Circle option below)
Bored Angry Frustrated Anxious Depressed Happy Relaxed Tired
4. How important is this cigarette? (Circle option below)
Most important Moderately important Least important
Middle of the Day Cigarette
1. What time is it? ___________________
2. What I am doing? (Circle activity or write in an activity)
Waking up Eating or drinking Socializing Driving Write in other____________
3. What is your mood? (Circle option below)
Bored Angry Frustrated Anxious Depressed Happy Relaxed Tired
4. How important is this cigarette? (Circle option below)
Most important Moderately important Least important
Evening Cigarette
1. What time is it? ___________________
2. What I am doing? (Circle activity or write in an activity)
Waking up Eating or drinking Socializing Driving Write in other____________
3. What is your mood? (Circle option below)
Bored Angry Frustrated Anxious Depressed Happy Relaxed Tired
4. How important is this cigarette? (Circle option below)
Most important Moderately important Least important
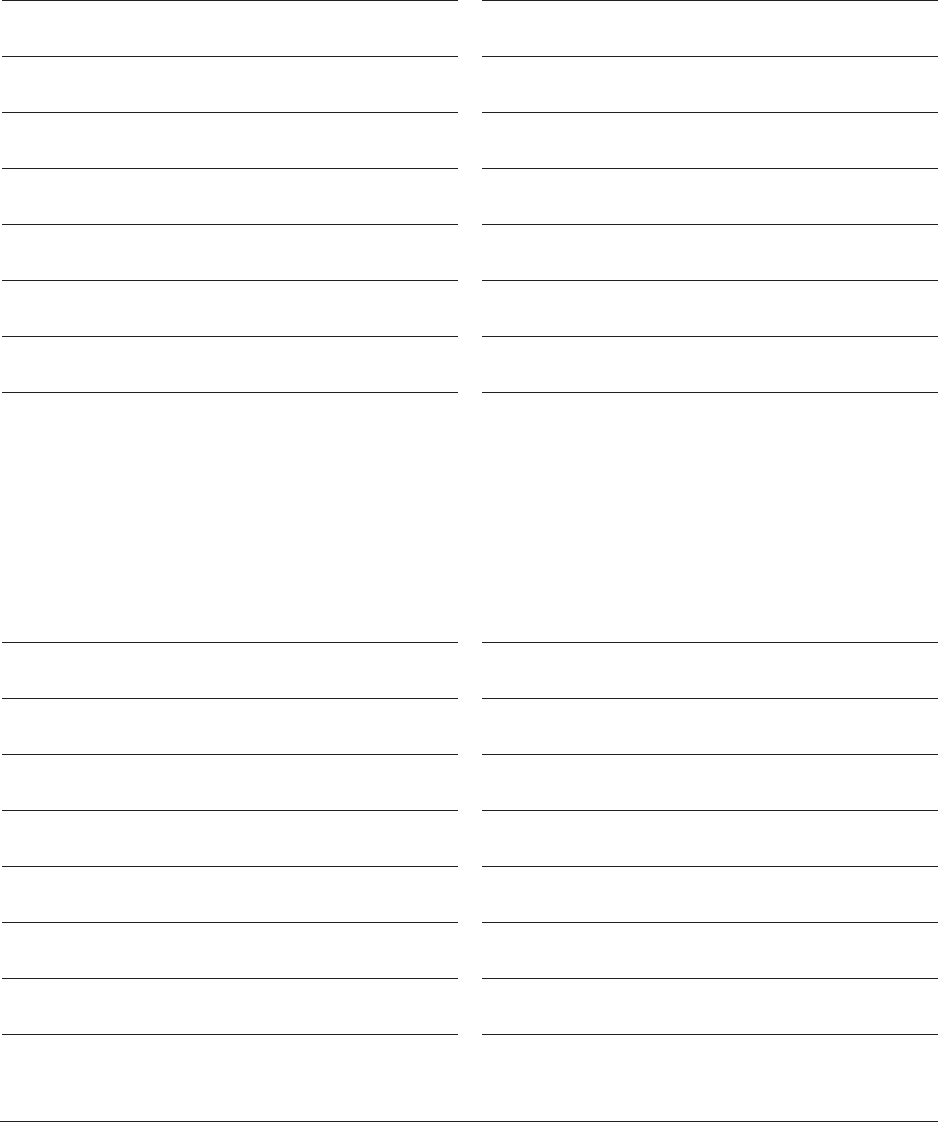
Module #4B
Handout
Integrated Illness Management
and Recovery Manual
Page 126
Balancing My Decision to Quit Smoking
Continuing Smoking
Costs Benets
Quitting Smoking
Costs Benets
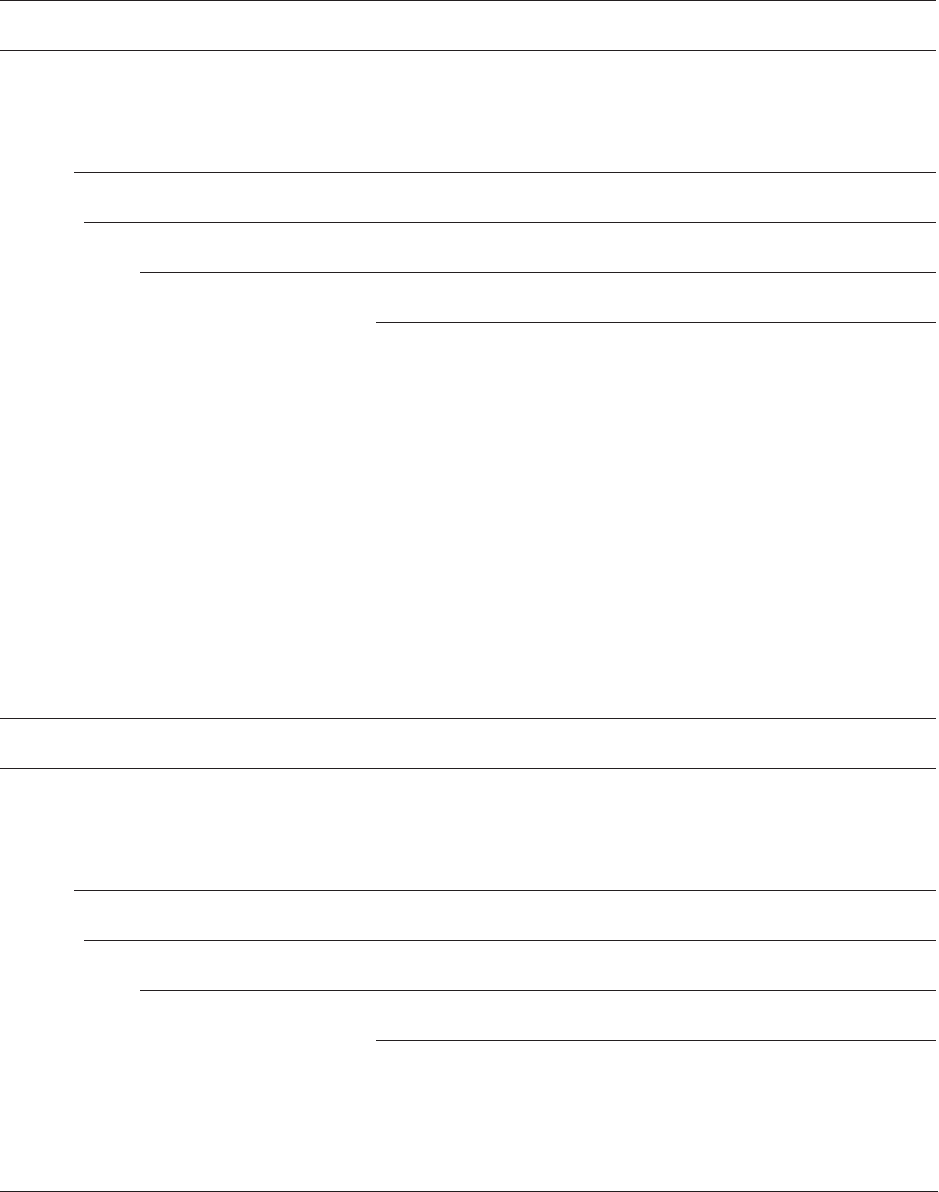
Module #4B
Handout
Integrated Illness Management
and Recovery Manual
Page 127
Integrated Illness Management and Recovery
Home Practice Sheet
My home practice for this week is:
To complete this home practice, I will use the following plan:
When:
Where:
With Whom:
What do I need to do the practice?
Today’s Date: _ _ / _ _ /_ _ _ _
Participant: ____________________ IIMR Specialist:_________________________
Integrated Illness Management and Recovery
Home Practice Sheet
My home practice for this week is:
To complete this home practice, I will use the following plan:
When:
Where:
With Whom:
What do I need to do the practice?
Today’s Date: _ _ / _ _ /_ _ _ _
Participant: ____________________ IIMR Specialist:_________________________

Module #5
Guidelines
Integrated Illness Management
and Recovery Manual
Page 129
Practitioner Guidelines for Handout #5:
Using Medication Effectively
Goals
This topic area can be covered in 3-4 sessions. The purpose of this topic is to medications for mental
illness and medical issues. Explore how taking medication may help with
reaching wellness and recovery goals. Help people make an informed decision about
taking medications including asking prescriber questions about medications.
Suggestions for Teaching
• When discussing medications, take opportunities to draw connections between taking medications as
prescribed and reaching meaningful goals.
• Encourage clients to examine beliefs about medication.
• Role-play how a client might ask their prescriber questions. Homework could include setting up an
appointment with the person’s doctor in order to ask questions.
• The practitioner could ask people to identify which medications they are currently
taking and which side effects they have experienced. If people have not talked to
their doctors about these side effects, they can role-play what they might say to
their doctor.
• The practitioner can model how to use a strategy for coping with side effects in the session (e.g., mus-
cle stretching exercise to help cope with muscle stiffness) and role-play with the person how to use the
strategy himself or herself.
• While discussing how to get the best results from medications, it may be appropriate to explore options
to improve adherence including: visual cues, electronic reminders, and pill boxes.
• Some individuals may not be able to fill a pill organizer box because of dexterity problems, vision
impairments, etc., and may not have someone at home to assist them. Help them explore local agencies
for programs that may help with medication-related tasks. Some pharmacies offer bubble packs or pre-
filled organizers as a service.
• People who have difficulty remembering whether or not they have taken their medication (and may
skip or take extra doses) should be encouraged to use a variety of tools including: pill organizers, cal-
endars or other strategies.
Review Questions
Do you know what medication you are taking for _______________?
How do you think it is working?
How do you make informed decisions about medications?
What is a symptom? What is a side effect?
What can you do if you are having bothersome side effects from medication?
What are your options?

Module #5
Guidelines
Integrated Illness Management
and Recovery Manual
Page 130
Suggestions for Home Practice
1. Ask the prescriber or nurse specific questions about medication. Develop a list of questions and any
upcoming appointments.
2. Implement a strategy for taking medication on a routine basis that was developed as part of behavior-
al tailoring. Involve family members and other supportive people whenever possible.
3. Encourage people to carry a list of medications with them at all times. Help the person develop a list
that they can carry with them.
Additional Resources
NAMI Hearts and Minds: A Roadmap to Wellness for People Living with Mental
Illness. There is a section on Medical Self-Advocacy that provides strategies for engaging in primary health
care and information about the impact of psychiatric medications and physical health.
http://www.nami.org/Content/NavigationMenu/Hearts_and_Minds/FINALfinal
RoadmaptoWellness.pdf
Download digital poster from SAMHSA on ways to promote wellness that includes working with primary
care doctor and asking questions.
http://store.samhsa.gov/product/SAMHSA-s-Wellness-Initiative-Three-Ways-to-
Promote-Wellness/SMA12-4569
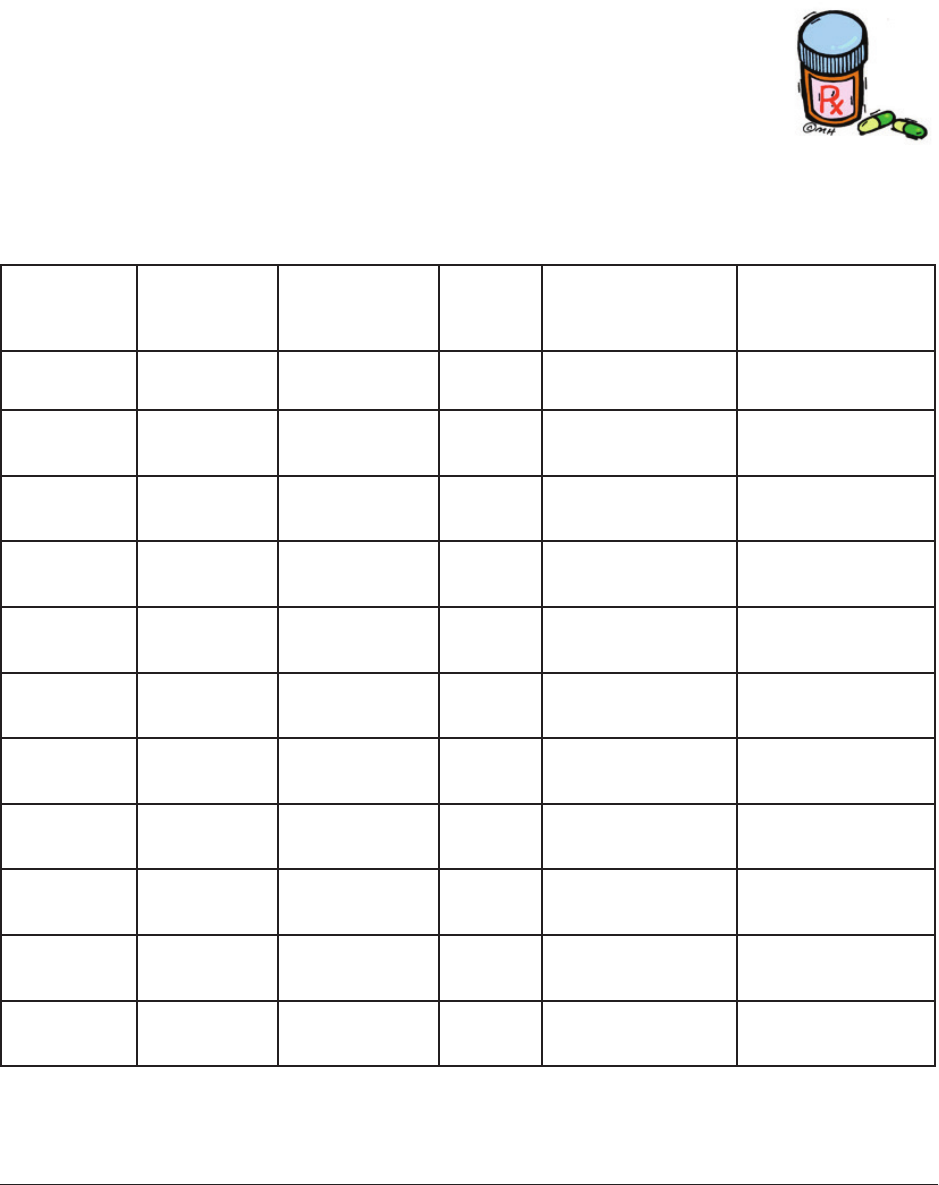
Module #5
Handout
Integrated Illness Management
and Recovery Manual
Page 131
Integrated Illness Management and Recovery
Handout #5:
Using Medication Effectively
This handout discusses medications for medical and psychiatric disorders.
Information is provided about the effects of medications, including their
advantages and disadvantages. People are encouraged to make their own
choices about taking medications. Strategies for getting the most out of
medications are described.
Make a list of all of your prescribed medications and the purpose of each one.
Medication List
Name of
Medication
I take this
medication
for…
Doctor’s
name
Dosage Medication
instructions
I started taking
this medication…
Atenolol High blood
pressure
Dr. Jane
Smith
1 mg Take 1 tablet
twice a day
January 2006
Learning More About Medications for Psychiatric Symptoms and Medical Disorders

Module #5
Handout
Integrated Illness Management
and Recovery Manual
Page 132
The medications and their benets for psychiatric symptoms and common medical
disorders are summarized on the following chart:
Medications and their benets
Category Medication I used Possible benets
Antipsychotics Can reduce symptoms of psychosis:
• Hallucinations
• Delusions
• Disorganized speech or behavior
Mood Stabilizers Can help reduce extremes of moods:
• Mania
• Depression
Antidepressants Can reduce the symptoms of depression:
• Low mood
• Poor appetite
• Sleep problems
• Low energy
• Difculty concentrating
• Helpful in treating anxiety disorders
Antianxiety or seda-
tives
Can reduce:
• Anxiety
• Feeling over-stimulated
• Difculty sleeping
Antihypertensives Can lower blood pressure
Cholesterol-lowering
medications
• Can raise HDL, “good cholesterol”
• Lower LDL, “bad cholesterol”
• Lower triglycerides
COPD medicines • Helps open the airway and bronchial
tubes
• Reduce swelling and inammation
Diabetes medicines
and Insulin
Can increase the amount of insulin in
the body
• Helps the cells use insulin more
effectively
• Helps the body’s cells to release more
insulin
• Decreases the amount of sugar
(glucose) released by the liver
• Increases the sensitivity of the body’s
tissue to insulin, increasing absorption
Pain medicines
(Appendix #9)
• Can reduce:
• Inammation (swelling) and pain
Other category:
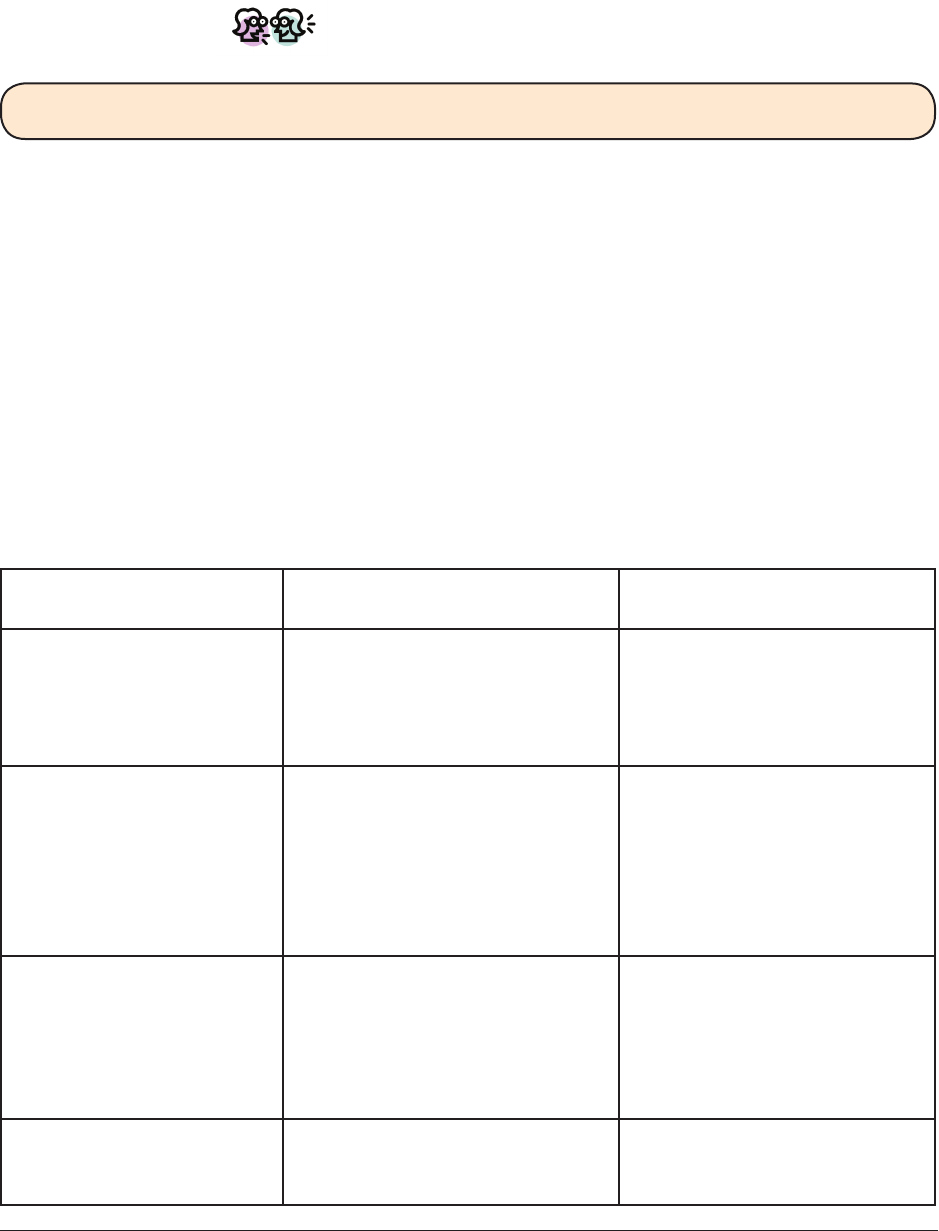
Module #5
Handout
Integrated Illness Management
and Recovery Manual
Page 133
At the end of this handout there are handouts with information about each type of
medication. Review the sheets that relate to the illnesses you have. Keep in mind, however,
that new medications are being developed all the time. Therefore, it is important to talk to
your doctor about what may have become available since these materials were printed.
Let’s Discuss!
What are “side effects” of medication?
Medications for mental illness and medical disorders can cause “side effects,” which are
undesired physical feelings that can be mild or severe. In most cases, side effects are
temporary, and improve over time as your body adjusts to medication. Some side effects
are very serious. If you recognize that you are having side effects, it is important to
contact your doctor as soon as possible. After evaluating how serious they are, your
doctor may recommend one of the following: reduce the dose of the medication, add
a side effect medication, or switch to another medication. The doctor may also suggest
some things that you can do to help reduce the discomfort or counteract the side
effects. There is also a handout with a list of strategies for coping with side effects.
The following table lists common side effects associated with medications (more
information about specic side effects is included in the information sheets on specic
types of medications).
Common side effects associated with medication
Medication Category Possible side effects Plan to cope with side
effect(s)
Antipsychotics • Muscle stiffness
• Mild tremors
• Restlessness
• Weight gain
• Diabetes
• Discuss with Prescriber
• Other:
Mood Stabilizers • Mild tremors
• Fatigue
• Nausea
• Muscle achiness
• Dry mouth
• Headaches
• Dizziness
• Discuss with Prescriber
• Other:
Antidepressants • Nausea
• Excitement
• Sexual problems
• Dry mouth
• Weight gain
• Dizziness
• Discuss with Prescriber
• Other:
Antianxiety or sedatives • Over-sedation
• Fatigue
• Problems with memory
• Discuss with Prescriber
• Other:
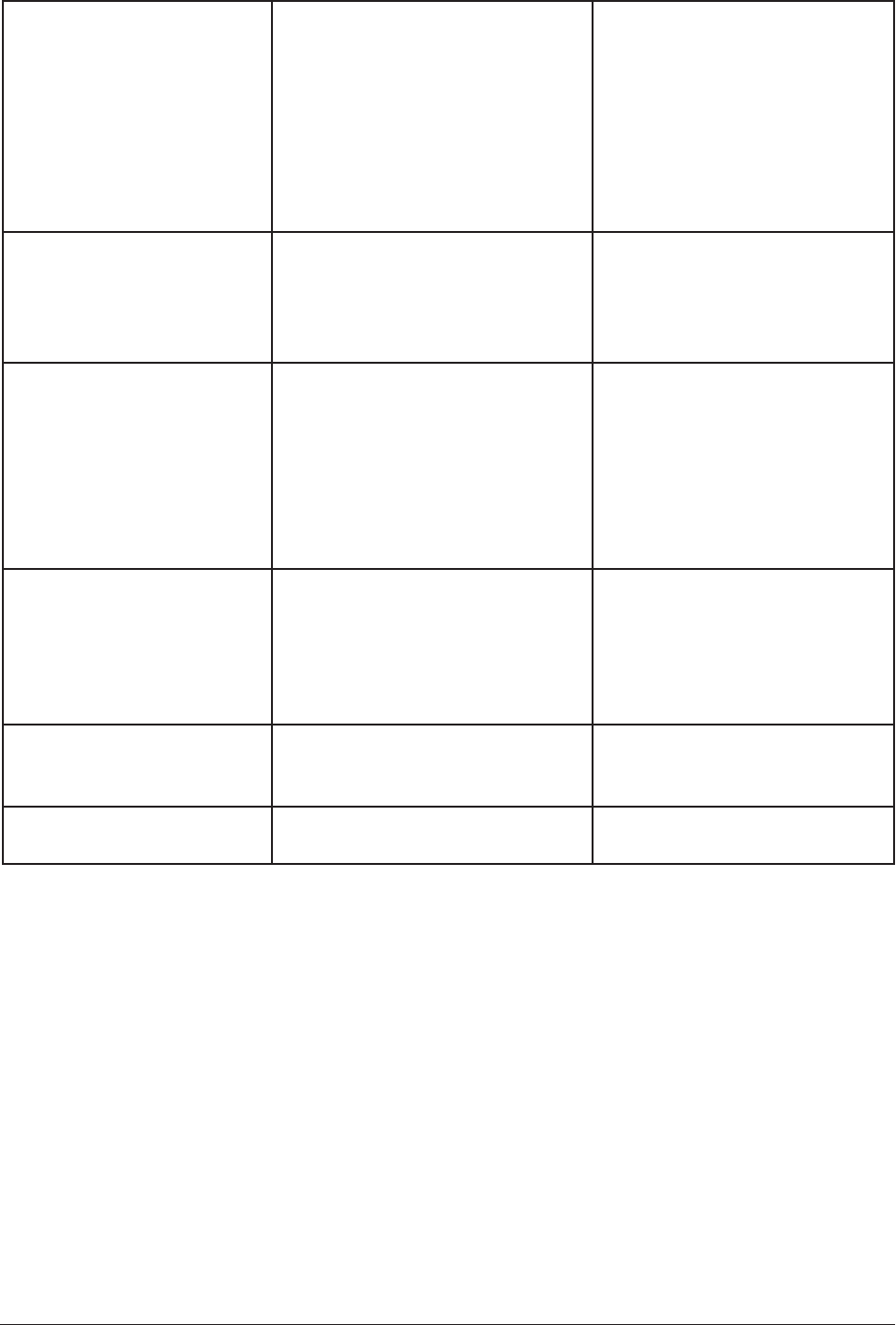
Module #5
Handout
Integrated Illness Management
and Recovery Manual
Page 134
Antihypertensives • Dehydration
• Fatigue
• Weakness
• Changes in sleep
• Sexual problems
• Cold hands/feet
• Headache
• Cough
• Constipation
• Discuss with Prescriber
• Other:
Cholesterol-lowering
medicines
• Gas
• Upset stomach
• Constipation
• Muscle problems
• Elevated liver enzymes
• Discuss with Prescriber
• Other:
Chronic obstructive pul-
monary disease medicines
• Rapid heartbeat
• Stomach upset
• Dry mouth
• Headache
• Increase in appetite
• Changes in blood sugar
• Retention of uid
• Depression
• Discuss with Prescriber
• Other:
Diabetes medicines and
Insulin
• Weight gain
• Headache
• Stomach upset
• Low blood sugar
• Metallic taste in mouth
• Gas
• Discuss with Prescriber
• Other:
Pain medicines • Stomach upset
• Bleeding problems
• Ulcers
• Discuss with Prescriber
• Other:
Other category: • Discuss with Prescriber
• Other:
Getting the most from your medications
Learning more about the medications you take is an important part of making good deci-
sions about your treatment. Working together with your doctor as in a partnership can be
helpful in making progress towards your recovery.
You should use you and your doctor’s expertise to make decisions about your medications
and your treatment. It helps to have some questions in mind when you are deciding about
taking medication or switching medications.
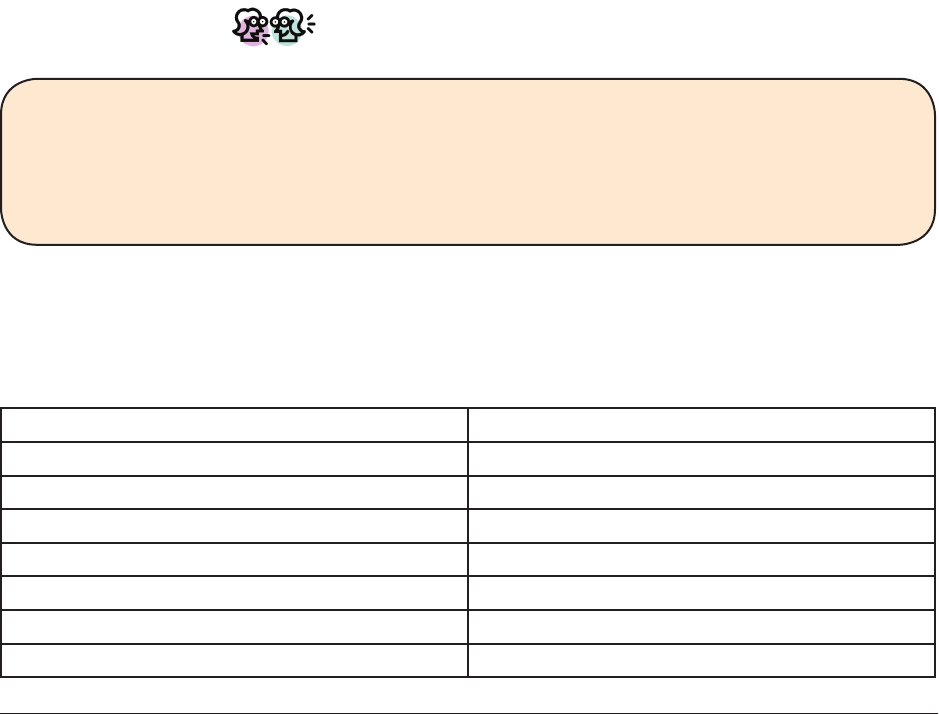
Module #5
Handout
Integrated Illness Management
and Recovery Manual
Page 135
Review the questions below and check off which questions you would like to bring with you
to your next meeting with your prescriber.
How will this medication benet me? What will it help me with?
How long does it take the medication to work?
What side effects might I get from the medicine?
What should I do if I notice side effects?
Is it ok to use the medicine for a long time (years)?
Why am I taking more than one medication for the same problem?
What if the medication doesn’t work for me?
Review the list of questions you want to ask your doctor then practice having the
conversation with your IMR practitioner or another group member. Follow these steps:
1. Make a list of the questions you want to ask your doctor
2. Tell your doctor that you want to talk about your medications
3. Tell your doctor about the medications you are taking
4. Ask the doctor the questions you have written down or talk about concerns that
you have about your medications
5. Thank your doctor for listening and helping
Let’s Discuss!
Now that you have reviewed the benets of medications, potential side effects, and
discussed questions you have about medications with your prescriber, it can be helpful
to summarize all of the information you have learned.
What are the most important things you have learned about your medication?
It can be helpful to think about how your medications are working well for you and ways
that they might not be working for you so that you can provide the best possible feedback
to your doctor. Fill out the chart below to summarize how your medications are working/
not working.
Ways medications are working for me Ways medications are not working for me

Module #5
Handout
Integrated Illness Management
and Recovery Manual
Page 136
Many people nd that it can be difcult to remember to take medications regularly. Below
are some strategies that can help you to take medications as part of your regular routine.
Simplify your medication schedule as much as possible.
When you take several medications several time search day, it is hard to
keep track of all the doses. Talk to your doctor about making your
medication schedule as simple as possible without losing any of the
benets (such switching to a long-acting medicine that is injected).
Take medications at the same time every day.
Taking medications at the same time (or times) every day makes it easier to remember.
Build taking medication into your daily routine.
It is often easier to remember to take medication if you do it right before or after anoth-
er daily activity. Examples of daily activities include brushing your teeth, showering, eating
breakfast, and getting ready to go to work.
Use cues to help yourself remember.
Many people have developed their own ways to help remember to take their medications
regularly. Examples include: using a pill container that is organized into daily doses, using
a calendar, making notes to yourself, asking a relative or other supporter to help you
remember.
Make a plan to use a strategy to help you get the best results from your medicaitons.
Share your strategy with a friend or family member and ask him or her to help you over
the next week to use your strategy. Keep track of how often you remember to take your
medication as prescribed.
Module #5
Handout
Integrated Illness Management
and Recovery Manual
Page 137
Integrated Illness Management and Recovery
Home Practice Sheet
My home practice for this week is:
To complete this home practice, I will use the following plan:
When:
Where:
With Whom:
What do I need to do the practice?
Today’s Date: _ _ / _ _ /_ _ _ _
Participant: ____________________ IIMR Specialist:_________________________
Integrated Illness Management and Recovery
Home Practice Sheet
My home practice for this week is:
To complete this home practice, I will use the following plan:
When:
Where:
With Whom:
What do I need to do the practice?
Today’s Date: _ _ / _ _ /_ _ _ _
Participant: ____________________ IIMR Specialist:_________________________
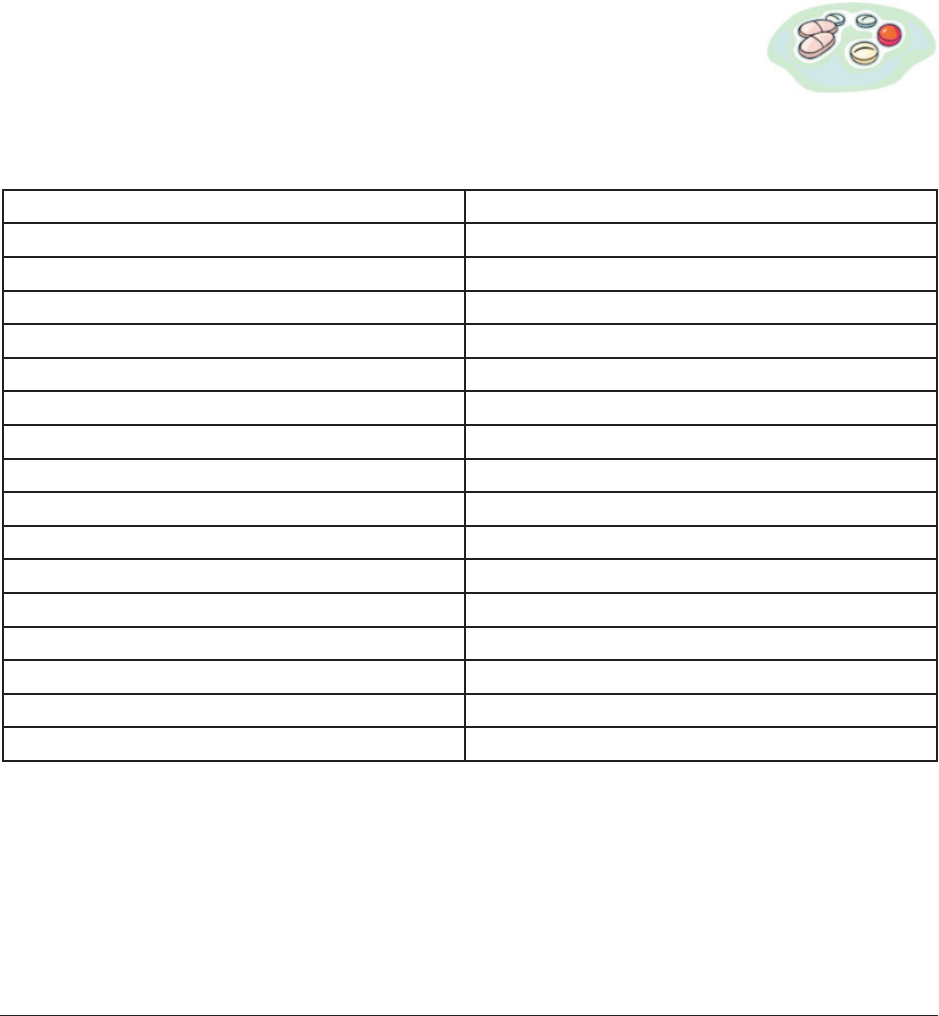
Module #5
Handout
Integrated Illness Management
and Recovery Manual
Page 138
Antipsychotic medications
Antipsychotic medications are sometimes called “major tranquilizers” or “neuroleptics.”
They reduce the symptoms of psychosis, including hearing or seeing things that aren’t
there (hallucinations), mistaken beliefs (delusions), and confused thinking (thought
disorders).
Antipsychotic medications are not addictive. They not only help reduce psychotic symp-
toms during and after a relapse, but also help prevent relapses and rehospitalizations.
Some of the newer medications also help reduce negative symptoms, including lack of
energy, motivation, pleasure, and emotional expressiveness. More medications are being
developed all the time, so it is important to keep up to-date with your doctor about what
medications are available.
The following chart contains the brand names and chemical names of
the antipsychotic medications that are currently available. Blank spaces
are provided to write in the names of new medications as they become
available.
Antipsychotic medications
Brand name Chemical name
Abilify aripiprazole
Clozaril clozapine
Geodon ziprasidone
Haldol haloperidol
Loxitane loxapine
Mellaril thioridazine
Moban molindone
Navane thiothixene
Prolixin uphenazine
Risperdal risperidone
Serentil mesoridazine
Seroquel quetiapine
Stelazine triuoperazine
Thorazine chlorpromazine
Trilafon perphenazine
Zyprexa olanzapine
Side effects of antipsychotic medications
People have very different reactions to medications. Some people who take antipsychotic
medications have side effects and some do not. Some antipsychotics cause muscle stiff-
ness, mild tremors, restlessness, and muscle spasms. Some can also cause sexual problems
or irregular menstrual periods. Many can cause weight gain, high blood sugar, and diabetes.

Module #5
Handout
Integrated Illness Management
and Recovery Manual
Page 139
“Tardive dyskinesia” is an undesirable side effect that involves muscle movements,
primarily in the face, mouth, tongue and hands, that cannot be controlled. Tardive
dyskinesia ranges from mild to severe. Let your doctor know if you notice any abnormal
muscle movements, so that he or she can evaluate for tardive dyskinesia. Not all
antipsychotics cause this.
“Agranulocytosis” is when people stop making white blood cells, which your body needs to
ght infections. It is a dangerous side effect of clozaril. Luckily, most people do not get
this side effect. People who take clozaril have regular blood tests to monitor white blood
cell levels.
Treatment of side effects
When you have side effects, contact your doctor immediately. After discussing the
side effects and evaluating how serious they are, he or she may recommend one of the
following: reduce the dose of the medication, add a side effect medication, or switch to
another medication. The doctor may also suggest some things that you can do to help
reduce the discomfort or counteract the side effects. See the “Coping with Medication
Side Effects” handout for other ideas.
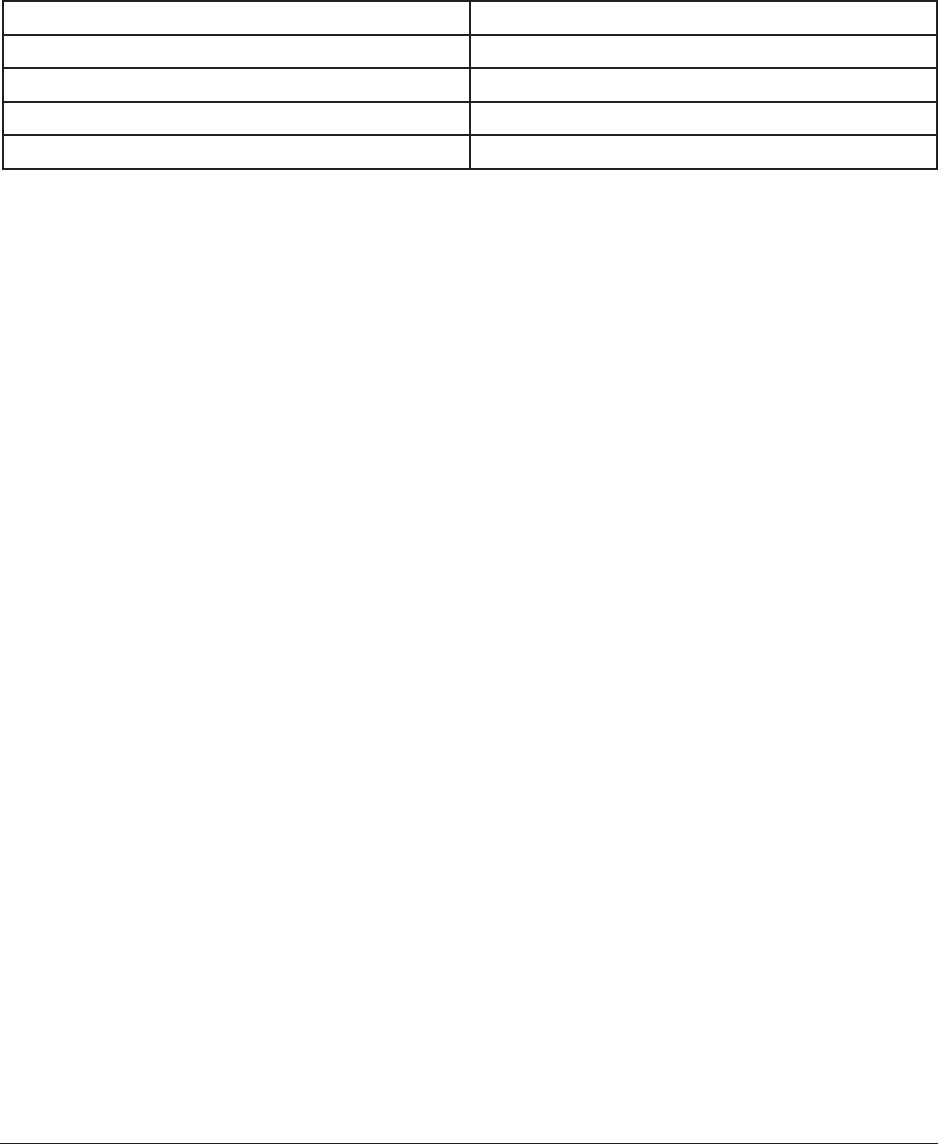
Module #5
Handout
Integrated Illness Management
and Recovery Manual
Page 140
Mood stabilizers
Mood stabilizing medications help treat problems with very low (depression) and very high
(mania) moods. They help to reduce symptoms and to prevent relapses and re-hospitaliza-
tions. They are not addictive. The following chart lists the most common mood stabilizers.
Mood stabilizing medications
Brand Name Chemical Name
Eskalith, Eskalith controlled release Lithium carbonate
Tegretol carbamazepine
Depakote, Depakene valproic acid
Lamictal lamotrigine
Side effects of mood stabilizers
Not everyone who takes mood stabilizers experiences side effects. However, it is
important to be aware of possible side effects and to contact your doctor as soon as
you notice them.
Lithium
Possible side effects include nausea, stomach cramps, thirst, fatigue, headache, and mild
tremors. More serious side effects include: vomiting, diarrhea, extreme thirst, muscle
twitching, slurred speech, confusion, dizziness, or stupor.
Although lithium is a natural chemical element, like oxygen or iron, it can be harmful
if there is too much of it in your body. To prevent this, the doctor must monitor the
amount of lithium in the body by taking regular blood tests.
It is also important to have enough salt in your diet while taking lithium, because
the sodium in salt helps to get rid of excess lithium. This means you should avoid
prescription and over-the-counter medications that get rid of excess water in your
body (diuretics) such as Fluidex with Pamabrom, Aqua-Ban, Tri-Aqua, or Aqua-rid.
Tegretol and Depakote
Possible side effects include: fatigue, muscle ache or weakness, dry mouth, constipation
or diarrhea, loss of appetite, nausea, skin rash, headache, dizziness, decreased sexual
interest, and temporary hair loss.
Some side effects are more serious, including: confusion, fever, jaundice, abnormal
bruising or bleeding, swelling of lymph glands, vomiting, and vision problems (such as
double vision). It is important to have regular blood tests to monitor the level of these
medications, and to check for any changes in blood cells and liver function.

Module #5
Handout
Integrated Illness Management
and Recovery Manual
Page 141
Lamictal
Possible side effects of Lamictal include dizziness, headaches, double vision,
unsteadiness, nausea, blurred vision, sleepiness, vomiting and a mild rash. These
symptoms usually occur when rst starting the medication and shortly after an
increase in dosage and then often fade. A severe rash should be reported to your
doctor immediately.
Because these medications can cause sleepiness, you must be cautious when driving
or using heavy machinery. It is recommended to limit drinking to one alcoholic drink
per week.
Treatment for side effects
When you have side effects, contact your doctor immediately. After discussing the
side effects and evaluating how serious they are, he or she may recommend one of the
following: reduce the dose of the medication, add a side effect medication, or switch
to another medication. The doctor may also suggest some things that you can do to help
reduce the discomfort or counteract the side effects. See the “Coping with Medication
Side Effects” handout for other ideas.
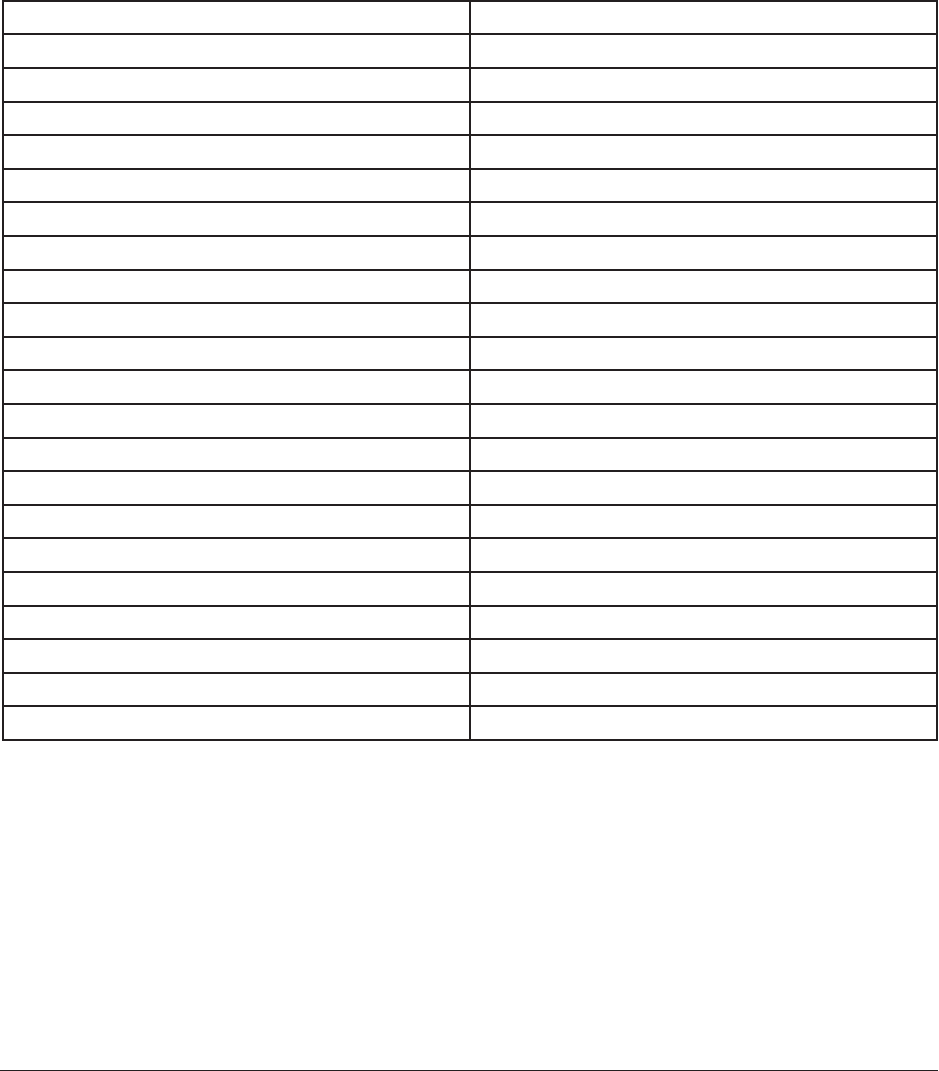
Module #5
Handout
Integrated Illness Management
and Recovery Manual
Page 142
Antidepressants
Antidepressants treat the symptoms of depression, including low mood, low energy,
appetite problems, sleep problems, and poor concentration. They help to reduce symptoms
and prevent relapses and hospitalizations. Antidepressants can also be effective for the
treatment of anxiety disorders such as panic disorder, obsessive compulsive disorder
and phobias. They are not addictive. The following chart lists the most common
antidepressants.
Antidepressant medications
Brand Name Chemical Name
Anafranil clomipramine
Celexa citalopram hydrobromide
Cymbalta duloxetine
Desyrel trazodone
Effexor venlafaxine
Elavil amitriptyline
Lexapro escitalopram oxalate
Ludiomil maptrotiline
Luvox uvoxamine
Marplan isocarboxazid
Nardil phenelzine
Norpramin desipramine
Pamelor, Aventyl nortriptyline
Paxil paraxitine
Prozac uoxetine
Serzone nefazadone
Sinequan, Adapin doxepin
Tofranil imipramine
Vivactil protriptyline
Wellbutrin buproprion
Zoloft sertraline
Side effects of antidepressants
Not everyone has side effects from antidepressants. Tell your doctor about any of the
following side effects: nausea, vomiting, excitement, agitation, headache, sexual problems,
dry mouth, dizziness, sleepiness, weight gain, constipation, heart palpitations, insomnia,
memory problems, overstimulation, extremely high blood pressure.
Hypomania, mania and antidepressants
A small percentage of people who take antidepressants develop symptoms of hypomania
or mania, including irritability, argumentativeness, agitation, decreased need for sleep,

Module #5
Handout
Integrated Illness Management
and Recovery Manual
Page 143
excessive talking, grandiosity, euphoria, hostility, extreme goal-directed behavior, and
behaving in ways that could be risky (hitchhiking, unprotected sex, spending more money
than you have). If you experience these symptoms, notify your doctor immediately. He or
she may lower your dosage of medication or stop it altogether.
Precautions when taking Marplan and Nardil
There are many foods and drugs that should be avoided when
taking Marplan and Nardil, including foods that are high in
tyramine, such as aged cheeses, aged meats (like salami and
pepperoni), and yeast extracts (except when they are baked into
breads). You should also avoid drinking beer, Chianti wine, sherry
wine and vermouth and taking certain medications such as
Tegretol, Dopar, Sinemet, Demerol, Aldomet, Ritalin,
decongestants and stimulants. It is important to obtain a
complete list from your doctor of drugs and foods to avoid. Although it is unusual,
occasionally people develop carpal tunnel syndrome when they take Marplan or Nardil.
This can be corrected by appropriate vitamin
supplements.
Treatment of side effects
When you have side effects, contact your doctor immediately. After discussing the
side effects and evaluating how serious they are, he or she may recommend one of the
following: reduce the dose of the medication, add a side effect medication, or switch
to another medication. The doctor may also suggest some things that you can do to help
reduce the discomfort or counteract the side effects. See the “Coping with Medication
Side Effects” handout for other ideas.
Module #5
Handout
Integrated Illness Management
and Recovery Manual
Page 144
Antianxiety and sleep medications
Antianxiety and sleep medications help reduce anxiety. Some of these medications also
help people sleep. Unlike other psychiatric medications, these medications take only
1-2 hours to work. Some antianxiety and sleep medications can be addictive and you should
try not to use them for months or years. Your doctor will carefully monitor your use of
these medicines.
The following chart lists the most common antianxiety and sleep
medications. Some of the medications can be used to help both anxiety
and sleep problems, while others are used to help only one of these
problems. Some of these medications are addictive, while others are not.
Antianxiety and sleep medications
Brand Name Chemical Name
Ativan lorazepam
Benadryl diphenhydramine
Buspar buspirone
Centrax prazepam
Dalmane urazepam
Halcion triazolam
Klonopin clonazepam
Librium chlordiazepoxide
Noctec Chloral hydrate
Restoril temazepam
Serax oxazepam
Valium diazepam
Xanax alprazolam
Side effects of antianxiety and sleep medications
Not everyone has side effects of these medications. The most common side effects
are sleepiness, fatigue, and poor memory (or other thinking problems). Because these
medicines cause sleepiness, limit drinking (no more than one drink /week). Also, be careful
when driving.
Treatment of side effects
If you have side effects, contact your doctor immediately. After discussing the side
effects and evaluating how serious they are, he or she may recommend one of the
following: reduce the dose of the medication, add a side effect medication, or switch
to another medication. The doctor may also suggest some things that you can do to help
reduce the discomfort or counteract the side effects. See the “Coping with Medication
Side Effects” handout for other ideas.
Module #5
Handout
Integrated Illness Management
and Recovery Manual
Page 145
Antihypertensive medications
The main purpose of antihypertensive medications is to lower blood pressure, however
there are several categories of these medications (listed below) and they work in
different ways.
• Diuretics
• Beta-blockers
• Angiotensin receptor blockers
• Angiotensin converting enzyme (ACE) inhibitors
• Calcium channel blockers
• Alpha-blockers99
Diuretics
• These medications get rid of water and salt from the body, making it easier for the
heart to pump your blood.
• Side effects are not having enough water in your body, weakness, and fatigue.
Sometimes the doctor will prescribe potassium pills to treat this side effect.
Beta-blockers
• These medications slow the rate that the heart beats.
• Side effects include: changes in sleep patterns, cold hands/feet, dry eyes/mouth,
impotence, fatigue, and occasionally depression.
Angiotensin antagonists
• These medications protect blood vessels from the hormone angiotensin II. This keeps
blood vessels wider which lowers pressure in the blood vessels.
• Side effects include: headache, cough, sore throat and swelling.
Angiotensin converting enzyme (ACE) inhibitors
• These medications prevent the production of hormone angiotensin II, a hormone that
causes narrowing of the blood vessels.
• Side effects include: skin rash, cough, decreased ability to taste food and, rarely,
kidney damage.
Calcium channel blockers
• These medications prevent calcium from entering the cells. This lowers blood pressure
by relaxing blood vessels.
• Side effects include: constipation, dizziness/headache, and increased or irregular
heart rate.
Module #5
Handout
Integrated Illness Management
and Recovery Manual
Page 146
Alpha-blockers
• These medications allow blood to pass easily through the vessels by reducing the nerve
impulses to the blood vessels.
• Side effects include: change in heart rate and dizziness.
Antihypertensive Medications
Brand Name Chemical Name Category
Tenormin Atenolol Beta-blocker
Sectraol Acebutolol Beta-blocker
Zestril Lisinopril ACE inhibitor
Lozol Indapamide Diuretic
Lasix Furosemide Diuretic
Vasotec Enalapril Maleate ACE inhibitor
Altace Ramipril ACE inhibitor
Avapro Irbesarten Angiotensin reception
blocker
Cardizem Diltiazem Hydrochloride Calcium channel blocker
Plendil Felodipine Calcium channel blocker
Lotensin Benazepril Hydrochlo-
ride
ACE inhibitor
Capoten Captopril ACE inhibitor
Treatment of side effects
If you have side effects, contact your doctor immediately. After discussing the side
effects and evaluating how serious they are, he or she may recommend one of the
following: reduce the dose of the medication, add a side effect medication, or switch
to another medication. The doctor may also suggest some things that you can do to help
reduce the discomfort or counteract the side effects. See the “Coping with Medication
Side Effects” handout for other ideas.
Module #5
Handout
Integrated Illness Management
and Recovery Manual
Page 147
Cholesterol-lowering medications
Medications for cholesterol do three things: raise HDL, “good cholesterol,” lower LDL,
“bad cholesterol,” and lower triglycerides (another type of fat in the blood).
Statins
These medications lower low-density lipoprotein, LDL, by lowering cholesterol production.
Bile acid sequestrates
These medications lower LDL by helping to eliminate cholesterol in the bowels.
Fibrates
These medications lower triglyceride and may increase HDL.
Niacin (nicotinic acid)
This is a B-vitamin that your doctor might prescribe in a higher amount than what is found
in over-the-counter pills. Niacin can lower LDL and triglycerides as well as increase HDL.
High doses of niacin can have many side effects such as hot ashes, gastrointestinal
symptoms such as nausea, gas, vomiting, peptic ulcers, and diarrhea, liver problems, gout,
and high blood sugar. Doctors try not to prescribe niacin to lower cholesterol because it
can raise blood sugar.
Side effects of cholesterol-lowering medications
Side effects include: gas, upset stomach, cramps and constipation, elevated liver enzymes,
muscle problems, and increased risk for cholesterol gall stones.
Medications for high cholesterol
Brand Name Chemical Name Category
Lipitor Atorvastatin Statin
Lescol Fluvastatin HMG CoA reductase
inhibitor
Crestor Rosuvastatin Statin
Tricor Fenobrate Bile acid sequestrants
Welchol Colesevelam Bile acid sequestrants
Colestid Colestipol Bile acid sequestrants
Lopid Gembrozil Fibrates
Questran Cholestyramine Bile acid sequestrants
Niacin/Nicotonic Acid Niacin/Nicotonic Acid RX strength B-vitamin

Module #5
Handout
Integrated Illness Management
and Recovery Manual
Page 148
Treatment of side effects
If you have side effects, contact your doctor immediately. After discussing the side
effects and evaluating how serious they are, he or she may recommend one of the
following: reduce the dose of the medication, add a side effect medication, or switch
to another medication. The doctor may also suggest some things that you can do to help
reduce the discomfort or counteract the side effects. See the “Coping with Medication
Side Effects” handout for other ideas.
Module #5
Handout
Integrated Illness Management
and Recovery Manual
Page 149
COPD medications
There are two main types of medications used for the treatment of COPD: bronchodilators
and corticosteroids. Both can be taken in the form of a pill or inhaled through an inhaler
or nebulizer.
Bronchodilators work to open the airway, bronchial tubes,
to the lungs. Side effects differ depending on the type of
bronchodilator but may include: rapid heartbeat, stomach
upset, dry mouth (inhaled anticholinergic), headache, high blood
pressure and hand tremors.
Corticosteroids reduce swelling and inammation. Side effects of
inhaled corticosteroids include thrush (yeast overgrowth in the
mouth) and dry mouth. Side effects of oral corticosteroids can be serious and should
be reported to your doctor. Effects of short-term use include: stomach upset, increase
in appetite, changes in blood sugar, too much uid in the body (swelling), depression,
irritability, and insomnia. Long-term effects include: high blood pressure, softening
of the bones, cataracts (clouding of the lens in your eye), and reduced ability to heal
(skin wounds).
In addition, expectorants or mucolytics may be prescribed to reduce the amount of mucus
in the airways and lungs.
COPD medications
Brand Name Chemical Name Category
Flovent Fluticasone Inhaled Corticosteroid
Xopenex Levalbuterol Bronchodilator
Serevent Salmeterol Xinafoate Bronchodilator
Theo-Dur, Respid Theophylline Broncodilator
Prednisone Prednisone Oral Corticosteroid
Mucomyst Acetylcysteine Mucolytic
Treatment of side effects
If you have side effects, contact your doctor immediately. After discussing the side
effects and evaluating how serious they are, he or she may recommend one of the
following: reduce the dose of the medication, add a side effect medication, or switch
to another medication. The doctor may also suggest some things that you can do to help
reduce the discomfort or counteract the side effects. See the “Coping with Medication
Side Effects” handout for other ideas.

Module #5
Handout
Integrated Illness Management
and Recovery Manual
Page 150
Diabetes medications and insulin
For people with Type 2 diabetes, treatment always involves increasing exercise and
changing eating habits. If blood glucose is still too high, medication is prescribed in
addition to maintaining healthy exercise and eating habits. These medications help with
one of two problems associated with Type 2 diabetes:
1. The body may not make enough insulin.
2. The cells don’t take in glucose as quickly and easily as they should.
There are six classes of medications for type 2 diabetes.
Sulfonylureas
• Increase the amount of insulin made in the body and help the cells use insulin better.
• Side effects include: weight gain, headache, gastrointestinal problems and low blood
sugar
Megliltinides
• Help the body’s cells to release more insulin.
• The most important side effect to watch for is low blood sugar.
Biguanides
• These medications, including metformin (or Glucophage), decrease the amount of
sugar (glucose) released by the liver and help the body’s tissue to use insulin, increasing
absorption. Metformin sometimes helps with weight loss.
• Side effects include belly problems and a metallic taste in the mouth. Lactic acidosis
(build-up of lactic acid in the blood) is a rare but serious side effect that may also
occur. Symptoms of lactic acidosis are nausea, vomiting, tiredness, or irregular heart
rate.
Alpha-glucosidase inhibitors
• These medications cause the body to absorb starches (like bread and potatoes), and
other carbohydrates (found in sugar, fruit, vegetables) more slowly.
• These medications need to be taken with food and may cause gas and diarrhea.
Thiazolidinediones or glitazones
• These medications help the body’s cells to use insulin. Before taking these medications,
people need to have liver function tests to check for any liver problems.
Module #5
Handout
Integrated Illness Management
and Recovery Manual
Page 151
Insulin
People with type 1 diabetes have to take insulin injections because
their bodies do not make insulin (the hormone that helps people use
blood sugar for energy). People with type 2 diabetes may or may not
need insulin shots. There are different types of insulin: fast-acting,
short-acting, intermediate acting, and long-acting. The different
types of insulin vary in the time they take to start working and in how
long their effects last. People may use more than one type of insulin in
different situations.
New medication for diabetes
The Federal Drug Administration has recently approved a new medication for diabetes.
Pramlintide or Symlin is a synthetic form of Amlyin, a hormone that works with insulin to
maintain blood glucose levels. Symlin, which must be used in addition to insulin but must be
injected separately, improves hemoglobin A1C tests (a measure of the long-term control
of sugar in the blood), reduces the risk of very low blood sugar, and may help with weight
loss.
Diabetes medications
Brand Name Chemical Name Category
Actos Pioglitazone Thiazolidinediones
Glucotrol Glipizide Sulfonylureas
Micronase Glyburide Sulfonylureas
Glyset Miglitol Alpha-glucosidase inhibitors
Starlix Nateglinide Meglitinides
Glucophage Metformin Biguanides
Prandin Repaglinide Meglitinides
Treatment of side effects
If you have side effects, contact your doctor immediately. After discussing the side
effects and evaluating how serious they are, he or she may recommend one of the
following: reduce the dose of the medication, add a side effect medication, or switch
to another medication. The doctor may also suggest some things that you can do to help
reduce the discomfort or counteract the side effects. See the “Coping with Medication
Side Effects” handout for other ideas.
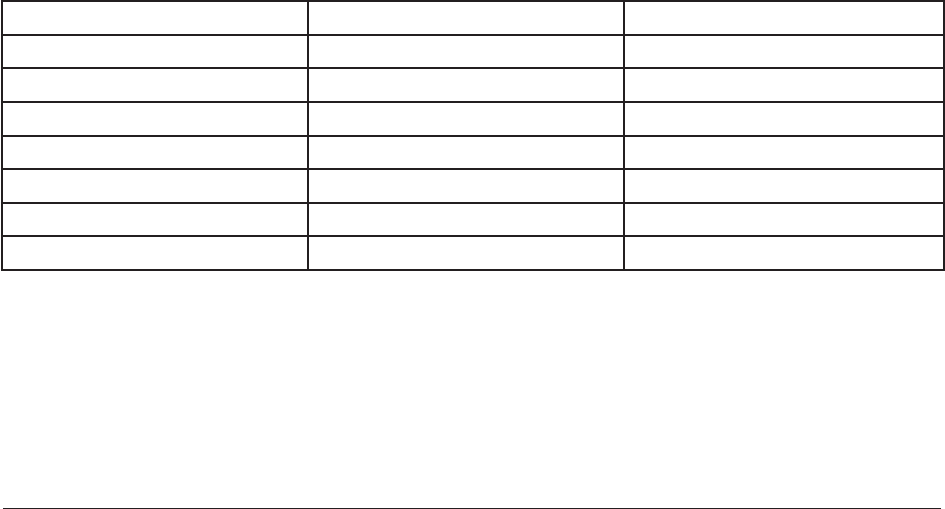
Module #5
Handout
Integrated Illness Management
and Recovery Manual
Page 152
Medications for chronic pain
There are many different kinds of prescription and over-the-counter medications used
to treat pain. Most of these medications aim to reduce inammation (swelling). Although
medications can provide relief, they have side effects and are most effective when used
with other treatments such as weight reduction, exercise, physical therapy, etc.
Analgesics
Analgesics are often recommended by doctors as the rst medication to try for pain
because they are well-tolerated and have minimal side effects if taken properly.
Salicylates
Salicylates are medications containing aspirin. Aspirin reduces pain AND inammation
however, it does have side effects such as stomach upset and bleeding problems. Doctors
consider a person’s medical history and other medications before recommending aspirin.
Non-steroidal anti-inammatory drugs (NSAID)s
NSAIDs are the most commonly prescribed medication for reducing pain and inammation.
Prostaglandins are substances in the body that make inammation and pain worse.
Prostaglandins are blocked by NSAIDS, causing pain and inammation to decrease.
Side effects can include: stomach problems, ulcers, and bleeding (if used for a long period
of time).
Opioids
Opioids are sometimes used to treat severe chronic pain. These medications need to be
taken as prescribed because there is a risk of addiction, tolerance, and dependence.
Medications for chronic pain
Brand Name Chemical Name Category
Aspirin (i.e. Bayer) Acetylsalicylic Acid Salicylate
Tylenol Acetaminophen Analgesic
Advil, Motrin, etc Ibuprofen NSAID
Feldene Piroxicam NSAID
Celebrex Celecoxib NSAID
Vicodin Hydrocodone Opioid
Oxycontin Oxycodone Opioid
Treatment of side effects
If you have side effects, contact your doctor immediately. After discussing the side
effects and evaluating how serious they are, he or she may recommend one of the
following: reduce the dose of the medication, add a side effect medication, or switch
to another medication. The doctor may also suggest some things that you can do to help
reduce the discomfort or counteract the side effects. See the “Coping with Medication
Side Effects” handout for other ideas
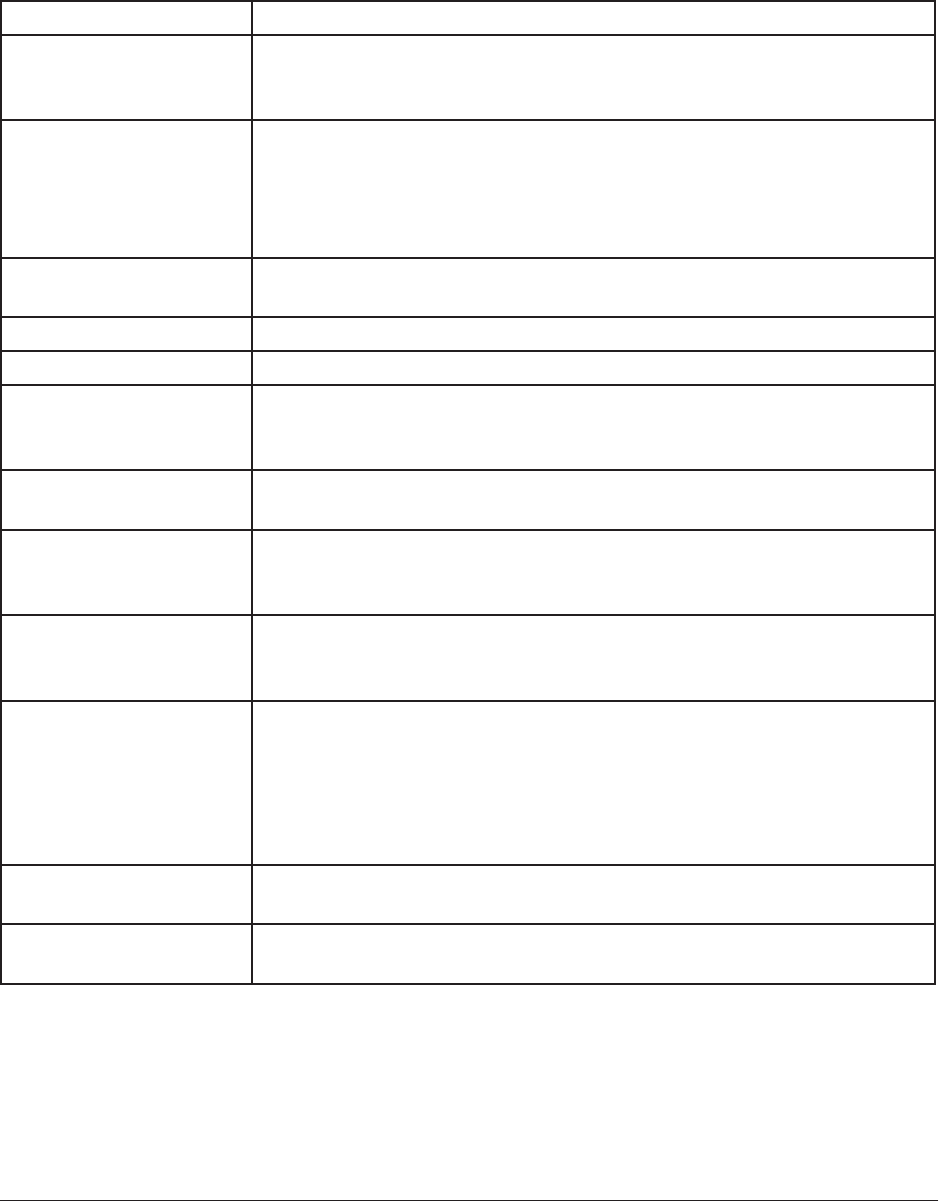
Module #5
Handout
Integrated Illness Management
and Recovery Manual
Page 153
Coping with medication side effects
The following charts list some of the common side effects of different categories of med-
ications and some suggestions for coping with them or counteracting them. Blank spaces
are provided for additional strategies that you nd useful.
Side effect Strategy
Drowsiness • Schedule a brief nap during the day.
• Get some mild, outdoor exercise, such as walking.
• Ask your doctor about taking medication in the evening
Increased appetite
and weight gain
• Eat healthy foods, such as fruits,
vegetables and grains.
• Cut down on sodas, desserts and fast foods.
• Engage in regular exercise.
• Join a weight reduction program.
Extreme restlessness • Find a vigorous activity that you enjoy, such as jogging, skating,
aerobics, sports, outdoor gardening, swimming, bicycling
Muscle stiffness • Do regular stretching exercises, yoga, or isometric exercises
Dizziness • Avoid getting up quickly from a sitting or lying down position.
Blurry vision • Talk to your doctor about getting reading glasses, which you
can buy without a
prescription at a local drug store.
Sensitivity to the sun • Stay in the shade, use sunscreen and wear protective clothing.
• Avoid going out at the sunniest time of day.
Shakiness or tremors • Ask your doctor about medications to treat tremors. Avoid
lling cups and
glasses to the brim.
Dry mouth • Chew sugarless gum, suck on sugarless hard candy, or take
frequent sips of
water.
Constipation • Drink 6-8 glasses of water daily.
• Eat high ber foods such as bran cereals, whole grain breads,
fruits and vegetables.
• Do light exercise daily.
• Take Senna (vegetable laxative) and/or Colace (docusate
sodium), which you can buy at a drug store.
Other:
Other:
Select a strategy you would like to practice to help cope with a side effect that you are
experiencing. Make a plan with your doctor for trying out this strategy. Ask a friend or
family member to help you with this coping strategy such as eating healthier, spending
time outdoors, or taking a short walk.
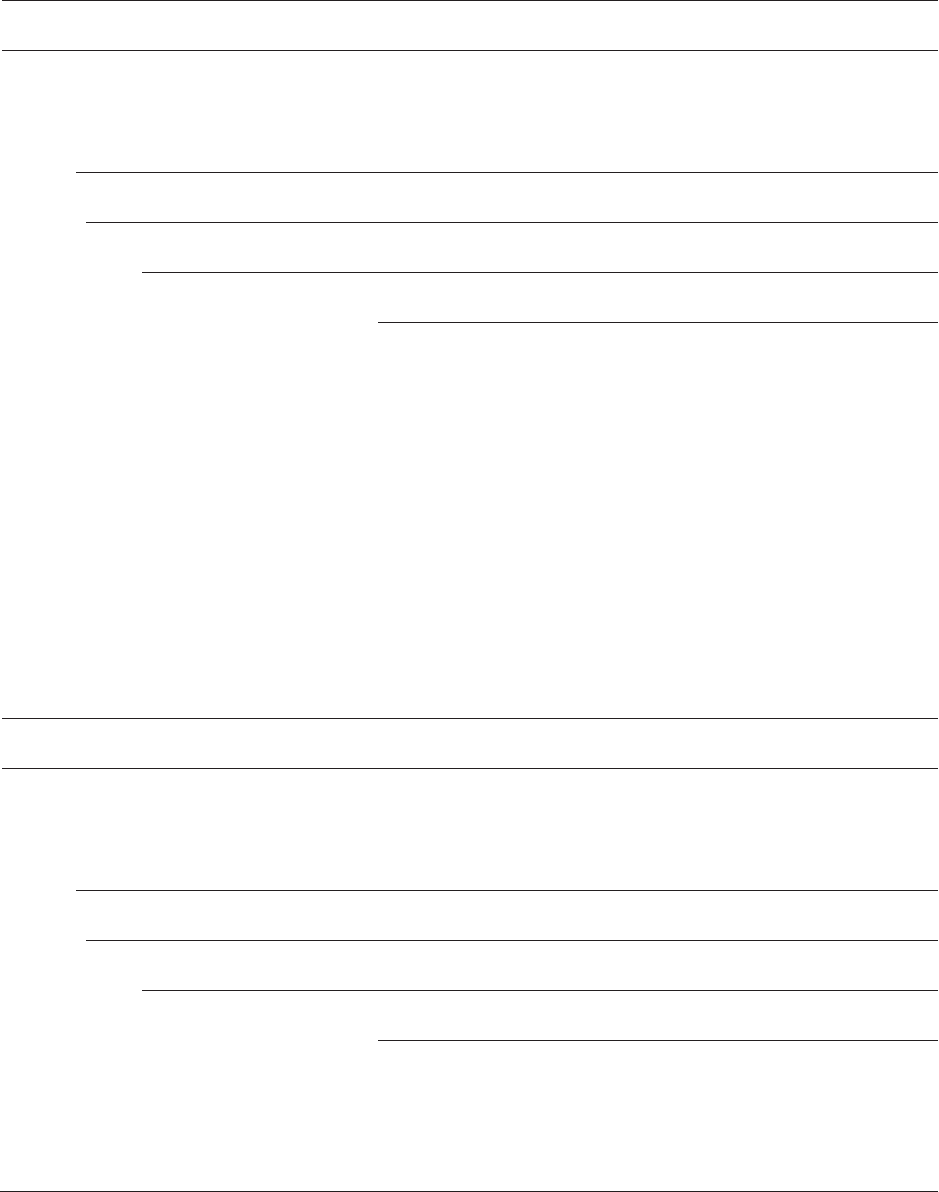
Module #5
Handout
Integrated Illness Management
and Recovery Manual
Page 154
Integrated Illness Management and Recovery
Home Practice Sheet
My home practice for this week is:
To complete this home practice, I will use the following plan:
When:
Where:
With Whom:
What do I need to do the practice?
Today’s Date: _ _ / _ _ /_ _ _ _
Participant: ____________________ IIMR Specialist:_________________________
Integrated Illness Management and Recovery
Home Practice Sheet
My home practice for this week is:
To complete this home practice, I will use the following plan:
When:
Where:
With Whom:
What do I need to do the practice?
Today’s Date: _ _ / _ _ /_ _ _ _
Participant: ____________________ IIMR Specialist:_________________________

Module #6
Guidelines
Integrated Illness Management
and Recovery Manual
Page 155
Practitioner Guidelines for Handout #6:
Social Support
Goals
This topic area can be covered in 2-3 sessions. The purpose of this topic is to help people identify and
practice strategies for connecting with people we see they see. This topic area will also address asking
for help and support for working towards a healthier life. Many consumers will identify goals related to
expanding social networks or enhancing their existing relationships. If a social support goal is identified,
covering the additional curriculum from Illness Management and Recovery is recommended.
Suggestions for Teaching
• Explore how increasing social support may be helpful in improving mental and physical health. Ask
people how increasing social support may be helpful in making a lifestyle change. For example, it can
be helpful to have someone to talk to about the difficulties of changing eating habits or inviting some-
one to be a “walking buddy.”
• Explore how joining an organization such as the local senior center or the YMCA can be a great way to
work towards multiple goals. Organizations that offer exercise, dance or other physical activities can be
great places to meet new people, to spend time with people, and to help them reach health goals.
• If people would like to try talking to someone that they see, review the common
situations where they may encounter people and also consider how they might be encountering new
people as part of making a change in their healthy behavior. For example, they may be interested in
taking an exercise or cooking class or joining a new support group. You could help the person make a
plan for going to the place and initiating
a conversation.
• If clients identify an organization that they would like to join to meet people and work on wellness
goals, develop a plan for how they will start the activity.
• Use role-plays to help clients practice asking for help from others to accomplish health-related activ-
ities, i.e. getting a ride to a doctor’s appointment. If people enroll in an exercise class in order to meet
others, you could set up a role-plays to help them practice starting a conversation with someone from
class.
• Many people may have experienced a loss or losses in their social network and may have difficulty
thinking about expanding or strengthening their social network. Explore with people how expanding
their social network may help them reach their goals for wellness. Discuss ways that relationships with
friends and family can be strengthened by asking them to help with wellness goals.
Review Questions
How might your friends or family be helpful in helping you reach your wellness goals or make life-
style changes?
How might engaging in a healthy lifestyle activity also be a good way to meet new
people?

Module #6
Guidelines
Integrated Illness Management
and Recovery Manual
Page 156
Suggestions for Home Practice
1. Clients could compile a list of wellness activities that they could do with other people or might be
good activities for meeting new people.
2. Make a list of activities or areas that would be helpful to ask for a helping hand. Consider areas relat-
ed to both mental and physical health.
3. Client could identify organizations that offer group exercise and make phone calls to obtain informa-
tion about joining.
Additional Resources
A Step-by-Step to Planning and Conducting a Successful Health Fair. Suggestions
for conducting a health fair that could be useful in promoting healthy activities and
encouraging support among people interested in making healthy lifestyle changes. http://www.integration.
samhsa.gov/health-wellness/wellness-strategies/uic_cspnj_health_fair_manual.pdf
Module #6
Handout
Integrated Illness Management
and Recovery Manual
Page 157
Integrated Illness Management and Recovery
Handout #6: Social Support
Having social support means that you feel connected and cared for by other people. This is
especially important for helping you to live a healthier and happier life.
There are two main topics in this section:
1. Recognizing the importance of social support and talking to people you see
2. Asking for a helping hand
Let’s Discuss!
What social support do you have?
How can social support help with physical health?
How can social support help with mental health?
How can social support help you reach your life goals?
Recognizing the importance of social support and talking to people
you see
The Mind-Body Connection:
The mind-body connection focuses on how emotions, mental health, relationships, spiritual-
ity, and health are inter-connected. There are several ways that having social support can
improve mental and physical health:
1. Talking to a supportive person when you are feeling down
because of mental health or physical health problems can
reduce stress and make you feel better and more able to
cope.
2. Developing a network of support can provide support for
making and maintaining a lifestyle change.
3. Having people in your life who are willing to help you
do things such as take you to appointments, pick up
medications at the pharmacy, help change a dressing on a
wound, can make it easier for you to manage your illnesses.
Module #6
Handout
Integrated Illness Management
and Recovery Manual
Page 158
What is social support?
“Social support” refers to having relationships that are rewarding, enriching and helpful.
The best relationships are those in which each person gives something to the relationship
and each person receives something from it. Social support can come from relationships
with many different people. Check each box where you have relationships.
Family members
Friends
Peers
Spouses
Boyfriends/girlfriends
Co-workers
Topic 1: Talking to people you see
During times of stress, illness, or relapse, people may spend more time alone because they
don’t feel like socializing. If this happens for a long time, people can lose touch with people.
Most people see others as they go about their daily lives, although they may not be in the
habit of talking to them. Talking with other people, even for very short periods, can be a
good way to build conversation skills and become more social. This can eventually lead to
forming relationships that can become supportive.
Here are some situations where you may encounter people you can talk to:
• at home (family members, roommates)
• at school or in a class
• in programs or groups you attend
• at work
• at church or other religious/spiritual gatherings
• as you go about your business (for example, coffee shop or appointments)
Let’s Discuss!
What help managing your mental illness would you like to have from a supportive
person (such as help remembering to take medications)?
What help managing your medical problems would you like to have from a supportive
person (such as help cooking healthy recipes)?
Members of religious or other
spiritual groups
Classmates
Mental health professionals
Peer support group members
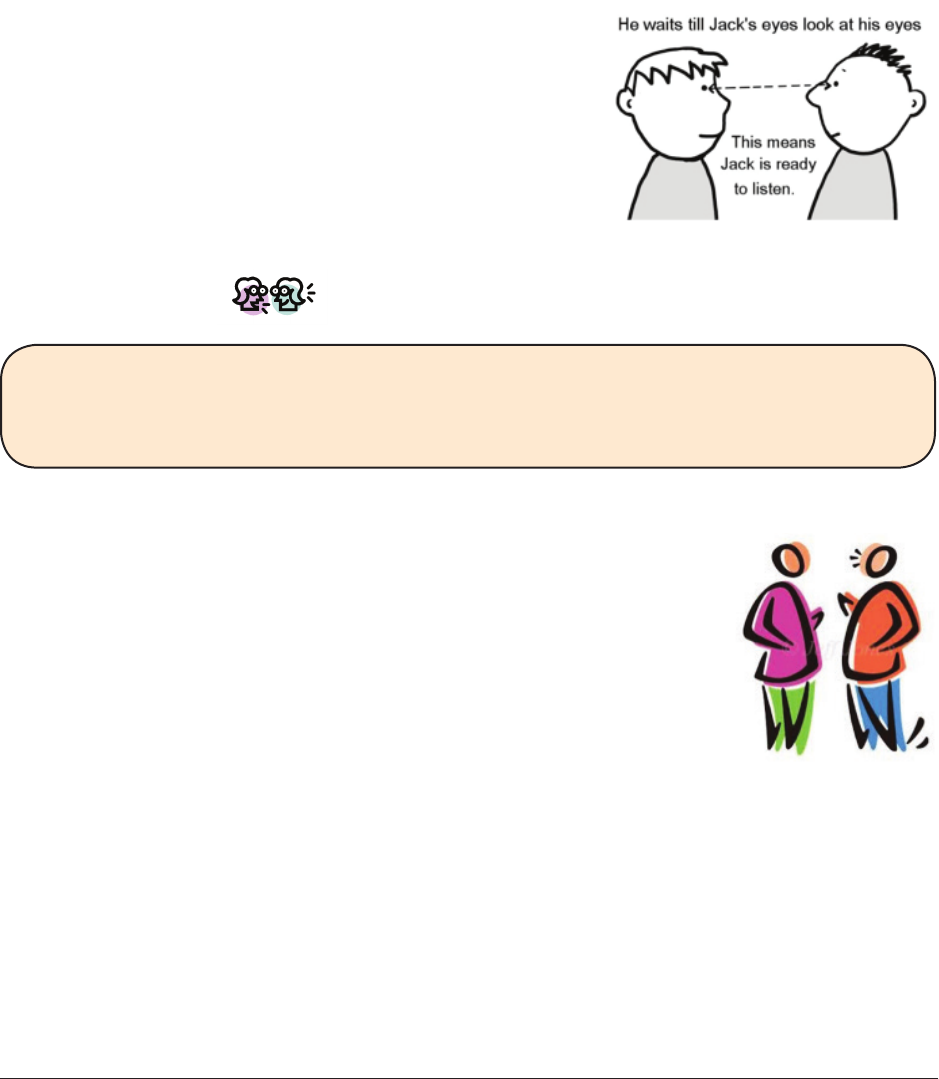
Module #6
Handout
Integrated Illness Management
and Recovery Manual
Page 159
It’s common to worry that you may have nothing to talk about. Some topics that are
relatively easy to talk about include:
Weather Pets
Sports Food
The activity that you are both doing Music
Television or movies Business you are taking care of
Steps that may be helpful in starting conversations with people you see:
• Find someone who isn’t occupied.
• Choose an interesting topic.
• Look at the person.
• Smile and nod your head to show you are listening.
• Tune in to what the other person is saying.
• Avoid telling very personal things about yourself.
Let’s Discuss!
Are you interested in having more conversations with people you see regularly?
If so, who is the person, and when and where do you usually see him or her?
Re-connecting with friends and family members
It’s up to you how much personal information you want to share. When
you rst reconnect with friends, it’s often better to start off sharing
things that are not highly personal such as where you are living, classes
you are taking, your job, or what you like to do in your spare time.
You might have lost contact because of something unpleasant that hap-
pened in the past. Here are a couple of suggestions for dealing
with unpleasant events:
1. If the unpleasant event was minor, you may choose to discuss it briey and move on, or
you may not need to discuss it in detail.
2. Speak openly about what happened. It is often best to apologize for something such as
losing your temper and then tell the person about the positive things in your life.
3. Keep in mind that not everyone will be interested in reconnecting. That’s okay. Some
people may be very busy or at a different place in their lives. Don’t get discouraged.

Module #6
Handout
Integrated Illness Management
and Recovery Manual
Page 160
Topic 2: Asking for a helping hand
Being able to ask for help is as important to successfully managing medical problems as
it is to managing emotional challenges. Below is a list of different ways you may consider
asking for a helping hand. Review the list and circle any of the examples that you may be
helpful to you.
• Remembering to take medication for mental illness or medical problems
• Joining in activities associated with a lifestyle change such as walking buddy
• Talking to someone when you feel down or frustrated
about your mental or physical illness
• Providing encouragement for a lifestyle change such as
stopping smoking
• Bringing someone along to medical or psychiatric
appointments to help remember instructions and
information
• Understanding technology tools associated with a lifestyle change such as searching the
internet for healthy recipes
• Completing tasks that you may not be able to do because of physical limitations or
worsening of a medical condition
• Attending a group or meeting supporting your mental health or healthy lifestyle such
as transportation to a Dual Recovery Group or Weight Watchers
• Introducing yourself or speaking at a support group
• Supporting you in weighing the pros and cons of an important treatment decision
• Providing transportation to a medical or psychiatric appointment
Steps for making a request
Making a request is often necessary to ask a person for help to do something or help to
complete a task. Making a request in a positive way can result in receiving help from
another person and strengthen a relationship between two people.
1. Find someone who could help you with your request. Choose someone who isn’t obviously
occupied. If the person is in the middle of doing something, they may not want to stop
what they are doing in order to talk to you.
2. Look at the person. Eye contact is important when you are talking to people. If you
feel uncomfortable looking into someone’s eyes, you can look somewhere close to their
eyes, such as their forehead or nose.
3. Say what you would like the person to do for you and why you need help. It can be
helpful to let the person know exactly what help you are requesting. Telling the person
why you need help allows the person to understand the reasons why their help is so
important to you.
4. Tell the person how it would make you feel. Telling the person how it would make you
feel can increase the chance that the person will say yes.
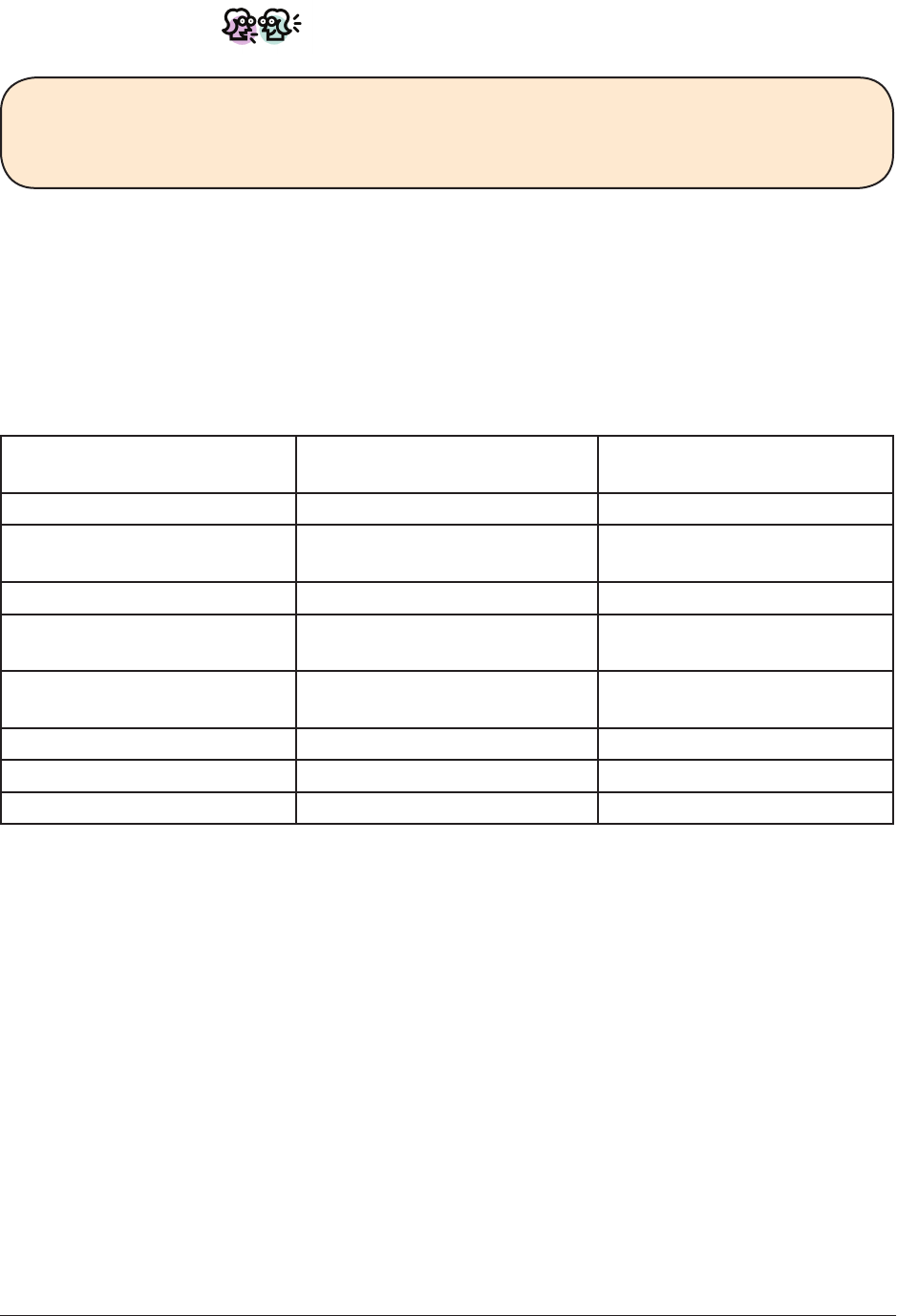
Module #6
Handout
Integrated Illness Management
and Recovery Manual
Page 161
Let’s Discuss!
How do you feel about making requests?
Do you follow these steps when making a request?
Do a role-play to practice making a request. Practicing helps you feel more prepared.
Making a connection to support a healthy lifestyle behavior
Having support can be incredibly helpful when trying to make a healthy lifestyle change
such as quitting smoking, beginning to exercise more regularly, or cooking more healthy
recipes. Use the following table to think about ways you might use social supports to take
a step forward in living a happier and healthier life.
Topic I might try this What I could say when I
see the person?
Fun things to do
Support in starting a new
hobby or lifestyle change
Asking for someone’s opinion
Mutual support for a
lifestyle change
Feedback about solving a
problem
Sharing common interests
Sharing a common goal
Other:
Practice how you might bring up a topic of interest you selected from the Common Areas
of Interest Table. This can help you feel more prepared and condent when strengthening
your connections with other people.
Module #6
Handout
Integrated Illness Management
and Recovery Manual
Page 162
Integrated Illness Management and Recovery
Home Practice Sheet
My home practice for this week is:
To complete this home practice, I will use the following plan:
When:
Where:
With Whom:
What do I need to do the practice?
Today’s Date: _ _ / _ _ /_ _ _ _
Participant: ____________________ IIMR Specialist:_________________________
Integrated Illness Management and Recovery
Home Practice Sheet
My home practice for this week is:
To complete this home practice, I will use the following plan:
When:
Where:
With Whom:
What do I need to do the practice?
Today’s Date: _ _ / _ _ /_ _ _ _
Participant: ____________________ IIMR Specialist:_________________________

Module #7
Guidelines
Integrated Illness Management
and Recovery Manual
Page 163
Practitioner Guidelines for Handout #7:
Managing Stress
Goals
This topic can be covered in 2 sessions. The purpose of this topic area is to help people identify things
that can cause them stress. Learn and practice strategies for preventing some sources of stress and strate-
gies for reducing the effects of stress.
Suggestions for Teaching
• Practitioners should keep in mind the recovery or health related goals identified by people in earlier
sessions. For many people, reducing stress may facilitate the ability to pursue personal or healthy life-
style goals.
• If someone wanted to try the strategy of talking to someone else about feeling stressed out, the prac-
titioner could help him choose whom he would talk to and role-play how he might approach the
person.
• If someone wanted to practice maintaining her sense of humor, the practitioner could help her decide
if she wanted to watch a particular television show or video or if she liked to read funny books or com-
ics. If she wanted to spend time with someone who has a good sense of humor, the practitioner could
help her role-play how she might approach the person.
• If someone wanted to use relaxation techniques to cope with stress, the practitioner could help her
practice one or more of the techniques described in the Appendix (relaxed breathing, muscle relax-
ation, and imagining a peaceful scene.)
• When someone can’t identify signs of stress, it may be helpful for the person to talk to family members
or other supportive people about what signs they noticed in the past when the person was under stress.
For example, family members might have noticed that the person had a decrease in appetite, slept
more, or was more irritable over small things that happened.
Review Questions
What are the signs you experience that help you know you are “under” stress?
What is the difference between preventing stress and coping with stress?
How do you think stress affects your physical health? Mental health?
Suggestions for Home Practice
1. Asking family members, friends and other supportive people to play a role in a prevention or coping
strategy. For example, a person might like someone to join her on a daily walk as part of a plan for
reducing stress.
2. Practicing a strategy for preventing stress, such as scheduling time for relaxation, and keeping track
of how it affects the person’s stress level.
3. Practicing a coping strategy, such as listening to music, and keeping track of how it affects the per-
son’s stress level.

Module #7
Guidelines
Integrated Illness Management
and Recovery Manual
Page 164
Additional Resources
Positive Coping with Health Conditions-Relaxation Worksheet-tips for teaching relaxation associated with a medical
health condition
http://www.comh.ca/publications/resources/pub_pchc/PCHC%20Skills%2001%20Relaxation.pdf
Module #7
Handout
Integrated Illness Management
and Recovery Manual
Page 165
Integrated Illness Management and Recovery
Handout #7: Managing Stress
In order to cope effectively with stress, it is important to know what situations you nd
stressful and what the experience of stress is like for you. Specic strategies for dealing
with stress are suggested, such as using relaxation techniques, talking with others,
exercising, and creative expression.
There are two main topics in this section:
1. Understanding and preventing stress for medical problems and mental illness
2. Strategies for coping with stress
Topic 1: Understanding and preventing stress for medical problems
and mental illness
What is stress?
“Stress” is a term people use to describe a feeling of pressure, strain, or
tension. People often say they are “under stress” or feel “stressed out”
when they are dealing with challenging situations or events. Stress is a
normal part of life. Everyone encounters stressful situations. Stress can
come from something positive (like moving to a new apartment, getting a
new job or being in a new relationship), or from something negative (like
worsening medical problems, getting into an argument with someone or
being the victim of a crime).
Let’s Discuss!
What kinds of situations make you feel stressed?
Why is stress relevant to medical problems and mental illness?
According to the stress-vulnerability model, stress is an important factor
in mental and medical illnesses because it can worsen symptoms and lead to
relapses. In addition, medical problems and symptoms of mental illness can
cause stress that makes it more difcult to deal with everyday life situations.
However, if you can decrease stress, you can decrease symptoms.
• Nobody has a stress-free life. Stress is a natural part of life.
• When people are under stress, it affects them physically and emotionally. Some people
show only physical signs of stress, such as tense muscles, headaches or sleep problems.
Others have trouble concentrating or become irritable, anxious or depressed.
• Being able to cope effectively with stressful situations can minimize the effects of
stress on you and your symptoms. This can enable you to continue to pursue your goals
and enjoy life.

Module #7
Handout
Integrated Illness Management
and Recovery Manual
Page 166
Let’s Discuss!
Have you noticed any signs of stress in the past week?
What makes you feel stressed?
Different people nd different things stressful. For example, some people enjoy the hus-
tle and bustle of a big city, while others don’t like the crowds and noise and nd it stress-
ful. Some people experience a lot of physical symptoms from a medical condition such
as arthritis while others may have very few symptoms that interfere in their daily lives.
Knowing what you personally nd stressful will help you cope better.
Let’s Discuss!
What is the most stressful life event you have experienced in the past year?
What are the most stressful daily hassles you have experienced in the past week?
How can you prevent stress?
Putting energy into preventing stress can pay off. If you get rid of some of the stress in
your life, it frees you up to enjoy yourself more and to accomplish more of your goals.
There are many things people can do to prevent stress from developing in the rst place.
This handout provides four examples of strategies you can use to prevent stress.
1. Figuring out strategies for situations that caused stress in the
past
If you found a situation stressful in the past, it will probably cause problems in the future.
It’s a good idea to think of different ways to handle stressful situations so that they won’t
be as stressful in the future.
Examples:
• If you get irritable when riding the bus at rush hour, try catching it at a less busy time.
• If you feel nervous before going to a doctor’s ofce, you could try practicing deep
breathing.
Let’s Discuss!
What is an example of a situation that caused stress for you in the past?
What strategies can you use so that it won’t be as stressful in the future?
Module #7
Handout
Integrated Illness Management
and Recovery Manual
Page 167
2. Developing a routine of doing activities that you enjoy
Having activities that you enjoy on a regular basis helps to prevent stress from building up.
Different people enjoy different things, so it’s important to nd out what you like doing.
Examples:
• Exercise, such as taking a walk or lifting weights
• Listening to music
• Doing artwork
• Reading
• Cooking
• Hobbies, such as knitting or building models or putting together puzzles
Make a plan to do things you enjoy regularly, either daily or 2-3 times per week.
Let’s Discuss!
What activities on the list do you enjoy doing or nd relaxing?
How can you participate in this activity once a week or more often?
3. Taking care of your health
Eating well, getting enough sleep, exercising regularly, and avoiding alcohol or drug abuse
help prevent stress. These habits are not easy to maintain, but they pay off.
Examples:
• Watching what you eat such as including fruits and vegetables with every meal
• Planning your sleep schedule to get enough sleep
Let’s Discuss!
What is one way you could take better care of your health to help you prevent stress.
4. Using relaxation techniques on a regular basis
When people practice relaxation techniques regularly they can keep stress
from building up. Three relaxation exercises that you can try are:
• Relaxed breathing
• Muscle relaxation
• Imagining a peaceful scene
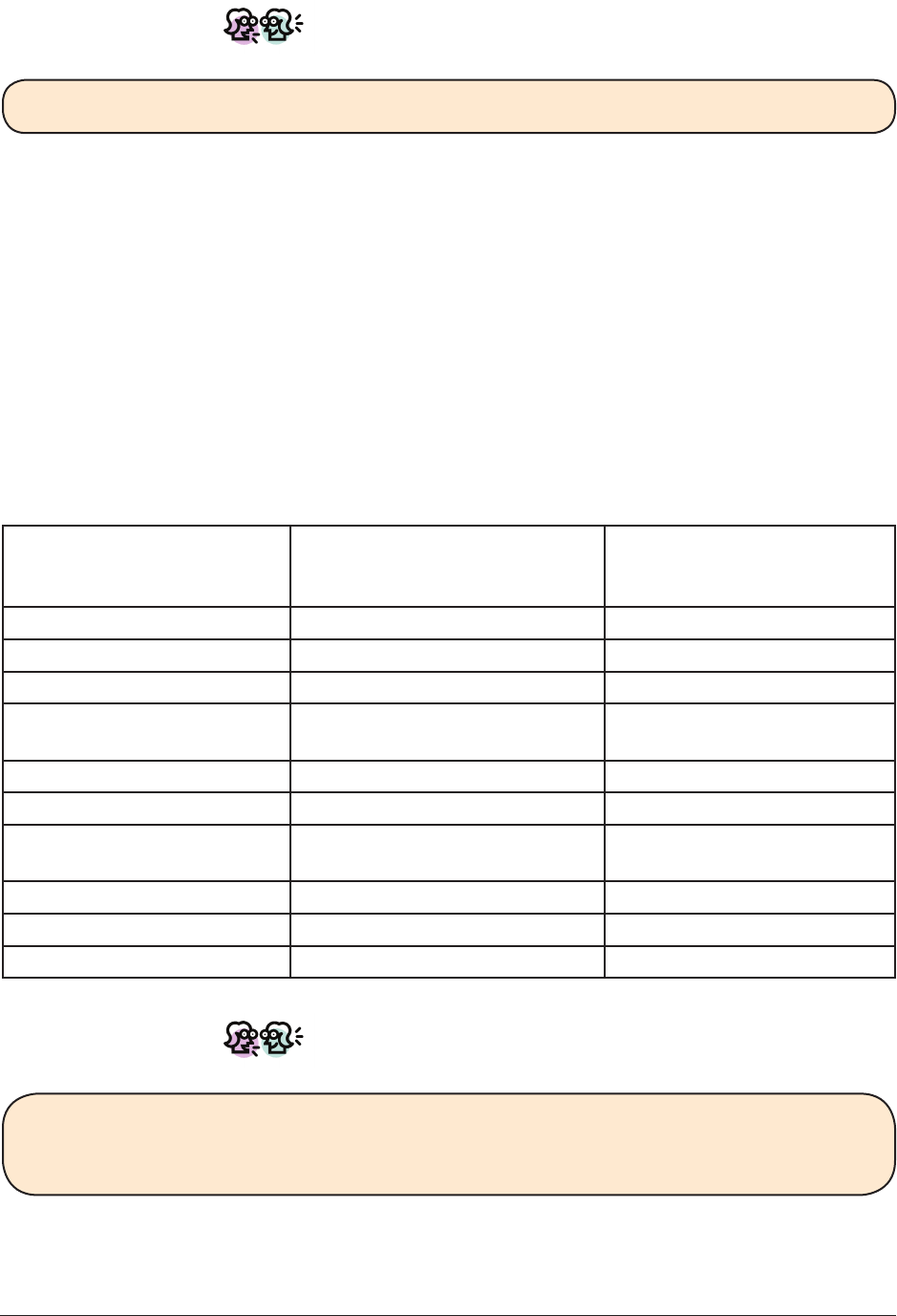
Module #7
Handout
Integrated Illness Management
and Recovery Manual
Page 168
Let’s Discuss!
Which stress prevention strategies would be most helpful to you?
It can be helpful to make a plan and to demonstrate how you can use a stress prevention
strategy in your daily life. Select a prevention strategy and make a plan to use it in the
next few days. Practice the prevention strategy in session if you are able.
Topic 2: Strategies for coping with stress
How can you cope with stress effectively?
Coping effectively with stress is a key to living a successful and rewarding life and being
able to pursue your personal goals. Use the following table to review common strategies
for coping with stress and place a check next to strategies you already use and strategies
you would like to try.
Strategies for coping with stress checklist
Strategy I already use this strategy I would like to try this
strategy or develop it
further
Talking to someone
Using relaxation techniques
Using positive self-talk
Participating in religion or
other form of spirituality
Exercising
Listening to music
Doing artwork or going to
see artwork
Participating in a hobby
Other:
Other:
Let’s Discuss!
What strategies do you use to cope with stress?
What strategies help you cope better with your physical or mental illness?

Module #7
Handout
Integrated Illness Management
and Recovery Manual
Page 169
What you can do if you notice you are under stress?
The rst step is to gure out whether you are experiencing a sign of stress or a symptom
of an illness (a medical or a psychiatric illness). Stress often affects the body so it can
feel the same as some physical symptoms like chest pain, fatigue, or even muscle ache.
Take some time to try to determine what is causing your distress. Try using stress
reduction strategies if you conclude that what you are experiencing is NOT a physical
symptom of a medical problem. Ask someone you trust if you have difculty guring out
whether you are having a medical symptom or stress.
Relaxation techniques
Three types of relaxation techniques are described below:
• Relaxed breathing
• Muscle relaxation
• Imagining a peaceful scene
Relaxation techniques are most effective when they are practiced on a regular basis.
When you are rst learning a technique, you usually concentrate on doing the steps
according to the instructions. As you become familiar with the instructions, you will
be able to concentrate more on the relaxation you are experiencing. Choose one of the
following techniques and try practicing it daily. After a week, evaluate whether you think
the technique is effective for you.
Relaxed breathing
The goal of this exercise is to slow down your breathing, especially your exhaling.
• Choose a word that you associate with relaxation, such as CALM, RELAX, or PEACEFUL.
• Inhale through your nose and exhale slowly through your mouth. Take normal breaths,
not deep ones.
• While you exhale, say the relaxing word you have chosen. Say it very slowly, like this,
“c-a-a-a-a-a-a-l-m” or “r-e-e-e-l-a-a-a-x.”
• Pause after exhaling before taking your next breath. If it’s not too distracting, count
to four before inhaling each new breath.
• Repeat the entire sequence 10 to 15 times.
Muscle relaxation
The goal of this technique is to gently stretch your muscles to reduce stiffness and
tension. The exercises start at your head and work down to your feet. You can do these
exercises while sitting in a chair.
• Shoulder shrugs. Lift both shoulders in a shrugging motion. Try to touch your ears with
your shoulders. Let your shoulders drop down after each shrug. Repeat 3-5 times.
• Overhead arm stretches. Raise both arms straight above your head. Interlace your
ngers, like you’re making a basket, with your palms facing down (towards the oor).
Stretch your arms towards the ceiling. Then, keeping your ngers interlaced, rotate
your palms to face upwards (towards the ceiling). Stretch towards the ceiling. Repeat
3-5 times.
Module #7
Handout
Integrated Illness Management
and Recovery Manual
Page 170
• Stomach tension. Pull your stomach muscles toward your back as tight as you can
tolerate. Feel the tension and hold on to it for ten seconds. Then let go of the muscles
and let your stomach relax, further and further. Then focus on the release from the
tension. Notice the heavy yet comfortable sensation in your stomach.
• Knee raises. Reach down and grab your right knee with one or both hands. Pull your
knee up towards your chest (as close to your chest as is comfortable). Hold your knee
there for a few seconds, before returning your foot to the oor. Reach down and grab
your left knee with one or both hands and bring it up towards your chest. Hold it there
for a few seconds. Repeat the sequence 3-5 times.
• Foot and ankle rolls. Lift your feet and stretch your legs out. Rotate your ankles and
feet, 3-5 times in one direction, then 3-5 times in the other direction.
Imagining a peaceful scene
The goal of this technique is to “take yourself away” from stress and picture yourself in a
more relaxed, calm situation.
1. Choose a scene that you nd peaceful, calm and restful. If you have trouble thinking of
a scene, consider the following:
• the beach • a river
• a walk in the woods • a farm
• a park • a log cabin
• a mountain path • a waterfall
• a canoe or sailboat on the water • a meadow
2. After choosing a peaceful scene, imagine as many details as possible, using all your
senses.
3. What does the scene look like?
What are the colors? Is it light or dark? What shapes are in the scene?
If it’s a nature scene, what kinds of trees or owers do you see?
If it’s a city scene, what kind of buildings? What kind of vehicles?
4. What sounds are in your peaceful scene?
Can you hear water or the sounds of waves?
Are there sounds from animals or birds?
From the breeze? From people?
5. What could you feel with your sense of touch?
Are there textures?
Is it cool or warm? Can you feel a breeze?
6. What smells are there in your peaceful scene?
Could you smell owers? The smell of the ocean? The smell of food cooking?
7. Disregard any stressful thoughts and keep your attention on the peaceful scene.
8. Allow at least ve minutes for this relaxation technique.
Module #7
Handout
Integrated Illness Management
and Recovery Manual
Page 171
Integrated Illness Management and Recovery
Home Practice Sheet
My home practice for this week is:
To complete this home practice, I will use the following plan:
When:
Where:
With Whom:
What do I need to do the practice?
Today’s Date: _ _ / _ _ /_ _ _ _
Participant: ____________________ IIMR Specialist:_________________________
Integrated Illness Management and Recovery
Home Practice Sheet
My home practice for this week is:
To complete this home practice, I will use the following plan:
When:
Where:
With Whom:
What do I need to do the practice?
Today’s Date: _ _ / _ _ /_ _ _ _
Participant: ____________________ IIMR Specialist:_________________________

Module #8
Guidelines
Integrated Illness Management
and Recovery Manual
Page 173
Practitioner Guidelines for Handout #8:
Managing Physical and Mental Health
Goals
Topic 8 should be covered in 2-3 sessions. The handouts introduce strategies for coping
with symptoms that are causing distress and interfering with management of mental/health problems,
ultimately getting in the way of progress towards goals.
Suggestions for Teaching
• Discuss the definition of a symptom and how symptoms have interfered with functioning?
• Use role-plays to practice positive self-talk and/or sharing experiences of symptoms with
a family member or friend.
• Practice a relaxation technique or mindfulness exercise in session and develop a plan for practicing the
technique as a home practice.
• Using a role-play, practice paraphrasing and reflection in conversation as a strategy to
reducing forgetfulness when conversing with others.
• During discussion of the topic, explore the relationship between physical symptoms and
the impact of poor management on mental health. Conversely, discuss how psychiatric
symptoms might impact management of health issues.
Review Questions
What is a symptom? How might symptoms interfere with progress towards goals?
What are some examples of effective coping strategies? Ineffective coping strategies?
What is positive self-talk? How can it be used to cope with symptoms?
What is mindfulness? How can mindfulness techniques be used as a coping strategy?
How can a family member or other supportive person be part of a relapse prevention plan?
Suggestions for Home Practice
1. Brainstorm a list of the symptoms you are experience or have experienced in the past
that have interfered the most with management of a health issue or progress towards
a goal.
2. Practice using positive self-talk and monitor your experience. Write some notes and
bring to next session for discussion.
3. Practice a relaxation technique or a mindfulness exercise as a strategy for coping with
an identified symptom. Think about the symptom and if the coping strategy was
effective.
4. Schedule a rest break over the week during a project or at work to see if periodic
breaks can help with concentration and focus.
Module #8
Handout
Integrated Illness Management
and Recovery Manual
Page 175
Integrated Illness Management and Recovery
Handout #8: Managing Persistent
Physical and Mental Health Symptoms
Common symptoms or problems such as depression, anxiety, sleep problems, pain, and
fatigue can be distressing. Coping strategies can be effective at reducing distressing
symptoms, and helping people life a healthier and happier life.
There are two main topics for this module:
1. Identifying distressing symptoms and improving overall coping.
2. Speciccopingstrategiesforsymptomsandotherproblems.
Topic 1: Identifying distressing symptoms and improving
management
Let’s Discuss!
What are “symptoms”?
What symptoms do you have?
“Symptoms” are physical or mental problems that are related to having a disease or illness.
For example, pain is a common symptom of many physical illnesses, such as some heart
conditions (angina or cardiac pain) or arthritis. Depression is a common symptom in many
mental illnesses, which can include problems such as feeling sad or blue, low self-esteem,
hopelessness, thoughts about death or dying, loss of energy and concentration, and
difcultieswithappetiteandsleep(eithertoomuchortoolittle).Sometimesitishard
togureoutwhetherasymptomiscausedbyamedicaloramentalhealthproblem.
Symptoms can be distressing. They can also interfere with day-to-day functioning. Dealing
with symptoms effectively can improve the quality of your life.
Let’s Discuss!
Whatkindsofsymptomsdoyoundupsettingorinterferewithyourfunctioning?
Mental health symptoms? Physical symptoms?
Module #8
Handout
Integrated Illness Management
and Recovery Manual
Page 176
Interactions between physical and mental health symptoms
Just as the body and mind are connected, the symptoms of physical and mental health
condition can interact with one-another. This means that the symptoms of one type of
illness can affect the other illness. Consider these examples:
• Pain related to arthritis can lead to restricted movement, and engaging less often in
enjoyable activities, such as going on nature walks or visiting friends and relatives. If
people stop participating in enjoyable activities, they can experience depression from
the loss of fun in their lives.
• Persistent feelings of anxiety, or having anxiety attacks, can be very distressing, and
can distract people from other important things, including managing a physical condition.
Forexample,insomeonewithdiabetes,anxietycaninterferewithmonitoringone’sblood
sugar level or following their diet, increasing their risk of negative consequences.
Let’s Discuss!
Have you noticed any interactions between the symptoms of your physical and mental
disorders?
What symptoms or problems interfere most with your life?
Although everybody with a physical or mental health condition experiences some
symptomsatsomepoint,peopledifferinthespecicsymptomstheyhave,howoften
they have them, and how troubling they are. Some symptoms may come and go, and may
onlybeaproblemsometimes.Othersymptomsmaybemoreconstant.Onepersonmaynd
that a particular symptom is very distressing or interferes with functioning, but another
person may not be so bothered.
In order to cope more effectively with symptoms, it can be helpful to identify which
symptoms are most troubling to you. Use the Problematic Symptoms Checklist below to
indicatewithofthefollowingsymptomsyouexperienceandwhichonesyoundmost
upsetting or disruptive.
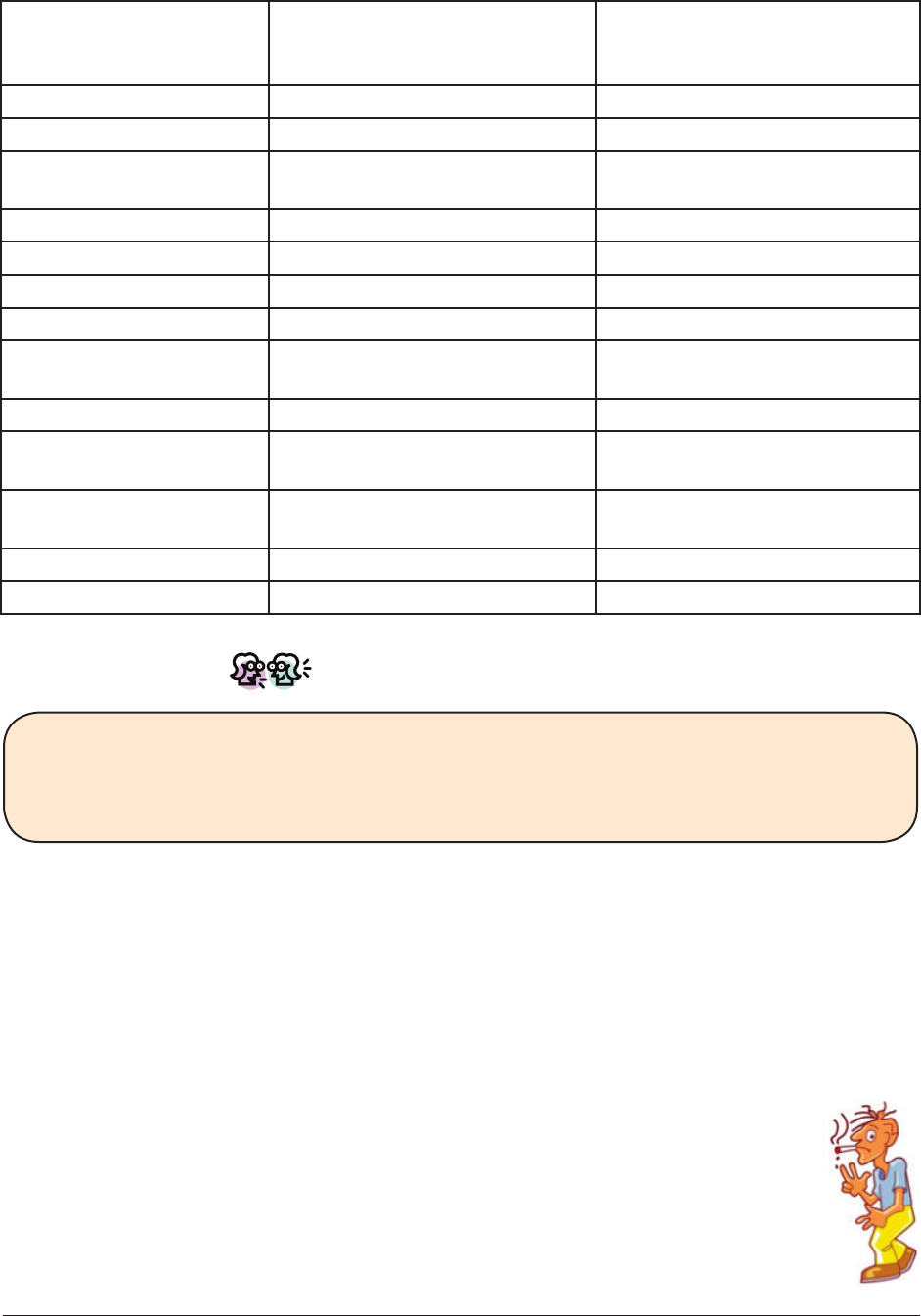
Module #8
Handout
Integrated Illness Management
and Recovery Manual
Page 177
Problematic symptoms checklist
Symptom I experience this symptom This symptom is distressing
or interferes with my
functioning
Physical pain
Restricted movement
Fatigue/easily tired/
low motivation
Shortness of breath
Depression
Anxiety fear, worry
Upsetting memories
Attention/concentration
problems
Difcultysleeping
Hallucinations (hearing
voices, seeing things)
Paranoid thoughts or
feelings
Other:
Other:
Let’s Discuss!
What symptoms or other problems do you experience related to your physical and
mental health conditions?
Which of these are distressing or interfere with your functioning?
Coping with symptoms and problems
When people are troubled by symptoms or other problems related to a mental health or
physicalcondition,theytrytonddifferentwaysofcopingwiththem.Somestrategies
may be more effective than others. Effective coping can reduce the burden of symptoms
or problems. But ineffective coping can actually make things worse.
Ineffective coping strategies
Ineffective coping strategies often provide immediate relief, or escape from the
problem, but in the long run are not helpful. Consider the following strategies
people sometimes use to cope with symptoms or problems:
• Drinking or using drugs to cope with pain, depression, anxiety, or hallucinations.
• Not moving or leaving the house to try to cope with pain, reduced energy,
shortness of breath, or becoming easily fatigued.
Module #8
Handout
Integrated Illness Management
and Recovery Manual
Page 178
First, Let’s Discuss!
Which of these strategies have you tried to use to cope with symptoms or problems?
What happened in the short-term? What happened over the long-run?
What other strategies have you tried to use for symptoms or problems that were not
effective?
Effective coping strategies
Effective strategies for coping with symptoms or problems can have many positive ef-
fects, including:
• Reducing the severity of the symptom itself
• Reducing distress related to the symptom
• Improving functioning by eliminating interference caused by the symptom or problem
The more effective strategies that a person has for coping with their symptoms or prob-
lems, the more effective their overall coping will be. Some coping strategies can be helpful
when dealing with any symptom or problem. These coping strategies are addressed below.
Othercopingstrategiesmaybeeffectivefordealingwithspecicsymptomsorproblems.
These strategies are addressed in the next topic.
Positive self-talk
People are often too hard on themselves—they are often their own worst critics! Having
compassion towards yourself is as important as having understanding for other people.
Positive Self-talk (what you say to yourself, about yourself) can reduce distress related to
symptoms and problems by reminding you of your strengths.
• Remind yourself of what you have accomplished and steps you
have taken rather than focusing only on setbacks
• Identify several of your strengths
• Be your own coach or cheerleader by telling yourself that you
are strong, that you can handle challenges, that you can accom-
plish your goals, that you are in charge of your own life
• Give yourself credit, and a pat on the back, for trying your very
best
• Tell yourself that you will not allow your symptoms to control you or your life
Module #8
Handout
Integrated Illness Management
and Recovery Manual
Page 179
Let’s Discuss!
Do you use positive self-talk to cope with symptoms or problems? Which ones?
How does it work?
Would you like to use positive self-talk more often, or use it to address other symp-
toms or problems?
Getting social support
Talking to other people can be a huge source of support when coping
with distressing symptoms or problems. Other people can help by
letting you know they care, suggesting useful strategies for dealing
with symptoms, or distracting you from your worries. Module 6
provides strategies for building social supports.
Ways people can help:
• Talk to someone and express your feelings about your concerns
• Arrange to do something fun with someone
• Show the person you appreciate them for caring
• Take your mind off yourself by thinking about what might please the other person
• Ask for suggestions about how to deal with symptoms or problem
Let’s Discuss!
Do you use social support to help you cope with symptoms or problems? How does it
work?
Would you like to use social support more often, or to address other symptoms or
problems?
Relaxation and stress management techniques
As reviewed in the Stress-Vulnerability module of this program, stress can increase
symptoms of both mental and physical illnesses. Thus, effective skills for coping with
stress can also reduce distress and the severity of symptoms and related problems.
Module 7 in this program describes relaxation techniques for coping with stress,
including relaxed breathing, positive imagery, and muscular relaxation. Some tips for
using relaxation to cope with symptoms include:
• Select a relaxation strategy (such as one of the above or your own combination of
methods) that you will be able to use in situations in which you experience distressing
symptoms or problems
Module #8
Handout
Integrated Illness Management
and Recovery Manual
Page 180
• Practice this relaxation strategy DAILY in calm situations in order to good at it BEFORE
trying to use it to cope with symptoms or other problems
• Give yourself time and practice for relaxation strategies to work when you are experi-
encing a symptom or problem—remember, “practice makes perfect!”
Let’s Discuss!
Do you use relaxation strategies to help you cope with symptoms or problems?
Which ones? Do they work?
Would you like to use relaxation strategies more often, or to address other symptoms
or problems?
Topic 2: Coping strategies for specic symptoms
In addition to the coping strategies described in Topic 1, which can be used to deal with
almost any distressing symptom or problem, there are many coping strategies that are
especially helpful with particular symptoms. Several of these strategies are described in
the next section.
Unwanted thoughts, feelings, memories, or sensations
Two general strategies are effective at reducing distress and interference caused
by frequent unwanted thoughts, feelings, memories, or sensations (such as pain or
discomfort) that are hard to ignore: 1) distraction and 2) mindfulness/acceptance.
1. Distraction
Sometimes the worst thing people can do is to pay it too much attention to distressing
symptoms or problems — to dwell on them too much. For example, focusing on pain,
depressive thoughts and feelings, worry or anxious thoughts and feelings, or hallucinations
(such as hearing voices) can actually make those symptoms worse, and increase distress.
Learning how to distract yourself from distressing symptoms can be a healthy coping
strategy that provides much relief.
Some tips for distracting yourself:
• Work on a puzzle or word game, reading a magazine or book, listen to music or talk
radio, or have a conversation with someone
• Engage in something invigorating that stimulates your body, such as taking a walk
or jog, doing some household chores, participating in an exercise or dance class, or
doing calisthenics
• Participate in fun activities, things that you enjoy and will give you a deserved
break—consider scheduling enjoyable time for yourself every day, and every week
to do something fun with someone else
Module #8
Handout
Integrated Illness Management
and Recovery Manual
Page 181
Let’s Discuss!
Have you ever used distraction to help you cope with symptoms or problems?
How did it work?
Would you like to use distraction more often, or to address another symptom or
problem?
2. Mindfulness/acceptance techniques
While distraction can often be helpful, trying not to think about something can sometimes
be downright impossible! Mindfulness or acceptance techniques are based on the fact that
youcan’tcontroleverythingthatgoesoninyourmindorbody,butyoudon’thavetolet
yourmindorbodycontrolyou.Thatmeansyoudon’thavetoletyourthoughts,feelings,or
senses, such as pain, dominate your life. These techniques can be useful for the same types
of symptoms as distraction methods.
Some tips on mindfulness/acceptance strategies:
• Acceptthatyoucan’tcontroleverythingthatgoesoninyourmindoryourbody,
butthat’sOK,you’retheoneinchargeofyourownlife.
• Practice “just noticing” distressing thoughts, feelings, or sensations without dwelling
on them and instead moving on with your day.
• Come up with something you can say to yourself in good humor that recognizes
thethought,feeling,orsensation,butdoesn’tgiveitpoweroveryourlife(suchas
“thanking your brain/body” for that thought/feeling/sensation)
• Imagineyourthoughts,feelings,orsensationsasariverorstream,alwaysowing
downandpastyou,ratherthansomethingxedintime.
Let’s Discuss!
Have you ever used mindfulness/acceptance techniques to help you cope with
symptoms or problems? Which ones? How did they work?
Would you like to use mindfulness/acceptance techniques more often, or to address
another symptom or problem?
Improving attention and concentration
Beingabletofocusone’sattentionandconcentrateonsomethingisanimportantskillwhen
interacting with people, getting things done, and getting the full enjoyment out of activi-
ties. You can improve your concentration through a combination of removing distractions,
repeating or paraphrasing verbal information, and scheduling rest breaks.
Module #8
Handout
Integrated Illness Management
and Recovery Manual
Page 182
Minimize distractions
It is easier to concentrate on something when there a fewer things around that can dis-
tract your attention.
• Avoidtryingto“multitask”—it’softeninefcientbecauseoneorbothtasksarepoorly
done and have to be done again.
• Turn the radio or TV off in order to concentrate when having a conversation, reading, or
doing another important task.
• If you are trying to do something on the computer, close down programs you are not
using (such as e-mail) and turn off automatic reminders (such as chimes for new email,
appointment reminders).
• Remove distractions when you are concentrating on something, such as noises in the
room, other papers on the desk, your cell phone, to help focus your attention
Paraphrase or repeat back verbal information
Difcultyrememberingthingswhentalkingwithpeopleifoftenduetolapsesinattention
wheretheinformationwasneverprocessedorattendedtointherstplace.Tohelpyou
pay attention to important information, try:
• Whenyoumeetanewpersonandrstheartheirname,usetheirnameassoonas
possible when you respond:
Person#1:Hi,mynameisJohn.It’snicetomeetyou.
Person #2: Hi, nice to meet you John. My name is Mary.
• Repeat back or paraphrase something some tells you to make sure you got it right:
Person#1:Whenyougotothestore,I’dlikeyoutogettissues,bananas,andice.
Person#2:OK,soyouwantmetogetbananas,ice,andtissuesatthestore?
Person #1: Right!
Schedule rest breaks
It can be frustrating and tiring to work on something until you lose your concentration.
Working for a set period of time (such as 15 minutes) and then taking a brief break (such
as 5 minutes) can help you maintain good attention and concentration. You may be able to
gradually increase the periods of time you spend concentrating.
Let’s Discuss!
Have you ever used any of these techniques to improve your attention or
concentration? Which ones? How did they work?
Would you like to use some of these techniques more often to improve your attention
or concentration?
Module #8
Handout
Integrated Illness Management
and Recovery Manual
Page 183
Coping with fatigue, low energy, or reduced motivation
Getting tired easily, or having low energy or motivation, can be discouraging and can get in
the way of getting things done and enjoying life. Effective coping strategies can help you
accomplish things at a pace that feels comfortable to you.
• Focus on taking one step at a time.
• “Program for success” by making your short-term goals or steps small enough that you
arecondentyouwillsucceedifyoutry.
• Congratulate yourself when you achieve a step towards a goal
• Invite people to do things with you, such as shopping, taking a walk, or going to the
movies. People are often more likely to go somewhere if they know someone else will be
there.
• Plan for breaks if you are going to engage in a long activity that could be tiring.
• Be patient and recognize that change will come slowly if you stick to it
Let’s Discuss!
Have you ever used any of these techniques to deal with fatigue, low energy, or
reduced motivation? Which ones? How did they work?
Would you like to use some of these techniques more often to improve your energy or
motivation?
Improving sleep
Difcultygettingagoodnight’ssleepcanmakeabigdifferencein
feeling rested and ready to take on a new day. Although it may feel
like your sleep is not under your control, you can actually improve your
sleepbychangingyourhabits.Scienticresearchhasshownthata
developing a set of habits can improve sleep and restfulness. It takes
timeandpatiencetochangeyourhabits,butit’sworthitinthelong
run. Revisit the handouts about Healthy Lifestyle to learn more about
improving your sleep.
Module #8
Handout
Integrated Illness Management
and Recovery Manual
Page 184
Integrated Illness Management and Recovery
Home Practice Sheet
My home practice for this week is:
To complete this home practice, I will use the following plan:
When:
Where:
With Whom:
What do I need to do the practice?
Today’sDate:__/__/____
Participant:____________________IIMRSpecialist:_________________________
Integrated Illness Management and Recovery
Home Practice Sheet
My home practice for this week is:
To complete this home practice, I will use the following plan:
When:
Where:
With Whom:
What do I need to do the practice?
Today’sDate:__/__/____
Participant:____________________IIMRSpecialist:_________________________

Module #9
Guidelines
Integrated Illness Management
and Recovery Manual
Page 185
Practitioner Guidelines for Handout #9:
Relapse Prevention
Goals
This topic area helps people examine their previous experience with relapse in order to develop a relapse
prevention plan. Help people identify triggers, early warning signs, and steps they can take to help pre-
vent relapses and hospitalizations. Though past negative experiences are discussed, the overriding ques-
tion is “What can be done so that you will have better health in the future?”
Suggestions for Teaching
• Help people to identify what their own experiences have been so they can identify important early
warning signs. The checklists can help people relate the information to their own experience.
• Connect relapses of psychiatric and medical illness. Encourage people to talk about
how a relapse in one (medical or psychiatric illness) can cause a relapse in the other.
• For diabetes, COPD, and chronic pain, in particular, help people learn to identify
exacerbations of these medical problems when they are happening.
• Keep in mind the recovery goals identified by people in earlier sessions. Help people to connect relapse
prevention with goal achievement. There are also opportunities to set new goals.
• If people have difficulty identifying triggering events or early warning signs of relapse, encourage them
to get input from family members or other supportive people. Help people role-play what kinds of
questions they might ask someone to find out information about early warning signs and triggers.
• People may find that talking about relapses brings back unpleasant memories. Focus the discussion
on identifying important information for the future, and help people avoid self-blame. If people berate
themselves, remind them that it can be very difficult to predict relapse, point out their strengths in
managing their illness, and praise them for developing a relapse prevention plan.
• Use cognitive-behavioral strategies when helping people develop their relapse prevention plans. For
example, if people decide that decreasing stress is part of their relapse
prevention plan, practitioners can help them role-play deep breathing or muscle
relaxation. If calling a friend is part of their plan, they can role-play what they would say when they
made the call. If increasing medication is part of their plan, they can role-play talking to their doctor.
Review Questions
What is an example of a something that might trigger a relapse?
What is an early warning sign?
What can people do to prevent an early warning sign from becoming a relapse?
How can a family member or other supportive person be part of a relapse prevention plan?

Module #9
Guidelines
Integrated Illness Management
and Recovery Manual
Page 186
Suggestions for Home Practice
1. Talking to family members and supporters about early warning signs of relapse they have observed.
2. Reviewing what helped and what did not help during past relapses or impending relapses.
3. Drafting or revising a Relapse Prevention Plan.
4. Asking family members, friends and others to play a specific role in the Relapse Prevention Plan.
5. Collecting necessary phone numbers or other needed resources for the Relapse Prevention Plan.
6. Posting a copy of the person’s Relapse Prevention Plan in an accessible (but private) place.
7. Initiating a component of the Relapse Prevention Plan that is more effective if done on a regular basis,
such as going to a support group.
8. Develop a plan to monitor increases in symptoms and to minimize exacerbating factors.

Module #9
Handout
Integrated Illness Management
and Recovery Manual
Page 187
Integrated Illness Management and Recovery
Handout #9: Relapse Prevention
What is a “relapse”?
Symptoms of mental and physical illnesses can change over time. Sometimes symptoms may
be gone; sometimes they may be mild or moderate. Sometimes they may be severe; this
is usually called a “relapse.” Some relapses can be managed at home, but other relapses
require hospitalization.
When was the last time you had a relapse of your medical symptoms?
When was the last time you had a relapse of your mental health symptoms?
What effect have relapses had on your ability to work on your personal goals?
What causes relapse?
It is sometimes hard to know why people have relapses of their mental or physical illness-
es. Research shows, however, that relapses are more likely to occur when people:
• Are under more stress (money problems, changing jobs or losing a job, having a new
baby, relationship problems)
• Stop taking their medications
• Stop monitoring the signs of their illness
• Use alcohol or drugs
• Are not managing their illnesses the way they are supposed to
What has caused your illnesses to relapse in the past?
How do relapses in psychiatric and medical illnesses affect each
other?
• Poor physical health can lead to increased stress, anxiety, and/or depression, making the
mental illness worse.
• For example, an increase in back pain could cause someone to become depressed or
ve ry irritated, potentially causing a psychiatric relapse.
• An increase in mental illness symptoms makes it harder to take care of physical
illnesses.
• For example, an increase in the negative symptoms of schizophrenia may cause
someone to stop monitoring blood sugars properly, increasing symptoms of diabetes
or causing even more serious problems (for example, poor kidney functioning).
How have relapses in your psychiatric and medical illness affected each other?

Module #9
Handout
Integrated Illness Management
and Recovery Manual
Page 188
How can you prevent or reduce the number of relapses you have?
• Recognize events or situations that caused relapses in the past.
• Recognize the “early warning signs” that you might be starting to have a relapse.
• Develop your own relapse prevention plan to respond to early warning signs.
• Use the help of other people, such as family members, professionals, and friends, to
prevent early warning signs from becoming full-blown relapses.
What are “early warning signs”?
The slight changes in behavior or feelings that often start to happen several weeks or
days before a relapse. Some early warning signs are relatively common, such as:
• Feeling tense or nervous
• Eating less or eating more
• Trouble sleeping or sleeping too much
• Decreased need for sleep
• Feeling depressed or low
• Feeling like not being around people
• Feeling irritable
• Stopping treatment
• Trouble concentrating
• Increased drug or alcohol use or abuse
Have you experienced any of these common early warning signs? Which ones?
Some early warning signs are quite unusual, such as:
• “Before my last two episodes of depression, I cut my hair very, very short.”
• “My brother noticed that I was whistling all the time.”
• “I started buying lottery tickets two or three times a day.”
• “I started wearing the same clothes every day.”
Have you experienced early warning signs that were relatively unique?
Do you always recognize your early warning signs?
You are not always aware when your behavior has changed and you are experiencing an
early warning sign of relapse. For example, you might not realize that you are feeling
unusually irritable. But, people around you may notice this. Friends, family members,
co-workers, healthcare practitioners and other supportive people often notice when
someone seems different or is acting out of character. They can help you recognize
early warning signs of both mental and physical illness. You could tell them what early
warning signs to look for, and let them know that you would like them to inform you when
they notice these signs.
Whom would you like to help you recognize early warning signs?

Module #9
Handout
Integrated Illness Management
and Recovery Manual
Page 189
How can you make a Relapse Prevention Plan?
You may nd it helpful to consult with the supportive people in your life. Peers, practi-
tioners, family members, and others can help you remember details about what helped in
past situations. After you have identied a situation that caused a relapse in the past,
think about how you might handle the situation differently in the future. For example, if
you notice that you have relapses of your depression whenever you are not getting enough
sleep or when you are not making time to get out for your daily walk, you should make sure
to get extra sleep and perhaps ask a friend to walk with you so that you will be sure to get
in the habit of doing it again. If you notice that being under stress tends to cause a re-
lapse of your chronic back pain, you could plan to use a specic relaxation technique, such
as guided imagery, or a yoga DVD to reduce stress.
What would you include in your Relapse Prevention Plan?
The next page has a form you can use to write your Relapse Prevention Plan.
Module #9
Handout
Integrated Illness Management
and Recovery Manual
Page 190
Relapse Prevention Plan
Reminder of events or situations that triggered relapses in the past:
1.
2.
3.
4.
Reminder of early warning signs that I experienced in the past:
1.
2.
3.
4
What I think would help me if I am experiencing an early warning sign:
1.
2.
3.
4.
Who I would like to assist me, and what I would like them to do:
1.
2.
3.
4.
Who would I like to be contacted in case of an emergency?
1.
2.
3.
4.

Module #9
Handout
Integrated Illness Management
and Recovery Manual
Page 191
Integrated Illness Management and Recovery
Home Practice Sheet
My home practice for this week is:
To complete this home practice, I will use the following plan:
When:
Where:
With Whom:
What do I need to do the practice?
Today’s Date: _ _ / _ _ /_ _ _ _
Participant: ____________________ IIMR Specialist:_________________________
Integrated Illness Management and Recovery
Home Practice Sheet
My home practice for this week is:
To complete this home practice, I will use the following plan:
When:
Where:
With Whom:
What do I need to do the practice?
Today’s Date: _ _ / _ _ /_ _ _ _
Participant: ____________________ IIMR Specialist:_________________________

Module #10
Guidelines
Integrated Illness Management
and Recovery Manual
Page 193
Practitioner Guidelines for Handout #10:
Getting Your Needs Met in the Health Care
System
Goals
This topic area, which can usually be covered in 2 sessions, focuses on getting resources needed for opti-
mal health care. It covers a description of services offered at community mental health centers and how to
advocate for services the client wants and needs. It also addresses getting primary care needs met as part
of self-managing medical issues. Finally, accessing resources for building a healthy lifestyle is covered in
more detail in follow-up to Topic 4.
Suggestions for Teaching
• After discussion of services/resources (mental health, medical, or lifestyle) clients
may want to develop a plan in session for accessing a new service. Review the list of
resources in the handout for guidance.
• Role-play a conversation between client advocating for a service and a professional at the mental health
center
• Practice making an appointment through a role-play and developing a list of questions
for the doctor in session.
• It is possible that visiting a gym or fitness center for a tour with the client may help him or her feel
comfortable enough to return to the facility on their own.
Review Questions
What does it mean to “advocate” for services?
What are some examples of health concerns that would require a visit to the
emergency room?
Why is it best to see your primary care physician for non-emergency health concerns?
How can you find out about resources in your area for exercise, nutrition, etc.?
Suggestions for Home Practice
1. Think about the services currently being received at the community mental health
centers. Brainstorm a list of other services that the client might be interested in
and why.
2. Develop a list of questions for an upcoming primary care doctor appointment or
a first-time appointment with a new provider.
3. Call exercise centers in the community and compare prices and other features such as hours of oper-
ation and group exercise opportunities. Write down the options and details down and bring the list
to next session for discussion.
4. Attend a nutrition class in the community. Write down back 2 or 3 pieces of new
information to share during the next session.

Module #10
Handout
Integrated Illness Management
and Recovery Manual
Page 195
Integrated Illness Management and Recovery
Handout #10: Getting Your Needs
Met in the Health Care System
Because physical and mental health are so inter-connected and crucial to achieving
recovery and wellness, it is very important for you to receive regular, on-going care for
BOTH your mental and physical health problems. Some mental health centers also offer
medical services so you can receive care in one place, but many do not. If you do not
have a regular medical doctor, you should make it a priority to nd one and to have an
appointment with him or her as soon as possible.
Steps for nding a medical doctor (Primary Care Provider)
Your relationship with your regular doctor is important and will hopefully last for many
years so it is crucial to work with someone you like and respect. There are several possible
ways to nd a good doctor.
1. Ask someone to suggest a good doctor: Get a recommendation from someone you
trust such as a friend, family member, or another care provider. Think about the
qualities you would like in a good doctor (kind, smart, good listener, easy to talk to).
Ask the person questions about the doctor and the experience of working with him or
her in order to have a good idea of what the doctor is like (for example, “How much
time does he/she spend with you during appointments?” “Does he/she involve you in
treatment decisions?” “Does he/she explain things well?”
2. Look for clinics in your neighborhood: If transportation will limit where you can get
medical care, observe what medical clinics are within walking distance. You can walk
into a clinic and tell the receptionist that you are looking for a primary care doctor.
He or she will tell you whether any of the clinic doctors are taking new patients and
may also be able to give you a brochure with the names of the doctors and possibly
information about each one. You could then go online to look for more information.
3. Call your insurance company: Your insurance company may require you to choose a
medical doctor from a list of the primary care providers that are covered under your
insurance plan. Or, you might be able to get a suggestion from the representatives on
the phone. There is usually a telephone number for your insurance company on the back
of your insurance card. Even if you get a recommendation from a friend you should call
your insurance company to make sure the doctor is on your company’s approved list of
doctors.
Getting healthcare or services for specic problems or needs
It seems like health care and community services in the United States change a lot. It is
easy to get confused about what services are available, who is eligible for them, and how
to get access to them. Case managers and social workers usually have current information,
so ask them if you are unsure. There is also information on the internet, but make sure it
is from a trustworthy source. Having a doctor who takes care of general medical health
issues is a basic necessity for everyone; however, you might have specic problems or
needs that require specialty health care or services.
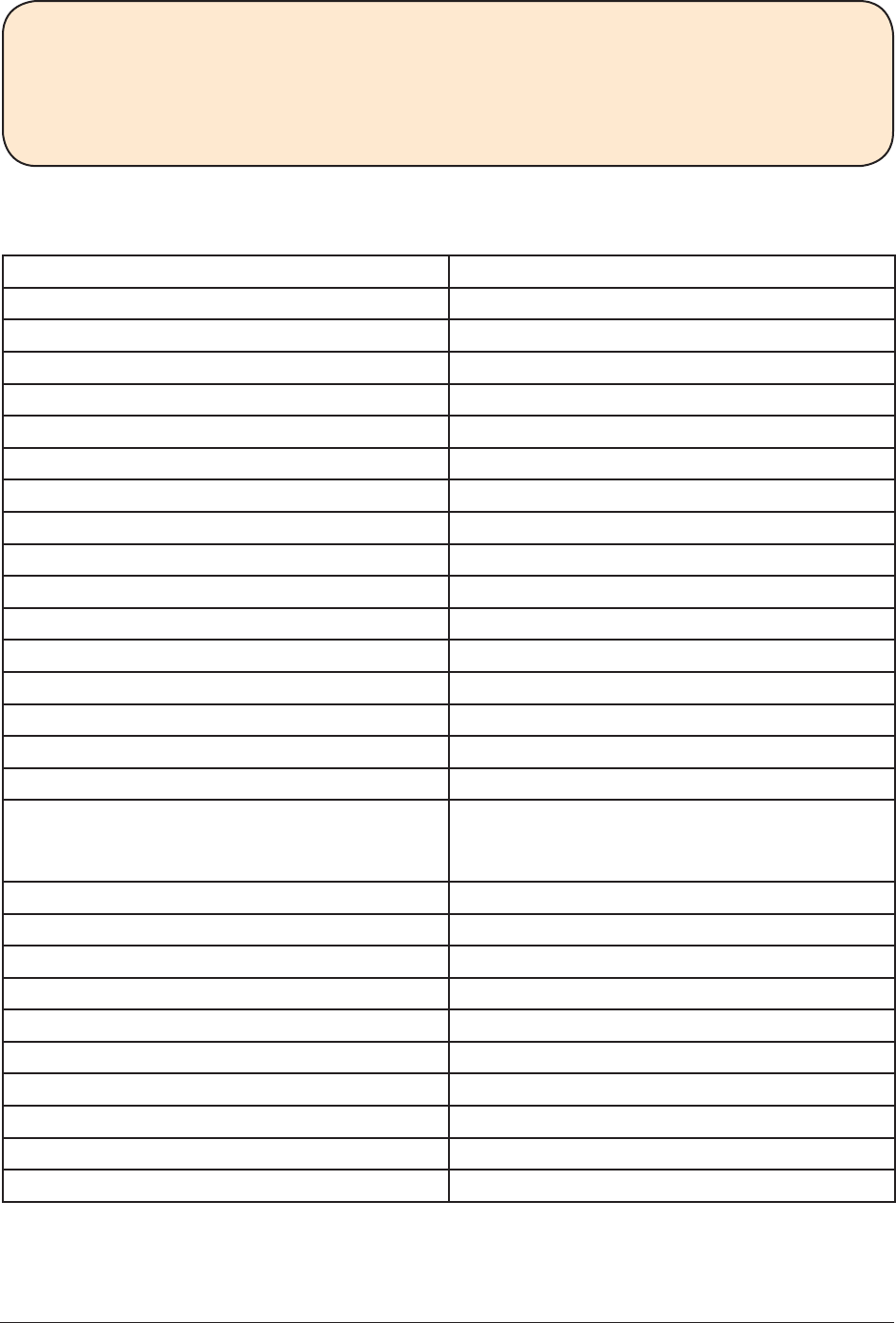
Module #10
Handout
Integrated Illness Management
and Recovery Manual
Page 196
What health care and/or services are you currently receiving? How helpful are they?
What other health care or services do you think would be helpful?
Complete the checklist below to make sure you are getting what you need and make a
plan to get the care or services you need.
Health Care and Community Services Checklist
Type of Health Care or Service I need
Mental Health Care
Case management
Medication management
Peer support/consumer-led programs
Individual therapy
Group therapy
Skills training
Family services
Day treatment
Support groups
Integrated substance use treatment
Employment services
Assertive Community Treatment (ACT)
Crisis Line
Medical Care or Services
Primary Care Physician
Specialist Provider (such as endocrinolo-
gist, cardiologist, podiatrist, sleep spe-
cialist)
Optometrist or Ophthalmologist
Dental Care
Nutritionist
Community Services
Smoking Cessation Support
Gym or Exercise Facility
Occupational therapy
Recreational therapy
Housing assistance
Other:
Module #10
Handout
Integrated Illness Management
and Recovery Manual
Page 197
Making an appointment
Making an appointment for a health care visits is an important skill to have so that you can
be more in charge of your own health. Before making an appointment with a health care
professional, think about the reason for the appointment and collect some things you will
need for the phone call including:
• Pen and paper - To take notes and write down appointment date/time.
• Calendar or Appointment Book - To check when you are available.
• Phone number and name of doctor
Steps for making an appointment
1. Say your rst and last name and the reason for your call.
For example:
“Hello. This is Susan Jones. I need an appointment with Dr. Smith for a
new patient appointment.”
2. Listen to the appointment date/time offered and repeat it.
For example:
“Ok, Dr. Smith could see me on Monday July 10 at 9:00 am? Let me
check…”
3. Check your calendar for availability.
4. Write down the date, time and special instructions for the appointment.
5. Repeat information back to the person.
For example:
“So, that’s Monday July 10 at 9:00 am and I should not eat for 12 hours
before the appointment so you can do a blood test?”
6. Thank the person for making the appointment.
For example: “Thanks very much.”
Steps for preparing for a health care appointment
1. Make a list of concerns or questions: Before going to a health care
appointment, think about your goals for the visit and make a list of
concerns and questions for your health care provider. Put the most
important concerns or questions at the top of the list in case you there
is not enough time to address every item. Bring a list of your medications
for you and your doctor to review. Look at your medications before the
appointment and think about any side effects you may need to report to the doctor.
If you are having a problem with a medication it is important to tell the doctor
because he or she may need to make a change.
2. Gather important items: Put all the things you will need for the appointment
(list of concerns, medication list, glasses or hearing aid, insurance card, pen and paper)
together in an obvious place so that you won’t leave for the appointment without them.
3. Ask for help: Ask a family member or friend to come to the appointment if you need
support or help. If you think you might have trouble remembering or hearing, having
someone accompany you can be helpful. After the appointment review what the doctor
said with the person to make sure you have all the information you need.
Module #10
Handout
Integrated Illness Management
and Recovery Manual
Page 198
4. Arrange for Transportation: Make sure you have a ride if you need one so that you
can arrive at your appointment on time or even a little early. Some transportation
services require advance notice so make arrangements ahead of time.
Sharing health information with your doctor
An important part of getting the best health care possible is knowing how to share health
information with your doctor or other health care providers.
Let’s Discuss!
Why is it important to be skilled at sharing health information with your doctor?
What are the types of information your doctor needs to know to diagnose a problem
or recommend a treatment? Tell me about the last time you shared health information
with your doctor.
Steps for sharing health information
1. At the beginning of an appointment, tell the doctor that you have a concern.
2. Describe in detail your concern or question and stay on topic. See below for what
details to provide.
3. Listen to the doctor’s recommendations and repeat back the information.
4. Thank the doctor.
Details to mention when you are reporting concerns or symptoms:
• Location - Say where the problem is. For example, “I have pain in my right knee.”
• Duration and frequency - Tell the doctor how long you have been having the symptom and
how often. For example, “I have had the pain every morning for the past two weeks.”
• Severity - Describe how bad the pain is. For example, “I would rate the pain an 8 on a
scale of 1-10.”
• Timing - Say when the symptom happens. For example, “I always have the pain when I
try to stand up after I have been sitting for more than an hour.”
• Things that make it better or worse - Tell the doctor what you have tried to cope with
the symptom or what makes the symptom worse. For example, “If I take two ibupro-
fen in the morning it keeps the pain at about a 6 versus an 8 during the day, however at
night the ibuprofen doesn’t seem to help.”
• Functioning - Explain the impact that the symptoms is having on your functioning. For
example: “The pain is making it hard for me to sleep and to carry anything heavy.”
Use the chart on the following page to track symptoms and record details for the doctor.
It may be helpful to bring the chart to the appointment with the doctor.
*Practice Sharing Health Information with Your Doctor*
Module #10
Handout
Integrated Illness Management
and Recovery Manual
Page 199
Symptom How long? How often? How severe? Where?
Effect on
Functioning? What makes it better/worse?
HEADACHE TWO WEEKS EVERYDAY 7 on a
SCALE from
1-10
MIDDLE OF
FOREHEAD
ADVIL HELPS. BRIGHT LIGHT
MAKES IT WORSE

Module #10
Handout
Integrated Illness Management
and Recovery Manual
Page 200
Let’s Discuss!
Have you encountered problems getting the health care or services you needed?
How did you handle the problem? How would learning to advocate for yourself help
you to reach your personal goals?
Advocating for yourself and solving problems in the health care
system
• Seek out someone who has a lot of experience with this type of problem.
For example, imagine that your doctor prescribed a medicine for an infection but when
you went to the pharmacy to get it, the clerk told you your Medicaid was not open and
it would cost you $150. In this situation, you might talk to a case manager or a benets
specialist because they usually know a lot about insurance coverage. You could also talk
to a family member or friend (if they also have Medicaid).
• Talk about your concerns calmly and clearly.
Even if your problem is the result of someone else’s mistake, you will get the situation
xed much faster, and it will cause you less stress, if you try to remain calm and use a
polite, even tone to talk about it. If you raise your voice or say negative things about the
person who might have made a mistake, you could make other people mad and then they
might be less likely to help you right away. It is also important to be very clear and to
try to talk only about the problem you want help with, not other problems you might be
having. It helps to practice what you are going to say before you say it.
• If you are not satised after talking to the rst person, take additional action.
If your problem does not get solved after talking to the rst person, talk to someone
else. In the example above, you might have to speak to your case manager’s supervisor
or you might have to call a consumer advocacy group such as the National Alliance for
Mental Illness.
• Take responsibility for things you can do to solve the problem.
If there are things you can do to solve the problem, offer to do them. In the example
above, you might have to send some paperwork to the local Medicaid ofce or you might
have to call the number on the back of your Medicaid card to get information about why
your insurance coverage is not active.
• Let people know that you appreciate their efforts.
When people try to help you solve your problem, remember to thank them sincerely for
their efforts. This will make them want to help in the future.
• Keep a record of the details of the problem and what you tried to do about it.
Keep whatever documents relate to the problem in a folder. Make notes of conversations
you have with people about the problem.
• If at rst you don’t succeed, try, try again.
Obstacles are a part of life, but sticking with a problem can pay off in a good way!
*Practice Advocating for Yourself and Solving Health Care Problems*

Module #10
Handout
Integrated Illness Management
and Recovery Manual
Page 201
Let’s Discuss!
When do you go to the doctor’s ofce versus urgent care versus the emergency room?
What is an example of a medical emergency?
Making decisions about where to seek care when you don’t feel well
Most medical concerns, with the exception of emergencies (which are discussed below),
should be handled by your regular doctor. This is because they know you and your health
history. Doctors and other health care providers can usually schedule an appointment on
the same day or the following day if you suddenly need to see someone. Even if it is after
hours (after 5pm) or a weekend day (Sat or Sun), you can still call your doctor or psychia-
trist. Most health care ofces have someone answering the phone and have a nurse and/or
doctor on call who can be reached and who will call you back to discuss your problem.
Emergencies that require immediate care
There are a limited number of symptoms or problems that cannot wait for a doctor’s ap-
pointment. These include:
1. Serious chest pain
2. Bleeding that will not stop from a serious cut
3. Serious plan to harm or kill yourself or someone else
4. Coughing up blood
5. Severe burn that is causing swelling or blistering
6. Extreme difculty breathing (allergic reaction, COPD, Asthma)
7. Symptoms of stroke (arm weakness, drooping face, slurred speech, difculty talking)
If you experience one of these 7 symptoms and you live with someone (or there is someone
in your building) who can drive you to the emergency room, you should immediately go.
Do not wait for someone who lives in a different place to come and pick you up. If you do
not have someone to drive you to the ER, you will have to call 911 and they will send an
ambulance.
Preventive health care
Preventive healthcare involves getting tests and exams to prevent medical problems from
developing or getting worse. The tests you should receive depend on your age, gender, and
medical history. Talk to a nurse or doctor or your I-IMR Specialist about which ones you
need.
Physical exam: Everyone should have a physical exam every year at their primary care
ofce. At the exam, your provider may order blood work, and will take your weight and
blood pressure and will listen to your heart and lungs and discuss any concerns you have
about your health.

Module #10
Handout
Integrated Illness Management
and Recovery Manual
Page 202
Screening for HIV/Sexually Transmitted Infections (STIs): Sexually active people should
be screened for HIV/STIs whenever they have a new partner and once a year. Depending on
sexual behaviors and number of partners, your provider may do screening more or less often.
Cholesterol test: This is a blood test that checks for levels of lipids (fats). It is recom-
mended for both women and men, but the frequency of the test depends on your age,
gender, and medical history. The test includes Total Cholesterol, which should be <200, LDL,
which should be <100, HDL, which should be >50, and Triglycerides, which should be <150.
Diabetes ccreening. If you have risk factors for diabetes such as high cholesterol, high
blood pressure, or if you are overweight or obese, a provider may order a fasting blood
sugar (glucose) test to check for diabetes. If you have diabetes, you will likely have a
hemoglobin A1c blood test 4 times a year. This test measures average blood sugar for the
past 3 months.
Flu shot: protects people from the inuenza virus and is recommended to everyone over the
age of 6 months. You should get it yearly and early in the u season if possible such as Sep-
tember or October.
Pneumonia vaccine: helps prevent getting certain kinds of pneumonia. Talk to your doctor
about whether you need to get this vaccine.
Tetanus shot: Everyone should have a shot to protect against tetanus at least every
10 years or if you have a serious cut or injury. Tetanus is a serious disease that causes
painful tightening of the muscles all over the body.
Eye exam: Everyone should have an eye exam by an optometrist or opthamologist every
2-3 years. You might need exams more often if you don’t see well, you wear contacts, or you
have a diagnosed eye condition like glaucoma or macular degeneration. In an eye exam, the
doctor will see how healthy your eye is and also look for problems with near and
farsightedness.
Hearing exam: a basic hearing test should be done as part of your yearly physical exam or a
more detiled hearing test may be done for older adults or if you are having trouble hearing.
Dental exam: Everyone should have a visit to the dentist at least once a year, even if you
do not have teeth or wear dentures. Dentists will check for mouth cancer, gingivitis, and
periodontitis.
Bone density screening: Women age 65 or older should have a bone density scan, which is
a special kind of x-ray, usually of the hips and back bone and forearm. This tests for
osteopenia and osteoporosis, which involves thinning of the bones in the body.
Cancer screening: Everyone should have a colonoscopy when they turn 50 to check for
colon cancer. People need to prepare for this test by drinking a special drink that helps move
the bowels. A doctor places a scope into the rectum that allows him/her to see the inside
walls of the colon. You are asleep for this test. Women age 21-65 should have PAP smear
tests regularly, but the frequency varies depending on your age, sexual practices, and re-
sults of prior tests. This is where the doctor takes some cells from the cervix, inside the
vagina. Women age 50-74 should get a mammogram, a special x-ray of the breasts, at least
every 2 years. But, all women should do self breast exams monthly to check for lumps. If you
do not know how to do a self exam, ask your doctor or nurse. If you feel a lump your doctor
may send you for further testing including an ultrasound or a mammogram. Men who are 50
or older should talk to their doctor about getting a PSA test to screen for prostate cancer.
The prostate is a gland behind the bladder that only males have.
Module #10
Handout
Integrated Illness Management
and Recovery Manual
Page 203
Building a healthy lifestyle
Changes to lifestyle such as getting more exercise, eating healthier, quitting or reducing
smoking, and avoiding alcohol and drugs are an important part of managing your overall
health, reaching your personal goals and living the best life possible. There are resources
in the community that might help you with these lifestyle changes.
Exercise and physical activity resources
Gyms and tness centers can help you get more exercise if you live in a part of the
country where cold weather would prevent you from exercising outside many months of the
year. Gyms also have things like special exercise equipment, swimming pools, and basketball
courts if you are someone who likes variety in exercise. Gyms require a membership fee
that may range from $8 - $200 per month. Some gyms, such as the YMCA, offer reduced
rates or even scholarships for people on a limited income. Or, you can is talk with some-
one at the tness center in your community to see if there are ways to get a break on the
membership fee in exchange for a service, such as cleaning, at the facility.
Community recreation centers and senior centers offer affordable or even free access
to exercise equipment, basketball courts, and possibly other facilities such as swimming
pools. These types of facilities may not be available in every community, but if available,
might be the rst place to start to nd an inexpensive indoor option for exercise and
physical activity.
Yoga studios, martial arts studios, and other private exercise studios sometimes offer
exchange for service programs. For example, you may be able to clean a yoga studio
once a week in exchange for free classes. Call the studio owner to nd out about such
opportunities.
Hospitals in your community may offer classes aimed at improving
tness such as yoga, or Zumba, or strength training. These classes
are not usually offered for free, but may be covered by your
insurance. Hospitals may also offer scholarships.
Healthy eating and diet resources
Weight Watchers has a meeting or multiple meetings in most areas. Membership costs
around $44 a month and includes in-person meetings and access to the online resources.
It costs around $20 per month to use only the online resources. Weight Watchers does
not offer scholarships, but you may be able to nd a special offer or sale.
Overeaters Anonymous may have meetings in your area. This organization focuses on
support and recovery for people who are struggling with uncontrolled overeating. Check
the website http://www.oa.org/or call 505-891-2664 for information.
Grocery store nutrition classes are available at some grocery stores and are often
offered for free. Topics may include: reading nutrition labels, shopping on a budget, and
healthy cooking demonstrations.
Food banks often partner with other local organizations to provide free nutrition
education.
Farmer’s markets are great places to nd fresh and local fruits and vegetables. Many
farmer’s markets accept food assistance cards for fresh produce, but it varies by state.

Module #10
Handout
Integrated Illness Management
and Recovery Manual
Page 204
Websites that might be helpful:
www.nutrition.gov
www.choosemyplate.gov
http://www.hsph.harvard.edu/nutritionsource/
Tobacco dependence treatment resources
Hospitals and health clinics may offer counseling for people interested in reducing or
quitting smoking. These resources are often described on the hospital/clinic website or by
calling the organization.
Quitlines are available in every state. Quitlines offer counseling and support by people
trained in helping people quit smoking. You can be directed to the quitline in your state by
calling 1-800-QUIT-NOW (1-800-784-8669).
Websites that might be helpful:
http://smokefree.gov/
www.lung.gov
http://www.nicotine-anonymous.org/
Making a plan for a healthy lifestyle change
After you have identied a healthy lifestyle change or goal that you want to achieve,
develop a plan to take the rst step toward reaching it. For example, if you want to lose
weight so that you can feel more comfortable in social situations, making a plan to get the
resources and support you need may increase the likelihood that you will be successful.
1. What is the goal you have set?
2. What is the rst step?
3. What resources do I need?
Cost. _________________________________________________
Transportation. _________________________________________
Time. _________________________________________________
Personal Support. ________________________________________
Other. ________________________________________________
4. When will you take the rst step? Date __/__/____

Module #10
Handout
Integrated Illness Management
and Recovery Manual
Page 205
Integrated Illness Management and Recovery
Home Practice Sheet
My home practice for this week is:
To complete this home practice, I will use the following plan:
When:
Where:
With Whom:
What do I need to do the practice?
Today’s Date: _ _ / _ _ /_ _ _ _
Participant: ____________________ IIMR Specialist:_________________________
Integrated Illness Management and Recovery
Home Practice Sheet
My home practice for this week is:
To complete this home practice, I will use the following plan:
When:
Where:
With Whom:
What do I need to do the practice?
Today’s Date: _ _ / _ _ /_ _ _ _
Participant: ____________________ IIMR Specialist:_________________________

Appendix
Integrated Illness Management
and Recovery Manual
Page 207
Appendix
A. Guide to Thoughts and Feelings
B. Common Styles of Thinking
C. The 5 Steps of Cognitive Restructuring Worksheet
D. Action Planning Worksheet
E. The 5 Steps of CR Note Card
F. Readiness Ruler for Changes in Behavior
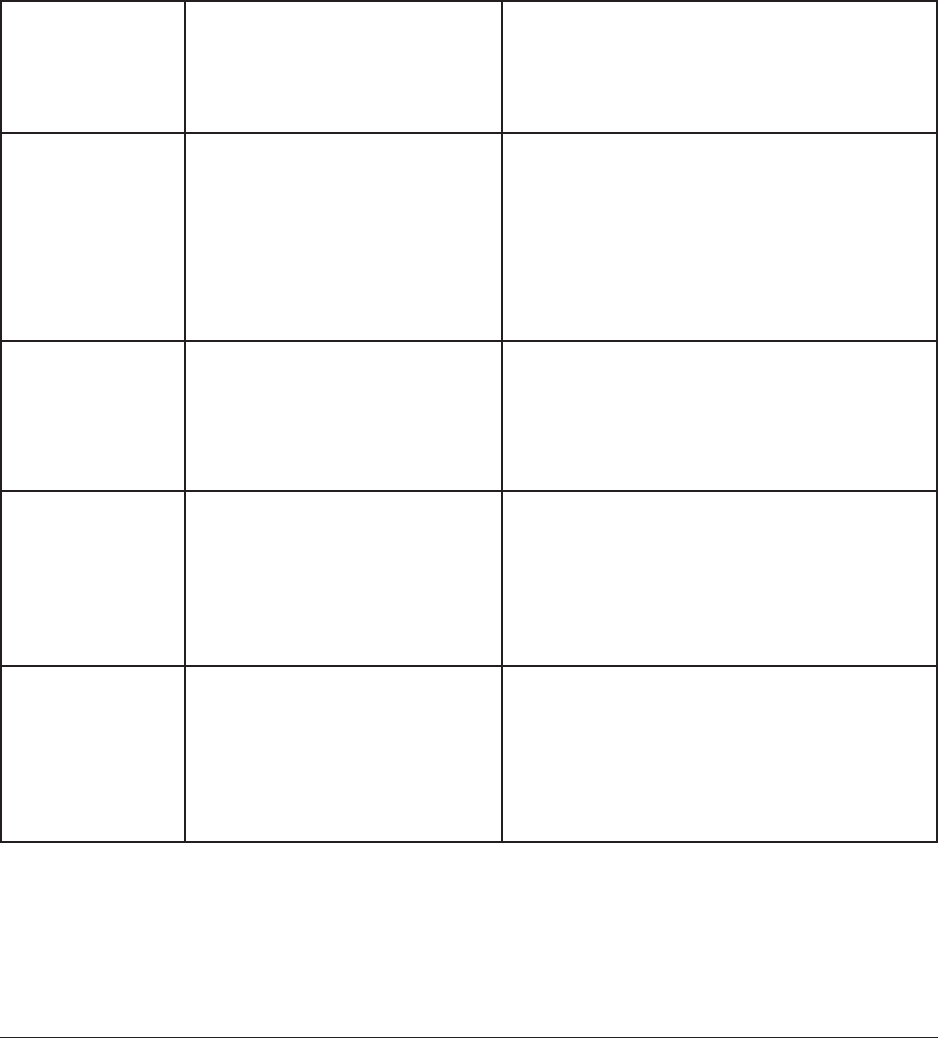
Appendix A
Integrated Illness Management
and Recovery Manual
Page 209
Guide To Thoughts And Feelings
Directions
If you are having a negative or upsetting feeling, first find the feeling on the chart. Then ask yourself
whether any of the questions in the second column apply to your thinking about the upsetting situa-
tion. If so, see the third column for some specific examples of thoughts that may apply to your upsetting
situation. If the questions in the second column don’t match up with your current thought process, then
perhaps you may be experiencing a different emotion after all. This sheet can help you hone in on which
feelings are most distressing to you and help you understand the thoughts that may be connected to those
feelings.
Negative Feeling Examples of questions you can
ask yourself to identify your
own underlying thoughts or
beliefs
Examples of thoughts or beliefs related to
the feeling
Fear or anxiety What bad things do I expect to
happen?
What am I scared is going to
happen?
Am I afraid I am going to lose
control or go crazy?
Thoughts that something bad will happen,
such as:
• Some terrible thing is going to happen
• I am going to be attacked or hurt
• I am going to be rejected or abandoned
• I am going to lose control or go crazy
Sadness or
depression
What have I lost in my life?
What is missing in me or in my
life?
Thoughts of loss, such as:
• I am worthless
• I don’t have anyone I can depend on
• Nothing will ever get better
Guilt or shame What bad thing have I done?
What is wrong with me?
Thoughts of having done something wrong
or being lacking in some way, such as:
• I am a failure
• I am to blame for what happened to me
• I am a bad person
Anger What is unfair about this
situation?
Who has wronged me?
Thoughts of being treated unfairly or having
been wronged, such as:
• I am being treated unfairly
• I am being taken advantage of
• Someone has done something wrong to me

Appendix B
Integrated Illness Management
and Recovery Manual
Page 211
Common Styles of Thinking
(Adapted from Burns, 1989 and Davidson et al., 1999)
Overgeneralization – A single distressing event is seen as a never-ending pattern. When something bad
happens, it is assumed that it will happen again and again.
Examples – My wife didn’t smile and say hello when she came home last night. She must be unhappy.
He was really nice to me today. This means he’s a wonderful person and I can trust him completely.
Mental Filter or Focus on the negative (“doom and gloom”) – A person selectively attends to negative
information; this is the “glass-half-empty” view of the world. By focusing on the negative, the person does
not see the “whole picture” and feels worse than necessary.
Examples – Jane focuses on the 5 items she missed on a 100-item exam and feels like a total failure.
Emotional reasoning – This occurs when the person’s feelings determine what he or she thinks or
believes, even when there is no ‘hard’ evidence to support it. Just because a person feels something, it
doesn’t mean it’s true.
Examples – A person who is afraid of elevators concludes on the basis of his fear reaction when he
gets in an elevator that elevators are dangerous.
A depressed client who concludes from his feelings of hopelessness about recovery from his illness
that he is hopeless and will never get better
All-or-nothing thinking (also “dichotomous thinking”) – A person who views things in extremes or
“black and white” terms, ignoring the “grays”.
Examples – Joe didn’t return my call promptly. He’s a totally unreliable person
I got a mediocre grade on my first case conceptualization write up; I fail at everything I try
“Must”, “Should”, and “Never” statements – translating one’s wishes and preferences into moral
imperatives for oneself and others
Examples – She should be on time for meetings with me. If she’s not, she’s not a responsible,
professional person
People should drive courteously. If they don’t, they shouldn’t be allowed to drive.
I should always be on time.
I must finish this task. If not, I will never be able to do anything.
I will never be good enough to be her friend.
Catastrophiszing – drawing conclusions, usually about the future, that involve exaggerated horrendous
outcomes
Examples – I overdrew my checking account. This means my credit rating will be ruined.
I failed that exam. That means I’ll fail out of graduate school.
Overestimation of Risk – The person thinks the risk of something is much greater than the evidence
supports.
Example – I’m not going to take a walk because I might be attacked.
Inaccurate or Excessive Self-Blame – The person blames himself or herself for something he or she had
little or no control over or responsibility for.
Example – It’s all my fault that I am alone and have no friends.

Appendix C
Integrated Illness Management
and Recovery Manual
Page 213
The 5 Steps Of Cognitive Restructuring Worksheet
(Adapted and modified from Mueser, Rosenberg, and Rosenberg 2009)
1. Situation
Ask yourself, “What happened that made me upset?” Write down a brief description of the situation.
Situation:
2. Feeling
Circle your strongest feeling (if more than one, use a separate sheet for each
feeling):
Fear/Anxiety Sadness/Depression Guilt/Shame Anger
3. Thought
Ask yourself, “What am I thinking that is leading me to feel this way?” Use your Guide to Thoughts
and Feelings handout to identify thoughts related to the feeling circled above. You may identi-
fy more than one thought related to the feeling. Write down your thoughts below, and circle the
thought most strongly related to the feeling.
Thoughts:
Is this thought a Common Style of Thinking? If yes, circle the one:
All-or-Nothing Over-Generalizing Must/Should/Never
Catastrophizing Emotional Reasoning Overestimation of Risk
Self-Blame Mental Filter

Appendix C
Integrated Illness Management
and Recovery Manual
Page 214
4. Evaluate Your Thought
Now ask yourself, “What evidence do I have for this thought?” “Is there an alternative way to look at
this situation?” “How would someone else think about the situation?” Write down the answers that
do support your thought and the answers that do not support your thought.
Things that DO support my thought:
Things that DO NOT support my thought:
5. Take Action!
Next, ask yourself, “Do things mostly support my thought or do things mostly NOT support my
thought?”
p NO, the evidence does not support my thought.
If the evidence does NOT support your thought, come up with a new thought that is supported by
the evidence. These thoughts are usually more balanced and helpful. Write your new, more helpful
thought in the space below. And remember, when you think of this upsetting situation in the future,
replace your unhelpful (“automatic”) thought with the new, more accurate thought.
New Thought:
p YES, the evidence does support my thought.
If the evidence DOES support your thought, decide what you need to do next in order to deal with
the situation. Ask yourself, “Do I need to get more information about what to do?” “Do I need to
get some help?” “Do I need to take steps to make sure I am safe?” Write down your action plan for
dealing with the upsetting situation below or complete the Action Plan Worksheet.
Action Plan:

Appendix D
Integrated Illness Management
and Recovery Manual
Page 215
Action Planning Worksheet
1. Define the Goal
What situation requires action?
Consider what change you would like to see in your situation.
Be as specific as possible.
2. Brainstorm Possible Strategies
What can you do to change the situation?
Using your problem-solving skills, think of all the possible ways
of effectively achieving your goal. Be creative.
3. Evaluate each solution
After you have identified a list of different strategies in step 2,
evaluate each one and place a + next to the best ones on the list.
Consider the following:
What information do you need?
Do you need help to implement the strategy?
Who is going to support you in taking this action?
What obstacles could interfere with the plan?
How could I prevent or deal with these obstacles?
4. Choose a solution
5. Plan how to implement the strategies you chose
I will take the following actions (Describe your plan):
6. Set a time or situation to follow up your plan
When and how are you going to take this action?
When do you want to use your plan?
1.
2.
3.
4.

Appendix E
Integrated Illness Management
and Recovery Manual
Page 217
The 5 Steps of CR Note Card
The 5 Steps of CR:
What is:
1. The Situation?
2. My upsetting Feeling?
3. My upsetting Thought?
4. Evidence FOR the thought?
Evidence AGAINST the thought?
_________________________________
5. Take Action!
Does the Evidence support thought?
NO: What is a more accurate Thought?
YES: Make an Action Plan for situation.
The 5 Steps of CR:
What is:
1. The Situation?
2. My upsetting Feeling?
3. My upsetting Thought?
4. Evidence FOR the thought?
Evidence AGAINST the thought?
_________________________________
5. Take Action!
Does the Evidence support thought?
NO: What is a more accurate Thought?
YES: Make an Action Plan for situation.
The 5 Steps of CR:
What is:
1. The Situation?
2. My upsetting Feeling?
3. My upsetting Thought?
4. Evidence FOR the thought?
Evidence AGAINST the thought?
_________________________________
5. Take Action!
Does the Evidence support thought?
NO: What is a more accurate Thought?
YES: Make an Action Plan for situation.
The 5 Steps of CR:
What is:
1. The Situation?
2. My upsetting Feeling?
3. My upsetting Thought?
4. Evidence FOR the thought?
Evidence AGAINST the thought?
_________________________________
5. Take Action!
Does the Evidence support thought?
NO: What is a more accurate Thought?
YES: Make an Action Plan for situation.
The 5 Steps of CR:
What is:
1. The Situation?
2. My upsetting Feeling?
3. My upsetting Thought?
4. Evidence FOR the thought?
Evidence AGAINST the thought?
_________________________________
5. Take Action!
Does the Evidence support thought?
NO: What is a more accurate Thought?
YES: Make an Action Plan for situation.
The 5 Steps of CR:
What is:
1. The Situation?
2. My upsetting Feeling?
3. My upsetting Thought?
4. Evidence FOR the thought?
Evidence AGAINST the thought?
_________________________________
5. Take Action!
Does the Evidence support thought?
NO: What is a more accurate Thought?
YES: Make an Action Plan for situation.
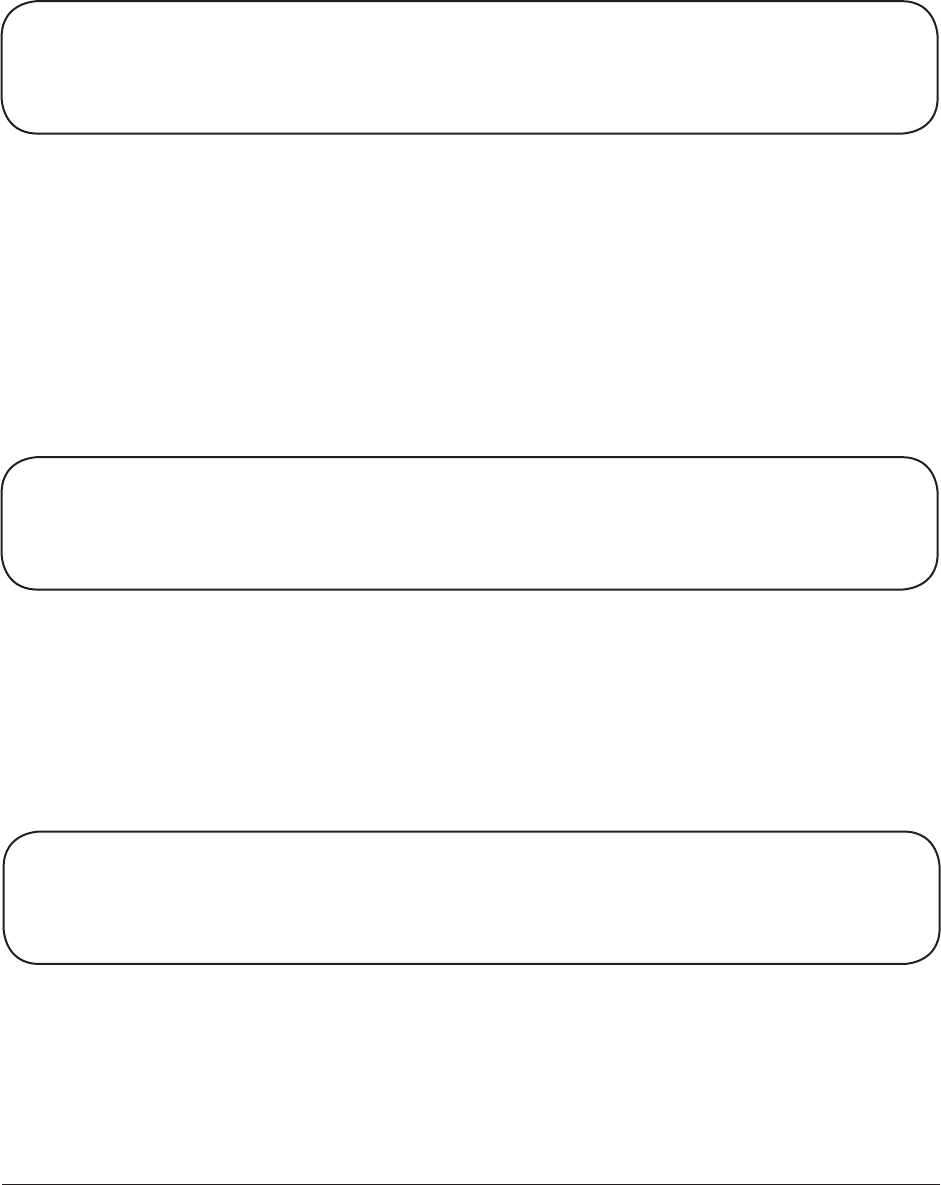
Appendix F
Integrated Illness Management
and Recovery Manual
Page 219
Using the Readiness Ruler to Explore Changes
in Behavior
How important would you say it is to make this change?
Not at all Somewhat Extremely
Important Important Important
1 2 3 4 5 6 7 8 9 10
• Why did you pick a ____ and not a lower number?
• What would it take for you to be at a higher number?
• What concerns do you have about changing your behavior?
If you were to decide right now to make a change in your behavior, how
confident are you that you could succeed?
Not at all Somewhat Extremely
Important Important Important
1 2 3 4 5 6 7 8 9 10
• Why did you pick a ____ and not a lower number?
• What would help you to have a higher number?
How ready are you right now to make a change in your behavior?
Not at all Ready Trying
Ready Unsure to Change
1 2 3 4 5 6 7 8 9 10
• What changes are you interested in making?
• Please list your goal for making a change.
• Is there a first step you can take now that could take now to make the change you identified? If so,
what is it and when could you do it?
